User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
AMA president calls on Congress to stabilize Medicare payments to physicians
Physician practices around the country took an unprecedented financial hit with the arrival of the COVID-19 pandemic in March 2020. Recent research from the American Medical Association reveals an estimated pandemic-related shortfall in Medicare physician fee spending of $13.9 billion, or a 14% reduction, across all states and all major specialties in 2020.
While the report pointed to a “strong recovery” in May and June, that recovery stalled in the second half of 2020, and spending never returned to pre–COVID-19 levels.
“Physicians experienced a significant and sustained drop in Medicare revenue during the first 10 months of the pandemic,” said AMA President Gerald Harmon, MD, in a statement. “Medical practices that have not buckled under financial strain continue to be stretched clinically, emotionally, and fiscally as the pandemic persists. Yet physicians face an array of planned cuts that would reduce Medicare physician payments by nearly 10% for 2022.”
The reduction in the Medicare physician fee schedule payments means providers may face payment cuts of more than 9% starting Jan. 1, 2022, when the cuts take effect. That is, unless Congress makes changes.
Medicare physician fee schedule spending on telehealth stood at $4.1 billion, or 5% of the total Medicare spent in 2020. From March 16 to June 30, $1.8 billion of this amount was on telehealth, while $1.1 billion came in during third and fourth quarters of 2020, respectively, per the report.
According to AMA’s research:
- Medicare physician fee schedule spending for 2020, relative to expected 2020 spending, dipped 32% between March 16 and June 30; spending was down during the last 6 months of the year by between 9% and 10%.
- The care settings hit the worst were ambulatory surgical centers, outpatient hospitals, and physician offices; the next worst off were hospital emergency departments, inpatient hospitals, and skilled nursing facilities.
- The specialties that fared worst included physical therapists (-28%), opthamologists (-19%), podiatrists (-18%), and dermatologists (-18%).
- Cumulative spending was down the most in Minnesota (-22%), Maine (-19%), and New York (-19%); less affected states included Idaho (-9%), Oklahoma (-9%), and South Carolina (9%).
AMA: Budget neutrality hurting physicians’ financial stability
Dr. Harmon is calling for financial stability in Medicare spending. In particular, the AMA is “strongly urging Congress to avert the planned payment cuts,” he said in a statement.
The challenge: The Medicare physician fee schedule is currently “budget neutral,” meaning that the budget is fixed, Dr. Harmon, a family medicine specialist in South Carolina, told this news organization.
“If you rob from Peter to pay Paul, Paul is going to be less efficient or less rewarded. It continues to be that there’s always a ‘pay for’ in these things. So budget neutrality is probably one of the first things we need to address,” he said.
Lack of routine care expected to affect health outcomes
The result of reduced screening and treatment during the pandemic could be as many as 10,000 excess deaths due to cancers of the breast and colon during the next 10 years, wrote Norman Sharpless, MD, director of the National Cancer Institute, in Science in June. Combined, breast cancer and colon cancer account for one-sixth of all cancers in the U.S., he wrote.
In addition, blood pressure control has gotten worse since the start of the pandemic, said Michael Rakotz, MD, FAHA, FAAFP, vice president of improving health outcomes at the AMA, in an AMA blog post.
Dr. Harmon’s advice for physician practices on getting patients in for routine care:
- Educate the area’s largest employers to encourage their employees.
- Engage with hospital employees, since hospitals are often the largest employers in many communities.
- Partner with health insurers.
- Show up at athletic events, which is a particularly good fit for “small town America,” said Dr. Harmon.
The AMA’s research doesn’t consider reimbursement from other public and private payers. It also doesn’t account for funding sources such as Provider Relief Fund grants, Paycheck Protection Program loans, and the temporary suspension of the Medicare sequester, per the report.
A version of this article first appeared on Medscape.com.
Physician practices around the country took an unprecedented financial hit with the arrival of the COVID-19 pandemic in March 2020. Recent research from the American Medical Association reveals an estimated pandemic-related shortfall in Medicare physician fee spending of $13.9 billion, or a 14% reduction, across all states and all major specialties in 2020.
While the report pointed to a “strong recovery” in May and June, that recovery stalled in the second half of 2020, and spending never returned to pre–COVID-19 levels.
“Physicians experienced a significant and sustained drop in Medicare revenue during the first 10 months of the pandemic,” said AMA President Gerald Harmon, MD, in a statement. “Medical practices that have not buckled under financial strain continue to be stretched clinically, emotionally, and fiscally as the pandemic persists. Yet physicians face an array of planned cuts that would reduce Medicare physician payments by nearly 10% for 2022.”
The reduction in the Medicare physician fee schedule payments means providers may face payment cuts of more than 9% starting Jan. 1, 2022, when the cuts take effect. That is, unless Congress makes changes.
Medicare physician fee schedule spending on telehealth stood at $4.1 billion, or 5% of the total Medicare spent in 2020. From March 16 to June 30, $1.8 billion of this amount was on telehealth, while $1.1 billion came in during third and fourth quarters of 2020, respectively, per the report.
According to AMA’s research:
- Medicare physician fee schedule spending for 2020, relative to expected 2020 spending, dipped 32% between March 16 and June 30; spending was down during the last 6 months of the year by between 9% and 10%.
- The care settings hit the worst were ambulatory surgical centers, outpatient hospitals, and physician offices; the next worst off were hospital emergency departments, inpatient hospitals, and skilled nursing facilities.
- The specialties that fared worst included physical therapists (-28%), opthamologists (-19%), podiatrists (-18%), and dermatologists (-18%).
- Cumulative spending was down the most in Minnesota (-22%), Maine (-19%), and New York (-19%); less affected states included Idaho (-9%), Oklahoma (-9%), and South Carolina (9%).
AMA: Budget neutrality hurting physicians’ financial stability
Dr. Harmon is calling for financial stability in Medicare spending. In particular, the AMA is “strongly urging Congress to avert the planned payment cuts,” he said in a statement.
The challenge: The Medicare physician fee schedule is currently “budget neutral,” meaning that the budget is fixed, Dr. Harmon, a family medicine specialist in South Carolina, told this news organization.
“If you rob from Peter to pay Paul, Paul is going to be less efficient or less rewarded. It continues to be that there’s always a ‘pay for’ in these things. So budget neutrality is probably one of the first things we need to address,” he said.
Lack of routine care expected to affect health outcomes
The result of reduced screening and treatment during the pandemic could be as many as 10,000 excess deaths due to cancers of the breast and colon during the next 10 years, wrote Norman Sharpless, MD, director of the National Cancer Institute, in Science in June. Combined, breast cancer and colon cancer account for one-sixth of all cancers in the U.S., he wrote.
In addition, blood pressure control has gotten worse since the start of the pandemic, said Michael Rakotz, MD, FAHA, FAAFP, vice president of improving health outcomes at the AMA, in an AMA blog post.
Dr. Harmon’s advice for physician practices on getting patients in for routine care:
- Educate the area’s largest employers to encourage their employees.
- Engage with hospital employees, since hospitals are often the largest employers in many communities.
- Partner with health insurers.
- Show up at athletic events, which is a particularly good fit for “small town America,” said Dr. Harmon.
The AMA’s research doesn’t consider reimbursement from other public and private payers. It also doesn’t account for funding sources such as Provider Relief Fund grants, Paycheck Protection Program loans, and the temporary suspension of the Medicare sequester, per the report.
A version of this article first appeared on Medscape.com.
Physician practices around the country took an unprecedented financial hit with the arrival of the COVID-19 pandemic in March 2020. Recent research from the American Medical Association reveals an estimated pandemic-related shortfall in Medicare physician fee spending of $13.9 billion, or a 14% reduction, across all states and all major specialties in 2020.
While the report pointed to a “strong recovery” in May and June, that recovery stalled in the second half of 2020, and spending never returned to pre–COVID-19 levels.
“Physicians experienced a significant and sustained drop in Medicare revenue during the first 10 months of the pandemic,” said AMA President Gerald Harmon, MD, in a statement. “Medical practices that have not buckled under financial strain continue to be stretched clinically, emotionally, and fiscally as the pandemic persists. Yet physicians face an array of planned cuts that would reduce Medicare physician payments by nearly 10% for 2022.”
The reduction in the Medicare physician fee schedule payments means providers may face payment cuts of more than 9% starting Jan. 1, 2022, when the cuts take effect. That is, unless Congress makes changes.
Medicare physician fee schedule spending on telehealth stood at $4.1 billion, or 5% of the total Medicare spent in 2020. From March 16 to June 30, $1.8 billion of this amount was on telehealth, while $1.1 billion came in during third and fourth quarters of 2020, respectively, per the report.
According to AMA’s research:
- Medicare physician fee schedule spending for 2020, relative to expected 2020 spending, dipped 32% between March 16 and June 30; spending was down during the last 6 months of the year by between 9% and 10%.
- The care settings hit the worst were ambulatory surgical centers, outpatient hospitals, and physician offices; the next worst off were hospital emergency departments, inpatient hospitals, and skilled nursing facilities.
- The specialties that fared worst included physical therapists (-28%), opthamologists (-19%), podiatrists (-18%), and dermatologists (-18%).
- Cumulative spending was down the most in Minnesota (-22%), Maine (-19%), and New York (-19%); less affected states included Idaho (-9%), Oklahoma (-9%), and South Carolina (9%).
AMA: Budget neutrality hurting physicians’ financial stability
Dr. Harmon is calling for financial stability in Medicare spending. In particular, the AMA is “strongly urging Congress to avert the planned payment cuts,” he said in a statement.
The challenge: The Medicare physician fee schedule is currently “budget neutral,” meaning that the budget is fixed, Dr. Harmon, a family medicine specialist in South Carolina, told this news organization.
“If you rob from Peter to pay Paul, Paul is going to be less efficient or less rewarded. It continues to be that there’s always a ‘pay for’ in these things. So budget neutrality is probably one of the first things we need to address,” he said.
Lack of routine care expected to affect health outcomes
The result of reduced screening and treatment during the pandemic could be as many as 10,000 excess deaths due to cancers of the breast and colon during the next 10 years, wrote Norman Sharpless, MD, director of the National Cancer Institute, in Science in June. Combined, breast cancer and colon cancer account for one-sixth of all cancers in the U.S., he wrote.
In addition, blood pressure control has gotten worse since the start of the pandemic, said Michael Rakotz, MD, FAHA, FAAFP, vice president of improving health outcomes at the AMA, in an AMA blog post.
Dr. Harmon’s advice for physician practices on getting patients in for routine care:
- Educate the area’s largest employers to encourage their employees.
- Engage with hospital employees, since hospitals are often the largest employers in many communities.
- Partner with health insurers.
- Show up at athletic events, which is a particularly good fit for “small town America,” said Dr. Harmon.
The AMA’s research doesn’t consider reimbursement from other public and private payers. It also doesn’t account for funding sources such as Provider Relief Fund grants, Paycheck Protection Program loans, and the temporary suspension of the Medicare sequester, per the report.
A version of this article first appeared on Medscape.com.
Differences in response to immunotherapy in men versus women
.
In a population-based cohort study, women with advanced melanoma and prior ipilimumab treatment who then received combination nivolumab and ipilimumab immunotherapy had a more than twofold increase in the risk for death in comparison with their male counterparts.
The hazard ratio (HR) for mortality among women versus men treated with the combination immunotherapy after prior ipilimumab treatment was 2.06 (P = .003). No such difference was observed among those receiving single-agent therapy with pembrolizumab or nivolumab (HR for mortality in women vs. men, 0.97; P = .85) or among patients without prior ipilimumab use (HR, 0.85; P = .16).
Women with prior ipilimumab use also had a nearly threefold increase in the risk for death with combination immunotherapy versus with single-agent anti–programmed cell death protein–1 (anti-PD-1) therapy (HR, 2.82), but no such difference was seen among the men in the study.
The findings were published online Dec. 2 in JAMA Network Open.
They come from an analysis of Surveillance, Epidemiology, and End Results (SEERS)–Medicare linked data for 982 men and 387 women with stage III or IV melanoma whose median age was 75 years.
The findings suggest that the patient’s sex should be considered in treatment planning to optimize outcomes, the authors noted.
“These novel findings suggest that, for women with a prior history of ipilimumab, treatment with anti-PD-1 therapy may be preferable to combination therapy, whereas for men, it is unclear which treatment is better,” they wrote.
In a press release, principal author Grace Lu-Yao, PhD, a professor at Thomas Jefferson University, Philadelphia, acknowledged that it remains unclear whether the increased risk for death in women is a result of treatment side effects or lack of efficacy, but she stressed that “this is a powerful signal in real-world data that we need to investigate further.
“This data is a wake-up call based on the experience of hundreds of patients on these drugs,” said Dr. Lu-Yao. “This real-world data demonstrates that the results derived from men might not be applicable to women and it is critical to design studies with sufficient power to evaluate treatment effectiveness by sex.”
Relevance for routine practice is unclear
The relevance of the findings for routine practice is unclear, given the median age of the cohort and a lack of data on whether excess mortality was cancer- or toxicity-related or due to another cause, Jeffrey S. Weber, MD, PhD, told this news organization. Dr. Weber is a professor and deputy director of the Laura and Isaac Perlmutter Cancer Center at New York University.
“The study is interesting and detailed, but it is a rather narrowly defined cohort that is over 65 and has a median of age 75, [which is] very different than most melanoma patient cohorts of patients treated with immunotherapy, whose median age is 10 years younger,” Dr. Weber said in an interview.
Furthermore, “in practice, almost no current patients will have been previously treated with ipilimumab and then receive combination immunotherapy,” he said. “Overall, these data would not impact on how I treat patients,” he said.
Gender differences in response
This study is not the first to show a gender-based difference in outcomes after immunotherapy. As previously reported by this news organization, a meta-analysis published in The Lancet Oncology in 2018 showed that immune checkpoint inhibitors are twice as effective as standard cancer therapies in men with advanced solid tumors, compared with their female counterparts.
However, sex-based differences remain under-assessed despite “accumulating evidence of the potential role played by sex in drug effectiveness owing to the biological differences between men and women,” wrote the authors of the latest study in melanoma.
“This lack of attention on the association of sex with the effectiveness of immune checkpoint inhibitor (ICI)–based immunotherapy may have significant negative consequences, especially because these treatments are associated with high toxicity and high treatment cost. For future trials, it would be crucial to examine effect modification by sex,” they added.
The study was funded by the Sidney Kimmel Cancer Center. Dr. Lu-Yao and coauthors have disclosed no relevant financial relationships. Dr. Weber is a regular contributor to Medscape. He reports relationships with Bristol-Myers Squibb, GlaxoSmithKline, Genentech BioOncology, Merck & Co, Novartis, EMD Serono, Celldex, CytomX, Nektar, Roche, Altor, Daiichi-Sankyo, and Eli Lilly and is named on patents filed for biomarkers for ipilimumab and nivolumab.
A version of this article first appeared on Medscape.com.
.
In a population-based cohort study, women with advanced melanoma and prior ipilimumab treatment who then received combination nivolumab and ipilimumab immunotherapy had a more than twofold increase in the risk for death in comparison with their male counterparts.
The hazard ratio (HR) for mortality among women versus men treated with the combination immunotherapy after prior ipilimumab treatment was 2.06 (P = .003). No such difference was observed among those receiving single-agent therapy with pembrolizumab or nivolumab (HR for mortality in women vs. men, 0.97; P = .85) or among patients without prior ipilimumab use (HR, 0.85; P = .16).
Women with prior ipilimumab use also had a nearly threefold increase in the risk for death with combination immunotherapy versus with single-agent anti–programmed cell death protein–1 (anti-PD-1) therapy (HR, 2.82), but no such difference was seen among the men in the study.
The findings were published online Dec. 2 in JAMA Network Open.
They come from an analysis of Surveillance, Epidemiology, and End Results (SEERS)–Medicare linked data for 982 men and 387 women with stage III or IV melanoma whose median age was 75 years.
The findings suggest that the patient’s sex should be considered in treatment planning to optimize outcomes, the authors noted.
“These novel findings suggest that, for women with a prior history of ipilimumab, treatment with anti-PD-1 therapy may be preferable to combination therapy, whereas for men, it is unclear which treatment is better,” they wrote.
In a press release, principal author Grace Lu-Yao, PhD, a professor at Thomas Jefferson University, Philadelphia, acknowledged that it remains unclear whether the increased risk for death in women is a result of treatment side effects or lack of efficacy, but she stressed that “this is a powerful signal in real-world data that we need to investigate further.
“This data is a wake-up call based on the experience of hundreds of patients on these drugs,” said Dr. Lu-Yao. “This real-world data demonstrates that the results derived from men might not be applicable to women and it is critical to design studies with sufficient power to evaluate treatment effectiveness by sex.”
Relevance for routine practice is unclear
The relevance of the findings for routine practice is unclear, given the median age of the cohort and a lack of data on whether excess mortality was cancer- or toxicity-related or due to another cause, Jeffrey S. Weber, MD, PhD, told this news organization. Dr. Weber is a professor and deputy director of the Laura and Isaac Perlmutter Cancer Center at New York University.
“The study is interesting and detailed, but it is a rather narrowly defined cohort that is over 65 and has a median of age 75, [which is] very different than most melanoma patient cohorts of patients treated with immunotherapy, whose median age is 10 years younger,” Dr. Weber said in an interview.
Furthermore, “in practice, almost no current patients will have been previously treated with ipilimumab and then receive combination immunotherapy,” he said. “Overall, these data would not impact on how I treat patients,” he said.
Gender differences in response
This study is not the first to show a gender-based difference in outcomes after immunotherapy. As previously reported by this news organization, a meta-analysis published in The Lancet Oncology in 2018 showed that immune checkpoint inhibitors are twice as effective as standard cancer therapies in men with advanced solid tumors, compared with their female counterparts.
However, sex-based differences remain under-assessed despite “accumulating evidence of the potential role played by sex in drug effectiveness owing to the biological differences between men and women,” wrote the authors of the latest study in melanoma.
“This lack of attention on the association of sex with the effectiveness of immune checkpoint inhibitor (ICI)–based immunotherapy may have significant negative consequences, especially because these treatments are associated with high toxicity and high treatment cost. For future trials, it would be crucial to examine effect modification by sex,” they added.
The study was funded by the Sidney Kimmel Cancer Center. Dr. Lu-Yao and coauthors have disclosed no relevant financial relationships. Dr. Weber is a regular contributor to Medscape. He reports relationships with Bristol-Myers Squibb, GlaxoSmithKline, Genentech BioOncology, Merck & Co, Novartis, EMD Serono, Celldex, CytomX, Nektar, Roche, Altor, Daiichi-Sankyo, and Eli Lilly and is named on patents filed for biomarkers for ipilimumab and nivolumab.
A version of this article first appeared on Medscape.com.
.
In a population-based cohort study, women with advanced melanoma and prior ipilimumab treatment who then received combination nivolumab and ipilimumab immunotherapy had a more than twofold increase in the risk for death in comparison with their male counterparts.
The hazard ratio (HR) for mortality among women versus men treated with the combination immunotherapy after prior ipilimumab treatment was 2.06 (P = .003). No such difference was observed among those receiving single-agent therapy with pembrolizumab or nivolumab (HR for mortality in women vs. men, 0.97; P = .85) or among patients without prior ipilimumab use (HR, 0.85; P = .16).
Women with prior ipilimumab use also had a nearly threefold increase in the risk for death with combination immunotherapy versus with single-agent anti–programmed cell death protein–1 (anti-PD-1) therapy (HR, 2.82), but no such difference was seen among the men in the study.
The findings were published online Dec. 2 in JAMA Network Open.
They come from an analysis of Surveillance, Epidemiology, and End Results (SEERS)–Medicare linked data for 982 men and 387 women with stage III or IV melanoma whose median age was 75 years.
The findings suggest that the patient’s sex should be considered in treatment planning to optimize outcomes, the authors noted.
“These novel findings suggest that, for women with a prior history of ipilimumab, treatment with anti-PD-1 therapy may be preferable to combination therapy, whereas for men, it is unclear which treatment is better,” they wrote.
In a press release, principal author Grace Lu-Yao, PhD, a professor at Thomas Jefferson University, Philadelphia, acknowledged that it remains unclear whether the increased risk for death in women is a result of treatment side effects or lack of efficacy, but she stressed that “this is a powerful signal in real-world data that we need to investigate further.
“This data is a wake-up call based on the experience of hundreds of patients on these drugs,” said Dr. Lu-Yao. “This real-world data demonstrates that the results derived from men might not be applicable to women and it is critical to design studies with sufficient power to evaluate treatment effectiveness by sex.”
Relevance for routine practice is unclear
The relevance of the findings for routine practice is unclear, given the median age of the cohort and a lack of data on whether excess mortality was cancer- or toxicity-related or due to another cause, Jeffrey S. Weber, MD, PhD, told this news organization. Dr. Weber is a professor and deputy director of the Laura and Isaac Perlmutter Cancer Center at New York University.
“The study is interesting and detailed, but it is a rather narrowly defined cohort that is over 65 and has a median of age 75, [which is] very different than most melanoma patient cohorts of patients treated with immunotherapy, whose median age is 10 years younger,” Dr. Weber said in an interview.
Furthermore, “in practice, almost no current patients will have been previously treated with ipilimumab and then receive combination immunotherapy,” he said. “Overall, these data would not impact on how I treat patients,” he said.
Gender differences in response
This study is not the first to show a gender-based difference in outcomes after immunotherapy. As previously reported by this news organization, a meta-analysis published in The Lancet Oncology in 2018 showed that immune checkpoint inhibitors are twice as effective as standard cancer therapies in men with advanced solid tumors, compared with their female counterparts.
However, sex-based differences remain under-assessed despite “accumulating evidence of the potential role played by sex in drug effectiveness owing to the biological differences between men and women,” wrote the authors of the latest study in melanoma.
“This lack of attention on the association of sex with the effectiveness of immune checkpoint inhibitor (ICI)–based immunotherapy may have significant negative consequences, especially because these treatments are associated with high toxicity and high treatment cost. For future trials, it would be crucial to examine effect modification by sex,” they added.
The study was funded by the Sidney Kimmel Cancer Center. Dr. Lu-Yao and coauthors have disclosed no relevant financial relationships. Dr. Weber is a regular contributor to Medscape. He reports relationships with Bristol-Myers Squibb, GlaxoSmithKline, Genentech BioOncology, Merck & Co, Novartis, EMD Serono, Celldex, CytomX, Nektar, Roche, Altor, Daiichi-Sankyo, and Eli Lilly and is named on patents filed for biomarkers for ipilimumab and nivolumab.
A version of this article first appeared on Medscape.com.
International panel backs energy-based devices as first-line treatment of acne scars
International consensus .
Peter R. Shumaker, MD, a dermatologist and dermatologic surgeon at the VA San Diego Healthcare System and one of the authors of the paper, noted that a panel of 24 international experts in dermatology and plastic surgery assembled to develop the recommendations for integrating EBDs into the management of acne scarring.
“The advent of fractional laser technology in the mid-2000s ushered in an exciting new period of exploration and advances in scar treatment with EBDs,” Dr. Shumaker said in an interview. “Despite intense interest and a wealth of available literature, international treatment guidelines and patient access to these potentially life-changing treatments are currently lagging behind our capabilities.”
One of the key recommendations of the paper is that EBDs should have an expanded role in the treatment of acne scars, according to Dr. Shumaker, associate clinical professor of dermatology at the University of California, San Diego. “Panel members were unanimous in their view that EBDs, particularly ablative and nonablative fractional lasers, vascular lasers, and fractional radiofrequency devices, have an important role in the management of acne scars and should be considered a first-line treatment for a variety of scar types,” he said.
The process leading to the recommendations included developing clinical questions, based on input from the panelists and a literature review, and using a two-step modified Delphi method, “an iterative process used to achieve consensus for a defined clinical problem where there is little or conflicting published evidence and where expert opinion is decisive,” the authors wrote. This involved email questionnaires highlighting different topics, including the role of EBDs in mitigating and treating acne scars in patients with active acne, the use of different EBDs for treating different types of acne scars, and considerations in treating skin of color.
The panel noted considerations in the treatment of acne scars in skin of color. “Regardless of the platform, patients with darker skin types may require treatment modifications including: a reduction in fluence/pulse energy; decreased microcolumn density; greater intervals between treatments; longer pulse durations; epidermal cooling with fastidious technique to ensure appropriate cooling, additional cooling in between passes to decrease bulk heating; and pretreatment and posttreatment topical regimens (e.g., retinoids, bleaching creams, etc.) and strict sun precautions,” wrote the authors.
Panelists agreed that there is an absence of large, well-controlled, multicenter comparative trials of various laser and energy treatments for acne scars. “Such trials would be helpful in establishing the relative utility and persistence of benefit of various laser treatments and also in comparing their effectiveness versus that of nonenergy treatments,” the authors noted.
Asked to comment on the paper, Andrei Metelitsa, MD, a dermatologist in Calgary, Alta., and clinical associate professor at the University of Calgary, said the consensus recommendations on EBDs in acne scarring are “providing an international expert perspective, potentially changing a long-perceived paradigm of treatments.”
Dr. Metelitsa pointed out that the authors are taking a solid position with respect to reducing the delay to initiation of laser treatment following isotretinoin therapy. “The authors take a strong stance against the old dogma of postponing laser resurfacing for at least 6 months post isotretinoin,” he said. “According to the authors, there is sufficient evidence to support the idea of safely starting laser therapies, including fractional ablative and nonablative, within 1 month post isotretinoin, much sooner than previously suggested.”
He added that the authors point to the fact most experts utilize vascular lasers, such as pulsed-dye, to treat active acne in combination with medical therapy, thus reducing duration and severity of inflammation and potentially reducing further scar formation. “According to this published consensus, such laser therapies can even be used while the patient is actively treated with isotretinoin,” he said.
Dr. Metelitsa noted that the consensus recommendations outline how the choice of device should be guided by the clinical subtype of acne scars.
Dr. Shumaker, Dr. Metelitsa, and the authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
International consensus .
Peter R. Shumaker, MD, a dermatologist and dermatologic surgeon at the VA San Diego Healthcare System and one of the authors of the paper, noted that a panel of 24 international experts in dermatology and plastic surgery assembled to develop the recommendations for integrating EBDs into the management of acne scarring.
“The advent of fractional laser technology in the mid-2000s ushered in an exciting new period of exploration and advances in scar treatment with EBDs,” Dr. Shumaker said in an interview. “Despite intense interest and a wealth of available literature, international treatment guidelines and patient access to these potentially life-changing treatments are currently lagging behind our capabilities.”
One of the key recommendations of the paper is that EBDs should have an expanded role in the treatment of acne scars, according to Dr. Shumaker, associate clinical professor of dermatology at the University of California, San Diego. “Panel members were unanimous in their view that EBDs, particularly ablative and nonablative fractional lasers, vascular lasers, and fractional radiofrequency devices, have an important role in the management of acne scars and should be considered a first-line treatment for a variety of scar types,” he said.
The process leading to the recommendations included developing clinical questions, based on input from the panelists and a literature review, and using a two-step modified Delphi method, “an iterative process used to achieve consensus for a defined clinical problem where there is little or conflicting published evidence and where expert opinion is decisive,” the authors wrote. This involved email questionnaires highlighting different topics, including the role of EBDs in mitigating and treating acne scars in patients with active acne, the use of different EBDs for treating different types of acne scars, and considerations in treating skin of color.
The panel noted considerations in the treatment of acne scars in skin of color. “Regardless of the platform, patients with darker skin types may require treatment modifications including: a reduction in fluence/pulse energy; decreased microcolumn density; greater intervals between treatments; longer pulse durations; epidermal cooling with fastidious technique to ensure appropriate cooling, additional cooling in between passes to decrease bulk heating; and pretreatment and posttreatment topical regimens (e.g., retinoids, bleaching creams, etc.) and strict sun precautions,” wrote the authors.
Panelists agreed that there is an absence of large, well-controlled, multicenter comparative trials of various laser and energy treatments for acne scars. “Such trials would be helpful in establishing the relative utility and persistence of benefit of various laser treatments and also in comparing their effectiveness versus that of nonenergy treatments,” the authors noted.
Asked to comment on the paper, Andrei Metelitsa, MD, a dermatologist in Calgary, Alta., and clinical associate professor at the University of Calgary, said the consensus recommendations on EBDs in acne scarring are “providing an international expert perspective, potentially changing a long-perceived paradigm of treatments.”
Dr. Metelitsa pointed out that the authors are taking a solid position with respect to reducing the delay to initiation of laser treatment following isotretinoin therapy. “The authors take a strong stance against the old dogma of postponing laser resurfacing for at least 6 months post isotretinoin,” he said. “According to the authors, there is sufficient evidence to support the idea of safely starting laser therapies, including fractional ablative and nonablative, within 1 month post isotretinoin, much sooner than previously suggested.”
He added that the authors point to the fact most experts utilize vascular lasers, such as pulsed-dye, to treat active acne in combination with medical therapy, thus reducing duration and severity of inflammation and potentially reducing further scar formation. “According to this published consensus, such laser therapies can even be used while the patient is actively treated with isotretinoin,” he said.
Dr. Metelitsa noted that the consensus recommendations outline how the choice of device should be guided by the clinical subtype of acne scars.
Dr. Shumaker, Dr. Metelitsa, and the authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
International consensus .
Peter R. Shumaker, MD, a dermatologist and dermatologic surgeon at the VA San Diego Healthcare System and one of the authors of the paper, noted that a panel of 24 international experts in dermatology and plastic surgery assembled to develop the recommendations for integrating EBDs into the management of acne scarring.
“The advent of fractional laser technology in the mid-2000s ushered in an exciting new period of exploration and advances in scar treatment with EBDs,” Dr. Shumaker said in an interview. “Despite intense interest and a wealth of available literature, international treatment guidelines and patient access to these potentially life-changing treatments are currently lagging behind our capabilities.”
One of the key recommendations of the paper is that EBDs should have an expanded role in the treatment of acne scars, according to Dr. Shumaker, associate clinical professor of dermatology at the University of California, San Diego. “Panel members were unanimous in their view that EBDs, particularly ablative and nonablative fractional lasers, vascular lasers, and fractional radiofrequency devices, have an important role in the management of acne scars and should be considered a first-line treatment for a variety of scar types,” he said.
The process leading to the recommendations included developing clinical questions, based on input from the panelists and a literature review, and using a two-step modified Delphi method, “an iterative process used to achieve consensus for a defined clinical problem where there is little or conflicting published evidence and where expert opinion is decisive,” the authors wrote. This involved email questionnaires highlighting different topics, including the role of EBDs in mitigating and treating acne scars in patients with active acne, the use of different EBDs for treating different types of acne scars, and considerations in treating skin of color.
The panel noted considerations in the treatment of acne scars in skin of color. “Regardless of the platform, patients with darker skin types may require treatment modifications including: a reduction in fluence/pulse energy; decreased microcolumn density; greater intervals between treatments; longer pulse durations; epidermal cooling with fastidious technique to ensure appropriate cooling, additional cooling in between passes to decrease bulk heating; and pretreatment and posttreatment topical regimens (e.g., retinoids, bleaching creams, etc.) and strict sun precautions,” wrote the authors.
Panelists agreed that there is an absence of large, well-controlled, multicenter comparative trials of various laser and energy treatments for acne scars. “Such trials would be helpful in establishing the relative utility and persistence of benefit of various laser treatments and also in comparing their effectiveness versus that of nonenergy treatments,” the authors noted.
Asked to comment on the paper, Andrei Metelitsa, MD, a dermatologist in Calgary, Alta., and clinical associate professor at the University of Calgary, said the consensus recommendations on EBDs in acne scarring are “providing an international expert perspective, potentially changing a long-perceived paradigm of treatments.”
Dr. Metelitsa pointed out that the authors are taking a solid position with respect to reducing the delay to initiation of laser treatment following isotretinoin therapy. “The authors take a strong stance against the old dogma of postponing laser resurfacing for at least 6 months post isotretinoin,” he said. “According to the authors, there is sufficient evidence to support the idea of safely starting laser therapies, including fractional ablative and nonablative, within 1 month post isotretinoin, much sooner than previously suggested.”
He added that the authors point to the fact most experts utilize vascular lasers, such as pulsed-dye, to treat active acne in combination with medical therapy, thus reducing duration and severity of inflammation and potentially reducing further scar formation. “According to this published consensus, such laser therapies can even be used while the patient is actively treated with isotretinoin,” he said.
Dr. Metelitsa noted that the consensus recommendations outline how the choice of device should be guided by the clinical subtype of acne scars.
Dr. Shumaker, Dr. Metelitsa, and the authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Dust mite immunotherapy may help some with eczema
, but improvement in the primary outcome was not significant, new data show.
Results of the small, randomized, double-blind, placebo-controlled trial were published recently in The Journal of Allergy and Clinical Immunology: In Practice.
Lead author Sarah Sella Langer, MD, of the department of medicine, Ribeirão Preto (Brazil) Medical School, University of São Paulo, and colleagues said their results suggest HDM SLIT is safe and effective as an add-on treatment.
The dust mite extract therapy had no major side effects after 18 months of treatment, the authors reported.
The researchers included data from 66 patients who completed the study. The participants were at least 3 years old, registered at least 15 on the SCORing Atopic Dermatitis (SCORAD) measure, and had a skin prick test and/or immunoglobulin E (IgE) test for sensitization to dust mites.
Patients were grouped by age (younger than 12 years or 12 years and older) to receive HDM SLIT (n = 35) or placebo (n = 31) 3 days a week for the study period – between May 2018 and June 2020 – at the Clinical Research Unit of Ribeirão Preto Medical School Hospital.
At baseline, the mean SCORAD was 46.9 (range, 17-87).
After 18 months, 74.2% and 58% of patients in HDM SLIT and placebo groups, respectively, showed at least a15-point decrease in SCORAD (relative risk, 1.28; 95% confidence interval, 0.89-1.83). However, those primary outcome results did not reach statistical significance.
On the other hand, some secondary outcomes did show significant results.
At 95% CI, the researchers reported significant objective-SCORAD decreases of 56.8% and 34.9% in HDM SLIT and placebo groups (average difference, 21.3). Significantly more patients had a score of 0 or 1 on the 5-point Investigator’s Global Assessment scale in the intervention group than in the placebo group (14/35 vs. 5/31; RR, 2.63).
There were no significant changes in the Eczema Area and Severity Index, the visual analogue scale for symptoms, the pruritus scale, or the Dermatology Life Quality Index.
Patients in the trial, most of whom had moderate to severe disease, continued to be treated with usual, individualized therapy for AD, in accordance with current guidelines and experts’ recommendations.
Tina Sindher, MD, an allergist with the Sean N. Parker Center for Allergy and Asthma Research at Stanford (Calif.) University, , told this news organization that the results are not robust enough to recommend the immunotherapy widely.
She pointed out that even in the placebo group, more than half the patients met the primary endpoint.
However, she did say HDM SLIT could be considered as an add-on treatment for the right patients, especially since risk for an allergic reaction or other adverse condition is small. The most common adverse effects were headache and abdominal pain, and they were reported in both the treatment and placebo groups.
With AD, she said, “there is no one drug that’s right for everyone,” because genetics and environment make the kind of symptoms and severity and duration different for each patient.
It all comes down to risk and benefits, she said.
She said if she had a patient with an environmental allergy who’s trying to manage nasal congestion and also happened to have eczema, “I think they’re a great candidate for sublingual dust mite therapy because then not only am I treating their nasal congestions, their other symptoms, it may also help their eczema,” Dr. Sindher said.
Without those concurrent conditions, she said, the benefits of dust mite immunotherapy would not outweigh the risks or the potential burden on the patient of having to take the SLIT.
She said she would present the choice to the patient, and if other treatments haven’t been successful and the patient wants to try it, she would be open to a trial period.
The study was supported by the Brazilian National Council for Scientific and Technological Development, the Institute of Investigation in Immunology, the National Institutes of Science and Technology, the Brazilian National Council for Scientific and Technological Development, and the São Paulo Research Foundation. The mite extract for immunotherapy was provided by the laboratory IPI-ASAC Brasil/ASAC Pharma Brasil. Dr. Langer received a doctoral scholarship from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES). Dr. Sindher reported no relevant financial relationships.
Commentary by Lawrence F. Eichenfield, MD
Environmental triggers of atopic dermatitis (AD) may be difficult to assess, especially as children with AD commonly develop “overlap” conditions of allergic rhinitis, food allergy, and asthma. The place of immunotherapy in treatment of AD has been controversial over the years, with mixed results from studies on its effect on eczema in different subpopulations. However, a holistic view of allergy care makes consideration of environmental allergies reasonable. The study by Dr. Langer and colleagues was a well-designed double-blind placebo-controlled trial of house dust mite sublingual immunotherapy in mite-sensitized AD patients aged 3 and older with at least mild AD, though the mean eczema severity was severe. After 18 months, there was an impressive 74% decrease in eczema score (SCORAD), but also a 58% decrease in the placebo group. While the primary outcome measure wasn’t statistically significant, some secondary ones were. I agree with the commentary in the article that the data doesn’t support immunotherapy being advised to everyone, while its use as an add-on treatment for certain patients in whom the eczema may overlap with other allergic manifestations is reasonable. For several years at Rady Children’s Hospital, San Diego, we have run a multidisciplinary atopic dermatitis program where patients are comanaged by dermatology and allergy. We have learned to appreciate that a broad perspective on managing comorbid conditions in children with AD really helps the patients and families to understand the many effects of inflammatory and allergic conditions, with improved outcomes and quality of life.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children's Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. He disclosed that he has served as an investigator and/or consultant to AbbVie, Lilly, Pfizer, Regeneron, Sanofi-Genzyme, and Verrica.
A version of this article first appeared on Medscape.com.
This article was updated 6/18/22.
, but improvement in the primary outcome was not significant, new data show.
Results of the small, randomized, double-blind, placebo-controlled trial were published recently in The Journal of Allergy and Clinical Immunology: In Practice.
Lead author Sarah Sella Langer, MD, of the department of medicine, Ribeirão Preto (Brazil) Medical School, University of São Paulo, and colleagues said their results suggest HDM SLIT is safe and effective as an add-on treatment.
The dust mite extract therapy had no major side effects after 18 months of treatment, the authors reported.
The researchers included data from 66 patients who completed the study. The participants were at least 3 years old, registered at least 15 on the SCORing Atopic Dermatitis (SCORAD) measure, and had a skin prick test and/or immunoglobulin E (IgE) test for sensitization to dust mites.
Patients were grouped by age (younger than 12 years or 12 years and older) to receive HDM SLIT (n = 35) or placebo (n = 31) 3 days a week for the study period – between May 2018 and June 2020 – at the Clinical Research Unit of Ribeirão Preto Medical School Hospital.
At baseline, the mean SCORAD was 46.9 (range, 17-87).
After 18 months, 74.2% and 58% of patients in HDM SLIT and placebo groups, respectively, showed at least a15-point decrease in SCORAD (relative risk, 1.28; 95% confidence interval, 0.89-1.83). However, those primary outcome results did not reach statistical significance.
On the other hand, some secondary outcomes did show significant results.
At 95% CI, the researchers reported significant objective-SCORAD decreases of 56.8% and 34.9% in HDM SLIT and placebo groups (average difference, 21.3). Significantly more patients had a score of 0 or 1 on the 5-point Investigator’s Global Assessment scale in the intervention group than in the placebo group (14/35 vs. 5/31; RR, 2.63).
There were no significant changes in the Eczema Area and Severity Index, the visual analogue scale for symptoms, the pruritus scale, or the Dermatology Life Quality Index.
Patients in the trial, most of whom had moderate to severe disease, continued to be treated with usual, individualized therapy for AD, in accordance with current guidelines and experts’ recommendations.
Tina Sindher, MD, an allergist with the Sean N. Parker Center for Allergy and Asthma Research at Stanford (Calif.) University, , told this news organization that the results are not robust enough to recommend the immunotherapy widely.
She pointed out that even in the placebo group, more than half the patients met the primary endpoint.
However, she did say HDM SLIT could be considered as an add-on treatment for the right patients, especially since risk for an allergic reaction or other adverse condition is small. The most common adverse effects were headache and abdominal pain, and they were reported in both the treatment and placebo groups.
With AD, she said, “there is no one drug that’s right for everyone,” because genetics and environment make the kind of symptoms and severity and duration different for each patient.
It all comes down to risk and benefits, she said.
She said if she had a patient with an environmental allergy who’s trying to manage nasal congestion and also happened to have eczema, “I think they’re a great candidate for sublingual dust mite therapy because then not only am I treating their nasal congestions, their other symptoms, it may also help their eczema,” Dr. Sindher said.
Without those concurrent conditions, she said, the benefits of dust mite immunotherapy would not outweigh the risks or the potential burden on the patient of having to take the SLIT.
She said she would present the choice to the patient, and if other treatments haven’t been successful and the patient wants to try it, she would be open to a trial period.
The study was supported by the Brazilian National Council for Scientific and Technological Development, the Institute of Investigation in Immunology, the National Institutes of Science and Technology, the Brazilian National Council for Scientific and Technological Development, and the São Paulo Research Foundation. The mite extract for immunotherapy was provided by the laboratory IPI-ASAC Brasil/ASAC Pharma Brasil. Dr. Langer received a doctoral scholarship from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES). Dr. Sindher reported no relevant financial relationships.
Commentary by Lawrence F. Eichenfield, MD
Environmental triggers of atopic dermatitis (AD) may be difficult to assess, especially as children with AD commonly develop “overlap” conditions of allergic rhinitis, food allergy, and asthma. The place of immunotherapy in treatment of AD has been controversial over the years, with mixed results from studies on its effect on eczema in different subpopulations. However, a holistic view of allergy care makes consideration of environmental allergies reasonable. The study by Dr. Langer and colleagues was a well-designed double-blind placebo-controlled trial of house dust mite sublingual immunotherapy in mite-sensitized AD patients aged 3 and older with at least mild AD, though the mean eczema severity was severe. After 18 months, there was an impressive 74% decrease in eczema score (SCORAD), but also a 58% decrease in the placebo group. While the primary outcome measure wasn’t statistically significant, some secondary ones were. I agree with the commentary in the article that the data doesn’t support immunotherapy being advised to everyone, while its use as an add-on treatment for certain patients in whom the eczema may overlap with other allergic manifestations is reasonable. For several years at Rady Children’s Hospital, San Diego, we have run a multidisciplinary atopic dermatitis program where patients are comanaged by dermatology and allergy. We have learned to appreciate that a broad perspective on managing comorbid conditions in children with AD really helps the patients and families to understand the many effects of inflammatory and allergic conditions, with improved outcomes and quality of life.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children's Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. He disclosed that he has served as an investigator and/or consultant to AbbVie, Lilly, Pfizer, Regeneron, Sanofi-Genzyme, and Verrica.
A version of this article first appeared on Medscape.com.
This article was updated 6/18/22.
, but improvement in the primary outcome was not significant, new data show.
Results of the small, randomized, double-blind, placebo-controlled trial were published recently in The Journal of Allergy and Clinical Immunology: In Practice.
Lead author Sarah Sella Langer, MD, of the department of medicine, Ribeirão Preto (Brazil) Medical School, University of São Paulo, and colleagues said their results suggest HDM SLIT is safe and effective as an add-on treatment.
The dust mite extract therapy had no major side effects after 18 months of treatment, the authors reported.
The researchers included data from 66 patients who completed the study. The participants were at least 3 years old, registered at least 15 on the SCORing Atopic Dermatitis (SCORAD) measure, and had a skin prick test and/or immunoglobulin E (IgE) test for sensitization to dust mites.
Patients were grouped by age (younger than 12 years or 12 years and older) to receive HDM SLIT (n = 35) or placebo (n = 31) 3 days a week for the study period – between May 2018 and June 2020 – at the Clinical Research Unit of Ribeirão Preto Medical School Hospital.
At baseline, the mean SCORAD was 46.9 (range, 17-87).
After 18 months, 74.2% and 58% of patients in HDM SLIT and placebo groups, respectively, showed at least a15-point decrease in SCORAD (relative risk, 1.28; 95% confidence interval, 0.89-1.83). However, those primary outcome results did not reach statistical significance.
On the other hand, some secondary outcomes did show significant results.
At 95% CI, the researchers reported significant objective-SCORAD decreases of 56.8% and 34.9% in HDM SLIT and placebo groups (average difference, 21.3). Significantly more patients had a score of 0 or 1 on the 5-point Investigator’s Global Assessment scale in the intervention group than in the placebo group (14/35 vs. 5/31; RR, 2.63).
There were no significant changes in the Eczema Area and Severity Index, the visual analogue scale for symptoms, the pruritus scale, or the Dermatology Life Quality Index.
Patients in the trial, most of whom had moderate to severe disease, continued to be treated with usual, individualized therapy for AD, in accordance with current guidelines and experts’ recommendations.
Tina Sindher, MD, an allergist with the Sean N. Parker Center for Allergy and Asthma Research at Stanford (Calif.) University, , told this news organization that the results are not robust enough to recommend the immunotherapy widely.
She pointed out that even in the placebo group, more than half the patients met the primary endpoint.
However, she did say HDM SLIT could be considered as an add-on treatment for the right patients, especially since risk for an allergic reaction or other adverse condition is small. The most common adverse effects were headache and abdominal pain, and they were reported in both the treatment and placebo groups.
With AD, she said, “there is no one drug that’s right for everyone,” because genetics and environment make the kind of symptoms and severity and duration different for each patient.
It all comes down to risk and benefits, she said.
She said if she had a patient with an environmental allergy who’s trying to manage nasal congestion and also happened to have eczema, “I think they’re a great candidate for sublingual dust mite therapy because then not only am I treating their nasal congestions, their other symptoms, it may also help their eczema,” Dr. Sindher said.
Without those concurrent conditions, she said, the benefits of dust mite immunotherapy would not outweigh the risks or the potential burden on the patient of having to take the SLIT.
She said she would present the choice to the patient, and if other treatments haven’t been successful and the patient wants to try it, she would be open to a trial period.
The study was supported by the Brazilian National Council for Scientific and Technological Development, the Institute of Investigation in Immunology, the National Institutes of Science and Technology, the Brazilian National Council for Scientific and Technological Development, and the São Paulo Research Foundation. The mite extract for immunotherapy was provided by the laboratory IPI-ASAC Brasil/ASAC Pharma Brasil. Dr. Langer received a doctoral scholarship from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES). Dr. Sindher reported no relevant financial relationships.
Commentary by Lawrence F. Eichenfield, MD
Environmental triggers of atopic dermatitis (AD) may be difficult to assess, especially as children with AD commonly develop “overlap” conditions of allergic rhinitis, food allergy, and asthma. The place of immunotherapy in treatment of AD has been controversial over the years, with mixed results from studies on its effect on eczema in different subpopulations. However, a holistic view of allergy care makes consideration of environmental allergies reasonable. The study by Dr. Langer and colleagues was a well-designed double-blind placebo-controlled trial of house dust mite sublingual immunotherapy in mite-sensitized AD patients aged 3 and older with at least mild AD, though the mean eczema severity was severe. After 18 months, there was an impressive 74% decrease in eczema score (SCORAD), but also a 58% decrease in the placebo group. While the primary outcome measure wasn’t statistically significant, some secondary ones were. I agree with the commentary in the article that the data doesn’t support immunotherapy being advised to everyone, while its use as an add-on treatment for certain patients in whom the eczema may overlap with other allergic manifestations is reasonable. For several years at Rady Children’s Hospital, San Diego, we have run a multidisciplinary atopic dermatitis program where patients are comanaged by dermatology and allergy. We have learned to appreciate that a broad perspective on managing comorbid conditions in children with AD really helps the patients and families to understand the many effects of inflammatory and allergic conditions, with improved outcomes and quality of life.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children's Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. He disclosed that he has served as an investigator and/or consultant to AbbVie, Lilly, Pfizer, Regeneron, Sanofi-Genzyme, and Verrica.
A version of this article first appeared on Medscape.com.
This article was updated 6/18/22.
Online reviews most important factor in choosing a doctor: Survey
from Press Ganey, a provider of patient satisfaction surveys. According to the data, this online information is more important to consumers in selecting a physician than another doctor’s referral and is more than twice as important when choosing a primary care physician.
In fact, 83% of respondents said they went online to read reviews of a physician after receiving a referral from another provider.
The online research trend reflects not only the increased familiarity of all generations with the internet but also the growing consumerization of health care, Thomas Jeffrey, president of the Sullivan/Luallin Group, a patient experience consulting firm, told this news organization.
“According to patient satisfaction surveys, people are becoming health care consumers more than in the past,” he noted. “Historically, we didn’t look at health care as a consumer product. But, with high deductibles and copays, doctor visits can represent a pretty significant out-of-pocket expense. As it begins to hit folks’ pocketbooks, they become more savvy shoppers.”
Digital preferences for providers were gaining “positive momentum” even before the COVID-19 pandemic, but the crisis “drove upticks in some consumer digital behaviors,” the Press Ganey report pointed out.
Mr. Jeffrey agreed, noting that this finding matches what Sullivan/Luallin has discovered in its research. “I think the pandemic pushed people to engage more online,” he said. “The highest net promoter score [likelihood to recommend in market surveys] for a pharmacy is the Amazon pharmacy, which is an online-based delivery service. Then you have telehealth visits, which are more convenient in many ways.”
How patients search online
In choosing a new primary care doctor, 51.1% go on the web first, 23.8% seek a referral from another health care provider, and 4.4% get information from an insurer or a benefits manager, according to the survey.
The factors that matter most to consumers when they pick any provider, in order, are online ratings and reviews of the physician, referral from a current doctor, ratings and reviews of the facility, and the quality and completeness of a doctor’s profile on a website or online directory. The doctor’s online presence and the quality of their website are also important.
According to Press Ganey, search engines like Google are the most used digital resources, with 65.4% of consumers employing them to find a doctor. However, consumers now use an average of 2.7 sites in their search. The leading destinations are a hospital or a clinic site, WebMD, Healthgrades, and Facebook. (This news organization is owned by WebMD.)
Compared with 2019, the report said, there has been a 22.8% decline in the use of search engines for seeking a doctor and a 53.7% increase in the use of health care review sites such as Healthgrades and Vitals.
When reading provider reviews, consumers look for more recent reviews and want the reviews to be “authentic and informative.” They also value the star ratings. About 84%of respondents said they wouldn’t book an appointment with a referred provider that had a rating of less than four stars.
Overall, the top reasons why people are deterred from making an appointment are difficulty contacting the office, the poor quality of online reviews, and an average online rating of less than four stars.
The vast majority of respondents (77%) said they believe internet reviews reflect their own experience with a provider organization, and only 2.6% said the reviews were inaccurate. Another finding of the survey indicates that this attention of patients to reviews of their own provider doesn’t represent idle curiosity: About 57% of Baby Boomers and 45% of millennials/Gen Z’ers said they’d written online reviews of a doctor or a hospital.
Factors in patient loyalty
The Press Ganey survey asked which of several factors, besides excellent care, patients weighed when giving a five-star review to a health care provider.
Quality of customer service was rated first by 70.8% of respondents, followed by cleanliness of facilities (67.5%), communication (63.4%), the provider’s bedside manner (63%), ease of appointment booking (58.8%), ease of patient intake/registration (52.3%), quality and accuracy of information (40.1%), availability of telehealth services (21.7%), and waiting room amenities (21.8%).
The report explained that “quality of customer service” means “demeanor, attentiveness, and helpfulness of staff and practitioners.” “Communication” refers to things like follow-up appointment reminders and annual checkup reminders.
According to Mr. Jeffrey, these factors were considered more important than a doctor’s bedside manner because of the team care approach in most physician offices. “We see a lot more folks derive their notion of quality from continuity of care. And if they feel the physician they love is being supported by a less than competent team, that can impact significantly their sense of the quality of care,” he said.
Online appointment booking is a must
To win over the online consumer, Press Ganey emphasized, practices should ensure that provider listings are accurate and complete. In addition, offering online appointment booking can avoid the top challenge in making a new appointment, which is getting through to the office.
Mr. Jeffrey concurred, although he notes that practices have to be careful about how they enable patients to select appointment slots online. He suggests that an appointment request form on a patient portal first ask what the purpose of the visit is and that it offer five or so options. If the request fits into a routine visit category, the provider’s calendar pops up and the patient can select a convenient time slot. If it’s something else, an appointment scheduler calls the patient back.
“There needs to be greater access to standard appointments online,” he said. “While privacy is an issue, you can use the patient portal that most EHRs have to provide online booking. If you want to succeed going forward, that’s going to be a major plus.”
Of course, to do any of this, including reading provider reviews, a consumer needs a good internet connection and a mobile or desktop device. While broadband internet access is still not available in some communities, the breakdown of the survey respondents by demographics shows that low-income people were included.
Mr. Jeffrey doesn’t believe that a lack of internet access or digital devices prevents many Americans from going online today. “Even in poor communities, most people have internet access through their smartphones. Even baby boomers are familiar with smartphones. I haven’t seen internet access be a big barrier for low-income households, because they all have access to phones.”
A version of this article first appeared on Medscape.com.
from Press Ganey, a provider of patient satisfaction surveys. According to the data, this online information is more important to consumers in selecting a physician than another doctor’s referral and is more than twice as important when choosing a primary care physician.
In fact, 83% of respondents said they went online to read reviews of a physician after receiving a referral from another provider.
The online research trend reflects not only the increased familiarity of all generations with the internet but also the growing consumerization of health care, Thomas Jeffrey, president of the Sullivan/Luallin Group, a patient experience consulting firm, told this news organization.
“According to patient satisfaction surveys, people are becoming health care consumers more than in the past,” he noted. “Historically, we didn’t look at health care as a consumer product. But, with high deductibles and copays, doctor visits can represent a pretty significant out-of-pocket expense. As it begins to hit folks’ pocketbooks, they become more savvy shoppers.”
Digital preferences for providers were gaining “positive momentum” even before the COVID-19 pandemic, but the crisis “drove upticks in some consumer digital behaviors,” the Press Ganey report pointed out.
Mr. Jeffrey agreed, noting that this finding matches what Sullivan/Luallin has discovered in its research. “I think the pandemic pushed people to engage more online,” he said. “The highest net promoter score [likelihood to recommend in market surveys] for a pharmacy is the Amazon pharmacy, which is an online-based delivery service. Then you have telehealth visits, which are more convenient in many ways.”
How patients search online
In choosing a new primary care doctor, 51.1% go on the web first, 23.8% seek a referral from another health care provider, and 4.4% get information from an insurer or a benefits manager, according to the survey.
The factors that matter most to consumers when they pick any provider, in order, are online ratings and reviews of the physician, referral from a current doctor, ratings and reviews of the facility, and the quality and completeness of a doctor’s profile on a website or online directory. The doctor’s online presence and the quality of their website are also important.
According to Press Ganey, search engines like Google are the most used digital resources, with 65.4% of consumers employing them to find a doctor. However, consumers now use an average of 2.7 sites in their search. The leading destinations are a hospital or a clinic site, WebMD, Healthgrades, and Facebook. (This news organization is owned by WebMD.)
Compared with 2019, the report said, there has been a 22.8% decline in the use of search engines for seeking a doctor and a 53.7% increase in the use of health care review sites such as Healthgrades and Vitals.
When reading provider reviews, consumers look for more recent reviews and want the reviews to be “authentic and informative.” They also value the star ratings. About 84%of respondents said they wouldn’t book an appointment with a referred provider that had a rating of less than four stars.
Overall, the top reasons why people are deterred from making an appointment are difficulty contacting the office, the poor quality of online reviews, and an average online rating of less than four stars.
The vast majority of respondents (77%) said they believe internet reviews reflect their own experience with a provider organization, and only 2.6% said the reviews were inaccurate. Another finding of the survey indicates that this attention of patients to reviews of their own provider doesn’t represent idle curiosity: About 57% of Baby Boomers and 45% of millennials/Gen Z’ers said they’d written online reviews of a doctor or a hospital.
Factors in patient loyalty
The Press Ganey survey asked which of several factors, besides excellent care, patients weighed when giving a five-star review to a health care provider.
Quality of customer service was rated first by 70.8% of respondents, followed by cleanliness of facilities (67.5%), communication (63.4%), the provider’s bedside manner (63%), ease of appointment booking (58.8%), ease of patient intake/registration (52.3%), quality and accuracy of information (40.1%), availability of telehealth services (21.7%), and waiting room amenities (21.8%).
The report explained that “quality of customer service” means “demeanor, attentiveness, and helpfulness of staff and practitioners.” “Communication” refers to things like follow-up appointment reminders and annual checkup reminders.
According to Mr. Jeffrey, these factors were considered more important than a doctor’s bedside manner because of the team care approach in most physician offices. “We see a lot more folks derive their notion of quality from continuity of care. And if they feel the physician they love is being supported by a less than competent team, that can impact significantly their sense of the quality of care,” he said.
Online appointment booking is a must
To win over the online consumer, Press Ganey emphasized, practices should ensure that provider listings are accurate and complete. In addition, offering online appointment booking can avoid the top challenge in making a new appointment, which is getting through to the office.
Mr. Jeffrey concurred, although he notes that practices have to be careful about how they enable patients to select appointment slots online. He suggests that an appointment request form on a patient portal first ask what the purpose of the visit is and that it offer five or so options. If the request fits into a routine visit category, the provider’s calendar pops up and the patient can select a convenient time slot. If it’s something else, an appointment scheduler calls the patient back.
“There needs to be greater access to standard appointments online,” he said. “While privacy is an issue, you can use the patient portal that most EHRs have to provide online booking. If you want to succeed going forward, that’s going to be a major plus.”
Of course, to do any of this, including reading provider reviews, a consumer needs a good internet connection and a mobile or desktop device. While broadband internet access is still not available in some communities, the breakdown of the survey respondents by demographics shows that low-income people were included.
Mr. Jeffrey doesn’t believe that a lack of internet access or digital devices prevents many Americans from going online today. “Even in poor communities, most people have internet access through their smartphones. Even baby boomers are familiar with smartphones. I haven’t seen internet access be a big barrier for low-income households, because they all have access to phones.”
A version of this article first appeared on Medscape.com.
from Press Ganey, a provider of patient satisfaction surveys. According to the data, this online information is more important to consumers in selecting a physician than another doctor’s referral and is more than twice as important when choosing a primary care physician.
In fact, 83% of respondents said they went online to read reviews of a physician after receiving a referral from another provider.
The online research trend reflects not only the increased familiarity of all generations with the internet but also the growing consumerization of health care, Thomas Jeffrey, president of the Sullivan/Luallin Group, a patient experience consulting firm, told this news organization.
“According to patient satisfaction surveys, people are becoming health care consumers more than in the past,” he noted. “Historically, we didn’t look at health care as a consumer product. But, with high deductibles and copays, doctor visits can represent a pretty significant out-of-pocket expense. As it begins to hit folks’ pocketbooks, they become more savvy shoppers.”
Digital preferences for providers were gaining “positive momentum” even before the COVID-19 pandemic, but the crisis “drove upticks in some consumer digital behaviors,” the Press Ganey report pointed out.
Mr. Jeffrey agreed, noting that this finding matches what Sullivan/Luallin has discovered in its research. “I think the pandemic pushed people to engage more online,” he said. “The highest net promoter score [likelihood to recommend in market surveys] for a pharmacy is the Amazon pharmacy, which is an online-based delivery service. Then you have telehealth visits, which are more convenient in many ways.”
How patients search online
In choosing a new primary care doctor, 51.1% go on the web first, 23.8% seek a referral from another health care provider, and 4.4% get information from an insurer or a benefits manager, according to the survey.
The factors that matter most to consumers when they pick any provider, in order, are online ratings and reviews of the physician, referral from a current doctor, ratings and reviews of the facility, and the quality and completeness of a doctor’s profile on a website or online directory. The doctor’s online presence and the quality of their website are also important.
According to Press Ganey, search engines like Google are the most used digital resources, with 65.4% of consumers employing them to find a doctor. However, consumers now use an average of 2.7 sites in their search. The leading destinations are a hospital or a clinic site, WebMD, Healthgrades, and Facebook. (This news organization is owned by WebMD.)
Compared with 2019, the report said, there has been a 22.8% decline in the use of search engines for seeking a doctor and a 53.7% increase in the use of health care review sites such as Healthgrades and Vitals.
When reading provider reviews, consumers look for more recent reviews and want the reviews to be “authentic and informative.” They also value the star ratings. About 84%of respondents said they wouldn’t book an appointment with a referred provider that had a rating of less than four stars.
Overall, the top reasons why people are deterred from making an appointment are difficulty contacting the office, the poor quality of online reviews, and an average online rating of less than four stars.
The vast majority of respondents (77%) said they believe internet reviews reflect their own experience with a provider organization, and only 2.6% said the reviews were inaccurate. Another finding of the survey indicates that this attention of patients to reviews of their own provider doesn’t represent idle curiosity: About 57% of Baby Boomers and 45% of millennials/Gen Z’ers said they’d written online reviews of a doctor or a hospital.
Factors in patient loyalty
The Press Ganey survey asked which of several factors, besides excellent care, patients weighed when giving a five-star review to a health care provider.
Quality of customer service was rated first by 70.8% of respondents, followed by cleanliness of facilities (67.5%), communication (63.4%), the provider’s bedside manner (63%), ease of appointment booking (58.8%), ease of patient intake/registration (52.3%), quality and accuracy of information (40.1%), availability of telehealth services (21.7%), and waiting room amenities (21.8%).
The report explained that “quality of customer service” means “demeanor, attentiveness, and helpfulness of staff and practitioners.” “Communication” refers to things like follow-up appointment reminders and annual checkup reminders.
According to Mr. Jeffrey, these factors were considered more important than a doctor’s bedside manner because of the team care approach in most physician offices. “We see a lot more folks derive their notion of quality from continuity of care. And if they feel the physician they love is being supported by a less than competent team, that can impact significantly their sense of the quality of care,” he said.
Online appointment booking is a must
To win over the online consumer, Press Ganey emphasized, practices should ensure that provider listings are accurate and complete. In addition, offering online appointment booking can avoid the top challenge in making a new appointment, which is getting through to the office.
Mr. Jeffrey concurred, although he notes that practices have to be careful about how they enable patients to select appointment slots online. He suggests that an appointment request form on a patient portal first ask what the purpose of the visit is and that it offer five or so options. If the request fits into a routine visit category, the provider’s calendar pops up and the patient can select a convenient time slot. If it’s something else, an appointment scheduler calls the patient back.
“There needs to be greater access to standard appointments online,” he said. “While privacy is an issue, you can use the patient portal that most EHRs have to provide online booking. If you want to succeed going forward, that’s going to be a major plus.”
Of course, to do any of this, including reading provider reviews, a consumer needs a good internet connection and a mobile or desktop device. While broadband internet access is still not available in some communities, the breakdown of the survey respondents by demographics shows that low-income people were included.
Mr. Jeffrey doesn’t believe that a lack of internet access or digital devices prevents many Americans from going online today. “Even in poor communities, most people have internet access through their smartphones. Even baby boomers are familiar with smartphones. I haven’t seen internet access be a big barrier for low-income households, because they all have access to phones.”
A version of this article first appeared on Medscape.com.
Tender Subcutaneous Nodule in a Prepubescent Boy
The Diagnosis: Dermatomyofibroma
Dermatomyofibroma is an uncommon, benign, cutaneous mesenchymal neoplasm composed of fibroblasts and myofibroblasts.1-3 This skin tumor was first described in 1991 by Hugel4 in the German literature as plaquelike fibromatosis. Pediatric dermatomyofibromas are exceedingly rare, with pediatric patients ranging in age from infants to teenagers.1
Clinically, dermatomyofibromas appear as long-standing, isolated, ill-demarcated, flesh-colored, slightly hyperpigmented or erythematous nodules or plaques that may be raised or indurated.1 Dermatomyofibromas may present with constant mild pain or pruritus, though in most cases the lesions are asymptomatic.1,3 The clinical presentation of dermatomyofibroma has a few distinct differences in children compared to adults. In adulthood, dermatomyofibroma has a strong female predominance and most commonly is located on the shoulder and adjacent upper body regions, including the axilla, neck, upper arm, and upper trunk.1-3 In childhood, the majority of dermatomyofibromas occur in young boys and usually are located on the neck with other upper body regions occurring less frequently.1,2 A shared characteristic includes the tendency for dermatomyofibromas to have an initial period of enlargement followed by stabilization or slow growth.1 Reported pediatric lesions have ranged in size from 4 to 60 mm with an average size of 14.9 mm (median, 12 mm).2
The diagnosis of dermatomyofibroma is based on histopathologic features in addition to clinical presentation. Histology from punch biopsy usually reveals a noninvasive dermal proliferation of bland, uniform, slender spindle cells oriented parallel to the overlying epidermis with increased and fragmented elastic fibers.1,3 Infiltration into the mid or deep dermis is common. The adnexal structures usually are spared; the stroma contains collagen and increased small blood vessels; and there typically is no inflammatory infiltrate, except for occasional scattered mast cells.2 Cytologically, the monomorphic spindleshaped tumor cells have an ill-defined, pale, eosinophilic cytoplasm and nuclei that are elongated with tapered edges.3 Dermatomyofibroma has a variable immunohistochemical profile, as it may stain focally positive for CD34 or smooth muscle actin, with occasional staining of factor XIIIa, desmin, calponin, or vimentin.1-3 Normal to increased levels of often fragmented elastic fibers is a helpful clue in distinguishing dermatomyofibroma from dermatofibroma, hypertrophic scar, dermatofibrosarcoma protuberans, and pilar leiomyoma, in which elastic fibers typically are reduced.3 Differential diagnoses of mesenchymal tumors in children include desmoid fibromatosis, connective tissue nevus, myofibromatosis, and smooth muscle hamartoma.1
A punch biopsy with clinical observation and followup is recommended for the management of lesions in cosmetically sensitive areas or in very young children who may not tolerate surgery. In symptomatic or cosmetically unappealing cases of dermatomyofibroma, simple surgical excision remains a viable treatment option. Recurrence is uncommon, even if only partially excised, and no instances of metastasis have been reported.1-5
Dermatomyofibromas may be mistaken for several other entities both benign and malignant. For example, the benign dermatofibroma is the second most common fibrohistiocytic tumor of the skin and presents as a firm, nontender, minimally elevated to dome-shaped papule that usually measures less than or equal to 1 cm in diameter with or without overlying skin changes.5,6 It primarily is seen in adults with a slight female predominance and favors the lower extremities.5 Patients usually are asymptomatic but often report a history of local trauma at the lesion site.6 Histologically, dermatofibroma is characterized by a nodular dermal proliferation of spindleshaped fibrous cells and histiocytes in a storiform pattern (Figure 1).6 Epidermal induction with acanthosis overlying the tumor often is found with occasional basilar hyperpigmentation.5 Dermatofibroma also characteristically has trapped collagen (“collagen balls”) seen at the periphery.5,6
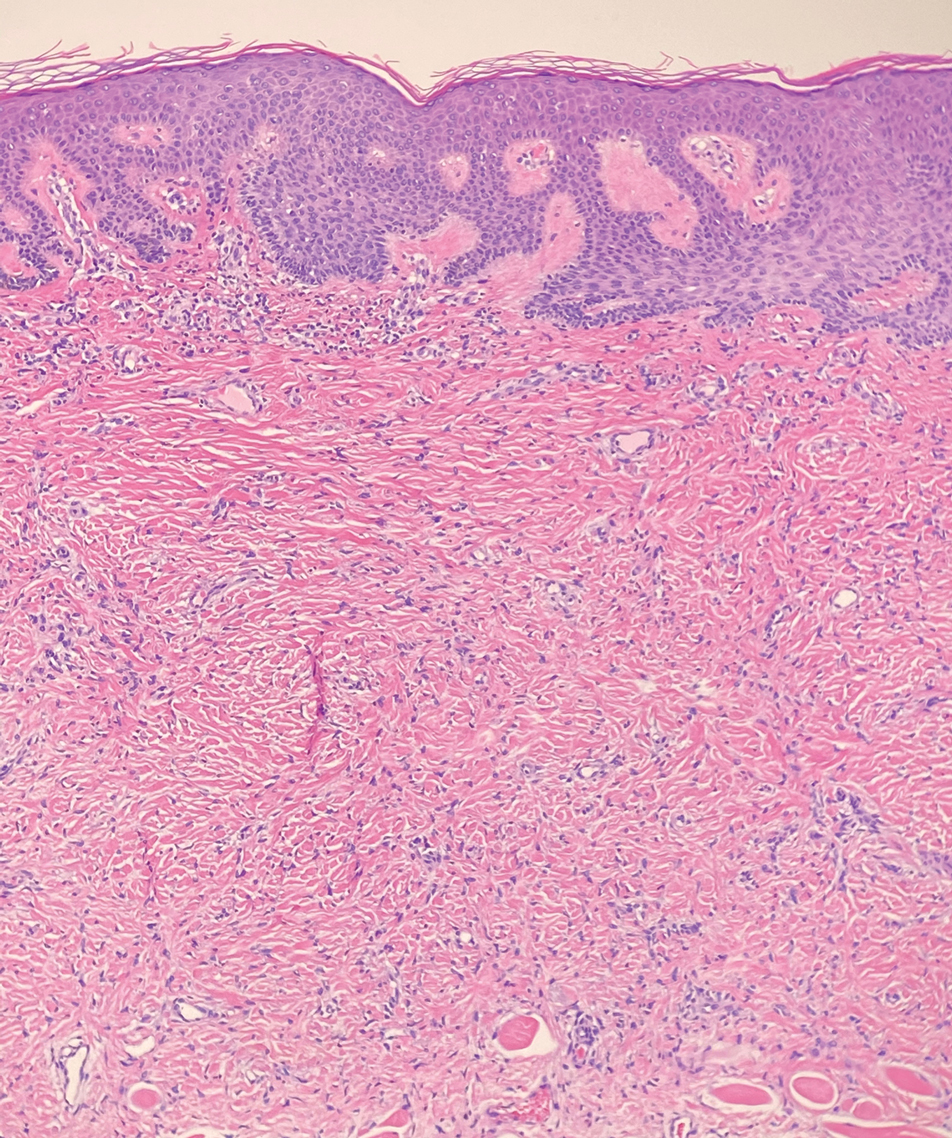
Piloleiomyomas are benign smooth muscle tumors arising from arrector pili muscles that may be solitary or multiple.5 Clinically, they typically present as firm, reddish-brown to flesh-colored papules or nodules that develop more commonly in adulthood.5,7 Piloleiomyomas favor the extremities and trunk, particularly the shoulder, and can be associated with spontaneous or induced pain. Histologically, piloleiomyomas are well circumscribed and centered within the reticular dermis situated closely to hair follicles (Figure 2).5 They are composed of numerous interlacing fascicles or whorls of smooth muscle cells with abundant eosinophilic cytoplasm and blunt-ended, cigar-shaped nuclei.5,7
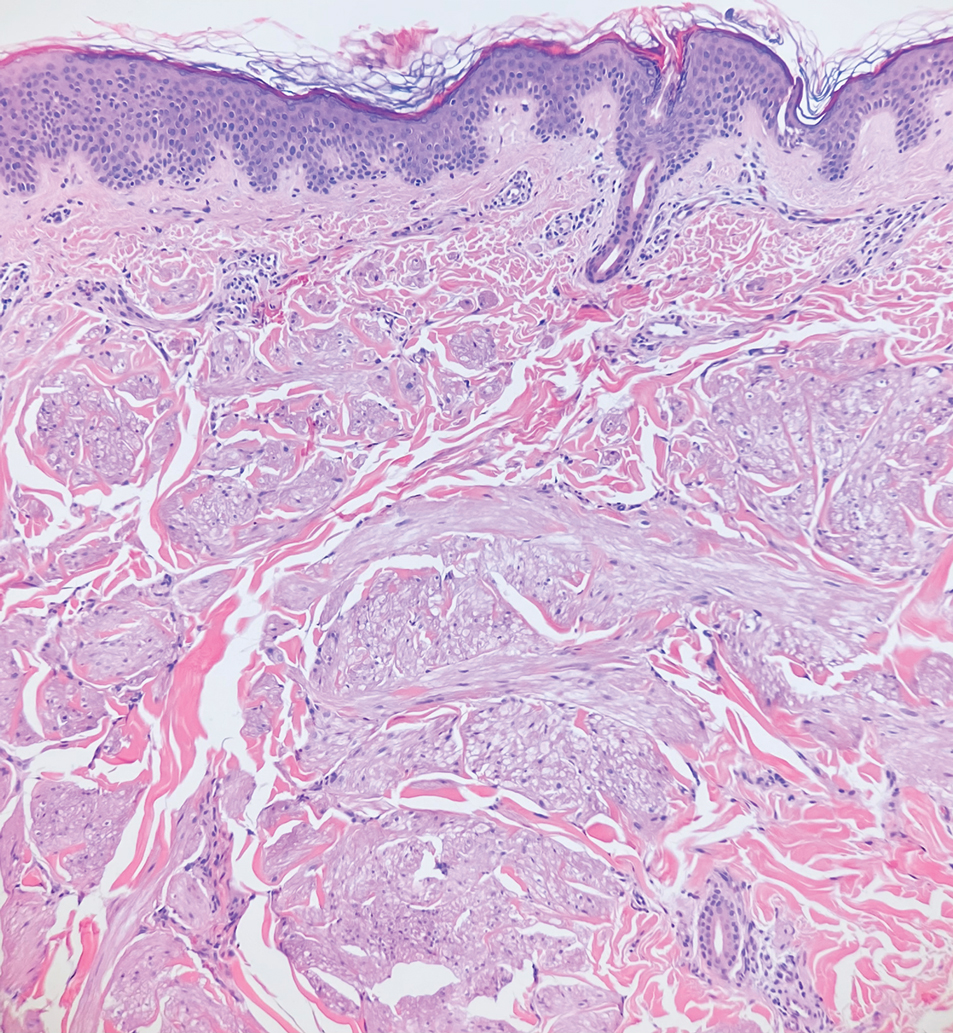
Solitary cutaneous myofibroma is a benign fibrous tumor found in adolescents and adults and is the counterpart to infantile myofibromatosis.8 Clinically, myofibromas typically present as painless, slow-growing, firm nodules with an occasional bluish hue. Histologically, solitary cutaneous myofibromas appear in a biphasic pattern, with hemangiopericytomatous components as well as spindle cells arranged in short bundles and fascicles resembling leiomyoma (Figure 3). The spindle cells also have abundant eosinophilic cytoplasm with short plump nuclei; the random, irregularly intersecting angles can be used to help differentiate myofibromas from smooth muscle lesions.8 Solitary cutaneous myofibroma is in the differential diagnosis for dermatomyofibroma because of their shared myofibroblastic nature.9
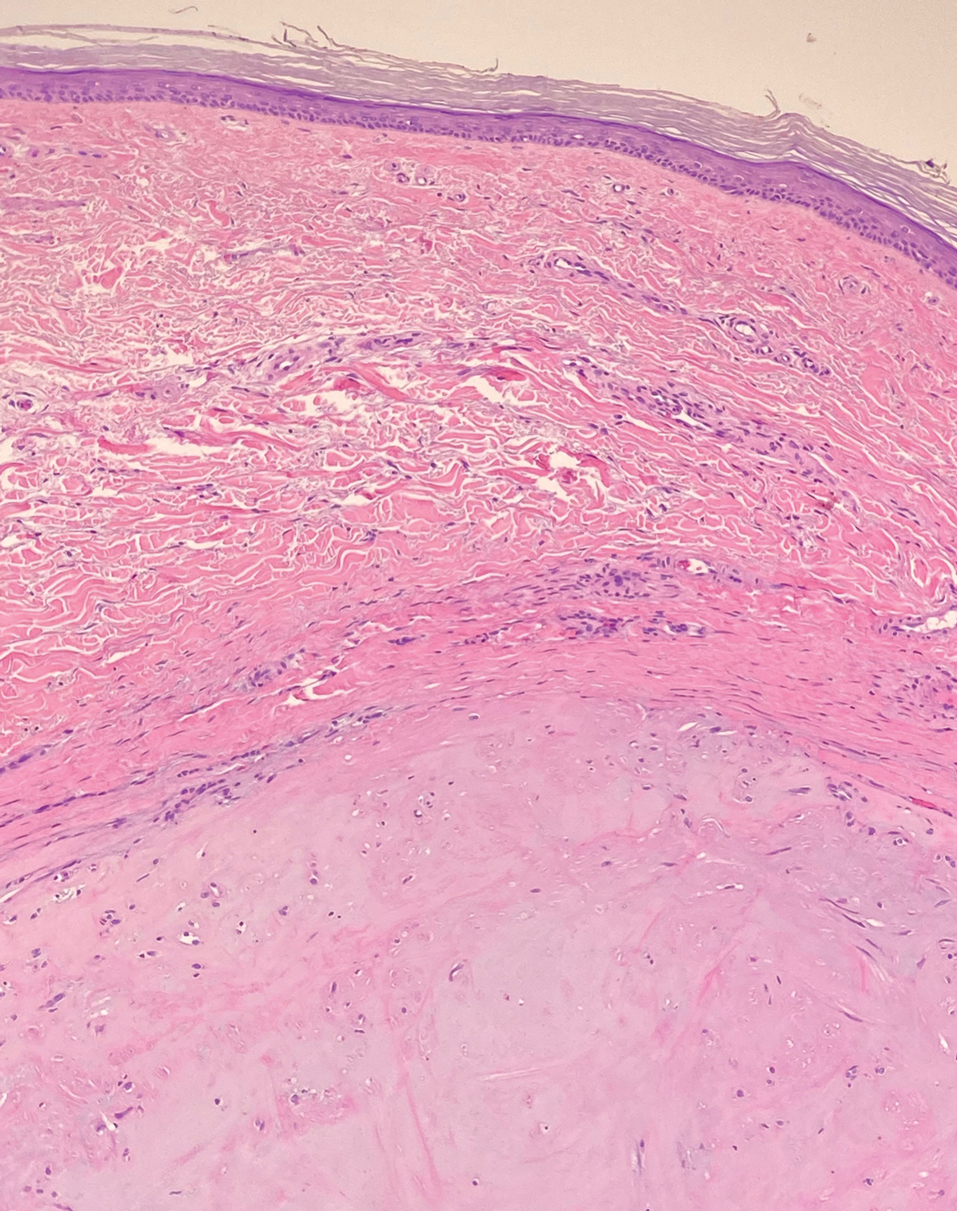
Dermatofibrosarcoma protuberans (DFSP) is an uncommon, locally invasive sarcoma with a high recurrence rate that favors young to middle-aged adults, with rare childhood onset reported.5,10,11 Clinically, DFSP typically presents as an asymptomatic, slow-growing, firm, flesh-colored, indurated plaque that develops into a violaceous to reddish-brown nodule.5 The atrophic variant of DFSP is characterized by a nonprotuberant lesion and can be especially difficult to distinguish from other entities such as dermatomyofibroma.11 The majority of DFSP lesions occur on the trunk, particularly in the shoulder or pelvic region.5 Histologically, early plaque lesions are comprised of monomorphic spindle cells arranged in long fascicles (parallel to the skin surface), infiltrating adnexal structures, and subcutaneous adipocytes in a multilayered honeycomb pattern; the spindle cells of late nodular lesions are arranged in short fascicles in a matted or storiform pattern (Figure 4).5,10 Early stages of DFSP as well as variations in childhood-onset DFSP can easily be misdiagnosed and incompletely excised.5
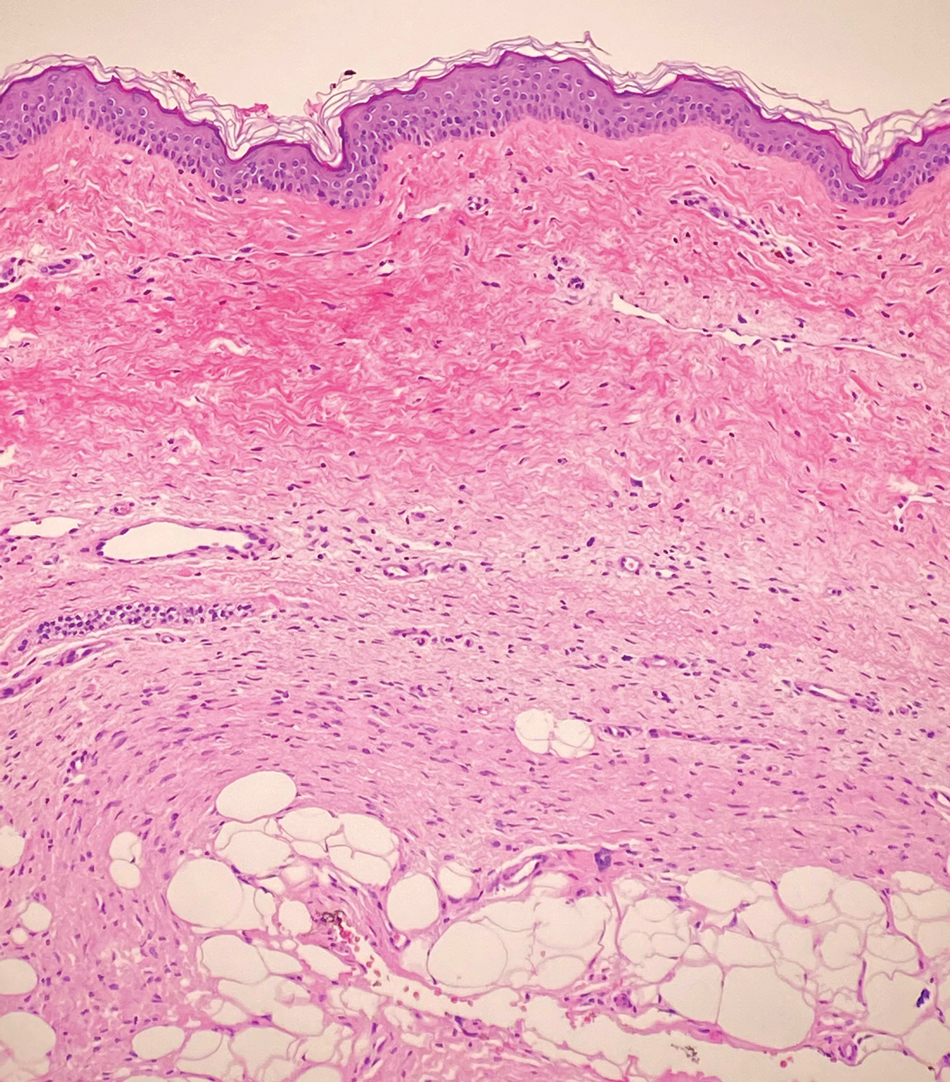
- Ma JE, Wieland CN, Tollefson MM. Dermatomyofibromas arising in children: report of two new cases and review of the literature. Pediatr Dermatol. 2017;34:347-351.
- Tardio JC, Azorin D, Hernandez-Nunez A, et al. Dermatomyofibromas presenting in pediatric patients: clinicopathologic characteristics and differential diagnosis. J Cutan Pathol. 2011;38:967-972.
- Mentzel T, Kutzner H. Dermatomyofibroma: clinicopathologic and immunohistochemical analysis of 56 cases and reappraisal of a rare and distinct cutaneous neoplasm. Am J Dermatopathol. 2009;31:44-49.
- Hugel H. Plaque-like dermal fibromatosis. Hautarzt. 1991;42:223-226.
- Bolognia JL, Jorizzo JL, Schaffer JV, eds. Dermatology. WB Saunders Co; 2012.
- Myers DJ, Fillman EP. Dermatofibroma. StatPearls [Internet]. StatPearls Publishing; 2020.
- Dilek N, Yuksel D, Sehitoglu I, et al. Cutaneous leiomyoma in a child: a case report. Oncol Lett. 2013;5:1163-1164.
- Roh HS, Paek JO, Yu HJ, et al. Solitary cutaneous myofibroma on the sole: an unusual localization. Ann Dermatol. 2012;24:220-222.
- Weedon D, Strutton G, Rubin AI, et al. Weedon’s Skin Pathology. Churchill Livingstone/Elsevier; 2010.
- Mendenhall WM, Zlotecki RA, Scarborough MT. Dermatofibrosarcoma protuberans. Cancer. 2004;101:2503-2508.
- Akay BN, Unlu E, Erdem C, et al. Dermatoscopic findings of atrophic dermatofibrosarcoma protuberans. Dermatol Pract Concept. 2015;5:71-73.
The Diagnosis: Dermatomyofibroma
Dermatomyofibroma is an uncommon, benign, cutaneous mesenchymal neoplasm composed of fibroblasts and myofibroblasts.1-3 This skin tumor was first described in 1991 by Hugel4 in the German literature as plaquelike fibromatosis. Pediatric dermatomyofibromas are exceedingly rare, with pediatric patients ranging in age from infants to teenagers.1
Clinically, dermatomyofibromas appear as long-standing, isolated, ill-demarcated, flesh-colored, slightly hyperpigmented or erythematous nodules or plaques that may be raised or indurated.1 Dermatomyofibromas may present with constant mild pain or pruritus, though in most cases the lesions are asymptomatic.1,3 The clinical presentation of dermatomyofibroma has a few distinct differences in children compared to adults. In adulthood, dermatomyofibroma has a strong female predominance and most commonly is located on the shoulder and adjacent upper body regions, including the axilla, neck, upper arm, and upper trunk.1-3 In childhood, the majority of dermatomyofibromas occur in young boys and usually are located on the neck with other upper body regions occurring less frequently.1,2 A shared characteristic includes the tendency for dermatomyofibromas to have an initial period of enlargement followed by stabilization or slow growth.1 Reported pediatric lesions have ranged in size from 4 to 60 mm with an average size of 14.9 mm (median, 12 mm).2
The diagnosis of dermatomyofibroma is based on histopathologic features in addition to clinical presentation. Histology from punch biopsy usually reveals a noninvasive dermal proliferation of bland, uniform, slender spindle cells oriented parallel to the overlying epidermis with increased and fragmented elastic fibers.1,3 Infiltration into the mid or deep dermis is common. The adnexal structures usually are spared; the stroma contains collagen and increased small blood vessels; and there typically is no inflammatory infiltrate, except for occasional scattered mast cells.2 Cytologically, the monomorphic spindleshaped tumor cells have an ill-defined, pale, eosinophilic cytoplasm and nuclei that are elongated with tapered edges.3 Dermatomyofibroma has a variable immunohistochemical profile, as it may stain focally positive for CD34 or smooth muscle actin, with occasional staining of factor XIIIa, desmin, calponin, or vimentin.1-3 Normal to increased levels of often fragmented elastic fibers is a helpful clue in distinguishing dermatomyofibroma from dermatofibroma, hypertrophic scar, dermatofibrosarcoma protuberans, and pilar leiomyoma, in which elastic fibers typically are reduced.3 Differential diagnoses of mesenchymal tumors in children include desmoid fibromatosis, connective tissue nevus, myofibromatosis, and smooth muscle hamartoma.1
A punch biopsy with clinical observation and followup is recommended for the management of lesions in cosmetically sensitive areas or in very young children who may not tolerate surgery. In symptomatic or cosmetically unappealing cases of dermatomyofibroma, simple surgical excision remains a viable treatment option. Recurrence is uncommon, even if only partially excised, and no instances of metastasis have been reported.1-5
Dermatomyofibromas may be mistaken for several other entities both benign and malignant. For example, the benign dermatofibroma is the second most common fibrohistiocytic tumor of the skin and presents as a firm, nontender, minimally elevated to dome-shaped papule that usually measures less than or equal to 1 cm in diameter with or without overlying skin changes.5,6 It primarily is seen in adults with a slight female predominance and favors the lower extremities.5 Patients usually are asymptomatic but often report a history of local trauma at the lesion site.6 Histologically, dermatofibroma is characterized by a nodular dermal proliferation of spindleshaped fibrous cells and histiocytes in a storiform pattern (Figure 1).6 Epidermal induction with acanthosis overlying the tumor often is found with occasional basilar hyperpigmentation.5 Dermatofibroma also characteristically has trapped collagen (“collagen balls”) seen at the periphery.5,6
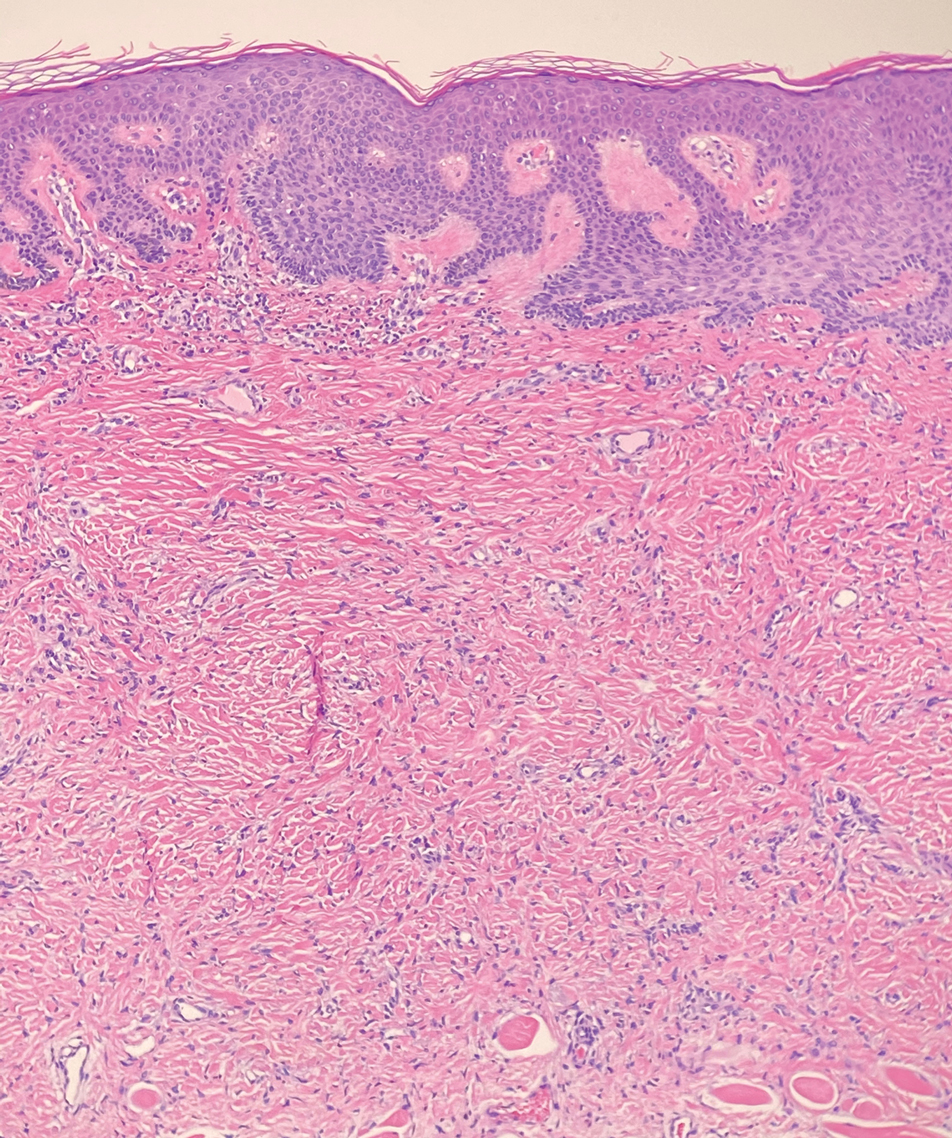
Piloleiomyomas are benign smooth muscle tumors arising from arrector pili muscles that may be solitary or multiple.5 Clinically, they typically present as firm, reddish-brown to flesh-colored papules or nodules that develop more commonly in adulthood.5,7 Piloleiomyomas favor the extremities and trunk, particularly the shoulder, and can be associated with spontaneous or induced pain. Histologically, piloleiomyomas are well circumscribed and centered within the reticular dermis situated closely to hair follicles (Figure 2).5 They are composed of numerous interlacing fascicles or whorls of smooth muscle cells with abundant eosinophilic cytoplasm and blunt-ended, cigar-shaped nuclei.5,7
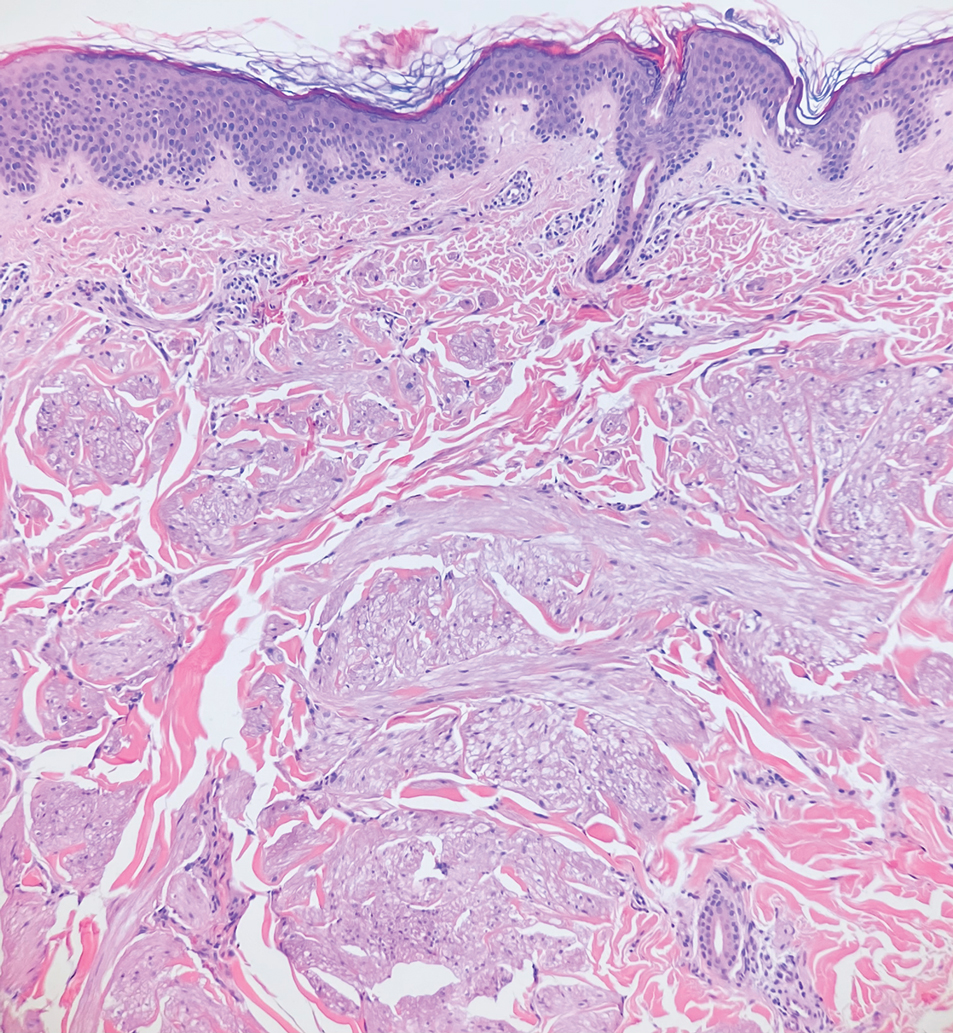
Solitary cutaneous myofibroma is a benign fibrous tumor found in adolescents and adults and is the counterpart to infantile myofibromatosis.8 Clinically, myofibromas typically present as painless, slow-growing, firm nodules with an occasional bluish hue. Histologically, solitary cutaneous myofibromas appear in a biphasic pattern, with hemangiopericytomatous components as well as spindle cells arranged in short bundles and fascicles resembling leiomyoma (Figure 3). The spindle cells also have abundant eosinophilic cytoplasm with short plump nuclei; the random, irregularly intersecting angles can be used to help differentiate myofibromas from smooth muscle lesions.8 Solitary cutaneous myofibroma is in the differential diagnosis for dermatomyofibroma because of their shared myofibroblastic nature.9
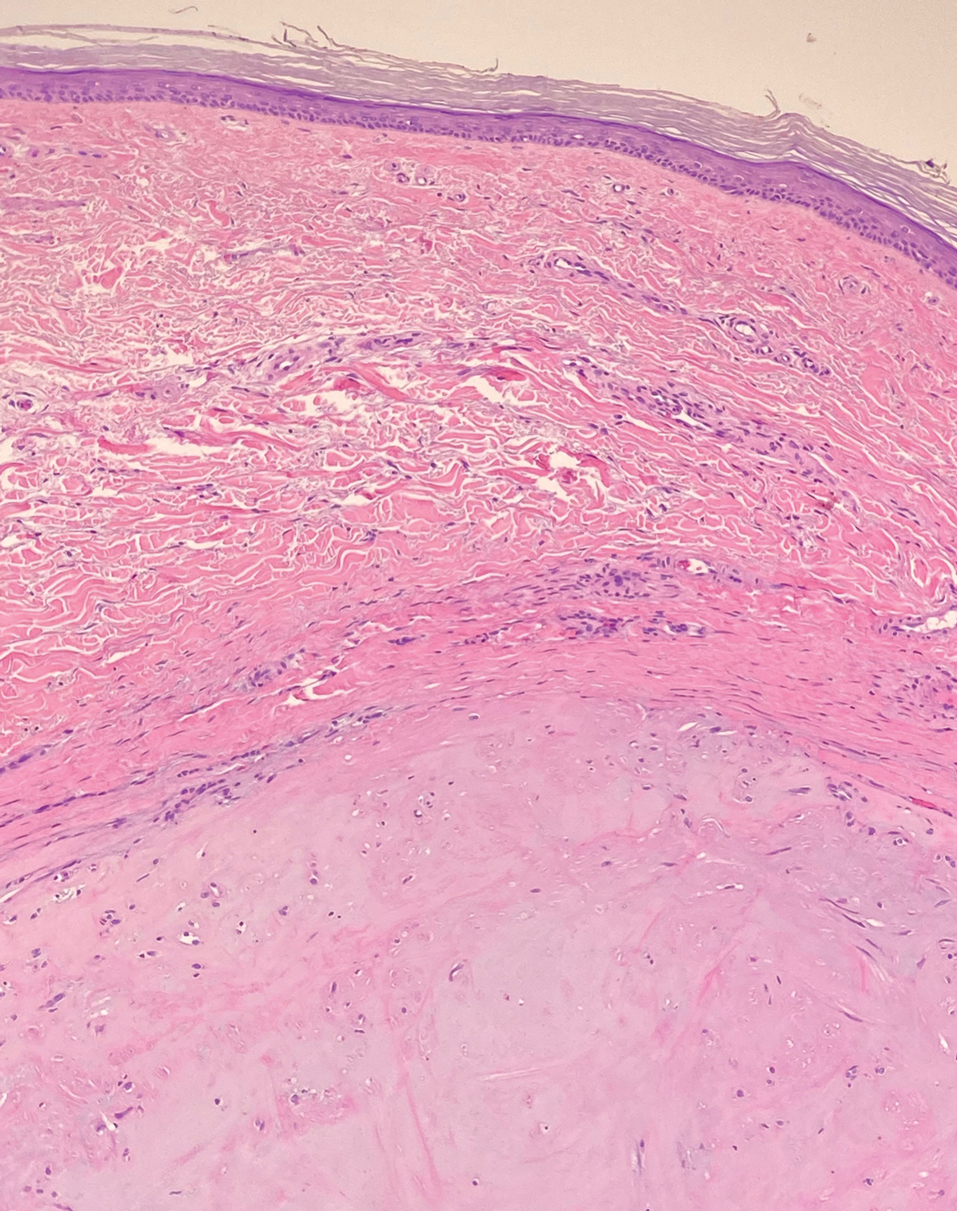
Dermatofibrosarcoma protuberans (DFSP) is an uncommon, locally invasive sarcoma with a high recurrence rate that favors young to middle-aged adults, with rare childhood onset reported.5,10,11 Clinically, DFSP typically presents as an asymptomatic, slow-growing, firm, flesh-colored, indurated plaque that develops into a violaceous to reddish-brown nodule.5 The atrophic variant of DFSP is characterized by a nonprotuberant lesion and can be especially difficult to distinguish from other entities such as dermatomyofibroma.11 The majority of DFSP lesions occur on the trunk, particularly in the shoulder or pelvic region.5 Histologically, early plaque lesions are comprised of monomorphic spindle cells arranged in long fascicles (parallel to the skin surface), infiltrating adnexal structures, and subcutaneous adipocytes in a multilayered honeycomb pattern; the spindle cells of late nodular lesions are arranged in short fascicles in a matted or storiform pattern (Figure 4).5,10 Early stages of DFSP as well as variations in childhood-onset DFSP can easily be misdiagnosed and incompletely excised.5
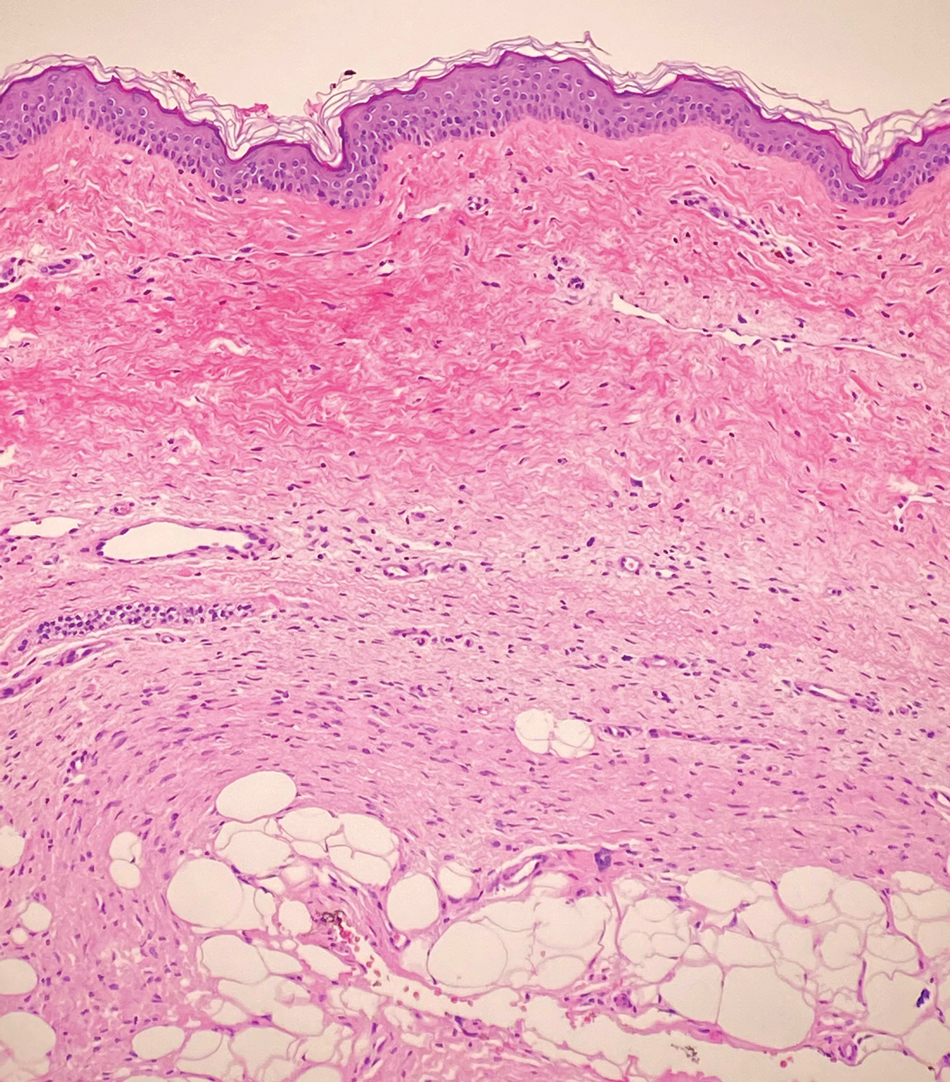
The Diagnosis: Dermatomyofibroma
Dermatomyofibroma is an uncommon, benign, cutaneous mesenchymal neoplasm composed of fibroblasts and myofibroblasts.1-3 This skin tumor was first described in 1991 by Hugel4 in the German literature as plaquelike fibromatosis. Pediatric dermatomyofibromas are exceedingly rare, with pediatric patients ranging in age from infants to teenagers.1
Clinically, dermatomyofibromas appear as long-standing, isolated, ill-demarcated, flesh-colored, slightly hyperpigmented or erythematous nodules or plaques that may be raised or indurated.1 Dermatomyofibromas may present with constant mild pain or pruritus, though in most cases the lesions are asymptomatic.1,3 The clinical presentation of dermatomyofibroma has a few distinct differences in children compared to adults. In adulthood, dermatomyofibroma has a strong female predominance and most commonly is located on the shoulder and adjacent upper body regions, including the axilla, neck, upper arm, and upper trunk.1-3 In childhood, the majority of dermatomyofibromas occur in young boys and usually are located on the neck with other upper body regions occurring less frequently.1,2 A shared characteristic includes the tendency for dermatomyofibromas to have an initial period of enlargement followed by stabilization or slow growth.1 Reported pediatric lesions have ranged in size from 4 to 60 mm with an average size of 14.9 mm (median, 12 mm).2
The diagnosis of dermatomyofibroma is based on histopathologic features in addition to clinical presentation. Histology from punch biopsy usually reveals a noninvasive dermal proliferation of bland, uniform, slender spindle cells oriented parallel to the overlying epidermis with increased and fragmented elastic fibers.1,3 Infiltration into the mid or deep dermis is common. The adnexal structures usually are spared; the stroma contains collagen and increased small blood vessels; and there typically is no inflammatory infiltrate, except for occasional scattered mast cells.2 Cytologically, the monomorphic spindleshaped tumor cells have an ill-defined, pale, eosinophilic cytoplasm and nuclei that are elongated with tapered edges.3 Dermatomyofibroma has a variable immunohistochemical profile, as it may stain focally positive for CD34 or smooth muscle actin, with occasional staining of factor XIIIa, desmin, calponin, or vimentin.1-3 Normal to increased levels of often fragmented elastic fibers is a helpful clue in distinguishing dermatomyofibroma from dermatofibroma, hypertrophic scar, dermatofibrosarcoma protuberans, and pilar leiomyoma, in which elastic fibers typically are reduced.3 Differential diagnoses of mesenchymal tumors in children include desmoid fibromatosis, connective tissue nevus, myofibromatosis, and smooth muscle hamartoma.1
A punch biopsy with clinical observation and followup is recommended for the management of lesions in cosmetically sensitive areas or in very young children who may not tolerate surgery. In symptomatic or cosmetically unappealing cases of dermatomyofibroma, simple surgical excision remains a viable treatment option. Recurrence is uncommon, even if only partially excised, and no instances of metastasis have been reported.1-5
Dermatomyofibromas may be mistaken for several other entities both benign and malignant. For example, the benign dermatofibroma is the second most common fibrohistiocytic tumor of the skin and presents as a firm, nontender, minimally elevated to dome-shaped papule that usually measures less than or equal to 1 cm in diameter with or without overlying skin changes.5,6 It primarily is seen in adults with a slight female predominance and favors the lower extremities.5 Patients usually are asymptomatic but often report a history of local trauma at the lesion site.6 Histologically, dermatofibroma is characterized by a nodular dermal proliferation of spindleshaped fibrous cells and histiocytes in a storiform pattern (Figure 1).6 Epidermal induction with acanthosis overlying the tumor often is found with occasional basilar hyperpigmentation.5 Dermatofibroma also characteristically has trapped collagen (“collagen balls”) seen at the periphery.5,6
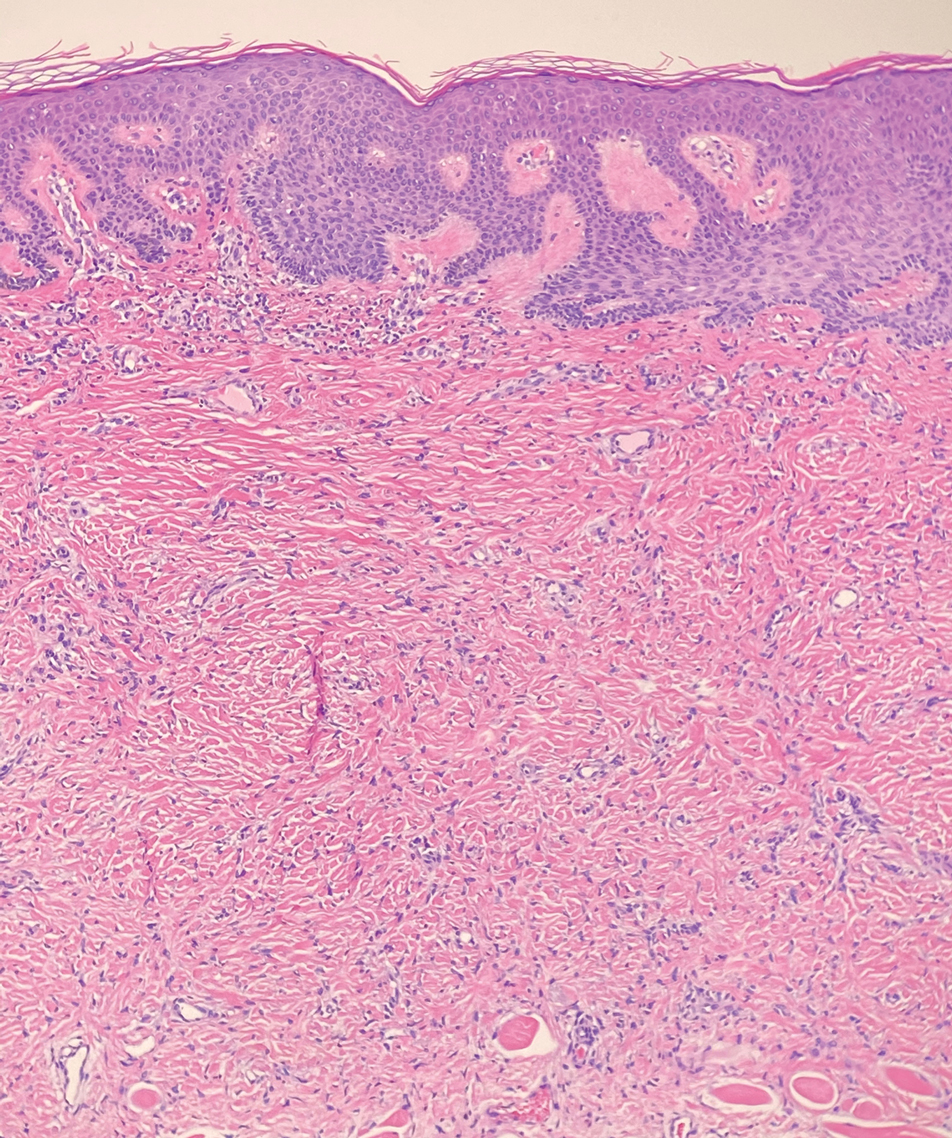
Piloleiomyomas are benign smooth muscle tumors arising from arrector pili muscles that may be solitary or multiple.5 Clinically, they typically present as firm, reddish-brown to flesh-colored papules or nodules that develop more commonly in adulthood.5,7 Piloleiomyomas favor the extremities and trunk, particularly the shoulder, and can be associated with spontaneous or induced pain. Histologically, piloleiomyomas are well circumscribed and centered within the reticular dermis situated closely to hair follicles (Figure 2).5 They are composed of numerous interlacing fascicles or whorls of smooth muscle cells with abundant eosinophilic cytoplasm and blunt-ended, cigar-shaped nuclei.5,7
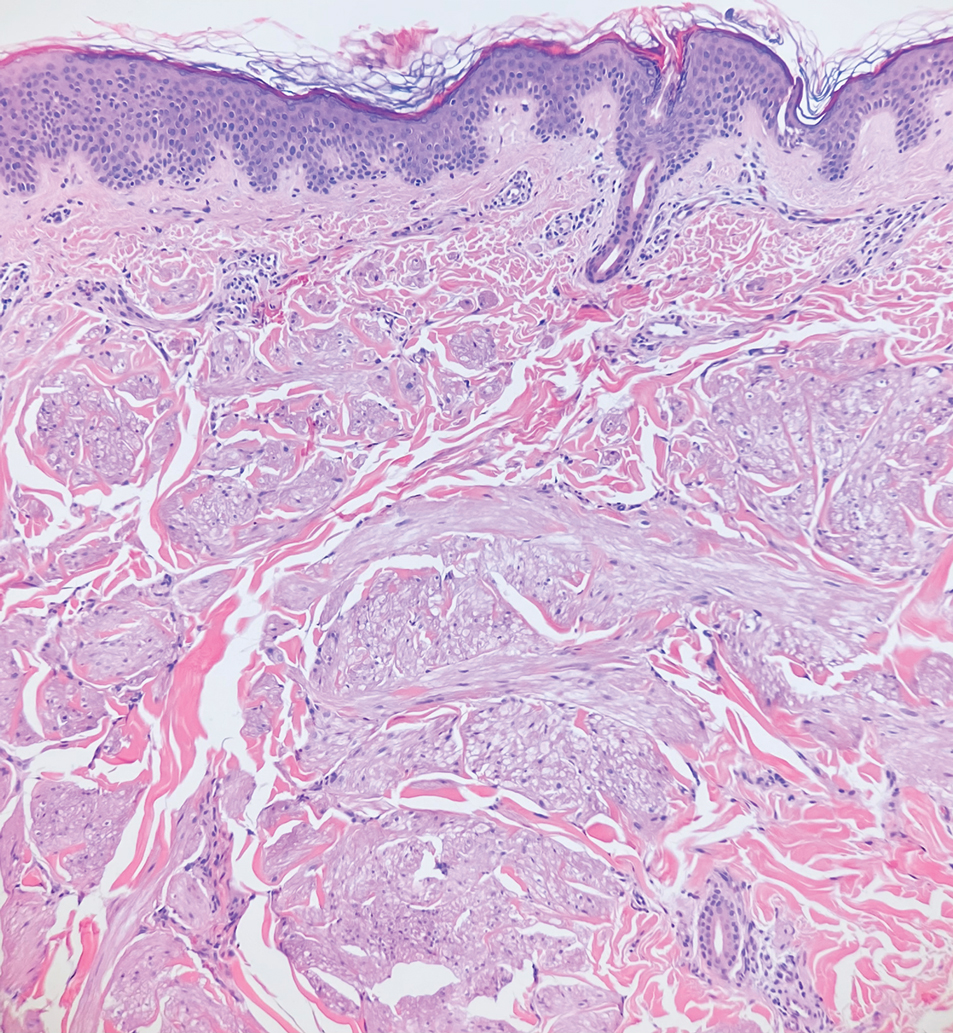
Solitary cutaneous myofibroma is a benign fibrous tumor found in adolescents and adults and is the counterpart to infantile myofibromatosis.8 Clinically, myofibromas typically present as painless, slow-growing, firm nodules with an occasional bluish hue. Histologically, solitary cutaneous myofibromas appear in a biphasic pattern, with hemangiopericytomatous components as well as spindle cells arranged in short bundles and fascicles resembling leiomyoma (Figure 3). The spindle cells also have abundant eosinophilic cytoplasm with short plump nuclei; the random, irregularly intersecting angles can be used to help differentiate myofibromas from smooth muscle lesions.8 Solitary cutaneous myofibroma is in the differential diagnosis for dermatomyofibroma because of their shared myofibroblastic nature.9
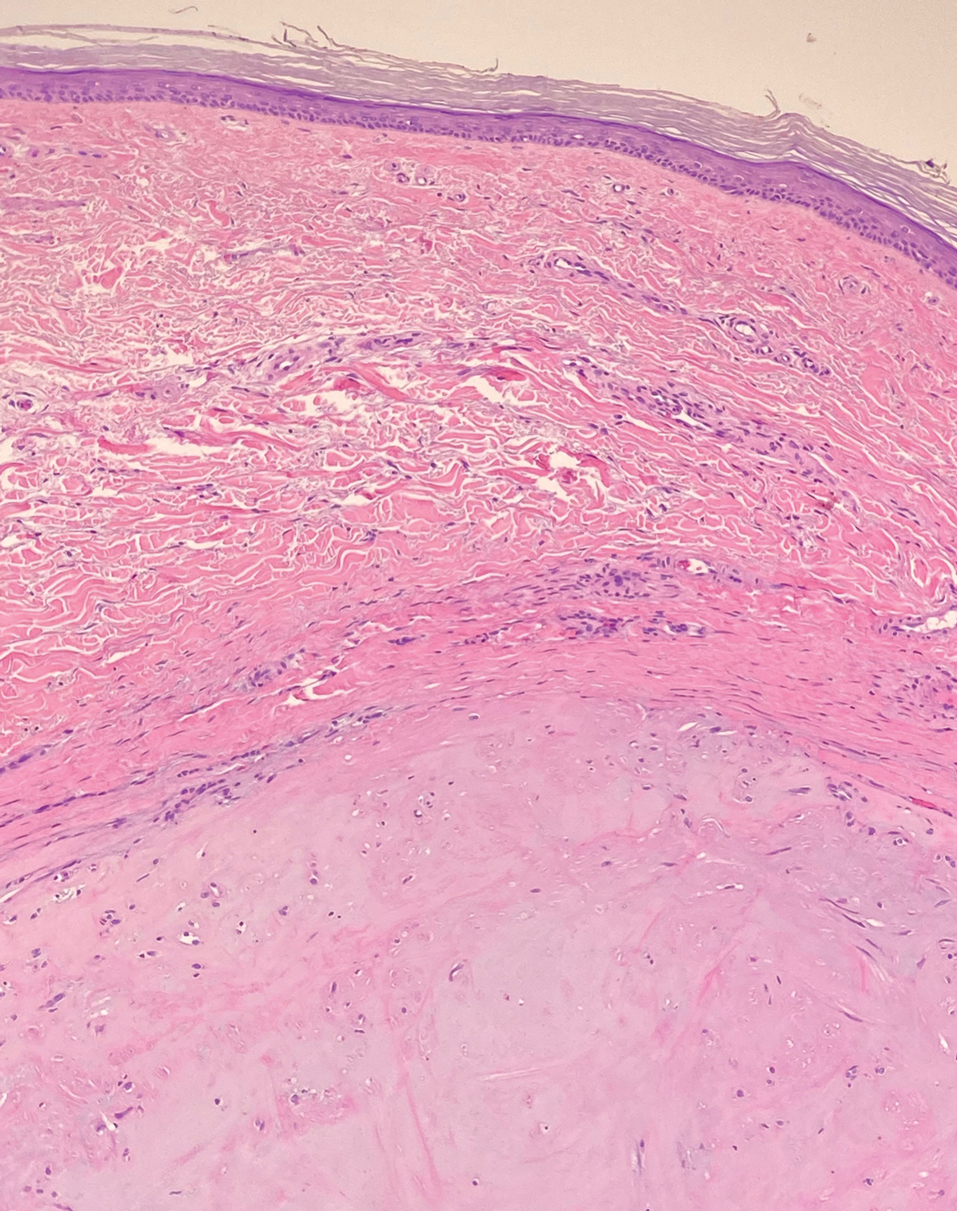
Dermatofibrosarcoma protuberans (DFSP) is an uncommon, locally invasive sarcoma with a high recurrence rate that favors young to middle-aged adults, with rare childhood onset reported.5,10,11 Clinically, DFSP typically presents as an asymptomatic, slow-growing, firm, flesh-colored, indurated plaque that develops into a violaceous to reddish-brown nodule.5 The atrophic variant of DFSP is characterized by a nonprotuberant lesion and can be especially difficult to distinguish from other entities such as dermatomyofibroma.11 The majority of DFSP lesions occur on the trunk, particularly in the shoulder or pelvic region.5 Histologically, early plaque lesions are comprised of monomorphic spindle cells arranged in long fascicles (parallel to the skin surface), infiltrating adnexal structures, and subcutaneous adipocytes in a multilayered honeycomb pattern; the spindle cells of late nodular lesions are arranged in short fascicles in a matted or storiform pattern (Figure 4).5,10 Early stages of DFSP as well as variations in childhood-onset DFSP can easily be misdiagnosed and incompletely excised.5
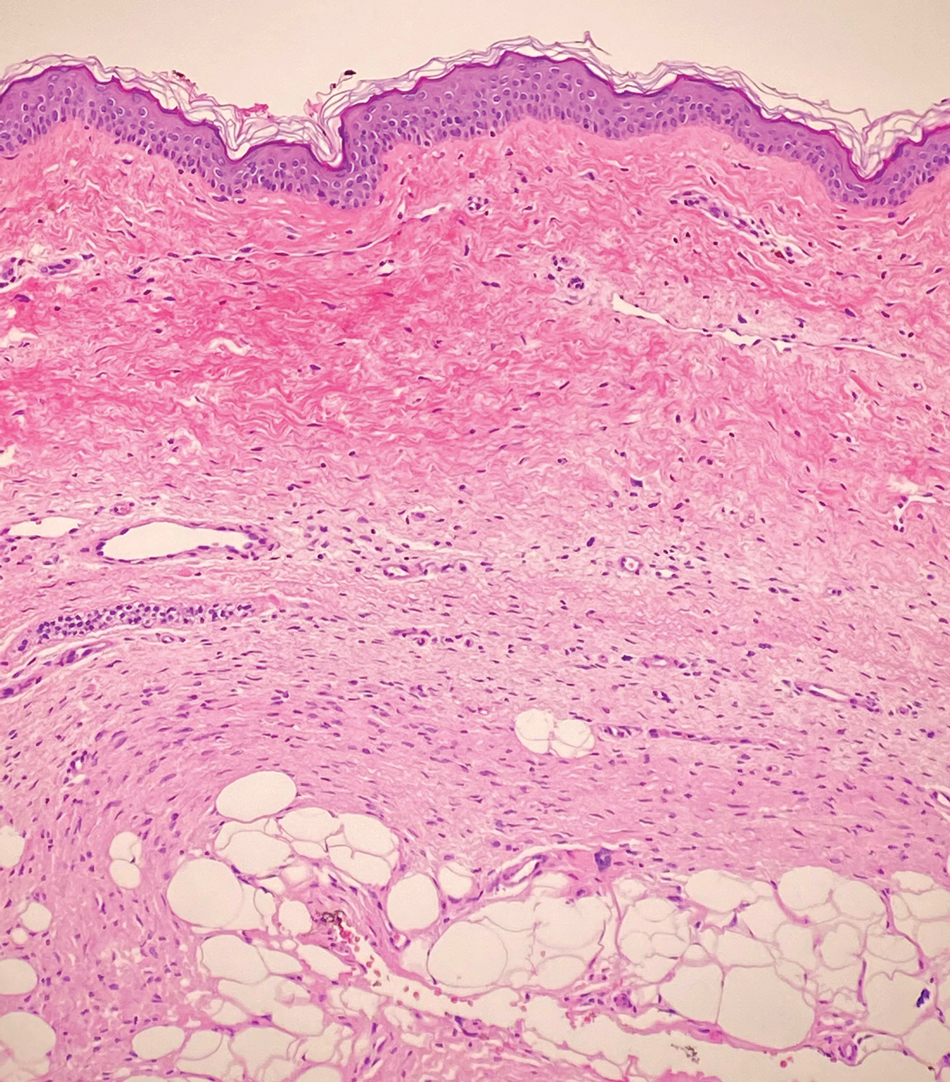
- Ma JE, Wieland CN, Tollefson MM. Dermatomyofibromas arising in children: report of two new cases and review of the literature. Pediatr Dermatol. 2017;34:347-351.
- Tardio JC, Azorin D, Hernandez-Nunez A, et al. Dermatomyofibromas presenting in pediatric patients: clinicopathologic characteristics and differential diagnosis. J Cutan Pathol. 2011;38:967-972.
- Mentzel T, Kutzner H. Dermatomyofibroma: clinicopathologic and immunohistochemical analysis of 56 cases and reappraisal of a rare and distinct cutaneous neoplasm. Am J Dermatopathol. 2009;31:44-49.
- Hugel H. Plaque-like dermal fibromatosis. Hautarzt. 1991;42:223-226.
- Bolognia JL, Jorizzo JL, Schaffer JV, eds. Dermatology. WB Saunders Co; 2012.
- Myers DJ, Fillman EP. Dermatofibroma. StatPearls [Internet]. StatPearls Publishing; 2020.
- Dilek N, Yuksel D, Sehitoglu I, et al. Cutaneous leiomyoma in a child: a case report. Oncol Lett. 2013;5:1163-1164.
- Roh HS, Paek JO, Yu HJ, et al. Solitary cutaneous myofibroma on the sole: an unusual localization. Ann Dermatol. 2012;24:220-222.
- Weedon D, Strutton G, Rubin AI, et al. Weedon’s Skin Pathology. Churchill Livingstone/Elsevier; 2010.
- Mendenhall WM, Zlotecki RA, Scarborough MT. Dermatofibrosarcoma protuberans. Cancer. 2004;101:2503-2508.
- Akay BN, Unlu E, Erdem C, et al. Dermatoscopic findings of atrophic dermatofibrosarcoma protuberans. Dermatol Pract Concept. 2015;5:71-73.
- Ma JE, Wieland CN, Tollefson MM. Dermatomyofibromas arising in children: report of two new cases and review of the literature. Pediatr Dermatol. 2017;34:347-351.
- Tardio JC, Azorin D, Hernandez-Nunez A, et al. Dermatomyofibromas presenting in pediatric patients: clinicopathologic characteristics and differential diagnosis. J Cutan Pathol. 2011;38:967-972.
- Mentzel T, Kutzner H. Dermatomyofibroma: clinicopathologic and immunohistochemical analysis of 56 cases and reappraisal of a rare and distinct cutaneous neoplasm. Am J Dermatopathol. 2009;31:44-49.
- Hugel H. Plaque-like dermal fibromatosis. Hautarzt. 1991;42:223-226.
- Bolognia JL, Jorizzo JL, Schaffer JV, eds. Dermatology. WB Saunders Co; 2012.
- Myers DJ, Fillman EP. Dermatofibroma. StatPearls [Internet]. StatPearls Publishing; 2020.
- Dilek N, Yuksel D, Sehitoglu I, et al. Cutaneous leiomyoma in a child: a case report. Oncol Lett. 2013;5:1163-1164.
- Roh HS, Paek JO, Yu HJ, et al. Solitary cutaneous myofibroma on the sole: an unusual localization. Ann Dermatol. 2012;24:220-222.
- Weedon D, Strutton G, Rubin AI, et al. Weedon’s Skin Pathology. Churchill Livingstone/Elsevier; 2010.
- Mendenhall WM, Zlotecki RA, Scarborough MT. Dermatofibrosarcoma protuberans. Cancer. 2004;101:2503-2508.
- Akay BN, Unlu E, Erdem C, et al. Dermatoscopic findings of atrophic dermatofibrosarcoma protuberans. Dermatol Pract Concept. 2015;5:71-73.
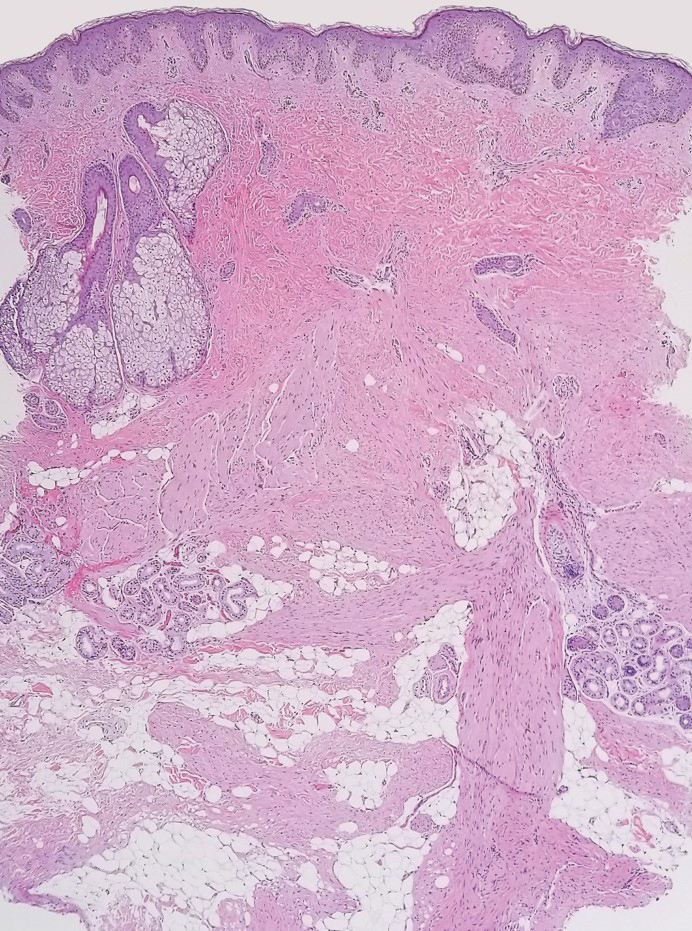

A 12-year-old boy with olive skin presented with a tender subcutaneous nodule on the back of 6 months’ duration. He reported the lesion initially grew rapidly with increasing pain for approximately 3 months with subsequent stabilization in size and modest resolution of his symptoms. Physical examination revealed a solitary, 15-mm, ill-defined, indurated, tender, subcutaneous nodule with subtle overlying hyperpigmentation on the left side of the upper back. Hematoxylin and eosin staining of a 4-mm punch biopsy revealed a nonencapsulated mass of monomorphic eosinophilic spindle cells organized into fascicles arranged predominantly parallel to the skin surface. The mass extended from the mid reticular dermis to the upper subcutis, sparing adnexal structures.
Care via video teleconferencing can be as effective as in-person for some conditions
This was a finding of a new study published in Annals of Internal Medicine involving a review of literature on video teleconferencing (VTC) visits, which was authored by Jordan Albritton, PhD, MPH and his colleagues.
The authors found generally comparable patient outcomes as well as no differences in health care use, patient satisfaction, and quality of life when visits conducted using VTC were compared with usual care.
While VTC may work best for monitoring patients with chronic conditions, it can also be effective for acute care, said Dr. Albritton, who is a research public health analyst at RTI International in Research Triangle Park, N.C., in an interview.
The investigators analyzed 20 randomized controlled trials of at least 50 patients and acceptable risk of bias in which VTC was used either for main or adjunct care delivery. Published from 2013 to 2019, these studies looked at care for diabetes and pain management, as well as some respiratory, neurologic, and cardiovascular conditions. Studies comparing VTC with usual care that did not involve any added in-person care were more likely to favor the VTC group, the investigators found.
“We excluded conditions such as substance use disorders, maternal care, and weight management for which there was sufficient prior evidence of the benefit of VTC,” Dr. Albritton said in an interview. “But I don’t think our results would have been substantially different if we had included these other diseases. We found general evidence in the literature that VTC is effective for a broader range of conditions.”
In some cases, such as if changes in a patient’s condition triggered an automatic virtual visit, the author said he thinks VTC may lead to even greater effectiveness.
“The doctor and patient could figure out on the spot what’s going on and perhaps change the medication,” Dr. Albritton explained.
In general agreement is Julia L. Frydman, MD, assistant professor in the Brookdale Department of Geriatric and Palliative Medicine at Icahn School of Medicine at Mount Sinai in New York, who was not involved in the RTI research.
“Telemedicine has promise across many medical subspecialties, and what we need now are more studies to understand the perspectives of patients, caregivers, and clinicians as well as the impact of telemedicine on health outcomes and healthcare utilization.”
In acknowledgment of their utility, video visits are on the rise in the United States. A 2020 survey found that 22% of patients and 80% of physicians reported having participated in a video visit, three times the rate of the previous year. The authors noted that policy changes enacted to support telehealth strategies during the pandemic are expected to remain in place, and although patients are returning to in-person care, the virtual visit market will likely continue growing.
Increased telemedicine use by older adults
“We’ve seen an exciting expansion of telemedicine use among older adults, and we need to focus on continuing to meet their needs,” Dr. Frydman said.
In a recent study of televisits during the pandemic, Dr. Frydman’s group found a fivefold greater uptake of remote consultations by seniors – from 5% to 25%. Although in-person visits were far more common among older adults.
A specific advantage of video-based over audio-only telehealth, noted Dr. Albritton, is that physicians can directly observe patients in their home environment. Sharing that view is Deepa Iyengar, MBBS/MD,MPH, professor of family medicine at McGovern Medical School at The University of Texas Health Science Center at Houston, where, she said, “the pandemic has put VTC use into overdrive.”
According to Dr. Iyengar, who was not involved in the RTI research, the video component definitely represents value-added over phone calls. “You can pick up visual cues on video that you might not see if the patient came in and you can see what the home environment is like – whether there are a lot of loose rugs on the floor or broken or missing light bulbs,” she said in an interview.
‘VTC is here to stay’
In other parts of the country, doctors are finding virtual care useful – and more common. “VTC is here to stay, for sure – the horse is out of the barn,” said Cheryl L. Wilkes, MD, an internist at Northwestern Medicine and assistant professor of medicine at Northwestern University in Chicago. “The RTI study shows no harm from VTC and also shows it may even improve clinical outcomes.”
Video visits can also save patients high parking fees at clinics and spare the sick or elderly from having to hire caregivers to bring them into the office or from having to walk blocks in dangerous weather conditions, she added. “And I can do a virtual visit on the fly or at night when a relative or caregiver is home from work to be there with the patient.”
In addition to being beneficial for following up with patients with chronic diseases such as hypertension or diabetes, VTC may be able to replace some visits that have traditionally required hands-on care, said Dr. Wilkes.
She said she knows a cardiologist who has refined a process whereby a patient – say, one who may have edema – is asked to perform a maneuver via VTC and then display the result to the doctor: The doctor says, “put your leg up and press on it hard for 10 seconds and then show me what it looks like,” according to Dr. Wilkes.
The key now is to identify the best persons across specialties from neurology to rheumatology to videotape ways they’ve created to help their patients participate virtually in consults traditionally done at the office, Dr. Wilkes noted.
But some conditions will always require palpation and the use of a stethoscope, according Dr. Iyengar.
“If someone has an ulcer, I have to be able to feel it,” she said.
And while some maternity care can be given virtually – for instance, if a mother-to be develops a bad cold – hands-on obstetrical care to check the position and health of the baby obviously has to be done in person. “So VTC is definitely going to be a welcome addition but not a replacement,” Dr. Iyengar said.
Gaps in research on VTC visits
Many questions remain regarding the overall usefulness of VTC visits for certain patient groups, according to the authors.
They highlighted, for example, the dearth of data on subgroups or on underserved and vulnerable populations, with no head-to-head studies identified in their review. In addition, they found no studies examining VTC versus usual care for patients with concurrent conditions or on its effect on health equity and disparities.
“It’s now our job to understand the ongoing barriers to telemedicine access, including the digital divide and the usability of telemedicine platforms, and design interventions that overcome them,” Dr. Frydman said. “At the same time, we need to make sure we’re understanding and respecting the preferences of older adults in terms of how they access health care.”
This study was supported by the Patient-Centered Outcomes Research Institute (PCORI). Dr. Albritton is employed by RTI International, the contractor responsible for conducting the research and developing the manuscript. Several coauthors disclosed support from or contracts with PCORI. One coauthor’s spouse holds stock in private health companies. Dr. Frydman, Dr. Iyengar, and Dr. Wilkes disclosed no competing interests relevant to their comments.
This was a finding of a new study published in Annals of Internal Medicine involving a review of literature on video teleconferencing (VTC) visits, which was authored by Jordan Albritton, PhD, MPH and his colleagues.
The authors found generally comparable patient outcomes as well as no differences in health care use, patient satisfaction, and quality of life when visits conducted using VTC were compared with usual care.
While VTC may work best for monitoring patients with chronic conditions, it can also be effective for acute care, said Dr. Albritton, who is a research public health analyst at RTI International in Research Triangle Park, N.C., in an interview.
The investigators analyzed 20 randomized controlled trials of at least 50 patients and acceptable risk of bias in which VTC was used either for main or adjunct care delivery. Published from 2013 to 2019, these studies looked at care for diabetes and pain management, as well as some respiratory, neurologic, and cardiovascular conditions. Studies comparing VTC with usual care that did not involve any added in-person care were more likely to favor the VTC group, the investigators found.
“We excluded conditions such as substance use disorders, maternal care, and weight management for which there was sufficient prior evidence of the benefit of VTC,” Dr. Albritton said in an interview. “But I don’t think our results would have been substantially different if we had included these other diseases. We found general evidence in the literature that VTC is effective for a broader range of conditions.”
In some cases, such as if changes in a patient’s condition triggered an automatic virtual visit, the author said he thinks VTC may lead to even greater effectiveness.
“The doctor and patient could figure out on the spot what’s going on and perhaps change the medication,” Dr. Albritton explained.
In general agreement is Julia L. Frydman, MD, assistant professor in the Brookdale Department of Geriatric and Palliative Medicine at Icahn School of Medicine at Mount Sinai in New York, who was not involved in the RTI research.
“Telemedicine has promise across many medical subspecialties, and what we need now are more studies to understand the perspectives of patients, caregivers, and clinicians as well as the impact of telemedicine on health outcomes and healthcare utilization.”
In acknowledgment of their utility, video visits are on the rise in the United States. A 2020 survey found that 22% of patients and 80% of physicians reported having participated in a video visit, three times the rate of the previous year. The authors noted that policy changes enacted to support telehealth strategies during the pandemic are expected to remain in place, and although patients are returning to in-person care, the virtual visit market will likely continue growing.
Increased telemedicine use by older adults
“We’ve seen an exciting expansion of telemedicine use among older adults, and we need to focus on continuing to meet their needs,” Dr. Frydman said.
In a recent study of televisits during the pandemic, Dr. Frydman’s group found a fivefold greater uptake of remote consultations by seniors – from 5% to 25%. Although in-person visits were far more common among older adults.
A specific advantage of video-based over audio-only telehealth, noted Dr. Albritton, is that physicians can directly observe patients in their home environment. Sharing that view is Deepa Iyengar, MBBS/MD,MPH, professor of family medicine at McGovern Medical School at The University of Texas Health Science Center at Houston, where, she said, “the pandemic has put VTC use into overdrive.”
According to Dr. Iyengar, who was not involved in the RTI research, the video component definitely represents value-added over phone calls. “You can pick up visual cues on video that you might not see if the patient came in and you can see what the home environment is like – whether there are a lot of loose rugs on the floor or broken or missing light bulbs,” she said in an interview.
‘VTC is here to stay’
In other parts of the country, doctors are finding virtual care useful – and more common. “VTC is here to stay, for sure – the horse is out of the barn,” said Cheryl L. Wilkes, MD, an internist at Northwestern Medicine and assistant professor of medicine at Northwestern University in Chicago. “The RTI study shows no harm from VTC and also shows it may even improve clinical outcomes.”
Video visits can also save patients high parking fees at clinics and spare the sick or elderly from having to hire caregivers to bring them into the office or from having to walk blocks in dangerous weather conditions, she added. “And I can do a virtual visit on the fly or at night when a relative or caregiver is home from work to be there with the patient.”
In addition to being beneficial for following up with patients with chronic diseases such as hypertension or diabetes, VTC may be able to replace some visits that have traditionally required hands-on care, said Dr. Wilkes.
She said she knows a cardiologist who has refined a process whereby a patient – say, one who may have edema – is asked to perform a maneuver via VTC and then display the result to the doctor: The doctor says, “put your leg up and press on it hard for 10 seconds and then show me what it looks like,” according to Dr. Wilkes.
The key now is to identify the best persons across specialties from neurology to rheumatology to videotape ways they’ve created to help their patients participate virtually in consults traditionally done at the office, Dr. Wilkes noted.
But some conditions will always require palpation and the use of a stethoscope, according Dr. Iyengar.
“If someone has an ulcer, I have to be able to feel it,” she said.
And while some maternity care can be given virtually – for instance, if a mother-to be develops a bad cold – hands-on obstetrical care to check the position and health of the baby obviously has to be done in person. “So VTC is definitely going to be a welcome addition but not a replacement,” Dr. Iyengar said.
Gaps in research on VTC visits
Many questions remain regarding the overall usefulness of VTC visits for certain patient groups, according to the authors.
They highlighted, for example, the dearth of data on subgroups or on underserved and vulnerable populations, with no head-to-head studies identified in their review. In addition, they found no studies examining VTC versus usual care for patients with concurrent conditions or on its effect on health equity and disparities.
“It’s now our job to understand the ongoing barriers to telemedicine access, including the digital divide and the usability of telemedicine platforms, and design interventions that overcome them,” Dr. Frydman said. “At the same time, we need to make sure we’re understanding and respecting the preferences of older adults in terms of how they access health care.”
This study was supported by the Patient-Centered Outcomes Research Institute (PCORI). Dr. Albritton is employed by RTI International, the contractor responsible for conducting the research and developing the manuscript. Several coauthors disclosed support from or contracts with PCORI. One coauthor’s spouse holds stock in private health companies. Dr. Frydman, Dr. Iyengar, and Dr. Wilkes disclosed no competing interests relevant to their comments.
This was a finding of a new study published in Annals of Internal Medicine involving a review of literature on video teleconferencing (VTC) visits, which was authored by Jordan Albritton, PhD, MPH and his colleagues.
The authors found generally comparable patient outcomes as well as no differences in health care use, patient satisfaction, and quality of life when visits conducted using VTC were compared with usual care.
While VTC may work best for monitoring patients with chronic conditions, it can also be effective for acute care, said Dr. Albritton, who is a research public health analyst at RTI International in Research Triangle Park, N.C., in an interview.
The investigators analyzed 20 randomized controlled trials of at least 50 patients and acceptable risk of bias in which VTC was used either for main or adjunct care delivery. Published from 2013 to 2019, these studies looked at care for diabetes and pain management, as well as some respiratory, neurologic, and cardiovascular conditions. Studies comparing VTC with usual care that did not involve any added in-person care were more likely to favor the VTC group, the investigators found.
“We excluded conditions such as substance use disorders, maternal care, and weight management for which there was sufficient prior evidence of the benefit of VTC,” Dr. Albritton said in an interview. “But I don’t think our results would have been substantially different if we had included these other diseases. We found general evidence in the literature that VTC is effective for a broader range of conditions.”
In some cases, such as if changes in a patient’s condition triggered an automatic virtual visit, the author said he thinks VTC may lead to even greater effectiveness.
“The doctor and patient could figure out on the spot what’s going on and perhaps change the medication,” Dr. Albritton explained.
In general agreement is Julia L. Frydman, MD, assistant professor in the Brookdale Department of Geriatric and Palliative Medicine at Icahn School of Medicine at Mount Sinai in New York, who was not involved in the RTI research.
“Telemedicine has promise across many medical subspecialties, and what we need now are more studies to understand the perspectives of patients, caregivers, and clinicians as well as the impact of telemedicine on health outcomes and healthcare utilization.”
In acknowledgment of their utility, video visits are on the rise in the United States. A 2020 survey found that 22% of patients and 80% of physicians reported having participated in a video visit, three times the rate of the previous year. The authors noted that policy changes enacted to support telehealth strategies during the pandemic are expected to remain in place, and although patients are returning to in-person care, the virtual visit market will likely continue growing.
Increased telemedicine use by older adults
“We’ve seen an exciting expansion of telemedicine use among older adults, and we need to focus on continuing to meet their needs,” Dr. Frydman said.
In a recent study of televisits during the pandemic, Dr. Frydman’s group found a fivefold greater uptake of remote consultations by seniors – from 5% to 25%. Although in-person visits were far more common among older adults.
A specific advantage of video-based over audio-only telehealth, noted Dr. Albritton, is that physicians can directly observe patients in their home environment. Sharing that view is Deepa Iyengar, MBBS/MD,MPH, professor of family medicine at McGovern Medical School at The University of Texas Health Science Center at Houston, where, she said, “the pandemic has put VTC use into overdrive.”
According to Dr. Iyengar, who was not involved in the RTI research, the video component definitely represents value-added over phone calls. “You can pick up visual cues on video that you might not see if the patient came in and you can see what the home environment is like – whether there are a lot of loose rugs on the floor or broken or missing light bulbs,” she said in an interview.
‘VTC is here to stay’
In other parts of the country, doctors are finding virtual care useful – and more common. “VTC is here to stay, for sure – the horse is out of the barn,” said Cheryl L. Wilkes, MD, an internist at Northwestern Medicine and assistant professor of medicine at Northwestern University in Chicago. “The RTI study shows no harm from VTC and also shows it may even improve clinical outcomes.”
Video visits can also save patients high parking fees at clinics and spare the sick or elderly from having to hire caregivers to bring them into the office or from having to walk blocks in dangerous weather conditions, she added. “And I can do a virtual visit on the fly or at night when a relative or caregiver is home from work to be there with the patient.”
In addition to being beneficial for following up with patients with chronic diseases such as hypertension or diabetes, VTC may be able to replace some visits that have traditionally required hands-on care, said Dr. Wilkes.
She said she knows a cardiologist who has refined a process whereby a patient – say, one who may have edema – is asked to perform a maneuver via VTC and then display the result to the doctor: The doctor says, “put your leg up and press on it hard for 10 seconds and then show me what it looks like,” according to Dr. Wilkes.
The key now is to identify the best persons across specialties from neurology to rheumatology to videotape ways they’ve created to help their patients participate virtually in consults traditionally done at the office, Dr. Wilkes noted.
But some conditions will always require palpation and the use of a stethoscope, according Dr. Iyengar.
“If someone has an ulcer, I have to be able to feel it,” she said.
And while some maternity care can be given virtually – for instance, if a mother-to be develops a bad cold – hands-on obstetrical care to check the position and health of the baby obviously has to be done in person. “So VTC is definitely going to be a welcome addition but not a replacement,” Dr. Iyengar said.
Gaps in research on VTC visits
Many questions remain regarding the overall usefulness of VTC visits for certain patient groups, according to the authors.
They highlighted, for example, the dearth of data on subgroups or on underserved and vulnerable populations, with no head-to-head studies identified in their review. In addition, they found no studies examining VTC versus usual care for patients with concurrent conditions or on its effect on health equity and disparities.
“It’s now our job to understand the ongoing barriers to telemedicine access, including the digital divide and the usability of telemedicine platforms, and design interventions that overcome them,” Dr. Frydman said. “At the same time, we need to make sure we’re understanding and respecting the preferences of older adults in terms of how they access health care.”
This study was supported by the Patient-Centered Outcomes Research Institute (PCORI). Dr. Albritton is employed by RTI International, the contractor responsible for conducting the research and developing the manuscript. Several coauthors disclosed support from or contracts with PCORI. One coauthor’s spouse holds stock in private health companies. Dr. Frydman, Dr. Iyengar, and Dr. Wilkes disclosed no competing interests relevant to their comments.
FROM ANNALS OF INTERNAL MEDICINE
Characterizing Counterfeit Dermatologic Devices Sold on Popular E-commerce Websites
To the Editor:
Approved medical devices on the market are substantial capital investments for practitioners. E-commerce websites, such as Alibaba.com (https://www.alibaba.com/) and DHgate.com (https://www.dhgate.com/), sell sham medical devices at a fraction of the cost of authentic products, with sellers often echoing the same treatment claims as legitimate devices that have been cleared by the US Food and Drug Administration (FDA).
In dermatology, devices claiming to perform cryolipolysis, laser skin resurfacing, radiofrequency skin tightening, and more exist on e-commerce websites. These counterfeit medical devices might differ from legitimate devices in ways that affect patient safety and treatment efficacy.1,2 The degree of difference between counterfeit and legitimate devices remains unknown, and potential harm from so-called knockoff devices needs to be critically examined by providers.
In this exploratory study, we characterize counterfeit listings of devices commonly used in dermatology. Using the trademark name of devices as the key terms, we searched Alibaba.com and DHgate.com for listings of counterfeit products. We recorded the total number of listings; the listing name, catalog number, and unit price; and claims of FDA certification. Characteristics of counterfeit listings were summarized using standard descriptive statistics in Microsoft Excel. Continuous variables were summarized with means and ranges.
Six medical devices that had been cleared by the FDA between 2002 and 2012 for use in dermatology were explored, including systems for picosecond and fractionated lasers, monopolar and bipolar radiofrequency skin tightening, cryolipolysis, and nonablative radiofrequency skin resurfacing. Our search of these 6 representative dermatologic devices revealed 47,055 counterfeit product listings on Alibaba.com and DHgate.com. Upon searching these popular e-commerce websites using the device name as the search term, the number of listings varied considerably between the 2 e-commerce websites for the same device and from device to device on the same e-commerce website. On Alibaba.com, the greatest number of listings resulted for picosecond laser (23,622 listings), fractionated laser (15,269), and radiofrequency skin tightening devices (3555); cryolipolysis and nonablative radiofrequency resurfacing devices had notably fewer listings (35 and 38, respectively). On DHGate.com, a similar trend was noted with the most numerous listings for picosecond and fractionated laser systems (2429 and 1345, respectively).
Among the first 10 listings of products on Alibaba.com and DHgate.com for these 6 devices, 10.7% (11 of 103) had advertised claims of FDA clearance on the listing page. Of 103 counterfeit products, China was the country of origin for 100; South Korea for 2; and Thailand for 1. Unit pricing was heterogeneous between the 2 e-commerce websites for the counterfeit listings; pricing for duplicate fractionated laser systems was particularly dissimilar, with an average price on Alibab.com of US $8105.80 and an average price on DHgate.com of US $3409.14. Even on the same e-commerce website, the range of unit pricing differed greatly for dermatologic devices. For example, among the first 10 listings on Alibaba.com for a fractionated laser system, the price ranged from US $2300 to US $32,000.
Counterfeit medical devices are on the rise in dermatology.1,3 Although devices such as radiofrequency and laser systems had thousands of knockoff listings on 2 e-commerce websites, other devices, such as cryolipolysis and body contouring systems, had fewer listings, suggesting heterogeneity in the prevalence of different counterfeit dermatologic devices on the market.
The varied pricing of the top 10 listings for each product and spurious claims of FDA clearance for some listings highlight the lack of regulatory authority over consistent product information on e-commerce websites. Furthermore, differences between characteristics of counterfeit device listings can impede efforts to trace suppliers and increase the opacity of counterfeit purchasing.
Three criteria have been proposed for a device to be considered counterfeit3:
• The device has no proven safety or efficacy among consumers. For example, the substantial threat of copycat devices in dermatology has been demonstrated by reports of burns caused by fake cryolipolysis devices.2
• The device violates patent rights or copy trademarks. Due to the regional nature of intellectual property rights, country-specific filings of patents and trademarks are required if protections are sought internationally. In this study, counterfeit devices originated in China, South Korea, and Thailand, where patent and trademark protections for the original devices do not extend.
• The device is falsely claimed to have been cleared by the FDA or other clinical regulatory authorities. Legitimate medical devices are subject to rounds of safety and compatibility testing using standards set by regulatory bodies, such as the FDA’s Center for Devices and Radiological Health, the International Organization of Standardization, and the International Electrotechnical Commission. Compliance with these safety standards is lost, however, among unregulated internet sales of medical devices. Our search revealed that 10.7% of the top 10 counterfeit device listings for each product explicitly mentioned FDA clearance in the product description. Among the thousands of listings on e-commerce sites, even a fraction that make spurious FDA-clearance claims can mislead consumers.
The issue of counterfeit medical devices has not gone unrecognized globally. In 2013, the World Health Organization created the Global Surveillance and Monitoring System to unify international efforts for reporting substandard, unlicensed, or falsified medical products.4 Although universal monitoring systems can improve detection of counterfeit products, we highlight the alarming continuing ease of purchasing counterfeit dermatologic devices through e-commerce websites. Due to the widespread nature of counterfeiting across all domains of medicine, the onus of curbing counterfeit dermatologic devices might be on dermatology providers to recognize and report such occurrences.
This exploration of counterfeit dermatologic devices revealed a lack of consistency throughout product listings on 2 popular e-commerce websites, Alibaba.com and DHgate.com. Given the alarming availability of these devices on the internet, practitioners should approach the purchase of any device with concern about counterfeiting. Future avenues of study might explore the prevalence of counterfeit devices used in dermatology practices and offer insight on regulation and consumer safety efforts.
- Wang JV, Zachary CB, Saedi N. Counterfeit esthetic devices and patient safety in dermatology. J Cosmet Dermatol. 2018;17:396-397. doi:10.1111/jocd.12526
- Biesman BS, Patel N. Physician alert: beware of counterfeit medical devices. Lasers Surg Med. 2014;46:528‐530. doi:10.1002/lsm.22275
- Stevens WG, Spring MA, Macias LH. Counterfeit medical devices: the money you save up front will cost you big in the end. Aesthet Surg J. 2014;34:786‐788. doi:10.1177/1090820X14529960
- Pisani E. WHO Global Surveillance and Monitoring System for Substandard and Falsified Medical Products. World Health Organization; 2017. Accessed November 21, 2021. https://www.who.int/medicines/regulation/ssffc/publications/GSMSreport_EN.pdf?ua=1
To the Editor:
Approved medical devices on the market are substantial capital investments for practitioners. E-commerce websites, such as Alibaba.com (https://www.alibaba.com/) and DHgate.com (https://www.dhgate.com/), sell sham medical devices at a fraction of the cost of authentic products, with sellers often echoing the same treatment claims as legitimate devices that have been cleared by the US Food and Drug Administration (FDA).
In dermatology, devices claiming to perform cryolipolysis, laser skin resurfacing, radiofrequency skin tightening, and more exist on e-commerce websites. These counterfeit medical devices might differ from legitimate devices in ways that affect patient safety and treatment efficacy.1,2 The degree of difference between counterfeit and legitimate devices remains unknown, and potential harm from so-called knockoff devices needs to be critically examined by providers.
In this exploratory study, we characterize counterfeit listings of devices commonly used in dermatology. Using the trademark name of devices as the key terms, we searched Alibaba.com and DHgate.com for listings of counterfeit products. We recorded the total number of listings; the listing name, catalog number, and unit price; and claims of FDA certification. Characteristics of counterfeit listings were summarized using standard descriptive statistics in Microsoft Excel. Continuous variables were summarized with means and ranges.
Six medical devices that had been cleared by the FDA between 2002 and 2012 for use in dermatology were explored, including systems for picosecond and fractionated lasers, monopolar and bipolar radiofrequency skin tightening, cryolipolysis, and nonablative radiofrequency skin resurfacing. Our search of these 6 representative dermatologic devices revealed 47,055 counterfeit product listings on Alibaba.com and DHgate.com. Upon searching these popular e-commerce websites using the device name as the search term, the number of listings varied considerably between the 2 e-commerce websites for the same device and from device to device on the same e-commerce website. On Alibaba.com, the greatest number of listings resulted for picosecond laser (23,622 listings), fractionated laser (15,269), and radiofrequency skin tightening devices (3555); cryolipolysis and nonablative radiofrequency resurfacing devices had notably fewer listings (35 and 38, respectively). On DHGate.com, a similar trend was noted with the most numerous listings for picosecond and fractionated laser systems (2429 and 1345, respectively).
Among the first 10 listings of products on Alibaba.com and DHgate.com for these 6 devices, 10.7% (11 of 103) had advertised claims of FDA clearance on the listing page. Of 103 counterfeit products, China was the country of origin for 100; South Korea for 2; and Thailand for 1. Unit pricing was heterogeneous between the 2 e-commerce websites for the counterfeit listings; pricing for duplicate fractionated laser systems was particularly dissimilar, with an average price on Alibab.com of US $8105.80 and an average price on DHgate.com of US $3409.14. Even on the same e-commerce website, the range of unit pricing differed greatly for dermatologic devices. For example, among the first 10 listings on Alibaba.com for a fractionated laser system, the price ranged from US $2300 to US $32,000.
Counterfeit medical devices are on the rise in dermatology.1,3 Although devices such as radiofrequency and laser systems had thousands of knockoff listings on 2 e-commerce websites, other devices, such as cryolipolysis and body contouring systems, had fewer listings, suggesting heterogeneity in the prevalence of different counterfeit dermatologic devices on the market.
The varied pricing of the top 10 listings for each product and spurious claims of FDA clearance for some listings highlight the lack of regulatory authority over consistent product information on e-commerce websites. Furthermore, differences between characteristics of counterfeit device listings can impede efforts to trace suppliers and increase the opacity of counterfeit purchasing.
Three criteria have been proposed for a device to be considered counterfeit3:
• The device has no proven safety or efficacy among consumers. For example, the substantial threat of copycat devices in dermatology has been demonstrated by reports of burns caused by fake cryolipolysis devices.2
• The device violates patent rights or copy trademarks. Due to the regional nature of intellectual property rights, country-specific filings of patents and trademarks are required if protections are sought internationally. In this study, counterfeit devices originated in China, South Korea, and Thailand, where patent and trademark protections for the original devices do not extend.
• The device is falsely claimed to have been cleared by the FDA or other clinical regulatory authorities. Legitimate medical devices are subject to rounds of safety and compatibility testing using standards set by regulatory bodies, such as the FDA’s Center for Devices and Radiological Health, the International Organization of Standardization, and the International Electrotechnical Commission. Compliance with these safety standards is lost, however, among unregulated internet sales of medical devices. Our search revealed that 10.7% of the top 10 counterfeit device listings for each product explicitly mentioned FDA clearance in the product description. Among the thousands of listings on e-commerce sites, even a fraction that make spurious FDA-clearance claims can mislead consumers.
The issue of counterfeit medical devices has not gone unrecognized globally. In 2013, the World Health Organization created the Global Surveillance and Monitoring System to unify international efforts for reporting substandard, unlicensed, or falsified medical products.4 Although universal monitoring systems can improve detection of counterfeit products, we highlight the alarming continuing ease of purchasing counterfeit dermatologic devices through e-commerce websites. Due to the widespread nature of counterfeiting across all domains of medicine, the onus of curbing counterfeit dermatologic devices might be on dermatology providers to recognize and report such occurrences.
This exploration of counterfeit dermatologic devices revealed a lack of consistency throughout product listings on 2 popular e-commerce websites, Alibaba.com and DHgate.com. Given the alarming availability of these devices on the internet, practitioners should approach the purchase of any device with concern about counterfeiting. Future avenues of study might explore the prevalence of counterfeit devices used in dermatology practices and offer insight on regulation and consumer safety efforts.
To the Editor:
Approved medical devices on the market are substantial capital investments for practitioners. E-commerce websites, such as Alibaba.com (https://www.alibaba.com/) and DHgate.com (https://www.dhgate.com/), sell sham medical devices at a fraction of the cost of authentic products, with sellers often echoing the same treatment claims as legitimate devices that have been cleared by the US Food and Drug Administration (FDA).
In dermatology, devices claiming to perform cryolipolysis, laser skin resurfacing, radiofrequency skin tightening, and more exist on e-commerce websites. These counterfeit medical devices might differ from legitimate devices in ways that affect patient safety and treatment efficacy.1,2 The degree of difference between counterfeit and legitimate devices remains unknown, and potential harm from so-called knockoff devices needs to be critically examined by providers.
In this exploratory study, we characterize counterfeit listings of devices commonly used in dermatology. Using the trademark name of devices as the key terms, we searched Alibaba.com and DHgate.com for listings of counterfeit products. We recorded the total number of listings; the listing name, catalog number, and unit price; and claims of FDA certification. Characteristics of counterfeit listings were summarized using standard descriptive statistics in Microsoft Excel. Continuous variables were summarized with means and ranges.
Six medical devices that had been cleared by the FDA between 2002 and 2012 for use in dermatology were explored, including systems for picosecond and fractionated lasers, monopolar and bipolar radiofrequency skin tightening, cryolipolysis, and nonablative radiofrequency skin resurfacing. Our search of these 6 representative dermatologic devices revealed 47,055 counterfeit product listings on Alibaba.com and DHgate.com. Upon searching these popular e-commerce websites using the device name as the search term, the number of listings varied considerably between the 2 e-commerce websites for the same device and from device to device on the same e-commerce website. On Alibaba.com, the greatest number of listings resulted for picosecond laser (23,622 listings), fractionated laser (15,269), and radiofrequency skin tightening devices (3555); cryolipolysis and nonablative radiofrequency resurfacing devices had notably fewer listings (35 and 38, respectively). On DHGate.com, a similar trend was noted with the most numerous listings for picosecond and fractionated laser systems (2429 and 1345, respectively).
Among the first 10 listings of products on Alibaba.com and DHgate.com for these 6 devices, 10.7% (11 of 103) had advertised claims of FDA clearance on the listing page. Of 103 counterfeit products, China was the country of origin for 100; South Korea for 2; and Thailand for 1. Unit pricing was heterogeneous between the 2 e-commerce websites for the counterfeit listings; pricing for duplicate fractionated laser systems was particularly dissimilar, with an average price on Alibab.com of US $8105.80 and an average price on DHgate.com of US $3409.14. Even on the same e-commerce website, the range of unit pricing differed greatly for dermatologic devices. For example, among the first 10 listings on Alibaba.com for a fractionated laser system, the price ranged from US $2300 to US $32,000.
Counterfeit medical devices are on the rise in dermatology.1,3 Although devices such as radiofrequency and laser systems had thousands of knockoff listings on 2 e-commerce websites, other devices, such as cryolipolysis and body contouring systems, had fewer listings, suggesting heterogeneity in the prevalence of different counterfeit dermatologic devices on the market.
The varied pricing of the top 10 listings for each product and spurious claims of FDA clearance for some listings highlight the lack of regulatory authority over consistent product information on e-commerce websites. Furthermore, differences between characteristics of counterfeit device listings can impede efforts to trace suppliers and increase the opacity of counterfeit purchasing.
Three criteria have been proposed for a device to be considered counterfeit3:
• The device has no proven safety or efficacy among consumers. For example, the substantial threat of copycat devices in dermatology has been demonstrated by reports of burns caused by fake cryolipolysis devices.2
• The device violates patent rights or copy trademarks. Due to the regional nature of intellectual property rights, country-specific filings of patents and trademarks are required if protections are sought internationally. In this study, counterfeit devices originated in China, South Korea, and Thailand, where patent and trademark protections for the original devices do not extend.
• The device is falsely claimed to have been cleared by the FDA or other clinical regulatory authorities. Legitimate medical devices are subject to rounds of safety and compatibility testing using standards set by regulatory bodies, such as the FDA’s Center for Devices and Radiological Health, the International Organization of Standardization, and the International Electrotechnical Commission. Compliance with these safety standards is lost, however, among unregulated internet sales of medical devices. Our search revealed that 10.7% of the top 10 counterfeit device listings for each product explicitly mentioned FDA clearance in the product description. Among the thousands of listings on e-commerce sites, even a fraction that make spurious FDA-clearance claims can mislead consumers.
The issue of counterfeit medical devices has not gone unrecognized globally. In 2013, the World Health Organization created the Global Surveillance and Monitoring System to unify international efforts for reporting substandard, unlicensed, or falsified medical products.4 Although universal monitoring systems can improve detection of counterfeit products, we highlight the alarming continuing ease of purchasing counterfeit dermatologic devices through e-commerce websites. Due to the widespread nature of counterfeiting across all domains of medicine, the onus of curbing counterfeit dermatologic devices might be on dermatology providers to recognize and report such occurrences.
This exploration of counterfeit dermatologic devices revealed a lack of consistency throughout product listings on 2 popular e-commerce websites, Alibaba.com and DHgate.com. Given the alarming availability of these devices on the internet, practitioners should approach the purchase of any device with concern about counterfeiting. Future avenues of study might explore the prevalence of counterfeit devices used in dermatology practices and offer insight on regulation and consumer safety efforts.
- Wang JV, Zachary CB, Saedi N. Counterfeit esthetic devices and patient safety in dermatology. J Cosmet Dermatol. 2018;17:396-397. doi:10.1111/jocd.12526
- Biesman BS, Patel N. Physician alert: beware of counterfeit medical devices. Lasers Surg Med. 2014;46:528‐530. doi:10.1002/lsm.22275
- Stevens WG, Spring MA, Macias LH. Counterfeit medical devices: the money you save up front will cost you big in the end. Aesthet Surg J. 2014;34:786‐788. doi:10.1177/1090820X14529960
- Pisani E. WHO Global Surveillance and Monitoring System for Substandard and Falsified Medical Products. World Health Organization; 2017. Accessed November 21, 2021. https://www.who.int/medicines/regulation/ssffc/publications/GSMSreport_EN.pdf?ua=1
- Wang JV, Zachary CB, Saedi N. Counterfeit esthetic devices and patient safety in dermatology. J Cosmet Dermatol. 2018;17:396-397. doi:10.1111/jocd.12526
- Biesman BS, Patel N. Physician alert: beware of counterfeit medical devices. Lasers Surg Med. 2014;46:528‐530. doi:10.1002/lsm.22275
- Stevens WG, Spring MA, Macias LH. Counterfeit medical devices: the money you save up front will cost you big in the end. Aesthet Surg J. 2014;34:786‐788. doi:10.1177/1090820X14529960
- Pisani E. WHO Global Surveillance and Monitoring System for Substandard and Falsified Medical Products. World Health Organization; 2017. Accessed November 21, 2021. https://www.who.int/medicines/regulation/ssffc/publications/GSMSreport_EN.pdf?ua=1
Practice Points
- Among thousands of counterfeit dermatologic listings, there is great heterogeneity in the number of listings per different subtypes of dermatologic devices, device descriptions, and unit pricing, along with false claims of US Food and Drug Administration clearance.
- Given the prevalence of counterfeit medical devices readily available for purchase online, dermatology practitioners should be wary of the authenticity of any medical device purchased for clinical use.
What’s Eating You? Caterpillars
Causes of Lepidopterism
Caterpillars are wormlike organisms that serve as the larval stage of moths and butterflies, which belong to the order Lepidoptera. There are almost 165,000 discovered species, with 13,000 found in the United States.1,2 Roughly 150 species are known to have the potential to cause an adverse reaction in humans, with 50 of these in the United States.1Lepidopterism describes systemic and cutaneous reactions to moths, butterflies, and caterpillars; erucism describes strictly cutaneous reactions.1
Although the rate of lepidopterism is thought to be underreported because it often is self-limited and of a mild nature, a review found caterpillars to be the cause of roughly 2.2% of reported bites and stings annually.2 Cases increase in number with seasonal increases in caterpillars, which vary by region and species. For example, the Megalopyge opercularis (southern flannel moth) caterpillar was noted to have 2 peaks in a Texas-based study: 12% of reported stings occurred in July; 59% from October through November.3 In general, the likelihood of exposure increases during warmer months, and exposure is more common in people who work outdoors in a rural area or in a suburban area where there are many caterpillar-infested trees.4
Most cases of lepidopterism are caused by caterpillars, not by adult butterflies and moths, because the former have many tubular, or porous, hairlike structures called setae that are embedded in the integument. Setae were once thought to be connected to poison-secreting glandular cells, but current belief is that venomous caterpillars lack specialized gland cells and instead produce venom through secretory epithelial cells located above the integument.1 Venom accumulates in the hemolymph and is stored in the setae or other types of bristles, such as scoli (wartlike bumps that bear setae) or spines.5 With a large amount of chitin, bristles have a tendency to fracture and release venom upon contact.1 It is thought that some species of caterpillars formulate venom by ingesting toxins or toxin precursors from plants; for example, the tiger moth (family Arctiidae) is known to produce venom containing biogenic amines, pyrrolizidine, alkaloids, and cardiac glycosides obtained through food sources.5
Even if a caterpillar does not produce venom, its setae might embed into skin or mucous membranes and cause an adverse irritant reaction.1 Setae also might dislodge and be transported in the air to embed in objects—some remaining stable in the environment for longer than a year.2 In contrast to setae, spines are permanently fixed into the integument; for that reason, only direct contact with the caterpillar can result in an adverse reaction. Although it is mostly caterpillars that contain setae and spines, certain species of moths also might contain these structures or might acquire them as they emerge from the cocoon, which often contains incorporated setae.2
Reactions in Humans
Lepidopterism encompasses 3 principal reactions in humans: sting reaction, hypersensitivity reaction, and lonomism (a hemorrhagic diathesis produced by Lonomia caterpillars). The type and severity of the reaction depends on (1) the species of caterpillar or moth and (2) the individual patient.2 There are approximately 12 families of caterpillars, mainly of the moth variety, that can cause an adverse reaction in humans.1 Tables 1 and 2 list examples of species that cause each type of reaction.6
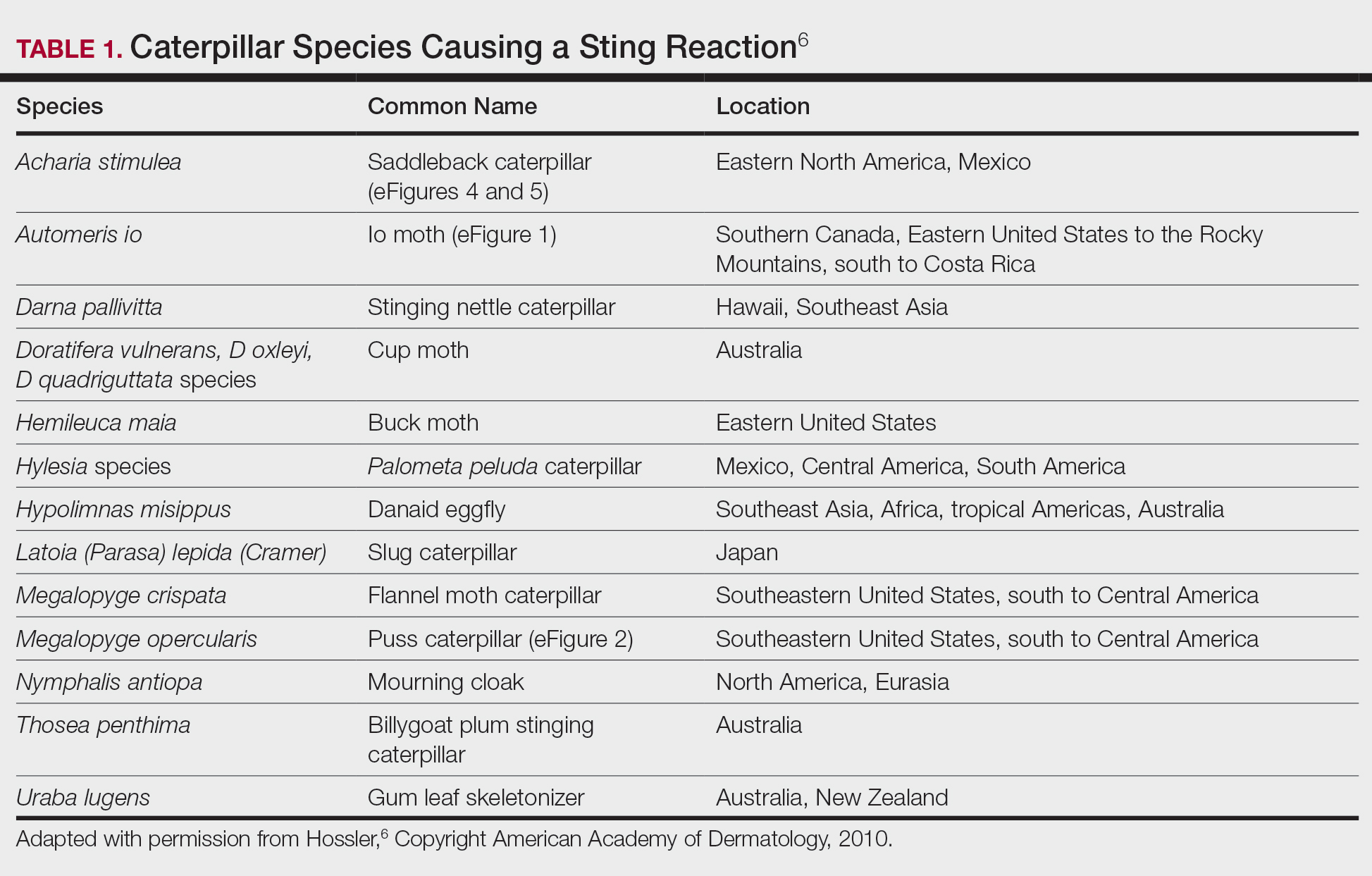

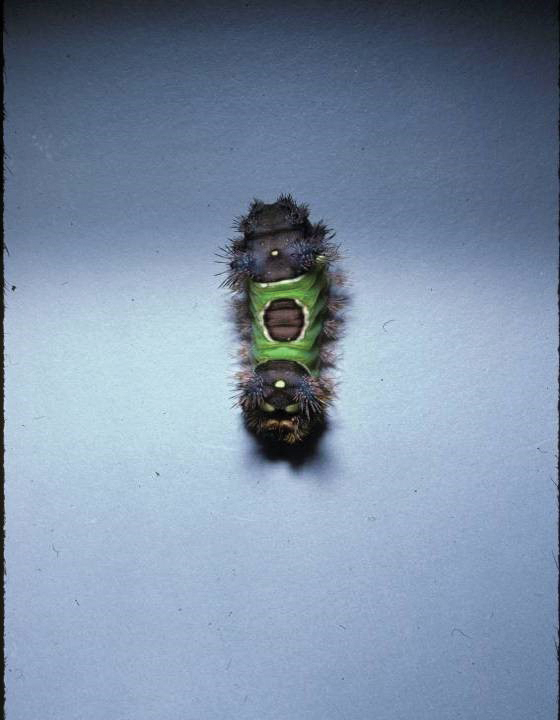
Chemicals and toxins contained in the poison of setae and spines vary by species of caterpillar. Numerous kinds have been isolated from different venoms,1,2 including several peptides, histamine, histamine-releasing substances, acetylcholine, phospholipase A, hyaluronidase, formic acid, proteins with trypsinlike activity, serine proteases such as kallikrein, and other enzymes with vasodegenerative and fibrinolytic properties
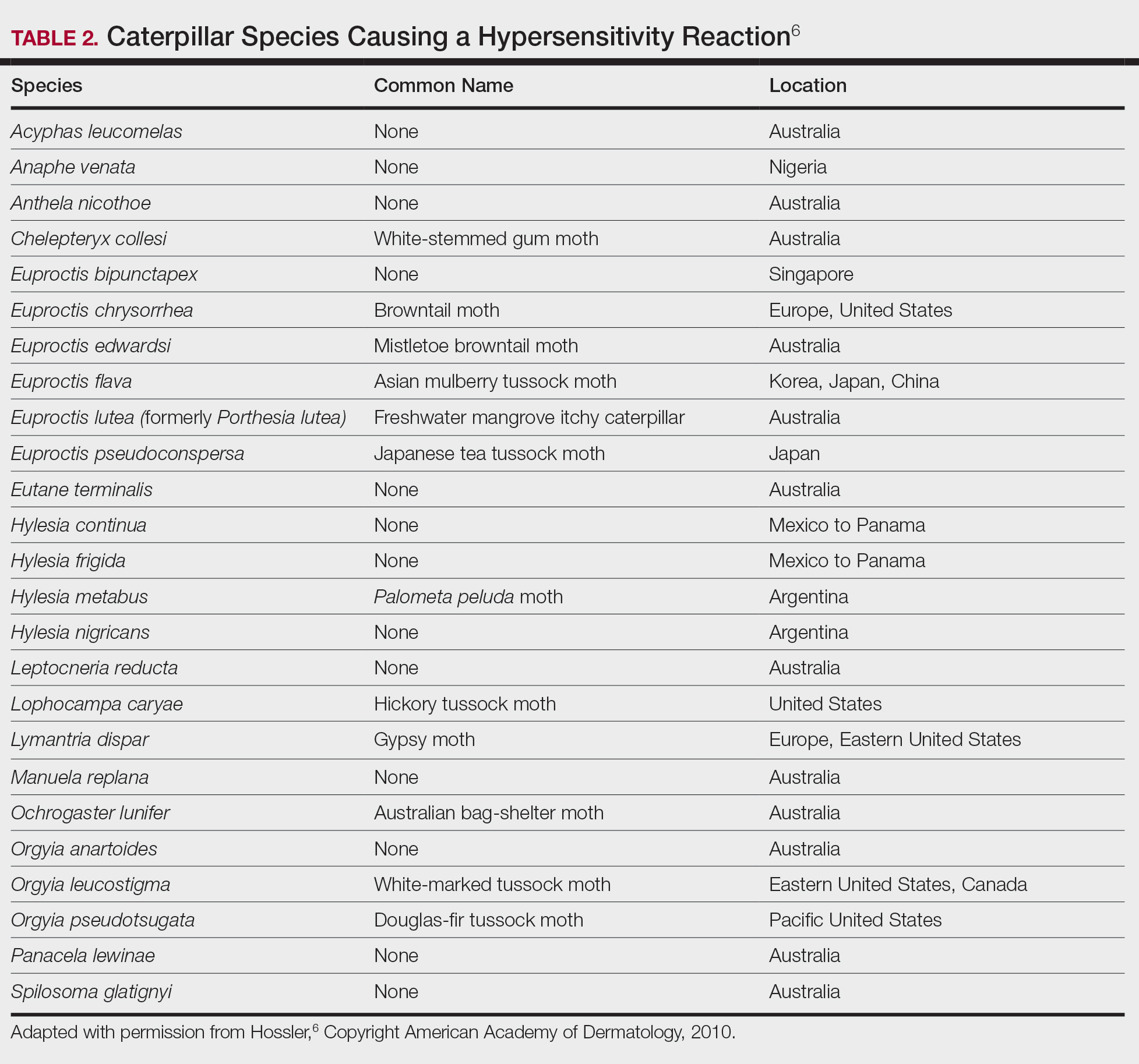
Stings: An Immediate Adverse Reaction—Depending on the venom, a sting might result in mild to severe burning pain, accompanied by welts, vesicles, and red papules or plaques.2 Figure 1 demonstrates a particularly mild sting from a caterpillar of the family Automeris, examples of which are seen in Figures 2 and 3 and eFigure 1. Components of the venom determine the mechanism of the sting and the pain that accompanies it. For example, a recent study demonstrated that the venom of the Latoia consocia caterpillar induces pain through the ion-channel receptor known as transient receptor potential vanilloid 1, which integrates and sends painful stimuli from the peripheral nervous system to the central nervous system.7 It is thought that a variety of ion channels are targets of the venom of caterpillars.




One of the most characteristic sting patterns is that of the caterpillar of family Megalopygidae (flannel moth)(eFigures 2 and 3). The stings of these caterpillars create a unique tram-track pattern of hemorrhagic macules or papules (Figure 4).4 A study found that 90% of reported M opercularis envenomations consist primarily of cutaneous symptoms, with 84% of those symptoms being irritation or pain; 45% a puncture or wound; 29% erythema; and 15% edema.3 Systemic findings can include headache, fever, adenopathy, nausea, vomiting, abdominal pain, and chest pain.4 Symptoms normally are self-limited, though they can last minutes or hours.



Hypersensitivity Reaction—Studies demonstrate that the symptoms of this reaction are a mixture of type I hypersensitivity, type IV hypersensitivity, and a foreign-body response.2 The specific hypersensitivity reaction depends on the venom and the exposed individual—most commonly including a combination of pruritic papules, urticarial wheals, flares, and dermatitis.2 A reaction that is a result of direct contact with the caterpillar or moth will appear on exposed areas; however, because setae embed in linens and clothing, they might cause a reaction anywhere on the body. Although usually self-limited, a hypersensitivity reaction might develop within minutes and can last for days or weeks.
Stings and hypersensitivity reactions to caterpillars and moths tend to lead to a nonspecific histologic presentation characterized by epidermal edema and a superficial perivascular lymphocytic infiltrate, often with eosinophils.6 After approximately 1 week, a foreign-body response to setae can lead to tuberculoid granulomas accompanied by neutrophils in the dermis and occasionally in subcutaneous tissues (Figures 5 and 6).8 If setae have not yet been removed, they also might be visible in skin scrapings.
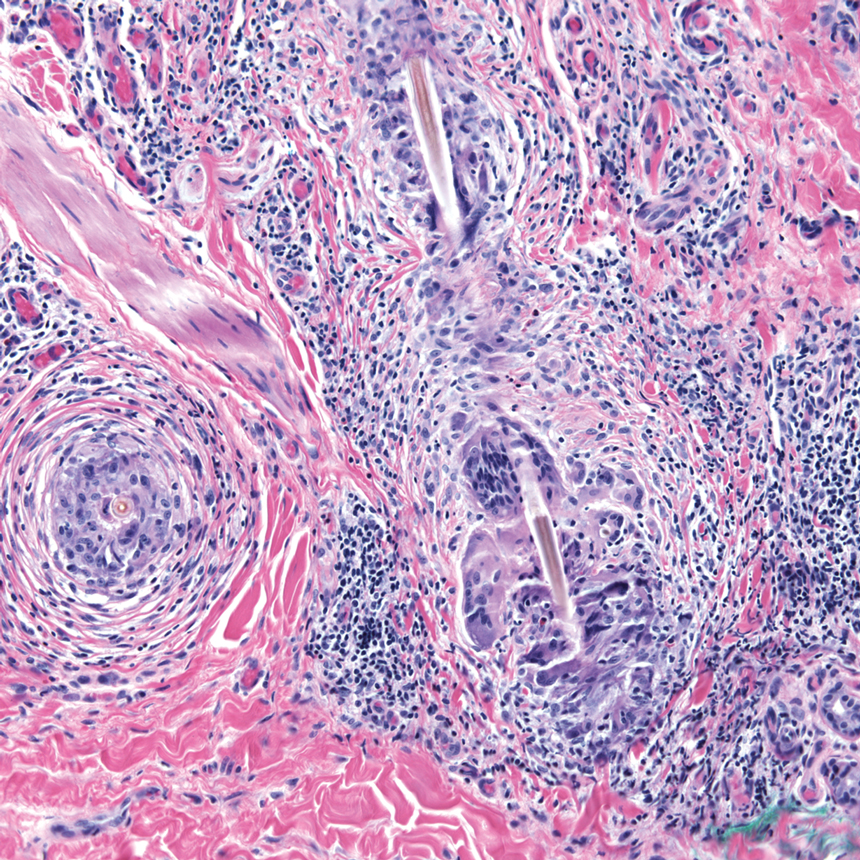
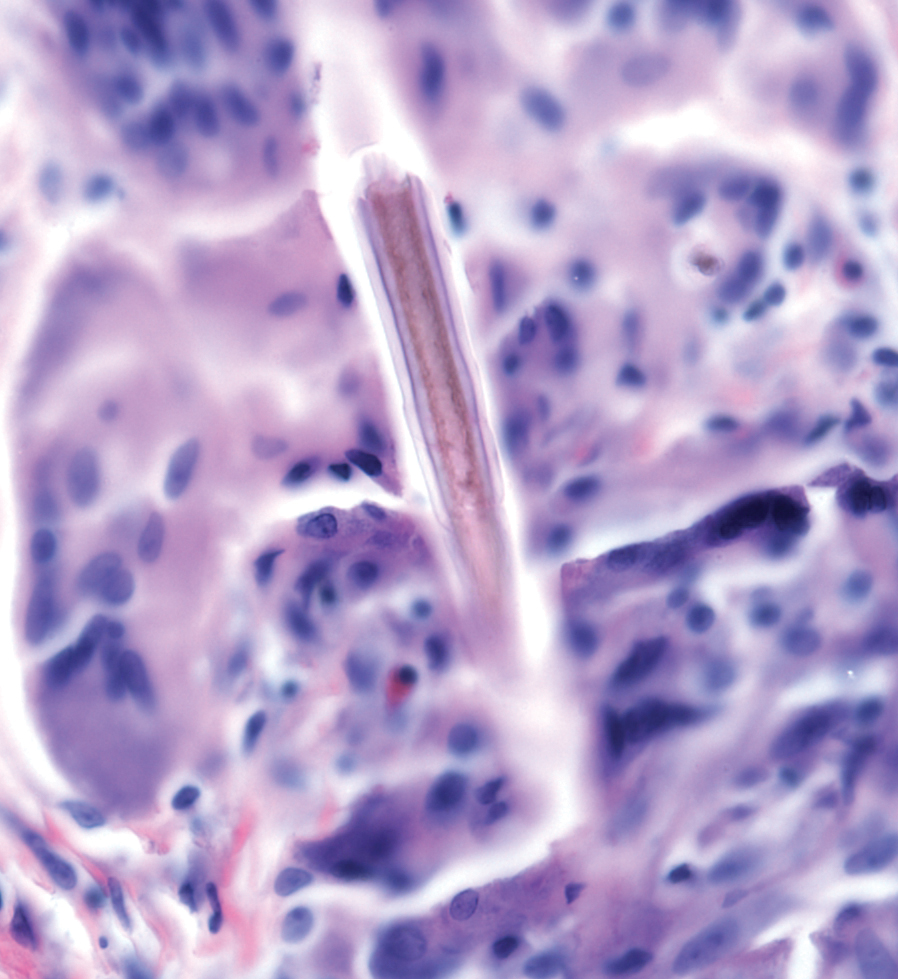
Additional complications can accompany the hypersensitivity reaction to setae or spines. Type I hypersensitivity reactions can lead to severe reactions on second contact due to previously sensitized IgE antibodies. Although the first reaction appears mild, second contact might result in angioedema, wheezing, dyspnea, or anaphylaxis, or a combination of these findings.9 In addition, some patients who come in contact with Dendrolimus caterpillars might develop a condition known as dendrolimiasis, characterized by dermatitis in addition to arthritis or chondritis.6 The arthritis is normally monoarticular and can result in complete destruction of the joint. Pararamose, a condition with a similar presentation, is caused by the Brazilian moth Premolis semirufa.6
Contact of setae or spines with mucous membranes or inhalation of setae also might result in edema, dysphagia, dyspnea, drooling, rhinitis, or conjunctivitis, or a combination of these findings.6 In addition, setae can embed in the eye and cause an inflammatory reaction—ophthalmia nodosa—most commonly caused by caterpillars of the pine processionary moth (Thaumetopoea pityocampa) and characterized by immediate chemosis, which can progress to liquefactive necrosis and hypopyon, later developing into a granulomatous foreign-body response.2,10 The process is thought to be the result of a combination of the thaumetopoein toxin in the setae and an IgE-mediated response to other proteins.10
Due to their harpoon shape and forward-only motion, setae might migrate deeper, potentially even to the optic nerve.11 Because migration might take years and the barbed shape of setae does not always allow removal, some patients require lifetime monitoring with slit-lamp examination.Chronic problems, such as cataracts and persistent posterior uveitis, have been reported.10,11
Lonomism—One of the most serious (though rarest) reactions to caterpillars is lonomism, a condition caused by the caterpillars of Lonomia achelous and Lonomia obliqua moths. These caterpillars have a unique combination of toxins filling their branched spines, which ultimately leads to the same outcome: a hemorrhagic diathesis.
The toxin of L achelous comprises several proteases that degrade fibrin, fibrinogen, and factor XIII while activating prothrombin. In contrast, L obliqua poison causes a hemorrhagic diathesis by promoting a consumptive coagulopathy through enzymes that activate factor X and prothrombin.
With initial contact with either of these Lonomia caterpillars, the patient experiences severe pain accompanied by systemic symptoms, including headache, nausea, and vomiting. Shortly afterward, symptoms of a hemorrhagic diathesis manifest, including bleeding gums, hematuria, bleeding from prior wounds, and epistaxis.5 Serious complications of the hemorrhagic diathesis, such as hemorrhage of major organs, leads to death in 4% of patients.5 A reported case of a patient whose Lonomia caterpillar sting went unrecognized until a week after the accident ended with progression to stage V chronic renal disease.12
Recent research has focused on the specific mechanism of injury caused by Lonomia species. A study found that the venom of L obliqua causes cytoskeleton rearrangement and migration in vascular smooth muscle cells (VSMCs) by inducing formation of reactive oxygen species through activation of nicotinamide adenine dinucleotide phosphate oxidase.13 Thus, the venom directly contributes to the proinflammatory phenotype of endothelial cells seen following envenomation. The same study also demonstrated that elevated reactive oxygen species trigger extracellular signal-regulated kinase pathway activation in VSMCs, leading to cell proliferation, re-stenosis, and ischemia.13 This finding was confirmed by another study,14 which demonstrated an increase in Rac1, a signaling protein involved in the extracellular signal-regulated kinase pathway, in VSMCs upon exposure to L obliqua venom. These studies propose potential new targets for treatment to prevent vascular damage.
Reactions to Adult Organisms—Although it is more common for the caterpillar form of these organisms to cause an adverse reaction, the adult moth also might be capable of causing a similar reaction by retaining setae from the cocoon or by their own spines. The most notable example of this is female moths of the genus Hylesia, which possess spines attached to glands on the abdomen. The poison in these spines—a mixture of proteases and chitinase—causes a dermatitis known as Caripito itch—the name derived from a river port in Venezuela where this moth caused a memorable epidemic of moth-induced dermatitis.7,15 Caripito itch is known for intense pruritus that most commonly lasts days or weeks, possibly longer than 1 year.
Diagnostic Difficulties
The challenge of diagnosing a caterpillar- or moth-induced reaction in humans arises from (1) the lack of clinical history (the caterpillar might not be seen at all by the patient or the examiner) and (2) the similarity of these reactions to those with more common triggers.
When setae remain embedded in the skin or mucous membranes, skin scrapings allow accelerated diagnosis. On a skin scraping prepared with 20% potassium hydroxide, setae appear as tapered and barbed hairlike structures, which allows them to be distinguished from other similar-appearing but differently shaped structures, such as glass fibers.
When setae do not remain embedded in the skin or when the cause of the reaction is due to spines, the physician is left with a nonspecific histologic picture and a large differential diagnosis to be narrowed down based on the history and occasionally the pattern of the skin lesion.
A challenge in sting diagnosis is differentiating a caterpillar or moth sting from that of another organism. In certain cases, such as those of the family Megalopygidae, specific patterns of stings might assist in making the diagnosis. Hypersensitivity reactions are associated with a wider differential diagnosis, including irritant or allergic dermatitis from other causes, scabies, eczema, lichen planus, lichen simplex chronicus, seborrheic dermatitis, and tinea corporis, to name a few.6 Skin scrapings can be examined for other features, such as burrows in the case of scabies, to further narrow the differential.
Stings and hypersensitivity reactions lacking a proper history and associated with more severe systemic symptoms have caused misdiagnosis or led to a workup for the wrong condition; for example, the picture of abdominal pain, nausea, vomiting, tachycardia, leukocytosis, hypokalemia, and metabolic acidosis can simulate appendicitis.16 Upon discovery of a puss caterpillar sting in a patient, her symptoms resolved after treatment with ondansetron, morphine, and intravenous fluids.16
In lonomism, the diagnosis must be established by laboratory measurement of the fibrinogen level, clotting factors, prothrombin time, and activated partial thromboplastin time.4 The differential diagnosis associated with lonomism includes disseminated intravascular coagulation (DIC), snakebite, and a hereditary bleeding disorder.4 The combination of laboratory tests and an extensive medical history allows a diagnosis. Absence of a personal or family history of bleeding excludes a diagnosis of hereditary bleeding disorder, whereas the absence of known causes of DIC or thrombocytopenia allows DIC to be excluded from the differential.
Treatment Options and Prevention
Treatment—The first step is to remove any embedded setae from the skin or mucous membranes. The stepwise recommendation is to remove any constricted clothing, detach setae with adhesive tape, wash with soap and water, and dry without touching the skin.1 Any remaining setae can be removed with additional tape or forceps; setae tend to be fragile and are difficult to remove in their entirety.
Other than removal of the setae, skin reactions are treated symptomatically. Ice packs and isopropyl alcohol have been utilized to cool burning or stinging areas. Pain, pruritus, and inflammation have been alleviated with antihistamines and topical corticosteroids.1 When pain is severe, oral codeine or local injection of anesthetic can be used. For severe and persistent skin lesions, a course of an oral glucocorticoid can be administered. Intramuscular triamcinolone acetonide has been shown to treat pain, dermatitis, and subcutaneous nodules otherwise refractory to treatment.8
Antivenin specific for L obliqua exists to treat lonomism and is therefore effective only when lonomism is caused by that species. Lonomism caused by L achelous is treated with cryoprecipitate, purified fibrinogen, and antifibrinolytic drugs, such as aprotinin.6 Whole blood and fresh-frozen plasma have been noted to make hemorrhage worse when utilized to treat lonomism. Because the mechanism of action of the venom of Lonomia species is based, in part, on inducing a proinflammatory profile in endothelial cells, studies have demonstrated that inhibition of kallikrein might prevent vascular injury and thus prevent serious adverse effects, such as renal failure.17
Prevention—People should wear proper protective clothing when outdoors in potentially infested areas. Measures should be taken to ensure that linens and clothing are not left outside in areas where setae might be carried on the wind. Infestation control is necessary if the population of caterpillars reaches a high enough level.
Conclusion
Several species of caterpillars and moths cause adverse reactions in humans: stings, hypersensitivity reactions, and lonomism. Although most reactions are self-limited, some might have more serious effects, including organ failure and death. Mechanisms of injury vary by species of caterpillar, moth, and butterfly; current research is focused on further defining venom components and signaling pathways to isolate potential targets to aid in the diagnosis and treatment of lepidopterism.
- Goldman BS, Bragg BN. Caterpillar and moth bites. Stat Pearls [Internet]. StatPearls Publishing. Updated August 3, 2021. Accessed November 4, 2021. https://www.ncbi.nlm.nih.gov/books/NBK539851/
- Hossler EW. Caterpillars and moths: part I. Dermatologic manifestations of encounters with Lepidoptera. J Am Acad Dermatol. 2010;62:1-10. doi:10.1016/j.jaad.2009.08.060
- Forrester MB. Megalopyge opercularis caterpillar stings reported to Texas poison centers. Wilderness Environ Med. 2018;29:215-220. doi:10.1016/j.wem.2018.02.002
- Hossler EW. Lepidopterism: skin disorders secondary to caterpillars and moths. UpToDate website. Published October 20, 2021. Accessed November 18, 2021. https://www.uptodate.com/contents/lepidopterism-skin-disorders-secondary-to-caterpillars-and-moths
- Villas-Boas IM, Bonfá G, Tambourgi DV. Venomous caterpillars: from inoculation apparatus to venom composition and envenomation. Toxicon. 2018;153:39-52. doi:10.1016/j.toxicon.2018.08.007
- Hossler EW. Caterpillars and moths: part II. dermatologic manifestations of encounters with Lepidoptera. J Am Acad Dermatol. 2010;62:13-28. doi:10.1016/j.jaad.2009.08.061
- Yao Z, Kamau PM, Han Y, et al. The Latoia consocia caterpillar induces pain by targeting nociceptive ion channel TRPV1. Toxins (Basel). 2019;11:695. doi:10.3390/toxins11120695
- Paniz-Mondolfi AE, Pérez-Alvarez AM, Lundberg U, et al. Cutaneous lepidopterism: dermatitis from contact with moths of Hylesia metabus (Cramer 1775) (Lepidoptera: Saturniidae), the causative agent of caripito itch. Int J Dermatol. 2011;50:535-541. doi:10.1111/j.1365-4632.2010.04683.x
- Santos-Magadán S, González de Olano D, Bartolomé-Zavala B, et al. Adverse reactions to the processionary caterpillar: irritant or allergic mechanism? Contact Dermatitis. 2009;60:109-110. doi:10.1111/j.1600-0536.2008.01464.x
- González-Martín-Moro J, Contreras-Martín I, Castro-Rebollo M, et al. Focal cortical cataract due to caterpillar hair migration. Clin Exp Optom. 2019;102:89-90. doi:10.1111/cxo.12809
- Singh A, Behera UC, Agrawal H. Intra-lenticular caterpillar seta in ophthalmia nodosa. Eur J Ophthalmol. 2021;31:NP109-NP111. doi:10.1177/1120672119858899
- Schmitberger PA, Fernandes TC, Santos RC, et al. Probable chronic renal failure caused by Lonomia caterpillar envenomation. J Venom Anim Toxins Incl Trop Dis. 2013;19:14. doi:10.1186/1678-9199-19-14
- Moraes JA, Rodrigues G, Nascimento-Silva V, et al. Effects of Lonomia obliqua venom on vascular smooth muscle cells: contribution of NADPH oxidase-derived reactive oxygen species. Toxins (Basel). 2017;9:360. doi:10.3390/toxins9110360
- Bernardi L, Pinto AFM, Mendes E, et al. Lonomia obliqua bristle extract modulates Rac1 activation, membrane dynamics and cell adhesion properties. Toxicon. 2019;162:32-39. doi:10.1016/j.toxicon.2019.02.019
- Cabrera G, Lundberg U, Rodríguez-Ulloa A, et al. Protein content of the Hylesia metabus egg nest setae (Cramer [1775]) (Lepidoptera: Saturniidae) and its association with the parental investment for the reproductive success and lepidopterism. J Proteomics. 2017;150:183-200. doi:10.1016/j.jprot.2016.08.010
- Greene SC, Carey JM. Puss caterpillar envenomation: erucism mimicking appendicitis in a young child. Pediatr Emerg Care. 2020;36:E732-E734. doi:10.1097/PEC.0000000000001514
- Berger M, de Moraes JA, Beys-da-Silva WO, et al. Renal and vascular effects of kallikrein inhibition in a model of Lonomia obliqua venom-induced acute kidney injury. PLoS Negl Trop Dis. 2019;13:e0007197. doi:10.1371/journal.pntd.0007197
Causes of Lepidopterism
Caterpillars are wormlike organisms that serve as the larval stage of moths and butterflies, which belong to the order Lepidoptera. There are almost 165,000 discovered species, with 13,000 found in the United States.1,2 Roughly 150 species are known to have the potential to cause an adverse reaction in humans, with 50 of these in the United States.1Lepidopterism describes systemic and cutaneous reactions to moths, butterflies, and caterpillars; erucism describes strictly cutaneous reactions.1
Although the rate of lepidopterism is thought to be underreported because it often is self-limited and of a mild nature, a review found caterpillars to be the cause of roughly 2.2% of reported bites and stings annually.2 Cases increase in number with seasonal increases in caterpillars, which vary by region and species. For example, the Megalopyge opercularis (southern flannel moth) caterpillar was noted to have 2 peaks in a Texas-based study: 12% of reported stings occurred in July; 59% from October through November.3 In general, the likelihood of exposure increases during warmer months, and exposure is more common in people who work outdoors in a rural area or in a suburban area where there are many caterpillar-infested trees.4
Most cases of lepidopterism are caused by caterpillars, not by adult butterflies and moths, because the former have many tubular, or porous, hairlike structures called setae that are embedded in the integument. Setae were once thought to be connected to poison-secreting glandular cells, but current belief is that venomous caterpillars lack specialized gland cells and instead produce venom through secretory epithelial cells located above the integument.1 Venom accumulates in the hemolymph and is stored in the setae or other types of bristles, such as scoli (wartlike bumps that bear setae) or spines.5 With a large amount of chitin, bristles have a tendency to fracture and release venom upon contact.1 It is thought that some species of caterpillars formulate venom by ingesting toxins or toxin precursors from plants; for example, the tiger moth (family Arctiidae) is known to produce venom containing biogenic amines, pyrrolizidine, alkaloids, and cardiac glycosides obtained through food sources.5
Even if a caterpillar does not produce venom, its setae might embed into skin or mucous membranes and cause an adverse irritant reaction.1 Setae also might dislodge and be transported in the air to embed in objects—some remaining stable in the environment for longer than a year.2 In contrast to setae, spines are permanently fixed into the integument; for that reason, only direct contact with the caterpillar can result in an adverse reaction. Although it is mostly caterpillars that contain setae and spines, certain species of moths also might contain these structures or might acquire them as they emerge from the cocoon, which often contains incorporated setae.2
Reactions in Humans
Lepidopterism encompasses 3 principal reactions in humans: sting reaction, hypersensitivity reaction, and lonomism (a hemorrhagic diathesis produced by Lonomia caterpillars). The type and severity of the reaction depends on (1) the species of caterpillar or moth and (2) the individual patient.2 There are approximately 12 families of caterpillars, mainly of the moth variety, that can cause an adverse reaction in humans.1 Tables 1 and 2 list examples of species that cause each type of reaction.6
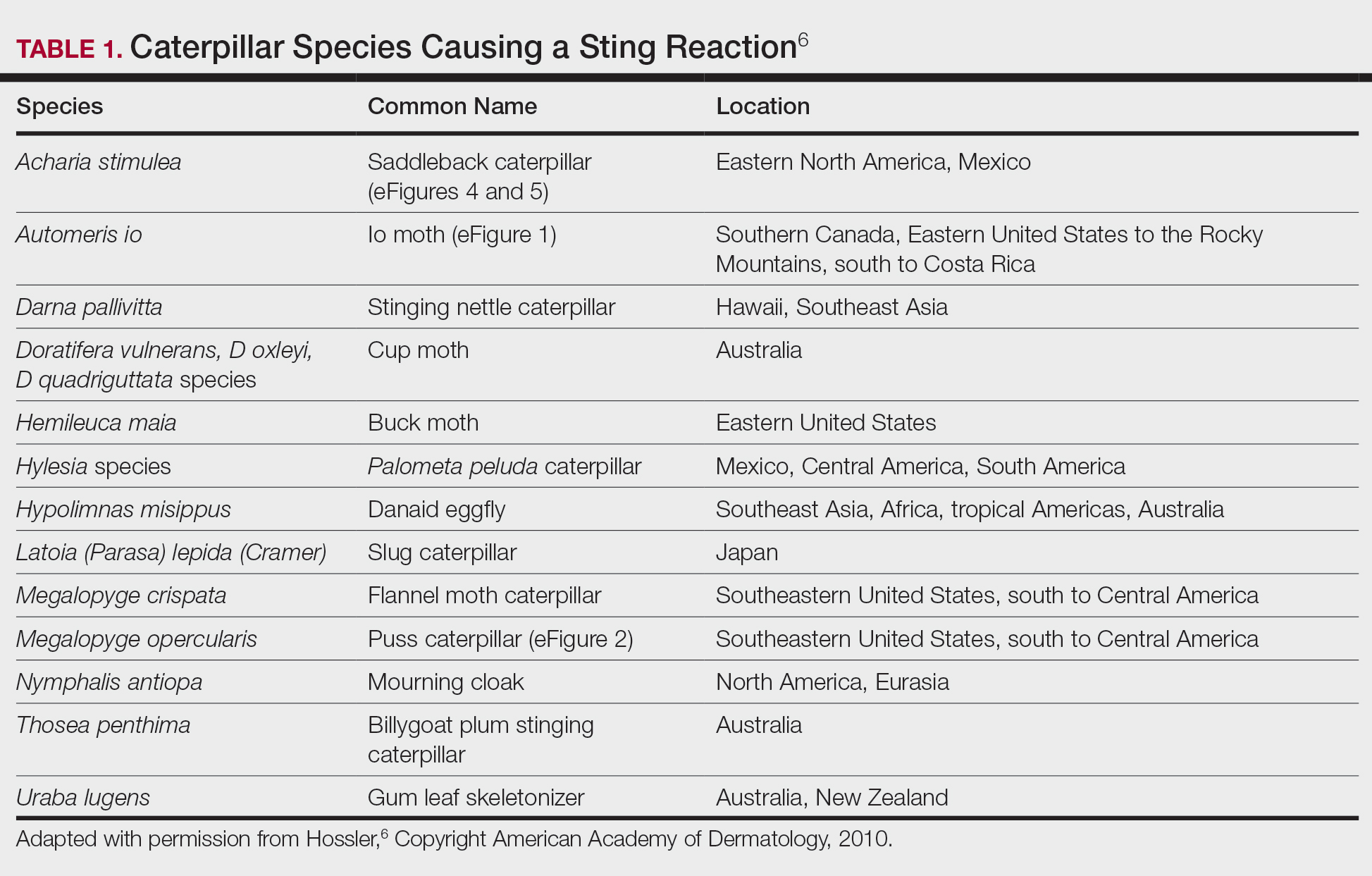

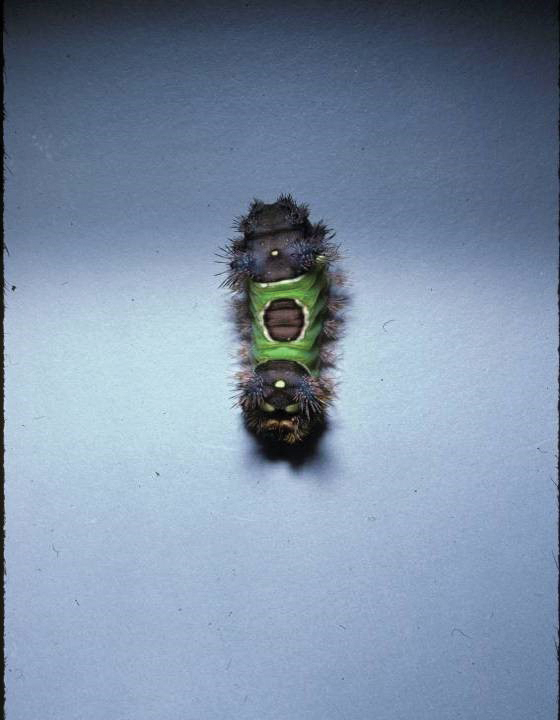
Chemicals and toxins contained in the poison of setae and spines vary by species of caterpillar. Numerous kinds have been isolated from different venoms,1,2 including several peptides, histamine, histamine-releasing substances, acetylcholine, phospholipase A, hyaluronidase, formic acid, proteins with trypsinlike activity, serine proteases such as kallikrein, and other enzymes with vasodegenerative and fibrinolytic properties
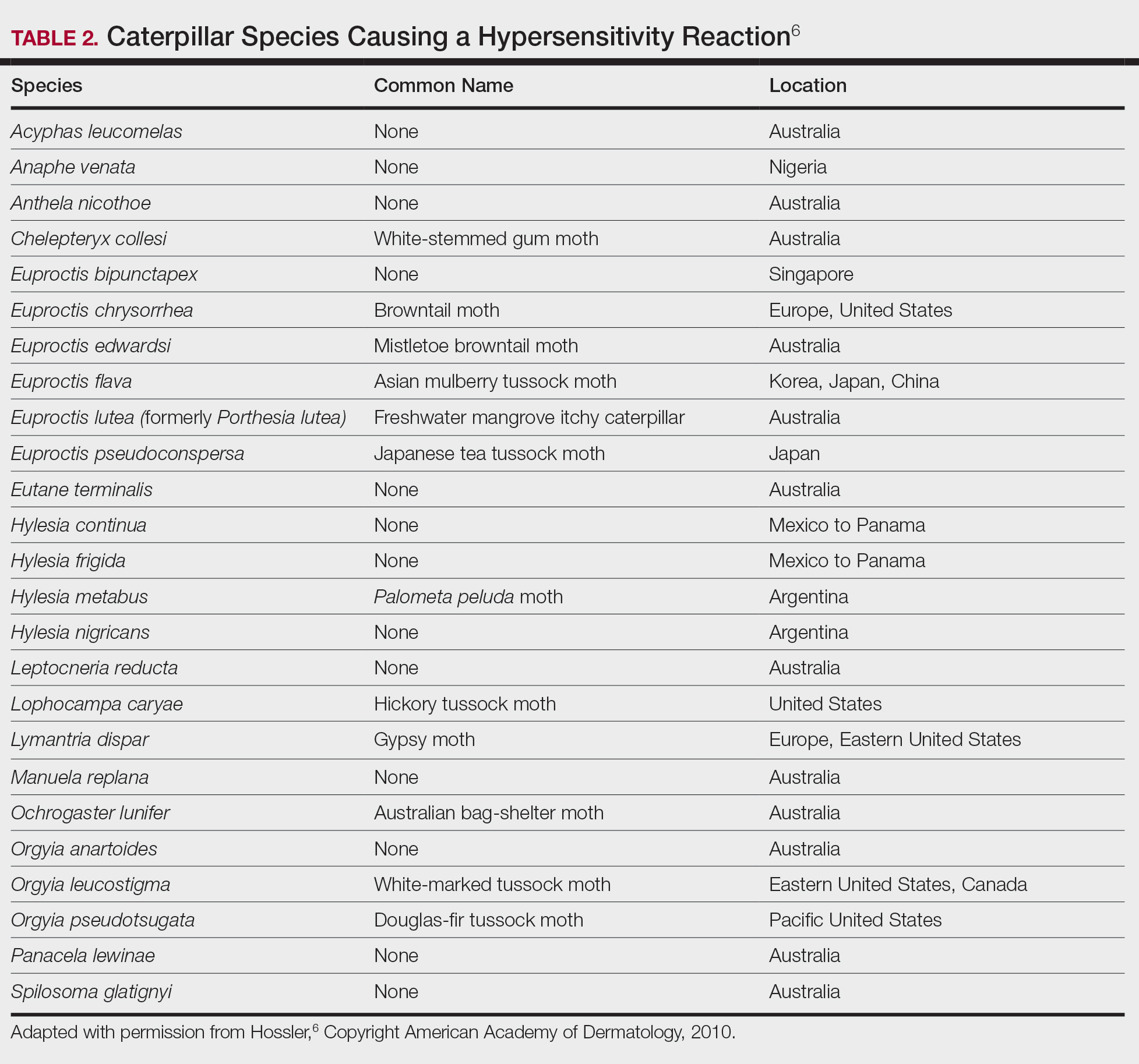
Stings: An Immediate Adverse Reaction—Depending on the venom, a sting might result in mild to severe burning pain, accompanied by welts, vesicles, and red papules or plaques.2 Figure 1 demonstrates a particularly mild sting from a caterpillar of the family Automeris, examples of which are seen in Figures 2 and 3 and eFigure 1. Components of the venom determine the mechanism of the sting and the pain that accompanies it. For example, a recent study demonstrated that the venom of the Latoia consocia caterpillar induces pain through the ion-channel receptor known as transient receptor potential vanilloid 1, which integrates and sends painful stimuli from the peripheral nervous system to the central nervous system.7 It is thought that a variety of ion channels are targets of the venom of caterpillars.




One of the most characteristic sting patterns is that of the caterpillar of family Megalopygidae (flannel moth)(eFigures 2 and 3). The stings of these caterpillars create a unique tram-track pattern of hemorrhagic macules or papules (Figure 4).4 A study found that 90% of reported M opercularis envenomations consist primarily of cutaneous symptoms, with 84% of those symptoms being irritation or pain; 45% a puncture or wound; 29% erythema; and 15% edema.3 Systemic findings can include headache, fever, adenopathy, nausea, vomiting, abdominal pain, and chest pain.4 Symptoms normally are self-limited, though they can last minutes or hours.



Hypersensitivity Reaction—Studies demonstrate that the symptoms of this reaction are a mixture of type I hypersensitivity, type IV hypersensitivity, and a foreign-body response.2 The specific hypersensitivity reaction depends on the venom and the exposed individual—most commonly including a combination of pruritic papules, urticarial wheals, flares, and dermatitis.2 A reaction that is a result of direct contact with the caterpillar or moth will appear on exposed areas; however, because setae embed in linens and clothing, they might cause a reaction anywhere on the body. Although usually self-limited, a hypersensitivity reaction might develop within minutes and can last for days or weeks.
Stings and hypersensitivity reactions to caterpillars and moths tend to lead to a nonspecific histologic presentation characterized by epidermal edema and a superficial perivascular lymphocytic infiltrate, often with eosinophils.6 After approximately 1 week, a foreign-body response to setae can lead to tuberculoid granulomas accompanied by neutrophils in the dermis and occasionally in subcutaneous tissues (Figures 5 and 6).8 If setae have not yet been removed, they also might be visible in skin scrapings.
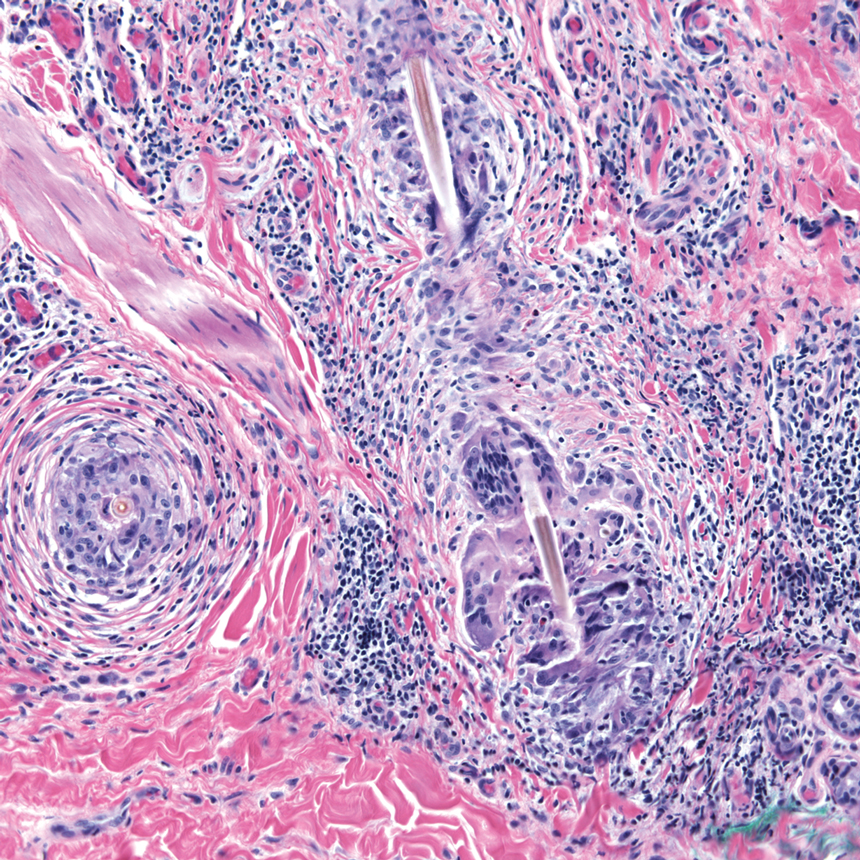
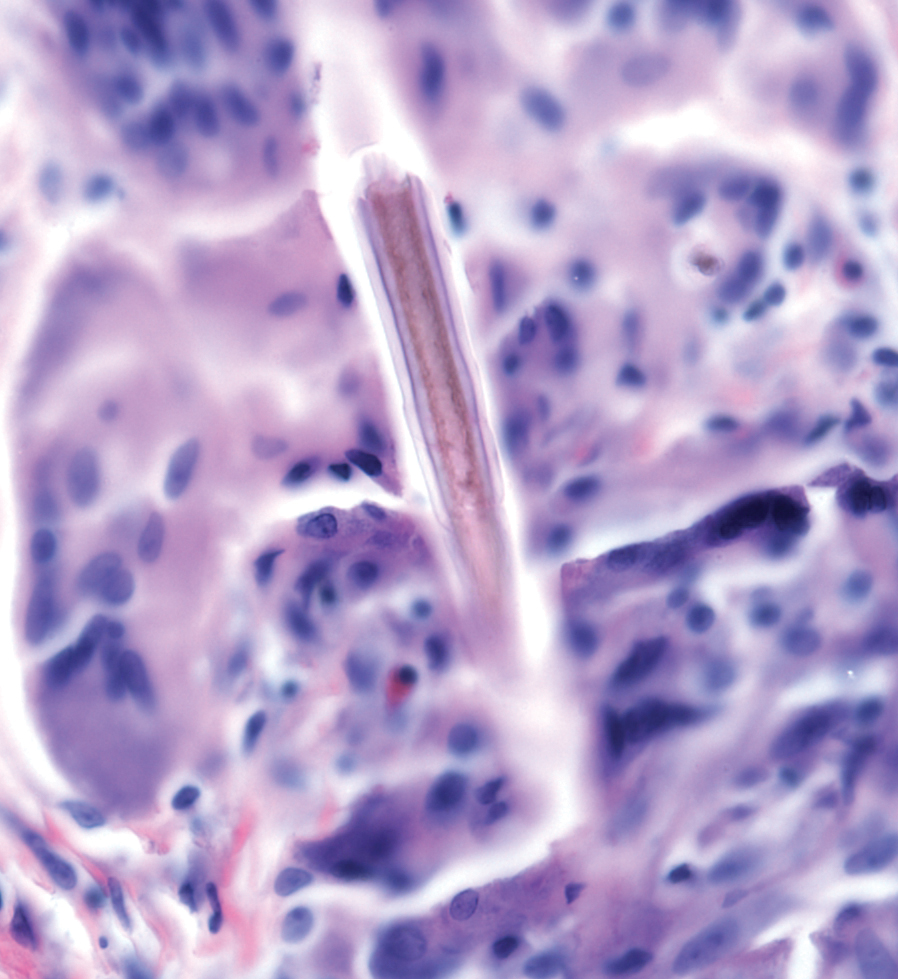
Additional complications can accompany the hypersensitivity reaction to setae or spines. Type I hypersensitivity reactions can lead to severe reactions on second contact due to previously sensitized IgE antibodies. Although the first reaction appears mild, second contact might result in angioedema, wheezing, dyspnea, or anaphylaxis, or a combination of these findings.9 In addition, some patients who come in contact with Dendrolimus caterpillars might develop a condition known as dendrolimiasis, characterized by dermatitis in addition to arthritis or chondritis.6 The arthritis is normally monoarticular and can result in complete destruction of the joint. Pararamose, a condition with a similar presentation, is caused by the Brazilian moth Premolis semirufa.6
Contact of setae or spines with mucous membranes or inhalation of setae also might result in edema, dysphagia, dyspnea, drooling, rhinitis, or conjunctivitis, or a combination of these findings.6 In addition, setae can embed in the eye and cause an inflammatory reaction—ophthalmia nodosa—most commonly caused by caterpillars of the pine processionary moth (Thaumetopoea pityocampa) and characterized by immediate chemosis, which can progress to liquefactive necrosis and hypopyon, later developing into a granulomatous foreign-body response.2,10 The process is thought to be the result of a combination of the thaumetopoein toxin in the setae and an IgE-mediated response to other proteins.10
Due to their harpoon shape and forward-only motion, setae might migrate deeper, potentially even to the optic nerve.11 Because migration might take years and the barbed shape of setae does not always allow removal, some patients require lifetime monitoring with slit-lamp examination.Chronic problems, such as cataracts and persistent posterior uveitis, have been reported.10,11
Lonomism—One of the most serious (though rarest) reactions to caterpillars is lonomism, a condition caused by the caterpillars of Lonomia achelous and Lonomia obliqua moths. These caterpillars have a unique combination of toxins filling their branched spines, which ultimately leads to the same outcome: a hemorrhagic diathesis.
The toxin of L achelous comprises several proteases that degrade fibrin, fibrinogen, and factor XIII while activating prothrombin. In contrast, L obliqua poison causes a hemorrhagic diathesis by promoting a consumptive coagulopathy through enzymes that activate factor X and prothrombin.
With initial contact with either of these Lonomia caterpillars, the patient experiences severe pain accompanied by systemic symptoms, including headache, nausea, and vomiting. Shortly afterward, symptoms of a hemorrhagic diathesis manifest, including bleeding gums, hematuria, bleeding from prior wounds, and epistaxis.5 Serious complications of the hemorrhagic diathesis, such as hemorrhage of major organs, leads to death in 4% of patients.5 A reported case of a patient whose Lonomia caterpillar sting went unrecognized until a week after the accident ended with progression to stage V chronic renal disease.12
Recent research has focused on the specific mechanism of injury caused by Lonomia species. A study found that the venom of L obliqua causes cytoskeleton rearrangement and migration in vascular smooth muscle cells (VSMCs) by inducing formation of reactive oxygen species through activation of nicotinamide adenine dinucleotide phosphate oxidase.13 Thus, the venom directly contributes to the proinflammatory phenotype of endothelial cells seen following envenomation. The same study also demonstrated that elevated reactive oxygen species trigger extracellular signal-regulated kinase pathway activation in VSMCs, leading to cell proliferation, re-stenosis, and ischemia.13 This finding was confirmed by another study,14 which demonstrated an increase in Rac1, a signaling protein involved in the extracellular signal-regulated kinase pathway, in VSMCs upon exposure to L obliqua venom. These studies propose potential new targets for treatment to prevent vascular damage.
Reactions to Adult Organisms—Although it is more common for the caterpillar form of these organisms to cause an adverse reaction, the adult moth also might be capable of causing a similar reaction by retaining setae from the cocoon or by their own spines. The most notable example of this is female moths of the genus Hylesia, which possess spines attached to glands on the abdomen. The poison in these spines—a mixture of proteases and chitinase—causes a dermatitis known as Caripito itch—the name derived from a river port in Venezuela where this moth caused a memorable epidemic of moth-induced dermatitis.7,15 Caripito itch is known for intense pruritus that most commonly lasts days or weeks, possibly longer than 1 year.
Diagnostic Difficulties
The challenge of diagnosing a caterpillar- or moth-induced reaction in humans arises from (1) the lack of clinical history (the caterpillar might not be seen at all by the patient or the examiner) and (2) the similarity of these reactions to those with more common triggers.
When setae remain embedded in the skin or mucous membranes, skin scrapings allow accelerated diagnosis. On a skin scraping prepared with 20% potassium hydroxide, setae appear as tapered and barbed hairlike structures, which allows them to be distinguished from other similar-appearing but differently shaped structures, such as glass fibers.
When setae do not remain embedded in the skin or when the cause of the reaction is due to spines, the physician is left with a nonspecific histologic picture and a large differential diagnosis to be narrowed down based on the history and occasionally the pattern of the skin lesion.
A challenge in sting diagnosis is differentiating a caterpillar or moth sting from that of another organism. In certain cases, such as those of the family Megalopygidae, specific patterns of stings might assist in making the diagnosis. Hypersensitivity reactions are associated with a wider differential diagnosis, including irritant or allergic dermatitis from other causes, scabies, eczema, lichen planus, lichen simplex chronicus, seborrheic dermatitis, and tinea corporis, to name a few.6 Skin scrapings can be examined for other features, such as burrows in the case of scabies, to further narrow the differential.
Stings and hypersensitivity reactions lacking a proper history and associated with more severe systemic symptoms have caused misdiagnosis or led to a workup for the wrong condition; for example, the picture of abdominal pain, nausea, vomiting, tachycardia, leukocytosis, hypokalemia, and metabolic acidosis can simulate appendicitis.16 Upon discovery of a puss caterpillar sting in a patient, her symptoms resolved after treatment with ondansetron, morphine, and intravenous fluids.16
In lonomism, the diagnosis must be established by laboratory measurement of the fibrinogen level, clotting factors, prothrombin time, and activated partial thromboplastin time.4 The differential diagnosis associated with lonomism includes disseminated intravascular coagulation (DIC), snakebite, and a hereditary bleeding disorder.4 The combination of laboratory tests and an extensive medical history allows a diagnosis. Absence of a personal or family history of bleeding excludes a diagnosis of hereditary bleeding disorder, whereas the absence of known causes of DIC or thrombocytopenia allows DIC to be excluded from the differential.
Treatment Options and Prevention
Treatment—The first step is to remove any embedded setae from the skin or mucous membranes. The stepwise recommendation is to remove any constricted clothing, detach setae with adhesive tape, wash with soap and water, and dry without touching the skin.1 Any remaining setae can be removed with additional tape or forceps; setae tend to be fragile and are difficult to remove in their entirety.
Other than removal of the setae, skin reactions are treated symptomatically. Ice packs and isopropyl alcohol have been utilized to cool burning or stinging areas. Pain, pruritus, and inflammation have been alleviated with antihistamines and topical corticosteroids.1 When pain is severe, oral codeine or local injection of anesthetic can be used. For severe and persistent skin lesions, a course of an oral glucocorticoid can be administered. Intramuscular triamcinolone acetonide has been shown to treat pain, dermatitis, and subcutaneous nodules otherwise refractory to treatment.8
Antivenin specific for L obliqua exists to treat lonomism and is therefore effective only when lonomism is caused by that species. Lonomism caused by L achelous is treated with cryoprecipitate, purified fibrinogen, and antifibrinolytic drugs, such as aprotinin.6 Whole blood and fresh-frozen plasma have been noted to make hemorrhage worse when utilized to treat lonomism. Because the mechanism of action of the venom of Lonomia species is based, in part, on inducing a proinflammatory profile in endothelial cells, studies have demonstrated that inhibition of kallikrein might prevent vascular injury and thus prevent serious adverse effects, such as renal failure.17
Prevention—People should wear proper protective clothing when outdoors in potentially infested areas. Measures should be taken to ensure that linens and clothing are not left outside in areas where setae might be carried on the wind. Infestation control is necessary if the population of caterpillars reaches a high enough level.
Conclusion
Several species of caterpillars and moths cause adverse reactions in humans: stings, hypersensitivity reactions, and lonomism. Although most reactions are self-limited, some might have more serious effects, including organ failure and death. Mechanisms of injury vary by species of caterpillar, moth, and butterfly; current research is focused on further defining venom components and signaling pathways to isolate potential targets to aid in the diagnosis and treatment of lepidopterism.
Causes of Lepidopterism
Caterpillars are wormlike organisms that serve as the larval stage of moths and butterflies, which belong to the order Lepidoptera. There are almost 165,000 discovered species, with 13,000 found in the United States.1,2 Roughly 150 species are known to have the potential to cause an adverse reaction in humans, with 50 of these in the United States.1Lepidopterism describes systemic and cutaneous reactions to moths, butterflies, and caterpillars; erucism describes strictly cutaneous reactions.1
Although the rate of lepidopterism is thought to be underreported because it often is self-limited and of a mild nature, a review found caterpillars to be the cause of roughly 2.2% of reported bites and stings annually.2 Cases increase in number with seasonal increases in caterpillars, which vary by region and species. For example, the Megalopyge opercularis (southern flannel moth) caterpillar was noted to have 2 peaks in a Texas-based study: 12% of reported stings occurred in July; 59% from October through November.3 In general, the likelihood of exposure increases during warmer months, and exposure is more common in people who work outdoors in a rural area or in a suburban area where there are many caterpillar-infested trees.4
Most cases of lepidopterism are caused by caterpillars, not by adult butterflies and moths, because the former have many tubular, or porous, hairlike structures called setae that are embedded in the integument. Setae were once thought to be connected to poison-secreting glandular cells, but current belief is that venomous caterpillars lack specialized gland cells and instead produce venom through secretory epithelial cells located above the integument.1 Venom accumulates in the hemolymph and is stored in the setae or other types of bristles, such as scoli (wartlike bumps that bear setae) or spines.5 With a large amount of chitin, bristles have a tendency to fracture and release venom upon contact.1 It is thought that some species of caterpillars formulate venom by ingesting toxins or toxin precursors from plants; for example, the tiger moth (family Arctiidae) is known to produce venom containing biogenic amines, pyrrolizidine, alkaloids, and cardiac glycosides obtained through food sources.5
Even if a caterpillar does not produce venom, its setae might embed into skin or mucous membranes and cause an adverse irritant reaction.1 Setae also might dislodge and be transported in the air to embed in objects—some remaining stable in the environment for longer than a year.2 In contrast to setae, spines are permanently fixed into the integument; for that reason, only direct contact with the caterpillar can result in an adverse reaction. Although it is mostly caterpillars that contain setae and spines, certain species of moths also might contain these structures or might acquire them as they emerge from the cocoon, which often contains incorporated setae.2
Reactions in Humans
Lepidopterism encompasses 3 principal reactions in humans: sting reaction, hypersensitivity reaction, and lonomism (a hemorrhagic diathesis produced by Lonomia caterpillars). The type and severity of the reaction depends on (1) the species of caterpillar or moth and (2) the individual patient.2 There are approximately 12 families of caterpillars, mainly of the moth variety, that can cause an adverse reaction in humans.1 Tables 1 and 2 list examples of species that cause each type of reaction.6
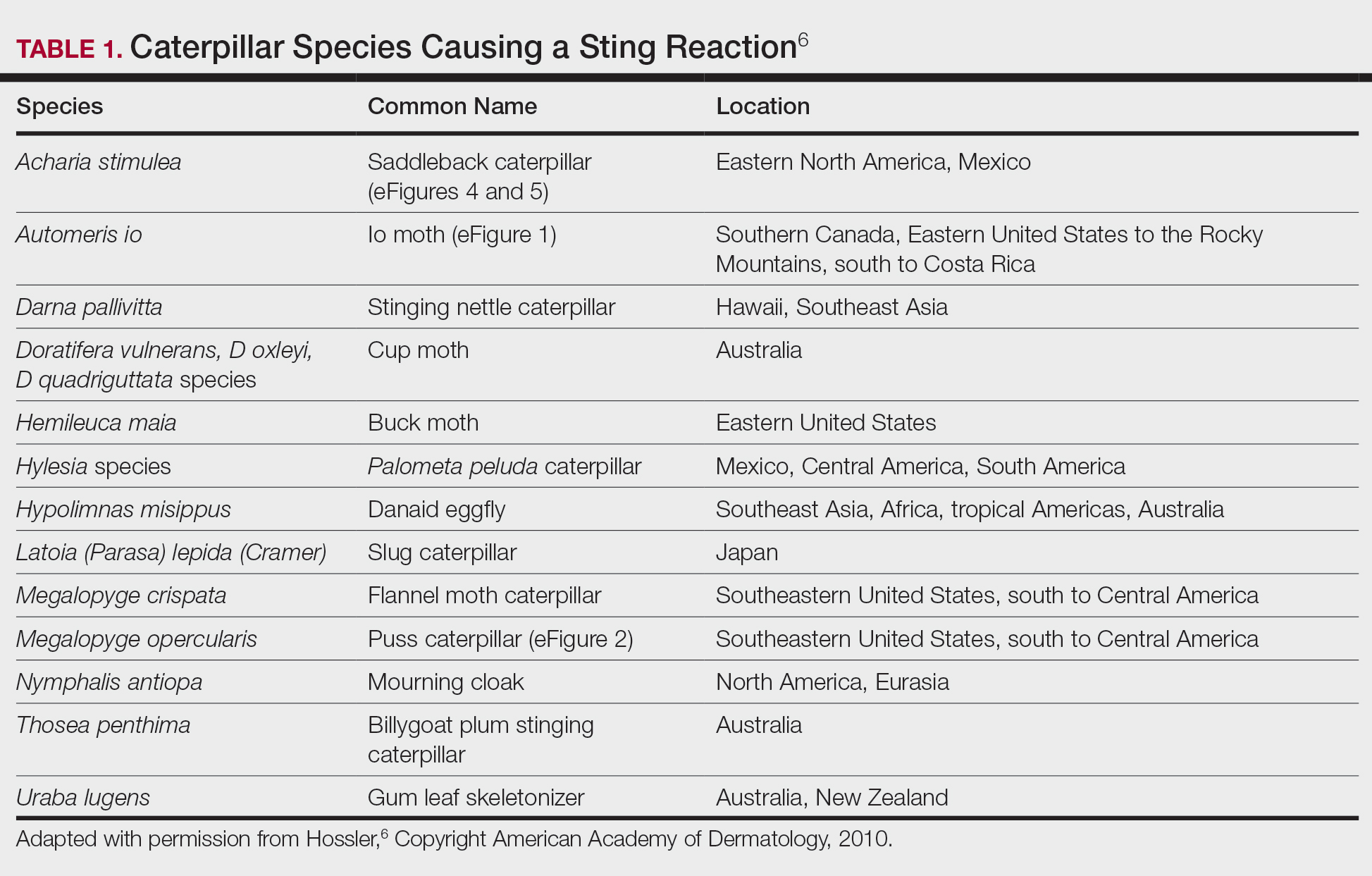

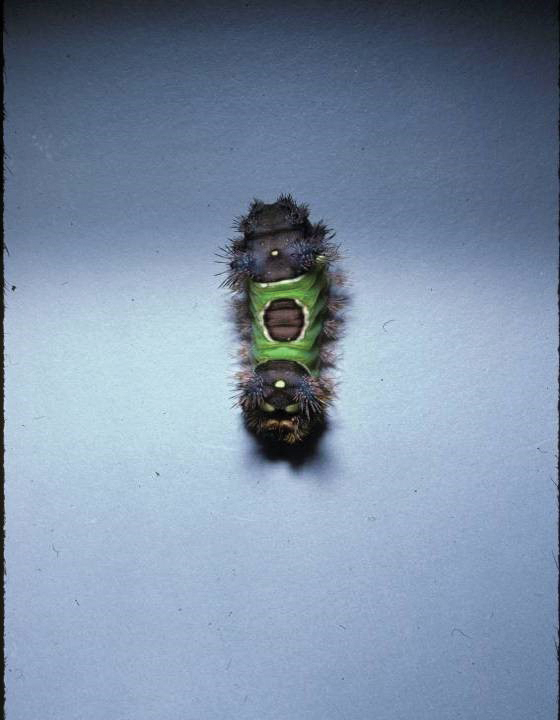
Chemicals and toxins contained in the poison of setae and spines vary by species of caterpillar. Numerous kinds have been isolated from different venoms,1,2 including several peptides, histamine, histamine-releasing substances, acetylcholine, phospholipase A, hyaluronidase, formic acid, proteins with trypsinlike activity, serine proteases such as kallikrein, and other enzymes with vasodegenerative and fibrinolytic properties
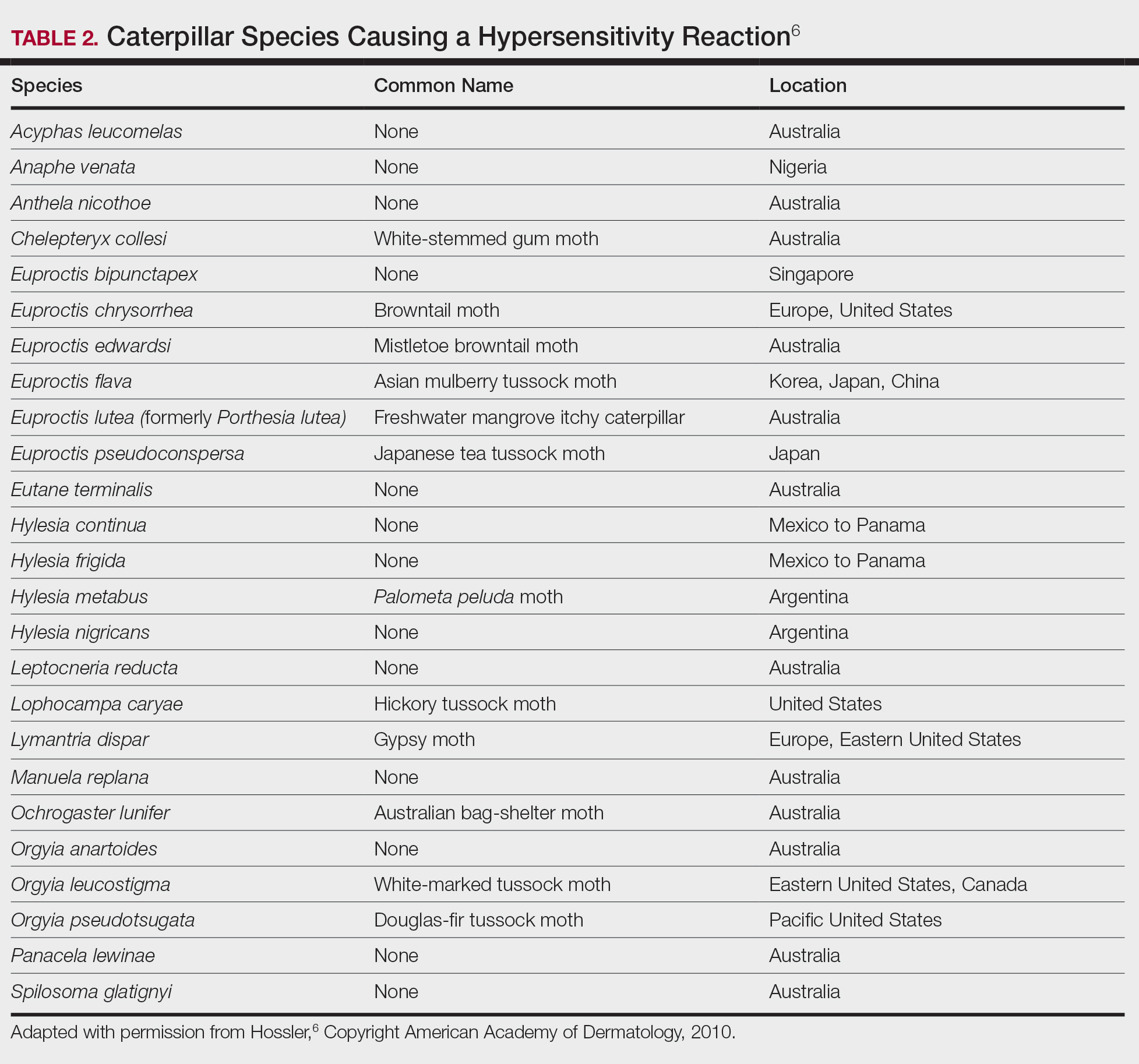
Stings: An Immediate Adverse Reaction—Depending on the venom, a sting might result in mild to severe burning pain, accompanied by welts, vesicles, and red papules or plaques.2 Figure 1 demonstrates a particularly mild sting from a caterpillar of the family Automeris, examples of which are seen in Figures 2 and 3 and eFigure 1. Components of the venom determine the mechanism of the sting and the pain that accompanies it. For example, a recent study demonstrated that the venom of the Latoia consocia caterpillar induces pain through the ion-channel receptor known as transient receptor potential vanilloid 1, which integrates and sends painful stimuli from the peripheral nervous system to the central nervous system.7 It is thought that a variety of ion channels are targets of the venom of caterpillars.




One of the most characteristic sting patterns is that of the caterpillar of family Megalopygidae (flannel moth)(eFigures 2 and 3). The stings of these caterpillars create a unique tram-track pattern of hemorrhagic macules or papules (Figure 4).4 A study found that 90% of reported M opercularis envenomations consist primarily of cutaneous symptoms, with 84% of those symptoms being irritation or pain; 45% a puncture or wound; 29% erythema; and 15% edema.3 Systemic findings can include headache, fever, adenopathy, nausea, vomiting, abdominal pain, and chest pain.4 Symptoms normally are self-limited, though they can last minutes or hours.



Hypersensitivity Reaction—Studies demonstrate that the symptoms of this reaction are a mixture of type I hypersensitivity, type IV hypersensitivity, and a foreign-body response.2 The specific hypersensitivity reaction depends on the venom and the exposed individual—most commonly including a combination of pruritic papules, urticarial wheals, flares, and dermatitis.2 A reaction that is a result of direct contact with the caterpillar or moth will appear on exposed areas; however, because setae embed in linens and clothing, they might cause a reaction anywhere on the body. Although usually self-limited, a hypersensitivity reaction might develop within minutes and can last for days or weeks.
Stings and hypersensitivity reactions to caterpillars and moths tend to lead to a nonspecific histologic presentation characterized by epidermal edema and a superficial perivascular lymphocytic infiltrate, often with eosinophils.6 After approximately 1 week, a foreign-body response to setae can lead to tuberculoid granulomas accompanied by neutrophils in the dermis and occasionally in subcutaneous tissues (Figures 5 and 6).8 If setae have not yet been removed, they also might be visible in skin scrapings.
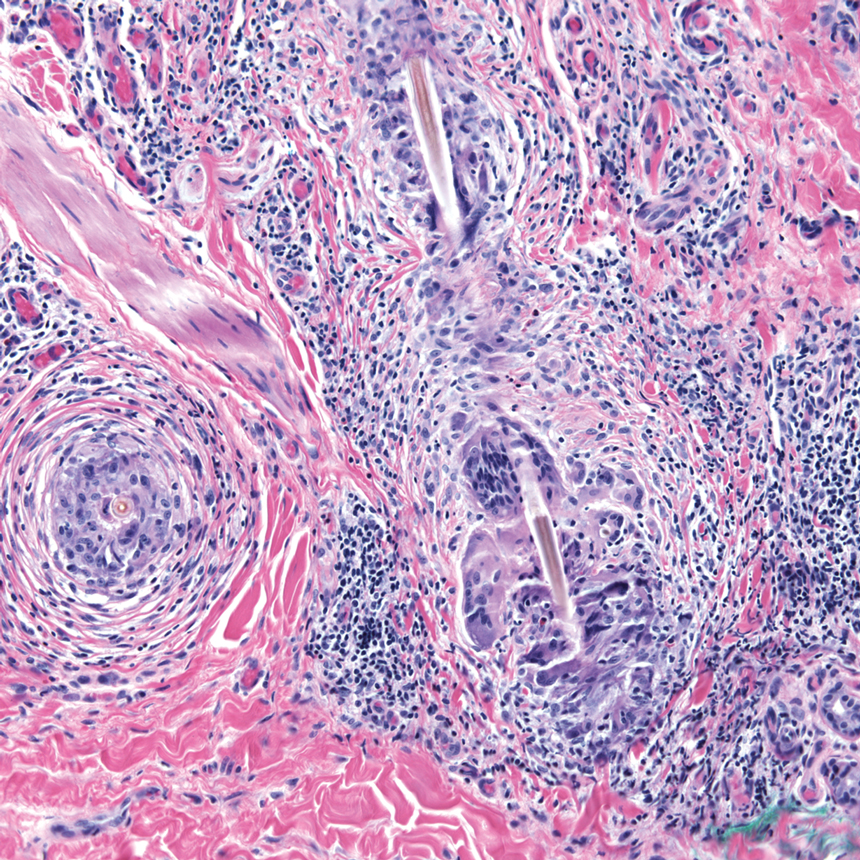
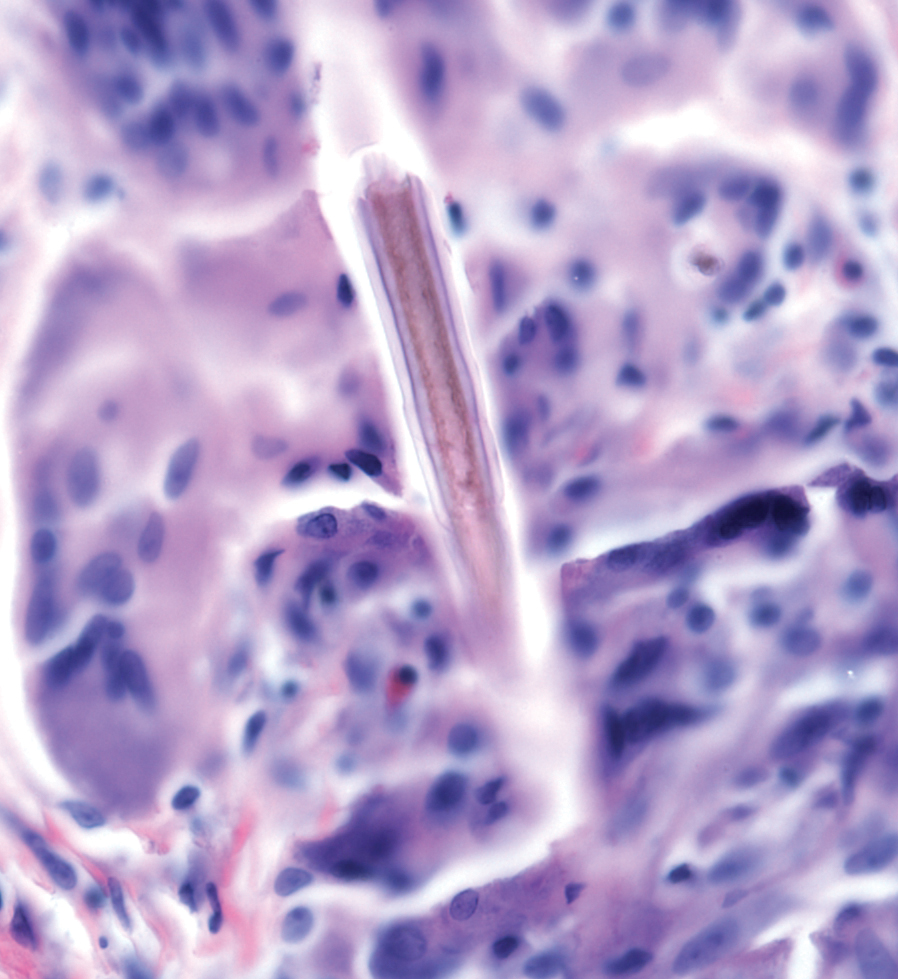
Additional complications can accompany the hypersensitivity reaction to setae or spines. Type I hypersensitivity reactions can lead to severe reactions on second contact due to previously sensitized IgE antibodies. Although the first reaction appears mild, second contact might result in angioedema, wheezing, dyspnea, or anaphylaxis, or a combination of these findings.9 In addition, some patients who come in contact with Dendrolimus caterpillars might develop a condition known as dendrolimiasis, characterized by dermatitis in addition to arthritis or chondritis.6 The arthritis is normally monoarticular and can result in complete destruction of the joint. Pararamose, a condition with a similar presentation, is caused by the Brazilian moth Premolis semirufa.6
Contact of setae or spines with mucous membranes or inhalation of setae also might result in edema, dysphagia, dyspnea, drooling, rhinitis, or conjunctivitis, or a combination of these findings.6 In addition, setae can embed in the eye and cause an inflammatory reaction—ophthalmia nodosa—most commonly caused by caterpillars of the pine processionary moth (Thaumetopoea pityocampa) and characterized by immediate chemosis, which can progress to liquefactive necrosis and hypopyon, later developing into a granulomatous foreign-body response.2,10 The process is thought to be the result of a combination of the thaumetopoein toxin in the setae and an IgE-mediated response to other proteins.10
Due to their harpoon shape and forward-only motion, setae might migrate deeper, potentially even to the optic nerve.11 Because migration might take years and the barbed shape of setae does not always allow removal, some patients require lifetime monitoring with slit-lamp examination.Chronic problems, such as cataracts and persistent posterior uveitis, have been reported.10,11
Lonomism—One of the most serious (though rarest) reactions to caterpillars is lonomism, a condition caused by the caterpillars of Lonomia achelous and Lonomia obliqua moths. These caterpillars have a unique combination of toxins filling their branched spines, which ultimately leads to the same outcome: a hemorrhagic diathesis.
The toxin of L achelous comprises several proteases that degrade fibrin, fibrinogen, and factor XIII while activating prothrombin. In contrast, L obliqua poison causes a hemorrhagic diathesis by promoting a consumptive coagulopathy through enzymes that activate factor X and prothrombin.
With initial contact with either of these Lonomia caterpillars, the patient experiences severe pain accompanied by systemic symptoms, including headache, nausea, and vomiting. Shortly afterward, symptoms of a hemorrhagic diathesis manifest, including bleeding gums, hematuria, bleeding from prior wounds, and epistaxis.5 Serious complications of the hemorrhagic diathesis, such as hemorrhage of major organs, leads to death in 4% of patients.5 A reported case of a patient whose Lonomia caterpillar sting went unrecognized until a week after the accident ended with progression to stage V chronic renal disease.12
Recent research has focused on the specific mechanism of injury caused by Lonomia species. A study found that the venom of L obliqua causes cytoskeleton rearrangement and migration in vascular smooth muscle cells (VSMCs) by inducing formation of reactive oxygen species through activation of nicotinamide adenine dinucleotide phosphate oxidase.13 Thus, the venom directly contributes to the proinflammatory phenotype of endothelial cells seen following envenomation. The same study also demonstrated that elevated reactive oxygen species trigger extracellular signal-regulated kinase pathway activation in VSMCs, leading to cell proliferation, re-stenosis, and ischemia.13 This finding was confirmed by another study,14 which demonstrated an increase in Rac1, a signaling protein involved in the extracellular signal-regulated kinase pathway, in VSMCs upon exposure to L obliqua venom. These studies propose potential new targets for treatment to prevent vascular damage.
Reactions to Adult Organisms—Although it is more common for the caterpillar form of these organisms to cause an adverse reaction, the adult moth also might be capable of causing a similar reaction by retaining setae from the cocoon or by their own spines. The most notable example of this is female moths of the genus Hylesia, which possess spines attached to glands on the abdomen. The poison in these spines—a mixture of proteases and chitinase—causes a dermatitis known as Caripito itch—the name derived from a river port in Venezuela where this moth caused a memorable epidemic of moth-induced dermatitis.7,15 Caripito itch is known for intense pruritus that most commonly lasts days or weeks, possibly longer than 1 year.
Diagnostic Difficulties
The challenge of diagnosing a caterpillar- or moth-induced reaction in humans arises from (1) the lack of clinical history (the caterpillar might not be seen at all by the patient or the examiner) and (2) the similarity of these reactions to those with more common triggers.
When setae remain embedded in the skin or mucous membranes, skin scrapings allow accelerated diagnosis. On a skin scraping prepared with 20% potassium hydroxide, setae appear as tapered and barbed hairlike structures, which allows them to be distinguished from other similar-appearing but differently shaped structures, such as glass fibers.
When setae do not remain embedded in the skin or when the cause of the reaction is due to spines, the physician is left with a nonspecific histologic picture and a large differential diagnosis to be narrowed down based on the history and occasionally the pattern of the skin lesion.
A challenge in sting diagnosis is differentiating a caterpillar or moth sting from that of another organism. In certain cases, such as those of the family Megalopygidae, specific patterns of stings might assist in making the diagnosis. Hypersensitivity reactions are associated with a wider differential diagnosis, including irritant or allergic dermatitis from other causes, scabies, eczema, lichen planus, lichen simplex chronicus, seborrheic dermatitis, and tinea corporis, to name a few.6 Skin scrapings can be examined for other features, such as burrows in the case of scabies, to further narrow the differential.
Stings and hypersensitivity reactions lacking a proper history and associated with more severe systemic symptoms have caused misdiagnosis or led to a workup for the wrong condition; for example, the picture of abdominal pain, nausea, vomiting, tachycardia, leukocytosis, hypokalemia, and metabolic acidosis can simulate appendicitis.16 Upon discovery of a puss caterpillar sting in a patient, her symptoms resolved after treatment with ondansetron, morphine, and intravenous fluids.16
In lonomism, the diagnosis must be established by laboratory measurement of the fibrinogen level, clotting factors, prothrombin time, and activated partial thromboplastin time.4 The differential diagnosis associated with lonomism includes disseminated intravascular coagulation (DIC), snakebite, and a hereditary bleeding disorder.4 The combination of laboratory tests and an extensive medical history allows a diagnosis. Absence of a personal or family history of bleeding excludes a diagnosis of hereditary bleeding disorder, whereas the absence of known causes of DIC or thrombocytopenia allows DIC to be excluded from the differential.
Treatment Options and Prevention
Treatment—The first step is to remove any embedded setae from the skin or mucous membranes. The stepwise recommendation is to remove any constricted clothing, detach setae with adhesive tape, wash with soap and water, and dry without touching the skin.1 Any remaining setae can be removed with additional tape or forceps; setae tend to be fragile and are difficult to remove in their entirety.
Other than removal of the setae, skin reactions are treated symptomatically. Ice packs and isopropyl alcohol have been utilized to cool burning or stinging areas. Pain, pruritus, and inflammation have been alleviated with antihistamines and topical corticosteroids.1 When pain is severe, oral codeine or local injection of anesthetic can be used. For severe and persistent skin lesions, a course of an oral glucocorticoid can be administered. Intramuscular triamcinolone acetonide has been shown to treat pain, dermatitis, and subcutaneous nodules otherwise refractory to treatment.8
Antivenin specific for L obliqua exists to treat lonomism and is therefore effective only when lonomism is caused by that species. Lonomism caused by L achelous is treated with cryoprecipitate, purified fibrinogen, and antifibrinolytic drugs, such as aprotinin.6 Whole blood and fresh-frozen plasma have been noted to make hemorrhage worse when utilized to treat lonomism. Because the mechanism of action of the venom of Lonomia species is based, in part, on inducing a proinflammatory profile in endothelial cells, studies have demonstrated that inhibition of kallikrein might prevent vascular injury and thus prevent serious adverse effects, such as renal failure.17
Prevention—People should wear proper protective clothing when outdoors in potentially infested areas. Measures should be taken to ensure that linens and clothing are not left outside in areas where setae might be carried on the wind. Infestation control is necessary if the population of caterpillars reaches a high enough level.
Conclusion
Several species of caterpillars and moths cause adverse reactions in humans: stings, hypersensitivity reactions, and lonomism. Although most reactions are self-limited, some might have more serious effects, including organ failure and death. Mechanisms of injury vary by species of caterpillar, moth, and butterfly; current research is focused on further defining venom components and signaling pathways to isolate potential targets to aid in the diagnosis and treatment of lepidopterism.
- Goldman BS, Bragg BN. Caterpillar and moth bites. Stat Pearls [Internet]. StatPearls Publishing. Updated August 3, 2021. Accessed November 4, 2021. https://www.ncbi.nlm.nih.gov/books/NBK539851/
- Hossler EW. Caterpillars and moths: part I. Dermatologic manifestations of encounters with Lepidoptera. J Am Acad Dermatol. 2010;62:1-10. doi:10.1016/j.jaad.2009.08.060
- Forrester MB. Megalopyge opercularis caterpillar stings reported to Texas poison centers. Wilderness Environ Med. 2018;29:215-220. doi:10.1016/j.wem.2018.02.002
- Hossler EW. Lepidopterism: skin disorders secondary to caterpillars and moths. UpToDate website. Published October 20, 2021. Accessed November 18, 2021. https://www.uptodate.com/contents/lepidopterism-skin-disorders-secondary-to-caterpillars-and-moths
- Villas-Boas IM, Bonfá G, Tambourgi DV. Venomous caterpillars: from inoculation apparatus to venom composition and envenomation. Toxicon. 2018;153:39-52. doi:10.1016/j.toxicon.2018.08.007
- Hossler EW. Caterpillars and moths: part II. dermatologic manifestations of encounters with Lepidoptera. J Am Acad Dermatol. 2010;62:13-28. doi:10.1016/j.jaad.2009.08.061
- Yao Z, Kamau PM, Han Y, et al. The Latoia consocia caterpillar induces pain by targeting nociceptive ion channel TRPV1. Toxins (Basel). 2019;11:695. doi:10.3390/toxins11120695
- Paniz-Mondolfi AE, Pérez-Alvarez AM, Lundberg U, et al. Cutaneous lepidopterism: dermatitis from contact with moths of Hylesia metabus (Cramer 1775) (Lepidoptera: Saturniidae), the causative agent of caripito itch. Int J Dermatol. 2011;50:535-541. doi:10.1111/j.1365-4632.2010.04683.x
- Santos-Magadán S, González de Olano D, Bartolomé-Zavala B, et al. Adverse reactions to the processionary caterpillar: irritant or allergic mechanism? Contact Dermatitis. 2009;60:109-110. doi:10.1111/j.1600-0536.2008.01464.x
- González-Martín-Moro J, Contreras-Martín I, Castro-Rebollo M, et al. Focal cortical cataract due to caterpillar hair migration. Clin Exp Optom. 2019;102:89-90. doi:10.1111/cxo.12809
- Singh A, Behera UC, Agrawal H. Intra-lenticular caterpillar seta in ophthalmia nodosa. Eur J Ophthalmol. 2021;31:NP109-NP111. doi:10.1177/1120672119858899
- Schmitberger PA, Fernandes TC, Santos RC, et al. Probable chronic renal failure caused by Lonomia caterpillar envenomation. J Venom Anim Toxins Incl Trop Dis. 2013;19:14. doi:10.1186/1678-9199-19-14
- Moraes JA, Rodrigues G, Nascimento-Silva V, et al. Effects of Lonomia obliqua venom on vascular smooth muscle cells: contribution of NADPH oxidase-derived reactive oxygen species. Toxins (Basel). 2017;9:360. doi:10.3390/toxins9110360
- Bernardi L, Pinto AFM, Mendes E, et al. Lonomia obliqua bristle extract modulates Rac1 activation, membrane dynamics and cell adhesion properties. Toxicon. 2019;162:32-39. doi:10.1016/j.toxicon.2019.02.019
- Cabrera G, Lundberg U, Rodríguez-Ulloa A, et al. Protein content of the Hylesia metabus egg nest setae (Cramer [1775]) (Lepidoptera: Saturniidae) and its association with the parental investment for the reproductive success and lepidopterism. J Proteomics. 2017;150:183-200. doi:10.1016/j.jprot.2016.08.010
- Greene SC, Carey JM. Puss caterpillar envenomation: erucism mimicking appendicitis in a young child. Pediatr Emerg Care. 2020;36:E732-E734. doi:10.1097/PEC.0000000000001514
- Berger M, de Moraes JA, Beys-da-Silva WO, et al. Renal and vascular effects of kallikrein inhibition in a model of Lonomia obliqua venom-induced acute kidney injury. PLoS Negl Trop Dis. 2019;13:e0007197. doi:10.1371/journal.pntd.0007197
- Goldman BS, Bragg BN. Caterpillar and moth bites. Stat Pearls [Internet]. StatPearls Publishing. Updated August 3, 2021. Accessed November 4, 2021. https://www.ncbi.nlm.nih.gov/books/NBK539851/
- Hossler EW. Caterpillars and moths: part I. Dermatologic manifestations of encounters with Lepidoptera. J Am Acad Dermatol. 2010;62:1-10. doi:10.1016/j.jaad.2009.08.060
- Forrester MB. Megalopyge opercularis caterpillar stings reported to Texas poison centers. Wilderness Environ Med. 2018;29:215-220. doi:10.1016/j.wem.2018.02.002
- Hossler EW. Lepidopterism: skin disorders secondary to caterpillars and moths. UpToDate website. Published October 20, 2021. Accessed November 18, 2021. https://www.uptodate.com/contents/lepidopterism-skin-disorders-secondary-to-caterpillars-and-moths
- Villas-Boas IM, Bonfá G, Tambourgi DV. Venomous caterpillars: from inoculation apparatus to venom composition and envenomation. Toxicon. 2018;153:39-52. doi:10.1016/j.toxicon.2018.08.007
- Hossler EW. Caterpillars and moths: part II. dermatologic manifestations of encounters with Lepidoptera. J Am Acad Dermatol. 2010;62:13-28. doi:10.1016/j.jaad.2009.08.061
- Yao Z, Kamau PM, Han Y, et al. The Latoia consocia caterpillar induces pain by targeting nociceptive ion channel TRPV1. Toxins (Basel). 2019;11:695. doi:10.3390/toxins11120695
- Paniz-Mondolfi AE, Pérez-Alvarez AM, Lundberg U, et al. Cutaneous lepidopterism: dermatitis from contact with moths of Hylesia metabus (Cramer 1775) (Lepidoptera: Saturniidae), the causative agent of caripito itch. Int J Dermatol. 2011;50:535-541. doi:10.1111/j.1365-4632.2010.04683.x
- Santos-Magadán S, González de Olano D, Bartolomé-Zavala B, et al. Adverse reactions to the processionary caterpillar: irritant or allergic mechanism? Contact Dermatitis. 2009;60:109-110. doi:10.1111/j.1600-0536.2008.01464.x
- González-Martín-Moro J, Contreras-Martín I, Castro-Rebollo M, et al. Focal cortical cataract due to caterpillar hair migration. Clin Exp Optom. 2019;102:89-90. doi:10.1111/cxo.12809
- Singh A, Behera UC, Agrawal H. Intra-lenticular caterpillar seta in ophthalmia nodosa. Eur J Ophthalmol. 2021;31:NP109-NP111. doi:10.1177/1120672119858899
- Schmitberger PA, Fernandes TC, Santos RC, et al. Probable chronic renal failure caused by Lonomia caterpillar envenomation. J Venom Anim Toxins Incl Trop Dis. 2013;19:14. doi:10.1186/1678-9199-19-14
- Moraes JA, Rodrigues G, Nascimento-Silva V, et al. Effects of Lonomia obliqua venom on vascular smooth muscle cells: contribution of NADPH oxidase-derived reactive oxygen species. Toxins (Basel). 2017;9:360. doi:10.3390/toxins9110360
- Bernardi L, Pinto AFM, Mendes E, et al. Lonomia obliqua bristle extract modulates Rac1 activation, membrane dynamics and cell adhesion properties. Toxicon. 2019;162:32-39. doi:10.1016/j.toxicon.2019.02.019
- Cabrera G, Lundberg U, Rodríguez-Ulloa A, et al. Protein content of the Hylesia metabus egg nest setae (Cramer [1775]) (Lepidoptera: Saturniidae) and its association with the parental investment for the reproductive success and lepidopterism. J Proteomics. 2017;150:183-200. doi:10.1016/j.jprot.2016.08.010
- Greene SC, Carey JM. Puss caterpillar envenomation: erucism mimicking appendicitis in a young child. Pediatr Emerg Care. 2020;36:E732-E734. doi:10.1097/PEC.0000000000001514
- Berger M, de Moraes JA, Beys-da-Silva WO, et al. Renal and vascular effects of kallikrein inhibition in a model of Lonomia obliqua venom-induced acute kidney injury. PLoS Negl Trop Dis. 2019;13:e0007197. doi:10.1371/journal.pntd.0007197
Practice Points
- Lepidopterism describes adverse reactions caused by the stings, hypersensitivity reactions, and lonomism (a hemorrhagic diathesis) of caterpillars, moths, and butterflies.
- Caterpillars can induce an adverse reaction by injecting venom stored in their bristles, inducing a foreign-body reaction to embedded bristles, or a combination of these mechanisms.
- A thorough history, skin scrapings, relevant examination of affected body parts (such as slit-lamp examination, in the case of eyes), and laboratory testing should be conducted to narrow the wide differential diagnosis associated with lepidopterism.
Diet in Wound Care: Can Nutrition Impact Healing?
Dermatologists commonly manage a variety of wounds in the outpatient setting. Wound healing requires a multifaceted approach that often includes topical and oral therapies, adjustment of mechanical factors, and behavioral and lifestyle modifications. Physiologically, wound healing requires an inflammatory phase, a proliferative phase, and a remodeling phase. Chronic wounds undergo a prolonged inflammatory response hindered by decreased growth factors and increased wound bioburden.1 Malnutrition has been routinely associated with wound chronicity and serves as a modifiable risk factor that may improve wound healing outcomes.2
Although the causes of wounds encountered in dermatology vary extensively, the importance of nutrition underlies all wound healing. Caloric needs in wound healing have been estimated at 30 to 40 kcal/kg dependent on baseline body weight, age, medical comorbidities, activity level, stage of wound healing, wound size, and number of wounds.1,3,4 Nutritional supplementation is patient dependent, but this article serves to review the existing literature on macronutrient and micronutrient supplementation to clarify the potentially complementary role for nutritional support in chronic wounds. All patients should be screened with a thorough history, review of systems, and physical examination for existing nutrient deficiencies. Patients with age-related or chronic diseases are at increased risk for nutritional deficiency, and focused laboratory testing may be warranted. Supplementation for specific deficiencies with help from a registered dietician is recommended.
Macronutrients for Wound Healing
Protein—Protein is the most widely known macronutrient required for wound healing. The primary function of dietary protein is to provide amino acids to perform physiologic functions.5 Not only does cutaneous injury increase the metabolic needs of the wounded area, but large amounts of protein can be continually lost through wound exudates. Protein is necessary for the immune response required to transition from inflammatory to proliferative phases of wound healing.6 Protein energy deficiency has been reported to reduce fibroblast activity, delay angiogenesis, and decrease collagen formation.7 Additionally, protein is required for the formation of inflammatory cells and maintenance of oncotic pressure, specifically in venous insufficiency wounds.1
The current recommended dietary allowance for protein in healthy adults is 0.8 g/kg daily of body weight. In patients with pressure ulcerations, a goal recommended dietary allowance of 1.25 to 2.0 g/kg daily of body weight, dependent on ulceration size, has been recommended by the National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel.8 This recommendation was based on a series of studies that reported enhanced healing rates in patients with pressure ulcers receiving higher-protein diets.9 The largest study to date was double-blinded and included 89 residents of long-term care facilities with stage II to stage IV pressure ulcers.10 Participants were randomized to receive commercial protein supplementation vs placebo. At the end of 8 weeks, a statistically significant difference was seen in mean (SD) pressure ulcer scale for healing scores (3.55 [4.66] vs 3.22 [4.11]; P<.05).10 A 2014 Cochrane review failed to identify benefit associated with nutritional interventions for either the prevention and/or treatment of pressure ulcers.11 Specific recommendations on protein intake for other types of chronic wounds have not been proposed. Protein supplementation generally is provided orally, if tolerated. Liquid supplements such as Boost (Nestlé), Carnation Breakfast Essentials (Nestlé), NuBasics (SupremeMed), Resource (Nestlé Health Science), and Ensure (Abbott Laboratories) are frequently used to supplement both protein and caloric intake. Protein oversupplementation has not been associated with improved outcomes and may cause or exacerbate other medical comorbidities.
Fatty Acids for Wound Healing
Wound healing is an anabolic process that requires adequate intake of substrates such as glucose and fat. Carbohydrates serve as the major energy source required for wound healing, while fats are thought to play roles in cell membrane development and modulation of cellular signaling.1 Fats utilize a unique pathway for energy production through beta-oxidation and the production of adenosine triphosphate, allowing available protein to be harnessed for wound healing.1 Omega-3 and omega-6 fatty acids serve as precursors to prostaglandins, leukotrienes, and thromboxane—all key mediators of the inflammatory phase of wound healing.3 Omega-3 fatty acids are thought to downregulate genes involved in proinflammatory pathways,12 as well as to diminish lymphocyte proliferation and levels of IL-1β, tumor necrosis factor α, and IL-6 in vitro.13 In vivo studies assessing the impact of omega-3 fatty acid supplementation on wound healing are minimal, and the role of dietary supplementation for this indication remains unknown. Fish oil contains the omega-3 fatty acid–rich eicosapentaenoic acid and docosahexaenoic acid, which has been compared to mineral oil supplementation for wound healing in healthy adults. When fish oil was supplemented for 4 weeks, no significant differences were identified in time to complete wound healing between groups. Interestingly, significantly higher levels of the proinflammatory cytokine IL-1β were identified in blister fluid at 24 hours after blistering vs the placebo group (t=2.52, df=25, P<.05).14 Prior studies evaluating wound healing in animal models similarly identified longer times to re-epithelialization after omega-3 polyunsaturated fatty acid supplementation orally and topically.15,16 The fatty acid quality and composition consumed also may impact wound healing, as high-fat diets that are not rich in omega-3 fatty acids have been shown to promote inflammation and impair wound healing in rats, but this has not been thoroughly explored in human trials.17 Although adequate intake of these macronutrients is important, excessive intake may be harmful. Larger prospective trials are needed to shed light on the dose and composition of fatty acid supplementation that may optimize wound healing.
Vitamins and Micronutrients Required for Wound Healing
Vitamin A—Many vitamins serve as cofactors for the enzymatic processes required in wound healing. Vitamin A is an essential fat-soluble vitamin that serves a variety of dermatologic functions and promotes wound healing through stimulation of fibroblasts and ground substance, and it facilitates epithelial cell differentiation when applied topically.3,18 Vitamin A works through the activation of retinoid receptors on endothelial cells, fibroblasts, keratinocytes, melanocytes, and sebocytes, and has purported anti-inflammatory effects that aid the healing of open wounds.3 Additionally, vitamin A is thought to enhance cytokine release in the inflammatory phase of wound healing.19 Supplemental vitamin A has been associated with positive effects on acute wound healing, burns, and radiation injuries.3 The utility of vitamin A supplementation in chronic wounds remains unknown; however, it has been shown to be beneficial in patients with inflammatory disease, such as rheumatoid arthritis, on corticosteroid therapy. Vitamin A supplementation in this population has been shown to counteract the negative effects of corticosteroids on wound healing via downregulation of transforming growth factor β and insulinlike growth factor 1.20 Vitamin A deficiency has been associated with impaired progression through inflammatory and remodeling phases of healing due to altered B-cell and T-cell function and antibody production.1 Some experts recommend short courses of oral vitamin A supplementation to enhance wound healing at doses between 10,000 and 25,000 IU daily.2,3 Large, population-based studies are needed, and the safety supporting this recommendation in all patients remains unknown.
Vitamin C—Vitamin C is widely known for its role in collagen formation, immunomodulation, and antioxidant capacity.1 Although vitamin C deficiency is associated with decreased collagen synthesis and impaired wound healing,21 the utility of long-term supplementation in patients who are not deficient remains unexplored. A systematic review evaluating interventional studies utilizing vitamin C supplementation on pressure ulcerations and surgical wound healing concluded that convincing evidence exists only for supplementation with at least 500 mg of vitamin C. The authors noted, “There is little evidence for improved healing of surgical wounds by high-dose single vitamin C supplementation (1–3 g/day).”22 In a prospective, randomized, controlled trial, 20 patients with pressure ulcerations were supplemented with vitamin C vs placebo with a mean reduction in pressure-sore area of 84% after 1 month in the vitamin C–supplemented group compared to 42.7% in the placebo group (P<.005). A limitation of this study is the small population.23 One current recommendation for vitamin C supplementation in chronic wounds is for 500 mg daily in uncomplicated wounds to 2 g daily in severe wounds.3 Additional studies have suggested that the benefits of vitamin C supplementation are maximized when given in combination with zinc and arginine.22 At this time, evaluation for vitamin C deficiency and appropriate supplementation in patients with chronic wounds is needed.
Zinc—Minerals similarly play important roles in enzymatic regulation. Hundreds of zinc-containing enzymes are involved in wound healing and are required in tissue repair, growth, antioxidant capacity, and immune function.1,24 Zinc is specifically critical to collagen, DNA, RNA, and protein synthesis, as well as cellular proliferation.4 Zinc deficiency has been encountered in the setting of chronic wounds with extensive drainage, decreased dietary intake, or excessive gastrointestinal losses.25 Although many studies exist evaluating the utility of zinc supplementation on wound healing, many are confounded by multinutrient supplementation. No studies to date support zinc supplementation when zinc deficiency is absent. Patient assessment for medications or conditions that may impact zinc metabolism should be completed. Importantly, zinc supplementation can interfere with the absorption of other cations, so excessive supplementation should be avoided.1
Amino Acids for Wound Healing
Arginine—Arginine is an essential amino acid that serves as a substrate for cellular proliferation, collagen deposition, and lymphocyte function.8,26,27 Arginine serves as the biologic precursor for nitric oxide (NO), a substrate that has important wound healing properties. Nitric oxide metabolites have been shown to positively regulate wound repair while NO metabolites are reduced in wound environments in diabetic ulcerations.28,29 Arginine also is a proline precursor, an essential building block for collagen synthesis,6,30 and a stimulator of growth hormone and T cells.30,31 Animal studies have suggested L-arginine supplementation may reverse impaired NO synthesis in diabetic wounds.28 A single randomized trial assessing differing doses of arginine supplementation on stage II or stage IV pressure ulcers noted an almost two-fold improvement in healing time.32 However, human studies have not shown increased rates of re-epithelialization of skin graft donor sites when provided oral or parenteral arginine supplementation.33 Inadequate data currently exist to support regular arginine supplementation for all types of wounds, and no safe dose of daily arginine intake has been established.
Glutamine—Similarly, glutamine supplementation has been proposed to accelerate wound healing due to its role as a primary metabolic fuel source for rapidly proliferating cells such as epithelial cells and fibroblasts.8 Glutamine is thought to induce expression of heat-shock proteins and protect against inflammatory and infectious wound complications.34 Additionally, glutamine is thought to increase tissue insulin sensitivity, which may prove beneficial in wounds, as topical insulin previously has been shown in animal and human models to promote healing.35 Glutamine is thought to play a role in the inflammatory phase of wound healing via superoxide production, leukocyte apoptosis, and phagocytosis.6,34,36 Unfortunately, numerous randomized trials on glutamine supplementation have resulted in conflicting evidence confounded by multisupplementation within the same trial.37,38 A double-blind, randomized, controlled trial of 270 participants assessed the effect of oral supplementation with arginine, glutamine, or β-hydroxy-β-methylbutyrate vs control in the healing time of diabetic foot ulcerations. Significant differences in wound closure time at week 16 were only identified in participants with low albumin levels (≤40 g/L) who were supplemented (50.8%) vs the control group (34.9%; P=.0325) and in those with poor limb perfusion (ankle-brachial index of <1.0) who were supplemented (60.3%) vs the control group (39.3%; P=.0079).39 Ongoing clinical trials evaluating the effects of glutamine supplementation on differing wound types will hopefully shed light on the efficacy of supplementation.
Final Thoughts
Wound healing is multifactorial and should consider the health status and medical comorbidities of each patient treated. We propose an individualized approach to wound healing that includes exploration of specific macronutrient and micronutrient deficiencies, as malnutrition has been associated with wound chronicity and serves as a modifiable risk factor to improve healing.2 The evidence backing specific nutrient supplementation in patients with deficiencies is strong and should be considered in patients with chronic wounds. Adequate caloric intake and protein content should be recommended for most wound patients; however, excessive protein intake has not been beneficial in wound healing. The data behind specific amino acid and vitamin supplementation are limited at this time. As with other therapeutics, there is likely an appropriate dose for supplementation that has not yet been elucidated. Consideration of wound type, size, depth, exudate, and underlying cause are important to optimize healing and tailor nutritional supplementation to each patient. We hope future studies will illuminate the complementary role of dietary intake and nutrient supplementation for the treatment of chronic nonhealing wounds.
- Quain AM, Khardori NM. Nutrition in wound care management: a comprehensive overview. Wounds. 2015;27:327-335.
- Stechmiller JK. Understanding the role of nutrition and wound healing. Nutr Clin Pract. 2010;25:61-68. doi:10.1177/0884533609358997
- Molnar JA, Underdown MJ, Clark WA. Nutrition and chronic wounds. Adv Wound Care (New Rochelle). 2014;3:663-681. doi:10.1089/wound.2014.0530
- Dorner B, Posthauer ME, Thomas D; Panel NPUA. The role of nutrition in pressure ulcer prevention and treatment: National Pressure Ulcer Advisory Panel white paper. Adv Skin Wound Care. 2009;22:212-221. doi:10.1097/01.ASW.0000350838.11854.0a
- Collins N. Protein and wound healing. Adv Skin Wound Care. 2001;14:288-289. doi:10.1097/00129334-200111000-00008
- Barchitta M, Maugeri A, Favara G, et al. Nutrition and wound healing: an overview focusing on the beneficial effects of curcumin [published online March 5, 2019]. Int J Mol Sci. doi:10.3390/ijms20051119
- Harris CL, Fraser C. Malnutrition in the institutionalized elderly: the effects on wound healing. Ostomy Wound Manage. 2004;50:54-63.
- Saghaleini SH, Dehghan K, Shadvar K, et al. Pressure ulcer and nutrition. Indian J Crit Care Med. 2018;22:283-289. doi:10.4103/ijccm.IJCCM_277_17
- Breslow RA, Hallfrisch J, Guy DG, et al. The importance of dietary protein in healing pressure ulcers. J Am Geriatr Soc. 1993;41:357-362. doi:10.1111/j.1532-5415.1993.tb06940.x
- Lee SK, Posthauer ME, Dorner B, et al. Pressure ulcer healing with a concentrated, fortified, collagen protein hydrolysate supplement: a randomized controlled trial. Adv Skin Wound Care. 2006;19:92-96. doi:10.1097/00129334-200603000-00011
- Langer G, Fink A. Nutritional interventions for preventing and treating pressure ulcers. Cochrane Database Syst Rev. 2014;6:CD003216. doi:10.1002/14651858.CD003216.pub2
- Bouwens M, van de Rest O, Dellschaft N, et al. Fish-oil supplementation induces antiinflammatory gene expression profiles in human blood mononuclear cells. Am J Clin Nutr. 2009;90:415-424. doi:10.3945/ajcn.2009.27680
- Meydani SN, Endres S, Woods MM, et al. Oral (n-3) fatty acid supplementation suppresses cytokine production and lymphocyte proliferation: comparison between young and older women. J Nutr. 1991;121:547-555. doi:10.1093/jn/121.4.547
- McDaniel JC, Belury M, Ahijevych K, et al. Omega-3 fatty acids effect on wound healing. Wound Repair Regen. 2008;16:337-345. doi:10.1111/j.1524-475X.2008.00388.x
- Mooney MA, Vaughn DM, Reinhart GA, et al. Evaluation of the effects of omega-3 fatty acid-containing diets on the inflammatory stage of wound healing in dogs. Am J Vet Res. 1998;59:859-863.
- Cardoso CR, Souza MA, Ferro EA, et al. Influence of topical administration of n-3 and n-6 essential and n-9 nonessential fatty acids on the healing of cutaneous wounds. Wound Repair Regen. 2004;12:235-243. doi:10.1111/j.1067-1927.2004.012216.x
- Rosa DF, Sarandy MM, Novaes RD, et al. High-fat diet and alcohol intake promotes inflammation and impairs skin wound healing in Wistar rats. Mediators Inflamm. 2018;2018:4658583. doi:10.1155/2018/4658583
- Levenson SM, Gruber CA, Rettura G, et al. Supplemental vitamin A prevents the acute radiation-induced defect in wound healing. Ann Surg. 1984;200:494-512. doi:10.1097/00000658-198410000-00011
- Palmieri B, Vadalà M, Laurino C. Nutrition in wound healing: investigation of the molecular mechanisms, a narrative review. J Wound Care. 2019;28:683-693. doi:10.12968/jowc.2019.28.10.683
- Ehrlich HP, Hunt TK. Effects of cortisone and vitamin A on wound healing. Ann Surg. 1968;167:324-328. doi:10.1097/00000658-196803000-00004
- Pullar JM, Carr AC, Vissers MCM. The roles of vitamin C in skin health [published online August 12, 2017]. Nutrients. doi:10.3390/nu9080866
- Ellinger S, Stehle P. Efficacy of vitamin supplementation in situations with wound healing disorders: results from clinical intervention studies. Curr Opin Clin Nutr Metab Care. 2009;12:588-595. doi:10.1097/MCO.0b013e328331a5b5
- Taylor TV, Rimmer S, Day B, et al. Ascorbic acid supplementation in the treatment of pressure-sores. Lancet. 1974;2:544-546. doi:10.1016/s0140-6736(74)91874-1
- Ibs KH, Rink L. Zinc-altered immune function. J Nutr. 2003;133(5 suppl 1):1452S-1456S. doi:10.1093/jn/133.5.1452S
- Hoffman M, Micheletti RG, Shields BE. Nutritional dermatoses in the hospitalized patient. Cutis. 2020;105:296-302, 308, E1-E5.
- Chow O, Barbul A. Immunonutrition: role in wound healing and tissue regeneration. Adv Wound Care (New Rochelle). 2014;3:46-53. doi:10.1089/wound.2012.0415
- Singh K, Coburn LA, Barry DP, et al. L-arginine uptake by cationic amino acid transporter 2 is essential for colonic epithelial cell restitution. Am J Physiol Gastrointest Liver Physiol. 2012;302:G1061-G1073. doi:10.1152/ajpgi.00544.2011
- Witte MB, Thornton FJ, Tantry U, et al. L-Arginine supplementation enhances diabetic wound healing: involvement of the nitric oxide synthase and arginase pathways. Metabolism. 2002;51:1269-1273. doi:10.1053/meta.2002.35185
- Witte MB, Barbul A. Role of nitric oxide in wound repair. Am J Surg. 2002;183:406-412. doi:10.1016/s0002-9610(02)00815-2
- Barbul A. Proline precursors to sustain Mammalian collagen synthesis. J Nutr. 2008;138:2021S-2024S. doi:10.1093/jn/138.10.2021S
- Wu G, Bazer FW, Davis TA, et al. Arginine metabolism and nutrition in growth, health and disease. Amino Acids. 2009;37:153-168. doi:10.1007/s00726-008-0210-y
- Leigh B, Desneves K, Rafferty J, et al. The effect of different doses of an arginine-containing supplement on the healing of pressure ulcers. J Wound Care. 2012;21:150-156. doi:10.12968/jowc.2012.21.3.150
- Debats IB, Koeneman MM, Booi DI, et al. Intravenous arginine and human skin graft donor site healing: a randomized controlled trial. Burns. 2011;37:420-426. doi:10.1016/j.burns.2010.06.003
- Wischmeyer PE. Glutamine and heat shock protein expression. Nutrition. 2002;18:225-228. doi:10.1016/s0899-9007(01)00796-1
- Wang J, Xu J. Effects of topical insulin on wound healing: a review of animal and human evidences. Diabetes Metab Syndr Obes. 2020;13:719-727. doi:10.2147/DMSO.S237294
- Newsholme P. Why is L-glutamine metabolism important to cells of the immune system in health, postinjury, surgery or infection?J Nutr. 2001;131(9 suppl):2515S-2522S; discussion 2523S-2524S. doi:10.1093/jn/131.9.2515S
- Aquino VM, Harvey AR, Garvin JH, et al. A double-blind randomized placebo-controlled study of oral glutamine in the prevention of mucositis in children undergoing hematopoietic stem cell transplantation: a pediatric blood and marrow transplant consortium study. Bone Marrow Transplant. 2005;36:611-616. doi:10.1038/sj.bmt.1705084
- Ward E, Smith M, Henderson M, et al. The effect of high-dose enteral glutamine on the incidence and severity of mucositis in paediatric oncology patients. Eur J Clin Nutr. 2009;63:134-140. doi:10.1038/sj.ejcn.1602894
- Armstrong DG, Hanft JR, Driver VR, et al. Effect of oral nutritional supplementation on wound healing in diabetic foot ulcers: a prospective randomized controlled trial. Diabet Med. 2014;31:1069-1077. doi:10.1111/dme.12509
Dermatologists commonly manage a variety of wounds in the outpatient setting. Wound healing requires a multifaceted approach that often includes topical and oral therapies, adjustment of mechanical factors, and behavioral and lifestyle modifications. Physiologically, wound healing requires an inflammatory phase, a proliferative phase, and a remodeling phase. Chronic wounds undergo a prolonged inflammatory response hindered by decreased growth factors and increased wound bioburden.1 Malnutrition has been routinely associated with wound chronicity and serves as a modifiable risk factor that may improve wound healing outcomes.2
Although the causes of wounds encountered in dermatology vary extensively, the importance of nutrition underlies all wound healing. Caloric needs in wound healing have been estimated at 30 to 40 kcal/kg dependent on baseline body weight, age, medical comorbidities, activity level, stage of wound healing, wound size, and number of wounds.1,3,4 Nutritional supplementation is patient dependent, but this article serves to review the existing literature on macronutrient and micronutrient supplementation to clarify the potentially complementary role for nutritional support in chronic wounds. All patients should be screened with a thorough history, review of systems, and physical examination for existing nutrient deficiencies. Patients with age-related or chronic diseases are at increased risk for nutritional deficiency, and focused laboratory testing may be warranted. Supplementation for specific deficiencies with help from a registered dietician is recommended.
Macronutrients for Wound Healing
Protein—Protein is the most widely known macronutrient required for wound healing. The primary function of dietary protein is to provide amino acids to perform physiologic functions.5 Not only does cutaneous injury increase the metabolic needs of the wounded area, but large amounts of protein can be continually lost through wound exudates. Protein is necessary for the immune response required to transition from inflammatory to proliferative phases of wound healing.6 Protein energy deficiency has been reported to reduce fibroblast activity, delay angiogenesis, and decrease collagen formation.7 Additionally, protein is required for the formation of inflammatory cells and maintenance of oncotic pressure, specifically in venous insufficiency wounds.1
The current recommended dietary allowance for protein in healthy adults is 0.8 g/kg daily of body weight. In patients with pressure ulcerations, a goal recommended dietary allowance of 1.25 to 2.0 g/kg daily of body weight, dependent on ulceration size, has been recommended by the National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel.8 This recommendation was based on a series of studies that reported enhanced healing rates in patients with pressure ulcers receiving higher-protein diets.9 The largest study to date was double-blinded and included 89 residents of long-term care facilities with stage II to stage IV pressure ulcers.10 Participants were randomized to receive commercial protein supplementation vs placebo. At the end of 8 weeks, a statistically significant difference was seen in mean (SD) pressure ulcer scale for healing scores (3.55 [4.66] vs 3.22 [4.11]; P<.05).10 A 2014 Cochrane review failed to identify benefit associated with nutritional interventions for either the prevention and/or treatment of pressure ulcers.11 Specific recommendations on protein intake for other types of chronic wounds have not been proposed. Protein supplementation generally is provided orally, if tolerated. Liquid supplements such as Boost (Nestlé), Carnation Breakfast Essentials (Nestlé), NuBasics (SupremeMed), Resource (Nestlé Health Science), and Ensure (Abbott Laboratories) are frequently used to supplement both protein and caloric intake. Protein oversupplementation has not been associated with improved outcomes and may cause or exacerbate other medical comorbidities.
Fatty Acids for Wound Healing
Wound healing is an anabolic process that requires adequate intake of substrates such as glucose and fat. Carbohydrates serve as the major energy source required for wound healing, while fats are thought to play roles in cell membrane development and modulation of cellular signaling.1 Fats utilize a unique pathway for energy production through beta-oxidation and the production of adenosine triphosphate, allowing available protein to be harnessed for wound healing.1 Omega-3 and omega-6 fatty acids serve as precursors to prostaglandins, leukotrienes, and thromboxane—all key mediators of the inflammatory phase of wound healing.3 Omega-3 fatty acids are thought to downregulate genes involved in proinflammatory pathways,12 as well as to diminish lymphocyte proliferation and levels of IL-1β, tumor necrosis factor α, and IL-6 in vitro.13 In vivo studies assessing the impact of omega-3 fatty acid supplementation on wound healing are minimal, and the role of dietary supplementation for this indication remains unknown. Fish oil contains the omega-3 fatty acid–rich eicosapentaenoic acid and docosahexaenoic acid, which has been compared to mineral oil supplementation for wound healing in healthy adults. When fish oil was supplemented for 4 weeks, no significant differences were identified in time to complete wound healing between groups. Interestingly, significantly higher levels of the proinflammatory cytokine IL-1β were identified in blister fluid at 24 hours after blistering vs the placebo group (t=2.52, df=25, P<.05).14 Prior studies evaluating wound healing in animal models similarly identified longer times to re-epithelialization after omega-3 polyunsaturated fatty acid supplementation orally and topically.15,16 The fatty acid quality and composition consumed also may impact wound healing, as high-fat diets that are not rich in omega-3 fatty acids have been shown to promote inflammation and impair wound healing in rats, but this has not been thoroughly explored in human trials.17 Although adequate intake of these macronutrients is important, excessive intake may be harmful. Larger prospective trials are needed to shed light on the dose and composition of fatty acid supplementation that may optimize wound healing.
Vitamins and Micronutrients Required for Wound Healing
Vitamin A—Many vitamins serve as cofactors for the enzymatic processes required in wound healing. Vitamin A is an essential fat-soluble vitamin that serves a variety of dermatologic functions and promotes wound healing through stimulation of fibroblasts and ground substance, and it facilitates epithelial cell differentiation when applied topically.3,18 Vitamin A works through the activation of retinoid receptors on endothelial cells, fibroblasts, keratinocytes, melanocytes, and sebocytes, and has purported anti-inflammatory effects that aid the healing of open wounds.3 Additionally, vitamin A is thought to enhance cytokine release in the inflammatory phase of wound healing.19 Supplemental vitamin A has been associated with positive effects on acute wound healing, burns, and radiation injuries.3 The utility of vitamin A supplementation in chronic wounds remains unknown; however, it has been shown to be beneficial in patients with inflammatory disease, such as rheumatoid arthritis, on corticosteroid therapy. Vitamin A supplementation in this population has been shown to counteract the negative effects of corticosteroids on wound healing via downregulation of transforming growth factor β and insulinlike growth factor 1.20 Vitamin A deficiency has been associated with impaired progression through inflammatory and remodeling phases of healing due to altered B-cell and T-cell function and antibody production.1 Some experts recommend short courses of oral vitamin A supplementation to enhance wound healing at doses between 10,000 and 25,000 IU daily.2,3 Large, population-based studies are needed, and the safety supporting this recommendation in all patients remains unknown.
Vitamin C—Vitamin C is widely known for its role in collagen formation, immunomodulation, and antioxidant capacity.1 Although vitamin C deficiency is associated with decreased collagen synthesis and impaired wound healing,21 the utility of long-term supplementation in patients who are not deficient remains unexplored. A systematic review evaluating interventional studies utilizing vitamin C supplementation on pressure ulcerations and surgical wound healing concluded that convincing evidence exists only for supplementation with at least 500 mg of vitamin C. The authors noted, “There is little evidence for improved healing of surgical wounds by high-dose single vitamin C supplementation (1–3 g/day).”22 In a prospective, randomized, controlled trial, 20 patients with pressure ulcerations were supplemented with vitamin C vs placebo with a mean reduction in pressure-sore area of 84% after 1 month in the vitamin C–supplemented group compared to 42.7% in the placebo group (P<.005). A limitation of this study is the small population.23 One current recommendation for vitamin C supplementation in chronic wounds is for 500 mg daily in uncomplicated wounds to 2 g daily in severe wounds.3 Additional studies have suggested that the benefits of vitamin C supplementation are maximized when given in combination with zinc and arginine.22 At this time, evaluation for vitamin C deficiency and appropriate supplementation in patients with chronic wounds is needed.
Zinc—Minerals similarly play important roles in enzymatic regulation. Hundreds of zinc-containing enzymes are involved in wound healing and are required in tissue repair, growth, antioxidant capacity, and immune function.1,24 Zinc is specifically critical to collagen, DNA, RNA, and protein synthesis, as well as cellular proliferation.4 Zinc deficiency has been encountered in the setting of chronic wounds with extensive drainage, decreased dietary intake, or excessive gastrointestinal losses.25 Although many studies exist evaluating the utility of zinc supplementation on wound healing, many are confounded by multinutrient supplementation. No studies to date support zinc supplementation when zinc deficiency is absent. Patient assessment for medications or conditions that may impact zinc metabolism should be completed. Importantly, zinc supplementation can interfere with the absorption of other cations, so excessive supplementation should be avoided.1
Amino Acids for Wound Healing
Arginine—Arginine is an essential amino acid that serves as a substrate for cellular proliferation, collagen deposition, and lymphocyte function.8,26,27 Arginine serves as the biologic precursor for nitric oxide (NO), a substrate that has important wound healing properties. Nitric oxide metabolites have been shown to positively regulate wound repair while NO metabolites are reduced in wound environments in diabetic ulcerations.28,29 Arginine also is a proline precursor, an essential building block for collagen synthesis,6,30 and a stimulator of growth hormone and T cells.30,31 Animal studies have suggested L-arginine supplementation may reverse impaired NO synthesis in diabetic wounds.28 A single randomized trial assessing differing doses of arginine supplementation on stage II or stage IV pressure ulcers noted an almost two-fold improvement in healing time.32 However, human studies have not shown increased rates of re-epithelialization of skin graft donor sites when provided oral or parenteral arginine supplementation.33 Inadequate data currently exist to support regular arginine supplementation for all types of wounds, and no safe dose of daily arginine intake has been established.
Glutamine—Similarly, glutamine supplementation has been proposed to accelerate wound healing due to its role as a primary metabolic fuel source for rapidly proliferating cells such as epithelial cells and fibroblasts.8 Glutamine is thought to induce expression of heat-shock proteins and protect against inflammatory and infectious wound complications.34 Additionally, glutamine is thought to increase tissue insulin sensitivity, which may prove beneficial in wounds, as topical insulin previously has been shown in animal and human models to promote healing.35 Glutamine is thought to play a role in the inflammatory phase of wound healing via superoxide production, leukocyte apoptosis, and phagocytosis.6,34,36 Unfortunately, numerous randomized trials on glutamine supplementation have resulted in conflicting evidence confounded by multisupplementation within the same trial.37,38 A double-blind, randomized, controlled trial of 270 participants assessed the effect of oral supplementation with arginine, glutamine, or β-hydroxy-β-methylbutyrate vs control in the healing time of diabetic foot ulcerations. Significant differences in wound closure time at week 16 were only identified in participants with low albumin levels (≤40 g/L) who were supplemented (50.8%) vs the control group (34.9%; P=.0325) and in those with poor limb perfusion (ankle-brachial index of <1.0) who were supplemented (60.3%) vs the control group (39.3%; P=.0079).39 Ongoing clinical trials evaluating the effects of glutamine supplementation on differing wound types will hopefully shed light on the efficacy of supplementation.
Final Thoughts
Wound healing is multifactorial and should consider the health status and medical comorbidities of each patient treated. We propose an individualized approach to wound healing that includes exploration of specific macronutrient and micronutrient deficiencies, as malnutrition has been associated with wound chronicity and serves as a modifiable risk factor to improve healing.2 The evidence backing specific nutrient supplementation in patients with deficiencies is strong and should be considered in patients with chronic wounds. Adequate caloric intake and protein content should be recommended for most wound patients; however, excessive protein intake has not been beneficial in wound healing. The data behind specific amino acid and vitamin supplementation are limited at this time. As with other therapeutics, there is likely an appropriate dose for supplementation that has not yet been elucidated. Consideration of wound type, size, depth, exudate, and underlying cause are important to optimize healing and tailor nutritional supplementation to each patient. We hope future studies will illuminate the complementary role of dietary intake and nutrient supplementation for the treatment of chronic nonhealing wounds.
Dermatologists commonly manage a variety of wounds in the outpatient setting. Wound healing requires a multifaceted approach that often includes topical and oral therapies, adjustment of mechanical factors, and behavioral and lifestyle modifications. Physiologically, wound healing requires an inflammatory phase, a proliferative phase, and a remodeling phase. Chronic wounds undergo a prolonged inflammatory response hindered by decreased growth factors and increased wound bioburden.1 Malnutrition has been routinely associated with wound chronicity and serves as a modifiable risk factor that may improve wound healing outcomes.2
Although the causes of wounds encountered in dermatology vary extensively, the importance of nutrition underlies all wound healing. Caloric needs in wound healing have been estimated at 30 to 40 kcal/kg dependent on baseline body weight, age, medical comorbidities, activity level, stage of wound healing, wound size, and number of wounds.1,3,4 Nutritional supplementation is patient dependent, but this article serves to review the existing literature on macronutrient and micronutrient supplementation to clarify the potentially complementary role for nutritional support in chronic wounds. All patients should be screened with a thorough history, review of systems, and physical examination for existing nutrient deficiencies. Patients with age-related or chronic diseases are at increased risk for nutritional deficiency, and focused laboratory testing may be warranted. Supplementation for specific deficiencies with help from a registered dietician is recommended.
Macronutrients for Wound Healing
Protein—Protein is the most widely known macronutrient required for wound healing. The primary function of dietary protein is to provide amino acids to perform physiologic functions.5 Not only does cutaneous injury increase the metabolic needs of the wounded area, but large amounts of protein can be continually lost through wound exudates. Protein is necessary for the immune response required to transition from inflammatory to proliferative phases of wound healing.6 Protein energy deficiency has been reported to reduce fibroblast activity, delay angiogenesis, and decrease collagen formation.7 Additionally, protein is required for the formation of inflammatory cells and maintenance of oncotic pressure, specifically in venous insufficiency wounds.1
The current recommended dietary allowance for protein in healthy adults is 0.8 g/kg daily of body weight. In patients with pressure ulcerations, a goal recommended dietary allowance of 1.25 to 2.0 g/kg daily of body weight, dependent on ulceration size, has been recommended by the National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel.8 This recommendation was based on a series of studies that reported enhanced healing rates in patients with pressure ulcers receiving higher-protein diets.9 The largest study to date was double-blinded and included 89 residents of long-term care facilities with stage II to stage IV pressure ulcers.10 Participants were randomized to receive commercial protein supplementation vs placebo. At the end of 8 weeks, a statistically significant difference was seen in mean (SD) pressure ulcer scale for healing scores (3.55 [4.66] vs 3.22 [4.11]; P<.05).10 A 2014 Cochrane review failed to identify benefit associated with nutritional interventions for either the prevention and/or treatment of pressure ulcers.11 Specific recommendations on protein intake for other types of chronic wounds have not been proposed. Protein supplementation generally is provided orally, if tolerated. Liquid supplements such as Boost (Nestlé), Carnation Breakfast Essentials (Nestlé), NuBasics (SupremeMed), Resource (Nestlé Health Science), and Ensure (Abbott Laboratories) are frequently used to supplement both protein and caloric intake. Protein oversupplementation has not been associated with improved outcomes and may cause or exacerbate other medical comorbidities.
Fatty Acids for Wound Healing
Wound healing is an anabolic process that requires adequate intake of substrates such as glucose and fat. Carbohydrates serve as the major energy source required for wound healing, while fats are thought to play roles in cell membrane development and modulation of cellular signaling.1 Fats utilize a unique pathway for energy production through beta-oxidation and the production of adenosine triphosphate, allowing available protein to be harnessed for wound healing.1 Omega-3 and omega-6 fatty acids serve as precursors to prostaglandins, leukotrienes, and thromboxane—all key mediators of the inflammatory phase of wound healing.3 Omega-3 fatty acids are thought to downregulate genes involved in proinflammatory pathways,12 as well as to diminish lymphocyte proliferation and levels of IL-1β, tumor necrosis factor α, and IL-6 in vitro.13 In vivo studies assessing the impact of omega-3 fatty acid supplementation on wound healing are minimal, and the role of dietary supplementation for this indication remains unknown. Fish oil contains the omega-3 fatty acid–rich eicosapentaenoic acid and docosahexaenoic acid, which has been compared to mineral oil supplementation for wound healing in healthy adults. When fish oil was supplemented for 4 weeks, no significant differences were identified in time to complete wound healing between groups. Interestingly, significantly higher levels of the proinflammatory cytokine IL-1β were identified in blister fluid at 24 hours after blistering vs the placebo group (t=2.52, df=25, P<.05).14 Prior studies evaluating wound healing in animal models similarly identified longer times to re-epithelialization after omega-3 polyunsaturated fatty acid supplementation orally and topically.15,16 The fatty acid quality and composition consumed also may impact wound healing, as high-fat diets that are not rich in omega-3 fatty acids have been shown to promote inflammation and impair wound healing in rats, but this has not been thoroughly explored in human trials.17 Although adequate intake of these macronutrients is important, excessive intake may be harmful. Larger prospective trials are needed to shed light on the dose and composition of fatty acid supplementation that may optimize wound healing.
Vitamins and Micronutrients Required for Wound Healing
Vitamin A—Many vitamins serve as cofactors for the enzymatic processes required in wound healing. Vitamin A is an essential fat-soluble vitamin that serves a variety of dermatologic functions and promotes wound healing through stimulation of fibroblasts and ground substance, and it facilitates epithelial cell differentiation when applied topically.3,18 Vitamin A works through the activation of retinoid receptors on endothelial cells, fibroblasts, keratinocytes, melanocytes, and sebocytes, and has purported anti-inflammatory effects that aid the healing of open wounds.3 Additionally, vitamin A is thought to enhance cytokine release in the inflammatory phase of wound healing.19 Supplemental vitamin A has been associated with positive effects on acute wound healing, burns, and radiation injuries.3 The utility of vitamin A supplementation in chronic wounds remains unknown; however, it has been shown to be beneficial in patients with inflammatory disease, such as rheumatoid arthritis, on corticosteroid therapy. Vitamin A supplementation in this population has been shown to counteract the negative effects of corticosteroids on wound healing via downregulation of transforming growth factor β and insulinlike growth factor 1.20 Vitamin A deficiency has been associated with impaired progression through inflammatory and remodeling phases of healing due to altered B-cell and T-cell function and antibody production.1 Some experts recommend short courses of oral vitamin A supplementation to enhance wound healing at doses between 10,000 and 25,000 IU daily.2,3 Large, population-based studies are needed, and the safety supporting this recommendation in all patients remains unknown.
Vitamin C—Vitamin C is widely known for its role in collagen formation, immunomodulation, and antioxidant capacity.1 Although vitamin C deficiency is associated with decreased collagen synthesis and impaired wound healing,21 the utility of long-term supplementation in patients who are not deficient remains unexplored. A systematic review evaluating interventional studies utilizing vitamin C supplementation on pressure ulcerations and surgical wound healing concluded that convincing evidence exists only for supplementation with at least 500 mg of vitamin C. The authors noted, “There is little evidence for improved healing of surgical wounds by high-dose single vitamin C supplementation (1–3 g/day).”22 In a prospective, randomized, controlled trial, 20 patients with pressure ulcerations were supplemented with vitamin C vs placebo with a mean reduction in pressure-sore area of 84% after 1 month in the vitamin C–supplemented group compared to 42.7% in the placebo group (P<.005). A limitation of this study is the small population.23 One current recommendation for vitamin C supplementation in chronic wounds is for 500 mg daily in uncomplicated wounds to 2 g daily in severe wounds.3 Additional studies have suggested that the benefits of vitamin C supplementation are maximized when given in combination with zinc and arginine.22 At this time, evaluation for vitamin C deficiency and appropriate supplementation in patients with chronic wounds is needed.
Zinc—Minerals similarly play important roles in enzymatic regulation. Hundreds of zinc-containing enzymes are involved in wound healing and are required in tissue repair, growth, antioxidant capacity, and immune function.1,24 Zinc is specifically critical to collagen, DNA, RNA, and protein synthesis, as well as cellular proliferation.4 Zinc deficiency has been encountered in the setting of chronic wounds with extensive drainage, decreased dietary intake, or excessive gastrointestinal losses.25 Although many studies exist evaluating the utility of zinc supplementation on wound healing, many are confounded by multinutrient supplementation. No studies to date support zinc supplementation when zinc deficiency is absent. Patient assessment for medications or conditions that may impact zinc metabolism should be completed. Importantly, zinc supplementation can interfere with the absorption of other cations, so excessive supplementation should be avoided.1
Amino Acids for Wound Healing
Arginine—Arginine is an essential amino acid that serves as a substrate for cellular proliferation, collagen deposition, and lymphocyte function.8,26,27 Arginine serves as the biologic precursor for nitric oxide (NO), a substrate that has important wound healing properties. Nitric oxide metabolites have been shown to positively regulate wound repair while NO metabolites are reduced in wound environments in diabetic ulcerations.28,29 Arginine also is a proline precursor, an essential building block for collagen synthesis,6,30 and a stimulator of growth hormone and T cells.30,31 Animal studies have suggested L-arginine supplementation may reverse impaired NO synthesis in diabetic wounds.28 A single randomized trial assessing differing doses of arginine supplementation on stage II or stage IV pressure ulcers noted an almost two-fold improvement in healing time.32 However, human studies have not shown increased rates of re-epithelialization of skin graft donor sites when provided oral or parenteral arginine supplementation.33 Inadequate data currently exist to support regular arginine supplementation for all types of wounds, and no safe dose of daily arginine intake has been established.
Glutamine—Similarly, glutamine supplementation has been proposed to accelerate wound healing due to its role as a primary metabolic fuel source for rapidly proliferating cells such as epithelial cells and fibroblasts.8 Glutamine is thought to induce expression of heat-shock proteins and protect against inflammatory and infectious wound complications.34 Additionally, glutamine is thought to increase tissue insulin sensitivity, which may prove beneficial in wounds, as topical insulin previously has been shown in animal and human models to promote healing.35 Glutamine is thought to play a role in the inflammatory phase of wound healing via superoxide production, leukocyte apoptosis, and phagocytosis.6,34,36 Unfortunately, numerous randomized trials on glutamine supplementation have resulted in conflicting evidence confounded by multisupplementation within the same trial.37,38 A double-blind, randomized, controlled trial of 270 participants assessed the effect of oral supplementation with arginine, glutamine, or β-hydroxy-β-methylbutyrate vs control in the healing time of diabetic foot ulcerations. Significant differences in wound closure time at week 16 were only identified in participants with low albumin levels (≤40 g/L) who were supplemented (50.8%) vs the control group (34.9%; P=.0325) and in those with poor limb perfusion (ankle-brachial index of <1.0) who were supplemented (60.3%) vs the control group (39.3%; P=.0079).39 Ongoing clinical trials evaluating the effects of glutamine supplementation on differing wound types will hopefully shed light on the efficacy of supplementation.
Final Thoughts
Wound healing is multifactorial and should consider the health status and medical comorbidities of each patient treated. We propose an individualized approach to wound healing that includes exploration of specific macronutrient and micronutrient deficiencies, as malnutrition has been associated with wound chronicity and serves as a modifiable risk factor to improve healing.2 The evidence backing specific nutrient supplementation in patients with deficiencies is strong and should be considered in patients with chronic wounds. Adequate caloric intake and protein content should be recommended for most wound patients; however, excessive protein intake has not been beneficial in wound healing. The data behind specific amino acid and vitamin supplementation are limited at this time. As with other therapeutics, there is likely an appropriate dose for supplementation that has not yet been elucidated. Consideration of wound type, size, depth, exudate, and underlying cause are important to optimize healing and tailor nutritional supplementation to each patient. We hope future studies will illuminate the complementary role of dietary intake and nutrient supplementation for the treatment of chronic nonhealing wounds.
- Quain AM, Khardori NM. Nutrition in wound care management: a comprehensive overview. Wounds. 2015;27:327-335.
- Stechmiller JK. Understanding the role of nutrition and wound healing. Nutr Clin Pract. 2010;25:61-68. doi:10.1177/0884533609358997
- Molnar JA, Underdown MJ, Clark WA. Nutrition and chronic wounds. Adv Wound Care (New Rochelle). 2014;3:663-681. doi:10.1089/wound.2014.0530
- Dorner B, Posthauer ME, Thomas D; Panel NPUA. The role of nutrition in pressure ulcer prevention and treatment: National Pressure Ulcer Advisory Panel white paper. Adv Skin Wound Care. 2009;22:212-221. doi:10.1097/01.ASW.0000350838.11854.0a
- Collins N. Protein and wound healing. Adv Skin Wound Care. 2001;14:288-289. doi:10.1097/00129334-200111000-00008
- Barchitta M, Maugeri A, Favara G, et al. Nutrition and wound healing: an overview focusing on the beneficial effects of curcumin [published online March 5, 2019]. Int J Mol Sci. doi:10.3390/ijms20051119
- Harris CL, Fraser C. Malnutrition in the institutionalized elderly: the effects on wound healing. Ostomy Wound Manage. 2004;50:54-63.
- Saghaleini SH, Dehghan K, Shadvar K, et al. Pressure ulcer and nutrition. Indian J Crit Care Med. 2018;22:283-289. doi:10.4103/ijccm.IJCCM_277_17
- Breslow RA, Hallfrisch J, Guy DG, et al. The importance of dietary protein in healing pressure ulcers. J Am Geriatr Soc. 1993;41:357-362. doi:10.1111/j.1532-5415.1993.tb06940.x
- Lee SK, Posthauer ME, Dorner B, et al. Pressure ulcer healing with a concentrated, fortified, collagen protein hydrolysate supplement: a randomized controlled trial. Adv Skin Wound Care. 2006;19:92-96. doi:10.1097/00129334-200603000-00011
- Langer G, Fink A. Nutritional interventions for preventing and treating pressure ulcers. Cochrane Database Syst Rev. 2014;6:CD003216. doi:10.1002/14651858.CD003216.pub2
- Bouwens M, van de Rest O, Dellschaft N, et al. Fish-oil supplementation induces antiinflammatory gene expression profiles in human blood mononuclear cells. Am J Clin Nutr. 2009;90:415-424. doi:10.3945/ajcn.2009.27680
- Meydani SN, Endres S, Woods MM, et al. Oral (n-3) fatty acid supplementation suppresses cytokine production and lymphocyte proliferation: comparison between young and older women. J Nutr. 1991;121:547-555. doi:10.1093/jn/121.4.547
- McDaniel JC, Belury M, Ahijevych K, et al. Omega-3 fatty acids effect on wound healing. Wound Repair Regen. 2008;16:337-345. doi:10.1111/j.1524-475X.2008.00388.x
- Mooney MA, Vaughn DM, Reinhart GA, et al. Evaluation of the effects of omega-3 fatty acid-containing diets on the inflammatory stage of wound healing in dogs. Am J Vet Res. 1998;59:859-863.
- Cardoso CR, Souza MA, Ferro EA, et al. Influence of topical administration of n-3 and n-6 essential and n-9 nonessential fatty acids on the healing of cutaneous wounds. Wound Repair Regen. 2004;12:235-243. doi:10.1111/j.1067-1927.2004.012216.x
- Rosa DF, Sarandy MM, Novaes RD, et al. High-fat diet and alcohol intake promotes inflammation and impairs skin wound healing in Wistar rats. Mediators Inflamm. 2018;2018:4658583. doi:10.1155/2018/4658583
- Levenson SM, Gruber CA, Rettura G, et al. Supplemental vitamin A prevents the acute radiation-induced defect in wound healing. Ann Surg. 1984;200:494-512. doi:10.1097/00000658-198410000-00011
- Palmieri B, Vadalà M, Laurino C. Nutrition in wound healing: investigation of the molecular mechanisms, a narrative review. J Wound Care. 2019;28:683-693. doi:10.12968/jowc.2019.28.10.683
- Ehrlich HP, Hunt TK. Effects of cortisone and vitamin A on wound healing. Ann Surg. 1968;167:324-328. doi:10.1097/00000658-196803000-00004
- Pullar JM, Carr AC, Vissers MCM. The roles of vitamin C in skin health [published online August 12, 2017]. Nutrients. doi:10.3390/nu9080866
- Ellinger S, Stehle P. Efficacy of vitamin supplementation in situations with wound healing disorders: results from clinical intervention studies. Curr Opin Clin Nutr Metab Care. 2009;12:588-595. doi:10.1097/MCO.0b013e328331a5b5
- Taylor TV, Rimmer S, Day B, et al. Ascorbic acid supplementation in the treatment of pressure-sores. Lancet. 1974;2:544-546. doi:10.1016/s0140-6736(74)91874-1
- Ibs KH, Rink L. Zinc-altered immune function. J Nutr. 2003;133(5 suppl 1):1452S-1456S. doi:10.1093/jn/133.5.1452S
- Hoffman M, Micheletti RG, Shields BE. Nutritional dermatoses in the hospitalized patient. Cutis. 2020;105:296-302, 308, E1-E5.
- Chow O, Barbul A. Immunonutrition: role in wound healing and tissue regeneration. Adv Wound Care (New Rochelle). 2014;3:46-53. doi:10.1089/wound.2012.0415
- Singh K, Coburn LA, Barry DP, et al. L-arginine uptake by cationic amino acid transporter 2 is essential for colonic epithelial cell restitution. Am J Physiol Gastrointest Liver Physiol. 2012;302:G1061-G1073. doi:10.1152/ajpgi.00544.2011
- Witte MB, Thornton FJ, Tantry U, et al. L-Arginine supplementation enhances diabetic wound healing: involvement of the nitric oxide synthase and arginase pathways. Metabolism. 2002;51:1269-1273. doi:10.1053/meta.2002.35185
- Witte MB, Barbul A. Role of nitric oxide in wound repair. Am J Surg. 2002;183:406-412. doi:10.1016/s0002-9610(02)00815-2
- Barbul A. Proline precursors to sustain Mammalian collagen synthesis. J Nutr. 2008;138:2021S-2024S. doi:10.1093/jn/138.10.2021S
- Wu G, Bazer FW, Davis TA, et al. Arginine metabolism and nutrition in growth, health and disease. Amino Acids. 2009;37:153-168. doi:10.1007/s00726-008-0210-y
- Leigh B, Desneves K, Rafferty J, et al. The effect of different doses of an arginine-containing supplement on the healing of pressure ulcers. J Wound Care. 2012;21:150-156. doi:10.12968/jowc.2012.21.3.150
- Debats IB, Koeneman MM, Booi DI, et al. Intravenous arginine and human skin graft donor site healing: a randomized controlled trial. Burns. 2011;37:420-426. doi:10.1016/j.burns.2010.06.003
- Wischmeyer PE. Glutamine and heat shock protein expression. Nutrition. 2002;18:225-228. doi:10.1016/s0899-9007(01)00796-1
- Wang J, Xu J. Effects of topical insulin on wound healing: a review of animal and human evidences. Diabetes Metab Syndr Obes. 2020;13:719-727. doi:10.2147/DMSO.S237294
- Newsholme P. Why is L-glutamine metabolism important to cells of the immune system in health, postinjury, surgery or infection?J Nutr. 2001;131(9 suppl):2515S-2522S; discussion 2523S-2524S. doi:10.1093/jn/131.9.2515S
- Aquino VM, Harvey AR, Garvin JH, et al. A double-blind randomized placebo-controlled study of oral glutamine in the prevention of mucositis in children undergoing hematopoietic stem cell transplantation: a pediatric blood and marrow transplant consortium study. Bone Marrow Transplant. 2005;36:611-616. doi:10.1038/sj.bmt.1705084
- Ward E, Smith M, Henderson M, et al. The effect of high-dose enteral glutamine on the incidence and severity of mucositis in paediatric oncology patients. Eur J Clin Nutr. 2009;63:134-140. doi:10.1038/sj.ejcn.1602894
- Armstrong DG, Hanft JR, Driver VR, et al. Effect of oral nutritional supplementation on wound healing in diabetic foot ulcers: a prospective randomized controlled trial. Diabet Med. 2014;31:1069-1077. doi:10.1111/dme.12509
- Quain AM, Khardori NM. Nutrition in wound care management: a comprehensive overview. Wounds. 2015;27:327-335.
- Stechmiller JK. Understanding the role of nutrition and wound healing. Nutr Clin Pract. 2010;25:61-68. doi:10.1177/0884533609358997
- Molnar JA, Underdown MJ, Clark WA. Nutrition and chronic wounds. Adv Wound Care (New Rochelle). 2014;3:663-681. doi:10.1089/wound.2014.0530
- Dorner B, Posthauer ME, Thomas D; Panel NPUA. The role of nutrition in pressure ulcer prevention and treatment: National Pressure Ulcer Advisory Panel white paper. Adv Skin Wound Care. 2009;22:212-221. doi:10.1097/01.ASW.0000350838.11854.0a
- Collins N. Protein and wound healing. Adv Skin Wound Care. 2001;14:288-289. doi:10.1097/00129334-200111000-00008
- Barchitta M, Maugeri A, Favara G, et al. Nutrition and wound healing: an overview focusing on the beneficial effects of curcumin [published online March 5, 2019]. Int J Mol Sci. doi:10.3390/ijms20051119
- Harris CL, Fraser C. Malnutrition in the institutionalized elderly: the effects on wound healing. Ostomy Wound Manage. 2004;50:54-63.
- Saghaleini SH, Dehghan K, Shadvar K, et al. Pressure ulcer and nutrition. Indian J Crit Care Med. 2018;22:283-289. doi:10.4103/ijccm.IJCCM_277_17
- Breslow RA, Hallfrisch J, Guy DG, et al. The importance of dietary protein in healing pressure ulcers. J Am Geriatr Soc. 1993;41:357-362. doi:10.1111/j.1532-5415.1993.tb06940.x
- Lee SK, Posthauer ME, Dorner B, et al. Pressure ulcer healing with a concentrated, fortified, collagen protein hydrolysate supplement: a randomized controlled trial. Adv Skin Wound Care. 2006;19:92-96. doi:10.1097/00129334-200603000-00011
- Langer G, Fink A. Nutritional interventions for preventing and treating pressure ulcers. Cochrane Database Syst Rev. 2014;6:CD003216. doi:10.1002/14651858.CD003216.pub2
- Bouwens M, van de Rest O, Dellschaft N, et al. Fish-oil supplementation induces antiinflammatory gene expression profiles in human blood mononuclear cells. Am J Clin Nutr. 2009;90:415-424. doi:10.3945/ajcn.2009.27680
- Meydani SN, Endres S, Woods MM, et al. Oral (n-3) fatty acid supplementation suppresses cytokine production and lymphocyte proliferation: comparison between young and older women. J Nutr. 1991;121:547-555. doi:10.1093/jn/121.4.547
- McDaniel JC, Belury M, Ahijevych K, et al. Omega-3 fatty acids effect on wound healing. Wound Repair Regen. 2008;16:337-345. doi:10.1111/j.1524-475X.2008.00388.x
- Mooney MA, Vaughn DM, Reinhart GA, et al. Evaluation of the effects of omega-3 fatty acid-containing diets on the inflammatory stage of wound healing in dogs. Am J Vet Res. 1998;59:859-863.
- Cardoso CR, Souza MA, Ferro EA, et al. Influence of topical administration of n-3 and n-6 essential and n-9 nonessential fatty acids on the healing of cutaneous wounds. Wound Repair Regen. 2004;12:235-243. doi:10.1111/j.1067-1927.2004.012216.x
- Rosa DF, Sarandy MM, Novaes RD, et al. High-fat diet and alcohol intake promotes inflammation and impairs skin wound healing in Wistar rats. Mediators Inflamm. 2018;2018:4658583. doi:10.1155/2018/4658583
- Levenson SM, Gruber CA, Rettura G, et al. Supplemental vitamin A prevents the acute radiation-induced defect in wound healing. Ann Surg. 1984;200:494-512. doi:10.1097/00000658-198410000-00011
- Palmieri B, Vadalà M, Laurino C. Nutrition in wound healing: investigation of the molecular mechanisms, a narrative review. J Wound Care. 2019;28:683-693. doi:10.12968/jowc.2019.28.10.683
- Ehrlich HP, Hunt TK. Effects of cortisone and vitamin A on wound healing. Ann Surg. 1968;167:324-328. doi:10.1097/00000658-196803000-00004
- Pullar JM, Carr AC, Vissers MCM. The roles of vitamin C in skin health [published online August 12, 2017]. Nutrients. doi:10.3390/nu9080866
- Ellinger S, Stehle P. Efficacy of vitamin supplementation in situations with wound healing disorders: results from clinical intervention studies. Curr Opin Clin Nutr Metab Care. 2009;12:588-595. doi:10.1097/MCO.0b013e328331a5b5
- Taylor TV, Rimmer S, Day B, et al. Ascorbic acid supplementation in the treatment of pressure-sores. Lancet. 1974;2:544-546. doi:10.1016/s0140-6736(74)91874-1
- Ibs KH, Rink L. Zinc-altered immune function. J Nutr. 2003;133(5 suppl 1):1452S-1456S. doi:10.1093/jn/133.5.1452S
- Hoffman M, Micheletti RG, Shields BE. Nutritional dermatoses in the hospitalized patient. Cutis. 2020;105:296-302, 308, E1-E5.
- Chow O, Barbul A. Immunonutrition: role in wound healing and tissue regeneration. Adv Wound Care (New Rochelle). 2014;3:46-53. doi:10.1089/wound.2012.0415
- Singh K, Coburn LA, Barry DP, et al. L-arginine uptake by cationic amino acid transporter 2 is essential for colonic epithelial cell restitution. Am J Physiol Gastrointest Liver Physiol. 2012;302:G1061-G1073. doi:10.1152/ajpgi.00544.2011
- Witte MB, Thornton FJ, Tantry U, et al. L-Arginine supplementation enhances diabetic wound healing: involvement of the nitric oxide synthase and arginase pathways. Metabolism. 2002;51:1269-1273. doi:10.1053/meta.2002.35185
- Witte MB, Barbul A. Role of nitric oxide in wound repair. Am J Surg. 2002;183:406-412. doi:10.1016/s0002-9610(02)00815-2
- Barbul A. Proline precursors to sustain Mammalian collagen synthesis. J Nutr. 2008;138:2021S-2024S. doi:10.1093/jn/138.10.2021S
- Wu G, Bazer FW, Davis TA, et al. Arginine metabolism and nutrition in growth, health and disease. Amino Acids. 2009;37:153-168. doi:10.1007/s00726-008-0210-y
- Leigh B, Desneves K, Rafferty J, et al. The effect of different doses of an arginine-containing supplement on the healing of pressure ulcers. J Wound Care. 2012;21:150-156. doi:10.12968/jowc.2012.21.3.150
- Debats IB, Koeneman MM, Booi DI, et al. Intravenous arginine and human skin graft donor site healing: a randomized controlled trial. Burns. 2011;37:420-426. doi:10.1016/j.burns.2010.06.003
- Wischmeyer PE. Glutamine and heat shock protein expression. Nutrition. 2002;18:225-228. doi:10.1016/s0899-9007(01)00796-1
- Wang J, Xu J. Effects of topical insulin on wound healing: a review of animal and human evidences. Diabetes Metab Syndr Obes. 2020;13:719-727. doi:10.2147/DMSO.S237294
- Newsholme P. Why is L-glutamine metabolism important to cells of the immune system in health, postinjury, surgery or infection?J Nutr. 2001;131(9 suppl):2515S-2522S; discussion 2523S-2524S. doi:10.1093/jn/131.9.2515S
- Aquino VM, Harvey AR, Garvin JH, et al. A double-blind randomized placebo-controlled study of oral glutamine in the prevention of mucositis in children undergoing hematopoietic stem cell transplantation: a pediatric blood and marrow transplant consortium study. Bone Marrow Transplant. 2005;36:611-616. doi:10.1038/sj.bmt.1705084
- Ward E, Smith M, Henderson M, et al. The effect of high-dose enteral glutamine on the incidence and severity of mucositis in paediatric oncology patients. Eur J Clin Nutr. 2009;63:134-140. doi:10.1038/sj.ejcn.1602894
- Armstrong DG, Hanft JR, Driver VR, et al. Effect of oral nutritional supplementation on wound healing in diabetic foot ulcers: a prospective randomized controlled trial. Diabet Med. 2014;31:1069-1077. doi:10.1111/dme.12509
Practice Points
- Optimizing wound healing requires local and systemic therapies as well as adequate nutritional support.
- Malnutrition is a potentially modifiable risk factor that may contribute to impaired wound healing.
- Patients with chronic wounds and specific nutrient deficiencies should supplement to optimize healing.








