User login
Early gestational diabetes treatment may improve neonatal outcomes
Screening and treatment for gestational diabetes are currently recommended at 24-28 weeks’ gestation, with earlier testing recommended for women at increased risk, but the potential benefits of earlier intervention remain debatable, wrote David Simmons, MD, of Western Sydney University, Campbelltown, Australia, and colleagues.
“Until now, there has been complete equipoise over whether to treat hyperglycemia below that of overt diabetes early in pregnancy,” Dr. Simmons said in an interview. The conflicting questions: “Would early treatment reduce the excess deposition of fat on the baby with all of its sequelae; but would early treatment reduce fuel supply to some babies at a critical time and lead to SGA [small for gestational age]?” Dr. Simmons noted.
In a study published in the New England Journal of Medicine, Dr. Simmons and colleagues randomized 406 women aged 18 years and older with singleton pregnancies to immediate treatment for gestational diabetes. Another 396 women were randomized to a control group for deferred treatment or no treatment, based on results of an oral glucose tolerance test at 24-28 weeks’ gestation. All participants had at least one risk factor for hyperglycemia, and met the World Health Organization criteria for gestational diabetes. Women with preexisting diabetes or contraindicating comorbid medical conditions were excluded.
The study had three primary outcomes. The first was a composite of neonatal outcomes including birth before 37 weeks’ gestation, birth weight of 4,500 g or higher, birth trauma, neonatal respiratory distress, phototherapy, stillbirth or neonatal death, or shoulder dystocia.
The final sample included 748 women for adverse neonatal outcomes, 750 for pregnancy-related hypertension, and 492 for neonatal lean body mass. The mean age of the participants was 32 years; approximately one-third were white European and another third were South Asian. Overall baseline demographics were similar between the groups, and the initial oral glucose tolerance tests were performed at a mean of 15.6 weeks’ gestation.
Overall, 24.9% of women in the early treatment group experienced an adverse neonatal event vs. 30.5% of controls, for an adjusted risk difference of –5.6% and adjusted relative risk of 0.82.
Notably, in an exploratory subgroup analysis, respiratory distress occurred in 9.8% of infants born to women in the immediate treatment group vs. 17.0% of infants in the control group. “Neonatal respiratory distress was the main driver of the between-group difference observed for the first primary outcome,” the researchers wrote. A prespecified subgroup analysis suggested that the impact of an earlier intervention on adverse neonatal outcomes might be greater among women with a higher glycemic value and those whose oral glucose tolerance tests occurred at less than 14 weeks’ gestation, they noted. Stillbirths or neonatal deaths were similar and infrequent in both groups.
Pregnancy-related hypertension occurred in 10.6% of the immediate-treatment group and 9.9% of the controls group (adjusted risk difference, 0.7%). For the third outcome, the mean neonatal lean body mass was 2.86 g in the immediate-treatment group and 2.91 g for the controls (adjusted mean difference, −0.04 g).
No differences in serious adverse events related to either screening or treatment were noted between the groups.
Impact on neonatal outcomes merits further study
Dr. Simmons said that he was surprised by the study findings. “We thought if there was an effect, it would be small, but it isn’t,” he told this publication.
“If you combine the severe adverse outcomes, the perineal trauma and the reduction in days in NICU/special care unit, this is a significant impact on morbidity and likely on cost,” and researchers are currently examining data for cost-effectiveness, he said.
“We did not expect the likely large impact on reducing respiratory distress and perineal trauma,” he noted. “These findings have not been previously reported, perhaps because they were not looked for.” By contrast, “we thought here might be reductions in lower gestational age and cesarean delivery, but there was not,” he added.
The findings were limited by several factors including the nonstandardized approach to gestational diabetes treatment and the use of third-trimester treatment targets that had not been tested in earlier trimesters, the researchers noted. Other limitations included the focus on women already at high risk for hyperglycemia; therefore, the results might not generalize to women not at risk, they wrote.
The current study represents a beginning of answers, with data suggesting that early treatment for gestational diabetes reduces severe adverse pregnancy outcomes, days in NICU/special care unit, and perineal trauma, likely from the first trimester, said Dr. Simmons. However, the findings must be interpreted with caution, as criteria that are too low “might lead to more small babies,” he said. “We look forward to working with others to translate these findings into practice,” he added.
Much more research is needed to answer the many questions prompted by the current study, including who did and did not have complications, Dr. Simmons told this publication. Other studies are needed to collect data on cost-effectiveness, as well as consumer views, especially “different perspectives from different parts of the globe,” he said. Although there is not enough evidence yet to draw conclusions about the role of continuous glucose monitoring (CGM) in managing gestational diabetes, many studies are underway; “we look forward to the results,” of these studies, Dr. Simmons added.
Findings support early screening
Gestational diabetes is one of the most common medical complications of pregnancy, and accounts for more than 80% of diabetes-related diagnoses in pregnancy, said Emily Fay, MD, a maternal-fetal medicine specialist at the University of Washington, Seattle, in an interview.
“Previous studies have found that women with gestational diabetes are at higher risk in their pregnancy, including higher chance of developing preeclampsia, higher chance of cesarean delivery, and higher risks for their baby, including risk of shoulder dystocia, birth trauma, and jaundice, and higher birth weights,” she said. “Fortunately, studies have also shown that treatment of gestational diabetes helps lower these risks,” she noted. Currently, patients undergo routine screening for gestational diabetes between 24 and 28 weeks of pregnancy, but some who have risk factors for gestational diabetes may have screening in the early part of pregnancy, said Dr. Fay.
The current findings were not surprising overall, said Dr. Fay, who was not involved in the study. “The study authors looked at a variety of outcomes including neonatal adverse outcomes, neonatal body weight, and pregnancy-related hypertension,” she said.
The researchers found that patients treated early had a lower rate of adverse neonatal outcomes, which was to be expected, Dr. Fay said. “They did not find a difference in neonatal body weight; this also was not surprising, as the women who were not in the early treatment group still received treatment at the time of diagnosis later in pregnancy, which likely helped normalize the weights,” she explained.
“My takeaway from this study is that we should continue to screen patients with risk factors for gestational diabetes early in pregnancy and treat them at the time of diagnosis,” Dr. Fay told this publication. However, barriers that may exist to early treatment involve access to care, including being able to see a provider early in pregnancy, she said. “The treatment for gestational diabetes includes dietary education with diet changes and checking blood sugars frequently. Access to nutrition education can be limited and access to healthy foods can be expensive and difficult to obtain,” she noted. “Checking blood sugars throughout the day can also be difficult for those who are busy or working and who may not have the ability to take time to do this,” she said. However, “these barriers may be overcome by health care reform that improves patient access to and coverage of pregnancy care, improved access and affordability of healthy foods, and employer flexibility to allow the time and space to check blood sugars if needed,” she added.
Looking ahead, the use of continuous glucose monitors in pregnancy is an expanding area of research, said Dr. Fay. “Patients can quickly view their blood sugar without the use of finger sticks, which may help overcome some of the barriers patients may have with using finger sticks,” she noted. “Continuous glucose monitors have been used for those with type 1 and type 2 diabetes with success, and we need to better understand if these can also be helpful in gestational diabetes,” she said. Dr. Fay and colleagues at the University of Washington are currently conducting an ongoing study to explore the use of CGM in gestational diabetes.
The study was supported by the National Health and Medical Research Council, the Region Örebro Research Committee, the Medical Scientific Fund of the Mayor of Vienna, the South Western Sydney Local Health District Academic Unit, and a Western Sydney University Ainsworth Trust Grant. The researchers had no financial conflicts to disclose. Dr. Fay had no relevant financial conflicts to disclose.
Screening and treatment for gestational diabetes are currently recommended at 24-28 weeks’ gestation, with earlier testing recommended for women at increased risk, but the potential benefits of earlier intervention remain debatable, wrote David Simmons, MD, of Western Sydney University, Campbelltown, Australia, and colleagues.
“Until now, there has been complete equipoise over whether to treat hyperglycemia below that of overt diabetes early in pregnancy,” Dr. Simmons said in an interview. The conflicting questions: “Would early treatment reduce the excess deposition of fat on the baby with all of its sequelae; but would early treatment reduce fuel supply to some babies at a critical time and lead to SGA [small for gestational age]?” Dr. Simmons noted.
In a study published in the New England Journal of Medicine, Dr. Simmons and colleagues randomized 406 women aged 18 years and older with singleton pregnancies to immediate treatment for gestational diabetes. Another 396 women were randomized to a control group for deferred treatment or no treatment, based on results of an oral glucose tolerance test at 24-28 weeks’ gestation. All participants had at least one risk factor for hyperglycemia, and met the World Health Organization criteria for gestational diabetes. Women with preexisting diabetes or contraindicating comorbid medical conditions were excluded.
The study had three primary outcomes. The first was a composite of neonatal outcomes including birth before 37 weeks’ gestation, birth weight of 4,500 g or higher, birth trauma, neonatal respiratory distress, phototherapy, stillbirth or neonatal death, or shoulder dystocia.
The final sample included 748 women for adverse neonatal outcomes, 750 for pregnancy-related hypertension, and 492 for neonatal lean body mass. The mean age of the participants was 32 years; approximately one-third were white European and another third were South Asian. Overall baseline demographics were similar between the groups, and the initial oral glucose tolerance tests were performed at a mean of 15.6 weeks’ gestation.
Overall, 24.9% of women in the early treatment group experienced an adverse neonatal event vs. 30.5% of controls, for an adjusted risk difference of –5.6% and adjusted relative risk of 0.82.
Notably, in an exploratory subgroup analysis, respiratory distress occurred in 9.8% of infants born to women in the immediate treatment group vs. 17.0% of infants in the control group. “Neonatal respiratory distress was the main driver of the between-group difference observed for the first primary outcome,” the researchers wrote. A prespecified subgroup analysis suggested that the impact of an earlier intervention on adverse neonatal outcomes might be greater among women with a higher glycemic value and those whose oral glucose tolerance tests occurred at less than 14 weeks’ gestation, they noted. Stillbirths or neonatal deaths were similar and infrequent in both groups.
Pregnancy-related hypertension occurred in 10.6% of the immediate-treatment group and 9.9% of the controls group (adjusted risk difference, 0.7%). For the third outcome, the mean neonatal lean body mass was 2.86 g in the immediate-treatment group and 2.91 g for the controls (adjusted mean difference, −0.04 g).
No differences in serious adverse events related to either screening or treatment were noted between the groups.
Impact on neonatal outcomes merits further study
Dr. Simmons said that he was surprised by the study findings. “We thought if there was an effect, it would be small, but it isn’t,” he told this publication.
“If you combine the severe adverse outcomes, the perineal trauma and the reduction in days in NICU/special care unit, this is a significant impact on morbidity and likely on cost,” and researchers are currently examining data for cost-effectiveness, he said.
“We did not expect the likely large impact on reducing respiratory distress and perineal trauma,” he noted. “These findings have not been previously reported, perhaps because they were not looked for.” By contrast, “we thought here might be reductions in lower gestational age and cesarean delivery, but there was not,” he added.
The findings were limited by several factors including the nonstandardized approach to gestational diabetes treatment and the use of third-trimester treatment targets that had not been tested in earlier trimesters, the researchers noted. Other limitations included the focus on women already at high risk for hyperglycemia; therefore, the results might not generalize to women not at risk, they wrote.
The current study represents a beginning of answers, with data suggesting that early treatment for gestational diabetes reduces severe adverse pregnancy outcomes, days in NICU/special care unit, and perineal trauma, likely from the first trimester, said Dr. Simmons. However, the findings must be interpreted with caution, as criteria that are too low “might lead to more small babies,” he said. “We look forward to working with others to translate these findings into practice,” he added.
Much more research is needed to answer the many questions prompted by the current study, including who did and did not have complications, Dr. Simmons told this publication. Other studies are needed to collect data on cost-effectiveness, as well as consumer views, especially “different perspectives from different parts of the globe,” he said. Although there is not enough evidence yet to draw conclusions about the role of continuous glucose monitoring (CGM) in managing gestational diabetes, many studies are underway; “we look forward to the results,” of these studies, Dr. Simmons added.
Findings support early screening
Gestational diabetes is one of the most common medical complications of pregnancy, and accounts for more than 80% of diabetes-related diagnoses in pregnancy, said Emily Fay, MD, a maternal-fetal medicine specialist at the University of Washington, Seattle, in an interview.
“Previous studies have found that women with gestational diabetes are at higher risk in their pregnancy, including higher chance of developing preeclampsia, higher chance of cesarean delivery, and higher risks for their baby, including risk of shoulder dystocia, birth trauma, and jaundice, and higher birth weights,” she said. “Fortunately, studies have also shown that treatment of gestational diabetes helps lower these risks,” she noted. Currently, patients undergo routine screening for gestational diabetes between 24 and 28 weeks of pregnancy, but some who have risk factors for gestational diabetes may have screening in the early part of pregnancy, said Dr. Fay.
The current findings were not surprising overall, said Dr. Fay, who was not involved in the study. “The study authors looked at a variety of outcomes including neonatal adverse outcomes, neonatal body weight, and pregnancy-related hypertension,” she said.
The researchers found that patients treated early had a lower rate of adverse neonatal outcomes, which was to be expected, Dr. Fay said. “They did not find a difference in neonatal body weight; this also was not surprising, as the women who were not in the early treatment group still received treatment at the time of diagnosis later in pregnancy, which likely helped normalize the weights,” she explained.
“My takeaway from this study is that we should continue to screen patients with risk factors for gestational diabetes early in pregnancy and treat them at the time of diagnosis,” Dr. Fay told this publication. However, barriers that may exist to early treatment involve access to care, including being able to see a provider early in pregnancy, she said. “The treatment for gestational diabetes includes dietary education with diet changes and checking blood sugars frequently. Access to nutrition education can be limited and access to healthy foods can be expensive and difficult to obtain,” she noted. “Checking blood sugars throughout the day can also be difficult for those who are busy or working and who may not have the ability to take time to do this,” she said. However, “these barriers may be overcome by health care reform that improves patient access to and coverage of pregnancy care, improved access and affordability of healthy foods, and employer flexibility to allow the time and space to check blood sugars if needed,” she added.
Looking ahead, the use of continuous glucose monitors in pregnancy is an expanding area of research, said Dr. Fay. “Patients can quickly view their blood sugar without the use of finger sticks, which may help overcome some of the barriers patients may have with using finger sticks,” she noted. “Continuous glucose monitors have been used for those with type 1 and type 2 diabetes with success, and we need to better understand if these can also be helpful in gestational diabetes,” she said. Dr. Fay and colleagues at the University of Washington are currently conducting an ongoing study to explore the use of CGM in gestational diabetes.
The study was supported by the National Health and Medical Research Council, the Region Örebro Research Committee, the Medical Scientific Fund of the Mayor of Vienna, the South Western Sydney Local Health District Academic Unit, and a Western Sydney University Ainsworth Trust Grant. The researchers had no financial conflicts to disclose. Dr. Fay had no relevant financial conflicts to disclose.
Screening and treatment for gestational diabetes are currently recommended at 24-28 weeks’ gestation, with earlier testing recommended for women at increased risk, but the potential benefits of earlier intervention remain debatable, wrote David Simmons, MD, of Western Sydney University, Campbelltown, Australia, and colleagues.
“Until now, there has been complete equipoise over whether to treat hyperglycemia below that of overt diabetes early in pregnancy,” Dr. Simmons said in an interview. The conflicting questions: “Would early treatment reduce the excess deposition of fat on the baby with all of its sequelae; but would early treatment reduce fuel supply to some babies at a critical time and lead to SGA [small for gestational age]?” Dr. Simmons noted.
In a study published in the New England Journal of Medicine, Dr. Simmons and colleagues randomized 406 women aged 18 years and older with singleton pregnancies to immediate treatment for gestational diabetes. Another 396 women were randomized to a control group for deferred treatment or no treatment, based on results of an oral glucose tolerance test at 24-28 weeks’ gestation. All participants had at least one risk factor for hyperglycemia, and met the World Health Organization criteria for gestational diabetes. Women with preexisting diabetes or contraindicating comorbid medical conditions were excluded.
The study had three primary outcomes. The first was a composite of neonatal outcomes including birth before 37 weeks’ gestation, birth weight of 4,500 g or higher, birth trauma, neonatal respiratory distress, phototherapy, stillbirth or neonatal death, or shoulder dystocia.
The final sample included 748 women for adverse neonatal outcomes, 750 for pregnancy-related hypertension, and 492 for neonatal lean body mass. The mean age of the participants was 32 years; approximately one-third were white European and another third were South Asian. Overall baseline demographics were similar between the groups, and the initial oral glucose tolerance tests were performed at a mean of 15.6 weeks’ gestation.
Overall, 24.9% of women in the early treatment group experienced an adverse neonatal event vs. 30.5% of controls, for an adjusted risk difference of –5.6% and adjusted relative risk of 0.82.
Notably, in an exploratory subgroup analysis, respiratory distress occurred in 9.8% of infants born to women in the immediate treatment group vs. 17.0% of infants in the control group. “Neonatal respiratory distress was the main driver of the between-group difference observed for the first primary outcome,” the researchers wrote. A prespecified subgroup analysis suggested that the impact of an earlier intervention on adverse neonatal outcomes might be greater among women with a higher glycemic value and those whose oral glucose tolerance tests occurred at less than 14 weeks’ gestation, they noted. Stillbirths or neonatal deaths were similar and infrequent in both groups.
Pregnancy-related hypertension occurred in 10.6% of the immediate-treatment group and 9.9% of the controls group (adjusted risk difference, 0.7%). For the third outcome, the mean neonatal lean body mass was 2.86 g in the immediate-treatment group and 2.91 g for the controls (adjusted mean difference, −0.04 g).
No differences in serious adverse events related to either screening or treatment were noted between the groups.
Impact on neonatal outcomes merits further study
Dr. Simmons said that he was surprised by the study findings. “We thought if there was an effect, it would be small, but it isn’t,” he told this publication.
“If you combine the severe adverse outcomes, the perineal trauma and the reduction in days in NICU/special care unit, this is a significant impact on morbidity and likely on cost,” and researchers are currently examining data for cost-effectiveness, he said.
“We did not expect the likely large impact on reducing respiratory distress and perineal trauma,” he noted. “These findings have not been previously reported, perhaps because they were not looked for.” By contrast, “we thought here might be reductions in lower gestational age and cesarean delivery, but there was not,” he added.
The findings were limited by several factors including the nonstandardized approach to gestational diabetes treatment and the use of third-trimester treatment targets that had not been tested in earlier trimesters, the researchers noted. Other limitations included the focus on women already at high risk for hyperglycemia; therefore, the results might not generalize to women not at risk, they wrote.
The current study represents a beginning of answers, with data suggesting that early treatment for gestational diabetes reduces severe adverse pregnancy outcomes, days in NICU/special care unit, and perineal trauma, likely from the first trimester, said Dr. Simmons. However, the findings must be interpreted with caution, as criteria that are too low “might lead to more small babies,” he said. “We look forward to working with others to translate these findings into practice,” he added.
Much more research is needed to answer the many questions prompted by the current study, including who did and did not have complications, Dr. Simmons told this publication. Other studies are needed to collect data on cost-effectiveness, as well as consumer views, especially “different perspectives from different parts of the globe,” he said. Although there is not enough evidence yet to draw conclusions about the role of continuous glucose monitoring (CGM) in managing gestational diabetes, many studies are underway; “we look forward to the results,” of these studies, Dr. Simmons added.
Findings support early screening
Gestational diabetes is one of the most common medical complications of pregnancy, and accounts for more than 80% of diabetes-related diagnoses in pregnancy, said Emily Fay, MD, a maternal-fetal medicine specialist at the University of Washington, Seattle, in an interview.
“Previous studies have found that women with gestational diabetes are at higher risk in their pregnancy, including higher chance of developing preeclampsia, higher chance of cesarean delivery, and higher risks for their baby, including risk of shoulder dystocia, birth trauma, and jaundice, and higher birth weights,” she said. “Fortunately, studies have also shown that treatment of gestational diabetes helps lower these risks,” she noted. Currently, patients undergo routine screening for gestational diabetes between 24 and 28 weeks of pregnancy, but some who have risk factors for gestational diabetes may have screening in the early part of pregnancy, said Dr. Fay.
The current findings were not surprising overall, said Dr. Fay, who was not involved in the study. “The study authors looked at a variety of outcomes including neonatal adverse outcomes, neonatal body weight, and pregnancy-related hypertension,” she said.
The researchers found that patients treated early had a lower rate of adverse neonatal outcomes, which was to be expected, Dr. Fay said. “They did not find a difference in neonatal body weight; this also was not surprising, as the women who were not in the early treatment group still received treatment at the time of diagnosis later in pregnancy, which likely helped normalize the weights,” she explained.
“My takeaway from this study is that we should continue to screen patients with risk factors for gestational diabetes early in pregnancy and treat them at the time of diagnosis,” Dr. Fay told this publication. However, barriers that may exist to early treatment involve access to care, including being able to see a provider early in pregnancy, she said. “The treatment for gestational diabetes includes dietary education with diet changes and checking blood sugars frequently. Access to nutrition education can be limited and access to healthy foods can be expensive and difficult to obtain,” she noted. “Checking blood sugars throughout the day can also be difficult for those who are busy or working and who may not have the ability to take time to do this,” she said. However, “these barriers may be overcome by health care reform that improves patient access to and coverage of pregnancy care, improved access and affordability of healthy foods, and employer flexibility to allow the time and space to check blood sugars if needed,” she added.
Looking ahead, the use of continuous glucose monitors in pregnancy is an expanding area of research, said Dr. Fay. “Patients can quickly view their blood sugar without the use of finger sticks, which may help overcome some of the barriers patients may have with using finger sticks,” she noted. “Continuous glucose monitors have been used for those with type 1 and type 2 diabetes with success, and we need to better understand if these can also be helpful in gestational diabetes,” she said. Dr. Fay and colleagues at the University of Washington are currently conducting an ongoing study to explore the use of CGM in gestational diabetes.
The study was supported by the National Health and Medical Research Council, the Region Örebro Research Committee, the Medical Scientific Fund of the Mayor of Vienna, the South Western Sydney Local Health District Academic Unit, and a Western Sydney University Ainsworth Trust Grant. The researchers had no financial conflicts to disclose. Dr. Fay had no relevant financial conflicts to disclose.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Boys may carry the weight, or overweight, of adults’ infertility
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
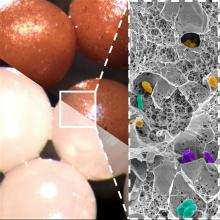
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
New protocol could cut fasting period to detect insulinomas
SEATTLE – , therefore yielding significant hospital cost savings, new data suggest.
Insulinomas are small, rare types of pancreatic tumors that are benign but secrete excess insulin, leading to hypoglycemia. More than 99% of people with insulinomas develop hypoglycemia within 72 hours, hence, the use of a 72-hour fast to detect these tumors.
But most people who are evaluated for hypoglycemia do not have an insulinoma and fasting in hospital for 3 days is burdensome and costly.
As part of a quality improvement project, Cleveland Clinic endocrinology fellow Michelle D. Lundholm, MD, and colleagues modified their hospital’s protocol to include measurement of beta-hydroxybutyrate (BHB), a marker of insulin suppression, every 12 hours with a cutoff of ≥ 2.7mmol/L for stopping the fast if hypoglycemia (venous glucose ≤ 45mg/dL) hasn’t occurred. This intervention cut in half the number of patients who needed to fast for the full 72 hours, without missing any insulinomas.
“We are excited to share how a relatively simple adjustment to our protocol allowed us to successfully reduce the burden of fasting on patients and more effectively utilize hospital resources. We hope that this encourages other centers to consider doing the same,” Dr. Lundholm said in an interview.
“These data support a 48-hour fast. The literature supports that’s sufficient to detect 95% of insulinomas. ... But, given our small insulinoma cohort, we are looking forward to learning from other studies,” she added.
Dr. Lundholm presented the late-breaking oral abstract at the annual scientific & clinical congress of the American Association of Clinical Endocrinology.
Asked to comment, session moderator Jenna Sarvaideo, MD, said: “We’re often steeped in tradition. That’s why this abstract and this quality improvement project is so exciting to me because it challenges the history. … and I think it’s ultimately helping patients.”
Dr. Sarvaideo, of Clement J. Zablocki VA Medical Center, Milwaukee, noted that, typically, although the fast will be stopped before 72 hours if the patient develops hypoglycemia, “often they don’t, so we keep going on and on. If we just paid more attention to the beta-hydroxybutyrate, I think that would be practice changing.”
She added that more data would be optimal, given that there were under 100 patients in the study, “but I do think that devising protocols is … very much still at the hands of the endocrinologists. I think that this work could make groups reevaluate their protocol and change it, maybe even with a small dataset and then move on from there and see what they see.”
Indeed, Dr. Lundholm pointed out that some institutions, such as the Mayo Clinic, already include 6-hour BHB measurements (along with glucose and insulin) in their protocols.
“For any institution that already draws regular BHB levels like this, it would be very easy to implement a new stopping criterion without adding any additional costs,” she said in an interview.
All insulinomas became apparent in less than 48 hours
The first report to look at the value of testing BHB at regular intervals was published by the Mayo Clinic in 2005 after they noticed patients without insulinoma were complaining of ketosis symptoms such as foul breath and digestive problems toward the end of the fast.
However, although BHB testing is used today as part of the evaluation, it’s typically only drawn at the start of the protocol and again at the time of hypoglycemia or at the end of 72 hours because more frequent values hadn’t been thought to be useful for guiding clinical management, Dr. Lundholm explained.
Between January 2018 and June 2020, Dr. Lundholm and colleagues followed 34 Cleveland Clinic patients who completed the usual 72-hour fast protocol. Overall, 71% were female, and 26% had undergone prior bariatric surgery procedures. Eleven (32%) developed hypoglycemia and stopped fasting. The other 23 (68%) fasted for the full 72 hours.
Dr. Lundholm and colleagues determined that the fast could have ended earlier in 35% of patients based on an elevated BHB without missing any insulinomas.
And so, in June 2020 the group revised their protocol to include the BHB ≥ 2.7mmol/L stopping criterion. Of the 30 patients evaluated from June 2020 to January 2023, 87% were female and 17% had undergone a bariatric procedure.
Here, 15 (50%) reached a BHB ≥ 2.7mmol/L and ended their fast at an average of 43.8 hours. Another seven (23%) ended the fast after developing hypoglycemia. Just eight patients (27%) fasted for the full 72 hours.
Overall, this resulted in approximately 376 fewer cumulative hours of inpatient admission than if patients had fasted for the full time.
Of the 64 patients who have completed the fasting protocol since 2018, seven (11%) who did have an insulinoma developed hypoglycemia within 48 hours and with a BHB < 2.7 mmol/L (median, 0.15).
Advantages: cost, adherence
A day in a general medicine bed at Cleveland Clinic was quoted as costing $2,420, based on publicly available information as of Jan. 1, 2023. “If half of patients leave 1 day earlier, this equates to about $1,210 per patient in savings from bed costs alone,” Dr. Lundholm told this news organization.
The revised protocol required an additional two to four blood draws, depending on the length of the fast. “The cost of these extra blood tests varies by lab and by count, but even at its highest does not exceed the amount of savings from bed costs,” she noted.
Patient adherence is another potential benefit of the revised protocol.
“Any study that requires 72 hours of patient cooperation is a challenge, particularly in an uncomfortable position like fasting. When we looked at these adherence numbers, we found that the percentage of patients who prematurely ended their fast decreased from 35% to 17% with the updated protocol,” Dr. Lundholm continued.
“This translates to fewer inconclusive results and fewer readmissions for repeat 72-hour fasting. While this was not our primary outcome, it was another noted benefit of our change,” she said.
Dr. Lundholm and Dr. Sarvaideo have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
SEATTLE – , therefore yielding significant hospital cost savings, new data suggest.
Insulinomas are small, rare types of pancreatic tumors that are benign but secrete excess insulin, leading to hypoglycemia. More than 99% of people with insulinomas develop hypoglycemia within 72 hours, hence, the use of a 72-hour fast to detect these tumors.
But most people who are evaluated for hypoglycemia do not have an insulinoma and fasting in hospital for 3 days is burdensome and costly.
As part of a quality improvement project, Cleveland Clinic endocrinology fellow Michelle D. Lundholm, MD, and colleagues modified their hospital’s protocol to include measurement of beta-hydroxybutyrate (BHB), a marker of insulin suppression, every 12 hours with a cutoff of ≥ 2.7mmol/L for stopping the fast if hypoglycemia (venous glucose ≤ 45mg/dL) hasn’t occurred. This intervention cut in half the number of patients who needed to fast for the full 72 hours, without missing any insulinomas.
“We are excited to share how a relatively simple adjustment to our protocol allowed us to successfully reduce the burden of fasting on patients and more effectively utilize hospital resources. We hope that this encourages other centers to consider doing the same,” Dr. Lundholm said in an interview.
“These data support a 48-hour fast. The literature supports that’s sufficient to detect 95% of insulinomas. ... But, given our small insulinoma cohort, we are looking forward to learning from other studies,” she added.
Dr. Lundholm presented the late-breaking oral abstract at the annual scientific & clinical congress of the American Association of Clinical Endocrinology.
Asked to comment, session moderator Jenna Sarvaideo, MD, said: “We’re often steeped in tradition. That’s why this abstract and this quality improvement project is so exciting to me because it challenges the history. … and I think it’s ultimately helping patients.”
Dr. Sarvaideo, of Clement J. Zablocki VA Medical Center, Milwaukee, noted that, typically, although the fast will be stopped before 72 hours if the patient develops hypoglycemia, “often they don’t, so we keep going on and on. If we just paid more attention to the beta-hydroxybutyrate, I think that would be practice changing.”
She added that more data would be optimal, given that there were under 100 patients in the study, “but I do think that devising protocols is … very much still at the hands of the endocrinologists. I think that this work could make groups reevaluate their protocol and change it, maybe even with a small dataset and then move on from there and see what they see.”
Indeed, Dr. Lundholm pointed out that some institutions, such as the Mayo Clinic, already include 6-hour BHB measurements (along with glucose and insulin) in their protocols.
“For any institution that already draws regular BHB levels like this, it would be very easy to implement a new stopping criterion without adding any additional costs,” she said in an interview.
All insulinomas became apparent in less than 48 hours
The first report to look at the value of testing BHB at regular intervals was published by the Mayo Clinic in 2005 after they noticed patients without insulinoma were complaining of ketosis symptoms such as foul breath and digestive problems toward the end of the fast.
However, although BHB testing is used today as part of the evaluation, it’s typically only drawn at the start of the protocol and again at the time of hypoglycemia or at the end of 72 hours because more frequent values hadn’t been thought to be useful for guiding clinical management, Dr. Lundholm explained.
Between January 2018 and June 2020, Dr. Lundholm and colleagues followed 34 Cleveland Clinic patients who completed the usual 72-hour fast protocol. Overall, 71% were female, and 26% had undergone prior bariatric surgery procedures. Eleven (32%) developed hypoglycemia and stopped fasting. The other 23 (68%) fasted for the full 72 hours.
Dr. Lundholm and colleagues determined that the fast could have ended earlier in 35% of patients based on an elevated BHB without missing any insulinomas.
And so, in June 2020 the group revised their protocol to include the BHB ≥ 2.7mmol/L stopping criterion. Of the 30 patients evaluated from June 2020 to January 2023, 87% were female and 17% had undergone a bariatric procedure.
Here, 15 (50%) reached a BHB ≥ 2.7mmol/L and ended their fast at an average of 43.8 hours. Another seven (23%) ended the fast after developing hypoglycemia. Just eight patients (27%) fasted for the full 72 hours.
Overall, this resulted in approximately 376 fewer cumulative hours of inpatient admission than if patients had fasted for the full time.
Of the 64 patients who have completed the fasting protocol since 2018, seven (11%) who did have an insulinoma developed hypoglycemia within 48 hours and with a BHB < 2.7 mmol/L (median, 0.15).
Advantages: cost, adherence
A day in a general medicine bed at Cleveland Clinic was quoted as costing $2,420, based on publicly available information as of Jan. 1, 2023. “If half of patients leave 1 day earlier, this equates to about $1,210 per patient in savings from bed costs alone,” Dr. Lundholm told this news organization.
The revised protocol required an additional two to four blood draws, depending on the length of the fast. “The cost of these extra blood tests varies by lab and by count, but even at its highest does not exceed the amount of savings from bed costs,” she noted.
Patient adherence is another potential benefit of the revised protocol.
“Any study that requires 72 hours of patient cooperation is a challenge, particularly in an uncomfortable position like fasting. When we looked at these adherence numbers, we found that the percentage of patients who prematurely ended their fast decreased from 35% to 17% with the updated protocol,” Dr. Lundholm continued.
“This translates to fewer inconclusive results and fewer readmissions for repeat 72-hour fasting. While this was not our primary outcome, it was another noted benefit of our change,” she said.
Dr. Lundholm and Dr. Sarvaideo have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
SEATTLE – , therefore yielding significant hospital cost savings, new data suggest.
Insulinomas are small, rare types of pancreatic tumors that are benign but secrete excess insulin, leading to hypoglycemia. More than 99% of people with insulinomas develop hypoglycemia within 72 hours, hence, the use of a 72-hour fast to detect these tumors.
But most people who are evaluated for hypoglycemia do not have an insulinoma and fasting in hospital for 3 days is burdensome and costly.
As part of a quality improvement project, Cleveland Clinic endocrinology fellow Michelle D. Lundholm, MD, and colleagues modified their hospital’s protocol to include measurement of beta-hydroxybutyrate (BHB), a marker of insulin suppression, every 12 hours with a cutoff of ≥ 2.7mmol/L for stopping the fast if hypoglycemia (venous glucose ≤ 45mg/dL) hasn’t occurred. This intervention cut in half the number of patients who needed to fast for the full 72 hours, without missing any insulinomas.
“We are excited to share how a relatively simple adjustment to our protocol allowed us to successfully reduce the burden of fasting on patients and more effectively utilize hospital resources. We hope that this encourages other centers to consider doing the same,” Dr. Lundholm said in an interview.
“These data support a 48-hour fast. The literature supports that’s sufficient to detect 95% of insulinomas. ... But, given our small insulinoma cohort, we are looking forward to learning from other studies,” she added.
Dr. Lundholm presented the late-breaking oral abstract at the annual scientific & clinical congress of the American Association of Clinical Endocrinology.
Asked to comment, session moderator Jenna Sarvaideo, MD, said: “We’re often steeped in tradition. That’s why this abstract and this quality improvement project is so exciting to me because it challenges the history. … and I think it’s ultimately helping patients.”
Dr. Sarvaideo, of Clement J. Zablocki VA Medical Center, Milwaukee, noted that, typically, although the fast will be stopped before 72 hours if the patient develops hypoglycemia, “often they don’t, so we keep going on and on. If we just paid more attention to the beta-hydroxybutyrate, I think that would be practice changing.”
She added that more data would be optimal, given that there were under 100 patients in the study, “but I do think that devising protocols is … very much still at the hands of the endocrinologists. I think that this work could make groups reevaluate their protocol and change it, maybe even with a small dataset and then move on from there and see what they see.”
Indeed, Dr. Lundholm pointed out that some institutions, such as the Mayo Clinic, already include 6-hour BHB measurements (along with glucose and insulin) in their protocols.
“For any institution that already draws regular BHB levels like this, it would be very easy to implement a new stopping criterion without adding any additional costs,” she said in an interview.
All insulinomas became apparent in less than 48 hours
The first report to look at the value of testing BHB at regular intervals was published by the Mayo Clinic in 2005 after they noticed patients without insulinoma were complaining of ketosis symptoms such as foul breath and digestive problems toward the end of the fast.
However, although BHB testing is used today as part of the evaluation, it’s typically only drawn at the start of the protocol and again at the time of hypoglycemia or at the end of 72 hours because more frequent values hadn’t been thought to be useful for guiding clinical management, Dr. Lundholm explained.
Between January 2018 and June 2020, Dr. Lundholm and colleagues followed 34 Cleveland Clinic patients who completed the usual 72-hour fast protocol. Overall, 71% were female, and 26% had undergone prior bariatric surgery procedures. Eleven (32%) developed hypoglycemia and stopped fasting. The other 23 (68%) fasted for the full 72 hours.
Dr. Lundholm and colleagues determined that the fast could have ended earlier in 35% of patients based on an elevated BHB without missing any insulinomas.
And so, in June 2020 the group revised their protocol to include the BHB ≥ 2.7mmol/L stopping criterion. Of the 30 patients evaluated from June 2020 to January 2023, 87% were female and 17% had undergone a bariatric procedure.
Here, 15 (50%) reached a BHB ≥ 2.7mmol/L and ended their fast at an average of 43.8 hours. Another seven (23%) ended the fast after developing hypoglycemia. Just eight patients (27%) fasted for the full 72 hours.
Overall, this resulted in approximately 376 fewer cumulative hours of inpatient admission than if patients had fasted for the full time.
Of the 64 patients who have completed the fasting protocol since 2018, seven (11%) who did have an insulinoma developed hypoglycemia within 48 hours and with a BHB < 2.7 mmol/L (median, 0.15).
Advantages: cost, adherence
A day in a general medicine bed at Cleveland Clinic was quoted as costing $2,420, based on publicly available information as of Jan. 1, 2023. “If half of patients leave 1 day earlier, this equates to about $1,210 per patient in savings from bed costs alone,” Dr. Lundholm told this news organization.
The revised protocol required an additional two to four blood draws, depending on the length of the fast. “The cost of these extra blood tests varies by lab and by count, but even at its highest does not exceed the amount of savings from bed costs,” she noted.
Patient adherence is another potential benefit of the revised protocol.
“Any study that requires 72 hours of patient cooperation is a challenge, particularly in an uncomfortable position like fasting. When we looked at these adherence numbers, we found that the percentage of patients who prematurely ended their fast decreased from 35% to 17% with the updated protocol,” Dr. Lundholm continued.
“This translates to fewer inconclusive results and fewer readmissions for repeat 72-hour fasting. While this was not our primary outcome, it was another noted benefit of our change,” she said.
Dr. Lundholm and Dr. Sarvaideo have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
AT AACE 2023
Statin misinformation on social media flagged by AI
Using artificial intelligence to analyze large amounts of information from social media platforms generated some novel insights into public perceptions about statins, results of a new study show.
The study, which used AI to analyze discussions about statins on the social media platform Reddit, corroborated previously documented reasons for statin hesitancy, including adverse effect profiles and general disenfranchisement with health care.
But it also found novel points of discourse, including linking statins to COVID-19 outcomes and the role of cholesterol, statins, and the ketogenic diet.
“We used AI to tell us what is being discussed about statins on social media and to quantify the information in topics that people think are important,” senior study author Fatima Rodriguez, MD, MPH, Stanford (Calif.) University School of Medicine, said in an interview.
“Some of the themes were surprising to us. While we expected discussion on side effects, we were surprised to see so much discussion refuting the idea that increased levels of LDL were detrimental. There were also a large amount of posts on statin use being correlated to COVID outcomes. Our findings show how widespread this misinformation is,” she said.
“As a preventative cardiologist, I spend a lot of my time trying to get patients to take statins, but patients often rely on social media for information, and this can contain a lot of misinformation. People tend to be more honest on online forums than they are in the doctor’s office, so they are probably asking the questions and having discussions on subjects they really care about. So, understanding what is being discussed on social media is very valuable information for us as clinicians.”
The study was published online in JAMA Network Open.
The researchers analyzed all statin-related discussions on Reddit that were dated between Jan. 1, 2009, and July 12, 2022. Statin- and cholesterol-focused communities were identified to create a list of statin-related discussions. An AI pipeline was developed to cluster these discussions into specific topics and overarching thematic groups.
A total of 10,233 unique statin-related discussions and 5,188 unique authors were identified. A total of 100 discussion topics were identified and classified into six overarching thematic groups: (1) ketogenic diets, diabetes, supplements, and statins; (2) statin adverse effects; (3) statin hesitancy; (4) clinical trial appraisals; (5) pharmaceutical industry bias and statins; and (6) red yeast rice and statins.
Several examples of statin-related misinformation were identified, including distrust of the hypothesis that LDL-C has a causal association with heart disease. Discussions included quotes such as, “I think LDL is pretty much irrelevant. Your HDL and triglycerides are far more important.”
Other topics suggested that certain natural supplements would be an acceptable alternative to statins. Quotes included: “Red yeast rice is a statin basically, by the way,” and “statins are basically mycotoxins and deplete you of fat-soluble nutrients, like coQ10, vit D, K, A and E, and in all likelihood through these depletions worsen cardiovascular health.”
The researchers also looked at temporal trends and found that these sorts of discussions have increased over time.
One of the common themes identified was using the ketogenic diet phenomenon as an argument against increased cholesterol levels being bad for health.
Dr. Rodriguez elaborated: “People think the ketogenic diet is healthy as they lose weight on it. And as it can be associated with a small increase in LDL cholesterol, there was a lot of opinion that this meant increasing LDL was a good thing.”
The researchers also conducted a sentiment analysis, which designated topics as positive, negative, or neutral with regard to statins.
“We found that almost no topic was positive. Everything was either neutral or negative. This is pretty consistent with what we are seeing around hesitancy in clinical practice, but you would think that maybe a few people may have a positive view on statins,” Dr. Rodriguez commented.
“One of the problems with statins and lowering cholesterol is that it takes a long time to see a benefit, but this misinformation will result in some people not taking their medication,” she added.
Dr. Rodriguez noted that in this study AI is augmenting, not replacing, what clinicians and researchers do. “But it is a valuable tool to scan a large volume of information, and we have shown here it can generate new insights that we may not have thought of. It’s important to know what’s out there so we can try and combat it.”
She pointed out that patients don’t read the medical literature showing the benefits of statins but rather rely on social media for their information.
“We need to understand all sorts of patient engagement and use the same tools to combat this misinformation. We have a responsibility to try and stop dangerous and false information from being propagated,” she commented.
“These drugs are clearly not dangerous when used in line with clinical guidelines, and they have been proven to have multiple benefits again and again, but we don’t see those kinds of discussions in the community at all. We as clinicians need to use social media and AI to give out the right information. This could start to combat all the misinformation out there.”
A version of this article first appeared on Medscape.com.
Using artificial intelligence to analyze large amounts of information from social media platforms generated some novel insights into public perceptions about statins, results of a new study show.
The study, which used AI to analyze discussions about statins on the social media platform Reddit, corroborated previously documented reasons for statin hesitancy, including adverse effect profiles and general disenfranchisement with health care.
But it also found novel points of discourse, including linking statins to COVID-19 outcomes and the role of cholesterol, statins, and the ketogenic diet.
“We used AI to tell us what is being discussed about statins on social media and to quantify the information in topics that people think are important,” senior study author Fatima Rodriguez, MD, MPH, Stanford (Calif.) University School of Medicine, said in an interview.
“Some of the themes were surprising to us. While we expected discussion on side effects, we were surprised to see so much discussion refuting the idea that increased levels of LDL were detrimental. There were also a large amount of posts on statin use being correlated to COVID outcomes. Our findings show how widespread this misinformation is,” she said.
“As a preventative cardiologist, I spend a lot of my time trying to get patients to take statins, but patients often rely on social media for information, and this can contain a lot of misinformation. People tend to be more honest on online forums than they are in the doctor’s office, so they are probably asking the questions and having discussions on subjects they really care about. So, understanding what is being discussed on social media is very valuable information for us as clinicians.”
The study was published online in JAMA Network Open.
The researchers analyzed all statin-related discussions on Reddit that were dated between Jan. 1, 2009, and July 12, 2022. Statin- and cholesterol-focused communities were identified to create a list of statin-related discussions. An AI pipeline was developed to cluster these discussions into specific topics and overarching thematic groups.
A total of 10,233 unique statin-related discussions and 5,188 unique authors were identified. A total of 100 discussion topics were identified and classified into six overarching thematic groups: (1) ketogenic diets, diabetes, supplements, and statins; (2) statin adverse effects; (3) statin hesitancy; (4) clinical trial appraisals; (5) pharmaceutical industry bias and statins; and (6) red yeast rice and statins.
Several examples of statin-related misinformation were identified, including distrust of the hypothesis that LDL-C has a causal association with heart disease. Discussions included quotes such as, “I think LDL is pretty much irrelevant. Your HDL and triglycerides are far more important.”
Other topics suggested that certain natural supplements would be an acceptable alternative to statins. Quotes included: “Red yeast rice is a statin basically, by the way,” and “statins are basically mycotoxins and deplete you of fat-soluble nutrients, like coQ10, vit D, K, A and E, and in all likelihood through these depletions worsen cardiovascular health.”
The researchers also looked at temporal trends and found that these sorts of discussions have increased over time.
One of the common themes identified was using the ketogenic diet phenomenon as an argument against increased cholesterol levels being bad for health.
Dr. Rodriguez elaborated: “People think the ketogenic diet is healthy as they lose weight on it. And as it can be associated with a small increase in LDL cholesterol, there was a lot of opinion that this meant increasing LDL was a good thing.”
The researchers also conducted a sentiment analysis, which designated topics as positive, negative, or neutral with regard to statins.
“We found that almost no topic was positive. Everything was either neutral or negative. This is pretty consistent with what we are seeing around hesitancy in clinical practice, but you would think that maybe a few people may have a positive view on statins,” Dr. Rodriguez commented.
“One of the problems with statins and lowering cholesterol is that it takes a long time to see a benefit, but this misinformation will result in some people not taking their medication,” she added.
Dr. Rodriguez noted that in this study AI is augmenting, not replacing, what clinicians and researchers do. “But it is a valuable tool to scan a large volume of information, and we have shown here it can generate new insights that we may not have thought of. It’s important to know what’s out there so we can try and combat it.”
She pointed out that patients don’t read the medical literature showing the benefits of statins but rather rely on social media for their information.
“We need to understand all sorts of patient engagement and use the same tools to combat this misinformation. We have a responsibility to try and stop dangerous and false information from being propagated,” she commented.
“These drugs are clearly not dangerous when used in line with clinical guidelines, and they have been proven to have multiple benefits again and again, but we don’t see those kinds of discussions in the community at all. We as clinicians need to use social media and AI to give out the right information. This could start to combat all the misinformation out there.”
A version of this article first appeared on Medscape.com.
Using artificial intelligence to analyze large amounts of information from social media platforms generated some novel insights into public perceptions about statins, results of a new study show.
The study, which used AI to analyze discussions about statins on the social media platform Reddit, corroborated previously documented reasons for statin hesitancy, including adverse effect profiles and general disenfranchisement with health care.
But it also found novel points of discourse, including linking statins to COVID-19 outcomes and the role of cholesterol, statins, and the ketogenic diet.
“We used AI to tell us what is being discussed about statins on social media and to quantify the information in topics that people think are important,” senior study author Fatima Rodriguez, MD, MPH, Stanford (Calif.) University School of Medicine, said in an interview.
“Some of the themes were surprising to us. While we expected discussion on side effects, we were surprised to see so much discussion refuting the idea that increased levels of LDL were detrimental. There were also a large amount of posts on statin use being correlated to COVID outcomes. Our findings show how widespread this misinformation is,” she said.
“As a preventative cardiologist, I spend a lot of my time trying to get patients to take statins, but patients often rely on social media for information, and this can contain a lot of misinformation. People tend to be more honest on online forums than they are in the doctor’s office, so they are probably asking the questions and having discussions on subjects they really care about. So, understanding what is being discussed on social media is very valuable information for us as clinicians.”
The study was published online in JAMA Network Open.
The researchers analyzed all statin-related discussions on Reddit that were dated between Jan. 1, 2009, and July 12, 2022. Statin- and cholesterol-focused communities were identified to create a list of statin-related discussions. An AI pipeline was developed to cluster these discussions into specific topics and overarching thematic groups.
A total of 10,233 unique statin-related discussions and 5,188 unique authors were identified. A total of 100 discussion topics were identified and classified into six overarching thematic groups: (1) ketogenic diets, diabetes, supplements, and statins; (2) statin adverse effects; (3) statin hesitancy; (4) clinical trial appraisals; (5) pharmaceutical industry bias and statins; and (6) red yeast rice and statins.
Several examples of statin-related misinformation were identified, including distrust of the hypothesis that LDL-C has a causal association with heart disease. Discussions included quotes such as, “I think LDL is pretty much irrelevant. Your HDL and triglycerides are far more important.”
Other topics suggested that certain natural supplements would be an acceptable alternative to statins. Quotes included: “Red yeast rice is a statin basically, by the way,” and “statins are basically mycotoxins and deplete you of fat-soluble nutrients, like coQ10, vit D, K, A and E, and in all likelihood through these depletions worsen cardiovascular health.”
The researchers also looked at temporal trends and found that these sorts of discussions have increased over time.
One of the common themes identified was using the ketogenic diet phenomenon as an argument against increased cholesterol levels being bad for health.
Dr. Rodriguez elaborated: “People think the ketogenic diet is healthy as they lose weight on it. And as it can be associated with a small increase in LDL cholesterol, there was a lot of opinion that this meant increasing LDL was a good thing.”
The researchers also conducted a sentiment analysis, which designated topics as positive, negative, or neutral with regard to statins.
“We found that almost no topic was positive. Everything was either neutral or negative. This is pretty consistent with what we are seeing around hesitancy in clinical practice, but you would think that maybe a few people may have a positive view on statins,” Dr. Rodriguez commented.
“One of the problems with statins and lowering cholesterol is that it takes a long time to see a benefit, but this misinformation will result in some people not taking their medication,” she added.
Dr. Rodriguez noted that in this study AI is augmenting, not replacing, what clinicians and researchers do. “But it is a valuable tool to scan a large volume of information, and we have shown here it can generate new insights that we may not have thought of. It’s important to know what’s out there so we can try and combat it.”
She pointed out that patients don’t read the medical literature showing the benefits of statins but rather rely on social media for their information.
“We need to understand all sorts of patient engagement and use the same tools to combat this misinformation. We have a responsibility to try and stop dangerous and false information from being propagated,” she commented.
“These drugs are clearly not dangerous when used in line with clinical guidelines, and they have been proven to have multiple benefits again and again, but we don’t see those kinds of discussions in the community at all. We as clinicians need to use social media and AI to give out the right information. This could start to combat all the misinformation out there.”
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Expert discusses which diets are best, based on the evidence
according to a speaker at the annual meeting of the American College of Physicians.
“Evidence from studies can help clinicians and their patients develop a successful dietary management plan and achieve optimal health,” said internist Michelle Hauser, MD, clinical associate professor at Stanford (Calif.) University. She also discussed evidence-based techniques to support patients in maintaining dietary modifications.
Predominantly plant‐based diets
Popular predominantly plant‐based diets include a Mediterranean diet, healthy vegetarian diet, predominantly whole-food plant‐based (WFPB) diet, and a dietary approach to stop hypertension (DASH).
The DASH diet was originally designed to help patients manage their blood pressure, but evidence suggests that it also can help adults with obesity lose weight. In contrast to the DASH diet, the Mediterranean diet is not low-fat and not very restrictive. Yet the evidence suggests that the Mediterranean diet is not only helpful for losing weight but also can reduce the risk of various chronic diseases, including obesity, type 2 diabetes, cardiovascular disease (CVD), and cancer, Dr. Hauser said. In addition, data suggest that the Mediterranean diet may reduce the risk of all-cause mortality and lower the levels of cholesterol.
“I like to highlight all these protective effects to my patients, because even if their goal is to lose weight, knowing that hard work pays off in additional ways can keep them motivated,” Dr. Hauser stated.
A healthy vegetarian diet and a WFPB diet are similar, and both are helpful in weight loss and management of total cholesterol and LDL‐C levels. Furthermore, healthy vegetarian and WFPB diets may reduce the risk of type 2 diabetes, CVD, and some cancers. Cohort study data suggest that progressively more vegetarian diets are associated with lower BMIs.
“My interpretation of these data is that predominantly plant-based diets rich in whole foods are healthful and can be done in a way that is sustainable for most,” said Dr. Hauser. However, this generally requires a lot of support at the outset to address gaps in knowledge, skills, and other potential barriers.
For example, she referred one obese patient at risk of diabetes and cardiovascular disease to a registered dietitian to develop a dietary plan. The patient also attended a behavioral medicine weight management program to learn strategies such as using smaller plates, and his family attended a healthy cooking class together to improve meal planning and cooking skills.
Time‐restricted feeding
There are numerous variations of time-restricted feeding, commonly referred to as intermittent fasting, but the principles are similar – limiting food intake to a specific window of time each day or week.
Although some studies have shown that time-restricted feeding may help patients reduce adiposity and improve lipid markers, most studies comparing time-restricted feeding to a calorie-restricted diet have shown little to no difference in weight-related outcomes, Dr. Hauser said.
These data suggest that time-restricted feeding may help patients with weight loss only if time restriction helps them reduce calorie intake. She also warned that time-restrictive feeding might cause late-night cravings and might not be helpful in individuals prone to food cravings.
Low‐carbohydrate and ketogenic diets
Losing muscle mass can prevent some people from dieting, but evidence suggests that a high-fat, very low-carbohydrate diet – also called a ketogenic diet – may help patients reduce weight and fat mass while preserving fat‐free mass, Dr. Hauser said.
The evidence regarding the usefulness of a low-carbohydrate (non-keto) diet is less clear because most studies compared it to a low-fat diet, and these two diets might lead to a similar extent of weight loss.
Rating the level of scientific evidence behind different diet options
Nutrition studies do no provide the same level of evidence as drug studies, said Dr. Hauser, because it is easier to conduct a randomized controlled trial of a drug versus placebo. Diets have many more variables, and it also takes much longer to observe most outcomes of a dietary change.
In addition, clinical trials of dietary interventions are typically short and focus on disease markers such as serum lipids and hemoglobin A1c levels. To obtain reliable information on the usefulness of a diet, researchers need to collect detailed health and lifestyle information from hundreds of thousands of people over several decades, which is not always feasible. “This is why meta-analyses of pooled dietary study data are more likely to yield dependable findings,” she noted.
Getting to know patients is essential to help them maintain diet modifications
When developing a diet plan for a patient, it is important to consider the sustainability of a dietary pattern. “The benefits of any healthy dietary change will only last as long as they can be maintained,” said Dr. Hauser. “Counseling someone on choosing an appropriate long-term dietary pattern requires getting to know them – taste preferences, food traditions, barriers, facilitators, food access, and time and cost restrictions.”
In an interview after the session, David Bittleman, MD, an internist at Veterans Affairs San Diego Health Care System, agreed that getting to know patients is essential for successfully advising them on diet.
“I always start developing a diet plan by trying to find out what [a patient’s] diet is like and what their goals are. I need to know what they are already doing in order to make suggestions about what they can do to make their diet healthier,” he said.
When asked about her approach to supporting patients in the long term, Dr. Hauser said that she recommends sequential, gradual changes. Dr. Hauser added that she suggests her patients prioritize implementing dietary changes that they are confident they can maintain.
Dr. Hauser and Dr. Bittleman report no relevant financial relationships.
according to a speaker at the annual meeting of the American College of Physicians.
“Evidence from studies can help clinicians and their patients develop a successful dietary management plan and achieve optimal health,” said internist Michelle Hauser, MD, clinical associate professor at Stanford (Calif.) University. She also discussed evidence-based techniques to support patients in maintaining dietary modifications.
Predominantly plant‐based diets
Popular predominantly plant‐based diets include a Mediterranean diet, healthy vegetarian diet, predominantly whole-food plant‐based (WFPB) diet, and a dietary approach to stop hypertension (DASH).
The DASH diet was originally designed to help patients manage their blood pressure, but evidence suggests that it also can help adults with obesity lose weight. In contrast to the DASH diet, the Mediterranean diet is not low-fat and not very restrictive. Yet the evidence suggests that the Mediterranean diet is not only helpful for losing weight but also can reduce the risk of various chronic diseases, including obesity, type 2 diabetes, cardiovascular disease (CVD), and cancer, Dr. Hauser said. In addition, data suggest that the Mediterranean diet may reduce the risk of all-cause mortality and lower the levels of cholesterol.
“I like to highlight all these protective effects to my patients, because even if their goal is to lose weight, knowing that hard work pays off in additional ways can keep them motivated,” Dr. Hauser stated.
A healthy vegetarian diet and a WFPB diet are similar, and both are helpful in weight loss and management of total cholesterol and LDL‐C levels. Furthermore, healthy vegetarian and WFPB diets may reduce the risk of type 2 diabetes, CVD, and some cancers. Cohort study data suggest that progressively more vegetarian diets are associated with lower BMIs.
“My interpretation of these data is that predominantly plant-based diets rich in whole foods are healthful and can be done in a way that is sustainable for most,” said Dr. Hauser. However, this generally requires a lot of support at the outset to address gaps in knowledge, skills, and other potential barriers.
For example, she referred one obese patient at risk of diabetes and cardiovascular disease to a registered dietitian to develop a dietary plan. The patient also attended a behavioral medicine weight management program to learn strategies such as using smaller plates, and his family attended a healthy cooking class together to improve meal planning and cooking skills.
Time‐restricted feeding
There are numerous variations of time-restricted feeding, commonly referred to as intermittent fasting, but the principles are similar – limiting food intake to a specific window of time each day or week.
Although some studies have shown that time-restricted feeding may help patients reduce adiposity and improve lipid markers, most studies comparing time-restricted feeding to a calorie-restricted diet have shown little to no difference in weight-related outcomes, Dr. Hauser said.
These data suggest that time-restricted feeding may help patients with weight loss only if time restriction helps them reduce calorie intake. She also warned that time-restrictive feeding might cause late-night cravings and might not be helpful in individuals prone to food cravings.
Low‐carbohydrate and ketogenic diets
Losing muscle mass can prevent some people from dieting, but evidence suggests that a high-fat, very low-carbohydrate diet – also called a ketogenic diet – may help patients reduce weight and fat mass while preserving fat‐free mass, Dr. Hauser said.
The evidence regarding the usefulness of a low-carbohydrate (non-keto) diet is less clear because most studies compared it to a low-fat diet, and these two diets might lead to a similar extent of weight loss.
Rating the level of scientific evidence behind different diet options
Nutrition studies do no provide the same level of evidence as drug studies, said Dr. Hauser, because it is easier to conduct a randomized controlled trial of a drug versus placebo. Diets have many more variables, and it also takes much longer to observe most outcomes of a dietary change.
In addition, clinical trials of dietary interventions are typically short and focus on disease markers such as serum lipids and hemoglobin A1c levels. To obtain reliable information on the usefulness of a diet, researchers need to collect detailed health and lifestyle information from hundreds of thousands of people over several decades, which is not always feasible. “This is why meta-analyses of pooled dietary study data are more likely to yield dependable findings,” she noted.
Getting to know patients is essential to help them maintain diet modifications
When developing a diet plan for a patient, it is important to consider the sustainability of a dietary pattern. “The benefits of any healthy dietary change will only last as long as they can be maintained,” said Dr. Hauser. “Counseling someone on choosing an appropriate long-term dietary pattern requires getting to know them – taste preferences, food traditions, barriers, facilitators, food access, and time and cost restrictions.”
In an interview after the session, David Bittleman, MD, an internist at Veterans Affairs San Diego Health Care System, agreed that getting to know patients is essential for successfully advising them on diet.
“I always start developing a diet plan by trying to find out what [a patient’s] diet is like and what their goals are. I need to know what they are already doing in order to make suggestions about what they can do to make their diet healthier,” he said.
When asked about her approach to supporting patients in the long term, Dr. Hauser said that she recommends sequential, gradual changes. Dr. Hauser added that she suggests her patients prioritize implementing dietary changes that they are confident they can maintain.
Dr. Hauser and Dr. Bittleman report no relevant financial relationships.
according to a speaker at the annual meeting of the American College of Physicians.
“Evidence from studies can help clinicians and their patients develop a successful dietary management plan and achieve optimal health,” said internist Michelle Hauser, MD, clinical associate professor at Stanford (Calif.) University. She also discussed evidence-based techniques to support patients in maintaining dietary modifications.
Predominantly plant‐based diets
Popular predominantly plant‐based diets include a Mediterranean diet, healthy vegetarian diet, predominantly whole-food plant‐based (WFPB) diet, and a dietary approach to stop hypertension (DASH).
The DASH diet was originally designed to help patients manage their blood pressure, but evidence suggests that it also can help adults with obesity lose weight. In contrast to the DASH diet, the Mediterranean diet is not low-fat and not very restrictive. Yet the evidence suggests that the Mediterranean diet is not only helpful for losing weight but also can reduce the risk of various chronic diseases, including obesity, type 2 diabetes, cardiovascular disease (CVD), and cancer, Dr. Hauser said. In addition, data suggest that the Mediterranean diet may reduce the risk of all-cause mortality and lower the levels of cholesterol.
“I like to highlight all these protective effects to my patients, because even if their goal is to lose weight, knowing that hard work pays off in additional ways can keep them motivated,” Dr. Hauser stated.
A healthy vegetarian diet and a WFPB diet are similar, and both are helpful in weight loss and management of total cholesterol and LDL‐C levels. Furthermore, healthy vegetarian and WFPB diets may reduce the risk of type 2 diabetes, CVD, and some cancers. Cohort study data suggest that progressively more vegetarian diets are associated with lower BMIs.
“My interpretation of these data is that predominantly plant-based diets rich in whole foods are healthful and can be done in a way that is sustainable for most,” said Dr. Hauser. However, this generally requires a lot of support at the outset to address gaps in knowledge, skills, and other potential barriers.
For example, she referred one obese patient at risk of diabetes and cardiovascular disease to a registered dietitian to develop a dietary plan. The patient also attended a behavioral medicine weight management program to learn strategies such as using smaller plates, and his family attended a healthy cooking class together to improve meal planning and cooking skills.
Time‐restricted feeding
There are numerous variations of time-restricted feeding, commonly referred to as intermittent fasting, but the principles are similar – limiting food intake to a specific window of time each day or week.
Although some studies have shown that time-restricted feeding may help patients reduce adiposity and improve lipid markers, most studies comparing time-restricted feeding to a calorie-restricted diet have shown little to no difference in weight-related outcomes, Dr. Hauser said.
These data suggest that time-restricted feeding may help patients with weight loss only if time restriction helps them reduce calorie intake. She also warned that time-restrictive feeding might cause late-night cravings and might not be helpful in individuals prone to food cravings.
Low‐carbohydrate and ketogenic diets
Losing muscle mass can prevent some people from dieting, but evidence suggests that a high-fat, very low-carbohydrate diet – also called a ketogenic diet – may help patients reduce weight and fat mass while preserving fat‐free mass, Dr. Hauser said.
The evidence regarding the usefulness of a low-carbohydrate (non-keto) diet is less clear because most studies compared it to a low-fat diet, and these two diets might lead to a similar extent of weight loss.
Rating the level of scientific evidence behind different diet options
Nutrition studies do no provide the same level of evidence as drug studies, said Dr. Hauser, because it is easier to conduct a randomized controlled trial of a drug versus placebo. Diets have many more variables, and it also takes much longer to observe most outcomes of a dietary change.
In addition, clinical trials of dietary interventions are typically short and focus on disease markers such as serum lipids and hemoglobin A1c levels. To obtain reliable information on the usefulness of a diet, researchers need to collect detailed health and lifestyle information from hundreds of thousands of people over several decades, which is not always feasible. “This is why meta-analyses of pooled dietary study data are more likely to yield dependable findings,” she noted.
Getting to know patients is essential to help them maintain diet modifications
When developing a diet plan for a patient, it is important to consider the sustainability of a dietary pattern. “The benefits of any healthy dietary change will only last as long as they can be maintained,” said Dr. Hauser. “Counseling someone on choosing an appropriate long-term dietary pattern requires getting to know them – taste preferences, food traditions, barriers, facilitators, food access, and time and cost restrictions.”
In an interview after the session, David Bittleman, MD, an internist at Veterans Affairs San Diego Health Care System, agreed that getting to know patients is essential for successfully advising them on diet.
“I always start developing a diet plan by trying to find out what [a patient’s] diet is like and what their goals are. I need to know what they are already doing in order to make suggestions about what they can do to make their diet healthier,” he said.
When asked about her approach to supporting patients in the long term, Dr. Hauser said that she recommends sequential, gradual changes. Dr. Hauser added that she suggests her patients prioritize implementing dietary changes that they are confident they can maintain.
Dr. Hauser and Dr. Bittleman report no relevant financial relationships.
AT INTERNAL MEDICINE 2023
Medications provide best risk-to-benefit ratio for weight loss, says expert
Lifestyle changes result in the least weight loss and may be safest, while surgery provides the most weight loss and has the greatest risk. Antiobesity medications, especially the newer ones used in combination with lifestyle changes, can provide significant and sustained weight loss with manageable side effects, said Daniel Bessesen, MD, a professor in the endocrinology, diabetes, and metabolism at University of Colorado at Denver, Aurora.
New and more effective antiobesity medications have given internists more potential options to discuss with their patients, Dr. Bessesen said. He reviewed the pros and cons of the different options.
Medications are indicated for patients with a body mass index greater than 30, including those with a weight-related comorbidity, Dr. Bessesen said. The average weight loss is 5%-15% over 3-6 months but may vary greatly. Insurance often does not cover the medication costs.
Older FDA-approved antiobesity medications
Phentermine is the most widely prescribed antiobesity medication, partly because it is the only option most people can afford out of pocket. Dr. Bessesen presented recent data showing that long-term use of phentermine was associated with greater weight loss and that patients continuously taking phentermine for 24 months lost 7.5% of their weight.
Phentermine suppresses appetite by increasing norepinephrine production. Dr. Bessesen warned that internists should be careful when prescribing it to patients with mental conditions, because it acts as a stimulant. Early studies raised concerns about the risk of cardiovascular disease (CVD) in patients taking phentermine. However, analysis of data from over 13,000 individuals showed no evidence of a relationship between phentermine exposure and CVD events.
“These data provide some reassurance that it could be used in patients with CVD risk,” he noted. Phentermine can also be combined with topiramate extended release, a combination that provides greater efficacy (up to 10% weight loss) with fewer side effects. However, this combination is less effective in patients with diabetes than in those without.
Additional treatment options included orlistat and naltrexone sustained release/bupropion SR. Orlistat is a good treatment alternative for patients with constipation and is the safest option among older anti-obesity medications, whereas naltrexone SR/bupropion SR may be useful in patients with food cravings. However, there is more variability in the individual-level benefit from these agents compared to phentermine and phentermine/topiramate ER, Dr. Bessesen said.
Newer anti‐obesity medications
Liraglutide, an agent used for the management of type 2 diabetes, has recently been approved for weight loss. Liraglutide causes moderate weight loss, and it may reduce the risk of CVD. However, there are tolerability issues, such as nausea and other risks, and Dr. Bessesen advises internists to “start at low doses and increase slowly.”
Semaglutide is the newest and most effective antiobesity drug approved by the Food and Drug Administration, providing sustained weight loss of 8% for up to 48 weeks after starting treatment. Although its efficacy is lower in patients with diabetes, Dr. Bessesen noted that “this is common for antiobesity agents, and clinicians should not refrain from prescribing it in this population.”
Setmelanotide is another new medication approved for chronic weight management in patients with monogenic obesity. This medication can be considered for patients with early-onset severe obesity with abnormal feeding behavior.
Commenting on barriers to access to new antiobesity medications, Dr. Bessesen said that “the high cost of these medications is a substantial problem, but as more companies become involved and products are on the market for a longer period of time, I am hopeful that prices will come down.”
Emerging antiobesity medications
Dr. Bessesen presented recent phase 3 data showing that treatment with tirzepatide provided sustained chronic loss and improved cardiometabolic measures with no diet. Tirzepatide, which targets receptors for glucagonlike peptide–1 and glucose-dependent insulinotropic polypeptide, is used for the management of type 2 diabetes and is expected to be reviewed soon by the FDA for its use in weight management.
A semaglutide/cagrilintide combination may also provide a new treatment option for patients with obesity. In a phase 1b trial, semaglutide/cagrilintide treatment resulted in up to 17% weight loss in patients with obesity who were otherwise healthy; however, phase 2 and 3 data are needed to confirm its efficacy.
A ‘holistic approach’
When deciding whether to prescribe antiobesity medications, Dr. Bessesen noted that medications are better than exercise alone. Factors to consider when deciding whether to prescribe drugs, as well as which ones, include costs, local regulatory guidelines, requirement for long-term use, and patient comorbidities.
He also stated that lifestyle changes, such as adopting healthy nutrition and exercising regularly, are also important and can enhance weight loss when combined with medications.
Richele Corrado, DO, MPH, agreed that lifestyle management in combination with medications may provide greater weight loss than each of these interventions alone.
“If you look at the data, exercise doesn’t help you lose much weight,” said Dr. Corrado, a staff internist and obesity medicine specialist at Walter Reed National Military Medical Center in Bethesda, Md., who spoke at the same session. She added that she has many patients who struggle to lose weight despite having a healthy lifestyle. “It’s important to discuss with these patients about medications and surgery.”
Dr. Bessesen noted that management of mental health and emotional well-being should also be an integral part of obesity management. “Treatment for obesity may be more successful when underlying psychological conditions such as depression, childhood sexual trauma, or anxiety are addressed and treated,” he said.
Dr. Bessesen was involved in the study of the efficacy of semaglutide/cagrilintide. He does not have any financial conflicts with the companies that make other mentioned medications. He has received research grants or contracts from Novo Nordisk, honoraria from Novo Nordisk, and consultantship from Eli Lilly. Dr. Corrado reported no relevant financial conflicts.
Lifestyle changes result in the least weight loss and may be safest, while surgery provides the most weight loss and has the greatest risk. Antiobesity medications, especially the newer ones used in combination with lifestyle changes, can provide significant and sustained weight loss with manageable side effects, said Daniel Bessesen, MD, a professor in the endocrinology, diabetes, and metabolism at University of Colorado at Denver, Aurora.
New and more effective antiobesity medications have given internists more potential options to discuss with their patients, Dr. Bessesen said. He reviewed the pros and cons of the different options.
Medications are indicated for patients with a body mass index greater than 30, including those with a weight-related comorbidity, Dr. Bessesen said. The average weight loss is 5%-15% over 3-6 months but may vary greatly. Insurance often does not cover the medication costs.
Older FDA-approved antiobesity medications
Phentermine is the most widely prescribed antiobesity medication, partly because it is the only option most people can afford out of pocket. Dr. Bessesen presented recent data showing that long-term use of phentermine was associated with greater weight loss and that patients continuously taking phentermine for 24 months lost 7.5% of their weight.
Phentermine suppresses appetite by increasing norepinephrine production. Dr. Bessesen warned that internists should be careful when prescribing it to patients with mental conditions, because it acts as a stimulant. Early studies raised concerns about the risk of cardiovascular disease (CVD) in patients taking phentermine. However, analysis of data from over 13,000 individuals showed no evidence of a relationship between phentermine exposure and CVD events.
“These data provide some reassurance that it could be used in patients with CVD risk,” he noted. Phentermine can also be combined with topiramate extended release, a combination that provides greater efficacy (up to 10% weight loss) with fewer side effects. However, this combination is less effective in patients with diabetes than in those without.
Additional treatment options included orlistat and naltrexone sustained release/bupropion SR. Orlistat is a good treatment alternative for patients with constipation and is the safest option among older anti-obesity medications, whereas naltrexone SR/bupropion SR may be useful in patients with food cravings. However, there is more variability in the individual-level benefit from these agents compared to phentermine and phentermine/topiramate ER, Dr. Bessesen said.
Newer anti‐obesity medications
Liraglutide, an agent used for the management of type 2 diabetes, has recently been approved for weight loss. Liraglutide causes moderate weight loss, and it may reduce the risk of CVD. However, there are tolerability issues, such as nausea and other risks, and Dr. Bessesen advises internists to “start at low doses and increase slowly.”
Semaglutide is the newest and most effective antiobesity drug approved by the Food and Drug Administration, providing sustained weight loss of 8% for up to 48 weeks after starting treatment. Although its efficacy is lower in patients with diabetes, Dr. Bessesen noted that “this is common for antiobesity agents, and clinicians should not refrain from prescribing it in this population.”
Setmelanotide is another new medication approved for chronic weight management in patients with monogenic obesity. This medication can be considered for patients with early-onset severe obesity with abnormal feeding behavior.
Commenting on barriers to access to new antiobesity medications, Dr. Bessesen said that “the high cost of these medications is a substantial problem, but as more companies become involved and products are on the market for a longer period of time, I am hopeful that prices will come down.”
Emerging antiobesity medications
Dr. Bessesen presented recent phase 3 data showing that treatment with tirzepatide provided sustained chronic loss and improved cardiometabolic measures with no diet. Tirzepatide, which targets receptors for glucagonlike peptide–1 and glucose-dependent insulinotropic polypeptide, is used for the management of type 2 diabetes and is expected to be reviewed soon by the FDA for its use in weight management.
A semaglutide/cagrilintide combination may also provide a new treatment option for patients with obesity. In a phase 1b trial, semaglutide/cagrilintide treatment resulted in up to 17% weight loss in patients with obesity who were otherwise healthy; however, phase 2 and 3 data are needed to confirm its efficacy.
A ‘holistic approach’
When deciding whether to prescribe antiobesity medications, Dr. Bessesen noted that medications are better than exercise alone. Factors to consider when deciding whether to prescribe drugs, as well as which ones, include costs, local regulatory guidelines, requirement for long-term use, and patient comorbidities.
He also stated that lifestyle changes, such as adopting healthy nutrition and exercising regularly, are also important and can enhance weight loss when combined with medications.
Richele Corrado, DO, MPH, agreed that lifestyle management in combination with medications may provide greater weight loss than each of these interventions alone.
“If you look at the data, exercise doesn’t help you lose much weight,” said Dr. Corrado, a staff internist and obesity medicine specialist at Walter Reed National Military Medical Center in Bethesda, Md., who spoke at the same session. She added that she has many patients who struggle to lose weight despite having a healthy lifestyle. “It’s important to discuss with these patients about medications and surgery.”
Dr. Bessesen noted that management of mental health and emotional well-being should also be an integral part of obesity management. “Treatment for obesity may be more successful when underlying psychological conditions such as depression, childhood sexual trauma, or anxiety are addressed and treated,” he said.
Dr. Bessesen was involved in the study of the efficacy of semaglutide/cagrilintide. He does not have any financial conflicts with the companies that make other mentioned medications. He has received research grants or contracts from Novo Nordisk, honoraria from Novo Nordisk, and consultantship from Eli Lilly. Dr. Corrado reported no relevant financial conflicts.
Lifestyle changes result in the least weight loss and may be safest, while surgery provides the most weight loss and has the greatest risk. Antiobesity medications, especially the newer ones used in combination with lifestyle changes, can provide significant and sustained weight loss with manageable side effects, said Daniel Bessesen, MD, a professor in the endocrinology, diabetes, and metabolism at University of Colorado at Denver, Aurora.
New and more effective antiobesity medications have given internists more potential options to discuss with their patients, Dr. Bessesen said. He reviewed the pros and cons of the different options.
Medications are indicated for patients with a body mass index greater than 30, including those with a weight-related comorbidity, Dr. Bessesen said. The average weight loss is 5%-15% over 3-6 months but may vary greatly. Insurance often does not cover the medication costs.
Older FDA-approved antiobesity medications
Phentermine is the most widely prescribed antiobesity medication, partly because it is the only option most people can afford out of pocket. Dr. Bessesen presented recent data showing that long-term use of phentermine was associated with greater weight loss and that patients continuously taking phentermine for 24 months lost 7.5% of their weight.
Phentermine suppresses appetite by increasing norepinephrine production. Dr. Bessesen warned that internists should be careful when prescribing it to patients with mental conditions, because it acts as a stimulant. Early studies raised concerns about the risk of cardiovascular disease (CVD) in patients taking phentermine. However, analysis of data from over 13,000 individuals showed no evidence of a relationship between phentermine exposure and CVD events.
“These data provide some reassurance that it could be used in patients with CVD risk,” he noted. Phentermine can also be combined with topiramate extended release, a combination that provides greater efficacy (up to 10% weight loss) with fewer side effects. However, this combination is less effective in patients with diabetes than in those without.
Additional treatment options included orlistat and naltrexone sustained release/bupropion SR. Orlistat is a good treatment alternative for patients with constipation and is the safest option among older anti-obesity medications, whereas naltrexone SR/bupropion SR may be useful in patients with food cravings. However, there is more variability in the individual-level benefit from these agents compared to phentermine and phentermine/topiramate ER, Dr. Bessesen said.
Newer anti‐obesity medications
Liraglutide, an agent used for the management of type 2 diabetes, has recently been approved for weight loss. Liraglutide causes moderate weight loss, and it may reduce the risk of CVD. However, there are tolerability issues, such as nausea and other risks, and Dr. Bessesen advises internists to “start at low doses and increase slowly.”
Semaglutide is the newest and most effective antiobesity drug approved by the Food and Drug Administration, providing sustained weight loss of 8% for up to 48 weeks after starting treatment. Although its efficacy is lower in patients with diabetes, Dr. Bessesen noted that “this is common for antiobesity agents, and clinicians should not refrain from prescribing it in this population.”
Setmelanotide is another new medication approved for chronic weight management in patients with monogenic obesity. This medication can be considered for patients with early-onset severe obesity with abnormal feeding behavior.
Commenting on barriers to access to new antiobesity medications, Dr. Bessesen said that “the high cost of these medications is a substantial problem, but as more companies become involved and products are on the market for a longer period of time, I am hopeful that prices will come down.”
Emerging antiobesity medications
Dr. Bessesen presented recent phase 3 data showing that treatment with tirzepatide provided sustained chronic loss and improved cardiometabolic measures with no diet. Tirzepatide, which targets receptors for glucagonlike peptide–1 and glucose-dependent insulinotropic polypeptide, is used for the management of type 2 diabetes and is expected to be reviewed soon by the FDA for its use in weight management.
A semaglutide/cagrilintide combination may also provide a new treatment option for patients with obesity. In a phase 1b trial, semaglutide/cagrilintide treatment resulted in up to 17% weight loss in patients with obesity who were otherwise healthy; however, phase 2 and 3 data are needed to confirm its efficacy.
A ‘holistic approach’
When deciding whether to prescribe antiobesity medications, Dr. Bessesen noted that medications are better than exercise alone. Factors to consider when deciding whether to prescribe drugs, as well as which ones, include costs, local regulatory guidelines, requirement for long-term use, and patient comorbidities.
He also stated that lifestyle changes, such as adopting healthy nutrition and exercising regularly, are also important and can enhance weight loss when combined with medications.
Richele Corrado, DO, MPH, agreed that lifestyle management in combination with medications may provide greater weight loss than each of these interventions alone.
“If you look at the data, exercise doesn’t help you lose much weight,” said Dr. Corrado, a staff internist and obesity medicine specialist at Walter Reed National Military Medical Center in Bethesda, Md., who spoke at the same session. She added that she has many patients who struggle to lose weight despite having a healthy lifestyle. “It’s important to discuss with these patients about medications and surgery.”
Dr. Bessesen noted that management of mental health and emotional well-being should also be an integral part of obesity management. “Treatment for obesity may be more successful when underlying psychological conditions such as depression, childhood sexual trauma, or anxiety are addressed and treated,” he said.
Dr. Bessesen was involved in the study of the efficacy of semaglutide/cagrilintide. He does not have any financial conflicts with the companies that make other mentioned medications. He has received research grants or contracts from Novo Nordisk, honoraria from Novo Nordisk, and consultantship from Eli Lilly. Dr. Corrado reported no relevant financial conflicts.
AT INTERNAL MEDICINE 2023
Seasonal variation in thyroid hormone TSH may lead to overprescribing
Seasonal variation in one of the hormones used to monitor thyroid function could in turn lead to false diagnoses of subclinical hypothyroidism and unnecessary prescriptions of levothyroxine, according to Yale clinical chemist Joe M. El-Khoury, PhD.
A Japanese study of more than 7,000 healthy individuals showed that thyrotropin-stimulating hormone (TSH) varies widely throughout the seasons, he said, peaking in the northern hemisphere’s winter months (January to February) with its low in the summer months (June to August). That paper was published last year in the Journal of the Endocrine Society.
But free thyroxine (FT4) levels in the Japanese population remained relatively stable, he wrote in a letter recently published in Clinical Chemistry.
“If you end up with a mildly elevated TSH result and a normal FT4, try getting retested 2-3 months later to make sure this is not a seasonal artifact or transient increase before prescribing/taking levothyroxine unnecessarily,” advised Dr. El-Khoury, director of Yale University’s Clinical Chemistry Laboratory, New Haven, Conn.
“Because the [population-based, laboratory] reference ranges don’t account for seasonal variation, we’re flagging a significant number of people as high TSH when they’re normal, and physicians are prescribing levothyroxine inappropriately to healthy people who don’t need it,” he told this news organization, adding that overtreatment can be harmful, particularly for elderly people.
This seasonal variation in TSH could account for between a third to a half of the 90% of all levothyroxine prescriptions that were found to be unnecessary, according to a U.S. study in 2021, Dr. El-Khoury added.
In a comment, Trisha Cubb, MD, said that Dr. El-Khoury’s letter “raises a good point, that we really need to look at our reference ranges, especially when more and more studies are showing that so many thyroid hormone prescriptions may not be necessary.”
Dr. Cubb, thyroid section director and assistant professor of clinical medicine at Weill Cornell Medical College/Houston Methodist Academic Institute, Texas, also agrees with Dr. El-Khoury’s suggestion to repeat lab results in some instances.
“I think repeating results, especially in our patients with subclinical disease, is important,” she noted.
And she pointed out that seasonal variation isn’t the only relevant variable. “We also know that multiple clinical factors like pregnancy status, coexisting comorbidities, or age can all influence what we as clinicians consider an acceptable TSH range in an individual patient.” And other medications, such as steroids, or supplements like biotin, “can all affect thyroid lab values,” she noted.
“Ensuring that minor abnormalities aren’t transient is important prior to initiating medical therapy. With any medical therapy there are possible side effects, along with time, cost, [and] monitoring, all of which can be associated with thyroid hormone replacement.”
TSH reference ranges should be adapted for subpopulations
Dr. El-Khoury explained that to get an idea of how big the seasonal differences in TSH observed in the Japanese study were, “the upper end of the population they tracked goes from 5.2 [mIU/L] in January to 3.4 [mIU/L] in August. So you have almost a 2-unit change in concentration that can happen in the reference population. But laboratory reference ranges, or ‘normal ranges,’ are usually fixed and don’t change by season.”
The higher the TSH, the more likely a person is to have hypothyroidism. Major recent studies have found no benefit of levothyroxine treatment with TSH levels below 7.0-10.0 mIU/L, he said.
“So, I suggest that the limit should be 7.0 [mIU/L] to be safe, but it could be as high as 10 [mIU/L]. In any case, let’s shift the mindset to clinical outcome–based treatment cutoffs,” he said, noting that this approach is currently used for decisions on cholesterol-lowering therapy or vitamin D supplementation, for example.
Regarding this suggestion of using a TSH cutoff of 7 mIU/L to diagnose subclinical hypothyroidism, Dr. Cubb said: “It really depends on the specific population. In an elderly patient, a higher TSH may be of less clinical concern when compared to a female who is actively trying to get pregnant.
“Overall, I think we do need to better understand what appropriate TSH ranges are in specific subpopulations, and then with time, make this more understandable and available for general medicine as well as subspecialty providers to be able to utilize,” she noted.
Regarding the particular Japanese findings cited by Dr. El-Khoury, Dr. Cubb observed that this was a very specific study population, “so we would need more data showing that this is more generalizable.”
And she noted that there’s also diurnal variation in TSH. “In the [Japanese] paper, patients had their thyroid labs drawn between 8:00 a.m. and 9:00 a.m. in a fasting state. Oftentimes in the U.S., thyroid labs are not drawn at specific times or [during] fasting. I think this is one of many factors that should be considered.”
Acknowledging seasonal variation would be a start
But overall, Dr. Cubb said that both the Japanese study and Dr. El-Khoury’s letter highlight “how season, in and of itself, which is not something we usually think about, can affect thyroid lab results. I believe as more data come out, more generalizable data, that’s how evidence-based guidelines are generated over time.”
According to Dr. El-Khoury, fixing the laboratory reference range issues would likely require a joint effort of professional medical societies, reference laboratories, and assay manufacturers. But with seasonal variation, that might be a difficult task.
“The problem is, in laboratory medicine, we don’t have rules for an analyte that changes by season to do anything different. My goal is to get people to at least acknowledge this is a problem and do something,” he concluded.
Dr. El-Khoury and Dr. Cubb have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Seasonal variation in one of the hormones used to monitor thyroid function could in turn lead to false diagnoses of subclinical hypothyroidism and unnecessary prescriptions of levothyroxine, according to Yale clinical chemist Joe M. El-Khoury, PhD.
A Japanese study of more than 7,000 healthy individuals showed that thyrotropin-stimulating hormone (TSH) varies widely throughout the seasons, he said, peaking in the northern hemisphere’s winter months (January to February) with its low in the summer months (June to August). That paper was published last year in the Journal of the Endocrine Society.
But free thyroxine (FT4) levels in the Japanese population remained relatively stable, he wrote in a letter recently published in Clinical Chemistry.
“If you end up with a mildly elevated TSH result and a normal FT4, try getting retested 2-3 months later to make sure this is not a seasonal artifact or transient increase before prescribing/taking levothyroxine unnecessarily,” advised Dr. El-Khoury, director of Yale University’s Clinical Chemistry Laboratory, New Haven, Conn.
“Because the [population-based, laboratory] reference ranges don’t account for seasonal variation, we’re flagging a significant number of people as high TSH when they’re normal, and physicians are prescribing levothyroxine inappropriately to healthy people who don’t need it,” he told this news organization, adding that overtreatment can be harmful, particularly for elderly people.
This seasonal variation in TSH could account for between a third to a half of the 90% of all levothyroxine prescriptions that were found to be unnecessary, according to a U.S. study in 2021, Dr. El-Khoury added.
In a comment, Trisha Cubb, MD, said that Dr. El-Khoury’s letter “raises a good point, that we really need to look at our reference ranges, especially when more and more studies are showing that so many thyroid hormone prescriptions may not be necessary.”
Dr. Cubb, thyroid section director and assistant professor of clinical medicine at Weill Cornell Medical College/Houston Methodist Academic Institute, Texas, also agrees with Dr. El-Khoury’s suggestion to repeat lab results in some instances.
“I think repeating results, especially in our patients with subclinical disease, is important,” she noted.
And she pointed out that seasonal variation isn’t the only relevant variable. “We also know that multiple clinical factors like pregnancy status, coexisting comorbidities, or age can all influence what we as clinicians consider an acceptable TSH range in an individual patient.” And other medications, such as steroids, or supplements like biotin, “can all affect thyroid lab values,” she noted.
“Ensuring that minor abnormalities aren’t transient is important prior to initiating medical therapy. With any medical therapy there are possible side effects, along with time, cost, [and] monitoring, all of which can be associated with thyroid hormone replacement.”
TSH reference ranges should be adapted for subpopulations
Dr. El-Khoury explained that to get an idea of how big the seasonal differences in TSH observed in the Japanese study were, “the upper end of the population they tracked goes from 5.2 [mIU/L] in January to 3.4 [mIU/L] in August. So you have almost a 2-unit change in concentration that can happen in the reference population. But laboratory reference ranges, or ‘normal ranges,’ are usually fixed and don’t change by season.”
The higher the TSH, the more likely a person is to have hypothyroidism. Major recent studies have found no benefit of levothyroxine treatment with TSH levels below 7.0-10.0 mIU/L, he said.
“So, I suggest that the limit should be 7.0 [mIU/L] to be safe, but it could be as high as 10 [mIU/L]. In any case, let’s shift the mindset to clinical outcome–based treatment cutoffs,” he said, noting that this approach is currently used for decisions on cholesterol-lowering therapy or vitamin D supplementation, for example.
Regarding this suggestion of using a TSH cutoff of 7 mIU/L to diagnose subclinical hypothyroidism, Dr. Cubb said: “It really depends on the specific population. In an elderly patient, a higher TSH may be of less clinical concern when compared to a female who is actively trying to get pregnant.
“Overall, I think we do need to better understand what appropriate TSH ranges are in specific subpopulations, and then with time, make this more understandable and available for general medicine as well as subspecialty providers to be able to utilize,” she noted.
Regarding the particular Japanese findings cited by Dr. El-Khoury, Dr. Cubb observed that this was a very specific study population, “so we would need more data showing that this is more generalizable.”
And she noted that there’s also diurnal variation in TSH. “In the [Japanese] paper, patients had their thyroid labs drawn between 8:00 a.m. and 9:00 a.m. in a fasting state. Oftentimes in the U.S., thyroid labs are not drawn at specific times or [during] fasting. I think this is one of many factors that should be considered.”
Acknowledging seasonal variation would be a start
But overall, Dr. Cubb said that both the Japanese study and Dr. El-Khoury’s letter highlight “how season, in and of itself, which is not something we usually think about, can affect thyroid lab results. I believe as more data come out, more generalizable data, that’s how evidence-based guidelines are generated over time.”
According to Dr. El-Khoury, fixing the laboratory reference range issues would likely require a joint effort of professional medical societies, reference laboratories, and assay manufacturers. But with seasonal variation, that might be a difficult task.
“The problem is, in laboratory medicine, we don’t have rules for an analyte that changes by season to do anything different. My goal is to get people to at least acknowledge this is a problem and do something,” he concluded.
Dr. El-Khoury and Dr. Cubb have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Seasonal variation in one of the hormones used to monitor thyroid function could in turn lead to false diagnoses of subclinical hypothyroidism and unnecessary prescriptions of levothyroxine, according to Yale clinical chemist Joe M. El-Khoury, PhD.
A Japanese study of more than 7,000 healthy individuals showed that thyrotropin-stimulating hormone (TSH) varies widely throughout the seasons, he said, peaking in the northern hemisphere’s winter months (January to February) with its low in the summer months (June to August). That paper was published last year in the Journal of the Endocrine Society.
But free thyroxine (FT4) levels in the Japanese population remained relatively stable, he wrote in a letter recently published in Clinical Chemistry.
“If you end up with a mildly elevated TSH result and a normal FT4, try getting retested 2-3 months later to make sure this is not a seasonal artifact or transient increase before prescribing/taking levothyroxine unnecessarily,” advised Dr. El-Khoury, director of Yale University’s Clinical Chemistry Laboratory, New Haven, Conn.
“Because the [population-based, laboratory] reference ranges don’t account for seasonal variation, we’re flagging a significant number of people as high TSH when they’re normal, and physicians are prescribing levothyroxine inappropriately to healthy people who don’t need it,” he told this news organization, adding that overtreatment can be harmful, particularly for elderly people.
This seasonal variation in TSH could account for between a third to a half of the 90% of all levothyroxine prescriptions that were found to be unnecessary, according to a U.S. study in 2021, Dr. El-Khoury added.
In a comment, Trisha Cubb, MD, said that Dr. El-Khoury’s letter “raises a good point, that we really need to look at our reference ranges, especially when more and more studies are showing that so many thyroid hormone prescriptions may not be necessary.”
Dr. Cubb, thyroid section director and assistant professor of clinical medicine at Weill Cornell Medical College/Houston Methodist Academic Institute, Texas, also agrees with Dr. El-Khoury’s suggestion to repeat lab results in some instances.
“I think repeating results, especially in our patients with subclinical disease, is important,” she noted.
And she pointed out that seasonal variation isn’t the only relevant variable. “We also know that multiple clinical factors like pregnancy status, coexisting comorbidities, or age can all influence what we as clinicians consider an acceptable TSH range in an individual patient.” And other medications, such as steroids, or supplements like biotin, “can all affect thyroid lab values,” she noted.
“Ensuring that minor abnormalities aren’t transient is important prior to initiating medical therapy. With any medical therapy there are possible side effects, along with time, cost, [and] monitoring, all of which can be associated with thyroid hormone replacement.”
TSH reference ranges should be adapted for subpopulations
Dr. El-Khoury explained that to get an idea of how big the seasonal differences in TSH observed in the Japanese study were, “the upper end of the population they tracked goes from 5.2 [mIU/L] in January to 3.4 [mIU/L] in August. So you have almost a 2-unit change in concentration that can happen in the reference population. But laboratory reference ranges, or ‘normal ranges,’ are usually fixed and don’t change by season.”
The higher the TSH, the more likely a person is to have hypothyroidism. Major recent studies have found no benefit of levothyroxine treatment with TSH levels below 7.0-10.0 mIU/L, he said.
“So, I suggest that the limit should be 7.0 [mIU/L] to be safe, but it could be as high as 10 [mIU/L]. In any case, let’s shift the mindset to clinical outcome–based treatment cutoffs,” he said, noting that this approach is currently used for decisions on cholesterol-lowering therapy or vitamin D supplementation, for example.
Regarding this suggestion of using a TSH cutoff of 7 mIU/L to diagnose subclinical hypothyroidism, Dr. Cubb said: “It really depends on the specific population. In an elderly patient, a higher TSH may be of less clinical concern when compared to a female who is actively trying to get pregnant.
“Overall, I think we do need to better understand what appropriate TSH ranges are in specific subpopulations, and then with time, make this more understandable and available for general medicine as well as subspecialty providers to be able to utilize,” she noted.
Regarding the particular Japanese findings cited by Dr. El-Khoury, Dr. Cubb observed that this was a very specific study population, “so we would need more data showing that this is more generalizable.”
And she noted that there’s also diurnal variation in TSH. “In the [Japanese] paper, patients had their thyroid labs drawn between 8:00 a.m. and 9:00 a.m. in a fasting state. Oftentimes in the U.S., thyroid labs are not drawn at specific times or [during] fasting. I think this is one of many factors that should be considered.”
Acknowledging seasonal variation would be a start
But overall, Dr. Cubb said that both the Japanese study and Dr. El-Khoury’s letter highlight “how season, in and of itself, which is not something we usually think about, can affect thyroid lab results. I believe as more data come out, more generalizable data, that’s how evidence-based guidelines are generated over time.”
According to Dr. El-Khoury, fixing the laboratory reference range issues would likely require a joint effort of professional medical societies, reference laboratories, and assay manufacturers. But with seasonal variation, that might be a difficult task.
“The problem is, in laboratory medicine, we don’t have rules for an analyte that changes by season to do anything different. My goal is to get people to at least acknowledge this is a problem and do something,” he concluded.
Dr. El-Khoury and Dr. Cubb have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CLINICAL CHEMISTRY
Parathyroidectomy does not preserve kidney function in seniors
Early parathyroidectomy within 1 year of diagnosis of primary hyperparathyroidism (PHPT) did not reduce the risk of a sustained decline in kidney function, measured by a decline in estimated glomerular filtration rate (eGFR) of at least 50%, compared with observation (no surgery) in adults aged 60 and older.
Early parathyroidectomy was, however, associated with a reduced adjusted risk of this decline in kidney function in patients with newly diagnosed PHPT who were younger than age 60.
The findings, based on data from close to 43,000 veterans, were published online in Annals of Internal Medicine.
“The important takeaway from our study is that for older adults [age 60 or older] with primary hyperparathyroidism, preservation of kidney function should not be a primary consideration when making decisions about whether to undergo parathyroidectomy,” lead author Carolyn D. Seib, MD, told this news organization.
“It is important that physicians also discuss with their patients the potential long-term benefits of parathyroidectomy related to a reduced risk of fractures, kidney stones, and cardiovascular disease, and improved quality of life, in addition to the need for lifelong surveillance if surgery is declined, weighing these against an individual patient’s risk of surgery,” said Dr. Seib, a surgeon at Palo Alto (Calif.) VA Medical Center.
“However, in patients younger than 60, early parathyroidectomy may prevent progression to chronic kidney disease (CKD) and should be more strongly considered,” she noted.
Parathyroidectomy, she observed, is a low-risk outpatient surgery for most adults.
“Potential complications of surgery include temporary or permanent hoarseness, hypoparathyroidism (low postoperative parathyroid function), bleeding requiring return to the operating room, and complications related to general anesthesia, all of which are rare,” said Dr. Seib.
“Surgery by a high-volume surgeon is associated with a reduced risk of complications, so patients should seek out an experienced parathyroid surgeon,” she emphasized.
Moreover, parathyroidectomy is the only treatment for primary hyperparathyroidism.
Does parathyroidectomy slow loss of kidney function?
Multidisciplinary guidelines recommend parathyroidectomy, at least in part to mitigate the risk for, and effects related to, the progression of CKD in patients with PHPT and an eGFR below 60 mL/min per 1.73 m2, the researchers wrote.
However, whether parathyroidectomy slows the loss of kidney function in adults with PHPT is not clear.
Guidelines also state that “observation for PHPT disease progression can be considered when patients have no obvious end organ damage (i.e., eGFR > 60 mL/min per 1.73 m2, normal bone mineral density, and no history of kidney stones or fractures),” Dr. Seib noted.
To address the evidence gap, the researchers emulated a randomized target trial using observational data.
In this type of study, Dr. Seib explained, “although patients aren’t randomly assigned to a treatment, complex statistical methods are used to adjust for baseline confounders in an attempt to emulate random treatment assignment and account for bias that may affect the timing of when patients receive treatment.”
Using national Veterans Health Administration data, researchers identified 43,697 veterans with a new biochemical diagnosis of PHPT, defined as elevated parathyroid hormone (> 65 ng/mL) within 6 months of an elevated serum calcium level (> 32.55 mmol/L or >10.2 mg/dL), from 2000 to 2019.
Of these patients, 3,804 underwent parathyroidectomy within 1 year of diagnosis of PHPT, and 39,893 did not, and instead, a watchful waiting approach was adopted.
To be included in the analysis, patients had to have an eGFR above 30 mL/min per 1.73 m2 for 12 months before PHPT diagnosis to exclude secondary or tertiary hyperparathyroidism.
The primary outcome was a sustained decline in eGFR of at least 50% from baseline.
In the overall cohort, patients had a mean pretreatment eGFR of 71.8 mL/min per 1.73 m2. The mean age of patients was 67, 88% were men, and 68% were White.
After a median follow-up of 4.9 years, 6.7% of the patients had a decline in eGFR of at least 50%.
The cumulative incidence of this decline in eGFR was 5.1% at 5 years and 10.8% at 10 years in patients who had had early parathyroidectomy compared with 5.1% and 12.0%, respectively, in patients who did not undergo surgery.
In the overall population, the risk of at least a 50% decline in eGFR was similar in the early parathyroidectomy group versus the observation group (adjusted hazard ratio [HR], 0.98, 95% confidence interval [CI], 0.82-1.16).
However, diving deeper showed that parathyroidectomy was associated with a reduced risk of the primary outcome among patients younger than 60 years (adjusted HR, 0.75, 95% CI, 0.59-0.93) but not among those aged 60 or older (adjusted HR, 1.08, 95% CI, 0.87-1.34).
“When participating in shared decision-making for older adults [age 60 and older] with PHPT, clinicians should not consider parathyroidectomy for potential benefits of preservation of kidney function,” the researchers reiterated.
“For younger patients, clinicians should discuss the potential benefit of parathyroidectomy to reduce the risk for CKD and associated complications in adults with PHPT,” they concluded.
The study was funded by the National Institute on Aging. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Early parathyroidectomy within 1 year of diagnosis of primary hyperparathyroidism (PHPT) did not reduce the risk of a sustained decline in kidney function, measured by a decline in estimated glomerular filtration rate (eGFR) of at least 50%, compared with observation (no surgery) in adults aged 60 and older.
Early parathyroidectomy was, however, associated with a reduced adjusted risk of this decline in kidney function in patients with newly diagnosed PHPT who were younger than age 60.
The findings, based on data from close to 43,000 veterans, were published online in Annals of Internal Medicine.
“The important takeaway from our study is that for older adults [age 60 or older] with primary hyperparathyroidism, preservation of kidney function should not be a primary consideration when making decisions about whether to undergo parathyroidectomy,” lead author Carolyn D. Seib, MD, told this news organization.
“It is important that physicians also discuss with their patients the potential long-term benefits of parathyroidectomy related to a reduced risk of fractures, kidney stones, and cardiovascular disease, and improved quality of life, in addition to the need for lifelong surveillance if surgery is declined, weighing these against an individual patient’s risk of surgery,” said Dr. Seib, a surgeon at Palo Alto (Calif.) VA Medical Center.
“However, in patients younger than 60, early parathyroidectomy may prevent progression to chronic kidney disease (CKD) and should be more strongly considered,” she noted.
Parathyroidectomy, she observed, is a low-risk outpatient surgery for most adults.
“Potential complications of surgery include temporary or permanent hoarseness, hypoparathyroidism (low postoperative parathyroid function), bleeding requiring return to the operating room, and complications related to general anesthesia, all of which are rare,” said Dr. Seib.
“Surgery by a high-volume surgeon is associated with a reduced risk of complications, so patients should seek out an experienced parathyroid surgeon,” she emphasized.
Moreover, parathyroidectomy is the only treatment for primary hyperparathyroidism.
Does parathyroidectomy slow loss of kidney function?
Multidisciplinary guidelines recommend parathyroidectomy, at least in part to mitigate the risk for, and effects related to, the progression of CKD in patients with PHPT and an eGFR below 60 mL/min per 1.73 m2, the researchers wrote.
However, whether parathyroidectomy slows the loss of kidney function in adults with PHPT is not clear.
Guidelines also state that “observation for PHPT disease progression can be considered when patients have no obvious end organ damage (i.e., eGFR > 60 mL/min per 1.73 m2, normal bone mineral density, and no history of kidney stones or fractures),” Dr. Seib noted.
To address the evidence gap, the researchers emulated a randomized target trial using observational data.
In this type of study, Dr. Seib explained, “although patients aren’t randomly assigned to a treatment, complex statistical methods are used to adjust for baseline confounders in an attempt to emulate random treatment assignment and account for bias that may affect the timing of when patients receive treatment.”
Using national Veterans Health Administration data, researchers identified 43,697 veterans with a new biochemical diagnosis of PHPT, defined as elevated parathyroid hormone (> 65 ng/mL) within 6 months of an elevated serum calcium level (> 32.55 mmol/L or >10.2 mg/dL), from 2000 to 2019.
Of these patients, 3,804 underwent parathyroidectomy within 1 year of diagnosis of PHPT, and 39,893 did not, and instead, a watchful waiting approach was adopted.
To be included in the analysis, patients had to have an eGFR above 30 mL/min per 1.73 m2 for 12 months before PHPT diagnosis to exclude secondary or tertiary hyperparathyroidism.
The primary outcome was a sustained decline in eGFR of at least 50% from baseline.
In the overall cohort, patients had a mean pretreatment eGFR of 71.8 mL/min per 1.73 m2. The mean age of patients was 67, 88% were men, and 68% were White.
After a median follow-up of 4.9 years, 6.7% of the patients had a decline in eGFR of at least 50%.
The cumulative incidence of this decline in eGFR was 5.1% at 5 years and 10.8% at 10 years in patients who had had early parathyroidectomy compared with 5.1% and 12.0%, respectively, in patients who did not undergo surgery.
In the overall population, the risk of at least a 50% decline in eGFR was similar in the early parathyroidectomy group versus the observation group (adjusted hazard ratio [HR], 0.98, 95% confidence interval [CI], 0.82-1.16).
However, diving deeper showed that parathyroidectomy was associated with a reduced risk of the primary outcome among patients younger than 60 years (adjusted HR, 0.75, 95% CI, 0.59-0.93) but not among those aged 60 or older (adjusted HR, 1.08, 95% CI, 0.87-1.34).
“When participating in shared decision-making for older adults [age 60 and older] with PHPT, clinicians should not consider parathyroidectomy for potential benefits of preservation of kidney function,” the researchers reiterated.
“For younger patients, clinicians should discuss the potential benefit of parathyroidectomy to reduce the risk for CKD and associated complications in adults with PHPT,” they concluded.
The study was funded by the National Institute on Aging. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Early parathyroidectomy within 1 year of diagnosis of primary hyperparathyroidism (PHPT) did not reduce the risk of a sustained decline in kidney function, measured by a decline in estimated glomerular filtration rate (eGFR) of at least 50%, compared with observation (no surgery) in adults aged 60 and older.
Early parathyroidectomy was, however, associated with a reduced adjusted risk of this decline in kidney function in patients with newly diagnosed PHPT who were younger than age 60.
The findings, based on data from close to 43,000 veterans, were published online in Annals of Internal Medicine.
“The important takeaway from our study is that for older adults [age 60 or older] with primary hyperparathyroidism, preservation of kidney function should not be a primary consideration when making decisions about whether to undergo parathyroidectomy,” lead author Carolyn D. Seib, MD, told this news organization.
“It is important that physicians also discuss with their patients the potential long-term benefits of parathyroidectomy related to a reduced risk of fractures, kidney stones, and cardiovascular disease, and improved quality of life, in addition to the need for lifelong surveillance if surgery is declined, weighing these against an individual patient’s risk of surgery,” said Dr. Seib, a surgeon at Palo Alto (Calif.) VA Medical Center.
“However, in patients younger than 60, early parathyroidectomy may prevent progression to chronic kidney disease (CKD) and should be more strongly considered,” she noted.
Parathyroidectomy, she observed, is a low-risk outpatient surgery for most adults.
“Potential complications of surgery include temporary or permanent hoarseness, hypoparathyroidism (low postoperative parathyroid function), bleeding requiring return to the operating room, and complications related to general anesthesia, all of which are rare,” said Dr. Seib.
“Surgery by a high-volume surgeon is associated with a reduced risk of complications, so patients should seek out an experienced parathyroid surgeon,” she emphasized.
Moreover, parathyroidectomy is the only treatment for primary hyperparathyroidism.
Does parathyroidectomy slow loss of kidney function?
Multidisciplinary guidelines recommend parathyroidectomy, at least in part to mitigate the risk for, and effects related to, the progression of CKD in patients with PHPT and an eGFR below 60 mL/min per 1.73 m2, the researchers wrote.
However, whether parathyroidectomy slows the loss of kidney function in adults with PHPT is not clear.
Guidelines also state that “observation for PHPT disease progression can be considered when patients have no obvious end organ damage (i.e., eGFR > 60 mL/min per 1.73 m2, normal bone mineral density, and no history of kidney stones or fractures),” Dr. Seib noted.
To address the evidence gap, the researchers emulated a randomized target trial using observational data.
In this type of study, Dr. Seib explained, “although patients aren’t randomly assigned to a treatment, complex statistical methods are used to adjust for baseline confounders in an attempt to emulate random treatment assignment and account for bias that may affect the timing of when patients receive treatment.”
Using national Veterans Health Administration data, researchers identified 43,697 veterans with a new biochemical diagnosis of PHPT, defined as elevated parathyroid hormone (> 65 ng/mL) within 6 months of an elevated serum calcium level (> 32.55 mmol/L or >10.2 mg/dL), from 2000 to 2019.
Of these patients, 3,804 underwent parathyroidectomy within 1 year of diagnosis of PHPT, and 39,893 did not, and instead, a watchful waiting approach was adopted.
To be included in the analysis, patients had to have an eGFR above 30 mL/min per 1.73 m2 for 12 months before PHPT diagnosis to exclude secondary or tertiary hyperparathyroidism.
The primary outcome was a sustained decline in eGFR of at least 50% from baseline.
In the overall cohort, patients had a mean pretreatment eGFR of 71.8 mL/min per 1.73 m2. The mean age of patients was 67, 88% were men, and 68% were White.
After a median follow-up of 4.9 years, 6.7% of the patients had a decline in eGFR of at least 50%.
The cumulative incidence of this decline in eGFR was 5.1% at 5 years and 10.8% at 10 years in patients who had had early parathyroidectomy compared with 5.1% and 12.0%, respectively, in patients who did not undergo surgery.
In the overall population, the risk of at least a 50% decline in eGFR was similar in the early parathyroidectomy group versus the observation group (adjusted hazard ratio [HR], 0.98, 95% confidence interval [CI], 0.82-1.16).
However, diving deeper showed that parathyroidectomy was associated with a reduced risk of the primary outcome among patients younger than 60 years (adjusted HR, 0.75, 95% CI, 0.59-0.93) but not among those aged 60 or older (adjusted HR, 1.08, 95% CI, 0.87-1.34).
“When participating in shared decision-making for older adults [age 60 and older] with PHPT, clinicians should not consider parathyroidectomy for potential benefits of preservation of kidney function,” the researchers reiterated.
“For younger patients, clinicians should discuss the potential benefit of parathyroidectomy to reduce the risk for CKD and associated complications in adults with PHPT,” they concluded.
The study was funded by the National Institute on Aging. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
TikTok offers to ‘balance your hormones’ are pure hokum
With more than 306 million views, #hormonebalance and #hormonebalancing are among the latest hacks to take over the social media platform TikTok, on which users post short videos. Influencers offer advice such as eating raw carrots for “happy hormones,” eating protein followed by fat for breakfast to regulate blood glucose, or taking vitamin B2 supplements for thyroid health.
Have you ever wondered if you were asleep during the lecture on “hormone balancing” in medical school? No, you weren’t. It was never a class for good reason, and you didn’t fail to read any such breakthrough studies in The New England Journal of Medicine either.
There are over 50 different hormones produced by humans and animals, regulating sleep, growth, metabolism and reproduction, among many other biological processes, so there is certainly no one-size-fits-all solution to ensure these are all working in perfect harmony.
When someone mentions “hormone balancing,” my mind wanders to the last time I took my car to have my tires rotated and balanced. If only it were as simple to balance hormones in real life. The best we can hope for is to get a specific hormone within the ideal physiologic range for that person’s age.
The term “hormone” can mean many things to different people. When a woman comes in with a hormone question, for example, it is often related to estrogen, followed by thyroid hormones. A wealth of misinformation exists in popular literature regarding these hormones alone.
Estrogen can be replaced, but not everyone needs it replaced. It depends on variables including age, underlying medical conditions, the time of day a test was drawn, and concomitant medications. Having low levels of a given hormone does not necessarily call for replacement either.
Insulin is another example of a hormone that can never completely be replaced in people with diabetes in a way that exactly mimics the normal physiologic release.
There are many lesser-known hormones that are measurable and replaceable but are also more difficult to reset to original manufacturer specifications.
A Google search for “hormone balancing” often sends you to “naturopaths” or “integrative medicine” practitioners, who often propose similar solutions to the TikTok influencers. Users are told that their hormones are out of whack and that restoring this “balance” can be achieved by purchasing whatever “natural products” or concoction they are selling.
These TikTok videos and online “experts” are the home-brewed versions of the strip-mall hormone specialists. TikTok videos claiming to help “balance hormones” typically don’t name a specific hormone either, or the end organs that each would have an impact on. Rather, they lump all hormones into a monolithic entity, implying that there is a single solution for all health problems. And personal testimonials extolling the benefits of a TikTok intervention don’t constitute proof of efficacy no matter how many “likes” they get. These influencers assume that viewers can “sense” their hormones are out of tune and no lab tests can convince them otherwise.
In these inflationary times, the cost of seeking medical care from conventional channels is increasingly prohibitive. It’s easy to understand the appeal of getting free advice from TikTok or some other Internet site. At best, following the advice will not have much impact; at worst, it could be harmful.
Don’t try this at home
There are some things that should never be tried at home, and do-it-yourself hormone replacement or remediation both fall under this umbrella.
Generally, the body does a good job of balancing its own hormones. Most patients don’t need to be worried if they’re in good health. If they’re in doubt, they should seek advice from a doctor, ideally an endocrinologist, but an ob.gyn. or general practitioner are also good options.
One of the first questions to ask a patient is “Which hormone are you worried about?” or “What health issue is it specifically that is bothering you?” Narrowing the focus to a single thing, if possible, will lead to a more efficient evaluation.
Often, patients arrive with multiple concerns written on little pieces of paper. These ubiquitous pieces of paper are the red flag for the flood of questions to follow.
Ordering the appropriate tests for the conditions they are concerned about can help put their minds at ease. If there are any specific deficiencies, or excesses in any hormones, then appropriate solutions can be discussed.
TikTok hormone-balancing solutions are simply the 21st-century version of the snake oil sold on late-night cable TV in the 1990s.
Needless to say, you should gently encourage your patients to stay away from these non–FDA-approved products, without making them feel stupid. Off-label use of hormones when these are not indicated is also to be avoided, unless a medical practitioner feels it is warranted.
Dr. de la Rosa is an endocrinologist in Englewood, Fla. He disclosed no conflicts of interest.
A version of this article first appeared on Medscape.com.
With more than 306 million views, #hormonebalance and #hormonebalancing are among the latest hacks to take over the social media platform TikTok, on which users post short videos. Influencers offer advice such as eating raw carrots for “happy hormones,” eating protein followed by fat for breakfast to regulate blood glucose, or taking vitamin B2 supplements for thyroid health.
Have you ever wondered if you were asleep during the lecture on “hormone balancing” in medical school? No, you weren’t. It was never a class for good reason, and you didn’t fail to read any such breakthrough studies in The New England Journal of Medicine either.
There are over 50 different hormones produced by humans and animals, regulating sleep, growth, metabolism and reproduction, among many other biological processes, so there is certainly no one-size-fits-all solution to ensure these are all working in perfect harmony.
When someone mentions “hormone balancing,” my mind wanders to the last time I took my car to have my tires rotated and balanced. If only it were as simple to balance hormones in real life. The best we can hope for is to get a specific hormone within the ideal physiologic range for that person’s age.
The term “hormone” can mean many things to different people. When a woman comes in with a hormone question, for example, it is often related to estrogen, followed by thyroid hormones. A wealth of misinformation exists in popular literature regarding these hormones alone.
Estrogen can be replaced, but not everyone needs it replaced. It depends on variables including age, underlying medical conditions, the time of day a test was drawn, and concomitant medications. Having low levels of a given hormone does not necessarily call for replacement either.
Insulin is another example of a hormone that can never completely be replaced in people with diabetes in a way that exactly mimics the normal physiologic release.
There are many lesser-known hormones that are measurable and replaceable but are also more difficult to reset to original manufacturer specifications.
A Google search for “hormone balancing” often sends you to “naturopaths” or “integrative medicine” practitioners, who often propose similar solutions to the TikTok influencers. Users are told that their hormones are out of whack and that restoring this “balance” can be achieved by purchasing whatever “natural products” or concoction they are selling.
These TikTok videos and online “experts” are the home-brewed versions of the strip-mall hormone specialists. TikTok videos claiming to help “balance hormones” typically don’t name a specific hormone either, or the end organs that each would have an impact on. Rather, they lump all hormones into a monolithic entity, implying that there is a single solution for all health problems. And personal testimonials extolling the benefits of a TikTok intervention don’t constitute proof of efficacy no matter how many “likes” they get. These influencers assume that viewers can “sense” their hormones are out of tune and no lab tests can convince them otherwise.
In these inflationary times, the cost of seeking medical care from conventional channels is increasingly prohibitive. It’s easy to understand the appeal of getting free advice from TikTok or some other Internet site. At best, following the advice will not have much impact; at worst, it could be harmful.
Don’t try this at home
There are some things that should never be tried at home, and do-it-yourself hormone replacement or remediation both fall under this umbrella.
Generally, the body does a good job of balancing its own hormones. Most patients don’t need to be worried if they’re in good health. If they’re in doubt, they should seek advice from a doctor, ideally an endocrinologist, but an ob.gyn. or general practitioner are also good options.
One of the first questions to ask a patient is “Which hormone are you worried about?” or “What health issue is it specifically that is bothering you?” Narrowing the focus to a single thing, if possible, will lead to a more efficient evaluation.
Often, patients arrive with multiple concerns written on little pieces of paper. These ubiquitous pieces of paper are the red flag for the flood of questions to follow.
Ordering the appropriate tests for the conditions they are concerned about can help put their minds at ease. If there are any specific deficiencies, or excesses in any hormones, then appropriate solutions can be discussed.
TikTok hormone-balancing solutions are simply the 21st-century version of the snake oil sold on late-night cable TV in the 1990s.
Needless to say, you should gently encourage your patients to stay away from these non–FDA-approved products, without making them feel stupid. Off-label use of hormones when these are not indicated is also to be avoided, unless a medical practitioner feels it is warranted.
Dr. de la Rosa is an endocrinologist in Englewood, Fla. He disclosed no conflicts of interest.
A version of this article first appeared on Medscape.com.
With more than 306 million views, #hormonebalance and #hormonebalancing are among the latest hacks to take over the social media platform TikTok, on which users post short videos. Influencers offer advice such as eating raw carrots for “happy hormones,” eating protein followed by fat for breakfast to regulate blood glucose, or taking vitamin B2 supplements for thyroid health.
Have you ever wondered if you were asleep during the lecture on “hormone balancing” in medical school? No, you weren’t. It was never a class for good reason, and you didn’t fail to read any such breakthrough studies in The New England Journal of Medicine either.
There are over 50 different hormones produced by humans and animals, regulating sleep, growth, metabolism and reproduction, among many other biological processes, so there is certainly no one-size-fits-all solution to ensure these are all working in perfect harmony.
When someone mentions “hormone balancing,” my mind wanders to the last time I took my car to have my tires rotated and balanced. If only it were as simple to balance hormones in real life. The best we can hope for is to get a specific hormone within the ideal physiologic range for that person’s age.
The term “hormone” can mean many things to different people. When a woman comes in with a hormone question, for example, it is often related to estrogen, followed by thyroid hormones. A wealth of misinformation exists in popular literature regarding these hormones alone.
Estrogen can be replaced, but not everyone needs it replaced. It depends on variables including age, underlying medical conditions, the time of day a test was drawn, and concomitant medications. Having low levels of a given hormone does not necessarily call for replacement either.
Insulin is another example of a hormone that can never completely be replaced in people with diabetes in a way that exactly mimics the normal physiologic release.
There are many lesser-known hormones that are measurable and replaceable but are also more difficult to reset to original manufacturer specifications.
A Google search for “hormone balancing” often sends you to “naturopaths” or “integrative medicine” practitioners, who often propose similar solutions to the TikTok influencers. Users are told that their hormones are out of whack and that restoring this “balance” can be achieved by purchasing whatever “natural products” or concoction they are selling.
These TikTok videos and online “experts” are the home-brewed versions of the strip-mall hormone specialists. TikTok videos claiming to help “balance hormones” typically don’t name a specific hormone either, or the end organs that each would have an impact on. Rather, they lump all hormones into a monolithic entity, implying that there is a single solution for all health problems. And personal testimonials extolling the benefits of a TikTok intervention don’t constitute proof of efficacy no matter how many “likes” they get. These influencers assume that viewers can “sense” their hormones are out of tune and no lab tests can convince them otherwise.
In these inflationary times, the cost of seeking medical care from conventional channels is increasingly prohibitive. It’s easy to understand the appeal of getting free advice from TikTok or some other Internet site. At best, following the advice will not have much impact; at worst, it could be harmful.
Don’t try this at home
There are some things that should never be tried at home, and do-it-yourself hormone replacement or remediation both fall under this umbrella.
Generally, the body does a good job of balancing its own hormones. Most patients don’t need to be worried if they’re in good health. If they’re in doubt, they should seek advice from a doctor, ideally an endocrinologist, but an ob.gyn. or general practitioner are also good options.
One of the first questions to ask a patient is “Which hormone are you worried about?” or “What health issue is it specifically that is bothering you?” Narrowing the focus to a single thing, if possible, will lead to a more efficient evaluation.
Often, patients arrive with multiple concerns written on little pieces of paper. These ubiquitous pieces of paper are the red flag for the flood of questions to follow.
Ordering the appropriate tests for the conditions they are concerned about can help put their minds at ease. If there are any specific deficiencies, or excesses in any hormones, then appropriate solutions can be discussed.
TikTok hormone-balancing solutions are simply the 21st-century version of the snake oil sold on late-night cable TV in the 1990s.
Needless to say, you should gently encourage your patients to stay away from these non–FDA-approved products, without making them feel stupid. Off-label use of hormones when these are not indicated is also to be avoided, unless a medical practitioner feels it is warranted.
Dr. de la Rosa is an endocrinologist in Englewood, Fla. He disclosed no conflicts of interest.
A version of this article first appeared on Medscape.com.
Statins don’t worsen muscle injury from moderately intense exercise
People who are physically active and on statins may have one less potential concern about the drugs. Despite their reputation for causing muscle injury, a study suggests statins won’t worsen the toll that sustained, moderately intensive exercise already takes on patients’ muscles.
Statin therapy in this prospective, controlled study wasn’t seen to aggravate normal muscle fatigue or pain from sustained exercise or adversely affect enzymes or other biomarkers associated with muscle injury.
The findings come from 100 individuals, of whom about two-thirds were on statins, participating in a public, 4-day, long-distance walking event held annually in the Netherlands. Results were published in the Journal of the American College of Cardiology with Neeltje A.E. Allard, MD, Radboud University Medical Center, Nijmegen, the Netherlands, as lead author.
For all of statins’ common use in adults with cardiovascular (CV) risk factors, the drugs are often blamed for causing excessive muscle pain or injury as a side effect. Yet there is a predominance of evidence to the contrary based on meta-analyses and clinical trials, suggesting that the drugs are taking the rap for many entirely unrelated muscle symptoms.
The new findings, from people ranging widely in fitness levels, suggest that “exercise of moderate intensity is feasible and safe” in statin users, that the drugs won’t exacerbate normal muscle symptoms from exercise, Dr. Allard told this news organization.
And that exercise doesn’t have to be on an unusual scale. Regular exercise in statin users can simply be consistent with broader guidelines, say 30 minutes of walking per day, she noted.
The study has such broad applicability, Dr. Allard said, because participants represented the spectrum of the thousands who signed up for the walking event, who varied in age, level of physical fitness, and number of CV risk factors. They included CV patients, the physically fit, “recreational walkers who didn’t really exercise regularly,” and “habitual nonexercisers.”
It enrolled three groups of participants in the Four Days Marches in Nijmegen, which in a typical year attracts tens of thousands of participants who walk up to 30 km, 40 km, or 50 km per day for 4 consecutive days.
They included 35 statin users who walked the event despite muscle symptoms, 34 on statins but without such symptoms, and 31 non–statin-using controls. Their mean ages ranged from 65 to 68 years.
Statin users were overwhelmingly on simvastatin or atorvastatin. The average statin therapy durations were 60 months and 96 months for those with and without symptoms, respectively.
Assessments were performed several days before the event, at baseline, and after the end of walking on days 1, 2, and 3.
Scores for muscle pain on the Brief Pain Inventory were higher at baseline for the symptomatic-on-statins group (P < .001) compared with the other two groups, and went up (P < .001) similarly across the three groups during each of the 3 days, the report notes. Fatigue scores on the Brief Fatigue Inventory followed the same pattern.
All biomarkers of muscle injury or stress were at comparable levels at baseline in the three groups and went up similarly (P < .001) with no significant differences at the end of day 3. Biomarkers included lactate dehydrogenase, creatine kinase, myoglobin, cardiac troponin I, and N-terminal pro-brain natriuretic peptide.
Statin-related reductions in levels of coenzyme Q 10 (CoQ10) have been thought to exacerbate muscle injury, the authors note. But levels of CoQ10 weren’t significantly different across the three groups at any point in the study, and they did not show any significant associations with measures of muscle injury, symptoms, or fatigue.
Patients with statin-associated muscle symptoms (SAMS) often limit physical activity because of muscle pain or weakness, but also “concerns that exercise will exacerbate muscle injury,” an accompanying editorial notes. “Therefore, exercise, a foundation of improving and maintaining cardiometabolic health, is often avoided or limited.”
But the current study, writes Robert S. Rosenson, MD, of Mount Sinai Heart, New York, indeed suggests that “many patients who develop SAMS may engage in a moderately intensive walking program without concern for worsened muscle biomarkers or performance.”
The exercise didn’t seem to improve muscle function in symptomatic statin users, compared with the other groups over the study’s very short follow-up, Dr. Rosenson observes. But “it remains uncertain from this study whether sustained exercise in SAMS patients will effectuate improved metabolic biomarkers or exercise capacity in the long term.”
Dr. Allard is supported by a grant from the Radboud Institute for Health Sciences; the other authors have disclosed no relevant financial relationships. Dr. Rosenson disclosed receiving research funding to his institution from Amgen, Arrowhead, Lilly, Novartis, and Regeneron; consulting fees from Amgen, Arrowhead, Lilly, Lipigon, Novartis, CRISPR Therapeutics, Precision BioSciences, Verve, Ultragenyx Pharmaceutical, and Regeneron; speaking fees from Amgen, Kowa, and Regeneron; and royalties from Wolters Kluwer (UpToDate); and that he holds stock in MediMergent.
A version of this article first appeared on Medscape.com.
People who are physically active and on statins may have one less potential concern about the drugs. Despite their reputation for causing muscle injury, a study suggests statins won’t worsen the toll that sustained, moderately intensive exercise already takes on patients’ muscles.
Statin therapy in this prospective, controlled study wasn’t seen to aggravate normal muscle fatigue or pain from sustained exercise or adversely affect enzymes or other biomarkers associated with muscle injury.
The findings come from 100 individuals, of whom about two-thirds were on statins, participating in a public, 4-day, long-distance walking event held annually in the Netherlands. Results were published in the Journal of the American College of Cardiology with Neeltje A.E. Allard, MD, Radboud University Medical Center, Nijmegen, the Netherlands, as lead author.
For all of statins’ common use in adults with cardiovascular (CV) risk factors, the drugs are often blamed for causing excessive muscle pain or injury as a side effect. Yet there is a predominance of evidence to the contrary based on meta-analyses and clinical trials, suggesting that the drugs are taking the rap for many entirely unrelated muscle symptoms.
The new findings, from people ranging widely in fitness levels, suggest that “exercise of moderate intensity is feasible and safe” in statin users, that the drugs won’t exacerbate normal muscle symptoms from exercise, Dr. Allard told this news organization.
And that exercise doesn’t have to be on an unusual scale. Regular exercise in statin users can simply be consistent with broader guidelines, say 30 minutes of walking per day, she noted.
The study has such broad applicability, Dr. Allard said, because participants represented the spectrum of the thousands who signed up for the walking event, who varied in age, level of physical fitness, and number of CV risk factors. They included CV patients, the physically fit, “recreational walkers who didn’t really exercise regularly,” and “habitual nonexercisers.”
It enrolled three groups of participants in the Four Days Marches in Nijmegen, which in a typical year attracts tens of thousands of participants who walk up to 30 km, 40 km, or 50 km per day for 4 consecutive days.
They included 35 statin users who walked the event despite muscle symptoms, 34 on statins but without such symptoms, and 31 non–statin-using controls. Their mean ages ranged from 65 to 68 years.
Statin users were overwhelmingly on simvastatin or atorvastatin. The average statin therapy durations were 60 months and 96 months for those with and without symptoms, respectively.
Assessments were performed several days before the event, at baseline, and after the end of walking on days 1, 2, and 3.
Scores for muscle pain on the Brief Pain Inventory were higher at baseline for the symptomatic-on-statins group (P < .001) compared with the other two groups, and went up (P < .001) similarly across the three groups during each of the 3 days, the report notes. Fatigue scores on the Brief Fatigue Inventory followed the same pattern.
All biomarkers of muscle injury or stress were at comparable levels at baseline in the three groups and went up similarly (P < .001) with no significant differences at the end of day 3. Biomarkers included lactate dehydrogenase, creatine kinase, myoglobin, cardiac troponin I, and N-terminal pro-brain natriuretic peptide.
Statin-related reductions in levels of coenzyme Q 10 (CoQ10) have been thought to exacerbate muscle injury, the authors note. But levels of CoQ10 weren’t significantly different across the three groups at any point in the study, and they did not show any significant associations with measures of muscle injury, symptoms, or fatigue.
Patients with statin-associated muscle symptoms (SAMS) often limit physical activity because of muscle pain or weakness, but also “concerns that exercise will exacerbate muscle injury,” an accompanying editorial notes. “Therefore, exercise, a foundation of improving and maintaining cardiometabolic health, is often avoided or limited.”
But the current study, writes Robert S. Rosenson, MD, of Mount Sinai Heart, New York, indeed suggests that “many patients who develop SAMS may engage in a moderately intensive walking program without concern for worsened muscle biomarkers or performance.”
The exercise didn’t seem to improve muscle function in symptomatic statin users, compared with the other groups over the study’s very short follow-up, Dr. Rosenson observes. But “it remains uncertain from this study whether sustained exercise in SAMS patients will effectuate improved metabolic biomarkers or exercise capacity in the long term.”
Dr. Allard is supported by a grant from the Radboud Institute for Health Sciences; the other authors have disclosed no relevant financial relationships. Dr. Rosenson disclosed receiving research funding to his institution from Amgen, Arrowhead, Lilly, Novartis, and Regeneron; consulting fees from Amgen, Arrowhead, Lilly, Lipigon, Novartis, CRISPR Therapeutics, Precision BioSciences, Verve, Ultragenyx Pharmaceutical, and Regeneron; speaking fees from Amgen, Kowa, and Regeneron; and royalties from Wolters Kluwer (UpToDate); and that he holds stock in MediMergent.
A version of this article first appeared on Medscape.com.
People who are physically active and on statins may have one less potential concern about the drugs. Despite their reputation for causing muscle injury, a study suggests statins won’t worsen the toll that sustained, moderately intensive exercise already takes on patients’ muscles.
Statin therapy in this prospective, controlled study wasn’t seen to aggravate normal muscle fatigue or pain from sustained exercise or adversely affect enzymes or other biomarkers associated with muscle injury.
The findings come from 100 individuals, of whom about two-thirds were on statins, participating in a public, 4-day, long-distance walking event held annually in the Netherlands. Results were published in the Journal of the American College of Cardiology with Neeltje A.E. Allard, MD, Radboud University Medical Center, Nijmegen, the Netherlands, as lead author.
For all of statins’ common use in adults with cardiovascular (CV) risk factors, the drugs are often blamed for causing excessive muscle pain or injury as a side effect. Yet there is a predominance of evidence to the contrary based on meta-analyses and clinical trials, suggesting that the drugs are taking the rap for many entirely unrelated muscle symptoms.
The new findings, from people ranging widely in fitness levels, suggest that “exercise of moderate intensity is feasible and safe” in statin users, that the drugs won’t exacerbate normal muscle symptoms from exercise, Dr. Allard told this news organization.
And that exercise doesn’t have to be on an unusual scale. Regular exercise in statin users can simply be consistent with broader guidelines, say 30 minutes of walking per day, she noted.
The study has such broad applicability, Dr. Allard said, because participants represented the spectrum of the thousands who signed up for the walking event, who varied in age, level of physical fitness, and number of CV risk factors. They included CV patients, the physically fit, “recreational walkers who didn’t really exercise regularly,” and “habitual nonexercisers.”
It enrolled three groups of participants in the Four Days Marches in Nijmegen, which in a typical year attracts tens of thousands of participants who walk up to 30 km, 40 km, or 50 km per day for 4 consecutive days.
They included 35 statin users who walked the event despite muscle symptoms, 34 on statins but without such symptoms, and 31 non–statin-using controls. Their mean ages ranged from 65 to 68 years.
Statin users were overwhelmingly on simvastatin or atorvastatin. The average statin therapy durations were 60 months and 96 months for those with and without symptoms, respectively.
Assessments were performed several days before the event, at baseline, and after the end of walking on days 1, 2, and 3.
Scores for muscle pain on the Brief Pain Inventory were higher at baseline for the symptomatic-on-statins group (P < .001) compared with the other two groups, and went up (P < .001) similarly across the three groups during each of the 3 days, the report notes. Fatigue scores on the Brief Fatigue Inventory followed the same pattern.
All biomarkers of muscle injury or stress were at comparable levels at baseline in the three groups and went up similarly (P < .001) with no significant differences at the end of day 3. Biomarkers included lactate dehydrogenase, creatine kinase, myoglobin, cardiac troponin I, and N-terminal pro-brain natriuretic peptide.
Statin-related reductions in levels of coenzyme Q 10 (CoQ10) have been thought to exacerbate muscle injury, the authors note. But levels of CoQ10 weren’t significantly different across the three groups at any point in the study, and they did not show any significant associations with measures of muscle injury, symptoms, or fatigue.
Patients with statin-associated muscle symptoms (SAMS) often limit physical activity because of muscle pain or weakness, but also “concerns that exercise will exacerbate muscle injury,” an accompanying editorial notes. “Therefore, exercise, a foundation of improving and maintaining cardiometabolic health, is often avoided or limited.”
But the current study, writes Robert S. Rosenson, MD, of Mount Sinai Heart, New York, indeed suggests that “many patients who develop SAMS may engage in a moderately intensive walking program without concern for worsened muscle biomarkers or performance.”
The exercise didn’t seem to improve muscle function in symptomatic statin users, compared with the other groups over the study’s very short follow-up, Dr. Rosenson observes. But “it remains uncertain from this study whether sustained exercise in SAMS patients will effectuate improved metabolic biomarkers or exercise capacity in the long term.”
Dr. Allard is supported by a grant from the Radboud Institute for Health Sciences; the other authors have disclosed no relevant financial relationships. Dr. Rosenson disclosed receiving research funding to his institution from Amgen, Arrowhead, Lilly, Novartis, and Regeneron; consulting fees from Amgen, Arrowhead, Lilly, Lipigon, Novartis, CRISPR Therapeutics, Precision BioSciences, Verve, Ultragenyx Pharmaceutical, and Regeneron; speaking fees from Amgen, Kowa, and Regeneron; and royalties from Wolters Kluwer (UpToDate); and that he holds stock in MediMergent.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY