User login
Standard measure may underestimate OSA in Black patients
Measurement error may be the culprit in underdiagnosing obstructive sleep apnea in Black patients, compared with White patients, based on data from nearly 2,000 individuals.
, according to Ali Azarbarzin, PhD, of Harvard Medical School, Boston.
“We wanted to examine the implications for obstructive sleep apnea,” which is often caused by a reduction in air flow, Dr. Azarbarzin said in an interview.
In a study presented at the American Thoracic Society’s international conference, Dr. Azarbarzin and colleagues examined data from 1,955 adults who were enrolled in the Multi-Ethnic Study of Atherosclerosis (MESA) Exam 5. The study participants underwent unattended 15-channel polysomnography that included a finger pulse oximeter. The mean age of the participants was 68.3 years, and 53.7% were women. A total of 12.1%, 23.7%, 27.7%, and 36.5% of the participants were Asian, Hispanic, Black, and White, respectively.
Apnea hypopnea index (AHI3P) was similar between Black and White patients, at approximately 19 events per hour. Black participants had higher wake SpO2, higher current smoking rates, and higher body mass index, compared with White participants, but these differences were not significant.
Severity of obstructive sleep apnea (OSA) was based on the hypoxic burden, which was defined as the total area under the respiratory curve. The total ventilatory burden was defined as the event-specific area under the ventilation signal and identified by amplitude changes in the nasal pressure signal. The researchers then calculated desaturation sensitivity (the primary outcome) as hypoxic burden divided by ventilatory burden.
In an unadjusted analysis, desaturation sensitivity was significantly lower in Black patients and Asian patients, compared with White patients (P < .001 and P < .02, respectively). After adjusting for age, sex, body mass index, and time spent in a supine position, desaturation sensitivity was lower only in Black patients, compared with White patients, and this difference persisted in both men and women.
The difference in desaturation sensitivity by race could be caused by differences in physiology or in measurement error, Dr. Azarbarzin told this news organization. If measurement error is the culprit, “we may be underestimating OSA severity in [Black people],” especially in Black women, he said.
However, more research is needed to understand the potential impact of both physiology and device accuracy on differences in oxygen saturation across ethnicities and to effectively identify and treat OSA in all patients, Dr. Azarbarzin said.
The MESA Study was supported by the National Institutes of Health and the National Institute on Aging. Data from MESA were obtained through support from the National Heart, Lung, and Blood Institute and the National Center for Advancing Translational Sciences. Dr. Azarbarzin disclosed funding from the National Institutes of Health, the American Health Association, and the American Academy of Sleep Medicine.
A version of this article first appeared on Medscape.com.
Measurement error may be the culprit in underdiagnosing obstructive sleep apnea in Black patients, compared with White patients, based on data from nearly 2,000 individuals.
, according to Ali Azarbarzin, PhD, of Harvard Medical School, Boston.
“We wanted to examine the implications for obstructive sleep apnea,” which is often caused by a reduction in air flow, Dr. Azarbarzin said in an interview.
In a study presented at the American Thoracic Society’s international conference, Dr. Azarbarzin and colleagues examined data from 1,955 adults who were enrolled in the Multi-Ethnic Study of Atherosclerosis (MESA) Exam 5. The study participants underwent unattended 15-channel polysomnography that included a finger pulse oximeter. The mean age of the participants was 68.3 years, and 53.7% were women. A total of 12.1%, 23.7%, 27.7%, and 36.5% of the participants were Asian, Hispanic, Black, and White, respectively.
Apnea hypopnea index (AHI3P) was similar between Black and White patients, at approximately 19 events per hour. Black participants had higher wake SpO2, higher current smoking rates, and higher body mass index, compared with White participants, but these differences were not significant.
Severity of obstructive sleep apnea (OSA) was based on the hypoxic burden, which was defined as the total area under the respiratory curve. The total ventilatory burden was defined as the event-specific area under the ventilation signal and identified by amplitude changes in the nasal pressure signal. The researchers then calculated desaturation sensitivity (the primary outcome) as hypoxic burden divided by ventilatory burden.
In an unadjusted analysis, desaturation sensitivity was significantly lower in Black patients and Asian patients, compared with White patients (P < .001 and P < .02, respectively). After adjusting for age, sex, body mass index, and time spent in a supine position, desaturation sensitivity was lower only in Black patients, compared with White patients, and this difference persisted in both men and women.
The difference in desaturation sensitivity by race could be caused by differences in physiology or in measurement error, Dr. Azarbarzin told this news organization. If measurement error is the culprit, “we may be underestimating OSA severity in [Black people],” especially in Black women, he said.
However, more research is needed to understand the potential impact of both physiology and device accuracy on differences in oxygen saturation across ethnicities and to effectively identify and treat OSA in all patients, Dr. Azarbarzin said.
The MESA Study was supported by the National Institutes of Health and the National Institute on Aging. Data from MESA were obtained through support from the National Heart, Lung, and Blood Institute and the National Center for Advancing Translational Sciences. Dr. Azarbarzin disclosed funding from the National Institutes of Health, the American Health Association, and the American Academy of Sleep Medicine.
A version of this article first appeared on Medscape.com.
Measurement error may be the culprit in underdiagnosing obstructive sleep apnea in Black patients, compared with White patients, based on data from nearly 2,000 individuals.
, according to Ali Azarbarzin, PhD, of Harvard Medical School, Boston.
“We wanted to examine the implications for obstructive sleep apnea,” which is often caused by a reduction in air flow, Dr. Azarbarzin said in an interview.
In a study presented at the American Thoracic Society’s international conference, Dr. Azarbarzin and colleagues examined data from 1,955 adults who were enrolled in the Multi-Ethnic Study of Atherosclerosis (MESA) Exam 5. The study participants underwent unattended 15-channel polysomnography that included a finger pulse oximeter. The mean age of the participants was 68.3 years, and 53.7% were women. A total of 12.1%, 23.7%, 27.7%, and 36.5% of the participants were Asian, Hispanic, Black, and White, respectively.
Apnea hypopnea index (AHI3P) was similar between Black and White patients, at approximately 19 events per hour. Black participants had higher wake SpO2, higher current smoking rates, and higher body mass index, compared with White participants, but these differences were not significant.
Severity of obstructive sleep apnea (OSA) was based on the hypoxic burden, which was defined as the total area under the respiratory curve. The total ventilatory burden was defined as the event-specific area under the ventilation signal and identified by amplitude changes in the nasal pressure signal. The researchers then calculated desaturation sensitivity (the primary outcome) as hypoxic burden divided by ventilatory burden.
In an unadjusted analysis, desaturation sensitivity was significantly lower in Black patients and Asian patients, compared with White patients (P < .001 and P < .02, respectively). After adjusting for age, sex, body mass index, and time spent in a supine position, desaturation sensitivity was lower only in Black patients, compared with White patients, and this difference persisted in both men and women.
The difference in desaturation sensitivity by race could be caused by differences in physiology or in measurement error, Dr. Azarbarzin told this news organization. If measurement error is the culprit, “we may be underestimating OSA severity in [Black people],” especially in Black women, he said.
However, more research is needed to understand the potential impact of both physiology and device accuracy on differences in oxygen saturation across ethnicities and to effectively identify and treat OSA in all patients, Dr. Azarbarzin said.
The MESA Study was supported by the National Institutes of Health and the National Institute on Aging. Data from MESA were obtained through support from the National Heart, Lung, and Blood Institute and the National Center for Advancing Translational Sciences. Dr. Azarbarzin disclosed funding from the National Institutes of Health, the American Health Association, and the American Academy of Sleep Medicine.
A version of this article first appeared on Medscape.com.
FROM ATS 2023
Which drug best reduces sleepiness in patients with OSA?
Solriamfetol who have residual daytime sleepiness after conventional treatment, according to a systematic review and meta-analysis.
In a systematic review of 14 trials that included more than 3,000 patients, solriamfetol was associated with improvements of 3.85 points on the Epworth Sleepiness Scale (ESS) score, compared with placebo.
“We found that solriamfetol is almost twice as effective as modafinil-armodafinil – the cheaper, older option – in improving the ESS score and much more effective at improving the Maintenance of Wakefulness Test (MWT),” study author Tyler Pitre, MD, an internal medicine physician at McMaster University, Hamilton, Ont., said in an interview.
The findings were published online in Annals of Internal Medicine.
High-certainty evidence
The analysis included 3,085 adults with excessive daytime sleepiness (EDS) who were receiving or were eligible for conventional OSA treatment such as positive airway pressure. Participants were randomly assigned to either placebo or any EDS pharmacotherapy (armodafinil, modafinil, solriamfetol, or pitolisant). The primary outcomes of the analysis were change in ESS and MWT. Secondary outcomes were drug-related adverse events.
The trials had a median follow-up time of 4 weeks. The meta-analysis showed that solriamfetol improves ESS to a greater extent than placebo (high certainty), armodafinil-modafinil and pitolisant (moderate certainty). Compared with placebo, the mean difference in ESS scores for solriamfetol, armodafinil-modafinil, and pitolisant was –3.85, –2.25, and –2.78, respectively.
The analysis yielded high-certainty evidence that solriamfetol and armodafinil-modafinil improved MWT, compared with placebo. The former was “probably superior,” while pitolisant “may have little to no effect on MWT, compared with placebo,” write the authors. The standardized mean difference in MWT scores, compared with placebo, was 0.90 for solriamfetol and 0.41 for armodafinil-modafinil. “Solriamfetol is probably superior to armodafinil-modafinil in improving MWT (SMD, 0.49),” say the authors.
Compared with placebo, armodafinil-modafinil probably increases the risk for discontinuation due to adverse events (relative risk, 2.01), and solriamfetol may increase the risk for discontinuation (RR, 2.04), according to the authors. Pitolisant “may have little to no effect on drug discontinuations due to adverse events,” write the authors.
Although solriamfetol may have led to more discontinuations than armodafinil-modafinil, “we did not find convincing evidence of serious adverse events, albeit with very short-term follow-up,” they add.
The most common side effects for all interventions were headaches, insomnia, and anxiety. Headaches were most likely with armodafinil-modafinil (RR, 1.87), and insomnia was most likely with pitolisant (RR, 7.25).
“Although solriamfetol appears most effective, comorbid hypertension and costs may be barriers to its use,” say the researchers. “Furthermore, there are potentially effective candidate therapies such as methylphenidate, atomoxetine, or caffeine, which have not been examined in randomized clinical trials.”
Although EDS is reported in 40%-58% of patients with OSA and can persist in 6%-18% despite PAP therapy, most non-sleep specialists may not be aware of pharmacologic options, said Dr. Pitre. “I have not seen a study that looks at the prescribing habits of physicians for this condition, but I suspect that primary care physicians are not prescribing modafinil-armodafinil frequently for this and less so for solriamfetol,” he said. “I hope this paper builds awareness of this condition and also informs clinicians on the options available to patients, as well as common side effects to counsel them on before starting treatment.”
Dr. Pitre was surprised at the magnitude of solriamfetol’s superiority to modafinil-armodafinil but cautioned that solriamfetol has been shown to increase blood pressure in higher doses. It therefore must be prescribed carefully, “especially to a population of patients who often have comorbid hypertension,” he said.
Some limitations of the analysis were that all trials were conducted in high-income countries (most commonly the United States). Moreover, 77% of participants were White, and 71% were male.
Beneficial adjunctive therapy
Commenting on the findings, Sogol Javaheri, MD, MPH, who was not involved in the research, said that they confirm those of prior studies and are “consistent with what my colleagues and I experience in our clinical practices.”
Dr. Javaheri is associate program director of the sleep medicine fellowship at Brigham and Women’s Hospital and assistant professor of medicine at Harvard Medical School, both in Boston.
While sleep medicine specialists are more likely than others to prescribe these medications, “any clinician may use these medications, ideally if they have ruled out other potential reversible causes of EDS,” said Dr. Javaheri. “The medications do not treat the underlying cause, which is why it’s important to use them as an adjunct to conventional therapy that actually treats the underlying sleep disorder and to rule out additional potential causes of sleepiness that are treatable.”
These potential causes might include insufficient sleep (less than 7 hours per night), untreated anemia, and incompletely treated sleep disorders, she explained. In sleep medicine, modafinil is usually the treatment of choice because of its lower cost, but it may reduce the efficacy of hormonal contraception. Solriamfetol, however, does not. “Additionally, I look forward to validation of pitolisant for treatment of EDS in OSA patients, as it is not a controlled substance and may benefit patients with a history of substance abuse or who may be at higher risk of addiction,” said Dr. Javaheri.
The study was conducted without outside funding. Dr. Pitre and Dr. Javaheri report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Solriamfetol who have residual daytime sleepiness after conventional treatment, according to a systematic review and meta-analysis.
In a systematic review of 14 trials that included more than 3,000 patients, solriamfetol was associated with improvements of 3.85 points on the Epworth Sleepiness Scale (ESS) score, compared with placebo.
“We found that solriamfetol is almost twice as effective as modafinil-armodafinil – the cheaper, older option – in improving the ESS score and much more effective at improving the Maintenance of Wakefulness Test (MWT),” study author Tyler Pitre, MD, an internal medicine physician at McMaster University, Hamilton, Ont., said in an interview.
The findings were published online in Annals of Internal Medicine.
High-certainty evidence
The analysis included 3,085 adults with excessive daytime sleepiness (EDS) who were receiving or were eligible for conventional OSA treatment such as positive airway pressure. Participants were randomly assigned to either placebo or any EDS pharmacotherapy (armodafinil, modafinil, solriamfetol, or pitolisant). The primary outcomes of the analysis were change in ESS and MWT. Secondary outcomes were drug-related adverse events.
The trials had a median follow-up time of 4 weeks. The meta-analysis showed that solriamfetol improves ESS to a greater extent than placebo (high certainty), armodafinil-modafinil and pitolisant (moderate certainty). Compared with placebo, the mean difference in ESS scores for solriamfetol, armodafinil-modafinil, and pitolisant was –3.85, –2.25, and –2.78, respectively.
The analysis yielded high-certainty evidence that solriamfetol and armodafinil-modafinil improved MWT, compared with placebo. The former was “probably superior,” while pitolisant “may have little to no effect on MWT, compared with placebo,” write the authors. The standardized mean difference in MWT scores, compared with placebo, was 0.90 for solriamfetol and 0.41 for armodafinil-modafinil. “Solriamfetol is probably superior to armodafinil-modafinil in improving MWT (SMD, 0.49),” say the authors.
Compared with placebo, armodafinil-modafinil probably increases the risk for discontinuation due to adverse events (relative risk, 2.01), and solriamfetol may increase the risk for discontinuation (RR, 2.04), according to the authors. Pitolisant “may have little to no effect on drug discontinuations due to adverse events,” write the authors.
Although solriamfetol may have led to more discontinuations than armodafinil-modafinil, “we did not find convincing evidence of serious adverse events, albeit with very short-term follow-up,” they add.
The most common side effects for all interventions were headaches, insomnia, and anxiety. Headaches were most likely with armodafinil-modafinil (RR, 1.87), and insomnia was most likely with pitolisant (RR, 7.25).
“Although solriamfetol appears most effective, comorbid hypertension and costs may be barriers to its use,” say the researchers. “Furthermore, there are potentially effective candidate therapies such as methylphenidate, atomoxetine, or caffeine, which have not been examined in randomized clinical trials.”
Although EDS is reported in 40%-58% of patients with OSA and can persist in 6%-18% despite PAP therapy, most non-sleep specialists may not be aware of pharmacologic options, said Dr. Pitre. “I have not seen a study that looks at the prescribing habits of physicians for this condition, but I suspect that primary care physicians are not prescribing modafinil-armodafinil frequently for this and less so for solriamfetol,” he said. “I hope this paper builds awareness of this condition and also informs clinicians on the options available to patients, as well as common side effects to counsel them on before starting treatment.”
Dr. Pitre was surprised at the magnitude of solriamfetol’s superiority to modafinil-armodafinil but cautioned that solriamfetol has been shown to increase blood pressure in higher doses. It therefore must be prescribed carefully, “especially to a population of patients who often have comorbid hypertension,” he said.
Some limitations of the analysis were that all trials were conducted in high-income countries (most commonly the United States). Moreover, 77% of participants were White, and 71% were male.
Beneficial adjunctive therapy
Commenting on the findings, Sogol Javaheri, MD, MPH, who was not involved in the research, said that they confirm those of prior studies and are “consistent with what my colleagues and I experience in our clinical practices.”
Dr. Javaheri is associate program director of the sleep medicine fellowship at Brigham and Women’s Hospital and assistant professor of medicine at Harvard Medical School, both in Boston.
While sleep medicine specialists are more likely than others to prescribe these medications, “any clinician may use these medications, ideally if they have ruled out other potential reversible causes of EDS,” said Dr. Javaheri. “The medications do not treat the underlying cause, which is why it’s important to use them as an adjunct to conventional therapy that actually treats the underlying sleep disorder and to rule out additional potential causes of sleepiness that are treatable.”
These potential causes might include insufficient sleep (less than 7 hours per night), untreated anemia, and incompletely treated sleep disorders, she explained. In sleep medicine, modafinil is usually the treatment of choice because of its lower cost, but it may reduce the efficacy of hormonal contraception. Solriamfetol, however, does not. “Additionally, I look forward to validation of pitolisant for treatment of EDS in OSA patients, as it is not a controlled substance and may benefit patients with a history of substance abuse or who may be at higher risk of addiction,” said Dr. Javaheri.
The study was conducted without outside funding. Dr. Pitre and Dr. Javaheri report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Solriamfetol who have residual daytime sleepiness after conventional treatment, according to a systematic review and meta-analysis.
In a systematic review of 14 trials that included more than 3,000 patients, solriamfetol was associated with improvements of 3.85 points on the Epworth Sleepiness Scale (ESS) score, compared with placebo.
“We found that solriamfetol is almost twice as effective as modafinil-armodafinil – the cheaper, older option – in improving the ESS score and much more effective at improving the Maintenance of Wakefulness Test (MWT),” study author Tyler Pitre, MD, an internal medicine physician at McMaster University, Hamilton, Ont., said in an interview.
The findings were published online in Annals of Internal Medicine.
High-certainty evidence
The analysis included 3,085 adults with excessive daytime sleepiness (EDS) who were receiving or were eligible for conventional OSA treatment such as positive airway pressure. Participants were randomly assigned to either placebo or any EDS pharmacotherapy (armodafinil, modafinil, solriamfetol, or pitolisant). The primary outcomes of the analysis were change in ESS and MWT. Secondary outcomes were drug-related adverse events.
The trials had a median follow-up time of 4 weeks. The meta-analysis showed that solriamfetol improves ESS to a greater extent than placebo (high certainty), armodafinil-modafinil and pitolisant (moderate certainty). Compared with placebo, the mean difference in ESS scores for solriamfetol, armodafinil-modafinil, and pitolisant was –3.85, –2.25, and –2.78, respectively.
The analysis yielded high-certainty evidence that solriamfetol and armodafinil-modafinil improved MWT, compared with placebo. The former was “probably superior,” while pitolisant “may have little to no effect on MWT, compared with placebo,” write the authors. The standardized mean difference in MWT scores, compared with placebo, was 0.90 for solriamfetol and 0.41 for armodafinil-modafinil. “Solriamfetol is probably superior to armodafinil-modafinil in improving MWT (SMD, 0.49),” say the authors.
Compared with placebo, armodafinil-modafinil probably increases the risk for discontinuation due to adverse events (relative risk, 2.01), and solriamfetol may increase the risk for discontinuation (RR, 2.04), according to the authors. Pitolisant “may have little to no effect on drug discontinuations due to adverse events,” write the authors.
Although solriamfetol may have led to more discontinuations than armodafinil-modafinil, “we did not find convincing evidence of serious adverse events, albeit with very short-term follow-up,” they add.
The most common side effects for all interventions were headaches, insomnia, and anxiety. Headaches were most likely with armodafinil-modafinil (RR, 1.87), and insomnia was most likely with pitolisant (RR, 7.25).
“Although solriamfetol appears most effective, comorbid hypertension and costs may be barriers to its use,” say the researchers. “Furthermore, there are potentially effective candidate therapies such as methylphenidate, atomoxetine, or caffeine, which have not been examined in randomized clinical trials.”
Although EDS is reported in 40%-58% of patients with OSA and can persist in 6%-18% despite PAP therapy, most non-sleep specialists may not be aware of pharmacologic options, said Dr. Pitre. “I have not seen a study that looks at the prescribing habits of physicians for this condition, but I suspect that primary care physicians are not prescribing modafinil-armodafinil frequently for this and less so for solriamfetol,” he said. “I hope this paper builds awareness of this condition and also informs clinicians on the options available to patients, as well as common side effects to counsel them on before starting treatment.”
Dr. Pitre was surprised at the magnitude of solriamfetol’s superiority to modafinil-armodafinil but cautioned that solriamfetol has been shown to increase blood pressure in higher doses. It therefore must be prescribed carefully, “especially to a population of patients who often have comorbid hypertension,” he said.
Some limitations of the analysis were that all trials were conducted in high-income countries (most commonly the United States). Moreover, 77% of participants were White, and 71% were male.
Beneficial adjunctive therapy
Commenting on the findings, Sogol Javaheri, MD, MPH, who was not involved in the research, said that they confirm those of prior studies and are “consistent with what my colleagues and I experience in our clinical practices.”
Dr. Javaheri is associate program director of the sleep medicine fellowship at Brigham and Women’s Hospital and assistant professor of medicine at Harvard Medical School, both in Boston.
While sleep medicine specialists are more likely than others to prescribe these medications, “any clinician may use these medications, ideally if they have ruled out other potential reversible causes of EDS,” said Dr. Javaheri. “The medications do not treat the underlying cause, which is why it’s important to use them as an adjunct to conventional therapy that actually treats the underlying sleep disorder and to rule out additional potential causes of sleepiness that are treatable.”
These potential causes might include insufficient sleep (less than 7 hours per night), untreated anemia, and incompletely treated sleep disorders, she explained. In sleep medicine, modafinil is usually the treatment of choice because of its lower cost, but it may reduce the efficacy of hormonal contraception. Solriamfetol, however, does not. “Additionally, I look forward to validation of pitolisant for treatment of EDS in OSA patients, as it is not a controlled substance and may benefit patients with a history of substance abuse or who may be at higher risk of addiction,” said Dr. Javaheri.
The study was conducted without outside funding. Dr. Pitre and Dr. Javaheri report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
Deep sleep may mitigate the impact of Alzheimer’s pathology
Investigators found that deep sleep, also known as non-REM (NREM) slow-wave sleep, can protect memory function in cognitively normal adults with a high beta-amyloid burden.
“Think of deep sleep almost like a life raft that keeps memory afloat, rather than memory getting dragged down by the weight of Alzheimer’s disease pathology,” senior investigator Matthew Walker, PhD, professor of neuroscience and psychology, University of California, Berkeley, said in a news release.
The study was published online in BMC Medicine.
Resilience factor
Studying resilience to existing brain pathology is “an exciting new research direction,” lead author Zsófia Zavecz, PhD, with the Center for Human Sleep Science at the University of California, Berkeley, said in an interview.
“That is, what factors explain the individual differences in cognitive function despite the same level of brain pathology, and how do some people with significant pathology have largely preserved memory?” she added.
The study included 62 cognitively normal older adults from the Berkeley Aging Cohort Study.
Sleep EEG recordings were obtained over 2 nights in a sleep lab and PET scans were used to quantify beta-amyloid. Half of the participants had high beta-amyloid burden and half were beta-amyloid negative.
After the sleep studies, all participants completed a memory task involving matching names to faces.
The results suggest that deep NREM slow-wave sleep significantly moderates the effect of beta-amyloid status on memory function.
Specifically, NREM slow-wave activity selectively supported superior memory function in adults with high beta-amyloid burden, who are most in need of cognitive reserve (B = 2.694, P = .019), the researchers report.
In contrast, adults without significant beta-amyloid pathological burden – and thus without the same need for cognitive reserve – did not similarly benefit from NREM slow-wave activity (B = –0.115, P = .876).
The findings remained significant after adjusting for age, sex, body mass index, gray matter atrophy, and previously identified cognitive reserve factors, such as education and physical activity.
Dr. Zavecz said there are several potential reasons why deep sleep may support cognitive reserve.
One is that during deep sleep specifically, memories are replayed in the brain, and this results in a “neural reorganization” that helps stabilize the memory and make it more permanent.
“Other explanations include deep sleep’s role in maintaining homeostasis in the brain’s capacity to form new neural connections and providing an optimal brain state for the clearance of toxins interfering with healthy brain functioning,” she noted.
“The extent to which sleep could offer a protective buffer against severe cognitive impairment remains to be tested. However, this study is the first step in hopefully a series of new research that will investigate sleep as a cognitive reserve factor,” said Dr. Zavecz.
Encouraging data
Reached for comment, Percy Griffin, PhD, Alzheimer’s Association director of scientific engagement, said although the study sample is small, the results are “encouraging because sleep is a modifiable factor and can therefore be targeted.”
“More work is needed in a larger population before we can fully leverage this stage of sleep to reduce the risk of developing cognitive decline,” Dr. Griffin said.
Also weighing in on this research, Shaheen Lakhan, MD, PhD, a neurologist and researcher in Boston, said the study is “exciting on two fronts – we may have an additional marker for the development of Alzheimer’s disease to predict risk and track disease, but also targets for early intervention with sleep architecture–enhancing therapies, be they drug, device, or digital.”
“For the sake of our brain health, we all must get very familiar with the concept of cognitive or brain reserve,” said Dr. Lakhan, who was not involved in the study.
“Brain reserve refers to our ability to buttress against the threat of dementia and classically it’s been associated with ongoing brain stimulation (i.e., higher education, cognitively demanding job),” he noted.
“This line of research now opens the door that optimal sleep health – especially deep NREM slow wave sleep – correlates with greater brain reserve against Alzheimer’s disease,” Dr. Lakhan said.
The study was supported by the National Institutes of Health and the University of California, Berkeley. Dr. Walker serves as an advisor to and has equity interest in Bryte, Shuni, Oura, and StimScience. Dr. Zavecz and Dr. Lakhan report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Investigators found that deep sleep, also known as non-REM (NREM) slow-wave sleep, can protect memory function in cognitively normal adults with a high beta-amyloid burden.
“Think of deep sleep almost like a life raft that keeps memory afloat, rather than memory getting dragged down by the weight of Alzheimer’s disease pathology,” senior investigator Matthew Walker, PhD, professor of neuroscience and psychology, University of California, Berkeley, said in a news release.
The study was published online in BMC Medicine.
Resilience factor
Studying resilience to existing brain pathology is “an exciting new research direction,” lead author Zsófia Zavecz, PhD, with the Center for Human Sleep Science at the University of California, Berkeley, said in an interview.
“That is, what factors explain the individual differences in cognitive function despite the same level of brain pathology, and how do some people with significant pathology have largely preserved memory?” she added.
The study included 62 cognitively normal older adults from the Berkeley Aging Cohort Study.
Sleep EEG recordings were obtained over 2 nights in a sleep lab and PET scans were used to quantify beta-amyloid. Half of the participants had high beta-amyloid burden and half were beta-amyloid negative.
After the sleep studies, all participants completed a memory task involving matching names to faces.
The results suggest that deep NREM slow-wave sleep significantly moderates the effect of beta-amyloid status on memory function.
Specifically, NREM slow-wave activity selectively supported superior memory function in adults with high beta-amyloid burden, who are most in need of cognitive reserve (B = 2.694, P = .019), the researchers report.
In contrast, adults without significant beta-amyloid pathological burden – and thus without the same need for cognitive reserve – did not similarly benefit from NREM slow-wave activity (B = –0.115, P = .876).
The findings remained significant after adjusting for age, sex, body mass index, gray matter atrophy, and previously identified cognitive reserve factors, such as education and physical activity.
Dr. Zavecz said there are several potential reasons why deep sleep may support cognitive reserve.
One is that during deep sleep specifically, memories are replayed in the brain, and this results in a “neural reorganization” that helps stabilize the memory and make it more permanent.
“Other explanations include deep sleep’s role in maintaining homeostasis in the brain’s capacity to form new neural connections and providing an optimal brain state for the clearance of toxins interfering with healthy brain functioning,” she noted.
“The extent to which sleep could offer a protective buffer against severe cognitive impairment remains to be tested. However, this study is the first step in hopefully a series of new research that will investigate sleep as a cognitive reserve factor,” said Dr. Zavecz.
Encouraging data
Reached for comment, Percy Griffin, PhD, Alzheimer’s Association director of scientific engagement, said although the study sample is small, the results are “encouraging because sleep is a modifiable factor and can therefore be targeted.”
“More work is needed in a larger population before we can fully leverage this stage of sleep to reduce the risk of developing cognitive decline,” Dr. Griffin said.
Also weighing in on this research, Shaheen Lakhan, MD, PhD, a neurologist and researcher in Boston, said the study is “exciting on two fronts – we may have an additional marker for the development of Alzheimer’s disease to predict risk and track disease, but also targets for early intervention with sleep architecture–enhancing therapies, be they drug, device, or digital.”
“For the sake of our brain health, we all must get very familiar with the concept of cognitive or brain reserve,” said Dr. Lakhan, who was not involved in the study.
“Brain reserve refers to our ability to buttress against the threat of dementia and classically it’s been associated with ongoing brain stimulation (i.e., higher education, cognitively demanding job),” he noted.
“This line of research now opens the door that optimal sleep health – especially deep NREM slow wave sleep – correlates with greater brain reserve against Alzheimer’s disease,” Dr. Lakhan said.
The study was supported by the National Institutes of Health and the University of California, Berkeley. Dr. Walker serves as an advisor to and has equity interest in Bryte, Shuni, Oura, and StimScience. Dr. Zavecz and Dr. Lakhan report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Investigators found that deep sleep, also known as non-REM (NREM) slow-wave sleep, can protect memory function in cognitively normal adults with a high beta-amyloid burden.
“Think of deep sleep almost like a life raft that keeps memory afloat, rather than memory getting dragged down by the weight of Alzheimer’s disease pathology,” senior investigator Matthew Walker, PhD, professor of neuroscience and psychology, University of California, Berkeley, said in a news release.
The study was published online in BMC Medicine.
Resilience factor
Studying resilience to existing brain pathology is “an exciting new research direction,” lead author Zsófia Zavecz, PhD, with the Center for Human Sleep Science at the University of California, Berkeley, said in an interview.
“That is, what factors explain the individual differences in cognitive function despite the same level of brain pathology, and how do some people with significant pathology have largely preserved memory?” she added.
The study included 62 cognitively normal older adults from the Berkeley Aging Cohort Study.
Sleep EEG recordings were obtained over 2 nights in a sleep lab and PET scans were used to quantify beta-amyloid. Half of the participants had high beta-amyloid burden and half were beta-amyloid negative.
After the sleep studies, all participants completed a memory task involving matching names to faces.
The results suggest that deep NREM slow-wave sleep significantly moderates the effect of beta-amyloid status on memory function.
Specifically, NREM slow-wave activity selectively supported superior memory function in adults with high beta-amyloid burden, who are most in need of cognitive reserve (B = 2.694, P = .019), the researchers report.
In contrast, adults without significant beta-amyloid pathological burden – and thus without the same need for cognitive reserve – did not similarly benefit from NREM slow-wave activity (B = –0.115, P = .876).
The findings remained significant after adjusting for age, sex, body mass index, gray matter atrophy, and previously identified cognitive reserve factors, such as education and physical activity.
Dr. Zavecz said there are several potential reasons why deep sleep may support cognitive reserve.
One is that during deep sleep specifically, memories are replayed in the brain, and this results in a “neural reorganization” that helps stabilize the memory and make it more permanent.
“Other explanations include deep sleep’s role in maintaining homeostasis in the brain’s capacity to form new neural connections and providing an optimal brain state for the clearance of toxins interfering with healthy brain functioning,” she noted.
“The extent to which sleep could offer a protective buffer against severe cognitive impairment remains to be tested. However, this study is the first step in hopefully a series of new research that will investigate sleep as a cognitive reserve factor,” said Dr. Zavecz.
Encouraging data
Reached for comment, Percy Griffin, PhD, Alzheimer’s Association director of scientific engagement, said although the study sample is small, the results are “encouraging because sleep is a modifiable factor and can therefore be targeted.”
“More work is needed in a larger population before we can fully leverage this stage of sleep to reduce the risk of developing cognitive decline,” Dr. Griffin said.
Also weighing in on this research, Shaheen Lakhan, MD, PhD, a neurologist and researcher in Boston, said the study is “exciting on two fronts – we may have an additional marker for the development of Alzheimer’s disease to predict risk and track disease, but also targets for early intervention with sleep architecture–enhancing therapies, be they drug, device, or digital.”
“For the sake of our brain health, we all must get very familiar with the concept of cognitive or brain reserve,” said Dr. Lakhan, who was not involved in the study.
“Brain reserve refers to our ability to buttress against the threat of dementia and classically it’s been associated with ongoing brain stimulation (i.e., higher education, cognitively demanding job),” he noted.
“This line of research now opens the door that optimal sleep health – especially deep NREM slow wave sleep – correlates with greater brain reserve against Alzheimer’s disease,” Dr. Lakhan said.
The study was supported by the National Institutes of Health and the University of California, Berkeley. Dr. Walker serves as an advisor to and has equity interest in Bryte, Shuni, Oura, and StimScience. Dr. Zavecz and Dr. Lakhan report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM BMC MEDICINE
Medical-level empathy? Yup, ChatGPT can fake that
Caution: Robotic uprisings in the rearview mirror are closer than they appear
ChatGPT. If you’ve been even in the proximity of the Internet lately, you may have heard of it. It’s quite an incredible piece of technology, an artificial intelligence that really could up-end a lot of industries. And lest doctors believe they’re safe from robotic replacement, consider this: ChatGPT took a test commonly used as a study resource by ophthalmologists and scored a 46%. Obviously, that’s not a passing grade. Job safe, right?
A month later, the researchers tried again. This time, ChatGPT got a 58%. Still not passing, and ChatGPT did especially poorly on ophthalmology specialty questions (it got 80% of general medicine questions right), but still, the jump in quality after just a month is ... concerning. It’s not like an AI will forget things. That score can only go up, and it’ll go up faster than you think.
“Sure, the robot is smart,” the doctors out there are thinking, “but how can an AI compete with human compassion, understanding, and bedside manner?”
And they’d be right. When it comes to bedside manner, there’s no competition between man and bot. ChatGPT is already winning.
In another study, researchers sampled nearly 200 questions from the subreddit r/AskDocs, which received verified physician responses. The researchers fed ChatGPT the questions – without the doctor’s answer – and a panel of health care professionals evaluated both the human doctor and ChatGPT in terms of quality and empathy.
Perhaps not surprisingly, the robot did better when it came to quality, providing a high-quality response 79% of the time, versus 22% for the human. But empathy? It was a bloodbath. ChatGPT provided an empathetic or very empathetic response 45% of the time, while humans could only do so 4.6% of the time. So much for bedside manner.
The researchers were suspiciously quick to note that ChatGPT isn’t a legitimate replacement for physicians, but could represent a tool to better provide care for patients. But let’s be honest, given ChatGPT’s quick advancement, how long before some intrepid stockholder says: “Hey, instead of paying doctors, why don’t we just use the free robot instead?” We give it a week. Or 11 minutes.
This week, on ‘As the sperm turns’
We’ve got a lot of spermy ground to cover, so let’s get right to it, starting with the small and working our way up.
We’re all pretty familiar with the basic structure of a sperm cell, yes? Bulbous head that contains all the important genetic information and a tail-like flagellum to propel it to its ultimate destination. Not much to work with there, you’d think, but what if Mother Nature, who clearly has a robust sense of humor, had something else in mind?
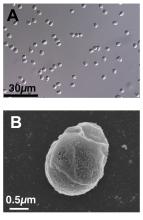
We present exhibit A, Paramormyorps kingsleyae, also known as the electric elephantfish, which happens to be the only known vertebrate species with tailless sperm. Sounds crazy to us, too, but Jason Gallant, PhD, of
Michigan State University, Lansing, has a theory: “A general notion in biology is that sperm are cheap, and eggs are expensive – but these fish may be telling us that sperm are more expensive than we might think. They could be saving energy by cutting back on sperm tails.”
He and his team think that finding the gene that turns off development of the flagellum in the elephant fish could benefit humans, specifically those with a genetic disorder called primary ciliary dyskinesia, whose lack of normally functioning cilia and flagella leads to chronic respiratory infection, abnormally positioned organs, fluid on the brain, and infertility.
And that – with “that” being infertility – brings us to exhibit B, a 41-year-old Dutch man named Jonathan Meijer who clearly has too much time on his hands.
A court in the Netherlands recently ordered him, and not for the first time, to stop donating sperm to fertility clinics after it was discovered that he had fathered between 500 and 600 children around the world. He had been banned from donating to Dutch clinics in 2017, at which point he had already fathered 100 children, but managed a workaround by donating internationally and online, sometimes using another name.
The judge ordered Mr. Meijer to contact all of the clinics abroad and ask them to destroy any of his sperm they still had in stock and threatened to fine him over $100,000 for each future violation.
Okay, so here’s the thing. We have been, um, let’s call it ... warned, about the evils of tastelessness in journalism, so we’re going to do what Mr. Meijer should have done and abstain. And we can last for longer than 11 minutes.
The realm of lost luggage and lost sleep
It may be convenient to live near an airport if you’re a frequent flyer, but it really doesn’t help your sleep numbers.
The first look at how such a common sound affects sleep duration showed that people exposed to even 45 decibels of airplane noise were less likely to get the 7-9 hours of sleep needed for healthy functioning, investigators said in Environmental Health Perspectives.
How loud is 45 dB exactly? A normal conversation is about 50 dB, while a whisper is 30 dB, to give you an idea. Airplane noise at 45 dB? You might not even notice it amongst the other noises in daily life.
The researchers looked at data from about 35,000 participants in the Nurses’ Health Study who live around 90 major U.S. airports. They examined plane noise every 5 years between 1995 and 2005, focusing on estimates of nighttime and daytime levels. Short sleep was most common among the nurses who lived on the West Coast, near major cargo airports or large bodies of water, and also among those who reported no hearing loss.
The investigators noted, however, that there was no consistent association between airplane noise and quality of sleep and stopped short of making any policy recommendations. Still, sleep is a very important, yet slept-on (pun intended) factor for our overall health, so it’s good to know if anything has the potential to cause disruption.
Caution: Robotic uprisings in the rearview mirror are closer than they appear
ChatGPT. If you’ve been even in the proximity of the Internet lately, you may have heard of it. It’s quite an incredible piece of technology, an artificial intelligence that really could up-end a lot of industries. And lest doctors believe they’re safe from robotic replacement, consider this: ChatGPT took a test commonly used as a study resource by ophthalmologists and scored a 46%. Obviously, that’s not a passing grade. Job safe, right?
A month later, the researchers tried again. This time, ChatGPT got a 58%. Still not passing, and ChatGPT did especially poorly on ophthalmology specialty questions (it got 80% of general medicine questions right), but still, the jump in quality after just a month is ... concerning. It’s not like an AI will forget things. That score can only go up, and it’ll go up faster than you think.
“Sure, the robot is smart,” the doctors out there are thinking, “but how can an AI compete with human compassion, understanding, and bedside manner?”
And they’d be right. When it comes to bedside manner, there’s no competition between man and bot. ChatGPT is already winning.
In another study, researchers sampled nearly 200 questions from the subreddit r/AskDocs, which received verified physician responses. The researchers fed ChatGPT the questions – without the doctor’s answer – and a panel of health care professionals evaluated both the human doctor and ChatGPT in terms of quality and empathy.
Perhaps not surprisingly, the robot did better when it came to quality, providing a high-quality response 79% of the time, versus 22% for the human. But empathy? It was a bloodbath. ChatGPT provided an empathetic or very empathetic response 45% of the time, while humans could only do so 4.6% of the time. So much for bedside manner.
The researchers were suspiciously quick to note that ChatGPT isn’t a legitimate replacement for physicians, but could represent a tool to better provide care for patients. But let’s be honest, given ChatGPT’s quick advancement, how long before some intrepid stockholder says: “Hey, instead of paying doctors, why don’t we just use the free robot instead?” We give it a week. Or 11 minutes.
This week, on ‘As the sperm turns’
We’ve got a lot of spermy ground to cover, so let’s get right to it, starting with the small and working our way up.
We’re all pretty familiar with the basic structure of a sperm cell, yes? Bulbous head that contains all the important genetic information and a tail-like flagellum to propel it to its ultimate destination. Not much to work with there, you’d think, but what if Mother Nature, who clearly has a robust sense of humor, had something else in mind?
We present exhibit A, Paramormyorps kingsleyae, also known as the electric elephantfish, which happens to be the only known vertebrate species with tailless sperm. Sounds crazy to us, too, but Jason Gallant, PhD, of
Michigan State University, Lansing, has a theory: “A general notion in biology is that sperm are cheap, and eggs are expensive – but these fish may be telling us that sperm are more expensive than we might think. They could be saving energy by cutting back on sperm tails.”
He and his team think that finding the gene that turns off development of the flagellum in the elephant fish could benefit humans, specifically those with a genetic disorder called primary ciliary dyskinesia, whose lack of normally functioning cilia and flagella leads to chronic respiratory infection, abnormally positioned organs, fluid on the brain, and infertility.
And that – with “that” being infertility – brings us to exhibit B, a 41-year-old Dutch man named Jonathan Meijer who clearly has too much time on his hands.
A court in the Netherlands recently ordered him, and not for the first time, to stop donating sperm to fertility clinics after it was discovered that he had fathered between 500 and 600 children around the world. He had been banned from donating to Dutch clinics in 2017, at which point he had already fathered 100 children, but managed a workaround by donating internationally and online, sometimes using another name.
The judge ordered Mr. Meijer to contact all of the clinics abroad and ask them to destroy any of his sperm they still had in stock and threatened to fine him over $100,000 for each future violation.
Okay, so here’s the thing. We have been, um, let’s call it ... warned, about the evils of tastelessness in journalism, so we’re going to do what Mr. Meijer should have done and abstain. And we can last for longer than 11 minutes.
The realm of lost luggage and lost sleep
It may be convenient to live near an airport if you’re a frequent flyer, but it really doesn’t help your sleep numbers.
The first look at how such a common sound affects sleep duration showed that people exposed to even 45 decibels of airplane noise were less likely to get the 7-9 hours of sleep needed for healthy functioning, investigators said in Environmental Health Perspectives.
How loud is 45 dB exactly? A normal conversation is about 50 dB, while a whisper is 30 dB, to give you an idea. Airplane noise at 45 dB? You might not even notice it amongst the other noises in daily life.
The researchers looked at data from about 35,000 participants in the Nurses’ Health Study who live around 90 major U.S. airports. They examined plane noise every 5 years between 1995 and 2005, focusing on estimates of nighttime and daytime levels. Short sleep was most common among the nurses who lived on the West Coast, near major cargo airports or large bodies of water, and also among those who reported no hearing loss.
The investigators noted, however, that there was no consistent association between airplane noise and quality of sleep and stopped short of making any policy recommendations. Still, sleep is a very important, yet slept-on (pun intended) factor for our overall health, so it’s good to know if anything has the potential to cause disruption.
Caution: Robotic uprisings in the rearview mirror are closer than they appear
ChatGPT. If you’ve been even in the proximity of the Internet lately, you may have heard of it. It’s quite an incredible piece of technology, an artificial intelligence that really could up-end a lot of industries. And lest doctors believe they’re safe from robotic replacement, consider this: ChatGPT took a test commonly used as a study resource by ophthalmologists and scored a 46%. Obviously, that’s not a passing grade. Job safe, right?
A month later, the researchers tried again. This time, ChatGPT got a 58%. Still not passing, and ChatGPT did especially poorly on ophthalmology specialty questions (it got 80% of general medicine questions right), but still, the jump in quality after just a month is ... concerning. It’s not like an AI will forget things. That score can only go up, and it’ll go up faster than you think.
“Sure, the robot is smart,” the doctors out there are thinking, “but how can an AI compete with human compassion, understanding, and bedside manner?”
And they’d be right. When it comes to bedside manner, there’s no competition between man and bot. ChatGPT is already winning.
In another study, researchers sampled nearly 200 questions from the subreddit r/AskDocs, which received verified physician responses. The researchers fed ChatGPT the questions – without the doctor’s answer – and a panel of health care professionals evaluated both the human doctor and ChatGPT in terms of quality and empathy.
Perhaps not surprisingly, the robot did better when it came to quality, providing a high-quality response 79% of the time, versus 22% for the human. But empathy? It was a bloodbath. ChatGPT provided an empathetic or very empathetic response 45% of the time, while humans could only do so 4.6% of the time. So much for bedside manner.
The researchers were suspiciously quick to note that ChatGPT isn’t a legitimate replacement for physicians, but could represent a tool to better provide care for patients. But let’s be honest, given ChatGPT’s quick advancement, how long before some intrepid stockholder says: “Hey, instead of paying doctors, why don’t we just use the free robot instead?” We give it a week. Or 11 minutes.
This week, on ‘As the sperm turns’
We’ve got a lot of spermy ground to cover, so let’s get right to it, starting with the small and working our way up.
We’re all pretty familiar with the basic structure of a sperm cell, yes? Bulbous head that contains all the important genetic information and a tail-like flagellum to propel it to its ultimate destination. Not much to work with there, you’d think, but what if Mother Nature, who clearly has a robust sense of humor, had something else in mind?
We present exhibit A, Paramormyorps kingsleyae, also known as the electric elephantfish, which happens to be the only known vertebrate species with tailless sperm. Sounds crazy to us, too, but Jason Gallant, PhD, of
Michigan State University, Lansing, has a theory: “A general notion in biology is that sperm are cheap, and eggs are expensive – but these fish may be telling us that sperm are more expensive than we might think. They could be saving energy by cutting back on sperm tails.”
He and his team think that finding the gene that turns off development of the flagellum in the elephant fish could benefit humans, specifically those with a genetic disorder called primary ciliary dyskinesia, whose lack of normally functioning cilia and flagella leads to chronic respiratory infection, abnormally positioned organs, fluid on the brain, and infertility.
And that – with “that” being infertility – brings us to exhibit B, a 41-year-old Dutch man named Jonathan Meijer who clearly has too much time on his hands.
A court in the Netherlands recently ordered him, and not for the first time, to stop donating sperm to fertility clinics after it was discovered that he had fathered between 500 and 600 children around the world. He had been banned from donating to Dutch clinics in 2017, at which point he had already fathered 100 children, but managed a workaround by donating internationally and online, sometimes using another name.
The judge ordered Mr. Meijer to contact all of the clinics abroad and ask them to destroy any of his sperm they still had in stock and threatened to fine him over $100,000 for each future violation.
Okay, so here’s the thing. We have been, um, let’s call it ... warned, about the evils of tastelessness in journalism, so we’re going to do what Mr. Meijer should have done and abstain. And we can last for longer than 11 minutes.
The realm of lost luggage and lost sleep
It may be convenient to live near an airport if you’re a frequent flyer, but it really doesn’t help your sleep numbers.
The first look at how such a common sound affects sleep duration showed that people exposed to even 45 decibels of airplane noise were less likely to get the 7-9 hours of sleep needed for healthy functioning, investigators said in Environmental Health Perspectives.
How loud is 45 dB exactly? A normal conversation is about 50 dB, while a whisper is 30 dB, to give you an idea. Airplane noise at 45 dB? You might not even notice it amongst the other noises in daily life.
The researchers looked at data from about 35,000 participants in the Nurses’ Health Study who live around 90 major U.S. airports. They examined plane noise every 5 years between 1995 and 2005, focusing on estimates of nighttime and daytime levels. Short sleep was most common among the nurses who lived on the West Coast, near major cargo airports or large bodies of water, and also among those who reported no hearing loss.
The investigators noted, however, that there was no consistent association between airplane noise and quality of sleep and stopped short of making any policy recommendations. Still, sleep is a very important, yet slept-on (pun intended) factor for our overall health, so it’s good to know if anything has the potential to cause disruption.
CPAP not only solution for sleep apnea
Although continuous positive airway pressure (CPAP) machines are the gold standard in the management of sleep apnea, several other treatments should be considered.
“Just because you have a hammer doesn’t mean everything is a nail,” Kimberly Hardin, MD, professor of clinical internal medicine at University of California, Davis, said at the annual meeting of the American College of Physicians.
“Sleep has been underestimated in the health arena for many, many years,” said Dr. Hardin, who likened sound sleep to the “sixth vital sign.” “We know that sleep plays an integral role in our health.”
Surgical options include nasal surgery and maxillomandibular advancement surgery, also known as double-jaw surgery. Such procedures should be considered only for patients who are unwilling or unable to use CPAP or other nonsurgical treatments.
Sleep apnea occurs in 4% of adult men and 2% of adult women aged 30-60. Most commonly, obstructive sleep apnea involves the cessation or significant decrease in airflow while sleeping. The Apnea Hypopnea Index (AHI) is the number of times a patient experiences apnea or hypopnea during one night divided by the hours of sleep. Normal sleep AHI is fewer than five events per hour on average; mild sleep apnea is five to 14 events; moderate, 15-29; and severe, at least 30 events.
To identify sleep apnea, physicians have several tools at their disposal, starting with preliminary questionnaires that query patients as to whether they are having trouble falling asleep, staying asleep, or are tired during the day. Additional assessment tools include sleep lab testing and at-home testing.
At-home testing has come to include more than the common devices that are worn around the chest and nose for a night.
“It’s not very fun looking,” Dr. Hardin said of the weighty, obtrusive monitoring devices. “So lots of folks have come up with some new ways of doing things.”
These new options incorporate headbands, wrist and finger devices, arterial tonometry, and sleep rings.
Studies show that U.S. adults do not get enough sleep, and poor-quality sleep is as inadequate as insufficient sleep. Barely a third of adults get the minimum 7 hours recommended by the Centers for Disease Control and Prevention. Non-Hispanic Black adults are less likely to report sleeping 7-9 hours and are more likely to report sleeping 6 or fewer hours than are non-Hispanic White and Hispanic adults.
Dr. Hardin said doctors can advise patients to keep their bedrooms quiet, dark, and cool with no TVs or electronics, to maintain regular wake and sleep times, and to stop consuming caffeine late in the day.
Insufficient or poor sleep can have wide-ranging implications on medical conditions such as diabetes, heart disease, obesity, immunodeficiency, cognitive function, mental health, and, ultimately, mortality, according to Dr. Hardin.
“Some people say, ‘Oh, never mind, I can sleep when I’m dead,’ “ Dr. Hardin said. But such a mentality can have a bearing on life expectancy.
A version of this article first appeared on Medscape.com.
Although continuous positive airway pressure (CPAP) machines are the gold standard in the management of sleep apnea, several other treatments should be considered.
“Just because you have a hammer doesn’t mean everything is a nail,” Kimberly Hardin, MD, professor of clinical internal medicine at University of California, Davis, said at the annual meeting of the American College of Physicians.
“Sleep has been underestimated in the health arena for many, many years,” said Dr. Hardin, who likened sound sleep to the “sixth vital sign.” “We know that sleep plays an integral role in our health.”
Surgical options include nasal surgery and maxillomandibular advancement surgery, also known as double-jaw surgery. Such procedures should be considered only for patients who are unwilling or unable to use CPAP or other nonsurgical treatments.
Sleep apnea occurs in 4% of adult men and 2% of adult women aged 30-60. Most commonly, obstructive sleep apnea involves the cessation or significant decrease in airflow while sleeping. The Apnea Hypopnea Index (AHI) is the number of times a patient experiences apnea or hypopnea during one night divided by the hours of sleep. Normal sleep AHI is fewer than five events per hour on average; mild sleep apnea is five to 14 events; moderate, 15-29; and severe, at least 30 events.
To identify sleep apnea, physicians have several tools at their disposal, starting with preliminary questionnaires that query patients as to whether they are having trouble falling asleep, staying asleep, or are tired during the day. Additional assessment tools include sleep lab testing and at-home testing.
At-home testing has come to include more than the common devices that are worn around the chest and nose for a night.
“It’s not very fun looking,” Dr. Hardin said of the weighty, obtrusive monitoring devices. “So lots of folks have come up with some new ways of doing things.”
These new options incorporate headbands, wrist and finger devices, arterial tonometry, and sleep rings.
Studies show that U.S. adults do not get enough sleep, and poor-quality sleep is as inadequate as insufficient sleep. Barely a third of adults get the minimum 7 hours recommended by the Centers for Disease Control and Prevention. Non-Hispanic Black adults are less likely to report sleeping 7-9 hours and are more likely to report sleeping 6 or fewer hours than are non-Hispanic White and Hispanic adults.
Dr. Hardin said doctors can advise patients to keep their bedrooms quiet, dark, and cool with no TVs or electronics, to maintain regular wake and sleep times, and to stop consuming caffeine late in the day.
Insufficient or poor sleep can have wide-ranging implications on medical conditions such as diabetes, heart disease, obesity, immunodeficiency, cognitive function, mental health, and, ultimately, mortality, according to Dr. Hardin.
“Some people say, ‘Oh, never mind, I can sleep when I’m dead,’ “ Dr. Hardin said. But such a mentality can have a bearing on life expectancy.
A version of this article first appeared on Medscape.com.
Although continuous positive airway pressure (CPAP) machines are the gold standard in the management of sleep apnea, several other treatments should be considered.
“Just because you have a hammer doesn’t mean everything is a nail,” Kimberly Hardin, MD, professor of clinical internal medicine at University of California, Davis, said at the annual meeting of the American College of Physicians.
“Sleep has been underestimated in the health arena for many, many years,” said Dr. Hardin, who likened sound sleep to the “sixth vital sign.” “We know that sleep plays an integral role in our health.”
Surgical options include nasal surgery and maxillomandibular advancement surgery, also known as double-jaw surgery. Such procedures should be considered only for patients who are unwilling or unable to use CPAP or other nonsurgical treatments.
Sleep apnea occurs in 4% of adult men and 2% of adult women aged 30-60. Most commonly, obstructive sleep apnea involves the cessation or significant decrease in airflow while sleeping. The Apnea Hypopnea Index (AHI) is the number of times a patient experiences apnea or hypopnea during one night divided by the hours of sleep. Normal sleep AHI is fewer than five events per hour on average; mild sleep apnea is five to 14 events; moderate, 15-29; and severe, at least 30 events.
To identify sleep apnea, physicians have several tools at their disposal, starting with preliminary questionnaires that query patients as to whether they are having trouble falling asleep, staying asleep, or are tired during the day. Additional assessment tools include sleep lab testing and at-home testing.
At-home testing has come to include more than the common devices that are worn around the chest and nose for a night.
“It’s not very fun looking,” Dr. Hardin said of the weighty, obtrusive monitoring devices. “So lots of folks have come up with some new ways of doing things.”
These new options incorporate headbands, wrist and finger devices, arterial tonometry, and sleep rings.
Studies show that U.S. adults do not get enough sleep, and poor-quality sleep is as inadequate as insufficient sleep. Barely a third of adults get the minimum 7 hours recommended by the Centers for Disease Control and Prevention. Non-Hispanic Black adults are less likely to report sleeping 7-9 hours and are more likely to report sleeping 6 or fewer hours than are non-Hispanic White and Hispanic adults.
Dr. Hardin said doctors can advise patients to keep their bedrooms quiet, dark, and cool with no TVs or electronics, to maintain regular wake and sleep times, and to stop consuming caffeine late in the day.
Insufficient or poor sleep can have wide-ranging implications on medical conditions such as diabetes, heart disease, obesity, immunodeficiency, cognitive function, mental health, and, ultimately, mortality, according to Dr. Hardin.
“Some people say, ‘Oh, never mind, I can sleep when I’m dead,’ “ Dr. Hardin said. But such a mentality can have a bearing on life expectancy.
A version of this article first appeared on Medscape.com.
FROM INTERNAL MEDICINE 2023
Erratic sleep, lack of activity tied to worsening schizophrenia symptoms
The findings also showed that people with schizophrenia spectrum disorders (SSDs) who lived in residential facilities experienced rigid routines, which correlated with a higher degree of negative symptoms.
The rigid routines were problematic for the patients living in residential settings, lead investigator Fabio Ferrarelli, MD, PhD, told this news organization. Dr. Ferrarelli is an associate professor of psychiatry at the University of Pittsburgh.
“Engaging in different activities at different times in activities associated with motivation and social interaction – this helps to ameliorate difficult-to-treat negative symptoms,” he said.
The findings were published online in Molecular Psychiatry.
Need to increase activity levels
While there is no shortage of research on sleep disturbances among people with schizophrenia, research focusing specifically on rest-activity rhythm disturbances and their relationships to symptoms of schizophrenia has been limited by small sample sizes or the lack of a control group, the investigators note.
To address this research gap, the investigators recruited 230 patients with SSD from participating residential facilities and communities throughout Italy. The participants included 108 healthy control participants, 54 community-dwelling patients with SSD who were receiving outpatient services, and 68 patients with SSD who were living in residential facilities.
All participants wore an actigraph for 7 consecutive days so that investigators could monitor sleep-wake patterns.
Compared with healthy control participants, both SSD groups had more total sleep time and spent more time resting or being passive (P < .001). In contrast, healthy control participants were much more active.
Part of the explanation for this may be that most of the control participants had jobs or attended school. In addition, the investigators note that many medications used to treat SSD can be highly sedating, causing some patients to sleep up to 15 hours per day.
Among residential participants with SSD, there was a higher level of inter-daily stability and higher daily rest-activity-rest fragmentation than occurred among healthy control participants or community-dwelling patients with SSD (P < .001). There was also a higher level of negative symptoms among residential participants with SSD than among the community-dwelling group with SSD.
When the findings were taken together, Dr. Ferrarelli and his team interpreted them to mean that inter-daily stability could reflect premature aging or neurodegenerative processes in patients with more severe forms of schizophrenia.
Another explanation could be that the rigid routine of the residential facility was making negative symptoms worse, Dr. Ferrarelli said. It is important to add variety into the mix – getting people to engage in different activities at different times of day would likely help residential SSD patients overcome negative symptoms of the disorder.
Although participants were recruited in Italy, Dr. Ferrarelli said he believes the findings are generalizable.
Bidirectional relationship?
Commenting on the findings, Matcheri Keshavan, MD, professor of psychiatry at Harvard Medical School in Boston, said the results are consistent with “well-known clinical observations that SSD patients tend to spend more time in bed and have more dysregulated sleep.
“Negative symptoms are also common, especially in residential patients. However, it is difficult to determine causality, as we do not know whether excessive sleepiness and decreased physical activity cause negative symptoms, or vice versa, or whether this is a bidirectional relationship,” Dr. Keshavan said.
He emphasized that physical exercise is known to increase sleep quality for people with mental illness and may also improve negative symptoms. “A useful approach in clinical practice is to increase activity levels, especially physical activities like walking and gardening.”
Dr. Keshavan said he would like to see future research that focuses on whether an intervention such as aerobic exercise would improve sleep quality as well as negative symptoms.
He also said that future research should ideally examine the characteristics of sleep alterations in schizophrenia.
“For example, while sleep duration is increased in schizophrenia, studies suggest that time spent in deep sleep is reduced; sleep spindles, which are important for consolidating memory during sleep, are also reduced. Correcting these deficits may improve negative symptoms and cognitive deficits,” he added.
The study was funded by the Italian Ministry of Health and the National Institute of Mental Health. There were no conflicts of interest.
A version of this article first appeared on Medscape.com.
The findings also showed that people with schizophrenia spectrum disorders (SSDs) who lived in residential facilities experienced rigid routines, which correlated with a higher degree of negative symptoms.
The rigid routines were problematic for the patients living in residential settings, lead investigator Fabio Ferrarelli, MD, PhD, told this news organization. Dr. Ferrarelli is an associate professor of psychiatry at the University of Pittsburgh.
“Engaging in different activities at different times in activities associated with motivation and social interaction – this helps to ameliorate difficult-to-treat negative symptoms,” he said.
The findings were published online in Molecular Psychiatry.
Need to increase activity levels
While there is no shortage of research on sleep disturbances among people with schizophrenia, research focusing specifically on rest-activity rhythm disturbances and their relationships to symptoms of schizophrenia has been limited by small sample sizes or the lack of a control group, the investigators note.
To address this research gap, the investigators recruited 230 patients with SSD from participating residential facilities and communities throughout Italy. The participants included 108 healthy control participants, 54 community-dwelling patients with SSD who were receiving outpatient services, and 68 patients with SSD who were living in residential facilities.
All participants wore an actigraph for 7 consecutive days so that investigators could monitor sleep-wake patterns.
Compared with healthy control participants, both SSD groups had more total sleep time and spent more time resting or being passive (P < .001). In contrast, healthy control participants were much more active.
Part of the explanation for this may be that most of the control participants had jobs or attended school. In addition, the investigators note that many medications used to treat SSD can be highly sedating, causing some patients to sleep up to 15 hours per day.
Among residential participants with SSD, there was a higher level of inter-daily stability and higher daily rest-activity-rest fragmentation than occurred among healthy control participants or community-dwelling patients with SSD (P < .001). There was also a higher level of negative symptoms among residential participants with SSD than among the community-dwelling group with SSD.
When the findings were taken together, Dr. Ferrarelli and his team interpreted them to mean that inter-daily stability could reflect premature aging or neurodegenerative processes in patients with more severe forms of schizophrenia.
Another explanation could be that the rigid routine of the residential facility was making negative symptoms worse, Dr. Ferrarelli said. It is important to add variety into the mix – getting people to engage in different activities at different times of day would likely help residential SSD patients overcome negative symptoms of the disorder.
Although participants were recruited in Italy, Dr. Ferrarelli said he believes the findings are generalizable.
Bidirectional relationship?
Commenting on the findings, Matcheri Keshavan, MD, professor of psychiatry at Harvard Medical School in Boston, said the results are consistent with “well-known clinical observations that SSD patients tend to spend more time in bed and have more dysregulated sleep.
“Negative symptoms are also common, especially in residential patients. However, it is difficult to determine causality, as we do not know whether excessive sleepiness and decreased physical activity cause negative symptoms, or vice versa, or whether this is a bidirectional relationship,” Dr. Keshavan said.
He emphasized that physical exercise is known to increase sleep quality for people with mental illness and may also improve negative symptoms. “A useful approach in clinical practice is to increase activity levels, especially physical activities like walking and gardening.”
Dr. Keshavan said he would like to see future research that focuses on whether an intervention such as aerobic exercise would improve sleep quality as well as negative symptoms.
He also said that future research should ideally examine the characteristics of sleep alterations in schizophrenia.
“For example, while sleep duration is increased in schizophrenia, studies suggest that time spent in deep sleep is reduced; sleep spindles, which are important for consolidating memory during sleep, are also reduced. Correcting these deficits may improve negative symptoms and cognitive deficits,” he added.
The study was funded by the Italian Ministry of Health and the National Institute of Mental Health. There were no conflicts of interest.
A version of this article first appeared on Medscape.com.
The findings also showed that people with schizophrenia spectrum disorders (SSDs) who lived in residential facilities experienced rigid routines, which correlated with a higher degree of negative symptoms.
The rigid routines were problematic for the patients living in residential settings, lead investigator Fabio Ferrarelli, MD, PhD, told this news organization. Dr. Ferrarelli is an associate professor of psychiatry at the University of Pittsburgh.
“Engaging in different activities at different times in activities associated with motivation and social interaction – this helps to ameliorate difficult-to-treat negative symptoms,” he said.
The findings were published online in Molecular Psychiatry.
Need to increase activity levels
While there is no shortage of research on sleep disturbances among people with schizophrenia, research focusing specifically on rest-activity rhythm disturbances and their relationships to symptoms of schizophrenia has been limited by small sample sizes or the lack of a control group, the investigators note.
To address this research gap, the investigators recruited 230 patients with SSD from participating residential facilities and communities throughout Italy. The participants included 108 healthy control participants, 54 community-dwelling patients with SSD who were receiving outpatient services, and 68 patients with SSD who were living in residential facilities.
All participants wore an actigraph for 7 consecutive days so that investigators could monitor sleep-wake patterns.
Compared with healthy control participants, both SSD groups had more total sleep time and spent more time resting or being passive (P < .001). In contrast, healthy control participants were much more active.
Part of the explanation for this may be that most of the control participants had jobs or attended school. In addition, the investigators note that many medications used to treat SSD can be highly sedating, causing some patients to sleep up to 15 hours per day.
Among residential participants with SSD, there was a higher level of inter-daily stability and higher daily rest-activity-rest fragmentation than occurred among healthy control participants or community-dwelling patients with SSD (P < .001). There was also a higher level of negative symptoms among residential participants with SSD than among the community-dwelling group with SSD.
When the findings were taken together, Dr. Ferrarelli and his team interpreted them to mean that inter-daily stability could reflect premature aging or neurodegenerative processes in patients with more severe forms of schizophrenia.
Another explanation could be that the rigid routine of the residential facility was making negative symptoms worse, Dr. Ferrarelli said. It is important to add variety into the mix – getting people to engage in different activities at different times of day would likely help residential SSD patients overcome negative symptoms of the disorder.
Although participants were recruited in Italy, Dr. Ferrarelli said he believes the findings are generalizable.
Bidirectional relationship?
Commenting on the findings, Matcheri Keshavan, MD, professor of psychiatry at Harvard Medical School in Boston, said the results are consistent with “well-known clinical observations that SSD patients tend to spend more time in bed and have more dysregulated sleep.
“Negative symptoms are also common, especially in residential patients. However, it is difficult to determine causality, as we do not know whether excessive sleepiness and decreased physical activity cause negative symptoms, or vice versa, or whether this is a bidirectional relationship,” Dr. Keshavan said.
He emphasized that physical exercise is known to increase sleep quality for people with mental illness and may also improve negative symptoms. “A useful approach in clinical practice is to increase activity levels, especially physical activities like walking and gardening.”
Dr. Keshavan said he would like to see future research that focuses on whether an intervention such as aerobic exercise would improve sleep quality as well as negative symptoms.
He also said that future research should ideally examine the characteristics of sleep alterations in schizophrenia.
“For example, while sleep duration is increased in schizophrenia, studies suggest that time spent in deep sleep is reduced; sleep spindles, which are important for consolidating memory during sleep, are also reduced. Correcting these deficits may improve negative symptoms and cognitive deficits,” he added.
The study was funded by the Italian Ministry of Health and the National Institute of Mental Health. There were no conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM MOLECULAR PSYCHIATRY
‘Shocking’ data on what’s really in melatonin gummies
New data may explain the recent massive jump in pediatric hospitalizations.
Thenvestigators found that consuming some products as directed could expose consumers, including children, to doses that are 40-130 times greater than what’s recommended.
“The results were quite shocking,” lead researcher Pieter Cohen, MD, with Harvard Medical School, Boston, and Cambridge Health Alliance, Somerville, Mass., said in an interview.
“Melatonin gummies contained up to 347% more melatonin than what was listed on the label, and some products also contained cannabidiol; in one brand of melatonin gummies, there was zero melatonin, just CBD,” Dr. Cohen said.
The study was published online in JAMA.
530% jump in pediatric hospitalizations
Melatonin products are not approved by the Food and Drug Administration but are sold over the counter or online.
Previous research from JAMA has shown the use of melatonin has increased over the past 2 decades among people of all ages.
With increased use has come a spike in reports of melatonin overdose, calls to poison control centers, and related ED visits for children.
Federal data show the number of U.S. children who unintentionally ingested melatonin supplements jumped 530% from 2012 to 2021. More than 4,000 of the reported ingestions led to a hospital stay; 287 children required intensive care, and two children died.
It was unclear why melatonin supplements were causing these harms, which led Dr. Cohen’s team to analyze 25 unique brands of “melatonin” gummies purchased online.
One product didn’t contain any melatonin but did contain 31.3 mg of CBD.
In the remaining products, the quantity of melatonin ranged from 1.3 mg to 13.1 mg per serving. The actual quantity of melatonin ranged from 74% to 347% of the labeled quantity, the researchers found.
They note that for a young adult who takes as little as 0.1-0.3 mg of melatonin, plasma concentrations can increase into the normal night-time range.
Of the 25 products (88%) analyzed, 22 were inaccurately labeled, and only 3 (12%) contained a quantity of melatonin that was within 10% (plus or minus) of the declared quantity.
Five products listed CBD as an ingredient. The listed quantity ranged from 10.6 mg to 31.3 mg per serving, although the actual quantity of CBD ranged from 104% to 118% of the labeled quantity.
Inquire about use in kids
A limitation of the study is that only one sample of each brand was analyzed, and only gummies were analyzed. It is not known whether the results are generalizable to melatonin products sold as tablets and capsules in the United States or whether the quantity of melatonin within an individual brand may vary from batch to batch.
A recent study from Canada showed similar results. In an analysis of 16 Canadian melatonin brands, the actual dose of melatonin ranged from 17% to 478% of the declared quantity.
It’s estimated that more than 1% of all U.S. children use melatonin supplements, most commonly for sleep, stress, and relaxation.
“Given new research as to the excessive quantities of melatonin in gummies, caution should be used if considering their use,” said Dr. Cohen.
“It’s important to inquire about melatonin use when caring for children, particularly when parents express concerns about their child’s sleep,” he added.
The American Academy of Sleep Medicine recently issued a health advisory encouraging parents to talk to a health care professional before giving melatonin or any supplement to children.
Children don’t need melatonin
Commenting on the study, Michael Breus, PhD, clinical psychologist and founder of TheSleepDoctor.com, agreed that analyzing only one sample of each brand is a key limitation “because supplements are made in batches, and gummies in particular are difficult to distribute the active ingredient evenly.
“But even with that being said, 88% of them were labeled incorrectly, so even if there were a few single-sample issues, I kind of doubt its all of them,” Dr. Breus said.
“Kids as a general rule do not need melatonin. Their brains make almost four times the necessary amount already. If you start giving kids pills to help them sleep, then they start to have a pill problem, causing another issue,” Dr. Breus added.
“Most children’s falling asleep and staying sleep issues can be treated with behavioral measures like cognitive-behavioral therapy for insomnia,” he said.
The study had no specific funding. Dr. Cohen has received research support from Consumers Union and PEW Charitable Trusts and royalties from UptoDate. Dr. Breus disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New data may explain the recent massive jump in pediatric hospitalizations.
Thenvestigators found that consuming some products as directed could expose consumers, including children, to doses that are 40-130 times greater than what’s recommended.
“The results were quite shocking,” lead researcher Pieter Cohen, MD, with Harvard Medical School, Boston, and Cambridge Health Alliance, Somerville, Mass., said in an interview.
“Melatonin gummies contained up to 347% more melatonin than what was listed on the label, and some products also contained cannabidiol; in one brand of melatonin gummies, there was zero melatonin, just CBD,” Dr. Cohen said.
The study was published online in JAMA.
530% jump in pediatric hospitalizations
Melatonin products are not approved by the Food and Drug Administration but are sold over the counter or online.
Previous research from JAMA has shown the use of melatonin has increased over the past 2 decades among people of all ages.
With increased use has come a spike in reports of melatonin overdose, calls to poison control centers, and related ED visits for children.
Federal data show the number of U.S. children who unintentionally ingested melatonin supplements jumped 530% from 2012 to 2021. More than 4,000 of the reported ingestions led to a hospital stay; 287 children required intensive care, and two children died.
It was unclear why melatonin supplements were causing these harms, which led Dr. Cohen’s team to analyze 25 unique brands of “melatonin” gummies purchased online.
One product didn’t contain any melatonin but did contain 31.3 mg of CBD.
In the remaining products, the quantity of melatonin ranged from 1.3 mg to 13.1 mg per serving. The actual quantity of melatonin ranged from 74% to 347% of the labeled quantity, the researchers found.
They note that for a young adult who takes as little as 0.1-0.3 mg of melatonin, plasma concentrations can increase into the normal night-time range.
Of the 25 products (88%) analyzed, 22 were inaccurately labeled, and only 3 (12%) contained a quantity of melatonin that was within 10% (plus or minus) of the declared quantity.
Five products listed CBD as an ingredient. The listed quantity ranged from 10.6 mg to 31.3 mg per serving, although the actual quantity of CBD ranged from 104% to 118% of the labeled quantity.
Inquire about use in kids
A limitation of the study is that only one sample of each brand was analyzed, and only gummies were analyzed. It is not known whether the results are generalizable to melatonin products sold as tablets and capsules in the United States or whether the quantity of melatonin within an individual brand may vary from batch to batch.
A recent study from Canada showed similar results. In an analysis of 16 Canadian melatonin brands, the actual dose of melatonin ranged from 17% to 478% of the declared quantity.
It’s estimated that more than 1% of all U.S. children use melatonin supplements, most commonly for sleep, stress, and relaxation.
“Given new research as to the excessive quantities of melatonin in gummies, caution should be used if considering their use,” said Dr. Cohen.
“It’s important to inquire about melatonin use when caring for children, particularly when parents express concerns about their child’s sleep,” he added.
The American Academy of Sleep Medicine recently issued a health advisory encouraging parents to talk to a health care professional before giving melatonin or any supplement to children.
Children don’t need melatonin
Commenting on the study, Michael Breus, PhD, clinical psychologist and founder of TheSleepDoctor.com, agreed that analyzing only one sample of each brand is a key limitation “because supplements are made in batches, and gummies in particular are difficult to distribute the active ingredient evenly.
“But even with that being said, 88% of them were labeled incorrectly, so even if there were a few single-sample issues, I kind of doubt its all of them,” Dr. Breus said.
“Kids as a general rule do not need melatonin. Their brains make almost four times the necessary amount already. If you start giving kids pills to help them sleep, then they start to have a pill problem, causing another issue,” Dr. Breus added.
“Most children’s falling asleep and staying sleep issues can be treated with behavioral measures like cognitive-behavioral therapy for insomnia,” he said.
The study had no specific funding. Dr. Cohen has received research support from Consumers Union and PEW Charitable Trusts and royalties from UptoDate. Dr. Breus disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New data may explain the recent massive jump in pediatric hospitalizations.
Thenvestigators found that consuming some products as directed could expose consumers, including children, to doses that are 40-130 times greater than what’s recommended.
“The results were quite shocking,” lead researcher Pieter Cohen, MD, with Harvard Medical School, Boston, and Cambridge Health Alliance, Somerville, Mass., said in an interview.
“Melatonin gummies contained up to 347% more melatonin than what was listed on the label, and some products also contained cannabidiol; in one brand of melatonin gummies, there was zero melatonin, just CBD,” Dr. Cohen said.
The study was published online in JAMA.
530% jump in pediatric hospitalizations
Melatonin products are not approved by the Food and Drug Administration but are sold over the counter or online.
Previous research from JAMA has shown the use of melatonin has increased over the past 2 decades among people of all ages.
With increased use has come a spike in reports of melatonin overdose, calls to poison control centers, and related ED visits for children.
Federal data show the number of U.S. children who unintentionally ingested melatonin supplements jumped 530% from 2012 to 2021. More than 4,000 of the reported ingestions led to a hospital stay; 287 children required intensive care, and two children died.
It was unclear why melatonin supplements were causing these harms, which led Dr. Cohen’s team to analyze 25 unique brands of “melatonin” gummies purchased online.
One product didn’t contain any melatonin but did contain 31.3 mg of CBD.
In the remaining products, the quantity of melatonin ranged from 1.3 mg to 13.1 mg per serving. The actual quantity of melatonin ranged from 74% to 347% of the labeled quantity, the researchers found.
They note that for a young adult who takes as little as 0.1-0.3 mg of melatonin, plasma concentrations can increase into the normal night-time range.
Of the 25 products (88%) analyzed, 22 were inaccurately labeled, and only 3 (12%) contained a quantity of melatonin that was within 10% (plus or minus) of the declared quantity.
Five products listed CBD as an ingredient. The listed quantity ranged from 10.6 mg to 31.3 mg per serving, although the actual quantity of CBD ranged from 104% to 118% of the labeled quantity.
Inquire about use in kids
A limitation of the study is that only one sample of each brand was analyzed, and only gummies were analyzed. It is not known whether the results are generalizable to melatonin products sold as tablets and capsules in the United States or whether the quantity of melatonin within an individual brand may vary from batch to batch.
A recent study from Canada showed similar results. In an analysis of 16 Canadian melatonin brands, the actual dose of melatonin ranged from 17% to 478% of the declared quantity.
It’s estimated that more than 1% of all U.S. children use melatonin supplements, most commonly for sleep, stress, and relaxation.
“Given new research as to the excessive quantities of melatonin in gummies, caution should be used if considering their use,” said Dr. Cohen.
“It’s important to inquire about melatonin use when caring for children, particularly when parents express concerns about their child’s sleep,” he added.
The American Academy of Sleep Medicine recently issued a health advisory encouraging parents to talk to a health care professional before giving melatonin or any supplement to children.
Children don’t need melatonin
Commenting on the study, Michael Breus, PhD, clinical psychologist and founder of TheSleepDoctor.com, agreed that analyzing only one sample of each brand is a key limitation “because supplements are made in batches, and gummies in particular are difficult to distribute the active ingredient evenly.
“But even with that being said, 88% of them were labeled incorrectly, so even if there were a few single-sample issues, I kind of doubt its all of them,” Dr. Breus said.
“Kids as a general rule do not need melatonin. Their brains make almost four times the necessary amount already. If you start giving kids pills to help them sleep, then they start to have a pill problem, causing another issue,” Dr. Breus added.
“Most children’s falling asleep and staying sleep issues can be treated with behavioral measures like cognitive-behavioral therapy for insomnia,” he said.
The study had no specific funding. Dr. Cohen has received research support from Consumers Union and PEW Charitable Trusts and royalties from UptoDate. Dr. Breus disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA
Obstructive sleep apnea linked to early cognitive decline
In a pilot study out of King’s College London, participants with severe OSA experienced worse executive functioning as well as social and emotional recognition versus healthy controls.
Major risk factors for OSA include obesity, high blood pressure, smoking, high cholesterol, and being middle-aged or older. Because some researchers have hypothesized that cognitive deficits could be driven by such comorbidities, the study investigators recruited middle-aged men with no medical comorbidities.
“Traditionally, we were more concerned with sleep apnea’s metabolic and cardiovascular comorbidities, and indeed, when cognitive deficits were demonstrated, most were attributed to them, and yet, our patients and their partners/families commonly tell us differently,” lead investigator Ivana Rosenzweig, MD, PhD, of King’s College London, who is also a consultant in sleep medicine and neuropsychiatry at Guy’s and St Thomas’ Hospital, London, said in an interview.
“Our findings provide a very important first step towards challenging the long-standing dogma that sleep apnea has little to do with the brain – apart from causing sleepiness – and that it is a predominantly nonneuro/psychiatric illness,” added Dr. Rosenzweig.
The findings were published online in Frontiers in Sleep.
Brain changes
The researchers wanted to understand how OSA may be linked to cognitive decline in the absence of cardiovascular and metabolic conditions.
To accomplish this, the investigators studied 27 men between the ages of 35 and 70 with a new diagnosis of mild to severe OSA without any comorbidities (16 with mild OSA and 11 with severe OSA). They also studied a control group of seven men matched for age, body mass index, and education level.
The team tested participants’ cognitive performance using the Cambridge Neuropsychological Test Automated Battery and found that the most significant deficits for the OSA group, compared with controls, were in areas of visual matching ability (P < .0001), short-term visual recognition memory, nonverbal patterns, executive functioning and attentional set-shifting (P < .001), psychomotor functioning, and social cognition and emotional recognition (P < .05).
On the latter two tests, impaired participants were less likely to accurately identify the emotion on computer-generated faces. Those with mild OSA performed better than those with severe OSA on these tasks, but rarely worse than controls.
Dr. Rosenzweig noted that the findings were one-of-a-kind because of the recruitment of patients with OSA who were otherwise healthy and nonobese, “something one rarely sees in the sleep clinic, where we commonly encounter patients with already developed comorbidities.
“In order to truly revolutionize the treatment for our patients, it is important to understand how much the accompanying comorbidities, such as systemic hypertension, obesity, diabetes, hyperlipidemia, and other various serious cardiovascular and metabolic diseases and how much the illness itself may shape the demonstrated cognitive deficits,” she said.
She also said that “it is widely agreed that medical problems in middle age may predispose to increased prevalence of dementia in later years.
Moreover, the very link between sleep apnea and Alzheimer’s, vascular and mixed dementia is increasingly demonstrated,” said Dr. Rosenzweig.
Although women typically have a lower prevalence of OSA than men, Dr. Rosenzweig said women were not included in the study “because we are too complex. As a lifelong feminist it pains me to say this, but to get any authoritative answer on our physiology, we need decent funding in place so that we can take into account all the intricacies of the changes of our sleep, physiology, and metabolism.
“While there is always lots of noise about how important it is to answer these questions, there are only very limited funds available for the sleep research,” she added.
Dr. Rosenzweig’s future research will focus on the potential link between OSA and neuroinflammation.
In a comment, Liza Ashbrook, MD, associate professor of neurology at the University of California, San Francisco, said the findings “add to the growing list of negative health consequences associated with sleep apnea.”
She said that, if the cognitive changes found in the study are, in fact, caused by OSA, it is unclear whether they are the beginning of long-term cognitive changes or a symptom of fragmented sleep that may be reversible.
Dr. Ashbrook said she would be interested in seeing research on understanding the effect of OSA treatment on the affected cognitive domains.
The study was funded by the Wellcome Trust. No relevant financial relationships were reported.
A version of this article originally appeared on Medscape.com.
In a pilot study out of King’s College London, participants with severe OSA experienced worse executive functioning as well as social and emotional recognition versus healthy controls.
Major risk factors for OSA include obesity, high blood pressure, smoking, high cholesterol, and being middle-aged or older. Because some researchers have hypothesized that cognitive deficits could be driven by such comorbidities, the study investigators recruited middle-aged men with no medical comorbidities.
“Traditionally, we were more concerned with sleep apnea’s metabolic and cardiovascular comorbidities, and indeed, when cognitive deficits were demonstrated, most were attributed to them, and yet, our patients and their partners/families commonly tell us differently,” lead investigator Ivana Rosenzweig, MD, PhD, of King’s College London, who is also a consultant in sleep medicine and neuropsychiatry at Guy’s and St Thomas’ Hospital, London, said in an interview.
“Our findings provide a very important first step towards challenging the long-standing dogma that sleep apnea has little to do with the brain – apart from causing sleepiness – and that it is a predominantly nonneuro/psychiatric illness,” added Dr. Rosenzweig.
The findings were published online in Frontiers in Sleep.
Brain changes
The researchers wanted to understand how OSA may be linked to cognitive decline in the absence of cardiovascular and metabolic conditions.
To accomplish this, the investigators studied 27 men between the ages of 35 and 70 with a new diagnosis of mild to severe OSA without any comorbidities (16 with mild OSA and 11 with severe OSA). They also studied a control group of seven men matched for age, body mass index, and education level.
The team tested participants’ cognitive performance using the Cambridge Neuropsychological Test Automated Battery and found that the most significant deficits for the OSA group, compared with controls, were in areas of visual matching ability (P < .0001), short-term visual recognition memory, nonverbal patterns, executive functioning and attentional set-shifting (P < .001), psychomotor functioning, and social cognition and emotional recognition (P < .05).
On the latter two tests, impaired participants were less likely to accurately identify the emotion on computer-generated faces. Those with mild OSA performed better than those with severe OSA on these tasks, but rarely worse than controls.
Dr. Rosenzweig noted that the findings were one-of-a-kind because of the recruitment of patients with OSA who were otherwise healthy and nonobese, “something one rarely sees in the sleep clinic, where we commonly encounter patients with already developed comorbidities.
“In order to truly revolutionize the treatment for our patients, it is important to understand how much the accompanying comorbidities, such as systemic hypertension, obesity, diabetes, hyperlipidemia, and other various serious cardiovascular and metabolic diseases and how much the illness itself may shape the demonstrated cognitive deficits,” she said.
She also said that “it is widely agreed that medical problems in middle age may predispose to increased prevalence of dementia in later years.
Moreover, the very link between sleep apnea and Alzheimer’s, vascular and mixed dementia is increasingly demonstrated,” said Dr. Rosenzweig.
Although women typically have a lower prevalence of OSA than men, Dr. Rosenzweig said women were not included in the study “because we are too complex. As a lifelong feminist it pains me to say this, but to get any authoritative answer on our physiology, we need decent funding in place so that we can take into account all the intricacies of the changes of our sleep, physiology, and metabolism.
“While there is always lots of noise about how important it is to answer these questions, there are only very limited funds available for the sleep research,” she added.
Dr. Rosenzweig’s future research will focus on the potential link between OSA and neuroinflammation.
In a comment, Liza Ashbrook, MD, associate professor of neurology at the University of California, San Francisco, said the findings “add to the growing list of negative health consequences associated with sleep apnea.”
She said that, if the cognitive changes found in the study are, in fact, caused by OSA, it is unclear whether they are the beginning of long-term cognitive changes or a symptom of fragmented sleep that may be reversible.
Dr. Ashbrook said she would be interested in seeing research on understanding the effect of OSA treatment on the affected cognitive domains.
The study was funded by the Wellcome Trust. No relevant financial relationships were reported.
A version of this article originally appeared on Medscape.com.
In a pilot study out of King’s College London, participants with severe OSA experienced worse executive functioning as well as social and emotional recognition versus healthy controls.
Major risk factors for OSA include obesity, high blood pressure, smoking, high cholesterol, and being middle-aged or older. Because some researchers have hypothesized that cognitive deficits could be driven by such comorbidities, the study investigators recruited middle-aged men with no medical comorbidities.
“Traditionally, we were more concerned with sleep apnea’s metabolic and cardiovascular comorbidities, and indeed, when cognitive deficits were demonstrated, most were attributed to them, and yet, our patients and their partners/families commonly tell us differently,” lead investigator Ivana Rosenzweig, MD, PhD, of King’s College London, who is also a consultant in sleep medicine and neuropsychiatry at Guy’s and St Thomas’ Hospital, London, said in an interview.
“Our findings provide a very important first step towards challenging the long-standing dogma that sleep apnea has little to do with the brain – apart from causing sleepiness – and that it is a predominantly nonneuro/psychiatric illness,” added Dr. Rosenzweig.
The findings were published online in Frontiers in Sleep.
Brain changes
The researchers wanted to understand how OSA may be linked to cognitive decline in the absence of cardiovascular and metabolic conditions.
To accomplish this, the investigators studied 27 men between the ages of 35 and 70 with a new diagnosis of mild to severe OSA without any comorbidities (16 with mild OSA and 11 with severe OSA). They also studied a control group of seven men matched for age, body mass index, and education level.
The team tested participants’ cognitive performance using the Cambridge Neuropsychological Test Automated Battery and found that the most significant deficits for the OSA group, compared with controls, were in areas of visual matching ability (P < .0001), short-term visual recognition memory, nonverbal patterns, executive functioning and attentional set-shifting (P < .001), psychomotor functioning, and social cognition and emotional recognition (P < .05).
On the latter two tests, impaired participants were less likely to accurately identify the emotion on computer-generated faces. Those with mild OSA performed better than those with severe OSA on these tasks, but rarely worse than controls.
Dr. Rosenzweig noted that the findings were one-of-a-kind because of the recruitment of patients with OSA who were otherwise healthy and nonobese, “something one rarely sees in the sleep clinic, where we commonly encounter patients with already developed comorbidities.
“In order to truly revolutionize the treatment for our patients, it is important to understand how much the accompanying comorbidities, such as systemic hypertension, obesity, diabetes, hyperlipidemia, and other various serious cardiovascular and metabolic diseases and how much the illness itself may shape the demonstrated cognitive deficits,” she said.
She also said that “it is widely agreed that medical problems in middle age may predispose to increased prevalence of dementia in later years.
Moreover, the very link between sleep apnea and Alzheimer’s, vascular and mixed dementia is increasingly demonstrated,” said Dr. Rosenzweig.
Although women typically have a lower prevalence of OSA than men, Dr. Rosenzweig said women were not included in the study “because we are too complex. As a lifelong feminist it pains me to say this, but to get any authoritative answer on our physiology, we need decent funding in place so that we can take into account all the intricacies of the changes of our sleep, physiology, and metabolism.
“While there is always lots of noise about how important it is to answer these questions, there are only very limited funds available for the sleep research,” she added.
Dr. Rosenzweig’s future research will focus on the potential link between OSA and neuroinflammation.
In a comment, Liza Ashbrook, MD, associate professor of neurology at the University of California, San Francisco, said the findings “add to the growing list of negative health consequences associated with sleep apnea.”
She said that, if the cognitive changes found in the study are, in fact, caused by OSA, it is unclear whether they are the beginning of long-term cognitive changes or a symptom of fragmented sleep that may be reversible.
Dr. Ashbrook said she would be interested in seeing research on understanding the effect of OSA treatment on the affected cognitive domains.
The study was funded by the Wellcome Trust. No relevant financial relationships were reported.
A version of this article originally appeared on Medscape.com.
FROM FRONTIERS IN SLEEP
Napping and AFib risk: The long and the short of it
Napping for more than half an hour during the day was associated with a 90% increased risk of atrial fibrillation (AFib), but shorter naps were linked to a reduced risk, based on data from more than 20,000 individuals.
“Short daytime napping is a common, healthy habit, especially in Mediterranean countries,” Jesus Diaz-Gutierrez, MD, of Juan Ramon Jimenez University Hospital, Huelva, Spain, said in a presentation at the annual congress of the European Association of Preventive Cardiology (EAPC).
Previous studies have shown a potential link between sleep patterns and AFib risk, but the association between specific duration of daytime naps and AFib risk has not been explored, he said.
Dr. Diaz-Gutierrez and colleagues used data from the University of Navarra Follow-up (SUN) Project, a prospective cohort of Spanish university graduates, to explore the possible link between naps and AFib. The study population included 20,348 individuals without AFib at baseline who were followed for a median of 13.8 years. The average age of participants at baseline was 38 years; 61% were women.
Daytime napping patterns were assessed at baseline, and participants were divided into nap groups of short nappers (defined as less than 30 minutes per day), and longer nappers (30 minutes or more per day), and those who reported no napping.
The researchers identified 131 incident cases of AFib during the follow-up period. Overall, the relative risk of incident AFib was significantly higher for the long nappers (adjusted hazard ratio 1.90) compared with short nappers in a multivariate analysis, while no significant risk appeared among non-nappers compared to short nappers (aHR 1.26).
The researchers then excluded the non-nappers in a secondary analysis to explore the impact of more specific daily nap duration on AFib risk. In a multivariate analysis, they found a 42% reduced risk of AF among those who napped for less than 15 minutes, and a 56% reduced risk for those who napped for 15-30 minutes, compared with those who napped for more than 30 minutes (aHR 0.56 and 0.42, respectively).
Potential explanations for the associations include the role of circadian rhythms, Dr. Diaz-Gutierrez said in a press release accompanying the presentation at the meeting. “Long daytime naps may disrupt the body’s internal clock (circadian rhythm), leading to shorter nighttime sleep, more nocturnal awakening, and reduced physical activity. In contrast, short daytime napping may improve circadian rhythm, lower blood pressure levels, and reduce stress.” More research is needed to validate the findings and the optimum nap duration, and whether a short nap is more advantageous than not napping in terms of AFib risk reduction, he said.
The study results suggest that naps of 15-30 minutes represent “a potential novel healthy lifestyle habit in the primary prevention of AFib,” Dr. Diaz-Gutierrez said in his presentation. However, the results also suggest that daily naps be limited to less than 30 minutes, he concluded.
Sleep habits may serve as red flag
“As we age, most if not all of us will develop sleep disturbances, such as insomnia, obstructive sleep apnea (OSA), and other sleep issues,” Lawrence S. Rosenthal, MD, of the University of Massachusetts, Worcester, said in an interview.
Therefore, “this study is near and dear to most people, and most would agree that poor sleeping habits affect our health.” In particular, OSA has been linked to AFib, although that was not measured in the current study, he added.
Dr. Rosenthal said he was not surprised by the current study findings. “It seems that a quick recharge of your ‘battery’ during the day is healthier than a long, deep sleep daytime nap,” he said. In addition, “Longer naps may be a marker of OSA,” he noted.
For clinicians, the take-home message of the current study is the need to consider underlying medical conditions in patients who regularly take long afternoon naps, and to consider these longer naps as a potential marker for AFib, said Dr. Rosenthal.
Looking ahead, a “deeper dive into the makeup of the populations studied” would be useful as a foundation for additional research, he said.
The SUN Project disclosed funding from the Spanish Government-Instituto de Salud Carlos III and the European Regional Development Fund (FEDER), the Navarra Regional Government, Plan Nacional Sobre Drogas, the University of Navarra, and the European Research Council. The researchers, and Dr. Rosenthal, had no financial conflicts to disclose.
Napping for more than half an hour during the day was associated with a 90% increased risk of atrial fibrillation (AFib), but shorter naps were linked to a reduced risk, based on data from more than 20,000 individuals.
“Short daytime napping is a common, healthy habit, especially in Mediterranean countries,” Jesus Diaz-Gutierrez, MD, of Juan Ramon Jimenez University Hospital, Huelva, Spain, said in a presentation at the annual congress of the European Association of Preventive Cardiology (EAPC).
Previous studies have shown a potential link between sleep patterns and AFib risk, but the association between specific duration of daytime naps and AFib risk has not been explored, he said.
Dr. Diaz-Gutierrez and colleagues used data from the University of Navarra Follow-up (SUN) Project, a prospective cohort of Spanish university graduates, to explore the possible link between naps and AFib. The study population included 20,348 individuals without AFib at baseline who were followed for a median of 13.8 years. The average age of participants at baseline was 38 years; 61% were women.
Daytime napping patterns were assessed at baseline, and participants were divided into nap groups of short nappers (defined as less than 30 minutes per day), and longer nappers (30 minutes or more per day), and those who reported no napping.
The researchers identified 131 incident cases of AFib during the follow-up period. Overall, the relative risk of incident AFib was significantly higher for the long nappers (adjusted hazard ratio 1.90) compared with short nappers in a multivariate analysis, while no significant risk appeared among non-nappers compared to short nappers (aHR 1.26).
The researchers then excluded the non-nappers in a secondary analysis to explore the impact of more specific daily nap duration on AFib risk. In a multivariate analysis, they found a 42% reduced risk of AF among those who napped for less than 15 minutes, and a 56% reduced risk for those who napped for 15-30 minutes, compared with those who napped for more than 30 minutes (aHR 0.56 and 0.42, respectively).
Potential explanations for the associations include the role of circadian rhythms, Dr. Diaz-Gutierrez said in a press release accompanying the presentation at the meeting. “Long daytime naps may disrupt the body’s internal clock (circadian rhythm), leading to shorter nighttime sleep, more nocturnal awakening, and reduced physical activity. In contrast, short daytime napping may improve circadian rhythm, lower blood pressure levels, and reduce stress.” More research is needed to validate the findings and the optimum nap duration, and whether a short nap is more advantageous than not napping in terms of AFib risk reduction, he said.
The study results suggest that naps of 15-30 minutes represent “a potential novel healthy lifestyle habit in the primary prevention of AFib,” Dr. Diaz-Gutierrez said in his presentation. However, the results also suggest that daily naps be limited to less than 30 minutes, he concluded.
Sleep habits may serve as red flag
“As we age, most if not all of us will develop sleep disturbances, such as insomnia, obstructive sleep apnea (OSA), and other sleep issues,” Lawrence S. Rosenthal, MD, of the University of Massachusetts, Worcester, said in an interview.
Therefore, “this study is near and dear to most people, and most would agree that poor sleeping habits affect our health.” In particular, OSA has been linked to AFib, although that was not measured in the current study, he added.
Dr. Rosenthal said he was not surprised by the current study findings. “It seems that a quick recharge of your ‘battery’ during the day is healthier than a long, deep sleep daytime nap,” he said. In addition, “Longer naps may be a marker of OSA,” he noted.
For clinicians, the take-home message of the current study is the need to consider underlying medical conditions in patients who regularly take long afternoon naps, and to consider these longer naps as a potential marker for AFib, said Dr. Rosenthal.
Looking ahead, a “deeper dive into the makeup of the populations studied” would be useful as a foundation for additional research, he said.
The SUN Project disclosed funding from the Spanish Government-Instituto de Salud Carlos III and the European Regional Development Fund (FEDER), the Navarra Regional Government, Plan Nacional Sobre Drogas, the University of Navarra, and the European Research Council. The researchers, and Dr. Rosenthal, had no financial conflicts to disclose.
Napping for more than half an hour during the day was associated with a 90% increased risk of atrial fibrillation (AFib), but shorter naps were linked to a reduced risk, based on data from more than 20,000 individuals.
“Short daytime napping is a common, healthy habit, especially in Mediterranean countries,” Jesus Diaz-Gutierrez, MD, of Juan Ramon Jimenez University Hospital, Huelva, Spain, said in a presentation at the annual congress of the European Association of Preventive Cardiology (EAPC).
Previous studies have shown a potential link between sleep patterns and AFib risk, but the association between specific duration of daytime naps and AFib risk has not been explored, he said.
Dr. Diaz-Gutierrez and colleagues used data from the University of Navarra Follow-up (SUN) Project, a prospective cohort of Spanish university graduates, to explore the possible link between naps and AFib. The study population included 20,348 individuals without AFib at baseline who were followed for a median of 13.8 years. The average age of participants at baseline was 38 years; 61% were women.
Daytime napping patterns were assessed at baseline, and participants were divided into nap groups of short nappers (defined as less than 30 minutes per day), and longer nappers (30 minutes or more per day), and those who reported no napping.
The researchers identified 131 incident cases of AFib during the follow-up period. Overall, the relative risk of incident AFib was significantly higher for the long nappers (adjusted hazard ratio 1.90) compared with short nappers in a multivariate analysis, while no significant risk appeared among non-nappers compared to short nappers (aHR 1.26).
The researchers then excluded the non-nappers in a secondary analysis to explore the impact of more specific daily nap duration on AFib risk. In a multivariate analysis, they found a 42% reduced risk of AF among those who napped for less than 15 minutes, and a 56% reduced risk for those who napped for 15-30 minutes, compared with those who napped for more than 30 minutes (aHR 0.56 and 0.42, respectively).
Potential explanations for the associations include the role of circadian rhythms, Dr. Diaz-Gutierrez said in a press release accompanying the presentation at the meeting. “Long daytime naps may disrupt the body’s internal clock (circadian rhythm), leading to shorter nighttime sleep, more nocturnal awakening, and reduced physical activity. In contrast, short daytime napping may improve circadian rhythm, lower blood pressure levels, and reduce stress.” More research is needed to validate the findings and the optimum nap duration, and whether a short nap is more advantageous than not napping in terms of AFib risk reduction, he said.
The study results suggest that naps of 15-30 minutes represent “a potential novel healthy lifestyle habit in the primary prevention of AFib,” Dr. Diaz-Gutierrez said in his presentation. However, the results also suggest that daily naps be limited to less than 30 minutes, he concluded.
Sleep habits may serve as red flag
“As we age, most if not all of us will develop sleep disturbances, such as insomnia, obstructive sleep apnea (OSA), and other sleep issues,” Lawrence S. Rosenthal, MD, of the University of Massachusetts, Worcester, said in an interview.
Therefore, “this study is near and dear to most people, and most would agree that poor sleeping habits affect our health.” In particular, OSA has been linked to AFib, although that was not measured in the current study, he added.
Dr. Rosenthal said he was not surprised by the current study findings. “It seems that a quick recharge of your ‘battery’ during the day is healthier than a long, deep sleep daytime nap,” he said. In addition, “Longer naps may be a marker of OSA,” he noted.
For clinicians, the take-home message of the current study is the need to consider underlying medical conditions in patients who regularly take long afternoon naps, and to consider these longer naps as a potential marker for AFib, said Dr. Rosenthal.
Looking ahead, a “deeper dive into the makeup of the populations studied” would be useful as a foundation for additional research, he said.
The SUN Project disclosed funding from the Spanish Government-Instituto de Salud Carlos III and the European Regional Development Fund (FEDER), the Navarra Regional Government, Plan Nacional Sobre Drogas, the University of Navarra, and the European Research Council. The researchers, and Dr. Rosenthal, had no financial conflicts to disclose.
FROM ESC PREVENTIVE CARDIOLOGY 2023
Sleep disturbances linked to post-COVID dyspnea
according to data from the U.K.’s CircCOVID study.
The researchers, led by John Blaikley, MRCP, PhD, respiratory physician and clinical scientist from the University of Manchester (England), found that sleep disturbance is a common problem after hospital admission for COVID-19 and may last for at least 1 year.
The study also showed that sleep disturbance after COVID hospitalization was associated with dyspnea and lower lung function. Further in-depth analysis revealed that the effects of sleep disturbance on dyspnea were partially mediated through both anxiety and muscle weakness; however, “this does not fully explain the association, suggesting other pathways are involved,” said Dr. Blaikley.
The study was jointly conducted by researchers from the University of Leicester (England), as well as 20 other U.K. institutes and the University of Helsinki. It was presented at the European Congress of Clinical Microbiology & Infectious Diseases and was simultaneously published in The Lancet Respiratory Medicine.
“Sleep disturbance is a common problem after hospitalization for COVID-19 and is associated with several symptoms in the post-COVID syndrome,” said Dr. Blaikley. “Clinicians should be aware of this association in their post-COVID syndrome clinics.”
He added that further work needs to be done to define the mechanism and to see whether the links are causal. “However, if they are, then treating sleep disturbance could have beneficial effects beyond improving sleep quality,” he said in an interview.
A large study recently showed that 4 in 10 people with post-COVID syndrome had moderate to severe sleep problems. Black people were at least three times more likely than White people to experience sleep problems. A total of 59% of all participants with long COVID reported having normal sleep or mild sleep disturbances, and 41% reported having moderate to severe sleep disturbances.
Unlike prior studies that evaluated sleep quality after COVID-19, which used either objective or subjective measures of sleep disturbance, the current study used both. “Using both measures revealed previously poorly described associations between sleep disturbance, breathlessness, reduced lung function, anxiety, and muscle weakness,” Dr. Blaikley pointed out.
Subjective and objective measures of sleep
The multicenter CircCOVID cohort study aimed to shed light on the prevalence and nature of sleep disturbance after patients are discharged from hospital for COVID-19 and to assess whether this was associated with dyspnea.
The study recruited a total of 2,320 participants who were part of a larger parent PHOSP-COVID study. After attending an early follow-up visit (at a median of 5 months after discharge from 83 U.K. hospitals for COVID-19), 638 participants provided data for analysis as measured by the Pittsburgh Sleep Quality Index (a subjective measure of sleep quality); 729 participants provided data for analysis as measured by actigraphy (an objective, wrist-worn, device-based measure of sleep quality) at a median of 7 months.
Breathlessness, the primary outcome, was assessed using the Dyspnea-12 validated questionnaire.
Actigraphy measurements were compared with an age-matched, sex-matched, body mass index (BMI)–matched, and time from discharge–matched cohort from the UK Biobank (a prepandemic comparator longitudinal cohort of 502,540 individuals, one-fifth of whom wore actigraphy devices). Sleep regularity was found to be 19% less in previously hospitalized patients with post-COVID syndrome, compared with matched controls who had been hospitalized for other reasons.
This “revealed that the actigraphy changes may be, in part, due to COVID-19 rather than hospitalization alone,” said Dr. Blaikley.
Data were collected at two time points after hospital discharge: 2-7 months (early), and 10-14 months (late). At the early time point, participants were clinically assessed with respect to anxiety, muscle function, and dyspnea, and lung function.
After discharge from hospital, the majority (62%) of post–COVID-19 participants reported poor sleep quality on the Pittsburgh Sleep Quality Index questionnaire. A “comparable” proportion (53%) felt that their quality of sleep had deteriorated following hospital discharge according to the numerical rating scale (subjective measure).
Also, sleep disturbance was found likely to persist for at least 12 months, since subjective sleep quality hardly changed between the early and late time points after hospital discharge.
Both subjective metrics (sleep quality and sleep quality deterioration after hospital discharge) and objective, device-based metrics (sleep regularity) were found to be associated with dyspnea and reduced lung function in patients with post-COVID syndrome.
“One of the striking findings in our study is the consistency with breathlessness and reduced lung function across different methods used to evaluate sleep,” highlighted Dr. Blaikley.
“The other striking finding was that participants following COVID-19 hospitalization actually slept longer [65 min; 95% confidence interval, 59-71 min] than participants hospitalized for non-COVID; however, their bedtimes were irregular, and it was this irregularity that was associated with breathlessness,” he added.
In comparison with nonhospitalized controls, also from the UK Biobank, study participants with lower sleep regularity had higher Dyspnea-12 scores (unadjusted effect estimate, 4.38; 95%: CI, 2.10-6.65). Those with poor sleep quality overall also had higher Dyspnea-12 scores (unadjusted effect estimate, 3.94; 95% CI, 2.78-5.10), and those who reported sleep quality deterioration had higher Dyspnea-12 scores (unadjusted effect estimate, 3,00; 95% CI, 1.82-4.28).
In comparison with hospitalized controls, CircCOVID participants had lower sleep regularity index (–19%; 95% CI, –20 to –16) and lower sleep efficiency (3.83 percentage points; 95% CI, 3.40-4.26).
Sleep disturbance after COVID hospitalization was also associated with lower lung function, from a 7% to a 14% reduction in predicted forced vital capacity, depending on which sleep measure used.
In an analysis of mediating factors active in the relationship between sleep disturbance and dyspnea/decreased lung function, the researchers found that reduced muscle function and anxiety, which are both recognized causes of dyspnea, could partially contribute to the association.
Regarding anxiety, and depending on the sleep metric, anxiety mediated 18%-39% of the effect of sleep disturbance on dyspnea, while muscle weakness mediated 27%-41% of this effect, reported Dr. Blaikley. Those with poor sleep quality were more likely to have mild, moderate, or severe anxiety, compared with participants who reported good-quality sleep.
A similar association was observed between anxiety and sleep quality deterioration.
“Two key questions are raised by our study: Do sleep interventions have a beneficial effect in post–COVID-19 syndrome, and are the associations causal?” asked Dr. Blaikley. “We hope to do a sleep intervention trial to answer these questions to explore if this is an effective treatment for post–COVID-19 syndrome.”
‘Underlying mechanisms remain unclear’
Amitava Banerjee, MD, professor of clinical data science and honorary consultant cardiologist, Institute of Health Informatics, UCL, London, welcomed the study but noted that it did not include nonhospitalized post-COVID patients.
“The majority of people with long COVID were not hospitalized for COVID, so the results may not be generalizable to this larger group,” she said in an interview. “Good-quality sleep is important for health and reduces risk of chronic diseases; quality of sleep is therefore likely to be important for those with long COVID in reducing their risk of chronic disease, but the role of sleep in the mechanism of long COVID needs further research.”
In a commentary also published in The Lancet Respiratory Medicine, W. Cameron McGuire, MD, pulmonary and critical care specialist from San Diego, California, and colleagues wrote: “These findings suggest that sleep disturbance, dyspnea, and anxiety are common after COVID-19 and are associated with one another, although the underlying mechanisms remain unclear.”
The commentators “applauded” the work overall but noted that the findings represent correlation rather than causation. “It is unclear whether sleep disturbance is causing anxiety or whether anxiety is contributing to poor sleep. ... For the sleep disturbances, increased BMI in the cohort reporting poor sleep, compared with those reporting good sleep might suggest underlying obstructive sleep apnea,” they wrote.
Dr. McGuire and colleagues added that many questions remain for researchers and clinicians, including “whether anxiety and dyspnoea are contributing to a low arousal threshold [disrupting sleep] ... whether the observed abnormalities (e.g., in dyspnea score) are clinically significant,” and “whether therapies such as glucocorticoids, anticoagulants, or previous vaccinations mitigate the observed abnormalities during COVID-19 recovery.”
Dr. Blaikley has received support to his institute from an MRC Transition Fellowship, Asthma + Lung UK, NIHR Manchester BRC, and UKRI; grants to his institution from the Small Business Research Initiative Home Spirometer and the National Institute of Academic Anaesthesia; and support from TEVA and Therakos for attending meetings. He is a committee member of the Royal Society of Medicine. A coauthor received funding from the National Institutes of Health and income for medical education from Zoll, Livanova, Jazz, and Eli Lilly. Dr. Banerjee is the chief investigator of STIMULATE-ICP (an NIHR-funded study) and has received research funding from AstraZeneca.
A version of this article first appeared on Medscape.com.
according to data from the U.K.’s CircCOVID study.
The researchers, led by John Blaikley, MRCP, PhD, respiratory physician and clinical scientist from the University of Manchester (England), found that sleep disturbance is a common problem after hospital admission for COVID-19 and may last for at least 1 year.
The study also showed that sleep disturbance after COVID hospitalization was associated with dyspnea and lower lung function. Further in-depth analysis revealed that the effects of sleep disturbance on dyspnea were partially mediated through both anxiety and muscle weakness; however, “this does not fully explain the association, suggesting other pathways are involved,” said Dr. Blaikley.
The study was jointly conducted by researchers from the University of Leicester (England), as well as 20 other U.K. institutes and the University of Helsinki. It was presented at the European Congress of Clinical Microbiology & Infectious Diseases and was simultaneously published in The Lancet Respiratory Medicine.
“Sleep disturbance is a common problem after hospitalization for COVID-19 and is associated with several symptoms in the post-COVID syndrome,” said Dr. Blaikley. “Clinicians should be aware of this association in their post-COVID syndrome clinics.”
He added that further work needs to be done to define the mechanism and to see whether the links are causal. “However, if they are, then treating sleep disturbance could have beneficial effects beyond improving sleep quality,” he said in an interview.
A large study recently showed that 4 in 10 people with post-COVID syndrome had moderate to severe sleep problems. Black people were at least three times more likely than White people to experience sleep problems. A total of 59% of all participants with long COVID reported having normal sleep or mild sleep disturbances, and 41% reported having moderate to severe sleep disturbances.
Unlike prior studies that evaluated sleep quality after COVID-19, which used either objective or subjective measures of sleep disturbance, the current study used both. “Using both measures revealed previously poorly described associations between sleep disturbance, breathlessness, reduced lung function, anxiety, and muscle weakness,” Dr. Blaikley pointed out.
Subjective and objective measures of sleep
The multicenter CircCOVID cohort study aimed to shed light on the prevalence and nature of sleep disturbance after patients are discharged from hospital for COVID-19 and to assess whether this was associated with dyspnea.
The study recruited a total of 2,320 participants who were part of a larger parent PHOSP-COVID study. After attending an early follow-up visit (at a median of 5 months after discharge from 83 U.K. hospitals for COVID-19), 638 participants provided data for analysis as measured by the Pittsburgh Sleep Quality Index (a subjective measure of sleep quality); 729 participants provided data for analysis as measured by actigraphy (an objective, wrist-worn, device-based measure of sleep quality) at a median of 7 months.
Breathlessness, the primary outcome, was assessed using the Dyspnea-12 validated questionnaire.
Actigraphy measurements were compared with an age-matched, sex-matched, body mass index (BMI)–matched, and time from discharge–matched cohort from the UK Biobank (a prepandemic comparator longitudinal cohort of 502,540 individuals, one-fifth of whom wore actigraphy devices). Sleep regularity was found to be 19% less in previously hospitalized patients with post-COVID syndrome, compared with matched controls who had been hospitalized for other reasons.
This “revealed that the actigraphy changes may be, in part, due to COVID-19 rather than hospitalization alone,” said Dr. Blaikley.
Data were collected at two time points after hospital discharge: 2-7 months (early), and 10-14 months (late). At the early time point, participants were clinically assessed with respect to anxiety, muscle function, and dyspnea, and lung function.
After discharge from hospital, the majority (62%) of post–COVID-19 participants reported poor sleep quality on the Pittsburgh Sleep Quality Index questionnaire. A “comparable” proportion (53%) felt that their quality of sleep had deteriorated following hospital discharge according to the numerical rating scale (subjective measure).
Also, sleep disturbance was found likely to persist for at least 12 months, since subjective sleep quality hardly changed between the early and late time points after hospital discharge.
Both subjective metrics (sleep quality and sleep quality deterioration after hospital discharge) and objective, device-based metrics (sleep regularity) were found to be associated with dyspnea and reduced lung function in patients with post-COVID syndrome.
“One of the striking findings in our study is the consistency with breathlessness and reduced lung function across different methods used to evaluate sleep,” highlighted Dr. Blaikley.
“The other striking finding was that participants following COVID-19 hospitalization actually slept longer [65 min; 95% confidence interval, 59-71 min] than participants hospitalized for non-COVID; however, their bedtimes were irregular, and it was this irregularity that was associated with breathlessness,” he added.
In comparison with nonhospitalized controls, also from the UK Biobank, study participants with lower sleep regularity had higher Dyspnea-12 scores (unadjusted effect estimate, 4.38; 95%: CI, 2.10-6.65). Those with poor sleep quality overall also had higher Dyspnea-12 scores (unadjusted effect estimate, 3.94; 95% CI, 2.78-5.10), and those who reported sleep quality deterioration had higher Dyspnea-12 scores (unadjusted effect estimate, 3,00; 95% CI, 1.82-4.28).
In comparison with hospitalized controls, CircCOVID participants had lower sleep regularity index (–19%; 95% CI, –20 to –16) and lower sleep efficiency (3.83 percentage points; 95% CI, 3.40-4.26).
Sleep disturbance after COVID hospitalization was also associated with lower lung function, from a 7% to a 14% reduction in predicted forced vital capacity, depending on which sleep measure used.
In an analysis of mediating factors active in the relationship between sleep disturbance and dyspnea/decreased lung function, the researchers found that reduced muscle function and anxiety, which are both recognized causes of dyspnea, could partially contribute to the association.
Regarding anxiety, and depending on the sleep metric, anxiety mediated 18%-39% of the effect of sleep disturbance on dyspnea, while muscle weakness mediated 27%-41% of this effect, reported Dr. Blaikley. Those with poor sleep quality were more likely to have mild, moderate, or severe anxiety, compared with participants who reported good-quality sleep.
A similar association was observed between anxiety and sleep quality deterioration.
“Two key questions are raised by our study: Do sleep interventions have a beneficial effect in post–COVID-19 syndrome, and are the associations causal?” asked Dr. Blaikley. “We hope to do a sleep intervention trial to answer these questions to explore if this is an effective treatment for post–COVID-19 syndrome.”
‘Underlying mechanisms remain unclear’
Amitava Banerjee, MD, professor of clinical data science and honorary consultant cardiologist, Institute of Health Informatics, UCL, London, welcomed the study but noted that it did not include nonhospitalized post-COVID patients.
“The majority of people with long COVID were not hospitalized for COVID, so the results may not be generalizable to this larger group,” she said in an interview. “Good-quality sleep is important for health and reduces risk of chronic diseases; quality of sleep is therefore likely to be important for those with long COVID in reducing their risk of chronic disease, but the role of sleep in the mechanism of long COVID needs further research.”
In a commentary also published in The Lancet Respiratory Medicine, W. Cameron McGuire, MD, pulmonary and critical care specialist from San Diego, California, and colleagues wrote: “These findings suggest that sleep disturbance, dyspnea, and anxiety are common after COVID-19 and are associated with one another, although the underlying mechanisms remain unclear.”
The commentators “applauded” the work overall but noted that the findings represent correlation rather than causation. “It is unclear whether sleep disturbance is causing anxiety or whether anxiety is contributing to poor sleep. ... For the sleep disturbances, increased BMI in the cohort reporting poor sleep, compared with those reporting good sleep might suggest underlying obstructive sleep apnea,” they wrote.
Dr. McGuire and colleagues added that many questions remain for researchers and clinicians, including “whether anxiety and dyspnoea are contributing to a low arousal threshold [disrupting sleep] ... whether the observed abnormalities (e.g., in dyspnea score) are clinically significant,” and “whether therapies such as glucocorticoids, anticoagulants, or previous vaccinations mitigate the observed abnormalities during COVID-19 recovery.”
Dr. Blaikley has received support to his institute from an MRC Transition Fellowship, Asthma + Lung UK, NIHR Manchester BRC, and UKRI; grants to his institution from the Small Business Research Initiative Home Spirometer and the National Institute of Academic Anaesthesia; and support from TEVA and Therakos for attending meetings. He is a committee member of the Royal Society of Medicine. A coauthor received funding from the National Institutes of Health and income for medical education from Zoll, Livanova, Jazz, and Eli Lilly. Dr. Banerjee is the chief investigator of STIMULATE-ICP (an NIHR-funded study) and has received research funding from AstraZeneca.
A version of this article first appeared on Medscape.com.
according to data from the U.K.’s CircCOVID study.
The researchers, led by John Blaikley, MRCP, PhD, respiratory physician and clinical scientist from the University of Manchester (England), found that sleep disturbance is a common problem after hospital admission for COVID-19 and may last for at least 1 year.
The study also showed that sleep disturbance after COVID hospitalization was associated with dyspnea and lower lung function. Further in-depth analysis revealed that the effects of sleep disturbance on dyspnea were partially mediated through both anxiety and muscle weakness; however, “this does not fully explain the association, suggesting other pathways are involved,” said Dr. Blaikley.
The study was jointly conducted by researchers from the University of Leicester (England), as well as 20 other U.K. institutes and the University of Helsinki. It was presented at the European Congress of Clinical Microbiology & Infectious Diseases and was simultaneously published in The Lancet Respiratory Medicine.
“Sleep disturbance is a common problem after hospitalization for COVID-19 and is associated with several symptoms in the post-COVID syndrome,” said Dr. Blaikley. “Clinicians should be aware of this association in their post-COVID syndrome clinics.”
He added that further work needs to be done to define the mechanism and to see whether the links are causal. “However, if they are, then treating sleep disturbance could have beneficial effects beyond improving sleep quality,” he said in an interview.
A large study recently showed that 4 in 10 people with post-COVID syndrome had moderate to severe sleep problems. Black people were at least three times more likely than White people to experience sleep problems. A total of 59% of all participants with long COVID reported having normal sleep or mild sleep disturbances, and 41% reported having moderate to severe sleep disturbances.
Unlike prior studies that evaluated sleep quality after COVID-19, which used either objective or subjective measures of sleep disturbance, the current study used both. “Using both measures revealed previously poorly described associations between sleep disturbance, breathlessness, reduced lung function, anxiety, and muscle weakness,” Dr. Blaikley pointed out.
Subjective and objective measures of sleep
The multicenter CircCOVID cohort study aimed to shed light on the prevalence and nature of sleep disturbance after patients are discharged from hospital for COVID-19 and to assess whether this was associated with dyspnea.
The study recruited a total of 2,320 participants who were part of a larger parent PHOSP-COVID study. After attending an early follow-up visit (at a median of 5 months after discharge from 83 U.K. hospitals for COVID-19), 638 participants provided data for analysis as measured by the Pittsburgh Sleep Quality Index (a subjective measure of sleep quality); 729 participants provided data for analysis as measured by actigraphy (an objective, wrist-worn, device-based measure of sleep quality) at a median of 7 months.
Breathlessness, the primary outcome, was assessed using the Dyspnea-12 validated questionnaire.
Actigraphy measurements were compared with an age-matched, sex-matched, body mass index (BMI)–matched, and time from discharge–matched cohort from the UK Biobank (a prepandemic comparator longitudinal cohort of 502,540 individuals, one-fifth of whom wore actigraphy devices). Sleep regularity was found to be 19% less in previously hospitalized patients with post-COVID syndrome, compared with matched controls who had been hospitalized for other reasons.
This “revealed that the actigraphy changes may be, in part, due to COVID-19 rather than hospitalization alone,” said Dr. Blaikley.
Data were collected at two time points after hospital discharge: 2-7 months (early), and 10-14 months (late). At the early time point, participants were clinically assessed with respect to anxiety, muscle function, and dyspnea, and lung function.
After discharge from hospital, the majority (62%) of post–COVID-19 participants reported poor sleep quality on the Pittsburgh Sleep Quality Index questionnaire. A “comparable” proportion (53%) felt that their quality of sleep had deteriorated following hospital discharge according to the numerical rating scale (subjective measure).
Also, sleep disturbance was found likely to persist for at least 12 months, since subjective sleep quality hardly changed between the early and late time points after hospital discharge.
Both subjective metrics (sleep quality and sleep quality deterioration after hospital discharge) and objective, device-based metrics (sleep regularity) were found to be associated with dyspnea and reduced lung function in patients with post-COVID syndrome.
“One of the striking findings in our study is the consistency with breathlessness and reduced lung function across different methods used to evaluate sleep,” highlighted Dr. Blaikley.
“The other striking finding was that participants following COVID-19 hospitalization actually slept longer [65 min; 95% confidence interval, 59-71 min] than participants hospitalized for non-COVID; however, their bedtimes were irregular, and it was this irregularity that was associated with breathlessness,” he added.
In comparison with nonhospitalized controls, also from the UK Biobank, study participants with lower sleep regularity had higher Dyspnea-12 scores (unadjusted effect estimate, 4.38; 95%: CI, 2.10-6.65). Those with poor sleep quality overall also had higher Dyspnea-12 scores (unadjusted effect estimate, 3.94; 95% CI, 2.78-5.10), and those who reported sleep quality deterioration had higher Dyspnea-12 scores (unadjusted effect estimate, 3,00; 95% CI, 1.82-4.28).
In comparison with hospitalized controls, CircCOVID participants had lower sleep regularity index (–19%; 95% CI, –20 to –16) and lower sleep efficiency (3.83 percentage points; 95% CI, 3.40-4.26).
Sleep disturbance after COVID hospitalization was also associated with lower lung function, from a 7% to a 14% reduction in predicted forced vital capacity, depending on which sleep measure used.
In an analysis of mediating factors active in the relationship between sleep disturbance and dyspnea/decreased lung function, the researchers found that reduced muscle function and anxiety, which are both recognized causes of dyspnea, could partially contribute to the association.
Regarding anxiety, and depending on the sleep metric, anxiety mediated 18%-39% of the effect of sleep disturbance on dyspnea, while muscle weakness mediated 27%-41% of this effect, reported Dr. Blaikley. Those with poor sleep quality were more likely to have mild, moderate, or severe anxiety, compared with participants who reported good-quality sleep.
A similar association was observed between anxiety and sleep quality deterioration.
“Two key questions are raised by our study: Do sleep interventions have a beneficial effect in post–COVID-19 syndrome, and are the associations causal?” asked Dr. Blaikley. “We hope to do a sleep intervention trial to answer these questions to explore if this is an effective treatment for post–COVID-19 syndrome.”
‘Underlying mechanisms remain unclear’
Amitava Banerjee, MD, professor of clinical data science and honorary consultant cardiologist, Institute of Health Informatics, UCL, London, welcomed the study but noted that it did not include nonhospitalized post-COVID patients.
“The majority of people with long COVID were not hospitalized for COVID, so the results may not be generalizable to this larger group,” she said in an interview. “Good-quality sleep is important for health and reduces risk of chronic diseases; quality of sleep is therefore likely to be important for those with long COVID in reducing their risk of chronic disease, but the role of sleep in the mechanism of long COVID needs further research.”
In a commentary also published in The Lancet Respiratory Medicine, W. Cameron McGuire, MD, pulmonary and critical care specialist from San Diego, California, and colleagues wrote: “These findings suggest that sleep disturbance, dyspnea, and anxiety are common after COVID-19 and are associated with one another, although the underlying mechanisms remain unclear.”
The commentators “applauded” the work overall but noted that the findings represent correlation rather than causation. “It is unclear whether sleep disturbance is causing anxiety or whether anxiety is contributing to poor sleep. ... For the sleep disturbances, increased BMI in the cohort reporting poor sleep, compared with those reporting good sleep might suggest underlying obstructive sleep apnea,” they wrote.
Dr. McGuire and colleagues added that many questions remain for researchers and clinicians, including “whether anxiety and dyspnoea are contributing to a low arousal threshold [disrupting sleep] ... whether the observed abnormalities (e.g., in dyspnea score) are clinically significant,” and “whether therapies such as glucocorticoids, anticoagulants, or previous vaccinations mitigate the observed abnormalities during COVID-19 recovery.”
Dr. Blaikley has received support to his institute from an MRC Transition Fellowship, Asthma + Lung UK, NIHR Manchester BRC, and UKRI; grants to his institution from the Small Business Research Initiative Home Spirometer and the National Institute of Academic Anaesthesia; and support from TEVA and Therakos for attending meetings. He is a committee member of the Royal Society of Medicine. A coauthor received funding from the National Institutes of Health and income for medical education from Zoll, Livanova, Jazz, and Eli Lilly. Dr. Banerjee is the chief investigator of STIMULATE-ICP (an NIHR-funded study) and has received research funding from AstraZeneca.
A version of this article first appeared on Medscape.com.
FROM ECCMID 2023