User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
JAK-inhibitor safety in adolescents with AD: Long-term analyses reported
WASHINGTON – and over 1,000 patient-years of exposure, Lawrence F. Eichenfield, MD, reported at the annual Revolutionizing Atopic Dermatitis conference.
In March 2023, the oral Janus kinase 1 (JAK1) inhibitor was approved by the Food and Drug Administration for treating adolescents aged 12-17 with refractory moderate to severe AD – an expanded indication from the approval in adults in 2022.
The new analysis evaluated data from patients who participated in the phase 3 JADE clinical trials – MONO-1, MONO-2, TEEN, and REGIMEN – and were subsequently enrolled in the ongoing phase 3 extension trial JADE EXTEND. Compared with a previous post hoc analysis in which adolescent patients had approximately 1 year of exposure, this updated analysis includes a sizable portion of patients with more than 96 weeks of exposure.
“We’re starting to get good numbers of [adolescents] who’ve had about 2 years of exposure,” said Dr. Eichenfield, professor of dermatology and pediatrics and vice chair of the department of dermatology at the University of California, San Diego, during a late-breaking research session.
With a data cut for this analysis of September 2021, “we haven’t seen additive long-term [adverse] effects” with longer exposures, he said. In addition, “there were no unique safety concerns related to adolescents compared to the findings observed [in an] integrated safety analysis using the same data cut in which most patients were adults.”
(The analysis in adults covered 3,802 patients with over 5,000 patient-years of exposure, and was presented at the annual American Academy of Dermatology meeting in March 2023.)
Also presented in the late-breaking abstract session at RAD 2023 was a long-term safety study of upadacitinib (Rinvoq), the other JAK1 inhibitor approved for adolescents with AD – approved by the FDA for both adolescents and adults with moderate to severe AD in 2022. The new analysis captures exposure of up to 4 years and shows no “worsening or accumulation of events,” compared with 1-year data, reported Christopher G. Bunick, MD, PhD, of the department of dermatology and the program in translational biomedicine at Yale University, New Haven, Conn.
Abrocitinib in adolescents
For the safety analysis of abrocitinib (Cibinqo), data were pooled into two cohorts: A consistent-dose cohort of 490 adolescents who received the same dose (200 mg or 100 mg) during the entire duration of the qualifying JADE trials, and a variable-dose cohort of 145 adolescents who received different doses (200 mg or 100 mg) during the JADE REGIMEN qualifying trial.
Duration of exposure was 96 weeks or more in 37%-38% of the consistent-dose cohort and 68% of the variable-dose cohort.
In the consistent-dose cohort, adverse events occurred in 243 (84%) and 153 (76%) of patients receiving 200-mg doses and 100-mg doses, respectively. Incidence rates for severe adverse events were 5.87 per 100 patient-years at both doses, and rates for adverse events leading to study discontinuation were 6.96/100 patient-years at 200 mg and 5.13/100 patient-years at 100 mg.
“No meaningful dose-response relationship was observed for serious adverse events, or adverse events leading to discontinuation, or adverse events of special interest,” said Dr. Eichenfield, also chief of pediatric and adolescent dermatology at Rady Children’s Hospital, San Diego.
The IRs of adverse events of special interest were 1.84/100 patient-years and 1.28/100 patient-years for serious infection; 2.11/100 patient-years, and 1.62/100 patient-years for all herpes zoster infections; and 0.69/100 patient-years and 0.32/100 patient-years for opportunistic herpes zoster infections in the 200-mg and 100-mg arms, respectively.
“Other than herpes zoster, there were no opportunistic infections observed and no tuberculosis cases,” he said. “There was one nonfatal venous thromboembolism in an adolescent who had a very strong family history of [pulmonary embolism], one retinal detachment [with a concurrent diagnosis of cataracts and of left eyebrow folliculitis], and no events of nonmelanoma skin cancer or other malignancies, major adverse cardiovascular events, or deaths.” The thromboembolism case was reported in the previous post hoc analysis.
In the variable-dose cohort, data were similar, Dr. Eichenfield said. The IRs for severe adverse events, adverse events leading to study withdrawal, and adverse events of special interest were consistent with those in the other cohort. And similarly, there were no reports of tuberculosis or other opportunistic infections (excluding herpes zoster), and no reports of nonmelanoma skin cancer (NMSC) or other malignancies, major adverse cardiovascular events (MACE), or death. In this cohort, there were no venous thromboembolism (VTE) reports.
Upadacitinib in adolescents, adults
The new analysis looked at up to 4 years of upadacitinib treatment in almost 2,700 adolescents and adults– and over 6,200 patient-years – using integrated data from three ongoing pivotal phase 3 studies: Measure Up 1, Measure Up 2, and AD Up. (Of these patients, 539 were adolescents, Dr. Bunick said after the meeting.)
In the Measure Up studies, patients were randomized 1:1:1 to receive a 15-mg dose, a 30-mg dose, or placebo once daily. In AD Up, patients in each arm received concomitant topical corticosteroids. At week 16, patients receiving the drug continued their assigned treatment during the ongoing blinded extension period, and those receiving placebo were rerandomized to upadacitinib 15 mg or 30 mg.
The exposure-adjusted event rates for any adverse event leading to discontinuation were 4.1/100 patient-years and 4.7/100 patient-years in patients receiving 15 mg and 30 mg, respectively, and the rates of any serious adverse event were 6.5/100 patient-years and 7.5/100 patient-years, Dr. Bunick reported. Three deaths occurred in the 30-mg group; all deaths were related to COVID infection and occurred in adults with cardiovascular risk factors.
Incidence rates of adverse events of special interest were similar to those in a previous 1-year analysis. The rate of serious infections per 100 patient years, for instance, was 2.3 and 2.8 in the 15-mg and 30-mg groups, respectively, compared with 2.2 and 2.8 in the 1-year analysis.
The rate of opportunistic infections, including eczema herpeticum (and excluding TB and herpes zoster), saw a slight bump in the new analysis to 2.4/100 patient-years with the 30-mg dose. Other event rates, across both dosages and durations, were less than 0.1/100 patient-years for active TB; 0.3-0.4/100 patient-years for NMSC, and 0.1/100 patient-years or below for other malignancies, MACE, and VTE. Herpes zoster had the highest event rate in both the 1- and 4-year analyses of between 3.1/100 patient-years and 5.8/100 patient-years, Dr. Bunick reported.
The adverse event rates for adolescents and adults “show consistency and are very low,” Dr. Bunick said. At 4 years, no new safety risks were identified.
‘The more data ... the better’
Data on the safety of new medications in children and adolescents is always important, and with systemic JAK inhibitors in particular, “the more data we can accumulate in [younger] patients with AD ... the better,” said Robert Sidbury, MD, MPH, professor in the department of pediatrics at the University of Washington, Seattle, and chief of the division of dermatology at Seattle Children’s Hospital, who was asked to comment on the two studies.
Dermatologists have taken comfort in the fact that the “daunting” boxed warning on JAK inhibitors “was generated in a very different population than we generally propose to treat, certainly when talking about children and adolescents,” said Dr. Sidbury, who was not involved in either of the new safety analyses.
The JAK inhibitor boxed warning “reflects a study of tofacitinib – a different JAK inhibitor with arguably more risk of adverse effects – in adults over the age of 50 with rheumatoid arthritis and multiple risk factors for comorbidities included in the boxed warning,” he said.
“This allows dermatologists to reasonably conclude that the boxed warning – while critical to discuss and consider in every patient – is likely less concerning than might otherwise by implied.”
With more patient experience, “the more our assessment of risk, and of the ‘legitimacy’ of the boxed warning in our patient population, becomes evidence-based as opposed to extrapolation,” Dr. Sidbury said.
The two studies reported, he said, “detail an experience that is not adverse effect free –I have yet to find that medication – but is a reasonable profile considering the robust efficacy results they accompany.”
The abrocitinib safety analysis was sponsored by Pfizer. Regarding the study of upadacitinib, AbbVie contributed to the design of the safety analysis and participated in data collection. No honoria or payments were made to the authors, according to the study abstract. Dr. Eichenfield is a consultant/advisory board member for Pfizer and other companies, and has served on the speakers bureau/received honoria for Pfizer and other companies. Dr. Bunick is a consultant for AbbVie and other companies, and has served as an speaker/received honoraria or served as an investigator for several companies. Dr. Sidbury disclosed being a consultant/advisory board member for Lilly and Leo and serving on the speakers bureau/honoraria for Beiersdorf. All reported receiving grant/research support from various companies.
WASHINGTON – and over 1,000 patient-years of exposure, Lawrence F. Eichenfield, MD, reported at the annual Revolutionizing Atopic Dermatitis conference.
In March 2023, the oral Janus kinase 1 (JAK1) inhibitor was approved by the Food and Drug Administration for treating adolescents aged 12-17 with refractory moderate to severe AD – an expanded indication from the approval in adults in 2022.
The new analysis evaluated data from patients who participated in the phase 3 JADE clinical trials – MONO-1, MONO-2, TEEN, and REGIMEN – and were subsequently enrolled in the ongoing phase 3 extension trial JADE EXTEND. Compared with a previous post hoc analysis in which adolescent patients had approximately 1 year of exposure, this updated analysis includes a sizable portion of patients with more than 96 weeks of exposure.
“We’re starting to get good numbers of [adolescents] who’ve had about 2 years of exposure,” said Dr. Eichenfield, professor of dermatology and pediatrics and vice chair of the department of dermatology at the University of California, San Diego, during a late-breaking research session.
With a data cut for this analysis of September 2021, “we haven’t seen additive long-term [adverse] effects” with longer exposures, he said. In addition, “there were no unique safety concerns related to adolescents compared to the findings observed [in an] integrated safety analysis using the same data cut in which most patients were adults.”
(The analysis in adults covered 3,802 patients with over 5,000 patient-years of exposure, and was presented at the annual American Academy of Dermatology meeting in March 2023.)
Also presented in the late-breaking abstract session at RAD 2023 was a long-term safety study of upadacitinib (Rinvoq), the other JAK1 inhibitor approved for adolescents with AD – approved by the FDA for both adolescents and adults with moderate to severe AD in 2022. The new analysis captures exposure of up to 4 years and shows no “worsening or accumulation of events,” compared with 1-year data, reported Christopher G. Bunick, MD, PhD, of the department of dermatology and the program in translational biomedicine at Yale University, New Haven, Conn.
Abrocitinib in adolescents
For the safety analysis of abrocitinib (Cibinqo), data were pooled into two cohorts: A consistent-dose cohort of 490 adolescents who received the same dose (200 mg or 100 mg) during the entire duration of the qualifying JADE trials, and a variable-dose cohort of 145 adolescents who received different doses (200 mg or 100 mg) during the JADE REGIMEN qualifying trial.
Duration of exposure was 96 weeks or more in 37%-38% of the consistent-dose cohort and 68% of the variable-dose cohort.
In the consistent-dose cohort, adverse events occurred in 243 (84%) and 153 (76%) of patients receiving 200-mg doses and 100-mg doses, respectively. Incidence rates for severe adverse events were 5.87 per 100 patient-years at both doses, and rates for adverse events leading to study discontinuation were 6.96/100 patient-years at 200 mg and 5.13/100 patient-years at 100 mg.
“No meaningful dose-response relationship was observed for serious adverse events, or adverse events leading to discontinuation, or adverse events of special interest,” said Dr. Eichenfield, also chief of pediatric and adolescent dermatology at Rady Children’s Hospital, San Diego.
The IRs of adverse events of special interest were 1.84/100 patient-years and 1.28/100 patient-years for serious infection; 2.11/100 patient-years, and 1.62/100 patient-years for all herpes zoster infections; and 0.69/100 patient-years and 0.32/100 patient-years for opportunistic herpes zoster infections in the 200-mg and 100-mg arms, respectively.
“Other than herpes zoster, there were no opportunistic infections observed and no tuberculosis cases,” he said. “There was one nonfatal venous thromboembolism in an adolescent who had a very strong family history of [pulmonary embolism], one retinal detachment [with a concurrent diagnosis of cataracts and of left eyebrow folliculitis], and no events of nonmelanoma skin cancer or other malignancies, major adverse cardiovascular events, or deaths.” The thromboembolism case was reported in the previous post hoc analysis.
In the variable-dose cohort, data were similar, Dr. Eichenfield said. The IRs for severe adverse events, adverse events leading to study withdrawal, and adverse events of special interest were consistent with those in the other cohort. And similarly, there were no reports of tuberculosis or other opportunistic infections (excluding herpes zoster), and no reports of nonmelanoma skin cancer (NMSC) or other malignancies, major adverse cardiovascular events (MACE), or death. In this cohort, there were no venous thromboembolism (VTE) reports.
Upadacitinib in adolescents, adults
The new analysis looked at up to 4 years of upadacitinib treatment in almost 2,700 adolescents and adults– and over 6,200 patient-years – using integrated data from three ongoing pivotal phase 3 studies: Measure Up 1, Measure Up 2, and AD Up. (Of these patients, 539 were adolescents, Dr. Bunick said after the meeting.)
In the Measure Up studies, patients were randomized 1:1:1 to receive a 15-mg dose, a 30-mg dose, or placebo once daily. In AD Up, patients in each arm received concomitant topical corticosteroids. At week 16, patients receiving the drug continued their assigned treatment during the ongoing blinded extension period, and those receiving placebo were rerandomized to upadacitinib 15 mg or 30 mg.
The exposure-adjusted event rates for any adverse event leading to discontinuation were 4.1/100 patient-years and 4.7/100 patient-years in patients receiving 15 mg and 30 mg, respectively, and the rates of any serious adverse event were 6.5/100 patient-years and 7.5/100 patient-years, Dr. Bunick reported. Three deaths occurred in the 30-mg group; all deaths were related to COVID infection and occurred in adults with cardiovascular risk factors.
Incidence rates of adverse events of special interest were similar to those in a previous 1-year analysis. The rate of serious infections per 100 patient years, for instance, was 2.3 and 2.8 in the 15-mg and 30-mg groups, respectively, compared with 2.2 and 2.8 in the 1-year analysis.
The rate of opportunistic infections, including eczema herpeticum (and excluding TB and herpes zoster), saw a slight bump in the new analysis to 2.4/100 patient-years with the 30-mg dose. Other event rates, across both dosages and durations, were less than 0.1/100 patient-years for active TB; 0.3-0.4/100 patient-years for NMSC, and 0.1/100 patient-years or below for other malignancies, MACE, and VTE. Herpes zoster had the highest event rate in both the 1- and 4-year analyses of between 3.1/100 patient-years and 5.8/100 patient-years, Dr. Bunick reported.
The adverse event rates for adolescents and adults “show consistency and are very low,” Dr. Bunick said. At 4 years, no new safety risks were identified.
‘The more data ... the better’
Data on the safety of new medications in children and adolescents is always important, and with systemic JAK inhibitors in particular, “the more data we can accumulate in [younger] patients with AD ... the better,” said Robert Sidbury, MD, MPH, professor in the department of pediatrics at the University of Washington, Seattle, and chief of the division of dermatology at Seattle Children’s Hospital, who was asked to comment on the two studies.
Dermatologists have taken comfort in the fact that the “daunting” boxed warning on JAK inhibitors “was generated in a very different population than we generally propose to treat, certainly when talking about children and adolescents,” said Dr. Sidbury, who was not involved in either of the new safety analyses.
The JAK inhibitor boxed warning “reflects a study of tofacitinib – a different JAK inhibitor with arguably more risk of adverse effects – in adults over the age of 50 with rheumatoid arthritis and multiple risk factors for comorbidities included in the boxed warning,” he said.
“This allows dermatologists to reasonably conclude that the boxed warning – while critical to discuss and consider in every patient – is likely less concerning than might otherwise by implied.”
With more patient experience, “the more our assessment of risk, and of the ‘legitimacy’ of the boxed warning in our patient population, becomes evidence-based as opposed to extrapolation,” Dr. Sidbury said.
The two studies reported, he said, “detail an experience that is not adverse effect free –I have yet to find that medication – but is a reasonable profile considering the robust efficacy results they accompany.”
The abrocitinib safety analysis was sponsored by Pfizer. Regarding the study of upadacitinib, AbbVie contributed to the design of the safety analysis and participated in data collection. No honoria or payments were made to the authors, according to the study abstract. Dr. Eichenfield is a consultant/advisory board member for Pfizer and other companies, and has served on the speakers bureau/received honoria for Pfizer and other companies. Dr. Bunick is a consultant for AbbVie and other companies, and has served as an speaker/received honoraria or served as an investigator for several companies. Dr. Sidbury disclosed being a consultant/advisory board member for Lilly and Leo and serving on the speakers bureau/honoraria for Beiersdorf. All reported receiving grant/research support from various companies.
WASHINGTON – and over 1,000 patient-years of exposure, Lawrence F. Eichenfield, MD, reported at the annual Revolutionizing Atopic Dermatitis conference.
In March 2023, the oral Janus kinase 1 (JAK1) inhibitor was approved by the Food and Drug Administration for treating adolescents aged 12-17 with refractory moderate to severe AD – an expanded indication from the approval in adults in 2022.
The new analysis evaluated data from patients who participated in the phase 3 JADE clinical trials – MONO-1, MONO-2, TEEN, and REGIMEN – and were subsequently enrolled in the ongoing phase 3 extension trial JADE EXTEND. Compared with a previous post hoc analysis in which adolescent patients had approximately 1 year of exposure, this updated analysis includes a sizable portion of patients with more than 96 weeks of exposure.
“We’re starting to get good numbers of [adolescents] who’ve had about 2 years of exposure,” said Dr. Eichenfield, professor of dermatology and pediatrics and vice chair of the department of dermatology at the University of California, San Diego, during a late-breaking research session.
With a data cut for this analysis of September 2021, “we haven’t seen additive long-term [adverse] effects” with longer exposures, he said. In addition, “there were no unique safety concerns related to adolescents compared to the findings observed [in an] integrated safety analysis using the same data cut in which most patients were adults.”
(The analysis in adults covered 3,802 patients with over 5,000 patient-years of exposure, and was presented at the annual American Academy of Dermatology meeting in March 2023.)
Also presented in the late-breaking abstract session at RAD 2023 was a long-term safety study of upadacitinib (Rinvoq), the other JAK1 inhibitor approved for adolescents with AD – approved by the FDA for both adolescents and adults with moderate to severe AD in 2022. The new analysis captures exposure of up to 4 years and shows no “worsening or accumulation of events,” compared with 1-year data, reported Christopher G. Bunick, MD, PhD, of the department of dermatology and the program in translational biomedicine at Yale University, New Haven, Conn.
Abrocitinib in adolescents
For the safety analysis of abrocitinib (Cibinqo), data were pooled into two cohorts: A consistent-dose cohort of 490 adolescents who received the same dose (200 mg or 100 mg) during the entire duration of the qualifying JADE trials, and a variable-dose cohort of 145 adolescents who received different doses (200 mg or 100 mg) during the JADE REGIMEN qualifying trial.
Duration of exposure was 96 weeks or more in 37%-38% of the consistent-dose cohort and 68% of the variable-dose cohort.
In the consistent-dose cohort, adverse events occurred in 243 (84%) and 153 (76%) of patients receiving 200-mg doses and 100-mg doses, respectively. Incidence rates for severe adverse events were 5.87 per 100 patient-years at both doses, and rates for adverse events leading to study discontinuation were 6.96/100 patient-years at 200 mg and 5.13/100 patient-years at 100 mg.
“No meaningful dose-response relationship was observed for serious adverse events, or adverse events leading to discontinuation, or adverse events of special interest,” said Dr. Eichenfield, also chief of pediatric and adolescent dermatology at Rady Children’s Hospital, San Diego.
The IRs of adverse events of special interest were 1.84/100 patient-years and 1.28/100 patient-years for serious infection; 2.11/100 patient-years, and 1.62/100 patient-years for all herpes zoster infections; and 0.69/100 patient-years and 0.32/100 patient-years for opportunistic herpes zoster infections in the 200-mg and 100-mg arms, respectively.
“Other than herpes zoster, there were no opportunistic infections observed and no tuberculosis cases,” he said. “There was one nonfatal venous thromboembolism in an adolescent who had a very strong family history of [pulmonary embolism], one retinal detachment [with a concurrent diagnosis of cataracts and of left eyebrow folliculitis], and no events of nonmelanoma skin cancer or other malignancies, major adverse cardiovascular events, or deaths.” The thromboembolism case was reported in the previous post hoc analysis.
In the variable-dose cohort, data were similar, Dr. Eichenfield said. The IRs for severe adverse events, adverse events leading to study withdrawal, and adverse events of special interest were consistent with those in the other cohort. And similarly, there were no reports of tuberculosis or other opportunistic infections (excluding herpes zoster), and no reports of nonmelanoma skin cancer (NMSC) or other malignancies, major adverse cardiovascular events (MACE), or death. In this cohort, there were no venous thromboembolism (VTE) reports.
Upadacitinib in adolescents, adults
The new analysis looked at up to 4 years of upadacitinib treatment in almost 2,700 adolescents and adults– and over 6,200 patient-years – using integrated data from three ongoing pivotal phase 3 studies: Measure Up 1, Measure Up 2, and AD Up. (Of these patients, 539 were adolescents, Dr. Bunick said after the meeting.)
In the Measure Up studies, patients were randomized 1:1:1 to receive a 15-mg dose, a 30-mg dose, or placebo once daily. In AD Up, patients in each arm received concomitant topical corticosteroids. At week 16, patients receiving the drug continued their assigned treatment during the ongoing blinded extension period, and those receiving placebo were rerandomized to upadacitinib 15 mg or 30 mg.
The exposure-adjusted event rates for any adverse event leading to discontinuation were 4.1/100 patient-years and 4.7/100 patient-years in patients receiving 15 mg and 30 mg, respectively, and the rates of any serious adverse event were 6.5/100 patient-years and 7.5/100 patient-years, Dr. Bunick reported. Three deaths occurred in the 30-mg group; all deaths were related to COVID infection and occurred in adults with cardiovascular risk factors.
Incidence rates of adverse events of special interest were similar to those in a previous 1-year analysis. The rate of serious infections per 100 patient years, for instance, was 2.3 and 2.8 in the 15-mg and 30-mg groups, respectively, compared with 2.2 and 2.8 in the 1-year analysis.
The rate of opportunistic infections, including eczema herpeticum (and excluding TB and herpes zoster), saw a slight bump in the new analysis to 2.4/100 patient-years with the 30-mg dose. Other event rates, across both dosages and durations, were less than 0.1/100 patient-years for active TB; 0.3-0.4/100 patient-years for NMSC, and 0.1/100 patient-years or below for other malignancies, MACE, and VTE. Herpes zoster had the highest event rate in both the 1- and 4-year analyses of between 3.1/100 patient-years and 5.8/100 patient-years, Dr. Bunick reported.
The adverse event rates for adolescents and adults “show consistency and are very low,” Dr. Bunick said. At 4 years, no new safety risks were identified.
‘The more data ... the better’
Data on the safety of new medications in children and adolescents is always important, and with systemic JAK inhibitors in particular, “the more data we can accumulate in [younger] patients with AD ... the better,” said Robert Sidbury, MD, MPH, professor in the department of pediatrics at the University of Washington, Seattle, and chief of the division of dermatology at Seattle Children’s Hospital, who was asked to comment on the two studies.
Dermatologists have taken comfort in the fact that the “daunting” boxed warning on JAK inhibitors “was generated in a very different population than we generally propose to treat, certainly when talking about children and adolescents,” said Dr. Sidbury, who was not involved in either of the new safety analyses.
The JAK inhibitor boxed warning “reflects a study of tofacitinib – a different JAK inhibitor with arguably more risk of adverse effects – in adults over the age of 50 with rheumatoid arthritis and multiple risk factors for comorbidities included in the boxed warning,” he said.
“This allows dermatologists to reasonably conclude that the boxed warning – while critical to discuss and consider in every patient – is likely less concerning than might otherwise by implied.”
With more patient experience, “the more our assessment of risk, and of the ‘legitimacy’ of the boxed warning in our patient population, becomes evidence-based as opposed to extrapolation,” Dr. Sidbury said.
The two studies reported, he said, “detail an experience that is not adverse effect free –I have yet to find that medication – but is a reasonable profile considering the robust efficacy results they accompany.”
The abrocitinib safety analysis was sponsored by Pfizer. Regarding the study of upadacitinib, AbbVie contributed to the design of the safety analysis and participated in data collection. No honoria or payments were made to the authors, according to the study abstract. Dr. Eichenfield is a consultant/advisory board member for Pfizer and other companies, and has served on the speakers bureau/received honoria for Pfizer and other companies. Dr. Bunick is a consultant for AbbVie and other companies, and has served as an speaker/received honoraria or served as an investigator for several companies. Dr. Sidbury disclosed being a consultant/advisory board member for Lilly and Leo and serving on the speakers bureau/honoraria for Beiersdorf. All reported receiving grant/research support from various companies.
AT RAD 2023
States move to curb insurers’ prior authorization requirements as federal reforms lag
Amid growing criticism of health insurers’ onerous prior authorization practices, lawmakers in 30 states have introduced bills this year that aim to rein in insurer gatekeeping and improve patient care.
“This is something that goes on in every doctor’s office every day; the frustrations, the delays, and the use of office staff time are just unbelievable,” said Steven Orland, MD, a board-certified urologist and president of the Medical Society of New Jersey.
The bills, which cover private health plans and insurers that states regulate, may provide some relief for physicians as federal efforts to streamline prior authorization for some Medicare patients have lagged.
Last year, Congress failed to pass the Improving Seniors’ Timely Access to Care Act of 2021, despite 326 co-sponsors. The bill would have compelled insurers covering Medicare Advantage enrollees to speed up prior authorizations, make the process more transparent, and remove obstacles such as requiring fax machine submissions.
Last month, however, the Centers for Medicare & Medicaid Services issued a final rule that will improve some aspects of prior authorizations in Medicare Advantage insurance plans and ensure that enrollees have the same access to necessary care as traditional Medicare enrollees.
The insurance industry has long defended prior authorization requirements and opposed legislation that would limit them.
America’s Health Insurance Plans (AHIP) and the Blue Cross Blue Shield Association said in a 2019 letter to a congressional committee when the federal legislation was first introduced, “Prior authorizations enforce best practices and guidelines for care management and help physicians identify and avoid care techniques that would harm patient outcomes, such as designating prescriptions that could feed into an opioid addiction.” AHIP didn’t respond to repeated requests for comment.
But some major insurers now appear willing to compromise and voluntarily reduce the volume of prior authorizations they require. Days before the federal final rule was released, three major insurers – United HealthCare, Cigna, and Aetna CVS Health – announced they plan to drop some prior authorization requirements and automate processes.
United HealthCare said it will eliminate almost 20% of its prior authorizations for some nonurgent surgeries and procedures starting this summer. It also will create a national Gold Card program in 2024 for physicians who meet its eligibility requirements, which would eliminate prior authorization requirements for most procedures. Both initiatives will apply to commercial, Medicare Advantage, and Medicaid businesses, said the insurer in a statement.
However, United HealthCare also announced that in June it will start requiring prior authorization for diagnostic (not screening) gastrointestinal endoscopies for its nearly 27 million privately insured patients, citing data it says shows potentially harmful overuse of scopes. Physician groups have publicly criticized the move, saying it could delay lifesaving treatment, and have asked the insurer to reconsider.
Cigna and Aetna also have moved to pare back prior authorization processes. Scott Josephs, national medical officer for Cigna, told Healthcare Dive that Cigna has removed prior authorization reviews from nearly 500 services since 2020.
An Aetna spokesperson told Healthcare Dive that the CVS-owned payer has implemented a gold card program and rolled back prior authorization requirements on cataract surgeries, video EEGs, and home infusion for some drugs, according to Healthcare Dive.
Cigna has faced increased scrutiny from some state regulators since a ProPublica/The Capitol Forum article revealed in March that its doctors were denying claims without opening patients’ files, contrary to what insurance laws and regulations require in many states.
Over a period of 2 months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the investigation found. In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
States aim to reduce prior authorization volume
The American Medical Association said it has been tracking nearly 90 prior authorization reform bills in 30 states. More than a dozen bills are still being considered in this legislative session, including in Arkansas, California, New Jersey, North Carolina, Maryland, and Washington, D.C.
“The groundswell of activity in the states reflects how big a problem this is,” said an AMA legislative expert. “The issue used to be ‘how can we automate and streamline processes’; now the issue is focused on reducing the volume of prior authorizations and the harm that can cause patients.”
The state bills use different strategies to reduce excessive prior authorization requirements. Maryland’s proposed bill, for example, would require just one prior authorization to stay on a prescription drug, if the insurer has previously approved the drug and the patient continues to successfully be treated by the drug.
Washington, D.C. and New Jersey have introduced comprehensive reform bills that include a “grace period” of 60 days, to ensure continuity of care when a patient switches health plans. They also would eliminate repeat authorizations for chronic and long-term conditions, set explicit timelines for insurers to respond to prior authorization requests and appeals, and require that practicing physicians review denials that are appealed.
Many state bills also would require insurers to be more transparent by posting information on their websites about which services and drugs require prior authorization and what their approval rates are for them, said AMA’s legislative expert.
“There’s a black hole of information that insurers have access to. We would really like to know how many prior authorization requests are denied, the time it takes to deny them, and the reasons for denial,” said Josh Bengal, JD, the director of government relations for the Medical Society of New Jersey.
The legislation in New Jersey and other states faces stiff opposition from the insurance lobby, especially state associations of health plans affiliated with AHIP. The California Association of Health Plans, for example, opposes a “gold card” bill (SB 598), introduced in February, that would allow a select group of high-performing doctors to skip prior authorizations for 1 year.
The CAHP states, “Californians deserve safe, high quality, high-value health care. Yet SB 598 will derail the progress we have made in our health care system by lowering the value and safety that Californians should expect from their health care providers,” according to a fact sheet.
The fact-sheet defines “low-value care” as medical services for which there is little to no benefit and poses potential physical or financial harm to patients, such as unnecessary CT scans or MRIs for uncomplicated conditions.
California is one of about a dozen states that have introduced gold card legislation this year. If enacted, they would join five states with gold card laws: West Virginia, Texas, Vermont, Michigan, and Louisiana.
How do gold cards work?
Physicians who achieve a high approval rate of prior authorizations from insurers for 1 year are eligible to be exempted from obtaining prior authorizations the following year.
The approval rate is at least 90% for a certain number of eligible health services, but the number of prior authorizations required to qualify can range from 5 to 30, depending on the state law.
Gold card legislation typically also gives the treating physician the right to have an appeal of a prior authorization denial by a physician peer of the same or similar specialty.
California’s bill would also apply to all covered health services, which is broader than what United HealthCare has proposed for its gold card exemption. The bill would also require a plan or insurer to annually monitor rates of prior authorization approval, modification, appeal, and denial, and to discontinue services, items, and supplies that are approved 95% of the time.
“These are important reforms that will help ensure that patients can receive the care they need, when they need it,” said CMA president Donaldo Hernandez, MD.
However, it’s not clear how many physicians will meet “gold card” status based on Texas’ recent experience with its own “gold card” law.
The Texas Department of Insurance estimated that only 3.3% of licensed physicians in the state have met “gold card” status since the bill became law in 2021, said Zeke Silva, MD, an interventional radiologist who serves on the Council of Legislation for the Texas Medical Association.
He noted that the legislation has had a limited effect for several reasons. Commercial health plans only make up only about 20% of all health plans in Texas. Also, the final regulations didn’t go into effect until last May and physicians are evaluated by health plans for “gold card” status every 6 months, said Dr. Silva.
In addition, physicians must have at least five prior authorizations approved for the same health service, which the law left up to the health plans to define, said Dr. Silva.
Now, the Texas Medical Association is lobbying for legislative improvements. “We want to reduce the number of eligible services that health plans require for prior authorizations and have more oversight of prior authorization denials by the Texas Department of Insurance and the Texas Medical Board,” said Dr. Silva.
He’s optimistic that if the bill becomes law, the number of physicians eligible for gold cards may increase.
Meanwhile, the AMA’s legislative expert, who declined to be identified because of organization policy, acknowledged the possibility that some prior authorization bills will die in state legislatures this year.
“We remain hopeful, but it’s an uphill battle. The state medical associations face a lot of opposition from health plans who don’t want to see these reforms become law.”
A version of this article originally appeared on Medscape.com.
Amid growing criticism of health insurers’ onerous prior authorization practices, lawmakers in 30 states have introduced bills this year that aim to rein in insurer gatekeeping and improve patient care.
“This is something that goes on in every doctor’s office every day; the frustrations, the delays, and the use of office staff time are just unbelievable,” said Steven Orland, MD, a board-certified urologist and president of the Medical Society of New Jersey.
The bills, which cover private health plans and insurers that states regulate, may provide some relief for physicians as federal efforts to streamline prior authorization for some Medicare patients have lagged.
Last year, Congress failed to pass the Improving Seniors’ Timely Access to Care Act of 2021, despite 326 co-sponsors. The bill would have compelled insurers covering Medicare Advantage enrollees to speed up prior authorizations, make the process more transparent, and remove obstacles such as requiring fax machine submissions.
Last month, however, the Centers for Medicare & Medicaid Services issued a final rule that will improve some aspects of prior authorizations in Medicare Advantage insurance plans and ensure that enrollees have the same access to necessary care as traditional Medicare enrollees.
The insurance industry has long defended prior authorization requirements and opposed legislation that would limit them.
America’s Health Insurance Plans (AHIP) and the Blue Cross Blue Shield Association said in a 2019 letter to a congressional committee when the federal legislation was first introduced, “Prior authorizations enforce best practices and guidelines for care management and help physicians identify and avoid care techniques that would harm patient outcomes, such as designating prescriptions that could feed into an opioid addiction.” AHIP didn’t respond to repeated requests for comment.
But some major insurers now appear willing to compromise and voluntarily reduce the volume of prior authorizations they require. Days before the federal final rule was released, three major insurers – United HealthCare, Cigna, and Aetna CVS Health – announced they plan to drop some prior authorization requirements and automate processes.
United HealthCare said it will eliminate almost 20% of its prior authorizations for some nonurgent surgeries and procedures starting this summer. It also will create a national Gold Card program in 2024 for physicians who meet its eligibility requirements, which would eliminate prior authorization requirements for most procedures. Both initiatives will apply to commercial, Medicare Advantage, and Medicaid businesses, said the insurer in a statement.
However, United HealthCare also announced that in June it will start requiring prior authorization for diagnostic (not screening) gastrointestinal endoscopies for its nearly 27 million privately insured patients, citing data it says shows potentially harmful overuse of scopes. Physician groups have publicly criticized the move, saying it could delay lifesaving treatment, and have asked the insurer to reconsider.
Cigna and Aetna also have moved to pare back prior authorization processes. Scott Josephs, national medical officer for Cigna, told Healthcare Dive that Cigna has removed prior authorization reviews from nearly 500 services since 2020.
An Aetna spokesperson told Healthcare Dive that the CVS-owned payer has implemented a gold card program and rolled back prior authorization requirements on cataract surgeries, video EEGs, and home infusion for some drugs, according to Healthcare Dive.
Cigna has faced increased scrutiny from some state regulators since a ProPublica/The Capitol Forum article revealed in March that its doctors were denying claims without opening patients’ files, contrary to what insurance laws and regulations require in many states.
Over a period of 2 months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the investigation found. In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
States aim to reduce prior authorization volume
The American Medical Association said it has been tracking nearly 90 prior authorization reform bills in 30 states. More than a dozen bills are still being considered in this legislative session, including in Arkansas, California, New Jersey, North Carolina, Maryland, and Washington, D.C.
“The groundswell of activity in the states reflects how big a problem this is,” said an AMA legislative expert. “The issue used to be ‘how can we automate and streamline processes’; now the issue is focused on reducing the volume of prior authorizations and the harm that can cause patients.”
The state bills use different strategies to reduce excessive prior authorization requirements. Maryland’s proposed bill, for example, would require just one prior authorization to stay on a prescription drug, if the insurer has previously approved the drug and the patient continues to successfully be treated by the drug.
Washington, D.C. and New Jersey have introduced comprehensive reform bills that include a “grace period” of 60 days, to ensure continuity of care when a patient switches health plans. They also would eliminate repeat authorizations for chronic and long-term conditions, set explicit timelines for insurers to respond to prior authorization requests and appeals, and require that practicing physicians review denials that are appealed.
Many state bills also would require insurers to be more transparent by posting information on their websites about which services and drugs require prior authorization and what their approval rates are for them, said AMA’s legislative expert.
“There’s a black hole of information that insurers have access to. We would really like to know how many prior authorization requests are denied, the time it takes to deny them, and the reasons for denial,” said Josh Bengal, JD, the director of government relations for the Medical Society of New Jersey.
The legislation in New Jersey and other states faces stiff opposition from the insurance lobby, especially state associations of health plans affiliated with AHIP. The California Association of Health Plans, for example, opposes a “gold card” bill (SB 598), introduced in February, that would allow a select group of high-performing doctors to skip prior authorizations for 1 year.
The CAHP states, “Californians deserve safe, high quality, high-value health care. Yet SB 598 will derail the progress we have made in our health care system by lowering the value and safety that Californians should expect from their health care providers,” according to a fact sheet.
The fact-sheet defines “low-value care” as medical services for which there is little to no benefit and poses potential physical or financial harm to patients, such as unnecessary CT scans or MRIs for uncomplicated conditions.
California is one of about a dozen states that have introduced gold card legislation this year. If enacted, they would join five states with gold card laws: West Virginia, Texas, Vermont, Michigan, and Louisiana.
How do gold cards work?
Physicians who achieve a high approval rate of prior authorizations from insurers for 1 year are eligible to be exempted from obtaining prior authorizations the following year.
The approval rate is at least 90% for a certain number of eligible health services, but the number of prior authorizations required to qualify can range from 5 to 30, depending on the state law.
Gold card legislation typically also gives the treating physician the right to have an appeal of a prior authorization denial by a physician peer of the same or similar specialty.
California’s bill would also apply to all covered health services, which is broader than what United HealthCare has proposed for its gold card exemption. The bill would also require a plan or insurer to annually monitor rates of prior authorization approval, modification, appeal, and denial, and to discontinue services, items, and supplies that are approved 95% of the time.
“These are important reforms that will help ensure that patients can receive the care they need, when they need it,” said CMA president Donaldo Hernandez, MD.
However, it’s not clear how many physicians will meet “gold card” status based on Texas’ recent experience with its own “gold card” law.
The Texas Department of Insurance estimated that only 3.3% of licensed physicians in the state have met “gold card” status since the bill became law in 2021, said Zeke Silva, MD, an interventional radiologist who serves on the Council of Legislation for the Texas Medical Association.
He noted that the legislation has had a limited effect for several reasons. Commercial health plans only make up only about 20% of all health plans in Texas. Also, the final regulations didn’t go into effect until last May and physicians are evaluated by health plans for “gold card” status every 6 months, said Dr. Silva.
In addition, physicians must have at least five prior authorizations approved for the same health service, which the law left up to the health plans to define, said Dr. Silva.
Now, the Texas Medical Association is lobbying for legislative improvements. “We want to reduce the number of eligible services that health plans require for prior authorizations and have more oversight of prior authorization denials by the Texas Department of Insurance and the Texas Medical Board,” said Dr. Silva.
He’s optimistic that if the bill becomes law, the number of physicians eligible for gold cards may increase.
Meanwhile, the AMA’s legislative expert, who declined to be identified because of organization policy, acknowledged the possibility that some prior authorization bills will die in state legislatures this year.
“We remain hopeful, but it’s an uphill battle. The state medical associations face a lot of opposition from health plans who don’t want to see these reforms become law.”
A version of this article originally appeared on Medscape.com.
Amid growing criticism of health insurers’ onerous prior authorization practices, lawmakers in 30 states have introduced bills this year that aim to rein in insurer gatekeeping and improve patient care.
“This is something that goes on in every doctor’s office every day; the frustrations, the delays, and the use of office staff time are just unbelievable,” said Steven Orland, MD, a board-certified urologist and president of the Medical Society of New Jersey.
The bills, which cover private health plans and insurers that states regulate, may provide some relief for physicians as federal efforts to streamline prior authorization for some Medicare patients have lagged.
Last year, Congress failed to pass the Improving Seniors’ Timely Access to Care Act of 2021, despite 326 co-sponsors. The bill would have compelled insurers covering Medicare Advantage enrollees to speed up prior authorizations, make the process more transparent, and remove obstacles such as requiring fax machine submissions.
Last month, however, the Centers for Medicare & Medicaid Services issued a final rule that will improve some aspects of prior authorizations in Medicare Advantage insurance plans and ensure that enrollees have the same access to necessary care as traditional Medicare enrollees.
The insurance industry has long defended prior authorization requirements and opposed legislation that would limit them.
America’s Health Insurance Plans (AHIP) and the Blue Cross Blue Shield Association said in a 2019 letter to a congressional committee when the federal legislation was first introduced, “Prior authorizations enforce best practices and guidelines for care management and help physicians identify and avoid care techniques that would harm patient outcomes, such as designating prescriptions that could feed into an opioid addiction.” AHIP didn’t respond to repeated requests for comment.
But some major insurers now appear willing to compromise and voluntarily reduce the volume of prior authorizations they require. Days before the federal final rule was released, three major insurers – United HealthCare, Cigna, and Aetna CVS Health – announced they plan to drop some prior authorization requirements and automate processes.
United HealthCare said it will eliminate almost 20% of its prior authorizations for some nonurgent surgeries and procedures starting this summer. It also will create a national Gold Card program in 2024 for physicians who meet its eligibility requirements, which would eliminate prior authorization requirements for most procedures. Both initiatives will apply to commercial, Medicare Advantage, and Medicaid businesses, said the insurer in a statement.
However, United HealthCare also announced that in June it will start requiring prior authorization for diagnostic (not screening) gastrointestinal endoscopies for its nearly 27 million privately insured patients, citing data it says shows potentially harmful overuse of scopes. Physician groups have publicly criticized the move, saying it could delay lifesaving treatment, and have asked the insurer to reconsider.
Cigna and Aetna also have moved to pare back prior authorization processes. Scott Josephs, national medical officer for Cigna, told Healthcare Dive that Cigna has removed prior authorization reviews from nearly 500 services since 2020.
An Aetna spokesperson told Healthcare Dive that the CVS-owned payer has implemented a gold card program and rolled back prior authorization requirements on cataract surgeries, video EEGs, and home infusion for some drugs, according to Healthcare Dive.
Cigna has faced increased scrutiny from some state regulators since a ProPublica/The Capitol Forum article revealed in March that its doctors were denying claims without opening patients’ files, contrary to what insurance laws and regulations require in many states.
Over a period of 2 months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the investigation found. In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
States aim to reduce prior authorization volume
The American Medical Association said it has been tracking nearly 90 prior authorization reform bills in 30 states. More than a dozen bills are still being considered in this legislative session, including in Arkansas, California, New Jersey, North Carolina, Maryland, and Washington, D.C.
“The groundswell of activity in the states reflects how big a problem this is,” said an AMA legislative expert. “The issue used to be ‘how can we automate and streamline processes’; now the issue is focused on reducing the volume of prior authorizations and the harm that can cause patients.”
The state bills use different strategies to reduce excessive prior authorization requirements. Maryland’s proposed bill, for example, would require just one prior authorization to stay on a prescription drug, if the insurer has previously approved the drug and the patient continues to successfully be treated by the drug.
Washington, D.C. and New Jersey have introduced comprehensive reform bills that include a “grace period” of 60 days, to ensure continuity of care when a patient switches health plans. They also would eliminate repeat authorizations for chronic and long-term conditions, set explicit timelines for insurers to respond to prior authorization requests and appeals, and require that practicing physicians review denials that are appealed.
Many state bills also would require insurers to be more transparent by posting information on their websites about which services and drugs require prior authorization and what their approval rates are for them, said AMA’s legislative expert.
“There’s a black hole of information that insurers have access to. We would really like to know how many prior authorization requests are denied, the time it takes to deny them, and the reasons for denial,” said Josh Bengal, JD, the director of government relations for the Medical Society of New Jersey.
The legislation in New Jersey and other states faces stiff opposition from the insurance lobby, especially state associations of health plans affiliated with AHIP. The California Association of Health Plans, for example, opposes a “gold card” bill (SB 598), introduced in February, that would allow a select group of high-performing doctors to skip prior authorizations for 1 year.
The CAHP states, “Californians deserve safe, high quality, high-value health care. Yet SB 598 will derail the progress we have made in our health care system by lowering the value and safety that Californians should expect from their health care providers,” according to a fact sheet.
The fact-sheet defines “low-value care” as medical services for which there is little to no benefit and poses potential physical or financial harm to patients, such as unnecessary CT scans or MRIs for uncomplicated conditions.
California is one of about a dozen states that have introduced gold card legislation this year. If enacted, they would join five states with gold card laws: West Virginia, Texas, Vermont, Michigan, and Louisiana.
How do gold cards work?
Physicians who achieve a high approval rate of prior authorizations from insurers for 1 year are eligible to be exempted from obtaining prior authorizations the following year.
The approval rate is at least 90% for a certain number of eligible health services, but the number of prior authorizations required to qualify can range from 5 to 30, depending on the state law.
Gold card legislation typically also gives the treating physician the right to have an appeal of a prior authorization denial by a physician peer of the same or similar specialty.
California’s bill would also apply to all covered health services, which is broader than what United HealthCare has proposed for its gold card exemption. The bill would also require a plan or insurer to annually monitor rates of prior authorization approval, modification, appeal, and denial, and to discontinue services, items, and supplies that are approved 95% of the time.
“These are important reforms that will help ensure that patients can receive the care they need, when they need it,” said CMA president Donaldo Hernandez, MD.
However, it’s not clear how many physicians will meet “gold card” status based on Texas’ recent experience with its own “gold card” law.
The Texas Department of Insurance estimated that only 3.3% of licensed physicians in the state have met “gold card” status since the bill became law in 2021, said Zeke Silva, MD, an interventional radiologist who serves on the Council of Legislation for the Texas Medical Association.
He noted that the legislation has had a limited effect for several reasons. Commercial health plans only make up only about 20% of all health plans in Texas. Also, the final regulations didn’t go into effect until last May and physicians are evaluated by health plans for “gold card” status every 6 months, said Dr. Silva.
In addition, physicians must have at least five prior authorizations approved for the same health service, which the law left up to the health plans to define, said Dr. Silva.
Now, the Texas Medical Association is lobbying for legislative improvements. “We want to reduce the number of eligible services that health plans require for prior authorizations and have more oversight of prior authorization denials by the Texas Department of Insurance and the Texas Medical Board,” said Dr. Silva.
He’s optimistic that if the bill becomes law, the number of physicians eligible for gold cards may increase.
Meanwhile, the AMA’s legislative expert, who declined to be identified because of organization policy, acknowledged the possibility that some prior authorization bills will die in state legislatures this year.
“We remain hopeful, but it’s an uphill battle. The state medical associations face a lot of opposition from health plans who don’t want to see these reforms become law.”
A version of this article originally appeared on Medscape.com.
Investigational lupus drug cenerimod moves to phase 3 studies after equivocal phase 2 results
SEOUL, SOUTH KOREA – A once-daily, oral dose of the investigational drug cenerimod, developed for the treatment of systemic lupus erythematosus, has shown a greater response rate among individuals with more severe disease, according to data presented at an international congress on SLE.
Cenerimod is a potent, highly-selective sphingosine 1–phosphate receptor 1 (S1P1) modulator with attenuated calcium signaling, which targets an important signaling molecule in immunity and cell migration, said rheumatologist Sandra Navarra, MD, of the University of Santo Tomas Hospital and St. Luke’s Medical Center in Manila, Philippines.
“It reduces the migration of T cells and B cells from the lymph nodes to the circulation into the tissues,” Dr. Navarra told the conference. S1P1 receptor modulators are already approved for treatment of multiple sclerosis, but cenerimod is the first to be explored for the treatment of lupus.
Dr. Navarra presented data from the international CARE study, a randomized, placebo-controlled, phase 2 study involving 427 patients with moderate to severe SLE.
Patients had to have been diagnosed at least 6 months before screening, be on stable lupus medications, and have abnormal antinuclear or anti–double stranded DNA antibodies. They were randomized to either 0.5 mg, 1 mg, 2 mg, or 4 mg of cenerimod daily or placebo for 12 months. At 6 months, the patients who had initially been randomized to 4 mg daily were rerandomized either to 2 mg daily or placebo.
While the study found that 4 mg of cenerimod was associated with a reduction in disease activity from baseline to month 6 on the modified Systemic Lupus Erythematosus Disease Activity Index–2000 score (excluding leukopenia), compared with placebo (P = .029). However, the final result was not statistically significant after adjustment for the multiplicity of tests for the four doses against placebo.
But the researchers saw a greater response among individuals with higher levels of interferon type 1 gene expression at baseline, as well as those with higher anti-dsDNA and lower C4 levels, which “makes sense,” Dr. Navarra said in an interview, because those were the sicker patients with “more inflammatory, more active disease.”
The study did exclude patients with active lupus nephritis, severe active central nervous system lupus, or severe cardiovascular disorders.
Dr. Navarra said the findings are now factored into patient selection for two phase 3 trials, called OPUS-1 and OPUS-2, which are now underway. The OPUS trials have revised eligibility criteria, as well as a screening period of up to 60 days to ensure that only patients with true moderate to severe SLE are enrolled.
The drug was well tolerated, with the rate of adverse events similar across all study groups. The adverse events of particular interest – hypertension, infections and infestations, and eye disorders – were all mild and transient. There were a greater number of reports of hypertension among those taking 1-mg and 4-mg doses of cenerimod, but Dr. Navarra said monthly measurements of systolic or diastolic blood pressure didn’t show any change.
The study was funded by cenerimod manufacturer Idorsia Pharmaceuticals. Dr. Navarra has financial relationships with Biogen, Astellas, Janssen, Novartis, Pfizer, Boehringer-Ingelheim, and GlaxoSmithKline.
SEOUL, SOUTH KOREA – A once-daily, oral dose of the investigational drug cenerimod, developed for the treatment of systemic lupus erythematosus, has shown a greater response rate among individuals with more severe disease, according to data presented at an international congress on SLE.
Cenerimod is a potent, highly-selective sphingosine 1–phosphate receptor 1 (S1P1) modulator with attenuated calcium signaling, which targets an important signaling molecule in immunity and cell migration, said rheumatologist Sandra Navarra, MD, of the University of Santo Tomas Hospital and St. Luke’s Medical Center in Manila, Philippines.
“It reduces the migration of T cells and B cells from the lymph nodes to the circulation into the tissues,” Dr. Navarra told the conference. S1P1 receptor modulators are already approved for treatment of multiple sclerosis, but cenerimod is the first to be explored for the treatment of lupus.
Dr. Navarra presented data from the international CARE study, a randomized, placebo-controlled, phase 2 study involving 427 patients with moderate to severe SLE.
Patients had to have been diagnosed at least 6 months before screening, be on stable lupus medications, and have abnormal antinuclear or anti–double stranded DNA antibodies. They were randomized to either 0.5 mg, 1 mg, 2 mg, or 4 mg of cenerimod daily or placebo for 12 months. At 6 months, the patients who had initially been randomized to 4 mg daily were rerandomized either to 2 mg daily or placebo.
While the study found that 4 mg of cenerimod was associated with a reduction in disease activity from baseline to month 6 on the modified Systemic Lupus Erythematosus Disease Activity Index–2000 score (excluding leukopenia), compared with placebo (P = .029). However, the final result was not statistically significant after adjustment for the multiplicity of tests for the four doses against placebo.
But the researchers saw a greater response among individuals with higher levels of interferon type 1 gene expression at baseline, as well as those with higher anti-dsDNA and lower C4 levels, which “makes sense,” Dr. Navarra said in an interview, because those were the sicker patients with “more inflammatory, more active disease.”
The study did exclude patients with active lupus nephritis, severe active central nervous system lupus, or severe cardiovascular disorders.
Dr. Navarra said the findings are now factored into patient selection for two phase 3 trials, called OPUS-1 and OPUS-2, which are now underway. The OPUS trials have revised eligibility criteria, as well as a screening period of up to 60 days to ensure that only patients with true moderate to severe SLE are enrolled.
The drug was well tolerated, with the rate of adverse events similar across all study groups. The adverse events of particular interest – hypertension, infections and infestations, and eye disorders – were all mild and transient. There were a greater number of reports of hypertension among those taking 1-mg and 4-mg doses of cenerimod, but Dr. Navarra said monthly measurements of systolic or diastolic blood pressure didn’t show any change.
The study was funded by cenerimod manufacturer Idorsia Pharmaceuticals. Dr. Navarra has financial relationships with Biogen, Astellas, Janssen, Novartis, Pfizer, Boehringer-Ingelheim, and GlaxoSmithKline.
SEOUL, SOUTH KOREA – A once-daily, oral dose of the investigational drug cenerimod, developed for the treatment of systemic lupus erythematosus, has shown a greater response rate among individuals with more severe disease, according to data presented at an international congress on SLE.
Cenerimod is a potent, highly-selective sphingosine 1–phosphate receptor 1 (S1P1) modulator with attenuated calcium signaling, which targets an important signaling molecule in immunity and cell migration, said rheumatologist Sandra Navarra, MD, of the University of Santo Tomas Hospital and St. Luke’s Medical Center in Manila, Philippines.
“It reduces the migration of T cells and B cells from the lymph nodes to the circulation into the tissues,” Dr. Navarra told the conference. S1P1 receptor modulators are already approved for treatment of multiple sclerosis, but cenerimod is the first to be explored for the treatment of lupus.
Dr. Navarra presented data from the international CARE study, a randomized, placebo-controlled, phase 2 study involving 427 patients with moderate to severe SLE.
Patients had to have been diagnosed at least 6 months before screening, be on stable lupus medications, and have abnormal antinuclear or anti–double stranded DNA antibodies. They were randomized to either 0.5 mg, 1 mg, 2 mg, or 4 mg of cenerimod daily or placebo for 12 months. At 6 months, the patients who had initially been randomized to 4 mg daily were rerandomized either to 2 mg daily or placebo.
While the study found that 4 mg of cenerimod was associated with a reduction in disease activity from baseline to month 6 on the modified Systemic Lupus Erythematosus Disease Activity Index–2000 score (excluding leukopenia), compared with placebo (P = .029). However, the final result was not statistically significant after adjustment for the multiplicity of tests for the four doses against placebo.
But the researchers saw a greater response among individuals with higher levels of interferon type 1 gene expression at baseline, as well as those with higher anti-dsDNA and lower C4 levels, which “makes sense,” Dr. Navarra said in an interview, because those were the sicker patients with “more inflammatory, more active disease.”
The study did exclude patients with active lupus nephritis, severe active central nervous system lupus, or severe cardiovascular disorders.
Dr. Navarra said the findings are now factored into patient selection for two phase 3 trials, called OPUS-1 and OPUS-2, which are now underway. The OPUS trials have revised eligibility criteria, as well as a screening period of up to 60 days to ensure that only patients with true moderate to severe SLE are enrolled.
The drug was well tolerated, with the rate of adverse events similar across all study groups. The adverse events of particular interest – hypertension, infections and infestations, and eye disorders – were all mild and transient. There were a greater number of reports of hypertension among those taking 1-mg and 4-mg doses of cenerimod, but Dr. Navarra said monthly measurements of systolic or diastolic blood pressure didn’t show any change.
The study was funded by cenerimod manufacturer Idorsia Pharmaceuticals. Dr. Navarra has financial relationships with Biogen, Astellas, Janssen, Novartis, Pfizer, Boehringer-Ingelheim, and GlaxoSmithKline.
AT LUPUS 2023
Severe hydroxychloroquine nonadherence linked to worse SLE outcomes
SEOUL, SOUTH KOREA – Regular testing of hydroxychloroquine levels in patients with systemic lupus erythematosus – especially those who are experiencing a disease flare – could help to identify patients who are not taking their treatment and are at risk of worse outcomes.
Data presented at an international congress on systemic lupus erythematosus showed that 7.3% of patients with SLE are severely nonadherent to their medication and have a higher risk of flare, early damage, and mortality.
Rheumatologist Nathalie Costedoat-Chalumeau, MD, PhD, professor of internal medicine at Cochin Hospital, Paris, presented data from 660 patients enrolled in the international longitudinal SLICC Inception Cohort, who had all been on hydroxychloroquine therapy for at least 3 months at baseline.
Patients’ serum hydroxychloroquine levels were measured at baseline and follow-up, and severe nonadherence was defined as below 106 ng/mL for those on 400 mg/day or 53 ng/mL for those on 200 mg/day.
Dr. Costedoat-Chalumeau said that those thresholds were chosen based on earlier work that analyzed the blood concentration of hydroxychloroquine in a group of patients and identified a group with very low concentrations corresponding to severe nonadherence.
“Since then, it has been reproduced by others with the same threshold,” she said. “When you have very low levels of hydroxychloroquine in their blood, you know that your patients don’t take their treatment.”
In the present study, the 7.3% of patients who met the criteria for severe nonadherence had a significant 3.3-fold higher risk of disease flare within a year of enrollment than did those who were adherent. They also had significantly higher mortality at 5 years after enrollment.
While the study didn’t show a significant difference in the level of damage at 5 years – defined as a worsening of their SLICC damage index – Dr. Costedoat-Chalumeau said they saw significantly greater damage occurring at 1, 2, and 3 years after enrollment among those who were severely nonadherent.
The challenge with recognizing these nonadherent patients is that they have no obvious differences at baseline from those who are adherent, Dr. Costedoat-Chalumeau said. The rates of nonadherence were similar regardless of what dose the patient was on, their ethnicity, gender, education level, or other demographic variables.
“I believe strongly that there is a benefit of testing hydroxychloroquine levels in the blood or serum to detect severe nonadherence,” she said.
At Dr. Costedoat-Chalumeau’s clinic, patients’ hydroxychloroquine levels are tested at every clinic visit, she said in an interview, and especially if they are experiencing a disease flare. “We want to know if the flare is because the patient is not taking the treatment or if it’s because the treatment is not effective, which is very different in terms of management,” she said. She recommended waiting at least 1 month after patients start treatment before measuring their hydroxychloroquine levels.
As to why some patients choose to stop taking their medication, Dr. Costedoat-Chalumeau said sometimes it was because patients were worried about side effects, but others were also unclear about why they needed to keep taking hydroxychloroquine.
“They think steroids are effective because when they take it they are better, but they don’t see the effect of hydroxychloroquine,” she said. “You have to explain that it doesn’t work the same.”
Commenting on the findings, session chair Joan Merrill, MD, professor of medicine at the University of Oklahoma Health Sciences Center, Oklahoma City, said the data show that severe nonadherence does have prognostic significance. “Many patients with SLE have low-grade disease or inflammation in the blood vessels that may not be clinically apparent and which hydroxychloroquine can help, so it might be wise to routinely get blood levels,” she said.
Dr. Costedoat-Chalumeau reported no relevant financial relationships apart from unrestricted institutional research grants from UCB and Roche.
SEOUL, SOUTH KOREA – Regular testing of hydroxychloroquine levels in patients with systemic lupus erythematosus – especially those who are experiencing a disease flare – could help to identify patients who are not taking their treatment and are at risk of worse outcomes.
Data presented at an international congress on systemic lupus erythematosus showed that 7.3% of patients with SLE are severely nonadherent to their medication and have a higher risk of flare, early damage, and mortality.
Rheumatologist Nathalie Costedoat-Chalumeau, MD, PhD, professor of internal medicine at Cochin Hospital, Paris, presented data from 660 patients enrolled in the international longitudinal SLICC Inception Cohort, who had all been on hydroxychloroquine therapy for at least 3 months at baseline.
Patients’ serum hydroxychloroquine levels were measured at baseline and follow-up, and severe nonadherence was defined as below 106 ng/mL for those on 400 mg/day or 53 ng/mL for those on 200 mg/day.
Dr. Costedoat-Chalumeau said that those thresholds were chosen based on earlier work that analyzed the blood concentration of hydroxychloroquine in a group of patients and identified a group with very low concentrations corresponding to severe nonadherence.
“Since then, it has been reproduced by others with the same threshold,” she said. “When you have very low levels of hydroxychloroquine in their blood, you know that your patients don’t take their treatment.”
In the present study, the 7.3% of patients who met the criteria for severe nonadherence had a significant 3.3-fold higher risk of disease flare within a year of enrollment than did those who were adherent. They also had significantly higher mortality at 5 years after enrollment.
While the study didn’t show a significant difference in the level of damage at 5 years – defined as a worsening of their SLICC damage index – Dr. Costedoat-Chalumeau said they saw significantly greater damage occurring at 1, 2, and 3 years after enrollment among those who were severely nonadherent.
The challenge with recognizing these nonadherent patients is that they have no obvious differences at baseline from those who are adherent, Dr. Costedoat-Chalumeau said. The rates of nonadherence were similar regardless of what dose the patient was on, their ethnicity, gender, education level, or other demographic variables.
“I believe strongly that there is a benefit of testing hydroxychloroquine levels in the blood or serum to detect severe nonadherence,” she said.
At Dr. Costedoat-Chalumeau’s clinic, patients’ hydroxychloroquine levels are tested at every clinic visit, she said in an interview, and especially if they are experiencing a disease flare. “We want to know if the flare is because the patient is not taking the treatment or if it’s because the treatment is not effective, which is very different in terms of management,” she said. She recommended waiting at least 1 month after patients start treatment before measuring their hydroxychloroquine levels.
As to why some patients choose to stop taking their medication, Dr. Costedoat-Chalumeau said sometimes it was because patients were worried about side effects, but others were also unclear about why they needed to keep taking hydroxychloroquine.
“They think steroids are effective because when they take it they are better, but they don’t see the effect of hydroxychloroquine,” she said. “You have to explain that it doesn’t work the same.”
Commenting on the findings, session chair Joan Merrill, MD, professor of medicine at the University of Oklahoma Health Sciences Center, Oklahoma City, said the data show that severe nonadherence does have prognostic significance. “Many patients with SLE have low-grade disease or inflammation in the blood vessels that may not be clinically apparent and which hydroxychloroquine can help, so it might be wise to routinely get blood levels,” she said.
Dr. Costedoat-Chalumeau reported no relevant financial relationships apart from unrestricted institutional research grants from UCB and Roche.
SEOUL, SOUTH KOREA – Regular testing of hydroxychloroquine levels in patients with systemic lupus erythematosus – especially those who are experiencing a disease flare – could help to identify patients who are not taking their treatment and are at risk of worse outcomes.
Data presented at an international congress on systemic lupus erythematosus showed that 7.3% of patients with SLE are severely nonadherent to their medication and have a higher risk of flare, early damage, and mortality.
Rheumatologist Nathalie Costedoat-Chalumeau, MD, PhD, professor of internal medicine at Cochin Hospital, Paris, presented data from 660 patients enrolled in the international longitudinal SLICC Inception Cohort, who had all been on hydroxychloroquine therapy for at least 3 months at baseline.
Patients’ serum hydroxychloroquine levels were measured at baseline and follow-up, and severe nonadherence was defined as below 106 ng/mL for those on 400 mg/day or 53 ng/mL for those on 200 mg/day.
Dr. Costedoat-Chalumeau said that those thresholds were chosen based on earlier work that analyzed the blood concentration of hydroxychloroquine in a group of patients and identified a group with very low concentrations corresponding to severe nonadherence.
“Since then, it has been reproduced by others with the same threshold,” she said. “When you have very low levels of hydroxychloroquine in their blood, you know that your patients don’t take their treatment.”
In the present study, the 7.3% of patients who met the criteria for severe nonadherence had a significant 3.3-fold higher risk of disease flare within a year of enrollment than did those who were adherent. They also had significantly higher mortality at 5 years after enrollment.
While the study didn’t show a significant difference in the level of damage at 5 years – defined as a worsening of their SLICC damage index – Dr. Costedoat-Chalumeau said they saw significantly greater damage occurring at 1, 2, and 3 years after enrollment among those who were severely nonadherent.
The challenge with recognizing these nonadherent patients is that they have no obvious differences at baseline from those who are adherent, Dr. Costedoat-Chalumeau said. The rates of nonadherence were similar regardless of what dose the patient was on, their ethnicity, gender, education level, or other demographic variables.
“I believe strongly that there is a benefit of testing hydroxychloroquine levels in the blood or serum to detect severe nonadherence,” she said.
At Dr. Costedoat-Chalumeau’s clinic, patients’ hydroxychloroquine levels are tested at every clinic visit, she said in an interview, and especially if they are experiencing a disease flare. “We want to know if the flare is because the patient is not taking the treatment or if it’s because the treatment is not effective, which is very different in terms of management,” she said. She recommended waiting at least 1 month after patients start treatment before measuring their hydroxychloroquine levels.
As to why some patients choose to stop taking their medication, Dr. Costedoat-Chalumeau said sometimes it was because patients were worried about side effects, but others were also unclear about why they needed to keep taking hydroxychloroquine.
“They think steroids are effective because when they take it they are better, but they don’t see the effect of hydroxychloroquine,” she said. “You have to explain that it doesn’t work the same.”
Commenting on the findings, session chair Joan Merrill, MD, professor of medicine at the University of Oklahoma Health Sciences Center, Oklahoma City, said the data show that severe nonadherence does have prognostic significance. “Many patients with SLE have low-grade disease or inflammation in the blood vessels that may not be clinically apparent and which hydroxychloroquine can help, so it might be wise to routinely get blood levels,” she said.
Dr. Costedoat-Chalumeau reported no relevant financial relationships apart from unrestricted institutional research grants from UCB and Roche.
AT LUPUS 2023
Can online mindfulness and self-compassion training improve quality of life for patients with atopic dermatitis?
, according to results of a small randomized controlled trial in Japan.
“We found that skin disease–specific QOL improved over time with a large effect size,” lead study author Sanae Kishimoto, MHS, MPH, of the School of Public Health, Graduate School of Medicine at Kyoto University and colleagues write in JAMA Dermatology. “These findings suggest that mindfulness and self-compassion training is an effective treatment option for adults with AD.”
A bothersome disease that worsens quality of life
AD, a chronic, relapsing, inflammatory, multifactorial skin disease involving intense itching, affects an estimated 15%-30% of children and 2%-10% of adults, with the incidence increasing in industrialized countries, the authors state.
Measured by disability-adjusted life years, AD has the highest disease burden among skin diseases, and people with AD commonly have anxiety, depression, and sleep problems. Treatments include medications, other skin care, and lifestyle changes. New biologics appear to be effective but are expensive and need to be studied for their long-term safety, the authors add.
“Stress can make the skin worse, but at the same time the skin disease and symptoms cause stress,” Peter A. Lio, MD, who was not involved in the study, told this news organization by email. “This vicious cycle contributes greatly to impairing quality of life.”
A program focused on wise, kind self-care
In the SMiLE study, the authors recruited adults with moderate to severe AD and Dermatology Life Quality Index (DLQI) score above 6 from dermatology clinics and through online announcements over 1 year beginning in July 2019.
Participants averaged 36.3 years of age, 80% were women, and their mean AD duration was 26.6 years. Everyone was allowed to receive usual care during the study, except for dupilumab (a newly marketed drug when the study started), psychotherapy, or other mindfulness training.
The researchers randomly assigned 56 adults to receive mindfulness training in addition to their usual care and 51 to the wait list plus usual care. Those in the training group received eight weekly 90-minute online mindfulness and self-compassion sessions. Each group-based session was conducted at the same time and day of the week and included meditation, informal psychoeducation, inquiry, and a short lecture, along with an optional 1-day silent meditation retreat at week 7 and an optional 2-hour videoconferencing booster session at week 13.
The intervention encouraged a nonjudgmental relationship with stress using mindfulness-based stress reduction (MBSR) and emphasized a compassionate relationship with oneself during suffering using mindful self-compassion (MSC). The program was developed and taught by lead author Dr. Kishimoto, a Japanese licensed clinical psychologist who has a history of AD, the paper notes.
At 13 weeks, after completing electronic assessments, patients in the training group showed greater improvement in the DLQI score than those on the wait list (between-group difference estimate, –6.34; 95% confidence interval, –8.27 to –4.41; P < .001). The standardized effect size (Cohen’s d) at 13 weeks was –1.06 (95% CI, –1.39 to –0.74).
Patients in the training group also improved more in all secondary outcomes: severity, itch- and scratch-related visual analog scales, self-compassion, mindfulness, psychological symptoms, and adherence to dermatologist-advised treatments.
They were also more likely to follow their dermatologist’s medical treatment plans, including moisturizer and topical steroid use.
One serious adverse event, endometrial cancer in one patient, was judged to be unrelated to the intervention.
Online format may give more patients access to treatment
“With relatively limited data in the literature, this particularly well-done, important study is likely to positively shape thinking around this topic,” said Dr. Lio, of the departments of dermatology and pediatrics at Northwestern University, Chicago. “This study nicely demonstrates that an online approach can be effective.
“In theory, these methods or techniques could democratize treatments like this, and open them up to many more patients,” he added. He would like to see partially or entirely automated apps (free of cost), similar to meditation “apps,” to treat patients more cost-effectively.
Dr. Lio explained that excluding participants on dupilumab (Dupixent) makes the results slightly less generalizable to patients with moderate to severe AD, who may have the most serious QOL challenges and who are often candidates for dupilumab.
“However, given that we almost never have all the known variables for a study, we are generally comfortable extrapolating that the intervention would likely be helpful for patients taking dupilumab as well, despite it not being specifically evaluated in that group,” he said.
Susan Massick, MD, of the department of dermatology at the Ohio State University Wexner Medical Center in Columbus, advises clinicians to take a multipronged approach to treating the physical and behavioral components of AD and to embrace therapies beyond prescription medications.
“Self-compassion training is another tool in our toolbox toward finding the right fix for our patients,” Dr. Massick said by email. She was not involved with this research.
“I applaud the focus of this study on behavioral health training as a means toward wellness and improved mindfulness,” she added. “I was impressed by the extent to which these simple measures helped improve the quality of life for patients who used the training.”
U.S. patients can benefit from these findings
“My sense is that AD patients the world over have many similar characteristics and concerns, so I would anticipate that the results would be comparable in a U.S. population,” Dr. Lio said. “Other studies performed in the U.S. also support this line of thinking.”
Although the study involved highly motivated patients in Japan, the suffering that patients with AD experience is universal regardless of race or ethnicity, Dr. Massick said. “Americans may be even more willing to embrace mindfulness and self-compassion training as a path toward better health and wellness.”
The study was funded by the Japan Agency for Medical Research and Development and the Mental Health Okamoto Memorial Foundation, the KDDI Foundation, the Pfizer Health Research Foundation, and the Japan Society for the Promotion of Science.
Dr. Kishimoto and several coauthors report relevant financial relationships with pharmaceutical companies. Dr. Lio reports financial relationships with Sanofi and Regeneron, the joint developers of dupilumab. Dr. Massick reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to results of a small randomized controlled trial in Japan.
“We found that skin disease–specific QOL improved over time with a large effect size,” lead study author Sanae Kishimoto, MHS, MPH, of the School of Public Health, Graduate School of Medicine at Kyoto University and colleagues write in JAMA Dermatology. “These findings suggest that mindfulness and self-compassion training is an effective treatment option for adults with AD.”
A bothersome disease that worsens quality of life
AD, a chronic, relapsing, inflammatory, multifactorial skin disease involving intense itching, affects an estimated 15%-30% of children and 2%-10% of adults, with the incidence increasing in industrialized countries, the authors state.
Measured by disability-adjusted life years, AD has the highest disease burden among skin diseases, and people with AD commonly have anxiety, depression, and sleep problems. Treatments include medications, other skin care, and lifestyle changes. New biologics appear to be effective but are expensive and need to be studied for their long-term safety, the authors add.
“Stress can make the skin worse, but at the same time the skin disease and symptoms cause stress,” Peter A. Lio, MD, who was not involved in the study, told this news organization by email. “This vicious cycle contributes greatly to impairing quality of life.”
A program focused on wise, kind self-care
In the SMiLE study, the authors recruited adults with moderate to severe AD and Dermatology Life Quality Index (DLQI) score above 6 from dermatology clinics and through online announcements over 1 year beginning in July 2019.
Participants averaged 36.3 years of age, 80% were women, and their mean AD duration was 26.6 years. Everyone was allowed to receive usual care during the study, except for dupilumab (a newly marketed drug when the study started), psychotherapy, or other mindfulness training.
The researchers randomly assigned 56 adults to receive mindfulness training in addition to their usual care and 51 to the wait list plus usual care. Those in the training group received eight weekly 90-minute online mindfulness and self-compassion sessions. Each group-based session was conducted at the same time and day of the week and included meditation, informal psychoeducation, inquiry, and a short lecture, along with an optional 1-day silent meditation retreat at week 7 and an optional 2-hour videoconferencing booster session at week 13.
The intervention encouraged a nonjudgmental relationship with stress using mindfulness-based stress reduction (MBSR) and emphasized a compassionate relationship with oneself during suffering using mindful self-compassion (MSC). The program was developed and taught by lead author Dr. Kishimoto, a Japanese licensed clinical psychologist who has a history of AD, the paper notes.
At 13 weeks, after completing electronic assessments, patients in the training group showed greater improvement in the DLQI score than those on the wait list (between-group difference estimate, –6.34; 95% confidence interval, –8.27 to –4.41; P < .001). The standardized effect size (Cohen’s d) at 13 weeks was –1.06 (95% CI, –1.39 to –0.74).
Patients in the training group also improved more in all secondary outcomes: severity, itch- and scratch-related visual analog scales, self-compassion, mindfulness, psychological symptoms, and adherence to dermatologist-advised treatments.
They were also more likely to follow their dermatologist’s medical treatment plans, including moisturizer and topical steroid use.
One serious adverse event, endometrial cancer in one patient, was judged to be unrelated to the intervention.
Online format may give more patients access to treatment
“With relatively limited data in the literature, this particularly well-done, important study is likely to positively shape thinking around this topic,” said Dr. Lio, of the departments of dermatology and pediatrics at Northwestern University, Chicago. “This study nicely demonstrates that an online approach can be effective.
“In theory, these methods or techniques could democratize treatments like this, and open them up to many more patients,” he added. He would like to see partially or entirely automated apps (free of cost), similar to meditation “apps,” to treat patients more cost-effectively.
Dr. Lio explained that excluding participants on dupilumab (Dupixent) makes the results slightly less generalizable to patients with moderate to severe AD, who may have the most serious QOL challenges and who are often candidates for dupilumab.
“However, given that we almost never have all the known variables for a study, we are generally comfortable extrapolating that the intervention would likely be helpful for patients taking dupilumab as well, despite it not being specifically evaluated in that group,” he said.
Susan Massick, MD, of the department of dermatology at the Ohio State University Wexner Medical Center in Columbus, advises clinicians to take a multipronged approach to treating the physical and behavioral components of AD and to embrace therapies beyond prescription medications.
“Self-compassion training is another tool in our toolbox toward finding the right fix for our patients,” Dr. Massick said by email. She was not involved with this research.
“I applaud the focus of this study on behavioral health training as a means toward wellness and improved mindfulness,” she added. “I was impressed by the extent to which these simple measures helped improve the quality of life for patients who used the training.”
U.S. patients can benefit from these findings
“My sense is that AD patients the world over have many similar characteristics and concerns, so I would anticipate that the results would be comparable in a U.S. population,” Dr. Lio said. “Other studies performed in the U.S. also support this line of thinking.”
Although the study involved highly motivated patients in Japan, the suffering that patients with AD experience is universal regardless of race or ethnicity, Dr. Massick said. “Americans may be even more willing to embrace mindfulness and self-compassion training as a path toward better health and wellness.”
The study was funded by the Japan Agency for Medical Research and Development and the Mental Health Okamoto Memorial Foundation, the KDDI Foundation, the Pfizer Health Research Foundation, and the Japan Society for the Promotion of Science.
Dr. Kishimoto and several coauthors report relevant financial relationships with pharmaceutical companies. Dr. Lio reports financial relationships with Sanofi and Regeneron, the joint developers of dupilumab. Dr. Massick reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to results of a small randomized controlled trial in Japan.
“We found that skin disease–specific QOL improved over time with a large effect size,” lead study author Sanae Kishimoto, MHS, MPH, of the School of Public Health, Graduate School of Medicine at Kyoto University and colleagues write in JAMA Dermatology. “These findings suggest that mindfulness and self-compassion training is an effective treatment option for adults with AD.”
A bothersome disease that worsens quality of life
AD, a chronic, relapsing, inflammatory, multifactorial skin disease involving intense itching, affects an estimated 15%-30% of children and 2%-10% of adults, with the incidence increasing in industrialized countries, the authors state.
Measured by disability-adjusted life years, AD has the highest disease burden among skin diseases, and people with AD commonly have anxiety, depression, and sleep problems. Treatments include medications, other skin care, and lifestyle changes. New biologics appear to be effective but are expensive and need to be studied for their long-term safety, the authors add.
“Stress can make the skin worse, but at the same time the skin disease and symptoms cause stress,” Peter A. Lio, MD, who was not involved in the study, told this news organization by email. “This vicious cycle contributes greatly to impairing quality of life.”
A program focused on wise, kind self-care
In the SMiLE study, the authors recruited adults with moderate to severe AD and Dermatology Life Quality Index (DLQI) score above 6 from dermatology clinics and through online announcements over 1 year beginning in July 2019.
Participants averaged 36.3 years of age, 80% were women, and their mean AD duration was 26.6 years. Everyone was allowed to receive usual care during the study, except for dupilumab (a newly marketed drug when the study started), psychotherapy, or other mindfulness training.
The researchers randomly assigned 56 adults to receive mindfulness training in addition to their usual care and 51 to the wait list plus usual care. Those in the training group received eight weekly 90-minute online mindfulness and self-compassion sessions. Each group-based session was conducted at the same time and day of the week and included meditation, informal psychoeducation, inquiry, and a short lecture, along with an optional 1-day silent meditation retreat at week 7 and an optional 2-hour videoconferencing booster session at week 13.
The intervention encouraged a nonjudgmental relationship with stress using mindfulness-based stress reduction (MBSR) and emphasized a compassionate relationship with oneself during suffering using mindful self-compassion (MSC). The program was developed and taught by lead author Dr. Kishimoto, a Japanese licensed clinical psychologist who has a history of AD, the paper notes.
At 13 weeks, after completing electronic assessments, patients in the training group showed greater improvement in the DLQI score than those on the wait list (between-group difference estimate, –6.34; 95% confidence interval, –8.27 to –4.41; P < .001). The standardized effect size (Cohen’s d) at 13 weeks was –1.06 (95% CI, –1.39 to –0.74).
Patients in the training group also improved more in all secondary outcomes: severity, itch- and scratch-related visual analog scales, self-compassion, mindfulness, psychological symptoms, and adherence to dermatologist-advised treatments.
They were also more likely to follow their dermatologist’s medical treatment plans, including moisturizer and topical steroid use.
One serious adverse event, endometrial cancer in one patient, was judged to be unrelated to the intervention.
Online format may give more patients access to treatment
“With relatively limited data in the literature, this particularly well-done, important study is likely to positively shape thinking around this topic,” said Dr. Lio, of the departments of dermatology and pediatrics at Northwestern University, Chicago. “This study nicely demonstrates that an online approach can be effective.
“In theory, these methods or techniques could democratize treatments like this, and open them up to many more patients,” he added. He would like to see partially or entirely automated apps (free of cost), similar to meditation “apps,” to treat patients more cost-effectively.
Dr. Lio explained that excluding participants on dupilumab (Dupixent) makes the results slightly less generalizable to patients with moderate to severe AD, who may have the most serious QOL challenges and who are often candidates for dupilumab.
“However, given that we almost never have all the known variables for a study, we are generally comfortable extrapolating that the intervention would likely be helpful for patients taking dupilumab as well, despite it not being specifically evaluated in that group,” he said.
Susan Massick, MD, of the department of dermatology at the Ohio State University Wexner Medical Center in Columbus, advises clinicians to take a multipronged approach to treating the physical and behavioral components of AD and to embrace therapies beyond prescription medications.
“Self-compassion training is another tool in our toolbox toward finding the right fix for our patients,” Dr. Massick said by email. She was not involved with this research.
“I applaud the focus of this study on behavioral health training as a means toward wellness and improved mindfulness,” she added. “I was impressed by the extent to which these simple measures helped improve the quality of life for patients who used the training.”
U.S. patients can benefit from these findings
“My sense is that AD patients the world over have many similar characteristics and concerns, so I would anticipate that the results would be comparable in a U.S. population,” Dr. Lio said. “Other studies performed in the U.S. also support this line of thinking.”
Although the study involved highly motivated patients in Japan, the suffering that patients with AD experience is universal regardless of race or ethnicity, Dr. Massick said. “Americans may be even more willing to embrace mindfulness and self-compassion training as a path toward better health and wellness.”
The study was funded by the Japan Agency for Medical Research and Development and the Mental Health Okamoto Memorial Foundation, the KDDI Foundation, the Pfizer Health Research Foundation, and the Japan Society for the Promotion of Science.
Dr. Kishimoto and several coauthors report relevant financial relationships with pharmaceutical companies. Dr. Lio reports financial relationships with Sanofi and Regeneron, the joint developers of dupilumab. Dr. Massick reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA DERMATOLOGY
Does Ozempic cause hair loss?
Should people be concerned about possible hair loss when taking Wegovy, Ozempic, or Mounjaro for weight loss (where the latter two drugs are being used off label) – as was recently claimed by some people on social media and reported in news stories?
The consensus among dermatologists and endocrinologists is no.
It’s up to the individual to weigh the benefits of treating obesity against the risks of the therapy, including the low risk of developing temporary hair loss, says one expert.
Wegovy, Ozempic, and Mounjaro
Of these three newer medications, only the glucagonlike peptide–1 (GLP-1) receptor agonist semaglutide (Wegovy) is approved by the Food and Drug Administration (since June 2021) for weight management – specifically for people with either obesity (body mass index ≥ 30 kg/m2) or overweight (BMI ≥ 27) plus at least one weight-related comorbidity such as hypertension, type 2 diabetes, and high cholesterol – with a dosage up to a 2.4-mg weekly injection.
When there was a short supply of Wegovy soon after it became available, some people turned to the same drug – semaglutide, but marketed as Ozempic for type 2 diabetes, which is titrated up to a 2-mg weekly injection. Still others opted for tirzepatide (Mounjaro), a dual GLP-1 agonist and glucose-dependent insulinotropic polypeptide (GIP) agonist. Tirzepatide is approved for type 2 diabetes in the United States but is not yet approved for weight loss.
Wegovy shortages continue to be reported.
; of interest, it was more common after bariatric surgery.
In clinical trials, 3% of patients receiving Wegovy (a 2.4-mg/wk injection) versus 1% of patients receiving placebo reported alopecia. Hair loss was not reported as a side effect in clinical trials of Ozempic (a 2-mg/wk injection) for type 2 diabetes. In a clinical trial of tirzepatide for weight loss in obesity, 5.7% of patients taking the highest dose (a 15-mg once-weekly injection) reported alopecia vs 1% of those who got a placebo.
In contrast, a review of 18 mostly observational studies reported that 57% of patients had hair loss after bariatric surgery.
Is it the drug or the rapid weight loss?
None of the experts consulted for this article had seen patients who came to them about hair loss while taking these drugs for weight loss.
“I have not seen patients complaining of hair loss from these medications, but perhaps it is just a matter of time,” said Lynne J. Goldberg, MD, a professor of dermatology and pathology and laboratory medicine, at Boston University, and director of the hair clinic at Boston Medical Center.
“Some of my patients lose hair when they lose weight, generally as a result of the weight loss itself and not as a side effect of these medications,” said Katharine H. Saunders, MD, an obesity medicine physician, cofounder of Intellihealth, and an assistant professor of medicine at Weill Cornell Medicine, New York.
“Hair loss from rapid weight loss is very common [and] not necessarily a side effect of the medication itself but more as a result of how quickly the weight loss occurs,” echoed Susan Massick, MD, associate professor of dermatology, Ohio State University, and a dermatologist at Ohio State’s Wexner Medical Center, both in Columbus.
“Hair loss is tricky,” observed Anne Peters, MD, director of clinical diabetes programs at the University of Southern California, Los Angeles. “Losing weight and/or changing your diet causes hair loss. Stress can cause hair loss. So, it is hard to separate weight loss from medication effect.”
Telogen effluvium (stress shedding) with rapid weight loss
The hair loss seems to be associated with rapid weight loss, the experts agreed.
“It is rare, but we can see patients who have a period of diffuse hair loss, called telogen effluvium, or ‘stress shedding’ with rapid weight loss,” said Michael A. Weintraub, MD, an endocrinologist at NYU Langone Health, New York.
This hair loss occurs in relation to either physical (surgery, pregnancy, illness) or emotional stress, added Dr. Weintraub, who is an assistant professor at NYU Grossman School of Medicine.
Hair loss caused by rapid weight loss could be caused by an antiobesity medication, but it could also occur with other obesity treatments, such as bariatric surgery or drastic dietary changes, he said. The hair shedding is typically short lived and reversible.
About 80%-85% of hair is in the anagen (growth) phase, about 5% is in a transitional (catagen) phase, and the rest is in telogen (resting, or shedding) phase, Dr. Massick explained. In telogen effluvium, hairs that are normally in the growth phase get suddenly shifted to telogen phase and are shed rapidly.
“Telogen effluvium can be caused by rapid weight loss, major surgery, severe COVID infection, high fever, or death in the family,” she noted. “You will not go bald with telogen effluvium, but you might find that you may lose a good volume of hair,” much more than the normal loss of up to 100 hairs a day.
“I counsel my patients about the possibility of losing hair before they undergo bariatric surgery,” Dr. Saunders said. “Generally, the health benefits of weight loss and weight maintenance outweigh the risk of temporary hair loss.”
Nutritional deficiencies and malnutrition can contribute to hair loss as well, and iron deficiency is sometimes a culprit, she added.
“If someone is worried” about hair loss associated with weight loss, “they should see their doctor,” Dr. Peters said. “If they are on thyroid hormone, in particular, the levels should be retested after weight loss.”
Hair loss appears more common after bariatric surgery than with antiobesity medications,” Dr. Weintraub observed, and it is unclear whether this is because the weight loss is more dramatic after surgery and thus a greater stressor, or whether it is caused by nutrient deficiency or a different mechanism entirely.
“Unlike certain forms of bariatric surgery, which can lead to malabsorption (e.g., Roux-en-Y gastric bypass), medications such as GLP-1 agonists and GLP-1/GIP dual agonists do not cause malabsorption,” Dr. Weintraub noted. “So nutritional deficiencies are less likely to be the cause of new hair loss in those taking antiobesity medications than [in] someone who underwent bariatric surgery.”
Iron and vitamin D deficiencies are the most common nutritional deficiencies that can cause hair loss, he noted.
Slow and steady weight loss rather than rapid
“I would suggest that patients try to keep the weight loss slow and steady, rather than rapid,” Dr. Goldberg said, “and follow any vitamin/mineral supplementation plan that they are given. Patients with bariatric surgery have nutritional guidance and a supplementation plan.”
“Follow a well-balanced dietary strategy with ample protein, vegetables, and some fruit,” Dr. Saunders said. Health care providers should monitor lab tests to check for and treat vitamin deficiencies, and registered dietitians can be crucial to ensure proper nutrition. She advises patients: “Find coping strategies to reduce stress and get enough sleep. If iron levels are low, start an iron supplement under your provider’s supervision.”
“Some of my patients swear by biotin supplements, prenatal vitamins or ‘hair, skin, and nails’ vitamins,” she added. If hair loss doesn’t stop, a dermatologist can look for other contributors and discuss strategies for hair restoration.
Individuals who undergo bariatric surgery require lifelong vitamin supplementation and yearly (or more frequent) lab testing, she noted.
“With, for example, bariatric surgery or any type of diet change you want to make sure you still maintain a balanced diet, whether its calories, protein, iron, zinc, vitamins (vitamin D for example),” Dr. Massick echoed.
Similarly, Dr. Peters advised: “I would say to maintain a normal healthy diet even if eating less. Exercise. Do all those healthy things. Taking a daily multivitamin isn’t a bad idea. Talk with a nutritionist. Use the appetite suppression of the medication to combine with healthy eating.”
“If someone is having new hair loss, they should see their clinician to evaluate for all possible causes,” Dr. Weintraub said. “Their provider can evaluate for underlying causes like thyroid dysfunction, iron deficiency, and vitamin D deficiency.”
However, if a patient’s pattern of hair loss is not diffuse but occurs in patches, this has an entirely different set of etiologies probably unrelated to antiobesity medication and should be evaluated.
Working with a nutritionist to ensure that patients have sufficient protein and micronutrient intake can lower the risk of developing hair loss and other complications, Dr. Weintraub said. “This is particularly important for certain forms of bariatric surgery such as Roux-en-Y gastric bypass, since that can lead to malabsorption of specific vitamins and minerals that need to be periodically measured and supplemented.”
In individuals starting an antiobesity medication, beginning a daily multivitamin has little harm, he added, and can ensure they are getting essential minerals and vitamins. However, no studies have specifically investigated this yet.
“Ultimately, it’s important to weigh the benefits of antiobesity medications against the potential risks, as we do with any medical intervention,” according to Dr. Weintraub.
“The purpose of treating obesity,” he stressed, “is to reduce the risk of heart disease, stroke, and multiple types of cancers. It’s up to the individual to weigh these benefits against the risks of the treatment, including the low risk of developing temporary hair loss.”
Dr. Peters writes a column for Medscape and disclosed that she served as a consultant for Blue Circle Health, Vertex, and Abbott Diabetes Care; received a research grant from Abbott Diabetes Care; and received stock options from Teladoc and Omada Health. Dr. Goldberg, Dr. Saunders, Dr. Massick, and Dr. Weintraub declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Should people be concerned about possible hair loss when taking Wegovy, Ozempic, or Mounjaro for weight loss (where the latter two drugs are being used off label) – as was recently claimed by some people on social media and reported in news stories?
The consensus among dermatologists and endocrinologists is no.
It’s up to the individual to weigh the benefits of treating obesity against the risks of the therapy, including the low risk of developing temporary hair loss, says one expert.
Wegovy, Ozempic, and Mounjaro
Of these three newer medications, only the glucagonlike peptide–1 (GLP-1) receptor agonist semaglutide (Wegovy) is approved by the Food and Drug Administration (since June 2021) for weight management – specifically for people with either obesity (body mass index ≥ 30 kg/m2) or overweight (BMI ≥ 27) plus at least one weight-related comorbidity such as hypertension, type 2 diabetes, and high cholesterol – with a dosage up to a 2.4-mg weekly injection.
When there was a short supply of Wegovy soon after it became available, some people turned to the same drug – semaglutide, but marketed as Ozempic for type 2 diabetes, which is titrated up to a 2-mg weekly injection. Still others opted for tirzepatide (Mounjaro), a dual GLP-1 agonist and glucose-dependent insulinotropic polypeptide (GIP) agonist. Tirzepatide is approved for type 2 diabetes in the United States but is not yet approved for weight loss.
Wegovy shortages continue to be reported.
; of interest, it was more common after bariatric surgery.
In clinical trials, 3% of patients receiving Wegovy (a 2.4-mg/wk injection) versus 1% of patients receiving placebo reported alopecia. Hair loss was not reported as a side effect in clinical trials of Ozempic (a 2-mg/wk injection) for type 2 diabetes. In a clinical trial of tirzepatide for weight loss in obesity, 5.7% of patients taking the highest dose (a 15-mg once-weekly injection) reported alopecia vs 1% of those who got a placebo.
In contrast, a review of 18 mostly observational studies reported that 57% of patients had hair loss after bariatric surgery.
Is it the drug or the rapid weight loss?
None of the experts consulted for this article had seen patients who came to them about hair loss while taking these drugs for weight loss.
“I have not seen patients complaining of hair loss from these medications, but perhaps it is just a matter of time,” said Lynne J. Goldberg, MD, a professor of dermatology and pathology and laboratory medicine, at Boston University, and director of the hair clinic at Boston Medical Center.
“Some of my patients lose hair when they lose weight, generally as a result of the weight loss itself and not as a side effect of these medications,” said Katharine H. Saunders, MD, an obesity medicine physician, cofounder of Intellihealth, and an assistant professor of medicine at Weill Cornell Medicine, New York.
“Hair loss from rapid weight loss is very common [and] not necessarily a side effect of the medication itself but more as a result of how quickly the weight loss occurs,” echoed Susan Massick, MD, associate professor of dermatology, Ohio State University, and a dermatologist at Ohio State’s Wexner Medical Center, both in Columbus.
“Hair loss is tricky,” observed Anne Peters, MD, director of clinical diabetes programs at the University of Southern California, Los Angeles. “Losing weight and/or changing your diet causes hair loss. Stress can cause hair loss. So, it is hard to separate weight loss from medication effect.”
Telogen effluvium (stress shedding) with rapid weight loss
The hair loss seems to be associated with rapid weight loss, the experts agreed.
“It is rare, but we can see patients who have a period of diffuse hair loss, called telogen effluvium, or ‘stress shedding’ with rapid weight loss,” said Michael A. Weintraub, MD, an endocrinologist at NYU Langone Health, New York.
This hair loss occurs in relation to either physical (surgery, pregnancy, illness) or emotional stress, added Dr. Weintraub, who is an assistant professor at NYU Grossman School of Medicine.
Hair loss caused by rapid weight loss could be caused by an antiobesity medication, but it could also occur with other obesity treatments, such as bariatric surgery or drastic dietary changes, he said. The hair shedding is typically short lived and reversible.
About 80%-85% of hair is in the anagen (growth) phase, about 5% is in a transitional (catagen) phase, and the rest is in telogen (resting, or shedding) phase, Dr. Massick explained. In telogen effluvium, hairs that are normally in the growth phase get suddenly shifted to telogen phase and are shed rapidly.
“Telogen effluvium can be caused by rapid weight loss, major surgery, severe COVID infection, high fever, or death in the family,” she noted. “You will not go bald with telogen effluvium, but you might find that you may lose a good volume of hair,” much more than the normal loss of up to 100 hairs a day.
“I counsel my patients about the possibility of losing hair before they undergo bariatric surgery,” Dr. Saunders said. “Generally, the health benefits of weight loss and weight maintenance outweigh the risk of temporary hair loss.”
Nutritional deficiencies and malnutrition can contribute to hair loss as well, and iron deficiency is sometimes a culprit, she added.
“If someone is worried” about hair loss associated with weight loss, “they should see their doctor,” Dr. Peters said. “If they are on thyroid hormone, in particular, the levels should be retested after weight loss.”
Hair loss appears more common after bariatric surgery than with antiobesity medications,” Dr. Weintraub observed, and it is unclear whether this is because the weight loss is more dramatic after surgery and thus a greater stressor, or whether it is caused by nutrient deficiency or a different mechanism entirely.
“Unlike certain forms of bariatric surgery, which can lead to malabsorption (e.g., Roux-en-Y gastric bypass), medications such as GLP-1 agonists and GLP-1/GIP dual agonists do not cause malabsorption,” Dr. Weintraub noted. “So nutritional deficiencies are less likely to be the cause of new hair loss in those taking antiobesity medications than [in] someone who underwent bariatric surgery.”
Iron and vitamin D deficiencies are the most common nutritional deficiencies that can cause hair loss, he noted.
Slow and steady weight loss rather than rapid
“I would suggest that patients try to keep the weight loss slow and steady, rather than rapid,” Dr. Goldberg said, “and follow any vitamin/mineral supplementation plan that they are given. Patients with bariatric surgery have nutritional guidance and a supplementation plan.”
“Follow a well-balanced dietary strategy with ample protein, vegetables, and some fruit,” Dr. Saunders said. Health care providers should monitor lab tests to check for and treat vitamin deficiencies, and registered dietitians can be crucial to ensure proper nutrition. She advises patients: “Find coping strategies to reduce stress and get enough sleep. If iron levels are low, start an iron supplement under your provider’s supervision.”
“Some of my patients swear by biotin supplements, prenatal vitamins or ‘hair, skin, and nails’ vitamins,” she added. If hair loss doesn’t stop, a dermatologist can look for other contributors and discuss strategies for hair restoration.
Individuals who undergo bariatric surgery require lifelong vitamin supplementation and yearly (or more frequent) lab testing, she noted.
“With, for example, bariatric surgery or any type of diet change you want to make sure you still maintain a balanced diet, whether its calories, protein, iron, zinc, vitamins (vitamin D for example),” Dr. Massick echoed.
Similarly, Dr. Peters advised: “I would say to maintain a normal healthy diet even if eating less. Exercise. Do all those healthy things. Taking a daily multivitamin isn’t a bad idea. Talk with a nutritionist. Use the appetite suppression of the medication to combine with healthy eating.”
“If someone is having new hair loss, they should see their clinician to evaluate for all possible causes,” Dr. Weintraub said. “Their provider can evaluate for underlying causes like thyroid dysfunction, iron deficiency, and vitamin D deficiency.”
However, if a patient’s pattern of hair loss is not diffuse but occurs in patches, this has an entirely different set of etiologies probably unrelated to antiobesity medication and should be evaluated.
Working with a nutritionist to ensure that patients have sufficient protein and micronutrient intake can lower the risk of developing hair loss and other complications, Dr. Weintraub said. “This is particularly important for certain forms of bariatric surgery such as Roux-en-Y gastric bypass, since that can lead to malabsorption of specific vitamins and minerals that need to be periodically measured and supplemented.”
In individuals starting an antiobesity medication, beginning a daily multivitamin has little harm, he added, and can ensure they are getting essential minerals and vitamins. However, no studies have specifically investigated this yet.
“Ultimately, it’s important to weigh the benefits of antiobesity medications against the potential risks, as we do with any medical intervention,” according to Dr. Weintraub.
“The purpose of treating obesity,” he stressed, “is to reduce the risk of heart disease, stroke, and multiple types of cancers. It’s up to the individual to weigh these benefits against the risks of the treatment, including the low risk of developing temporary hair loss.”
Dr. Peters writes a column for Medscape and disclosed that she served as a consultant for Blue Circle Health, Vertex, and Abbott Diabetes Care; received a research grant from Abbott Diabetes Care; and received stock options from Teladoc and Omada Health. Dr. Goldberg, Dr. Saunders, Dr. Massick, and Dr. Weintraub declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Should people be concerned about possible hair loss when taking Wegovy, Ozempic, or Mounjaro for weight loss (where the latter two drugs are being used off label) – as was recently claimed by some people on social media and reported in news stories?
The consensus among dermatologists and endocrinologists is no.
It’s up to the individual to weigh the benefits of treating obesity against the risks of the therapy, including the low risk of developing temporary hair loss, says one expert.
Wegovy, Ozempic, and Mounjaro
Of these three newer medications, only the glucagonlike peptide–1 (GLP-1) receptor agonist semaglutide (Wegovy) is approved by the Food and Drug Administration (since June 2021) for weight management – specifically for people with either obesity (body mass index ≥ 30 kg/m2) or overweight (BMI ≥ 27) plus at least one weight-related comorbidity such as hypertension, type 2 diabetes, and high cholesterol – with a dosage up to a 2.4-mg weekly injection.
When there was a short supply of Wegovy soon after it became available, some people turned to the same drug – semaglutide, but marketed as Ozempic for type 2 diabetes, which is titrated up to a 2-mg weekly injection. Still others opted for tirzepatide (Mounjaro), a dual GLP-1 agonist and glucose-dependent insulinotropic polypeptide (GIP) agonist. Tirzepatide is approved for type 2 diabetes in the United States but is not yet approved for weight loss.
Wegovy shortages continue to be reported.
; of interest, it was more common after bariatric surgery.
In clinical trials, 3% of patients receiving Wegovy (a 2.4-mg/wk injection) versus 1% of patients receiving placebo reported alopecia. Hair loss was not reported as a side effect in clinical trials of Ozempic (a 2-mg/wk injection) for type 2 diabetes. In a clinical trial of tirzepatide for weight loss in obesity, 5.7% of patients taking the highest dose (a 15-mg once-weekly injection) reported alopecia vs 1% of those who got a placebo.
In contrast, a review of 18 mostly observational studies reported that 57% of patients had hair loss after bariatric surgery.
Is it the drug or the rapid weight loss?
None of the experts consulted for this article had seen patients who came to them about hair loss while taking these drugs for weight loss.
“I have not seen patients complaining of hair loss from these medications, but perhaps it is just a matter of time,” said Lynne J. Goldberg, MD, a professor of dermatology and pathology and laboratory medicine, at Boston University, and director of the hair clinic at Boston Medical Center.
“Some of my patients lose hair when they lose weight, generally as a result of the weight loss itself and not as a side effect of these medications,” said Katharine H. Saunders, MD, an obesity medicine physician, cofounder of Intellihealth, and an assistant professor of medicine at Weill Cornell Medicine, New York.
“Hair loss from rapid weight loss is very common [and] not necessarily a side effect of the medication itself but more as a result of how quickly the weight loss occurs,” echoed Susan Massick, MD, associate professor of dermatology, Ohio State University, and a dermatologist at Ohio State’s Wexner Medical Center, both in Columbus.
“Hair loss is tricky,” observed Anne Peters, MD, director of clinical diabetes programs at the University of Southern California, Los Angeles. “Losing weight and/or changing your diet causes hair loss. Stress can cause hair loss. So, it is hard to separate weight loss from medication effect.”
Telogen effluvium (stress shedding) with rapid weight loss
The hair loss seems to be associated with rapid weight loss, the experts agreed.
“It is rare, but we can see patients who have a period of diffuse hair loss, called telogen effluvium, or ‘stress shedding’ with rapid weight loss,” said Michael A. Weintraub, MD, an endocrinologist at NYU Langone Health, New York.
This hair loss occurs in relation to either physical (surgery, pregnancy, illness) or emotional stress, added Dr. Weintraub, who is an assistant professor at NYU Grossman School of Medicine.
Hair loss caused by rapid weight loss could be caused by an antiobesity medication, but it could also occur with other obesity treatments, such as bariatric surgery or drastic dietary changes, he said. The hair shedding is typically short lived and reversible.
About 80%-85% of hair is in the anagen (growth) phase, about 5% is in a transitional (catagen) phase, and the rest is in telogen (resting, or shedding) phase, Dr. Massick explained. In telogen effluvium, hairs that are normally in the growth phase get suddenly shifted to telogen phase and are shed rapidly.
“Telogen effluvium can be caused by rapid weight loss, major surgery, severe COVID infection, high fever, or death in the family,” she noted. “You will not go bald with telogen effluvium, but you might find that you may lose a good volume of hair,” much more than the normal loss of up to 100 hairs a day.
“I counsel my patients about the possibility of losing hair before they undergo bariatric surgery,” Dr. Saunders said. “Generally, the health benefits of weight loss and weight maintenance outweigh the risk of temporary hair loss.”
Nutritional deficiencies and malnutrition can contribute to hair loss as well, and iron deficiency is sometimes a culprit, she added.
“If someone is worried” about hair loss associated with weight loss, “they should see their doctor,” Dr. Peters said. “If they are on thyroid hormone, in particular, the levels should be retested after weight loss.”
Hair loss appears more common after bariatric surgery than with antiobesity medications,” Dr. Weintraub observed, and it is unclear whether this is because the weight loss is more dramatic after surgery and thus a greater stressor, or whether it is caused by nutrient deficiency or a different mechanism entirely.
“Unlike certain forms of bariatric surgery, which can lead to malabsorption (e.g., Roux-en-Y gastric bypass), medications such as GLP-1 agonists and GLP-1/GIP dual agonists do not cause malabsorption,” Dr. Weintraub noted. “So nutritional deficiencies are less likely to be the cause of new hair loss in those taking antiobesity medications than [in] someone who underwent bariatric surgery.”
Iron and vitamin D deficiencies are the most common nutritional deficiencies that can cause hair loss, he noted.
Slow and steady weight loss rather than rapid
“I would suggest that patients try to keep the weight loss slow and steady, rather than rapid,” Dr. Goldberg said, “and follow any vitamin/mineral supplementation plan that they are given. Patients with bariatric surgery have nutritional guidance and a supplementation plan.”
“Follow a well-balanced dietary strategy with ample protein, vegetables, and some fruit,” Dr. Saunders said. Health care providers should monitor lab tests to check for and treat vitamin deficiencies, and registered dietitians can be crucial to ensure proper nutrition. She advises patients: “Find coping strategies to reduce stress and get enough sleep. If iron levels are low, start an iron supplement under your provider’s supervision.”
“Some of my patients swear by biotin supplements, prenatal vitamins or ‘hair, skin, and nails’ vitamins,” she added. If hair loss doesn’t stop, a dermatologist can look for other contributors and discuss strategies for hair restoration.
Individuals who undergo bariatric surgery require lifelong vitamin supplementation and yearly (or more frequent) lab testing, she noted.
“With, for example, bariatric surgery or any type of diet change you want to make sure you still maintain a balanced diet, whether its calories, protein, iron, zinc, vitamins (vitamin D for example),” Dr. Massick echoed.
Similarly, Dr. Peters advised: “I would say to maintain a normal healthy diet even if eating less. Exercise. Do all those healthy things. Taking a daily multivitamin isn’t a bad idea. Talk with a nutritionist. Use the appetite suppression of the medication to combine with healthy eating.”
“If someone is having new hair loss, they should see their clinician to evaluate for all possible causes,” Dr. Weintraub said. “Their provider can evaluate for underlying causes like thyroid dysfunction, iron deficiency, and vitamin D deficiency.”
However, if a patient’s pattern of hair loss is not diffuse but occurs in patches, this has an entirely different set of etiologies probably unrelated to antiobesity medication and should be evaluated.
Working with a nutritionist to ensure that patients have sufficient protein and micronutrient intake can lower the risk of developing hair loss and other complications, Dr. Weintraub said. “This is particularly important for certain forms of bariatric surgery such as Roux-en-Y gastric bypass, since that can lead to malabsorption of specific vitamins and minerals that need to be periodically measured and supplemented.”
In individuals starting an antiobesity medication, beginning a daily multivitamin has little harm, he added, and can ensure they are getting essential minerals and vitamins. However, no studies have specifically investigated this yet.
“Ultimately, it’s important to weigh the benefits of antiobesity medications against the potential risks, as we do with any medical intervention,” according to Dr. Weintraub.
“The purpose of treating obesity,” he stressed, “is to reduce the risk of heart disease, stroke, and multiple types of cancers. It’s up to the individual to weigh these benefits against the risks of the treatment, including the low risk of developing temporary hair loss.”
Dr. Peters writes a column for Medscape and disclosed that she served as a consultant for Blue Circle Health, Vertex, and Abbott Diabetes Care; received a research grant from Abbott Diabetes Care; and received stock options from Teladoc and Omada Health. Dr. Goldberg, Dr. Saunders, Dr. Massick, and Dr. Weintraub declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People still want their medical intelligence in human form
Doctors or AI? Lukewarm vote of confidence goes to …
Well, we’ve got some good news for the physicians out there, and we’ve got some bad news. Which do you want first? Okay, we’re mostly hearing good news, so here goes: Most people would choose a human doctor over artificial intelligence for the diagnosis and treatment of their medical conditions.
And the bad news? In the survey we’re talking about, “most” was 53%, so not exactly a huge victory for the carbon-based life forms. Yup, about 47% of the 2,472 respondents said they would prefer an AI-based clinic over a human specialist, and that number went up if individuals were told that their primary care physicians were on board with AI, “or otherwise nudged to consider AI as good,” the research team said in a written statement released by the University of Arizona, Tucson.
They went on to add that “this signaled the significance of the human physician in guiding a patient’s decision.” So patients will still need their doctors in the future to … um … this is a bit awkward … tell them how good the AI is?
And yes, we know that ChatGPT is already doing the same thing to journalists, but could it write a medical-humor column? Not a chance. Probably can’t even tell a joke.
How do ghosts get rid of wrinkles? Boo-tox. There, let’s see ChatGPT do that.
Explaining the joke makes it funnier, right?
Here at LOTME headquarters, we live by one simple rule, passed down directly from the Buddha himself: “Never let a good presurgical assessment of refractory epilepsy go to waste. Also, don’t believe everything you read on the Internet.”
This human-created joke has been brought to you by the leading theory of humor, which states that comedy stems from our brain reacting to an incongruous part of reality in a positive way. These positive emotions light up our neurons in a specific fashion, and boom, comedy is achieved.
Previous studies into the science of comedy have typically used functional MRI to analyze the brain while it was gripped in the throes of a comedic reaction. Unfortunately, fMRI cannot detect the entirety of the electromagnetic spectrum generated by the brain during these moments, so observing scientists have been, quite literally, missing out on some of the joke. And that’s where a new study from France comes in.
In the study, the researchers showed a group of patients with epilepsy who were hooked up to deep brain electrodes and a high-tech neuroimaging machine – part of the aforementioned presurgical assessment – a 3-minute excerpt from a Charlie Chaplin movie and analyzed their brain activity. Why Charlie Chaplin? Simple. Slapstick is perhaps the most accessible form of comedy across cultures. We can all appreciate a man getting hit in the head with a coconut. The world’s oldest bar joke or whatever this is? Not so much.
During the funniest scenes, all study participants showed increased high-frequency gamma waves (indicating high cognitive engagement) and a decrease in low-frequency waves (indicating reduced inattention and introspection). During unfunny scenes, such as transition moments, the opposite occurred. Importantly, this inverse relationship occurred in the temporal lobe but not in other regions, supporting previous research that indicated humor was mainly processed in the temporal lobe.
The investigators suggested future research should focus on longer videos with more complex forms of comedy, such as jokes, irony, sarcasm, or reference humor. So, uh, a guy getting hit in the head with two coconuts? That’s high-brow stuff right there.
Hot take: Humans aren’t that special
We humans have always prided ourselves on being different from “the animals” in an exceptional way. News flash! We aren’t. We may be the apex predator, but new research shows that humans, as part of the animal kingdom, just aren’t special.
Not special? How can they say that? Are gorillas doing open-heart surgery? Do wolverines tell jokes? At a more basic level, though, the way we operate as mammals in societies is not unique or even new. Elephants are known to mourn their deceased and to have funeral-like practices, ants invented agriculture, and we’re certainly not the only species that has figured out how to use tools.
This new research just demonstrates another way we aren’t exceptional, and that’s in our mating practices and outcomes.
“Humans appear to resemble mammals that live in monogamous partnerships and to some extent, those classified as cooperative breeders, where breeding individuals have to rely on the help of others to raise their offspring,” Monique Borgerhoff Mulder, PhD, professor emerita of anthropology at the University of California, Davis, said in a written statement.
The research team, which consisted of over 100 investigators, looked at 90 human populations based on data from over 80,000 people globally and compared the human data with 49 different nonhuman mammal species. In polygynous societies in which men take several wives, they found, women have more access to resources like food, shelter, and parenting help. Monogamy, on the other hand, “can drive significant inequalities among women,” Dr. Borgerhoff Mulder said, by promoting large differences in the number of children couples produce.
Human day-to-day behavior and child-rearing habits – one parent taking a daughter to ballet class and fixing dinner so the other parent can get to exercise class before picking up the son from soccer practice – may have us thinking that we are part of an evolved society, but really we are not much different than other mammals that hunt, forage for food, and rear and teach their children, the researchers suggested.
So, yes, humans can travel to the moon, create a vaccine for smallpox, and hit other humans with coconuts, but when it comes to simply having offspring or raising them, we’re not all that special. Get over it.
Doctors or AI? Lukewarm vote of confidence goes to …
Well, we’ve got some good news for the physicians out there, and we’ve got some bad news. Which do you want first? Okay, we’re mostly hearing good news, so here goes: Most people would choose a human doctor over artificial intelligence for the diagnosis and treatment of their medical conditions.
And the bad news? In the survey we’re talking about, “most” was 53%, so not exactly a huge victory for the carbon-based life forms. Yup, about 47% of the 2,472 respondents said they would prefer an AI-based clinic over a human specialist, and that number went up if individuals were told that their primary care physicians were on board with AI, “or otherwise nudged to consider AI as good,” the research team said in a written statement released by the University of Arizona, Tucson.
They went on to add that “this signaled the significance of the human physician in guiding a patient’s decision.” So patients will still need their doctors in the future to … um … this is a bit awkward … tell them how good the AI is?
And yes, we know that ChatGPT is already doing the same thing to journalists, but could it write a medical-humor column? Not a chance. Probably can’t even tell a joke.
How do ghosts get rid of wrinkles? Boo-tox. There, let’s see ChatGPT do that.
Explaining the joke makes it funnier, right?
Here at LOTME headquarters, we live by one simple rule, passed down directly from the Buddha himself: “Never let a good presurgical assessment of refractory epilepsy go to waste. Also, don’t believe everything you read on the Internet.”
This human-created joke has been brought to you by the leading theory of humor, which states that comedy stems from our brain reacting to an incongruous part of reality in a positive way. These positive emotions light up our neurons in a specific fashion, and boom, comedy is achieved.
Previous studies into the science of comedy have typically used functional MRI to analyze the brain while it was gripped in the throes of a comedic reaction. Unfortunately, fMRI cannot detect the entirety of the electromagnetic spectrum generated by the brain during these moments, so observing scientists have been, quite literally, missing out on some of the joke. And that’s where a new study from France comes in.
In the study, the researchers showed a group of patients with epilepsy who were hooked up to deep brain electrodes and a high-tech neuroimaging machine – part of the aforementioned presurgical assessment – a 3-minute excerpt from a Charlie Chaplin movie and analyzed their brain activity. Why Charlie Chaplin? Simple. Slapstick is perhaps the most accessible form of comedy across cultures. We can all appreciate a man getting hit in the head with a coconut. The world’s oldest bar joke or whatever this is? Not so much.
During the funniest scenes, all study participants showed increased high-frequency gamma waves (indicating high cognitive engagement) and a decrease in low-frequency waves (indicating reduced inattention and introspection). During unfunny scenes, such as transition moments, the opposite occurred. Importantly, this inverse relationship occurred in the temporal lobe but not in other regions, supporting previous research that indicated humor was mainly processed in the temporal lobe.
The investigators suggested future research should focus on longer videos with more complex forms of comedy, such as jokes, irony, sarcasm, or reference humor. So, uh, a guy getting hit in the head with two coconuts? That’s high-brow stuff right there.
Hot take: Humans aren’t that special
We humans have always prided ourselves on being different from “the animals” in an exceptional way. News flash! We aren’t. We may be the apex predator, but new research shows that humans, as part of the animal kingdom, just aren’t special.
Not special? How can they say that? Are gorillas doing open-heart surgery? Do wolverines tell jokes? At a more basic level, though, the way we operate as mammals in societies is not unique or even new. Elephants are known to mourn their deceased and to have funeral-like practices, ants invented agriculture, and we’re certainly not the only species that has figured out how to use tools.
This new research just demonstrates another way we aren’t exceptional, and that’s in our mating practices and outcomes.
“Humans appear to resemble mammals that live in monogamous partnerships and to some extent, those classified as cooperative breeders, where breeding individuals have to rely on the help of others to raise their offspring,” Monique Borgerhoff Mulder, PhD, professor emerita of anthropology at the University of California, Davis, said in a written statement.
The research team, which consisted of over 100 investigators, looked at 90 human populations based on data from over 80,000 people globally and compared the human data with 49 different nonhuman mammal species. In polygynous societies in which men take several wives, they found, women have more access to resources like food, shelter, and parenting help. Monogamy, on the other hand, “can drive significant inequalities among women,” Dr. Borgerhoff Mulder said, by promoting large differences in the number of children couples produce.
Human day-to-day behavior and child-rearing habits – one parent taking a daughter to ballet class and fixing dinner so the other parent can get to exercise class before picking up the son from soccer practice – may have us thinking that we are part of an evolved society, but really we are not much different than other mammals that hunt, forage for food, and rear and teach their children, the researchers suggested.
So, yes, humans can travel to the moon, create a vaccine for smallpox, and hit other humans with coconuts, but when it comes to simply having offspring or raising them, we’re not all that special. Get over it.
Doctors or AI? Lukewarm vote of confidence goes to …
Well, we’ve got some good news for the physicians out there, and we’ve got some bad news. Which do you want first? Okay, we’re mostly hearing good news, so here goes: Most people would choose a human doctor over artificial intelligence for the diagnosis and treatment of their medical conditions.
And the bad news? In the survey we’re talking about, “most” was 53%, so not exactly a huge victory for the carbon-based life forms. Yup, about 47% of the 2,472 respondents said they would prefer an AI-based clinic over a human specialist, and that number went up if individuals were told that their primary care physicians were on board with AI, “or otherwise nudged to consider AI as good,” the research team said in a written statement released by the University of Arizona, Tucson.
They went on to add that “this signaled the significance of the human physician in guiding a patient’s decision.” So patients will still need their doctors in the future to … um … this is a bit awkward … tell them how good the AI is?
And yes, we know that ChatGPT is already doing the same thing to journalists, but could it write a medical-humor column? Not a chance. Probably can’t even tell a joke.
How do ghosts get rid of wrinkles? Boo-tox. There, let’s see ChatGPT do that.
Explaining the joke makes it funnier, right?
Here at LOTME headquarters, we live by one simple rule, passed down directly from the Buddha himself: “Never let a good presurgical assessment of refractory epilepsy go to waste. Also, don’t believe everything you read on the Internet.”
This human-created joke has been brought to you by the leading theory of humor, which states that comedy stems from our brain reacting to an incongruous part of reality in a positive way. These positive emotions light up our neurons in a specific fashion, and boom, comedy is achieved.
Previous studies into the science of comedy have typically used functional MRI to analyze the brain while it was gripped in the throes of a comedic reaction. Unfortunately, fMRI cannot detect the entirety of the electromagnetic spectrum generated by the brain during these moments, so observing scientists have been, quite literally, missing out on some of the joke. And that’s where a new study from France comes in.
In the study, the researchers showed a group of patients with epilepsy who were hooked up to deep brain electrodes and a high-tech neuroimaging machine – part of the aforementioned presurgical assessment – a 3-minute excerpt from a Charlie Chaplin movie and analyzed their brain activity. Why Charlie Chaplin? Simple. Slapstick is perhaps the most accessible form of comedy across cultures. We can all appreciate a man getting hit in the head with a coconut. The world’s oldest bar joke or whatever this is? Not so much.
During the funniest scenes, all study participants showed increased high-frequency gamma waves (indicating high cognitive engagement) and a decrease in low-frequency waves (indicating reduced inattention and introspection). During unfunny scenes, such as transition moments, the opposite occurred. Importantly, this inverse relationship occurred in the temporal lobe but not in other regions, supporting previous research that indicated humor was mainly processed in the temporal lobe.
The investigators suggested future research should focus on longer videos with more complex forms of comedy, such as jokes, irony, sarcasm, or reference humor. So, uh, a guy getting hit in the head with two coconuts? That’s high-brow stuff right there.
Hot take: Humans aren’t that special
We humans have always prided ourselves on being different from “the animals” in an exceptional way. News flash! We aren’t. We may be the apex predator, but new research shows that humans, as part of the animal kingdom, just aren’t special.
Not special? How can they say that? Are gorillas doing open-heart surgery? Do wolverines tell jokes? At a more basic level, though, the way we operate as mammals in societies is not unique or even new. Elephants are known to mourn their deceased and to have funeral-like practices, ants invented agriculture, and we’re certainly not the only species that has figured out how to use tools.
This new research just demonstrates another way we aren’t exceptional, and that’s in our mating practices and outcomes.
“Humans appear to resemble mammals that live in monogamous partnerships and to some extent, those classified as cooperative breeders, where breeding individuals have to rely on the help of others to raise their offspring,” Monique Borgerhoff Mulder, PhD, professor emerita of anthropology at the University of California, Davis, said in a written statement.
The research team, which consisted of over 100 investigators, looked at 90 human populations based on data from over 80,000 people globally and compared the human data with 49 different nonhuman mammal species. In polygynous societies in which men take several wives, they found, women have more access to resources like food, shelter, and parenting help. Monogamy, on the other hand, “can drive significant inequalities among women,” Dr. Borgerhoff Mulder said, by promoting large differences in the number of children couples produce.
Human day-to-day behavior and child-rearing habits – one parent taking a daughter to ballet class and fixing dinner so the other parent can get to exercise class before picking up the son from soccer practice – may have us thinking that we are part of an evolved society, but really we are not much different than other mammals that hunt, forage for food, and rear and teach their children, the researchers suggested.
So, yes, humans can travel to the moon, create a vaccine for smallpox, and hit other humans with coconuts, but when it comes to simply having offspring or raising them, we’re not all that special. Get over it.
Extracellular Matrix–Based Collagen Dressings for Scalp Repair Following Mohs Micrographic Surgery
To the Editor:
Squamous cell carcinoma (SCC) is the second most common cancer of the scalp.1 Mohs micrographic surgery is used to treat SCC, and it commonly generates a 2.5×2.5-cm open wound with exposed bone.2 Although Mohs micrographic surgery effectively treats cutaneous lesions, it carries a high risk for complications such as infection, wound dehiscence, and partial or full-thickness skin graft necrosis.3 Recommended therapies to decrease these complications include linear closures, flaps, and peripheral autograft tissue.4 However, these procedures do not come without risks and carry their own complications. Therefore, we suggest a safe, less-invasive initial approach using a synthetic extracellular matrix (ECM)–based collagen dressing for secondary wound closure.
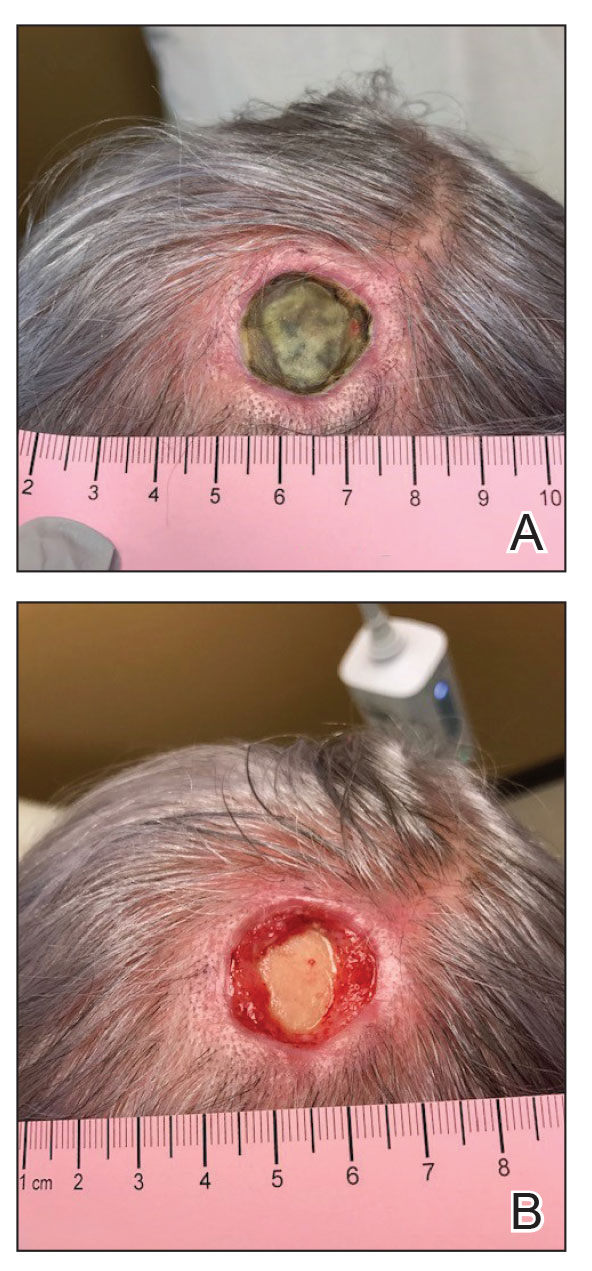
A 76-year-old woman presented to the infectious disease clinic at Monument Health Rapid City Clinic (Rapid City, South Dakota) for evaluation of a dehisced scalp wound 3 months following Mohs micrographic surgery for scalp SCC. The wound underwent primary closure following surgery and dehisced shortly after (Figure 1A). Various oral antimicrobials were used by the dermatologist to assist with wound closure but without success. The patient was referred to the wound clinic for management. At the first appointment, all necrotic tissue was debrided and the cranium was exposed in the wound base (Figure 1B). The wound measured 2.3×2.3×0.2 cm. An ECM-containing collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was used to provide a scaffold for wound closure (Figure 2A). It was dressed with the petroleum-based gauze Xeroform (Cardinal Health) and covered with dry gauze to prevent evaporation and provide moist wound healing. The wound developed some budding tissue islands 3 weeks after weekly ECM-based collagen dressing applications (Figure 3A). The wound continued to decrease in size and formed an isthmus by the second month of therapy (Figure 3B). The wound fully closed within 3 months and showed minimal scarring after 3 years (Figure 2B).
![A, An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound. B, The wound showed minimal scarring 3 years after closure. A, An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound. B, The wound showed minimal scarring 3 years after closure.](https://cdn.mdedge.com/files/s3fs-public/CT111005033_e_Fig2_AB.jpg)
Chronic wounds usually get trapped in the inflammatory stage of wound healing due to destruction of growth factors and ECM by metalloproteases (MMPs), which creates a vicious cycle and wound stalling. Wound debridement converts a chronic wound back into an acute wound, which is the first step of healing. Following wound debridement, collagen-based dressings can assist with healing by binding the destructive MMPs, and ECM matrix promotes the building of new tissue. The 3 most commonly used ECM-based collagen dressings are Endoform, PuraPly AM (Organogenesis Inc), and Puracol Ultra ECM (Medline Industries, Inc).
![A, Budding tissue islands developed on a scalp wound 3 weeks after application of an extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]). B, An isthmus developed 7 weeks after application A, Budding tissue islands developed on a scalp wound 3 weeks after application of an extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]). B, An isthmus developed 7 weeks after application](https://cdn.mdedge.com/files/s3fs-public/CT111005033_e_Fig3_AB.jpg)
Endoform is ovine-based collagen and provides a natural porous bioscaffold for rapid cell infiltration.5 It contains more than 150 ECM proteins along with residual vascular channels that help re-establish new vasculature. Ovine-based collagen contains collagen types I, III, and IV arranged as native fibers that retain the 3-dimensional architecture present in tissue ECM.5 Although MMPs are essential in normal healing, the elevated presence of MMPs has been linked to stalled wound healing. Clinical observation and assessment may not be sufficient to identify a wound with elevated protease activity that can break down ECM, affect wound fibroblasts, and impair growth factor response. Although collagen ECM itself does not contain any growth factors, it preserves the destruction of native ECM and growth factors by MMPs by functioning as a sacrificial substrate. The addition of 0.3% ionic silver to the ECM has been shown to decrease bacterial growth and prevent biofilm formation.6
PuraPly AM is a native, type I porcine collagen matrix embedded with the
Puracol Ultra ECM is made of porcine mesothelium and is comprised of types I, III, and IV collagens; elastin; fibronectin; laminin; and proteoglycans. It also contains fibroblast growth factors, contributing to angiogenesis in the wound.9
Application of ECM-based collagen dressings on debrided wounds requires moisture for absorption. Because cranium wounds lack sufficient exudate production, dermal templates need to be hydrated with sterile normal saline before application and covered with a moisture-retaining dressing. Extracellular matrix–based dressings are biodegradable and can be reapplied every 5 to 7 days. For chronic wounds, application of collagen dressings, such as Endoform, is essential and could be considered as the first step prior to switching to more advanced wound care modalities.6,10 Additional studies investigating ECM-containing may determine their comparative efficacy.
- Burton KA, Ashack KA, Khachemoune A. Cutaneous squamous cell carcinoma: a review of high-risk and metastatic disease. Am J Clin Dermatol. 2016;17:491-508. doi:10.1007/s40257-016-0207-3
- Kimyai-Asadi A, Goldberg LH, Peterson SR, et al. The incidence of major complications from Mohs micrographic surgery performed in office-based and hospital-based settings. J Am Acad Dermatol. 2005;53:628-634. doi:10.1016/j.jaad.2005.03.023
- Merritt BG, Lee NY, Brodland DG, et al. The safety of Mohs surgery: a prospective multicenter cohort study. J Am Acad Dermatol. 2012;67:1302-1309. doi:10.1016/j.jaad.2012.05.041
- Yu WY, Salmon P, Thuener J, et al. Mohs surgery for advanced tumors of the scalp. Dermatol Surg. 2019;45(suppl 2):S110-S117.
- Endoform. Aroa Biosurgery Limited website. Accessed May 22, 2023. https://aroa.com/product/endoform/
- Liden BA, May BC. Clinical outcomes following the use of ovine forestomach matrix (endoform dermal template) to treat chronic wounds. Adv Skin Wound Care. 2013;26:164-167. doi:10.1097/01.ASW.0000428862.34294.d4
- PuraPly AM. Organogenesis website. Accessed May 22, 2023. https://organogenesis.com/surgical-sports-medicine/puraplyam/
- Bain MA, Koullias GJ, Morse K, et al. Type I collagen matrix plus polyhexamethylene biguanide antimicrobial for the treatment of cutaneous wounds. J Comp Eff Res. 2020;9:691-703. doi:10.2217/cer-2020-0058
- Puracol Ultra ECM Collagen Wound Dressings. Medical Industries, LP website. May 22, 2023. https://punchout.medline.com/product/Puracol-Ultra-Extracellular-Matrix-ECM-Collagen-Wound-Dressing/Collagen-Dressings/Z05-PF188619?question=&index=P4&indexCount=4
- Raizman R, Hill R, Woo K. Prospective multicenter evaluation of an advanced extracellular matrix for wound management. Adv Skin Wound Care. 2020;33:437-444. doi:10.1097/01.ASW.0000667052.74087.d6
To the Editor:
Squamous cell carcinoma (SCC) is the second most common cancer of the scalp.1 Mohs micrographic surgery is used to treat SCC, and it commonly generates a 2.5×2.5-cm open wound with exposed bone.2 Although Mohs micrographic surgery effectively treats cutaneous lesions, it carries a high risk for complications such as infection, wound dehiscence, and partial or full-thickness skin graft necrosis.3 Recommended therapies to decrease these complications include linear closures, flaps, and peripheral autograft tissue.4 However, these procedures do not come without risks and carry their own complications. Therefore, we suggest a safe, less-invasive initial approach using a synthetic extracellular matrix (ECM)–based collagen dressing for secondary wound closure.
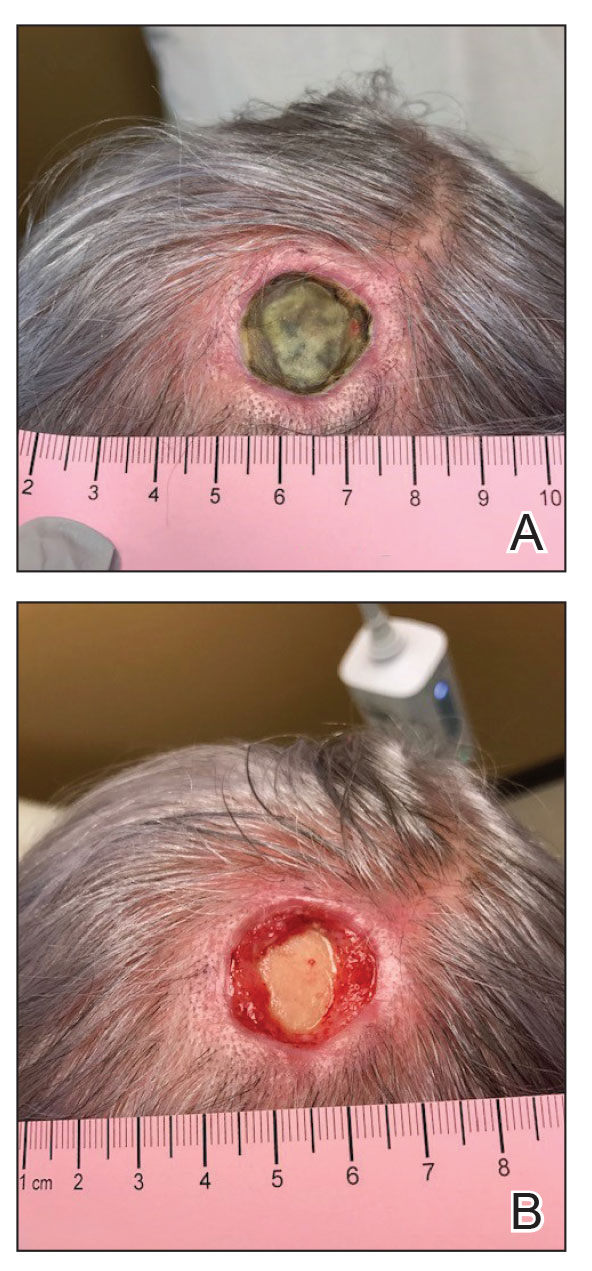
A 76-year-old woman presented to the infectious disease clinic at Monument Health Rapid City Clinic (Rapid City, South Dakota) for evaluation of a dehisced scalp wound 3 months following Mohs micrographic surgery for scalp SCC. The wound underwent primary closure following surgery and dehisced shortly after (Figure 1A). Various oral antimicrobials were used by the dermatologist to assist with wound closure but without success. The patient was referred to the wound clinic for management. At the first appointment, all necrotic tissue was debrided and the cranium was exposed in the wound base (Figure 1B). The wound measured 2.3×2.3×0.2 cm. An ECM-containing collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was used to provide a scaffold for wound closure (Figure 2A). It was dressed with the petroleum-based gauze Xeroform (Cardinal Health) and covered with dry gauze to prevent evaporation and provide moist wound healing. The wound developed some budding tissue islands 3 weeks after weekly ECM-based collagen dressing applications (Figure 3A). The wound continued to decrease in size and formed an isthmus by the second month of therapy (Figure 3B). The wound fully closed within 3 months and showed minimal scarring after 3 years (Figure 2B).
![A, An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound. B, The wound showed minimal scarring 3 years after closure. A, An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound. B, The wound showed minimal scarring 3 years after closure.](https://cdn.mdedge.com/files/s3fs-public/CT111005033_e_Fig2_AB.jpg)
Chronic wounds usually get trapped in the inflammatory stage of wound healing due to destruction of growth factors and ECM by metalloproteases (MMPs), which creates a vicious cycle and wound stalling. Wound debridement converts a chronic wound back into an acute wound, which is the first step of healing. Following wound debridement, collagen-based dressings can assist with healing by binding the destructive MMPs, and ECM matrix promotes the building of new tissue. The 3 most commonly used ECM-based collagen dressings are Endoform, PuraPly AM (Organogenesis Inc), and Puracol Ultra ECM (Medline Industries, Inc).
![A, Budding tissue islands developed on a scalp wound 3 weeks after application of an extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]). B, An isthmus developed 7 weeks after application A, Budding tissue islands developed on a scalp wound 3 weeks after application of an extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]). B, An isthmus developed 7 weeks after application](https://cdn.mdedge.com/files/s3fs-public/CT111005033_e_Fig3_AB.jpg)
Endoform is ovine-based collagen and provides a natural porous bioscaffold for rapid cell infiltration.5 It contains more than 150 ECM proteins along with residual vascular channels that help re-establish new vasculature. Ovine-based collagen contains collagen types I, III, and IV arranged as native fibers that retain the 3-dimensional architecture present in tissue ECM.5 Although MMPs are essential in normal healing, the elevated presence of MMPs has been linked to stalled wound healing. Clinical observation and assessment may not be sufficient to identify a wound with elevated protease activity that can break down ECM, affect wound fibroblasts, and impair growth factor response. Although collagen ECM itself does not contain any growth factors, it preserves the destruction of native ECM and growth factors by MMPs by functioning as a sacrificial substrate. The addition of 0.3% ionic silver to the ECM has been shown to decrease bacterial growth and prevent biofilm formation.6
PuraPly AM is a native, type I porcine collagen matrix embedded with the
Puracol Ultra ECM is made of porcine mesothelium and is comprised of types I, III, and IV collagens; elastin; fibronectin; laminin; and proteoglycans. It also contains fibroblast growth factors, contributing to angiogenesis in the wound.9
Application of ECM-based collagen dressings on debrided wounds requires moisture for absorption. Because cranium wounds lack sufficient exudate production, dermal templates need to be hydrated with sterile normal saline before application and covered with a moisture-retaining dressing. Extracellular matrix–based dressings are biodegradable and can be reapplied every 5 to 7 days. For chronic wounds, application of collagen dressings, such as Endoform, is essential and could be considered as the first step prior to switching to more advanced wound care modalities.6,10 Additional studies investigating ECM-containing may determine their comparative efficacy.
To the Editor:
Squamous cell carcinoma (SCC) is the second most common cancer of the scalp.1 Mohs micrographic surgery is used to treat SCC, and it commonly generates a 2.5×2.5-cm open wound with exposed bone.2 Although Mohs micrographic surgery effectively treats cutaneous lesions, it carries a high risk for complications such as infection, wound dehiscence, and partial or full-thickness skin graft necrosis.3 Recommended therapies to decrease these complications include linear closures, flaps, and peripheral autograft tissue.4 However, these procedures do not come without risks and carry their own complications. Therefore, we suggest a safe, less-invasive initial approach using a synthetic extracellular matrix (ECM)–based collagen dressing for secondary wound closure.
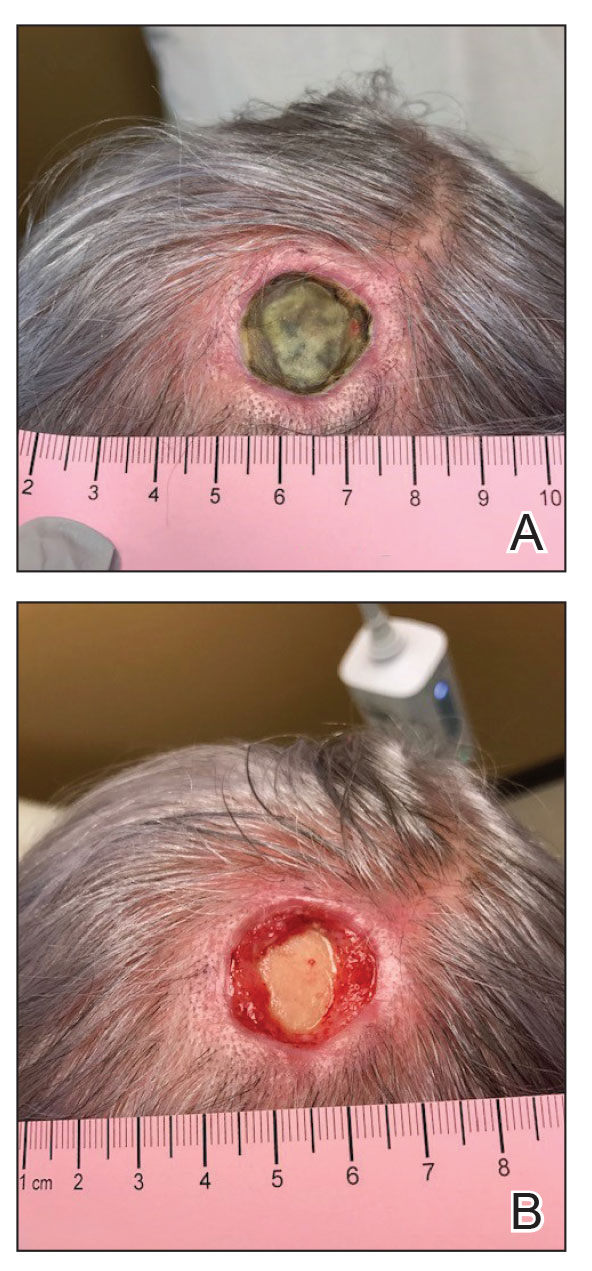
A 76-year-old woman presented to the infectious disease clinic at Monument Health Rapid City Clinic (Rapid City, South Dakota) for evaluation of a dehisced scalp wound 3 months following Mohs micrographic surgery for scalp SCC. The wound underwent primary closure following surgery and dehisced shortly after (Figure 1A). Various oral antimicrobials were used by the dermatologist to assist with wound closure but without success. The patient was referred to the wound clinic for management. At the first appointment, all necrotic tissue was debrided and the cranium was exposed in the wound base (Figure 1B). The wound measured 2.3×2.3×0.2 cm. An ECM-containing collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was used to provide a scaffold for wound closure (Figure 2A). It was dressed with the petroleum-based gauze Xeroform (Cardinal Health) and covered with dry gauze to prevent evaporation and provide moist wound healing. The wound developed some budding tissue islands 3 weeks after weekly ECM-based collagen dressing applications (Figure 3A). The wound continued to decrease in size and formed an isthmus by the second month of therapy (Figure 3B). The wound fully closed within 3 months and showed minimal scarring after 3 years (Figure 2B).
![A, An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound. B, The wound showed minimal scarring 3 years after closure. A, An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound. B, The wound showed minimal scarring 3 years after closure.](https://cdn.mdedge.com/files/s3fs-public/CT111005033_e_Fig2_AB.jpg)
Chronic wounds usually get trapped in the inflammatory stage of wound healing due to destruction of growth factors and ECM by metalloproteases (MMPs), which creates a vicious cycle and wound stalling. Wound debridement converts a chronic wound back into an acute wound, which is the first step of healing. Following wound debridement, collagen-based dressings can assist with healing by binding the destructive MMPs, and ECM matrix promotes the building of new tissue. The 3 most commonly used ECM-based collagen dressings are Endoform, PuraPly AM (Organogenesis Inc), and Puracol Ultra ECM (Medline Industries, Inc).
![A, Budding tissue islands developed on a scalp wound 3 weeks after application of an extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]). B, An isthmus developed 7 weeks after application A, Budding tissue islands developed on a scalp wound 3 weeks after application of an extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]). B, An isthmus developed 7 weeks after application](https://cdn.mdedge.com/files/s3fs-public/CT111005033_e_Fig3_AB.jpg)
Endoform is ovine-based collagen and provides a natural porous bioscaffold for rapid cell infiltration.5 It contains more than 150 ECM proteins along with residual vascular channels that help re-establish new vasculature. Ovine-based collagen contains collagen types I, III, and IV arranged as native fibers that retain the 3-dimensional architecture present in tissue ECM.5 Although MMPs are essential in normal healing, the elevated presence of MMPs has been linked to stalled wound healing. Clinical observation and assessment may not be sufficient to identify a wound with elevated protease activity that can break down ECM, affect wound fibroblasts, and impair growth factor response. Although collagen ECM itself does not contain any growth factors, it preserves the destruction of native ECM and growth factors by MMPs by functioning as a sacrificial substrate. The addition of 0.3% ionic silver to the ECM has been shown to decrease bacterial growth and prevent biofilm formation.6
PuraPly AM is a native, type I porcine collagen matrix embedded with the
Puracol Ultra ECM is made of porcine mesothelium and is comprised of types I, III, and IV collagens; elastin; fibronectin; laminin; and proteoglycans. It also contains fibroblast growth factors, contributing to angiogenesis in the wound.9
Application of ECM-based collagen dressings on debrided wounds requires moisture for absorption. Because cranium wounds lack sufficient exudate production, dermal templates need to be hydrated with sterile normal saline before application and covered with a moisture-retaining dressing. Extracellular matrix–based dressings are biodegradable and can be reapplied every 5 to 7 days. For chronic wounds, application of collagen dressings, such as Endoform, is essential and could be considered as the first step prior to switching to more advanced wound care modalities.6,10 Additional studies investigating ECM-containing may determine their comparative efficacy.
- Burton KA, Ashack KA, Khachemoune A. Cutaneous squamous cell carcinoma: a review of high-risk and metastatic disease. Am J Clin Dermatol. 2016;17:491-508. doi:10.1007/s40257-016-0207-3
- Kimyai-Asadi A, Goldberg LH, Peterson SR, et al. The incidence of major complications from Mohs micrographic surgery performed in office-based and hospital-based settings. J Am Acad Dermatol. 2005;53:628-634. doi:10.1016/j.jaad.2005.03.023
- Merritt BG, Lee NY, Brodland DG, et al. The safety of Mohs surgery: a prospective multicenter cohort study. J Am Acad Dermatol. 2012;67:1302-1309. doi:10.1016/j.jaad.2012.05.041
- Yu WY, Salmon P, Thuener J, et al. Mohs surgery for advanced tumors of the scalp. Dermatol Surg. 2019;45(suppl 2):S110-S117.
- Endoform. Aroa Biosurgery Limited website. Accessed May 22, 2023. https://aroa.com/product/endoform/
- Liden BA, May BC. Clinical outcomes following the use of ovine forestomach matrix (endoform dermal template) to treat chronic wounds. Adv Skin Wound Care. 2013;26:164-167. doi:10.1097/01.ASW.0000428862.34294.d4
- PuraPly AM. Organogenesis website. Accessed May 22, 2023. https://organogenesis.com/surgical-sports-medicine/puraplyam/
- Bain MA, Koullias GJ, Morse K, et al. Type I collagen matrix plus polyhexamethylene biguanide antimicrobial for the treatment of cutaneous wounds. J Comp Eff Res. 2020;9:691-703. doi:10.2217/cer-2020-0058
- Puracol Ultra ECM Collagen Wound Dressings. Medical Industries, LP website. May 22, 2023. https://punchout.medline.com/product/Puracol-Ultra-Extracellular-Matrix-ECM-Collagen-Wound-Dressing/Collagen-Dressings/Z05-PF188619?question=&index=P4&indexCount=4
- Raizman R, Hill R, Woo K. Prospective multicenter evaluation of an advanced extracellular matrix for wound management. Adv Skin Wound Care. 2020;33:437-444. doi:10.1097/01.ASW.0000667052.74087.d6
- Burton KA, Ashack KA, Khachemoune A. Cutaneous squamous cell carcinoma: a review of high-risk and metastatic disease. Am J Clin Dermatol. 2016;17:491-508. doi:10.1007/s40257-016-0207-3
- Kimyai-Asadi A, Goldberg LH, Peterson SR, et al. The incidence of major complications from Mohs micrographic surgery performed in office-based and hospital-based settings. J Am Acad Dermatol. 2005;53:628-634. doi:10.1016/j.jaad.2005.03.023
- Merritt BG, Lee NY, Brodland DG, et al. The safety of Mohs surgery: a prospective multicenter cohort study. J Am Acad Dermatol. 2012;67:1302-1309. doi:10.1016/j.jaad.2012.05.041
- Yu WY, Salmon P, Thuener J, et al. Mohs surgery for advanced tumors of the scalp. Dermatol Surg. 2019;45(suppl 2):S110-S117.
- Endoform. Aroa Biosurgery Limited website. Accessed May 22, 2023. https://aroa.com/product/endoform/
- Liden BA, May BC. Clinical outcomes following the use of ovine forestomach matrix (endoform dermal template) to treat chronic wounds. Adv Skin Wound Care. 2013;26:164-167. doi:10.1097/01.ASW.0000428862.34294.d4
- PuraPly AM. Organogenesis website. Accessed May 22, 2023. https://organogenesis.com/surgical-sports-medicine/puraplyam/
- Bain MA, Koullias GJ, Morse K, et al. Type I collagen matrix plus polyhexamethylene biguanide antimicrobial for the treatment of cutaneous wounds. J Comp Eff Res. 2020;9:691-703. doi:10.2217/cer-2020-0058
- Puracol Ultra ECM Collagen Wound Dressings. Medical Industries, LP website. May 22, 2023. https://punchout.medline.com/product/Puracol-Ultra-Extracellular-Matrix-ECM-Collagen-Wound-Dressing/Collagen-Dressings/Z05-PF188619?question=&index=P4&indexCount=4
- Raizman R, Hill R, Woo K. Prospective multicenter evaluation of an advanced extracellular matrix for wound management. Adv Skin Wound Care. 2020;33:437-444. doi:10.1097/01.ASW.0000667052.74087.d6
Practice Points
- Patients who undergo Mohs micrographic surgery on the scalp are prone to developing complications such as infection, wound dehiscence, and partial or full-thickness skin graft necrosis.
- Use of extracellular matrix–based dressings may assist with deep wound healing on the scalp.
Nevus Sebaceus With Novel HRAS Sequence Variant Mutation Misdiagnosed as Alopecia Areata
To the Editor:
A 12-year-old girl presented to the dermatology clinic for evaluation of a congenital scalp lesion. The patient was diagnosed with alopecia areata by a dermatologist at 4 years of age, and she was treated with topical corticosteroids and minoxidil, which failed to resolve her condition. Physical examination revealed an 8×10-cm, well-demarcated, yellowish-pink plaque located over the vertex and right parietal scalp (Figure 1A), extending down to the right preauricular cheek (Figure 1B) in a linear configuration with blaschkoid features. The scalp plaque appeared bald and completely lacking in terminal hairs but contained numerous fine vellus hairs (Figure 1A). A 6-mm, oval-appearing, pigmented papule was present in the plaque, and a few smaller, scattered, pigmented papules were noted in the vertex region (Figure 1A).
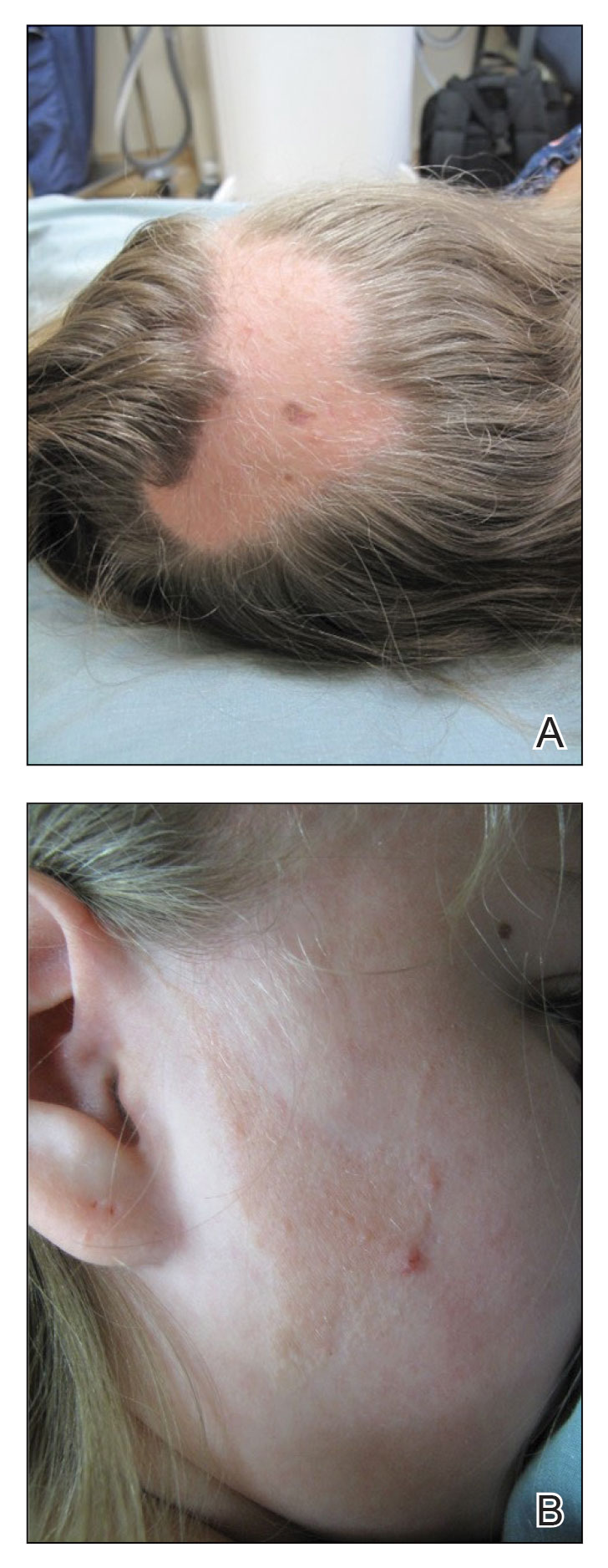
The cutaneous examination was otherwise unremarkable. A review of systems was negative, except for a history of attention-deficit/hyperactivity disorder. There was no history of seizures or other neurocognitive developmental abnormalities.

A 4-mm punch biopsy of the vertex scalp included the pigmented lesion but excluded an adnexal neoplasm. Epidermal acanthosis and mild papillomatosis were reported on microscopic examination. Multiple prominent sebaceous glands without associated hair follicles, which emptied directly onto the epidermal surface, were noted in the dermis (Figure 2). Several apocrine glands were observed (Figure 3). Epidermal and dermal melanocytic nests were highlighted with SOX-10 and Melan-A immunohistochemical stains, confirming the presence of a benign compound nevus. The punch biopsy analysis confirmed the diagnosis of a nevus sebaceus (NS) of Jadassohn (organoid nevus) with incidental compound nevus. Additional 4-mm punch biopsies were obtained for genetic testing, performed by the Genomics and Pathology Services at Washington University (St. Louis, Missouri). A missense HRAS p.G12V variant was observed in the tissue. A negative blood test result ruled out a germline mutation. The patient was managed with active observation of the lesion to evaluate for potential formation of neoplasms, as well as continuity of care with the dermatology clinic, considering the extent of the lesions, to monitor the development of any new medical conditions that would be concerning for syndromes associated with NS.
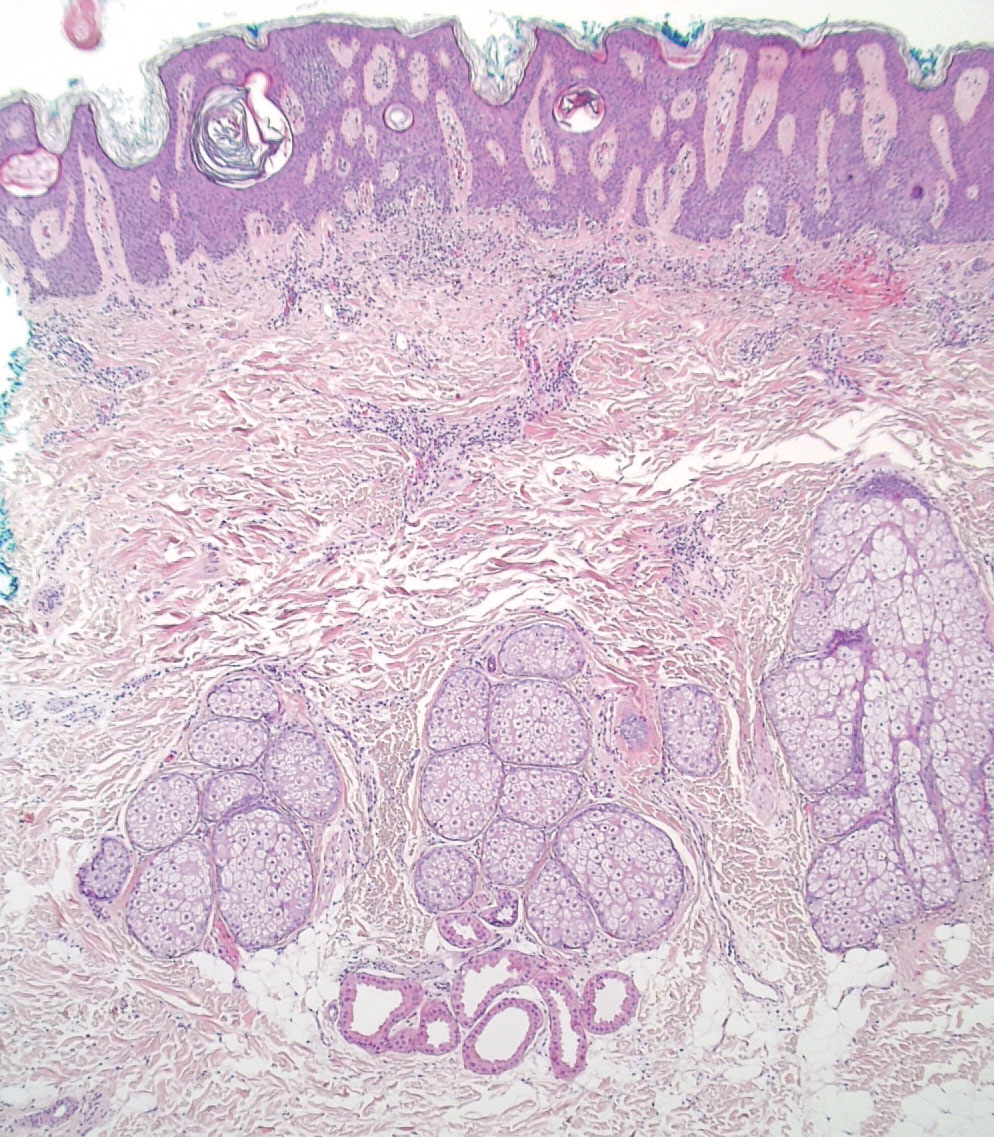
Nevus sebaceus is a benign skin hamartoma caused by a congenital defect in the pilosebaceous follicular unit and consists of epidermal, sebaceous, and apocrine elements.1,2 In dermatology patients, the prevalence of NS ranges from 0.05% to 1%.1 In 90% of cases, NS presents at birth as a 1- to 10-cm, round or linear, yellowish-orange, hairless plaque located on the scalp. It also may appear on the face, neck, trunk, oral mucosa, or labia minora.1,3 Although NS is a benign condition, secondary tumors may form within the lesion.3
The physical and histologic characteristics of NS evolve as the patient ages. In childhood, NS typically appears as a yellow-pink macule or patch with mild to moderate epidermal hyperplasia. Patients exhibit underdeveloped sebaceous glands, immature hair follicles, hyperkeratosis, and acanthosis.1,3,4 The development of early lesions can be quite subtle and can lead to diagnostic uncertainty, as described in our patient. During puberty, lesions thicken due to papillomatous hyperplasia in the epidermis, and the number and size of sebaceous and apocrine glands increase.4 In adults, the risk for secondary tumor formation increases. These physical and histologic transformations, including secondary tumor formation, are thought to be stimulated by the action of postpubertal androgens.1
Nevus sebaceus is associated with both benign and malignant secondary tumor formation; however, fewer than 1% of tumors are malignant.1 In a retrospective analysis, Idriss and Elston5 (N=707) reported that 21.4% of patients with NS had secondary neoplasms; 18.9% of the secondary neoplasms were benign, and 2.5% were malignant. Additionally, this study showed that secondary tumor formation can occur in children, though it typically occurs in adults. Benign neoplasms were reported in 5 children in the subset aged 0 to 10 years and 10 children in the subset aged 11 to 17 years; 1 child developed a malignant neoplasm in the latter subset.5 The most common NS-associated benign neoplasms include trichoblastoma and syringocystadenoma papilliferum. Others include trichilemmoma, apocrine/eccrine adenoma, and sebaceoma.1 Nevus sebaceus–associated malignant neoplasms include basal cell carcinoma, squamous cell carcinoma, adenocarcinoma, carcinosarcoma, and sebaceous carcinoma.3
Our patient was incorrectly diagnosed and treated for alopecia areata before an eventual diagnosis of NS was confirmed by biopsy. Additional genetic studies revealed a novel mutation in the HRAS gene, the most commonly affected gene in NS. The most common mutation location seen in more than 90% of NS lesions is HRAS c.37G>C (p.G13R), while KRAS mutations account for almost all the remaining cases.3 In our patient, a pathogenic missense HRAS p.G12V variant of somatic origin was detected with DNA extraction and sequencing from a fresh tissue sample acquired from two 4-mm punch biopsies performed on the lesion. The following genes were sequenced and found to be uninvolved: BRAF, FGFR1, FGFR2, FGFR3, GNA11, GNAQ, KRAS, MAP3K3, NRAS, PIK3CA, and TEK. The Sanger sequencing method for comparative analysis performed on peripheral blood was negative.
Nevus sebaceus typically is caused by a sporadic mutation, though familial cases have been reported.1 Additionally, germline HRAS mutations can lead to Costello syndrome, an autosomal-dominant disorder characterized by short stature; intellectual disabilities; coarse facial features; facial and perianal papillomata; cardiac defects; loose skin; joint hyperflexibility; and an increased risk for malignant tumors including rhabdomyosarcoma, neuroblastoma, and transitional cell carcinoma of the bladder.6
The diagnosis of NS often can be made clinically but can be difficult to confirm in underdeveloped lesions in young children. The differential diagnosis can include alopecia areata, aplasia cutis congenita, juvenile xanthogranuloma, epidermal nevus, de novo syringocystadenoma papilliferum, and solitary mastocytoma.1 Nevus sebaceus can be associated with 4 additional syndromes: Schimmelpenning syndrome; phacomatosis pigmentokeratotica; didymosis aplasticosebacea; and SCALP (sebaceus nevus, central nervous system malformations, aplasia cutis congenital, limbal dermoid, pigmented nevus) syndrome.1 Approximately 7% of NS cases may be associated with Schimmelpenning-Feuerstein-Mims (SFM) syndrome, a more severe condition that leads to systemic involvement and abnormalities in the neurological, ophthalmological, cardiovascular, genitourological, and skeletal systems.1,3 Phacomatosis pigmentokeratotica has speckled lentiginous nevi, as well as abnormalities in the neurological, ophthalmological, cardiovascular, genitourological, and skeletal systems.1 Didymosis aplasticosebacea is the concurrence of NS and aplasia cutis congenita.
The definitive treatment of NS is surgical excision. Alternative therapies include photodynamic therapy, fractional laser resurfacing, and dermabrasion; these are not definitive treatments, and patients must be monitored for the development of secondary neoplasms. Multiple variables must be considered when determining treatment, including patient age, risk potential for malignancy, and surgery-associated risks.1 In our patient, given the extent of the lesions, active observation and follow-up was agreed upon for management.
This case demonstrates the importance of considering NS as an alternative diagnosis when alopecia areata has been diagnosed in a child who is unresponsive to treatments. After the diagnosis of NS is confirmed, more serious associated syndromes should be ruled out, and treatment should be tailored to each case.
- Patel P, Malik K, Khachemoune A. Sebaceus and Becker’s nevus: overview of their presentation, pathogenesis, associations, and treatment. Am J Clin Dermatol. 2015;16:197-204. doi:10.1007/s40257-015-0123-y
- Azzam MJ, Beutler BD, Calame A, et al. Osteoma cutis associated with nevus sebaceus: case report and review of cutaneous osteoma-associated skin tumors (COASTs). Cureus. 2019;11:E4959. doi:10.7759/cureus.4959
- Aslam A, Salam A, Griffiths CEM, et al. Naevus sebaceus: a mosaic RASopathy. Clin Exp Dermatol. 2014;39:1-6. doi:10.1111/ced.12209
- Basu P, Erickson CP, Calame A, et al. Nevus sebaceus with syringocystadenoma papilliferum, prurigo nodularis, apocrine cystadenoma, basaloid follicular proliferation, and sebaceoma: case report and review of nevus sebaceus-associated conditions. Dermatol Online J. 2020;26:13030/qt85k968bk.
- Idriss MH, Elston DM. Secondary neoplasms associated with nevus sebaceus of Jadassohn: a study of 707 cases. J Am Acad Dermatol. 2014;70:332-337. doi:10.1016/j.jaad.2013.10.004
- Gripp KW, Rauen KA. Costello syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al, eds. GeneReviews [Internet]. University of Washington, Seattle; 1993-2020. August 29, 2006. Updated August 29, 2019. https://pubmed.ncbi.nlm.nih.gov/20301680
To the Editor:
A 12-year-old girl presented to the dermatology clinic for evaluation of a congenital scalp lesion. The patient was diagnosed with alopecia areata by a dermatologist at 4 years of age, and she was treated with topical corticosteroids and minoxidil, which failed to resolve her condition. Physical examination revealed an 8×10-cm, well-demarcated, yellowish-pink plaque located over the vertex and right parietal scalp (Figure 1A), extending down to the right preauricular cheek (Figure 1B) in a linear configuration with blaschkoid features. The scalp plaque appeared bald and completely lacking in terminal hairs but contained numerous fine vellus hairs (Figure 1A). A 6-mm, oval-appearing, pigmented papule was present in the plaque, and a few smaller, scattered, pigmented papules were noted in the vertex region (Figure 1A).
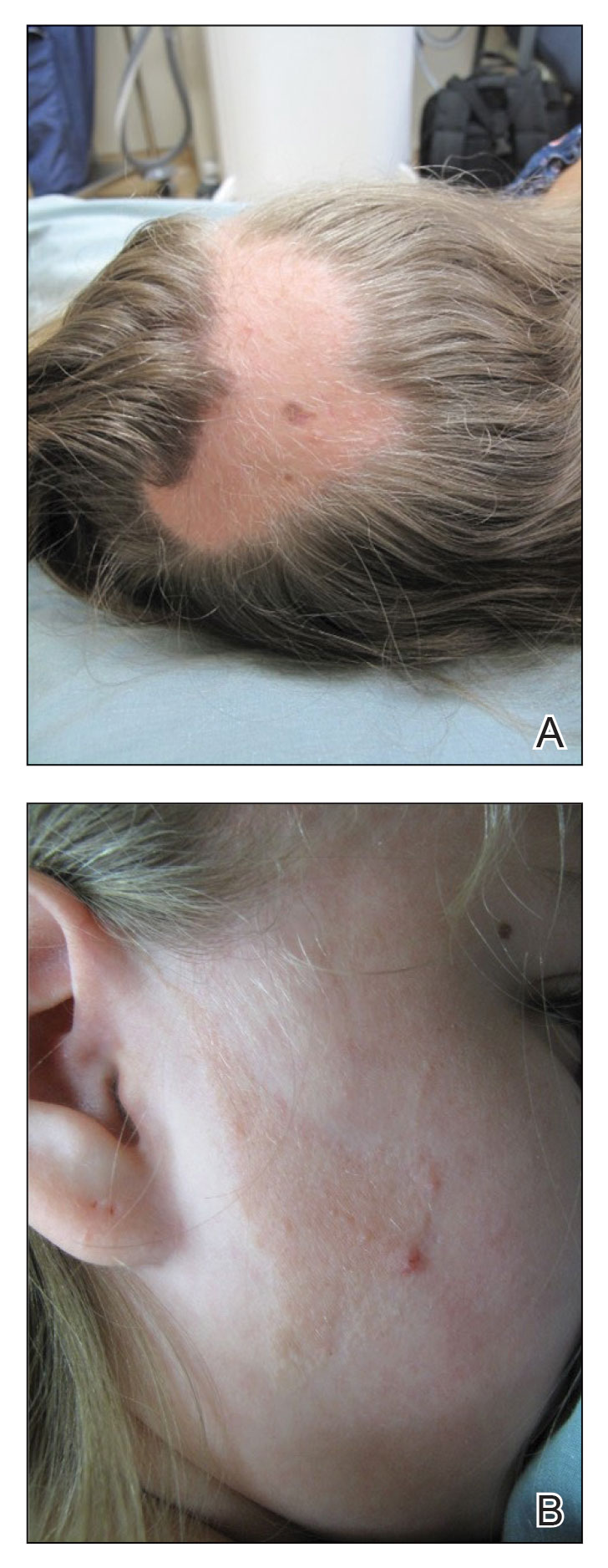
The cutaneous examination was otherwise unremarkable. A review of systems was negative, except for a history of attention-deficit/hyperactivity disorder. There was no history of seizures or other neurocognitive developmental abnormalities.

A 4-mm punch biopsy of the vertex scalp included the pigmented lesion but excluded an adnexal neoplasm. Epidermal acanthosis and mild papillomatosis were reported on microscopic examination. Multiple prominent sebaceous glands without associated hair follicles, which emptied directly onto the epidermal surface, were noted in the dermis (Figure 2). Several apocrine glands were observed (Figure 3). Epidermal and dermal melanocytic nests were highlighted with SOX-10 and Melan-A immunohistochemical stains, confirming the presence of a benign compound nevus. The punch biopsy analysis confirmed the diagnosis of a nevus sebaceus (NS) of Jadassohn (organoid nevus) with incidental compound nevus. Additional 4-mm punch biopsies were obtained for genetic testing, performed by the Genomics and Pathology Services at Washington University (St. Louis, Missouri). A missense HRAS p.G12V variant was observed in the tissue. A negative blood test result ruled out a germline mutation. The patient was managed with active observation of the lesion to evaluate for potential formation of neoplasms, as well as continuity of care with the dermatology clinic, considering the extent of the lesions, to monitor the development of any new medical conditions that would be concerning for syndromes associated with NS.
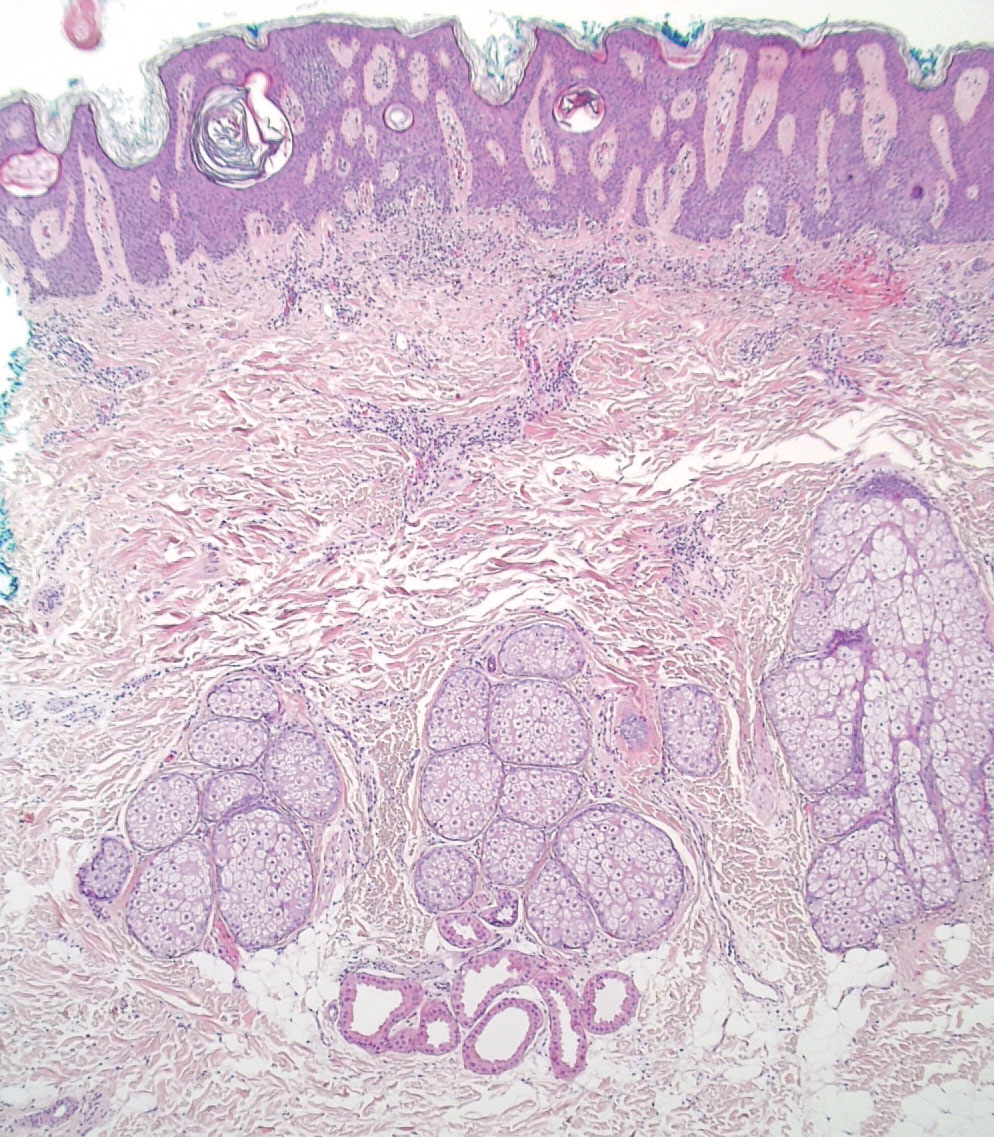
Nevus sebaceus is a benign skin hamartoma caused by a congenital defect in the pilosebaceous follicular unit and consists of epidermal, sebaceous, and apocrine elements.1,2 In dermatology patients, the prevalence of NS ranges from 0.05% to 1%.1 In 90% of cases, NS presents at birth as a 1- to 10-cm, round or linear, yellowish-orange, hairless plaque located on the scalp. It also may appear on the face, neck, trunk, oral mucosa, or labia minora.1,3 Although NS is a benign condition, secondary tumors may form within the lesion.3
The physical and histologic characteristics of NS evolve as the patient ages. In childhood, NS typically appears as a yellow-pink macule or patch with mild to moderate epidermal hyperplasia. Patients exhibit underdeveloped sebaceous glands, immature hair follicles, hyperkeratosis, and acanthosis.1,3,4 The development of early lesions can be quite subtle and can lead to diagnostic uncertainty, as described in our patient. During puberty, lesions thicken due to papillomatous hyperplasia in the epidermis, and the number and size of sebaceous and apocrine glands increase.4 In adults, the risk for secondary tumor formation increases. These physical and histologic transformations, including secondary tumor formation, are thought to be stimulated by the action of postpubertal androgens.1
Nevus sebaceus is associated with both benign and malignant secondary tumor formation; however, fewer than 1% of tumors are malignant.1 In a retrospective analysis, Idriss and Elston5 (N=707) reported that 21.4% of patients with NS had secondary neoplasms; 18.9% of the secondary neoplasms were benign, and 2.5% were malignant. Additionally, this study showed that secondary tumor formation can occur in children, though it typically occurs in adults. Benign neoplasms were reported in 5 children in the subset aged 0 to 10 years and 10 children in the subset aged 11 to 17 years; 1 child developed a malignant neoplasm in the latter subset.5 The most common NS-associated benign neoplasms include trichoblastoma and syringocystadenoma papilliferum. Others include trichilemmoma, apocrine/eccrine adenoma, and sebaceoma.1 Nevus sebaceus–associated malignant neoplasms include basal cell carcinoma, squamous cell carcinoma, adenocarcinoma, carcinosarcoma, and sebaceous carcinoma.3
Our patient was incorrectly diagnosed and treated for alopecia areata before an eventual diagnosis of NS was confirmed by biopsy. Additional genetic studies revealed a novel mutation in the HRAS gene, the most commonly affected gene in NS. The most common mutation location seen in more than 90% of NS lesions is HRAS c.37G>C (p.G13R), while KRAS mutations account for almost all the remaining cases.3 In our patient, a pathogenic missense HRAS p.G12V variant of somatic origin was detected with DNA extraction and sequencing from a fresh tissue sample acquired from two 4-mm punch biopsies performed on the lesion. The following genes were sequenced and found to be uninvolved: BRAF, FGFR1, FGFR2, FGFR3, GNA11, GNAQ, KRAS, MAP3K3, NRAS, PIK3CA, and TEK. The Sanger sequencing method for comparative analysis performed on peripheral blood was negative.
Nevus sebaceus typically is caused by a sporadic mutation, though familial cases have been reported.1 Additionally, germline HRAS mutations can lead to Costello syndrome, an autosomal-dominant disorder characterized by short stature; intellectual disabilities; coarse facial features; facial and perianal papillomata; cardiac defects; loose skin; joint hyperflexibility; and an increased risk for malignant tumors including rhabdomyosarcoma, neuroblastoma, and transitional cell carcinoma of the bladder.6
The diagnosis of NS often can be made clinically but can be difficult to confirm in underdeveloped lesions in young children. The differential diagnosis can include alopecia areata, aplasia cutis congenita, juvenile xanthogranuloma, epidermal nevus, de novo syringocystadenoma papilliferum, and solitary mastocytoma.1 Nevus sebaceus can be associated with 4 additional syndromes: Schimmelpenning syndrome; phacomatosis pigmentokeratotica; didymosis aplasticosebacea; and SCALP (sebaceus nevus, central nervous system malformations, aplasia cutis congenital, limbal dermoid, pigmented nevus) syndrome.1 Approximately 7% of NS cases may be associated with Schimmelpenning-Feuerstein-Mims (SFM) syndrome, a more severe condition that leads to systemic involvement and abnormalities in the neurological, ophthalmological, cardiovascular, genitourological, and skeletal systems.1,3 Phacomatosis pigmentokeratotica has speckled lentiginous nevi, as well as abnormalities in the neurological, ophthalmological, cardiovascular, genitourological, and skeletal systems.1 Didymosis aplasticosebacea is the concurrence of NS and aplasia cutis congenita.
The definitive treatment of NS is surgical excision. Alternative therapies include photodynamic therapy, fractional laser resurfacing, and dermabrasion; these are not definitive treatments, and patients must be monitored for the development of secondary neoplasms. Multiple variables must be considered when determining treatment, including patient age, risk potential for malignancy, and surgery-associated risks.1 In our patient, given the extent of the lesions, active observation and follow-up was agreed upon for management.
This case demonstrates the importance of considering NS as an alternative diagnosis when alopecia areata has been diagnosed in a child who is unresponsive to treatments. After the diagnosis of NS is confirmed, more serious associated syndromes should be ruled out, and treatment should be tailored to each case.
To the Editor:
A 12-year-old girl presented to the dermatology clinic for evaluation of a congenital scalp lesion. The patient was diagnosed with alopecia areata by a dermatologist at 4 years of age, and she was treated with topical corticosteroids and minoxidil, which failed to resolve her condition. Physical examination revealed an 8×10-cm, well-demarcated, yellowish-pink plaque located over the vertex and right parietal scalp (Figure 1A), extending down to the right preauricular cheek (Figure 1B) in a linear configuration with blaschkoid features. The scalp plaque appeared bald and completely lacking in terminal hairs but contained numerous fine vellus hairs (Figure 1A). A 6-mm, oval-appearing, pigmented papule was present in the plaque, and a few smaller, scattered, pigmented papules were noted in the vertex region (Figure 1A).
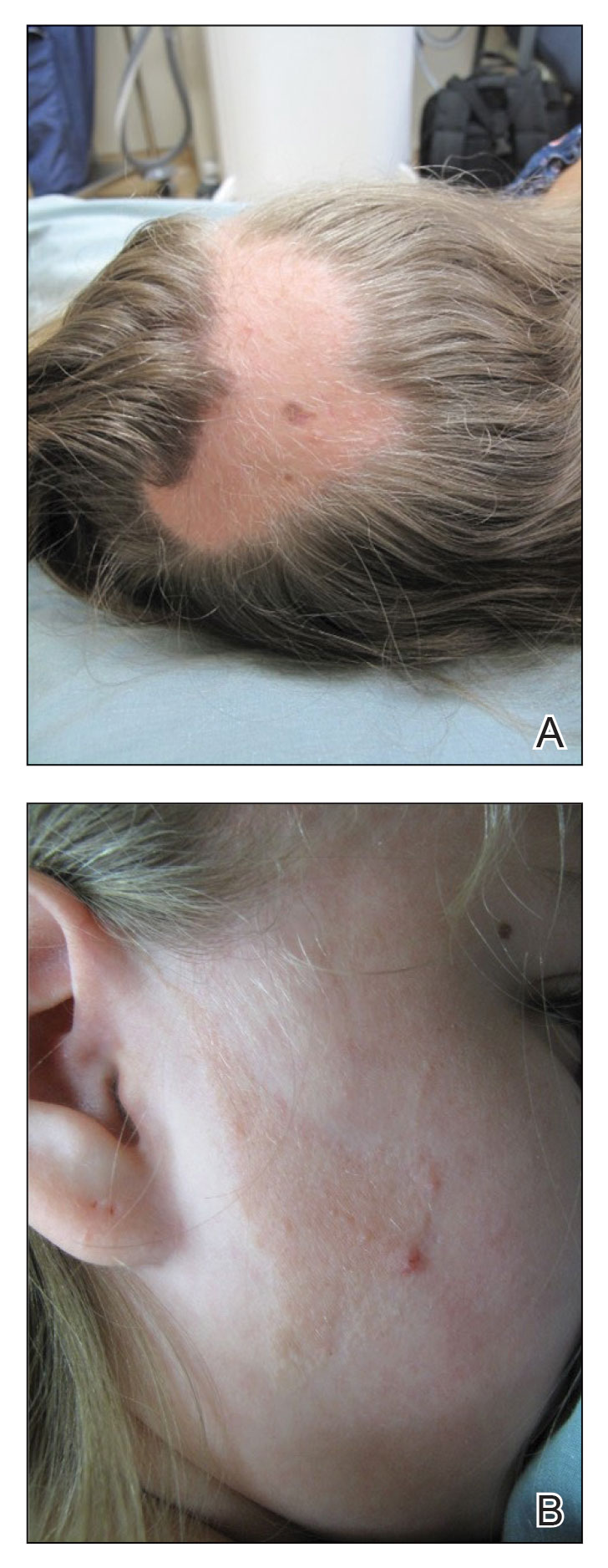
The cutaneous examination was otherwise unremarkable. A review of systems was negative, except for a history of attention-deficit/hyperactivity disorder. There was no history of seizures or other neurocognitive developmental abnormalities.

A 4-mm punch biopsy of the vertex scalp included the pigmented lesion but excluded an adnexal neoplasm. Epidermal acanthosis and mild papillomatosis were reported on microscopic examination. Multiple prominent sebaceous glands without associated hair follicles, which emptied directly onto the epidermal surface, were noted in the dermis (Figure 2). Several apocrine glands were observed (Figure 3). Epidermal and dermal melanocytic nests were highlighted with SOX-10 and Melan-A immunohistochemical stains, confirming the presence of a benign compound nevus. The punch biopsy analysis confirmed the diagnosis of a nevus sebaceus (NS) of Jadassohn (organoid nevus) with incidental compound nevus. Additional 4-mm punch biopsies were obtained for genetic testing, performed by the Genomics and Pathology Services at Washington University (St. Louis, Missouri). A missense HRAS p.G12V variant was observed in the tissue. A negative blood test result ruled out a germline mutation. The patient was managed with active observation of the lesion to evaluate for potential formation of neoplasms, as well as continuity of care with the dermatology clinic, considering the extent of the lesions, to monitor the development of any new medical conditions that would be concerning for syndromes associated with NS.
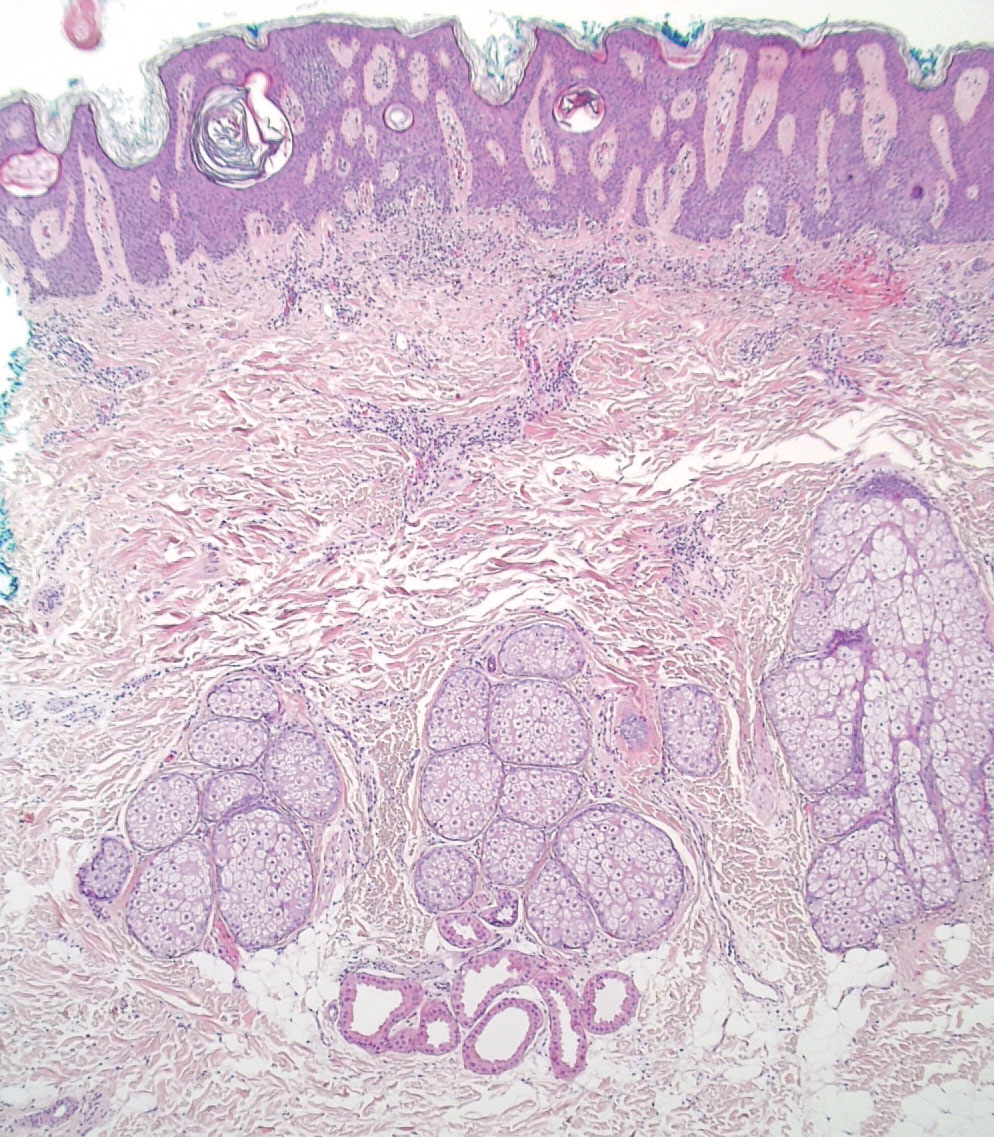
Nevus sebaceus is a benign skin hamartoma caused by a congenital defect in the pilosebaceous follicular unit and consists of epidermal, sebaceous, and apocrine elements.1,2 In dermatology patients, the prevalence of NS ranges from 0.05% to 1%.1 In 90% of cases, NS presents at birth as a 1- to 10-cm, round or linear, yellowish-orange, hairless plaque located on the scalp. It also may appear on the face, neck, trunk, oral mucosa, or labia minora.1,3 Although NS is a benign condition, secondary tumors may form within the lesion.3
The physical and histologic characteristics of NS evolve as the patient ages. In childhood, NS typically appears as a yellow-pink macule or patch with mild to moderate epidermal hyperplasia. Patients exhibit underdeveloped sebaceous glands, immature hair follicles, hyperkeratosis, and acanthosis.1,3,4 The development of early lesions can be quite subtle and can lead to diagnostic uncertainty, as described in our patient. During puberty, lesions thicken due to papillomatous hyperplasia in the epidermis, and the number and size of sebaceous and apocrine glands increase.4 In adults, the risk for secondary tumor formation increases. These physical and histologic transformations, including secondary tumor formation, are thought to be stimulated by the action of postpubertal androgens.1
Nevus sebaceus is associated with both benign and malignant secondary tumor formation; however, fewer than 1% of tumors are malignant.1 In a retrospective analysis, Idriss and Elston5 (N=707) reported that 21.4% of patients with NS had secondary neoplasms; 18.9% of the secondary neoplasms were benign, and 2.5% were malignant. Additionally, this study showed that secondary tumor formation can occur in children, though it typically occurs in adults. Benign neoplasms were reported in 5 children in the subset aged 0 to 10 years and 10 children in the subset aged 11 to 17 years; 1 child developed a malignant neoplasm in the latter subset.5 The most common NS-associated benign neoplasms include trichoblastoma and syringocystadenoma papilliferum. Others include trichilemmoma, apocrine/eccrine adenoma, and sebaceoma.1 Nevus sebaceus–associated malignant neoplasms include basal cell carcinoma, squamous cell carcinoma, adenocarcinoma, carcinosarcoma, and sebaceous carcinoma.3
Our patient was incorrectly diagnosed and treated for alopecia areata before an eventual diagnosis of NS was confirmed by biopsy. Additional genetic studies revealed a novel mutation in the HRAS gene, the most commonly affected gene in NS. The most common mutation location seen in more than 90% of NS lesions is HRAS c.37G>C (p.G13R), while KRAS mutations account for almost all the remaining cases.3 In our patient, a pathogenic missense HRAS p.G12V variant of somatic origin was detected with DNA extraction and sequencing from a fresh tissue sample acquired from two 4-mm punch biopsies performed on the lesion. The following genes were sequenced and found to be uninvolved: BRAF, FGFR1, FGFR2, FGFR3, GNA11, GNAQ, KRAS, MAP3K3, NRAS, PIK3CA, and TEK. The Sanger sequencing method for comparative analysis performed on peripheral blood was negative.
Nevus sebaceus typically is caused by a sporadic mutation, though familial cases have been reported.1 Additionally, germline HRAS mutations can lead to Costello syndrome, an autosomal-dominant disorder characterized by short stature; intellectual disabilities; coarse facial features; facial and perianal papillomata; cardiac defects; loose skin; joint hyperflexibility; and an increased risk for malignant tumors including rhabdomyosarcoma, neuroblastoma, and transitional cell carcinoma of the bladder.6
The diagnosis of NS often can be made clinically but can be difficult to confirm in underdeveloped lesions in young children. The differential diagnosis can include alopecia areata, aplasia cutis congenita, juvenile xanthogranuloma, epidermal nevus, de novo syringocystadenoma papilliferum, and solitary mastocytoma.1 Nevus sebaceus can be associated with 4 additional syndromes: Schimmelpenning syndrome; phacomatosis pigmentokeratotica; didymosis aplasticosebacea; and SCALP (sebaceus nevus, central nervous system malformations, aplasia cutis congenital, limbal dermoid, pigmented nevus) syndrome.1 Approximately 7% of NS cases may be associated with Schimmelpenning-Feuerstein-Mims (SFM) syndrome, a more severe condition that leads to systemic involvement and abnormalities in the neurological, ophthalmological, cardiovascular, genitourological, and skeletal systems.1,3 Phacomatosis pigmentokeratotica has speckled lentiginous nevi, as well as abnormalities in the neurological, ophthalmological, cardiovascular, genitourological, and skeletal systems.1 Didymosis aplasticosebacea is the concurrence of NS and aplasia cutis congenita.
The definitive treatment of NS is surgical excision. Alternative therapies include photodynamic therapy, fractional laser resurfacing, and dermabrasion; these are not definitive treatments, and patients must be monitored for the development of secondary neoplasms. Multiple variables must be considered when determining treatment, including patient age, risk potential for malignancy, and surgery-associated risks.1 In our patient, given the extent of the lesions, active observation and follow-up was agreed upon for management.
This case demonstrates the importance of considering NS as an alternative diagnosis when alopecia areata has been diagnosed in a child who is unresponsive to treatments. After the diagnosis of NS is confirmed, more serious associated syndromes should be ruled out, and treatment should be tailored to each case.
- Patel P, Malik K, Khachemoune A. Sebaceus and Becker’s nevus: overview of their presentation, pathogenesis, associations, and treatment. Am J Clin Dermatol. 2015;16:197-204. doi:10.1007/s40257-015-0123-y
- Azzam MJ, Beutler BD, Calame A, et al. Osteoma cutis associated with nevus sebaceus: case report and review of cutaneous osteoma-associated skin tumors (COASTs). Cureus. 2019;11:E4959. doi:10.7759/cureus.4959
- Aslam A, Salam A, Griffiths CEM, et al. Naevus sebaceus: a mosaic RASopathy. Clin Exp Dermatol. 2014;39:1-6. doi:10.1111/ced.12209
- Basu P, Erickson CP, Calame A, et al. Nevus sebaceus with syringocystadenoma papilliferum, prurigo nodularis, apocrine cystadenoma, basaloid follicular proliferation, and sebaceoma: case report and review of nevus sebaceus-associated conditions. Dermatol Online J. 2020;26:13030/qt85k968bk.
- Idriss MH, Elston DM. Secondary neoplasms associated with nevus sebaceus of Jadassohn: a study of 707 cases. J Am Acad Dermatol. 2014;70:332-337. doi:10.1016/j.jaad.2013.10.004
- Gripp KW, Rauen KA. Costello syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al, eds. GeneReviews [Internet]. University of Washington, Seattle; 1993-2020. August 29, 2006. Updated August 29, 2019. https://pubmed.ncbi.nlm.nih.gov/20301680
- Patel P, Malik K, Khachemoune A. Sebaceus and Becker’s nevus: overview of their presentation, pathogenesis, associations, and treatment. Am J Clin Dermatol. 2015;16:197-204. doi:10.1007/s40257-015-0123-y
- Azzam MJ, Beutler BD, Calame A, et al. Osteoma cutis associated with nevus sebaceus: case report and review of cutaneous osteoma-associated skin tumors (COASTs). Cureus. 2019;11:E4959. doi:10.7759/cureus.4959
- Aslam A, Salam A, Griffiths CEM, et al. Naevus sebaceus: a mosaic RASopathy. Clin Exp Dermatol. 2014;39:1-6. doi:10.1111/ced.12209
- Basu P, Erickson CP, Calame A, et al. Nevus sebaceus with syringocystadenoma papilliferum, prurigo nodularis, apocrine cystadenoma, basaloid follicular proliferation, and sebaceoma: case report and review of nevus sebaceus-associated conditions. Dermatol Online J. 2020;26:13030/qt85k968bk.
- Idriss MH, Elston DM. Secondary neoplasms associated with nevus sebaceus of Jadassohn: a study of 707 cases. J Am Acad Dermatol. 2014;70:332-337. doi:10.1016/j.jaad.2013.10.004
- Gripp KW, Rauen KA. Costello syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al, eds. GeneReviews [Internet]. University of Washington, Seattle; 1993-2020. August 29, 2006. Updated August 29, 2019. https://pubmed.ncbi.nlm.nih.gov/20301680
Practice Points
- Nevus sebaceus (NS), commonly referred to as NS of Jadassohn or organoid nevus, is a benign skin hamartoma that consists of epidermal, sebaceous, and apocrine elements and is caused by a congenital defect in the pilosebaceous follicular unit.
- Early stages of NS can be mistaken for alopecia areata.
- Once the diagnosis of NS is confirmed, the presence of associated syndromes should be evaluated.
- The definitive treatment of NS is surgical excision; however, multiple variables must be considered when determining treatment, including patient age, risk for developing malignancy, and surgery-associated risks.
FDA approves Yuflyma as ninth adalimumab biosimilar
The U.S. Food and Drug Administration has approved the biosimilar adalimumab-aaty (Yuflyma) in a citrate-free, high-concentration formulation, the manufacturer, Celltrion USA, announced today. It is the ninth biosimilar of adalimumab (Humira) to be approved in the United States.
Yuflyma is approved for the treatment of adult patients with rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, ulcerative colitis, plaque psoriasis, and hidradenitis suppurativa. It is also approved for polyarticular juvenile idiopathic arthritis for patients aged 2 years or older, as well as for Crohn’s disease in adults and in pediatric patients aged 6 years or older.
The formulation was approved on the basis of a comprehensive data package of analytic, preclinical, and clinical studies, according to Celltrion USA, “demonstrating that Yuflyma is comparable to the reference product Humira in terms of efficacy, safety, pharmacokinetics, and immunogenicity up to 24 weeks and 1 year following treatment.”
The company conducted a double-blind, randomized phase 3 trial that compared switching from reference adalimumab to Yuflyma with continuing either reference adalimumab or Yuflyma for patients with active rheumatoid arthritis. In that trial, the efficacy, pharmacokinetics, safety, and immunogenicity of Yuflyma and reference adalimumab were comparable after 1 year of treatment, including after switching from reference adalimumab to Yuflyma.
“Currently, more than 80% of patients treated with Humira in the United States rely on a high-concentration and citrate-free formulation of this medication. The availability of a high-concentration and citrate-free formulation adalimumab biosimilar provides an important treatment option for patients with inflammatory diseases who benefit from this effective therapy,” said Jonathan Kay, MD, of the University of Massachusetts, Worcester, in the press release.
The citrate-free formulation is thought to lead to less pain on injection.
Yuflyma will be available in prefilled syringe and autoinjector administration options.
Celltrion USA plans to market the drug in the United States in July 2023. Following the initial launch of 40 mg/0.4 mL, the company plans to launch dose forms of 80 mg/0.8 mL and 20 mg/0.2 mL.
Celltrion USA is also seeking an interchangeability designation from the FDA following the completion of an interchangeability trial of 366 patients with chronic plaque psoriasis. The interchangeability designation would mean that patients successfully switched from Humira to Yuflyma multiple times in the trial. The interchangeability designation would allow pharmacists to autosubstitute Humira with Yuflyma. In these cases, individual state laws control how and whether physicians will be notified of this switch.
If interchangeability is approved for Yuflyma, which the company tentatively expects in the fourth quarter of 2024, it would be just the third interchangeable biosimilar approved by the FDA overall and the second adalimumab biosimilar to be designated as such, after adalimumab-adbm (Cyltezo) in October 2021.
Yuflyma was approved in Canada in December 2021 for 10 indications: rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, adult Crohn’s disease, adult ulcerative colitis, hidradenitis suppurativa, plaque psoriasis, adult uveitis, and pediatric uveitis.
In February 2022, the European Commission granted marketing authorization for Yuflyma across those 10 indications, as well as for nonradiographic axial spondyloarthritis, pediatric plaque psoriasis, and pediatric Crohn’s disease.
In April 2022, Celltrion USA signed a licensing agreement with AbbVie, the manufacturer of Humira. Under that agreement, Celltrion will pay royalties to AbbVie on sales of their individual biosimilars, and AbbVie agreed to drop all patent litigation.
The full prescribing information for Yuflyma is available here.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved the biosimilar adalimumab-aaty (Yuflyma) in a citrate-free, high-concentration formulation, the manufacturer, Celltrion USA, announced today. It is the ninth biosimilar of adalimumab (Humira) to be approved in the United States.
Yuflyma is approved for the treatment of adult patients with rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, ulcerative colitis, plaque psoriasis, and hidradenitis suppurativa. It is also approved for polyarticular juvenile idiopathic arthritis for patients aged 2 years or older, as well as for Crohn’s disease in adults and in pediatric patients aged 6 years or older.
The formulation was approved on the basis of a comprehensive data package of analytic, preclinical, and clinical studies, according to Celltrion USA, “demonstrating that Yuflyma is comparable to the reference product Humira in terms of efficacy, safety, pharmacokinetics, and immunogenicity up to 24 weeks and 1 year following treatment.”
The company conducted a double-blind, randomized phase 3 trial that compared switching from reference adalimumab to Yuflyma with continuing either reference adalimumab or Yuflyma for patients with active rheumatoid arthritis. In that trial, the efficacy, pharmacokinetics, safety, and immunogenicity of Yuflyma and reference adalimumab were comparable after 1 year of treatment, including after switching from reference adalimumab to Yuflyma.
“Currently, more than 80% of patients treated with Humira in the United States rely on a high-concentration and citrate-free formulation of this medication. The availability of a high-concentration and citrate-free formulation adalimumab biosimilar provides an important treatment option for patients with inflammatory diseases who benefit from this effective therapy,” said Jonathan Kay, MD, of the University of Massachusetts, Worcester, in the press release.
The citrate-free formulation is thought to lead to less pain on injection.
Yuflyma will be available in prefilled syringe and autoinjector administration options.
Celltrion USA plans to market the drug in the United States in July 2023. Following the initial launch of 40 mg/0.4 mL, the company plans to launch dose forms of 80 mg/0.8 mL and 20 mg/0.2 mL.
Celltrion USA is also seeking an interchangeability designation from the FDA following the completion of an interchangeability trial of 366 patients with chronic plaque psoriasis. The interchangeability designation would mean that patients successfully switched from Humira to Yuflyma multiple times in the trial. The interchangeability designation would allow pharmacists to autosubstitute Humira with Yuflyma. In these cases, individual state laws control how and whether physicians will be notified of this switch.
If interchangeability is approved for Yuflyma, which the company tentatively expects in the fourth quarter of 2024, it would be just the third interchangeable biosimilar approved by the FDA overall and the second adalimumab biosimilar to be designated as such, after adalimumab-adbm (Cyltezo) in October 2021.
Yuflyma was approved in Canada in December 2021 for 10 indications: rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, adult Crohn’s disease, adult ulcerative colitis, hidradenitis suppurativa, plaque psoriasis, adult uveitis, and pediatric uveitis.
In February 2022, the European Commission granted marketing authorization for Yuflyma across those 10 indications, as well as for nonradiographic axial spondyloarthritis, pediatric plaque psoriasis, and pediatric Crohn’s disease.
In April 2022, Celltrion USA signed a licensing agreement with AbbVie, the manufacturer of Humira. Under that agreement, Celltrion will pay royalties to AbbVie on sales of their individual biosimilars, and AbbVie agreed to drop all patent litigation.
The full prescribing information for Yuflyma is available here.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved the biosimilar adalimumab-aaty (Yuflyma) in a citrate-free, high-concentration formulation, the manufacturer, Celltrion USA, announced today. It is the ninth biosimilar of adalimumab (Humira) to be approved in the United States.
Yuflyma is approved for the treatment of adult patients with rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, ulcerative colitis, plaque psoriasis, and hidradenitis suppurativa. It is also approved for polyarticular juvenile idiopathic arthritis for patients aged 2 years or older, as well as for Crohn’s disease in adults and in pediatric patients aged 6 years or older.
The formulation was approved on the basis of a comprehensive data package of analytic, preclinical, and clinical studies, according to Celltrion USA, “demonstrating that Yuflyma is comparable to the reference product Humira in terms of efficacy, safety, pharmacokinetics, and immunogenicity up to 24 weeks and 1 year following treatment.”
The company conducted a double-blind, randomized phase 3 trial that compared switching from reference adalimumab to Yuflyma with continuing either reference adalimumab or Yuflyma for patients with active rheumatoid arthritis. In that trial, the efficacy, pharmacokinetics, safety, and immunogenicity of Yuflyma and reference adalimumab were comparable after 1 year of treatment, including after switching from reference adalimumab to Yuflyma.
“Currently, more than 80% of patients treated with Humira in the United States rely on a high-concentration and citrate-free formulation of this medication. The availability of a high-concentration and citrate-free formulation adalimumab biosimilar provides an important treatment option for patients with inflammatory diseases who benefit from this effective therapy,” said Jonathan Kay, MD, of the University of Massachusetts, Worcester, in the press release.
The citrate-free formulation is thought to lead to less pain on injection.
Yuflyma will be available in prefilled syringe and autoinjector administration options.
Celltrion USA plans to market the drug in the United States in July 2023. Following the initial launch of 40 mg/0.4 mL, the company plans to launch dose forms of 80 mg/0.8 mL and 20 mg/0.2 mL.
Celltrion USA is also seeking an interchangeability designation from the FDA following the completion of an interchangeability trial of 366 patients with chronic plaque psoriasis. The interchangeability designation would mean that patients successfully switched from Humira to Yuflyma multiple times in the trial. The interchangeability designation would allow pharmacists to autosubstitute Humira with Yuflyma. In these cases, individual state laws control how and whether physicians will be notified of this switch.
If interchangeability is approved for Yuflyma, which the company tentatively expects in the fourth quarter of 2024, it would be just the third interchangeable biosimilar approved by the FDA overall and the second adalimumab biosimilar to be designated as such, after adalimumab-adbm (Cyltezo) in October 2021.
Yuflyma was approved in Canada in December 2021 for 10 indications: rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, adult Crohn’s disease, adult ulcerative colitis, hidradenitis suppurativa, plaque psoriasis, adult uveitis, and pediatric uveitis.
In February 2022, the European Commission granted marketing authorization for Yuflyma across those 10 indications, as well as for nonradiographic axial spondyloarthritis, pediatric plaque psoriasis, and pediatric Crohn’s disease.
In April 2022, Celltrion USA signed a licensing agreement with AbbVie, the manufacturer of Humira. Under that agreement, Celltrion will pay royalties to AbbVie on sales of their individual biosimilars, and AbbVie agreed to drop all patent litigation.
The full prescribing information for Yuflyma is available here.
A version of this article first appeared on Medscape.com.

















![An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound. An extracellular matrix–based collagen dressing (Endoform Natural Restorative Bioscaffold [Aroa Biosurgery Inc]) was applied to the wound.](https://cdn.mdedge.com/files/s3fs-public/CT111005033_e_300x300.jpg)
