User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Cumulative exposure to high-potency topical steroid doses drives osteoporosis fractures
In support of previously published case reports, in a dose-response relationship.
In a stepwise manner, the hazard ratios for major osteoporotic fracture (MOF) were found to start climbing incrementally for those with a cumulative topical steroid dose equivalent of more than 500 g of mometasone furoate when compared with exposure of 200-499 g, according to the team of investigators from the University of Copenhagen.
“Use of these drugs is very common, and we found an estimated population-attributable risk of as much as 4.3%,” the investigators reported in the study, published in JAMA Dermatology.
The retrospective cohort study drew data from the Danish National Patient Registry, which covers 99% of the country’s population. It was linked to the Danish National Prescription Registry, which captures data on pharmacy-dispensed medications. Data collected from the beginning of 2003 to the end of 2017 were evaluated.
Exposures to potent or very potent topical corticosteroids were converted into a single standard with potency equivalent to 1 mg/g of mometasone furoate. Four strata of exposure were compared to a reference exposure of 200-499 g. These were 500-999 g, 1,000-1,999 g, 2,000-9,999 g, and 10,000 g or greater.
For the first strata, the small increased risk for MOF did not reach significance (HR, 1.01; 95% confidence interval, 0.99-1.03), but each of the others did. These climbed from a 5% greater risk (HR 1.05 95% CI 1.02-1.08) for a cumulative exposure of 1,000 to 1,999 g, to a 10% greater risk (HR, 1.10; 95% CI, 1.07-1.13) for a cumulative exposure of 2,000-9,999 g, and finally to a 27% greater risk (HR, 1.27; 95% CI, 1.19-1.35) for a cumulative exposure of 10,000 g or higher.
The study included more than 700,000 individuals exposed to topical mometasone at a potency equivalent of 200 g or more over the study period. The reference group (200-499 g) was the largest (317,907 individuals). The first strata (500-999 g) included 186,359 patients; the second (1,000-1,999 g), 111,203 patients; the third (2,000-9,999 g), 94,334 patients; and the fifth (10,000 g or more), 13,448 patients.
“A 3% increase in the relative risk of osteoporosis and MOF was observed per doubling of the TCS dose,” according to the investigators.
Patients exposed to doses of high-potency topical steroids that put them at risk of MOF is limited but substantial, according to the senior author, Alexander Egeberg, MD, PhD, of the department of dermatology and allergy at Herlev and Gentofte Hospital, Copenhagen.
“It is true that the risk is modest for the average user of topical steroids,” Dr. Egeberg said in an interview. However, despite the fact that topical steroids are intended for short-term use, “2% of all our users had been exposed to the equivalent of 10,000 g of mometasone, which mean 100 tubes of 100 g.”
If the other two strata at significantly increased risk of MOF (greater than 1,000 g) are included, an additional 28% of all users are facing the potential for clinically significant osteoporosis, according to the Danish data.
The adverse effect of steroids on bone metabolism has been established previously, and several studies have linked systemic corticosteroid exposure, including inhaled corticosteroids, with increased risk of osteoporotic fracture. For example, one study showed that patients with chronic obstructive pulmonary disease on daily inhaled doses of the equivalent of fluticasone at or above 1,000 mcg for more than 4 years had about a 10% increased risk of MOF relative to those not exposed.
The data associate topical steroids with increased risk of osteoporotic fracture, but Dr. Egeberg said osteoporosis is not the only reason to use topical steroids prudently.
“It is important to keep in mind that osteoporosis and fractures are at the extreme end of the side-effect profile and that other side effects, such as striae formation, skin thinning, and dysregulated diabetes, can occur with much lower quantities of topical steroids,” Dr. Egeberg said
For avoiding this risk, “there are no specific cutoffs” recommended for topical steroids in current guidelines, but dermatologists should be aware that many of the indications for topical steroids, such as psoriasis and atopic dermatitis, involve skin with an impaired barrier function, exposing patients to an increased likelihood of absorption, according to Dr. Egeberg.
“A general rule of thumb that we use is that, if a patient with persistent disease activity requires a new prescription of the equivalent of 100 g mometasone every 1-2 months, it might be worth considering if there is a suitable alternative,” Dr. Egeberg said.
In an accompanying editorial, Rebecca D. Jackson, MD, of the division of endocrinology, diabetes, and metabolism in the department of internal medicine at Ohio State University, Columbus, agreed that no guidelines specific to avoiding the risks of topical corticosteroids are currently available, but she advised clinicians to be considering these risks nonetheless. In general, she suggested that topical steroids, like oral steroids, should be used at “the lowest dose for the shortest duration necessary to manage the underlying medical condition.”
The correlation between topical corticosteroids and increased risk of osteoporotic fracture, although not established previously in a large study, is not surprising, according to Victoria Werth, MD, chief of dermatology at the Philadelphia Veterans Affairs Hospital and professor of dermatology at the University of Pennsylvania, also in Philadelphia.
“Systemic absorption of potent topical steroids has previously been demonstrated with a rapid decrease in serum cortisol levels,” Dr. Werth said in an interview. She indicated that concern about the risk of osteoporosis imposed by use of potent steroids over large body surface areas is appropriate.
To minimize this risk, “it is reasonable to use the lowest dose of steroid possible and to try to substitute other medications when possible,” she said.
Dr. Egeberg reported financial relationships with Abbvie, Almirall, Bristol-Myers Squibb, Dermavant Sciences, Galderma, Janssen Pharmaceuticals, Eli Lilly, Novartis, Pfizer, Samsung, Bioepis, and UCB. Five authors had disclosures related to some of those pharmaceutical companies and/or others. Dr. Jackson had no disclosures.
In support of previously published case reports, in a dose-response relationship.
In a stepwise manner, the hazard ratios for major osteoporotic fracture (MOF) were found to start climbing incrementally for those with a cumulative topical steroid dose equivalent of more than 500 g of mometasone furoate when compared with exposure of 200-499 g, according to the team of investigators from the University of Copenhagen.
“Use of these drugs is very common, and we found an estimated population-attributable risk of as much as 4.3%,” the investigators reported in the study, published in JAMA Dermatology.
The retrospective cohort study drew data from the Danish National Patient Registry, which covers 99% of the country’s population. It was linked to the Danish National Prescription Registry, which captures data on pharmacy-dispensed medications. Data collected from the beginning of 2003 to the end of 2017 were evaluated.
Exposures to potent or very potent topical corticosteroids were converted into a single standard with potency equivalent to 1 mg/g of mometasone furoate. Four strata of exposure were compared to a reference exposure of 200-499 g. These were 500-999 g, 1,000-1,999 g, 2,000-9,999 g, and 10,000 g or greater.
For the first strata, the small increased risk for MOF did not reach significance (HR, 1.01; 95% confidence interval, 0.99-1.03), but each of the others did. These climbed from a 5% greater risk (HR 1.05 95% CI 1.02-1.08) for a cumulative exposure of 1,000 to 1,999 g, to a 10% greater risk (HR, 1.10; 95% CI, 1.07-1.13) for a cumulative exposure of 2,000-9,999 g, and finally to a 27% greater risk (HR, 1.27; 95% CI, 1.19-1.35) for a cumulative exposure of 10,000 g or higher.
The study included more than 700,000 individuals exposed to topical mometasone at a potency equivalent of 200 g or more over the study period. The reference group (200-499 g) was the largest (317,907 individuals). The first strata (500-999 g) included 186,359 patients; the second (1,000-1,999 g), 111,203 patients; the third (2,000-9,999 g), 94,334 patients; and the fifth (10,000 g or more), 13,448 patients.
“A 3% increase in the relative risk of osteoporosis and MOF was observed per doubling of the TCS dose,” according to the investigators.
Patients exposed to doses of high-potency topical steroids that put them at risk of MOF is limited but substantial, according to the senior author, Alexander Egeberg, MD, PhD, of the department of dermatology and allergy at Herlev and Gentofte Hospital, Copenhagen.
“It is true that the risk is modest for the average user of topical steroids,” Dr. Egeberg said in an interview. However, despite the fact that topical steroids are intended for short-term use, “2% of all our users had been exposed to the equivalent of 10,000 g of mometasone, which mean 100 tubes of 100 g.”
If the other two strata at significantly increased risk of MOF (greater than 1,000 g) are included, an additional 28% of all users are facing the potential for clinically significant osteoporosis, according to the Danish data.
The adverse effect of steroids on bone metabolism has been established previously, and several studies have linked systemic corticosteroid exposure, including inhaled corticosteroids, with increased risk of osteoporotic fracture. For example, one study showed that patients with chronic obstructive pulmonary disease on daily inhaled doses of the equivalent of fluticasone at or above 1,000 mcg for more than 4 years had about a 10% increased risk of MOF relative to those not exposed.
The data associate topical steroids with increased risk of osteoporotic fracture, but Dr. Egeberg said osteoporosis is not the only reason to use topical steroids prudently.
“It is important to keep in mind that osteoporosis and fractures are at the extreme end of the side-effect profile and that other side effects, such as striae formation, skin thinning, and dysregulated diabetes, can occur with much lower quantities of topical steroids,” Dr. Egeberg said
For avoiding this risk, “there are no specific cutoffs” recommended for topical steroids in current guidelines, but dermatologists should be aware that many of the indications for topical steroids, such as psoriasis and atopic dermatitis, involve skin with an impaired barrier function, exposing patients to an increased likelihood of absorption, according to Dr. Egeberg.
“A general rule of thumb that we use is that, if a patient with persistent disease activity requires a new prescription of the equivalent of 100 g mometasone every 1-2 months, it might be worth considering if there is a suitable alternative,” Dr. Egeberg said.
In an accompanying editorial, Rebecca D. Jackson, MD, of the division of endocrinology, diabetes, and metabolism in the department of internal medicine at Ohio State University, Columbus, agreed that no guidelines specific to avoiding the risks of topical corticosteroids are currently available, but she advised clinicians to be considering these risks nonetheless. In general, she suggested that topical steroids, like oral steroids, should be used at “the lowest dose for the shortest duration necessary to manage the underlying medical condition.”
The correlation between topical corticosteroids and increased risk of osteoporotic fracture, although not established previously in a large study, is not surprising, according to Victoria Werth, MD, chief of dermatology at the Philadelphia Veterans Affairs Hospital and professor of dermatology at the University of Pennsylvania, also in Philadelphia.
“Systemic absorption of potent topical steroids has previously been demonstrated with a rapid decrease in serum cortisol levels,” Dr. Werth said in an interview. She indicated that concern about the risk of osteoporosis imposed by use of potent steroids over large body surface areas is appropriate.
To minimize this risk, “it is reasonable to use the lowest dose of steroid possible and to try to substitute other medications when possible,” she said.
Dr. Egeberg reported financial relationships with Abbvie, Almirall, Bristol-Myers Squibb, Dermavant Sciences, Galderma, Janssen Pharmaceuticals, Eli Lilly, Novartis, Pfizer, Samsung, Bioepis, and UCB. Five authors had disclosures related to some of those pharmaceutical companies and/or others. Dr. Jackson had no disclosures.
In support of previously published case reports, in a dose-response relationship.
In a stepwise manner, the hazard ratios for major osteoporotic fracture (MOF) were found to start climbing incrementally for those with a cumulative topical steroid dose equivalent of more than 500 g of mometasone furoate when compared with exposure of 200-499 g, according to the team of investigators from the University of Copenhagen.
“Use of these drugs is very common, and we found an estimated population-attributable risk of as much as 4.3%,” the investigators reported in the study, published in JAMA Dermatology.
The retrospective cohort study drew data from the Danish National Patient Registry, which covers 99% of the country’s population. It was linked to the Danish National Prescription Registry, which captures data on pharmacy-dispensed medications. Data collected from the beginning of 2003 to the end of 2017 were evaluated.
Exposures to potent or very potent topical corticosteroids were converted into a single standard with potency equivalent to 1 mg/g of mometasone furoate. Four strata of exposure were compared to a reference exposure of 200-499 g. These were 500-999 g, 1,000-1,999 g, 2,000-9,999 g, and 10,000 g or greater.
For the first strata, the small increased risk for MOF did not reach significance (HR, 1.01; 95% confidence interval, 0.99-1.03), but each of the others did. These climbed from a 5% greater risk (HR 1.05 95% CI 1.02-1.08) for a cumulative exposure of 1,000 to 1,999 g, to a 10% greater risk (HR, 1.10; 95% CI, 1.07-1.13) for a cumulative exposure of 2,000-9,999 g, and finally to a 27% greater risk (HR, 1.27; 95% CI, 1.19-1.35) for a cumulative exposure of 10,000 g or higher.
The study included more than 700,000 individuals exposed to topical mometasone at a potency equivalent of 200 g or more over the study period. The reference group (200-499 g) was the largest (317,907 individuals). The first strata (500-999 g) included 186,359 patients; the second (1,000-1,999 g), 111,203 patients; the third (2,000-9,999 g), 94,334 patients; and the fifth (10,000 g or more), 13,448 patients.
“A 3% increase in the relative risk of osteoporosis and MOF was observed per doubling of the TCS dose,” according to the investigators.
Patients exposed to doses of high-potency topical steroids that put them at risk of MOF is limited but substantial, according to the senior author, Alexander Egeberg, MD, PhD, of the department of dermatology and allergy at Herlev and Gentofte Hospital, Copenhagen.
“It is true that the risk is modest for the average user of topical steroids,” Dr. Egeberg said in an interview. However, despite the fact that topical steroids are intended for short-term use, “2% of all our users had been exposed to the equivalent of 10,000 g of mometasone, which mean 100 tubes of 100 g.”
If the other two strata at significantly increased risk of MOF (greater than 1,000 g) are included, an additional 28% of all users are facing the potential for clinically significant osteoporosis, according to the Danish data.
The adverse effect of steroids on bone metabolism has been established previously, and several studies have linked systemic corticosteroid exposure, including inhaled corticosteroids, with increased risk of osteoporotic fracture. For example, one study showed that patients with chronic obstructive pulmonary disease on daily inhaled doses of the equivalent of fluticasone at or above 1,000 mcg for more than 4 years had about a 10% increased risk of MOF relative to those not exposed.
The data associate topical steroids with increased risk of osteoporotic fracture, but Dr. Egeberg said osteoporosis is not the only reason to use topical steroids prudently.
“It is important to keep in mind that osteoporosis and fractures are at the extreme end of the side-effect profile and that other side effects, such as striae formation, skin thinning, and dysregulated diabetes, can occur with much lower quantities of topical steroids,” Dr. Egeberg said
For avoiding this risk, “there are no specific cutoffs” recommended for topical steroids in current guidelines, but dermatologists should be aware that many of the indications for topical steroids, such as psoriasis and atopic dermatitis, involve skin with an impaired barrier function, exposing patients to an increased likelihood of absorption, according to Dr. Egeberg.
“A general rule of thumb that we use is that, if a patient with persistent disease activity requires a new prescription of the equivalent of 100 g mometasone every 1-2 months, it might be worth considering if there is a suitable alternative,” Dr. Egeberg said.
In an accompanying editorial, Rebecca D. Jackson, MD, of the division of endocrinology, diabetes, and metabolism in the department of internal medicine at Ohio State University, Columbus, agreed that no guidelines specific to avoiding the risks of topical corticosteroids are currently available, but she advised clinicians to be considering these risks nonetheless. In general, she suggested that topical steroids, like oral steroids, should be used at “the lowest dose for the shortest duration necessary to manage the underlying medical condition.”
The correlation between topical corticosteroids and increased risk of osteoporotic fracture, although not established previously in a large study, is not surprising, according to Victoria Werth, MD, chief of dermatology at the Philadelphia Veterans Affairs Hospital and professor of dermatology at the University of Pennsylvania, also in Philadelphia.
“Systemic absorption of potent topical steroids has previously been demonstrated with a rapid decrease in serum cortisol levels,” Dr. Werth said in an interview. She indicated that concern about the risk of osteoporosis imposed by use of potent steroids over large body surface areas is appropriate.
To minimize this risk, “it is reasonable to use the lowest dose of steroid possible and to try to substitute other medications when possible,” she said.
Dr. Egeberg reported financial relationships with Abbvie, Almirall, Bristol-Myers Squibb, Dermavant Sciences, Galderma, Janssen Pharmaceuticals, Eli Lilly, Novartis, Pfizer, Samsung, Bioepis, and UCB. Five authors had disclosures related to some of those pharmaceutical companies and/or others. Dr. Jackson had no disclosures.
FROM JAMA DERMATOLOGY
Infectious diseases ‘giant’ John Bartlett: His ‘impact will endure’
The cause of death was not immediately disclosed.
Dr. Bartlett is remembered by colleagues for his wide range of infectious disease expertise, an ability to repeatedly predict emerging issues in the field, and for inspiring students and trainees to choose the same specialty.
“What I consistently found so extraordinary about John was his excitement for ID – the whole field. He had a wonderful sixth sense about what was going to be the next ‘big thing,’” Paul Edward Sax, MD, clinical director of the Infectious Disease Clinic at Brigham and Women’s Hospital in Boston, told this news organization.
“He thoroughly absorbed the emerging research on the topic and then provided the most wonderful clinical summaries,” Dr. Sax said. “His range of expert content areas was unbelievably broad.” Dr. Bartlett was “a true ID polymath.”
Dr. Bartlett was “a giant in the field of infectious diseases,” David Lee Thomas, MD, MPH, said in an interview. He agreed that Dr. Bartlett was a visionary who could anticipate the most exciting developments in the specialty.
Dr. Bartlett also “led the efforts to combat the foes, from HIV to antimicrobial resistance,” said Dr. Thomas, director of the division of infectious diseases and professor of medicine at Johns Hopkins University.
A pioneer in HIV research and care
Dr. Bartlett’s early research focused on anaerobic pulmonary and other infections, Bacteroides fragilis pathogenesis, and colitis caused by Clostridioides difficile.
Shortly after joining Johns Hopkins in 1980, he focused on HIV/AIDS research and caring for people with HIV. Dr. Bartlett led clinical trials of new treatments and developed years of HIV clinical treatment guidelines.
“Back when most hospitals, university medical centers, and ID divisions were running away from the AIDS epidemic, John took it on, both as a scientific priority and a moral imperative,” Dr. Sax writes in a blog post for NEJM Journal Watch. “With the help of Frank Polk and the Hopkins president, he established an outpatient AIDS clinic and an inpatient AIDS ward – both of which were way ahead of their time.”
In the same post, Dr. Sax points out that Dr. Bartlett was an expert in multiple areas – any one of which could be a sole career focus. “How many ID doctors are true experts in all of the following distinct topics? HIV, Clostridium difficile, respiratory tract infections, antimicrobial resistance, and anaerobic pulmonary infections.” Dr. Sax writes.
Expertise that defined an era
In a piece reviewing the long history of infectious disease medicine at Johns Hopkins published in Clinical Infectious Diseases in 2014, Paul Auwaerter, MD, and colleagues describe his tenure at the institution from 1980 to 2006 as “The Bartlett Era,” notable for the many advances he spearheaded.
“It is nearly impossible to find someone trained in infectious diseases in the past 30 years who has not been impacted by John Bartlett,” Dr. Auwaerter and colleagues note. “His tireless devotion to scholarship, teaching, and patient care remains an inspiration to his faculty members at Johns Hopkins, his colleagues, and coworkers around the world.”
Dr. Bartlett was not only a faculty member in the division of infectious diseases, he also helped establish it. When he joined Johns Hopkins, the infectious disease department featured just three faculty members with a research budget of less than $285,000. By the time he left 26 years later, the division had 44 faculty members on tenure track and a research budget exceeding $40 million.
Sharing memories via social media
Reactions to Dr. Bartlett’s passing on Twitter were swift.
“We have lost one of the greatest physicians I have ever met or had the privilege to learn from. Saddened to hear of Dr. John G. Bartlett’s passing. He inspired so many, including me, to choose the field of infectious diseases,” David Fisk, MD, infectious disease specialist in Santa Barbara, Calif., wrote on Twitter.
“John Bartlett just died – a true visionary and the classic ‘Renaissance’ person in clinical ID. Such a nice guy, too! His IDSA/IDWeek literature summaries (among other things) were amazing. We’ll miss him!” Dr. Sax tweeted on Jan. 19.
A colleague at Johns Hopkins, transplant infectious disease specialist Shmuel Shoham, MD, shared an anecdote about Dr. Bartlett on Twitter: “Year ago. My office is across from his. I ask him what he is doing. He tells me he is reviewing a file from the Vatican to adjudicate whether a miracle happened. True story.”
Infectious disease specialist Graeme Forrest, MBBS, also shared a story about Dr. Bartlett via Twitter. “He described to me in 2001 how the U.S. model of health care would not cope with a pandemic or serious bioterror attack as it’s not connected to disseminate information. How prescient from 20 years ago.”
Dr. Bartlett shared his expertise at many national and international infectious disease conferences over the years. He also authored 470 articles, 282 book chapters, and 61 editions of 14 books.
Dr. Bartlett was also a regular contributor to this news organization. For example, he shared his expertise in perspective pieces that addressed priorities in antibiotic stewardship, upcoming infectious disease predictions, and critical infectious disease topics in a three-part series.
Dr. Bartlett’s education includes a bachelor’s degree from Dartmouth College in Hanover, N.H., in 1959 and an MD from Upstate Medical Center in Syracuse, N.Y., in 1963. He did his first 2 years of residency at Brigham and Women’s Hospital.
He also served as an Army captain from 1965 to 1967, treating patients in fever wards in Vietnam. He then returned to the United States to finish his internal medicine training at the University of Alabama in 1968.
Dr. Bartlett completed his fellowship in infectious diseases at the University of California, Los Angeles. In 1975, he joined the faculty at Tufts University, Boston.
Leaving a legacy
Dr. Bartlett’s influence will likely live on in many ways at Johns Hopkins.
“John is a larger-than-life legend whose impact will endure and after whom we are so proud to have named our clinical service, The Bartlett Specialty Practice,” Dr. Thomas said.
The specialty practice clinic named for him has 23 exam rooms and features multidisciplinary care for people with HIV, hepatitis, bone infections, general infectious diseases, and more. Furthermore, friends, family, and colleagues joined forces to create the “Dr. John G. Bartlett HIV/AIDS Fund.”
They note that it is “only appropriate that we honor him by creating an endowment that will provide support for young trainees and junior faculty in the division, helping them transition to their independent careers.”
In addition to all his professional accomplishments, “He was also a genuinely nice person, approachable and humble,” Dr. Sax said. “We really lost a great one!”
A version of this article first appeared on Medscape.com.
The cause of death was not immediately disclosed.
Dr. Bartlett is remembered by colleagues for his wide range of infectious disease expertise, an ability to repeatedly predict emerging issues in the field, and for inspiring students and trainees to choose the same specialty.
“What I consistently found so extraordinary about John was his excitement for ID – the whole field. He had a wonderful sixth sense about what was going to be the next ‘big thing,’” Paul Edward Sax, MD, clinical director of the Infectious Disease Clinic at Brigham and Women’s Hospital in Boston, told this news organization.
“He thoroughly absorbed the emerging research on the topic and then provided the most wonderful clinical summaries,” Dr. Sax said. “His range of expert content areas was unbelievably broad.” Dr. Bartlett was “a true ID polymath.”
Dr. Bartlett was “a giant in the field of infectious diseases,” David Lee Thomas, MD, MPH, said in an interview. He agreed that Dr. Bartlett was a visionary who could anticipate the most exciting developments in the specialty.
Dr. Bartlett also “led the efforts to combat the foes, from HIV to antimicrobial resistance,” said Dr. Thomas, director of the division of infectious diseases and professor of medicine at Johns Hopkins University.
A pioneer in HIV research and care
Dr. Bartlett’s early research focused on anaerobic pulmonary and other infections, Bacteroides fragilis pathogenesis, and colitis caused by Clostridioides difficile.
Shortly after joining Johns Hopkins in 1980, he focused on HIV/AIDS research and caring for people with HIV. Dr. Bartlett led clinical trials of new treatments and developed years of HIV clinical treatment guidelines.
“Back when most hospitals, university medical centers, and ID divisions were running away from the AIDS epidemic, John took it on, both as a scientific priority and a moral imperative,” Dr. Sax writes in a blog post for NEJM Journal Watch. “With the help of Frank Polk and the Hopkins president, he established an outpatient AIDS clinic and an inpatient AIDS ward – both of which were way ahead of their time.”
In the same post, Dr. Sax points out that Dr. Bartlett was an expert in multiple areas – any one of which could be a sole career focus. “How many ID doctors are true experts in all of the following distinct topics? HIV, Clostridium difficile, respiratory tract infections, antimicrobial resistance, and anaerobic pulmonary infections.” Dr. Sax writes.
Expertise that defined an era
In a piece reviewing the long history of infectious disease medicine at Johns Hopkins published in Clinical Infectious Diseases in 2014, Paul Auwaerter, MD, and colleagues describe his tenure at the institution from 1980 to 2006 as “The Bartlett Era,” notable for the many advances he spearheaded.
“It is nearly impossible to find someone trained in infectious diseases in the past 30 years who has not been impacted by John Bartlett,” Dr. Auwaerter and colleagues note. “His tireless devotion to scholarship, teaching, and patient care remains an inspiration to his faculty members at Johns Hopkins, his colleagues, and coworkers around the world.”
Dr. Bartlett was not only a faculty member in the division of infectious diseases, he also helped establish it. When he joined Johns Hopkins, the infectious disease department featured just three faculty members with a research budget of less than $285,000. By the time he left 26 years later, the division had 44 faculty members on tenure track and a research budget exceeding $40 million.
Sharing memories via social media
Reactions to Dr. Bartlett’s passing on Twitter were swift.
“We have lost one of the greatest physicians I have ever met or had the privilege to learn from. Saddened to hear of Dr. John G. Bartlett’s passing. He inspired so many, including me, to choose the field of infectious diseases,” David Fisk, MD, infectious disease specialist in Santa Barbara, Calif., wrote on Twitter.
“John Bartlett just died – a true visionary and the classic ‘Renaissance’ person in clinical ID. Such a nice guy, too! His IDSA/IDWeek literature summaries (among other things) were amazing. We’ll miss him!” Dr. Sax tweeted on Jan. 19.
A colleague at Johns Hopkins, transplant infectious disease specialist Shmuel Shoham, MD, shared an anecdote about Dr. Bartlett on Twitter: “Year ago. My office is across from his. I ask him what he is doing. He tells me he is reviewing a file from the Vatican to adjudicate whether a miracle happened. True story.”
Infectious disease specialist Graeme Forrest, MBBS, also shared a story about Dr. Bartlett via Twitter. “He described to me in 2001 how the U.S. model of health care would not cope with a pandemic or serious bioterror attack as it’s not connected to disseminate information. How prescient from 20 years ago.”
Dr. Bartlett shared his expertise at many national and international infectious disease conferences over the years. He also authored 470 articles, 282 book chapters, and 61 editions of 14 books.
Dr. Bartlett was also a regular contributor to this news organization. For example, he shared his expertise in perspective pieces that addressed priorities in antibiotic stewardship, upcoming infectious disease predictions, and critical infectious disease topics in a three-part series.
Dr. Bartlett’s education includes a bachelor’s degree from Dartmouth College in Hanover, N.H., in 1959 and an MD from Upstate Medical Center in Syracuse, N.Y., in 1963. He did his first 2 years of residency at Brigham and Women’s Hospital.
He also served as an Army captain from 1965 to 1967, treating patients in fever wards in Vietnam. He then returned to the United States to finish his internal medicine training at the University of Alabama in 1968.
Dr. Bartlett completed his fellowship in infectious diseases at the University of California, Los Angeles. In 1975, he joined the faculty at Tufts University, Boston.
Leaving a legacy
Dr. Bartlett’s influence will likely live on in many ways at Johns Hopkins.
“John is a larger-than-life legend whose impact will endure and after whom we are so proud to have named our clinical service, The Bartlett Specialty Practice,” Dr. Thomas said.
The specialty practice clinic named for him has 23 exam rooms and features multidisciplinary care for people with HIV, hepatitis, bone infections, general infectious diseases, and more. Furthermore, friends, family, and colleagues joined forces to create the “Dr. John G. Bartlett HIV/AIDS Fund.”
They note that it is “only appropriate that we honor him by creating an endowment that will provide support for young trainees and junior faculty in the division, helping them transition to their independent careers.”
In addition to all his professional accomplishments, “He was also a genuinely nice person, approachable and humble,” Dr. Sax said. “We really lost a great one!”
A version of this article first appeared on Medscape.com.
The cause of death was not immediately disclosed.
Dr. Bartlett is remembered by colleagues for his wide range of infectious disease expertise, an ability to repeatedly predict emerging issues in the field, and for inspiring students and trainees to choose the same specialty.
“What I consistently found so extraordinary about John was his excitement for ID – the whole field. He had a wonderful sixth sense about what was going to be the next ‘big thing,’” Paul Edward Sax, MD, clinical director of the Infectious Disease Clinic at Brigham and Women’s Hospital in Boston, told this news organization.
“He thoroughly absorbed the emerging research on the topic and then provided the most wonderful clinical summaries,” Dr. Sax said. “His range of expert content areas was unbelievably broad.” Dr. Bartlett was “a true ID polymath.”
Dr. Bartlett was “a giant in the field of infectious diseases,” David Lee Thomas, MD, MPH, said in an interview. He agreed that Dr. Bartlett was a visionary who could anticipate the most exciting developments in the specialty.
Dr. Bartlett also “led the efforts to combat the foes, from HIV to antimicrobial resistance,” said Dr. Thomas, director of the division of infectious diseases and professor of medicine at Johns Hopkins University.
A pioneer in HIV research and care
Dr. Bartlett’s early research focused on anaerobic pulmonary and other infections, Bacteroides fragilis pathogenesis, and colitis caused by Clostridioides difficile.
Shortly after joining Johns Hopkins in 1980, he focused on HIV/AIDS research and caring for people with HIV. Dr. Bartlett led clinical trials of new treatments and developed years of HIV clinical treatment guidelines.
“Back when most hospitals, university medical centers, and ID divisions were running away from the AIDS epidemic, John took it on, both as a scientific priority and a moral imperative,” Dr. Sax writes in a blog post for NEJM Journal Watch. “With the help of Frank Polk and the Hopkins president, he established an outpatient AIDS clinic and an inpatient AIDS ward – both of which were way ahead of their time.”
In the same post, Dr. Sax points out that Dr. Bartlett was an expert in multiple areas – any one of which could be a sole career focus. “How many ID doctors are true experts in all of the following distinct topics? HIV, Clostridium difficile, respiratory tract infections, antimicrobial resistance, and anaerobic pulmonary infections.” Dr. Sax writes.
Expertise that defined an era
In a piece reviewing the long history of infectious disease medicine at Johns Hopkins published in Clinical Infectious Diseases in 2014, Paul Auwaerter, MD, and colleagues describe his tenure at the institution from 1980 to 2006 as “The Bartlett Era,” notable for the many advances he spearheaded.
“It is nearly impossible to find someone trained in infectious diseases in the past 30 years who has not been impacted by John Bartlett,” Dr. Auwaerter and colleagues note. “His tireless devotion to scholarship, teaching, and patient care remains an inspiration to his faculty members at Johns Hopkins, his colleagues, and coworkers around the world.”
Dr. Bartlett was not only a faculty member in the division of infectious diseases, he also helped establish it. When he joined Johns Hopkins, the infectious disease department featured just three faculty members with a research budget of less than $285,000. By the time he left 26 years later, the division had 44 faculty members on tenure track and a research budget exceeding $40 million.
Sharing memories via social media
Reactions to Dr. Bartlett’s passing on Twitter were swift.
“We have lost one of the greatest physicians I have ever met or had the privilege to learn from. Saddened to hear of Dr. John G. Bartlett’s passing. He inspired so many, including me, to choose the field of infectious diseases,” David Fisk, MD, infectious disease specialist in Santa Barbara, Calif., wrote on Twitter.
“John Bartlett just died – a true visionary and the classic ‘Renaissance’ person in clinical ID. Such a nice guy, too! His IDSA/IDWeek literature summaries (among other things) were amazing. We’ll miss him!” Dr. Sax tweeted on Jan. 19.
A colleague at Johns Hopkins, transplant infectious disease specialist Shmuel Shoham, MD, shared an anecdote about Dr. Bartlett on Twitter: “Year ago. My office is across from his. I ask him what he is doing. He tells me he is reviewing a file from the Vatican to adjudicate whether a miracle happened. True story.”
Infectious disease specialist Graeme Forrest, MBBS, also shared a story about Dr. Bartlett via Twitter. “He described to me in 2001 how the U.S. model of health care would not cope with a pandemic or serious bioterror attack as it’s not connected to disseminate information. How prescient from 20 years ago.”
Dr. Bartlett shared his expertise at many national and international infectious disease conferences over the years. He also authored 470 articles, 282 book chapters, and 61 editions of 14 books.
Dr. Bartlett was also a regular contributor to this news organization. For example, he shared his expertise in perspective pieces that addressed priorities in antibiotic stewardship, upcoming infectious disease predictions, and critical infectious disease topics in a three-part series.
Dr. Bartlett’s education includes a bachelor’s degree from Dartmouth College in Hanover, N.H., in 1959 and an MD from Upstate Medical Center in Syracuse, N.Y., in 1963. He did his first 2 years of residency at Brigham and Women’s Hospital.
He also served as an Army captain from 1965 to 1967, treating patients in fever wards in Vietnam. He then returned to the United States to finish his internal medicine training at the University of Alabama in 1968.
Dr. Bartlett completed his fellowship in infectious diseases at the University of California, Los Angeles. In 1975, he joined the faculty at Tufts University, Boston.
Leaving a legacy
Dr. Bartlett’s influence will likely live on in many ways at Johns Hopkins.
“John is a larger-than-life legend whose impact will endure and after whom we are so proud to have named our clinical service, The Bartlett Specialty Practice,” Dr. Thomas said.
The specialty practice clinic named for him has 23 exam rooms and features multidisciplinary care for people with HIV, hepatitis, bone infections, general infectious diseases, and more. Furthermore, friends, family, and colleagues joined forces to create the “Dr. John G. Bartlett HIV/AIDS Fund.”
They note that it is “only appropriate that we honor him by creating an endowment that will provide support for young trainees and junior faculty in the division, helping them transition to their independent careers.”
In addition to all his professional accomplishments, “He was also a genuinely nice person, approachable and humble,” Dr. Sax said. “We really lost a great one!”
A version of this article first appeared on Medscape.com.
USPSTF plan for revising breast screening guidance questioned
The U.S. Preventive Services Task Force is planning to update its breast cancer screening guidelines, which were last issued in 2016. For transparency, it has released the draft research plan it will use for formulating the update, and this draft plan is open for comment until Feb. 17.
However, an expert in breast screening has taken issue with the whole plan.
Daniel Kopans, MD, professor of radiology at Harvard Medical School and founder of the Breast Imaging Division at Massachusetts General Hospital, Boston, argues that previous USPSTF guidelines on breast cancer screening “have been based on flawed analyses of scientific data” and the research plan, as outlined, perpetuates this.
He has also objected, yet again, to the USPSTF panel not having any experts in breast screening on the panel.
Writing in a commentary on Aunt Minnie, a radiology website, he warns about the dangers of not listening to experts: “The COVID-19 pandemic has demonstrated the tragic consequences that result from ignoring science, evidence, and the analysis and advice of experts while being guided by inexpert advice.”
Controversy over previous guidelines
The current USPSTF guidelines on breast cancer screening, which were issued in 2016, were largely unchanged from the previous guidelines that had been issued in 2009. They recommended mammography screening every 2 years for women 50-74 years of age but said that women aged 40-49 should make individual decisions about screening in partnership with their doctors.
The guidance on younger women was met with severe criticism from many experts, as previously reported by this news organization, and the every-2-year interval has also been questioned.
The American College of Radiology and Society of Breast Imaging both recommend annual mammograms starting at age 40.
In the update the USPSTF is now planning, it has an opportunity to “revisit the group’s flawed decision in 2009” about not recommending screening for women in their 40s, argues Dr. Kopans.
But to do that, a number of factors need to be addressed to present a fair and impartial review of the science and evidence in favor of breast screening, he continues, while worrying the draft plan, as currently outlined, will not do so.
One big problem, he argues, is that USPSTF, in its draft plan, has not included statistical models from the U.S. National Cancer Institute and Cancer Intervention and Surveillance Modeling Network to project the potential outcomes of various screening protocols. These NCI/CISNET models all predict that the most lives are saved by annual screening starting at age 40, he points out.
Without these models, the USPSTF will be “guessing in their predictions,” he argues.
Second, even though a reduction in advanced-stage disease is a potentially useful “surrogate endpoint,” Dr. Kopans points out that it is still crucial to remember that women diagnosed at all stages of breast cancer die of the disease. “It has been shown that reducing the size of cancers within stages is also a major benefit from screening that reduces deaths,” he says.
Third, he contends in his commentary that there is a “false claim that the background incidence of breast cancer has not increased over time.” Dr. Kopans says this has been the primary source of misinformation that has been used to promote “the false concepts of massive overdiagnosis” as well as a “false claim that there has not been a reduction in advanced cancers.”
To emphasize his point, Dr. Kopans explains that data clearly demonstrate that the baseline incidence of breast cancer has steadily risen by 1%-1.3% per year, going back at least 80 years. This increase predates screening, which didn’t really begin until the mid-1980s.
“If the correct increasing baseline is used, not only is there no apparent ‘overdiagnosis’ of invasive cancers, but it appears that there has been a major reduction in the incidence of invasive cancers,” he writes. “By using the correct baseline incidence and extrapolation, it is also clear that there has been a major reduction in the rate of advanced cancers.”
To date, there have not been any randomized controlled trials comparing screening intervals (for example, annual vs. every second or third year). But based on the CISNET models, Dr. Kopans emphasized that annual screening is estimated to provide the greatest reduction in deaths. “All women ages 40-74 should be encouraged to be screened every year,” he says.
A version of this article first appeared on Medscape.com.
The U.S. Preventive Services Task Force is planning to update its breast cancer screening guidelines, which were last issued in 2016. For transparency, it has released the draft research plan it will use for formulating the update, and this draft plan is open for comment until Feb. 17.
However, an expert in breast screening has taken issue with the whole plan.
Daniel Kopans, MD, professor of radiology at Harvard Medical School and founder of the Breast Imaging Division at Massachusetts General Hospital, Boston, argues that previous USPSTF guidelines on breast cancer screening “have been based on flawed analyses of scientific data” and the research plan, as outlined, perpetuates this.
He has also objected, yet again, to the USPSTF panel not having any experts in breast screening on the panel.
Writing in a commentary on Aunt Minnie, a radiology website, he warns about the dangers of not listening to experts: “The COVID-19 pandemic has demonstrated the tragic consequences that result from ignoring science, evidence, and the analysis and advice of experts while being guided by inexpert advice.”
Controversy over previous guidelines
The current USPSTF guidelines on breast cancer screening, which were issued in 2016, were largely unchanged from the previous guidelines that had been issued in 2009. They recommended mammography screening every 2 years for women 50-74 years of age but said that women aged 40-49 should make individual decisions about screening in partnership with their doctors.
The guidance on younger women was met with severe criticism from many experts, as previously reported by this news organization, and the every-2-year interval has also been questioned.
The American College of Radiology and Society of Breast Imaging both recommend annual mammograms starting at age 40.
In the update the USPSTF is now planning, it has an opportunity to “revisit the group’s flawed decision in 2009” about not recommending screening for women in their 40s, argues Dr. Kopans.
But to do that, a number of factors need to be addressed to present a fair and impartial review of the science and evidence in favor of breast screening, he continues, while worrying the draft plan, as currently outlined, will not do so.
One big problem, he argues, is that USPSTF, in its draft plan, has not included statistical models from the U.S. National Cancer Institute and Cancer Intervention and Surveillance Modeling Network to project the potential outcomes of various screening protocols. These NCI/CISNET models all predict that the most lives are saved by annual screening starting at age 40, he points out.
Without these models, the USPSTF will be “guessing in their predictions,” he argues.
Second, even though a reduction in advanced-stage disease is a potentially useful “surrogate endpoint,” Dr. Kopans points out that it is still crucial to remember that women diagnosed at all stages of breast cancer die of the disease. “It has been shown that reducing the size of cancers within stages is also a major benefit from screening that reduces deaths,” he says.
Third, he contends in his commentary that there is a “false claim that the background incidence of breast cancer has not increased over time.” Dr. Kopans says this has been the primary source of misinformation that has been used to promote “the false concepts of massive overdiagnosis” as well as a “false claim that there has not been a reduction in advanced cancers.”
To emphasize his point, Dr. Kopans explains that data clearly demonstrate that the baseline incidence of breast cancer has steadily risen by 1%-1.3% per year, going back at least 80 years. This increase predates screening, which didn’t really begin until the mid-1980s.
“If the correct increasing baseline is used, not only is there no apparent ‘overdiagnosis’ of invasive cancers, but it appears that there has been a major reduction in the incidence of invasive cancers,” he writes. “By using the correct baseline incidence and extrapolation, it is also clear that there has been a major reduction in the rate of advanced cancers.”
To date, there have not been any randomized controlled trials comparing screening intervals (for example, annual vs. every second or third year). But based on the CISNET models, Dr. Kopans emphasized that annual screening is estimated to provide the greatest reduction in deaths. “All women ages 40-74 should be encouraged to be screened every year,” he says.
A version of this article first appeared on Medscape.com.
The U.S. Preventive Services Task Force is planning to update its breast cancer screening guidelines, which were last issued in 2016. For transparency, it has released the draft research plan it will use for formulating the update, and this draft plan is open for comment until Feb. 17.
However, an expert in breast screening has taken issue with the whole plan.
Daniel Kopans, MD, professor of radiology at Harvard Medical School and founder of the Breast Imaging Division at Massachusetts General Hospital, Boston, argues that previous USPSTF guidelines on breast cancer screening “have been based on flawed analyses of scientific data” and the research plan, as outlined, perpetuates this.
He has also objected, yet again, to the USPSTF panel not having any experts in breast screening on the panel.
Writing in a commentary on Aunt Minnie, a radiology website, he warns about the dangers of not listening to experts: “The COVID-19 pandemic has demonstrated the tragic consequences that result from ignoring science, evidence, and the analysis and advice of experts while being guided by inexpert advice.”
Controversy over previous guidelines
The current USPSTF guidelines on breast cancer screening, which were issued in 2016, were largely unchanged from the previous guidelines that had been issued in 2009. They recommended mammography screening every 2 years for women 50-74 years of age but said that women aged 40-49 should make individual decisions about screening in partnership with their doctors.
The guidance on younger women was met with severe criticism from many experts, as previously reported by this news organization, and the every-2-year interval has also been questioned.
The American College of Radiology and Society of Breast Imaging both recommend annual mammograms starting at age 40.
In the update the USPSTF is now planning, it has an opportunity to “revisit the group’s flawed decision in 2009” about not recommending screening for women in their 40s, argues Dr. Kopans.
But to do that, a number of factors need to be addressed to present a fair and impartial review of the science and evidence in favor of breast screening, he continues, while worrying the draft plan, as currently outlined, will not do so.
One big problem, he argues, is that USPSTF, in its draft plan, has not included statistical models from the U.S. National Cancer Institute and Cancer Intervention and Surveillance Modeling Network to project the potential outcomes of various screening protocols. These NCI/CISNET models all predict that the most lives are saved by annual screening starting at age 40, he points out.
Without these models, the USPSTF will be “guessing in their predictions,” he argues.
Second, even though a reduction in advanced-stage disease is a potentially useful “surrogate endpoint,” Dr. Kopans points out that it is still crucial to remember that women diagnosed at all stages of breast cancer die of the disease. “It has been shown that reducing the size of cancers within stages is also a major benefit from screening that reduces deaths,” he says.
Third, he contends in his commentary that there is a “false claim that the background incidence of breast cancer has not increased over time.” Dr. Kopans says this has been the primary source of misinformation that has been used to promote “the false concepts of massive overdiagnosis” as well as a “false claim that there has not been a reduction in advanced cancers.”
To emphasize his point, Dr. Kopans explains that data clearly demonstrate that the baseline incidence of breast cancer has steadily risen by 1%-1.3% per year, going back at least 80 years. This increase predates screening, which didn’t really begin until the mid-1980s.
“If the correct increasing baseline is used, not only is there no apparent ‘overdiagnosis’ of invasive cancers, but it appears that there has been a major reduction in the incidence of invasive cancers,” he writes. “By using the correct baseline incidence and extrapolation, it is also clear that there has been a major reduction in the rate of advanced cancers.”
To date, there have not been any randomized controlled trials comparing screening intervals (for example, annual vs. every second or third year). But based on the CISNET models, Dr. Kopans emphasized that annual screening is estimated to provide the greatest reduction in deaths. “All women ages 40-74 should be encouraged to be screened every year,” he says.
A version of this article first appeared on Medscape.com.
BY ROXANNE NELSON, RN, BSN
Super Bowl ad for diabetes device prompts debate
A commercial for the continuous glucose monitor (CGM) Dexcom G6 shown during the Super Bowl has provoked strong reactions in the diabetes community, both positive and negative.
The 30-second ad, which aired between the first two quarters of the American football game yesterday, features singer-songwriter-actor Nick Jonas, who has type 1 diabetes. During the ad, Mr. Jonas asks – with so much technology available today, including drones that deliver packages and self-driving cars – why are people with diabetes still pricking their fingers to test their blood sugar?
Mr. Jonas goes on to demonstrate the Dexcom G6 smartphone glucose app as it displays three different glucose levels including two trending upward, explaining: “It shows your glucose right in your phone, and where it’s heading, without fingersticks. Finally, technology that makes it easier to manage our diabetes.”
Diabetes type or insulin treatment are not mentioned in the ad, despite the fact that most insurance plans typically only cover CGMs for people with type 1 diabetes and sometimes for those with type 2 diabetes who take multiple daily insulin doses (given the risk for hypoglycemia).
Ad prompts mixed reaction on social media
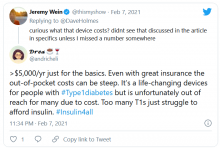
Reactions rolled in on Twitter after the ad debuted Feb. 2, and then again after it aired during the game.
Some people who have type 1 diabetes themselves or have children with the disease who use the product were thrilled.
“Thanks to @NickJonas for his advocacy on T1. My 11-year old has been on the Dexcom for 3 weeks. For a newly diagnosed kid, it removes a lot of anxiety (and for his parents, too!) Plus, he is thrilled his meter has a Super Bowl commercial!” tweeted @KatisJewell.
Another positive tweet, from @rturnerroy, read: “@nickjonas Thank you for bringing representation to #type1diabetes. And hey #Dexcom, you’re the best.”
But many others were critical, both of Jonas and Dexcom. @hb_herrick tweeted: “Diabetes awareness is fantastic. Dexcom being able to afford Nick Jonas for a #SuperBowl commercial is not. This is a health care product. Make it more affordable for those who need it.”
Another Twitter user, @universeofdust, tweeted: “Feeling ambivalent about the #Dexcom ad tbh. I love the awareness & representation. But also not a big fan of dexcom spending $5.5 mill+ to make the CGM seem like this ~cool & trendy~ thing when many type 1s can’t afford their insulin, let alone a CGM.”
And @andricheli wrote: “Only people lucky enough to have excellent insurance and be able to afford the out-of-pocket costs have access. Many others do not.”
And in another tweet the same user said, “The #Dexcom is an amazing device. It’s literally lifesaving and life extending. But it’s also very expensive and not available to everyone. Maybe instead of spending $5 mil on a Super Bowl ad, @dexcom should spend that on getting Dex into the handle of people who need it.”
Others, including @1hitwonderdate, criticized Mr. Jonas directly, asking him: “As someone who has struggled with diabetes and is trying to support themselves along with millions of others, why not use this platform to help those who can’t afford their supplies or are rationing them?!”
Dexcom and Jonas’ organization respond
This news organization reached out to both Dexcom and to Beyond Type 1, a nonprofit organization cofounded by Mr. Jonas, for comment. Both emailed responses.
Regarding the intended audience for the ad, Dexcom acknowledged that it hoped to reach a much wider group than just people with type 1 diabetes or even just insulin users.
“We believe our CGM technology has the ability to empower any person with diabetes and significantly improve their treatment and quality of life, whether they are using insulin or not,” the company said, adding that the ad was also aimed at “loved ones, caregivers, and even health care professionals who need to know about this technology.”
According to Dexcom, the G6 is covered by 99% of commercial insurance in the United States, in addition to Medicare, and by Medicaid in more than 40 states. Over 70% of Dexcom patients with pharmacy coverage in the United States pay under $60 per month for CGM, and a third pay $0 out-of-pocket.
“That said, we know there’s more to be done to improve access, and we are working with several partners to broaden access to Dexcom CGM, especially for people with type 2 diabetes not on mealtime insulin,” the company noted.
Beyond Type 1 responded to the criticisms about Mr. Jonas personally, noting that the celebrity is, in fact, heavily involved in advocacy.
“Nick was involved in the launch of GetInsulin.org this past October,” they said. “GetInsulin.org is a tool created by Beyond Type 1 to connect people with diabetes in the United States to the insulin access and affordability options that match their unique circumstances. ... Beyond Type 1 will continue driving awareness of short-term solutions related to insulin access and affordability while fighting for systemic change.”
The organization “is also advocating for systemic payment policies that will make devices less expensive and avoid the same pitfalls (and rising prices) as the drug pricing system in the U.S.”
Mr. Jonas himself appears aware of the concerns.
Is 2021’s most expensive Super Bowl ad justified?
Meanwhile, in a piece in Esquire, Dave Holmes, who has type 1 diabetes, weighs up the pros and cons of the ad.
He writes: “While Jonas makes it look fun and easy to use a Dexcom G6 – a program to just get with like you would a drone or LED eyelashes – the process of acquiring one is complicated and often very expensive, even for people with good insurance. Which makes the year’s most expensive ad buy, for a product that only a small percentage of the U.S. population needs, confusing to me and others.”
Mr. Holmes also spoke with Craig Stubing, founder of the Beta Cell Foundation, a nonprofit that aims to educate and empower those with type 1 diabetes.
“Spending all this money on an ad, when people’s lives are at stake. I don’t know if offensive is the right word, but it seems out of touch with the reality that their patients are facing,” Mr. Stubing told Mr. Holmes.
A version of this article first appeared on Medscape.com.
A commercial for the continuous glucose monitor (CGM) Dexcom G6 shown during the Super Bowl has provoked strong reactions in the diabetes community, both positive and negative.
The 30-second ad, which aired between the first two quarters of the American football game yesterday, features singer-songwriter-actor Nick Jonas, who has type 1 diabetes. During the ad, Mr. Jonas asks – with so much technology available today, including drones that deliver packages and self-driving cars – why are people with diabetes still pricking their fingers to test their blood sugar?
Mr. Jonas goes on to demonstrate the Dexcom G6 smartphone glucose app as it displays three different glucose levels including two trending upward, explaining: “It shows your glucose right in your phone, and where it’s heading, without fingersticks. Finally, technology that makes it easier to manage our diabetes.”
Diabetes type or insulin treatment are not mentioned in the ad, despite the fact that most insurance plans typically only cover CGMs for people with type 1 diabetes and sometimes for those with type 2 diabetes who take multiple daily insulin doses (given the risk for hypoglycemia).
Ad prompts mixed reaction on social media
Reactions rolled in on Twitter after the ad debuted Feb. 2, and then again after it aired during the game.
Some people who have type 1 diabetes themselves or have children with the disease who use the product were thrilled.
“Thanks to @NickJonas for his advocacy on T1. My 11-year old has been on the Dexcom for 3 weeks. For a newly diagnosed kid, it removes a lot of anxiety (and for his parents, too!) Plus, he is thrilled his meter has a Super Bowl commercial!” tweeted @KatisJewell.
Another positive tweet, from @rturnerroy, read: “@nickjonas Thank you for bringing representation to #type1diabetes. And hey #Dexcom, you’re the best.”
But many others were critical, both of Jonas and Dexcom. @hb_herrick tweeted: “Diabetes awareness is fantastic. Dexcom being able to afford Nick Jonas for a #SuperBowl commercial is not. This is a health care product. Make it more affordable for those who need it.”
Another Twitter user, @universeofdust, tweeted: “Feeling ambivalent about the #Dexcom ad tbh. I love the awareness & representation. But also not a big fan of dexcom spending $5.5 mill+ to make the CGM seem like this ~cool & trendy~ thing when many type 1s can’t afford their insulin, let alone a CGM.”
And @andricheli wrote: “Only people lucky enough to have excellent insurance and be able to afford the out-of-pocket costs have access. Many others do not.”
And in another tweet the same user said, “The #Dexcom is an amazing device. It’s literally lifesaving and life extending. But it’s also very expensive and not available to everyone. Maybe instead of spending $5 mil on a Super Bowl ad, @dexcom should spend that on getting Dex into the handle of people who need it.”
Others, including @1hitwonderdate, criticized Mr. Jonas directly, asking him: “As someone who has struggled with diabetes and is trying to support themselves along with millions of others, why not use this platform to help those who can’t afford their supplies or are rationing them?!”
Dexcom and Jonas’ organization respond
This news organization reached out to both Dexcom and to Beyond Type 1, a nonprofit organization cofounded by Mr. Jonas, for comment. Both emailed responses.
Regarding the intended audience for the ad, Dexcom acknowledged that it hoped to reach a much wider group than just people with type 1 diabetes or even just insulin users.
“We believe our CGM technology has the ability to empower any person with diabetes and significantly improve their treatment and quality of life, whether they are using insulin or not,” the company said, adding that the ad was also aimed at “loved ones, caregivers, and even health care professionals who need to know about this technology.”
According to Dexcom, the G6 is covered by 99% of commercial insurance in the United States, in addition to Medicare, and by Medicaid in more than 40 states. Over 70% of Dexcom patients with pharmacy coverage in the United States pay under $60 per month for CGM, and a third pay $0 out-of-pocket.
“That said, we know there’s more to be done to improve access, and we are working with several partners to broaden access to Dexcom CGM, especially for people with type 2 diabetes not on mealtime insulin,” the company noted.
Beyond Type 1 responded to the criticisms about Mr. Jonas personally, noting that the celebrity is, in fact, heavily involved in advocacy.
“Nick was involved in the launch of GetInsulin.org this past October,” they said. “GetInsulin.org is a tool created by Beyond Type 1 to connect people with diabetes in the United States to the insulin access and affordability options that match their unique circumstances. ... Beyond Type 1 will continue driving awareness of short-term solutions related to insulin access and affordability while fighting for systemic change.”
The organization “is also advocating for systemic payment policies that will make devices less expensive and avoid the same pitfalls (and rising prices) as the drug pricing system in the U.S.”
Mr. Jonas himself appears aware of the concerns.
Is 2021’s most expensive Super Bowl ad justified?
Meanwhile, in a piece in Esquire, Dave Holmes, who has type 1 diabetes, weighs up the pros and cons of the ad.
He writes: “While Jonas makes it look fun and easy to use a Dexcom G6 – a program to just get with like you would a drone or LED eyelashes – the process of acquiring one is complicated and often very expensive, even for people with good insurance. Which makes the year’s most expensive ad buy, for a product that only a small percentage of the U.S. population needs, confusing to me and others.”
Mr. Holmes also spoke with Craig Stubing, founder of the Beta Cell Foundation, a nonprofit that aims to educate and empower those with type 1 diabetes.
“Spending all this money on an ad, when people’s lives are at stake. I don’t know if offensive is the right word, but it seems out of touch with the reality that their patients are facing,” Mr. Stubing told Mr. Holmes.
A version of this article first appeared on Medscape.com.
A commercial for the continuous glucose monitor (CGM) Dexcom G6 shown during the Super Bowl has provoked strong reactions in the diabetes community, both positive and negative.
The 30-second ad, which aired between the first two quarters of the American football game yesterday, features singer-songwriter-actor Nick Jonas, who has type 1 diabetes. During the ad, Mr. Jonas asks – with so much technology available today, including drones that deliver packages and self-driving cars – why are people with diabetes still pricking their fingers to test their blood sugar?
Mr. Jonas goes on to demonstrate the Dexcom G6 smartphone glucose app as it displays three different glucose levels including two trending upward, explaining: “It shows your glucose right in your phone, and where it’s heading, without fingersticks. Finally, technology that makes it easier to manage our diabetes.”
Diabetes type or insulin treatment are not mentioned in the ad, despite the fact that most insurance plans typically only cover CGMs for people with type 1 diabetes and sometimes for those with type 2 diabetes who take multiple daily insulin doses (given the risk for hypoglycemia).
Ad prompts mixed reaction on social media
Reactions rolled in on Twitter after the ad debuted Feb. 2, and then again after it aired during the game.
Some people who have type 1 diabetes themselves or have children with the disease who use the product were thrilled.
“Thanks to @NickJonas for his advocacy on T1. My 11-year old has been on the Dexcom for 3 weeks. For a newly diagnosed kid, it removes a lot of anxiety (and for his parents, too!) Plus, he is thrilled his meter has a Super Bowl commercial!” tweeted @KatisJewell.
Another positive tweet, from @rturnerroy, read: “@nickjonas Thank you for bringing representation to #type1diabetes. And hey #Dexcom, you’re the best.”
But many others were critical, both of Jonas and Dexcom. @hb_herrick tweeted: “Diabetes awareness is fantastic. Dexcom being able to afford Nick Jonas for a #SuperBowl commercial is not. This is a health care product. Make it more affordable for those who need it.”
Another Twitter user, @universeofdust, tweeted: “Feeling ambivalent about the #Dexcom ad tbh. I love the awareness & representation. But also not a big fan of dexcom spending $5.5 mill+ to make the CGM seem like this ~cool & trendy~ thing when many type 1s can’t afford their insulin, let alone a CGM.”
And @andricheli wrote: “Only people lucky enough to have excellent insurance and be able to afford the out-of-pocket costs have access. Many others do not.”
And in another tweet the same user said, “The #Dexcom is an amazing device. It’s literally lifesaving and life extending. But it’s also very expensive and not available to everyone. Maybe instead of spending $5 mil on a Super Bowl ad, @dexcom should spend that on getting Dex into the handle of people who need it.”
Others, including @1hitwonderdate, criticized Mr. Jonas directly, asking him: “As someone who has struggled with diabetes and is trying to support themselves along with millions of others, why not use this platform to help those who can’t afford their supplies or are rationing them?!”
Dexcom and Jonas’ organization respond
This news organization reached out to both Dexcom and to Beyond Type 1, a nonprofit organization cofounded by Mr. Jonas, for comment. Both emailed responses.
Regarding the intended audience for the ad, Dexcom acknowledged that it hoped to reach a much wider group than just people with type 1 diabetes or even just insulin users.
“We believe our CGM technology has the ability to empower any person with diabetes and significantly improve their treatment and quality of life, whether they are using insulin or not,” the company said, adding that the ad was also aimed at “loved ones, caregivers, and even health care professionals who need to know about this technology.”
According to Dexcom, the G6 is covered by 99% of commercial insurance in the United States, in addition to Medicare, and by Medicaid in more than 40 states. Over 70% of Dexcom patients with pharmacy coverage in the United States pay under $60 per month for CGM, and a third pay $0 out-of-pocket.
“That said, we know there’s more to be done to improve access, and we are working with several partners to broaden access to Dexcom CGM, especially for people with type 2 diabetes not on mealtime insulin,” the company noted.
Beyond Type 1 responded to the criticisms about Mr. Jonas personally, noting that the celebrity is, in fact, heavily involved in advocacy.
“Nick was involved in the launch of GetInsulin.org this past October,” they said. “GetInsulin.org is a tool created by Beyond Type 1 to connect people with diabetes in the United States to the insulin access and affordability options that match their unique circumstances. ... Beyond Type 1 will continue driving awareness of short-term solutions related to insulin access and affordability while fighting for systemic change.”
The organization “is also advocating for systemic payment policies that will make devices less expensive and avoid the same pitfalls (and rising prices) as the drug pricing system in the U.S.”
Mr. Jonas himself appears aware of the concerns.
Is 2021’s most expensive Super Bowl ad justified?
Meanwhile, in a piece in Esquire, Dave Holmes, who has type 1 diabetes, weighs up the pros and cons of the ad.
He writes: “While Jonas makes it look fun and easy to use a Dexcom G6 – a program to just get with like you would a drone or LED eyelashes – the process of acquiring one is complicated and often very expensive, even for people with good insurance. Which makes the year’s most expensive ad buy, for a product that only a small percentage of the U.S. population needs, confusing to me and others.”
Mr. Holmes also spoke with Craig Stubing, founder of the Beta Cell Foundation, a nonprofit that aims to educate and empower those with type 1 diabetes.
“Spending all this money on an ad, when people’s lives are at stake. I don’t know if offensive is the right word, but it seems out of touch with the reality that their patients are facing,” Mr. Stubing told Mr. Holmes.
A version of this article first appeared on Medscape.com.
The changing brain signature of HIV
“This shift in subcortical signatures may be contributing to the increasing range of neuropsychiatric and cognitive outcomes,” write Neda Jahanshad, PhD, University of Southern California, Los Angeles, and colleagues.
The study was published online Jan. 15 in JAMA Network Open.
Brain signature of HIV
The researchers with the HIV Working Group within the Enhancing Neuro Imaging Genetics Through Meta Analysis (ENIGMA) consortium examined structural brain associations with CD4+ T cell counts and HIV viral load.
These clinical markers are the most consistently available in studies of HIV and generalize across demographically and clinically diverse HIV-infected individuals, they point out. However, the degree to which they capture central nervous system injury is not fully understood.
In this cross-sectional study of 1,203 HIV-infected adults from 13 HIV neuroimaging studies, a lower CD4+ T-cell count was associated with smaller hippocampal and thalamic volume independent of treatment status. However, in a subset of adults not on cART, a lower CD4+ T-cell count was associated with smaller putamen volume.
Across all participants, detectable viral load was associated with smaller hippocampal volume, but in the subset on cART, detectable viral load was also associated with smaller amygdala volume.
The findings indicate that plasma markers universally used to monitor immune function and response to treatment in patients with HIV infection are associated with subcortical brain volume.
“Our findings,” they add, “extend beyond the classically implicated regions of the basal ganglia and may represent a generalizable brain signature of HIV infection in the cART era.”
A limitation of the analysis is that most of the participants were men (n = 880, 73%). “A more extensive international effort assessing the neurologic effects of HIV infection in women is needed,” they conclude.
This analysis, they add, demonstrates the feasibility and utility of a global collaborative initiative to understand the neurologic signatures of HIV infection. They invite other HIV researchers to join the ENIGMA-HIV consortium.
“With a greater collaborative effort, we will be able to assess factors that may modulate neurologic outcomes, including cART treatment regimens, comorbidities, coinfections, substance use, socioeconomic factors, and demographic factors, as well as the functional implications of such structural brain differences, in well-powered analyses,” the researchers say.
“Understanding the neurobiological changes that may contribute to neuropsychiatric and cognitive outcomes in HIV-positive individuals is critical for identifying individuals at risk for neurologic symptoms, driving novel treatments that may protect the CNS, and monitoring treatment response,” they add.
Support for this research was provided by grants from the National Institutes of Health, the SA Medical Research Council, the National Health and Medical Research Council, and the European Research Council. Dr. Jahanshad received partial research support from Biogen for work unrelated to the topic of this article. A complete list of author disclosures is in the original article.
A version of this article first appeared on Medscape.com.
“This shift in subcortical signatures may be contributing to the increasing range of neuropsychiatric and cognitive outcomes,” write Neda Jahanshad, PhD, University of Southern California, Los Angeles, and colleagues.
The study was published online Jan. 15 in JAMA Network Open.
Brain signature of HIV
The researchers with the HIV Working Group within the Enhancing Neuro Imaging Genetics Through Meta Analysis (ENIGMA) consortium examined structural brain associations with CD4+ T cell counts and HIV viral load.
These clinical markers are the most consistently available in studies of HIV and generalize across demographically and clinically diverse HIV-infected individuals, they point out. However, the degree to which they capture central nervous system injury is not fully understood.
In this cross-sectional study of 1,203 HIV-infected adults from 13 HIV neuroimaging studies, a lower CD4+ T-cell count was associated with smaller hippocampal and thalamic volume independent of treatment status. However, in a subset of adults not on cART, a lower CD4+ T-cell count was associated with smaller putamen volume.
Across all participants, detectable viral load was associated with smaller hippocampal volume, but in the subset on cART, detectable viral load was also associated with smaller amygdala volume.
The findings indicate that plasma markers universally used to monitor immune function and response to treatment in patients with HIV infection are associated with subcortical brain volume.
“Our findings,” they add, “extend beyond the classically implicated regions of the basal ganglia and may represent a generalizable brain signature of HIV infection in the cART era.”
A limitation of the analysis is that most of the participants were men (n = 880, 73%). “A more extensive international effort assessing the neurologic effects of HIV infection in women is needed,” they conclude.
This analysis, they add, demonstrates the feasibility and utility of a global collaborative initiative to understand the neurologic signatures of HIV infection. They invite other HIV researchers to join the ENIGMA-HIV consortium.
“With a greater collaborative effort, we will be able to assess factors that may modulate neurologic outcomes, including cART treatment regimens, comorbidities, coinfections, substance use, socioeconomic factors, and demographic factors, as well as the functional implications of such structural brain differences, in well-powered analyses,” the researchers say.
“Understanding the neurobiological changes that may contribute to neuropsychiatric and cognitive outcomes in HIV-positive individuals is critical for identifying individuals at risk for neurologic symptoms, driving novel treatments that may protect the CNS, and monitoring treatment response,” they add.
Support for this research was provided by grants from the National Institutes of Health, the SA Medical Research Council, the National Health and Medical Research Council, and the European Research Council. Dr. Jahanshad received partial research support from Biogen for work unrelated to the topic of this article. A complete list of author disclosures is in the original article.
A version of this article first appeared on Medscape.com.
“This shift in subcortical signatures may be contributing to the increasing range of neuropsychiatric and cognitive outcomes,” write Neda Jahanshad, PhD, University of Southern California, Los Angeles, and colleagues.
The study was published online Jan. 15 in JAMA Network Open.
Brain signature of HIV
The researchers with the HIV Working Group within the Enhancing Neuro Imaging Genetics Through Meta Analysis (ENIGMA) consortium examined structural brain associations with CD4+ T cell counts and HIV viral load.
These clinical markers are the most consistently available in studies of HIV and generalize across demographically and clinically diverse HIV-infected individuals, they point out. However, the degree to which they capture central nervous system injury is not fully understood.
In this cross-sectional study of 1,203 HIV-infected adults from 13 HIV neuroimaging studies, a lower CD4+ T-cell count was associated with smaller hippocampal and thalamic volume independent of treatment status. However, in a subset of adults not on cART, a lower CD4+ T-cell count was associated with smaller putamen volume.
Across all participants, detectable viral load was associated with smaller hippocampal volume, but in the subset on cART, detectable viral load was also associated with smaller amygdala volume.
The findings indicate that plasma markers universally used to monitor immune function and response to treatment in patients with HIV infection are associated with subcortical brain volume.
“Our findings,” they add, “extend beyond the classically implicated regions of the basal ganglia and may represent a generalizable brain signature of HIV infection in the cART era.”
A limitation of the analysis is that most of the participants were men (n = 880, 73%). “A more extensive international effort assessing the neurologic effects of HIV infection in women is needed,” they conclude.
This analysis, they add, demonstrates the feasibility and utility of a global collaborative initiative to understand the neurologic signatures of HIV infection. They invite other HIV researchers to join the ENIGMA-HIV consortium.
“With a greater collaborative effort, we will be able to assess factors that may modulate neurologic outcomes, including cART treatment regimens, comorbidities, coinfections, substance use, socioeconomic factors, and demographic factors, as well as the functional implications of such structural brain differences, in well-powered analyses,” the researchers say.
“Understanding the neurobiological changes that may contribute to neuropsychiatric and cognitive outcomes in HIV-positive individuals is critical for identifying individuals at risk for neurologic symptoms, driving novel treatments that may protect the CNS, and monitoring treatment response,” they add.
Support for this research was provided by grants from the National Institutes of Health, the SA Medical Research Council, the National Health and Medical Research Council, and the European Research Council. Dr. Jahanshad received partial research support from Biogen for work unrelated to the topic of this article. A complete list of author disclosures is in the original article.
A version of this article first appeared on Medscape.com.
Semaglutide for weight loss? A good first STEP, with caveats
The phase 3a STEP 1 trial that investigated the use of semaglutide (Novo Nordisk), a glucagonlike peptide–1 (GLP-1) agonist, for weight loss is aptly named, some say.
“In sum, we have a long way to go to control the obesity epidemic ... but on the face of it, the STEP 1 trial (like its name) is a good beginning,” wrote coeditorialists Julie R. Ingelfinger, MD, from Harvard Medical School, Boston, and a deputy editor of the New England Journal of Medicine, and Clifford J. Rosen, MD, from Tufts University School of Medicine, also in Boston.
The trial findings by John P.H. Wilding, DM, University of Liverpool (England), and colleagues and an accompanying editorial were published online Feb. 10, 2021, in the New England Journal of Medicine.
“The results are encouraging, with significantly more patients in the semaglutide group having clinically important weight loss,” Dr. Ingelfinger and Dr. Rosen stressed.
However, they also cautioned that “despite the positive results of this trial, the present study has some important limitations” and “there are concerns, including adverse events (mostly gastrointestinal – nausea, sometimes vomiting, and diarrhea) related primarily to the class of the agent.”
Two U.K. experts drew similar takeaways, speaking to the U.K. Science Media Centre.
“This was a well-designed study with unequivocal findings,” which showed that semaglutide “is indeed likely to be a game-changer in the fight against obesity,” according to Baptiste Leurent, PhD, London School of Hygiene and Tropical Medicine.
However, if the drug is approved at this dose for this use, patients would need close monitoring for gastrointestinal disorders, and “we also need to better understand what is happening once the treatment is stopped, and whether it could be taken for a shorter period of time.”
Sir Stephen O’Rahilly, MD, MRC Metabolic Diseases Unit, University of Cambridge (England), pointed out that “GLP-1 is made by cells in the intestine and levels increase in the blood after a meal, providing some of the signal to the brain that tells us we are ‘full,’ ” so GLP-1 agonists have been studied as appetite suppressants, in addition to their approved use to treat type 2 diabetes.
Only about 4.5% of participants in STEP 1 stopped taking semaglutide because of gastrointestinal issues, he noted, although more participants in that group reported problems with gallstones, which can follow rapid weight loss.
And “unlike some previous appetite suppressant drugs which caused significant psychological and psychiatric side effects, there is no evidence that semaglutide has any adverse effects of that nature,” Dr. O’Rahilly noted.
In sum, he said, “this is the start of a new era for obesity drug development with the future direction being to achieve levels of weight loss comparable to semaglutide, while having fewer side effects.”
‘Pressing need’ to address obesity; semaglutide filed for obesity
There is a “pressing need” to address the worldwide increase in obesity and weight-related coexisting conditions, Dr. Ingelfinger and Dr. Rosen noted.
Sustained long-term weight loss with diet and exercise is challenging; behavioral weight-loss strategies “fail more often than not,” bariatric surgery is invasive and often followed by eventual weight regain, they wrote.
In addition, said Dr. Wilding and colleagues, the “use of available [weight-loss] medications remains limited by modest efficacy, safety concerns, and cost.”
Subcutaneous semaglutide, approved for treating type 2 diabetes (as Ozempic) in adults at doses of up to 1 mg/week, induced weight loss at higher doses. The current study is part of the global Semaglutide Treatment Effect in People With Obesity program of four trials (STEP 1, 2, 3, and 4) that aimed to test the safety and efficacy of subcutaneous semaglutide 2.4 mg/week for weight loss.
Topline results from STEP 1 were presented June 4, 2020.
And as reported earlier, results from STEP 3 – a 68-week trial of semaglutide versus placebo in 611 participants who all received very intensive diet and exercise counseling – were presented at the virtual ObesityWeek 2020 meeting.
The four trials of semaglutide for weight loss have been completed and the data were submitted to the Food and Drug Administration on Dec. 4, 2020 (with a decision expected within 6 months) and to the European Medicines Agency on Dec. 18, 2020.
Most patients had 5% weight loss with semaglutide
The STEP 1 trial enrolled 1,961 adults with a body mass index (BMI) of at least 30 kg/m2 or at least 27 with at least one weight-related coexisting condition, but without type 2 diabetes, at 129 sites in 16 countries in Asia, Europe, North America, and South America.
Participants were a mean age of 47 and three-quarters were women. Most participants were White (76%), followed by Asian (13%), Black or African American (6%), or other (5%).
On average, they had a BMI of 38 and weighed 105 kg. Three-quarters had one or more coexisting conditions.
Participants were randomized to receive semaglutide (1,306 patients) or placebo (655 patients), added to lifestyle intervention.
Everyone received 17 monthly individual counseling sessions during which they learned about adhering to a diet with a 500-calorie/day deficit, were encouraged to build up to walking 150 minutes each week, and recorded their daily diet and exercise (in a diary or using an app).
Semaglutide was administered with a prefilled pen injector at a dose of 0.25 mg/week for the first 4 weeks, escalated to 2.4 mg/week by week 16 (or lower if the patient had unacceptable side effects).
At 68 weeks, participants in the semaglutide versus placebo group had greater mean weight loss (14.9% vs. 2.4%, or 15.3 kg vs. 2.6 kg).
Participants in the semaglutide versus placebo group were much more likely to have lost at least 5% of their initial weight (86% vs. 31.5%) or at least 10% of their initial weight (69.1% vs. 12.0%), or at least 15% of their initial weight (50.5% vs. 4.9%; P < .001 for all three comparisons).
About 80% of participants adhered to the study treatment. A third of participants in the semaglutide group who completed the study lost at least 20% of their initial weight, which approaches the 20%-30% reported weight loss 1-3 years after sleeve gastrectomy, the researchers noted.
Participants in the semaglutide group also had greater improvements in waist circumference and levels of hemoglobin A1c, C-reactive protein (a marker of inflammation), and fasting lipids, as well as in physical function scores on SF-36 and IWQOL-Lite-CT questionnaires.
In their editorial, Dr. Ingelfinger and Dr. Rosen noted that “daily oral semaglutide [already approved in 7-mg and 14-mg doses for the treatment of type 2 diabetes as Rybelsus] might be more appealing to many people,” as a weight-loss medication than a once-weekly subcutaneous dose. Semaglutide is the first GLP-1 agonist available as an oral agent.
The ongoing Semaglutide Effects on Heart Disease and Stroke in Patients With Overweight or Obesity (SELECT) trial (with expected completion in 2023) will shed light on cardiovascular outcomes after 2.5-5 years.
GI disorders and ‘important limitations’
More participants in the semaglutide than the placebo group reported gastrointestinal disorders (typically nausea, diarrhea, vomiting, and constipation; 74.2% vs. 47.9%), which were mostly transient and mild to moderate in severity, but also led to more treatment discontinuation (7.0% vs. 3.1%).
More patients in the semaglutide versus placebo group had a gall bladder–related disorder (2.6% vs. 1.2%, mostly cholelithiasis) and mild acute pancreatitis (3 vs. 0 participants), but there were no between-group differences in neoplasms.
Dr. Wilding and colleagues acknowledge the limitations of the study, including the fact that it enrolled mainly women, mainly non-White participants, was relatively short, and excluded patients with type 2 diabetes.
Mean placebo-corrected weight loss with 2.4 mg/weekly subcutaneous semaglutide was greater than with 3.0 mg once-daily subcutaneous liraglutide (Saxenda, Novo Nordisk) – the only GLP-1 agonist approved for weight management – in the 56-week SCALE trial (12.4% vs. 4.5%); however, the two studies had different populations.
The study was supported by Novo Nordisk. Dr. Ingelfinger is a deputy editor and Dr. Rosen is an associate editor of the New England Journal of Medicine. Dr. Ingelfinger, Dr. Rosen, and Dr. Leurent have reported no relevant financial relationships. Dr. O’Rahilly has a current research collaboration with Novo Nordisk scientists in an unrelated area and has been a consultant for the company.
A version of this article first appeared on Medscape.com.
The phase 3a STEP 1 trial that investigated the use of semaglutide (Novo Nordisk), a glucagonlike peptide–1 (GLP-1) agonist, for weight loss is aptly named, some say.
“In sum, we have a long way to go to control the obesity epidemic ... but on the face of it, the STEP 1 trial (like its name) is a good beginning,” wrote coeditorialists Julie R. Ingelfinger, MD, from Harvard Medical School, Boston, and a deputy editor of the New England Journal of Medicine, and Clifford J. Rosen, MD, from Tufts University School of Medicine, also in Boston.
The trial findings by John P.H. Wilding, DM, University of Liverpool (England), and colleagues and an accompanying editorial were published online Feb. 10, 2021, in the New England Journal of Medicine.
“The results are encouraging, with significantly more patients in the semaglutide group having clinically important weight loss,” Dr. Ingelfinger and Dr. Rosen stressed.
However, they also cautioned that “despite the positive results of this trial, the present study has some important limitations” and “there are concerns, including adverse events (mostly gastrointestinal – nausea, sometimes vomiting, and diarrhea) related primarily to the class of the agent.”
Two U.K. experts drew similar takeaways, speaking to the U.K. Science Media Centre.
“This was a well-designed study with unequivocal findings,” which showed that semaglutide “is indeed likely to be a game-changer in the fight against obesity,” according to Baptiste Leurent, PhD, London School of Hygiene and Tropical Medicine.
However, if the drug is approved at this dose for this use, patients would need close monitoring for gastrointestinal disorders, and “we also need to better understand what is happening once the treatment is stopped, and whether it could be taken for a shorter period of time.”
Sir Stephen O’Rahilly, MD, MRC Metabolic Diseases Unit, University of Cambridge (England), pointed out that “GLP-1 is made by cells in the intestine and levels increase in the blood after a meal, providing some of the signal to the brain that tells us we are ‘full,’ ” so GLP-1 agonists have been studied as appetite suppressants, in addition to their approved use to treat type 2 diabetes.
Only about 4.5% of participants in STEP 1 stopped taking semaglutide because of gastrointestinal issues, he noted, although more participants in that group reported problems with gallstones, which can follow rapid weight loss.
And “unlike some previous appetite suppressant drugs which caused significant psychological and psychiatric side effects, there is no evidence that semaglutide has any adverse effects of that nature,” Dr. O’Rahilly noted.
In sum, he said, “this is the start of a new era for obesity drug development with the future direction being to achieve levels of weight loss comparable to semaglutide, while having fewer side effects.”
‘Pressing need’ to address obesity; semaglutide filed for obesity
There is a “pressing need” to address the worldwide increase in obesity and weight-related coexisting conditions, Dr. Ingelfinger and Dr. Rosen noted.
Sustained long-term weight loss with diet and exercise is challenging; behavioral weight-loss strategies “fail more often than not,” bariatric surgery is invasive and often followed by eventual weight regain, they wrote.
In addition, said Dr. Wilding and colleagues, the “use of available [weight-loss] medications remains limited by modest efficacy, safety concerns, and cost.”
Subcutaneous semaglutide, approved for treating type 2 diabetes (as Ozempic) in adults at doses of up to 1 mg/week, induced weight loss at higher doses. The current study is part of the global Semaglutide Treatment Effect in People With Obesity program of four trials (STEP 1, 2, 3, and 4) that aimed to test the safety and efficacy of subcutaneous semaglutide 2.4 mg/week for weight loss.
Topline results from STEP 1 were presented June 4, 2020.
And as reported earlier, results from STEP 3 – a 68-week trial of semaglutide versus placebo in 611 participants who all received very intensive diet and exercise counseling – were presented at the virtual ObesityWeek 2020 meeting.
The four trials of semaglutide for weight loss have been completed and the data were submitted to the Food and Drug Administration on Dec. 4, 2020 (with a decision expected within 6 months) and to the European Medicines Agency on Dec. 18, 2020.
Most patients had 5% weight loss with semaglutide
The STEP 1 trial enrolled 1,961 adults with a body mass index (BMI) of at least 30 kg/m2 or at least 27 with at least one weight-related coexisting condition, but without type 2 diabetes, at 129 sites in 16 countries in Asia, Europe, North America, and South America.
Participants were a mean age of 47 and three-quarters were women. Most participants were White (76%), followed by Asian (13%), Black or African American (6%), or other (5%).
On average, they had a BMI of 38 and weighed 105 kg. Three-quarters had one or more coexisting conditions.
Participants were randomized to receive semaglutide (1,306 patients) or placebo (655 patients), added to lifestyle intervention.
Everyone received 17 monthly individual counseling sessions during which they learned about adhering to a diet with a 500-calorie/day deficit, were encouraged to build up to walking 150 minutes each week, and recorded their daily diet and exercise (in a diary or using an app).
Semaglutide was administered with a prefilled pen injector at a dose of 0.25 mg/week for the first 4 weeks, escalated to 2.4 mg/week by week 16 (or lower if the patient had unacceptable side effects).
At 68 weeks, participants in the semaglutide versus placebo group had greater mean weight loss (14.9% vs. 2.4%, or 15.3 kg vs. 2.6 kg).
Participants in the semaglutide versus placebo group were much more likely to have lost at least 5% of their initial weight (86% vs. 31.5%) or at least 10% of their initial weight (69.1% vs. 12.0%), or at least 15% of their initial weight (50.5% vs. 4.9%; P < .001 for all three comparisons).
About 80% of participants adhered to the study treatment. A third of participants in the semaglutide group who completed the study lost at least 20% of their initial weight, which approaches the 20%-30% reported weight loss 1-3 years after sleeve gastrectomy, the researchers noted.
Participants in the semaglutide group also had greater improvements in waist circumference and levels of hemoglobin A1c, C-reactive protein (a marker of inflammation), and fasting lipids, as well as in physical function scores on SF-36 and IWQOL-Lite-CT questionnaires.
In their editorial, Dr. Ingelfinger and Dr. Rosen noted that “daily oral semaglutide [already approved in 7-mg and 14-mg doses for the treatment of type 2 diabetes as Rybelsus] might be more appealing to many people,” as a weight-loss medication than a once-weekly subcutaneous dose. Semaglutide is the first GLP-1 agonist available as an oral agent.
The ongoing Semaglutide Effects on Heart Disease and Stroke in Patients With Overweight or Obesity (SELECT) trial (with expected completion in 2023) will shed light on cardiovascular outcomes after 2.5-5 years.
GI disorders and ‘important limitations’
More participants in the semaglutide than the placebo group reported gastrointestinal disorders (typically nausea, diarrhea, vomiting, and constipation; 74.2% vs. 47.9%), which were mostly transient and mild to moderate in severity, but also led to more treatment discontinuation (7.0% vs. 3.1%).
More patients in the semaglutide versus placebo group had a gall bladder–related disorder (2.6% vs. 1.2%, mostly cholelithiasis) and mild acute pancreatitis (3 vs. 0 participants), but there were no between-group differences in neoplasms.
Dr. Wilding and colleagues acknowledge the limitations of the study, including the fact that it enrolled mainly women, mainly non-White participants, was relatively short, and excluded patients with type 2 diabetes.
Mean placebo-corrected weight loss with 2.4 mg/weekly subcutaneous semaglutide was greater than with 3.0 mg once-daily subcutaneous liraglutide (Saxenda, Novo Nordisk) – the only GLP-1 agonist approved for weight management – in the 56-week SCALE trial (12.4% vs. 4.5%); however, the two studies had different populations.
The study was supported by Novo Nordisk. Dr. Ingelfinger is a deputy editor and Dr. Rosen is an associate editor of the New England Journal of Medicine. Dr. Ingelfinger, Dr. Rosen, and Dr. Leurent have reported no relevant financial relationships. Dr. O’Rahilly has a current research collaboration with Novo Nordisk scientists in an unrelated area and has been a consultant for the company.
A version of this article first appeared on Medscape.com.
The phase 3a STEP 1 trial that investigated the use of semaglutide (Novo Nordisk), a glucagonlike peptide–1 (GLP-1) agonist, for weight loss is aptly named, some say.
“In sum, we have a long way to go to control the obesity epidemic ... but on the face of it, the STEP 1 trial (like its name) is a good beginning,” wrote coeditorialists Julie R. Ingelfinger, MD, from Harvard Medical School, Boston, and a deputy editor of the New England Journal of Medicine, and Clifford J. Rosen, MD, from Tufts University School of Medicine, also in Boston.
The trial findings by John P.H. Wilding, DM, University of Liverpool (England), and colleagues and an accompanying editorial were published online Feb. 10, 2021, in the New England Journal of Medicine.
“The results are encouraging, with significantly more patients in the semaglutide group having clinically important weight loss,” Dr. Ingelfinger and Dr. Rosen stressed.
However, they also cautioned that “despite the positive results of this trial, the present study has some important limitations” and “there are concerns, including adverse events (mostly gastrointestinal – nausea, sometimes vomiting, and diarrhea) related primarily to the class of the agent.”
Two U.K. experts drew similar takeaways, speaking to the U.K. Science Media Centre.
“This was a well-designed study with unequivocal findings,” which showed that semaglutide “is indeed likely to be a game-changer in the fight against obesity,” according to Baptiste Leurent, PhD, London School of Hygiene and Tropical Medicine.
However, if the drug is approved at this dose for this use, patients would need close monitoring for gastrointestinal disorders, and “we also need to better understand what is happening once the treatment is stopped, and whether it could be taken for a shorter period of time.”
Sir Stephen O’Rahilly, MD, MRC Metabolic Diseases Unit, University of Cambridge (England), pointed out that “GLP-1 is made by cells in the intestine and levels increase in the blood after a meal, providing some of the signal to the brain that tells us we are ‘full,’ ” so GLP-1 agonists have been studied as appetite suppressants, in addition to their approved use to treat type 2 diabetes.
Only about 4.5% of participants in STEP 1 stopped taking semaglutide because of gastrointestinal issues, he noted, although more participants in that group reported problems with gallstones, which can follow rapid weight loss.
And “unlike some previous appetite suppressant drugs which caused significant psychological and psychiatric side effects, there is no evidence that semaglutide has any adverse effects of that nature,” Dr. O’Rahilly noted.
In sum, he said, “this is the start of a new era for obesity drug development with the future direction being to achieve levels of weight loss comparable to semaglutide, while having fewer side effects.”
‘Pressing need’ to address obesity; semaglutide filed for obesity
There is a “pressing need” to address the worldwide increase in obesity and weight-related coexisting conditions, Dr. Ingelfinger and Dr. Rosen noted.
Sustained long-term weight loss with diet and exercise is challenging; behavioral weight-loss strategies “fail more often than not,” bariatric surgery is invasive and often followed by eventual weight regain, they wrote.
In addition, said Dr. Wilding and colleagues, the “use of available [weight-loss] medications remains limited by modest efficacy, safety concerns, and cost.”
Subcutaneous semaglutide, approved for treating type 2 diabetes (as Ozempic) in adults at doses of up to 1 mg/week, induced weight loss at higher doses. The current study is part of the global Semaglutide Treatment Effect in People With Obesity program of four trials (STEP 1, 2, 3, and 4) that aimed to test the safety and efficacy of subcutaneous semaglutide 2.4 mg/week for weight loss.
Topline results from STEP 1 were presented June 4, 2020.
And as reported earlier, results from STEP 3 – a 68-week trial of semaglutide versus placebo in 611 participants who all received very intensive diet and exercise counseling – were presented at the virtual ObesityWeek 2020 meeting.
The four trials of semaglutide for weight loss have been completed and the data were submitted to the Food and Drug Administration on Dec. 4, 2020 (with a decision expected within 6 months) and to the European Medicines Agency on Dec. 18, 2020.
Most patients had 5% weight loss with semaglutide
The STEP 1 trial enrolled 1,961 adults with a body mass index (BMI) of at least 30 kg/m2 or at least 27 with at least one weight-related coexisting condition, but without type 2 diabetes, at 129 sites in 16 countries in Asia, Europe, North America, and South America.
Participants were a mean age of 47 and three-quarters were women. Most participants were White (76%), followed by Asian (13%), Black or African American (6%), or other (5%).
On average, they had a BMI of 38 and weighed 105 kg. Three-quarters had one or more coexisting conditions.
Participants were randomized to receive semaglutide (1,306 patients) or placebo (655 patients), added to lifestyle intervention.
Everyone received 17 monthly individual counseling sessions during which they learned about adhering to a diet with a 500-calorie/day deficit, were encouraged to build up to walking 150 minutes each week, and recorded their daily diet and exercise (in a diary or using an app).
Semaglutide was administered with a prefilled pen injector at a dose of 0.25 mg/week for the first 4 weeks, escalated to 2.4 mg/week by week 16 (or lower if the patient had unacceptable side effects).
At 68 weeks, participants in the semaglutide versus placebo group had greater mean weight loss (14.9% vs. 2.4%, or 15.3 kg vs. 2.6 kg).
Participants in the semaglutide versus placebo group were much more likely to have lost at least 5% of their initial weight (86% vs. 31.5%) or at least 10% of their initial weight (69.1% vs. 12.0%), or at least 15% of their initial weight (50.5% vs. 4.9%; P < .001 for all three comparisons).
About 80% of participants adhered to the study treatment. A third of participants in the semaglutide group who completed the study lost at least 20% of their initial weight, which approaches the 20%-30% reported weight loss 1-3 years after sleeve gastrectomy, the researchers noted.
Participants in the semaglutide group also had greater improvements in waist circumference and levels of hemoglobin A1c, C-reactive protein (a marker of inflammation), and fasting lipids, as well as in physical function scores on SF-36 and IWQOL-Lite-CT questionnaires.
In their editorial, Dr. Ingelfinger and Dr. Rosen noted that “daily oral semaglutide [already approved in 7-mg and 14-mg doses for the treatment of type 2 diabetes as Rybelsus] might be more appealing to many people,” as a weight-loss medication than a once-weekly subcutaneous dose. Semaglutide is the first GLP-1 agonist available as an oral agent.
The ongoing Semaglutide Effects on Heart Disease and Stroke in Patients With Overweight or Obesity (SELECT) trial (with expected completion in 2023) will shed light on cardiovascular outcomes after 2.5-5 years.
GI disorders and ‘important limitations’
More participants in the semaglutide than the placebo group reported gastrointestinal disorders (typically nausea, diarrhea, vomiting, and constipation; 74.2% vs. 47.9%), which were mostly transient and mild to moderate in severity, but also led to more treatment discontinuation (7.0% vs. 3.1%).
More patients in the semaglutide versus placebo group had a gall bladder–related disorder (2.6% vs. 1.2%, mostly cholelithiasis) and mild acute pancreatitis (3 vs. 0 participants), but there were no between-group differences in neoplasms.
Dr. Wilding and colleagues acknowledge the limitations of the study, including the fact that it enrolled mainly women, mainly non-White participants, was relatively short, and excluded patients with type 2 diabetes.
Mean placebo-corrected weight loss with 2.4 mg/weekly subcutaneous semaglutide was greater than with 3.0 mg once-daily subcutaneous liraglutide (Saxenda, Novo Nordisk) – the only GLP-1 agonist approved for weight management – in the 56-week SCALE trial (12.4% vs. 4.5%); however, the two studies had different populations.
The study was supported by Novo Nordisk. Dr. Ingelfinger is a deputy editor and Dr. Rosen is an associate editor of the New England Journal of Medicine. Dr. Ingelfinger, Dr. Rosen, and Dr. Leurent have reported no relevant financial relationships. Dr. O’Rahilly has a current research collaboration with Novo Nordisk scientists in an unrelated area and has been a consultant for the company.
A version of this article first appeared on Medscape.com.
FDA approves orphan drug evinacumab-dgnb for homozygous FH
The Food and Drug Administration has approved the fully human monoclonal antibody evinacumab-dgnb (Evkeeza, Regeneron Pharmaceuticals) for use on top of other cholesterol-modifying medication in patients aged 12 years and older with homozygous familial hypercholesterolemia (HoFH), the agency and Regeneron have announced.
Evinacumab had received orphan drug designation and underwent priority regulatory review based primarily on the phase 3 ELIPSE trial, presented at a meeting in March 2020 and published in August 2020 in the New England Journal of Medicine (doi: 10.1056/NEJMoa2004215).
In the trial with 65 patients with HoFH on guideline-based lipid-modifying therapy, those who also received evinacumab 15 mg/kg intravenously every 4 weeks showed a nearly 50% drop in LDL cholesterol levels after 24 weeks, compared with patients given a placebo. Only 2% of patients in both groups discontinued therapy because of adverse reactions.
The drug blocks angiopoietin-like 3, itself an inhibitor of lipoprotein lipase and endothelial lipase. It therefore lowers LDL cholesterol levels by mechanisms that don’t directly involve the LDL receptor.
Regeneron estimates that about 1300 people in the United States have the homozygous genetic disorder, which can lead to LDL cholesterol levels of a 1,000 mg/dL or higher, advanced premature atherosclerosis, and extreme risk for cardiovascular events.
The drug’s average wholesale acquisition cost per patient in the United States is expected to be about $450,000 per year, the company said, adding that it has a financial support program to help qualified patients with out-of-pocket costs.
Regeneron’s announcement included a comment from dyslipidemia-therapy expert Daniel J. Rader, MD, University of Pennsylvania, Philadelphia, who called evinacumab “a potentially transformational new treatment for people with HoFH.”
The drug is currently under regulatory review for the same indication in Europe, the company said.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved the fully human monoclonal antibody evinacumab-dgnb (Evkeeza, Regeneron Pharmaceuticals) for use on top of other cholesterol-modifying medication in patients aged 12 years and older with homozygous familial hypercholesterolemia (HoFH), the agency and Regeneron have announced.
Evinacumab had received orphan drug designation and underwent priority regulatory review based primarily on the phase 3 ELIPSE trial, presented at a meeting in March 2020 and published in August 2020 in the New England Journal of Medicine (doi: 10.1056/NEJMoa2004215).
In the trial with 65 patients with HoFH on guideline-based lipid-modifying therapy, those who also received evinacumab 15 mg/kg intravenously every 4 weeks showed a nearly 50% drop in LDL cholesterol levels after 24 weeks, compared with patients given a placebo. Only 2% of patients in both groups discontinued therapy because of adverse reactions.
The drug blocks angiopoietin-like 3, itself an inhibitor of lipoprotein lipase and endothelial lipase. It therefore lowers LDL cholesterol levels by mechanisms that don’t directly involve the LDL receptor.
Regeneron estimates that about 1300 people in the United States have the homozygous genetic disorder, which can lead to LDL cholesterol levels of a 1,000 mg/dL or higher, advanced premature atherosclerosis, and extreme risk for cardiovascular events.
The drug’s average wholesale acquisition cost per patient in the United States is expected to be about $450,000 per year, the company said, adding that it has a financial support program to help qualified patients with out-of-pocket costs.
Regeneron’s announcement included a comment from dyslipidemia-therapy expert Daniel J. Rader, MD, University of Pennsylvania, Philadelphia, who called evinacumab “a potentially transformational new treatment for people with HoFH.”
The drug is currently under regulatory review for the same indication in Europe, the company said.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved the fully human monoclonal antibody evinacumab-dgnb (Evkeeza, Regeneron Pharmaceuticals) for use on top of other cholesterol-modifying medication in patients aged 12 years and older with homozygous familial hypercholesterolemia (HoFH), the agency and Regeneron have announced.
Evinacumab had received orphan drug designation and underwent priority regulatory review based primarily on the phase 3 ELIPSE trial, presented at a meeting in March 2020 and published in August 2020 in the New England Journal of Medicine (doi: 10.1056/NEJMoa2004215).
In the trial with 65 patients with HoFH on guideline-based lipid-modifying therapy, those who also received evinacumab 15 mg/kg intravenously every 4 weeks showed a nearly 50% drop in LDL cholesterol levels after 24 weeks, compared with patients given a placebo. Only 2% of patients in both groups discontinued therapy because of adverse reactions.
The drug blocks angiopoietin-like 3, itself an inhibitor of lipoprotein lipase and endothelial lipase. It therefore lowers LDL cholesterol levels by mechanisms that don’t directly involve the LDL receptor.
Regeneron estimates that about 1300 people in the United States have the homozygous genetic disorder, which can lead to LDL cholesterol levels of a 1,000 mg/dL or higher, advanced premature atherosclerosis, and extreme risk for cardiovascular events.
The drug’s average wholesale acquisition cost per patient in the United States is expected to be about $450,000 per year, the company said, adding that it has a financial support program to help qualified patients with out-of-pocket costs.
Regeneron’s announcement included a comment from dyslipidemia-therapy expert Daniel J. Rader, MD, University of Pennsylvania, Philadelphia, who called evinacumab “a potentially transformational new treatment for people with HoFH.”
The drug is currently under regulatory review for the same indication in Europe, the company said.
A version of this article first appeared on Medscape.com.
Menopause transition affects heart health risks
Menopause is a key time to monitor women for the development or increase of cardiovascular risk factors, according to a new consensus statement developed by the Task Force on Gender of the European Society of Cardiology and a multidisciplinary ESC working group on Women’s Health in Menopause.
“After menopause, traditional cardiovascular risk factors are adversely affected – particularly hypertension,” wrote Angela H.E.M. Maas, MD, of Radboud University Medical Center, Nijmegen, Netherlands, and colleagues.
“Since the first ESC consensus paper on the management of cardiovascular risk in perimenopausal women was published in 2007, we have a greater understanding on the role of female-specific risk factors for cardiovascular disease (CVD),” they said.
In a consensus statement published in the European Heart Journal, the authors presented clinical guidance for diagnosis and management of cardiovascular risk factors during the menopause transition. The transition to menopause increases a woman’s risk for developing several CVD risk factors, including central adiposity, increased insulin resistance, a proatherogenic lipid profile, and autonomic dysfunction that can contribute to increased heart rate variability, according to the statement.
Estrogen changes may affect ischemic disease
In general, obstructive coronary artery disease (CAD) strikes women later than men, but coronary vasomotor conditions are a common cause of ischemic heart disease in women with or without CAD, the authors noted.
“Lower estrogen levels after menopause are related to altered vascular function, enhanced inflammation, and up-regulation of other hormonal systems such as the renin–angiotensin–aldosterone system, the sympathetic nervous system, and reduced nitric oxide–dependent vasodilation,” they wrote. They recommended use of the coronary artery calcium score for screening middle-aged women who are symptomatic or at intermediate cardiovascular risk.
The transition to menopause causes changes in lipid profiles, and a rise in blood pressure in particular “may be both a direct effect of hormonal changes on the vasculature and metabolic changes with aging,” but hypertension in early post menopause is “often poorly managed,” the authors noted.
Compared with asymptomatic women, women who suffer from severe menopausal symptoms often have increased cardiovascular disease risk factors. For example, the Women’s Health Initiative (WHI) study showed a 48% increased risk of incident diabetes at follow-up in women with severe symptoms of hot flashes and night sweats, the authors wrote. Clinicians should also be aware of the increased immune reactivity that occurs during and after menopause and the increased CVD risk associated with autoimmune and endocrine disorders, they said.
Multiple strategies to reduce risk
Strategies to address the cardiovascular risk in menopause include assessing glucose, lipid levels, and blood pressure during the transition to menopause, according to the statement.
In addition, they recommended increasing employer awareness of menopause, as changes may interfere with working ability. A healthy lifestyle including healthy diet and regular exercise can help reduce cardiovascular risks and relieve symptoms. Menopausal hormone therapy (MHT) may be indicated to relieve symptoms, including symptoms of depression, and provide cardioprotection for younger women around the time of menopause, according to the statement.
However, “MHT is not recommended in women at high CV risk and after a previous CVD event,” and all women should be assessed for cardiovascular risk factors before starting MHT, they emphasized.
Results raise awareness of cardiovascular health and menopause link
“Over the past 20 years, our knowledge of how menopause might contribute to cardiovascular disease has dramatically evolved,” said Samar El Khoudary, MD, of the University of Pittsburg, in an interview.
“We have accumulated data that consistently point to the menopause transition as a time of change in cardiovascular health. As such, there is a compelling need to discuss the implications of the accumulating body of literature on this topic,” she said. “The goal is to raise awareness for both health care providers and women of the significant adverse cardiovascular health changes accompanying the menopause transition and to point out the importance of adopting prevention strategies early during this stage,” she explained.
The impact of the hormonal changes of menopause on CVD risk “is very complex,” Dr. El Khoudary said. “Until now, we could not prove that using estrogen therapy is cardioprotective,” she emphasized. “Studies point to the need to consider the timing of hormone use, as well as types and route of administration,” she noted. “The truth is that, although the menopause transition is associated with an acceleration in CVD risk, the exact mechanism still is not completely clear. Hormone changes contribute, but they are not the ultimate contributor,” she added.
Research gaps include data on lifestyle and behavioral interventions
“Irrespective of the accumulating findings showing adverse changes in multiple cardiovascular health parameters, as women transition through menopause, we do not have data documenting current status of ideal cardiovascular health components during the menopause transition among women,” said Dr. El Khoudary. “The limited data we have [suggest] that a very small proportion of women transitioning through menopause eat a healthy diet (less than 20%) or practice physical activity (about7.2%) at a level that matches the current recommendations,” she noted.
“Lifestyle and behavioral interventions are critical to maintain a healthy heart and reduce heart disease; we do not have adequate randomized clinical trials testing these interventions specifically during the menopause transition,” she said.
“Similarly, we are in need of randomized clinical trials of therapeutic interventions such as lipid-lowering medications and menopause hormone therapy in women transitioning through menopause,” said Dr. El Khoudary. “This high-risk population has not been the focus of previous clinical trials, leaving us with questions of how the results from these studies might apply to women during the menopause transition,” she said.
Consensus invites collaboration
“I commend the group for putting together a statement that crosses practice and specialty boundaries,” said Lubna Pal, MD, of Yale School of Medicine, New Haven, Conn., in an interview. Although the statement does not present novel information, it “has the power of unifying the various providers by bringing focus on the individual elements spanning a woman’s life that cumulatively determine her lifetime health risk,” she said. Preeclampsia may be a risk factor for cardiovascular disease later in life, and events in reproductive age may determine a woman’s trajectory during the transition to menopause and beyond, Dr. Pal noted.
“The consensus statement will likely be read by internists and family medicine providers as well as ob.gyns.; it encourages all those involved in caring for female patients to take on the responsibility of ‘passing on the baton,’ such that all women who are deemed at an enhanced risk for cardiovascular disease are assured due diligence in care through stringent surveillance and timely interventions,” said Dr. Pal. “It is a call for the various providers who care for women at distinct stages of life to work together toward a shared goal of optimizing every woman’s health across her lifespan,” she said.
“More research is needed for us to better understand the mechanisms at play” in the development of cardiovascular risk and in understanding the continuity of changes across women’s lifespans, Dr. Pal said. “We have associations, but not much information about causation,” she emphasized. However, the statement promotes the dissemination of information about women’s health and sensitizes providers to the potential and the power of preventive care. “We should be much more liberal and loud in holding conversations about risk quantification and risk reduction, and this statement is a resounding effort toward identifying and mitigating long-term cardiovascular risk, even if only through promoting a healthier lifestyle in those deemed at risk,” she added.
The statement received no outside funding. Lead author Dr. Maas had no financial conflicts to disclose. Dr. El Khoudary had no financial conflicts to disclose. Dr. Pal had no relevant financial conflicts to disclose.
Menopause is a key time to monitor women for the development or increase of cardiovascular risk factors, according to a new consensus statement developed by the Task Force on Gender of the European Society of Cardiology and a multidisciplinary ESC working group on Women’s Health in Menopause.
“After menopause, traditional cardiovascular risk factors are adversely affected – particularly hypertension,” wrote Angela H.E.M. Maas, MD, of Radboud University Medical Center, Nijmegen, Netherlands, and colleagues.
“Since the first ESC consensus paper on the management of cardiovascular risk in perimenopausal women was published in 2007, we have a greater understanding on the role of female-specific risk factors for cardiovascular disease (CVD),” they said.
In a consensus statement published in the European Heart Journal, the authors presented clinical guidance for diagnosis and management of cardiovascular risk factors during the menopause transition. The transition to menopause increases a woman’s risk for developing several CVD risk factors, including central adiposity, increased insulin resistance, a proatherogenic lipid profile, and autonomic dysfunction that can contribute to increased heart rate variability, according to the statement.
Estrogen changes may affect ischemic disease
In general, obstructive coronary artery disease (CAD) strikes women later than men, but coronary vasomotor conditions are a common cause of ischemic heart disease in women with or without CAD, the authors noted.
“Lower estrogen levels after menopause are related to altered vascular function, enhanced inflammation, and up-regulation of other hormonal systems such as the renin–angiotensin–aldosterone system, the sympathetic nervous system, and reduced nitric oxide–dependent vasodilation,” they wrote. They recommended use of the coronary artery calcium score for screening middle-aged women who are symptomatic or at intermediate cardiovascular risk.
The transition to menopause causes changes in lipid profiles, and a rise in blood pressure in particular “may be both a direct effect of hormonal changes on the vasculature and metabolic changes with aging,” but hypertension in early post menopause is “often poorly managed,” the authors noted.
Compared with asymptomatic women, women who suffer from severe menopausal symptoms often have increased cardiovascular disease risk factors. For example, the Women’s Health Initiative (WHI) study showed a 48% increased risk of incident diabetes at follow-up in women with severe symptoms of hot flashes and night sweats, the authors wrote. Clinicians should also be aware of the increased immune reactivity that occurs during and after menopause and the increased CVD risk associated with autoimmune and endocrine disorders, they said.
Multiple strategies to reduce risk
Strategies to address the cardiovascular risk in menopause include assessing glucose, lipid levels, and blood pressure during the transition to menopause, according to the statement.
In addition, they recommended increasing employer awareness of menopause, as changes may interfere with working ability. A healthy lifestyle including healthy diet and regular exercise can help reduce cardiovascular risks and relieve symptoms. Menopausal hormone therapy (MHT) may be indicated to relieve symptoms, including symptoms of depression, and provide cardioprotection for younger women around the time of menopause, according to the statement.
However, “MHT is not recommended in women at high CV risk and after a previous CVD event,” and all women should be assessed for cardiovascular risk factors before starting MHT, they emphasized.
Results raise awareness of cardiovascular health and menopause link
“Over the past 20 years, our knowledge of how menopause might contribute to cardiovascular disease has dramatically evolved,” said Samar El Khoudary, MD, of the University of Pittsburg, in an interview.
“We have accumulated data that consistently point to the menopause transition as a time of change in cardiovascular health. As such, there is a compelling need to discuss the implications of the accumulating body of literature on this topic,” she said. “The goal is to raise awareness for both health care providers and women of the significant adverse cardiovascular health changes accompanying the menopause transition and to point out the importance of adopting prevention strategies early during this stage,” she explained.
The impact of the hormonal changes of menopause on CVD risk “is very complex,” Dr. El Khoudary said. “Until now, we could not prove that using estrogen therapy is cardioprotective,” she emphasized. “Studies point to the need to consider the timing of hormone use, as well as types and route of administration,” she noted. “The truth is that, although the menopause transition is associated with an acceleration in CVD risk, the exact mechanism still is not completely clear. Hormone changes contribute, but they are not the ultimate contributor,” she added.
Research gaps include data on lifestyle and behavioral interventions
“Irrespective of the accumulating findings showing adverse changes in multiple cardiovascular health parameters, as women transition through menopause, we do not have data documenting current status of ideal cardiovascular health components during the menopause transition among women,” said Dr. El Khoudary. “The limited data we have [suggest] that a very small proportion of women transitioning through menopause eat a healthy diet (less than 20%) or practice physical activity (about7.2%) at a level that matches the current recommendations,” she noted.
“Lifestyle and behavioral interventions are critical to maintain a healthy heart and reduce heart disease; we do not have adequate randomized clinical trials testing these interventions specifically during the menopause transition,” she said.
“Similarly, we are in need of randomized clinical trials of therapeutic interventions such as lipid-lowering medications and menopause hormone therapy in women transitioning through menopause,” said Dr. El Khoudary. “This high-risk population has not been the focus of previous clinical trials, leaving us with questions of how the results from these studies might apply to women during the menopause transition,” she said.
Consensus invites collaboration
“I commend the group for putting together a statement that crosses practice and specialty boundaries,” said Lubna Pal, MD, of Yale School of Medicine, New Haven, Conn., in an interview. Although the statement does not present novel information, it “has the power of unifying the various providers by bringing focus on the individual elements spanning a woman’s life that cumulatively determine her lifetime health risk,” she said. Preeclampsia may be a risk factor for cardiovascular disease later in life, and events in reproductive age may determine a woman’s trajectory during the transition to menopause and beyond, Dr. Pal noted.
“The consensus statement will likely be read by internists and family medicine providers as well as ob.gyns.; it encourages all those involved in caring for female patients to take on the responsibility of ‘passing on the baton,’ such that all women who are deemed at an enhanced risk for cardiovascular disease are assured due diligence in care through stringent surveillance and timely interventions,” said Dr. Pal. “It is a call for the various providers who care for women at distinct stages of life to work together toward a shared goal of optimizing every woman’s health across her lifespan,” she said.
“More research is needed for us to better understand the mechanisms at play” in the development of cardiovascular risk and in understanding the continuity of changes across women’s lifespans, Dr. Pal said. “We have associations, but not much information about causation,” she emphasized. However, the statement promotes the dissemination of information about women’s health and sensitizes providers to the potential and the power of preventive care. “We should be much more liberal and loud in holding conversations about risk quantification and risk reduction, and this statement is a resounding effort toward identifying and mitigating long-term cardiovascular risk, even if only through promoting a healthier lifestyle in those deemed at risk,” she added.
The statement received no outside funding. Lead author Dr. Maas had no financial conflicts to disclose. Dr. El Khoudary had no financial conflicts to disclose. Dr. Pal had no relevant financial conflicts to disclose.
Menopause is a key time to monitor women for the development or increase of cardiovascular risk factors, according to a new consensus statement developed by the Task Force on Gender of the European Society of Cardiology and a multidisciplinary ESC working group on Women’s Health in Menopause.
“After menopause, traditional cardiovascular risk factors are adversely affected – particularly hypertension,” wrote Angela H.E.M. Maas, MD, of Radboud University Medical Center, Nijmegen, Netherlands, and colleagues.
“Since the first ESC consensus paper on the management of cardiovascular risk in perimenopausal women was published in 2007, we have a greater understanding on the role of female-specific risk factors for cardiovascular disease (CVD),” they said.
In a consensus statement published in the European Heart Journal, the authors presented clinical guidance for diagnosis and management of cardiovascular risk factors during the menopause transition. The transition to menopause increases a woman’s risk for developing several CVD risk factors, including central adiposity, increased insulin resistance, a proatherogenic lipid profile, and autonomic dysfunction that can contribute to increased heart rate variability, according to the statement.
Estrogen changes may affect ischemic disease
In general, obstructive coronary artery disease (CAD) strikes women later than men, but coronary vasomotor conditions are a common cause of ischemic heart disease in women with or without CAD, the authors noted.
“Lower estrogen levels after menopause are related to altered vascular function, enhanced inflammation, and up-regulation of other hormonal systems such as the renin–angiotensin–aldosterone system, the sympathetic nervous system, and reduced nitric oxide–dependent vasodilation,” they wrote. They recommended use of the coronary artery calcium score for screening middle-aged women who are symptomatic or at intermediate cardiovascular risk.
The transition to menopause causes changes in lipid profiles, and a rise in blood pressure in particular “may be both a direct effect of hormonal changes on the vasculature and metabolic changes with aging,” but hypertension in early post menopause is “often poorly managed,” the authors noted.
Compared with asymptomatic women, women who suffer from severe menopausal symptoms often have increased cardiovascular disease risk factors. For example, the Women’s Health Initiative (WHI) study showed a 48% increased risk of incident diabetes at follow-up in women with severe symptoms of hot flashes and night sweats, the authors wrote. Clinicians should also be aware of the increased immune reactivity that occurs during and after menopause and the increased CVD risk associated with autoimmune and endocrine disorders, they said.
Multiple strategies to reduce risk
Strategies to address the cardiovascular risk in menopause include assessing glucose, lipid levels, and blood pressure during the transition to menopause, according to the statement.
In addition, they recommended increasing employer awareness of menopause, as changes may interfere with working ability. A healthy lifestyle including healthy diet and regular exercise can help reduce cardiovascular risks and relieve symptoms. Menopausal hormone therapy (MHT) may be indicated to relieve symptoms, including symptoms of depression, and provide cardioprotection for younger women around the time of menopause, according to the statement.
However, “MHT is not recommended in women at high CV risk and after a previous CVD event,” and all women should be assessed for cardiovascular risk factors before starting MHT, they emphasized.
Results raise awareness of cardiovascular health and menopause link
“Over the past 20 years, our knowledge of how menopause might contribute to cardiovascular disease has dramatically evolved,” said Samar El Khoudary, MD, of the University of Pittsburg, in an interview.
“We have accumulated data that consistently point to the menopause transition as a time of change in cardiovascular health. As such, there is a compelling need to discuss the implications of the accumulating body of literature on this topic,” she said. “The goal is to raise awareness for both health care providers and women of the significant adverse cardiovascular health changes accompanying the menopause transition and to point out the importance of adopting prevention strategies early during this stage,” she explained.
The impact of the hormonal changes of menopause on CVD risk “is very complex,” Dr. El Khoudary said. “Until now, we could not prove that using estrogen therapy is cardioprotective,” she emphasized. “Studies point to the need to consider the timing of hormone use, as well as types and route of administration,” she noted. “The truth is that, although the menopause transition is associated with an acceleration in CVD risk, the exact mechanism still is not completely clear. Hormone changes contribute, but they are not the ultimate contributor,” she added.
Research gaps include data on lifestyle and behavioral interventions
“Irrespective of the accumulating findings showing adverse changes in multiple cardiovascular health parameters, as women transition through menopause, we do not have data documenting current status of ideal cardiovascular health components during the menopause transition among women,” said Dr. El Khoudary. “The limited data we have [suggest] that a very small proportion of women transitioning through menopause eat a healthy diet (less than 20%) or practice physical activity (about7.2%) at a level that matches the current recommendations,” she noted.
“Lifestyle and behavioral interventions are critical to maintain a healthy heart and reduce heart disease; we do not have adequate randomized clinical trials testing these interventions specifically during the menopause transition,” she said.
“Similarly, we are in need of randomized clinical trials of therapeutic interventions such as lipid-lowering medications and menopause hormone therapy in women transitioning through menopause,” said Dr. El Khoudary. “This high-risk population has not been the focus of previous clinical trials, leaving us with questions of how the results from these studies might apply to women during the menopause transition,” she said.
Consensus invites collaboration
“I commend the group for putting together a statement that crosses practice and specialty boundaries,” said Lubna Pal, MD, of Yale School of Medicine, New Haven, Conn., in an interview. Although the statement does not present novel information, it “has the power of unifying the various providers by bringing focus on the individual elements spanning a woman’s life that cumulatively determine her lifetime health risk,” she said. Preeclampsia may be a risk factor for cardiovascular disease later in life, and events in reproductive age may determine a woman’s trajectory during the transition to menopause and beyond, Dr. Pal noted.
“The consensus statement will likely be read by internists and family medicine providers as well as ob.gyns.; it encourages all those involved in caring for female patients to take on the responsibility of ‘passing on the baton,’ such that all women who are deemed at an enhanced risk for cardiovascular disease are assured due diligence in care through stringent surveillance and timely interventions,” said Dr. Pal. “It is a call for the various providers who care for women at distinct stages of life to work together toward a shared goal of optimizing every woman’s health across her lifespan,” she said.
“More research is needed for us to better understand the mechanisms at play” in the development of cardiovascular risk and in understanding the continuity of changes across women’s lifespans, Dr. Pal said. “We have associations, but not much information about causation,” she emphasized. However, the statement promotes the dissemination of information about women’s health and sensitizes providers to the potential and the power of preventive care. “We should be much more liberal and loud in holding conversations about risk quantification and risk reduction, and this statement is a resounding effort toward identifying and mitigating long-term cardiovascular risk, even if only through promoting a healthier lifestyle in those deemed at risk,” she added.
The statement received no outside funding. Lead author Dr. Maas had no financial conflicts to disclose. Dr. El Khoudary had no financial conflicts to disclose. Dr. Pal had no relevant financial conflicts to disclose.
FROM THE EUROPEAN HEART JOURNAL
Vedolizumab looks safer than anti-TNF drugs in older adults with IBD
A large analysis of Medicare data from all 50 states suggests that vedolizumab may be just as effective as anti–tumor necrosis factor (anti-TNF) agents in controlling inflammatory bowel disease (IBD) in patients aged over 65 years, with fewer infectious disease hospitalizations.
The study was prompted by the fact that older adults are greatly underrepresented in clinical trials of approved IBD medications. There is a second peak in IBD diagnosis among people in their 50s and 60s, and IBD patients are living longer with more effective medications. So although a significant number of IBD patients are aged 65 years or older, that group encompasses less than 1% of adults in clinical trials, Bharati Kochar, MD, reported at the annual congress of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
“Therefore, we don’t know how well these medications work and how safe they are specifically in older adults,” said Dr. Kochar, a gastroenterologist at Massachusetts General Hospital and assistant professor of medicine at Harvard Medical School, both in Boston.
The data largely support what had been known mechanistically about vedolizumab. “It suggests that both drugs work well enough to prevent [IBD-related] hospitalizations, but clearly there was a benefit toward the safer medication, Entyvio [vedolizumab], in the infection-related hospitalizations. That’s not the only readout in infections, but it is an important readout because infections that get hospitalized are the ones that predict mortality and disability,” said Matthew Ciorba, MD, who attended the session. Dr. Ciorba is director of the IBD Center at Washington University in St. Louis and was not involved in the study.
“I think this study is reassuring to clinicians. It provides important clinical data that support what we know about the mechanisms of vedolizumab. The safety data we predicted is borne out in this large and well-done study,” said Dr. Ciorba.
The researchers collected a 20% random sample from a 50-state Medicare claims database, including patients who were aged 65 years or older, who had two or more codes for Crohn’s disease or ulcerative colitis, and had 18 months of continuous enrollment. It excluded Medicare Part C patients; those who used ustekinumab, natalizumab, cyclosporine, or tacrolimus during the look back and study period; and those with two or more codes for rheumatoid arthritis, plaque psoriasis, psoriatic arthritis, or ankylosing spondylitis during the study period.
Among those included, 480 patients were on vedolizumab, while 1,152 were on anti-TNF medications. The two groups were broadly similar in their characteristics: Twenty-nine percent of both groups took budesonide, although the anti-TNF group had a higher frequency use of systemic corticosteroids (68% vs. 57%), 5-ASA drugs (62% vs. 42%), and immunomodulators (32% vs. 28%).
There were no significant differences between the two groups with respect to frequency of IBD-related hospitalizations, IBD-related surgery, steroid prescription rate after induction, or all-cause hospitalization. However, infection-related hospitalizations were less frequent in the vedolizumab group (crude incidence, 0.03 vs. 0.05 per person-year; adjusted hazard ratio, 0.47; 95% confidence interval, 0.25-0.86).
“I think it’s important to use your clinical judgment to treat the patient in front of you, and these data should simply help contextualize risk for older IBD patients newly initiating vedolizumab and anti-TNF agents,” said Dr. Kochar. However, recognizing the limitations of any retrospective study based on administrative data, she called for additional research. “There is a vast need for additional large and robust comparative effectiveness and safety studies in older adults of the rapidly proliferating arsenal of IBD medications,” Dr. Kochar concluded.
Dr. Kochar and Dr. Ciorba have no relevant financial disclosures.
A large analysis of Medicare data from all 50 states suggests that vedolizumab may be just as effective as anti–tumor necrosis factor (anti-TNF) agents in controlling inflammatory bowel disease (IBD) in patients aged over 65 years, with fewer infectious disease hospitalizations.
The study was prompted by the fact that older adults are greatly underrepresented in clinical trials of approved IBD medications. There is a second peak in IBD diagnosis among people in their 50s and 60s, and IBD patients are living longer with more effective medications. So although a significant number of IBD patients are aged 65 years or older, that group encompasses less than 1% of adults in clinical trials, Bharati Kochar, MD, reported at the annual congress of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
“Therefore, we don’t know how well these medications work and how safe they are specifically in older adults,” said Dr. Kochar, a gastroenterologist at Massachusetts General Hospital and assistant professor of medicine at Harvard Medical School, both in Boston.
The data largely support what had been known mechanistically about vedolizumab. “It suggests that both drugs work well enough to prevent [IBD-related] hospitalizations, but clearly there was a benefit toward the safer medication, Entyvio [vedolizumab], in the infection-related hospitalizations. That’s not the only readout in infections, but it is an important readout because infections that get hospitalized are the ones that predict mortality and disability,” said Matthew Ciorba, MD, who attended the session. Dr. Ciorba is director of the IBD Center at Washington University in St. Louis and was not involved in the study.
“I think this study is reassuring to clinicians. It provides important clinical data that support what we know about the mechanisms of vedolizumab. The safety data we predicted is borne out in this large and well-done study,” said Dr. Ciorba.
The researchers collected a 20% random sample from a 50-state Medicare claims database, including patients who were aged 65 years or older, who had two or more codes for Crohn’s disease or ulcerative colitis, and had 18 months of continuous enrollment. It excluded Medicare Part C patients; those who used ustekinumab, natalizumab, cyclosporine, or tacrolimus during the look back and study period; and those with two or more codes for rheumatoid arthritis, plaque psoriasis, psoriatic arthritis, or ankylosing spondylitis during the study period.
Among those included, 480 patients were on vedolizumab, while 1,152 were on anti-TNF medications. The two groups were broadly similar in their characteristics: Twenty-nine percent of both groups took budesonide, although the anti-TNF group had a higher frequency use of systemic corticosteroids (68% vs. 57%), 5-ASA drugs (62% vs. 42%), and immunomodulators (32% vs. 28%).
There were no significant differences between the two groups with respect to frequency of IBD-related hospitalizations, IBD-related surgery, steroid prescription rate after induction, or all-cause hospitalization. However, infection-related hospitalizations were less frequent in the vedolizumab group (crude incidence, 0.03 vs. 0.05 per person-year; adjusted hazard ratio, 0.47; 95% confidence interval, 0.25-0.86).
“I think it’s important to use your clinical judgment to treat the patient in front of you, and these data should simply help contextualize risk for older IBD patients newly initiating vedolizumab and anti-TNF agents,” said Dr. Kochar. However, recognizing the limitations of any retrospective study based on administrative data, she called for additional research. “There is a vast need for additional large and robust comparative effectiveness and safety studies in older adults of the rapidly proliferating arsenal of IBD medications,” Dr. Kochar concluded.
Dr. Kochar and Dr. Ciorba have no relevant financial disclosures.
A large analysis of Medicare data from all 50 states suggests that vedolizumab may be just as effective as anti–tumor necrosis factor (anti-TNF) agents in controlling inflammatory bowel disease (IBD) in patients aged over 65 years, with fewer infectious disease hospitalizations.
The study was prompted by the fact that older adults are greatly underrepresented in clinical trials of approved IBD medications. There is a second peak in IBD diagnosis among people in their 50s and 60s, and IBD patients are living longer with more effective medications. So although a significant number of IBD patients are aged 65 years or older, that group encompasses less than 1% of adults in clinical trials, Bharati Kochar, MD, reported at the annual congress of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
“Therefore, we don’t know how well these medications work and how safe they are specifically in older adults,” said Dr. Kochar, a gastroenterologist at Massachusetts General Hospital and assistant professor of medicine at Harvard Medical School, both in Boston.
The data largely support what had been known mechanistically about vedolizumab. “It suggests that both drugs work well enough to prevent [IBD-related] hospitalizations, but clearly there was a benefit toward the safer medication, Entyvio [vedolizumab], in the infection-related hospitalizations. That’s not the only readout in infections, but it is an important readout because infections that get hospitalized are the ones that predict mortality and disability,” said Matthew Ciorba, MD, who attended the session. Dr. Ciorba is director of the IBD Center at Washington University in St. Louis and was not involved in the study.
“I think this study is reassuring to clinicians. It provides important clinical data that support what we know about the mechanisms of vedolizumab. The safety data we predicted is borne out in this large and well-done study,” said Dr. Ciorba.
The researchers collected a 20% random sample from a 50-state Medicare claims database, including patients who were aged 65 years or older, who had two or more codes for Crohn’s disease or ulcerative colitis, and had 18 months of continuous enrollment. It excluded Medicare Part C patients; those who used ustekinumab, natalizumab, cyclosporine, or tacrolimus during the look back and study period; and those with two or more codes for rheumatoid arthritis, plaque psoriasis, psoriatic arthritis, or ankylosing spondylitis during the study period.
Among those included, 480 patients were on vedolizumab, while 1,152 were on anti-TNF medications. The two groups were broadly similar in their characteristics: Twenty-nine percent of both groups took budesonide, although the anti-TNF group had a higher frequency use of systemic corticosteroids (68% vs. 57%), 5-ASA drugs (62% vs. 42%), and immunomodulators (32% vs. 28%).
There were no significant differences between the two groups with respect to frequency of IBD-related hospitalizations, IBD-related surgery, steroid prescription rate after induction, or all-cause hospitalization. However, infection-related hospitalizations were less frequent in the vedolizumab group (crude incidence, 0.03 vs. 0.05 per person-year; adjusted hazard ratio, 0.47; 95% confidence interval, 0.25-0.86).
“I think it’s important to use your clinical judgment to treat the patient in front of you, and these data should simply help contextualize risk for older IBD patients newly initiating vedolizumab and anti-TNF agents,” said Dr. Kochar. However, recognizing the limitations of any retrospective study based on administrative data, she called for additional research. “There is a vast need for additional large and robust comparative effectiveness and safety studies in older adults of the rapidly proliferating arsenal of IBD medications,” Dr. Kochar concluded.
Dr. Kochar and Dr. Ciorba have no relevant financial disclosures.
FROM THE CROHN’S & COLITIS CONGRESS
Women and ACS: Focus on typical symptoms to improve outcomes
There are some differences in how women relative to men report symptoms of an acute coronary syndrome (ACS), but they should not be permitted to get in the way of prompt diagnosis and treatment, according to an expert review at the virtual Going Back to the Heart of Cardiology meeting.
“We need to get away from the idea that symptoms of a myocardial infarction in women are atypical, because women are also having typical symptoms,” said Martha Gulati, MD, chief of cardiology at the University of Arizona, Phoenix.
Sexes share key symptoms, but not treatment
Although “women are more likely to report additional symptoms,” chest pain “is pretty much equal between men and women” presenting with an ACS, according to Dr. Gulati.
There are several studies that have shown this, including the Variation in Recovery: Role of Gender on Outcomes of Young AMI patients (VIRGO). In VIRGO, which looked at ACS symptom presentation in younger patients (ages 18-55 years), 87.0% of women versus 89.5% of men presented with chest pain defined as pain, pressure, tightness, or discomfort.
Even among those who recognize that more women die of cardiovascular disease (CVD) disease than any other cause, nothing seems to erase the bias that women in an ED are less likely than men to be having a heart attack. About 60 million women in the United States have CVD, so no threat imposes a higher toll in morbidity and mortality.
In comparison, there are only about 3.5 million women with breast cancer. Even though this is a major cause of morbidity and mortality in women, it is dwarfed by CVD, according to statistics cited by Dr. Gulati. Yet, the data show women get inferior care by guideline-based standards.
“After a myocardial infarction, women relative to men are less likely to get aspirin or beta-blockers within 24 hours, they are less likely to undergo any type of invasive procedure, and they are less likely to meet the door-to-balloon time or receive any reperfusion therapy,” Dr. Gulati said. After a CVD event, “the only thing women do better is to die.”
Additional symptoms may muddy the diagnostic waters
In the setting of ACS, the problem is not that women fail to report symptoms that should lead clinicians to consider CVD, but that they report additional symptoms. For the clinician less inclined to consider CVD in women, particularly younger women, there is a greater risk of going down the wrong diagnostic pathway.
In other words, women report symptoms consistent with CVD, “but it is a question of whether we are hearing it,” Dr. Gulati said.
In the VIRGO study, 61.9% of women versus 54.8% of men (P < .001) presented three or more symptoms in addition to chest pain, such as epigastric symptoms, discomfort in the arms or neck, or palpitations. Women were more likely than men to attribute the symptoms to stress or anxiety (20.9% vs. 11.8%; P < .001), while less likely to consider them a result of muscle pain (15.4% vs. 21.2%; P = .029).
There are other gender differences for ACS. For example, women are more likely than men to presented ischemia without obstruction, but Dr. Gulati emphasized that lack of obstruction is not a reason to dismiss the potential for an underlying CV cause.
‘Yentl syndrome’ persists
“Women should not need to present exactly like men to be taken seriously,” she said, describing the “Yentl syndrome,” which now has its own Wikipedia page. A cardiovascular version of this syndrome was first described 30 years ago. Based on a movie of a woman who cross dresses in order to be allowed to undertake Jewish studies, the term captures the societal failure to adapt care for women who do not present disease the same way that men do.
Overall, inadequate urgency to pursue potential symptoms of ACS in women is just another manifestation of the “bikini approach to women’s health,” according to Dr. Gulati. This describes the focus on the breast and reproductive system to the exclusion or other organs and anatomy. Dr. Gulati speculated that this might be the reason that clinicians have failed to apply ACS guidelines to women with the same rigor that they apply to men.
This is hardly a new issue. Calls for improving cardiovascular care in women have been increasing in volume for more than past 20 years, but the issue has proven persistent, according to Dr. Gulati. As an example, she noted that the same types of gaps in care and in outcome reported in a 2008 registry study had not much changed in an article published 8 years later.
The solution is not complex, according to Dr. Gulati. In the ED, guideline-directed diagnostic tests should be offered to any man or woman, including younger women, who present with chest pain, ignoring gender bias that threatens misinterpretation of patient history and symptoms. Once CVD is diagnosed as promptly in women as it is in men, guideline-directed intervention would be expected to reduce the gender gap in outcomes.
“By applying standardized protocols, it will help us to the same for women as we do for men,” Dr. Gulati said.
The meeting was sponsored by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
There are some differences in how women relative to men report symptoms of an acute coronary syndrome (ACS), but they should not be permitted to get in the way of prompt diagnosis and treatment, according to an expert review at the virtual Going Back to the Heart of Cardiology meeting.
“We need to get away from the idea that symptoms of a myocardial infarction in women are atypical, because women are also having typical symptoms,” said Martha Gulati, MD, chief of cardiology at the University of Arizona, Phoenix.
Sexes share key symptoms, but not treatment
Although “women are more likely to report additional symptoms,” chest pain “is pretty much equal between men and women” presenting with an ACS, according to Dr. Gulati.
There are several studies that have shown this, including the Variation in Recovery: Role of Gender on Outcomes of Young AMI patients (VIRGO). In VIRGO, which looked at ACS symptom presentation in younger patients (ages 18-55 years), 87.0% of women versus 89.5% of men presented with chest pain defined as pain, pressure, tightness, or discomfort.
Even among those who recognize that more women die of cardiovascular disease (CVD) disease than any other cause, nothing seems to erase the bias that women in an ED are less likely than men to be having a heart attack. About 60 million women in the United States have CVD, so no threat imposes a higher toll in morbidity and mortality.
In comparison, there are only about 3.5 million women with breast cancer. Even though this is a major cause of morbidity and mortality in women, it is dwarfed by CVD, according to statistics cited by Dr. Gulati. Yet, the data show women get inferior care by guideline-based standards.
“After a myocardial infarction, women relative to men are less likely to get aspirin or beta-blockers within 24 hours, they are less likely to undergo any type of invasive procedure, and they are less likely to meet the door-to-balloon time or receive any reperfusion therapy,” Dr. Gulati said. After a CVD event, “the only thing women do better is to die.”
Additional symptoms may muddy the diagnostic waters
In the setting of ACS, the problem is not that women fail to report symptoms that should lead clinicians to consider CVD, but that they report additional symptoms. For the clinician less inclined to consider CVD in women, particularly younger women, there is a greater risk of going down the wrong diagnostic pathway.
In other words, women report symptoms consistent with CVD, “but it is a question of whether we are hearing it,” Dr. Gulati said.
In the VIRGO study, 61.9% of women versus 54.8% of men (P < .001) presented three or more symptoms in addition to chest pain, such as epigastric symptoms, discomfort in the arms or neck, or palpitations. Women were more likely than men to attribute the symptoms to stress or anxiety (20.9% vs. 11.8%; P < .001), while less likely to consider them a result of muscle pain (15.4% vs. 21.2%; P = .029).
There are other gender differences for ACS. For example, women are more likely than men to presented ischemia without obstruction, but Dr. Gulati emphasized that lack of obstruction is not a reason to dismiss the potential for an underlying CV cause.
‘Yentl syndrome’ persists
“Women should not need to present exactly like men to be taken seriously,” she said, describing the “Yentl syndrome,” which now has its own Wikipedia page. A cardiovascular version of this syndrome was first described 30 years ago. Based on a movie of a woman who cross dresses in order to be allowed to undertake Jewish studies, the term captures the societal failure to adapt care for women who do not present disease the same way that men do.
Overall, inadequate urgency to pursue potential symptoms of ACS in women is just another manifestation of the “bikini approach to women’s health,” according to Dr. Gulati. This describes the focus on the breast and reproductive system to the exclusion or other organs and anatomy. Dr. Gulati speculated that this might be the reason that clinicians have failed to apply ACS guidelines to women with the same rigor that they apply to men.
This is hardly a new issue. Calls for improving cardiovascular care in women have been increasing in volume for more than past 20 years, but the issue has proven persistent, according to Dr. Gulati. As an example, she noted that the same types of gaps in care and in outcome reported in a 2008 registry study had not much changed in an article published 8 years later.
The solution is not complex, according to Dr. Gulati. In the ED, guideline-directed diagnostic tests should be offered to any man or woman, including younger women, who present with chest pain, ignoring gender bias that threatens misinterpretation of patient history and symptoms. Once CVD is diagnosed as promptly in women as it is in men, guideline-directed intervention would be expected to reduce the gender gap in outcomes.
“By applying standardized protocols, it will help us to the same for women as we do for men,” Dr. Gulati said.
The meeting was sponsored by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
There are some differences in how women relative to men report symptoms of an acute coronary syndrome (ACS), but they should not be permitted to get in the way of prompt diagnosis and treatment, according to an expert review at the virtual Going Back to the Heart of Cardiology meeting.
“We need to get away from the idea that symptoms of a myocardial infarction in women are atypical, because women are also having typical symptoms,” said Martha Gulati, MD, chief of cardiology at the University of Arizona, Phoenix.
Sexes share key symptoms, but not treatment
Although “women are more likely to report additional symptoms,” chest pain “is pretty much equal between men and women” presenting with an ACS, according to Dr. Gulati.
There are several studies that have shown this, including the Variation in Recovery: Role of Gender on Outcomes of Young AMI patients (VIRGO). In VIRGO, which looked at ACS symptom presentation in younger patients (ages 18-55 years), 87.0% of women versus 89.5% of men presented with chest pain defined as pain, pressure, tightness, or discomfort.
Even among those who recognize that more women die of cardiovascular disease (CVD) disease than any other cause, nothing seems to erase the bias that women in an ED are less likely than men to be having a heart attack. About 60 million women in the United States have CVD, so no threat imposes a higher toll in morbidity and mortality.
In comparison, there are only about 3.5 million women with breast cancer. Even though this is a major cause of morbidity and mortality in women, it is dwarfed by CVD, according to statistics cited by Dr. Gulati. Yet, the data show women get inferior care by guideline-based standards.
“After a myocardial infarction, women relative to men are less likely to get aspirin or beta-blockers within 24 hours, they are less likely to undergo any type of invasive procedure, and they are less likely to meet the door-to-balloon time or receive any reperfusion therapy,” Dr. Gulati said. After a CVD event, “the only thing women do better is to die.”
Additional symptoms may muddy the diagnostic waters
In the setting of ACS, the problem is not that women fail to report symptoms that should lead clinicians to consider CVD, but that they report additional symptoms. For the clinician less inclined to consider CVD in women, particularly younger women, there is a greater risk of going down the wrong diagnostic pathway.
In other words, women report symptoms consistent with CVD, “but it is a question of whether we are hearing it,” Dr. Gulati said.
In the VIRGO study, 61.9% of women versus 54.8% of men (P < .001) presented three or more symptoms in addition to chest pain, such as epigastric symptoms, discomfort in the arms or neck, or palpitations. Women were more likely than men to attribute the symptoms to stress or anxiety (20.9% vs. 11.8%; P < .001), while less likely to consider them a result of muscle pain (15.4% vs. 21.2%; P = .029).
There are other gender differences for ACS. For example, women are more likely than men to presented ischemia without obstruction, but Dr. Gulati emphasized that lack of obstruction is not a reason to dismiss the potential for an underlying CV cause.
‘Yentl syndrome’ persists
“Women should not need to present exactly like men to be taken seriously,” she said, describing the “Yentl syndrome,” which now has its own Wikipedia page. A cardiovascular version of this syndrome was first described 30 years ago. Based on a movie of a woman who cross dresses in order to be allowed to undertake Jewish studies, the term captures the societal failure to adapt care for women who do not present disease the same way that men do.
Overall, inadequate urgency to pursue potential symptoms of ACS in women is just another manifestation of the “bikini approach to women’s health,” according to Dr. Gulati. This describes the focus on the breast and reproductive system to the exclusion or other organs and anatomy. Dr. Gulati speculated that this might be the reason that clinicians have failed to apply ACS guidelines to women with the same rigor that they apply to men.
This is hardly a new issue. Calls for improving cardiovascular care in women have been increasing in volume for more than past 20 years, but the issue has proven persistent, according to Dr. Gulati. As an example, she noted that the same types of gaps in care and in outcome reported in a 2008 registry study had not much changed in an article published 8 years later.
The solution is not complex, according to Dr. Gulati. In the ED, guideline-directed diagnostic tests should be offered to any man or woman, including younger women, who present with chest pain, ignoring gender bias that threatens misinterpretation of patient history and symptoms. Once CVD is diagnosed as promptly in women as it is in men, guideline-directed intervention would be expected to reduce the gender gap in outcomes.
“By applying standardized protocols, it will help us to the same for women as we do for men,” Dr. Gulati said.
The meeting was sponsored by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
FROM GOING BACK TO THE HEART OF CARDIOLOGY