User login
Early surgery for intracerebral bleeds may benefit a select few
LONDON – Approximately 2%-3% of patients with spontaneous intracerebral hemorrhage may benefit from early surgical removal of hematoma, according to the results of the second Surgical Trial in Lobar Intracerebral Hemorrhage.
As reported at the annual European Stroke Conference and published simultaneously in the Lancet, patients with superficial lesions and an unfavorable prognostic score appeared to benefit from early surgical intervention, compared with those given conservative medical treatment (odds ratio [OR] = 0.49, P =.02). Conversely, those with a good prognostic score did not seem to benefit (OR = 1.12, P = .57).
The primary analysis showed no significant benefit of early surgery overall, with 41.4% of 297 patients in the early surgery group and 37.7% of 286 patients in the conservative treatment group having a favorable outcome at 6 months, as determined by the 8-point extended Glasgow Outcome Scale (GOS-E) (P = .367).
"That’s a 3.7% absolute benefit, which is not enough to change surgical practice on its own," said Dr. A. David Mendelow, professor of neurosurgery at Newcastle University in Newcastle upon Tyne, England. "We were looking for a 12% benefit when we set out to do this trial," he added during a press conference.
A 6% decrease in mortality at 6 months was seen favoring surgery (18% vs. 24% for conservative therapy), but this was not statistically significant (P = .095).
"Intracerebral hemorrhage is not a homogenous condition," Dr. Mendelow said, adding that it can be a difficult decision to operate. Clinical manifestations can range from no apparent effects to severe disability and rapid death. "STICH [Surgical Trial in Lobar Intracerebral Hemorrhage] focused on patients that we are not quite sure about whether to operate or not," he said.
The hypothesis for the trial was based on the findings of the first STICH trial (Acta Neurochir. Suppl. 2006;96:65-8). The results of the trial were again neutral overall, but subgroup analyses showed that some groups of patients did worse with surgery, such as those with deep-seated bleeds, and some may fare better, such as those with superficial lobar hematomas.
STICH II therefore specifically recruited this latter group of patients to see if the effect was real or an artifact of the scientific analysis. In total, 601 conscious ICH patients with a median age of 65 years were recruited at 78 centers in 27 countries. Patients had to have a superficial lesion (1 cm or less from the cortical surface of the brain) that was between 10 mL and 100 mL in volume, and with no sign of intraventricular hemorrhage on CT scanning. Patients had to be recruited within 48 hours of the stroke and surgical intervention had to be performed within 12 hours (Lancet 2013 May 29 [doi:10.1016/S0140-6736(13)60986-1]). (A total of 6 patients were excluded or withdrew from the study before intervention, and after intervention another 12 withdrew, were lost to follow-up, or were alive but had an unknown status.)
The GOS-E was calculated from the answers to a questionnaire sent out to patients and their relatives 6 months following their stroke. A cutoff score of approximately 27 was used to categorize patients as having a good or bad prognosis. At baseline, about two-thirds of patients had a good prognosis, and the remainder had a poor prognosis.
"The notion that early surgery might be beneficial in this subgroup of patients is supported by the results of the investigator’s updated meta-analysis of 15 trials,"
"One of the reasons, perhaps, for a lack of significance was the [number of] crossovers from initial conservative therapy to surgery," Dr. Mendelow said. Indeed, 21% of patients who were originally randomized to conservative treatment crossed over to the surgical arm. These patients had "clearly deteriorated" prior to having surgery, he said when presenting the findings. Furthermore, only 37% of these crossovers received surgery within the specified 12-hour time limit.
STICH provides the best, albeit insufficient, evidence to date on the role of surgery in ICH, Dr. Oliver Gautschi and Dr. Karl Schaller, both of the University of Geneva, commented in an editorial about the trial (Lancet 2013 May 29 [doi:10.1016/S0140-6736(13)61087-9]) .
"The notion that early surgery might be beneficial in this subgroup of patients is supported by the results of the investigator’s updated meta-analysis of 15 trials," they wrote. "The overall result of this meta-analysis of patients with different types of intracerebral hemorrhage favors surgery."
The results of two other surgical studies, CLEAR III and MISTIE III, "are eagerly awaited," Dr. Gautschi and Dr. Schaller said, noting that, "decompressive hemicraniectomy might be a[nother] promising surgical procedure."
The U.K. Medical Research Council funded STICH II. Dr. Mendelow reported having no relevant financial disclosures.
LONDON – Approximately 2%-3% of patients with spontaneous intracerebral hemorrhage may benefit from early surgical removal of hematoma, according to the results of the second Surgical Trial in Lobar Intracerebral Hemorrhage.
As reported at the annual European Stroke Conference and published simultaneously in the Lancet, patients with superficial lesions and an unfavorable prognostic score appeared to benefit from early surgical intervention, compared with those given conservative medical treatment (odds ratio [OR] = 0.49, P =.02). Conversely, those with a good prognostic score did not seem to benefit (OR = 1.12, P = .57).
The primary analysis showed no significant benefit of early surgery overall, with 41.4% of 297 patients in the early surgery group and 37.7% of 286 patients in the conservative treatment group having a favorable outcome at 6 months, as determined by the 8-point extended Glasgow Outcome Scale (GOS-E) (P = .367).
"That’s a 3.7% absolute benefit, which is not enough to change surgical practice on its own," said Dr. A. David Mendelow, professor of neurosurgery at Newcastle University in Newcastle upon Tyne, England. "We were looking for a 12% benefit when we set out to do this trial," he added during a press conference.
A 6% decrease in mortality at 6 months was seen favoring surgery (18% vs. 24% for conservative therapy), but this was not statistically significant (P = .095).
"Intracerebral hemorrhage is not a homogenous condition," Dr. Mendelow said, adding that it can be a difficult decision to operate. Clinical manifestations can range from no apparent effects to severe disability and rapid death. "STICH [Surgical Trial in Lobar Intracerebral Hemorrhage] focused on patients that we are not quite sure about whether to operate or not," he said.
The hypothesis for the trial was based on the findings of the first STICH trial (Acta Neurochir. Suppl. 2006;96:65-8). The results of the trial were again neutral overall, but subgroup analyses showed that some groups of patients did worse with surgery, such as those with deep-seated bleeds, and some may fare better, such as those with superficial lobar hematomas.
STICH II therefore specifically recruited this latter group of patients to see if the effect was real or an artifact of the scientific analysis. In total, 601 conscious ICH patients with a median age of 65 years were recruited at 78 centers in 27 countries. Patients had to have a superficial lesion (1 cm or less from the cortical surface of the brain) that was between 10 mL and 100 mL in volume, and with no sign of intraventricular hemorrhage on CT scanning. Patients had to be recruited within 48 hours of the stroke and surgical intervention had to be performed within 12 hours (Lancet 2013 May 29 [doi:10.1016/S0140-6736(13)60986-1]). (A total of 6 patients were excluded or withdrew from the study before intervention, and after intervention another 12 withdrew, were lost to follow-up, or were alive but had an unknown status.)
The GOS-E was calculated from the answers to a questionnaire sent out to patients and their relatives 6 months following their stroke. A cutoff score of approximately 27 was used to categorize patients as having a good or bad prognosis. At baseline, about two-thirds of patients had a good prognosis, and the remainder had a poor prognosis.
"The notion that early surgery might be beneficial in this subgroup of patients is supported by the results of the investigator’s updated meta-analysis of 15 trials,"
"One of the reasons, perhaps, for a lack of significance was the [number of] crossovers from initial conservative therapy to surgery," Dr. Mendelow said. Indeed, 21% of patients who were originally randomized to conservative treatment crossed over to the surgical arm. These patients had "clearly deteriorated" prior to having surgery, he said when presenting the findings. Furthermore, only 37% of these crossovers received surgery within the specified 12-hour time limit.
STICH provides the best, albeit insufficient, evidence to date on the role of surgery in ICH, Dr. Oliver Gautschi and Dr. Karl Schaller, both of the University of Geneva, commented in an editorial about the trial (Lancet 2013 May 29 [doi:10.1016/S0140-6736(13)61087-9]) .
"The notion that early surgery might be beneficial in this subgroup of patients is supported by the results of the investigator’s updated meta-analysis of 15 trials," they wrote. "The overall result of this meta-analysis of patients with different types of intracerebral hemorrhage favors surgery."
The results of two other surgical studies, CLEAR III and MISTIE III, "are eagerly awaited," Dr. Gautschi and Dr. Schaller said, noting that, "decompressive hemicraniectomy might be a[nother] promising surgical procedure."
The U.K. Medical Research Council funded STICH II. Dr. Mendelow reported having no relevant financial disclosures.
LONDON – Approximately 2%-3% of patients with spontaneous intracerebral hemorrhage may benefit from early surgical removal of hematoma, according to the results of the second Surgical Trial in Lobar Intracerebral Hemorrhage.
As reported at the annual European Stroke Conference and published simultaneously in the Lancet, patients with superficial lesions and an unfavorable prognostic score appeared to benefit from early surgical intervention, compared with those given conservative medical treatment (odds ratio [OR] = 0.49, P =.02). Conversely, those with a good prognostic score did not seem to benefit (OR = 1.12, P = .57).
The primary analysis showed no significant benefit of early surgery overall, with 41.4% of 297 patients in the early surgery group and 37.7% of 286 patients in the conservative treatment group having a favorable outcome at 6 months, as determined by the 8-point extended Glasgow Outcome Scale (GOS-E) (P = .367).
"That’s a 3.7% absolute benefit, which is not enough to change surgical practice on its own," said Dr. A. David Mendelow, professor of neurosurgery at Newcastle University in Newcastle upon Tyne, England. "We were looking for a 12% benefit when we set out to do this trial," he added during a press conference.
A 6% decrease in mortality at 6 months was seen favoring surgery (18% vs. 24% for conservative therapy), but this was not statistically significant (P = .095).
"Intracerebral hemorrhage is not a homogenous condition," Dr. Mendelow said, adding that it can be a difficult decision to operate. Clinical manifestations can range from no apparent effects to severe disability and rapid death. "STICH [Surgical Trial in Lobar Intracerebral Hemorrhage] focused on patients that we are not quite sure about whether to operate or not," he said.
The hypothesis for the trial was based on the findings of the first STICH trial (Acta Neurochir. Suppl. 2006;96:65-8). The results of the trial were again neutral overall, but subgroup analyses showed that some groups of patients did worse with surgery, such as those with deep-seated bleeds, and some may fare better, such as those with superficial lobar hematomas.
STICH II therefore specifically recruited this latter group of patients to see if the effect was real or an artifact of the scientific analysis. In total, 601 conscious ICH patients with a median age of 65 years were recruited at 78 centers in 27 countries. Patients had to have a superficial lesion (1 cm or less from the cortical surface of the brain) that was between 10 mL and 100 mL in volume, and with no sign of intraventricular hemorrhage on CT scanning. Patients had to be recruited within 48 hours of the stroke and surgical intervention had to be performed within 12 hours (Lancet 2013 May 29 [doi:10.1016/S0140-6736(13)60986-1]). (A total of 6 patients were excluded or withdrew from the study before intervention, and after intervention another 12 withdrew, were lost to follow-up, or were alive but had an unknown status.)
The GOS-E was calculated from the answers to a questionnaire sent out to patients and their relatives 6 months following their stroke. A cutoff score of approximately 27 was used to categorize patients as having a good or bad prognosis. At baseline, about two-thirds of patients had a good prognosis, and the remainder had a poor prognosis.
"The notion that early surgery might be beneficial in this subgroup of patients is supported by the results of the investigator’s updated meta-analysis of 15 trials,"
"One of the reasons, perhaps, for a lack of significance was the [number of] crossovers from initial conservative therapy to surgery," Dr. Mendelow said. Indeed, 21% of patients who were originally randomized to conservative treatment crossed over to the surgical arm. These patients had "clearly deteriorated" prior to having surgery, he said when presenting the findings. Furthermore, only 37% of these crossovers received surgery within the specified 12-hour time limit.
STICH provides the best, albeit insufficient, evidence to date on the role of surgery in ICH, Dr. Oliver Gautschi and Dr. Karl Schaller, both of the University of Geneva, commented in an editorial about the trial (Lancet 2013 May 29 [doi:10.1016/S0140-6736(13)61087-9]) .
"The notion that early surgery might be beneficial in this subgroup of patients is supported by the results of the investigator’s updated meta-analysis of 15 trials," they wrote. "The overall result of this meta-analysis of patients with different types of intracerebral hemorrhage favors surgery."
The results of two other surgical studies, CLEAR III and MISTIE III, "are eagerly awaited," Dr. Gautschi and Dr. Schaller said, noting that, "decompressive hemicraniectomy might be a[nother] promising surgical procedure."
The U.K. Medical Research Council funded STICH II. Dr. Mendelow reported having no relevant financial disclosures.
AT THE EUROPEAN STROKE CONFERENCE
Major finding: A favorable outcome at 6 months was seen in 41% of the early surgery group and 38% of the conservative treatment group (P = .367).
Data source: STICH II, an international, multicenter prospective trial of 601 patients randomized to early surgery (within 12 hours) or medical treatment within 48 hours of a spontaneous superficial intracerebral hemorrhage.
Disclosures: The U.K. Medical Research Council funded STICH II. Dr. Mendelow reported having no relevant financial disclosures.
Headgear comes off for amateur boxers
This summer, amateur, elite male boxers are back to competing without headgear after nearly 3 decades of being required to wear it during competition. The headgear rule was put in place by the International Boxing Association (AIBA) before the 1984 Olympics, but now elite, male boxers are beginning to compete in much more professional style.
So what will this mean for concussion rates and concussion risk?
At first glance, it may seem to put boxers at greater risk; however, clinical evidence has shown that headgear does not necessarily reduce the incidence of concussion. The advantage of headgear is that it protects the face and decreases eye injuries, nose injuries, and facial lacerations. It does not stop the head from spinning, the primary cause of concussion in boxers.
There are four ways that boxers can get brain injury, but none of them can be prevented by wearing headgear. These mechanisms include:
• Rotational acceleration. This occurs when the head twists/spins – usually from a blow to the side of the jaw, cheek, or chin – and the brain follows, resulting in the stretching and tearing of axons. (This is why knockouts usually come from a severe blow to the chin.)
• Linear acceleration. This happens when the brain moves forward/backward – usually from a direct blow to the face – and strikes the skull, resulting in the stretching or tearing of neurons in the brain and brain stem.
• Injury to the carotid arteries. This occurs after a sudden flexion of the neck – usually from a direct blow to it – resulting in tears in one or both carotid arteries, causing a stroke.
• Impact deceleration. This is the rapid slowing of the brain inside the skull and is usually caused by hitting an immovable object like the ring floor, resulting in cerebral contusions.
In fact, there is a new, still unpublished AIBA study that suggests the removal of headgear would decrease head injuries, such as concussions. According to the study spearheaded by AIBA medical commission chairman Dr. Charles Butler, the rate of concussion was 0.38% in 7,352 rounds for boxers wearing headgear, compared with 0.17% in 7,545 rounds for those without headgear.
On the other hand, another recent study by the Cleveland Clinic found that headgear can help decrease linear acceleration and the potential for injury from it.
Clearly, there is still much debate on this issue. As amateur boxers start this new phase of competition, experts will be better able to observe changes in concussion rates, if any, and hopefully come to a definitive conclusion as to whether headgear use has any impact at all.
Dr. Jordan is the director of the brain injury program and the memory evaluation treatment service at Burke Rehabilitation Hospital in White Plains, N.Y. He currently serves as the chief medical officer of the New York State Athletic Commission, as a team physician for USA Boxing, and as a member of the NFL Players Association Mackey-White Traumatic Brain Injury Committee and the NFL Neuro-Cognitive Disability Committee.
This summer, amateur, elite male boxers are back to competing without headgear after nearly 3 decades of being required to wear it during competition. The headgear rule was put in place by the International Boxing Association (AIBA) before the 1984 Olympics, but now elite, male boxers are beginning to compete in much more professional style.
So what will this mean for concussion rates and concussion risk?
At first glance, it may seem to put boxers at greater risk; however, clinical evidence has shown that headgear does not necessarily reduce the incidence of concussion. The advantage of headgear is that it protects the face and decreases eye injuries, nose injuries, and facial lacerations. It does not stop the head from spinning, the primary cause of concussion in boxers.
There are four ways that boxers can get brain injury, but none of them can be prevented by wearing headgear. These mechanisms include:
• Rotational acceleration. This occurs when the head twists/spins – usually from a blow to the side of the jaw, cheek, or chin – and the brain follows, resulting in the stretching and tearing of axons. (This is why knockouts usually come from a severe blow to the chin.)
• Linear acceleration. This happens when the brain moves forward/backward – usually from a direct blow to the face – and strikes the skull, resulting in the stretching or tearing of neurons in the brain and brain stem.
• Injury to the carotid arteries. This occurs after a sudden flexion of the neck – usually from a direct blow to it – resulting in tears in one or both carotid arteries, causing a stroke.
• Impact deceleration. This is the rapid slowing of the brain inside the skull and is usually caused by hitting an immovable object like the ring floor, resulting in cerebral contusions.
In fact, there is a new, still unpublished AIBA study that suggests the removal of headgear would decrease head injuries, such as concussions. According to the study spearheaded by AIBA medical commission chairman Dr. Charles Butler, the rate of concussion was 0.38% in 7,352 rounds for boxers wearing headgear, compared with 0.17% in 7,545 rounds for those without headgear.
On the other hand, another recent study by the Cleveland Clinic found that headgear can help decrease linear acceleration and the potential for injury from it.
Clearly, there is still much debate on this issue. As amateur boxers start this new phase of competition, experts will be better able to observe changes in concussion rates, if any, and hopefully come to a definitive conclusion as to whether headgear use has any impact at all.
Dr. Jordan is the director of the brain injury program and the memory evaluation treatment service at Burke Rehabilitation Hospital in White Plains, N.Y. He currently serves as the chief medical officer of the New York State Athletic Commission, as a team physician for USA Boxing, and as a member of the NFL Players Association Mackey-White Traumatic Brain Injury Committee and the NFL Neuro-Cognitive Disability Committee.
This summer, amateur, elite male boxers are back to competing without headgear after nearly 3 decades of being required to wear it during competition. The headgear rule was put in place by the International Boxing Association (AIBA) before the 1984 Olympics, but now elite, male boxers are beginning to compete in much more professional style.
So what will this mean for concussion rates and concussion risk?
At first glance, it may seem to put boxers at greater risk; however, clinical evidence has shown that headgear does not necessarily reduce the incidence of concussion. The advantage of headgear is that it protects the face and decreases eye injuries, nose injuries, and facial lacerations. It does not stop the head from spinning, the primary cause of concussion in boxers.
There are four ways that boxers can get brain injury, but none of them can be prevented by wearing headgear. These mechanisms include:
• Rotational acceleration. This occurs when the head twists/spins – usually from a blow to the side of the jaw, cheek, or chin – and the brain follows, resulting in the stretching and tearing of axons. (This is why knockouts usually come from a severe blow to the chin.)
• Linear acceleration. This happens when the brain moves forward/backward – usually from a direct blow to the face – and strikes the skull, resulting in the stretching or tearing of neurons in the brain and brain stem.
• Injury to the carotid arteries. This occurs after a sudden flexion of the neck – usually from a direct blow to it – resulting in tears in one or both carotid arteries, causing a stroke.
• Impact deceleration. This is the rapid slowing of the brain inside the skull and is usually caused by hitting an immovable object like the ring floor, resulting in cerebral contusions.
In fact, there is a new, still unpublished AIBA study that suggests the removal of headgear would decrease head injuries, such as concussions. According to the study spearheaded by AIBA medical commission chairman Dr. Charles Butler, the rate of concussion was 0.38% in 7,352 rounds for boxers wearing headgear, compared with 0.17% in 7,545 rounds for those without headgear.
On the other hand, another recent study by the Cleveland Clinic found that headgear can help decrease linear acceleration and the potential for injury from it.
Clearly, there is still much debate on this issue. As amateur boxers start this new phase of competition, experts will be better able to observe changes in concussion rates, if any, and hopefully come to a definitive conclusion as to whether headgear use has any impact at all.
Dr. Jordan is the director of the brain injury program and the memory evaluation treatment service at Burke Rehabilitation Hospital in White Plains, N.Y. He currently serves as the chief medical officer of the New York State Athletic Commission, as a team physician for USA Boxing, and as a member of the NFL Players Association Mackey-White Traumatic Brain Injury Committee and the NFL Neuro-Cognitive Disability Committee.
Decompression for malignant stroke in elderly lowers death, disability
LONDON – Decompressive surgery dramatically increased the survival chances of older adult patients who had massive brain swelling after a middle cerebral artery stroke, according to the results of a randomized clinical trial.
After 1 year of follow-up, 57% of patients aged 61 years or older were still alive if they had undergone hemicraniectomy, compared with 24% (P less than .001) of those who received standard intensive care alone in the DESTINY II trial. The increase in survival did not lead to an increase in severe disability, study investigator Dr. Werner Hacke of the University of Heidelberg, Germany, reported at the annual European Stroke Conference.
"Malignant infarction of the middle cerebral artery [MCA] is the deadliest type of ischemic brain infarction," Dr. Hacke noted. It is associated with rapid neurological deterioration caused by cerebral edema (Postgrad. Med. J. 2010;86:235-42) and is responsible for 70%-80% of in-hospital mortality if treated conservatively using mechanical ventilation and intracranial pressure reduction.
Evidence supporting decompressive surgery
Previous pooled research, including the DESTINY I study (Decompressive Surgery for the Treatment of Malignant Infarction of the Middle Cerebral Artery), showed that relieving the pressure on the brain by temporarily removing part of the skull within the first 48 hours of ischemic injury reduces the risk of death and poor clinical outcome by almost 50% in patients under the age of 60 years (Lancet Neurol. 2007;6:215-22). The DESTINY II data now show that older patients also can benefit from decompressive surgery, perhaps as much as their younger counterparts.
A total of 112 patients with malignant MCA infarction aged 61 years and older were recruited into the study and randomized to receive maximum conservative treatment alone or in addition to hemicraniectomy within 48 hours after symptom onset (Int. J. Stroke 2011;6:79-86). The mean age was 70 years, and 60%-67% had infarctions affecting the nondominant cerebral hemisphere. The mean National Institutes of Health Stroke Scale (NIHSS) score was 20-22 at admission.
The primary endpoint was the proportion of patients achieving a modified Rankin Scale (mRS) score of 0-4 versus 5-6 at 6 months. A score of 6 on this scale signifies death and a score of 5 represents severe disability, such as being bedridden and incontinent and requiring constant nursing care and attention.
Dr. Hacke noted that the trial’s data and safety monitoring board halted the trial at the 6-month assessment after reviewing data on 82 patients. The exact reasons were undisclosed, but part of the study’s protocol was to stop the trial once statistical significance was reached. At the time the trial has halted, a further 30 patients had already been randomized and were included in the intention-to-treat analysis (ITT).
DESTINY II results
Significantly more patients who underwent surgery had a mRS of 0-4 than did those who had standard intensive care treatment (40.5% vs. 18.6%, P = .039) using the DSMB data set. The percentages of surgically and conservatively treated patients with an mRS of 5 or 6 were 59.5% and 81.4%, respectively. Performing an ITT analysis did not change the findings.
The number needed to treat was just 4, Dr. Hacke reported.
At 12 months in the ITT population, he noted that 38% of surgically and 16% of conservatively managed patients with an mRS of 0-4 were alive, as were 62% versus 84% of those, respectively, who had a mRS of 5-6 (P =.009).
An ITT analysis of multiple secondary endpoints at 1 year – which included the NIHSS score, Barthel Activities of Daily Living Index, Short Form-36 physical and mental domains, Hamilton Rating Scale for Depression, and the EuroQoL-5D – was also significantly in favor of early hemicraniectomy. This was perhaps a statistical artifact, Dr. Hacke observed, as the significance disappeared when data were examined in only the patients who had survived to 1 year.
Retrospective consent to surgery
When survivors and their caregivers were asked if they would undergo the same procedure again, given the knowledge of the final outcome, the majority of both surgically treated (77%, n = 27) and conservatively managed survivors (73%, n = 15) said that they would.
This finding shows that most patients, including those with moderately severe disability (mRS of 4) would rather have the procedures than be dead.
Dr. Christine Roffe, professor of medicine at Keele University in Stoke-on-Trent, England, commented that a person’s point of view of disability often changes after having a stroke.
"We’ve always assumed that if you asked someone before they had a stroke, ‘Would you rather have a stroke or be dead?’ that people would say, ‘I’d rather be dead,’ " she said in an interview. It’s not unreasonable that most people would probably say they would rather be dead than be severely incapacitated for the rest of their lives, she added.
However, after having a stroke, people often report that they are able to continue to live their lives reasonably happily despite often being quite disabled and having lost their independence.
The DESTINY II data show that people who had surgery were quite happy despite any disability, and this was at a similar level to those who were treated conservatively but with higher survival rates, Dr. Roffe noted.
The ethical implications of this could be considerable, she suggested. It shows that people who have living wills or who decide that they do not want treatment in the event of a stroke could live just as happy a life after the event as before. It therefore begs the question of whether patients should be allowed to decide on this aspect of their care, she added.
The German Research Foundation and the German Ministry of Science and Education financially supported the study. Dr. Hacke had no disclosures. Dr. Roffe was not involved in the study and had no relevant conflicts of interest.
LONDON – Decompressive surgery dramatically increased the survival chances of older adult patients who had massive brain swelling after a middle cerebral artery stroke, according to the results of a randomized clinical trial.
After 1 year of follow-up, 57% of patients aged 61 years or older were still alive if they had undergone hemicraniectomy, compared with 24% (P less than .001) of those who received standard intensive care alone in the DESTINY II trial. The increase in survival did not lead to an increase in severe disability, study investigator Dr. Werner Hacke of the University of Heidelberg, Germany, reported at the annual European Stroke Conference.
"Malignant infarction of the middle cerebral artery [MCA] is the deadliest type of ischemic brain infarction," Dr. Hacke noted. It is associated with rapid neurological deterioration caused by cerebral edema (Postgrad. Med. J. 2010;86:235-42) and is responsible for 70%-80% of in-hospital mortality if treated conservatively using mechanical ventilation and intracranial pressure reduction.
Evidence supporting decompressive surgery
Previous pooled research, including the DESTINY I study (Decompressive Surgery for the Treatment of Malignant Infarction of the Middle Cerebral Artery), showed that relieving the pressure on the brain by temporarily removing part of the skull within the first 48 hours of ischemic injury reduces the risk of death and poor clinical outcome by almost 50% in patients under the age of 60 years (Lancet Neurol. 2007;6:215-22). The DESTINY II data now show that older patients also can benefit from decompressive surgery, perhaps as much as their younger counterparts.
A total of 112 patients with malignant MCA infarction aged 61 years and older were recruited into the study and randomized to receive maximum conservative treatment alone or in addition to hemicraniectomy within 48 hours after symptom onset (Int. J. Stroke 2011;6:79-86). The mean age was 70 years, and 60%-67% had infarctions affecting the nondominant cerebral hemisphere. The mean National Institutes of Health Stroke Scale (NIHSS) score was 20-22 at admission.
The primary endpoint was the proportion of patients achieving a modified Rankin Scale (mRS) score of 0-4 versus 5-6 at 6 months. A score of 6 on this scale signifies death and a score of 5 represents severe disability, such as being bedridden and incontinent and requiring constant nursing care and attention.
Dr. Hacke noted that the trial’s data and safety monitoring board halted the trial at the 6-month assessment after reviewing data on 82 patients. The exact reasons were undisclosed, but part of the study’s protocol was to stop the trial once statistical significance was reached. At the time the trial has halted, a further 30 patients had already been randomized and were included in the intention-to-treat analysis (ITT).
DESTINY II results
Significantly more patients who underwent surgery had a mRS of 0-4 than did those who had standard intensive care treatment (40.5% vs. 18.6%, P = .039) using the DSMB data set. The percentages of surgically and conservatively treated patients with an mRS of 5 or 6 were 59.5% and 81.4%, respectively. Performing an ITT analysis did not change the findings.
The number needed to treat was just 4, Dr. Hacke reported.
At 12 months in the ITT population, he noted that 38% of surgically and 16% of conservatively managed patients with an mRS of 0-4 were alive, as were 62% versus 84% of those, respectively, who had a mRS of 5-6 (P =.009).
An ITT analysis of multiple secondary endpoints at 1 year – which included the NIHSS score, Barthel Activities of Daily Living Index, Short Form-36 physical and mental domains, Hamilton Rating Scale for Depression, and the EuroQoL-5D – was also significantly in favor of early hemicraniectomy. This was perhaps a statistical artifact, Dr. Hacke observed, as the significance disappeared when data were examined in only the patients who had survived to 1 year.
Retrospective consent to surgery
When survivors and their caregivers were asked if they would undergo the same procedure again, given the knowledge of the final outcome, the majority of both surgically treated (77%, n = 27) and conservatively managed survivors (73%, n = 15) said that they would.
This finding shows that most patients, including those with moderately severe disability (mRS of 4) would rather have the procedures than be dead.
Dr. Christine Roffe, professor of medicine at Keele University in Stoke-on-Trent, England, commented that a person’s point of view of disability often changes after having a stroke.
"We’ve always assumed that if you asked someone before they had a stroke, ‘Would you rather have a stroke or be dead?’ that people would say, ‘I’d rather be dead,’ " she said in an interview. It’s not unreasonable that most people would probably say they would rather be dead than be severely incapacitated for the rest of their lives, she added.
However, after having a stroke, people often report that they are able to continue to live their lives reasonably happily despite often being quite disabled and having lost their independence.
The DESTINY II data show that people who had surgery were quite happy despite any disability, and this was at a similar level to those who were treated conservatively but with higher survival rates, Dr. Roffe noted.
The ethical implications of this could be considerable, she suggested. It shows that people who have living wills or who decide that they do not want treatment in the event of a stroke could live just as happy a life after the event as before. It therefore begs the question of whether patients should be allowed to decide on this aspect of their care, she added.
The German Research Foundation and the German Ministry of Science and Education financially supported the study. Dr. Hacke had no disclosures. Dr. Roffe was not involved in the study and had no relevant conflicts of interest.
LONDON – Decompressive surgery dramatically increased the survival chances of older adult patients who had massive brain swelling after a middle cerebral artery stroke, according to the results of a randomized clinical trial.
After 1 year of follow-up, 57% of patients aged 61 years or older were still alive if they had undergone hemicraniectomy, compared with 24% (P less than .001) of those who received standard intensive care alone in the DESTINY II trial. The increase in survival did not lead to an increase in severe disability, study investigator Dr. Werner Hacke of the University of Heidelberg, Germany, reported at the annual European Stroke Conference.
"Malignant infarction of the middle cerebral artery [MCA] is the deadliest type of ischemic brain infarction," Dr. Hacke noted. It is associated with rapid neurological deterioration caused by cerebral edema (Postgrad. Med. J. 2010;86:235-42) and is responsible for 70%-80% of in-hospital mortality if treated conservatively using mechanical ventilation and intracranial pressure reduction.
Evidence supporting decompressive surgery
Previous pooled research, including the DESTINY I study (Decompressive Surgery for the Treatment of Malignant Infarction of the Middle Cerebral Artery), showed that relieving the pressure on the brain by temporarily removing part of the skull within the first 48 hours of ischemic injury reduces the risk of death and poor clinical outcome by almost 50% in patients under the age of 60 years (Lancet Neurol. 2007;6:215-22). The DESTINY II data now show that older patients also can benefit from decompressive surgery, perhaps as much as their younger counterparts.
A total of 112 patients with malignant MCA infarction aged 61 years and older were recruited into the study and randomized to receive maximum conservative treatment alone or in addition to hemicraniectomy within 48 hours after symptom onset (Int. J. Stroke 2011;6:79-86). The mean age was 70 years, and 60%-67% had infarctions affecting the nondominant cerebral hemisphere. The mean National Institutes of Health Stroke Scale (NIHSS) score was 20-22 at admission.
The primary endpoint was the proportion of patients achieving a modified Rankin Scale (mRS) score of 0-4 versus 5-6 at 6 months. A score of 6 on this scale signifies death and a score of 5 represents severe disability, such as being bedridden and incontinent and requiring constant nursing care and attention.
Dr. Hacke noted that the trial’s data and safety monitoring board halted the trial at the 6-month assessment after reviewing data on 82 patients. The exact reasons were undisclosed, but part of the study’s protocol was to stop the trial once statistical significance was reached. At the time the trial has halted, a further 30 patients had already been randomized and were included in the intention-to-treat analysis (ITT).
DESTINY II results
Significantly more patients who underwent surgery had a mRS of 0-4 than did those who had standard intensive care treatment (40.5% vs. 18.6%, P = .039) using the DSMB data set. The percentages of surgically and conservatively treated patients with an mRS of 5 or 6 were 59.5% and 81.4%, respectively. Performing an ITT analysis did not change the findings.
The number needed to treat was just 4, Dr. Hacke reported.
At 12 months in the ITT population, he noted that 38% of surgically and 16% of conservatively managed patients with an mRS of 0-4 were alive, as were 62% versus 84% of those, respectively, who had a mRS of 5-6 (P =.009).
An ITT analysis of multiple secondary endpoints at 1 year – which included the NIHSS score, Barthel Activities of Daily Living Index, Short Form-36 physical and mental domains, Hamilton Rating Scale for Depression, and the EuroQoL-5D – was also significantly in favor of early hemicraniectomy. This was perhaps a statistical artifact, Dr. Hacke observed, as the significance disappeared when data were examined in only the patients who had survived to 1 year.
Retrospective consent to surgery
When survivors and their caregivers were asked if they would undergo the same procedure again, given the knowledge of the final outcome, the majority of both surgically treated (77%, n = 27) and conservatively managed survivors (73%, n = 15) said that they would.
This finding shows that most patients, including those with moderately severe disability (mRS of 4) would rather have the procedures than be dead.
Dr. Christine Roffe, professor of medicine at Keele University in Stoke-on-Trent, England, commented that a person’s point of view of disability often changes after having a stroke.
"We’ve always assumed that if you asked someone before they had a stroke, ‘Would you rather have a stroke or be dead?’ that people would say, ‘I’d rather be dead,’ " she said in an interview. It’s not unreasonable that most people would probably say they would rather be dead than be severely incapacitated for the rest of their lives, she added.
However, after having a stroke, people often report that they are able to continue to live their lives reasonably happily despite often being quite disabled and having lost their independence.
The DESTINY II data show that people who had surgery were quite happy despite any disability, and this was at a similar level to those who were treated conservatively but with higher survival rates, Dr. Roffe noted.
The ethical implications of this could be considerable, she suggested. It shows that people who have living wills or who decide that they do not want treatment in the event of a stroke could live just as happy a life after the event as before. It therefore begs the question of whether patients should be allowed to decide on this aspect of their care, she added.
The German Research Foundation and the German Ministry of Science and Education financially supported the study. Dr. Hacke had no disclosures. Dr. Roffe was not involved in the study and had no relevant conflicts of interest.
AT THE EUROPEAN STROKE CONFERENCE
Major finding: At 1 year, 57% of surgically managed versus 24% of conservatively managed patients were alive (P less than .001).
Data source: DESTINY II, a multicenter, randomized controlled clinical trial of decompressive surgery or conservative intensive care treatment in 112 patients aged 61 years or older with malignant infarction of the middle cerebral artery.
Disclosures: The German Research Foundation and the German Ministry of Science and Education financially supported the study. Dr. Hacke had no disclosures. Dr. Roffe was not involved in the study and had no relevant conflicts of interest.
Improved presurgery impulse control screening needed in Parkinson’s
SYDNEY, AUSTRALIA – Many Parkinson’s disease centers performing deep brain stimulation surgery are not using formal, standardized screening for impulse control disorders in pre- or postsurgical patients, according to a large survey of Parkinson Study Group centers.
Deep brain stimulation surgery is known to increase impulsivity, and standard practice is to identify and treat impulse control disorders in patients before surgery, according to lead author Dr. Nawaz Hack, a junior fellow in movement disorders at the University of Florida, Gainesville, and his colleagues.
"Surgery will improve their motor symptoms, but it may make their impulsivity worse, especially if you don’t screen and appropriately identify it," Dr. Hack said. "But if you catch it early through a standardized screening, you can address it."
The researchers surveyed 48 Parkinson Study Group centers, 97% of which performed deep brain stimulation surgery and 67% of which said they served a population of over 500 patients a year.
The results showed that only 23% of sites employed a formal battery of tests for impulsive and compulsive behavior and that 7% did not report screening for impulse control disorders.
Speaking at a poster session at the international congress of Parkinson’s Disease and Movement Disorders, Dr. Hack said that the majority of sites were employing a more ad-hoc approach to screening for impulse control disorders, using questions that were not necessarily standardized.
The survey found that 80% of responding centers used a neuropsychologist to screen for potential behavioral issues but only 32% used a psychiatrist, suggesting that most are focused on identifying the problem but do not necessarily have the facilities to manage and treat it.
There was also a wide variety of approaches taken to manage impulse control issues in presurgical patients.
Seventy-nine percent of patients with an impulse control disorder were treated with medication reduction, although there were 10 different strategies employed across centers, the survey’s authors reported.
"This is what happens in the centers that understand Parkinson’s disease – these are centers that are knowledgeable – so if we’re deficient there, what’s happening?" Dr. Hack said.
The concern was that patients whose impulsivity becomes exacerbated by surgery were more likely to be lost to follow up because of the potential financial consequences of their behavioral disorder.
"If you’re impulsive before, and you’re not treated or screened, you will be seriously impulsive after, so they’ll leave the operating room, they’ll go home, and they’ll start doing behaviors that are literally destroying their family, their lives, and their finances," Dr. Hack said.
However, he said that identifying patients with impulse control disorders could be difficult because patients were sometimes reluctant to volunteer information on behaviors that might indicate the presence of impulsivity, such as hypersexuality or problem gambling.
Nearly three-quarters of centers (72%) reported observing impulse control disorders among deep brain stimulation surgery patients, and 68% reported it in postoperative patients.
Most centers (79%) did not feel that the choice of brain target, whether subthalamic nucleus or globus pallidus, was influential in behavioral disorders.
Dr. Hack did not declare any financial conflicts of interest with the research.
SYDNEY, AUSTRALIA – Many Parkinson’s disease centers performing deep brain stimulation surgery are not using formal, standardized screening for impulse control disorders in pre- or postsurgical patients, according to a large survey of Parkinson Study Group centers.
Deep brain stimulation surgery is known to increase impulsivity, and standard practice is to identify and treat impulse control disorders in patients before surgery, according to lead author Dr. Nawaz Hack, a junior fellow in movement disorders at the University of Florida, Gainesville, and his colleagues.
"Surgery will improve their motor symptoms, but it may make their impulsivity worse, especially if you don’t screen and appropriately identify it," Dr. Hack said. "But if you catch it early through a standardized screening, you can address it."
The researchers surveyed 48 Parkinson Study Group centers, 97% of which performed deep brain stimulation surgery and 67% of which said they served a population of over 500 patients a year.
The results showed that only 23% of sites employed a formal battery of tests for impulsive and compulsive behavior and that 7% did not report screening for impulse control disorders.
Speaking at a poster session at the international congress of Parkinson’s Disease and Movement Disorders, Dr. Hack said that the majority of sites were employing a more ad-hoc approach to screening for impulse control disorders, using questions that were not necessarily standardized.
The survey found that 80% of responding centers used a neuropsychologist to screen for potential behavioral issues but only 32% used a psychiatrist, suggesting that most are focused on identifying the problem but do not necessarily have the facilities to manage and treat it.
There was also a wide variety of approaches taken to manage impulse control issues in presurgical patients.
Seventy-nine percent of patients with an impulse control disorder were treated with medication reduction, although there were 10 different strategies employed across centers, the survey’s authors reported.
"This is what happens in the centers that understand Parkinson’s disease – these are centers that are knowledgeable – so if we’re deficient there, what’s happening?" Dr. Hack said.
The concern was that patients whose impulsivity becomes exacerbated by surgery were more likely to be lost to follow up because of the potential financial consequences of their behavioral disorder.
"If you’re impulsive before, and you’re not treated or screened, you will be seriously impulsive after, so they’ll leave the operating room, they’ll go home, and they’ll start doing behaviors that are literally destroying their family, their lives, and their finances," Dr. Hack said.
However, he said that identifying patients with impulse control disorders could be difficult because patients were sometimes reluctant to volunteer information on behaviors that might indicate the presence of impulsivity, such as hypersexuality or problem gambling.
Nearly three-quarters of centers (72%) reported observing impulse control disorders among deep brain stimulation surgery patients, and 68% reported it in postoperative patients.
Most centers (79%) did not feel that the choice of brain target, whether subthalamic nucleus or globus pallidus, was influential in behavioral disorders.
Dr. Hack did not declare any financial conflicts of interest with the research.
SYDNEY, AUSTRALIA – Many Parkinson’s disease centers performing deep brain stimulation surgery are not using formal, standardized screening for impulse control disorders in pre- or postsurgical patients, according to a large survey of Parkinson Study Group centers.
Deep brain stimulation surgery is known to increase impulsivity, and standard practice is to identify and treat impulse control disorders in patients before surgery, according to lead author Dr. Nawaz Hack, a junior fellow in movement disorders at the University of Florida, Gainesville, and his colleagues.
"Surgery will improve their motor symptoms, but it may make their impulsivity worse, especially if you don’t screen and appropriately identify it," Dr. Hack said. "But if you catch it early through a standardized screening, you can address it."
The researchers surveyed 48 Parkinson Study Group centers, 97% of which performed deep brain stimulation surgery and 67% of which said they served a population of over 500 patients a year.
The results showed that only 23% of sites employed a formal battery of tests for impulsive and compulsive behavior and that 7% did not report screening for impulse control disorders.
Speaking at a poster session at the international congress of Parkinson’s Disease and Movement Disorders, Dr. Hack said that the majority of sites were employing a more ad-hoc approach to screening for impulse control disorders, using questions that were not necessarily standardized.
The survey found that 80% of responding centers used a neuropsychologist to screen for potential behavioral issues but only 32% used a psychiatrist, suggesting that most are focused on identifying the problem but do not necessarily have the facilities to manage and treat it.
There was also a wide variety of approaches taken to manage impulse control issues in presurgical patients.
Seventy-nine percent of patients with an impulse control disorder were treated with medication reduction, although there were 10 different strategies employed across centers, the survey’s authors reported.
"This is what happens in the centers that understand Parkinson’s disease – these are centers that are knowledgeable – so if we’re deficient there, what’s happening?" Dr. Hack said.
The concern was that patients whose impulsivity becomes exacerbated by surgery were more likely to be lost to follow up because of the potential financial consequences of their behavioral disorder.
"If you’re impulsive before, and you’re not treated or screened, you will be seriously impulsive after, so they’ll leave the operating room, they’ll go home, and they’ll start doing behaviors that are literally destroying their family, their lives, and their finances," Dr. Hack said.
However, he said that identifying patients with impulse control disorders could be difficult because patients were sometimes reluctant to volunteer information on behaviors that might indicate the presence of impulsivity, such as hypersexuality or problem gambling.
Nearly three-quarters of centers (72%) reported observing impulse control disorders among deep brain stimulation surgery patients, and 68% reported it in postoperative patients.
Most centers (79%) did not feel that the choice of brain target, whether subthalamic nucleus or globus pallidus, was influential in behavioral disorders.
Dr. Hack did not declare any financial conflicts of interest with the research.
AT THE 2013 MDS INTERNATIONAL CONGRESS
Major finding: Only 23% of sites employed a formal battery of tests for impulsive and compulsive behavior and 7% did not report screening for impulse control disorders.
Data source: Survey of 48 Parkinson Study Group centers.
Disclosures: Dr. Hack did not declare any financial conflicts of interest.
Concussion recovery takes longer if children have had one before
Children and teenagers take longer to recover from a concussion if they’ve had one before, especially within the past year, Boston Children’s Hospital emergency department physicians found in a study of 280 of their concussed patients published June 10 in Pediatrics.
The median duration of symptoms, assessed by the serial Rivermead Post-Concussion Symptoms Questionnaire (RPSQ) over a period of 3 months, climbed from 12 days in patients who hadn’t been concussed before to 24 days in those who had. The median symptom duration was 28 days in patients with multiple previous concussions, and 35 days in those who’d been concussed within the previous year, "nearly three times the median duration [for] those who had no previous concussions," according to Dr. Matthew A. Eisenberg and his associates at the hospital (Pediatrics 2013 [doi:10.1542/peds.2013-0432]).
"Similarly, patients with two or more previous concussions had more than double the median symptom duration [of] patients with zero or one previous concussion," they found.
On multivariate analysis, previous concussion, maintaining consciousness, being 13 years or older, and an initial RPSQ of 18 or higher all predicted prolonged recovery. Among all comers, 77% had symptoms at 1 week, 32% at 4 weeks, and 15% at 3 months. The mean age in the trial was 14.3 years (range, 11-22 years).
The findings were statistically significant and have "direct implications on the management of athletes and other at-risk individuals who sustain concussions, supporting the concept that sufficient time to recover from a concussion may improve long-term outcomes," the investigators said.
"However, we did not find an association between physician-advised cognitive or physical rest and duration of symptoms, which may reflect the limitations of our observational study," they added. "A randomized [controlled] trial will likely be necessary to address the utility of this intervention."
Sixty-six percent of the subjects were enrolled the day they were injured; 24.7% were enrolled 1 day later, 7.2% 2 days later, and 1.7% 3 days later. The majority (63.8%) had been injured playing hockey, soccer, football, basketball or some other sport.
The investigators defined concussion broadly to include either altered mental status following blunt head trauma or, within 4 hours of it, any of the following symptoms that were not present before the injury: headache, nausea, vomiting, dizziness/balance problems, fatigue, drowsiness, blurred vision, memory difficulty, or trouble concentrating.
The most common symptoms in the study were headache (85.1%), fatigue (64.7%), and dizziness (63.0%); 4.3% of subjects had altered gait or balance, and 2.4% had altered mental status. There were no abnormalities in the 20.8% of kids who got neuroimaging.
On discharge, 65.9% were prescribed a period of cognitive rest and 92.4% were told to take time off from sports; 63.8% were also told to follow up with their primary care doctor, 45.5% with a sports concussion clinic, and 6.2% with a specialist.
In contrast to prior studies, loss of consciousness seemed to protect against a prolonged recovery (HR, 0.648; P = .02). Maybe the 22% of kids who got knocked out were more likely to follow their doctors’ advice to rest, "thus speeding recovery from their injury. We cannot, however, eliminate the possibility that there is a biological basis to this finding," the team noted.
Subjects who were 13 years or older might have taken longer to recover (HR, 1.404; P = .04) because games "between older children involve more contact and higher-force impacts," although neurobiologic differences between older and younger kids might have played a role, as well, the investigators said.
"Female patients" – about 43% of the study total – "had more severe symptoms at presentation in our study (mean initial RPSQ of 21.3 vs. 17.0 in male patients, P = .02). ... Whether this finding is indicative of the fact that female patients have more severe symptoms from concussion in general, as suggested in several previous studies, or is due to referral bias in which female individuals preferentially present to the ED when symptoms are more severe ... cannot be ascertained from our data," they noted.
Female gender fell out on multivariate analysis as a predictor of prolonged recovery (HR, 1.294; P= 0.11).
The investigators said they had no relevant financial disclosures.
This study is "incredibly interesting. It’s amazing to think that as recently as 5-7 years ago, people were still operating under the advice that 90% of concussion patients get better within a week. You can still find that online every now and then. But clearly, whether they’ve had multiple concussions or not, recovery time is longer for teens and preteens than anyone has expected in the past. This backs up what I see in the clinic," said Dr. Kevin Walter.
So, if kids come to the office a week or 2 after a concussion and say they’re all better, they are "going to be the exception to the rule." More likely, they are not being honest with themselves or are a bit too eager to get back into the game or classroom, he said.
"You don’t want to let the athlete make the decision on their own that they’re better. [Sometimes] ERs [still] send them out saying that ‘if you still feel bad in a week, then go get seen. Otherwise, get back into sport[s],’ " he said.
Follow-up is critical to prevent that from happening. "The gold standard is moving towards multidisciplinary care with physicians and neuropsychologists, with the input of a school athletic trainer. [In my clinic,] the luxury of having a neuropsychologist is wonderful; they’ve got the cognitive function testing" to uncover subtle problems, "and they’ve got more time [to work with patients] and expertise on how to deliver the tests appropriately," Dr. Walter said.
No matter how hard it is for young patients to power down for a bit, "we know without a doubt that kids need some degree of cognitive rest and physical rest from activity and sports" after a concussion. It’s troubling in the study "that only 92% of people who had a concussion were told to refrain from athletics. That should be 100%; that’s the goal we need to shoot for," he said.
For now, it’s unclear if there’s a gap between when kids feel better and when they are truly physiologically recovered, and if they are especially vulnerable to another concussion in between. Also, although it’s been recognized before that kid concussions are different than ones in adults, what exactly that means for treatment is uncertain at this point.
Even so, "for most kids, we need to move a little bit more slowly" than in the past, he said.
Dr. Walter is an associate professor in the departments of orthopedic surgery and pediatrics at the Medical College of Wisconsin in Milwaukee, cofounder of the college’s Sports Concussion Program, and a member of the Institute of Medicine’s Committee on Sports-Related Concussions in Youth. He was lead author of the American Academy of Pediatrics’ clinical report "Sport-Related Concussion in Children and Adolescents."
This study is "incredibly interesting. It’s amazing to think that as recently as 5-7 years ago, people were still operating under the advice that 90% of concussion patients get better within a week. You can still find that online every now and then. But clearly, whether they’ve had multiple concussions or not, recovery time is longer for teens and preteens than anyone has expected in the past. This backs up what I see in the clinic," said Dr. Kevin Walter.
So, if kids come to the office a week or 2 after a concussion and say they’re all better, they are "going to be the exception to the rule." More likely, they are not being honest with themselves or are a bit too eager to get back into the game or classroom, he said.
"You don’t want to let the athlete make the decision on their own that they’re better. [Sometimes] ERs [still] send them out saying that ‘if you still feel bad in a week, then go get seen. Otherwise, get back into sport[s],’ " he said.
Follow-up is critical to prevent that from happening. "The gold standard is moving towards multidisciplinary care with physicians and neuropsychologists, with the input of a school athletic trainer. [In my clinic,] the luxury of having a neuropsychologist is wonderful; they’ve got the cognitive function testing" to uncover subtle problems, "and they’ve got more time [to work with patients] and expertise on how to deliver the tests appropriately," Dr. Walter said.
No matter how hard it is for young patients to power down for a bit, "we know without a doubt that kids need some degree of cognitive rest and physical rest from activity and sports" after a concussion. It’s troubling in the study "that only 92% of people who had a concussion were told to refrain from athletics. That should be 100%; that’s the goal we need to shoot for," he said.
For now, it’s unclear if there’s a gap between when kids feel better and when they are truly physiologically recovered, and if they are especially vulnerable to another concussion in between. Also, although it’s been recognized before that kid concussions are different than ones in adults, what exactly that means for treatment is uncertain at this point.
Even so, "for most kids, we need to move a little bit more slowly" than in the past, he said.
Dr. Walter is an associate professor in the departments of orthopedic surgery and pediatrics at the Medical College of Wisconsin in Milwaukee, cofounder of the college’s Sports Concussion Program, and a member of the Institute of Medicine’s Committee on Sports-Related Concussions in Youth. He was lead author of the American Academy of Pediatrics’ clinical report "Sport-Related Concussion in Children and Adolescents."
This study is "incredibly interesting. It’s amazing to think that as recently as 5-7 years ago, people were still operating under the advice that 90% of concussion patients get better within a week. You can still find that online every now and then. But clearly, whether they’ve had multiple concussions or not, recovery time is longer for teens and preteens than anyone has expected in the past. This backs up what I see in the clinic," said Dr. Kevin Walter.
So, if kids come to the office a week or 2 after a concussion and say they’re all better, they are "going to be the exception to the rule." More likely, they are not being honest with themselves or are a bit too eager to get back into the game or classroom, he said.
"You don’t want to let the athlete make the decision on their own that they’re better. [Sometimes] ERs [still] send them out saying that ‘if you still feel bad in a week, then go get seen. Otherwise, get back into sport[s],’ " he said.
Follow-up is critical to prevent that from happening. "The gold standard is moving towards multidisciplinary care with physicians and neuropsychologists, with the input of a school athletic trainer. [In my clinic,] the luxury of having a neuropsychologist is wonderful; they’ve got the cognitive function testing" to uncover subtle problems, "and they’ve got more time [to work with patients] and expertise on how to deliver the tests appropriately," Dr. Walter said.
No matter how hard it is for young patients to power down for a bit, "we know without a doubt that kids need some degree of cognitive rest and physical rest from activity and sports" after a concussion. It’s troubling in the study "that only 92% of people who had a concussion were told to refrain from athletics. That should be 100%; that’s the goal we need to shoot for," he said.
For now, it’s unclear if there’s a gap between when kids feel better and when they are truly physiologically recovered, and if they are especially vulnerable to another concussion in between. Also, although it’s been recognized before that kid concussions are different than ones in adults, what exactly that means for treatment is uncertain at this point.
Even so, "for most kids, we need to move a little bit more slowly" than in the past, he said.
Dr. Walter is an associate professor in the departments of orthopedic surgery and pediatrics at the Medical College of Wisconsin in Milwaukee, cofounder of the college’s Sports Concussion Program, and a member of the Institute of Medicine’s Committee on Sports-Related Concussions in Youth. He was lead author of the American Academy of Pediatrics’ clinical report "Sport-Related Concussion in Children and Adolescents."
Children and teenagers take longer to recover from a concussion if they’ve had one before, especially within the past year, Boston Children’s Hospital emergency department physicians found in a study of 280 of their concussed patients published June 10 in Pediatrics.
The median duration of symptoms, assessed by the serial Rivermead Post-Concussion Symptoms Questionnaire (RPSQ) over a period of 3 months, climbed from 12 days in patients who hadn’t been concussed before to 24 days in those who had. The median symptom duration was 28 days in patients with multiple previous concussions, and 35 days in those who’d been concussed within the previous year, "nearly three times the median duration [for] those who had no previous concussions," according to Dr. Matthew A. Eisenberg and his associates at the hospital (Pediatrics 2013 [doi:10.1542/peds.2013-0432]).
"Similarly, patients with two or more previous concussions had more than double the median symptom duration [of] patients with zero or one previous concussion," they found.
On multivariate analysis, previous concussion, maintaining consciousness, being 13 years or older, and an initial RPSQ of 18 or higher all predicted prolonged recovery. Among all comers, 77% had symptoms at 1 week, 32% at 4 weeks, and 15% at 3 months. The mean age in the trial was 14.3 years (range, 11-22 years).
The findings were statistically significant and have "direct implications on the management of athletes and other at-risk individuals who sustain concussions, supporting the concept that sufficient time to recover from a concussion may improve long-term outcomes," the investigators said.
"However, we did not find an association between physician-advised cognitive or physical rest and duration of symptoms, which may reflect the limitations of our observational study," they added. "A randomized [controlled] trial will likely be necessary to address the utility of this intervention."
Sixty-six percent of the subjects were enrolled the day they were injured; 24.7% were enrolled 1 day later, 7.2% 2 days later, and 1.7% 3 days later. The majority (63.8%) had been injured playing hockey, soccer, football, basketball or some other sport.
The investigators defined concussion broadly to include either altered mental status following blunt head trauma or, within 4 hours of it, any of the following symptoms that were not present before the injury: headache, nausea, vomiting, dizziness/balance problems, fatigue, drowsiness, blurred vision, memory difficulty, or trouble concentrating.
The most common symptoms in the study were headache (85.1%), fatigue (64.7%), and dizziness (63.0%); 4.3% of subjects had altered gait or balance, and 2.4% had altered mental status. There were no abnormalities in the 20.8% of kids who got neuroimaging.
On discharge, 65.9% were prescribed a period of cognitive rest and 92.4% were told to take time off from sports; 63.8% were also told to follow up with their primary care doctor, 45.5% with a sports concussion clinic, and 6.2% with a specialist.
In contrast to prior studies, loss of consciousness seemed to protect against a prolonged recovery (HR, 0.648; P = .02). Maybe the 22% of kids who got knocked out were more likely to follow their doctors’ advice to rest, "thus speeding recovery from their injury. We cannot, however, eliminate the possibility that there is a biological basis to this finding," the team noted.
Subjects who were 13 years or older might have taken longer to recover (HR, 1.404; P = .04) because games "between older children involve more contact and higher-force impacts," although neurobiologic differences between older and younger kids might have played a role, as well, the investigators said.
"Female patients" – about 43% of the study total – "had more severe symptoms at presentation in our study (mean initial RPSQ of 21.3 vs. 17.0 in male patients, P = .02). ... Whether this finding is indicative of the fact that female patients have more severe symptoms from concussion in general, as suggested in several previous studies, or is due to referral bias in which female individuals preferentially present to the ED when symptoms are more severe ... cannot be ascertained from our data," they noted.
Female gender fell out on multivariate analysis as a predictor of prolonged recovery (HR, 1.294; P= 0.11).
The investigators said they had no relevant financial disclosures.
Children and teenagers take longer to recover from a concussion if they’ve had one before, especially within the past year, Boston Children’s Hospital emergency department physicians found in a study of 280 of their concussed patients published June 10 in Pediatrics.
The median duration of symptoms, assessed by the serial Rivermead Post-Concussion Symptoms Questionnaire (RPSQ) over a period of 3 months, climbed from 12 days in patients who hadn’t been concussed before to 24 days in those who had. The median symptom duration was 28 days in patients with multiple previous concussions, and 35 days in those who’d been concussed within the previous year, "nearly three times the median duration [for] those who had no previous concussions," according to Dr. Matthew A. Eisenberg and his associates at the hospital (Pediatrics 2013 [doi:10.1542/peds.2013-0432]).
"Similarly, patients with two or more previous concussions had more than double the median symptom duration [of] patients with zero or one previous concussion," they found.
On multivariate analysis, previous concussion, maintaining consciousness, being 13 years or older, and an initial RPSQ of 18 or higher all predicted prolonged recovery. Among all comers, 77% had symptoms at 1 week, 32% at 4 weeks, and 15% at 3 months. The mean age in the trial was 14.3 years (range, 11-22 years).
The findings were statistically significant and have "direct implications on the management of athletes and other at-risk individuals who sustain concussions, supporting the concept that sufficient time to recover from a concussion may improve long-term outcomes," the investigators said.
"However, we did not find an association between physician-advised cognitive or physical rest and duration of symptoms, which may reflect the limitations of our observational study," they added. "A randomized [controlled] trial will likely be necessary to address the utility of this intervention."
Sixty-six percent of the subjects were enrolled the day they were injured; 24.7% were enrolled 1 day later, 7.2% 2 days later, and 1.7% 3 days later. The majority (63.8%) had been injured playing hockey, soccer, football, basketball or some other sport.
The investigators defined concussion broadly to include either altered mental status following blunt head trauma or, within 4 hours of it, any of the following symptoms that were not present before the injury: headache, nausea, vomiting, dizziness/balance problems, fatigue, drowsiness, blurred vision, memory difficulty, or trouble concentrating.
The most common symptoms in the study were headache (85.1%), fatigue (64.7%), and dizziness (63.0%); 4.3% of subjects had altered gait or balance, and 2.4% had altered mental status. There were no abnormalities in the 20.8% of kids who got neuroimaging.
On discharge, 65.9% were prescribed a period of cognitive rest and 92.4% were told to take time off from sports; 63.8% were also told to follow up with their primary care doctor, 45.5% with a sports concussion clinic, and 6.2% with a specialist.
In contrast to prior studies, loss of consciousness seemed to protect against a prolonged recovery (HR, 0.648; P = .02). Maybe the 22% of kids who got knocked out were more likely to follow their doctors’ advice to rest, "thus speeding recovery from their injury. We cannot, however, eliminate the possibility that there is a biological basis to this finding," the team noted.
Subjects who were 13 years or older might have taken longer to recover (HR, 1.404; P = .04) because games "between older children involve more contact and higher-force impacts," although neurobiologic differences between older and younger kids might have played a role, as well, the investigators said.
"Female patients" – about 43% of the study total – "had more severe symptoms at presentation in our study (mean initial RPSQ of 21.3 vs. 17.0 in male patients, P = .02). ... Whether this finding is indicative of the fact that female patients have more severe symptoms from concussion in general, as suggested in several previous studies, or is due to referral bias in which female individuals preferentially present to the ED when symptoms are more severe ... cannot be ascertained from our data," they noted.
Female gender fell out on multivariate analysis as a predictor of prolonged recovery (HR, 1.294; P= 0.11).
The investigators said they had no relevant financial disclosures.
FROM PEDIATRICS
Major finding: The median duration of concussion symptoms was 12 days in children and teens who hadn’t been concussed before, 24 days in those who had, and 35 days in those who had been concussed within the previous year.
Data source: A prospective cohort study of 280 concussed patients aged 11-22 years.
Disclosures: The study was funded by Boston Children’s Hospital, where it was conducted. The investigators said they had no relevant financial disclosures.
Getting back in the game
"When can I go back to play, doc?" is a question you’ll hear often when treating athletes with concussions. For many of them, the answer would be in 7-10 days, but for more moderate or severe cases, that could go up to a month or more. It all depends on the athlete and his or her concussion history. However, there are some general guidelines to follow to determine when an athlete is ready to get back on the field.
First of all, athletes should not be allowed to return to play in the current game or practice in which they were injured. From there, they should be medically managed and given adequate physical and cognitive rest until they are asymptomatic.
This means that all symptoms have resolved, the neurologic examination is normal and their cognitive function has returned to baseline, if this was established prior to injury. They also should not be on any medications for concussion, that is, they should not be popping acetaminophen for headaches.
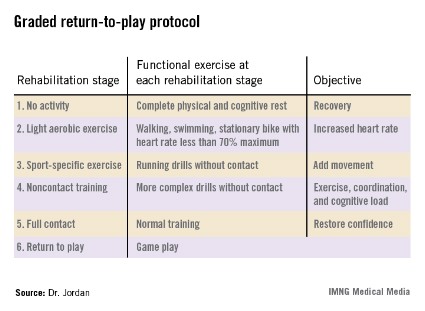
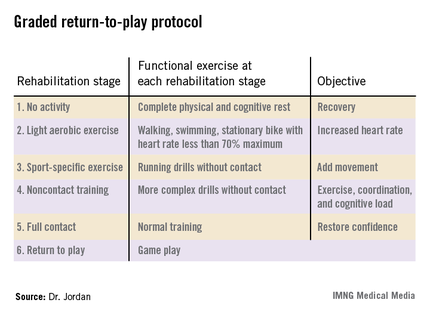
Another way to determine if the athlete is ready to get back in the game is by using the graded return-to-play protocol.
Typically, athletes move up the stages one level a day, although that is not necessary. You can certainly accelerate the process depending on the sport and the athlete. Those who are in noncontact sports like swimming can probably go through the levels quicker than someone who plays soccer.
I would suggest documenting how the athlete is doing throughout the process so everyone has a record of the athlete’s progress. I don’t think you can ever overdocument, and it’s a good habit to get into.
Along with the protocol, there’s also a computerized neuropsychological testing tool that’s fairly short and really focuses on what functions are affected. People tend to rely on this tool but you have to keep in mind that this is only one tool and should not be used alone.
Tools cannot replace a thorough cognitive evaluation. Just as there are no tests that can diagnose a concussion, there’s no tool that’ll say the athlete is ok to return to play. Ultimately, it is up to you to make that call, but the evaluation tools should certainly be used to help.
Dr. Barry Jordan is the director of the brain injury program and the memory evaluation treatment service at Burke Rehabilitation Hospital in White Plains, N.Y. He currently serves as the chief medical officer of the New York State Athletic Commission, a team physician for U.S.A. Boxing, and as a member of the NFL Players Association Mackey-White Traumatic Brain Injury Committee and the NFL Neuro-Cognitive Disability Committee.
"When can I go back to play, doc?" is a question you’ll hear often when treating athletes with concussions. For many of them, the answer would be in 7-10 days, but for more moderate or severe cases, that could go up to a month or more. It all depends on the athlete and his or her concussion history. However, there are some general guidelines to follow to determine when an athlete is ready to get back on the field.
First of all, athletes should not be allowed to return to play in the current game or practice in which they were injured. From there, they should be medically managed and given adequate physical and cognitive rest until they are asymptomatic.
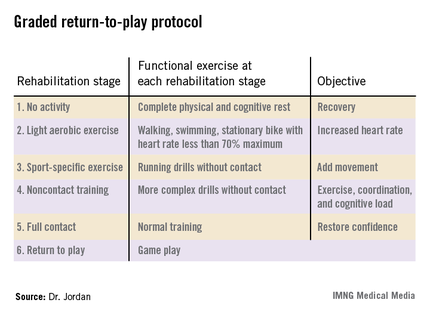
This means that all symptoms have resolved, the neurologic examination is normal and their cognitive function has returned to baseline, if this was established prior to injury. They also should not be on any medications for concussion, that is, they should not be popping acetaminophen for headaches.
Another way to determine if the athlete is ready to get back in the game is by using the graded return-to-play protocol.
Typically, athletes move up the stages one level a day, although that is not necessary. You can certainly accelerate the process depending on the sport and the athlete. Those who are in noncontact sports like swimming can probably go through the levels quicker than someone who plays soccer.
I would suggest documenting how the athlete is doing throughout the process so everyone has a record of the athlete’s progress. I don’t think you can ever overdocument, and it’s a good habit to get into.
Along with the protocol, there’s also a computerized neuropsychological testing tool that’s fairly short and really focuses on what functions are affected. People tend to rely on this tool but you have to keep in mind that this is only one tool and should not be used alone.
Tools cannot replace a thorough cognitive evaluation. Just as there are no tests that can diagnose a concussion, there’s no tool that’ll say the athlete is ok to return to play. Ultimately, it is up to you to make that call, but the evaluation tools should certainly be used to help.
Dr. Barry Jordan is the director of the brain injury program and the memory evaluation treatment service at Burke Rehabilitation Hospital in White Plains, N.Y. He currently serves as the chief medical officer of the New York State Athletic Commission, a team physician for U.S.A. Boxing, and as a member of the NFL Players Association Mackey-White Traumatic Brain Injury Committee and the NFL Neuro-Cognitive Disability Committee.
"When can I go back to play, doc?" is a question you’ll hear often when treating athletes with concussions. For many of them, the answer would be in 7-10 days, but for more moderate or severe cases, that could go up to a month or more. It all depends on the athlete and his or her concussion history. However, there are some general guidelines to follow to determine when an athlete is ready to get back on the field.
First of all, athletes should not be allowed to return to play in the current game or practice in which they were injured. From there, they should be medically managed and given adequate physical and cognitive rest until they are asymptomatic.
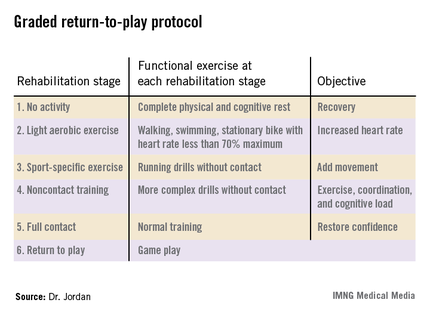
This means that all symptoms have resolved, the neurologic examination is normal and their cognitive function has returned to baseline, if this was established prior to injury. They also should not be on any medications for concussion, that is, they should not be popping acetaminophen for headaches.
Another way to determine if the athlete is ready to get back in the game is by using the graded return-to-play protocol.
Typically, athletes move up the stages one level a day, although that is not necessary. You can certainly accelerate the process depending on the sport and the athlete. Those who are in noncontact sports like swimming can probably go through the levels quicker than someone who plays soccer.
I would suggest documenting how the athlete is doing throughout the process so everyone has a record of the athlete’s progress. I don’t think you can ever overdocument, and it’s a good habit to get into.
Along with the protocol, there’s also a computerized neuropsychological testing tool that’s fairly short and really focuses on what functions are affected. People tend to rely on this tool but you have to keep in mind that this is only one tool and should not be used alone.
Tools cannot replace a thorough cognitive evaluation. Just as there are no tests that can diagnose a concussion, there’s no tool that’ll say the athlete is ok to return to play. Ultimately, it is up to you to make that call, but the evaluation tools should certainly be used to help.
Dr. Barry Jordan is the director of the brain injury program and the memory evaluation treatment service at Burke Rehabilitation Hospital in White Plains, N.Y. He currently serves as the chief medical officer of the New York State Athletic Commission, a team physician for U.S.A. Boxing, and as a member of the NFL Players Association Mackey-White Traumatic Brain Injury Committee and the NFL Neuro-Cognitive Disability Committee.
Surgical fellowship directors: General surgery trainees arrive ill prepared
INDIANAPOLIS – The nation’s elite surgical educators are up in arms over reported widespread deficiencies in the skill set and judgment of recent graduates of 5-year general surgery residencies.
Many trainees arrive at surgical subspecialty fellowships unprepared in their basic skills, according to a detailed new survey of the nation’s subspecialty fellowship program directors. The underlying theme of the responses is that many fellows are pursuing fellowship positions to make up for inadequacies in their general surgery residency rather than to push their skills to the next level, according to Dr. Samer Mattar.
About 80% of graduating general surgery residents now seek fellowships to obtain advanced training in bariatric, colorectal, thoracic, hepatobiliary, or other surgical specialty areas.
"Many new fellows must gain basic and fundamental skills at the beginning of their fellowship before they can commence to benefit from the advanced skills that they originally came to obtain. The current high demand for fellowship training and the lack of readiness upon completion of general surgery residencies should be a call to action for all stakeholders in surgical training," Dr. Mattar said in presenting the survey results at the annual meeting of the American Surgical Association.
Constructive changes are afoot, according to Dr. Mattar of Indiana University, Indianapolis. Plans are well underway to change the fourth year of medical school so that students interested in a career in surgery can begin preparing for it. And there are also efforts to custom tailor the final year of general surgery residency so residents can focus on their planned fellowship year. Toward that end, the Fellowship Council has moved the fellowship match date up to June so residents who know they are fellowship-bound can put their fifth year to the best use.
The survey was conducted by the Fellowship Council, an umbrella organization in charge of standardizing curricula, accrediting programs, and matching residents to fellowships. The group distributed the surveys to all 145 subspecialty fellowship program directors and drew a 63% response rate. That’s considered high for such a lengthy survey, said Dr. Mattar, and is an indication of the importance educators place on the subject.
The survey assessed five key educational domains: professionalism, independent practice, psychomotor skills, expertise in their chosen disease state, and scholarly focus.
"Incoming fellows exhibited high levels of professionalism, but there were deficiencies in autonomy and independence, psychomotor abilities, and – most profoundly – in academics and scholarship," Dr. Mattar said.
Among the key survey findings:
• Incoming fellows were unable to independently perform half an hour of a major procedure, according to 43% of program directors.
• Of incoming fellows, 30% couldn’t independently perform basic operations such as laparoscopic cholecystectomy.
• Of incoming fellows, 56% were able to laparoscopically suture and tie knots properly; 26% couldn’t recognize anatomic planes through the laparoscope.
• One-quarter was deemed unable to recognize early signs of complications.
In other findings, nearly 40% of program directors said new fellows display a lack of "patient ownership." "We promote patient ownership in our programs. We are somewhat disappointed and dismayed that the fellows feel that the patient is part of a service and not their own," Dr. Mattar commented. Half of the program directors indicated their incoming fellows demonstrated independence in the operating room and on call, although they reported the fellows showed marked improvement in these areas as the year went on.
A large majority of program directors felt their fellows were disinterested in research and in advancing the field, even though, as Dr. Mattar noted, "This is a mandate in our curriculum."
He reported having no financial conflicts.
No one should be surprised by the Fellowship Council survey results. During the past decade, the failure rate on the American Board of Surgery’s oral exam has climbed steadily from 16% to 28%. At present, the percentage of examinees who fail either the oral or written American Board of Surgery exam the first time around is in the mid-30s. That’s arguably an absurd failure rate for a 5-year training program in a group of people who should have mastered the subject.
The 80-hour work limit has effectively subtracted 6-12 months from the general surgery residency, yet I do not believe this emotional and contentious issue is the explanation.
At present, the average number of operations done by a first-year resident is less than two per week, while second-year residents average two to three per week. Our residents are spending 80 hours a week while doing two or three operations per week, which arguably could be done in half a day. It would be hard to imagine a less efficient educational process.
Dr. Frank R. Lewis is executive director of the American Board of Surgery. He was an invited discussant of the presentation.
No one should be surprised by the Fellowship Council survey results. During the past decade, the failure rate on the American Board of Surgery’s oral exam has climbed steadily from 16% to 28%. At present, the percentage of examinees who fail either the oral or written American Board of Surgery exam the first time around is in the mid-30s. That’s arguably an absurd failure rate for a 5-year training program in a group of people who should have mastered the subject.
The 80-hour work limit has effectively subtracted 6-12 months from the general surgery residency, yet I do not believe this emotional and contentious issue is the explanation.
At present, the average number of operations done by a first-year resident is less than two per week, while second-year residents average two to three per week. Our residents are spending 80 hours a week while doing two or three operations per week, which arguably could be done in half a day. It would be hard to imagine a less efficient educational process.
Dr. Frank R. Lewis is executive director of the American Board of Surgery. He was an invited discussant of the presentation.
No one should be surprised by the Fellowship Council survey results. During the past decade, the failure rate on the American Board of Surgery’s oral exam has climbed steadily from 16% to 28%. At present, the percentage of examinees who fail either the oral or written American Board of Surgery exam the first time around is in the mid-30s. That’s arguably an absurd failure rate for a 5-year training program in a group of people who should have mastered the subject.
The 80-hour work limit has effectively subtracted 6-12 months from the general surgery residency, yet I do not believe this emotional and contentious issue is the explanation.
At present, the average number of operations done by a first-year resident is less than two per week, while second-year residents average two to three per week. Our residents are spending 80 hours a week while doing two or three operations per week, which arguably could be done in half a day. It would be hard to imagine a less efficient educational process.
Dr. Frank R. Lewis is executive director of the American Board of Surgery. He was an invited discussant of the presentation.
INDIANAPOLIS – The nation’s elite surgical educators are up in arms over reported widespread deficiencies in the skill set and judgment of recent graduates of 5-year general surgery residencies.
Many trainees arrive at surgical subspecialty fellowships unprepared in their basic skills, according to a detailed new survey of the nation’s subspecialty fellowship program directors. The underlying theme of the responses is that many fellows are pursuing fellowship positions to make up for inadequacies in their general surgery residency rather than to push their skills to the next level, according to Dr. Samer Mattar.
About 80% of graduating general surgery residents now seek fellowships to obtain advanced training in bariatric, colorectal, thoracic, hepatobiliary, or other surgical specialty areas.
"Many new fellows must gain basic and fundamental skills at the beginning of their fellowship before they can commence to benefit from the advanced skills that they originally came to obtain. The current high demand for fellowship training and the lack of readiness upon completion of general surgery residencies should be a call to action for all stakeholders in surgical training," Dr. Mattar said in presenting the survey results at the annual meeting of the American Surgical Association.
Constructive changes are afoot, according to Dr. Mattar of Indiana University, Indianapolis. Plans are well underway to change the fourth year of medical school so that students interested in a career in surgery can begin preparing for it. And there are also efforts to custom tailor the final year of general surgery residency so residents can focus on their planned fellowship year. Toward that end, the Fellowship Council has moved the fellowship match date up to June so residents who know they are fellowship-bound can put their fifth year to the best use.
The survey was conducted by the Fellowship Council, an umbrella organization in charge of standardizing curricula, accrediting programs, and matching residents to fellowships. The group distributed the surveys to all 145 subspecialty fellowship program directors and drew a 63% response rate. That’s considered high for such a lengthy survey, said Dr. Mattar, and is an indication of the importance educators place on the subject.
The survey assessed five key educational domains: professionalism, independent practice, psychomotor skills, expertise in their chosen disease state, and scholarly focus.
"Incoming fellows exhibited high levels of professionalism, but there were deficiencies in autonomy and independence, psychomotor abilities, and – most profoundly – in academics and scholarship," Dr. Mattar said.
Among the key survey findings:
• Incoming fellows were unable to independently perform half an hour of a major procedure, according to 43% of program directors.
• Of incoming fellows, 30% couldn’t independently perform basic operations such as laparoscopic cholecystectomy.
• Of incoming fellows, 56% were able to laparoscopically suture and tie knots properly; 26% couldn’t recognize anatomic planes through the laparoscope.
• One-quarter was deemed unable to recognize early signs of complications.
In other findings, nearly 40% of program directors said new fellows display a lack of "patient ownership." "We promote patient ownership in our programs. We are somewhat disappointed and dismayed that the fellows feel that the patient is part of a service and not their own," Dr. Mattar commented. Half of the program directors indicated their incoming fellows demonstrated independence in the operating room and on call, although they reported the fellows showed marked improvement in these areas as the year went on.
A large majority of program directors felt their fellows were disinterested in research and in advancing the field, even though, as Dr. Mattar noted, "This is a mandate in our curriculum."
He reported having no financial conflicts.
INDIANAPOLIS – The nation’s elite surgical educators are up in arms over reported widespread deficiencies in the skill set and judgment of recent graduates of 5-year general surgery residencies.
Many trainees arrive at surgical subspecialty fellowships unprepared in their basic skills, according to a detailed new survey of the nation’s subspecialty fellowship program directors. The underlying theme of the responses is that many fellows are pursuing fellowship positions to make up for inadequacies in their general surgery residency rather than to push their skills to the next level, according to Dr. Samer Mattar.
About 80% of graduating general surgery residents now seek fellowships to obtain advanced training in bariatric, colorectal, thoracic, hepatobiliary, or other surgical specialty areas.
"Many new fellows must gain basic and fundamental skills at the beginning of their fellowship before they can commence to benefit from the advanced skills that they originally came to obtain. The current high demand for fellowship training and the lack of readiness upon completion of general surgery residencies should be a call to action for all stakeholders in surgical training," Dr. Mattar said in presenting the survey results at the annual meeting of the American Surgical Association.
Constructive changes are afoot, according to Dr. Mattar of Indiana University, Indianapolis. Plans are well underway to change the fourth year of medical school so that students interested in a career in surgery can begin preparing for it. And there are also efforts to custom tailor the final year of general surgery residency so residents can focus on their planned fellowship year. Toward that end, the Fellowship Council has moved the fellowship match date up to June so residents who know they are fellowship-bound can put their fifth year to the best use.
The survey was conducted by the Fellowship Council, an umbrella organization in charge of standardizing curricula, accrediting programs, and matching residents to fellowships. The group distributed the surveys to all 145 subspecialty fellowship program directors and drew a 63% response rate. That’s considered high for such a lengthy survey, said Dr. Mattar, and is an indication of the importance educators place on the subject.
The survey assessed five key educational domains: professionalism, independent practice, psychomotor skills, expertise in their chosen disease state, and scholarly focus.
"Incoming fellows exhibited high levels of professionalism, but there were deficiencies in autonomy and independence, psychomotor abilities, and – most profoundly – in academics and scholarship," Dr. Mattar said.
Among the key survey findings:
• Incoming fellows were unable to independently perform half an hour of a major procedure, according to 43% of program directors.
• Of incoming fellows, 30% couldn’t independently perform basic operations such as laparoscopic cholecystectomy.
• Of incoming fellows, 56% were able to laparoscopically suture and tie knots properly; 26% couldn’t recognize anatomic planes through the laparoscope.
• One-quarter was deemed unable to recognize early signs of complications.
In other findings, nearly 40% of program directors said new fellows display a lack of "patient ownership." "We promote patient ownership in our programs. We are somewhat disappointed and dismayed that the fellows feel that the patient is part of a service and not their own," Dr. Mattar commented. Half of the program directors indicated their incoming fellows demonstrated independence in the operating room and on call, although they reported the fellows showed marked improvement in these areas as the year went on.
A large majority of program directors felt their fellows were disinterested in research and in advancing the field, even though, as Dr. Mattar noted, "This is a mandate in our curriculum."
He reported having no financial conflicts.
AT THE ASA ANNUAL MEETING
Major finding: Surgical subspecialty program directors said that 43% of incoming fellows were unable to independently perform half an hour of a major procedure.
Data source: Survey responses from 91 of the nation’s 145 surgical subspecialty program directors.
Disclosures: The survey was conducted by the Fellowship Council, an umbrella organization with oversight over surgical subspecialty fellowships. The presenter reported having no financial conflicts.
Despite new approaches, surgery underused for epilepsy
BETHESDA, MD. – Surgery is curative in half of patients with refractory temporal lobe epilepsy, yet it is still highly underused – in part because of misperceptions about the risks and benefits, according to Dr. Edward F. Chang.
Dr. Chang, assistant professor of neurological surgery and physiology at the University of California, San Francisco, said that numerous studies have shown that 60%-70% of patients are free of seizures 1 year after surgery and that at least half have seizure freedom over the long term. Also, there are "well-documented quality of life improvements," he said at the meeting sponsored by the National Institute of Neurological Disorders and Stroke.
Sixty percent of people with epilepsy have focal seizures, and the temporal lobe form is the most common type of epilepsy that is characterized by focal seizures, according to NINDS. The Epilepsy Foundation estimates that there are at least 200,000 new cases of epilepsy (any type) in the United States each year.
Based on the totality of the evidence, in 2003 the American Academy of Neurology, the American Epilepsy Society, and the American Association of Neurological Surgeons jointly published a guideline statement (Neurology 2003;60:538-47), urging referral of refractory patients for surgery.
But physicians are still not heeding that guidance, said Dr. Chang. His own survey of clinicians (Neurology 2012;78:1200-6) showed that there had been no increase in surgery in a 5-year period after the joint recommendation. Dr. Chang characterized that as "very depressing in terms of how we are using evidence," especially since there has been an increasing burden of epilepsy. In some cases, patients have lived with epilepsy for 20-30 years before being referred for surgery, he said.
Surgery is safe and effective and the side effects are predictable, he noted, adding that the number needed to treat for one patient with refractory temporal lobe epilepsy to become free of disabling seizures is only two – a number that parallels the use of antibiotics for pneumonia.
"We are below the standard of care," Dr. Chang said. Clinicians and patients shy away from surgery because "of the idea that brain surgery is too dangerous," he said. And physicians don’t understand the data. Drug and device makers also are "spending millions of dollars a year telling patients there are other options," he said, but if "we address this basic utilization problem we’d see an immediate and substantial reduction ... in the burden of epilepsy worldwide."
There have been several advances in surgical technique in the last few years that might make neurologists and patients – who might be spooked by looking at photos and videos of temporal lobe surgery on the Internet – more comfortable. For instance, there are transcortical approaches, which use a small incision to go through the white matter to the hippocampus. With the subtemporal approach, "you don’t have to go through any lateral cortex at all," he noted.
"Even for relatively large lesions that are quite deep in the brain we can actually do these minimally invasive approaches by just going underneath the lateral temporal cortex and selectively removing the hippocampus," Dr. Chang said.
On the horizon, there are nonsurgical minimally invasive techniques under development that have the potential to yield outcomes similar to surgery, he added. NINDS is funding a pivotal trial of stereotactic radiosurgery. The device selectively delivers radiation to the hippocampus and mesial lobe and spares the lateral temporal areas en route. Overall, it is fairly safe, but some patients have severe swelling as long as a year after the procedure and most have no effect for at least a year.
Another approach under study is using MRI to guide laser thermoablation. "A lot of us are quite excited about this," Dr. Chang said. The MRI allows the clinician to accurately place the laser and study how much the tissue is heated, which can help researchers determine whether there is damage and if it might be irreversible.
Finally, there is MRI-guided focused ultrasound, which uses the same principles as radiosurgery to target structures deep in the brain, he said. The procedure is currently in phase III trials for essential tremor.
There is, however, "a lot of irrational exuberance with these technologies," he pointed out.
It is not clear how to validate them, especially since clinicians are currently struggling with how to validate different surgical approaches. A big issue for the surgery trials is that it is difficult to recruit patients. Many have said that they don’t want to participate because they don’t want to be randomized.
Researchers also are trying to better understand epileptogenesis and how to reduce procedural side effects, including how to predict effects on cognitive function. To get there, "we need to understand more about how human cognition works," Dr. Chang said. Brain-mapping studies are showing that most aspects of cognition are not centered in one specific, focused area.
"Just like we’re thinking now that seizures are part of a distributed network, we also need to understand comorbidities and morbidity from surgical approaches in the same kind of framework," he said.
Until surgery is better used and studied, it is unlikely that neurology can move forward to truly understand the safety and effectiveness of the minimally invasive approaches, Dr. Chang said.
Dr. Chang has received grants from the National Institutes of Health and the Esther A. and Joseph Klingenstein Fund.
On Twitter @aliciaault
BETHESDA, MD. – Surgery is curative in half of patients with refractory temporal lobe epilepsy, yet it is still highly underused – in part because of misperceptions about the risks and benefits, according to Dr. Edward F. Chang.
Dr. Chang, assistant professor of neurological surgery and physiology at the University of California, San Francisco, said that numerous studies have shown that 60%-70% of patients are free of seizures 1 year after surgery and that at least half have seizure freedom over the long term. Also, there are "well-documented quality of life improvements," he said at the meeting sponsored by the National Institute of Neurological Disorders and Stroke.
Sixty percent of people with epilepsy have focal seizures, and the temporal lobe form is the most common type of epilepsy that is characterized by focal seizures, according to NINDS. The Epilepsy Foundation estimates that there are at least 200,000 new cases of epilepsy (any type) in the United States each year.
Based on the totality of the evidence, in 2003 the American Academy of Neurology, the American Epilepsy Society, and the American Association of Neurological Surgeons jointly published a guideline statement (Neurology 2003;60:538-47), urging referral of refractory patients for surgery.
But physicians are still not heeding that guidance, said Dr. Chang. His own survey of clinicians (Neurology 2012;78:1200-6) showed that there had been no increase in surgery in a 5-year period after the joint recommendation. Dr. Chang characterized that as "very depressing in terms of how we are using evidence," especially since there has been an increasing burden of epilepsy. In some cases, patients have lived with epilepsy for 20-30 years before being referred for surgery, he said.
Surgery is safe and effective and the side effects are predictable, he noted, adding that the number needed to treat for one patient with refractory temporal lobe epilepsy to become free of disabling seizures is only two – a number that parallels the use of antibiotics for pneumonia.
"We are below the standard of care," Dr. Chang said. Clinicians and patients shy away from surgery because "of the idea that brain surgery is too dangerous," he said. And physicians don’t understand the data. Drug and device makers also are "spending millions of dollars a year telling patients there are other options," he said, but if "we address this basic utilization problem we’d see an immediate and substantial reduction ... in the burden of epilepsy worldwide."
There have been several advances in surgical technique in the last few years that might make neurologists and patients – who might be spooked by looking at photos and videos of temporal lobe surgery on the Internet – more comfortable. For instance, there are transcortical approaches, which use a small incision to go through the white matter to the hippocampus. With the subtemporal approach, "you don’t have to go through any lateral cortex at all," he noted.
"Even for relatively large lesions that are quite deep in the brain we can actually do these minimally invasive approaches by just going underneath the lateral temporal cortex and selectively removing the hippocampus," Dr. Chang said.
On the horizon, there are nonsurgical minimally invasive techniques under development that have the potential to yield outcomes similar to surgery, he added. NINDS is funding a pivotal trial of stereotactic radiosurgery. The device selectively delivers radiation to the hippocampus and mesial lobe and spares the lateral temporal areas en route. Overall, it is fairly safe, but some patients have severe swelling as long as a year after the procedure and most have no effect for at least a year.
Another approach under study is using MRI to guide laser thermoablation. "A lot of us are quite excited about this," Dr. Chang said. The MRI allows the clinician to accurately place the laser and study how much the tissue is heated, which can help researchers determine whether there is damage and if it might be irreversible.
Finally, there is MRI-guided focused ultrasound, which uses the same principles as radiosurgery to target structures deep in the brain, he said. The procedure is currently in phase III trials for essential tremor.
There is, however, "a lot of irrational exuberance with these technologies," he pointed out.
It is not clear how to validate them, especially since clinicians are currently struggling with how to validate different surgical approaches. A big issue for the surgery trials is that it is difficult to recruit patients. Many have said that they don’t want to participate because they don’t want to be randomized.
Researchers also are trying to better understand epileptogenesis and how to reduce procedural side effects, including how to predict effects on cognitive function. To get there, "we need to understand more about how human cognition works," Dr. Chang said. Brain-mapping studies are showing that most aspects of cognition are not centered in one specific, focused area.
"Just like we’re thinking now that seizures are part of a distributed network, we also need to understand comorbidities and morbidity from surgical approaches in the same kind of framework," he said.
Until surgery is better used and studied, it is unlikely that neurology can move forward to truly understand the safety and effectiveness of the minimally invasive approaches, Dr. Chang said.
Dr. Chang has received grants from the National Institutes of Health and the Esther A. and Joseph Klingenstein Fund.
On Twitter @aliciaault
BETHESDA, MD. – Surgery is curative in half of patients with refractory temporal lobe epilepsy, yet it is still highly underused – in part because of misperceptions about the risks and benefits, according to Dr. Edward F. Chang.
Dr. Chang, assistant professor of neurological surgery and physiology at the University of California, San Francisco, said that numerous studies have shown that 60%-70% of patients are free of seizures 1 year after surgery and that at least half have seizure freedom over the long term. Also, there are "well-documented quality of life improvements," he said at the meeting sponsored by the National Institute of Neurological Disorders and Stroke.
Sixty percent of people with epilepsy have focal seizures, and the temporal lobe form is the most common type of epilepsy that is characterized by focal seizures, according to NINDS. The Epilepsy Foundation estimates that there are at least 200,000 new cases of epilepsy (any type) in the United States each year.
Based on the totality of the evidence, in 2003 the American Academy of Neurology, the American Epilepsy Society, and the American Association of Neurological Surgeons jointly published a guideline statement (Neurology 2003;60:538-47), urging referral of refractory patients for surgery.
But physicians are still not heeding that guidance, said Dr. Chang. His own survey of clinicians (Neurology 2012;78:1200-6) showed that there had been no increase in surgery in a 5-year period after the joint recommendation. Dr. Chang characterized that as "very depressing in terms of how we are using evidence," especially since there has been an increasing burden of epilepsy. In some cases, patients have lived with epilepsy for 20-30 years before being referred for surgery, he said.
Surgery is safe and effective and the side effects are predictable, he noted, adding that the number needed to treat for one patient with refractory temporal lobe epilepsy to become free of disabling seizures is only two – a number that parallels the use of antibiotics for pneumonia.
"We are below the standard of care," Dr. Chang said. Clinicians and patients shy away from surgery because "of the idea that brain surgery is too dangerous," he said. And physicians don’t understand the data. Drug and device makers also are "spending millions of dollars a year telling patients there are other options," he said, but if "we address this basic utilization problem we’d see an immediate and substantial reduction ... in the burden of epilepsy worldwide."
There have been several advances in surgical technique in the last few years that might make neurologists and patients – who might be spooked by looking at photos and videos of temporal lobe surgery on the Internet – more comfortable. For instance, there are transcortical approaches, which use a small incision to go through the white matter to the hippocampus. With the subtemporal approach, "you don’t have to go through any lateral cortex at all," he noted.
"Even for relatively large lesions that are quite deep in the brain we can actually do these minimally invasive approaches by just going underneath the lateral temporal cortex and selectively removing the hippocampus," Dr. Chang said.
On the horizon, there are nonsurgical minimally invasive techniques under development that have the potential to yield outcomes similar to surgery, he added. NINDS is funding a pivotal trial of stereotactic radiosurgery. The device selectively delivers radiation to the hippocampus and mesial lobe and spares the lateral temporal areas en route. Overall, it is fairly safe, but some patients have severe swelling as long as a year after the procedure and most have no effect for at least a year.
Another approach under study is using MRI to guide laser thermoablation. "A lot of us are quite excited about this," Dr. Chang said. The MRI allows the clinician to accurately place the laser and study how much the tissue is heated, which can help researchers determine whether there is damage and if it might be irreversible.
Finally, there is MRI-guided focused ultrasound, which uses the same principles as radiosurgery to target structures deep in the brain, he said. The procedure is currently in phase III trials for essential tremor.
There is, however, "a lot of irrational exuberance with these technologies," he pointed out.
It is not clear how to validate them, especially since clinicians are currently struggling with how to validate different surgical approaches. A big issue for the surgery trials is that it is difficult to recruit patients. Many have said that they don’t want to participate because they don’t want to be randomized.
Researchers also are trying to better understand epileptogenesis and how to reduce procedural side effects, including how to predict effects on cognitive function. To get there, "we need to understand more about how human cognition works," Dr. Chang said. Brain-mapping studies are showing that most aspects of cognition are not centered in one specific, focused area.
"Just like we’re thinking now that seizures are part of a distributed network, we also need to understand comorbidities and morbidity from surgical approaches in the same kind of framework," he said.
Until surgery is better used and studied, it is unlikely that neurology can move forward to truly understand the safety and effectiveness of the minimally invasive approaches, Dr. Chang said.
Dr. Chang has received grants from the National Institutes of Health and the Esther A. and Joseph Klingenstein Fund.
On Twitter @aliciaault
EXPERT ANALYSIS FROM CURING THE EPILEPSIES 2013
Manage most SEGAs with rapamycin analogs, not surgery
SAN DIEGO – Medical management with sirolimus or everolimus for pediatric patients with tuberous sclerosis complex and subependymal giant cell astrocytomas is more effective and safer than surgery, researchers from the University of Cincinnati and University of California, Los Angeles, have found.
Although the benign tumors have traditionally been left to surgeons, it’s become clear in recent years that rapamycin analogs are effective, too. The question has been "which [approach] is best? Medical management "is known to be pretty mild compared to the surgery," but it’s not curative, explained lead investigator Susanne Yoon, the University of Cincinnati medical student who presented the results at the annual meeting of the American Academy of Neurology.
The team compared outcomes for 23 SEGA (subependymal giant cell astrocytoma) patients who underwent surgery, 81 who took sirolimus or everolimus, and 9 who got both. The surgery patients were diagnosed when they were about 10 years old and were followed for a median of 8.9 years; the medical patients were about 7 years old when diagnosed, and were followed for a median of 2.8 years. Boys made up the majority of both groups.
None of the children who took a rapamycin analog needed surgery; tumors shrank by more than half in 61% (45). The drugs caused infections, weight change, or hyperlipidemia in some, but only 13% (11) needed to stop the drug or go to the hospital because of side effects.
Meanwhile, surgery cured just 39% (9) of the children who got it, sometimes after two or three operations; 61% (14) of those patients had prolonged hospitalizations or were hospitalized due to postoperative complications that included intracranial hemorrhage in 8, hydrocephalus/shunt malfunction in 6, neurologic impairment, and seizures.
"Not only does medical management win in efficacy, but it also wins in the safety issues. Rapalog [rapamycin] therapy, alone or in combination, is becoming a cornerstone of tumor management" in neurocutaneous disorders, said Dr. David H. Viskochil, professor of pediatrics at the University of Utah, Salt Lake City, commenting on the study.
"Of course, there are emergent situations where you’ve just got to go in and get the tumor out; you can’t wait 3 months to see" if drugs work. "But if a child is just starting to show some symptoms and not deteriorating, then you can start with medicine first and see what happens," he said.
"The question is if you got [SEGAs] really early, would surgical cure be much more likely? The studies aren’t quite there yet," he said in an interview.
Ms. Yoon and Dr. Viskochil said they have no disclosures.
SAN DIEGO – Medical management with sirolimus or everolimus for pediatric patients with tuberous sclerosis complex and subependymal giant cell astrocytomas is more effective and safer than surgery, researchers from the University of Cincinnati and University of California, Los Angeles, have found.
Although the benign tumors have traditionally been left to surgeons, it’s become clear in recent years that rapamycin analogs are effective, too. The question has been "which [approach] is best? Medical management "is known to be pretty mild compared to the surgery," but it’s not curative, explained lead investigator Susanne Yoon, the University of Cincinnati medical student who presented the results at the annual meeting of the American Academy of Neurology.
The team compared outcomes for 23 SEGA (subependymal giant cell astrocytoma) patients who underwent surgery, 81 who took sirolimus or everolimus, and 9 who got both. The surgery patients were diagnosed when they were about 10 years old and were followed for a median of 8.9 years; the medical patients were about 7 years old when diagnosed, and were followed for a median of 2.8 years. Boys made up the majority of both groups.
None of the children who took a rapamycin analog needed surgery; tumors shrank by more than half in 61% (45). The drugs caused infections, weight change, or hyperlipidemia in some, but only 13% (11) needed to stop the drug or go to the hospital because of side effects.
Meanwhile, surgery cured just 39% (9) of the children who got it, sometimes after two or three operations; 61% (14) of those patients had prolonged hospitalizations or were hospitalized due to postoperative complications that included intracranial hemorrhage in 8, hydrocephalus/shunt malfunction in 6, neurologic impairment, and seizures.
"Not only does medical management win in efficacy, but it also wins in the safety issues. Rapalog [rapamycin] therapy, alone or in combination, is becoming a cornerstone of tumor management" in neurocutaneous disorders, said Dr. David H. Viskochil, professor of pediatrics at the University of Utah, Salt Lake City, commenting on the study.
"Of course, there are emergent situations where you’ve just got to go in and get the tumor out; you can’t wait 3 months to see" if drugs work. "But if a child is just starting to show some symptoms and not deteriorating, then you can start with medicine first and see what happens," he said.
"The question is if you got [SEGAs] really early, would surgical cure be much more likely? The studies aren’t quite there yet," he said in an interview.
Ms. Yoon and Dr. Viskochil said they have no disclosures.
SAN DIEGO – Medical management with sirolimus or everolimus for pediatric patients with tuberous sclerosis complex and subependymal giant cell astrocytomas is more effective and safer than surgery, researchers from the University of Cincinnati and University of California, Los Angeles, have found.
Although the benign tumors have traditionally been left to surgeons, it’s become clear in recent years that rapamycin analogs are effective, too. The question has been "which [approach] is best? Medical management "is known to be pretty mild compared to the surgery," but it’s not curative, explained lead investigator Susanne Yoon, the University of Cincinnati medical student who presented the results at the annual meeting of the American Academy of Neurology.
The team compared outcomes for 23 SEGA (subependymal giant cell astrocytoma) patients who underwent surgery, 81 who took sirolimus or everolimus, and 9 who got both. The surgery patients were diagnosed when they were about 10 years old and were followed for a median of 8.9 years; the medical patients were about 7 years old when diagnosed, and were followed for a median of 2.8 years. Boys made up the majority of both groups.
None of the children who took a rapamycin analog needed surgery; tumors shrank by more than half in 61% (45). The drugs caused infections, weight change, or hyperlipidemia in some, but only 13% (11) needed to stop the drug or go to the hospital because of side effects.
Meanwhile, surgery cured just 39% (9) of the children who got it, sometimes after two or three operations; 61% (14) of those patients had prolonged hospitalizations or were hospitalized due to postoperative complications that included intracranial hemorrhage in 8, hydrocephalus/shunt malfunction in 6, neurologic impairment, and seizures.
"Not only does medical management win in efficacy, but it also wins in the safety issues. Rapalog [rapamycin] therapy, alone or in combination, is becoming a cornerstone of tumor management" in neurocutaneous disorders, said Dr. David H. Viskochil, professor of pediatrics at the University of Utah, Salt Lake City, commenting on the study.
"Of course, there are emergent situations where you’ve just got to go in and get the tumor out; you can’t wait 3 months to see" if drugs work. "But if a child is just starting to show some symptoms and not deteriorating, then you can start with medicine first and see what happens," he said.
"The question is if you got [SEGAs] really early, would surgical cure be much more likely? The studies aren’t quite there yet," he said in an interview.
Ms. Yoon and Dr. Viskochil said they have no disclosures.
AT THE 2013 AAN ANNUAL MEETING
Major finding: Rapamycin analogs shrink SEGA tumors by more than 50% in a majority of children, and obviate the need for surgery.
Data source: Comparison of surgical and medical treatment of SEGA tumors in 113 children.
Disclosures: Ms. Yoon and Dr. Viskochil said they have no disclosures.
Stereotactic laser ablation found feasible for hypothalamic hamartoma
SAN DIEGO – Magnetic resonance-guided stereotactic laser ablation is a safe and effective option in the treatment of hypothalamic hamartoma, results from a multicenter pilot study showed.
At the annual meeting of the American Academy of Neurology, Dr. Daniel J. Curry reported results from 20 patients who have undergone treatment with a Food and Drug Administration–cleared neurosurgical tissue coagulation system called Visualase. Hypothalamic hamartoma (HH) is a rare disorder of pediatric epilepsy with an estimated prevalence of 1:50,000-100,000, said Dr. Curry, director of pediatric surgical epilepsy and functional neurosurgery at Texas Children’s Hospital, Houston.
"The main presentation is the mirthless laughter of gelastic seizures, but patients can have other seizure types," he said. "The diagnosis is frequently delayed, and high seizure burden in the brain can lead to epileptic encephalopathy. Seizures are notoriously resistant to medical managements necessitating surgical intervention ... open, endoscopic, or ablative."
To date, surgical intervention has been limited due to modest outcomes, with 37%-50% achieving seizure freedom. The location of HH tumors makes surgical intervention difficult, and as a result 7%-10% of patients have permanent surgical morbidity.
For the technique using the Visualase, Dr. Curry and his associates at four other medical centers in the United States performed the surgical technique through a single 4-mm incision, a 3.2-mm burr hole, and a 1.65-mm cannula trajectory with Visualase under real-time MR thermography, first with a confirmation test at about 3 W, followed by higher doses of 6-10 W for 50-120 seconds. Temperature limits were set to protect the hypothalamus and basilar artery and optic tract. The surgery had an immediate effect, and patients stayed in the hospital for a mean of 2 days.
The primary measure was seizure frequency at 1 year while the secondary measure was the complication profile of stereotactic laser ablation in epilepsy.
Of the 20 patients, 5 were adults, and the entire study population ranged in age from 22 months to 34 years. A total of 21 ablations were performed in the 20 patients. Dr. Curry reported that all but four patients were seizure free after the procedure. However, the rate of seizures diminished among the four who were not seizure free.
Seizures recurred in one of the pediatric patients. "We re-ablated him and he is now seizure free," Dr. Curry said.
Complications to date have included two missed targets, one case of IV phenytoin toxicity, one case of transient diabetes insipidus, two cases of transient hemiparesis, and one subarachnoid hemorrhage. Perioperative, temporary weight gain was detected in most patients. "With lack of hormonal disturbance, this is thought to be due to the perioperative, high-dose steroid use," Dr. Curry explained.
Postoperative interviews with parents of study participants "have revealed significant improvements in intellectual development, concentration, and interactiveness," he said. "Most families report improvement of mood, decreased behavioral disorders, and rage attacks."
To date, only two patients have completed formal postoperative neuropsychological testing. "There were no significant declines in memory in either patient," Dr. Curry said. One had improved math skills and reading comprehension while the other complained of memory dysfunction but was not below normal on testing.
"We have learned that laser ablation of hypothalamic hamartoma can be accomplished safely," Dr. Curry concluded. "More studies are needed to explain the antiepileptic effect in settings of incomplete radiologic destruction of the target and to advance thermal planning."
Dr. Curry said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Magnetic resonance-guided stereotactic laser ablation is a safe and effective option in the treatment of hypothalamic hamartoma, results from a multicenter pilot study showed.
At the annual meeting of the American Academy of Neurology, Dr. Daniel J. Curry reported results from 20 patients who have undergone treatment with a Food and Drug Administration–cleared neurosurgical tissue coagulation system called Visualase. Hypothalamic hamartoma (HH) is a rare disorder of pediatric epilepsy with an estimated prevalence of 1:50,000-100,000, said Dr. Curry, director of pediatric surgical epilepsy and functional neurosurgery at Texas Children’s Hospital, Houston.
"The main presentation is the mirthless laughter of gelastic seizures, but patients can have other seizure types," he said. "The diagnosis is frequently delayed, and high seizure burden in the brain can lead to epileptic encephalopathy. Seizures are notoriously resistant to medical managements necessitating surgical intervention ... open, endoscopic, or ablative."
To date, surgical intervention has been limited due to modest outcomes, with 37%-50% achieving seizure freedom. The location of HH tumors makes surgical intervention difficult, and as a result 7%-10% of patients have permanent surgical morbidity.
For the technique using the Visualase, Dr. Curry and his associates at four other medical centers in the United States performed the surgical technique through a single 4-mm incision, a 3.2-mm burr hole, and a 1.65-mm cannula trajectory with Visualase under real-time MR thermography, first with a confirmation test at about 3 W, followed by higher doses of 6-10 W for 50-120 seconds. Temperature limits were set to protect the hypothalamus and basilar artery and optic tract. The surgery had an immediate effect, and patients stayed in the hospital for a mean of 2 days.
The primary measure was seizure frequency at 1 year while the secondary measure was the complication profile of stereotactic laser ablation in epilepsy.
Of the 20 patients, 5 were adults, and the entire study population ranged in age from 22 months to 34 years. A total of 21 ablations were performed in the 20 patients. Dr. Curry reported that all but four patients were seizure free after the procedure. However, the rate of seizures diminished among the four who were not seizure free.
Seizures recurred in one of the pediatric patients. "We re-ablated him and he is now seizure free," Dr. Curry said.
Complications to date have included two missed targets, one case of IV phenytoin toxicity, one case of transient diabetes insipidus, two cases of transient hemiparesis, and one subarachnoid hemorrhage. Perioperative, temporary weight gain was detected in most patients. "With lack of hormonal disturbance, this is thought to be due to the perioperative, high-dose steroid use," Dr. Curry explained.
Postoperative interviews with parents of study participants "have revealed significant improvements in intellectual development, concentration, and interactiveness," he said. "Most families report improvement of mood, decreased behavioral disorders, and rage attacks."
To date, only two patients have completed formal postoperative neuropsychological testing. "There were no significant declines in memory in either patient," Dr. Curry said. One had improved math skills and reading comprehension while the other complained of memory dysfunction but was not below normal on testing.
"We have learned that laser ablation of hypothalamic hamartoma can be accomplished safely," Dr. Curry concluded. "More studies are needed to explain the antiepileptic effect in settings of incomplete radiologic destruction of the target and to advance thermal planning."
Dr. Curry said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Magnetic resonance-guided stereotactic laser ablation is a safe and effective option in the treatment of hypothalamic hamartoma, results from a multicenter pilot study showed.
At the annual meeting of the American Academy of Neurology, Dr. Daniel J. Curry reported results from 20 patients who have undergone treatment with a Food and Drug Administration–cleared neurosurgical tissue coagulation system called Visualase. Hypothalamic hamartoma (HH) is a rare disorder of pediatric epilepsy with an estimated prevalence of 1:50,000-100,000, said Dr. Curry, director of pediatric surgical epilepsy and functional neurosurgery at Texas Children’s Hospital, Houston.
"The main presentation is the mirthless laughter of gelastic seizures, but patients can have other seizure types," he said. "The diagnosis is frequently delayed, and high seizure burden in the brain can lead to epileptic encephalopathy. Seizures are notoriously resistant to medical managements necessitating surgical intervention ... open, endoscopic, or ablative."
To date, surgical intervention has been limited due to modest outcomes, with 37%-50% achieving seizure freedom. The location of HH tumors makes surgical intervention difficult, and as a result 7%-10% of patients have permanent surgical morbidity.
For the technique using the Visualase, Dr. Curry and his associates at four other medical centers in the United States performed the surgical technique through a single 4-mm incision, a 3.2-mm burr hole, and a 1.65-mm cannula trajectory with Visualase under real-time MR thermography, first with a confirmation test at about 3 W, followed by higher doses of 6-10 W for 50-120 seconds. Temperature limits were set to protect the hypothalamus and basilar artery and optic tract. The surgery had an immediate effect, and patients stayed in the hospital for a mean of 2 days.
The primary measure was seizure frequency at 1 year while the secondary measure was the complication profile of stereotactic laser ablation in epilepsy.
Of the 20 patients, 5 were adults, and the entire study population ranged in age from 22 months to 34 years. A total of 21 ablations were performed in the 20 patients. Dr. Curry reported that all but four patients were seizure free after the procedure. However, the rate of seizures diminished among the four who were not seizure free.
Seizures recurred in one of the pediatric patients. "We re-ablated him and he is now seizure free," Dr. Curry said.
Complications to date have included two missed targets, one case of IV phenytoin toxicity, one case of transient diabetes insipidus, two cases of transient hemiparesis, and one subarachnoid hemorrhage. Perioperative, temporary weight gain was detected in most patients. "With lack of hormonal disturbance, this is thought to be due to the perioperative, high-dose steroid use," Dr. Curry explained.
Postoperative interviews with parents of study participants "have revealed significant improvements in intellectual development, concentration, and interactiveness," he said. "Most families report improvement of mood, decreased behavioral disorders, and rage attacks."
To date, only two patients have completed formal postoperative neuropsychological testing. "There were no significant declines in memory in either patient," Dr. Curry said. One had improved math skills and reading comprehension while the other complained of memory dysfunction but was not below normal on testing.
"We have learned that laser ablation of hypothalamic hamartoma can be accomplished safely," Dr. Curry concluded. "More studies are needed to explain the antiepileptic effect in settings of incomplete radiologic destruction of the target and to advance thermal planning."
Dr. Curry said that he had no relevant financial conflicts to disclose.
AT THE 2013 AAN ANNUAL MEETING
Major finding: After 20 patients with hypothalamic hamartoma underwent MR-guided stereotactic laser ablation, all but 4 were seizure free.
Data source: A multicenter pilot study of 21 ablations performed in patients who ranged in age from 22 months to 34 years.
Disclosures: Dr. Curry said that he had no relevant financial conflicts to disclose.