User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
AI in Medicine: Are Large Language Models Ready for the Exam Room?
In seconds, Ravi Parikh, MD, an oncologist at the Emory University School of Medicine in Atlanta, had a summary of his patient’s entire medical history. Normally, Parikh skimmed the cumbersome files before seeing a patient. However, the artificial intelligence (AI) tool his institution was testing could list the highlights he needed in a fraction of the time.
“On the whole, I like it ... it saves me time,” Parikh said of the tool. “But I’d be lying if I told you it was perfect all the time. It’s interpreting the [patient] history in some ways that may be inaccurate,” he said.
Within the first week of testing the tool, Parikh started to notice that the large language model (LLM) made a particular mistake in his patients with prostate cancer. If their prostate-specific antigen test results came back slightly elevated — which is part of normal variation — the LLM recorded it as disease progression. Because Parikh reviews all his notes — with or without using an AI tool — after a visit, he easily caught the mistake before it was added to the chart. “The problem, I think, is if these mistakes go under the hood,” he said.
In the data science world, these mistakes are called hallucinations. And a growing body of research suggests they’re happening more frequently than is safe for healthcare. The industry promised LLMs would alleviate administrative burden and reduce physician burnout. But so far, studies show these AI-tool mistakes often create more work for doctors, not less. To truly help physicians and be safe for patients, some experts say healthcare needs to build its own LLMs from the ground up. And all agree that the field desperately needs a way to vet these algorithms more thoroughly.
Prone to Error
Right now, “I think the industry is focused on taking existing LLMs and forcing them into usage for healthcare,” said Nigam H. Shah, MBBS, PhD, chief data scientist for Stanford Health. However, the value of deploying general LLMs in the healthcare space is questionable. “People are starting to wonder if we’re using these tools wrong,” he told this news organization.
In 2023, Shah and his colleagues evaluated seven LLMs on their ability to answer electronic health record–based questions. For realistic tasks, the error rate in the best cases was about 35%, he said. “To me, that rate seems a bit high ... to adopt for routine use.”
A study earlier this year by the UC San Diego School of Medicine showed that using LLMs to respond to patient messages increased the time doctors spent on messages. And this summer, a study by the clinical AI firm Mendel found that when GPT-4o or Llama-3 were used to summarize patient medical records, almost every summary contained at least one type of hallucination.
“We’ve seen cases where a patient does have drug allergies, but the system says ‘no known drug allergies’ ” in the medical history summary, said Wael Salloum, PhD, cofounder and chief science officer at Mendel. “That’s a serious hallucination.” And if physicians have to constantly verify what the system is telling them, that “defeats the purpose [of summarization],” he said.
A Higher Quality Diet
Part of the trouble with LLMs is that there’s just not enough high-quality information to feed them. The algorithms are insatiable, requiring vast swaths of data for training. GPT-3.5, for instance, was trained on 570 GB of data from the internet, more than 300 billion words. And to train GPT-4o, OpenAI reportedly transcribed more than 1 million hours of YouTube content.
However, the strategies that built these general LLMs don’t always translate well to healthcare. The internet is full of low-quality or misleading health information from wellness sites and supplement advertisements. And even data that are trustworthy, like the millions of clinical studies and the US Food and Drug Administration (FDA) statements, can be outdated, Salloum said. And “an LLM in training can’t distinguish good from bad,” he added.
The good news is that clinicians don’t rely on controversial information in the real world. Medical knowledge is standardized. “Healthcare is a domain rich with explicit knowledge,” Salloum said. So there’s potential to build a more reliable LLM that is guided by robust medical standards and guidelines.
It’s possible that healthcare could use small language models, which are LLM’s pocket-sized cousins, and perform tasks needing only bite-sized datasets requiring fewer resources and easier fine-tuning, according to Microsoft’s website. Shah said training these smaller models on real medical data might be an option, like an LLM meant to respond to patient messages that could be trained with real messages sent by physicians.
Several groups are already working on databases of standardized human medical knowledge or real physician responses. “Perhaps that will work better than using LLMs trained on the general internet. Those studies need to be done,” Shah said.
Jon Tamir, assistant professor of electrical and computer engineering and co-lead of the AI Health Lab at The University of Texas at Austin, said, “The community has recognized that we are entering a new era of AI where the dataset itself is the most important aspect. We need training sets that are highly curated and highly specialized.
“If the dataset is highly specialized, it will definitely help reduce hallucinations,” he said.
Cutting Overconfidence
A major problem with LLM mistakes is that they are often hard to detect. Hallucinations can be highly convincing even if they’re highly inaccurate, according to Tamir.
When Shah, for instance, was recently testing an LLM on de-identified patient data, he asked the LLM which blood test the patient last had. The model responded with “complete blood count [CBC].” But when he asked for the results, the model gave him white blood count and other values. “Turns out that record did not have a CBC done at all! The result was entirely made up,” he said.
Making healthcare LLMs safer and more reliable will mean training AI to acknowledge potential mistakes and uncertainty. Existing LLMs are trained to project confidence and produce a lot of answers, even when there isn’t one, Salloum said. They rarely respond with “I don’t know” even when their prediction has low confidence, he added.
Healthcare stands to benefit from a system that highlights uncertainty and potential errors. For instance, if a patient’s history shows they have smoked, stopped smoking, vaped, and started smoking again. The LLM might call them a smoker but flag the comment as uncertain because the chronology is complicated, Salloum said.
Tamir added that this strategy could improve LLM and doctor collaboration by honing in on where human expertise is needed most.
Too Little Evaluation
For any improvement strategy to work, LLMs — and all AI-assisted healthcare tools — first need a better evaluation framework. So far, LLMs have “been used in really exciting ways but not really well-vetted ways,” Tamir said.
While some AI-assisted tools, particularly in medical imaging, have undergone rigorous FDA evaluations and earned approval, most haven’t. And because the FDA only regulates algorithms that are considered medical devices, Parikh said that most LLMs used for administrative tasks and efficiency don’t fall under the regulatory agency’s purview.
But these algorithms still have access to patient information and can directly influence patient and doctor decisions. Third-party regulatory agencies are expected to emerge, but it’s still unclear who those will be. Before developers can build a safer and more efficient LLM for healthcare, they’ll need better guidelines and guardrails. “Unless we figure out evaluation, how would we know whether the healthcare-appropriate large language models are better or worse?” Shah asked.
A version of this article appeared on Medscape.com.
In seconds, Ravi Parikh, MD, an oncologist at the Emory University School of Medicine in Atlanta, had a summary of his patient’s entire medical history. Normally, Parikh skimmed the cumbersome files before seeing a patient. However, the artificial intelligence (AI) tool his institution was testing could list the highlights he needed in a fraction of the time.
“On the whole, I like it ... it saves me time,” Parikh said of the tool. “But I’d be lying if I told you it was perfect all the time. It’s interpreting the [patient] history in some ways that may be inaccurate,” he said.
Within the first week of testing the tool, Parikh started to notice that the large language model (LLM) made a particular mistake in his patients with prostate cancer. If their prostate-specific antigen test results came back slightly elevated — which is part of normal variation — the LLM recorded it as disease progression. Because Parikh reviews all his notes — with or without using an AI tool — after a visit, he easily caught the mistake before it was added to the chart. “The problem, I think, is if these mistakes go under the hood,” he said.
In the data science world, these mistakes are called hallucinations. And a growing body of research suggests they’re happening more frequently than is safe for healthcare. The industry promised LLMs would alleviate administrative burden and reduce physician burnout. But so far, studies show these AI-tool mistakes often create more work for doctors, not less. To truly help physicians and be safe for patients, some experts say healthcare needs to build its own LLMs from the ground up. And all agree that the field desperately needs a way to vet these algorithms more thoroughly.
Prone to Error
Right now, “I think the industry is focused on taking existing LLMs and forcing them into usage for healthcare,” said Nigam H. Shah, MBBS, PhD, chief data scientist for Stanford Health. However, the value of deploying general LLMs in the healthcare space is questionable. “People are starting to wonder if we’re using these tools wrong,” he told this news organization.
In 2023, Shah and his colleagues evaluated seven LLMs on their ability to answer electronic health record–based questions. For realistic tasks, the error rate in the best cases was about 35%, he said. “To me, that rate seems a bit high ... to adopt for routine use.”
A study earlier this year by the UC San Diego School of Medicine showed that using LLMs to respond to patient messages increased the time doctors spent on messages. And this summer, a study by the clinical AI firm Mendel found that when GPT-4o or Llama-3 were used to summarize patient medical records, almost every summary contained at least one type of hallucination.
“We’ve seen cases where a patient does have drug allergies, but the system says ‘no known drug allergies’ ” in the medical history summary, said Wael Salloum, PhD, cofounder and chief science officer at Mendel. “That’s a serious hallucination.” And if physicians have to constantly verify what the system is telling them, that “defeats the purpose [of summarization],” he said.
A Higher Quality Diet
Part of the trouble with LLMs is that there’s just not enough high-quality information to feed them. The algorithms are insatiable, requiring vast swaths of data for training. GPT-3.5, for instance, was trained on 570 GB of data from the internet, more than 300 billion words. And to train GPT-4o, OpenAI reportedly transcribed more than 1 million hours of YouTube content.
However, the strategies that built these general LLMs don’t always translate well to healthcare. The internet is full of low-quality or misleading health information from wellness sites and supplement advertisements. And even data that are trustworthy, like the millions of clinical studies and the US Food and Drug Administration (FDA) statements, can be outdated, Salloum said. And “an LLM in training can’t distinguish good from bad,” he added.
The good news is that clinicians don’t rely on controversial information in the real world. Medical knowledge is standardized. “Healthcare is a domain rich with explicit knowledge,” Salloum said. So there’s potential to build a more reliable LLM that is guided by robust medical standards and guidelines.
It’s possible that healthcare could use small language models, which are LLM’s pocket-sized cousins, and perform tasks needing only bite-sized datasets requiring fewer resources and easier fine-tuning, according to Microsoft’s website. Shah said training these smaller models on real medical data might be an option, like an LLM meant to respond to patient messages that could be trained with real messages sent by physicians.
Several groups are already working on databases of standardized human medical knowledge or real physician responses. “Perhaps that will work better than using LLMs trained on the general internet. Those studies need to be done,” Shah said.
Jon Tamir, assistant professor of electrical and computer engineering and co-lead of the AI Health Lab at The University of Texas at Austin, said, “The community has recognized that we are entering a new era of AI where the dataset itself is the most important aspect. We need training sets that are highly curated and highly specialized.
“If the dataset is highly specialized, it will definitely help reduce hallucinations,” he said.
Cutting Overconfidence
A major problem with LLM mistakes is that they are often hard to detect. Hallucinations can be highly convincing even if they’re highly inaccurate, according to Tamir.
When Shah, for instance, was recently testing an LLM on de-identified patient data, he asked the LLM which blood test the patient last had. The model responded with “complete blood count [CBC].” But when he asked for the results, the model gave him white blood count and other values. “Turns out that record did not have a CBC done at all! The result was entirely made up,” he said.
Making healthcare LLMs safer and more reliable will mean training AI to acknowledge potential mistakes and uncertainty. Existing LLMs are trained to project confidence and produce a lot of answers, even when there isn’t one, Salloum said. They rarely respond with “I don’t know” even when their prediction has low confidence, he added.
Healthcare stands to benefit from a system that highlights uncertainty and potential errors. For instance, if a patient’s history shows they have smoked, stopped smoking, vaped, and started smoking again. The LLM might call them a smoker but flag the comment as uncertain because the chronology is complicated, Salloum said.
Tamir added that this strategy could improve LLM and doctor collaboration by honing in on where human expertise is needed most.
Too Little Evaluation
For any improvement strategy to work, LLMs — and all AI-assisted healthcare tools — first need a better evaluation framework. So far, LLMs have “been used in really exciting ways but not really well-vetted ways,” Tamir said.
While some AI-assisted tools, particularly in medical imaging, have undergone rigorous FDA evaluations and earned approval, most haven’t. And because the FDA only regulates algorithms that are considered medical devices, Parikh said that most LLMs used for administrative tasks and efficiency don’t fall under the regulatory agency’s purview.
But these algorithms still have access to patient information and can directly influence patient and doctor decisions. Third-party regulatory agencies are expected to emerge, but it’s still unclear who those will be. Before developers can build a safer and more efficient LLM for healthcare, they’ll need better guidelines and guardrails. “Unless we figure out evaluation, how would we know whether the healthcare-appropriate large language models are better or worse?” Shah asked.
A version of this article appeared on Medscape.com.
In seconds, Ravi Parikh, MD, an oncologist at the Emory University School of Medicine in Atlanta, had a summary of his patient’s entire medical history. Normally, Parikh skimmed the cumbersome files before seeing a patient. However, the artificial intelligence (AI) tool his institution was testing could list the highlights he needed in a fraction of the time.
“On the whole, I like it ... it saves me time,” Parikh said of the tool. “But I’d be lying if I told you it was perfect all the time. It’s interpreting the [patient] history in some ways that may be inaccurate,” he said.
Within the first week of testing the tool, Parikh started to notice that the large language model (LLM) made a particular mistake in his patients with prostate cancer. If their prostate-specific antigen test results came back slightly elevated — which is part of normal variation — the LLM recorded it as disease progression. Because Parikh reviews all his notes — with or without using an AI tool — after a visit, he easily caught the mistake before it was added to the chart. “The problem, I think, is if these mistakes go under the hood,” he said.
In the data science world, these mistakes are called hallucinations. And a growing body of research suggests they’re happening more frequently than is safe for healthcare. The industry promised LLMs would alleviate administrative burden and reduce physician burnout. But so far, studies show these AI-tool mistakes often create more work for doctors, not less. To truly help physicians and be safe for patients, some experts say healthcare needs to build its own LLMs from the ground up. And all agree that the field desperately needs a way to vet these algorithms more thoroughly.
Prone to Error
Right now, “I think the industry is focused on taking existing LLMs and forcing them into usage for healthcare,” said Nigam H. Shah, MBBS, PhD, chief data scientist for Stanford Health. However, the value of deploying general LLMs in the healthcare space is questionable. “People are starting to wonder if we’re using these tools wrong,” he told this news organization.
In 2023, Shah and his colleagues evaluated seven LLMs on their ability to answer electronic health record–based questions. For realistic tasks, the error rate in the best cases was about 35%, he said. “To me, that rate seems a bit high ... to adopt for routine use.”
A study earlier this year by the UC San Diego School of Medicine showed that using LLMs to respond to patient messages increased the time doctors spent on messages. And this summer, a study by the clinical AI firm Mendel found that when GPT-4o or Llama-3 were used to summarize patient medical records, almost every summary contained at least one type of hallucination.
“We’ve seen cases where a patient does have drug allergies, but the system says ‘no known drug allergies’ ” in the medical history summary, said Wael Salloum, PhD, cofounder and chief science officer at Mendel. “That’s a serious hallucination.” And if physicians have to constantly verify what the system is telling them, that “defeats the purpose [of summarization],” he said.
A Higher Quality Diet
Part of the trouble with LLMs is that there’s just not enough high-quality information to feed them. The algorithms are insatiable, requiring vast swaths of data for training. GPT-3.5, for instance, was trained on 570 GB of data from the internet, more than 300 billion words. And to train GPT-4o, OpenAI reportedly transcribed more than 1 million hours of YouTube content.
However, the strategies that built these general LLMs don’t always translate well to healthcare. The internet is full of low-quality or misleading health information from wellness sites and supplement advertisements. And even data that are trustworthy, like the millions of clinical studies and the US Food and Drug Administration (FDA) statements, can be outdated, Salloum said. And “an LLM in training can’t distinguish good from bad,” he added.
The good news is that clinicians don’t rely on controversial information in the real world. Medical knowledge is standardized. “Healthcare is a domain rich with explicit knowledge,” Salloum said. So there’s potential to build a more reliable LLM that is guided by robust medical standards and guidelines.
It’s possible that healthcare could use small language models, which are LLM’s pocket-sized cousins, and perform tasks needing only bite-sized datasets requiring fewer resources and easier fine-tuning, according to Microsoft’s website. Shah said training these smaller models on real medical data might be an option, like an LLM meant to respond to patient messages that could be trained with real messages sent by physicians.
Several groups are already working on databases of standardized human medical knowledge or real physician responses. “Perhaps that will work better than using LLMs trained on the general internet. Those studies need to be done,” Shah said.
Jon Tamir, assistant professor of electrical and computer engineering and co-lead of the AI Health Lab at The University of Texas at Austin, said, “The community has recognized that we are entering a new era of AI where the dataset itself is the most important aspect. We need training sets that are highly curated and highly specialized.
“If the dataset is highly specialized, it will definitely help reduce hallucinations,” he said.
Cutting Overconfidence
A major problem with LLM mistakes is that they are often hard to detect. Hallucinations can be highly convincing even if they’re highly inaccurate, according to Tamir.
When Shah, for instance, was recently testing an LLM on de-identified patient data, he asked the LLM which blood test the patient last had. The model responded with “complete blood count [CBC].” But when he asked for the results, the model gave him white blood count and other values. “Turns out that record did not have a CBC done at all! The result was entirely made up,” he said.
Making healthcare LLMs safer and more reliable will mean training AI to acknowledge potential mistakes and uncertainty. Existing LLMs are trained to project confidence and produce a lot of answers, even when there isn’t one, Salloum said. They rarely respond with “I don’t know” even when their prediction has low confidence, he added.
Healthcare stands to benefit from a system that highlights uncertainty and potential errors. For instance, if a patient’s history shows they have smoked, stopped smoking, vaped, and started smoking again. The LLM might call them a smoker but flag the comment as uncertain because the chronology is complicated, Salloum said.
Tamir added that this strategy could improve LLM and doctor collaboration by honing in on where human expertise is needed most.
Too Little Evaluation
For any improvement strategy to work, LLMs — and all AI-assisted healthcare tools — first need a better evaluation framework. So far, LLMs have “been used in really exciting ways but not really well-vetted ways,” Tamir said.
While some AI-assisted tools, particularly in medical imaging, have undergone rigorous FDA evaluations and earned approval, most haven’t. And because the FDA only regulates algorithms that are considered medical devices, Parikh said that most LLMs used for administrative tasks and efficiency don’t fall under the regulatory agency’s purview.
But these algorithms still have access to patient information and can directly influence patient and doctor decisions. Third-party regulatory agencies are expected to emerge, but it’s still unclear who those will be. Before developers can build a safer and more efficient LLM for healthcare, they’ll need better guidelines and guardrails. “Unless we figure out evaluation, how would we know whether the healthcare-appropriate large language models are better or worse?” Shah asked.
A version of this article appeared on Medscape.com.
Cybersecurity Concerns Continue to Rise With Ransom, Data Manipulation, AI Risks
From the largest healthcare companies to solo practices, just every organization in medicine faces a risk for costly cyberattacks. In recent years, hackers have threatened to release the personal information of patients and employees — or paralyze online systems — unless they’re paid a ransom.
Should companies pay? It’s not an easy answer, a pair of experts told colleagues in an American Medical Association (AMA) cybersecurity webinar on October 18. It turns out that each choice — pay or don’t pay — can end up being costly.
This is just one of the new challenges facing the American medical system on the cybersecurity front, the speakers said. Others include the possibility that hackers will manipulate patient data — turning a medical test negative, for example, when it’s actually positive — and take advantage of the powers of artificial intelligence (AI).
The AMA held the webinar to educate physicians about cybersecurity risks and defenses, an especially hot topic in the wake of February’s Change Healthcare hack, which cost UnitedHealth Group an estimated $2.5 billion — so far — and deeply disrupted the American healthcare system.
Cautionary tales abound. Greg Garcia, executive director for cybersecurity of the Health Sector Coordinating Council, a coalition of medical industry organizations, pointed to a Pennsylvania clinic that refused to pay a ransom to prevent the release of hundreds of images of patients with breast cancer undressed from the waist up. Garcia told webinar participants that the ransom was $5 million.
Risky Choices
While the Federal Bureau of Investigation recommends against paying a ransom, this can be a risky choice, Garcia said. Hackers released the images, and the center has reportedly agreed to settle a class-action lawsuit for $65 million. “They traded $5 million for $60 million,” Garcia added, slightly misstating the settlement amount.
Health systems have been cagey about whether they’ve paid ransoms to prevent private data from being made public in cyberattacks. If a ransom is demanded, “it’s every organization for itself,” Garcia said.
He highlighted the case of a chain of psychiatry practices in Finland that suffered a ransomware attack in 2020. The hackers “contacted the patients and said: ‘Hey, call your clinic and tell them to pay the ransom. Otherwise, we’re going to release all your psychiatric notes to the public.’ ”
Cyberattacks continue. In October, Boston Children’s Health Physicians announced that it had suffered a “ recent security incident” involving data — possibly including Social Security numbers and treatment information — regarding patients and employees. A hacker group reportedly claimed responsibility and wants the system, which boasts more than 300 clinicians, to pay a ransom or else it will release the stolen information.
Should Paying Ransom Be a Crime?
Christian Dameff, MD, MS, an emergency medicine physician and director of the Center for Healthcare Cybersecurity at the University of California (UC), San Diego, noted that there are efforts to turn paying ransom into a crime. “If people aren’t paying ransoms, then ransomware operators will move to something else that makes them money.”
Dameff urged colleagues to understand we no longer live in a world where clinicians only bother to think of technology when they call the IT department to help them reset their password.
New challenges face clinicians, he said. “How do we develop better strategies, downtime procedures, and safe clinical care in an era where our vital technology may be gone, not just for an hour or 2, but as is the case with these ransomware attacks, sometimes weeks to months.”
Garcia said “cybersecurity is everybody’s responsibility, including frontline clinicians. Because you’re touching data, you’re touching technology, you’re touching patients, and all of those things combine to present some vulnerabilities in the digital world.”
Next Frontier: Hackers May Manipulate Patient Data
Dameff said future hackers may use AI to manipulate individual patient data in ways that threaten patient health. AI makes this easier to accomplish.
“What if I delete your allergies in your electronic health record, or I manipulate your chest x-ray, or I change your lab values so it looks like you’re in diabetic ketoacidosis when you’re not so a clinician gives you insulin when you don’t need it?”
Garcia highlighted another new threat: Phishing efforts that are harder to ignore thanks to AI.
“One of the most successful way that hackers get in, disrupt systems, and steal data is through email phishing, and it’s only going to get better because of artificial intelligence,” he said. “No longer are you going to have typos in that email written by a hacking group in Nigeria or in China. It’s going to be perfect looking.”
What can practices and healthcare systems do? Garcia highlighted federal health agency efforts to encourage organizations to adopt best practices in cybersecurity.
“If you’ve got a data breach, and you can show to the US Department of Health & Human Services [HHS] you have implemented generally recognized cybersecurity controls over the past year, that you have done your best, you did the right thing, and you still got hit, HHS is directed to essentially take it easy on you,” he said. “That’s a positive incentive.”
Ransomware Guide in the Works
Dameff said UC San Diego’s Center for Healthcare Cybersecurity plans to publish a free cybersecurity guide in 2025 that will include specific information about ransomware attacks for medical specialties such as cardiology, trauma surgery, and pediatrics.
“Then, should you ever be ransomed, you can pull out this guide. You’ll know what’s going to kind of happen, and you can better prepare for those effects.”
Will the future president prioritize healthcare cybersecurity? That remains to be seen, but crises do have the capacity to concentrate the mind, experts said.
The nation’s capital “has a very short memory, a short attention span. The policymakers tend to be reactive,” Dameff said. “All it takes is yet another Change Healthcare–like attack that disrupts 30% or more of the nation’s healthcare system for the policymakers to sit up, take notice, and try to come up with solutions.”
In addition, he said, an estimated two data breaches/ransomware attacks are occurring per day. “The fact is that we’re all patients, up to the President of the United States and every member of the Congress is a patient.”
There’s a “very existential, very palpable understanding that cyber safety is patient safety and cyber insecurity is patient insecurity,” Dameff said.
A version of this article appeared on Medscape.com.
From the largest healthcare companies to solo practices, just every organization in medicine faces a risk for costly cyberattacks. In recent years, hackers have threatened to release the personal information of patients and employees — or paralyze online systems — unless they’re paid a ransom.
Should companies pay? It’s not an easy answer, a pair of experts told colleagues in an American Medical Association (AMA) cybersecurity webinar on October 18. It turns out that each choice — pay or don’t pay — can end up being costly.
This is just one of the new challenges facing the American medical system on the cybersecurity front, the speakers said. Others include the possibility that hackers will manipulate patient data — turning a medical test negative, for example, when it’s actually positive — and take advantage of the powers of artificial intelligence (AI).
The AMA held the webinar to educate physicians about cybersecurity risks and defenses, an especially hot topic in the wake of February’s Change Healthcare hack, which cost UnitedHealth Group an estimated $2.5 billion — so far — and deeply disrupted the American healthcare system.
Cautionary tales abound. Greg Garcia, executive director for cybersecurity of the Health Sector Coordinating Council, a coalition of medical industry organizations, pointed to a Pennsylvania clinic that refused to pay a ransom to prevent the release of hundreds of images of patients with breast cancer undressed from the waist up. Garcia told webinar participants that the ransom was $5 million.
Risky Choices
While the Federal Bureau of Investigation recommends against paying a ransom, this can be a risky choice, Garcia said. Hackers released the images, and the center has reportedly agreed to settle a class-action lawsuit for $65 million. “They traded $5 million for $60 million,” Garcia added, slightly misstating the settlement amount.
Health systems have been cagey about whether they’ve paid ransoms to prevent private data from being made public in cyberattacks. If a ransom is demanded, “it’s every organization for itself,” Garcia said.
He highlighted the case of a chain of psychiatry practices in Finland that suffered a ransomware attack in 2020. The hackers “contacted the patients and said: ‘Hey, call your clinic and tell them to pay the ransom. Otherwise, we’re going to release all your psychiatric notes to the public.’ ”
Cyberattacks continue. In October, Boston Children’s Health Physicians announced that it had suffered a “ recent security incident” involving data — possibly including Social Security numbers and treatment information — regarding patients and employees. A hacker group reportedly claimed responsibility and wants the system, which boasts more than 300 clinicians, to pay a ransom or else it will release the stolen information.
Should Paying Ransom Be a Crime?
Christian Dameff, MD, MS, an emergency medicine physician and director of the Center for Healthcare Cybersecurity at the University of California (UC), San Diego, noted that there are efforts to turn paying ransom into a crime. “If people aren’t paying ransoms, then ransomware operators will move to something else that makes them money.”
Dameff urged colleagues to understand we no longer live in a world where clinicians only bother to think of technology when they call the IT department to help them reset their password.
New challenges face clinicians, he said. “How do we develop better strategies, downtime procedures, and safe clinical care in an era where our vital technology may be gone, not just for an hour or 2, but as is the case with these ransomware attacks, sometimes weeks to months.”
Garcia said “cybersecurity is everybody’s responsibility, including frontline clinicians. Because you’re touching data, you’re touching technology, you’re touching patients, and all of those things combine to present some vulnerabilities in the digital world.”
Next Frontier: Hackers May Manipulate Patient Data
Dameff said future hackers may use AI to manipulate individual patient data in ways that threaten patient health. AI makes this easier to accomplish.
“What if I delete your allergies in your electronic health record, or I manipulate your chest x-ray, or I change your lab values so it looks like you’re in diabetic ketoacidosis when you’re not so a clinician gives you insulin when you don’t need it?”
Garcia highlighted another new threat: Phishing efforts that are harder to ignore thanks to AI.
“One of the most successful way that hackers get in, disrupt systems, and steal data is through email phishing, and it’s only going to get better because of artificial intelligence,” he said. “No longer are you going to have typos in that email written by a hacking group in Nigeria or in China. It’s going to be perfect looking.”
What can practices and healthcare systems do? Garcia highlighted federal health agency efforts to encourage organizations to adopt best practices in cybersecurity.
“If you’ve got a data breach, and you can show to the US Department of Health & Human Services [HHS] you have implemented generally recognized cybersecurity controls over the past year, that you have done your best, you did the right thing, and you still got hit, HHS is directed to essentially take it easy on you,” he said. “That’s a positive incentive.”
Ransomware Guide in the Works
Dameff said UC San Diego’s Center for Healthcare Cybersecurity plans to publish a free cybersecurity guide in 2025 that will include specific information about ransomware attacks for medical specialties such as cardiology, trauma surgery, and pediatrics.
“Then, should you ever be ransomed, you can pull out this guide. You’ll know what’s going to kind of happen, and you can better prepare for those effects.”
Will the future president prioritize healthcare cybersecurity? That remains to be seen, but crises do have the capacity to concentrate the mind, experts said.
The nation’s capital “has a very short memory, a short attention span. The policymakers tend to be reactive,” Dameff said. “All it takes is yet another Change Healthcare–like attack that disrupts 30% or more of the nation’s healthcare system for the policymakers to sit up, take notice, and try to come up with solutions.”
In addition, he said, an estimated two data breaches/ransomware attacks are occurring per day. “The fact is that we’re all patients, up to the President of the United States and every member of the Congress is a patient.”
There’s a “very existential, very palpable understanding that cyber safety is patient safety and cyber insecurity is patient insecurity,” Dameff said.
A version of this article appeared on Medscape.com.
From the largest healthcare companies to solo practices, just every organization in medicine faces a risk for costly cyberattacks. In recent years, hackers have threatened to release the personal information of patients and employees — or paralyze online systems — unless they’re paid a ransom.
Should companies pay? It’s not an easy answer, a pair of experts told colleagues in an American Medical Association (AMA) cybersecurity webinar on October 18. It turns out that each choice — pay or don’t pay — can end up being costly.
This is just one of the new challenges facing the American medical system on the cybersecurity front, the speakers said. Others include the possibility that hackers will manipulate patient data — turning a medical test negative, for example, when it’s actually positive — and take advantage of the powers of artificial intelligence (AI).
The AMA held the webinar to educate physicians about cybersecurity risks and defenses, an especially hot topic in the wake of February’s Change Healthcare hack, which cost UnitedHealth Group an estimated $2.5 billion — so far — and deeply disrupted the American healthcare system.
Cautionary tales abound. Greg Garcia, executive director for cybersecurity of the Health Sector Coordinating Council, a coalition of medical industry organizations, pointed to a Pennsylvania clinic that refused to pay a ransom to prevent the release of hundreds of images of patients with breast cancer undressed from the waist up. Garcia told webinar participants that the ransom was $5 million.
Risky Choices
While the Federal Bureau of Investigation recommends against paying a ransom, this can be a risky choice, Garcia said. Hackers released the images, and the center has reportedly agreed to settle a class-action lawsuit for $65 million. “They traded $5 million for $60 million,” Garcia added, slightly misstating the settlement amount.
Health systems have been cagey about whether they’ve paid ransoms to prevent private data from being made public in cyberattacks. If a ransom is demanded, “it’s every organization for itself,” Garcia said.
He highlighted the case of a chain of psychiatry practices in Finland that suffered a ransomware attack in 2020. The hackers “contacted the patients and said: ‘Hey, call your clinic and tell them to pay the ransom. Otherwise, we’re going to release all your psychiatric notes to the public.’ ”
Cyberattacks continue. In October, Boston Children’s Health Physicians announced that it had suffered a “ recent security incident” involving data — possibly including Social Security numbers and treatment information — regarding patients and employees. A hacker group reportedly claimed responsibility and wants the system, which boasts more than 300 clinicians, to pay a ransom or else it will release the stolen information.
Should Paying Ransom Be a Crime?
Christian Dameff, MD, MS, an emergency medicine physician and director of the Center for Healthcare Cybersecurity at the University of California (UC), San Diego, noted that there are efforts to turn paying ransom into a crime. “If people aren’t paying ransoms, then ransomware operators will move to something else that makes them money.”
Dameff urged colleagues to understand we no longer live in a world where clinicians only bother to think of technology when they call the IT department to help them reset their password.
New challenges face clinicians, he said. “How do we develop better strategies, downtime procedures, and safe clinical care in an era where our vital technology may be gone, not just for an hour or 2, but as is the case with these ransomware attacks, sometimes weeks to months.”
Garcia said “cybersecurity is everybody’s responsibility, including frontline clinicians. Because you’re touching data, you’re touching technology, you’re touching patients, and all of those things combine to present some vulnerabilities in the digital world.”
Next Frontier: Hackers May Manipulate Patient Data
Dameff said future hackers may use AI to manipulate individual patient data in ways that threaten patient health. AI makes this easier to accomplish.
“What if I delete your allergies in your electronic health record, or I manipulate your chest x-ray, or I change your lab values so it looks like you’re in diabetic ketoacidosis when you’re not so a clinician gives you insulin when you don’t need it?”
Garcia highlighted another new threat: Phishing efforts that are harder to ignore thanks to AI.
“One of the most successful way that hackers get in, disrupt systems, and steal data is through email phishing, and it’s only going to get better because of artificial intelligence,” he said. “No longer are you going to have typos in that email written by a hacking group in Nigeria or in China. It’s going to be perfect looking.”
What can practices and healthcare systems do? Garcia highlighted federal health agency efforts to encourage organizations to adopt best practices in cybersecurity.
“If you’ve got a data breach, and you can show to the US Department of Health & Human Services [HHS] you have implemented generally recognized cybersecurity controls over the past year, that you have done your best, you did the right thing, and you still got hit, HHS is directed to essentially take it easy on you,” he said. “That’s a positive incentive.”
Ransomware Guide in the Works
Dameff said UC San Diego’s Center for Healthcare Cybersecurity plans to publish a free cybersecurity guide in 2025 that will include specific information about ransomware attacks for medical specialties such as cardiology, trauma surgery, and pediatrics.
“Then, should you ever be ransomed, you can pull out this guide. You’ll know what’s going to kind of happen, and you can better prepare for those effects.”
Will the future president prioritize healthcare cybersecurity? That remains to be seen, but crises do have the capacity to concentrate the mind, experts said.
The nation’s capital “has a very short memory, a short attention span. The policymakers tend to be reactive,” Dameff said. “All it takes is yet another Change Healthcare–like attack that disrupts 30% or more of the nation’s healthcare system for the policymakers to sit up, take notice, and try to come up with solutions.”
In addition, he said, an estimated two data breaches/ransomware attacks are occurring per day. “The fact is that we’re all patients, up to the President of the United States and every member of the Congress is a patient.”
There’s a “very existential, very palpable understanding that cyber safety is patient safety and cyber insecurity is patient insecurity,” Dameff said.
A version of this article appeared on Medscape.com.
ICD-10-CM Codes for CCCA, FFA Now Available
in the field of hair loss disorders.
“CCCA and FFA are conditions that require early diagnosis and intervention to prevent irreversible hair loss,” Maria Hordinsky, MD, professor of dermatology at the University of Minnesota, Minneapolis, and a member of the Board of Directors, Scarring Alopecia Foundation (SAF), said in an interview.
“The use of these new codes will make it easier for clinicians to identify affected patients and improve treatment outcomes. It also opens the door for more robust research efforts aimed at understanding the etiology and progression of CCCA and FFA, which could lead to new and more effective treatments in the future. Overall, this development represents a positive step toward improving care for individuals affected by these challenging conditions.”
The new codes — L66.81 for CCCA and L66.12 for FFA — were approved by the Centers for Disease Control and Prevention (CDC) on June 15, 2023, but not implemented until October 1, 2024.
Amy J. McMichael, MD, professor of dermatology at Wake Forest University School of Medicine, Winston-Salem, North Carolina, and a scientific advisor to SAF, told this news organization that Itisha Jefferson, a medical student at Loyola University Chicago’s Stritch School of Medicine, and her peers on the SAF’s Medical Student Executive Board, played a pivotal role in advocating for the codes.
In 2022, Jefferson, who has CCCA, and her fellow medical students helped create the proposals that were ultimately submitted to the CDC.
“They were critical in working with the CDC leaders to get the necessary information submitted and processed,” McMichael said. “They were also amazing at corralling our dermatologist group for the development of the necessary presentations and helped to shepherd us to the finish line for all logistic issues.”
On March 8, 2023, McMichael and Hordinsky made their pitch for the codes in person at the CDC’s ICD-10 Coordination and Maintenance Committee meeting, with McMichael discussing CCCA and Hordinsky discussing FFA.
“We also discussed the lack of standardized tracking, which has contributed to misdiagnoses and inadequate treatment options,” Hordinsky recalled. “We highlighted the importance of having distinct codes for these conditions to improve clinical outcomes, ensure that patients have access to appropriate care, better tracking of disease prevalence, and greater epidemiologic monitoring with access to electronic medical records and other large real-world evidence datasets and databases, the results of which could contribute to health policy decision-making.”
To spread the word about the new codes, McMichael, Hordinsky, and other members of the SAF are working with the original team of medical students, some of whom who are now dermatology residents, to develop an information guide to send to societies and organizations that were supportive of the codes. A publication in the dermatology literature is also planned.
For her part, Jefferson said that she will continue to advocate for patients with scarring alopecia as a medical student and when she becomes a physician. “I hope in the near future we will see an externally led FDA Patient-Focused Drug Development meeting for both CCCA and FFA, further advancing care and research for these conditions,” she said in an interview.
McMichael, Hordinsky, and Jefferson had no relevant disclosures to report.
A version of this article appeared on Medscape.com.
in the field of hair loss disorders.
“CCCA and FFA are conditions that require early diagnosis and intervention to prevent irreversible hair loss,” Maria Hordinsky, MD, professor of dermatology at the University of Minnesota, Minneapolis, and a member of the Board of Directors, Scarring Alopecia Foundation (SAF), said in an interview.
“The use of these new codes will make it easier for clinicians to identify affected patients and improve treatment outcomes. It also opens the door for more robust research efforts aimed at understanding the etiology and progression of CCCA and FFA, which could lead to new and more effective treatments in the future. Overall, this development represents a positive step toward improving care for individuals affected by these challenging conditions.”
The new codes — L66.81 for CCCA and L66.12 for FFA — were approved by the Centers for Disease Control and Prevention (CDC) on June 15, 2023, but not implemented until October 1, 2024.
Amy J. McMichael, MD, professor of dermatology at Wake Forest University School of Medicine, Winston-Salem, North Carolina, and a scientific advisor to SAF, told this news organization that Itisha Jefferson, a medical student at Loyola University Chicago’s Stritch School of Medicine, and her peers on the SAF’s Medical Student Executive Board, played a pivotal role in advocating for the codes.
In 2022, Jefferson, who has CCCA, and her fellow medical students helped create the proposals that were ultimately submitted to the CDC.
“They were critical in working with the CDC leaders to get the necessary information submitted and processed,” McMichael said. “They were also amazing at corralling our dermatologist group for the development of the necessary presentations and helped to shepherd us to the finish line for all logistic issues.”
On March 8, 2023, McMichael and Hordinsky made their pitch for the codes in person at the CDC’s ICD-10 Coordination and Maintenance Committee meeting, with McMichael discussing CCCA and Hordinsky discussing FFA.
“We also discussed the lack of standardized tracking, which has contributed to misdiagnoses and inadequate treatment options,” Hordinsky recalled. “We highlighted the importance of having distinct codes for these conditions to improve clinical outcomes, ensure that patients have access to appropriate care, better tracking of disease prevalence, and greater epidemiologic monitoring with access to electronic medical records and other large real-world evidence datasets and databases, the results of which could contribute to health policy decision-making.”
To spread the word about the new codes, McMichael, Hordinsky, and other members of the SAF are working with the original team of medical students, some of whom who are now dermatology residents, to develop an information guide to send to societies and organizations that were supportive of the codes. A publication in the dermatology literature is also planned.
For her part, Jefferson said that she will continue to advocate for patients with scarring alopecia as a medical student and when she becomes a physician. “I hope in the near future we will see an externally led FDA Patient-Focused Drug Development meeting for both CCCA and FFA, further advancing care and research for these conditions,” she said in an interview.
McMichael, Hordinsky, and Jefferson had no relevant disclosures to report.
A version of this article appeared on Medscape.com.
in the field of hair loss disorders.
“CCCA and FFA are conditions that require early diagnosis and intervention to prevent irreversible hair loss,” Maria Hordinsky, MD, professor of dermatology at the University of Minnesota, Minneapolis, and a member of the Board of Directors, Scarring Alopecia Foundation (SAF), said in an interview.
“The use of these new codes will make it easier for clinicians to identify affected patients and improve treatment outcomes. It also opens the door for more robust research efforts aimed at understanding the etiology and progression of CCCA and FFA, which could lead to new and more effective treatments in the future. Overall, this development represents a positive step toward improving care for individuals affected by these challenging conditions.”
The new codes — L66.81 for CCCA and L66.12 for FFA — were approved by the Centers for Disease Control and Prevention (CDC) on June 15, 2023, but not implemented until October 1, 2024.
Amy J. McMichael, MD, professor of dermatology at Wake Forest University School of Medicine, Winston-Salem, North Carolina, and a scientific advisor to SAF, told this news organization that Itisha Jefferson, a medical student at Loyola University Chicago’s Stritch School of Medicine, and her peers on the SAF’s Medical Student Executive Board, played a pivotal role in advocating for the codes.
In 2022, Jefferson, who has CCCA, and her fellow medical students helped create the proposals that were ultimately submitted to the CDC.
“They were critical in working with the CDC leaders to get the necessary information submitted and processed,” McMichael said. “They were also amazing at corralling our dermatologist group for the development of the necessary presentations and helped to shepherd us to the finish line for all logistic issues.”
On March 8, 2023, McMichael and Hordinsky made their pitch for the codes in person at the CDC’s ICD-10 Coordination and Maintenance Committee meeting, with McMichael discussing CCCA and Hordinsky discussing FFA.
“We also discussed the lack of standardized tracking, which has contributed to misdiagnoses and inadequate treatment options,” Hordinsky recalled. “We highlighted the importance of having distinct codes for these conditions to improve clinical outcomes, ensure that patients have access to appropriate care, better tracking of disease prevalence, and greater epidemiologic monitoring with access to electronic medical records and other large real-world evidence datasets and databases, the results of which could contribute to health policy decision-making.”
To spread the word about the new codes, McMichael, Hordinsky, and other members of the SAF are working with the original team of medical students, some of whom who are now dermatology residents, to develop an information guide to send to societies and organizations that were supportive of the codes. A publication in the dermatology literature is also planned.
For her part, Jefferson said that she will continue to advocate for patients with scarring alopecia as a medical student and when she becomes a physician. “I hope in the near future we will see an externally led FDA Patient-Focused Drug Development meeting for both CCCA and FFA, further advancing care and research for these conditions,” she said in an interview.
McMichael, Hordinsky, and Jefferson had no relevant disclosures to report.
A version of this article appeared on Medscape.com.
Community Outreach Benefits Dermatology Residents and Their Patients
The sun often is rising in the rearview mirror as I travel with the University of New Mexico dermatology team from Albuquerque to our satellite clinic in Gallup, New Mexico. This twice-monthly trip—with a group usually comprising an attending physician, residents, and medical students—provides an invaluable opportunity for me to take part in delivering care to a majority Native American population and connects our institution and its trainees to the state’s rural and indigenous cultures and communities.
Community outreach is an important initiative for many dermatology residency training programs. Engaging with the community outside the clinic setting allows residents to hone their clinical skills, interact with and meet new people, and help to improve access to health care, especially for members of underserved populations.
Limited access to health care remains a pressing issue in the United States, especially for underserved and rural communities. There currently is no standardized way to measure access to care, but multiple contributing factors have been identified, including but not limited to patient wait times and throughput, provider turnover, ratio of dermatologists to patient population, insurance type, and patient outcomes.1 Fortunately, there are many ways for dermatology residents to get involved and improve access to dermatologic services in their communities, including skin cancer screenings, free clinics, and teledermatology.
Skin Cancer Screenings
More than 40% of community outreach initiatives offered by dermatology residency programs are related to skin cancer screening and prevention.2 The American Academy of Dermatology’s free skin cancer check program (https://www.aad.org/member/career/volunteer/spot) offers a way to participate in or even host a skin cancer screening in your community. Since 1985, this program has identified nearly 300,000 suspicious lesions and more than 30,000 suspected melanomas. Resources for setting up a skin cancer screening in your community are available on the program’s website. Residents may take this opportunity to teach medical students how to perform full-body skin examinations and/or practice making independent decisions as the supervisor for medical trainees. Skin cancer screening events not only expand access to care in underserved communities but also help residents feel more connected to the local community, especially if they have moved to a new location for their residency training.
Free Clinics
Engaging in educational opportunities offered through residency programs is another way to participate in community outreach. In particular, many programs are affiliated with a School of Medicine within their institution that allows residents to spearhead volunteer opportunities such as working at a free clinic. In fact, more than 30% of initiatives offered at dermatology residency programs are free general dermatology clinics.2 Residents are in the unique position of being both learners themselves as well as educators to trainees.3 As part of our role, we can provide crucial specialty care to the community by working in concert with medical students and while also familiarizing ourselves with treating populations that we may not reach in our daily clinical work. For example, by participating in free clinics, we can provide care to vulnerable populations who typically may have financial or time barriers that prevent them from seeking care at the institution-associated clinic, including individuals experiencing homelessness, patients who are uninsured, and individuals who cannot take time off work to pursue medical care. Our presence in the community helps to reduce barriers to specialty care, particularly in the field of dermatology where the access shortage in the context of rising skin cancer rates prompts public health concerns.4
Teledermatology
Teledermatology became a way to extend our reach in the community more than ever before during the COVID-19 pandemic. Advances in audio, visual, and data telecommunication have been particularly helpful in dermatology, a specialty that relies heavily on visual cues for diagnosis. Synchronous, asynchronous, and hybrid teledermatology services implemented during the pandemic have gained favor among patients and dermatologists and are still applied in current practice.5,6
For example, in the state of New Mexico (where there is a severe shortage of board-certified dermatologists to care for the state’s population), teledermatology has allowed rural providers of all specialties to consult University of New Mexico dermatologists by sending clinical photographs along with patient information and history via secure messaging. Instead of having the patient travel hundreds of miles to see the nearest dermatologist for their skin condition or endure long wait times to get in to see a specialist, primary providers now can initiate treatment or work-up for their patient’s skin issue in a timely manner with the use of teledermatology to consult specialists.
Teledermatology has demonstrated cost-effectiveness, accuracy, and efficiency in conveniently expanding access to care. It offers patients and dermatologists flexibility in receiving and delivering health care, respectively.7 As residents, learning how to navigate this technologic frontier in health care delivery is imperative, as it will remain a prevalent tool in the future care of our communities, particularly in underserved areas.
Final Thoughts
Through community outreach initiatives, dermatology residents have an opportunity not only to enrich our education but also to connect with and become closer to our patients. Skin cancer screenings, free clinics, and teledermatology have provided ways to reach more communities and remain important aspects of dermatology residency.
- Patel B, Blalock TW. Defining “access to care” for dermatology at academic medical institutions. J Am Acad Dermatol. 2023;89:627-628. doi:10.1016/j.jaad.2023.03.014
- Fritsche M, Maglakelidze N, Zaenglein A, et al. Community outreach initiatives in dermatology: cross-sectional study. Arch Dermatol Res. 2023;315:2693-2695. doi:10.1007/s00403-023-02629-y
- Chiu LW. Teaching tips for dermatology residents. Cutis. 2024;113:E17-E19. doi:10.12788/cutis.1046
- Duniphin DD. Limited access to dermatology specialty care: barriers and teledermatology. Dermatol Pract Concept. 2023;13:E2023031. doi:10.5826/dpc.1301a31
- Ibrahim AE, Magdy M, Khalaf EM, et al. Teledermatology in the time of COVID-19. Int J Clin Pract. 2021;75:e15000. doi:10.1111/ijcp.15000
- Farr MA, Duvic M, Joshi TP. Teledermatology during COVID-19: an updated review. Am J Clin Dermatol. 2021;22:467-475. doi:10.1007/s40257-021-00601-y
- Lipner SR. Optimizing patient care with teledermatology: improving access, efficiency, and satisfaction. Cutis. 2024;114:63-64. doi:10.12788/cutis.1073
The sun often is rising in the rearview mirror as I travel with the University of New Mexico dermatology team from Albuquerque to our satellite clinic in Gallup, New Mexico. This twice-monthly trip—with a group usually comprising an attending physician, residents, and medical students—provides an invaluable opportunity for me to take part in delivering care to a majority Native American population and connects our institution and its trainees to the state’s rural and indigenous cultures and communities.
Community outreach is an important initiative for many dermatology residency training programs. Engaging with the community outside the clinic setting allows residents to hone their clinical skills, interact with and meet new people, and help to improve access to health care, especially for members of underserved populations.
Limited access to health care remains a pressing issue in the United States, especially for underserved and rural communities. There currently is no standardized way to measure access to care, but multiple contributing factors have been identified, including but not limited to patient wait times and throughput, provider turnover, ratio of dermatologists to patient population, insurance type, and patient outcomes.1 Fortunately, there are many ways for dermatology residents to get involved and improve access to dermatologic services in their communities, including skin cancer screenings, free clinics, and teledermatology.
Skin Cancer Screenings
More than 40% of community outreach initiatives offered by dermatology residency programs are related to skin cancer screening and prevention.2 The American Academy of Dermatology’s free skin cancer check program (https://www.aad.org/member/career/volunteer/spot) offers a way to participate in or even host a skin cancer screening in your community. Since 1985, this program has identified nearly 300,000 suspicious lesions and more than 30,000 suspected melanomas. Resources for setting up a skin cancer screening in your community are available on the program’s website. Residents may take this opportunity to teach medical students how to perform full-body skin examinations and/or practice making independent decisions as the supervisor for medical trainees. Skin cancer screening events not only expand access to care in underserved communities but also help residents feel more connected to the local community, especially if they have moved to a new location for their residency training.
Free Clinics
Engaging in educational opportunities offered through residency programs is another way to participate in community outreach. In particular, many programs are affiliated with a School of Medicine within their institution that allows residents to spearhead volunteer opportunities such as working at a free clinic. In fact, more than 30% of initiatives offered at dermatology residency programs are free general dermatology clinics.2 Residents are in the unique position of being both learners themselves as well as educators to trainees.3 As part of our role, we can provide crucial specialty care to the community by working in concert with medical students and while also familiarizing ourselves with treating populations that we may not reach in our daily clinical work. For example, by participating in free clinics, we can provide care to vulnerable populations who typically may have financial or time barriers that prevent them from seeking care at the institution-associated clinic, including individuals experiencing homelessness, patients who are uninsured, and individuals who cannot take time off work to pursue medical care. Our presence in the community helps to reduce barriers to specialty care, particularly in the field of dermatology where the access shortage in the context of rising skin cancer rates prompts public health concerns.4
Teledermatology
Teledermatology became a way to extend our reach in the community more than ever before during the COVID-19 pandemic. Advances in audio, visual, and data telecommunication have been particularly helpful in dermatology, a specialty that relies heavily on visual cues for diagnosis. Synchronous, asynchronous, and hybrid teledermatology services implemented during the pandemic have gained favor among patients and dermatologists and are still applied in current practice.5,6
For example, in the state of New Mexico (where there is a severe shortage of board-certified dermatologists to care for the state’s population), teledermatology has allowed rural providers of all specialties to consult University of New Mexico dermatologists by sending clinical photographs along with patient information and history via secure messaging. Instead of having the patient travel hundreds of miles to see the nearest dermatologist for their skin condition or endure long wait times to get in to see a specialist, primary providers now can initiate treatment or work-up for their patient’s skin issue in a timely manner with the use of teledermatology to consult specialists.
Teledermatology has demonstrated cost-effectiveness, accuracy, and efficiency in conveniently expanding access to care. It offers patients and dermatologists flexibility in receiving and delivering health care, respectively.7 As residents, learning how to navigate this technologic frontier in health care delivery is imperative, as it will remain a prevalent tool in the future care of our communities, particularly in underserved areas.
Final Thoughts
Through community outreach initiatives, dermatology residents have an opportunity not only to enrich our education but also to connect with and become closer to our patients. Skin cancer screenings, free clinics, and teledermatology have provided ways to reach more communities and remain important aspects of dermatology residency.
The sun often is rising in the rearview mirror as I travel with the University of New Mexico dermatology team from Albuquerque to our satellite clinic in Gallup, New Mexico. This twice-monthly trip—with a group usually comprising an attending physician, residents, and medical students—provides an invaluable opportunity for me to take part in delivering care to a majority Native American population and connects our institution and its trainees to the state’s rural and indigenous cultures and communities.
Community outreach is an important initiative for many dermatology residency training programs. Engaging with the community outside the clinic setting allows residents to hone their clinical skills, interact with and meet new people, and help to improve access to health care, especially for members of underserved populations.
Limited access to health care remains a pressing issue in the United States, especially for underserved and rural communities. There currently is no standardized way to measure access to care, but multiple contributing factors have been identified, including but not limited to patient wait times and throughput, provider turnover, ratio of dermatologists to patient population, insurance type, and patient outcomes.1 Fortunately, there are many ways for dermatology residents to get involved and improve access to dermatologic services in their communities, including skin cancer screenings, free clinics, and teledermatology.
Skin Cancer Screenings
More than 40% of community outreach initiatives offered by dermatology residency programs are related to skin cancer screening and prevention.2 The American Academy of Dermatology’s free skin cancer check program (https://www.aad.org/member/career/volunteer/spot) offers a way to participate in or even host a skin cancer screening in your community. Since 1985, this program has identified nearly 300,000 suspicious lesions and more than 30,000 suspected melanomas. Resources for setting up a skin cancer screening in your community are available on the program’s website. Residents may take this opportunity to teach medical students how to perform full-body skin examinations and/or practice making independent decisions as the supervisor for medical trainees. Skin cancer screening events not only expand access to care in underserved communities but also help residents feel more connected to the local community, especially if they have moved to a new location for their residency training.
Free Clinics
Engaging in educational opportunities offered through residency programs is another way to participate in community outreach. In particular, many programs are affiliated with a School of Medicine within their institution that allows residents to spearhead volunteer opportunities such as working at a free clinic. In fact, more than 30% of initiatives offered at dermatology residency programs are free general dermatology clinics.2 Residents are in the unique position of being both learners themselves as well as educators to trainees.3 As part of our role, we can provide crucial specialty care to the community by working in concert with medical students and while also familiarizing ourselves with treating populations that we may not reach in our daily clinical work. For example, by participating in free clinics, we can provide care to vulnerable populations who typically may have financial or time barriers that prevent them from seeking care at the institution-associated clinic, including individuals experiencing homelessness, patients who are uninsured, and individuals who cannot take time off work to pursue medical care. Our presence in the community helps to reduce barriers to specialty care, particularly in the field of dermatology where the access shortage in the context of rising skin cancer rates prompts public health concerns.4
Teledermatology
Teledermatology became a way to extend our reach in the community more than ever before during the COVID-19 pandemic. Advances in audio, visual, and data telecommunication have been particularly helpful in dermatology, a specialty that relies heavily on visual cues for diagnosis. Synchronous, asynchronous, and hybrid teledermatology services implemented during the pandemic have gained favor among patients and dermatologists and are still applied in current practice.5,6
For example, in the state of New Mexico (where there is a severe shortage of board-certified dermatologists to care for the state’s population), teledermatology has allowed rural providers of all specialties to consult University of New Mexico dermatologists by sending clinical photographs along with patient information and history via secure messaging. Instead of having the patient travel hundreds of miles to see the nearest dermatologist for their skin condition or endure long wait times to get in to see a specialist, primary providers now can initiate treatment or work-up for their patient’s skin issue in a timely manner with the use of teledermatology to consult specialists.
Teledermatology has demonstrated cost-effectiveness, accuracy, and efficiency in conveniently expanding access to care. It offers patients and dermatologists flexibility in receiving and delivering health care, respectively.7 As residents, learning how to navigate this technologic frontier in health care delivery is imperative, as it will remain a prevalent tool in the future care of our communities, particularly in underserved areas.
Final Thoughts
Through community outreach initiatives, dermatology residents have an opportunity not only to enrich our education but also to connect with and become closer to our patients. Skin cancer screenings, free clinics, and teledermatology have provided ways to reach more communities and remain important aspects of dermatology residency.
- Patel B, Blalock TW. Defining “access to care” for dermatology at academic medical institutions. J Am Acad Dermatol. 2023;89:627-628. doi:10.1016/j.jaad.2023.03.014
- Fritsche M, Maglakelidze N, Zaenglein A, et al. Community outreach initiatives in dermatology: cross-sectional study. Arch Dermatol Res. 2023;315:2693-2695. doi:10.1007/s00403-023-02629-y
- Chiu LW. Teaching tips for dermatology residents. Cutis. 2024;113:E17-E19. doi:10.12788/cutis.1046
- Duniphin DD. Limited access to dermatology specialty care: barriers and teledermatology. Dermatol Pract Concept. 2023;13:E2023031. doi:10.5826/dpc.1301a31
- Ibrahim AE, Magdy M, Khalaf EM, et al. Teledermatology in the time of COVID-19. Int J Clin Pract. 2021;75:e15000. doi:10.1111/ijcp.15000
- Farr MA, Duvic M, Joshi TP. Teledermatology during COVID-19: an updated review. Am J Clin Dermatol. 2021;22:467-475. doi:10.1007/s40257-021-00601-y
- Lipner SR. Optimizing patient care with teledermatology: improving access, efficiency, and satisfaction. Cutis. 2024;114:63-64. doi:10.12788/cutis.1073
- Patel B, Blalock TW. Defining “access to care” for dermatology at academic medical institutions. J Am Acad Dermatol. 2023;89:627-628. doi:10.1016/j.jaad.2023.03.014
- Fritsche M, Maglakelidze N, Zaenglein A, et al. Community outreach initiatives in dermatology: cross-sectional study. Arch Dermatol Res. 2023;315:2693-2695. doi:10.1007/s00403-023-02629-y
- Chiu LW. Teaching tips for dermatology residents. Cutis. 2024;113:E17-E19. doi:10.12788/cutis.1046
- Duniphin DD. Limited access to dermatology specialty care: barriers and teledermatology. Dermatol Pract Concept. 2023;13:E2023031. doi:10.5826/dpc.1301a31
- Ibrahim AE, Magdy M, Khalaf EM, et al. Teledermatology in the time of COVID-19. Int J Clin Pract. 2021;75:e15000. doi:10.1111/ijcp.15000
- Farr MA, Duvic M, Joshi TP. Teledermatology during COVID-19: an updated review. Am J Clin Dermatol. 2021;22:467-475. doi:10.1007/s40257-021-00601-y
- Lipner SR. Optimizing patient care with teledermatology: improving access, efficiency, and satisfaction. Cutis. 2024;114:63-64. doi:10.12788/cutis.1073
Resident Pearls
- Outreach initiatives can help residents feel more connected to their community and expand access to care.
- Skin cancer screenings, free clinics, and teledermatology are a few ways residents may get involved in their local communities.
Eruption of Multiple Linear Hyperpigmented Plaques
THE DIAGNOSIS: Chemotherapy-Induced Flagellate Dermatitis
Based on the clinical presentation and temporal relation with chemotherapy, a diagnosis of bleomycininduced flagellate dermatitis (FD) was made, as bleomycin is the only chemotherapeutic agent from this regimen that has been linked with FD.1,2 Laboratory findings revealed eosinophilia, further supporting a druginduced dermatitis. The patient was treated with oral steroids and diphenhydramine to alleviate itching and discomfort. The chemotherapy was temporarily discontinued until symptomatic improvement was observed within 2 to 3 days.
Flagellate dermatitis is characterized by unique erythematous, linear, intermingled streaks of adjoining firm papules—often preceded by a prodrome of global pruritus—that eventually become hyperpigmented as the erythema subsides. The clinical manifestation of FD can be idiopathic; true/mechanical (dermatitis artefacta, abuse, sadomasochism); chemotherapy induced (peplomycin, trastuzumab, cisplatin, docetaxel, bendamustine); toxin induced (shiitake mushroom, cnidarian stings, Paederus insects); related to rheumatologic diseases (dermatomyositis, adult-onset Still disease), dermatographism, phytophotodermatitis, or poison ivy dermatitis; or induced by chikungunya fever.1
The term flagellate originates from the Latin word flagellum, which pertains to the distinctive whiplike pattern. It was first described by Moulin et al3 in 1970 in reference to bleomycin-induced linear hyperpigmentation. Bleomycin, a glycopeptide antibiotic derived from Streptomyces verticillus, is used to treat Hodgkin lymphoma, squamous cell carcinoma, and germ cell tumors. The worldwide incidence of bleomycin-induced FD is 8% to 22% and commonly is associated with a cumulative dose greater than 100 U.2 Clinical presentation is variable in terms of onset, distribution, and morphology of the eruption and could be independent of dose, route of administration, or type of malignancy being treated. The flagellate rash commonly involves the trunk, arms, and legs; can develop within hours to 6 months of starting bleomycin therapy; often is preceded by generalized itching; and eventually heals with hyperpigmentation.
Possible mechanisms of bleomycin-induced FD include localized melanogenesis, inflammatory pigmentary incontinence, alterations to normal pigmentation patterns, cytotoxic effects of the drug itself, minor trauma/ scratching leading to increased blood flow and causing local accumulation of bleomycin, heat recall, and reduced epidermal turnover leading to extended interaction between keratinocytes and melanocytes.2 Heat exposure can act as a trigger for bleomycin-induced skin rash recall even months after the treatment is stopped.
Apart from discontinuing the drug, there is no specific treatment available for bleomycin-induced FD. The primary objective of treatment is to alleviate pruritus, which often involves the use of topical or systemic corticosteroids and oral antihistamines. The duration of treatment depends on the patient’s clinical response. Once treatment is discontinued, FD typically resolves within 6 to 8 months. However, there can be a permanent postinflammatory hyperpigmentation in the affected area.4 Although there is a concern for increased mortality after postponement of chemotherapy,5 the decision to proceed with or discontinue the chemotherapy regimen necessitates a comprehensive interdisciplinary discussion and a meticulous assessment of the risks and benefits that is customized to each individual patient. Flagellate dermatitis can reoccur with bleomycin re-exposure; a combined approach of proactive topical and systemic steroid treatment seems to diminish the likelihood of FD recurrence.5
Our case underscores the importance of recognizing, detecting, and managing FD promptly in individuals undergoing bleomycin-based chemotherapy. Medical professionals should familiarize themselves with this distinct adverse effect linked to bleomycin, enabling prompt discontinuation if necessary, and educate patients about the condition’s typically temporary nature, thereby alleviating their concerns.
- Bhushan P, Manjul P, Baliyan V. Flagellate dermatoses. Indian J Dermatol Venereol Leprol. 2014;80:149-152.
- Ziemer M, Goetze S, Juhasz K, et al. Flagellate dermatitis as a bleomycinspecific adverse effect of cytostatic therapy: a clinical-histopathologic correlation. Am J Clin Dermatol. 2011;12:68-76. doi:10.2165/11537080-000000000-00000
- Moulin G, Fière B, Beyvin A. Cutaneous pigmentation caused by bleomycin. Article in French. Bull Soc Fr Dermatol Syphiligr. 1970;77:293-296.
- Biswas A, Chaudhari PB, Sharma P, et al. Bleomycin induced flagellate erythema: revisiting a unique complication. J Cancer Res Ther. 2013;9:500-503. doi:10.4103/0973-1482.119358
- Hanna TP, King WD, Thibodeau S, et al. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ. 2020;371:m4087. doi:10.1136/bmj.m4087
THE DIAGNOSIS: Chemotherapy-Induced Flagellate Dermatitis
Based on the clinical presentation and temporal relation with chemotherapy, a diagnosis of bleomycininduced flagellate dermatitis (FD) was made, as bleomycin is the only chemotherapeutic agent from this regimen that has been linked with FD.1,2 Laboratory findings revealed eosinophilia, further supporting a druginduced dermatitis. The patient was treated with oral steroids and diphenhydramine to alleviate itching and discomfort. The chemotherapy was temporarily discontinued until symptomatic improvement was observed within 2 to 3 days.
Flagellate dermatitis is characterized by unique erythematous, linear, intermingled streaks of adjoining firm papules—often preceded by a prodrome of global pruritus—that eventually become hyperpigmented as the erythema subsides. The clinical manifestation of FD can be idiopathic; true/mechanical (dermatitis artefacta, abuse, sadomasochism); chemotherapy induced (peplomycin, trastuzumab, cisplatin, docetaxel, bendamustine); toxin induced (shiitake mushroom, cnidarian stings, Paederus insects); related to rheumatologic diseases (dermatomyositis, adult-onset Still disease), dermatographism, phytophotodermatitis, or poison ivy dermatitis; or induced by chikungunya fever.1
The term flagellate originates from the Latin word flagellum, which pertains to the distinctive whiplike pattern. It was first described by Moulin et al3 in 1970 in reference to bleomycin-induced linear hyperpigmentation. Bleomycin, a glycopeptide antibiotic derived from Streptomyces verticillus, is used to treat Hodgkin lymphoma, squamous cell carcinoma, and germ cell tumors. The worldwide incidence of bleomycin-induced FD is 8% to 22% and commonly is associated with a cumulative dose greater than 100 U.2 Clinical presentation is variable in terms of onset, distribution, and morphology of the eruption and could be independent of dose, route of administration, or type of malignancy being treated. The flagellate rash commonly involves the trunk, arms, and legs; can develop within hours to 6 months of starting bleomycin therapy; often is preceded by generalized itching; and eventually heals with hyperpigmentation.
Possible mechanisms of bleomycin-induced FD include localized melanogenesis, inflammatory pigmentary incontinence, alterations to normal pigmentation patterns, cytotoxic effects of the drug itself, minor trauma/ scratching leading to increased blood flow and causing local accumulation of bleomycin, heat recall, and reduced epidermal turnover leading to extended interaction between keratinocytes and melanocytes.2 Heat exposure can act as a trigger for bleomycin-induced skin rash recall even months after the treatment is stopped.
Apart from discontinuing the drug, there is no specific treatment available for bleomycin-induced FD. The primary objective of treatment is to alleviate pruritus, which often involves the use of topical or systemic corticosteroids and oral antihistamines. The duration of treatment depends on the patient’s clinical response. Once treatment is discontinued, FD typically resolves within 6 to 8 months. However, there can be a permanent postinflammatory hyperpigmentation in the affected area.4 Although there is a concern for increased mortality after postponement of chemotherapy,5 the decision to proceed with or discontinue the chemotherapy regimen necessitates a comprehensive interdisciplinary discussion and a meticulous assessment of the risks and benefits that is customized to each individual patient. Flagellate dermatitis can reoccur with bleomycin re-exposure; a combined approach of proactive topical and systemic steroid treatment seems to diminish the likelihood of FD recurrence.5
Our case underscores the importance of recognizing, detecting, and managing FD promptly in individuals undergoing bleomycin-based chemotherapy. Medical professionals should familiarize themselves with this distinct adverse effect linked to bleomycin, enabling prompt discontinuation if necessary, and educate patients about the condition’s typically temporary nature, thereby alleviating their concerns.
THE DIAGNOSIS: Chemotherapy-Induced Flagellate Dermatitis
Based on the clinical presentation and temporal relation with chemotherapy, a diagnosis of bleomycininduced flagellate dermatitis (FD) was made, as bleomycin is the only chemotherapeutic agent from this regimen that has been linked with FD.1,2 Laboratory findings revealed eosinophilia, further supporting a druginduced dermatitis. The patient was treated with oral steroids and diphenhydramine to alleviate itching and discomfort. The chemotherapy was temporarily discontinued until symptomatic improvement was observed within 2 to 3 days.
Flagellate dermatitis is characterized by unique erythematous, linear, intermingled streaks of adjoining firm papules—often preceded by a prodrome of global pruritus—that eventually become hyperpigmented as the erythema subsides. The clinical manifestation of FD can be idiopathic; true/mechanical (dermatitis artefacta, abuse, sadomasochism); chemotherapy induced (peplomycin, trastuzumab, cisplatin, docetaxel, bendamustine); toxin induced (shiitake mushroom, cnidarian stings, Paederus insects); related to rheumatologic diseases (dermatomyositis, adult-onset Still disease), dermatographism, phytophotodermatitis, or poison ivy dermatitis; or induced by chikungunya fever.1
The term flagellate originates from the Latin word flagellum, which pertains to the distinctive whiplike pattern. It was first described by Moulin et al3 in 1970 in reference to bleomycin-induced linear hyperpigmentation. Bleomycin, a glycopeptide antibiotic derived from Streptomyces verticillus, is used to treat Hodgkin lymphoma, squamous cell carcinoma, and germ cell tumors. The worldwide incidence of bleomycin-induced FD is 8% to 22% and commonly is associated with a cumulative dose greater than 100 U.2 Clinical presentation is variable in terms of onset, distribution, and morphology of the eruption and could be independent of dose, route of administration, or type of malignancy being treated. The flagellate rash commonly involves the trunk, arms, and legs; can develop within hours to 6 months of starting bleomycin therapy; often is preceded by generalized itching; and eventually heals with hyperpigmentation.
Possible mechanisms of bleomycin-induced FD include localized melanogenesis, inflammatory pigmentary incontinence, alterations to normal pigmentation patterns, cytotoxic effects of the drug itself, minor trauma/ scratching leading to increased blood flow and causing local accumulation of bleomycin, heat recall, and reduced epidermal turnover leading to extended interaction between keratinocytes and melanocytes.2 Heat exposure can act as a trigger for bleomycin-induced skin rash recall even months after the treatment is stopped.
Apart from discontinuing the drug, there is no specific treatment available for bleomycin-induced FD. The primary objective of treatment is to alleviate pruritus, which often involves the use of topical or systemic corticosteroids and oral antihistamines. The duration of treatment depends on the patient’s clinical response. Once treatment is discontinued, FD typically resolves within 6 to 8 months. However, there can be a permanent postinflammatory hyperpigmentation in the affected area.4 Although there is a concern for increased mortality after postponement of chemotherapy,5 the decision to proceed with or discontinue the chemotherapy regimen necessitates a comprehensive interdisciplinary discussion and a meticulous assessment of the risks and benefits that is customized to each individual patient. Flagellate dermatitis can reoccur with bleomycin re-exposure; a combined approach of proactive topical and systemic steroid treatment seems to diminish the likelihood of FD recurrence.5
Our case underscores the importance of recognizing, detecting, and managing FD promptly in individuals undergoing bleomycin-based chemotherapy. Medical professionals should familiarize themselves with this distinct adverse effect linked to bleomycin, enabling prompt discontinuation if necessary, and educate patients about the condition’s typically temporary nature, thereby alleviating their concerns.
- Bhushan P, Manjul P, Baliyan V. Flagellate dermatoses. Indian J Dermatol Venereol Leprol. 2014;80:149-152.
- Ziemer M, Goetze S, Juhasz K, et al. Flagellate dermatitis as a bleomycinspecific adverse effect of cytostatic therapy: a clinical-histopathologic correlation. Am J Clin Dermatol. 2011;12:68-76. doi:10.2165/11537080-000000000-00000
- Moulin G, Fière B, Beyvin A. Cutaneous pigmentation caused by bleomycin. Article in French. Bull Soc Fr Dermatol Syphiligr. 1970;77:293-296.
- Biswas A, Chaudhari PB, Sharma P, et al. Bleomycin induced flagellate erythema: revisiting a unique complication. J Cancer Res Ther. 2013;9:500-503. doi:10.4103/0973-1482.119358
- Hanna TP, King WD, Thibodeau S, et al. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ. 2020;371:m4087. doi:10.1136/bmj.m4087
- Bhushan P, Manjul P, Baliyan V. Flagellate dermatoses. Indian J Dermatol Venereol Leprol. 2014;80:149-152.
- Ziemer M, Goetze S, Juhasz K, et al. Flagellate dermatitis as a bleomycinspecific adverse effect of cytostatic therapy: a clinical-histopathologic correlation. Am J Clin Dermatol. 2011;12:68-76. doi:10.2165/11537080-000000000-00000
- Moulin G, Fière B, Beyvin A. Cutaneous pigmentation caused by bleomycin. Article in French. Bull Soc Fr Dermatol Syphiligr. 1970;77:293-296.
- Biswas A, Chaudhari PB, Sharma P, et al. Bleomycin induced flagellate erythema: revisiting a unique complication. J Cancer Res Ther. 2013;9:500-503. doi:10.4103/0973-1482.119358
- Hanna TP, King WD, Thibodeau S, et al. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ. 2020;371:m4087. doi:10.1136/bmj.m4087
A 28-year-old man presented for evaluation of an intensely itchy rash of 5 days’ duration involving the face, trunk, arms, and legs. The patient recently had been diagnosed with classical Hodgkin lymphoma and was started on a biweekly chemotherapy regimen of adriamycin, bleomycin, vinblastine, and dacarbazine 3 weeks prior. He reported that a red, itchy, papular rash had developed on the hands 1 week after starting chemotherapy and improved with antihistamines. Symptoms of the current rash included night sweats, occasional fever, substantial unintentional weight loss, and fatigue. He had no history of urticaria, angioedema, anaphylaxis, or nail changes.
Physical examination revealed widespread, itchy, linear and curvilinear hyperpigmented plaques on the upper arms, shoulders, back (top), face, and thighs, as well as erythematous grouped papules on the bilateral palms (bottom). There was no mucosal or systemic involvement.

Six Tips for Media Interviews
As a physician, you might be contacted by the media to provide your professional opinion and advice. Or you might be looking for media interview opportunities to market your practice or side project. And if you do research, media interviews can be an effective way to spread the word. It’s important to prepare for a media interview so that you achieve the outcome you are looking for.
Keep your message simple. When you are a subject expert, you might think that the basics are obvious or even boring, and that the nuances are more important. However, most of the audience is looking for big-picture information that they can apply to their lives. Consider a few key takeaways, keeping in mind that your interview is likely to be edited to short sound bites or a few quotes. It may help to jot down notes so that you cover the fundamentals clearly. You could even write and rehearse a script beforehand. If there is something complicated or subtle that you want to convey, you can preface it by saying, “This is confusing but very important …” to let the audience know to give extra consideration to what you are about to say.
Avoid extremes and hyperbole. Sometimes, exaggerated statements make their way into medical discussions. Statements such as “it doesn’t matter how many calories you consume — it’s all about the quality” are common oversimplifications. But you might be upset to see your name next to a comment like this because it is not actually correct. Check the phrasing of your key takeaways to avoid being stuck defending or explaining an inaccurate statement when your patients ask you about it later.
Ask the interviewers what they are looking for. Many medical topics have some controversial element, so it is good to know what you’re getting into. Find out the purpose of the article or interview before you decide whether it is right for you. It could be about another doctor in town who is being sued; if you don’t want to be associated with that story, it might be best to decline the interview.
Explain your goals. You might accept or pursue an interview to raise awareness about an underrecognized condition. You might want the public to identify and get help for early symptoms, or you might want to create empathy for people coping with a disease you treat. Consider why you are participating in an interview, and communicate that to the interviewer to ensure that your objective can be part of the final product.
Know whom you’re dealing with. It is good to learn about the publication/media channel before you agree to participate. It may have a political bias, or perhaps the interview is intended to promote a specific product. If you agree with and support their purposes, then you may be happy to lend your opinion. But learning about the “voice” of the publication in advance allows you to make an informed decision about whether you want to be identified with a particular political ideology or product endorsement.
Ask to see your quotes before publication. It’s good to have the opportunity to make corrections in case you are accidentally misquoted or misunderstood. It is best to ask to see quotes before you agree to the interview. Some reporters may agree to (or even prefer) a written question-and-answer format so that they can directly quote your responses without rephrasing your words. You could suggest this, especially if you are too busy for a call or live meeting.
As a physician, your insights and advice can be highly beneficial to others. You can also use media interviews to propel your career forward. Doing your homework can ensure that you will be pleased with the final product and how your words were used.
Dr. Moawad, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
As a physician, you might be contacted by the media to provide your professional opinion and advice. Or you might be looking for media interview opportunities to market your practice or side project. And if you do research, media interviews can be an effective way to spread the word. It’s important to prepare for a media interview so that you achieve the outcome you are looking for.
Keep your message simple. When you are a subject expert, you might think that the basics are obvious or even boring, and that the nuances are more important. However, most of the audience is looking for big-picture information that they can apply to their lives. Consider a few key takeaways, keeping in mind that your interview is likely to be edited to short sound bites or a few quotes. It may help to jot down notes so that you cover the fundamentals clearly. You could even write and rehearse a script beforehand. If there is something complicated or subtle that you want to convey, you can preface it by saying, “This is confusing but very important …” to let the audience know to give extra consideration to what you are about to say.
Avoid extremes and hyperbole. Sometimes, exaggerated statements make their way into medical discussions. Statements such as “it doesn’t matter how many calories you consume — it’s all about the quality” are common oversimplifications. But you might be upset to see your name next to a comment like this because it is not actually correct. Check the phrasing of your key takeaways to avoid being stuck defending or explaining an inaccurate statement when your patients ask you about it later.
Ask the interviewers what they are looking for. Many medical topics have some controversial element, so it is good to know what you’re getting into. Find out the purpose of the article or interview before you decide whether it is right for you. It could be about another doctor in town who is being sued; if you don’t want to be associated with that story, it might be best to decline the interview.
Explain your goals. You might accept or pursue an interview to raise awareness about an underrecognized condition. You might want the public to identify and get help for early symptoms, or you might want to create empathy for people coping with a disease you treat. Consider why you are participating in an interview, and communicate that to the interviewer to ensure that your objective can be part of the final product.
Know whom you’re dealing with. It is good to learn about the publication/media channel before you agree to participate. It may have a political bias, or perhaps the interview is intended to promote a specific product. If you agree with and support their purposes, then you may be happy to lend your opinion. But learning about the “voice” of the publication in advance allows you to make an informed decision about whether you want to be identified with a particular political ideology or product endorsement.
Ask to see your quotes before publication. It’s good to have the opportunity to make corrections in case you are accidentally misquoted or misunderstood. It is best to ask to see quotes before you agree to the interview. Some reporters may agree to (or even prefer) a written question-and-answer format so that they can directly quote your responses without rephrasing your words. You could suggest this, especially if you are too busy for a call or live meeting.
As a physician, your insights and advice can be highly beneficial to others. You can also use media interviews to propel your career forward. Doing your homework can ensure that you will be pleased with the final product and how your words were used.
Dr. Moawad, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
As a physician, you might be contacted by the media to provide your professional opinion and advice. Or you might be looking for media interview opportunities to market your practice or side project. And if you do research, media interviews can be an effective way to spread the word. It’s important to prepare for a media interview so that you achieve the outcome you are looking for.
Keep your message simple. When you are a subject expert, you might think that the basics are obvious or even boring, and that the nuances are more important. However, most of the audience is looking for big-picture information that they can apply to their lives. Consider a few key takeaways, keeping in mind that your interview is likely to be edited to short sound bites or a few quotes. It may help to jot down notes so that you cover the fundamentals clearly. You could even write and rehearse a script beforehand. If there is something complicated or subtle that you want to convey, you can preface it by saying, “This is confusing but very important …” to let the audience know to give extra consideration to what you are about to say.
Avoid extremes and hyperbole. Sometimes, exaggerated statements make their way into medical discussions. Statements such as “it doesn’t matter how many calories you consume — it’s all about the quality” are common oversimplifications. But you might be upset to see your name next to a comment like this because it is not actually correct. Check the phrasing of your key takeaways to avoid being stuck defending or explaining an inaccurate statement when your patients ask you about it later.
Ask the interviewers what they are looking for. Many medical topics have some controversial element, so it is good to know what you’re getting into. Find out the purpose of the article or interview before you decide whether it is right for you. It could be about another doctor in town who is being sued; if you don’t want to be associated with that story, it might be best to decline the interview.
Explain your goals. You might accept or pursue an interview to raise awareness about an underrecognized condition. You might want the public to identify and get help for early symptoms, or you might want to create empathy for people coping with a disease you treat. Consider why you are participating in an interview, and communicate that to the interviewer to ensure that your objective can be part of the final product.
Know whom you’re dealing with. It is good to learn about the publication/media channel before you agree to participate. It may have a political bias, or perhaps the interview is intended to promote a specific product. If you agree with and support their purposes, then you may be happy to lend your opinion. But learning about the “voice” of the publication in advance allows you to make an informed decision about whether you want to be identified with a particular political ideology or product endorsement.
Ask to see your quotes before publication. It’s good to have the opportunity to make corrections in case you are accidentally misquoted or misunderstood. It is best to ask to see quotes before you agree to the interview. Some reporters may agree to (or even prefer) a written question-and-answer format so that they can directly quote your responses without rephrasing your words. You could suggest this, especially if you are too busy for a call or live meeting.
As a physician, your insights and advice can be highly beneficial to others. You can also use media interviews to propel your career forward. Doing your homework can ensure that you will be pleased with the final product and how your words were used.
Dr. Moawad, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Study Finds Elevated Skin Cancer Risk Among US Veterans
of recent national data.
“US veterans are known to have increased risk of cancers and cancer morbidity compared to the general US population,” one of the study authors, Sepideh Ashrafzadeh, MD, a third-year dermatology resident at Massachusetts General Hospital, Boston, told this news organization following the annual meeting of the American Society for Dermatologic Surgery, where the results were presented. “There have been several studies that have shown that US veterans have an increased prevalence of melanoma compared to nonveterans,” she said, noting, however, that no study has investigated the prevalence of nonmelanoma skin cancers (NMSCs), which include basal cell carcinomas and squamous cell carcinomas, compared with the general population.
To address this knowledge gap, the researchers performed a national cross-sectional study of adults aged 18 years or older from the 2019-2023 National Health Interview Surveys to examine the prevalence of melanoma and NMSCs among veterans compared with the general US population. They aggregated and tabulated the data by veteran status, defined as having served at any point in the US armed forces, reserves, or national guard, and by demographic and socioeconomic status variables. Next, they performed multivariate logistic regression for skin cancer risk adjusted for age, sex, race, ethnicity, urbanicity, and disability status.
The study population consisted of 14,301 veterans and 209,936 nonveterans. Compared with nonveterans, veterans were more likely to have been diagnosed with skin cancer at some point in their lives (7% vs 2.4%; P < .001); had a higher mean age of skin cancer diagnosis (61.1 vs 55.8 years; P < .001); were more likely to have been diagnosed with melanoma (2.8% vs 0.9%; P < .001), and were more likely to have been diagnosed with NMSC (4.4% vs 1.6%; P < .001).
The researchers found that older age, White race, non-Hispanic ethnicity, and veteran status were all associated with higher odds of developing NMSCs, even after adjusting for relevant covariates. Specifically, veterans had 1.23 higher odds of developing NMSC than the general population, while two factors were protective for developing NMSCs: Living in a rural setting (adjusted odds ratio [aOR], 0.78) and receiving supplemental security income or disability income (aOR, 0.69).
In another part of the study, the researchers evaluated demographic and socioeconomic variables associated with developing melanoma among veterans. These included the following: Male (aOR, 1.16), older age (50-64 years: aOR, 6.82; 65-74 years: aOR, 12.55; and 75 years or older: aOR, 16.16), White race (aOR, 9.24), and non-Hispanic ethnicity (aOR, 7.15).
“Veterans may have occupational risks such as sun and chemical exposure, as well as behavioral habits for sun protection, that may contribute to their elevated risk of melanoma and NMSCs,” Ashrafzadeh said. “Therefore, US veterans would benefit from targeted and regular skin cancer screenings, sun protective preventative resources such as hats and sunscreen, and access to medical and surgical care for diagnosis and treatment of skin cancers.”
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Connecticut, who was asked to comment on the findings, said that a key strength of the study is that it drew from a nationally representative sample. “A limitation is that skin cancer was self-reported rather than based on documented medical histories,” Ko said. “The study confirms that skin cancer risk is higher in older individuals (> 75 as compared to < 50) and in individuals of self-reported white race and non-Hispanic ethnicity,” she added.
Neither the researchers nor Ko reported having relevant disclosures.
A version of this article first appeared on Medscape.com.
of recent national data.
“US veterans are known to have increased risk of cancers and cancer morbidity compared to the general US population,” one of the study authors, Sepideh Ashrafzadeh, MD, a third-year dermatology resident at Massachusetts General Hospital, Boston, told this news organization following the annual meeting of the American Society for Dermatologic Surgery, where the results were presented. “There have been several studies that have shown that US veterans have an increased prevalence of melanoma compared to nonveterans,” she said, noting, however, that no study has investigated the prevalence of nonmelanoma skin cancers (NMSCs), which include basal cell carcinomas and squamous cell carcinomas, compared with the general population.
To address this knowledge gap, the researchers performed a national cross-sectional study of adults aged 18 years or older from the 2019-2023 National Health Interview Surveys to examine the prevalence of melanoma and NMSCs among veterans compared with the general US population. They aggregated and tabulated the data by veteran status, defined as having served at any point in the US armed forces, reserves, or national guard, and by demographic and socioeconomic status variables. Next, they performed multivariate logistic regression for skin cancer risk adjusted for age, sex, race, ethnicity, urbanicity, and disability status.
The study population consisted of 14,301 veterans and 209,936 nonveterans. Compared with nonveterans, veterans were more likely to have been diagnosed with skin cancer at some point in their lives (7% vs 2.4%; P < .001); had a higher mean age of skin cancer diagnosis (61.1 vs 55.8 years; P < .001); were more likely to have been diagnosed with melanoma (2.8% vs 0.9%; P < .001), and were more likely to have been diagnosed with NMSC (4.4% vs 1.6%; P < .001).
The researchers found that older age, White race, non-Hispanic ethnicity, and veteran status were all associated with higher odds of developing NMSCs, even after adjusting for relevant covariates. Specifically, veterans had 1.23 higher odds of developing NMSC than the general population, while two factors were protective for developing NMSCs: Living in a rural setting (adjusted odds ratio [aOR], 0.78) and receiving supplemental security income or disability income (aOR, 0.69).
In another part of the study, the researchers evaluated demographic and socioeconomic variables associated with developing melanoma among veterans. These included the following: Male (aOR, 1.16), older age (50-64 years: aOR, 6.82; 65-74 years: aOR, 12.55; and 75 years or older: aOR, 16.16), White race (aOR, 9.24), and non-Hispanic ethnicity (aOR, 7.15).
“Veterans may have occupational risks such as sun and chemical exposure, as well as behavioral habits for sun protection, that may contribute to their elevated risk of melanoma and NMSCs,” Ashrafzadeh said. “Therefore, US veterans would benefit from targeted and regular skin cancer screenings, sun protective preventative resources such as hats and sunscreen, and access to medical and surgical care for diagnosis and treatment of skin cancers.”
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Connecticut, who was asked to comment on the findings, said that a key strength of the study is that it drew from a nationally representative sample. “A limitation is that skin cancer was self-reported rather than based on documented medical histories,” Ko said. “The study confirms that skin cancer risk is higher in older individuals (> 75 as compared to < 50) and in individuals of self-reported white race and non-Hispanic ethnicity,” she added.
Neither the researchers nor Ko reported having relevant disclosures.
A version of this article first appeared on Medscape.com.
of recent national data.
“US veterans are known to have increased risk of cancers and cancer morbidity compared to the general US population,” one of the study authors, Sepideh Ashrafzadeh, MD, a third-year dermatology resident at Massachusetts General Hospital, Boston, told this news organization following the annual meeting of the American Society for Dermatologic Surgery, where the results were presented. “There have been several studies that have shown that US veterans have an increased prevalence of melanoma compared to nonveterans,” she said, noting, however, that no study has investigated the prevalence of nonmelanoma skin cancers (NMSCs), which include basal cell carcinomas and squamous cell carcinomas, compared with the general population.
To address this knowledge gap, the researchers performed a national cross-sectional study of adults aged 18 years or older from the 2019-2023 National Health Interview Surveys to examine the prevalence of melanoma and NMSCs among veterans compared with the general US population. They aggregated and tabulated the data by veteran status, defined as having served at any point in the US armed forces, reserves, or national guard, and by demographic and socioeconomic status variables. Next, they performed multivariate logistic regression for skin cancer risk adjusted for age, sex, race, ethnicity, urbanicity, and disability status.
The study population consisted of 14,301 veterans and 209,936 nonveterans. Compared with nonveterans, veterans were more likely to have been diagnosed with skin cancer at some point in their lives (7% vs 2.4%; P < .001); had a higher mean age of skin cancer diagnosis (61.1 vs 55.8 years; P < .001); were more likely to have been diagnosed with melanoma (2.8% vs 0.9%; P < .001), and were more likely to have been diagnosed with NMSC (4.4% vs 1.6%; P < .001).
The researchers found that older age, White race, non-Hispanic ethnicity, and veteran status were all associated with higher odds of developing NMSCs, even after adjusting for relevant covariates. Specifically, veterans had 1.23 higher odds of developing NMSC than the general population, while two factors were protective for developing NMSCs: Living in a rural setting (adjusted odds ratio [aOR], 0.78) and receiving supplemental security income or disability income (aOR, 0.69).
In another part of the study, the researchers evaluated demographic and socioeconomic variables associated with developing melanoma among veterans. These included the following: Male (aOR, 1.16), older age (50-64 years: aOR, 6.82; 65-74 years: aOR, 12.55; and 75 years or older: aOR, 16.16), White race (aOR, 9.24), and non-Hispanic ethnicity (aOR, 7.15).
“Veterans may have occupational risks such as sun and chemical exposure, as well as behavioral habits for sun protection, that may contribute to their elevated risk of melanoma and NMSCs,” Ashrafzadeh said. “Therefore, US veterans would benefit from targeted and regular skin cancer screenings, sun protective preventative resources such as hats and sunscreen, and access to medical and surgical care for diagnosis and treatment of skin cancers.”
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Connecticut, who was asked to comment on the findings, said that a key strength of the study is that it drew from a nationally representative sample. “A limitation is that skin cancer was self-reported rather than based on documented medical histories,” Ko said. “The study confirms that skin cancer risk is higher in older individuals (> 75 as compared to < 50) and in individuals of self-reported white race and non-Hispanic ethnicity,” she added.
Neither the researchers nor Ko reported having relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM ASDS 2024
Cancer’s Other Toll: Long-Term Financial Fallout for Survivors
Overall, patients with cancer tend to face higher rates of debt collection, medical collections, and bankruptcies, as well as lower credit scores, according to two new studies presented at the American College of Surgeons Clinical Congress 2024.
“These are the first studies to provide numerical evidence of financial toxicity among cancer survivors,” Benjamin C. James, MD, with Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, Massachusetts, who worked on both studies, said in a statement. “Previous data on this topic largely relies on subjective survey reviews.”
In one study, researchers used the Massachusetts Cancer Registry to identify 99,175 patients diagnosed with cancer between 2010 and 2019 and matched them with 188,875 control individuals without cancer. Researchers then assessed financial toxicity using Experian credit bureau data for participants.
Overall, patients with cancer faced a range of financial challenges that often lasted years following their diagnosis.
Patients were nearly five times more likely to experience bankruptcy and had average credit scores nearly 80 points lower than control individuals without cancer. The drop in credit scores was more pronounced for survivors of bladder, liver, lung, and colorectal cancer (CRC) and persisted for up to 9.5 years.
For certain cancer types, in particular, “we are looking years after a diagnosis, and we see that the credit score goes down and it never comes back up,” James said.
The other study, which used a sample of 7227 patients with CRC from Massachusetts, identified several factors that correlated with lower credit scores.
Compared with patients who only had surgery, peers who underwent radiation only experienced a 62-point drop in their credit score after their diagnosis, while those who had chemotherapy alone had just over a 14-point drop in their credit score. Among patients who had combination treatments, those who underwent both surgery and radiation experienced a nearly 16-point drop in their credit score and those who had surgery and chemoradiation actually experienced a 2.59 bump, compared with those who had surgery alone.
Financial toxicity was worse for patients younger than 62 years, those identifying as Black or Hispanic individuals, unmarried individuals, those with an annual income below $52,000, and those living in deprived areas.
The studies add to findings from the 2015 North American Thyroid Cancer Survivorship Study, which reported that 50% of thyroid cancer survivors encountered financial toxicity because of their diagnosis.
James said the persistent financial strain of cancer care, even in a state like Massachusetts, which mandates universal healthcare, underscores the need for “broader policy changes and reforms, including reconsidering debt collection practices.”
“Financial security should be a priority in cancer care,” he added.
The studies had no specific funding. The authors have disclosed no relevant conflict of interest.
A version of this article first appeared on Medscape.com.
Overall, patients with cancer tend to face higher rates of debt collection, medical collections, and bankruptcies, as well as lower credit scores, according to two new studies presented at the American College of Surgeons Clinical Congress 2024.
“These are the first studies to provide numerical evidence of financial toxicity among cancer survivors,” Benjamin C. James, MD, with Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, Massachusetts, who worked on both studies, said in a statement. “Previous data on this topic largely relies on subjective survey reviews.”
In one study, researchers used the Massachusetts Cancer Registry to identify 99,175 patients diagnosed with cancer between 2010 and 2019 and matched them with 188,875 control individuals without cancer. Researchers then assessed financial toxicity using Experian credit bureau data for participants.
Overall, patients with cancer faced a range of financial challenges that often lasted years following their diagnosis.
Patients were nearly five times more likely to experience bankruptcy and had average credit scores nearly 80 points lower than control individuals without cancer. The drop in credit scores was more pronounced for survivors of bladder, liver, lung, and colorectal cancer (CRC) and persisted for up to 9.5 years.
For certain cancer types, in particular, “we are looking years after a diagnosis, and we see that the credit score goes down and it never comes back up,” James said.
The other study, which used a sample of 7227 patients with CRC from Massachusetts, identified several factors that correlated with lower credit scores.
Compared with patients who only had surgery, peers who underwent radiation only experienced a 62-point drop in their credit score after their diagnosis, while those who had chemotherapy alone had just over a 14-point drop in their credit score. Among patients who had combination treatments, those who underwent both surgery and radiation experienced a nearly 16-point drop in their credit score and those who had surgery and chemoradiation actually experienced a 2.59 bump, compared with those who had surgery alone.
Financial toxicity was worse for patients younger than 62 years, those identifying as Black or Hispanic individuals, unmarried individuals, those with an annual income below $52,000, and those living in deprived areas.
The studies add to findings from the 2015 North American Thyroid Cancer Survivorship Study, which reported that 50% of thyroid cancer survivors encountered financial toxicity because of their diagnosis.
James said the persistent financial strain of cancer care, even in a state like Massachusetts, which mandates universal healthcare, underscores the need for “broader policy changes and reforms, including reconsidering debt collection practices.”
“Financial security should be a priority in cancer care,” he added.
The studies had no specific funding. The authors have disclosed no relevant conflict of interest.
A version of this article first appeared on Medscape.com.
Overall, patients with cancer tend to face higher rates of debt collection, medical collections, and bankruptcies, as well as lower credit scores, according to two new studies presented at the American College of Surgeons Clinical Congress 2024.
“These are the first studies to provide numerical evidence of financial toxicity among cancer survivors,” Benjamin C. James, MD, with Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, Massachusetts, who worked on both studies, said in a statement. “Previous data on this topic largely relies on subjective survey reviews.”
In one study, researchers used the Massachusetts Cancer Registry to identify 99,175 patients diagnosed with cancer between 2010 and 2019 and matched them with 188,875 control individuals without cancer. Researchers then assessed financial toxicity using Experian credit bureau data for participants.
Overall, patients with cancer faced a range of financial challenges that often lasted years following their diagnosis.
Patients were nearly five times more likely to experience bankruptcy and had average credit scores nearly 80 points lower than control individuals without cancer. The drop in credit scores was more pronounced for survivors of bladder, liver, lung, and colorectal cancer (CRC) and persisted for up to 9.5 years.
For certain cancer types, in particular, “we are looking years after a diagnosis, and we see that the credit score goes down and it never comes back up,” James said.
The other study, which used a sample of 7227 patients with CRC from Massachusetts, identified several factors that correlated with lower credit scores.
Compared with patients who only had surgery, peers who underwent radiation only experienced a 62-point drop in their credit score after their diagnosis, while those who had chemotherapy alone had just over a 14-point drop in their credit score. Among patients who had combination treatments, those who underwent both surgery and radiation experienced a nearly 16-point drop in their credit score and those who had surgery and chemoradiation actually experienced a 2.59 bump, compared with those who had surgery alone.
Financial toxicity was worse for patients younger than 62 years, those identifying as Black or Hispanic individuals, unmarried individuals, those with an annual income below $52,000, and those living in deprived areas.
The studies add to findings from the 2015 North American Thyroid Cancer Survivorship Study, which reported that 50% of thyroid cancer survivors encountered financial toxicity because of their diagnosis.
James said the persistent financial strain of cancer care, even in a state like Massachusetts, which mandates universal healthcare, underscores the need for “broader policy changes and reforms, including reconsidering debt collection practices.”
“Financial security should be a priority in cancer care,” he added.
The studies had no specific funding. The authors have disclosed no relevant conflict of interest.
A version of this article first appeared on Medscape.com.
FROM ACSCS 2024
Asteraceae Dermatitis: Everyday Plants With Allergenic Potential
The Asteraceae (formerly Compositae) family of plants is derived from the ancient Greek word aster, meaning “star,” referring to the starlike arrangement of flower petals around a central disc known as a capitulum. What initially appears as a single flower is actually a composite of several smaller flowers, hence the former name Compositae.1 Well-known members of the Asteraceae family include ornamental annuals (eg, sunflowers, marigolds, cosmos), herbaceous perennials (eg, chrysanthemums, dandelions), vegetables (eg, lettuce, chicory, artichokes), herbs (eg, chamomile, tarragon), and weeds (eg, ragweed, horseweed, capeweed)(Figure 1).2

There are more than 25,000 species of Asteraceae plants that thrive in a wide range of climates worldwide. Cases of Asteraceae-induced skin reactions have been reported in North America, Europe, Asia, and Australia.3 Members of the Asteraceae family are ubiquitous in gardens, along roadsides, and in the wilderness. Occupational exposure commonly affects gardeners, florists, farmers, and forestry workers through either direct contact with plants or via airborne pollen. Furthermore, plants of the Asteraceae family are used in various products, including pediculicides (eg, insect repellents), cosmetics (eg, eye creams, body washes), and food products (eg, cooking oils, sweetening agents, coffee substitutes, herbal teas).4-6 These plants have substantial allergic potential, resulting in numerous cutaneous reactions.
Allergic Potential
Asteraceae plants can elicit both immediate and delayed hypersensitivity reactions (HSRs); for instance, exposure to ragweed pollen may cause an IgE-mediated type 1 HSR manifesting as allergic rhinitis or a type IV HSR manifesting as airborne allergic contact dermatitis.7,8 The main contact allergens present in Asteraceae plants are sesquiterpene lactones, which are found in the leaves, stems, flowers, and pollen.9-11 Sesquiterpene lactones consist of an α-methyl group attached to a lactone ring combined with a sesquiterpene.12 Patch testing can be used to diagnose Asteraceae allergy; however, the results are not consistently reliable because there is no perfect screening allergen. Patch test preparations commonly used to detect Asteraceae allergy include Compositae mix (consisting of Anthemis nobilis extract, Chamomilla recutita extract, Achillea millefolium extract, Tanacetum vulgare extract, Arnica montana extract, and parthenolide) and sesquiterpene lactone mix (consisting of alantolactone, dehydrocostus lactone, and costunolide). In North America, the prevalence of positive patch tests to Compositae mix and sesquiterpene lactone mix is approximately 2% and 0.5%, respectively.13 When patch testing is performed, both Compositae mix and sesquiterpene lactone mix should be utilized to minimize the risk of missing Asteraceae allergy, as sesquiterpene lactone mix alone does not detect all Compositae-sensitized patients. Additionally, it may be necessary to test supplemental Asteraceae allergens, including preparations from specific plants to which the patient has been exposed. Exposure to Asteraceae-containing cosmetic products may lead to dermatitis, though this is highly dependent on the particular plant species involved. For instance, the prevalence of sensitization is high in arnica (tincture) and elecampane but low with more commonly used species such as German chamomile.14
Cutaneous Manifestations
Asteraceae dermatitis, which also is known as Australian bush dermatitis, weed dermatitis, and chrysanthemum dermatitis,2 can manifest on any area of the body that directly contacts the plant or is exposed to the pollen. Asteraceae dermatitis historically was reported in older adults with a recent history of plant exposure.6,15 However, recent data have shown a female preponderance and a younger mean age of onset (46–49 years).16
There are multiple distinct clinical manifestations of Asteraceae dermatitis. The most common cutaneous finding is localized vesicular or eczematous patches on the hands or wrists. Other variations include eczematous rashes on the exposed skin of the hands, arms, face, and neck; generalized eczema; and isolated facial eczema.16,17 These variations can be attributed to contact dermatitis caused by airborne pollen, which may mimic photodermatitis. However, airborne Asteraceae dermatitis can be distinguished clinically from photodermatitis by the involvement of sun-protected areas such as the skinfolds of the eyelids, retroauricular sulci, and nasolabial folds (Figure 2).2,9 In rare cases, systemic allergic contact dermatitis can occur if the Asteraceae allergen is ingested.2,18
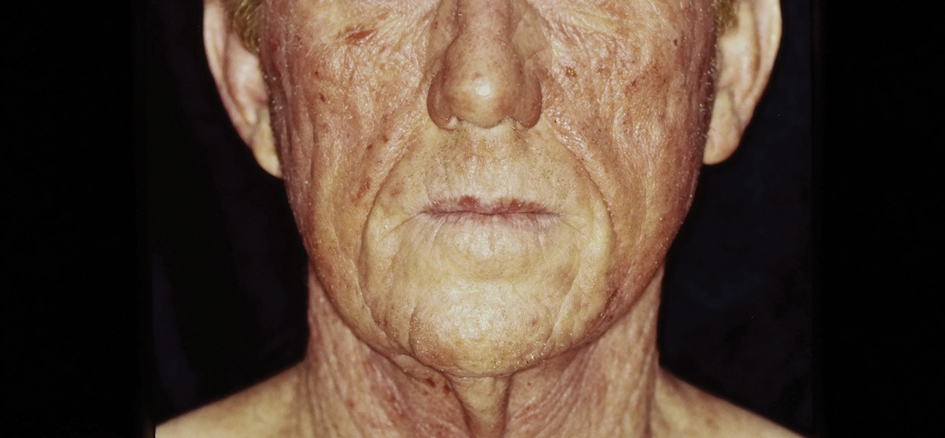
Other diagnostic clues include dermatitis that flares during the summer, at the peak of the growing season, with remission in the cooler months. Potential risk factors include a childhood history of atopic dermatitis and allergic rhinitis.16 With prolonged exposure, patients may develop chronic actinic dermatitis, an immunologically mediated photodermatosis characterized by lichenified and pruritic eczematous plaques located predominantly on sun-exposed areas with notable sparing of the skin folds.19 The association between Asteraceae dermatitis and chronic actinic dermatitis is highly variable, with some studies reporting a 25% correlation and others finding a stronger association of up to 80%.2,15,20 Asteraceae allergy appears to be a relatively uncommon cause of photoallergy in North America. In one recent study, 16% (3/19) of patients with chronic actinic dermatitis had positive patch or photopatch tests to sesquiterpene lactone mix, but in another large study of photopatch testing it was reported to be a rare photoallergen.21,22
Parthenium dermatitis is an allergic contact dermatitis caused by exposure to Parthenium hysterophorus, a weed of the Asteraceae family that is responsible for 30% of cases of contact dermatitis in India.23,24 Unlike the more classic manifestation of Asteraceae dermatitis, which primarily affects the upper extremities in cases from North America and Europe, Parthenium dermatitis typically occurs in an airborne pattern distribution.24
Management
While complete avoidance of Asteraceae plants is ideal, it often is unrealistic due to their abundance in nature. Therefore, minimizing exposure to the causative plants is recommended. Primary preventive measures such as wearing protective gloves and clothing and applying bentonite clay prior to exposure should be taken when working outdoors. Promptly showering after contact with plants also can reduce the risk for Asteraceae dermatitis.
Symptomatic treatment is appropriate for mild cases and includes topical corticosteroids and calcineurin inhibitors. For severe cases, systemic corticosteroids may be needed for acute flares, with azathioprine, mycophenolate, cyclosporine, or methotrexate available for recalcitrant disease. Verma et al25 found that treatment with azathioprine for 6 months resulted in greater than 60% clearance in all 12 patients, with a majority achieving 80% to 100% clearance. Methotrexate has been used at doses of 15 mg once weekly.26 Narrowband UVB and psoralen plus UVA have been effective in extensive cases; however, care should be exercised in patients with photosensitive dermatitis, who instead should practice strict photoprotection.27-29 Lakshmi et al30 reported the use of cyclosporine during the acute phase of Asteraceae dermatitis at a dose of 2.5 mg/kg daily for 4 to 8 weeks. There have been several case reports of dupilumab treating allergic contact dermatitis; however, there have been 3 cases of patients with atopic dermatitis developing Asteraceae dermatitis while taking dupilumab.31,32 Recently, oral Janus kinase inhibitors have shown success in treating refractory cases of airborne Asteraceae dermatitis.33,34 Further research is needed to determine the safety and efficacy of dupilumab and Janus kinase inhibitors for treatment of Asteraceae dermatitis.
Final Thoughts
The Asteraceae plant family is vast and diverse, with more than 200 species reported to cause allergic contact dermatitis.12 Common modes of contact include gardening, occupational exposure, airborne pollen, and use of pediculicides and cosmetics that contain components of Asteraceae plants. Educating patients on how to minimize contact with Asteraceae plants is the most effective management strategy; topical agents and oral immunosuppressives can be used for symptomatic treatment.
- Morhardt S, Morhardt E. California Desert Flowers: An Introduction to Families, Genera, and Species. University of California Press; 2004.
- Gordon LA. Compositae dermatitis. Australas J Dermatol. 1999;40:123-130. doi:10.1046/j.1440-0960.1999.00341.x
- Denisow-Pietrzyk M, Pietrzyk Ł, Denisow B. Asteraceae species as potential environmental factors of allergy. Environ Sci Pollut Res Int. 2019;26:6290-6300. doi:10.1007/s11356-019-04146-w
- Paulsen E, Chistensen LP, Andersen KE. Cosmetics and herbal remedies with Compositae plant extracts—are they tolerated by Compositae-allergic patients? Contact Dermatitis. 2008;58:15-23. doi:10.1111/j.1600-0536.2007.01250.x
- Burry JN, Reid JG, Kirk J. Australian bush dermatitis. Contact Dermatitis. 1975;1:263-264. doi:10.1111/j.1600-0536.1975.tb05422.x
- Punchihewa N, Palmer A, Nixon R. Allergic contact dermatitis to Compositae: an Australian case series. Contact Dermatitis. 2022;87:356-362. doi:10.1111/cod.14162
- Chen KW, Marusciac L, Tamas PT, et al. Ragweed pollen allergy: burden, characteristics, and management of an imported allergen source in Europe. Int Arch Allergy Immunol. 2018;176:163-180. doi:10.1159/000487997
- Schloemer JA, Zirwas MJ, Burkhart CG. Airborne contact dermatitis: common causes in the USA. Int J Dermatol. 2015;54:271-274. doi:10.1111/ijd.12692
- Arlette J, Mitchell JC. Compositae dermatitis. current aspects. Contact Dermatitis. 1981;7:129-136. doi:10.1111/j.1600-0536.1981.tb04584.x
- Mitchell JC, Dupuis G. Allergic contact dermatitis from sesquiterpenoids of the Compositae family of plants. Br J Dermatol. 1971;84:139-150. doi:10.1111/j.1365-2133.1971.tb06857.x
- Salapovic H, Geier J, Reznicek G. Quantification of Sesquiterpene lactones in Asteraceae plant extracts: evaluation of their allergenic potential. Sci Pharm. 2013;81:807-818. doi:10.3797/scipharm.1306-17
- Paulsen E. Compositae dermatitis: a survey. Contact Dermatitis. 1992;26:76-86. doi:10.1111/j.1600-0536.1992.tb00888.x. Published correction appears in Contact Dermatitis. 1992;27:208.
- DeKoven JG, Silverberg JI, Warshaw EM, et al. North American Contact Dermatitis Group patch test results: 2017-2018. Dermatitis. 2021;32:111-123. doi:10.1097/DER.0000000000000729
- Paulsen E. Contact sensitization from Compositae-containing herbal remedies and cosmetics. Contact Dermatitis. 2002;47:189-198. doi:10.1034/j.1600-0536.2002.470401.x
- Frain-Bell W, Johnson BE. Contact allergic sensitivity to plants and the photosensitivity dermatitis and actinic reticuloid syndrome. Br J Dermatol. 1979;101:503-512.
- Paulsen E, Andersen KE. Clinical patterns of Compositae dermatitis in Danish monosensitized patients. Contact Dermatitis. 2018;78:185-193. doi:10.1111/cod.12916
- Jovanovic´ M, Poljacki M. Compositae dermatitis. Med Pregl. 2003;56:43-49. doi:10.2298/mpns0302043j
- Krook G. Occupational dermatitis from Lactuca sativa (lettuce) and Cichorium (endive). simultaneous occurrence of immediate and delayed allergy as a cause of contact dermatitis. Contact Dermatitis. 1977;3:27-36. doi:10.1111/j.1600-0536.1977.tb03583.x
- Paek SY, Lim HW. Chronic actinic dermatitis. Dermatol Clin. 2014;32:355-361, viii-ix. doi:10.1016/j.det.2014.03.007
- du P Menagé H, Hawk JL, White IR. Sesquiterpene lactone mix contact sensitivity and its relationship to chronic actinic dermatitis: a follow-up study. Contact Dermatitis. 1998;39:119-122. doi:10.1111/j.1600-0536.1998.tb05859.x
- Wang CX, Belsito DV. Chronic actinic dermatitis revisited. Dermatitis. 2020;31:68-74. doi:10.1097/DER.0000000000000531
- DeLeo VA, Adler BL, Warshaw EM, et al. Photopatch test results of the North American contact dermatitis group, 1999-2009. Photodermatol Photoimmunol Photomed. 2022;38:288-291. doi:10.1111/phpp.12742
- McGovern TW, LaWarre S. Botanical briefs: the scourge of India—Parthenium hysterophorus L. Cutis. 2001;67:27-34. Published correction appears in Cutis. 2001;67:154.
- Sharma VK, Verma P, Maharaja K. Parthenium dermatitis. Photochem Photobiol Sci. 2013;12:85-94. doi:10.1039/c2pp25186h
- Verma KK, Bansal A, Sethuraman G. Parthenium dermatitis treated with azathioprine weekly pulse doses. Indian J Dermatol Venereol Leprol. 2006;72:24-27. doi:10.4103/0378-6323.19713
- Sharma VK, Bhat R, Sethuraman G, et al. Treatment of Parthenium dermatitis with methotrexate. Contact Dermatitis. 2007;57:118-119. doi:10.1111/j.1600-0536.2006.00950.x
- Burke DA, Corey G, Storrs FJ. Psoralen plus UVA protocol for Compositae photosensitivity. Am J Contact Dermat. 1996;7:171-176.
- Lovell CR. Allergic contact dermatitis due to plants. In: Plants and the Skin. Blackwell Scientific Publications; 1993:96-254.
- Dogra S, Parsad D, Handa S. Narrowband ultraviolet B in airborne contact dermatitis: a ray of hope! Br J Dermatol. 2004;150:373-374. doi:10.1111/j.1365-2133.2004.05724.x
- Lakshmi C, Srinivas CR, Jayaraman A. Ciclosporin in Parthenium dermatitis—a report of 2 cases. Contact Dermatitis. 2008;59:245-248. doi:10.1111/j.1600-0536.2007.01208.x
- Hendricks AJ, Yosipovitch G, Shi VY. Dupilumab use in dermatologic conditions beyond atopic dermatitis—a systematic review. J Dermatolog Treat. 2021;32:19-28. doi:10.1080/09546634.2019.1689227
- Napolitano M, Fabbrocini G, Patruno C. Allergic contact dermatitis to Compositae: a possible cause of dupilumab-associated facial and neck dermatitis in atopic dermatitis patients? Contact Dermatitis. 2021;85:473-474. doi:10.1111/cod.13898
- Muddebihal A, Sardana K, Sinha S, et al. Tofacitinib in refractory Parthenium-induced airborne allergic contact dermatitis. Contact Dermatitis. 2023;88:150-152. doi:10.1111/cod.14234
- Baltazar D, Shinamoto SR, Hamann CP, et al. Occupational airborne allergic contact dermatitis to invasive Compositae species treated with abrocitinib: a case report. Contact Dermatitis. 2022;87:542-544. doi:10.1111/cod.14204
The Asteraceae (formerly Compositae) family of plants is derived from the ancient Greek word aster, meaning “star,” referring to the starlike arrangement of flower petals around a central disc known as a capitulum. What initially appears as a single flower is actually a composite of several smaller flowers, hence the former name Compositae.1 Well-known members of the Asteraceae family include ornamental annuals (eg, sunflowers, marigolds, cosmos), herbaceous perennials (eg, chrysanthemums, dandelions), vegetables (eg, lettuce, chicory, artichokes), herbs (eg, chamomile, tarragon), and weeds (eg, ragweed, horseweed, capeweed)(Figure 1).2

There are more than 25,000 species of Asteraceae plants that thrive in a wide range of climates worldwide. Cases of Asteraceae-induced skin reactions have been reported in North America, Europe, Asia, and Australia.3 Members of the Asteraceae family are ubiquitous in gardens, along roadsides, and in the wilderness. Occupational exposure commonly affects gardeners, florists, farmers, and forestry workers through either direct contact with plants or via airborne pollen. Furthermore, plants of the Asteraceae family are used in various products, including pediculicides (eg, insect repellents), cosmetics (eg, eye creams, body washes), and food products (eg, cooking oils, sweetening agents, coffee substitutes, herbal teas).4-6 These plants have substantial allergic potential, resulting in numerous cutaneous reactions.
Allergic Potential
Asteraceae plants can elicit both immediate and delayed hypersensitivity reactions (HSRs); for instance, exposure to ragweed pollen may cause an IgE-mediated type 1 HSR manifesting as allergic rhinitis or a type IV HSR manifesting as airborne allergic contact dermatitis.7,8 The main contact allergens present in Asteraceae plants are sesquiterpene lactones, which are found in the leaves, stems, flowers, and pollen.9-11 Sesquiterpene lactones consist of an α-methyl group attached to a lactone ring combined with a sesquiterpene.12 Patch testing can be used to diagnose Asteraceae allergy; however, the results are not consistently reliable because there is no perfect screening allergen. Patch test preparations commonly used to detect Asteraceae allergy include Compositae mix (consisting of Anthemis nobilis extract, Chamomilla recutita extract, Achillea millefolium extract, Tanacetum vulgare extract, Arnica montana extract, and parthenolide) and sesquiterpene lactone mix (consisting of alantolactone, dehydrocostus lactone, and costunolide). In North America, the prevalence of positive patch tests to Compositae mix and sesquiterpene lactone mix is approximately 2% and 0.5%, respectively.13 When patch testing is performed, both Compositae mix and sesquiterpene lactone mix should be utilized to minimize the risk of missing Asteraceae allergy, as sesquiterpene lactone mix alone does not detect all Compositae-sensitized patients. Additionally, it may be necessary to test supplemental Asteraceae allergens, including preparations from specific plants to which the patient has been exposed. Exposure to Asteraceae-containing cosmetic products may lead to dermatitis, though this is highly dependent on the particular plant species involved. For instance, the prevalence of sensitization is high in arnica (tincture) and elecampane but low with more commonly used species such as German chamomile.14
Cutaneous Manifestations
Asteraceae dermatitis, which also is known as Australian bush dermatitis, weed dermatitis, and chrysanthemum dermatitis,2 can manifest on any area of the body that directly contacts the plant or is exposed to the pollen. Asteraceae dermatitis historically was reported in older adults with a recent history of plant exposure.6,15 However, recent data have shown a female preponderance and a younger mean age of onset (46–49 years).16
There are multiple distinct clinical manifestations of Asteraceae dermatitis. The most common cutaneous finding is localized vesicular or eczematous patches on the hands or wrists. Other variations include eczematous rashes on the exposed skin of the hands, arms, face, and neck; generalized eczema; and isolated facial eczema.16,17 These variations can be attributed to contact dermatitis caused by airborne pollen, which may mimic photodermatitis. However, airborne Asteraceae dermatitis can be distinguished clinically from photodermatitis by the involvement of sun-protected areas such as the skinfolds of the eyelids, retroauricular sulci, and nasolabial folds (Figure 2).2,9 In rare cases, systemic allergic contact dermatitis can occur if the Asteraceae allergen is ingested.2,18
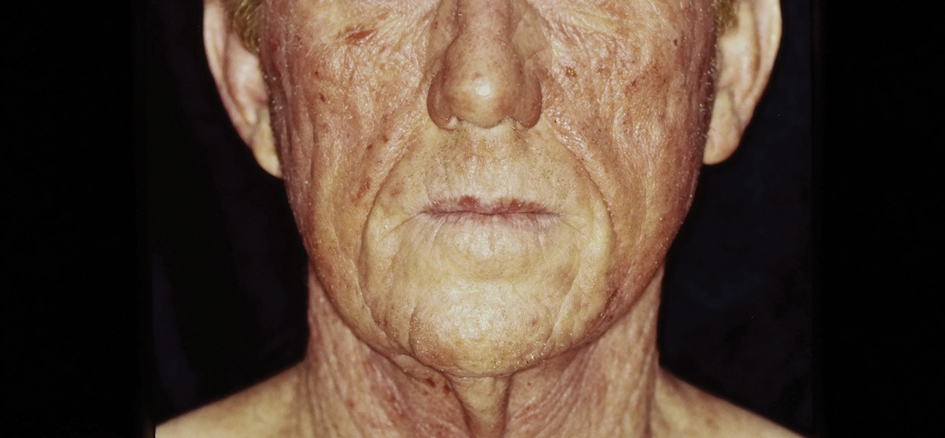
Other diagnostic clues include dermatitis that flares during the summer, at the peak of the growing season, with remission in the cooler months. Potential risk factors include a childhood history of atopic dermatitis and allergic rhinitis.16 With prolonged exposure, patients may develop chronic actinic dermatitis, an immunologically mediated photodermatosis characterized by lichenified and pruritic eczematous plaques located predominantly on sun-exposed areas with notable sparing of the skin folds.19 The association between Asteraceae dermatitis and chronic actinic dermatitis is highly variable, with some studies reporting a 25% correlation and others finding a stronger association of up to 80%.2,15,20 Asteraceae allergy appears to be a relatively uncommon cause of photoallergy in North America. In one recent study, 16% (3/19) of patients with chronic actinic dermatitis had positive patch or photopatch tests to sesquiterpene lactone mix, but in another large study of photopatch testing it was reported to be a rare photoallergen.21,22
Parthenium dermatitis is an allergic contact dermatitis caused by exposure to Parthenium hysterophorus, a weed of the Asteraceae family that is responsible for 30% of cases of contact dermatitis in India.23,24 Unlike the more classic manifestation of Asteraceae dermatitis, which primarily affects the upper extremities in cases from North America and Europe, Parthenium dermatitis typically occurs in an airborne pattern distribution.24
Management
While complete avoidance of Asteraceae plants is ideal, it often is unrealistic due to their abundance in nature. Therefore, minimizing exposure to the causative plants is recommended. Primary preventive measures such as wearing protective gloves and clothing and applying bentonite clay prior to exposure should be taken when working outdoors. Promptly showering after contact with plants also can reduce the risk for Asteraceae dermatitis.
Symptomatic treatment is appropriate for mild cases and includes topical corticosteroids and calcineurin inhibitors. For severe cases, systemic corticosteroids may be needed for acute flares, with azathioprine, mycophenolate, cyclosporine, or methotrexate available for recalcitrant disease. Verma et al25 found that treatment with azathioprine for 6 months resulted in greater than 60% clearance in all 12 patients, with a majority achieving 80% to 100% clearance. Methotrexate has been used at doses of 15 mg once weekly.26 Narrowband UVB and psoralen plus UVA have been effective in extensive cases; however, care should be exercised in patients with photosensitive dermatitis, who instead should practice strict photoprotection.27-29 Lakshmi et al30 reported the use of cyclosporine during the acute phase of Asteraceae dermatitis at a dose of 2.5 mg/kg daily for 4 to 8 weeks. There have been several case reports of dupilumab treating allergic contact dermatitis; however, there have been 3 cases of patients with atopic dermatitis developing Asteraceae dermatitis while taking dupilumab.31,32 Recently, oral Janus kinase inhibitors have shown success in treating refractory cases of airborne Asteraceae dermatitis.33,34 Further research is needed to determine the safety and efficacy of dupilumab and Janus kinase inhibitors for treatment of Asteraceae dermatitis.
Final Thoughts
The Asteraceae plant family is vast and diverse, with more than 200 species reported to cause allergic contact dermatitis.12 Common modes of contact include gardening, occupational exposure, airborne pollen, and use of pediculicides and cosmetics that contain components of Asteraceae plants. Educating patients on how to minimize contact with Asteraceae plants is the most effective management strategy; topical agents and oral immunosuppressives can be used for symptomatic treatment.
The Asteraceae (formerly Compositae) family of plants is derived from the ancient Greek word aster, meaning “star,” referring to the starlike arrangement of flower petals around a central disc known as a capitulum. What initially appears as a single flower is actually a composite of several smaller flowers, hence the former name Compositae.1 Well-known members of the Asteraceae family include ornamental annuals (eg, sunflowers, marigolds, cosmos), herbaceous perennials (eg, chrysanthemums, dandelions), vegetables (eg, lettuce, chicory, artichokes), herbs (eg, chamomile, tarragon), and weeds (eg, ragweed, horseweed, capeweed)(Figure 1).2

There are more than 25,000 species of Asteraceae plants that thrive in a wide range of climates worldwide. Cases of Asteraceae-induced skin reactions have been reported in North America, Europe, Asia, and Australia.3 Members of the Asteraceae family are ubiquitous in gardens, along roadsides, and in the wilderness. Occupational exposure commonly affects gardeners, florists, farmers, and forestry workers through either direct contact with plants or via airborne pollen. Furthermore, plants of the Asteraceae family are used in various products, including pediculicides (eg, insect repellents), cosmetics (eg, eye creams, body washes), and food products (eg, cooking oils, sweetening agents, coffee substitutes, herbal teas).4-6 These plants have substantial allergic potential, resulting in numerous cutaneous reactions.
Allergic Potential
Asteraceae plants can elicit both immediate and delayed hypersensitivity reactions (HSRs); for instance, exposure to ragweed pollen may cause an IgE-mediated type 1 HSR manifesting as allergic rhinitis or a type IV HSR manifesting as airborne allergic contact dermatitis.7,8 The main contact allergens present in Asteraceae plants are sesquiterpene lactones, which are found in the leaves, stems, flowers, and pollen.9-11 Sesquiterpene lactones consist of an α-methyl group attached to a lactone ring combined with a sesquiterpene.12 Patch testing can be used to diagnose Asteraceae allergy; however, the results are not consistently reliable because there is no perfect screening allergen. Patch test preparations commonly used to detect Asteraceae allergy include Compositae mix (consisting of Anthemis nobilis extract, Chamomilla recutita extract, Achillea millefolium extract, Tanacetum vulgare extract, Arnica montana extract, and parthenolide) and sesquiterpene lactone mix (consisting of alantolactone, dehydrocostus lactone, and costunolide). In North America, the prevalence of positive patch tests to Compositae mix and sesquiterpene lactone mix is approximately 2% and 0.5%, respectively.13 When patch testing is performed, both Compositae mix and sesquiterpene lactone mix should be utilized to minimize the risk of missing Asteraceae allergy, as sesquiterpene lactone mix alone does not detect all Compositae-sensitized patients. Additionally, it may be necessary to test supplemental Asteraceae allergens, including preparations from specific plants to which the patient has been exposed. Exposure to Asteraceae-containing cosmetic products may lead to dermatitis, though this is highly dependent on the particular plant species involved. For instance, the prevalence of sensitization is high in arnica (tincture) and elecampane but low with more commonly used species such as German chamomile.14
Cutaneous Manifestations
Asteraceae dermatitis, which also is known as Australian bush dermatitis, weed dermatitis, and chrysanthemum dermatitis,2 can manifest on any area of the body that directly contacts the plant or is exposed to the pollen. Asteraceae dermatitis historically was reported in older adults with a recent history of plant exposure.6,15 However, recent data have shown a female preponderance and a younger mean age of onset (46–49 years).16
There are multiple distinct clinical manifestations of Asteraceae dermatitis. The most common cutaneous finding is localized vesicular or eczematous patches on the hands or wrists. Other variations include eczematous rashes on the exposed skin of the hands, arms, face, and neck; generalized eczema; and isolated facial eczema.16,17 These variations can be attributed to contact dermatitis caused by airborne pollen, which may mimic photodermatitis. However, airborne Asteraceae dermatitis can be distinguished clinically from photodermatitis by the involvement of sun-protected areas such as the skinfolds of the eyelids, retroauricular sulci, and nasolabial folds (Figure 2).2,9 In rare cases, systemic allergic contact dermatitis can occur if the Asteraceae allergen is ingested.2,18
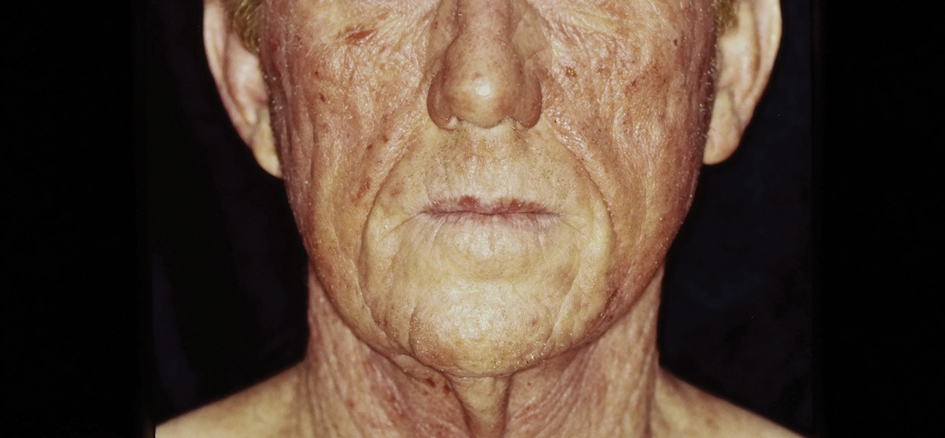
Other diagnostic clues include dermatitis that flares during the summer, at the peak of the growing season, with remission in the cooler months. Potential risk factors include a childhood history of atopic dermatitis and allergic rhinitis.16 With prolonged exposure, patients may develop chronic actinic dermatitis, an immunologically mediated photodermatosis characterized by lichenified and pruritic eczematous plaques located predominantly on sun-exposed areas with notable sparing of the skin folds.19 The association between Asteraceae dermatitis and chronic actinic dermatitis is highly variable, with some studies reporting a 25% correlation and others finding a stronger association of up to 80%.2,15,20 Asteraceae allergy appears to be a relatively uncommon cause of photoallergy in North America. In one recent study, 16% (3/19) of patients with chronic actinic dermatitis had positive patch or photopatch tests to sesquiterpene lactone mix, but in another large study of photopatch testing it was reported to be a rare photoallergen.21,22
Parthenium dermatitis is an allergic contact dermatitis caused by exposure to Parthenium hysterophorus, a weed of the Asteraceae family that is responsible for 30% of cases of contact dermatitis in India.23,24 Unlike the more classic manifestation of Asteraceae dermatitis, which primarily affects the upper extremities in cases from North America and Europe, Parthenium dermatitis typically occurs in an airborne pattern distribution.24
Management
While complete avoidance of Asteraceae plants is ideal, it often is unrealistic due to their abundance in nature. Therefore, minimizing exposure to the causative plants is recommended. Primary preventive measures such as wearing protective gloves and clothing and applying bentonite clay prior to exposure should be taken when working outdoors. Promptly showering after contact with plants also can reduce the risk for Asteraceae dermatitis.
Symptomatic treatment is appropriate for mild cases and includes topical corticosteroids and calcineurin inhibitors. For severe cases, systemic corticosteroids may be needed for acute flares, with azathioprine, mycophenolate, cyclosporine, or methotrexate available for recalcitrant disease. Verma et al25 found that treatment with azathioprine for 6 months resulted in greater than 60% clearance in all 12 patients, with a majority achieving 80% to 100% clearance. Methotrexate has been used at doses of 15 mg once weekly.26 Narrowband UVB and psoralen plus UVA have been effective in extensive cases; however, care should be exercised in patients with photosensitive dermatitis, who instead should practice strict photoprotection.27-29 Lakshmi et al30 reported the use of cyclosporine during the acute phase of Asteraceae dermatitis at a dose of 2.5 mg/kg daily for 4 to 8 weeks. There have been several case reports of dupilumab treating allergic contact dermatitis; however, there have been 3 cases of patients with atopic dermatitis developing Asteraceae dermatitis while taking dupilumab.31,32 Recently, oral Janus kinase inhibitors have shown success in treating refractory cases of airborne Asteraceae dermatitis.33,34 Further research is needed to determine the safety and efficacy of dupilumab and Janus kinase inhibitors for treatment of Asteraceae dermatitis.
Final Thoughts
The Asteraceae plant family is vast and diverse, with more than 200 species reported to cause allergic contact dermatitis.12 Common modes of contact include gardening, occupational exposure, airborne pollen, and use of pediculicides and cosmetics that contain components of Asteraceae plants. Educating patients on how to minimize contact with Asteraceae plants is the most effective management strategy; topical agents and oral immunosuppressives can be used for symptomatic treatment.
- Morhardt S, Morhardt E. California Desert Flowers: An Introduction to Families, Genera, and Species. University of California Press; 2004.
- Gordon LA. Compositae dermatitis. Australas J Dermatol. 1999;40:123-130. doi:10.1046/j.1440-0960.1999.00341.x
- Denisow-Pietrzyk M, Pietrzyk Ł, Denisow B. Asteraceae species as potential environmental factors of allergy. Environ Sci Pollut Res Int. 2019;26:6290-6300. doi:10.1007/s11356-019-04146-w
- Paulsen E, Chistensen LP, Andersen KE. Cosmetics and herbal remedies with Compositae plant extracts—are they tolerated by Compositae-allergic patients? Contact Dermatitis. 2008;58:15-23. doi:10.1111/j.1600-0536.2007.01250.x
- Burry JN, Reid JG, Kirk J. Australian bush dermatitis. Contact Dermatitis. 1975;1:263-264. doi:10.1111/j.1600-0536.1975.tb05422.x
- Punchihewa N, Palmer A, Nixon R. Allergic contact dermatitis to Compositae: an Australian case series. Contact Dermatitis. 2022;87:356-362. doi:10.1111/cod.14162
- Chen KW, Marusciac L, Tamas PT, et al. Ragweed pollen allergy: burden, characteristics, and management of an imported allergen source in Europe. Int Arch Allergy Immunol. 2018;176:163-180. doi:10.1159/000487997
- Schloemer JA, Zirwas MJ, Burkhart CG. Airborne contact dermatitis: common causes in the USA. Int J Dermatol. 2015;54:271-274. doi:10.1111/ijd.12692
- Arlette J, Mitchell JC. Compositae dermatitis. current aspects. Contact Dermatitis. 1981;7:129-136. doi:10.1111/j.1600-0536.1981.tb04584.x
- Mitchell JC, Dupuis G. Allergic contact dermatitis from sesquiterpenoids of the Compositae family of plants. Br J Dermatol. 1971;84:139-150. doi:10.1111/j.1365-2133.1971.tb06857.x
- Salapovic H, Geier J, Reznicek G. Quantification of Sesquiterpene lactones in Asteraceae plant extracts: evaluation of their allergenic potential. Sci Pharm. 2013;81:807-818. doi:10.3797/scipharm.1306-17
- Paulsen E. Compositae dermatitis: a survey. Contact Dermatitis. 1992;26:76-86. doi:10.1111/j.1600-0536.1992.tb00888.x. Published correction appears in Contact Dermatitis. 1992;27:208.
- DeKoven JG, Silverberg JI, Warshaw EM, et al. North American Contact Dermatitis Group patch test results: 2017-2018. Dermatitis. 2021;32:111-123. doi:10.1097/DER.0000000000000729
- Paulsen E. Contact sensitization from Compositae-containing herbal remedies and cosmetics. Contact Dermatitis. 2002;47:189-198. doi:10.1034/j.1600-0536.2002.470401.x
- Frain-Bell W, Johnson BE. Contact allergic sensitivity to plants and the photosensitivity dermatitis and actinic reticuloid syndrome. Br J Dermatol. 1979;101:503-512.
- Paulsen E, Andersen KE. Clinical patterns of Compositae dermatitis in Danish monosensitized patients. Contact Dermatitis. 2018;78:185-193. doi:10.1111/cod.12916
- Jovanovic´ M, Poljacki M. Compositae dermatitis. Med Pregl. 2003;56:43-49. doi:10.2298/mpns0302043j
- Krook G. Occupational dermatitis from Lactuca sativa (lettuce) and Cichorium (endive). simultaneous occurrence of immediate and delayed allergy as a cause of contact dermatitis. Contact Dermatitis. 1977;3:27-36. doi:10.1111/j.1600-0536.1977.tb03583.x
- Paek SY, Lim HW. Chronic actinic dermatitis. Dermatol Clin. 2014;32:355-361, viii-ix. doi:10.1016/j.det.2014.03.007
- du P Menagé H, Hawk JL, White IR. Sesquiterpene lactone mix contact sensitivity and its relationship to chronic actinic dermatitis: a follow-up study. Contact Dermatitis. 1998;39:119-122. doi:10.1111/j.1600-0536.1998.tb05859.x
- Wang CX, Belsito DV. Chronic actinic dermatitis revisited. Dermatitis. 2020;31:68-74. doi:10.1097/DER.0000000000000531
- DeLeo VA, Adler BL, Warshaw EM, et al. Photopatch test results of the North American contact dermatitis group, 1999-2009. Photodermatol Photoimmunol Photomed. 2022;38:288-291. doi:10.1111/phpp.12742
- McGovern TW, LaWarre S. Botanical briefs: the scourge of India—Parthenium hysterophorus L. Cutis. 2001;67:27-34. Published correction appears in Cutis. 2001;67:154.
- Sharma VK, Verma P, Maharaja K. Parthenium dermatitis. Photochem Photobiol Sci. 2013;12:85-94. doi:10.1039/c2pp25186h
- Verma KK, Bansal A, Sethuraman G. Parthenium dermatitis treated with azathioprine weekly pulse doses. Indian J Dermatol Venereol Leprol. 2006;72:24-27. doi:10.4103/0378-6323.19713
- Sharma VK, Bhat R, Sethuraman G, et al. Treatment of Parthenium dermatitis with methotrexate. Contact Dermatitis. 2007;57:118-119. doi:10.1111/j.1600-0536.2006.00950.x
- Burke DA, Corey G, Storrs FJ. Psoralen plus UVA protocol for Compositae photosensitivity. Am J Contact Dermat. 1996;7:171-176.
- Lovell CR. Allergic contact dermatitis due to plants. In: Plants and the Skin. Blackwell Scientific Publications; 1993:96-254.
- Dogra S, Parsad D, Handa S. Narrowband ultraviolet B in airborne contact dermatitis: a ray of hope! Br J Dermatol. 2004;150:373-374. doi:10.1111/j.1365-2133.2004.05724.x
- Lakshmi C, Srinivas CR, Jayaraman A. Ciclosporin in Parthenium dermatitis—a report of 2 cases. Contact Dermatitis. 2008;59:245-248. doi:10.1111/j.1600-0536.2007.01208.x
- Hendricks AJ, Yosipovitch G, Shi VY. Dupilumab use in dermatologic conditions beyond atopic dermatitis—a systematic review. J Dermatolog Treat. 2021;32:19-28. doi:10.1080/09546634.2019.1689227
- Napolitano M, Fabbrocini G, Patruno C. Allergic contact dermatitis to Compositae: a possible cause of dupilumab-associated facial and neck dermatitis in atopic dermatitis patients? Contact Dermatitis. 2021;85:473-474. doi:10.1111/cod.13898
- Muddebihal A, Sardana K, Sinha S, et al. Tofacitinib in refractory Parthenium-induced airborne allergic contact dermatitis. Contact Dermatitis. 2023;88:150-152. doi:10.1111/cod.14234
- Baltazar D, Shinamoto SR, Hamann CP, et al. Occupational airborne allergic contact dermatitis to invasive Compositae species treated with abrocitinib: a case report. Contact Dermatitis. 2022;87:542-544. doi:10.1111/cod.14204
- Morhardt S, Morhardt E. California Desert Flowers: An Introduction to Families, Genera, and Species. University of California Press; 2004.
- Gordon LA. Compositae dermatitis. Australas J Dermatol. 1999;40:123-130. doi:10.1046/j.1440-0960.1999.00341.x
- Denisow-Pietrzyk M, Pietrzyk Ł, Denisow B. Asteraceae species as potential environmental factors of allergy. Environ Sci Pollut Res Int. 2019;26:6290-6300. doi:10.1007/s11356-019-04146-w
- Paulsen E, Chistensen LP, Andersen KE. Cosmetics and herbal remedies with Compositae plant extracts—are they tolerated by Compositae-allergic patients? Contact Dermatitis. 2008;58:15-23. doi:10.1111/j.1600-0536.2007.01250.x
- Burry JN, Reid JG, Kirk J. Australian bush dermatitis. Contact Dermatitis. 1975;1:263-264. doi:10.1111/j.1600-0536.1975.tb05422.x
- Punchihewa N, Palmer A, Nixon R. Allergic contact dermatitis to Compositae: an Australian case series. Contact Dermatitis. 2022;87:356-362. doi:10.1111/cod.14162
- Chen KW, Marusciac L, Tamas PT, et al. Ragweed pollen allergy: burden, characteristics, and management of an imported allergen source in Europe. Int Arch Allergy Immunol. 2018;176:163-180. doi:10.1159/000487997
- Schloemer JA, Zirwas MJ, Burkhart CG. Airborne contact dermatitis: common causes in the USA. Int J Dermatol. 2015;54:271-274. doi:10.1111/ijd.12692
- Arlette J, Mitchell JC. Compositae dermatitis. current aspects. Contact Dermatitis. 1981;7:129-136. doi:10.1111/j.1600-0536.1981.tb04584.x
- Mitchell JC, Dupuis G. Allergic contact dermatitis from sesquiterpenoids of the Compositae family of plants. Br J Dermatol. 1971;84:139-150. doi:10.1111/j.1365-2133.1971.tb06857.x
- Salapovic H, Geier J, Reznicek G. Quantification of Sesquiterpene lactones in Asteraceae plant extracts: evaluation of their allergenic potential. Sci Pharm. 2013;81:807-818. doi:10.3797/scipharm.1306-17
- Paulsen E. Compositae dermatitis: a survey. Contact Dermatitis. 1992;26:76-86. doi:10.1111/j.1600-0536.1992.tb00888.x. Published correction appears in Contact Dermatitis. 1992;27:208.
- DeKoven JG, Silverberg JI, Warshaw EM, et al. North American Contact Dermatitis Group patch test results: 2017-2018. Dermatitis. 2021;32:111-123. doi:10.1097/DER.0000000000000729
- Paulsen E. Contact sensitization from Compositae-containing herbal remedies and cosmetics. Contact Dermatitis. 2002;47:189-198. doi:10.1034/j.1600-0536.2002.470401.x
- Frain-Bell W, Johnson BE. Contact allergic sensitivity to plants and the photosensitivity dermatitis and actinic reticuloid syndrome. Br J Dermatol. 1979;101:503-512.
- Paulsen E, Andersen KE. Clinical patterns of Compositae dermatitis in Danish monosensitized patients. Contact Dermatitis. 2018;78:185-193. doi:10.1111/cod.12916
- Jovanovic´ M, Poljacki M. Compositae dermatitis. Med Pregl. 2003;56:43-49. doi:10.2298/mpns0302043j
- Krook G. Occupational dermatitis from Lactuca sativa (lettuce) and Cichorium (endive). simultaneous occurrence of immediate and delayed allergy as a cause of contact dermatitis. Contact Dermatitis. 1977;3:27-36. doi:10.1111/j.1600-0536.1977.tb03583.x
- Paek SY, Lim HW. Chronic actinic dermatitis. Dermatol Clin. 2014;32:355-361, viii-ix. doi:10.1016/j.det.2014.03.007
- du P Menagé H, Hawk JL, White IR. Sesquiterpene lactone mix contact sensitivity and its relationship to chronic actinic dermatitis: a follow-up study. Contact Dermatitis. 1998;39:119-122. doi:10.1111/j.1600-0536.1998.tb05859.x
- Wang CX, Belsito DV. Chronic actinic dermatitis revisited. Dermatitis. 2020;31:68-74. doi:10.1097/DER.0000000000000531
- DeLeo VA, Adler BL, Warshaw EM, et al. Photopatch test results of the North American contact dermatitis group, 1999-2009. Photodermatol Photoimmunol Photomed. 2022;38:288-291. doi:10.1111/phpp.12742
- McGovern TW, LaWarre S. Botanical briefs: the scourge of India—Parthenium hysterophorus L. Cutis. 2001;67:27-34. Published correction appears in Cutis. 2001;67:154.
- Sharma VK, Verma P, Maharaja K. Parthenium dermatitis. Photochem Photobiol Sci. 2013;12:85-94. doi:10.1039/c2pp25186h
- Verma KK, Bansal A, Sethuraman G. Parthenium dermatitis treated with azathioprine weekly pulse doses. Indian J Dermatol Venereol Leprol. 2006;72:24-27. doi:10.4103/0378-6323.19713
- Sharma VK, Bhat R, Sethuraman G, et al. Treatment of Parthenium dermatitis with methotrexate. Contact Dermatitis. 2007;57:118-119. doi:10.1111/j.1600-0536.2006.00950.x
- Burke DA, Corey G, Storrs FJ. Psoralen plus UVA protocol for Compositae photosensitivity. Am J Contact Dermat. 1996;7:171-176.
- Lovell CR. Allergic contact dermatitis due to plants. In: Plants and the Skin. Blackwell Scientific Publications; 1993:96-254.
- Dogra S, Parsad D, Handa S. Narrowband ultraviolet B in airborne contact dermatitis: a ray of hope! Br J Dermatol. 2004;150:373-374. doi:10.1111/j.1365-2133.2004.05724.x
- Lakshmi C, Srinivas CR, Jayaraman A. Ciclosporin in Parthenium dermatitis—a report of 2 cases. Contact Dermatitis. 2008;59:245-248. doi:10.1111/j.1600-0536.2007.01208.x
- Hendricks AJ, Yosipovitch G, Shi VY. Dupilumab use in dermatologic conditions beyond atopic dermatitis—a systematic review. J Dermatolog Treat. 2021;32:19-28. doi:10.1080/09546634.2019.1689227
- Napolitano M, Fabbrocini G, Patruno C. Allergic contact dermatitis to Compositae: a possible cause of dupilumab-associated facial and neck dermatitis in atopic dermatitis patients? Contact Dermatitis. 2021;85:473-474. doi:10.1111/cod.13898
- Muddebihal A, Sardana K, Sinha S, et al. Tofacitinib in refractory Parthenium-induced airborne allergic contact dermatitis. Contact Dermatitis. 2023;88:150-152. doi:10.1111/cod.14234
- Baltazar D, Shinamoto SR, Hamann CP, et al. Occupational airborne allergic contact dermatitis to invasive Compositae species treated with abrocitinib: a case report. Contact Dermatitis. 2022;87:542-544. doi:10.1111/cod.14204
Practice Points
- Asteraceae dermatitis can occur from direct contact with plants of the Asteraceae family; through airborne pollen; or from exposure to topical medications, cooking products, and cosmetics.
- Patient education on primary prevention, especially protective clothing, is crucial, as these plants are ubiquitous outdoors and have diverse phenotypes.
- Management of mild Asteraceae dermatitis consists primarily of topical corticosteroids and calcineurin inhibitors, while systemic corticosteroids and other immunosuppressive agents are utilized for severe or recalcitrant cases.
Atopic Dermatitis: Upadacitinib Effectiveness Maintained Through 76 weeks Among Adolescents
TOPLINE:
across three phase 3 trials.
METHODOLOGY:
- Researchers conducted three double-blind, placebo-controlled phase 3 randomized clinical trials (Measure Up 1, Measure Up 2, and AD Up) involving 542 adolescents aged 12-17 years with moderate to severe AD.
- Participants were randomized to receive the oral Janus kinase inhibitor upadacitinib (15 mg or 30 mg once daily) or placebo, with or without topical corticosteroids, for 16 weeks, followed by rerandomization of patients in the placebo group to upadacitinib for up to 76 weeks.
- Study endpoints were at least a 75%, 90%, or 100% reduction in the Eczema Area and Severity Index (EASI-75, EASI-90, and EASI-100, respectively), Validated Investigator Global Assessment for AD (vIGA-AD) score of 0 or 1, and a ≥ 4-point improvement in the Worst Pruritus Numerical Rating Scale (WP-NRS).
- Adverse events were monitored, including serious infections, herpes zoster, and creatine kinase elevation.
TAKEAWAY:
- Among those who continued treatment on upadacitinib, 15 mg and 30 mg, EASI-75 response rates were maintained or improved through week 76 in all three studies. Patients who switched from placebo to upadacitinib also experienced improvements in EASI-75 through week 76.
- The proportion of patients who achieved EASI-90 and EASI-100 responses increased, and in general, were maintained from week 16 through week 76 in all three studies; the proportion was numerically higher among patients on 30 mg for all three studies.
- The proportion of adolescents achieving vIGA-AD score of 0 or 1 and WP-NRS improvement of ≥ 4 points was sustained or improved through 76 weeks.
- Serious infections were reported in five patients or fewer in each treatment group for all three studies. All opportunistic infections were eczema herpeticum; most cases were not serious, or were mild or moderate, and in general, did not require stopping treatment.
IN PRACTICE:
“These results through 76 weeks demonstrated that upadacitinib, with a favorable benefit-risk profile, was an effective long-term treatment option for adolescents with moderate to severe AD,” the authors wrote.
SOURCE:
The study was led by Amy S. Paller, MD, professor and chair of dermatology, Northwestern University, Chicago, and was published online on October 23 in JAMA Dermatology.
LIMITATIONS:
The study limitations included a small sample size, and the findings did not extend to patients under 12 years or those weighing < 40 kg.
DISCLOSURES:
This study was supported by AbbVie. Paller received grants and personal fees from pharmaceutical companies including AbbVie during the conduct of the study. Several authors reported financial ties with various sources, including AbbVie.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
across three phase 3 trials.
METHODOLOGY:
- Researchers conducted three double-blind, placebo-controlled phase 3 randomized clinical trials (Measure Up 1, Measure Up 2, and AD Up) involving 542 adolescents aged 12-17 years with moderate to severe AD.
- Participants were randomized to receive the oral Janus kinase inhibitor upadacitinib (15 mg or 30 mg once daily) or placebo, with or without topical corticosteroids, for 16 weeks, followed by rerandomization of patients in the placebo group to upadacitinib for up to 76 weeks.
- Study endpoints were at least a 75%, 90%, or 100% reduction in the Eczema Area and Severity Index (EASI-75, EASI-90, and EASI-100, respectively), Validated Investigator Global Assessment for AD (vIGA-AD) score of 0 or 1, and a ≥ 4-point improvement in the Worst Pruritus Numerical Rating Scale (WP-NRS).
- Adverse events were monitored, including serious infections, herpes zoster, and creatine kinase elevation.
TAKEAWAY:
- Among those who continued treatment on upadacitinib, 15 mg and 30 mg, EASI-75 response rates were maintained or improved through week 76 in all three studies. Patients who switched from placebo to upadacitinib also experienced improvements in EASI-75 through week 76.
- The proportion of patients who achieved EASI-90 and EASI-100 responses increased, and in general, were maintained from week 16 through week 76 in all three studies; the proportion was numerically higher among patients on 30 mg for all three studies.
- The proportion of adolescents achieving vIGA-AD score of 0 or 1 and WP-NRS improvement of ≥ 4 points was sustained or improved through 76 weeks.
- Serious infections were reported in five patients or fewer in each treatment group for all three studies. All opportunistic infections were eczema herpeticum; most cases were not serious, or were mild or moderate, and in general, did not require stopping treatment.
IN PRACTICE:
“These results through 76 weeks demonstrated that upadacitinib, with a favorable benefit-risk profile, was an effective long-term treatment option for adolescents with moderate to severe AD,” the authors wrote.
SOURCE:
The study was led by Amy S. Paller, MD, professor and chair of dermatology, Northwestern University, Chicago, and was published online on October 23 in JAMA Dermatology.
LIMITATIONS:
The study limitations included a small sample size, and the findings did not extend to patients under 12 years or those weighing < 40 kg.
DISCLOSURES:
This study was supported by AbbVie. Paller received grants and personal fees from pharmaceutical companies including AbbVie during the conduct of the study. Several authors reported financial ties with various sources, including AbbVie.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
across three phase 3 trials.
METHODOLOGY:
- Researchers conducted three double-blind, placebo-controlled phase 3 randomized clinical trials (Measure Up 1, Measure Up 2, and AD Up) involving 542 adolescents aged 12-17 years with moderate to severe AD.
- Participants were randomized to receive the oral Janus kinase inhibitor upadacitinib (15 mg or 30 mg once daily) or placebo, with or without topical corticosteroids, for 16 weeks, followed by rerandomization of patients in the placebo group to upadacitinib for up to 76 weeks.
- Study endpoints were at least a 75%, 90%, or 100% reduction in the Eczema Area and Severity Index (EASI-75, EASI-90, and EASI-100, respectively), Validated Investigator Global Assessment for AD (vIGA-AD) score of 0 or 1, and a ≥ 4-point improvement in the Worst Pruritus Numerical Rating Scale (WP-NRS).
- Adverse events were monitored, including serious infections, herpes zoster, and creatine kinase elevation.
TAKEAWAY:
- Among those who continued treatment on upadacitinib, 15 mg and 30 mg, EASI-75 response rates were maintained or improved through week 76 in all three studies. Patients who switched from placebo to upadacitinib also experienced improvements in EASI-75 through week 76.
- The proportion of patients who achieved EASI-90 and EASI-100 responses increased, and in general, were maintained from week 16 through week 76 in all three studies; the proportion was numerically higher among patients on 30 mg for all three studies.
- The proportion of adolescents achieving vIGA-AD score of 0 or 1 and WP-NRS improvement of ≥ 4 points was sustained or improved through 76 weeks.
- Serious infections were reported in five patients or fewer in each treatment group for all three studies. All opportunistic infections were eczema herpeticum; most cases were not serious, or were mild or moderate, and in general, did not require stopping treatment.
IN PRACTICE:
“These results through 76 weeks demonstrated that upadacitinib, with a favorable benefit-risk profile, was an effective long-term treatment option for adolescents with moderate to severe AD,” the authors wrote.
SOURCE:
The study was led by Amy S. Paller, MD, professor and chair of dermatology, Northwestern University, Chicago, and was published online on October 23 in JAMA Dermatology.
LIMITATIONS:
The study limitations included a small sample size, and the findings did not extend to patients under 12 years or those weighing < 40 kg.
DISCLOSURES:
This study was supported by AbbVie. Paller received grants and personal fees from pharmaceutical companies including AbbVie during the conduct of the study. Several authors reported financial ties with various sources, including AbbVie.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.








