User login
Delayed first contraception use raises unwanted pregnancy risk
Young women who delay starting contraception when they start sexual activity are at increased risk of unwanted pregnancy, according to data from a cross-sectional study of more than 26,000 women in the United States.
Unintended pregnancy in the United States is associated with delayed prenatal care, premature birth, and low birth weight and remains more common among African American and Hispanic women than among white women, and it also is more common among low-income women than among high income women, wrote Mara E. Murray Horwitz, MD, of Harvard Pilgrim Health Care Institute in Boston and her colleagues.
“Reducing unintended pregnancy and the associated socioeconomic disparities is a national public health priority,” they wrote.
In a study published in Pediatrics, the researchers reviewed data from four cycles of the National Survey of Family Growth between 2002 and 2015. They examined self-reported responses from 26,359 women aged 15-44 years with sexual debuts during 1970-2014, including the dates of sexual debut, initiation of contraceptives, and rates of unwanted pregnancy. Timely contraceptive initiation was defined as use within a month of starting sexual activity.
Overall, one in five women reported delayed initiation of contraception. This delay was significantly associated with an increased unwanted pregnancy risk within 3 months of starting sexual activity, compared with timely use of contraception (adjusted risk ratio, 3.7). The average age of sexual debut was 17 years.
When the researchers examined subgroups, they found that one in four respondents who were African American, Hispanic, or low income reported delayed contraceptive initiation.
No association with unwanted pregnancy was found between effective versus less effective contraception methods. Timely contraceptive use increased during the study period from less than 10% in the 1970s to more than 25% in the 2000s, but condoms accounted for most of this increase. Use of other methods including long-acting reversible and short-acting hormonal options was low, especially among African American, Hispanic, and low-income women, Dr. Murray Horwitz and her colleagues noted.
The study was limited by several factors including the use of self-reports, lack of data on the exact start of contraceptive initiation, and the lack of association between contraceptive method and unwanted pregnancy, the researchers noted. However, the findings suggest that clinicians can help by intervening with young patients and educating them about early adoption of pregnancy prevention strategies.
The study was funded by the National Institutes of Health; Dr. Murray Horwitz was supported by an award from the NIH and Harvard Pilgrim Health Care Institute. Another researcher received support from Harvard Pilgrim Health Care Institute to provide mentorship for the study. The remaining researcher had no relevant financial disclosures.
SOURCE: Murray Horwitz M et al. Pediatrics. 2019;143(2):e20182463.
Despite a declining teen birth rate in the last several decades, the United States has the highest teen birth rate among industrialized nations. While many factors play into this rate, we know that, in many European countries with low teen birth rates, adolescents often initiate contraceptive methods before their sexual debut. As we often tell teenagers, they can become pregnant the “first time,” which makes initiating contraception early – and preferably before sexual debut – an important strategy to preventing unplanned pregnancy.
This study identifies the trends over time in the initiation of contraception in relationship to sexual debut and examines its effects on unplanned teen pregnancy. Understanding these trends can help clinicians more effectively target teen pregnancy.
I was pleasantly surprised to see that rates of timely contraceptive initiation have increased since 1970. Sadly, this rise is largely because of condom use. Use of effective forms of contraception – especially long-acting reversible forms of contraception (LARC), such as the IUD or the etonogestrel rod – still remain low at the time of sexual debut. While we continue to encourage LARCs as first line for pregnancy prevention, many patients are not getting the message about these highly effective, safe methods. Unsurprisingly, there are significant differences based on race/ethnicity and socioeconomic status on timely initiation of contraceptive methods, especially highly effective methods. This supports prior research which has shown significant barriers in access to contraception to these groups, which leads to higher rates of unplanned pregnancies.
Dr. Kelly Curran, MD, specializes in adolescent medicine at the University of Oklahoma, Oklahoma City. She is a member of the Pediatric News editorial advisory board and was asked to comment on the study by Murray Horwitz et al. Dr. Curran had no relevant financial disclosures.
Despite a declining teen birth rate in the last several decades, the United States has the highest teen birth rate among industrialized nations. While many factors play into this rate, we know that, in many European countries with low teen birth rates, adolescents often initiate contraceptive methods before their sexual debut. As we often tell teenagers, they can become pregnant the “first time,” which makes initiating contraception early – and preferably before sexual debut – an important strategy to preventing unplanned pregnancy.
This study identifies the trends over time in the initiation of contraception in relationship to sexual debut and examines its effects on unplanned teen pregnancy. Understanding these trends can help clinicians more effectively target teen pregnancy.
I was pleasantly surprised to see that rates of timely contraceptive initiation have increased since 1970. Sadly, this rise is largely because of condom use. Use of effective forms of contraception – especially long-acting reversible forms of contraception (LARC), such as the IUD or the etonogestrel rod – still remain low at the time of sexual debut. While we continue to encourage LARCs as first line for pregnancy prevention, many patients are not getting the message about these highly effective, safe methods. Unsurprisingly, there are significant differences based on race/ethnicity and socioeconomic status on timely initiation of contraceptive methods, especially highly effective methods. This supports prior research which has shown significant barriers in access to contraception to these groups, which leads to higher rates of unplanned pregnancies.
Dr. Kelly Curran, MD, specializes in adolescent medicine at the University of Oklahoma, Oklahoma City. She is a member of the Pediatric News editorial advisory board and was asked to comment on the study by Murray Horwitz et al. Dr. Curran had no relevant financial disclosures.
Despite a declining teen birth rate in the last several decades, the United States has the highest teen birth rate among industrialized nations. While many factors play into this rate, we know that, in many European countries with low teen birth rates, adolescents often initiate contraceptive methods before their sexual debut. As we often tell teenagers, they can become pregnant the “first time,” which makes initiating contraception early – and preferably before sexual debut – an important strategy to preventing unplanned pregnancy.
This study identifies the trends over time in the initiation of contraception in relationship to sexual debut and examines its effects on unplanned teen pregnancy. Understanding these trends can help clinicians more effectively target teen pregnancy.
I was pleasantly surprised to see that rates of timely contraceptive initiation have increased since 1970. Sadly, this rise is largely because of condom use. Use of effective forms of contraception – especially long-acting reversible forms of contraception (LARC), such as the IUD or the etonogestrel rod – still remain low at the time of sexual debut. While we continue to encourage LARCs as first line for pregnancy prevention, many patients are not getting the message about these highly effective, safe methods. Unsurprisingly, there are significant differences based on race/ethnicity and socioeconomic status on timely initiation of contraceptive methods, especially highly effective methods. This supports prior research which has shown significant barriers in access to contraception to these groups, which leads to higher rates of unplanned pregnancies.
Dr. Kelly Curran, MD, specializes in adolescent medicine at the University of Oklahoma, Oklahoma City. She is a member of the Pediatric News editorial advisory board and was asked to comment on the study by Murray Horwitz et al. Dr. Curran had no relevant financial disclosures.
Young women who delay starting contraception when they start sexual activity are at increased risk of unwanted pregnancy, according to data from a cross-sectional study of more than 26,000 women in the United States.
Unintended pregnancy in the United States is associated with delayed prenatal care, premature birth, and low birth weight and remains more common among African American and Hispanic women than among white women, and it also is more common among low-income women than among high income women, wrote Mara E. Murray Horwitz, MD, of Harvard Pilgrim Health Care Institute in Boston and her colleagues.
“Reducing unintended pregnancy and the associated socioeconomic disparities is a national public health priority,” they wrote.
In a study published in Pediatrics, the researchers reviewed data from four cycles of the National Survey of Family Growth between 2002 and 2015. They examined self-reported responses from 26,359 women aged 15-44 years with sexual debuts during 1970-2014, including the dates of sexual debut, initiation of contraceptives, and rates of unwanted pregnancy. Timely contraceptive initiation was defined as use within a month of starting sexual activity.
Overall, one in five women reported delayed initiation of contraception. This delay was significantly associated with an increased unwanted pregnancy risk within 3 months of starting sexual activity, compared with timely use of contraception (adjusted risk ratio, 3.7). The average age of sexual debut was 17 years.
When the researchers examined subgroups, they found that one in four respondents who were African American, Hispanic, or low income reported delayed contraceptive initiation.
No association with unwanted pregnancy was found between effective versus less effective contraception methods. Timely contraceptive use increased during the study period from less than 10% in the 1970s to more than 25% in the 2000s, but condoms accounted for most of this increase. Use of other methods including long-acting reversible and short-acting hormonal options was low, especially among African American, Hispanic, and low-income women, Dr. Murray Horwitz and her colleagues noted.
The study was limited by several factors including the use of self-reports, lack of data on the exact start of contraceptive initiation, and the lack of association between contraceptive method and unwanted pregnancy, the researchers noted. However, the findings suggest that clinicians can help by intervening with young patients and educating them about early adoption of pregnancy prevention strategies.
The study was funded by the National Institutes of Health; Dr. Murray Horwitz was supported by an award from the NIH and Harvard Pilgrim Health Care Institute. Another researcher received support from Harvard Pilgrim Health Care Institute to provide mentorship for the study. The remaining researcher had no relevant financial disclosures.
SOURCE: Murray Horwitz M et al. Pediatrics. 2019;143(2):e20182463.
Young women who delay starting contraception when they start sexual activity are at increased risk of unwanted pregnancy, according to data from a cross-sectional study of more than 26,000 women in the United States.
Unintended pregnancy in the United States is associated with delayed prenatal care, premature birth, and low birth weight and remains more common among African American and Hispanic women than among white women, and it also is more common among low-income women than among high income women, wrote Mara E. Murray Horwitz, MD, of Harvard Pilgrim Health Care Institute in Boston and her colleagues.
“Reducing unintended pregnancy and the associated socioeconomic disparities is a national public health priority,” they wrote.
In a study published in Pediatrics, the researchers reviewed data from four cycles of the National Survey of Family Growth between 2002 and 2015. They examined self-reported responses from 26,359 women aged 15-44 years with sexual debuts during 1970-2014, including the dates of sexual debut, initiation of contraceptives, and rates of unwanted pregnancy. Timely contraceptive initiation was defined as use within a month of starting sexual activity.
Overall, one in five women reported delayed initiation of contraception. This delay was significantly associated with an increased unwanted pregnancy risk within 3 months of starting sexual activity, compared with timely use of contraception (adjusted risk ratio, 3.7). The average age of sexual debut was 17 years.
When the researchers examined subgroups, they found that one in four respondents who were African American, Hispanic, or low income reported delayed contraceptive initiation.
No association with unwanted pregnancy was found between effective versus less effective contraception methods. Timely contraceptive use increased during the study period from less than 10% in the 1970s to more than 25% in the 2000s, but condoms accounted for most of this increase. Use of other methods including long-acting reversible and short-acting hormonal options was low, especially among African American, Hispanic, and low-income women, Dr. Murray Horwitz and her colleagues noted.
The study was limited by several factors including the use of self-reports, lack of data on the exact start of contraceptive initiation, and the lack of association between contraceptive method and unwanted pregnancy, the researchers noted. However, the findings suggest that clinicians can help by intervening with young patients and educating them about early adoption of pregnancy prevention strategies.
The study was funded by the National Institutes of Health; Dr. Murray Horwitz was supported by an award from the NIH and Harvard Pilgrim Health Care Institute. Another researcher received support from Harvard Pilgrim Health Care Institute to provide mentorship for the study. The remaining researcher had no relevant financial disclosures.
SOURCE: Murray Horwitz M et al. Pediatrics. 2019;143(2):e20182463.
FROM PEDIATRICS
Key clinical point: Women who delayed using contraception were significantly more likely to become pregnant within 3 months of starting sexual activity than were those who had initiated contraception use, especially black, Hispanic, and low-income women.
Major finding: Unwanted pregnancy within 3 months of sexual debut was 3.7 times more likely in women who delayed initial contraception use, compared with those who had timely initiation.
Study details: The data come from a cross-sectional study including 26,359 women with sexual debuts between 1970 and 2014.
Disclosures: The study was funded by the National Institutes of Health; Dr. Murray Horwitz was supported by an award from the NIH and Harvard Pilgrim Health Care Institute. Another researcher received support from Harvard Pilgrim Health Care Institute to provide mentorship for the study. The remaining researcher had no relevant financial disclosures.
Source: Horwitz M et al. Pediatrics. 2019;143(2):e20182463.
SMFM and ACOG team up for interpregnancy care guidance
A new consensus statement places renewed focus on maternal interpregnancy care, with a goal of extending care past the postpartum period to provide a wellness-maximizing continuum of care.
The document, developed by the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine (SMFM), recognizes that pregnancy is part of the lifelong continuum of health and wellness. Although not all women will go on to have another pregnancy, the concept of interpregnancy care recognizes that ob.gyns. have a vital role that extends past the postpartum period.
“This is a shift in what we used to think was our job. We used to think that our job ended when the baby came out,” said the first author of the obstetric care consensus statement, Judette Marie Louis, MD, an ob.gyn. faculty member at the University of South Florida, Tampa, and a SMFM board member. “For too long, our focus was just the baby; we need to tell women, ‘You’re important too,’ ” she said in an interview.
“The interpregnancy period is an opportunity to address these complications of medical issues that have developed during pregnancy, to assess a woman’s mental and physical well-being, and to optimize her health along her life course,” Dr. Louis and her coauthors wrote in Obstetrics & Gynecology.
Conceptually, the opportunity for interpregnancy care arises after any pregnancy, no matter the outcome, and is part of the continuum of care for women of reproductive age. For women who do not intend a future pregnancy, well-woman care is the focus, while women who currently intend to become pregnant again receive interpregnancy care. Women may move from one arm of the continuum to the other if their intentions change or if they become pregnant, explained Dr. Louis and her coauthors.
Birth spacing
The new consensus document includes an emphasis on long-term health outcomes as well as maternal and neonatal outcomes in future pregnancies. Although the evidence is of no more than moderate quality, women should be advised to have an interpregnancy interval of at least 6 months and offered counseling about family planning before delivery. Risks and benefits of an interpregnancy interval of less than 18 months should be reviewed as well.
For women with a history of preterm birth and those who have had a prior cesarean delivery and desire a subsequent trial of labor, birth spacing is particularly important, noted Dr. Louis and her colleagues. There is higher-risk evidence for uterine rupture after cesarean delivery if delivery-to-delivery intervals are 18-24 months or less.
Recommendations regarding the length of the interpregnancy interval generally should not be affected by a history of prior infertility.
Other recommendations
High-quality evidence supports breast feeding’s salutary effects on maternal and child health, so women should receive anticipatory support and guidance to enable breastfeeding, according to the document.
In accordance with other guidelines, the document recommends that all women be screened for depression post partum and as part of well-woman care in the interpregnancy interval. Procedures for effective diagnosis, treatment, and follow-up should accompany the screening.
Best practices dictate that women are asked about alcohol, prescription, and nonprescription drug use as a routine matter. High-quality evidence supports offering smoking cessation support to women who smoke and giving specific advice about nutrition and physical activity that’s based on “proven behavioral techniques.”
Evidence is of moderate quality that women should be encouraged to reach their prepregnancy weight by a year after delivery, with the ultimate goal of having a body mass index of 18.5-24.9.
High-quality evidence backs encouragement to engage in safe sex practices, with care providers also advised to facilitate partner screening and treatment for STIs.
Screening for STIs should follow guidance put forward by the Centers for Disease Control and Prevention and should be offered to women at high risk for STIs; those with a history of STI should have a careful history taken to determine risks for current or repeat infections, wrote Dr. Louis and her coauthors. These strong recommendations have high-quality evidence behind them.
The consensus statement recommends screening women for intimate partner violence, with moderate-quality evidence to support the recommendation. Patient navigators, expert medical interpretation, and other health educators can be offered to women with health literacy or language and communication challenges, but the evidence backing the recommendation is of low quality.
A subset of the interpregnancy care recommendations gives additional guidance regarding women with a history of high-risk pregnancy. All women planning pregnancy – or who could become pregnant – should take 500 mcg of folic acid daily beginning 1 month before fertilization and continuing through the 12th week of pregnancy. Folic acid supplementation for women who have had children with neural tube defects should begin at least 3 months before fertilization and continue through 12 weeks of pregnancy, at a dose of 400 mg.
All prescription and nonprescription medications, as well as potential environmental teratogens, should be reviewed before a repeat pregnancy. This, as well as the folic acid recommendations, are strong recommendations backed by high-quality evidence.
When appropriate, genetic counseling should be offered to women who have had prior pregnancies with genetic disorders or congenital anomalies. Asymptomatic genitourinary infections should not be treated in women with a history of preterm birth during the interpregnancy interval. These are strong recommendations, but are backed by low to moderate quality evidence, wrote Dr. Louis and her colleagues.
Another section of the consensus document specifically addresses specific health conditions, including diabetes, gestational diabetes, gestational and chronic hypertension, and preeclampsia, as well as mental health disorders and overweight or obesity.
For each, Dr. Louis and her coauthors recommend counseling that reviews complications and risk for future disease; for example, not only does prior preeclampsia increase risk for that complication in future pregnancies, risk for later cardiovascular disease is also doubled. The document outlines recommended interpregnancy testing, management considerations and medications of concern for health care providers caring for women with these conditions, and condition-specific goals.
Of the association between gestational diabetes, hypertension, and preeclampsia with later disease, Dr. Louis said in the interview, “We don’t know. ... It may be that pregnancy accelerates these diseases. We do know that normal changes in pregnancy stress your body, and that preeclampsia damages your vessels. Pregnancy can give you a warning, but we don’t have enough information to predict the outcome” in later life. “We do know there is some advice we can give: stop smoking and maintain a normal body weight.”
Other conditions such as HIV, renal disease, epilepsy, autoimmune and thyroid disease, and thrombophilias and antiphospholipid antibody syndrome are also addressed in this section of the consensus document.
Specific attention also is given to psychosocial risks, such as socioeconomic disadvantages and being a member of a racial or ethnic minority. Social determinants of health are complex, said Dr. Louis, but socioeconomic and racial stressors can include the added burden of caring for loved ones with constrained resources. Additionally, there can be access issues: Women can get emergent care by presenting to the ED but receiving continued primary and specialty care can be much more of a challenge.
Regarding racism, Dr. Louis said, “We all come into caring for these women with certain ideas.” For example, it’s not enough to say of a patient, “She’s noncompliant. You need to ask why.” When the “why” question is asked, then you may discover, “there’s something you can help the patient with,” she said. “We need to ask why, and then take steps to help our patients.”
Document building
The working group for the consensus document felt it was important to include nonphysicians who care for women, Dr. Louis said, so drafts were reviewed by and input received from the American College of Nurse-Midwives and the National Association of Nurse Practitioners in Women’s Health. Both groups endorsed the document.
The collaborative process of putting drafts together and then reviewing and revising the document was a big part of the reason it took 2 years to produce the interpregnancy care consensus statement. “It was the equivalent of two full gestations with a short interpregnancy interval!” said Dr. Louis, laughing. But seeking input from all stakeholders strengthened the final product.
Dr. Louis reported no conflicts of interest and no outside sources of funding were reported.
SOURCE: Louis JM et al. Obstet Gynecol. 2019;133:e51-72.
A new consensus statement places renewed focus on maternal interpregnancy care, with a goal of extending care past the postpartum period to provide a wellness-maximizing continuum of care.
The document, developed by the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine (SMFM), recognizes that pregnancy is part of the lifelong continuum of health and wellness. Although not all women will go on to have another pregnancy, the concept of interpregnancy care recognizes that ob.gyns. have a vital role that extends past the postpartum period.
“This is a shift in what we used to think was our job. We used to think that our job ended when the baby came out,” said the first author of the obstetric care consensus statement, Judette Marie Louis, MD, an ob.gyn. faculty member at the University of South Florida, Tampa, and a SMFM board member. “For too long, our focus was just the baby; we need to tell women, ‘You’re important too,’ ” she said in an interview.
“The interpregnancy period is an opportunity to address these complications of medical issues that have developed during pregnancy, to assess a woman’s mental and physical well-being, and to optimize her health along her life course,” Dr. Louis and her coauthors wrote in Obstetrics & Gynecology.
Conceptually, the opportunity for interpregnancy care arises after any pregnancy, no matter the outcome, and is part of the continuum of care for women of reproductive age. For women who do not intend a future pregnancy, well-woman care is the focus, while women who currently intend to become pregnant again receive interpregnancy care. Women may move from one arm of the continuum to the other if their intentions change or if they become pregnant, explained Dr. Louis and her coauthors.
Birth spacing
The new consensus document includes an emphasis on long-term health outcomes as well as maternal and neonatal outcomes in future pregnancies. Although the evidence is of no more than moderate quality, women should be advised to have an interpregnancy interval of at least 6 months and offered counseling about family planning before delivery. Risks and benefits of an interpregnancy interval of less than 18 months should be reviewed as well.
For women with a history of preterm birth and those who have had a prior cesarean delivery and desire a subsequent trial of labor, birth spacing is particularly important, noted Dr. Louis and her colleagues. There is higher-risk evidence for uterine rupture after cesarean delivery if delivery-to-delivery intervals are 18-24 months or less.
Recommendations regarding the length of the interpregnancy interval generally should not be affected by a history of prior infertility.
Other recommendations
High-quality evidence supports breast feeding’s salutary effects on maternal and child health, so women should receive anticipatory support and guidance to enable breastfeeding, according to the document.
In accordance with other guidelines, the document recommends that all women be screened for depression post partum and as part of well-woman care in the interpregnancy interval. Procedures for effective diagnosis, treatment, and follow-up should accompany the screening.
Best practices dictate that women are asked about alcohol, prescription, and nonprescription drug use as a routine matter. High-quality evidence supports offering smoking cessation support to women who smoke and giving specific advice about nutrition and physical activity that’s based on “proven behavioral techniques.”
Evidence is of moderate quality that women should be encouraged to reach their prepregnancy weight by a year after delivery, with the ultimate goal of having a body mass index of 18.5-24.9.
High-quality evidence backs encouragement to engage in safe sex practices, with care providers also advised to facilitate partner screening and treatment for STIs.
Screening for STIs should follow guidance put forward by the Centers for Disease Control and Prevention and should be offered to women at high risk for STIs; those with a history of STI should have a careful history taken to determine risks for current or repeat infections, wrote Dr. Louis and her coauthors. These strong recommendations have high-quality evidence behind them.
The consensus statement recommends screening women for intimate partner violence, with moderate-quality evidence to support the recommendation. Patient navigators, expert medical interpretation, and other health educators can be offered to women with health literacy or language and communication challenges, but the evidence backing the recommendation is of low quality.
A subset of the interpregnancy care recommendations gives additional guidance regarding women with a history of high-risk pregnancy. All women planning pregnancy – or who could become pregnant – should take 500 mcg of folic acid daily beginning 1 month before fertilization and continuing through the 12th week of pregnancy. Folic acid supplementation for women who have had children with neural tube defects should begin at least 3 months before fertilization and continue through 12 weeks of pregnancy, at a dose of 400 mg.
All prescription and nonprescription medications, as well as potential environmental teratogens, should be reviewed before a repeat pregnancy. This, as well as the folic acid recommendations, are strong recommendations backed by high-quality evidence.
When appropriate, genetic counseling should be offered to women who have had prior pregnancies with genetic disorders or congenital anomalies. Asymptomatic genitourinary infections should not be treated in women with a history of preterm birth during the interpregnancy interval. These are strong recommendations, but are backed by low to moderate quality evidence, wrote Dr. Louis and her colleagues.
Another section of the consensus document specifically addresses specific health conditions, including diabetes, gestational diabetes, gestational and chronic hypertension, and preeclampsia, as well as mental health disorders and overweight or obesity.
For each, Dr. Louis and her coauthors recommend counseling that reviews complications and risk for future disease; for example, not only does prior preeclampsia increase risk for that complication in future pregnancies, risk for later cardiovascular disease is also doubled. The document outlines recommended interpregnancy testing, management considerations and medications of concern for health care providers caring for women with these conditions, and condition-specific goals.
Of the association between gestational diabetes, hypertension, and preeclampsia with later disease, Dr. Louis said in the interview, “We don’t know. ... It may be that pregnancy accelerates these diseases. We do know that normal changes in pregnancy stress your body, and that preeclampsia damages your vessels. Pregnancy can give you a warning, but we don’t have enough information to predict the outcome” in later life. “We do know there is some advice we can give: stop smoking and maintain a normal body weight.”
Other conditions such as HIV, renal disease, epilepsy, autoimmune and thyroid disease, and thrombophilias and antiphospholipid antibody syndrome are also addressed in this section of the consensus document.
Specific attention also is given to psychosocial risks, such as socioeconomic disadvantages and being a member of a racial or ethnic minority. Social determinants of health are complex, said Dr. Louis, but socioeconomic and racial stressors can include the added burden of caring for loved ones with constrained resources. Additionally, there can be access issues: Women can get emergent care by presenting to the ED but receiving continued primary and specialty care can be much more of a challenge.
Regarding racism, Dr. Louis said, “We all come into caring for these women with certain ideas.” For example, it’s not enough to say of a patient, “She’s noncompliant. You need to ask why.” When the “why” question is asked, then you may discover, “there’s something you can help the patient with,” she said. “We need to ask why, and then take steps to help our patients.”
Document building
The working group for the consensus document felt it was important to include nonphysicians who care for women, Dr. Louis said, so drafts were reviewed by and input received from the American College of Nurse-Midwives and the National Association of Nurse Practitioners in Women’s Health. Both groups endorsed the document.
The collaborative process of putting drafts together and then reviewing and revising the document was a big part of the reason it took 2 years to produce the interpregnancy care consensus statement. “It was the equivalent of two full gestations with a short interpregnancy interval!” said Dr. Louis, laughing. But seeking input from all stakeholders strengthened the final product.
Dr. Louis reported no conflicts of interest and no outside sources of funding were reported.
SOURCE: Louis JM et al. Obstet Gynecol. 2019;133:e51-72.
A new consensus statement places renewed focus on maternal interpregnancy care, with a goal of extending care past the postpartum period to provide a wellness-maximizing continuum of care.
The document, developed by the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine (SMFM), recognizes that pregnancy is part of the lifelong continuum of health and wellness. Although not all women will go on to have another pregnancy, the concept of interpregnancy care recognizes that ob.gyns. have a vital role that extends past the postpartum period.
“This is a shift in what we used to think was our job. We used to think that our job ended when the baby came out,” said the first author of the obstetric care consensus statement, Judette Marie Louis, MD, an ob.gyn. faculty member at the University of South Florida, Tampa, and a SMFM board member. “For too long, our focus was just the baby; we need to tell women, ‘You’re important too,’ ” she said in an interview.
“The interpregnancy period is an opportunity to address these complications of medical issues that have developed during pregnancy, to assess a woman’s mental and physical well-being, and to optimize her health along her life course,” Dr. Louis and her coauthors wrote in Obstetrics & Gynecology.
Conceptually, the opportunity for interpregnancy care arises after any pregnancy, no matter the outcome, and is part of the continuum of care for women of reproductive age. For women who do not intend a future pregnancy, well-woman care is the focus, while women who currently intend to become pregnant again receive interpregnancy care. Women may move from one arm of the continuum to the other if their intentions change or if they become pregnant, explained Dr. Louis and her coauthors.
Birth spacing
The new consensus document includes an emphasis on long-term health outcomes as well as maternal and neonatal outcomes in future pregnancies. Although the evidence is of no more than moderate quality, women should be advised to have an interpregnancy interval of at least 6 months and offered counseling about family planning before delivery. Risks and benefits of an interpregnancy interval of less than 18 months should be reviewed as well.
For women with a history of preterm birth and those who have had a prior cesarean delivery and desire a subsequent trial of labor, birth spacing is particularly important, noted Dr. Louis and her colleagues. There is higher-risk evidence for uterine rupture after cesarean delivery if delivery-to-delivery intervals are 18-24 months or less.
Recommendations regarding the length of the interpregnancy interval generally should not be affected by a history of prior infertility.
Other recommendations
High-quality evidence supports breast feeding’s salutary effects on maternal and child health, so women should receive anticipatory support and guidance to enable breastfeeding, according to the document.
In accordance with other guidelines, the document recommends that all women be screened for depression post partum and as part of well-woman care in the interpregnancy interval. Procedures for effective diagnosis, treatment, and follow-up should accompany the screening.
Best practices dictate that women are asked about alcohol, prescription, and nonprescription drug use as a routine matter. High-quality evidence supports offering smoking cessation support to women who smoke and giving specific advice about nutrition and physical activity that’s based on “proven behavioral techniques.”
Evidence is of moderate quality that women should be encouraged to reach their prepregnancy weight by a year after delivery, with the ultimate goal of having a body mass index of 18.5-24.9.
High-quality evidence backs encouragement to engage in safe sex practices, with care providers also advised to facilitate partner screening and treatment for STIs.
Screening for STIs should follow guidance put forward by the Centers for Disease Control and Prevention and should be offered to women at high risk for STIs; those with a history of STI should have a careful history taken to determine risks for current or repeat infections, wrote Dr. Louis and her coauthors. These strong recommendations have high-quality evidence behind them.
The consensus statement recommends screening women for intimate partner violence, with moderate-quality evidence to support the recommendation. Patient navigators, expert medical interpretation, and other health educators can be offered to women with health literacy or language and communication challenges, but the evidence backing the recommendation is of low quality.
A subset of the interpregnancy care recommendations gives additional guidance regarding women with a history of high-risk pregnancy. All women planning pregnancy – or who could become pregnant – should take 500 mcg of folic acid daily beginning 1 month before fertilization and continuing through the 12th week of pregnancy. Folic acid supplementation for women who have had children with neural tube defects should begin at least 3 months before fertilization and continue through 12 weeks of pregnancy, at a dose of 400 mg.
All prescription and nonprescription medications, as well as potential environmental teratogens, should be reviewed before a repeat pregnancy. This, as well as the folic acid recommendations, are strong recommendations backed by high-quality evidence.
When appropriate, genetic counseling should be offered to women who have had prior pregnancies with genetic disorders or congenital anomalies. Asymptomatic genitourinary infections should not be treated in women with a history of preterm birth during the interpregnancy interval. These are strong recommendations, but are backed by low to moderate quality evidence, wrote Dr. Louis and her colleagues.
Another section of the consensus document specifically addresses specific health conditions, including diabetes, gestational diabetes, gestational and chronic hypertension, and preeclampsia, as well as mental health disorders and overweight or obesity.
For each, Dr. Louis and her coauthors recommend counseling that reviews complications and risk for future disease; for example, not only does prior preeclampsia increase risk for that complication in future pregnancies, risk for later cardiovascular disease is also doubled. The document outlines recommended interpregnancy testing, management considerations and medications of concern for health care providers caring for women with these conditions, and condition-specific goals.
Of the association between gestational diabetes, hypertension, and preeclampsia with later disease, Dr. Louis said in the interview, “We don’t know. ... It may be that pregnancy accelerates these diseases. We do know that normal changes in pregnancy stress your body, and that preeclampsia damages your vessels. Pregnancy can give you a warning, but we don’t have enough information to predict the outcome” in later life. “We do know there is some advice we can give: stop smoking and maintain a normal body weight.”
Other conditions such as HIV, renal disease, epilepsy, autoimmune and thyroid disease, and thrombophilias and antiphospholipid antibody syndrome are also addressed in this section of the consensus document.
Specific attention also is given to psychosocial risks, such as socioeconomic disadvantages and being a member of a racial or ethnic minority. Social determinants of health are complex, said Dr. Louis, but socioeconomic and racial stressors can include the added burden of caring for loved ones with constrained resources. Additionally, there can be access issues: Women can get emergent care by presenting to the ED but receiving continued primary and specialty care can be much more of a challenge.
Regarding racism, Dr. Louis said, “We all come into caring for these women with certain ideas.” For example, it’s not enough to say of a patient, “She’s noncompliant. You need to ask why.” When the “why” question is asked, then you may discover, “there’s something you can help the patient with,” she said. “We need to ask why, and then take steps to help our patients.”
Document building
The working group for the consensus document felt it was important to include nonphysicians who care for women, Dr. Louis said, so drafts were reviewed by and input received from the American College of Nurse-Midwives and the National Association of Nurse Practitioners in Women’s Health. Both groups endorsed the document.
The collaborative process of putting drafts together and then reviewing and revising the document was a big part of the reason it took 2 years to produce the interpregnancy care consensus statement. “It was the equivalent of two full gestations with a short interpregnancy interval!” said Dr. Louis, laughing. But seeking input from all stakeholders strengthened the final product.
Dr. Louis reported no conflicts of interest and no outside sources of funding were reported.
SOURCE: Louis JM et al. Obstet Gynecol. 2019;133:e51-72.
FROM OBSTETRICS & GYNECOLOGY
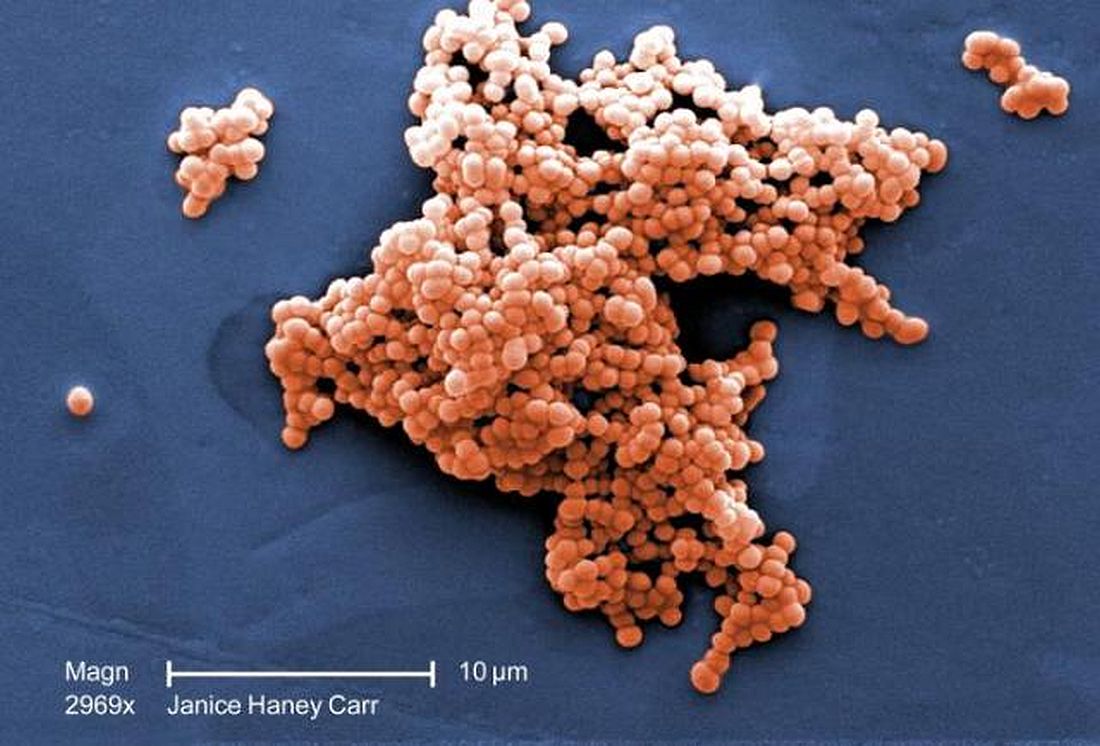
Incidence of late-onset GBS cases are higher than early-onset disease
according to a multistate study of invasive group B streptococcal disease published in JAMA Pediatrics.
Using data from the Active Bacterial Core surveillance (ABCs) program, Srinivas Acharya Nanduri, MD, MPH, at the Centers for Disease Control and Prevention, and colleagues performed an analysis of early-onset disease (EOD) and late-onset disease (LOD) cases of group B Streptococcus (GBS) in infants from 10 different states between 2006 and 2015, and whether mothers of infants with EOD received intrapartum antibiotic prophylaxis (IAP). EOD was defined as between 0 and 6 days old, while LOD occurred between 7 days and 89 days old.
They found 1,277 cases of EOD and 1,387 cases of LOD in total, with a decrease in incidence of EOD from 0.37 per 1,000 live births in 2006 to 0.23 per 1,000 live births in 2015 (P less than .001); LOD incidence remained stable at a mean 0.31 per 1,000 live births during the same time period.
In 2015, the national burden for EOD and LOD was estimated at 840 and 1,265 cases, respectively. Mothers of infants with EOD did not have indications for and did not receive IAP in 617 cases (48%) and did not receive IAP despite indications in 278 (22%) cases.
“While the current culture-based screening strategy has been highly successful in reducing EOD burden, our data show that almost half of remaining infants with EOD were born to mothers with no indication for receiving IAP,” Dr. Nanduri and colleagues wrote.
Because there currently is no effective prevention strategy against LOS GBS, the investigators wrote that a maternal vaccine against the most common serotypes “holds promise to prevent a substantial portion of this remaining burden,” and noted several GBS candidate vaccines were in advanced stages of development.
The researchers also looked at GBS serotype data in 1,743 patients from seven different centers. The most commonly found serotype isolates of 887 EOD cases were Ia (242 cases, 27%) and III (242 cases, 27%) overall. Serotype III was most common for LOD cases (481 cases, 56%) and increased in incidence from 0.12 per 1,000 live births to 0.20 per 1,000 live births during the study period (P less than .001), while serotype IV was responsible for 53 cases (6%) of both EOD and LOD.
Dr. Nanduri and associates wrote that over 99% of the serotyped EOD (881 cases) and serotyped LOD (853 cases) cases were caused by serotypes Ia, Ib, II, III, IV, and V. With regard to antimicrobial resistance, there were no cases of beta-lactam resistance, but there was constitutive clindamycin resistance in 359 isolate test results (21%).
The researchers noted that they were limited in the study by 1 year of whole-genome sequencing data, the ABCs capturing only 10% of live birth data in the United States, and conclusions on EOD prevention restricted to data from labor and delivery records.
This study was funded in part by the CDC. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
SOURCE: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
Perinatal group B Streptococcus (GBS) disease prevention guidelines are credited for the low rate of early-onset disease (EOD) cases of GBS in the United States, but the practice of intrapartum antibiotic prophylaxis (IAP) remains controversial in places like the United Kingdom where the National Health Service does not recommend screening-based IAP for GBS, Sagori Mukhopadhyay, MD, MMSc, and Karen M. Puopolo, MD, PhD, wrote in a related editorial.
One reason for concern about GBS IAP policies is that, despite the decreased number of EOD cases after implementation of IAP, the rate of late-onset disease (LOD) cases remain the same, the authors wrote. And implementation of IAP is not perfect: In some cases IAP was used for less than the recommended duration, used less effective drugs, or given too late so fetal infections were already established.
In addition, some may be uncomfortable with increased perinatal exposure to antibiotics – “a long-held concern about the extent to which widespread perinatal antibiotic use may contribute to the emergence and expansion of antibiotic-resistant GBS,” they added. However, despite the concern, the fatality ratio for EOD was 7% in the study by Nanduri et al., and one complication of GBS in survivors is neurodevelopmental impairment, according to a meta-analysis of 18 studies.
One solution that could address both EOD and LOD cases of GBS is the development of a GBS vaccine. Although there is reluctance to vaccinate pregnant women, recent studies have shown success in vaccinating women for influenza, tetanus, diphtheria, and pertussis; these recent efforts have “reinvigorated” academia’s interest in vaccine research for this population.
“Vaccination certainly could be a first step to eliminating neonatal GBS disease in the United States and may be the only available approach to addressing the substantial international burden of GBS-associated stillbirth, preterm birth, and neonatal disease morbidity and mortality,” the authors wrote. “But for now, while GBS IAP may be imperfect, it is the success we have.”
Dr. Mukhopadhyay and Dr. Puopolo are from the division of neonatology at the Children’s Hospital of Philadelphia. Dr. Mukhopadhyay and Dr. Puopolo commented on the study by Nanduri et al. in an accompanying editorial (Mukhopadhyay et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.4824). They reported no relevant conflicts of interest.
Perinatal group B Streptococcus (GBS) disease prevention guidelines are credited for the low rate of early-onset disease (EOD) cases of GBS in the United States, but the practice of intrapartum antibiotic prophylaxis (IAP) remains controversial in places like the United Kingdom where the National Health Service does not recommend screening-based IAP for GBS, Sagori Mukhopadhyay, MD, MMSc, and Karen M. Puopolo, MD, PhD, wrote in a related editorial.
One reason for concern about GBS IAP policies is that, despite the decreased number of EOD cases after implementation of IAP, the rate of late-onset disease (LOD) cases remain the same, the authors wrote. And implementation of IAP is not perfect: In some cases IAP was used for less than the recommended duration, used less effective drugs, or given too late so fetal infections were already established.
In addition, some may be uncomfortable with increased perinatal exposure to antibiotics – “a long-held concern about the extent to which widespread perinatal antibiotic use may contribute to the emergence and expansion of antibiotic-resistant GBS,” they added. However, despite the concern, the fatality ratio for EOD was 7% in the study by Nanduri et al., and one complication of GBS in survivors is neurodevelopmental impairment, according to a meta-analysis of 18 studies.
One solution that could address both EOD and LOD cases of GBS is the development of a GBS vaccine. Although there is reluctance to vaccinate pregnant women, recent studies have shown success in vaccinating women for influenza, tetanus, diphtheria, and pertussis; these recent efforts have “reinvigorated” academia’s interest in vaccine research for this population.
“Vaccination certainly could be a first step to eliminating neonatal GBS disease in the United States and may be the only available approach to addressing the substantial international burden of GBS-associated stillbirth, preterm birth, and neonatal disease morbidity and mortality,” the authors wrote. “But for now, while GBS IAP may be imperfect, it is the success we have.”
Dr. Mukhopadhyay and Dr. Puopolo are from the division of neonatology at the Children’s Hospital of Philadelphia. Dr. Mukhopadhyay and Dr. Puopolo commented on the study by Nanduri et al. in an accompanying editorial (Mukhopadhyay et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.4824). They reported no relevant conflicts of interest.
Perinatal group B Streptococcus (GBS) disease prevention guidelines are credited for the low rate of early-onset disease (EOD) cases of GBS in the United States, but the practice of intrapartum antibiotic prophylaxis (IAP) remains controversial in places like the United Kingdom where the National Health Service does not recommend screening-based IAP for GBS, Sagori Mukhopadhyay, MD, MMSc, and Karen M. Puopolo, MD, PhD, wrote in a related editorial.
One reason for concern about GBS IAP policies is that, despite the decreased number of EOD cases after implementation of IAP, the rate of late-onset disease (LOD) cases remain the same, the authors wrote. And implementation of IAP is not perfect: In some cases IAP was used for less than the recommended duration, used less effective drugs, or given too late so fetal infections were already established.
In addition, some may be uncomfortable with increased perinatal exposure to antibiotics – “a long-held concern about the extent to which widespread perinatal antibiotic use may contribute to the emergence and expansion of antibiotic-resistant GBS,” they added. However, despite the concern, the fatality ratio for EOD was 7% in the study by Nanduri et al., and one complication of GBS in survivors is neurodevelopmental impairment, according to a meta-analysis of 18 studies.
One solution that could address both EOD and LOD cases of GBS is the development of a GBS vaccine. Although there is reluctance to vaccinate pregnant women, recent studies have shown success in vaccinating women for influenza, tetanus, diphtheria, and pertussis; these recent efforts have “reinvigorated” academia’s interest in vaccine research for this population.
“Vaccination certainly could be a first step to eliminating neonatal GBS disease in the United States and may be the only available approach to addressing the substantial international burden of GBS-associated stillbirth, preterm birth, and neonatal disease morbidity and mortality,” the authors wrote. “But for now, while GBS IAP may be imperfect, it is the success we have.”
Dr. Mukhopadhyay and Dr. Puopolo are from the division of neonatology at the Children’s Hospital of Philadelphia. Dr. Mukhopadhyay and Dr. Puopolo commented on the study by Nanduri et al. in an accompanying editorial (Mukhopadhyay et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.4824). They reported no relevant conflicts of interest.
according to a multistate study of invasive group B streptococcal disease published in JAMA Pediatrics.
Using data from the Active Bacterial Core surveillance (ABCs) program, Srinivas Acharya Nanduri, MD, MPH, at the Centers for Disease Control and Prevention, and colleagues performed an analysis of early-onset disease (EOD) and late-onset disease (LOD) cases of group B Streptococcus (GBS) in infants from 10 different states between 2006 and 2015, and whether mothers of infants with EOD received intrapartum antibiotic prophylaxis (IAP). EOD was defined as between 0 and 6 days old, while LOD occurred between 7 days and 89 days old.
They found 1,277 cases of EOD and 1,387 cases of LOD in total, with a decrease in incidence of EOD from 0.37 per 1,000 live births in 2006 to 0.23 per 1,000 live births in 2015 (P less than .001); LOD incidence remained stable at a mean 0.31 per 1,000 live births during the same time period.
In 2015, the national burden for EOD and LOD was estimated at 840 and 1,265 cases, respectively. Mothers of infants with EOD did not have indications for and did not receive IAP in 617 cases (48%) and did not receive IAP despite indications in 278 (22%) cases.
“While the current culture-based screening strategy has been highly successful in reducing EOD burden, our data show that almost half of remaining infants with EOD were born to mothers with no indication for receiving IAP,” Dr. Nanduri and colleagues wrote.
Because there currently is no effective prevention strategy against LOS GBS, the investigators wrote that a maternal vaccine against the most common serotypes “holds promise to prevent a substantial portion of this remaining burden,” and noted several GBS candidate vaccines were in advanced stages of development.
The researchers also looked at GBS serotype data in 1,743 patients from seven different centers. The most commonly found serotype isolates of 887 EOD cases were Ia (242 cases, 27%) and III (242 cases, 27%) overall. Serotype III was most common for LOD cases (481 cases, 56%) and increased in incidence from 0.12 per 1,000 live births to 0.20 per 1,000 live births during the study period (P less than .001), while serotype IV was responsible for 53 cases (6%) of both EOD and LOD.
Dr. Nanduri and associates wrote that over 99% of the serotyped EOD (881 cases) and serotyped LOD (853 cases) cases were caused by serotypes Ia, Ib, II, III, IV, and V. With regard to antimicrobial resistance, there were no cases of beta-lactam resistance, but there was constitutive clindamycin resistance in 359 isolate test results (21%).
The researchers noted that they were limited in the study by 1 year of whole-genome sequencing data, the ABCs capturing only 10% of live birth data in the United States, and conclusions on EOD prevention restricted to data from labor and delivery records.
This study was funded in part by the CDC. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
SOURCE: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
according to a multistate study of invasive group B streptococcal disease published in JAMA Pediatrics.
Using data from the Active Bacterial Core surveillance (ABCs) program, Srinivas Acharya Nanduri, MD, MPH, at the Centers for Disease Control and Prevention, and colleagues performed an analysis of early-onset disease (EOD) and late-onset disease (LOD) cases of group B Streptococcus (GBS) in infants from 10 different states between 2006 and 2015, and whether mothers of infants with EOD received intrapartum antibiotic prophylaxis (IAP). EOD was defined as between 0 and 6 days old, while LOD occurred between 7 days and 89 days old.
They found 1,277 cases of EOD and 1,387 cases of LOD in total, with a decrease in incidence of EOD from 0.37 per 1,000 live births in 2006 to 0.23 per 1,000 live births in 2015 (P less than .001); LOD incidence remained stable at a mean 0.31 per 1,000 live births during the same time period.
In 2015, the national burden for EOD and LOD was estimated at 840 and 1,265 cases, respectively. Mothers of infants with EOD did not have indications for and did not receive IAP in 617 cases (48%) and did not receive IAP despite indications in 278 (22%) cases.
“While the current culture-based screening strategy has been highly successful in reducing EOD burden, our data show that almost half of remaining infants with EOD were born to mothers with no indication for receiving IAP,” Dr. Nanduri and colleagues wrote.
Because there currently is no effective prevention strategy against LOS GBS, the investigators wrote that a maternal vaccine against the most common serotypes “holds promise to prevent a substantial portion of this remaining burden,” and noted several GBS candidate vaccines were in advanced stages of development.
The researchers also looked at GBS serotype data in 1,743 patients from seven different centers. The most commonly found serotype isolates of 887 EOD cases were Ia (242 cases, 27%) and III (242 cases, 27%) overall. Serotype III was most common for LOD cases (481 cases, 56%) and increased in incidence from 0.12 per 1,000 live births to 0.20 per 1,000 live births during the study period (P less than .001), while serotype IV was responsible for 53 cases (6%) of both EOD and LOD.
Dr. Nanduri and associates wrote that over 99% of the serotyped EOD (881 cases) and serotyped LOD (853 cases) cases were caused by serotypes Ia, Ib, II, III, IV, and V. With regard to antimicrobial resistance, there were no cases of beta-lactam resistance, but there was constitutive clindamycin resistance in 359 isolate test results (21%).
The researchers noted that they were limited in the study by 1 year of whole-genome sequencing data, the ABCs capturing only 10% of live birth data in the United States, and conclusions on EOD prevention restricted to data from labor and delivery records.
This study was funded in part by the CDC. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
SOURCE: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
FROM JAMA PEDIATRICS
Key clinical point: Between 2006 and 2015, early-onset disease cases of group B Streptococcus (GBS) declined, while the incidence of late-onset cases did not change.
Major finding: The rate of early-onset GBS declined from 0.37 to 0.23 per 1,000 live births and the rate of late-onset GBS cases remained at a mean 0.31 per 1,000 live births.
Study details: A population-based study of infants with early-onset disease and late-onset disease GBS from 10 different states in the Active Bacterial Core surveillance program between 2006 and 2015.
Disclosures: This study was funded in part by the Centers for Disease Control and Prevention. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
Source: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
Soy didn’t up all-cause mortality in breast cancer survivors
A cohort of Chinese women who are breast cancer survivors had no increased mortality from soy intake, according to a new study.
The work adds to the existing body of evidence that women with breast cancer, or risk for breast cancer, don’t need to modify their soy intake to mitigate risk, said the study’s first author, Suzanne C. Ho, PhD.
Speaking at the annual meeting of the North American Menopause Society, Dr. Ho noted that the combination of increasing breast cancer incidence and improved outcome has resulted in larger numbers of breast cancer survivors in Hong Kong, where she is professor emerita at the Chinese University of Hong Kong.
The prospective, ongoing study examines the association between soy intake pre- and postdiagnosis and total mortality for Chinese women who are breast cancer survivors. Dr. Ho said that she and her colleagues hypothesized that they would not see higher mortality among women who had higher soy intake – and this was the case.
Of 1,497 breast cancer survivors drawn from two facilities in Hong Kong, those who consumed higher quantities of dietary soy did not have increased risk of all-cause mortality, compared with those in the lowest tertile of soy consumption.
There are theoretical underpinnings for thinking that soy could be a player in cancer risk, but the biochemistry and epidemiology behind the studies are complicated. Estrogen plays a role in human breast cancer, and many modern breast cancer treatments actually dampen endogenous estrogens.
However, epidemiologic data have shown that consumption of soy-based foods – which contain phytoestrogens, primarily in the form of isoflavones – is inversely associated with developing breast cancer.
This is all part of why soy-based foods have been thought of as a mixed bag with regard to breast cancer: Soy isoflavones are, said Dr. Ho, “Natural estrogen receptor modulators that possess both estrogenlike and antiestrogenic properties.”
Other chemicals contained in soy may fight cancer, with effects that are antioxidative and strengthen immune response. Soy constituents also inhibit DNA topoisomerase I and II, proteases, tyrosine kinases, and inositol phosphate, effects that can slow tumor growth. Still, one soy isoflavone, genistein, actually can promote growth of estrogen-dependent tumors in rats, said Dr. Ho
Dr. Ho and her colleagues enrolled Hong Kong residents for the study of mortality among breast cancer survivors. Participants were included if they were Chinese, female, aged 24-77 years, and had their first primary breast cancer histologically confirmed within 12 months of entering the study. Cancer had to be graded below stage III.
Using a 109-item validated food questionnaire, investigators gathered information about participants’ soy intake and general diet for the year prior to breast cancer diagnosis. Other patient characteristics, relevant prognostic information from medical records, and anthropometric data were collected at baseline, and repeated at 18, 36, and 60 months.
The primary outcome measure – all-cause mortality during the follow-up period – was tracked for a mean 50.9 months, with a 78% retention rate for study participants, said Dr. Ho. In total, 96 patients died during follow-up, making up 5.9% of the premenopausal and 7% of the postmenopausal participants.
Statistical analysis corrected for potential confounders, including patient and disease characteristics and treatment modalities, as well as overall energy consumption.
Patients were evenly divided into tertiles of soy isoflavone intake, with cutpoints of 3.77 mg/1,000 kcal and 10.05 mg/1,000 kcal for the lower limit of the two higher tertiles. For the highest tertile, though, mean isoflavone intake was actually 20.87 mg/1,000 kcal.
Patient, disease, and treatment characteristics did not differ significantly among the tertiles.
An adjusted statistical analysis looked at pre- and postmenopausal women separately by tertile of soy isoflavone consumption, setting the hazard ratio for all-cause mortality at 1.00 for women in the lowest tertile of soy consumption.
For premenopausal women in the middle tertile, the HR was 0.45 (95% confidence interval, 0.20-1.00), and 0.86 for those in the highest tertile (95% CI, 0.43-1.72); 782 participants, in all, were premenopausal.
For the 715 postmenopausal women, the HR for those in the middle tertile of soy consumption was 0.94 (95% CI, 0.43-2.05), and 1.11 in the highest (95% CI, 0.54-2.29).
Taking all pre- and postmenopausal participants together, those in the middle tertile of soy isoflavone intake had an all-cause mortality HR of 0.63 (95% CI, 0.37-1.09). For the highest tertile of the full cohort, the HR was 0.95 (95% CI, 0.58-1.55).
Confidence intervals were wide in these findings, but Dr. Ho noted that “moderate soy food intake might be associated with better survival.”
“Prediagnosis soy intake did not increase the risk of all-cause mortality in breast cancer survivors,” said Dr. Ho, findings she called “consistent with the literature that soy consumption does not adversely effect breast cancer survival.”
The study is ongoing, she explained, and “longer follow-up will provide further evidence on the effect of pre- and postdiagnosis soy intake on breast cancer outcomes.”
The study had a homogeneous population of southern Chinese women, with fairly good retention and robust statistical adjustment for confounders. However, it wasn’t possible to assess bioavailability of isoflavones and their metabolites, which can vary according to individual microbiota. Also, researchers did not track whether patients used traditional Chinese medicine.
The World Cancer Research Fund International supported the study. Dr. Ho reported no conflicts of interest.
SOURCE: Ho S et al. NAMS 2018, Abstract S-23.
A cohort of Chinese women who are breast cancer survivors had no increased mortality from soy intake, according to a new study.
The work adds to the existing body of evidence that women with breast cancer, or risk for breast cancer, don’t need to modify their soy intake to mitigate risk, said the study’s first author, Suzanne C. Ho, PhD.
Speaking at the annual meeting of the North American Menopause Society, Dr. Ho noted that the combination of increasing breast cancer incidence and improved outcome has resulted in larger numbers of breast cancer survivors in Hong Kong, where she is professor emerita at the Chinese University of Hong Kong.
The prospective, ongoing study examines the association between soy intake pre- and postdiagnosis and total mortality for Chinese women who are breast cancer survivors. Dr. Ho said that she and her colleagues hypothesized that they would not see higher mortality among women who had higher soy intake – and this was the case.
Of 1,497 breast cancer survivors drawn from two facilities in Hong Kong, those who consumed higher quantities of dietary soy did not have increased risk of all-cause mortality, compared with those in the lowest tertile of soy consumption.
There are theoretical underpinnings for thinking that soy could be a player in cancer risk, but the biochemistry and epidemiology behind the studies are complicated. Estrogen plays a role in human breast cancer, and many modern breast cancer treatments actually dampen endogenous estrogens.
However, epidemiologic data have shown that consumption of soy-based foods – which contain phytoestrogens, primarily in the form of isoflavones – is inversely associated with developing breast cancer.
This is all part of why soy-based foods have been thought of as a mixed bag with regard to breast cancer: Soy isoflavones are, said Dr. Ho, “Natural estrogen receptor modulators that possess both estrogenlike and antiestrogenic properties.”
Other chemicals contained in soy may fight cancer, with effects that are antioxidative and strengthen immune response. Soy constituents also inhibit DNA topoisomerase I and II, proteases, tyrosine kinases, and inositol phosphate, effects that can slow tumor growth. Still, one soy isoflavone, genistein, actually can promote growth of estrogen-dependent tumors in rats, said Dr. Ho
Dr. Ho and her colleagues enrolled Hong Kong residents for the study of mortality among breast cancer survivors. Participants were included if they were Chinese, female, aged 24-77 years, and had their first primary breast cancer histologically confirmed within 12 months of entering the study. Cancer had to be graded below stage III.
Using a 109-item validated food questionnaire, investigators gathered information about participants’ soy intake and general diet for the year prior to breast cancer diagnosis. Other patient characteristics, relevant prognostic information from medical records, and anthropometric data were collected at baseline, and repeated at 18, 36, and 60 months.
The primary outcome measure – all-cause mortality during the follow-up period – was tracked for a mean 50.9 months, with a 78% retention rate for study participants, said Dr. Ho. In total, 96 patients died during follow-up, making up 5.9% of the premenopausal and 7% of the postmenopausal participants.
Statistical analysis corrected for potential confounders, including patient and disease characteristics and treatment modalities, as well as overall energy consumption.
Patients were evenly divided into tertiles of soy isoflavone intake, with cutpoints of 3.77 mg/1,000 kcal and 10.05 mg/1,000 kcal for the lower limit of the two higher tertiles. For the highest tertile, though, mean isoflavone intake was actually 20.87 mg/1,000 kcal.
Patient, disease, and treatment characteristics did not differ significantly among the tertiles.
An adjusted statistical analysis looked at pre- and postmenopausal women separately by tertile of soy isoflavone consumption, setting the hazard ratio for all-cause mortality at 1.00 for women in the lowest tertile of soy consumption.
For premenopausal women in the middle tertile, the HR was 0.45 (95% confidence interval, 0.20-1.00), and 0.86 for those in the highest tertile (95% CI, 0.43-1.72); 782 participants, in all, were premenopausal.
For the 715 postmenopausal women, the HR for those in the middle tertile of soy consumption was 0.94 (95% CI, 0.43-2.05), and 1.11 in the highest (95% CI, 0.54-2.29).
Taking all pre- and postmenopausal participants together, those in the middle tertile of soy isoflavone intake had an all-cause mortality HR of 0.63 (95% CI, 0.37-1.09). For the highest tertile of the full cohort, the HR was 0.95 (95% CI, 0.58-1.55).
Confidence intervals were wide in these findings, but Dr. Ho noted that “moderate soy food intake might be associated with better survival.”
“Prediagnosis soy intake did not increase the risk of all-cause mortality in breast cancer survivors,” said Dr. Ho, findings she called “consistent with the literature that soy consumption does not adversely effect breast cancer survival.”
The study is ongoing, she explained, and “longer follow-up will provide further evidence on the effect of pre- and postdiagnosis soy intake on breast cancer outcomes.”
The study had a homogeneous population of southern Chinese women, with fairly good retention and robust statistical adjustment for confounders. However, it wasn’t possible to assess bioavailability of isoflavones and their metabolites, which can vary according to individual microbiota. Also, researchers did not track whether patients used traditional Chinese medicine.
The World Cancer Research Fund International supported the study. Dr. Ho reported no conflicts of interest.
SOURCE: Ho S et al. NAMS 2018, Abstract S-23.
A cohort of Chinese women who are breast cancer survivors had no increased mortality from soy intake, according to a new study.
The work adds to the existing body of evidence that women with breast cancer, or risk for breast cancer, don’t need to modify their soy intake to mitigate risk, said the study’s first author, Suzanne C. Ho, PhD.
Speaking at the annual meeting of the North American Menopause Society, Dr. Ho noted that the combination of increasing breast cancer incidence and improved outcome has resulted in larger numbers of breast cancer survivors in Hong Kong, where she is professor emerita at the Chinese University of Hong Kong.
The prospective, ongoing study examines the association between soy intake pre- and postdiagnosis and total mortality for Chinese women who are breast cancer survivors. Dr. Ho said that she and her colleagues hypothesized that they would not see higher mortality among women who had higher soy intake – and this was the case.
Of 1,497 breast cancer survivors drawn from two facilities in Hong Kong, those who consumed higher quantities of dietary soy did not have increased risk of all-cause mortality, compared with those in the lowest tertile of soy consumption.
There are theoretical underpinnings for thinking that soy could be a player in cancer risk, but the biochemistry and epidemiology behind the studies are complicated. Estrogen plays a role in human breast cancer, and many modern breast cancer treatments actually dampen endogenous estrogens.
However, epidemiologic data have shown that consumption of soy-based foods – which contain phytoestrogens, primarily in the form of isoflavones – is inversely associated with developing breast cancer.
This is all part of why soy-based foods have been thought of as a mixed bag with regard to breast cancer: Soy isoflavones are, said Dr. Ho, “Natural estrogen receptor modulators that possess both estrogenlike and antiestrogenic properties.”
Other chemicals contained in soy may fight cancer, with effects that are antioxidative and strengthen immune response. Soy constituents also inhibit DNA topoisomerase I and II, proteases, tyrosine kinases, and inositol phosphate, effects that can slow tumor growth. Still, one soy isoflavone, genistein, actually can promote growth of estrogen-dependent tumors in rats, said Dr. Ho
Dr. Ho and her colleagues enrolled Hong Kong residents for the study of mortality among breast cancer survivors. Participants were included if they were Chinese, female, aged 24-77 years, and had their first primary breast cancer histologically confirmed within 12 months of entering the study. Cancer had to be graded below stage III.
Using a 109-item validated food questionnaire, investigators gathered information about participants’ soy intake and general diet for the year prior to breast cancer diagnosis. Other patient characteristics, relevant prognostic information from medical records, and anthropometric data were collected at baseline, and repeated at 18, 36, and 60 months.
The primary outcome measure – all-cause mortality during the follow-up period – was tracked for a mean 50.9 months, with a 78% retention rate for study participants, said Dr. Ho. In total, 96 patients died during follow-up, making up 5.9% of the premenopausal and 7% of the postmenopausal participants.
Statistical analysis corrected for potential confounders, including patient and disease characteristics and treatment modalities, as well as overall energy consumption.
Patients were evenly divided into tertiles of soy isoflavone intake, with cutpoints of 3.77 mg/1,000 kcal and 10.05 mg/1,000 kcal for the lower limit of the two higher tertiles. For the highest tertile, though, mean isoflavone intake was actually 20.87 mg/1,000 kcal.
Patient, disease, and treatment characteristics did not differ significantly among the tertiles.
An adjusted statistical analysis looked at pre- and postmenopausal women separately by tertile of soy isoflavone consumption, setting the hazard ratio for all-cause mortality at 1.00 for women in the lowest tertile of soy consumption.
For premenopausal women in the middle tertile, the HR was 0.45 (95% confidence interval, 0.20-1.00), and 0.86 for those in the highest tertile (95% CI, 0.43-1.72); 782 participants, in all, were premenopausal.
For the 715 postmenopausal women, the HR for those in the middle tertile of soy consumption was 0.94 (95% CI, 0.43-2.05), and 1.11 in the highest (95% CI, 0.54-2.29).
Taking all pre- and postmenopausal participants together, those in the middle tertile of soy isoflavone intake had an all-cause mortality HR of 0.63 (95% CI, 0.37-1.09). For the highest tertile of the full cohort, the HR was 0.95 (95% CI, 0.58-1.55).
Confidence intervals were wide in these findings, but Dr. Ho noted that “moderate soy food intake might be associated with better survival.”
“Prediagnosis soy intake did not increase the risk of all-cause mortality in breast cancer survivors,” said Dr. Ho, findings she called “consistent with the literature that soy consumption does not adversely effect breast cancer survival.”
The study is ongoing, she explained, and “longer follow-up will provide further evidence on the effect of pre- and postdiagnosis soy intake on breast cancer outcomes.”
The study had a homogeneous population of southern Chinese women, with fairly good retention and robust statistical adjustment for confounders. However, it wasn’t possible to assess bioavailability of isoflavones and their metabolites, which can vary according to individual microbiota. Also, researchers did not track whether patients used traditional Chinese medicine.
The World Cancer Research Fund International supported the study. Dr. Ho reported no conflicts of interest.
SOURCE: Ho S et al. NAMS 2018, Abstract S-23.
REPORTING FROM NAMS 2018
Key clinical point: Soy consumption did not increase mortality risk in breast cancer survivors.
Major finding: The hazard ratios for all-cause mortality were 0.63 and 0.95 for the two highest tertiles of soy consumption.
Study details: An ongoing prospective cohort study of 1,497 female breast cancer survivors in Hong Kong.
Disclosures: The World Cancer Research Fund International supported the study. Dr. Ho reported no conflicts of interest.
Source: Ho S et al. NAMS 2018, Abstract S-23.
Female Veterans’ Experiences With VHA Treatment for Military Sexual Trauma
Females are the fastest growing population to seek care at the Veterans Health Administration (VHA).1 Based on a 2014 study examining prevalence of military sexual trauma (MST), it is estimated that about one-third of females in the military screen positive for MST, and the rates are higher for younger veterans.2 Military sexual trauma includes both rape and any sexual activity that occurred without consent; offensive sexual remarks or advances can also represent MST. The issue of MST, therefore, is an important one to address adequately, especially for female veterans who are screened through the VHA system.
Since 1992, the VHA has been required to provide services for MST, defined as “sexual harassment that is threatening in character or physical assault of a sexual nature that occurred while the victim was in the military.”3 Despite this mandate, it has taken many years for all VHA hospitals to adopt recommended screening tools to identify survivors of MST and give them proper resources. Only half of VHA hospitals adopted screening 6 years after the policy change.4 In addition, the environment in which the survivors receive MST care may trigger posttraumatic stress symptoms as many of the other patients seeking care at the VHA hospital resemble the perpetrators.5 Thus, up to half of females who report a history of MST do not receive care for their MST through the VHA.6
Having a history of MST significantly increases the risks of developing mental health disorders, including posttraumatic stress disorder (PTSD), major depressive disorder, generalized anxiety disorder, and suicidal ideation.2 This group also has overall decreased quality of life (QOL). Female veterans have increased sexual dysfunction and dissatisfaction, which is heightened with a history of MST.7 Addressing MST requires treatment of all aspects of life affected by MST, such as mental health, sexual function, and QOL. The quality of treatment for MST through VHA hospitals deserves attention and likely still requires improvement with better incorporation of the patient’s perspective.
Qualitative research allows for incorporation of the patient’s perspective and is useful for exploring new ideas and themes.8 Current qualitative research using individual interviews of MST survivors focuses more on mental health treatment modalities through the VHA system and how resources are used within the system.9,10 While it is important to understand the quantity of these resources, their quality also should be explored. Research has identified unique gender-specific concerns such as female-only mental health groups.10 However, there has been less focus on how to improve current therapies and the treatment modalities (regardless of whether it is a community service or at the VHA system) females find most helpful. There is a gap in understanding the patient’s perspective and assessment of current MST treatments as well as the unmet needs both within and outside of the VHA system. Therefore, the purpose of this study is 2-fold: (1) examine the utilization of VHA services for MST, as well as outside services, through focusgroup sessions; and (2) to offer specific recommendations for improving MST treatment for female veterans from the patient’s perspective.
Methods
After obtaining institutional review board approval (16-H192), females who screened positive for a history of MST, using the validated MST screening questionnaire, were recruited from the Women’s Continuity Clinic, Urology clinic, and via a research flyer placed within key locations at the New Mexico Veterans Affairs (VA) Health Care System (NMVAHCS).11 Inclusion criteria were veterans aged > 18 years who could speak and understand English. Those who agreed to participate attended any 1 of 5 focus groups. Prior to initiation of the focus groups, the investigators generated a focus-group script, including specific questions or probes to explore treatment, unmet needs (such as other health conditions the veteran associated with MST that were not being addressed), and recommendations for care improvement.
Subjects granted consent privately prior to conduction of the focus group. Each participant completed a basic demographic (age, race, ethnicity) and clinical history (including pain conditions and therapy received for MST). These characteristics were evaluated with descriptive statistics, including means and frequencies.
The focus groups took place on the NM VAHCS Raymond G. Murphy VA Medical Center campus in a private conference room and were moderated by nonmedical research personnel experienced in focus-group moderation. Focus groups were recorded and transcribed. An iterative process was used with revisions to the script and probe questions as needed. Focus groups were planned for 2 hours but were allowed to continue at the participants’ discretion.
The de-identified transcripts were uploaded to the web-based qualitative engine Dedoose 6.2.21 software (Los Angeles, CA) and coded. Using grounded theory, the codes were grouped into themes and subsequently organized into emergent concepts.8,12 Following constant comparative methodology, ideas were compared and combined between each focus group.8,13 After completion of the focus groups, the generated ideas were organized and refined to create a conceptual framework that represented the collective ideas from the focus groups.
Results
Between January and June 2017, 5 focus groups with 17 participants were conducted; each session lasted about 3 hours. The average age was 52 ± 8.3 years, and were from a diverse racial and ethnic background. Most reported that > 20 years had passed since the first MST, and care-seeking for the first time was > 11 years after the trauma, although symptoms related to the MST most frequently began within 1 year of the trauma (Table 1).
Preliminary Themes
The Trauma
Focus-group participants noted improved therapies offered by the VA but challenges obtaining health care:
“…because I’m really trying to deal with it and just be happy and get my joy back and deal with the isolation.”
“Another way that the memories affected me was barricading myself in my own house, starting from the front door.”
Male-Dominated VA
Participants also noted that, along with screening improving the system, dedicated female staff and service connection are important:
“The Womens Clinic is nice, and it’s nice to know that I can go there and I’m not having to discuss everything with men all over the place.”
“The other thing... that would be really good for survivors of MST, is help with disability.”
While the focus-group participants found dedicated women’s clinics helpful and providing improved care, the overall VA environment remains male-dominated:
“Because it’s really hard to relax and be vulnerable and be in your body and in your emotions if there‘s a bunch of penises around. When I saw these guys on the floor I’m like, I ain’t going in there.”
This male-dominated sense also incorporated a feeling of being misunderstood by a system that has traditionally cared for male veterans:
“People don‘t understand. They think, oh, you‘re overreacting, but they don’t know what it feels like to be inside.”
“I wouldn’t say they treat you like a second citizen, but it’s like almost every appointment I go to that’s not in the Women’s Clinic, the secretaries or whatever will be like ‘Oh, are you looking for somebody, or...’
Assumption Females Are Not Veterans
“There was an older gentleman behind me, they were like ‘Are you checking him in?’ I said, ‘I’m sure he’ll check himself in, but I’m checking myself in.’”
Participants also reported that there is an assumption that you’re not a veteran when you’re female:
“All of the care should be geared to be the same. And we know we need to recognize that men have their issues, and women will have their issues. But we don’t need to just say ‘all women have this issue, throw them over there.’”
Self-Doubt
“The world doesn’t validate rape, you asked for it, it was what you were wearing, it was what you said.”
Ongoing efforts to have female-only spaces, therapy groups, and support networks were encouraged by all 5 focus groups. These themes, provided the foundation for emergent concepts regarding patients’ perceptions of their treatment for MST: (1) Improvement has been slow but measurable; (2) VA cares more about male veterans; (3) The isolation from MST is pervasive; (4) It’s hard to navigate the VA system or any health care when you’re traumatized; and (5) Sexual assault leaves lasting self-doubt that providers need to address.
Isolation
Because there are barriers to seeking care the overarching method for coping with the effects of MST was isolation.
Overcoming the isolation was essential to seeking any care. Participants reported years of living alone, avoiding social situations and contexts, and difficulty with basic tasks because of the isolation.
“That the coping skills, that the isolation is a coping skill and all these things, and that I had to do that to survive.”
Lack of family and provider support and the VHA’s perceived focus on male veterans perpetuated this sense of isolation. Additionally, feeding the isolation were other maladaptive behaviors, such as alcoholism, weight gain, and anger.
“I was always an athlete until my MST, and I still find myself drinking whisky and wanting to smoke pot. It’s not that I want to, I guess it gives me a sense of relief, because my MST made me an alcoholic.”
Participants reported that successful treatment of MST must include treatment of other maladaptive behaviors and specific provider-behavior changes.
At times, providers contribute to female MST survivors’ feeling undervalued:
“I had an hour session and she kept looking at her watch and blowing me off, and I finally said, okay, I’m done, good-bye, after 45 minutes.”
Validation
Participants’ suggestions to improve MST treatment, including goal sharing, validation, knowledge, and support:
“They should have staff awareness groups, or focus groups to teach them the same thing that the patients are receiving as far as how to handle yourself, how to interact with others. Don’t bring your sh** from home into your job. You’re an employee, don’t take it personal.” (
The need for provider-level support and validation likely stems from the sense that many females expressed that MST was their fault. As one participant said,
“It wasn’t violent for me. I froze. So that’s another reason that I feel guilty because it’s like I didn’t fight. I just froze and put up with it, so I feel like jeez it was my fault. I didn’t... Somehow I am responsible for this.”
Thus, the groups concluded that the most powerful support was provider validation:
“The most important for me was that I was told it was not my fault. Over and over and over. That is the most important thing that us females need to know. Because that is such a relief and that opened up so much more.”
At all of the focus groups, female veterans reported that physician validation of the assault was essential to healing. When providers communicated validation, the women experienced the most improvement in symptoms.
Therapies for MST
A variety of modalities was recommended as helpful in coping with symptoms associated with MST. One female noted her therapy dog allowed her to get her first Papanicolaou (Pap) smear in years:
“Pelvic exams are like the seventh circle of hell. Like, God, you’d think I was being abducted by aliens or something. Last time, up here, they let me bring my little dog, which was extraordinarily helpful for me.”
For others, more traditional therapy such as prolonged exposure therapy or cognitive behavioral therapy, was helpful.
“After my prolonged exposure therapy; it saved my life. I’m not suicidal, and the only thing that’s really, really affected is sometimes I still have to sleep with a night light. Over 80% of the symptoms that I had and the problems that I had were alleviated with the therapy.”
Other veterans noted alternative therapies as beneficial for overcoming trauma:
“Yoga has really helped me with dealing with chronic pain and letting go of things that no longer serve me, and remembering about the inhale, the exhale, there’s a pause between the exhale and an inhale, where that’s where I make my choices, my thoughts, catch it, check it, change it, challenge my thoughts, that’s really, really helped me.”
From these concepts, and the specific suggestions female veterans provided for improvement in care,
Discussion
This qualitative study of the quality of MST treatment with specific suggestions for improvement shows that the underlying force impacting health care in female survivors of MST is isolation. In turn, that isolation is perpetuated by personal beliefs, mental health, lack of support, and the VHA culture. While there was improvement in VHA care noted, female veterans offered many specific suggestions—simple ones that could be rapidly implemented—to enhance care. Many of these suggestions were targeted at provider-level behaviors such as validation, goal setting, knowledge (both about the military and about MST), and support.
Previous work showed that tangible (ie, words, being present) support rather than broad social support only generally helps reduces posttraumatic stress symptoms.15 These researchers found that tangible support moderated the relationship between number of lifetime traumas and PTSD. Schumm and colleagues also found that high social support predicted lower PTSD severity for inner-city women who experienced both child abuse and adult rape.16 A prior meta-analysis found social support was the strongest correlate of PTSD (effect size = 0.4).17
Our finding that female MST survivors desire verbal support from physicians may point to the inherent sense that validation helps healing, demonstrated by this meta-analysis. Importantly, the focus group participants did not specify the type of physician (psychiatrist, primary care provider, gynecologist, surgeon, etc) who needed to provide this support. Thus, we believe this suggestion is applicable to all physician interactions when the history of MST comes up. Physicians may be unaware of their profound impact in helping women recover from MST. This validation may also apply to survivors of other types of sexual trauma.
A second simple suggestion that arose from the focus groups was the need for broader options for MST therapy. Current data on the locations female veterans are treated for MST include specialty MST clinics, specialty PTSD clinics, psychosocial rehabilitation, and substance use disorder clinics, showing a wide range of settings.18 But female veterans are also asking for more services, including animal therapy, art therapy, yoga, and tai chi. While it may not be possible to offer every resource at every VHA facility, partnering with community services may help fulfill this veteran need.
The focus groups’ third suggestion for improvement in MST was better treatment for the health problems associated with sexual trauma, such as chronic pelvic pain, sexual dysfunction, and weight gain. It is important to note that the female veterans provided this list of associated health conditions from the broader facilitator question “What health problems do you think you have because of MST?” Females correctly identified common sequelae of sexual abuse, including pelvic pain and sexual dysfunction.14,19 Weight gain and obesity have been associated with childhood sexual trauma and abuse, but they are not well studied in MST and may be worth further exploration.20,21
Limitations
There are several inherent weaknesses in this study. The female veterans who agreed to participate in the focus group may not be representative of the entire population, particularly as survivors may be reluctant to talk about their MST experience. The participants in our focus groups were most commonly 2 decades past the MST and their experience with therapy may differ from that of women more recently traumatized and engaged in therapy. However, the fact that many of these females were still receiving some form of therapy 20 years after the traumatic event deserves attention.
Recall bias may have affected how female veterans described their experiences with MST treatment.
Strengths of the study included the inherent patient-centered approach and ability to analyze data not readily extracted from patient records or validated questionnaires. Additionally, this qualitative approach allows for the discovery of patient-driven ideas and concerns. Our focus groups also contained a majority of minority females (including Hispanic and American Indian) populations that are frequently underrepresented in research.
Conclusion
Our data show there is still substantial room for improvement in the therapies and in the physician-level care for MST. While each treatment experience was unique, the collective agreement was that multimodal therapy was beneficial. However, the isolation that often comes from MST makes accessing care and treatment challenging. A crucial component to combating this isolation is provider validation and support for the female’s experience with MST. The simple act of hearing “I believe you” from the provider can make a huge impact on continuing to seek care and overcoming the consequences of MST.
1. Rossiter AG, Smith S. The invisible wounds of war: caring for women veterans who have experienced military sexual trauma. J Am Assoc Nurse Pract. 2014;26(7):364-369.
2. Klingensmith K, Tsai J, Mota N, et al. Military sexual trauma in US veterans: results from the national health and resilience in veterans study. J Clin Psychiatry. 2014;75(10):e1133-e1139.
3. US. Department of Veterans Affairs, Veteran Health Administration. Military sexual trauma. https://www.publichealth.va.gov/docs/vhi/military_sexual_trauma.pdf. Published January 2004. Accessed July 16, 2018.
4. Suris AM, Davis LL, Kashner TM, et al. A survey of sexual trauma treatment provided by VA medical centers. Psychiatr Serv. 1998;49(3):382-384.
5. Gilmore AK, Davis MT, Grubaugh A, et al. “Do you expect me to receive PTSD care in a setting where most of the other patients remind me of the perpetrator?”: home-based telemedicine to address barriers to care unique to military sexual trauma and veterans affairs hospitals. Contemp Clin Trials. 2016;48:59-64.
6. Calhoun PS, Schry AR, Dennis PA, et al. The association between military sexual trauma and use of VA and non-VA health care services among female veterans with military service in Iraq or Afghanistan. J Interpers Violence. 2018;33(15):2439-2464.
7. Rosebrock L, Carroll R. Sexual function in female veterans: a review. J Sex Marital Ther. 2017;43(3):228-245.
8. Glaser BG, Strauss AL. The Discovery of Grounded Theory. Strategies for Qualitative Research. http://www.sxf.uevora.pt/wp-content/uploads/2013/03/Glaser_1967.pdf. Published 1999. Accessed July 16, 2018.
9. Kelly MM, Vogt DS, Scheiderer EM, et al. Effects of military trauma exposure on women veterans’ use and perceptions of Veterans Health Administration care. J Gen Intern Med. 2008;23(6):741-747.
10. Kehle-Forbes SM, Harwood EM, Spoont MR, et al. Experiences with VHA care: a qualitative study of U.S. women veterans with self-reported trauma histories. BMC Women Health. 2017;17(1):38.
11. McIntyre LM, Butterfield MI, Nanda K. Validation of trauma questionnaire in Veteran women. J Gen Int Med;1999;14(3):186-189.
12. Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ. 2000;320:114-116.
13. Maykut PMR. Beginning Qualitative Research. A Philosophic and Practical Guide. London, England: The Falmer Press; 1994.
14. Cichowski SB, Rogers RG, Clark EA, et al. Military sexual trauma in female veterans is associated with chronic pain conditions. Mil Med. 2017;182(9):e1895-e1899.
15. Glass N, Perrin N, Campbell JC, Soeken K. The protective role of tangible support on post-traumatic stress disorder symptoms in urban women survivors of violence. Res Nurs Health. 2007;30(5):558-568.
16. Schumm JA, Briggs-Phillips M, Hobfoll SE. Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among Inner-city women. J Trauma Stress. 2006;19(6):825-836.
17. Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. 2003;129(1):52-73.
18. Valdez C, Kimerling R, Hyun JK, et al. Veterans Health Administration mental health treatment settings of patients who report military sexual trauma. J Trauma Dissociation. 2011;12(3):232-243.
19. Maseroli E, Scavello I, Cipriani S, et al. Psychobiological correlates of vaginismus: an exploratory analysis. J Sex Med. 2017;14(11):1392-1402.
20. Imperatori C, Innamorati M, Lamis DA, et al. Childhood trauma in obese and overweight women with food addiction and clinical-level of binge eating. Child Abuse Negl. 2016;58:180-190.
21. Williamson DF, Thompson TJ, Anda RF, Dietz WH, Felitti V. Body weight and obesity in adults and self-reported abuse in childhood. Int J Obes Relat Metab Disord. 2002;26(8):1075-1082.
Females are the fastest growing population to seek care at the Veterans Health Administration (VHA).1 Based on a 2014 study examining prevalence of military sexual trauma (MST), it is estimated that about one-third of females in the military screen positive for MST, and the rates are higher for younger veterans.2 Military sexual trauma includes both rape and any sexual activity that occurred without consent; offensive sexual remarks or advances can also represent MST. The issue of MST, therefore, is an important one to address adequately, especially for female veterans who are screened through the VHA system.
Since 1992, the VHA has been required to provide services for MST, defined as “sexual harassment that is threatening in character or physical assault of a sexual nature that occurred while the victim was in the military.”3 Despite this mandate, it has taken many years for all VHA hospitals to adopt recommended screening tools to identify survivors of MST and give them proper resources. Only half of VHA hospitals adopted screening 6 years after the policy change.4 In addition, the environment in which the survivors receive MST care may trigger posttraumatic stress symptoms as many of the other patients seeking care at the VHA hospital resemble the perpetrators.5 Thus, up to half of females who report a history of MST do not receive care for their MST through the VHA.6
Having a history of MST significantly increases the risks of developing mental health disorders, including posttraumatic stress disorder (PTSD), major depressive disorder, generalized anxiety disorder, and suicidal ideation.2 This group also has overall decreased quality of life (QOL). Female veterans have increased sexual dysfunction and dissatisfaction, which is heightened with a history of MST.7 Addressing MST requires treatment of all aspects of life affected by MST, such as mental health, sexual function, and QOL. The quality of treatment for MST through VHA hospitals deserves attention and likely still requires improvement with better incorporation of the patient’s perspective.
Qualitative research allows for incorporation of the patient’s perspective and is useful for exploring new ideas and themes.8 Current qualitative research using individual interviews of MST survivors focuses more on mental health treatment modalities through the VHA system and how resources are used within the system.9,10 While it is important to understand the quantity of these resources, their quality also should be explored. Research has identified unique gender-specific concerns such as female-only mental health groups.10 However, there has been less focus on how to improve current therapies and the treatment modalities (regardless of whether it is a community service or at the VHA system) females find most helpful. There is a gap in understanding the patient’s perspective and assessment of current MST treatments as well as the unmet needs both within and outside of the VHA system. Therefore, the purpose of this study is 2-fold: (1) examine the utilization of VHA services for MST, as well as outside services, through focusgroup sessions; and (2) to offer specific recommendations for improving MST treatment for female veterans from the patient’s perspective.
Methods
After obtaining institutional review board approval (16-H192), females who screened positive for a history of MST, using the validated MST screening questionnaire, were recruited from the Women’s Continuity Clinic, Urology clinic, and via a research flyer placed within key locations at the New Mexico Veterans Affairs (VA) Health Care System (NMVAHCS).11 Inclusion criteria were veterans aged > 18 years who could speak and understand English. Those who agreed to participate attended any 1 of 5 focus groups. Prior to initiation of the focus groups, the investigators generated a focus-group script, including specific questions or probes to explore treatment, unmet needs (such as other health conditions the veteran associated with MST that were not being addressed), and recommendations for care improvement.
Subjects granted consent privately prior to conduction of the focus group. Each participant completed a basic demographic (age, race, ethnicity) and clinical history (including pain conditions and therapy received for MST). These characteristics were evaluated with descriptive statistics, including means and frequencies.
The focus groups took place on the NM VAHCS Raymond G. Murphy VA Medical Center campus in a private conference room and were moderated by nonmedical research personnel experienced in focus-group moderation. Focus groups were recorded and transcribed. An iterative process was used with revisions to the script and probe questions as needed. Focus groups were planned for 2 hours but were allowed to continue at the participants’ discretion.
The de-identified transcripts were uploaded to the web-based qualitative engine Dedoose 6.2.21 software (Los Angeles, CA) and coded. Using grounded theory, the codes were grouped into themes and subsequently organized into emergent concepts.8,12 Following constant comparative methodology, ideas were compared and combined between each focus group.8,13 After completion of the focus groups, the generated ideas were organized and refined to create a conceptual framework that represented the collective ideas from the focus groups.
Results
Between January and June 2017, 5 focus groups with 17 participants were conducted; each session lasted about 3 hours. The average age was 52 ± 8.3 years, and were from a diverse racial and ethnic background. Most reported that > 20 years had passed since the first MST, and care-seeking for the first time was > 11 years after the trauma, although symptoms related to the MST most frequently began within 1 year of the trauma (Table 1).
Preliminary Themes
The Trauma
Focus-group participants noted improved therapies offered by the VA but challenges obtaining health care:
“…because I’m really trying to deal with it and just be happy and get my joy back and deal with the isolation.”
“Another way that the memories affected me was barricading myself in my own house, starting from the front door.”
Male-Dominated VA
Participants also noted that, along with screening improving the system, dedicated female staff and service connection are important:
“The Womens Clinic is nice, and it’s nice to know that I can go there and I’m not having to discuss everything with men all over the place.”
“The other thing... that would be really good for survivors of MST, is help with disability.”
While the focus-group participants found dedicated women’s clinics helpful and providing improved care, the overall VA environment remains male-dominated:
“Because it’s really hard to relax and be vulnerable and be in your body and in your emotions if there‘s a bunch of penises around. When I saw these guys on the floor I’m like, I ain’t going in there.”
This male-dominated sense also incorporated a feeling of being misunderstood by a system that has traditionally cared for male veterans:
“People don‘t understand. They think, oh, you‘re overreacting, but they don’t know what it feels like to be inside.”
“I wouldn’t say they treat you like a second citizen, but it’s like almost every appointment I go to that’s not in the Women’s Clinic, the secretaries or whatever will be like ‘Oh, are you looking for somebody, or...’
Assumption Females Are Not Veterans
“There was an older gentleman behind me, they were like ‘Are you checking him in?’ I said, ‘I’m sure he’ll check himself in, but I’m checking myself in.’”
Participants also reported that there is an assumption that you’re not a veteran when you’re female:
“All of the care should be geared to be the same. And we know we need to recognize that men have their issues, and women will have their issues. But we don’t need to just say ‘all women have this issue, throw them over there.’”
Self-Doubt
“The world doesn’t validate rape, you asked for it, it was what you were wearing, it was what you said.”
Ongoing efforts to have female-only spaces, therapy groups, and support networks were encouraged by all 5 focus groups. These themes, provided the foundation for emergent concepts regarding patients’ perceptions of their treatment for MST: (1) Improvement has been slow but measurable; (2) VA cares more about male veterans; (3) The isolation from MST is pervasive; (4) It’s hard to navigate the VA system or any health care when you’re traumatized; and (5) Sexual assault leaves lasting self-doubt that providers need to address.
Isolation
Because there are barriers to seeking care the overarching method for coping with the effects of MST was isolation.
Overcoming the isolation was essential to seeking any care. Participants reported years of living alone, avoiding social situations and contexts, and difficulty with basic tasks because of the isolation.
“That the coping skills, that the isolation is a coping skill and all these things, and that I had to do that to survive.”
Lack of family and provider support and the VHA’s perceived focus on male veterans perpetuated this sense of isolation. Additionally, feeding the isolation were other maladaptive behaviors, such as alcoholism, weight gain, and anger.
“I was always an athlete until my MST, and I still find myself drinking whisky and wanting to smoke pot. It’s not that I want to, I guess it gives me a sense of relief, because my MST made me an alcoholic.”
Participants reported that successful treatment of MST must include treatment of other maladaptive behaviors and specific provider-behavior changes.
At times, providers contribute to female MST survivors’ feeling undervalued:
“I had an hour session and she kept looking at her watch and blowing me off, and I finally said, okay, I’m done, good-bye, after 45 minutes.”
Validation
Participants’ suggestions to improve MST treatment, including goal sharing, validation, knowledge, and support:
“They should have staff awareness groups, or focus groups to teach them the same thing that the patients are receiving as far as how to handle yourself, how to interact with others. Don’t bring your sh** from home into your job. You’re an employee, don’t take it personal.” (
The need for provider-level support and validation likely stems from the sense that many females expressed that MST was their fault. As one participant said,
“It wasn’t violent for me. I froze. So that’s another reason that I feel guilty because it’s like I didn’t fight. I just froze and put up with it, so I feel like jeez it was my fault. I didn’t... Somehow I am responsible for this.”
Thus, the groups concluded that the most powerful support was provider validation:
“The most important for me was that I was told it was not my fault. Over and over and over. That is the most important thing that us females need to know. Because that is such a relief and that opened up so much more.”
At all of the focus groups, female veterans reported that physician validation of the assault was essential to healing. When providers communicated validation, the women experienced the most improvement in symptoms.
Therapies for MST
A variety of modalities was recommended as helpful in coping with symptoms associated with MST. One female noted her therapy dog allowed her to get her first Papanicolaou (Pap) smear in years:
“Pelvic exams are like the seventh circle of hell. Like, God, you’d think I was being abducted by aliens or something. Last time, up here, they let me bring my little dog, which was extraordinarily helpful for me.”
For others, more traditional therapy such as prolonged exposure therapy or cognitive behavioral therapy, was helpful.
“After my prolonged exposure therapy; it saved my life. I’m not suicidal, and the only thing that’s really, really affected is sometimes I still have to sleep with a night light. Over 80% of the symptoms that I had and the problems that I had were alleviated with the therapy.”
Other veterans noted alternative therapies as beneficial for overcoming trauma:
“Yoga has really helped me with dealing with chronic pain and letting go of things that no longer serve me, and remembering about the inhale, the exhale, there’s a pause between the exhale and an inhale, where that’s where I make my choices, my thoughts, catch it, check it, change it, challenge my thoughts, that’s really, really helped me.”
From these concepts, and the specific suggestions female veterans provided for improvement in care,
Discussion
This qualitative study of the quality of MST treatment with specific suggestions for improvement shows that the underlying force impacting health care in female survivors of MST is isolation. In turn, that isolation is perpetuated by personal beliefs, mental health, lack of support, and the VHA culture. While there was improvement in VHA care noted, female veterans offered many specific suggestions—simple ones that could be rapidly implemented—to enhance care. Many of these suggestions were targeted at provider-level behaviors such as validation, goal setting, knowledge (both about the military and about MST), and support.
Previous work showed that tangible (ie, words, being present) support rather than broad social support only generally helps reduces posttraumatic stress symptoms.15 These researchers found that tangible support moderated the relationship between number of lifetime traumas and PTSD. Schumm and colleagues also found that high social support predicted lower PTSD severity for inner-city women who experienced both child abuse and adult rape.16 A prior meta-analysis found social support was the strongest correlate of PTSD (effect size = 0.4).17
Our finding that female MST survivors desire verbal support from physicians may point to the inherent sense that validation helps healing, demonstrated by this meta-analysis. Importantly, the focus group participants did not specify the type of physician (psychiatrist, primary care provider, gynecologist, surgeon, etc) who needed to provide this support. Thus, we believe this suggestion is applicable to all physician interactions when the history of MST comes up. Physicians may be unaware of their profound impact in helping women recover from MST. This validation may also apply to survivors of other types of sexual trauma.
A second simple suggestion that arose from the focus groups was the need for broader options for MST therapy. Current data on the locations female veterans are treated for MST include specialty MST clinics, specialty PTSD clinics, psychosocial rehabilitation, and substance use disorder clinics, showing a wide range of settings.18 But female veterans are also asking for more services, including animal therapy, art therapy, yoga, and tai chi. While it may not be possible to offer every resource at every VHA facility, partnering with community services may help fulfill this veteran need.
The focus groups’ third suggestion for improvement in MST was better treatment for the health problems associated with sexual trauma, such as chronic pelvic pain, sexual dysfunction, and weight gain. It is important to note that the female veterans provided this list of associated health conditions from the broader facilitator question “What health problems do you think you have because of MST?” Females correctly identified common sequelae of sexual abuse, including pelvic pain and sexual dysfunction.14,19 Weight gain and obesity have been associated with childhood sexual trauma and abuse, but they are not well studied in MST and may be worth further exploration.20,21
Limitations
There are several inherent weaknesses in this study. The female veterans who agreed to participate in the focus group may not be representative of the entire population, particularly as survivors may be reluctant to talk about their MST experience. The participants in our focus groups were most commonly 2 decades past the MST and their experience with therapy may differ from that of women more recently traumatized and engaged in therapy. However, the fact that many of these females were still receiving some form of therapy 20 years after the traumatic event deserves attention.
Recall bias may have affected how female veterans described their experiences with MST treatment.
Strengths of the study included the inherent patient-centered approach and ability to analyze data not readily extracted from patient records or validated questionnaires. Additionally, this qualitative approach allows for the discovery of patient-driven ideas and concerns. Our focus groups also contained a majority of minority females (including Hispanic and American Indian) populations that are frequently underrepresented in research.
Conclusion
Our data show there is still substantial room for improvement in the therapies and in the physician-level care for MST. While each treatment experience was unique, the collective agreement was that multimodal therapy was beneficial. However, the isolation that often comes from MST makes accessing care and treatment challenging. A crucial component to combating this isolation is provider validation and support for the female’s experience with MST. The simple act of hearing “I believe you” from the provider can make a huge impact on continuing to seek care and overcoming the consequences of MST.
Females are the fastest growing population to seek care at the Veterans Health Administration (VHA).1 Based on a 2014 study examining prevalence of military sexual trauma (MST), it is estimated that about one-third of females in the military screen positive for MST, and the rates are higher for younger veterans.2 Military sexual trauma includes both rape and any sexual activity that occurred without consent; offensive sexual remarks or advances can also represent MST. The issue of MST, therefore, is an important one to address adequately, especially for female veterans who are screened through the VHA system.
Since 1992, the VHA has been required to provide services for MST, defined as “sexual harassment that is threatening in character or physical assault of a sexual nature that occurred while the victim was in the military.”3 Despite this mandate, it has taken many years for all VHA hospitals to adopt recommended screening tools to identify survivors of MST and give them proper resources. Only half of VHA hospitals adopted screening 6 years after the policy change.4 In addition, the environment in which the survivors receive MST care may trigger posttraumatic stress symptoms as many of the other patients seeking care at the VHA hospital resemble the perpetrators.5 Thus, up to half of females who report a history of MST do not receive care for their MST through the VHA.6
Having a history of MST significantly increases the risks of developing mental health disorders, including posttraumatic stress disorder (PTSD), major depressive disorder, generalized anxiety disorder, and suicidal ideation.2 This group also has overall decreased quality of life (QOL). Female veterans have increased sexual dysfunction and dissatisfaction, which is heightened with a history of MST.7 Addressing MST requires treatment of all aspects of life affected by MST, such as mental health, sexual function, and QOL. The quality of treatment for MST through VHA hospitals deserves attention and likely still requires improvement with better incorporation of the patient’s perspective.
Qualitative research allows for incorporation of the patient’s perspective and is useful for exploring new ideas and themes.8 Current qualitative research using individual interviews of MST survivors focuses more on mental health treatment modalities through the VHA system and how resources are used within the system.9,10 While it is important to understand the quantity of these resources, their quality also should be explored. Research has identified unique gender-specific concerns such as female-only mental health groups.10 However, there has been less focus on how to improve current therapies and the treatment modalities (regardless of whether it is a community service or at the VHA system) females find most helpful. There is a gap in understanding the patient’s perspective and assessment of current MST treatments as well as the unmet needs both within and outside of the VHA system. Therefore, the purpose of this study is 2-fold: (1) examine the utilization of VHA services for MST, as well as outside services, through focusgroup sessions; and (2) to offer specific recommendations for improving MST treatment for female veterans from the patient’s perspective.
Methods
After obtaining institutional review board approval (16-H192), females who screened positive for a history of MST, using the validated MST screening questionnaire, were recruited from the Women’s Continuity Clinic, Urology clinic, and via a research flyer placed within key locations at the New Mexico Veterans Affairs (VA) Health Care System (NMVAHCS).11 Inclusion criteria were veterans aged > 18 years who could speak and understand English. Those who agreed to participate attended any 1 of 5 focus groups. Prior to initiation of the focus groups, the investigators generated a focus-group script, including specific questions or probes to explore treatment, unmet needs (such as other health conditions the veteran associated with MST that were not being addressed), and recommendations for care improvement.
Subjects granted consent privately prior to conduction of the focus group. Each participant completed a basic demographic (age, race, ethnicity) and clinical history (including pain conditions and therapy received for MST). These characteristics were evaluated with descriptive statistics, including means and frequencies.
The focus groups took place on the NM VAHCS Raymond G. Murphy VA Medical Center campus in a private conference room and were moderated by nonmedical research personnel experienced in focus-group moderation. Focus groups were recorded and transcribed. An iterative process was used with revisions to the script and probe questions as needed. Focus groups were planned for 2 hours but were allowed to continue at the participants’ discretion.
The de-identified transcripts were uploaded to the web-based qualitative engine Dedoose 6.2.21 software (Los Angeles, CA) and coded. Using grounded theory, the codes were grouped into themes and subsequently organized into emergent concepts.8,12 Following constant comparative methodology, ideas were compared and combined between each focus group.8,13 After completion of the focus groups, the generated ideas were organized and refined to create a conceptual framework that represented the collective ideas from the focus groups.
Results
Between January and June 2017, 5 focus groups with 17 participants were conducted; each session lasted about 3 hours. The average age was 52 ± 8.3 years, and were from a diverse racial and ethnic background. Most reported that > 20 years had passed since the first MST, and care-seeking for the first time was > 11 years after the trauma, although symptoms related to the MST most frequently began within 1 year of the trauma (Table 1).
Preliminary Themes
The Trauma
Focus-group participants noted improved therapies offered by the VA but challenges obtaining health care:
“…because I’m really trying to deal with it and just be happy and get my joy back and deal with the isolation.”
“Another way that the memories affected me was barricading myself in my own house, starting from the front door.”
Male-Dominated VA
Participants also noted that, along with screening improving the system, dedicated female staff and service connection are important:
“The Womens Clinic is nice, and it’s nice to know that I can go there and I’m not having to discuss everything with men all over the place.”
“The other thing... that would be really good for survivors of MST, is help with disability.”
While the focus-group participants found dedicated women’s clinics helpful and providing improved care, the overall VA environment remains male-dominated:
“Because it’s really hard to relax and be vulnerable and be in your body and in your emotions if there‘s a bunch of penises around. When I saw these guys on the floor I’m like, I ain’t going in there.”
This male-dominated sense also incorporated a feeling of being misunderstood by a system that has traditionally cared for male veterans:
“People don‘t understand. They think, oh, you‘re overreacting, but they don’t know what it feels like to be inside.”
“I wouldn’t say they treat you like a second citizen, but it’s like almost every appointment I go to that’s not in the Women’s Clinic, the secretaries or whatever will be like ‘Oh, are you looking for somebody, or...’
Assumption Females Are Not Veterans
“There was an older gentleman behind me, they were like ‘Are you checking him in?’ I said, ‘I’m sure he’ll check himself in, but I’m checking myself in.’”
Participants also reported that there is an assumption that you’re not a veteran when you’re female:
“All of the care should be geared to be the same. And we know we need to recognize that men have their issues, and women will have their issues. But we don’t need to just say ‘all women have this issue, throw them over there.’”
Self-Doubt
“The world doesn’t validate rape, you asked for it, it was what you were wearing, it was what you said.”
Ongoing efforts to have female-only spaces, therapy groups, and support networks were encouraged by all 5 focus groups. These themes, provided the foundation for emergent concepts regarding patients’ perceptions of their treatment for MST: (1) Improvement has been slow but measurable; (2) VA cares more about male veterans; (3) The isolation from MST is pervasive; (4) It’s hard to navigate the VA system or any health care when you’re traumatized; and (5) Sexual assault leaves lasting self-doubt that providers need to address.
Isolation
Because there are barriers to seeking care the overarching method for coping with the effects of MST was isolation.
Overcoming the isolation was essential to seeking any care. Participants reported years of living alone, avoiding social situations and contexts, and difficulty with basic tasks because of the isolation.
“That the coping skills, that the isolation is a coping skill and all these things, and that I had to do that to survive.”
Lack of family and provider support and the VHA’s perceived focus on male veterans perpetuated this sense of isolation. Additionally, feeding the isolation were other maladaptive behaviors, such as alcoholism, weight gain, and anger.
“I was always an athlete until my MST, and I still find myself drinking whisky and wanting to smoke pot. It’s not that I want to, I guess it gives me a sense of relief, because my MST made me an alcoholic.”
Participants reported that successful treatment of MST must include treatment of other maladaptive behaviors and specific provider-behavior changes.
At times, providers contribute to female MST survivors’ feeling undervalued:
“I had an hour session and she kept looking at her watch and blowing me off, and I finally said, okay, I’m done, good-bye, after 45 minutes.”
Validation
Participants’ suggestions to improve MST treatment, including goal sharing, validation, knowledge, and support:
“They should have staff awareness groups, or focus groups to teach them the same thing that the patients are receiving as far as how to handle yourself, how to interact with others. Don’t bring your sh** from home into your job. You’re an employee, don’t take it personal.” (
The need for provider-level support and validation likely stems from the sense that many females expressed that MST was their fault. As one participant said,
“It wasn’t violent for me. I froze. So that’s another reason that I feel guilty because it’s like I didn’t fight. I just froze and put up with it, so I feel like jeez it was my fault. I didn’t... Somehow I am responsible for this.”
Thus, the groups concluded that the most powerful support was provider validation:
“The most important for me was that I was told it was not my fault. Over and over and over. That is the most important thing that us females need to know. Because that is such a relief and that opened up so much more.”
At all of the focus groups, female veterans reported that physician validation of the assault was essential to healing. When providers communicated validation, the women experienced the most improvement in symptoms.
Therapies for MST
A variety of modalities was recommended as helpful in coping with symptoms associated with MST. One female noted her therapy dog allowed her to get her first Papanicolaou (Pap) smear in years:
“Pelvic exams are like the seventh circle of hell. Like, God, you’d think I was being abducted by aliens or something. Last time, up here, they let me bring my little dog, which was extraordinarily helpful for me.”
For others, more traditional therapy such as prolonged exposure therapy or cognitive behavioral therapy, was helpful.
“After my prolonged exposure therapy; it saved my life. I’m not suicidal, and the only thing that’s really, really affected is sometimes I still have to sleep with a night light. Over 80% of the symptoms that I had and the problems that I had were alleviated with the therapy.”
Other veterans noted alternative therapies as beneficial for overcoming trauma:
“Yoga has really helped me with dealing with chronic pain and letting go of things that no longer serve me, and remembering about the inhale, the exhale, there’s a pause between the exhale and an inhale, where that’s where I make my choices, my thoughts, catch it, check it, change it, challenge my thoughts, that’s really, really helped me.”
From these concepts, and the specific suggestions female veterans provided for improvement in care,
Discussion
This qualitative study of the quality of MST treatment with specific suggestions for improvement shows that the underlying force impacting health care in female survivors of MST is isolation. In turn, that isolation is perpetuated by personal beliefs, mental health, lack of support, and the VHA culture. While there was improvement in VHA care noted, female veterans offered many specific suggestions—simple ones that could be rapidly implemented—to enhance care. Many of these suggestions were targeted at provider-level behaviors such as validation, goal setting, knowledge (both about the military and about MST), and support.
Previous work showed that tangible (ie, words, being present) support rather than broad social support only generally helps reduces posttraumatic stress symptoms.15 These researchers found that tangible support moderated the relationship between number of lifetime traumas and PTSD. Schumm and colleagues also found that high social support predicted lower PTSD severity for inner-city women who experienced both child abuse and adult rape.16 A prior meta-analysis found social support was the strongest correlate of PTSD (effect size = 0.4).17
Our finding that female MST survivors desire verbal support from physicians may point to the inherent sense that validation helps healing, demonstrated by this meta-analysis. Importantly, the focus group participants did not specify the type of physician (psychiatrist, primary care provider, gynecologist, surgeon, etc) who needed to provide this support. Thus, we believe this suggestion is applicable to all physician interactions when the history of MST comes up. Physicians may be unaware of their profound impact in helping women recover from MST. This validation may also apply to survivors of other types of sexual trauma.
A second simple suggestion that arose from the focus groups was the need for broader options for MST therapy. Current data on the locations female veterans are treated for MST include specialty MST clinics, specialty PTSD clinics, psychosocial rehabilitation, and substance use disorder clinics, showing a wide range of settings.18 But female veterans are also asking for more services, including animal therapy, art therapy, yoga, and tai chi. While it may not be possible to offer every resource at every VHA facility, partnering with community services may help fulfill this veteran need.
The focus groups’ third suggestion for improvement in MST was better treatment for the health problems associated with sexual trauma, such as chronic pelvic pain, sexual dysfunction, and weight gain. It is important to note that the female veterans provided this list of associated health conditions from the broader facilitator question “What health problems do you think you have because of MST?” Females correctly identified common sequelae of sexual abuse, including pelvic pain and sexual dysfunction.14,19 Weight gain and obesity have been associated with childhood sexual trauma and abuse, but they are not well studied in MST and may be worth further exploration.20,21
Limitations
There are several inherent weaknesses in this study. The female veterans who agreed to participate in the focus group may not be representative of the entire population, particularly as survivors may be reluctant to talk about their MST experience. The participants in our focus groups were most commonly 2 decades past the MST and their experience with therapy may differ from that of women more recently traumatized and engaged in therapy. However, the fact that many of these females were still receiving some form of therapy 20 years after the traumatic event deserves attention.
Recall bias may have affected how female veterans described their experiences with MST treatment.
Strengths of the study included the inherent patient-centered approach and ability to analyze data not readily extracted from patient records or validated questionnaires. Additionally, this qualitative approach allows for the discovery of patient-driven ideas and concerns. Our focus groups also contained a majority of minority females (including Hispanic and American Indian) populations that are frequently underrepresented in research.
Conclusion
Our data show there is still substantial room for improvement in the therapies and in the physician-level care for MST. While each treatment experience was unique, the collective agreement was that multimodal therapy was beneficial. However, the isolation that often comes from MST makes accessing care and treatment challenging. A crucial component to combating this isolation is provider validation and support for the female’s experience with MST. The simple act of hearing “I believe you” from the provider can make a huge impact on continuing to seek care and overcoming the consequences of MST.
1. Rossiter AG, Smith S. The invisible wounds of war: caring for women veterans who have experienced military sexual trauma. J Am Assoc Nurse Pract. 2014;26(7):364-369.
2. Klingensmith K, Tsai J, Mota N, et al. Military sexual trauma in US veterans: results from the national health and resilience in veterans study. J Clin Psychiatry. 2014;75(10):e1133-e1139.
3. US. Department of Veterans Affairs, Veteran Health Administration. Military sexual trauma. https://www.publichealth.va.gov/docs/vhi/military_sexual_trauma.pdf. Published January 2004. Accessed July 16, 2018.
4. Suris AM, Davis LL, Kashner TM, et al. A survey of sexual trauma treatment provided by VA medical centers. Psychiatr Serv. 1998;49(3):382-384.
5. Gilmore AK, Davis MT, Grubaugh A, et al. “Do you expect me to receive PTSD care in a setting where most of the other patients remind me of the perpetrator?”: home-based telemedicine to address barriers to care unique to military sexual trauma and veterans affairs hospitals. Contemp Clin Trials. 2016;48:59-64.
6. Calhoun PS, Schry AR, Dennis PA, et al. The association between military sexual trauma and use of VA and non-VA health care services among female veterans with military service in Iraq or Afghanistan. J Interpers Violence. 2018;33(15):2439-2464.
7. Rosebrock L, Carroll R. Sexual function in female veterans: a review. J Sex Marital Ther. 2017;43(3):228-245.
8. Glaser BG, Strauss AL. The Discovery of Grounded Theory. Strategies for Qualitative Research. http://www.sxf.uevora.pt/wp-content/uploads/2013/03/Glaser_1967.pdf. Published 1999. Accessed July 16, 2018.
9. Kelly MM, Vogt DS, Scheiderer EM, et al. Effects of military trauma exposure on women veterans’ use and perceptions of Veterans Health Administration care. J Gen Intern Med. 2008;23(6):741-747.
10. Kehle-Forbes SM, Harwood EM, Spoont MR, et al. Experiences with VHA care: a qualitative study of U.S. women veterans with self-reported trauma histories. BMC Women Health. 2017;17(1):38.
11. McIntyre LM, Butterfield MI, Nanda K. Validation of trauma questionnaire in Veteran women. J Gen Int Med;1999;14(3):186-189.
12. Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ. 2000;320:114-116.
13. Maykut PMR. Beginning Qualitative Research. A Philosophic and Practical Guide. London, England: The Falmer Press; 1994.
14. Cichowski SB, Rogers RG, Clark EA, et al. Military sexual trauma in female veterans is associated with chronic pain conditions. Mil Med. 2017;182(9):e1895-e1899.
15. Glass N, Perrin N, Campbell JC, Soeken K. The protective role of tangible support on post-traumatic stress disorder symptoms in urban women survivors of violence. Res Nurs Health. 2007;30(5):558-568.
16. Schumm JA, Briggs-Phillips M, Hobfoll SE. Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among Inner-city women. J Trauma Stress. 2006;19(6):825-836.
17. Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. 2003;129(1):52-73.
18. Valdez C, Kimerling R, Hyun JK, et al. Veterans Health Administration mental health treatment settings of patients who report military sexual trauma. J Trauma Dissociation. 2011;12(3):232-243.
19. Maseroli E, Scavello I, Cipriani S, et al. Psychobiological correlates of vaginismus: an exploratory analysis. J Sex Med. 2017;14(11):1392-1402.
20. Imperatori C, Innamorati M, Lamis DA, et al. Childhood trauma in obese and overweight women with food addiction and clinical-level of binge eating. Child Abuse Negl. 2016;58:180-190.
21. Williamson DF, Thompson TJ, Anda RF, Dietz WH, Felitti V. Body weight and obesity in adults and self-reported abuse in childhood. Int J Obes Relat Metab Disord. 2002;26(8):1075-1082.
1. Rossiter AG, Smith S. The invisible wounds of war: caring for women veterans who have experienced military sexual trauma. J Am Assoc Nurse Pract. 2014;26(7):364-369.
2. Klingensmith K, Tsai J, Mota N, et al. Military sexual trauma in US veterans: results from the national health and resilience in veterans study. J Clin Psychiatry. 2014;75(10):e1133-e1139.
3. US. Department of Veterans Affairs, Veteran Health Administration. Military sexual trauma. https://www.publichealth.va.gov/docs/vhi/military_sexual_trauma.pdf. Published January 2004. Accessed July 16, 2018.
4. Suris AM, Davis LL, Kashner TM, et al. A survey of sexual trauma treatment provided by VA medical centers. Psychiatr Serv. 1998;49(3):382-384.
5. Gilmore AK, Davis MT, Grubaugh A, et al. “Do you expect me to receive PTSD care in a setting where most of the other patients remind me of the perpetrator?”: home-based telemedicine to address barriers to care unique to military sexual trauma and veterans affairs hospitals. Contemp Clin Trials. 2016;48:59-64.
6. Calhoun PS, Schry AR, Dennis PA, et al. The association between military sexual trauma and use of VA and non-VA health care services among female veterans with military service in Iraq or Afghanistan. J Interpers Violence. 2018;33(15):2439-2464.
7. Rosebrock L, Carroll R. Sexual function in female veterans: a review. J Sex Marital Ther. 2017;43(3):228-245.
8. Glaser BG, Strauss AL. The Discovery of Grounded Theory. Strategies for Qualitative Research. http://www.sxf.uevora.pt/wp-content/uploads/2013/03/Glaser_1967.pdf. Published 1999. Accessed July 16, 2018.
9. Kelly MM, Vogt DS, Scheiderer EM, et al. Effects of military trauma exposure on women veterans’ use and perceptions of Veterans Health Administration care. J Gen Intern Med. 2008;23(6):741-747.
10. Kehle-Forbes SM, Harwood EM, Spoont MR, et al. Experiences with VHA care: a qualitative study of U.S. women veterans with self-reported trauma histories. BMC Women Health. 2017;17(1):38.
11. McIntyre LM, Butterfield MI, Nanda K. Validation of trauma questionnaire in Veteran women. J Gen Int Med;1999;14(3):186-189.
12. Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ. 2000;320:114-116.
13. Maykut PMR. Beginning Qualitative Research. A Philosophic and Practical Guide. London, England: The Falmer Press; 1994.
14. Cichowski SB, Rogers RG, Clark EA, et al. Military sexual trauma in female veterans is associated with chronic pain conditions. Mil Med. 2017;182(9):e1895-e1899.
15. Glass N, Perrin N, Campbell JC, Soeken K. The protective role of tangible support on post-traumatic stress disorder symptoms in urban women survivors of violence. Res Nurs Health. 2007;30(5):558-568.
16. Schumm JA, Briggs-Phillips M, Hobfoll SE. Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among Inner-city women. J Trauma Stress. 2006;19(6):825-836.
17. Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. 2003;129(1):52-73.
18. Valdez C, Kimerling R, Hyun JK, et al. Veterans Health Administration mental health treatment settings of patients who report military sexual trauma. J Trauma Dissociation. 2011;12(3):232-243.
19. Maseroli E, Scavello I, Cipriani S, et al. Psychobiological correlates of vaginismus: an exploratory analysis. J Sex Med. 2017;14(11):1392-1402.
20. Imperatori C, Innamorati M, Lamis DA, et al. Childhood trauma in obese and overweight women with food addiction and clinical-level of binge eating. Child Abuse Negl. 2016;58:180-190.
21. Williamson DF, Thompson TJ, Anda RF, Dietz WH, Felitti V. Body weight and obesity in adults and self-reported abuse in childhood. Int J Obes Relat Metab Disord. 2002;26(8):1075-1082.
Think outside lower body for pelvic pain
Also today, treating obstructive sleep apnea with positive airway pressure decreased amyloid levels, spending on medical marketing increased by more than $12 billion over that past two decades, and one expert has advice on how you can get your work published.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, treating obstructive sleep apnea with positive airway pressure decreased amyloid levels, spending on medical marketing increased by more than $12 billion over that past two decades, and one expert has advice on how you can get your work published.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, treating obstructive sleep apnea with positive airway pressure decreased amyloid levels, spending on medical marketing increased by more than $12 billion over that past two decades, and one expert has advice on how you can get your work published.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Most oral HRT linked to increased VTE risk
Transdermal hormone replacement therapy is associated with the lowest risk of venous thromboembolism, yet still is relatively underused compared to oral preparations, researchers say.
Writing in the BMJ, Yana Vinogradova, PhD, of the University of Nottingham (England) and her associates reported the results of two nested case-control studies of hormone replacement therapy (HRT) and venous thromboembolism (VTE) from Jan. 1998 to Feb. 2017 that altogether included 80,396 women aged 40-79 years with a primary diagnosis of VTE matched to 391,494 female controls.
Overall, 7% of the women with VTE had been exposed to HRT in the 90 days before the index date versus 5.5% of controls.
The greatest increase in risk of VTE, compared with no exposure, was seen with oral conjugated equine estrogen with medroxyprogesterone acetate, which was associated with a more than twofold increase in risk (odds ratio, 2.10; 95% confidence interval, 1.92-2.31; P less than .01).
However transdermal HRT use was not associated with any increase in risk, compared with no HRT exposure. The data even pointed to a slight decrease in risk, which the authors suggested may be the result of some residual confounding or indication bias.
Oral HRT generally was associated with a 58% increased risk of VTE, which amounted to a number needed to harm of 1,076 and nine extra cases of VTE per 10,000 women taking oral HRT.
Dr. Vinogradova and her colleagues noted that the vast majority of women in the study were being prescribed oral HRT for menopausal symptoms despite previous studies showing transdermal HRT has much lower risk.
“When women with menopausal symptoms already have an increased VTE risk because of comorbidities or obesity, these women and their doctors should give greater consideration to transdermal HRT,” they wrote.
Lubna Pal, MBBS, director of the menopause program and professor of obstetrics, gynecology, and reproductive sciences at Yale University, New Haven, Conn., commented in an interview, “These data are tremendously reassuring. The reported findings are: 1) reaffirm what we have already known , i.e. that advancing age, higher body mass index, and higher doses of exogenous systemic estrogen therapy are associated with increased risk for VTE; 2) offer greater granularity in risk for VTE with different formulations of estrogens and progestins and different regimens than understood thus far, 3) reaffirm that, unlike oral estrogen, transdermal estrogen formulations in doses commonly utilized in clinical practice are not associated with VTE risk, and 4) provide reassurance that the absolute risk, while exaggerated with oral estrogen or combination estrogen and progestin use, is nonetheless small as reflected in the number needed to harm with oral hormone therapy being 1,076, and the number of extra VTE cases attributable to oral HT being 9 per 10,000 woman years.
“The authors are to be commended on this massive analytic undertaking that allows an improved understanding of HRT-related risk for VTE and offers meaningful guidance to the practitioner,” said Dr. Pal, who was not involved in the study.*
Estrogen-only preparations had a 40% higher risk and combined preparations had a 73% higher risk, compared with no exposure.
In estrogen-only preparations, the lowest risk was seen with estradiol, compared with conjugated equine estrogens or combined preparations.
The lowest risk of VTE among oral preparations was seen with estradiol plus dydrogesterone, which only showed a nonsignificant 18% increase in risk.
In an attempt to account for possible increased risk of VTE, the authors conducted a sensitivity analysis in a subgroup of women who had not previously used anticoagulants, but they found similar results to the main analysis.
“This sensitivity analysis indicates that most of the excluded women had probably used anticoagulants because of atrial fibrillation or hip replacement operations rather than an earlier unrecorded VTE,” they wrote.
One author declared directorship of a clinical software company, but no other conflicts of interest were declared. There was no external funding. Dr. Pal reported that she was a coinvestigator in the Kronos Early Estrogen Prevention Study and on an AMAG Pharmaceuticals advisory board and member of their speaker’s bureau.
SOURCE: Vinogradova Y et al. BMJ. 2019 Jan 9. doi: 10.1136/bmj.k4810.
*This article was updated 1/11/19.
Transdermal hormone replacement therapy is associated with the lowest risk of venous thromboembolism, yet still is relatively underused compared to oral preparations, researchers say.
Writing in the BMJ, Yana Vinogradova, PhD, of the University of Nottingham (England) and her associates reported the results of two nested case-control studies of hormone replacement therapy (HRT) and venous thromboembolism (VTE) from Jan. 1998 to Feb. 2017 that altogether included 80,396 women aged 40-79 years with a primary diagnosis of VTE matched to 391,494 female controls.
Overall, 7% of the women with VTE had been exposed to HRT in the 90 days before the index date versus 5.5% of controls.
The greatest increase in risk of VTE, compared with no exposure, was seen with oral conjugated equine estrogen with medroxyprogesterone acetate, which was associated with a more than twofold increase in risk (odds ratio, 2.10; 95% confidence interval, 1.92-2.31; P less than .01).
However transdermal HRT use was not associated with any increase in risk, compared with no HRT exposure. The data even pointed to a slight decrease in risk, which the authors suggested may be the result of some residual confounding or indication bias.
Oral HRT generally was associated with a 58% increased risk of VTE, which amounted to a number needed to harm of 1,076 and nine extra cases of VTE per 10,000 women taking oral HRT.
Dr. Vinogradova and her colleagues noted that the vast majority of women in the study were being prescribed oral HRT for menopausal symptoms despite previous studies showing transdermal HRT has much lower risk.
“When women with menopausal symptoms already have an increased VTE risk because of comorbidities or obesity, these women and their doctors should give greater consideration to transdermal HRT,” they wrote.
Lubna Pal, MBBS, director of the menopause program and professor of obstetrics, gynecology, and reproductive sciences at Yale University, New Haven, Conn., commented in an interview, “These data are tremendously reassuring. The reported findings are: 1) reaffirm what we have already known , i.e. that advancing age, higher body mass index, and higher doses of exogenous systemic estrogen therapy are associated with increased risk for VTE; 2) offer greater granularity in risk for VTE with different formulations of estrogens and progestins and different regimens than understood thus far, 3) reaffirm that, unlike oral estrogen, transdermal estrogen formulations in doses commonly utilized in clinical practice are not associated with VTE risk, and 4) provide reassurance that the absolute risk, while exaggerated with oral estrogen or combination estrogen and progestin use, is nonetheless small as reflected in the number needed to harm with oral hormone therapy being 1,076, and the number of extra VTE cases attributable to oral HT being 9 per 10,000 woman years.
“The authors are to be commended on this massive analytic undertaking that allows an improved understanding of HRT-related risk for VTE and offers meaningful guidance to the practitioner,” said Dr. Pal, who was not involved in the study.*
Estrogen-only preparations had a 40% higher risk and combined preparations had a 73% higher risk, compared with no exposure.
In estrogen-only preparations, the lowest risk was seen with estradiol, compared with conjugated equine estrogens or combined preparations.
The lowest risk of VTE among oral preparations was seen with estradiol plus dydrogesterone, which only showed a nonsignificant 18% increase in risk.
In an attempt to account for possible increased risk of VTE, the authors conducted a sensitivity analysis in a subgroup of women who had not previously used anticoagulants, but they found similar results to the main analysis.
“This sensitivity analysis indicates that most of the excluded women had probably used anticoagulants because of atrial fibrillation or hip replacement operations rather than an earlier unrecorded VTE,” they wrote.
One author declared directorship of a clinical software company, but no other conflicts of interest were declared. There was no external funding. Dr. Pal reported that she was a coinvestigator in the Kronos Early Estrogen Prevention Study and on an AMAG Pharmaceuticals advisory board and member of their speaker’s bureau.
SOURCE: Vinogradova Y et al. BMJ. 2019 Jan 9. doi: 10.1136/bmj.k4810.
*This article was updated 1/11/19.
Transdermal hormone replacement therapy is associated with the lowest risk of venous thromboembolism, yet still is relatively underused compared to oral preparations, researchers say.
Writing in the BMJ, Yana Vinogradova, PhD, of the University of Nottingham (England) and her associates reported the results of two nested case-control studies of hormone replacement therapy (HRT) and venous thromboembolism (VTE) from Jan. 1998 to Feb. 2017 that altogether included 80,396 women aged 40-79 years with a primary diagnosis of VTE matched to 391,494 female controls.
Overall, 7% of the women with VTE had been exposed to HRT in the 90 days before the index date versus 5.5% of controls.
The greatest increase in risk of VTE, compared with no exposure, was seen with oral conjugated equine estrogen with medroxyprogesterone acetate, which was associated with a more than twofold increase in risk (odds ratio, 2.10; 95% confidence interval, 1.92-2.31; P less than .01).
However transdermal HRT use was not associated with any increase in risk, compared with no HRT exposure. The data even pointed to a slight decrease in risk, which the authors suggested may be the result of some residual confounding or indication bias.
Oral HRT generally was associated with a 58% increased risk of VTE, which amounted to a number needed to harm of 1,076 and nine extra cases of VTE per 10,000 women taking oral HRT.
Dr. Vinogradova and her colleagues noted that the vast majority of women in the study were being prescribed oral HRT for menopausal symptoms despite previous studies showing transdermal HRT has much lower risk.
“When women with menopausal symptoms already have an increased VTE risk because of comorbidities or obesity, these women and their doctors should give greater consideration to transdermal HRT,” they wrote.
Lubna Pal, MBBS, director of the menopause program and professor of obstetrics, gynecology, and reproductive sciences at Yale University, New Haven, Conn., commented in an interview, “These data are tremendously reassuring. The reported findings are: 1) reaffirm what we have already known , i.e. that advancing age, higher body mass index, and higher doses of exogenous systemic estrogen therapy are associated with increased risk for VTE; 2) offer greater granularity in risk for VTE with different formulations of estrogens and progestins and different regimens than understood thus far, 3) reaffirm that, unlike oral estrogen, transdermal estrogen formulations in doses commonly utilized in clinical practice are not associated with VTE risk, and 4) provide reassurance that the absolute risk, while exaggerated with oral estrogen or combination estrogen and progestin use, is nonetheless small as reflected in the number needed to harm with oral hormone therapy being 1,076, and the number of extra VTE cases attributable to oral HT being 9 per 10,000 woman years.
“The authors are to be commended on this massive analytic undertaking that allows an improved understanding of HRT-related risk for VTE and offers meaningful guidance to the practitioner,” said Dr. Pal, who was not involved in the study.*
Estrogen-only preparations had a 40% higher risk and combined preparations had a 73% higher risk, compared with no exposure.
In estrogen-only preparations, the lowest risk was seen with estradiol, compared with conjugated equine estrogens or combined preparations.
The lowest risk of VTE among oral preparations was seen with estradiol plus dydrogesterone, which only showed a nonsignificant 18% increase in risk.
In an attempt to account for possible increased risk of VTE, the authors conducted a sensitivity analysis in a subgroup of women who had not previously used anticoagulants, but they found similar results to the main analysis.
“This sensitivity analysis indicates that most of the excluded women had probably used anticoagulants because of atrial fibrillation or hip replacement operations rather than an earlier unrecorded VTE,” they wrote.
One author declared directorship of a clinical software company, but no other conflicts of interest were declared. There was no external funding. Dr. Pal reported that she was a coinvestigator in the Kronos Early Estrogen Prevention Study and on an AMAG Pharmaceuticals advisory board and member of their speaker’s bureau.
SOURCE: Vinogradova Y et al. BMJ. 2019 Jan 9. doi: 10.1136/bmj.k4810.
*This article was updated 1/11/19.
FROM THE BMJ
Key clinical point: Transdermal HRT is not associated with any increase in VTE risk.
Major finding: Conjugated equine estrogen with medroxyprogesterone shows a twofold increase in VTE risk.
Study details: Nested case-control study in 80,396 women and 391,494 female controls.
Disclosures: One author declared directorship of a clinical software company, but no other conflicts of interest were declared. There was no external funding. Dr. Pal reported that she was a coinvestigator in the Kronos Early Estrogen Prevention Study and on an AMAG Pharmaceuticals advisory board and member of their speaker’s bureau.
Source: Vinogradova Y et al. BMJ. 2019 Jan 9. doi: 10.1136/bmj.k4810
ACOG updates guidance on chronic hypertension in pregnancy, gestational hypertension
Ob.gyns. will need to focus more on individualized care as they use the two new practice bulletins, one on chronic hypertension in pregnancy and one on gestational hypertension and preeclampsia, released by the American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins–Obstetrics.
The bulletins will replace the 2013 ACOG hypertension in pregnancy task force report and are published in the January issue of Obstetrics & Gynecology.
“The task force was a tour de force in creating a comprehensive view of hypertensive diseases of pregnancy, including research,” Christian M. Pettker, MD, who helped develop both practice bulletins, stated in a press release. “The updated guidance provides clearer recommendations for the management of gestational hypertension with severe-range blood pressure, an emphasis on and instructions for timely treatment of acutely elevated blood pressures, and more defined recommendations for the management of pain in postoperative patients with hypertension.”
“Ob.gyns. will need to focus more on individualized care and may find it’s best to err on the side of caution because the appropriate treatment of hypertensive diseases in pregnancy may be the most important focus of our attempts to improve maternal mortality and morbidity in the United States,” he said.*
Gestational hypertension or preeclampsia
For women with gestational hypertension or preeclampsia at 37 weeks of gestation or later without severe features, the guidelines recommend delivery rather than expectant management.
Those patients with severe features of gestational hypertension or preeclampsia or eclampsia should receive magnesium sulfate to prevent or treat seizures.
Patients should receive low-dose aspirin (81 mg/day) for preeclampsia prophylaxis between 12 weeks and 28 weeks of gestation if they have high-risk factors of preeclampsia such as multifetal gestation, a previous pregnancy with preeclampsia, renal disease, autoimmune disease, type 1 or type 2 diabetes mellitus, chronic hypertension, or a previous pregnancy with preeclampsia; or more than one moderate risk factor such as a family history of preeclampsia, maternal age greater than 35 years, first pregnancy, body mass index greater than 30, personal history factors, or sociodemographic characteristics.
NSAIDs should continue to be used in preference to opioid analgesics.
The guidance also discusses mode of delivery, antihypertensive drugs and thresholds for treatment, management of acute complications for preeclampsia with HELLP (hemolysis, elevated liver enzymes, low platelet count) syndrome, the optimal treatment for eclampsia, and postpartum hypertension and headache.
Chronic hypertension
Pregnant women with chronic hypertension also should receive low-dose aspirin between 12 weeks and 28 weeks of gestation. Antihypertensive therapy should be initiated for women with persistent chronic hypertension at systolic pressure of 160 mm Hg or higher and/or diastolic pressure of 110 mm Hg or higher. Consider treating patients at lower blood pressure (BP) thresholds depending on comorbidities or underlying impaired renal function.
ACOG has recommended treating pregnant patients as chronically hypertensive according to recently changed criteria from the American College of Cardiology and the American Heart Association, which call for classifying blood pressure into the following categories:
- Normal. Systolic BP less than 120 mm Hg; diastolic BP less than 80 mm Hg.
- Elevated. Systolic BP greater than or equal to 120-129 mm Hg; diastolic BP greater than 80 mm Hg.
- Stage 1 hypertension. Systolic BP, 130-139 mm Hg; diastolic BP, 80-89 mm Hg.
- Stage 2 hypertension. Systolic BP greater than or equal to 140 mm Hg; diastolic BP greater than or equal to 90 mm Hg.
“The new blood pressure ranges for nonpregnant women have a lower threshold for hypertension diagnosis compared to ACOG’s criteria,” Dr. Pettker said. “This will likely cause a general increase in patients classified as chronic hypertensive and will require shared decision making by the ob.gyn. and the patient regarding appropriate management in pregnancy.”
The guideline also discusses chronic hypertension with superimposed preeclampsia; tests for baseline evaluation of chronic hypertension in pregnancy; common oral antihypertensive agents to use in pregnancy and those to use for urgent blood pressure control in pregnancy; control of acute-onset severe-range hypertension; and postpartum considerations in patients with chronic hypertension.
SOURCE: Gestational hypertension and preeclampsia. ACOG Practice Bulletin No. 202. Obstet Gynecol. 2019;133:e1-25; Chronic hypertension in pregnancy. ACOG Practice Bulletin No. 203. Obstet Gynecol. 2019;133:e26-50.
This article was updated 1/11/19 and 11/19/19.
Ob.gyns. will need to focus more on individualized care as they use the two new practice bulletins, one on chronic hypertension in pregnancy and one on gestational hypertension and preeclampsia, released by the American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins–Obstetrics.
The bulletins will replace the 2013 ACOG hypertension in pregnancy task force report and are published in the January issue of Obstetrics & Gynecology.
“The task force was a tour de force in creating a comprehensive view of hypertensive diseases of pregnancy, including research,” Christian M. Pettker, MD, who helped develop both practice bulletins, stated in a press release. “The updated guidance provides clearer recommendations for the management of gestational hypertension with severe-range blood pressure, an emphasis on and instructions for timely treatment of acutely elevated blood pressures, and more defined recommendations for the management of pain in postoperative patients with hypertension.”
“Ob.gyns. will need to focus more on individualized care and may find it’s best to err on the side of caution because the appropriate treatment of hypertensive diseases in pregnancy may be the most important focus of our attempts to improve maternal mortality and morbidity in the United States,” he said.*
Gestational hypertension or preeclampsia
For women with gestational hypertension or preeclampsia at 37 weeks of gestation or later without severe features, the guidelines recommend delivery rather than expectant management.
Those patients with severe features of gestational hypertension or preeclampsia or eclampsia should receive magnesium sulfate to prevent or treat seizures.
Patients should receive low-dose aspirin (81 mg/day) for preeclampsia prophylaxis between 12 weeks and 28 weeks of gestation if they have high-risk factors of preeclampsia such as multifetal gestation, a previous pregnancy with preeclampsia, renal disease, autoimmune disease, type 1 or type 2 diabetes mellitus, chronic hypertension, or a previous pregnancy with preeclampsia; or more than one moderate risk factor such as a family history of preeclampsia, maternal age greater than 35 years, first pregnancy, body mass index greater than 30, personal history factors, or sociodemographic characteristics.
NSAIDs should continue to be used in preference to opioid analgesics.
The guidance also discusses mode of delivery, antihypertensive drugs and thresholds for treatment, management of acute complications for preeclampsia with HELLP (hemolysis, elevated liver enzymes, low platelet count) syndrome, the optimal treatment for eclampsia, and postpartum hypertension and headache.
Chronic hypertension
Pregnant women with chronic hypertension also should receive low-dose aspirin between 12 weeks and 28 weeks of gestation. Antihypertensive therapy should be initiated for women with persistent chronic hypertension at systolic pressure of 160 mm Hg or higher and/or diastolic pressure of 110 mm Hg or higher. Consider treating patients at lower blood pressure (BP) thresholds depending on comorbidities or underlying impaired renal function.
ACOG has recommended treating pregnant patients as chronically hypertensive according to recently changed criteria from the American College of Cardiology and the American Heart Association, which call for classifying blood pressure into the following categories:
- Normal. Systolic BP less than 120 mm Hg; diastolic BP less than 80 mm Hg.
- Elevated. Systolic BP greater than or equal to 120-129 mm Hg; diastolic BP greater than 80 mm Hg.
- Stage 1 hypertension. Systolic BP, 130-139 mm Hg; diastolic BP, 80-89 mm Hg.
- Stage 2 hypertension. Systolic BP greater than or equal to 140 mm Hg; diastolic BP greater than or equal to 90 mm Hg.
“The new blood pressure ranges for nonpregnant women have a lower threshold for hypertension diagnosis compared to ACOG’s criteria,” Dr. Pettker said. “This will likely cause a general increase in patients classified as chronic hypertensive and will require shared decision making by the ob.gyn. and the patient regarding appropriate management in pregnancy.”
The guideline also discusses chronic hypertension with superimposed preeclampsia; tests for baseline evaluation of chronic hypertension in pregnancy; common oral antihypertensive agents to use in pregnancy and those to use for urgent blood pressure control in pregnancy; control of acute-onset severe-range hypertension; and postpartum considerations in patients with chronic hypertension.
SOURCE: Gestational hypertension and preeclampsia. ACOG Practice Bulletin No. 202. Obstet Gynecol. 2019;133:e1-25; Chronic hypertension in pregnancy. ACOG Practice Bulletin No. 203. Obstet Gynecol. 2019;133:e26-50.
This article was updated 1/11/19 and 11/19/19.
Ob.gyns. will need to focus more on individualized care as they use the two new practice bulletins, one on chronic hypertension in pregnancy and one on gestational hypertension and preeclampsia, released by the American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins–Obstetrics.
The bulletins will replace the 2013 ACOG hypertension in pregnancy task force report and are published in the January issue of Obstetrics & Gynecology.
“The task force was a tour de force in creating a comprehensive view of hypertensive diseases of pregnancy, including research,” Christian M. Pettker, MD, who helped develop both practice bulletins, stated in a press release. “The updated guidance provides clearer recommendations for the management of gestational hypertension with severe-range blood pressure, an emphasis on and instructions for timely treatment of acutely elevated blood pressures, and more defined recommendations for the management of pain in postoperative patients with hypertension.”
“Ob.gyns. will need to focus more on individualized care and may find it’s best to err on the side of caution because the appropriate treatment of hypertensive diseases in pregnancy may be the most important focus of our attempts to improve maternal mortality and morbidity in the United States,” he said.*
Gestational hypertension or preeclampsia
For women with gestational hypertension or preeclampsia at 37 weeks of gestation or later without severe features, the guidelines recommend delivery rather than expectant management.
Those patients with severe features of gestational hypertension or preeclampsia or eclampsia should receive magnesium sulfate to prevent or treat seizures.
Patients should receive low-dose aspirin (81 mg/day) for preeclampsia prophylaxis between 12 weeks and 28 weeks of gestation if they have high-risk factors of preeclampsia such as multifetal gestation, a previous pregnancy with preeclampsia, renal disease, autoimmune disease, type 1 or type 2 diabetes mellitus, chronic hypertension, or a previous pregnancy with preeclampsia; or more than one moderate risk factor such as a family history of preeclampsia, maternal age greater than 35 years, first pregnancy, body mass index greater than 30, personal history factors, or sociodemographic characteristics.
NSAIDs should continue to be used in preference to opioid analgesics.
The guidance also discusses mode of delivery, antihypertensive drugs and thresholds for treatment, management of acute complications for preeclampsia with HELLP (hemolysis, elevated liver enzymes, low platelet count) syndrome, the optimal treatment for eclampsia, and postpartum hypertension and headache.
Chronic hypertension
Pregnant women with chronic hypertension also should receive low-dose aspirin between 12 weeks and 28 weeks of gestation. Antihypertensive therapy should be initiated for women with persistent chronic hypertension at systolic pressure of 160 mm Hg or higher and/or diastolic pressure of 110 mm Hg or higher. Consider treating patients at lower blood pressure (BP) thresholds depending on comorbidities or underlying impaired renal function.
ACOG has recommended treating pregnant patients as chronically hypertensive according to recently changed criteria from the American College of Cardiology and the American Heart Association, which call for classifying blood pressure into the following categories:
- Normal. Systolic BP less than 120 mm Hg; diastolic BP less than 80 mm Hg.
- Elevated. Systolic BP greater than or equal to 120-129 mm Hg; diastolic BP greater than 80 mm Hg.
- Stage 1 hypertension. Systolic BP, 130-139 mm Hg; diastolic BP, 80-89 mm Hg.
- Stage 2 hypertension. Systolic BP greater than or equal to 140 mm Hg; diastolic BP greater than or equal to 90 mm Hg.
“The new blood pressure ranges for nonpregnant women have a lower threshold for hypertension diagnosis compared to ACOG’s criteria,” Dr. Pettker said. “This will likely cause a general increase in patients classified as chronic hypertensive and will require shared decision making by the ob.gyn. and the patient regarding appropriate management in pregnancy.”
The guideline also discusses chronic hypertension with superimposed preeclampsia; tests for baseline evaluation of chronic hypertension in pregnancy; common oral antihypertensive agents to use in pregnancy and those to use for urgent blood pressure control in pregnancy; control of acute-onset severe-range hypertension; and postpartum considerations in patients with chronic hypertension.
SOURCE: Gestational hypertension and preeclampsia. ACOG Practice Bulletin No. 202. Obstet Gynecol. 2019;133:e1-25; Chronic hypertension in pregnancy. ACOG Practice Bulletin No. 203. Obstet Gynecol. 2019;133:e26-50.
This article was updated 1/11/19 and 11/19/19.
FROM OBSTETRICS & GYNECOLOGY
Proposed triple I criteria may overlook febrile women at risk post partum
A large proportion of laboring febrile women are not meeting proposed criteria for intrauterine inflammation or infection or both (triple I), but still may be at risk, according to an analysis of expert recommendations for clinical diagnosis published in Obstetrics & Gynecology.
“Our data suggest caution in universal implementation of the triple I criteria to guide clinical management of febrile women in the intrapartum period,” according to lead author Samsiya Ona, MD, of Brigham and Women’s Hospital in Boston, and her coauthors.
In early 2015, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) established criteria for diagnosing triple I in an effort to “decrease overtreatment of intrapartum women and low-risk newborns.” To assess the validity of those criteria, Dr. Ona and her colleagues analyzed 339 women with a temperature taken of 100.4°F or greater (38.0°C) during labor or within 1 hour post partum from June 2015 to September 2017.
The women were split into two groups: 212 met criteria for suspected triple I (documented fever plus clinical signs of intrauterine infection such as maternal leukocytosis greater than 15,000 per mm3, fetal tachycardia greater than 160 beats per minute, and purulent amniotic fluid) and 127 met criteria for isolated maternal fever. Among the suspected triple I group, incidence of adverse clinical infectious outcomes was 12%, comparable with 10% in the isolated maternal fever group (P = .50). When it came to predicting confirmed triple I, the sensitivity and specificity of the suspected triple I criteria were 71% (95% confidence interval, 61.4%-80.1%) and 41% (95% CI, 33.6%-47.8%), respectively. For predicting adverse clinical infectious outcomes, the sensitivity and specificity of the suspected triple I criteria were 68% (95% CI, 50.2%-82.0%) and 38% (95% CI, 32.6%-43.8%).
The authors cited among study limitations their including only women who had blood cultures sent at initial fever and excluding women who did not have repeat febrile temperature taken within 45 minutes. However, they noted the benefits of working with “a unique, large database with physiologic, laboratory, and microbiological parameters” and emphasized the need for an improved method of diagnosis, suggesting “a simple bedside minimally invasive marker of infection may be ideal.”
The study was supported by an Expanding the Boundaries Faculty Grant from the department of obstetrics, gynecology, and reproductive biology at the Brigham and Women’s Hospital in Boston. No conflicts of interest were reported.
SOURCE: Ona S et al. Obstet Gynecol. 2019 Jan. doi: 10.1097/AOG.0000000000003008.
A large proportion of laboring febrile women are not meeting proposed criteria for intrauterine inflammation or infection or both (triple I), but still may be at risk, according to an analysis of expert recommendations for clinical diagnosis published in Obstetrics & Gynecology.
“Our data suggest caution in universal implementation of the triple I criteria to guide clinical management of febrile women in the intrapartum period,” according to lead author Samsiya Ona, MD, of Brigham and Women’s Hospital in Boston, and her coauthors.
In early 2015, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) established criteria for diagnosing triple I in an effort to “decrease overtreatment of intrapartum women and low-risk newborns.” To assess the validity of those criteria, Dr. Ona and her colleagues analyzed 339 women with a temperature taken of 100.4°F or greater (38.0°C) during labor or within 1 hour post partum from June 2015 to September 2017.
The women were split into two groups: 212 met criteria for suspected triple I (documented fever plus clinical signs of intrauterine infection such as maternal leukocytosis greater than 15,000 per mm3, fetal tachycardia greater than 160 beats per minute, and purulent amniotic fluid) and 127 met criteria for isolated maternal fever. Among the suspected triple I group, incidence of adverse clinical infectious outcomes was 12%, comparable with 10% in the isolated maternal fever group (P = .50). When it came to predicting confirmed triple I, the sensitivity and specificity of the suspected triple I criteria were 71% (95% confidence interval, 61.4%-80.1%) and 41% (95% CI, 33.6%-47.8%), respectively. For predicting adverse clinical infectious outcomes, the sensitivity and specificity of the suspected triple I criteria were 68% (95% CI, 50.2%-82.0%) and 38% (95% CI, 32.6%-43.8%).
The authors cited among study limitations their including only women who had blood cultures sent at initial fever and excluding women who did not have repeat febrile temperature taken within 45 minutes. However, they noted the benefits of working with “a unique, large database with physiologic, laboratory, and microbiological parameters” and emphasized the need for an improved method of diagnosis, suggesting “a simple bedside minimally invasive marker of infection may be ideal.”
The study was supported by an Expanding the Boundaries Faculty Grant from the department of obstetrics, gynecology, and reproductive biology at the Brigham and Women’s Hospital in Boston. No conflicts of interest were reported.
SOURCE: Ona S et al. Obstet Gynecol. 2019 Jan. doi: 10.1097/AOG.0000000000003008.
A large proportion of laboring febrile women are not meeting proposed criteria for intrauterine inflammation or infection or both (triple I), but still may be at risk, according to an analysis of expert recommendations for clinical diagnosis published in Obstetrics & Gynecology.
“Our data suggest caution in universal implementation of the triple I criteria to guide clinical management of febrile women in the intrapartum period,” according to lead author Samsiya Ona, MD, of Brigham and Women’s Hospital in Boston, and her coauthors.
In early 2015, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) established criteria for diagnosing triple I in an effort to “decrease overtreatment of intrapartum women and low-risk newborns.” To assess the validity of those criteria, Dr. Ona and her colleagues analyzed 339 women with a temperature taken of 100.4°F or greater (38.0°C) during labor or within 1 hour post partum from June 2015 to September 2017.
The women were split into two groups: 212 met criteria for suspected triple I (documented fever plus clinical signs of intrauterine infection such as maternal leukocytosis greater than 15,000 per mm3, fetal tachycardia greater than 160 beats per minute, and purulent amniotic fluid) and 127 met criteria for isolated maternal fever. Among the suspected triple I group, incidence of adverse clinical infectious outcomes was 12%, comparable with 10% in the isolated maternal fever group (P = .50). When it came to predicting confirmed triple I, the sensitivity and specificity of the suspected triple I criteria were 71% (95% confidence interval, 61.4%-80.1%) and 41% (95% CI, 33.6%-47.8%), respectively. For predicting adverse clinical infectious outcomes, the sensitivity and specificity of the suspected triple I criteria were 68% (95% CI, 50.2%-82.0%) and 38% (95% CI, 32.6%-43.8%).
The authors cited among study limitations their including only women who had blood cultures sent at initial fever and excluding women who did not have repeat febrile temperature taken within 45 minutes. However, they noted the benefits of working with “a unique, large database with physiologic, laboratory, and microbiological parameters” and emphasized the need for an improved method of diagnosis, suggesting “a simple bedside minimally invasive marker of infection may be ideal.”
The study was supported by an Expanding the Boundaries Faculty Grant from the department of obstetrics, gynecology, and reproductive biology at the Brigham and Women’s Hospital in Boston. No conflicts of interest were reported.
SOURCE: Ona S et al. Obstet Gynecol. 2019 Jan. doi: 10.1097/AOG.0000000000003008.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point:
Major finding: The sensitivity and specificity of the suspected triple I criteria to predict an adverse clinical infectious outcome were 68% for the suspected triple I group and 38% for the isolated maternal fever group.
Study details: A retrospective cohort study of 339 women with intrapartum fever from June 2015 to September 2017.
Disclosures: The study was supported by an Expanding the Boundaries Faculty Grant from the department of obstetrics, gynecology, and reproductive biology at the Brigham and Women’s Hospital in Boston. No conflicts of interest were reported.
Source: Ona S et al. Obstet Gynecol. 2019 Jan. doi: 10.1097/AOG.0000000000003008.
Danish study finds reassuring data on pregnancy outcomes in atopic dermatitis patients
PARIS – over an 18-year period, which showed no increased risk of pregnancy and birth problems other than modestly increased risks of premature rupture of membranes and neonatal staphylococcal septicemia, according to Jacob P. Thyssen, MD, PhD.
At a session of the European Task Force of Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology, he presented a case control study of 10,668 births to Danish women with atopic dermatitis (AD) during 1997-2014. They were matched 1:10 by age, parity, and birth year to mothers without AD.
The risk of premature rupture of membranes was 15% higher in mothers with AD. And while the increased relative risk of neonatal staphylococcal septicemia was more substantial – a 145% increase – this was in fact a rare complication, observed Dr. Thyssen, a dermatologist at the University of Copenhagen.
There was no significant difference between women with or without AD in rates of preeclampsia, prematurity, pregnancy-induced hypertension, placenta previa, placental abruption, neonatal nonstaphylococcal septicemia, or other complications. The two groups had a similar number of visits to physicians and midwives during pregnancy.
Moreover, although the body mass index was similar in women with or without AD, the risk of gestational diabetes in women with the disease was significantly reduced by 21%; their risk of having a large-for-gestational-age baby with a birth weight of 4,500 g or more was also significantly lower than in controls.
Women received less treatment for AD during their pregnancy than they did beforehand. While pregnant, their disease was managed predominantly with topical corticosteroids and UV therapy. There was very little use of superpotent topical steroids, topical calcineurin inhibitors, or immunosuppressants, although 10% of pregnant women received systemic corticosteroids for their AD.
Dr. Thyssen reported serving as a scientific adviser and paid speaker for Leo Pharma, Roche, Eli Lilly, and Sanofi-Genzyme, although this study was conducted without commercial support.
PARIS – over an 18-year period, which showed no increased risk of pregnancy and birth problems other than modestly increased risks of premature rupture of membranes and neonatal staphylococcal septicemia, according to Jacob P. Thyssen, MD, PhD.
At a session of the European Task Force of Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology, he presented a case control study of 10,668 births to Danish women with atopic dermatitis (AD) during 1997-2014. They were matched 1:10 by age, parity, and birth year to mothers without AD.
The risk of premature rupture of membranes was 15% higher in mothers with AD. And while the increased relative risk of neonatal staphylococcal septicemia was more substantial – a 145% increase – this was in fact a rare complication, observed Dr. Thyssen, a dermatologist at the University of Copenhagen.
There was no significant difference between women with or without AD in rates of preeclampsia, prematurity, pregnancy-induced hypertension, placenta previa, placental abruption, neonatal nonstaphylococcal septicemia, or other complications. The two groups had a similar number of visits to physicians and midwives during pregnancy.
Moreover, although the body mass index was similar in women with or without AD, the risk of gestational diabetes in women with the disease was significantly reduced by 21%; their risk of having a large-for-gestational-age baby with a birth weight of 4,500 g or more was also significantly lower than in controls.
Women received less treatment for AD during their pregnancy than they did beforehand. While pregnant, their disease was managed predominantly with topical corticosteroids and UV therapy. There was very little use of superpotent topical steroids, topical calcineurin inhibitors, or immunosuppressants, although 10% of pregnant women received systemic corticosteroids for their AD.
Dr. Thyssen reported serving as a scientific adviser and paid speaker for Leo Pharma, Roche, Eli Lilly, and Sanofi-Genzyme, although this study was conducted without commercial support.
PARIS – over an 18-year period, which showed no increased risk of pregnancy and birth problems other than modestly increased risks of premature rupture of membranes and neonatal staphylococcal septicemia, according to Jacob P. Thyssen, MD, PhD.
At a session of the European Task Force of Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology, he presented a case control study of 10,668 births to Danish women with atopic dermatitis (AD) during 1997-2014. They were matched 1:10 by age, parity, and birth year to mothers without AD.
The risk of premature rupture of membranes was 15% higher in mothers with AD. And while the increased relative risk of neonatal staphylococcal septicemia was more substantial – a 145% increase – this was in fact a rare complication, observed Dr. Thyssen, a dermatologist at the University of Copenhagen.
There was no significant difference between women with or without AD in rates of preeclampsia, prematurity, pregnancy-induced hypertension, placenta previa, placental abruption, neonatal nonstaphylococcal septicemia, or other complications. The two groups had a similar number of visits to physicians and midwives during pregnancy.
Moreover, although the body mass index was similar in women with or without AD, the risk of gestational diabetes in women with the disease was significantly reduced by 21%; their risk of having a large-for-gestational-age baby with a birth weight of 4,500 g or more was also significantly lower than in controls.
Women received less treatment for AD during their pregnancy than they did beforehand. While pregnant, their disease was managed predominantly with topical corticosteroids and UV therapy. There was very little use of superpotent topical steroids, topical calcineurin inhibitors, or immunosuppressants, although 10% of pregnant women received systemic corticosteroids for their AD.
Dr. Thyssen reported serving as a scientific adviser and paid speaker for Leo Pharma, Roche, Eli Lilly, and Sanofi-Genzyme, although this study was conducted without commercial support.
REPORTING FROM THE EADV CONGRESS
Key clinical point: Birth complications are uncommon for women with atopic dermatitis in pregnancy.
Major finding: The risk of premature rupture of membranes was increased by 15% in women with atopic dermatitis in pregnancy, but their risk of gestational diabetes was reduced by 21%.
Study details: This case control study included 10,668 births to Danish women with atopic dermatitis and 10 times as many matched controls without the disease.
Disclosures: The study presenter reported serving as a scientific adviser and paid speaker for Leo Pharma, Roche, Eli Lilly, and Sanofi-Genzyme, although this study was conducted without commercial support.