User login
Making one key connection may increase HPV vax uptake
The understanding that human papillomavirus (HPV) causes oropharyngeal squamous cell carcinoma (OPSCC) has been linked with increased likelihood of adults having been vaccinated for HPV, new research indicates.
In a study published online in JAMA Otolaryngology–Head and Neck Surgery, most of the 288 adults surveyed with validated questions were not aware that HPV causes OPSCC and had not been told of the relationship by their health care provider.
Researchers found that when participants knew about the relationship between HPV infection and OPSCC they were more than three times as likely to be vaccinated (odds ratio, 3.7; 95% confidence interval, 1.8-7.6) as those without the knowledge.
The survey was paired with a novel point-of-care adult vaccination program within an otolaryngology clinic.
“Targeted education aimed at unvaccinated adults establishing the relationship between HPV infection and OPSCC, paired with point-of-care vaccination, may be an innovative strategy for increasing HPV vaccination rates in adults,” write the authors, led by Jacob C. Bloom, MD, with the department of otolaryngology–head and neck surgery at Boston Medical Center.
Current HPV vaccination recommendations include three parts:
- Routine vaccination at age 11 or 12 years
- Catch-up vaccination at ages 13-26 years if not adequately vaccinated
- Shared clinical decision-making in adults aged 27-45 years if the vaccine series has not been completed.
Despite proven efficacy and safety of the HPV vaccine, vaccination rates are low for adults. Although 75% of adolescents aged 13-17 years have initiated the HPV vaccine, recent studies show only 16% of U.S. men aged 18-21 years have received at least 1 dose of the HPV vaccine, the authors write.
Christiana Zhang, MD, with the division of internal medicine at Johns Hopkins University in Baltimore, who was not part of the study, said she was not surprised by the lack of knowledge about the HPV-OPSCC link.
Patients are often counseled on the relationship between HPV and genital warts or anogenital cancers like cervical cancer, she says, but there is less patient education surrounding the relationship between HPV and oropharyngeal cancers.
She says she does counsel patients on the link with OPSCC, but not all providers do and provider knowledge in general surrounding HPV is low.
“Research has shown that knowledge and confidence among health care providers surrounding HPV vaccination is generally low, and this corresponds with a low vaccination recommendation rate,” she says.
She adds, “Patient education on HPV infection and its relationship with OPSCC, paired with point-of-care vaccination for qualifying patients, is a great approach.”
But the education needs to go beyond patients, she says.
“Given the important role that health care providers play in vaccine uptake, I think further efforts are needed to educate providers on HPV vaccination as well,” she says.
The study included patients aged 18-45 years who sought routine outpatient care at the otolaryngology clinic at Boston Medical Center from Sept. 1, 2020, to May 19, 2021.
Limitations of this study include studying a population from a single otolaryngology clinic in an urban, academic medical center. The population was more racially and ethnically diverse than the U.S. population with 60.3% identifying as racial and ethnic minorities. Gender and educational levels were also not reflective of U.S. demographics as half (50.8%) of the participants had a college degree or higher and 58.3% were women.
Dr. Bloom reports grants from the American Head and Neck Cancer Society during the conduct of the study. Coauthor Dr. Faden reports personal fees from Merck, Neotic, Focus, BMS, Chrystalis Biomedical Advisors, and Guidepoint; receiving nonfinancial support from BostonGene and Predicine; and receiving grants from Calico outside the submitted work. Dr. Zhang reports no relevant financial relationships.
The understanding that human papillomavirus (HPV) causes oropharyngeal squamous cell carcinoma (OPSCC) has been linked with increased likelihood of adults having been vaccinated for HPV, new research indicates.
In a study published online in JAMA Otolaryngology–Head and Neck Surgery, most of the 288 adults surveyed with validated questions were not aware that HPV causes OPSCC and had not been told of the relationship by their health care provider.
Researchers found that when participants knew about the relationship between HPV infection and OPSCC they were more than three times as likely to be vaccinated (odds ratio, 3.7; 95% confidence interval, 1.8-7.6) as those without the knowledge.
The survey was paired with a novel point-of-care adult vaccination program within an otolaryngology clinic.
“Targeted education aimed at unvaccinated adults establishing the relationship between HPV infection and OPSCC, paired with point-of-care vaccination, may be an innovative strategy for increasing HPV vaccination rates in adults,” write the authors, led by Jacob C. Bloom, MD, with the department of otolaryngology–head and neck surgery at Boston Medical Center.
Current HPV vaccination recommendations include three parts:
- Routine vaccination at age 11 or 12 years
- Catch-up vaccination at ages 13-26 years if not adequately vaccinated
- Shared clinical decision-making in adults aged 27-45 years if the vaccine series has not been completed.
Despite proven efficacy and safety of the HPV vaccine, vaccination rates are low for adults. Although 75% of adolescents aged 13-17 years have initiated the HPV vaccine, recent studies show only 16% of U.S. men aged 18-21 years have received at least 1 dose of the HPV vaccine, the authors write.
Christiana Zhang, MD, with the division of internal medicine at Johns Hopkins University in Baltimore, who was not part of the study, said she was not surprised by the lack of knowledge about the HPV-OPSCC link.
Patients are often counseled on the relationship between HPV and genital warts or anogenital cancers like cervical cancer, she says, but there is less patient education surrounding the relationship between HPV and oropharyngeal cancers.
She says she does counsel patients on the link with OPSCC, but not all providers do and provider knowledge in general surrounding HPV is low.
“Research has shown that knowledge and confidence among health care providers surrounding HPV vaccination is generally low, and this corresponds with a low vaccination recommendation rate,” she says.
She adds, “Patient education on HPV infection and its relationship with OPSCC, paired with point-of-care vaccination for qualifying patients, is a great approach.”
But the education needs to go beyond patients, she says.
“Given the important role that health care providers play in vaccine uptake, I think further efforts are needed to educate providers on HPV vaccination as well,” she says.
The study included patients aged 18-45 years who sought routine outpatient care at the otolaryngology clinic at Boston Medical Center from Sept. 1, 2020, to May 19, 2021.
Limitations of this study include studying a population from a single otolaryngology clinic in an urban, academic medical center. The population was more racially and ethnically diverse than the U.S. population with 60.3% identifying as racial and ethnic minorities. Gender and educational levels were also not reflective of U.S. demographics as half (50.8%) of the participants had a college degree or higher and 58.3% were women.
Dr. Bloom reports grants from the American Head and Neck Cancer Society during the conduct of the study. Coauthor Dr. Faden reports personal fees from Merck, Neotic, Focus, BMS, Chrystalis Biomedical Advisors, and Guidepoint; receiving nonfinancial support from BostonGene and Predicine; and receiving grants from Calico outside the submitted work. Dr. Zhang reports no relevant financial relationships.
The understanding that human papillomavirus (HPV) causes oropharyngeal squamous cell carcinoma (OPSCC) has been linked with increased likelihood of adults having been vaccinated for HPV, new research indicates.
In a study published online in JAMA Otolaryngology–Head and Neck Surgery, most of the 288 adults surveyed with validated questions were not aware that HPV causes OPSCC and had not been told of the relationship by their health care provider.
Researchers found that when participants knew about the relationship between HPV infection and OPSCC they were more than three times as likely to be vaccinated (odds ratio, 3.7; 95% confidence interval, 1.8-7.6) as those without the knowledge.
The survey was paired with a novel point-of-care adult vaccination program within an otolaryngology clinic.
“Targeted education aimed at unvaccinated adults establishing the relationship between HPV infection and OPSCC, paired with point-of-care vaccination, may be an innovative strategy for increasing HPV vaccination rates in adults,” write the authors, led by Jacob C. Bloom, MD, with the department of otolaryngology–head and neck surgery at Boston Medical Center.
Current HPV vaccination recommendations include three parts:
- Routine vaccination at age 11 or 12 years
- Catch-up vaccination at ages 13-26 years if not adequately vaccinated
- Shared clinical decision-making in adults aged 27-45 years if the vaccine series has not been completed.
Despite proven efficacy and safety of the HPV vaccine, vaccination rates are low for adults. Although 75% of adolescents aged 13-17 years have initiated the HPV vaccine, recent studies show only 16% of U.S. men aged 18-21 years have received at least 1 dose of the HPV vaccine, the authors write.
Christiana Zhang, MD, with the division of internal medicine at Johns Hopkins University in Baltimore, who was not part of the study, said she was not surprised by the lack of knowledge about the HPV-OPSCC link.
Patients are often counseled on the relationship between HPV and genital warts or anogenital cancers like cervical cancer, she says, but there is less patient education surrounding the relationship between HPV and oropharyngeal cancers.
She says she does counsel patients on the link with OPSCC, but not all providers do and provider knowledge in general surrounding HPV is low.
“Research has shown that knowledge and confidence among health care providers surrounding HPV vaccination is generally low, and this corresponds with a low vaccination recommendation rate,” she says.
She adds, “Patient education on HPV infection and its relationship with OPSCC, paired with point-of-care vaccination for qualifying patients, is a great approach.”
But the education needs to go beyond patients, she says.
“Given the important role that health care providers play in vaccine uptake, I think further efforts are needed to educate providers on HPV vaccination as well,” she says.
The study included patients aged 18-45 years who sought routine outpatient care at the otolaryngology clinic at Boston Medical Center from Sept. 1, 2020, to May 19, 2021.
Limitations of this study include studying a population from a single otolaryngology clinic in an urban, academic medical center. The population was more racially and ethnically diverse than the U.S. population with 60.3% identifying as racial and ethnic minorities. Gender and educational levels were also not reflective of U.S. demographics as half (50.8%) of the participants had a college degree or higher and 58.3% were women.
Dr. Bloom reports grants from the American Head and Neck Cancer Society during the conduct of the study. Coauthor Dr. Faden reports personal fees from Merck, Neotic, Focus, BMS, Chrystalis Biomedical Advisors, and Guidepoint; receiving nonfinancial support from BostonGene and Predicine; and receiving grants from Calico outside the submitted work. Dr. Zhang reports no relevant financial relationships.
FROM JAMA OTOLARYNGOLOGY–HEAD AND NECK SURGERY
Industry funding falls for rheumatology research
Industry-sponsored research funding has fallen by more than 20% from 2014 to 2022, according to a new analysis.
“Despite the growing partnerships and networks between rheumatologists, the public sector, and the health care industry to optimize research funding allocations, the declining trend in industry-sponsored research payments is a concerning sign for all rheumatologists,” writes study author Anju Murayama, an undergraduate medical student at the Tohoku University School of Medicine in Sendai City, Japan. The data suggest that “more and more rheumatologists are facing difficulties in obtaining research funding from the health care industry.”
Dr. Murayama used the Open Payments Database, which contains records of payments made by drug and pharmaceutical companies to health care providers. The analysis included research payments provided directly to rheumatologists (direct-research payments) and payments given to clinicians or health care organizations related to research whose principal investigator was a rheumatologist (associated-research payments). These associated payments included costs for study enrollment and screening, safety monitoring committees, research publication, and more.
The research was published August 15 in The Journal of Rheumatology .
In 2014, the total direct payments to rheumatologists from industry were $1.4 million. These payments jumped to nearly $4.6 million in 2016 but have declined since. In 2022, there were $976,481 in total payments, a 31% drop from 9 years before.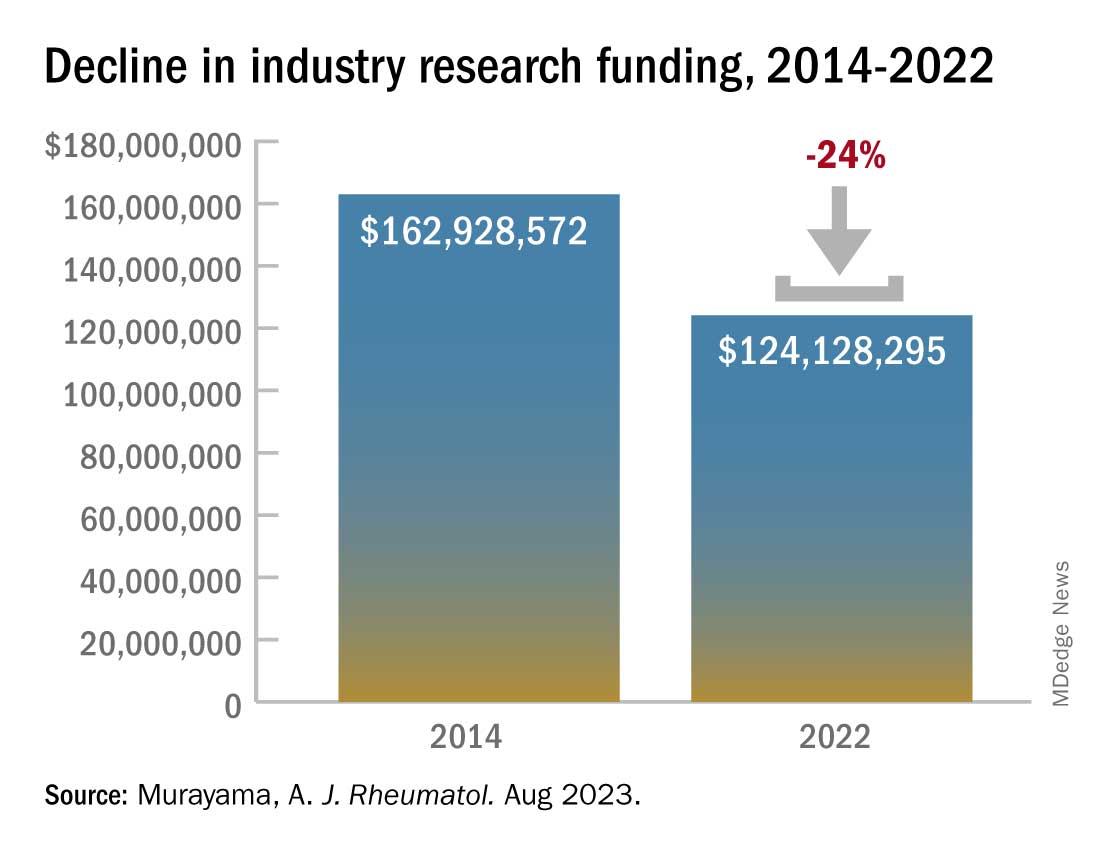
This decline comes after an observed drop in research funding from the public sector. From 2014 to 2017, public-sector research funding to members of the American College of Rheumatology fell by 7.5%. Timothy Niewold, MD, a rheumatologist and vice chair for research in the department of medicine at Hospital for Special Surgery, New York, said that he and colleagues have felt the funding squeeze from both public and industry sectors. “The budgets for trials have seemed tight,” he told this news organization. With the overhead and cost of doing a trial at an academic institution like HSS, “sometimes you can’t make the budget work,” and researchers must pass on industry-funded trials.
The analysis also found a larger discrepancy between average and median associated-research payments. Of the $1.4 billion in associated-research payments combined over the 9-year period, the median payments per physician ($173,022) were much smaller than the mean payments ($989,753), which indicates that “only a very small number of rheumatologists received substantial amounts of research funding from the industry,” Dr. Murayama wrote in an email to this news organization. “This finding might support statements published by Scher and Schett in Nature Review Rheumatology suggesting that many industry-initiated clinical trials are conducted and authored by a small number of influential rheumatologists, often referred to as key opinion leaders.”
The analysis also found that of all associated payments, less than 3% ($39.2 million) went to funding preclinical research, which is “more disappointing than surprising,” Dr. Niewold said. Though clinical trials are expensive and require larger amounts of investment, industry partnerships at preclinical phases of research are important for devising novel solutions for these complex rheumatic diseases, he noted. “The clinical trials are one piece,” he added, “but you need the whole [research] continuum.”
Dr. Niewold reports receiving research grants from EMD Serono and Zenas Biopharma and consulting for Thermo Fisher Scientific, Progentec Diagnostics, Roivant Sciences, Ventus, S3 Connected Health, AstraZeneca, and Inova. Dr. Murayama reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Industry-sponsored research funding has fallen by more than 20% from 2014 to 2022, according to a new analysis.
“Despite the growing partnerships and networks between rheumatologists, the public sector, and the health care industry to optimize research funding allocations, the declining trend in industry-sponsored research payments is a concerning sign for all rheumatologists,” writes study author Anju Murayama, an undergraduate medical student at the Tohoku University School of Medicine in Sendai City, Japan. The data suggest that “more and more rheumatologists are facing difficulties in obtaining research funding from the health care industry.”
Dr. Murayama used the Open Payments Database, which contains records of payments made by drug and pharmaceutical companies to health care providers. The analysis included research payments provided directly to rheumatologists (direct-research payments) and payments given to clinicians or health care organizations related to research whose principal investigator was a rheumatologist (associated-research payments). These associated payments included costs for study enrollment and screening, safety monitoring committees, research publication, and more.
The research was published August 15 in The Journal of Rheumatology .
In 2014, the total direct payments to rheumatologists from industry were $1.4 million. These payments jumped to nearly $4.6 million in 2016 but have declined since. In 2022, there were $976,481 in total payments, a 31% drop from 9 years before.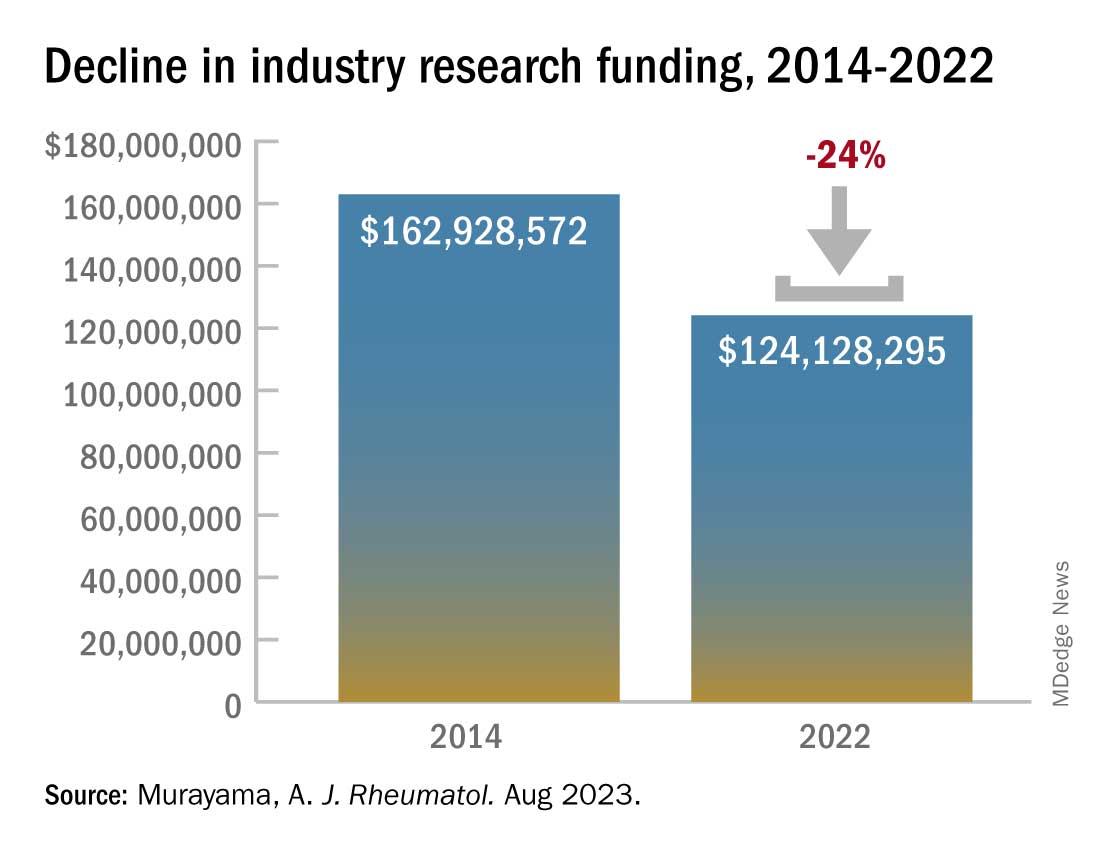
This decline comes after an observed drop in research funding from the public sector. From 2014 to 2017, public-sector research funding to members of the American College of Rheumatology fell by 7.5%. Timothy Niewold, MD, a rheumatologist and vice chair for research in the department of medicine at Hospital for Special Surgery, New York, said that he and colleagues have felt the funding squeeze from both public and industry sectors. “The budgets for trials have seemed tight,” he told this news organization. With the overhead and cost of doing a trial at an academic institution like HSS, “sometimes you can’t make the budget work,” and researchers must pass on industry-funded trials.
The analysis also found a larger discrepancy between average and median associated-research payments. Of the $1.4 billion in associated-research payments combined over the 9-year period, the median payments per physician ($173,022) were much smaller than the mean payments ($989,753), which indicates that “only a very small number of rheumatologists received substantial amounts of research funding from the industry,” Dr. Murayama wrote in an email to this news organization. “This finding might support statements published by Scher and Schett in Nature Review Rheumatology suggesting that many industry-initiated clinical trials are conducted and authored by a small number of influential rheumatologists, often referred to as key opinion leaders.”
The analysis also found that of all associated payments, less than 3% ($39.2 million) went to funding preclinical research, which is “more disappointing than surprising,” Dr. Niewold said. Though clinical trials are expensive and require larger amounts of investment, industry partnerships at preclinical phases of research are important for devising novel solutions for these complex rheumatic diseases, he noted. “The clinical trials are one piece,” he added, “but you need the whole [research] continuum.”
Dr. Niewold reports receiving research grants from EMD Serono and Zenas Biopharma and consulting for Thermo Fisher Scientific, Progentec Diagnostics, Roivant Sciences, Ventus, S3 Connected Health, AstraZeneca, and Inova. Dr. Murayama reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Industry-sponsored research funding has fallen by more than 20% from 2014 to 2022, according to a new analysis.
“Despite the growing partnerships and networks between rheumatologists, the public sector, and the health care industry to optimize research funding allocations, the declining trend in industry-sponsored research payments is a concerning sign for all rheumatologists,” writes study author Anju Murayama, an undergraduate medical student at the Tohoku University School of Medicine in Sendai City, Japan. The data suggest that “more and more rheumatologists are facing difficulties in obtaining research funding from the health care industry.”
Dr. Murayama used the Open Payments Database, which contains records of payments made by drug and pharmaceutical companies to health care providers. The analysis included research payments provided directly to rheumatologists (direct-research payments) and payments given to clinicians or health care organizations related to research whose principal investigator was a rheumatologist (associated-research payments). These associated payments included costs for study enrollment and screening, safety monitoring committees, research publication, and more.
The research was published August 15 in The Journal of Rheumatology .
In 2014, the total direct payments to rheumatologists from industry were $1.4 million. These payments jumped to nearly $4.6 million in 2016 but have declined since. In 2022, there were $976,481 in total payments, a 31% drop from 9 years before.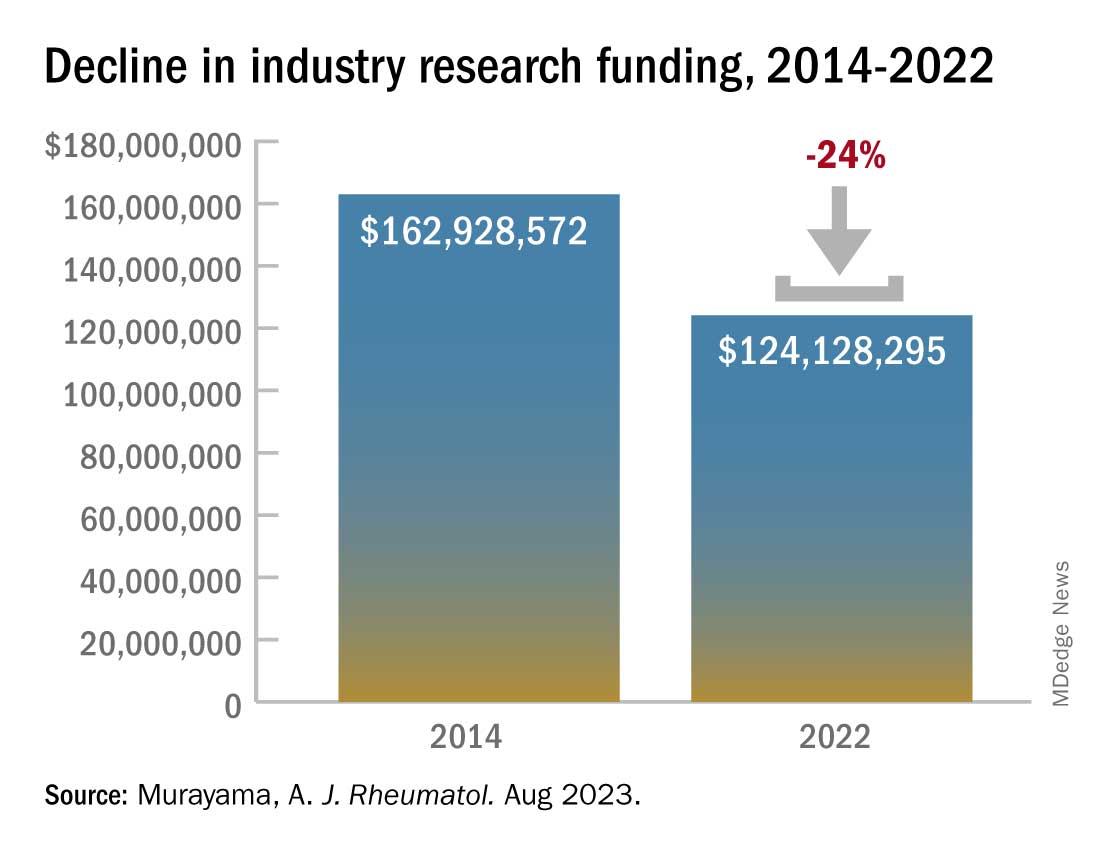
This decline comes after an observed drop in research funding from the public sector. From 2014 to 2017, public-sector research funding to members of the American College of Rheumatology fell by 7.5%. Timothy Niewold, MD, a rheumatologist and vice chair for research in the department of medicine at Hospital for Special Surgery, New York, said that he and colleagues have felt the funding squeeze from both public and industry sectors. “The budgets for trials have seemed tight,” he told this news organization. With the overhead and cost of doing a trial at an academic institution like HSS, “sometimes you can’t make the budget work,” and researchers must pass on industry-funded trials.
The analysis also found a larger discrepancy between average and median associated-research payments. Of the $1.4 billion in associated-research payments combined over the 9-year period, the median payments per physician ($173,022) were much smaller than the mean payments ($989,753), which indicates that “only a very small number of rheumatologists received substantial amounts of research funding from the industry,” Dr. Murayama wrote in an email to this news organization. “This finding might support statements published by Scher and Schett in Nature Review Rheumatology suggesting that many industry-initiated clinical trials are conducted and authored by a small number of influential rheumatologists, often referred to as key opinion leaders.”
The analysis also found that of all associated payments, less than 3% ($39.2 million) went to funding preclinical research, which is “more disappointing than surprising,” Dr. Niewold said. Though clinical trials are expensive and require larger amounts of investment, industry partnerships at preclinical phases of research are important for devising novel solutions for these complex rheumatic diseases, he noted. “The clinical trials are one piece,” he added, “but you need the whole [research] continuum.”
Dr. Niewold reports receiving research grants from EMD Serono and Zenas Biopharma and consulting for Thermo Fisher Scientific, Progentec Diagnostics, Roivant Sciences, Ventus, S3 Connected Health, AstraZeneca, and Inova. Dr. Murayama reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF RHEUMATOLOGY
Medicare announces 10 drugs targeted for price cuts in 2026
People on Medicare may in 2026 see prices drop for 10 medicines, including pricey diabetes, cancer, blood clot, and arthritis treatments, if advocates for federal drug-price negotiations can implement their plans amid tough opposition.
It’s unclear at this time, though, how these negotiations will play out. The Chamber of Commerce has sided with pharmaceutical companies in bids to block direct Medicare negotiation of drug prices. Many influential Republicans in Congress oppose this plan, which has deep support from both Democrats and AARP.
While facing strong opposition to negotiations, the Centers for Medicare & Medicaid Services sought in its announcement to illustrate the high costs of the selected medicines.
CMS provided data on total Part D costs for selected medicines for the period from June 2022 to May 2023, along with tallies of the number of people taking these drugs. The 10 selected medicines are as follows:
- Eliquis (generic name: apixaban), used to prevent and treat serious blood clots. It is taken by about 3.7 million people through Part D plans. The estimated cost is $16.4 billion.
- Jardiance (generic name: empagliflozin), used for diabetes and heart failure. It is taken by almost 1.6 million people through Part D plans. The estimated cost is $7.06 billion.
- Xarelto (generic name: rivaroxaban), used for blood clots. It is taken by about 1.3 million people through Part D plans. The estimated cost is $6 billion.
- Januvia (generic name: sitagliptin), used for diabetes. It is taken by about 869,00 people through Part D plans. The estimated cost is $4.1 billion.
- Farxiga (generic name: dapagliflozin), used for diabetes, heart failure, and chronic kidney disease. It is taken by about 799,000 people through Part D plans. The estimated cost is almost $3.3 billion.
- Entresto (generic name: sacubitril/valsartan), used to treat heart failure. It is taken by 587,000 people through Part D plans. The estimated cost is $2.9 billion.
- Enbrel( generic name: etanercept), used for rheumatoid arthritis, psoriasis, and psoriatic arthritis. It is taken by 48,000 people through Part D plans. The estimated cost is $2.8 billion.
- Imbruvica (generic name: ibrutinib), used to treat some blood cancers. It is taken by about 20,000 people in Part D plans. The estimated cost is $2.7 billion.
- Stelara (generic name: ustekinumab), used to treat plaque psoriasis, psoriatic arthritis, or certain bowel conditions (Crohn’s disease, ulcerative colitis). It is used by about 22,000 people through Part D plans. The estimated cost is $2.6 billion.
- Fiasp; Fiasp FlexTouch; Fiasp PenFill; NovoLog; NovoLog FlexPen; NovoLog PenFill. These are forms of insulin used to treat diabetes. They are used by about 777,000 people through Part D plans. The estimated cost is $2.6 billion.
A vocal critic of Medicare drug negotiations, Joel White, president of the Council for Affordable Health Coverage, called the announcement of the 10 drugs selected for negotiation “a hollow victory lap.” A former Republican staffer on the House Ways and Means Committee, Mr. White aided with the development of the Medicare Part D plans and has kept tabs on the pharmacy programs since its launch in 2006.
“No one’s costs will go down now or for years because of this announcement” about Part D negotiations, Mr. White said in a statement.
According to its website, CAHC includes among its members the American Academy of Ophthalmology as well as some patient groups, drugmakers, such as Johnson & Johnson, and insurers and industry groups, such as the National Association of Manufacturers.
Separately, the influential Chamber of Commerce is making a strong push to at least delay the implementation of the Medicare Part D drug negotiations. On Aug. 28, the chamber released a letter sent to the Biden administration, raising concerns about a “rush” to implement the provisions of the Inflation Reduction Act.
The chamber also has filed suit to challenge the drug negotiation provisions of the Inflation Reduction Act, requesting that the court issue a preliminary injunction by Oct. 1, 2023.
Other pending legal challenges to direct Medicare drug negotiations include suits filed by Merck, Bristol-Myers Squibb, Johnson & Johnson, Boehringer Ingelheim, and AstraZeneca, according to an email from Pharmaceutical Research and Manufacturers of America. PhRMA also said it is a party to a case.
In addition, the three congressional Republicans with most direct influence over Medicare policy issued on Aug. 29 a joint statement outlining their objections to the planned negotiations on drug prices.
This drug-negotiation proposal is “an unworkable, legally dubious scheme that will lead to higher prices for new drugs coming to market, stifle the development of new cures, and destroy jobs,” said House Energy and Commerce Committee Chair Cathy McMorris Rodgers (R-Wash.), House Ways and Means Committee Chair Jason Smith (R-Mo.), and Senate Finance Committee Ranking Member Mike Crapo (R-Idaho).
Democrats were equally firm and vocal in their support of the negotiations. Senate Finance Chairman Ron Wyden (D-Ore.) issued a statement on Aug. 29 that said the release of the list of the 10 drugs selected for Medicare drug negotiations is part of a “seismic shift in the relationship between Big Pharma, the federal government, and seniors who are counting on lower prices.
“I will be following the negotiation process closely and will fight any attempt by Big Pharma to undo or undermine the progress that’s been made,” Mr. Wyden said.
In addition, AARP issued a statement of its continued support for Medicare drug negotiations.
“The No. 1 reason seniors skip or ration their prescriptions is because they can’t afford them. This must stop,” said AARP executive vice president and chief advocacy and engagement officer Nancy LeaMond in the statement. “The big drug companies and their allies continue suing to overturn the Medicare drug price negotiation program to keep up their price gouging. We can’t allow seniors to be Big Pharma’s cash machine anymore.”
A version of this article first appeared on Medscape.com.
People on Medicare may in 2026 see prices drop for 10 medicines, including pricey diabetes, cancer, blood clot, and arthritis treatments, if advocates for federal drug-price negotiations can implement their plans amid tough opposition.
It’s unclear at this time, though, how these negotiations will play out. The Chamber of Commerce has sided with pharmaceutical companies in bids to block direct Medicare negotiation of drug prices. Many influential Republicans in Congress oppose this plan, which has deep support from both Democrats and AARP.
While facing strong opposition to negotiations, the Centers for Medicare & Medicaid Services sought in its announcement to illustrate the high costs of the selected medicines.
CMS provided data on total Part D costs for selected medicines for the period from June 2022 to May 2023, along with tallies of the number of people taking these drugs. The 10 selected medicines are as follows:
- Eliquis (generic name: apixaban), used to prevent and treat serious blood clots. It is taken by about 3.7 million people through Part D plans. The estimated cost is $16.4 billion.
- Jardiance (generic name: empagliflozin), used for diabetes and heart failure. It is taken by almost 1.6 million people through Part D plans. The estimated cost is $7.06 billion.
- Xarelto (generic name: rivaroxaban), used for blood clots. It is taken by about 1.3 million people through Part D plans. The estimated cost is $6 billion.
- Januvia (generic name: sitagliptin), used for diabetes. It is taken by about 869,00 people through Part D plans. The estimated cost is $4.1 billion.
- Farxiga (generic name: dapagliflozin), used for diabetes, heart failure, and chronic kidney disease. It is taken by about 799,000 people through Part D plans. The estimated cost is almost $3.3 billion.
- Entresto (generic name: sacubitril/valsartan), used to treat heart failure. It is taken by 587,000 people through Part D plans. The estimated cost is $2.9 billion.
- Enbrel( generic name: etanercept), used for rheumatoid arthritis, psoriasis, and psoriatic arthritis. It is taken by 48,000 people through Part D plans. The estimated cost is $2.8 billion.
- Imbruvica (generic name: ibrutinib), used to treat some blood cancers. It is taken by about 20,000 people in Part D plans. The estimated cost is $2.7 billion.
- Stelara (generic name: ustekinumab), used to treat plaque psoriasis, psoriatic arthritis, or certain bowel conditions (Crohn’s disease, ulcerative colitis). It is used by about 22,000 people through Part D plans. The estimated cost is $2.6 billion.
- Fiasp; Fiasp FlexTouch; Fiasp PenFill; NovoLog; NovoLog FlexPen; NovoLog PenFill. These are forms of insulin used to treat diabetes. They are used by about 777,000 people through Part D plans. The estimated cost is $2.6 billion.
A vocal critic of Medicare drug negotiations, Joel White, president of the Council for Affordable Health Coverage, called the announcement of the 10 drugs selected for negotiation “a hollow victory lap.” A former Republican staffer on the House Ways and Means Committee, Mr. White aided with the development of the Medicare Part D plans and has kept tabs on the pharmacy programs since its launch in 2006.
“No one’s costs will go down now or for years because of this announcement” about Part D negotiations, Mr. White said in a statement.
According to its website, CAHC includes among its members the American Academy of Ophthalmology as well as some patient groups, drugmakers, such as Johnson & Johnson, and insurers and industry groups, such as the National Association of Manufacturers.
Separately, the influential Chamber of Commerce is making a strong push to at least delay the implementation of the Medicare Part D drug negotiations. On Aug. 28, the chamber released a letter sent to the Biden administration, raising concerns about a “rush” to implement the provisions of the Inflation Reduction Act.
The chamber also has filed suit to challenge the drug negotiation provisions of the Inflation Reduction Act, requesting that the court issue a preliminary injunction by Oct. 1, 2023.
Other pending legal challenges to direct Medicare drug negotiations include suits filed by Merck, Bristol-Myers Squibb, Johnson & Johnson, Boehringer Ingelheim, and AstraZeneca, according to an email from Pharmaceutical Research and Manufacturers of America. PhRMA also said it is a party to a case.
In addition, the three congressional Republicans with most direct influence over Medicare policy issued on Aug. 29 a joint statement outlining their objections to the planned negotiations on drug prices.
This drug-negotiation proposal is “an unworkable, legally dubious scheme that will lead to higher prices for new drugs coming to market, stifle the development of new cures, and destroy jobs,” said House Energy and Commerce Committee Chair Cathy McMorris Rodgers (R-Wash.), House Ways and Means Committee Chair Jason Smith (R-Mo.), and Senate Finance Committee Ranking Member Mike Crapo (R-Idaho).
Democrats were equally firm and vocal in their support of the negotiations. Senate Finance Chairman Ron Wyden (D-Ore.) issued a statement on Aug. 29 that said the release of the list of the 10 drugs selected for Medicare drug negotiations is part of a “seismic shift in the relationship between Big Pharma, the federal government, and seniors who are counting on lower prices.
“I will be following the negotiation process closely and will fight any attempt by Big Pharma to undo or undermine the progress that’s been made,” Mr. Wyden said.
In addition, AARP issued a statement of its continued support for Medicare drug negotiations.
“The No. 1 reason seniors skip or ration their prescriptions is because they can’t afford them. This must stop,” said AARP executive vice president and chief advocacy and engagement officer Nancy LeaMond in the statement. “The big drug companies and their allies continue suing to overturn the Medicare drug price negotiation program to keep up their price gouging. We can’t allow seniors to be Big Pharma’s cash machine anymore.”
A version of this article first appeared on Medscape.com.
People on Medicare may in 2026 see prices drop for 10 medicines, including pricey diabetes, cancer, blood clot, and arthritis treatments, if advocates for federal drug-price negotiations can implement their plans amid tough opposition.
It’s unclear at this time, though, how these negotiations will play out. The Chamber of Commerce has sided with pharmaceutical companies in bids to block direct Medicare negotiation of drug prices. Many influential Republicans in Congress oppose this plan, which has deep support from both Democrats and AARP.
While facing strong opposition to negotiations, the Centers for Medicare & Medicaid Services sought in its announcement to illustrate the high costs of the selected medicines.
CMS provided data on total Part D costs for selected medicines for the period from June 2022 to May 2023, along with tallies of the number of people taking these drugs. The 10 selected medicines are as follows:
- Eliquis (generic name: apixaban), used to prevent and treat serious blood clots. It is taken by about 3.7 million people through Part D plans. The estimated cost is $16.4 billion.
- Jardiance (generic name: empagliflozin), used for diabetes and heart failure. It is taken by almost 1.6 million people through Part D plans. The estimated cost is $7.06 billion.
- Xarelto (generic name: rivaroxaban), used for blood clots. It is taken by about 1.3 million people through Part D plans. The estimated cost is $6 billion.
- Januvia (generic name: sitagliptin), used for diabetes. It is taken by about 869,00 people through Part D plans. The estimated cost is $4.1 billion.
- Farxiga (generic name: dapagliflozin), used for diabetes, heart failure, and chronic kidney disease. It is taken by about 799,000 people through Part D plans. The estimated cost is almost $3.3 billion.
- Entresto (generic name: sacubitril/valsartan), used to treat heart failure. It is taken by 587,000 people through Part D plans. The estimated cost is $2.9 billion.
- Enbrel( generic name: etanercept), used for rheumatoid arthritis, psoriasis, and psoriatic arthritis. It is taken by 48,000 people through Part D plans. The estimated cost is $2.8 billion.
- Imbruvica (generic name: ibrutinib), used to treat some blood cancers. It is taken by about 20,000 people in Part D plans. The estimated cost is $2.7 billion.
- Stelara (generic name: ustekinumab), used to treat plaque psoriasis, psoriatic arthritis, or certain bowel conditions (Crohn’s disease, ulcerative colitis). It is used by about 22,000 people through Part D plans. The estimated cost is $2.6 billion.
- Fiasp; Fiasp FlexTouch; Fiasp PenFill; NovoLog; NovoLog FlexPen; NovoLog PenFill. These are forms of insulin used to treat diabetes. They are used by about 777,000 people through Part D plans. The estimated cost is $2.6 billion.
A vocal critic of Medicare drug negotiations, Joel White, president of the Council for Affordable Health Coverage, called the announcement of the 10 drugs selected for negotiation “a hollow victory lap.” A former Republican staffer on the House Ways and Means Committee, Mr. White aided with the development of the Medicare Part D plans and has kept tabs on the pharmacy programs since its launch in 2006.
“No one’s costs will go down now or for years because of this announcement” about Part D negotiations, Mr. White said in a statement.
According to its website, CAHC includes among its members the American Academy of Ophthalmology as well as some patient groups, drugmakers, such as Johnson & Johnson, and insurers and industry groups, such as the National Association of Manufacturers.
Separately, the influential Chamber of Commerce is making a strong push to at least delay the implementation of the Medicare Part D drug negotiations. On Aug. 28, the chamber released a letter sent to the Biden administration, raising concerns about a “rush” to implement the provisions of the Inflation Reduction Act.
The chamber also has filed suit to challenge the drug negotiation provisions of the Inflation Reduction Act, requesting that the court issue a preliminary injunction by Oct. 1, 2023.
Other pending legal challenges to direct Medicare drug negotiations include suits filed by Merck, Bristol-Myers Squibb, Johnson & Johnson, Boehringer Ingelheim, and AstraZeneca, according to an email from Pharmaceutical Research and Manufacturers of America. PhRMA also said it is a party to a case.
In addition, the three congressional Republicans with most direct influence over Medicare policy issued on Aug. 29 a joint statement outlining their objections to the planned negotiations on drug prices.
This drug-negotiation proposal is “an unworkable, legally dubious scheme that will lead to higher prices for new drugs coming to market, stifle the development of new cures, and destroy jobs,” said House Energy and Commerce Committee Chair Cathy McMorris Rodgers (R-Wash.), House Ways and Means Committee Chair Jason Smith (R-Mo.), and Senate Finance Committee Ranking Member Mike Crapo (R-Idaho).
Democrats were equally firm and vocal in their support of the negotiations. Senate Finance Chairman Ron Wyden (D-Ore.) issued a statement on Aug. 29 that said the release of the list of the 10 drugs selected for Medicare drug negotiations is part of a “seismic shift in the relationship between Big Pharma, the federal government, and seniors who are counting on lower prices.
“I will be following the negotiation process closely and will fight any attempt by Big Pharma to undo or undermine the progress that’s been made,” Mr. Wyden said.
In addition, AARP issued a statement of its continued support for Medicare drug negotiations.
“The No. 1 reason seniors skip or ration their prescriptions is because they can’t afford them. This must stop,” said AARP executive vice president and chief advocacy and engagement officer Nancy LeaMond in the statement. “The big drug companies and their allies continue suing to overturn the Medicare drug price negotiation program to keep up their price gouging. We can’t allow seniors to be Big Pharma’s cash machine anymore.”
A version of this article first appeared on Medscape.com.
It’s not an assembly line
A lot of businesses benefit from being in private equity funds.
Health care isn’t one of them, and a recent report found that
This really shouldn’t surprise anyone. Such funds may offer glittering phrases like “improved technology” and “greater efficiency” but the bottom line is that they’re run by – and for – the shareholders. The majority of them aren’t going to be medical people or realize that you can’t run a medical practice like it’s a clothing retailer or electronic car manufacturer.
I’m not saying medicine isn’t a business – it is. I depend on my little practice to support three families, so keeping it in the black is important. But it also needs to run well to do that. Measures to increase revenue, like cutting my staff down (there are only two of them) or overbooking patients would seriously impact me effectively doing my part, which is playing doctor.
You can predict pretty accurately how long it will take to put a motor and bumper assembly on a specific model of car, but you can’t do that in medicine because people aren’t standardized. Even if you control variables such as same sex, age, and diagnosis, personalities vary widely, as do treatment decisions, questions they’ll have, and the “oh, another thing” factor.
That doesn’t happen at a bottling plant.
In the business model of health care, you’re hoping revenue will pay overhead and a reasonable salary for everyone. But when you add a private equity firm in, the shareholders also expect to be paid. Which means either revenue has to go up significantly, or costs have to be cut (layoffs, short staffing, reduced benefits, etc.), or a combination of both.
Regardless of which option is chosen, it isn’t good for the medical staff or the patients. Increasing the number of people seen in a given amount of time per doctor may be good for the shareholders, but it’s not good for the doctor or the person being cared for. Think of Lucy and Ethyl at the chocolate factory.
Even in an auto factory, if you speed up the rate of cars going through the assembly line, sooner or later mistakes will be made. Humans can’t keep up, and even robots will make errors if things aren’t aligned correctly, or are a few seconds ahead or behind the program. This is why they (hopefully) have quality control, to try and catch those things before they’re on the road.
Of course, cars are more easily fixable. When the mistake is found you repair or replace the part. You can’t do that as easily in people, and when serious mistakes happen it’s the doctor who’s held at fault – not the shareholders who pressured him or her to see patients faster and with less support.
Unfortunately, this is the way the current trend is going. The more people who are involved in the practice of medicine, in person or behind the scenes, the smaller each slice of the pie gets.
That’s not good for the patient, who’s the person at the center of it all and the reason why we’re here.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A lot of businesses benefit from being in private equity funds.
Health care isn’t one of them, and a recent report found that
This really shouldn’t surprise anyone. Such funds may offer glittering phrases like “improved technology” and “greater efficiency” but the bottom line is that they’re run by – and for – the shareholders. The majority of them aren’t going to be medical people or realize that you can’t run a medical practice like it’s a clothing retailer or electronic car manufacturer.
I’m not saying medicine isn’t a business – it is. I depend on my little practice to support three families, so keeping it in the black is important. But it also needs to run well to do that. Measures to increase revenue, like cutting my staff down (there are only two of them) or overbooking patients would seriously impact me effectively doing my part, which is playing doctor.
You can predict pretty accurately how long it will take to put a motor and bumper assembly on a specific model of car, but you can’t do that in medicine because people aren’t standardized. Even if you control variables such as same sex, age, and diagnosis, personalities vary widely, as do treatment decisions, questions they’ll have, and the “oh, another thing” factor.
That doesn’t happen at a bottling plant.
In the business model of health care, you’re hoping revenue will pay overhead and a reasonable salary for everyone. But when you add a private equity firm in, the shareholders also expect to be paid. Which means either revenue has to go up significantly, or costs have to be cut (layoffs, short staffing, reduced benefits, etc.), or a combination of both.
Regardless of which option is chosen, it isn’t good for the medical staff or the patients. Increasing the number of people seen in a given amount of time per doctor may be good for the shareholders, but it’s not good for the doctor or the person being cared for. Think of Lucy and Ethyl at the chocolate factory.
Even in an auto factory, if you speed up the rate of cars going through the assembly line, sooner or later mistakes will be made. Humans can’t keep up, and even robots will make errors if things aren’t aligned correctly, or are a few seconds ahead or behind the program. This is why they (hopefully) have quality control, to try and catch those things before they’re on the road.
Of course, cars are more easily fixable. When the mistake is found you repair or replace the part. You can’t do that as easily in people, and when serious mistakes happen it’s the doctor who’s held at fault – not the shareholders who pressured him or her to see patients faster and with less support.
Unfortunately, this is the way the current trend is going. The more people who are involved in the practice of medicine, in person or behind the scenes, the smaller each slice of the pie gets.
That’s not good for the patient, who’s the person at the center of it all and the reason why we’re here.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A lot of businesses benefit from being in private equity funds.
Health care isn’t one of them, and a recent report found that
This really shouldn’t surprise anyone. Such funds may offer glittering phrases like “improved technology” and “greater efficiency” but the bottom line is that they’re run by – and for – the shareholders. The majority of them aren’t going to be medical people or realize that you can’t run a medical practice like it’s a clothing retailer or electronic car manufacturer.
I’m not saying medicine isn’t a business – it is. I depend on my little practice to support three families, so keeping it in the black is important. But it also needs to run well to do that. Measures to increase revenue, like cutting my staff down (there are only two of them) or overbooking patients would seriously impact me effectively doing my part, which is playing doctor.
You can predict pretty accurately how long it will take to put a motor and bumper assembly on a specific model of car, but you can’t do that in medicine because people aren’t standardized. Even if you control variables such as same sex, age, and diagnosis, personalities vary widely, as do treatment decisions, questions they’ll have, and the “oh, another thing” factor.
That doesn’t happen at a bottling plant.
In the business model of health care, you’re hoping revenue will pay overhead and a reasonable salary for everyone. But when you add a private equity firm in, the shareholders also expect to be paid. Which means either revenue has to go up significantly, or costs have to be cut (layoffs, short staffing, reduced benefits, etc.), or a combination of both.
Regardless of which option is chosen, it isn’t good for the medical staff or the patients. Increasing the number of people seen in a given amount of time per doctor may be good for the shareholders, but it’s not good for the doctor or the person being cared for. Think of Lucy and Ethyl at the chocolate factory.
Even in an auto factory, if you speed up the rate of cars going through the assembly line, sooner or later mistakes will be made. Humans can’t keep up, and even robots will make errors if things aren’t aligned correctly, or are a few seconds ahead or behind the program. This is why they (hopefully) have quality control, to try and catch those things before they’re on the road.
Of course, cars are more easily fixable. When the mistake is found you repair or replace the part. You can’t do that as easily in people, and when serious mistakes happen it’s the doctor who’s held at fault – not the shareholders who pressured him or her to see patients faster and with less support.
Unfortunately, this is the way the current trend is going. The more people who are involved in the practice of medicine, in person or behind the scenes, the smaller each slice of the pie gets.
That’s not good for the patient, who’s the person at the center of it all and the reason why we’re here.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Use of mental health services soared during pandemic
By the end of August 2022, overall use of mental health services was almost 40% higher than before the COVID-19 pandemic, while spending increased by 54%, according to a new study by researchers at the RAND Corporation.
During the early phase of the pandemic, from mid-March to mid-December 2020, before the vaccine was available, in-person visits decreased by 40%, while telehealth visits increased by 1,000%, reported Jonathan H. Cantor, PhD, and colleagues at RAND, and at Castlight Health, a benefit coordination provider, in a paper published online in JAMA Health Forum.
Between December 2020 and August 2022, telehealth visits stayed stable, but in-person visits creeped back up, eventually reaching 80% of prepandemic levels. However, “total utilization was higher than before the pandemic,” Dr. Cantor, a policy researcher at RAND, told this news organization.
“It could be that it’s easier for individuals to receive care via telehealth, but it could also just be that there’s a greater demand or need since the pandemic,” said Dr. Cantor. “We’ll just need more research to actually unpack what’s going on,” he said.
Initial per capita spending increased by about a third and was up overall by more than half. But it’s not clear how much of that is due to utilization or to price of services, said Dr. Cantor. Spending for telehealth services remained stable in the post-vaccine period, while spending on in-person visits returned to prepandemic levels.
Dr. Cantor and his colleagues were not able to determine whether utilization was by new or existing patients, but he said that would be good data to have. “It would be really important to know whether or not folks are initiating care because telehealth is making it easier,” he said.
The authors analyzed about 1.5 million claims for anxiety disorders, major depressive disorder, bipolar disorder, schizophrenia, and posttraumatic stress disorder, out of claims submitted by 7 million commercially insured adults whose self-insured employers used the Castlight benefit.
Dr. Cantor noted that this is just a small subset of the U.S. population. He said he’d like to have data from Medicare and Medicaid to fully assess the impact of the COVID-19 pandemic on mental health and of telehealth visits.
“This is a still-burgeoning field,” he said about telehealth. “We’re still trying to get a handle on how things are operating, given that there’s been so much change so rapidly.”
Meanwhile, 152 major employers responding to a large national survey this summer said that they’ve been grappling with how COVID-19 has affected workers. The employers include 72 Fortune 100 companies and provide health coverage for more than 60 million workers, retirees, and their families.
Seventy-seven percent said they are currently seeing an increase in depression, anxiety, and substance use disorders as a result of the pandemic, according to the Business Group on Health’s survey. That’s up from 44% in 2022.
Going forward, employers will focus on increasing access to mental health services, the survey reported.
“Our survey found that in 2024 and for the near future, employers will be acutely focused on addressing employees’ mental health needs while ensuring access and lowering cost barriers,” Ellen Kelsay, president and CEO of Business Group on Health, said in a statement.
The study was supported by grants from the National Institute of Mental Health and the National Institute on Aging. Coauthor Dena Bravata, MD, a Castlight employee, reported receiving personal fees from Castlight Health during the conduct of the study. Coauthor Christopher M. Whaley, a RAND employee, reported receiving personal fees from Castlight Health outside the submitted work.
A version of this article appeared on Medscape.com.
By the end of August 2022, overall use of mental health services was almost 40% higher than before the COVID-19 pandemic, while spending increased by 54%, according to a new study by researchers at the RAND Corporation.
During the early phase of the pandemic, from mid-March to mid-December 2020, before the vaccine was available, in-person visits decreased by 40%, while telehealth visits increased by 1,000%, reported Jonathan H. Cantor, PhD, and colleagues at RAND, and at Castlight Health, a benefit coordination provider, in a paper published online in JAMA Health Forum.
Between December 2020 and August 2022, telehealth visits stayed stable, but in-person visits creeped back up, eventually reaching 80% of prepandemic levels. However, “total utilization was higher than before the pandemic,” Dr. Cantor, a policy researcher at RAND, told this news organization.
“It could be that it’s easier for individuals to receive care via telehealth, but it could also just be that there’s a greater demand or need since the pandemic,” said Dr. Cantor. “We’ll just need more research to actually unpack what’s going on,” he said.
Initial per capita spending increased by about a third and was up overall by more than half. But it’s not clear how much of that is due to utilization or to price of services, said Dr. Cantor. Spending for telehealth services remained stable in the post-vaccine period, while spending on in-person visits returned to prepandemic levels.
Dr. Cantor and his colleagues were not able to determine whether utilization was by new or existing patients, but he said that would be good data to have. “It would be really important to know whether or not folks are initiating care because telehealth is making it easier,” he said.
The authors analyzed about 1.5 million claims for anxiety disorders, major depressive disorder, bipolar disorder, schizophrenia, and posttraumatic stress disorder, out of claims submitted by 7 million commercially insured adults whose self-insured employers used the Castlight benefit.
Dr. Cantor noted that this is just a small subset of the U.S. population. He said he’d like to have data from Medicare and Medicaid to fully assess the impact of the COVID-19 pandemic on mental health and of telehealth visits.
“This is a still-burgeoning field,” he said about telehealth. “We’re still trying to get a handle on how things are operating, given that there’s been so much change so rapidly.”
Meanwhile, 152 major employers responding to a large national survey this summer said that they’ve been grappling with how COVID-19 has affected workers. The employers include 72 Fortune 100 companies and provide health coverage for more than 60 million workers, retirees, and their families.
Seventy-seven percent said they are currently seeing an increase in depression, anxiety, and substance use disorders as a result of the pandemic, according to the Business Group on Health’s survey. That’s up from 44% in 2022.
Going forward, employers will focus on increasing access to mental health services, the survey reported.
“Our survey found that in 2024 and for the near future, employers will be acutely focused on addressing employees’ mental health needs while ensuring access and lowering cost barriers,” Ellen Kelsay, president and CEO of Business Group on Health, said in a statement.
The study was supported by grants from the National Institute of Mental Health and the National Institute on Aging. Coauthor Dena Bravata, MD, a Castlight employee, reported receiving personal fees from Castlight Health during the conduct of the study. Coauthor Christopher M. Whaley, a RAND employee, reported receiving personal fees from Castlight Health outside the submitted work.
A version of this article appeared on Medscape.com.
By the end of August 2022, overall use of mental health services was almost 40% higher than before the COVID-19 pandemic, while spending increased by 54%, according to a new study by researchers at the RAND Corporation.
During the early phase of the pandemic, from mid-March to mid-December 2020, before the vaccine was available, in-person visits decreased by 40%, while telehealth visits increased by 1,000%, reported Jonathan H. Cantor, PhD, and colleagues at RAND, and at Castlight Health, a benefit coordination provider, in a paper published online in JAMA Health Forum.
Between December 2020 and August 2022, telehealth visits stayed stable, but in-person visits creeped back up, eventually reaching 80% of prepandemic levels. However, “total utilization was higher than before the pandemic,” Dr. Cantor, a policy researcher at RAND, told this news organization.
“It could be that it’s easier for individuals to receive care via telehealth, but it could also just be that there’s a greater demand or need since the pandemic,” said Dr. Cantor. “We’ll just need more research to actually unpack what’s going on,” he said.
Initial per capita spending increased by about a third and was up overall by more than half. But it’s not clear how much of that is due to utilization or to price of services, said Dr. Cantor. Spending for telehealth services remained stable in the post-vaccine period, while spending on in-person visits returned to prepandemic levels.
Dr. Cantor and his colleagues were not able to determine whether utilization was by new or existing patients, but he said that would be good data to have. “It would be really important to know whether or not folks are initiating care because telehealth is making it easier,” he said.
The authors analyzed about 1.5 million claims for anxiety disorders, major depressive disorder, bipolar disorder, schizophrenia, and posttraumatic stress disorder, out of claims submitted by 7 million commercially insured adults whose self-insured employers used the Castlight benefit.
Dr. Cantor noted that this is just a small subset of the U.S. population. He said he’d like to have data from Medicare and Medicaid to fully assess the impact of the COVID-19 pandemic on mental health and of telehealth visits.
“This is a still-burgeoning field,” he said about telehealth. “We’re still trying to get a handle on how things are operating, given that there’s been so much change so rapidly.”
Meanwhile, 152 major employers responding to a large national survey this summer said that they’ve been grappling with how COVID-19 has affected workers. The employers include 72 Fortune 100 companies and provide health coverage for more than 60 million workers, retirees, and their families.
Seventy-seven percent said they are currently seeing an increase in depression, anxiety, and substance use disorders as a result of the pandemic, according to the Business Group on Health’s survey. That’s up from 44% in 2022.
Going forward, employers will focus on increasing access to mental health services, the survey reported.
“Our survey found that in 2024 and for the near future, employers will be acutely focused on addressing employees’ mental health needs while ensuring access and lowering cost barriers,” Ellen Kelsay, president and CEO of Business Group on Health, said in a statement.
The study was supported by grants from the National Institute of Mental Health and the National Institute on Aging. Coauthor Dena Bravata, MD, a Castlight employee, reported receiving personal fees from Castlight Health during the conduct of the study. Coauthor Christopher M. Whaley, a RAND employee, reported receiving personal fees from Castlight Health outside the submitted work.
A version of this article appeared on Medscape.com.
National Practitioner Data Bank should go public, group says
arguing that extra public scrutiny could pressure state medical boards to be more aggressive watchdogs.
Public Citizen’s report includes an analysis of how frequently medical boards sanctioned physicians in 2019, 2020, and 2021. These sanctions include license revocations, suspensions, voluntary surrenders of licenses, and limitations on practice while under investigation.
The report used data from the National Practitioner Data Bank (NPDB), a federal repository of reports about state licensure, discipline, and certification actions as well as medical malpractice payments. The database is closed to the public, but hospitals, malpractice insurers, and investigators can query it.
According to Public Citizen’s calculations, states most likely to take serious disciplinary action against physicians were:
- Michigan: 1.74 serious disciplinary actions per 1,000 physicians per year
- Ohio: 1.61
- North Dakota: 1.60
- Colorado: 1.55
- Arizona: 1.53
- The states least likely to do so were:
- Nevada: 0.24 serious disciplinary actions per 1,000 physicians per year
- New Hampshire: 0.25
- Georgia: 0.27
- Indiana: 0.28
- Nebraska: 0.32
- California, the largest U.S. state by both population and number of physicians, landed near the middle, ranking 27th with a rate of 0.83 serious actions per 1,000 physicians, Public Citizen said.
“There is no evidence that physicians in any state are, overall, more or less likely to be incompetent or miscreant than the physicians in any other state,” said Robert Oshel, PhD, a former NPDB associate director for research and an author of the report.
The differences instead reflect variations in boards’ enforcement of medical practice laws, domination of licensing boards by physicians, and inadequate budgets, he noted.
Public Citizen said Congress should change federal law to let members of the public get information from the NPDB to do a background check on physicians whom they are considering seeing or are already seeing. This would not only help individuals but also would spur state licensing boards to do their own checks with the NPDB, the group said.
“If licensing boards routinely queried the NPDB, they would not be faulted by the public and state legislators for not knowing about malpractice payments or disciplinary actions affecting their licensees and therefore not taking reasonable actions concerning their licensees found to have poor records,” the report said.
Questioning NPDB access for consumers
Michelle Mello, JD, PhD, a professor of law and health policy at Stanford (Calif.) University, has studied the current applications of the NPDB. In 2019, she published an article in The New England Journal of Medicine examining changes in practice patterns for clinicians who faced multiple malpractice claims.
Dr. Mello questioned what benefit consumers would get from direct access to the NPDB’s information.
“It provides almost no context for the information it reports, making it even harder for patients to make sense of what they see there,” Dr. Mello said in an interview.
Hospitals are already required to routinely query the NPDB. This legal requirement should be expanded to include licensing boards, which the report called “the last line of defense for the public from incompetent and miscreant physicians,” Public Citizen said.
“Ideally, this amendment should include free continuous query access by medical boards for all their licensees,” the report said. “In the absence of any action by Congress, individual state legislatures should require their licensing boards to query all their licensees or enroll in continuous query, as a few states already do.”
The Federation of State Medical Boards agreed with some of the other suggestions Public Citizen offered in the report. The two concur on the need for increased funding to state medical boards to ensure that they have adequate resources and staffing to fulfill their duties, FSMB said in a statement.
But FSMB disagreed with Public Citizens’ approach to ranking boards, saying it could mislead. The report lacks context about how boards’ funding and authority vary, Humayun Chaudhry, DO, FSMB’s chief executive officer, said. He also questioned the decision to focus only on serious disciplinary actions.
“The Public Citizen report does not take into account the wide range of disciplinary steps boards can take such as letters of reprimand or fines, which are often enough to stop problem behaviors – preempting further problems in the future,” Dr. Chaudhry said.
D.C. gets worst rating
The District of Columbia earned the worst mark in the Public Citizen ranking, holding the 51st spot, the same place it held in the group’s similar ranking on actions taken in the 2017-2019 period. There were 0.19 serious disciplinary actions per 1,000 physicians a year in Washington, Public Citizen said.
In an email to this news organization, Dr. Oshel said that the Public Citizen analysis focused on the number of licensed physicians in each state and D.C. that can be obtained and compared reliably. It avoided using the term “practicing physicians” owing in part to doubts about the reliability of these counts, he said.
As many as 20% of physicians nationwide are focused primarily on work outside of clinical care, Dr. Oshel estimated. In D.C., perhaps 40% of physicians may fall into this category. Of the more than 13,700 physicians licensed in D.C., there may be only about 8,126 actively practicing, according to Dr. Oshel.
But even using that lower estimate of practicing physicians would only raise D.C.’s ranking to 46, signaling a need for stepped-up enforcement, Dr. Oshel said.
“[Whether it’s] 46th or 51st, both are bad,” Dr. Oshel said.
A version of this article first appeared on Medscape.com.
arguing that extra public scrutiny could pressure state medical boards to be more aggressive watchdogs.
Public Citizen’s report includes an analysis of how frequently medical boards sanctioned physicians in 2019, 2020, and 2021. These sanctions include license revocations, suspensions, voluntary surrenders of licenses, and limitations on practice while under investigation.
The report used data from the National Practitioner Data Bank (NPDB), a federal repository of reports about state licensure, discipline, and certification actions as well as medical malpractice payments. The database is closed to the public, but hospitals, malpractice insurers, and investigators can query it.
According to Public Citizen’s calculations, states most likely to take serious disciplinary action against physicians were:
- Michigan: 1.74 serious disciplinary actions per 1,000 physicians per year
- Ohio: 1.61
- North Dakota: 1.60
- Colorado: 1.55
- Arizona: 1.53
- The states least likely to do so were:
- Nevada: 0.24 serious disciplinary actions per 1,000 physicians per year
- New Hampshire: 0.25
- Georgia: 0.27
- Indiana: 0.28
- Nebraska: 0.32
- California, the largest U.S. state by both population and number of physicians, landed near the middle, ranking 27th with a rate of 0.83 serious actions per 1,000 physicians, Public Citizen said.
“There is no evidence that physicians in any state are, overall, more or less likely to be incompetent or miscreant than the physicians in any other state,” said Robert Oshel, PhD, a former NPDB associate director for research and an author of the report.
The differences instead reflect variations in boards’ enforcement of medical practice laws, domination of licensing boards by physicians, and inadequate budgets, he noted.
Public Citizen said Congress should change federal law to let members of the public get information from the NPDB to do a background check on physicians whom they are considering seeing or are already seeing. This would not only help individuals but also would spur state licensing boards to do their own checks with the NPDB, the group said.
“If licensing boards routinely queried the NPDB, they would not be faulted by the public and state legislators for not knowing about malpractice payments or disciplinary actions affecting their licensees and therefore not taking reasonable actions concerning their licensees found to have poor records,” the report said.
Questioning NPDB access for consumers
Michelle Mello, JD, PhD, a professor of law and health policy at Stanford (Calif.) University, has studied the current applications of the NPDB. In 2019, she published an article in The New England Journal of Medicine examining changes in practice patterns for clinicians who faced multiple malpractice claims.
Dr. Mello questioned what benefit consumers would get from direct access to the NPDB’s information.
“It provides almost no context for the information it reports, making it even harder for patients to make sense of what they see there,” Dr. Mello said in an interview.
Hospitals are already required to routinely query the NPDB. This legal requirement should be expanded to include licensing boards, which the report called “the last line of defense for the public from incompetent and miscreant physicians,” Public Citizen said.
“Ideally, this amendment should include free continuous query access by medical boards for all their licensees,” the report said. “In the absence of any action by Congress, individual state legislatures should require their licensing boards to query all their licensees or enroll in continuous query, as a few states already do.”
The Federation of State Medical Boards agreed with some of the other suggestions Public Citizen offered in the report. The two concur on the need for increased funding to state medical boards to ensure that they have adequate resources and staffing to fulfill their duties, FSMB said in a statement.
But FSMB disagreed with Public Citizens’ approach to ranking boards, saying it could mislead. The report lacks context about how boards’ funding and authority vary, Humayun Chaudhry, DO, FSMB’s chief executive officer, said. He also questioned the decision to focus only on serious disciplinary actions.
“The Public Citizen report does not take into account the wide range of disciplinary steps boards can take such as letters of reprimand or fines, which are often enough to stop problem behaviors – preempting further problems in the future,” Dr. Chaudhry said.
D.C. gets worst rating
The District of Columbia earned the worst mark in the Public Citizen ranking, holding the 51st spot, the same place it held in the group’s similar ranking on actions taken in the 2017-2019 period. There were 0.19 serious disciplinary actions per 1,000 physicians a year in Washington, Public Citizen said.
In an email to this news organization, Dr. Oshel said that the Public Citizen analysis focused on the number of licensed physicians in each state and D.C. that can be obtained and compared reliably. It avoided using the term “practicing physicians” owing in part to doubts about the reliability of these counts, he said.
As many as 20% of physicians nationwide are focused primarily on work outside of clinical care, Dr. Oshel estimated. In D.C., perhaps 40% of physicians may fall into this category. Of the more than 13,700 physicians licensed in D.C., there may be only about 8,126 actively practicing, according to Dr. Oshel.
But even using that lower estimate of practicing physicians would only raise D.C.’s ranking to 46, signaling a need for stepped-up enforcement, Dr. Oshel said.
“[Whether it’s] 46th or 51st, both are bad,” Dr. Oshel said.
A version of this article first appeared on Medscape.com.
arguing that extra public scrutiny could pressure state medical boards to be more aggressive watchdogs.
Public Citizen’s report includes an analysis of how frequently medical boards sanctioned physicians in 2019, 2020, and 2021. These sanctions include license revocations, suspensions, voluntary surrenders of licenses, and limitations on practice while under investigation.
The report used data from the National Practitioner Data Bank (NPDB), a federal repository of reports about state licensure, discipline, and certification actions as well as medical malpractice payments. The database is closed to the public, but hospitals, malpractice insurers, and investigators can query it.
According to Public Citizen’s calculations, states most likely to take serious disciplinary action against physicians were:
- Michigan: 1.74 serious disciplinary actions per 1,000 physicians per year
- Ohio: 1.61
- North Dakota: 1.60
- Colorado: 1.55
- Arizona: 1.53
- The states least likely to do so were:
- Nevada: 0.24 serious disciplinary actions per 1,000 physicians per year
- New Hampshire: 0.25
- Georgia: 0.27
- Indiana: 0.28
- Nebraska: 0.32
- California, the largest U.S. state by both population and number of physicians, landed near the middle, ranking 27th with a rate of 0.83 serious actions per 1,000 physicians, Public Citizen said.
“There is no evidence that physicians in any state are, overall, more or less likely to be incompetent or miscreant than the physicians in any other state,” said Robert Oshel, PhD, a former NPDB associate director for research and an author of the report.
The differences instead reflect variations in boards’ enforcement of medical practice laws, domination of licensing boards by physicians, and inadequate budgets, he noted.
Public Citizen said Congress should change federal law to let members of the public get information from the NPDB to do a background check on physicians whom they are considering seeing or are already seeing. This would not only help individuals but also would spur state licensing boards to do their own checks with the NPDB, the group said.
“If licensing boards routinely queried the NPDB, they would not be faulted by the public and state legislators for not knowing about malpractice payments or disciplinary actions affecting their licensees and therefore not taking reasonable actions concerning their licensees found to have poor records,” the report said.
Questioning NPDB access for consumers
Michelle Mello, JD, PhD, a professor of law and health policy at Stanford (Calif.) University, has studied the current applications of the NPDB. In 2019, she published an article in The New England Journal of Medicine examining changes in practice patterns for clinicians who faced multiple malpractice claims.
Dr. Mello questioned what benefit consumers would get from direct access to the NPDB’s information.
“It provides almost no context for the information it reports, making it even harder for patients to make sense of what they see there,” Dr. Mello said in an interview.
Hospitals are already required to routinely query the NPDB. This legal requirement should be expanded to include licensing boards, which the report called “the last line of defense for the public from incompetent and miscreant physicians,” Public Citizen said.
“Ideally, this amendment should include free continuous query access by medical boards for all their licensees,” the report said. “In the absence of any action by Congress, individual state legislatures should require their licensing boards to query all their licensees or enroll in continuous query, as a few states already do.”
The Federation of State Medical Boards agreed with some of the other suggestions Public Citizen offered in the report. The two concur on the need for increased funding to state medical boards to ensure that they have adequate resources and staffing to fulfill their duties, FSMB said in a statement.
But FSMB disagreed with Public Citizens’ approach to ranking boards, saying it could mislead. The report lacks context about how boards’ funding and authority vary, Humayun Chaudhry, DO, FSMB’s chief executive officer, said. He also questioned the decision to focus only on serious disciplinary actions.
“The Public Citizen report does not take into account the wide range of disciplinary steps boards can take such as letters of reprimand or fines, which are often enough to stop problem behaviors – preempting further problems in the future,” Dr. Chaudhry said.
D.C. gets worst rating
The District of Columbia earned the worst mark in the Public Citizen ranking, holding the 51st spot, the same place it held in the group’s similar ranking on actions taken in the 2017-2019 period. There were 0.19 serious disciplinary actions per 1,000 physicians a year in Washington, Public Citizen said.
In an email to this news organization, Dr. Oshel said that the Public Citizen analysis focused on the number of licensed physicians in each state and D.C. that can be obtained and compared reliably. It avoided using the term “practicing physicians” owing in part to doubts about the reliability of these counts, he said.
As many as 20% of physicians nationwide are focused primarily on work outside of clinical care, Dr. Oshel estimated. In D.C., perhaps 40% of physicians may fall into this category. Of the more than 13,700 physicians licensed in D.C., there may be only about 8,126 actively practicing, according to Dr. Oshel.
But even using that lower estimate of practicing physicians would only raise D.C.’s ranking to 46, signaling a need for stepped-up enforcement, Dr. Oshel said.
“[Whether it’s] 46th or 51st, both are bad,” Dr. Oshel said.
A version of this article first appeared on Medscape.com.
Consider housing insecurity, other issues when managing challenging skin diseases in children, expert says
ASHEVILLE, N.C. – , according to a pediatric dermatologist who addressed the annual meeting of the Society for Pediatric Dermatology.
As a general principle for treating chronic skin conditions in children who are not doing well, it is reasonable to draw out information about a patient’s access to adequate housing, nutrition, and other basic needs, George Hightower, MD, PhD, of the division of pediatric and adolescent dermatology, University of California, San Diego, said at the meeting.
“We need conversations about where patients play, learn, and rest their heads at night,” said Dr. Hightower, who conducts research in this area. Fundamental components of well-being, such as stable housing and secure access to nutrition “are inseparable” from a child’s health, he noted.
“What are the stakes?” he asked. For many children, these factors might mean the difference between effective and poor control of the diseases for which the patient is seeking care.
To illustrate the point, Dr. Hightower used hidradenitis suppurativa (HS), a disease that appears to be on the rise among adolescents, as an example of why patient circumstances matter and should be considered. A complex disorder that is more prevalent in resource-poor communities, HS is difficult to control, often requiring extended periods of treatment with medications that can involve complex dosing or regular infusions.
“There is a need for medical providers to help the patient plan for this chronic illness,” said Dr. Hightower, referring to the importance of close follow-up. In adolescents, HS can be sufficiently disruptive from both the physical and psychological perspective that poor control can “derail future aspirations” by complicating educational endeavors and social interactions.
Dr. Hightower acknowledged that simply documenting housing insecurity or other issues does not solve these problems, but he does believe that developing a sensitivity to these obstacles to health care is a first step. It is a process that should permeate into medical training, health care research, and strategies to improve outcomes.
“The connections between fair housing and clinical practice may appear tenuous and inconsequential to the care provided by medical specialists,” Dr. Hightower said, but he emphasized that there are clear consequences when these factors contribute to inadequate control of such diseases as HS. As a source of missed appointments and disjointed care, an unstable home life can be an important barrier to disease control – and because of scarring nodules, fistulae, pain, school absences, and social isolation, complications can be dire.
Solutions to insecure housing are not typically available to an individual clinician, but the awareness that this can be a factor can help both physicians and patients begin to think about the role this plays in impairing recovery and what solutions might be found to modify the impact. Awareness not just among individual clinicians but a broader consortium of those working to improve health care outcomes is needed to “challenge the way we are doing medicine,” he said.
While conversations about the social determinants of health, including access to resources within patients’ neighborhoods, schools, and environment, can demonstrate concern about how to address obstacles, it can also be part of a reorientation to think beyond treatment for the underlying pathology alone. Eliciting trust and emphasizing the importance of environmental barriers to adequate care can be positive steps on the path to solutions.
Participatory action research
Relevant to this orientation, Dr. Hightower spoke about participatory action research (PAR), which provides a framework for patients to participate in the planning of clinical studies to effect change, not just serve as subjects in these studies.
The assumption of PAR is that “all people have valuable knowledge about their lives and experiences,” Dr. Hightower said. From this assumption, individuals who have been historically marginalized by race, income, or other factors can help define the problems from the patient’s perspective and, from there, create studies to seek solutions.
PAR is consistent with a patient-centered approach to medical care, which Dr. Hightower called “the future of medicine.” It involves a big-picture approach to look beyond disease pathology and symptoms to factors that might be creating susceptibility to disease and undermining health care.
Organized medicine alone cannot solve the cause of social inequities leading to disparate risks for disease and risks of inadequate health care, but Dr. Hightower argued that these inequities should not be ignored. He believes medical trainees should learn how to elicit information about the barriers to adequate health care and be aware of solutions, such as fair housing policies.
While he believes that PAR is an example of a pathway to problem solving, he suggested that a comprehensive approach requires an effective method of communication between providers and patients that would lead to a collaborative and mutually reinforcing approach.
“How do we ensure that individuals from communities most impacted by health disparities are treated fairly and empowered to address these disparities?” Dr. Hightower asked. He said that this is the direction of his own research and the issues that inhibit adequate treatment of many dermatologic diseases, as well as other types of disease, in childhood.
Craig Burkhart, MD, director of a private pediatric and adolescent dermatology practice in Cary, N.C., said that Dr. Hightower’s message is relevant. The value of considering and addressing the psychological well-being of patients of any age is not a new concept, but he acknowledged that he, for one, has not routinely inquired about obstacles to follow-up care if there is a signal that this might be an issue.
“As dermatologists, we focus on the acute complaints. We want to make the patient better,” said Dr. Burkhart, who moderated the session in which Dr. Hightower spoke. He agreed with Dr. Hightower that environmental factors make a difference on the road to recovery for a patient, and his presentation was a good reminder, he said, to consider the patient’s circumstances when response to treatment is inadequate, particularly in chronic diseases like HS, for which comprehensive care and close follow-up are needed.
Dr. Hightower and Dr. Burkhart report no potential conflicts of interest.
ASHEVILLE, N.C. – , according to a pediatric dermatologist who addressed the annual meeting of the Society for Pediatric Dermatology.
As a general principle for treating chronic skin conditions in children who are not doing well, it is reasonable to draw out information about a patient’s access to adequate housing, nutrition, and other basic needs, George Hightower, MD, PhD, of the division of pediatric and adolescent dermatology, University of California, San Diego, said at the meeting.
“We need conversations about where patients play, learn, and rest their heads at night,” said Dr. Hightower, who conducts research in this area. Fundamental components of well-being, such as stable housing and secure access to nutrition “are inseparable” from a child’s health, he noted.
“What are the stakes?” he asked. For many children, these factors might mean the difference between effective and poor control of the diseases for which the patient is seeking care.
To illustrate the point, Dr. Hightower used hidradenitis suppurativa (HS), a disease that appears to be on the rise among adolescents, as an example of why patient circumstances matter and should be considered. A complex disorder that is more prevalent in resource-poor communities, HS is difficult to control, often requiring extended periods of treatment with medications that can involve complex dosing or regular infusions.
“There is a need for medical providers to help the patient plan for this chronic illness,” said Dr. Hightower, referring to the importance of close follow-up. In adolescents, HS can be sufficiently disruptive from both the physical and psychological perspective that poor control can “derail future aspirations” by complicating educational endeavors and social interactions.
Dr. Hightower acknowledged that simply documenting housing insecurity or other issues does not solve these problems, but he does believe that developing a sensitivity to these obstacles to health care is a first step. It is a process that should permeate into medical training, health care research, and strategies to improve outcomes.
“The connections between fair housing and clinical practice may appear tenuous and inconsequential to the care provided by medical specialists,” Dr. Hightower said, but he emphasized that there are clear consequences when these factors contribute to inadequate control of such diseases as HS. As a source of missed appointments and disjointed care, an unstable home life can be an important barrier to disease control – and because of scarring nodules, fistulae, pain, school absences, and social isolation, complications can be dire.
Solutions to insecure housing are not typically available to an individual clinician, but the awareness that this can be a factor can help both physicians and patients begin to think about the role this plays in impairing recovery and what solutions might be found to modify the impact. Awareness not just among individual clinicians but a broader consortium of those working to improve health care outcomes is needed to “challenge the way we are doing medicine,” he said.
While conversations about the social determinants of health, including access to resources within patients’ neighborhoods, schools, and environment, can demonstrate concern about how to address obstacles, it can also be part of a reorientation to think beyond treatment for the underlying pathology alone. Eliciting trust and emphasizing the importance of environmental barriers to adequate care can be positive steps on the path to solutions.
Participatory action research
Relevant to this orientation, Dr. Hightower spoke about participatory action research (PAR), which provides a framework for patients to participate in the planning of clinical studies to effect change, not just serve as subjects in these studies.
The assumption of PAR is that “all people have valuable knowledge about their lives and experiences,” Dr. Hightower said. From this assumption, individuals who have been historically marginalized by race, income, or other factors can help define the problems from the patient’s perspective and, from there, create studies to seek solutions.
PAR is consistent with a patient-centered approach to medical care, which Dr. Hightower called “the future of medicine.” It involves a big-picture approach to look beyond disease pathology and symptoms to factors that might be creating susceptibility to disease and undermining health care.
Organized medicine alone cannot solve the cause of social inequities leading to disparate risks for disease and risks of inadequate health care, but Dr. Hightower argued that these inequities should not be ignored. He believes medical trainees should learn how to elicit information about the barriers to adequate health care and be aware of solutions, such as fair housing policies.
While he believes that PAR is an example of a pathway to problem solving, he suggested that a comprehensive approach requires an effective method of communication between providers and patients that would lead to a collaborative and mutually reinforcing approach.
“How do we ensure that individuals from communities most impacted by health disparities are treated fairly and empowered to address these disparities?” Dr. Hightower asked. He said that this is the direction of his own research and the issues that inhibit adequate treatment of many dermatologic diseases, as well as other types of disease, in childhood.
Craig Burkhart, MD, director of a private pediatric and adolescent dermatology practice in Cary, N.C., said that Dr. Hightower’s message is relevant. The value of considering and addressing the psychological well-being of patients of any age is not a new concept, but he acknowledged that he, for one, has not routinely inquired about obstacles to follow-up care if there is a signal that this might be an issue.
“As dermatologists, we focus on the acute complaints. We want to make the patient better,” said Dr. Burkhart, who moderated the session in which Dr. Hightower spoke. He agreed with Dr. Hightower that environmental factors make a difference on the road to recovery for a patient, and his presentation was a good reminder, he said, to consider the patient’s circumstances when response to treatment is inadequate, particularly in chronic diseases like HS, for which comprehensive care and close follow-up are needed.
Dr. Hightower and Dr. Burkhart report no potential conflicts of interest.
ASHEVILLE, N.C. – , according to a pediatric dermatologist who addressed the annual meeting of the Society for Pediatric Dermatology.
As a general principle for treating chronic skin conditions in children who are not doing well, it is reasonable to draw out information about a patient’s access to adequate housing, nutrition, and other basic needs, George Hightower, MD, PhD, of the division of pediatric and adolescent dermatology, University of California, San Diego, said at the meeting.
“We need conversations about where patients play, learn, and rest their heads at night,” said Dr. Hightower, who conducts research in this area. Fundamental components of well-being, such as stable housing and secure access to nutrition “are inseparable” from a child’s health, he noted.
“What are the stakes?” he asked. For many children, these factors might mean the difference between effective and poor control of the diseases for which the patient is seeking care.
To illustrate the point, Dr. Hightower used hidradenitis suppurativa (HS), a disease that appears to be on the rise among adolescents, as an example of why patient circumstances matter and should be considered. A complex disorder that is more prevalent in resource-poor communities, HS is difficult to control, often requiring extended periods of treatment with medications that can involve complex dosing or regular infusions.
“There is a need for medical providers to help the patient plan for this chronic illness,” said Dr. Hightower, referring to the importance of close follow-up. In adolescents, HS can be sufficiently disruptive from both the physical and psychological perspective that poor control can “derail future aspirations” by complicating educational endeavors and social interactions.
Dr. Hightower acknowledged that simply documenting housing insecurity or other issues does not solve these problems, but he does believe that developing a sensitivity to these obstacles to health care is a first step. It is a process that should permeate into medical training, health care research, and strategies to improve outcomes.
“The connections between fair housing and clinical practice may appear tenuous and inconsequential to the care provided by medical specialists,” Dr. Hightower said, but he emphasized that there are clear consequences when these factors contribute to inadequate control of such diseases as HS. As a source of missed appointments and disjointed care, an unstable home life can be an important barrier to disease control – and because of scarring nodules, fistulae, pain, school absences, and social isolation, complications can be dire.
Solutions to insecure housing are not typically available to an individual clinician, but the awareness that this can be a factor can help both physicians and patients begin to think about the role this plays in impairing recovery and what solutions might be found to modify the impact. Awareness not just among individual clinicians but a broader consortium of those working to improve health care outcomes is needed to “challenge the way we are doing medicine,” he said.
While conversations about the social determinants of health, including access to resources within patients’ neighborhoods, schools, and environment, can demonstrate concern about how to address obstacles, it can also be part of a reorientation to think beyond treatment for the underlying pathology alone. Eliciting trust and emphasizing the importance of environmental barriers to adequate care can be positive steps on the path to solutions.
Participatory action research
Relevant to this orientation, Dr. Hightower spoke about participatory action research (PAR), which provides a framework for patients to participate in the planning of clinical studies to effect change, not just serve as subjects in these studies.
The assumption of PAR is that “all people have valuable knowledge about their lives and experiences,” Dr. Hightower said. From this assumption, individuals who have been historically marginalized by race, income, or other factors can help define the problems from the patient’s perspective and, from there, create studies to seek solutions.
PAR is consistent with a patient-centered approach to medical care, which Dr. Hightower called “the future of medicine.” It involves a big-picture approach to look beyond disease pathology and symptoms to factors that might be creating susceptibility to disease and undermining health care.
Organized medicine alone cannot solve the cause of social inequities leading to disparate risks for disease and risks of inadequate health care, but Dr. Hightower argued that these inequities should not be ignored. He believes medical trainees should learn how to elicit information about the barriers to adequate health care and be aware of solutions, such as fair housing policies.
While he believes that PAR is an example of a pathway to problem solving, he suggested that a comprehensive approach requires an effective method of communication between providers and patients that would lead to a collaborative and mutually reinforcing approach.
“How do we ensure that individuals from communities most impacted by health disparities are treated fairly and empowered to address these disparities?” Dr. Hightower asked. He said that this is the direction of his own research and the issues that inhibit adequate treatment of many dermatologic diseases, as well as other types of disease, in childhood.
Craig Burkhart, MD, director of a private pediatric and adolescent dermatology practice in Cary, N.C., said that Dr. Hightower’s message is relevant. The value of considering and addressing the psychological well-being of patients of any age is not a new concept, but he acknowledged that he, for one, has not routinely inquired about obstacles to follow-up care if there is a signal that this might be an issue.
“As dermatologists, we focus on the acute complaints. We want to make the patient better,” said Dr. Burkhart, who moderated the session in which Dr. Hightower spoke. He agreed with Dr. Hightower that environmental factors make a difference on the road to recovery for a patient, and his presentation was a good reminder, he said, to consider the patient’s circumstances when response to treatment is inadequate, particularly in chronic diseases like HS, for which comprehensive care and close follow-up are needed.
Dr. Hightower and Dr. Burkhart report no potential conflicts of interest.
AT SPD 2023
Mothers in medicine: What can we learn when worlds collide?
Across all industries, studies by the U.S. Department of Labor have shown that women, on average, earn 83.7 percent of what their male peers earn. While a lot has been written about the struggles women face in medicine, there have been decidedly fewer analyses that focus on women who choose to become mothers while working in medicine.
I’ve been privileged to work with medical students and residents for the last 8 years as the director of graduate and medical student mental health at Rowan-Virtua School of Osteopathic Medicine in Mt. Laurel, N.J. Often, the women I see as patients speak about their struggles with the elusive goal of “having it all.” While both men and women in medicine have difficulty maintaining a work-life balance, I’ve learned, both personally and professionally, that many women face a unique set of challenges.
No matter what their professional status, our society often views a woman as the default parent. For example, the teacher often calls the mothers first. The camp nurse calls me first, not my husband, when our child scrapes a knee. After-school play dates are arranged by the mothers, not fathers.
But mothers also bring to medicine a wealth of unique experiences, ideas, and viewpoints. They learn firsthand how to foster affect regulation and frustration tolerance in their kids and become efficient at managing the constant, conflicting tug of war of demands.
Some may argue that, over time, women end up earning significantly less than their male counterparts because they leave the workforce while on maternity leave, ultimately delaying their upward career progression. It’s likely a much more complex problem. Many of my patients believe that, in our male-dominated society (and workforce), women are punished for being aggressive or stating bold opinions, while men are rewarded for the same actions. While a man may sound forceful and in charge, a women will likely be thought of as brusque and unappreciative.
Outside of work, many women may have more on their plate. A 2020 Gallup poll of more than 3,000 heterosexual couples found that women are responsible for the majority of household chores. Women continue to handle more of the emotional labor within their families, regardless of income, age, or professional status. This is sometimes called the “Mental Load’ or “Second Shift.” As our society continues to view women as the default parent for childcare, medical issues, and overarching social and emotional tasks vital to raising happy, healthy children, the struggle a female medical professional feels is palpable.
Raising kids requires a parent to consistently dole out control, predictability, and reassurance for a child to thrive. Good limit and boundary setting leads to healthy development from a young age.
Psychiatric patients (and perhaps all patients) also require control, predictability, and reassurance from their doctor. The lessons learned in being a good mother can be directly applied in patient care, and vice versa. The cross-pollination of this relationship continues to grow more powerful as a woman’s children grow and her career matures.
Pediatrician and psychoanalyst Donald Winnicott’s idea of a “good enough” mother cannot be a one-size-fits-all approach. Women who self-select into the world of medicine often hold themselves to a higher standard than “good enough.” Acknowledging that the demands from both home and work will fluctuate is key to achieving success both personally and professionally, and lessons from home can and should be utilized to become a more effective physician. The notion of having it all, and the definition of success, must evolve over time.
Dr. Maymind is director of medical and graduate student mental health at Rowan-Virtua School of Osteopathic Medicine in Mt. Laurel, N.J. She has no relevant disclosures.
Across all industries, studies by the U.S. Department of Labor have shown that women, on average, earn 83.7 percent of what their male peers earn. While a lot has been written about the struggles women face in medicine, there have been decidedly fewer analyses that focus on women who choose to become mothers while working in medicine.
I’ve been privileged to work with medical students and residents for the last 8 years as the director of graduate and medical student mental health at Rowan-Virtua School of Osteopathic Medicine in Mt. Laurel, N.J. Often, the women I see as patients speak about their struggles with the elusive goal of “having it all.” While both men and women in medicine have difficulty maintaining a work-life balance, I’ve learned, both personally and professionally, that many women face a unique set of challenges.
No matter what their professional status, our society often views a woman as the default parent. For example, the teacher often calls the mothers first. The camp nurse calls me first, not my husband, when our child scrapes a knee. After-school play dates are arranged by the mothers, not fathers.
But mothers also bring to medicine a wealth of unique experiences, ideas, and viewpoints. They learn firsthand how to foster affect regulation and frustration tolerance in their kids and become efficient at managing the constant, conflicting tug of war of demands.
Some may argue that, over time, women end up earning significantly less than their male counterparts because they leave the workforce while on maternity leave, ultimately delaying their upward career progression. It’s likely a much more complex problem. Many of my patients believe that, in our male-dominated society (and workforce), women are punished for being aggressive or stating bold opinions, while men are rewarded for the same actions. While a man may sound forceful and in charge, a women will likely be thought of as brusque and unappreciative.
Outside of work, many women may have more on their plate. A 2020 Gallup poll of more than 3,000 heterosexual couples found that women are responsible for the majority of household chores. Women continue to handle more of the emotional labor within their families, regardless of income, age, or professional status. This is sometimes called the “Mental Load’ or “Second Shift.” As our society continues to view women as the default parent for childcare, medical issues, and overarching social and emotional tasks vital to raising happy, healthy children, the struggle a female medical professional feels is palpable.
Raising kids requires a parent to consistently dole out control, predictability, and reassurance for a child to thrive. Good limit and boundary setting leads to healthy development from a young age.
Psychiatric patients (and perhaps all patients) also require control, predictability, and reassurance from their doctor. The lessons learned in being a good mother can be directly applied in patient care, and vice versa. The cross-pollination of this relationship continues to grow more powerful as a woman’s children grow and her career matures.
Pediatrician and psychoanalyst Donald Winnicott’s idea of a “good enough” mother cannot be a one-size-fits-all approach. Women who self-select into the world of medicine often hold themselves to a higher standard than “good enough.” Acknowledging that the demands from both home and work will fluctuate is key to achieving success both personally and professionally, and lessons from home can and should be utilized to become a more effective physician. The notion of having it all, and the definition of success, must evolve over time.
Dr. Maymind is director of medical and graduate student mental health at Rowan-Virtua School of Osteopathic Medicine in Mt. Laurel, N.J. She has no relevant disclosures.
Across all industries, studies by the U.S. Department of Labor have shown that women, on average, earn 83.7 percent of what their male peers earn. While a lot has been written about the struggles women face in medicine, there have been decidedly fewer analyses that focus on women who choose to become mothers while working in medicine.
I’ve been privileged to work with medical students and residents for the last 8 years as the director of graduate and medical student mental health at Rowan-Virtua School of Osteopathic Medicine in Mt. Laurel, N.J. Often, the women I see as patients speak about their struggles with the elusive goal of “having it all.” While both men and women in medicine have difficulty maintaining a work-life balance, I’ve learned, both personally and professionally, that many women face a unique set of challenges.
No matter what their professional status, our society often views a woman as the default parent. For example, the teacher often calls the mothers first. The camp nurse calls me first, not my husband, when our child scrapes a knee. After-school play dates are arranged by the mothers, not fathers.
But mothers also bring to medicine a wealth of unique experiences, ideas, and viewpoints. They learn firsthand how to foster affect regulation and frustration tolerance in their kids and become efficient at managing the constant, conflicting tug of war of demands.
Some may argue that, over time, women end up earning significantly less than their male counterparts because they leave the workforce while on maternity leave, ultimately delaying their upward career progression. It’s likely a much more complex problem. Many of my patients believe that, in our male-dominated society (and workforce), women are punished for being aggressive or stating bold opinions, while men are rewarded for the same actions. While a man may sound forceful and in charge, a women will likely be thought of as brusque and unappreciative.
Outside of work, many women may have more on their plate. A 2020 Gallup poll of more than 3,000 heterosexual couples found that women are responsible for the majority of household chores. Women continue to handle more of the emotional labor within their families, regardless of income, age, or professional status. This is sometimes called the “Mental Load’ or “Second Shift.” As our society continues to view women as the default parent for childcare, medical issues, and overarching social and emotional tasks vital to raising happy, healthy children, the struggle a female medical professional feels is palpable.
Raising kids requires a parent to consistently dole out control, predictability, and reassurance for a child to thrive. Good limit and boundary setting leads to healthy development from a young age.
Psychiatric patients (and perhaps all patients) also require control, predictability, and reassurance from their doctor. The lessons learned in being a good mother can be directly applied in patient care, and vice versa. The cross-pollination of this relationship continues to grow more powerful as a woman’s children grow and her career matures.
Pediatrician and psychoanalyst Donald Winnicott’s idea of a “good enough” mother cannot be a one-size-fits-all approach. Women who self-select into the world of medicine often hold themselves to a higher standard than “good enough.” Acknowledging that the demands from both home and work will fluctuate is key to achieving success both personally and professionally, and lessons from home can and should be utilized to become a more effective physician. The notion of having it all, and the definition of success, must evolve over time.
Dr. Maymind is director of medical and graduate student mental health at Rowan-Virtua School of Osteopathic Medicine in Mt. Laurel, N.J. She has no relevant disclosures.
As MOC debate heats up, cardiology societies weigh in
It’s no secret that many physicians question the value of Maintenance of Certification requirements and are concerned about the amount of time, effort, and money the process takes. Now, they and at least two cardiology societies are starting to speak up.
MOC is an initiative from the American Board of Internal Medicine that requires an initial certification that costs thousands of dollars and must be repeated every 10 years. Annual MOC requirements involve tests that cost $220 for the first certificate a physician holds and about $120 for each subsequent one.
Interventional cardiologists (ICs) and other subspecialists have additional fees and requirements.
MOC ‘burdensome,’ ‘costly,’ ‘complex’
On July 21, hematologist-oncologist Aaron Goodman, MD, an associate professor at the University of California, San Diego, posted a petition on behalf of ABIM diplomates.
As of August 22, the petition had garnered more than 18,000 signatures.
Dr. Goodman recently debated ABIM President and CEO Richard J. Baron, MD, in a Healthcare Unfiltered podcast. Before the debate, host Chadi Nabhan, MD, MBA, tweeted that he could not find a single physician who would defend the MOC and recertification.
The debate touched on topics such as fees, evidence of value, the certification test format, and the cost and requirements to maintain more than one board certification. Overall, Dr. Goodman made the analogy to giving a patient chemotherapy: Because there are harms, he better know that there are also benefits. He cited that the harms associated with MOC include “financial toxicity, time toxicity, and stress toxicity,” with the latter being particularly toxic to him personally.
Though the podcast gave both participants ample opportunities to express their views, it’s not clear that either participant persuaded the other.
Cardiologists who are unhappy with MOC are speaking up on X, formerly known as Twitter. IC Matthew Sample, MD, listed five things he’s done to improve his practice since IC graduation, for which he received no MOC points.
In response, internist Artem Minalyan, MD, asked: “Hypothetically, if Dr. Baron required an IC procedure, I wonder if he would request you to get all your MOC points prior to consenting.”
SCAI and HRS weigh in
Some professional societies have responded to the ABIM’s threat to revoke the certifications of cardiologists who don’t participate in periodic MOC activities.
The Society for Cardiovascular Angiography & Interventions published its “Position on ABIM Revocation of Certification for Not Participating in MOC.” In it, SCAI states that ABIM diplomates who pass their exams and report procedural volumes as required should be “indisputably” recognized as “certified” for the relevant time frame (for example, 10 years), regardless of whether they participate in any other MOC activities.
SCAI President George D. Dangas, MD, PhD, said in an interview that “many of our members have expressed their frustration surrounding the confusion regarding their MOC requirements, including myself. We felt that this confusion could endanger the certified status of members, which would inevitably impact patient care, which is our greatest concern.”
The society has received an “overwhelmingly positive response” to its statement, he said. “Our hope is that ABIM will consider simpler, transparent regulations that are reflective of the feedback received from their constituents.”
In response to the COVID-19 pandemic, ABIM extended the deadline for diplomates whose certificate expired in 2020 or 2021 until the end of 2022; Dr. Dangas suggested ABIM further extend the deadline to enroll in or renew the MOC to the end of 2024 and that ABIM should “develop a recertification program that can be explained in a single slide/page.”
Other subspecialty groups are following SCAI’s lead including the EP Advocacy Foundation, and the Heart Rhythm Society.
MOC alternatives
The ABIM touts the value of MOC on its website, stating: “There is compelling evidence showing that MOC improves value of care without sacrificing quality and that board certified physicians command higher salaries.”
Alternative options that are arguably less arduous are available.
In collaboration with ABIM, the American College of Cardiology launched the ABIM/ACC Collaborative Maintenance Pathway in 2019 as an alternative MOC assessment option.
The CMP “focuses on one or a small group of topics within cardiology each year, incorporating learning activities as well as a pre-/postformative knowledge assessment,” Janice Sibley, ACC’s executive vice president of education and publishing said in an interview, adding that the program continues to evolve.
In 2022, she noted that the ACC increased the flexibility of the CMP by removing the 7-hour learning engagement requirement, allowing users to choose how much time to spend learning in the CMP program. They also extended the performance assessment windows from 7 to 9 days each, covering 2 weekends for each.
She said that, to date, more than “6,400 learners” are enrolled in the CMP program.
Though the collaboration seems to make MOC less onerous, some cardiologists think it makes the ACC “complicit.”
A certification program that is independent of the ABIM launched in 2015. The National Board of Physicians and Surgeons is a nonprofit organization led by an advisory board of unpaid physicians. NBPAS seems to be gaining momentum and acceptance.
Cardiologist Melissa Walton-Shirley, MD, recounted her recertification experience with the NBPAS late in 2022. She now maintains a “hybrid” certification with both ABIM and NBPAS. Though she wants to support the latter, she found that the alternative certification option still requires an initial ABIM certification and is not recognized in all states or by many insurers and hospitals.
Will MOC ever disappear? Ms. Sibley said that the ACC is always looking to improve and enhance their offerings. “It is time to lead a change in the conversation from certification to continuous competency, from punitive to supportive options, from random knowledge testing to focused assessing knowledge gaps and lifelong learning. This will require innovation, technology, and new ways of thinking that offer cardiologists flexibility, relevance, and value and ultimately benefit the patients they serve.”
Many physicians, including cardiologists, are hoping that Dr. Goodman’s petition and further pressure from professional societies may finally translate into action.
A version of this article first appeared on Medscape.com.
It’s no secret that many physicians question the value of Maintenance of Certification requirements and are concerned about the amount of time, effort, and money the process takes. Now, they and at least two cardiology societies are starting to speak up.
MOC is an initiative from the American Board of Internal Medicine that requires an initial certification that costs thousands of dollars and must be repeated every 10 years. Annual MOC requirements involve tests that cost $220 for the first certificate a physician holds and about $120 for each subsequent one.
Interventional cardiologists (ICs) and other subspecialists have additional fees and requirements.
MOC ‘burdensome,’ ‘costly,’ ‘complex’
On July 21, hematologist-oncologist Aaron Goodman, MD, an associate professor at the University of California, San Diego, posted a petition on behalf of ABIM diplomates.
As of August 22, the petition had garnered more than 18,000 signatures.
Dr. Goodman recently debated ABIM President and CEO Richard J. Baron, MD, in a Healthcare Unfiltered podcast. Before the debate, host Chadi Nabhan, MD, MBA, tweeted that he could not find a single physician who would defend the MOC and recertification.
The debate touched on topics such as fees, evidence of value, the certification test format, and the cost and requirements to maintain more than one board certification. Overall, Dr. Goodman made the analogy to giving a patient chemotherapy: Because there are harms, he better know that there are also benefits. He cited that the harms associated with MOC include “financial toxicity, time toxicity, and stress toxicity,” with the latter being particularly toxic to him personally.
Though the podcast gave both participants ample opportunities to express their views, it’s not clear that either participant persuaded the other.
Cardiologists who are unhappy with MOC are speaking up on X, formerly known as Twitter. IC Matthew Sample, MD, listed five things he’s done to improve his practice since IC graduation, for which he received no MOC points.
In response, internist Artem Minalyan, MD, asked: “Hypothetically, if Dr. Baron required an IC procedure, I wonder if he would request you to get all your MOC points prior to consenting.”
SCAI and HRS weigh in
Some professional societies have responded to the ABIM’s threat to revoke the certifications of cardiologists who don’t participate in periodic MOC activities.
The Society for Cardiovascular Angiography & Interventions published its “Position on ABIM Revocation of Certification for Not Participating in MOC.” In it, SCAI states that ABIM diplomates who pass their exams and report procedural volumes as required should be “indisputably” recognized as “certified” for the relevant time frame (for example, 10 years), regardless of whether they participate in any other MOC activities.
SCAI President George D. Dangas, MD, PhD, said in an interview that “many of our members have expressed their frustration surrounding the confusion regarding their MOC requirements, including myself. We felt that this confusion could endanger the certified status of members, which would inevitably impact patient care, which is our greatest concern.”
The society has received an “overwhelmingly positive response” to its statement, he said. “Our hope is that ABIM will consider simpler, transparent regulations that are reflective of the feedback received from their constituents.”
In response to the COVID-19 pandemic, ABIM extended the deadline for diplomates whose certificate expired in 2020 or 2021 until the end of 2022; Dr. Dangas suggested ABIM further extend the deadline to enroll in or renew the MOC to the end of 2024 and that ABIM should “develop a recertification program that can be explained in a single slide/page.”
Other subspecialty groups are following SCAI’s lead including the EP Advocacy Foundation, and the Heart Rhythm Society.
MOC alternatives
The ABIM touts the value of MOC on its website, stating: “There is compelling evidence showing that MOC improves value of care without sacrificing quality and that board certified physicians command higher salaries.”
Alternative options that are arguably less arduous are available.
In collaboration with ABIM, the American College of Cardiology launched the ABIM/ACC Collaborative Maintenance Pathway in 2019 as an alternative MOC assessment option.
The CMP “focuses on one or a small group of topics within cardiology each year, incorporating learning activities as well as a pre-/postformative knowledge assessment,” Janice Sibley, ACC’s executive vice president of education and publishing said in an interview, adding that the program continues to evolve.
In 2022, she noted that the ACC increased the flexibility of the CMP by removing the 7-hour learning engagement requirement, allowing users to choose how much time to spend learning in the CMP program. They also extended the performance assessment windows from 7 to 9 days each, covering 2 weekends for each.
She said that, to date, more than “6,400 learners” are enrolled in the CMP program.
Though the collaboration seems to make MOC less onerous, some cardiologists think it makes the ACC “complicit.”
A certification program that is independent of the ABIM launched in 2015. The National Board of Physicians and Surgeons is a nonprofit organization led by an advisory board of unpaid physicians. NBPAS seems to be gaining momentum and acceptance.
Cardiologist Melissa Walton-Shirley, MD, recounted her recertification experience with the NBPAS late in 2022. She now maintains a “hybrid” certification with both ABIM and NBPAS. Though she wants to support the latter, she found that the alternative certification option still requires an initial ABIM certification and is not recognized in all states or by many insurers and hospitals.
Will MOC ever disappear? Ms. Sibley said that the ACC is always looking to improve and enhance their offerings. “It is time to lead a change in the conversation from certification to continuous competency, from punitive to supportive options, from random knowledge testing to focused assessing knowledge gaps and lifelong learning. This will require innovation, technology, and new ways of thinking that offer cardiologists flexibility, relevance, and value and ultimately benefit the patients they serve.”
Many physicians, including cardiologists, are hoping that Dr. Goodman’s petition and further pressure from professional societies may finally translate into action.
A version of this article first appeared on Medscape.com.
It’s no secret that many physicians question the value of Maintenance of Certification requirements and are concerned about the amount of time, effort, and money the process takes. Now, they and at least two cardiology societies are starting to speak up.
MOC is an initiative from the American Board of Internal Medicine that requires an initial certification that costs thousands of dollars and must be repeated every 10 years. Annual MOC requirements involve tests that cost $220 for the first certificate a physician holds and about $120 for each subsequent one.
Interventional cardiologists (ICs) and other subspecialists have additional fees and requirements.
MOC ‘burdensome,’ ‘costly,’ ‘complex’
On July 21, hematologist-oncologist Aaron Goodman, MD, an associate professor at the University of California, San Diego, posted a petition on behalf of ABIM diplomates.
As of August 22, the petition had garnered more than 18,000 signatures.
Dr. Goodman recently debated ABIM President and CEO Richard J. Baron, MD, in a Healthcare Unfiltered podcast. Before the debate, host Chadi Nabhan, MD, MBA, tweeted that he could not find a single physician who would defend the MOC and recertification.
The debate touched on topics such as fees, evidence of value, the certification test format, and the cost and requirements to maintain more than one board certification. Overall, Dr. Goodman made the analogy to giving a patient chemotherapy: Because there are harms, he better know that there are also benefits. He cited that the harms associated with MOC include “financial toxicity, time toxicity, and stress toxicity,” with the latter being particularly toxic to him personally.
Though the podcast gave both participants ample opportunities to express their views, it’s not clear that either participant persuaded the other.
Cardiologists who are unhappy with MOC are speaking up on X, formerly known as Twitter. IC Matthew Sample, MD, listed five things he’s done to improve his practice since IC graduation, for which he received no MOC points.
In response, internist Artem Minalyan, MD, asked: “Hypothetically, if Dr. Baron required an IC procedure, I wonder if he would request you to get all your MOC points prior to consenting.”
SCAI and HRS weigh in
Some professional societies have responded to the ABIM’s threat to revoke the certifications of cardiologists who don’t participate in periodic MOC activities.
The Society for Cardiovascular Angiography & Interventions published its “Position on ABIM Revocation of Certification for Not Participating in MOC.” In it, SCAI states that ABIM diplomates who pass their exams and report procedural volumes as required should be “indisputably” recognized as “certified” for the relevant time frame (for example, 10 years), regardless of whether they participate in any other MOC activities.
SCAI President George D. Dangas, MD, PhD, said in an interview that “many of our members have expressed their frustration surrounding the confusion regarding their MOC requirements, including myself. We felt that this confusion could endanger the certified status of members, which would inevitably impact patient care, which is our greatest concern.”
The society has received an “overwhelmingly positive response” to its statement, he said. “Our hope is that ABIM will consider simpler, transparent regulations that are reflective of the feedback received from their constituents.”
In response to the COVID-19 pandemic, ABIM extended the deadline for diplomates whose certificate expired in 2020 or 2021 until the end of 2022; Dr. Dangas suggested ABIM further extend the deadline to enroll in or renew the MOC to the end of 2024 and that ABIM should “develop a recertification program that can be explained in a single slide/page.”
Other subspecialty groups are following SCAI’s lead including the EP Advocacy Foundation, and the Heart Rhythm Society.
MOC alternatives
The ABIM touts the value of MOC on its website, stating: “There is compelling evidence showing that MOC improves value of care without sacrificing quality and that board certified physicians command higher salaries.”
Alternative options that are arguably less arduous are available.
In collaboration with ABIM, the American College of Cardiology launched the ABIM/ACC Collaborative Maintenance Pathway in 2019 as an alternative MOC assessment option.
The CMP “focuses on one or a small group of topics within cardiology each year, incorporating learning activities as well as a pre-/postformative knowledge assessment,” Janice Sibley, ACC’s executive vice president of education and publishing said in an interview, adding that the program continues to evolve.
In 2022, she noted that the ACC increased the flexibility of the CMP by removing the 7-hour learning engagement requirement, allowing users to choose how much time to spend learning in the CMP program. They also extended the performance assessment windows from 7 to 9 days each, covering 2 weekends for each.
She said that, to date, more than “6,400 learners” are enrolled in the CMP program.
Though the collaboration seems to make MOC less onerous, some cardiologists think it makes the ACC “complicit.”
A certification program that is independent of the ABIM launched in 2015. The National Board of Physicians and Surgeons is a nonprofit organization led by an advisory board of unpaid physicians. NBPAS seems to be gaining momentum and acceptance.
Cardiologist Melissa Walton-Shirley, MD, recounted her recertification experience with the NBPAS late in 2022. She now maintains a “hybrid” certification with both ABIM and NBPAS. Though she wants to support the latter, she found that the alternative certification option still requires an initial ABIM certification and is not recognized in all states or by many insurers and hospitals.
Will MOC ever disappear? Ms. Sibley said that the ACC is always looking to improve and enhance their offerings. “It is time to lead a change in the conversation from certification to continuous competency, from punitive to supportive options, from random knowledge testing to focused assessing knowledge gaps and lifelong learning. This will require innovation, technology, and new ways of thinking that offer cardiologists flexibility, relevance, and value and ultimately benefit the patients they serve.”
Many physicians, including cardiologists, are hoping that Dr. Goodman’s petition and further pressure from professional societies may finally translate into action.
A version of this article first appeared on Medscape.com.
Buyer beware
The invitation came to my house, addressed to “residential customer.” It was for my wife and me to attend a free dinner at a swanky local restaurant to learn about “revolutionary” treatments for memory loss. It was presented by a “wellness expert.”
Of course, I just had to check out the website.
The dinner was hosted by an internist pushing an unproven (except for the usual small noncontrolled studies) treatment. Although not stated, I’m sure when you call you’ll find out this is not covered by insurance; not Food and Drug Administration approved to treat, cure, diagnose, prevent any disease; your mileage may vary, etc.
The website was full of testimonials as to how well the treatments worked, primarily from people in their 20s-40s who are, realistically, unlikely to have a pathologically serious cause for memory problems. The site also mentions that you can use it to treat traumatic brain injury, ADHD, learning disorders, obsessive-compulsive disorder, PTSD, Parkinson’s disease, autism, dementia, and stroke, though it does clearly state that such use is not FDA approved.
Prices (I assume all cash pay) for the treatment weren’t listed. I guess you have to come to the “free” dinner for those, or submit an online form to the office.
I’m not going to say the advertised treatment doesn’t work. It might, for at least some of those things. A PubMed search tells me it’s under investigation for several of them.
But that doesn’t mean it works. It might, but a lot of things that look promising in early trials end up failing in the long run. So, at least to me, this is no different than people selling various over-the-counter supplements online with all kinds of extravagant claims and testimonials.
I also have to question a treatment targeting young people for memory loss. In neurology we see a lot of that, and know that true pathology is rare. Most of these patients have root issues with depression, or anxiety, or stress that are affecting their memory. That doesn’t make their memory issues any less real, but they shouldn’t be lumped in with neurodegenerative diseases. They need to be correctly diagnosed and treated for what they are.
Maybe it’s just me, but I often see this sort of thing as kind of sketchy – generating business for unproven treatments by selling fear – you need to do something NOW to keep from getting worse. And, of course there’s always the mysterious “they.” The treatments “they” offer don’t work. Why aren’t “they” telling you what really does?
Looking at the restaurant’s online menu, dinners are around $75 per person and the invitation says “seats are limited.” Doing some mental math gives you an idea how many diners need to come, what percentage of them need to sign up for the treatment, and how much it costs to recoup the investment.
Let the buyer beware.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The invitation came to my house, addressed to “residential customer.” It was for my wife and me to attend a free dinner at a swanky local restaurant to learn about “revolutionary” treatments for memory loss. It was presented by a “wellness expert.”
Of course, I just had to check out the website.
The dinner was hosted by an internist pushing an unproven (except for the usual small noncontrolled studies) treatment. Although not stated, I’m sure when you call you’ll find out this is not covered by insurance; not Food and Drug Administration approved to treat, cure, diagnose, prevent any disease; your mileage may vary, etc.
The website was full of testimonials as to how well the treatments worked, primarily from people in their 20s-40s who are, realistically, unlikely to have a pathologically serious cause for memory problems. The site also mentions that you can use it to treat traumatic brain injury, ADHD, learning disorders, obsessive-compulsive disorder, PTSD, Parkinson’s disease, autism, dementia, and stroke, though it does clearly state that such use is not FDA approved.
Prices (I assume all cash pay) for the treatment weren’t listed. I guess you have to come to the “free” dinner for those, or submit an online form to the office.
I’m not going to say the advertised treatment doesn’t work. It might, for at least some of those things. A PubMed search tells me it’s under investigation for several of them.
But that doesn’t mean it works. It might, but a lot of things that look promising in early trials end up failing in the long run. So, at least to me, this is no different than people selling various over-the-counter supplements online with all kinds of extravagant claims and testimonials.
I also have to question a treatment targeting young people for memory loss. In neurology we see a lot of that, and know that true pathology is rare. Most of these patients have root issues with depression, or anxiety, or stress that are affecting their memory. That doesn’t make their memory issues any less real, but they shouldn’t be lumped in with neurodegenerative diseases. They need to be correctly diagnosed and treated for what they are.
Maybe it’s just me, but I often see this sort of thing as kind of sketchy – generating business for unproven treatments by selling fear – you need to do something NOW to keep from getting worse. And, of course there’s always the mysterious “they.” The treatments “they” offer don’t work. Why aren’t “they” telling you what really does?
Looking at the restaurant’s online menu, dinners are around $75 per person and the invitation says “seats are limited.” Doing some mental math gives you an idea how many diners need to come, what percentage of them need to sign up for the treatment, and how much it costs to recoup the investment.
Let the buyer beware.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The invitation came to my house, addressed to “residential customer.” It was for my wife and me to attend a free dinner at a swanky local restaurant to learn about “revolutionary” treatments for memory loss. It was presented by a “wellness expert.”
Of course, I just had to check out the website.
The dinner was hosted by an internist pushing an unproven (except for the usual small noncontrolled studies) treatment. Although not stated, I’m sure when you call you’ll find out this is not covered by insurance; not Food and Drug Administration approved to treat, cure, diagnose, prevent any disease; your mileage may vary, etc.
The website was full of testimonials as to how well the treatments worked, primarily from people in their 20s-40s who are, realistically, unlikely to have a pathologically serious cause for memory problems. The site also mentions that you can use it to treat traumatic brain injury, ADHD, learning disorders, obsessive-compulsive disorder, PTSD, Parkinson’s disease, autism, dementia, and stroke, though it does clearly state that such use is not FDA approved.
Prices (I assume all cash pay) for the treatment weren’t listed. I guess you have to come to the “free” dinner for those, or submit an online form to the office.
I’m not going to say the advertised treatment doesn’t work. It might, for at least some of those things. A PubMed search tells me it’s under investigation for several of them.
But that doesn’t mean it works. It might, but a lot of things that look promising in early trials end up failing in the long run. So, at least to me, this is no different than people selling various over-the-counter supplements online with all kinds of extravagant claims and testimonials.
I also have to question a treatment targeting young people for memory loss. In neurology we see a lot of that, and know that true pathology is rare. Most of these patients have root issues with depression, or anxiety, or stress that are affecting their memory. That doesn’t make their memory issues any less real, but they shouldn’t be lumped in with neurodegenerative diseases. They need to be correctly diagnosed and treated for what they are.
Maybe it’s just me, but I often see this sort of thing as kind of sketchy – generating business for unproven treatments by selling fear – you need to do something NOW to keep from getting worse. And, of course there’s always the mysterious “they.” The treatments “they” offer don’t work. Why aren’t “they” telling you what really does?
Looking at the restaurant’s online menu, dinners are around $75 per person and the invitation says “seats are limited.” Doing some mental math gives you an idea how many diners need to come, what percentage of them need to sign up for the treatment, and how much it costs to recoup the investment.
Let the buyer beware.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.



