User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Physician recruitment drops by 30% because of pandemic
the firm reported.
“Rather than having many practice opportunities to choose from, physicians now may have to compete to secure practice opportunities that meet their needs,” the authors wrote in Merritt Hawkins’ report on the impact of COVID-19.
Most of the report concerns physician recruitment from April 1, 2019, to March 31, 2020. The data were mostly derived from searches that Merritt Hawkins conducted before the effects of the pandemic was fully felt.
Family medicine was again the most sought-after specialty, as it has been for the past 14 years. But demand for primary care doctors – including family physicians, internists, and pediatricians – leveled off, and average starting salaries for primary care doctors dropped during 2019-2020. In contrast, the number of searches conducted for nurse practitioners (NPs) and physician assistants (PAs) increased by 54%, and their salaries increased slightly.
To explain the lackluster prospects for primary care before the pandemic, the authors cited research showing that patients were turning away from the traditional office visit model. At the same time, there was a rise in visits to NPs and PAs, including those in urgent care centers and retail clinics.
As a result of decreased demand for primary care physicians and the rising prevalence of telehealth, Merritt Hawkins expects primary care salaries to drop overall. With telehealth generating a larger portion of revenues, “it is uncertain whether primary care physicians will be able to sustain levels of reimbursement that were prevalent pre-COVID even at such time as the economy is improved and utilization increases,” the authors reported.
Demand for specialists was increasing prior to the COVID-19 crisis, partly as a result of the aging of the population. Seventy-eight percent of all searches were for medical specialists, compared with 67% 5 years ago. However, the pandemic has set back specialist searches. “Demand and compensation for specialists also will change as a result of COVID-19 in response to declines in the volume of medical procedures,” according to the authors.
In contrast, the recruitment of doctors who are on the front line of COVID-19 care is expected to increase. Among the fields anticipated to be in demand are emergency department specialists, infectious disease specialists, and pulmonology/critical care physicians. Travis Singleton, executive vice president of Merritt Hawkins, said in an interview that this trend is already happening and will accelerate as COVID-19 hot spots arise across the country.
Specialists in different fields received either higher or lower offers than during the previous year. Starting salaries for noninvasive cardiologists, for example, dropped 7.3%; gastroenterologists earned 7.7% less; and neurologists, 6.9% less. In contrast, orthopedic surgeons saw offers surge 16.7%; radiologists, 9.3%; and pulmonologists/critical care specialists, 7.7%.
Physicians were offered salaries plus bonuses in three-quarters of searches. Relative value unit–based production remained the most common basis for bonuses. Quality/value-based metrics were used in computing 64% of bonuses – up from 56% the previous year – but still determined only 11% of total physician compensation.
Pandemic outlook
Whereas health care helped drive the U.S. economy in 2018-2019, the pace of job growth in health care has decreased since March. As a result of the pandemic, health care spending in the United States declined by 18% in the first quarter of 2020. Physician practice revenue dropped by 55% during the first quarter, and many small and solo practices are still struggling.
In a 2018 Merritt Hawkins survey, 18% of physicians said they had used telehealth to treat patients. Because of the pandemic, that percentage jumped to 48% in April 2020. But telehealth hasn’t made up for the loss of patient revenue from in-office procedures, tests, and other services, and it still isn’t being reimbursed at the same level as in-office visits.
With practices under severe financial strain, the authors explained, “A majority of private practices have curtailed most physician recruiting activity since the virus emerged.”
In some states, many specialty practices have been adversely affected by the suspension of elective procedures, and specialty practices that rely on nonessential procedures are unlikely to recruit additional physicians.
One-third of practices could close
The survival of many private practices is now in question. “Based on the losses physician practices have sustained as a result of COVID-19, some markets could lose up to 35% or more of their most vulnerable group practices while a large percent of others will be acquired,” the authors wrote.
Hospitals and health systems will acquire the bulk of these practices, in many cases at fire-sale prices, Mr. Singleton predicted. This enormous shift from private practice to employment, he added, “will have as much to do with the [physician] income levels we’re going to see as the demand for the specialties themselves.”
Right now, he said, Merritt Hawkins is fielding a huge number of requests from doctors seeking employment, but there aren’t many jobs out there. “We haven’t seen an employer-friendly market like this since the 1970s,” he noted. “Before the pandemic, a physician might have had five to 10 jobs to choose from. Now it’s the opposite: We have one job, and 5 to 10 physicians are applying for it.”
Singleton believes the market will adjust by the second quarter of next year. Even if the pandemic worsens, he said, the system will have made the necessary corrections and adjustments “because we have to start seeing patients again, both in terms of demand and economics. So these doctors will be in demand again and will have work.”
Contingent employment
Although the COVID-related falloff in revenue has hit private practices the hardest, some employed physicians have also found themselves in a bind. According to a Merritt Hawkins/Physicians Foundation survey conducted in April, 21% of physicians said they had been furloughed or had taken a pay cut.
Mr. Singleton views this trend as part of hospitals’ reassessment of how they’re going to deal with labor going forward. To cope with utilization ebbs and flows in response to the virus, hospitals are now considering what the report calls a “contingent labor/flex staffing model.”
Under this type of arrangement, which some hospitals have already adopted, physicians may no longer work full time in a single setting, Mr. Singleton said. They may be asked to conduct telehealth visits on nights and weekends and work 20 hours a week in the clinic, or they may have shifts in multiple hospitals or clinics.
“You can make as much or more on a temporary basis as on a permanent basis,” he said. “But you have to be more flexible. You may have to travel or do a different scope of work, or work in different settings.”
A version of this article originally appeared on Medscape.com.
the firm reported.
“Rather than having many practice opportunities to choose from, physicians now may have to compete to secure practice opportunities that meet their needs,” the authors wrote in Merritt Hawkins’ report on the impact of COVID-19.
Most of the report concerns physician recruitment from April 1, 2019, to March 31, 2020. The data were mostly derived from searches that Merritt Hawkins conducted before the effects of the pandemic was fully felt.
Family medicine was again the most sought-after specialty, as it has been for the past 14 years. But demand for primary care doctors – including family physicians, internists, and pediatricians – leveled off, and average starting salaries for primary care doctors dropped during 2019-2020. In contrast, the number of searches conducted for nurse practitioners (NPs) and physician assistants (PAs) increased by 54%, and their salaries increased slightly.
To explain the lackluster prospects for primary care before the pandemic, the authors cited research showing that patients were turning away from the traditional office visit model. At the same time, there was a rise in visits to NPs and PAs, including those in urgent care centers and retail clinics.
As a result of decreased demand for primary care physicians and the rising prevalence of telehealth, Merritt Hawkins expects primary care salaries to drop overall. With telehealth generating a larger portion of revenues, “it is uncertain whether primary care physicians will be able to sustain levels of reimbursement that were prevalent pre-COVID even at such time as the economy is improved and utilization increases,” the authors reported.
Demand for specialists was increasing prior to the COVID-19 crisis, partly as a result of the aging of the population. Seventy-eight percent of all searches were for medical specialists, compared with 67% 5 years ago. However, the pandemic has set back specialist searches. “Demand and compensation for specialists also will change as a result of COVID-19 in response to declines in the volume of medical procedures,” according to the authors.
In contrast, the recruitment of doctors who are on the front line of COVID-19 care is expected to increase. Among the fields anticipated to be in demand are emergency department specialists, infectious disease specialists, and pulmonology/critical care physicians. Travis Singleton, executive vice president of Merritt Hawkins, said in an interview that this trend is already happening and will accelerate as COVID-19 hot spots arise across the country.
Specialists in different fields received either higher or lower offers than during the previous year. Starting salaries for noninvasive cardiologists, for example, dropped 7.3%; gastroenterologists earned 7.7% less; and neurologists, 6.9% less. In contrast, orthopedic surgeons saw offers surge 16.7%; radiologists, 9.3%; and pulmonologists/critical care specialists, 7.7%.
Physicians were offered salaries plus bonuses in three-quarters of searches. Relative value unit–based production remained the most common basis for bonuses. Quality/value-based metrics were used in computing 64% of bonuses – up from 56% the previous year – but still determined only 11% of total physician compensation.
Pandemic outlook
Whereas health care helped drive the U.S. economy in 2018-2019, the pace of job growth in health care has decreased since March. As a result of the pandemic, health care spending in the United States declined by 18% in the first quarter of 2020. Physician practice revenue dropped by 55% during the first quarter, and many small and solo practices are still struggling.
In a 2018 Merritt Hawkins survey, 18% of physicians said they had used telehealth to treat patients. Because of the pandemic, that percentage jumped to 48% in April 2020. But telehealth hasn’t made up for the loss of patient revenue from in-office procedures, tests, and other services, and it still isn’t being reimbursed at the same level as in-office visits.
With practices under severe financial strain, the authors explained, “A majority of private practices have curtailed most physician recruiting activity since the virus emerged.”
In some states, many specialty practices have been adversely affected by the suspension of elective procedures, and specialty practices that rely on nonessential procedures are unlikely to recruit additional physicians.
One-third of practices could close
The survival of many private practices is now in question. “Based on the losses physician practices have sustained as a result of COVID-19, some markets could lose up to 35% or more of their most vulnerable group practices while a large percent of others will be acquired,” the authors wrote.
Hospitals and health systems will acquire the bulk of these practices, in many cases at fire-sale prices, Mr. Singleton predicted. This enormous shift from private practice to employment, he added, “will have as much to do with the [physician] income levels we’re going to see as the demand for the specialties themselves.”
Right now, he said, Merritt Hawkins is fielding a huge number of requests from doctors seeking employment, but there aren’t many jobs out there. “We haven’t seen an employer-friendly market like this since the 1970s,” he noted. “Before the pandemic, a physician might have had five to 10 jobs to choose from. Now it’s the opposite: We have one job, and 5 to 10 physicians are applying for it.”
Singleton believes the market will adjust by the second quarter of next year. Even if the pandemic worsens, he said, the system will have made the necessary corrections and adjustments “because we have to start seeing patients again, both in terms of demand and economics. So these doctors will be in demand again and will have work.”
Contingent employment
Although the COVID-related falloff in revenue has hit private practices the hardest, some employed physicians have also found themselves in a bind. According to a Merritt Hawkins/Physicians Foundation survey conducted in April, 21% of physicians said they had been furloughed or had taken a pay cut.
Mr. Singleton views this trend as part of hospitals’ reassessment of how they’re going to deal with labor going forward. To cope with utilization ebbs and flows in response to the virus, hospitals are now considering what the report calls a “contingent labor/flex staffing model.”
Under this type of arrangement, which some hospitals have already adopted, physicians may no longer work full time in a single setting, Mr. Singleton said. They may be asked to conduct telehealth visits on nights and weekends and work 20 hours a week in the clinic, or they may have shifts in multiple hospitals or clinics.
“You can make as much or more on a temporary basis as on a permanent basis,” he said. “But you have to be more flexible. You may have to travel or do a different scope of work, or work in different settings.”
A version of this article originally appeared on Medscape.com.
the firm reported.
“Rather than having many practice opportunities to choose from, physicians now may have to compete to secure practice opportunities that meet their needs,” the authors wrote in Merritt Hawkins’ report on the impact of COVID-19.
Most of the report concerns physician recruitment from April 1, 2019, to March 31, 2020. The data were mostly derived from searches that Merritt Hawkins conducted before the effects of the pandemic was fully felt.
Family medicine was again the most sought-after specialty, as it has been for the past 14 years. But demand for primary care doctors – including family physicians, internists, and pediatricians – leveled off, and average starting salaries for primary care doctors dropped during 2019-2020. In contrast, the number of searches conducted for nurse practitioners (NPs) and physician assistants (PAs) increased by 54%, and their salaries increased slightly.
To explain the lackluster prospects for primary care before the pandemic, the authors cited research showing that patients were turning away from the traditional office visit model. At the same time, there was a rise in visits to NPs and PAs, including those in urgent care centers and retail clinics.
As a result of decreased demand for primary care physicians and the rising prevalence of telehealth, Merritt Hawkins expects primary care salaries to drop overall. With telehealth generating a larger portion of revenues, “it is uncertain whether primary care physicians will be able to sustain levels of reimbursement that were prevalent pre-COVID even at such time as the economy is improved and utilization increases,” the authors reported.
Demand for specialists was increasing prior to the COVID-19 crisis, partly as a result of the aging of the population. Seventy-eight percent of all searches were for medical specialists, compared with 67% 5 years ago. However, the pandemic has set back specialist searches. “Demand and compensation for specialists also will change as a result of COVID-19 in response to declines in the volume of medical procedures,” according to the authors.
In contrast, the recruitment of doctors who are on the front line of COVID-19 care is expected to increase. Among the fields anticipated to be in demand are emergency department specialists, infectious disease specialists, and pulmonology/critical care physicians. Travis Singleton, executive vice president of Merritt Hawkins, said in an interview that this trend is already happening and will accelerate as COVID-19 hot spots arise across the country.
Specialists in different fields received either higher or lower offers than during the previous year. Starting salaries for noninvasive cardiologists, for example, dropped 7.3%; gastroenterologists earned 7.7% less; and neurologists, 6.9% less. In contrast, orthopedic surgeons saw offers surge 16.7%; radiologists, 9.3%; and pulmonologists/critical care specialists, 7.7%.
Physicians were offered salaries plus bonuses in three-quarters of searches. Relative value unit–based production remained the most common basis for bonuses. Quality/value-based metrics were used in computing 64% of bonuses – up from 56% the previous year – but still determined only 11% of total physician compensation.
Pandemic outlook
Whereas health care helped drive the U.S. economy in 2018-2019, the pace of job growth in health care has decreased since March. As a result of the pandemic, health care spending in the United States declined by 18% in the first quarter of 2020. Physician practice revenue dropped by 55% during the first quarter, and many small and solo practices are still struggling.
In a 2018 Merritt Hawkins survey, 18% of physicians said they had used telehealth to treat patients. Because of the pandemic, that percentage jumped to 48% in April 2020. But telehealth hasn’t made up for the loss of patient revenue from in-office procedures, tests, and other services, and it still isn’t being reimbursed at the same level as in-office visits.
With practices under severe financial strain, the authors explained, “A majority of private practices have curtailed most physician recruiting activity since the virus emerged.”
In some states, many specialty practices have been adversely affected by the suspension of elective procedures, and specialty practices that rely on nonessential procedures are unlikely to recruit additional physicians.
One-third of practices could close
The survival of many private practices is now in question. “Based on the losses physician practices have sustained as a result of COVID-19, some markets could lose up to 35% or more of their most vulnerable group practices while a large percent of others will be acquired,” the authors wrote.
Hospitals and health systems will acquire the bulk of these practices, in many cases at fire-sale prices, Mr. Singleton predicted. This enormous shift from private practice to employment, he added, “will have as much to do with the [physician] income levels we’re going to see as the demand for the specialties themselves.”
Right now, he said, Merritt Hawkins is fielding a huge number of requests from doctors seeking employment, but there aren’t many jobs out there. “We haven’t seen an employer-friendly market like this since the 1970s,” he noted. “Before the pandemic, a physician might have had five to 10 jobs to choose from. Now it’s the opposite: We have one job, and 5 to 10 physicians are applying for it.”
Singleton believes the market will adjust by the second quarter of next year. Even if the pandemic worsens, he said, the system will have made the necessary corrections and adjustments “because we have to start seeing patients again, both in terms of demand and economics. So these doctors will be in demand again and will have work.”
Contingent employment
Although the COVID-related falloff in revenue has hit private practices the hardest, some employed physicians have also found themselves in a bind. According to a Merritt Hawkins/Physicians Foundation survey conducted in April, 21% of physicians said they had been furloughed or had taken a pay cut.
Mr. Singleton views this trend as part of hospitals’ reassessment of how they’re going to deal with labor going forward. To cope with utilization ebbs and flows in response to the virus, hospitals are now considering what the report calls a “contingent labor/flex staffing model.”
Under this type of arrangement, which some hospitals have already adopted, physicians may no longer work full time in a single setting, Mr. Singleton said. They may be asked to conduct telehealth visits on nights and weekends and work 20 hours a week in the clinic, or they may have shifts in multiple hospitals or clinics.
“You can make as much or more on a temporary basis as on a permanent basis,” he said. “But you have to be more flexible. You may have to travel or do a different scope of work, or work in different settings.”
A version of this article originally appeared on Medscape.com.
Provide support in uncertain times
A sense of safety and stability, both emotional and physical, is crucial in promoting the healthy development of youth. Between the global pandemic, need for social distancing, economic downturn, and increased awareness of racial disparities, for many this sense of stability has been rattled.
School closures have led to a loss of social interaction, challenges to continued academic growth, and, for some students, lack of access to nutrition and increased food insecurity. For students with learning or mental health challenges, closures may have eliminated or significantly reduced desperately needed supports received in school.1 While these trying circumstances have been difficult for many, the transition back to school in the fall also may be challenging because of the uncertainty about what this will look like and possible change in routine. Some students or their families may have anxiety about returning, either because of a history of adverse experiences at school such as bullying, or because of fears about exposure for themselves or others to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The past several months also brought about greater awareness of systemic racial disparities, whether as reflected in health care, education, or the criminal justice system. According to the Centers for Disease Control and Prevention data, Latinx and African-American individuals in the United States have had a threefold greater chance of contracting SARS-CoV-2 and have a twofold greater risk of death, compared with white people in the same communities.2 Other social determinants of health – economic stability, education, social factors such as incarceration and discrimination, and neighborhood factors including access to healthy food – play a role in this vulnerability.
The pandemic has resulted in a need for social distancing, and as a result, isolation. Children and teens exposed to the news may have anxiety about what they see or hear. Additional pressures in the family can include economic uncertainty, loss of employment for the primary wage earner of the household, or stress related to family members being first responders.
Any one of these factors is a potentially significant stressor, so how do we best support youth to help them survive and hopefully thrive during this time?
- It is important to establish a sense of routine; this can help create a sense of stability and safety. Recognizing that circumstances are not the same as they were 5 or 6 months ago, encouraging structure should not come at the cost of preserving connection.
- Note positive behavior and choices made by children and make sure they know it was observed.
- Many children have experienced increased screen time with the lack of structure of the traditional school day or summer camp and extracurricular activities. Limiting screen time and being mindful of its potential impact on mood is prudent.
- Self-care for parents and guardians is important. This time is stressful for the adults of the household, let alone children who are learning self-regulation skills.
- Listen to children’s or teens’ concerns and share information in developmentally appropriate ways. It is okay to not have all of the answers.
- Balance fostering a sense of gratitude with not invalidating a child’s or teen’s experience. Showing empathy during this time is vital. While there may be other soccer seasons, it is normal to experience grief about the loss of experiences during this time.
- Parents and guardians know their children best, so it is prudent for them to be mindful of concerning changes such as an increase in sadness, anxiety, or irritability that negatively impacts daily functioning such as sleeping, eating, or relationships with family and friends.
- Promote social interactions with appropriate safeguards in place. Unfortunately, the number of SARS-CoV-2 infections is increasing in multiple states, and there is the potential to return to some of the previous restrictions. However, encouraging social interaction while following local guidelines and with cautions such as limiting the number of people present, meeting outside, or considering interacting with others who are similarly social distancing can help foster social connection and development.
- Maintain connection digitally when in-person contact is not an option.3 Social groups, places of worship, and other activities have been agile in developing virtual communities. Communication by voice and/or video is thought to be more powerful than by written communication (text, email) alone.4 However, it is important to consider those who may have limited to no access to electronic methods.
- Encourage open communication with children about diversity and bias, and consider how our interactions with others may affect our children’s perspectives.5
- As providers, it is crucial that we address structural and institutional systems that negatively impact the health, safety, and access to care including our Black, indigenous, and people of color (BIPOC) and lesbian, gay, bisexual, transgender/transsexual, queer/questioning, intersex, and allied/asexual/aromantic/agender (LGBTQIA) patients.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. Dr. Strange has no relevant financial disclosures. Email her at [email protected].
Online resources for parents and families
- Child Mind Institute: Coping With the Coronavirus Crisis: Supporting Your Kids.
- American Psychological Association: Talking with children about discrimination.
- Common Sense Media: Help with determining appropriateness of media for children.
Hotlines
- National Suicide Prevention Hotline: 1-800-273-8255
- GLBT National Hotline: 888-843-4564
- The California Peer-Run Warm Line: 1-855-845-7415
- Trevor Project: 866-488-7386 or text TREVOR to 1-202-304-1200
- Trans Lifeline: 877-565-8860
- Crisis Text Line: Text HOME to 741741
References
1. JAMA Pediatr. 2020 Apr 14. doi: 10.1001/jamapediatrics.2020.1456.
2. CDC: COVID-19 in Racial and Ethnic Minority Groups.
3. JAMA. 2020 Mar 23. doi: 10.1001/jama.2020.4469.
4. JAMA Intern Med. 2020 Apr 10. doi: 10.1001/jamainternmed.2020.1562.
5. American Psychological Association: Talking with children about discrimination.
A sense of safety and stability, both emotional and physical, is crucial in promoting the healthy development of youth. Between the global pandemic, need for social distancing, economic downturn, and increased awareness of racial disparities, for many this sense of stability has been rattled.
School closures have led to a loss of social interaction, challenges to continued academic growth, and, for some students, lack of access to nutrition and increased food insecurity. For students with learning or mental health challenges, closures may have eliminated or significantly reduced desperately needed supports received in school.1 While these trying circumstances have been difficult for many, the transition back to school in the fall also may be challenging because of the uncertainty about what this will look like and possible change in routine. Some students or their families may have anxiety about returning, either because of a history of adverse experiences at school such as bullying, or because of fears about exposure for themselves or others to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The past several months also brought about greater awareness of systemic racial disparities, whether as reflected in health care, education, or the criminal justice system. According to the Centers for Disease Control and Prevention data, Latinx and African-American individuals in the United States have had a threefold greater chance of contracting SARS-CoV-2 and have a twofold greater risk of death, compared with white people in the same communities.2 Other social determinants of health – economic stability, education, social factors such as incarceration and discrimination, and neighborhood factors including access to healthy food – play a role in this vulnerability.
The pandemic has resulted in a need for social distancing, and as a result, isolation. Children and teens exposed to the news may have anxiety about what they see or hear. Additional pressures in the family can include economic uncertainty, loss of employment for the primary wage earner of the household, or stress related to family members being first responders.
Any one of these factors is a potentially significant stressor, so how do we best support youth to help them survive and hopefully thrive during this time?
- It is important to establish a sense of routine; this can help create a sense of stability and safety. Recognizing that circumstances are not the same as they were 5 or 6 months ago, encouraging structure should not come at the cost of preserving connection.
- Note positive behavior and choices made by children and make sure they know it was observed.
- Many children have experienced increased screen time with the lack of structure of the traditional school day or summer camp and extracurricular activities. Limiting screen time and being mindful of its potential impact on mood is prudent.
- Self-care for parents and guardians is important. This time is stressful for the adults of the household, let alone children who are learning self-regulation skills.
- Listen to children’s or teens’ concerns and share information in developmentally appropriate ways. It is okay to not have all of the answers.
- Balance fostering a sense of gratitude with not invalidating a child’s or teen’s experience. Showing empathy during this time is vital. While there may be other soccer seasons, it is normal to experience grief about the loss of experiences during this time.
- Parents and guardians know their children best, so it is prudent for them to be mindful of concerning changes such as an increase in sadness, anxiety, or irritability that negatively impacts daily functioning such as sleeping, eating, or relationships with family and friends.
- Promote social interactions with appropriate safeguards in place. Unfortunately, the number of SARS-CoV-2 infections is increasing in multiple states, and there is the potential to return to some of the previous restrictions. However, encouraging social interaction while following local guidelines and with cautions such as limiting the number of people present, meeting outside, or considering interacting with others who are similarly social distancing can help foster social connection and development.
- Maintain connection digitally when in-person contact is not an option.3 Social groups, places of worship, and other activities have been agile in developing virtual communities. Communication by voice and/or video is thought to be more powerful than by written communication (text, email) alone.4 However, it is important to consider those who may have limited to no access to electronic methods.
- Encourage open communication with children about diversity and bias, and consider how our interactions with others may affect our children’s perspectives.5
- As providers, it is crucial that we address structural and institutional systems that negatively impact the health, safety, and access to care including our Black, indigenous, and people of color (BIPOC) and lesbian, gay, bisexual, transgender/transsexual, queer/questioning, intersex, and allied/asexual/aromantic/agender (LGBTQIA) patients.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. Dr. Strange has no relevant financial disclosures. Email her at [email protected].
Online resources for parents and families
- Child Mind Institute: Coping With the Coronavirus Crisis: Supporting Your Kids.
- American Psychological Association: Talking with children about discrimination.
- Common Sense Media: Help with determining appropriateness of media for children.
Hotlines
- National Suicide Prevention Hotline: 1-800-273-8255
- GLBT National Hotline: 888-843-4564
- The California Peer-Run Warm Line: 1-855-845-7415
- Trevor Project: 866-488-7386 or text TREVOR to 1-202-304-1200
- Trans Lifeline: 877-565-8860
- Crisis Text Line: Text HOME to 741741
References
1. JAMA Pediatr. 2020 Apr 14. doi: 10.1001/jamapediatrics.2020.1456.
2. CDC: COVID-19 in Racial and Ethnic Minority Groups.
3. JAMA. 2020 Mar 23. doi: 10.1001/jama.2020.4469.
4. JAMA Intern Med. 2020 Apr 10. doi: 10.1001/jamainternmed.2020.1562.
5. American Psychological Association: Talking with children about discrimination.
A sense of safety and stability, both emotional and physical, is crucial in promoting the healthy development of youth. Between the global pandemic, need for social distancing, economic downturn, and increased awareness of racial disparities, for many this sense of stability has been rattled.
School closures have led to a loss of social interaction, challenges to continued academic growth, and, for some students, lack of access to nutrition and increased food insecurity. For students with learning or mental health challenges, closures may have eliminated or significantly reduced desperately needed supports received in school.1 While these trying circumstances have been difficult for many, the transition back to school in the fall also may be challenging because of the uncertainty about what this will look like and possible change in routine. Some students or their families may have anxiety about returning, either because of a history of adverse experiences at school such as bullying, or because of fears about exposure for themselves or others to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The past several months also brought about greater awareness of systemic racial disparities, whether as reflected in health care, education, or the criminal justice system. According to the Centers for Disease Control and Prevention data, Latinx and African-American individuals in the United States have had a threefold greater chance of contracting SARS-CoV-2 and have a twofold greater risk of death, compared with white people in the same communities.2 Other social determinants of health – economic stability, education, social factors such as incarceration and discrimination, and neighborhood factors including access to healthy food – play a role in this vulnerability.
The pandemic has resulted in a need for social distancing, and as a result, isolation. Children and teens exposed to the news may have anxiety about what they see or hear. Additional pressures in the family can include economic uncertainty, loss of employment for the primary wage earner of the household, or stress related to family members being first responders.
Any one of these factors is a potentially significant stressor, so how do we best support youth to help them survive and hopefully thrive during this time?
- It is important to establish a sense of routine; this can help create a sense of stability and safety. Recognizing that circumstances are not the same as they were 5 or 6 months ago, encouraging structure should not come at the cost of preserving connection.
- Note positive behavior and choices made by children and make sure they know it was observed.
- Many children have experienced increased screen time with the lack of structure of the traditional school day or summer camp and extracurricular activities. Limiting screen time and being mindful of its potential impact on mood is prudent.
- Self-care for parents and guardians is important. This time is stressful for the adults of the household, let alone children who are learning self-regulation skills.
- Listen to children’s or teens’ concerns and share information in developmentally appropriate ways. It is okay to not have all of the answers.
- Balance fostering a sense of gratitude with not invalidating a child’s or teen’s experience. Showing empathy during this time is vital. While there may be other soccer seasons, it is normal to experience grief about the loss of experiences during this time.
- Parents and guardians know their children best, so it is prudent for them to be mindful of concerning changes such as an increase in sadness, anxiety, or irritability that negatively impacts daily functioning such as sleeping, eating, or relationships with family and friends.
- Promote social interactions with appropriate safeguards in place. Unfortunately, the number of SARS-CoV-2 infections is increasing in multiple states, and there is the potential to return to some of the previous restrictions. However, encouraging social interaction while following local guidelines and with cautions such as limiting the number of people present, meeting outside, or considering interacting with others who are similarly social distancing can help foster social connection and development.
- Maintain connection digitally when in-person contact is not an option.3 Social groups, places of worship, and other activities have been agile in developing virtual communities. Communication by voice and/or video is thought to be more powerful than by written communication (text, email) alone.4 However, it is important to consider those who may have limited to no access to electronic methods.
- Encourage open communication with children about diversity and bias, and consider how our interactions with others may affect our children’s perspectives.5
- As providers, it is crucial that we address structural and institutional systems that negatively impact the health, safety, and access to care including our Black, indigenous, and people of color (BIPOC) and lesbian, gay, bisexual, transgender/transsexual, queer/questioning, intersex, and allied/asexual/aromantic/agender (LGBTQIA) patients.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. Dr. Strange has no relevant financial disclosures. Email her at [email protected].
Online resources for parents and families
- Child Mind Institute: Coping With the Coronavirus Crisis: Supporting Your Kids.
- American Psychological Association: Talking with children about discrimination.
- Common Sense Media: Help with determining appropriateness of media for children.
Hotlines
- National Suicide Prevention Hotline: 1-800-273-8255
- GLBT National Hotline: 888-843-4564
- The California Peer-Run Warm Line: 1-855-845-7415
- Trevor Project: 866-488-7386 or text TREVOR to 1-202-304-1200
- Trans Lifeline: 877-565-8860
- Crisis Text Line: Text HOME to 741741
References
1. JAMA Pediatr. 2020 Apr 14. doi: 10.1001/jamapediatrics.2020.1456.
2. CDC: COVID-19 in Racial and Ethnic Minority Groups.
3. JAMA. 2020 Mar 23. doi: 10.1001/jama.2020.4469.
4. JAMA Intern Med. 2020 Apr 10. doi: 10.1001/jamainternmed.2020.1562.
5. American Psychological Association: Talking with children about discrimination.
Medical societies advise on vitamin D in midst of COVID-19
Six medical societies from across the globe are emphasizing the importance of individuals obtaining the daily recommended dose of vitamin D, especially given the impact of the COVID-19 pandemic on outdoor time.
The statement, “Joint Guidance on Vitamin D in the Era of COVID-19,” is supported by the American Society for Bone and Mineral Research, the Endocrine Society, and the American Association of Clinical Endocrinologists, among others.
They felt the need to clarify the recommendations for clinicians. Central to the guidance is the recommendation to directly expose the skin to sunlight for 15-30 minutes per day, while taking care to avoid sunburn.
The statement noted that “vitamin D is very safe when taken at reasonable dosages and is important for musculoskeletal health. Levels are likely to decline as individuals reduce outside activity (sun exposure) during the pandemic.”
It added that “most older and younger adults can safely take 400-1000 IU daily to keep vitamin D levels within the optimal range as recommended by [the US] Institute of Medicine guidelines.”
The statement also noted that the scientific evidence clearly supports the benefits that vitamin D (in combination with calcium intake) plays in building a strong skeleton and preventing bone loss.
Other societies supporting the statement are the European Calcified Tissue Society, the National Osteoporosis Foundation, and the International Osteoporosis Foundation.
What role for vitamin D in COVID-19?
Over recent months, the role of vitamin D in relation to prevention of COVID-19 has been the subject of intense debate. Now, these societies have joined forces and endorsed evidence-based guidance to clarify the issue around obtaining the daily recommended dosage of vitamin D.
During the pandemic, orders to stay at home meant individuals were likely to spend less time outdoors and have less opportunity to draw their vitamin D directly from sunlight, which is its main source, other than a limited number of foods or as a dietary supplement, the societies explained.
However, they acknowledged that the role of vitamin D in COVID-19 remains unclear.
“The current data do not provide any evidence that vitamin D supplementation will help prevent or treat COVID-19 infection; however, our guidance does not preclude further study of the potential effects of vitamin D on COVID-19,” the joint statement said.
Research to date suggests that vitamin D may play a role in enhancing the immune response, and given prior work demonstrating a role for the activated form of vitamin D – 1,25(OH)2D – in immune responses, “further research into vitamin D supplementation in COVID-19 disease is warranted,” it added. “Trials to date have been observational and there have been no randomized, controlled trials from which firm conclusions about causal relationships can be drawn. Observational studies suggest associations between low vitamin D concentrations and higher rates of COVID-19 infection.”
Medscape Medical News previously reported on the existing observational data regarding vitamin D in COVID-19. A recent rapid evidence review by the National Institute for Health and Care Excellence failed to find any evidence that vitamin D supplementation reduces the risk or severity of COVID-19.
A version of this article originally appeared on Medscape.com.
Six medical societies from across the globe are emphasizing the importance of individuals obtaining the daily recommended dose of vitamin D, especially given the impact of the COVID-19 pandemic on outdoor time.
The statement, “Joint Guidance on Vitamin D in the Era of COVID-19,” is supported by the American Society for Bone and Mineral Research, the Endocrine Society, and the American Association of Clinical Endocrinologists, among others.
They felt the need to clarify the recommendations for clinicians. Central to the guidance is the recommendation to directly expose the skin to sunlight for 15-30 minutes per day, while taking care to avoid sunburn.
The statement noted that “vitamin D is very safe when taken at reasonable dosages and is important for musculoskeletal health. Levels are likely to decline as individuals reduce outside activity (sun exposure) during the pandemic.”
It added that “most older and younger adults can safely take 400-1000 IU daily to keep vitamin D levels within the optimal range as recommended by [the US] Institute of Medicine guidelines.”
The statement also noted that the scientific evidence clearly supports the benefits that vitamin D (in combination with calcium intake) plays in building a strong skeleton and preventing bone loss.
Other societies supporting the statement are the European Calcified Tissue Society, the National Osteoporosis Foundation, and the International Osteoporosis Foundation.
What role for vitamin D in COVID-19?
Over recent months, the role of vitamin D in relation to prevention of COVID-19 has been the subject of intense debate. Now, these societies have joined forces and endorsed evidence-based guidance to clarify the issue around obtaining the daily recommended dosage of vitamin D.
During the pandemic, orders to stay at home meant individuals were likely to spend less time outdoors and have less opportunity to draw their vitamin D directly from sunlight, which is its main source, other than a limited number of foods or as a dietary supplement, the societies explained.
However, they acknowledged that the role of vitamin D in COVID-19 remains unclear.
“The current data do not provide any evidence that vitamin D supplementation will help prevent or treat COVID-19 infection; however, our guidance does not preclude further study of the potential effects of vitamin D on COVID-19,” the joint statement said.
Research to date suggests that vitamin D may play a role in enhancing the immune response, and given prior work demonstrating a role for the activated form of vitamin D – 1,25(OH)2D – in immune responses, “further research into vitamin D supplementation in COVID-19 disease is warranted,” it added. “Trials to date have been observational and there have been no randomized, controlled trials from which firm conclusions about causal relationships can be drawn. Observational studies suggest associations between low vitamin D concentrations and higher rates of COVID-19 infection.”
Medscape Medical News previously reported on the existing observational data regarding vitamin D in COVID-19. A recent rapid evidence review by the National Institute for Health and Care Excellence failed to find any evidence that vitamin D supplementation reduces the risk or severity of COVID-19.
A version of this article originally appeared on Medscape.com.
Six medical societies from across the globe are emphasizing the importance of individuals obtaining the daily recommended dose of vitamin D, especially given the impact of the COVID-19 pandemic on outdoor time.
The statement, “Joint Guidance on Vitamin D in the Era of COVID-19,” is supported by the American Society for Bone and Mineral Research, the Endocrine Society, and the American Association of Clinical Endocrinologists, among others.
They felt the need to clarify the recommendations for clinicians. Central to the guidance is the recommendation to directly expose the skin to sunlight for 15-30 minutes per day, while taking care to avoid sunburn.
The statement noted that “vitamin D is very safe when taken at reasonable dosages and is important for musculoskeletal health. Levels are likely to decline as individuals reduce outside activity (sun exposure) during the pandemic.”
It added that “most older and younger adults can safely take 400-1000 IU daily to keep vitamin D levels within the optimal range as recommended by [the US] Institute of Medicine guidelines.”
The statement also noted that the scientific evidence clearly supports the benefits that vitamin D (in combination with calcium intake) plays in building a strong skeleton and preventing bone loss.
Other societies supporting the statement are the European Calcified Tissue Society, the National Osteoporosis Foundation, and the International Osteoporosis Foundation.
What role for vitamin D in COVID-19?
Over recent months, the role of vitamin D in relation to prevention of COVID-19 has been the subject of intense debate. Now, these societies have joined forces and endorsed evidence-based guidance to clarify the issue around obtaining the daily recommended dosage of vitamin D.
During the pandemic, orders to stay at home meant individuals were likely to spend less time outdoors and have less opportunity to draw their vitamin D directly from sunlight, which is its main source, other than a limited number of foods or as a dietary supplement, the societies explained.
However, they acknowledged that the role of vitamin D in COVID-19 remains unclear.
“The current data do not provide any evidence that vitamin D supplementation will help prevent or treat COVID-19 infection; however, our guidance does not preclude further study of the potential effects of vitamin D on COVID-19,” the joint statement said.
Research to date suggests that vitamin D may play a role in enhancing the immune response, and given prior work demonstrating a role for the activated form of vitamin D – 1,25(OH)2D – in immune responses, “further research into vitamin D supplementation in COVID-19 disease is warranted,” it added. “Trials to date have been observational and there have been no randomized, controlled trials from which firm conclusions about causal relationships can be drawn. Observational studies suggest associations between low vitamin D concentrations and higher rates of COVID-19 infection.”
Medscape Medical News previously reported on the existing observational data regarding vitamin D in COVID-19. A recent rapid evidence review by the National Institute for Health and Care Excellence failed to find any evidence that vitamin D supplementation reduces the risk or severity of COVID-19.
A version of this article originally appeared on Medscape.com.
Daily Recap: Hospitalized COVID patients need MRIs; Americans vote for face masks
Here are the stories our MDedge editors across specialties think you need to know about today:
Three stages to COVID-19 brain damage, new review suggests
A new review outlined a three-stage classification of the impact of COVID-19 on the central nervous system and recommended all hospitalized patients with the virus undergo MRI to flag potential neurologic damage and inform postdischarge monitoring.
In stage 1, viral damage is limited to epithelial cells of the nose and mouth, and in stage 2 blood clots that form in the lungs may travel to the brain, leading to stroke. In stage 3, the virus crosses the blood-brain barrier and invades the brain.
“Our major take-home points are that patients with COVID-19 symptoms, such as shortness of breath, headache, or dizziness, may have neurological symptoms that, at the time of hospitalization, might not be noticed or prioritized, or whose neurological symptoms may become apparent only after they leave the hospital,” said lead author Majid Fotuhi, MD, PhD. The review was published online in the Journal of Alzheimer’s Disease. Read more.
Topline results for novel intranasal med to treat opioid overdose
Topline results show positive results for the experimental intranasal nalmefene product OX125 for opioid overdose reversal, Orexo, the drug’s manufacturer, announced.
A crossover, comparative bioavailability study was conducted in healthy volunteers to assess nalmefene absorption of three development formulations of OX125. Preliminary results showed “extensive and rapid absorption” across all three formulations versus an intramuscular injection of nalmefene, Orexo reported.
“As the U.S. heroin crisis has developed to a fentanyl crisis, the medical need for novel and more powerful opioid rescue medications is vast,” Nikolaj Sørensen, president and CEO of Orexo, said in a press release. Read more.
Republican or Democrat, Americans vote for face masks
Most Americans support the required use of face masks in public, along with universal COVID-19 testing, to provide a safe work environment during the pandemic, according to a new report from the Commonwealth Fund.
Results of a recent survey show that 85% of adults believe that it is very or somewhat important to require everyone to wear a face mask “at work, when shopping, and on public transportation,” said Sara R. Collins, PhD, vice president for health care coverage and access at the fund, and associates.
Regarding regular testing, 66% of Republicans and those leaning Republican said that such testing was very/somewhat important to ensure a safe work environment, as did 91% on the Democratic side. Read more.
Weight loss failures drive bariatric surgery regrets
Not all weight loss surgery patients “live happily ever after,” according to Daniel B. Jones, MD.
A 2014 study of 22 women who underwent weight loss surgery reported lower energy, worse quality of life, and persistent eating disorders.
Of gastric band patients, “almost 20% did not think they made the right decision,” he said. As for RYGP patients, 13% of patients at 1 year and 4 years reported that weight loss surgery caused “some” or “a lot” of negative effects. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Three stages to COVID-19 brain damage, new review suggests
A new review outlined a three-stage classification of the impact of COVID-19 on the central nervous system and recommended all hospitalized patients with the virus undergo MRI to flag potential neurologic damage and inform postdischarge monitoring.
In stage 1, viral damage is limited to epithelial cells of the nose and mouth, and in stage 2 blood clots that form in the lungs may travel to the brain, leading to stroke. In stage 3, the virus crosses the blood-brain barrier and invades the brain.
“Our major take-home points are that patients with COVID-19 symptoms, such as shortness of breath, headache, or dizziness, may have neurological symptoms that, at the time of hospitalization, might not be noticed or prioritized, or whose neurological symptoms may become apparent only after they leave the hospital,” said lead author Majid Fotuhi, MD, PhD. The review was published online in the Journal of Alzheimer’s Disease. Read more.
Topline results for novel intranasal med to treat opioid overdose
Topline results show positive results for the experimental intranasal nalmefene product OX125 for opioid overdose reversal, Orexo, the drug’s manufacturer, announced.
A crossover, comparative bioavailability study was conducted in healthy volunteers to assess nalmefene absorption of three development formulations of OX125. Preliminary results showed “extensive and rapid absorption” across all three formulations versus an intramuscular injection of nalmefene, Orexo reported.
“As the U.S. heroin crisis has developed to a fentanyl crisis, the medical need for novel and more powerful opioid rescue medications is vast,” Nikolaj Sørensen, president and CEO of Orexo, said in a press release. Read more.
Republican or Democrat, Americans vote for face masks
Most Americans support the required use of face masks in public, along with universal COVID-19 testing, to provide a safe work environment during the pandemic, according to a new report from the Commonwealth Fund.
Results of a recent survey show that 85% of adults believe that it is very or somewhat important to require everyone to wear a face mask “at work, when shopping, and on public transportation,” said Sara R. Collins, PhD, vice president for health care coverage and access at the fund, and associates.
Regarding regular testing, 66% of Republicans and those leaning Republican said that such testing was very/somewhat important to ensure a safe work environment, as did 91% on the Democratic side. Read more.
Weight loss failures drive bariatric surgery regrets
Not all weight loss surgery patients “live happily ever after,” according to Daniel B. Jones, MD.
A 2014 study of 22 women who underwent weight loss surgery reported lower energy, worse quality of life, and persistent eating disorders.
Of gastric band patients, “almost 20% did not think they made the right decision,” he said. As for RYGP patients, 13% of patients at 1 year and 4 years reported that weight loss surgery caused “some” or “a lot” of negative effects. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Three stages to COVID-19 brain damage, new review suggests
A new review outlined a three-stage classification of the impact of COVID-19 on the central nervous system and recommended all hospitalized patients with the virus undergo MRI to flag potential neurologic damage and inform postdischarge monitoring.
In stage 1, viral damage is limited to epithelial cells of the nose and mouth, and in stage 2 blood clots that form in the lungs may travel to the brain, leading to stroke. In stage 3, the virus crosses the blood-brain barrier and invades the brain.
“Our major take-home points are that patients with COVID-19 symptoms, such as shortness of breath, headache, or dizziness, may have neurological symptoms that, at the time of hospitalization, might not be noticed or prioritized, or whose neurological symptoms may become apparent only after they leave the hospital,” said lead author Majid Fotuhi, MD, PhD. The review was published online in the Journal of Alzheimer’s Disease. Read more.
Topline results for novel intranasal med to treat opioid overdose
Topline results show positive results for the experimental intranasal nalmefene product OX125 for opioid overdose reversal, Orexo, the drug’s manufacturer, announced.
A crossover, comparative bioavailability study was conducted in healthy volunteers to assess nalmefene absorption of three development formulations of OX125. Preliminary results showed “extensive and rapid absorption” across all three formulations versus an intramuscular injection of nalmefene, Orexo reported.
“As the U.S. heroin crisis has developed to a fentanyl crisis, the medical need for novel and more powerful opioid rescue medications is vast,” Nikolaj Sørensen, president and CEO of Orexo, said in a press release. Read more.
Republican or Democrat, Americans vote for face masks
Most Americans support the required use of face masks in public, along with universal COVID-19 testing, to provide a safe work environment during the pandemic, according to a new report from the Commonwealth Fund.
Results of a recent survey show that 85% of adults believe that it is very or somewhat important to require everyone to wear a face mask “at work, when shopping, and on public transportation,” said Sara R. Collins, PhD, vice president for health care coverage and access at the fund, and associates.
Regarding regular testing, 66% of Republicans and those leaning Republican said that such testing was very/somewhat important to ensure a safe work environment, as did 91% on the Democratic side. Read more.
Weight loss failures drive bariatric surgery regrets
Not all weight loss surgery patients “live happily ever after,” according to Daniel B. Jones, MD.
A 2014 study of 22 women who underwent weight loss surgery reported lower energy, worse quality of life, and persistent eating disorders.
Of gastric band patients, “almost 20% did not think they made the right decision,” he said. As for RYGP patients, 13% of patients at 1 year and 4 years reported that weight loss surgery caused “some” or “a lot” of negative effects. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Daily Recap: Docs are good at saving money; SARS-CoV-2 vaccine trials advance
Here are the stories our MDedge editors across specialties think you need to know about today:
Many physicians live within their means and save
Although about two of five physicians report a net worth of between $1 million and $5 million, about half report that they are living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.
Net worth figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%). Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000. Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
Asked about saving habits, 43% of physicians reported they live below their means. Just 7% said they live above their means. How do they save money? Survey respondents reported putting bonus money into an investment account, putting extra money toward paying down the mortgage, and bringing lunch to work everyday.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic. Read more.
Phase 3 COVID-19 vaccine trials launching in July
There are now 120 Investigational New Drug applications to the Food and Drug Administration for a SARS-CoV-2 vaccine, and researchers at more than 70 companies across the globe are interested in making a vaccine, according to Paul A. Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.” Read more.
FDA approves in-home breast cancer treatment
The Food and Drug Administration has approved a combination of subcutaneous breast cancer treatments that could be administered at home, following completion of chemotherapy.
The agency gave the green light to pertuzumab (Perjeta, Genentech/Roche), trastuzumab (Herceptin, Genentech/Roche) and hyaluronidase (Phesgo, Genentech/Roche), administered subcutaneously rather than intravenously, for the treatment of early and metastatic HER2-positive breast cancers.
Phesgo is initially used in combination with chemotherapy at an infusion center but could continue to be administered in a patient’s home by a qualified health care professional once chemotherapy is complete. Read more.
Could a visual tool aid migraine management?
A new visual tool aims to streamline patient-clinician communication about risk factors for progression from episodic to chronic migraines.
The tool is still just a prototype, but it could eventually synthesize patient responses to an integrated questionnaire and produce a chart illustrating where the patient stands with respect to a range of modifiable risk factors from depression to insomnia.
Physicians must see patients in short appointment periods, making it difficult to communicate all of the risk factors and behavioral characteristics that can contribute to risk of progression. “If you have a patient and you’re able to look at a visualization tool quickly and say: ‘Okay, my patient really is having insomnia and sleep issues,’ you can focus the session talking about sleep, cognitive-behavioral therapy for insomnia, and all the things we can help patients with,” lead researcher Ami Cuneo, MD, who is a headache fellow at the University of Washington, Seattle, said in an interview.
Dr. Cuneo presented a poster describing the concept at the virtual annual meeting of the American Headache Society. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Many physicians live within their means and save
Although about two of five physicians report a net worth of between $1 million and $5 million, about half report that they are living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.
Net worth figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%). Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000. Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
Asked about saving habits, 43% of physicians reported they live below their means. Just 7% said they live above their means. How do they save money? Survey respondents reported putting bonus money into an investment account, putting extra money toward paying down the mortgage, and bringing lunch to work everyday.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic. Read more.
Phase 3 COVID-19 vaccine trials launching in July
There are now 120 Investigational New Drug applications to the Food and Drug Administration for a SARS-CoV-2 vaccine, and researchers at more than 70 companies across the globe are interested in making a vaccine, according to Paul A. Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.” Read more.
FDA approves in-home breast cancer treatment
The Food and Drug Administration has approved a combination of subcutaneous breast cancer treatments that could be administered at home, following completion of chemotherapy.
The agency gave the green light to pertuzumab (Perjeta, Genentech/Roche), trastuzumab (Herceptin, Genentech/Roche) and hyaluronidase (Phesgo, Genentech/Roche), administered subcutaneously rather than intravenously, for the treatment of early and metastatic HER2-positive breast cancers.
Phesgo is initially used in combination with chemotherapy at an infusion center but could continue to be administered in a patient’s home by a qualified health care professional once chemotherapy is complete. Read more.
Could a visual tool aid migraine management?
A new visual tool aims to streamline patient-clinician communication about risk factors for progression from episodic to chronic migraines.
The tool is still just a prototype, but it could eventually synthesize patient responses to an integrated questionnaire and produce a chart illustrating where the patient stands with respect to a range of modifiable risk factors from depression to insomnia.
Physicians must see patients in short appointment periods, making it difficult to communicate all of the risk factors and behavioral characteristics that can contribute to risk of progression. “If you have a patient and you’re able to look at a visualization tool quickly and say: ‘Okay, my patient really is having insomnia and sleep issues,’ you can focus the session talking about sleep, cognitive-behavioral therapy for insomnia, and all the things we can help patients with,” lead researcher Ami Cuneo, MD, who is a headache fellow at the University of Washington, Seattle, said in an interview.
Dr. Cuneo presented a poster describing the concept at the virtual annual meeting of the American Headache Society. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Many physicians live within their means and save
Although about two of five physicians report a net worth of between $1 million and $5 million, about half report that they are living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.
Net worth figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%). Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000. Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
Asked about saving habits, 43% of physicians reported they live below their means. Just 7% said they live above their means. How do they save money? Survey respondents reported putting bonus money into an investment account, putting extra money toward paying down the mortgage, and bringing lunch to work everyday.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic. Read more.
Phase 3 COVID-19 vaccine trials launching in July
There are now 120 Investigational New Drug applications to the Food and Drug Administration for a SARS-CoV-2 vaccine, and researchers at more than 70 companies across the globe are interested in making a vaccine, according to Paul A. Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.” Read more.
FDA approves in-home breast cancer treatment
The Food and Drug Administration has approved a combination of subcutaneous breast cancer treatments that could be administered at home, following completion of chemotherapy.
The agency gave the green light to pertuzumab (Perjeta, Genentech/Roche), trastuzumab (Herceptin, Genentech/Roche) and hyaluronidase (Phesgo, Genentech/Roche), administered subcutaneously rather than intravenously, for the treatment of early and metastatic HER2-positive breast cancers.
Phesgo is initially used in combination with chemotherapy at an infusion center but could continue to be administered in a patient’s home by a qualified health care professional once chemotherapy is complete. Read more.
Could a visual tool aid migraine management?
A new visual tool aims to streamline patient-clinician communication about risk factors for progression from episodic to chronic migraines.
The tool is still just a prototype, but it could eventually synthesize patient responses to an integrated questionnaire and produce a chart illustrating where the patient stands with respect to a range of modifiable risk factors from depression to insomnia.
Physicians must see patients in short appointment periods, making it difficult to communicate all of the risk factors and behavioral characteristics that can contribute to risk of progression. “If you have a patient and you’re able to look at a visualization tool quickly and say: ‘Okay, my patient really is having insomnia and sleep issues,’ you can focus the session talking about sleep, cognitive-behavioral therapy for insomnia, and all the things we can help patients with,” lead researcher Ami Cuneo, MD, who is a headache fellow at the University of Washington, Seattle, said in an interview.
Dr. Cuneo presented a poster describing the concept at the virtual annual meeting of the American Headache Society. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Guidance on infection prevention for health care personnel
As we reopen our offices we are faced with the challenge of determining the best way to do it safely – protecting ourselves, our staff, and our patients.
In this column we will focus on selected details of the recommendations from IDSA and the CDC that may be helpful in primary care offices.
Face masks
Many clinicians have asked whether a physician should use a mask while seeing patients without COVID-19 in the office, and if yes, which type. The IDSA guideline states that mask usage is imperative for reducing the risk of health care workers contracting COVID-19.1 The evidence is derived from a number of sources, including a retrospective study from Wuhan (China) University that examined two groups of health care workers during the outbreak. The first group wore N95 masks and washed their hands frequently, while the second group did not wear masks and washed their hands less frequently. In the group that took greater actions to protect themselves, none of the 493 staff members contracted COVID-19, compared with 10 of 213 staff members in the other group. The decrease in infection rate occurred in the group that wore masks despite the fact that this group had 733% more exposure to COVID-19 patients.2 Further evidence came from a case-control study done in hospitals in Hong Kong during the 2003 SARS-CoV outbreak.3 This study showed that mask wearing was the most significant intervention for reducing infection, followed by gowning, and then handwashing. These findings make it clear that mask usage is a must for all health care providers who may be caring for patients who could have COVID-19.
The guideline also reviews evidence about the use of surgical masks versus N95 masks. On reviewing indirect evidence from the SARS-CoV epidemic, IDSA found that wearing any mask – surgical or N95 – led to a large reduction in the risk of developing an infection. In this systematic review of five observational studies in health care personnel, for those wearing surgical masks, the odds ratio for developing an infection was 0.13 (95% CI, 0.03-0.62), and for those wearing N95 masks, the odds ratio was 0.12 (95% CI, 0.06-0.26). There was not a significant difference between risk reductions for those who wore surgical masks and N95 masks, respectively.1,4 The IDSA guideline panel recommended “that health care personnel caring for patients with suspected or known COVID-19 use either a surgical mask or N95 respirator ... as part of appropriate PPE.” Since there is not a significant difference in outcomes between those who use surgical masks and those who use N95 respirators, and the IDSA guideline states either type of mask is considered appropriate when taking care of patients with suspected or known COVID-19, in our opinion, use of surgical masks rather than N95s is sufficient when performing low-risk activities. Such activities include seeing patients who do not have a high likelihood of COVID-19 in the office setting.
The IDSA recommendation also discusses universal masking, defined as both patients and clinicians wearing masks. The recommendation is supported by the findings of a study in which universal mask usage was used to prevent the spread of H1N 1 during the 2009 outbreak. In this study of staff members and patients exposed to H1N1 who all wore masks, only 0.48% of 836 acquired infection. In the same study, not wearing a mask by either the provider or patient increased the risk of infection.5 Also, in a prospective study of hematopoietic stem cell transplant patients, universal masking caused infection rates to drop from 10.3% to 4.4%.6
The IDSA guideline states the following: “There may be some, albeit uncertain, benefit to universal masking in the absence of resource constraints. However, the benefits of universal masking with surgical masks should be weighed against the risk of increasing the PPE burn rate and contextualized to the background COVID-19 prevalence rate for asymptomatic or minimally symptomatic HCPs [health care providers] and visitors.”1
The CDC’s guidance statement says the following: “Continued community transmission has increased the number of individuals potentially exposed to and infectious with SARS-CoV-2. Fever and symptom screening have proven to be relatively ineffective in identifying all infected individuals, including HCPs. Symptom screening also will not identify individuals who are infected but otherwise asymptomatic or pre-symptomatic; additional interventions are needed to limit the unrecognized introduction of SARS-CoV-2 into healthcare settings by these individuals. As part of aggressive source control measures, healthcare facilities should consider implementing policies requiring everyone entering the facility to wear a cloth face covering (if tolerated) while in the building, regardless of symptoms.”7
It is our opinion, based on the CDC and IDSA recommendations, that both clinicians and patients should be required to wear masks when patients are seen in the office if possible. Many offices have instituted a policy that says, if a patient refuses to wear a mask during an office visit, then the patient will not be seen.
Eye protection
Many clinicians are uncertain about whether eye protection needs to be used when seeing asymptomatic patients. The IDSA acknowledges that there are not studies that have looked critically at eye protection, but the society also acknowledges “appropriate personal protective equipment includes, in addition to a mask or respirator, eye protection, gown and gloves.”1 In addition, the CDC recommends that, for healthcare workers located in areas with moderate or higher prevalence of COVID-19, HCPs should wear eye protection in addition to facemasks since they may encounter asymptomatic individuals with COVID-19.
Gowns and gloves
Gowns and gloves are recommended as a part of personal protective gear when caring for patients who have COVID-19. The IDSA guideline is clear in its recommendations, but does not cite evidence for having no gloves versus having gloves. Furthermore, they state that the evidence is insufficient to recommend double gloves, with the top glove used to take off a personal protective gown, and the inner glove discarded after the gown is removed. The CDC do not make recommendations for routine use of gloves in the care of patients who do not have COVID-19, even in areas where there may be asymptomatic COVID-19, and recommends standard precautions, specifically practicing hand hygiene before and after patient contact.8
The Bottom Line
When seeing patients with COVID-19, N-95 masks, goggles or face shields, gowns, and gloves should be used, with hand hygiene routinely practiced before and after seeing patients. For offices seeing patients not suspected of having COVID-19, the IDSA guideline clarifies that there is not a statistical difference in acquisition of infection with the use of surgical face masks vs N95 respirators. According to the CDC recommendations, eye protection in addition to facemasks should be used by the health care provider, and masks should be worn by patients. Hand hygiene should be used routinely before and after all patient contact. With use of these approaches, it should be safe for offices to reopen and see patients.
Neil Skolnik, MD, is professor of family and community medicine at the Thomas Jefferson University, Philadelphia, and associate director of the Family Medicine Residency Program at Abington (Pa.) Jefferson Health. Jeffrey Matthews, DO, is a second-year resident in the Family Medicine Residency at Abington Jefferson Health. For questions or comments, feel free to contact Dr. Skolnik on Twitter @NeilSkolnik.
References
1. Lynch JB, Davitkov P, Anderson DJ, et al. COVID-19 Guideline, Part 2: Infection Prevention. IDSA Home. https://www.idsociety.org/practice-guideline/covid-19-guideline-infection-prevention/. April 27, 2020. Accessed June 10, 2020.
2. J Hosp Infect. 2020 May;105(1):104-5.
3. Lancet. 2003;361(9368):1519-20.
4. Influenza Other Respir Viruses. 2020 Apr 4. doi: 2020;10.1111/irv.12745.
5. J Hosp Infect. 2010;74(3):271-7.
6. Clin Infect Dis. 2016;63(8):999-1006.
7. Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Accessed Jun 16, 2020.
8. Centers for Disease Control and Prevention. Healthcare Infection Prevention and Control FAQs for COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-faq.html. Accessed June 15, 2020.
As we reopen our offices we are faced with the challenge of determining the best way to do it safely – protecting ourselves, our staff, and our patients.
In this column we will focus on selected details of the recommendations from IDSA and the CDC that may be helpful in primary care offices.
Face masks
Many clinicians have asked whether a physician should use a mask while seeing patients without COVID-19 in the office, and if yes, which type. The IDSA guideline states that mask usage is imperative for reducing the risk of health care workers contracting COVID-19.1 The evidence is derived from a number of sources, including a retrospective study from Wuhan (China) University that examined two groups of health care workers during the outbreak. The first group wore N95 masks and washed their hands frequently, while the second group did not wear masks and washed their hands less frequently. In the group that took greater actions to protect themselves, none of the 493 staff members contracted COVID-19, compared with 10 of 213 staff members in the other group. The decrease in infection rate occurred in the group that wore masks despite the fact that this group had 733% more exposure to COVID-19 patients.2 Further evidence came from a case-control study done in hospitals in Hong Kong during the 2003 SARS-CoV outbreak.3 This study showed that mask wearing was the most significant intervention for reducing infection, followed by gowning, and then handwashing. These findings make it clear that mask usage is a must for all health care providers who may be caring for patients who could have COVID-19.
The guideline also reviews evidence about the use of surgical masks versus N95 masks. On reviewing indirect evidence from the SARS-CoV epidemic, IDSA found that wearing any mask – surgical or N95 – led to a large reduction in the risk of developing an infection. In this systematic review of five observational studies in health care personnel, for those wearing surgical masks, the odds ratio for developing an infection was 0.13 (95% CI, 0.03-0.62), and for those wearing N95 masks, the odds ratio was 0.12 (95% CI, 0.06-0.26). There was not a significant difference between risk reductions for those who wore surgical masks and N95 masks, respectively.1,4 The IDSA guideline panel recommended “that health care personnel caring for patients with suspected or known COVID-19 use either a surgical mask or N95 respirator ... as part of appropriate PPE.” Since there is not a significant difference in outcomes between those who use surgical masks and those who use N95 respirators, and the IDSA guideline states either type of mask is considered appropriate when taking care of patients with suspected or known COVID-19, in our opinion, use of surgical masks rather than N95s is sufficient when performing low-risk activities. Such activities include seeing patients who do not have a high likelihood of COVID-19 in the office setting.
The IDSA recommendation also discusses universal masking, defined as both patients and clinicians wearing masks. The recommendation is supported by the findings of a study in which universal mask usage was used to prevent the spread of H1N 1 during the 2009 outbreak. In this study of staff members and patients exposed to H1N1 who all wore masks, only 0.48% of 836 acquired infection. In the same study, not wearing a mask by either the provider or patient increased the risk of infection.5 Also, in a prospective study of hematopoietic stem cell transplant patients, universal masking caused infection rates to drop from 10.3% to 4.4%.6
The IDSA guideline states the following: “There may be some, albeit uncertain, benefit to universal masking in the absence of resource constraints. However, the benefits of universal masking with surgical masks should be weighed against the risk of increasing the PPE burn rate and contextualized to the background COVID-19 prevalence rate for asymptomatic or minimally symptomatic HCPs [health care providers] and visitors.”1
The CDC’s guidance statement says the following: “Continued community transmission has increased the number of individuals potentially exposed to and infectious with SARS-CoV-2. Fever and symptom screening have proven to be relatively ineffective in identifying all infected individuals, including HCPs. Symptom screening also will not identify individuals who are infected but otherwise asymptomatic or pre-symptomatic; additional interventions are needed to limit the unrecognized introduction of SARS-CoV-2 into healthcare settings by these individuals. As part of aggressive source control measures, healthcare facilities should consider implementing policies requiring everyone entering the facility to wear a cloth face covering (if tolerated) while in the building, regardless of symptoms.”7
It is our opinion, based on the CDC and IDSA recommendations, that both clinicians and patients should be required to wear masks when patients are seen in the office if possible. Many offices have instituted a policy that says, if a patient refuses to wear a mask during an office visit, then the patient will not be seen.
Eye protection
Many clinicians are uncertain about whether eye protection needs to be used when seeing asymptomatic patients. The IDSA acknowledges that there are not studies that have looked critically at eye protection, but the society also acknowledges “appropriate personal protective equipment includes, in addition to a mask or respirator, eye protection, gown and gloves.”1 In addition, the CDC recommends that, for healthcare workers located in areas with moderate or higher prevalence of COVID-19, HCPs should wear eye protection in addition to facemasks since they may encounter asymptomatic individuals with COVID-19.
Gowns and gloves
Gowns and gloves are recommended as a part of personal protective gear when caring for patients who have COVID-19. The IDSA guideline is clear in its recommendations, but does not cite evidence for having no gloves versus having gloves. Furthermore, they state that the evidence is insufficient to recommend double gloves, with the top glove used to take off a personal protective gown, and the inner glove discarded after the gown is removed. The CDC do not make recommendations for routine use of gloves in the care of patients who do not have COVID-19, even in areas where there may be asymptomatic COVID-19, and recommends standard precautions, specifically practicing hand hygiene before and after patient contact.8
The Bottom Line
When seeing patients with COVID-19, N-95 masks, goggles or face shields, gowns, and gloves should be used, with hand hygiene routinely practiced before and after seeing patients. For offices seeing patients not suspected of having COVID-19, the IDSA guideline clarifies that there is not a statistical difference in acquisition of infection with the use of surgical face masks vs N95 respirators. According to the CDC recommendations, eye protection in addition to facemasks should be used by the health care provider, and masks should be worn by patients. Hand hygiene should be used routinely before and after all patient contact. With use of these approaches, it should be safe for offices to reopen and see patients.
Neil Skolnik, MD, is professor of family and community medicine at the Thomas Jefferson University, Philadelphia, and associate director of the Family Medicine Residency Program at Abington (Pa.) Jefferson Health. Jeffrey Matthews, DO, is a second-year resident in the Family Medicine Residency at Abington Jefferson Health. For questions or comments, feel free to contact Dr. Skolnik on Twitter @NeilSkolnik.
References
1. Lynch JB, Davitkov P, Anderson DJ, et al. COVID-19 Guideline, Part 2: Infection Prevention. IDSA Home. https://www.idsociety.org/practice-guideline/covid-19-guideline-infection-prevention/. April 27, 2020. Accessed June 10, 2020.
2. J Hosp Infect. 2020 May;105(1):104-5.
3. Lancet. 2003;361(9368):1519-20.
4. Influenza Other Respir Viruses. 2020 Apr 4. doi: 2020;10.1111/irv.12745.
5. J Hosp Infect. 2010;74(3):271-7.
6. Clin Infect Dis. 2016;63(8):999-1006.
7. Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Accessed Jun 16, 2020.
8. Centers for Disease Control and Prevention. Healthcare Infection Prevention and Control FAQs for COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-faq.html. Accessed June 15, 2020.
As we reopen our offices we are faced with the challenge of determining the best way to do it safely – protecting ourselves, our staff, and our patients.
In this column we will focus on selected details of the recommendations from IDSA and the CDC that may be helpful in primary care offices.
Face masks
Many clinicians have asked whether a physician should use a mask while seeing patients without COVID-19 in the office, and if yes, which type. The IDSA guideline states that mask usage is imperative for reducing the risk of health care workers contracting COVID-19.1 The evidence is derived from a number of sources, including a retrospective study from Wuhan (China) University that examined two groups of health care workers during the outbreak. The first group wore N95 masks and washed their hands frequently, while the second group did not wear masks and washed their hands less frequently. In the group that took greater actions to protect themselves, none of the 493 staff members contracted COVID-19, compared with 10 of 213 staff members in the other group. The decrease in infection rate occurred in the group that wore masks despite the fact that this group had 733% more exposure to COVID-19 patients.2 Further evidence came from a case-control study done in hospitals in Hong Kong during the 2003 SARS-CoV outbreak.3 This study showed that mask wearing was the most significant intervention for reducing infection, followed by gowning, and then handwashing. These findings make it clear that mask usage is a must for all health care providers who may be caring for patients who could have COVID-19.
The guideline also reviews evidence about the use of surgical masks versus N95 masks. On reviewing indirect evidence from the SARS-CoV epidemic, IDSA found that wearing any mask – surgical or N95 – led to a large reduction in the risk of developing an infection. In this systematic review of five observational studies in health care personnel, for those wearing surgical masks, the odds ratio for developing an infection was 0.13 (95% CI, 0.03-0.62), and for those wearing N95 masks, the odds ratio was 0.12 (95% CI, 0.06-0.26). There was not a significant difference between risk reductions for those who wore surgical masks and N95 masks, respectively.1,4 The IDSA guideline panel recommended “that health care personnel caring for patients with suspected or known COVID-19 use either a surgical mask or N95 respirator ... as part of appropriate PPE.” Since there is not a significant difference in outcomes between those who use surgical masks and those who use N95 respirators, and the IDSA guideline states either type of mask is considered appropriate when taking care of patients with suspected or known COVID-19, in our opinion, use of surgical masks rather than N95s is sufficient when performing low-risk activities. Such activities include seeing patients who do not have a high likelihood of COVID-19 in the office setting.
The IDSA recommendation also discusses universal masking, defined as both patients and clinicians wearing masks. The recommendation is supported by the findings of a study in which universal mask usage was used to prevent the spread of H1N 1 during the 2009 outbreak. In this study of staff members and patients exposed to H1N1 who all wore masks, only 0.48% of 836 acquired infection. In the same study, not wearing a mask by either the provider or patient increased the risk of infection.5 Also, in a prospective study of hematopoietic stem cell transplant patients, universal masking caused infection rates to drop from 10.3% to 4.4%.6
The IDSA guideline states the following: “There may be some, albeit uncertain, benefit to universal masking in the absence of resource constraints. However, the benefits of universal masking with surgical masks should be weighed against the risk of increasing the PPE burn rate and contextualized to the background COVID-19 prevalence rate for asymptomatic or minimally symptomatic HCPs [health care providers] and visitors.”1
The CDC’s guidance statement says the following: “Continued community transmission has increased the number of individuals potentially exposed to and infectious with SARS-CoV-2. Fever and symptom screening have proven to be relatively ineffective in identifying all infected individuals, including HCPs. Symptom screening also will not identify individuals who are infected but otherwise asymptomatic or pre-symptomatic; additional interventions are needed to limit the unrecognized introduction of SARS-CoV-2 into healthcare settings by these individuals. As part of aggressive source control measures, healthcare facilities should consider implementing policies requiring everyone entering the facility to wear a cloth face covering (if tolerated) while in the building, regardless of symptoms.”7
It is our opinion, based on the CDC and IDSA recommendations, that both clinicians and patients should be required to wear masks when patients are seen in the office if possible. Many offices have instituted a policy that says, if a patient refuses to wear a mask during an office visit, then the patient will not be seen.
Eye protection
Many clinicians are uncertain about whether eye protection needs to be used when seeing asymptomatic patients. The IDSA acknowledges that there are not studies that have looked critically at eye protection, but the society also acknowledges “appropriate personal protective equipment includes, in addition to a mask or respirator, eye protection, gown and gloves.”1 In addition, the CDC recommends that, for healthcare workers located in areas with moderate or higher prevalence of COVID-19, HCPs should wear eye protection in addition to facemasks since they may encounter asymptomatic individuals with COVID-19.
Gowns and gloves
Gowns and gloves are recommended as a part of personal protective gear when caring for patients who have COVID-19. The IDSA guideline is clear in its recommendations, but does not cite evidence for having no gloves versus having gloves. Furthermore, they state that the evidence is insufficient to recommend double gloves, with the top glove used to take off a personal protective gown, and the inner glove discarded after the gown is removed. The CDC do not make recommendations for routine use of gloves in the care of patients who do not have COVID-19, even in areas where there may be asymptomatic COVID-19, and recommends standard precautions, specifically practicing hand hygiene before and after patient contact.8
The Bottom Line
When seeing patients with COVID-19, N-95 masks, goggles or face shields, gowns, and gloves should be used, with hand hygiene routinely practiced before and after seeing patients. For offices seeing patients not suspected of having COVID-19, the IDSA guideline clarifies that there is not a statistical difference in acquisition of infection with the use of surgical face masks vs N95 respirators. According to the CDC recommendations, eye protection in addition to facemasks should be used by the health care provider, and masks should be worn by patients. Hand hygiene should be used routinely before and after all patient contact. With use of these approaches, it should be safe for offices to reopen and see patients.
Neil Skolnik, MD, is professor of family and community medicine at the Thomas Jefferson University, Philadelphia, and associate director of the Family Medicine Residency Program at Abington (Pa.) Jefferson Health. Jeffrey Matthews, DO, is a second-year resident in the Family Medicine Residency at Abington Jefferson Health. For questions or comments, feel free to contact Dr. Skolnik on Twitter @NeilSkolnik.
References
1. Lynch JB, Davitkov P, Anderson DJ, et al. COVID-19 Guideline, Part 2: Infection Prevention. IDSA Home. https://www.idsociety.org/practice-guideline/covid-19-guideline-infection-prevention/. April 27, 2020. Accessed June 10, 2020.
2. J Hosp Infect. 2020 May;105(1):104-5.
3. Lancet. 2003;361(9368):1519-20.
4. Influenza Other Respir Viruses. 2020 Apr 4. doi: 2020;10.1111/irv.12745.
5. J Hosp Infect. 2010;74(3):271-7.
6. Clin Infect Dis. 2016;63(8):999-1006.
7. Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Accessed Jun 16, 2020.
8. Centers for Disease Control and Prevention. Healthcare Infection Prevention and Control FAQs for COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-faq.html. Accessed June 15, 2020.
Cortisol levels on COVID-19 admission may be a marker of severity
Patients with COVID-19 who have high levels of the steroid hormone cortisol on admission to hospital have a substantially increased risk of dying, U.K. researchers have discovered.
Waljit S. Dhillo, MBBS, PhD, head of the division of diabetes, endocrinology and metabolism at Imperial College London, and colleagues studied 535 patients admitted to major London hospitals. Their article was published online June 18 in Lancet Diabetes & Endocrinology.
“Our analyses show for the first time that patients with COVID-19 mount a marked and appropriate acute cortisol stress response,” said Dr. Dhillo and colleagues.
Moreover, “high cortisol concentrations were associated with increased mortality and a reduced median survival, probably because this is a marker of the severity of illness.”
So measuring cortisol on admission is potentially “another simple marker to use alongside oxygen saturation levels to help us identify which patients need to be admitted immediately, and which may not,” Dr. Dhillo noted in a statement from his institution.
“Having an early indicator of which patients may deteriorate more quickly will help us with providing the best level of care as quickly as possible. In addition, we can also take cortisol levels into account when we are working out how best to treat our patients,” he said.
However, it’s important to note that this means – particularly in the wake of the RECOVERY trial reported last week – that “in the early part of the disease you don’t need steroids,” he said.
In contrast to SARS, no adrenal insufficiency with COVID-19
Cortisol levels when healthy and resting are 100-200 nmol/L and nearly zero when sleeping, the researchers explained.
They decided to examine cortisol levels because, although physiological stress from critical illness normally increases levels of the hormone, the prior coronavirus, severe acute respiratory syndrome coronavirus (SARS-CoV), had the opposite effect and induced cortisol insufficiency in some patients.
“We would have said we’re not quite sure” what effect SARS-CoV-2 is having on cortisol levels, “so that’s why we collected the data,” Dr. Dhillo said in an interview.
The researchers studied patients admitted to three large London teaching hospitals between March 9 and April 22 with a clinical suspicion of SARS-CoV-2 infection. All patients had a standard set of blood tests, including full blood count, creatinine, C-reactive protein, D-dimer, and serum cortisol.
After exclusions, the team assessed 535 patients admitted over the study period who had baseline cortisol measured within 48 hours of admission.
Of these, 403 patients were diagnosed with COVID-19 based on a positive result on real-time polymerase chain reaction testing (88%) or a strong clinical and radiological suspicion, despite a negative test (12%).
In total, 132 (25%) individuals were not diagnosed with COVID-19.
Patients with COVID-19 were a mean age of 66.3 years, and 59.6% were men.
Mean cortisol concentrations in patients with COVID-19 were significantly higher than those not diagnosed with the virus (619 vs 519 nmol/L; P < .0001).
And by May 8, significantly more patients with COVID-19 died than those without (27.8% vs 6.8%; P < .0001).
Doubling of cortisol levels associated with 40% higher mortality
Multivariate analysis taking into account age, presence of comorbidities, and laboratory tests revealed that a doubling of cortisol concentrations among those with COVID-19 was associated with a significant increase in mortality, at a hazard ratio of 1.42 (P = .014).
And patients with COVID-19 whose baseline cortisol level was >744 nmol/L had a median survival of just 15 days, compared with those with a level ≤744 nmol/L, who had a median survival of 36 days (P < .0001).
The team notes that the cortisol stress responses in their patients with COVID-19 ranged up to 3,241 nmol/L, which is “a marked cortisol stress response, perhaps higher than is observed in patients undergoing major surgery.”
Of interest, there was no interaction between cortisol levels and ethnicity in their study; a subsequent analysis of the data stratified by black, Asian, and other minority ethnicities revealed no significant differences.
The team note that their results will need to be reproduced in other populations.
“Any potential role for cortisol measurement at baseline and later during an inpatient stay with COVID-19 as a prognostic biomarker, either by itself or in combination with other biomarkers, will require validation in a prospective study.”
Implications for treatment: Reserve dexamethasone for critically ill
Dr. Dhillo explained that, because their findings indicate that people initially infected with COVID-19 do mount an appropriate stress (cortisol) response, it is important that people properly understand this in the wake of the RECOVERY trial, reported last week.
The trial showed that the widely available steroid dexamethasone significantly reduced mortality among severely ill COVID-19 patients in the intensive care unit when given at a supraphysiologic dose of 6 mg.
But it would be hazardous for anyone to self-medicate with steroids at an early stage of COVID-19 because that would further increase cortisol levels and could suppress the immune system.
“For the average person on the street with COVID-19,” excess steroids will make their symptoms worse, Dr. Dhillo explained, adding this is important to emphasize because dexamethasone, and similar steroids, “are cheap and likely available on the Internet, and so misunderstanding of the RECOVERY trial could have serious implications.”
But once patients are very sick, with “inflammation in their lungs” and are in the intensive care unit, and often on ventilators – which is a very small subgroup of those with COVID-19 – it becomes a very different story, he stressed.
“RECOVERY shows clearly there seems to be a benefit once you need oxygen or are on a ventilator, and that makes sense because [dexamethasone] is going to be an anti-inflammatory,” in this instance when the “lungs are full of water.”
“But in the early days you definitely don’t need it and it could be harmful,” he reiterated.
The study is funded by the U.K. National Institute for Health Research and Medical Research Council. The authors have reported no relevant financial relationships.
This article first appeared on Medscape.com.
Patients with COVID-19 who have high levels of the steroid hormone cortisol on admission to hospital have a substantially increased risk of dying, U.K. researchers have discovered.
Waljit S. Dhillo, MBBS, PhD, head of the division of diabetes, endocrinology and metabolism at Imperial College London, and colleagues studied 535 patients admitted to major London hospitals. Their article was published online June 18 in Lancet Diabetes & Endocrinology.
“Our analyses show for the first time that patients with COVID-19 mount a marked and appropriate acute cortisol stress response,” said Dr. Dhillo and colleagues.
Moreover, “high cortisol concentrations were associated with increased mortality and a reduced median survival, probably because this is a marker of the severity of illness.”
So measuring cortisol on admission is potentially “another simple marker to use alongside oxygen saturation levels to help us identify which patients need to be admitted immediately, and which may not,” Dr. Dhillo noted in a statement from his institution.
“Having an early indicator of which patients may deteriorate more quickly will help us with providing the best level of care as quickly as possible. In addition, we can also take cortisol levels into account when we are working out how best to treat our patients,” he said.
However, it’s important to note that this means – particularly in the wake of the RECOVERY trial reported last week – that “in the early part of the disease you don’t need steroids,” he said.
In contrast to SARS, no adrenal insufficiency with COVID-19
Cortisol levels when healthy and resting are 100-200 nmol/L and nearly zero when sleeping, the researchers explained.
They decided to examine cortisol levels because, although physiological stress from critical illness normally increases levels of the hormone, the prior coronavirus, severe acute respiratory syndrome coronavirus (SARS-CoV), had the opposite effect and induced cortisol insufficiency in some patients.
“We would have said we’re not quite sure” what effect SARS-CoV-2 is having on cortisol levels, “so that’s why we collected the data,” Dr. Dhillo said in an interview.
The researchers studied patients admitted to three large London teaching hospitals between March 9 and April 22 with a clinical suspicion of SARS-CoV-2 infection. All patients had a standard set of blood tests, including full blood count, creatinine, C-reactive protein, D-dimer, and serum cortisol.
After exclusions, the team assessed 535 patients admitted over the study period who had baseline cortisol measured within 48 hours of admission.
Of these, 403 patients were diagnosed with COVID-19 based on a positive result on real-time polymerase chain reaction testing (88%) or a strong clinical and radiological suspicion, despite a negative test (12%).
In total, 132 (25%) individuals were not diagnosed with COVID-19.
Patients with COVID-19 were a mean age of 66.3 years, and 59.6% were men.
Mean cortisol concentrations in patients with COVID-19 were significantly higher than those not diagnosed with the virus (619 vs 519 nmol/L; P < .0001).
And by May 8, significantly more patients with COVID-19 died than those without (27.8% vs 6.8%; P < .0001).
Doubling of cortisol levels associated with 40% higher mortality
Multivariate analysis taking into account age, presence of comorbidities, and laboratory tests revealed that a doubling of cortisol concentrations among those with COVID-19 was associated with a significant increase in mortality, at a hazard ratio of 1.42 (P = .014).
And patients with COVID-19 whose baseline cortisol level was >744 nmol/L had a median survival of just 15 days, compared with those with a level ≤744 nmol/L, who had a median survival of 36 days (P < .0001).
The team notes that the cortisol stress responses in their patients with COVID-19 ranged up to 3,241 nmol/L, which is “a marked cortisol stress response, perhaps higher than is observed in patients undergoing major surgery.”
Of interest, there was no interaction between cortisol levels and ethnicity in their study; a subsequent analysis of the data stratified by black, Asian, and other minority ethnicities revealed no significant differences.
The team note that their results will need to be reproduced in other populations.
“Any potential role for cortisol measurement at baseline and later during an inpatient stay with COVID-19 as a prognostic biomarker, either by itself or in combination with other biomarkers, will require validation in a prospective study.”
Implications for treatment: Reserve dexamethasone for critically ill
Dr. Dhillo explained that, because their findings indicate that people initially infected with COVID-19 do mount an appropriate stress (cortisol) response, it is important that people properly understand this in the wake of the RECOVERY trial, reported last week.
The trial showed that the widely available steroid dexamethasone significantly reduced mortality among severely ill COVID-19 patients in the intensive care unit when given at a supraphysiologic dose of 6 mg.
But it would be hazardous for anyone to self-medicate with steroids at an early stage of COVID-19 because that would further increase cortisol levels and could suppress the immune system.
“For the average person on the street with COVID-19,” excess steroids will make their symptoms worse, Dr. Dhillo explained, adding this is important to emphasize because dexamethasone, and similar steroids, “are cheap and likely available on the Internet, and so misunderstanding of the RECOVERY trial could have serious implications.”
But once patients are very sick, with “inflammation in their lungs” and are in the intensive care unit, and often on ventilators – which is a very small subgroup of those with COVID-19 – it becomes a very different story, he stressed.
“RECOVERY shows clearly there seems to be a benefit once you need oxygen or are on a ventilator, and that makes sense because [dexamethasone] is going to be an anti-inflammatory,” in this instance when the “lungs are full of water.”
“But in the early days you definitely don’t need it and it could be harmful,” he reiterated.
The study is funded by the U.K. National Institute for Health Research and Medical Research Council. The authors have reported no relevant financial relationships.
This article first appeared on Medscape.com.
Patients with COVID-19 who have high levels of the steroid hormone cortisol on admission to hospital have a substantially increased risk of dying, U.K. researchers have discovered.
Waljit S. Dhillo, MBBS, PhD, head of the division of diabetes, endocrinology and metabolism at Imperial College London, and colleagues studied 535 patients admitted to major London hospitals. Their article was published online June 18 in Lancet Diabetes & Endocrinology.
“Our analyses show for the first time that patients with COVID-19 mount a marked and appropriate acute cortisol stress response,” said Dr. Dhillo and colleagues.
Moreover, “high cortisol concentrations were associated with increased mortality and a reduced median survival, probably because this is a marker of the severity of illness.”
So measuring cortisol on admission is potentially “another simple marker to use alongside oxygen saturation levels to help us identify which patients need to be admitted immediately, and which may not,” Dr. Dhillo noted in a statement from his institution.
“Having an early indicator of which patients may deteriorate more quickly will help us with providing the best level of care as quickly as possible. In addition, we can also take cortisol levels into account when we are working out how best to treat our patients,” he said.
However, it’s important to note that this means – particularly in the wake of the RECOVERY trial reported last week – that “in the early part of the disease you don’t need steroids,” he said.
In contrast to SARS, no adrenal insufficiency with COVID-19
Cortisol levels when healthy and resting are 100-200 nmol/L and nearly zero when sleeping, the researchers explained.
They decided to examine cortisol levels because, although physiological stress from critical illness normally increases levels of the hormone, the prior coronavirus, severe acute respiratory syndrome coronavirus (SARS-CoV), had the opposite effect and induced cortisol insufficiency in some patients.
“We would have said we’re not quite sure” what effect SARS-CoV-2 is having on cortisol levels, “so that’s why we collected the data,” Dr. Dhillo said in an interview.
The researchers studied patients admitted to three large London teaching hospitals between March 9 and April 22 with a clinical suspicion of SARS-CoV-2 infection. All patients had a standard set of blood tests, including full blood count, creatinine, C-reactive protein, D-dimer, and serum cortisol.
After exclusions, the team assessed 535 patients admitted over the study period who had baseline cortisol measured within 48 hours of admission.
Of these, 403 patients were diagnosed with COVID-19 based on a positive result on real-time polymerase chain reaction testing (88%) or a strong clinical and radiological suspicion, despite a negative test (12%).
In total, 132 (25%) individuals were not diagnosed with COVID-19.
Patients with COVID-19 were a mean age of 66.3 years, and 59.6% were men.
Mean cortisol concentrations in patients with COVID-19 were significantly higher than those not diagnosed with the virus (619 vs 519 nmol/L; P < .0001).
And by May 8, significantly more patients with COVID-19 died than those without (27.8% vs 6.8%; P < .0001).
Doubling of cortisol levels associated with 40% higher mortality
Multivariate analysis taking into account age, presence of comorbidities, and laboratory tests revealed that a doubling of cortisol concentrations among those with COVID-19 was associated with a significant increase in mortality, at a hazard ratio of 1.42 (P = .014).
And patients with COVID-19 whose baseline cortisol level was >744 nmol/L had a median survival of just 15 days, compared with those with a level ≤744 nmol/L, who had a median survival of 36 days (P < .0001).
The team notes that the cortisol stress responses in their patients with COVID-19 ranged up to 3,241 nmol/L, which is “a marked cortisol stress response, perhaps higher than is observed in patients undergoing major surgery.”
Of interest, there was no interaction between cortisol levels and ethnicity in their study; a subsequent analysis of the data stratified by black, Asian, and other minority ethnicities revealed no significant differences.
The team note that their results will need to be reproduced in other populations.
“Any potential role for cortisol measurement at baseline and later during an inpatient stay with COVID-19 as a prognostic biomarker, either by itself or in combination with other biomarkers, will require validation in a prospective study.”
Implications for treatment: Reserve dexamethasone for critically ill
Dr. Dhillo explained that, because their findings indicate that people initially infected with COVID-19 do mount an appropriate stress (cortisol) response, it is important that people properly understand this in the wake of the RECOVERY trial, reported last week.
The trial showed that the widely available steroid dexamethasone significantly reduced mortality among severely ill COVID-19 patients in the intensive care unit when given at a supraphysiologic dose of 6 mg.
But it would be hazardous for anyone to self-medicate with steroids at an early stage of COVID-19 because that would further increase cortisol levels and could suppress the immune system.
“For the average person on the street with COVID-19,” excess steroids will make their symptoms worse, Dr. Dhillo explained, adding this is important to emphasize because dexamethasone, and similar steroids, “are cheap and likely available on the Internet, and so misunderstanding of the RECOVERY trial could have serious implications.”
But once patients are very sick, with “inflammation in their lungs” and are in the intensive care unit, and often on ventilators – which is a very small subgroup of those with COVID-19 – it becomes a very different story, he stressed.
“RECOVERY shows clearly there seems to be a benefit once you need oxygen or are on a ventilator, and that makes sense because [dexamethasone] is going to be an anti-inflammatory,” in this instance when the “lungs are full of water.”
“But in the early days you definitely don’t need it and it could be harmful,” he reiterated.
The study is funded by the U.K. National Institute for Health Research and Medical Research Council. The authors have reported no relevant financial relationships.
This article first appeared on Medscape.com.
ED visits for life-threatening conditions declined early in COVID-19 pandemic
ED visits for myocardial infarction, stroke, and hyperglycemic crisis dropped substantially in the 10 weeks after COVID-19 was declared a national emergency on March 13, according to the Centers for Disease Control and Prevention.
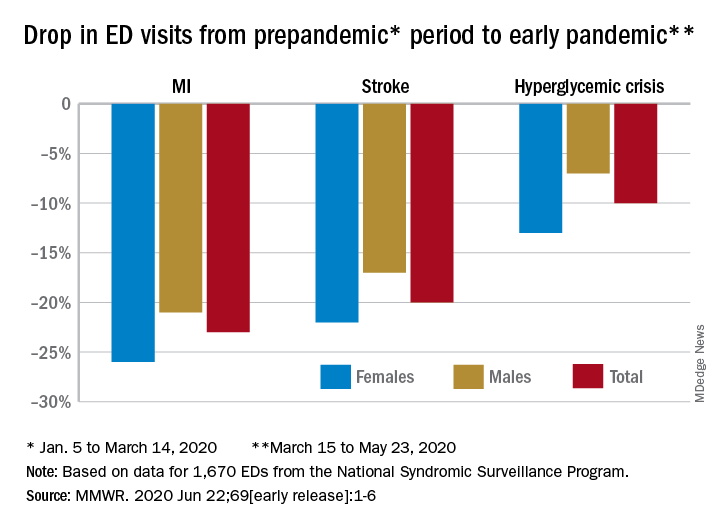
Compared with the 10-week period from Jan. 5 to March 14, ED visits were down by 23% for MI, 20% for stroke, and 10% for hyperglycemic crisis from March 15 to May 23, Samantha J. Lange, MPH, and associates at the CDC reported June 22 in the Morbidity and Mortality Weekly Report.
“A short-term decline of this magnitude … is biologically implausible for MI and stroke, especially for older adults, and unlikely for hyperglycemic crisis, and the finding suggests that patients with these conditions either could not access care or were delaying or avoiding seeking care during the early pandemic period,” they wrote.
The largest decreases in the actual number of visits for MI occurred among both men (down by 2,114, –24%) and women (down by 1,459, –25%) aged 65-74 years. For stroke, men aged 65-74 years had 1,406 (–19%) fewer visits to the ED and women 75-84 years had 1,642 (–23%) fewer visits, the CDC researchers said.
For hypoglycemic crisis, the largest declines during the early pandemic period occurred among younger adults: ED visits for men and women aged 18-44 years were down, respectively, by 419 (–8%) and 775 (–16%), they reported based on data from the National Syndromic Surveillance Program.
“Decreases in ED visits for hyperglycemic crisis might be less striking because patient recognition of this crisis is typically augmented by home glucose monitoring and not reliant upon symptoms alone, as is the case for MI and stroke,” Ms. Lange and her associates noted.
Charting weekly visit numbers showed that the drop for all three conditions actually started the week before the emergency was declared and reached its nadir the week after (March 22) for MI and 2 weeks later (March 29) for stroke and hypoglycemic crisis.
Visits for hypoglycemic crisis have largely returned to normal since those low points, but MI and stroke visits “remain below prepandemic levels” despite gradual increases through April and May, they said.
It has been reported that “deaths not associated with confirmed or probable COVID-19 might have been directly or indirectly attributed to the pandemic. The striking decline in ED visits for acute life-threatening conditions might partially explain observed excess mortality not associated with COVID-19,” the investigators wrote.
ED visits for myocardial infarction, stroke, and hyperglycemic crisis dropped substantially in the 10 weeks after COVID-19 was declared a national emergency on March 13, according to the Centers for Disease Control and Prevention.
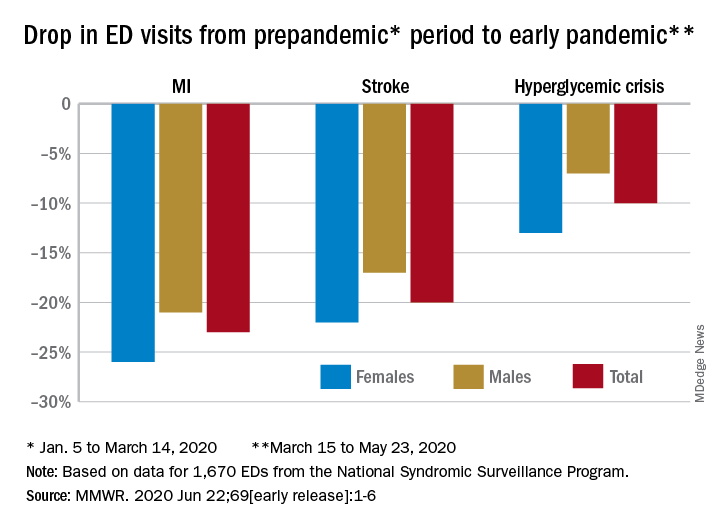
Compared with the 10-week period from Jan. 5 to March 14, ED visits were down by 23% for MI, 20% for stroke, and 10% for hyperglycemic crisis from March 15 to May 23, Samantha J. Lange, MPH, and associates at the CDC reported June 22 in the Morbidity and Mortality Weekly Report.
“A short-term decline of this magnitude … is biologically implausible for MI and stroke, especially for older adults, and unlikely for hyperglycemic crisis, and the finding suggests that patients with these conditions either could not access care or were delaying or avoiding seeking care during the early pandemic period,” they wrote.
The largest decreases in the actual number of visits for MI occurred among both men (down by 2,114, –24%) and women (down by 1,459, –25%) aged 65-74 years. For stroke, men aged 65-74 years had 1,406 (–19%) fewer visits to the ED and women 75-84 years had 1,642 (–23%) fewer visits, the CDC researchers said.
For hypoglycemic crisis, the largest declines during the early pandemic period occurred among younger adults: ED visits for men and women aged 18-44 years were down, respectively, by 419 (–8%) and 775 (–16%), they reported based on data from the National Syndromic Surveillance Program.
“Decreases in ED visits for hyperglycemic crisis might be less striking because patient recognition of this crisis is typically augmented by home glucose monitoring and not reliant upon symptoms alone, as is the case for MI and stroke,” Ms. Lange and her associates noted.
Charting weekly visit numbers showed that the drop for all three conditions actually started the week before the emergency was declared and reached its nadir the week after (March 22) for MI and 2 weeks later (March 29) for stroke and hypoglycemic crisis.
Visits for hypoglycemic crisis have largely returned to normal since those low points, but MI and stroke visits “remain below prepandemic levels” despite gradual increases through April and May, they said.
It has been reported that “deaths not associated with confirmed or probable COVID-19 might have been directly or indirectly attributed to the pandemic. The striking decline in ED visits for acute life-threatening conditions might partially explain observed excess mortality not associated with COVID-19,” the investigators wrote.
ED visits for myocardial infarction, stroke, and hyperglycemic crisis dropped substantially in the 10 weeks after COVID-19 was declared a national emergency on March 13, according to the Centers for Disease Control and Prevention.
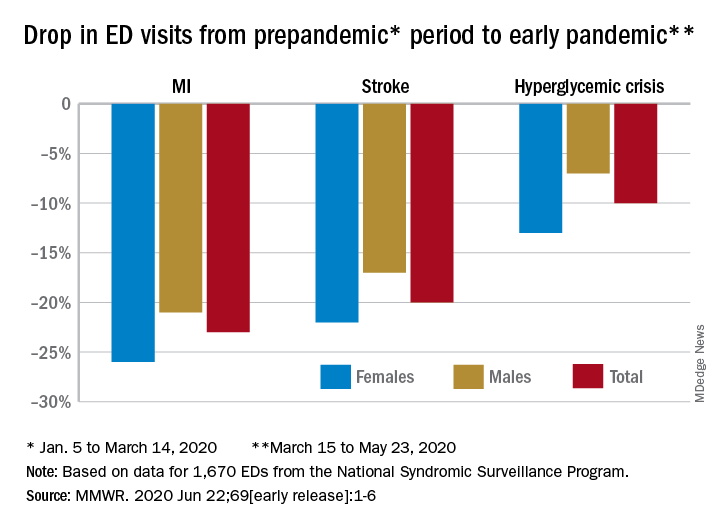
Compared with the 10-week period from Jan. 5 to March 14, ED visits were down by 23% for MI, 20% for stroke, and 10% for hyperglycemic crisis from March 15 to May 23, Samantha J. Lange, MPH, and associates at the CDC reported June 22 in the Morbidity and Mortality Weekly Report.
“A short-term decline of this magnitude … is biologically implausible for MI and stroke, especially for older adults, and unlikely for hyperglycemic crisis, and the finding suggests that patients with these conditions either could not access care or were delaying or avoiding seeking care during the early pandemic period,” they wrote.
The largest decreases in the actual number of visits for MI occurred among both men (down by 2,114, –24%) and women (down by 1,459, –25%) aged 65-74 years. For stroke, men aged 65-74 years had 1,406 (–19%) fewer visits to the ED and women 75-84 years had 1,642 (–23%) fewer visits, the CDC researchers said.
For hypoglycemic crisis, the largest declines during the early pandemic period occurred among younger adults: ED visits for men and women aged 18-44 years were down, respectively, by 419 (–8%) and 775 (–16%), they reported based on data from the National Syndromic Surveillance Program.
“Decreases in ED visits for hyperglycemic crisis might be less striking because patient recognition of this crisis is typically augmented by home glucose monitoring and not reliant upon symptoms alone, as is the case for MI and stroke,” Ms. Lange and her associates noted.
Charting weekly visit numbers showed that the drop for all three conditions actually started the week before the emergency was declared and reached its nadir the week after (March 22) for MI and 2 weeks later (March 29) for stroke and hypoglycemic crisis.
Visits for hypoglycemic crisis have largely returned to normal since those low points, but MI and stroke visits “remain below prepandemic levels” despite gradual increases through April and May, they said.
It has been reported that “deaths not associated with confirmed or probable COVID-19 might have been directly or indirectly attributed to the pandemic. The striking decline in ED visits for acute life-threatening conditions might partially explain observed excess mortality not associated with COVID-19,” the investigators wrote.
FROM MMWR
Where does dexamethasone fit in with diabetic ketoacidosis in COVID-19?
A new article in the Journal of Clinical Endocrinology & Metabolism (JCEM) addresses unique concerns and considerations regarding diabetic ketoacidosis (DKA) in the setting of COVID-19.
Corresponding author Marie E. McDonnell, MD, director of the diabetes program at Brigham and Women’s Hospital, Boston, Massachusetts, discussed the recommendations with Medscape Medical News and also spoke about the news this week that the corticosteroid dexamethasone reduced death rates in severely ill patients with COVID-19.
The full JCEM article, by lead author Nadine E. Palermo, DO, Division of Endocrinology, Diabetes, and Hypertension, also at Brigham and Women’s Hospital, covers DKA diagnosis and triage, and emphasizes that usual hospital protocols for DKA management may need to be adjusted during COVID-19 to help preserve personal protective equipment and ICU beds.
“Hospitals and clinicians need to be able to quickly identify and manage DKA in COVID patients to save lives. This involves determining the options for management, including when less intensive subcutaneous insulin is indicated, and understanding how to guide patients on avoiding this serious complication,” McDonnell said in an Endocrine Society statement.
What about dexamethasone for severe COVID-19 in diabetes?
The new article briefly touches on the fact that upward adjustments to intensive intravenous insulin therapy for DKA may be necessary in patients with COVID-19 who are receiving concomitant corticosteroids or vasopressors.
But it was written prior to the June 16 announcement of the “RECOVERY” trial results with dexamethasone. The UK National Health Service immediately approved the drug’s use in the COVID-19 setting, despite the fact that there has been no published article on the findings yet.
McDonnell told Medscape Medical News that she would need to see formal results to better understand exactly which patients were studied and which ones benefited.
“The peer review will be critical. It looks as if it only benefits people who need respiratory support, but I want to understand that in much more detail,” she said. “If they all had acute respiratory distress syndrome [ARDS],” that’s different.
“There are already some data supporting steroid use in ARDS,” she noted, but added that not all of it suggests benefit.
She pointed to one of several studies now showing that diabetes, and hyperglycemia among people without a prior diabetes diagnosis, are both strong predictors of mortality in hospitalized patients with COVID-19.
“There was a very clear relationship between hyperglycemia and outcomes. We really shouldn’t put people at risk until we have clear data,” she said.
If, once the data are reviewed and appropriate dexamethasone becomes an established treatment for severe COVID-19, hyperglycemia would be a concern among all patients, not just those with previously diagnosed diabetes, she noted.
“We know a good number of people with prediabetes develop hyperglycemia when put on steroids. They can push people over the edge. We’re not going to miss anybody, but treating steroid-induced hyperglycemia is really hard,” McDonnell explained.
She also recommended 2014 guidance from Diabetes UK and the Association of British Clinical Diabetologists, which addresses management of inpatient steroid-induced DKA in patients with and without pre-existing diabetes.
Another major concern, she said, is “patients trying to get dexamethasone when they start to get sick” because this is not the right population to use this agent.
“We worry about people who do not need this drug. If they have diabetes, they put themselves at risk of hyperglycemia, which then increases the risk of severe COVID-19. And then they’re also putting themselves at risk of DKA. It would just be bad medicine,” she said.
Managing DKA in the face of COVID-19: Flexibility is key
In the JCEM article, Palermo and colleagues emphasize that the usual hospital protocols for DKA management may need to be adjusted during COVID-19 in the interest of reducing transmission risk and preserving scare resources.
They provide evidence for alternative treatment strategies, such as the use of subcutaneous rather than intravenous insulin when appropriate.
“We wanted to outline when exactly you should consider nonintensive management strategies for DKA,” McDonnell further explained to Medscape Medical News.
“That would include those with mild or some with moderate DKA. ... The idea is to remind our colleagues about that because hospitals tend to operate on a protocol-driven algorithmic methodology, they can forget to step off the usual care pathway even if evidence supports that,” she said.
But on the other hand, she also said that, in some very complex or severely ill patients with COVID-19, classical intravenous insulin therapy makes the most sense even if their DKA is mild.
The outpatient setting: Prevention and preparation
The new article also addresses several concerns regarding DKA prevention in the outpatient setting.
As with other guidelines, it includes a reminder that patients with diabetes should be advised to discontinue sodium-glucose cotransporter 2 (SGLT2) inhibitors if they become ill with COVID-19, especially if they’re not eating or drinking normally, because they raise the risk for DKA.
Also, for patients with type 1 diabetes, particularly those with a history of repeated DKA, “this is the time to make sure we reach out to patients to refill their insulin prescriptions and address issues related to cost and other access difficulties,” McDonnell said.
The authors also emphasize that insulin starts and education should not be postponed during the pandemic. “Patients identified as meeting criteria to start insulin should be referred for urgent education, either in person or, whenever possible and practical, via video teleconferencing,” they urge.
McDonnell has reported receiving research funding from Novo Nordisk. The other two authors have reported no relevant financial relationships.
This article first appeared on Medscape.com.
A new article in the Journal of Clinical Endocrinology & Metabolism (JCEM) addresses unique concerns and considerations regarding diabetic ketoacidosis (DKA) in the setting of COVID-19.
Corresponding author Marie E. McDonnell, MD, director of the diabetes program at Brigham and Women’s Hospital, Boston, Massachusetts, discussed the recommendations with Medscape Medical News and also spoke about the news this week that the corticosteroid dexamethasone reduced death rates in severely ill patients with COVID-19.
The full JCEM article, by lead author Nadine E. Palermo, DO, Division of Endocrinology, Diabetes, and Hypertension, also at Brigham and Women’s Hospital, covers DKA diagnosis and triage, and emphasizes that usual hospital protocols for DKA management may need to be adjusted during COVID-19 to help preserve personal protective equipment and ICU beds.
“Hospitals and clinicians need to be able to quickly identify and manage DKA in COVID patients to save lives. This involves determining the options for management, including when less intensive subcutaneous insulin is indicated, and understanding how to guide patients on avoiding this serious complication,” McDonnell said in an Endocrine Society statement.
What about dexamethasone for severe COVID-19 in diabetes?
The new article briefly touches on the fact that upward adjustments to intensive intravenous insulin therapy for DKA may be necessary in patients with COVID-19 who are receiving concomitant corticosteroids or vasopressors.
But it was written prior to the June 16 announcement of the “RECOVERY” trial results with dexamethasone. The UK National Health Service immediately approved the drug’s use in the COVID-19 setting, despite the fact that there has been no published article on the findings yet.
McDonnell told Medscape Medical News that she would need to see formal results to better understand exactly which patients were studied and which ones benefited.
“The peer review will be critical. It looks as if it only benefits people who need respiratory support, but I want to understand that in much more detail,” she said. “If they all had acute respiratory distress syndrome [ARDS],” that’s different.
“There are already some data supporting steroid use in ARDS,” she noted, but added that not all of it suggests benefit.
She pointed to one of several studies now showing that diabetes, and hyperglycemia among people without a prior diabetes diagnosis, are both strong predictors of mortality in hospitalized patients with COVID-19.
“There was a very clear relationship between hyperglycemia and outcomes. We really shouldn’t put people at risk until we have clear data,” she said.
If, once the data are reviewed and appropriate dexamethasone becomes an established treatment for severe COVID-19, hyperglycemia would be a concern among all patients, not just those with previously diagnosed diabetes, she noted.
“We know a good number of people with prediabetes develop hyperglycemia when put on steroids. They can push people over the edge. We’re not going to miss anybody, but treating steroid-induced hyperglycemia is really hard,” McDonnell explained.
She also recommended 2014 guidance from Diabetes UK and the Association of British Clinical Diabetologists, which addresses management of inpatient steroid-induced DKA in patients with and without pre-existing diabetes.
Another major concern, she said, is “patients trying to get dexamethasone when they start to get sick” because this is not the right population to use this agent.
“We worry about people who do not need this drug. If they have diabetes, they put themselves at risk of hyperglycemia, which then increases the risk of severe COVID-19. And then they’re also putting themselves at risk of DKA. It would just be bad medicine,” she said.
Managing DKA in the face of COVID-19: Flexibility is key
In the JCEM article, Palermo and colleagues emphasize that the usual hospital protocols for DKA management may need to be adjusted during COVID-19 in the interest of reducing transmission risk and preserving scare resources.
They provide evidence for alternative treatment strategies, such as the use of subcutaneous rather than intravenous insulin when appropriate.
“We wanted to outline when exactly you should consider nonintensive management strategies for DKA,” McDonnell further explained to Medscape Medical News.
“That would include those with mild or some with moderate DKA. ... The idea is to remind our colleagues about that because hospitals tend to operate on a protocol-driven algorithmic methodology, they can forget to step off the usual care pathway even if evidence supports that,” she said.
But on the other hand, she also said that, in some very complex or severely ill patients with COVID-19, classical intravenous insulin therapy makes the most sense even if their DKA is mild.
The outpatient setting: Prevention and preparation
The new article also addresses several concerns regarding DKA prevention in the outpatient setting.
As with other guidelines, it includes a reminder that patients with diabetes should be advised to discontinue sodium-glucose cotransporter 2 (SGLT2) inhibitors if they become ill with COVID-19, especially if they’re not eating or drinking normally, because they raise the risk for DKA.
Also, for patients with type 1 diabetes, particularly those with a history of repeated DKA, “this is the time to make sure we reach out to patients to refill their insulin prescriptions and address issues related to cost and other access difficulties,” McDonnell said.
The authors also emphasize that insulin starts and education should not be postponed during the pandemic. “Patients identified as meeting criteria to start insulin should be referred for urgent education, either in person or, whenever possible and practical, via video teleconferencing,” they urge.
McDonnell has reported receiving research funding from Novo Nordisk. The other two authors have reported no relevant financial relationships.
This article first appeared on Medscape.com.
A new article in the Journal of Clinical Endocrinology & Metabolism (JCEM) addresses unique concerns and considerations regarding diabetic ketoacidosis (DKA) in the setting of COVID-19.
Corresponding author Marie E. McDonnell, MD, director of the diabetes program at Brigham and Women’s Hospital, Boston, Massachusetts, discussed the recommendations with Medscape Medical News and also spoke about the news this week that the corticosteroid dexamethasone reduced death rates in severely ill patients with COVID-19.
The full JCEM article, by lead author Nadine E. Palermo, DO, Division of Endocrinology, Diabetes, and Hypertension, also at Brigham and Women’s Hospital, covers DKA diagnosis and triage, and emphasizes that usual hospital protocols for DKA management may need to be adjusted during COVID-19 to help preserve personal protective equipment and ICU beds.
“Hospitals and clinicians need to be able to quickly identify and manage DKA in COVID patients to save lives. This involves determining the options for management, including when less intensive subcutaneous insulin is indicated, and understanding how to guide patients on avoiding this serious complication,” McDonnell said in an Endocrine Society statement.
What about dexamethasone for severe COVID-19 in diabetes?
The new article briefly touches on the fact that upward adjustments to intensive intravenous insulin therapy for DKA may be necessary in patients with COVID-19 who are receiving concomitant corticosteroids or vasopressors.
But it was written prior to the June 16 announcement of the “RECOVERY” trial results with dexamethasone. The UK National Health Service immediately approved the drug’s use in the COVID-19 setting, despite the fact that there has been no published article on the findings yet.
McDonnell told Medscape Medical News that she would need to see formal results to better understand exactly which patients were studied and which ones benefited.
“The peer review will be critical. It looks as if it only benefits people who need respiratory support, but I want to understand that in much more detail,” she said. “If they all had acute respiratory distress syndrome [ARDS],” that’s different.
“There are already some data supporting steroid use in ARDS,” she noted, but added that not all of it suggests benefit.
She pointed to one of several studies now showing that diabetes, and hyperglycemia among people without a prior diabetes diagnosis, are both strong predictors of mortality in hospitalized patients with COVID-19.
“There was a very clear relationship between hyperglycemia and outcomes. We really shouldn’t put people at risk until we have clear data,” she said.
If, once the data are reviewed and appropriate dexamethasone becomes an established treatment for severe COVID-19, hyperglycemia would be a concern among all patients, not just those with previously diagnosed diabetes, she noted.
“We know a good number of people with prediabetes develop hyperglycemia when put on steroids. They can push people over the edge. We’re not going to miss anybody, but treating steroid-induced hyperglycemia is really hard,” McDonnell explained.
She also recommended 2014 guidance from Diabetes UK and the Association of British Clinical Diabetologists, which addresses management of inpatient steroid-induced DKA in patients with and without pre-existing diabetes.
Another major concern, she said, is “patients trying to get dexamethasone when they start to get sick” because this is not the right population to use this agent.
“We worry about people who do not need this drug. If they have diabetes, they put themselves at risk of hyperglycemia, which then increases the risk of severe COVID-19. And then they’re also putting themselves at risk of DKA. It would just be bad medicine,” she said.
Managing DKA in the face of COVID-19: Flexibility is key
In the JCEM article, Palermo and colleagues emphasize that the usual hospital protocols for DKA management may need to be adjusted during COVID-19 in the interest of reducing transmission risk and preserving scare resources.
They provide evidence for alternative treatment strategies, such as the use of subcutaneous rather than intravenous insulin when appropriate.
“We wanted to outline when exactly you should consider nonintensive management strategies for DKA,” McDonnell further explained to Medscape Medical News.
“That would include those with mild or some with moderate DKA. ... The idea is to remind our colleagues about that because hospitals tend to operate on a protocol-driven algorithmic methodology, they can forget to step off the usual care pathway even if evidence supports that,” she said.
But on the other hand, she also said that, in some very complex or severely ill patients with COVID-19, classical intravenous insulin therapy makes the most sense even if their DKA is mild.
The outpatient setting: Prevention and preparation
The new article also addresses several concerns regarding DKA prevention in the outpatient setting.
As with other guidelines, it includes a reminder that patients with diabetes should be advised to discontinue sodium-glucose cotransporter 2 (SGLT2) inhibitors if they become ill with COVID-19, especially if they’re not eating or drinking normally, because they raise the risk for DKA.
Also, for patients with type 1 diabetes, particularly those with a history of repeated DKA, “this is the time to make sure we reach out to patients to refill their insulin prescriptions and address issues related to cost and other access difficulties,” McDonnell said.
The authors also emphasize that insulin starts and education should not be postponed during the pandemic. “Patients identified as meeting criteria to start insulin should be referred for urgent education, either in person or, whenever possible and practical, via video teleconferencing,” they urge.
McDonnell has reported receiving research funding from Novo Nordisk. The other two authors have reported no relevant financial relationships.
This article first appeared on Medscape.com.
Face mask type matters when sterilizing, study finds
according to researchers. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks.
With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%.
In a research letter published online June 15 in JAMA Network Open, researchers from the University of Oklahoma Health Sciences Center, Oklahoma City, report the results of a study of the two sterilization techniques on the pressure drop and filtration efficiency of N95, KN95, and surgical face masks.
“The H2O2 treatment showed a small effect on the overall filtration efficiency of the tested masks, but the ClO2 treatment showed marked reduction in the overall filtration efficiency of the KN95s and surgical face masks. All pressure drop changes were within the acceptable range,” the researchers write.
The study did not evaluate the effect of repeated sterilizations on face masks.
Five masks of each type were sterilized with either H2O2 or ClO2. Masks were then placed in a test chamber, and a salt aerosol was nebulized to assess both upstream and downstream filtration as well as pressure drop. The researchers used a mobility particle sizer to measure particle number concentration from 16.8 nm to 514 nm. An acceptable pressure drop was defined as a drop of less than 1.38 inches of water (35 mm) for inhalation.
Although pressure drop changes were within the acceptable range for all three mask types following sterilization with either method, H2O2 sterilization yielded the least reduction in filtration efficacy in all cases. After sterilization with H2O2, filtration efficiencies were 96.6%, 97.1%, and 91.6% for the N95s, KN95s, and the surgical face masks, respectively. In contrast, filtration efficiencies after ClO2 sterilization were 95.1%, 76.2%, and 77.9%, respectively.
The researchers note that, although overall filtration efficiency was maintained with ClO2 sterilization, there was a significant drop in efficiency with respect to particles of approximately 300 nm (0.3 microns) in size. For particles of that size, mean filtration efficiency decreased to 86.2% for N95s, 40.8% for KN95s, and 47.1% for surgical face masks.
The testing described in the report is “quite affordable at $350 per mask type, so it is hard to imagine any health care provider cannot set aside a small budget to conduct such an important test,” author Evan Floyd, PhD, told Medscape Medical News.
Given the high demand for effective face masks and the current risk for counterfeit products, Floyd suggested that individual facilities test all masks intended for use by healthcare workers before and after sterilization procedures.
“However, if for some reason testing is not an option, we would recommend sticking to established brands and suppliers, perhaps reach out to your state health department or a local representative of the strategic stockpile of PPE,” he noted.
The authors acknowledge that further studies using a larger sample size and a greater variety of masks, as well as studies to evaluate different sterilization techniques, are required. Further, “measuring the respirator’s filtration efficiency by aerosol size instead of only measuring the overall filtration efficiency” should also be considered. Such an approach would enable researchers to evaluate the degree to which masks protect against specific infectious agents.
This article first appeared on Medscape.com.
according to researchers. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks.
With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%.
In a research letter published online June 15 in JAMA Network Open, researchers from the University of Oklahoma Health Sciences Center, Oklahoma City, report the results of a study of the two sterilization techniques on the pressure drop and filtration efficiency of N95, KN95, and surgical face masks.
“The H2O2 treatment showed a small effect on the overall filtration efficiency of the tested masks, but the ClO2 treatment showed marked reduction in the overall filtration efficiency of the KN95s and surgical face masks. All pressure drop changes were within the acceptable range,” the researchers write.
The study did not evaluate the effect of repeated sterilizations on face masks.
Five masks of each type were sterilized with either H2O2 or ClO2. Masks were then placed in a test chamber, and a salt aerosol was nebulized to assess both upstream and downstream filtration as well as pressure drop. The researchers used a mobility particle sizer to measure particle number concentration from 16.8 nm to 514 nm. An acceptable pressure drop was defined as a drop of less than 1.38 inches of water (35 mm) for inhalation.
Although pressure drop changes were within the acceptable range for all three mask types following sterilization with either method, H2O2 sterilization yielded the least reduction in filtration efficacy in all cases. After sterilization with H2O2, filtration efficiencies were 96.6%, 97.1%, and 91.6% for the N95s, KN95s, and the surgical face masks, respectively. In contrast, filtration efficiencies after ClO2 sterilization were 95.1%, 76.2%, and 77.9%, respectively.
The researchers note that, although overall filtration efficiency was maintained with ClO2 sterilization, there was a significant drop in efficiency with respect to particles of approximately 300 nm (0.3 microns) in size. For particles of that size, mean filtration efficiency decreased to 86.2% for N95s, 40.8% for KN95s, and 47.1% for surgical face masks.
The testing described in the report is “quite affordable at $350 per mask type, so it is hard to imagine any health care provider cannot set aside a small budget to conduct such an important test,” author Evan Floyd, PhD, told Medscape Medical News.
Given the high demand for effective face masks and the current risk for counterfeit products, Floyd suggested that individual facilities test all masks intended for use by healthcare workers before and after sterilization procedures.
“However, if for some reason testing is not an option, we would recommend sticking to established brands and suppliers, perhaps reach out to your state health department or a local representative of the strategic stockpile of PPE,” he noted.
The authors acknowledge that further studies using a larger sample size and a greater variety of masks, as well as studies to evaluate different sterilization techniques, are required. Further, “measuring the respirator’s filtration efficiency by aerosol size instead of only measuring the overall filtration efficiency” should also be considered. Such an approach would enable researchers to evaluate the degree to which masks protect against specific infectious agents.
This article first appeared on Medscape.com.
according to researchers. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks.
With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%.
In a research letter published online June 15 in JAMA Network Open, researchers from the University of Oklahoma Health Sciences Center, Oklahoma City, report the results of a study of the two sterilization techniques on the pressure drop and filtration efficiency of N95, KN95, and surgical face masks.
“The H2O2 treatment showed a small effect on the overall filtration efficiency of the tested masks, but the ClO2 treatment showed marked reduction in the overall filtration efficiency of the KN95s and surgical face masks. All pressure drop changes were within the acceptable range,” the researchers write.
The study did not evaluate the effect of repeated sterilizations on face masks.
Five masks of each type were sterilized with either H2O2 or ClO2. Masks were then placed in a test chamber, and a salt aerosol was nebulized to assess both upstream and downstream filtration as well as pressure drop. The researchers used a mobility particle sizer to measure particle number concentration from 16.8 nm to 514 nm. An acceptable pressure drop was defined as a drop of less than 1.38 inches of water (35 mm) for inhalation.
Although pressure drop changes were within the acceptable range for all three mask types following sterilization with either method, H2O2 sterilization yielded the least reduction in filtration efficacy in all cases. After sterilization with H2O2, filtration efficiencies were 96.6%, 97.1%, and 91.6% for the N95s, KN95s, and the surgical face masks, respectively. In contrast, filtration efficiencies after ClO2 sterilization were 95.1%, 76.2%, and 77.9%, respectively.
The researchers note that, although overall filtration efficiency was maintained with ClO2 sterilization, there was a significant drop in efficiency with respect to particles of approximately 300 nm (0.3 microns) in size. For particles of that size, mean filtration efficiency decreased to 86.2% for N95s, 40.8% for KN95s, and 47.1% for surgical face masks.
The testing described in the report is “quite affordable at $350 per mask type, so it is hard to imagine any health care provider cannot set aside a small budget to conduct such an important test,” author Evan Floyd, PhD, told Medscape Medical News.
Given the high demand for effective face masks and the current risk for counterfeit products, Floyd suggested that individual facilities test all masks intended for use by healthcare workers before and after sterilization procedures.
“However, if for some reason testing is not an option, we would recommend sticking to established brands and suppliers, perhaps reach out to your state health department or a local representative of the strategic stockpile of PPE,” he noted.
The authors acknowledge that further studies using a larger sample size and a greater variety of masks, as well as studies to evaluate different sterilization techniques, are required. Further, “measuring the respirator’s filtration efficiency by aerosol size instead of only measuring the overall filtration efficiency” should also be considered. Such an approach would enable researchers to evaluate the degree to which masks protect against specific infectious agents.
This article first appeared on Medscape.com.





