User login
NCCN survey shows ongoing chemo drug shortages
Although access to carboplatin and cisplatin has improved slightly since June, when 93% and 70% of 27 NCCN member institutions reported shortages of the two agents, supplies remain limited and other anticancer drugs remain scarce, an NCCN follow-up survey shows.
Of 29 institutions surveyed last month, 86% reported having difficulty obtaining at least one anticancer drug, and 72% and 59% reported ongoing shortages of carboplatin and cisplatin, respectively – drugs recommended for treating patients involved in hundreds of different cancer scenarios, according to the NCCN.
“Drug shortages aren’t new, but the widespread impact makes this one particularly alarming,” NCCN’s chief executive officer, Robert W. Carlson, MD, said in a press statement. “It is extremely concerning that this situation continues despite significant attention and effort over the past few months.”
The latest survey, conducted between Sept. 6 and 27, was sent to the 33 NCCN member institutions. Overall, most respondents reported “being able to continue treating every patient who needs carboplatin or cisplatin, despite lowered supply, primarily by implementing strict waste management strategies,” the network noted, adding that “the responses may not reflect any additional challenges experienced by smaller community practices serving rural and marginalized patients.”
In addition to carboplatin and cisplatin shortages, the survey results also revealed that centers are experiencing shortages of a host of other drugs, including methotrexate (66%), 5-flourouracil (55%), fludarabine (45%), hydrocortisone (41%), and dacarbazine (28%), according to the press release.
“These drug shortages are the result of decades of systemic challenges,” noted Alyssa Schatz, senior director of policy and advocacy for NCCN, in a press release. “We recognize that comprehensive solutions take time, and we appreciate everyone who has put forth proposals to improve investment in generics and our data infrastructure. At the same time, we have to acknowledge that the cancer drug shortage has been ongoing for months, which is unacceptable for anyone impacted by cancer today.”
Following the June survey, the NCCN called for action from the federal government, the pharmaceutical industry, providers, and payers, encouraging them “to work together to ensure quality, effective, equitable, and accessible cancer care” and has since worked with multiple stakeholders and policymaking organizations to “advocate for short- and long-term fixes.”
“These new survey results remind us that we are still in an ongoing crisis and must respond with appropriate urgency,” Ms. Shatz added.
A version of this article first appeared on Medscape.com.
Although access to carboplatin and cisplatin has improved slightly since June, when 93% and 70% of 27 NCCN member institutions reported shortages of the two agents, supplies remain limited and other anticancer drugs remain scarce, an NCCN follow-up survey shows.
Of 29 institutions surveyed last month, 86% reported having difficulty obtaining at least one anticancer drug, and 72% and 59% reported ongoing shortages of carboplatin and cisplatin, respectively – drugs recommended for treating patients involved in hundreds of different cancer scenarios, according to the NCCN.
“Drug shortages aren’t new, but the widespread impact makes this one particularly alarming,” NCCN’s chief executive officer, Robert W. Carlson, MD, said in a press statement. “It is extremely concerning that this situation continues despite significant attention and effort over the past few months.”
The latest survey, conducted between Sept. 6 and 27, was sent to the 33 NCCN member institutions. Overall, most respondents reported “being able to continue treating every patient who needs carboplatin or cisplatin, despite lowered supply, primarily by implementing strict waste management strategies,” the network noted, adding that “the responses may not reflect any additional challenges experienced by smaller community practices serving rural and marginalized patients.”
In addition to carboplatin and cisplatin shortages, the survey results also revealed that centers are experiencing shortages of a host of other drugs, including methotrexate (66%), 5-flourouracil (55%), fludarabine (45%), hydrocortisone (41%), and dacarbazine (28%), according to the press release.
“These drug shortages are the result of decades of systemic challenges,” noted Alyssa Schatz, senior director of policy and advocacy for NCCN, in a press release. “We recognize that comprehensive solutions take time, and we appreciate everyone who has put forth proposals to improve investment in generics and our data infrastructure. At the same time, we have to acknowledge that the cancer drug shortage has been ongoing for months, which is unacceptable for anyone impacted by cancer today.”
Following the June survey, the NCCN called for action from the federal government, the pharmaceutical industry, providers, and payers, encouraging them “to work together to ensure quality, effective, equitable, and accessible cancer care” and has since worked with multiple stakeholders and policymaking organizations to “advocate for short- and long-term fixes.”
“These new survey results remind us that we are still in an ongoing crisis and must respond with appropriate urgency,” Ms. Shatz added.
A version of this article first appeared on Medscape.com.
Although access to carboplatin and cisplatin has improved slightly since June, when 93% and 70% of 27 NCCN member institutions reported shortages of the two agents, supplies remain limited and other anticancer drugs remain scarce, an NCCN follow-up survey shows.
Of 29 institutions surveyed last month, 86% reported having difficulty obtaining at least one anticancer drug, and 72% and 59% reported ongoing shortages of carboplatin and cisplatin, respectively – drugs recommended for treating patients involved in hundreds of different cancer scenarios, according to the NCCN.
“Drug shortages aren’t new, but the widespread impact makes this one particularly alarming,” NCCN’s chief executive officer, Robert W. Carlson, MD, said in a press statement. “It is extremely concerning that this situation continues despite significant attention and effort over the past few months.”
The latest survey, conducted between Sept. 6 and 27, was sent to the 33 NCCN member institutions. Overall, most respondents reported “being able to continue treating every patient who needs carboplatin or cisplatin, despite lowered supply, primarily by implementing strict waste management strategies,” the network noted, adding that “the responses may not reflect any additional challenges experienced by smaller community practices serving rural and marginalized patients.”
In addition to carboplatin and cisplatin shortages, the survey results also revealed that centers are experiencing shortages of a host of other drugs, including methotrexate (66%), 5-flourouracil (55%), fludarabine (45%), hydrocortisone (41%), and dacarbazine (28%), according to the press release.
“These drug shortages are the result of decades of systemic challenges,” noted Alyssa Schatz, senior director of policy and advocacy for NCCN, in a press release. “We recognize that comprehensive solutions take time, and we appreciate everyone who has put forth proposals to improve investment in generics and our data infrastructure. At the same time, we have to acknowledge that the cancer drug shortage has been ongoing for months, which is unacceptable for anyone impacted by cancer today.”
Following the June survey, the NCCN called for action from the federal government, the pharmaceutical industry, providers, and payers, encouraging them “to work together to ensure quality, effective, equitable, and accessible cancer care” and has since worked with multiple stakeholders and policymaking organizations to “advocate for short- and long-term fixes.”
“These new survey results remind us that we are still in an ongoing crisis and must respond with appropriate urgency,” Ms. Shatz added.
A version of this article first appeared on Medscape.com.
From scrubs to screens: Growing your patient base with social media
With physicians under increasing pressure to see more patients in shorter office visits, developing a social media presence may offer valuable opportunities to connect with patients, explain procedures, combat misinformation, talk through a published article, and even share a joke or meme.
But there are caveats for doctors posting on social media platforms. This news organization spoke to four doctors who successfully use social media.
Use social media for the right reasons
While you’re under no obligation to build a social media presence, if you’re going to do it, be sure your intentions are solid, said Don S. Dizon, MD, professor of medicine and professor of surgery at Brown University, Providence, R.I. Dr. Dizon, as @DoctorDon, has 44,700 TikTok followers and uses the platform to answer cancer-related questions.
“It should be your altruism that motivates you to post,” said Dr. Dizon, who is also associate director of community outreach and engagement at the Legorreta Cancer Center in Providence, R.I., and director of medical oncology at Rhode Island Hospital. “What we can do for society at large is to provide our input into issues, add informed opinions where there’s controversy, and address misinformation.”
If you don’t know where to start, consider seeking a digital mentor to talk through your options.
“You may never meet this person, but you should choose them if you like their style, their content, their delivery, and their perspective,” Dr. Dizon said. “Find another doctor out there on social media whom you feel you can emulate. Take your time, too. Soon enough, you’ll develop your own style and your own online persona.”
Post clear, accurate information
If you want to be lighthearted on social media, that’s your choice. But Jennifer Trachtenberg, a pediatrician with nearly 7,000 Instagram followers in New York who posts as @askdrjen, prefers to offer vaccine scheduling tips, alert parents about COVID-19 rates, and offer advice on cold and flu prevention.
“Right now, I’m mainly doing this to educate patients and make them aware of topics that I think are important and that I see my patients needing more information on,” she said. “We have to be clear: People take what we say seriously. So, while it’s important to be relatable, it’s even more important to share evidence-based information.”
Many patients get their information on social media
While patients once came to the doctor armed with information sourced via “Doctor Google,” today, just as many patients use social media to learn about their condition or the medications they’re taking.
Unfortunately, a recent Ohio State University, Columbus, study found that the majority of gynecologic cancer advice on TikTok, for example, was either misleading or inaccurate.
“This misinformation should be a motivator for physicians to explore the social media space,” Dr. Dizon said. “Our voices need to be on there.”
Break down barriers – and make connections
Mike Natter, MD, an endocrinologist in New York, has type 1 diabetes. This informs his work – and his life – and he’s passionate about sharing it with his 117,000 followers as @mike.natter on Instagram.
“A lot of type 1s follow me, so there’s an advocacy component to what I do,” he said. “I enjoy being able to raise awareness and keep people up to date on the newest research and treatment.”
But that’s not all: Dr. Natter is also an artist who went to art school before he went to medical school, and his account is rife with his cartoons and illustrations about everything from valvular disease to diabetic ketoacidosis.
“I found that I was drawing a lot of my notes in medical school,” he said. “When I drew my notes, I did quite well, and I think that using art and illustration is a great tool. It breaks down barriers and makes health information all the more accessible to everyone.”
Share your expertise as a doctor – and a person
As a mom and pediatrician, Krupa Playforth, MD, who practices in Vienna, Va., knows that what she posts carries weight. So, whether she’s writing about backpack safety tips, choking hazards, or separation anxiety, her followers can rest assured that she’s posting responsibly.
“Pediatricians often underestimate how smart parents are,” said Dr. Playforth, who has three kids, ages 8, 5, and 2, and has 137,000 followers on @thepediatricianmom, her Instagram account. “Their anxiety comes from an understandable place, which is why I see my role as that of a parent and pediatrician who can translate the knowledge pediatricians have into something parents can understand.”
Dr. Playforth, who jumped on social media during COVID-19 and experienced a positive response in her local community, said being on social media is imperative if you’re a pediatrician.
“This is the future of pediatric medicine in particular,” she said. “A lot of pediatricians don’t want to embrace social media, but I think that’s a mistake. After all, while parents think pediatricians have all the answers, when we think of our own children, most doctors are like other parents – we can’t think objectively about our kids. It’s helpful for me to share that and to help parents feel less alone.”
If you’re not yet using social media to the best of your physician abilities, you might take a shot at becoming widely recognizable. Pick a preferred platform, answer common patient questions, dispel medical myths, provide pertinent information, and let your personality shine.
A version of this article first appeared on Medscape.com.
With physicians under increasing pressure to see more patients in shorter office visits, developing a social media presence may offer valuable opportunities to connect with patients, explain procedures, combat misinformation, talk through a published article, and even share a joke or meme.
But there are caveats for doctors posting on social media platforms. This news organization spoke to four doctors who successfully use social media.
Use social media for the right reasons
While you’re under no obligation to build a social media presence, if you’re going to do it, be sure your intentions are solid, said Don S. Dizon, MD, professor of medicine and professor of surgery at Brown University, Providence, R.I. Dr. Dizon, as @DoctorDon, has 44,700 TikTok followers and uses the platform to answer cancer-related questions.
“It should be your altruism that motivates you to post,” said Dr. Dizon, who is also associate director of community outreach and engagement at the Legorreta Cancer Center in Providence, R.I., and director of medical oncology at Rhode Island Hospital. “What we can do for society at large is to provide our input into issues, add informed opinions where there’s controversy, and address misinformation.”
If you don’t know where to start, consider seeking a digital mentor to talk through your options.
“You may never meet this person, but you should choose them if you like their style, their content, their delivery, and their perspective,” Dr. Dizon said. “Find another doctor out there on social media whom you feel you can emulate. Take your time, too. Soon enough, you’ll develop your own style and your own online persona.”
Post clear, accurate information
If you want to be lighthearted on social media, that’s your choice. But Jennifer Trachtenberg, a pediatrician with nearly 7,000 Instagram followers in New York who posts as @askdrjen, prefers to offer vaccine scheduling tips, alert parents about COVID-19 rates, and offer advice on cold and flu prevention.
“Right now, I’m mainly doing this to educate patients and make them aware of topics that I think are important and that I see my patients needing more information on,” she said. “We have to be clear: People take what we say seriously. So, while it’s important to be relatable, it’s even more important to share evidence-based information.”
Many patients get their information on social media
While patients once came to the doctor armed with information sourced via “Doctor Google,” today, just as many patients use social media to learn about their condition or the medications they’re taking.
Unfortunately, a recent Ohio State University, Columbus, study found that the majority of gynecologic cancer advice on TikTok, for example, was either misleading or inaccurate.
“This misinformation should be a motivator for physicians to explore the social media space,” Dr. Dizon said. “Our voices need to be on there.”
Break down barriers – and make connections
Mike Natter, MD, an endocrinologist in New York, has type 1 diabetes. This informs his work – and his life – and he’s passionate about sharing it with his 117,000 followers as @mike.natter on Instagram.
“A lot of type 1s follow me, so there’s an advocacy component to what I do,” he said. “I enjoy being able to raise awareness and keep people up to date on the newest research and treatment.”
But that’s not all: Dr. Natter is also an artist who went to art school before he went to medical school, and his account is rife with his cartoons and illustrations about everything from valvular disease to diabetic ketoacidosis.
“I found that I was drawing a lot of my notes in medical school,” he said. “When I drew my notes, I did quite well, and I think that using art and illustration is a great tool. It breaks down barriers and makes health information all the more accessible to everyone.”
Share your expertise as a doctor – and a person
As a mom and pediatrician, Krupa Playforth, MD, who practices in Vienna, Va., knows that what she posts carries weight. So, whether she’s writing about backpack safety tips, choking hazards, or separation anxiety, her followers can rest assured that she’s posting responsibly.
“Pediatricians often underestimate how smart parents are,” said Dr. Playforth, who has three kids, ages 8, 5, and 2, and has 137,000 followers on @thepediatricianmom, her Instagram account. “Their anxiety comes from an understandable place, which is why I see my role as that of a parent and pediatrician who can translate the knowledge pediatricians have into something parents can understand.”
Dr. Playforth, who jumped on social media during COVID-19 and experienced a positive response in her local community, said being on social media is imperative if you’re a pediatrician.
“This is the future of pediatric medicine in particular,” she said. “A lot of pediatricians don’t want to embrace social media, but I think that’s a mistake. After all, while parents think pediatricians have all the answers, when we think of our own children, most doctors are like other parents – we can’t think objectively about our kids. It’s helpful for me to share that and to help parents feel less alone.”
If you’re not yet using social media to the best of your physician abilities, you might take a shot at becoming widely recognizable. Pick a preferred platform, answer common patient questions, dispel medical myths, provide pertinent information, and let your personality shine.
A version of this article first appeared on Medscape.com.
With physicians under increasing pressure to see more patients in shorter office visits, developing a social media presence may offer valuable opportunities to connect with patients, explain procedures, combat misinformation, talk through a published article, and even share a joke or meme.
But there are caveats for doctors posting on social media platforms. This news organization spoke to four doctors who successfully use social media.
Use social media for the right reasons
While you’re under no obligation to build a social media presence, if you’re going to do it, be sure your intentions are solid, said Don S. Dizon, MD, professor of medicine and professor of surgery at Brown University, Providence, R.I. Dr. Dizon, as @DoctorDon, has 44,700 TikTok followers and uses the platform to answer cancer-related questions.
“It should be your altruism that motivates you to post,” said Dr. Dizon, who is also associate director of community outreach and engagement at the Legorreta Cancer Center in Providence, R.I., and director of medical oncology at Rhode Island Hospital. “What we can do for society at large is to provide our input into issues, add informed opinions where there’s controversy, and address misinformation.”
If you don’t know where to start, consider seeking a digital mentor to talk through your options.
“You may never meet this person, but you should choose them if you like their style, their content, their delivery, and their perspective,” Dr. Dizon said. “Find another doctor out there on social media whom you feel you can emulate. Take your time, too. Soon enough, you’ll develop your own style and your own online persona.”
Post clear, accurate information
If you want to be lighthearted on social media, that’s your choice. But Jennifer Trachtenberg, a pediatrician with nearly 7,000 Instagram followers in New York who posts as @askdrjen, prefers to offer vaccine scheduling tips, alert parents about COVID-19 rates, and offer advice on cold and flu prevention.
“Right now, I’m mainly doing this to educate patients and make them aware of topics that I think are important and that I see my patients needing more information on,” she said. “We have to be clear: People take what we say seriously. So, while it’s important to be relatable, it’s even more important to share evidence-based information.”
Many patients get their information on social media
While patients once came to the doctor armed with information sourced via “Doctor Google,” today, just as many patients use social media to learn about their condition or the medications they’re taking.
Unfortunately, a recent Ohio State University, Columbus, study found that the majority of gynecologic cancer advice on TikTok, for example, was either misleading or inaccurate.
“This misinformation should be a motivator for physicians to explore the social media space,” Dr. Dizon said. “Our voices need to be on there.”
Break down barriers – and make connections
Mike Natter, MD, an endocrinologist in New York, has type 1 diabetes. This informs his work – and his life – and he’s passionate about sharing it with his 117,000 followers as @mike.natter on Instagram.
“A lot of type 1s follow me, so there’s an advocacy component to what I do,” he said. “I enjoy being able to raise awareness and keep people up to date on the newest research and treatment.”
But that’s not all: Dr. Natter is also an artist who went to art school before he went to medical school, and his account is rife with his cartoons and illustrations about everything from valvular disease to diabetic ketoacidosis.
“I found that I was drawing a lot of my notes in medical school,” he said. “When I drew my notes, I did quite well, and I think that using art and illustration is a great tool. It breaks down barriers and makes health information all the more accessible to everyone.”
Share your expertise as a doctor – and a person
As a mom and pediatrician, Krupa Playforth, MD, who practices in Vienna, Va., knows that what she posts carries weight. So, whether she’s writing about backpack safety tips, choking hazards, or separation anxiety, her followers can rest assured that she’s posting responsibly.
“Pediatricians often underestimate how smart parents are,” said Dr. Playforth, who has three kids, ages 8, 5, and 2, and has 137,000 followers on @thepediatricianmom, her Instagram account. “Their anxiety comes from an understandable place, which is why I see my role as that of a parent and pediatrician who can translate the knowledge pediatricians have into something parents can understand.”
Dr. Playforth, who jumped on social media during COVID-19 and experienced a positive response in her local community, said being on social media is imperative if you’re a pediatrician.
“This is the future of pediatric medicine in particular,” she said. “A lot of pediatricians don’t want to embrace social media, but I think that’s a mistake. After all, while parents think pediatricians have all the answers, when we think of our own children, most doctors are like other parents – we can’t think objectively about our kids. It’s helpful for me to share that and to help parents feel less alone.”
If you’re not yet using social media to the best of your physician abilities, you might take a shot at becoming widely recognizable. Pick a preferred platform, answer common patient questions, dispel medical myths, provide pertinent information, and let your personality shine.
A version of this article first appeared on Medscape.com.
Advanced practice radiation therapists: Are they worth it?
An innovative care model involving in the radiation oncology department of Mount Sinai Health System in New York.
At a time when clinician burnout is rampant, a novel approach that brings value to both patients and health systems – and helps advance the careers of highly educated and skilled practitioners – represents a welcome step forward, according to Samantha Skubish, MS, RT, chief technical director of radiation oncology and Mount Sinai.
In the new care model, APRTs work alongside radiation oncologists and support “the care of resource-intensive patient populations,” according to the Association of Community Cancer Centers, which recently recognized the Mount Sinai Health System program as a 2023 ACCC Innovator Award winner.
The new and improved “model for continuity of care” with the APRT role has “helped improve the patient experience and create a more streamlined, efficient process while also alleviating some of the burden on our physicians,” Ms. Skubish said in the ACCC press release. She explained that APRTs possess the skills, knowledge, and judgment to provide an elevated level of care, as evidenced by decades of international research.
A 2022 systematic review of APRT-based care models outside the United States explored how the models have worked. Overall, the research shows that such models improve quality, efficiency, wellness, and administrative outcomes, according to investigators.
At Mount Sinai, the first health system to develop the APRT role in the United States, research to demonstrate the benefits of APRT model continues. In 2021, an APRT working group was established to “garner a network of individuals across the country focused on the work to prove the advanced practice radiation therapy model in the U.S.,” according to Danielle McDonagh, MS, RT, Mount Sinai’s clinical coordinator of radiation sciences education and research.
A paper published in May by Ms. McDonagh and colleagues underscored the potential for “positive change and impact” of the APRT care model in radiation oncology.
“We’re all in this current and longstanding crisis of clinician shortages,” Kimberly Smith, MPA, explained in a video introducing the Mount Sinai program.
“If you look at your therapists’ skill set and allow them to work at the top of their license, you can provide a cost-saving solution that lends itself to value-based care,” said Ms. Smith, vice president of radiation oncology services at Mount Sinai.
Indeed, Sheryl Green, MBBCh, professor and medical director of radiation oncology at Mount Sinai, noted that “the APRT has allowed us to really improve the quality of care that we deliver, primarily in the aspects of optimizing and personalizing the patient experience.”
Ms. Skubish and Ms. Smith will share details of the new care model at the ACCC’s upcoming National Oncology Conference.
An innovative care model involving in the radiation oncology department of Mount Sinai Health System in New York.
At a time when clinician burnout is rampant, a novel approach that brings value to both patients and health systems – and helps advance the careers of highly educated and skilled practitioners – represents a welcome step forward, according to Samantha Skubish, MS, RT, chief technical director of radiation oncology and Mount Sinai.
In the new care model, APRTs work alongside radiation oncologists and support “the care of resource-intensive patient populations,” according to the Association of Community Cancer Centers, which recently recognized the Mount Sinai Health System program as a 2023 ACCC Innovator Award winner.
The new and improved “model for continuity of care” with the APRT role has “helped improve the patient experience and create a more streamlined, efficient process while also alleviating some of the burden on our physicians,” Ms. Skubish said in the ACCC press release. She explained that APRTs possess the skills, knowledge, and judgment to provide an elevated level of care, as evidenced by decades of international research.
A 2022 systematic review of APRT-based care models outside the United States explored how the models have worked. Overall, the research shows that such models improve quality, efficiency, wellness, and administrative outcomes, according to investigators.
At Mount Sinai, the first health system to develop the APRT role in the United States, research to demonstrate the benefits of APRT model continues. In 2021, an APRT working group was established to “garner a network of individuals across the country focused on the work to prove the advanced practice radiation therapy model in the U.S.,” according to Danielle McDonagh, MS, RT, Mount Sinai’s clinical coordinator of radiation sciences education and research.
A paper published in May by Ms. McDonagh and colleagues underscored the potential for “positive change and impact” of the APRT care model in radiation oncology.
“We’re all in this current and longstanding crisis of clinician shortages,” Kimberly Smith, MPA, explained in a video introducing the Mount Sinai program.
“If you look at your therapists’ skill set and allow them to work at the top of their license, you can provide a cost-saving solution that lends itself to value-based care,” said Ms. Smith, vice president of radiation oncology services at Mount Sinai.
Indeed, Sheryl Green, MBBCh, professor and medical director of radiation oncology at Mount Sinai, noted that “the APRT has allowed us to really improve the quality of care that we deliver, primarily in the aspects of optimizing and personalizing the patient experience.”
Ms. Skubish and Ms. Smith will share details of the new care model at the ACCC’s upcoming National Oncology Conference.
An innovative care model involving in the radiation oncology department of Mount Sinai Health System in New York.
At a time when clinician burnout is rampant, a novel approach that brings value to both patients and health systems – and helps advance the careers of highly educated and skilled practitioners – represents a welcome step forward, according to Samantha Skubish, MS, RT, chief technical director of radiation oncology and Mount Sinai.
In the new care model, APRTs work alongside radiation oncologists and support “the care of resource-intensive patient populations,” according to the Association of Community Cancer Centers, which recently recognized the Mount Sinai Health System program as a 2023 ACCC Innovator Award winner.
The new and improved “model for continuity of care” with the APRT role has “helped improve the patient experience and create a more streamlined, efficient process while also alleviating some of the burden on our physicians,” Ms. Skubish said in the ACCC press release. She explained that APRTs possess the skills, knowledge, and judgment to provide an elevated level of care, as evidenced by decades of international research.
A 2022 systematic review of APRT-based care models outside the United States explored how the models have worked. Overall, the research shows that such models improve quality, efficiency, wellness, and administrative outcomes, according to investigators.
At Mount Sinai, the first health system to develop the APRT role in the United States, research to demonstrate the benefits of APRT model continues. In 2021, an APRT working group was established to “garner a network of individuals across the country focused on the work to prove the advanced practice radiation therapy model in the U.S.,” according to Danielle McDonagh, MS, RT, Mount Sinai’s clinical coordinator of radiation sciences education and research.
A paper published in May by Ms. McDonagh and colleagues underscored the potential for “positive change and impact” of the APRT care model in radiation oncology.
“We’re all in this current and longstanding crisis of clinician shortages,” Kimberly Smith, MPA, explained in a video introducing the Mount Sinai program.
“If you look at your therapists’ skill set and allow them to work at the top of their license, you can provide a cost-saving solution that lends itself to value-based care,” said Ms. Smith, vice president of radiation oncology services at Mount Sinai.
Indeed, Sheryl Green, MBBCh, professor and medical director of radiation oncology at Mount Sinai, noted that “the APRT has allowed us to really improve the quality of care that we deliver, primarily in the aspects of optimizing and personalizing the patient experience.”
Ms. Skubish and Ms. Smith will share details of the new care model at the ACCC’s upcoming National Oncology Conference.
What’s right and wrong for doctors on social media
She went by the name “Dr. Roxy” on social media and became something of a sensation on TikTok, where she livestreamed her patients’ operations. Ultimately, however, plastic surgeon Katharine Roxanne Grawe, MD, lost her medical license based partly on her “life-altering, reckless treatment,” heightened by her social media fame. In July, the Ohio state medical board permanently revoked Dr. Grawe’s license after twice reprimanding her for her failure to meet the standard of care. The board also determined that, by livestreaming procedures, she placed her patients in danger of immediate and serious harm.
Although most doctors don’t use social media to the degree that Dr. Grawe did, using the various platforms – from X (formerly Twitter) to Facebook, Instagram, and TikTok – can be a slippery slope. Medscape’s Physician Behavior Report 2023 revealed that doctors have seen their share of unprofessional or offensive social media use from their peers. Nearly 7 in 10 said it is unethical for a doctor to act rudely, offensively, or unprofessionally on social media, even if their medical practice isn’t mentioned. As one physician put it: “Professional is not a 9-to-5 descriptor.”
“There’s still a stigma attached,” said Liudmila Schafer, MD, an oncologist with The Doctor Connect, a career consulting firm. “Physicians face a tougher challenge due to societal expectations of perfection, with greater consequences for mistakes. We’re under constant ‘observation’ from peers, employers, and patients.”
Beverly Hills plastic surgeon Jay Calvert, MD, says he holds firm boundaries with how he uses social media. “I do comedy on the side, but it’s not acceptable for me as a doctor to share that on social media,” he said. “People want doctors who are professional, and I’m always concerned about how I present myself.”
Dr. Calvert said it is fairly easy to spot doctors who cross the line with social media. “You have to hold yourself back when posting. Doing things like dancing in the OR are out of whack with the profession.”
According to Dr. Schafer, a definite line to avoid crossing is offering medical advice or guidance on social media. “You also can’t discuss confidential practice details, respond to unfamiliar contacts, or discuss institutional policies without permission,” she said. “It’s important to add disclaimers if a personal scientific opinion is shared without reference [or] research or with unchecked sources.”
Navigating the many social media sites
Each social media platform has its pros and cons. Doctors need to determine why to use them and what the payback of each might be. Dr. Schafer uses multiple sites, including LinkedIn, Facebook, Instagram, X, Threads, YouTube, and, to a lesser degree, Clubhouse. How and what she posts on each varies. “I use them almost 95% professionally,” she said. “It’s challenging to meet and engage in person, so that is where social media helps.”
Stephen Pribut, MD, a Washington-based podiatrist, likes to use X as an information source. He follows pretty simple rules when it comes to what he tweets and shares on various sites: “I stay away from politics and religion,” he said. “I also avoid controversial topics online, such as vaccines.”
Joseph Daibes, DO, who specializes in cardiovascular medicine at New Jersey Heart and Vein, Clifton, said he has changed how he uses social media. “Initially, I was a passive consumer, but as I recognized the importance of accurate medical information online, I became more active in weighing in responsibly, occasionally sharing studies, debunking myths, and engaging in meaningful conversations,” he said. “Social media can get dangerous, so we have a duty to use it responsibly, and I cannot stress that enough.”
For plastic surgeons like Dr. Calvert, the visual platforms such as Instagram can prove invaluable for marketing purposes. “I’ve been using Instagram since 2012, and it’s been my most positive experience,” he said. “I don’t generate business from it, but I use it to back up my qualifications as a surgeon.”
Potential patients like to scroll through posts by plastic surgeons to learn what their finished product looks like, Dr. Calvert said. In many cases, plastic surgeons hire social media experts to cultivate their content. “I’ve hired and fired social media managers over the years, ultimately deciding I should develop my own content,” he said. “I want people to see the same doctor on social media that they will see in the office. I like an authentic presentation, not glitzy.”
Social media gone wrong
Dr. Calvert said that in the world of plastic surgery, some doctors use social media to present “before and after” compilations that in his opinion aren’t necessarily fully authentic, and this rubs him wrong. “There’s a bit of ‘cheating’ in some of these posts, using filters, making the ‘befores’ particularly bad, and other tricks,” he said.
Dr. Daibes has also seen his share of social media misuse: ”Red flags include oversharing personal indulgences, engaging in online spats, or making unfounded medical claims,” he said. “It’s essential to remember our role as educators and advocates, and to present ourselves in a way that upholds the dignity of our profession.”
At the end of the day, social media can have positive uses for physicians, and it is clearly here to stay. The onus for responsible use ultimately falls to the physicians using it.
Dr. Daibes emphasizes the fact that a doctor’s words carry weight – perhaps more so than those of other professionals. “The added scrutiny is good because it keeps us accountable; it’s crucial that our information is accurate,” he said. “The downside is that the scrutiny can be stifling at times and lead to self-censorship, even on nonmedical matters.”
Physicians have suggested eight guidelines for doctors to follow when using social media:
- Remember that you represent your profession, even if posting on personal accounts.
- Never post from the operating room, the emergency department, or any sort of medical space.
- If you’re employed, before you post, check with your employer to see whether they have any rules or guidance surrounding social media.
- Never use social media to badmouth colleagues, hospitals, or other healthcare organizations.
- Never use social media to dispense medical advice.
- Steer clear of the obvious hot-button issues, like religion and politics.
- Always protect patient privacy when posting.
- Be careful with how and whom you engage on social media.
A version of this article first appeared on Medscape.com.
She went by the name “Dr. Roxy” on social media and became something of a sensation on TikTok, where she livestreamed her patients’ operations. Ultimately, however, plastic surgeon Katharine Roxanne Grawe, MD, lost her medical license based partly on her “life-altering, reckless treatment,” heightened by her social media fame. In July, the Ohio state medical board permanently revoked Dr. Grawe’s license after twice reprimanding her for her failure to meet the standard of care. The board also determined that, by livestreaming procedures, she placed her patients in danger of immediate and serious harm.
Although most doctors don’t use social media to the degree that Dr. Grawe did, using the various platforms – from X (formerly Twitter) to Facebook, Instagram, and TikTok – can be a slippery slope. Medscape’s Physician Behavior Report 2023 revealed that doctors have seen their share of unprofessional or offensive social media use from their peers. Nearly 7 in 10 said it is unethical for a doctor to act rudely, offensively, or unprofessionally on social media, even if their medical practice isn’t mentioned. As one physician put it: “Professional is not a 9-to-5 descriptor.”
“There’s still a stigma attached,” said Liudmila Schafer, MD, an oncologist with The Doctor Connect, a career consulting firm. “Physicians face a tougher challenge due to societal expectations of perfection, with greater consequences for mistakes. We’re under constant ‘observation’ from peers, employers, and patients.”
Beverly Hills plastic surgeon Jay Calvert, MD, says he holds firm boundaries with how he uses social media. “I do comedy on the side, but it’s not acceptable for me as a doctor to share that on social media,” he said. “People want doctors who are professional, and I’m always concerned about how I present myself.”
Dr. Calvert said it is fairly easy to spot doctors who cross the line with social media. “You have to hold yourself back when posting. Doing things like dancing in the OR are out of whack with the profession.”
According to Dr. Schafer, a definite line to avoid crossing is offering medical advice or guidance on social media. “You also can’t discuss confidential practice details, respond to unfamiliar contacts, or discuss institutional policies without permission,” she said. “It’s important to add disclaimers if a personal scientific opinion is shared without reference [or] research or with unchecked sources.”
Navigating the many social media sites
Each social media platform has its pros and cons. Doctors need to determine why to use them and what the payback of each might be. Dr. Schafer uses multiple sites, including LinkedIn, Facebook, Instagram, X, Threads, YouTube, and, to a lesser degree, Clubhouse. How and what she posts on each varies. “I use them almost 95% professionally,” she said. “It’s challenging to meet and engage in person, so that is where social media helps.”
Stephen Pribut, MD, a Washington-based podiatrist, likes to use X as an information source. He follows pretty simple rules when it comes to what he tweets and shares on various sites: “I stay away from politics and religion,” he said. “I also avoid controversial topics online, such as vaccines.”
Joseph Daibes, DO, who specializes in cardiovascular medicine at New Jersey Heart and Vein, Clifton, said he has changed how he uses social media. “Initially, I was a passive consumer, but as I recognized the importance of accurate medical information online, I became more active in weighing in responsibly, occasionally sharing studies, debunking myths, and engaging in meaningful conversations,” he said. “Social media can get dangerous, so we have a duty to use it responsibly, and I cannot stress that enough.”
For plastic surgeons like Dr. Calvert, the visual platforms such as Instagram can prove invaluable for marketing purposes. “I’ve been using Instagram since 2012, and it’s been my most positive experience,” he said. “I don’t generate business from it, but I use it to back up my qualifications as a surgeon.”
Potential patients like to scroll through posts by plastic surgeons to learn what their finished product looks like, Dr. Calvert said. In many cases, plastic surgeons hire social media experts to cultivate their content. “I’ve hired and fired social media managers over the years, ultimately deciding I should develop my own content,” he said. “I want people to see the same doctor on social media that they will see in the office. I like an authentic presentation, not glitzy.”
Social media gone wrong
Dr. Calvert said that in the world of plastic surgery, some doctors use social media to present “before and after” compilations that in his opinion aren’t necessarily fully authentic, and this rubs him wrong. “There’s a bit of ‘cheating’ in some of these posts, using filters, making the ‘befores’ particularly bad, and other tricks,” he said.
Dr. Daibes has also seen his share of social media misuse: ”Red flags include oversharing personal indulgences, engaging in online spats, or making unfounded medical claims,” he said. “It’s essential to remember our role as educators and advocates, and to present ourselves in a way that upholds the dignity of our profession.”
At the end of the day, social media can have positive uses for physicians, and it is clearly here to stay. The onus for responsible use ultimately falls to the physicians using it.
Dr. Daibes emphasizes the fact that a doctor’s words carry weight – perhaps more so than those of other professionals. “The added scrutiny is good because it keeps us accountable; it’s crucial that our information is accurate,” he said. “The downside is that the scrutiny can be stifling at times and lead to self-censorship, even on nonmedical matters.”
Physicians have suggested eight guidelines for doctors to follow when using social media:
- Remember that you represent your profession, even if posting on personal accounts.
- Never post from the operating room, the emergency department, or any sort of medical space.
- If you’re employed, before you post, check with your employer to see whether they have any rules or guidance surrounding social media.
- Never use social media to badmouth colleagues, hospitals, or other healthcare organizations.
- Never use social media to dispense medical advice.
- Steer clear of the obvious hot-button issues, like religion and politics.
- Always protect patient privacy when posting.
- Be careful with how and whom you engage on social media.
A version of this article first appeared on Medscape.com.
She went by the name “Dr. Roxy” on social media and became something of a sensation on TikTok, where she livestreamed her patients’ operations. Ultimately, however, plastic surgeon Katharine Roxanne Grawe, MD, lost her medical license based partly on her “life-altering, reckless treatment,” heightened by her social media fame. In July, the Ohio state medical board permanently revoked Dr. Grawe’s license after twice reprimanding her for her failure to meet the standard of care. The board also determined that, by livestreaming procedures, she placed her patients in danger of immediate and serious harm.
Although most doctors don’t use social media to the degree that Dr. Grawe did, using the various platforms – from X (formerly Twitter) to Facebook, Instagram, and TikTok – can be a slippery slope. Medscape’s Physician Behavior Report 2023 revealed that doctors have seen their share of unprofessional or offensive social media use from their peers. Nearly 7 in 10 said it is unethical for a doctor to act rudely, offensively, or unprofessionally on social media, even if their medical practice isn’t mentioned. As one physician put it: “Professional is not a 9-to-5 descriptor.”
“There’s still a stigma attached,” said Liudmila Schafer, MD, an oncologist with The Doctor Connect, a career consulting firm. “Physicians face a tougher challenge due to societal expectations of perfection, with greater consequences for mistakes. We’re under constant ‘observation’ from peers, employers, and patients.”
Beverly Hills plastic surgeon Jay Calvert, MD, says he holds firm boundaries with how he uses social media. “I do comedy on the side, but it’s not acceptable for me as a doctor to share that on social media,” he said. “People want doctors who are professional, and I’m always concerned about how I present myself.”
Dr. Calvert said it is fairly easy to spot doctors who cross the line with social media. “You have to hold yourself back when posting. Doing things like dancing in the OR are out of whack with the profession.”
According to Dr. Schafer, a definite line to avoid crossing is offering medical advice or guidance on social media. “You also can’t discuss confidential practice details, respond to unfamiliar contacts, or discuss institutional policies without permission,” she said. “It’s important to add disclaimers if a personal scientific opinion is shared without reference [or] research or with unchecked sources.”
Navigating the many social media sites
Each social media platform has its pros and cons. Doctors need to determine why to use them and what the payback of each might be. Dr. Schafer uses multiple sites, including LinkedIn, Facebook, Instagram, X, Threads, YouTube, and, to a lesser degree, Clubhouse. How and what she posts on each varies. “I use them almost 95% professionally,” she said. “It’s challenging to meet and engage in person, so that is where social media helps.”
Stephen Pribut, MD, a Washington-based podiatrist, likes to use X as an information source. He follows pretty simple rules when it comes to what he tweets and shares on various sites: “I stay away from politics and religion,” he said. “I also avoid controversial topics online, such as vaccines.”
Joseph Daibes, DO, who specializes in cardiovascular medicine at New Jersey Heart and Vein, Clifton, said he has changed how he uses social media. “Initially, I was a passive consumer, but as I recognized the importance of accurate medical information online, I became more active in weighing in responsibly, occasionally sharing studies, debunking myths, and engaging in meaningful conversations,” he said. “Social media can get dangerous, so we have a duty to use it responsibly, and I cannot stress that enough.”
For plastic surgeons like Dr. Calvert, the visual platforms such as Instagram can prove invaluable for marketing purposes. “I’ve been using Instagram since 2012, and it’s been my most positive experience,” he said. “I don’t generate business from it, but I use it to back up my qualifications as a surgeon.”
Potential patients like to scroll through posts by plastic surgeons to learn what their finished product looks like, Dr. Calvert said. In many cases, plastic surgeons hire social media experts to cultivate their content. “I’ve hired and fired social media managers over the years, ultimately deciding I should develop my own content,” he said. “I want people to see the same doctor on social media that they will see in the office. I like an authentic presentation, not glitzy.”
Social media gone wrong
Dr. Calvert said that in the world of plastic surgery, some doctors use social media to present “before and after” compilations that in his opinion aren’t necessarily fully authentic, and this rubs him wrong. “There’s a bit of ‘cheating’ in some of these posts, using filters, making the ‘befores’ particularly bad, and other tricks,” he said.
Dr. Daibes has also seen his share of social media misuse: ”Red flags include oversharing personal indulgences, engaging in online spats, or making unfounded medical claims,” he said. “It’s essential to remember our role as educators and advocates, and to present ourselves in a way that upholds the dignity of our profession.”
At the end of the day, social media can have positive uses for physicians, and it is clearly here to stay. The onus for responsible use ultimately falls to the physicians using it.
Dr. Daibes emphasizes the fact that a doctor’s words carry weight – perhaps more so than those of other professionals. “The added scrutiny is good because it keeps us accountable; it’s crucial that our information is accurate,” he said. “The downside is that the scrutiny can be stifling at times and lead to self-censorship, even on nonmedical matters.”
Physicians have suggested eight guidelines for doctors to follow when using social media:
- Remember that you represent your profession, even if posting on personal accounts.
- Never post from the operating room, the emergency department, or any sort of medical space.
- If you’re employed, before you post, check with your employer to see whether they have any rules or guidance surrounding social media.
- Never use social media to badmouth colleagues, hospitals, or other healthcare organizations.
- Never use social media to dispense medical advice.
- Steer clear of the obvious hot-button issues, like religion and politics.
- Always protect patient privacy when posting.
- Be careful with how and whom you engage on social media.
A version of this article first appeared on Medscape.com.
Update on Dermatology Reimbursement in 2024
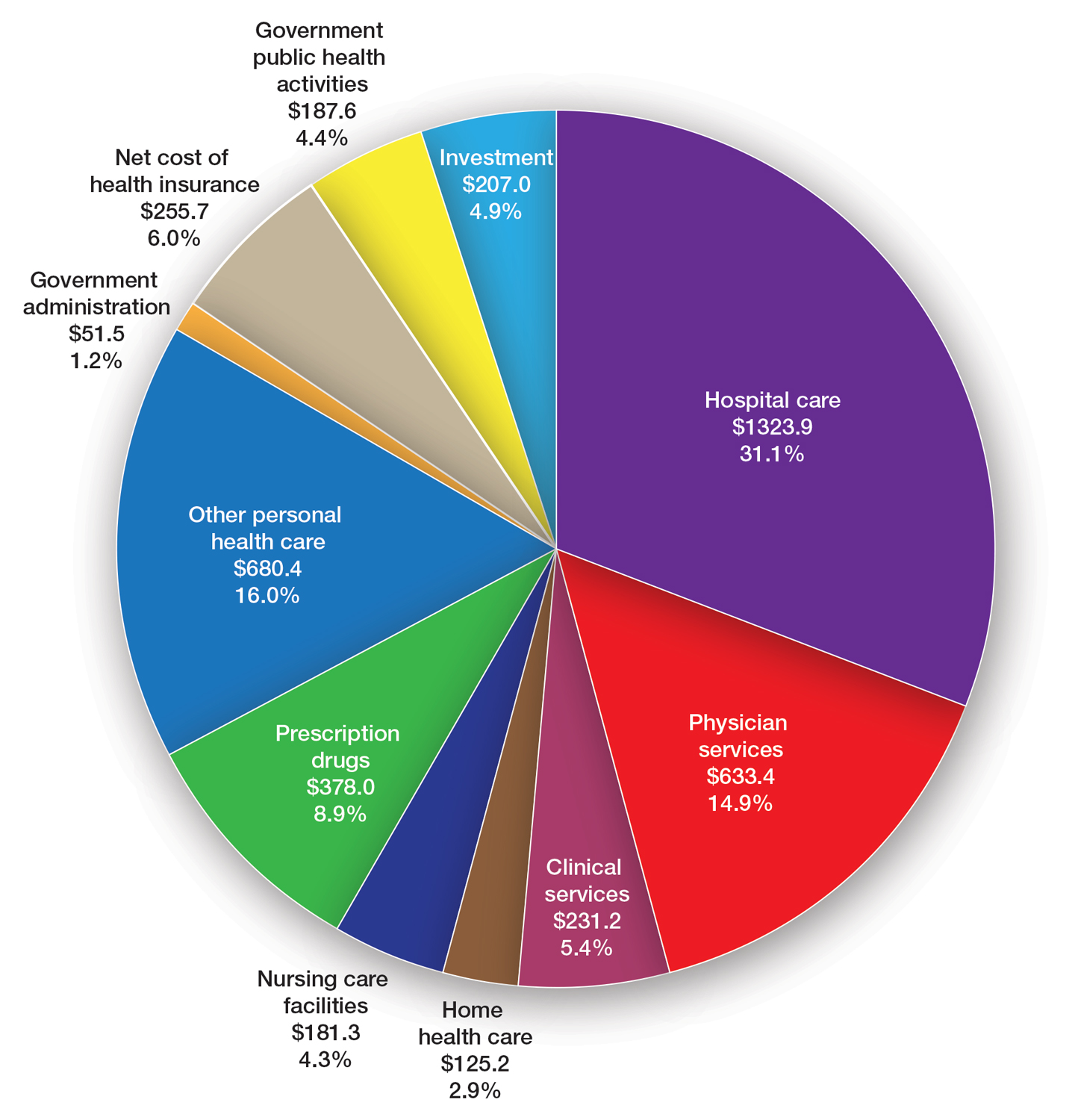
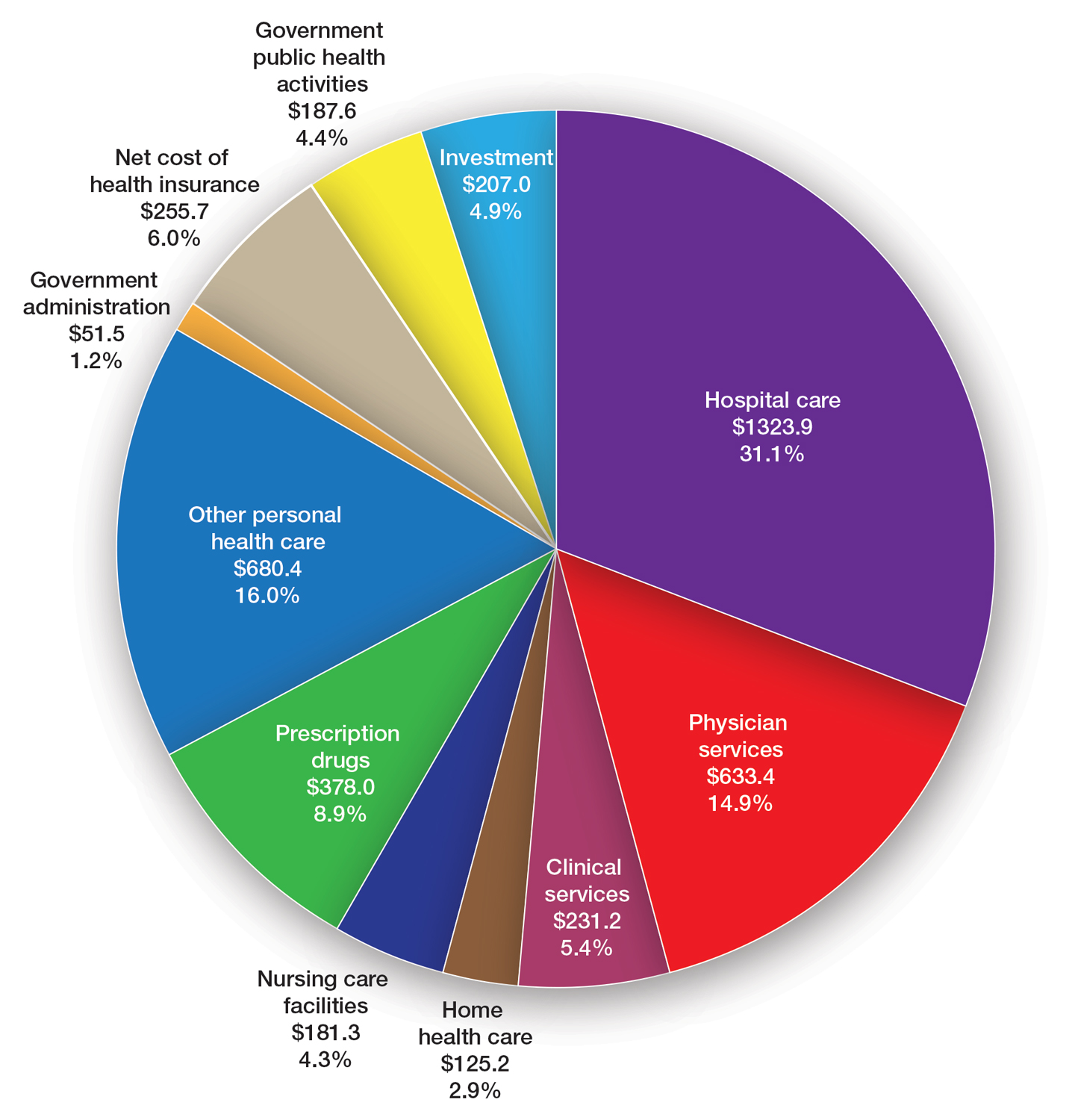
Health care spending in the United States remained relatively flat from 2019 to 2021 and only increased 2.7% in 2021, reaching $4.3 billion or $12,914 per person. Physician services account for 15% of health care spending (Figure). Relative value units (RVUs) signify the time it took a physician to complete a task multiplied by a conversion factor (CF). When RVUs initially were created in 1992 by what is now the Centers for Medicare &Medicaid Services (CMS), the CF was $32.00. Thirty-one years later, the CF is $33.89 in 2023; however, it would be $66.00 if the CF had increased with inflation.1 If the proposed 2024 Medicare physician fee schedule (MPFS) is adopted, the payment formula would decrease by 3.4% ($32.75) relative to the 2023 fee schedule ($33.89), which would be a 9% decrease relative to 2019 ($36.04).2,3 This reduction is due to the budget neutrality adjustment required by changes in RVUs, implementation of the evaluation and management (E/M) add-on code G2211, and proposed increases in primary are services.2,3 Since 2001, Medicare physician payment has declined by 26%.4 Adjustments to the CF typically are made based on 3 factors: (1) the Medicare Economic Index (MEI); (2) an expenditure target performance adjustment; and (3) miscellaneous adjustments, including those for budget neutrality required by law. Despite continued substantial increases in practice expenses, physicians’ reimbursement has remained flat while other service providers, such as those in skilled nursing facilities and hospitals, have received favorable payment increases compared to practice cost inflation and the Consumer Price Index.4
The CMS will not incorporate 2017 MEI cost weights for the RVUs in the MPFS rate setting for 2024 because all key measures of practice expenses in the MEI accelerated in 2022. Instead, the CMS is updating data on practice expense per hour to calculate payment for physician services with a survey for physician practices that launched on July 31, 2023.5 The American Medical Association contracted with Mathematica, an independent research company, to conduct a physician practice information survey that will be used to determine indirect practice expenses. Physicians should be on the lookout for emails regarding completion of these surveys and the appropriate financial expert in their practice should be contacted so the responses are accurate, as these data are key to future updates in the Medicare pay formula used to reimburse physicians.
Impact of Medicare Cuts
The recent congressional debt limit deal set spending caps for the next 2 fiscal years. Dermatology is facing an overall payment reduction of 1.87% (range, 1%–4%).2,3 The impact will depend on the services offered in an individual practice; for example, payment for a punch biopsy (Current Procedural Terminology [CPT] code 11104) would decrease by 3.9%. Payment for benign destruction (CPT code 17110) would decrease by 2.8%, and payment for even simple E/M of an established patient (CPT code 99213) would decrease by 1.6%. Overall, there would be a reduction of 2.75% for dermatopathology services, with a decrease of 2% for CPT code 88305 global and decreases for the technical component of 1% and professional component of 3%.2,3
Medicare cuts have reached a critical level, and physicians cannot continue to absorb the costs to own and operate their practices.4 This has led to health market consolidation, which in turn limits competition and patient access while driving up health care costs and driving down the quality of care. Small independent rural practices as well as those caring for historically marginalized patients will be disproportionately affected.
Proposed Addition of E/M Code G2211
In the calendar year (CY) 2021 final rule, the CMS tried to adopt a new add-on code—G2211—patients with a serious or complex condition that typically require referral and coordination of multispecialty care. Per the CMS, the primary policy goal of G2211 is to increase payments to primary care physicians and to reimburse them more appropriately for the care provided to patients with a serious or complex condition.2,3 It can be reported in conjunction with all office and outpatient E/M visits to better account for additional resources associated with primary care, or similarly ongoing medical care related to a patient’s single, serious condition, or complex condition.3 Typically, G2211 would not be used by dermatologists, as this add-on code requires visit complexity inherent to E/M associated with medical care services that serve as the continuing focal point for all needed health care services and/or with medical care services that are part of ongoing care related to a patient’s single serious condition or a complex condition.2,3
Initially, the CMS assumed that G2211 would be reported with 90% of all office and outpatient E/M visit claims, which would account for a considerable portion of total MPFS schedule spending; however, the House of Medicine disagreed and believed it would be 75%.2,3 Given the extremely high utilization estimate, G2211 would have had a substantial effect on budget neutrality, accounting for an estimated increase of $3.3 billion and a corresponding 3.0% cut to the CY 2021 MPFS. Because of the potential payment reductions to physicians and a successful advocacy effort by organized medicine, including the American Academy of Dermatology Association (AADA), Congress delayed implementation of G2211 until CY 2024. Modifier -25 cannot be reported with G2211. The CMS revised its utilization assumptions from 90% of all E/M services to an initial utilization of 38% and then 54% when fully adopted. The proposed 2024 payment for G2211 is an additional $16.05.2,3
Advancing Health Equity With Healthcare Common Procedure Coding System G Codes
The CMS is proposing coding and payment for several new services to help underserved populations, including addressing unmet health-related social needs that can potentially interfere with the diagnosis and treatment of medical conditions, which includes paying for certain caregiver training services as well as payment for community health integration services.2,3 These are the first MPFS services designed to include care involving community health workers, who link underserved communities with critical health care and social services in the community. Additionally, the rule also proposes coding and payment for evaluating the risks related to social factors that affect a patient’s health, such as access to affordable quality health care, that can take place during an annual wellness visit or in combination with an E/M visit.2,3 As dermatologists, we should be familiar with this set of G codes, as we will likely use them in practice for patients with transportation needs.
Advocacy Efforts on Medicare Payment Reform
Medicare physician payment reform needs to happen at a national level. Advocacy efforts by the AADA and other groups have been underway to mitigate the proposed 2024 cuts. The Strengthening Medicare for Patients and Providers Act (HR 2474) is a bill that was introduced by a bipartisan coalition of physicians to provide an inflation-based increase in Medicare payments in 2024 and beyond.6
Other Legislative Updates Affecting Dermatology
Modifier -25—Cigna’s policy requiring dermatologists to submit documentation to use modifier -25 when billing with E/M CPT codes 99212 through 99215 has been delayed indefinitely.7 If a payer denies a dermatologist payment, contact the AADA Patient Access and Payer Relations committee ([email protected]) for assistance.
Telehealth and Digital Pathology—Recent legislation authorized extension of many of the Medicare telehealth and digital pathology flexibilities that were put in place during the COVID-19 public health emergency through December 31, 2024.8,9 Seventeen newly approved CPT telemedicine codes for new and established patient audio-visual and audio-only visits recently were surveyed.2,3 The data from the survey will be used as a key element in assigning a specific RVU to the CMS and will be included in the MPFS.
Thirty additional new digital pathology add-on CPT category III codes for 2024 were added to the ones from 2023.2,3 These codes can be used to report additional clinical staff work and service requirements associated with digitizing glass microscope slides for primary diagnosis. They cannot be used for archival or educational purposes, clinical conferences, training, or validating artificial intelligence algorithms. Category III codes used for emerging technologies have no assigned RVUs or reimbursement.2,3
The Cures Act—The Cures Act aims to ensure that patients have timely access to their health information.10 It requires all physicians to make their office notes, laboratory results, and other diagnostic reports available to patients as soon as the office receives them. The rules went into effect on April 5, 2021, with a limited definition of electronic health information; on October 6, 2022, the Cures Act rule expanded to include all electronic health information. The AADA has urged the Office of the National Coordinator for Health Information Technology to collaborate with stakeholder organizations to re-evaluate federal policies concerning the immediate release of electronic health information and information blocking, particularly in cases with life-altering diagnoses.10 They stressed the importance of prioritizing the well-being and emotional stability of patients and enhancing care by providing patients adequate time and support to process, comprehend, and discuss findings with their physician.
Proposed 2024 Medicare Quality Payment Program Requirements
The CMS proposed to increase the performance threshold in the quality payment program from 75 to 82 points for the 2024 Merit-based Incentive Payment System (MIPS) performance period, impacting the 2026 payment year.2,3,11 As a result of this increase, there could be more MIPS-eligible clinicians receiving penalties, which could be a reduction of up to 9%. The AADA will firmly oppose any increase in the threshold and strongly urge CMS to maintain the 75-point threshold. The performance category weights for the 2024 performance year will remain unchanged from the 2023 performance year.2,3,11
2024 Proposed Quality MIPS Measures Set—The CMS proposed to remove the topped-out MIPS measure 138 (coordination of care for melanoma).2,3,11 Additionally, it proposed to remove MIPS measure 402 (tobacco use and help with quitting among adolescents) as a quality measure from MIPS because the agency believes it is duplicative of measure 226 (preventive care and screening: tobacco use: screening and cessation intervention).2,3,11
MIPS Value Pathways—The CMS consolidated 2 previously established MIPS value pathways (MVPs): the Promoting Wellness MVP and the Optimizing Chronic Disease Management MVP.2,3,11 Proposed new MVPs for 2024 include Focusing on Women’s Health; Quality Care for the Treatment of Ear, Nose, and Throat Disorders; Prevention and Treatment of Infectious Disorders Including Hepatitis C and HIV; Quality Care in Mental Health and Substance Use Disorders; and Rehabilitative Support for Musculoskeletal Care. Dermatology is not impacted; however, the CMS plans to sunset traditional MIPS and replace it with MVPs—the future of MIPS.2,3,11 The AADA maintains that traditional MIPS should continue to be an option because MVPs have a limited number of measures for dermatologists.
Update on Reporting Suture Removal
There are 2 new CPT add-on codes—15853 and 15854—for the removal of sutures or staples not requiring anesthesia to be listed separately in addition to an appropriate E/M service. These add-on codes went into effect on January 1, 2023.12 These codes were created with the intent to capture and ensure remuneration for practice expenses that are not included in a stand-alone E/M encounter that occur after a 0-day procedure (eg, services reported with CPT codes 11102–11107 and 11300–11313) for wound check and suture removal where appropriate. These new add-on codes do not have physician work RVUs assigned to them because they are only for practice expenses (eg, clinical staff time, disposable supplies, use of equipment); CPT code 15853 is reported for the removal of sutures or staples, and CPT code 15854 is reported when both sutures and staples are removed. These codes can only be reported if an E/M service also is reported for the patient encounter.12
Final Thoughts
The AADA is working with the House of Medicine and the medical specialty community to develop specific proposals to reform the Medicare payment system.4 The proposed 2024 MPFS was released on July 13, 2023, and final regulations are expected in the late fall of 2023. The AADA will continue to engage with the CMS, but it is important for physicians to learn about and support advocacy priorities and efforts as well as join forces to protect their practices. As health care professionals, we have unique insights into the challenges and needs of our patients and the health care system. Advocacy can take various forms, such as supporting or opposing specific legislations, participating in grassroots campaigns, engaging with policymakers, and/or joining professional organizations that advocate for health care–related issues. Get involved, stay informed, and stay engaged through dermatology medical societies; together we can make a difference.
- Centers for Medicare & Medicaid Services. NHE fact sheet. Updated September 6, 2023. Accessed September 18, 2023. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NHE-Fact-Sheet
- Medicare and Medicaid Programs; CY 2024 payment policies under the physician fee schedule and other changes to part B payment and coverage policies; Medicare shared savings program requirements; Medicare advantage; Medicare and Medicaid provider and supplier enrollment policies; and basic health program. Fed Regist. 2023;88:52262-53197. To be codified at 42 CFR §405, §410, §411, §414, §415, §418, §422, §423, §424, §425, §455, §489, §491, §495, §498, and §600. https://www.federalregister.gov/documents/2023/08/07/2023-14624/medicare-and-medicaid-programs-cy-2024-payment-policies-under-the-physician-fee-schedule-and-other
- Centers for Medicare & Medicaid Services. Calendar year (CY) 2024 Medicare physician fee schedule proposed rule. Published July 13, 2023. Accessed September 18, 2023. https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2024-medicare-physician-fee-schedule-proposed-rule
- American Medical Association. Payment reform. Accessed September 18, 2023. https://www.ama-assn.org/health-care-advocacypayment-reform
- American Medical Association. Physician answers on this survey will shape future Medicare pay. Published July 31, 2023. Accessed September 18, 2023. https://www.ama-assn.org/practice-management/medicare-medicaid/physician-answers-survey-will-shape-future -medicare-pay
- Strengthening Medicare for Patients and Providers Act, HR 2474, 118 Congress (2023-2024). https://www.congress.gov/bill/118th-congress/house-bill/2474
- American Academy of Dermatology Association. Academy advocacy priorities. Accessed September 18, 2023. https://www.aad.org/member/advocacy/priorities
- College of American Pathologists. Remote sign-out of cases with digital pathology FAQs. Accessed September 18, 2023. https://www.cap.org/covid-19/remote-sign-out-faqs
- Centers for Medicare & Medicaid Services. Telehealth. Updated September 6, 2023. Accessed September 18, 2023. https://www.cms.gov/medicare/coverage/telehealth
- The Office of the National Coordinator for Health Information Technology. ONC’s Cures Act final rule. Accessed September 18, 2023. https://www.healthit.gov/topic/oncs-cures-act-final-rule
- Centers for Medicare & Medicaid Services. Calendar Year (CY) 2024 Medicare Physician Fee Schedule (PFS) Notice of Proposed Rule Making Quality Payment Program Policy Overview: Proposals and Requests for Information. Accessed September 12, 2023. https://email.aadresources.org/e3t/Ctc/I6+113/cVKqx04/VVWzj43dDbctW8c23GW1ZLnJHW1xTZ7Q50Y DYN89Qzy5nCVhV3Zsc37CgFV9W5Ck4-D42qs9BW38PtXn4LSlNLW1QKpPL4xT8BMW6Mcwww3FdwCHN3vfGTMXbtF-W2-Zzfy5WHDg6W88tx1F1KgsgxW7zDzT46C2sFXW800vQJ3lLsS_W5D6f1d30-f3cN1njgZ_dX7xkW447ldH2-kgc5VCs7Xg1GY6dsN87pLVJqJG5XW8VWwD-7VxVkJN777f5fJL7jBW8RxkQM1lcSDjVV746T3C-stpN52V_S5xj7q6W3_vldf3p1Yk2Vbd4ZD3cPrHqW5Pwv9m567fkzW1vfDm51H-T7rW1jVrxl8gstXyW5RVTn8863CVFW8g6LgK2YdhpkW34HC4z3_pGYgW8V_qWH3g-tTlW4S3RD-1dKry7W4_rW8d1ssZ1fVwXQjQ9krVMW8Y0bTt8Nr5CNW6vbG0h3wyx59W8WCrNW50p5n6W1r-VBC2rKh93N4W2RyYr7vvm3kxG1
- Centers for Medicare & Medicaid Services. Chapter III surgery: integumentary system CPT codes 10000-19999 for Medicare national correct coding initiative policy manual. Updated January 1, 2023. Accessed September 26, 2023. https://www.cms.gov/files/document/medicare-ncci-policy-manual-2023-chapter-3.pdf
Health care spending in the United States remained relatively flat from 2019 to 2021 and only increased 2.7% in 2021, reaching $4.3 billion or $12,914 per person. Physician services account for 15% of health care spending (Figure). Relative value units (RVUs) signify the time it took a physician to complete a task multiplied by a conversion factor (CF). When RVUs initially were created in 1992 by what is now the Centers for Medicare &Medicaid Services (CMS), the CF was $32.00. Thirty-one years later, the CF is $33.89 in 2023; however, it would be $66.00 if the CF had increased with inflation.1 If the proposed 2024 Medicare physician fee schedule (MPFS) is adopted, the payment formula would decrease by 3.4% ($32.75) relative to the 2023 fee schedule ($33.89), which would be a 9% decrease relative to 2019 ($36.04).2,3 This reduction is due to the budget neutrality adjustment required by changes in RVUs, implementation of the evaluation and management (E/M) add-on code G2211, and proposed increases in primary are services.2,3 Since 2001, Medicare physician payment has declined by 26%.4 Adjustments to the CF typically are made based on 3 factors: (1) the Medicare Economic Index (MEI); (2) an expenditure target performance adjustment; and (3) miscellaneous adjustments, including those for budget neutrality required by law. Despite continued substantial increases in practice expenses, physicians’ reimbursement has remained flat while other service providers, such as those in skilled nursing facilities and hospitals, have received favorable payment increases compared to practice cost inflation and the Consumer Price Index.4
The CMS will not incorporate 2017 MEI cost weights for the RVUs in the MPFS rate setting for 2024 because all key measures of practice expenses in the MEI accelerated in 2022. Instead, the CMS is updating data on practice expense per hour to calculate payment for physician services with a survey for physician practices that launched on July 31, 2023.5 The American Medical Association contracted with Mathematica, an independent research company, to conduct a physician practice information survey that will be used to determine indirect practice expenses. Physicians should be on the lookout for emails regarding completion of these surveys and the appropriate financial expert in their practice should be contacted so the responses are accurate, as these data are key to future updates in the Medicare pay formula used to reimburse physicians.
Impact of Medicare Cuts
The recent congressional debt limit deal set spending caps for the next 2 fiscal years. Dermatology is facing an overall payment reduction of 1.87% (range, 1%–4%).2,3 The impact will depend on the services offered in an individual practice; for example, payment for a punch biopsy (Current Procedural Terminology [CPT] code 11104) would decrease by 3.9%. Payment for benign destruction (CPT code 17110) would decrease by 2.8%, and payment for even simple E/M of an established patient (CPT code 99213) would decrease by 1.6%. Overall, there would be a reduction of 2.75% for dermatopathology services, with a decrease of 2% for CPT code 88305 global and decreases for the technical component of 1% and professional component of 3%.2,3
Medicare cuts have reached a critical level, and physicians cannot continue to absorb the costs to own and operate their practices.4 This has led to health market consolidation, which in turn limits competition and patient access while driving up health care costs and driving down the quality of care. Small independent rural practices as well as those caring for historically marginalized patients will be disproportionately affected.
Proposed Addition of E/M Code G2211
In the calendar year (CY) 2021 final rule, the CMS tried to adopt a new add-on code—G2211—patients with a serious or complex condition that typically require referral and coordination of multispecialty care. Per the CMS, the primary policy goal of G2211 is to increase payments to primary care physicians and to reimburse them more appropriately for the care provided to patients with a serious or complex condition.2,3 It can be reported in conjunction with all office and outpatient E/M visits to better account for additional resources associated with primary care, or similarly ongoing medical care related to a patient’s single, serious condition, or complex condition.3 Typically, G2211 would not be used by dermatologists, as this add-on code requires visit complexity inherent to E/M associated with medical care services that serve as the continuing focal point for all needed health care services and/or with medical care services that are part of ongoing care related to a patient’s single serious condition or a complex condition.2,3
Initially, the CMS assumed that G2211 would be reported with 90% of all office and outpatient E/M visit claims, which would account for a considerable portion of total MPFS schedule spending; however, the House of Medicine disagreed and believed it would be 75%.2,3 Given the extremely high utilization estimate, G2211 would have had a substantial effect on budget neutrality, accounting for an estimated increase of $3.3 billion and a corresponding 3.0% cut to the CY 2021 MPFS. Because of the potential payment reductions to physicians and a successful advocacy effort by organized medicine, including the American Academy of Dermatology Association (AADA), Congress delayed implementation of G2211 until CY 2024. Modifier -25 cannot be reported with G2211. The CMS revised its utilization assumptions from 90% of all E/M services to an initial utilization of 38% and then 54% when fully adopted. The proposed 2024 payment for G2211 is an additional $16.05.2,3
Advancing Health Equity With Healthcare Common Procedure Coding System G Codes
The CMS is proposing coding and payment for several new services to help underserved populations, including addressing unmet health-related social needs that can potentially interfere with the diagnosis and treatment of medical conditions, which includes paying for certain caregiver training services as well as payment for community health integration services.2,3 These are the first MPFS services designed to include care involving community health workers, who link underserved communities with critical health care and social services in the community. Additionally, the rule also proposes coding and payment for evaluating the risks related to social factors that affect a patient’s health, such as access to affordable quality health care, that can take place during an annual wellness visit or in combination with an E/M visit.2,3 As dermatologists, we should be familiar with this set of G codes, as we will likely use them in practice for patients with transportation needs.
Advocacy Efforts on Medicare Payment Reform
Medicare physician payment reform needs to happen at a national level. Advocacy efforts by the AADA and other groups have been underway to mitigate the proposed 2024 cuts. The Strengthening Medicare for Patients and Providers Act (HR 2474) is a bill that was introduced by a bipartisan coalition of physicians to provide an inflation-based increase in Medicare payments in 2024 and beyond.6
Other Legislative Updates Affecting Dermatology
Modifier -25—Cigna’s policy requiring dermatologists to submit documentation to use modifier -25 when billing with E/M CPT codes 99212 through 99215 has been delayed indefinitely.7 If a payer denies a dermatologist payment, contact the AADA Patient Access and Payer Relations committee ([email protected]) for assistance.
Telehealth and Digital Pathology—Recent legislation authorized extension of many of the Medicare telehealth and digital pathology flexibilities that were put in place during the COVID-19 public health emergency through December 31, 2024.8,9 Seventeen newly approved CPT telemedicine codes for new and established patient audio-visual and audio-only visits recently were surveyed.2,3 The data from the survey will be used as a key element in assigning a specific RVU to the CMS and will be included in the MPFS.
Thirty additional new digital pathology add-on CPT category III codes for 2024 were added to the ones from 2023.2,3 These codes can be used to report additional clinical staff work and service requirements associated with digitizing glass microscope slides for primary diagnosis. They cannot be used for archival or educational purposes, clinical conferences, training, or validating artificial intelligence algorithms. Category III codes used for emerging technologies have no assigned RVUs or reimbursement.2,3
The Cures Act—The Cures Act aims to ensure that patients have timely access to their health information.10 It requires all physicians to make their office notes, laboratory results, and other diagnostic reports available to patients as soon as the office receives them. The rules went into effect on April 5, 2021, with a limited definition of electronic health information; on October 6, 2022, the Cures Act rule expanded to include all electronic health information. The AADA has urged the Office of the National Coordinator for Health Information Technology to collaborate with stakeholder organizations to re-evaluate federal policies concerning the immediate release of electronic health information and information blocking, particularly in cases with life-altering diagnoses.10 They stressed the importance of prioritizing the well-being and emotional stability of patients and enhancing care by providing patients adequate time and support to process, comprehend, and discuss findings with their physician.
Proposed 2024 Medicare Quality Payment Program Requirements
The CMS proposed to increase the performance threshold in the quality payment program from 75 to 82 points for the 2024 Merit-based Incentive Payment System (MIPS) performance period, impacting the 2026 payment year.2,3,11 As a result of this increase, there could be more MIPS-eligible clinicians receiving penalties, which could be a reduction of up to 9%. The AADA will firmly oppose any increase in the threshold and strongly urge CMS to maintain the 75-point threshold. The performance category weights for the 2024 performance year will remain unchanged from the 2023 performance year.2,3,11
2024 Proposed Quality MIPS Measures Set—The CMS proposed to remove the topped-out MIPS measure 138 (coordination of care for melanoma).2,3,11 Additionally, it proposed to remove MIPS measure 402 (tobacco use and help with quitting among adolescents) as a quality measure from MIPS because the agency believes it is duplicative of measure 226 (preventive care and screening: tobacco use: screening and cessation intervention).2,3,11
MIPS Value Pathways—The CMS consolidated 2 previously established MIPS value pathways (MVPs): the Promoting Wellness MVP and the Optimizing Chronic Disease Management MVP.2,3,11 Proposed new MVPs for 2024 include Focusing on Women’s Health; Quality Care for the Treatment of Ear, Nose, and Throat Disorders; Prevention and Treatment of Infectious Disorders Including Hepatitis C and HIV; Quality Care in Mental Health and Substance Use Disorders; and Rehabilitative Support for Musculoskeletal Care. Dermatology is not impacted; however, the CMS plans to sunset traditional MIPS and replace it with MVPs—the future of MIPS.2,3,11 The AADA maintains that traditional MIPS should continue to be an option because MVPs have a limited number of measures for dermatologists.
Update on Reporting Suture Removal
There are 2 new CPT add-on codes—15853 and 15854—for the removal of sutures or staples not requiring anesthesia to be listed separately in addition to an appropriate E/M service. These add-on codes went into effect on January 1, 2023.12 These codes were created with the intent to capture and ensure remuneration for practice expenses that are not included in a stand-alone E/M encounter that occur after a 0-day procedure (eg, services reported with CPT codes 11102–11107 and 11300–11313) for wound check and suture removal where appropriate. These new add-on codes do not have physician work RVUs assigned to them because they are only for practice expenses (eg, clinical staff time, disposable supplies, use of equipment); CPT code 15853 is reported for the removal of sutures or staples, and CPT code 15854 is reported when both sutures and staples are removed. These codes can only be reported if an E/M service also is reported for the patient encounter.12
Final Thoughts
The AADA is working with the House of Medicine and the medical specialty community to develop specific proposals to reform the Medicare payment system.4 The proposed 2024 MPFS was released on July 13, 2023, and final regulations are expected in the late fall of 2023. The AADA will continue to engage with the CMS, but it is important for physicians to learn about and support advocacy priorities and efforts as well as join forces to protect their practices. As health care professionals, we have unique insights into the challenges and needs of our patients and the health care system. Advocacy can take various forms, such as supporting or opposing specific legislations, participating in grassroots campaigns, engaging with policymakers, and/or joining professional organizations that advocate for health care–related issues. Get involved, stay informed, and stay engaged through dermatology medical societies; together we can make a difference.
Health care spending in the United States remained relatively flat from 2019 to 2021 and only increased 2.7% in 2021, reaching $4.3 billion or $12,914 per person. Physician services account for 15% of health care spending (Figure). Relative value units (RVUs) signify the time it took a physician to complete a task multiplied by a conversion factor (CF). When RVUs initially were created in 1992 by what is now the Centers for Medicare &Medicaid Services (CMS), the CF was $32.00. Thirty-one years later, the CF is $33.89 in 2023; however, it would be $66.00 if the CF had increased with inflation.1 If the proposed 2024 Medicare physician fee schedule (MPFS) is adopted, the payment formula would decrease by 3.4% ($32.75) relative to the 2023 fee schedule ($33.89), which would be a 9% decrease relative to 2019 ($36.04).2,3 This reduction is due to the budget neutrality adjustment required by changes in RVUs, implementation of the evaluation and management (E/M) add-on code G2211, and proposed increases in primary are services.2,3 Since 2001, Medicare physician payment has declined by 26%.4 Adjustments to the CF typically are made based on 3 factors: (1) the Medicare Economic Index (MEI); (2) an expenditure target performance adjustment; and (3) miscellaneous adjustments, including those for budget neutrality required by law. Despite continued substantial increases in practice expenses, physicians’ reimbursement has remained flat while other service providers, such as those in skilled nursing facilities and hospitals, have received favorable payment increases compared to practice cost inflation and the Consumer Price Index.4
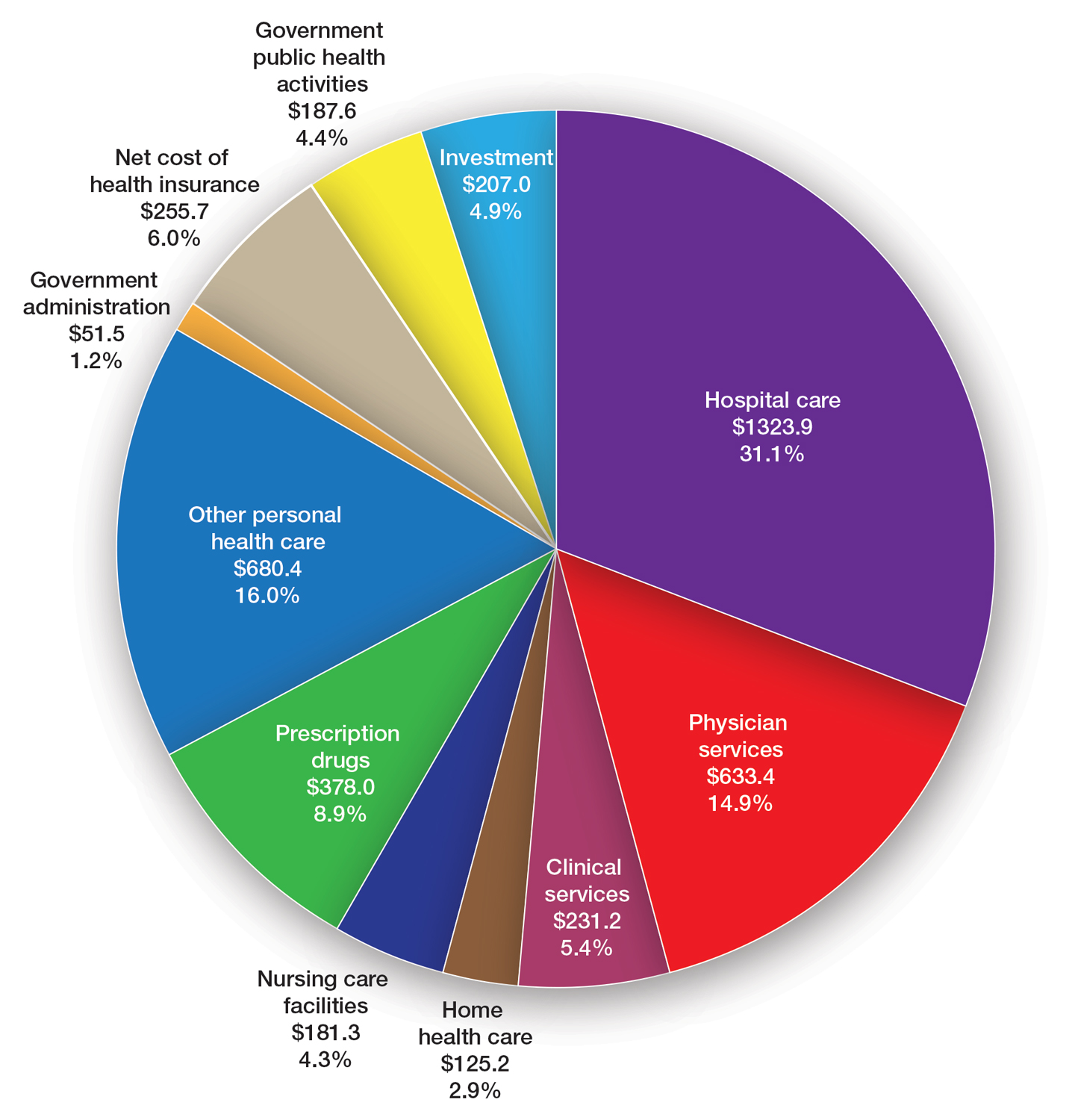
The CMS will not incorporate 2017 MEI cost weights for the RVUs in the MPFS rate setting for 2024 because all key measures of practice expenses in the MEI accelerated in 2022. Instead, the CMS is updating data on practice expense per hour to calculate payment for physician services with a survey for physician practices that launched on July 31, 2023.5 The American Medical Association contracted with Mathematica, an independent research company, to conduct a physician practice information survey that will be used to determine indirect practice expenses. Physicians should be on the lookout for emails regarding completion of these surveys and the appropriate financial expert in their practice should be contacted so the responses are accurate, as these data are key to future updates in the Medicare pay formula used to reimburse physicians.
Impact of Medicare Cuts
The recent congressional debt limit deal set spending caps for the next 2 fiscal years. Dermatology is facing an overall payment reduction of 1.87% (range, 1%–4%).2,3 The impact will depend on the services offered in an individual practice; for example, payment for a punch biopsy (Current Procedural Terminology [CPT] code 11104) would decrease by 3.9%. Payment for benign destruction (CPT code 17110) would decrease by 2.8%, and payment for even simple E/M of an established patient (CPT code 99213) would decrease by 1.6%. Overall, there would be a reduction of 2.75% for dermatopathology services, with a decrease of 2% for CPT code 88305 global and decreases for the technical component of 1% and professional component of 3%.2,3
Medicare cuts have reached a critical level, and physicians cannot continue to absorb the costs to own and operate their practices.4 This has led to health market consolidation, which in turn limits competition and patient access while driving up health care costs and driving down the quality of care. Small independent rural practices as well as those caring for historically marginalized patients will be disproportionately affected.
Proposed Addition of E/M Code G2211
In the calendar year (CY) 2021 final rule, the CMS tried to adopt a new add-on code—G2211—patients with a serious or complex condition that typically require referral and coordination of multispecialty care. Per the CMS, the primary policy goal of G2211 is to increase payments to primary care physicians and to reimburse them more appropriately for the care provided to patients with a serious or complex condition.2,3 It can be reported in conjunction with all office and outpatient E/M visits to better account for additional resources associated with primary care, or similarly ongoing medical care related to a patient’s single, serious condition, or complex condition.3 Typically, G2211 would not be used by dermatologists, as this add-on code requires visit complexity inherent to E/M associated with medical care services that serve as the continuing focal point for all needed health care services and/or with medical care services that are part of ongoing care related to a patient’s single serious condition or a complex condition.2,3
Initially, the CMS assumed that G2211 would be reported with 90% of all office and outpatient E/M visit claims, which would account for a considerable portion of total MPFS schedule spending; however, the House of Medicine disagreed and believed it would be 75%.2,3 Given the extremely high utilization estimate, G2211 would have had a substantial effect on budget neutrality, accounting for an estimated increase of $3.3 billion and a corresponding 3.0% cut to the CY 2021 MPFS. Because of the potential payment reductions to physicians and a successful advocacy effort by organized medicine, including the American Academy of Dermatology Association (AADA), Congress delayed implementation of G2211 until CY 2024. Modifier -25 cannot be reported with G2211. The CMS revised its utilization assumptions from 90% of all E/M services to an initial utilization of 38% and then 54% when fully adopted. The proposed 2024 payment for G2211 is an additional $16.05.2,3
Advancing Health Equity With Healthcare Common Procedure Coding System G Codes
The CMS is proposing coding and payment for several new services to help underserved populations, including addressing unmet health-related social needs that can potentially interfere with the diagnosis and treatment of medical conditions, which includes paying for certain caregiver training services as well as payment for community health integration services.2,3 These are the first MPFS services designed to include care involving community health workers, who link underserved communities with critical health care and social services in the community. Additionally, the rule also proposes coding and payment for evaluating the risks related to social factors that affect a patient’s health, such as access to affordable quality health care, that can take place during an annual wellness visit or in combination with an E/M visit.2,3 As dermatologists, we should be familiar with this set of G codes, as we will likely use them in practice for patients with transportation needs.
Advocacy Efforts on Medicare Payment Reform
Medicare physician payment reform needs to happen at a national level. Advocacy efforts by the AADA and other groups have been underway to mitigate the proposed 2024 cuts. The Strengthening Medicare for Patients and Providers Act (HR 2474) is a bill that was introduced by a bipartisan coalition of physicians to provide an inflation-based increase in Medicare payments in 2024 and beyond.6
Other Legislative Updates Affecting Dermatology
Modifier -25—Cigna’s policy requiring dermatologists to submit documentation to use modifier -25 when billing with E/M CPT codes 99212 through 99215 has been delayed indefinitely.7 If a payer denies a dermatologist payment, contact the AADA Patient Access and Payer Relations committee ([email protected]) for assistance.
Telehealth and Digital Pathology—Recent legislation authorized extension of many of the Medicare telehealth and digital pathology flexibilities that were put in place during the COVID-19 public health emergency through December 31, 2024.8,9 Seventeen newly approved CPT telemedicine codes for new and established patient audio-visual and audio-only visits recently were surveyed.2,3 The data from the survey will be used as a key element in assigning a specific RVU to the CMS and will be included in the MPFS.
Thirty additional new digital pathology add-on CPT category III codes for 2024 were added to the ones from 2023.2,3 These codes can be used to report additional clinical staff work and service requirements associated with digitizing glass microscope slides for primary diagnosis. They cannot be used for archival or educational purposes, clinical conferences, training, or validating artificial intelligence algorithms. Category III codes used for emerging technologies have no assigned RVUs or reimbursement.2,3
The Cures Act—The Cures Act aims to ensure that patients have timely access to their health information.10 It requires all physicians to make their office notes, laboratory results, and other diagnostic reports available to patients as soon as the office receives them. The rules went into effect on April 5, 2021, with a limited definition of electronic health information; on October 6, 2022, the Cures Act rule expanded to include all electronic health information. The AADA has urged the Office of the National Coordinator for Health Information Technology to collaborate with stakeholder organizations to re-evaluate federal policies concerning the immediate release of electronic health information and information blocking, particularly in cases with life-altering diagnoses.10 They stressed the importance of prioritizing the well-being and emotional stability of patients and enhancing care by providing patients adequate time and support to process, comprehend, and discuss findings with their physician.
Proposed 2024 Medicare Quality Payment Program Requirements
The CMS proposed to increase the performance threshold in the quality payment program from 75 to 82 points for the 2024 Merit-based Incentive Payment System (MIPS) performance period, impacting the 2026 payment year.2,3,11 As a result of this increase, there could be more MIPS-eligible clinicians receiving penalties, which could be a reduction of up to 9%. The AADA will firmly oppose any increase in the threshold and strongly urge CMS to maintain the 75-point threshold. The performance category weights for the 2024 performance year will remain unchanged from the 2023 performance year.2,3,11
2024 Proposed Quality MIPS Measures Set—The CMS proposed to remove the topped-out MIPS measure 138 (coordination of care for melanoma).2,3,11 Additionally, it proposed to remove MIPS measure 402 (tobacco use and help with quitting among adolescents) as a quality measure from MIPS because the agency believes it is duplicative of measure 226 (preventive care and screening: tobacco use: screening and cessation intervention).2,3,11
MIPS Value Pathways—The CMS consolidated 2 previously established MIPS value pathways (MVPs): the Promoting Wellness MVP and the Optimizing Chronic Disease Management MVP.2,3,11 Proposed new MVPs for 2024 include Focusing on Women’s Health; Quality Care for the Treatment of Ear, Nose, and Throat Disorders; Prevention and Treatment of Infectious Disorders Including Hepatitis C and HIV; Quality Care in Mental Health and Substance Use Disorders; and Rehabilitative Support for Musculoskeletal Care. Dermatology is not impacted; however, the CMS plans to sunset traditional MIPS and replace it with MVPs—the future of MIPS.2,3,11 The AADA maintains that traditional MIPS should continue to be an option because MVPs have a limited number of measures for dermatologists.
Update on Reporting Suture Removal
There are 2 new CPT add-on codes—15853 and 15854—for the removal of sutures or staples not requiring anesthesia to be listed separately in addition to an appropriate E/M service. These add-on codes went into effect on January 1, 2023.12 These codes were created with the intent to capture and ensure remuneration for practice expenses that are not included in a stand-alone E/M encounter that occur after a 0-day procedure (eg, services reported with CPT codes 11102–11107 and 11300–11313) for wound check and suture removal where appropriate. These new add-on codes do not have physician work RVUs assigned to them because they are only for practice expenses (eg, clinical staff time, disposable supplies, use of equipment); CPT code 15853 is reported for the removal of sutures or staples, and CPT code 15854 is reported when both sutures and staples are removed. These codes can only be reported if an E/M service also is reported for the patient encounter.12
Final Thoughts
The AADA is working with the House of Medicine and the medical specialty community to develop specific proposals to reform the Medicare payment system.4 The proposed 2024 MPFS was released on July 13, 2023, and final regulations are expected in the late fall of 2023. The AADA will continue to engage with the CMS, but it is important for physicians to learn about and support advocacy priorities and efforts as well as join forces to protect their practices. As health care professionals, we have unique insights into the challenges and needs of our patients and the health care system. Advocacy can take various forms, such as supporting or opposing specific legislations, participating in grassroots campaigns, engaging with policymakers, and/or joining professional organizations that advocate for health care–related issues. Get involved, stay informed, and stay engaged through dermatology medical societies; together we can make a difference.
- Centers for Medicare & Medicaid Services. NHE fact sheet. Updated September 6, 2023. Accessed September 18, 2023. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NHE-Fact-Sheet
- Medicare and Medicaid Programs; CY 2024 payment policies under the physician fee schedule and other changes to part B payment and coverage policies; Medicare shared savings program requirements; Medicare advantage; Medicare and Medicaid provider and supplier enrollment policies; and basic health program. Fed Regist. 2023;88:52262-53197. To be codified at 42 CFR §405, §410, §411, §414, §415, §418, §422, §423, §424, §425, §455, §489, §491, §495, §498, and §600. https://www.federalregister.gov/documents/2023/08/07/2023-14624/medicare-and-medicaid-programs-cy-2024-payment-policies-under-the-physician-fee-schedule-and-other
- Centers for Medicare & Medicaid Services. Calendar year (CY) 2024 Medicare physician fee schedule proposed rule. Published July 13, 2023. Accessed September 18, 2023. https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2024-medicare-physician-fee-schedule-proposed-rule
- American Medical Association. Payment reform. Accessed September 18, 2023. https://www.ama-assn.org/health-care-advocacypayment-reform
- American Medical Association. Physician answers on this survey will shape future Medicare pay. Published July 31, 2023. Accessed September 18, 2023. https://www.ama-assn.org/practice-management/medicare-medicaid/physician-answers-survey-will-shape-future -medicare-pay
- Strengthening Medicare for Patients and Providers Act, HR 2474, 118 Congress (2023-2024). https://www.congress.gov/bill/118th-congress/house-bill/2474
- American Academy of Dermatology Association. Academy advocacy priorities. Accessed September 18, 2023. https://www.aad.org/member/advocacy/priorities
- College of American Pathologists. Remote sign-out of cases with digital pathology FAQs. Accessed September 18, 2023. https://www.cap.org/covid-19/remote-sign-out-faqs
- Centers for Medicare & Medicaid Services. Telehealth. Updated September 6, 2023. Accessed September 18, 2023. https://www.cms.gov/medicare/coverage/telehealth
- The Office of the National Coordinator for Health Information Technology. ONC’s Cures Act final rule. Accessed September 18, 2023. https://www.healthit.gov/topic/oncs-cures-act-final-rule
- Centers for Medicare & Medicaid Services. Calendar Year (CY) 2024 Medicare Physician Fee Schedule (PFS) Notice of Proposed Rule Making Quality Payment Program Policy Overview: Proposals and Requests for Information. Accessed September 12, 2023. https://email.aadresources.org/e3t/Ctc/I6+113/cVKqx04/VVWzj43dDbctW8c23GW1ZLnJHW1xTZ7Q50Y DYN89Qzy5nCVhV3Zsc37CgFV9W5Ck4-D42qs9BW38PtXn4LSlNLW1QKpPL4xT8BMW6Mcwww3FdwCHN3vfGTMXbtF-W2-Zzfy5WHDg6W88tx1F1KgsgxW7zDzT46C2sFXW800vQJ3lLsS_W5D6f1d30-f3cN1njgZ_dX7xkW447ldH2-kgc5VCs7Xg1GY6dsN87pLVJqJG5XW8VWwD-7VxVkJN777f5fJL7jBW8RxkQM1lcSDjVV746T3C-stpN52V_S5xj7q6W3_vldf3p1Yk2Vbd4ZD3cPrHqW5Pwv9m567fkzW1vfDm51H-T7rW1jVrxl8gstXyW5RVTn8863CVFW8g6LgK2YdhpkW34HC4z3_pGYgW8V_qWH3g-tTlW4S3RD-1dKry7W4_rW8d1ssZ1fVwXQjQ9krVMW8Y0bTt8Nr5CNW6vbG0h3wyx59W8WCrNW50p5n6W1r-VBC2rKh93N4W2RyYr7vvm3kxG1
- Centers for Medicare & Medicaid Services. Chapter III surgery: integumentary system CPT codes 10000-19999 for Medicare national correct coding initiative policy manual. Updated January 1, 2023. Accessed September 26, 2023. https://www.cms.gov/files/document/medicare-ncci-policy-manual-2023-chapter-3.pdf
- Centers for Medicare & Medicaid Services. NHE fact sheet. Updated September 6, 2023. Accessed September 18, 2023. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NHE-Fact-Sheet
- Medicare and Medicaid Programs; CY 2024 payment policies under the physician fee schedule and other changes to part B payment and coverage policies; Medicare shared savings program requirements; Medicare advantage; Medicare and Medicaid provider and supplier enrollment policies; and basic health program. Fed Regist. 2023;88:52262-53197. To be codified at 42 CFR §405, §410, §411, §414, §415, §418, §422, §423, §424, §425, §455, §489, §491, §495, §498, and §600. https://www.federalregister.gov/documents/2023/08/07/2023-14624/medicare-and-medicaid-programs-cy-2024-payment-policies-under-the-physician-fee-schedule-and-other
- Centers for Medicare & Medicaid Services. Calendar year (CY) 2024 Medicare physician fee schedule proposed rule. Published July 13, 2023. Accessed September 18, 2023. https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2024-medicare-physician-fee-schedule-proposed-rule
- American Medical Association. Payment reform. Accessed September 18, 2023. https://www.ama-assn.org/health-care-advocacypayment-reform
- American Medical Association. Physician answers on this survey will shape future Medicare pay. Published July 31, 2023. Accessed September 18, 2023. https://www.ama-assn.org/practice-management/medicare-medicaid/physician-answers-survey-will-shape-future -medicare-pay
- Strengthening Medicare for Patients and Providers Act, HR 2474, 118 Congress (2023-2024). https://www.congress.gov/bill/118th-congress/house-bill/2474
- American Academy of Dermatology Association. Academy advocacy priorities. Accessed September 18, 2023. https://www.aad.org/member/advocacy/priorities
- College of American Pathologists. Remote sign-out of cases with digital pathology FAQs. Accessed September 18, 2023. https://www.cap.org/covid-19/remote-sign-out-faqs
- Centers for Medicare & Medicaid Services. Telehealth. Updated September 6, 2023. Accessed September 18, 2023. https://www.cms.gov/medicare/coverage/telehealth
- The Office of the National Coordinator for Health Information Technology. ONC’s Cures Act final rule. Accessed September 18, 2023. https://www.healthit.gov/topic/oncs-cures-act-final-rule
- Centers for Medicare & Medicaid Services. Calendar Year (CY) 2024 Medicare Physician Fee Schedule (PFS) Notice of Proposed Rule Making Quality Payment Program Policy Overview: Proposals and Requests for Information. Accessed September 12, 2023. https://email.aadresources.org/e3t/Ctc/I6+113/cVKqx04/VVWzj43dDbctW8c23GW1ZLnJHW1xTZ7Q50Y DYN89Qzy5nCVhV3Zsc37CgFV9W5Ck4-D42qs9BW38PtXn4LSlNLW1QKpPL4xT8BMW6Mcwww3FdwCHN3vfGTMXbtF-W2-Zzfy5WHDg6W88tx1F1KgsgxW7zDzT46C2sFXW800vQJ3lLsS_W5D6f1d30-f3cN1njgZ_dX7xkW447ldH2-kgc5VCs7Xg1GY6dsN87pLVJqJG5XW8VWwD-7VxVkJN777f5fJL7jBW8RxkQM1lcSDjVV746T3C-stpN52V_S5xj7q6W3_vldf3p1Yk2Vbd4ZD3cPrHqW5Pwv9m567fkzW1vfDm51H-T7rW1jVrxl8gstXyW5RVTn8863CVFW8g6LgK2YdhpkW34HC4z3_pGYgW8V_qWH3g-tTlW4S3RD-1dKry7W4_rW8d1ssZ1fVwXQjQ9krVMW8Y0bTt8Nr5CNW6vbG0h3wyx59W8WCrNW50p5n6W1r-VBC2rKh93N4W2RyYr7vvm3kxG1
- Centers for Medicare & Medicaid Services. Chapter III surgery: integumentary system CPT codes 10000-19999 for Medicare national correct coding initiative policy manual. Updated January 1, 2023. Accessed September 26, 2023. https://www.cms.gov/files/document/medicare-ncci-policy-manual-2023-chapter-3.pdf
PRACTICE POINTS
- The proposed 2024 Medicare physician fee schedule published by the Centers for Medicare & Medicaid Services in July 2023 will negatively impact dermatology practices.
- The final regulations are expected in November 2023.
New York GI advocates for team approach in GI care
“I was a little kid, so I wasn’t helping him,” but he said he learned a great deal by sitting in the hallways and listening to his father talk to patients. “I could clearly hear the human suffering on the other side.”
This experience had a big impact on Dr. Berry, who continues the family trade. Like his father, talking with patients about their condition is his favorite part of the job, but especially talking about the role of diet, lifestyle, and stress on GI health, said Dr. Berry, who is a gastroenterologist and clinical assistant professor of medicine at New York University’s Grossman School of Medicine.
In addition to his clinical practice, Dr.Berry serves as the co-founder & chief medical officer at Oshi Health. Oshi is an integrative healthcare clinic that is entirely virtual and entirely and solely about GI health. The clinic works with GI clinicians and other healthcare providers, allowing patients access to multidisciplinary care that has proven to reduce healthcare costs and improve patient outcomes. The company was recently named a recipient of funding through the American College of Gastroenterology and the American Gastroenterological Association’s Center for GI Innovation & Technology’s GI Opportunity Fund.
The Oshi model is a whole-person, multidisciplinary GI care model, which includes traditional medical care for GI conditions but also provides access to health coaching, nutrition and diet support, and behavioral and mental health services. Research shows the approach is effective in mitigating symptoms. A 2020 randomized controlled trial published in Lancet Gastroenterology and Hepatology demonstrated that integrated multidisciplinary care led to improvement in symptoms, quality of life, and cost of care for complex GI conditions, as compared with the traditional GI specialist care model. Numerous similar studies have found that integrated care teams were better equipped to meet the needs of patients with inflammatory bowel disease (IBD) and patients with disorders of gut-brain interaction (DGBIs), patient outcomes and satisfaction were better, overall direct and indirect costs were lower and psychological health needs better addressed.
Q: What was the inspiration behind Oshi Health?
Dr. Berry: Gastroenterologists continue to witness unnecessary patient suffering due to antiquated care delivery models and perverse incentives in our healthcare system. Oshi’s care model was designed to align incentives and provide patients with access to clinicians who are traditionally not reimbursed in fee-for-service healthcare while also helping GI practices provide this care to their patients. During my clinical training it was easy for me to order expensive and invasive testing for my patients, but very difficult for me to get them the multidisciplinary care they needed. Many of the patients I would see didn’t need more MRIs, CT scans, or expensive medications. They needed access to a team of clinicians to help with all the aspects of GI care, including diet, behavioral, and medical.
Q: Why is multidisciplinary care the right approach?
Dr. Berry: GI is a very complex field with many nuances that can impact a patient’s symptoms. As physicians, our role is now evolving to oversee a team of clinicians working together to maximize expertise in nutrition and the gut-brain axis. With these new multidisciplinary care models, GI practices can expand their capabilities. At Oshi Health, every single patient has access to a nurse practitioner, dietician, psychologist, and health coach — all overseen by a gastroenterologist — as a covered benefit through their health plan. Providing multidisciplinary care through a virtual-first model solves some of the scalability challenges of these intensive care models and can significantly improve access to care.
Q: What grant-funded clinical research are you doing right now?
Dr. Berry: Most of my research focuses on evaluating the impact of novel care delivery models in GI and the evaluation of digital technologies in GI and how we can incorporate those digital technologies into clinical practice. How can we determine what type of care can be done remotely via video visits? What can be done on the phone or via text messaging? How can we get these new services paid for so patients can reap the benefits of seeing their doctor more frequently?
Q: What teacher or mentor had the greatest impact on you?
Dr. Berry: Dr. John Allen, MD, MBA has had an incredible impact on my career. He’s the former president of the American Gastroenterological Association, and was the chief clinical officer and a professor at the University of Michigan. He’s one of the rare GI doctors that has both a strong clinical and leadership role in GI. I can’t thank him enough for planting the seeds to encourage me to focus on improving the ways we deliver care to patients.
Q: Describe how you would spend a free Saturday afternoon.
Dr. Berry: Roaming around and exploring a new neighborhood either in New York City or anywhere in the world. If I wasn’t going to be a doctor, I’d probably be an anthropologist. I love observing people in their element, and exploring new neighborhoods that are off the beaten path is a great way to do that.
Lightning round! Do you prefer texting or talking?
Texting
What’s high on your list of travel destinations?
Antarctica
Where was your most memorable vacation?
Patagonia
How many cups of coffee do you drink daily?
Four
What’s your favorite holiday?
Halloween
What’s your favorite junk food?
In-N-Out Burger
If you weren’t a gastroenterologist, what would you be?
Anthropologist
“I was a little kid, so I wasn’t helping him,” but he said he learned a great deal by sitting in the hallways and listening to his father talk to patients. “I could clearly hear the human suffering on the other side.”
This experience had a big impact on Dr. Berry, who continues the family trade. Like his father, talking with patients about their condition is his favorite part of the job, but especially talking about the role of diet, lifestyle, and stress on GI health, said Dr. Berry, who is a gastroenterologist and clinical assistant professor of medicine at New York University’s Grossman School of Medicine.
In addition to his clinical practice, Dr.Berry serves as the co-founder & chief medical officer at Oshi Health. Oshi is an integrative healthcare clinic that is entirely virtual and entirely and solely about GI health. The clinic works with GI clinicians and other healthcare providers, allowing patients access to multidisciplinary care that has proven to reduce healthcare costs and improve patient outcomes. The company was recently named a recipient of funding through the American College of Gastroenterology and the American Gastroenterological Association’s Center for GI Innovation & Technology’s GI Opportunity Fund.
The Oshi model is a whole-person, multidisciplinary GI care model, which includes traditional medical care for GI conditions but also provides access to health coaching, nutrition and diet support, and behavioral and mental health services. Research shows the approach is effective in mitigating symptoms. A 2020 randomized controlled trial published in Lancet Gastroenterology and Hepatology demonstrated that integrated multidisciplinary care led to improvement in symptoms, quality of life, and cost of care for complex GI conditions, as compared with the traditional GI specialist care model. Numerous similar studies have found that integrated care teams were better equipped to meet the needs of patients with inflammatory bowel disease (IBD) and patients with disorders of gut-brain interaction (DGBIs), patient outcomes and satisfaction were better, overall direct and indirect costs were lower and psychological health needs better addressed.
Q: What was the inspiration behind Oshi Health?
Dr. Berry: Gastroenterologists continue to witness unnecessary patient suffering due to antiquated care delivery models and perverse incentives in our healthcare system. Oshi’s care model was designed to align incentives and provide patients with access to clinicians who are traditionally not reimbursed in fee-for-service healthcare while also helping GI practices provide this care to their patients. During my clinical training it was easy for me to order expensive and invasive testing for my patients, but very difficult for me to get them the multidisciplinary care they needed. Many of the patients I would see didn’t need more MRIs, CT scans, or expensive medications. They needed access to a team of clinicians to help with all the aspects of GI care, including diet, behavioral, and medical.
Q: Why is multidisciplinary care the right approach?
Dr. Berry: GI is a very complex field with many nuances that can impact a patient’s symptoms. As physicians, our role is now evolving to oversee a team of clinicians working together to maximize expertise in nutrition and the gut-brain axis. With these new multidisciplinary care models, GI practices can expand their capabilities. At Oshi Health, every single patient has access to a nurse practitioner, dietician, psychologist, and health coach — all overseen by a gastroenterologist — as a covered benefit through their health plan. Providing multidisciplinary care through a virtual-first model solves some of the scalability challenges of these intensive care models and can significantly improve access to care.
Q: What grant-funded clinical research are you doing right now?
Dr. Berry: Most of my research focuses on evaluating the impact of novel care delivery models in GI and the evaluation of digital technologies in GI and how we can incorporate those digital technologies into clinical practice. How can we determine what type of care can be done remotely via video visits? What can be done on the phone or via text messaging? How can we get these new services paid for so patients can reap the benefits of seeing their doctor more frequently?
Q: What teacher or mentor had the greatest impact on you?
Dr. Berry: Dr. John Allen, MD, MBA has had an incredible impact on my career. He’s the former president of the American Gastroenterological Association, and was the chief clinical officer and a professor at the University of Michigan. He’s one of the rare GI doctors that has both a strong clinical and leadership role in GI. I can’t thank him enough for planting the seeds to encourage me to focus on improving the ways we deliver care to patients.
Q: Describe how you would spend a free Saturday afternoon.
Dr. Berry: Roaming around and exploring a new neighborhood either in New York City or anywhere in the world. If I wasn’t going to be a doctor, I’d probably be an anthropologist. I love observing people in their element, and exploring new neighborhoods that are off the beaten path is a great way to do that.
Lightning round! Do you prefer texting or talking?
Texting
What’s high on your list of travel destinations?
Antarctica
Where was your most memorable vacation?
Patagonia
How many cups of coffee do you drink daily?
Four
What’s your favorite holiday?
Halloween
What’s your favorite junk food?
In-N-Out Burger
If you weren’t a gastroenterologist, what would you be?
Anthropologist
“I was a little kid, so I wasn’t helping him,” but he said he learned a great deal by sitting in the hallways and listening to his father talk to patients. “I could clearly hear the human suffering on the other side.”
This experience had a big impact on Dr. Berry, who continues the family trade. Like his father, talking with patients about their condition is his favorite part of the job, but especially talking about the role of diet, lifestyle, and stress on GI health, said Dr. Berry, who is a gastroenterologist and clinical assistant professor of medicine at New York University’s Grossman School of Medicine.
In addition to his clinical practice, Dr.Berry serves as the co-founder & chief medical officer at Oshi Health. Oshi is an integrative healthcare clinic that is entirely virtual and entirely and solely about GI health. The clinic works with GI clinicians and other healthcare providers, allowing patients access to multidisciplinary care that has proven to reduce healthcare costs and improve patient outcomes. The company was recently named a recipient of funding through the American College of Gastroenterology and the American Gastroenterological Association’s Center for GI Innovation & Technology’s GI Opportunity Fund.
The Oshi model is a whole-person, multidisciplinary GI care model, which includes traditional medical care for GI conditions but also provides access to health coaching, nutrition and diet support, and behavioral and mental health services. Research shows the approach is effective in mitigating symptoms. A 2020 randomized controlled trial published in Lancet Gastroenterology and Hepatology demonstrated that integrated multidisciplinary care led to improvement in symptoms, quality of life, and cost of care for complex GI conditions, as compared with the traditional GI specialist care model. Numerous similar studies have found that integrated care teams were better equipped to meet the needs of patients with inflammatory bowel disease (IBD) and patients with disorders of gut-brain interaction (DGBIs), patient outcomes and satisfaction were better, overall direct and indirect costs were lower and psychological health needs better addressed.
Q: What was the inspiration behind Oshi Health?
Dr. Berry: Gastroenterologists continue to witness unnecessary patient suffering due to antiquated care delivery models and perverse incentives in our healthcare system. Oshi’s care model was designed to align incentives and provide patients with access to clinicians who are traditionally not reimbursed in fee-for-service healthcare while also helping GI practices provide this care to their patients. During my clinical training it was easy for me to order expensive and invasive testing for my patients, but very difficult for me to get them the multidisciplinary care they needed. Many of the patients I would see didn’t need more MRIs, CT scans, or expensive medications. They needed access to a team of clinicians to help with all the aspects of GI care, including diet, behavioral, and medical.
Q: Why is multidisciplinary care the right approach?
Dr. Berry: GI is a very complex field with many nuances that can impact a patient’s symptoms. As physicians, our role is now evolving to oversee a team of clinicians working together to maximize expertise in nutrition and the gut-brain axis. With these new multidisciplinary care models, GI practices can expand their capabilities. At Oshi Health, every single patient has access to a nurse practitioner, dietician, psychologist, and health coach — all overseen by a gastroenterologist — as a covered benefit through their health plan. Providing multidisciplinary care through a virtual-first model solves some of the scalability challenges of these intensive care models and can significantly improve access to care.
Q: What grant-funded clinical research are you doing right now?
Dr. Berry: Most of my research focuses on evaluating the impact of novel care delivery models in GI and the evaluation of digital technologies in GI and how we can incorporate those digital technologies into clinical practice. How can we determine what type of care can be done remotely via video visits? What can be done on the phone or via text messaging? How can we get these new services paid for so patients can reap the benefits of seeing their doctor more frequently?
Q: What teacher or mentor had the greatest impact on you?
Dr. Berry: Dr. John Allen, MD, MBA has had an incredible impact on my career. He’s the former president of the American Gastroenterological Association, and was the chief clinical officer and a professor at the University of Michigan. He’s one of the rare GI doctors that has both a strong clinical and leadership role in GI. I can’t thank him enough for planting the seeds to encourage me to focus on improving the ways we deliver care to patients.
Q: Describe how you would spend a free Saturday afternoon.
Dr. Berry: Roaming around and exploring a new neighborhood either in New York City or anywhere in the world. If I wasn’t going to be a doctor, I’d probably be an anthropologist. I love observing people in their element, and exploring new neighborhoods that are off the beaten path is a great way to do that.
Lightning round! Do you prefer texting or talking?
Texting
What’s high on your list of travel destinations?
Antarctica
Where was your most memorable vacation?
Patagonia
How many cups of coffee do you drink daily?
Four
What’s your favorite holiday?
Halloween
What’s your favorite junk food?
In-N-Out Burger
If you weren’t a gastroenterologist, what would you be?
Anthropologist
ACP addresses ethical issues for ‘grateful patients’ physician fundraising
Patients sometimes want to give back to their physician or hospital. In recent years, the practice of soliciting donations from these patients has grown into structured fundraising initiatives at some health care organizations. Some employers mandate clinicians solicit donations, while other doctors participate voluntarily.
“In recent decades, more physician practices have become part of large health systems: these arrangements can offer benefits to care but can also lead to interference in the patient-physician relationship and challenges to the physician’s ethical responsibilities to patients,” said Omar T. Atiq, MD, president of the American College of Physicians.
Grateful patient fundraising (GPF) is largely based on models of charitable giving outside of health care and is relatively new to the industry. Simply defined, it is the solicitation of donations by doctors from current and former patients. Funds may be used for operating costs, clinical research, equipment upgrades, or facility improvements.
In a newly published position paper, the ACP, which represents roughly 161,000 physicians, is clear that clinicians should not try to convert their patients into donors.
“Physicians who directly solicit funds from their own patients do risk interfering with the physician-patient relationship, which is supposed to be based on the patient’s best interests, not the physicians’ interests,” said Stacey A. Tovino, JD, PhD, director of health care law programs at the University of Oklahoma, Norman.
Once involved in fundraising, patients may also develop an unrealistic expectation of what kind of care they should receive, according to the ACP.
Another pitfall clinicians may fall into is the HIPAA Privacy Rule. In 2013, HIPAA was expanded to allow hospital fundraisers to access privileged health information, including demographic, health insurance, treating clinician, and data on outcomes. Dr. Atiq said that, since then, electronic health records have been used as tools to aide fundraising efforts. For instance, some health care organizations have embedded a feature inside EHRs to allow physicians to flag development officers when a patient or family member might be a potential donor.
Patients may be unaware that hospital fundraising departments have access to their electronic health records, or that they have the right to opt out of fundraising solicitations.
“Physicians should not use or reveal patient information for fundraising,” Dr. Atiq said. “Even acknowledging that a person is under one’s care can make it possible for protected health information to be revealed.”
Data-mining EHRs may be legal, Ms. Tovino said, but it hugs a fine ethical line.
“A patient may not expect that their information will be used for these purposes and may not know how to opt out of having their information used in these ways,” Ms. Tovino said.
A clinician’s employment contract, whether it be a full-time position or for specific admitting privileges, may make it hard for them to push back against expectations to ask patients for money or screen for donors. Metrics or expectations to approach potential donors create ethical snares for clinicians – and it pits them between their patient and place of employment.
“GPF does raise ethical concerns, including those surrounding confidentiality and privacy, and whether physicians are being remunerated or evaluated based on their participation,” Ms. Tovino said.
Asked how doctors can avoid being involved in GPF, Dr. Atiq referred to the ACP ethics manual, which separates clinicians from fundraising.
“Redirecting the patient to discuss donations with institutional administrators provides the appropriate venue and firewall,” he said.
An author of the ACP paper reported a paid position on the board of the Government Employees Health Association.
A version of this article first appeared on Medscape.com.
Patients sometimes want to give back to their physician or hospital. In recent years, the practice of soliciting donations from these patients has grown into structured fundraising initiatives at some health care organizations. Some employers mandate clinicians solicit donations, while other doctors participate voluntarily.
“In recent decades, more physician practices have become part of large health systems: these arrangements can offer benefits to care but can also lead to interference in the patient-physician relationship and challenges to the physician’s ethical responsibilities to patients,” said Omar T. Atiq, MD, president of the American College of Physicians.
Grateful patient fundraising (GPF) is largely based on models of charitable giving outside of health care and is relatively new to the industry. Simply defined, it is the solicitation of donations by doctors from current and former patients. Funds may be used for operating costs, clinical research, equipment upgrades, or facility improvements.
In a newly published position paper, the ACP, which represents roughly 161,000 physicians, is clear that clinicians should not try to convert their patients into donors.
“Physicians who directly solicit funds from their own patients do risk interfering with the physician-patient relationship, which is supposed to be based on the patient’s best interests, not the physicians’ interests,” said Stacey A. Tovino, JD, PhD, director of health care law programs at the University of Oklahoma, Norman.
Once involved in fundraising, patients may also develop an unrealistic expectation of what kind of care they should receive, according to the ACP.
Another pitfall clinicians may fall into is the HIPAA Privacy Rule. In 2013, HIPAA was expanded to allow hospital fundraisers to access privileged health information, including demographic, health insurance, treating clinician, and data on outcomes. Dr. Atiq said that, since then, electronic health records have been used as tools to aide fundraising efforts. For instance, some health care organizations have embedded a feature inside EHRs to allow physicians to flag development officers when a patient or family member might be a potential donor.
Patients may be unaware that hospital fundraising departments have access to their electronic health records, or that they have the right to opt out of fundraising solicitations.
“Physicians should not use or reveal patient information for fundraising,” Dr. Atiq said. “Even acknowledging that a person is under one’s care can make it possible for protected health information to be revealed.”
Data-mining EHRs may be legal, Ms. Tovino said, but it hugs a fine ethical line.
“A patient may not expect that their information will be used for these purposes and may not know how to opt out of having their information used in these ways,” Ms. Tovino said.
A clinician’s employment contract, whether it be a full-time position or for specific admitting privileges, may make it hard for them to push back against expectations to ask patients for money or screen for donors. Metrics or expectations to approach potential donors create ethical snares for clinicians – and it pits them between their patient and place of employment.
“GPF does raise ethical concerns, including those surrounding confidentiality and privacy, and whether physicians are being remunerated or evaluated based on their participation,” Ms. Tovino said.
Asked how doctors can avoid being involved in GPF, Dr. Atiq referred to the ACP ethics manual, which separates clinicians from fundraising.
“Redirecting the patient to discuss donations with institutional administrators provides the appropriate venue and firewall,” he said.
An author of the ACP paper reported a paid position on the board of the Government Employees Health Association.
A version of this article first appeared on Medscape.com.
Patients sometimes want to give back to their physician or hospital. In recent years, the practice of soliciting donations from these patients has grown into structured fundraising initiatives at some health care organizations. Some employers mandate clinicians solicit donations, while other doctors participate voluntarily.
“In recent decades, more physician practices have become part of large health systems: these arrangements can offer benefits to care but can also lead to interference in the patient-physician relationship and challenges to the physician’s ethical responsibilities to patients,” said Omar T. Atiq, MD, president of the American College of Physicians.
Grateful patient fundraising (GPF) is largely based on models of charitable giving outside of health care and is relatively new to the industry. Simply defined, it is the solicitation of donations by doctors from current and former patients. Funds may be used for operating costs, clinical research, equipment upgrades, or facility improvements.
In a newly published position paper, the ACP, which represents roughly 161,000 physicians, is clear that clinicians should not try to convert their patients into donors.
“Physicians who directly solicit funds from their own patients do risk interfering with the physician-patient relationship, which is supposed to be based on the patient’s best interests, not the physicians’ interests,” said Stacey A. Tovino, JD, PhD, director of health care law programs at the University of Oklahoma, Norman.
Once involved in fundraising, patients may also develop an unrealistic expectation of what kind of care they should receive, according to the ACP.
Another pitfall clinicians may fall into is the HIPAA Privacy Rule. In 2013, HIPAA was expanded to allow hospital fundraisers to access privileged health information, including demographic, health insurance, treating clinician, and data on outcomes. Dr. Atiq said that, since then, electronic health records have been used as tools to aide fundraising efforts. For instance, some health care organizations have embedded a feature inside EHRs to allow physicians to flag development officers when a patient or family member might be a potential donor.
Patients may be unaware that hospital fundraising departments have access to their electronic health records, or that they have the right to opt out of fundraising solicitations.
“Physicians should not use or reveal patient information for fundraising,” Dr. Atiq said. “Even acknowledging that a person is under one’s care can make it possible for protected health information to be revealed.”
Data-mining EHRs may be legal, Ms. Tovino said, but it hugs a fine ethical line.
“A patient may not expect that their information will be used for these purposes and may not know how to opt out of having their information used in these ways,” Ms. Tovino said.
A clinician’s employment contract, whether it be a full-time position or for specific admitting privileges, may make it hard for them to push back against expectations to ask patients for money or screen for donors. Metrics or expectations to approach potential donors create ethical snares for clinicians – and it pits them between their patient and place of employment.
“GPF does raise ethical concerns, including those surrounding confidentiality and privacy, and whether physicians are being remunerated or evaluated based on their participation,” Ms. Tovino said.
Asked how doctors can avoid being involved in GPF, Dr. Atiq referred to the ACP ethics manual, which separates clinicians from fundraising.
“Redirecting the patient to discuss donations with institutional administrators provides the appropriate venue and firewall,” he said.
An author of the ACP paper reported a paid position on the board of the Government Employees Health Association.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
How to get paid if your patient passes on
The death of a patient comes with many challenges for physicians, including a range of emotional and professional issues. Beyond those concerns,
“When a patient passes away, obviously there is, unfortunately, a lot of paperwork and stress for families, and it’s a very difficult situation,” says Shikha Jain, MD, an oncologist and associate professor of medicine at the University of Illinois at Chicago. “Talking about finances in that moment can be difficult and uncomfortable, and one thing I’d recommend is that the physicians themselves not get involved.”
Instead, Dr. Jain said, someone in the billing department in the practice or the hospital should take a lead on dealing with any outstanding debts.
“That doctor-patient relationship is a very precious relationship, so you don’t want to mix that financial aspect of providing care with the doctor-patient relationship,” Dr. Jain said. “That’s one thing that’s really important.”
The best approach in such situations is for practices to have a standing policy in place that dictates how to handle bills once a patient has died.
In most cases, the executor of the patient’s will must inform all creditors, including doctors, that the decedent has died, but sometimes there’s a delay.
Hoping the doctor’s office writes it off
“Even though the person in charge of the estate is supposed to contact the doctor’s office and let them know when a patient has passed, that doesn’t always happen,” says Hope Wen, head of billing at practice management platform Soundry Health. “It can be very challenging to track down that information, and sometimes they’re just crossing their fingers hoping that the doctor’s office will just write off the balance, which they often do.”
Some offices use a service that compares accounts receivable lists to Social Security death files and state records to identify deaths more quickly. Some physicians might also use a debt collection agency or an attorney who has experience collecting decedent debts and dealing with executors and probate courts.
Once the practice becomes aware that a patient has died, it can no longer send communications to the name and address on file, although it can continue to go through the billing process with the insurer for any bills incurred up to the date of the death.
At that point, the estate becomes responsible for the debt, and all communication must go to the executor of the estate (in some states, this might be called a personal representative). The office can reach out to any contacts on file to see if they are able to identify the executor.
“You want to do that in a compassionate way,” says Jack Brown III, JD, MBA, president of Gulf Coast Collection Bureau. “You’ll tell them you’re sorry for their loss, but you’re wondering who is responsible for the estate. Once you’ve identified that person and gotten their letter of administration from the probate court or a power of attorney, then you can speak with that person as if they were the patient.”
The names of executors are also public record and are available through the probate court (sometimes called the surrogate court) in the county where the decedent lived.
“Even if there’s no will or no executive named, the court will appoint an administrator for the estate, which is usually a family member,” said Robert Bernstein, an estate lawyer in Parsippany, N.J. “Their information will be on file in the court.”
Insurance coverage
Typically, insurance will pay for treatment (after deductibles and copays) up until the date of the patient’s death. But, of course, it can take months for some insurance companies to make their final payments, allowing physicians to know exactly how much they’re owed by that estate. In such cases, it’s important for physicians to know the rules in the decedent’s state for how long they have to file a claim.
Most states require that claims occur within 6-9 months of the person’s death. However, in some states, claimants can continue to file for much longer if the estate has not yet paid out all of its assets.
“Sometimes there is real estate to sell or a business to wind down, and it can take years for the estate to distribute all of the assets,” Mr. Bernstein says. “If it’s a year later and they still haven’t distributed the assets, the physician can still file the claim and should be paid.”
In some cases, especially if the decedent received compassionate, quality care, their family will want to make good on any outstanding debts to the health care providers who took care of their loved ones in their final days. In other cases, especially when a family member has had a long illness, their assets have been depleted over time or were transferred to other family members so that there is little left in the estate itself when the patient dies.
Regardless of other circumstances, the estate alone is responsible for such payments, and family members, including spouses and children, typically have no liability. (Though rarely enforced, some states do have filial responsibility laws that could hold children responsible for their parents’ debts, including unpaid medical bills. In addition, states with community property laws might require a surviving spouse to cover their partner’s debt, even after death.)
The probate process varies from state to state, but in general, the probate system and the executor will gather all existing assets and then notify all creditors about how to submit a claim. Typically, the claim will need to include information about how much is owed and documentation, such as bills and an explanation of benefits to back up the claim. It should be borne in mind that even those who’ve passed away have privacy protections under the Health Insurance Portability and Accountability Act, so practices must be careful as to how much information they’re sharing through their claim.
Once the estate has received all the claims, the executor will follow a priority of claims, starting with secured creditors. Typically, medical bills, especially those incurred in the last 90 days of the decedent’s life, have priority in the probate process, Mr. Brown says.
How to minimize losses
In that case, the practice would write off the unpaid debt as a business loss. If there are not enough assets in the estate to pay all claims, the executor will follow a state schedule that apportions those assets that are available.
There are some steps that practices can take to protect themselves from incurring such losses. For example, before beginning treatment, practices might consider asking patients to name a guarantor, who will essentially promise to cover any outstanding debts that the patient incurs.
To be binding, the office will need a signature from both the patient and the guarantor. Some offices may also keep a patient credit card number on file with written authorization that they can use to pay bills that are past due, although this payment method would no longer be valid after a patient dies.
While it’s important for all physicians to document and verify the financial information for their patients, oncologists often must consider an additional layer of fiduciary responsibility when it comes to their patients. Ms. Wen suggests that oncology offices check in with insurance companies to determine whether a patient has exhausted their benefits.
“That can happen with cancer patients, depending on how long they’ve been receiving treatment and what type of treatment they’ve been getting,” she said. “Some of the clinical trials, insurance will pay for them, but they’re really expensive and can get toward that max. So knowing where they are with their insurance coverage is big.”
When time is of the essence, some patients will choose to go forward with a treatment before receiving insurance approval. In those cases, the office must have an additional conversation in which the costs of the treatment are discussed. The office should obtain written confirmation of who will pay if the insurer does not, Ms. Wen said. While it’s the patient’s responsibility to keep track of their insurance benefits, oncology practices and hospitals must also exercise due diligence in monitoring the benefits that are available.
“That’s part of their contract with insurance companies if they’re in network, helping patients understand their benefits,” Ms. Wen saids.
It’s also important for practices to keep clear, consistent records to make it easier to identify outstanding bills and the correct contact information for them. If bills had gone unpaid prior to a patient’s death and the office started legal action and received a judgment, that claim would typically go ahead of other creditors’ claims.
Dr. Jain says that some practices might also consider keeping a financial adviser or social worker on staff who can assist patients and their families with understanding their out-of-pocket costs for treatment.
“Financial toxicity in oncology and medical care is a very real problem,” she says. “At the beginning of the relationship, I recommend that my patients get set up with a financial specialist that can help them navigate that aspect, not only when a patient passes away but during the process of receiving treatment, so they’re not shocked by the bills.”
A version of this article first appeared on Medscape.com.
The death of a patient comes with many challenges for physicians, including a range of emotional and professional issues. Beyond those concerns,
“When a patient passes away, obviously there is, unfortunately, a lot of paperwork and stress for families, and it’s a very difficult situation,” says Shikha Jain, MD, an oncologist and associate professor of medicine at the University of Illinois at Chicago. “Talking about finances in that moment can be difficult and uncomfortable, and one thing I’d recommend is that the physicians themselves not get involved.”
Instead, Dr. Jain said, someone in the billing department in the practice or the hospital should take a lead on dealing with any outstanding debts.
“That doctor-patient relationship is a very precious relationship, so you don’t want to mix that financial aspect of providing care with the doctor-patient relationship,” Dr. Jain said. “That’s one thing that’s really important.”
The best approach in such situations is for practices to have a standing policy in place that dictates how to handle bills once a patient has died.
In most cases, the executor of the patient’s will must inform all creditors, including doctors, that the decedent has died, but sometimes there’s a delay.
Hoping the doctor’s office writes it off
“Even though the person in charge of the estate is supposed to contact the doctor’s office and let them know when a patient has passed, that doesn’t always happen,” says Hope Wen, head of billing at practice management platform Soundry Health. “It can be very challenging to track down that information, and sometimes they’re just crossing their fingers hoping that the doctor’s office will just write off the balance, which they often do.”
Some offices use a service that compares accounts receivable lists to Social Security death files and state records to identify deaths more quickly. Some physicians might also use a debt collection agency or an attorney who has experience collecting decedent debts and dealing with executors and probate courts.
Once the practice becomes aware that a patient has died, it can no longer send communications to the name and address on file, although it can continue to go through the billing process with the insurer for any bills incurred up to the date of the death.
At that point, the estate becomes responsible for the debt, and all communication must go to the executor of the estate (in some states, this might be called a personal representative). The office can reach out to any contacts on file to see if they are able to identify the executor.
“You want to do that in a compassionate way,” says Jack Brown III, JD, MBA, president of Gulf Coast Collection Bureau. “You’ll tell them you’re sorry for their loss, but you’re wondering who is responsible for the estate. Once you’ve identified that person and gotten their letter of administration from the probate court or a power of attorney, then you can speak with that person as if they were the patient.”
The names of executors are also public record and are available through the probate court (sometimes called the surrogate court) in the county where the decedent lived.
“Even if there’s no will or no executive named, the court will appoint an administrator for the estate, which is usually a family member,” said Robert Bernstein, an estate lawyer in Parsippany, N.J. “Their information will be on file in the court.”
Insurance coverage
Typically, insurance will pay for treatment (after deductibles and copays) up until the date of the patient’s death. But, of course, it can take months for some insurance companies to make their final payments, allowing physicians to know exactly how much they’re owed by that estate. In such cases, it’s important for physicians to know the rules in the decedent’s state for how long they have to file a claim.
Most states require that claims occur within 6-9 months of the person’s death. However, in some states, claimants can continue to file for much longer if the estate has not yet paid out all of its assets.
“Sometimes there is real estate to sell or a business to wind down, and it can take years for the estate to distribute all of the assets,” Mr. Bernstein says. “If it’s a year later and they still haven’t distributed the assets, the physician can still file the claim and should be paid.”
In some cases, especially if the decedent received compassionate, quality care, their family will want to make good on any outstanding debts to the health care providers who took care of their loved ones in their final days. In other cases, especially when a family member has had a long illness, their assets have been depleted over time or were transferred to other family members so that there is little left in the estate itself when the patient dies.
Regardless of other circumstances, the estate alone is responsible for such payments, and family members, including spouses and children, typically have no liability. (Though rarely enforced, some states do have filial responsibility laws that could hold children responsible for their parents’ debts, including unpaid medical bills. In addition, states with community property laws might require a surviving spouse to cover their partner’s debt, even after death.)
The probate process varies from state to state, but in general, the probate system and the executor will gather all existing assets and then notify all creditors about how to submit a claim. Typically, the claim will need to include information about how much is owed and documentation, such as bills and an explanation of benefits to back up the claim. It should be borne in mind that even those who’ve passed away have privacy protections under the Health Insurance Portability and Accountability Act, so practices must be careful as to how much information they’re sharing through their claim.
Once the estate has received all the claims, the executor will follow a priority of claims, starting with secured creditors. Typically, medical bills, especially those incurred in the last 90 days of the decedent’s life, have priority in the probate process, Mr. Brown says.
How to minimize losses
In that case, the practice would write off the unpaid debt as a business loss. If there are not enough assets in the estate to pay all claims, the executor will follow a state schedule that apportions those assets that are available.
There are some steps that practices can take to protect themselves from incurring such losses. For example, before beginning treatment, practices might consider asking patients to name a guarantor, who will essentially promise to cover any outstanding debts that the patient incurs.
To be binding, the office will need a signature from both the patient and the guarantor. Some offices may also keep a patient credit card number on file with written authorization that they can use to pay bills that are past due, although this payment method would no longer be valid after a patient dies.
While it’s important for all physicians to document and verify the financial information for their patients, oncologists often must consider an additional layer of fiduciary responsibility when it comes to their patients. Ms. Wen suggests that oncology offices check in with insurance companies to determine whether a patient has exhausted their benefits.
“That can happen with cancer patients, depending on how long they’ve been receiving treatment and what type of treatment they’ve been getting,” she said. “Some of the clinical trials, insurance will pay for them, but they’re really expensive and can get toward that max. So knowing where they are with their insurance coverage is big.”
When time is of the essence, some patients will choose to go forward with a treatment before receiving insurance approval. In those cases, the office must have an additional conversation in which the costs of the treatment are discussed. The office should obtain written confirmation of who will pay if the insurer does not, Ms. Wen said. While it’s the patient’s responsibility to keep track of their insurance benefits, oncology practices and hospitals must also exercise due diligence in monitoring the benefits that are available.
“That’s part of their contract with insurance companies if they’re in network, helping patients understand their benefits,” Ms. Wen saids.
It’s also important for practices to keep clear, consistent records to make it easier to identify outstanding bills and the correct contact information for them. If bills had gone unpaid prior to a patient’s death and the office started legal action and received a judgment, that claim would typically go ahead of other creditors’ claims.
Dr. Jain says that some practices might also consider keeping a financial adviser or social worker on staff who can assist patients and their families with understanding their out-of-pocket costs for treatment.
“Financial toxicity in oncology and medical care is a very real problem,” she says. “At the beginning of the relationship, I recommend that my patients get set up with a financial specialist that can help them navigate that aspect, not only when a patient passes away but during the process of receiving treatment, so they’re not shocked by the bills.”
A version of this article first appeared on Medscape.com.
The death of a patient comes with many challenges for physicians, including a range of emotional and professional issues. Beyond those concerns,
“When a patient passes away, obviously there is, unfortunately, a lot of paperwork and stress for families, and it’s a very difficult situation,” says Shikha Jain, MD, an oncologist and associate professor of medicine at the University of Illinois at Chicago. “Talking about finances in that moment can be difficult and uncomfortable, and one thing I’d recommend is that the physicians themselves not get involved.”
Instead, Dr. Jain said, someone in the billing department in the practice or the hospital should take a lead on dealing with any outstanding debts.
“That doctor-patient relationship is a very precious relationship, so you don’t want to mix that financial aspect of providing care with the doctor-patient relationship,” Dr. Jain said. “That’s one thing that’s really important.”
The best approach in such situations is for practices to have a standing policy in place that dictates how to handle bills once a patient has died.
In most cases, the executor of the patient’s will must inform all creditors, including doctors, that the decedent has died, but sometimes there’s a delay.
Hoping the doctor’s office writes it off
“Even though the person in charge of the estate is supposed to contact the doctor’s office and let them know when a patient has passed, that doesn’t always happen,” says Hope Wen, head of billing at practice management platform Soundry Health. “It can be very challenging to track down that information, and sometimes they’re just crossing their fingers hoping that the doctor’s office will just write off the balance, which they often do.”
Some offices use a service that compares accounts receivable lists to Social Security death files and state records to identify deaths more quickly. Some physicians might also use a debt collection agency or an attorney who has experience collecting decedent debts and dealing with executors and probate courts.
Once the practice becomes aware that a patient has died, it can no longer send communications to the name and address on file, although it can continue to go through the billing process with the insurer for any bills incurred up to the date of the death.
At that point, the estate becomes responsible for the debt, and all communication must go to the executor of the estate (in some states, this might be called a personal representative). The office can reach out to any contacts on file to see if they are able to identify the executor.
“You want to do that in a compassionate way,” says Jack Brown III, JD, MBA, president of Gulf Coast Collection Bureau. “You’ll tell them you’re sorry for their loss, but you’re wondering who is responsible for the estate. Once you’ve identified that person and gotten their letter of administration from the probate court or a power of attorney, then you can speak with that person as if they were the patient.”
The names of executors are also public record and are available through the probate court (sometimes called the surrogate court) in the county where the decedent lived.
“Even if there’s no will or no executive named, the court will appoint an administrator for the estate, which is usually a family member,” said Robert Bernstein, an estate lawyer in Parsippany, N.J. “Their information will be on file in the court.”
Insurance coverage
Typically, insurance will pay for treatment (after deductibles and copays) up until the date of the patient’s death. But, of course, it can take months for some insurance companies to make their final payments, allowing physicians to know exactly how much they’re owed by that estate. In such cases, it’s important for physicians to know the rules in the decedent’s state for how long they have to file a claim.
Most states require that claims occur within 6-9 months of the person’s death. However, in some states, claimants can continue to file for much longer if the estate has not yet paid out all of its assets.
“Sometimes there is real estate to sell or a business to wind down, and it can take years for the estate to distribute all of the assets,” Mr. Bernstein says. “If it’s a year later and they still haven’t distributed the assets, the physician can still file the claim and should be paid.”
In some cases, especially if the decedent received compassionate, quality care, their family will want to make good on any outstanding debts to the health care providers who took care of their loved ones in their final days. In other cases, especially when a family member has had a long illness, their assets have been depleted over time or were transferred to other family members so that there is little left in the estate itself when the patient dies.
Regardless of other circumstances, the estate alone is responsible for such payments, and family members, including spouses and children, typically have no liability. (Though rarely enforced, some states do have filial responsibility laws that could hold children responsible for their parents’ debts, including unpaid medical bills. In addition, states with community property laws might require a surviving spouse to cover their partner’s debt, even after death.)
The probate process varies from state to state, but in general, the probate system and the executor will gather all existing assets and then notify all creditors about how to submit a claim. Typically, the claim will need to include information about how much is owed and documentation, such as bills and an explanation of benefits to back up the claim. It should be borne in mind that even those who’ve passed away have privacy protections under the Health Insurance Portability and Accountability Act, so practices must be careful as to how much information they’re sharing through their claim.
Once the estate has received all the claims, the executor will follow a priority of claims, starting with secured creditors. Typically, medical bills, especially those incurred in the last 90 days of the decedent’s life, have priority in the probate process, Mr. Brown says.
How to minimize losses
In that case, the practice would write off the unpaid debt as a business loss. If there are not enough assets in the estate to pay all claims, the executor will follow a state schedule that apportions those assets that are available.
There are some steps that practices can take to protect themselves from incurring such losses. For example, before beginning treatment, practices might consider asking patients to name a guarantor, who will essentially promise to cover any outstanding debts that the patient incurs.
To be binding, the office will need a signature from both the patient and the guarantor. Some offices may also keep a patient credit card number on file with written authorization that they can use to pay bills that are past due, although this payment method would no longer be valid after a patient dies.
While it’s important for all physicians to document and verify the financial information for their patients, oncologists often must consider an additional layer of fiduciary responsibility when it comes to their patients. Ms. Wen suggests that oncology offices check in with insurance companies to determine whether a patient has exhausted their benefits.
“That can happen with cancer patients, depending on how long they’ve been receiving treatment and what type of treatment they’ve been getting,” she said. “Some of the clinical trials, insurance will pay for them, but they’re really expensive and can get toward that max. So knowing where they are with their insurance coverage is big.”
When time is of the essence, some patients will choose to go forward with a treatment before receiving insurance approval. In those cases, the office must have an additional conversation in which the costs of the treatment are discussed. The office should obtain written confirmation of who will pay if the insurer does not, Ms. Wen said. While it’s the patient’s responsibility to keep track of their insurance benefits, oncology practices and hospitals must also exercise due diligence in monitoring the benefits that are available.
“That’s part of their contract with insurance companies if they’re in network, helping patients understand their benefits,” Ms. Wen saids.
It’s also important for practices to keep clear, consistent records to make it easier to identify outstanding bills and the correct contact information for them. If bills had gone unpaid prior to a patient’s death and the office started legal action and received a judgment, that claim would typically go ahead of other creditors’ claims.
Dr. Jain says that some practices might also consider keeping a financial adviser or social worker on staff who can assist patients and their families with understanding their out-of-pocket costs for treatment.
“Financial toxicity in oncology and medical care is a very real problem,” she says. “At the beginning of the relationship, I recommend that my patients get set up with a financial specialist that can help them navigate that aspect, not only when a patient passes away but during the process of receiving treatment, so they’re not shocked by the bills.”
A version of this article first appeared on Medscape.com.
Do you agree with recent authors that patient satisfaction questionnaires should be modified to account for inherent societal biases, such as gender inequality and racism, to improve patient feedback?
[polldaddy:12782738]
[polldaddy:12782738]
[polldaddy:12782738]
Do doctors have a legal right to work from home because of health issues or disability?
A radiologist who claims he was forced to resign after requesting to work from home has settled his discrimination lawsuit with a New York hospital.
Although the case was resolved without a definitive win, legal analysts say the complaint raises important questions about whether some physicians have the right to work from home.
Since the pandemic, employers across the country have become more accepting of professionals working remotely.
Richard Heiden, MD, sued New York City Health and Hospitals in 2020, claiming discrimination and retaliation violations under the American with Disabilities Act (ADA) and the New York State Human Rights Law. Dr. Heiden, who has ulcerative colitis, had asked to work off-site during the start of the pandemic, but the hospital denied his accommodation request. Shortly later, administrators accused Dr. Heiden of poor performance and requested he resign or administrators would terminate him, according to his lawsuit.
Attorneys for New York City Health and Hospitals contended that Dr. Heiden was a poorly performing radiologist who was undergoing a performance review at the time of his accommodation request. The radiologist’s departure was related to the results of the review and had nothing to do with his disability or accommodation request, according to the hospital.
The undisclosed settlement ends a 3-year court battle between Dr. Heiden and the hospital corporation.
In an email, Laura Williams, an attorney for the hospital corporation, said that “the settlement was in the best interest of all parties.”
Dr. Heiden and his attorneys also did not respond to requests for comment.
A critical piece to the puzzle is understanding who is protected under the ADA and is therefore entitled to reasonable accommodations, said Doron Dorfman, JSD, an associate professor at Seton Hall University Law School in Newark, N.J., who focuses on disability law.
A common misconception is that only physicians with a physical disability are “disabled,” he said. However, under the law, a disabled individual is anyone with a physical or mental impairment – including mental illness – that limits major life activities; a person with a history of such impairment; or a person who is perceived by others as having an impairment.
“The law is much broader than many people think,” he said. “I think a lot of people don’t think about those with invisible disabilities, such as people with allergies, those who are immunocompromised, those with chronic illnesses. A lot of people don’t see themselves as disabled, and a lot of employers don’t see them as disabled.”
Working from home has not historically been considered a “reasonable accommodation” under the ADA, Mr. Dorfman said. However, that appears to be changing.
“There has been a sea change,” Mr. Dorfman said. “The question is coming before the courts more frequently, and recent legal decisions show judges may be altering their views on the subject.”
What led to the doctor’s lawsuit?
Dr. Heiden, a longtime radiologist, had practiced at Lincoln Medical and Mental Health Center for about a year when he requested to work remotely. (Lincoln is operated by New York City Health and Hospitals.) At the time, the governor of New York had ordered a statewide lockdown because of COVID-19, and Dr. Heiden expressed concern that his ulcerative colitis made him a high-risk individual for the virus, according to court documents.
In his March 22, 2020, request, Dr. Heiden said that, except for fluoroscopy, his job could be done entirely from his home, according to a district court summary of the case. He also offered to pay for any costs associated with the remote work setup.
Around the same time, New York City Health and Hospitals permitted its facilities to issue a limited number of workstations to radiologists to facilitate remote work in the event of COVID-related staffing shortages. Administrators were in the process of acquiring remote radiology workstations and determining which radiologists at Lincoln would receive them, according to the case summary.
On March 24, the chair of radiology at Lincoln met with Dr. Heiden to review the results of a recent focused professional practice evaluation (FPPE). An FPPE refers to an intensive review of an expansive selection of patient cases handled by the subject physician. During the meeting, the chair that claimed Dr. Heiden was a poor performer and was accurate in his assessments 93.8% of the time, which was below the hospital’s 97% threshold, according to Dr. Heiden’s lawsuit. Dr. Heiden disagreed with the results, and the two engaged in several more meetings.
Meanwhile, Dr. Heiden’s accommodation request was forwarded to other administrators. In an email introduced into court evidence, the chair indicated he did not support the accommodation, writing that Dr. Heiden’s “skill set does not meet the criteria for the initial installations” of the workstations.
On March 26, 2020, the chair allegedly asked Dr. Heiden to either resign or he would be terminated and reported to the New York State Office of Professional Medical Conduct. Four days later, Dr. Heiden learned that his accommodation request had been denied. He resigned on April 2, 2020.
In his lawsuit, Dr. Heiden claimed that the hospital discriminated against him on the basis of his disability in violation of ADA by denying him equal terms and conditions of employment and failing to provide a reasonable accommodation.
The defendants, who included the radiology chair, did not dispute that Dr. Heiden was asked to resign or that administrators warned termination, but they argued the impetus was his FPPE results and a history of inaccurate interpretations. Other clinicians and physicians had expressed concerns about Dr. Heiden’s “lack of clarity [and] interpretive errors,” according to deposition testimony. The hospital emphasized the FPPE had concluded before Dr. Heiden’s accommodation request was made.
New York City Health and Hospitals requested a federal judge dismiss the lawsuit for lack of valid claims. In January 2023, U.S. District Judge Lewis Liman allowed the case to proceed, ruling that some of Dr. Heiden’s claims had merit.
“Plaintiff has satisfied his obligation to proffer sufficient evidence to create an inference of retaliatory or discriminatory intent,” Judge Liman wrote in his decision. “[The chair] had not always planned to ask for plaintiff’s resignation based on the results of the FPPE completed on March 10, 2020. The decision to ask for that resignation arose shortly after the request for the accommodation. And there is evidence from which the jury could find that [the chair] was not receptive to making the accommodation.”
A jury trial was scheduled for July 2023, but the parties reached a settlement on May 31, 2023.
Is working from home reasonable for physicians?
The widespread swing to remote work in recent years has paved a smoother road for physicians who request the accommodation, said Peter Poullos, MD, clinical associate professor of radiology, gastroenterology, and hepatology at Stanford (Calif.) University and founder and cochair of the Stanford Medicine Alliance for Disability Inclusion and Equity.
“There is now a precedent and examples all over that working from home for some is a viable alternative to working in the hospital or a clinic,” Dr. Poullos said. “If a lawyer can point to instances of other people having received the same accommodation, even if the accommodation was given to someone without a disability, it’s much harder for an employer to say: ‘It’s not possible.’ Because clearly, it is.”
A key factor is the employee’s job duties and whether the employee can complete them remotely, said Mr. Dorfman. With physicians, the reasonableness would heavily depend on their specialty.
A radiologist, for example, would probably have a stronger case for performing their duties remotely compared with a surgeon, Dr. Poullos said.
In general, whether an accommodation is reasonable is decided on a case-by-case basis and usually includes reviewing supporting documentation from a medical provider, said Emily Harvey, a Denver-based disability law attorney. Employers are allowed to deny accommodations if they would cause an undue burden to the employer or fundamentally alter the nature or operation of the job or business.
“When it comes to the ADA, and disability rights in general, the analysis is based on the need of the individual,” she said. “Two people with identical diagnoses could need vastly different accommodations to be successful in the same job.”
Mr. Dorfman added that employers are only required to provide an accommodation that is reasonable under the circumstances, whether or not that accommodation meets the preferred request of the employee. For instance, if an immunocompromised physician asked to work from home, but the employer could ensure that all those working around the physician will mask, that could be reasonable enough.
A recent case analysis by Bloomberg Law shows that more courts are siding with employees who request remote work, compared with in past years. Employees who made disability-related remote work requests prevailed in 40% of federal court rulings from 2021 to 2023 versusa success rate of 30% from 2017 to 2019, according to the July 2023 analysis.
The analysis shows that employers still win the majority of the time, but that the gap is closing, Mr. Dorfman said.
In a September 2020 decision, for example, a Massachusetts District Court ruled in favor of an employee with asthma who was precluding from working at home by a behavioral and mental health agency. U.S. Magistrate Judge Katherine Robertson said that the manager was entitled to telework as a reasonable accommodation under the ADA for 60 days or until further notice. The lawsuit was settled in 2021.
“I think judges are much more used to working from home themselves,” Mr. Dorfman said. “That may affect their sense of accepting remote work as a reasonable accommodation. Their personal experience with it [may] actually inform their view of the topic.”
Your accommodation request was denied: Now what?
If you are unsure about your rights under the ADA, a first step is understanding the law’s protections and learning the obligations of your employer.
Keep in mind that not everyone at your workplace may understand the law and what is required, said Dr. Poullos. When making a request to work from home, ensure that you’re using the right words and asking the right people, he advised. Some physicians, for instance, may only discuss the request with their direct supervisor and give up when the request is denied. “The employee might say, ‘I’ve been dealing with some medical issues and I’m really tired and need to adjust my schedule.’ They don’t mention the word ‘disability,’ they don’t mention the ADA, they don’t mention the word ‘accommodation,’ and so that might not trigger the appropriate response.”
Lisa Meeks, PhD, an expert and researcher in disabilities in medical education, encourages physicians and others to follow the appeals process at their institution if they feel their accommodation request has been unjustly denied.
Research shows that physicians who make accommodation requests rarely escalate denials to an appeal, grievance, or complaint, said Dr. Meeks, cohost of the Docs With Disabilities podcast and director of the Docs With Disabilities Initiative. The initiative aims to use research, education, and stories to drive change in perceptions, disability policy, and procedures in health professions and in biomedical and science education.
If an accommodation cannot be agreed on, doctors can reach out the Equal Employment Opportunity Commission and file a discrimination charge. The agency will review the case and provide an opinion on whether the charge has merit. The EEOC’s decision is not binding in court, and even if the agency believes the charge has no merit, employees still have the right to sue, he said.
Ms. Harvey added that the EEOC has many resources on its website, and that most states also have civil rights agencies that have additional resources. Every state and U.S. territory also has a protection and advocacy organization that may be able to help. Physicians can also review their state bar to locate and consult with disability rights attorneys.
Although it may seem like an uphill battle to push for an accommodation, it can be worth it in the end, said Michael Argenyi, MD, an addiction medicine specialist and assistant professor at the University of Massachusetts, Worcester. Dr. Argenyi, who has hearing loss, was featured on the Docs With Disabilities podcast.
“It’s difficult to ‘rock the boat’ and ask for support from the C-suite for employees with disabilities, or to rearrange a small medical office budget to establish a byline just for accommodations,” Dr. Argenyi said. “Yet, the payoff is worthwhile – patients and fellow colleagues notice commitments to diversity building and inclusion.”
A version of this article appeared on Medscape.com.
A radiologist who claims he was forced to resign after requesting to work from home has settled his discrimination lawsuit with a New York hospital.
Although the case was resolved without a definitive win, legal analysts say the complaint raises important questions about whether some physicians have the right to work from home.
Since the pandemic, employers across the country have become more accepting of professionals working remotely.
Richard Heiden, MD, sued New York City Health and Hospitals in 2020, claiming discrimination and retaliation violations under the American with Disabilities Act (ADA) and the New York State Human Rights Law. Dr. Heiden, who has ulcerative colitis, had asked to work off-site during the start of the pandemic, but the hospital denied his accommodation request. Shortly later, administrators accused Dr. Heiden of poor performance and requested he resign or administrators would terminate him, according to his lawsuit.
Attorneys for New York City Health and Hospitals contended that Dr. Heiden was a poorly performing radiologist who was undergoing a performance review at the time of his accommodation request. The radiologist’s departure was related to the results of the review and had nothing to do with his disability or accommodation request, according to the hospital.
The undisclosed settlement ends a 3-year court battle between Dr. Heiden and the hospital corporation.
In an email, Laura Williams, an attorney for the hospital corporation, said that “the settlement was in the best interest of all parties.”
Dr. Heiden and his attorneys also did not respond to requests for comment.
A critical piece to the puzzle is understanding who is protected under the ADA and is therefore entitled to reasonable accommodations, said Doron Dorfman, JSD, an associate professor at Seton Hall University Law School in Newark, N.J., who focuses on disability law.
A common misconception is that only physicians with a physical disability are “disabled,” he said. However, under the law, a disabled individual is anyone with a physical or mental impairment – including mental illness – that limits major life activities; a person with a history of such impairment; or a person who is perceived by others as having an impairment.
“The law is much broader than many people think,” he said. “I think a lot of people don’t think about those with invisible disabilities, such as people with allergies, those who are immunocompromised, those with chronic illnesses. A lot of people don’t see themselves as disabled, and a lot of employers don’t see them as disabled.”
Working from home has not historically been considered a “reasonable accommodation” under the ADA, Mr. Dorfman said. However, that appears to be changing.
“There has been a sea change,” Mr. Dorfman said. “The question is coming before the courts more frequently, and recent legal decisions show judges may be altering their views on the subject.”
What led to the doctor’s lawsuit?
Dr. Heiden, a longtime radiologist, had practiced at Lincoln Medical and Mental Health Center for about a year when he requested to work remotely. (Lincoln is operated by New York City Health and Hospitals.) At the time, the governor of New York had ordered a statewide lockdown because of COVID-19, and Dr. Heiden expressed concern that his ulcerative colitis made him a high-risk individual for the virus, according to court documents.
In his March 22, 2020, request, Dr. Heiden said that, except for fluoroscopy, his job could be done entirely from his home, according to a district court summary of the case. He also offered to pay for any costs associated with the remote work setup.
Around the same time, New York City Health and Hospitals permitted its facilities to issue a limited number of workstations to radiologists to facilitate remote work in the event of COVID-related staffing shortages. Administrators were in the process of acquiring remote radiology workstations and determining which radiologists at Lincoln would receive them, according to the case summary.
On March 24, the chair of radiology at Lincoln met with Dr. Heiden to review the results of a recent focused professional practice evaluation (FPPE). An FPPE refers to an intensive review of an expansive selection of patient cases handled by the subject physician. During the meeting, the chair that claimed Dr. Heiden was a poor performer and was accurate in his assessments 93.8% of the time, which was below the hospital’s 97% threshold, according to Dr. Heiden’s lawsuit. Dr. Heiden disagreed with the results, and the two engaged in several more meetings.
Meanwhile, Dr. Heiden’s accommodation request was forwarded to other administrators. In an email introduced into court evidence, the chair indicated he did not support the accommodation, writing that Dr. Heiden’s “skill set does not meet the criteria for the initial installations” of the workstations.
On March 26, 2020, the chair allegedly asked Dr. Heiden to either resign or he would be terminated and reported to the New York State Office of Professional Medical Conduct. Four days later, Dr. Heiden learned that his accommodation request had been denied. He resigned on April 2, 2020.
In his lawsuit, Dr. Heiden claimed that the hospital discriminated against him on the basis of his disability in violation of ADA by denying him equal terms and conditions of employment and failing to provide a reasonable accommodation.
The defendants, who included the radiology chair, did not dispute that Dr. Heiden was asked to resign or that administrators warned termination, but they argued the impetus was his FPPE results and a history of inaccurate interpretations. Other clinicians and physicians had expressed concerns about Dr. Heiden’s “lack of clarity [and] interpretive errors,” according to deposition testimony. The hospital emphasized the FPPE had concluded before Dr. Heiden’s accommodation request was made.
New York City Health and Hospitals requested a federal judge dismiss the lawsuit for lack of valid claims. In January 2023, U.S. District Judge Lewis Liman allowed the case to proceed, ruling that some of Dr. Heiden’s claims had merit.
“Plaintiff has satisfied his obligation to proffer sufficient evidence to create an inference of retaliatory or discriminatory intent,” Judge Liman wrote in his decision. “[The chair] had not always planned to ask for plaintiff’s resignation based on the results of the FPPE completed on March 10, 2020. The decision to ask for that resignation arose shortly after the request for the accommodation. And there is evidence from which the jury could find that [the chair] was not receptive to making the accommodation.”
A jury trial was scheduled for July 2023, but the parties reached a settlement on May 31, 2023.
Is working from home reasonable for physicians?
The widespread swing to remote work in recent years has paved a smoother road for physicians who request the accommodation, said Peter Poullos, MD, clinical associate professor of radiology, gastroenterology, and hepatology at Stanford (Calif.) University and founder and cochair of the Stanford Medicine Alliance for Disability Inclusion and Equity.
“There is now a precedent and examples all over that working from home for some is a viable alternative to working in the hospital or a clinic,” Dr. Poullos said. “If a lawyer can point to instances of other people having received the same accommodation, even if the accommodation was given to someone without a disability, it’s much harder for an employer to say: ‘It’s not possible.’ Because clearly, it is.”
A key factor is the employee’s job duties and whether the employee can complete them remotely, said Mr. Dorfman. With physicians, the reasonableness would heavily depend on their specialty.
A radiologist, for example, would probably have a stronger case for performing their duties remotely compared with a surgeon, Dr. Poullos said.
In general, whether an accommodation is reasonable is decided on a case-by-case basis and usually includes reviewing supporting documentation from a medical provider, said Emily Harvey, a Denver-based disability law attorney. Employers are allowed to deny accommodations if they would cause an undue burden to the employer or fundamentally alter the nature or operation of the job or business.
“When it comes to the ADA, and disability rights in general, the analysis is based on the need of the individual,” she said. “Two people with identical diagnoses could need vastly different accommodations to be successful in the same job.”
Mr. Dorfman added that employers are only required to provide an accommodation that is reasonable under the circumstances, whether or not that accommodation meets the preferred request of the employee. For instance, if an immunocompromised physician asked to work from home, but the employer could ensure that all those working around the physician will mask, that could be reasonable enough.
A recent case analysis by Bloomberg Law shows that more courts are siding with employees who request remote work, compared with in past years. Employees who made disability-related remote work requests prevailed in 40% of federal court rulings from 2021 to 2023 versusa success rate of 30% from 2017 to 2019, according to the July 2023 analysis.
The analysis shows that employers still win the majority of the time, but that the gap is closing, Mr. Dorfman said.
In a September 2020 decision, for example, a Massachusetts District Court ruled in favor of an employee with asthma who was precluding from working at home by a behavioral and mental health agency. U.S. Magistrate Judge Katherine Robertson said that the manager was entitled to telework as a reasonable accommodation under the ADA for 60 days or until further notice. The lawsuit was settled in 2021.
“I think judges are much more used to working from home themselves,” Mr. Dorfman said. “That may affect their sense of accepting remote work as a reasonable accommodation. Their personal experience with it [may] actually inform their view of the topic.”
Your accommodation request was denied: Now what?
If you are unsure about your rights under the ADA, a first step is understanding the law’s protections and learning the obligations of your employer.
Keep in mind that not everyone at your workplace may understand the law and what is required, said Dr. Poullos. When making a request to work from home, ensure that you’re using the right words and asking the right people, he advised. Some physicians, for instance, may only discuss the request with their direct supervisor and give up when the request is denied. “The employee might say, ‘I’ve been dealing with some medical issues and I’m really tired and need to adjust my schedule.’ They don’t mention the word ‘disability,’ they don’t mention the ADA, they don’t mention the word ‘accommodation,’ and so that might not trigger the appropriate response.”
Lisa Meeks, PhD, an expert and researcher in disabilities in medical education, encourages physicians and others to follow the appeals process at their institution if they feel their accommodation request has been unjustly denied.
Research shows that physicians who make accommodation requests rarely escalate denials to an appeal, grievance, or complaint, said Dr. Meeks, cohost of the Docs With Disabilities podcast and director of the Docs With Disabilities Initiative. The initiative aims to use research, education, and stories to drive change in perceptions, disability policy, and procedures in health professions and in biomedical and science education.
If an accommodation cannot be agreed on, doctors can reach out the Equal Employment Opportunity Commission and file a discrimination charge. The agency will review the case and provide an opinion on whether the charge has merit. The EEOC’s decision is not binding in court, and even if the agency believes the charge has no merit, employees still have the right to sue, he said.
Ms. Harvey added that the EEOC has many resources on its website, and that most states also have civil rights agencies that have additional resources. Every state and U.S. territory also has a protection and advocacy organization that may be able to help. Physicians can also review their state bar to locate and consult with disability rights attorneys.
Although it may seem like an uphill battle to push for an accommodation, it can be worth it in the end, said Michael Argenyi, MD, an addiction medicine specialist and assistant professor at the University of Massachusetts, Worcester. Dr. Argenyi, who has hearing loss, was featured on the Docs With Disabilities podcast.
“It’s difficult to ‘rock the boat’ and ask for support from the C-suite for employees with disabilities, or to rearrange a small medical office budget to establish a byline just for accommodations,” Dr. Argenyi said. “Yet, the payoff is worthwhile – patients and fellow colleagues notice commitments to diversity building and inclusion.”
A version of this article appeared on Medscape.com.
A radiologist who claims he was forced to resign after requesting to work from home has settled his discrimination lawsuit with a New York hospital.
Although the case was resolved without a definitive win, legal analysts say the complaint raises important questions about whether some physicians have the right to work from home.
Since the pandemic, employers across the country have become more accepting of professionals working remotely.
Richard Heiden, MD, sued New York City Health and Hospitals in 2020, claiming discrimination and retaliation violations under the American with Disabilities Act (ADA) and the New York State Human Rights Law. Dr. Heiden, who has ulcerative colitis, had asked to work off-site during the start of the pandemic, but the hospital denied his accommodation request. Shortly later, administrators accused Dr. Heiden of poor performance and requested he resign or administrators would terminate him, according to his lawsuit.
Attorneys for New York City Health and Hospitals contended that Dr. Heiden was a poorly performing radiologist who was undergoing a performance review at the time of his accommodation request. The radiologist’s departure was related to the results of the review and had nothing to do with his disability or accommodation request, according to the hospital.
The undisclosed settlement ends a 3-year court battle between Dr. Heiden and the hospital corporation.
In an email, Laura Williams, an attorney for the hospital corporation, said that “the settlement was in the best interest of all parties.”
Dr. Heiden and his attorneys also did not respond to requests for comment.
A critical piece to the puzzle is understanding who is protected under the ADA and is therefore entitled to reasonable accommodations, said Doron Dorfman, JSD, an associate professor at Seton Hall University Law School in Newark, N.J., who focuses on disability law.
A common misconception is that only physicians with a physical disability are “disabled,” he said. However, under the law, a disabled individual is anyone with a physical or mental impairment – including mental illness – that limits major life activities; a person with a history of such impairment; or a person who is perceived by others as having an impairment.
“The law is much broader than many people think,” he said. “I think a lot of people don’t think about those with invisible disabilities, such as people with allergies, those who are immunocompromised, those with chronic illnesses. A lot of people don’t see themselves as disabled, and a lot of employers don’t see them as disabled.”
Working from home has not historically been considered a “reasonable accommodation” under the ADA, Mr. Dorfman said. However, that appears to be changing.
“There has been a sea change,” Mr. Dorfman said. “The question is coming before the courts more frequently, and recent legal decisions show judges may be altering their views on the subject.”
What led to the doctor’s lawsuit?
Dr. Heiden, a longtime radiologist, had practiced at Lincoln Medical and Mental Health Center for about a year when he requested to work remotely. (Lincoln is operated by New York City Health and Hospitals.) At the time, the governor of New York had ordered a statewide lockdown because of COVID-19, and Dr. Heiden expressed concern that his ulcerative colitis made him a high-risk individual for the virus, according to court documents.
In his March 22, 2020, request, Dr. Heiden said that, except for fluoroscopy, his job could be done entirely from his home, according to a district court summary of the case. He also offered to pay for any costs associated with the remote work setup.
Around the same time, New York City Health and Hospitals permitted its facilities to issue a limited number of workstations to radiologists to facilitate remote work in the event of COVID-related staffing shortages. Administrators were in the process of acquiring remote radiology workstations and determining which radiologists at Lincoln would receive them, according to the case summary.
On March 24, the chair of radiology at Lincoln met with Dr. Heiden to review the results of a recent focused professional practice evaluation (FPPE). An FPPE refers to an intensive review of an expansive selection of patient cases handled by the subject physician. During the meeting, the chair that claimed Dr. Heiden was a poor performer and was accurate in his assessments 93.8% of the time, which was below the hospital’s 97% threshold, according to Dr. Heiden’s lawsuit. Dr. Heiden disagreed with the results, and the two engaged in several more meetings.
Meanwhile, Dr. Heiden’s accommodation request was forwarded to other administrators. In an email introduced into court evidence, the chair indicated he did not support the accommodation, writing that Dr. Heiden’s “skill set does not meet the criteria for the initial installations” of the workstations.
On March 26, 2020, the chair allegedly asked Dr. Heiden to either resign or he would be terminated and reported to the New York State Office of Professional Medical Conduct. Four days later, Dr. Heiden learned that his accommodation request had been denied. He resigned on April 2, 2020.
In his lawsuit, Dr. Heiden claimed that the hospital discriminated against him on the basis of his disability in violation of ADA by denying him equal terms and conditions of employment and failing to provide a reasonable accommodation.
The defendants, who included the radiology chair, did not dispute that Dr. Heiden was asked to resign or that administrators warned termination, but they argued the impetus was his FPPE results and a history of inaccurate interpretations. Other clinicians and physicians had expressed concerns about Dr. Heiden’s “lack of clarity [and] interpretive errors,” according to deposition testimony. The hospital emphasized the FPPE had concluded before Dr. Heiden’s accommodation request was made.
New York City Health and Hospitals requested a federal judge dismiss the lawsuit for lack of valid claims. In January 2023, U.S. District Judge Lewis Liman allowed the case to proceed, ruling that some of Dr. Heiden’s claims had merit.
“Plaintiff has satisfied his obligation to proffer sufficient evidence to create an inference of retaliatory or discriminatory intent,” Judge Liman wrote in his decision. “[The chair] had not always planned to ask for plaintiff’s resignation based on the results of the FPPE completed on March 10, 2020. The decision to ask for that resignation arose shortly after the request for the accommodation. And there is evidence from which the jury could find that [the chair] was not receptive to making the accommodation.”
A jury trial was scheduled for July 2023, but the parties reached a settlement on May 31, 2023.
Is working from home reasonable for physicians?
The widespread swing to remote work in recent years has paved a smoother road for physicians who request the accommodation, said Peter Poullos, MD, clinical associate professor of radiology, gastroenterology, and hepatology at Stanford (Calif.) University and founder and cochair of the Stanford Medicine Alliance for Disability Inclusion and Equity.
“There is now a precedent and examples all over that working from home for some is a viable alternative to working in the hospital or a clinic,” Dr. Poullos said. “If a lawyer can point to instances of other people having received the same accommodation, even if the accommodation was given to someone without a disability, it’s much harder for an employer to say: ‘It’s not possible.’ Because clearly, it is.”
A key factor is the employee’s job duties and whether the employee can complete them remotely, said Mr. Dorfman. With physicians, the reasonableness would heavily depend on their specialty.
A radiologist, for example, would probably have a stronger case for performing their duties remotely compared with a surgeon, Dr. Poullos said.
In general, whether an accommodation is reasonable is decided on a case-by-case basis and usually includes reviewing supporting documentation from a medical provider, said Emily Harvey, a Denver-based disability law attorney. Employers are allowed to deny accommodations if they would cause an undue burden to the employer or fundamentally alter the nature or operation of the job or business.
“When it comes to the ADA, and disability rights in general, the analysis is based on the need of the individual,” she said. “Two people with identical diagnoses could need vastly different accommodations to be successful in the same job.”
Mr. Dorfman added that employers are only required to provide an accommodation that is reasonable under the circumstances, whether or not that accommodation meets the preferred request of the employee. For instance, if an immunocompromised physician asked to work from home, but the employer could ensure that all those working around the physician will mask, that could be reasonable enough.
A recent case analysis by Bloomberg Law shows that more courts are siding with employees who request remote work, compared with in past years. Employees who made disability-related remote work requests prevailed in 40% of federal court rulings from 2021 to 2023 versusa success rate of 30% from 2017 to 2019, according to the July 2023 analysis.
The analysis shows that employers still win the majority of the time, but that the gap is closing, Mr. Dorfman said.
In a September 2020 decision, for example, a Massachusetts District Court ruled in favor of an employee with asthma who was precluding from working at home by a behavioral and mental health agency. U.S. Magistrate Judge Katherine Robertson said that the manager was entitled to telework as a reasonable accommodation under the ADA for 60 days or until further notice. The lawsuit was settled in 2021.
“I think judges are much more used to working from home themselves,” Mr. Dorfman said. “That may affect their sense of accepting remote work as a reasonable accommodation. Their personal experience with it [may] actually inform their view of the topic.”
Your accommodation request was denied: Now what?
If you are unsure about your rights under the ADA, a first step is understanding the law’s protections and learning the obligations of your employer.
Keep in mind that not everyone at your workplace may understand the law and what is required, said Dr. Poullos. When making a request to work from home, ensure that you’re using the right words and asking the right people, he advised. Some physicians, for instance, may only discuss the request with their direct supervisor and give up when the request is denied. “The employee might say, ‘I’ve been dealing with some medical issues and I’m really tired and need to adjust my schedule.’ They don’t mention the word ‘disability,’ they don’t mention the ADA, they don’t mention the word ‘accommodation,’ and so that might not trigger the appropriate response.”
Lisa Meeks, PhD, an expert and researcher in disabilities in medical education, encourages physicians and others to follow the appeals process at their institution if they feel their accommodation request has been unjustly denied.
Research shows that physicians who make accommodation requests rarely escalate denials to an appeal, grievance, or complaint, said Dr. Meeks, cohost of the Docs With Disabilities podcast and director of the Docs With Disabilities Initiative. The initiative aims to use research, education, and stories to drive change in perceptions, disability policy, and procedures in health professions and in biomedical and science education.
If an accommodation cannot be agreed on, doctors can reach out the Equal Employment Opportunity Commission and file a discrimination charge. The agency will review the case and provide an opinion on whether the charge has merit. The EEOC’s decision is not binding in court, and even if the agency believes the charge has no merit, employees still have the right to sue, he said.
Ms. Harvey added that the EEOC has many resources on its website, and that most states also have civil rights agencies that have additional resources. Every state and U.S. territory also has a protection and advocacy organization that may be able to help. Physicians can also review their state bar to locate and consult with disability rights attorneys.
Although it may seem like an uphill battle to push for an accommodation, it can be worth it in the end, said Michael Argenyi, MD, an addiction medicine specialist and assistant professor at the University of Massachusetts, Worcester. Dr. Argenyi, who has hearing loss, was featured on the Docs With Disabilities podcast.
“It’s difficult to ‘rock the boat’ and ask for support from the C-suite for employees with disabilities, or to rearrange a small medical office budget to establish a byline just for accommodations,” Dr. Argenyi said. “Yet, the payoff is worthwhile – patients and fellow colleagues notice commitments to diversity building and inclusion.”
A version of this article appeared on Medscape.com.

