User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


No rise in major hemorrhagic events with antiplatelet therapy after ICH
Background: Antiplatelet agents reduce the risk of major vascular events in patient with established vaso-occlusive disease, but they may increase the risk of ICH. Patients with prior ICH are at risk for both vaso-occlusive and hemorrhagic events. Clarification of the relative risk and benefit of antiplatelet agent use in this clinical scenario would serve to guide therapy.
Study design: Prospective, open-label, randomized parallel group trial.
Setting: 122 hospitals located in the United Kingdom.
Synopsis: The study included 537 adult patients with imaging-confirmed, nontraumatic intracerebral hemorrhage who were previously prescribed antithrombotic medications were randomized in 1:1 fashion to either start or avoid antiplatelet therapy. Participants were followed up on an annual basis with postal questionnaires both to the participants and their primary care providers. No significant difference was identified in rates of recurrent ICH (adjusted hazard ratio, 0.51; 95% confidence interval, 0.25-1.03), major hemorrhagic events (aHR, 0.71; 95% CI, 0.39-1.30), or major occlusive vascular events (aHR, 1.02; 95% CI, 0.65-1.60) between groups.
Hospitalists should be aware that these data suggest that the risk assessment for resumption of antiplatelet agents should not be affected by a history of nontraumatic intracerebral hemorrhage when weighed against the benefit of these medications in patients with occlusive vascular disease.
Bottom line: Resumption of antiplatelet agents following intracerebral hemorrhage showed no evidence of increased risk of recurrent intracerebral hemorrhage or major hemorrhagic events.
Citation: RESTART Collaboration. Effects of antiplatelet therapy after stroke due to intracerebral haemorrhage (RESTART): A randomized, open-label trial. Lancet. 2019. doi: 10.1016/S0140-6736(19)30840-2.
Dr. Deitelzweig is system department chair of hospital medicine at Ochsner Health System, New Orleans.
Background: Antiplatelet agents reduce the risk of major vascular events in patient with established vaso-occlusive disease, but they may increase the risk of ICH. Patients with prior ICH are at risk for both vaso-occlusive and hemorrhagic events. Clarification of the relative risk and benefit of antiplatelet agent use in this clinical scenario would serve to guide therapy.
Study design: Prospective, open-label, randomized parallel group trial.
Setting: 122 hospitals located in the United Kingdom.
Synopsis: The study included 537 adult patients with imaging-confirmed, nontraumatic intracerebral hemorrhage who were previously prescribed antithrombotic medications were randomized in 1:1 fashion to either start or avoid antiplatelet therapy. Participants were followed up on an annual basis with postal questionnaires both to the participants and their primary care providers. No significant difference was identified in rates of recurrent ICH (adjusted hazard ratio, 0.51; 95% confidence interval, 0.25-1.03), major hemorrhagic events (aHR, 0.71; 95% CI, 0.39-1.30), or major occlusive vascular events (aHR, 1.02; 95% CI, 0.65-1.60) between groups.
Hospitalists should be aware that these data suggest that the risk assessment for resumption of antiplatelet agents should not be affected by a history of nontraumatic intracerebral hemorrhage when weighed against the benefit of these medications in patients with occlusive vascular disease.
Bottom line: Resumption of antiplatelet agents following intracerebral hemorrhage showed no evidence of increased risk of recurrent intracerebral hemorrhage or major hemorrhagic events.
Citation: RESTART Collaboration. Effects of antiplatelet therapy after stroke due to intracerebral haemorrhage (RESTART): A randomized, open-label trial. Lancet. 2019. doi: 10.1016/S0140-6736(19)30840-2.
Dr. Deitelzweig is system department chair of hospital medicine at Ochsner Health System, New Orleans.
Background: Antiplatelet agents reduce the risk of major vascular events in patient with established vaso-occlusive disease, but they may increase the risk of ICH. Patients with prior ICH are at risk for both vaso-occlusive and hemorrhagic events. Clarification of the relative risk and benefit of antiplatelet agent use in this clinical scenario would serve to guide therapy.
Study design: Prospective, open-label, randomized parallel group trial.
Setting: 122 hospitals located in the United Kingdom.
Synopsis: The study included 537 adult patients with imaging-confirmed, nontraumatic intracerebral hemorrhage who were previously prescribed antithrombotic medications were randomized in 1:1 fashion to either start or avoid antiplatelet therapy. Participants were followed up on an annual basis with postal questionnaires both to the participants and their primary care providers. No significant difference was identified in rates of recurrent ICH (adjusted hazard ratio, 0.51; 95% confidence interval, 0.25-1.03), major hemorrhagic events (aHR, 0.71; 95% CI, 0.39-1.30), or major occlusive vascular events (aHR, 1.02; 95% CI, 0.65-1.60) between groups.
Hospitalists should be aware that these data suggest that the risk assessment for resumption of antiplatelet agents should not be affected by a history of nontraumatic intracerebral hemorrhage when weighed against the benefit of these medications in patients with occlusive vascular disease.
Bottom line: Resumption of antiplatelet agents following intracerebral hemorrhage showed no evidence of increased risk of recurrent intracerebral hemorrhage or major hemorrhagic events.
Citation: RESTART Collaboration. Effects of antiplatelet therapy after stroke due to intracerebral haemorrhage (RESTART): A randomized, open-label trial. Lancet. 2019. doi: 10.1016/S0140-6736(19)30840-2.
Dr. Deitelzweig is system department chair of hospital medicine at Ochsner Health System, New Orleans.
Infection ups mortality risk in patients with dementia
Infection increases mortality risk among patients with dementia, new research suggests. A large, registry-based cohort study showed that
“This is the first study to our knowledge to show that increased mortality is observed across all infection types in people with dementia and that increased mortality is seen both short and long term,” said coinvestigator Janet Janbek, a PhD student at the Danish Dementia Research Center, Rigshospitalet, University of Copenhagen.
The findings were presented at the virtual annual meeting of the Alzheimer’s Association International Conference.
Large Danish cohort
The investigators analyzed data from Danish national health registries for nearly 1.5 million individuals aged 65 years and older who had visited the hospital with an infection. There were 575,260 deaths during more than 12.7 million person-years of follow-up.
Patients with dementia who also had a hospital visit for infection died at a 6.5 times higher rate than participants without dementia or an infection. Those with either dementia alone or infection-related contacts alone had a threefold increased rate of death.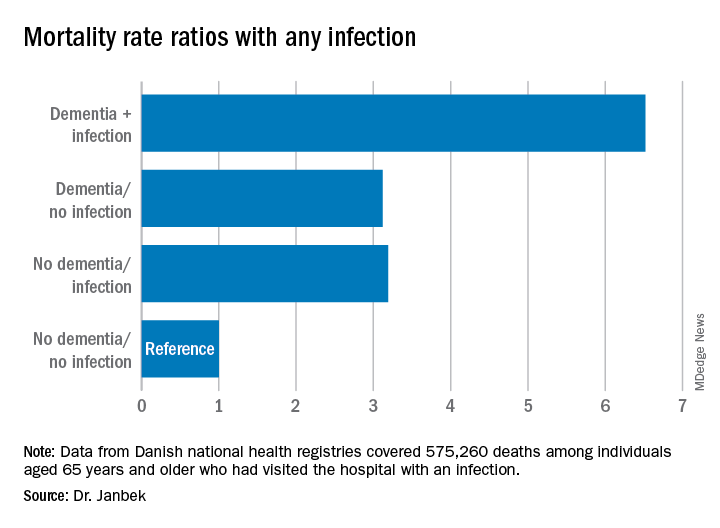
The mortality rate was highest within the first 30 days following the hospital visit for infection. However, the rate remained elevated for 10 years after the initial infection-related hospital visit.
Mortality rates from all infections, including major infections, such as sepsis, down to minor ear infections were elevated in patients with dementia, compared with people who did not have dementia or an infection-related hospital visit.
Ms. Janbek said there are several possible explanations for the association of infection and increased mortality risk in those with dementia. “After a hospital contact with a severe infection, people with dementia may become more reliant on external care, become more frail, and have declined functional levels, which might explain the observed association.”
It might also be that patients with dementia have more severe infections than those without dementia at the time of hospital contact, possibly because of delayed diagnosis, which could explain the higher mortality rates, said Ms. Janbek.
“It is also plausible that infections play a role in worsening dementia and subsequently lead to increased mortality,” she noted.
“Clinicians and health care personnel need to pay closer attention to infections of all types in people with dementia, and steps toward better clinical management and improved posthospital care need to be explored and undertaken. We need to identify possible preventive measures and targeted interventions in people with dementia and infections,” Ms. Janbek said.
‘Interesting observation’
Commenting on the study, Rebecca M. Edelmayer, PhD, director of scientific engagement for the Alzheimer’s Association, said it presents “an interesting observation.” However, “we can’t make any direct assumptions from this research per se about infections and dementia and whether they are causative in any way,” noted Dr. Edelmayer, who was not involved with the study.
Instead, the study highlighted the importance of “taking care of our overall health and making sure that individuals that might be vulnerable to infection, like those who are already living with dementia, are getting the best care possible,” she said.
Ms. Janbek and Dr. Edelmayer have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Infection increases mortality risk among patients with dementia, new research suggests. A large, registry-based cohort study showed that
“This is the first study to our knowledge to show that increased mortality is observed across all infection types in people with dementia and that increased mortality is seen both short and long term,” said coinvestigator Janet Janbek, a PhD student at the Danish Dementia Research Center, Rigshospitalet, University of Copenhagen.
The findings were presented at the virtual annual meeting of the Alzheimer’s Association International Conference.
Large Danish cohort
The investigators analyzed data from Danish national health registries for nearly 1.5 million individuals aged 65 years and older who had visited the hospital with an infection. There were 575,260 deaths during more than 12.7 million person-years of follow-up.
Patients with dementia who also had a hospital visit for infection died at a 6.5 times higher rate than participants without dementia or an infection. Those with either dementia alone or infection-related contacts alone had a threefold increased rate of death.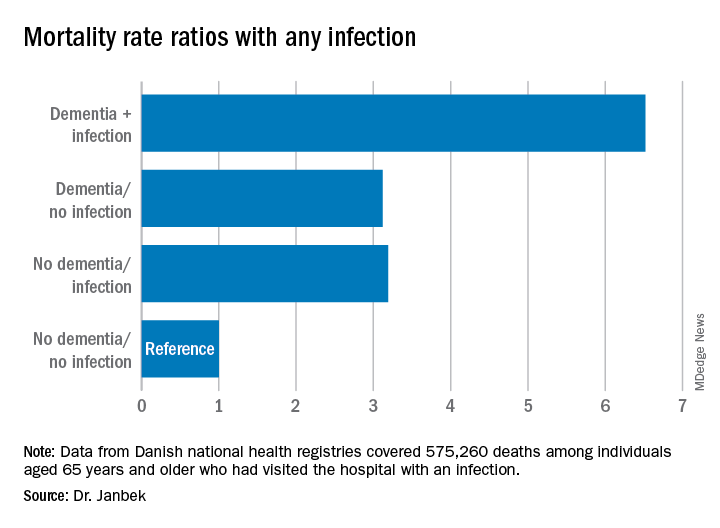
The mortality rate was highest within the first 30 days following the hospital visit for infection. However, the rate remained elevated for 10 years after the initial infection-related hospital visit.
Mortality rates from all infections, including major infections, such as sepsis, down to minor ear infections were elevated in patients with dementia, compared with people who did not have dementia or an infection-related hospital visit.
Ms. Janbek said there are several possible explanations for the association of infection and increased mortality risk in those with dementia. “After a hospital contact with a severe infection, people with dementia may become more reliant on external care, become more frail, and have declined functional levels, which might explain the observed association.”
It might also be that patients with dementia have more severe infections than those without dementia at the time of hospital contact, possibly because of delayed diagnosis, which could explain the higher mortality rates, said Ms. Janbek.
“It is also plausible that infections play a role in worsening dementia and subsequently lead to increased mortality,” she noted.
“Clinicians and health care personnel need to pay closer attention to infections of all types in people with dementia, and steps toward better clinical management and improved posthospital care need to be explored and undertaken. We need to identify possible preventive measures and targeted interventions in people with dementia and infections,” Ms. Janbek said.
‘Interesting observation’
Commenting on the study, Rebecca M. Edelmayer, PhD, director of scientific engagement for the Alzheimer’s Association, said it presents “an interesting observation.” However, “we can’t make any direct assumptions from this research per se about infections and dementia and whether they are causative in any way,” noted Dr. Edelmayer, who was not involved with the study.
Instead, the study highlighted the importance of “taking care of our overall health and making sure that individuals that might be vulnerable to infection, like those who are already living with dementia, are getting the best care possible,” she said.
Ms. Janbek and Dr. Edelmayer have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Infection increases mortality risk among patients with dementia, new research suggests. A large, registry-based cohort study showed that
“This is the first study to our knowledge to show that increased mortality is observed across all infection types in people with dementia and that increased mortality is seen both short and long term,” said coinvestigator Janet Janbek, a PhD student at the Danish Dementia Research Center, Rigshospitalet, University of Copenhagen.
The findings were presented at the virtual annual meeting of the Alzheimer’s Association International Conference.
Large Danish cohort
The investigators analyzed data from Danish national health registries for nearly 1.5 million individuals aged 65 years and older who had visited the hospital with an infection. There were 575,260 deaths during more than 12.7 million person-years of follow-up.
Patients with dementia who also had a hospital visit for infection died at a 6.5 times higher rate than participants without dementia or an infection. Those with either dementia alone or infection-related contacts alone had a threefold increased rate of death.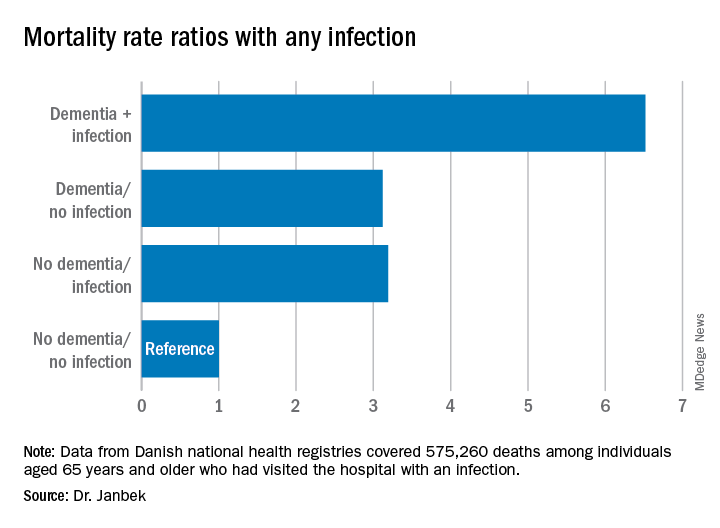
The mortality rate was highest within the first 30 days following the hospital visit for infection. However, the rate remained elevated for 10 years after the initial infection-related hospital visit.
Mortality rates from all infections, including major infections, such as sepsis, down to minor ear infections were elevated in patients with dementia, compared with people who did not have dementia or an infection-related hospital visit.
Ms. Janbek said there are several possible explanations for the association of infection and increased mortality risk in those with dementia. “After a hospital contact with a severe infection, people with dementia may become more reliant on external care, become more frail, and have declined functional levels, which might explain the observed association.”
It might also be that patients with dementia have more severe infections than those without dementia at the time of hospital contact, possibly because of delayed diagnosis, which could explain the higher mortality rates, said Ms. Janbek.
“It is also plausible that infections play a role in worsening dementia and subsequently lead to increased mortality,” she noted.
“Clinicians and health care personnel need to pay closer attention to infections of all types in people with dementia, and steps toward better clinical management and improved posthospital care need to be explored and undertaken. We need to identify possible preventive measures and targeted interventions in people with dementia and infections,” Ms. Janbek said.
‘Interesting observation’
Commenting on the study, Rebecca M. Edelmayer, PhD, director of scientific engagement for the Alzheimer’s Association, said it presents “an interesting observation.” However, “we can’t make any direct assumptions from this research per se about infections and dementia and whether they are causative in any way,” noted Dr. Edelmayer, who was not involved with the study.
Instead, the study highlighted the importance of “taking care of our overall health and making sure that individuals that might be vulnerable to infection, like those who are already living with dementia, are getting the best care possible,” she said.
Ms. Janbek and Dr. Edelmayer have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM AAIC 2020
Early palliative care fails to improve QOL in advanced heart failure
A new palliative care intervention for U.S. patients with advanced heart failure did not improve quality of life or mood after 16 weeks of participation in a randomized trial.
“Future analyses and studies will examine both the patient factors and intervention components to find the right palliative care dose, for the right patient, at the right time,” wrote Marie A. Bakitas, DNSc, of the University of Alabama at Birmingham, and coauthors. The study was published in JAMA Internal Medicine.
“My first reaction is disappointment,” Larry Allen, MD, of the University of Colorado in Denver, said in an interview. “We had hoped to see the ENABLE program, which had been successful in cancer, translate to the heart failure setting.”
Improvement of palliative care in heart failure patients might rest on who needs it most
“One thing to note,” Dr. Allen added in an interview, “is that, in this population of patients, some of the measures they were trying to improve were already relatively mild to start with. It may not be that the intervention didn’t help but that they picked a patient population that wasn’t particularly in need. If you treat someone who doesn’t have a problem, it’s hard to make them better.”
In a separate interview, Dr. Bakitas acknowledged a similar sentiment. “We were a little surprised until we looked at our sample,” she said. “We realized that we had recruited all these very high-functioning, good quality-of-life patients. What we then did was look at a subsample of patients who had low quality of life at baseline. Low and behold, the intervention had an effect. The patients who started with a poor quality of life had a statistically and clinically significant benefit. Their KCCQ score increased by over 5 points.”
As for next steps. Dr. Bakitas noted that they’re twofold: “One is refining the patient population who can benefit, and the second is working on the intervention and figuring out which pieces are the ones that provide the most benefit.
“Because of logistics and practical issues, not everyone in the study got all the intervention that they should have. Think of it like a drug trial; if someone misses a pill, they don’t get the full dose that we thought would work. We need to make sure our interventions have the right pieces in place. We don’t want to develop a great intervention that’s not practical for patients.”
Study design and outcomes
To determine the benefits of early palliative care for patients with heart failure, the researchers developed the ENABLE CHF-PC (Educate, Nurture, Advise, Before Life Ends Comprehensive Heartcare for Patients and Caregivers) intervention. This nurse-led program includes an in-person consultant followed by six telehealth nurse coaching sessions lasting 30-40 minutes and then monthly follow-up calls through either 48 weeks or the patient’s death.
To test the effectiveness of their intervention after 16 weeks, the researchers launched a two-site, single-blind randomized clinical trial made up of 415 patients who were 50 years or older with advanced heart failure. Among the patients, 53% were men and the mean age was 64 years; 55% were African American, 26% lived in a rural area, and 46% had a high school education or less. The average length of time since heart failure diagnosis was 5.1 years.
Patients were randomized evenly to receive either the ENABLE CHF-PC intervention (208) or usual care. The primary outcomes were quality of life (QOL), which was measured by the heart failure–specific 23-item Kansas City Cardiomyopathy Questionnaire (KCCQ) and the 14-item Functional Assessment of Chronic Illness Therapy–Palliative-14 (FACIT Pal-14), and mood, which was measured by the 14-item Hospital Anxiety and Depression Scale (HADS). Pain was measured via 3-item pain intensity and 2-item pain interference scales.
Effect size was measured as Cohen d or d-equivalent, where a small effect is 0.2, medium is 0.5, and large is about 0.854.
At baseline, the mean KCCQ score of 52.6 at baseline indicated a “fairly good” QOL across all patients. After 16 weeks, the mean KCCQ score improved 3.9 points in the intervention group, compared with 2.3 points in the usual care group (d = 0.07; [95% confidence interval, –0.09-0.24]). In addition, the mean FACIT-Pal-14 score improved 1.4 points in the intervention group compared to 0.2 points in the usual care group (d = 0.12 [95% CI, –0.03-0.28]). Only small differences were observed between groups regarding anxiety and depression, but pain intensity (difference, –2.8; SE, 0.9; d = –0.26 [95% CI, –0.43-0.09]) and pain interference (difference, –2.3; SE, 1; d = –0.21 [95% CI, –0.40 to –0.02]) demonstrated a statistically significant and clinically important decrease.
As heart failure care evolves, so must palliative care
Though the study and intervention developed by Dr. Bakitas and colleagues is commendable, it is only somewhat surprising that it did not drastically improve patients’ quality of life, Nathan E. Goldstein, MD, of the Icahn School of Medicine at Mount Sinai in New York, wrote in an accompanying editorial.
He noted several reasons for the lack of improvement, including a large proportion of patients still being in the early stages of the disease. Ultimately, however, he wonders if innovation in heart failure care ultimately impacted the study while it was occurring. Medications and technological advancements evolve rapidly in this field, he said, especially over the course of a 3-year study period.
To continue this work and produce real benefits in patients with advanced heart failure, Dr. Goldstein emphasized the need for “dynamic palliative care interventions that can adapt to the constantly changing landscape of the patient’s needs caused by the underlying nature of the disease, as well as the innovations in the field of cardiology.”
The authors acknowledged their study’s limitations, including data attrition at 16 weeks that was higher than expected – a turn of events they attributed to “unique socioeconomic factors … and lack of regular health care appointments” among some participants. In addition, a minority of patients were unable to stick to the study protocol, which has led the researchers to begin investigating video alternatives to in-person consultation.
The study was supported by the National Institutes of Health/National Institutes of Nursing Research. Four of the authors reported received grants from the National Institutes of Nursing Research outside the submitted work or during the study. Dr. Goldstein reported no conflicts of interest.
SOURCE: Bakitas MA et al. JAMA Intern Med. 2020 July 27. doi: 10.1001/jamainternmed.2020.2861.
A new palliative care intervention for U.S. patients with advanced heart failure did not improve quality of life or mood after 16 weeks of participation in a randomized trial.
“Future analyses and studies will examine both the patient factors and intervention components to find the right palliative care dose, for the right patient, at the right time,” wrote Marie A. Bakitas, DNSc, of the University of Alabama at Birmingham, and coauthors. The study was published in JAMA Internal Medicine.
“My first reaction is disappointment,” Larry Allen, MD, of the University of Colorado in Denver, said in an interview. “We had hoped to see the ENABLE program, which had been successful in cancer, translate to the heart failure setting.”
Improvement of palliative care in heart failure patients might rest on who needs it most
“One thing to note,” Dr. Allen added in an interview, “is that, in this population of patients, some of the measures they were trying to improve were already relatively mild to start with. It may not be that the intervention didn’t help but that they picked a patient population that wasn’t particularly in need. If you treat someone who doesn’t have a problem, it’s hard to make them better.”
In a separate interview, Dr. Bakitas acknowledged a similar sentiment. “We were a little surprised until we looked at our sample,” she said. “We realized that we had recruited all these very high-functioning, good quality-of-life patients. What we then did was look at a subsample of patients who had low quality of life at baseline. Low and behold, the intervention had an effect. The patients who started with a poor quality of life had a statistically and clinically significant benefit. Their KCCQ score increased by over 5 points.”
As for next steps. Dr. Bakitas noted that they’re twofold: “One is refining the patient population who can benefit, and the second is working on the intervention and figuring out which pieces are the ones that provide the most benefit.
“Because of logistics and practical issues, not everyone in the study got all the intervention that they should have. Think of it like a drug trial; if someone misses a pill, they don’t get the full dose that we thought would work. We need to make sure our interventions have the right pieces in place. We don’t want to develop a great intervention that’s not practical for patients.”
Study design and outcomes
To determine the benefits of early palliative care for patients with heart failure, the researchers developed the ENABLE CHF-PC (Educate, Nurture, Advise, Before Life Ends Comprehensive Heartcare for Patients and Caregivers) intervention. This nurse-led program includes an in-person consultant followed by six telehealth nurse coaching sessions lasting 30-40 minutes and then monthly follow-up calls through either 48 weeks or the patient’s death.
To test the effectiveness of their intervention after 16 weeks, the researchers launched a two-site, single-blind randomized clinical trial made up of 415 patients who were 50 years or older with advanced heart failure. Among the patients, 53% were men and the mean age was 64 years; 55% were African American, 26% lived in a rural area, and 46% had a high school education or less. The average length of time since heart failure diagnosis was 5.1 years.
Patients were randomized evenly to receive either the ENABLE CHF-PC intervention (208) or usual care. The primary outcomes were quality of life (QOL), which was measured by the heart failure–specific 23-item Kansas City Cardiomyopathy Questionnaire (KCCQ) and the 14-item Functional Assessment of Chronic Illness Therapy–Palliative-14 (FACIT Pal-14), and mood, which was measured by the 14-item Hospital Anxiety and Depression Scale (HADS). Pain was measured via 3-item pain intensity and 2-item pain interference scales.
Effect size was measured as Cohen d or d-equivalent, where a small effect is 0.2, medium is 0.5, and large is about 0.854.
At baseline, the mean KCCQ score of 52.6 at baseline indicated a “fairly good” QOL across all patients. After 16 weeks, the mean KCCQ score improved 3.9 points in the intervention group, compared with 2.3 points in the usual care group (d = 0.07; [95% confidence interval, –0.09-0.24]). In addition, the mean FACIT-Pal-14 score improved 1.4 points in the intervention group compared to 0.2 points in the usual care group (d = 0.12 [95% CI, –0.03-0.28]). Only small differences were observed between groups regarding anxiety and depression, but pain intensity (difference, –2.8; SE, 0.9; d = –0.26 [95% CI, –0.43-0.09]) and pain interference (difference, –2.3; SE, 1; d = –0.21 [95% CI, –0.40 to –0.02]) demonstrated a statistically significant and clinically important decrease.
As heart failure care evolves, so must palliative care
Though the study and intervention developed by Dr. Bakitas and colleagues is commendable, it is only somewhat surprising that it did not drastically improve patients’ quality of life, Nathan E. Goldstein, MD, of the Icahn School of Medicine at Mount Sinai in New York, wrote in an accompanying editorial.
He noted several reasons for the lack of improvement, including a large proportion of patients still being in the early stages of the disease. Ultimately, however, he wonders if innovation in heart failure care ultimately impacted the study while it was occurring. Medications and technological advancements evolve rapidly in this field, he said, especially over the course of a 3-year study period.
To continue this work and produce real benefits in patients with advanced heart failure, Dr. Goldstein emphasized the need for “dynamic palliative care interventions that can adapt to the constantly changing landscape of the patient’s needs caused by the underlying nature of the disease, as well as the innovations in the field of cardiology.”
The authors acknowledged their study’s limitations, including data attrition at 16 weeks that was higher than expected – a turn of events they attributed to “unique socioeconomic factors … and lack of regular health care appointments” among some participants. In addition, a minority of patients were unable to stick to the study protocol, which has led the researchers to begin investigating video alternatives to in-person consultation.
The study was supported by the National Institutes of Health/National Institutes of Nursing Research. Four of the authors reported received grants from the National Institutes of Nursing Research outside the submitted work or during the study. Dr. Goldstein reported no conflicts of interest.
SOURCE: Bakitas MA et al. JAMA Intern Med. 2020 July 27. doi: 10.1001/jamainternmed.2020.2861.
A new palliative care intervention for U.S. patients with advanced heart failure did not improve quality of life or mood after 16 weeks of participation in a randomized trial.
“Future analyses and studies will examine both the patient factors and intervention components to find the right palliative care dose, for the right patient, at the right time,” wrote Marie A. Bakitas, DNSc, of the University of Alabama at Birmingham, and coauthors. The study was published in JAMA Internal Medicine.
“My first reaction is disappointment,” Larry Allen, MD, of the University of Colorado in Denver, said in an interview. “We had hoped to see the ENABLE program, which had been successful in cancer, translate to the heart failure setting.”
Improvement of palliative care in heart failure patients might rest on who needs it most
“One thing to note,” Dr. Allen added in an interview, “is that, in this population of patients, some of the measures they were trying to improve were already relatively mild to start with. It may not be that the intervention didn’t help but that they picked a patient population that wasn’t particularly in need. If you treat someone who doesn’t have a problem, it’s hard to make them better.”
In a separate interview, Dr. Bakitas acknowledged a similar sentiment. “We were a little surprised until we looked at our sample,” she said. “We realized that we had recruited all these very high-functioning, good quality-of-life patients. What we then did was look at a subsample of patients who had low quality of life at baseline. Low and behold, the intervention had an effect. The patients who started with a poor quality of life had a statistically and clinically significant benefit. Their KCCQ score increased by over 5 points.”
As for next steps. Dr. Bakitas noted that they’re twofold: “One is refining the patient population who can benefit, and the second is working on the intervention and figuring out which pieces are the ones that provide the most benefit.
“Because of logistics and practical issues, not everyone in the study got all the intervention that they should have. Think of it like a drug trial; if someone misses a pill, they don’t get the full dose that we thought would work. We need to make sure our interventions have the right pieces in place. We don’t want to develop a great intervention that’s not practical for patients.”
Study design and outcomes
To determine the benefits of early palliative care for patients with heart failure, the researchers developed the ENABLE CHF-PC (Educate, Nurture, Advise, Before Life Ends Comprehensive Heartcare for Patients and Caregivers) intervention. This nurse-led program includes an in-person consultant followed by six telehealth nurse coaching sessions lasting 30-40 minutes and then monthly follow-up calls through either 48 weeks or the patient’s death.
To test the effectiveness of their intervention after 16 weeks, the researchers launched a two-site, single-blind randomized clinical trial made up of 415 patients who were 50 years or older with advanced heart failure. Among the patients, 53% were men and the mean age was 64 years; 55% were African American, 26% lived in a rural area, and 46% had a high school education or less. The average length of time since heart failure diagnosis was 5.1 years.
Patients were randomized evenly to receive either the ENABLE CHF-PC intervention (208) or usual care. The primary outcomes were quality of life (QOL), which was measured by the heart failure–specific 23-item Kansas City Cardiomyopathy Questionnaire (KCCQ) and the 14-item Functional Assessment of Chronic Illness Therapy–Palliative-14 (FACIT Pal-14), and mood, which was measured by the 14-item Hospital Anxiety and Depression Scale (HADS). Pain was measured via 3-item pain intensity and 2-item pain interference scales.
Effect size was measured as Cohen d or d-equivalent, where a small effect is 0.2, medium is 0.5, and large is about 0.854.
At baseline, the mean KCCQ score of 52.6 at baseline indicated a “fairly good” QOL across all patients. After 16 weeks, the mean KCCQ score improved 3.9 points in the intervention group, compared with 2.3 points in the usual care group (d = 0.07; [95% confidence interval, –0.09-0.24]). In addition, the mean FACIT-Pal-14 score improved 1.4 points in the intervention group compared to 0.2 points in the usual care group (d = 0.12 [95% CI, –0.03-0.28]). Only small differences were observed between groups regarding anxiety and depression, but pain intensity (difference, –2.8; SE, 0.9; d = –0.26 [95% CI, –0.43-0.09]) and pain interference (difference, –2.3; SE, 1; d = –0.21 [95% CI, –0.40 to –0.02]) demonstrated a statistically significant and clinically important decrease.
As heart failure care evolves, so must palliative care
Though the study and intervention developed by Dr. Bakitas and colleagues is commendable, it is only somewhat surprising that it did not drastically improve patients’ quality of life, Nathan E. Goldstein, MD, of the Icahn School of Medicine at Mount Sinai in New York, wrote in an accompanying editorial.
He noted several reasons for the lack of improvement, including a large proportion of patients still being in the early stages of the disease. Ultimately, however, he wonders if innovation in heart failure care ultimately impacted the study while it was occurring. Medications and technological advancements evolve rapidly in this field, he said, especially over the course of a 3-year study period.
To continue this work and produce real benefits in patients with advanced heart failure, Dr. Goldstein emphasized the need for “dynamic palliative care interventions that can adapt to the constantly changing landscape of the patient’s needs caused by the underlying nature of the disease, as well as the innovations in the field of cardiology.”
The authors acknowledged their study’s limitations, including data attrition at 16 weeks that was higher than expected – a turn of events they attributed to “unique socioeconomic factors … and lack of regular health care appointments” among some participants. In addition, a minority of patients were unable to stick to the study protocol, which has led the researchers to begin investigating video alternatives to in-person consultation.
The study was supported by the National Institutes of Health/National Institutes of Nursing Research. Four of the authors reported received grants from the National Institutes of Nursing Research outside the submitted work or during the study. Dr. Goldstein reported no conflicts of interest.
SOURCE: Bakitas MA et al. JAMA Intern Med. 2020 July 27. doi: 10.1001/jamainternmed.2020.2861.
FROM JAMA INTERNAL MEDICINE
COVID-19–related skin changes: The hidden racism in documentation
Belatedly, the disproportionate impact of COVID-19 on patients of color is getting attention. By now, we’ve read the headlines. Black people in the United States make up about 13% of the population but account for almost three times (34%) as many deaths. This story repeats – in other countries and in other minority communities.
Early detection is critical both to initiate supportive care and to isolate affected individuals and limit spread. Skin manifestations of COVID-19, especially those that occur early in the disease (eg, vesicular eruptions) or have prognostic significance (livedo, retiform purpura, necrosis), are critical to this goal of early recognition.
In this context, a recent systematic literature review looked at all articles describing skin manifestations associated with COVID-19. The investigators identified 46 articles published between March and May 2020 which included a total of 130 clinical images.
The following findings from this study are striking:
- 92% of the published images of COVID-associated skin manifestations were in I-III.
- Only 6% of COVID skin lesions included in the articles were in patients with skin type IV.
- None showed COVID skin lesions in skin types V or VI.
- Only six of the articles reported race and ethnicity demographics. In those, 91% of the patients were White and 9% were Hispanic.
These results reveal a critical lack of representative clinical images of COVID-associated skin manifestations in patients of color. This deficiency is made all the more egregious given the fact that patients of color, including those who are Black, Latinx, and Native American, have been especially hard hit by the COVID-19 pandemic and suffer disproportionate disease-related morbidity and mortality.
As the study authors point out, skin manifestations in people of color often differ significantly from findings in White skin (for example, look at the figure depicting the rash typical of Kawasaki disease in a dark-skinned child compared with a light-skinned child). It is not a stretch to suggest that skin manifestations associated with COVID-19 may look very different in darker skin.
This isn’t a new phenomenon. Almost half of dermatologists feel that they’ve had insufficient exposure to skin disease in darker skin types. Skin of color remains underrepresented in medical journals.
Like other forms of passive, institutional racism, this deficiency will only be improved if dermatologists and dermatology publications actively seek out COVID-associated skin manifestations in patients of color and prioritize sharing these images. A medical student in the United Kingdom has gotten the ball rolling, compiling a handbook of clinical signs in darker skin types as part of a student-staff partnership at St. George’s Hospital and the University of London. At this time, Mind the Gap is looking for a publisher.
Dr. Lipper is an assistant clinical professor at the University of Vermont, Burlington, and a staff physician in the department of dermatology at Danbury (Conn.) Hospital. He has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Belatedly, the disproportionate impact of COVID-19 on patients of color is getting attention. By now, we’ve read the headlines. Black people in the United States make up about 13% of the population but account for almost three times (34%) as many deaths. This story repeats – in other countries and in other minority communities.
Early detection is critical both to initiate supportive care and to isolate affected individuals and limit spread. Skin manifestations of COVID-19, especially those that occur early in the disease (eg, vesicular eruptions) or have prognostic significance (livedo, retiform purpura, necrosis), are critical to this goal of early recognition.
In this context, a recent systematic literature review looked at all articles describing skin manifestations associated with COVID-19. The investigators identified 46 articles published between March and May 2020 which included a total of 130 clinical images.
The following findings from this study are striking:
- 92% of the published images of COVID-associated skin manifestations were in I-III.
- Only 6% of COVID skin lesions included in the articles were in patients with skin type IV.
- None showed COVID skin lesions in skin types V or VI.
- Only six of the articles reported race and ethnicity demographics. In those, 91% of the patients were White and 9% were Hispanic.
These results reveal a critical lack of representative clinical images of COVID-associated skin manifestations in patients of color. This deficiency is made all the more egregious given the fact that patients of color, including those who are Black, Latinx, and Native American, have been especially hard hit by the COVID-19 pandemic and suffer disproportionate disease-related morbidity and mortality.
As the study authors point out, skin manifestations in people of color often differ significantly from findings in White skin (for example, look at the figure depicting the rash typical of Kawasaki disease in a dark-skinned child compared with a light-skinned child). It is not a stretch to suggest that skin manifestations associated with COVID-19 may look very different in darker skin.
This isn’t a new phenomenon. Almost half of dermatologists feel that they’ve had insufficient exposure to skin disease in darker skin types. Skin of color remains underrepresented in medical journals.
Like other forms of passive, institutional racism, this deficiency will only be improved if dermatologists and dermatology publications actively seek out COVID-associated skin manifestations in patients of color and prioritize sharing these images. A medical student in the United Kingdom has gotten the ball rolling, compiling a handbook of clinical signs in darker skin types as part of a student-staff partnership at St. George’s Hospital and the University of London. At this time, Mind the Gap is looking for a publisher.
Dr. Lipper is an assistant clinical professor at the University of Vermont, Burlington, and a staff physician in the department of dermatology at Danbury (Conn.) Hospital. He has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Belatedly, the disproportionate impact of COVID-19 on patients of color is getting attention. By now, we’ve read the headlines. Black people in the United States make up about 13% of the population but account for almost three times (34%) as many deaths. This story repeats – in other countries and in other minority communities.
Early detection is critical both to initiate supportive care and to isolate affected individuals and limit spread. Skin manifestations of COVID-19, especially those that occur early in the disease (eg, vesicular eruptions) or have prognostic significance (livedo, retiform purpura, necrosis), are critical to this goal of early recognition.
In this context, a recent systematic literature review looked at all articles describing skin manifestations associated with COVID-19. The investigators identified 46 articles published between March and May 2020 which included a total of 130 clinical images.
The following findings from this study are striking:
- 92% of the published images of COVID-associated skin manifestations were in I-III.
- Only 6% of COVID skin lesions included in the articles were in patients with skin type IV.
- None showed COVID skin lesions in skin types V or VI.
- Only six of the articles reported race and ethnicity demographics. In those, 91% of the patients were White and 9% were Hispanic.
These results reveal a critical lack of representative clinical images of COVID-associated skin manifestations in patients of color. This deficiency is made all the more egregious given the fact that patients of color, including those who are Black, Latinx, and Native American, have been especially hard hit by the COVID-19 pandemic and suffer disproportionate disease-related morbidity and mortality.
As the study authors point out, skin manifestations in people of color often differ significantly from findings in White skin (for example, look at the figure depicting the rash typical of Kawasaki disease in a dark-skinned child compared with a light-skinned child). It is not a stretch to suggest that skin manifestations associated with COVID-19 may look very different in darker skin.
This isn’t a new phenomenon. Almost half of dermatologists feel that they’ve had insufficient exposure to skin disease in darker skin types. Skin of color remains underrepresented in medical journals.
Like other forms of passive, institutional racism, this deficiency will only be improved if dermatologists and dermatology publications actively seek out COVID-associated skin manifestations in patients of color and prioritize sharing these images. A medical student in the United Kingdom has gotten the ball rolling, compiling a handbook of clinical signs in darker skin types as part of a student-staff partnership at St. George’s Hospital and the University of London. At this time, Mind the Gap is looking for a publisher.
Dr. Lipper is an assistant clinical professor at the University of Vermont, Burlington, and a staff physician in the department of dermatology at Danbury (Conn.) Hospital. He has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
‘Staggering’ increase in COVID-linked depression, anxiety
Since the start of the COVID-19 pandemic, there has been a dramatic increase in depression, anxiety, psychosis, and suicidality, new research shows.
The new data, released by Mental Health America (MHA), came from individuals who completed a voluntary online mental health screen.
As of the end of June, over 169,000 additional participants reported having moderate to severe depression or anxiety, compared with participants who completed the screen prior to the pandemic.
In June alone, 18,000 additional participants were found to be at risk for psychosis, continuing a rising pattern that began in May, when 16,000 reported psychosis risk.
“We continue to see staggering numbers that indicate increased rates in depression and anxiety because of COVID-19,” Paul Gionfriddo, president and CEO of MHA, said in a release.
“In fact, the problem is bigger than anyone imagined, making it clear how the pandemic is affecting people now and will continue to affect people who mourn loved ones and whose serious mental conditions are left untreated. So we need to take this very seriously,” Mr. Gionfriddo said in an interview.
Real-time data
MHA has been conducting online screenings for 6 years. To date, nearly 5.5 million screenings have been completed, making it the largest screening program of its kind in the United States, Mr. Gionfriddo reported.
“At the beginning of the pandemic, we were asked by a member of the media if we could offer any insight about how anxiety in particular was affecting people during the pandemic since we were the only ones with a database that could give quantitative detail,” he said.
The results of their screen could also help find that information “in real time,” he added.
More people are now undergoing mental health screenings, Mr. Gionfriddo noted.
At roughly 7,000 per day in May and June, the number of anxiety and depression screenings that were completed per day were 406% and 457% higher, respectively, than the number completed in January.
The youngest group of participants were those aged 11-17 years; the oldest age group consisted of individuals 65 years and older.
The Patient Health Questionnaire–9 was used to identify those at risk for depression, the General Anxiety Disorder–7 was used to identify those at risk for anxiety, and the Prodromal Questionnaire Brief Version was used to identify those at high risk for psychosis.
Current events
Roughly 90% screened positive for moderate to severe depression, and 80% screened positive for moderate to severe anxiety.
“Kids between the ages of 11 and 17 years have been the most stressed, but it seems to be easier to bear as you get older,” Mr. Gionfriddo said.
Loneliness and isolation were cited as contributors to depression and anxiety by the largest percentage of individuals with these conditions (74% and 65%, respectively).
In June, roughly one quarter of participants also cited grief or loss and financial concerns as contributors to anxiety (25.31% and 24.18%, respectively) and to depression (26.53% and 23.36%).
Current events were cited as an important contributor, leading to more mental health problems in June, compared with May (36.11% vs 29.41 for anxiety; 29.13% vs 21.77% for depression).
The June screen added the category of racism as a potential contributor. Close to 8% reported it as a reason for anxiety, and roughly 5% considered it a reason for depression.
“We will be releasing more data at the end of July, and it will be interesting to see how the racism category compares to data we collected at the end of June,” Mr. Gionfriddo noted.
Dramatic increase
The screen also showed a “dramatic increase” in the number of people who reported being at risk for psychosis, with 18,000 participants screening positive. This represented more than four times the baseline figures recorded through March.
“We were not surprised to see a spike in depression and anxiety, but why were we seeing a spike in psychosis in May/June?” Mr. Gionfriddo asked. He suggested that stress may play a role in driving this increased risk.
“These data, we hope, will get policymakers to pay attention, take it seriously, and intervene to prevent psychosis at an earlier stage before signs and symptoms emerge,” said Mr. Gionfriddo.
One of the most alarming findings was that in June, 25,498 participants who screened positive for depression reported thinking of suicide or self-harm on “more than half of days to nearly every day.” A total of 14,607 participants said they had these thoughts every day.
Overall, the results should reinforce the recommendations of the US Preventive Services Task Force to routinely screen for depression in any clinical setting on a regular basis, Mr. Gionfriddo said.
In addition, policymakers “need to balance reopening vs. quarantining and isolating, and we need to think about what the next 2-4 years look like in terms of balancing physical health risks and mental health risks,” he noted.
“We’ve been treating the pandemic like a sprint and now, 4 or 5 months into it, perhaps as a middle-distance run, when in fact it’s a marathon,” he added.
Advocates needed
The increase in anxiety and depression often centers on the changes and uncertainties in the college experience, such as whether classes will be held in person, online, or a hybrid of the two, said Dr. Ritchie, who was not involved with the research.
Additionally, some college students who have “left the nest” have been forced to “return to the nest,” which compounds stress, she said.
LGBTQ youngsters may be particularly affected because some have “come out of the closet” while away from home and now must negotiate going back to their home of record. They are uncertain whether or not “to go back into the closet,” added Dr. Ritchie, who is also vice chair of psychiatry at Georgetown University, Washington.
Psychiatrists and other mental health professionals should be advocates for “getting services to more people for the greatest good,” she noted.
For example, the MHA data “might be useful in advocating for keeping telehealth accessible and even promoting it,” she said.
The full report is available on MHA’s website.
Mr. Gionfriddo and Dr. Ritchie report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Since the start of the COVID-19 pandemic, there has been a dramatic increase in depression, anxiety, psychosis, and suicidality, new research shows.
The new data, released by Mental Health America (MHA), came from individuals who completed a voluntary online mental health screen.
As of the end of June, over 169,000 additional participants reported having moderate to severe depression or anxiety, compared with participants who completed the screen prior to the pandemic.
In June alone, 18,000 additional participants were found to be at risk for psychosis, continuing a rising pattern that began in May, when 16,000 reported psychosis risk.
“We continue to see staggering numbers that indicate increased rates in depression and anxiety because of COVID-19,” Paul Gionfriddo, president and CEO of MHA, said in a release.
“In fact, the problem is bigger than anyone imagined, making it clear how the pandemic is affecting people now and will continue to affect people who mourn loved ones and whose serious mental conditions are left untreated. So we need to take this very seriously,” Mr. Gionfriddo said in an interview.
Real-time data
MHA has been conducting online screenings for 6 years. To date, nearly 5.5 million screenings have been completed, making it the largest screening program of its kind in the United States, Mr. Gionfriddo reported.
“At the beginning of the pandemic, we were asked by a member of the media if we could offer any insight about how anxiety in particular was affecting people during the pandemic since we were the only ones with a database that could give quantitative detail,” he said.
The results of their screen could also help find that information “in real time,” he added.
More people are now undergoing mental health screenings, Mr. Gionfriddo noted.
At roughly 7,000 per day in May and June, the number of anxiety and depression screenings that were completed per day were 406% and 457% higher, respectively, than the number completed in January.
The youngest group of participants were those aged 11-17 years; the oldest age group consisted of individuals 65 years and older.
The Patient Health Questionnaire–9 was used to identify those at risk for depression, the General Anxiety Disorder–7 was used to identify those at risk for anxiety, and the Prodromal Questionnaire Brief Version was used to identify those at high risk for psychosis.
Current events
Roughly 90% screened positive for moderate to severe depression, and 80% screened positive for moderate to severe anxiety.
“Kids between the ages of 11 and 17 years have been the most stressed, but it seems to be easier to bear as you get older,” Mr. Gionfriddo said.
Loneliness and isolation were cited as contributors to depression and anxiety by the largest percentage of individuals with these conditions (74% and 65%, respectively).
In June, roughly one quarter of participants also cited grief or loss and financial concerns as contributors to anxiety (25.31% and 24.18%, respectively) and to depression (26.53% and 23.36%).
Current events were cited as an important contributor, leading to more mental health problems in June, compared with May (36.11% vs 29.41 for anxiety; 29.13% vs 21.77% for depression).
The June screen added the category of racism as a potential contributor. Close to 8% reported it as a reason for anxiety, and roughly 5% considered it a reason for depression.
“We will be releasing more data at the end of July, and it will be interesting to see how the racism category compares to data we collected at the end of June,” Mr. Gionfriddo noted.
Dramatic increase
The screen also showed a “dramatic increase” in the number of people who reported being at risk for psychosis, with 18,000 participants screening positive. This represented more than four times the baseline figures recorded through March.
“We were not surprised to see a spike in depression and anxiety, but why were we seeing a spike in psychosis in May/June?” Mr. Gionfriddo asked. He suggested that stress may play a role in driving this increased risk.
“These data, we hope, will get policymakers to pay attention, take it seriously, and intervene to prevent psychosis at an earlier stage before signs and symptoms emerge,” said Mr. Gionfriddo.
One of the most alarming findings was that in June, 25,498 participants who screened positive for depression reported thinking of suicide or self-harm on “more than half of days to nearly every day.” A total of 14,607 participants said they had these thoughts every day.
Overall, the results should reinforce the recommendations of the US Preventive Services Task Force to routinely screen for depression in any clinical setting on a regular basis, Mr. Gionfriddo said.
In addition, policymakers “need to balance reopening vs. quarantining and isolating, and we need to think about what the next 2-4 years look like in terms of balancing physical health risks and mental health risks,” he noted.
“We’ve been treating the pandemic like a sprint and now, 4 or 5 months into it, perhaps as a middle-distance run, when in fact it’s a marathon,” he added.
Advocates needed
The increase in anxiety and depression often centers on the changes and uncertainties in the college experience, such as whether classes will be held in person, online, or a hybrid of the two, said Dr. Ritchie, who was not involved with the research.
Additionally, some college students who have “left the nest” have been forced to “return to the nest,” which compounds stress, she said.
LGBTQ youngsters may be particularly affected because some have “come out of the closet” while away from home and now must negotiate going back to their home of record. They are uncertain whether or not “to go back into the closet,” added Dr. Ritchie, who is also vice chair of psychiatry at Georgetown University, Washington.
Psychiatrists and other mental health professionals should be advocates for “getting services to more people for the greatest good,” she noted.
For example, the MHA data “might be useful in advocating for keeping telehealth accessible and even promoting it,” she said.
The full report is available on MHA’s website.
Mr. Gionfriddo and Dr. Ritchie report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Since the start of the COVID-19 pandemic, there has been a dramatic increase in depression, anxiety, psychosis, and suicidality, new research shows.
The new data, released by Mental Health America (MHA), came from individuals who completed a voluntary online mental health screen.
As of the end of June, over 169,000 additional participants reported having moderate to severe depression or anxiety, compared with participants who completed the screen prior to the pandemic.
In June alone, 18,000 additional participants were found to be at risk for psychosis, continuing a rising pattern that began in May, when 16,000 reported psychosis risk.
“We continue to see staggering numbers that indicate increased rates in depression and anxiety because of COVID-19,” Paul Gionfriddo, president and CEO of MHA, said in a release.
“In fact, the problem is bigger than anyone imagined, making it clear how the pandemic is affecting people now and will continue to affect people who mourn loved ones and whose serious mental conditions are left untreated. So we need to take this very seriously,” Mr. Gionfriddo said in an interview.
Real-time data
MHA has been conducting online screenings for 6 years. To date, nearly 5.5 million screenings have been completed, making it the largest screening program of its kind in the United States, Mr. Gionfriddo reported.
“At the beginning of the pandemic, we were asked by a member of the media if we could offer any insight about how anxiety in particular was affecting people during the pandemic since we were the only ones with a database that could give quantitative detail,” he said.
The results of their screen could also help find that information “in real time,” he added.
More people are now undergoing mental health screenings, Mr. Gionfriddo noted.
At roughly 7,000 per day in May and June, the number of anxiety and depression screenings that were completed per day were 406% and 457% higher, respectively, than the number completed in January.
The youngest group of participants were those aged 11-17 years; the oldest age group consisted of individuals 65 years and older.
The Patient Health Questionnaire–9 was used to identify those at risk for depression, the General Anxiety Disorder–7 was used to identify those at risk for anxiety, and the Prodromal Questionnaire Brief Version was used to identify those at high risk for psychosis.
Current events
Roughly 90% screened positive for moderate to severe depression, and 80% screened positive for moderate to severe anxiety.
“Kids between the ages of 11 and 17 years have been the most stressed, but it seems to be easier to bear as you get older,” Mr. Gionfriddo said.
Loneliness and isolation were cited as contributors to depression and anxiety by the largest percentage of individuals with these conditions (74% and 65%, respectively).
In June, roughly one quarter of participants also cited grief or loss and financial concerns as contributors to anxiety (25.31% and 24.18%, respectively) and to depression (26.53% and 23.36%).
Current events were cited as an important contributor, leading to more mental health problems in June, compared with May (36.11% vs 29.41 for anxiety; 29.13% vs 21.77% for depression).
The June screen added the category of racism as a potential contributor. Close to 8% reported it as a reason for anxiety, and roughly 5% considered it a reason for depression.
“We will be releasing more data at the end of July, and it will be interesting to see how the racism category compares to data we collected at the end of June,” Mr. Gionfriddo noted.
Dramatic increase
The screen also showed a “dramatic increase” in the number of people who reported being at risk for psychosis, with 18,000 participants screening positive. This represented more than four times the baseline figures recorded through March.
“We were not surprised to see a spike in depression and anxiety, but why were we seeing a spike in psychosis in May/June?” Mr. Gionfriddo asked. He suggested that stress may play a role in driving this increased risk.
“These data, we hope, will get policymakers to pay attention, take it seriously, and intervene to prevent psychosis at an earlier stage before signs and symptoms emerge,” said Mr. Gionfriddo.
One of the most alarming findings was that in June, 25,498 participants who screened positive for depression reported thinking of suicide or self-harm on “more than half of days to nearly every day.” A total of 14,607 participants said they had these thoughts every day.
Overall, the results should reinforce the recommendations of the US Preventive Services Task Force to routinely screen for depression in any clinical setting on a regular basis, Mr. Gionfriddo said.
In addition, policymakers “need to balance reopening vs. quarantining and isolating, and we need to think about what the next 2-4 years look like in terms of balancing physical health risks and mental health risks,” he noted.
“We’ve been treating the pandemic like a sprint and now, 4 or 5 months into it, perhaps as a middle-distance run, when in fact it’s a marathon,” he added.
Advocates needed
The increase in anxiety and depression often centers on the changes and uncertainties in the college experience, such as whether classes will be held in person, online, or a hybrid of the two, said Dr. Ritchie, who was not involved with the research.
Additionally, some college students who have “left the nest” have been forced to “return to the nest,” which compounds stress, she said.
LGBTQ youngsters may be particularly affected because some have “come out of the closet” while away from home and now must negotiate going back to their home of record. They are uncertain whether or not “to go back into the closet,” added Dr. Ritchie, who is also vice chair of psychiatry at Georgetown University, Washington.
Psychiatrists and other mental health professionals should be advocates for “getting services to more people for the greatest good,” she noted.
For example, the MHA data “might be useful in advocating for keeping telehealth accessible and even promoting it,” she said.
The full report is available on MHA’s website.
Mr. Gionfriddo and Dr. Ritchie report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Heart damage even after COVID-19 ‘recovery’ evokes specter of later heart failure
Evidence that the heart can take a major hit in patients hospitalized with COVID-19, especially those already with cardiovascular disease (CV) or its risk factors, has been sadly apparent from the pandemic’s earliest days.
Less clear from case studies and small series to date has been whether SARS-CoV-2 directly attacks the heart and whether acute cardiac effects of the illness may lead to some kind of lingering cardiomyopathy.
The field’s grasp of those issues advanced a bit in two new reports published July 27 in JAMA Cardiology that seem to validate concerns the virus can infect the myocardium, without necessarily causing myocarditis and the possibility that some “recovered” patients may be left with persisting myocardial injury and inflammation that potentially could later manifest as heart failure.
Persisting inflammation by cardiac magnetic resonance
A prospective cohort study with 100 patients recovered from a recent bout of the disease showed evidence of ventricular dysfunction, greater ventricular mass, and in 78% of the cohort, signs of myocardial inflammation by cardiac magnetic resonance (CMR) imaging. The CMR findings correlated with elevations in troponin T by high-sensitivity assay (hs-TnT).
Two-thirds of the cohort, whose acute COVID-19 severity had “ranged from asymptomatic to minor-to-moderate symptoms,” had recovered at home, whereas the remaining “severely unwell patients” had been hospitalized, wrote the authors, led by Valentina O. Püntmann, MD, PhD, University Hospital Frankfurt (Germany).
None of the patients had a history of heart failure or cardiomyopathy, although some had hypertension, diabetes, or evidence of coronary disease.
“Our findings demonstrate that participants with a relative paucity of preexisting cardiovascular condition and with mostly home-based recovery had frequent cardiac inflammatory involvement, which was similar to the hospitalized subgroup with regards to severity and extent,” the group noted.
“There is a considerable ongoing myocardial inflammation in the heart muscle weeks after recovery from COVID-19 illness. This finding is important because it may herald a considerable burden of heart failure in a few years down the line,” Dr. Püntmann said in an interview.
Early diagnosis would offer “a good chance that early treatment could reduce the relentless course of inflammatory damage or even halt it,” she said.
“The relatively clear onset of COVID-19 illness provides an opportunity, which we often do not have with other conditions, to take a proactive action and to look for heart involvement early, within a few weeks of recovery.”
The study’s CMR evidence of inflammation edema, scarring, and pericardial effusion are among “the major diagnostic criteria for inflammatory and viral myocarditis,” observed Biykem Bozkurt, MD, PhD, from Baylor College of Medicine, Houston, who wasn’t part of either new study.
The findings suggest – consistent with previous evidence – that some patients with recent COVID-19 may be left with ongoing myocardial inflammation, and this study further adds that it could potentially become subacute or even chronic and in some may not be totally reversible, she said in an interview. How long the effects are likely to persist “remains to be determined. We need longer-term outcomes data.”
Viral presence without myocarditis
The accompanying report featured a postmortem analysis of hearts from 39 patients with mostly severe COVID-19 that pointed to a significant SARS-CoV-2 presence and signs that the virus vigorously replicated in the myocardium.
But there was no evidence that the infection led to fulminant myocarditis. Rather, the virus had apparently infiltrated the heart by localizing in interstitial cells or in macrophages that took up in the myocardium without actually entering myocytes, concluded the report’s authors, led by Diana Lindner, PhD, from the University Heart and Vascular Centre, Hamburg (Germany).
The findings suggest “that the presence of SARS-CoV-2 in cardiac tissue does not necessarily cause an inflammatory reaction consistent with clinical myocarditis,” the group wrote.
Previously in the literature, in “cases in which myocardial inflammation was present, there was also evidence of clinical myocarditis, and therefore the current cases underlie a different pathophysiology,” they concluded.
No evidence of the virus was seen in 15 cases, about 61% of the group. In 16 of the remaining 24 hearts, the viral load exceeded 1,000 copies per mcg of RNA, a substantial presence. Those 16 showed increased expression of inflammatory cytokines but no inflammatory cell infiltrates or changes in leukocyte counts, the researchers noted.
“Findings of suggested viral replication in the cases with a very high viral load are showing that we need to do more studies to find out long-term consequences, which we do not know right now,” senior author Dirk Westermann, MD, also from the University Heart and Vascular Centre, Hamburg, said.
Implications for heart failure
The postmortem findings from Dr. Lindner and associates “provide intriguing evidence that COVID-19 is associated with at least some component of myocardial injury, perhaps as the result of direct viral infection of the heart,” wrote Clyde W. Yancy, MD, MSc, from Northwestern University, Chicago, and Gregg C. Fonarow, MD, from the University of California, Los Angeles, in an editorial accompanying both reports.
The CMR study from Dr. Püntmann and colleagues – on the backdrop of earlier COVID-19 observations – suggests the potential for “residual left ventricular dysfunction and ongoing inflammation” in the months following a COVID-19 diagnosis. Both developments may be “of sufficient concern to represent a nidus for new-onset heart failure and other cardiovascular complications,” contend Dr. Yancy and Dr. Fonarow.
“When added to the postmortem pathological findings from Lindner et al, we see the plot thickening and we are inclined to raise a new and very evident concern that cardiomyopathy and heart failure related to COVID-19 may potentially evolve as the natural history of this infection becomes clearer,” they wrote.
Some patients, having recovered from the acute illness, may be left with a chronic inflammatory state that probably puts them at increased risk for future heart failure, agreed Dr. Bozkurt when interviewed. “They could show further decline in cardiac function, and their recovery might take longer than with the usual viral illnesses that we see,” she said.
“There could also be a risk of sudden death. Inflammation sometimes gives rise to sudden death and ventricular arrhythmia, which I would be very worried about, especially if the myocardium is stressed,” Dr. Bozkurt said. “So competitive sports in those patients potentially could be risky.”
COVID-19 cohort vs. matched control subjects
The CMR study from Dr. Püntmann and colleagues prospectively entered 100 patients recently recovered from an acute bout of COVID-19, either at home or at a hospital, who were followed in a registry based at University Hospital Frankfurt. Their median age was 49 years; 47% were female. They were compared with 50 age- and sex-matched control patients and 50 apparently healthy volunteers matched for risk factors, the group noted.
On the same day as the CMR assessment, the recently recovered patients, compared with the healthy control subjects and risk-factor matched control subjects, respectively, showed (P ≤ .001 in each case):
- A reduced left ventricular (LV) ejection fraction: 56% vs. 60% and 61%.
- A higher LV end-diastolic volume index: 86 mL/m2 vs. 80 mL/m2 and 75 mL/m2.
- A greater LV mass index: 51 g/m2 vs. 47 g/m2 and 53 g/m2.
- A higher hs-TnT level: 5.6 pg/mL vs. 3.2 pg/mL and 3.9 pg/mL.
- A greater prevalence of hs-TnT levels 3 pg/mL or more: 71% vs. 11% and 31%.
At CMR, 78% of the recovered COVID-19 patients showed abnormalities that included raised myocardial native T1 and T2 mapping, which is suggestive of fibrosis and edema from inflammation, compared with the two control groups (P < .001 for all differences), “independent of preexisting conditions, severity and overall course of the acute illness, and the time from the original diagnosis,” the group wrote. Native T1 and T2 mapping correlated significantly with hs-TnT.
“We now have the diagnostic means to detect cardiac inflammation early, and we need make every effort to apply them in every day practice,”Dr. Püntmann said in the interview.
“Using cardiac MRI will allow us to raise our game against COVID-19 and proactively develop efficient cardioprotective treatments,” she said. “Until we have effective means of protecting from the infection, that is vaccination, we must act swiftly and within the means at hand.”
The analysis evokes several other ways patients with COVID-19 might be screened for significant myocardial involvement.
“Strategies could include checking troponins, not only at admission but maybe at discharge and perhaps even those individuals who are at home and are not necessarily requiring care,” Dr. Bozkurt said.
“Biomarker profiling and screening for ongoing inflammation probably are going to be important components of COVID-19, especially for those with subclinical risk and disease.”
Dr. Westermann proposed that troponin elevations at discharge “might be a good starting point” for selecting COVID-19 patients for functional testing or imaging to screen for cardiac sequelae. Performing such tests routinely now “would be overwhelming given the massive increase in patients we still see today.”
Dr. Püntmann had no disclosures; statements of potential conflict for the other authors are in the report. Dr. Bozkurt has previously disclosed receiving consultant fees or honoraria from Bayer Healthcare, Bristol-Myers Squibb, Lantheus Medical Imaging, and Respicardia; serving on a data safety monitoring board for LivaNova USA ; and having unspecified relationships with Abbott Laboratories. Dr. Lindner had no disclosures; Dr. Westermann reported receiving personal fees from AstraZeneca, Bayer, Novartis, and Medtronic. Dr. Yancy is a deputy editor and Dr. Fonarow a section editor for JAMA Cardiology. Dr. Yancy had no other disclosures. Dr. Fonarow reported receiving personal fees from Abbott Laboratories, Amgen, AstraZeneca, Bayer, CHF Solutions, Edwards Lifesciences, Janssen, Medtronic, Merck, and Novartis.
A version of this article originally appeared on Medscape.com.
Evidence that the heart can take a major hit in patients hospitalized with COVID-19, especially those already with cardiovascular disease (CV) or its risk factors, has been sadly apparent from the pandemic’s earliest days.
Less clear from case studies and small series to date has been whether SARS-CoV-2 directly attacks the heart and whether acute cardiac effects of the illness may lead to some kind of lingering cardiomyopathy.
The field’s grasp of those issues advanced a bit in two new reports published July 27 in JAMA Cardiology that seem to validate concerns the virus can infect the myocardium, without necessarily causing myocarditis and the possibility that some “recovered” patients may be left with persisting myocardial injury and inflammation that potentially could later manifest as heart failure.
Persisting inflammation by cardiac magnetic resonance
A prospective cohort study with 100 patients recovered from a recent bout of the disease showed evidence of ventricular dysfunction, greater ventricular mass, and in 78% of the cohort, signs of myocardial inflammation by cardiac magnetic resonance (CMR) imaging. The CMR findings correlated with elevations in troponin T by high-sensitivity assay (hs-TnT).
Two-thirds of the cohort, whose acute COVID-19 severity had “ranged from asymptomatic to minor-to-moderate symptoms,” had recovered at home, whereas the remaining “severely unwell patients” had been hospitalized, wrote the authors, led by Valentina O. Püntmann, MD, PhD, University Hospital Frankfurt (Germany).
None of the patients had a history of heart failure or cardiomyopathy, although some had hypertension, diabetes, or evidence of coronary disease.
“Our findings demonstrate that participants with a relative paucity of preexisting cardiovascular condition and with mostly home-based recovery had frequent cardiac inflammatory involvement, which was similar to the hospitalized subgroup with regards to severity and extent,” the group noted.
“There is a considerable ongoing myocardial inflammation in the heart muscle weeks after recovery from COVID-19 illness. This finding is important because it may herald a considerable burden of heart failure in a few years down the line,” Dr. Püntmann said in an interview.
Early diagnosis would offer “a good chance that early treatment could reduce the relentless course of inflammatory damage or even halt it,” she said.
“The relatively clear onset of COVID-19 illness provides an opportunity, which we often do not have with other conditions, to take a proactive action and to look for heart involvement early, within a few weeks of recovery.”
The study’s CMR evidence of inflammation edema, scarring, and pericardial effusion are among “the major diagnostic criteria for inflammatory and viral myocarditis,” observed Biykem Bozkurt, MD, PhD, from Baylor College of Medicine, Houston, who wasn’t part of either new study.
The findings suggest – consistent with previous evidence – that some patients with recent COVID-19 may be left with ongoing myocardial inflammation, and this study further adds that it could potentially become subacute or even chronic and in some may not be totally reversible, she said in an interview. How long the effects are likely to persist “remains to be determined. We need longer-term outcomes data.”
Viral presence without myocarditis
The accompanying report featured a postmortem analysis of hearts from 39 patients with mostly severe COVID-19 that pointed to a significant SARS-CoV-2 presence and signs that the virus vigorously replicated in the myocardium.
But there was no evidence that the infection led to fulminant myocarditis. Rather, the virus had apparently infiltrated the heart by localizing in interstitial cells or in macrophages that took up in the myocardium without actually entering myocytes, concluded the report’s authors, led by Diana Lindner, PhD, from the University Heart and Vascular Centre, Hamburg (Germany).
The findings suggest “that the presence of SARS-CoV-2 in cardiac tissue does not necessarily cause an inflammatory reaction consistent with clinical myocarditis,” the group wrote.
Previously in the literature, in “cases in which myocardial inflammation was present, there was also evidence of clinical myocarditis, and therefore the current cases underlie a different pathophysiology,” they concluded.
No evidence of the virus was seen in 15 cases, about 61% of the group. In 16 of the remaining 24 hearts, the viral load exceeded 1,000 copies per mcg of RNA, a substantial presence. Those 16 showed increased expression of inflammatory cytokines but no inflammatory cell infiltrates or changes in leukocyte counts, the researchers noted.
“Findings of suggested viral replication in the cases with a very high viral load are showing that we need to do more studies to find out long-term consequences, which we do not know right now,” senior author Dirk Westermann, MD, also from the University Heart and Vascular Centre, Hamburg, said.
Implications for heart failure
The postmortem findings from Dr. Lindner and associates “provide intriguing evidence that COVID-19 is associated with at least some component of myocardial injury, perhaps as the result of direct viral infection of the heart,” wrote Clyde W. Yancy, MD, MSc, from Northwestern University, Chicago, and Gregg C. Fonarow, MD, from the University of California, Los Angeles, in an editorial accompanying both reports.
The CMR study from Dr. Püntmann and colleagues – on the backdrop of earlier COVID-19 observations – suggests the potential for “residual left ventricular dysfunction and ongoing inflammation” in the months following a COVID-19 diagnosis. Both developments may be “of sufficient concern to represent a nidus for new-onset heart failure and other cardiovascular complications,” contend Dr. Yancy and Dr. Fonarow.
“When added to the postmortem pathological findings from Lindner et al, we see the plot thickening and we are inclined to raise a new and very evident concern that cardiomyopathy and heart failure related to COVID-19 may potentially evolve as the natural history of this infection becomes clearer,” they wrote.
Some patients, having recovered from the acute illness, may be left with a chronic inflammatory state that probably puts them at increased risk for future heart failure, agreed Dr. Bozkurt when interviewed. “They could show further decline in cardiac function, and their recovery might take longer than with the usual viral illnesses that we see,” she said.
“There could also be a risk of sudden death. Inflammation sometimes gives rise to sudden death and ventricular arrhythmia, which I would be very worried about, especially if the myocardium is stressed,” Dr. Bozkurt said. “So competitive sports in those patients potentially could be risky.”
COVID-19 cohort vs. matched control subjects
The CMR study from Dr. Püntmann and colleagues prospectively entered 100 patients recently recovered from an acute bout of COVID-19, either at home or at a hospital, who were followed in a registry based at University Hospital Frankfurt. Their median age was 49 years; 47% were female. They were compared with 50 age- and sex-matched control patients and 50 apparently healthy volunteers matched for risk factors, the group noted.
On the same day as the CMR assessment, the recently recovered patients, compared with the healthy control subjects and risk-factor matched control subjects, respectively, showed (P ≤ .001 in each case):
- A reduced left ventricular (LV) ejection fraction: 56% vs. 60% and 61%.
- A higher LV end-diastolic volume index: 86 mL/m2 vs. 80 mL/m2 and 75 mL/m2.
- A greater LV mass index: 51 g/m2 vs. 47 g/m2 and 53 g/m2.
- A higher hs-TnT level: 5.6 pg/mL vs. 3.2 pg/mL and 3.9 pg/mL.
- A greater prevalence of hs-TnT levels 3 pg/mL or more: 71% vs. 11% and 31%.
At CMR, 78% of the recovered COVID-19 patients showed abnormalities that included raised myocardial native T1 and T2 mapping, which is suggestive of fibrosis and edema from inflammation, compared with the two control groups (P < .001 for all differences), “independent of preexisting conditions, severity and overall course of the acute illness, and the time from the original diagnosis,” the group wrote. Native T1 and T2 mapping correlated significantly with hs-TnT.
“We now have the diagnostic means to detect cardiac inflammation early, and we need make every effort to apply them in every day practice,”Dr. Püntmann said in the interview.
“Using cardiac MRI will allow us to raise our game against COVID-19 and proactively develop efficient cardioprotective treatments,” she said. “Until we have effective means of protecting from the infection, that is vaccination, we must act swiftly and within the means at hand.”
The analysis evokes several other ways patients with COVID-19 might be screened for significant myocardial involvement.
“Strategies could include checking troponins, not only at admission but maybe at discharge and perhaps even those individuals who are at home and are not necessarily requiring care,” Dr. Bozkurt said.
“Biomarker profiling and screening for ongoing inflammation probably are going to be important components of COVID-19, especially for those with subclinical risk and disease.”
Dr. Westermann proposed that troponin elevations at discharge “might be a good starting point” for selecting COVID-19 patients for functional testing or imaging to screen for cardiac sequelae. Performing such tests routinely now “would be overwhelming given the massive increase in patients we still see today.”
Dr. Püntmann had no disclosures; statements of potential conflict for the other authors are in the report. Dr. Bozkurt has previously disclosed receiving consultant fees or honoraria from Bayer Healthcare, Bristol-Myers Squibb, Lantheus Medical Imaging, and Respicardia; serving on a data safety monitoring board for LivaNova USA ; and having unspecified relationships with Abbott Laboratories. Dr. Lindner had no disclosures; Dr. Westermann reported receiving personal fees from AstraZeneca, Bayer, Novartis, and Medtronic. Dr. Yancy is a deputy editor and Dr. Fonarow a section editor for JAMA Cardiology. Dr. Yancy had no other disclosures. Dr. Fonarow reported receiving personal fees from Abbott Laboratories, Amgen, AstraZeneca, Bayer, CHF Solutions, Edwards Lifesciences, Janssen, Medtronic, Merck, and Novartis.
A version of this article originally appeared on Medscape.com.
Evidence that the heart can take a major hit in patients hospitalized with COVID-19, especially those already with cardiovascular disease (CV) or its risk factors, has been sadly apparent from the pandemic’s earliest days.
Less clear from case studies and small series to date has been whether SARS-CoV-2 directly attacks the heart and whether acute cardiac effects of the illness may lead to some kind of lingering cardiomyopathy.
The field’s grasp of those issues advanced a bit in two new reports published July 27 in JAMA Cardiology that seem to validate concerns the virus can infect the myocardium, without necessarily causing myocarditis and the possibility that some “recovered” patients may be left with persisting myocardial injury and inflammation that potentially could later manifest as heart failure.
Persisting inflammation by cardiac magnetic resonance
A prospective cohort study with 100 patients recovered from a recent bout of the disease showed evidence of ventricular dysfunction, greater ventricular mass, and in 78% of the cohort, signs of myocardial inflammation by cardiac magnetic resonance (CMR) imaging. The CMR findings correlated with elevations in troponin T by high-sensitivity assay (hs-TnT).
Two-thirds of the cohort, whose acute COVID-19 severity had “ranged from asymptomatic to minor-to-moderate symptoms,” had recovered at home, whereas the remaining “severely unwell patients” had been hospitalized, wrote the authors, led by Valentina O. Püntmann, MD, PhD, University Hospital Frankfurt (Germany).
None of the patients had a history of heart failure or cardiomyopathy, although some had hypertension, diabetes, or evidence of coronary disease.
“Our findings demonstrate that participants with a relative paucity of preexisting cardiovascular condition and with mostly home-based recovery had frequent cardiac inflammatory involvement, which was similar to the hospitalized subgroup with regards to severity and extent,” the group noted.
“There is a considerable ongoing myocardial inflammation in the heart muscle weeks after recovery from COVID-19 illness. This finding is important because it may herald a considerable burden of heart failure in a few years down the line,” Dr. Püntmann said in an interview.
Early diagnosis would offer “a good chance that early treatment could reduce the relentless course of inflammatory damage or even halt it,” she said.
“The relatively clear onset of COVID-19 illness provides an opportunity, which we often do not have with other conditions, to take a proactive action and to look for heart involvement early, within a few weeks of recovery.”
The study’s CMR evidence of inflammation edema, scarring, and pericardial effusion are among “the major diagnostic criteria for inflammatory and viral myocarditis,” observed Biykem Bozkurt, MD, PhD, from Baylor College of Medicine, Houston, who wasn’t part of either new study.
The findings suggest – consistent with previous evidence – that some patients with recent COVID-19 may be left with ongoing myocardial inflammation, and this study further adds that it could potentially become subacute or even chronic and in some may not be totally reversible, she said in an interview. How long the effects are likely to persist “remains to be determined. We need longer-term outcomes data.”
Viral presence without myocarditis
The accompanying report featured a postmortem analysis of hearts from 39 patients with mostly severe COVID-19 that pointed to a significant SARS-CoV-2 presence and signs that the virus vigorously replicated in the myocardium.
But there was no evidence that the infection led to fulminant myocarditis. Rather, the virus had apparently infiltrated the heart by localizing in interstitial cells or in macrophages that took up in the myocardium without actually entering myocytes, concluded the report’s authors, led by Diana Lindner, PhD, from the University Heart and Vascular Centre, Hamburg (Germany).
The findings suggest “that the presence of SARS-CoV-2 in cardiac tissue does not necessarily cause an inflammatory reaction consistent with clinical myocarditis,” the group wrote.
Previously in the literature, in “cases in which myocardial inflammation was present, there was also evidence of clinical myocarditis, and therefore the current cases underlie a different pathophysiology,” they concluded.
No evidence of the virus was seen in 15 cases, about 61% of the group. In 16 of the remaining 24 hearts, the viral load exceeded 1,000 copies per mcg of RNA, a substantial presence. Those 16 showed increased expression of inflammatory cytokines but no inflammatory cell infiltrates or changes in leukocyte counts, the researchers noted.
“Findings of suggested viral replication in the cases with a very high viral load are showing that we need to do more studies to find out long-term consequences, which we do not know right now,” senior author Dirk Westermann, MD, also from the University Heart and Vascular Centre, Hamburg, said.
Implications for heart failure
The postmortem findings from Dr. Lindner and associates “provide intriguing evidence that COVID-19 is associated with at least some component of myocardial injury, perhaps as the result of direct viral infection of the heart,” wrote Clyde W. Yancy, MD, MSc, from Northwestern University, Chicago, and Gregg C. Fonarow, MD, from the University of California, Los Angeles, in an editorial accompanying both reports.
The CMR study from Dr. Püntmann and colleagues – on the backdrop of earlier COVID-19 observations – suggests the potential for “residual left ventricular dysfunction and ongoing inflammation” in the months following a COVID-19 diagnosis. Both developments may be “of sufficient concern to represent a nidus for new-onset heart failure and other cardiovascular complications,” contend Dr. Yancy and Dr. Fonarow.
“When added to the postmortem pathological findings from Lindner et al, we see the plot thickening and we are inclined to raise a new and very evident concern that cardiomyopathy and heart failure related to COVID-19 may potentially evolve as the natural history of this infection becomes clearer,” they wrote.
Some patients, having recovered from the acute illness, may be left with a chronic inflammatory state that probably puts them at increased risk for future heart failure, agreed Dr. Bozkurt when interviewed. “They could show further decline in cardiac function, and their recovery might take longer than with the usual viral illnesses that we see,” she said.
“There could also be a risk of sudden death. Inflammation sometimes gives rise to sudden death and ventricular arrhythmia, which I would be very worried about, especially if the myocardium is stressed,” Dr. Bozkurt said. “So competitive sports in those patients potentially could be risky.”
COVID-19 cohort vs. matched control subjects
The CMR study from Dr. Püntmann and colleagues prospectively entered 100 patients recently recovered from an acute bout of COVID-19, either at home or at a hospital, who were followed in a registry based at University Hospital Frankfurt. Their median age was 49 years; 47% were female. They were compared with 50 age- and sex-matched control patients and 50 apparently healthy volunteers matched for risk factors, the group noted.
On the same day as the CMR assessment, the recently recovered patients, compared with the healthy control subjects and risk-factor matched control subjects, respectively, showed (P ≤ .001 in each case):
- A reduced left ventricular (LV) ejection fraction: 56% vs. 60% and 61%.
- A higher LV end-diastolic volume index: 86 mL/m2 vs. 80 mL/m2 and 75 mL/m2.
- A greater LV mass index: 51 g/m2 vs. 47 g/m2 and 53 g/m2.
- A higher hs-TnT level: 5.6 pg/mL vs. 3.2 pg/mL and 3.9 pg/mL.
- A greater prevalence of hs-TnT levels 3 pg/mL or more: 71% vs. 11% and 31%.
At CMR, 78% of the recovered COVID-19 patients showed abnormalities that included raised myocardial native T1 and T2 mapping, which is suggestive of fibrosis and edema from inflammation, compared with the two control groups (P < .001 for all differences), “independent of preexisting conditions, severity and overall course of the acute illness, and the time from the original diagnosis,” the group wrote. Native T1 and T2 mapping correlated significantly with hs-TnT.
“We now have the diagnostic means to detect cardiac inflammation early, and we need make every effort to apply them in every day practice,”Dr. Püntmann said in the interview.
“Using cardiac MRI will allow us to raise our game against COVID-19 and proactively develop efficient cardioprotective treatments,” she said. “Until we have effective means of protecting from the infection, that is vaccination, we must act swiftly and within the means at hand.”
The analysis evokes several other ways patients with COVID-19 might be screened for significant myocardial involvement.
“Strategies could include checking troponins, not only at admission but maybe at discharge and perhaps even those individuals who are at home and are not necessarily requiring care,” Dr. Bozkurt said.
“Biomarker profiling and screening for ongoing inflammation probably are going to be important components of COVID-19, especially for those with subclinical risk and disease.”
Dr. Westermann proposed that troponin elevations at discharge “might be a good starting point” for selecting COVID-19 patients for functional testing or imaging to screen for cardiac sequelae. Performing such tests routinely now “would be overwhelming given the massive increase in patients we still see today.”
Dr. Püntmann had no disclosures; statements of potential conflict for the other authors are in the report. Dr. Bozkurt has previously disclosed receiving consultant fees or honoraria from Bayer Healthcare, Bristol-Myers Squibb, Lantheus Medical Imaging, and Respicardia; serving on a data safety monitoring board for LivaNova USA ; and having unspecified relationships with Abbott Laboratories. Dr. Lindner had no disclosures; Dr. Westermann reported receiving personal fees from AstraZeneca, Bayer, Novartis, and Medtronic. Dr. Yancy is a deputy editor and Dr. Fonarow a section editor for JAMA Cardiology. Dr. Yancy had no other disclosures. Dr. Fonarow reported receiving personal fees from Abbott Laboratories, Amgen, AstraZeneca, Bayer, CHF Solutions, Edwards Lifesciences, Janssen, Medtronic, Merck, and Novartis.
A version of this article originally appeared on Medscape.com.
More data needed to better understand COVID-19 skin manifestations
Qing Zhao, MD, Xiaokai Fang, MD, and their colleagues at the Shandong Provincial Hospital for Skin Diseases & Shandong Provincial Institute of Dermatology and Venereology, in Jinan, China, reported the results of a literature review of 44 articles published through May 2020 that included 507 patients with cutaneous manifestations of COVID-19. The review was published in the Journal of The European Academy of Dermatology and Venereology.
Nearly all of the patients (96%) were from Europe, and more than half were women (60%), with an average age of 49 years. Most patients had multiple skin symptoms, with the most common being erythema (44%), chilblain-like lesions (20%), urticaria-like lesions (16%), vesicular manifestations (13%), livedo/necrosis (6%), and petechiae (almost 2%). The authors described erythema as being present in specific sites, such as the trunk, extremities, flexural regions, face, and mucous membranes. Slightly less than half of all patients had significant pruritus.
Data on systemic COVID-19 symptoms were available for 431 patients and included fever in about two-thirds of patients and cough in almost 70%, with dyspnea in almost half of patients. Almost 60% had fatigue, and almost 60% had asthenia. Information about the onset of skin symptoms was available in 88 patients; of these patients, lesions were seen an average of almost 10 days after systemic symptoms appeared and, in almost 15%, were the first symptoms noted.
Histopathologic exams were done for only 23 patients and, in all cases, showed “inflammatory features without specific pathological changes, such as lymphocyte infiltration.” In one study, reverse transcription polymerase chain reaction testing of skin biopsy specimens tested negative for SARS-CoV-2.
Expression of ACE2, the receptor of SARS-CoV-2, in the skin was evaluated in six of the studies. “Higher ACE2 expression was identified in keratinocytes, mainly in differentiating keratinocytes and basal cells compared to the other cells of skin tissues,” the authors wrote. These results were confirmed with immunohistochemistry, which, they said, found “ACE2-positive keratinocytes in the stratum basal, the stratum spinosum, and the stratum granulosum of epiderma.” They added that this provides evidence “for percutaneous infection or the entry of virus into patients through skin tissues,” but cautioned that more research is needed.
The authors acknowledged that there are still many unanswered questions about COVID-19, and that more clinical data and research are needed, to improve the understanding of the cutaneous manifestations associated with COVID-19.
In an interview, Alisa N. Femia, MD, director of inpatient dermatology in the department of dermatology at New York University, said that the cutaneous signs described in the review align well with what she has seen in patients with COVID-19.
At this point, it is unclear whether cutaneous manifestations of COVID-19 are a result of SARS-CoV-2 invading the skin or an immune response related to SARS-CoV-2, noted Dr. Femia, who was not involved in the research. One method of entry could be through transmitting virus present on the skin to another part of the body where infection is more likely.
While it is possible COVID-19 could be contracted through the skin, she noted, it is much more likely an individual would be infected by SARS-CoV-2 through more traditionally understood means of transmission, such as through respiratory droplets in person-to-person contact. “I think we are far away from drawing that conclusion, that one could touch a surface or a person who has COVID and contract it through their skin,” Dr. Femia said. “The skin has a lot of other ways to protect against that from occurring,” she added.
“SAR-CoV-2 obviously enters through the ACE2 receptor, which is fairly ubiquitous, and it has been seen in keratinocytes,” she said. “But the skin is one of our biggest barriers ... and further, studies to date have shown that that receptor is expressed in relatively low levels of the keratinocytes.”
Pathogenesis of different cutaneous manifestations may be different, Dr. Femia said. For example, urticaria and morbilliform eruption were described by the authors of the review as more benign eruptions, but pathogenesis may differ from that of so-called COVID toes and from the pathogenesis of purpura and ulcerations seen in patients with more severe disease, she noted. It is plausible, she added, that purpura and ulcerations may be a “direct invasion of SARS-CoV-2 into endothelial cells,” which creates secondary processes “that ultimately destroy the skin.”
Urticaria and morbilliform eruptions, on the other hand, “are more simply that the immune system is recognizing COVID, and in doing so, is also recognizing some antigens in the skin and creating a hypersensitive response to the skin” and has “nothing to do with the SARS-CoV-2 virus actually being in that location,” she said.
It is important to differentiate between patients who have skin manifestations attributed to COVID-19 and those with manifestations independent of COVID-19, which is difficult, Dr. Femia noted. A patient with COVID-19 and a cutaneous manifestation may be having a reaction to a medication. “It’s important to have a critical eye and to remember that, when we see these manifestations, we should always be investigating whether there was an alternative cause so that we can better learn what exactly we should be attributing to this infection,” she said
Adam Friedman, MD, professor and interim chair of dermatology at George Washington University, Washington, said the authors of the review had presented interesting work, but made some “assumptions that need to be proven.” Dr. Friedman also was not involved in the research, but agreed in an interview with the assessment that it is unlikely SARS-CoV-2 would penetrate the skin. While some viruses – such as the poxvirus that causes molluscum contagiosum and the herpes simplex virus – invade keratinocytes specifically, there is a particular clinical phenotype that results that is associated with changes in the epidermis. However, “the skin manifestations of COVID-19 do not fit with direct skin invasion, [but] rather the immune response to systemic disease,” he said.
“[I]n terms of systemic invasion through the skin, it is possible, but this study certainly doesn’t show that. The presence/expression of ACE2 in the epidermis doesn’t translate to route of infection,” Dr. Friedman said..
The study received financial support from Shandong First Medical University, the Innovation Project of Shandong Academy of Medical Sciences and the Shandong Province Taishan Scholar Project. The authors report no relevant financial disclosures. Dr. Femia and Dr. Friedman had no relevant financial disclosures.
SOURCE: Zhao Q et al. J Eur Acad Dermatol Venereol. 2020 Jun 28. doi: 10.1111/jdv.16778.
Qing Zhao, MD, Xiaokai Fang, MD, and their colleagues at the Shandong Provincial Hospital for Skin Diseases & Shandong Provincial Institute of Dermatology and Venereology, in Jinan, China, reported the results of a literature review of 44 articles published through May 2020 that included 507 patients with cutaneous manifestations of COVID-19. The review was published in the Journal of The European Academy of Dermatology and Venereology.
Nearly all of the patients (96%) were from Europe, and more than half were women (60%), with an average age of 49 years. Most patients had multiple skin symptoms, with the most common being erythema (44%), chilblain-like lesions (20%), urticaria-like lesions (16%), vesicular manifestations (13%), livedo/necrosis (6%), and petechiae (almost 2%). The authors described erythema as being present in specific sites, such as the trunk, extremities, flexural regions, face, and mucous membranes. Slightly less than half of all patients had significant pruritus.
Data on systemic COVID-19 symptoms were available for 431 patients and included fever in about two-thirds of patients and cough in almost 70%, with dyspnea in almost half of patients. Almost 60% had fatigue, and almost 60% had asthenia. Information about the onset of skin symptoms was available in 88 patients; of these patients, lesions were seen an average of almost 10 days after systemic symptoms appeared and, in almost 15%, were the first symptoms noted.
Histopathologic exams were done for only 23 patients and, in all cases, showed “inflammatory features without specific pathological changes, such as lymphocyte infiltration.” In one study, reverse transcription polymerase chain reaction testing of skin biopsy specimens tested negative for SARS-CoV-2.
Expression of ACE2, the receptor of SARS-CoV-2, in the skin was evaluated in six of the studies. “Higher ACE2 expression was identified in keratinocytes, mainly in differentiating keratinocytes and basal cells compared to the other cells of skin tissues,” the authors wrote. These results were confirmed with immunohistochemistry, which, they said, found “ACE2-positive keratinocytes in the stratum basal, the stratum spinosum, and the stratum granulosum of epiderma.” They added that this provides evidence “for percutaneous infection or the entry of virus into patients through skin tissues,” but cautioned that more research is needed.
The authors acknowledged that there are still many unanswered questions about COVID-19, and that more clinical data and research are needed, to improve the understanding of the cutaneous manifestations associated with COVID-19.
In an interview, Alisa N. Femia, MD, director of inpatient dermatology in the department of dermatology at New York University, said that the cutaneous signs described in the review align well with what she has seen in patients with COVID-19.
At this point, it is unclear whether cutaneous manifestations of COVID-19 are a result of SARS-CoV-2 invading the skin or an immune response related to SARS-CoV-2, noted Dr. Femia, who was not involved in the research. One method of entry could be through transmitting virus present on the skin to another part of the body where infection is more likely.
While it is possible COVID-19 could be contracted through the skin, she noted, it is much more likely an individual would be infected by SARS-CoV-2 through more traditionally understood means of transmission, such as through respiratory droplets in person-to-person contact. “I think we are far away from drawing that conclusion, that one could touch a surface or a person who has COVID and contract it through their skin,” Dr. Femia said. “The skin has a lot of other ways to protect against that from occurring,” she added.
“SAR-CoV-2 obviously enters through the ACE2 receptor, which is fairly ubiquitous, and it has been seen in keratinocytes,” she said. “But the skin is one of our biggest barriers ... and further, studies to date have shown that that receptor is expressed in relatively low levels of the keratinocytes.”
Pathogenesis of different cutaneous manifestations may be different, Dr. Femia said. For example, urticaria and morbilliform eruption were described by the authors of the review as more benign eruptions, but pathogenesis may differ from that of so-called COVID toes and from the pathogenesis of purpura and ulcerations seen in patients with more severe disease, she noted. It is plausible, she added, that purpura and ulcerations may be a “direct invasion of SARS-CoV-2 into endothelial cells,” which creates secondary processes “that ultimately destroy the skin.”
Urticaria and morbilliform eruptions, on the other hand, “are more simply that the immune system is recognizing COVID, and in doing so, is also recognizing some antigens in the skin and creating a hypersensitive response to the skin” and has “nothing to do with the SARS-CoV-2 virus actually being in that location,” she said.
It is important to differentiate between patients who have skin manifestations attributed to COVID-19 and those with manifestations independent of COVID-19, which is difficult, Dr. Femia noted. A patient with COVID-19 and a cutaneous manifestation may be having a reaction to a medication. “It’s important to have a critical eye and to remember that, when we see these manifestations, we should always be investigating whether there was an alternative cause so that we can better learn what exactly we should be attributing to this infection,” she said
Adam Friedman, MD, professor and interim chair of dermatology at George Washington University, Washington, said the authors of the review had presented interesting work, but made some “assumptions that need to be proven.” Dr. Friedman also was not involved in the research, but agreed in an interview with the assessment that it is unlikely SARS-CoV-2 would penetrate the skin. While some viruses – such as the poxvirus that causes molluscum contagiosum and the herpes simplex virus – invade keratinocytes specifically, there is a particular clinical phenotype that results that is associated with changes in the epidermis. However, “the skin manifestations of COVID-19 do not fit with direct skin invasion, [but] rather the immune response to systemic disease,” he said.
“[I]n terms of systemic invasion through the skin, it is possible, but this study certainly doesn’t show that. The presence/expression of ACE2 in the epidermis doesn’t translate to route of infection,” Dr. Friedman said..
The study received financial support from Shandong First Medical University, the Innovation Project of Shandong Academy of Medical Sciences and the Shandong Province Taishan Scholar Project. The authors report no relevant financial disclosures. Dr. Femia and Dr. Friedman had no relevant financial disclosures.
SOURCE: Zhao Q et al. J Eur Acad Dermatol Venereol. 2020 Jun 28. doi: 10.1111/jdv.16778.
Qing Zhao, MD, Xiaokai Fang, MD, and their colleagues at the Shandong Provincial Hospital for Skin Diseases & Shandong Provincial Institute of Dermatology and Venereology, in Jinan, China, reported the results of a literature review of 44 articles published through May 2020 that included 507 patients with cutaneous manifestations of COVID-19. The review was published in the Journal of The European Academy of Dermatology and Venereology.
Nearly all of the patients (96%) were from Europe, and more than half were women (60%), with an average age of 49 years. Most patients had multiple skin symptoms, with the most common being erythema (44%), chilblain-like lesions (20%), urticaria-like lesions (16%), vesicular manifestations (13%), livedo/necrosis (6%), and petechiae (almost 2%). The authors described erythema as being present in specific sites, such as the trunk, extremities, flexural regions, face, and mucous membranes. Slightly less than half of all patients had significant pruritus.
Data on systemic COVID-19 symptoms were available for 431 patients and included fever in about two-thirds of patients and cough in almost 70%, with dyspnea in almost half of patients. Almost 60% had fatigue, and almost 60% had asthenia. Information about the onset of skin symptoms was available in 88 patients; of these patients, lesions were seen an average of almost 10 days after systemic symptoms appeared and, in almost 15%, were the first symptoms noted.
Histopathologic exams were done for only 23 patients and, in all cases, showed “inflammatory features without specific pathological changes, such as lymphocyte infiltration.” In one study, reverse transcription polymerase chain reaction testing of skin biopsy specimens tested negative for SARS-CoV-2.
Expression of ACE2, the receptor of SARS-CoV-2, in the skin was evaluated in six of the studies. “Higher ACE2 expression was identified in keratinocytes, mainly in differentiating keratinocytes and basal cells compared to the other cells of skin tissues,” the authors wrote. These results were confirmed with immunohistochemistry, which, they said, found “ACE2-positive keratinocytes in the stratum basal, the stratum spinosum, and the stratum granulosum of epiderma.” They added that this provides evidence “for percutaneous infection or the entry of virus into patients through skin tissues,” but cautioned that more research is needed.
The authors acknowledged that there are still many unanswered questions about COVID-19, and that more clinical data and research are needed, to improve the understanding of the cutaneous manifestations associated with COVID-19.
In an interview, Alisa N. Femia, MD, director of inpatient dermatology in the department of dermatology at New York University, said that the cutaneous signs described in the review align well with what she has seen in patients with COVID-19.
At this point, it is unclear whether cutaneous manifestations of COVID-19 are a result of SARS-CoV-2 invading the skin or an immune response related to SARS-CoV-2, noted Dr. Femia, who was not involved in the research. One method of entry could be through transmitting virus present on the skin to another part of the body where infection is more likely.
While it is possible COVID-19 could be contracted through the skin, she noted, it is much more likely an individual would be infected by SARS-CoV-2 through more traditionally understood means of transmission, such as through respiratory droplets in person-to-person contact. “I think we are far away from drawing that conclusion, that one could touch a surface or a person who has COVID and contract it through their skin,” Dr. Femia said. “The skin has a lot of other ways to protect against that from occurring,” she added.
“SAR-CoV-2 obviously enters through the ACE2 receptor, which is fairly ubiquitous, and it has been seen in keratinocytes,” she said. “But the skin is one of our biggest barriers ... and further, studies to date have shown that that receptor is expressed in relatively low levels of the keratinocytes.”
Pathogenesis of different cutaneous manifestations may be different, Dr. Femia said. For example, urticaria and morbilliform eruption were described by the authors of the review as more benign eruptions, but pathogenesis may differ from that of so-called COVID toes and from the pathogenesis of purpura and ulcerations seen in patients with more severe disease, she noted. It is plausible, she added, that purpura and ulcerations may be a “direct invasion of SARS-CoV-2 into endothelial cells,” which creates secondary processes “that ultimately destroy the skin.”
Urticaria and morbilliform eruptions, on the other hand, “are more simply that the immune system is recognizing COVID, and in doing so, is also recognizing some antigens in the skin and creating a hypersensitive response to the skin” and has “nothing to do with the SARS-CoV-2 virus actually being in that location,” she said.
It is important to differentiate between patients who have skin manifestations attributed to COVID-19 and those with manifestations independent of COVID-19, which is difficult, Dr. Femia noted. A patient with COVID-19 and a cutaneous manifestation may be having a reaction to a medication. “It’s important to have a critical eye and to remember that, when we see these manifestations, we should always be investigating whether there was an alternative cause so that we can better learn what exactly we should be attributing to this infection,” she said
Adam Friedman, MD, professor and interim chair of dermatology at George Washington University, Washington, said the authors of the review had presented interesting work, but made some “assumptions that need to be proven.” Dr. Friedman also was not involved in the research, but agreed in an interview with the assessment that it is unlikely SARS-CoV-2 would penetrate the skin. While some viruses – such as the poxvirus that causes molluscum contagiosum and the herpes simplex virus – invade keratinocytes specifically, there is a particular clinical phenotype that results that is associated with changes in the epidermis. However, “the skin manifestations of COVID-19 do not fit with direct skin invasion, [but] rather the immune response to systemic disease,” he said.
“[I]n terms of systemic invasion through the skin, it is possible, but this study certainly doesn’t show that. The presence/expression of ACE2 in the epidermis doesn’t translate to route of infection,” Dr. Friedman said..
The study received financial support from Shandong First Medical University, the Innovation Project of Shandong Academy of Medical Sciences and the Shandong Province Taishan Scholar Project. The authors report no relevant financial disclosures. Dr. Femia and Dr. Friedman had no relevant financial disclosures.
SOURCE: Zhao Q et al. J Eur Acad Dermatol Venereol. 2020 Jun 28. doi: 10.1111/jdv.16778.
FROM THE JOURNAL OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY
Are you SARS-CoV-2 vaccine hesitant?
When the pandemic was just emerging from its infancy and we were just beginning to think about social distancing, I was sitting around enjoying an adult beverage and some gluten free (not my choice) snacks with some friends. A retired nurse who had just celebrated her 80th birthday said, “I can’t wait until they’ve developed a vaccine.” A former electrical engineer sitting just short of 2 meters to her left responded, “Don’t save me a place near the front of the line for something that is being developed in a program called Warp Speed.”
How do you feel about the potential SARS-CoV-2 vaccine? Are you going to roll up your sleeve as soon as the vaccine becomes available in your community? What are you going to suggest to your patients, your children? I suspect many of you will answer, “It depends.”
Will it make any difference to you which biochemical-immune-bending strategy is being used to make the vaccine? All of them will probably be the result of a clever sounding but novel technique, all of them with a track record that is measured in months and not years. Will you be swayed by how large the trials were? Or how long the follow-up lasted? How effective must the vaccine be to convince you that it is worth receiving or recommending? Do you have the tools and experience to make a decision like that? I know I don’t. And should you and I even be put in a position to make that decision?
In the past, you and I may have relied on the Centers for Disease Control and Prevention for advice. But given the somewhat murky and stormy relationship between the CDC and the president, the vaccine recommendation may be issued by the White House and not the CDC.
For those of us who were practicing medicine during the Swine Flu fiasco of 1976, the pace and the politics surrounding the development of a SARS-CoV-2 vaccine has a discomforting déjà vu quality about it. The fact that like this year 1976 was an election year that infused the development process with a sense of urgency above and beyond any of the concerns about the pandemic that never happened. Although causality was never proven, there was a surge in Guillain-Barré syndrome cases that had been linked temporally to the vaccine.
Of course, our pandemic is real, and it would be imprudent to wait a year or more to watch for long-term vaccine sequelae. However, I am more than a little concerned that fast tracking the development process may result in unfortunate consequences in the short term that could have been avoided with a more measured approach to trialing the vaccines.
The sad reality is that as a nation we tend to be impatient. We are drawn to quick fixes that come in a vial or a capsule. We are learning that simple measures like mask wearing and social distancing can make a difference in slowing the spread of the virus. It would be tragic to rush a vaccine into production that at best turns out to simply be an expensive alternative to the measures that we know work or at worst injures more of us than it saves.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
When the pandemic was just emerging from its infancy and we were just beginning to think about social distancing, I was sitting around enjoying an adult beverage and some gluten free (not my choice) snacks with some friends. A retired nurse who had just celebrated her 80th birthday said, “I can’t wait until they’ve developed a vaccine.” A former electrical engineer sitting just short of 2 meters to her left responded, “Don’t save me a place near the front of the line for something that is being developed in a program called Warp Speed.”
How do you feel about the potential SARS-CoV-2 vaccine? Are you going to roll up your sleeve as soon as the vaccine becomes available in your community? What are you going to suggest to your patients, your children? I suspect many of you will answer, “It depends.”
Will it make any difference to you which biochemical-immune-bending strategy is being used to make the vaccine? All of them will probably be the result of a clever sounding but novel technique, all of them with a track record that is measured in months and not years. Will you be swayed by how large the trials were? Or how long the follow-up lasted? How effective must the vaccine be to convince you that it is worth receiving or recommending? Do you have the tools and experience to make a decision like that? I know I don’t. And should you and I even be put in a position to make that decision?
In the past, you and I may have relied on the Centers for Disease Control and Prevention for advice. But given the somewhat murky and stormy relationship between the CDC and the president, the vaccine recommendation may be issued by the White House and not the CDC.
For those of us who were practicing medicine during the Swine Flu fiasco of 1976, the pace and the politics surrounding the development of a SARS-CoV-2 vaccine has a discomforting déjà vu quality about it. The fact that like this year 1976 was an election year that infused the development process with a sense of urgency above and beyond any of the concerns about the pandemic that never happened. Although causality was never proven, there was a surge in Guillain-Barré syndrome cases that had been linked temporally to the vaccine.
Of course, our pandemic is real, and it would be imprudent to wait a year or more to watch for long-term vaccine sequelae. However, I am more than a little concerned that fast tracking the development process may result in unfortunate consequences in the short term that could have been avoided with a more measured approach to trialing the vaccines.
The sad reality is that as a nation we tend to be impatient. We are drawn to quick fixes that come in a vial or a capsule. We are learning that simple measures like mask wearing and social distancing can make a difference in slowing the spread of the virus. It would be tragic to rush a vaccine into production that at best turns out to simply be an expensive alternative to the measures that we know work or at worst injures more of us than it saves.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
When the pandemic was just emerging from its infancy and we were just beginning to think about social distancing, I was sitting around enjoying an adult beverage and some gluten free (not my choice) snacks with some friends. A retired nurse who had just celebrated her 80th birthday said, “I can’t wait until they’ve developed a vaccine.” A former electrical engineer sitting just short of 2 meters to her left responded, “Don’t save me a place near the front of the line for something that is being developed in a program called Warp Speed.”
How do you feel about the potential SARS-CoV-2 vaccine? Are you going to roll up your sleeve as soon as the vaccine becomes available in your community? What are you going to suggest to your patients, your children? I suspect many of you will answer, “It depends.”
Will it make any difference to you which biochemical-immune-bending strategy is being used to make the vaccine? All of them will probably be the result of a clever sounding but novel technique, all of them with a track record that is measured in months and not years. Will you be swayed by how large the trials were? Or how long the follow-up lasted? How effective must the vaccine be to convince you that it is worth receiving or recommending? Do you have the tools and experience to make a decision like that? I know I don’t. And should you and I even be put in a position to make that decision?
In the past, you and I may have relied on the Centers for Disease Control and Prevention for advice. But given the somewhat murky and stormy relationship between the CDC and the president, the vaccine recommendation may be issued by the White House and not the CDC.
For those of us who were practicing medicine during the Swine Flu fiasco of 1976, the pace and the politics surrounding the development of a SARS-CoV-2 vaccine has a discomforting déjà vu quality about it. The fact that like this year 1976 was an election year that infused the development process with a sense of urgency above and beyond any of the concerns about the pandemic that never happened. Although causality was never proven, there was a surge in Guillain-Barré syndrome cases that had been linked temporally to the vaccine.
Of course, our pandemic is real, and it would be imprudent to wait a year or more to watch for long-term vaccine sequelae. However, I am more than a little concerned that fast tracking the development process may result in unfortunate consequences in the short term that could have been avoided with a more measured approach to trialing the vaccines.
The sad reality is that as a nation we tend to be impatient. We are drawn to quick fixes that come in a vial or a capsule. We are learning that simple measures like mask wearing and social distancing can make a difference in slowing the spread of the virus. It would be tragic to rush a vaccine into production that at best turns out to simply be an expensive alternative to the measures that we know work or at worst injures more of us than it saves.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
COVID-19 bits and pieces
It turns out that a pandemic, at least this COVID-19 version, can be a challenge for folks like me who are seldom at a loss for words. The pandemic has so overwhelmed every corner of our lives that it is hard to think of another topic on which to pontificate and still not tromp on someone’s political toes. One can always write about the pandemic itself, and I’ve tried that, but as the curtain is gradually being pulled back on this crafty little germ one runs the risk of making an observation today that will be disproved in a week or 2. However, I can’t suppress my urge to write, and so I have decided to share a few brief random observations. Of course they are related to the pandemic. And of course I realize that there is a better than fifty percent chance that they will be proved wrong by the time you read my next Letters from Maine.
Under the radar
Two of the many mysteries about SARS-CoV-2 involve young children who as a group appear to be less easily infected than adults and even when infected seem to be less likely to spread the disease to other people, particularly adults. One explanation posited by some researchers in France is that young children are less likely to have symptoms such as cough and are less powerful speakers and so might be less likely to spew out a significant number of infected aerosolized droplets (“How to Reopen Schools: What Science and Other Countries Teach Us.” By Pam Belluck, Apoorva Mandavill, and Benedict Carey. New York Times, July 11, 2020). While there are probably several factors to explain this observation, one may be that young children are short, seldom taller than an adult waistline. I suspect the majority of aerosols they emit fall and inactivate harmlessly to the floor several feet below an adult’s nose and mouth. Regardless of the explanation, it appears to be good news for the opening of schools, at least for the early grades.
Forget the deep cleaning
There has been a glut of news stories about reopening schools, and many of these stories are accompanied by images of school custodians with buckets, mops, spray bottles, and sponges scouring desks and walls. The most recent image in our local newspaper was of someone scrubbing the underside of a desk. I know it’s taking the World Health Organization an unconscionable period of time to acknowledge that SARS-CoV-2 is airborne, but the rest of us should have gotten the message long ago and been directing our attention to air handling and ventilation. The urge to scrub and deep clean is a hard habit to break, but this nasty bug is not like influenza or a flesh eating bacteria in which deep cleaning might help. A better image to attach to a story on school reopening would be one of a custodian with a screwdriver struggling to pry open a classroom window that had been painted shut a decade ago.
Managing the inevitable
Middlebury College in Vermont and Bowdoin College here in Brunswick, Maine, are similar in many respects because they are small and situated in relatively isolated small New England towns with good track records for pandemic management. Middlebury has elected to invite all its 2,750 students back to campus, whereas Bowdoin has decided to allow only incoming first years and transfer students (for a total of about 600) to return. Both schools will institute similar testing and social distancing protocols and restrict students from access to their respective towns (“A Tale of 2 Colleges.” By Bill Burger. Inside Higher Ed, June 29,2020). It will be an interesting experiment. I’m voting for Middlebury and not because my son and daughter-in-law are alums, but because I think Middlebury seems to have acknowledged that no matter how diligent one is in creating a SARS-CoV-2–free environment at the outset, these are college kids and there will be some cases on both campuses. It is on how those inevitable realities are managed and contained that an institution should be judged.
Patience
Unfortunately, We always have been a restless and impatient population eager to get moving and it has driven us to greatness. Hopefully, patience will be a lesson that we will learn, along with many others.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
It turns out that a pandemic, at least this COVID-19 version, can be a challenge for folks like me who are seldom at a loss for words. The pandemic has so overwhelmed every corner of our lives that it is hard to think of another topic on which to pontificate and still not tromp on someone’s political toes. One can always write about the pandemic itself, and I’ve tried that, but as the curtain is gradually being pulled back on this crafty little germ one runs the risk of making an observation today that will be disproved in a week or 2. However, I can’t suppress my urge to write, and so I have decided to share a few brief random observations. Of course they are related to the pandemic. And of course I realize that there is a better than fifty percent chance that they will be proved wrong by the time you read my next Letters from Maine.
Under the radar
Two of the many mysteries about SARS-CoV-2 involve young children who as a group appear to be less easily infected than adults and even when infected seem to be less likely to spread the disease to other people, particularly adults. One explanation posited by some researchers in France is that young children are less likely to have symptoms such as cough and are less powerful speakers and so might be less likely to spew out a significant number of infected aerosolized droplets (“How to Reopen Schools: What Science and Other Countries Teach Us.” By Pam Belluck, Apoorva Mandavill, and Benedict Carey. New York Times, July 11, 2020). While there are probably several factors to explain this observation, one may be that young children are short, seldom taller than an adult waistline. I suspect the majority of aerosols they emit fall and inactivate harmlessly to the floor several feet below an adult’s nose and mouth. Regardless of the explanation, it appears to be good news for the opening of schools, at least for the early grades.
Forget the deep cleaning
There has been a glut of news stories about reopening schools, and many of these stories are accompanied by images of school custodians with buckets, mops, spray bottles, and sponges scouring desks and walls. The most recent image in our local newspaper was of someone scrubbing the underside of a desk. I know it’s taking the World Health Organization an unconscionable period of time to acknowledge that SARS-CoV-2 is airborne, but the rest of us should have gotten the message long ago and been directing our attention to air handling and ventilation. The urge to scrub and deep clean is a hard habit to break, but this nasty bug is not like influenza or a flesh eating bacteria in which deep cleaning might help. A better image to attach to a story on school reopening would be one of a custodian with a screwdriver struggling to pry open a classroom window that had been painted shut a decade ago.
Managing the inevitable
Middlebury College in Vermont and Bowdoin College here in Brunswick, Maine, are similar in many respects because they are small and situated in relatively isolated small New England towns with good track records for pandemic management. Middlebury has elected to invite all its 2,750 students back to campus, whereas Bowdoin has decided to allow only incoming first years and transfer students (for a total of about 600) to return. Both schools will institute similar testing and social distancing protocols and restrict students from access to their respective towns (“A Tale of 2 Colleges.” By Bill Burger. Inside Higher Ed, June 29,2020). It will be an interesting experiment. I’m voting for Middlebury and not because my son and daughter-in-law are alums, but because I think Middlebury seems to have acknowledged that no matter how diligent one is in creating a SARS-CoV-2–free environment at the outset, these are college kids and there will be some cases on both campuses. It is on how those inevitable realities are managed and contained that an institution should be judged.
Patience
Unfortunately, We always have been a restless and impatient population eager to get moving and it has driven us to greatness. Hopefully, patience will be a lesson that we will learn, along with many others.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
It turns out that a pandemic, at least this COVID-19 version, can be a challenge for folks like me who are seldom at a loss for words. The pandemic has so overwhelmed every corner of our lives that it is hard to think of another topic on which to pontificate and still not tromp on someone’s political toes. One can always write about the pandemic itself, and I’ve tried that, but as the curtain is gradually being pulled back on this crafty little germ one runs the risk of making an observation today that will be disproved in a week or 2. However, I can’t suppress my urge to write, and so I have decided to share a few brief random observations. Of course they are related to the pandemic. And of course I realize that there is a better than fifty percent chance that they will be proved wrong by the time you read my next Letters from Maine.
Under the radar
Two of the many mysteries about SARS-CoV-2 involve young children who as a group appear to be less easily infected than adults and even when infected seem to be less likely to spread the disease to other people, particularly adults. One explanation posited by some researchers in France is that young children are less likely to have symptoms such as cough and are less powerful speakers and so might be less likely to spew out a significant number of infected aerosolized droplets (“How to Reopen Schools: What Science and Other Countries Teach Us.” By Pam Belluck, Apoorva Mandavill, and Benedict Carey. New York Times, July 11, 2020). While there are probably several factors to explain this observation, one may be that young children are short, seldom taller than an adult waistline. I suspect the majority of aerosols they emit fall and inactivate harmlessly to the floor several feet below an adult’s nose and mouth. Regardless of the explanation, it appears to be good news for the opening of schools, at least for the early grades.
Forget the deep cleaning
There has been a glut of news stories about reopening schools, and many of these stories are accompanied by images of school custodians with buckets, mops, spray bottles, and sponges scouring desks and walls. The most recent image in our local newspaper was of someone scrubbing the underside of a desk. I know it’s taking the World Health Organization an unconscionable period of time to acknowledge that SARS-CoV-2 is airborne, but the rest of us should have gotten the message long ago and been directing our attention to air handling and ventilation. The urge to scrub and deep clean is a hard habit to break, but this nasty bug is not like influenza or a flesh eating bacteria in which deep cleaning might help. A better image to attach to a story on school reopening would be one of a custodian with a screwdriver struggling to pry open a classroom window that had been painted shut a decade ago.
Managing the inevitable
Middlebury College in Vermont and Bowdoin College here in Brunswick, Maine, are similar in many respects because they are small and situated in relatively isolated small New England towns with good track records for pandemic management. Middlebury has elected to invite all its 2,750 students back to campus, whereas Bowdoin has decided to allow only incoming first years and transfer students (for a total of about 600) to return. Both schools will institute similar testing and social distancing protocols and restrict students from access to their respective towns (“A Tale of 2 Colleges.” By Bill Burger. Inside Higher Ed, June 29,2020). It will be an interesting experiment. I’m voting for Middlebury and not because my son and daughter-in-law are alums, but because I think Middlebury seems to have acknowledged that no matter how diligent one is in creating a SARS-CoV-2–free environment at the outset, these are college kids and there will be some cases on both campuses. It is on how those inevitable realities are managed and contained that an institution should be judged.
Patience
Unfortunately, We always have been a restless and impatient population eager to get moving and it has driven us to greatness. Hopefully, patience will be a lesson that we will learn, along with many others.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Higher death rate seen in cancer patients with nosocomial COVID-19
, according to researchers.
In an observational study of patients with COVID-19 and cancer, 19% of patients had COVID-19 acquired during a non-COVID-related hospital stay, and 81% had community-acquired COVID-19.
At a median follow-up of 23 days, the overall mortality rate was 28%. However, the all-cause mortality rate in patients with nosocomial COVID-19 was more than double that of patients with community-acquired COVID-19, at 47% and 23%, respectively.
Arielle Elkrief, MD, of the University of Montreal, reported these results during the AACR virtual meeting: COVID-19 and Cancer.
“This is the first report that describes a high rate of hospital-acquired COVID-19 in patients with cancer, at a rate of 19%,” Dr. Elkrief said. “This was associated with high mortality in both univariate and multivariate analyses.”
The study included 250 adults and 3 children with COVID-19 and cancer who were identified between March 3 and May 23, 2020. They ranged in age from 4 to 95 years, but the median age was 73 years.
All patients had either laboratory-confirmed (95%) or presumed COVID-19 (5%) and invasive cancer. The most common cancer types were similar to those seen in the general population. Lung and breast cancer were the most common, followed by lymphoma, prostate cancer, and colorectal cancer. Most patients were on active anticancer therapy, most often chemotherapy.
Most patients (n = 236) were residents of Quebec, but 17 patients were residents of British Columbia.
“It is important to note that Quebec was one of the most heavily affected areas in North America at the time of the study,” Dr. Elkrief said.
Outcomes by group
There were 206 patients (81%) who had community-acquired COVID-19 and 47 (19%) who had nosocomial COVID-19. The two groups were similar with respect to sex, performance status, and cancer stage. A small trend toward more patients on active therapy was seen in the nosocomial group, but the difference did not reach statistical significance.
The median overall survival was 27 days in the nosocomial group and 71 days in the community-acquired group (hazard ratio, 2.2; P = .002).
A multivariate analysis showed that nosocomial infection was “strongly and independently associated with death,” Dr. Elkrief said. “Other risk factors for poor prognosis included age, poor [performance] status, and advanced stage of cancer.”
There were no significant differences between the hospital-acquired and community-acquired groups for other outcomes, including oxygen requirements (43% and 47%, respectively), ICU admission (13% and 11%), need for mechanical ventilation (6% and 5%), or length of stay (median, 9.5 days and 8.5 days).
The low rate of ICU admission, considering the mortality rate of 28%, “could reflect that patients with cancer are less likely to be admitted to the ICU,” Dr. Elkrief noted.
Applying the findings to practice
The findings reinforce the importance of adherence to stringent infection control guidelines to protect vulnerable patients, such as those with cancer, Dr. Elkrief said.
In ambulatory settings, this means decreasing in-person visits through increased use of teleconsultations, and for those who need to be seen in person, screening for symptoms or use of polymerase chain reaction testing should be used when resources are available, she said.
“Similar principles apply to chemotherapy treatment units,” Dr. Elkrief said. She added that staff must avoid cross-contamination between COVID and COVID-free zones, and that “dedicated personnel and equipment should be maintained and separate between these two zones.
“Adequate protective personal equipment and strict hand hygiene protocols are also of utmost importance,” Dr. Elkrief said. “The threat of COVID-19 is not behind us, and so we continue to enforce these strategies to protect our patients.”
Session moderator Gypsyamber D’Souza, PhD, an infectious disease epidemiologist at Johns Hopkins University in Baltimore, raised the question of whether the high nosocomial infection and death rate in this study was related to patients having more severe disease because of underlying comorbidities.
Dr. Elkrief explained that the overall mortality rate was indeed higher than the 13% reported in other studies, and it may reflect an overrepresentation of hospitalized or more severely ill patients in the cohort.
However, the investigators made every effort to include all patients with both cancer and COVID-19 by using systematic screening of inpatient and outpatients lists and registries.
Further, the multivariate analysis included both inpatients and outpatients and adjusted for known negative prognostic factors for COVID-19 outcomes. These included increasing age, poor performance status, and different comorbidities.
The finding that nosocomial infection was an independent predictor of death “pushed us to look at nosocomial infection as a new independent risk factor,” Dr. Elkrief said.
Dr. Elkrief reported grant support from AstraZeneca. Dr. D’Souza did not report any disclosures.
SOURCE: Elkrief A et al. AACR: COVID and Cancer, Abstract S12-01.
, according to researchers.
In an observational study of patients with COVID-19 and cancer, 19% of patients had COVID-19 acquired during a non-COVID-related hospital stay, and 81% had community-acquired COVID-19.
At a median follow-up of 23 days, the overall mortality rate was 28%. However, the all-cause mortality rate in patients with nosocomial COVID-19 was more than double that of patients with community-acquired COVID-19, at 47% and 23%, respectively.
Arielle Elkrief, MD, of the University of Montreal, reported these results during the AACR virtual meeting: COVID-19 and Cancer.
“This is the first report that describes a high rate of hospital-acquired COVID-19 in patients with cancer, at a rate of 19%,” Dr. Elkrief said. “This was associated with high mortality in both univariate and multivariate analyses.”
The study included 250 adults and 3 children with COVID-19 and cancer who were identified between March 3 and May 23, 2020. They ranged in age from 4 to 95 years, but the median age was 73 years.
All patients had either laboratory-confirmed (95%) or presumed COVID-19 (5%) and invasive cancer. The most common cancer types were similar to those seen in the general population. Lung and breast cancer were the most common, followed by lymphoma, prostate cancer, and colorectal cancer. Most patients were on active anticancer therapy, most often chemotherapy.
Most patients (n = 236) were residents of Quebec, but 17 patients were residents of British Columbia.
“It is important to note that Quebec was one of the most heavily affected areas in North America at the time of the study,” Dr. Elkrief said.
Outcomes by group
There were 206 patients (81%) who had community-acquired COVID-19 and 47 (19%) who had nosocomial COVID-19. The two groups were similar with respect to sex, performance status, and cancer stage. A small trend toward more patients on active therapy was seen in the nosocomial group, but the difference did not reach statistical significance.
The median overall survival was 27 days in the nosocomial group and 71 days in the community-acquired group (hazard ratio, 2.2; P = .002).
A multivariate analysis showed that nosocomial infection was “strongly and independently associated with death,” Dr. Elkrief said. “Other risk factors for poor prognosis included age, poor [performance] status, and advanced stage of cancer.”
There were no significant differences between the hospital-acquired and community-acquired groups for other outcomes, including oxygen requirements (43% and 47%, respectively), ICU admission (13% and 11%), need for mechanical ventilation (6% and 5%), or length of stay (median, 9.5 days and 8.5 days).
The low rate of ICU admission, considering the mortality rate of 28%, “could reflect that patients with cancer are less likely to be admitted to the ICU,” Dr. Elkrief noted.
Applying the findings to practice
The findings reinforce the importance of adherence to stringent infection control guidelines to protect vulnerable patients, such as those with cancer, Dr. Elkrief said.
In ambulatory settings, this means decreasing in-person visits through increased use of teleconsultations, and for those who need to be seen in person, screening for symptoms or use of polymerase chain reaction testing should be used when resources are available, she said.
“Similar principles apply to chemotherapy treatment units,” Dr. Elkrief said. She added that staff must avoid cross-contamination between COVID and COVID-free zones, and that “dedicated personnel and equipment should be maintained and separate between these two zones.
“Adequate protective personal equipment and strict hand hygiene protocols are also of utmost importance,” Dr. Elkrief said. “The threat of COVID-19 is not behind us, and so we continue to enforce these strategies to protect our patients.”
Session moderator Gypsyamber D’Souza, PhD, an infectious disease epidemiologist at Johns Hopkins University in Baltimore, raised the question of whether the high nosocomial infection and death rate in this study was related to patients having more severe disease because of underlying comorbidities.
Dr. Elkrief explained that the overall mortality rate was indeed higher than the 13% reported in other studies, and it may reflect an overrepresentation of hospitalized or more severely ill patients in the cohort.
However, the investigators made every effort to include all patients with both cancer and COVID-19 by using systematic screening of inpatient and outpatients lists and registries.
Further, the multivariate analysis included both inpatients and outpatients and adjusted for known negative prognostic factors for COVID-19 outcomes. These included increasing age, poor performance status, and different comorbidities.
The finding that nosocomial infection was an independent predictor of death “pushed us to look at nosocomial infection as a new independent risk factor,” Dr. Elkrief said.
Dr. Elkrief reported grant support from AstraZeneca. Dr. D’Souza did not report any disclosures.
SOURCE: Elkrief A et al. AACR: COVID and Cancer, Abstract S12-01.
, according to researchers.
In an observational study of patients with COVID-19 and cancer, 19% of patients had COVID-19 acquired during a non-COVID-related hospital stay, and 81% had community-acquired COVID-19.
At a median follow-up of 23 days, the overall mortality rate was 28%. However, the all-cause mortality rate in patients with nosocomial COVID-19 was more than double that of patients with community-acquired COVID-19, at 47% and 23%, respectively.
Arielle Elkrief, MD, of the University of Montreal, reported these results during the AACR virtual meeting: COVID-19 and Cancer.
“This is the first report that describes a high rate of hospital-acquired COVID-19 in patients with cancer, at a rate of 19%,” Dr. Elkrief said. “This was associated with high mortality in both univariate and multivariate analyses.”
The study included 250 adults and 3 children with COVID-19 and cancer who were identified between March 3 and May 23, 2020. They ranged in age from 4 to 95 years, but the median age was 73 years.
All patients had either laboratory-confirmed (95%) or presumed COVID-19 (5%) and invasive cancer. The most common cancer types were similar to those seen in the general population. Lung and breast cancer were the most common, followed by lymphoma, prostate cancer, and colorectal cancer. Most patients were on active anticancer therapy, most often chemotherapy.
Most patients (n = 236) were residents of Quebec, but 17 patients were residents of British Columbia.
“It is important to note that Quebec was one of the most heavily affected areas in North America at the time of the study,” Dr. Elkrief said.
Outcomes by group
There were 206 patients (81%) who had community-acquired COVID-19 and 47 (19%) who had nosocomial COVID-19. The two groups were similar with respect to sex, performance status, and cancer stage. A small trend toward more patients on active therapy was seen in the nosocomial group, but the difference did not reach statistical significance.
The median overall survival was 27 days in the nosocomial group and 71 days in the community-acquired group (hazard ratio, 2.2; P = .002).
A multivariate analysis showed that nosocomial infection was “strongly and independently associated with death,” Dr. Elkrief said. “Other risk factors for poor prognosis included age, poor [performance] status, and advanced stage of cancer.”
There were no significant differences between the hospital-acquired and community-acquired groups for other outcomes, including oxygen requirements (43% and 47%, respectively), ICU admission (13% and 11%), need for mechanical ventilation (6% and 5%), or length of stay (median, 9.5 days and 8.5 days).
The low rate of ICU admission, considering the mortality rate of 28%, “could reflect that patients with cancer are less likely to be admitted to the ICU,” Dr. Elkrief noted.
Applying the findings to practice
The findings reinforce the importance of adherence to stringent infection control guidelines to protect vulnerable patients, such as those with cancer, Dr. Elkrief said.
In ambulatory settings, this means decreasing in-person visits through increased use of teleconsultations, and for those who need to be seen in person, screening for symptoms or use of polymerase chain reaction testing should be used when resources are available, she said.
“Similar principles apply to chemotherapy treatment units,” Dr. Elkrief said. She added that staff must avoid cross-contamination between COVID and COVID-free zones, and that “dedicated personnel and equipment should be maintained and separate between these two zones.
“Adequate protective personal equipment and strict hand hygiene protocols are also of utmost importance,” Dr. Elkrief said. “The threat of COVID-19 is not behind us, and so we continue to enforce these strategies to protect our patients.”
Session moderator Gypsyamber D’Souza, PhD, an infectious disease epidemiologist at Johns Hopkins University in Baltimore, raised the question of whether the high nosocomial infection and death rate in this study was related to patients having more severe disease because of underlying comorbidities.
Dr. Elkrief explained that the overall mortality rate was indeed higher than the 13% reported in other studies, and it may reflect an overrepresentation of hospitalized or more severely ill patients in the cohort.
However, the investigators made every effort to include all patients with both cancer and COVID-19 by using systematic screening of inpatient and outpatients lists and registries.
Further, the multivariate analysis included both inpatients and outpatients and adjusted for known negative prognostic factors for COVID-19 outcomes. These included increasing age, poor performance status, and different comorbidities.
The finding that nosocomial infection was an independent predictor of death “pushed us to look at nosocomial infection as a new independent risk factor,” Dr. Elkrief said.
Dr. Elkrief reported grant support from AstraZeneca. Dr. D’Souza did not report any disclosures.
SOURCE: Elkrief A et al. AACR: COVID and Cancer, Abstract S12-01.
FROM AACR: COVID-19 AND CANCER
















