User login
Patients with hypermobile Ehlers-Danlos syndrome report skin laxity, scarring
.
The genetic cause of hEDS, a common inherited connective tissue disorder, remains unknown, wrote Alan Snyder, MD, of the department of dermatology and dermatologic surgery at Medical University of South Carolina, Charleston, and colleagues.
Previous research suggests that changes in dermal mechanics predispose these patients to a range of skin conditions including mast cell activation disorder (MCAD) spectrum and chronic spontaneous urticaria, abnormal scars or wound healing, piezogenic papules, dyshidrosis, skin laxity or softness, easy bruising, local anesthesia resistance, keratosis pilaris, striae, and hidradenitis suppurativa, the researchers wrote.
However, data on these and other dermatologic manifestations of hEDS are limited, they said.
The diagnosis of hEDS will continue to be made more frequently and carefully, as the condition becomes more recognized and understood in the medical community, especially with anticipated capabilities of genetic testing, Dr. Snyder said in an interview.
“Being able to be aware of disease-specific comorbidities, such as those discovered in this study, allows providers to better stratify phenotypes and improve patient disease co-management,” he said.
In the study, published in the Journal of the American Academy of Dermatology, the researchers reviewed data on 1,364 patients with ICD-10 or ICD-9 codes for hEDS or EDS unspecified who were seen at a single institution between June 2005 and May 2022. Most of the patients were White (95.4%) and female (86.7%); the average age was 29.2 years.
Of the 1,364 patients included in the chart review, 497 (36.4%) had documented skin manifestations. Of these, 118 (24.2%) had disorders of follicular occlusion (12 had hidradenitis suppurativa, 32 had folliculitis, and 74 had acne); 112 (23%) had eczema or atopic dermatitis, 98 (19.7%) had mast cell disorder, 32 (6.4%) had psoriasis, and 32 (6.4%) had wound healing issues (16 had hypertrophic keloids/scarring, 5 had abscesses, 3 had abnormal bruising, and 8 had other would healing issues).
The study also included results of a multiple-choice patient survey from 1,354 individuals. In the survey, approximately two-thirds of patients reported abnormal scarring, abnormal wound healing, and cutaneous laxity (61.7%, 69.0%, and 71.0%, respectively).
The findings were limited by several factors including the retrospective study design, lack of testing to confirm hEDS diagnosis, and the potential interdisciplinary selection bias for diagnoses, the authors noted.
However, the results support previous studies showing increased rates of occlusive conditions in hEDS and higher rates of acne, folliculitis, and psoriasis, and highlight the need for clinician education to manage patients and promote better outcomes, the researchers concluded.
Data Enhance Clinical Awareness
“Given the increasingly understood relation between TH2-directed and mast-cell mediated diseases and hEDS, it was not necessarily a surprise to find the increased prevalence of atopy and mast cell disease, but rather an interesting confirmation, within the limitations that exist with retrospective chart review,” Dr. Snyder told this news organization. “While it may make some intuitive sense that certain cohorts with higher risk of HS may have a higher risk of acne, this had not been reported in the literature to date,” he noted. “Given the high levels of patient reported issues with scarring and wound healing, I was surprised that so few analogous diagnoses were physician-reported in the medical records.”
In clinical practice, “health care professionals and patients need to be aware hEDS is associated with high rates of eczematous, mast-cell mediated and follicular occlusive cutaneous disorders,” Dr. Snyder said in an interview. “There seems to be a discrepancy between patients and physician awareness of scarring or wound healing issues in this patient population,” he added.
Looking ahead, “we need to better research and characterize the various hEDS phenotypes to understand who is at highest risk for various TH2-mediated or follicular occlusive disorders,” said Dr. Snyder. “Moreover, a greater understanding is needed of the wound healing inadequacies that predispose these patients to poor outcomes during dermatologic surgery,” he said.
The study was supported by the Ehlers-Danlos Society and the Milton and Tamar Maltz Family Foundation. The researchers had no financial conflicts to disclose.
.
The genetic cause of hEDS, a common inherited connective tissue disorder, remains unknown, wrote Alan Snyder, MD, of the department of dermatology and dermatologic surgery at Medical University of South Carolina, Charleston, and colleagues.
Previous research suggests that changes in dermal mechanics predispose these patients to a range of skin conditions including mast cell activation disorder (MCAD) spectrum and chronic spontaneous urticaria, abnormal scars or wound healing, piezogenic papules, dyshidrosis, skin laxity or softness, easy bruising, local anesthesia resistance, keratosis pilaris, striae, and hidradenitis suppurativa, the researchers wrote.
However, data on these and other dermatologic manifestations of hEDS are limited, they said.
The diagnosis of hEDS will continue to be made more frequently and carefully, as the condition becomes more recognized and understood in the medical community, especially with anticipated capabilities of genetic testing, Dr. Snyder said in an interview.
“Being able to be aware of disease-specific comorbidities, such as those discovered in this study, allows providers to better stratify phenotypes and improve patient disease co-management,” he said.
In the study, published in the Journal of the American Academy of Dermatology, the researchers reviewed data on 1,364 patients with ICD-10 or ICD-9 codes for hEDS or EDS unspecified who were seen at a single institution between June 2005 and May 2022. Most of the patients were White (95.4%) and female (86.7%); the average age was 29.2 years.
Of the 1,364 patients included in the chart review, 497 (36.4%) had documented skin manifestations. Of these, 118 (24.2%) had disorders of follicular occlusion (12 had hidradenitis suppurativa, 32 had folliculitis, and 74 had acne); 112 (23%) had eczema or atopic dermatitis, 98 (19.7%) had mast cell disorder, 32 (6.4%) had psoriasis, and 32 (6.4%) had wound healing issues (16 had hypertrophic keloids/scarring, 5 had abscesses, 3 had abnormal bruising, and 8 had other would healing issues).
The study also included results of a multiple-choice patient survey from 1,354 individuals. In the survey, approximately two-thirds of patients reported abnormal scarring, abnormal wound healing, and cutaneous laxity (61.7%, 69.0%, and 71.0%, respectively).
The findings were limited by several factors including the retrospective study design, lack of testing to confirm hEDS diagnosis, and the potential interdisciplinary selection bias for diagnoses, the authors noted.
However, the results support previous studies showing increased rates of occlusive conditions in hEDS and higher rates of acne, folliculitis, and psoriasis, and highlight the need for clinician education to manage patients and promote better outcomes, the researchers concluded.
Data Enhance Clinical Awareness
“Given the increasingly understood relation between TH2-directed and mast-cell mediated diseases and hEDS, it was not necessarily a surprise to find the increased prevalence of atopy and mast cell disease, but rather an interesting confirmation, within the limitations that exist with retrospective chart review,” Dr. Snyder told this news organization. “While it may make some intuitive sense that certain cohorts with higher risk of HS may have a higher risk of acne, this had not been reported in the literature to date,” he noted. “Given the high levels of patient reported issues with scarring and wound healing, I was surprised that so few analogous diagnoses were physician-reported in the medical records.”
In clinical practice, “health care professionals and patients need to be aware hEDS is associated with high rates of eczematous, mast-cell mediated and follicular occlusive cutaneous disorders,” Dr. Snyder said in an interview. “There seems to be a discrepancy between patients and physician awareness of scarring or wound healing issues in this patient population,” he added.
Looking ahead, “we need to better research and characterize the various hEDS phenotypes to understand who is at highest risk for various TH2-mediated or follicular occlusive disorders,” said Dr. Snyder. “Moreover, a greater understanding is needed of the wound healing inadequacies that predispose these patients to poor outcomes during dermatologic surgery,” he said.
The study was supported by the Ehlers-Danlos Society and the Milton and Tamar Maltz Family Foundation. The researchers had no financial conflicts to disclose.
.
The genetic cause of hEDS, a common inherited connective tissue disorder, remains unknown, wrote Alan Snyder, MD, of the department of dermatology and dermatologic surgery at Medical University of South Carolina, Charleston, and colleagues.
Previous research suggests that changes in dermal mechanics predispose these patients to a range of skin conditions including mast cell activation disorder (MCAD) spectrum and chronic spontaneous urticaria, abnormal scars or wound healing, piezogenic papules, dyshidrosis, skin laxity or softness, easy bruising, local anesthesia resistance, keratosis pilaris, striae, and hidradenitis suppurativa, the researchers wrote.
However, data on these and other dermatologic manifestations of hEDS are limited, they said.
The diagnosis of hEDS will continue to be made more frequently and carefully, as the condition becomes more recognized and understood in the medical community, especially with anticipated capabilities of genetic testing, Dr. Snyder said in an interview.
“Being able to be aware of disease-specific comorbidities, such as those discovered in this study, allows providers to better stratify phenotypes and improve patient disease co-management,” he said.
In the study, published in the Journal of the American Academy of Dermatology, the researchers reviewed data on 1,364 patients with ICD-10 or ICD-9 codes for hEDS or EDS unspecified who were seen at a single institution between June 2005 and May 2022. Most of the patients were White (95.4%) and female (86.7%); the average age was 29.2 years.
Of the 1,364 patients included in the chart review, 497 (36.4%) had documented skin manifestations. Of these, 118 (24.2%) had disorders of follicular occlusion (12 had hidradenitis suppurativa, 32 had folliculitis, and 74 had acne); 112 (23%) had eczema or atopic dermatitis, 98 (19.7%) had mast cell disorder, 32 (6.4%) had psoriasis, and 32 (6.4%) had wound healing issues (16 had hypertrophic keloids/scarring, 5 had abscesses, 3 had abnormal bruising, and 8 had other would healing issues).
The study also included results of a multiple-choice patient survey from 1,354 individuals. In the survey, approximately two-thirds of patients reported abnormal scarring, abnormal wound healing, and cutaneous laxity (61.7%, 69.0%, and 71.0%, respectively).
The findings were limited by several factors including the retrospective study design, lack of testing to confirm hEDS diagnosis, and the potential interdisciplinary selection bias for diagnoses, the authors noted.
However, the results support previous studies showing increased rates of occlusive conditions in hEDS and higher rates of acne, folliculitis, and psoriasis, and highlight the need for clinician education to manage patients and promote better outcomes, the researchers concluded.
Data Enhance Clinical Awareness
“Given the increasingly understood relation between TH2-directed and mast-cell mediated diseases and hEDS, it was not necessarily a surprise to find the increased prevalence of atopy and mast cell disease, but rather an interesting confirmation, within the limitations that exist with retrospective chart review,” Dr. Snyder told this news organization. “While it may make some intuitive sense that certain cohorts with higher risk of HS may have a higher risk of acne, this had not been reported in the literature to date,” he noted. “Given the high levels of patient reported issues with scarring and wound healing, I was surprised that so few analogous diagnoses were physician-reported in the medical records.”
In clinical practice, “health care professionals and patients need to be aware hEDS is associated with high rates of eczematous, mast-cell mediated and follicular occlusive cutaneous disorders,” Dr. Snyder said in an interview. “There seems to be a discrepancy between patients and physician awareness of scarring or wound healing issues in this patient population,” he added.
Looking ahead, “we need to better research and characterize the various hEDS phenotypes to understand who is at highest risk for various TH2-mediated or follicular occlusive disorders,” said Dr. Snyder. “Moreover, a greater understanding is needed of the wound healing inadequacies that predispose these patients to poor outcomes during dermatologic surgery,” he said.
The study was supported by the Ehlers-Danlos Society and the Milton and Tamar Maltz Family Foundation. The researchers had no financial conflicts to disclose.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Rheumatology Match Day results for 2024 follow trends of past years
While adult rheumatology programs continue to have high match rates, pediatric rheumatology programs remain less popular.
The National Residency Matching Program (NRMP) reported on Nov. 29 that rheumatology filled 124 of 127 programs (97.6%), with 273 (98.9%) of 276 positions filled. Comparatively, pediatric rheumatology filled 21 out of 38 programs (55%) and 32 (61.5%) of 52 positions.
This year, the number of programs and positions across all specialties rose by 3%, whereas the number of applications only rose by 0.4% (35 additional applicants).
“The growth of fellowship programs and positions in the Match reflect training opportunities and the future workforce trends of medical subspecialties,” said NRMP President Donna Lamb, DHSc, MBA, BSN, in a statement. “While the increase in applicant numbers did not keep pace with the increase in positions this year, the Match rate for applicants remains strong at 82%.”
In adult rheumatology, matched applicants included 117 MD graduates, 86 foreign applicants, 38 DO graduates, and 32 U.S. citizen international medical graduates. A total of 348 applicants preferred the specialty, and 78% matched to rheumatology, whereas 2% matched to a different specialty. Another 70 applicants (20%) did not match to any program.
In pediatric rheumatology, matched applicants included 23 MD graduates, 6 DO graduates, and 3 foreign applicants. All applicants who preferred pediatric rheumatology matched to a program.
Adult rheumatology was one of several specialties that filled over 95% of positions. The other specialties that matched at that rate were allergy and immunology, cardiovascular disease, clinical cardiac electrophysiology, critical care medicine, gastroenterology, hematology and oncology, and pulmonary/critical care. Interventional Pulmonology and Oncology was the only specialty to achieve a 100% fill rate.
A version of this article first appeared on Medscape.com.
While adult rheumatology programs continue to have high match rates, pediatric rheumatology programs remain less popular.
The National Residency Matching Program (NRMP) reported on Nov. 29 that rheumatology filled 124 of 127 programs (97.6%), with 273 (98.9%) of 276 positions filled. Comparatively, pediatric rheumatology filled 21 out of 38 programs (55%) and 32 (61.5%) of 52 positions.
This year, the number of programs and positions across all specialties rose by 3%, whereas the number of applications only rose by 0.4% (35 additional applicants).
“The growth of fellowship programs and positions in the Match reflect training opportunities and the future workforce trends of medical subspecialties,” said NRMP President Donna Lamb, DHSc, MBA, BSN, in a statement. “While the increase in applicant numbers did not keep pace with the increase in positions this year, the Match rate for applicants remains strong at 82%.”
In adult rheumatology, matched applicants included 117 MD graduates, 86 foreign applicants, 38 DO graduates, and 32 U.S. citizen international medical graduates. A total of 348 applicants preferred the specialty, and 78% matched to rheumatology, whereas 2% matched to a different specialty. Another 70 applicants (20%) did not match to any program.
In pediatric rheumatology, matched applicants included 23 MD graduates, 6 DO graduates, and 3 foreign applicants. All applicants who preferred pediatric rheumatology matched to a program.
Adult rheumatology was one of several specialties that filled over 95% of positions. The other specialties that matched at that rate were allergy and immunology, cardiovascular disease, clinical cardiac electrophysiology, critical care medicine, gastroenterology, hematology and oncology, and pulmonary/critical care. Interventional Pulmonology and Oncology was the only specialty to achieve a 100% fill rate.
A version of this article first appeared on Medscape.com.
While adult rheumatology programs continue to have high match rates, pediatric rheumatology programs remain less popular.
The National Residency Matching Program (NRMP) reported on Nov. 29 that rheumatology filled 124 of 127 programs (97.6%), with 273 (98.9%) of 276 positions filled. Comparatively, pediatric rheumatology filled 21 out of 38 programs (55%) and 32 (61.5%) of 52 positions.
This year, the number of programs and positions across all specialties rose by 3%, whereas the number of applications only rose by 0.4% (35 additional applicants).
“The growth of fellowship programs and positions in the Match reflect training opportunities and the future workforce trends of medical subspecialties,” said NRMP President Donna Lamb, DHSc, MBA, BSN, in a statement. “While the increase in applicant numbers did not keep pace with the increase in positions this year, the Match rate for applicants remains strong at 82%.”
In adult rheumatology, matched applicants included 117 MD graduates, 86 foreign applicants, 38 DO graduates, and 32 U.S. citizen international medical graduates. A total of 348 applicants preferred the specialty, and 78% matched to rheumatology, whereas 2% matched to a different specialty. Another 70 applicants (20%) did not match to any program.
In pediatric rheumatology, matched applicants included 23 MD graduates, 6 DO graduates, and 3 foreign applicants. All applicants who preferred pediatric rheumatology matched to a program.
Adult rheumatology was one of several specialties that filled over 95% of positions. The other specialties that matched at that rate were allergy and immunology, cardiovascular disease, clinical cardiac electrophysiology, critical care medicine, gastroenterology, hematology and oncology, and pulmonary/critical care. Interventional Pulmonology and Oncology was the only specialty to achieve a 100% fill rate.
A version of this article first appeared on Medscape.com.
First referral guide issued for axial spondyloarthritis
SAN DIEGO – The Spondyloarthritis Research and Treatment Network (SPARTAN) has created the first referral recommendations for axial spondyloarthritis (axSpA).
The draft recommendations use a points scoring system, with the goal that at least one in three patients referred would be diagnosed with axSpA, an inflammatory arthritis that affects the central skeleton and shares a genetic overlap with skin psoriasis, inflammatory bowel disease, and inflammatory eye disease.
Patients with axSpA can wait 10 years after symptom onset to be diagnosed with the condition. There are currently no guidelines to advise clinicians on when to refer to a rheumatologist, and with the rheumatology workforce shortage, “it is impossible for rheumatologists to evaluate the 20% of adults in the U.S. who have chronic back pain,” said Maureen Dubreuil, MD, a rheumatologist at Boston University. She presented the work at the annual meeting of the American College of Rheumatology.
To address this issue, Dr. Dubreuil and colleagues conducted a literature review to determine how predictive different spondyloarthritis features were of eventual axSpA diagnosis. The interdisciplinary team identified 38 studies published before March 2022, and uncovered 28 individual potential features associated with axSpA, including pain sites, family history of axSpA and related conditions, blood markers of inflammation, genetic testing, and imaging findings.
Inflammatory back pain elements had the lower predictive values, with positive likelihood ratios (LR+) ranging from 1.15 to 2.32, while imaging findings were the most predictive (LR+s from 6.40 to 10.02).
Using a Delphi exercise and discrete choice experiments, members narrowed the checklist down to 10 features. These 10 features were assigned points, with a score of 3 points qualifying for a referral of adults 45 years or younger with chronic pain (3 or more months) in the back, hip, or buttock.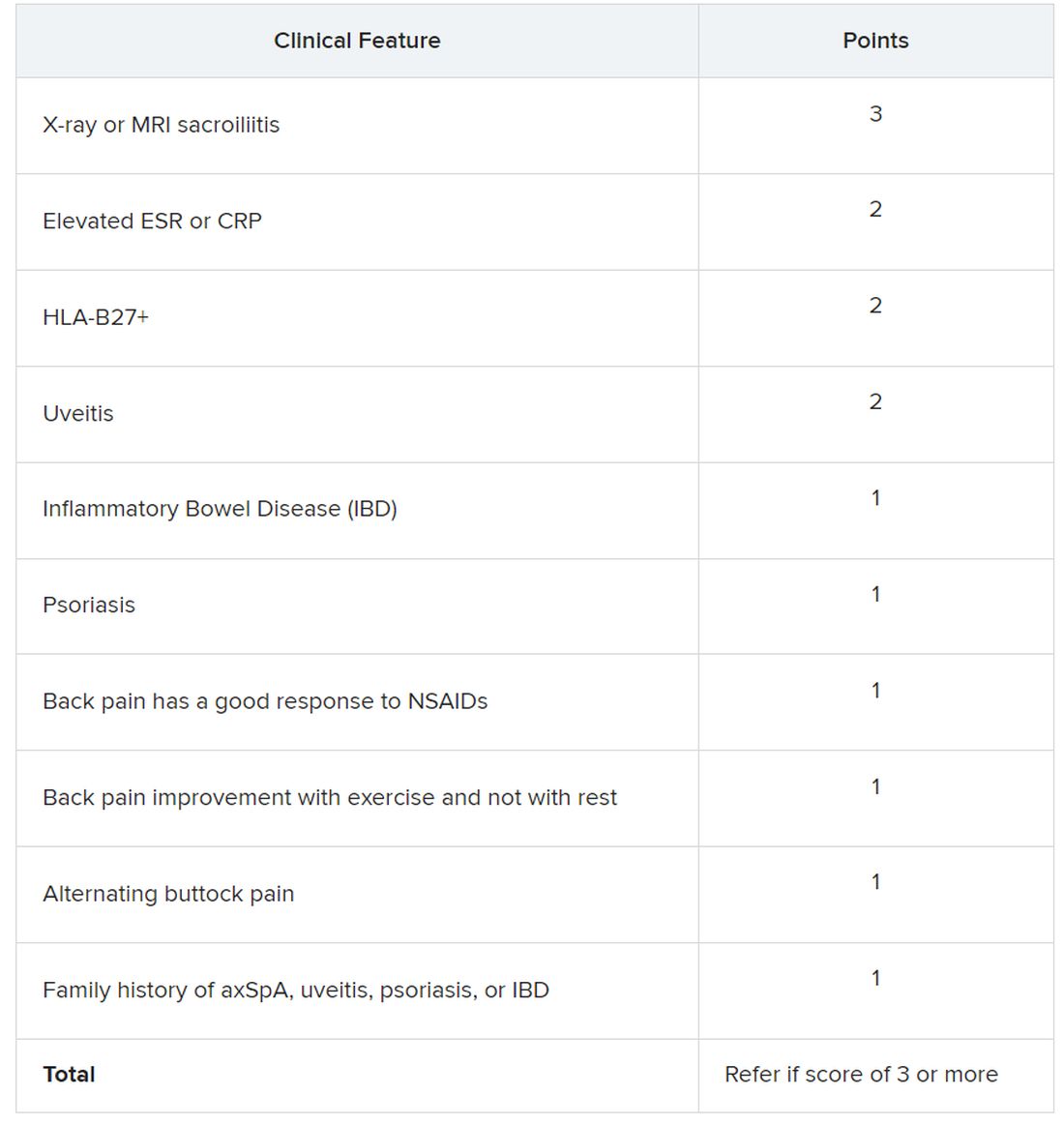
Sacroiliitis seen on imaging, either by x-ray or MRI, received the highest score of 3 points. Dr. Dubreuil emphasized that imaging was not required for a referral, but if a patient has received imaging “that shows sacroiliitis, that is sufficient for referral to a rheumatologist,” she said in her presentation.
Elevated erythrocyte sedimentation rate or C-reactive protein, HLA-B27 positivity, and uveitis score 2 points. Inflammatory bowel disease; psoriasis; back pain with good response to NSAIDs; back pain improvement with exercise and not with rest; alternating buttock pain; and family history of axial spondyloarthritis, uveitis, psoriasis, or IBD score 1 point.
Dr. Dubreuil and colleagues expect that these criteria for referral will result in about one in three referred adults aged 45 years or younger with chronic back pain being diagnosed with axSpA. They also say additional research is necessary to understand if these recommendations increase probability of axSpA diagnosis and reduce diagnostic delays.
“We’re now getting to the stage where we are creating this screening tool, but [testing the] performance of the screening tool is going to be the major next step,” said Mark Hwang, MD, of UTHealth Houston in an interview with this news organization. He is a member of SPARTAN but was not involved with authoring the recommendations. “Will the screening tool enhance the ability on the back end to identify axSpA? We don’t know yet.”
Jon Chan, MD, a rheumatologist at the University of British Columbia, Vancouver, agreed that these recommendations “are a good first step,” but that more awareness about axSpA from nonrheumatologists would also be helpful in identifying new axSpA patients. He is also a member of SPARTAN and comoderated with Dr. Hwang the session where the new recommendations were presented. “I think other diseases like rheumatoid arthritis or lupus have a lot more recognition in the nonrheumatology community,” he told this news organization.
Connecting with other health professionals who see a lot of patients with back pain – physiotherapists, chiropractors, and chronic pain physicians – could also be helpful, he added. “A lot of times, patients go straight to a physio and circumvent the doctor,” he said.
Dr. Chan reports success in educating other departments. “I put up a poster in the emergency department saying, ‘If you’re young with back pain and uveitis, you need to be seen by rheumatology,’ and we’ve identified a ton of axSpA patients that way,” he said. “Maybe their uveitis was very mild, but their back pain was quite severe, and no one really clued in.”
Dr. Dubreuil disclosed financial relationships with Amgen, Pfizer, and UCB Pharma. Her abstract coauthors disclosed financial relationships with multiple pharmaceutical companies. Dr. Hwang consults for UCB and has received research support from Janssen. Dr. Chan has relationships with AbbVie/Abbott, Eli Lilly, Janssen, Novartis, and UCB.
SAN DIEGO – The Spondyloarthritis Research and Treatment Network (SPARTAN) has created the first referral recommendations for axial spondyloarthritis (axSpA).
The draft recommendations use a points scoring system, with the goal that at least one in three patients referred would be diagnosed with axSpA, an inflammatory arthritis that affects the central skeleton and shares a genetic overlap with skin psoriasis, inflammatory bowel disease, and inflammatory eye disease.
Patients with axSpA can wait 10 years after symptom onset to be diagnosed with the condition. There are currently no guidelines to advise clinicians on when to refer to a rheumatologist, and with the rheumatology workforce shortage, “it is impossible for rheumatologists to evaluate the 20% of adults in the U.S. who have chronic back pain,” said Maureen Dubreuil, MD, a rheumatologist at Boston University. She presented the work at the annual meeting of the American College of Rheumatology.
To address this issue, Dr. Dubreuil and colleagues conducted a literature review to determine how predictive different spondyloarthritis features were of eventual axSpA diagnosis. The interdisciplinary team identified 38 studies published before March 2022, and uncovered 28 individual potential features associated with axSpA, including pain sites, family history of axSpA and related conditions, blood markers of inflammation, genetic testing, and imaging findings.
Inflammatory back pain elements had the lower predictive values, with positive likelihood ratios (LR+) ranging from 1.15 to 2.32, while imaging findings were the most predictive (LR+s from 6.40 to 10.02).
Using a Delphi exercise and discrete choice experiments, members narrowed the checklist down to 10 features. These 10 features were assigned points, with a score of 3 points qualifying for a referral of adults 45 years or younger with chronic pain (3 or more months) in the back, hip, or buttock.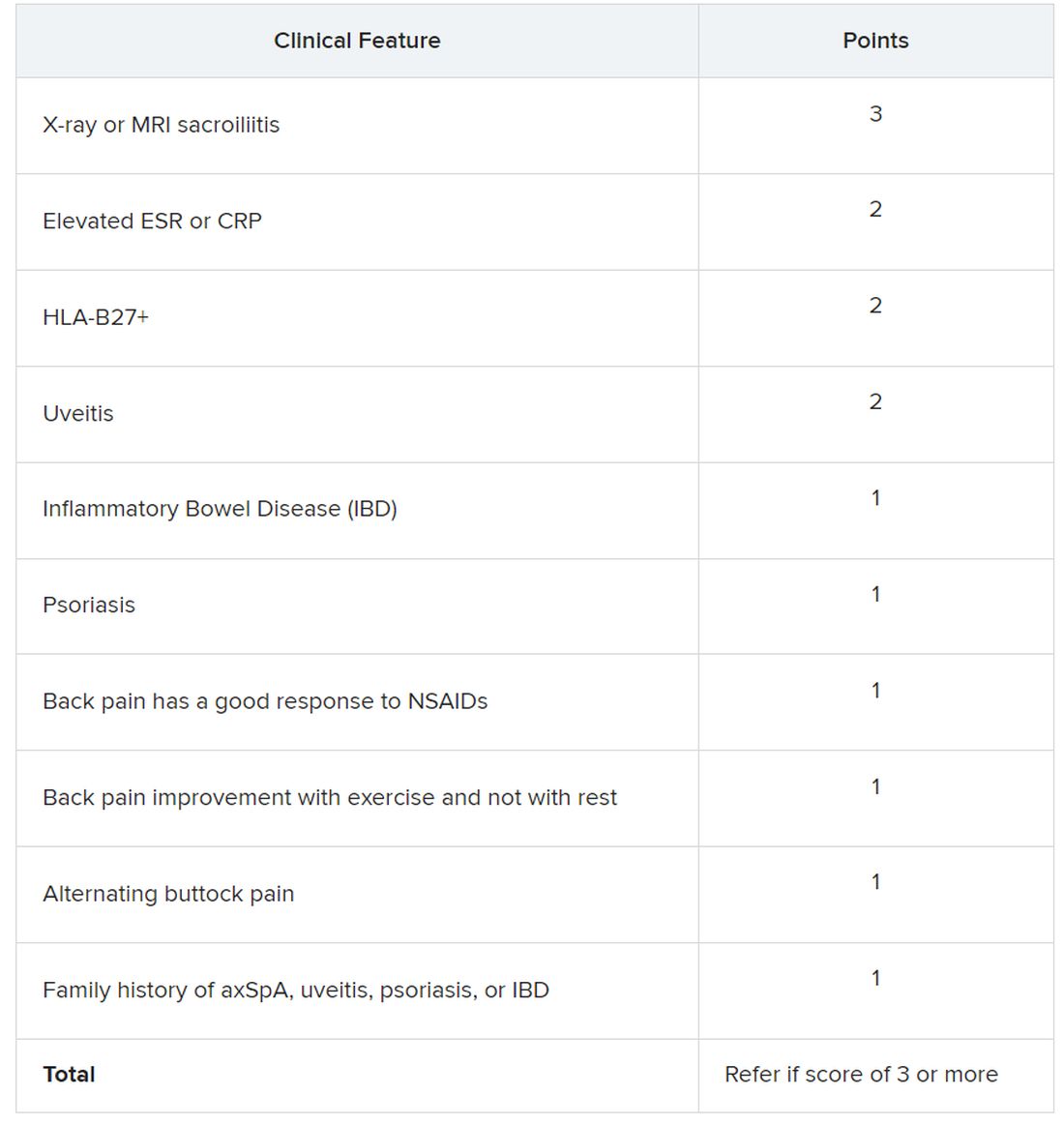
Sacroiliitis seen on imaging, either by x-ray or MRI, received the highest score of 3 points. Dr. Dubreuil emphasized that imaging was not required for a referral, but if a patient has received imaging “that shows sacroiliitis, that is sufficient for referral to a rheumatologist,” she said in her presentation.
Elevated erythrocyte sedimentation rate or C-reactive protein, HLA-B27 positivity, and uveitis score 2 points. Inflammatory bowel disease; psoriasis; back pain with good response to NSAIDs; back pain improvement with exercise and not with rest; alternating buttock pain; and family history of axial spondyloarthritis, uveitis, psoriasis, or IBD score 1 point.
Dr. Dubreuil and colleagues expect that these criteria for referral will result in about one in three referred adults aged 45 years or younger with chronic back pain being diagnosed with axSpA. They also say additional research is necessary to understand if these recommendations increase probability of axSpA diagnosis and reduce diagnostic delays.
“We’re now getting to the stage where we are creating this screening tool, but [testing the] performance of the screening tool is going to be the major next step,” said Mark Hwang, MD, of UTHealth Houston in an interview with this news organization. He is a member of SPARTAN but was not involved with authoring the recommendations. “Will the screening tool enhance the ability on the back end to identify axSpA? We don’t know yet.”
Jon Chan, MD, a rheumatologist at the University of British Columbia, Vancouver, agreed that these recommendations “are a good first step,” but that more awareness about axSpA from nonrheumatologists would also be helpful in identifying new axSpA patients. He is also a member of SPARTAN and comoderated with Dr. Hwang the session where the new recommendations were presented. “I think other diseases like rheumatoid arthritis or lupus have a lot more recognition in the nonrheumatology community,” he told this news organization.
Connecting with other health professionals who see a lot of patients with back pain – physiotherapists, chiropractors, and chronic pain physicians – could also be helpful, he added. “A lot of times, patients go straight to a physio and circumvent the doctor,” he said.
Dr. Chan reports success in educating other departments. “I put up a poster in the emergency department saying, ‘If you’re young with back pain and uveitis, you need to be seen by rheumatology,’ and we’ve identified a ton of axSpA patients that way,” he said. “Maybe their uveitis was very mild, but their back pain was quite severe, and no one really clued in.”
Dr. Dubreuil disclosed financial relationships with Amgen, Pfizer, and UCB Pharma. Her abstract coauthors disclosed financial relationships with multiple pharmaceutical companies. Dr. Hwang consults for UCB and has received research support from Janssen. Dr. Chan has relationships with AbbVie/Abbott, Eli Lilly, Janssen, Novartis, and UCB.
SAN DIEGO – The Spondyloarthritis Research and Treatment Network (SPARTAN) has created the first referral recommendations for axial spondyloarthritis (axSpA).
The draft recommendations use a points scoring system, with the goal that at least one in three patients referred would be diagnosed with axSpA, an inflammatory arthritis that affects the central skeleton and shares a genetic overlap with skin psoriasis, inflammatory bowel disease, and inflammatory eye disease.
Patients with axSpA can wait 10 years after symptom onset to be diagnosed with the condition. There are currently no guidelines to advise clinicians on when to refer to a rheumatologist, and with the rheumatology workforce shortage, “it is impossible for rheumatologists to evaluate the 20% of adults in the U.S. who have chronic back pain,” said Maureen Dubreuil, MD, a rheumatologist at Boston University. She presented the work at the annual meeting of the American College of Rheumatology.
To address this issue, Dr. Dubreuil and colleagues conducted a literature review to determine how predictive different spondyloarthritis features were of eventual axSpA diagnosis. The interdisciplinary team identified 38 studies published before March 2022, and uncovered 28 individual potential features associated with axSpA, including pain sites, family history of axSpA and related conditions, blood markers of inflammation, genetic testing, and imaging findings.
Inflammatory back pain elements had the lower predictive values, with positive likelihood ratios (LR+) ranging from 1.15 to 2.32, while imaging findings were the most predictive (LR+s from 6.40 to 10.02).
Using a Delphi exercise and discrete choice experiments, members narrowed the checklist down to 10 features. These 10 features were assigned points, with a score of 3 points qualifying for a referral of adults 45 years or younger with chronic pain (3 or more months) in the back, hip, or buttock.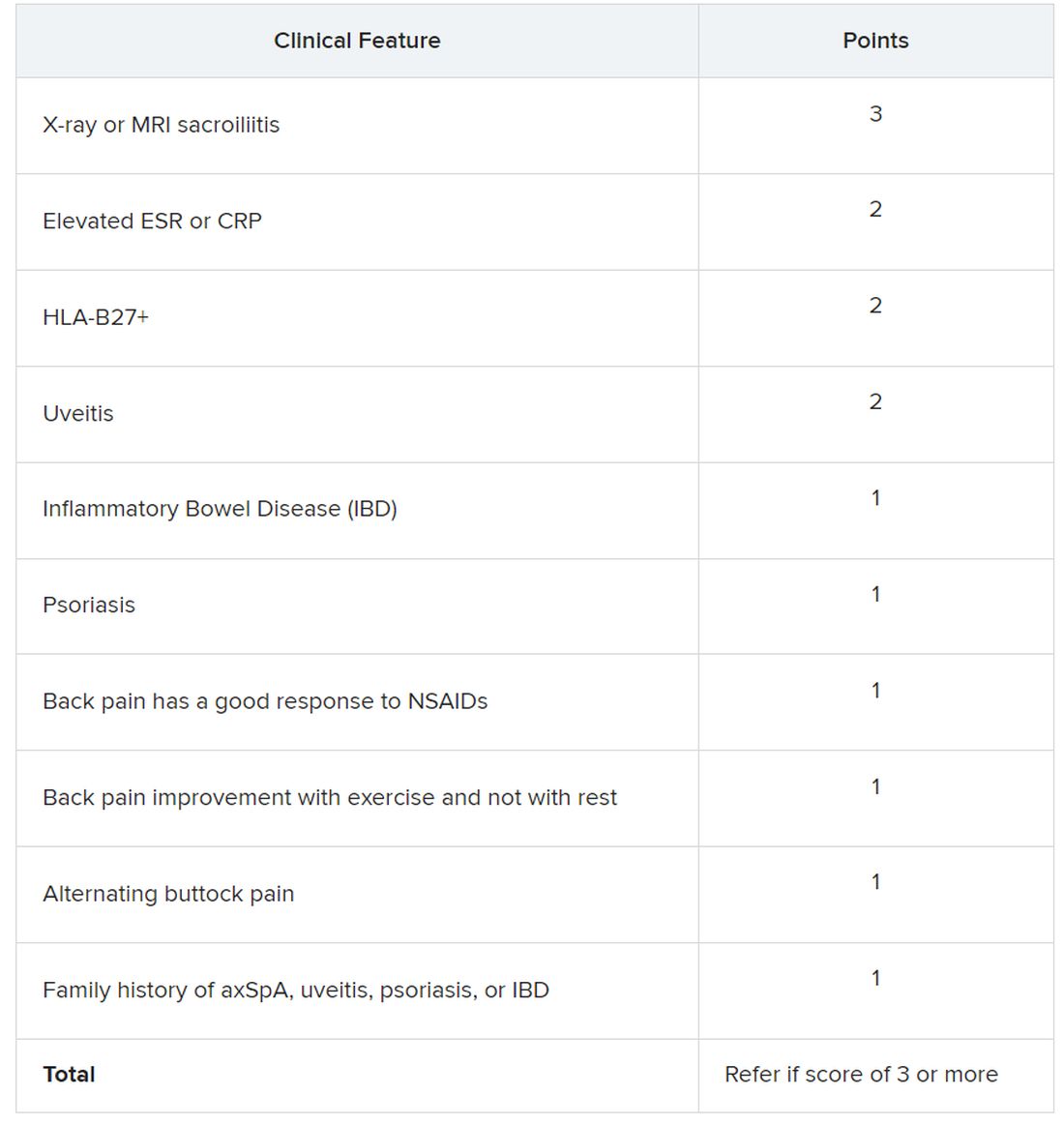
Sacroiliitis seen on imaging, either by x-ray or MRI, received the highest score of 3 points. Dr. Dubreuil emphasized that imaging was not required for a referral, but if a patient has received imaging “that shows sacroiliitis, that is sufficient for referral to a rheumatologist,” she said in her presentation.
Elevated erythrocyte sedimentation rate or C-reactive protein, HLA-B27 positivity, and uveitis score 2 points. Inflammatory bowel disease; psoriasis; back pain with good response to NSAIDs; back pain improvement with exercise and not with rest; alternating buttock pain; and family history of axial spondyloarthritis, uveitis, psoriasis, or IBD score 1 point.
Dr. Dubreuil and colleagues expect that these criteria for referral will result in about one in three referred adults aged 45 years or younger with chronic back pain being diagnosed with axSpA. They also say additional research is necessary to understand if these recommendations increase probability of axSpA diagnosis and reduce diagnostic delays.
“We’re now getting to the stage where we are creating this screening tool, but [testing the] performance of the screening tool is going to be the major next step,” said Mark Hwang, MD, of UTHealth Houston in an interview with this news organization. He is a member of SPARTAN but was not involved with authoring the recommendations. “Will the screening tool enhance the ability on the back end to identify axSpA? We don’t know yet.”
Jon Chan, MD, a rheumatologist at the University of British Columbia, Vancouver, agreed that these recommendations “are a good first step,” but that more awareness about axSpA from nonrheumatologists would also be helpful in identifying new axSpA patients. He is also a member of SPARTAN and comoderated with Dr. Hwang the session where the new recommendations were presented. “I think other diseases like rheumatoid arthritis or lupus have a lot more recognition in the nonrheumatology community,” he told this news organization.
Connecting with other health professionals who see a lot of patients with back pain – physiotherapists, chiropractors, and chronic pain physicians – could also be helpful, he added. “A lot of times, patients go straight to a physio and circumvent the doctor,” he said.
Dr. Chan reports success in educating other departments. “I put up a poster in the emergency department saying, ‘If you’re young with back pain and uveitis, you need to be seen by rheumatology,’ and we’ve identified a ton of axSpA patients that way,” he said. “Maybe their uveitis was very mild, but their back pain was quite severe, and no one really clued in.”
Dr. Dubreuil disclosed financial relationships with Amgen, Pfizer, and UCB Pharma. Her abstract coauthors disclosed financial relationships with multiple pharmaceutical companies. Dr. Hwang consults for UCB and has received research support from Janssen. Dr. Chan has relationships with AbbVie/Abbott, Eli Lilly, Janssen, Novartis, and UCB.
AT ACR 2023
A new standard for treatment of torus fractures of the wrist?
ILLUSTRATIVE CASE
A 9-year-old girl presents to your urgent care clinic after a fall while snowboarding for the first time. She reports falling forward onto her outstretched right hand and describes pain in her distal right forearm. She denies paresthesias, weakness, or lacerations. Physical examination reveals mild edema of the dorsal aspect of her distal right forearm and tenderness to palpation of the dorsal aspect of her distal radius. She denies tenderness to palpation of her ulna, anatomic snuffbox, hand, and elbow. Range of motion of the wrist is full on passive testing, but she declines active testing due to pain. Wrist radiographs reveal an uncomplicated torus fracture of the distal radius. Can immobilization with a soft bandage alone sufficiently treat this fracture?
Fractures of the distal radius are among the most common fractures of the upper extremity and commonly occur from a fall onto an outstretched hand.2 In the pediatric population, torus fractures, also known as buckle fractures, are the most common type of distal radius fracture, comprising an estimated 50% of pediatric wrist fractures.3,4 This is due to the presence of a
Pediatric torus fractures of the distal radius generally are treated with immobilization,2 traditionally through a
Despite common use of immobilization, torus fractures of the distal radius are anatomically stable, and displacement is unlikely to occur.7,8 As such, many studies have suggested that treatment of torus fractures with rigid immobilization in a cast or splint may not be necessary.9,10 However, a 2018 Cochrane review concluded that the quality of evidence illustrating similar recovery between treatments was low, leaving uncertainty as to the most appropriate management strategy.6 Less casting and follow-up imaging could have positive implications for patient satisfaction, health care–associated costs, and radiation exposure.10
This study, the Forearm Fracture Recovery in Children Evaluation (FORCE) trial, compared the traditional treatment of distal radius torus fractures with rigid immobilization to soft immobilization and immediate discharge.
STUDY SUMMARY
Providing quality evidence for a standard of care
FORCE was a randomized controlled equivalence trial (N = 965) across 23 emergency departments (EDs) in the United Kingdom that compared pain and function in pediatric patients with distal radius torus fractures treated with a soft bandage and immediate discharge vs rigid immobilization and routine follow-up.1 Patients included children ages 4 to 15 years presenting to the ED with a distal radius torus fracture, which was confirmed radiologically.
Patients with concomitant
Continue to: Patients were randomly assigned...
Patients were randomly assigned in a 1:1 ratio to receive treatment with either a soft bandage such as a gauze roller bandage (n = 489) or rigid immobilization (n = 476). For patients in the bandage group, a soft bandage was applied in the ED or provided for home application without planned clinical follow-up. Patients in the rigid immobilization group were treated in the ED with either a removable manufactured splint or a molded splint or cast, followed by the standard follow-up practice of the treating center. Patients in the soft bandage group were advised not to wear the bandage for more than 3 weeks. Blinding was not possible, but the treatment team did not take part in patient follow-up.
The primary outcome was change in pain 3 days after treatment, measured on the Wong-Baker FACES Pain Rating Scale (an ordinal assessment using 6 illustrated facial expressions translated to a numeric rating on a scale of 0-10, with higher scores indicating worse pain). This scale has an established minimum clinically important difference (MCID) value of 1 face (2 points).11 Per standard practice in equivalence trials, the equivalence margin was defined as half the MCID, with a value of 1.0 used in this study.
Secondary outcomes measured over the 6-week follow-up period included additional pain measurements using the Wong-Baker scale, measures of function and health-related quality of life, analgesia use, days of absence from school or childcare, complication rates, and patient satisfaction. This study used modified intention-to-treat and per-protocol analyses.
The mean age of participants was 9.6 years; 39% were girls and 61% were boys. In the bandage group, 94% opted to have the soft bandage applied in the ED, and 95% of the rigid immobilization group were treated with a removable wrist splint in the ED. At 3 days, pain scores improved by 3.2 points (standard deviation [SD] = 2.1) in the soft bandage group and 3.1 points (SD = 2.1) in the rigid immobilization group. The adjusted difference was –0.1 (95% CI, –0.37 to 0.17) in the intention-to-treat analysis and –0.06 (95% CI, –0.34 to 0.21) in the per-protocol analysis, which were both less than the predetermined equivalence margin. This equivalence margin also was met at all secondary time points (1 day, 7 days, 3 weeks, and 6 weeks after treatment) and in subgroup analysis of those 4 to 7 years and 8 to 15 years.
Use of any analgesia in the prior 24 hours was slightly higher in the soft bandage group on Day 1 (83% vs 78%; P = .04) and Day 3 (57% vs 51%; P = .05), but this difference was not seen on Day 7. Satisfaction, measured via a 7-point Likert scale (range from “extremely satisfied” to “extremely unsatisfied”), was slightly lower in the soft bandage group on Day 1 (median 2 [interquartile range = 1, 2] vs median 1 [interquartile range = 1, 2]; P < .0001) but was not different after 6 weeks. There were no measured differences in any other secondary outcomes, including function, quality of life, and complication rates.
Continue to: By the primary end point...
By the primary end point of 3 days, 36 patients (7%) in the soft bandage group returned to medical care requesting a change to rigid immobilization, compared with 1 patient (0.2%) in the rigid immobilization group declining intervention.
WHAT’S NEW
Equivalence in pain and function scores
This trial showed equivalence in pain at 3 days’ follow-up in children with distal radius torus fractures who were offered bandaging and then immediately discharged from the ED, compared with rigid immobilization and clinical follow-up. There were no significant differences in pain or function between groups during the 6 weeks following the initial injury. De-escalation of treatment offers an equivalent, resource-sparing alternative to traditional treatment of these fractures.
CAVEATS
Lack of masking likely introduced bias
There are no major caveats associated with managing distal radius torus fractures with a soft bandage and discharge from the ED, compared with the traditional treatment of rigid immobilization. However, bias was likely introduced in patient-reported outcomes due to the inability to mask patients and families to the treatment allocation. This may have led to overstating the severity of outcomes in the bandage group, given the strong preference for rigid immobilization, although equivalence was illustrated despite this potential bias.
CHALLENGES TO IMPLEMENTATION
Preferences may be difficult to change
Parents and clinicians demonstrated a preference for rigid immobilization, as shown in the imbalance in treatment crossovers, with 7% of children changing to the rigid immobilization group by the primary study end point of 3 days. The study authors hypothesized that crossovers may have been due to the perception by some parents that rigid immobilization is the gold standard of treatment, as well as clinicians’ seeking to escalate care for patients returning for follow-up. Policy and guideline changes, as well as physician efforts to educate patients on outcomes with soft bandage treatment, are likely to improve these misconceptions.
1. Perry DC, Achten J, Knight R, et al; FORCE Collaborators in collaboration with PERUKI. Immobilisation of torus fractures of the wrist in children (FORCE): a randomised controlled equivalence trial in the UK. Lancet. 2022;400:39-47. doi: 10.1016/S0140-6736(22)01015-7
2. Patel DS, Statuta SM, Ahmed N. Common fractures of the radius and ulna. Am Fam Physician. 2021;103:345-354.
3. Asokan A, Kheir N. Pediatric Torus Buckle Fracture. StatPearls Publishing; 2023.
4. Naranje SM, Erali RA, Warner WC Jr, et al. Epidemiology of pediatric fractures presenting to emergency departments in the United States. J Pediatr Orthop. 2016;36:e45-e48. doi: 10.1097/BPO.0000000000000595
5. Kennedy SA, Slobogean GP, Mulpuri K. Does degree of immobilization influence refracture rate in the forearm buckle fracture? J Pediatr Orthop B. 2010;19:77-81. doi: 10.1097/BPB.0b013e32832f067a
6. Handoll HHG, Elliott J, Iheozor-Ejiofor Z, et al. Interventions for treating wrist fractures in children. Cochrane Database Syst Rev. 2018;12:CD012470. doi: 10.1002/14651858.CD012470.pub2
7. Perry DC, Gibson P, Roland D, et al. What level of immobilisation is necessary for treatment of torus (buckle) fractures of the distal radius in children? BMJ. 2021;372:m4862. doi: 10.1136/bmj.m4862
8. Williams KG, Smith G, Luhmann SJ, et al. A randomized controlled trial of cast versus splint for distal radial buckle fracture: an evaluation of satisfaction, convenience, and preference. Pediatr Emerg Care. 2013;29:555-559. doi: 10.1097/PEC.0b013e31828e56fb
9. Jiang N, Cao ZH, Ma YF, et al. Management of pediatric forearm torus fractures: a systematic review and meta-analysis. Pediatr Emerg Care. 2016;32:773-778. doi: 10.1097/PEC.0000000000000579
10. Williams BA, Alvarado CA, Montoya-Williams DC, et al. Buckling down on torus fractures: has evolving evidence affected practice? J Child Orthop. 2018;12:123-128. doi: 10.1302/1863-2548.12.170122
11. Garra G, Singer AJ, Taira BR, et al. Validation of the Wong-Baker FACES Pain Rating Scale in pediatric emergency department patients. Acad Emerg Med. 2010;17:50-54. doi: 10.1111/j.1553-2712.2009.00620.x
ILLUSTRATIVE CASE
A 9-year-old girl presents to your urgent care clinic after a fall while snowboarding for the first time. She reports falling forward onto her outstretched right hand and describes pain in her distal right forearm. She denies paresthesias, weakness, or lacerations. Physical examination reveals mild edema of the dorsal aspect of her distal right forearm and tenderness to palpation of the dorsal aspect of her distal radius. She denies tenderness to palpation of her ulna, anatomic snuffbox, hand, and elbow. Range of motion of the wrist is full on passive testing, but she declines active testing due to pain. Wrist radiographs reveal an uncomplicated torus fracture of the distal radius. Can immobilization with a soft bandage alone sufficiently treat this fracture?
Fractures of the distal radius are among the most common fractures of the upper extremity and commonly occur from a fall onto an outstretched hand.2 In the pediatric population, torus fractures, also known as buckle fractures, are the most common type of distal radius fracture, comprising an estimated 50% of pediatric wrist fractures.3,4 This is due to the presence of a
Pediatric torus fractures of the distal radius generally are treated with immobilization,2 traditionally through a
Despite common use of immobilization, torus fractures of the distal radius are anatomically stable, and displacement is unlikely to occur.7,8 As such, many studies have suggested that treatment of torus fractures with rigid immobilization in a cast or splint may not be necessary.9,10 However, a 2018 Cochrane review concluded that the quality of evidence illustrating similar recovery between treatments was low, leaving uncertainty as to the most appropriate management strategy.6 Less casting and follow-up imaging could have positive implications for patient satisfaction, health care–associated costs, and radiation exposure.10
This study, the Forearm Fracture Recovery in Children Evaluation (FORCE) trial, compared the traditional treatment of distal radius torus fractures with rigid immobilization to soft immobilization and immediate discharge.
STUDY SUMMARY
Providing quality evidence for a standard of care
FORCE was a randomized controlled equivalence trial (N = 965) across 23 emergency departments (EDs) in the United Kingdom that compared pain and function in pediatric patients with distal radius torus fractures treated with a soft bandage and immediate discharge vs rigid immobilization and routine follow-up.1 Patients included children ages 4 to 15 years presenting to the ED with a distal radius torus fracture, which was confirmed radiologically.
Patients with concomitant
Continue to: Patients were randomly assigned...
Patients were randomly assigned in a 1:1 ratio to receive treatment with either a soft bandage such as a gauze roller bandage (n = 489) or rigid immobilization (n = 476). For patients in the bandage group, a soft bandage was applied in the ED or provided for home application without planned clinical follow-up. Patients in the rigid immobilization group were treated in the ED with either a removable manufactured splint or a molded splint or cast, followed by the standard follow-up practice of the treating center. Patients in the soft bandage group were advised not to wear the bandage for more than 3 weeks. Blinding was not possible, but the treatment team did not take part in patient follow-up.
The primary outcome was change in pain 3 days after treatment, measured on the Wong-Baker FACES Pain Rating Scale (an ordinal assessment using 6 illustrated facial expressions translated to a numeric rating on a scale of 0-10, with higher scores indicating worse pain). This scale has an established minimum clinically important difference (MCID) value of 1 face (2 points).11 Per standard practice in equivalence trials, the equivalence margin was defined as half the MCID, with a value of 1.0 used in this study.
Secondary outcomes measured over the 6-week follow-up period included additional pain measurements using the Wong-Baker scale, measures of function and health-related quality of life, analgesia use, days of absence from school or childcare, complication rates, and patient satisfaction. This study used modified intention-to-treat and per-protocol analyses.
The mean age of participants was 9.6 years; 39% were girls and 61% were boys. In the bandage group, 94% opted to have the soft bandage applied in the ED, and 95% of the rigid immobilization group were treated with a removable wrist splint in the ED. At 3 days, pain scores improved by 3.2 points (standard deviation [SD] = 2.1) in the soft bandage group and 3.1 points (SD = 2.1) in the rigid immobilization group. The adjusted difference was –0.1 (95% CI, –0.37 to 0.17) in the intention-to-treat analysis and –0.06 (95% CI, –0.34 to 0.21) in the per-protocol analysis, which were both less than the predetermined equivalence margin. This equivalence margin also was met at all secondary time points (1 day, 7 days, 3 weeks, and 6 weeks after treatment) and in subgroup analysis of those 4 to 7 years and 8 to 15 years.
Use of any analgesia in the prior 24 hours was slightly higher in the soft bandage group on Day 1 (83% vs 78%; P = .04) and Day 3 (57% vs 51%; P = .05), but this difference was not seen on Day 7. Satisfaction, measured via a 7-point Likert scale (range from “extremely satisfied” to “extremely unsatisfied”), was slightly lower in the soft bandage group on Day 1 (median 2 [interquartile range = 1, 2] vs median 1 [interquartile range = 1, 2]; P < .0001) but was not different after 6 weeks. There were no measured differences in any other secondary outcomes, including function, quality of life, and complication rates.
Continue to: By the primary end point...
By the primary end point of 3 days, 36 patients (7%) in the soft bandage group returned to medical care requesting a change to rigid immobilization, compared with 1 patient (0.2%) in the rigid immobilization group declining intervention.
WHAT’S NEW
Equivalence in pain and function scores
This trial showed equivalence in pain at 3 days’ follow-up in children with distal radius torus fractures who were offered bandaging and then immediately discharged from the ED, compared with rigid immobilization and clinical follow-up. There were no significant differences in pain or function between groups during the 6 weeks following the initial injury. De-escalation of treatment offers an equivalent, resource-sparing alternative to traditional treatment of these fractures.
CAVEATS
Lack of masking likely introduced bias
There are no major caveats associated with managing distal radius torus fractures with a soft bandage and discharge from the ED, compared with the traditional treatment of rigid immobilization. However, bias was likely introduced in patient-reported outcomes due to the inability to mask patients and families to the treatment allocation. This may have led to overstating the severity of outcomes in the bandage group, given the strong preference for rigid immobilization, although equivalence was illustrated despite this potential bias.
CHALLENGES TO IMPLEMENTATION
Preferences may be difficult to change
Parents and clinicians demonstrated a preference for rigid immobilization, as shown in the imbalance in treatment crossovers, with 7% of children changing to the rigid immobilization group by the primary study end point of 3 days. The study authors hypothesized that crossovers may have been due to the perception by some parents that rigid immobilization is the gold standard of treatment, as well as clinicians’ seeking to escalate care for patients returning for follow-up. Policy and guideline changes, as well as physician efforts to educate patients on outcomes with soft bandage treatment, are likely to improve these misconceptions.
ILLUSTRATIVE CASE
A 9-year-old girl presents to your urgent care clinic after a fall while snowboarding for the first time. She reports falling forward onto her outstretched right hand and describes pain in her distal right forearm. She denies paresthesias, weakness, or lacerations. Physical examination reveals mild edema of the dorsal aspect of her distal right forearm and tenderness to palpation of the dorsal aspect of her distal radius. She denies tenderness to palpation of her ulna, anatomic snuffbox, hand, and elbow. Range of motion of the wrist is full on passive testing, but she declines active testing due to pain. Wrist radiographs reveal an uncomplicated torus fracture of the distal radius. Can immobilization with a soft bandage alone sufficiently treat this fracture?
Fractures of the distal radius are among the most common fractures of the upper extremity and commonly occur from a fall onto an outstretched hand.2 In the pediatric population, torus fractures, also known as buckle fractures, are the most common type of distal radius fracture, comprising an estimated 50% of pediatric wrist fractures.3,4 This is due to the presence of a
Pediatric torus fractures of the distal radius generally are treated with immobilization,2 traditionally through a
Despite common use of immobilization, torus fractures of the distal radius are anatomically stable, and displacement is unlikely to occur.7,8 As such, many studies have suggested that treatment of torus fractures with rigid immobilization in a cast or splint may not be necessary.9,10 However, a 2018 Cochrane review concluded that the quality of evidence illustrating similar recovery between treatments was low, leaving uncertainty as to the most appropriate management strategy.6 Less casting and follow-up imaging could have positive implications for patient satisfaction, health care–associated costs, and radiation exposure.10
This study, the Forearm Fracture Recovery in Children Evaluation (FORCE) trial, compared the traditional treatment of distal radius torus fractures with rigid immobilization to soft immobilization and immediate discharge.
STUDY SUMMARY
Providing quality evidence for a standard of care
FORCE was a randomized controlled equivalence trial (N = 965) across 23 emergency departments (EDs) in the United Kingdom that compared pain and function in pediatric patients with distal radius torus fractures treated with a soft bandage and immediate discharge vs rigid immobilization and routine follow-up.1 Patients included children ages 4 to 15 years presenting to the ED with a distal radius torus fracture, which was confirmed radiologically.
Patients with concomitant
Continue to: Patients were randomly assigned...
Patients were randomly assigned in a 1:1 ratio to receive treatment with either a soft bandage such as a gauze roller bandage (n = 489) or rigid immobilization (n = 476). For patients in the bandage group, a soft bandage was applied in the ED or provided for home application without planned clinical follow-up. Patients in the rigid immobilization group were treated in the ED with either a removable manufactured splint or a molded splint or cast, followed by the standard follow-up practice of the treating center. Patients in the soft bandage group were advised not to wear the bandage for more than 3 weeks. Blinding was not possible, but the treatment team did not take part in patient follow-up.
The primary outcome was change in pain 3 days after treatment, measured on the Wong-Baker FACES Pain Rating Scale (an ordinal assessment using 6 illustrated facial expressions translated to a numeric rating on a scale of 0-10, with higher scores indicating worse pain). This scale has an established minimum clinically important difference (MCID) value of 1 face (2 points).11 Per standard practice in equivalence trials, the equivalence margin was defined as half the MCID, with a value of 1.0 used in this study.
Secondary outcomes measured over the 6-week follow-up period included additional pain measurements using the Wong-Baker scale, measures of function and health-related quality of life, analgesia use, days of absence from school or childcare, complication rates, and patient satisfaction. This study used modified intention-to-treat and per-protocol analyses.
The mean age of participants was 9.6 years; 39% were girls and 61% were boys. In the bandage group, 94% opted to have the soft bandage applied in the ED, and 95% of the rigid immobilization group were treated with a removable wrist splint in the ED. At 3 days, pain scores improved by 3.2 points (standard deviation [SD] = 2.1) in the soft bandage group and 3.1 points (SD = 2.1) in the rigid immobilization group. The adjusted difference was –0.1 (95% CI, –0.37 to 0.17) in the intention-to-treat analysis and –0.06 (95% CI, –0.34 to 0.21) in the per-protocol analysis, which were both less than the predetermined equivalence margin. This equivalence margin also was met at all secondary time points (1 day, 7 days, 3 weeks, and 6 weeks after treatment) and in subgroup analysis of those 4 to 7 years and 8 to 15 years.
Use of any analgesia in the prior 24 hours was slightly higher in the soft bandage group on Day 1 (83% vs 78%; P = .04) and Day 3 (57% vs 51%; P = .05), but this difference was not seen on Day 7. Satisfaction, measured via a 7-point Likert scale (range from “extremely satisfied” to “extremely unsatisfied”), was slightly lower in the soft bandage group on Day 1 (median 2 [interquartile range = 1, 2] vs median 1 [interquartile range = 1, 2]; P < .0001) but was not different after 6 weeks. There were no measured differences in any other secondary outcomes, including function, quality of life, and complication rates.
Continue to: By the primary end point...
By the primary end point of 3 days, 36 patients (7%) in the soft bandage group returned to medical care requesting a change to rigid immobilization, compared with 1 patient (0.2%) in the rigid immobilization group declining intervention.
WHAT’S NEW
Equivalence in pain and function scores
This trial showed equivalence in pain at 3 days’ follow-up in children with distal radius torus fractures who were offered bandaging and then immediately discharged from the ED, compared with rigid immobilization and clinical follow-up. There were no significant differences in pain or function between groups during the 6 weeks following the initial injury. De-escalation of treatment offers an equivalent, resource-sparing alternative to traditional treatment of these fractures.
CAVEATS
Lack of masking likely introduced bias
There are no major caveats associated with managing distal radius torus fractures with a soft bandage and discharge from the ED, compared with the traditional treatment of rigid immobilization. However, bias was likely introduced in patient-reported outcomes due to the inability to mask patients and families to the treatment allocation. This may have led to overstating the severity of outcomes in the bandage group, given the strong preference for rigid immobilization, although equivalence was illustrated despite this potential bias.
CHALLENGES TO IMPLEMENTATION
Preferences may be difficult to change
Parents and clinicians demonstrated a preference for rigid immobilization, as shown in the imbalance in treatment crossovers, with 7% of children changing to the rigid immobilization group by the primary study end point of 3 days. The study authors hypothesized that crossovers may have been due to the perception by some parents that rigid immobilization is the gold standard of treatment, as well as clinicians’ seeking to escalate care for patients returning for follow-up. Policy and guideline changes, as well as physician efforts to educate patients on outcomes with soft bandage treatment, are likely to improve these misconceptions.
1. Perry DC, Achten J, Knight R, et al; FORCE Collaborators in collaboration with PERUKI. Immobilisation of torus fractures of the wrist in children (FORCE): a randomised controlled equivalence trial in the UK. Lancet. 2022;400:39-47. doi: 10.1016/S0140-6736(22)01015-7
2. Patel DS, Statuta SM, Ahmed N. Common fractures of the radius and ulna. Am Fam Physician. 2021;103:345-354.
3. Asokan A, Kheir N. Pediatric Torus Buckle Fracture. StatPearls Publishing; 2023.
4. Naranje SM, Erali RA, Warner WC Jr, et al. Epidemiology of pediatric fractures presenting to emergency departments in the United States. J Pediatr Orthop. 2016;36:e45-e48. doi: 10.1097/BPO.0000000000000595
5. Kennedy SA, Slobogean GP, Mulpuri K. Does degree of immobilization influence refracture rate in the forearm buckle fracture? J Pediatr Orthop B. 2010;19:77-81. doi: 10.1097/BPB.0b013e32832f067a
6. Handoll HHG, Elliott J, Iheozor-Ejiofor Z, et al. Interventions for treating wrist fractures in children. Cochrane Database Syst Rev. 2018;12:CD012470. doi: 10.1002/14651858.CD012470.pub2
7. Perry DC, Gibson P, Roland D, et al. What level of immobilisation is necessary for treatment of torus (buckle) fractures of the distal radius in children? BMJ. 2021;372:m4862. doi: 10.1136/bmj.m4862
8. Williams KG, Smith G, Luhmann SJ, et al. A randomized controlled trial of cast versus splint for distal radial buckle fracture: an evaluation of satisfaction, convenience, and preference. Pediatr Emerg Care. 2013;29:555-559. doi: 10.1097/PEC.0b013e31828e56fb
9. Jiang N, Cao ZH, Ma YF, et al. Management of pediatric forearm torus fractures: a systematic review and meta-analysis. Pediatr Emerg Care. 2016;32:773-778. doi: 10.1097/PEC.0000000000000579
10. Williams BA, Alvarado CA, Montoya-Williams DC, et al. Buckling down on torus fractures: has evolving evidence affected practice? J Child Orthop. 2018;12:123-128. doi: 10.1302/1863-2548.12.170122
11. Garra G, Singer AJ, Taira BR, et al. Validation of the Wong-Baker FACES Pain Rating Scale in pediatric emergency department patients. Acad Emerg Med. 2010;17:50-54. doi: 10.1111/j.1553-2712.2009.00620.x
1. Perry DC, Achten J, Knight R, et al; FORCE Collaborators in collaboration with PERUKI. Immobilisation of torus fractures of the wrist in children (FORCE): a randomised controlled equivalence trial in the UK. Lancet. 2022;400:39-47. doi: 10.1016/S0140-6736(22)01015-7
2. Patel DS, Statuta SM, Ahmed N. Common fractures of the radius and ulna. Am Fam Physician. 2021;103:345-354.
3. Asokan A, Kheir N. Pediatric Torus Buckle Fracture. StatPearls Publishing; 2023.
4. Naranje SM, Erali RA, Warner WC Jr, et al. Epidemiology of pediatric fractures presenting to emergency departments in the United States. J Pediatr Orthop. 2016;36:e45-e48. doi: 10.1097/BPO.0000000000000595
5. Kennedy SA, Slobogean GP, Mulpuri K. Does degree of immobilization influence refracture rate in the forearm buckle fracture? J Pediatr Orthop B. 2010;19:77-81. doi: 10.1097/BPB.0b013e32832f067a
6. Handoll HHG, Elliott J, Iheozor-Ejiofor Z, et al. Interventions for treating wrist fractures in children. Cochrane Database Syst Rev. 2018;12:CD012470. doi: 10.1002/14651858.CD012470.pub2
7. Perry DC, Gibson P, Roland D, et al. What level of immobilisation is necessary for treatment of torus (buckle) fractures of the distal radius in children? BMJ. 2021;372:m4862. doi: 10.1136/bmj.m4862
8. Williams KG, Smith G, Luhmann SJ, et al. A randomized controlled trial of cast versus splint for distal radial buckle fracture: an evaluation of satisfaction, convenience, and preference. Pediatr Emerg Care. 2013;29:555-559. doi: 10.1097/PEC.0b013e31828e56fb
9. Jiang N, Cao ZH, Ma YF, et al. Management of pediatric forearm torus fractures: a systematic review and meta-analysis. Pediatr Emerg Care. 2016;32:773-778. doi: 10.1097/PEC.0000000000000579
10. Williams BA, Alvarado CA, Montoya-Williams DC, et al. Buckling down on torus fractures: has evolving evidence affected practice? J Child Orthop. 2018;12:123-128. doi: 10.1302/1863-2548.12.170122
11. Garra G, Singer AJ, Taira BR, et al. Validation of the Wong-Baker FACES Pain Rating Scale in pediatric emergency department patients. Acad Emerg Med. 2010;17:50-54. doi: 10.1111/j.1553-2712.2009.00620.x
PRACTICE CHANGER
For uncomplicated pediatric torus fractures of the distal radius, consider definitive management with soft bandage immobilization until pain resolution, rather than rigid immobilization and clinical follow-up.
STRENGTH OF RECOMMENDATION
B: Based on a single randomized controlled trial with patient-oriented outcomes.1
Perry DC, Achten J, Knight R, et al; FORCE Collaborators in collaboration with PERUKI. Immobilisation of torus fractures of the wrist in children (FORCE): a randomised controlled equivalence trial in the UK. Lancet. 2022;400:39-47. doi: 10.1016/S0140-6736(22)01015-7
‘Hidden’ cognitive impairments in DMD may worsen outcomes
A new tool from the National Institutes of Health, called NIH Toolbox, could improve that outcome, according to Mathula Thangarajh, MD, PhD, who has conducted research in the field.
“When we talk to families and parents, they are able to identify that even during infancy that [children with DMD] have delayed cognitive function. This includes speech delay, but also language and adaptive skills. We also know that those children with speech delay, which is really a very commonly reported phenotype in up to 50%, go on to have school-based needs. They may repeat [grades] in elementary years, but they also use more resources at school,” said Dr. Thangarajh, who is an assistant professor of neurology at the Children’s Hospital of Richmond at Virginia Commonwealth University, Richmond, during a talk at the 2023 annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine (AANEM).
A previous natural history study that utilized the Pediatric Quality of Life assessment also showed that DMD patients reported the lowest scores in brain health, including emotional health and school performance.
Other research has shown a correlation between cognitive function and survival in DMD. “This suggests that health maintenance may play an important role [in outcomes],” said Dr. Thangarajh. Another study found a correlation between psychomotor delay that required school-based interventions and earlier loss of ambulation, lower cardiac ejection fraction, and worse pulmonary function. The researchers also found that boys with cognitive delay were diagnosed at an earlier age, and yet had delays in diagnosis and worse motor function, pulmonary health, and cardiac health outcomes. On average, they lost ambulatory ability 2 years earlier.
A study by Dr. Thangarajh’s group showed that patients with speech delay and lower IQ had lower performance in timed tests, including 6-minute walk test distance and scored an average of 2 points lower on the North Star Ambulatory Assessment.
A tool for continuous cognitive assessment
The Centers for Disease Control and Prevention–supported DMD CARE guidelines only say that neuropsychological evaluations should be considered at diagnosis, but is essential if concerns arise about developmental progress. However, the Muscular Dystrophy Association has found barriers both in access to specialists, with an average wait time of 1-2 years, and burdensome out-of-pocket costs.
Those issues prompted Dr. Thangarajh to look for an alternative solution. At the time that she embarked on this work, the NIH was interested in technologies to assess neurobehavioral issues across different diseases. The resulting NIH Toolbox iPad app was driven largely by failed clinical trials in dementia, and the aim was to be able to provide continuous assessment over time. “It will allow for assessments across the lifespan, so you can use the same construct from age 3 to 80-plus,” said Dr. Thangarajh. It can also normalize population factors, such as annual household income and mother’s IQ.
She set out to validate the NIH Toolbox in children with DMD. The toolbox includes measures of crystalized cognition and fluid cognition. The former encompasses vocabulary and reading ability, which are strongly predicted by socioeconomic status and maternal IQ. On the other hand, fluid cognition includes cognitive features that develop across the lifespan and is directly related to academic underperformance in DMD patients.
Dr. Thangarajh’s group assessed 30 boys with DMD and found that crystallized cognition was normal, but they had a deficit in fluid cognition. They found deficits within several subdomains of fluid cognition. “This tells us that the NIH Toolbox was able to replicate what we had known in the literature, that these boys really have lower intellectual capacity, but they also have significant weakness in fluid cognition,” she said.
She also wanted to examine changes over time by testing the boys at a 1-year interview. “What we found was that they are not making as much gain in fluid cognition as we would like. They are just making marginal improvements over time. This has implications on how often we should screen them, but also not be over reliant on using school-based resources for them to get tested,” said Dr. Thangarajh.
Her group’s analysis of a dataset of 55 boys provided by PTC Therapeutics revealed a difference by age in a test of working memory. “What we found was that boys who are actually greater than 9 years, compared with those who are less than 9 years, they actually had a reversal of development-based improvement. The older they get, they were not making as much gains as you would expect,” said Dr. Thangarajh.
She went on to discuss psychosocial determinants of cognitive health in DMD. It is known that women who are carriers of the dystrophin mutation can underperform in cognitively stressful tasks, leading her to wonder if this could lead to transgenerational risk to offspring with DMD. Her group tested women who were carriers of the mutation with the NIH Toolbox and found that they had lower fluid cognition than noncarriers. They then tested 65 dyads of mothers and children, and found a correlation, but only when it came to inhibitory control, which required the individual to note the direction of an arrow while ignoring surrounding arrows pointing in various directions.
Next, the researchers examined neighborhoods and their impact on cognitive health, which can be affected by the presence of green spaces, access to public transportation and good nutrition, and other factors. There were significant deficits associated with residence zip codes. “We were pretty shocked. Someone who is not in a socially vulnerable region is scoring slightly below average, but someone who is in a very socially vulnerable neighborhood is only scoring 75 [age-adjusted score] on the NIH toolbox. So with this, we can conclude that carrier women are vulnerable in certain cognitive domains, but also children who come from socially vulnerable [situations] have poor cognitive control. This, again, has implications on how often we should screen and how much we should overly rely on school-based resources for these individuals,” said Dr. Thangarajh.
Overcoming a significant barrier
The NIH Toolbox has a lot of potential to improve DMD care, according to Dianna Quan, MD, who is the incoming president of AANEM, and professor of neurology at the University of Colorado at Denver, Aurora. “There’s this huge problem in terms of getting people in to see neuropsychologists and having formal evaluations. I think that’s a huge barrier. If we have people able to access this toolkit, which is simple and easily and universally accessible, how wonderful is that? I think that will be a really great improvement on what’s going on right now. It allows people to easily screen for these cognitive disabilities and make sure that we address them,” Dr. Quan said in an interview.
Asked how the tool could specifically improve care, Dr. Quan suggested that the first step is to understand the contributing factors to cognitive issues, whether they are biological, social, or a combination. “Some of them we can modify, potentially, through addressing the social environment. Some of those biologic factors may also be modifiable with many of the new drug studies that are coming.”
Dr. Thangarajh has received speaker honoraria from NS Pharma and PTC Therapeutics. Dr. Quan has received funding from Alnylam, Pfizer, Cytokinetics, Momenta, and Argenx.
A new tool from the National Institutes of Health, called NIH Toolbox, could improve that outcome, according to Mathula Thangarajh, MD, PhD, who has conducted research in the field.
“When we talk to families and parents, they are able to identify that even during infancy that [children with DMD] have delayed cognitive function. This includes speech delay, but also language and adaptive skills. We also know that those children with speech delay, which is really a very commonly reported phenotype in up to 50%, go on to have school-based needs. They may repeat [grades] in elementary years, but they also use more resources at school,” said Dr. Thangarajh, who is an assistant professor of neurology at the Children’s Hospital of Richmond at Virginia Commonwealth University, Richmond, during a talk at the 2023 annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine (AANEM).
A previous natural history study that utilized the Pediatric Quality of Life assessment also showed that DMD patients reported the lowest scores in brain health, including emotional health and school performance.
Other research has shown a correlation between cognitive function and survival in DMD. “This suggests that health maintenance may play an important role [in outcomes],” said Dr. Thangarajh. Another study found a correlation between psychomotor delay that required school-based interventions and earlier loss of ambulation, lower cardiac ejection fraction, and worse pulmonary function. The researchers also found that boys with cognitive delay were diagnosed at an earlier age, and yet had delays in diagnosis and worse motor function, pulmonary health, and cardiac health outcomes. On average, they lost ambulatory ability 2 years earlier.
A study by Dr. Thangarajh’s group showed that patients with speech delay and lower IQ had lower performance in timed tests, including 6-minute walk test distance and scored an average of 2 points lower on the North Star Ambulatory Assessment.
A tool for continuous cognitive assessment
The Centers for Disease Control and Prevention–supported DMD CARE guidelines only say that neuropsychological evaluations should be considered at diagnosis, but is essential if concerns arise about developmental progress. However, the Muscular Dystrophy Association has found barriers both in access to specialists, with an average wait time of 1-2 years, and burdensome out-of-pocket costs.
Those issues prompted Dr. Thangarajh to look for an alternative solution. At the time that she embarked on this work, the NIH was interested in technologies to assess neurobehavioral issues across different diseases. The resulting NIH Toolbox iPad app was driven largely by failed clinical trials in dementia, and the aim was to be able to provide continuous assessment over time. “It will allow for assessments across the lifespan, so you can use the same construct from age 3 to 80-plus,” said Dr. Thangarajh. It can also normalize population factors, such as annual household income and mother’s IQ.
She set out to validate the NIH Toolbox in children with DMD. The toolbox includes measures of crystalized cognition and fluid cognition. The former encompasses vocabulary and reading ability, which are strongly predicted by socioeconomic status and maternal IQ. On the other hand, fluid cognition includes cognitive features that develop across the lifespan and is directly related to academic underperformance in DMD patients.
Dr. Thangarajh’s group assessed 30 boys with DMD and found that crystallized cognition was normal, but they had a deficit in fluid cognition. They found deficits within several subdomains of fluid cognition. “This tells us that the NIH Toolbox was able to replicate what we had known in the literature, that these boys really have lower intellectual capacity, but they also have significant weakness in fluid cognition,” she said.
She also wanted to examine changes over time by testing the boys at a 1-year interview. “What we found was that they are not making as much gain in fluid cognition as we would like. They are just making marginal improvements over time. This has implications on how often we should screen them, but also not be over reliant on using school-based resources for them to get tested,” said Dr. Thangarajh.
Her group’s analysis of a dataset of 55 boys provided by PTC Therapeutics revealed a difference by age in a test of working memory. “What we found was that boys who are actually greater than 9 years, compared with those who are less than 9 years, they actually had a reversal of development-based improvement. The older they get, they were not making as much gains as you would expect,” said Dr. Thangarajh.
She went on to discuss psychosocial determinants of cognitive health in DMD. It is known that women who are carriers of the dystrophin mutation can underperform in cognitively stressful tasks, leading her to wonder if this could lead to transgenerational risk to offspring with DMD. Her group tested women who were carriers of the mutation with the NIH Toolbox and found that they had lower fluid cognition than noncarriers. They then tested 65 dyads of mothers and children, and found a correlation, but only when it came to inhibitory control, which required the individual to note the direction of an arrow while ignoring surrounding arrows pointing in various directions.
Next, the researchers examined neighborhoods and their impact on cognitive health, which can be affected by the presence of green spaces, access to public transportation and good nutrition, and other factors. There were significant deficits associated with residence zip codes. “We were pretty shocked. Someone who is not in a socially vulnerable region is scoring slightly below average, but someone who is in a very socially vulnerable neighborhood is only scoring 75 [age-adjusted score] on the NIH toolbox. So with this, we can conclude that carrier women are vulnerable in certain cognitive domains, but also children who come from socially vulnerable [situations] have poor cognitive control. This, again, has implications on how often we should screen and how much we should overly rely on school-based resources for these individuals,” said Dr. Thangarajh.
Overcoming a significant barrier
The NIH Toolbox has a lot of potential to improve DMD care, according to Dianna Quan, MD, who is the incoming president of AANEM, and professor of neurology at the University of Colorado at Denver, Aurora. “There’s this huge problem in terms of getting people in to see neuropsychologists and having formal evaluations. I think that’s a huge barrier. If we have people able to access this toolkit, which is simple and easily and universally accessible, how wonderful is that? I think that will be a really great improvement on what’s going on right now. It allows people to easily screen for these cognitive disabilities and make sure that we address them,” Dr. Quan said in an interview.
Asked how the tool could specifically improve care, Dr. Quan suggested that the first step is to understand the contributing factors to cognitive issues, whether they are biological, social, or a combination. “Some of them we can modify, potentially, through addressing the social environment. Some of those biologic factors may also be modifiable with many of the new drug studies that are coming.”
Dr. Thangarajh has received speaker honoraria from NS Pharma and PTC Therapeutics. Dr. Quan has received funding from Alnylam, Pfizer, Cytokinetics, Momenta, and Argenx.
A new tool from the National Institutes of Health, called NIH Toolbox, could improve that outcome, according to Mathula Thangarajh, MD, PhD, who has conducted research in the field.
“When we talk to families and parents, they are able to identify that even during infancy that [children with DMD] have delayed cognitive function. This includes speech delay, but also language and adaptive skills. We also know that those children with speech delay, which is really a very commonly reported phenotype in up to 50%, go on to have school-based needs. They may repeat [grades] in elementary years, but they also use more resources at school,” said Dr. Thangarajh, who is an assistant professor of neurology at the Children’s Hospital of Richmond at Virginia Commonwealth University, Richmond, during a talk at the 2023 annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine (AANEM).
A previous natural history study that utilized the Pediatric Quality of Life assessment also showed that DMD patients reported the lowest scores in brain health, including emotional health and school performance.
Other research has shown a correlation between cognitive function and survival in DMD. “This suggests that health maintenance may play an important role [in outcomes],” said Dr. Thangarajh. Another study found a correlation between psychomotor delay that required school-based interventions and earlier loss of ambulation, lower cardiac ejection fraction, and worse pulmonary function. The researchers also found that boys with cognitive delay were diagnosed at an earlier age, and yet had delays in diagnosis and worse motor function, pulmonary health, and cardiac health outcomes. On average, they lost ambulatory ability 2 years earlier.
A study by Dr. Thangarajh’s group showed that patients with speech delay and lower IQ had lower performance in timed tests, including 6-minute walk test distance and scored an average of 2 points lower on the North Star Ambulatory Assessment.
A tool for continuous cognitive assessment
The Centers for Disease Control and Prevention–supported DMD CARE guidelines only say that neuropsychological evaluations should be considered at diagnosis, but is essential if concerns arise about developmental progress. However, the Muscular Dystrophy Association has found barriers both in access to specialists, with an average wait time of 1-2 years, and burdensome out-of-pocket costs.
Those issues prompted Dr. Thangarajh to look for an alternative solution. At the time that she embarked on this work, the NIH was interested in technologies to assess neurobehavioral issues across different diseases. The resulting NIH Toolbox iPad app was driven largely by failed clinical trials in dementia, and the aim was to be able to provide continuous assessment over time. “It will allow for assessments across the lifespan, so you can use the same construct from age 3 to 80-plus,” said Dr. Thangarajh. It can also normalize population factors, such as annual household income and mother’s IQ.
She set out to validate the NIH Toolbox in children with DMD. The toolbox includes measures of crystalized cognition and fluid cognition. The former encompasses vocabulary and reading ability, which are strongly predicted by socioeconomic status and maternal IQ. On the other hand, fluid cognition includes cognitive features that develop across the lifespan and is directly related to academic underperformance in DMD patients.
Dr. Thangarajh’s group assessed 30 boys with DMD and found that crystallized cognition was normal, but they had a deficit in fluid cognition. They found deficits within several subdomains of fluid cognition. “This tells us that the NIH Toolbox was able to replicate what we had known in the literature, that these boys really have lower intellectual capacity, but they also have significant weakness in fluid cognition,” she said.
She also wanted to examine changes over time by testing the boys at a 1-year interview. “What we found was that they are not making as much gain in fluid cognition as we would like. They are just making marginal improvements over time. This has implications on how often we should screen them, but also not be over reliant on using school-based resources for them to get tested,” said Dr. Thangarajh.
Her group’s analysis of a dataset of 55 boys provided by PTC Therapeutics revealed a difference by age in a test of working memory. “What we found was that boys who are actually greater than 9 years, compared with those who are less than 9 years, they actually had a reversal of development-based improvement. The older they get, they were not making as much gains as you would expect,” said Dr. Thangarajh.
She went on to discuss psychosocial determinants of cognitive health in DMD. It is known that women who are carriers of the dystrophin mutation can underperform in cognitively stressful tasks, leading her to wonder if this could lead to transgenerational risk to offspring with DMD. Her group tested women who were carriers of the mutation with the NIH Toolbox and found that they had lower fluid cognition than noncarriers. They then tested 65 dyads of mothers and children, and found a correlation, but only when it came to inhibitory control, which required the individual to note the direction of an arrow while ignoring surrounding arrows pointing in various directions.
Next, the researchers examined neighborhoods and their impact on cognitive health, which can be affected by the presence of green spaces, access to public transportation and good nutrition, and other factors. There were significant deficits associated with residence zip codes. “We were pretty shocked. Someone who is not in a socially vulnerable region is scoring slightly below average, but someone who is in a very socially vulnerable neighborhood is only scoring 75 [age-adjusted score] on the NIH toolbox. So with this, we can conclude that carrier women are vulnerable in certain cognitive domains, but also children who come from socially vulnerable [situations] have poor cognitive control. This, again, has implications on how often we should screen and how much we should overly rely on school-based resources for these individuals,” said Dr. Thangarajh.
Overcoming a significant barrier
The NIH Toolbox has a lot of potential to improve DMD care, according to Dianna Quan, MD, who is the incoming president of AANEM, and professor of neurology at the University of Colorado at Denver, Aurora. “There’s this huge problem in terms of getting people in to see neuropsychologists and having formal evaluations. I think that’s a huge barrier. If we have people able to access this toolkit, which is simple and easily and universally accessible, how wonderful is that? I think that will be a really great improvement on what’s going on right now. It allows people to easily screen for these cognitive disabilities and make sure that we address them,” Dr. Quan said in an interview.
Asked how the tool could specifically improve care, Dr. Quan suggested that the first step is to understand the contributing factors to cognitive issues, whether they are biological, social, or a combination. “Some of them we can modify, potentially, through addressing the social environment. Some of those biologic factors may also be modifiable with many of the new drug studies that are coming.”
Dr. Thangarajh has received speaker honoraria from NS Pharma and PTC Therapeutics. Dr. Quan has received funding from Alnylam, Pfizer, Cytokinetics, Momenta, and Argenx.
FROM AANEM 2023
Strength training promotes knee health, lowers OA risk
TOPLINE:
Strength training at any point in life is associated with a lower risk of knee pain and osteoarthritis, contrary to persistent assumptions of adverse effects.
METHODOLOGY:
- Researchers reviewed data on strength training and knee pain from 2,607 adults. They used the Historical Physical Activity Survey Instrument to assess the impact of strength training during four periods (ages 12-18 years, 19-34 years, 35-49 years, and 50 years and older).
- The participants were enrolled in the Osteoarthritis Initiative, a multicenter, prospective, longitudinal study; 44% were male, the average age was 64.3 years, and the mean body mass index was 28.5 kg/m2.
- Strength training was defined as those exposed and not exposed, as well as divided into low, medium, and high tertiles for those exposed. A total of 818 individuals were exposed to strength training, and 1,789 were not exposed to strength training.
- The primary outcomes were frequent knee pain, radiographic OA (ROA), and symptomatic radiographic OA (SOA).
TAKEAWAY:
- The study is the first to examine the effect of strength training on knee health in a community population sample not selected for a history of elite weight lifting.
- Overall, strength training at any point in life was associated with lower incidence of frequent knee pain, ROA, and SOA, compared with no strength training (odds ratios, 0.82, 0.83, and 0.77, respectively).
- When separated by tertiles, only the high-exposure group had significantly reduced odds of frequent knee pain, ROA, and SOA, with odds ratios of 0.74, 0.70, and 0.69, respectively. A dose-response relationship appeared for all three conditions, with the lowest odds ratios in the highest strength training exposure groups.
- Findings were similar for different age ranges, but the association between strength training and less frequent knee pain, less ROA, and less SOA was strongest in the older age groups.
IN PRACTICE:
“Our findings support the idea that the medical community should proactively encourage more people to participate in strength training to help reduce their risk of osteoarthritis and other chronic conditions,” the researchers write.
SOURCE:
The study, with first author Grace H. Lo, MD, of Baylor College of Medicine, Houston, and colleagues, was published in Arthritis and Rheumatology.
LIMITATIONS:
The observational design and self-selected study population of strength training participants might bias the results, including participants’ recall of their activity level levels and changes in exercise trends over time. More research is needed to explore associations between strength training and knee OA among those who started strength training at a younger age.
DISCLOSURES:
The study was funded in part by the VA Health Services Research and Development Center for Innovations in Quality, Effectiveness, and Safety at the Michael E. DeBakey VA Medical Center, Houston, and by donations to the Tupper Research Fund at Tufts Medical Center. The Osteoarthritis Initiative is supported by the National Institutes of Health; private funding partners include Merck Research Laboratories, Novartis, GlaxoSmithKline, and Pfizer. Three authors report having financial relationships with multiple pharmaceutical companies.
A version of this article first appeared on Medscape.com.
TOPLINE:
Strength training at any point in life is associated with a lower risk of knee pain and osteoarthritis, contrary to persistent assumptions of adverse effects.
METHODOLOGY:
- Researchers reviewed data on strength training and knee pain from 2,607 adults. They used the Historical Physical Activity Survey Instrument to assess the impact of strength training during four periods (ages 12-18 years, 19-34 years, 35-49 years, and 50 years and older).
- The participants were enrolled in the Osteoarthritis Initiative, a multicenter, prospective, longitudinal study; 44% were male, the average age was 64.3 years, and the mean body mass index was 28.5 kg/m2.
- Strength training was defined as those exposed and not exposed, as well as divided into low, medium, and high tertiles for those exposed. A total of 818 individuals were exposed to strength training, and 1,789 were not exposed to strength training.
- The primary outcomes were frequent knee pain, radiographic OA (ROA), and symptomatic radiographic OA (SOA).
TAKEAWAY:
- The study is the first to examine the effect of strength training on knee health in a community population sample not selected for a history of elite weight lifting.
- Overall, strength training at any point in life was associated with lower incidence of frequent knee pain, ROA, and SOA, compared with no strength training (odds ratios, 0.82, 0.83, and 0.77, respectively).
- When separated by tertiles, only the high-exposure group had significantly reduced odds of frequent knee pain, ROA, and SOA, with odds ratios of 0.74, 0.70, and 0.69, respectively. A dose-response relationship appeared for all three conditions, with the lowest odds ratios in the highest strength training exposure groups.
- Findings were similar for different age ranges, but the association between strength training and less frequent knee pain, less ROA, and less SOA was strongest in the older age groups.
IN PRACTICE:
“Our findings support the idea that the medical community should proactively encourage more people to participate in strength training to help reduce their risk of osteoarthritis and other chronic conditions,” the researchers write.
SOURCE:
The study, with first author Grace H. Lo, MD, of Baylor College of Medicine, Houston, and colleagues, was published in Arthritis and Rheumatology.
LIMITATIONS:
The observational design and self-selected study population of strength training participants might bias the results, including participants’ recall of their activity level levels and changes in exercise trends over time. More research is needed to explore associations between strength training and knee OA among those who started strength training at a younger age.
DISCLOSURES:
The study was funded in part by the VA Health Services Research and Development Center for Innovations in Quality, Effectiveness, and Safety at the Michael E. DeBakey VA Medical Center, Houston, and by donations to the Tupper Research Fund at Tufts Medical Center. The Osteoarthritis Initiative is supported by the National Institutes of Health; private funding partners include Merck Research Laboratories, Novartis, GlaxoSmithKline, and Pfizer. Three authors report having financial relationships with multiple pharmaceutical companies.
A version of this article first appeared on Medscape.com.
TOPLINE:
Strength training at any point in life is associated with a lower risk of knee pain and osteoarthritis, contrary to persistent assumptions of adverse effects.
METHODOLOGY:
- Researchers reviewed data on strength training and knee pain from 2,607 adults. They used the Historical Physical Activity Survey Instrument to assess the impact of strength training during four periods (ages 12-18 years, 19-34 years, 35-49 years, and 50 years and older).
- The participants were enrolled in the Osteoarthritis Initiative, a multicenter, prospective, longitudinal study; 44% were male, the average age was 64.3 years, and the mean body mass index was 28.5 kg/m2.
- Strength training was defined as those exposed and not exposed, as well as divided into low, medium, and high tertiles for those exposed. A total of 818 individuals were exposed to strength training, and 1,789 were not exposed to strength training.
- The primary outcomes were frequent knee pain, radiographic OA (ROA), and symptomatic radiographic OA (SOA).
TAKEAWAY:
- The study is the first to examine the effect of strength training on knee health in a community population sample not selected for a history of elite weight lifting.
- Overall, strength training at any point in life was associated with lower incidence of frequent knee pain, ROA, and SOA, compared with no strength training (odds ratios, 0.82, 0.83, and 0.77, respectively).
- When separated by tertiles, only the high-exposure group had significantly reduced odds of frequent knee pain, ROA, and SOA, with odds ratios of 0.74, 0.70, and 0.69, respectively. A dose-response relationship appeared for all three conditions, with the lowest odds ratios in the highest strength training exposure groups.
- Findings were similar for different age ranges, but the association between strength training and less frequent knee pain, less ROA, and less SOA was strongest in the older age groups.
IN PRACTICE:
“Our findings support the idea that the medical community should proactively encourage more people to participate in strength training to help reduce their risk of osteoarthritis and other chronic conditions,” the researchers write.
SOURCE:
The study, with first author Grace H. Lo, MD, of Baylor College of Medicine, Houston, and colleagues, was published in Arthritis and Rheumatology.
LIMITATIONS:
The observational design and self-selected study population of strength training participants might bias the results, including participants’ recall of their activity level levels and changes in exercise trends over time. More research is needed to explore associations between strength training and knee OA among those who started strength training at a younger age.
DISCLOSURES:
The study was funded in part by the VA Health Services Research and Development Center for Innovations in Quality, Effectiveness, and Safety at the Michael E. DeBakey VA Medical Center, Houston, and by donations to the Tupper Research Fund at Tufts Medical Center. The Osteoarthritis Initiative is supported by the National Institutes of Health; private funding partners include Merck Research Laboratories, Novartis, GlaxoSmithKline, and Pfizer. Three authors report having financial relationships with multiple pharmaceutical companies.
A version of this article first appeared on Medscape.com.
FDA OKs first ustekinumab biosimilar
The U.S. Food and Drug Administration has approved ustekinumab-auub (Wezlana) as a biosimilar to ustekinumab (Stelara) for the treatment of multiple inflammatory conditions. This is the first approval for a ustekinumab biosimilar in the United States.
Ustekinumab-auub was also granted an interchangeability designation, meaning that, depending on state law, a pharmacist may substitute the biosimilar for the reference product without consulting the prescribing provider.
“Today’s approval exemplifies the FDA’s longstanding commitment to support a competitive marketplace for biological products,” Sarah Yim, MD, director of the Office of Therapeutic Biologics and Biosimilars in the FDA’s Center for Drug Evaluation and Research, said in a statement. “This approval can empower patients by helping to increase access to safe, effective, and high-quality medications at potentially lower cost.”
Ustekinumab, manufactured by Johnson & Johnson, targets interleukin-12 and IL-23 and was first approved in 2009. Ustekinumab-auub was developed by Amgen.
Ustekinumab-auub is approved for the treatment of adult patients with moderate to severe plaque psoriasis who are candidates for phototherapy or systemic therapy, active psoriatic arthritis, moderate to severely active Crohn’s disease, and moderate to severely active ulcerative colitis. It is also approved for pediatric patients aged 6 years and older with moderate to severe plaque psoriasis who are candidates for phototherapy or systemic therapy and active psoriatic arthritis.
The approval was based on “comprehensive review of scientific evidence,” including “comparisons of the products on an analytical level using an extensive battery of chemical and biological tests and biological assays that confirmed similarity in the structural and functional features of Wezlana and Stelara (including those known to impact safety and efficacy), and comparative human pharmacokinetic data, clinical immunogenicity data, and other clinical safety and effectiveness data,” the FDA said.
Some common side effects of ustekinumab-auub include nasopharyngitis, upper respiratory tract infection, headache, fatigue, and nausea. The most severe side effect of the biosimilar, as with the reference drug ustekinumab, is infection.
The product launch of ustekinumab-auub will be delayed as a part of a settlement of Johnson & Johnson’s lawsuit against Amgen, according to Reuters. The details of the settlement are confidential, but it was stated that the biosimilar would be available by Jan. 1, 2025.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved ustekinumab-auub (Wezlana) as a biosimilar to ustekinumab (Stelara) for the treatment of multiple inflammatory conditions. This is the first approval for a ustekinumab biosimilar in the United States.
Ustekinumab-auub was also granted an interchangeability designation, meaning that, depending on state law, a pharmacist may substitute the biosimilar for the reference product without consulting the prescribing provider.
“Today’s approval exemplifies the FDA’s longstanding commitment to support a competitive marketplace for biological products,” Sarah Yim, MD, director of the Office of Therapeutic Biologics and Biosimilars in the FDA’s Center for Drug Evaluation and Research, said in a statement. “This approval can empower patients by helping to increase access to safe, effective, and high-quality medications at potentially lower cost.”
Ustekinumab, manufactured by Johnson & Johnson, targets interleukin-12 and IL-23 and was first approved in 2009. Ustekinumab-auub was developed by Amgen.
Ustekinumab-auub is approved for the treatment of adult patients with moderate to severe plaque psoriasis who are candidates for phototherapy or systemic therapy, active psoriatic arthritis, moderate to severely active Crohn’s disease, and moderate to severely active ulcerative colitis. It is also approved for pediatric patients aged 6 years and older with moderate to severe plaque psoriasis who are candidates for phototherapy or systemic therapy and active psoriatic arthritis.
The approval was based on “comprehensive review of scientific evidence,” including “comparisons of the products on an analytical level using an extensive battery of chemical and biological tests and biological assays that confirmed similarity in the structural and functional features of Wezlana and Stelara (including those known to impact safety and efficacy), and comparative human pharmacokinetic data, clinical immunogenicity data, and other clinical safety and effectiveness data,” the FDA said.
Some common side effects of ustekinumab-auub include nasopharyngitis, upper respiratory tract infection, headache, fatigue, and nausea. The most severe side effect of the biosimilar, as with the reference drug ustekinumab, is infection.
The product launch of ustekinumab-auub will be delayed as a part of a settlement of Johnson & Johnson’s lawsuit against Amgen, according to Reuters. The details of the settlement are confidential, but it was stated that the biosimilar would be available by Jan. 1, 2025.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved ustekinumab-auub (Wezlana) as a biosimilar to ustekinumab (Stelara) for the treatment of multiple inflammatory conditions. This is the first approval for a ustekinumab biosimilar in the United States.
Ustekinumab-auub was also granted an interchangeability designation, meaning that, depending on state law, a pharmacist may substitute the biosimilar for the reference product without consulting the prescribing provider.
“Today’s approval exemplifies the FDA’s longstanding commitment to support a competitive marketplace for biological products,” Sarah Yim, MD, director of the Office of Therapeutic Biologics and Biosimilars in the FDA’s Center for Drug Evaluation and Research, said in a statement. “This approval can empower patients by helping to increase access to safe, effective, and high-quality medications at potentially lower cost.”
Ustekinumab, manufactured by Johnson & Johnson, targets interleukin-12 and IL-23 and was first approved in 2009. Ustekinumab-auub was developed by Amgen.
Ustekinumab-auub is approved for the treatment of adult patients with moderate to severe plaque psoriasis who are candidates for phototherapy or systemic therapy, active psoriatic arthritis, moderate to severely active Crohn’s disease, and moderate to severely active ulcerative colitis. It is also approved for pediatric patients aged 6 years and older with moderate to severe plaque psoriasis who are candidates for phototherapy or systemic therapy and active psoriatic arthritis.
The approval was based on “comprehensive review of scientific evidence,” including “comparisons of the products on an analytical level using an extensive battery of chemical and biological tests and biological assays that confirmed similarity in the structural and functional features of Wezlana and Stelara (including those known to impact safety and efficacy), and comparative human pharmacokinetic data, clinical immunogenicity data, and other clinical safety and effectiveness data,” the FDA said.
Some common side effects of ustekinumab-auub include nasopharyngitis, upper respiratory tract infection, headache, fatigue, and nausea. The most severe side effect of the biosimilar, as with the reference drug ustekinumab, is infection.
The product launch of ustekinumab-auub will be delayed as a part of a settlement of Johnson & Johnson’s lawsuit against Amgen, according to Reuters. The details of the settlement are confidential, but it was stated that the biosimilar would be available by Jan. 1, 2025.
A version of this article first appeared on Medscape.com.
FDA approves ninth Humira biosimilar, with interchangeability
The Food and Drug Administration has granted an interchangeability designation to adalimumab-afzb (Abrilada), according to an announcement from Pfizer.
This is the second adalimumab biosimilar granted interchangeability. The first, adalimumab-adbm (Cyltezo), became available in July.
Biosimilars introduce market competition that can help lower drug prices. Adalimumab-afzb is one of nine approved biosimilars for Humira, and the last to launch in 2023.
Adalimumab-afzb is indicated for:
- Adults with rheumatoid arthritis.
- Polyarticular juvenile idiopathic arthritis in patients 2 years of age and older.
- Adults with psoriatic arthritis.
- Adults with ankylosing spondylitis.
- Crohn’s disease in adults and children 6 years of age and older.
- Adults with ulcerative colitis.
- Adults with plaque psoriasis.
- Adults with hidradenitis suppurativa.
- Adults with noninfectious intermediate and posterior uveitis and panuveitis.
“With this designation, Abrilada is now both biosimilar to and interchangeable with Humira, reinforcing confidence among physicians and pharmacists that there is no decrease in effectiveness or increase in safety risk associated with switching between Abrilada and the reference product,” Roy Fleischmann, MD, clinical professor of medicine, University of Texas Southwestern Medical Center, Dallas, said in Pfizer’s statement.
An interchangeability designation allows pharmacists to substitute the biosimilar for the reference product without involving the prescribing clinician (according to state law). To achieve this designation, Pfizer submitted data from a phase 3 study led by Dr. Fleischmann that evaluated adalimumab-afzb in patients with RA. Patients who were switched three times between the biosimilar and the reference product had outcomes similar to those of patients continuously treated with the reference product.
Adalimumab-afzb will be available later in October at a 5% discount from Humira’s price. Later this year, the drug will launch at a second price, a 60% discount from Humira.
Full prescribing information for adalimumab-afzb is available here.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has granted an interchangeability designation to adalimumab-afzb (Abrilada), according to an announcement from Pfizer.
This is the second adalimumab biosimilar granted interchangeability. The first, adalimumab-adbm (Cyltezo), became available in July.
Biosimilars introduce market competition that can help lower drug prices. Adalimumab-afzb is one of nine approved biosimilars for Humira, and the last to launch in 2023.
Adalimumab-afzb is indicated for:
- Adults with rheumatoid arthritis.
- Polyarticular juvenile idiopathic arthritis in patients 2 years of age and older.
- Adults with psoriatic arthritis.
- Adults with ankylosing spondylitis.
- Crohn’s disease in adults and children 6 years of age and older.
- Adults with ulcerative colitis.
- Adults with plaque psoriasis.
- Adults with hidradenitis suppurativa.
- Adults with noninfectious intermediate and posterior uveitis and panuveitis.
“With this designation, Abrilada is now both biosimilar to and interchangeable with Humira, reinforcing confidence among physicians and pharmacists that there is no decrease in effectiveness or increase in safety risk associated with switching between Abrilada and the reference product,” Roy Fleischmann, MD, clinical professor of medicine, University of Texas Southwestern Medical Center, Dallas, said in Pfizer’s statement.
An interchangeability designation allows pharmacists to substitute the biosimilar for the reference product without involving the prescribing clinician (according to state law). To achieve this designation, Pfizer submitted data from a phase 3 study led by Dr. Fleischmann that evaluated adalimumab-afzb in patients with RA. Patients who were switched three times between the biosimilar and the reference product had outcomes similar to those of patients continuously treated with the reference product.
Adalimumab-afzb will be available later in October at a 5% discount from Humira’s price. Later this year, the drug will launch at a second price, a 60% discount from Humira.
Full prescribing information for adalimumab-afzb is available here.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has granted an interchangeability designation to adalimumab-afzb (Abrilada), according to an announcement from Pfizer.
This is the second adalimumab biosimilar granted interchangeability. The first, adalimumab-adbm (Cyltezo), became available in July.
Biosimilars introduce market competition that can help lower drug prices. Adalimumab-afzb is one of nine approved biosimilars for Humira, and the last to launch in 2023.
Adalimumab-afzb is indicated for:
- Adults with rheumatoid arthritis.
- Polyarticular juvenile idiopathic arthritis in patients 2 years of age and older.
- Adults with psoriatic arthritis.
- Adults with ankylosing spondylitis.
- Crohn’s disease in adults and children 6 years of age and older.
- Adults with ulcerative colitis.
- Adults with plaque psoriasis.
- Adults with hidradenitis suppurativa.
- Adults with noninfectious intermediate and posterior uveitis and panuveitis.
“With this designation, Abrilada is now both biosimilar to and interchangeable with Humira, reinforcing confidence among physicians and pharmacists that there is no decrease in effectiveness or increase in safety risk associated with switching between Abrilada and the reference product,” Roy Fleischmann, MD, clinical professor of medicine, University of Texas Southwestern Medical Center, Dallas, said in Pfizer’s statement.
An interchangeability designation allows pharmacists to substitute the biosimilar for the reference product without involving the prescribing clinician (according to state law). To achieve this designation, Pfizer submitted data from a phase 3 study led by Dr. Fleischmann that evaluated adalimumab-afzb in patients with RA. Patients who were switched three times between the biosimilar and the reference product had outcomes similar to those of patients continuously treated with the reference product.
Adalimumab-afzb will be available later in October at a 5% discount from Humira’s price. Later this year, the drug will launch at a second price, a 60% discount from Humira.
Full prescribing information for adalimumab-afzb is available here.
A version of this article first appeared on Medscape.com.
FDA approves first tocilizumab biosimilar
The Food and Drug Administration has approved the biosimilar tocilizumab-bavi (Tofidence), Biogen, the drug’s manufacturer, announced on Sept. 29.
It is the first tocilizumab biosimilar approved by the FDA. The reference product, Actemra (Genentech), was first approved by the agency in 2010.
“The approval of Tofidence in the U.S. marks another positive step toward helping more people with chronic autoimmune conditions gain access to leading therapies,” Ian Henshaw, global head of biosimilars at Biogen, said in a statement. “With the increasing numbers of approved biosimilars, we expect increased savings and sustainability for health care systems and an increase in physician choice and patient access to biologics.”
Biogen’s pricing for tocilizumab-bavi will be available closer to the product’s launch date, which has yet to be determined, a company spokesman said. The U.S. average monthly cost of Actemra for rheumatoid arthritis, administered intravenously, is $2,134-$4,268 depending on dosage, according to a Genentech spokesperson.
Tocilizumab-bavi is an intravenous formulation (20 mg/mL) indicated for treatment of moderately to severely active RA, polyarticular juvenile idiopathic arthritis (PJIA), and systemic juvenile idiopathic arthritis (SJIA). The medication is administered every 4 weeks in RA and PJIA and every 8 weeks in SJIA as a single intravenous drip infusion over 1 hour.
The European Commission approved its first tocilizumab biosimilar, Tyenne (Fresenius Kabi), earlier in 2023 in both subcutaneous and intravenous formulations. Biogen did not comment on whether the company is working on a subcutaneous formulation for tocilizumab-bavi.
A version of this article appeared on Medscape.com.
The Food and Drug Administration has approved the biosimilar tocilizumab-bavi (Tofidence), Biogen, the drug’s manufacturer, announced on Sept. 29.
It is the first tocilizumab biosimilar approved by the FDA. The reference product, Actemra (Genentech), was first approved by the agency in 2010.
“The approval of Tofidence in the U.S. marks another positive step toward helping more people with chronic autoimmune conditions gain access to leading therapies,” Ian Henshaw, global head of biosimilars at Biogen, said in a statement. “With the increasing numbers of approved biosimilars, we expect increased savings and sustainability for health care systems and an increase in physician choice and patient access to biologics.”
Biogen’s pricing for tocilizumab-bavi will be available closer to the product’s launch date, which has yet to be determined, a company spokesman said. The U.S. average monthly cost of Actemra for rheumatoid arthritis, administered intravenously, is $2,134-$4,268 depending on dosage, according to a Genentech spokesperson.
Tocilizumab-bavi is an intravenous formulation (20 mg/mL) indicated for treatment of moderately to severely active RA, polyarticular juvenile idiopathic arthritis (PJIA), and systemic juvenile idiopathic arthritis (SJIA). The medication is administered every 4 weeks in RA and PJIA and every 8 weeks in SJIA as a single intravenous drip infusion over 1 hour.
The European Commission approved its first tocilizumab biosimilar, Tyenne (Fresenius Kabi), earlier in 2023 in both subcutaneous and intravenous formulations. Biogen did not comment on whether the company is working on a subcutaneous formulation for tocilizumab-bavi.
A version of this article appeared on Medscape.com.
The Food and Drug Administration has approved the biosimilar tocilizumab-bavi (Tofidence), Biogen, the drug’s manufacturer, announced on Sept. 29.
It is the first tocilizumab biosimilar approved by the FDA. The reference product, Actemra (Genentech), was first approved by the agency in 2010.
“The approval of Tofidence in the U.S. marks another positive step toward helping more people with chronic autoimmune conditions gain access to leading therapies,” Ian Henshaw, global head of biosimilars at Biogen, said in a statement. “With the increasing numbers of approved biosimilars, we expect increased savings and sustainability for health care systems and an increase in physician choice and patient access to biologics.”
Biogen’s pricing for tocilizumab-bavi will be available closer to the product’s launch date, which has yet to be determined, a company spokesman said. The U.S. average monthly cost of Actemra for rheumatoid arthritis, administered intravenously, is $2,134-$4,268 depending on dosage, according to a Genentech spokesperson.
Tocilizumab-bavi is an intravenous formulation (20 mg/mL) indicated for treatment of moderately to severely active RA, polyarticular juvenile idiopathic arthritis (PJIA), and systemic juvenile idiopathic arthritis (SJIA). The medication is administered every 4 weeks in RA and PJIA and every 8 weeks in SJIA as a single intravenous drip infusion over 1 hour.
The European Commission approved its first tocilizumab biosimilar, Tyenne (Fresenius Kabi), earlier in 2023 in both subcutaneous and intravenous formulations. Biogen did not comment on whether the company is working on a subcutaneous formulation for tocilizumab-bavi.
A version of this article appeared on Medscape.com.
Should people who play sports pay higher medical insurance premiums?
This transcript has been edited for clarity.
If you’re anywhere near Seattle, anywhere near Florida, or anywhere where it might be not oppressively hot outside but encouraging some people who might want to go out and get a little exercise, you’ve undoubtedly seen or heard of pickleball.
This took off, I think, out of Bainbridge Island, Wash. It was meant as a gentlemanly game where people didn’t exert themselves too much. The joke is you could play it while holding a drink in one hand. It’s gotten more popular and more competitive. It’s kind of a miniature version of tennis, with a smaller court, a plastic ball, and a wooden paddle. The ball can go back and forth rapidly, but you’re always playing doubles and it doesn’t take as much energy, exertion, and, if you will, fitness as a game like singles tennis.
The upside is it’s gotten many people outdoors getting some exercise and socializing. That’s all to the good. But a recent study suggested that there are about $500 million worth of injuries coming into the health care system associated with pickleball. There have been leg sprains, broken bones, people getting hit in the eye, hamstring pulls, and many other problems. I’ve been told that many of the spectators who show up for pickleball matches are there with a cast or have some kind of a wrap on because they were injured.
Well, many people have argued in the past about what we are going to do about health care costs. Some suggest if you voluntarily incur health care damage, you ought to pay for that yourself and you ought to have a big copay.
If you decide you’re going to do cross-country skiing or downhill skiing and you injure yourself, you chose to do it, so you pay. If you’re not going to maintain your weight, you’re going to smoke, or you’re going to ride around without a helmet, that’s your choice. You ought to pay.
I think the pickleball example is really a good challenge to these views. You obviously want people to go out and get some exercise. Here, we’re talking about a population that’s a little older and oftentimes doesn’t get out there as much as doctors would like to get the exercise that’s still important that they need, and yet it does incur injuries and problems.
My suggestion would be to make the game a little safer. Let’s try to encourage people to warm up more before they get out there and jump out of the car and engage in their pickleball battles. Goggles might be important to prevent the eye injuries in a game that’s played up close. Maybe we want to make sure that people look out for one another out there. If they think they’re getting dehydrated or tired, they should say, “Let’s sit down.”
I’m not willing to put a tax or a copay on the pickleball players of America. I know they choose to do it. It’s got an upside and benefits, as many things like skiing and other behaviors that have some risk do, but I think we want to be encouraging, not discouraging, of it.
I don’t like a society where anybody who tries to do something that takes risk winds up bearing extra cost for doing that. I understand that that gets people irritated when it comes to dangerous, hyper-risky behavior like smoking and not wearing a motorcycle helmet. I think the way to engage is not to call out the sinner or to try and punish those who are trying to do things that bring them enjoyment, reward, or in some of these cases, physical fitness, but to try to make things safer and try to gradually improve and get rid of the risk side to capture the full benefit side.
I’m not sure I’ve come up with all the best ways to make pickleball safer, but I think that’s where our thinking in health care should go. My view is to get out there and play pickleball. If you do pull your hamstring, raise my insurance premium a little bit. I’ll help to pay for it. Better you get some enjoyment and some exercise.
I get the downside, but come on, folks, we ought to be, as a community, somewhat supportive of the fun and recreation that our fellow citizens engage in.
Dr. Caplan is director, division of medical ethics, New York University Langone Medical Center. He disclosed serving as a director, officer, partner, employee, adviser, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position); and as a contributing author and adviser for Medscape.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
If you’re anywhere near Seattle, anywhere near Florida, or anywhere where it might be not oppressively hot outside but encouraging some people who might want to go out and get a little exercise, you’ve undoubtedly seen or heard of pickleball.
This took off, I think, out of Bainbridge Island, Wash. It was meant as a gentlemanly game where people didn’t exert themselves too much. The joke is you could play it while holding a drink in one hand. It’s gotten more popular and more competitive. It’s kind of a miniature version of tennis, with a smaller court, a plastic ball, and a wooden paddle. The ball can go back and forth rapidly, but you’re always playing doubles and it doesn’t take as much energy, exertion, and, if you will, fitness as a game like singles tennis.
The upside is it’s gotten many people outdoors getting some exercise and socializing. That’s all to the good. But a recent study suggested that there are about $500 million worth of injuries coming into the health care system associated with pickleball. There have been leg sprains, broken bones, people getting hit in the eye, hamstring pulls, and many other problems. I’ve been told that many of the spectators who show up for pickleball matches are there with a cast or have some kind of a wrap on because they were injured.
Well, many people have argued in the past about what we are going to do about health care costs. Some suggest if you voluntarily incur health care damage, you ought to pay for that yourself and you ought to have a big copay.
If you decide you’re going to do cross-country skiing or downhill skiing and you injure yourself, you chose to do it, so you pay. If you’re not going to maintain your weight, you’re going to smoke, or you’re going to ride around without a helmet, that’s your choice. You ought to pay.
I think the pickleball example is really a good challenge to these views. You obviously want people to go out and get some exercise. Here, we’re talking about a population that’s a little older and oftentimes doesn’t get out there as much as doctors would like to get the exercise that’s still important that they need, and yet it does incur injuries and problems.
My suggestion would be to make the game a little safer. Let’s try to encourage people to warm up more before they get out there and jump out of the car and engage in their pickleball battles. Goggles might be important to prevent the eye injuries in a game that’s played up close. Maybe we want to make sure that people look out for one another out there. If they think they’re getting dehydrated or tired, they should say, “Let’s sit down.”
I’m not willing to put a tax or a copay on the pickleball players of America. I know they choose to do it. It’s got an upside and benefits, as many things like skiing and other behaviors that have some risk do, but I think we want to be encouraging, not discouraging, of it.
I don’t like a society where anybody who tries to do something that takes risk winds up bearing extra cost for doing that. I understand that that gets people irritated when it comes to dangerous, hyper-risky behavior like smoking and not wearing a motorcycle helmet. I think the way to engage is not to call out the sinner or to try and punish those who are trying to do things that bring them enjoyment, reward, or in some of these cases, physical fitness, but to try to make things safer and try to gradually improve and get rid of the risk side to capture the full benefit side.
I’m not sure I’ve come up with all the best ways to make pickleball safer, but I think that’s where our thinking in health care should go. My view is to get out there and play pickleball. If you do pull your hamstring, raise my insurance premium a little bit. I’ll help to pay for it. Better you get some enjoyment and some exercise.
I get the downside, but come on, folks, we ought to be, as a community, somewhat supportive of the fun and recreation that our fellow citizens engage in.
Dr. Caplan is director, division of medical ethics, New York University Langone Medical Center. He disclosed serving as a director, officer, partner, employee, adviser, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position); and as a contributing author and adviser for Medscape.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
If you’re anywhere near Seattle, anywhere near Florida, or anywhere where it might be not oppressively hot outside but encouraging some people who might want to go out and get a little exercise, you’ve undoubtedly seen or heard of pickleball.
This took off, I think, out of Bainbridge Island, Wash. It was meant as a gentlemanly game where people didn’t exert themselves too much. The joke is you could play it while holding a drink in one hand. It’s gotten more popular and more competitive. It’s kind of a miniature version of tennis, with a smaller court, a plastic ball, and a wooden paddle. The ball can go back and forth rapidly, but you’re always playing doubles and it doesn’t take as much energy, exertion, and, if you will, fitness as a game like singles tennis.
The upside is it’s gotten many people outdoors getting some exercise and socializing. That’s all to the good. But a recent study suggested that there are about $500 million worth of injuries coming into the health care system associated with pickleball. There have been leg sprains, broken bones, people getting hit in the eye, hamstring pulls, and many other problems. I’ve been told that many of the spectators who show up for pickleball matches are there with a cast or have some kind of a wrap on because they were injured.
Well, many people have argued in the past about what we are going to do about health care costs. Some suggest if you voluntarily incur health care damage, you ought to pay for that yourself and you ought to have a big copay.
If you decide you’re going to do cross-country skiing or downhill skiing and you injure yourself, you chose to do it, so you pay. If you’re not going to maintain your weight, you’re going to smoke, or you’re going to ride around without a helmet, that’s your choice. You ought to pay.
I think the pickleball example is really a good challenge to these views. You obviously want people to go out and get some exercise. Here, we’re talking about a population that’s a little older and oftentimes doesn’t get out there as much as doctors would like to get the exercise that’s still important that they need, and yet it does incur injuries and problems.
My suggestion would be to make the game a little safer. Let’s try to encourage people to warm up more before they get out there and jump out of the car and engage in their pickleball battles. Goggles might be important to prevent the eye injuries in a game that’s played up close. Maybe we want to make sure that people look out for one another out there. If they think they’re getting dehydrated or tired, they should say, “Let’s sit down.”
I’m not willing to put a tax or a copay on the pickleball players of America. I know they choose to do it. It’s got an upside and benefits, as many things like skiing and other behaviors that have some risk do, but I think we want to be encouraging, not discouraging, of it.
I don’t like a society where anybody who tries to do something that takes risk winds up bearing extra cost for doing that. I understand that that gets people irritated when it comes to dangerous, hyper-risky behavior like smoking and not wearing a motorcycle helmet. I think the way to engage is not to call out the sinner or to try and punish those who are trying to do things that bring them enjoyment, reward, or in some of these cases, physical fitness, but to try to make things safer and try to gradually improve and get rid of the risk side to capture the full benefit side.
I’m not sure I’ve come up with all the best ways to make pickleball safer, but I think that’s where our thinking in health care should go. My view is to get out there and play pickleball. If you do pull your hamstring, raise my insurance premium a little bit. I’ll help to pay for it. Better you get some enjoyment and some exercise.
I get the downside, but come on, folks, we ought to be, as a community, somewhat supportive of the fun and recreation that our fellow citizens engage in.
Dr. Caplan is director, division of medical ethics, New York University Langone Medical Center. He disclosed serving as a director, officer, partner, employee, adviser, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position); and as a contributing author and adviser for Medscape.
A version of this article appeared on Medscape.com.