User login
Treating fractures in elderly patients: Beyond the broken bone
While half the fracture-prevention battle is getting people diagnosed with low bone density, nearly 80% of older Americans who suffer bone breaks are not tested or treated for osteoporosis. Fractures associated with aging and diminished bone mineral density exact an enormous toll on patients’ lives and cost the health care system billions of dollars annually according to Bone Health and Osteoporosis: A Report of the Surgeon General. But current gaps in patient education and bone density screening are huge.
“It’s concerning that older patients at risk for fracture are often not screened to determine their risk factors contributing to osteoporosis and patients are not educated about fracture prevention,” said Meryl S. LeBoff, MD, an endocrinologist at Brigham and Women’s Hospital, and chief of calcium and bone section, and professor of medicine, at Harvard Medical School, Boston. “Furthermore, the majority of highest-risk women and men who do have fractures are not screened and they do not receive effective, [Food and Drug Administration]–approved therapies.”
Recent guidelines
Screening with dual-energy x-ray absorptiometry (DEXA) is recommended for all women at age 65 and all men at age 70. But the occasion of a fracture in an older person who has not yet met these age thresholds should prompt a bone density assessment.
“Doctors need to stress that one in two women and one in four men over age 50 will have a fracture in their remaining lifetimes,” Dr. LeBoff said. ”Primary care doctors play a critical role in ordering timely bone densitometry for both sexes.
If an older patient has been treated for a fracture, the main goal going forward is to prevent another one, for which the risk is highest in the 2 years after the incident fracture.”
According to Kendall F. Moseley, MD, clinical director of the division of endocrinology, diabetes & metabolism at Johns Hopkins Medicine in Baltimore, “Elderly patients need to understand that a fracture at their age is like a heart attack of the bone,” she said, adding that just as cardiovascular risk factors such as high blood pressure and blood lipids are silent before a stroke or infarction, the bone thinning of old age is also silent.
Endocrinologist Jennifer J. Kelly, DO, director of the metabolic bone program and an associate professor at the University of Vermont Medical Center in Burlington, said a fracture in anyone over age 50 that appears not to have resulted from a traumatic blow, is a compelling reason to order a DEXA exam.
Nahid J. Rianon, MBBS/MD, DrPH, assistant professor of the division of geriatric medicine at the UTHealth McGovern Medical School, Houston, goes further: “Any fracture in someone age 50 and older warrants screening for osteoporosis. And if the fracture is nontraumatic, that is by definition a clinical diagnosis of osteoporosis regardless of normal results on bone density tests and they should be treated medically. There are aspects of bone that we still can’t measure in the clinical setting.”
If DEXA is not accessible, fracture risk over the next 10 years can be evaluated based on multiple patient characteristics and medical history using the online FRAX calculator.
Just a 3% risk of hip fracture on FRAX is considered an indication to begin medical osteoporosis treatment in the United States regardless of bone density test results, Dr. Rianon said.
Fracture management
Whether a senior suffers a traumatic fracture or an osteoporosis-related fragility fracture, older age can impede the healing process in some. Senescence may also increase systemic proinflammatory status, according to Clark and colleagues, writing in Current Osteoporosis Reports.
They called for research to develop more directed treatment options for the elderly population.
Dr. Rianon noted that healing may also be affected by a decrease in muscle mass, which plays a role in holding the bone in place. “But it is still controversial how changing metabolic factors affect bone healing in the elderly.”
However, countered Dr. Kelly, fractures in elderly patients are not necessarily less likely to mend – if osteoporosis is not present. “Many heal very well – it really depends more upon their overall health and medical history. Whether or not a person requires surgery depends more upon the extent of the fracture and if the bone is able to align and heal appropriately without surgery.”
Fracture sites
Spine. According to the American Academy of Orthopedic Surgeons the earliest and most frequent site of fragility fractures in the elderly is the spine. Most vertebral fracture pain improves within 3 months without specific treatment. A short period of rest, limited analgesic use, and possible back bracing may help as the fractures heal on their own. But if pain is severe and persistent, vertebral augmentation with percutaneous kyphoplasty or vertebroplasty may be an option. These procedures, however, can destabilize surrounding discs because of the greater thickness of the injected cement.
Hip. The most dangerous fractures occur in the hip. These carry at least a 20% risk of death in the first postoperative year and must be treated surgically. Those in the proximal femur, the head, or the femoral neck will usually need hip replacement, but if the break is farther down, it may be repaired with cement, screws, plates, and rods.
Distal radius. Outcomes of wrist fractures may be positive without surgical intervention, according to a recent retrospective analysis from Turkey by Yalin and colleagues. In a comparison of clinical outcomes in seniors aged 70-89 and assigned to cast immobilization or various surgical treatments for distal radius fractures, no statistically significant difference was found in patient-reported disability scores and range of motion values between casting and surgery in the first postoperative year.
Other sites. Fractures in the elderly are not uncommon in the shoulder, distal radius, cubitus, proximal humerus, and humerus. These fractures are often treated without surgery, but nevertheless signal a high risk for additional fractures.
Bone-enhancing medications
Even in the absence of diagnosed low bone density or osteoporosis, anabolic agents such as the synthetic human parathyroid hormones abaloparatide (Tymlos) and teriparatide (Forteo) may be used to help in some cases with a bad healing prognosis and may also be used for people undergoing surgeries such as a spinal fusion, but there are not clinical guidelines. “We receive referrals regularly for this treatment from our orthopedics colleagues, but it is considered an off-label use,” Dr. Kelly said.
The anabolics teriparatide and romosozumab (Evenity) have proved effective in lowering fractures in high-risk older women.
Post fracture
After recovering from a fracture, elderly people are strongly advised to make lifestyle changes to boost bone health and reduce risk of further fractures, said Willy M. Valencia, MD, a geriatrician-endocrinologist at the Cleveland Clinic. Apart from active daily living, he recommends several types of formal exercise to promote bone formation; increase muscle mass, strength, and flexibility; and improve endurance, balance, and gait. The National Institute on Aging outlines suitable exercise programs for seniors.
“These exercises will help reduce the risk of falling and to avoid more fractures,” he said. “Whether a patient has been exercising before the fracture or not, they may feel some reticence or reluctance to take up exercise afterwards because they’re afraid of having another fracture, but they should understand that their fracture risk increases if they remain sedentary. They should start slowly but they can’t be sitting all day.”
Even before it’s possible to exercise at the healing fracture site, added Dr. Rianon, its advisable to work other areas of the body. “Overall mobility is important, and exercising other parts of the body can stimulate strength and help prevent falling.”
In other postsurgical measures, a bone-friendly diet rich in calcium and vitamin D, as well as supplementation with these vital nutrients, is essential to lower the risk of falling.
Fall prevention is paramount, said Dr. Valencia. While exercise can improve, gait, balance, and endurance, logistical measures may also be necessary. Seniors may have to move to a one-floor domicile with no stairs to negotiate. At the very least, they need to fall-proof their daily lives by upgrading their eyeglasses and home lighting, eliminating obstacles and loose carpets, fixing bannisters, and installing bathroom handrails. Some may need assistive devices for walking, especially outdoors in slippery conditions.
At the end of the day, the role of the primary physician in screening for bone problems before fracture and postsurgical care is key. “Risk factors for osteoporosis and fracture risk must be added to the patient’s chart,” said Dr. Rianon. Added Dr. Moseley. “No matter how busy they are, my hope is that primary care physicians will not put patients’ bone health at the bottom of the clinical agenda.”
While half the fracture-prevention battle is getting people diagnosed with low bone density, nearly 80% of older Americans who suffer bone breaks are not tested or treated for osteoporosis. Fractures associated with aging and diminished bone mineral density exact an enormous toll on patients’ lives and cost the health care system billions of dollars annually according to Bone Health and Osteoporosis: A Report of the Surgeon General. But current gaps in patient education and bone density screening are huge.
“It’s concerning that older patients at risk for fracture are often not screened to determine their risk factors contributing to osteoporosis and patients are not educated about fracture prevention,” said Meryl S. LeBoff, MD, an endocrinologist at Brigham and Women’s Hospital, and chief of calcium and bone section, and professor of medicine, at Harvard Medical School, Boston. “Furthermore, the majority of highest-risk women and men who do have fractures are not screened and they do not receive effective, [Food and Drug Administration]–approved therapies.”
Recent guidelines
Screening with dual-energy x-ray absorptiometry (DEXA) is recommended for all women at age 65 and all men at age 70. But the occasion of a fracture in an older person who has not yet met these age thresholds should prompt a bone density assessment.
“Doctors need to stress that one in two women and one in four men over age 50 will have a fracture in their remaining lifetimes,” Dr. LeBoff said. ”Primary care doctors play a critical role in ordering timely bone densitometry for both sexes.
If an older patient has been treated for a fracture, the main goal going forward is to prevent another one, for which the risk is highest in the 2 years after the incident fracture.”
According to Kendall F. Moseley, MD, clinical director of the division of endocrinology, diabetes & metabolism at Johns Hopkins Medicine in Baltimore, “Elderly patients need to understand that a fracture at their age is like a heart attack of the bone,” she said, adding that just as cardiovascular risk factors such as high blood pressure and blood lipids are silent before a stroke or infarction, the bone thinning of old age is also silent.
Endocrinologist Jennifer J. Kelly, DO, director of the metabolic bone program and an associate professor at the University of Vermont Medical Center in Burlington, said a fracture in anyone over age 50 that appears not to have resulted from a traumatic blow, is a compelling reason to order a DEXA exam.
Nahid J. Rianon, MBBS/MD, DrPH, assistant professor of the division of geriatric medicine at the UTHealth McGovern Medical School, Houston, goes further: “Any fracture in someone age 50 and older warrants screening for osteoporosis. And if the fracture is nontraumatic, that is by definition a clinical diagnosis of osteoporosis regardless of normal results on bone density tests and they should be treated medically. There are aspects of bone that we still can’t measure in the clinical setting.”
If DEXA is not accessible, fracture risk over the next 10 years can be evaluated based on multiple patient characteristics and medical history using the online FRAX calculator.
Just a 3% risk of hip fracture on FRAX is considered an indication to begin medical osteoporosis treatment in the United States regardless of bone density test results, Dr. Rianon said.
Fracture management
Whether a senior suffers a traumatic fracture or an osteoporosis-related fragility fracture, older age can impede the healing process in some. Senescence may also increase systemic proinflammatory status, according to Clark and colleagues, writing in Current Osteoporosis Reports.
They called for research to develop more directed treatment options for the elderly population.
Dr. Rianon noted that healing may also be affected by a decrease in muscle mass, which plays a role in holding the bone in place. “But it is still controversial how changing metabolic factors affect bone healing in the elderly.”
However, countered Dr. Kelly, fractures in elderly patients are not necessarily less likely to mend – if osteoporosis is not present. “Many heal very well – it really depends more upon their overall health and medical history. Whether or not a person requires surgery depends more upon the extent of the fracture and if the bone is able to align and heal appropriately without surgery.”
Fracture sites
Spine. According to the American Academy of Orthopedic Surgeons the earliest and most frequent site of fragility fractures in the elderly is the spine. Most vertebral fracture pain improves within 3 months without specific treatment. A short period of rest, limited analgesic use, and possible back bracing may help as the fractures heal on their own. But if pain is severe and persistent, vertebral augmentation with percutaneous kyphoplasty or vertebroplasty may be an option. These procedures, however, can destabilize surrounding discs because of the greater thickness of the injected cement.
Hip. The most dangerous fractures occur in the hip. These carry at least a 20% risk of death in the first postoperative year and must be treated surgically. Those in the proximal femur, the head, or the femoral neck will usually need hip replacement, but if the break is farther down, it may be repaired with cement, screws, plates, and rods.
Distal radius. Outcomes of wrist fractures may be positive without surgical intervention, according to a recent retrospective analysis from Turkey by Yalin and colleagues. In a comparison of clinical outcomes in seniors aged 70-89 and assigned to cast immobilization or various surgical treatments for distal radius fractures, no statistically significant difference was found in patient-reported disability scores and range of motion values between casting and surgery in the first postoperative year.
Other sites. Fractures in the elderly are not uncommon in the shoulder, distal radius, cubitus, proximal humerus, and humerus. These fractures are often treated without surgery, but nevertheless signal a high risk for additional fractures.
Bone-enhancing medications
Even in the absence of diagnosed low bone density or osteoporosis, anabolic agents such as the synthetic human parathyroid hormones abaloparatide (Tymlos) and teriparatide (Forteo) may be used to help in some cases with a bad healing prognosis and may also be used for people undergoing surgeries such as a spinal fusion, but there are not clinical guidelines. “We receive referrals regularly for this treatment from our orthopedics colleagues, but it is considered an off-label use,” Dr. Kelly said.
The anabolics teriparatide and romosozumab (Evenity) have proved effective in lowering fractures in high-risk older women.
Post fracture
After recovering from a fracture, elderly people are strongly advised to make lifestyle changes to boost bone health and reduce risk of further fractures, said Willy M. Valencia, MD, a geriatrician-endocrinologist at the Cleveland Clinic. Apart from active daily living, he recommends several types of formal exercise to promote bone formation; increase muscle mass, strength, and flexibility; and improve endurance, balance, and gait. The National Institute on Aging outlines suitable exercise programs for seniors.
“These exercises will help reduce the risk of falling and to avoid more fractures,” he said. “Whether a patient has been exercising before the fracture or not, they may feel some reticence or reluctance to take up exercise afterwards because they’re afraid of having another fracture, but they should understand that their fracture risk increases if they remain sedentary. They should start slowly but they can’t be sitting all day.”
Even before it’s possible to exercise at the healing fracture site, added Dr. Rianon, its advisable to work other areas of the body. “Overall mobility is important, and exercising other parts of the body can stimulate strength and help prevent falling.”
In other postsurgical measures, a bone-friendly diet rich in calcium and vitamin D, as well as supplementation with these vital nutrients, is essential to lower the risk of falling.
Fall prevention is paramount, said Dr. Valencia. While exercise can improve, gait, balance, and endurance, logistical measures may also be necessary. Seniors may have to move to a one-floor domicile with no stairs to negotiate. At the very least, they need to fall-proof their daily lives by upgrading their eyeglasses and home lighting, eliminating obstacles and loose carpets, fixing bannisters, and installing bathroom handrails. Some may need assistive devices for walking, especially outdoors in slippery conditions.
At the end of the day, the role of the primary physician in screening for bone problems before fracture and postsurgical care is key. “Risk factors for osteoporosis and fracture risk must be added to the patient’s chart,” said Dr. Rianon. Added Dr. Moseley. “No matter how busy they are, my hope is that primary care physicians will not put patients’ bone health at the bottom of the clinical agenda.”
While half the fracture-prevention battle is getting people diagnosed with low bone density, nearly 80% of older Americans who suffer bone breaks are not tested or treated for osteoporosis. Fractures associated with aging and diminished bone mineral density exact an enormous toll on patients’ lives and cost the health care system billions of dollars annually according to Bone Health and Osteoporosis: A Report of the Surgeon General. But current gaps in patient education and bone density screening are huge.
“It’s concerning that older patients at risk for fracture are often not screened to determine their risk factors contributing to osteoporosis and patients are not educated about fracture prevention,” said Meryl S. LeBoff, MD, an endocrinologist at Brigham and Women’s Hospital, and chief of calcium and bone section, and professor of medicine, at Harvard Medical School, Boston. “Furthermore, the majority of highest-risk women and men who do have fractures are not screened and they do not receive effective, [Food and Drug Administration]–approved therapies.”
Recent guidelines
Screening with dual-energy x-ray absorptiometry (DEXA) is recommended for all women at age 65 and all men at age 70. But the occasion of a fracture in an older person who has not yet met these age thresholds should prompt a bone density assessment.
“Doctors need to stress that one in two women and one in four men over age 50 will have a fracture in their remaining lifetimes,” Dr. LeBoff said. ”Primary care doctors play a critical role in ordering timely bone densitometry for both sexes.
If an older patient has been treated for a fracture, the main goal going forward is to prevent another one, for which the risk is highest in the 2 years after the incident fracture.”
According to Kendall F. Moseley, MD, clinical director of the division of endocrinology, diabetes & metabolism at Johns Hopkins Medicine in Baltimore, “Elderly patients need to understand that a fracture at their age is like a heart attack of the bone,” she said, adding that just as cardiovascular risk factors such as high blood pressure and blood lipids are silent before a stroke or infarction, the bone thinning of old age is also silent.
Endocrinologist Jennifer J. Kelly, DO, director of the metabolic bone program and an associate professor at the University of Vermont Medical Center in Burlington, said a fracture in anyone over age 50 that appears not to have resulted from a traumatic blow, is a compelling reason to order a DEXA exam.
Nahid J. Rianon, MBBS/MD, DrPH, assistant professor of the division of geriatric medicine at the UTHealth McGovern Medical School, Houston, goes further: “Any fracture in someone age 50 and older warrants screening for osteoporosis. And if the fracture is nontraumatic, that is by definition a clinical diagnosis of osteoporosis regardless of normal results on bone density tests and they should be treated medically. There are aspects of bone that we still can’t measure in the clinical setting.”
If DEXA is not accessible, fracture risk over the next 10 years can be evaluated based on multiple patient characteristics and medical history using the online FRAX calculator.
Just a 3% risk of hip fracture on FRAX is considered an indication to begin medical osteoporosis treatment in the United States regardless of bone density test results, Dr. Rianon said.
Fracture management
Whether a senior suffers a traumatic fracture or an osteoporosis-related fragility fracture, older age can impede the healing process in some. Senescence may also increase systemic proinflammatory status, according to Clark and colleagues, writing in Current Osteoporosis Reports.
They called for research to develop more directed treatment options for the elderly population.
Dr. Rianon noted that healing may also be affected by a decrease in muscle mass, which plays a role in holding the bone in place. “But it is still controversial how changing metabolic factors affect bone healing in the elderly.”
However, countered Dr. Kelly, fractures in elderly patients are not necessarily less likely to mend – if osteoporosis is not present. “Many heal very well – it really depends more upon their overall health and medical history. Whether or not a person requires surgery depends more upon the extent of the fracture and if the bone is able to align and heal appropriately without surgery.”
Fracture sites
Spine. According to the American Academy of Orthopedic Surgeons the earliest and most frequent site of fragility fractures in the elderly is the spine. Most vertebral fracture pain improves within 3 months without specific treatment. A short period of rest, limited analgesic use, and possible back bracing may help as the fractures heal on their own. But if pain is severe and persistent, vertebral augmentation with percutaneous kyphoplasty or vertebroplasty may be an option. These procedures, however, can destabilize surrounding discs because of the greater thickness of the injected cement.
Hip. The most dangerous fractures occur in the hip. These carry at least a 20% risk of death in the first postoperative year and must be treated surgically. Those in the proximal femur, the head, or the femoral neck will usually need hip replacement, but if the break is farther down, it may be repaired with cement, screws, plates, and rods.
Distal radius. Outcomes of wrist fractures may be positive without surgical intervention, according to a recent retrospective analysis from Turkey by Yalin and colleagues. In a comparison of clinical outcomes in seniors aged 70-89 and assigned to cast immobilization or various surgical treatments for distal radius fractures, no statistically significant difference was found in patient-reported disability scores and range of motion values between casting and surgery in the first postoperative year.
Other sites. Fractures in the elderly are not uncommon in the shoulder, distal radius, cubitus, proximal humerus, and humerus. These fractures are often treated without surgery, but nevertheless signal a high risk for additional fractures.
Bone-enhancing medications
Even in the absence of diagnosed low bone density or osteoporosis, anabolic agents such as the synthetic human parathyroid hormones abaloparatide (Tymlos) and teriparatide (Forteo) may be used to help in some cases with a bad healing prognosis and may also be used for people undergoing surgeries such as a spinal fusion, but there are not clinical guidelines. “We receive referrals regularly for this treatment from our orthopedics colleagues, but it is considered an off-label use,” Dr. Kelly said.
The anabolics teriparatide and romosozumab (Evenity) have proved effective in lowering fractures in high-risk older women.
Post fracture
After recovering from a fracture, elderly people are strongly advised to make lifestyle changes to boost bone health and reduce risk of further fractures, said Willy M. Valencia, MD, a geriatrician-endocrinologist at the Cleveland Clinic. Apart from active daily living, he recommends several types of formal exercise to promote bone formation; increase muscle mass, strength, and flexibility; and improve endurance, balance, and gait. The National Institute on Aging outlines suitable exercise programs for seniors.
“These exercises will help reduce the risk of falling and to avoid more fractures,” he said. “Whether a patient has been exercising before the fracture or not, they may feel some reticence or reluctance to take up exercise afterwards because they’re afraid of having another fracture, but they should understand that their fracture risk increases if they remain sedentary. They should start slowly but they can’t be sitting all day.”
Even before it’s possible to exercise at the healing fracture site, added Dr. Rianon, its advisable to work other areas of the body. “Overall mobility is important, and exercising other parts of the body can stimulate strength and help prevent falling.”
In other postsurgical measures, a bone-friendly diet rich in calcium and vitamin D, as well as supplementation with these vital nutrients, is essential to lower the risk of falling.
Fall prevention is paramount, said Dr. Valencia. While exercise can improve, gait, balance, and endurance, logistical measures may also be necessary. Seniors may have to move to a one-floor domicile with no stairs to negotiate. At the very least, they need to fall-proof their daily lives by upgrading their eyeglasses and home lighting, eliminating obstacles and loose carpets, fixing bannisters, and installing bathroom handrails. Some may need assistive devices for walking, especially outdoors in slippery conditions.
At the end of the day, the role of the primary physician in screening for bone problems before fracture and postsurgical care is key. “Risk factors for osteoporosis and fracture risk must be added to the patient’s chart,” said Dr. Rianon. Added Dr. Moseley. “No matter how busy they are, my hope is that primary care physicians will not put patients’ bone health at the bottom of the clinical agenda.”
Pain mismanagement by the numbers
Despite my best efforts to cultivate acquaintances across a broader age group, my social circle still has the somewhat musty odor of septuagenarians. We try to talk about things beyond the weather and grandchildren but pain scenarios surface with unfortunate frequency. Arthritic joints ache, body parts wear out or become diseased and have to be removed or replaced. That stuff can hurt.
There are two pain-related themes that seem to crop up more frequently than you might expect. The first is the unfortunate side effects of opioid medication – most often gastric distress and vomiting, then of course there’s constipation. They seem so common that a good many of my acquaintances just plain refuse to take opioids when they have been prescribed postoperatively because of their vivid memories of the consequences or horror stories friends have told.
The second theme is the general annoyance with the damn “Please rate your pain from one to ten” request issued by every well-intentioned nurse. Do you mean the pain I am having right now, this second, or last night, or the average over the last day and a half? Or should I be comparing it with when I gave birth 70 years ago, or when I stubbed my toe getting out of the shower last week? And then what are you going to do with my guesstimated number?
It may surprise some of you that 40 years ago there wasn’t a pain scale fetish. But a few observant health care professionals realized that many of our patients were suffering because we weren’t adequately managing their pain. In postoperative situations this was slowing recovery and effecting outcomes. Like good pseudoscientists, they realized that we should first quantify the pain and the notion that no pain should go unrated came into being. Nor should pain go untreated, which is too frequently interpreted as meaning unmedicated.
For example a systematic review of 61 studies of juvenile idiopathic arthritis (JIA) published in the journal Pediatric Rheumatology found that there was positive relationship between pain and a child’s belief that pain causes harm, disability, and lack of control. Not surprisingly, stress was also associated with pain intensity.
It is a long paper and touches on numerous other associations of varying degrees of strength between parental, social, and other external factors. But, in general, they were not as consistent as those related to a child’s beliefs.
Before, or at least at the same time, we treat a patient’s pain, we should learn more about that patient – his or her concerns, beliefs, and stressors. You and I may have exactly the same hernia operation, but if you have a better understanding of why you are going to feel uncomfortable after the surgery, and understand that not every pain is the result of a complication, I suspect you are more likely to complain of less pain.
The recent JIA study doesn’t claim to suggest therapeutic methods. However, one wonders what the result would be if we could somehow alter a patient’s belief system so that he or she no longer sees pain as always harmful, nor does the patient see himself or herself as powerless to do anything about the pain. To do this experiment we must follow up our robotic request to “rate your pain” with a dialogue in which we learn more about the patient. Which means probing believes, fears, and stressors.
You can tell me this exercise would be unrealistic and time consuming. But I bet in the long run it will save time. Even if it doesn’t it is the better way to manage pain.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Despite my best efforts to cultivate acquaintances across a broader age group, my social circle still has the somewhat musty odor of septuagenarians. We try to talk about things beyond the weather and grandchildren but pain scenarios surface with unfortunate frequency. Arthritic joints ache, body parts wear out or become diseased and have to be removed or replaced. That stuff can hurt.
There are two pain-related themes that seem to crop up more frequently than you might expect. The first is the unfortunate side effects of opioid medication – most often gastric distress and vomiting, then of course there’s constipation. They seem so common that a good many of my acquaintances just plain refuse to take opioids when they have been prescribed postoperatively because of their vivid memories of the consequences or horror stories friends have told.
The second theme is the general annoyance with the damn “Please rate your pain from one to ten” request issued by every well-intentioned nurse. Do you mean the pain I am having right now, this second, or last night, or the average over the last day and a half? Or should I be comparing it with when I gave birth 70 years ago, or when I stubbed my toe getting out of the shower last week? And then what are you going to do with my guesstimated number?
It may surprise some of you that 40 years ago there wasn’t a pain scale fetish. But a few observant health care professionals realized that many of our patients were suffering because we weren’t adequately managing their pain. In postoperative situations this was slowing recovery and effecting outcomes. Like good pseudoscientists, they realized that we should first quantify the pain and the notion that no pain should go unrated came into being. Nor should pain go untreated, which is too frequently interpreted as meaning unmedicated.
For example a systematic review of 61 studies of juvenile idiopathic arthritis (JIA) published in the journal Pediatric Rheumatology found that there was positive relationship between pain and a child’s belief that pain causes harm, disability, and lack of control. Not surprisingly, stress was also associated with pain intensity.
It is a long paper and touches on numerous other associations of varying degrees of strength between parental, social, and other external factors. But, in general, they were not as consistent as those related to a child’s beliefs.
Before, or at least at the same time, we treat a patient’s pain, we should learn more about that patient – his or her concerns, beliefs, and stressors. You and I may have exactly the same hernia operation, but if you have a better understanding of why you are going to feel uncomfortable after the surgery, and understand that not every pain is the result of a complication, I suspect you are more likely to complain of less pain.
The recent JIA study doesn’t claim to suggest therapeutic methods. However, one wonders what the result would be if we could somehow alter a patient’s belief system so that he or she no longer sees pain as always harmful, nor does the patient see himself or herself as powerless to do anything about the pain. To do this experiment we must follow up our robotic request to “rate your pain” with a dialogue in which we learn more about the patient. Which means probing believes, fears, and stressors.
You can tell me this exercise would be unrealistic and time consuming. But I bet in the long run it will save time. Even if it doesn’t it is the better way to manage pain.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Despite my best efforts to cultivate acquaintances across a broader age group, my social circle still has the somewhat musty odor of septuagenarians. We try to talk about things beyond the weather and grandchildren but pain scenarios surface with unfortunate frequency. Arthritic joints ache, body parts wear out or become diseased and have to be removed or replaced. That stuff can hurt.
There are two pain-related themes that seem to crop up more frequently than you might expect. The first is the unfortunate side effects of opioid medication – most often gastric distress and vomiting, then of course there’s constipation. They seem so common that a good many of my acquaintances just plain refuse to take opioids when they have been prescribed postoperatively because of their vivid memories of the consequences or horror stories friends have told.
The second theme is the general annoyance with the damn “Please rate your pain from one to ten” request issued by every well-intentioned nurse. Do you mean the pain I am having right now, this second, or last night, or the average over the last day and a half? Or should I be comparing it with when I gave birth 70 years ago, or when I stubbed my toe getting out of the shower last week? And then what are you going to do with my guesstimated number?
It may surprise some of you that 40 years ago there wasn’t a pain scale fetish. But a few observant health care professionals realized that many of our patients were suffering because we weren’t adequately managing their pain. In postoperative situations this was slowing recovery and effecting outcomes. Like good pseudoscientists, they realized that we should first quantify the pain and the notion that no pain should go unrated came into being. Nor should pain go untreated, which is too frequently interpreted as meaning unmedicated.
For example a systematic review of 61 studies of juvenile idiopathic arthritis (JIA) published in the journal Pediatric Rheumatology found that there was positive relationship between pain and a child’s belief that pain causes harm, disability, and lack of control. Not surprisingly, stress was also associated with pain intensity.
It is a long paper and touches on numerous other associations of varying degrees of strength between parental, social, and other external factors. But, in general, they were not as consistent as those related to a child’s beliefs.
Before, or at least at the same time, we treat a patient’s pain, we should learn more about that patient – his or her concerns, beliefs, and stressors. You and I may have exactly the same hernia operation, but if you have a better understanding of why you are going to feel uncomfortable after the surgery, and understand that not every pain is the result of a complication, I suspect you are more likely to complain of less pain.
The recent JIA study doesn’t claim to suggest therapeutic methods. However, one wonders what the result would be if we could somehow alter a patient’s belief system so that he or she no longer sees pain as always harmful, nor does the patient see himself or herself as powerless to do anything about the pain. To do this experiment we must follow up our robotic request to “rate your pain” with a dialogue in which we learn more about the patient. Which means probing believes, fears, and stressors.
You can tell me this exercise would be unrealistic and time consuming. But I bet in the long run it will save time. Even if it doesn’t it is the better way to manage pain.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Knee pain and injury: When is a surgical consult needed?
Evidence supports what family physicians know to be true: Knee pain is an exceedingly common presenting problem in the primary care office. Estimates of lifetime incidence reach as high as 54%,1 and the prevalence of knee pain in the general population is increasing.2 Knee disability can result from acute or traumatic injuries as well as chronic, degenerative conditions such as osteoarthritis (OA). The decision to pursue orthopedic consultation for a particular injury or painful knee condition can be challenging. To address this, we highlight specific knee diagnoses known to cause pain, with the aim of describing which conditions likely will necessitate surgical consultation—and which won’t.
Acute or nondegenerative knee injuries and pain
Acute knee injuries range in severity from simple contusions and sprains to high-energy, traumatic injuries with resulting joint instability and potential neurovascular compromise. While conservative treatment often is successful for many simple injuries, surgical management—sometimes urgently or emergently—is needed in other cases, as will be detailed shortly.
Neurovascular injury associated with knee dislocations
Acute neurovascular injuries often require emergent surgical intervention. Although rare, tibiofemoral (knee) dislocations pose a significant challenge to the clinician in both diagnosis and management. The reported frequency of popliteal artery injury or rupture following a dislocation varies widely, with rates ranging from 5% to 64%, according to older studies; more recent data, however, suggest the rate is actually as low as 3.3%.3
Immediate immobilization and emergency department transport for monitoring, orthopedics consultation, and vascular studies or vascular surgery consultation is recommended in the case of a suspected knee dislocation. In one cross-sectional cohort study, the surgical management of knee dislocations yielded favorable outcomes in > 75% of cases.5
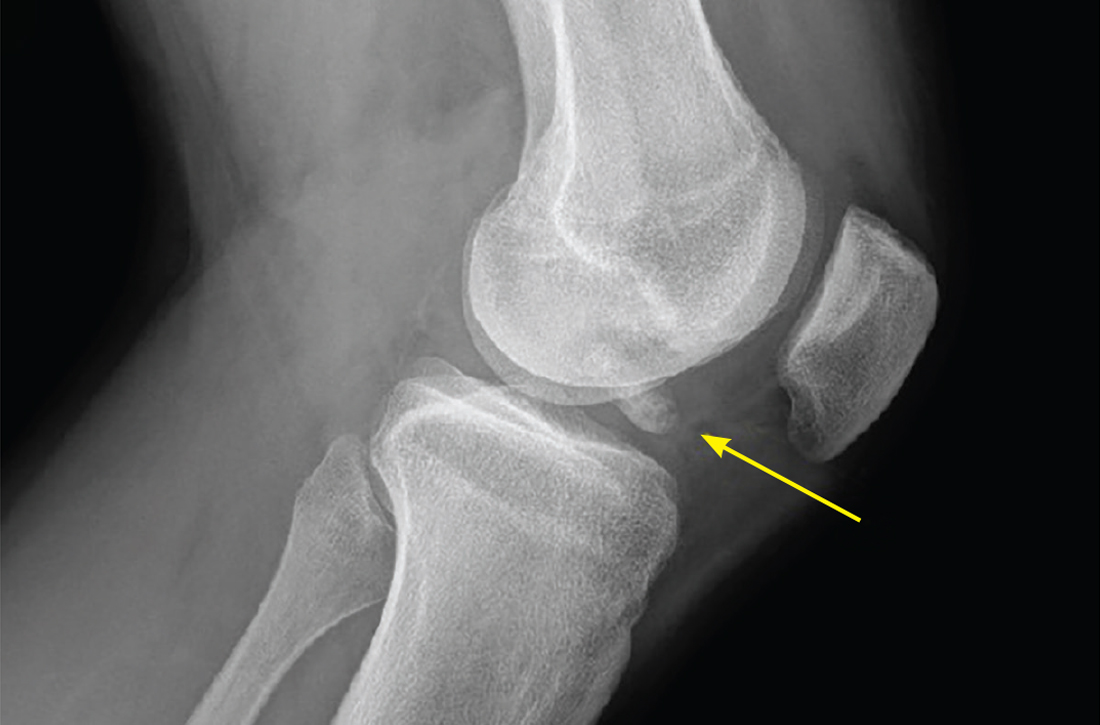
Tibial plateau fracture
This fracture often occurs as a result of high-energy trauma, such as contact sports or motor vehicle accidents, and is characterized by a proximal tibial fracture line with extension to the articular surface. X-rays often are sufficient for initial diagnosis. Computed tomography can help rule out a fracture line when clinical suspicion is high and x-rays are nondiagnostic. As noted earlier, any suggestion of neurovascular compromise on physical exam requires an emergent orthopedic surgeon consultation for a possible displaced and unstable (or more complex) injury (FIGURE 1).6-8
Nondisplaced tibial plateau fractures without supraphysiologic ligamentous laxity on valgus or varus stress testing can be managed safely with protection and early mobilization, gradual progression of weight-bearing, and serial x-rays to ensure fracture healing and stability.
Gross joint instability identified by positive valgus or varus stress testing, positive anterior or posterior drawer testing, or patient inability to tolerate these maneuvers due to pain similarly should raise suspicion for a more significant fracture at risk for concurrent neurovascular injury. Acute compartment syndrome also is a known complication of tibial plateau fractures and similarly requires emergent operative management. Urgent surgical consultation is recommended for fractures with displaced fracture fragments, tibial articular surface step-off or depression, fractures with concurrent joint laxity, or medial plateau fractures.6-8
Continue to: Patella fractures
Patella fractures
These fractures occur as a direct blow to the front of the knee, such as falling forward onto a hard surface, or indirectly due to a sudden extreme eccentric contraction of the quadriceps muscle. Nondisplaced fractures with an intact knee extension mechanism, which is examined via a supine straight-leg raise or seated knee extension, are managed with weight-bearing as tolerated in strict immobilization in full extension for 4 to 6 weeks, with active range-of-motion and isometric quadriceps exercises beginning in 1 to 2 weeks. Serial x-rays also are obtained to ensure fracture displacement does not occur during the rehabilitation process.9
High-quality evidence guiding follow-up care and comparing outcomes of surgical and nonsurgical management of patella fractures is lacking, and studies comparing different surgical techniques are of lower methodological quality.10 Nevertheless, displaced or comminuted patellar fractures are referred urgently to orthopedic surgical care for fixation, as are those with concurrent loose bodies, chondral surface injuries or articular step-off, or osteochondral fractures.9 Inability to perform a straight-leg raise (ie, clinical loss of the knee extension mechanism) suggests a fracture under tension that likely also requires surgical fixation for successful recovery. Neurovascular injuries are unlikely in most patellar fractures but would require emergent surgical consultation.9
Ligamentous injury
Tibiofemoral joint laxity occurs as a result of ligamentous injury, with or without tibial plateau fracture. The anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL) comprise the 4 main ligaments of the knee. The ACL resists anterior tibial translation and rotational forces, while the PCL resists posterior tibial translation. The MCL and LCL resist valgus and varus stress, respectively.
Ligament injuries are classified as Grades 1 to 311:
- Grade 1 sprains. The ligament is stretched, but there is no macroscopic tearing; joint stability is maintained.
- Grade 2 sprains. There are partial macroscopic ligament tears. There is joint laxity due to the partial loss of the ligament’s structural integrity.
- Grade 3 sprains. The ligament is fully avulsed or ruptured with resultant gross joint instability.
Continue to: ACL tears
ACL tears occur most commonly via a noncontact event, as when an individual plants their foot and suddenly changes direction during sport or other physical activity. Treatment hinges on patient activity levels and participation in sports. Patients who do not plan to engage in athletic movements (that require changes in direction or planting and twisting) and who otherwise maintain satisfactory joint stability during activities of daily living may elect to defer or even altogether avoid surgical reconstruction of isolated ACL tears. One pair of studies demonstrated equivalent outcomes in surgical and nonsurgical management in 121 young, nonelite athletes at 2- and 5-year follow-up, although the crossover from the nonsurgical to surgical groups was high.12,13 Athletes who regain satisfactory function and stability nonoperatively can defer surgical intervention. However, the majority of active patients and athletes will require surgical ACL reconstruction to return to pre-injury functional levels.14
PCL sprains occur as a result of sudden posteriorly directed force on the tibia, such as when the knee is hyperextended or a patient falls directly onto a flexed knee. Patients with Grade 1 and 2 isolated sprains generally will recover with conservative care, as will patients with some Grade 3 complete tears that do not fully compromise joint stability. However, high-grade PCL injuries often are comorbid with posterolateral corner or other injuries, leading to a higher likelihood of joint instability and thus the need for surgical intervention for the best chance at an optimal outcome.15
MCL sprain. Surgical management is not required in an isolated Grade 1 or 2 MCL sprain, as the hallmarks of recovery—return of joint stability, knee strength and range of motion, and pain reduction—can be achieved successfully with conservative management. Isolated Grade 3 MCL sprains are also successfully managed nonoperatively16 except in specific cases, such as a concurrent large avulsion fracture.17
LCL sprain. Similarly, isolated Grade 1 and 2 LCL sprains generally do not require surgical intervention. However, Grade 3 LCL injuries usually do, as persistent joint instability and poor functional outcomes are more common with nonsurgical management.18-20 Additionally, high-grade LCL injuries frequently manifest with comorbid meniscus injuries or sprains of the posterolateral corner of the knee, a complex anatomic structure that provides both static and dynamic tibiofemoral joint stability. Surgical repair or reconstruction of the posterolateral corner frequently is necessary for optimal functional outcomes.21
Multiligamentous sprains frequently lead to gross joint instability and necessitate orthopedic surgeon consultation to determine the best treatment plan; this should be done emergently if neurovascular compromise is suspected. A common injury combination is simultaneous ACL and MCL sprains with or without meniscus injury. In these cases, some surgeons will choose to defer ACL reconstruction until after MCL healing is achieved. This allows the patient to regain valgus stability of the joint prior to performing ACL reconstruction to regain rotational and anterior stability.20
Continue to: Patellar dislocations
Patellar dislocations represent a relatively common knee injury in young active patients, often occurring in a noncontact fashion when a valgus force is applied to an externally rotated and planted lower leg.
Major tendon rupture
Patellar tendon ruptures occur when a sudden eccentric force is applied to the knee, such as when landing from a jump with the knee flexed. Patellar tendon ruptures frequently are clinically apparent, with patients demonstrating a high-riding patella and loss of active knee extension. Quadriceps tendon ruptures often result from a similar injury mechanism in older patients, with a similar loss of active knee extension and a palpable gap superior to the patella.24
Partial tears in patients who can maintain full extension of the knee against gravity are treated nonoperatively, but early surgical repair is indicated for complete quadriceps or patellar tendon ruptures to achieve optimal outcomes.
Even with prompt treatment, return to sport is not guaranteed. According to a recent systematic review, athletes returned to play 88.9% and 89.8% of the time following patellar and quadriceps tendon repairs, respectively. However, returning to the same level of play was less common and achieved 80.8% (patellar tendon repair) and 70% (quadriceps tendon repair) of the time. Return-to-work rates were higher, at 96% for both surgical treatments.29
Locked knee and acute meniscus tears in younger patients
In some acute knee injuries, meniscus tears, loose cartilage bodies or osteochondral defects, or other internal structures can become interposed between the femoral and tibial surfaces, preventing both active and passive knee extension. Such injuries are often severely painful and functionally debilitating. While manipulation under anesthesia can acutely restore joint function,30 diagnostic and therapeutic arthroscopy often is pursued for definitive treatment.31 Compared to the gold standard of diagnostic arthroscopy, preoperative magnetic resonance imaging (MRI) carries positive and negative predictive values of 85% and 77%, respectively, in identifying or ruling out the anatomic structure responsible for a locked knee. 32 As such,
Continue to: Depending on the location...
Depending on the location, size, and shape of an acute meniscus tear in younger patients, surgical repair may be an option to preserve long-term joint function. In one case series of patients younger than 20 years, 62% of meniscus repairs yielded good outcomes after a mean follow-up period of 16.8 years.33
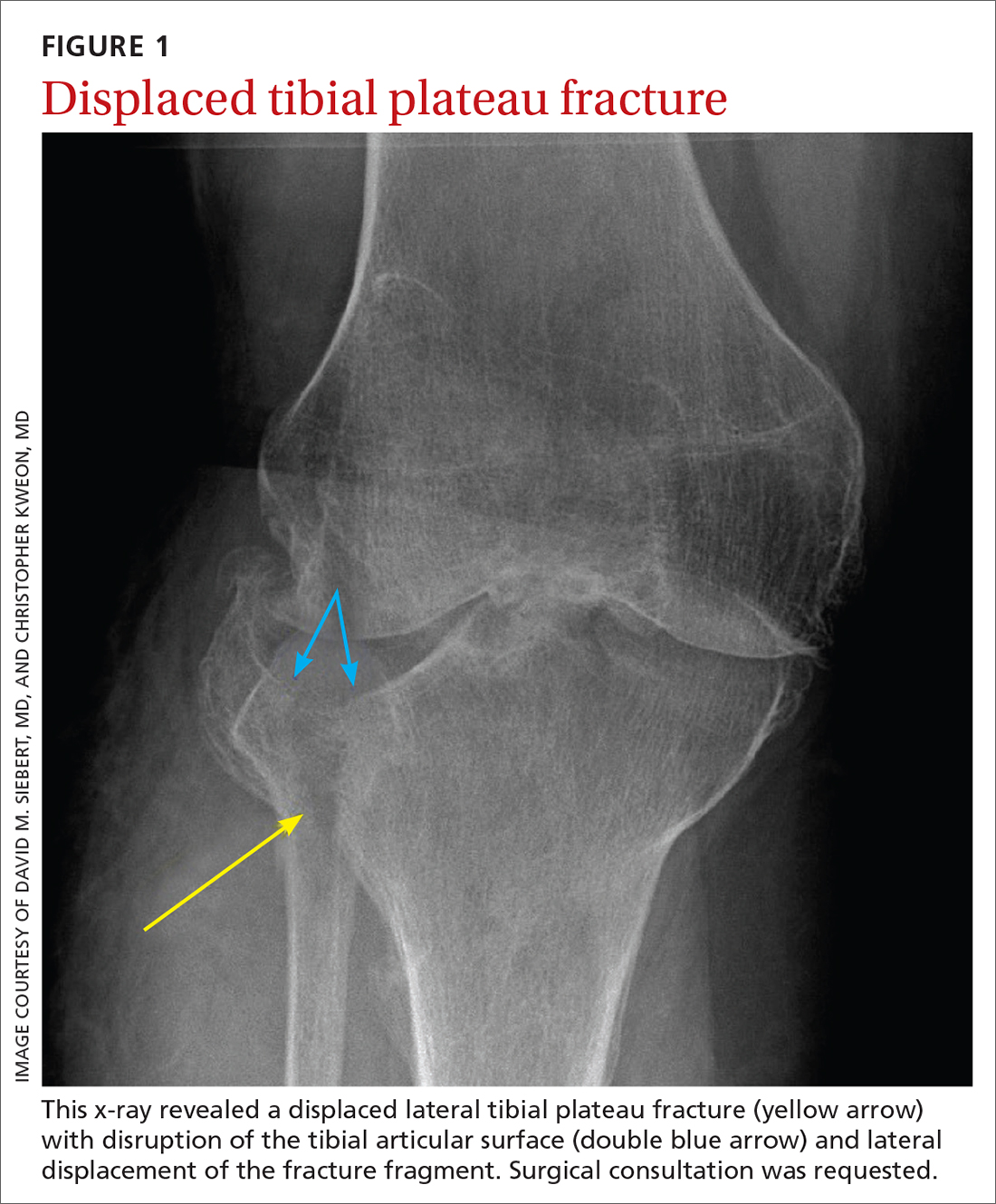
Osteochondritis dissecans
Osteochondritis dissecans is characterized by subchondral bone osteonecrosis that most often occurs in pediatric patients, potentially causing the separation of a fragment of articular cartilage and subchondral bone into the joint space (FIGURE 2). In early stages, nonoperative treatment consisting of prolonged rest followed by physical therapy to gradually return to activity is recommended to prevent small, low-grade lesions from progressing to unstable or separated fragments. Arthroscopy, which consists of microfracture or other surgical resurfacing techniques to restore joint integrity, is pursued in more advanced cases of unstable or separated fragments.

High-quality data guiding the management of osteochondritis dissecans are lacking, and these recommendations are based on consensus guidelines.34
Septic arthritis
Septic arthritis is a medical emergency caused by the hematogenous spread of microorganisms, most often staphylococci and streptococci species. Less commonly, it arises from direct inoculation through an open wound or, rarely, iatrogenically following a joint injection procedure. Clinical signs of septic arthritis include joint pain, joint swelling, and fever. Passive range of motion of the joint is often severely painful. Synovial fluid studies consistent with septic arthritis include an elevated white blood cell count greater than 25,000/mcL with polymorphonuclear cell predominance.35 The knee accounts for more than 50% of septic arthritis cases, and surgical drainage usually is required to achieve infection source control and decrease morbidity and mortality due to destruction of articular cartilage when treatment is delayed.36
Chronic knee injuries and pain
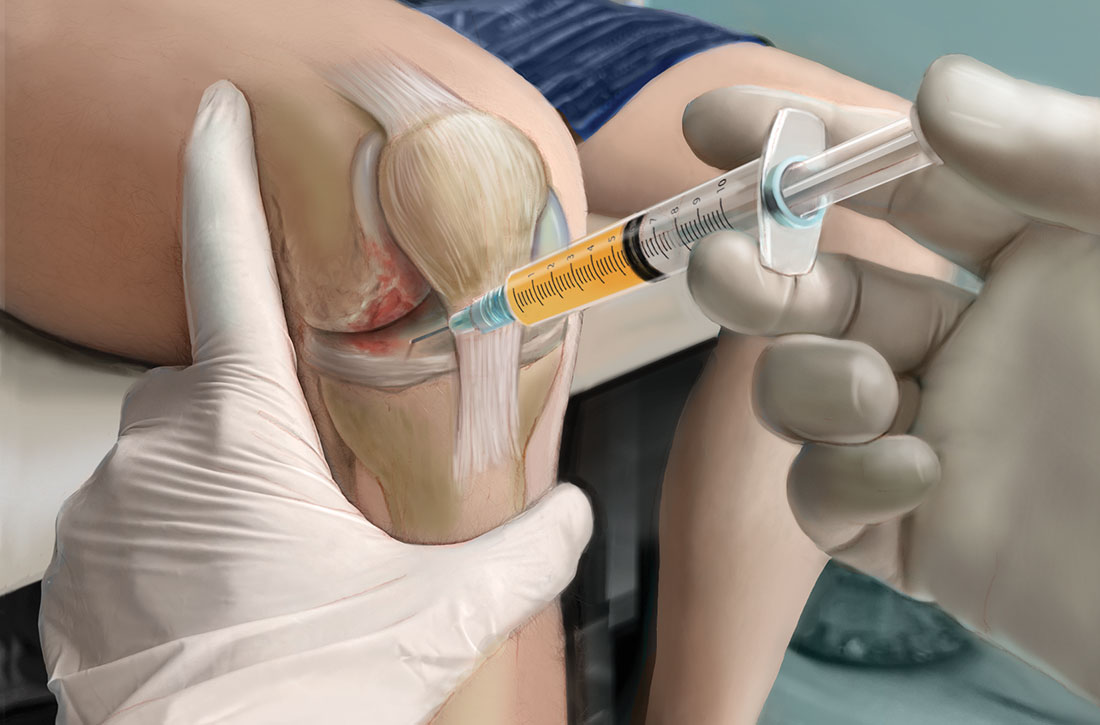
Surgical intervention for chronic knee injuries and pain generally is considered when patients demonstrate significant functional impairment and persistent symptoms despite pursuing numerous nonsurgical treatment options. A significant portion of chronic knee pain is due to degenerative processes such as OA or meniscus injuries, or tears without a history of trauma that do not cause locking of the knee. Treatments for degenerative knee pain include supervised exercise, physical therapy, bracing, offloading with a cane or other equipment, topical or oral anti-inflammatories or analgesics, and injectable therapies such as intra-articular corticosteroids.37
Continue to: Other common causes...
Other common causes of chronic knee pain include chronic tendinopathy or biomechanical syndromes such as patellofemoral pain syndrome or iliotibial band syndrome. Surgical treatment of these conditions is pursued in select cases and only after exhausting nonoperative treatment programs, as recommended by international consensus statements,38 societal guidelines,39 and expert opinion.40 High-quality data on the effectiveness, or ineffectiveness, of surgical intervention for these conditions are lacking.
Despite being one of the most commonly performed surgical procedures in the United States,41 arthroscopic partial meniscectomy treatment of degenerative meniscus tears does not lead to improved outcomes compared to nonsurgical management, according to multiple recent studies.42-45 Evidence does not support routine arthroscopic intervention for degenerative meniscus tears or OA,42 and recent guidelines recommend against it46 or to pursue it only after nonsurgical treatments have failed.37
Surgical management of degenerative knee conditions generally consists of partial or total arthroplasty and is similarly considered after failure of conservative measures. Appropriate use criteria that account for multiple clinical and patient factors are used to enhance patient selection for the procedure.47
Takeaways
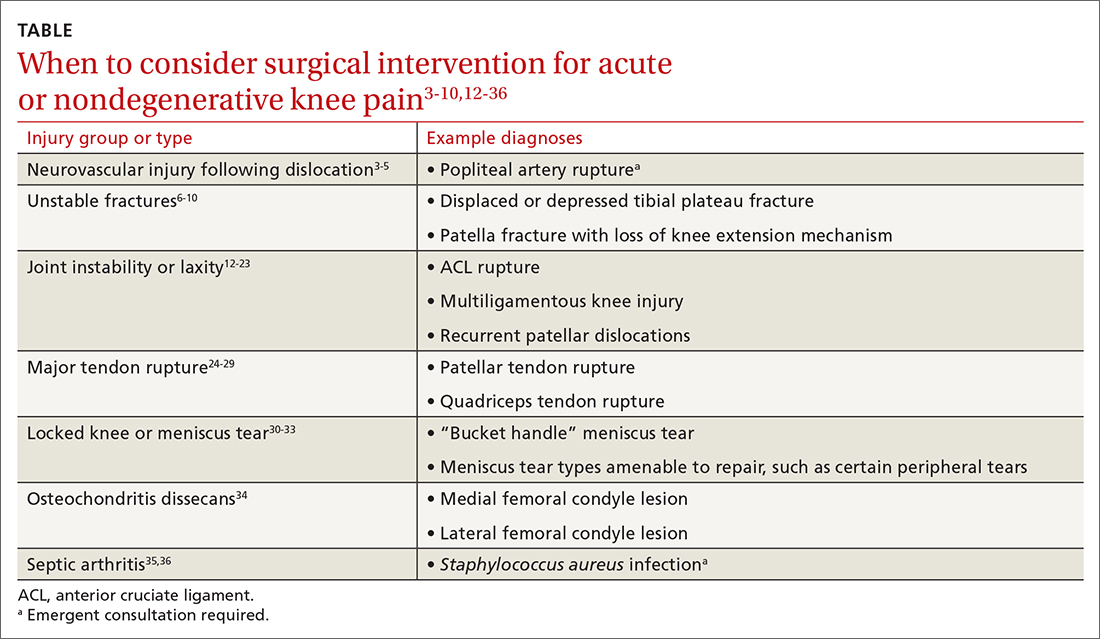
Primary care clinicians will treat patients sustaining knee injuries and see many patients with knee pain in the outpatient setting. Treatment options vary considerably depending on the underlying diagnosis and resulting functional losses. Several categories of clinical presentation, including neurovascular injury, unstable or displaced fractures, joint instability, major tendon rupture, significant mechanical symptoms such as a locked knee, certain osteochondral injuries, and septic arthritis, likely or almost always warrant surgical consultation (TABLE3-10,12-36). Occasionally, as in the case of neurovascular injury or septic arthritis, such consultation should be emergent.
CORRESPONDENCE
David M. Siebert, MD, Sports Medicine Center at Husky Stadium, 3800 Montlake Boulevard NE, Seattle, WA 98195; [email protected]
1. Baker P, Reading I, Cooper C, et al. Knee disorders in the general population and their relation to occupation. Occup Environ Med. 2003;60:794-797. doi: 10.1136/oem.60.10.794
2. Nguyen UD, Zhang Y, Zhu Y, et al. Increasing prevalence of knee pain and symptomatic knee osteoarthritis: survey and cohort data. Ann Intern Med. 20116;155:725-732. doi: 10.7326/0003-4819-155-11-201112060-00004
3. Natsuhara KM, Yeranosian MG, Cohen JR, et al. What is the frequency of vascular injury after knee dislocation? Clin Orthop Relat Res. 2014;472:2615-2620. doi: 10.1007/s11999-014-3566-1
4. Seroyer ST, Musahl V, Harner CD. Management of the acute knee dislocation: the Pittsburgh experience. Injury. 2008;39:710-718. doi: 10.1016/j.injury.2007.11.022
5. Sinan SM, Elsoe R, Mikkelsen C, et al. Clinical, functional, and patient-reported outcome of traumatic knee dislocations: a retrospective cohort study of 75 patients with 6.5-year follow up. Arch Orthop Trauma Surg. 2023;143:2589-2597. doi: 10.1007/s00402-022-04578-z
6. Schatzker J, Kfuri M. Revisiting the management of tibial plateau fractures. Injury. 2022;53:2207-2218. doi: 10.1016/j.injury.2022.04.006
7. Rudran B, Little C, Wiik A, et al. Tibial plateau fracture: anatomy, diagnosis and management. Br J Hosp Med (Lond). 2020;81:1-9. doi: 10.12968/hmed.2020.0339
8. Tscherne H, Lobenhoffer P. Tibial plateau fractures: management and expected results. Clin Orthop Relat Res. 1993;(292):87-100.
9. Melvin JS, Mehta S. Patellar fractures in adults. J Am Acad Orthop Surg. 2011;19:198-207. doi: 10.5435/00124635-201104000-00004
10. Filho JS, Lenza M, Tamaoki MJ, et al. Interventions for treating fractures of the patella in adults. Cochrane Database Syst Rev. 2021;2:CD009651. doi: 10.1002/14651858.CD009651.pub3
11. Palmer W, Bancroft L, Bonar F, et al. Glossary of terms for musculoskeletal radiology. Skeletal Radiol. 2020;49(suppl 1):1-33. doi: 10.1007/s00256-020-03465-1
12. Frobell RB, Roos EM, Roos HP, et al. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363:331-342. doi: 10.1056/NEJMoa0907797
13. Frobell RB, Roos HP, Roos EM, et al. Treatment for acute anterior cruciate ligament tear: five year outcome of randomized trial. Br J Sports Med. 2015;49:700. doi: 10.1136/bmj.f232
14. Diermeier TA, Rothrauff BB, Engebretsen L, et al; Panther Symposium ACL Treatment Consensus Group. Treatment after anterior cruciate ligament injury: Panther Symposium ACL Treatment Consensus Group. Br J Sports Med. 2021;55:14-22. doi: 10.1136/bjsports-2020-102200
15. Bedi A, Musahl V, Cowan JB. Management of posterior cruciate ligament injuries: an evidence-based review. J Am Acad Orthop Surg. 2016;24:277-289. doi: 10.5435/JAAOS-D-14-00326
16. Edson CJ. Conservative and postoperative rehabilitation of isolated and combined injuries of the medial collateral ligament. Sports Med Arthrosc Rev. 2006;14:105-110. doi: 10.1097/01.jsa.0000212308.32076.f2
17. Vosoughi F, Dogahe RR, Nuri A, et al. Medial collateral ligament injury of the knee: a review on current concept and management. Arch Bone Jt Surg. 2021;9:255-262. doi: 10.22038/abjs.2021.48458.2401
18. Kannus P. Nonoperative treatment of grade II and III sprains of the lateral ligament compartment of the knee. Am J Sports Med. 1989;17:83-88. doi: 10.1177/036354658901700114
19. Krukhaug Y, Mølster A, Rodt A, et al. Lateral ligament injuries of the knee. Knee Surg Sports Traumatol Arthrosc. 1998;6:21-25. doi: 10.1007/s001670050067
20. Grawe B, Schroeder AJ, Kakazu R, et al. Lateral collateral ligament injury about the knee: anatomy, evaluation, and management. J Am Acad Orthop Surg. 2018 15;26:e120-127. doi: 10.5435/JAAOS-D-16-00028
21. Ranawat A, Baker III CL, Henry S, et al. Posterolateral corner injury of the knee: evaluation and management. J Am Acad Orthop Surg. 2008;16:506-518.
22. Palmu S, Kallio PE, Donell ST, et al. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90:463-470. doi: 10.2106/JBJS.G.00072
23. Cohen D, Le N, Zakharia A, et al. MPFL reconstruction results in lower redislocation rates and higher functional outcomes than rehabilitation: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2022;30:3784-3795. doi: 10.1007/s00167-022-07003-5
24. Siwek CW, Rao JP. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am. 1981;63:932-937.
25. Konrath GA, Chen D, Lock T, et al. Outcomes following repair of quadriceps tendon ruptures. J Orthop Trauma. 1998;12:273-279. doi: 10.1097/00005131-199805000-00010
26. Rasul Jr. AT, Fischer DA. Primary repair of quadriceps tendon ruptures: results of treatment. Clin Orthop Relat Res. 1993;(289):205-207.
27. Rougraff BT, Reeck CC, Essenmacher J. Complete quadriceps tendon ruptures. Orthopedics. 1996;19:509-514.
28. Bui CN, Learned JR, Scolaro JA. Treatment of patellar fractures and injuries to the extensor mechanism of the knee: a critical analysis review. JBJS Rev. 2018;6:e1. doi: 10.2106/JBJS.RVW.17.00172
29. Haskel JD, Fried JW, Hurley ET, et al. High rates of return to play and work follow knee extensor tendon ruptures but low rate of return to pre-injury level of play. Knee Surg Sports Traumatol Arthrosc. 2021;29:2695-2700. doi: 10.1007/s00167-021-06537-4
30. Critchley IJ, Bracey DJ. The acutely locked knee—is a manipulation worth while? Injury. 1985;16:281-283. doi: 10.1016/s0020-1383(85)80020-6
31. Allum RL, Jones JR. The locked knee. Injury. 1986;17:256-258. doi: 10.1016/0020-1383(86)90231-7
32. Helmark IC, Neergaard K, Krogsgaard MR. Traumatic knee extension deficit (the locked knee): can MRI reduce the need for arthroscopy? Knee Surg Sports Traumatol Arthrosc. 2007;15:863-868. doi: 10.1007/s00167-006-0244-1
33. Noyes FR, Chen RC, Barber-Westin SD, et al. Greater than 10-year results of red-white longitudinal meniscal repairs in patients 20 years of age or younger. Am J Sports Med. 2011;39:1008-1017. doi: 10.1177/0363546510392014
34. Chambers HG, Shea KG, Anderson AF, et al; American Academy of Orthopedic Surgeons. Diagnosis and treatment of osteochondritis dissecans. J Am Acad Orthop Surg. 2011;19:297-306. doi: 10.5435/00124635-201105000-00007
35. Margaretten ME, Kohlwes J, Moore D, et al. Does this adult patient have septic arthritis? JAMA. 2007;297:1478-1488. doi: 10.1001/jama.297.13.1478
36. Gupta MN, Sturrock RD, Field M. A prospective 2-year study of 75 patients with adult-onset septic arthritis. Rheumatology (Oxford). 2001;40:24-30. doi: 10.1093/rheumatology/40.1.24
37. Brophy RH, Fillingham YA. AAOS clinical practice guideline summary: management of osteoarthritis of the knee (nonarthroplasty), 3rd edition. J Am Acad Orthop Surg. 2022;30:e721-729. doi: 10.5435/JAAOS-D-21-01233
38. Collins NJ, Barton CJ, van Middelkoop M, et al. 2018 Consensus statement on exercise therapy and physical interventions (orthoses, taping and manual therapy) to treat patellofemoral pain: recommendations from the 5th International Patellofemoral Pain Research Retreat, Gold Coast, Australia, 2017. Br J Sports Med. 2018;52:1170-1178. doi: 10.1136/bjsports-2018-099397
39. Strauss EJ, Kim S, Calcei JG, et al. Iliotibial band syndrome: evaluation and management. J Am Acad Orthop Surg. 2011;19:728-736. doi: 10.5435/00124635-201112000-00003
40. Millar NL, Murrell GAC, Kirwan P. Time to put down the scalpel? The role of surgery in tendinopathy. Br J Sports Med. 2020;54:441-442. doi: 10.1136/bjsports-2019-101084
41. Hall MJ, Schwartzman A, Zhang J, et al. Ambulatory surgery data from hospitals and ambulatory surgery centers: United States, 2010. Natl Health Stat Report. 2017;(102):1-15.
42. Kise NJ, Risberg MA, Stensrud S, et al. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomized controlled trial with two year follow-up. BMJ. 2016;354:i3740. doi: 10.1136/bmj.i3740
43. Sihvonen R, Paavola M, Malmivaara A, et al, FIDELITY (Finnish Degenerative Meniscus Lesion Study) Investigators. Arthroscopic partial meniscectomy for a degenerative meniscus tear: a 5 year follow-up of the placebo-surgery controlled FIDELITY (Finnish Degenerative Meniscus Lesion Study) trial. Br J Sports Med. 2020;54:1332-1339. doi: 10.1136/bjsports-2020-102813
44. Pihl K, Ensor J, Peat G, et al. Wild goose chase—no predictable patient subgroups benefit from meniscal surgery: patient-reported outcomes of 641 patients 1 year after surgery. Br J Sports Med. 2020;54:13-22. doi: 10.1136/bjsports-2018-100321
45. O’Connor D, Johnston RV, Brignardello-Petersen R, et al. Athroscopic surgery for degenerative knee disease (osteoarthritis including degenerative meniscal tears). Cochrane Database Syst Rev. 2022;3:CD014328. doi: 10.1002/14651858.CD014328
46. Siemieniuk RAC, Harris IA, Agoritsas T, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. Br J Sports Med. 2018;52:313. doi: 10.1136/bjsports-2017-j1982rep
47. Manner PA, Tubb CC, Levine BR. AAOS appropriate use criteria: surgical management of osteoarthritis of the knee. J Am Acad Orthop Surg. 2018;26:e194-197. doi: 10.5435/JAAOS-D-17-00425
Evidence supports what family physicians know to be true: Knee pain is an exceedingly common presenting problem in the primary care office. Estimates of lifetime incidence reach as high as 54%,1 and the prevalence of knee pain in the general population is increasing.2 Knee disability can result from acute or traumatic injuries as well as chronic, degenerative conditions such as osteoarthritis (OA). The decision to pursue orthopedic consultation for a particular injury or painful knee condition can be challenging. To address this, we highlight specific knee diagnoses known to cause pain, with the aim of describing which conditions likely will necessitate surgical consultation—and which won’t.
Acute or nondegenerative knee injuries and pain
Acute knee injuries range in severity from simple contusions and sprains to high-energy, traumatic injuries with resulting joint instability and potential neurovascular compromise. While conservative treatment often is successful for many simple injuries, surgical management—sometimes urgently or emergently—is needed in other cases, as will be detailed shortly.
Neurovascular injury associated with knee dislocations
Acute neurovascular injuries often require emergent surgical intervention. Although rare, tibiofemoral (knee) dislocations pose a significant challenge to the clinician in both diagnosis and management. The reported frequency of popliteal artery injury or rupture following a dislocation varies widely, with rates ranging from 5% to 64%, according to older studies; more recent data, however, suggest the rate is actually as low as 3.3%.3
Immediate immobilization and emergency department transport for monitoring, orthopedics consultation, and vascular studies or vascular surgery consultation is recommended in the case of a suspected knee dislocation. In one cross-sectional cohort study, the surgical management of knee dislocations yielded favorable outcomes in > 75% of cases.5
Tibial plateau fracture
This fracture often occurs as a result of high-energy trauma, such as contact sports or motor vehicle accidents, and is characterized by a proximal tibial fracture line with extension to the articular surface. X-rays often are sufficient for initial diagnosis. Computed tomography can help rule out a fracture line when clinical suspicion is high and x-rays are nondiagnostic. As noted earlier, any suggestion of neurovascular compromise on physical exam requires an emergent orthopedic surgeon consultation for a possible displaced and unstable (or more complex) injury (FIGURE 1).6-8
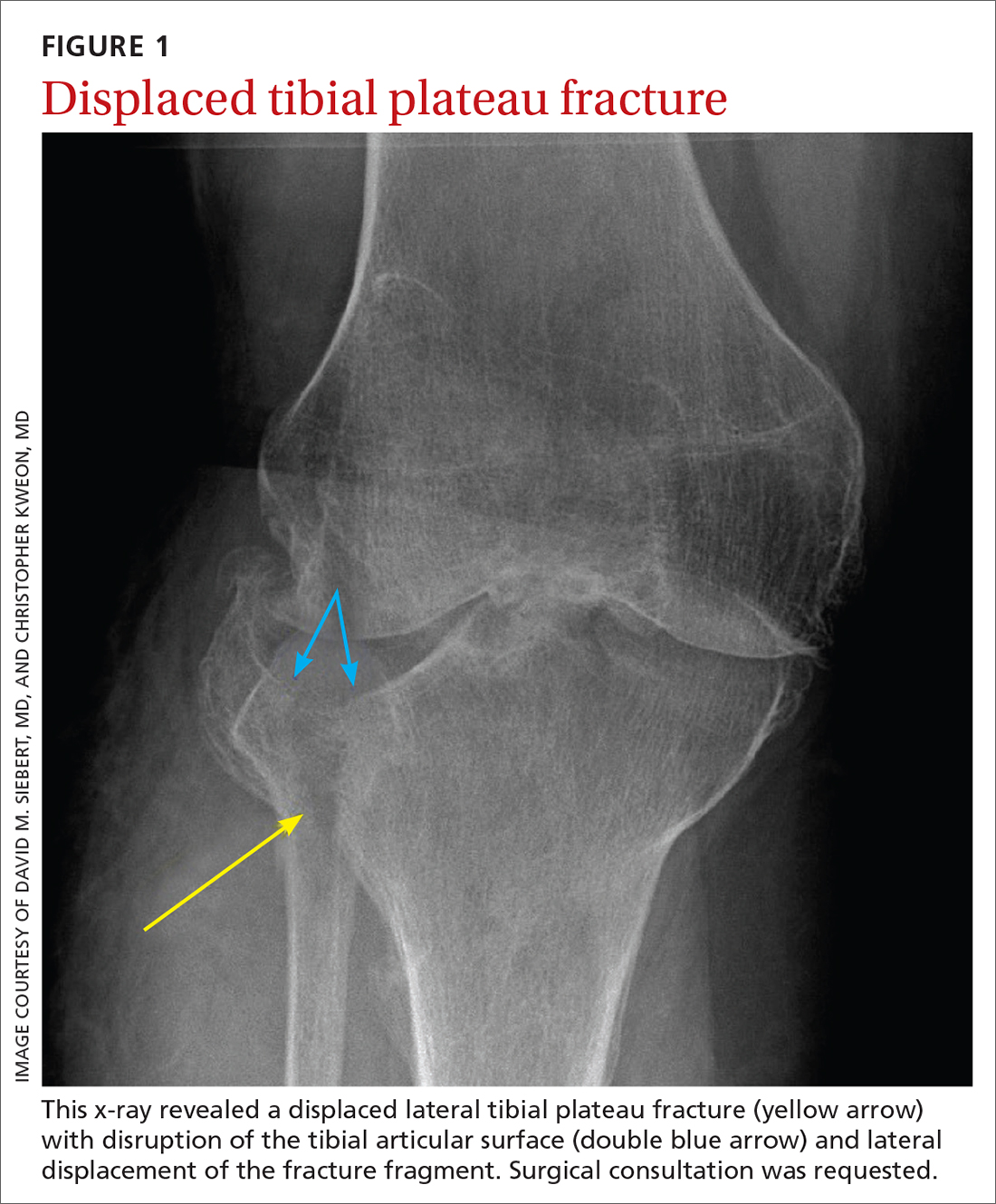
Nondisplaced tibial plateau fractures without supraphysiologic ligamentous laxity on valgus or varus stress testing can be managed safely with protection and early mobilization, gradual progression of weight-bearing, and serial x-rays to ensure fracture healing and stability.
Gross joint instability identified by positive valgus or varus stress testing, positive anterior or posterior drawer testing, or patient inability to tolerate these maneuvers due to pain similarly should raise suspicion for a more significant fracture at risk for concurrent neurovascular injury. Acute compartment syndrome also is a known complication of tibial plateau fractures and similarly requires emergent operative management. Urgent surgical consultation is recommended for fractures with displaced fracture fragments, tibial articular surface step-off or depression, fractures with concurrent joint laxity, or medial plateau fractures.6-8
Continue to: Patella fractures
Patella fractures
These fractures occur as a direct blow to the front of the knee, such as falling forward onto a hard surface, or indirectly due to a sudden extreme eccentric contraction of the quadriceps muscle. Nondisplaced fractures with an intact knee extension mechanism, which is examined via a supine straight-leg raise or seated knee extension, are managed with weight-bearing as tolerated in strict immobilization in full extension for 4 to 6 weeks, with active range-of-motion and isometric quadriceps exercises beginning in 1 to 2 weeks. Serial x-rays also are obtained to ensure fracture displacement does not occur during the rehabilitation process.9
High-quality evidence guiding follow-up care and comparing outcomes of surgical and nonsurgical management of patella fractures is lacking, and studies comparing different surgical techniques are of lower methodological quality.10 Nevertheless, displaced or comminuted patellar fractures are referred urgently to orthopedic surgical care for fixation, as are those with concurrent loose bodies, chondral surface injuries or articular step-off, or osteochondral fractures.9 Inability to perform a straight-leg raise (ie, clinical loss of the knee extension mechanism) suggests a fracture under tension that likely also requires surgical fixation for successful recovery. Neurovascular injuries are unlikely in most patellar fractures but would require emergent surgical consultation.9
Ligamentous injury
Tibiofemoral joint laxity occurs as a result of ligamentous injury, with or without tibial plateau fracture. The anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL) comprise the 4 main ligaments of the knee. The ACL resists anterior tibial translation and rotational forces, while the PCL resists posterior tibial translation. The MCL and LCL resist valgus and varus stress, respectively.
Ligament injuries are classified as Grades 1 to 311:
- Grade 1 sprains. The ligament is stretched, but there is no macroscopic tearing; joint stability is maintained.
- Grade 2 sprains. There are partial macroscopic ligament tears. There is joint laxity due to the partial loss of the ligament’s structural integrity.
- Grade 3 sprains. The ligament is fully avulsed or ruptured with resultant gross joint instability.
Continue to: ACL tears
ACL tears occur most commonly via a noncontact event, as when an individual plants their foot and suddenly changes direction during sport or other physical activity. Treatment hinges on patient activity levels and participation in sports. Patients who do not plan to engage in athletic movements (that require changes in direction or planting and twisting) and who otherwise maintain satisfactory joint stability during activities of daily living may elect to defer or even altogether avoid surgical reconstruction of isolated ACL tears. One pair of studies demonstrated equivalent outcomes in surgical and nonsurgical management in 121 young, nonelite athletes at 2- and 5-year follow-up, although the crossover from the nonsurgical to surgical groups was high.12,13 Athletes who regain satisfactory function and stability nonoperatively can defer surgical intervention. However, the majority of active patients and athletes will require surgical ACL reconstruction to return to pre-injury functional levels.14
PCL sprains occur as a result of sudden posteriorly directed force on the tibia, such as when the knee is hyperextended or a patient falls directly onto a flexed knee. Patients with Grade 1 and 2 isolated sprains generally will recover with conservative care, as will patients with some Grade 3 complete tears that do not fully compromise joint stability. However, high-grade PCL injuries often are comorbid with posterolateral corner or other injuries, leading to a higher likelihood of joint instability and thus the need for surgical intervention for the best chance at an optimal outcome.15
MCL sprain. Surgical management is not required in an isolated Grade 1 or 2 MCL sprain, as the hallmarks of recovery—return of joint stability, knee strength and range of motion, and pain reduction—can be achieved successfully with conservative management. Isolated Grade 3 MCL sprains are also successfully managed nonoperatively16 except in specific cases, such as a concurrent large avulsion fracture.17
LCL sprain. Similarly, isolated Grade 1 and 2 LCL sprains generally do not require surgical intervention. However, Grade 3 LCL injuries usually do, as persistent joint instability and poor functional outcomes are more common with nonsurgical management.18-20 Additionally, high-grade LCL injuries frequently manifest with comorbid meniscus injuries or sprains of the posterolateral corner of the knee, a complex anatomic structure that provides both static and dynamic tibiofemoral joint stability. Surgical repair or reconstruction of the posterolateral corner frequently is necessary for optimal functional outcomes.21
Multiligamentous sprains frequently lead to gross joint instability and necessitate orthopedic surgeon consultation to determine the best treatment plan; this should be done emergently if neurovascular compromise is suspected. A common injury combination is simultaneous ACL and MCL sprains with or without meniscus injury. In these cases, some surgeons will choose to defer ACL reconstruction until after MCL healing is achieved. This allows the patient to regain valgus stability of the joint prior to performing ACL reconstruction to regain rotational and anterior stability.20
Continue to: Patellar dislocations
Patellar dislocations represent a relatively common knee injury in young active patients, often occurring in a noncontact fashion when a valgus force is applied to an externally rotated and planted lower leg.
Major tendon rupture
Patellar tendon ruptures occur when a sudden eccentric force is applied to the knee, such as when landing from a jump with the knee flexed. Patellar tendon ruptures frequently are clinically apparent, with patients demonstrating a high-riding patella and loss of active knee extension. Quadriceps tendon ruptures often result from a similar injury mechanism in older patients, with a similar loss of active knee extension and a palpable gap superior to the patella.24
Partial tears in patients who can maintain full extension of the knee against gravity are treated nonoperatively, but early surgical repair is indicated for complete quadriceps or patellar tendon ruptures to achieve optimal outcomes.
Even with prompt treatment, return to sport is not guaranteed. According to a recent systematic review, athletes returned to play 88.9% and 89.8% of the time following patellar and quadriceps tendon repairs, respectively. However, returning to the same level of play was less common and achieved 80.8% (patellar tendon repair) and 70% (quadriceps tendon repair) of the time. Return-to-work rates were higher, at 96% for both surgical treatments.29
Locked knee and acute meniscus tears in younger patients
In some acute knee injuries, meniscus tears, loose cartilage bodies or osteochondral defects, or other internal structures can become interposed between the femoral and tibial surfaces, preventing both active and passive knee extension. Such injuries are often severely painful and functionally debilitating. While manipulation under anesthesia can acutely restore joint function,30 diagnostic and therapeutic arthroscopy often is pursued for definitive treatment.31 Compared to the gold standard of diagnostic arthroscopy, preoperative magnetic resonance imaging (MRI) carries positive and negative predictive values of 85% and 77%, respectively, in identifying or ruling out the anatomic structure responsible for a locked knee. 32 As such,
Continue to: Depending on the location...
Depending on the location, size, and shape of an acute meniscus tear in younger patients, surgical repair may be an option to preserve long-term joint function. In one case series of patients younger than 20 years, 62% of meniscus repairs yielded good outcomes after a mean follow-up period of 16.8 years.33
Osteochondritis dissecans
Osteochondritis dissecans is characterized by subchondral bone osteonecrosis that most often occurs in pediatric patients, potentially causing the separation of a fragment of articular cartilage and subchondral bone into the joint space (FIGURE 2). In early stages, nonoperative treatment consisting of prolonged rest followed by physical therapy to gradually return to activity is recommended to prevent small, low-grade lesions from progressing to unstable or separated fragments. Arthroscopy, which consists of microfracture or other surgical resurfacing techniques to restore joint integrity, is pursued in more advanced cases of unstable or separated fragments.

High-quality data guiding the management of osteochondritis dissecans are lacking, and these recommendations are based on consensus guidelines.34
Septic arthritis
Septic arthritis is a medical emergency caused by the hematogenous spread of microorganisms, most often staphylococci and streptococci species. Less commonly, it arises from direct inoculation through an open wound or, rarely, iatrogenically following a joint injection procedure. Clinical signs of septic arthritis include joint pain, joint swelling, and fever. Passive range of motion of the joint is often severely painful. Synovial fluid studies consistent with septic arthritis include an elevated white blood cell count greater than 25,000/mcL with polymorphonuclear cell predominance.35 The knee accounts for more than 50% of septic arthritis cases, and surgical drainage usually is required to achieve infection source control and decrease morbidity and mortality due to destruction of articular cartilage when treatment is delayed.36
Chronic knee injuries and pain
Surgical intervention for chronic knee injuries and pain generally is considered when patients demonstrate significant functional impairment and persistent symptoms despite pursuing numerous nonsurgical treatment options. A significant portion of chronic knee pain is due to degenerative processes such as OA or meniscus injuries, or tears without a history of trauma that do not cause locking of the knee. Treatments for degenerative knee pain include supervised exercise, physical therapy, bracing, offloading with a cane or other equipment, topical or oral anti-inflammatories or analgesics, and injectable therapies such as intra-articular corticosteroids.37
Continue to: Other common causes...
Other common causes of chronic knee pain include chronic tendinopathy or biomechanical syndromes such as patellofemoral pain syndrome or iliotibial band syndrome. Surgical treatment of these conditions is pursued in select cases and only after exhausting nonoperative treatment programs, as recommended by international consensus statements,38 societal guidelines,39 and expert opinion.40 High-quality data on the effectiveness, or ineffectiveness, of surgical intervention for these conditions are lacking.
Despite being one of the most commonly performed surgical procedures in the United States,41 arthroscopic partial meniscectomy treatment of degenerative meniscus tears does not lead to improved outcomes compared to nonsurgical management, according to multiple recent studies.42-45 Evidence does not support routine arthroscopic intervention for degenerative meniscus tears or OA,42 and recent guidelines recommend against it46 or to pursue it only after nonsurgical treatments have failed.37
Surgical management of degenerative knee conditions generally consists of partial or total arthroplasty and is similarly considered after failure of conservative measures. Appropriate use criteria that account for multiple clinical and patient factors are used to enhance patient selection for the procedure.47
Takeaways
Primary care clinicians will treat patients sustaining knee injuries and see many patients with knee pain in the outpatient setting. Treatment options vary considerably depending on the underlying diagnosis and resulting functional losses. Several categories of clinical presentation, including neurovascular injury, unstable or displaced fractures, joint instability, major tendon rupture, significant mechanical symptoms such as a locked knee, certain osteochondral injuries, and septic arthritis, likely or almost always warrant surgical consultation (TABLE3-10,12-36). Occasionally, as in the case of neurovascular injury or septic arthritis, such consultation should be emergent.
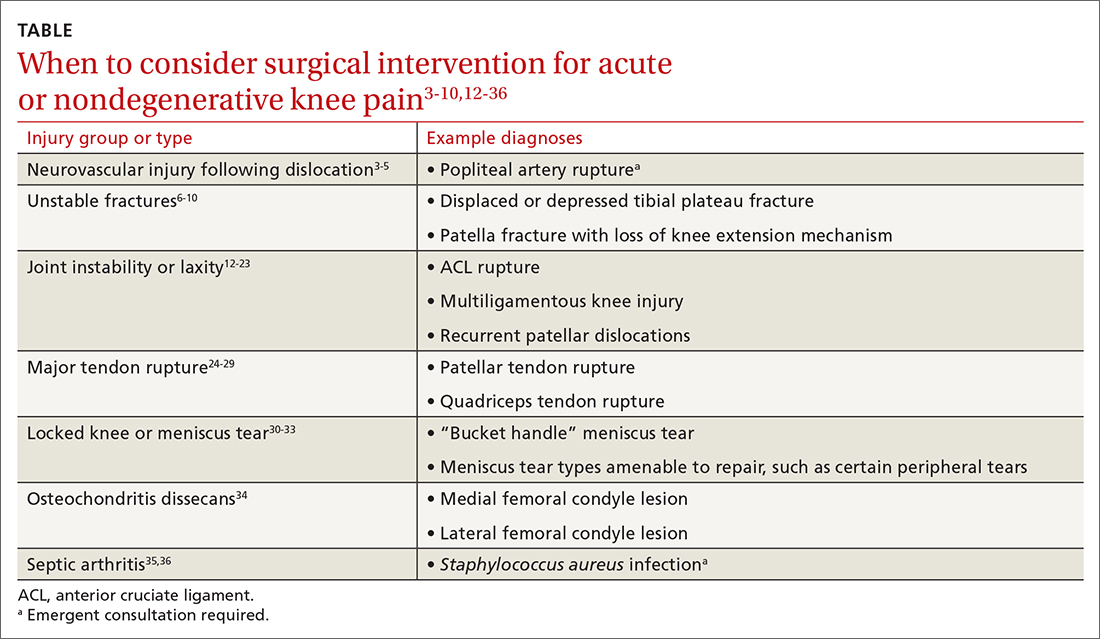
CORRESPONDENCE
David M. Siebert, MD, Sports Medicine Center at Husky Stadium, 3800 Montlake Boulevard NE, Seattle, WA 98195; [email protected]
Evidence supports what family physicians know to be true: Knee pain is an exceedingly common presenting problem in the primary care office. Estimates of lifetime incidence reach as high as 54%,1 and the prevalence of knee pain in the general population is increasing.2 Knee disability can result from acute or traumatic injuries as well as chronic, degenerative conditions such as osteoarthritis (OA). The decision to pursue orthopedic consultation for a particular injury or painful knee condition can be challenging. To address this, we highlight specific knee diagnoses known to cause pain, with the aim of describing which conditions likely will necessitate surgical consultation—and which won’t.
Acute or nondegenerative knee injuries and pain
Acute knee injuries range in severity from simple contusions and sprains to high-energy, traumatic injuries with resulting joint instability and potential neurovascular compromise. While conservative treatment often is successful for many simple injuries, surgical management—sometimes urgently or emergently—is needed in other cases, as will be detailed shortly.
Neurovascular injury associated with knee dislocations
Acute neurovascular injuries often require emergent surgical intervention. Although rare, tibiofemoral (knee) dislocations pose a significant challenge to the clinician in both diagnosis and management. The reported frequency of popliteal artery injury or rupture following a dislocation varies widely, with rates ranging from 5% to 64%, according to older studies; more recent data, however, suggest the rate is actually as low as 3.3%.3
Immediate immobilization and emergency department transport for monitoring, orthopedics consultation, and vascular studies or vascular surgery consultation is recommended in the case of a suspected knee dislocation. In one cross-sectional cohort study, the surgical management of knee dislocations yielded favorable outcomes in > 75% of cases.5
Tibial plateau fracture
This fracture often occurs as a result of high-energy trauma, such as contact sports or motor vehicle accidents, and is characterized by a proximal tibial fracture line with extension to the articular surface. X-rays often are sufficient for initial diagnosis. Computed tomography can help rule out a fracture line when clinical suspicion is high and x-rays are nondiagnostic. As noted earlier, any suggestion of neurovascular compromise on physical exam requires an emergent orthopedic surgeon consultation for a possible displaced and unstable (or more complex) injury (FIGURE 1).6-8
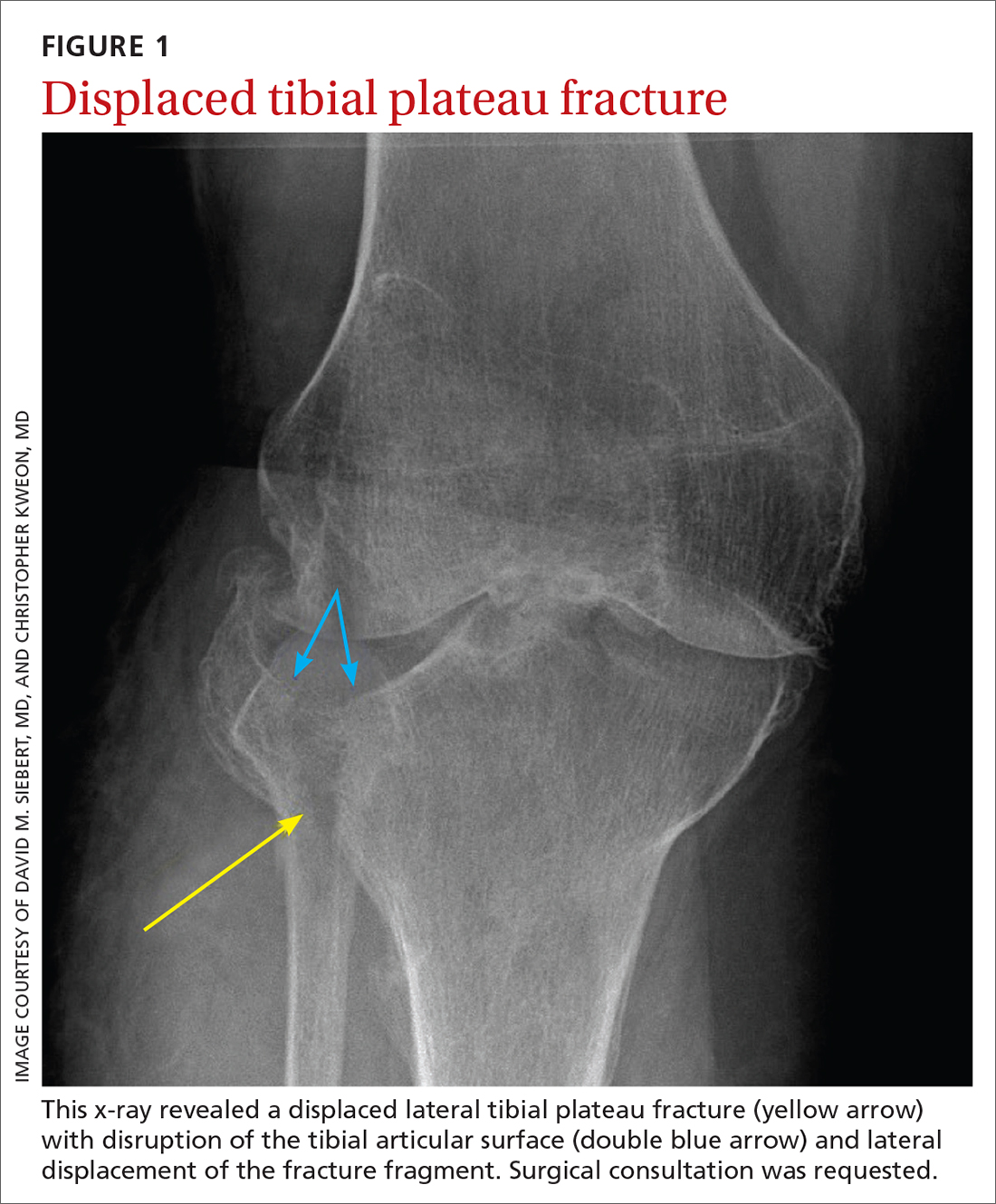
Nondisplaced tibial plateau fractures without supraphysiologic ligamentous laxity on valgus or varus stress testing can be managed safely with protection and early mobilization, gradual progression of weight-bearing, and serial x-rays to ensure fracture healing and stability.
Gross joint instability identified by positive valgus or varus stress testing, positive anterior or posterior drawer testing, or patient inability to tolerate these maneuvers due to pain similarly should raise suspicion for a more significant fracture at risk for concurrent neurovascular injury. Acute compartment syndrome also is a known complication of tibial plateau fractures and similarly requires emergent operative management. Urgent surgical consultation is recommended for fractures with displaced fracture fragments, tibial articular surface step-off or depression, fractures with concurrent joint laxity, or medial plateau fractures.6-8
Continue to: Patella fractures
Patella fractures
These fractures occur as a direct blow to the front of the knee, such as falling forward onto a hard surface, or indirectly due to a sudden extreme eccentric contraction of the quadriceps muscle. Nondisplaced fractures with an intact knee extension mechanism, which is examined via a supine straight-leg raise or seated knee extension, are managed with weight-bearing as tolerated in strict immobilization in full extension for 4 to 6 weeks, with active range-of-motion and isometric quadriceps exercises beginning in 1 to 2 weeks. Serial x-rays also are obtained to ensure fracture displacement does not occur during the rehabilitation process.9
High-quality evidence guiding follow-up care and comparing outcomes of surgical and nonsurgical management of patella fractures is lacking, and studies comparing different surgical techniques are of lower methodological quality.10 Nevertheless, displaced or comminuted patellar fractures are referred urgently to orthopedic surgical care for fixation, as are those with concurrent loose bodies, chondral surface injuries or articular step-off, or osteochondral fractures.9 Inability to perform a straight-leg raise (ie, clinical loss of the knee extension mechanism) suggests a fracture under tension that likely also requires surgical fixation for successful recovery. Neurovascular injuries are unlikely in most patellar fractures but would require emergent surgical consultation.9
Ligamentous injury
Tibiofemoral joint laxity occurs as a result of ligamentous injury, with or without tibial plateau fracture. The anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL) comprise the 4 main ligaments of the knee. The ACL resists anterior tibial translation and rotational forces, while the PCL resists posterior tibial translation. The MCL and LCL resist valgus and varus stress, respectively.
Ligament injuries are classified as Grades 1 to 311:
- Grade 1 sprains. The ligament is stretched, but there is no macroscopic tearing; joint stability is maintained.
- Grade 2 sprains. There are partial macroscopic ligament tears. There is joint laxity due to the partial loss of the ligament’s structural integrity.
- Grade 3 sprains. The ligament is fully avulsed or ruptured with resultant gross joint instability.
Continue to: ACL tears
ACL tears occur most commonly via a noncontact event, as when an individual plants their foot and suddenly changes direction during sport or other physical activity. Treatment hinges on patient activity levels and participation in sports. Patients who do not plan to engage in athletic movements (that require changes in direction or planting and twisting) and who otherwise maintain satisfactory joint stability during activities of daily living may elect to defer or even altogether avoid surgical reconstruction of isolated ACL tears. One pair of studies demonstrated equivalent outcomes in surgical and nonsurgical management in 121 young, nonelite athletes at 2- and 5-year follow-up, although the crossover from the nonsurgical to surgical groups was high.12,13 Athletes who regain satisfactory function and stability nonoperatively can defer surgical intervention. However, the majority of active patients and athletes will require surgical ACL reconstruction to return to pre-injury functional levels.14
PCL sprains occur as a result of sudden posteriorly directed force on the tibia, such as when the knee is hyperextended or a patient falls directly onto a flexed knee. Patients with Grade 1 and 2 isolated sprains generally will recover with conservative care, as will patients with some Grade 3 complete tears that do not fully compromise joint stability. However, high-grade PCL injuries often are comorbid with posterolateral corner or other injuries, leading to a higher likelihood of joint instability and thus the need for surgical intervention for the best chance at an optimal outcome.15
MCL sprain. Surgical management is not required in an isolated Grade 1 or 2 MCL sprain, as the hallmarks of recovery—return of joint stability, knee strength and range of motion, and pain reduction—can be achieved successfully with conservative management. Isolated Grade 3 MCL sprains are also successfully managed nonoperatively16 except in specific cases, such as a concurrent large avulsion fracture.17
LCL sprain. Similarly, isolated Grade 1 and 2 LCL sprains generally do not require surgical intervention. However, Grade 3 LCL injuries usually do, as persistent joint instability and poor functional outcomes are more common with nonsurgical management.18-20 Additionally, high-grade LCL injuries frequently manifest with comorbid meniscus injuries or sprains of the posterolateral corner of the knee, a complex anatomic structure that provides both static and dynamic tibiofemoral joint stability. Surgical repair or reconstruction of the posterolateral corner frequently is necessary for optimal functional outcomes.21
Multiligamentous sprains frequently lead to gross joint instability and necessitate orthopedic surgeon consultation to determine the best treatment plan; this should be done emergently if neurovascular compromise is suspected. A common injury combination is simultaneous ACL and MCL sprains with or without meniscus injury. In these cases, some surgeons will choose to defer ACL reconstruction until after MCL healing is achieved. This allows the patient to regain valgus stability of the joint prior to performing ACL reconstruction to regain rotational and anterior stability.20
Continue to: Patellar dislocations
Patellar dislocations represent a relatively common knee injury in young active patients, often occurring in a noncontact fashion when a valgus force is applied to an externally rotated and planted lower leg.
Major tendon rupture
Patellar tendon ruptures occur when a sudden eccentric force is applied to the knee, such as when landing from a jump with the knee flexed. Patellar tendon ruptures frequently are clinically apparent, with patients demonstrating a high-riding patella and loss of active knee extension. Quadriceps tendon ruptures often result from a similar injury mechanism in older patients, with a similar loss of active knee extension and a palpable gap superior to the patella.24
Partial tears in patients who can maintain full extension of the knee against gravity are treated nonoperatively, but early surgical repair is indicated for complete quadriceps or patellar tendon ruptures to achieve optimal outcomes.
Even with prompt treatment, return to sport is not guaranteed. According to a recent systematic review, athletes returned to play 88.9% and 89.8% of the time following patellar and quadriceps tendon repairs, respectively. However, returning to the same level of play was less common and achieved 80.8% (patellar tendon repair) and 70% (quadriceps tendon repair) of the time. Return-to-work rates were higher, at 96% for both surgical treatments.29
Locked knee and acute meniscus tears in younger patients
In some acute knee injuries, meniscus tears, loose cartilage bodies or osteochondral defects, or other internal structures can become interposed between the femoral and tibial surfaces, preventing both active and passive knee extension. Such injuries are often severely painful and functionally debilitating. While manipulation under anesthesia can acutely restore joint function,30 diagnostic and therapeutic arthroscopy often is pursued for definitive treatment.31 Compared to the gold standard of diagnostic arthroscopy, preoperative magnetic resonance imaging (MRI) carries positive and negative predictive values of 85% and 77%, respectively, in identifying or ruling out the anatomic structure responsible for a locked knee. 32 As such,
Continue to: Depending on the location...
Depending on the location, size, and shape of an acute meniscus tear in younger patients, surgical repair may be an option to preserve long-term joint function. In one case series of patients younger than 20 years, 62% of meniscus repairs yielded good outcomes after a mean follow-up period of 16.8 years.33
Osteochondritis dissecans
Osteochondritis dissecans is characterized by subchondral bone osteonecrosis that most often occurs in pediatric patients, potentially causing the separation of a fragment of articular cartilage and subchondral bone into the joint space (FIGURE 2). In early stages, nonoperative treatment consisting of prolonged rest followed by physical therapy to gradually return to activity is recommended to prevent small, low-grade lesions from progressing to unstable or separated fragments. Arthroscopy, which consists of microfracture or other surgical resurfacing techniques to restore joint integrity, is pursued in more advanced cases of unstable or separated fragments.

High-quality data guiding the management of osteochondritis dissecans are lacking, and these recommendations are based on consensus guidelines.34
Septic arthritis
Septic arthritis is a medical emergency caused by the hematogenous spread of microorganisms, most often staphylococci and streptococci species. Less commonly, it arises from direct inoculation through an open wound or, rarely, iatrogenically following a joint injection procedure. Clinical signs of septic arthritis include joint pain, joint swelling, and fever. Passive range of motion of the joint is often severely painful. Synovial fluid studies consistent with septic arthritis include an elevated white blood cell count greater than 25,000/mcL with polymorphonuclear cell predominance.35 The knee accounts for more than 50% of septic arthritis cases, and surgical drainage usually is required to achieve infection source control and decrease morbidity and mortality due to destruction of articular cartilage when treatment is delayed.36
Chronic knee injuries and pain
Surgical intervention for chronic knee injuries and pain generally is considered when patients demonstrate significant functional impairment and persistent symptoms despite pursuing numerous nonsurgical treatment options. A significant portion of chronic knee pain is due to degenerative processes such as OA or meniscus injuries, or tears without a history of trauma that do not cause locking of the knee. Treatments for degenerative knee pain include supervised exercise, physical therapy, bracing, offloading with a cane or other equipment, topical or oral anti-inflammatories or analgesics, and injectable therapies such as intra-articular corticosteroids.37
Continue to: Other common causes...
Other common causes of chronic knee pain include chronic tendinopathy or biomechanical syndromes such as patellofemoral pain syndrome or iliotibial band syndrome. Surgical treatment of these conditions is pursued in select cases and only after exhausting nonoperative treatment programs, as recommended by international consensus statements,38 societal guidelines,39 and expert opinion.40 High-quality data on the effectiveness, or ineffectiveness, of surgical intervention for these conditions are lacking.
Despite being one of the most commonly performed surgical procedures in the United States,41 arthroscopic partial meniscectomy treatment of degenerative meniscus tears does not lead to improved outcomes compared to nonsurgical management, according to multiple recent studies.42-45 Evidence does not support routine arthroscopic intervention for degenerative meniscus tears or OA,42 and recent guidelines recommend against it46 or to pursue it only after nonsurgical treatments have failed.37
Surgical management of degenerative knee conditions generally consists of partial or total arthroplasty and is similarly considered after failure of conservative measures. Appropriate use criteria that account for multiple clinical and patient factors are used to enhance patient selection for the procedure.47
Takeaways
Primary care clinicians will treat patients sustaining knee injuries and see many patients with knee pain in the outpatient setting. Treatment options vary considerably depending on the underlying diagnosis and resulting functional losses. Several categories of clinical presentation, including neurovascular injury, unstable or displaced fractures, joint instability, major tendon rupture, significant mechanical symptoms such as a locked knee, certain osteochondral injuries, and septic arthritis, likely or almost always warrant surgical consultation (TABLE3-10,12-36). Occasionally, as in the case of neurovascular injury or septic arthritis, such consultation should be emergent.
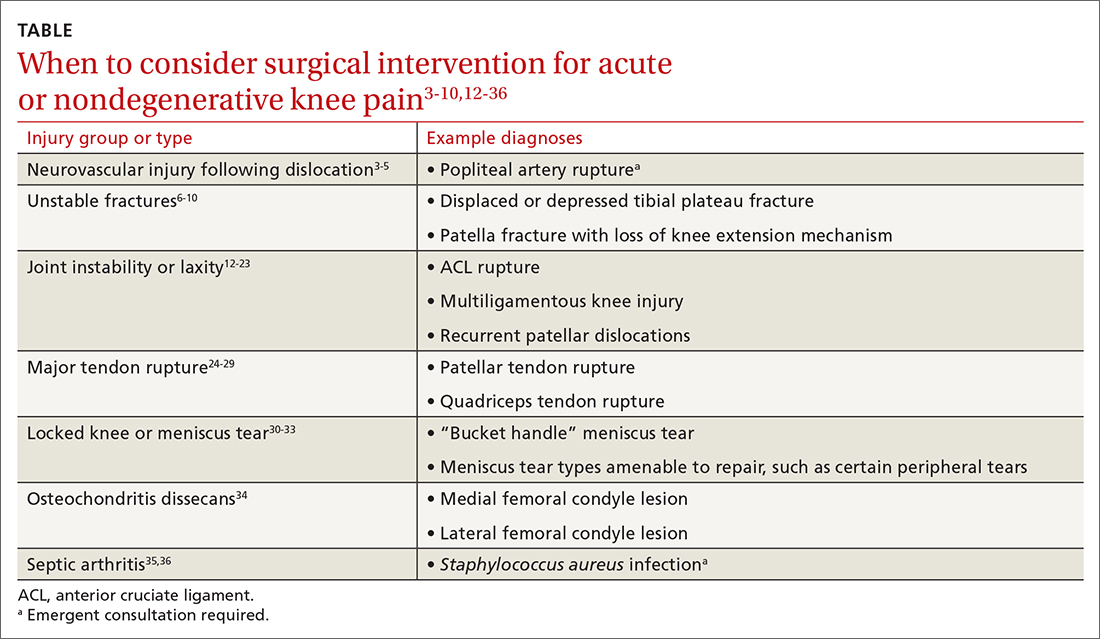
CORRESPONDENCE
David M. Siebert, MD, Sports Medicine Center at Husky Stadium, 3800 Montlake Boulevard NE, Seattle, WA 98195; [email protected]
1. Baker P, Reading I, Cooper C, et al. Knee disorders in the general population and their relation to occupation. Occup Environ Med. 2003;60:794-797. doi: 10.1136/oem.60.10.794
2. Nguyen UD, Zhang Y, Zhu Y, et al. Increasing prevalence of knee pain and symptomatic knee osteoarthritis: survey and cohort data. Ann Intern Med. 20116;155:725-732. doi: 10.7326/0003-4819-155-11-201112060-00004
3. Natsuhara KM, Yeranosian MG, Cohen JR, et al. What is the frequency of vascular injury after knee dislocation? Clin Orthop Relat Res. 2014;472:2615-2620. doi: 10.1007/s11999-014-3566-1
4. Seroyer ST, Musahl V, Harner CD. Management of the acute knee dislocation: the Pittsburgh experience. Injury. 2008;39:710-718. doi: 10.1016/j.injury.2007.11.022
5. Sinan SM, Elsoe R, Mikkelsen C, et al. Clinical, functional, and patient-reported outcome of traumatic knee dislocations: a retrospective cohort study of 75 patients with 6.5-year follow up. Arch Orthop Trauma Surg. 2023;143:2589-2597. doi: 10.1007/s00402-022-04578-z
6. Schatzker J, Kfuri M. Revisiting the management of tibial plateau fractures. Injury. 2022;53:2207-2218. doi: 10.1016/j.injury.2022.04.006
7. Rudran B, Little C, Wiik A, et al. Tibial plateau fracture: anatomy, diagnosis and management. Br J Hosp Med (Lond). 2020;81:1-9. doi: 10.12968/hmed.2020.0339
8. Tscherne H, Lobenhoffer P. Tibial plateau fractures: management and expected results. Clin Orthop Relat Res. 1993;(292):87-100.
9. Melvin JS, Mehta S. Patellar fractures in adults. J Am Acad Orthop Surg. 2011;19:198-207. doi: 10.5435/00124635-201104000-00004
10. Filho JS, Lenza M, Tamaoki MJ, et al. Interventions for treating fractures of the patella in adults. Cochrane Database Syst Rev. 2021;2:CD009651. doi: 10.1002/14651858.CD009651.pub3
11. Palmer W, Bancroft L, Bonar F, et al. Glossary of terms for musculoskeletal radiology. Skeletal Radiol. 2020;49(suppl 1):1-33. doi: 10.1007/s00256-020-03465-1
12. Frobell RB, Roos EM, Roos HP, et al. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363:331-342. doi: 10.1056/NEJMoa0907797
13. Frobell RB, Roos HP, Roos EM, et al. Treatment for acute anterior cruciate ligament tear: five year outcome of randomized trial. Br J Sports Med. 2015;49:700. doi: 10.1136/bmj.f232
14. Diermeier TA, Rothrauff BB, Engebretsen L, et al; Panther Symposium ACL Treatment Consensus Group. Treatment after anterior cruciate ligament injury: Panther Symposium ACL Treatment Consensus Group. Br J Sports Med. 2021;55:14-22. doi: 10.1136/bjsports-2020-102200
15. Bedi A, Musahl V, Cowan JB. Management of posterior cruciate ligament injuries: an evidence-based review. J Am Acad Orthop Surg. 2016;24:277-289. doi: 10.5435/JAAOS-D-14-00326
16. Edson CJ. Conservative and postoperative rehabilitation of isolated and combined injuries of the medial collateral ligament. Sports Med Arthrosc Rev. 2006;14:105-110. doi: 10.1097/01.jsa.0000212308.32076.f2
17. Vosoughi F, Dogahe RR, Nuri A, et al. Medial collateral ligament injury of the knee: a review on current concept and management. Arch Bone Jt Surg. 2021;9:255-262. doi: 10.22038/abjs.2021.48458.2401
18. Kannus P. Nonoperative treatment of grade II and III sprains of the lateral ligament compartment of the knee. Am J Sports Med. 1989;17:83-88. doi: 10.1177/036354658901700114
19. Krukhaug Y, Mølster A, Rodt A, et al. Lateral ligament injuries of the knee. Knee Surg Sports Traumatol Arthrosc. 1998;6:21-25. doi: 10.1007/s001670050067
20. Grawe B, Schroeder AJ, Kakazu R, et al. Lateral collateral ligament injury about the knee: anatomy, evaluation, and management. J Am Acad Orthop Surg. 2018 15;26:e120-127. doi: 10.5435/JAAOS-D-16-00028
21. Ranawat A, Baker III CL, Henry S, et al. Posterolateral corner injury of the knee: evaluation and management. J Am Acad Orthop Surg. 2008;16:506-518.
22. Palmu S, Kallio PE, Donell ST, et al. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90:463-470. doi: 10.2106/JBJS.G.00072
23. Cohen D, Le N, Zakharia A, et al. MPFL reconstruction results in lower redislocation rates and higher functional outcomes than rehabilitation: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2022;30:3784-3795. doi: 10.1007/s00167-022-07003-5
24. Siwek CW, Rao JP. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am. 1981;63:932-937.
25. Konrath GA, Chen D, Lock T, et al. Outcomes following repair of quadriceps tendon ruptures. J Orthop Trauma. 1998;12:273-279. doi: 10.1097/00005131-199805000-00010
26. Rasul Jr. AT, Fischer DA. Primary repair of quadriceps tendon ruptures: results of treatment. Clin Orthop Relat Res. 1993;(289):205-207.
27. Rougraff BT, Reeck CC, Essenmacher J. Complete quadriceps tendon ruptures. Orthopedics. 1996;19:509-514.
28. Bui CN, Learned JR, Scolaro JA. Treatment of patellar fractures and injuries to the extensor mechanism of the knee: a critical analysis review. JBJS Rev. 2018;6:e1. doi: 10.2106/JBJS.RVW.17.00172
29. Haskel JD, Fried JW, Hurley ET, et al. High rates of return to play and work follow knee extensor tendon ruptures but low rate of return to pre-injury level of play. Knee Surg Sports Traumatol Arthrosc. 2021;29:2695-2700. doi: 10.1007/s00167-021-06537-4
30. Critchley IJ, Bracey DJ. The acutely locked knee—is a manipulation worth while? Injury. 1985;16:281-283. doi: 10.1016/s0020-1383(85)80020-6
31. Allum RL, Jones JR. The locked knee. Injury. 1986;17:256-258. doi: 10.1016/0020-1383(86)90231-7
32. Helmark IC, Neergaard K, Krogsgaard MR. Traumatic knee extension deficit (the locked knee): can MRI reduce the need for arthroscopy? Knee Surg Sports Traumatol Arthrosc. 2007;15:863-868. doi: 10.1007/s00167-006-0244-1
33. Noyes FR, Chen RC, Barber-Westin SD, et al. Greater than 10-year results of red-white longitudinal meniscal repairs in patients 20 years of age or younger. Am J Sports Med. 2011;39:1008-1017. doi: 10.1177/0363546510392014
34. Chambers HG, Shea KG, Anderson AF, et al; American Academy of Orthopedic Surgeons. Diagnosis and treatment of osteochondritis dissecans. J Am Acad Orthop Surg. 2011;19:297-306. doi: 10.5435/00124635-201105000-00007
35. Margaretten ME, Kohlwes J, Moore D, et al. Does this adult patient have septic arthritis? JAMA. 2007;297:1478-1488. doi: 10.1001/jama.297.13.1478
36. Gupta MN, Sturrock RD, Field M. A prospective 2-year study of 75 patients with adult-onset septic arthritis. Rheumatology (Oxford). 2001;40:24-30. doi: 10.1093/rheumatology/40.1.24
37. Brophy RH, Fillingham YA. AAOS clinical practice guideline summary: management of osteoarthritis of the knee (nonarthroplasty), 3rd edition. J Am Acad Orthop Surg. 2022;30:e721-729. doi: 10.5435/JAAOS-D-21-01233
38. Collins NJ, Barton CJ, van Middelkoop M, et al. 2018 Consensus statement on exercise therapy and physical interventions (orthoses, taping and manual therapy) to treat patellofemoral pain: recommendations from the 5th International Patellofemoral Pain Research Retreat, Gold Coast, Australia, 2017. Br J Sports Med. 2018;52:1170-1178. doi: 10.1136/bjsports-2018-099397
39. Strauss EJ, Kim S, Calcei JG, et al. Iliotibial band syndrome: evaluation and management. J Am Acad Orthop Surg. 2011;19:728-736. doi: 10.5435/00124635-201112000-00003
40. Millar NL, Murrell GAC, Kirwan P. Time to put down the scalpel? The role of surgery in tendinopathy. Br J Sports Med. 2020;54:441-442. doi: 10.1136/bjsports-2019-101084
41. Hall MJ, Schwartzman A, Zhang J, et al. Ambulatory surgery data from hospitals and ambulatory surgery centers: United States, 2010. Natl Health Stat Report. 2017;(102):1-15.
42. Kise NJ, Risberg MA, Stensrud S, et al. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomized controlled trial with two year follow-up. BMJ. 2016;354:i3740. doi: 10.1136/bmj.i3740
43. Sihvonen R, Paavola M, Malmivaara A, et al, FIDELITY (Finnish Degenerative Meniscus Lesion Study) Investigators. Arthroscopic partial meniscectomy for a degenerative meniscus tear: a 5 year follow-up of the placebo-surgery controlled FIDELITY (Finnish Degenerative Meniscus Lesion Study) trial. Br J Sports Med. 2020;54:1332-1339. doi: 10.1136/bjsports-2020-102813
44. Pihl K, Ensor J, Peat G, et al. Wild goose chase—no predictable patient subgroups benefit from meniscal surgery: patient-reported outcomes of 641 patients 1 year after surgery. Br J Sports Med. 2020;54:13-22. doi: 10.1136/bjsports-2018-100321
45. O’Connor D, Johnston RV, Brignardello-Petersen R, et al. Athroscopic surgery for degenerative knee disease (osteoarthritis including degenerative meniscal tears). Cochrane Database Syst Rev. 2022;3:CD014328. doi: 10.1002/14651858.CD014328
46. Siemieniuk RAC, Harris IA, Agoritsas T, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. Br J Sports Med. 2018;52:313. doi: 10.1136/bjsports-2017-j1982rep
47. Manner PA, Tubb CC, Levine BR. AAOS appropriate use criteria: surgical management of osteoarthritis of the knee. J Am Acad Orthop Surg. 2018;26:e194-197. doi: 10.5435/JAAOS-D-17-00425
1. Baker P, Reading I, Cooper C, et al. Knee disorders in the general population and their relation to occupation. Occup Environ Med. 2003;60:794-797. doi: 10.1136/oem.60.10.794
2. Nguyen UD, Zhang Y, Zhu Y, et al. Increasing prevalence of knee pain and symptomatic knee osteoarthritis: survey and cohort data. Ann Intern Med. 20116;155:725-732. doi: 10.7326/0003-4819-155-11-201112060-00004
3. Natsuhara KM, Yeranosian MG, Cohen JR, et al. What is the frequency of vascular injury after knee dislocation? Clin Orthop Relat Res. 2014;472:2615-2620. doi: 10.1007/s11999-014-3566-1
4. Seroyer ST, Musahl V, Harner CD. Management of the acute knee dislocation: the Pittsburgh experience. Injury. 2008;39:710-718. doi: 10.1016/j.injury.2007.11.022
5. Sinan SM, Elsoe R, Mikkelsen C, et al. Clinical, functional, and patient-reported outcome of traumatic knee dislocations: a retrospective cohort study of 75 patients with 6.5-year follow up. Arch Orthop Trauma Surg. 2023;143:2589-2597. doi: 10.1007/s00402-022-04578-z
6. Schatzker J, Kfuri M. Revisiting the management of tibial plateau fractures. Injury. 2022;53:2207-2218. doi: 10.1016/j.injury.2022.04.006
7. Rudran B, Little C, Wiik A, et al. Tibial plateau fracture: anatomy, diagnosis and management. Br J Hosp Med (Lond). 2020;81:1-9. doi: 10.12968/hmed.2020.0339
8. Tscherne H, Lobenhoffer P. Tibial plateau fractures: management and expected results. Clin Orthop Relat Res. 1993;(292):87-100.
9. Melvin JS, Mehta S. Patellar fractures in adults. J Am Acad Orthop Surg. 2011;19:198-207. doi: 10.5435/00124635-201104000-00004
10. Filho JS, Lenza M, Tamaoki MJ, et al. Interventions for treating fractures of the patella in adults. Cochrane Database Syst Rev. 2021;2:CD009651. doi: 10.1002/14651858.CD009651.pub3
11. Palmer W, Bancroft L, Bonar F, et al. Glossary of terms for musculoskeletal radiology. Skeletal Radiol. 2020;49(suppl 1):1-33. doi: 10.1007/s00256-020-03465-1
12. Frobell RB, Roos EM, Roos HP, et al. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363:331-342. doi: 10.1056/NEJMoa0907797
13. Frobell RB, Roos HP, Roos EM, et al. Treatment for acute anterior cruciate ligament tear: five year outcome of randomized trial. Br J Sports Med. 2015;49:700. doi: 10.1136/bmj.f232
14. Diermeier TA, Rothrauff BB, Engebretsen L, et al; Panther Symposium ACL Treatment Consensus Group. Treatment after anterior cruciate ligament injury: Panther Symposium ACL Treatment Consensus Group. Br J Sports Med. 2021;55:14-22. doi: 10.1136/bjsports-2020-102200
15. Bedi A, Musahl V, Cowan JB. Management of posterior cruciate ligament injuries: an evidence-based review. J Am Acad Orthop Surg. 2016;24:277-289. doi: 10.5435/JAAOS-D-14-00326
16. Edson CJ. Conservative and postoperative rehabilitation of isolated and combined injuries of the medial collateral ligament. Sports Med Arthrosc Rev. 2006;14:105-110. doi: 10.1097/01.jsa.0000212308.32076.f2
17. Vosoughi F, Dogahe RR, Nuri A, et al. Medial collateral ligament injury of the knee: a review on current concept and management. Arch Bone Jt Surg. 2021;9:255-262. doi: 10.22038/abjs.2021.48458.2401
18. Kannus P. Nonoperative treatment of grade II and III sprains of the lateral ligament compartment of the knee. Am J Sports Med. 1989;17:83-88. doi: 10.1177/036354658901700114
19. Krukhaug Y, Mølster A, Rodt A, et al. Lateral ligament injuries of the knee. Knee Surg Sports Traumatol Arthrosc. 1998;6:21-25. doi: 10.1007/s001670050067
20. Grawe B, Schroeder AJ, Kakazu R, et al. Lateral collateral ligament injury about the knee: anatomy, evaluation, and management. J Am Acad Orthop Surg. 2018 15;26:e120-127. doi: 10.5435/JAAOS-D-16-00028
21. Ranawat A, Baker III CL, Henry S, et al. Posterolateral corner injury of the knee: evaluation and management. J Am Acad Orthop Surg. 2008;16:506-518.
22. Palmu S, Kallio PE, Donell ST, et al. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90:463-470. doi: 10.2106/JBJS.G.00072
23. Cohen D, Le N, Zakharia A, et al. MPFL reconstruction results in lower redislocation rates and higher functional outcomes than rehabilitation: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2022;30:3784-3795. doi: 10.1007/s00167-022-07003-5
24. Siwek CW, Rao JP. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am. 1981;63:932-937.
25. Konrath GA, Chen D, Lock T, et al. Outcomes following repair of quadriceps tendon ruptures. J Orthop Trauma. 1998;12:273-279. doi: 10.1097/00005131-199805000-00010
26. Rasul Jr. AT, Fischer DA. Primary repair of quadriceps tendon ruptures: results of treatment. Clin Orthop Relat Res. 1993;(289):205-207.
27. Rougraff BT, Reeck CC, Essenmacher J. Complete quadriceps tendon ruptures. Orthopedics. 1996;19:509-514.
28. Bui CN, Learned JR, Scolaro JA. Treatment of patellar fractures and injuries to the extensor mechanism of the knee: a critical analysis review. JBJS Rev. 2018;6:e1. doi: 10.2106/JBJS.RVW.17.00172
29. Haskel JD, Fried JW, Hurley ET, et al. High rates of return to play and work follow knee extensor tendon ruptures but low rate of return to pre-injury level of play. Knee Surg Sports Traumatol Arthrosc. 2021;29:2695-2700. doi: 10.1007/s00167-021-06537-4
30. Critchley IJ, Bracey DJ. The acutely locked knee—is a manipulation worth while? Injury. 1985;16:281-283. doi: 10.1016/s0020-1383(85)80020-6
31. Allum RL, Jones JR. The locked knee. Injury. 1986;17:256-258. doi: 10.1016/0020-1383(86)90231-7
32. Helmark IC, Neergaard K, Krogsgaard MR. Traumatic knee extension deficit (the locked knee): can MRI reduce the need for arthroscopy? Knee Surg Sports Traumatol Arthrosc. 2007;15:863-868. doi: 10.1007/s00167-006-0244-1
33. Noyes FR, Chen RC, Barber-Westin SD, et al. Greater than 10-year results of red-white longitudinal meniscal repairs in patients 20 years of age or younger. Am J Sports Med. 2011;39:1008-1017. doi: 10.1177/0363546510392014
34. Chambers HG, Shea KG, Anderson AF, et al; American Academy of Orthopedic Surgeons. Diagnosis and treatment of osteochondritis dissecans. J Am Acad Orthop Surg. 2011;19:297-306. doi: 10.5435/00124635-201105000-00007
35. Margaretten ME, Kohlwes J, Moore D, et al. Does this adult patient have septic arthritis? JAMA. 2007;297:1478-1488. doi: 10.1001/jama.297.13.1478
36. Gupta MN, Sturrock RD, Field M. A prospective 2-year study of 75 patients with adult-onset septic arthritis. Rheumatology (Oxford). 2001;40:24-30. doi: 10.1093/rheumatology/40.1.24
37. Brophy RH, Fillingham YA. AAOS clinical practice guideline summary: management of osteoarthritis of the knee (nonarthroplasty), 3rd edition. J Am Acad Orthop Surg. 2022;30:e721-729. doi: 10.5435/JAAOS-D-21-01233
38. Collins NJ, Barton CJ, van Middelkoop M, et al. 2018 Consensus statement on exercise therapy and physical interventions (orthoses, taping and manual therapy) to treat patellofemoral pain: recommendations from the 5th International Patellofemoral Pain Research Retreat, Gold Coast, Australia, 2017. Br J Sports Med. 2018;52:1170-1178. doi: 10.1136/bjsports-2018-099397
39. Strauss EJ, Kim S, Calcei JG, et al. Iliotibial band syndrome: evaluation and management. J Am Acad Orthop Surg. 2011;19:728-736. doi: 10.5435/00124635-201112000-00003
40. Millar NL, Murrell GAC, Kirwan P. Time to put down the scalpel? The role of surgery in tendinopathy. Br J Sports Med. 2020;54:441-442. doi: 10.1136/bjsports-2019-101084
41. Hall MJ, Schwartzman A, Zhang J, et al. Ambulatory surgery data from hospitals and ambulatory surgery centers: United States, 2010. Natl Health Stat Report. 2017;(102):1-15.
42. Kise NJ, Risberg MA, Stensrud S, et al. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomized controlled trial with two year follow-up. BMJ. 2016;354:i3740. doi: 10.1136/bmj.i3740
43. Sihvonen R, Paavola M, Malmivaara A, et al, FIDELITY (Finnish Degenerative Meniscus Lesion Study) Investigators. Arthroscopic partial meniscectomy for a degenerative meniscus tear: a 5 year follow-up of the placebo-surgery controlled FIDELITY (Finnish Degenerative Meniscus Lesion Study) trial. Br J Sports Med. 2020;54:1332-1339. doi: 10.1136/bjsports-2020-102813
44. Pihl K, Ensor J, Peat G, et al. Wild goose chase—no predictable patient subgroups benefit from meniscal surgery: patient-reported outcomes of 641 patients 1 year after surgery. Br J Sports Med. 2020;54:13-22. doi: 10.1136/bjsports-2018-100321
45. O’Connor D, Johnston RV, Brignardello-Petersen R, et al. Athroscopic surgery for degenerative knee disease (osteoarthritis including degenerative meniscal tears). Cochrane Database Syst Rev. 2022;3:CD014328. doi: 10.1002/14651858.CD014328
46. Siemieniuk RAC, Harris IA, Agoritsas T, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. Br J Sports Med. 2018;52:313. doi: 10.1136/bjsports-2017-j1982rep
47. Manner PA, Tubb CC, Levine BR. AAOS appropriate use criteria: surgical management of osteoarthritis of the knee. J Am Acad Orthop Surg. 2018;26:e194-197. doi: 10.5435/JAAOS-D-17-00425
PRACTICE RECOMMENDATIONS
› Consider surgical management, potentially emergently, for acute knee injuries that result in significant joint instability, unstable fractures, or neurovascular compromise. A
› Avoid arthroscopy for chronic, degenerative sources of knee pain, such as osteoarthritis and degenerative meniscus tears, as it is no longer routinely recommended. A
› Treat osteoarthritis surgically after nonsurgical treatments have failed. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Humira biosimilars: Five things to know
The best-selling drug Humira (adalimumab) now faces competition in the United States after a 20-year monopoly. The first adalimumab biosimilar, Amjevita, launched in the United States on January 31, and in July, seven additional biosimilars became available. These drugs have the potential to lower prescription drug prices, but when and by how much remains to be seen.
Here’s what you need to know about adalimumab biosimilars.
What Humira biosimilars are now available?
Eight different biosimilars have launched in 2023 with discounts as large at 85% from Humira’s list price of $6,922. A few companies also offer two price points.

Three of these biosimilars – Hadlima, Hyrimoz, and Yuflyma – are available in high concentration formulations. This high concentration formulation makes up 85% of Humira prescriptions, according to a report from Goodroot, a collection of companies focused on lowering health care costs.
Cyltezo is currently the only adalimumab biosimilar with an interchangeability designation, meaning that a pharmacist can substitute the biosimilar for an equivalent Humira prescription without the intervention of a clinician. A total of 47 states allow for these substitutions without prior approval from a clinician, according to Goodroot, and the clinician must be notified of the switch within a certain time frame. A total of 40 states require that patients be notified of the switch before substitution.
However, it’s not clear if this interchangeability designation will prove an advantage for Cyltezo, as it is interchangeable with the lower concentration version of Humira that makes up just 15% of prescriptions.
Most of the companies behind these biosimilars are pursuing interchangeability designations for their drugs, except for Fresenius Kabi (Idacio) and Coherus (Yusimry).
A ninth biosimilar, Pfizer’s adalimumab-afzb (Abrilada), is not yet on the market and is currently awaiting an approval decision from the Food and Drug Administration to add an interchangeability designation to its prior approval for a low-concentration formulation.
Why are they priced differently?
The two price points offer different deals to payers. Pharmacy benefit managers make confidential agreements with drug manufacturers to get a discount – called a rebate – to get the drug on the PBM’s formulary. The PBM keeps a portion of that rebate, and the rest is passed on to the insurance company and patients. Biosimilars at a higher price point will likely offer larger rebates. Biosimilars offered at lower price points incorporate this discount up front in their list pricing and likely will not offer large rebates.
Will biosimilars be covered by payers?
Currently, biosimilars are being offered on formularies at parity with Humira, meaning they are on the same tier. The PBM companies OptumRx and Cigna Group’s Express Scripts will offer Amjevita (at both price points), Cyltezo, and Hyrimoz (at both price points).
“This decision allows our clients flexibility to provide access to the lower list price, so members in high-deductible plans and benefit designs with coinsurance can experience lower out-of-pocket costs,” said OptumRx spokesperson Isaac Sorensen in an email.
Mark Cuban Cost Plus Drug Company, which uses a direct-to-consumer model, will offer Yusimry for $567.27 on its website. SmithRx, a PBM based in San Francisco, announced it would partner with Cost Plus Drugs to offer Yusimry, adding that SmithRx members can use their insurance benefits to further reduce out-of-pocket costs. RxPreferred, another PBM, will also offer Yusimry through its partnership with Cuban’s company.
The news website Formulary Watch previously reported that CVS Caremark, another of the biggest PBMs, will be offering Amjevita, but as a nonpreferred brand, while Humira remains the preferred brand. CVS Caremark did not respond to a request for comment.
Will patients pay less?
Biosimilars have been touted as a potential solution to lower spending on biologic drugs, but it’s unknown if patients will ultimately benefit with lower out-of-pocket costs. It’s “impossible to predict” if the discount that third-party payers pay will be passed on to consumers, said Mark Fendrick, MD, who directs the University of Michigan Center for Value-based Insurance Design in Ann Arbor.
Generally, a consumer’s copay is a percentage of a drug’s list price, so it stands to reason that a low drug price would result in lower out-of-pocket payments. While this is mostly true, Humira has a successful copay assistance program to lower prescription costs for consumers. According to a 2022 IQVIA report, 82% of commercial prescriptions cost patients less than $10 for Humira because of this program.
To appeal to patients, biosimilar companies will need to offer similar savings, Dr. Fendrick added. “There will be some discontent if patients are actually asked to pay more out-of-pocket for a less expensive drug,” he said.
All eight companies behind these biosimilars are offering or will be launching copay saving programs, many which advertise copays as low as $0 per month for eligible patients.
How will Humira respond?
Marta Wosińska, PhD, a health care economist at the Brookings Institute, Washington, predicts payers will use these lower biosimilar prices to negotiate better deals with AbbVie, Humira’s manufacturer. “We have a lot of players coming into [the market] right now, so the competition is really fierce,” she said. In response, AbbVie will need to increase rebates on Humira and/or lower its price to compete with these biosimilars.
“The ball is in AbbVie’s court,” she said. “If [the company] is not willing to drop price sufficiently, then payers will start switching to biosimilars.”
Dr. Fendrick reported past financial relationships and consulting arrangements with AbbVie, Amgen, Arnold Ventures, Bayer, CareFirst, BlueCross BlueShield, and many other companies. Dr. Wosińska has received funding from Arnold Ventures and serves as an expert witness on antitrust cases involving generic medication.
A version of this article first appeared on Medscape.com.
The best-selling drug Humira (adalimumab) now faces competition in the United States after a 20-year monopoly. The first adalimumab biosimilar, Amjevita, launched in the United States on January 31, and in July, seven additional biosimilars became available. These drugs have the potential to lower prescription drug prices, but when and by how much remains to be seen.
Here’s what you need to know about adalimumab biosimilars.
What Humira biosimilars are now available?
Eight different biosimilars have launched in 2023 with discounts as large at 85% from Humira’s list price of $6,922. A few companies also offer two price points.

Three of these biosimilars – Hadlima, Hyrimoz, and Yuflyma – are available in high concentration formulations. This high concentration formulation makes up 85% of Humira prescriptions, according to a report from Goodroot, a collection of companies focused on lowering health care costs.
Cyltezo is currently the only adalimumab biosimilar with an interchangeability designation, meaning that a pharmacist can substitute the biosimilar for an equivalent Humira prescription without the intervention of a clinician. A total of 47 states allow for these substitutions without prior approval from a clinician, according to Goodroot, and the clinician must be notified of the switch within a certain time frame. A total of 40 states require that patients be notified of the switch before substitution.
However, it’s not clear if this interchangeability designation will prove an advantage for Cyltezo, as it is interchangeable with the lower concentration version of Humira that makes up just 15% of prescriptions.
Most of the companies behind these biosimilars are pursuing interchangeability designations for their drugs, except for Fresenius Kabi (Idacio) and Coherus (Yusimry).
A ninth biosimilar, Pfizer’s adalimumab-afzb (Abrilada), is not yet on the market and is currently awaiting an approval decision from the Food and Drug Administration to add an interchangeability designation to its prior approval for a low-concentration formulation.
Why are they priced differently?
The two price points offer different deals to payers. Pharmacy benefit managers make confidential agreements with drug manufacturers to get a discount – called a rebate – to get the drug on the PBM’s formulary. The PBM keeps a portion of that rebate, and the rest is passed on to the insurance company and patients. Biosimilars at a higher price point will likely offer larger rebates. Biosimilars offered at lower price points incorporate this discount up front in their list pricing and likely will not offer large rebates.
Will biosimilars be covered by payers?
Currently, biosimilars are being offered on formularies at parity with Humira, meaning they are on the same tier. The PBM companies OptumRx and Cigna Group’s Express Scripts will offer Amjevita (at both price points), Cyltezo, and Hyrimoz (at both price points).
“This decision allows our clients flexibility to provide access to the lower list price, so members in high-deductible plans and benefit designs with coinsurance can experience lower out-of-pocket costs,” said OptumRx spokesperson Isaac Sorensen in an email.
Mark Cuban Cost Plus Drug Company, which uses a direct-to-consumer model, will offer Yusimry for $567.27 on its website. SmithRx, a PBM based in San Francisco, announced it would partner with Cost Plus Drugs to offer Yusimry, adding that SmithRx members can use their insurance benefits to further reduce out-of-pocket costs. RxPreferred, another PBM, will also offer Yusimry through its partnership with Cuban’s company.
The news website Formulary Watch previously reported that CVS Caremark, another of the biggest PBMs, will be offering Amjevita, but as a nonpreferred brand, while Humira remains the preferred brand. CVS Caremark did not respond to a request for comment.
Will patients pay less?
Biosimilars have been touted as a potential solution to lower spending on biologic drugs, but it’s unknown if patients will ultimately benefit with lower out-of-pocket costs. It’s “impossible to predict” if the discount that third-party payers pay will be passed on to consumers, said Mark Fendrick, MD, who directs the University of Michigan Center for Value-based Insurance Design in Ann Arbor.
Generally, a consumer’s copay is a percentage of a drug’s list price, so it stands to reason that a low drug price would result in lower out-of-pocket payments. While this is mostly true, Humira has a successful copay assistance program to lower prescription costs for consumers. According to a 2022 IQVIA report, 82% of commercial prescriptions cost patients less than $10 for Humira because of this program.
To appeal to patients, biosimilar companies will need to offer similar savings, Dr. Fendrick added. “There will be some discontent if patients are actually asked to pay more out-of-pocket for a less expensive drug,” he said.
All eight companies behind these biosimilars are offering or will be launching copay saving programs, many which advertise copays as low as $0 per month for eligible patients.
How will Humira respond?
Marta Wosińska, PhD, a health care economist at the Brookings Institute, Washington, predicts payers will use these lower biosimilar prices to negotiate better deals with AbbVie, Humira’s manufacturer. “We have a lot of players coming into [the market] right now, so the competition is really fierce,” she said. In response, AbbVie will need to increase rebates on Humira and/or lower its price to compete with these biosimilars.
“The ball is in AbbVie’s court,” she said. “If [the company] is not willing to drop price sufficiently, then payers will start switching to biosimilars.”
Dr. Fendrick reported past financial relationships and consulting arrangements with AbbVie, Amgen, Arnold Ventures, Bayer, CareFirst, BlueCross BlueShield, and many other companies. Dr. Wosińska has received funding from Arnold Ventures and serves as an expert witness on antitrust cases involving generic medication.
A version of this article first appeared on Medscape.com.
The best-selling drug Humira (adalimumab) now faces competition in the United States after a 20-year monopoly. The first adalimumab biosimilar, Amjevita, launched in the United States on January 31, and in July, seven additional biosimilars became available. These drugs have the potential to lower prescription drug prices, but when and by how much remains to be seen.
Here’s what you need to know about adalimumab biosimilars.
What Humira biosimilars are now available?
Eight different biosimilars have launched in 2023 with discounts as large at 85% from Humira’s list price of $6,922. A few companies also offer two price points.

Three of these biosimilars – Hadlima, Hyrimoz, and Yuflyma – are available in high concentration formulations. This high concentration formulation makes up 85% of Humira prescriptions, according to a report from Goodroot, a collection of companies focused on lowering health care costs.
Cyltezo is currently the only adalimumab biosimilar with an interchangeability designation, meaning that a pharmacist can substitute the biosimilar for an equivalent Humira prescription without the intervention of a clinician. A total of 47 states allow for these substitutions without prior approval from a clinician, according to Goodroot, and the clinician must be notified of the switch within a certain time frame. A total of 40 states require that patients be notified of the switch before substitution.
However, it’s not clear if this interchangeability designation will prove an advantage for Cyltezo, as it is interchangeable with the lower concentration version of Humira that makes up just 15% of prescriptions.
Most of the companies behind these biosimilars are pursuing interchangeability designations for their drugs, except for Fresenius Kabi (Idacio) and Coherus (Yusimry).
A ninth biosimilar, Pfizer’s adalimumab-afzb (Abrilada), is not yet on the market and is currently awaiting an approval decision from the Food and Drug Administration to add an interchangeability designation to its prior approval for a low-concentration formulation.
Why are they priced differently?
The two price points offer different deals to payers. Pharmacy benefit managers make confidential agreements with drug manufacturers to get a discount – called a rebate – to get the drug on the PBM’s formulary. The PBM keeps a portion of that rebate, and the rest is passed on to the insurance company and patients. Biosimilars at a higher price point will likely offer larger rebates. Biosimilars offered at lower price points incorporate this discount up front in their list pricing and likely will not offer large rebates.
Will biosimilars be covered by payers?
Currently, biosimilars are being offered on formularies at parity with Humira, meaning they are on the same tier. The PBM companies OptumRx and Cigna Group’s Express Scripts will offer Amjevita (at both price points), Cyltezo, and Hyrimoz (at both price points).
“This decision allows our clients flexibility to provide access to the lower list price, so members in high-deductible plans and benefit designs with coinsurance can experience lower out-of-pocket costs,” said OptumRx spokesperson Isaac Sorensen in an email.
Mark Cuban Cost Plus Drug Company, which uses a direct-to-consumer model, will offer Yusimry for $567.27 on its website. SmithRx, a PBM based in San Francisco, announced it would partner with Cost Plus Drugs to offer Yusimry, adding that SmithRx members can use their insurance benefits to further reduce out-of-pocket costs. RxPreferred, another PBM, will also offer Yusimry through its partnership with Cuban’s company.
The news website Formulary Watch previously reported that CVS Caremark, another of the biggest PBMs, will be offering Amjevita, but as a nonpreferred brand, while Humira remains the preferred brand. CVS Caremark did not respond to a request for comment.
Will patients pay less?
Biosimilars have been touted as a potential solution to lower spending on biologic drugs, but it’s unknown if patients will ultimately benefit with lower out-of-pocket costs. It’s “impossible to predict” if the discount that third-party payers pay will be passed on to consumers, said Mark Fendrick, MD, who directs the University of Michigan Center for Value-based Insurance Design in Ann Arbor.
Generally, a consumer’s copay is a percentage of a drug’s list price, so it stands to reason that a low drug price would result in lower out-of-pocket payments. While this is mostly true, Humira has a successful copay assistance program to lower prescription costs for consumers. According to a 2022 IQVIA report, 82% of commercial prescriptions cost patients less than $10 for Humira because of this program.
To appeal to patients, biosimilar companies will need to offer similar savings, Dr. Fendrick added. “There will be some discontent if patients are actually asked to pay more out-of-pocket for a less expensive drug,” he said.
All eight companies behind these biosimilars are offering or will be launching copay saving programs, many which advertise copays as low as $0 per month for eligible patients.
How will Humira respond?
Marta Wosińska, PhD, a health care economist at the Brookings Institute, Washington, predicts payers will use these lower biosimilar prices to negotiate better deals with AbbVie, Humira’s manufacturer. “We have a lot of players coming into [the market] right now, so the competition is really fierce,” she said. In response, AbbVie will need to increase rebates on Humira and/or lower its price to compete with these biosimilars.
“The ball is in AbbVie’s court,” she said. “If [the company] is not willing to drop price sufficiently, then payers will start switching to biosimilars.”
Dr. Fendrick reported past financial relationships and consulting arrangements with AbbVie, Amgen, Arnold Ventures, Bayer, CareFirst, BlueCross BlueShield, and many other companies. Dr. Wosińska has received funding from Arnold Ventures and serves as an expert witness on antitrust cases involving generic medication.
A version of this article first appeared on Medscape.com.
All in stride: Few age limitations for joint replacement
Kathy Blackwell is not going to allow a couple of aching joints stop her from living her best life.
The 73-year-old resident of Simi Valley, Calif., a bedroom community about 30 miles northwest of downtown Los Angeles, organizes regular activities for her group of seniors. The 20- to 30-member-strong band of seasoned citizens, mostly women, keep active. Over the coming weeks, they plan to catch the Beach Boys at the historic Hollywood Bowl and take a cruise to Alaska.
The busy schedule is why Ms. Blackwell intends to delay her second hip replacement surgery, opting instead for a cortisone shot in hopes of easing the pain enough to enjoy the upcoming excursions.
Not that she is shy about joint replacement. If her orthopedic surgeon offered a frequent customer punch card like the ones you get at the local coffee shop, hers would be nearly full. Ms. Blackwell’s knees and a hip have been replaced, and her other hip will be, too, once her calendar clears up.
“If you go on enough with chronic pain where there’s no relief, you get cranky,” Ms. Blackwell said.
More than 1 million new knees, hips
Joint replacements are getting more common, with about 790,000 total knee replacements and more than 450,000 hip replacements performed annually in the United States, according to the American College of Rheumatology.
Experts agree age is not a factor when considering candidates for joint replacement. Rafael Sierra, MD, of the Mayo Clinic, Rochester, Minn., said he’s done hip replacements on patients as young as 12 and as old as 102. Orthopedic surgeon John Wang, MD, of the Hospital for Special Surgery, New York, has performed a total knee arthroscopy on a patient in their mid-90s. At 73, Ms. Blackwell is on the older side of the average age of 66 for a hip replacement.
“A lot of research and studies have shown that no matter what the age ranges, people end up doing great,” Dr. Wang said.
More importantly than age, older patients should be prepared for postsurgery therapy and treatment. For younger patients, the biggest drawback is outliving the estimated 25-year life span of a joint replacement. Complications are rare and occur in about 2% of procedures. These include infection, dislocation of the joint, and blood clots; other health issues you also have are not a factor.
Considering Ms. Blackwell’s hard time with her first knee replacement, it’s no small wonder that she ever set foot in a surgeon’s office again.
After putting it off for 7 years, Ms. Blackwell finally agreed to her doctor’s advice to replace her left knee in 2017 to relieve what she described as a “grinding,” chronic, bone-on-bone pain.
“It got to the point where there were no alternatives,” she said.
But her first orthopedic surgeon did a “lousy job,” leaving her with a gaping, festering wound that resulted in sepsis and required wound vacuum therapy to close the lesion. She eventually found another surgeon who removed and cleaned up her artificial knee before replacing the prosthesis. Luckily, the sepsis didn’t spread, and eight surgeries later, she was in the clear.
Ms. Blackwell’s second knee replacement in 2018 was a textbook surgery, as was a hip replacement in late 2019 .
“Your whole attitude changes,” she said.
What generalists should know
Orthopedic surgeons recommend that primary care doctors ask two things when weighing joint replacements: Have they exhausted nonsurgical treatments, and is the pain intolerable? They also advise avoiding narcotics to treat the symptoms.
The top issue to consider for a primary care doctor when weighing whether their patient may be a candidate for joint replacement is if the pain and the imaging are bad enough to warrant surgery.
“You don’t want to do it too soon,” Dr. Sierra said.
Dr. Sierra likes to tell the story of the golfer whose knee stiffens after playing 18 holes. To those patients, he recommends dialing back the activity; in this case, using a cart or playing only nine holes.
Dr. Wang agrees, asking if the pain is “lifestyle altering” and if the patient was unresponsive to nonsurgical treatments such as over-the-counter medications, anti-inflammatory medication and shots, home exercises or physical therapy, wearing a brace or sleeve, or simply changing their activity.
And no addictive pain pills to treat arthritis that can lead to other serious issues.
“This is not going to heal itself,” Dr. Wang said. “It’s not going to improve on its own. So, we don’t want to throw narcotics at it just to cover it up.”
Karen Smith, MD, has been a family doctor in rural North Carolina for more than 30 years. When she sees patients complaining about their joints, she first looks at function and pain. From there, she explores why they’re having discomfort. For example, is the problem an ergonomic issue at work or the result of carrying a lot of body weight?
“We look at those areas to determine what can be modified,” she said. “All of that’s done even before we get to having the orthopedic involvement.”
Dr. Smith said she also considers things beyond basic medicine: What is the patient’s mental status and tolerance for pain? Do they have a support system at home for post-operative care? And can they afford to miss work?
“We look at all of those factors together because that is going to determine the outcome that we’re hoping to achieve,” Dr. Smith said.
Great expectations
A recent study shows that older patients respond better to knee replacements than younger patients, particularly with pain relief and quality of life. The reason for this is believed to boil down to expectations. Whereas a younger person may want to return to the racquetball court and perform like they used to, older patients may just wish to walk down the hall without discomfort.
“It’s possible that these under 55-age-old patients may just take a little longer to heal to be satisfied,” Dr. Wang said. “We really can’t speak to why this is happening, but it’s possible that the younger patients are more active, and they expect more out of their knee.”
Jeevan Sall, MD, is a primary care sports medicine doctor with Providence Mission Heritage Medical Group in Laguna Niguel, Calif. He first discusses conservative management for patients struggling with arthritis in their joints. These measures include rehabilitation exercises, braces, shoe inserts, medication, and weight loss efforts. If these steps don’t improve a patient’s pain or lifestyle, surgery is on the table. Managing expectations is a significant factor.
“Is the patient mentally ready for surgery?” Dr. Sall said. “This includes what they hope to achieve with surgery as well as the risk and benefits of the procedure.”
Ms. Blackwell’s hip and knee pain came simply from a life well lived, with no marathon running or life-changing accident to speak of. She worked as a housewife raising her two children and owned an elevator company with her late husband, Robert Blackwell.
Yes, the elevator construction business has jokes.
“We have our ups and downs,” Ms. Blackwell said.
And with her new joints, so does she.
A version of this article first appeared on WebMD.com.
Kathy Blackwell is not going to allow a couple of aching joints stop her from living her best life.
The 73-year-old resident of Simi Valley, Calif., a bedroom community about 30 miles northwest of downtown Los Angeles, organizes regular activities for her group of seniors. The 20- to 30-member-strong band of seasoned citizens, mostly women, keep active. Over the coming weeks, they plan to catch the Beach Boys at the historic Hollywood Bowl and take a cruise to Alaska.
The busy schedule is why Ms. Blackwell intends to delay her second hip replacement surgery, opting instead for a cortisone shot in hopes of easing the pain enough to enjoy the upcoming excursions.
Not that she is shy about joint replacement. If her orthopedic surgeon offered a frequent customer punch card like the ones you get at the local coffee shop, hers would be nearly full. Ms. Blackwell’s knees and a hip have been replaced, and her other hip will be, too, once her calendar clears up.
“If you go on enough with chronic pain where there’s no relief, you get cranky,” Ms. Blackwell said.
More than 1 million new knees, hips
Joint replacements are getting more common, with about 790,000 total knee replacements and more than 450,000 hip replacements performed annually in the United States, according to the American College of Rheumatology.
Experts agree age is not a factor when considering candidates for joint replacement. Rafael Sierra, MD, of the Mayo Clinic, Rochester, Minn., said he’s done hip replacements on patients as young as 12 and as old as 102. Orthopedic surgeon John Wang, MD, of the Hospital for Special Surgery, New York, has performed a total knee arthroscopy on a patient in their mid-90s. At 73, Ms. Blackwell is on the older side of the average age of 66 for a hip replacement.
“A lot of research and studies have shown that no matter what the age ranges, people end up doing great,” Dr. Wang said.
More importantly than age, older patients should be prepared for postsurgery therapy and treatment. For younger patients, the biggest drawback is outliving the estimated 25-year life span of a joint replacement. Complications are rare and occur in about 2% of procedures. These include infection, dislocation of the joint, and blood clots; other health issues you also have are not a factor.
Considering Ms. Blackwell’s hard time with her first knee replacement, it’s no small wonder that she ever set foot in a surgeon’s office again.
After putting it off for 7 years, Ms. Blackwell finally agreed to her doctor’s advice to replace her left knee in 2017 to relieve what she described as a “grinding,” chronic, bone-on-bone pain.
“It got to the point where there were no alternatives,” she said.
But her first orthopedic surgeon did a “lousy job,” leaving her with a gaping, festering wound that resulted in sepsis and required wound vacuum therapy to close the lesion. She eventually found another surgeon who removed and cleaned up her artificial knee before replacing the prosthesis. Luckily, the sepsis didn’t spread, and eight surgeries later, she was in the clear.
Ms. Blackwell’s second knee replacement in 2018 was a textbook surgery, as was a hip replacement in late 2019 .
“Your whole attitude changes,” she said.
What generalists should know
Orthopedic surgeons recommend that primary care doctors ask two things when weighing joint replacements: Have they exhausted nonsurgical treatments, and is the pain intolerable? They also advise avoiding narcotics to treat the symptoms.
The top issue to consider for a primary care doctor when weighing whether their patient may be a candidate for joint replacement is if the pain and the imaging are bad enough to warrant surgery.
“You don’t want to do it too soon,” Dr. Sierra said.
Dr. Sierra likes to tell the story of the golfer whose knee stiffens after playing 18 holes. To those patients, he recommends dialing back the activity; in this case, using a cart or playing only nine holes.
Dr. Wang agrees, asking if the pain is “lifestyle altering” and if the patient was unresponsive to nonsurgical treatments such as over-the-counter medications, anti-inflammatory medication and shots, home exercises or physical therapy, wearing a brace or sleeve, or simply changing their activity.
And no addictive pain pills to treat arthritis that can lead to other serious issues.
“This is not going to heal itself,” Dr. Wang said. “It’s not going to improve on its own. So, we don’t want to throw narcotics at it just to cover it up.”
Karen Smith, MD, has been a family doctor in rural North Carolina for more than 30 years. When she sees patients complaining about their joints, she first looks at function and pain. From there, she explores why they’re having discomfort. For example, is the problem an ergonomic issue at work or the result of carrying a lot of body weight?
“We look at those areas to determine what can be modified,” she said. “All of that’s done even before we get to having the orthopedic involvement.”
Dr. Smith said she also considers things beyond basic medicine: What is the patient’s mental status and tolerance for pain? Do they have a support system at home for post-operative care? And can they afford to miss work?
“We look at all of those factors together because that is going to determine the outcome that we’re hoping to achieve,” Dr. Smith said.
Great expectations
A recent study shows that older patients respond better to knee replacements than younger patients, particularly with pain relief and quality of life. The reason for this is believed to boil down to expectations. Whereas a younger person may want to return to the racquetball court and perform like they used to, older patients may just wish to walk down the hall without discomfort.
“It’s possible that these under 55-age-old patients may just take a little longer to heal to be satisfied,” Dr. Wang said. “We really can’t speak to why this is happening, but it’s possible that the younger patients are more active, and they expect more out of their knee.”
Jeevan Sall, MD, is a primary care sports medicine doctor with Providence Mission Heritage Medical Group in Laguna Niguel, Calif. He first discusses conservative management for patients struggling with arthritis in their joints. These measures include rehabilitation exercises, braces, shoe inserts, medication, and weight loss efforts. If these steps don’t improve a patient’s pain or lifestyle, surgery is on the table. Managing expectations is a significant factor.
“Is the patient mentally ready for surgery?” Dr. Sall said. “This includes what they hope to achieve with surgery as well as the risk and benefits of the procedure.”
Ms. Blackwell’s hip and knee pain came simply from a life well lived, with no marathon running or life-changing accident to speak of. She worked as a housewife raising her two children and owned an elevator company with her late husband, Robert Blackwell.
Yes, the elevator construction business has jokes.
“We have our ups and downs,” Ms. Blackwell said.
And with her new joints, so does she.
A version of this article first appeared on WebMD.com.
Kathy Blackwell is not going to allow a couple of aching joints stop her from living her best life.
The 73-year-old resident of Simi Valley, Calif., a bedroom community about 30 miles northwest of downtown Los Angeles, organizes regular activities for her group of seniors. The 20- to 30-member-strong band of seasoned citizens, mostly women, keep active. Over the coming weeks, they plan to catch the Beach Boys at the historic Hollywood Bowl and take a cruise to Alaska.
The busy schedule is why Ms. Blackwell intends to delay her second hip replacement surgery, opting instead for a cortisone shot in hopes of easing the pain enough to enjoy the upcoming excursions.
Not that she is shy about joint replacement. If her orthopedic surgeon offered a frequent customer punch card like the ones you get at the local coffee shop, hers would be nearly full. Ms. Blackwell’s knees and a hip have been replaced, and her other hip will be, too, once her calendar clears up.
“If you go on enough with chronic pain where there’s no relief, you get cranky,” Ms. Blackwell said.
More than 1 million new knees, hips
Joint replacements are getting more common, with about 790,000 total knee replacements and more than 450,000 hip replacements performed annually in the United States, according to the American College of Rheumatology.
Experts agree age is not a factor when considering candidates for joint replacement. Rafael Sierra, MD, of the Mayo Clinic, Rochester, Minn., said he’s done hip replacements on patients as young as 12 and as old as 102. Orthopedic surgeon John Wang, MD, of the Hospital for Special Surgery, New York, has performed a total knee arthroscopy on a patient in their mid-90s. At 73, Ms. Blackwell is on the older side of the average age of 66 for a hip replacement.
“A lot of research and studies have shown that no matter what the age ranges, people end up doing great,” Dr. Wang said.
More importantly than age, older patients should be prepared for postsurgery therapy and treatment. For younger patients, the biggest drawback is outliving the estimated 25-year life span of a joint replacement. Complications are rare and occur in about 2% of procedures. These include infection, dislocation of the joint, and blood clots; other health issues you also have are not a factor.
Considering Ms. Blackwell’s hard time with her first knee replacement, it’s no small wonder that she ever set foot in a surgeon’s office again.
After putting it off for 7 years, Ms. Blackwell finally agreed to her doctor’s advice to replace her left knee in 2017 to relieve what she described as a “grinding,” chronic, bone-on-bone pain.
“It got to the point where there were no alternatives,” she said.
But her first orthopedic surgeon did a “lousy job,” leaving her with a gaping, festering wound that resulted in sepsis and required wound vacuum therapy to close the lesion. She eventually found another surgeon who removed and cleaned up her artificial knee before replacing the prosthesis. Luckily, the sepsis didn’t spread, and eight surgeries later, she was in the clear.
Ms. Blackwell’s second knee replacement in 2018 was a textbook surgery, as was a hip replacement in late 2019 .
“Your whole attitude changes,” she said.
What generalists should know
Orthopedic surgeons recommend that primary care doctors ask two things when weighing joint replacements: Have they exhausted nonsurgical treatments, and is the pain intolerable? They also advise avoiding narcotics to treat the symptoms.
The top issue to consider for a primary care doctor when weighing whether their patient may be a candidate for joint replacement is if the pain and the imaging are bad enough to warrant surgery.
“You don’t want to do it too soon,” Dr. Sierra said.
Dr. Sierra likes to tell the story of the golfer whose knee stiffens after playing 18 holes. To those patients, he recommends dialing back the activity; in this case, using a cart or playing only nine holes.
Dr. Wang agrees, asking if the pain is “lifestyle altering” and if the patient was unresponsive to nonsurgical treatments such as over-the-counter medications, anti-inflammatory medication and shots, home exercises or physical therapy, wearing a brace or sleeve, or simply changing their activity.
And no addictive pain pills to treat arthritis that can lead to other serious issues.
“This is not going to heal itself,” Dr. Wang said. “It’s not going to improve on its own. So, we don’t want to throw narcotics at it just to cover it up.”
Karen Smith, MD, has been a family doctor in rural North Carolina for more than 30 years. When she sees patients complaining about their joints, she first looks at function and pain. From there, she explores why they’re having discomfort. For example, is the problem an ergonomic issue at work or the result of carrying a lot of body weight?
“We look at those areas to determine what can be modified,” she said. “All of that’s done even before we get to having the orthopedic involvement.”
Dr. Smith said she also considers things beyond basic medicine: What is the patient’s mental status and tolerance for pain? Do they have a support system at home for post-operative care? And can they afford to miss work?
“We look at all of those factors together because that is going to determine the outcome that we’re hoping to achieve,” Dr. Smith said.
Great expectations
A recent study shows that older patients respond better to knee replacements than younger patients, particularly with pain relief and quality of life. The reason for this is believed to boil down to expectations. Whereas a younger person may want to return to the racquetball court and perform like they used to, older patients may just wish to walk down the hall without discomfort.
“It’s possible that these under 55-age-old patients may just take a little longer to heal to be satisfied,” Dr. Wang said. “We really can’t speak to why this is happening, but it’s possible that the younger patients are more active, and they expect more out of their knee.”
Jeevan Sall, MD, is a primary care sports medicine doctor with Providence Mission Heritage Medical Group in Laguna Niguel, Calif. He first discusses conservative management for patients struggling with arthritis in their joints. These measures include rehabilitation exercises, braces, shoe inserts, medication, and weight loss efforts. If these steps don’t improve a patient’s pain or lifestyle, surgery is on the table. Managing expectations is a significant factor.
“Is the patient mentally ready for surgery?” Dr. Sall said. “This includes what they hope to achieve with surgery as well as the risk and benefits of the procedure.”
Ms. Blackwell’s hip and knee pain came simply from a life well lived, with no marathon running or life-changing accident to speak of. She worked as a housewife raising her two children and owned an elevator company with her late husband, Robert Blackwell.
Yes, the elevator construction business has jokes.
“We have our ups and downs,” Ms. Blackwell said.
And with her new joints, so does she.
A version of this article first appeared on WebMD.com.
‘Landmark’ trial shows opioids for back, neck pain no better than placebo
Opioids do not relieve acute low back or neck pain in the short term and lead to worse outcomes in the long term, results of the first randomized controlled trial testing the efficacy and safety of a short course of opioids for acute nonspecific low back/neck pain suggest.
After 6 weeks, there was no significant difference in pain scores of patients who took opioids, compared with those who took placebo. After 1 year, patients given the placebo had slightly lower pain scores. Also, patients using opioids were at greater risk of opioid misuse after 1 year.
This is a “landmark” trial with “practice-changing” results, senior author Christine Lin, PhD, with the University of Sydney, told this news organization.
“Before this trial, we did not have good evidence on whether opioids were effective for acute low back pain or neck pain, yet opioids were one of the most commonly used medicines for these conditions,” Dr. Lin explained.
On the basis of these results, “opioids should not be recommended at all for acute low back pain and neck pain,” Dr. Lin said.
Results of the OPAL study were published online in The Lancet.
Rigorous trial
The trial was conducted in 157 primary care or emergency department sites in Australia and involved 347 adults who had been experiencing low back pain, neck pain, or both for 12 weeks or less.
They were randomly allocated (1:1) to receive guideline-recommended care (reassurance and advice to stay active) plus an opioid (oxycodone up to 20 mg daily) or identical placebo for up to 6 weeks. Naloxone was provided to help prevent opioid-induced constipation and improve blinding.
The primary outcome was pain severity at 6 weeks, measured with the pain severity subscale of the Brief Pain Inventory (10-point scale).
After 6 weeks, opioid therapy offered no more relief for acute back/neck pain or functional improvement than placebo.
The mean pain score at 6 weeks was 2.78 in the opioid group, versus 2.25 in the placebo group (adjusted mean difference, 0.53; 95% confidence interval, –0.00 to 1.07; P = .051). At 1 year, mean pain scores in the placebo group were slightly lower than in the opioid group (1.8 vs. 2.4).
In addition, there was a doubling of the risk of opioid misuse at 1 year among patients randomly allocated to receive opioid therapy for 6 weeks, compared with those allocated to receive placebo for 6 weeks.
At 1 year, 24 (20%) of 123 of the patients who received opioids were at risk of misuse, as indicated by the Current Opioid Misuse Measure scale, compared with 13 (10%) of 128 patients in the placebo group (P = .049). The COMM is a widely used measure of current aberrant drug-related behavior among patients with chronic pain who are being prescribed opioid therapy.
Results raise ‘serious questions’
“I believe the findings of the study will need to be disseminated to the doctors and patients, so they receive this latest evidence on opioids,” Dr. Lin said in an interview.
“We need to reassure doctors and patients that most people with acute low back pain and neck pain recover well with time (usually by 6 weeks), so management is simple – staying active, avoiding bed rest, and, if necessary, using a heat pack for short term pain relief. If drugs are required, consider anti-inflammatory drugs,” Dr. Lin added.
The authors of a linked comment say the OPAL trial “raises serious questions about the use of opioid therapy for acute low back and neck pain.”
Mark Sullivan, MD, PhD, and Jane Ballantyne, MD, with the University of Washington, Seattle, note that current clinical guidelines recommend opioids for patients with acute back and neck pain when other drug treatments fail or are contraindicated.
“As many as two-thirds of patients might receive an opioid when presenting for care of back or neck pain. It is time to re-examine these guidelines and these practices,” Dr. Sullivan and Dr. Ballantyne conclude.
Funding for the OPAL study was provided by the National Health and Medical Research Council, the University of Sydney Faculty of Medicine and Health, and SafeWork SA. The study authors have disclosed no relevant financial relationships. Dr. Sullivan and Dr. Ballantyne are board members (unpaid) of Physicians for Responsible Opioid Prescribing and have been paid consultants in opioid litigation.
A version of this article originally appeared on Medscape.com.
Opioids do not relieve acute low back or neck pain in the short term and lead to worse outcomes in the long term, results of the first randomized controlled trial testing the efficacy and safety of a short course of opioids for acute nonspecific low back/neck pain suggest.
After 6 weeks, there was no significant difference in pain scores of patients who took opioids, compared with those who took placebo. After 1 year, patients given the placebo had slightly lower pain scores. Also, patients using opioids were at greater risk of opioid misuse after 1 year.
This is a “landmark” trial with “practice-changing” results, senior author Christine Lin, PhD, with the University of Sydney, told this news organization.
“Before this trial, we did not have good evidence on whether opioids were effective for acute low back pain or neck pain, yet opioids were one of the most commonly used medicines for these conditions,” Dr. Lin explained.
On the basis of these results, “opioids should not be recommended at all for acute low back pain and neck pain,” Dr. Lin said.
Results of the OPAL study were published online in The Lancet.
Rigorous trial
The trial was conducted in 157 primary care or emergency department sites in Australia and involved 347 adults who had been experiencing low back pain, neck pain, or both for 12 weeks or less.
They were randomly allocated (1:1) to receive guideline-recommended care (reassurance and advice to stay active) plus an opioid (oxycodone up to 20 mg daily) or identical placebo for up to 6 weeks. Naloxone was provided to help prevent opioid-induced constipation and improve blinding.
The primary outcome was pain severity at 6 weeks, measured with the pain severity subscale of the Brief Pain Inventory (10-point scale).
After 6 weeks, opioid therapy offered no more relief for acute back/neck pain or functional improvement than placebo.
The mean pain score at 6 weeks was 2.78 in the opioid group, versus 2.25 in the placebo group (adjusted mean difference, 0.53; 95% confidence interval, –0.00 to 1.07; P = .051). At 1 year, mean pain scores in the placebo group were slightly lower than in the opioid group (1.8 vs. 2.4).
In addition, there was a doubling of the risk of opioid misuse at 1 year among patients randomly allocated to receive opioid therapy for 6 weeks, compared with those allocated to receive placebo for 6 weeks.
At 1 year, 24 (20%) of 123 of the patients who received opioids were at risk of misuse, as indicated by the Current Opioid Misuse Measure scale, compared with 13 (10%) of 128 patients in the placebo group (P = .049). The COMM is a widely used measure of current aberrant drug-related behavior among patients with chronic pain who are being prescribed opioid therapy.
Results raise ‘serious questions’
“I believe the findings of the study will need to be disseminated to the doctors and patients, so they receive this latest evidence on opioids,” Dr. Lin said in an interview.
“We need to reassure doctors and patients that most people with acute low back pain and neck pain recover well with time (usually by 6 weeks), so management is simple – staying active, avoiding bed rest, and, if necessary, using a heat pack for short term pain relief. If drugs are required, consider anti-inflammatory drugs,” Dr. Lin added.
The authors of a linked comment say the OPAL trial “raises serious questions about the use of opioid therapy for acute low back and neck pain.”
Mark Sullivan, MD, PhD, and Jane Ballantyne, MD, with the University of Washington, Seattle, note that current clinical guidelines recommend opioids for patients with acute back and neck pain when other drug treatments fail or are contraindicated.
“As many as two-thirds of patients might receive an opioid when presenting for care of back or neck pain. It is time to re-examine these guidelines and these practices,” Dr. Sullivan and Dr. Ballantyne conclude.
Funding for the OPAL study was provided by the National Health and Medical Research Council, the University of Sydney Faculty of Medicine and Health, and SafeWork SA. The study authors have disclosed no relevant financial relationships. Dr. Sullivan and Dr. Ballantyne are board members (unpaid) of Physicians for Responsible Opioid Prescribing and have been paid consultants in opioid litigation.
A version of this article originally appeared on Medscape.com.
Opioids do not relieve acute low back or neck pain in the short term and lead to worse outcomes in the long term, results of the first randomized controlled trial testing the efficacy and safety of a short course of opioids for acute nonspecific low back/neck pain suggest.
After 6 weeks, there was no significant difference in pain scores of patients who took opioids, compared with those who took placebo. After 1 year, patients given the placebo had slightly lower pain scores. Also, patients using opioids were at greater risk of opioid misuse after 1 year.
This is a “landmark” trial with “practice-changing” results, senior author Christine Lin, PhD, with the University of Sydney, told this news organization.
“Before this trial, we did not have good evidence on whether opioids were effective for acute low back pain or neck pain, yet opioids were one of the most commonly used medicines for these conditions,” Dr. Lin explained.
On the basis of these results, “opioids should not be recommended at all for acute low back pain and neck pain,” Dr. Lin said.
Results of the OPAL study were published online in The Lancet.
Rigorous trial
The trial was conducted in 157 primary care or emergency department sites in Australia and involved 347 adults who had been experiencing low back pain, neck pain, or both for 12 weeks or less.
They were randomly allocated (1:1) to receive guideline-recommended care (reassurance and advice to stay active) plus an opioid (oxycodone up to 20 mg daily) or identical placebo for up to 6 weeks. Naloxone was provided to help prevent opioid-induced constipation and improve blinding.
The primary outcome was pain severity at 6 weeks, measured with the pain severity subscale of the Brief Pain Inventory (10-point scale).
After 6 weeks, opioid therapy offered no more relief for acute back/neck pain or functional improvement than placebo.
The mean pain score at 6 weeks was 2.78 in the opioid group, versus 2.25 in the placebo group (adjusted mean difference, 0.53; 95% confidence interval, –0.00 to 1.07; P = .051). At 1 year, mean pain scores in the placebo group were slightly lower than in the opioid group (1.8 vs. 2.4).
In addition, there was a doubling of the risk of opioid misuse at 1 year among patients randomly allocated to receive opioid therapy for 6 weeks, compared with those allocated to receive placebo for 6 weeks.
At 1 year, 24 (20%) of 123 of the patients who received opioids were at risk of misuse, as indicated by the Current Opioid Misuse Measure scale, compared with 13 (10%) of 128 patients in the placebo group (P = .049). The COMM is a widely used measure of current aberrant drug-related behavior among patients with chronic pain who are being prescribed opioid therapy.
Results raise ‘serious questions’
“I believe the findings of the study will need to be disseminated to the doctors and patients, so they receive this latest evidence on opioids,” Dr. Lin said in an interview.
“We need to reassure doctors and patients that most people with acute low back pain and neck pain recover well with time (usually by 6 weeks), so management is simple – staying active, avoiding bed rest, and, if necessary, using a heat pack for short term pain relief. If drugs are required, consider anti-inflammatory drugs,” Dr. Lin added.
The authors of a linked comment say the OPAL trial “raises serious questions about the use of opioid therapy for acute low back and neck pain.”
Mark Sullivan, MD, PhD, and Jane Ballantyne, MD, with the University of Washington, Seattle, note that current clinical guidelines recommend opioids for patients with acute back and neck pain when other drug treatments fail or are contraindicated.
“As many as two-thirds of patients might receive an opioid when presenting for care of back or neck pain. It is time to re-examine these guidelines and these practices,” Dr. Sullivan and Dr. Ballantyne conclude.
Funding for the OPAL study was provided by the National Health and Medical Research Council, the University of Sydney Faculty of Medicine and Health, and SafeWork SA. The study authors have disclosed no relevant financial relationships. Dr. Sullivan and Dr. Ballantyne are board members (unpaid) of Physicians for Responsible Opioid Prescribing and have been paid consultants in opioid litigation.
A version of this article originally appeared on Medscape.com.
Systemic JIA and AOSD are the same disease, EULAR says
Systemic juvenile idiopathic arthritis (sJIA) and adult-onset Still’s disease (AOSD) should be grouped into one disease, Still’s disease, according to new diagnosis and treatment recommendations presented at the annual European Congress of Rheumatology.
The recommendations, made in collaboration with EULAR and the Pediatric Rheumatology European Society, emphasized that the ultimate treatment target for Still’s disease should be drug-free remission in all patients and that macrophage activation syndrome (MAS) should be identified and treated as soon as possible.
The task force focused on MAS because despite effective, innovative therapies, “we continued to see MAS,” said presenter Bruno Fautrel, MD, Pitié-Salpêtrière University Hospital, Paris. “We have to be very concerned about this potential complication.”
Dr. Fautrel copresented the recommendations with Fabrizio De Benedetti, MD, PhD, head of the division of rheumatology, Bambino Gesù Hospital, Rome.
Diagnosis
Dr. Fautrel noted that the cutoff age of 16 that differentiates sJIA and AOSD is “arbitrary.” There are some differences in age: The frequency of the disease is higher in young children, but it plateaus in young adults. Children under 18 months old are also far more likely to develop MAS.
To diagnose and treat Still’s disease, the recommendations state that clinicians should consider four criteria:
- A fever spiking at or above 39° C (102.2° F) for at least 7 days.
- A transient rash, preferentially on the trunk, that coincides with fever spikes, rash is typically erythematous but other rashes, like urticaria, can be consistent with the diagnosis.
- Some musculoskeletal involvement is common, involving arthralgia/myalgia.
- High levels of inflammation identified by neutrophilic leukocytosis, increased serum C-reactive protein (CRP), and ferritin.
Dr. Fautrel noted that, while arthritis can be present, it is not necessary to make a diagnosis. In pediatrics, “arthritis is likely to happen after a few weeks of the evolution of the disease,” and waiting for arthritis to develop can lead to diagnostic delay, “which is a problem.”
For individuals with suspected Still’s disease, NSAIDs can be used as a “bridging therapy” before the diagnosis is confirmed.
Treatment
The recommendations emphasized that treatment and therapeutic strategy “should be based on shared decision-making between the parents/patients and the treating team,” with the ultimate goal of drug-free remission.
To achieve this goal, the document outlines time-based targets for clinically inactive disease (CID). At 4 weeks, patients should have no fever, reduction of active or swollen joint count by more than 50%, a normal CRP level, and a rating of less than 20 on a visual analog scale of 0-100. At 3 months, patients should maintain clinically inactive disease with a glucocorticoid dose of less than 0.1 or 0.2 mg/kg per day. At 6 months, CID should be maintained without glucocorticoids.
While the authors of the recommendations noted that glucocorticoids are efficacious, their long-term use should be avoided because of safety issues. An interleukin-1 or IL-6 inhibitor should be prioritized and initiated as soon as possible after diagnosis.
Patients should maintain CID between 3 and 6 months before tapering off biologics.
The recommendations are congruent with the 2021 American College of Rheumatology’s guidelines for sJIA, noted Karen Onel, MD, pediatric rheumatologist, Hospital for Special Surgery, New York, and the principle investigator for the ACR guidelines. One main difference is that the EULAR recommendations included time lines for treatment targets, while the ACR’s did not.
“It’s great to have these time lines in there,” she said in an interview, though there are still some unknowns. “We don’t actually know what the tapering frequency should be,” she said, “but these are definitely goals that we need to explore and see how they evolve.”
MAS and lung complications
The EULAR recommendations also touched on two concerning complications, particularly in children: MAS and lung disease. According to the document, MAS should be considered in patients with Still’s disease with these symptoms: fever, splenomegaly, elevated serum ferritin, low cell counts, abnormal liver function tests, elevated serum triglycerides, and intravascular activation of coagulation. The MAS 2016 criteria can also be used to facilitate diagnosis.
“MAS treatment must include high-dose glucocorticoids,” the document states. “In addition, treatments including anakinra, ciclosporin, and/or interferon-gamma inhibitors should be considered as a part of initial therapy.”
The recommendations also addressed the risk for lung disease, “which is an emerging issue, particularly in children, that the physician should be very well aware of,” Dr. De Benedetti said. This complication can arise at any time point of the disease, he added.
The document advised actively screening for lung disease by searching for clinical symptoms such as digital clubbing, persistent cough, and shortness of breath. Pulmonary function tests like pulse oximetry and diffusing capacity of the lungs for carbon monoxide may also be used, but these standard lung function tests are very difficult to do in children under 6 years old, Dr. De Benedetti noted. The recommendations advise performing high-resolution CT in “any patients with clinical concerns.”
“We have lowered the threshold for CT scan because of the emerging features of this lung disease that may actually be lethal and therefore require prompt attention,” Dr. De Benedetti noted.
The recommendations for lung disease are “broad,” as there is still much to learn about the risk for lung disease in a small portion of sJIA patients, Dr. Onel said.
“There’s a lot that we are trying to work out about this; exactly how to screen, who to screen, what to do, who to treat, and how to treat really remains unclear,” she said. “We absolutely agree that this is a major, major issue that we need to come to some sort of agreement upon, but we’re just not there yet.”
Dr. De Benedetti, Dr. Fautrel, and Dr. Onel disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Systemic juvenile idiopathic arthritis (sJIA) and adult-onset Still’s disease (AOSD) should be grouped into one disease, Still’s disease, according to new diagnosis and treatment recommendations presented at the annual European Congress of Rheumatology.
The recommendations, made in collaboration with EULAR and the Pediatric Rheumatology European Society, emphasized that the ultimate treatment target for Still’s disease should be drug-free remission in all patients and that macrophage activation syndrome (MAS) should be identified and treated as soon as possible.
The task force focused on MAS because despite effective, innovative therapies, “we continued to see MAS,” said presenter Bruno Fautrel, MD, Pitié-Salpêtrière University Hospital, Paris. “We have to be very concerned about this potential complication.”
Dr. Fautrel copresented the recommendations with Fabrizio De Benedetti, MD, PhD, head of the division of rheumatology, Bambino Gesù Hospital, Rome.
Diagnosis
Dr. Fautrel noted that the cutoff age of 16 that differentiates sJIA and AOSD is “arbitrary.” There are some differences in age: The frequency of the disease is higher in young children, but it plateaus in young adults. Children under 18 months old are also far more likely to develop MAS.
To diagnose and treat Still’s disease, the recommendations state that clinicians should consider four criteria:
- A fever spiking at or above 39° C (102.2° F) for at least 7 days.
- A transient rash, preferentially on the trunk, that coincides with fever spikes, rash is typically erythematous but other rashes, like urticaria, can be consistent with the diagnosis.
- Some musculoskeletal involvement is common, involving arthralgia/myalgia.
- High levels of inflammation identified by neutrophilic leukocytosis, increased serum C-reactive protein (CRP), and ferritin.
Dr. Fautrel noted that, while arthritis can be present, it is not necessary to make a diagnosis. In pediatrics, “arthritis is likely to happen after a few weeks of the evolution of the disease,” and waiting for arthritis to develop can lead to diagnostic delay, “which is a problem.”
For individuals with suspected Still’s disease, NSAIDs can be used as a “bridging therapy” before the diagnosis is confirmed.
Treatment
The recommendations emphasized that treatment and therapeutic strategy “should be based on shared decision-making between the parents/patients and the treating team,” with the ultimate goal of drug-free remission.
To achieve this goal, the document outlines time-based targets for clinically inactive disease (CID). At 4 weeks, patients should have no fever, reduction of active or swollen joint count by more than 50%, a normal CRP level, and a rating of less than 20 on a visual analog scale of 0-100. At 3 months, patients should maintain clinically inactive disease with a glucocorticoid dose of less than 0.1 or 0.2 mg/kg per day. At 6 months, CID should be maintained without glucocorticoids.
While the authors of the recommendations noted that glucocorticoids are efficacious, their long-term use should be avoided because of safety issues. An interleukin-1 or IL-6 inhibitor should be prioritized and initiated as soon as possible after diagnosis.
Patients should maintain CID between 3 and 6 months before tapering off biologics.
The recommendations are congruent with the 2021 American College of Rheumatology’s guidelines for sJIA, noted Karen Onel, MD, pediatric rheumatologist, Hospital for Special Surgery, New York, and the principle investigator for the ACR guidelines. One main difference is that the EULAR recommendations included time lines for treatment targets, while the ACR’s did not.
“It’s great to have these time lines in there,” she said in an interview, though there are still some unknowns. “We don’t actually know what the tapering frequency should be,” she said, “but these are definitely goals that we need to explore and see how they evolve.”
MAS and lung complications
The EULAR recommendations also touched on two concerning complications, particularly in children: MAS and lung disease. According to the document, MAS should be considered in patients with Still’s disease with these symptoms: fever, splenomegaly, elevated serum ferritin, low cell counts, abnormal liver function tests, elevated serum triglycerides, and intravascular activation of coagulation. The MAS 2016 criteria can also be used to facilitate diagnosis.
“MAS treatment must include high-dose glucocorticoids,” the document states. “In addition, treatments including anakinra, ciclosporin, and/or interferon-gamma inhibitors should be considered as a part of initial therapy.”
The recommendations also addressed the risk for lung disease, “which is an emerging issue, particularly in children, that the physician should be very well aware of,” Dr. De Benedetti said. This complication can arise at any time point of the disease, he added.
The document advised actively screening for lung disease by searching for clinical symptoms such as digital clubbing, persistent cough, and shortness of breath. Pulmonary function tests like pulse oximetry and diffusing capacity of the lungs for carbon monoxide may also be used, but these standard lung function tests are very difficult to do in children under 6 years old, Dr. De Benedetti noted. The recommendations advise performing high-resolution CT in “any patients with clinical concerns.”
“We have lowered the threshold for CT scan because of the emerging features of this lung disease that may actually be lethal and therefore require prompt attention,” Dr. De Benedetti noted.
The recommendations for lung disease are “broad,” as there is still much to learn about the risk for lung disease in a small portion of sJIA patients, Dr. Onel said.
“There’s a lot that we are trying to work out about this; exactly how to screen, who to screen, what to do, who to treat, and how to treat really remains unclear,” she said. “We absolutely agree that this is a major, major issue that we need to come to some sort of agreement upon, but we’re just not there yet.”
Dr. De Benedetti, Dr. Fautrel, and Dr. Onel disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Systemic juvenile idiopathic arthritis (sJIA) and adult-onset Still’s disease (AOSD) should be grouped into one disease, Still’s disease, according to new diagnosis and treatment recommendations presented at the annual European Congress of Rheumatology.
The recommendations, made in collaboration with EULAR and the Pediatric Rheumatology European Society, emphasized that the ultimate treatment target for Still’s disease should be drug-free remission in all patients and that macrophage activation syndrome (MAS) should be identified and treated as soon as possible.
The task force focused on MAS because despite effective, innovative therapies, “we continued to see MAS,” said presenter Bruno Fautrel, MD, Pitié-Salpêtrière University Hospital, Paris. “We have to be very concerned about this potential complication.”
Dr. Fautrel copresented the recommendations with Fabrizio De Benedetti, MD, PhD, head of the division of rheumatology, Bambino Gesù Hospital, Rome.
Diagnosis
Dr. Fautrel noted that the cutoff age of 16 that differentiates sJIA and AOSD is “arbitrary.” There are some differences in age: The frequency of the disease is higher in young children, but it plateaus in young adults. Children under 18 months old are also far more likely to develop MAS.
To diagnose and treat Still’s disease, the recommendations state that clinicians should consider four criteria:
- A fever spiking at or above 39° C (102.2° F) for at least 7 days.
- A transient rash, preferentially on the trunk, that coincides with fever spikes, rash is typically erythematous but other rashes, like urticaria, can be consistent with the diagnosis.
- Some musculoskeletal involvement is common, involving arthralgia/myalgia.
- High levels of inflammation identified by neutrophilic leukocytosis, increased serum C-reactive protein (CRP), and ferritin.
Dr. Fautrel noted that, while arthritis can be present, it is not necessary to make a diagnosis. In pediatrics, “arthritis is likely to happen after a few weeks of the evolution of the disease,” and waiting for arthritis to develop can lead to diagnostic delay, “which is a problem.”
For individuals with suspected Still’s disease, NSAIDs can be used as a “bridging therapy” before the diagnosis is confirmed.
Treatment
The recommendations emphasized that treatment and therapeutic strategy “should be based on shared decision-making between the parents/patients and the treating team,” with the ultimate goal of drug-free remission.
To achieve this goal, the document outlines time-based targets for clinically inactive disease (CID). At 4 weeks, patients should have no fever, reduction of active or swollen joint count by more than 50%, a normal CRP level, and a rating of less than 20 on a visual analog scale of 0-100. At 3 months, patients should maintain clinically inactive disease with a glucocorticoid dose of less than 0.1 or 0.2 mg/kg per day. At 6 months, CID should be maintained without glucocorticoids.
While the authors of the recommendations noted that glucocorticoids are efficacious, their long-term use should be avoided because of safety issues. An interleukin-1 or IL-6 inhibitor should be prioritized and initiated as soon as possible after diagnosis.
Patients should maintain CID between 3 and 6 months before tapering off biologics.
The recommendations are congruent with the 2021 American College of Rheumatology’s guidelines for sJIA, noted Karen Onel, MD, pediatric rheumatologist, Hospital for Special Surgery, New York, and the principle investigator for the ACR guidelines. One main difference is that the EULAR recommendations included time lines for treatment targets, while the ACR’s did not.
“It’s great to have these time lines in there,” she said in an interview, though there are still some unknowns. “We don’t actually know what the tapering frequency should be,” she said, “but these are definitely goals that we need to explore and see how they evolve.”
MAS and lung complications
The EULAR recommendations also touched on two concerning complications, particularly in children: MAS and lung disease. According to the document, MAS should be considered in patients with Still’s disease with these symptoms: fever, splenomegaly, elevated serum ferritin, low cell counts, abnormal liver function tests, elevated serum triglycerides, and intravascular activation of coagulation. The MAS 2016 criteria can also be used to facilitate diagnosis.
“MAS treatment must include high-dose glucocorticoids,” the document states. “In addition, treatments including anakinra, ciclosporin, and/or interferon-gamma inhibitors should be considered as a part of initial therapy.”
The recommendations also addressed the risk for lung disease, “which is an emerging issue, particularly in children, that the physician should be very well aware of,” Dr. De Benedetti said. This complication can arise at any time point of the disease, he added.
The document advised actively screening for lung disease by searching for clinical symptoms such as digital clubbing, persistent cough, and shortness of breath. Pulmonary function tests like pulse oximetry and diffusing capacity of the lungs for carbon monoxide may also be used, but these standard lung function tests are very difficult to do in children under 6 years old, Dr. De Benedetti noted. The recommendations advise performing high-resolution CT in “any patients with clinical concerns.”
“We have lowered the threshold for CT scan because of the emerging features of this lung disease that may actually be lethal and therefore require prompt attention,” Dr. De Benedetti noted.
The recommendations for lung disease are “broad,” as there is still much to learn about the risk for lung disease in a small portion of sJIA patients, Dr. Onel said.
“There’s a lot that we are trying to work out about this; exactly how to screen, who to screen, what to do, who to treat, and how to treat really remains unclear,” she said. “We absolutely agree that this is a major, major issue that we need to come to some sort of agreement upon, but we’re just not there yet.”
Dr. De Benedetti, Dr. Fautrel, and Dr. Onel disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM EULAR 2023
Acute Achilles tendon rupture: Skip the surgery?
ILLUSTRATIVE CASE
An otherwise healthy 45-year-old man sustained an acute right-side Achilles tendon rupture while playing tennis. He has not taken quinolones recently, has no history of previous Achilles tendon rupture, and prior to this injury had no difficulty walking. He presents initially to his primary care physician and wants advice: Does he need surgery?
Acute Achilles tendon rupture manifests as acute-onset pain and impaired plantar flexion.2 Older, active, male patients are at increased risk. There is disagreement among treating physicians regarding best practices for managing this common and debilitating injury. Prior clinical trials comparing operative to nonoperative management, as well as those comparing different surgical techniques, were limited by small sample sizes.3-5
A 2019 systematic review and meta-analysis that relied heavily on observational data suggested that nonoperative management carries greater risk for rerupture but lower risk for complications than surgical treatment, without differences in patient-reported functional outcomes.5 This 2022 RCT adds certainty to comparisons of surgical and nonoperative treatment.
STUDY SUMMARY
Equivalent outcomes but higher rates of rerupture for nonoperative patients
Norwegian investigators conducted a prospective, single-blind RCT at 4 treating facilities among patients ages 18 to 60 years with unilateral acute Achilles tendon rupture. A total of 554 patients were randomized in a 1:1:1 ratio to 1 of 3 groups: nonoperative treatment, open-repair surgery, or minimally invasive surgery. Ultimately, 526 patients who completed the intervention and at least 1 follow-up survey were included in the final analysis, which exceeded the number needed according to the pre-study 80% power calculation. Seventy-four percent of the patients were male, and the average age at time of injury was 40 years. Nearly all patients were classified as healthy or having only mild or well-controlled chronic illnesses.
Before randomization, patients completed the 10-item Achilles tendon Total Rupture Score (ATRS) questionnaire to gauge their pre-injury baseline function. ATRS is scored 0 to 100, with lower scores indicating more limitation in function; a clinically important difference is 8 to 10 points. There were no statistically significant differences in pre-injury baseline ATRS (92.7, 93.9, and 94.2 for the nonoperative, open-repair, and minimally invasive groups, respectively) or other patient characteristics among the 3 groups.
For all participants, application of a below-the-knee equinus cast with plantar flexion was performed within 72 hours after the injury. Patients in the surgical arms had surgery within 8 days, followed by application of a new cast. For all study groups, the cast was maintained for a total of 2 weeks, followed by 6 weeks of weight-bearing in an ankle-foot orthosis with heel wedges that were gradually reduced in number. All patients were treated with identical serial immobilization and physical therapy programs for 36 weeks.
The primary study outcome was change from baseline ATRS at 12 months after injury. Secondary outcomes included ATRS at 3 and 6 months and domain-specific quality-of-life scores (from the 36-Item Short Form Health Survey; SF-36) at 6 and 12 months. Patients also underwent physical testing of their Achilles tendon function at 6 and 12 months, during which they wore knee-high socks in order to blind the evaluators. Reruptures were recorded as secondary outcomes as well.
Continue to: There were no significant...
There were no significant differences between groups in the primary outcome. The mean changes in ATRS were −2.6 points (95% CI, −6.5 to 2.0) for nonoperative treatment compared with minimally invasive surgery, and 1.0 point (95% CI, −5.2 to 3.1) for nonoperative treatment compared with open repair.
All groups had similar secondary self-reported ATRS at 3 and 6 months and SF-36 scores at 6 and 12 months. Blinded physical test results also were similar between groups at 6 and 12 months.
Tendon rerupture within 12 months was more common in the nonoperative arm than in the 2 surgical arms (6.2% vs 0.6% in both operative groups; 5.6% difference; 95% CI for difference, 1.9-10.2 for open repair and 1.8-10.2 for minimally invasive surgery). Risk for nerve injury was higher in both the minimally invasive surgery group (5.2%) and the open-repair surgery group (2.8%) compared with the nonoperative group (0.6%; no P value given for comparison).
WHAT’S NEW
Largest RCT to date showed effectiveness of nonoperative Tx
This study is the largest well-powered and rigorously conducted RCT to show that nonoperative management of acute Achilles tendon rupture offers equivalent patient-reported outcomes at 12 months after injury. Nonoperative management was associated with a lower risk for nerve injury but higher risk for tendon rerupture.
These findings support previous studies on the topic. As previously mentioned, a 2019 systematic review and meta-analysis of 10 RCTs (N = 944) and 19 observational studies (N = 14,918) examined operative compared with nonoperative treatment of acute Achilles tendon rupture and found a lower rerupture rate in the operative group but a higher complication rate.5 An underpowered 2010 RCT (N = 97) of operative vs nonoperative treatment of acute Achilles tendon rupture found no statistical difference in ATRS.3 Another underpowered RCT conducted in 2013 (N = 100) compared surgical treatment, accelerated rehabilitation, and nonsurgical treatment in acute Achilles tendon rupture and found no statistical difference in ATRS.4
CAVEATS
Study results may not apply to some patient groups
These findings may not apply to patients older than 60 years, who were excluded from this RCT, or patients with debilitation or significant chronic disease. Patients with prior Achilles rupture also were excluded.
The study population in Norway, which is more physically active than nearby countries, may not be generalizable worldwide.6 Patients wishing to minimize the risk for rerupture may still prefer to have surgery after acute Achilles tendon rupture.
CHALLENGES TO IMPLEMENTATION
Potentially limited options for patients
Most patients with acute Achilles tendon rupture are evaluated by orthopedic surgeons, who may or may not offer nonoperative management. Availability of practitioners to provide serial casting, appropriate heel wedges, and rehabilitation may vary regionally. All patients in this study were evaluated within 72 hours of injury; these findings may not be applicable for patients at a longer time since injury.
1. Myhrvold SB, Brouwer EF, Andresen TKM, et al. Nonoperative or surgical treatment of acute Achilles’ tendon rupture. N Engl J Med. 2022;386:1409-1420. doi: 10.1056/NEJMoa2108447
2. Huttunen TT, Kannus P, Rolf C, et al. Acute achilles tendon ruptures: incidence of injury and surgery in Sweden between 2001 and 2012. Am J Sports Med. 2014;42:2419-2423. doi: 10.1177/0363546514540599
3. Nilsson-Helander K, Silbernagel KG, Thomeé R, et al. Acute achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010;38:2186-2193. doi: 10.1177/0363546510376052
4. Olsson N, Silbernagel KG, Eriksson BI, et al. Stable surgical repair with accelerated rehabilitation versus nonsurgical treatment for acute Achilles tendon ruptures: a randomized controlled study. Am J Sports Med. 2013;41:2867-2876. doi: 10.1177/0363546513503282
5. Ochen Y, Beks RB, van Heijl M, et al. Operative treatment versus nonoperative treatment of Achilles tendon ruptures: systematic review and meta-analysis. BMJ. 2019;364:k5120. doi: 10.1136/bmj.k5120
6. Urbaniak-Brekke AM, Pluta B, Krzykała M, et al. Physical activity of Polish and Norwegian local communities in the context of self-government authorities’ projects. Int J Environ Res Public Health. 2019;16:1710. doi: 10.3390/ijerph16101710
ILLUSTRATIVE CASE
An otherwise healthy 45-year-old man sustained an acute right-side Achilles tendon rupture while playing tennis. He has not taken quinolones recently, has no history of previous Achilles tendon rupture, and prior to this injury had no difficulty walking. He presents initially to his primary care physician and wants advice: Does he need surgery?
Acute Achilles tendon rupture manifests as acute-onset pain and impaired plantar flexion.2 Older, active, male patients are at increased risk. There is disagreement among treating physicians regarding best practices for managing this common and debilitating injury. Prior clinical trials comparing operative to nonoperative management, as well as those comparing different surgical techniques, were limited by small sample sizes.3-5
A 2019 systematic review and meta-analysis that relied heavily on observational data suggested that nonoperative management carries greater risk for rerupture but lower risk for complications than surgical treatment, without differences in patient-reported functional outcomes.5 This 2022 RCT adds certainty to comparisons of surgical and nonoperative treatment.
STUDY SUMMARY
Equivalent outcomes but higher rates of rerupture for nonoperative patients
Norwegian investigators conducted a prospective, single-blind RCT at 4 treating facilities among patients ages 18 to 60 years with unilateral acute Achilles tendon rupture. A total of 554 patients were randomized in a 1:1:1 ratio to 1 of 3 groups: nonoperative treatment, open-repair surgery, or minimally invasive surgery. Ultimately, 526 patients who completed the intervention and at least 1 follow-up survey were included in the final analysis, which exceeded the number needed according to the pre-study 80% power calculation. Seventy-four percent of the patients were male, and the average age at time of injury was 40 years. Nearly all patients were classified as healthy or having only mild or well-controlled chronic illnesses.
Before randomization, patients completed the 10-item Achilles tendon Total Rupture Score (ATRS) questionnaire to gauge their pre-injury baseline function. ATRS is scored 0 to 100, with lower scores indicating more limitation in function; a clinically important difference is 8 to 10 points. There were no statistically significant differences in pre-injury baseline ATRS (92.7, 93.9, and 94.2 for the nonoperative, open-repair, and minimally invasive groups, respectively) or other patient characteristics among the 3 groups.
For all participants, application of a below-the-knee equinus cast with plantar flexion was performed within 72 hours after the injury. Patients in the surgical arms had surgery within 8 days, followed by application of a new cast. For all study groups, the cast was maintained for a total of 2 weeks, followed by 6 weeks of weight-bearing in an ankle-foot orthosis with heel wedges that were gradually reduced in number. All patients were treated with identical serial immobilization and physical therapy programs for 36 weeks.
The primary study outcome was change from baseline ATRS at 12 months after injury. Secondary outcomes included ATRS at 3 and 6 months and domain-specific quality-of-life scores (from the 36-Item Short Form Health Survey; SF-36) at 6 and 12 months. Patients also underwent physical testing of their Achilles tendon function at 6 and 12 months, during which they wore knee-high socks in order to blind the evaluators. Reruptures were recorded as secondary outcomes as well.
Continue to: There were no significant...
There were no significant differences between groups in the primary outcome. The mean changes in ATRS were −2.6 points (95% CI, −6.5 to 2.0) for nonoperative treatment compared with minimally invasive surgery, and 1.0 point (95% CI, −5.2 to 3.1) for nonoperative treatment compared with open repair.
All groups had similar secondary self-reported ATRS at 3 and 6 months and SF-36 scores at 6 and 12 months. Blinded physical test results also were similar between groups at 6 and 12 months.
Tendon rerupture within 12 months was more common in the nonoperative arm than in the 2 surgical arms (6.2% vs 0.6% in both operative groups; 5.6% difference; 95% CI for difference, 1.9-10.2 for open repair and 1.8-10.2 for minimally invasive surgery). Risk for nerve injury was higher in both the minimally invasive surgery group (5.2%) and the open-repair surgery group (2.8%) compared with the nonoperative group (0.6%; no P value given for comparison).
WHAT’S NEW
Largest RCT to date showed effectiveness of nonoperative Tx
This study is the largest well-powered and rigorously conducted RCT to show that nonoperative management of acute Achilles tendon rupture offers equivalent patient-reported outcomes at 12 months after injury. Nonoperative management was associated with a lower risk for nerve injury but higher risk for tendon rerupture.
These findings support previous studies on the topic. As previously mentioned, a 2019 systematic review and meta-analysis of 10 RCTs (N = 944) and 19 observational studies (N = 14,918) examined operative compared with nonoperative treatment of acute Achilles tendon rupture and found a lower rerupture rate in the operative group but a higher complication rate.5 An underpowered 2010 RCT (N = 97) of operative vs nonoperative treatment of acute Achilles tendon rupture found no statistical difference in ATRS.3 Another underpowered RCT conducted in 2013 (N = 100) compared surgical treatment, accelerated rehabilitation, and nonsurgical treatment in acute Achilles tendon rupture and found no statistical difference in ATRS.4
CAVEATS
Study results may not apply to some patient groups
These findings may not apply to patients older than 60 years, who were excluded from this RCT, or patients with debilitation or significant chronic disease. Patients with prior Achilles rupture also were excluded.
The study population in Norway, which is more physically active than nearby countries, may not be generalizable worldwide.6 Patients wishing to minimize the risk for rerupture may still prefer to have surgery after acute Achilles tendon rupture.
CHALLENGES TO IMPLEMENTATION
Potentially limited options for patients
Most patients with acute Achilles tendon rupture are evaluated by orthopedic surgeons, who may or may not offer nonoperative management. Availability of practitioners to provide serial casting, appropriate heel wedges, and rehabilitation may vary regionally. All patients in this study were evaluated within 72 hours of injury; these findings may not be applicable for patients at a longer time since injury.
ILLUSTRATIVE CASE
An otherwise healthy 45-year-old man sustained an acute right-side Achilles tendon rupture while playing tennis. He has not taken quinolones recently, has no history of previous Achilles tendon rupture, and prior to this injury had no difficulty walking. He presents initially to his primary care physician and wants advice: Does he need surgery?
Acute Achilles tendon rupture manifests as acute-onset pain and impaired plantar flexion.2 Older, active, male patients are at increased risk. There is disagreement among treating physicians regarding best practices for managing this common and debilitating injury. Prior clinical trials comparing operative to nonoperative management, as well as those comparing different surgical techniques, were limited by small sample sizes.3-5
A 2019 systematic review and meta-analysis that relied heavily on observational data suggested that nonoperative management carries greater risk for rerupture but lower risk for complications than surgical treatment, without differences in patient-reported functional outcomes.5 This 2022 RCT adds certainty to comparisons of surgical and nonoperative treatment.
STUDY SUMMARY
Equivalent outcomes but higher rates of rerupture for nonoperative patients
Norwegian investigators conducted a prospective, single-blind RCT at 4 treating facilities among patients ages 18 to 60 years with unilateral acute Achilles tendon rupture. A total of 554 patients were randomized in a 1:1:1 ratio to 1 of 3 groups: nonoperative treatment, open-repair surgery, or minimally invasive surgery. Ultimately, 526 patients who completed the intervention and at least 1 follow-up survey were included in the final analysis, which exceeded the number needed according to the pre-study 80% power calculation. Seventy-four percent of the patients were male, and the average age at time of injury was 40 years. Nearly all patients were classified as healthy or having only mild or well-controlled chronic illnesses.
Before randomization, patients completed the 10-item Achilles tendon Total Rupture Score (ATRS) questionnaire to gauge their pre-injury baseline function. ATRS is scored 0 to 100, with lower scores indicating more limitation in function; a clinically important difference is 8 to 10 points. There were no statistically significant differences in pre-injury baseline ATRS (92.7, 93.9, and 94.2 for the nonoperative, open-repair, and minimally invasive groups, respectively) or other patient characteristics among the 3 groups.
For all participants, application of a below-the-knee equinus cast with plantar flexion was performed within 72 hours after the injury. Patients in the surgical arms had surgery within 8 days, followed by application of a new cast. For all study groups, the cast was maintained for a total of 2 weeks, followed by 6 weeks of weight-bearing in an ankle-foot orthosis with heel wedges that were gradually reduced in number. All patients were treated with identical serial immobilization and physical therapy programs for 36 weeks.
The primary study outcome was change from baseline ATRS at 12 months after injury. Secondary outcomes included ATRS at 3 and 6 months and domain-specific quality-of-life scores (from the 36-Item Short Form Health Survey; SF-36) at 6 and 12 months. Patients also underwent physical testing of their Achilles tendon function at 6 and 12 months, during which they wore knee-high socks in order to blind the evaluators. Reruptures were recorded as secondary outcomes as well.
Continue to: There were no significant...
There were no significant differences between groups in the primary outcome. The mean changes in ATRS were −2.6 points (95% CI, −6.5 to 2.0) for nonoperative treatment compared with minimally invasive surgery, and 1.0 point (95% CI, −5.2 to 3.1) for nonoperative treatment compared with open repair.
All groups had similar secondary self-reported ATRS at 3 and 6 months and SF-36 scores at 6 and 12 months. Blinded physical test results also were similar between groups at 6 and 12 months.
Tendon rerupture within 12 months was more common in the nonoperative arm than in the 2 surgical arms (6.2% vs 0.6% in both operative groups; 5.6% difference; 95% CI for difference, 1.9-10.2 for open repair and 1.8-10.2 for minimally invasive surgery). Risk for nerve injury was higher in both the minimally invasive surgery group (5.2%) and the open-repair surgery group (2.8%) compared with the nonoperative group (0.6%; no P value given for comparison).
WHAT’S NEW
Largest RCT to date showed effectiveness of nonoperative Tx
This study is the largest well-powered and rigorously conducted RCT to show that nonoperative management of acute Achilles tendon rupture offers equivalent patient-reported outcomes at 12 months after injury. Nonoperative management was associated with a lower risk for nerve injury but higher risk for tendon rerupture.
These findings support previous studies on the topic. As previously mentioned, a 2019 systematic review and meta-analysis of 10 RCTs (N = 944) and 19 observational studies (N = 14,918) examined operative compared with nonoperative treatment of acute Achilles tendon rupture and found a lower rerupture rate in the operative group but a higher complication rate.5 An underpowered 2010 RCT (N = 97) of operative vs nonoperative treatment of acute Achilles tendon rupture found no statistical difference in ATRS.3 Another underpowered RCT conducted in 2013 (N = 100) compared surgical treatment, accelerated rehabilitation, and nonsurgical treatment in acute Achilles tendon rupture and found no statistical difference in ATRS.4
CAVEATS
Study results may not apply to some patient groups
These findings may not apply to patients older than 60 years, who were excluded from this RCT, or patients with debilitation or significant chronic disease. Patients with prior Achilles rupture also were excluded.
The study population in Norway, which is more physically active than nearby countries, may not be generalizable worldwide.6 Patients wishing to minimize the risk for rerupture may still prefer to have surgery after acute Achilles tendon rupture.
CHALLENGES TO IMPLEMENTATION
Potentially limited options for patients
Most patients with acute Achilles tendon rupture are evaluated by orthopedic surgeons, who may or may not offer nonoperative management. Availability of practitioners to provide serial casting, appropriate heel wedges, and rehabilitation may vary regionally. All patients in this study were evaluated within 72 hours of injury; these findings may not be applicable for patients at a longer time since injury.
1. Myhrvold SB, Brouwer EF, Andresen TKM, et al. Nonoperative or surgical treatment of acute Achilles’ tendon rupture. N Engl J Med. 2022;386:1409-1420. doi: 10.1056/NEJMoa2108447
2. Huttunen TT, Kannus P, Rolf C, et al. Acute achilles tendon ruptures: incidence of injury and surgery in Sweden between 2001 and 2012. Am J Sports Med. 2014;42:2419-2423. doi: 10.1177/0363546514540599
3. Nilsson-Helander K, Silbernagel KG, Thomeé R, et al. Acute achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010;38:2186-2193. doi: 10.1177/0363546510376052
4. Olsson N, Silbernagel KG, Eriksson BI, et al. Stable surgical repair with accelerated rehabilitation versus nonsurgical treatment for acute Achilles tendon ruptures: a randomized controlled study. Am J Sports Med. 2013;41:2867-2876. doi: 10.1177/0363546513503282
5. Ochen Y, Beks RB, van Heijl M, et al. Operative treatment versus nonoperative treatment of Achilles tendon ruptures: systematic review and meta-analysis. BMJ. 2019;364:k5120. doi: 10.1136/bmj.k5120
6. Urbaniak-Brekke AM, Pluta B, Krzykała M, et al. Physical activity of Polish and Norwegian local communities in the context of self-government authorities’ projects. Int J Environ Res Public Health. 2019;16:1710. doi: 10.3390/ijerph16101710
1. Myhrvold SB, Brouwer EF, Andresen TKM, et al. Nonoperative or surgical treatment of acute Achilles’ tendon rupture. N Engl J Med. 2022;386:1409-1420. doi: 10.1056/NEJMoa2108447
2. Huttunen TT, Kannus P, Rolf C, et al. Acute achilles tendon ruptures: incidence of injury and surgery in Sweden between 2001 and 2012. Am J Sports Med. 2014;42:2419-2423. doi: 10.1177/0363546514540599
3. Nilsson-Helander K, Silbernagel KG, Thomeé R, et al. Acute achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010;38:2186-2193. doi: 10.1177/0363546510376052
4. Olsson N, Silbernagel KG, Eriksson BI, et al. Stable surgical repair with accelerated rehabilitation versus nonsurgical treatment for acute Achilles tendon ruptures: a randomized controlled study. Am J Sports Med. 2013;41:2867-2876. doi: 10.1177/0363546513503282
5. Ochen Y, Beks RB, van Heijl M, et al. Operative treatment versus nonoperative treatment of Achilles tendon ruptures: systematic review and meta-analysis. BMJ. 2019;364:k5120. doi: 10.1136/bmj.k5120
6. Urbaniak-Brekke AM, Pluta B, Krzykała M, et al. Physical activity of Polish and Norwegian local communities in the context of self-government authorities’ projects. Int J Environ Res Public Health. 2019;16:1710. doi: 10.3390/ijerph16101710
PRACTICE CHANGER
For healthy patients ages 18 to 60 years with acute Achilles tendon rupture, consider nonoperative immobilization, which offered a benefit in function comparable to open-repair or minimally invasive surgery in this randomized controlled trial (RCT).
STRENGTH OF RECOMMENDATION
B: Based on a single RCT.1
Myhrvold SB, Brouwer EF, Andresen TKM, et al. Nonoperative or surgical treatment of acute Achilles’ tendon rupture. N Engl J Med. 2022;386:1409-1420. doi: 10.1056/NEJMoa2108447
Which patients might benefit from platelet-rich plasma?
Platelet-rich plasma (PRP) injections have become a popular treatment option in a variety of specialties including sports medicine, maxillofacial surgery, dermatology, cosmetology, and reproductive medicine.1 PRP is an autologous blood product derived from whole blood, using a centrifuge to isolate a concentrated layer of platelets. The a-granules in platelets release transforming growth factor b 1, vascular endothelial growth factor, platelet-derived growth factor, basic fibroblast growth factor, epidermal growth factor, insulin-like growth factor 1, and other mediators that enhance the natural healing process.2
When patients ask. Familiarity with the use of PRP to treat specific musculoskeletal (MSK) conditions is essential for family physicians who frequently are asked by patients about whether PRP is right for them. These patients may have experienced failure of medication therapy or declined surgical intervention, or may not be surgical candidates. This review details the evidence surrounding common intra-articular and extra-articular applications of PRP. But first, a word about how PRP is prepared, its contraindications, and costs.
Preparation and types of PRP
Although there are many commercial systems for preparing PRP, there is no consensus on the optimal formulation.2 Other terms for PRP, such as autologous concentrated platelets and super-concentrated platelets, are based on concentration of red blood cells, leukocytes, and fibrin.3 PRP therapies usually are categorized as leukocyte-rich PRP (LR-PRP) or leukocyte-poor PRP (LP-PRP), based on neutrophil concentrations that are above and below baseline.2 Leukocyte concentration is one of the most debated topics in PRP therapy.4
Common commercially available preparation systems produce platelet concentrations between 3 to 6 times the baseline platelet count.5 Although there is no universally agreed upon PRP formulation, studies have shown 2 centrifugation cycles (“double-spun” or “dual centrifugation”) that yield platelet concentrations between 1.8 to 1.9 times the baseline values significantly improve MSK conditions.6-8
For MSK purposes, PRP may be injected into intratendinous, peritendinous, and intra-articular spaces. Currently, there is no consensus regarding injection frequency. Many studies have incorporated single-injection protocols, while some have used 2 to 3 injections repeated over several weeks to months. PRP commonly is injected at point-of-care without requiring storage.
Contraindications. PRP has been shown to be safe, with most adverse effects attributed to local injection site pain, bleeding, swelling, and bruising.9
Contraindications to PRP include active malignancy or recent remission from malignancy with the exception of nonmetastatic skin tumors.10 PRP is not recommended for patients with an allergy to manufacturing components (eg, dimethyl sulfoxide), thrombocytopenia, nonsteroidal anti-inflammatory drug use within 2 weeks, active infection causing fever, and local infection at the injection site.10 Since local anesthetics may impair platelet function, they should not be given at the same injection site as PRP.10
Continue to: Cost
Cost. PRP is not covered by most insurance plans.11,12 The cost for PRP may range from $500 to $2500 for a single injection.12
Evidence-based summary by condition
Knee osteoarthritis
❯❯❯ Consider using PRP
Knee osteoarthritis (OA) is a common cause of pain and disability. Treatment options include physical therapy, pharmacotherapy, and surgery. PRP has gained popularity as a nonsurgical option. A recent meta-analysis by Costa et al13 of 40 studies with 3035 participants comparing intra-articular PRP with hyaluronic acid (HA), corticosteroid, and saline injections, found that PRP appears to be more effective or as effective as other nonsurgical modalities. However, due to study heterogeneity and high risk for bias, the authors could not recommend PRP for knee OA in clinical practice.13
Despite Costa et al’s findings, reproducible data have demonstrated the superiority of PRP over other nonsurgical treatment options for knee OA. A 2021 systematic review and meta-analysis of 18 randomized controlled trials (RCTs; N = 811) by Belk et al6 comparing PRP to HA injections showed a higher mean improvement in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores in the PRP group compared to the HA group (44.7% vs 12.6%, respectively; P < .01).6 Six of 11 studies using the visual analog scale (VAS) for pain reported significantly less pain in the PRP group compared to the HA group (P < .05).6 The mean follow-up time was 11.1 months.6 Three of 6 studies reported improved subjective International Knee Documentation Committee (IKDC) scores (range from 0-100, with higher scores representing higher levels of function and lower levels of symptoms) in the PRP group compared to the HA group: 75.7 ± 15.1 vs 65.6 ± 16.9 (P = .004); 65.5 ± 3.6 vs 55.8 ± 3.8 (P = .01); and 60.8 ± 9.8 vs 48.4 ± 6.2 (P < .05).6 There was concern for moderate-to-high heterogeneity.6
Other systematic reviews and meta-analyses found similar efficacy of PRP for knee OA, including improved WOMAC scores and patient-reported outcomes (eg, pain, physical function, stiffness) compared to other injectable options.14,15 A systematic review of 14 RCTs (N = 1423) by Shen et al15 showed improved WOMAC scores at 3 months (mean differences [MD] = –14.53; 95% CI, –29.97 to –7.09; P < .001), 6 months
Despite a lack of consensus regarding the optimal preparation of PRP for knee OA, another recent RCT (N = 192) found significant improvement in mean subjective IKDC scores in the LR-PRP group (45.5 ± 15.5 to 60.7 ± 21.1; P < .0005) and the LP-PRP group (46.8 ± 15.8 to 62.9 ± 19.9; P < .0005), indicating efficacy regardless of PRP type.4
Continue to: Ankle osteoarthritis
Ankle osteoarthritis
❯ ❯ ❯ Additional research is needed
Ankle OA affects 3.4% of all adults and is more common in the younger population than knee or hip OA.16 An RCT (N = 100) investigating PRP vs placebo (saline) injections showed no statistically significant difference in American Orthopedic Foot and Ankle Society scores evaluating pain and function over 26 weeks (–2 points; 95% CI, –5 to 1; P = .16).16 Limitations to this study include its small sample size and the PRP formulation used. (The intervention group received 2 injections of 2 mL of PRP, and the platelet concentration was not reported.)16
Hip osteoarthritis
❯ ❯ ❯ Additional research is needed
Symptomatic hip OA occurs in 40% of adults older than 65 years, with a higher prevalence in women.18 Currently, corticosteroid injections are the only intra-articular therapy recommended by international guidelines for hip OA.19 A systematic review and meta-analysis comparing PRP to HA injections that included 4 RCTs (N = 303) showed a statistically significant reduction in VAS scores at 2 months in the PRP group compared to the HA group (weighted mean difference [WMD] = –0.376; 95% CI, –0.614 to –0.138; P = .002).18 However, there were no significant differences in VAS scores between the PRP and HA groups at 6 months (WMD = –0.141; 95% CI, –0.401 to 0.119; P = .289) and 12 months (WMD = –0.083; 95% CI, –0.343 to 0.117; P = .534). Likewise, no significant differences were found in WOMAC scores at 6 months (WMD = –2.841; 95% CI, –6.248 to 0.565; P = .102) and 12 months (WMD = –3.134; 95% CI, –6.624 to 0.356; P = .078) and Harris Hip Scores (HHS) at 6 months (WMD = 2.782; 95% CI, –6.639 to 12.203; P =.563) and 12 months (WMD = 0.706; 95% CI, –6.333 to 7.745; P = .844).18
A systematic review of 6 RCTs (N = 408) by Belk et al20 comparing PRP to HA for hip OA found similar short-term improvements in WOMAC scores (standardized mean differences [SMD] = 0.27; 95% CI, –0.05 to 0.59; P = .09), VAS scores (MD = 0.59; 95% CI, –0.741 to 1.92; P = .39), and HHS (MD = -0.81; 95% CI, –10.06 to 8.43; P = .93). The average follow-up time was 12.2 and 11.9 months for the PRP and HA groups, respectively.20
LR-PRP, which was used in 1 of the 6 RCTs, showed improvement in VAS scores and HHS from baseline, but no significant difference compared to HA at the latest follow-up.20 A pooled subanalysis of the 3 studies that used LP-PRP found no difference in WOMAC scores between the PRP and HA groups (SMD = 0.42; 95% CI, –0.01 to 0.86; P = .06).20 Future studies comparing the efficacy of intra-articular steroid vs PRP for hip OA would be beneficial.18
Continue to: Rotator cuff tendinopathy
Rotator cuff tendinopathy
❯ ❯ ❯ Consider PRP for short-term pain relief
Painful conditions of the rotator cuff include impingement syndrome, tendonitis, and partial and complete tears. A 2021 RCT (N = 58) by Dadgostar et al21 comparing PRP injection to corticosteroid therapy (methylprednisolone and lidocaine) for the treatment of rotator cuff tendinopathy showed significant improvement in VAS scores at 3 months in the PRP group compared to the corticosteroid group (6.66
Another RCT (N = 99) by Kwong et al22 comparing PRP to corticosteroids found similar short-term advantages of LP-PRP with an improved VAS score (–13.6 vs 0.4; P = .03), American Shoulder and Elbow Surgeons score (13.0 vs 2.9; P = .02), and Western Ontario Rotator Cuff Index score (16.8 vs 5.8; P = .03). However, there was no long-term benefit of PRP over corticosteroids found at 12 months.22
A 2021 systematic review and meta-analysis by Hamid et al23 that included 8 RCTs (N = 976) favored PRP over control (no injection, saline injections, and/or shoulder rehabilitation) with improved VAS scores at 12 months (SMD = –0.5; 95% CI, –0.7 to –0.2; P < .001). The evidence on functional outcome was mixed. Data pooled from 2 studies (n = 228) found better Shoulder Pain and Disability Index (SPADI) scores compared to controls at 3- and 6-month follow-ups. However, there were no significant differences in Disabilities of the Arm, Shoulder and Hand (DASH) scores between the 2 groups.23
Patellar tendinopathy
❯ ❯ ❯ Consider using PRP for return to sport
Patellar tendinopathy, a common MSK condition encountered in the primary care setting, has an overall prevalence of 22% in elite athletes at some point in their career.24 Nonsurgical management options include rest, ice, eccentric and isometric exercises, anti-inflammatory drugs, extracorporeal shock wave therapy (ESWT), and dry needling (DN).
A 2014 RCT (N = 23) evaluating DN vs PRP for patellar tendinopathy favored PRP with improved VAS scores (mean ± SD = 25.4 ± 23.2 points; P = .01 vs 5.2 ± 12.5 points; P = .20) at 12 weeks (P = .02). However, at ≥ 26 weeks, the improvement in pain and function scores was similar between the DN and PRP groups (33.2 ± 14.0 points; P = .001 vs 28.9 ± 25.2 points; P = .01). Notably, there was significantly more improvement in the PRP group at 12 weeks (P = .02) but not at 26 weeks (P = .66).25
Continue to: Another perspective study...
Another prospective study (N = 31) comparing PRP to physiotherapy showed a greater improvement in sport activity level reflected by the Tegner score in the PRP group (percentage improvement, 39 ± 22%) compared to control (20 ± 27%; P = .048) at 6 months.7
A recent RCT (N = 20) revealed improved VAS scores at 6 months with rehabilitation paired with either bone marrow mesenchymal stem cells (BM-MSC) or LP-PRP when compared with baseline (BM-MSC group: 4.23 ± 2.13 to 2.52 ± 2.37; P = .0621; LP-PRP group: 3.10 ± 1.20 to 1.13 ± 1.25; P = .0083). Pain was significantly reduced during sport play in both groups at 6 months when compared with baseline (BM-MSC group: 6.91 ± 1.11 to 3.06 ± 2.89, P = .0049; PRP group: 7.03 ± 1.42 to 1.94 ± 1.24, P = .0001).26
A 2019 systematic review and meta-analysis (N = 2530) demonstrated greater improvements in Victorian Institute of Sport Assessment scale for patellar tendinopathy (VISA-P) with multiple injections of PRP (38.7 points; 95% CI, 26.3-51.2 points) compared to single injections of PRP (24.3 points; 95% CI, 18.2-30.5 points), eccentric exercise (28.3 points; 95% CI, 18.9-37.8 points) and ESWT (27.4 points; 95% CI, 10.0-39.8 points) after 6 months.27 In contrast, an RCT (n = 57) comparing a single injection of LR-PRP or LP-PRP was no more effective than a single injection of saline for improvement in mean VISA-P scores (P > .05) at 1 year.28
Lateral epicondylitis
❯ ❯ ❯ Consider using PRP
Lateral epicondylitis (“tennis elbow”) is caused by overuse of the elbow extensors at the site of the lateral epicondyle. Chronic lateral epicondylosis involves tissue degeneration and microtrauma. Most cases of epicondylar tendinopathies are treated nonoperatively, with corticosteroid injections being a mainstay of treatment despite their short-term benefit29 and potential to deteriorate connective tissue over time. Recent studies suggest PRP therapy for epicondylitis and epicondylosis may increase long-term pain relief and improve function.
A 2017 systematic review and meta-analysis of 16 RCTs (N = 1018) concluded PRP was more efficacious than control injections (bupivacaine) for pain reduction in tendinopathies (effect size = 0.47; 95% CI, 0.22-0.72).30 In the review, lateral epicondylitis was evaluated in 12 studies and was most responsive to PRP (effect size = 0.57) when compared to control injection.30 In another systematic review (5 RCTs; 250 patients), corticosteroid injections improved pain within the first 6 weeks of treatment. However, PRP outperformed corticosteroid in VAS scores (21.3 ± 28.1 vs 42.4 ± 26.8) and DASH scores (17.6 ± 24.0 vs 36.5 ± 23.8) (P < .001) at 2 years.31
Continue to: A 2022 systematic review...
A 2022 systematic review and meta-analysis (26 studies; N = 1040) comparing scores at baseline vs 2 years post-PRP showed improvement in VAS scores (7.4 ± 1.30 vs 3.71 ± 2.35; P < .001), DASH scores (60.8 ± 12.5 vs 13.0 ± 18.5; P < .001), Patient-Rated Tennis Elbow Evaluation (55.6 ± 14.7 vs 48.8 ± 4.1; P < .001), and Mayo Clinic Performance Index (55.5 ± 6.1 vs 93.0 ± 6.7; P < .001).32
Regarding the therapeutic effects of different PRP types in lateral epicondylitis, a 2022 systematic review of 33 studies (N = 2420) found improved function and pain relief with LR-PRP and LP-PRP with no significant differences.33 Pretreatment VAS scores in the LR-PRP group, which ranged from 6.1 to 8.0, improved to 1.5 to 4.0 at 3 months and 0.6 to 3.3 after 1 year.33 Similarly, pretreatment VAS scores in the LP-PRP group, which ranged from 4.2 to 8.4, improved to 1.6 to 5.9 at 3 months and 0.7 to 2.7 after 1 year.34 DASH scores also improved in the LR-PRP and LP-PRP groups, with pretreatment scores (LR-PRP, 47.0 to 54.3; LP-PRP, 30.0 to 67.7) improving to 20.0 to 22.0 and 5.5 to 19.0, respectively, at 1 year.33
Achilles tendinopathy
❯ ❯ ❯ Do not use PRP; evidence is lacking
Achilles tendinopathy, caused by chronic overuse and overload resulting in microtrauma and poor tissue healing, typically occurs in the most poorly vascularized portion of the tendon and is common in runners. First-line treatments for Achilles tendinopathy include eccentric strength training and anti-inflammatory drugs.34,35 Corticosteroid injections are not recommended, given concern for degraded tendon tissue over time and worse function.34
A 2020 systematic review of 11 randomized and nonrandomized clinical trials (N = 406) found PRP improved Victorian Institute of Sports Assessment—Achilles (VISA-A) scores at 24 weeks compared to other nonsurgical treatment options (41.2 vs 70.12; P < .018).34 However, a higher-quality 2021 systematic review and meta-analysis of 4 RCTs (N = 170) comparing PRP injections with placebo showed no significant difference in VISA-A scores at 3 months (0.23; 95% CI, –0.45 to 0.91), 6 months (0.83; 95% CI, –0.26 to 1.92), and 12 months (0.83; 95% CI, –0.77 to 2.44).36 Therefore, further studies are warranted to evaluate the benefit of PRP injections for Achilles tendinopathy.
Conclusions
While high-quality studies support the use of PRP for knee OA and lateral epicondylitis, they have a moderate-to-high risk for bias. Several RCTs show that PRP provides superior short-term pain relief and range of motion compared to corticosteroids for rotator cuff tendinopathy. Multiple injections of PRP for patellar tendinopathy may accelerate return to sport and improve symptoms over the long term. However, current evidence does not support PRP therapy for Achilles tendinopathy. Given variability in PRP preparation, an accurate interpretation of the literature regarding its use in MSK conditions is recommended (TABLE4,6,7,14-18,20-23,25-28,30-34,36).
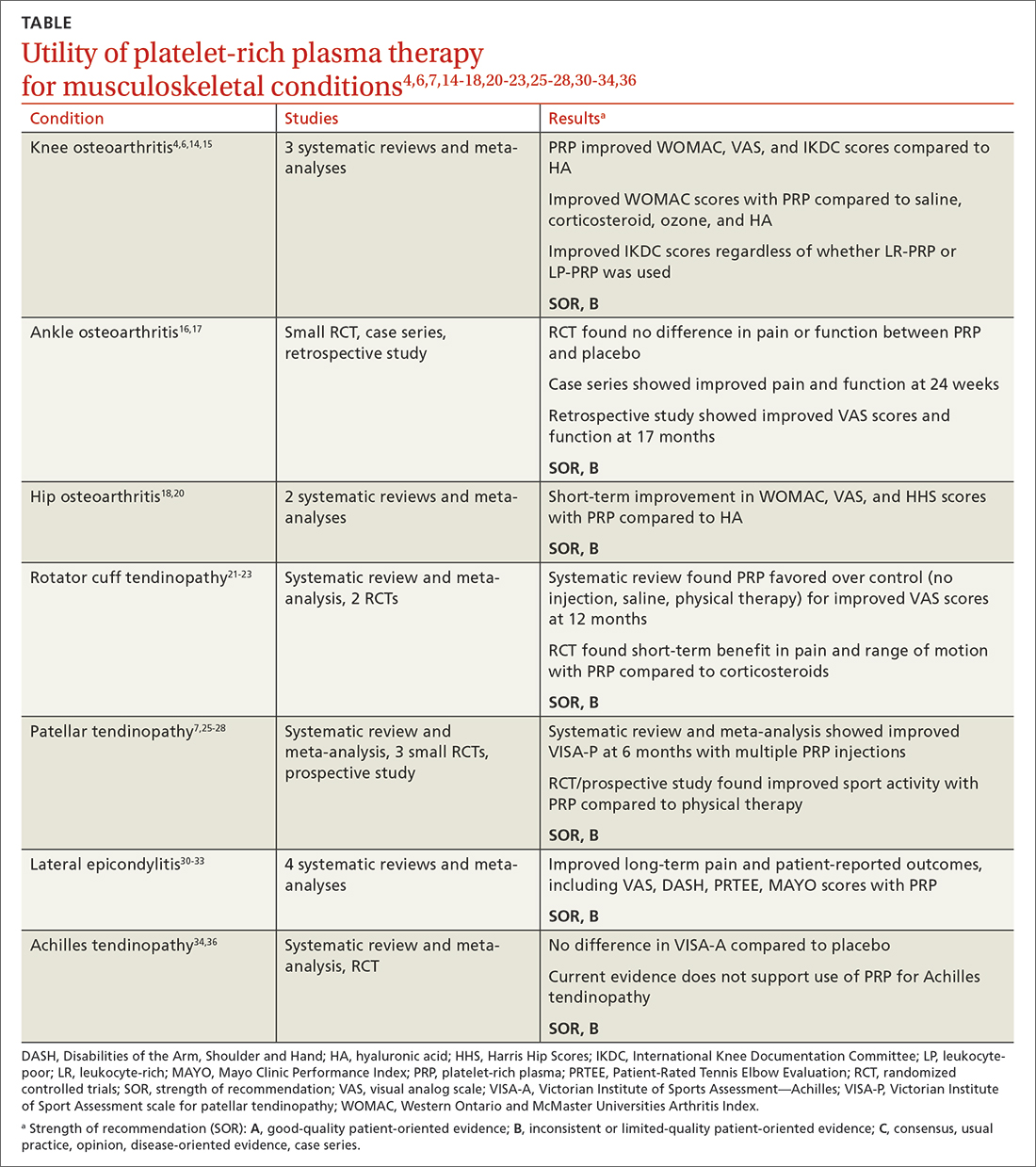
Continue to: Concerning the effectiveness of PRP...
Concerning the effectiveness of PRP, it is important to consider early publication bias. Although recent studies have shown its benefits,6,14,15,37 additional studies comparing PRP to placebo will help demonstrate its efficacy. Interestingly, a literature search by Bar-Or et al38 found intra-articular saline may have a therapeutic effect on knee OA and confound findings when used as a placebo.
Recognizing the presence or lack of clinically significant improvement in the literature is important. For example, while some recent studies have shown PRP exceeds the minimal clinically significant difference for knee OA and lateral epicondylitis, others have not.32,37 A 2021 systematic review of 11 clinical practice guidelines for the use of PRP in knee OA found that 9 were “uncertain or unable to make a recommendation” and 2 recommended against it.39
In its 2021 position statement for the responsible use of regenerative medicine, the American Medical Society for Sports Medicine includes guidance on integrating orthobiologics into clinical practice. The guideline emphasizes informed consent and provides an evidence-based rationale for using PRP in certain patient populations (lateral epicondylitis and younger patients with mild-to-moderate knee OA), recommending its use only after exhausting other conservative options.40 Patients should be referred to physicians with experience using PRP and image-guided procedures.
CORRESPONDENCE
Gregory D. Bentz Jr, MD, 3640 High Street Suite 3B, Portsmouth, VA 23707; [email protected]
1. Cecerska-Heryć E, Goszka M, Serwin N, et al. Applications of the regenerative capacity of platelets in modern medicine. Cytokine Growth Factor Rev. 2022;64:84-94. doi: 10.1016/j.cytogfr.2021.11.003
2. Le ADK, Enweze L, DeBaun MR, et al. Current clinical recommendations for use of platelet-rich plasma. Curr Rev Musculoskelet Med. 2018;11:624-634. doi: 10.1007/s12178-018-9527-7
3. Everts P, Onishi K, Jayaram P, et al. Platelet-rich plasma: new performance understandings and therapeutic considerations in 2020. Int J Mol Sci. 2020;21:7794. doi: 10.3390/ijms21207794
4. Di Martino A, Boffa A, Andriolo L, et al. Leukocyte-rich versus leukocyte-poor platelet-rich plasma for the treatment of knee osteoarthritis: a double-blind randomized trial. Am J Sports Med. 2022;50:609-617. doi: 10.1177/03635465211064303
5. Mariani E, Pulsatelli L. Platelet concentrates in musculoskeletal medicine. Int J Mol Sci. 2020;21:1328. doi: 10.3390/ijms21041328
6. Belk JW, Kraeutler MJ, Houck DA, et al. Platelet-rich plasma versus hyaluronic acid for knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Am J Sports Med. 2021;49:249-260. doi: 10.1177/0363546520909397
7. Filardo G, Kon E, Della Villa S, et al. Use of platelet-rich plasma for the treatment of refractory jumper’s knee. Int Orthop. 2010;34:909-915. doi: 10.1007/s00264-009-0845-7
8. Kon E, Filardo G, Delcogliano M, et al. Platelet-rich plasma: new clinical application: a pilot study for treatment of jumper’s knee. Injury. 2009;40:598-603. doi: 10.1016/j.injury.2008.11.026
9. Kanchanatawan W, Arirachakaran A, Chaijenkij K, et al. Short-term outcomes of platelet-rich plasma injection for treatment of osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2016;24:1665-1677. doi: 10.1007/s00167-015-3784-4
10. Cook J, Young M. Biologic therapies for tendon and muscle injury. UpToDate. Updated August 11, 2022. Accessed May 23, 2023. www.uptodate.com/contents/biologic-therapies-for-tendon-and-muscle-injury
11. Bendich I, Rubenstein WJ, Cole BJ, et al. What is the appropriate price for platelet-rich plasma injections for knee osteoarthritis? A cost-effectiveness analysis based on evidence from Level I randomized controlled trials. Arthroscopy. 2020;36:1983-1991.e1. doi: 10.1016/j.arthro.2020.02.004
12. Jones IA, Togashi RC, Thomas Vangsness C Jr. The economics and regulation of PRP in the evolving field of orthopedic biologics. Curr Rev Musculoskelet Med. 2018;11:558-565. doi: 10.1007/s12178-018-9514-z
13. Costa LAV, Lenza M, Irrgang JJ, et al. How does platelet-rich plasma compare clinically to other therapies in the treatment of knee osteoarthritis? A systematic review and meta-analysis. Am J Sports Med. 2023;51:1074-1086 doi: 10.1177/03635465211062243
14. Meheux CJ, McCulloch PC, Lintner DM, et al. Efficacy of intra-articular platelet-rich plasma injections in knee osteoarthritis: a systematic review. Arthroscopy. 2016;32:495-505. doi: 10.1016/j.arthro.2015.08.005
15. Shen L, Yuan T, Chen S, et al. The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. 2017;12:16. doi: 10.1186/s13018-017-0521-3
16. Paget LDA, Reurink G, de Vos RJ, et al; PRIMA Study Group. Effect of platelet-rich plasma injections vs. placebo on ankle symptoms and function in patients with ankle osteoarthritis: a randomized clinical trial. JAMA. 2021;326:1595-1605. doi: 10.1001/jama.2021.16602
17. Evans A, Ibrahim M, Pope R, et al. Treating hand and foot osteoarthritis using a patient’s own blood: a systematic review and meta-analysis of platelet-rich plasma. J Orthop. 2020;18:226-236. doi: 10.1016/j.jor.2020.01.037
18. Ye Y, Zhou X, Mao S, et al. Platelet rich plasma versus hyaluronic acid in patients with hip osteoarthritis: a meta-analysis of randomized controlled trials. Int J Surg. 2018;53:279-287. doi: 10.1016/j.ijsu.2018.03.078.
19. Berney M, McCarroll P, Glynn L, et al. Platelet-rich plasma injections for hip osteoarthritis: a review of the evidence. Ir J Med Sci. 2021;190:1021-1025. doi: 10.1007/s11845-020-02388-z
20. Belk JW, Houck DA, Littlefield CP, et al. Platelet-rich plasma versus hyaluronic acid for hip osteoarthritis yields similarly beneficial short-term clinical outcomes: a systematic review and meta-analysis of Level I and II randomized controlled trials. Arthroscopy. 2022;38:2035-2046. doi: 10.1016/j.arthro.2021.11.005
21. Dadgostar H, Fahimipour F, Pahlevan Sabagh A, et al. Corticosteroids or platelet-rich plasma injections for rotator cuff tendinopathy: a randomized clinical trial study. J Orthop Surg Res. 2021;16:333. doi: 10.1186/s13018-021-02470-x
22. Kwong CA, Woodmass JM, Gusnowski EM, et al. Platelet-rich plasma in patients with partial-thickness rotator cuff tears or tendinopathy leads to significantly improved short-term pain relief and function compared with corticosteroid injection: a double-blind randomized controlled trial. Arthroscopy. 2021;37:510-517. doi: 10.1016/j.arthro.2020.10.037
23. A Hamid MS, Sazlina SG. Platelet-rich plasma for rotator cuff tendinopathy: a systematic review and meta-analysis. PLoS One. 2021;16:e0251111. doi: 10.1371/journal.pone.0251111
24. Lian OB, Engebretsen L, Bahr R. Prevalence of jumper’s knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med. 2005;33:561-567. doi: 10.1177/0363546504270454
25. Dragoo JL, Wasterlain AS, Braun HJ, et al. Platelet-rich plasma as a treatment for patellar tendinopathy: a double-blind, randomized controlled trial. Am J Sports Med. 2014;42:610-618. doi: 10.1177/0363546513518416.
26. Rodas G, Soler-Rich R, Rius-Tarruella J, et al. Effect of autologous expanded bone marrow mesenchymal stem cells or leukocyte-poor platelet-rich plasma in chronic patellar tendinopathy (with gap >3 mm): preliminary outcomes after 6 months of a double-blind, randomized, prospective study. Am J Sports Med. 2021;49:1492-1504. doi: 10.1177/0363546521998725
27. Andriolo L, Altamura SA, Reale D, et al. Nonsurgical treatments of patellar tendinopathy: multiple injections of platelet-rich plasma are a suitable option: a systematic review and meta-analysis. Am J Sports Med. 2019;47:1001-1018. doi: 10.1177/0363546518759674
28. Scott A, LaPrade RF, Harmon KG, et al. Platelet-rich plasma for patellar tendinopathy: a randomized controlled trial of leukocyte-rich PRP or leukocyte-poor PRP versus saline. Am J Sports Med. 2019;47:1654-1661. doi: 10.1177/0363546519837954
29. Kemp JA, Olson MA, Tao MA, et al. Platelet-rich plasma versus corticosteroid injection for the treatment of lateral epicondylitis: a systematic review of systematic reviews. Int J Sports Phys Ther. 2021;16:597-605. doi: 10.26603/001c.24148
30. Miller LE, Parrish WR, Roides B, et al. Efficacy of platelet-rich plasma injections for symptomatic tendinopathy: systematic review and meta-analysis of randomised injection-controlled trials. BMJ Open Sport Exerc Med. 2017;3:e000237. doi: 10.1136/bmjsem-2017- 000237
31. Ben-Nafa W, Munro W. The effect of corticosteroid versus platelet-rich plasma injection therapies for the management of lateral epicondylitis: a systematic review. SICOT J. 2018;4:11.
32. Niemiec P, Szyluk K, Jarosz A, et al. Effectiveness of platelet-rich plasma for lateral epicondylitis: a systematic review and meta-analysis based on achievement of minimal clinically important difference. Orthop J Sports Med. 2022;10:23259671221086920. doi: 10.1177/23259671221086920
33. Li S, Yang G, Zhang H, et al. A systematic review on the efficacy of different types of platelet-rich plasma in the management of lateral epicondylitis. J Shoulder Elbow Surg. 2022;311533-1544. doi: 10.1016/j.jse.2022.02.017.
34. Madhi MI, Yausep OE, Khamdan K, et al. The use of PRP in treatment of Achilles tendinopathy: a systematic review of literature. Study design: systematic review of literature. Ann Med Surg (Lond). 2020;55:320-326. doi: 10.1016/j.amsu.2020.04.042
35. Loppini M, Maffulli N. Conservative management of tendinopathy: an evidence-based approach. Muscles Ligaments Tendons J. 2012;1:134-137.
36. Nauwelaers AK, Van Oost L, Peers K. Evidence for the use of PRP in chronic midsubstance Achilles tendinopathy: a systematic review with meta-analysis. Foot Ankle Surg. 2021;27:486-495. doi: 10.1016/j.fas.2020.07.009
37. Dai WL, Zhou AG, Zhang H, et al. Efficacy of platelet-rich plasma in the treatment of knee osteoarthritis: a meta-analysis of randomized controlled trials. Arthroscopy. 2017;33:659-670.e1. doi: 10.1016/j.arthro.2016.09.024
38. Bar-Or D, Rael LT, Brody EN. Use of saline as a placebo in intra-articular injections in osteoarthritis: potential contributions to nociceptive pain relief. Open Rheumatol J. 2017;11:16-22. doi: 10.2174/1874312901711010016
39. Phillips M, Bhandari M, Grant J, et al. A systematic review of current clinical practice guidelines on intra-articular hyaluronic acid, corticosteroid, and platelet-rich plasma injection for knee osteoarthritis: an international perspective. Orthop J Sports Med. 2021;9:23259671211030272. doi: 10.1177/23259671211030272
40. Finnoff JT, Awan TM, Borg-Stein J, et al. American Medical Society for Sports Medicine position statement: principles for the responsible use of regenerative medicine in sports medicine. Clin J Sport Med. 2021;31:530-541. doi: 10.1097/JSM.0000000000000973
Platelet-rich plasma (PRP) injections have become a popular treatment option in a variety of specialties including sports medicine, maxillofacial surgery, dermatology, cosmetology, and reproductive medicine.1 PRP is an autologous blood product derived from whole blood, using a centrifuge to isolate a concentrated layer of platelets. The a-granules in platelets release transforming growth factor b 1, vascular endothelial growth factor, platelet-derived growth factor, basic fibroblast growth factor, epidermal growth factor, insulin-like growth factor 1, and other mediators that enhance the natural healing process.2
When patients ask. Familiarity with the use of PRP to treat specific musculoskeletal (MSK) conditions is essential for family physicians who frequently are asked by patients about whether PRP is right for them. These patients may have experienced failure of medication therapy or declined surgical intervention, or may not be surgical candidates. This review details the evidence surrounding common intra-articular and extra-articular applications of PRP. But first, a word about how PRP is prepared, its contraindications, and costs.
Preparation and types of PRP
Although there are many commercial systems for preparing PRP, there is no consensus on the optimal formulation.2 Other terms for PRP, such as autologous concentrated platelets and super-concentrated platelets, are based on concentration of red blood cells, leukocytes, and fibrin.3 PRP therapies usually are categorized as leukocyte-rich PRP (LR-PRP) or leukocyte-poor PRP (LP-PRP), based on neutrophil concentrations that are above and below baseline.2 Leukocyte concentration is one of the most debated topics in PRP therapy.4
Common commercially available preparation systems produce platelet concentrations between 3 to 6 times the baseline platelet count.5 Although there is no universally agreed upon PRP formulation, studies have shown 2 centrifugation cycles (“double-spun” or “dual centrifugation”) that yield platelet concentrations between 1.8 to 1.9 times the baseline values significantly improve MSK conditions.6-8
For MSK purposes, PRP may be injected into intratendinous, peritendinous, and intra-articular spaces. Currently, there is no consensus regarding injection frequency. Many studies have incorporated single-injection protocols, while some have used 2 to 3 injections repeated over several weeks to months. PRP commonly is injected at point-of-care without requiring storage.
Contraindications. PRP has been shown to be safe, with most adverse effects attributed to local injection site pain, bleeding, swelling, and bruising.9
Contraindications to PRP include active malignancy or recent remission from malignancy with the exception of nonmetastatic skin tumors.10 PRP is not recommended for patients with an allergy to manufacturing components (eg, dimethyl sulfoxide), thrombocytopenia, nonsteroidal anti-inflammatory drug use within 2 weeks, active infection causing fever, and local infection at the injection site.10 Since local anesthetics may impair platelet function, they should not be given at the same injection site as PRP.10
Continue to: Cost
Cost. PRP is not covered by most insurance plans.11,12 The cost for PRP may range from $500 to $2500 for a single injection.12
Evidence-based summary by condition
Knee osteoarthritis
❯❯❯ Consider using PRP
Knee osteoarthritis (OA) is a common cause of pain and disability. Treatment options include physical therapy, pharmacotherapy, and surgery. PRP has gained popularity as a nonsurgical option. A recent meta-analysis by Costa et al13 of 40 studies with 3035 participants comparing intra-articular PRP with hyaluronic acid (HA), corticosteroid, and saline injections, found that PRP appears to be more effective or as effective as other nonsurgical modalities. However, due to study heterogeneity and high risk for bias, the authors could not recommend PRP for knee OA in clinical practice.13
Despite Costa et al’s findings, reproducible data have demonstrated the superiority of PRP over other nonsurgical treatment options for knee OA. A 2021 systematic review and meta-analysis of 18 randomized controlled trials (RCTs; N = 811) by Belk et al6 comparing PRP to HA injections showed a higher mean improvement in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores in the PRP group compared to the HA group (44.7% vs 12.6%, respectively; P < .01).6 Six of 11 studies using the visual analog scale (VAS) for pain reported significantly less pain in the PRP group compared to the HA group (P < .05).6 The mean follow-up time was 11.1 months.6 Three of 6 studies reported improved subjective International Knee Documentation Committee (IKDC) scores (range from 0-100, with higher scores representing higher levels of function and lower levels of symptoms) in the PRP group compared to the HA group: 75.7 ± 15.1 vs 65.6 ± 16.9 (P = .004); 65.5 ± 3.6 vs 55.8 ± 3.8 (P = .01); and 60.8 ± 9.8 vs 48.4 ± 6.2 (P < .05).6 There was concern for moderate-to-high heterogeneity.6
Other systematic reviews and meta-analyses found similar efficacy of PRP for knee OA, including improved WOMAC scores and patient-reported outcomes (eg, pain, physical function, stiffness) compared to other injectable options.14,15 A systematic review of 14 RCTs (N = 1423) by Shen et al15 showed improved WOMAC scores at 3 months (mean differences [MD] = –14.53; 95% CI, –29.97 to –7.09; P < .001), 6 months
Despite a lack of consensus regarding the optimal preparation of PRP for knee OA, another recent RCT (N = 192) found significant improvement in mean subjective IKDC scores in the LR-PRP group (45.5 ± 15.5 to 60.7 ± 21.1; P < .0005) and the LP-PRP group (46.8 ± 15.8 to 62.9 ± 19.9; P < .0005), indicating efficacy regardless of PRP type.4
Continue to: Ankle osteoarthritis
Ankle osteoarthritis
❯ ❯ ❯ Additional research is needed
Ankle OA affects 3.4% of all adults and is more common in the younger population than knee or hip OA.16 An RCT (N = 100) investigating PRP vs placebo (saline) injections showed no statistically significant difference in American Orthopedic Foot and Ankle Society scores evaluating pain and function over 26 weeks (–2 points; 95% CI, –5 to 1; P = .16).16 Limitations to this study include its small sample size and the PRP formulation used. (The intervention group received 2 injections of 2 mL of PRP, and the platelet concentration was not reported.)16
Hip osteoarthritis
❯ ❯ ❯ Additional research is needed
Symptomatic hip OA occurs in 40% of adults older than 65 years, with a higher prevalence in women.18 Currently, corticosteroid injections are the only intra-articular therapy recommended by international guidelines for hip OA.19 A systematic review and meta-analysis comparing PRP to HA injections that included 4 RCTs (N = 303) showed a statistically significant reduction in VAS scores at 2 months in the PRP group compared to the HA group (weighted mean difference [WMD] = –0.376; 95% CI, –0.614 to –0.138; P = .002).18 However, there were no significant differences in VAS scores between the PRP and HA groups at 6 months (WMD = –0.141; 95% CI, –0.401 to 0.119; P = .289) and 12 months (WMD = –0.083; 95% CI, –0.343 to 0.117; P = .534). Likewise, no significant differences were found in WOMAC scores at 6 months (WMD = –2.841; 95% CI, –6.248 to 0.565; P = .102) and 12 months (WMD = –3.134; 95% CI, –6.624 to 0.356; P = .078) and Harris Hip Scores (HHS) at 6 months (WMD = 2.782; 95% CI, –6.639 to 12.203; P =.563) and 12 months (WMD = 0.706; 95% CI, –6.333 to 7.745; P = .844).18
A systematic review of 6 RCTs (N = 408) by Belk et al20 comparing PRP to HA for hip OA found similar short-term improvements in WOMAC scores (standardized mean differences [SMD] = 0.27; 95% CI, –0.05 to 0.59; P = .09), VAS scores (MD = 0.59; 95% CI, –0.741 to 1.92; P = .39), and HHS (MD = -0.81; 95% CI, –10.06 to 8.43; P = .93). The average follow-up time was 12.2 and 11.9 months for the PRP and HA groups, respectively.20
LR-PRP, which was used in 1 of the 6 RCTs, showed improvement in VAS scores and HHS from baseline, but no significant difference compared to HA at the latest follow-up.20 A pooled subanalysis of the 3 studies that used LP-PRP found no difference in WOMAC scores between the PRP and HA groups (SMD = 0.42; 95% CI, –0.01 to 0.86; P = .06).20 Future studies comparing the efficacy of intra-articular steroid vs PRP for hip OA would be beneficial.18
Continue to: Rotator cuff tendinopathy
Rotator cuff tendinopathy
❯ ❯ ❯ Consider PRP for short-term pain relief
Painful conditions of the rotator cuff include impingement syndrome, tendonitis, and partial and complete tears. A 2021 RCT (N = 58) by Dadgostar et al21 comparing PRP injection to corticosteroid therapy (methylprednisolone and lidocaine) for the treatment of rotator cuff tendinopathy showed significant improvement in VAS scores at 3 months in the PRP group compared to the corticosteroid group (6.66
Another RCT (N = 99) by Kwong et al22 comparing PRP to corticosteroids found similar short-term advantages of LP-PRP with an improved VAS score (–13.6 vs 0.4; P = .03), American Shoulder and Elbow Surgeons score (13.0 vs 2.9; P = .02), and Western Ontario Rotator Cuff Index score (16.8 vs 5.8; P = .03). However, there was no long-term benefit of PRP over corticosteroids found at 12 months.22
A 2021 systematic review and meta-analysis by Hamid et al23 that included 8 RCTs (N = 976) favored PRP over control (no injection, saline injections, and/or shoulder rehabilitation) with improved VAS scores at 12 months (SMD = –0.5; 95% CI, –0.7 to –0.2; P < .001). The evidence on functional outcome was mixed. Data pooled from 2 studies (n = 228) found better Shoulder Pain and Disability Index (SPADI) scores compared to controls at 3- and 6-month follow-ups. However, there were no significant differences in Disabilities of the Arm, Shoulder and Hand (DASH) scores between the 2 groups.23
Patellar tendinopathy
❯ ❯ ❯ Consider using PRP for return to sport
Patellar tendinopathy, a common MSK condition encountered in the primary care setting, has an overall prevalence of 22% in elite athletes at some point in their career.24 Nonsurgical management options include rest, ice, eccentric and isometric exercises, anti-inflammatory drugs, extracorporeal shock wave therapy (ESWT), and dry needling (DN).
A 2014 RCT (N = 23) evaluating DN vs PRP for patellar tendinopathy favored PRP with improved VAS scores (mean ± SD = 25.4 ± 23.2 points; P = .01 vs 5.2 ± 12.5 points; P = .20) at 12 weeks (P = .02). However, at ≥ 26 weeks, the improvement in pain and function scores was similar between the DN and PRP groups (33.2 ± 14.0 points; P = .001 vs 28.9 ± 25.2 points; P = .01). Notably, there was significantly more improvement in the PRP group at 12 weeks (P = .02) but not at 26 weeks (P = .66).25
Continue to: Another perspective study...
Another prospective study (N = 31) comparing PRP to physiotherapy showed a greater improvement in sport activity level reflected by the Tegner score in the PRP group (percentage improvement, 39 ± 22%) compared to control (20 ± 27%; P = .048) at 6 months.7
A recent RCT (N = 20) revealed improved VAS scores at 6 months with rehabilitation paired with either bone marrow mesenchymal stem cells (BM-MSC) or LP-PRP when compared with baseline (BM-MSC group: 4.23 ± 2.13 to 2.52 ± 2.37; P = .0621; LP-PRP group: 3.10 ± 1.20 to 1.13 ± 1.25; P = .0083). Pain was significantly reduced during sport play in both groups at 6 months when compared with baseline (BM-MSC group: 6.91 ± 1.11 to 3.06 ± 2.89, P = .0049; PRP group: 7.03 ± 1.42 to 1.94 ± 1.24, P = .0001).26
A 2019 systematic review and meta-analysis (N = 2530) demonstrated greater improvements in Victorian Institute of Sport Assessment scale for patellar tendinopathy (VISA-P) with multiple injections of PRP (38.7 points; 95% CI, 26.3-51.2 points) compared to single injections of PRP (24.3 points; 95% CI, 18.2-30.5 points), eccentric exercise (28.3 points; 95% CI, 18.9-37.8 points) and ESWT (27.4 points; 95% CI, 10.0-39.8 points) after 6 months.27 In contrast, an RCT (n = 57) comparing a single injection of LR-PRP or LP-PRP was no more effective than a single injection of saline for improvement in mean VISA-P scores (P > .05) at 1 year.28
Lateral epicondylitis
❯ ❯ ❯ Consider using PRP
Lateral epicondylitis (“tennis elbow”) is caused by overuse of the elbow extensors at the site of the lateral epicondyle. Chronic lateral epicondylosis involves tissue degeneration and microtrauma. Most cases of epicondylar tendinopathies are treated nonoperatively, with corticosteroid injections being a mainstay of treatment despite their short-term benefit29 and potential to deteriorate connective tissue over time. Recent studies suggest PRP therapy for epicondylitis and epicondylosis may increase long-term pain relief and improve function.
A 2017 systematic review and meta-analysis of 16 RCTs (N = 1018) concluded PRP was more efficacious than control injections (bupivacaine) for pain reduction in tendinopathies (effect size = 0.47; 95% CI, 0.22-0.72).30 In the review, lateral epicondylitis was evaluated in 12 studies and was most responsive to PRP (effect size = 0.57) when compared to control injection.30 In another systematic review (5 RCTs; 250 patients), corticosteroid injections improved pain within the first 6 weeks of treatment. However, PRP outperformed corticosteroid in VAS scores (21.3 ± 28.1 vs 42.4 ± 26.8) and DASH scores (17.6 ± 24.0 vs 36.5 ± 23.8) (P < .001) at 2 years.31
Continue to: A 2022 systematic review...
A 2022 systematic review and meta-analysis (26 studies; N = 1040) comparing scores at baseline vs 2 years post-PRP showed improvement in VAS scores (7.4 ± 1.30 vs 3.71 ± 2.35; P < .001), DASH scores (60.8 ± 12.5 vs 13.0 ± 18.5; P < .001), Patient-Rated Tennis Elbow Evaluation (55.6 ± 14.7 vs 48.8 ± 4.1; P < .001), and Mayo Clinic Performance Index (55.5 ± 6.1 vs 93.0 ± 6.7; P < .001).32
Regarding the therapeutic effects of different PRP types in lateral epicondylitis, a 2022 systematic review of 33 studies (N = 2420) found improved function and pain relief with LR-PRP and LP-PRP with no significant differences.33 Pretreatment VAS scores in the LR-PRP group, which ranged from 6.1 to 8.0, improved to 1.5 to 4.0 at 3 months and 0.6 to 3.3 after 1 year.33 Similarly, pretreatment VAS scores in the LP-PRP group, which ranged from 4.2 to 8.4, improved to 1.6 to 5.9 at 3 months and 0.7 to 2.7 after 1 year.34 DASH scores also improved in the LR-PRP and LP-PRP groups, with pretreatment scores (LR-PRP, 47.0 to 54.3; LP-PRP, 30.0 to 67.7) improving to 20.0 to 22.0 and 5.5 to 19.0, respectively, at 1 year.33
Achilles tendinopathy
❯ ❯ ❯ Do not use PRP; evidence is lacking
Achilles tendinopathy, caused by chronic overuse and overload resulting in microtrauma and poor tissue healing, typically occurs in the most poorly vascularized portion of the tendon and is common in runners. First-line treatments for Achilles tendinopathy include eccentric strength training and anti-inflammatory drugs.34,35 Corticosteroid injections are not recommended, given concern for degraded tendon tissue over time and worse function.34
A 2020 systematic review of 11 randomized and nonrandomized clinical trials (N = 406) found PRP improved Victorian Institute of Sports Assessment—Achilles (VISA-A) scores at 24 weeks compared to other nonsurgical treatment options (41.2 vs 70.12; P < .018).34 However, a higher-quality 2021 systematic review and meta-analysis of 4 RCTs (N = 170) comparing PRP injections with placebo showed no significant difference in VISA-A scores at 3 months (0.23; 95% CI, –0.45 to 0.91), 6 months (0.83; 95% CI, –0.26 to 1.92), and 12 months (0.83; 95% CI, –0.77 to 2.44).36 Therefore, further studies are warranted to evaluate the benefit of PRP injections for Achilles tendinopathy.
Conclusions
While high-quality studies support the use of PRP for knee OA and lateral epicondylitis, they have a moderate-to-high risk for bias. Several RCTs show that PRP provides superior short-term pain relief and range of motion compared to corticosteroids for rotator cuff tendinopathy. Multiple injections of PRP for patellar tendinopathy may accelerate return to sport and improve symptoms over the long term. However, current evidence does not support PRP therapy for Achilles tendinopathy. Given variability in PRP preparation, an accurate interpretation of the literature regarding its use in MSK conditions is recommended (TABLE4,6,7,14-18,20-23,25-28,30-34,36).
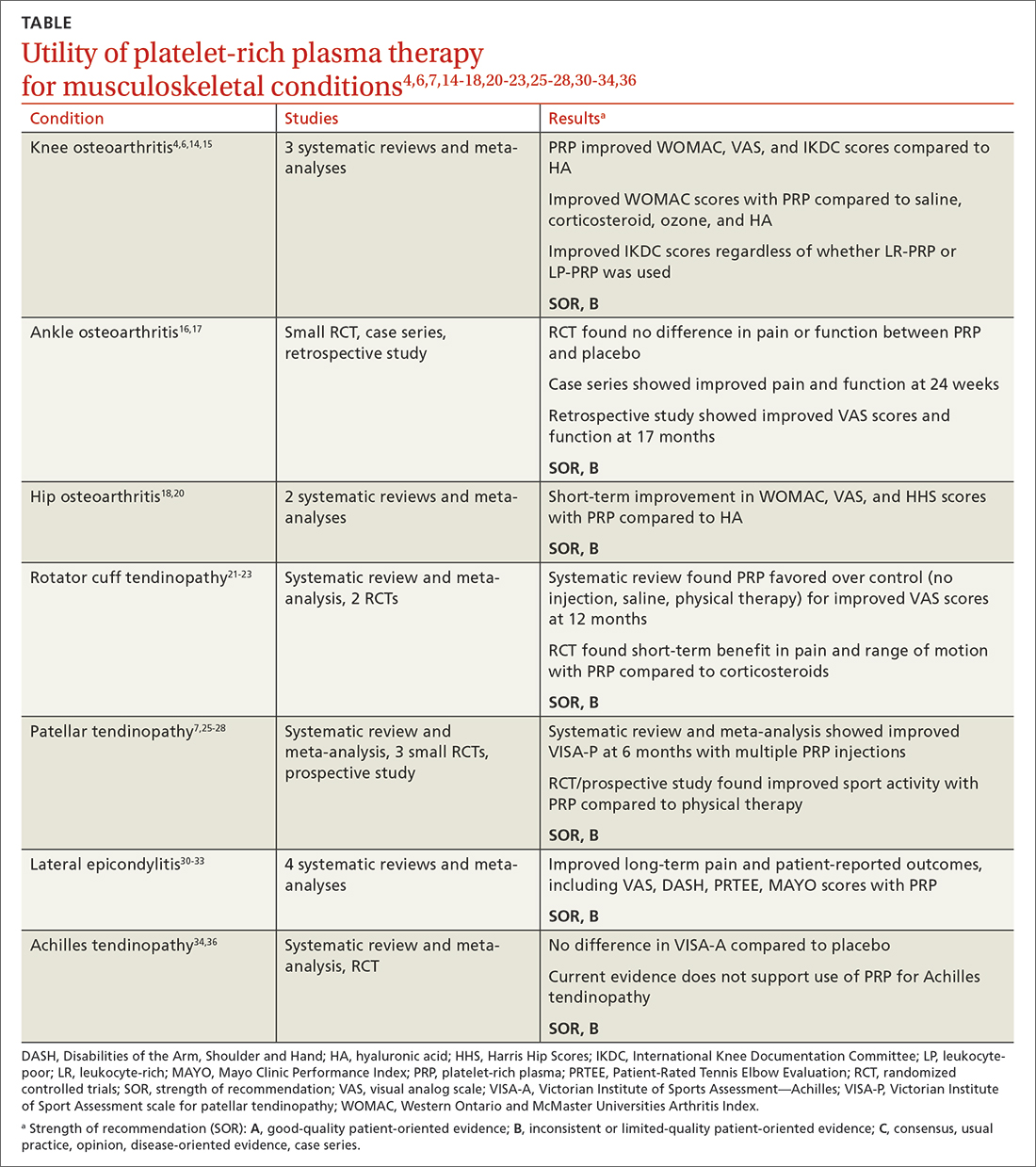
Continue to: Concerning the effectiveness of PRP...
Concerning the effectiveness of PRP, it is important to consider early publication bias. Although recent studies have shown its benefits,6,14,15,37 additional studies comparing PRP to placebo will help demonstrate its efficacy. Interestingly, a literature search by Bar-Or et al38 found intra-articular saline may have a therapeutic effect on knee OA and confound findings when used as a placebo.
Recognizing the presence or lack of clinically significant improvement in the literature is important. For example, while some recent studies have shown PRP exceeds the minimal clinically significant difference for knee OA and lateral epicondylitis, others have not.32,37 A 2021 systematic review of 11 clinical practice guidelines for the use of PRP in knee OA found that 9 were “uncertain or unable to make a recommendation” and 2 recommended against it.39
In its 2021 position statement for the responsible use of regenerative medicine, the American Medical Society for Sports Medicine includes guidance on integrating orthobiologics into clinical practice. The guideline emphasizes informed consent and provides an evidence-based rationale for using PRP in certain patient populations (lateral epicondylitis and younger patients with mild-to-moderate knee OA), recommending its use only after exhausting other conservative options.40 Patients should be referred to physicians with experience using PRP and image-guided procedures.
CORRESPONDENCE
Gregory D. Bentz Jr, MD, 3640 High Street Suite 3B, Portsmouth, VA 23707; [email protected]
Platelet-rich plasma (PRP) injections have become a popular treatment option in a variety of specialties including sports medicine, maxillofacial surgery, dermatology, cosmetology, and reproductive medicine.1 PRP is an autologous blood product derived from whole blood, using a centrifuge to isolate a concentrated layer of platelets. The a-granules in platelets release transforming growth factor b 1, vascular endothelial growth factor, platelet-derived growth factor, basic fibroblast growth factor, epidermal growth factor, insulin-like growth factor 1, and other mediators that enhance the natural healing process.2
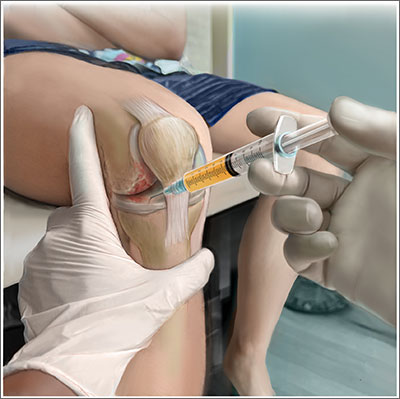
When patients ask. Familiarity with the use of PRP to treat specific musculoskeletal (MSK) conditions is essential for family physicians who frequently are asked by patients about whether PRP is right for them. These patients may have experienced failure of medication therapy or declined surgical intervention, or may not be surgical candidates. This review details the evidence surrounding common intra-articular and extra-articular applications of PRP. But first, a word about how PRP is prepared, its contraindications, and costs.
Preparation and types of PRP
Although there are many commercial systems for preparing PRP, there is no consensus on the optimal formulation.2 Other terms for PRP, such as autologous concentrated platelets and super-concentrated platelets, are based on concentration of red blood cells, leukocytes, and fibrin.3 PRP therapies usually are categorized as leukocyte-rich PRP (LR-PRP) or leukocyte-poor PRP (LP-PRP), based on neutrophil concentrations that are above and below baseline.2 Leukocyte concentration is one of the most debated topics in PRP therapy.4
Common commercially available preparation systems produce platelet concentrations between 3 to 6 times the baseline platelet count.5 Although there is no universally agreed upon PRP formulation, studies have shown 2 centrifugation cycles (“double-spun” or “dual centrifugation”) that yield platelet concentrations between 1.8 to 1.9 times the baseline values significantly improve MSK conditions.6-8
For MSK purposes, PRP may be injected into intratendinous, peritendinous, and intra-articular spaces. Currently, there is no consensus regarding injection frequency. Many studies have incorporated single-injection protocols, while some have used 2 to 3 injections repeated over several weeks to months. PRP commonly is injected at point-of-care without requiring storage.
Contraindications. PRP has been shown to be safe, with most adverse effects attributed to local injection site pain, bleeding, swelling, and bruising.9
Contraindications to PRP include active malignancy or recent remission from malignancy with the exception of nonmetastatic skin tumors.10 PRP is not recommended for patients with an allergy to manufacturing components (eg, dimethyl sulfoxide), thrombocytopenia, nonsteroidal anti-inflammatory drug use within 2 weeks, active infection causing fever, and local infection at the injection site.10 Since local anesthetics may impair platelet function, they should not be given at the same injection site as PRP.10
Continue to: Cost
Cost. PRP is not covered by most insurance plans.11,12 The cost for PRP may range from $500 to $2500 for a single injection.12
Evidence-based summary by condition
Knee osteoarthritis
❯❯❯ Consider using PRP
Knee osteoarthritis (OA) is a common cause of pain and disability. Treatment options include physical therapy, pharmacotherapy, and surgery. PRP has gained popularity as a nonsurgical option. A recent meta-analysis by Costa et al13 of 40 studies with 3035 participants comparing intra-articular PRP with hyaluronic acid (HA), corticosteroid, and saline injections, found that PRP appears to be more effective or as effective as other nonsurgical modalities. However, due to study heterogeneity and high risk for bias, the authors could not recommend PRP for knee OA in clinical practice.13
Despite Costa et al’s findings, reproducible data have demonstrated the superiority of PRP over other nonsurgical treatment options for knee OA. A 2021 systematic review and meta-analysis of 18 randomized controlled trials (RCTs; N = 811) by Belk et al6 comparing PRP to HA injections showed a higher mean improvement in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores in the PRP group compared to the HA group (44.7% vs 12.6%, respectively; P < .01).6 Six of 11 studies using the visual analog scale (VAS) for pain reported significantly less pain in the PRP group compared to the HA group (P < .05).6 The mean follow-up time was 11.1 months.6 Three of 6 studies reported improved subjective International Knee Documentation Committee (IKDC) scores (range from 0-100, with higher scores representing higher levels of function and lower levels of symptoms) in the PRP group compared to the HA group: 75.7 ± 15.1 vs 65.6 ± 16.9 (P = .004); 65.5 ± 3.6 vs 55.8 ± 3.8 (P = .01); and 60.8 ± 9.8 vs 48.4 ± 6.2 (P < .05).6 There was concern for moderate-to-high heterogeneity.6
Other systematic reviews and meta-analyses found similar efficacy of PRP for knee OA, including improved WOMAC scores and patient-reported outcomes (eg, pain, physical function, stiffness) compared to other injectable options.14,15 A systematic review of 14 RCTs (N = 1423) by Shen et al15 showed improved WOMAC scores at 3 months (mean differences [MD] = –14.53; 95% CI, –29.97 to –7.09; P < .001), 6 months
Despite a lack of consensus regarding the optimal preparation of PRP for knee OA, another recent RCT (N = 192) found significant improvement in mean subjective IKDC scores in the LR-PRP group (45.5 ± 15.5 to 60.7 ± 21.1; P < .0005) and the LP-PRP group (46.8 ± 15.8 to 62.9 ± 19.9; P < .0005), indicating efficacy regardless of PRP type.4
Continue to: Ankle osteoarthritis
Ankle osteoarthritis
❯ ❯ ❯ Additional research is needed
Ankle OA affects 3.4% of all adults and is more common in the younger population than knee or hip OA.16 An RCT (N = 100) investigating PRP vs placebo (saline) injections showed no statistically significant difference in American Orthopedic Foot and Ankle Society scores evaluating pain and function over 26 weeks (–2 points; 95% CI, –5 to 1; P = .16).16 Limitations to this study include its small sample size and the PRP formulation used. (The intervention group received 2 injections of 2 mL of PRP, and the platelet concentration was not reported.)16
Hip osteoarthritis
❯ ❯ ❯ Additional research is needed
Symptomatic hip OA occurs in 40% of adults older than 65 years, with a higher prevalence in women.18 Currently, corticosteroid injections are the only intra-articular therapy recommended by international guidelines for hip OA.19 A systematic review and meta-analysis comparing PRP to HA injections that included 4 RCTs (N = 303) showed a statistically significant reduction in VAS scores at 2 months in the PRP group compared to the HA group (weighted mean difference [WMD] = –0.376; 95% CI, –0.614 to –0.138; P = .002).18 However, there were no significant differences in VAS scores between the PRP and HA groups at 6 months (WMD = –0.141; 95% CI, –0.401 to 0.119; P = .289) and 12 months (WMD = –0.083; 95% CI, –0.343 to 0.117; P = .534). Likewise, no significant differences were found in WOMAC scores at 6 months (WMD = –2.841; 95% CI, –6.248 to 0.565; P = .102) and 12 months (WMD = –3.134; 95% CI, –6.624 to 0.356; P = .078) and Harris Hip Scores (HHS) at 6 months (WMD = 2.782; 95% CI, –6.639 to 12.203; P =.563) and 12 months (WMD = 0.706; 95% CI, –6.333 to 7.745; P = .844).18
A systematic review of 6 RCTs (N = 408) by Belk et al20 comparing PRP to HA for hip OA found similar short-term improvements in WOMAC scores (standardized mean differences [SMD] = 0.27; 95% CI, –0.05 to 0.59; P = .09), VAS scores (MD = 0.59; 95% CI, –0.741 to 1.92; P = .39), and HHS (MD = -0.81; 95% CI, –10.06 to 8.43; P = .93). The average follow-up time was 12.2 and 11.9 months for the PRP and HA groups, respectively.20
LR-PRP, which was used in 1 of the 6 RCTs, showed improvement in VAS scores and HHS from baseline, but no significant difference compared to HA at the latest follow-up.20 A pooled subanalysis of the 3 studies that used LP-PRP found no difference in WOMAC scores between the PRP and HA groups (SMD = 0.42; 95% CI, –0.01 to 0.86; P = .06).20 Future studies comparing the efficacy of intra-articular steroid vs PRP for hip OA would be beneficial.18
Continue to: Rotator cuff tendinopathy
Rotator cuff tendinopathy
❯ ❯ ❯ Consider PRP for short-term pain relief
Painful conditions of the rotator cuff include impingement syndrome, tendonitis, and partial and complete tears. A 2021 RCT (N = 58) by Dadgostar et al21 comparing PRP injection to corticosteroid therapy (methylprednisolone and lidocaine) for the treatment of rotator cuff tendinopathy showed significant improvement in VAS scores at 3 months in the PRP group compared to the corticosteroid group (6.66
Another RCT (N = 99) by Kwong et al22 comparing PRP to corticosteroids found similar short-term advantages of LP-PRP with an improved VAS score (–13.6 vs 0.4; P = .03), American Shoulder and Elbow Surgeons score (13.0 vs 2.9; P = .02), and Western Ontario Rotator Cuff Index score (16.8 vs 5.8; P = .03). However, there was no long-term benefit of PRP over corticosteroids found at 12 months.22
A 2021 systematic review and meta-analysis by Hamid et al23 that included 8 RCTs (N = 976) favored PRP over control (no injection, saline injections, and/or shoulder rehabilitation) with improved VAS scores at 12 months (SMD = –0.5; 95% CI, –0.7 to –0.2; P < .001). The evidence on functional outcome was mixed. Data pooled from 2 studies (n = 228) found better Shoulder Pain and Disability Index (SPADI) scores compared to controls at 3- and 6-month follow-ups. However, there were no significant differences in Disabilities of the Arm, Shoulder and Hand (DASH) scores between the 2 groups.23
Patellar tendinopathy
❯ ❯ ❯ Consider using PRP for return to sport
Patellar tendinopathy, a common MSK condition encountered in the primary care setting, has an overall prevalence of 22% in elite athletes at some point in their career.24 Nonsurgical management options include rest, ice, eccentric and isometric exercises, anti-inflammatory drugs, extracorporeal shock wave therapy (ESWT), and dry needling (DN).
A 2014 RCT (N = 23) evaluating DN vs PRP for patellar tendinopathy favored PRP with improved VAS scores (mean ± SD = 25.4 ± 23.2 points; P = .01 vs 5.2 ± 12.5 points; P = .20) at 12 weeks (P = .02). However, at ≥ 26 weeks, the improvement in pain and function scores was similar between the DN and PRP groups (33.2 ± 14.0 points; P = .001 vs 28.9 ± 25.2 points; P = .01). Notably, there was significantly more improvement in the PRP group at 12 weeks (P = .02) but not at 26 weeks (P = .66).25
Continue to: Another perspective study...
Another prospective study (N = 31) comparing PRP to physiotherapy showed a greater improvement in sport activity level reflected by the Tegner score in the PRP group (percentage improvement, 39 ± 22%) compared to control (20 ± 27%; P = .048) at 6 months.7
A recent RCT (N = 20) revealed improved VAS scores at 6 months with rehabilitation paired with either bone marrow mesenchymal stem cells (BM-MSC) or LP-PRP when compared with baseline (BM-MSC group: 4.23 ± 2.13 to 2.52 ± 2.37; P = .0621; LP-PRP group: 3.10 ± 1.20 to 1.13 ± 1.25; P = .0083). Pain was significantly reduced during sport play in both groups at 6 months when compared with baseline (BM-MSC group: 6.91 ± 1.11 to 3.06 ± 2.89, P = .0049; PRP group: 7.03 ± 1.42 to 1.94 ± 1.24, P = .0001).26
A 2019 systematic review and meta-analysis (N = 2530) demonstrated greater improvements in Victorian Institute of Sport Assessment scale for patellar tendinopathy (VISA-P) with multiple injections of PRP (38.7 points; 95% CI, 26.3-51.2 points) compared to single injections of PRP (24.3 points; 95% CI, 18.2-30.5 points), eccentric exercise (28.3 points; 95% CI, 18.9-37.8 points) and ESWT (27.4 points; 95% CI, 10.0-39.8 points) after 6 months.27 In contrast, an RCT (n = 57) comparing a single injection of LR-PRP or LP-PRP was no more effective than a single injection of saline for improvement in mean VISA-P scores (P > .05) at 1 year.28
Lateral epicondylitis
❯ ❯ ❯ Consider using PRP
Lateral epicondylitis (“tennis elbow”) is caused by overuse of the elbow extensors at the site of the lateral epicondyle. Chronic lateral epicondylosis involves tissue degeneration and microtrauma. Most cases of epicondylar tendinopathies are treated nonoperatively, with corticosteroid injections being a mainstay of treatment despite their short-term benefit29 and potential to deteriorate connective tissue over time. Recent studies suggest PRP therapy for epicondylitis and epicondylosis may increase long-term pain relief and improve function.
A 2017 systematic review and meta-analysis of 16 RCTs (N = 1018) concluded PRP was more efficacious than control injections (bupivacaine) for pain reduction in tendinopathies (effect size = 0.47; 95% CI, 0.22-0.72).30 In the review, lateral epicondylitis was evaluated in 12 studies and was most responsive to PRP (effect size = 0.57) when compared to control injection.30 In another systematic review (5 RCTs; 250 patients), corticosteroid injections improved pain within the first 6 weeks of treatment. However, PRP outperformed corticosteroid in VAS scores (21.3 ± 28.1 vs 42.4 ± 26.8) and DASH scores (17.6 ± 24.0 vs 36.5 ± 23.8) (P < .001) at 2 years.31
Continue to: A 2022 systematic review...
A 2022 systematic review and meta-analysis (26 studies; N = 1040) comparing scores at baseline vs 2 years post-PRP showed improvement in VAS scores (7.4 ± 1.30 vs 3.71 ± 2.35; P < .001), DASH scores (60.8 ± 12.5 vs 13.0 ± 18.5; P < .001), Patient-Rated Tennis Elbow Evaluation (55.6 ± 14.7 vs 48.8 ± 4.1; P < .001), and Mayo Clinic Performance Index (55.5 ± 6.1 vs 93.0 ± 6.7; P < .001).32
Regarding the therapeutic effects of different PRP types in lateral epicondylitis, a 2022 systematic review of 33 studies (N = 2420) found improved function and pain relief with LR-PRP and LP-PRP with no significant differences.33 Pretreatment VAS scores in the LR-PRP group, which ranged from 6.1 to 8.0, improved to 1.5 to 4.0 at 3 months and 0.6 to 3.3 after 1 year.33 Similarly, pretreatment VAS scores in the LP-PRP group, which ranged from 4.2 to 8.4, improved to 1.6 to 5.9 at 3 months and 0.7 to 2.7 after 1 year.34 DASH scores also improved in the LR-PRP and LP-PRP groups, with pretreatment scores (LR-PRP, 47.0 to 54.3; LP-PRP, 30.0 to 67.7) improving to 20.0 to 22.0 and 5.5 to 19.0, respectively, at 1 year.33
Achilles tendinopathy
❯ ❯ ❯ Do not use PRP; evidence is lacking
Achilles tendinopathy, caused by chronic overuse and overload resulting in microtrauma and poor tissue healing, typically occurs in the most poorly vascularized portion of the tendon and is common in runners. First-line treatments for Achilles tendinopathy include eccentric strength training and anti-inflammatory drugs.34,35 Corticosteroid injections are not recommended, given concern for degraded tendon tissue over time and worse function.34
A 2020 systematic review of 11 randomized and nonrandomized clinical trials (N = 406) found PRP improved Victorian Institute of Sports Assessment—Achilles (VISA-A) scores at 24 weeks compared to other nonsurgical treatment options (41.2 vs 70.12; P < .018).34 However, a higher-quality 2021 systematic review and meta-analysis of 4 RCTs (N = 170) comparing PRP injections with placebo showed no significant difference in VISA-A scores at 3 months (0.23; 95% CI, –0.45 to 0.91), 6 months (0.83; 95% CI, –0.26 to 1.92), and 12 months (0.83; 95% CI, –0.77 to 2.44).36 Therefore, further studies are warranted to evaluate the benefit of PRP injections for Achilles tendinopathy.
Conclusions
While high-quality studies support the use of PRP for knee OA and lateral epicondylitis, they have a moderate-to-high risk for bias. Several RCTs show that PRP provides superior short-term pain relief and range of motion compared to corticosteroids for rotator cuff tendinopathy. Multiple injections of PRP for patellar tendinopathy may accelerate return to sport and improve symptoms over the long term. However, current evidence does not support PRP therapy for Achilles tendinopathy. Given variability in PRP preparation, an accurate interpretation of the literature regarding its use in MSK conditions is recommended (TABLE4,6,7,14-18,20-23,25-28,30-34,36).
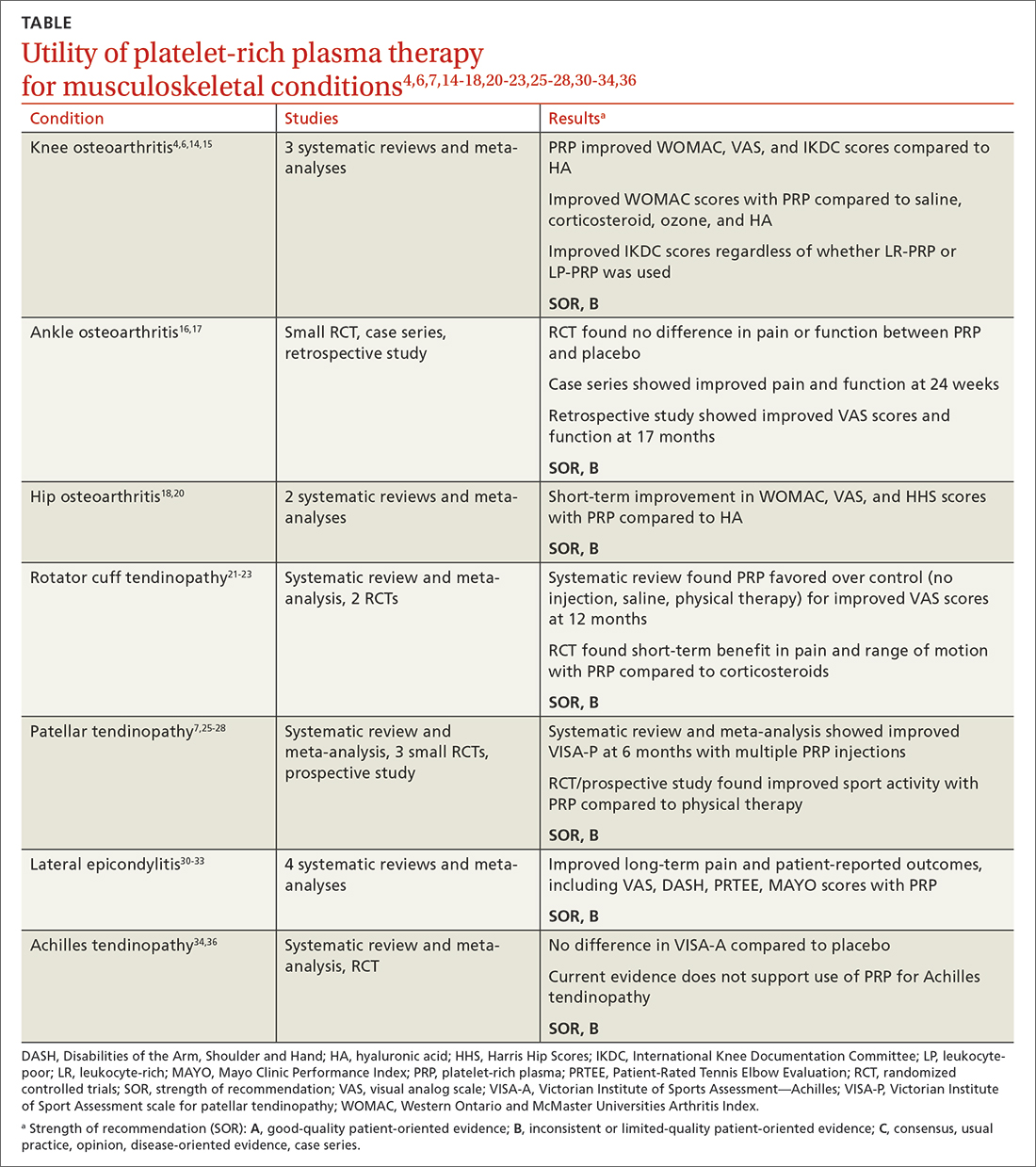
Continue to: Concerning the effectiveness of PRP...
Concerning the effectiveness of PRP, it is important to consider early publication bias. Although recent studies have shown its benefits,6,14,15,37 additional studies comparing PRP to placebo will help demonstrate its efficacy. Interestingly, a literature search by Bar-Or et al38 found intra-articular saline may have a therapeutic effect on knee OA and confound findings when used as a placebo.
Recognizing the presence or lack of clinically significant improvement in the literature is important. For example, while some recent studies have shown PRP exceeds the minimal clinically significant difference for knee OA and lateral epicondylitis, others have not.32,37 A 2021 systematic review of 11 clinical practice guidelines for the use of PRP in knee OA found that 9 were “uncertain or unable to make a recommendation” and 2 recommended against it.39
In its 2021 position statement for the responsible use of regenerative medicine, the American Medical Society for Sports Medicine includes guidance on integrating orthobiologics into clinical practice. The guideline emphasizes informed consent and provides an evidence-based rationale for using PRP in certain patient populations (lateral epicondylitis and younger patients with mild-to-moderate knee OA), recommending its use only after exhausting other conservative options.40 Patients should be referred to physicians with experience using PRP and image-guided procedures.
CORRESPONDENCE
Gregory D. Bentz Jr, MD, 3640 High Street Suite 3B, Portsmouth, VA 23707; [email protected]
1. Cecerska-Heryć E, Goszka M, Serwin N, et al. Applications of the regenerative capacity of platelets in modern medicine. Cytokine Growth Factor Rev. 2022;64:84-94. doi: 10.1016/j.cytogfr.2021.11.003
2. Le ADK, Enweze L, DeBaun MR, et al. Current clinical recommendations for use of platelet-rich plasma. Curr Rev Musculoskelet Med. 2018;11:624-634. doi: 10.1007/s12178-018-9527-7
3. Everts P, Onishi K, Jayaram P, et al. Platelet-rich plasma: new performance understandings and therapeutic considerations in 2020. Int J Mol Sci. 2020;21:7794. doi: 10.3390/ijms21207794
4. Di Martino A, Boffa A, Andriolo L, et al. Leukocyte-rich versus leukocyte-poor platelet-rich plasma for the treatment of knee osteoarthritis: a double-blind randomized trial. Am J Sports Med. 2022;50:609-617. doi: 10.1177/03635465211064303
5. Mariani E, Pulsatelli L. Platelet concentrates in musculoskeletal medicine. Int J Mol Sci. 2020;21:1328. doi: 10.3390/ijms21041328
6. Belk JW, Kraeutler MJ, Houck DA, et al. Platelet-rich plasma versus hyaluronic acid for knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Am J Sports Med. 2021;49:249-260. doi: 10.1177/0363546520909397
7. Filardo G, Kon E, Della Villa S, et al. Use of platelet-rich plasma for the treatment of refractory jumper’s knee. Int Orthop. 2010;34:909-915. doi: 10.1007/s00264-009-0845-7
8. Kon E, Filardo G, Delcogliano M, et al. Platelet-rich plasma: new clinical application: a pilot study for treatment of jumper’s knee. Injury. 2009;40:598-603. doi: 10.1016/j.injury.2008.11.026
9. Kanchanatawan W, Arirachakaran A, Chaijenkij K, et al. Short-term outcomes of platelet-rich plasma injection for treatment of osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2016;24:1665-1677. doi: 10.1007/s00167-015-3784-4
10. Cook J, Young M. Biologic therapies for tendon and muscle injury. UpToDate. Updated August 11, 2022. Accessed May 23, 2023. www.uptodate.com/contents/biologic-therapies-for-tendon-and-muscle-injury
11. Bendich I, Rubenstein WJ, Cole BJ, et al. What is the appropriate price for platelet-rich plasma injections for knee osteoarthritis? A cost-effectiveness analysis based on evidence from Level I randomized controlled trials. Arthroscopy. 2020;36:1983-1991.e1. doi: 10.1016/j.arthro.2020.02.004
12. Jones IA, Togashi RC, Thomas Vangsness C Jr. The economics and regulation of PRP in the evolving field of orthopedic biologics. Curr Rev Musculoskelet Med. 2018;11:558-565. doi: 10.1007/s12178-018-9514-z
13. Costa LAV, Lenza M, Irrgang JJ, et al. How does platelet-rich plasma compare clinically to other therapies in the treatment of knee osteoarthritis? A systematic review and meta-analysis. Am J Sports Med. 2023;51:1074-1086 doi: 10.1177/03635465211062243
14. Meheux CJ, McCulloch PC, Lintner DM, et al. Efficacy of intra-articular platelet-rich plasma injections in knee osteoarthritis: a systematic review. Arthroscopy. 2016;32:495-505. doi: 10.1016/j.arthro.2015.08.005
15. Shen L, Yuan T, Chen S, et al. The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. 2017;12:16. doi: 10.1186/s13018-017-0521-3
16. Paget LDA, Reurink G, de Vos RJ, et al; PRIMA Study Group. Effect of platelet-rich plasma injections vs. placebo on ankle symptoms and function in patients with ankle osteoarthritis: a randomized clinical trial. JAMA. 2021;326:1595-1605. doi: 10.1001/jama.2021.16602
17. Evans A, Ibrahim M, Pope R, et al. Treating hand and foot osteoarthritis using a patient’s own blood: a systematic review and meta-analysis of platelet-rich plasma. J Orthop. 2020;18:226-236. doi: 10.1016/j.jor.2020.01.037
18. Ye Y, Zhou X, Mao S, et al. Platelet rich plasma versus hyaluronic acid in patients with hip osteoarthritis: a meta-analysis of randomized controlled trials. Int J Surg. 2018;53:279-287. doi: 10.1016/j.ijsu.2018.03.078.
19. Berney M, McCarroll P, Glynn L, et al. Platelet-rich plasma injections for hip osteoarthritis: a review of the evidence. Ir J Med Sci. 2021;190:1021-1025. doi: 10.1007/s11845-020-02388-z
20. Belk JW, Houck DA, Littlefield CP, et al. Platelet-rich plasma versus hyaluronic acid for hip osteoarthritis yields similarly beneficial short-term clinical outcomes: a systematic review and meta-analysis of Level I and II randomized controlled trials. Arthroscopy. 2022;38:2035-2046. doi: 10.1016/j.arthro.2021.11.005
21. Dadgostar H, Fahimipour F, Pahlevan Sabagh A, et al. Corticosteroids or platelet-rich plasma injections for rotator cuff tendinopathy: a randomized clinical trial study. J Orthop Surg Res. 2021;16:333. doi: 10.1186/s13018-021-02470-x
22. Kwong CA, Woodmass JM, Gusnowski EM, et al. Platelet-rich plasma in patients with partial-thickness rotator cuff tears or tendinopathy leads to significantly improved short-term pain relief and function compared with corticosteroid injection: a double-blind randomized controlled trial. Arthroscopy. 2021;37:510-517. doi: 10.1016/j.arthro.2020.10.037
23. A Hamid MS, Sazlina SG. Platelet-rich plasma for rotator cuff tendinopathy: a systematic review and meta-analysis. PLoS One. 2021;16:e0251111. doi: 10.1371/journal.pone.0251111
24. Lian OB, Engebretsen L, Bahr R. Prevalence of jumper’s knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med. 2005;33:561-567. doi: 10.1177/0363546504270454
25. Dragoo JL, Wasterlain AS, Braun HJ, et al. Platelet-rich plasma as a treatment for patellar tendinopathy: a double-blind, randomized controlled trial. Am J Sports Med. 2014;42:610-618. doi: 10.1177/0363546513518416.
26. Rodas G, Soler-Rich R, Rius-Tarruella J, et al. Effect of autologous expanded bone marrow mesenchymal stem cells or leukocyte-poor platelet-rich plasma in chronic patellar tendinopathy (with gap >3 mm): preliminary outcomes after 6 months of a double-blind, randomized, prospective study. Am J Sports Med. 2021;49:1492-1504. doi: 10.1177/0363546521998725
27. Andriolo L, Altamura SA, Reale D, et al. Nonsurgical treatments of patellar tendinopathy: multiple injections of platelet-rich plasma are a suitable option: a systematic review and meta-analysis. Am J Sports Med. 2019;47:1001-1018. doi: 10.1177/0363546518759674
28. Scott A, LaPrade RF, Harmon KG, et al. Platelet-rich plasma for patellar tendinopathy: a randomized controlled trial of leukocyte-rich PRP or leukocyte-poor PRP versus saline. Am J Sports Med. 2019;47:1654-1661. doi: 10.1177/0363546519837954
29. Kemp JA, Olson MA, Tao MA, et al. Platelet-rich plasma versus corticosteroid injection for the treatment of lateral epicondylitis: a systematic review of systematic reviews. Int J Sports Phys Ther. 2021;16:597-605. doi: 10.26603/001c.24148
30. Miller LE, Parrish WR, Roides B, et al. Efficacy of platelet-rich plasma injections for symptomatic tendinopathy: systematic review and meta-analysis of randomised injection-controlled trials. BMJ Open Sport Exerc Med. 2017;3:e000237. doi: 10.1136/bmjsem-2017- 000237
31. Ben-Nafa W, Munro W. The effect of corticosteroid versus platelet-rich plasma injection therapies for the management of lateral epicondylitis: a systematic review. SICOT J. 2018;4:11.
32. Niemiec P, Szyluk K, Jarosz A, et al. Effectiveness of platelet-rich plasma for lateral epicondylitis: a systematic review and meta-analysis based on achievement of minimal clinically important difference. Orthop J Sports Med. 2022;10:23259671221086920. doi: 10.1177/23259671221086920
33. Li S, Yang G, Zhang H, et al. A systematic review on the efficacy of different types of platelet-rich plasma in the management of lateral epicondylitis. J Shoulder Elbow Surg. 2022;311533-1544. doi: 10.1016/j.jse.2022.02.017.
34. Madhi MI, Yausep OE, Khamdan K, et al. The use of PRP in treatment of Achilles tendinopathy: a systematic review of literature. Study design: systematic review of literature. Ann Med Surg (Lond). 2020;55:320-326. doi: 10.1016/j.amsu.2020.04.042
35. Loppini M, Maffulli N. Conservative management of tendinopathy: an evidence-based approach. Muscles Ligaments Tendons J. 2012;1:134-137.
36. Nauwelaers AK, Van Oost L, Peers K. Evidence for the use of PRP in chronic midsubstance Achilles tendinopathy: a systematic review with meta-analysis. Foot Ankle Surg. 2021;27:486-495. doi: 10.1016/j.fas.2020.07.009
37. Dai WL, Zhou AG, Zhang H, et al. Efficacy of platelet-rich plasma in the treatment of knee osteoarthritis: a meta-analysis of randomized controlled trials. Arthroscopy. 2017;33:659-670.e1. doi: 10.1016/j.arthro.2016.09.024
38. Bar-Or D, Rael LT, Brody EN. Use of saline as a placebo in intra-articular injections in osteoarthritis: potential contributions to nociceptive pain relief. Open Rheumatol J. 2017;11:16-22. doi: 10.2174/1874312901711010016
39. Phillips M, Bhandari M, Grant J, et al. A systematic review of current clinical practice guidelines on intra-articular hyaluronic acid, corticosteroid, and platelet-rich plasma injection for knee osteoarthritis: an international perspective. Orthop J Sports Med. 2021;9:23259671211030272. doi: 10.1177/23259671211030272
40. Finnoff JT, Awan TM, Borg-Stein J, et al. American Medical Society for Sports Medicine position statement: principles for the responsible use of regenerative medicine in sports medicine. Clin J Sport Med. 2021;31:530-541. doi: 10.1097/JSM.0000000000000973
1. Cecerska-Heryć E, Goszka M, Serwin N, et al. Applications of the regenerative capacity of platelets in modern medicine. Cytokine Growth Factor Rev. 2022;64:84-94. doi: 10.1016/j.cytogfr.2021.11.003
2. Le ADK, Enweze L, DeBaun MR, et al. Current clinical recommendations for use of platelet-rich plasma. Curr Rev Musculoskelet Med. 2018;11:624-634. doi: 10.1007/s12178-018-9527-7
3. Everts P, Onishi K, Jayaram P, et al. Platelet-rich plasma: new performance understandings and therapeutic considerations in 2020. Int J Mol Sci. 2020;21:7794. doi: 10.3390/ijms21207794
4. Di Martino A, Boffa A, Andriolo L, et al. Leukocyte-rich versus leukocyte-poor platelet-rich plasma for the treatment of knee osteoarthritis: a double-blind randomized trial. Am J Sports Med. 2022;50:609-617. doi: 10.1177/03635465211064303
5. Mariani E, Pulsatelli L. Platelet concentrates in musculoskeletal medicine. Int J Mol Sci. 2020;21:1328. doi: 10.3390/ijms21041328
6. Belk JW, Kraeutler MJ, Houck DA, et al. Platelet-rich plasma versus hyaluronic acid for knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Am J Sports Med. 2021;49:249-260. doi: 10.1177/0363546520909397
7. Filardo G, Kon E, Della Villa S, et al. Use of platelet-rich plasma for the treatment of refractory jumper’s knee. Int Orthop. 2010;34:909-915. doi: 10.1007/s00264-009-0845-7
8. Kon E, Filardo G, Delcogliano M, et al. Platelet-rich plasma: new clinical application: a pilot study for treatment of jumper’s knee. Injury. 2009;40:598-603. doi: 10.1016/j.injury.2008.11.026
9. Kanchanatawan W, Arirachakaran A, Chaijenkij K, et al. Short-term outcomes of platelet-rich plasma injection for treatment of osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2016;24:1665-1677. doi: 10.1007/s00167-015-3784-4
10. Cook J, Young M. Biologic therapies for tendon and muscle injury. UpToDate. Updated August 11, 2022. Accessed May 23, 2023. www.uptodate.com/contents/biologic-therapies-for-tendon-and-muscle-injury
11. Bendich I, Rubenstein WJ, Cole BJ, et al. What is the appropriate price for platelet-rich plasma injections for knee osteoarthritis? A cost-effectiveness analysis based on evidence from Level I randomized controlled trials. Arthroscopy. 2020;36:1983-1991.e1. doi: 10.1016/j.arthro.2020.02.004
12. Jones IA, Togashi RC, Thomas Vangsness C Jr. The economics and regulation of PRP in the evolving field of orthopedic biologics. Curr Rev Musculoskelet Med. 2018;11:558-565. doi: 10.1007/s12178-018-9514-z
13. Costa LAV, Lenza M, Irrgang JJ, et al. How does platelet-rich plasma compare clinically to other therapies in the treatment of knee osteoarthritis? A systematic review and meta-analysis. Am J Sports Med. 2023;51:1074-1086 doi: 10.1177/03635465211062243
14. Meheux CJ, McCulloch PC, Lintner DM, et al. Efficacy of intra-articular platelet-rich plasma injections in knee osteoarthritis: a systematic review. Arthroscopy. 2016;32:495-505. doi: 10.1016/j.arthro.2015.08.005
15. Shen L, Yuan T, Chen S, et al. The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. 2017;12:16. doi: 10.1186/s13018-017-0521-3
16. Paget LDA, Reurink G, de Vos RJ, et al; PRIMA Study Group. Effect of platelet-rich plasma injections vs. placebo on ankle symptoms and function in patients with ankle osteoarthritis: a randomized clinical trial. JAMA. 2021;326:1595-1605. doi: 10.1001/jama.2021.16602
17. Evans A, Ibrahim M, Pope R, et al. Treating hand and foot osteoarthritis using a patient’s own blood: a systematic review and meta-analysis of platelet-rich plasma. J Orthop. 2020;18:226-236. doi: 10.1016/j.jor.2020.01.037
18. Ye Y, Zhou X, Mao S, et al. Platelet rich plasma versus hyaluronic acid in patients with hip osteoarthritis: a meta-analysis of randomized controlled trials. Int J Surg. 2018;53:279-287. doi: 10.1016/j.ijsu.2018.03.078.
19. Berney M, McCarroll P, Glynn L, et al. Platelet-rich plasma injections for hip osteoarthritis: a review of the evidence. Ir J Med Sci. 2021;190:1021-1025. doi: 10.1007/s11845-020-02388-z
20. Belk JW, Houck DA, Littlefield CP, et al. Platelet-rich plasma versus hyaluronic acid for hip osteoarthritis yields similarly beneficial short-term clinical outcomes: a systematic review and meta-analysis of Level I and II randomized controlled trials. Arthroscopy. 2022;38:2035-2046. doi: 10.1016/j.arthro.2021.11.005
21. Dadgostar H, Fahimipour F, Pahlevan Sabagh A, et al. Corticosteroids or platelet-rich plasma injections for rotator cuff tendinopathy: a randomized clinical trial study. J Orthop Surg Res. 2021;16:333. doi: 10.1186/s13018-021-02470-x
22. Kwong CA, Woodmass JM, Gusnowski EM, et al. Platelet-rich plasma in patients with partial-thickness rotator cuff tears or tendinopathy leads to significantly improved short-term pain relief and function compared with corticosteroid injection: a double-blind randomized controlled trial. Arthroscopy. 2021;37:510-517. doi: 10.1016/j.arthro.2020.10.037
23. A Hamid MS, Sazlina SG. Platelet-rich plasma for rotator cuff tendinopathy: a systematic review and meta-analysis. PLoS One. 2021;16:e0251111. doi: 10.1371/journal.pone.0251111
24. Lian OB, Engebretsen L, Bahr R. Prevalence of jumper’s knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med. 2005;33:561-567. doi: 10.1177/0363546504270454
25. Dragoo JL, Wasterlain AS, Braun HJ, et al. Platelet-rich plasma as a treatment for patellar tendinopathy: a double-blind, randomized controlled trial. Am J Sports Med. 2014;42:610-618. doi: 10.1177/0363546513518416.
26. Rodas G, Soler-Rich R, Rius-Tarruella J, et al. Effect of autologous expanded bone marrow mesenchymal stem cells or leukocyte-poor platelet-rich plasma in chronic patellar tendinopathy (with gap >3 mm): preliminary outcomes after 6 months of a double-blind, randomized, prospective study. Am J Sports Med. 2021;49:1492-1504. doi: 10.1177/0363546521998725
27. Andriolo L, Altamura SA, Reale D, et al. Nonsurgical treatments of patellar tendinopathy: multiple injections of platelet-rich plasma are a suitable option: a systematic review and meta-analysis. Am J Sports Med. 2019;47:1001-1018. doi: 10.1177/0363546518759674
28. Scott A, LaPrade RF, Harmon KG, et al. Platelet-rich plasma for patellar tendinopathy: a randomized controlled trial of leukocyte-rich PRP or leukocyte-poor PRP versus saline. Am J Sports Med. 2019;47:1654-1661. doi: 10.1177/0363546519837954
29. Kemp JA, Olson MA, Tao MA, et al. Platelet-rich plasma versus corticosteroid injection for the treatment of lateral epicondylitis: a systematic review of systematic reviews. Int J Sports Phys Ther. 2021;16:597-605. doi: 10.26603/001c.24148
30. Miller LE, Parrish WR, Roides B, et al. Efficacy of platelet-rich plasma injections for symptomatic tendinopathy: systematic review and meta-analysis of randomised injection-controlled trials. BMJ Open Sport Exerc Med. 2017;3:e000237. doi: 10.1136/bmjsem-2017- 000237
31. Ben-Nafa W, Munro W. The effect of corticosteroid versus platelet-rich plasma injection therapies for the management of lateral epicondylitis: a systematic review. SICOT J. 2018;4:11.
32. Niemiec P, Szyluk K, Jarosz A, et al. Effectiveness of platelet-rich plasma for lateral epicondylitis: a systematic review and meta-analysis based on achievement of minimal clinically important difference. Orthop J Sports Med. 2022;10:23259671221086920. doi: 10.1177/23259671221086920
33. Li S, Yang G, Zhang H, et al. A systematic review on the efficacy of different types of platelet-rich plasma in the management of lateral epicondylitis. J Shoulder Elbow Surg. 2022;311533-1544. doi: 10.1016/j.jse.2022.02.017.
34. Madhi MI, Yausep OE, Khamdan K, et al. The use of PRP in treatment of Achilles tendinopathy: a systematic review of literature. Study design: systematic review of literature. Ann Med Surg (Lond). 2020;55:320-326. doi: 10.1016/j.amsu.2020.04.042
35. Loppini M, Maffulli N. Conservative management of tendinopathy: an evidence-based approach. Muscles Ligaments Tendons J. 2012;1:134-137.
36. Nauwelaers AK, Van Oost L, Peers K. Evidence for the use of PRP in chronic midsubstance Achilles tendinopathy: a systematic review with meta-analysis. Foot Ankle Surg. 2021;27:486-495. doi: 10.1016/j.fas.2020.07.009
37. Dai WL, Zhou AG, Zhang H, et al. Efficacy of platelet-rich plasma in the treatment of knee osteoarthritis: a meta-analysis of randomized controlled trials. Arthroscopy. 2017;33:659-670.e1. doi: 10.1016/j.arthro.2016.09.024
38. Bar-Or D, Rael LT, Brody EN. Use of saline as a placebo in intra-articular injections in osteoarthritis: potential contributions to nociceptive pain relief. Open Rheumatol J. 2017;11:16-22. doi: 10.2174/1874312901711010016
39. Phillips M, Bhandari M, Grant J, et al. A systematic review of current clinical practice guidelines on intra-articular hyaluronic acid, corticosteroid, and platelet-rich plasma injection for knee osteoarthritis: an international perspective. Orthop J Sports Med. 2021;9:23259671211030272. doi: 10.1177/23259671211030272
40. Finnoff JT, Awan TM, Borg-Stein J, et al. American Medical Society for Sports Medicine position statement: principles for the responsible use of regenerative medicine in sports medicine. Clin J Sport Med. 2021;31:530-541. doi: 10.1097/JSM.0000000000000973
PRACTICE RECOMMENDATIONS
› Consider plateletrich plasma (PRP) for conservative management of knee osteoarthritis and lateral epicondylitis. B
› Consider giving multiple injections of PRP for longterm pain relief and expedited return to sport in patellar tendinopathy. B
› Do not use PRP for Achilles tendinopathy due to a lack of clinical evidence. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Exercise and empathy can help back pain patients in primary care
Treatment of chronic back pain remains a challenge for primary care physicians, and a new Cochrane Review confirms previous studies suggesting that analgesics and antidepressants fall short in terms of relief.
Data from another Cochrane Review support the value of exercise for chronic low back pain, although it is often underused, and the Food and Drug Administration’s recent approval of a spinal cord stimulation device for chronic back pain opens the door for another alternative.
Regardless of treatment type, however, patients report that empathy and clear communication from their doctors go a long way in their satisfaction with pain management, according to another recent study.
Exercise helps when patients adhere
The objective of the Cochrane Review on “Exercise therapy for chronic low back pain” was to determine whether exercise improves pain and functioning for people with chronic low back pain, compared with no treatment, usual care, or other common treatments, corresponding author Jill Hayden, PhD, of Dalhousie University, Halifax, N.S., said in an interview.
When back pain is chronic, it is expensive in terms of health care costs and lost work hours, said Dr. Hayden. “Exercise is promoted in many guidelines and is often recommended for, and used by, people with chronic low back pain.” However, “systematic reviews have found only small treatment effects, with considerable variation across individual trials.”
The 2021 review is one of the largest in the Cochrane Library, and included 249 trials and 24,486 study participants. However, Dr. Hayden said she had been disappointed by the methodological limitations of many of the trials. “The field is saturated with small exercise trials, many of which suffer from poor planning, conduct, and reporting due to limited resources.”
In the current review, “we found that exercise is likely to be effective for chronic low back pain. Overall, 3 months after the start of treatment, people receiving exercise treatment rated their pain an average of 15 points better on a scale of 0-100, and functional limitations were 7 points better, compared to people who had no treatment or usual care,” said Dr. Hayden.
Barriers to the use of exercise to treat pain may include fear of movement on the part of patients, she noted.
“Although our related network meta-analysis found some differences between specific types of exercise, we found all exercise types are more effective than minimal treatment,” she said. “People with chronic low back pain should be encouraged to do exercises that they enjoy and will do consistently to promote adherence.”
Limitations of medications
Both the safety and effectiveness of analgesics and antidepressants for pain in general and back pain in particular have come under scrutiny in recent research. A study published online in the British Medical Journal of patients with acute low back pain found that, although some medications were associated with large reductions in pain intensity, compared with placebo, the quality of the studies was “low or very low confidence,” according to a Medscape report on the findings.
This conclusion was supported in a large-scale analysis of the safety and effectiveness of antidepressants in chronic pain conditions, including back pain.
A new Cochrane Review led by a team of researchers in the United Kingdom found inadequate evidence to support the effectiveness of most antidepressants used for chronic pain, including amitriptyline, fluoxetine, citalopram, paroxetine, sertraline, and duloxetine.
“While chronic pain remains one of the top causes of daily disability worldwide, clinicians’ choices at offering interventions are getting fewer, especially if they tend toward a medical model and want a pharmacological solution,” corresponding author Tamar Pincus, PhD, of the University of Southampton (England), said in an interview. “We now know that opioids harm patients, and the evidence for common analgesics such as paracetamol and ibuprofen, for some conditions such as back pain, suggest they are not effective and might cause harm. This leaves clinicians with few options, and the most common prescription, supported by guidelines, is antidepressants.”
The study found moderate evidence that duloxetine can reduce pain in the short term and improve physical activity and some evidence that milnacipran might also be effective, Dr. Pincus said. “For all other antidepressants, including the commonly prescribed amitriptyline, the evidence was poor. Of importance, the average length of trials was 10 weeks, so long-term effects for all antidepressants remain unknown, and side effects and adverse events were reported poorly, so we also don’t know if any antidepressants are harmful.”
The takeaway message for the management of back pain in particular? “If a clinician and a patient decide together that it would be a good idea to try an antidepressant to reduce pain, they should consider starting with duloxetine, the drug with supporting evidence,” she said.
Physician attitude matters
Antidepressants may not have much impact on chronic pain, but a physician’s empathy and support do, according to data from a registry study of more than 1,300 individuals.
Despite efforts and guidelines from multiple medical organizations to promote optimal pain management, “much remains unknown regarding how the patient-physician interaction affects the process of delivering medical care for chronic low back pain and, ultimately, patient satisfaction,” John C. Licciardone, DO, of the University of North Texas Health Science Center, Fort Worth, and colleagues wrote in Annals of Family Medicine.
Previous studies have examined the relationship between clinical outcomes and patient satisfaction, but data on patient satisfaction with medical care for chronic low back pain specifically are limited, they said.
The researchers reviewed data from a national pain registry of adults aged 21-79 years that included self-reported measures of physician communication and empathy, prescribing data for opioids, and outcomes data for pain intensity, physical function, and health-related quality of life.
In a multivariate analysis, physician empathy and physician communication showed the strongest associations with patient satisfaction (P < .001).
The researchers found a negligible correlation between opioid prescription and perceived physician empathy and communication, “although current physician prescribing of opioids was also associated with patient satisfaction,” they wrote.
“Our findings pertaining to physician empathy are intriguing because they do not necessarily involve a therapeutic alliance with the patient based on collaborative communication or the expectation of a therapeutic effect via pharmacotherapy,” the researchers wrote .
The findings were limited by several factors including the cross-sectional design that prevented conclusions about cause and effect, the researchers noted. “It is possible that prior improvements in pain intensity, physical function, or [health-related quality of life] might have prompted participants to report more favorable ratings for physician empathy, physician communication, or patient satisfaction at registry enrollment.” However, the study supports the view that patients with low back pain in particular value physicians who validate their concerns and symptoms, and who make an effort to communicate treatment plans clearly.
Back pain patients continue to challenge primary care
“Back pain is a major issue in U.S. health care, in part because too many people have tough physical jobs or longstanding injuries that become chronic,” William Golden, MD, professor of medicine and public health at the University of Arkansas for Medical Sciences, Little Rock, said in an interview.
“There are no magic bullets for a lot of back pain patients, so empathy and support are key drivers,” he noted. “Helping patients maximize functionality as opposed to seeking mythical cures is the stronger line of visit discussions, but that takes a bit of time and skill in interviewing.
“It is fairly well established that duloxetine is useful in pain management, especially when present with mood disorders, either primary or secondary to the back-related disability,” said Dr. Golden. “Greater dissemination of its utility is probably useful, as is the side effect profile of the drug as well,” given the “nasty discontinuation syndrome when the treatment is reduced or stopped.”
Looking ahead, “more research is needed about microsurgery, namely for whom and for what anatomic presentations,” said Dr. Golden. Other topics for further research include a better understanding about medical marijuana and pain management and its interactions and side effects with other opioids and muscle relaxants. “Polypharmacy is still an issue in this class of patient,” and many of these patients are frustrated and angry “so the psychosocial skills of the PCP can be greatly tested as well,” he said.
Empathy promotes patient adherence to treatment
The new opioid prescription guidelines have increased interest among clinicians in how to improve patient satisfaction with the care for back pain provided, Noel Deep, MD, said in an interview. “These studies address this concern and bring forth an important aspect of the physician-patient relationship, namely the human touch and empathy.”
“I have been a strong proponent of the trust and relationship between a physician and patient; displaying empathy and increased and transparent communication between the physician and the patient has always resulted in better relationships and better outcomes for patients, especially those dealing with chronic health concerns,” said Dr. Deep, who is a general internist in a multispecialty group practice with Aspirus Antigo (Wisc.) Clinic and the chief medical officer and a staff physician at Aspirus Langlade Hospital, also in Antigo.
Potential barriers to effective pain management include beliefs and attitudes on the part of patients, Dr. Deep noted. “Physicians lacking adequate time to communicate effectively with the patient and describe nonopioid and nonsurgical interventions would be another potential barrier.” Other issues include the time and effort, as well as cost, associated with interventions such as physical therapy and other nondrug and nonsurgical interventions. Issues with family and social support and health literacy are also potential barriers to pain management.
Clinical takeaways
Low back pain is one of the most common reasons for a visit in primary care and can be “chronic and debilitating,” Grace Lin, MD, an internal medicine physician and primary care provider at the University of California, San Francisco, said in an interview.
“One issue with the Cochrane Review on exercise is that the studies on exercise were heterogeneous, so it’s difficult to know whether there is a particular kind of exercise that would be most effective and should be recommended to patients,” she said.
Furthermore, she said, “there is a physical therapist shortage in the U.S. I practice in a major city with a large health care system, and it can still take months to get an appointment with a physical therapist.” Also, insurance coverage may limit which therapists a patient can see and how many visits they can have.
“On the clinician side, I think physicians need to be better informed about the evidence base for back pain treatment, namely that exercise is effective and that, long term, analgesics are not,” Dr. Lin said. “This might decrease overprescription of ineffective analgesics and encourage more education about and referrals to physical therapy.”
“Physicians should continue to educate patients that physical therapy is the first-line treatment for back pain and that pain medications are secondary,” she said. “I think that analgesics can be effective for the short term to get people to a point where they feel well enough to do physical therapy. Duloxetine also appears to be moderately effective for chronic low back pain, in part because it may also help address coexisting depression and anxiety,” but these options should be reserved for adjuncts to physical therapy for back pain.
The findings from the study on empathy and communication suggest that the main challenges to these behaviors are systemic, said Dr. Lin.
“Our health care system is not conducive to treating chronic back pain,” she said. Primary care visits that last for 15 or 20 minutes are not long enough to diagnose and counsel patients on such a complex problem as chronic low back pain. Since back pain is usually not the only issue the primary care physician is dealing with during that visit, this can lead to patients feeling like their doctor isn’t listening to them and doesn’t care about their pain.
“We need to better understand the mechanisms by which people develop chronic, debilitating back pain,” Dr. Lin said. “I think if we understood this better, more effective and targeted treatments, both pharmacological and nonpharmacological, could be developed.”
The Annals of Family Medicine study received no outside funding, and the researchers had no financial conflicts to disclose. The Cochrane Reviews was supported by the National Institute for Health and Care Research’s Health Technology Assessment program, and the authors had no financial conflicts to disclose. Dr. Golden and Dr. Deep had no financial conflicts to disclose and serve on the editorial advisory board of Internal Medicine News. Dr. Lin disclosed receiving research funding from the Institute for Clinical and Economic Review and the National Institutes of Health.
Treatment of chronic back pain remains a challenge for primary care physicians, and a new Cochrane Review confirms previous studies suggesting that analgesics and antidepressants fall short in terms of relief.
Data from another Cochrane Review support the value of exercise for chronic low back pain, although it is often underused, and the Food and Drug Administration’s recent approval of a spinal cord stimulation device for chronic back pain opens the door for another alternative.
Regardless of treatment type, however, patients report that empathy and clear communication from their doctors go a long way in their satisfaction with pain management, according to another recent study.
Exercise helps when patients adhere
The objective of the Cochrane Review on “Exercise therapy for chronic low back pain” was to determine whether exercise improves pain and functioning for people with chronic low back pain, compared with no treatment, usual care, or other common treatments, corresponding author Jill Hayden, PhD, of Dalhousie University, Halifax, N.S., said in an interview.
When back pain is chronic, it is expensive in terms of health care costs and lost work hours, said Dr. Hayden. “Exercise is promoted in many guidelines and is often recommended for, and used by, people with chronic low back pain.” However, “systematic reviews have found only small treatment effects, with considerable variation across individual trials.”
The 2021 review is one of the largest in the Cochrane Library, and included 249 trials and 24,486 study participants. However, Dr. Hayden said she had been disappointed by the methodological limitations of many of the trials. “The field is saturated with small exercise trials, many of which suffer from poor planning, conduct, and reporting due to limited resources.”
In the current review, “we found that exercise is likely to be effective for chronic low back pain. Overall, 3 months after the start of treatment, people receiving exercise treatment rated their pain an average of 15 points better on a scale of 0-100, and functional limitations were 7 points better, compared to people who had no treatment or usual care,” said Dr. Hayden.
Barriers to the use of exercise to treat pain may include fear of movement on the part of patients, she noted.
“Although our related network meta-analysis found some differences between specific types of exercise, we found all exercise types are more effective than minimal treatment,” she said. “People with chronic low back pain should be encouraged to do exercises that they enjoy and will do consistently to promote adherence.”
Limitations of medications
Both the safety and effectiveness of analgesics and antidepressants for pain in general and back pain in particular have come under scrutiny in recent research. A study published online in the British Medical Journal of patients with acute low back pain found that, although some medications were associated with large reductions in pain intensity, compared with placebo, the quality of the studies was “low or very low confidence,” according to a Medscape report on the findings.
This conclusion was supported in a large-scale analysis of the safety and effectiveness of antidepressants in chronic pain conditions, including back pain.
A new Cochrane Review led by a team of researchers in the United Kingdom found inadequate evidence to support the effectiveness of most antidepressants used for chronic pain, including amitriptyline, fluoxetine, citalopram, paroxetine, sertraline, and duloxetine.
“While chronic pain remains one of the top causes of daily disability worldwide, clinicians’ choices at offering interventions are getting fewer, especially if they tend toward a medical model and want a pharmacological solution,” corresponding author Tamar Pincus, PhD, of the University of Southampton (England), said in an interview. “We now know that opioids harm patients, and the evidence for common analgesics such as paracetamol and ibuprofen, for some conditions such as back pain, suggest they are not effective and might cause harm. This leaves clinicians with few options, and the most common prescription, supported by guidelines, is antidepressants.”
The study found moderate evidence that duloxetine can reduce pain in the short term and improve physical activity and some evidence that milnacipran might also be effective, Dr. Pincus said. “For all other antidepressants, including the commonly prescribed amitriptyline, the evidence was poor. Of importance, the average length of trials was 10 weeks, so long-term effects for all antidepressants remain unknown, and side effects and adverse events were reported poorly, so we also don’t know if any antidepressants are harmful.”
The takeaway message for the management of back pain in particular? “If a clinician and a patient decide together that it would be a good idea to try an antidepressant to reduce pain, they should consider starting with duloxetine, the drug with supporting evidence,” she said.
Physician attitude matters
Antidepressants may not have much impact on chronic pain, but a physician’s empathy and support do, according to data from a registry study of more than 1,300 individuals.
Despite efforts and guidelines from multiple medical organizations to promote optimal pain management, “much remains unknown regarding how the patient-physician interaction affects the process of delivering medical care for chronic low back pain and, ultimately, patient satisfaction,” John C. Licciardone, DO, of the University of North Texas Health Science Center, Fort Worth, and colleagues wrote in Annals of Family Medicine.
Previous studies have examined the relationship between clinical outcomes and patient satisfaction, but data on patient satisfaction with medical care for chronic low back pain specifically are limited, they said.
The researchers reviewed data from a national pain registry of adults aged 21-79 years that included self-reported measures of physician communication and empathy, prescribing data for opioids, and outcomes data for pain intensity, physical function, and health-related quality of life.
In a multivariate analysis, physician empathy and physician communication showed the strongest associations with patient satisfaction (P < .001).
The researchers found a negligible correlation between opioid prescription and perceived physician empathy and communication, “although current physician prescribing of opioids was also associated with patient satisfaction,” they wrote.
“Our findings pertaining to physician empathy are intriguing because they do not necessarily involve a therapeutic alliance with the patient based on collaborative communication or the expectation of a therapeutic effect via pharmacotherapy,” the researchers wrote .
The findings were limited by several factors including the cross-sectional design that prevented conclusions about cause and effect, the researchers noted. “It is possible that prior improvements in pain intensity, physical function, or [health-related quality of life] might have prompted participants to report more favorable ratings for physician empathy, physician communication, or patient satisfaction at registry enrollment.” However, the study supports the view that patients with low back pain in particular value physicians who validate their concerns and symptoms, and who make an effort to communicate treatment plans clearly.
Back pain patients continue to challenge primary care
“Back pain is a major issue in U.S. health care, in part because too many people have tough physical jobs or longstanding injuries that become chronic,” William Golden, MD, professor of medicine and public health at the University of Arkansas for Medical Sciences, Little Rock, said in an interview.
“There are no magic bullets for a lot of back pain patients, so empathy and support are key drivers,” he noted. “Helping patients maximize functionality as opposed to seeking mythical cures is the stronger line of visit discussions, but that takes a bit of time and skill in interviewing.
“It is fairly well established that duloxetine is useful in pain management, especially when present with mood disorders, either primary or secondary to the back-related disability,” said Dr. Golden. “Greater dissemination of its utility is probably useful, as is the side effect profile of the drug as well,” given the “nasty discontinuation syndrome when the treatment is reduced or stopped.”
Looking ahead, “more research is needed about microsurgery, namely for whom and for what anatomic presentations,” said Dr. Golden. Other topics for further research include a better understanding about medical marijuana and pain management and its interactions and side effects with other opioids and muscle relaxants. “Polypharmacy is still an issue in this class of patient,” and many of these patients are frustrated and angry “so the psychosocial skills of the PCP can be greatly tested as well,” he said.
Empathy promotes patient adherence to treatment
The new opioid prescription guidelines have increased interest among clinicians in how to improve patient satisfaction with the care for back pain provided, Noel Deep, MD, said in an interview. “These studies address this concern and bring forth an important aspect of the physician-patient relationship, namely the human touch and empathy.”
“I have been a strong proponent of the trust and relationship between a physician and patient; displaying empathy and increased and transparent communication between the physician and the patient has always resulted in better relationships and better outcomes for patients, especially those dealing with chronic health concerns,” said Dr. Deep, who is a general internist in a multispecialty group practice with Aspirus Antigo (Wisc.) Clinic and the chief medical officer and a staff physician at Aspirus Langlade Hospital, also in Antigo.
Potential barriers to effective pain management include beliefs and attitudes on the part of patients, Dr. Deep noted. “Physicians lacking adequate time to communicate effectively with the patient and describe nonopioid and nonsurgical interventions would be another potential barrier.” Other issues include the time and effort, as well as cost, associated with interventions such as physical therapy and other nondrug and nonsurgical interventions. Issues with family and social support and health literacy are also potential barriers to pain management.
Clinical takeaways
Low back pain is one of the most common reasons for a visit in primary care and can be “chronic and debilitating,” Grace Lin, MD, an internal medicine physician and primary care provider at the University of California, San Francisco, said in an interview.
“One issue with the Cochrane Review on exercise is that the studies on exercise were heterogeneous, so it’s difficult to know whether there is a particular kind of exercise that would be most effective and should be recommended to patients,” she said.
Furthermore, she said, “there is a physical therapist shortage in the U.S. I practice in a major city with a large health care system, and it can still take months to get an appointment with a physical therapist.” Also, insurance coverage may limit which therapists a patient can see and how many visits they can have.
“On the clinician side, I think physicians need to be better informed about the evidence base for back pain treatment, namely that exercise is effective and that, long term, analgesics are not,” Dr. Lin said. “This might decrease overprescription of ineffective analgesics and encourage more education about and referrals to physical therapy.”
“Physicians should continue to educate patients that physical therapy is the first-line treatment for back pain and that pain medications are secondary,” she said. “I think that analgesics can be effective for the short term to get people to a point where they feel well enough to do physical therapy. Duloxetine also appears to be moderately effective for chronic low back pain, in part because it may also help address coexisting depression and anxiety,” but these options should be reserved for adjuncts to physical therapy for back pain.
The findings from the study on empathy and communication suggest that the main challenges to these behaviors are systemic, said Dr. Lin.
“Our health care system is not conducive to treating chronic back pain,” she said. Primary care visits that last for 15 or 20 minutes are not long enough to diagnose and counsel patients on such a complex problem as chronic low back pain. Since back pain is usually not the only issue the primary care physician is dealing with during that visit, this can lead to patients feeling like their doctor isn’t listening to them and doesn’t care about their pain.
“We need to better understand the mechanisms by which people develop chronic, debilitating back pain,” Dr. Lin said. “I think if we understood this better, more effective and targeted treatments, both pharmacological and nonpharmacological, could be developed.”
The Annals of Family Medicine study received no outside funding, and the researchers had no financial conflicts to disclose. The Cochrane Reviews was supported by the National Institute for Health and Care Research’s Health Technology Assessment program, and the authors had no financial conflicts to disclose. Dr. Golden and Dr. Deep had no financial conflicts to disclose and serve on the editorial advisory board of Internal Medicine News. Dr. Lin disclosed receiving research funding from the Institute for Clinical and Economic Review and the National Institutes of Health.
Treatment of chronic back pain remains a challenge for primary care physicians, and a new Cochrane Review confirms previous studies suggesting that analgesics and antidepressants fall short in terms of relief.
Data from another Cochrane Review support the value of exercise for chronic low back pain, although it is often underused, and the Food and Drug Administration’s recent approval of a spinal cord stimulation device for chronic back pain opens the door for another alternative.
Regardless of treatment type, however, patients report that empathy and clear communication from their doctors go a long way in their satisfaction with pain management, according to another recent study.
Exercise helps when patients adhere
The objective of the Cochrane Review on “Exercise therapy for chronic low back pain” was to determine whether exercise improves pain and functioning for people with chronic low back pain, compared with no treatment, usual care, or other common treatments, corresponding author Jill Hayden, PhD, of Dalhousie University, Halifax, N.S., said in an interview.
When back pain is chronic, it is expensive in terms of health care costs and lost work hours, said Dr. Hayden. “Exercise is promoted in many guidelines and is often recommended for, and used by, people with chronic low back pain.” However, “systematic reviews have found only small treatment effects, with considerable variation across individual trials.”
The 2021 review is one of the largest in the Cochrane Library, and included 249 trials and 24,486 study participants. However, Dr. Hayden said she had been disappointed by the methodological limitations of many of the trials. “The field is saturated with small exercise trials, many of which suffer from poor planning, conduct, and reporting due to limited resources.”
In the current review, “we found that exercise is likely to be effective for chronic low back pain. Overall, 3 months after the start of treatment, people receiving exercise treatment rated their pain an average of 15 points better on a scale of 0-100, and functional limitations were 7 points better, compared to people who had no treatment or usual care,” said Dr. Hayden.
Barriers to the use of exercise to treat pain may include fear of movement on the part of patients, she noted.
“Although our related network meta-analysis found some differences between specific types of exercise, we found all exercise types are more effective than minimal treatment,” she said. “People with chronic low back pain should be encouraged to do exercises that they enjoy and will do consistently to promote adherence.”
Limitations of medications
Both the safety and effectiveness of analgesics and antidepressants for pain in general and back pain in particular have come under scrutiny in recent research. A study published online in the British Medical Journal of patients with acute low back pain found that, although some medications were associated with large reductions in pain intensity, compared with placebo, the quality of the studies was “low or very low confidence,” according to a Medscape report on the findings.
This conclusion was supported in a large-scale analysis of the safety and effectiveness of antidepressants in chronic pain conditions, including back pain.
A new Cochrane Review led by a team of researchers in the United Kingdom found inadequate evidence to support the effectiveness of most antidepressants used for chronic pain, including amitriptyline, fluoxetine, citalopram, paroxetine, sertraline, and duloxetine.
“While chronic pain remains one of the top causes of daily disability worldwide, clinicians’ choices at offering interventions are getting fewer, especially if they tend toward a medical model and want a pharmacological solution,” corresponding author Tamar Pincus, PhD, of the University of Southampton (England), said in an interview. “We now know that opioids harm patients, and the evidence for common analgesics such as paracetamol and ibuprofen, for some conditions such as back pain, suggest they are not effective and might cause harm. This leaves clinicians with few options, and the most common prescription, supported by guidelines, is antidepressants.”
The study found moderate evidence that duloxetine can reduce pain in the short term and improve physical activity and some evidence that milnacipran might also be effective, Dr. Pincus said. “For all other antidepressants, including the commonly prescribed amitriptyline, the evidence was poor. Of importance, the average length of trials was 10 weeks, so long-term effects for all antidepressants remain unknown, and side effects and adverse events were reported poorly, so we also don’t know if any antidepressants are harmful.”
The takeaway message for the management of back pain in particular? “If a clinician and a patient decide together that it would be a good idea to try an antidepressant to reduce pain, they should consider starting with duloxetine, the drug with supporting evidence,” she said.
Physician attitude matters
Antidepressants may not have much impact on chronic pain, but a physician’s empathy and support do, according to data from a registry study of more than 1,300 individuals.
Despite efforts and guidelines from multiple medical organizations to promote optimal pain management, “much remains unknown regarding how the patient-physician interaction affects the process of delivering medical care for chronic low back pain and, ultimately, patient satisfaction,” John C. Licciardone, DO, of the University of North Texas Health Science Center, Fort Worth, and colleagues wrote in Annals of Family Medicine.
Previous studies have examined the relationship between clinical outcomes and patient satisfaction, but data on patient satisfaction with medical care for chronic low back pain specifically are limited, they said.
The researchers reviewed data from a national pain registry of adults aged 21-79 years that included self-reported measures of physician communication and empathy, prescribing data for opioids, and outcomes data for pain intensity, physical function, and health-related quality of life.
In a multivariate analysis, physician empathy and physician communication showed the strongest associations with patient satisfaction (P < .001).
The researchers found a negligible correlation between opioid prescription and perceived physician empathy and communication, “although current physician prescribing of opioids was also associated with patient satisfaction,” they wrote.
“Our findings pertaining to physician empathy are intriguing because they do not necessarily involve a therapeutic alliance with the patient based on collaborative communication or the expectation of a therapeutic effect via pharmacotherapy,” the researchers wrote .
The findings were limited by several factors including the cross-sectional design that prevented conclusions about cause and effect, the researchers noted. “It is possible that prior improvements in pain intensity, physical function, or [health-related quality of life] might have prompted participants to report more favorable ratings for physician empathy, physician communication, or patient satisfaction at registry enrollment.” However, the study supports the view that patients with low back pain in particular value physicians who validate their concerns and symptoms, and who make an effort to communicate treatment plans clearly.
Back pain patients continue to challenge primary care
“Back pain is a major issue in U.S. health care, in part because too many people have tough physical jobs or longstanding injuries that become chronic,” William Golden, MD, professor of medicine and public health at the University of Arkansas for Medical Sciences, Little Rock, said in an interview.
“There are no magic bullets for a lot of back pain patients, so empathy and support are key drivers,” he noted. “Helping patients maximize functionality as opposed to seeking mythical cures is the stronger line of visit discussions, but that takes a bit of time and skill in interviewing.
“It is fairly well established that duloxetine is useful in pain management, especially when present with mood disorders, either primary or secondary to the back-related disability,” said Dr. Golden. “Greater dissemination of its utility is probably useful, as is the side effect profile of the drug as well,” given the “nasty discontinuation syndrome when the treatment is reduced or stopped.”
Looking ahead, “more research is needed about microsurgery, namely for whom and for what anatomic presentations,” said Dr. Golden. Other topics for further research include a better understanding about medical marijuana and pain management and its interactions and side effects with other opioids and muscle relaxants. “Polypharmacy is still an issue in this class of patient,” and many of these patients are frustrated and angry “so the psychosocial skills of the PCP can be greatly tested as well,” he said.
Empathy promotes patient adherence to treatment
The new opioid prescription guidelines have increased interest among clinicians in how to improve patient satisfaction with the care for back pain provided, Noel Deep, MD, said in an interview. “These studies address this concern and bring forth an important aspect of the physician-patient relationship, namely the human touch and empathy.”
“I have been a strong proponent of the trust and relationship between a physician and patient; displaying empathy and increased and transparent communication between the physician and the patient has always resulted in better relationships and better outcomes for patients, especially those dealing with chronic health concerns,” said Dr. Deep, who is a general internist in a multispecialty group practice with Aspirus Antigo (Wisc.) Clinic and the chief medical officer and a staff physician at Aspirus Langlade Hospital, also in Antigo.
Potential barriers to effective pain management include beliefs and attitudes on the part of patients, Dr. Deep noted. “Physicians lacking adequate time to communicate effectively with the patient and describe nonopioid and nonsurgical interventions would be another potential barrier.” Other issues include the time and effort, as well as cost, associated with interventions such as physical therapy and other nondrug and nonsurgical interventions. Issues with family and social support and health literacy are also potential barriers to pain management.
Clinical takeaways
Low back pain is one of the most common reasons for a visit in primary care and can be “chronic and debilitating,” Grace Lin, MD, an internal medicine physician and primary care provider at the University of California, San Francisco, said in an interview.
“One issue with the Cochrane Review on exercise is that the studies on exercise were heterogeneous, so it’s difficult to know whether there is a particular kind of exercise that would be most effective and should be recommended to patients,” she said.
Furthermore, she said, “there is a physical therapist shortage in the U.S. I practice in a major city with a large health care system, and it can still take months to get an appointment with a physical therapist.” Also, insurance coverage may limit which therapists a patient can see and how many visits they can have.
“On the clinician side, I think physicians need to be better informed about the evidence base for back pain treatment, namely that exercise is effective and that, long term, analgesics are not,” Dr. Lin said. “This might decrease overprescription of ineffective analgesics and encourage more education about and referrals to physical therapy.”
“Physicians should continue to educate patients that physical therapy is the first-line treatment for back pain and that pain medications are secondary,” she said. “I think that analgesics can be effective for the short term to get people to a point where they feel well enough to do physical therapy. Duloxetine also appears to be moderately effective for chronic low back pain, in part because it may also help address coexisting depression and anxiety,” but these options should be reserved for adjuncts to physical therapy for back pain.
The findings from the study on empathy and communication suggest that the main challenges to these behaviors are systemic, said Dr. Lin.
“Our health care system is not conducive to treating chronic back pain,” she said. Primary care visits that last for 15 or 20 minutes are not long enough to diagnose and counsel patients on such a complex problem as chronic low back pain. Since back pain is usually not the only issue the primary care physician is dealing with during that visit, this can lead to patients feeling like their doctor isn’t listening to them and doesn’t care about their pain.
“We need to better understand the mechanisms by which people develop chronic, debilitating back pain,” Dr. Lin said. “I think if we understood this better, more effective and targeted treatments, both pharmacological and nonpharmacological, could be developed.”
The Annals of Family Medicine study received no outside funding, and the researchers had no financial conflicts to disclose. The Cochrane Reviews was supported by the National Institute for Health and Care Research’s Health Technology Assessment program, and the authors had no financial conflicts to disclose. Dr. Golden and Dr. Deep had no financial conflicts to disclose and serve on the editorial advisory board of Internal Medicine News. Dr. Lin disclosed receiving research funding from the Institute for Clinical and Economic Review and the National Institutes of Health.