User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Simulation-based training effective for transesophageal echo
Simulation-based teaching of transesophageal echocardiography (TEE) improved cardiology fellows’ knowledge, skills, and comfort with the procedure, compared with traditional training, a new study shows.
“TEE learning may be hampered by the lack of availability of teachers and equipment and by the need for esophageal intubation, which is semi-invasive,” Augustin Coisne, MD, PhD, of the Cardiovascular Research Foundation in New York, said in an interview. “In this setting, simulation emerges as a key educational tool, but we were lacking evidence supporting simulation-based educational programs.”
Fellows in the simulation group achieved higher theoretical test scores and practical test scores after the training than did those in the traditional group.
Furthermore, Dr. Coisne said, “the results of the subgroup analyses were surprising and unexpected. The effect of the simulation-based training was greater among fellows at the beginning of fellowship – i.e., 2 years or less of training – in both theoretical and practical tests and in women [versus men] for the theoretical test.”
Their results, from the randomized SIMULATOR study, were published online in JAMA Cardiology.
More ready, more confident
The researchers randomly assigned 324 cardiology fellows (mean age, 26.4 years; about 30% women) inexperienced in TEE from 42 French university centers to TEE training with or without simulation support. Both groups participated in traditional didactic training using e-learning with an online course that is compulsory for all cardiology fellows in France.
The simulation group also participated in two 2-hour teaching sessions using a TEE simulator.
Each fellow completed a theoretical and a practical test prior to training to assess their baseline TEE level and again 3 months after the end of the training program. A TEE simulator (U/S Mentor Simulator; 3D Systems Simbionix) was used for all tests, and 24 certified echocardiography teachers served as both trainers and raters.
The theoretical tests included 20 online video-based questions to evaluate recognition of standard TEE views, normal anatomy, and some pathological cases. Fellows had 90 seconds to choose the best answer for each question from five multiple-choice options.
For the practical tests, fellows had 3 minutes to familiarize themselves with the handling of the simulator, without specific training and before the probe introduction.
They were asked to show 10 basic views on the simulator and had a maximum of 1 minute for each view.
The coprimary outcomes were the scores in the final theoretical and practical tests. TEE duration and the fellows’ self-assessment of their proficiency were also evaluated.
At baseline, the theoretical and practical test scores were similar between the groups (33.0 for the simulator group vs. 32.5 for the traditional group, and 44.2 vs. 46.1, respectively).
After training, the fellows in the simulation group had higher theoretical and practical test scores than those in the traditional group (47.2% vs. 38.3% and 74.5% vs. 59.0%, respectively).
Score changes were consistently higher when the pretraining scores were lower, an association that was stronger in the simulation group.
Dr. Coisne noted that subgroup analyses showed that the effectiveness of the simulation training was greater when performed at the beginning of the fellowship. On the theoretical test, the point increase was 11.9 for the simulation group versus 4.25 points for the traditional training group; for the practical test, the increases were 24.0 points versus 10.1 points.
After training, it took significantly less time for the simulation group to complete a TEE than it did the traditional group (8.3 vs. 9.4 minutes).
Furthermore, simulation group fellows reported that they felt more ready (mean score, 3.0 vs. 1.7) and more confident (mean score, 3.3 vs. 2.4) about performing a TEE alone after training.
“The simulation approach is definitively scalable to every institution,” Dr. Coisne said. “However, a medico-economic analysis should be interesting because the cost of the simulator and its maintenance might be a limitation to spread simulation-based teaching. The possibility for smaller hospitals to pool their financial input to share a TEE simulator could be considered to increase its cost-effectiveness.”
Real-world outcomes required
Commenting on the study, S. Justin Szawlewicz, MD, chair of cardiovascular medicine at Deborah Heart and Lung Center in Brown Mills, N.J., pointed out that the authors indicated that the number of TEEs performed by the trainees was not collected.
“This would be useful information to determine if those who received simulator training sought out and performed more TEEs, and also to determine if cardiology trainees in France perform a similar number of TEEs as cardiology trainees in the United States.”
In addition, he said, “the 4 hours of simulator training in TEE is extra education and experience that the standard trainees didn’t get. Would 4 extra hours of standard training didactics also improve trainees’ scores?”
Noting that the fellows’ ability to perform TEE in real patients was not assessed, Dr. Szawlewicz said, “a study could be designed that evaluated TEE images from real patients to see if trainees receiving simulator training performed better, more comprehensive and efficient TEEs than standard training.”
Nevertheless, he concluded, “Four hours of simulator training appears to improve TEE knowledge and skills. This is something we would consider at our institution.”
Like Dr. Szawlewicz, Michael Spooner, MD, MBA, of Mercy One North Iowa Heart Center in Mason City, and Kathryn Bertlacher, MD, of the University of Pittsburgh Medical Center, noted in a related editorial, “data are not provided about change in the learner’s behavior or performance on an actual TEE after the course, nor are there data about clinical outcomes such as patient safety or completeness of subsequent TEEs.
“This limitation, which is a limitation of most of the existing TEE simulation literature, is a high bar to cross,” they concluded. “Reaching this bar will require studies such as this to provide foundational understanding.”
Twin-Medical provided the TEE simulators. No relevant conflicts of interest were disclosed.
A version of this article first appeared on Medscape.com.
Simulation-based teaching of transesophageal echocardiography (TEE) improved cardiology fellows’ knowledge, skills, and comfort with the procedure, compared with traditional training, a new study shows.
“TEE learning may be hampered by the lack of availability of teachers and equipment and by the need for esophageal intubation, which is semi-invasive,” Augustin Coisne, MD, PhD, of the Cardiovascular Research Foundation in New York, said in an interview. “In this setting, simulation emerges as a key educational tool, but we were lacking evidence supporting simulation-based educational programs.”
Fellows in the simulation group achieved higher theoretical test scores and practical test scores after the training than did those in the traditional group.
Furthermore, Dr. Coisne said, “the results of the subgroup analyses were surprising and unexpected. The effect of the simulation-based training was greater among fellows at the beginning of fellowship – i.e., 2 years or less of training – in both theoretical and practical tests and in women [versus men] for the theoretical test.”
Their results, from the randomized SIMULATOR study, were published online in JAMA Cardiology.
More ready, more confident
The researchers randomly assigned 324 cardiology fellows (mean age, 26.4 years; about 30% women) inexperienced in TEE from 42 French university centers to TEE training with or without simulation support. Both groups participated in traditional didactic training using e-learning with an online course that is compulsory for all cardiology fellows in France.
The simulation group also participated in two 2-hour teaching sessions using a TEE simulator.
Each fellow completed a theoretical and a practical test prior to training to assess their baseline TEE level and again 3 months after the end of the training program. A TEE simulator (U/S Mentor Simulator; 3D Systems Simbionix) was used for all tests, and 24 certified echocardiography teachers served as both trainers and raters.
The theoretical tests included 20 online video-based questions to evaluate recognition of standard TEE views, normal anatomy, and some pathological cases. Fellows had 90 seconds to choose the best answer for each question from five multiple-choice options.
For the practical tests, fellows had 3 minutes to familiarize themselves with the handling of the simulator, without specific training and before the probe introduction.
They were asked to show 10 basic views on the simulator and had a maximum of 1 minute for each view.
The coprimary outcomes were the scores in the final theoretical and practical tests. TEE duration and the fellows’ self-assessment of their proficiency were also evaluated.
At baseline, the theoretical and practical test scores were similar between the groups (33.0 for the simulator group vs. 32.5 for the traditional group, and 44.2 vs. 46.1, respectively).
After training, the fellows in the simulation group had higher theoretical and practical test scores than those in the traditional group (47.2% vs. 38.3% and 74.5% vs. 59.0%, respectively).
Score changes were consistently higher when the pretraining scores were lower, an association that was stronger in the simulation group.
Dr. Coisne noted that subgroup analyses showed that the effectiveness of the simulation training was greater when performed at the beginning of the fellowship. On the theoretical test, the point increase was 11.9 for the simulation group versus 4.25 points for the traditional training group; for the practical test, the increases were 24.0 points versus 10.1 points.
After training, it took significantly less time for the simulation group to complete a TEE than it did the traditional group (8.3 vs. 9.4 minutes).
Furthermore, simulation group fellows reported that they felt more ready (mean score, 3.0 vs. 1.7) and more confident (mean score, 3.3 vs. 2.4) about performing a TEE alone after training.
“The simulation approach is definitively scalable to every institution,” Dr. Coisne said. “However, a medico-economic analysis should be interesting because the cost of the simulator and its maintenance might be a limitation to spread simulation-based teaching. The possibility for smaller hospitals to pool their financial input to share a TEE simulator could be considered to increase its cost-effectiveness.”
Real-world outcomes required
Commenting on the study, S. Justin Szawlewicz, MD, chair of cardiovascular medicine at Deborah Heart and Lung Center in Brown Mills, N.J., pointed out that the authors indicated that the number of TEEs performed by the trainees was not collected.
“This would be useful information to determine if those who received simulator training sought out and performed more TEEs, and also to determine if cardiology trainees in France perform a similar number of TEEs as cardiology trainees in the United States.”
In addition, he said, “the 4 hours of simulator training in TEE is extra education and experience that the standard trainees didn’t get. Would 4 extra hours of standard training didactics also improve trainees’ scores?”
Noting that the fellows’ ability to perform TEE in real patients was not assessed, Dr. Szawlewicz said, “a study could be designed that evaluated TEE images from real patients to see if trainees receiving simulator training performed better, more comprehensive and efficient TEEs than standard training.”
Nevertheless, he concluded, “Four hours of simulator training appears to improve TEE knowledge and skills. This is something we would consider at our institution.”
Like Dr. Szawlewicz, Michael Spooner, MD, MBA, of Mercy One North Iowa Heart Center in Mason City, and Kathryn Bertlacher, MD, of the University of Pittsburgh Medical Center, noted in a related editorial, “data are not provided about change in the learner’s behavior or performance on an actual TEE after the course, nor are there data about clinical outcomes such as patient safety or completeness of subsequent TEEs.
“This limitation, which is a limitation of most of the existing TEE simulation literature, is a high bar to cross,” they concluded. “Reaching this bar will require studies such as this to provide foundational understanding.”
Twin-Medical provided the TEE simulators. No relevant conflicts of interest were disclosed.
A version of this article first appeared on Medscape.com.
Simulation-based teaching of transesophageal echocardiography (TEE) improved cardiology fellows’ knowledge, skills, and comfort with the procedure, compared with traditional training, a new study shows.
“TEE learning may be hampered by the lack of availability of teachers and equipment and by the need for esophageal intubation, which is semi-invasive,” Augustin Coisne, MD, PhD, of the Cardiovascular Research Foundation in New York, said in an interview. “In this setting, simulation emerges as a key educational tool, but we were lacking evidence supporting simulation-based educational programs.”
Fellows in the simulation group achieved higher theoretical test scores and practical test scores after the training than did those in the traditional group.
Furthermore, Dr. Coisne said, “the results of the subgroup analyses were surprising and unexpected. The effect of the simulation-based training was greater among fellows at the beginning of fellowship – i.e., 2 years or less of training – in both theoretical and practical tests and in women [versus men] for the theoretical test.”
Their results, from the randomized SIMULATOR study, were published online in JAMA Cardiology.
More ready, more confident
The researchers randomly assigned 324 cardiology fellows (mean age, 26.4 years; about 30% women) inexperienced in TEE from 42 French university centers to TEE training with or without simulation support. Both groups participated in traditional didactic training using e-learning with an online course that is compulsory for all cardiology fellows in France.
The simulation group also participated in two 2-hour teaching sessions using a TEE simulator.
Each fellow completed a theoretical and a practical test prior to training to assess their baseline TEE level and again 3 months after the end of the training program. A TEE simulator (U/S Mentor Simulator; 3D Systems Simbionix) was used for all tests, and 24 certified echocardiography teachers served as both trainers and raters.
The theoretical tests included 20 online video-based questions to evaluate recognition of standard TEE views, normal anatomy, and some pathological cases. Fellows had 90 seconds to choose the best answer for each question from five multiple-choice options.
For the practical tests, fellows had 3 minutes to familiarize themselves with the handling of the simulator, without specific training and before the probe introduction.
They were asked to show 10 basic views on the simulator and had a maximum of 1 minute for each view.
The coprimary outcomes were the scores in the final theoretical and practical tests. TEE duration and the fellows’ self-assessment of their proficiency were also evaluated.
At baseline, the theoretical and practical test scores were similar between the groups (33.0 for the simulator group vs. 32.5 for the traditional group, and 44.2 vs. 46.1, respectively).
After training, the fellows in the simulation group had higher theoretical and practical test scores than those in the traditional group (47.2% vs. 38.3% and 74.5% vs. 59.0%, respectively).
Score changes were consistently higher when the pretraining scores were lower, an association that was stronger in the simulation group.
Dr. Coisne noted that subgroup analyses showed that the effectiveness of the simulation training was greater when performed at the beginning of the fellowship. On the theoretical test, the point increase was 11.9 for the simulation group versus 4.25 points for the traditional training group; for the practical test, the increases were 24.0 points versus 10.1 points.
After training, it took significantly less time for the simulation group to complete a TEE than it did the traditional group (8.3 vs. 9.4 minutes).
Furthermore, simulation group fellows reported that they felt more ready (mean score, 3.0 vs. 1.7) and more confident (mean score, 3.3 vs. 2.4) about performing a TEE alone after training.
“The simulation approach is definitively scalable to every institution,” Dr. Coisne said. “However, a medico-economic analysis should be interesting because the cost of the simulator and its maintenance might be a limitation to spread simulation-based teaching. The possibility for smaller hospitals to pool their financial input to share a TEE simulator could be considered to increase its cost-effectiveness.”
Real-world outcomes required
Commenting on the study, S. Justin Szawlewicz, MD, chair of cardiovascular medicine at Deborah Heart and Lung Center in Brown Mills, N.J., pointed out that the authors indicated that the number of TEEs performed by the trainees was not collected.
“This would be useful information to determine if those who received simulator training sought out and performed more TEEs, and also to determine if cardiology trainees in France perform a similar number of TEEs as cardiology trainees in the United States.”
In addition, he said, “the 4 hours of simulator training in TEE is extra education and experience that the standard trainees didn’t get. Would 4 extra hours of standard training didactics also improve trainees’ scores?”
Noting that the fellows’ ability to perform TEE in real patients was not assessed, Dr. Szawlewicz said, “a study could be designed that evaluated TEE images from real patients to see if trainees receiving simulator training performed better, more comprehensive and efficient TEEs than standard training.”
Nevertheless, he concluded, “Four hours of simulator training appears to improve TEE knowledge and skills. This is something we would consider at our institution.”
Like Dr. Szawlewicz, Michael Spooner, MD, MBA, of Mercy One North Iowa Heart Center in Mason City, and Kathryn Bertlacher, MD, of the University of Pittsburgh Medical Center, noted in a related editorial, “data are not provided about change in the learner’s behavior or performance on an actual TEE after the course, nor are there data about clinical outcomes such as patient safety or completeness of subsequent TEEs.
“This limitation, which is a limitation of most of the existing TEE simulation literature, is a high bar to cross,” they concluded. “Reaching this bar will require studies such as this to provide foundational understanding.”
Twin-Medical provided the TEE simulators. No relevant conflicts of interest were disclosed.
A version of this article first appeared on Medscape.com.
FROM JAMA CARDIOLOGY
Adverse events reported in one-quarter of inpatient admissions
as indicated from data from 2,809 admissions at 11 hospitals.
The 1991 Harvard Medical Practice Study, which focused on medical injury and litigation, documented an adverse event rate of 3.7 events per 100 admissions; 28% of those events were attributed to negligence, write David W. Bates, MD, of Brigham and Women’s Hospital, Boston, and colleagues.
Although patient safety has changed significantly since 1991, documenting improvements has been challenging, the researchers say. Several reports have shown a decrease in health care–associated infections. However, other aspects of safety – notably, adverse drug events, defined as injuries resulting from drugs taken – are not easily measured and tracked, the researchers say.
“We have not had good estimates of how much harm is being caused by care in hospitals in an ongoing way that looked across all types of adverse events,” and the current review is therefore important, Dr. Bates said in an interview.
In a study recently published in the New England Journal of Medicine, the researchers analyzed a random sample of 2,809 hospital admissions from 11 hospitals in Massachusetts during the 2018 calendar year. The hospitals ranged in size from fewer than 100 beds to more than 700 beds; all patients were aged 18 years and older. A panel of nine nurses reviewed the admissions records to identify potential adverse events, and eight physicians reviewed the adverse event summaries and either agreed or disagreed with the adverse event type. The severity of each event was ranked using a general severity scale into categories of significant, serious, life-threatening, or fatal.
Overall, at least one adverse event was identified in 23.6% of the hospital admissions. A total of 978 adverse events were deemed to have occurred during the index admission, and 222 of these (22.7%) were deemed preventable. Among the preventable adverse events, 19.7% were classified as serious, 3.3% as life-threatening, and 0.5% as fatal.
A total of 523 admissions (18.6%) involved at least one significant adverse event, defined as an event that caused unnecessary harm but from which recovery was rapid. A total of 211 admissions involved a serious adverse event, defined as harm resulting in substantial intervention or prolonged recovery; 34 included at least one life-threatening event; and seven admissions involved a fatal adverse event.
A total of 191 admissions involved at least one adverse event deemed preventable. Of those, 29 involved at least one preventable adverse event that was serious, life-threatening, or fatal, the researchers write. Of the seven deaths in the study population, one was deemed preventable.
The most common adverse events were adverse drug events, which accounted for 39.0% of the adverse events; surgical or other procedural events accounted for 30.4%; patient care events (including falls and pressure ulcers) accounted for 15.0%; and health care–associated infections accounted for 11.9%.
Overcoming barriers to better safety
“The overall level of harm, with nearly 1 in 4 patients suffering an adverse event, was higher than I expected it might be,” Dr. Bates told this news organization. However, techniques for identifying adverse events have improved, and “it is easier to find them in electronic records than in paper records,” he noted.
“Hospitals have many issues they are currently dealing with since COVID, and one issue is simply prioritization,” Dr. Bates said. “But it is now possible to measure harm for all patients using electronic tools, and if hospitals know how much harm they are having in specific areas, they can make choices about which ones to focus on.”
“We now have effective prevention strategies for most of the main kinds of harm,” he said. Generally, rates of harm are high because these strategies are not being used effectively, he said. “In addition, there are new tools that can be used – for example, to identify patients who are decompensating earlier,” he noted.
As for additional research, some specific types of harm that have been resistant to interventions, such as pressure ulcers, deserve more attention, said Dr. Bates. “In addition, diagnostic errors appear to cause a great deal of harm, but we don’t yet have good strategies for preventing these,” he said.
The study findings were limited by several factors, including the use of data from hospitals that might not represent hospitals at large and by the inclusion mainly of patients with private insurance, the researchers write. Other limitations include the likelihood that some adverse events were missed and the level of agreement on adverse events between adjudicators was only fair.
However, the findings serve as a reminder to health care professionals of the need for continued attention to improving patient safety, and measuring adverse events remains a critical part of guiding these improvements, the researchers conclude.
Timely reassessment and opportunities to improve
In the decades since the publication of the report, “To Err Is Human,” by the National Academies in 2000, significant attention has been paid to improving patient safety during hospitalizations, and health care systems have increased in both system and disease complexity, Said Suman Pal, MBBS, a specialist in hospital medicine at the University of New Mexico, Albuquerque, said in an interview. “Therefore, this study is important in reassessing the safety of inpatient care at the current time,” he said.
“The findings of this study showing preventable adverse events in approximately 7% of all admissions; while concerning, is not surprising, as it is consistent with other studies over time, as the authors have also noted in their discussion,” said Dr. Pal. The current findings “underscore the importance of continuous quality improvement efforts to increase the safety of patient care for hospitalized patients,” he noted.
“The increasing complexity of medical care, fragmentation of health care, structural inequities of health systems, and more recent widespread public health challenges such as the COVID-19 pandemic have been, in my opinion, barriers to improving patient safety,” Dr. Pal said. “The use of innovation and an interdisciplinary approach to patient safety and quality improvement in hospital-based care, such as the use of machine learning to monitor trends and predict the individualized risk of harm, could be a potential way out” to help reduce barriers and improve safety, he said.
“Additional research is needed to understand the key drivers of preventable harm for hospitalized patients in the United States,” said Dr. Pal. “When planning for change, keen attention must be paid to understanding how these [drivers] may differ for patients who have been historically marginalized or are otherwise underserved so as to not exacerbate health care inequities,” he added.
The study was funded by the Controlled Risk Insurance Company and the Risk Management Foundation of the Harvard Medical Institutions. Dr. Bates owns stock options with AESOP, Clew, FeelBetter, Guided Clinical Solutions, MDClone, and ValeraHealth and has grants/contracts from IBM Watson and EarlySense. He has also served as a consultant for CDI Negev. Dr. Pal has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
as indicated from data from 2,809 admissions at 11 hospitals.
The 1991 Harvard Medical Practice Study, which focused on medical injury and litigation, documented an adverse event rate of 3.7 events per 100 admissions; 28% of those events were attributed to negligence, write David W. Bates, MD, of Brigham and Women’s Hospital, Boston, and colleagues.
Although patient safety has changed significantly since 1991, documenting improvements has been challenging, the researchers say. Several reports have shown a decrease in health care–associated infections. However, other aspects of safety – notably, adverse drug events, defined as injuries resulting from drugs taken – are not easily measured and tracked, the researchers say.
“We have not had good estimates of how much harm is being caused by care in hospitals in an ongoing way that looked across all types of adverse events,” and the current review is therefore important, Dr. Bates said in an interview.
In a study recently published in the New England Journal of Medicine, the researchers analyzed a random sample of 2,809 hospital admissions from 11 hospitals in Massachusetts during the 2018 calendar year. The hospitals ranged in size from fewer than 100 beds to more than 700 beds; all patients were aged 18 years and older. A panel of nine nurses reviewed the admissions records to identify potential adverse events, and eight physicians reviewed the adverse event summaries and either agreed or disagreed with the adverse event type. The severity of each event was ranked using a general severity scale into categories of significant, serious, life-threatening, or fatal.
Overall, at least one adverse event was identified in 23.6% of the hospital admissions. A total of 978 adverse events were deemed to have occurred during the index admission, and 222 of these (22.7%) were deemed preventable. Among the preventable adverse events, 19.7% were classified as serious, 3.3% as life-threatening, and 0.5% as fatal.
A total of 523 admissions (18.6%) involved at least one significant adverse event, defined as an event that caused unnecessary harm but from which recovery was rapid. A total of 211 admissions involved a serious adverse event, defined as harm resulting in substantial intervention or prolonged recovery; 34 included at least one life-threatening event; and seven admissions involved a fatal adverse event.
A total of 191 admissions involved at least one adverse event deemed preventable. Of those, 29 involved at least one preventable adverse event that was serious, life-threatening, or fatal, the researchers write. Of the seven deaths in the study population, one was deemed preventable.
The most common adverse events were adverse drug events, which accounted for 39.0% of the adverse events; surgical or other procedural events accounted for 30.4%; patient care events (including falls and pressure ulcers) accounted for 15.0%; and health care–associated infections accounted for 11.9%.
Overcoming barriers to better safety
“The overall level of harm, with nearly 1 in 4 patients suffering an adverse event, was higher than I expected it might be,” Dr. Bates told this news organization. However, techniques for identifying adverse events have improved, and “it is easier to find them in electronic records than in paper records,” he noted.
“Hospitals have many issues they are currently dealing with since COVID, and one issue is simply prioritization,” Dr. Bates said. “But it is now possible to measure harm for all patients using electronic tools, and if hospitals know how much harm they are having in specific areas, they can make choices about which ones to focus on.”
“We now have effective prevention strategies for most of the main kinds of harm,” he said. Generally, rates of harm are high because these strategies are not being used effectively, he said. “In addition, there are new tools that can be used – for example, to identify patients who are decompensating earlier,” he noted.
As for additional research, some specific types of harm that have been resistant to interventions, such as pressure ulcers, deserve more attention, said Dr. Bates. “In addition, diagnostic errors appear to cause a great deal of harm, but we don’t yet have good strategies for preventing these,” he said.
The study findings were limited by several factors, including the use of data from hospitals that might not represent hospitals at large and by the inclusion mainly of patients with private insurance, the researchers write. Other limitations include the likelihood that some adverse events were missed and the level of agreement on adverse events between adjudicators was only fair.
However, the findings serve as a reminder to health care professionals of the need for continued attention to improving patient safety, and measuring adverse events remains a critical part of guiding these improvements, the researchers conclude.
Timely reassessment and opportunities to improve
In the decades since the publication of the report, “To Err Is Human,” by the National Academies in 2000, significant attention has been paid to improving patient safety during hospitalizations, and health care systems have increased in both system and disease complexity, Said Suman Pal, MBBS, a specialist in hospital medicine at the University of New Mexico, Albuquerque, said in an interview. “Therefore, this study is important in reassessing the safety of inpatient care at the current time,” he said.
“The findings of this study showing preventable adverse events in approximately 7% of all admissions; while concerning, is not surprising, as it is consistent with other studies over time, as the authors have also noted in their discussion,” said Dr. Pal. The current findings “underscore the importance of continuous quality improvement efforts to increase the safety of patient care for hospitalized patients,” he noted.
“The increasing complexity of medical care, fragmentation of health care, structural inequities of health systems, and more recent widespread public health challenges such as the COVID-19 pandemic have been, in my opinion, barriers to improving patient safety,” Dr. Pal said. “The use of innovation and an interdisciplinary approach to patient safety and quality improvement in hospital-based care, such as the use of machine learning to monitor trends and predict the individualized risk of harm, could be a potential way out” to help reduce barriers and improve safety, he said.
“Additional research is needed to understand the key drivers of preventable harm for hospitalized patients in the United States,” said Dr. Pal. “When planning for change, keen attention must be paid to understanding how these [drivers] may differ for patients who have been historically marginalized or are otherwise underserved so as to not exacerbate health care inequities,” he added.
The study was funded by the Controlled Risk Insurance Company and the Risk Management Foundation of the Harvard Medical Institutions. Dr. Bates owns stock options with AESOP, Clew, FeelBetter, Guided Clinical Solutions, MDClone, and ValeraHealth and has grants/contracts from IBM Watson and EarlySense. He has also served as a consultant for CDI Negev. Dr. Pal has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
as indicated from data from 2,809 admissions at 11 hospitals.
The 1991 Harvard Medical Practice Study, which focused on medical injury and litigation, documented an adverse event rate of 3.7 events per 100 admissions; 28% of those events were attributed to negligence, write David W. Bates, MD, of Brigham and Women’s Hospital, Boston, and colleagues.
Although patient safety has changed significantly since 1991, documenting improvements has been challenging, the researchers say. Several reports have shown a decrease in health care–associated infections. However, other aspects of safety – notably, adverse drug events, defined as injuries resulting from drugs taken – are not easily measured and tracked, the researchers say.
“We have not had good estimates of how much harm is being caused by care in hospitals in an ongoing way that looked across all types of adverse events,” and the current review is therefore important, Dr. Bates said in an interview.
In a study recently published in the New England Journal of Medicine, the researchers analyzed a random sample of 2,809 hospital admissions from 11 hospitals in Massachusetts during the 2018 calendar year. The hospitals ranged in size from fewer than 100 beds to more than 700 beds; all patients were aged 18 years and older. A panel of nine nurses reviewed the admissions records to identify potential adverse events, and eight physicians reviewed the adverse event summaries and either agreed or disagreed with the adverse event type. The severity of each event was ranked using a general severity scale into categories of significant, serious, life-threatening, or fatal.
Overall, at least one adverse event was identified in 23.6% of the hospital admissions. A total of 978 adverse events were deemed to have occurred during the index admission, and 222 of these (22.7%) were deemed preventable. Among the preventable adverse events, 19.7% were classified as serious, 3.3% as life-threatening, and 0.5% as fatal.
A total of 523 admissions (18.6%) involved at least one significant adverse event, defined as an event that caused unnecessary harm but from which recovery was rapid. A total of 211 admissions involved a serious adverse event, defined as harm resulting in substantial intervention or prolonged recovery; 34 included at least one life-threatening event; and seven admissions involved a fatal adverse event.
A total of 191 admissions involved at least one adverse event deemed preventable. Of those, 29 involved at least one preventable adverse event that was serious, life-threatening, or fatal, the researchers write. Of the seven deaths in the study population, one was deemed preventable.
The most common adverse events were adverse drug events, which accounted for 39.0% of the adverse events; surgical or other procedural events accounted for 30.4%; patient care events (including falls and pressure ulcers) accounted for 15.0%; and health care–associated infections accounted for 11.9%.
Overcoming barriers to better safety
“The overall level of harm, with nearly 1 in 4 patients suffering an adverse event, was higher than I expected it might be,” Dr. Bates told this news organization. However, techniques for identifying adverse events have improved, and “it is easier to find them in electronic records than in paper records,” he noted.
“Hospitals have many issues they are currently dealing with since COVID, and one issue is simply prioritization,” Dr. Bates said. “But it is now possible to measure harm for all patients using electronic tools, and if hospitals know how much harm they are having in specific areas, they can make choices about which ones to focus on.”
“We now have effective prevention strategies for most of the main kinds of harm,” he said. Generally, rates of harm are high because these strategies are not being used effectively, he said. “In addition, there are new tools that can be used – for example, to identify patients who are decompensating earlier,” he noted.
As for additional research, some specific types of harm that have been resistant to interventions, such as pressure ulcers, deserve more attention, said Dr. Bates. “In addition, diagnostic errors appear to cause a great deal of harm, but we don’t yet have good strategies for preventing these,” he said.
The study findings were limited by several factors, including the use of data from hospitals that might not represent hospitals at large and by the inclusion mainly of patients with private insurance, the researchers write. Other limitations include the likelihood that some adverse events were missed and the level of agreement on adverse events between adjudicators was only fair.
However, the findings serve as a reminder to health care professionals of the need for continued attention to improving patient safety, and measuring adverse events remains a critical part of guiding these improvements, the researchers conclude.
Timely reassessment and opportunities to improve
In the decades since the publication of the report, “To Err Is Human,” by the National Academies in 2000, significant attention has been paid to improving patient safety during hospitalizations, and health care systems have increased in both system and disease complexity, Said Suman Pal, MBBS, a specialist in hospital medicine at the University of New Mexico, Albuquerque, said in an interview. “Therefore, this study is important in reassessing the safety of inpatient care at the current time,” he said.
“The findings of this study showing preventable adverse events in approximately 7% of all admissions; while concerning, is not surprising, as it is consistent with other studies over time, as the authors have also noted in their discussion,” said Dr. Pal. The current findings “underscore the importance of continuous quality improvement efforts to increase the safety of patient care for hospitalized patients,” he noted.
“The increasing complexity of medical care, fragmentation of health care, structural inequities of health systems, and more recent widespread public health challenges such as the COVID-19 pandemic have been, in my opinion, barriers to improving patient safety,” Dr. Pal said. “The use of innovation and an interdisciplinary approach to patient safety and quality improvement in hospital-based care, such as the use of machine learning to monitor trends and predict the individualized risk of harm, could be a potential way out” to help reduce barriers and improve safety, he said.
“Additional research is needed to understand the key drivers of preventable harm for hospitalized patients in the United States,” said Dr. Pal. “When planning for change, keen attention must be paid to understanding how these [drivers] may differ for patients who have been historically marginalized or are otherwise underserved so as to not exacerbate health care inequities,” he added.
The study was funded by the Controlled Risk Insurance Company and the Risk Management Foundation of the Harvard Medical Institutions. Dr. Bates owns stock options with AESOP, Clew, FeelBetter, Guided Clinical Solutions, MDClone, and ValeraHealth and has grants/contracts from IBM Watson and EarlySense. He has also served as a consultant for CDI Negev. Dr. Pal has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Possible bivalent vaccine link to strokes in people over 65
who got the shot, the Centers for Disease Control and Prevention and the Food and Drug Administration said in a joint news release.
The release did not recommend people change their vaccine practices, saying the database finding probably did not represent a “true clinical risk.” The CDC said everybody, including people over 65, should stay up to date on their COVID vaccines, including the bivalent booster.
The news release said the Vaccine Safety Datalink (VSD), “a near real-time surveillance system,” raised a safety concern about the Pfizer/BioNTech booster.
“Rapid-response investigation of the signal in the VSD raised a question of whether people 65 and older who have received the Pfizer-BioNTech COVID-19 Vaccine, Bivalent were more likely to have an ischemic stroke in the 21 days following vaccination compared with days 22-44 following vaccination,” the news release said.
Ischemic strokes are blockages of blood to the brain, often caused by blood clots.
“Although the totality of the data currently suggests that it is very unlikely that the signal in VSD (Vaccine Safety Datalink) represents a true clinical risk, we believe it is important to share this information with the public, as we have in the past, when one of our safety monitoring systems detects a signal,” the release said.
No higher likelihood of strokes linked to the Pfizer bivalent vaccine had been found by Pfizer/BioNTech, the Department of Veterans Affairs, the Vaccine Adverse Event Reporting System maintained by the CDC and the FDA, or other agencies that monitor reactions of vaccines, the news release said. No safety issues about strokes have been identified with the Moderna bivalent vaccine.
CNN, citing a CDC official, reported that about 550,000 seniors who got Pfizer bivalent boosters were tracked by the VSD, and 130 of them had strokes within 3 weeks of getting the shot. None of those 130 people died, CNN said. The official spoke on the condition of anonymity because they weren’t authorized to share the data.
The issue will be discussed at the January meeting of the FDA’s Vaccines and Related Biological Products Advisory Committee.
In a joint statement, Pfizer and BioNTech said: “Neither Pfizer and BioNTech nor the CDC or FDA have observed similar findings across numerous other monitoring systems in the U.S. and globally and there is no evidence to conclude that ischemic stroke is associated with the use of the companies’ COVID-19 vaccines.”
Bivalent boosters contain two strains of vaccine – one to protect against the original COVID-19 virus and another targeting Omicron subvariants.
A version of this article first appeared on WebMD.com.
who got the shot, the Centers for Disease Control and Prevention and the Food and Drug Administration said in a joint news release.
The release did not recommend people change their vaccine practices, saying the database finding probably did not represent a “true clinical risk.” The CDC said everybody, including people over 65, should stay up to date on their COVID vaccines, including the bivalent booster.
The news release said the Vaccine Safety Datalink (VSD), “a near real-time surveillance system,” raised a safety concern about the Pfizer/BioNTech booster.
“Rapid-response investigation of the signal in the VSD raised a question of whether people 65 and older who have received the Pfizer-BioNTech COVID-19 Vaccine, Bivalent were more likely to have an ischemic stroke in the 21 days following vaccination compared with days 22-44 following vaccination,” the news release said.
Ischemic strokes are blockages of blood to the brain, often caused by blood clots.
“Although the totality of the data currently suggests that it is very unlikely that the signal in VSD (Vaccine Safety Datalink) represents a true clinical risk, we believe it is important to share this information with the public, as we have in the past, when one of our safety monitoring systems detects a signal,” the release said.
No higher likelihood of strokes linked to the Pfizer bivalent vaccine had been found by Pfizer/BioNTech, the Department of Veterans Affairs, the Vaccine Adverse Event Reporting System maintained by the CDC and the FDA, or other agencies that monitor reactions of vaccines, the news release said. No safety issues about strokes have been identified with the Moderna bivalent vaccine.
CNN, citing a CDC official, reported that about 550,000 seniors who got Pfizer bivalent boosters were tracked by the VSD, and 130 of them had strokes within 3 weeks of getting the shot. None of those 130 people died, CNN said. The official spoke on the condition of anonymity because they weren’t authorized to share the data.
The issue will be discussed at the January meeting of the FDA’s Vaccines and Related Biological Products Advisory Committee.
In a joint statement, Pfizer and BioNTech said: “Neither Pfizer and BioNTech nor the CDC or FDA have observed similar findings across numerous other monitoring systems in the U.S. and globally and there is no evidence to conclude that ischemic stroke is associated with the use of the companies’ COVID-19 vaccines.”
Bivalent boosters contain two strains of vaccine – one to protect against the original COVID-19 virus and another targeting Omicron subvariants.
A version of this article first appeared on WebMD.com.
who got the shot, the Centers for Disease Control and Prevention and the Food and Drug Administration said in a joint news release.
The release did not recommend people change their vaccine practices, saying the database finding probably did not represent a “true clinical risk.” The CDC said everybody, including people over 65, should stay up to date on their COVID vaccines, including the bivalent booster.
The news release said the Vaccine Safety Datalink (VSD), “a near real-time surveillance system,” raised a safety concern about the Pfizer/BioNTech booster.
“Rapid-response investigation of the signal in the VSD raised a question of whether people 65 and older who have received the Pfizer-BioNTech COVID-19 Vaccine, Bivalent were more likely to have an ischemic stroke in the 21 days following vaccination compared with days 22-44 following vaccination,” the news release said.
Ischemic strokes are blockages of blood to the brain, often caused by blood clots.
“Although the totality of the data currently suggests that it is very unlikely that the signal in VSD (Vaccine Safety Datalink) represents a true clinical risk, we believe it is important to share this information with the public, as we have in the past, when one of our safety monitoring systems detects a signal,” the release said.
No higher likelihood of strokes linked to the Pfizer bivalent vaccine had been found by Pfizer/BioNTech, the Department of Veterans Affairs, the Vaccine Adverse Event Reporting System maintained by the CDC and the FDA, or other agencies that monitor reactions of vaccines, the news release said. No safety issues about strokes have been identified with the Moderna bivalent vaccine.
CNN, citing a CDC official, reported that about 550,000 seniors who got Pfizer bivalent boosters were tracked by the VSD, and 130 of them had strokes within 3 weeks of getting the shot. None of those 130 people died, CNN said. The official spoke on the condition of anonymity because they weren’t authorized to share the data.
The issue will be discussed at the January meeting of the FDA’s Vaccines and Related Biological Products Advisory Committee.
In a joint statement, Pfizer and BioNTech said: “Neither Pfizer and BioNTech nor the CDC or FDA have observed similar findings across numerous other monitoring systems in the U.S. and globally and there is no evidence to conclude that ischemic stroke is associated with the use of the companies’ COVID-19 vaccines.”
Bivalent boosters contain two strains of vaccine – one to protect against the original COVID-19 virus and another targeting Omicron subvariants.
A version of this article first appeared on WebMD.com.
Nearly 50% of patients with dementia experience falls
, suggests new research that also identifies multiple risk factors for these falls.
In a study of more than 5,500 participants, 45.5% of those with dementia experienced one or more falls, compared with 30.9% of their peers without dementia.
Vision impairment and living with a spouse were among the strongest predictors of future fall risk among participants living with dementia. Interestingly, high neighborhood social deprivation, which is reflected by such things as income and education, was associated with lower odds of falling.
Overall, the results highlight the need for a multidisciplinary approach to preventing falls among elderly individuals with dementia, said lead author Safiyyah M. Okoye, PhD, assistant professor, College of Nursing and Health Professions, Drexel University, Philadelphia.
“We need to consider different dimensions and figure out how we can try to go beyond the clinic in our interactions,” she said.
Dr. Okoye noted that in addition to reviewing medications that may contribute to falls and screening for vision problems, clinicians might also consider resources to improve the home environment and ensure that families have appropriate caregiving.
The findings were published online in Alzheimer’s and Dementia: The Journal of the Alzheimer’s Association.
No ‘silver bullet’
Every year, falls cause millions of injuries in older adults, and those with dementia are especially vulnerable. This population has twice the risk of falling and up to three times the risk of incurring serious fall-related injuries, such as fractures, the researchers noted.
Falls are a leading cause of hospitalization among those with dementia. Previous evidence has shown that persons with dementia are more likely to experience negative health consequences, such as delirium, while in hospital, compared with those without dementia. Even minor fall-related injuries are associated with the patient’s being discharged to a nursing home rather than returning home.
Dr. Okoye stressed that many factors contribute to falls, including health status; function, such as the ability to walk and balance; medications; home environment; and activity level.
“There are multidimensional aspects, and we can’t just find one silver bullet to address falls. It should be addressed comprehensively,” she said.
Existing studies “overwhelmingly” focus on factors related to health and function that could be addressed in the doctor’s office or with a referral, rather than on environmental and social factors, Dr. Okoye noted.
And even though the risk of falling is high among community-dwelling seniors with dementia, very few studies have addressed the risk of falls among these adults, she added.
The new analysis included a nationally representative sample of 5,581 community-dwelling adults who participated in both the 2015 and 2016 National Health and Aging Trends Study (NHATS). The NHATS is a population-based survey of health and disability trends and trajectories among Americans aged 65 years and older.
During interviews, participants were asked, personally or by proxy, about falls during the previous 12 months. Having fallen at baseline was evaluated as a possible predictor of falls in the subsequent 12 months.
To determine probable dementia, researchers asked whether a doctor had ever told the participants that they had dementia or Alzheimer’s disease. They also used a dementia screening questionnaire and neuropsychological tests of memory, orientation, and executive function.
Of the total sample, most (n = 5,093) did not have dementia.
Physical environmental factors that were assessed included conditions at home, such as clutter, tripping hazards, and structural issues, as well as neighborhood social and economic deprivation – such as income, education levels, and employment status.
Fall rates and counterintuitive findings
Results showed that significantly more of those with dementia than without experienced one or more falls (45.5% vs. 30.9%; P < .001).
In addition, a history of falling was significantly associated with subsequent falls among those with dementia (odds ratio, 6.20; 95% confidence interval, 3.81-10.09), as was vision impairment (OR, 2.22; 95% CI, 1.12-4.40) and living with a spouse versus alone (OR, 2.43; 95% CI, 1.09-5.43).
A possible explanation for higher fall risk among those living with a partner is that those living alone usually have better functioning, the investigators noted. Also, live-in partners tend to be of a similar age as the person with dementia and may have challenges of their own.
Interestingly, high neighborhood social deprivation was associated with lower odds of falling (OR, 0.55 for the highest deprivation scores; 95% CI, 0.31-0.98), a finding Dr. Okoye said was “counterintuitive.”
This result could be related to the social environment, she noted. “Maybe there are more people around in the house, more people with eyes on the person, or more people in the community who know the person. Despite the low economic resources, there could be social resources there,” she said.
The new findings underscore the idea that falling is a multidimensional phenomenon among older adults with dementia as well as those without dementia, Dr. Okoye noted.
Doctors can play a role in reducing falls among patients with dementia by asking about falls, possibly eliminating medications that are associated with risk of falling, and screening for and correcting vision and hearing impairments, she suggested.
They may also help determine household hazards for a patient, such as clutter and poor lighting, and ensure that these are addressed, Dr. Okoye added.
No surprise
Commenting on the study, David S. Knopman, MD, a clinical neurologist at Mayo Clinic, Rochester, Minn., said the finding that visual impairment and a prior history of falling are predictive of subsequent falls “comes as no surprise.”
Dr. Knopman, whose research focuses on late-life cognitive disorders, was not involved with the current study.
Risk reduction is “of course” a key management goal, he said. “Vigilance and optimizing the patient’s living space to reduce fall risks are the major strategies,” he added.
Dr. Knopman reiterated that falls among those with dementia are associated with higher mortality and often lead to loss of the capacity to live outside of an institution.
The study was supported by the National Institute on Aging. The investigators and Dr. Knopman report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, suggests new research that also identifies multiple risk factors for these falls.
In a study of more than 5,500 participants, 45.5% of those with dementia experienced one or more falls, compared with 30.9% of their peers without dementia.
Vision impairment and living with a spouse were among the strongest predictors of future fall risk among participants living with dementia. Interestingly, high neighborhood social deprivation, which is reflected by such things as income and education, was associated with lower odds of falling.
Overall, the results highlight the need for a multidisciplinary approach to preventing falls among elderly individuals with dementia, said lead author Safiyyah M. Okoye, PhD, assistant professor, College of Nursing and Health Professions, Drexel University, Philadelphia.
“We need to consider different dimensions and figure out how we can try to go beyond the clinic in our interactions,” she said.
Dr. Okoye noted that in addition to reviewing medications that may contribute to falls and screening for vision problems, clinicians might also consider resources to improve the home environment and ensure that families have appropriate caregiving.
The findings were published online in Alzheimer’s and Dementia: The Journal of the Alzheimer’s Association.
No ‘silver bullet’
Every year, falls cause millions of injuries in older adults, and those with dementia are especially vulnerable. This population has twice the risk of falling and up to three times the risk of incurring serious fall-related injuries, such as fractures, the researchers noted.
Falls are a leading cause of hospitalization among those with dementia. Previous evidence has shown that persons with dementia are more likely to experience negative health consequences, such as delirium, while in hospital, compared with those without dementia. Even minor fall-related injuries are associated with the patient’s being discharged to a nursing home rather than returning home.
Dr. Okoye stressed that many factors contribute to falls, including health status; function, such as the ability to walk and balance; medications; home environment; and activity level.
“There are multidimensional aspects, and we can’t just find one silver bullet to address falls. It should be addressed comprehensively,” she said.
Existing studies “overwhelmingly” focus on factors related to health and function that could be addressed in the doctor’s office or with a referral, rather than on environmental and social factors, Dr. Okoye noted.
And even though the risk of falling is high among community-dwelling seniors with dementia, very few studies have addressed the risk of falls among these adults, she added.
The new analysis included a nationally representative sample of 5,581 community-dwelling adults who participated in both the 2015 and 2016 National Health and Aging Trends Study (NHATS). The NHATS is a population-based survey of health and disability trends and trajectories among Americans aged 65 years and older.
During interviews, participants were asked, personally or by proxy, about falls during the previous 12 months. Having fallen at baseline was evaluated as a possible predictor of falls in the subsequent 12 months.
To determine probable dementia, researchers asked whether a doctor had ever told the participants that they had dementia or Alzheimer’s disease. They also used a dementia screening questionnaire and neuropsychological tests of memory, orientation, and executive function.
Of the total sample, most (n = 5,093) did not have dementia.
Physical environmental factors that were assessed included conditions at home, such as clutter, tripping hazards, and structural issues, as well as neighborhood social and economic deprivation – such as income, education levels, and employment status.
Fall rates and counterintuitive findings
Results showed that significantly more of those with dementia than without experienced one or more falls (45.5% vs. 30.9%; P < .001).
In addition, a history of falling was significantly associated with subsequent falls among those with dementia (odds ratio, 6.20; 95% confidence interval, 3.81-10.09), as was vision impairment (OR, 2.22; 95% CI, 1.12-4.40) and living with a spouse versus alone (OR, 2.43; 95% CI, 1.09-5.43).
A possible explanation for higher fall risk among those living with a partner is that those living alone usually have better functioning, the investigators noted. Also, live-in partners tend to be of a similar age as the person with dementia and may have challenges of their own.
Interestingly, high neighborhood social deprivation was associated with lower odds of falling (OR, 0.55 for the highest deprivation scores; 95% CI, 0.31-0.98), a finding Dr. Okoye said was “counterintuitive.”
This result could be related to the social environment, she noted. “Maybe there are more people around in the house, more people with eyes on the person, or more people in the community who know the person. Despite the low economic resources, there could be social resources there,” she said.
The new findings underscore the idea that falling is a multidimensional phenomenon among older adults with dementia as well as those without dementia, Dr. Okoye noted.
Doctors can play a role in reducing falls among patients with dementia by asking about falls, possibly eliminating medications that are associated with risk of falling, and screening for and correcting vision and hearing impairments, she suggested.
They may also help determine household hazards for a patient, such as clutter and poor lighting, and ensure that these are addressed, Dr. Okoye added.
No surprise
Commenting on the study, David S. Knopman, MD, a clinical neurologist at Mayo Clinic, Rochester, Minn., said the finding that visual impairment and a prior history of falling are predictive of subsequent falls “comes as no surprise.”
Dr. Knopman, whose research focuses on late-life cognitive disorders, was not involved with the current study.
Risk reduction is “of course” a key management goal, he said. “Vigilance and optimizing the patient’s living space to reduce fall risks are the major strategies,” he added.
Dr. Knopman reiterated that falls among those with dementia are associated with higher mortality and often lead to loss of the capacity to live outside of an institution.
The study was supported by the National Institute on Aging. The investigators and Dr. Knopman report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, suggests new research that also identifies multiple risk factors for these falls.
In a study of more than 5,500 participants, 45.5% of those with dementia experienced one or more falls, compared with 30.9% of their peers without dementia.
Vision impairment and living with a spouse were among the strongest predictors of future fall risk among participants living with dementia. Interestingly, high neighborhood social deprivation, which is reflected by such things as income and education, was associated with lower odds of falling.
Overall, the results highlight the need for a multidisciplinary approach to preventing falls among elderly individuals with dementia, said lead author Safiyyah M. Okoye, PhD, assistant professor, College of Nursing and Health Professions, Drexel University, Philadelphia.
“We need to consider different dimensions and figure out how we can try to go beyond the clinic in our interactions,” she said.
Dr. Okoye noted that in addition to reviewing medications that may contribute to falls and screening for vision problems, clinicians might also consider resources to improve the home environment and ensure that families have appropriate caregiving.
The findings were published online in Alzheimer’s and Dementia: The Journal of the Alzheimer’s Association.
No ‘silver bullet’
Every year, falls cause millions of injuries in older adults, and those with dementia are especially vulnerable. This population has twice the risk of falling and up to three times the risk of incurring serious fall-related injuries, such as fractures, the researchers noted.
Falls are a leading cause of hospitalization among those with dementia. Previous evidence has shown that persons with dementia are more likely to experience negative health consequences, such as delirium, while in hospital, compared with those without dementia. Even minor fall-related injuries are associated with the patient’s being discharged to a nursing home rather than returning home.
Dr. Okoye stressed that many factors contribute to falls, including health status; function, such as the ability to walk and balance; medications; home environment; and activity level.
“There are multidimensional aspects, and we can’t just find one silver bullet to address falls. It should be addressed comprehensively,” she said.
Existing studies “overwhelmingly” focus on factors related to health and function that could be addressed in the doctor’s office or with a referral, rather than on environmental and social factors, Dr. Okoye noted.
And even though the risk of falling is high among community-dwelling seniors with dementia, very few studies have addressed the risk of falls among these adults, she added.
The new analysis included a nationally representative sample of 5,581 community-dwelling adults who participated in both the 2015 and 2016 National Health and Aging Trends Study (NHATS). The NHATS is a population-based survey of health and disability trends and trajectories among Americans aged 65 years and older.
During interviews, participants were asked, personally or by proxy, about falls during the previous 12 months. Having fallen at baseline was evaluated as a possible predictor of falls in the subsequent 12 months.
To determine probable dementia, researchers asked whether a doctor had ever told the participants that they had dementia or Alzheimer’s disease. They also used a dementia screening questionnaire and neuropsychological tests of memory, orientation, and executive function.
Of the total sample, most (n = 5,093) did not have dementia.
Physical environmental factors that were assessed included conditions at home, such as clutter, tripping hazards, and structural issues, as well as neighborhood social and economic deprivation – such as income, education levels, and employment status.
Fall rates and counterintuitive findings
Results showed that significantly more of those with dementia than without experienced one or more falls (45.5% vs. 30.9%; P < .001).
In addition, a history of falling was significantly associated with subsequent falls among those with dementia (odds ratio, 6.20; 95% confidence interval, 3.81-10.09), as was vision impairment (OR, 2.22; 95% CI, 1.12-4.40) and living with a spouse versus alone (OR, 2.43; 95% CI, 1.09-5.43).
A possible explanation for higher fall risk among those living with a partner is that those living alone usually have better functioning, the investigators noted. Also, live-in partners tend to be of a similar age as the person with dementia and may have challenges of their own.
Interestingly, high neighborhood social deprivation was associated with lower odds of falling (OR, 0.55 for the highest deprivation scores; 95% CI, 0.31-0.98), a finding Dr. Okoye said was “counterintuitive.”
This result could be related to the social environment, she noted. “Maybe there are more people around in the house, more people with eyes on the person, or more people in the community who know the person. Despite the low economic resources, there could be social resources there,” she said.
The new findings underscore the idea that falling is a multidimensional phenomenon among older adults with dementia as well as those without dementia, Dr. Okoye noted.
Doctors can play a role in reducing falls among patients with dementia by asking about falls, possibly eliminating medications that are associated with risk of falling, and screening for and correcting vision and hearing impairments, she suggested.
They may also help determine household hazards for a patient, such as clutter and poor lighting, and ensure that these are addressed, Dr. Okoye added.
No surprise
Commenting on the study, David S. Knopman, MD, a clinical neurologist at Mayo Clinic, Rochester, Minn., said the finding that visual impairment and a prior history of falling are predictive of subsequent falls “comes as no surprise.”
Dr. Knopman, whose research focuses on late-life cognitive disorders, was not involved with the current study.
Risk reduction is “of course” a key management goal, he said. “Vigilance and optimizing the patient’s living space to reduce fall risks are the major strategies,” he added.
Dr. Knopman reiterated that falls among those with dementia are associated with higher mortality and often lead to loss of the capacity to live outside of an institution.
The study was supported by the National Institute on Aging. The investigators and Dr. Knopman report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ALZHEIMER’S AND DEMENTIA
Children and COVID: ED visits and hospitalizations start to fall again
Emergency department visits and hospitalizations for COVID-19 in children appear to be following the declining trend set by weekly cases since early December, based on data from the Centers for Disease Control and Prevention.
. New cases took a different path that had the weekly total falling through November before taking a big jump during the week of Nov. 27 to Dec. 3 – the count doubled from 30,000 the previous week to 63,000 – and then decreased again, the CDC reported.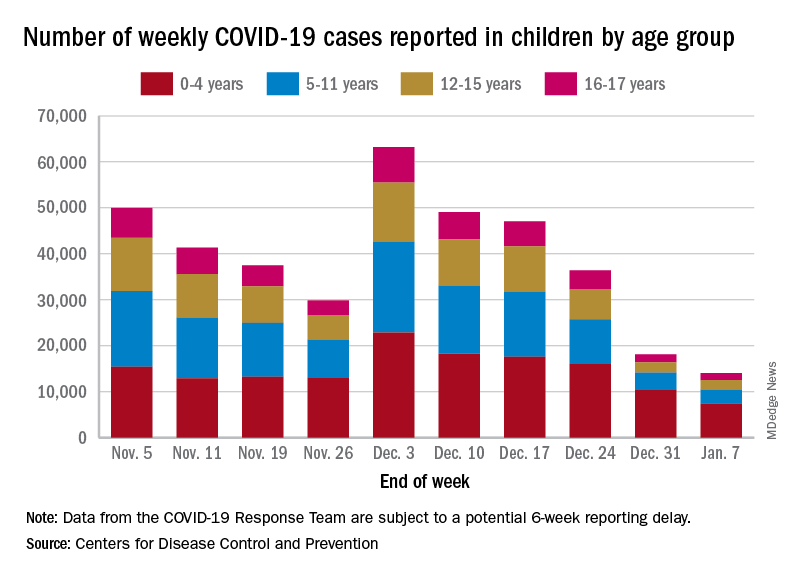
The proportion of ED visits with COVID, which was down to 1.0% of all ED visits (7-day average) for children aged 0-4 years on Nov. 4, was up to 3.2% on Jan. 3 but slipped to 2.5% as of Jan. 10. The patterns for older children are similar, with some differences in timing and lower peaks (1.7% for 12- to 15-year-olds and 1.9% for those aged 16-17), according to the CDC’s COVID Data Tracker.
The trend for new hospital admissions of children with confirmed COVID showed a similar rise through December, and the latest data for the very beginning of January suggest an even faster drop, although there is more of a reporting lag with hospitalization data, compared with ED visits, the CDC noted.
The most current data (Dec. 30 to Jan. 5) available from the American Academy of Pediatrics and the Children’s Hospital Association show less volatility in the number of weekly cases through November and December, with the peak being about 48,000 in mid-December. The AAP/CHA totals for the last 2 weeks, however, were both higher than the CDC’s corresponding counts, which are more preliminary and subject to revision.
The CDC puts the total number of COVID cases in children at 16.7 million – about 17.2% of all cases – as of Jan. 11, with 1,981 deaths reported so far. The AAP and CHA are not tracking deaths, but their case total as of Jan. 5 was 15.2 million, which represents 18.1% of cases in all ages. The AAP/CHA report is based on data reported publicly by an ever-decreasing number of states and territories.
Emergency department visits and hospitalizations for COVID-19 in children appear to be following the declining trend set by weekly cases since early December, based on data from the Centers for Disease Control and Prevention.
. New cases took a different path that had the weekly total falling through November before taking a big jump during the week of Nov. 27 to Dec. 3 – the count doubled from 30,000 the previous week to 63,000 – and then decreased again, the CDC reported.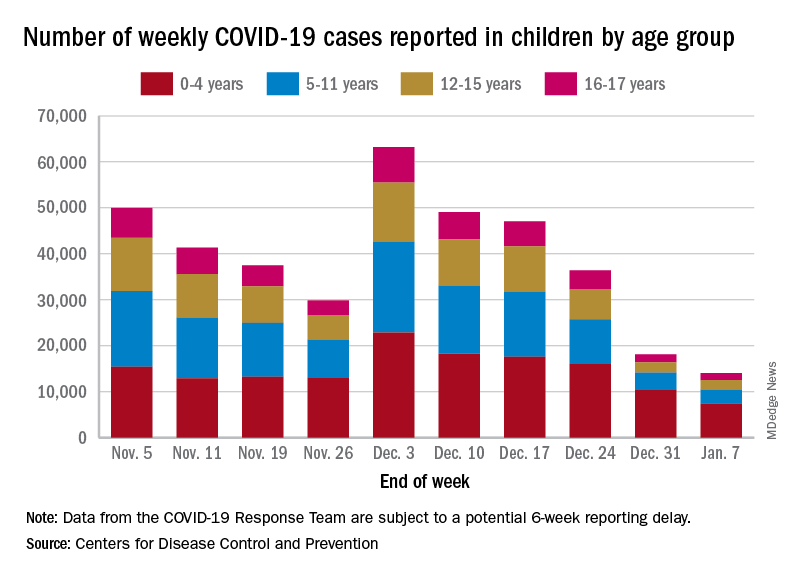
The proportion of ED visits with COVID, which was down to 1.0% of all ED visits (7-day average) for children aged 0-4 years on Nov. 4, was up to 3.2% on Jan. 3 but slipped to 2.5% as of Jan. 10. The patterns for older children are similar, with some differences in timing and lower peaks (1.7% for 12- to 15-year-olds and 1.9% for those aged 16-17), according to the CDC’s COVID Data Tracker.
The trend for new hospital admissions of children with confirmed COVID showed a similar rise through December, and the latest data for the very beginning of January suggest an even faster drop, although there is more of a reporting lag with hospitalization data, compared with ED visits, the CDC noted.
The most current data (Dec. 30 to Jan. 5) available from the American Academy of Pediatrics and the Children’s Hospital Association show less volatility in the number of weekly cases through November and December, with the peak being about 48,000 in mid-December. The AAP/CHA totals for the last 2 weeks, however, were both higher than the CDC’s corresponding counts, which are more preliminary and subject to revision.
The CDC puts the total number of COVID cases in children at 16.7 million – about 17.2% of all cases – as of Jan. 11, with 1,981 deaths reported so far. The AAP and CHA are not tracking deaths, but their case total as of Jan. 5 was 15.2 million, which represents 18.1% of cases in all ages. The AAP/CHA report is based on data reported publicly by an ever-decreasing number of states and territories.
Emergency department visits and hospitalizations for COVID-19 in children appear to be following the declining trend set by weekly cases since early December, based on data from the Centers for Disease Control and Prevention.
. New cases took a different path that had the weekly total falling through November before taking a big jump during the week of Nov. 27 to Dec. 3 – the count doubled from 30,000 the previous week to 63,000 – and then decreased again, the CDC reported.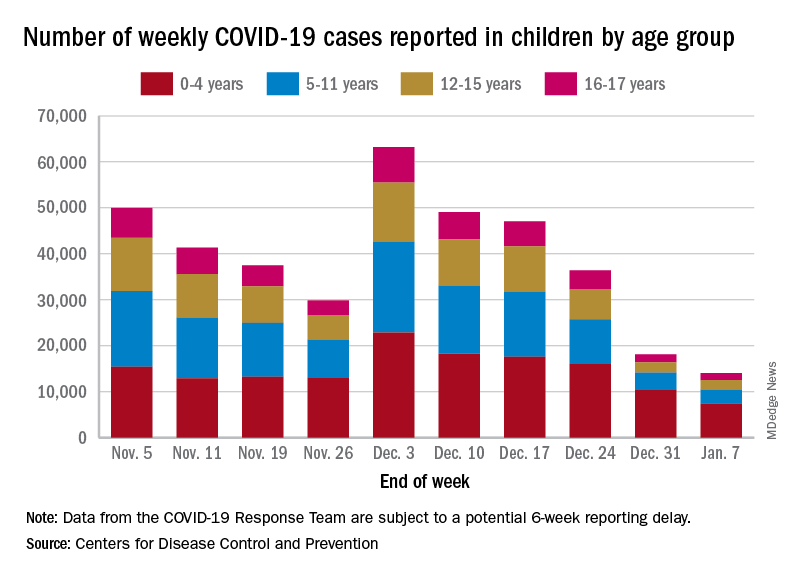
The proportion of ED visits with COVID, which was down to 1.0% of all ED visits (7-day average) for children aged 0-4 years on Nov. 4, was up to 3.2% on Jan. 3 but slipped to 2.5% as of Jan. 10. The patterns for older children are similar, with some differences in timing and lower peaks (1.7% for 12- to 15-year-olds and 1.9% for those aged 16-17), according to the CDC’s COVID Data Tracker.
The trend for new hospital admissions of children with confirmed COVID showed a similar rise through December, and the latest data for the very beginning of January suggest an even faster drop, although there is more of a reporting lag with hospitalization data, compared with ED visits, the CDC noted.
The most current data (Dec. 30 to Jan. 5) available from the American Academy of Pediatrics and the Children’s Hospital Association show less volatility in the number of weekly cases through November and December, with the peak being about 48,000 in mid-December. The AAP/CHA totals for the last 2 weeks, however, were both higher than the CDC’s corresponding counts, which are more preliminary and subject to revision.
The CDC puts the total number of COVID cases in children at 16.7 million – about 17.2% of all cases – as of Jan. 11, with 1,981 deaths reported so far. The AAP and CHA are not tracking deaths, but their case total as of Jan. 5 was 15.2 million, which represents 18.1% of cases in all ages. The AAP/CHA report is based on data reported publicly by an ever-decreasing number of states and territories.
Manicure gone wrong leads to cancer diagnosis
. Now, she and her doctor are spreading the word about her ordeal as a lesson that speed and persistence in seeking treatment are the keys that make her type of cancer – squamous cell carcinoma – completely curable.
“She cut me, and the cut wasn’t just a regular cuticle cut. She cut me deep, and that was one of the first times that happened to me,” Grace Garcia, 50, told TODAY.com, recalling the November 2021 incident.
Ms. Garcia had been getting her nails done regularly for 20 years, she said, but happened to go to a different salon than her usual spot because she couldn’t get an appointment during the busy pre-Thanksgiving season. She doesn’t recall whether the technician opened packaging that signals unused tools.
She put antibiotic ointment on the cut, but it didn’t heal after a few days. Eventually, the skin closed and a darkened bump formed. It was painful. She went to her doctor, who said it was a “callus from writing,” she told TODAY.com. But it was on her ring finger, which didn’t seem connected to writing. Her doctor said to keep an eye on it.
Five months after the cut occurred, she mentioned it during a gynecology appointment and was referred to a dermatologist, who also advised keeping an eye on it. A wart developed. She went back to her primary care physician and then to another dermatologist. The spot was biopsied.
Squamous cell carcinoma is a common type of skin cancer, according to the American Academy of Dermatology. It can have many causes, but the cause in Ms. Garcia’s case was both very common and very rare: human papillomavirus, or HPV. HPV is a virus that infects millions of people every year, but it’s not a typical cause of skin cancer.
“It’s pretty rare for several reasons. Generally speaking, the strains that cause cancer from an HPV standpoint tend to be more sexually transmitted,” dermatologist Teo Soleymani told TODAY.com. “In Grace’s case, she had an injury, which became the portal of entry. So that thick skin that we have on our hands and feet that acts as a natural barrier against infections and things like that was no longer the case, and the virus was able to infect her skin.”
Dr. Soleymani said Ms. Garcia’s persistence to get answers likely saved her from losing a finger.
“Your outcomes are entirely dictated by how early you catch them, and very often they’re completely curable,” he said. “Her persistence – not only was she able to have a great outcome, she probably saved herself from having her finger amputated.”
. Now, she and her doctor are spreading the word about her ordeal as a lesson that speed and persistence in seeking treatment are the keys that make her type of cancer – squamous cell carcinoma – completely curable.
“She cut me, and the cut wasn’t just a regular cuticle cut. She cut me deep, and that was one of the first times that happened to me,” Grace Garcia, 50, told TODAY.com, recalling the November 2021 incident.
Ms. Garcia had been getting her nails done regularly for 20 years, she said, but happened to go to a different salon than her usual spot because she couldn’t get an appointment during the busy pre-Thanksgiving season. She doesn’t recall whether the technician opened packaging that signals unused tools.
She put antibiotic ointment on the cut, but it didn’t heal after a few days. Eventually, the skin closed and a darkened bump formed. It was painful. She went to her doctor, who said it was a “callus from writing,” she told TODAY.com. But it was on her ring finger, which didn’t seem connected to writing. Her doctor said to keep an eye on it.
Five months after the cut occurred, she mentioned it during a gynecology appointment and was referred to a dermatologist, who also advised keeping an eye on it. A wart developed. She went back to her primary care physician and then to another dermatologist. The spot was biopsied.
Squamous cell carcinoma is a common type of skin cancer, according to the American Academy of Dermatology. It can have many causes, but the cause in Ms. Garcia’s case was both very common and very rare: human papillomavirus, or HPV. HPV is a virus that infects millions of people every year, but it’s not a typical cause of skin cancer.
“It’s pretty rare for several reasons. Generally speaking, the strains that cause cancer from an HPV standpoint tend to be more sexually transmitted,” dermatologist Teo Soleymani told TODAY.com. “In Grace’s case, she had an injury, which became the portal of entry. So that thick skin that we have on our hands and feet that acts as a natural barrier against infections and things like that was no longer the case, and the virus was able to infect her skin.”
Dr. Soleymani said Ms. Garcia’s persistence to get answers likely saved her from losing a finger.
“Your outcomes are entirely dictated by how early you catch them, and very often they’re completely curable,” he said. “Her persistence – not only was she able to have a great outcome, she probably saved herself from having her finger amputated.”
. Now, she and her doctor are spreading the word about her ordeal as a lesson that speed and persistence in seeking treatment are the keys that make her type of cancer – squamous cell carcinoma – completely curable.
“She cut me, and the cut wasn’t just a regular cuticle cut. She cut me deep, and that was one of the first times that happened to me,” Grace Garcia, 50, told TODAY.com, recalling the November 2021 incident.
Ms. Garcia had been getting her nails done regularly for 20 years, she said, but happened to go to a different salon than her usual spot because she couldn’t get an appointment during the busy pre-Thanksgiving season. She doesn’t recall whether the technician opened packaging that signals unused tools.
She put antibiotic ointment on the cut, but it didn’t heal after a few days. Eventually, the skin closed and a darkened bump formed. It was painful. She went to her doctor, who said it was a “callus from writing,” she told TODAY.com. But it was on her ring finger, which didn’t seem connected to writing. Her doctor said to keep an eye on it.
Five months after the cut occurred, she mentioned it during a gynecology appointment and was referred to a dermatologist, who also advised keeping an eye on it. A wart developed. She went back to her primary care physician and then to another dermatologist. The spot was biopsied.
Squamous cell carcinoma is a common type of skin cancer, according to the American Academy of Dermatology. It can have many causes, but the cause in Ms. Garcia’s case was both very common and very rare: human papillomavirus, or HPV. HPV is a virus that infects millions of people every year, but it’s not a typical cause of skin cancer.
“It’s pretty rare for several reasons. Generally speaking, the strains that cause cancer from an HPV standpoint tend to be more sexually transmitted,” dermatologist Teo Soleymani told TODAY.com. “In Grace’s case, she had an injury, which became the portal of entry. So that thick skin that we have on our hands and feet that acts as a natural barrier against infections and things like that was no longer the case, and the virus was able to infect her skin.”
Dr. Soleymani said Ms. Garcia’s persistence to get answers likely saved her from losing a finger.
“Your outcomes are entirely dictated by how early you catch them, and very often they’re completely curable,” he said. “Her persistence – not only was she able to have a great outcome, she probably saved herself from having her finger amputated.”
Add this to the list of long COVID symptoms: Stigma
Most people with long COVID find they’re facing stigma due to their condition, according to a new report from researchers in the United Kingdom. In short: Relatives and friends may not believe they’re truly sick.
The U.K. team found that more than three-quarters of people studied had experienced stigma often or always.
In fact, 95% of people with long COVID faced at least one type of stigma at least sometimes, according to the study, published in November in the journal PLOS One.
Those conclusions had surprised the study’s lead researcher, Marija Pantelic, PhD, a public health lecturer at Brighton and Sussex Medical School, England.
“After years of working on HIV-related stigma, I was shocked to see how many people were turning a blind eye to and dismissing the difficulties experienced by people with long COVID,” Dr. Pantelic says. “It has also been clear to me from the start that this stigma is detrimental not just for people’s dignity, but also public health.”
Even some doctors argue that the growing attention paid to long COVID is excessive.
“It’s often normal to experience mild fatigue or weaknesses for weeks after being sick and inactive and not eating well. Calling these cases long COVID is the medicalization of modern life,” Marty Makary, MD, a surgeon and public policy researcher at Johns Hopkins University, Baltimore, wrote in a commentary in the Wall Street Journal.
Other doctors strongly disagree, including Alba Azola, MD, codirector of the Johns Hopkins Post-Acute COVID-19 Team and an expert in the stigma surrounding long COVID.
“Putting that spin on things, it’s just hurting people,” she says.
One example is people who cannot return to work.
“A lot of their family members tell me that they’re being lazy,” Dr. Azola says. “That’s part of the public stigma, that these are people just trying to get out of work.”
Some experts say the U.K. study represents a landmark.
“When you have data like this on long COVID stigma, it becomes more difficult to deny its existence or address it,” says Naomi Torres-Mackie, PhD, a clinical psychologist at Lenox Hill Hospital in New York. She also is head of research at the New York–based Mental Health Coalition, a group of experts working to end the stigma surrounding mental health.
She recalls her first patient with long COVID.
“She experienced the discomfort and pain itself, and then she had this crushing feeling that it wasn’t valid, or real. She felt very alone in it,” Dr. Torres-Mackie says.
Another one of her patients is working at her job from home but facing doubt about her condition from her employers.
“Every month, her medical doctor has to produce a letter confirming her medical condition,” Dr. Torres-Mackie says.
Taking part in the British stigma survey were 1,166 people, including 966 residents of the United Kingdom, with the average age of 48. Nearly 85% were female, and more than three-quarters were educated at the university level or higher.
Half of them said they had a clinical diagnosis of long COVID.
More than 60% of them said that at least some of the time, they were cautious about who they talked to about their condition. And fully 34% of those who did disclose their diagnosis said that they regretted having done so.
That’s a difficult experience for those with long COVID, says Leonard Jason, PhD, a professor of psychology at DePaul University in Chicago.
“It’s like they’re traumatized by the initial experience of being sick, and retraumatized by the response of others to them,” he says.
Unexplained illnesses are not well-regarded by the general public, Dr. Jason says.
He gave the example of multiple sclerosis. Before the 1980s, those with MS were considered to have a psychological illness, he says. “Then, in the 1980s, there were biomarkers that said, ‘Here’s the evidence.’ ”
The British study described three types of stigma stemming from the long COVID diagnosis of those questioned:
- Enacted stigma: People were directly treated unfairly because of their condition.
- Internalized stigma: People felt embarrassed by that condition.
- Anticipated stigma: People expected they would be treated poorly because of their diagnosis.
Dr. Azola calls the medical community a major problem when it comes to dealing with long COVID.
“What I see with my patients is medical trauma,” she says. They may have symptoms that send them to the emergency room, and then the tests come back negative. “Instead of tracking the patients’ symptoms, patients get told, ‘Everything looks good, you can go home, this is a panic attack,’ ” she says.
Some people go online to search for treatments, sometimes launching GoFundMe campaigns to raise money for unreliable treatments.
Long COVID patients may have gone through 5 to 10 doctors before they arrive for treatment with the Johns Hopkins Post-Acute COVID-19 Team. The clinic began in April 2020 remotely and in August of that year in person.
Today, the clinic staff spends an hour with a first-time long COVID patient, hearing their stories and helping relieve anxiety, Dr. Azola says.
The phenomenon of long COVID is similar to what patients have had with chronic fatigue syndrome, lupus, or fibromyalgia, where people have symptoms that are hard to explain, says Jennifer Chevinsky, MD, deputy public health officer for Riverside County, Calif.
“Stigma within medicine or health care is nothing new,” she says.
In Chicago, Dr. Jason notes that the federal government’s decision to invest hundreds of millions of dollars in long COVID research “shows the government is helping destigmatize it.”
Dr. Pantelic says she and her colleagues are continuing their research.
“We are interested in understanding the impacts of this stigma, and how to mitigate any adverse outcomes for patients and services,” she says.
A version of this article first appeared on WebMD.com.
Most people with long COVID find they’re facing stigma due to their condition, according to a new report from researchers in the United Kingdom. In short: Relatives and friends may not believe they’re truly sick.
The U.K. team found that more than three-quarters of people studied had experienced stigma often or always.
In fact, 95% of people with long COVID faced at least one type of stigma at least sometimes, according to the study, published in November in the journal PLOS One.
Those conclusions had surprised the study’s lead researcher, Marija Pantelic, PhD, a public health lecturer at Brighton and Sussex Medical School, England.
“After years of working on HIV-related stigma, I was shocked to see how many people were turning a blind eye to and dismissing the difficulties experienced by people with long COVID,” Dr. Pantelic says. “It has also been clear to me from the start that this stigma is detrimental not just for people’s dignity, but also public health.”
Even some doctors argue that the growing attention paid to long COVID is excessive.
“It’s often normal to experience mild fatigue or weaknesses for weeks after being sick and inactive and not eating well. Calling these cases long COVID is the medicalization of modern life,” Marty Makary, MD, a surgeon and public policy researcher at Johns Hopkins University, Baltimore, wrote in a commentary in the Wall Street Journal.
Other doctors strongly disagree, including Alba Azola, MD, codirector of the Johns Hopkins Post-Acute COVID-19 Team and an expert in the stigma surrounding long COVID.
“Putting that spin on things, it’s just hurting people,” she says.
One example is people who cannot return to work.
“A lot of their family members tell me that they’re being lazy,” Dr. Azola says. “That’s part of the public stigma, that these are people just trying to get out of work.”
Some experts say the U.K. study represents a landmark.
“When you have data like this on long COVID stigma, it becomes more difficult to deny its existence or address it,” says Naomi Torres-Mackie, PhD, a clinical psychologist at Lenox Hill Hospital in New York. She also is head of research at the New York–based Mental Health Coalition, a group of experts working to end the stigma surrounding mental health.
She recalls her first patient with long COVID.
“She experienced the discomfort and pain itself, and then she had this crushing feeling that it wasn’t valid, or real. She felt very alone in it,” Dr. Torres-Mackie says.
Another one of her patients is working at her job from home but facing doubt about her condition from her employers.
“Every month, her medical doctor has to produce a letter confirming her medical condition,” Dr. Torres-Mackie says.
Taking part in the British stigma survey were 1,166 people, including 966 residents of the United Kingdom, with the average age of 48. Nearly 85% were female, and more than three-quarters were educated at the university level or higher.
Half of them said they had a clinical diagnosis of long COVID.
More than 60% of them said that at least some of the time, they were cautious about who they talked to about their condition. And fully 34% of those who did disclose their diagnosis said that they regretted having done so.
That’s a difficult experience for those with long COVID, says Leonard Jason, PhD, a professor of psychology at DePaul University in Chicago.
“It’s like they’re traumatized by the initial experience of being sick, and retraumatized by the response of others to them,” he says.
Unexplained illnesses are not well-regarded by the general public, Dr. Jason says.
He gave the example of multiple sclerosis. Before the 1980s, those with MS were considered to have a psychological illness, he says. “Then, in the 1980s, there were biomarkers that said, ‘Here’s the evidence.’ ”
The British study described three types of stigma stemming from the long COVID diagnosis of those questioned:
- Enacted stigma: People were directly treated unfairly because of their condition.
- Internalized stigma: People felt embarrassed by that condition.
- Anticipated stigma: People expected they would be treated poorly because of their diagnosis.
Dr. Azola calls the medical community a major problem when it comes to dealing with long COVID.
“What I see with my patients is medical trauma,” she says. They may have symptoms that send them to the emergency room, and then the tests come back negative. “Instead of tracking the patients’ symptoms, patients get told, ‘Everything looks good, you can go home, this is a panic attack,’ ” she says.
Some people go online to search for treatments, sometimes launching GoFundMe campaigns to raise money for unreliable treatments.
Long COVID patients may have gone through 5 to 10 doctors before they arrive for treatment with the Johns Hopkins Post-Acute COVID-19 Team. The clinic began in April 2020 remotely and in August of that year in person.
Today, the clinic staff spends an hour with a first-time long COVID patient, hearing their stories and helping relieve anxiety, Dr. Azola says.
The phenomenon of long COVID is similar to what patients have had with chronic fatigue syndrome, lupus, or fibromyalgia, where people have symptoms that are hard to explain, says Jennifer Chevinsky, MD, deputy public health officer for Riverside County, Calif.
“Stigma within medicine or health care is nothing new,” she says.
In Chicago, Dr. Jason notes that the federal government’s decision to invest hundreds of millions of dollars in long COVID research “shows the government is helping destigmatize it.”
Dr. Pantelic says she and her colleagues are continuing their research.
“We are interested in understanding the impacts of this stigma, and how to mitigate any adverse outcomes for patients and services,” she says.
A version of this article first appeared on WebMD.com.
Most people with long COVID find they’re facing stigma due to their condition, according to a new report from researchers in the United Kingdom. In short: Relatives and friends may not believe they’re truly sick.
The U.K. team found that more than three-quarters of people studied had experienced stigma often or always.
In fact, 95% of people with long COVID faced at least one type of stigma at least sometimes, according to the study, published in November in the journal PLOS One.
Those conclusions had surprised the study’s lead researcher, Marija Pantelic, PhD, a public health lecturer at Brighton and Sussex Medical School, England.
“After years of working on HIV-related stigma, I was shocked to see how many people were turning a blind eye to and dismissing the difficulties experienced by people with long COVID,” Dr. Pantelic says. “It has also been clear to me from the start that this stigma is detrimental not just for people’s dignity, but also public health.”
Even some doctors argue that the growing attention paid to long COVID is excessive.
“It’s often normal to experience mild fatigue or weaknesses for weeks after being sick and inactive and not eating well. Calling these cases long COVID is the medicalization of modern life,” Marty Makary, MD, a surgeon and public policy researcher at Johns Hopkins University, Baltimore, wrote in a commentary in the Wall Street Journal.
Other doctors strongly disagree, including Alba Azola, MD, codirector of the Johns Hopkins Post-Acute COVID-19 Team and an expert in the stigma surrounding long COVID.
“Putting that spin on things, it’s just hurting people,” she says.
One example is people who cannot return to work.
“A lot of their family members tell me that they’re being lazy,” Dr. Azola says. “That’s part of the public stigma, that these are people just trying to get out of work.”
Some experts say the U.K. study represents a landmark.
“When you have data like this on long COVID stigma, it becomes more difficult to deny its existence or address it,” says Naomi Torres-Mackie, PhD, a clinical psychologist at Lenox Hill Hospital in New York. She also is head of research at the New York–based Mental Health Coalition, a group of experts working to end the stigma surrounding mental health.
She recalls her first patient with long COVID.
“She experienced the discomfort and pain itself, and then she had this crushing feeling that it wasn’t valid, or real. She felt very alone in it,” Dr. Torres-Mackie says.
Another one of her patients is working at her job from home but facing doubt about her condition from her employers.
“Every month, her medical doctor has to produce a letter confirming her medical condition,” Dr. Torres-Mackie says.
Taking part in the British stigma survey were 1,166 people, including 966 residents of the United Kingdom, with the average age of 48. Nearly 85% were female, and more than three-quarters were educated at the university level or higher.
Half of them said they had a clinical diagnosis of long COVID.
More than 60% of them said that at least some of the time, they were cautious about who they talked to about their condition. And fully 34% of those who did disclose their diagnosis said that they regretted having done so.
That’s a difficult experience for those with long COVID, says Leonard Jason, PhD, a professor of psychology at DePaul University in Chicago.
“It’s like they’re traumatized by the initial experience of being sick, and retraumatized by the response of others to them,” he says.
Unexplained illnesses are not well-regarded by the general public, Dr. Jason says.
He gave the example of multiple sclerosis. Before the 1980s, those with MS were considered to have a psychological illness, he says. “Then, in the 1980s, there were biomarkers that said, ‘Here’s the evidence.’ ”
The British study described three types of stigma stemming from the long COVID diagnosis of those questioned:
- Enacted stigma: People were directly treated unfairly because of their condition.
- Internalized stigma: People felt embarrassed by that condition.
- Anticipated stigma: People expected they would be treated poorly because of their diagnosis.
Dr. Azola calls the medical community a major problem when it comes to dealing with long COVID.
“What I see with my patients is medical trauma,” she says. They may have symptoms that send them to the emergency room, and then the tests come back negative. “Instead of tracking the patients’ symptoms, patients get told, ‘Everything looks good, you can go home, this is a panic attack,’ ” she says.
Some people go online to search for treatments, sometimes launching GoFundMe campaigns to raise money for unreliable treatments.
Long COVID patients may have gone through 5 to 10 doctors before they arrive for treatment with the Johns Hopkins Post-Acute COVID-19 Team. The clinic began in April 2020 remotely and in August of that year in person.
Today, the clinic staff spends an hour with a first-time long COVID patient, hearing their stories and helping relieve anxiety, Dr. Azola says.
The phenomenon of long COVID is similar to what patients have had with chronic fatigue syndrome, lupus, or fibromyalgia, where people have symptoms that are hard to explain, says Jennifer Chevinsky, MD, deputy public health officer for Riverside County, Calif.
“Stigma within medicine or health care is nothing new,” she says.
In Chicago, Dr. Jason notes that the federal government’s decision to invest hundreds of millions of dollars in long COVID research “shows the government is helping destigmatize it.”
Dr. Pantelic says she and her colleagues are continuing their research.
“We are interested in understanding the impacts of this stigma, and how to mitigate any adverse outcomes for patients and services,” she says.
A version of this article first appeared on WebMD.com.
PLOS ONE
What the FTC’s proposed ban on noncompete agreements could mean for physicians, other clinicians
The proposed rule seeks to ban companies from enforcing noncompete clauses in employment contracts, a practice that represents an “unfair method of competition” with “exploitative and widespread” impacts, including suppression of wages, innovation, and entrepreneurial spirit, the FTC said. The public has 60 days to submit comments on the proposal before the FTC issues the final rule.
Employers often include noncompete clauses in physician contracts because they want to avoid having patients leave their health care system and follow a doctor to a competitor. A 2018 survey of primary care physicians found that about half of office-based physicians and 37% of physicians employed at hospitals or freestanding care centers were bound by restrictive covenants.
“A federal ban on noncompete agreements will ensure that physicians nationwide can finally change jobs without fear of being sued,” Erik B. Smith, MD, JD, clinical assistant professor of anesthesiology at the University of Southern California, Los Angeles, said in an interview.
Many doctors would like to see noncompete agreements vanish, but some physicians still favor them.
“As a small-practice owner, I am personally against this. The noncompete helps me take a risk and hire a physician. It typically takes 2-3 years for me to break even. I think this will further consolidate employment with large hospital systems unfortunately,” Texas cardiologist Rishin Shah, MD, recently tweeted in response to the FTC announcement.
Dr. Smith, who has advocated for noncompete reform, said about half of states currently allow the controversial clauses.
However, several states have recently passed laws restricting their use. California, North Dakota, and Oklahoma ban noncompetes, although some narrowly defined exceptions, such as the sale of a business, remain.
Other states, like Colorado, Illinois, and Oregon, broadly ban noncompete clauses, except for workers earning above a certain threshold. For example, in Colorado, noncompete agreements are permitted for highly compensated employees earning more than $101,250.
Despite additional restrictions on noncompete agreements for workers in the District of Columbia, the new legislation does not apply to physicians earning total compensation of $250,000 or more. However, their employers must define the geographic parameters of the noncompete and limit postemployment restrictions to 2 years.
Restrictive covenants are “uniquely challenging to family medicine’s emphasis on longitudinal care and the patient-physician relationship,” said Tochi Iroku-Malize, MD, MPH, president of the American Academy of Family Physicians. The limitations imposed by noncompete agreements “potentially reduce patient choice, lower the quality of care for patients, and ultimately harm the foundation of family medicine – our relationships with our patients.”
Although the proposed rule aligns with President Biden’s executive order promoting economic competition, Dr. Smith said a national ban on noncompete agreements may push the limits of FTC authority.
“This new rule will certainly result in a ‘major questions doctrine’ Supreme Court challenge,” said Dr. Smith, and possibly be struck down if the court determines an administrative overstep into areas of “vast economic or political significance.”
A controversial policy
The American Medical Association’s code of ethics discourages covenants that “unreasonably restrict” the ability of physicians to practice following contract termination. And in 2022, the AMA cited “overly broad” noncompete language as a red flag young physicians should watch out for during contract negotiations.
But in 2020, the AMA asked the FTC not to use its rulemaking authority to regulate noncompete clauses in physician employment contracts, and instead, relegate enforcement of such agreements to each state. The American Hospital Association expressed similar views.
Still, the FTC said that eliminating noncompete clauses will increase annual wages by $300 billion, allow 30 million Americans to pursue better job opportunities, and encourage hiring competition among employers. It will also save consumers up to $148 billion in health care costs annually.
“Noncompetes block workers from freely switching jobs, depriving them of higher wages and better working conditions, and depriving businesses of a talent pool that they need to build and expand,” Lina M. Khan, FTC chair, said in a press release about the proposal.
A national ban on noncompetes would keep more physicians in the industry and practicing in their communities, a win for patients and providers, said Dr. Smith. It could also compel employers to offer more competitive employment packages, including fair wages, better work conditions, and a culture of well-being and patient safety.
“Whatever the final rule is, I’m certain it will be legally challenged,” said Dr. Smith, adding that the nation’s most prominent business lobbying group, the Chamber of Commerce, has already issued a statement calling the rule “blatantly unlawful."
A version of this article first appeared on Medscape.com.
The proposed rule seeks to ban companies from enforcing noncompete clauses in employment contracts, a practice that represents an “unfair method of competition” with “exploitative and widespread” impacts, including suppression of wages, innovation, and entrepreneurial spirit, the FTC said. The public has 60 days to submit comments on the proposal before the FTC issues the final rule.
Employers often include noncompete clauses in physician contracts because they want to avoid having patients leave their health care system and follow a doctor to a competitor. A 2018 survey of primary care physicians found that about half of office-based physicians and 37% of physicians employed at hospitals or freestanding care centers were bound by restrictive covenants.
“A federal ban on noncompete agreements will ensure that physicians nationwide can finally change jobs without fear of being sued,” Erik B. Smith, MD, JD, clinical assistant professor of anesthesiology at the University of Southern California, Los Angeles, said in an interview.
Many doctors would like to see noncompete agreements vanish, but some physicians still favor them.
“As a small-practice owner, I am personally against this. The noncompete helps me take a risk and hire a physician. It typically takes 2-3 years for me to break even. I think this will further consolidate employment with large hospital systems unfortunately,” Texas cardiologist Rishin Shah, MD, recently tweeted in response to the FTC announcement.
Dr. Smith, who has advocated for noncompete reform, said about half of states currently allow the controversial clauses.
However, several states have recently passed laws restricting their use. California, North Dakota, and Oklahoma ban noncompetes, although some narrowly defined exceptions, such as the sale of a business, remain.
Other states, like Colorado, Illinois, and Oregon, broadly ban noncompete clauses, except for workers earning above a certain threshold. For example, in Colorado, noncompete agreements are permitted for highly compensated employees earning more than $101,250.
Despite additional restrictions on noncompete agreements for workers in the District of Columbia, the new legislation does not apply to physicians earning total compensation of $250,000 or more. However, their employers must define the geographic parameters of the noncompete and limit postemployment restrictions to 2 years.
Restrictive covenants are “uniquely challenging to family medicine’s emphasis on longitudinal care and the patient-physician relationship,” said Tochi Iroku-Malize, MD, MPH, president of the American Academy of Family Physicians. The limitations imposed by noncompete agreements “potentially reduce patient choice, lower the quality of care for patients, and ultimately harm the foundation of family medicine – our relationships with our patients.”
Although the proposed rule aligns with President Biden’s executive order promoting economic competition, Dr. Smith said a national ban on noncompete agreements may push the limits of FTC authority.
“This new rule will certainly result in a ‘major questions doctrine’ Supreme Court challenge,” said Dr. Smith, and possibly be struck down if the court determines an administrative overstep into areas of “vast economic or political significance.”
A controversial policy
The American Medical Association’s code of ethics discourages covenants that “unreasonably restrict” the ability of physicians to practice following contract termination. And in 2022, the AMA cited “overly broad” noncompete language as a red flag young physicians should watch out for during contract negotiations.
But in 2020, the AMA asked the FTC not to use its rulemaking authority to regulate noncompete clauses in physician employment contracts, and instead, relegate enforcement of such agreements to each state. The American Hospital Association expressed similar views.
Still, the FTC said that eliminating noncompete clauses will increase annual wages by $300 billion, allow 30 million Americans to pursue better job opportunities, and encourage hiring competition among employers. It will also save consumers up to $148 billion in health care costs annually.
“Noncompetes block workers from freely switching jobs, depriving them of higher wages and better working conditions, and depriving businesses of a talent pool that they need to build and expand,” Lina M. Khan, FTC chair, said in a press release about the proposal.
A national ban on noncompetes would keep more physicians in the industry and practicing in their communities, a win for patients and providers, said Dr. Smith. It could also compel employers to offer more competitive employment packages, including fair wages, better work conditions, and a culture of well-being and patient safety.
“Whatever the final rule is, I’m certain it will be legally challenged,” said Dr. Smith, adding that the nation’s most prominent business lobbying group, the Chamber of Commerce, has already issued a statement calling the rule “blatantly unlawful."
A version of this article first appeared on Medscape.com.
The proposed rule seeks to ban companies from enforcing noncompete clauses in employment contracts, a practice that represents an “unfair method of competition” with “exploitative and widespread” impacts, including suppression of wages, innovation, and entrepreneurial spirit, the FTC said. The public has 60 days to submit comments on the proposal before the FTC issues the final rule.
Employers often include noncompete clauses in physician contracts because they want to avoid having patients leave their health care system and follow a doctor to a competitor. A 2018 survey of primary care physicians found that about half of office-based physicians and 37% of physicians employed at hospitals or freestanding care centers were bound by restrictive covenants.
“A federal ban on noncompete agreements will ensure that physicians nationwide can finally change jobs without fear of being sued,” Erik B. Smith, MD, JD, clinical assistant professor of anesthesiology at the University of Southern California, Los Angeles, said in an interview.
Many doctors would like to see noncompete agreements vanish, but some physicians still favor them.
“As a small-practice owner, I am personally against this. The noncompete helps me take a risk and hire a physician. It typically takes 2-3 years for me to break even. I think this will further consolidate employment with large hospital systems unfortunately,” Texas cardiologist Rishin Shah, MD, recently tweeted in response to the FTC announcement.
Dr. Smith, who has advocated for noncompete reform, said about half of states currently allow the controversial clauses.
However, several states have recently passed laws restricting their use. California, North Dakota, and Oklahoma ban noncompetes, although some narrowly defined exceptions, such as the sale of a business, remain.
Other states, like Colorado, Illinois, and Oregon, broadly ban noncompete clauses, except for workers earning above a certain threshold. For example, in Colorado, noncompete agreements are permitted for highly compensated employees earning more than $101,250.
Despite additional restrictions on noncompete agreements for workers in the District of Columbia, the new legislation does not apply to physicians earning total compensation of $250,000 or more. However, their employers must define the geographic parameters of the noncompete and limit postemployment restrictions to 2 years.
Restrictive covenants are “uniquely challenging to family medicine’s emphasis on longitudinal care and the patient-physician relationship,” said Tochi Iroku-Malize, MD, MPH, president of the American Academy of Family Physicians. The limitations imposed by noncompete agreements “potentially reduce patient choice, lower the quality of care for patients, and ultimately harm the foundation of family medicine – our relationships with our patients.”
Although the proposed rule aligns with President Biden’s executive order promoting economic competition, Dr. Smith said a national ban on noncompete agreements may push the limits of FTC authority.
“This new rule will certainly result in a ‘major questions doctrine’ Supreme Court challenge,” said Dr. Smith, and possibly be struck down if the court determines an administrative overstep into areas of “vast economic or political significance.”
A controversial policy
The American Medical Association’s code of ethics discourages covenants that “unreasonably restrict” the ability of physicians to practice following contract termination. And in 2022, the AMA cited “overly broad” noncompete language as a red flag young physicians should watch out for during contract negotiations.
But in 2020, the AMA asked the FTC not to use its rulemaking authority to regulate noncompete clauses in physician employment contracts, and instead, relegate enforcement of such agreements to each state. The American Hospital Association expressed similar views.
Still, the FTC said that eliminating noncompete clauses will increase annual wages by $300 billion, allow 30 million Americans to pursue better job opportunities, and encourage hiring competition among employers. It will also save consumers up to $148 billion in health care costs annually.
“Noncompetes block workers from freely switching jobs, depriving them of higher wages and better working conditions, and depriving businesses of a talent pool that they need to build and expand,” Lina M. Khan, FTC chair, said in a press release about the proposal.
A national ban on noncompetes would keep more physicians in the industry and practicing in their communities, a win for patients and providers, said Dr. Smith. It could also compel employers to offer more competitive employment packages, including fair wages, better work conditions, and a culture of well-being and patient safety.
“Whatever the final rule is, I’m certain it will be legally challenged,” said Dr. Smith, adding that the nation’s most prominent business lobbying group, the Chamber of Commerce, has already issued a statement calling the rule “blatantly unlawful."
A version of this article first appeared on Medscape.com.
Atrial failure or insufficiency: A new syndrome
Atrial dysfunction, widely considered a marker or consequence of other heart diseases, is a relevant clinical entity, which is why it is justified to define atrial failure or insufficiency as “a new syndrome that all cardiologists should be aware of,” said Adrián Baranchuk, MD, PhD, professor of medicine at Queen’s University, Kingston, Ont., during the 2022 48th Argentine Congress of Cardiology in Buenos Aires.
“The atria are like the heart’s silly sisters and can fail just like the ventricle fails. Understanding their function and dysfunction helps us to understand heart failure. And as electrophysiologists and clinical cardiologists, we have to embrace this concept and understand it in depth,” Dr. Baranchuk, president-elect of the Inter-American Society of Cardiology, said in an interview.
The specialist first proposed atrial failure as an entity or syndrome in early 2020 in an article in the Journal of the American College of Cardiology. His four collaborators included the experienced Eugene Braunwald, MD, from Brigham and Women’s Hospital, Boston, and Antoni Bayés de Luna, PhD, from the department of medicine of the autonomous University of Barcelona.
Pathology despite function
“In many patients with heart failure, the pump function is preserved, but what causes the pathology? For the last 5-10 years, attention has been focused on the ventricle: whether it contracts poorly or whether it contracts properly and relaxes poorly. However, we have also seen patients in whom the ventricle contracts properly and relaxes properly. Where else can we look? We started looking at atrial contraction, especially the left atrium,” recalled Dr. Baranchuk.
He and his colleagues proposed the following consensus definition of atrial failure or insufficiency: any atrial dysfunction (anatomical, mechanical, electrical, and rheological, including blood homeostasis) that causes impaired function, heart symptoms, and a worsening of quality of life (or life expectancy) in the absence of significant valvular or ventricular abnormalities.
In his presentation, recorded and projected by video from Canada, Dr. Baranchuk pointed out that there are two large groups of causes of atrial failure: one that has to do with electrical disorders of atrial and interatrial contraction and another related to the progressive development of fibrosis, which gradually leads to dyssynchrony in interatrial contraction, pump failure, and impaired atrial function as a reservoir and as a conduit.
“In turn, these mechanisms trigger neurohormonal alterations that perpetuate atrial failure, so it is not just a matter of progressive fibrosis, which is very difficult to treat, but also of constant neurohormonal activation that guarantees that these phenomena never resolve,” said Dr. Baranchuk. The manifestations or end point of this cascade of events are the known ones: stroke, ischemia, and heart failure.
New entity necessary?
Defining atrial failure or insufficiency as a clinical entity not only restores the hierarchy of the atria in cardiac function, which was already postulated by William Harvey in 1628, but also enables new lines of research that would eventually allow timely preventive interventions.
One key is early recognition of partial or total interatrial block by analyzing the characteristics of the P wave on the electrocardiogram, which could serve to prevent progression to atrial fibrillation. Left atrial enlargement can also be detected by echocardiography.
“When the contractile impairment is severe and you are in atrial fibrillation, all that remains is to apply patches. The strategy is to correct risk factors beforehand, such as high blood pressure, sleep apnea, or high-dose alcohol consumption, as well as tirelessly searching for atrial fibrillation, with Holter electrocardiograms, continuous monitoring devices, such as Apple Watch, KardiaMobile, or an implantable loop recorder,” Dr. Baranchuk said in an interview.
Two ongoing or planned studies, ARCADIA and AMIABLE, will seek to determine whether anticoagulation in patients with elevated cardiovascular risk scores and any of these atrial disorders that have not yet led to atrial fibrillation could reduce the incidence of stroke.
The strategy has a rational basis. In a subanalysis of raw data from the NAVIGATE ESUS study in patients with embolic stroke of unknown cause, Dr. Baranchuk estimated that the presence of interatrial block was a tenfold higher predictor of the risk of experiencing a second stroke. Another 2018 observational study in which he participated found that in outpatients with heart failure, advanced interatrial block approximately tripled the risk of developing atrial fibrillation and ischemic stroke.
For Dr. Baranchuk, other questions that still need to be answered include whether drugs used for heart failure with preserved ejection fraction can be useful in primary atrial failure or whether specific drugs can be repositioned or developed to suppress or slow the process of fibrosis. “From generating the clinical concept, many lines of research are enabled.”
“The concept of atrial failure is very interesting and opens our eyes to treatments,” another speaker at the session, Alejo Tronconi, MD, a cardiologist and electrophysiologist at the Cardiovascular Institute of the South, Cipolletti, Argentina, said in an interview.
“It is necessary to cut circuits that have been extensively studied in heart failure models, and now we are beginning to see their participation in atrial dysfunction,” he said.
Dr. Baranchuk and Dr. Tronconi declared no relevant financial conflict of interest.
A version of this article first appeared on Medscape.com.
Atrial dysfunction, widely considered a marker or consequence of other heart diseases, is a relevant clinical entity, which is why it is justified to define atrial failure or insufficiency as “a new syndrome that all cardiologists should be aware of,” said Adrián Baranchuk, MD, PhD, professor of medicine at Queen’s University, Kingston, Ont., during the 2022 48th Argentine Congress of Cardiology in Buenos Aires.
“The atria are like the heart’s silly sisters and can fail just like the ventricle fails. Understanding their function and dysfunction helps us to understand heart failure. And as electrophysiologists and clinical cardiologists, we have to embrace this concept and understand it in depth,” Dr. Baranchuk, president-elect of the Inter-American Society of Cardiology, said in an interview.
The specialist first proposed atrial failure as an entity or syndrome in early 2020 in an article in the Journal of the American College of Cardiology. His four collaborators included the experienced Eugene Braunwald, MD, from Brigham and Women’s Hospital, Boston, and Antoni Bayés de Luna, PhD, from the department of medicine of the autonomous University of Barcelona.
Pathology despite function
“In many patients with heart failure, the pump function is preserved, but what causes the pathology? For the last 5-10 years, attention has been focused on the ventricle: whether it contracts poorly or whether it contracts properly and relaxes poorly. However, we have also seen patients in whom the ventricle contracts properly and relaxes properly. Where else can we look? We started looking at atrial contraction, especially the left atrium,” recalled Dr. Baranchuk.
He and his colleagues proposed the following consensus definition of atrial failure or insufficiency: any atrial dysfunction (anatomical, mechanical, electrical, and rheological, including blood homeostasis) that causes impaired function, heart symptoms, and a worsening of quality of life (or life expectancy) in the absence of significant valvular or ventricular abnormalities.
In his presentation, recorded and projected by video from Canada, Dr. Baranchuk pointed out that there are two large groups of causes of atrial failure: one that has to do with electrical disorders of atrial and interatrial contraction and another related to the progressive development of fibrosis, which gradually leads to dyssynchrony in interatrial contraction, pump failure, and impaired atrial function as a reservoir and as a conduit.
“In turn, these mechanisms trigger neurohormonal alterations that perpetuate atrial failure, so it is not just a matter of progressive fibrosis, which is very difficult to treat, but also of constant neurohormonal activation that guarantees that these phenomena never resolve,” said Dr. Baranchuk. The manifestations or end point of this cascade of events are the known ones: stroke, ischemia, and heart failure.
New entity necessary?
Defining atrial failure or insufficiency as a clinical entity not only restores the hierarchy of the atria in cardiac function, which was already postulated by William Harvey in 1628, but also enables new lines of research that would eventually allow timely preventive interventions.
One key is early recognition of partial or total interatrial block by analyzing the characteristics of the P wave on the electrocardiogram, which could serve to prevent progression to atrial fibrillation. Left atrial enlargement can also be detected by echocardiography.
“When the contractile impairment is severe and you are in atrial fibrillation, all that remains is to apply patches. The strategy is to correct risk factors beforehand, such as high blood pressure, sleep apnea, or high-dose alcohol consumption, as well as tirelessly searching for atrial fibrillation, with Holter electrocardiograms, continuous monitoring devices, such as Apple Watch, KardiaMobile, or an implantable loop recorder,” Dr. Baranchuk said in an interview.
Two ongoing or planned studies, ARCADIA and AMIABLE, will seek to determine whether anticoagulation in patients with elevated cardiovascular risk scores and any of these atrial disorders that have not yet led to atrial fibrillation could reduce the incidence of stroke.
The strategy has a rational basis. In a subanalysis of raw data from the NAVIGATE ESUS study in patients with embolic stroke of unknown cause, Dr. Baranchuk estimated that the presence of interatrial block was a tenfold higher predictor of the risk of experiencing a second stroke. Another 2018 observational study in which he participated found that in outpatients with heart failure, advanced interatrial block approximately tripled the risk of developing atrial fibrillation and ischemic stroke.
For Dr. Baranchuk, other questions that still need to be answered include whether drugs used for heart failure with preserved ejection fraction can be useful in primary atrial failure or whether specific drugs can be repositioned or developed to suppress or slow the process of fibrosis. “From generating the clinical concept, many lines of research are enabled.”
“The concept of atrial failure is very interesting and opens our eyes to treatments,” another speaker at the session, Alejo Tronconi, MD, a cardiologist and electrophysiologist at the Cardiovascular Institute of the South, Cipolletti, Argentina, said in an interview.
“It is necessary to cut circuits that have been extensively studied in heart failure models, and now we are beginning to see their participation in atrial dysfunction,” he said.
Dr. Baranchuk and Dr. Tronconi declared no relevant financial conflict of interest.
A version of this article first appeared on Medscape.com.
Atrial dysfunction, widely considered a marker or consequence of other heart diseases, is a relevant clinical entity, which is why it is justified to define atrial failure or insufficiency as “a new syndrome that all cardiologists should be aware of,” said Adrián Baranchuk, MD, PhD, professor of medicine at Queen’s University, Kingston, Ont., during the 2022 48th Argentine Congress of Cardiology in Buenos Aires.
“The atria are like the heart’s silly sisters and can fail just like the ventricle fails. Understanding their function and dysfunction helps us to understand heart failure. And as electrophysiologists and clinical cardiologists, we have to embrace this concept and understand it in depth,” Dr. Baranchuk, president-elect of the Inter-American Society of Cardiology, said in an interview.
The specialist first proposed atrial failure as an entity or syndrome in early 2020 in an article in the Journal of the American College of Cardiology. His four collaborators included the experienced Eugene Braunwald, MD, from Brigham and Women’s Hospital, Boston, and Antoni Bayés de Luna, PhD, from the department of medicine of the autonomous University of Barcelona.
Pathology despite function
“In many patients with heart failure, the pump function is preserved, but what causes the pathology? For the last 5-10 years, attention has been focused on the ventricle: whether it contracts poorly or whether it contracts properly and relaxes poorly. However, we have also seen patients in whom the ventricle contracts properly and relaxes properly. Where else can we look? We started looking at atrial contraction, especially the left atrium,” recalled Dr. Baranchuk.
He and his colleagues proposed the following consensus definition of atrial failure or insufficiency: any atrial dysfunction (anatomical, mechanical, electrical, and rheological, including blood homeostasis) that causes impaired function, heart symptoms, and a worsening of quality of life (or life expectancy) in the absence of significant valvular or ventricular abnormalities.
In his presentation, recorded and projected by video from Canada, Dr. Baranchuk pointed out that there are two large groups of causes of atrial failure: one that has to do with electrical disorders of atrial and interatrial contraction and another related to the progressive development of fibrosis, which gradually leads to dyssynchrony in interatrial contraction, pump failure, and impaired atrial function as a reservoir and as a conduit.
“In turn, these mechanisms trigger neurohormonal alterations that perpetuate atrial failure, so it is not just a matter of progressive fibrosis, which is very difficult to treat, but also of constant neurohormonal activation that guarantees that these phenomena never resolve,” said Dr. Baranchuk. The manifestations or end point of this cascade of events are the known ones: stroke, ischemia, and heart failure.
New entity necessary?
Defining atrial failure or insufficiency as a clinical entity not only restores the hierarchy of the atria in cardiac function, which was already postulated by William Harvey in 1628, but also enables new lines of research that would eventually allow timely preventive interventions.
One key is early recognition of partial or total interatrial block by analyzing the characteristics of the P wave on the electrocardiogram, which could serve to prevent progression to atrial fibrillation. Left atrial enlargement can also be detected by echocardiography.
“When the contractile impairment is severe and you are in atrial fibrillation, all that remains is to apply patches. The strategy is to correct risk factors beforehand, such as high blood pressure, sleep apnea, or high-dose alcohol consumption, as well as tirelessly searching for atrial fibrillation, with Holter electrocardiograms, continuous monitoring devices, such as Apple Watch, KardiaMobile, or an implantable loop recorder,” Dr. Baranchuk said in an interview.
Two ongoing or planned studies, ARCADIA and AMIABLE, will seek to determine whether anticoagulation in patients with elevated cardiovascular risk scores and any of these atrial disorders that have not yet led to atrial fibrillation could reduce the incidence of stroke.
The strategy has a rational basis. In a subanalysis of raw data from the NAVIGATE ESUS study in patients with embolic stroke of unknown cause, Dr. Baranchuk estimated that the presence of interatrial block was a tenfold higher predictor of the risk of experiencing a second stroke. Another 2018 observational study in which he participated found that in outpatients with heart failure, advanced interatrial block approximately tripled the risk of developing atrial fibrillation and ischemic stroke.
For Dr. Baranchuk, other questions that still need to be answered include whether drugs used for heart failure with preserved ejection fraction can be useful in primary atrial failure or whether specific drugs can be repositioned or developed to suppress or slow the process of fibrosis. “From generating the clinical concept, many lines of research are enabled.”
“The concept of atrial failure is very interesting and opens our eyes to treatments,” another speaker at the session, Alejo Tronconi, MD, a cardiologist and electrophysiologist at the Cardiovascular Institute of the South, Cipolletti, Argentina, said in an interview.
“It is necessary to cut circuits that have been extensively studied in heart failure models, and now we are beginning to see their participation in atrial dysfunction,” he said.
Dr. Baranchuk and Dr. Tronconi declared no relevant financial conflict of interest.
A version of this article first appeared on Medscape.com.
AAD unveils updated guidelines for topical AD treatment in adults
, and topical phosphodiesterase-4 (PDE-4) and Janus kinase (JAK) inhibitors. The guidelines also conditionally recommend the use of bathing and wet wrap therapy but recommend against the use of topical antimicrobials, antiseptics, and antihistamines.
The development updates the AAD’s 2014 recommendations for managing AD with topical therapies, published almost 9 years ago. “At that time, the only U.S. FDA–approved systemic medication for atopic dermatitis was prednisone – universally felt amongst dermatologists to be the least appropriate systemic medication for this condition, at least chronically,” Robert Sidbury, MD, MPH, who cochaired a 14-member multidisciplinary work group that assembled the updated guidelines, told this news organization in an interview.
“Since 2017, there have been two different biologic medications approved for moderate to severe AD (dupilumab and tralokinumab) with certainly a third or more right around the corner. There have been two new oral agents approved for moderate to severe AD – upadacitinib and abrocitinib – with others on the way,” he noted. While these are not topical therapies, the purview of the newly released guidelines, he said, “there have also been new topical medications approved since that time (crisaborole and ruxolitinib). It was high time for an update.”
For the new guidelines, which were published online in the Journal of the American Academy of Dermatology, Dr. Sidbury, chief of the division of dermatology at Seattle Children’s Hospital, guidelines cochair Dawn M. R. Davis, MD, a dermatologist at Mayo Clinic, Rochester, Minn., and colleagues conducted a systematic review of evidence regarding the use of nonprescription topical agents such as moisturizers, bathing practices, and wet wraps, as well as topical pharmacologic modalities such as corticosteroids, calcineurin inhibitors, JAK inhibitors, PDE-4 inhibitors, antimicrobials, and antihistamines.
Next, the work group applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach for assessing the certainty of the evidence and formulating and grading clinical recommendations based on relevant randomized trials in the medical literature.
12 recommendations
Of the 12 recommendations made for adults with AD, the work group ranked 7 as “strong” based on the evidence reviewed, and the rest as “conditional.” The “strong” recommendations include the use of moisturizers; the use of tacrolimus 0.03% or 0.1%; the use of pimecrolimus 1% cream for mild to moderate AD; use of topical steroids; intermittent use of medium-potency topical corticosteroids as maintenance therapy to reduce flares and relapse; the use of the topical PDE-4 inhibitor crisaborole, and the use of the topical JAK inhibitor ruxolitinib.
Regarding ruxolitinib cream 1.5%, the work group advised that the treatment area “should not exceed 20% body surface area, and a maximum of 60 grams should be applied per week; these stipulations are aimed at reducing systemic absorption, as black box warnings include serious infections, mortality, malignancies (for example, lymphoma), major adverse cardiovascular events, and thrombosis.”
Conditional recommendations in the guidelines include those for bathing for treatment and maintenance and the use of wet dressings, and those against the use of topical antimicrobials, topical antihistamines, and topical antiseptics.
According to Dr. Sidbury, the topic of bathing generated robust discussion among the work group members. “Though [each group member] has strong opinions and individual practice styles, they were also able to recognize that the evidence is all that matters in a project like this, which led to a ‘conditional’ recommendation regarding bathing frequency backed by ‘low’ evidence,” he said. “While this may seem like ‘guidance’ that doesn’t ‘guide,’ I would argue it informs the guideline consumer exactly where we are in terms of this question and allows them to use their best judgment and experience as their true north here.”
In the realm of topical steroids, Dr. Sidbury said that topical steroid addiction (TSA) and topical steroid withdrawal (TSW) have been a “controversial but persistent concern” from some patients and providers. “Two systematic reviews of this topic were mentioned, and it was made clear that the evidence base [for the concepts] is weak,” he said. “With that important caveat ,the guideline committee delineated both a definition of TSW/TSA and potential risk factors.”
Dr. Sidbury marveled at the potential impact of newer medicines such as crisaborole and ruxolitinib on younger AD patients as well. Crisaborole is now Food and Drug Administration approved down to 3 months of age for mild to moderate AD. “This is extraordinary and expands treatment options for all providers at an age when parents and providers are most conservative in their practice,” he said. “Ruxolitinib, also nonsteroidal, is FDA approved for mild to moderate AD down to 12 years of age. Having spent a good percentage of my practice years either being able to offer only topical steroids, or later topical steroids and topical calcineurin inhibitors like tacrolimus or pimecrolimus, having additional options is wonderful.”
In the guidelines, the work group noted that “significant gaps remain” in current understanding of various topical AD therapies. “Studies are needed which examine quality of life and other patient-important outcomes, changes to the cutaneous microbiome, as well as long term follow-up, and use in special and diverse populations (e.g., pregnancy, lactation, immunosuppression, multiple comorbidities, skin of color, pediatric),” they wrote. “Furthermore, increased use of new systemic AD treatment options (dupilumab, tralokinumab, abrocitinib, upadacitinib) in patients with moderate to severe disease may result in a selection bias toward milder disease in current and future AD topical therapy studies.”
Use of topical therapies to manage AD in pediatric patients will be covered in a forthcoming AAD guideline. The first updated AD guideline, on comorbidities associated with AD in adults, was released in January 2022.
Dr. Sidbury reported that he serves as an advisory board member for Pfizer, a principal investigator for Regeneron, an investigator for Brickell Biotech and Galderma USA, and a consultant for Galderma Global and Microes. Other work group members reported having financial disclosures with many pharmaceutical companies.
, and topical phosphodiesterase-4 (PDE-4) and Janus kinase (JAK) inhibitors. The guidelines also conditionally recommend the use of bathing and wet wrap therapy but recommend against the use of topical antimicrobials, antiseptics, and antihistamines.
The development updates the AAD’s 2014 recommendations for managing AD with topical therapies, published almost 9 years ago. “At that time, the only U.S. FDA–approved systemic medication for atopic dermatitis was prednisone – universally felt amongst dermatologists to be the least appropriate systemic medication for this condition, at least chronically,” Robert Sidbury, MD, MPH, who cochaired a 14-member multidisciplinary work group that assembled the updated guidelines, told this news organization in an interview.
“Since 2017, there have been two different biologic medications approved for moderate to severe AD (dupilumab and tralokinumab) with certainly a third or more right around the corner. There have been two new oral agents approved for moderate to severe AD – upadacitinib and abrocitinib – with others on the way,” he noted. While these are not topical therapies, the purview of the newly released guidelines, he said, “there have also been new topical medications approved since that time (crisaborole and ruxolitinib). It was high time for an update.”
For the new guidelines, which were published online in the Journal of the American Academy of Dermatology, Dr. Sidbury, chief of the division of dermatology at Seattle Children’s Hospital, guidelines cochair Dawn M. R. Davis, MD, a dermatologist at Mayo Clinic, Rochester, Minn., and colleagues conducted a systematic review of evidence regarding the use of nonprescription topical agents such as moisturizers, bathing practices, and wet wraps, as well as topical pharmacologic modalities such as corticosteroids, calcineurin inhibitors, JAK inhibitors, PDE-4 inhibitors, antimicrobials, and antihistamines.
Next, the work group applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach for assessing the certainty of the evidence and formulating and grading clinical recommendations based on relevant randomized trials in the medical literature.
12 recommendations
Of the 12 recommendations made for adults with AD, the work group ranked 7 as “strong” based on the evidence reviewed, and the rest as “conditional.” The “strong” recommendations include the use of moisturizers; the use of tacrolimus 0.03% or 0.1%; the use of pimecrolimus 1% cream for mild to moderate AD; use of topical steroids; intermittent use of medium-potency topical corticosteroids as maintenance therapy to reduce flares and relapse; the use of the topical PDE-4 inhibitor crisaborole, and the use of the topical JAK inhibitor ruxolitinib.
Regarding ruxolitinib cream 1.5%, the work group advised that the treatment area “should not exceed 20% body surface area, and a maximum of 60 grams should be applied per week; these stipulations are aimed at reducing systemic absorption, as black box warnings include serious infections, mortality, malignancies (for example, lymphoma), major adverse cardiovascular events, and thrombosis.”
Conditional recommendations in the guidelines include those for bathing for treatment and maintenance and the use of wet dressings, and those against the use of topical antimicrobials, topical antihistamines, and topical antiseptics.
According to Dr. Sidbury, the topic of bathing generated robust discussion among the work group members. “Though [each group member] has strong opinions and individual practice styles, they were also able to recognize that the evidence is all that matters in a project like this, which led to a ‘conditional’ recommendation regarding bathing frequency backed by ‘low’ evidence,” he said. “While this may seem like ‘guidance’ that doesn’t ‘guide,’ I would argue it informs the guideline consumer exactly where we are in terms of this question and allows them to use their best judgment and experience as their true north here.”
In the realm of topical steroids, Dr. Sidbury said that topical steroid addiction (TSA) and topical steroid withdrawal (TSW) have been a “controversial but persistent concern” from some patients and providers. “Two systematic reviews of this topic were mentioned, and it was made clear that the evidence base [for the concepts] is weak,” he said. “With that important caveat ,the guideline committee delineated both a definition of TSW/TSA and potential risk factors.”
Dr. Sidbury marveled at the potential impact of newer medicines such as crisaborole and ruxolitinib on younger AD patients as well. Crisaborole is now Food and Drug Administration approved down to 3 months of age for mild to moderate AD. “This is extraordinary and expands treatment options for all providers at an age when parents and providers are most conservative in their practice,” he said. “Ruxolitinib, also nonsteroidal, is FDA approved for mild to moderate AD down to 12 years of age. Having spent a good percentage of my practice years either being able to offer only topical steroids, or later topical steroids and topical calcineurin inhibitors like tacrolimus or pimecrolimus, having additional options is wonderful.”
In the guidelines, the work group noted that “significant gaps remain” in current understanding of various topical AD therapies. “Studies are needed which examine quality of life and other patient-important outcomes, changes to the cutaneous microbiome, as well as long term follow-up, and use in special and diverse populations (e.g., pregnancy, lactation, immunosuppression, multiple comorbidities, skin of color, pediatric),” they wrote. “Furthermore, increased use of new systemic AD treatment options (dupilumab, tralokinumab, abrocitinib, upadacitinib) in patients with moderate to severe disease may result in a selection bias toward milder disease in current and future AD topical therapy studies.”
Use of topical therapies to manage AD in pediatric patients will be covered in a forthcoming AAD guideline. The first updated AD guideline, on comorbidities associated with AD in adults, was released in January 2022.
Dr. Sidbury reported that he serves as an advisory board member for Pfizer, a principal investigator for Regeneron, an investigator for Brickell Biotech and Galderma USA, and a consultant for Galderma Global and Microes. Other work group members reported having financial disclosures with many pharmaceutical companies.
, and topical phosphodiesterase-4 (PDE-4) and Janus kinase (JAK) inhibitors. The guidelines also conditionally recommend the use of bathing and wet wrap therapy but recommend against the use of topical antimicrobials, antiseptics, and antihistamines.
The development updates the AAD’s 2014 recommendations for managing AD with topical therapies, published almost 9 years ago. “At that time, the only U.S. FDA–approved systemic medication for atopic dermatitis was prednisone – universally felt amongst dermatologists to be the least appropriate systemic medication for this condition, at least chronically,” Robert Sidbury, MD, MPH, who cochaired a 14-member multidisciplinary work group that assembled the updated guidelines, told this news organization in an interview.
“Since 2017, there have been two different biologic medications approved for moderate to severe AD (dupilumab and tralokinumab) with certainly a third or more right around the corner. There have been two new oral agents approved for moderate to severe AD – upadacitinib and abrocitinib – with others on the way,” he noted. While these are not topical therapies, the purview of the newly released guidelines, he said, “there have also been new topical medications approved since that time (crisaborole and ruxolitinib). It was high time for an update.”
For the new guidelines, which were published online in the Journal of the American Academy of Dermatology, Dr. Sidbury, chief of the division of dermatology at Seattle Children’s Hospital, guidelines cochair Dawn M. R. Davis, MD, a dermatologist at Mayo Clinic, Rochester, Minn., and colleagues conducted a systematic review of evidence regarding the use of nonprescription topical agents such as moisturizers, bathing practices, and wet wraps, as well as topical pharmacologic modalities such as corticosteroids, calcineurin inhibitors, JAK inhibitors, PDE-4 inhibitors, antimicrobials, and antihistamines.
Next, the work group applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach for assessing the certainty of the evidence and formulating and grading clinical recommendations based on relevant randomized trials in the medical literature.
12 recommendations
Of the 12 recommendations made for adults with AD, the work group ranked 7 as “strong” based on the evidence reviewed, and the rest as “conditional.” The “strong” recommendations include the use of moisturizers; the use of tacrolimus 0.03% or 0.1%; the use of pimecrolimus 1% cream for mild to moderate AD; use of topical steroids; intermittent use of medium-potency topical corticosteroids as maintenance therapy to reduce flares and relapse; the use of the topical PDE-4 inhibitor crisaborole, and the use of the topical JAK inhibitor ruxolitinib.
Regarding ruxolitinib cream 1.5%, the work group advised that the treatment area “should not exceed 20% body surface area, and a maximum of 60 grams should be applied per week; these stipulations are aimed at reducing systemic absorption, as black box warnings include serious infections, mortality, malignancies (for example, lymphoma), major adverse cardiovascular events, and thrombosis.”
Conditional recommendations in the guidelines include those for bathing for treatment and maintenance and the use of wet dressings, and those against the use of topical antimicrobials, topical antihistamines, and topical antiseptics.
According to Dr. Sidbury, the topic of bathing generated robust discussion among the work group members. “Though [each group member] has strong opinions and individual practice styles, they were also able to recognize that the evidence is all that matters in a project like this, which led to a ‘conditional’ recommendation regarding bathing frequency backed by ‘low’ evidence,” he said. “While this may seem like ‘guidance’ that doesn’t ‘guide,’ I would argue it informs the guideline consumer exactly where we are in terms of this question and allows them to use their best judgment and experience as their true north here.”
In the realm of topical steroids, Dr. Sidbury said that topical steroid addiction (TSA) and topical steroid withdrawal (TSW) have been a “controversial but persistent concern” from some patients and providers. “Two systematic reviews of this topic were mentioned, and it was made clear that the evidence base [for the concepts] is weak,” he said. “With that important caveat ,the guideline committee delineated both a definition of TSW/TSA and potential risk factors.”
Dr. Sidbury marveled at the potential impact of newer medicines such as crisaborole and ruxolitinib on younger AD patients as well. Crisaborole is now Food and Drug Administration approved down to 3 months of age for mild to moderate AD. “This is extraordinary and expands treatment options for all providers at an age when parents and providers are most conservative in their practice,” he said. “Ruxolitinib, also nonsteroidal, is FDA approved for mild to moderate AD down to 12 years of age. Having spent a good percentage of my practice years either being able to offer only topical steroids, or later topical steroids and topical calcineurin inhibitors like tacrolimus or pimecrolimus, having additional options is wonderful.”
In the guidelines, the work group noted that “significant gaps remain” in current understanding of various topical AD therapies. “Studies are needed which examine quality of life and other patient-important outcomes, changes to the cutaneous microbiome, as well as long term follow-up, and use in special and diverse populations (e.g., pregnancy, lactation, immunosuppression, multiple comorbidities, skin of color, pediatric),” they wrote. “Furthermore, increased use of new systemic AD treatment options (dupilumab, tralokinumab, abrocitinib, upadacitinib) in patients with moderate to severe disease may result in a selection bias toward milder disease in current and future AD topical therapy studies.”
Use of topical therapies to manage AD in pediatric patients will be covered in a forthcoming AAD guideline. The first updated AD guideline, on comorbidities associated with AD in adults, was released in January 2022.
Dr. Sidbury reported that he serves as an advisory board member for Pfizer, a principal investigator for Regeneron, an investigator for Brickell Biotech and Galderma USA, and a consultant for Galderma Global and Microes. Other work group members reported having financial disclosures with many pharmaceutical companies.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY

