User login
Formerly Skin & Allergy News
ass lick
assault rifle
balls
ballsac
black jack
bleach
Boko Haram
bondage
causas
cheap
child abuse
cocaine
compulsive behaviors
cost of miracles
cunt
Daech
display network stats
drug paraphernalia
explosion
fart
fda and death
fda AND warn
fda AND warning
fda AND warns
feom
fuck
gambling
gfc
gun
human trafficking
humira AND expensive
illegal
ISIL
ISIS
Islamic caliphate
Islamic state
madvocate
masturbation
mixed martial arts
MMA
molestation
national rifle association
NRA
nsfw
nuccitelli
pedophile
pedophilia
poker
porn
porn
pornography
psychedelic drug
recreational drug
sex slave rings
shit
slot machine
snort
substance abuse
terrorism
terrorist
texarkana
Texas hold 'em
UFC
section[contains(@class, 'nav-hidden')]
section[contains(@class, 'nav-hidden active')]
The leading independent newspaper covering dermatology news and commentary.
This doc still supports NP/PA-led care ... with caveats
Two years ago, I argued that independent care from nurse practitioners (NPs) and physician assistants (PAs) would not have ill effects on health outcomes. To the surprise of no one, NPs and PAs embraced the argument; physicians clobbered it.
My case had three pegs: One was that medicine isn’t rocket science and clinicians control a lot less than we think we do. The second peg was that technology levels the playing field of clinical care. High-sensitivity troponin assays, for instance, make missing MI a lot less likely. The third peg was empirical: Studies have found little difference in MD versus non–MD-led care. Looking back, I now see empiricism as the weakest part of the argument because the studies had so many limitations.
I update this viewpoint now because health care is increasingly delivered by NPs and PAs. And there are two concerning trends regarding NP education and experience. First is that nurses are turning to advanced practitioner training earlier in their careers – without gathering much bedside experience. And these training programs are increasingly likely to be online, with minimal hands-on clinical tutoring.
Education and experience pop in my head often. Not every day, but many days I think back to my lucky 7 years in Indiana learning under the supervision of master clinicians – at a time when trainees were allowed the leeway to make decisions ... and mistakes. Then, when I joined private practice, I continued to learn from experienced practitioners.
It would be foolish to argue that training and experience aren’t important.
But here’s the thing:
I will make three points: First, I will bolster two of my old arguments as to why we shouldn’t be worried about non-MD clinicians, then I will propose some ideas to increase confidence in NP and PA care.
Health care does not equal health
On the matter of how much clinicians affect outcomes, a recently published randomized controlled trial performed in India found that subsidizing insurance care led to increased utilization of hospital services but had no significant effect on health outcomes. This follows the RAND and Oregon Health Insurance studies in the United States, which largely reported similar results.
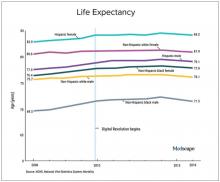
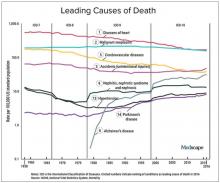
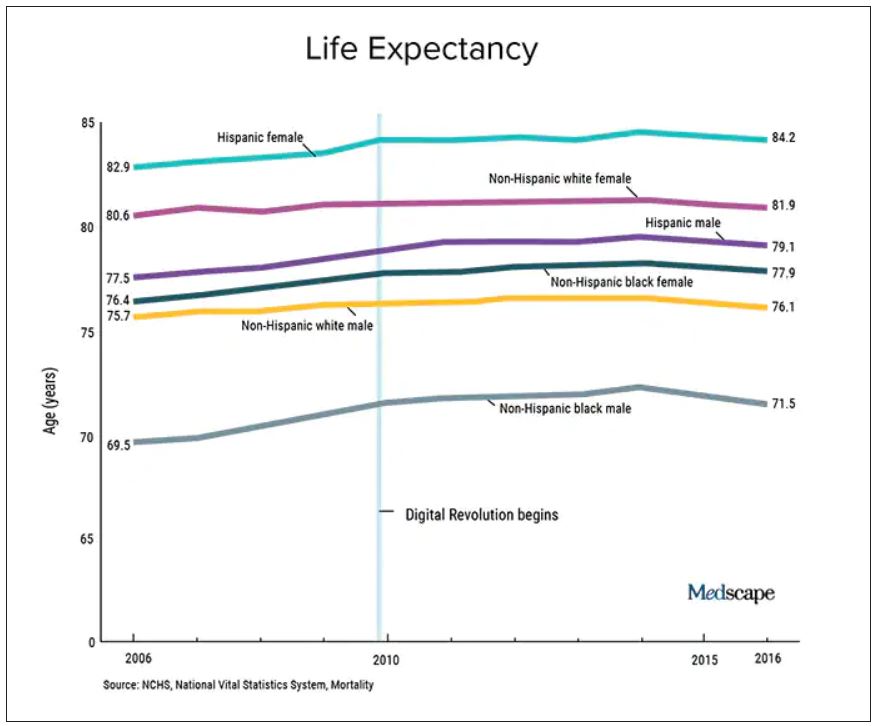
We should also not dismiss the fact that – despite the massive technology gains over the past half-century in digital health and artificial intelligence and increased use of quality measures, new drugs and procedures, and mega-medical centers – the average lifespan of Americans is flat to declining (in most ethnic and racial groups). Worse than no gains in longevity, perhaps, is that death from diseases like dementia and Parkinson’s disease are on the rise.
A neutral Martian would look down and wonder why all this health care hasn’t translated to longer and better lives. The causes of this paradox remain speculative, and are for another column, but the point remains that – on average – more health care is clearly not delivering more health. And if that is true, one may deduce that much of U.S. health care is marginal when it comes to affecting major outcomes.
It’s about the delta
Logos trumps pathos. Sure, my physician colleagues can tell scary anecdotes of bad outcomes caused by an inexperienced NP or PA. I would counter that by saying I have sat on our hospital’s peer review committee for 2 decades, including the era before NPs or PAs were practicing, and I have plenty of stories of physician errors. These include, of course, my own errors.
Logos: We must consider the difference between non–MD-led care and MD-led care.
My arguments from 2020 remain relevant today. Most medical problems are not engineering puzzles. Many, perhaps most, patients fall into an easy protocol – say, chest pain, dyspnea, or atrial fibrillation. With basic training, a motivated serious person quickly gains skill in recognizing and treating everyday problems.
And just 2 years on, technology further levels the playing field. Consider radiology in 2022 – it’s easy to take for granted the speed of the CT scan, the fidelity of the MRI, and the easy access to both in the U.S. hospital system. Less experienced clinicians have never had more tools to assist with diagnostics and therapeutics.
The expansion of team-based care has also mitigated the effects of inexperience. It took Americans longer than Canadians to figure out how helpful pharmacists could be. Pharmacists in my hospital now help us dose complicated medicines and protect us against prescribing errors.
Then there is the immediate access to online information. Gone are the days when you had to memorize long-QT syndromes. Book knowledge – that I spent years acquiring – now comes in seconds. The other day an NP corrected me. I asked, Are you sure? Boom, she took out her phone and showed me the evidence.
In sum, if it were even possible to measure the clinical competence of care from NP and PA versus physicians, there would be two bell-shaped curves with a tremendous amount of overlap. And that overlap would steadily increase as a given NP or PA gathered experience. (The NP in our electrophysiology division has more than 25 years’ experience in heart rhythm care, and it is common for colleagues to call her before one of us docs. Rightly so.)
Three basic proposals regarding NP and PA care
To ensure quality of care, I have three proposals.
It has always seemed strange to me that an NP or PA can flip from one field to another without a period of training. I can’t just change practice from electrophysiology to dermatology without doing a residency. But NPs and PAs can.
My first proposal would be that NPs and PAs spend a substantial period of training in a field before practice – a legit apprenticeship. The duration of this period is a matter of debate, but it ought to be standardized.
My second proposal is that, if physicians are required to pass certification exams, so should NPs. (PAs have an exam every 10 years.) The exam should be the same as (or very similar to) the physician exam, and it should be specific to their field of practice.
While I have argued (and still feel) that the American Board of Internal Medicine brand of certification is dubious, the fact remains that physicians must maintain proficiency in their field. Requiring NPs and PAs to do the same would help foster specialization. And while I can’t cite empirical evidence, specialization seems super-important. We have NPs at my hospital who have been in the same area for years, and they exude clinical competence.
Finally, I have come to believe that the best way for nearly any clinician to practice medicine is as part of a team. (The exception being primary care in rural areas where there are clinician shortages.)
On the matter of team care, I’ve practiced for a long time, but nearly every day I run situations by a colleague; often this person is an NP. The economist Friedrich Hayek proposed that dispersed knowledge always outpaces the wisdom of any individual. That notion pertains well to the increasing complexities and specialization of modern medical practice.
A person who commits to learning one area of medicine, enjoys helping people, asks often for help, and has the support of colleagues is set up to be a successful clinician – whether the letters after their name are APRN, PA, DO, or MD.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky. He did not report any relevant financial disclosures. A version of this article first appeared on Medscape.com.
Two years ago, I argued that independent care from nurse practitioners (NPs) and physician assistants (PAs) would not have ill effects on health outcomes. To the surprise of no one, NPs and PAs embraced the argument; physicians clobbered it.
My case had three pegs: One was that medicine isn’t rocket science and clinicians control a lot less than we think we do. The second peg was that technology levels the playing field of clinical care. High-sensitivity troponin assays, for instance, make missing MI a lot less likely. The third peg was empirical: Studies have found little difference in MD versus non–MD-led care. Looking back, I now see empiricism as the weakest part of the argument because the studies had so many limitations.
I update this viewpoint now because health care is increasingly delivered by NPs and PAs. And there are two concerning trends regarding NP education and experience. First is that nurses are turning to advanced practitioner training earlier in their careers – without gathering much bedside experience. And these training programs are increasingly likely to be online, with minimal hands-on clinical tutoring.
Education and experience pop in my head often. Not every day, but many days I think back to my lucky 7 years in Indiana learning under the supervision of master clinicians – at a time when trainees were allowed the leeway to make decisions ... and mistakes. Then, when I joined private practice, I continued to learn from experienced practitioners.
It would be foolish to argue that training and experience aren’t important.
But here’s the thing:
I will make three points: First, I will bolster two of my old arguments as to why we shouldn’t be worried about non-MD clinicians, then I will propose some ideas to increase confidence in NP and PA care.
Health care does not equal health
On the matter of how much clinicians affect outcomes, a recently published randomized controlled trial performed in India found that subsidizing insurance care led to increased utilization of hospital services but had no significant effect on health outcomes. This follows the RAND and Oregon Health Insurance studies in the United States, which largely reported similar results.
We should also not dismiss the fact that – despite the massive technology gains over the past half-century in digital health and artificial intelligence and increased use of quality measures, new drugs and procedures, and mega-medical centers – the average lifespan of Americans is flat to declining (in most ethnic and racial groups). Worse than no gains in longevity, perhaps, is that death from diseases like dementia and Parkinson’s disease are on the rise.
A neutral Martian would look down and wonder why all this health care hasn’t translated to longer and better lives. The causes of this paradox remain speculative, and are for another column, but the point remains that – on average – more health care is clearly not delivering more health. And if that is true, one may deduce that much of U.S. health care is marginal when it comes to affecting major outcomes.
It’s about the delta
Logos trumps pathos. Sure, my physician colleagues can tell scary anecdotes of bad outcomes caused by an inexperienced NP or PA. I would counter that by saying I have sat on our hospital’s peer review committee for 2 decades, including the era before NPs or PAs were practicing, and I have plenty of stories of physician errors. These include, of course, my own errors.
Logos: We must consider the difference between non–MD-led care and MD-led care.
My arguments from 2020 remain relevant today. Most medical problems are not engineering puzzles. Many, perhaps most, patients fall into an easy protocol – say, chest pain, dyspnea, or atrial fibrillation. With basic training, a motivated serious person quickly gains skill in recognizing and treating everyday problems.
And just 2 years on, technology further levels the playing field. Consider radiology in 2022 – it’s easy to take for granted the speed of the CT scan, the fidelity of the MRI, and the easy access to both in the U.S. hospital system. Less experienced clinicians have never had more tools to assist with diagnostics and therapeutics.
The expansion of team-based care has also mitigated the effects of inexperience. It took Americans longer than Canadians to figure out how helpful pharmacists could be. Pharmacists in my hospital now help us dose complicated medicines and protect us against prescribing errors.
Then there is the immediate access to online information. Gone are the days when you had to memorize long-QT syndromes. Book knowledge – that I spent years acquiring – now comes in seconds. The other day an NP corrected me. I asked, Are you sure? Boom, she took out her phone and showed me the evidence.
In sum, if it were even possible to measure the clinical competence of care from NP and PA versus physicians, there would be two bell-shaped curves with a tremendous amount of overlap. And that overlap would steadily increase as a given NP or PA gathered experience. (The NP in our electrophysiology division has more than 25 years’ experience in heart rhythm care, and it is common for colleagues to call her before one of us docs. Rightly so.)
Three basic proposals regarding NP and PA care
To ensure quality of care, I have three proposals.
It has always seemed strange to me that an NP or PA can flip from one field to another without a period of training. I can’t just change practice from electrophysiology to dermatology without doing a residency. But NPs and PAs can.
My first proposal would be that NPs and PAs spend a substantial period of training in a field before practice – a legit apprenticeship. The duration of this period is a matter of debate, but it ought to be standardized.
My second proposal is that, if physicians are required to pass certification exams, so should NPs. (PAs have an exam every 10 years.) The exam should be the same as (or very similar to) the physician exam, and it should be specific to their field of practice.
While I have argued (and still feel) that the American Board of Internal Medicine brand of certification is dubious, the fact remains that physicians must maintain proficiency in their field. Requiring NPs and PAs to do the same would help foster specialization. And while I can’t cite empirical evidence, specialization seems super-important. We have NPs at my hospital who have been in the same area for years, and they exude clinical competence.
Finally, I have come to believe that the best way for nearly any clinician to practice medicine is as part of a team. (The exception being primary care in rural areas where there are clinician shortages.)
On the matter of team care, I’ve practiced for a long time, but nearly every day I run situations by a colleague; often this person is an NP. The economist Friedrich Hayek proposed that dispersed knowledge always outpaces the wisdom of any individual. That notion pertains well to the increasing complexities and specialization of modern medical practice.
A person who commits to learning one area of medicine, enjoys helping people, asks often for help, and has the support of colleagues is set up to be a successful clinician – whether the letters after their name are APRN, PA, DO, or MD.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky. He did not report any relevant financial disclosures. A version of this article first appeared on Medscape.com.
Two years ago, I argued that independent care from nurse practitioners (NPs) and physician assistants (PAs) would not have ill effects on health outcomes. To the surprise of no one, NPs and PAs embraced the argument; physicians clobbered it.
My case had three pegs: One was that medicine isn’t rocket science and clinicians control a lot less than we think we do. The second peg was that technology levels the playing field of clinical care. High-sensitivity troponin assays, for instance, make missing MI a lot less likely. The third peg was empirical: Studies have found little difference in MD versus non–MD-led care. Looking back, I now see empiricism as the weakest part of the argument because the studies had so many limitations.
I update this viewpoint now because health care is increasingly delivered by NPs and PAs. And there are two concerning trends regarding NP education and experience. First is that nurses are turning to advanced practitioner training earlier in their careers – without gathering much bedside experience. And these training programs are increasingly likely to be online, with minimal hands-on clinical tutoring.
Education and experience pop in my head often. Not every day, but many days I think back to my lucky 7 years in Indiana learning under the supervision of master clinicians – at a time when trainees were allowed the leeway to make decisions ... and mistakes. Then, when I joined private practice, I continued to learn from experienced practitioners.
It would be foolish to argue that training and experience aren’t important.
But here’s the thing:
I will make three points: First, I will bolster two of my old arguments as to why we shouldn’t be worried about non-MD clinicians, then I will propose some ideas to increase confidence in NP and PA care.
Health care does not equal health
On the matter of how much clinicians affect outcomes, a recently published randomized controlled trial performed in India found that subsidizing insurance care led to increased utilization of hospital services but had no significant effect on health outcomes. This follows the RAND and Oregon Health Insurance studies in the United States, which largely reported similar results.
We should also not dismiss the fact that – despite the massive technology gains over the past half-century in digital health and artificial intelligence and increased use of quality measures, new drugs and procedures, and mega-medical centers – the average lifespan of Americans is flat to declining (in most ethnic and racial groups). Worse than no gains in longevity, perhaps, is that death from diseases like dementia and Parkinson’s disease are on the rise.
A neutral Martian would look down and wonder why all this health care hasn’t translated to longer and better lives. The causes of this paradox remain speculative, and are for another column, but the point remains that – on average – more health care is clearly not delivering more health. And if that is true, one may deduce that much of U.S. health care is marginal when it comes to affecting major outcomes.
It’s about the delta
Logos trumps pathos. Sure, my physician colleagues can tell scary anecdotes of bad outcomes caused by an inexperienced NP or PA. I would counter that by saying I have sat on our hospital’s peer review committee for 2 decades, including the era before NPs or PAs were practicing, and I have plenty of stories of physician errors. These include, of course, my own errors.
Logos: We must consider the difference between non–MD-led care and MD-led care.
My arguments from 2020 remain relevant today. Most medical problems are not engineering puzzles. Many, perhaps most, patients fall into an easy protocol – say, chest pain, dyspnea, or atrial fibrillation. With basic training, a motivated serious person quickly gains skill in recognizing and treating everyday problems.
And just 2 years on, technology further levels the playing field. Consider radiology in 2022 – it’s easy to take for granted the speed of the CT scan, the fidelity of the MRI, and the easy access to both in the U.S. hospital system. Less experienced clinicians have never had more tools to assist with diagnostics and therapeutics.
The expansion of team-based care has also mitigated the effects of inexperience. It took Americans longer than Canadians to figure out how helpful pharmacists could be. Pharmacists in my hospital now help us dose complicated medicines and protect us against prescribing errors.
Then there is the immediate access to online information. Gone are the days when you had to memorize long-QT syndromes. Book knowledge – that I spent years acquiring – now comes in seconds. The other day an NP corrected me. I asked, Are you sure? Boom, she took out her phone and showed me the evidence.
In sum, if it were even possible to measure the clinical competence of care from NP and PA versus physicians, there would be two bell-shaped curves with a tremendous amount of overlap. And that overlap would steadily increase as a given NP or PA gathered experience. (The NP in our electrophysiology division has more than 25 years’ experience in heart rhythm care, and it is common for colleagues to call her before one of us docs. Rightly so.)
Three basic proposals regarding NP and PA care
To ensure quality of care, I have three proposals.
It has always seemed strange to me that an NP or PA can flip from one field to another without a period of training. I can’t just change practice from electrophysiology to dermatology without doing a residency. But NPs and PAs can.
My first proposal would be that NPs and PAs spend a substantial period of training in a field before practice – a legit apprenticeship. The duration of this period is a matter of debate, but it ought to be standardized.
My second proposal is that, if physicians are required to pass certification exams, so should NPs. (PAs have an exam every 10 years.) The exam should be the same as (or very similar to) the physician exam, and it should be specific to their field of practice.
While I have argued (and still feel) that the American Board of Internal Medicine brand of certification is dubious, the fact remains that physicians must maintain proficiency in their field. Requiring NPs and PAs to do the same would help foster specialization. And while I can’t cite empirical evidence, specialization seems super-important. We have NPs at my hospital who have been in the same area for years, and they exude clinical competence.
Finally, I have come to believe that the best way for nearly any clinician to practice medicine is as part of a team. (The exception being primary care in rural areas where there are clinician shortages.)
On the matter of team care, I’ve practiced for a long time, but nearly every day I run situations by a colleague; often this person is an NP. The economist Friedrich Hayek proposed that dispersed knowledge always outpaces the wisdom of any individual. That notion pertains well to the increasing complexities and specialization of modern medical practice.
A person who commits to learning one area of medicine, enjoys helping people, asks often for help, and has the support of colleagues is set up to be a successful clinician – whether the letters after their name are APRN, PA, DO, or MD.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky. He did not report any relevant financial disclosures. A version of this article first appeared on Medscape.com.
Seven ways doctors could get better payment from insurers
, say experts in physician-payer contracts.
Many doctors sign long-term agreements and then forget about them, says Marcia Brauchler, president and founder of Physicians’ Ally, Littleton, Colorado, a health care consulting company. “The average doctor is trying to run a practice on 2010 rates because they haven’t touched their insurance contracts for 10 years,” she says.
Payers also make a lot of money by adopting dozens of unilateral policy and procedure changes every year that they know physicians are too busy to read. They are counting on the fact that few doctors will understand what the policy changes are and that even fewer will contest them, says Greg Brodek, JD, chair of the health law practice group and head of the managed care litigation practice at Duane Morris, who represents doctors in disputes with payers.
These experts say doctors can push back on one-sided payer contracts and negotiate changes. Mr. Brodek says some practices have more leverage than others to influence payers – if they are larger, in a specialty that the payer needs in its network, or located in a remote area where the payer has limited options.
Here are seven key areas to pay attention to:
1. Long-term contracts. Most doctors sign multiyear “evergreen” contracts that renew automatically every year. This allows insurers to continue to pay doctors the same rate for years.
To avoid this, doctors should negotiate new rates when their agreements renew or, if they prefer, ask that a cost-of-living adjustment be included in the multiyear contract that applies to subsequent years, says Ms. Brauchler.
2. Fee schedules. Payers will “whitewash” what they’re paying you by saying it’s 100% of the payer fee schedule. When it comes to Medicare, they may be paying you a lot less, says Ms. Brauchler.
“My biggest takeaway is to compare the CPT codes of the payer’s fee schedule against what Medicare allows. For example, for CPT code 99213, a 15-minute established office visit, if Medicare pays you $100 and Aetna pays you $75.00, you’re getting 75% of Medicare,” says Ms. Brauchler. To avoid this, doctors should ask that the contract state that reimbursement be made according to Medicare’s medical policies rather than the payer’s.
3. Audits. Commercial payers will claim they have a contractual right to conduct pre- and post-payment audits of physicians’ claims that can result in reduced payments. The contract only states that if doctors correctly submit claims, they will get paid, not that they will have to go through extra steps, which is a breach of their agreement, says Mr. Brodek.
In his experience, 90% of payers back down when asked to provide the contractual basis to conduct these audits. “Or, they take the position that it’s not in the contract but that they have a policy.”
4. Contract amendments versus policies and procedures. This is a huge area that needs to be clarified in contracts and monitored by providers throughout their relationships with payers. Contracts have three elements: the parties, the services provided, and the payment. Changing any one of those terms requires an amendment and advance written notice that has to be delivered to the other party in a certain way, such as by overnight delivery, says Mr. Brodek.
In addition, both parties have to sign that they agree to an amendment. “But, that’s too cumbersome and complicated for payers who have decided to adopt policies instead. These are unilateral changes made with no advance notice given, since the payer typically posts the change on its website,” says Mr. Brodek.
5. Recoupment efforts. Payers will review claims after they’re paid and contact the doctor saying they found a mistake, such as inappropriate coding. They will claim that the doctor now owes them a large sum of money based on a percentage of claims reviewed. “They typically send the doctor a letter that ends with, ‘If you do not pay this amount within 30 days, we will offset the amount due against future payments that we would otherwise make to you,’” says Mr. Brodek.
He recommends that contracts include the doctors’ right to contest an audit so the “payer doesn’t have the unilateral right to disregard the initial coding that the doctor appropriately assigned to the claim and recoup the money anyway,” says Mr. Brodek.
6. Medical network rentals and products. Most contracts say that payers can rent out their medical networks to other health plans, such as HMOs, and that the clinicians agree to comply with all of their policies and procedures. The agreement may also cover the products of other plans.
“The problem is that physicians are not given information about the other plans, including their terms and conditions for getting paid,” says Mr. Brodek. If a problem with payment arises, they have no written agreement with that plan, which makes it harder to enforce.
“That’s why we recommend that doctors negotiate agreements that only cover the main payer. Most of the time, the payer is amenable to putting that language in the contract,” he says.
7. Payer products. In the past several years, a typical contract has included appendices that list the payer’s products, such as Medicare, workers compensation, auto insurance liability, or health care exchange products. Many clinicians don’t realize they can pick the plans they want to participate in by accepting or opting out, says Mr. Brodek.
“We advise clients to limit the contract to what you want covered and to make informed decisions, because some products have low fees set by the states, such as workers compensation and health care exchanges,” says Mr. Brodek.
A version of this article first appeared on Medscape.com.
, say experts in physician-payer contracts.
Many doctors sign long-term agreements and then forget about them, says Marcia Brauchler, president and founder of Physicians’ Ally, Littleton, Colorado, a health care consulting company. “The average doctor is trying to run a practice on 2010 rates because they haven’t touched their insurance contracts for 10 years,” she says.
Payers also make a lot of money by adopting dozens of unilateral policy and procedure changes every year that they know physicians are too busy to read. They are counting on the fact that few doctors will understand what the policy changes are and that even fewer will contest them, says Greg Brodek, JD, chair of the health law practice group and head of the managed care litigation practice at Duane Morris, who represents doctors in disputes with payers.
These experts say doctors can push back on one-sided payer contracts and negotiate changes. Mr. Brodek says some practices have more leverage than others to influence payers – if they are larger, in a specialty that the payer needs in its network, or located in a remote area where the payer has limited options.
Here are seven key areas to pay attention to:
1. Long-term contracts. Most doctors sign multiyear “evergreen” contracts that renew automatically every year. This allows insurers to continue to pay doctors the same rate for years.
To avoid this, doctors should negotiate new rates when their agreements renew or, if they prefer, ask that a cost-of-living adjustment be included in the multiyear contract that applies to subsequent years, says Ms. Brauchler.
2. Fee schedules. Payers will “whitewash” what they’re paying you by saying it’s 100% of the payer fee schedule. When it comes to Medicare, they may be paying you a lot less, says Ms. Brauchler.
“My biggest takeaway is to compare the CPT codes of the payer’s fee schedule against what Medicare allows. For example, for CPT code 99213, a 15-minute established office visit, if Medicare pays you $100 and Aetna pays you $75.00, you’re getting 75% of Medicare,” says Ms. Brauchler. To avoid this, doctors should ask that the contract state that reimbursement be made according to Medicare’s medical policies rather than the payer’s.
3. Audits. Commercial payers will claim they have a contractual right to conduct pre- and post-payment audits of physicians’ claims that can result in reduced payments. The contract only states that if doctors correctly submit claims, they will get paid, not that they will have to go through extra steps, which is a breach of their agreement, says Mr. Brodek.
In his experience, 90% of payers back down when asked to provide the contractual basis to conduct these audits. “Or, they take the position that it’s not in the contract but that they have a policy.”
4. Contract amendments versus policies and procedures. This is a huge area that needs to be clarified in contracts and monitored by providers throughout their relationships with payers. Contracts have three elements: the parties, the services provided, and the payment. Changing any one of those terms requires an amendment and advance written notice that has to be delivered to the other party in a certain way, such as by overnight delivery, says Mr. Brodek.
In addition, both parties have to sign that they agree to an amendment. “But, that’s too cumbersome and complicated for payers who have decided to adopt policies instead. These are unilateral changes made with no advance notice given, since the payer typically posts the change on its website,” says Mr. Brodek.
5. Recoupment efforts. Payers will review claims after they’re paid and contact the doctor saying they found a mistake, such as inappropriate coding. They will claim that the doctor now owes them a large sum of money based on a percentage of claims reviewed. “They typically send the doctor a letter that ends with, ‘If you do not pay this amount within 30 days, we will offset the amount due against future payments that we would otherwise make to you,’” says Mr. Brodek.
He recommends that contracts include the doctors’ right to contest an audit so the “payer doesn’t have the unilateral right to disregard the initial coding that the doctor appropriately assigned to the claim and recoup the money anyway,” says Mr. Brodek.
6. Medical network rentals and products. Most contracts say that payers can rent out their medical networks to other health plans, such as HMOs, and that the clinicians agree to comply with all of their policies and procedures. The agreement may also cover the products of other plans.
“The problem is that physicians are not given information about the other plans, including their terms and conditions for getting paid,” says Mr. Brodek. If a problem with payment arises, they have no written agreement with that plan, which makes it harder to enforce.
“That’s why we recommend that doctors negotiate agreements that only cover the main payer. Most of the time, the payer is amenable to putting that language in the contract,” he says.
7. Payer products. In the past several years, a typical contract has included appendices that list the payer’s products, such as Medicare, workers compensation, auto insurance liability, or health care exchange products. Many clinicians don’t realize they can pick the plans they want to participate in by accepting or opting out, says Mr. Brodek.
“We advise clients to limit the contract to what you want covered and to make informed decisions, because some products have low fees set by the states, such as workers compensation and health care exchanges,” says Mr. Brodek.
A version of this article first appeared on Medscape.com.
, say experts in physician-payer contracts.
Many doctors sign long-term agreements and then forget about them, says Marcia Brauchler, president and founder of Physicians’ Ally, Littleton, Colorado, a health care consulting company. “The average doctor is trying to run a practice on 2010 rates because they haven’t touched their insurance contracts for 10 years,” she says.
Payers also make a lot of money by adopting dozens of unilateral policy and procedure changes every year that they know physicians are too busy to read. They are counting on the fact that few doctors will understand what the policy changes are and that even fewer will contest them, says Greg Brodek, JD, chair of the health law practice group and head of the managed care litigation practice at Duane Morris, who represents doctors in disputes with payers.
These experts say doctors can push back on one-sided payer contracts and negotiate changes. Mr. Brodek says some practices have more leverage than others to influence payers – if they are larger, in a specialty that the payer needs in its network, or located in a remote area where the payer has limited options.
Here are seven key areas to pay attention to:
1. Long-term contracts. Most doctors sign multiyear “evergreen” contracts that renew automatically every year. This allows insurers to continue to pay doctors the same rate for years.
To avoid this, doctors should negotiate new rates when their agreements renew or, if they prefer, ask that a cost-of-living adjustment be included in the multiyear contract that applies to subsequent years, says Ms. Brauchler.
2. Fee schedules. Payers will “whitewash” what they’re paying you by saying it’s 100% of the payer fee schedule. When it comes to Medicare, they may be paying you a lot less, says Ms. Brauchler.
“My biggest takeaway is to compare the CPT codes of the payer’s fee schedule against what Medicare allows. For example, for CPT code 99213, a 15-minute established office visit, if Medicare pays you $100 and Aetna pays you $75.00, you’re getting 75% of Medicare,” says Ms. Brauchler. To avoid this, doctors should ask that the contract state that reimbursement be made according to Medicare’s medical policies rather than the payer’s.
3. Audits. Commercial payers will claim they have a contractual right to conduct pre- and post-payment audits of physicians’ claims that can result in reduced payments. The contract only states that if doctors correctly submit claims, they will get paid, not that they will have to go through extra steps, which is a breach of their agreement, says Mr. Brodek.
In his experience, 90% of payers back down when asked to provide the contractual basis to conduct these audits. “Or, they take the position that it’s not in the contract but that they have a policy.”
4. Contract amendments versus policies and procedures. This is a huge area that needs to be clarified in contracts and monitored by providers throughout their relationships with payers. Contracts have three elements: the parties, the services provided, and the payment. Changing any one of those terms requires an amendment and advance written notice that has to be delivered to the other party in a certain way, such as by overnight delivery, says Mr. Brodek.
In addition, both parties have to sign that they agree to an amendment. “But, that’s too cumbersome and complicated for payers who have decided to adopt policies instead. These are unilateral changes made with no advance notice given, since the payer typically posts the change on its website,” says Mr. Brodek.
5. Recoupment efforts. Payers will review claims after they’re paid and contact the doctor saying they found a mistake, such as inappropriate coding. They will claim that the doctor now owes them a large sum of money based on a percentage of claims reviewed. “They typically send the doctor a letter that ends with, ‘If you do not pay this amount within 30 days, we will offset the amount due against future payments that we would otherwise make to you,’” says Mr. Brodek.
He recommends that contracts include the doctors’ right to contest an audit so the “payer doesn’t have the unilateral right to disregard the initial coding that the doctor appropriately assigned to the claim and recoup the money anyway,” says Mr. Brodek.
6. Medical network rentals and products. Most contracts say that payers can rent out their medical networks to other health plans, such as HMOs, and that the clinicians agree to comply with all of their policies and procedures. The agreement may also cover the products of other plans.
“The problem is that physicians are not given information about the other plans, including their terms and conditions for getting paid,” says Mr. Brodek. If a problem with payment arises, they have no written agreement with that plan, which makes it harder to enforce.
“That’s why we recommend that doctors negotiate agreements that only cover the main payer. Most of the time, the payer is amenable to putting that language in the contract,” he says.
7. Payer products. In the past several years, a typical contract has included appendices that list the payer’s products, such as Medicare, workers compensation, auto insurance liability, or health care exchange products. Many clinicians don’t realize they can pick the plans they want to participate in by accepting or opting out, says Mr. Brodek.
“We advise clients to limit the contract to what you want covered and to make informed decisions, because some products have low fees set by the states, such as workers compensation and health care exchanges,” says Mr. Brodek.
A version of this article first appeared on Medscape.com.
Ways to make sure 2022 doesn’t stink for docs
Depending on the data you’re looking at, 40%-60% of physicians are burned out.
Research studies and the eye test reveal the painfully obvious: Colleagues are tired, winded, spent, and at times way past burned out. People aren’t asking me if they’re burned out. They know they’re burned out; heck, they can even recite the Maslach burnout inventory, forward and backward, in a mask, or while completing a COVID quarantine. A fair share of people know the key steps to prevent burnout and promote recovery.
What I’m starting to see more of is, “Why should I even bother to recover from this? Why pick myself up again just to get another occupational stress injury (burnout, demoralization, moral injury, etc.)?” In other words, it’s not just simply about negating burnout; it’s about supporting and facilitating the motivation to work.
We’ve been through so much with COVID that it might be challenging to remember when you saw a truly engaged work environment. No doubt, we have outstanding professionals across medicine who answer the bell every day. However, if you’ve been looking closely, many teams/units have lost a bit of the zip and pep. The synergy and trust aren’t as smooth, and at noon, everyone counts the hours to the end of the shift.
You may be thinking, Well, of course, they are; we’re still amid a pandemic, and people have been through hell. Your observation would be correct, except I’ve personally seen some teams weather the pandemic storm and still remain engaged (some even more involved).
The No. 1 consult result for the GW Resiliency and Well-Being Center, where I work, has been on lectures for burnout. The R&WC has given so many of these lectures that my dreams take the form of a PowerPoint presentation. Overall the talks have gone very well. We’ve added skills sections on practices of whole-person care. We’ve blitzed the daylights out of restorative sleep, yet I know we are still searching for the correct narrative.
Motivated staff, faculty, and students will genuinely take in the information and follow the recommendations; however, they still struggle to find that drive and zest for work. Yes, moving from burnout to neutral is reasonable but likely won’t move the needle of your professional or personal life. We need to have the emotional energy and the clear desire to utilize that energy for a meaningful purpose.
Talking about burnout in specific ways is straightforward and, in my opinion, much easier than talking about engagement. Part of the challenge when trying to discuss engagement is that people can feel invalidated or that you’re telling them to be stoic. Or worse yet, that the problem of burnout primarily lies with them. It’s essential to recognize the role of an organizational factor in burnout (approximately 80%, depending on the study); still, even if you address burnout, people may not be miserable, but it doesn’t mean they will stay at their current job (please cue intro music for the Great Resignation).
Engagement models have existed for some time and certainly have gained much more attention in health care settings over the past 2 decades. Engagement can be described as having three components: dedication, vigor, and absorption. When a person is filling all three of these components over time, presto – you get the much-sought-after state of the supremely engaged professional.
These models definitely give us excellent starting points to approach engagement from a pre-COVID era. In COVID and beyond, I’m not sure how these models will stand up in a hybrid work environment, where autonomy and flexibility could be more valued than ever. Personally, COVID revealed some things I was missing in my work pre-COVID:
- Time to think and process. This was one of the great things about being a consultation-liaison psychiatrist; it was literally feast or famine.
- Doing what I’m talented at and really enjoy.
- Time is short, and I want to be more present in the life of my family.
The list above isn’t exhaustive, but I’ve found them to be my own personal recipe for being engaged. Over the next series of articles, I’m going to focus on engagement and factors related to key resilience. These articles will be informed by a front-line view from my colleagues, and hopefully start to separate the myth from reality on the subject of health professional engagement and resilience.
Everyone be safe and well!
A version of this article first appeared on Medscape.com.
Depending on the data you’re looking at, 40%-60% of physicians are burned out.
Research studies and the eye test reveal the painfully obvious: Colleagues are tired, winded, spent, and at times way past burned out. People aren’t asking me if they’re burned out. They know they’re burned out; heck, they can even recite the Maslach burnout inventory, forward and backward, in a mask, or while completing a COVID quarantine. A fair share of people know the key steps to prevent burnout and promote recovery.
What I’m starting to see more of is, “Why should I even bother to recover from this? Why pick myself up again just to get another occupational stress injury (burnout, demoralization, moral injury, etc.)?” In other words, it’s not just simply about negating burnout; it’s about supporting and facilitating the motivation to work.
We’ve been through so much with COVID that it might be challenging to remember when you saw a truly engaged work environment. No doubt, we have outstanding professionals across medicine who answer the bell every day. However, if you’ve been looking closely, many teams/units have lost a bit of the zip and pep. The synergy and trust aren’t as smooth, and at noon, everyone counts the hours to the end of the shift.
You may be thinking, Well, of course, they are; we’re still amid a pandemic, and people have been through hell. Your observation would be correct, except I’ve personally seen some teams weather the pandemic storm and still remain engaged (some even more involved).
The No. 1 consult result for the GW Resiliency and Well-Being Center, where I work, has been on lectures for burnout. The R&WC has given so many of these lectures that my dreams take the form of a PowerPoint presentation. Overall the talks have gone very well. We’ve added skills sections on practices of whole-person care. We’ve blitzed the daylights out of restorative sleep, yet I know we are still searching for the correct narrative.
Motivated staff, faculty, and students will genuinely take in the information and follow the recommendations; however, they still struggle to find that drive and zest for work. Yes, moving from burnout to neutral is reasonable but likely won’t move the needle of your professional or personal life. We need to have the emotional energy and the clear desire to utilize that energy for a meaningful purpose.
Talking about burnout in specific ways is straightforward and, in my opinion, much easier than talking about engagement. Part of the challenge when trying to discuss engagement is that people can feel invalidated or that you’re telling them to be stoic. Or worse yet, that the problem of burnout primarily lies with them. It’s essential to recognize the role of an organizational factor in burnout (approximately 80%, depending on the study); still, even if you address burnout, people may not be miserable, but it doesn’t mean they will stay at their current job (please cue intro music for the Great Resignation).
Engagement models have existed for some time and certainly have gained much more attention in health care settings over the past 2 decades. Engagement can be described as having three components: dedication, vigor, and absorption. When a person is filling all three of these components over time, presto – you get the much-sought-after state of the supremely engaged professional.
These models definitely give us excellent starting points to approach engagement from a pre-COVID era. In COVID and beyond, I’m not sure how these models will stand up in a hybrid work environment, where autonomy and flexibility could be more valued than ever. Personally, COVID revealed some things I was missing in my work pre-COVID:
- Time to think and process. This was one of the great things about being a consultation-liaison psychiatrist; it was literally feast or famine.
- Doing what I’m talented at and really enjoy.
- Time is short, and I want to be more present in the life of my family.
The list above isn’t exhaustive, but I’ve found them to be my own personal recipe for being engaged. Over the next series of articles, I’m going to focus on engagement and factors related to key resilience. These articles will be informed by a front-line view from my colleagues, and hopefully start to separate the myth from reality on the subject of health professional engagement and resilience.
Everyone be safe and well!
A version of this article first appeared on Medscape.com.
Depending on the data you’re looking at, 40%-60% of physicians are burned out.
Research studies and the eye test reveal the painfully obvious: Colleagues are tired, winded, spent, and at times way past burned out. People aren’t asking me if they’re burned out. They know they’re burned out; heck, they can even recite the Maslach burnout inventory, forward and backward, in a mask, or while completing a COVID quarantine. A fair share of people know the key steps to prevent burnout and promote recovery.
What I’m starting to see more of is, “Why should I even bother to recover from this? Why pick myself up again just to get another occupational stress injury (burnout, demoralization, moral injury, etc.)?” In other words, it’s not just simply about negating burnout; it’s about supporting and facilitating the motivation to work.
We’ve been through so much with COVID that it might be challenging to remember when you saw a truly engaged work environment. No doubt, we have outstanding professionals across medicine who answer the bell every day. However, if you’ve been looking closely, many teams/units have lost a bit of the zip and pep. The synergy and trust aren’t as smooth, and at noon, everyone counts the hours to the end of the shift.
You may be thinking, Well, of course, they are; we’re still amid a pandemic, and people have been through hell. Your observation would be correct, except I’ve personally seen some teams weather the pandemic storm and still remain engaged (some even more involved).
The No. 1 consult result for the GW Resiliency and Well-Being Center, where I work, has been on lectures for burnout. The R&WC has given so many of these lectures that my dreams take the form of a PowerPoint presentation. Overall the talks have gone very well. We’ve added skills sections on practices of whole-person care. We’ve blitzed the daylights out of restorative sleep, yet I know we are still searching for the correct narrative.
Motivated staff, faculty, and students will genuinely take in the information and follow the recommendations; however, they still struggle to find that drive and zest for work. Yes, moving from burnout to neutral is reasonable but likely won’t move the needle of your professional or personal life. We need to have the emotional energy and the clear desire to utilize that energy for a meaningful purpose.
Talking about burnout in specific ways is straightforward and, in my opinion, much easier than talking about engagement. Part of the challenge when trying to discuss engagement is that people can feel invalidated or that you’re telling them to be stoic. Or worse yet, that the problem of burnout primarily lies with them. It’s essential to recognize the role of an organizational factor in burnout (approximately 80%, depending on the study); still, even if you address burnout, people may not be miserable, but it doesn’t mean they will stay at their current job (please cue intro music for the Great Resignation).
Engagement models have existed for some time and certainly have gained much more attention in health care settings over the past 2 decades. Engagement can be described as having three components: dedication, vigor, and absorption. When a person is filling all three of these components over time, presto – you get the much-sought-after state of the supremely engaged professional.
These models definitely give us excellent starting points to approach engagement from a pre-COVID era. In COVID and beyond, I’m not sure how these models will stand up in a hybrid work environment, where autonomy and flexibility could be more valued than ever. Personally, COVID revealed some things I was missing in my work pre-COVID:
- Time to think and process. This was one of the great things about being a consultation-liaison psychiatrist; it was literally feast or famine.
- Doing what I’m talented at and really enjoy.
- Time is short, and I want to be more present in the life of my family.
The list above isn’t exhaustive, but I’ve found them to be my own personal recipe for being engaged. Over the next series of articles, I’m going to focus on engagement and factors related to key resilience. These articles will be informed by a front-line view from my colleagues, and hopefully start to separate the myth from reality on the subject of health professional engagement and resilience.
Everyone be safe and well!
A version of this article first appeared on Medscape.com.
Gut bacteria linked with long COVID
While links have been found between the gut’s microbiome and COVID-19, as well as other diseases, this is the first published research to show a link specifically to COVID’s long-term effects, the investigators, based at the Chinese University of Hong Kong, wrote in Gut.
“To our knowledge, this is the first study to show that altered gut microbiome composition is strongly associated with persistent symptoms in patients with COVID-19 up to 6 months after clearance of SARS-CoV-2 virus,” said Siew Ng, MBBS, PhD, associate director at the university’s Center for Gut Microbiota Research.
At three hospitals, the researchers enrolled 106 patients with COVID-19 from February to August 2020 with stool samples at admission and at 1 month and 6 months after discharge, and compared them with people who did not have COVID, recruited in 2019. The severity of COVID in the enrolled patients was mostly mild to moderate.
At 3 months, 86 of the patients with COVID had post–acute COVID-19 syndrome (PACS) – defined as at least one persistent, otherwise unexplained symptom 4 weeks after clearance of the virus. And 81 patients had PACS at 6 months, most commonly fatigue, poor memory, hair loss, anxiety, and trouble sleeping.
Using stool samples for their analysis, the researchers found that, broadly, the diversity of the types of bacteria, and the abundance of these bacteria, were significantly lower at 6 months for those with PACS, compared with those without PACS and with controls (P < .05 and P < .0001, respectively). Among those with PACS, 28 bacteria species were diminished and 14 were enriched, both at baseline and follow-up. Those patients who had COVID but not PACS showed just 25 alterations of bacteria species at the time of hospital admission, and they all normalized by 6 months.
Having respiratory symptoms at 6 months was linked with higher levels of opportunistic pathogens such as Streptococcus anginosus and S. vestibularis. Neuropsychiatric symptoms and fatigue were associated with nosocomial pathogens that are linked to opportunistic infections, such as Clostridium innocuum and Actinomyces naeslundii (P < .05).
Bacteria known for producing butyrate, a beneficial fatty acid, were significantly depleted in those patients with hair loss. And certain of these bacteria, including Bifidobacterium pseudocatenulatum and Faecalibacterium prausnitzii, had the largest inverse correlations with PACS at 6 months (P < .05), the researchers found.
“Particular gut microbial profiles may indicate heightened susceptibility,” Dr. Ng said.
Although the findings were drawn from patients with earlier strains of the COVID-19 virus, the findings still apply to new variants, including Omicron, since these pose the same problem of persistent disruption of the immune system, Dr. Ng said.
Her group is conducting trials to look at how modulating the microbiome might prevent long COVID and boost antibodies after vaccination in high-risk people, she said.
“Gut microbiota influences the health of the host,” Dr. Ng said. “It provides crucial benefits in the form of immune system development, prevention of infections, nutrient acquisition, and brain and nervous system functionality. Considering the millions of people infected during the ongoing pandemic, our findings are a strong impetus for consideration of microbiota modulation to facilitate timely recovery and reduce the burden of post–acute COVID-19 syndrome.”
John Haran, MD, PhD, associate professor of microbiology and physiological systems and emergency medicine at the University of Massachusetts, Worcester, said the research adds to the evidence base on the gut microbiome’s links to COVID, but there was likely be no clinical impact yet. Still, he said the findings linking specific species to specific symptoms was particularly interesting.
“Very early on during hospitalization, [the researchers] saw these differences and correlated out with people who have longer symptoms, and especially different groups of people that have longer symptoms, too,” said Dr. Haran, who has done research on the topic. “It’s very different if you have different symptoms, for example, you keep coughing for months versus you have brain fog and fatigue, or other debilitating symptoms.”
Dr. Haran noted that the findings didn’t identify bacteria types especially linked to COVID, but rather species that have already been found to be associated with a “bad” microbiome. He also pointed out that the patients enrolled in the study were not vaccinated, because vaccines weren’t available at the time. Still, further study to see whether modulation of gut bacteria can be a therapy seems worthwhile.
“Microbiome modulation is pretty safe, and that’s really the next big step that needs to be taken in this,” he said.
For now, the findings don’t give the clinician much new ammunition for treatment.
“We’re not there yet,” he added. “It’s not as if clinicians are going to tell their COVID patients: ‘Go out and buy some kale.’ ”
Eugene Chang, MD, professor of medicine at the University of Chicago, who has studied the gut microbiome and gastrointestinal disease, said it’s “too preliminary” to say whether the findings could lead to a clinical impact. The measures used merely identify the microbes present, but not what they are doing.
“These measures are unlikely to perform well enough to be useful for risk assessment or predicting clinical outcomes,” he said. “That being said, advances in technology are being made where next generations of metrics could be developed and useful as stratifiers and predictors of risk.”
Seeing shifting patterns associated with certain symptoms, he said, is “notable because it suggests that the disturbances of the gut microbiota in PACS are significant.”
But he said it’s important to know whether these changes are a cause of PACS in some way or just an effect of it.
“If causative or contributory – this has to be proven – then ‘microbiota modulation’ would make sense and could be a priority for development,” he said. “If merely an effect, these metrics and better ones to come could be useful as predictors or measures of the patient’s general state of health.”
As seen in his group’s work and other work, he said, “the gut microbiota is highly sensitive to changes in their ecosystem, which is influenced by the health state of the patient.”
Dr. Ng, Dr. Haran, and Dr. Chang reported no relevant disclosures.
This article was updated Jan. 27, 2022.
While links have been found between the gut’s microbiome and COVID-19, as well as other diseases, this is the first published research to show a link specifically to COVID’s long-term effects, the investigators, based at the Chinese University of Hong Kong, wrote in Gut.
“To our knowledge, this is the first study to show that altered gut microbiome composition is strongly associated with persistent symptoms in patients with COVID-19 up to 6 months after clearance of SARS-CoV-2 virus,” said Siew Ng, MBBS, PhD, associate director at the university’s Center for Gut Microbiota Research.
At three hospitals, the researchers enrolled 106 patients with COVID-19 from February to August 2020 with stool samples at admission and at 1 month and 6 months after discharge, and compared them with people who did not have COVID, recruited in 2019. The severity of COVID in the enrolled patients was mostly mild to moderate.
At 3 months, 86 of the patients with COVID had post–acute COVID-19 syndrome (PACS) – defined as at least one persistent, otherwise unexplained symptom 4 weeks after clearance of the virus. And 81 patients had PACS at 6 months, most commonly fatigue, poor memory, hair loss, anxiety, and trouble sleeping.
Using stool samples for their analysis, the researchers found that, broadly, the diversity of the types of bacteria, and the abundance of these bacteria, were significantly lower at 6 months for those with PACS, compared with those without PACS and with controls (P < .05 and P < .0001, respectively). Among those with PACS, 28 bacteria species were diminished and 14 were enriched, both at baseline and follow-up. Those patients who had COVID but not PACS showed just 25 alterations of bacteria species at the time of hospital admission, and they all normalized by 6 months.
Having respiratory symptoms at 6 months was linked with higher levels of opportunistic pathogens such as Streptococcus anginosus and S. vestibularis. Neuropsychiatric symptoms and fatigue were associated with nosocomial pathogens that are linked to opportunistic infections, such as Clostridium innocuum and Actinomyces naeslundii (P < .05).
Bacteria known for producing butyrate, a beneficial fatty acid, were significantly depleted in those patients with hair loss. And certain of these bacteria, including Bifidobacterium pseudocatenulatum and Faecalibacterium prausnitzii, had the largest inverse correlations with PACS at 6 months (P < .05), the researchers found.
“Particular gut microbial profiles may indicate heightened susceptibility,” Dr. Ng said.
Although the findings were drawn from patients with earlier strains of the COVID-19 virus, the findings still apply to new variants, including Omicron, since these pose the same problem of persistent disruption of the immune system, Dr. Ng said.
Her group is conducting trials to look at how modulating the microbiome might prevent long COVID and boost antibodies after vaccination in high-risk people, she said.
“Gut microbiota influences the health of the host,” Dr. Ng said. “It provides crucial benefits in the form of immune system development, prevention of infections, nutrient acquisition, and brain and nervous system functionality. Considering the millions of people infected during the ongoing pandemic, our findings are a strong impetus for consideration of microbiota modulation to facilitate timely recovery and reduce the burden of post–acute COVID-19 syndrome.”
John Haran, MD, PhD, associate professor of microbiology and physiological systems and emergency medicine at the University of Massachusetts, Worcester, said the research adds to the evidence base on the gut microbiome’s links to COVID, but there was likely be no clinical impact yet. Still, he said the findings linking specific species to specific symptoms was particularly interesting.
“Very early on during hospitalization, [the researchers] saw these differences and correlated out with people who have longer symptoms, and especially different groups of people that have longer symptoms, too,” said Dr. Haran, who has done research on the topic. “It’s very different if you have different symptoms, for example, you keep coughing for months versus you have brain fog and fatigue, or other debilitating symptoms.”
Dr. Haran noted that the findings didn’t identify bacteria types especially linked to COVID, but rather species that have already been found to be associated with a “bad” microbiome. He also pointed out that the patients enrolled in the study were not vaccinated, because vaccines weren’t available at the time. Still, further study to see whether modulation of gut bacteria can be a therapy seems worthwhile.
“Microbiome modulation is pretty safe, and that’s really the next big step that needs to be taken in this,” he said.
For now, the findings don’t give the clinician much new ammunition for treatment.
“We’re not there yet,” he added. “It’s not as if clinicians are going to tell their COVID patients: ‘Go out and buy some kale.’ ”
Eugene Chang, MD, professor of medicine at the University of Chicago, who has studied the gut microbiome and gastrointestinal disease, said it’s “too preliminary” to say whether the findings could lead to a clinical impact. The measures used merely identify the microbes present, but not what they are doing.
“These measures are unlikely to perform well enough to be useful for risk assessment or predicting clinical outcomes,” he said. “That being said, advances in technology are being made where next generations of metrics could be developed and useful as stratifiers and predictors of risk.”
Seeing shifting patterns associated with certain symptoms, he said, is “notable because it suggests that the disturbances of the gut microbiota in PACS are significant.”
But he said it’s important to know whether these changes are a cause of PACS in some way or just an effect of it.
“If causative or contributory – this has to be proven – then ‘microbiota modulation’ would make sense and could be a priority for development,” he said. “If merely an effect, these metrics and better ones to come could be useful as predictors or measures of the patient’s general state of health.”
As seen in his group’s work and other work, he said, “the gut microbiota is highly sensitive to changes in their ecosystem, which is influenced by the health state of the patient.”
Dr. Ng, Dr. Haran, and Dr. Chang reported no relevant disclosures.
This article was updated Jan. 27, 2022.
While links have been found between the gut’s microbiome and COVID-19, as well as other diseases, this is the first published research to show a link specifically to COVID’s long-term effects, the investigators, based at the Chinese University of Hong Kong, wrote in Gut.
“To our knowledge, this is the first study to show that altered gut microbiome composition is strongly associated with persistent symptoms in patients with COVID-19 up to 6 months after clearance of SARS-CoV-2 virus,” said Siew Ng, MBBS, PhD, associate director at the university’s Center for Gut Microbiota Research.
At three hospitals, the researchers enrolled 106 patients with COVID-19 from February to August 2020 with stool samples at admission and at 1 month and 6 months after discharge, and compared them with people who did not have COVID, recruited in 2019. The severity of COVID in the enrolled patients was mostly mild to moderate.
At 3 months, 86 of the patients with COVID had post–acute COVID-19 syndrome (PACS) – defined as at least one persistent, otherwise unexplained symptom 4 weeks after clearance of the virus. And 81 patients had PACS at 6 months, most commonly fatigue, poor memory, hair loss, anxiety, and trouble sleeping.
Using stool samples for their analysis, the researchers found that, broadly, the diversity of the types of bacteria, and the abundance of these bacteria, were significantly lower at 6 months for those with PACS, compared with those without PACS and with controls (P < .05 and P < .0001, respectively). Among those with PACS, 28 bacteria species were diminished and 14 were enriched, both at baseline and follow-up. Those patients who had COVID but not PACS showed just 25 alterations of bacteria species at the time of hospital admission, and they all normalized by 6 months.
Having respiratory symptoms at 6 months was linked with higher levels of opportunistic pathogens such as Streptococcus anginosus and S. vestibularis. Neuropsychiatric symptoms and fatigue were associated with nosocomial pathogens that are linked to opportunistic infections, such as Clostridium innocuum and Actinomyces naeslundii (P < .05).
Bacteria known for producing butyrate, a beneficial fatty acid, were significantly depleted in those patients with hair loss. And certain of these bacteria, including Bifidobacterium pseudocatenulatum and Faecalibacterium prausnitzii, had the largest inverse correlations with PACS at 6 months (P < .05), the researchers found.
“Particular gut microbial profiles may indicate heightened susceptibility,” Dr. Ng said.
Although the findings were drawn from patients with earlier strains of the COVID-19 virus, the findings still apply to new variants, including Omicron, since these pose the same problem of persistent disruption of the immune system, Dr. Ng said.
Her group is conducting trials to look at how modulating the microbiome might prevent long COVID and boost antibodies after vaccination in high-risk people, she said.
“Gut microbiota influences the health of the host,” Dr. Ng said. “It provides crucial benefits in the form of immune system development, prevention of infections, nutrient acquisition, and brain and nervous system functionality. Considering the millions of people infected during the ongoing pandemic, our findings are a strong impetus for consideration of microbiota modulation to facilitate timely recovery and reduce the burden of post–acute COVID-19 syndrome.”
John Haran, MD, PhD, associate professor of microbiology and physiological systems and emergency medicine at the University of Massachusetts, Worcester, said the research adds to the evidence base on the gut microbiome’s links to COVID, but there was likely be no clinical impact yet. Still, he said the findings linking specific species to specific symptoms was particularly interesting.
“Very early on during hospitalization, [the researchers] saw these differences and correlated out with people who have longer symptoms, and especially different groups of people that have longer symptoms, too,” said Dr. Haran, who has done research on the topic. “It’s very different if you have different symptoms, for example, you keep coughing for months versus you have brain fog and fatigue, or other debilitating symptoms.”
Dr. Haran noted that the findings didn’t identify bacteria types especially linked to COVID, but rather species that have already been found to be associated with a “bad” microbiome. He also pointed out that the patients enrolled in the study were not vaccinated, because vaccines weren’t available at the time. Still, further study to see whether modulation of gut bacteria can be a therapy seems worthwhile.
“Microbiome modulation is pretty safe, and that’s really the next big step that needs to be taken in this,” he said.
For now, the findings don’t give the clinician much new ammunition for treatment.
“We’re not there yet,” he added. “It’s not as if clinicians are going to tell their COVID patients: ‘Go out and buy some kale.’ ”
Eugene Chang, MD, professor of medicine at the University of Chicago, who has studied the gut microbiome and gastrointestinal disease, said it’s “too preliminary” to say whether the findings could lead to a clinical impact. The measures used merely identify the microbes present, but not what they are doing.
“These measures are unlikely to perform well enough to be useful for risk assessment or predicting clinical outcomes,” he said. “That being said, advances in technology are being made where next generations of metrics could be developed and useful as stratifiers and predictors of risk.”
Seeing shifting patterns associated with certain symptoms, he said, is “notable because it suggests that the disturbances of the gut microbiota in PACS are significant.”
But he said it’s important to know whether these changes are a cause of PACS in some way or just an effect of it.
“If causative or contributory – this has to be proven – then ‘microbiota modulation’ would make sense and could be a priority for development,” he said. “If merely an effect, these metrics and better ones to come could be useful as predictors or measures of the patient’s general state of health.”
As seen in his group’s work and other work, he said, “the gut microbiota is highly sensitive to changes in their ecosystem, which is influenced by the health state of the patient.”
Dr. Ng, Dr. Haran, and Dr. Chang reported no relevant disclosures.
This article was updated Jan. 27, 2022.
FROM GUT
‘Post-truth era’ hurts COVID-19 response, trust in science
Can you tell which of the following statements are true and which are false?
COVID-19 is not a threat to younger people, and only those who have other medical conditions are dying from it.
The mRNA vaccines developed to prevent the coronavirus alter your genes, can make your body “magnetic,” and are killing more people than the virus itself.
President Joe Biden’s climate change plan calls for a ban on meat consumption to cut greenhouse gas emissions.
The 2020 presidential election was rigged and stolen.
If you guessed that all of these claims are false, you’re right – take a bow. Not a single one of these statements has any factual support, according to scientific research, legal rulings, and legitimate government authorities.
And yet public opinion surveys show millions of Americans, and others around the world, believe some of these falsehoods are true and can’t be convinced otherwise.
Social media, politicians and partisan websites, TV programs, and commentators have widely circulated these and other unfounded claims so frequently that many people say they simply can’t tell what’s objectively true and not anymore.
So much so,
The new study – The Rise and Fall of Rationality in Language, published in the Proceedings of the National Academy of Sciences – found that facts have become less important in public discourse.
As a result, unsupported beliefs have taken precedent over readily identifiable truths in discussions of health, science, and politics. The upshot: “Feelings trump facts” in social media, news reports, books, and other sources of information.
And here’s the kicker: The trend did not begin with the rise of former President Donald Trump, the COVID-19 pandemic, or the advent of social media; in fact, it has been growing for much longer than you might think.
“While the current ‘post-truth era’ has taken many by surprise, the study shows that over the past 40 years, public interest has undergone an accelerating shift from the collective to the individual, and from rationality towards emotion,” concluded the researchers from Indiana University and Wageningen University & Research in the Netherlands.
“Our work suggests that the societal balance between emotion and reason has shifted back to what it used to be around 150 years ago,” says lead researcher Marten Scheffer, PhD, a professor in the department of environmental sciences at WUR. “This implies that scientists, experts, and policymakers will have to think about the best way to respond to that social change.”
Researchers surprised by findings
The findings are based on a very detailed analysis of language from millions of books, newspaper articles, Google searches, TV reports, social media posts, and other sources dating back to 1850.
The researchers analyzed how often the 5,000 most used words appeared over the past 170 years and found that the use of those having to do with facts and reasoning, such as “determine” and “conclusion,” has fallen dramatically since 1980. Meanwhile, the use of words related to human emotion, such as “feel” and “believe,” have skyrocketed.
Dr. Scheffer notes rapid developments in science and technology from 1850 to 1980 had profound social and economic benefits that helped boost the status of the scientific approach. That shift in public attitudes had ripple effects on culture, society, education, politics, and religion – and “the role of spiritualism dwindled” in the modern world, he says.
But since 1980, that trend has seen a major reversal, with beliefs becoming more important than facts to many people, he says. At the same time, trust in science and scientists has fallen.
Dr. Scheffer says the researchers expected to find some evidence of a swing toward more belief-based sentiments during the Trump era but were surprised to discover how strong it is and that the trend has actually been a long time coming.
“The shift in interest from rational to intuitive/emotional is pretty obvious now in the post-truth political and social media discussion,” he says. “However, our work shows that it already started in the 1980s. For me personally, that went under the radar, except perhaps for the rise of alternative (to religion) forms of spirituality.
“We were especially struck by how strong the patterns are and how universal they appear across languages, nonfiction and fiction, and even in The New York Times.”
In the political world, the implications are significant enough – impacting policies and politicians on both sides of the aisle and across the globe. Just look at the deepening political divisions during the Trump presidency.
But for health and science, the spread of misinformation and falsehoods can be matters of life or death, as we have seen in the politically charged debates over how best to combat COVID-19 and global climate change.
“Our public debate seems increasingly driven by what people want to be true rather than what is actually true. As a scientist, that worries me,” says study co-author Johan Bollen, PhD, a professor of informatics at Indiana University.
“As a society, we are now faced with major collective problems that we need to approach from a pragmatic, rational, and objective perspective to be successful,” he says. “After all, global warming doesn’t care about whether you believe in it or not … but we will all suffer as a society if we fail to take adequate measures.”
For WUR co-researcher Ingrid van de Leemput, the trend isn’t merely academic; she’s seen it play out in her personal life.
“I do speak to people that, for instance, think the vaccines are poison,” she says. “I’m also on Twitter, and there, I’m every day surprised about how easily many people form their opinions, based on feelings, on what others say, or on some unfounded source.”
Public health experts say the embrace of personal beliefs over facts is one reason only 63% of Americans have been vaccinated against COVID-19. The result: millions of preventable infections among those who downplay the risks of the virus and reject the strong scientific evidence of vaccine safety and effectiveness.
“None of this really surprises me,” Johns Hopkins University social and behavioral scientist Rupali Limaye, PhD, says of the new study findings. Dr. Limaye coauthored a paper in 2016 in JAMA Pediatrics about how to talk to parents about vaccine hesitancy and the fact that we’re living in what they called “this post-truth era.”
Dr. Limaye says the trend has made it difficult for doctors, scientists, and health authorities to make fact-based arguments for COVID-19 vaccination, mask-wearing, social distancing, and other measures to control the virus.
“It’s been really hard being a scientist to hear people say, ‘Well, that’s not true’ when we say something very basic that I think all of us can agree on – like the grass is green,” she says. “To be honest, I worry that a lot of scientists are going to quit being in science because they’re exhausted.”
What’s driving the trend?
So, what’s behind the embrace of “alternative facts,” as former White House counselor Kellyanne Conway put it so brazenly in 2017, in defending the White House’s false claims that Trump’s inauguration crowd was the largest ever?
Dr. Scheffer and colleagues identified a handful of things that have encouraged the embrace of falsehoods over facts in recent years.
- The Internet: Its rise in the late 1980s, and its growing role as a primary source of news and information, has allowed more belief-based misinformation to flourish and spread like wildfire.
- Social media: The new study found the use of sentiment- and intuition-related words accelerated around 2007, along with a global surge in social media that catapulted Facebook, Twitter, and others into the mainstream, replacing more traditional fact-based media (i.e., newspapers and magazines).
- The 2007 financial crisis: The downturn in the global economy meant more people were dealing with job stress, investment losses, and other problems that fed the interest in belief-based, anti-establishment social media posts.
- Conspiracy theories: Falsehoods involving hidden political agendas, shadow “elites,” and wealthy people with dark motives tend to thrive during times of crisis and societal anxiety. “Conspiracy theories originate particularly in times of uncertainty and crisis and generally depict established institutions as hiding the truth and sustaining an unfair situation,” the researchers noted. “As a result, they may find fertile grounds on social media platforms promulgating a sense of unfairness, subsequently feeding anti-system sentiments.”
Dr. Scheffer says that growing political divisions during the Trump era have widened the fact-vs.-fiction divide. The ex-president voiced many anti-science views on global climate change, for instance, and spread so many falsehoods about COVID-19 and the 2020 election that Facebook, Twitter, and YouTube suspended his accounts.
Yet Trump remains a popular figure among Republicans, with most saying in a December poll they believe his baseless claims that the 2020 election was “rigged” and “stolen,” despite all credible, easily accessible evidence that it was secure, according to a recent poll by the University of Massachusetts at Amherst.
More than 60 courts have rejected Trump’s lawsuits seeking to overturn the election results. All 50 states, the District of Columbia, and both branches of Congress have certified the election results, giving Biden the White House. Even Trump’s own Justice Department confirmed that the 2020 election was free and fair.
Nevertheless, the University of Massachusetts survey found that most Republicans believe one or more conspiracy theories floated by the former president and those pushing his “big lie” that Democrats rigged the election to elect Biden.
Ed Berliner, an Emmy Award-winning broadcast journalist and media consultant, suggests something else is driving the spread of misinformation: the pursuit of ratings by cable TV and media companies to boost ad and subscriber revenues.
As a former executive producer and syndicated cable TV show host, he says he has seen firsthand how facts are often lost in opinion-driven news programs, even on network programs claiming to offer “fair and balanced” journalism.
“Propaganda is the new currency in America, and those who do not fight back against it are doomed to be overrun by the misinformation,” says Mr. Berliner, host of The Man in the Arena and CEO of Entourage Media LLC.
“The broadcast news media has to stop this incessant ‘infotainment’ prattle, stop trying to nuzzle up to a soft side, and bear down on hard facts, exposing the lies and refusing to back down.”
Public health implications
Public health and media experts alike say the PNAS study findings are disheartening but underscore the need for doctors and scientists to do a better job of communicating about COVID-19 and other pressing issues.
Dr. Limaye, from Johns Hopkins, is particularly concerned about the rise in conspiracy theories that has led to COVID-19 vaccine hesitancy.
“When we speak to individuals about getting the COVID vaccine…the types of concerns that come up now are very different than they were 8 years ago,” she says. “The comments we used to hear were much more related to vaccine safety. [People] would say, ‘I’m worried about an ingredient in the vaccine’ or ‘I’m worried that my kiddo has to get three different shots within 6 months to have a series dose completed.’”
But now, a lot of comments they receive are about government and pharma conspiracies.
What that means is doctors and scientists must do more than simply say “here are the facts” and “trust me, I’m a doctor or a scientist,” she says. And these approaches don’t only apply to public health.
“It’s funny, because when we talk to climate change scientists, as vaccine [specialists], we’ll say we can’t believe that people think COVID is a hoax,” she says. “And they’re like, ‘Hold my beer, we’ve been dealing with this for 20 years. Hello, it’s just your guys’ turn to deal with this public denial of science.’”
Dr. Limaye is also concerned about the impacts on funding for scientific research.
“There’s always been a really strong bipartisan effort with regards to funding for science, when you look at Congress and when you look at appropriations,” she says. “But what ended up happening, especially with the Trump administration, was that there was a real shift in that. We’ve never really seen that before in past generations.”
So, what’s the big take-home message?
Dr. Limaye believes doctors and public health experts must show more empathy – and not be combative or arrogant – in communicating science in one-on-one conversations. This month, she’s launching a new course for parents, school administrators, and nurses on how to do precisely that.
“It’s really all about how to have hard conversations with people who might be anti-science,” she says. “It’s being empathetic and not being dismissive. But it’s hard work, and I think a lot of people are just not cut out for it and just don’t have the time for it…You can’t just say, ‘Well, this is science, and I’m a doctor’ – that doesn’t work anymore.”
Brendan Nyhan, PhD, a Dartmouth College political scientist, echoes those sentiments in a separate paper recently published in the Proceedings of the National Academy of Sciences. In fact, he suggests that providing accurate, fact-based information to counter false claims may actually backfire and reinforce some people’s unfounded beliefs.
“One response to the prevalence of mistaken beliefs is to try to set the record straight by providing accurate information – for instance, by providing evidence of the scientific consensus on climate change,” he writes. “The failures of this approach, which is sometimes referred to as the ‘deficit model’ in science communication, are well-known.”
Dr. Nyhan argues two things make some people more prone to believe falsehoods:
What scientists call “ingrouping,” a kind of tribal mentality that makes some people choose social identity or politics over truth-seeking and demonize others who don’t agree with their views
The rise of high-profile political figures, such as Trump, who encourage their followers to indulge in their desire for “identify-affirming misinformation”
Dr. Scheffer says the most important thing for doctors, health experts, and scientists to recognize is that it’s crucial to gain the trust of someone who may believe fictions over facts to make any persuasive argument on COVID-19 or any other issue.
He also has a standard response to those who present falsehoods to him as facts that he suggests anyone can use: “That is interesting. Would you mind helping me understand how you came to that opinion?”
A version of this article first appeared on WebMD.com.
Can you tell which of the following statements are true and which are false?
COVID-19 is not a threat to younger people, and only those who have other medical conditions are dying from it.
The mRNA vaccines developed to prevent the coronavirus alter your genes, can make your body “magnetic,” and are killing more people than the virus itself.
President Joe Biden’s climate change plan calls for a ban on meat consumption to cut greenhouse gas emissions.
The 2020 presidential election was rigged and stolen.
If you guessed that all of these claims are false, you’re right – take a bow. Not a single one of these statements has any factual support, according to scientific research, legal rulings, and legitimate government authorities.
And yet public opinion surveys show millions of Americans, and others around the world, believe some of these falsehoods are true and can’t be convinced otherwise.
Social media, politicians and partisan websites, TV programs, and commentators have widely circulated these and other unfounded claims so frequently that many people say they simply can’t tell what’s objectively true and not anymore.
So much so,
The new study – The Rise and Fall of Rationality in Language, published in the Proceedings of the National Academy of Sciences – found that facts have become less important in public discourse.
As a result, unsupported beliefs have taken precedent over readily identifiable truths in discussions of health, science, and politics. The upshot: “Feelings trump facts” in social media, news reports, books, and other sources of information.
And here’s the kicker: The trend did not begin with the rise of former President Donald Trump, the COVID-19 pandemic, or the advent of social media; in fact, it has been growing for much longer than you might think.
“While the current ‘post-truth era’ has taken many by surprise, the study shows that over the past 40 years, public interest has undergone an accelerating shift from the collective to the individual, and from rationality towards emotion,” concluded the researchers from Indiana University and Wageningen University & Research in the Netherlands.
“Our work suggests that the societal balance between emotion and reason has shifted back to what it used to be around 150 years ago,” says lead researcher Marten Scheffer, PhD, a professor in the department of environmental sciences at WUR. “This implies that scientists, experts, and policymakers will have to think about the best way to respond to that social change.”
Researchers surprised by findings
The findings are based on a very detailed analysis of language from millions of books, newspaper articles, Google searches, TV reports, social media posts, and other sources dating back to 1850.
The researchers analyzed how often the 5,000 most used words appeared over the past 170 years and found that the use of those having to do with facts and reasoning, such as “determine” and “conclusion,” has fallen dramatically since 1980. Meanwhile, the use of words related to human emotion, such as “feel” and “believe,” have skyrocketed.
Dr. Scheffer notes rapid developments in science and technology from 1850 to 1980 had profound social and economic benefits that helped boost the status of the scientific approach. That shift in public attitudes had ripple effects on culture, society, education, politics, and religion – and “the role of spiritualism dwindled” in the modern world, he says.
But since 1980, that trend has seen a major reversal, with beliefs becoming more important than facts to many people, he says. At the same time, trust in science and scientists has fallen.
Dr. Scheffer says the researchers expected to find some evidence of a swing toward more belief-based sentiments during the Trump era but were surprised to discover how strong it is and that the trend has actually been a long time coming.
“The shift in interest from rational to intuitive/emotional is pretty obvious now in the post-truth political and social media discussion,” he says. “However, our work shows that it already started in the 1980s. For me personally, that went under the radar, except perhaps for the rise of alternative (to religion) forms of spirituality.
“We were especially struck by how strong the patterns are and how universal they appear across languages, nonfiction and fiction, and even in The New York Times.”
In the political world, the implications are significant enough – impacting policies and politicians on both sides of the aisle and across the globe. Just look at the deepening political divisions during the Trump presidency.
But for health and science, the spread of misinformation and falsehoods can be matters of life or death, as we have seen in the politically charged debates over how best to combat COVID-19 and global climate change.
“Our public debate seems increasingly driven by what people want to be true rather than what is actually true. As a scientist, that worries me,” says study co-author Johan Bollen, PhD, a professor of informatics at Indiana University.
“As a society, we are now faced with major collective problems that we need to approach from a pragmatic, rational, and objective perspective to be successful,” he says. “After all, global warming doesn’t care about whether you believe in it or not … but we will all suffer as a society if we fail to take adequate measures.”
For WUR co-researcher Ingrid van de Leemput, the trend isn’t merely academic; she’s seen it play out in her personal life.
“I do speak to people that, for instance, think the vaccines are poison,” she says. “I’m also on Twitter, and there, I’m every day surprised about how easily many people form their opinions, based on feelings, on what others say, or on some unfounded source.”
Public health experts say the embrace of personal beliefs over facts is one reason only 63% of Americans have been vaccinated against COVID-19. The result: millions of preventable infections among those who downplay the risks of the virus and reject the strong scientific evidence of vaccine safety and effectiveness.
“None of this really surprises me,” Johns Hopkins University social and behavioral scientist Rupali Limaye, PhD, says of the new study findings. Dr. Limaye coauthored a paper in 2016 in JAMA Pediatrics about how to talk to parents about vaccine hesitancy and the fact that we’re living in what they called “this post-truth era.”
Dr. Limaye says the trend has made it difficult for doctors, scientists, and health authorities to make fact-based arguments for COVID-19 vaccination, mask-wearing, social distancing, and other measures to control the virus.
“It’s been really hard being a scientist to hear people say, ‘Well, that’s not true’ when we say something very basic that I think all of us can agree on – like the grass is green,” she says. “To be honest, I worry that a lot of scientists are going to quit being in science because they’re exhausted.”
What’s driving the trend?
So, what’s behind the embrace of “alternative facts,” as former White House counselor Kellyanne Conway put it so brazenly in 2017, in defending the White House’s false claims that Trump’s inauguration crowd was the largest ever?
Dr. Scheffer and colleagues identified a handful of things that have encouraged the embrace of falsehoods over facts in recent years.
- The Internet: Its rise in the late 1980s, and its growing role as a primary source of news and information, has allowed more belief-based misinformation to flourish and spread like wildfire.
- Social media: The new study found the use of sentiment- and intuition-related words accelerated around 2007, along with a global surge in social media that catapulted Facebook, Twitter, and others into the mainstream, replacing more traditional fact-based media (i.e., newspapers and magazines).
- The 2007 financial crisis: The downturn in the global economy meant more people were dealing with job stress, investment losses, and other problems that fed the interest in belief-based, anti-establishment social media posts.
- Conspiracy theories: Falsehoods involving hidden political agendas, shadow “elites,” and wealthy people with dark motives tend to thrive during times of crisis and societal anxiety. “Conspiracy theories originate particularly in times of uncertainty and crisis and generally depict established institutions as hiding the truth and sustaining an unfair situation,” the researchers noted. “As a result, they may find fertile grounds on social media platforms promulgating a sense of unfairness, subsequently feeding anti-system sentiments.”
Dr. Scheffer says that growing political divisions during the Trump era have widened the fact-vs.-fiction divide. The ex-president voiced many anti-science views on global climate change, for instance, and spread so many falsehoods about COVID-19 and the 2020 election that Facebook, Twitter, and YouTube suspended his accounts.
Yet Trump remains a popular figure among Republicans, with most saying in a December poll they believe his baseless claims that the 2020 election was “rigged” and “stolen,” despite all credible, easily accessible evidence that it was secure, according to a recent poll by the University of Massachusetts at Amherst.
More than 60 courts have rejected Trump’s lawsuits seeking to overturn the election results. All 50 states, the District of Columbia, and both branches of Congress have certified the election results, giving Biden the White House. Even Trump’s own Justice Department confirmed that the 2020 election was free and fair.
Nevertheless, the University of Massachusetts survey found that most Republicans believe one or more conspiracy theories floated by the former president and those pushing his “big lie” that Democrats rigged the election to elect Biden.
Ed Berliner, an Emmy Award-winning broadcast journalist and media consultant, suggests something else is driving the spread of misinformation: the pursuit of ratings by cable TV and media companies to boost ad and subscriber revenues.
As a former executive producer and syndicated cable TV show host, he says he has seen firsthand how facts are often lost in opinion-driven news programs, even on network programs claiming to offer “fair and balanced” journalism.
“Propaganda is the new currency in America, and those who do not fight back against it are doomed to be overrun by the misinformation,” says Mr. Berliner, host of The Man in the Arena and CEO of Entourage Media LLC.
“The broadcast news media has to stop this incessant ‘infotainment’ prattle, stop trying to nuzzle up to a soft side, and bear down on hard facts, exposing the lies and refusing to back down.”
Public health implications
Public health and media experts alike say the PNAS study findings are disheartening but underscore the need for doctors and scientists to do a better job of communicating about COVID-19 and other pressing issues.
Dr. Limaye, from Johns Hopkins, is particularly concerned about the rise in conspiracy theories that has led to COVID-19 vaccine hesitancy.
“When we speak to individuals about getting the COVID vaccine…the types of concerns that come up now are very different than they were 8 years ago,” she says. “The comments we used to hear were much more related to vaccine safety. [People] would say, ‘I’m worried about an ingredient in the vaccine’ or ‘I’m worried that my kiddo has to get three different shots within 6 months to have a series dose completed.’”
But now, a lot of comments they receive are about government and pharma conspiracies.
What that means is doctors and scientists must do more than simply say “here are the facts” and “trust me, I’m a doctor or a scientist,” she says. And these approaches don’t only apply to public health.
“It’s funny, because when we talk to climate change scientists, as vaccine [specialists], we’ll say we can’t believe that people think COVID is a hoax,” she says. “And they’re like, ‘Hold my beer, we’ve been dealing with this for 20 years. Hello, it’s just your guys’ turn to deal with this public denial of science.’”
Dr. Limaye is also concerned about the impacts on funding for scientific research.
“There’s always been a really strong bipartisan effort with regards to funding for science, when you look at Congress and when you look at appropriations,” she says. “But what ended up happening, especially with the Trump administration, was that there was a real shift in that. We’ve never really seen that before in past generations.”
So, what’s the big take-home message?
Dr. Limaye believes doctors and public health experts must show more empathy – and not be combative or arrogant – in communicating science in one-on-one conversations. This month, she’s launching a new course for parents, school administrators, and nurses on how to do precisely that.
“It’s really all about how to have hard conversations with people who might be anti-science,” she says. “It’s being empathetic and not being dismissive. But it’s hard work, and I think a lot of people are just not cut out for it and just don’t have the time for it…You can’t just say, ‘Well, this is science, and I’m a doctor’ – that doesn’t work anymore.”
Brendan Nyhan, PhD, a Dartmouth College political scientist, echoes those sentiments in a separate paper recently published in the Proceedings of the National Academy of Sciences. In fact, he suggests that providing accurate, fact-based information to counter false claims may actually backfire and reinforce some people’s unfounded beliefs.
“One response to the prevalence of mistaken beliefs is to try to set the record straight by providing accurate information – for instance, by providing evidence of the scientific consensus on climate change,” he writes. “The failures of this approach, which is sometimes referred to as the ‘deficit model’ in science communication, are well-known.”
Dr. Nyhan argues two things make some people more prone to believe falsehoods:
What scientists call “ingrouping,” a kind of tribal mentality that makes some people choose social identity or politics over truth-seeking and demonize others who don’t agree with their views
The rise of high-profile political figures, such as Trump, who encourage their followers to indulge in their desire for “identify-affirming misinformation”
Dr. Scheffer says the most important thing for doctors, health experts, and scientists to recognize is that it’s crucial to gain the trust of someone who may believe fictions over facts to make any persuasive argument on COVID-19 or any other issue.
He also has a standard response to those who present falsehoods to him as facts that he suggests anyone can use: “That is interesting. Would you mind helping me understand how you came to that opinion?”
A version of this article first appeared on WebMD.com.
Can you tell which of the following statements are true and which are false?
COVID-19 is not a threat to younger people, and only those who have other medical conditions are dying from it.
The mRNA vaccines developed to prevent the coronavirus alter your genes, can make your body “magnetic,” and are killing more people than the virus itself.
President Joe Biden’s climate change plan calls for a ban on meat consumption to cut greenhouse gas emissions.
The 2020 presidential election was rigged and stolen.
If you guessed that all of these claims are false, you’re right – take a bow. Not a single one of these statements has any factual support, according to scientific research, legal rulings, and legitimate government authorities.
And yet public opinion surveys show millions of Americans, and others around the world, believe some of these falsehoods are true and can’t be convinced otherwise.
Social media, politicians and partisan websites, TV programs, and commentators have widely circulated these and other unfounded claims so frequently that many people say they simply can’t tell what’s objectively true and not anymore.
So much so,
The new study – The Rise and Fall of Rationality in Language, published in the Proceedings of the National Academy of Sciences – found that facts have become less important in public discourse.
As a result, unsupported beliefs have taken precedent over readily identifiable truths in discussions of health, science, and politics. The upshot: “Feelings trump facts” in social media, news reports, books, and other sources of information.
And here’s the kicker: The trend did not begin with the rise of former President Donald Trump, the COVID-19 pandemic, or the advent of social media; in fact, it has been growing for much longer than you might think.
“While the current ‘post-truth era’ has taken many by surprise, the study shows that over the past 40 years, public interest has undergone an accelerating shift from the collective to the individual, and from rationality towards emotion,” concluded the researchers from Indiana University and Wageningen University & Research in the Netherlands.
“Our work suggests that the societal balance between emotion and reason has shifted back to what it used to be around 150 years ago,” says lead researcher Marten Scheffer, PhD, a professor in the department of environmental sciences at WUR. “This implies that scientists, experts, and policymakers will have to think about the best way to respond to that social change.”
Researchers surprised by findings
The findings are based on a very detailed analysis of language from millions of books, newspaper articles, Google searches, TV reports, social media posts, and other sources dating back to 1850.
The researchers analyzed how often the 5,000 most used words appeared over the past 170 years and found that the use of those having to do with facts and reasoning, such as “determine” and “conclusion,” has fallen dramatically since 1980. Meanwhile, the use of words related to human emotion, such as “feel” and “believe,” have skyrocketed.
Dr. Scheffer notes rapid developments in science and technology from 1850 to 1980 had profound social and economic benefits that helped boost the status of the scientific approach. That shift in public attitudes had ripple effects on culture, society, education, politics, and religion – and “the role of spiritualism dwindled” in the modern world, he says.
But since 1980, that trend has seen a major reversal, with beliefs becoming more important than facts to many people, he says. At the same time, trust in science and scientists has fallen.
Dr. Scheffer says the researchers expected to find some evidence of a swing toward more belief-based sentiments during the Trump era but were surprised to discover how strong it is and that the trend has actually been a long time coming.
“The shift in interest from rational to intuitive/emotional is pretty obvious now in the post-truth political and social media discussion,” he says. “However, our work shows that it already started in the 1980s. For me personally, that went under the radar, except perhaps for the rise of alternative (to religion) forms of spirituality.
“We were especially struck by how strong the patterns are and how universal they appear across languages, nonfiction and fiction, and even in The New York Times.”
In the political world, the implications are significant enough – impacting policies and politicians on both sides of the aisle and across the globe. Just look at the deepening political divisions during the Trump presidency.
But for health and science, the spread of misinformation and falsehoods can be matters of life or death, as we have seen in the politically charged debates over how best to combat COVID-19 and global climate change.
“Our public debate seems increasingly driven by what people want to be true rather than what is actually true. As a scientist, that worries me,” says study co-author Johan Bollen, PhD, a professor of informatics at Indiana University.
“As a society, we are now faced with major collective problems that we need to approach from a pragmatic, rational, and objective perspective to be successful,” he says. “After all, global warming doesn’t care about whether you believe in it or not … but we will all suffer as a society if we fail to take adequate measures.”
For WUR co-researcher Ingrid van de Leemput, the trend isn’t merely academic; she’s seen it play out in her personal life.
“I do speak to people that, for instance, think the vaccines are poison,” she says. “I’m also on Twitter, and there, I’m every day surprised about how easily many people form their opinions, based on feelings, on what others say, or on some unfounded source.”
Public health experts say the embrace of personal beliefs over facts is one reason only 63% of Americans have been vaccinated against COVID-19. The result: millions of preventable infections among those who downplay the risks of the virus and reject the strong scientific evidence of vaccine safety and effectiveness.
“None of this really surprises me,” Johns Hopkins University social and behavioral scientist Rupali Limaye, PhD, says of the new study findings. Dr. Limaye coauthored a paper in 2016 in JAMA Pediatrics about how to talk to parents about vaccine hesitancy and the fact that we’re living in what they called “this post-truth era.”
Dr. Limaye says the trend has made it difficult for doctors, scientists, and health authorities to make fact-based arguments for COVID-19 vaccination, mask-wearing, social distancing, and other measures to control the virus.
“It’s been really hard being a scientist to hear people say, ‘Well, that’s not true’ when we say something very basic that I think all of us can agree on – like the grass is green,” she says. “To be honest, I worry that a lot of scientists are going to quit being in science because they’re exhausted.”
What’s driving the trend?
So, what’s behind the embrace of “alternative facts,” as former White House counselor Kellyanne Conway put it so brazenly in 2017, in defending the White House’s false claims that Trump’s inauguration crowd was the largest ever?
Dr. Scheffer and colleagues identified a handful of things that have encouraged the embrace of falsehoods over facts in recent years.
- The Internet: Its rise in the late 1980s, and its growing role as a primary source of news and information, has allowed more belief-based misinformation to flourish and spread like wildfire.
- Social media: The new study found the use of sentiment- and intuition-related words accelerated around 2007, along with a global surge in social media that catapulted Facebook, Twitter, and others into the mainstream, replacing more traditional fact-based media (i.e., newspapers and magazines).
- The 2007 financial crisis: The downturn in the global economy meant more people were dealing with job stress, investment losses, and other problems that fed the interest in belief-based, anti-establishment social media posts.
- Conspiracy theories: Falsehoods involving hidden political agendas, shadow “elites,” and wealthy people with dark motives tend to thrive during times of crisis and societal anxiety. “Conspiracy theories originate particularly in times of uncertainty and crisis and generally depict established institutions as hiding the truth and sustaining an unfair situation,” the researchers noted. “As a result, they may find fertile grounds on social media platforms promulgating a sense of unfairness, subsequently feeding anti-system sentiments.”
Dr. Scheffer says that growing political divisions during the Trump era have widened the fact-vs.-fiction divide. The ex-president voiced many anti-science views on global climate change, for instance, and spread so many falsehoods about COVID-19 and the 2020 election that Facebook, Twitter, and YouTube suspended his accounts.
Yet Trump remains a popular figure among Republicans, with most saying in a December poll they believe his baseless claims that the 2020 election was “rigged” and “stolen,” despite all credible, easily accessible evidence that it was secure, according to a recent poll by the University of Massachusetts at Amherst.
More than 60 courts have rejected Trump’s lawsuits seeking to overturn the election results. All 50 states, the District of Columbia, and both branches of Congress have certified the election results, giving Biden the White House. Even Trump’s own Justice Department confirmed that the 2020 election was free and fair.
Nevertheless, the University of Massachusetts survey found that most Republicans believe one or more conspiracy theories floated by the former president and those pushing his “big lie” that Democrats rigged the election to elect Biden.
Ed Berliner, an Emmy Award-winning broadcast journalist and media consultant, suggests something else is driving the spread of misinformation: the pursuit of ratings by cable TV and media companies to boost ad and subscriber revenues.
As a former executive producer and syndicated cable TV show host, he says he has seen firsthand how facts are often lost in opinion-driven news programs, even on network programs claiming to offer “fair and balanced” journalism.
“Propaganda is the new currency in America, and those who do not fight back against it are doomed to be overrun by the misinformation,” says Mr. Berliner, host of The Man in the Arena and CEO of Entourage Media LLC.
“The broadcast news media has to stop this incessant ‘infotainment’ prattle, stop trying to nuzzle up to a soft side, and bear down on hard facts, exposing the lies and refusing to back down.”
Public health implications
Public health and media experts alike say the PNAS study findings are disheartening but underscore the need for doctors and scientists to do a better job of communicating about COVID-19 and other pressing issues.
Dr. Limaye, from Johns Hopkins, is particularly concerned about the rise in conspiracy theories that has led to COVID-19 vaccine hesitancy.
“When we speak to individuals about getting the COVID vaccine…the types of concerns that come up now are very different than they were 8 years ago,” she says. “The comments we used to hear were much more related to vaccine safety. [People] would say, ‘I’m worried about an ingredient in the vaccine’ or ‘I’m worried that my kiddo has to get three different shots within 6 months to have a series dose completed.’”
But now, a lot of comments they receive are about government and pharma conspiracies.
What that means is doctors and scientists must do more than simply say “here are the facts” and “trust me, I’m a doctor or a scientist,” she says. And these approaches don’t only apply to public health.
“It’s funny, because when we talk to climate change scientists, as vaccine [specialists], we’ll say we can’t believe that people think COVID is a hoax,” she says. “And they’re like, ‘Hold my beer, we’ve been dealing with this for 20 years. Hello, it’s just your guys’ turn to deal with this public denial of science.’”
Dr. Limaye is also concerned about the impacts on funding for scientific research.
“There’s always been a really strong bipartisan effort with regards to funding for science, when you look at Congress and when you look at appropriations,” she says. “But what ended up happening, especially with the Trump administration, was that there was a real shift in that. We’ve never really seen that before in past generations.”
So, what’s the big take-home message?
Dr. Limaye believes doctors and public health experts must show more empathy – and not be combative or arrogant – in communicating science in one-on-one conversations. This month, she’s launching a new course for parents, school administrators, and nurses on how to do precisely that.
“It’s really all about how to have hard conversations with people who might be anti-science,” she says. “It’s being empathetic and not being dismissive. But it’s hard work, and I think a lot of people are just not cut out for it and just don’t have the time for it…You can’t just say, ‘Well, this is science, and I’m a doctor’ – that doesn’t work anymore.”
Brendan Nyhan, PhD, a Dartmouth College political scientist, echoes those sentiments in a separate paper recently published in the Proceedings of the National Academy of Sciences. In fact, he suggests that providing accurate, fact-based information to counter false claims may actually backfire and reinforce some people’s unfounded beliefs.
“One response to the prevalence of mistaken beliefs is to try to set the record straight by providing accurate information – for instance, by providing evidence of the scientific consensus on climate change,” he writes. “The failures of this approach, which is sometimes referred to as the ‘deficit model’ in science communication, are well-known.”
Dr. Nyhan argues two things make some people more prone to believe falsehoods:
What scientists call “ingrouping,” a kind of tribal mentality that makes some people choose social identity or politics over truth-seeking and demonize others who don’t agree with their views
The rise of high-profile political figures, such as Trump, who encourage their followers to indulge in their desire for “identify-affirming misinformation”
Dr. Scheffer says the most important thing for doctors, health experts, and scientists to recognize is that it’s crucial to gain the trust of someone who may believe fictions over facts to make any persuasive argument on COVID-19 or any other issue.
He also has a standard response to those who present falsehoods to him as facts that he suggests anyone can use: “That is interesting. Would you mind helping me understand how you came to that opinion?”
A version of this article first appeared on WebMD.com.
OTC cannabidiol products tied to improved pain, sleep, anxiety
Interim findings from Advancing CBD Education and Science, a 100% virtual, open label, randomized, controlled trial, show study participants experienced various degrees of “clinically meaningful” improvements in sleep quality, anxiety, and pain.
“ACES is the largest clinical trial ever conducted on commercially available CBD products and provides first-of-its-kind real world evidence into what conditions users may experience benefit from CBD usage, whether these benefits are clinically meaningful, what attributes of CBD products may impact health outcomes, and what side effects may occur,” study coinvestigator Jessica Saleska, PhD, MPH, director of research at Radicle Science, the company that conducted the study, told this news organization.
Scant evidence
Despite the growing market size of commercially available CBD products “there is still scant data on the effectiveness of over-the-counter cannabinoid products due to the cost, speed, and scale limitations of the current approach to scientific research,” Jeff Chen, MD, MBA, cofounder and CEO of Radicle Science, told this news organization.
One of the study’s goals, said Ethan Russo, MD, a neurologist, founder/CEO of CReDO Science, and scientific adviser for Radicle, is to help consumers make informed decisions before purchasing and using commercially available oral CBD products.
Designed to eliminate all physical infrastructure, which minimizes costs and facilitates faster execution, ACES was conducted much like a phase 4 clinical trial, collating real-world data gathered over 4 weeks.
“The process that Radicle scientists [have] advanced is sort of a crowdsourcing approach to doing clinical science,” Dr. Russo said. “Hopefully, there is going to be a considerable amount of data generated that [will] affect people’s buying options.”
The study also aimed to evaluate product attributes, including composition, mode of use, dosage, dosage timing and frequency, and their correlation to degrees of outcomes.
Dr. Russo explained why product composition is an important factor, especially when dealing with CBD. “What happens with any given [CBD] preparation is going to be totally a function of other components, if any.
“For example, there’s this mistaken notion that cannabidiol is sedating; it is not. Pure cannabidiol is stimulating in low and moderate amounts. Where the confusion has arisen is that the early chemovars containing cannabidiol were also predominant in myrcene, the sedating terpene, [thereby] creating this misimpression that it is good for sleep,” he added.
However, CBD might also affect sleep by reducing anxiety that interferes with it. “What’s clear is that cannabidiol is an antianxiety agent, if you have a sufficient dose,” Dr. Russo said.
The 4-week study included 2,704 participants aged 21 years and older, self-reporting anxiety, chronic pain, or sleep disturbances as a primary reason for taking CBD. Study participants were randomly assigned to receive 1 of 13 commercially available oral CBD extracts.
Participants were allocated to 1 of 14 cohorts, comprising 13 treatment groups with 208 participants each who received a single CBD product, or a wait-list control group of 296 participants who received product at the study’s end.
The primary outcome focused on “clinically meaningful” changes, which were defined as “distinct and palpable improvements in quality of life through improvements in respective health outcomes.”
Secondary outcomes included changes in sleep, anxiety, and pain based on several validated indices, including the PROMIS (Patient-Reported Outcome Measurement Information System) Sleep Short Form; the PROMIS Anxiety Scale; the Patient Global Impression of Change; the Pain, Enjoyment, General Activity scale; and the General Anxiety Disorder–7 scale.
The interim study results are promising, with participants reporting, on average, a 71% improvement in well-being. Additionally, 63% reported clinically meaningful improvements in anxiety, and 61% in sleep quality. The CBD products provided smaller benefits in pain management, with less than half (47%) experiencing meaningful improvements.
In addition to improvement in sleep, pain, and anxiety, these data highlight how rapidly benefits occurred; most were realized during the first week of the study, with up to 61% of treatment group participants reporting a therapeutic effect within 1-4 hours of taking their assigned product.
Overcoming the placebo effect
Commenting on the research, Justin Strickland, PhD, an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, who was not involved in the research, said without knowing a lot about the pharmacology of the products being tested, early dramatic improvements in these measures, such as sleep impairment, are common.
“There are some data to suggest that there is an expectancy effect when we talk about the therapeutic benefit of cannabinoid products, (i.e., when someone has the expectation that they are going to experience a stronger effect) but this is true of any drug in an open label trial,” Dr. Strickland added.
Dr. Russo took the point a step further. “It’s getting near impossible to look at cannabinoid compounds, even with randomized, controlled trials because of the burgeoning placebo responses. When you couple it with the fact that consumers have the mistaken notion that cannabis-based drugs are miraculous, the expectations are so high that everyone thinks that they’re on the real stuff, even if it’s a placebo group.”
Still, both Dr. Strickland and Dr. Russo highlighted the fact that ACES mirrors real-world experience, which will they hope will inform the use of CBD and CBD-based preparations moving forward. By removing certain barriers like institutional bureaucracy or federal funding restrictions inherent to more traditional randomized controlled trial design, ACES might provide data that bridge the gap between efficacy and effectiveness.
ACES was funded by Radicle Science. Dr. Chen is cofounder and CEO of Radicle Science. Dr. Russo and Dr. Strickland disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Interim findings from Advancing CBD Education and Science, a 100% virtual, open label, randomized, controlled trial, show study participants experienced various degrees of “clinically meaningful” improvements in sleep quality, anxiety, and pain.
“ACES is the largest clinical trial ever conducted on commercially available CBD products and provides first-of-its-kind real world evidence into what conditions users may experience benefit from CBD usage, whether these benefits are clinically meaningful, what attributes of CBD products may impact health outcomes, and what side effects may occur,” study coinvestigator Jessica Saleska, PhD, MPH, director of research at Radicle Science, the company that conducted the study, told this news organization.
Scant evidence
Despite the growing market size of commercially available CBD products “there is still scant data on the effectiveness of over-the-counter cannabinoid products due to the cost, speed, and scale limitations of the current approach to scientific research,” Jeff Chen, MD, MBA, cofounder and CEO of Radicle Science, told this news organization.
One of the study’s goals, said Ethan Russo, MD, a neurologist, founder/CEO of CReDO Science, and scientific adviser for Radicle, is to help consumers make informed decisions before purchasing and using commercially available oral CBD products.
Designed to eliminate all physical infrastructure, which minimizes costs and facilitates faster execution, ACES was conducted much like a phase 4 clinical trial, collating real-world data gathered over 4 weeks.
“The process that Radicle scientists [have] advanced is sort of a crowdsourcing approach to doing clinical science,” Dr. Russo said. “Hopefully, there is going to be a considerable amount of data generated that [will] affect people’s buying options.”
The study also aimed to evaluate product attributes, including composition, mode of use, dosage, dosage timing and frequency, and their correlation to degrees of outcomes.
Dr. Russo explained why product composition is an important factor, especially when dealing with CBD. “What happens with any given [CBD] preparation is going to be totally a function of other components, if any.
“For example, there’s this mistaken notion that cannabidiol is sedating; it is not. Pure cannabidiol is stimulating in low and moderate amounts. Where the confusion has arisen is that the early chemovars containing cannabidiol were also predominant in myrcene, the sedating terpene, [thereby] creating this misimpression that it is good for sleep,” he added.
However, CBD might also affect sleep by reducing anxiety that interferes with it. “What’s clear is that cannabidiol is an antianxiety agent, if you have a sufficient dose,” Dr. Russo said.
The 4-week study included 2,704 participants aged 21 years and older, self-reporting anxiety, chronic pain, or sleep disturbances as a primary reason for taking CBD. Study participants were randomly assigned to receive 1 of 13 commercially available oral CBD extracts.
Participants were allocated to 1 of 14 cohorts, comprising 13 treatment groups with 208 participants each who received a single CBD product, or a wait-list control group of 296 participants who received product at the study’s end.
The primary outcome focused on “clinically meaningful” changes, which were defined as “distinct and palpable improvements in quality of life through improvements in respective health outcomes.”
Secondary outcomes included changes in sleep, anxiety, and pain based on several validated indices, including the PROMIS (Patient-Reported Outcome Measurement Information System) Sleep Short Form; the PROMIS Anxiety Scale; the Patient Global Impression of Change; the Pain, Enjoyment, General Activity scale; and the General Anxiety Disorder–7 scale.
The interim study results are promising, with participants reporting, on average, a 71% improvement in well-being. Additionally, 63% reported clinically meaningful improvements in anxiety, and 61% in sleep quality. The CBD products provided smaller benefits in pain management, with less than half (47%) experiencing meaningful improvements.
In addition to improvement in sleep, pain, and anxiety, these data highlight how rapidly benefits occurred; most were realized during the first week of the study, with up to 61% of treatment group participants reporting a therapeutic effect within 1-4 hours of taking their assigned product.
Overcoming the placebo effect
Commenting on the research, Justin Strickland, PhD, an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, who was not involved in the research, said without knowing a lot about the pharmacology of the products being tested, early dramatic improvements in these measures, such as sleep impairment, are common.
“There are some data to suggest that there is an expectancy effect when we talk about the therapeutic benefit of cannabinoid products, (i.e., when someone has the expectation that they are going to experience a stronger effect) but this is true of any drug in an open label trial,” Dr. Strickland added.
Dr. Russo took the point a step further. “It’s getting near impossible to look at cannabinoid compounds, even with randomized, controlled trials because of the burgeoning placebo responses. When you couple it with the fact that consumers have the mistaken notion that cannabis-based drugs are miraculous, the expectations are so high that everyone thinks that they’re on the real stuff, even if it’s a placebo group.”
Still, both Dr. Strickland and Dr. Russo highlighted the fact that ACES mirrors real-world experience, which will they hope will inform the use of CBD and CBD-based preparations moving forward. By removing certain barriers like institutional bureaucracy or federal funding restrictions inherent to more traditional randomized controlled trial design, ACES might provide data that bridge the gap between efficacy and effectiveness.
ACES was funded by Radicle Science. Dr. Chen is cofounder and CEO of Radicle Science. Dr. Russo and Dr. Strickland disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Interim findings from Advancing CBD Education and Science, a 100% virtual, open label, randomized, controlled trial, show study participants experienced various degrees of “clinically meaningful” improvements in sleep quality, anxiety, and pain.
“ACES is the largest clinical trial ever conducted on commercially available CBD products and provides first-of-its-kind real world evidence into what conditions users may experience benefit from CBD usage, whether these benefits are clinically meaningful, what attributes of CBD products may impact health outcomes, and what side effects may occur,” study coinvestigator Jessica Saleska, PhD, MPH, director of research at Radicle Science, the company that conducted the study, told this news organization.
Scant evidence
Despite the growing market size of commercially available CBD products “there is still scant data on the effectiveness of over-the-counter cannabinoid products due to the cost, speed, and scale limitations of the current approach to scientific research,” Jeff Chen, MD, MBA, cofounder and CEO of Radicle Science, told this news organization.
One of the study’s goals, said Ethan Russo, MD, a neurologist, founder/CEO of CReDO Science, and scientific adviser for Radicle, is to help consumers make informed decisions before purchasing and using commercially available oral CBD products.
Designed to eliminate all physical infrastructure, which minimizes costs and facilitates faster execution, ACES was conducted much like a phase 4 clinical trial, collating real-world data gathered over 4 weeks.
“The process that Radicle scientists [have] advanced is sort of a crowdsourcing approach to doing clinical science,” Dr. Russo said. “Hopefully, there is going to be a considerable amount of data generated that [will] affect people’s buying options.”
The study also aimed to evaluate product attributes, including composition, mode of use, dosage, dosage timing and frequency, and their correlation to degrees of outcomes.
Dr. Russo explained why product composition is an important factor, especially when dealing with CBD. “What happens with any given [CBD] preparation is going to be totally a function of other components, if any.
“For example, there’s this mistaken notion that cannabidiol is sedating; it is not. Pure cannabidiol is stimulating in low and moderate amounts. Where the confusion has arisen is that the early chemovars containing cannabidiol were also predominant in myrcene, the sedating terpene, [thereby] creating this misimpression that it is good for sleep,” he added.
However, CBD might also affect sleep by reducing anxiety that interferes with it. “What’s clear is that cannabidiol is an antianxiety agent, if you have a sufficient dose,” Dr. Russo said.
The 4-week study included 2,704 participants aged 21 years and older, self-reporting anxiety, chronic pain, or sleep disturbances as a primary reason for taking CBD. Study participants were randomly assigned to receive 1 of 13 commercially available oral CBD extracts.
Participants were allocated to 1 of 14 cohorts, comprising 13 treatment groups with 208 participants each who received a single CBD product, or a wait-list control group of 296 participants who received product at the study’s end.
The primary outcome focused on “clinically meaningful” changes, which were defined as “distinct and palpable improvements in quality of life through improvements in respective health outcomes.”
Secondary outcomes included changes in sleep, anxiety, and pain based on several validated indices, including the PROMIS (Patient-Reported Outcome Measurement Information System) Sleep Short Form; the PROMIS Anxiety Scale; the Patient Global Impression of Change; the Pain, Enjoyment, General Activity scale; and the General Anxiety Disorder–7 scale.
The interim study results are promising, with participants reporting, on average, a 71% improvement in well-being. Additionally, 63% reported clinically meaningful improvements in anxiety, and 61% in sleep quality. The CBD products provided smaller benefits in pain management, with less than half (47%) experiencing meaningful improvements.
In addition to improvement in sleep, pain, and anxiety, these data highlight how rapidly benefits occurred; most were realized during the first week of the study, with up to 61% of treatment group participants reporting a therapeutic effect within 1-4 hours of taking their assigned product.
Overcoming the placebo effect
Commenting on the research, Justin Strickland, PhD, an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, who was not involved in the research, said without knowing a lot about the pharmacology of the products being tested, early dramatic improvements in these measures, such as sleep impairment, are common.
“There are some data to suggest that there is an expectancy effect when we talk about the therapeutic benefit of cannabinoid products, (i.e., when someone has the expectation that they are going to experience a stronger effect) but this is true of any drug in an open label trial,” Dr. Strickland added.
Dr. Russo took the point a step further. “It’s getting near impossible to look at cannabinoid compounds, even with randomized, controlled trials because of the burgeoning placebo responses. When you couple it with the fact that consumers have the mistaken notion that cannabis-based drugs are miraculous, the expectations are so high that everyone thinks that they’re on the real stuff, even if it’s a placebo group.”
Still, both Dr. Strickland and Dr. Russo highlighted the fact that ACES mirrors real-world experience, which will they hope will inform the use of CBD and CBD-based preparations moving forward. By removing certain barriers like institutional bureaucracy or federal funding restrictions inherent to more traditional randomized controlled trial design, ACES might provide data that bridge the gap between efficacy and effectiveness.
ACES was funded by Radicle Science. Dr. Chen is cofounder and CEO of Radicle Science. Dr. Russo and Dr. Strickland disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Physician burnout, depression compounded by COVID: Survey
In 2020, it was hard to imagine that the situation could get worse for doctors.
But 2021 presented a new set of challenges. As quarantines lifted and physicians tried to get back to work, they were forced to deal with reduced staff, continuing COVID stress, and pandemic-related anxieties about family and loved ones.
Medscape’s National Burnout and Depression Report 2022 asked more than 13,000 physicians from 29 specialties to share details about their lives and struggles with burnout and depression in 2021. The results paint a picture of physicians trying to fulfill their mission to care for patients, but struggling to maintain their own well-being amid a global pandemic.
Burnout bump
In 2021’s report, 42% of physicians said they were burned out. In 2022, that number increased to 47%. Perhaps not surprisingly, burnout among emergency physicians took the biggest leap, increasing from 43% to 60%. Critical care (56%), ob.gyn. (53%), and infectious disease and family medicine (both at 51%) rounded out the top five specialties with doctors experiencing burnout in 2021.
Burnout has typically been a greater problem for women than men physicians, and the pandemic hasn’t changed that. “There’s no question that women have reported far more role strain during the pandemic than men,” says Carol A. Bernstein, MD, psychiatrist at Montefiore Health System and professor and vice chair for faculty development and well-being at the Albert Einstein College of Medicine, both in New York. And indeed, 56% of women and 41% of men reported burnout in the 2022 survey.
The causes, however, weren’t especially pandemic related – or at least not directly. As in previous surveys, the major contributing factor to burnout was too much paperwork (60%), such as charting and other bureaucratic tasks. Treating COVID-19 patients was cited as the major source of stress by 10% of respondents. About 34% said too many hours at work was the biggest contributing factor to burnout.
The nature of the beast
What is burnout like for these doctors? One described the conditions that lead to burnout like this: “I barely spend enough time with most patients, just running from one to the next; and then after work, I spend hours documenting, charting, dealing with reports. I feel like an overpaid clerk.” Another said: “Where’s the relationships with patients that used to make this worthwhile?” Others fingered staffing shortages at work or an overwhelming home life: “Staff calls in sick; we’re all running around trying to find things and get things done. It never ends.”
Of those who do experience burnout, the problem reaches beyond the workplace, with 54% saying that their burnout has a strong/severe impact on life and 68% reporting that burnout affects their relationships. One respondent said: “I’m always tired; I have trouble concentrating, no time for the children, more arguments with my hubby.” Another put it this way: “Home is just as busy and chaotic as work. I can never relax.”
It doesn’t help matters that physicians are likely to think they’re the only professionals experiencing job burnout. For example, only 36% of respondents believe teachers experience comparable burnout, yet more than 41% of teachers leave the profession within 5 years of starting – often because of burnout.
When it comes to methods for coping with burnout, exercise is the clear favorite, with 63% of respondents saying exercise helps maintain their mental health. About 41% talk with family members or close friends. However, less healthy coping mechanisms were cited as well, such as isolating themselves from others (45%), sleeping (41%), and eating junk food (35%) or drinking alcohol (24%).
When it comes to trying to alleviate burnout, 29% have tried meditation or similar stress-reduction techniques, while others have reduced their work hours (29%) or changed their work settings (19%).
‘Now I feel like there’s no hope’
About a fifth of physicians (21%) said they suffered from clinical depression, and 64% reported feeling “blue, down, or sad.” One physician characterized their depression this way: “I used to think my life would be great. Now I feel like there’s no hope, this will never get better, I’ll never be happy.”
Of doctors reporting depression, 53% said their illness did not affect their interactions with patients, while 34% said depression caused them to be more easily exasperated by patients.
When asked about seeking help for depression, about half (49%) said they believed they could deal with emotional stress on their own. Unfortunately, fear of medical boards finding out keeps 43% of physicians from reaching out for help, according to the survey.
A version of this article first appeared on Medscape.com.
In 2020, it was hard to imagine that the situation could get worse for doctors.
But 2021 presented a new set of challenges. As quarantines lifted and physicians tried to get back to work, they were forced to deal with reduced staff, continuing COVID stress, and pandemic-related anxieties about family and loved ones.
Medscape’s National Burnout and Depression Report 2022 asked more than 13,000 physicians from 29 specialties to share details about their lives and struggles with burnout and depression in 2021. The results paint a picture of physicians trying to fulfill their mission to care for patients, but struggling to maintain their own well-being amid a global pandemic.
Burnout bump
In 2021’s report, 42% of physicians said they were burned out. In 2022, that number increased to 47%. Perhaps not surprisingly, burnout among emergency physicians took the biggest leap, increasing from 43% to 60%. Critical care (56%), ob.gyn. (53%), and infectious disease and family medicine (both at 51%) rounded out the top five specialties with doctors experiencing burnout in 2021.
Burnout has typically been a greater problem for women than men physicians, and the pandemic hasn’t changed that. “There’s no question that women have reported far more role strain during the pandemic than men,” says Carol A. Bernstein, MD, psychiatrist at Montefiore Health System and professor and vice chair for faculty development and well-being at the Albert Einstein College of Medicine, both in New York. And indeed, 56% of women and 41% of men reported burnout in the 2022 survey.
The causes, however, weren’t especially pandemic related – or at least not directly. As in previous surveys, the major contributing factor to burnout was too much paperwork (60%), such as charting and other bureaucratic tasks. Treating COVID-19 patients was cited as the major source of stress by 10% of respondents. About 34% said too many hours at work was the biggest contributing factor to burnout.
The nature of the beast
What is burnout like for these doctors? One described the conditions that lead to burnout like this: “I barely spend enough time with most patients, just running from one to the next; and then after work, I spend hours documenting, charting, dealing with reports. I feel like an overpaid clerk.” Another said: “Where’s the relationships with patients that used to make this worthwhile?” Others fingered staffing shortages at work or an overwhelming home life: “Staff calls in sick; we’re all running around trying to find things and get things done. It never ends.”
Of those who do experience burnout, the problem reaches beyond the workplace, with 54% saying that their burnout has a strong/severe impact on life and 68% reporting that burnout affects their relationships. One respondent said: “I’m always tired; I have trouble concentrating, no time for the children, more arguments with my hubby.” Another put it this way: “Home is just as busy and chaotic as work. I can never relax.”
It doesn’t help matters that physicians are likely to think they’re the only professionals experiencing job burnout. For example, only 36% of respondents believe teachers experience comparable burnout, yet more than 41% of teachers leave the profession within 5 years of starting – often because of burnout.
When it comes to methods for coping with burnout, exercise is the clear favorite, with 63% of respondents saying exercise helps maintain their mental health. About 41% talk with family members or close friends. However, less healthy coping mechanisms were cited as well, such as isolating themselves from others (45%), sleeping (41%), and eating junk food (35%) or drinking alcohol (24%).
When it comes to trying to alleviate burnout, 29% have tried meditation or similar stress-reduction techniques, while others have reduced their work hours (29%) or changed their work settings (19%).
‘Now I feel like there’s no hope’
About a fifth of physicians (21%) said they suffered from clinical depression, and 64% reported feeling “blue, down, or sad.” One physician characterized their depression this way: “I used to think my life would be great. Now I feel like there’s no hope, this will never get better, I’ll never be happy.”
Of doctors reporting depression, 53% said their illness did not affect their interactions with patients, while 34% said depression caused them to be more easily exasperated by patients.
When asked about seeking help for depression, about half (49%) said they believed they could deal with emotional stress on their own. Unfortunately, fear of medical boards finding out keeps 43% of physicians from reaching out for help, according to the survey.
A version of this article first appeared on Medscape.com.
In 2020, it was hard to imagine that the situation could get worse for doctors.
But 2021 presented a new set of challenges. As quarantines lifted and physicians tried to get back to work, they were forced to deal with reduced staff, continuing COVID stress, and pandemic-related anxieties about family and loved ones.
Medscape’s National Burnout and Depression Report 2022 asked more than 13,000 physicians from 29 specialties to share details about their lives and struggles with burnout and depression in 2021. The results paint a picture of physicians trying to fulfill their mission to care for patients, but struggling to maintain their own well-being amid a global pandemic.
Burnout bump
In 2021’s report, 42% of physicians said they were burned out. In 2022, that number increased to 47%. Perhaps not surprisingly, burnout among emergency physicians took the biggest leap, increasing from 43% to 60%. Critical care (56%), ob.gyn. (53%), and infectious disease and family medicine (both at 51%) rounded out the top five specialties with doctors experiencing burnout in 2021.
Burnout has typically been a greater problem for women than men physicians, and the pandemic hasn’t changed that. “There’s no question that women have reported far more role strain during the pandemic than men,” says Carol A. Bernstein, MD, psychiatrist at Montefiore Health System and professor and vice chair for faculty development and well-being at the Albert Einstein College of Medicine, both in New York. And indeed, 56% of women and 41% of men reported burnout in the 2022 survey.
The causes, however, weren’t especially pandemic related – or at least not directly. As in previous surveys, the major contributing factor to burnout was too much paperwork (60%), such as charting and other bureaucratic tasks. Treating COVID-19 patients was cited as the major source of stress by 10% of respondents. About 34% said too many hours at work was the biggest contributing factor to burnout.
The nature of the beast
What is burnout like for these doctors? One described the conditions that lead to burnout like this: “I barely spend enough time with most patients, just running from one to the next; and then after work, I spend hours documenting, charting, dealing with reports. I feel like an overpaid clerk.” Another said: “Where’s the relationships with patients that used to make this worthwhile?” Others fingered staffing shortages at work or an overwhelming home life: “Staff calls in sick; we’re all running around trying to find things and get things done. It never ends.”
Of those who do experience burnout, the problem reaches beyond the workplace, with 54% saying that their burnout has a strong/severe impact on life and 68% reporting that burnout affects their relationships. One respondent said: “I’m always tired; I have trouble concentrating, no time for the children, more arguments with my hubby.” Another put it this way: “Home is just as busy and chaotic as work. I can never relax.”
It doesn’t help matters that physicians are likely to think they’re the only professionals experiencing job burnout. For example, only 36% of respondents believe teachers experience comparable burnout, yet more than 41% of teachers leave the profession within 5 years of starting – often because of burnout.
When it comes to methods for coping with burnout, exercise is the clear favorite, with 63% of respondents saying exercise helps maintain their mental health. About 41% talk with family members or close friends. However, less healthy coping mechanisms were cited as well, such as isolating themselves from others (45%), sleeping (41%), and eating junk food (35%) or drinking alcohol (24%).
When it comes to trying to alleviate burnout, 29% have tried meditation or similar stress-reduction techniques, while others have reduced their work hours (29%) or changed their work settings (19%).
‘Now I feel like there’s no hope’
About a fifth of physicians (21%) said they suffered from clinical depression, and 64% reported feeling “blue, down, or sad.” One physician characterized their depression this way: “I used to think my life would be great. Now I feel like there’s no hope, this will never get better, I’ll never be happy.”
Of doctors reporting depression, 53% said their illness did not affect their interactions with patients, while 34% said depression caused them to be more easily exasperated by patients.
When asked about seeking help for depression, about half (49%) said they believed they could deal with emotional stress on their own. Unfortunately, fear of medical boards finding out keeps 43% of physicians from reaching out for help, according to the survey.
A version of this article first appeared on Medscape.com.
Phase 2 studies of novel JAK1 inhibitor for HS show promise
results from two small phase 2 studies showed.
“INCB054707 is an oral, small-molecule JAK1 inhibitor with approximately 52-fold greater selectivity for JAK1 versus JAK2,” researchers led by Afsaneh Alavi, MD, of the Mayo Clinic in Rochester, Minn., wrote in an article published recently in the British Journal of Dermatology. “Specifically targeting JAK1, a critical regulator of proinflammatory cytokine signaling implicated in several immune-related diseases, may reduce cytokine signaling involved in HS pathogenesis while limiting JAK2-mediated cytopenias.”
For the first study, 10 patients received 15 mg INCB054707 once daily for 8 weeks (NCT03569371). For the second study, 35 patients were randomized to 30, 60, or 90 mg INCB054707 once daily or placebo (3:1 within each cohort) for 8 weeks (NCT03607487). Eligibility criteria for both studies included patients with Hurley stage II/III HS who aged 18-75 years with lesions present in two or more anatomic locations, and a total abscess and inflammatory nodule count of three or more. The primary endpoint for both studies was safety and tolerability. Secondary endpoints included HS Clinical Response (HiSCR) and other efficacy measures.
The researchers reported that 30% of patients in study 1 and 42.3% of patients who received INCB054707 in study 2 experienced one or more treatment-emergent adverse event, most commonly upper respiratory tract infection. Among evaluable patients, 3 patients (42.9%) in study 1 and 17 patients in study 2 (65.4%) achieved HiSCR at week 8, compared with 57.1% of those in the placebo group. By dosing, 55.6% in the 30-mg group achieved HiSCR at week 8, compared with 55.6% in the 60-mg group and 87.5% in the 90-mg group.
“In conclusion, safety and efficacy findings from these two phase 2 studies establish proof of concept for the JAK1 inhibitor INCB054707 in the treatment of moderate to severe HS,” the authors wrote. “A phase 2, dose-ranging, placebo-controlled study exploring three dose levels and including approximately 200 patients is ongoing (NCT04476043) and expected to provide additional evidence of the safety and efficacy profile of INCB054707 in patients with HS.”
INCB054707 is being developed by Incyte Corporation. Dr. Alavi disclosed that she has received honoraria as a consultant or advisory board participant from AbbVie, Janssen, Novartis, Boehringer Ingelheim, InflaRX, and UCB, and received honoraria as an investigator for Boehringer Ingelheim and Processa.
results from two small phase 2 studies showed.
“INCB054707 is an oral, small-molecule JAK1 inhibitor with approximately 52-fold greater selectivity for JAK1 versus JAK2,” researchers led by Afsaneh Alavi, MD, of the Mayo Clinic in Rochester, Minn., wrote in an article published recently in the British Journal of Dermatology. “Specifically targeting JAK1, a critical regulator of proinflammatory cytokine signaling implicated in several immune-related diseases, may reduce cytokine signaling involved in HS pathogenesis while limiting JAK2-mediated cytopenias.”
For the first study, 10 patients received 15 mg INCB054707 once daily for 8 weeks (NCT03569371). For the second study, 35 patients were randomized to 30, 60, or 90 mg INCB054707 once daily or placebo (3:1 within each cohort) for 8 weeks (NCT03607487). Eligibility criteria for both studies included patients with Hurley stage II/III HS who aged 18-75 years with lesions present in two or more anatomic locations, and a total abscess and inflammatory nodule count of three or more. The primary endpoint for both studies was safety and tolerability. Secondary endpoints included HS Clinical Response (HiSCR) and other efficacy measures.
The researchers reported that 30% of patients in study 1 and 42.3% of patients who received INCB054707 in study 2 experienced one or more treatment-emergent adverse event, most commonly upper respiratory tract infection. Among evaluable patients, 3 patients (42.9%) in study 1 and 17 patients in study 2 (65.4%) achieved HiSCR at week 8, compared with 57.1% of those in the placebo group. By dosing, 55.6% in the 30-mg group achieved HiSCR at week 8, compared with 55.6% in the 60-mg group and 87.5% in the 90-mg group.
“In conclusion, safety and efficacy findings from these two phase 2 studies establish proof of concept for the JAK1 inhibitor INCB054707 in the treatment of moderate to severe HS,” the authors wrote. “A phase 2, dose-ranging, placebo-controlled study exploring three dose levels and including approximately 200 patients is ongoing (NCT04476043) and expected to provide additional evidence of the safety and efficacy profile of INCB054707 in patients with HS.”
INCB054707 is being developed by Incyte Corporation. Dr. Alavi disclosed that she has received honoraria as a consultant or advisory board participant from AbbVie, Janssen, Novartis, Boehringer Ingelheim, InflaRX, and UCB, and received honoraria as an investigator for Boehringer Ingelheim and Processa.
results from two small phase 2 studies showed.
“INCB054707 is an oral, small-molecule JAK1 inhibitor with approximately 52-fold greater selectivity for JAK1 versus JAK2,” researchers led by Afsaneh Alavi, MD, of the Mayo Clinic in Rochester, Minn., wrote in an article published recently in the British Journal of Dermatology. “Specifically targeting JAK1, a critical regulator of proinflammatory cytokine signaling implicated in several immune-related diseases, may reduce cytokine signaling involved in HS pathogenesis while limiting JAK2-mediated cytopenias.”
For the first study, 10 patients received 15 mg INCB054707 once daily for 8 weeks (NCT03569371). For the second study, 35 patients were randomized to 30, 60, or 90 mg INCB054707 once daily or placebo (3:1 within each cohort) for 8 weeks (NCT03607487). Eligibility criteria for both studies included patients with Hurley stage II/III HS who aged 18-75 years with lesions present in two or more anatomic locations, and a total abscess and inflammatory nodule count of three or more. The primary endpoint for both studies was safety and tolerability. Secondary endpoints included HS Clinical Response (HiSCR) and other efficacy measures.
The researchers reported that 30% of patients in study 1 and 42.3% of patients who received INCB054707 in study 2 experienced one or more treatment-emergent adverse event, most commonly upper respiratory tract infection. Among evaluable patients, 3 patients (42.9%) in study 1 and 17 patients in study 2 (65.4%) achieved HiSCR at week 8, compared with 57.1% of those in the placebo group. By dosing, 55.6% in the 30-mg group achieved HiSCR at week 8, compared with 55.6% in the 60-mg group and 87.5% in the 90-mg group.
“In conclusion, safety and efficacy findings from these two phase 2 studies establish proof of concept for the JAK1 inhibitor INCB054707 in the treatment of moderate to severe HS,” the authors wrote. “A phase 2, dose-ranging, placebo-controlled study exploring three dose levels and including approximately 200 patients is ongoing (NCT04476043) and expected to provide additional evidence of the safety and efficacy profile of INCB054707 in patients with HS.”
INCB054707 is being developed by Incyte Corporation. Dr. Alavi disclosed that she has received honoraria as a consultant or advisory board participant from AbbVie, Janssen, Novartis, Boehringer Ingelheim, InflaRX, and UCB, and received honoraria as an investigator for Boehringer Ingelheim and Processa.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
More than a month after launch, iPLEDGE glitches persist
which mandates the program to prevent fetal exposure to the teratogenic effects of isotretinoin, and by the American Academy of Dermatology Association, whose members have repeatedly asked the FDA for meetings to discuss solutions. The AADA is the legislative and advocacy arm of AAD.
When the new program launched Dec. 13, 2021, the website crashed repeatedly, with physicians and patients complaining they got locked out or bounced off the platform when they tried to follow instructions to enter information. Hold times to talk to a live person stretched to hours.
The latest improvement attempt, announced Jan. 14 by the FDA, is a tool created by the Isotretinoin Products Manufacturers Group, the manufacturers responsible for the FDA-mandated REMS program. It is meant to allow prescribers and designees to send log-in links directly to patients’ email accounts through the iPLEDGE REMS portal, bypassing the troublesome call center.
And it’s not the answer, dermatologists said.
“The new tool does not solve issues such as prescribers or pharmacies not being able to access the site, unacceptably long call center wait times, inefficiencies caused by frequent attestation requirements for those who cannot become pregnant, patients becoming ‘locked out’ because they missed a window period through no fault of their own, among others,” said John Barbieri, MD, MBA, director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital and instructor in dermatology at Harvard Medical School, both in Boston.
The day after the FDA update about the new tool, Klint Peebles, MD, a dermatologist at Kaiser Permanente in Washington, D.C., tweeted: “Lip service and empty words.” He noted that the situation has been “disastrous from the start” as the new platform launched.
Under the iPLEDGE program in place for the acne drug, physicians, patients, and pharmacies prescribing, using, or dispensing the drug must all be registered, with requirements that include the use of two forms of an effective contraceptive and regular pregnancy testing for patients who can become pregnant.
The aim of the new gender-neutral approach to the risk mitigation program is to make the experience more inclusive for transgender patients. The previous three risk categories (females of reproductive potential, females not of reproductive potential, and males) are now reduced to just two (those capable of getting pregnant and those not capable of getting pregnant).
The problem is the execution of the new platform. The transition from the old website to the new was done quickly. By most accounts, the Dec. 13 rollout was chaotic, a failure, and disastrous, triggering numerous expressions of frustration on Twitter and other social media, with some calling for the program to be halted until the bugs could be worked out.
“While the new gender-neutral categories are a welcome improvement to the system, the new categorization approach was not the underlying reason for the new platform and its failed rollout, which was instead due to a change in vendor,” Dr. Barbieri told this news organization.
AADA: More recent efforts to improve the system
“We have a letter to the FDA asking for a stakeholders meeting to include us, the IPMG, and pharmacists because there are ongoing problems, though there have been some improvement in terms of certain elements,” Ilona Frieden, MD, chair of the AADA’s iPLEDGE Workgroup and professor of dermatology at the University of California, San Francisco, said in an interview shortly after the FDA posted the update on the new tool. “That said, there are many patients who have not gotten isotretinoin during the 1 month since the roll-out of the new platform.”
What still needs to be fixed? “We have ongoing concerns about the lack of transparency of the IPMG, about call center wait times, actual number of prescriptions on the hands of patients compared to the previous month, and those patients who can get pregnant who – despite complying with all of the REMS requirements – are being locked out because of the lack of timely attestation to their negative pregnancy status due to the website, not the patients themselves,” Dr. Frieden told this news organization.
“We are continuing to advocate to have decreased attestation requirements for individuals who cannot become pregnant – because this will improve the efficiency of the system for those patients for whom the REMS program goals are truly intended – those who can become pregnant, since the primary aim of the REMS program is to minimize fetal exposure.”
An AADA spokesperson said that the IPMG has invited the AADA to a joint stakeholders meeting on Jan. 26, along with representatives from the FDA and pharmacy industry.
Spotty progress
“The iPLEDGE situation is as frustrating as ever,” said Neil S. Goldberg, MD, a dermatologist in Westchester County, New York, after the FDA’s Jan. 14 update was released. “It’s like they never tested the new website before deploying it.”
Among the issues he has experienced in his practice, he said, is an instance in which iPLEDGE swapped the first names of a mother and daughter, so it was impossible to fill the prescription. “It happened twice in the same day,” Dr. Goldberg said. The patient had to call iPLEDGE to fix this, but the call center wasn’t taking calls.
In today’s technology environment, he said, it’s hard to believe that “we have to put up with this.”
Some have seen success. ‘’The tool is working fine on our end,” said Mitesh Patel, PharmD, pharmacy manager at Sunshine Pharmacy in White Plains, N.Y. However, he added that some doctors and patients are still having issues. He encourages dermatologists still having issues with the system to reach out to independent pharmacies that have processed iPLEDGE prescriptions and ‘’lean on them to assist.”
This news organization contacted CVS and Walgreens about how the system is working at their locations, but has not yet received a response.
Dr. Goldberg, Dr. Frieden, Dr. Barbieri, and Dr. Peebles have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This story was updated on 1/24/22.
which mandates the program to prevent fetal exposure to the teratogenic effects of isotretinoin, and by the American Academy of Dermatology Association, whose members have repeatedly asked the FDA for meetings to discuss solutions. The AADA is the legislative and advocacy arm of AAD.
When the new program launched Dec. 13, 2021, the website crashed repeatedly, with physicians and patients complaining they got locked out or bounced off the platform when they tried to follow instructions to enter information. Hold times to talk to a live person stretched to hours.
The latest improvement attempt, announced Jan. 14 by the FDA, is a tool created by the Isotretinoin Products Manufacturers Group, the manufacturers responsible for the FDA-mandated REMS program. It is meant to allow prescribers and designees to send log-in links directly to patients’ email accounts through the iPLEDGE REMS portal, bypassing the troublesome call center.
And it’s not the answer, dermatologists said.
“The new tool does not solve issues such as prescribers or pharmacies not being able to access the site, unacceptably long call center wait times, inefficiencies caused by frequent attestation requirements for those who cannot become pregnant, patients becoming ‘locked out’ because they missed a window period through no fault of their own, among others,” said John Barbieri, MD, MBA, director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital and instructor in dermatology at Harvard Medical School, both in Boston.
The day after the FDA update about the new tool, Klint Peebles, MD, a dermatologist at Kaiser Permanente in Washington, D.C., tweeted: “Lip service and empty words.” He noted that the situation has been “disastrous from the start” as the new platform launched.
Under the iPLEDGE program in place for the acne drug, physicians, patients, and pharmacies prescribing, using, or dispensing the drug must all be registered, with requirements that include the use of two forms of an effective contraceptive and regular pregnancy testing for patients who can become pregnant.
The aim of the new gender-neutral approach to the risk mitigation program is to make the experience more inclusive for transgender patients. The previous three risk categories (females of reproductive potential, females not of reproductive potential, and males) are now reduced to just two (those capable of getting pregnant and those not capable of getting pregnant).
The problem is the execution of the new platform. The transition from the old website to the new was done quickly. By most accounts, the Dec. 13 rollout was chaotic, a failure, and disastrous, triggering numerous expressions of frustration on Twitter and other social media, with some calling for the program to be halted until the bugs could be worked out.
“While the new gender-neutral categories are a welcome improvement to the system, the new categorization approach was not the underlying reason for the new platform and its failed rollout, which was instead due to a change in vendor,” Dr. Barbieri told this news organization.
AADA: More recent efforts to improve the system
“We have a letter to the FDA asking for a stakeholders meeting to include us, the IPMG, and pharmacists because there are ongoing problems, though there have been some improvement in terms of certain elements,” Ilona Frieden, MD, chair of the AADA’s iPLEDGE Workgroup and professor of dermatology at the University of California, San Francisco, said in an interview shortly after the FDA posted the update on the new tool. “That said, there are many patients who have not gotten isotretinoin during the 1 month since the roll-out of the new platform.”
What still needs to be fixed? “We have ongoing concerns about the lack of transparency of the IPMG, about call center wait times, actual number of prescriptions on the hands of patients compared to the previous month, and those patients who can get pregnant who – despite complying with all of the REMS requirements – are being locked out because of the lack of timely attestation to their negative pregnancy status due to the website, not the patients themselves,” Dr. Frieden told this news organization.
“We are continuing to advocate to have decreased attestation requirements for individuals who cannot become pregnant – because this will improve the efficiency of the system for those patients for whom the REMS program goals are truly intended – those who can become pregnant, since the primary aim of the REMS program is to minimize fetal exposure.”
An AADA spokesperson said that the IPMG has invited the AADA to a joint stakeholders meeting on Jan. 26, along with representatives from the FDA and pharmacy industry.
Spotty progress
“The iPLEDGE situation is as frustrating as ever,” said Neil S. Goldberg, MD, a dermatologist in Westchester County, New York, after the FDA’s Jan. 14 update was released. “It’s like they never tested the new website before deploying it.”
Among the issues he has experienced in his practice, he said, is an instance in which iPLEDGE swapped the first names of a mother and daughter, so it was impossible to fill the prescription. “It happened twice in the same day,” Dr. Goldberg said. The patient had to call iPLEDGE to fix this, but the call center wasn’t taking calls.
In today’s technology environment, he said, it’s hard to believe that “we have to put up with this.”
Some have seen success. ‘’The tool is working fine on our end,” said Mitesh Patel, PharmD, pharmacy manager at Sunshine Pharmacy in White Plains, N.Y. However, he added that some doctors and patients are still having issues. He encourages dermatologists still having issues with the system to reach out to independent pharmacies that have processed iPLEDGE prescriptions and ‘’lean on them to assist.”
This news organization contacted CVS and Walgreens about how the system is working at their locations, but has not yet received a response.
Dr. Goldberg, Dr. Frieden, Dr. Barbieri, and Dr. Peebles have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This story was updated on 1/24/22.
which mandates the program to prevent fetal exposure to the teratogenic effects of isotretinoin, and by the American Academy of Dermatology Association, whose members have repeatedly asked the FDA for meetings to discuss solutions. The AADA is the legislative and advocacy arm of AAD.
When the new program launched Dec. 13, 2021, the website crashed repeatedly, with physicians and patients complaining they got locked out or bounced off the platform when they tried to follow instructions to enter information. Hold times to talk to a live person stretched to hours.
The latest improvement attempt, announced Jan. 14 by the FDA, is a tool created by the Isotretinoin Products Manufacturers Group, the manufacturers responsible for the FDA-mandated REMS program. It is meant to allow prescribers and designees to send log-in links directly to patients’ email accounts through the iPLEDGE REMS portal, bypassing the troublesome call center.
And it’s not the answer, dermatologists said.
“The new tool does not solve issues such as prescribers or pharmacies not being able to access the site, unacceptably long call center wait times, inefficiencies caused by frequent attestation requirements for those who cannot become pregnant, patients becoming ‘locked out’ because they missed a window period through no fault of their own, among others,” said John Barbieri, MD, MBA, director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital and instructor in dermatology at Harvard Medical School, both in Boston.
The day after the FDA update about the new tool, Klint Peebles, MD, a dermatologist at Kaiser Permanente in Washington, D.C., tweeted: “Lip service and empty words.” He noted that the situation has been “disastrous from the start” as the new platform launched.
Under the iPLEDGE program in place for the acne drug, physicians, patients, and pharmacies prescribing, using, or dispensing the drug must all be registered, with requirements that include the use of two forms of an effective contraceptive and regular pregnancy testing for patients who can become pregnant.
The aim of the new gender-neutral approach to the risk mitigation program is to make the experience more inclusive for transgender patients. The previous three risk categories (females of reproductive potential, females not of reproductive potential, and males) are now reduced to just two (those capable of getting pregnant and those not capable of getting pregnant).
The problem is the execution of the new platform. The transition from the old website to the new was done quickly. By most accounts, the Dec. 13 rollout was chaotic, a failure, and disastrous, triggering numerous expressions of frustration on Twitter and other social media, with some calling for the program to be halted until the bugs could be worked out.
“While the new gender-neutral categories are a welcome improvement to the system, the new categorization approach was not the underlying reason for the new platform and its failed rollout, which was instead due to a change in vendor,” Dr. Barbieri told this news organization.
AADA: More recent efforts to improve the system
“We have a letter to the FDA asking for a stakeholders meeting to include us, the IPMG, and pharmacists because there are ongoing problems, though there have been some improvement in terms of certain elements,” Ilona Frieden, MD, chair of the AADA’s iPLEDGE Workgroup and professor of dermatology at the University of California, San Francisco, said in an interview shortly after the FDA posted the update on the new tool. “That said, there are many patients who have not gotten isotretinoin during the 1 month since the roll-out of the new platform.”
What still needs to be fixed? “We have ongoing concerns about the lack of transparency of the IPMG, about call center wait times, actual number of prescriptions on the hands of patients compared to the previous month, and those patients who can get pregnant who – despite complying with all of the REMS requirements – are being locked out because of the lack of timely attestation to their negative pregnancy status due to the website, not the patients themselves,” Dr. Frieden told this news organization.
“We are continuing to advocate to have decreased attestation requirements for individuals who cannot become pregnant – because this will improve the efficiency of the system for those patients for whom the REMS program goals are truly intended – those who can become pregnant, since the primary aim of the REMS program is to minimize fetal exposure.”
An AADA spokesperson said that the IPMG has invited the AADA to a joint stakeholders meeting on Jan. 26, along with representatives from the FDA and pharmacy industry.
Spotty progress
“The iPLEDGE situation is as frustrating as ever,” said Neil S. Goldberg, MD, a dermatologist in Westchester County, New York, after the FDA’s Jan. 14 update was released. “It’s like they never tested the new website before deploying it.”
Among the issues he has experienced in his practice, he said, is an instance in which iPLEDGE swapped the first names of a mother and daughter, so it was impossible to fill the prescription. “It happened twice in the same day,” Dr. Goldberg said. The patient had to call iPLEDGE to fix this, but the call center wasn’t taking calls.
In today’s technology environment, he said, it’s hard to believe that “we have to put up with this.”
Some have seen success. ‘’The tool is working fine on our end,” said Mitesh Patel, PharmD, pharmacy manager at Sunshine Pharmacy in White Plains, N.Y. However, he added that some doctors and patients are still having issues. He encourages dermatologists still having issues with the system to reach out to independent pharmacies that have processed iPLEDGE prescriptions and ‘’lean on them to assist.”
This news organization contacted CVS and Walgreens about how the system is working at their locations, but has not yet received a response.
Dr. Goldberg, Dr. Frieden, Dr. Barbieri, and Dr. Peebles have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This story was updated on 1/24/22.
Rituximab and COVID-19 vaccines: Studies begin to answer key questions
Rituximab has presented something of a conundrum for patients taking the monoclonal antibody during the COVID-19 pandemic.
Used to manage a variety of autoimmune diseases and cancers, rituximab acts against CD20 proteins expressed on the surface of B cells, causing B-cell depletion. However, it is this B-cell depletion that may put these patients at greater risk of COVID-19 development, progression to more severe disease, and in-hospital mortality. Evidence for this appears to be mixed, with studies showing both that patients using rituximab to manage various diseases are and are not at increased risk for SARS-CoV-2 infection, COVID-19 progression, and mortality.
As COVID-19 vaccine rollouts take place across the world, more questions have been raised about the relationship between B-cell depletion from anti-CD20 therapies and COVID-19 vaccines. Do rituximab and other anti-CD20 therapies affect a patient’s response to COVID-19 vaccines? If this is the case, does the timing of anti-CD20 treatment matter to maximize B-cell levels and improve the vaccine’s effectiveness? And how do COVID-19 vaccine booster doses factor into the equation?
Humoral and cell-mediated responses following COVID-19 vaccination
First, the bad news: The vaccine is unquestionably safe to administer in patients taking rituximab, but one thing that has been well established is that antibody response to COVID-19 vaccination in these individuals does is reduced. This isn’t entirely unprecedented, as previous studies have shown a weakened immune response to pneumococcal polysaccharide and keyhole limpet hemocyanin vaccines among patients taking rituximab.
“Compromised immunogenicity to the SARS-CoV-2 vaccines has been demonstrated in rituximab-treated patients, which is of particular concern given the observation that B-cell–depleting therapies may be associated with worse COVID outcomes,” Robert F. Spiera, MD, director of the Scleroderma, Vasculitis, and Myositis Center at the Hospital for Special Surgery in New York, said in an interview.
For example, in a recent study from the Medical University of Vienna, 29 (39%) of 74 patients receiving rituximab (43% as monotherapy, 57% with conventional-synthetic disease-modifying antirheumatic drugs) who were vaccinated with either the Comirnaty (Pfizer-BioNTech) or Spikevax (Moderna) COVID-19 vaccine achieved seroconversion, compared with 100% of patients in a healthy control group, and all but 1 patient without detectable CD19+ peripheral B cells did not develop anti–SARS-CoV-2 receptor-binding domain antibodies.
“There is an increasing number of studies in this field, and they confirm that patients treated with rituximab and other anti-CD20 agents have severely reduced serological responses to COVID-19 vaccines,” Ingrid Jyssum, MD, of the division of rheumatology and research at Diakonhjemmet Hospital in Oslo, said in an interview.
One silver lining is that patients treated with anti-CD20 therapies appear to have a cell-mediated response following vaccination even if they don’t develop SARS-CoV-2 antibodies. “Studies that also investigate T-cell responses are starting to emerge, and so far, they show that, even if the patients do not have antibodies, they may have T-cell responses,” Dr. Jyssum said.
One study of 24 patients with autoimmune diseases taking rituximab that evaluated humoral and T-cell responses following vaccination with the Comirnaty vaccine found that none had a humoral response to the vaccine, but the T-cell response from that group did not significantly differ from 35 patients receiving other immunosuppressants and 26 patients in a healthy control group. In another study of rituximab- or ocrelizumab-treated patients who received mRNA-based COVID-19 vaccines, 69.4% developed SARS-CoV-2–specific antibodies, compared with a control group, but 96.2% of patients taking ocrelizumab and 81.8% of patients taking rituximab mounted a spike-specific CD8+ T-cell response, compared with 66.7% in the control group, and there were comparable rates (85%-90%) of spike-specific CD4+ T cells in all groups. In the study from the Medical University of Vienna, T-cell response was detected in rituximab-treated patients who both did and did not mount an antibody response.
The clinical relevance of how a blunted humoral immune response but a respectable T-cell response to COVID-19 vaccines affects patients treated with anti-CD20 therapies isn’t currently known, Dr. Jyssum said.
While these data are reassuring, they’re also incomplete, Dr. Spiera noted. “The ultimate outcome of relevance to assess vaccine efficacy is protection from COVID and from severe outcomes of COVID infection (i.e., hospitalization, mechanical ventilation, death). That data will require assessment of very large numbers of rituximab-treated vaccinated patients to be compared with rituximab-treated unvaccinated patients, and is unlikely to be forthcoming in the very near future.
“In the meantime, however, achieving serologic positivity, meaning having evidence of serologic as well as cellular immunity following vaccination, is a desired outcome, and likely implies more robust immunity.”
Does treatment timing impact COVID-19 vaccine response?
Given enough time, B-cell reconstitution will occur in patients taking rituximab. With that in mind, is it beneficial to wait a certain amount of time after a patient has stopped rituximab therapy or time since their last dose before giving them a COVID-19 vaccine? In their guidance on COVID-19 vaccines for patients with rheumatic and musculoskeletal diseases, the American College of Rheumatology said there is moderate evidence to consider “optimal timing of dosing and vaccination with the rheumatology provider before proceeding.”
“Guidelines and preliminary studies of serologic response to COVID vaccine in rituximab-treated patients have suggested that longer time from last rituximab exposure is associated with a greater likelihood of a serologic response,” Dr. Spiera said.
In a brief report published in Arthritis & Rheumatology, Dr. Spiera and colleagues performed a retrospective chart review of 56 patients with varying levels of last exposure to rituximab who received a COVID-19 vaccine. Their results showed that, when patients were vaccinated 6-12 months after the last rituximab dose, 55% were seronegative, and when this was more than 12 months, only 13% were seronegative, compared with seronegativity in 86% who were vaccinated less than 6 months after their last rituximab dose.
The RituxiVac trial, conducted by researchers in Switzerland, also examined vaccine responses of 96 rituximab-treated patients who received Comirnaty or Spikevax; results recently published in The Lancet Rheumatology showed findings similar to other studies, with reduced humoral and cell-mediated responses. In the RituxiVac trial, the median time to last anti-CD20 treatment was 1.07 years.
“The typical interval between rituximab doses [for treatment of rheumatoid arthritis, as well as for remission maintenance in antineutrophil cytoplasmic antibody–associated vasculitis] is typically 6 months, and this has become widely used as the interval from last rituximab to time of COVID vaccination, with a recommendation to wait 4 weeks (if possible) from time of vaccination until the next rituximab administration,” Dr. Spiera explained. However, this window seems to vary depending on the study.
Recent research published in Arthritis & Rheumatology indicates B-cell levels could be a relevant indicator for humoral and cell-mediated response in patients with rheumatic diseases treated with rituximab, with a level of 10 B cells/mcL (0.4% of lymphocytes) identified as one potential marker for likely seroconversion following COVID-19 vaccination.
“In some smaller case series, it has been further recognized that rituximab-treated patients who were beginning to reconstitute peripheral B cells were most likely to respond serologically. Our present study confirmed those findings, demonstrating that the presence of detectable B cells was strongly associated with vaccine responsiveness, and affords complementary information to time from last [rituximab dose] in informing the likelihood of a vaccine response,” Dr. Spiera said.
However, the literature is limited in this area, and an exact cutoff for B-cell counts in these patients isn’t currently known, Dr. Jyssum said. A better metric is time away from anti-CD20 therapies, with CD19 cell count being highly correlated with last infusion.
Dr. Spiera agreed that there is no consistent B-cell percentage that works as a cutoff. “In our study, we looked at it as a binary variable, although we did find that a higher percentage of B cells in the peripheral lymphocyte population was associated with a higher likelihood of seroconversion. We did not, however, identify a ‘threshold’ for vaccine serologic responsiveness.”
Should clinicians measure antibodies?
The Food and Drug Administration and the Centers for Disease Control and Prevention have recommended that health care providers and the public not use COVID-19 antibody tests as a way to gauge immunity after exposure to SARS-CoV-2 and after receiving a COVID-19 vaccination. The ACR’s guidance on COVID-19 vaccination for patients with rheumatic and musculoskeletal diseases strongly recommends against ordering antibody tests for patients with autoimmune inflammatory rheumatic diseases as a way to measure immunity.
“Generally, such measurements are not recommended as the clinical correlate of various antibody levels are not known,” Dr. Jyssum said. “With regular infusions of rituximab or other anti-CD20 agents, one cannot expect that these patients will develop significant levels of antibodies.”
However, she said there might be situations where it’s useful to know whether a patient has developed antibodies at all. “Assessing the significance of specific antibody levels is difficult, and the subject of scientific studies. Patients lacking a humoral vaccine response are left to rely on their T-cell responses and on infectious control measures to prevent disease.”
Dr. Spiera said he disagreed with guidelines recommending against checking antibody levels after vaccination, “particularly in patients treated with immunosuppressive medications that might be expected to blunt their serologic response to the vaccines.
“Although we cannot be sure what level of measurable antibodies offer what level of protection, most clinicians would agree that patients who demonstrate no detectable antibodies (which is a common finding in rituximab-treated patients) should be considered at higher risk,” he said. “Indeed, recommendations regarding booster vaccine administration in general was initially based on the observation of declining antibody levels with longer time from vaccination.”
Do COVID-19 vaccine boosters help patients on anti-CD20 therapy?
As of January 2022, the FDA and CDC have recommended a third primary series shot of COVID-19 vaccines for some moderately to severely immunocompromised patients as young as 5 years old (for Comirnaty vaccine) or a booster shot of either Comirnaty or Spikevax for everyone aged 12 years and older, including immunocompromised people, while the ACR goes into more detail and recommends clinicians time a patient’s booster shot with temporary treatment interruption.
In The Lancet Rheumatology, Dr. Jyssum and colleagues recently published results from the prospective Nor-vaC study examining the humoral and cell-mediated immune responses of 87 patients with RA being treated with rituximab who received the Comirnaty, Spikevax, or Vaxzevria (AstraZeneca) COVID-19 vaccines; of these, 49 patients received a booster dose at a median of 70 days after completing their primary series. The results showed 19 patients (28.1%) had a serologic response after their primary series, while 8 of 49 patients (16.3%) who received their booster dose had a serologic response.
All patients who received a third dose in the study had a T-cell response, Dr. Jyssum said. “This is reassuring for patients and clinicians. T cells have been found to be important in countering COVID-19 disease, but whether we can rely on the T-cell response alone in the absence of antibodies to protect patients from infection or from serious COVID disease is still not determined,” she said.
When asked if she would recommend COVID-19 vaccine booster doses for patients on rituximab, Dr. Jyssum replied: “Absolutely.”
Another study, recently published in Annals of the Rheumatic Diseases, examined heterologous and homologous booster doses for 60 patients receiving rituximab without seroconversion after their COVID-19 vaccine primary series. The results showed no significant difference in new seroconversion at 4 weeks based on whether the patient received a vector or mRNA vaccine (22% vs. 32%), but all patients who received a booster dose with a vector vaccine had specific T-cell responses, compared with 81% of patients who received an mRNA vaccine booster. There was a new humoral and/or cellular response in 9 of 11 patients (82%), and most patients with peripheral B cells (12 of 18 patients; 67%) achieved seroconversion.
“Our data show that a cellular and/or humoral immune response can be achieved on a third COVID-19 vaccination in most of the patients who initially developed neither a humoral nor a cellular immune response,” the researchers concluded. “The efficacy data together with the safety data seen in our trial provide a favorable risk/benefit ratio and support the implementation of a third vaccination for nonseroconverted high-risk autoimmune disease patients treated with B-cell–depleting agents.”
Dr. Spiera said booster doses are an important part of the equation, and “it is important to consider factors that would be associated with a greater likelihood of achieving a serologic response, particularly in those patients who did not demonstrate a serologic response to the initial vaccines series.
“Preliminary data shows that the beginnings of B-cell reconstitution is also associated with a positive serologic response following a booster of the COVID-19 vaccine,” he said.
The authors of the cited studies reported numerous relevant financial disclosures. Dr. Spiera and Dr. Jyssum reported no relevant financial disclosures.
Rituximab has presented something of a conundrum for patients taking the monoclonal antibody during the COVID-19 pandemic.
Used to manage a variety of autoimmune diseases and cancers, rituximab acts against CD20 proteins expressed on the surface of B cells, causing B-cell depletion. However, it is this B-cell depletion that may put these patients at greater risk of COVID-19 development, progression to more severe disease, and in-hospital mortality. Evidence for this appears to be mixed, with studies showing both that patients using rituximab to manage various diseases are and are not at increased risk for SARS-CoV-2 infection, COVID-19 progression, and mortality.
As COVID-19 vaccine rollouts take place across the world, more questions have been raised about the relationship between B-cell depletion from anti-CD20 therapies and COVID-19 vaccines. Do rituximab and other anti-CD20 therapies affect a patient’s response to COVID-19 vaccines? If this is the case, does the timing of anti-CD20 treatment matter to maximize B-cell levels and improve the vaccine’s effectiveness? And how do COVID-19 vaccine booster doses factor into the equation?
Humoral and cell-mediated responses following COVID-19 vaccination
First, the bad news: The vaccine is unquestionably safe to administer in patients taking rituximab, but one thing that has been well established is that antibody response to COVID-19 vaccination in these individuals does is reduced. This isn’t entirely unprecedented, as previous studies have shown a weakened immune response to pneumococcal polysaccharide and keyhole limpet hemocyanin vaccines among patients taking rituximab.
“Compromised immunogenicity to the SARS-CoV-2 vaccines has been demonstrated in rituximab-treated patients, which is of particular concern given the observation that B-cell–depleting therapies may be associated with worse COVID outcomes,” Robert F. Spiera, MD, director of the Scleroderma, Vasculitis, and Myositis Center at the Hospital for Special Surgery in New York, said in an interview.
For example, in a recent study from the Medical University of Vienna, 29 (39%) of 74 patients receiving rituximab (43% as monotherapy, 57% with conventional-synthetic disease-modifying antirheumatic drugs) who were vaccinated with either the Comirnaty (Pfizer-BioNTech) or Spikevax (Moderna) COVID-19 vaccine achieved seroconversion, compared with 100% of patients in a healthy control group, and all but 1 patient without detectable CD19+ peripheral B cells did not develop anti–SARS-CoV-2 receptor-binding domain antibodies.
“There is an increasing number of studies in this field, and they confirm that patients treated with rituximab and other anti-CD20 agents have severely reduced serological responses to COVID-19 vaccines,” Ingrid Jyssum, MD, of the division of rheumatology and research at Diakonhjemmet Hospital in Oslo, said in an interview.
One silver lining is that patients treated with anti-CD20 therapies appear to have a cell-mediated response following vaccination even if they don’t develop SARS-CoV-2 antibodies. “Studies that also investigate T-cell responses are starting to emerge, and so far, they show that, even if the patients do not have antibodies, they may have T-cell responses,” Dr. Jyssum said.
One study of 24 patients with autoimmune diseases taking rituximab that evaluated humoral and T-cell responses following vaccination with the Comirnaty vaccine found that none had a humoral response to the vaccine, but the T-cell response from that group did not significantly differ from 35 patients receiving other immunosuppressants and 26 patients in a healthy control group. In another study of rituximab- or ocrelizumab-treated patients who received mRNA-based COVID-19 vaccines, 69.4% developed SARS-CoV-2–specific antibodies, compared with a control group, but 96.2% of patients taking ocrelizumab and 81.8% of patients taking rituximab mounted a spike-specific CD8+ T-cell response, compared with 66.7% in the control group, and there were comparable rates (85%-90%) of spike-specific CD4+ T cells in all groups. In the study from the Medical University of Vienna, T-cell response was detected in rituximab-treated patients who both did and did not mount an antibody response.
The clinical relevance of how a blunted humoral immune response but a respectable T-cell response to COVID-19 vaccines affects patients treated with anti-CD20 therapies isn’t currently known, Dr. Jyssum said.
While these data are reassuring, they’re also incomplete, Dr. Spiera noted. “The ultimate outcome of relevance to assess vaccine efficacy is protection from COVID and from severe outcomes of COVID infection (i.e., hospitalization, mechanical ventilation, death). That data will require assessment of very large numbers of rituximab-treated vaccinated patients to be compared with rituximab-treated unvaccinated patients, and is unlikely to be forthcoming in the very near future.
“In the meantime, however, achieving serologic positivity, meaning having evidence of serologic as well as cellular immunity following vaccination, is a desired outcome, and likely implies more robust immunity.”
Does treatment timing impact COVID-19 vaccine response?
Given enough time, B-cell reconstitution will occur in patients taking rituximab. With that in mind, is it beneficial to wait a certain amount of time after a patient has stopped rituximab therapy or time since their last dose before giving them a COVID-19 vaccine? In their guidance on COVID-19 vaccines for patients with rheumatic and musculoskeletal diseases, the American College of Rheumatology said there is moderate evidence to consider “optimal timing of dosing and vaccination with the rheumatology provider before proceeding.”
“Guidelines and preliminary studies of serologic response to COVID vaccine in rituximab-treated patients have suggested that longer time from last rituximab exposure is associated with a greater likelihood of a serologic response,” Dr. Spiera said.
In a brief report published in Arthritis & Rheumatology, Dr. Spiera and colleagues performed a retrospective chart review of 56 patients with varying levels of last exposure to rituximab who received a COVID-19 vaccine. Their results showed that, when patients were vaccinated 6-12 months after the last rituximab dose, 55% were seronegative, and when this was more than 12 months, only 13% were seronegative, compared with seronegativity in 86% who were vaccinated less than 6 months after their last rituximab dose.
The RituxiVac trial, conducted by researchers in Switzerland, also examined vaccine responses of 96 rituximab-treated patients who received Comirnaty or Spikevax; results recently published in The Lancet Rheumatology showed findings similar to other studies, with reduced humoral and cell-mediated responses. In the RituxiVac trial, the median time to last anti-CD20 treatment was 1.07 years.
“The typical interval between rituximab doses [for treatment of rheumatoid arthritis, as well as for remission maintenance in antineutrophil cytoplasmic antibody–associated vasculitis] is typically 6 months, and this has become widely used as the interval from last rituximab to time of COVID vaccination, with a recommendation to wait 4 weeks (if possible) from time of vaccination until the next rituximab administration,” Dr. Spiera explained. However, this window seems to vary depending on the study.
Recent research published in Arthritis & Rheumatology indicates B-cell levels could be a relevant indicator for humoral and cell-mediated response in patients with rheumatic diseases treated with rituximab, with a level of 10 B cells/mcL (0.4% of lymphocytes) identified as one potential marker for likely seroconversion following COVID-19 vaccination.
“In some smaller case series, it has been further recognized that rituximab-treated patients who were beginning to reconstitute peripheral B cells were most likely to respond serologically. Our present study confirmed those findings, demonstrating that the presence of detectable B cells was strongly associated with vaccine responsiveness, and affords complementary information to time from last [rituximab dose] in informing the likelihood of a vaccine response,” Dr. Spiera said.
However, the literature is limited in this area, and an exact cutoff for B-cell counts in these patients isn’t currently known, Dr. Jyssum said. A better metric is time away from anti-CD20 therapies, with CD19 cell count being highly correlated with last infusion.
Dr. Spiera agreed that there is no consistent B-cell percentage that works as a cutoff. “In our study, we looked at it as a binary variable, although we did find that a higher percentage of B cells in the peripheral lymphocyte population was associated with a higher likelihood of seroconversion. We did not, however, identify a ‘threshold’ for vaccine serologic responsiveness.”
Should clinicians measure antibodies?
The Food and Drug Administration and the Centers for Disease Control and Prevention have recommended that health care providers and the public not use COVID-19 antibody tests as a way to gauge immunity after exposure to SARS-CoV-2 and after receiving a COVID-19 vaccination. The ACR’s guidance on COVID-19 vaccination for patients with rheumatic and musculoskeletal diseases strongly recommends against ordering antibody tests for patients with autoimmune inflammatory rheumatic diseases as a way to measure immunity.
“Generally, such measurements are not recommended as the clinical correlate of various antibody levels are not known,” Dr. Jyssum said. “With regular infusions of rituximab or other anti-CD20 agents, one cannot expect that these patients will develop significant levels of antibodies.”
However, she said there might be situations where it’s useful to know whether a patient has developed antibodies at all. “Assessing the significance of specific antibody levels is difficult, and the subject of scientific studies. Patients lacking a humoral vaccine response are left to rely on their T-cell responses and on infectious control measures to prevent disease.”
Dr. Spiera said he disagreed with guidelines recommending against checking antibody levels after vaccination, “particularly in patients treated with immunosuppressive medications that might be expected to blunt their serologic response to the vaccines.
“Although we cannot be sure what level of measurable antibodies offer what level of protection, most clinicians would agree that patients who demonstrate no detectable antibodies (which is a common finding in rituximab-treated patients) should be considered at higher risk,” he said. “Indeed, recommendations regarding booster vaccine administration in general was initially based on the observation of declining antibody levels with longer time from vaccination.”
Do COVID-19 vaccine boosters help patients on anti-CD20 therapy?
As of January 2022, the FDA and CDC have recommended a third primary series shot of COVID-19 vaccines for some moderately to severely immunocompromised patients as young as 5 years old (for Comirnaty vaccine) or a booster shot of either Comirnaty or Spikevax for everyone aged 12 years and older, including immunocompromised people, while the ACR goes into more detail and recommends clinicians time a patient’s booster shot with temporary treatment interruption.
In The Lancet Rheumatology, Dr. Jyssum and colleagues recently published results from the prospective Nor-vaC study examining the humoral and cell-mediated immune responses of 87 patients with RA being treated with rituximab who received the Comirnaty, Spikevax, or Vaxzevria (AstraZeneca) COVID-19 vaccines; of these, 49 patients received a booster dose at a median of 70 days after completing their primary series. The results showed 19 patients (28.1%) had a serologic response after their primary series, while 8 of 49 patients (16.3%) who received their booster dose had a serologic response.
All patients who received a third dose in the study had a T-cell response, Dr. Jyssum said. “This is reassuring for patients and clinicians. T cells have been found to be important in countering COVID-19 disease, but whether we can rely on the T-cell response alone in the absence of antibodies to protect patients from infection or from serious COVID disease is still not determined,” she said.
When asked if she would recommend COVID-19 vaccine booster doses for patients on rituximab, Dr. Jyssum replied: “Absolutely.”
Another study, recently published in Annals of the Rheumatic Diseases, examined heterologous and homologous booster doses for 60 patients receiving rituximab without seroconversion after their COVID-19 vaccine primary series. The results showed no significant difference in new seroconversion at 4 weeks based on whether the patient received a vector or mRNA vaccine (22% vs. 32%), but all patients who received a booster dose with a vector vaccine had specific T-cell responses, compared with 81% of patients who received an mRNA vaccine booster. There was a new humoral and/or cellular response in 9 of 11 patients (82%), and most patients with peripheral B cells (12 of 18 patients; 67%) achieved seroconversion.
“Our data show that a cellular and/or humoral immune response can be achieved on a third COVID-19 vaccination in most of the patients who initially developed neither a humoral nor a cellular immune response,” the researchers concluded. “The efficacy data together with the safety data seen in our trial provide a favorable risk/benefit ratio and support the implementation of a third vaccination for nonseroconverted high-risk autoimmune disease patients treated with B-cell–depleting agents.”
Dr. Spiera said booster doses are an important part of the equation, and “it is important to consider factors that would be associated with a greater likelihood of achieving a serologic response, particularly in those patients who did not demonstrate a serologic response to the initial vaccines series.
“Preliminary data shows that the beginnings of B-cell reconstitution is also associated with a positive serologic response following a booster of the COVID-19 vaccine,” he said.
The authors of the cited studies reported numerous relevant financial disclosures. Dr. Spiera and Dr. Jyssum reported no relevant financial disclosures.
Rituximab has presented something of a conundrum for patients taking the monoclonal antibody during the COVID-19 pandemic.
Used to manage a variety of autoimmune diseases and cancers, rituximab acts against CD20 proteins expressed on the surface of B cells, causing B-cell depletion. However, it is this B-cell depletion that may put these patients at greater risk of COVID-19 development, progression to more severe disease, and in-hospital mortality. Evidence for this appears to be mixed, with studies showing both that patients using rituximab to manage various diseases are and are not at increased risk for SARS-CoV-2 infection, COVID-19 progression, and mortality.
As COVID-19 vaccine rollouts take place across the world, more questions have been raised about the relationship between B-cell depletion from anti-CD20 therapies and COVID-19 vaccines. Do rituximab and other anti-CD20 therapies affect a patient’s response to COVID-19 vaccines? If this is the case, does the timing of anti-CD20 treatment matter to maximize B-cell levels and improve the vaccine’s effectiveness? And how do COVID-19 vaccine booster doses factor into the equation?
Humoral and cell-mediated responses following COVID-19 vaccination
First, the bad news: The vaccine is unquestionably safe to administer in patients taking rituximab, but one thing that has been well established is that antibody response to COVID-19 vaccination in these individuals does is reduced. This isn’t entirely unprecedented, as previous studies have shown a weakened immune response to pneumococcal polysaccharide and keyhole limpet hemocyanin vaccines among patients taking rituximab.
“Compromised immunogenicity to the SARS-CoV-2 vaccines has been demonstrated in rituximab-treated patients, which is of particular concern given the observation that B-cell–depleting therapies may be associated with worse COVID outcomes,” Robert F. Spiera, MD, director of the Scleroderma, Vasculitis, and Myositis Center at the Hospital for Special Surgery in New York, said in an interview.
For example, in a recent study from the Medical University of Vienna, 29 (39%) of 74 patients receiving rituximab (43% as monotherapy, 57% with conventional-synthetic disease-modifying antirheumatic drugs) who were vaccinated with either the Comirnaty (Pfizer-BioNTech) or Spikevax (Moderna) COVID-19 vaccine achieved seroconversion, compared with 100% of patients in a healthy control group, and all but 1 patient without detectable CD19+ peripheral B cells did not develop anti–SARS-CoV-2 receptor-binding domain antibodies.
“There is an increasing number of studies in this field, and they confirm that patients treated with rituximab and other anti-CD20 agents have severely reduced serological responses to COVID-19 vaccines,” Ingrid Jyssum, MD, of the division of rheumatology and research at Diakonhjemmet Hospital in Oslo, said in an interview.
One silver lining is that patients treated with anti-CD20 therapies appear to have a cell-mediated response following vaccination even if they don’t develop SARS-CoV-2 antibodies. “Studies that also investigate T-cell responses are starting to emerge, and so far, they show that, even if the patients do not have antibodies, they may have T-cell responses,” Dr. Jyssum said.
One study of 24 patients with autoimmune diseases taking rituximab that evaluated humoral and T-cell responses following vaccination with the Comirnaty vaccine found that none had a humoral response to the vaccine, but the T-cell response from that group did not significantly differ from 35 patients receiving other immunosuppressants and 26 patients in a healthy control group. In another study of rituximab- or ocrelizumab-treated patients who received mRNA-based COVID-19 vaccines, 69.4% developed SARS-CoV-2–specific antibodies, compared with a control group, but 96.2% of patients taking ocrelizumab and 81.8% of patients taking rituximab mounted a spike-specific CD8+ T-cell response, compared with 66.7% in the control group, and there were comparable rates (85%-90%) of spike-specific CD4+ T cells in all groups. In the study from the Medical University of Vienna, T-cell response was detected in rituximab-treated patients who both did and did not mount an antibody response.
The clinical relevance of how a blunted humoral immune response but a respectable T-cell response to COVID-19 vaccines affects patients treated with anti-CD20 therapies isn’t currently known, Dr. Jyssum said.
While these data are reassuring, they’re also incomplete, Dr. Spiera noted. “The ultimate outcome of relevance to assess vaccine efficacy is protection from COVID and from severe outcomes of COVID infection (i.e., hospitalization, mechanical ventilation, death). That data will require assessment of very large numbers of rituximab-treated vaccinated patients to be compared with rituximab-treated unvaccinated patients, and is unlikely to be forthcoming in the very near future.
“In the meantime, however, achieving serologic positivity, meaning having evidence of serologic as well as cellular immunity following vaccination, is a desired outcome, and likely implies more robust immunity.”
Does treatment timing impact COVID-19 vaccine response?
Given enough time, B-cell reconstitution will occur in patients taking rituximab. With that in mind, is it beneficial to wait a certain amount of time after a patient has stopped rituximab therapy or time since their last dose before giving them a COVID-19 vaccine? In their guidance on COVID-19 vaccines for patients with rheumatic and musculoskeletal diseases, the American College of Rheumatology said there is moderate evidence to consider “optimal timing of dosing and vaccination with the rheumatology provider before proceeding.”
“Guidelines and preliminary studies of serologic response to COVID vaccine in rituximab-treated patients have suggested that longer time from last rituximab exposure is associated with a greater likelihood of a serologic response,” Dr. Spiera said.
In a brief report published in Arthritis & Rheumatology, Dr. Spiera and colleagues performed a retrospective chart review of 56 patients with varying levels of last exposure to rituximab who received a COVID-19 vaccine. Their results showed that, when patients were vaccinated 6-12 months after the last rituximab dose, 55% were seronegative, and when this was more than 12 months, only 13% were seronegative, compared with seronegativity in 86% who were vaccinated less than 6 months after their last rituximab dose.
The RituxiVac trial, conducted by researchers in Switzerland, also examined vaccine responses of 96 rituximab-treated patients who received Comirnaty or Spikevax; results recently published in The Lancet Rheumatology showed findings similar to other studies, with reduced humoral and cell-mediated responses. In the RituxiVac trial, the median time to last anti-CD20 treatment was 1.07 years.
“The typical interval between rituximab doses [for treatment of rheumatoid arthritis, as well as for remission maintenance in antineutrophil cytoplasmic antibody–associated vasculitis] is typically 6 months, and this has become widely used as the interval from last rituximab to time of COVID vaccination, with a recommendation to wait 4 weeks (if possible) from time of vaccination until the next rituximab administration,” Dr. Spiera explained. However, this window seems to vary depending on the study.
Recent research published in Arthritis & Rheumatology indicates B-cell levels could be a relevant indicator for humoral and cell-mediated response in patients with rheumatic diseases treated with rituximab, with a level of 10 B cells/mcL (0.4% of lymphocytes) identified as one potential marker for likely seroconversion following COVID-19 vaccination.
“In some smaller case series, it has been further recognized that rituximab-treated patients who were beginning to reconstitute peripheral B cells were most likely to respond serologically. Our present study confirmed those findings, demonstrating that the presence of detectable B cells was strongly associated with vaccine responsiveness, and affords complementary information to time from last [rituximab dose] in informing the likelihood of a vaccine response,” Dr. Spiera said.
However, the literature is limited in this area, and an exact cutoff for B-cell counts in these patients isn’t currently known, Dr. Jyssum said. A better metric is time away from anti-CD20 therapies, with CD19 cell count being highly correlated with last infusion.
Dr. Spiera agreed that there is no consistent B-cell percentage that works as a cutoff. “In our study, we looked at it as a binary variable, although we did find that a higher percentage of B cells in the peripheral lymphocyte population was associated with a higher likelihood of seroconversion. We did not, however, identify a ‘threshold’ for vaccine serologic responsiveness.”
Should clinicians measure antibodies?
The Food and Drug Administration and the Centers for Disease Control and Prevention have recommended that health care providers and the public not use COVID-19 antibody tests as a way to gauge immunity after exposure to SARS-CoV-2 and after receiving a COVID-19 vaccination. The ACR’s guidance on COVID-19 vaccination for patients with rheumatic and musculoskeletal diseases strongly recommends against ordering antibody tests for patients with autoimmune inflammatory rheumatic diseases as a way to measure immunity.
“Generally, such measurements are not recommended as the clinical correlate of various antibody levels are not known,” Dr. Jyssum said. “With regular infusions of rituximab or other anti-CD20 agents, one cannot expect that these patients will develop significant levels of antibodies.”
However, she said there might be situations where it’s useful to know whether a patient has developed antibodies at all. “Assessing the significance of specific antibody levels is difficult, and the subject of scientific studies. Patients lacking a humoral vaccine response are left to rely on their T-cell responses and on infectious control measures to prevent disease.”
Dr. Spiera said he disagreed with guidelines recommending against checking antibody levels after vaccination, “particularly in patients treated with immunosuppressive medications that might be expected to blunt their serologic response to the vaccines.
“Although we cannot be sure what level of measurable antibodies offer what level of protection, most clinicians would agree that patients who demonstrate no detectable antibodies (which is a common finding in rituximab-treated patients) should be considered at higher risk,” he said. “Indeed, recommendations regarding booster vaccine administration in general was initially based on the observation of declining antibody levels with longer time from vaccination.”
Do COVID-19 vaccine boosters help patients on anti-CD20 therapy?
As of January 2022, the FDA and CDC have recommended a third primary series shot of COVID-19 vaccines for some moderately to severely immunocompromised patients as young as 5 years old (for Comirnaty vaccine) or a booster shot of either Comirnaty or Spikevax for everyone aged 12 years and older, including immunocompromised people, while the ACR goes into more detail and recommends clinicians time a patient’s booster shot with temporary treatment interruption.
In The Lancet Rheumatology, Dr. Jyssum and colleagues recently published results from the prospective Nor-vaC study examining the humoral and cell-mediated immune responses of 87 patients with RA being treated with rituximab who received the Comirnaty, Spikevax, or Vaxzevria (AstraZeneca) COVID-19 vaccines; of these, 49 patients received a booster dose at a median of 70 days after completing their primary series. The results showed 19 patients (28.1%) had a serologic response after their primary series, while 8 of 49 patients (16.3%) who received their booster dose had a serologic response.
All patients who received a third dose in the study had a T-cell response, Dr. Jyssum said. “This is reassuring for patients and clinicians. T cells have been found to be important in countering COVID-19 disease, but whether we can rely on the T-cell response alone in the absence of antibodies to protect patients from infection or from serious COVID disease is still not determined,” she said.
When asked if she would recommend COVID-19 vaccine booster doses for patients on rituximab, Dr. Jyssum replied: “Absolutely.”
Another study, recently published in Annals of the Rheumatic Diseases, examined heterologous and homologous booster doses for 60 patients receiving rituximab without seroconversion after their COVID-19 vaccine primary series. The results showed no significant difference in new seroconversion at 4 weeks based on whether the patient received a vector or mRNA vaccine (22% vs. 32%), but all patients who received a booster dose with a vector vaccine had specific T-cell responses, compared with 81% of patients who received an mRNA vaccine booster. There was a new humoral and/or cellular response in 9 of 11 patients (82%), and most patients with peripheral B cells (12 of 18 patients; 67%) achieved seroconversion.
“Our data show that a cellular and/or humoral immune response can be achieved on a third COVID-19 vaccination in most of the patients who initially developed neither a humoral nor a cellular immune response,” the researchers concluded. “The efficacy data together with the safety data seen in our trial provide a favorable risk/benefit ratio and support the implementation of a third vaccination for nonseroconverted high-risk autoimmune disease patients treated with B-cell–depleting agents.”
Dr. Spiera said booster doses are an important part of the equation, and “it is important to consider factors that would be associated with a greater likelihood of achieving a serologic response, particularly in those patients who did not demonstrate a serologic response to the initial vaccines series.
“Preliminary data shows that the beginnings of B-cell reconstitution is also associated with a positive serologic response following a booster of the COVID-19 vaccine,” he said.
The authors of the cited studies reported numerous relevant financial disclosures. Dr. Spiera and Dr. Jyssum reported no relevant financial disclosures.