User login
News and Views that Matter to Physicians
Voice recognition software errors: Often silly, sometimes serious
How much is 15%?
Not that much, on paper. With any drug, at least 15% of people will get some kind of side effect. Usually they all list dizziness and headaches at the top.
Could the same be true of a seemingly harmless technology?
Voice recognition software has become pretty commonplace in modern medicine but is far from perfect. I try to be pretty careful about proofreading my dictations, but many docs, especially those in emergency room, don’t have the time to. So VR errors slip by, persisting in 71% of notes.
Most of these errors are just silly and obvious for what they are. But a recent study at a level I ER found that 15% of dictations contained one or more errors deemed as “critical,” with the potential to adversely affect patient care (Int J Med Inform. 2016 Sep;93:70-3).
Communication among doctors, nurses, and all the other key players in the hospital environment is one of the most critical areas in modern medicine. So many people often rely on the initial dictation for an idea of what’s going on that a critical error can affect the way they think about the case from the get-go.
Another issue, sadly, in today’s hospital is that no one takes (or has) the time to get a patient’s past medical history. It’s commonplace to pull the history out of previous admission notes. (Admittedly, sometimes in a demented or unconscious patient you don’t have a choice.) As a result, errors of this sort tend to propagate down the line, from an admission, to the consults, to the discharge summary, and into the next admission.
So let’s get back to that 15%.
I have to assume that 15% of people being admitted aren’t having catastrophic events from medical errors, hopefully because the doctors and nurses handling patient care are thinking for themselves, recognizing dictation errors, and addressing them appropriately.
But even if we dial it down to a tenth of that, say 1.5%, it’s still a serious concern. Bad outcomes in medicine are never entirely avoidable. That’s the nature of the job.
But bad outcomes caused by too much trust in a still-faulty technology are avoidable.
If 15% of people had a serious outcome from a medication, you’d be very cautious about using it. We need to treat these technological gadgets with the same concerns we extend to drugs and procedures. Avoidable bad outcomes, regardless of cause, are never good.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How much is 15%?
Not that much, on paper. With any drug, at least 15% of people will get some kind of side effect. Usually they all list dizziness and headaches at the top.
Could the same be true of a seemingly harmless technology?
Voice recognition software has become pretty commonplace in modern medicine but is far from perfect. I try to be pretty careful about proofreading my dictations, but many docs, especially those in emergency room, don’t have the time to. So VR errors slip by, persisting in 71% of notes.
Most of these errors are just silly and obvious for what they are. But a recent study at a level I ER found that 15% of dictations contained one or more errors deemed as “critical,” with the potential to adversely affect patient care (Int J Med Inform. 2016 Sep;93:70-3).
Communication among doctors, nurses, and all the other key players in the hospital environment is one of the most critical areas in modern medicine. So many people often rely on the initial dictation for an idea of what’s going on that a critical error can affect the way they think about the case from the get-go.
Another issue, sadly, in today’s hospital is that no one takes (or has) the time to get a patient’s past medical history. It’s commonplace to pull the history out of previous admission notes. (Admittedly, sometimes in a demented or unconscious patient you don’t have a choice.) As a result, errors of this sort tend to propagate down the line, from an admission, to the consults, to the discharge summary, and into the next admission.
So let’s get back to that 15%.
I have to assume that 15% of people being admitted aren’t having catastrophic events from medical errors, hopefully because the doctors and nurses handling patient care are thinking for themselves, recognizing dictation errors, and addressing them appropriately.
But even if we dial it down to a tenth of that, say 1.5%, it’s still a serious concern. Bad outcomes in medicine are never entirely avoidable. That’s the nature of the job.
But bad outcomes caused by too much trust in a still-faulty technology are avoidable.
If 15% of people had a serious outcome from a medication, you’d be very cautious about using it. We need to treat these technological gadgets with the same concerns we extend to drugs and procedures. Avoidable bad outcomes, regardless of cause, are never good.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How much is 15%?
Not that much, on paper. With any drug, at least 15% of people will get some kind of side effect. Usually they all list dizziness and headaches at the top.
Could the same be true of a seemingly harmless technology?
Voice recognition software has become pretty commonplace in modern medicine but is far from perfect. I try to be pretty careful about proofreading my dictations, but many docs, especially those in emergency room, don’t have the time to. So VR errors slip by, persisting in 71% of notes.
Most of these errors are just silly and obvious for what they are. But a recent study at a level I ER found that 15% of dictations contained one or more errors deemed as “critical,” with the potential to adversely affect patient care (Int J Med Inform. 2016 Sep;93:70-3).
Communication among doctors, nurses, and all the other key players in the hospital environment is one of the most critical areas in modern medicine. So many people often rely on the initial dictation for an idea of what’s going on that a critical error can affect the way they think about the case from the get-go.
Another issue, sadly, in today’s hospital is that no one takes (or has) the time to get a patient’s past medical history. It’s commonplace to pull the history out of previous admission notes. (Admittedly, sometimes in a demented or unconscious patient you don’t have a choice.) As a result, errors of this sort tend to propagate down the line, from an admission, to the consults, to the discharge summary, and into the next admission.
So let’s get back to that 15%.
I have to assume that 15% of people being admitted aren’t having catastrophic events from medical errors, hopefully because the doctors and nurses handling patient care are thinking for themselves, recognizing dictation errors, and addressing them appropriately.
But even if we dial it down to a tenth of that, say 1.5%, it’s still a serious concern. Bad outcomes in medicine are never entirely avoidable. That’s the nature of the job.
But bad outcomes caused by too much trust in a still-faulty technology are avoidable.
If 15% of people had a serious outcome from a medication, you’d be very cautious about using it. We need to treat these technological gadgets with the same concerns we extend to drugs and procedures. Avoidable bad outcomes, regardless of cause, are never good.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
IBD medical homes dramatically cut ED visits, hospitalizations
LAS VEGAS – A collaborative care approach to patients with inflammatory bowel disease (IBD) dramatically reduced emergency department visits and hospitalizations and also boosted quality of life.
The IBD patient-centered medical home employs open-access scheduling, remote monitoring, and telemedicine. A patient’s team includes a social worker, a nurse practitioner, a dietitian, a psychiatrist, and other specialists. The gastroenterologist acts as a primary care physician, according to Miguel Regueiro, MD, AGAF, medical director of the IBD Center at the University of Pittsburgh Medical Center, who presented the outcomes at the annual meeting of the American College of Gastroenterology.
Patients were eligible if at least 25% of their health care expenditures in the prior year were related to Crohn’s disease or ulcerative colitis.
The team enrolled 308 patients in the first year, with 290 remaining by the end of the year. Quality of life, as measured by the Short Inflammatory Bowel Disease Questionnaire, rose from a mean score of 7.1 to 9.1 points by the end of the study. There was a 51.9% decrease in ED visits (322 to 155), and a 53.1% reduction in hospitalizations (160 to 75), compared with the previous year.
Among patients who had been in the program for at least 6 months, ED visits dropped by 47% (197 to 116; P = .001) and hospitalizations dropped by 44% (100 to 56; P less than .005).
Physicians must also rise to the challenge. “The majority of gastroenterologists wouldn’t want to do this because it puts responsibility on them for the whole patient rather than just the disease,” said Dr. Regueiro.
But that discomfort shouldn’t sway them from making necessary changes. Rising health care costs could force specialists into new roles. “The way I look at it, if we don’t do something like this, the insurance companies will tell us what to do,” said Dr. Regueiro.
Dr. Regueiro is a member of advisory boards for AbbVie, Jansen, Takeda, UCB, and Pfizer. Dr. Quigley reported no conflicts of interest.
LAS VEGAS – A collaborative care approach to patients with inflammatory bowel disease (IBD) dramatically reduced emergency department visits and hospitalizations and also boosted quality of life.
The IBD patient-centered medical home employs open-access scheduling, remote monitoring, and telemedicine. A patient’s team includes a social worker, a nurse practitioner, a dietitian, a psychiatrist, and other specialists. The gastroenterologist acts as a primary care physician, according to Miguel Regueiro, MD, AGAF, medical director of the IBD Center at the University of Pittsburgh Medical Center, who presented the outcomes at the annual meeting of the American College of Gastroenterology.
Patients were eligible if at least 25% of their health care expenditures in the prior year were related to Crohn’s disease or ulcerative colitis.
The team enrolled 308 patients in the first year, with 290 remaining by the end of the year. Quality of life, as measured by the Short Inflammatory Bowel Disease Questionnaire, rose from a mean score of 7.1 to 9.1 points by the end of the study. There was a 51.9% decrease in ED visits (322 to 155), and a 53.1% reduction in hospitalizations (160 to 75), compared with the previous year.
Among patients who had been in the program for at least 6 months, ED visits dropped by 47% (197 to 116; P = .001) and hospitalizations dropped by 44% (100 to 56; P less than .005).
Physicians must also rise to the challenge. “The majority of gastroenterologists wouldn’t want to do this because it puts responsibility on them for the whole patient rather than just the disease,” said Dr. Regueiro.
But that discomfort shouldn’t sway them from making necessary changes. Rising health care costs could force specialists into new roles. “The way I look at it, if we don’t do something like this, the insurance companies will tell us what to do,” said Dr. Regueiro.
Dr. Regueiro is a member of advisory boards for AbbVie, Jansen, Takeda, UCB, and Pfizer. Dr. Quigley reported no conflicts of interest.
LAS VEGAS – A collaborative care approach to patients with inflammatory bowel disease (IBD) dramatically reduced emergency department visits and hospitalizations and also boosted quality of life.
The IBD patient-centered medical home employs open-access scheduling, remote monitoring, and telemedicine. A patient’s team includes a social worker, a nurse practitioner, a dietitian, a psychiatrist, and other specialists. The gastroenterologist acts as a primary care physician, according to Miguel Regueiro, MD, AGAF, medical director of the IBD Center at the University of Pittsburgh Medical Center, who presented the outcomes at the annual meeting of the American College of Gastroenterology.
Patients were eligible if at least 25% of their health care expenditures in the prior year were related to Crohn’s disease or ulcerative colitis.
The team enrolled 308 patients in the first year, with 290 remaining by the end of the year. Quality of life, as measured by the Short Inflammatory Bowel Disease Questionnaire, rose from a mean score of 7.1 to 9.1 points by the end of the study. There was a 51.9% decrease in ED visits (322 to 155), and a 53.1% reduction in hospitalizations (160 to 75), compared with the previous year.
Among patients who had been in the program for at least 6 months, ED visits dropped by 47% (197 to 116; P = .001) and hospitalizations dropped by 44% (100 to 56; P less than .005).
Physicians must also rise to the challenge. “The majority of gastroenterologists wouldn’t want to do this because it puts responsibility on them for the whole patient rather than just the disease,” said Dr. Regueiro.
But that discomfort shouldn’t sway them from making necessary changes. Rising health care costs could force specialists into new roles. “The way I look at it, if we don’t do something like this, the insurance companies will tell us what to do,” said Dr. Regueiro.
Dr. Regueiro is a member of advisory boards for AbbVie, Jansen, Takeda, UCB, and Pfizer. Dr. Quigley reported no conflicts of interest.
AT ACG 2016
Key clinical point:
Major finding: ED visits were cut by 51.9% and hospitalizations by 53.1% compared to the previous year.
Data source: Observational study.
Disclosures: Dr. Regueiro is a member of advisory boards for AbbVie, Jansen, Takeda, UCB, and Pfizer. Dr. Quigley reported no conflicts of interest.
Psych issues adding to pediatric hospitalization costs
Although pediatric hospitalizations are driven mostly by medical costs, comorbid psychiatric problems are increasingly adding to the expense, according to a review of 3,114,099 hospitalizations at 33 children’s hospitals in the United States from 2005 to 2014.
For pediatric hospitalizations without a psychiatric diagnosis, costs rose from $3,696 to $4,150 per day over the past decade. For medical stays with a psychiatric diagnosis, the price rose from $2,694 to $3,393 per day, a higher percent change. Overall, the cost of hospitalizing sick children with comorbid psychiatric diagnoses increased from $671 million to $1.6 billion.
The “strategic planning to meet the rising demand for psychiatric care in tertiary care children’s hospitals should place high priority on the needs of children with a primary medical condition and co-occurring psychiatric disorders,” said investigators led by Bonnie Zima, MD, from the University of California, Los Angeles, Semel Institute for Neuroscience and Human Behavior (Pediatrics. 2016 Oct 21. doi: 10.1542/peds.2016-0909).
“From 2005 through 2014 ... there was significant cumulative percent increase in total number of hospitalizations, hospital days, and hospital costs for all patients. Of the total hospitalizations, 18.3% (568,449) were associated with a psychiatric disorder, either primary or secondary,” they noted.
Meanwhile, hospitalizations for psychiatric-only diagnoses were minimal, just 3.6% of the total with the most common problems again being depression, anxiety, and suicide and self-injury. “Hospital resource use for only psychiatric disorders declined, consistent with the national shift to managed care for behavioral health services,” the investigators said.
“Collectively, these data will further guide strategic planning by children’s hospitals as they strive to integrate mental health care into their health care systems. Together, these findings … underscore the need for quality improvement interventions that target improving linkage with community mental health care after pediatric hospitalization,” they said.
The National Institutes of Health funded the study. Dr. Zima was supported by the National Institute of Mental Health and Behavioral Health Centers of Excellence for California. Dr. Naomi S. Bardach and Dr. Tumaini R. Coker were supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Jay G. Berry was supported by the Agency for Healthcare Research and Quality. The authors had no conflicts of interest.
Although pediatric hospitalizations are driven mostly by medical costs, comorbid psychiatric problems are increasingly adding to the expense, according to a review of 3,114,099 hospitalizations at 33 children’s hospitals in the United States from 2005 to 2014.
For pediatric hospitalizations without a psychiatric diagnosis, costs rose from $3,696 to $4,150 per day over the past decade. For medical stays with a psychiatric diagnosis, the price rose from $2,694 to $3,393 per day, a higher percent change. Overall, the cost of hospitalizing sick children with comorbid psychiatric diagnoses increased from $671 million to $1.6 billion.
The “strategic planning to meet the rising demand for psychiatric care in tertiary care children’s hospitals should place high priority on the needs of children with a primary medical condition and co-occurring psychiatric disorders,” said investigators led by Bonnie Zima, MD, from the University of California, Los Angeles, Semel Institute for Neuroscience and Human Behavior (Pediatrics. 2016 Oct 21. doi: 10.1542/peds.2016-0909).
“From 2005 through 2014 ... there was significant cumulative percent increase in total number of hospitalizations, hospital days, and hospital costs for all patients. Of the total hospitalizations, 18.3% (568,449) were associated with a psychiatric disorder, either primary or secondary,” they noted.
Meanwhile, hospitalizations for psychiatric-only diagnoses were minimal, just 3.6% of the total with the most common problems again being depression, anxiety, and suicide and self-injury. “Hospital resource use for only psychiatric disorders declined, consistent with the national shift to managed care for behavioral health services,” the investigators said.
“Collectively, these data will further guide strategic planning by children’s hospitals as they strive to integrate mental health care into their health care systems. Together, these findings … underscore the need for quality improvement interventions that target improving linkage with community mental health care after pediatric hospitalization,” they said.
The National Institutes of Health funded the study. Dr. Zima was supported by the National Institute of Mental Health and Behavioral Health Centers of Excellence for California. Dr. Naomi S. Bardach and Dr. Tumaini R. Coker were supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Jay G. Berry was supported by the Agency for Healthcare Research and Quality. The authors had no conflicts of interest.
Although pediatric hospitalizations are driven mostly by medical costs, comorbid psychiatric problems are increasingly adding to the expense, according to a review of 3,114,099 hospitalizations at 33 children’s hospitals in the United States from 2005 to 2014.
For pediatric hospitalizations without a psychiatric diagnosis, costs rose from $3,696 to $4,150 per day over the past decade. For medical stays with a psychiatric diagnosis, the price rose from $2,694 to $3,393 per day, a higher percent change. Overall, the cost of hospitalizing sick children with comorbid psychiatric diagnoses increased from $671 million to $1.6 billion.
The “strategic planning to meet the rising demand for psychiatric care in tertiary care children’s hospitals should place high priority on the needs of children with a primary medical condition and co-occurring psychiatric disorders,” said investigators led by Bonnie Zima, MD, from the University of California, Los Angeles, Semel Institute for Neuroscience and Human Behavior (Pediatrics. 2016 Oct 21. doi: 10.1542/peds.2016-0909).
“From 2005 through 2014 ... there was significant cumulative percent increase in total number of hospitalizations, hospital days, and hospital costs for all patients. Of the total hospitalizations, 18.3% (568,449) were associated with a psychiatric disorder, either primary or secondary,” they noted.
Meanwhile, hospitalizations for psychiatric-only diagnoses were minimal, just 3.6% of the total with the most common problems again being depression, anxiety, and suicide and self-injury. “Hospital resource use for only psychiatric disorders declined, consistent with the national shift to managed care for behavioral health services,” the investigators said.
“Collectively, these data will further guide strategic planning by children’s hospitals as they strive to integrate mental health care into their health care systems. Together, these findings … underscore the need for quality improvement interventions that target improving linkage with community mental health care after pediatric hospitalization,” they said.
The National Institutes of Health funded the study. Dr. Zima was supported by the National Institute of Mental Health and Behavioral Health Centers of Excellence for California. Dr. Naomi S. Bardach and Dr. Tumaini R. Coker were supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Jay G. Berry was supported by the Agency for Healthcare Research and Quality. The authors had no conflicts of interest.
FROM PEDIATRICS
Key clinical point:
Major finding: For pediatric hospitalizations without a psychiatric diagnosis, costs rose during the past decade from $3,696 to $4,150 per day. For medical stays with a psychiatric diagnosis, the price rose from $2,694 to $3,393 per day.
Data source: Review of 3,114,099 hospitalizations at 33 children’s hospitals in the United States during 2005-2014
Disclosures: The National Institutes of Health funded the study. Dr. Zima was supported by the National Institute of Mental Health and Behavioral Health Centers of Excellence for California. Dr. Naomi S. Bardach and Dr. Tumaini R. Coker were supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Jay G. Berry was supported by the Agency for Healthcare Research and Quality. The authors had no conflicts of interest.
Texas medical board drops appeal against Teladoc
The Texas Medical Board (TMB) has dropped an appeal that had challenged whether national telemedicine company Teladoc could sue over telemedicine restrictions enacted by the board. Both parties will now prepare to argue the merits behind the case in U.S. District Court in Austin, Texas.
TMB plans to vigorously defend its telemedicine rules in court, said Scott Freshour, interim executive director. He did not elaborate on the reasons behind the board’s Oct. 14 vote to withdraw its appeal in the case.
TMB withdrew its appeal because it didn’t want to suffer another loss to Teladoc in the courts, said Adam Vandervoort, Teladoc’s chief legal counsel. In a public meeting, a TMB official called the decision to withdraw “purely strategic,” according to Mr. Vandervoort.
This “raises troubling questions about the TMB’s motives in both filing, and subsequently retracting, the appeal,” Mr. Vandervoort said in a statement. “Teladoc and its amicus parties expended substantial resources on defending the appeal, which now will not result in a decision.”
The dispute stems from a medical board rule that requires Texas physicians to conduct a “face-to-face” evaluation before treating a patient via telemedicine. The face-to-face visit can be conducted through telemedicine at an established medical site, but it may not be established through an online questionnaire, e-mail, text, chat, or telephonic evaluation or consultation. In addition, the TMB requires that distant site providers establish a physician-patient relationship, which at a minimum includes: establishing that the person requesting the treatment is in fact who the person claims to be, establishing a diagnosis through the use of acceptable medical practices, discussing with the patient the risks and benefits of various treatment options, and ensuring the availability of the distant site provider or coverage of the patient for appropriate follow-up care.
Teladoc sued the medical board in April 2015 claiming the face-to-face rule violates federal antitrust laws. Teladoc provides access to medical care via phone or interactive video and treats patients for nonemergency conditions. A judge halted the rule’s enforcement until the litigation is resolved.
The TMB requested that a judge throw out the suit, arguing that the board is immune from antitrust liability as a state agency. A district court disagreed and allowed the case to proceed. The board then appealed to 5th U.S. Circuit Court of Appeals to overturn the district court’s decision.
It’s likely that the board’s decision not to pursue the appeal was affected by the recent backing of Teladoc by the U.S. Department of Justice (DOJ) and the Federal Trade Commission (FTC) regarding the application of the state action doctrine, said Paul W. Pitts, a San Francisco health law attorney who has closely followed the case. The doctrine protects the deliberate policy choices of sovereign states to displace competition with regulation or monopoly public service.
In a brief to the 5th Circuit, the DOJ and the FTC urged the appeals court to dismiss the board’s appeal. The agencies called TMB’s telemedicine rules anticompetitive and said the board was not protected by the state action doctrine because requirements under the doctrine were not satisfied. However, the America Medical Association and the Texas Medical Association sided with the TMB, telling the court the entity should be immune from federal antitrust liability.
Aside from the AMA and Texas Medical Association, the Texas board had few allies in the appeals dispute,” Mr. Pitts said in an interview.
“Many interested parties were lining up on the side of Teledoc by filing amici curiae arguing that the 5th Circuit lacked jurisdiction to hear this appeal and that the state action doctrine is not applicable,” he said. “As the market for telemedicine grows rapidly, there is an increasing number of parties with something at stake in this case.”
Now that the appeal has ended, the district court can get back to the primary issue at hand: whether the rule requiring a face-to-face exam can be justified or whether it’s just a means of protecting the traditional physician practice, Mr. Pitts said. The ultimate ruling in the case has broad implications for the practice of telemedicine in Texas and beyond.
“Medical boards in other states are revising their rules to be more accommodating of telemedicine as the use of this approach grows in acceptance around the country.” he said. “The Texas Medical Board is increasingly an outlier in this space. If Teledoc prevails, you can expect to see investors taking another look at the telemedicine space as the Texas market opens up and the role of the state medical board is diminished.”
[email protected]
On Twitter @legal_med
The Texas Medical Board (TMB) has dropped an appeal that had challenged whether national telemedicine company Teladoc could sue over telemedicine restrictions enacted by the board. Both parties will now prepare to argue the merits behind the case in U.S. District Court in Austin, Texas.
TMB plans to vigorously defend its telemedicine rules in court, said Scott Freshour, interim executive director. He did not elaborate on the reasons behind the board’s Oct. 14 vote to withdraw its appeal in the case.
TMB withdrew its appeal because it didn’t want to suffer another loss to Teladoc in the courts, said Adam Vandervoort, Teladoc’s chief legal counsel. In a public meeting, a TMB official called the decision to withdraw “purely strategic,” according to Mr. Vandervoort.
This “raises troubling questions about the TMB’s motives in both filing, and subsequently retracting, the appeal,” Mr. Vandervoort said in a statement. “Teladoc and its amicus parties expended substantial resources on defending the appeal, which now will not result in a decision.”
The dispute stems from a medical board rule that requires Texas physicians to conduct a “face-to-face” evaluation before treating a patient via telemedicine. The face-to-face visit can be conducted through telemedicine at an established medical site, but it may not be established through an online questionnaire, e-mail, text, chat, or telephonic evaluation or consultation. In addition, the TMB requires that distant site providers establish a physician-patient relationship, which at a minimum includes: establishing that the person requesting the treatment is in fact who the person claims to be, establishing a diagnosis through the use of acceptable medical practices, discussing with the patient the risks and benefits of various treatment options, and ensuring the availability of the distant site provider or coverage of the patient for appropriate follow-up care.
Teladoc sued the medical board in April 2015 claiming the face-to-face rule violates federal antitrust laws. Teladoc provides access to medical care via phone or interactive video and treats patients for nonemergency conditions. A judge halted the rule’s enforcement until the litigation is resolved.
The TMB requested that a judge throw out the suit, arguing that the board is immune from antitrust liability as a state agency. A district court disagreed and allowed the case to proceed. The board then appealed to 5th U.S. Circuit Court of Appeals to overturn the district court’s decision.
It’s likely that the board’s decision not to pursue the appeal was affected by the recent backing of Teladoc by the U.S. Department of Justice (DOJ) and the Federal Trade Commission (FTC) regarding the application of the state action doctrine, said Paul W. Pitts, a San Francisco health law attorney who has closely followed the case. The doctrine protects the deliberate policy choices of sovereign states to displace competition with regulation or monopoly public service.
In a brief to the 5th Circuit, the DOJ and the FTC urged the appeals court to dismiss the board’s appeal. The agencies called TMB’s telemedicine rules anticompetitive and said the board was not protected by the state action doctrine because requirements under the doctrine were not satisfied. However, the America Medical Association and the Texas Medical Association sided with the TMB, telling the court the entity should be immune from federal antitrust liability.
Aside from the AMA and Texas Medical Association, the Texas board had few allies in the appeals dispute,” Mr. Pitts said in an interview.
“Many interested parties were lining up on the side of Teledoc by filing amici curiae arguing that the 5th Circuit lacked jurisdiction to hear this appeal and that the state action doctrine is not applicable,” he said. “As the market for telemedicine grows rapidly, there is an increasing number of parties with something at stake in this case.”
Now that the appeal has ended, the district court can get back to the primary issue at hand: whether the rule requiring a face-to-face exam can be justified or whether it’s just a means of protecting the traditional physician practice, Mr. Pitts said. The ultimate ruling in the case has broad implications for the practice of telemedicine in Texas and beyond.
“Medical boards in other states are revising their rules to be more accommodating of telemedicine as the use of this approach grows in acceptance around the country.” he said. “The Texas Medical Board is increasingly an outlier in this space. If Teledoc prevails, you can expect to see investors taking another look at the telemedicine space as the Texas market opens up and the role of the state medical board is diminished.”
[email protected]
On Twitter @legal_med
The Texas Medical Board (TMB) has dropped an appeal that had challenged whether national telemedicine company Teladoc could sue over telemedicine restrictions enacted by the board. Both parties will now prepare to argue the merits behind the case in U.S. District Court in Austin, Texas.
TMB plans to vigorously defend its telemedicine rules in court, said Scott Freshour, interim executive director. He did not elaborate on the reasons behind the board’s Oct. 14 vote to withdraw its appeal in the case.
TMB withdrew its appeal because it didn’t want to suffer another loss to Teladoc in the courts, said Adam Vandervoort, Teladoc’s chief legal counsel. In a public meeting, a TMB official called the decision to withdraw “purely strategic,” according to Mr. Vandervoort.
This “raises troubling questions about the TMB’s motives in both filing, and subsequently retracting, the appeal,” Mr. Vandervoort said in a statement. “Teladoc and its amicus parties expended substantial resources on defending the appeal, which now will not result in a decision.”
The dispute stems from a medical board rule that requires Texas physicians to conduct a “face-to-face” evaluation before treating a patient via telemedicine. The face-to-face visit can be conducted through telemedicine at an established medical site, but it may not be established through an online questionnaire, e-mail, text, chat, or telephonic evaluation or consultation. In addition, the TMB requires that distant site providers establish a physician-patient relationship, which at a minimum includes: establishing that the person requesting the treatment is in fact who the person claims to be, establishing a diagnosis through the use of acceptable medical practices, discussing with the patient the risks and benefits of various treatment options, and ensuring the availability of the distant site provider or coverage of the patient for appropriate follow-up care.
Teladoc sued the medical board in April 2015 claiming the face-to-face rule violates federal antitrust laws. Teladoc provides access to medical care via phone or interactive video and treats patients for nonemergency conditions. A judge halted the rule’s enforcement until the litigation is resolved.
The TMB requested that a judge throw out the suit, arguing that the board is immune from antitrust liability as a state agency. A district court disagreed and allowed the case to proceed. The board then appealed to 5th U.S. Circuit Court of Appeals to overturn the district court’s decision.
It’s likely that the board’s decision not to pursue the appeal was affected by the recent backing of Teladoc by the U.S. Department of Justice (DOJ) and the Federal Trade Commission (FTC) regarding the application of the state action doctrine, said Paul W. Pitts, a San Francisco health law attorney who has closely followed the case. The doctrine protects the deliberate policy choices of sovereign states to displace competition with regulation or monopoly public service.
In a brief to the 5th Circuit, the DOJ and the FTC urged the appeals court to dismiss the board’s appeal. The agencies called TMB’s telemedicine rules anticompetitive and said the board was not protected by the state action doctrine because requirements under the doctrine were not satisfied. However, the America Medical Association and the Texas Medical Association sided with the TMB, telling the court the entity should be immune from federal antitrust liability.
Aside from the AMA and Texas Medical Association, the Texas board had few allies in the appeals dispute,” Mr. Pitts said in an interview.
“Many interested parties were lining up on the side of Teledoc by filing amici curiae arguing that the 5th Circuit lacked jurisdiction to hear this appeal and that the state action doctrine is not applicable,” he said. “As the market for telemedicine grows rapidly, there is an increasing number of parties with something at stake in this case.”
Now that the appeal has ended, the district court can get back to the primary issue at hand: whether the rule requiring a face-to-face exam can be justified or whether it’s just a means of protecting the traditional physician practice, Mr. Pitts said. The ultimate ruling in the case has broad implications for the practice of telemedicine in Texas and beyond.
“Medical boards in other states are revising their rules to be more accommodating of telemedicine as the use of this approach grows in acceptance around the country.” he said. “The Texas Medical Board is increasingly an outlier in this space. If Teledoc prevails, you can expect to see investors taking another look at the telemedicine space as the Texas market opens up and the role of the state medical board is diminished.”
[email protected]
On Twitter @legal_med
Analysis: CMS expects no MACRA pay cut for most small practices
Most small practices will see no change in their Medicare payments or perhaps even a bonus for participating in MACRA’s new Quality Payment Program (QPP) beginning in 2017.
Contrary to the initial proposed regulations from the Centers for Medicare & Medicaid Services, analysis of the final regulations shows that 90% of practices with one to nine clinicians should see no impact or even a pay increase in 2019 if they start participating in QPP next year, according to an agency analysis. The only way to fare worse would be to completely opt out of the program.
The sea change is based on two modifications to the proposed rule, according to Walter Gorski, director of regulatory affairs at the American College of Physicians. The first is the new flexibility for QPP participation for 2017. In September, CMS announced that any level of participation in the Merit-Based Incentive Payment System (MIPS) – from reporting “some data” as a low-level test to full participation in an Advanced Alternative Payment Model – would result in no penalty or pay cut for physicians and other health care providers.
The second key is the higher threshold for exemption from reporting requirements. Under the proposed rule, providers who receive Medicare payments of more than $10,000 for 100 and see fewer Medicare patients had to participate; the final rule raises that to $30,000 or more or 100 or fewer Medicare patients. Mr. Gorski said this could result in 30% of physicians being exempt and therefore not having to face the penalties associated with the program.
In comparison, CMS expect 98.5% of practices with more than 100 clinicians to receive either a bonus payment or no bonus/penalty.
Most small practices will see no change in their Medicare payments or perhaps even a bonus for participating in MACRA’s new Quality Payment Program (QPP) beginning in 2017.
Contrary to the initial proposed regulations from the Centers for Medicare & Medicaid Services, analysis of the final regulations shows that 90% of practices with one to nine clinicians should see no impact or even a pay increase in 2019 if they start participating in QPP next year, according to an agency analysis. The only way to fare worse would be to completely opt out of the program.
The sea change is based on two modifications to the proposed rule, according to Walter Gorski, director of regulatory affairs at the American College of Physicians. The first is the new flexibility for QPP participation for 2017. In September, CMS announced that any level of participation in the Merit-Based Incentive Payment System (MIPS) – from reporting “some data” as a low-level test to full participation in an Advanced Alternative Payment Model – would result in no penalty or pay cut for physicians and other health care providers.
The second key is the higher threshold for exemption from reporting requirements. Under the proposed rule, providers who receive Medicare payments of more than $10,000 for 100 and see fewer Medicare patients had to participate; the final rule raises that to $30,000 or more or 100 or fewer Medicare patients. Mr. Gorski said this could result in 30% of physicians being exempt and therefore not having to face the penalties associated with the program.
In comparison, CMS expect 98.5% of practices with more than 100 clinicians to receive either a bonus payment or no bonus/penalty.
Most small practices will see no change in their Medicare payments or perhaps even a bonus for participating in MACRA’s new Quality Payment Program (QPP) beginning in 2017.
Contrary to the initial proposed regulations from the Centers for Medicare & Medicaid Services, analysis of the final regulations shows that 90% of practices with one to nine clinicians should see no impact or even a pay increase in 2019 if they start participating in QPP next year, according to an agency analysis. The only way to fare worse would be to completely opt out of the program.
The sea change is based on two modifications to the proposed rule, according to Walter Gorski, director of regulatory affairs at the American College of Physicians. The first is the new flexibility for QPP participation for 2017. In September, CMS announced that any level of participation in the Merit-Based Incentive Payment System (MIPS) – from reporting “some data” as a low-level test to full participation in an Advanced Alternative Payment Model – would result in no penalty or pay cut for physicians and other health care providers.
The second key is the higher threshold for exemption from reporting requirements. Under the proposed rule, providers who receive Medicare payments of more than $10,000 for 100 and see fewer Medicare patients had to participate; the final rule raises that to $30,000 or more or 100 or fewer Medicare patients. Mr. Gorski said this could result in 30% of physicians being exempt and therefore not having to face the penalties associated with the program.
In comparison, CMS expect 98.5% of practices with more than 100 clinicians to receive either a bonus payment or no bonus/penalty.
Access issues looming as more docs eye exit from clinical practice
Almost half (47.8%) of physicians surveyed are considering a change in how they practice medicine within the next 1-3 years, including cutting back on hours, retiring, switching to cash/concierge practice, working locum tenens, seeking a nonclinical health care job, seeking employment, or working part time.
That’s according to responses to the 2016 Survey of America’s Physicians Practice Patterns & Perspectives, a biennial survey commissioned by The Physicians Foundation and conducted by Merritt Hawkins. A total of 17,236 physicians responded to the survey.
The percentage looking to change is up from 43.6% in the 2014 survey, but down from the 50.2% of physicians who responded the same way in 2012.
Dr. Ray pointed to a number of findings in the survey that could be driving the growth in those looking to make a change.
“If you think about the last year, the clinical, administrative, and financial changes that have occurred have occurred at a whirlwind pace,” Dr. Ray said. “For instance, continued expansion of the Affordable Care Act has included as many as 20 million new people to the rolls at the same time we have a documented physician shortage where 80% of physicians say that they have all the patients that they can take care of. They are either at capacity or they are overextended.”
Other factors influencing physicians’ employment decisions include the transition to value-based payments under the Medicare Access and CHIP Reauthorization Act (MACRA), the transition to ICD-10, the growth of physician employment, the continued sale of private practices to hospitals and health systems, and the “businessification” of heath care.
“If any of these [changes] occurred in a period of time, it would be impactful,” he said. “But to have all occur simultaneously, we say now that to be a physician is to feel the ground shaking under your feet. This is the landscape in which the survey was taken.”
Given the volume of change, it is no surprise that physician morale is low, Dr. Ray said. “One of the first things that jumps out is morale. The question was ‘what best describes your professional morale about your current feelings and the current state of the medical profession?’ and 54% were somewhat or very negative; 46% were positive/somewhat positive/very positive. The very negatives were twice what the very positives were,” he noted.
Inadequate time to deliver quality care also was cited.
“Only 14% [of respondents] said that they have all the time that they need to provide the highest standards of care; 86% said that their time was either always limited, often limited, or sometimes limited,” Dr. Ray said.
Dr. Ray highlighted another question that provides insight into physicians’ dissatisfaction with their practice environment.
The survey asked, “To what degree is patient care in your practice adversely impacted by external factors such as third party authorizations, treatment protocols, EHR design, etc.”
“The critical term here is ‘adversely impacted,’ not just influenced, but adversely impacted,” Dr. Ray said. “Only 2.3% said not at all; 10% total said either not at all or a little bit. The rest said either somewhat, a good deal, or a great deal. In fact, 72% said a good deal or a great deal.”
All of this is leading to physician burnout, he said.
“I think it all bounces back to interference with the doctor/patient relationship and the fact that [physicians] feel like there are distractions within the practice of medicine due to the regulatory environment,” he said “They are not allowed to make decisions like they want to make in the best interest of their patients based on their training and their studying and their special experience with that patient. It creates this barrier with this professional satisfaction that they want to receive from taking care of patients.”
Almost half (47.8%) of physicians surveyed are considering a change in how they practice medicine within the next 1-3 years, including cutting back on hours, retiring, switching to cash/concierge practice, working locum tenens, seeking a nonclinical health care job, seeking employment, or working part time.
That’s according to responses to the 2016 Survey of America’s Physicians Practice Patterns & Perspectives, a biennial survey commissioned by The Physicians Foundation and conducted by Merritt Hawkins. A total of 17,236 physicians responded to the survey.
The percentage looking to change is up from 43.6% in the 2014 survey, but down from the 50.2% of physicians who responded the same way in 2012.
Dr. Ray pointed to a number of findings in the survey that could be driving the growth in those looking to make a change.
“If you think about the last year, the clinical, administrative, and financial changes that have occurred have occurred at a whirlwind pace,” Dr. Ray said. “For instance, continued expansion of the Affordable Care Act has included as many as 20 million new people to the rolls at the same time we have a documented physician shortage where 80% of physicians say that they have all the patients that they can take care of. They are either at capacity or they are overextended.”
Other factors influencing physicians’ employment decisions include the transition to value-based payments under the Medicare Access and CHIP Reauthorization Act (MACRA), the transition to ICD-10, the growth of physician employment, the continued sale of private practices to hospitals and health systems, and the “businessification” of heath care.
“If any of these [changes] occurred in a period of time, it would be impactful,” he said. “But to have all occur simultaneously, we say now that to be a physician is to feel the ground shaking under your feet. This is the landscape in which the survey was taken.”
Given the volume of change, it is no surprise that physician morale is low, Dr. Ray said. “One of the first things that jumps out is morale. The question was ‘what best describes your professional morale about your current feelings and the current state of the medical profession?’ and 54% were somewhat or very negative; 46% were positive/somewhat positive/very positive. The very negatives were twice what the very positives were,” he noted.
Inadequate time to deliver quality care also was cited.
“Only 14% [of respondents] said that they have all the time that they need to provide the highest standards of care; 86% said that their time was either always limited, often limited, or sometimes limited,” Dr. Ray said.
Dr. Ray highlighted another question that provides insight into physicians’ dissatisfaction with their practice environment.
The survey asked, “To what degree is patient care in your practice adversely impacted by external factors such as third party authorizations, treatment protocols, EHR design, etc.”
“The critical term here is ‘adversely impacted,’ not just influenced, but adversely impacted,” Dr. Ray said. “Only 2.3% said not at all; 10% total said either not at all or a little bit. The rest said either somewhat, a good deal, or a great deal. In fact, 72% said a good deal or a great deal.”
All of this is leading to physician burnout, he said.
“I think it all bounces back to interference with the doctor/patient relationship and the fact that [physicians] feel like there are distractions within the practice of medicine due to the regulatory environment,” he said “They are not allowed to make decisions like they want to make in the best interest of their patients based on their training and their studying and their special experience with that patient. It creates this barrier with this professional satisfaction that they want to receive from taking care of patients.”
Almost half (47.8%) of physicians surveyed are considering a change in how they practice medicine within the next 1-3 years, including cutting back on hours, retiring, switching to cash/concierge practice, working locum tenens, seeking a nonclinical health care job, seeking employment, or working part time.
That’s according to responses to the 2016 Survey of America’s Physicians Practice Patterns & Perspectives, a biennial survey commissioned by The Physicians Foundation and conducted by Merritt Hawkins. A total of 17,236 physicians responded to the survey.
The percentage looking to change is up from 43.6% in the 2014 survey, but down from the 50.2% of physicians who responded the same way in 2012.
Dr. Ray pointed to a number of findings in the survey that could be driving the growth in those looking to make a change.
“If you think about the last year, the clinical, administrative, and financial changes that have occurred have occurred at a whirlwind pace,” Dr. Ray said. “For instance, continued expansion of the Affordable Care Act has included as many as 20 million new people to the rolls at the same time we have a documented physician shortage where 80% of physicians say that they have all the patients that they can take care of. They are either at capacity or they are overextended.”
Other factors influencing physicians’ employment decisions include the transition to value-based payments under the Medicare Access and CHIP Reauthorization Act (MACRA), the transition to ICD-10, the growth of physician employment, the continued sale of private practices to hospitals and health systems, and the “businessification” of heath care.
“If any of these [changes] occurred in a period of time, it would be impactful,” he said. “But to have all occur simultaneously, we say now that to be a physician is to feel the ground shaking under your feet. This is the landscape in which the survey was taken.”
Given the volume of change, it is no surprise that physician morale is low, Dr. Ray said. “One of the first things that jumps out is morale. The question was ‘what best describes your professional morale about your current feelings and the current state of the medical profession?’ and 54% were somewhat or very negative; 46% were positive/somewhat positive/very positive. The very negatives were twice what the very positives were,” he noted.
Inadequate time to deliver quality care also was cited.
“Only 14% [of respondents] said that they have all the time that they need to provide the highest standards of care; 86% said that their time was either always limited, often limited, or sometimes limited,” Dr. Ray said.
Dr. Ray highlighted another question that provides insight into physicians’ dissatisfaction with their practice environment.
The survey asked, “To what degree is patient care in your practice adversely impacted by external factors such as third party authorizations, treatment protocols, EHR design, etc.”
“The critical term here is ‘adversely impacted,’ not just influenced, but adversely impacted,” Dr. Ray said. “Only 2.3% said not at all; 10% total said either not at all or a little bit. The rest said either somewhat, a good deal, or a great deal. In fact, 72% said a good deal or a great deal.”
All of this is leading to physician burnout, he said.
“I think it all bounces back to interference with the doctor/patient relationship and the fact that [physicians] feel like there are distractions within the practice of medicine due to the regulatory environment,” he said “They are not allowed to make decisions like they want to make in the best interest of their patients based on their training and their studying and their special experience with that patient. It creates this barrier with this professional satisfaction that they want to receive from taking care of patients.”
A tool to assess comportment and communication for hospitalists
With the rise of hospital medicine in the United States, the lion’s share of inpatient care is delivered by hospitalists. Both hospitals and hospitalist providers are committed to delivering excellent patient care, but to accomplish this goal, specific feedback is essential.
Patient satisfaction surveys that assess provider performance, such as Press Ganey (PG)1 and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS),2 do not truly provide feedback at the encounter level with valid attribution, and these data are not sent to providers in a timely manner.
In the analyses, the HMCCOT scores were moderately correlated with the hospitalists’ PG scores. Higher scores on the HMCCOT took an average of 13 minutes per patient encounter, giving further credence to the fact that excellent communication and comportment can be rapidly established at the bedside.
Patients’ complaints about doctors often relate to comportment and communication; the grievances are most commonly about feeling rushed, not being heard, and that information was not conveyed in a clear manner.4 Patient-centeredness has been shown to improve patient satisfaction as well as clinical outcomes, in part because they feel like partners in the mutually agreed upon treatment plans.5 Many of the components of the HMCCOT are at the heart of patient-centered care. While comportment may not be a frequently used term in patient care, respectful behaviors performed at the opening of any encounter [etiquette-based medicine which includes introducing oneself to patients and smiling] set the tone for the doctor-patient interaction.
Demonstrating genuine interest in the patient as a person is a core component of excellent patient care. Sir William Osler famously observed “It is much more important to know what sort of a patient has a disease than what sort of a disease a patient has.”6 A common method of “demonstrating interest in the patient as a person” recorded by the HMCCOT was physicians asking about patient’s personal history and of their interests. It is not difficult to fathom how knowing about patients’ personal interests and perspectives can help to most effectively engage them in establishing their goals of care and with therapeutic decisions.
Because hospitalists spend only a small proportion of their clinical time in direct patient care at the bedside, they need to make every moment count. HMCCOT allows for the identification of providers who are excellent in communication and comportment. Once identified, these exemplars can watch their peers and become the trainers to establish a culture of excellence.
Larger studies will be needed in the future to assess whether interventions that translate into improved comportment and communication among hospitalists will definitively augment patient satisfaction and ameliorate clinical outcomes.
1. Press Ganey. Accessed Dec. 15, 2015.
2. HCAHPS. Accessed Feb. 2, 2016.
3. Kotwal S, Khaliq W, Landis R, Wright S. Developing a comportment and communication tool for use in hospital medicine. J Hosp Med. 2016 Aug 13. doi: 10.1002/jhm.2647.
4. Hickson GB, Clayton EW, Entman SS, Miller CS, Githens PB, Whetten-Goldstein K, Sloan FA. Obstetricians’ prior malpractice experience and patients’ satisfaction with care. JAMA. 1994 Nov 23-30;272(20):1583-7.
5. Epstein RM, Street RL. Patient-centered communication in cancer care: promoting healing and reducing suffering. National Cancer Institute, NIH Publication No. 07-6225. Bethesda, MD, 2007.
6. Taylor RB. White Coat Tales: Medicine’s Heroes, Heritage, and Misadventure. New York: Springer; 2007:126.
Susrutha Kotwal, MD, and Scott Wright, MD, are based in the department of medicine, division of hospital medicine, Johns Hopkins Bayview Medical Center and Johns Hopkins University, Baltimore.
With the rise of hospital medicine in the United States, the lion’s share of inpatient care is delivered by hospitalists. Both hospitals and hospitalist providers are committed to delivering excellent patient care, but to accomplish this goal, specific feedback is essential.
Patient satisfaction surveys that assess provider performance, such as Press Ganey (PG)1 and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS),2 do not truly provide feedback at the encounter level with valid attribution, and these data are not sent to providers in a timely manner.
In the analyses, the HMCCOT scores were moderately correlated with the hospitalists’ PG scores. Higher scores on the HMCCOT took an average of 13 minutes per patient encounter, giving further credence to the fact that excellent communication and comportment can be rapidly established at the bedside.
Patients’ complaints about doctors often relate to comportment and communication; the grievances are most commonly about feeling rushed, not being heard, and that information was not conveyed in a clear manner.4 Patient-centeredness has been shown to improve patient satisfaction as well as clinical outcomes, in part because they feel like partners in the mutually agreed upon treatment plans.5 Many of the components of the HMCCOT are at the heart of patient-centered care. While comportment may not be a frequently used term in patient care, respectful behaviors performed at the opening of any encounter [etiquette-based medicine which includes introducing oneself to patients and smiling] set the tone for the doctor-patient interaction.
Demonstrating genuine interest in the patient as a person is a core component of excellent patient care. Sir William Osler famously observed “It is much more important to know what sort of a patient has a disease than what sort of a disease a patient has.”6 A common method of “demonstrating interest in the patient as a person” recorded by the HMCCOT was physicians asking about patient’s personal history and of their interests. It is not difficult to fathom how knowing about patients’ personal interests and perspectives can help to most effectively engage them in establishing their goals of care and with therapeutic decisions.
Because hospitalists spend only a small proportion of their clinical time in direct patient care at the bedside, they need to make every moment count. HMCCOT allows for the identification of providers who are excellent in communication and comportment. Once identified, these exemplars can watch their peers and become the trainers to establish a culture of excellence.
Larger studies will be needed in the future to assess whether interventions that translate into improved comportment and communication among hospitalists will definitively augment patient satisfaction and ameliorate clinical outcomes.
1. Press Ganey. Accessed Dec. 15, 2015.
2. HCAHPS. Accessed Feb. 2, 2016.
3. Kotwal S, Khaliq W, Landis R, Wright S. Developing a comportment and communication tool for use in hospital medicine. J Hosp Med. 2016 Aug 13. doi: 10.1002/jhm.2647.
4. Hickson GB, Clayton EW, Entman SS, Miller CS, Githens PB, Whetten-Goldstein K, Sloan FA. Obstetricians’ prior malpractice experience and patients’ satisfaction with care. JAMA. 1994 Nov 23-30;272(20):1583-7.
5. Epstein RM, Street RL. Patient-centered communication in cancer care: promoting healing and reducing suffering. National Cancer Institute, NIH Publication No. 07-6225. Bethesda, MD, 2007.
6. Taylor RB. White Coat Tales: Medicine’s Heroes, Heritage, and Misadventure. New York: Springer; 2007:126.
Susrutha Kotwal, MD, and Scott Wright, MD, are based in the department of medicine, division of hospital medicine, Johns Hopkins Bayview Medical Center and Johns Hopkins University, Baltimore.
With the rise of hospital medicine in the United States, the lion’s share of inpatient care is delivered by hospitalists. Both hospitals and hospitalist providers are committed to delivering excellent patient care, but to accomplish this goal, specific feedback is essential.
Patient satisfaction surveys that assess provider performance, such as Press Ganey (PG)1 and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS),2 do not truly provide feedback at the encounter level with valid attribution, and these data are not sent to providers in a timely manner.
In the analyses, the HMCCOT scores were moderately correlated with the hospitalists’ PG scores. Higher scores on the HMCCOT took an average of 13 minutes per patient encounter, giving further credence to the fact that excellent communication and comportment can be rapidly established at the bedside.
Patients’ complaints about doctors often relate to comportment and communication; the grievances are most commonly about feeling rushed, not being heard, and that information was not conveyed in a clear manner.4 Patient-centeredness has been shown to improve patient satisfaction as well as clinical outcomes, in part because they feel like partners in the mutually agreed upon treatment plans.5 Many of the components of the HMCCOT are at the heart of patient-centered care. While comportment may not be a frequently used term in patient care, respectful behaviors performed at the opening of any encounter [etiquette-based medicine which includes introducing oneself to patients and smiling] set the tone for the doctor-patient interaction.
Demonstrating genuine interest in the patient as a person is a core component of excellent patient care. Sir William Osler famously observed “It is much more important to know what sort of a patient has a disease than what sort of a disease a patient has.”6 A common method of “demonstrating interest in the patient as a person” recorded by the HMCCOT was physicians asking about patient’s personal history and of their interests. It is not difficult to fathom how knowing about patients’ personal interests and perspectives can help to most effectively engage them in establishing their goals of care and with therapeutic decisions.
Because hospitalists spend only a small proportion of their clinical time in direct patient care at the bedside, they need to make every moment count. HMCCOT allows for the identification of providers who are excellent in communication and comportment. Once identified, these exemplars can watch their peers and become the trainers to establish a culture of excellence.
Larger studies will be needed in the future to assess whether interventions that translate into improved comportment and communication among hospitalists will definitively augment patient satisfaction and ameliorate clinical outcomes.
1. Press Ganey. Accessed Dec. 15, 2015.
2. HCAHPS. Accessed Feb. 2, 2016.
3. Kotwal S, Khaliq W, Landis R, Wright S. Developing a comportment and communication tool for use in hospital medicine. J Hosp Med. 2016 Aug 13. doi: 10.1002/jhm.2647.
4. Hickson GB, Clayton EW, Entman SS, Miller CS, Githens PB, Whetten-Goldstein K, Sloan FA. Obstetricians’ prior malpractice experience and patients’ satisfaction with care. JAMA. 1994 Nov 23-30;272(20):1583-7.
5. Epstein RM, Street RL. Patient-centered communication in cancer care: promoting healing and reducing suffering. National Cancer Institute, NIH Publication No. 07-6225. Bethesda, MD, 2007.
6. Taylor RB. White Coat Tales: Medicine’s Heroes, Heritage, and Misadventure. New York: Springer; 2007:126.
Susrutha Kotwal, MD, and Scott Wright, MD, are based in the department of medicine, division of hospital medicine, Johns Hopkins Bayview Medical Center and Johns Hopkins University, Baltimore.
CMS offering educational webinars on MACRA
The Centers for Medicare & Medicaid Services is offering a pair of webinars aimed at helping physicians navigate the new regulation that operationalizes the Medicare Access and CHIP Reauthorization Act (MACRA).
The first webinar, scheduled for Oct. 26, will provide an overview of the two components of the Quality Payment Program – the Merit-Based Incentive Payment System (MIPS) and advanced Alternative Payment Models (APMs).
The second webinar, scheduled for Nov. 15, is targeted to Medicare Part B fee-for-service clinicians, office managers and administrators, state and national associations that represent health care providers, and other stakeholders and will feature a question-and-answer session.
The webinars are part of the agency’s ongoing efforts to help educate practitioners on the provisions of the final MACRA regulation, which was issued on Oct. 14. CMS also recently launched a website to help in that regard.
The Centers for Medicare & Medicaid Services is offering a pair of webinars aimed at helping physicians navigate the new regulation that operationalizes the Medicare Access and CHIP Reauthorization Act (MACRA).
The first webinar, scheduled for Oct. 26, will provide an overview of the two components of the Quality Payment Program – the Merit-Based Incentive Payment System (MIPS) and advanced Alternative Payment Models (APMs).
The second webinar, scheduled for Nov. 15, is targeted to Medicare Part B fee-for-service clinicians, office managers and administrators, state and national associations that represent health care providers, and other stakeholders and will feature a question-and-answer session.
The webinars are part of the agency’s ongoing efforts to help educate practitioners on the provisions of the final MACRA regulation, which was issued on Oct. 14. CMS also recently launched a website to help in that regard.
The Centers for Medicare & Medicaid Services is offering a pair of webinars aimed at helping physicians navigate the new regulation that operationalizes the Medicare Access and CHIP Reauthorization Act (MACRA).
The first webinar, scheduled for Oct. 26, will provide an overview of the two components of the Quality Payment Program – the Merit-Based Incentive Payment System (MIPS) and advanced Alternative Payment Models (APMs).
The second webinar, scheduled for Nov. 15, is targeted to Medicare Part B fee-for-service clinicians, office managers and administrators, state and national associations that represent health care providers, and other stakeholders and will feature a question-and-answer session.
The webinars are part of the agency’s ongoing efforts to help educate practitioners on the provisions of the final MACRA regulation, which was issued on Oct. 14. CMS also recently launched a website to help in that regard.
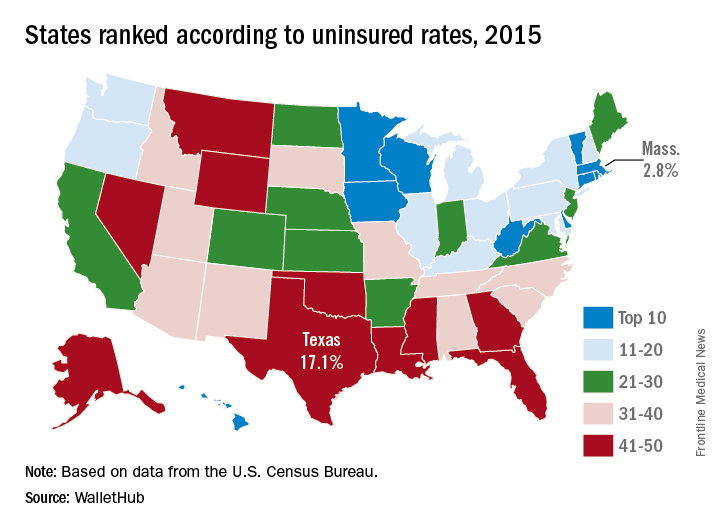
Uninsured rate lowest in Massachusetts
Massachusetts had the nation’s lowest uninsured rate in 2015, and Texas had the highest, according to the personal finance website WalletHub.
Massachusetts’ uninsured rate of 2.8% was followed by Vermont at 3.8%, Hawaii at 4%, Minnesota at 4.5%, and Iowa at 5%, WalletHub reported.
Nevada, which was 44th overall in 2015, had the largest reduction (–10.3%) in its uninsured rate from 2010 to 2015. Oregon had the next-largest drop (10.1%) and Massachusetts had the smallest decrease at –1.6%, meaning that no state saw an increase over the 5-year period, the WalletHub report showed.
A quick run through some subgroups shows that Vermont had the lowest percentage of uninsured children (1%) and Alaska had the highest (10.6%), Massachusetts was lowest for whites (2.2%) and Hispanics (5.3%) while Mississippi was highest (10.9% white and 37.6% Hispanic). Hawaii had the lowest rate (3.8%) for blacks, and Montana had the highest (17.4%), WalletHub said.
Massachusetts had the nation’s lowest uninsured rate in 2015, and Texas had the highest, according to the personal finance website WalletHub.
Massachusetts’ uninsured rate of 2.8% was followed by Vermont at 3.8%, Hawaii at 4%, Minnesota at 4.5%, and Iowa at 5%, WalletHub reported.
Nevada, which was 44th overall in 2015, had the largest reduction (–10.3%) in its uninsured rate from 2010 to 2015. Oregon had the next-largest drop (10.1%) and Massachusetts had the smallest decrease at –1.6%, meaning that no state saw an increase over the 5-year period, the WalletHub report showed.
A quick run through some subgroups shows that Vermont had the lowest percentage of uninsured children (1%) and Alaska had the highest (10.6%), Massachusetts was lowest for whites (2.2%) and Hispanics (5.3%) while Mississippi was highest (10.9% white and 37.6% Hispanic). Hawaii had the lowest rate (3.8%) for blacks, and Montana had the highest (17.4%), WalletHub said.
Massachusetts had the nation’s lowest uninsured rate in 2015, and Texas had the highest, according to the personal finance website WalletHub.
Massachusetts’ uninsured rate of 2.8% was followed by Vermont at 3.8%, Hawaii at 4%, Minnesota at 4.5%, and Iowa at 5%, WalletHub reported.
Nevada, which was 44th overall in 2015, had the largest reduction (–10.3%) in its uninsured rate from 2010 to 2015. Oregon had the next-largest drop (10.1%) and Massachusetts had the smallest decrease at –1.6%, meaning that no state saw an increase over the 5-year period, the WalletHub report showed.
A quick run through some subgroups shows that Vermont had the lowest percentage of uninsured children (1%) and Alaska had the highest (10.6%), Massachusetts was lowest for whites (2.2%) and Hispanics (5.3%) while Mississippi was highest (10.9% white and 37.6% Hispanic). Hawaii had the lowest rate (3.8%) for blacks, and Montana had the highest (17.4%), WalletHub said.
SAVR for radiation-induced aortic stenosis has high late mortality
ROME – Radiation-induced aortic stenosis is associated with markedly worse long-term outcome after surgical aortic valve replacement than when the operation is performed in patients without a history of radiotherapy, Milind Y. Desai, MD, reported at the annual congress of the European Society of Cardiology.
Moreover, the Society of Thoracic Surgeons (STS) score isn’t good at risk-stratifying patients with radiation-induced aortic stenosis who are under consideration for surgical aortic valve replacement (SAVR).
Radiation-induced heart disease is a late complication of thoracic radiotherapy. It’s particularly common in patients who got radiation for lymphomas or breast cancer. It can affect any cardiac structure, including the myocardium, pericardium, valves, coronary arteries, and the conduction system.
Aortic stenosis is the most common valvular manifestation, present in roughly 80% of patients with radiation-induced heart disease. At the Cleveland Clinic, the average time from radiotherapy to development of radiation-induced aortic stenosis (RIAS) is about 20 years. The condition is characterized by thickening of the junction between the base of the anterior mitral leaflet and aortic root, known as the aortomitral curtain, Dr. Desai explained.
He presented a retrospective observational cohort study involving 172 patients who underwent SAVR for RIAS and an equal number of SAVR patients with no such history. The groups were matched by age, sex, aortic valve area, and type and timing of SAVR. Of note, the group with RIAS had a mean preoperative STS score of 11, and the control group averaged a similar score of 10.
The key finding: During a mean follow-up of 6 years, the all-cause mortality rate was a hefty 48% in patients with RIAS, compared with just 7% in matched controls. Only about 5% of deaths in the group with RIAS were from recurrent malignancy. The low figure is not surprising given the average 20-year lag between radiotherapy and development of radiation-induced heart disease.
“In our experience, most of these patients develop a recurrent pleural effusion and nasty cardiopulmonary issues that result in their death,” according to Dr. Desai.
In a multivariate Cox proportional hazards analysis, a history of chest radiation therapy was by far the strongest predictor of all-cause mortality, conferring an 8.5-fold increase in risk.
The only other statistically significant predictor of mortality during follow-up in multivariate analysis was a high STS score, with an associated weak albeit statistically significant 1.15-fold increased risk. A total of 30 of 78 (39%) RIAS patients with an STS score below 4 died during follow-up, compared with none of 91 controls.
Thirty-four of 92 (37%) RIAS patients under age 65 died during follow-up, whereas none of 83 control SAVR patients did so.
Having coronary artery bypass surgery or other cardiac surgery at the time of SAVR was not associated with significantly increased risk of mortality compared with solo SAVR.
In-hospital outcomes were consistently worse after SAVR in the RIAS group. Half of the RIAS patients experienced in-hospital atrial fibrillation and 29% developed persistent atrial fibrillation, compared with 30% and 24% of controls. About 22% of RIAS patients were readmitted within 3 months after surgery, as were only 8% of controls. In-hospital mortality occurred in 2% of SAVR patients with RIAS; none of the matched controls did.
Dr. Desai reported having no financial interests relative to this study.
ROME – Radiation-induced aortic stenosis is associated with markedly worse long-term outcome after surgical aortic valve replacement than when the operation is performed in patients without a history of radiotherapy, Milind Y. Desai, MD, reported at the annual congress of the European Society of Cardiology.
Moreover, the Society of Thoracic Surgeons (STS) score isn’t good at risk-stratifying patients with radiation-induced aortic stenosis who are under consideration for surgical aortic valve replacement (SAVR).
Radiation-induced heart disease is a late complication of thoracic radiotherapy. It’s particularly common in patients who got radiation for lymphomas or breast cancer. It can affect any cardiac structure, including the myocardium, pericardium, valves, coronary arteries, and the conduction system.
Aortic stenosis is the most common valvular manifestation, present in roughly 80% of patients with radiation-induced heart disease. At the Cleveland Clinic, the average time from radiotherapy to development of radiation-induced aortic stenosis (RIAS) is about 20 years. The condition is characterized by thickening of the junction between the base of the anterior mitral leaflet and aortic root, known as the aortomitral curtain, Dr. Desai explained.
He presented a retrospective observational cohort study involving 172 patients who underwent SAVR for RIAS and an equal number of SAVR patients with no such history. The groups were matched by age, sex, aortic valve area, and type and timing of SAVR. Of note, the group with RIAS had a mean preoperative STS score of 11, and the control group averaged a similar score of 10.
The key finding: During a mean follow-up of 6 years, the all-cause mortality rate was a hefty 48% in patients with RIAS, compared with just 7% in matched controls. Only about 5% of deaths in the group with RIAS were from recurrent malignancy. The low figure is not surprising given the average 20-year lag between radiotherapy and development of radiation-induced heart disease.
“In our experience, most of these patients develop a recurrent pleural effusion and nasty cardiopulmonary issues that result in their death,” according to Dr. Desai.
In a multivariate Cox proportional hazards analysis, a history of chest radiation therapy was by far the strongest predictor of all-cause mortality, conferring an 8.5-fold increase in risk.
The only other statistically significant predictor of mortality during follow-up in multivariate analysis was a high STS score, with an associated weak albeit statistically significant 1.15-fold increased risk. A total of 30 of 78 (39%) RIAS patients with an STS score below 4 died during follow-up, compared with none of 91 controls.
Thirty-four of 92 (37%) RIAS patients under age 65 died during follow-up, whereas none of 83 control SAVR patients did so.
Having coronary artery bypass surgery or other cardiac surgery at the time of SAVR was not associated with significantly increased risk of mortality compared with solo SAVR.
In-hospital outcomes were consistently worse after SAVR in the RIAS group. Half of the RIAS patients experienced in-hospital atrial fibrillation and 29% developed persistent atrial fibrillation, compared with 30% and 24% of controls. About 22% of RIAS patients were readmitted within 3 months after surgery, as were only 8% of controls. In-hospital mortality occurred in 2% of SAVR patients with RIAS; none of the matched controls did.
Dr. Desai reported having no financial interests relative to this study.
ROME – Radiation-induced aortic stenosis is associated with markedly worse long-term outcome after surgical aortic valve replacement than when the operation is performed in patients without a history of radiotherapy, Milind Y. Desai, MD, reported at the annual congress of the European Society of Cardiology.
Moreover, the Society of Thoracic Surgeons (STS) score isn’t good at risk-stratifying patients with radiation-induced aortic stenosis who are under consideration for surgical aortic valve replacement (SAVR).
Radiation-induced heart disease is a late complication of thoracic radiotherapy. It’s particularly common in patients who got radiation for lymphomas or breast cancer. It can affect any cardiac structure, including the myocardium, pericardium, valves, coronary arteries, and the conduction system.
Aortic stenosis is the most common valvular manifestation, present in roughly 80% of patients with radiation-induced heart disease. At the Cleveland Clinic, the average time from radiotherapy to development of radiation-induced aortic stenosis (RIAS) is about 20 years. The condition is characterized by thickening of the junction between the base of the anterior mitral leaflet and aortic root, known as the aortomitral curtain, Dr. Desai explained.
He presented a retrospective observational cohort study involving 172 patients who underwent SAVR for RIAS and an equal number of SAVR patients with no such history. The groups were matched by age, sex, aortic valve area, and type and timing of SAVR. Of note, the group with RIAS had a mean preoperative STS score of 11, and the control group averaged a similar score of 10.
The key finding: During a mean follow-up of 6 years, the all-cause mortality rate was a hefty 48% in patients with RIAS, compared with just 7% in matched controls. Only about 5% of deaths in the group with RIAS were from recurrent malignancy. The low figure is not surprising given the average 20-year lag between radiotherapy and development of radiation-induced heart disease.
“In our experience, most of these patients develop a recurrent pleural effusion and nasty cardiopulmonary issues that result in their death,” according to Dr. Desai.
In a multivariate Cox proportional hazards analysis, a history of chest radiation therapy was by far the strongest predictor of all-cause mortality, conferring an 8.5-fold increase in risk.
The only other statistically significant predictor of mortality during follow-up in multivariate analysis was a high STS score, with an associated weak albeit statistically significant 1.15-fold increased risk. A total of 30 of 78 (39%) RIAS patients with an STS score below 4 died during follow-up, compared with none of 91 controls.
Thirty-four of 92 (37%) RIAS patients under age 65 died during follow-up, whereas none of 83 control SAVR patients did so.
Having coronary artery bypass surgery or other cardiac surgery at the time of SAVR was not associated with significantly increased risk of mortality compared with solo SAVR.
In-hospital outcomes were consistently worse after SAVR in the RIAS group. Half of the RIAS patients experienced in-hospital atrial fibrillation and 29% developed persistent atrial fibrillation, compared with 30% and 24% of controls. About 22% of RIAS patients were readmitted within 3 months after surgery, as were only 8% of controls. In-hospital mortality occurred in 2% of SAVR patients with RIAS; none of the matched controls did.
Dr. Desai reported having no financial interests relative to this study.
AT THE ESC CONGRESS 2016
Key clinical point:
Major finding: All-cause mortality occurred in 48% of 172 patients with radiation-induced severe aortic stenosis during a mean follow-up of 6 years after surgical aortic valve replacement, compared with just 7% of matched controls.
Data source: This was a retrospective observational study involving 172 closely matched pairs of surgical aortic valve replacement patients.
Disclosures: The presenter reported having no financial conflicts of interest regarding this study.