User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


The state of hospital medicine in 2018
Productivity, pay, and roles remain center stage
In a national health care environment undergoing unprecedented transformation, the specialty of hospital medicine appears to be an island of relative stability, a conclusion that is supported by the principal findings from SHM’s 2018 State of Hospital Medicine (SoHM) report.
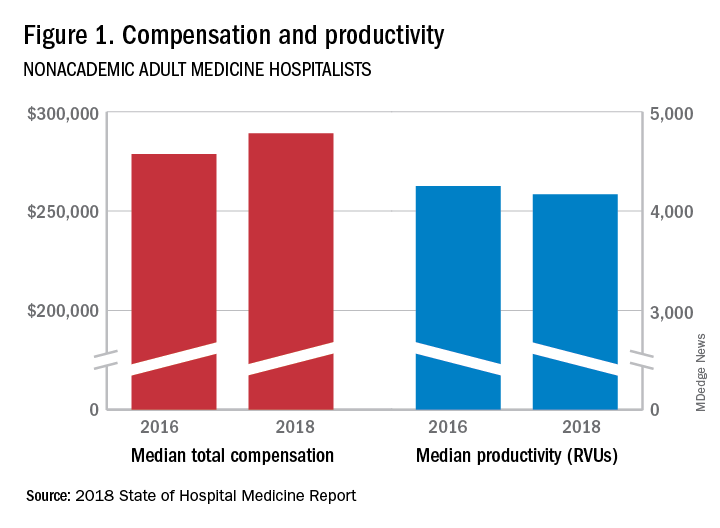
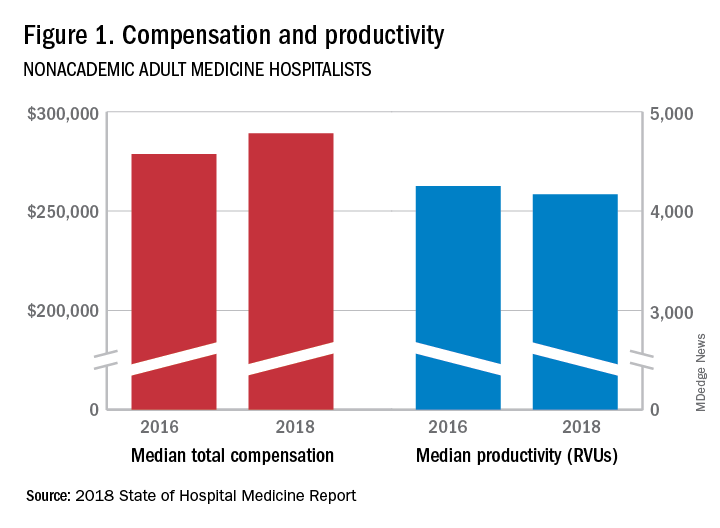
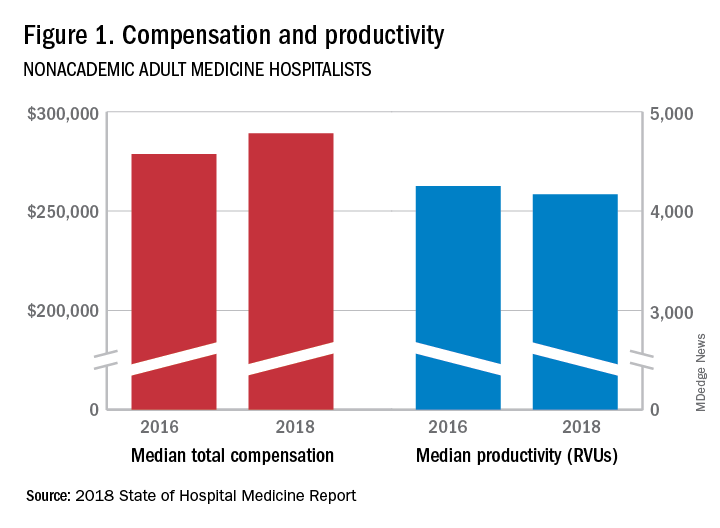
The report of hospitalist group practice characteristics, as well as other key data defining the field’s current status, that the Society of Hospital Medicine puts out every 2 years reveals that overall salaries for hospitalist physicians are up by 3.8% since 2016. Although productivity, as measured by work relative value units (RVUs), remained largely flat over the same period, financial support per full-time equivalent (FTE) physician position to hospitalist groups from their hospitals and health systems is up significantly.
Total support per FTE averaged $176,657 in 2018, 12% higher than in 2016, noted Leslie Flores, MHA, SFHM, of Nelson Flores Hospital Medicine Consultants, and a member of SHM’s Practice Analysis Committee, which oversees the biennial survey. Compensation and productivity data were collected by the Medical Group Management Association and licensed by SHM for inclusion in its report.
These findings – particularly the flat productivity – raise questions about long-term sustainability, Ms. Flores said. “What is going on? Do hospital administrators still recognize the value hospitalists bring to the operations and the quality of their hospitals? Or is paying the subsidy just a cost of doing business – a necessity for most hospitals in a setting where demand for hospitalist positions remains high?”
Andrew White, MD, FACP, SFHM, chair of SHM’s Practice Analysis Committee and director of the hospital medicine service at the University of Washington Medical Center, Seattle, said basic market forces dictate that it is “pretty much inconceivable” to run a modern hospital of any size without hospitalists.
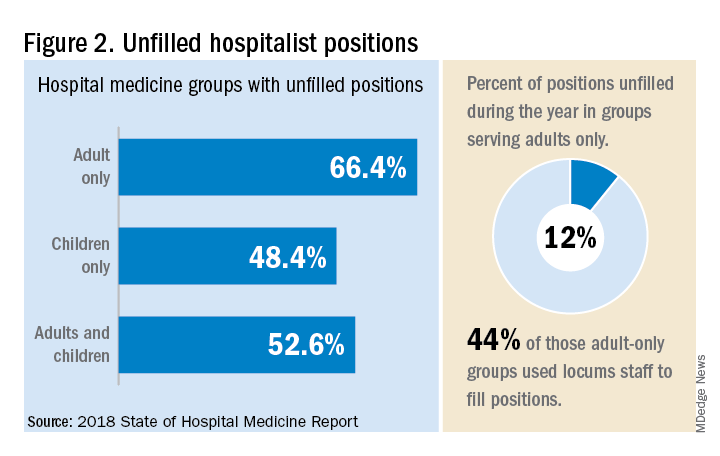
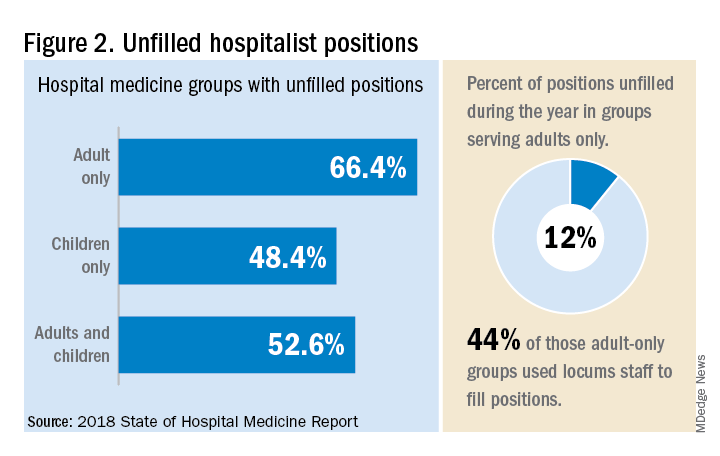
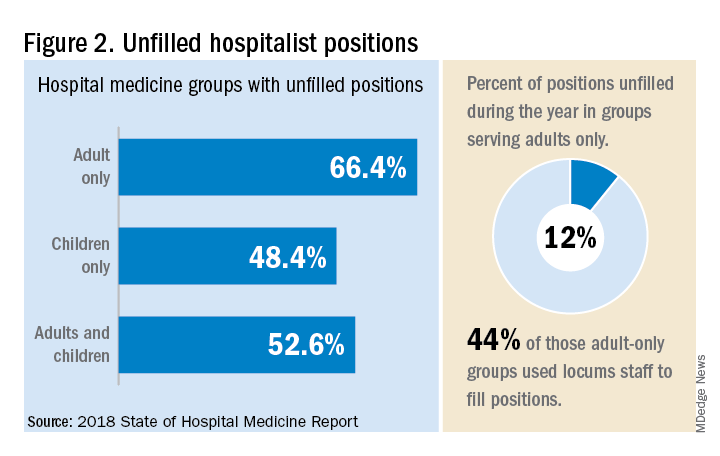
“Clearly, demand outstrips supply, which drives up salaries and support, whether CEOs feel that the hospitalist group is earning that support or not,” Dr. White said. “The unfilled hospitalist positions we identified speak to ongoing projected greater demand than supply. That said, hospitalists and group leaders can’t be complacent and must collaborate effectively with hospitals to provide highly valuable services.” Turnover of hospitalist positions was up slightly, he noted, at 7.4% in 2018, from 6.9% in 2016, reversing a trend of previous years.
But will these trends continue at a time when hospitals face continued pressure to cut costs, as the hospital medicine subsidy may represent one of their largest cost centers? Because the size of hospitalist groups continues to grow, hospitals’ total subsidy for hospital medicine is going up faster than the percentage increase in support per FTE.
How do hospitalists use the SoHM report?
Dr. White called the 2018 SoHM report the “most representative and balanced sample to date” of hospitalist group practices, with some of the highest quality data, thanks to more robust participation in the survey by pediatric groups and improved distribution among hospitalist management companies and academic programs.
“Not that past reports had major flaws, but this version is more authoritative, reflecting an intentional effort by our Practice Analysis Committee to bring in more participants from key groups,” he said.
The biennial report has been around long enough to achieve brand recognition in the field as the most authoritative source of information regarding hospitalist practice, he added. “We worked hard this year to balance the participants, with more of our responses than in the past coming from multi-hospital groups, whether 4 to 5 sites, or 20 to 30.”
Surveys were conducted online in January and February of 2018 in response to invitations mailed and emailed to targeted hospital medicine group leaders. A total of 569 groups completed the survey, representing 8,889 hospitalist FTEs, approximately 16% of the total hospitalist workforce. Responses were presented in several categories, including by size of program, region and employment model. Groups that care for adults only represented 87.9% of the surveys, while groups that care for children only were 6.7% and groups that care for both adults and children were 5.4%.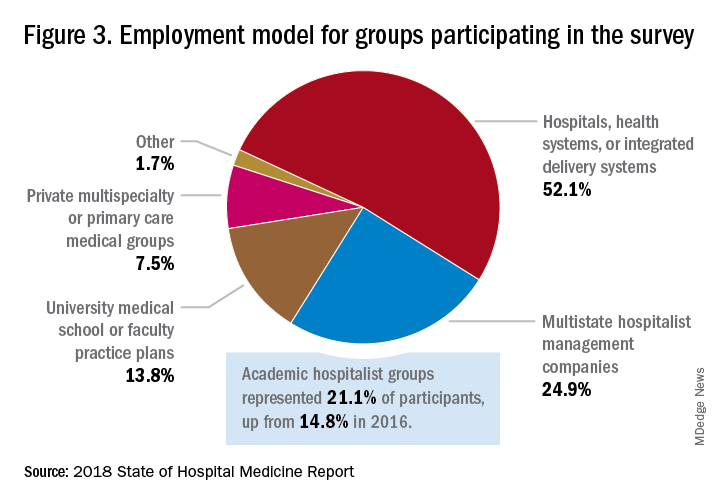
“This survey doesn’t tell us what should be best practice in hospital medicine,” Dr. White said, only what is actual current practice. He uses it in his own health system to not only contextualize and justify his group’s performance metrics for hospital administrators – relative to national and categorical averages – but also to see if the direction his group is following is consistent with what’s going on in the larger field.
“These data offer a very powerful resource regarding the trends in hospital medicine,” said Romil Chadha, MD, MPH, FACP, SFHM, associate division chief for operations in the division of hospital medicine at the University of Kentucky and UK Healthcare, Lexington. “It is my repository of data to go before my administrators for decisions that need to be made or to pilot new programs.”
Dr. Chadha also uses the data to help answer compensation, scheduling, and support questions from his group’s members.
Thomas McIlraith, MD, immediate past chairman of the hospital medicine department at Mercy Medical Group, Sacramento, Calif., said the report’s value is that it allows comparisons of salaries in different settings, and to see, for example, how night staffing is structured. “A lot of leaders I spoke to at SHM’s 2018 Leadership Academy in Vancouver were saying they didn’t feel up to parity with the national standards. You can use the report to look at the state of hospital medicine nationally and make comparisons,” he said.
Calls for more productivity
Roberta Himebaugh, MBA, SFHM, senior vice president of acute care services for the national hospitalist management company TeamHealth, and cochair of the SHM Practice Administrators Special Interest Group, said her company’s clients have traditionally asked for greater productivity from their hospitalist contracts as a way to decrease overall costs. Some markets are starting to see a change in that approach, she noted.
“Recently there’s been an increased focus on paying hospitalists to focus on quality rather than just productivity. Some of our clients are willing to pay for that, and we are trying to assign value to this non-billable time or adjust our productivity standards appropriately. I think hospitals definitely understand the value of non-billable services from hospitalists, but still will push us on the productivity targets,” Ms. Himebaugh said.
“I don’t believe hospital medicine can be sustainable long term on flat productivity or flat RVUs,” she added. “Yet the costs of burnout associated with pushing higher productivity are not sustainable, either.” So what are the answers? She said many inefficiencies are involved in responding to inquiries on the floor that could have been addressed another way, or waiting for the turnaround of diagnostic tests.
“Maybe we don’t need physicians to be in the hospital 24/7 if we have access to telehealth, or a partnership with the emergency department, or greater use of advanced care practice providers,” Ms. Himebaugh said. “Our hospitals are examining those options, and we have to look at how we can become more efficient and less costly. At TeamHealth, we are trying to staff for value – looking at patient flow patterns and adjusting our schedules accordingly. Is there a bolus of admissions tied to emergency department shift changes, or to certain days of the week? How can we move from the 12-hour shift that begins at 7 a.m. and ends at 7 p.m., and instead provide coverage for when the patients are there?”
Mark Williams, MD, MHM, chief of the division of hospital medicine at the University of Kentucky, Lexington, said he appreciates the volume of data in the report but wishes for even more survey participants, which could make the breakouts for subgroups such as academic hospitalists more robust. Other current sources of hospitalist salary data include the Association of American Medical Colleges (AAMC), which produces compensation reports to help medical schools and teaching hospitals with benchmarking, and the Faculty Practice Solution Center developed jointly by AAMC and Vizient to provide faculty practice plans with analytic tools. The Medical Group Management Association (MGMA) is another valuable source of information, some of which was licensed for inclusion in the SoHM report.
“There is no source of absolute truth that hospitalists can point to,” Dr. Williams said. “I will present my data and my administrators will reply: ‘We have our own data.’ Our institution has consistently ranked first or second nationwide for the sickest patients. We take more Medicaid and dually eligible patients, who have a lot of social issues. They take a lot of time to manage medically and the RVUs don’t reflect that. And yet I’m still judged by my RVUs generated per hospitalist. Hospital administrators understandably want to get the most productivity, and they are looking for their own data for average productivity numbers.”
Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., said that hospital medicine’s flat productivity trends would be difficult to sustain in the business world. But there aren’t easy or obvious ways to increase hospitalists’ productivity. The SoHM report also shows that as productivity increases, total compensation increases but at a lower rate, resulting in a gradual decrease in compensation per RVU.
Pressures to increase productivity can be a double-edged sword, Dr. Williams added. Demanding that doctors make more billable visits faster to generate more RVUs can be a recipe for burnout and turnover, with huge costs associated with recruiting replacements.
“If there was recent turnover of hospitalists at the hospital, with the need to find replacements, there may be institutional memory about that,” he said. “But where are hospitals spending their money? Bottom line, we still need to learn to cut our costs.”
How is hospitalist practice evolving?
In addition to payment and productivity data, the SoHM report provides a current picture of the evolving state of hospitalist group practices. A key thread is how the work hospitalists are doing, and the way they do it, is changing, with new information about comanagement roles, dedicated admitters, night coverage, geographic rounding, and the like.
Making greater use of nurse practitioners and physician assistants (NPs/PAs), may be one way to change the flat productivity trends, Dr. Brown said. With a cost per RVU that’s roughly half that of a doctor’s, NPs/PAs could contribute to the bottom line. But he sees surprisingly large variation in how hospitalist groups are using them. Typically, they are deployed at a ratio of four doctors to one NP/PA, but that ratio could be two to one or even one to one, he said.
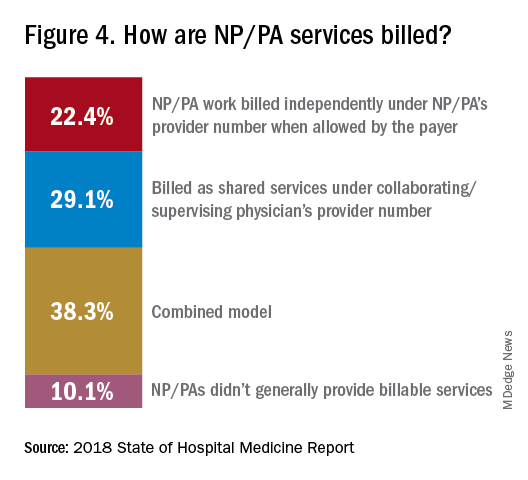
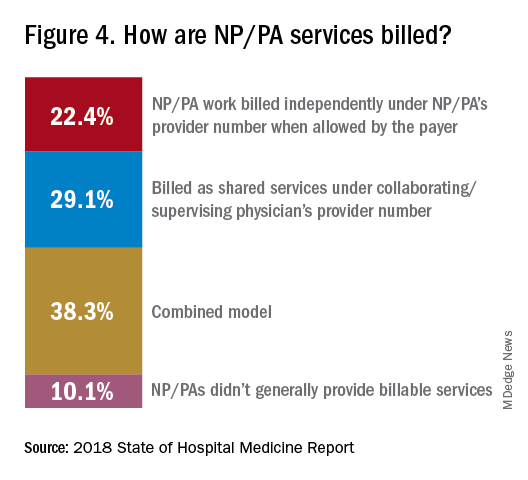
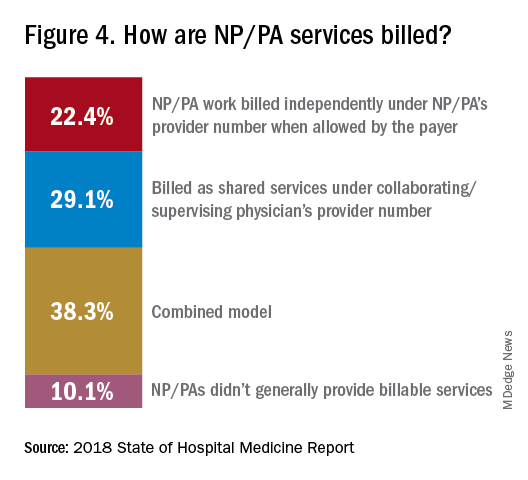
Use of NPs/PAs by academic hospitalist groups is up, from 52.1% in 2016 to 75.7% in 2018. For adult-only groups, 76.8% had NPs/PAs, with higher rates in hospitals and health systems and lower rates in the West region. But a lot of groups are using these practitioners for nonproductive work, and some are failing to generate any billing income, Dr. Brown said.
“The rate at which NPs/PAs performed billable services was higher in physician-owned practices, resulting in a lower cost per RVU, suggesting that many practices may be underutilizing their NPs/PAs or not sharing the work.” Not every NP or PA wants to or is able to care for very complex patients, Dr. Brown said, “but you want a system where the NP and PA can work at the highest level permitted by state law.”
The predominant scheduling model of hospital medicine, 7 days on duty followed by 7 days off, has diminished somewhat in recent years. There appears to be some fluctuation and a gradual move away from 7 on/7 off toward some kind of variable approach, since the former may not be physically sustainable for the doctor over the long haul, Dr. Brown said. Some groups are experimenting with a combined approach.
“I think balancing workload with manpower has always been a challenge for our field. Maybe we should be working shorter shifts or fewer days and making sure our hospitalists aren’t ever sitting around idle,” he said. “And could we come in on nonclinical days to do administrative tasks? I think the solution is out there, but we haven’t created the algorithms to define that yet. If you could somehow use the data for volume, number of beds, nurse staffing, etc., by year and seasonally, you might be able to reliably predict census. This is about applying data hospitals already have in their electronic health records, but utilizing the data in ways that are more helpful.”
Dr. McIlraith added that a big driver of the future of hospital medicine will be the evolution of the EHR and the digitalization of health care, as hospitals learn how to leverage more of what’s in their EHRs. “The impact will grow for hospitalists through the creation and maturation of big data systems – and the learning that can be extracted from what’s contained in the electronic health record.”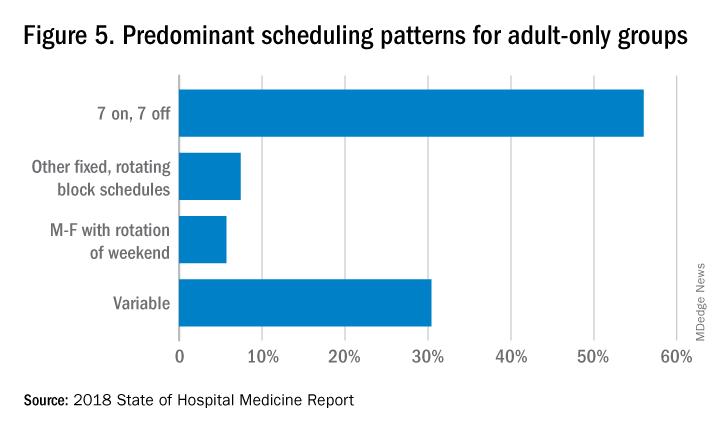
Another important question for hospitalist groups is their model of backup scheduling, to make sure there is a replacement available if a scheduled doctor calls in sick or if demand is unexpectedly high.
“In today’s world, this is how we have traditionally managed unpredictability,” Dr. Brown said. “You don’t know when you will need it, but if you need it, you want it immediately. So how do you pay for it – only when the doctor comes in, or also an amount just for being on call?” Some groups pay for both, he said, others for neither.
“We are a group of 70 hospitalists, and if someone is sick you can’t just shut down the service,” said Dr. Chadha. “We are one of the few to use incentives for both, which could include a 1-week decrease in clinical shifts in exchange for 2 weeks of backup. We have times with 25% usage of backup number 1, and 10% usage of backup number 2,” he noted. “But the goal is for our hospitalists to have assurances that there is a backup system and that it works.”
The presence of nocturnists in hospitals continues to rise, with 76.1% of adults-only groups having nocturnists, 27.6% of children-only groups, and 68.2% of adults and children groups. Geographic or unit-based hospital assignments have grown to 36.4% of adult-only groups.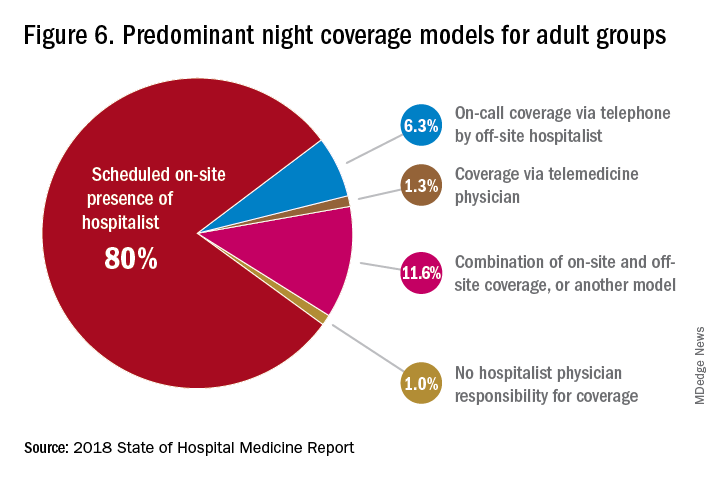
What are hospitalists’ other new roles?
“We have a large group of 50 doctors, with about 40 FTEs, and we are evolving from the traditional generalist role toward more subspecialty comanagement,” said Bryan Huang, MD, physician adviser and associate clinical professor in the division of hospital medicine at the University of California–San Diego. “Our hospitalists are asking what it means to be an academic hospitalist as our teaching roles have shrunk.”
Dr. Huang recently took on a new role as physician adviser for his hospital in such areas as utilization review, patient flow, and length of stay. “I’m spearheading a work group to address quality issues – all of which involve collaboration with other professionals. We also developed an admitting role here for a hospitalist whose sole role for the day is to admit patients.” Nationally up to 51.2% of hospitalist groups utilize a dedicated daytime admitter.
The report found that hospital services for which hospitalists are more likely to be attendings than consultants include GI/liver, 78.4%; palliative care, 77.3%; neurology/stroke, 73.6%; oncology, 67.8%; cardiology, 56.9%; and critical care, 50.7%. Conditions where hospitalists are more likely to consult rather than admit and attend include neurosurgery, orthopedics, general surgery, cardiovascular surgery, and other surgical subspecialties.
Other hospital services routinely provided by adult-only hospitalists include care of patients in an ICU setting (62.7%); primary responsibility for observation units (54.6%); primary clinical responsibility for rapid response teams (48.8%); primary responsibility for code blue or cardiac arrest teams (43.8%); nighttime admissions or tuck-in services (33.9%); and medical procedures (31.5%). For pediatric hospital medicine groups, care of healthy newborns and medical procedures were among the most common services provided, while for hospitalists serving adults and children, rapid response teams, ICUs, and specialty units were most common.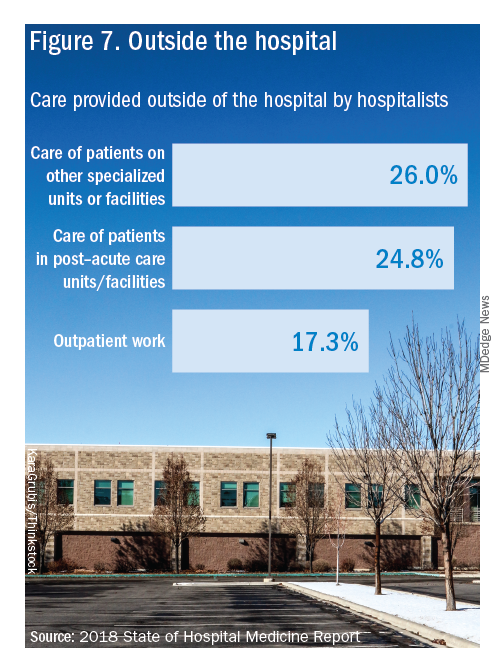
New models of payment for health care
As the larger health care system is being transformed by new payment models and benefit structures, including accountable care organizations (ACOs), value-based purchasing, bundled payments, and other forms of population-based coverage – which is described as a volume-to-value shift in health care – how are these new models affecting hospitalists?
Observers say penetration of these new models varies widely by locality but they haven’t had much direct impact on hospitalists’ practices – at least not yet. However, as hospitals and health systems find themselves needing to learn new ways to invest their resources differently in response to these trends, what matters to the hospital should be of great importance to the hospitalist group.
“I haven’t seen a lot of dramatic changes in how hospitalists engage with value-based purchasing,” Dr. White said. “If we know that someone is part of an ACO, the instinctual – and right – response is to treat them like any other patient. But we still need to be committed to not waste resources.”
Hospitalists are the best people to understand the intricacies of how the health care system works under value-based approaches, Dr. Huang said. “That’s why so many hospitalists have taken leadership positions in their hospitals. I think all of this translates to the practical, day-to-day work of hospitalists, reflected in our focus on readmissions and length of stay.”
Dr. Williams said the health care system still hasn’t turned the corner from fee-for-service to value-based purchasing. “It still represents a tiny fraction of the income of hospitalists. Hospitals still have to focus on the bottom line, as fee-for-service reimbursement for hospitalized patients continues to get squeezed, and ACOs aren’t exactly paying premium rates either. Ask almost any hospital CEO what drives their bottom line today and the answer is volume – along with optimizing productivity. Pretty much every place I look, the future does not look terribly rosy for hospitals.”
Ms. Himebaugh said she is bullish on hospital medicine, in the sense that it’s unlikely to go away anytime soon. “Hospitalists are needed and provide value. But I don’t think we have devised the right model yet. I’m not sure our current model is sustainable. We need to find new models we can afford that don’t require squeezing our providers.”
For more information about the 2018 State of Hospital Medicine Report, contact SHM’s Practice Management Department at: [email protected] or call 800-843-3360. See also: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/.
Productivity, pay, and roles remain center stage
Productivity, pay, and roles remain center stage
In a national health care environment undergoing unprecedented transformation, the specialty of hospital medicine appears to be an island of relative stability, a conclusion that is supported by the principal findings from SHM’s 2018 State of Hospital Medicine (SoHM) report.
The report of hospitalist group practice characteristics, as well as other key data defining the field’s current status, that the Society of Hospital Medicine puts out every 2 years reveals that overall salaries for hospitalist physicians are up by 3.8% since 2016. Although productivity, as measured by work relative value units (RVUs), remained largely flat over the same period, financial support per full-time equivalent (FTE) physician position to hospitalist groups from their hospitals and health systems is up significantly.
Total support per FTE averaged $176,657 in 2018, 12% higher than in 2016, noted Leslie Flores, MHA, SFHM, of Nelson Flores Hospital Medicine Consultants, and a member of SHM’s Practice Analysis Committee, which oversees the biennial survey. Compensation and productivity data were collected by the Medical Group Management Association and licensed by SHM for inclusion in its report.
These findings – particularly the flat productivity – raise questions about long-term sustainability, Ms. Flores said. “What is going on? Do hospital administrators still recognize the value hospitalists bring to the operations and the quality of their hospitals? Or is paying the subsidy just a cost of doing business – a necessity for most hospitals in a setting where demand for hospitalist positions remains high?”
Andrew White, MD, FACP, SFHM, chair of SHM’s Practice Analysis Committee and director of the hospital medicine service at the University of Washington Medical Center, Seattle, said basic market forces dictate that it is “pretty much inconceivable” to run a modern hospital of any size without hospitalists.
“Clearly, demand outstrips supply, which drives up salaries and support, whether CEOs feel that the hospitalist group is earning that support or not,” Dr. White said. “The unfilled hospitalist positions we identified speak to ongoing projected greater demand than supply. That said, hospitalists and group leaders can’t be complacent and must collaborate effectively with hospitals to provide highly valuable services.” Turnover of hospitalist positions was up slightly, he noted, at 7.4% in 2018, from 6.9% in 2016, reversing a trend of previous years.
But will these trends continue at a time when hospitals face continued pressure to cut costs, as the hospital medicine subsidy may represent one of their largest cost centers? Because the size of hospitalist groups continues to grow, hospitals’ total subsidy for hospital medicine is going up faster than the percentage increase in support per FTE.
How do hospitalists use the SoHM report?
Dr. White called the 2018 SoHM report the “most representative and balanced sample to date” of hospitalist group practices, with some of the highest quality data, thanks to more robust participation in the survey by pediatric groups and improved distribution among hospitalist management companies and academic programs.
“Not that past reports had major flaws, but this version is more authoritative, reflecting an intentional effort by our Practice Analysis Committee to bring in more participants from key groups,” he said.
The biennial report has been around long enough to achieve brand recognition in the field as the most authoritative source of information regarding hospitalist practice, he added. “We worked hard this year to balance the participants, with more of our responses than in the past coming from multi-hospital groups, whether 4 to 5 sites, or 20 to 30.”
Surveys were conducted online in January and February of 2018 in response to invitations mailed and emailed to targeted hospital medicine group leaders. A total of 569 groups completed the survey, representing 8,889 hospitalist FTEs, approximately 16% of the total hospitalist workforce. Responses were presented in several categories, including by size of program, region and employment model. Groups that care for adults only represented 87.9% of the surveys, while groups that care for children only were 6.7% and groups that care for both adults and children were 5.4%.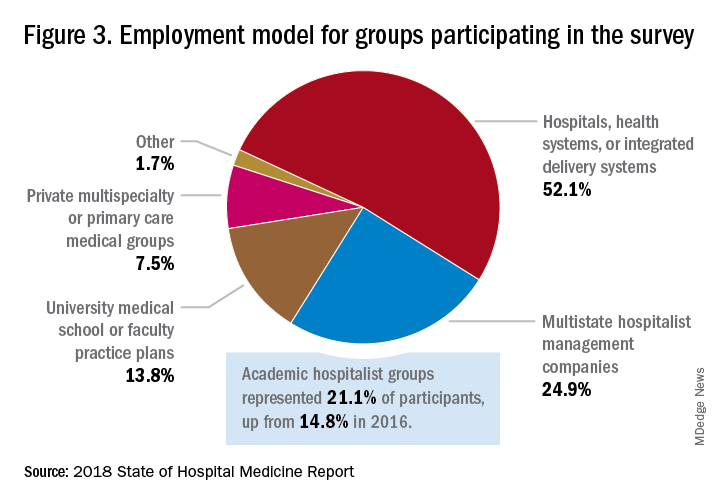
“This survey doesn’t tell us what should be best practice in hospital medicine,” Dr. White said, only what is actual current practice. He uses it in his own health system to not only contextualize and justify his group’s performance metrics for hospital administrators – relative to national and categorical averages – but also to see if the direction his group is following is consistent with what’s going on in the larger field.
“These data offer a very powerful resource regarding the trends in hospital medicine,” said Romil Chadha, MD, MPH, FACP, SFHM, associate division chief for operations in the division of hospital medicine at the University of Kentucky and UK Healthcare, Lexington. “It is my repository of data to go before my administrators for decisions that need to be made or to pilot new programs.”
Dr. Chadha also uses the data to help answer compensation, scheduling, and support questions from his group’s members.
Thomas McIlraith, MD, immediate past chairman of the hospital medicine department at Mercy Medical Group, Sacramento, Calif., said the report’s value is that it allows comparisons of salaries in different settings, and to see, for example, how night staffing is structured. “A lot of leaders I spoke to at SHM’s 2018 Leadership Academy in Vancouver were saying they didn’t feel up to parity with the national standards. You can use the report to look at the state of hospital medicine nationally and make comparisons,” he said.
Calls for more productivity
Roberta Himebaugh, MBA, SFHM, senior vice president of acute care services for the national hospitalist management company TeamHealth, and cochair of the SHM Practice Administrators Special Interest Group, said her company’s clients have traditionally asked for greater productivity from their hospitalist contracts as a way to decrease overall costs. Some markets are starting to see a change in that approach, she noted.
“Recently there’s been an increased focus on paying hospitalists to focus on quality rather than just productivity. Some of our clients are willing to pay for that, and we are trying to assign value to this non-billable time or adjust our productivity standards appropriately. I think hospitals definitely understand the value of non-billable services from hospitalists, but still will push us on the productivity targets,” Ms. Himebaugh said.
“I don’t believe hospital medicine can be sustainable long term on flat productivity or flat RVUs,” she added. “Yet the costs of burnout associated with pushing higher productivity are not sustainable, either.” So what are the answers? She said many inefficiencies are involved in responding to inquiries on the floor that could have been addressed another way, or waiting for the turnaround of diagnostic tests.
“Maybe we don’t need physicians to be in the hospital 24/7 if we have access to telehealth, or a partnership with the emergency department, or greater use of advanced care practice providers,” Ms. Himebaugh said. “Our hospitals are examining those options, and we have to look at how we can become more efficient and less costly. At TeamHealth, we are trying to staff for value – looking at patient flow patterns and adjusting our schedules accordingly. Is there a bolus of admissions tied to emergency department shift changes, or to certain days of the week? How can we move from the 12-hour shift that begins at 7 a.m. and ends at 7 p.m., and instead provide coverage for when the patients are there?”
Mark Williams, MD, MHM, chief of the division of hospital medicine at the University of Kentucky, Lexington, said he appreciates the volume of data in the report but wishes for even more survey participants, which could make the breakouts for subgroups such as academic hospitalists more robust. Other current sources of hospitalist salary data include the Association of American Medical Colleges (AAMC), which produces compensation reports to help medical schools and teaching hospitals with benchmarking, and the Faculty Practice Solution Center developed jointly by AAMC and Vizient to provide faculty practice plans with analytic tools. The Medical Group Management Association (MGMA) is another valuable source of information, some of which was licensed for inclusion in the SoHM report.
“There is no source of absolute truth that hospitalists can point to,” Dr. Williams said. “I will present my data and my administrators will reply: ‘We have our own data.’ Our institution has consistently ranked first or second nationwide for the sickest patients. We take more Medicaid and dually eligible patients, who have a lot of social issues. They take a lot of time to manage medically and the RVUs don’t reflect that. And yet I’m still judged by my RVUs generated per hospitalist. Hospital administrators understandably want to get the most productivity, and they are looking for their own data for average productivity numbers.”
Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., said that hospital medicine’s flat productivity trends would be difficult to sustain in the business world. But there aren’t easy or obvious ways to increase hospitalists’ productivity. The SoHM report also shows that as productivity increases, total compensation increases but at a lower rate, resulting in a gradual decrease in compensation per RVU.
Pressures to increase productivity can be a double-edged sword, Dr. Williams added. Demanding that doctors make more billable visits faster to generate more RVUs can be a recipe for burnout and turnover, with huge costs associated with recruiting replacements.
“If there was recent turnover of hospitalists at the hospital, with the need to find replacements, there may be institutional memory about that,” he said. “But where are hospitals spending their money? Bottom line, we still need to learn to cut our costs.”
How is hospitalist practice evolving?
In addition to payment and productivity data, the SoHM report provides a current picture of the evolving state of hospitalist group practices. A key thread is how the work hospitalists are doing, and the way they do it, is changing, with new information about comanagement roles, dedicated admitters, night coverage, geographic rounding, and the like.
Making greater use of nurse practitioners and physician assistants (NPs/PAs), may be one way to change the flat productivity trends, Dr. Brown said. With a cost per RVU that’s roughly half that of a doctor’s, NPs/PAs could contribute to the bottom line. But he sees surprisingly large variation in how hospitalist groups are using them. Typically, they are deployed at a ratio of four doctors to one NP/PA, but that ratio could be two to one or even one to one, he said.
Use of NPs/PAs by academic hospitalist groups is up, from 52.1% in 2016 to 75.7% in 2018. For adult-only groups, 76.8% had NPs/PAs, with higher rates in hospitals and health systems and lower rates in the West region. But a lot of groups are using these practitioners for nonproductive work, and some are failing to generate any billing income, Dr. Brown said.
“The rate at which NPs/PAs performed billable services was higher in physician-owned practices, resulting in a lower cost per RVU, suggesting that many practices may be underutilizing their NPs/PAs or not sharing the work.” Not every NP or PA wants to or is able to care for very complex patients, Dr. Brown said, “but you want a system where the NP and PA can work at the highest level permitted by state law.”
The predominant scheduling model of hospital medicine, 7 days on duty followed by 7 days off, has diminished somewhat in recent years. There appears to be some fluctuation and a gradual move away from 7 on/7 off toward some kind of variable approach, since the former may not be physically sustainable for the doctor over the long haul, Dr. Brown said. Some groups are experimenting with a combined approach.
“I think balancing workload with manpower has always been a challenge for our field. Maybe we should be working shorter shifts or fewer days and making sure our hospitalists aren’t ever sitting around idle,” he said. “And could we come in on nonclinical days to do administrative tasks? I think the solution is out there, but we haven’t created the algorithms to define that yet. If you could somehow use the data for volume, number of beds, nurse staffing, etc., by year and seasonally, you might be able to reliably predict census. This is about applying data hospitals already have in their electronic health records, but utilizing the data in ways that are more helpful.”
Dr. McIlraith added that a big driver of the future of hospital medicine will be the evolution of the EHR and the digitalization of health care, as hospitals learn how to leverage more of what’s in their EHRs. “The impact will grow for hospitalists through the creation and maturation of big data systems – and the learning that can be extracted from what’s contained in the electronic health record.”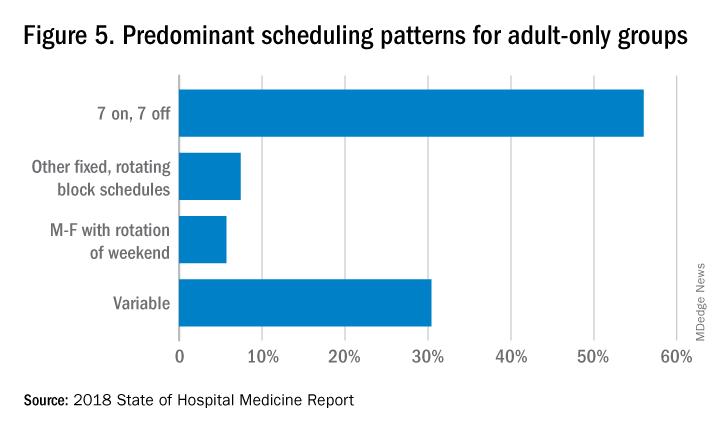
Another important question for hospitalist groups is their model of backup scheduling, to make sure there is a replacement available if a scheduled doctor calls in sick or if demand is unexpectedly high.
“In today’s world, this is how we have traditionally managed unpredictability,” Dr. Brown said. “You don’t know when you will need it, but if you need it, you want it immediately. So how do you pay for it – only when the doctor comes in, or also an amount just for being on call?” Some groups pay for both, he said, others for neither.
“We are a group of 70 hospitalists, and if someone is sick you can’t just shut down the service,” said Dr. Chadha. “We are one of the few to use incentives for both, which could include a 1-week decrease in clinical shifts in exchange for 2 weeks of backup. We have times with 25% usage of backup number 1, and 10% usage of backup number 2,” he noted. “But the goal is for our hospitalists to have assurances that there is a backup system and that it works.”
The presence of nocturnists in hospitals continues to rise, with 76.1% of adults-only groups having nocturnists, 27.6% of children-only groups, and 68.2% of adults and children groups. Geographic or unit-based hospital assignments have grown to 36.4% of adult-only groups.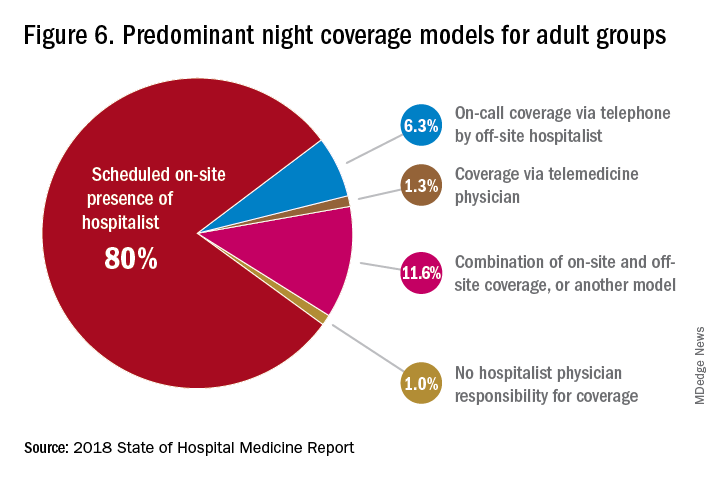
What are hospitalists’ other new roles?
“We have a large group of 50 doctors, with about 40 FTEs, and we are evolving from the traditional generalist role toward more subspecialty comanagement,” said Bryan Huang, MD, physician adviser and associate clinical professor in the division of hospital medicine at the University of California–San Diego. “Our hospitalists are asking what it means to be an academic hospitalist as our teaching roles have shrunk.”
Dr. Huang recently took on a new role as physician adviser for his hospital in such areas as utilization review, patient flow, and length of stay. “I’m spearheading a work group to address quality issues – all of which involve collaboration with other professionals. We also developed an admitting role here for a hospitalist whose sole role for the day is to admit patients.” Nationally up to 51.2% of hospitalist groups utilize a dedicated daytime admitter.
The report found that hospital services for which hospitalists are more likely to be attendings than consultants include GI/liver, 78.4%; palliative care, 77.3%; neurology/stroke, 73.6%; oncology, 67.8%; cardiology, 56.9%; and critical care, 50.7%. Conditions where hospitalists are more likely to consult rather than admit and attend include neurosurgery, orthopedics, general surgery, cardiovascular surgery, and other surgical subspecialties.
Other hospital services routinely provided by adult-only hospitalists include care of patients in an ICU setting (62.7%); primary responsibility for observation units (54.6%); primary clinical responsibility for rapid response teams (48.8%); primary responsibility for code blue or cardiac arrest teams (43.8%); nighttime admissions or tuck-in services (33.9%); and medical procedures (31.5%). For pediatric hospital medicine groups, care of healthy newborns and medical procedures were among the most common services provided, while for hospitalists serving adults and children, rapid response teams, ICUs, and specialty units were most common.
New models of payment for health care
As the larger health care system is being transformed by new payment models and benefit structures, including accountable care organizations (ACOs), value-based purchasing, bundled payments, and other forms of population-based coverage – which is described as a volume-to-value shift in health care – how are these new models affecting hospitalists?
Observers say penetration of these new models varies widely by locality but they haven’t had much direct impact on hospitalists’ practices – at least not yet. However, as hospitals and health systems find themselves needing to learn new ways to invest their resources differently in response to these trends, what matters to the hospital should be of great importance to the hospitalist group.
“I haven’t seen a lot of dramatic changes in how hospitalists engage with value-based purchasing,” Dr. White said. “If we know that someone is part of an ACO, the instinctual – and right – response is to treat them like any other patient. But we still need to be committed to not waste resources.”
Hospitalists are the best people to understand the intricacies of how the health care system works under value-based approaches, Dr. Huang said. “That’s why so many hospitalists have taken leadership positions in their hospitals. I think all of this translates to the practical, day-to-day work of hospitalists, reflected in our focus on readmissions and length of stay.”
Dr. Williams said the health care system still hasn’t turned the corner from fee-for-service to value-based purchasing. “It still represents a tiny fraction of the income of hospitalists. Hospitals still have to focus on the bottom line, as fee-for-service reimbursement for hospitalized patients continues to get squeezed, and ACOs aren’t exactly paying premium rates either. Ask almost any hospital CEO what drives their bottom line today and the answer is volume – along with optimizing productivity. Pretty much every place I look, the future does not look terribly rosy for hospitals.”
Ms. Himebaugh said she is bullish on hospital medicine, in the sense that it’s unlikely to go away anytime soon. “Hospitalists are needed and provide value. But I don’t think we have devised the right model yet. I’m not sure our current model is sustainable. We need to find new models we can afford that don’t require squeezing our providers.”
For more information about the 2018 State of Hospital Medicine Report, contact SHM’s Practice Management Department at: [email protected] or call 800-843-3360. See also: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/.
In a national health care environment undergoing unprecedented transformation, the specialty of hospital medicine appears to be an island of relative stability, a conclusion that is supported by the principal findings from SHM’s 2018 State of Hospital Medicine (SoHM) report.
The report of hospitalist group practice characteristics, as well as other key data defining the field’s current status, that the Society of Hospital Medicine puts out every 2 years reveals that overall salaries for hospitalist physicians are up by 3.8% since 2016. Although productivity, as measured by work relative value units (RVUs), remained largely flat over the same period, financial support per full-time equivalent (FTE) physician position to hospitalist groups from their hospitals and health systems is up significantly.
Total support per FTE averaged $176,657 in 2018, 12% higher than in 2016, noted Leslie Flores, MHA, SFHM, of Nelson Flores Hospital Medicine Consultants, and a member of SHM’s Practice Analysis Committee, which oversees the biennial survey. Compensation and productivity data were collected by the Medical Group Management Association and licensed by SHM for inclusion in its report.
These findings – particularly the flat productivity – raise questions about long-term sustainability, Ms. Flores said. “What is going on? Do hospital administrators still recognize the value hospitalists bring to the operations and the quality of their hospitals? Or is paying the subsidy just a cost of doing business – a necessity for most hospitals in a setting where demand for hospitalist positions remains high?”
Andrew White, MD, FACP, SFHM, chair of SHM’s Practice Analysis Committee and director of the hospital medicine service at the University of Washington Medical Center, Seattle, said basic market forces dictate that it is “pretty much inconceivable” to run a modern hospital of any size without hospitalists.
“Clearly, demand outstrips supply, which drives up salaries and support, whether CEOs feel that the hospitalist group is earning that support or not,” Dr. White said. “The unfilled hospitalist positions we identified speak to ongoing projected greater demand than supply. That said, hospitalists and group leaders can’t be complacent and must collaborate effectively with hospitals to provide highly valuable services.” Turnover of hospitalist positions was up slightly, he noted, at 7.4% in 2018, from 6.9% in 2016, reversing a trend of previous years.
But will these trends continue at a time when hospitals face continued pressure to cut costs, as the hospital medicine subsidy may represent one of their largest cost centers? Because the size of hospitalist groups continues to grow, hospitals’ total subsidy for hospital medicine is going up faster than the percentage increase in support per FTE.
How do hospitalists use the SoHM report?
Dr. White called the 2018 SoHM report the “most representative and balanced sample to date” of hospitalist group practices, with some of the highest quality data, thanks to more robust participation in the survey by pediatric groups and improved distribution among hospitalist management companies and academic programs.
“Not that past reports had major flaws, but this version is more authoritative, reflecting an intentional effort by our Practice Analysis Committee to bring in more participants from key groups,” he said.
The biennial report has been around long enough to achieve brand recognition in the field as the most authoritative source of information regarding hospitalist practice, he added. “We worked hard this year to balance the participants, with more of our responses than in the past coming from multi-hospital groups, whether 4 to 5 sites, or 20 to 30.”
Surveys were conducted online in January and February of 2018 in response to invitations mailed and emailed to targeted hospital medicine group leaders. A total of 569 groups completed the survey, representing 8,889 hospitalist FTEs, approximately 16% of the total hospitalist workforce. Responses were presented in several categories, including by size of program, region and employment model. Groups that care for adults only represented 87.9% of the surveys, while groups that care for children only were 6.7% and groups that care for both adults and children were 5.4%.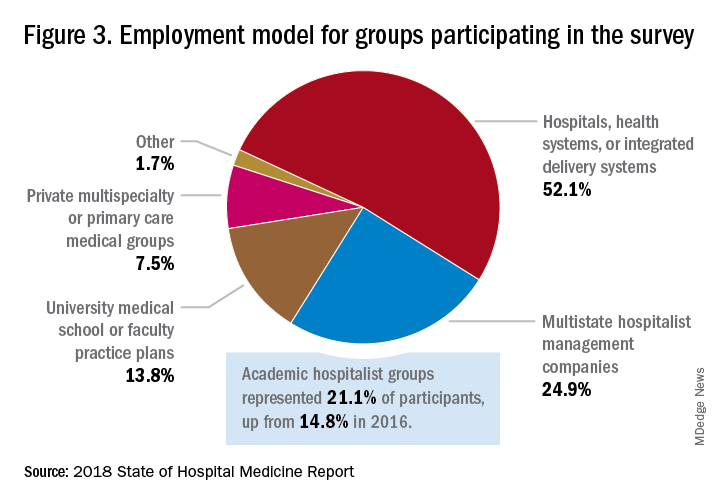
“This survey doesn’t tell us what should be best practice in hospital medicine,” Dr. White said, only what is actual current practice. He uses it in his own health system to not only contextualize and justify his group’s performance metrics for hospital administrators – relative to national and categorical averages – but also to see if the direction his group is following is consistent with what’s going on in the larger field.
“These data offer a very powerful resource regarding the trends in hospital medicine,” said Romil Chadha, MD, MPH, FACP, SFHM, associate division chief for operations in the division of hospital medicine at the University of Kentucky and UK Healthcare, Lexington. “It is my repository of data to go before my administrators for decisions that need to be made or to pilot new programs.”
Dr. Chadha also uses the data to help answer compensation, scheduling, and support questions from his group’s members.
Thomas McIlraith, MD, immediate past chairman of the hospital medicine department at Mercy Medical Group, Sacramento, Calif., said the report’s value is that it allows comparisons of salaries in different settings, and to see, for example, how night staffing is structured. “A lot of leaders I spoke to at SHM’s 2018 Leadership Academy in Vancouver were saying they didn’t feel up to parity with the national standards. You can use the report to look at the state of hospital medicine nationally and make comparisons,” he said.
Calls for more productivity
Roberta Himebaugh, MBA, SFHM, senior vice president of acute care services for the national hospitalist management company TeamHealth, and cochair of the SHM Practice Administrators Special Interest Group, said her company’s clients have traditionally asked for greater productivity from their hospitalist contracts as a way to decrease overall costs. Some markets are starting to see a change in that approach, she noted.
“Recently there’s been an increased focus on paying hospitalists to focus on quality rather than just productivity. Some of our clients are willing to pay for that, and we are trying to assign value to this non-billable time or adjust our productivity standards appropriately. I think hospitals definitely understand the value of non-billable services from hospitalists, but still will push us on the productivity targets,” Ms. Himebaugh said.
“I don’t believe hospital medicine can be sustainable long term on flat productivity or flat RVUs,” she added. “Yet the costs of burnout associated with pushing higher productivity are not sustainable, either.” So what are the answers? She said many inefficiencies are involved in responding to inquiries on the floor that could have been addressed another way, or waiting for the turnaround of diagnostic tests.
“Maybe we don’t need physicians to be in the hospital 24/7 if we have access to telehealth, or a partnership with the emergency department, or greater use of advanced care practice providers,” Ms. Himebaugh said. “Our hospitals are examining those options, and we have to look at how we can become more efficient and less costly. At TeamHealth, we are trying to staff for value – looking at patient flow patterns and adjusting our schedules accordingly. Is there a bolus of admissions tied to emergency department shift changes, or to certain days of the week? How can we move from the 12-hour shift that begins at 7 a.m. and ends at 7 p.m., and instead provide coverage for when the patients are there?”
Mark Williams, MD, MHM, chief of the division of hospital medicine at the University of Kentucky, Lexington, said he appreciates the volume of data in the report but wishes for even more survey participants, which could make the breakouts for subgroups such as academic hospitalists more robust. Other current sources of hospitalist salary data include the Association of American Medical Colleges (AAMC), which produces compensation reports to help medical schools and teaching hospitals with benchmarking, and the Faculty Practice Solution Center developed jointly by AAMC and Vizient to provide faculty practice plans with analytic tools. The Medical Group Management Association (MGMA) is another valuable source of information, some of which was licensed for inclusion in the SoHM report.
“There is no source of absolute truth that hospitalists can point to,” Dr. Williams said. “I will present my data and my administrators will reply: ‘We have our own data.’ Our institution has consistently ranked first or second nationwide for the sickest patients. We take more Medicaid and dually eligible patients, who have a lot of social issues. They take a lot of time to manage medically and the RVUs don’t reflect that. And yet I’m still judged by my RVUs generated per hospitalist. Hospital administrators understandably want to get the most productivity, and they are looking for their own data for average productivity numbers.”
Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., said that hospital medicine’s flat productivity trends would be difficult to sustain in the business world. But there aren’t easy or obvious ways to increase hospitalists’ productivity. The SoHM report also shows that as productivity increases, total compensation increases but at a lower rate, resulting in a gradual decrease in compensation per RVU.
Pressures to increase productivity can be a double-edged sword, Dr. Williams added. Demanding that doctors make more billable visits faster to generate more RVUs can be a recipe for burnout and turnover, with huge costs associated with recruiting replacements.
“If there was recent turnover of hospitalists at the hospital, with the need to find replacements, there may be institutional memory about that,” he said. “But where are hospitals spending their money? Bottom line, we still need to learn to cut our costs.”
How is hospitalist practice evolving?
In addition to payment and productivity data, the SoHM report provides a current picture of the evolving state of hospitalist group practices. A key thread is how the work hospitalists are doing, and the way they do it, is changing, with new information about comanagement roles, dedicated admitters, night coverage, geographic rounding, and the like.
Making greater use of nurse practitioners and physician assistants (NPs/PAs), may be one way to change the flat productivity trends, Dr. Brown said. With a cost per RVU that’s roughly half that of a doctor’s, NPs/PAs could contribute to the bottom line. But he sees surprisingly large variation in how hospitalist groups are using them. Typically, they are deployed at a ratio of four doctors to one NP/PA, but that ratio could be two to one or even one to one, he said.
Use of NPs/PAs by academic hospitalist groups is up, from 52.1% in 2016 to 75.7% in 2018. For adult-only groups, 76.8% had NPs/PAs, with higher rates in hospitals and health systems and lower rates in the West region. But a lot of groups are using these practitioners for nonproductive work, and some are failing to generate any billing income, Dr. Brown said.
“The rate at which NPs/PAs performed billable services was higher in physician-owned practices, resulting in a lower cost per RVU, suggesting that many practices may be underutilizing their NPs/PAs or not sharing the work.” Not every NP or PA wants to or is able to care for very complex patients, Dr. Brown said, “but you want a system where the NP and PA can work at the highest level permitted by state law.”
The predominant scheduling model of hospital medicine, 7 days on duty followed by 7 days off, has diminished somewhat in recent years. There appears to be some fluctuation and a gradual move away from 7 on/7 off toward some kind of variable approach, since the former may not be physically sustainable for the doctor over the long haul, Dr. Brown said. Some groups are experimenting with a combined approach.
“I think balancing workload with manpower has always been a challenge for our field. Maybe we should be working shorter shifts or fewer days and making sure our hospitalists aren’t ever sitting around idle,” he said. “And could we come in on nonclinical days to do administrative tasks? I think the solution is out there, but we haven’t created the algorithms to define that yet. If you could somehow use the data for volume, number of beds, nurse staffing, etc., by year and seasonally, you might be able to reliably predict census. This is about applying data hospitals already have in their electronic health records, but utilizing the data in ways that are more helpful.”
Dr. McIlraith added that a big driver of the future of hospital medicine will be the evolution of the EHR and the digitalization of health care, as hospitals learn how to leverage more of what’s in their EHRs. “The impact will grow for hospitalists through the creation and maturation of big data systems – and the learning that can be extracted from what’s contained in the electronic health record.”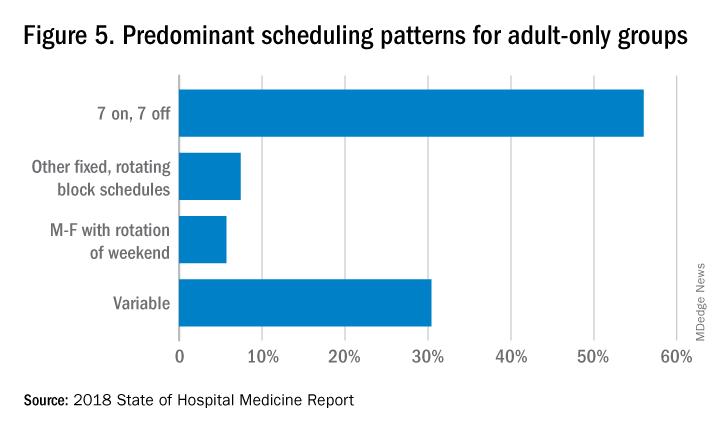
Another important question for hospitalist groups is their model of backup scheduling, to make sure there is a replacement available if a scheduled doctor calls in sick or if demand is unexpectedly high.
“In today’s world, this is how we have traditionally managed unpredictability,” Dr. Brown said. “You don’t know when you will need it, but if you need it, you want it immediately. So how do you pay for it – only when the doctor comes in, or also an amount just for being on call?” Some groups pay for both, he said, others for neither.
“We are a group of 70 hospitalists, and if someone is sick you can’t just shut down the service,” said Dr. Chadha. “We are one of the few to use incentives for both, which could include a 1-week decrease in clinical shifts in exchange for 2 weeks of backup. We have times with 25% usage of backup number 1, and 10% usage of backup number 2,” he noted. “But the goal is for our hospitalists to have assurances that there is a backup system and that it works.”
The presence of nocturnists in hospitals continues to rise, with 76.1% of adults-only groups having nocturnists, 27.6% of children-only groups, and 68.2% of adults and children groups. Geographic or unit-based hospital assignments have grown to 36.4% of adult-only groups.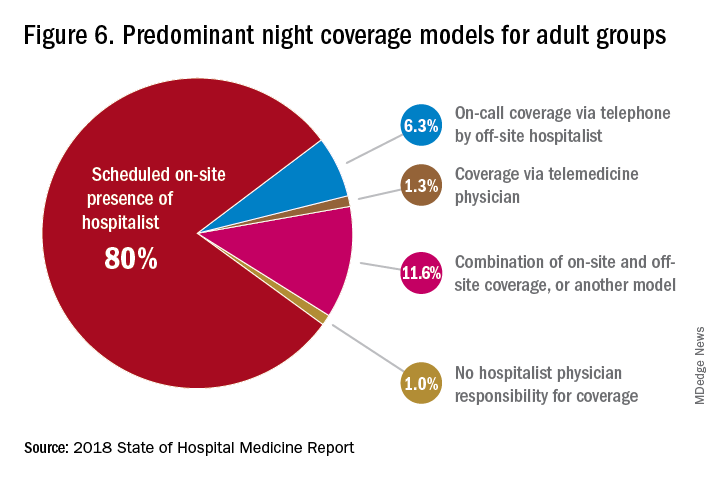
What are hospitalists’ other new roles?
“We have a large group of 50 doctors, with about 40 FTEs, and we are evolving from the traditional generalist role toward more subspecialty comanagement,” said Bryan Huang, MD, physician adviser and associate clinical professor in the division of hospital medicine at the University of California–San Diego. “Our hospitalists are asking what it means to be an academic hospitalist as our teaching roles have shrunk.”
Dr. Huang recently took on a new role as physician adviser for his hospital in such areas as utilization review, patient flow, and length of stay. “I’m spearheading a work group to address quality issues – all of which involve collaboration with other professionals. We also developed an admitting role here for a hospitalist whose sole role for the day is to admit patients.” Nationally up to 51.2% of hospitalist groups utilize a dedicated daytime admitter.
The report found that hospital services for which hospitalists are more likely to be attendings than consultants include GI/liver, 78.4%; palliative care, 77.3%; neurology/stroke, 73.6%; oncology, 67.8%; cardiology, 56.9%; and critical care, 50.7%. Conditions where hospitalists are more likely to consult rather than admit and attend include neurosurgery, orthopedics, general surgery, cardiovascular surgery, and other surgical subspecialties.
Other hospital services routinely provided by adult-only hospitalists include care of patients in an ICU setting (62.7%); primary responsibility for observation units (54.6%); primary clinical responsibility for rapid response teams (48.8%); primary responsibility for code blue or cardiac arrest teams (43.8%); nighttime admissions or tuck-in services (33.9%); and medical procedures (31.5%). For pediatric hospital medicine groups, care of healthy newborns and medical procedures were among the most common services provided, while for hospitalists serving adults and children, rapid response teams, ICUs, and specialty units were most common.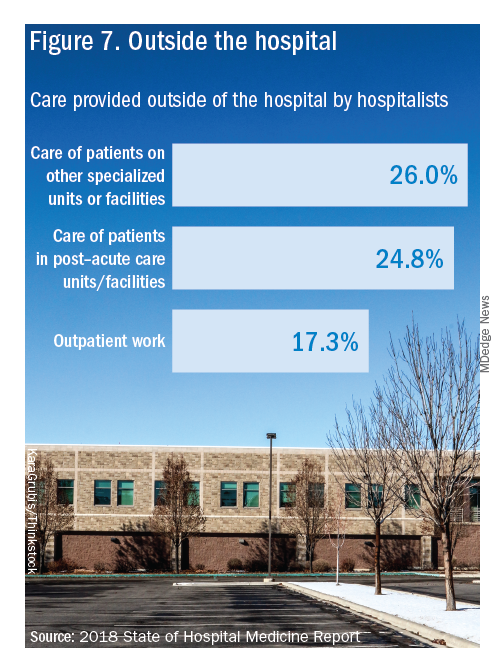
New models of payment for health care
As the larger health care system is being transformed by new payment models and benefit structures, including accountable care organizations (ACOs), value-based purchasing, bundled payments, and other forms of population-based coverage – which is described as a volume-to-value shift in health care – how are these new models affecting hospitalists?
Observers say penetration of these new models varies widely by locality but they haven’t had much direct impact on hospitalists’ practices – at least not yet. However, as hospitals and health systems find themselves needing to learn new ways to invest their resources differently in response to these trends, what matters to the hospital should be of great importance to the hospitalist group.
“I haven’t seen a lot of dramatic changes in how hospitalists engage with value-based purchasing,” Dr. White said. “If we know that someone is part of an ACO, the instinctual – and right – response is to treat them like any other patient. But we still need to be committed to not waste resources.”
Hospitalists are the best people to understand the intricacies of how the health care system works under value-based approaches, Dr. Huang said. “That’s why so many hospitalists have taken leadership positions in their hospitals. I think all of this translates to the practical, day-to-day work of hospitalists, reflected in our focus on readmissions and length of stay.”
Dr. Williams said the health care system still hasn’t turned the corner from fee-for-service to value-based purchasing. “It still represents a tiny fraction of the income of hospitalists. Hospitals still have to focus on the bottom line, as fee-for-service reimbursement for hospitalized patients continues to get squeezed, and ACOs aren’t exactly paying premium rates either. Ask almost any hospital CEO what drives their bottom line today and the answer is volume – along with optimizing productivity. Pretty much every place I look, the future does not look terribly rosy for hospitals.”
Ms. Himebaugh said she is bullish on hospital medicine, in the sense that it’s unlikely to go away anytime soon. “Hospitalists are needed and provide value. But I don’t think we have devised the right model yet. I’m not sure our current model is sustainable. We need to find new models we can afford that don’t require squeezing our providers.”
For more information about the 2018 State of Hospital Medicine Report, contact SHM’s Practice Management Department at: [email protected] or call 800-843-3360. See also: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/.
Appropriate use criteria for imaging in nonvalvular heart disease released
The American College of Cardiology, the American Heart Association, and other groups have jointly released an appropriate use criteria (AUC) document regarding the use of imaging modalities in diagnosing nonvalvular (that is, structural) heart disease.
Imaging plays an important role in diagnosing both valvular and nonvalvular heart diseases, so the goal of the document was to help clinicians provide high-quality care by standardizing the decision-making process. To do so, a committee was formed to devise scenarios that reflected situations in real-world practice; these scenarios were considered within categories to prevent the list from being too exhaustive. The scenarios were then reviewed by a rating panel in terms of how appropriate certain modalities were in each situation. The panel members first evaluated the scenarios independently then face to face as a panel before giving their final scores (from 1 to 9) independently.
For example, for the indication of nonsustained ventricular tachycardia, the panelists rated transthoracic echocardiography with or without 3-D and with contrast as needed as a 8, which means it’s an “appropriate test,” whereas they gave CT for the same indication a 3, which means “rarely appropriate.” For sustained ventricular tachycardia or ventricular fibrillation, they gave a 9 and a 6, respectively; this latter score indicates the test “may be appropriate.” These scenarios and the respective scores for any given test are organized into tables, such as initial evaluation or follow-up.
This AUC document “signals a shift from documents evaluating a single modality in various disease states to documents evaluating multiple imaging modalities and focusing on evidence and clinical experience within a given disease category,” the authors wrote. “We believe this approach better reflects clinical decision making in real-world scenarios and offers the diagnostic choices available to the clinician.”
The full document can be viewed in JACC.
The American College of Cardiology, the American Heart Association, and other groups have jointly released an appropriate use criteria (AUC) document regarding the use of imaging modalities in diagnosing nonvalvular (that is, structural) heart disease.
Imaging plays an important role in diagnosing both valvular and nonvalvular heart diseases, so the goal of the document was to help clinicians provide high-quality care by standardizing the decision-making process. To do so, a committee was formed to devise scenarios that reflected situations in real-world practice; these scenarios were considered within categories to prevent the list from being too exhaustive. The scenarios were then reviewed by a rating panel in terms of how appropriate certain modalities were in each situation. The panel members first evaluated the scenarios independently then face to face as a panel before giving their final scores (from 1 to 9) independently.
For example, for the indication of nonsustained ventricular tachycardia, the panelists rated transthoracic echocardiography with or without 3-D and with contrast as needed as a 8, which means it’s an “appropriate test,” whereas they gave CT for the same indication a 3, which means “rarely appropriate.” For sustained ventricular tachycardia or ventricular fibrillation, they gave a 9 and a 6, respectively; this latter score indicates the test “may be appropriate.” These scenarios and the respective scores for any given test are organized into tables, such as initial evaluation or follow-up.
This AUC document “signals a shift from documents evaluating a single modality in various disease states to documents evaluating multiple imaging modalities and focusing on evidence and clinical experience within a given disease category,” the authors wrote. “We believe this approach better reflects clinical decision making in real-world scenarios and offers the diagnostic choices available to the clinician.”
The full document can be viewed in JACC.
The American College of Cardiology, the American Heart Association, and other groups have jointly released an appropriate use criteria (AUC) document regarding the use of imaging modalities in diagnosing nonvalvular (that is, structural) heart disease.
Imaging plays an important role in diagnosing both valvular and nonvalvular heart diseases, so the goal of the document was to help clinicians provide high-quality care by standardizing the decision-making process. To do so, a committee was formed to devise scenarios that reflected situations in real-world practice; these scenarios were considered within categories to prevent the list from being too exhaustive. The scenarios were then reviewed by a rating panel in terms of how appropriate certain modalities were in each situation. The panel members first evaluated the scenarios independently then face to face as a panel before giving their final scores (from 1 to 9) independently.
For example, for the indication of nonsustained ventricular tachycardia, the panelists rated transthoracic echocardiography with or without 3-D and with contrast as needed as a 8, which means it’s an “appropriate test,” whereas they gave CT for the same indication a 3, which means “rarely appropriate.” For sustained ventricular tachycardia or ventricular fibrillation, they gave a 9 and a 6, respectively; this latter score indicates the test “may be appropriate.” These scenarios and the respective scores for any given test are organized into tables, such as initial evaluation or follow-up.
This AUC document “signals a shift from documents evaluating a single modality in various disease states to documents evaluating multiple imaging modalities and focusing on evidence and clinical experience within a given disease category,” the authors wrote. “We believe this approach better reflects clinical decision making in real-world scenarios and offers the diagnostic choices available to the clinician.”
The full document can be viewed in JACC.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
SHM announces National Hospitalist Day
Inaugural day of recognition to honor hospital medicine care team
The Society of Hospital Medicine is proud to announce the inaugural National Hospitalist Day, to be held on Thursday, March 7, 2019. Occurring the first Thursday in March annually, National Hospitalist Day will serve to celebrate the fastest-growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape.
National Hospitalist Day was recently approved by the National Day Calendar and was one of approximately 30 national days to be approved for the year out of an applicant pool of more than 18,000.
“As the only society dedicated to the specialty of hospital medicine, it is appropriate that SHM spearhead a national day to recognize the countless contributions of hospitalists to health care, from clinical, academic, and leadership perspectives and more,” said Larry Wellikson, MD, MHM, chief executive officer of SHM. “We look forward to hospitalists across the nation contributing to the festivities and making this a tradition for years to come.”
In addition to celebrating hospitalists’ contributions to patient care, SHM will also be highlighting the diverse career paths of hospital medicine professionals, from frontline hospitalist physicians, nurse practitioners, and physician assistants to practice administrators, C-suite executives, and academic hospitalists.
Highlights of SHM’s campaign include the following:
- Downloadable customizable posters and assets for hospitals and individuals’ offices to celebrate their hospital medicine team, available on SHM’s website, hospitalmedicine.org.
- A series of spotlights of hospitalists at all stages of their careers in The Hospitalist, SHM’s monthly newsmagazine.
- A social media campaign inviting hospitalists and their employers to share their success stories using the hashtag #HowWeHospitalist, including banner graphics, profile photo overlays, and more.
- A social media contest to determine the most creative ways of celebrating use of the hashtag.
- A Twitter chat for hospitalists to celebrate virtually with their colleagues and peers from around the world.
“Hospitalists innovate, lead, and push the boundaries of clinical care and deserve to be recognized for their transformative contributions to health care,” said Eric E. Howell, MD, MHM, chief operating officer of SHM. “We hope this is the beginning of a long-standing tradition in honoring hospitalists and the noteworthy work they do.”
For more information, visit www.hospitalmedicine.org/hospitalistday.
Mr. Radler is marketing communications manager at the Society of Hospital Medicine.
Inaugural day of recognition to honor hospital medicine care team
Inaugural day of recognition to honor hospital medicine care team
The Society of Hospital Medicine is proud to announce the inaugural National Hospitalist Day, to be held on Thursday, March 7, 2019. Occurring the first Thursday in March annually, National Hospitalist Day will serve to celebrate the fastest-growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape.
National Hospitalist Day was recently approved by the National Day Calendar and was one of approximately 30 national days to be approved for the year out of an applicant pool of more than 18,000.
“As the only society dedicated to the specialty of hospital medicine, it is appropriate that SHM spearhead a national day to recognize the countless contributions of hospitalists to health care, from clinical, academic, and leadership perspectives and more,” said Larry Wellikson, MD, MHM, chief executive officer of SHM. “We look forward to hospitalists across the nation contributing to the festivities and making this a tradition for years to come.”
In addition to celebrating hospitalists’ contributions to patient care, SHM will also be highlighting the diverse career paths of hospital medicine professionals, from frontline hospitalist physicians, nurse practitioners, and physician assistants to practice administrators, C-suite executives, and academic hospitalists.
Highlights of SHM’s campaign include the following:
- Downloadable customizable posters and assets for hospitals and individuals’ offices to celebrate their hospital medicine team, available on SHM’s website, hospitalmedicine.org.
- A series of spotlights of hospitalists at all stages of their careers in The Hospitalist, SHM’s monthly newsmagazine.
- A social media campaign inviting hospitalists and their employers to share their success stories using the hashtag #HowWeHospitalist, including banner graphics, profile photo overlays, and more.
- A social media contest to determine the most creative ways of celebrating use of the hashtag.
- A Twitter chat for hospitalists to celebrate virtually with their colleagues and peers from around the world.
“Hospitalists innovate, lead, and push the boundaries of clinical care and deserve to be recognized for their transformative contributions to health care,” said Eric E. Howell, MD, MHM, chief operating officer of SHM. “We hope this is the beginning of a long-standing tradition in honoring hospitalists and the noteworthy work they do.”
For more information, visit www.hospitalmedicine.org/hospitalistday.
Mr. Radler is marketing communications manager at the Society of Hospital Medicine.
The Society of Hospital Medicine is proud to announce the inaugural National Hospitalist Day, to be held on Thursday, March 7, 2019. Occurring the first Thursday in March annually, National Hospitalist Day will serve to celebrate the fastest-growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape.
National Hospitalist Day was recently approved by the National Day Calendar and was one of approximately 30 national days to be approved for the year out of an applicant pool of more than 18,000.
“As the only society dedicated to the specialty of hospital medicine, it is appropriate that SHM spearhead a national day to recognize the countless contributions of hospitalists to health care, from clinical, academic, and leadership perspectives and more,” said Larry Wellikson, MD, MHM, chief executive officer of SHM. “We look forward to hospitalists across the nation contributing to the festivities and making this a tradition for years to come.”
In addition to celebrating hospitalists’ contributions to patient care, SHM will also be highlighting the diverse career paths of hospital medicine professionals, from frontline hospitalist physicians, nurse practitioners, and physician assistants to practice administrators, C-suite executives, and academic hospitalists.
Highlights of SHM’s campaign include the following:
- Downloadable customizable posters and assets for hospitals and individuals’ offices to celebrate their hospital medicine team, available on SHM’s website, hospitalmedicine.org.
- A series of spotlights of hospitalists at all stages of their careers in The Hospitalist, SHM’s monthly newsmagazine.
- A social media campaign inviting hospitalists and their employers to share their success stories using the hashtag #HowWeHospitalist, including banner graphics, profile photo overlays, and more.
- A social media contest to determine the most creative ways of celebrating use of the hashtag.
- A Twitter chat for hospitalists to celebrate virtually with their colleagues and peers from around the world.
“Hospitalists innovate, lead, and push the boundaries of clinical care and deserve to be recognized for their transformative contributions to health care,” said Eric E. Howell, MD, MHM, chief operating officer of SHM. “We hope this is the beginning of a long-standing tradition in honoring hospitalists and the noteworthy work they do.”
For more information, visit www.hospitalmedicine.org/hospitalistday.
Mr. Radler is marketing communications manager at the Society of Hospital Medicine.
New diabetes drugs solidify their cardiovascular and renal benefits
CHICAGO – When the first results from a large trial that showed profound and unexpected benefits for preventing heart failure hospitalizations associated with use of the antihyperglycemic sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin came out – a little over 3 years ago – the general reaction from clinicians was some variant of “Could this be real?”
Since then, as results from some five other large, international trials have come out showing both similar benefits from two other drugs in the same SGLT2 inhibitor class, canagliflozin and dapagliflozin, as well as results showing clear cardiovascular disease benefits from three drugs in a second class of antihyperglycemics, the glucagonlike peptide–1 receptor agonists (GLP-1 RAs), the general consensus among cardiologists became: “The cardiovascular and renal benefits are real. How can we now best use these drugs to help patients?”
This change increasingly forces cardiologists, as well as the primary care physicians who often manage patients with type 2 diabetes mellitus, to become more comfortable prescribing these two classes of antihyperglycemic drugs. During a talk at the American Heart Association scientific sessions, Eugene Braunwald, MD, arguably the top thought leader in cardiology, coined a new name for the medical subspecialty that he foresees navigating this overlap between diabetes care and cardiovascular disease prevention: diabetocardiology (although a more euphonic alternative might be cardiodiabetology, while the more comprehensive name could be cardionephrodiabetology).
“I was certainly surprised” by the first report in 2015 from the EMPA-REG OUTCOME trial (N Engl J Med. 2015 Nov 26;373[22]:2117-28), said Dr. Braunwald, who is professor of medicine at Harvard Medical School in Boston. A lot of his colleagues were surprised and said, “It’s just one trial.”
“Now we have three trials,” with the addition of the CANVAS trial for canagliflozin (N Engl J Med. 2017 Aug 17;377[7]:644-57) and the DECLARE-TIMI 58 trial (N Engl J Med. 2018 Nov 10. doi:10.1056/NEJMoa1812389) for dapagliflozin reported at the AHA meeting in November.
“We are in the midst of two pandemics: heart failure and type 2 diabetes. As cardiologists, we have to learn how to deal with this,” said Dr. Braunwald, and the evidence now clearly shows that these drugs can help with that.
As another speaker at the meeting, Javed Butler, MD, a heart failure specialist, observed in a separate talk at the meeting, “Heart failure is one of the most common, if not the most common complication, of patients with diabetes.” This tight link between heart failure and diabetes helps make cardiovascular mortality “the number one cause of death” in patients with diabetes, said Dr. Butler, professor and chairman of medicine at the University of Mississippi in Jackson.
“Thanks to the cardiovascular outcome trials, we now have a much broader and deeper appreciation of heart failure and renal disease as integral components of the cardiovascular-renal spectrum in people with diabetes,” said Subodh Verma, MD, a professor at the University of Toronto and cardiac surgeon at St. Michael’s Hospital in Toronto. Dr. Braunwald spelled out in his talk some of the interrelationships of diabetes, heart failure, and renal dysfunction that together produce a downward-spiraling vicious circle for patients, a pathophysiological process that clinicians can now short-circuit by treatment with a SGLT2 inhibitor.
Cardiovascular outcome trials show the way
In the context of antihyperglycemic drugs, the “cardiovascular outcome trials” refers to a series of large trials mandated by the Food and Drug Administration in 2008 to assess the cardiovascular disease effects of new agents coming onto the U.S. market to treat type 2 diabetes mellitus (T2DM). By the time Dr. Verma spoke at the AHA meeting, he could cite reported results from 12 of these trials: 5 different drugs in the GLP-1 RA class, 4 drugs in the dipeptidyl peptidase-4 (DPP-4) inhibitor class, and 3 drugs from the SGLT2 inhibitor class. Dr. Verma summed what the findings have shown.
The four tested DDP-4 inhibitors (alogliptin, linagliptin, saxagliptin, and sitagliptin) consistently showed neutrality for the primary outcome of major adverse cardiovascular disease events (MACE), constituted by cardiovascular disease death, MI, or stroke.
The five tested GLP-1 RAs (albiglutide, exenatide, liraglutide, lixisenatide, and semaglutide) showed a mixed pattern of MACE results that seemed to be linked with the subclass the drug fell into. The two exedin-4–based drugs, exenatide and lixisenatide, each showed a statistically neutral effect for MACE, as well as collectively in a combined analysis. In contrast, three human GLP-1–based drugs, albiglutide, liraglutide, and semaglutide, each showed a consistent, statistically-significant MACE reduction in their respective outcome trials, and collectively they showed a highly significant 18% reduction in MACE, compared with placebo, Dr. Verma said. Further, recent analysis by Dr. Verma that used data from liraglutide treatment in the LEADER trial showed the MACE benefit occurred only among enrolled patients treated with liraglutide who had established atherosclerotic cardiovascular disease (ASCVD). Patients enrolled in the trial with only multiple risk factors (in addition to having T2DM) but without established ASCVD showed no significant benefit from liraglutide treatment for the MACE endpoint, compared with control patients.
Recently a press-release announcement of results from a sixth GLP-1 RA, dulaglutide, in the REWIND trial of MACE outcomes suggested that a drug in this class could have broader effect. The majority, 69%, of the 9,901 patients with T2DM enrolled in REWIND had risk factors but not established ASCVD at enrollment. A Nov. 5, 2018, statement from the company developing this drug, Lilly, reported that the study overall produced a statistically significant reduction in MACE, although it provided no additional details. As the released noted, this made REWIND the first trial to show a MACE benefit from a drug in the GLP-1 RA class in patients without established ASCVD.
The MACE outcome results from the three SGLT2 inhibitor trials showed a similar pattern as liraglutide: In patients with established ASCVD, the drugs individually each produced a MACE reduction, although dapagliflozin just missed having a statistically significant reduction. Collectively, the three drugs showed a statistically significant, 14% relative risk reduction for MACE, compared with control patients. But among patients with multiple risk factors only, but without established ASCVD, included in two of the three trials (CANVAS and DECLARE-TIMI 58), the results showed both individually and collectively a neutral MACE effect.
But unlike the other antihyperglycemic drugs tested in the cardiovascular outcome trials, the SGLT2 inhibitors have shown two additional, highly important secondary outcomes: a consistent reduction in hospitalization for heart failure and a consistent reduction in renal-disease progression.
A meta-analysis of the three SGLT2 inhibitor trials published coincident with the release of the DECLARE-TIMI 58 results showed that, for the outcome of either cardiovascular death or hospitalization for heart failure, the SGLT2 inhibitors collectively showed a significant 29% relative decrease in this incidence among patients with a history of heart failure, and a significant 21% relative decrease among patients without history of heart failure (Lancet. 2018 Nov 10. doi: 10.1016/S0140-6736(18)32590-X). Among the subset of patients with established ASCVD, treatment with a SGLT2 inhibitor across all three trials showed a significant 16% relative risk reduction, and in the subset with multiple risk factors but no established ASCVD, the two SGLT2 inhibitors collectively produced a 16% relative cut in cardiovascular death or heart failure hospitalization with a P value of .06. Finally, the Lancet meta-analysis showed that, for a combined endpoint that reflected renal worsening, the SGLT2 inhibitors showed a significant relative reduction of about 45% in both the subgroup of patients with established ASCVD and in the subgroup of those with just risk factors.
“This is a big step forward for patients with multiple risk factors and diabetes but without ASCVD, that both renal disease and hospitalization for heart failure are sensitive” to the SGLT2 inhibitors, Dr. Verma noted. “We see renal protection and reduction of heart failure hospitalization across both primary and secondary prevention patients, with no need to distinguish them based on ASCVD.” In contrast, he noted, the MACE benefit from the SGLT2 inhibitors seems limited to patients with ASCVD. The day before making this point in a talk during the meeting, Dr. Verma had published the same message in a commentary (Lancet. 2018 Nov 10. doi: 10.1016/S0140-6736(18)32824-1).
Although the “nomenclature of primary versus secondary prevention is appropriate for atherosclerotic outcomes, it is likely to be inappropriate for a person with type 2 diabetes who is at risk of hospitalization for heart failure and renal disease,” Dr. Verma wrote with his associates in the commentary.
What it means for clinicians
The upshot of all of these cardiovascular outcome trial results that came out over the past 3 years has been a new appreciation of how antihyperglycemic drugs can have cardiovascular and renal benefits that transcend their effects on glycemia. The evidence has put the SGLT2 inhibitors and GLP-1 RAs on track to challenge, and potentially displace, metformin as the top drug to prescribe for patients with T2DM.
Clinicians should realize that they should prescribe SGLT2 inhibitors and selected GLP-1 RAs “as early as metformin in patients with established ASCVD,” said Dr. Verma. “For patients with recalcitrant atherosclerotic disease and a history of MI and ischemia, I’d primarily treat with a GLP-1 RA. In a patient with left ventricular dysfunction or evidence of heart failure, I’d use an SGLT2 inhibitor. But it’s not a fight between these two. You could treat a patients with type 2 diabetes with both classes,” although the practicality of this approach is limited by the high cost of these drugs.
The SGLT2 inhibitors “should now be considered as first-line therapy after metformin in most people with type 2 diabetes, irrespective of whether or not they have established atherosclerotic vascular disease, chronic kidney disease, or heart failure,” he and his associates wrote in their recent commentary.
“What I struggle with the most is how we prioritize and individualize secondary-prevention therapies based on risk for ischemia and heart failure. Some therapies [the SGLT2 inhibitors] are predominantly for heart failure prevention, and some [the GLP-1 RAs] are primarily for ischemia. How do we choose when a patient cannot afford to take both? Does a combination of a SGLT2 inhibitor and a GLP-1 RA offer the greatest CVD benefit? We need to test this in a trial. And will metformin be displaced as first-line treatment?” Dr. Verma asked.
“The day will probably come when, for maximal protection, you treat with both classes. But right now we’re forced to choose because of the cost,” said John McMurray, MD, professor of cardiology at the University of Glasgow, in a talk during the meeting.
As to specifically which SGLT2 inhibitor to prescribe, “they all look pretty much the same” in the newly published meta-analysis, Dr. McMurray said, although he noted that safety differences among agents in the class remain possible.
“For patients similar to those studied in the three SGLT2 inhibitor trials, clinicians should use one of these drugs to reduce the risk for incident heart failure, irrespective of their effect on MACE,” said Dr. Butler. Reducing the risk for incident heart failure and of progressive renal dysfunction are two new goals for antihyperglycemic therapy that now overlay the long-standing goals of controlling glycemia and reducing cardiovascular disease risk and the more recent goals of cutting cardiovascular disease mortality and cutting the risk for a MACE event.
A current limitation for practice is that the none of the three drug companies that market the tested SGLT2 inhibitor drugs has sought regulatory approval for an indication of reducing the risk for heart failure hospitalization. Despite that, “these drugs should be used for renal protection and reducing heart failure hospitalizations,” Dr. Butler said. “We need to start thinking about this and not get lost thinking about only their MACE effect because, when you focus on MACE, there is a competition between the SGLT2 inhibitors and the GLP-1 RA. If we think of GLP-1 RAs as drugs to prevent MACE, and SGLT2 inhibitors as drugs that primarily prevent heart failure and renal dysfunction, then there is no competition. Perhaps combined treatment is where we need to go,” he said in an interview.
But the enthusiasm that experts like Dr. Butler, Dr. McMurray, and Dr. Verma have for wider use of both classes of drugs in appropriate patients is not necessarily matched right now among many community physicians. Cardiologist David J. Becker, MD, is an example of the clinicians who appreciate the growing evidence that supports wider use of these antihyperglycemic drugs but remain uneasy about applying this evidence in their practice.
Dr. Becker, associate director of the Preventive and Integrative Heart Health Program of the Temple Heart and Vascular Institute in Philadelphia, writes a column for the Philadelphia Inquirer on medical care. In a December 2018 piece, he said “like most cardiologists, I ‘don’t do diabetes’ – because it’s not my expertise. The new drugs, however, mean I need to learn more” about treating these patients. “The problem: There are so many of these medications that they present a bewildering choice for patients and doctors.”
Dr. Becker cited several barriers he sees for himself and his nonendocrinologist colleagues to prescribe these drugs – and for patients to take them:
- High cost, with prices that run close to $20/day for each medication.
- A thicket of names and choices that “lead to confusion and paralysis,” which has been exacerbated by “advertising wars” among competing drug companies.
- Cardiologists and primary care physicians usually defer to endocrinologists to prescribe these drugs, but most patients with T2DM aren’t seen by endocrinologists. The result: “Few doctors prescribe them.”
The cardiovascular disease benefits of these drugs have not been adequately promoted. Until that changes, “cardiologists like me will not realize their importance,” Dr. Becker concluded.
While christening the new diabetocardiology subspecialty, Dr. Braunwald placed the onus for managing this emerging facet of diabetes largely outside the scope of endocrinology.
“We can’t call in a consultant every time we have a patient with diabetes; it would bankrupt the system,” he said. Training of cardiologists now needs to include several months of treating patients with diabetes, Dr. Braunwald advised, just like 30 or so years ago when cardiologists like himself had to become more familiar with blood clotting to better manage thrombotic disease.
Dr. Braunwald has been a consultant to Cardurion, Myokardia, and Sanofi; an advisor to Endcardia; and has received research funding from AstraZeneca, Daiishi Sankyo, and Novartis. Dr. Butler has been a consultant or advisor to AstraZeneca, Amgen, Bayer, Boehringer Ingelheim, Janssen, Merck, Novartis, Novo Nordisk, and Sanofi. Dr. Verma has received honoraria and research funding from Abbott, Amgen, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Janssen, Merck, Novartis, NovoNordisk, Sanofi, and Valeant. Dr. McMurray has received research funding from 12 companies. Dr. Becker had no disclosures.
CHICAGO – When the first results from a large trial that showed profound and unexpected benefits for preventing heart failure hospitalizations associated with use of the antihyperglycemic sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin came out – a little over 3 years ago – the general reaction from clinicians was some variant of “Could this be real?”
Since then, as results from some five other large, international trials have come out showing both similar benefits from two other drugs in the same SGLT2 inhibitor class, canagliflozin and dapagliflozin, as well as results showing clear cardiovascular disease benefits from three drugs in a second class of antihyperglycemics, the glucagonlike peptide–1 receptor agonists (GLP-1 RAs), the general consensus among cardiologists became: “The cardiovascular and renal benefits are real. How can we now best use these drugs to help patients?”
This change increasingly forces cardiologists, as well as the primary care physicians who often manage patients with type 2 diabetes mellitus, to become more comfortable prescribing these two classes of antihyperglycemic drugs. During a talk at the American Heart Association scientific sessions, Eugene Braunwald, MD, arguably the top thought leader in cardiology, coined a new name for the medical subspecialty that he foresees navigating this overlap between diabetes care and cardiovascular disease prevention: diabetocardiology (although a more euphonic alternative might be cardiodiabetology, while the more comprehensive name could be cardionephrodiabetology).
“I was certainly surprised” by the first report in 2015 from the EMPA-REG OUTCOME trial (N Engl J Med. 2015 Nov 26;373[22]:2117-28), said Dr. Braunwald, who is professor of medicine at Harvard Medical School in Boston. A lot of his colleagues were surprised and said, “It’s just one trial.”
“Now we have three trials,” with the addition of the CANVAS trial for canagliflozin (N Engl J Med. 2017 Aug 17;377[7]:644-57) and the DECLARE-TIMI 58 trial (N Engl J Med. 2018 Nov 10. doi:10.1056/NEJMoa1812389) for dapagliflozin reported at the AHA meeting in November.
“We are in the midst of two pandemics: heart failure and type 2 diabetes. As cardiologists, we have to learn how to deal with this,” said Dr. Braunwald, and the evidence now clearly shows that these drugs can help with that.
As another speaker at the meeting, Javed Butler, MD, a heart failure specialist, observed in a separate talk at the meeting, “Heart failure is one of the most common, if not the most common complication, of patients with diabetes.” This tight link between heart failure and diabetes helps make cardiovascular mortality “the number one cause of death” in patients with diabetes, said Dr. Butler, professor and chairman of medicine at the University of Mississippi in Jackson.
“Thanks to the cardiovascular outcome trials, we now have a much broader and deeper appreciation of heart failure and renal disease as integral components of the cardiovascular-renal spectrum in people with diabetes,” said Subodh Verma, MD, a professor at the University of Toronto and cardiac surgeon at St. Michael’s Hospital in Toronto. Dr. Braunwald spelled out in his talk some of the interrelationships of diabetes, heart failure, and renal dysfunction that together produce a downward-spiraling vicious circle for patients, a pathophysiological process that clinicians can now short-circuit by treatment with a SGLT2 inhibitor.
Cardiovascular outcome trials show the way
In the context of antihyperglycemic drugs, the “cardiovascular outcome trials” refers to a series of large trials mandated by the Food and Drug Administration in 2008 to assess the cardiovascular disease effects of new agents coming onto the U.S. market to treat type 2 diabetes mellitus (T2DM). By the time Dr. Verma spoke at the AHA meeting, he could cite reported results from 12 of these trials: 5 different drugs in the GLP-1 RA class, 4 drugs in the dipeptidyl peptidase-4 (DPP-4) inhibitor class, and 3 drugs from the SGLT2 inhibitor class. Dr. Verma summed what the findings have shown.
The four tested DDP-4 inhibitors (alogliptin, linagliptin, saxagliptin, and sitagliptin) consistently showed neutrality for the primary outcome of major adverse cardiovascular disease events (MACE), constituted by cardiovascular disease death, MI, or stroke.
The five tested GLP-1 RAs (albiglutide, exenatide, liraglutide, lixisenatide, and semaglutide) showed a mixed pattern of MACE results that seemed to be linked with the subclass the drug fell into. The two exedin-4–based drugs, exenatide and lixisenatide, each showed a statistically neutral effect for MACE, as well as collectively in a combined analysis. In contrast, three human GLP-1–based drugs, albiglutide, liraglutide, and semaglutide, each showed a consistent, statistically-significant MACE reduction in their respective outcome trials, and collectively they showed a highly significant 18% reduction in MACE, compared with placebo, Dr. Verma said. Further, recent analysis by Dr. Verma that used data from liraglutide treatment in the LEADER trial showed the MACE benefit occurred only among enrolled patients treated with liraglutide who had established atherosclerotic cardiovascular disease (ASCVD). Patients enrolled in the trial with only multiple risk factors (in addition to having T2DM) but without established ASCVD showed no significant benefit from liraglutide treatment for the MACE endpoint, compared with control patients.
Recently a press-release announcement of results from a sixth GLP-1 RA, dulaglutide, in the REWIND trial of MACE outcomes suggested that a drug in this class could have broader effect. The majority, 69%, of the 9,901 patients with T2DM enrolled in REWIND had risk factors but not established ASCVD at enrollment. A Nov. 5, 2018, statement from the company developing this drug, Lilly, reported that the study overall produced a statistically significant reduction in MACE, although it provided no additional details. As the released noted, this made REWIND the first trial to show a MACE benefit from a drug in the GLP-1 RA class in patients without established ASCVD.
The MACE outcome results from the three SGLT2 inhibitor trials showed a similar pattern as liraglutide: In patients with established ASCVD, the drugs individually each produced a MACE reduction, although dapagliflozin just missed having a statistically significant reduction. Collectively, the three drugs showed a statistically significant, 14% relative risk reduction for MACE, compared with control patients. But among patients with multiple risk factors only, but without established ASCVD, included in two of the three trials (CANVAS and DECLARE-TIMI 58), the results showed both individually and collectively a neutral MACE effect.
But unlike the other antihyperglycemic drugs tested in the cardiovascular outcome trials, the SGLT2 inhibitors have shown two additional, highly important secondary outcomes: a consistent reduction in hospitalization for heart failure and a consistent reduction in renal-disease progression.
A meta-analysis of the three SGLT2 inhibitor trials published coincident with the release of the DECLARE-TIMI 58 results showed that, for the outcome of either cardiovascular death or hospitalization for heart failure, the SGLT2 inhibitors collectively showed a significant 29% relative decrease in this incidence among patients with a history of heart failure, and a significant 21% relative decrease among patients without history of heart failure (Lancet. 2018 Nov 10. doi: 10.1016/S0140-6736(18)32590-X). Among the subset of patients with established ASCVD, treatment with a SGLT2 inhibitor across all three trials showed a significant 16% relative risk reduction, and in the subset with multiple risk factors but no established ASCVD, the two SGLT2 inhibitors collectively produced a 16% relative cut in cardiovascular death or heart failure hospitalization with a P value of .06. Finally, the Lancet meta-analysis showed that, for a combined endpoint that reflected renal worsening, the SGLT2 inhibitors showed a significant relative reduction of about 45% in both the subgroup of patients with established ASCVD and in the subgroup of those with just risk factors.
“This is a big step forward for patients with multiple risk factors and diabetes but without ASCVD, that both renal disease and hospitalization for heart failure are sensitive” to the SGLT2 inhibitors, Dr. Verma noted. “We see renal protection and reduction of heart failure hospitalization across both primary and secondary prevention patients, with no need to distinguish them based on ASCVD.” In contrast, he noted, the MACE benefit from the SGLT2 inhibitors seems limited to patients with ASCVD. The day before making this point in a talk during the meeting, Dr. Verma had published the same message in a commentary (Lancet. 2018 Nov 10. doi: 10.1016/S0140-6736(18)32824-1).
Although the “nomenclature of primary versus secondary prevention is appropriate for atherosclerotic outcomes, it is likely to be inappropriate for a person with type 2 diabetes who is at risk of hospitalization for heart failure and renal disease,” Dr. Verma wrote with his associates in the commentary.
What it means for clinicians
The upshot of all of these cardiovascular outcome trial results that came out over the past 3 years has been a new appreciation of how antihyperglycemic drugs can have cardiovascular and renal benefits that transcend their effects on glycemia. The evidence has put the SGLT2 inhibitors and GLP-1 RAs on track to challenge, and potentially displace, metformin as the top drug to prescribe for patients with T2DM.
Clinicians should realize that they should prescribe SGLT2 inhibitors and selected GLP-1 RAs “as early as metformin in patients with established ASCVD,” said Dr. Verma. “For patients with recalcitrant atherosclerotic disease and a history of MI and ischemia, I’d primarily treat with a GLP-1 RA. In a patient with left ventricular dysfunction or evidence of heart failure, I’d use an SGLT2 inhibitor. But it’s not a fight between these two. You could treat a patients with type 2 diabetes with both classes,” although the practicality of this approach is limited by the high cost of these drugs.
The SGLT2 inhibitors “should now be considered as first-line therapy after metformin in most people with type 2 diabetes, irrespective of whether or not they have established atherosclerotic vascular disease, chronic kidney disease, or heart failure,” he and his associates wrote in their recent commentary.
“What I struggle with the most is how we prioritize and individualize secondary-prevention therapies based on risk for ischemia and heart failure. Some therapies [the SGLT2 inhibitors] are predominantly for heart failure prevention, and some [the GLP-1 RAs] are primarily for ischemia. How do we choose when a patient cannot afford to take both? Does a combination of a SGLT2 inhibitor and a GLP-1 RA offer the greatest CVD benefit? We need to test this in a trial. And will metformin be displaced as first-line treatment?” Dr. Verma asked.
“The day will probably come when, for maximal protection, you treat with both classes. But right now we’re forced to choose because of the cost,” said John McMurray, MD, professor of cardiology at the University of Glasgow, in a talk during the meeting.
As to specifically which SGLT2 inhibitor to prescribe, “they all look pretty much the same” in the newly published meta-analysis, Dr. McMurray said, although he noted that safety differences among agents in the class remain possible.
“For patients similar to those studied in the three SGLT2 inhibitor trials, clinicians should use one of these drugs to reduce the risk for incident heart failure, irrespective of their effect on MACE,” said Dr. Butler. Reducing the risk for incident heart failure and of progressive renal dysfunction are two new goals for antihyperglycemic therapy that now overlay the long-standing goals of controlling glycemia and reducing cardiovascular disease risk and the more recent goals of cutting cardiovascular disease mortality and cutting the risk for a MACE event.
A current limitation for practice is that the none of the three drug companies that market the tested SGLT2 inhibitor drugs has sought regulatory approval for an indication of reducing the risk for heart failure hospitalization. Despite that, “these drugs should be used for renal protection and reducing heart failure hospitalizations,” Dr. Butler said. “We need to start thinking about this and not get lost thinking about only their MACE effect because, when you focus on MACE, there is a competition between the SGLT2 inhibitors and the GLP-1 RA. If we think of GLP-1 RAs as drugs to prevent MACE, and SGLT2 inhibitors as drugs that primarily prevent heart failure and renal dysfunction, then there is no competition. Perhaps combined treatment is where we need to go,” he said in an interview.
But the enthusiasm that experts like Dr. Butler, Dr. McMurray, and Dr. Verma have for wider use of both classes of drugs in appropriate patients is not necessarily matched right now among many community physicians. Cardiologist David J. Becker, MD, is an example of the clinicians who appreciate the growing evidence that supports wider use of these antihyperglycemic drugs but remain uneasy about applying this evidence in their practice.
Dr. Becker, associate director of the Preventive and Integrative Heart Health Program of the Temple Heart and Vascular Institute in Philadelphia, writes a column for the Philadelphia Inquirer on medical care. In a December 2018 piece, he said “like most cardiologists, I ‘don’t do diabetes’ – because it’s not my expertise. The new drugs, however, mean I need to learn more” about treating these patients. “The problem: There are so many of these medications that they present a bewildering choice for patients and doctors.”
Dr. Becker cited several barriers he sees for himself and his nonendocrinologist colleagues to prescribe these drugs – and for patients to take them:
- High cost, with prices that run close to $20/day for each medication.
- A thicket of names and choices that “lead to confusion and paralysis,” which has been exacerbated by “advertising wars” among competing drug companies.
- Cardiologists and primary care physicians usually defer to endocrinologists to prescribe these drugs, but most patients with T2DM aren’t seen by endocrinologists. The result: “Few doctors prescribe them.”
The cardiovascular disease benefits of these drugs have not been adequately promoted. Until that changes, “cardiologists like me will not realize their importance,” Dr. Becker concluded.
While christening the new diabetocardiology subspecialty, Dr. Braunwald placed the onus for managing this emerging facet of diabetes largely outside the scope of endocrinology.
“We can’t call in a consultant every time we have a patient with diabetes; it would bankrupt the system,” he said. Training of cardiologists now needs to include several months of treating patients with diabetes, Dr. Braunwald advised, just like 30 or so years ago when cardiologists like himself had to become more familiar with blood clotting to better manage thrombotic disease.
Dr. Braunwald has been a consultant to Cardurion, Myokardia, and Sanofi; an advisor to Endcardia; and has received research funding from AstraZeneca, Daiishi Sankyo, and Novartis. Dr. Butler has been a consultant or advisor to AstraZeneca, Amgen, Bayer, Boehringer Ingelheim, Janssen, Merck, Novartis, Novo Nordisk, and Sanofi. Dr. Verma has received honoraria and research funding from Abbott, Amgen, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Janssen, Merck, Novartis, NovoNordisk, Sanofi, and Valeant. Dr. McMurray has received research funding from 12 companies. Dr. Becker had no disclosures.
CHICAGO – When the first results from a large trial that showed profound and unexpected benefits for preventing heart failure hospitalizations associated with use of the antihyperglycemic sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin came out – a little over 3 years ago – the general reaction from clinicians was some variant of “Could this be real?”
Since then, as results from some five other large, international trials have come out showing both similar benefits from two other drugs in the same SGLT2 inhibitor class, canagliflozin and dapagliflozin, as well as results showing clear cardiovascular disease benefits from three drugs in a second class of antihyperglycemics, the glucagonlike peptide–1 receptor agonists (GLP-1 RAs), the general consensus among cardiologists became: “The cardiovascular and renal benefits are real. How can we now best use these drugs to help patients?”
This change increasingly forces cardiologists, as well as the primary care physicians who often manage patients with type 2 diabetes mellitus, to become more comfortable prescribing these two classes of antihyperglycemic drugs. During a talk at the American Heart Association scientific sessions, Eugene Braunwald, MD, arguably the top thought leader in cardiology, coined a new name for the medical subspecialty that he foresees navigating this overlap between diabetes care and cardiovascular disease prevention: diabetocardiology (although a more euphonic alternative might be cardiodiabetology, while the more comprehensive name could be cardionephrodiabetology).
“I was certainly surprised” by the first report in 2015 from the EMPA-REG OUTCOME trial (N Engl J Med. 2015 Nov 26;373[22]:2117-28), said Dr. Braunwald, who is professor of medicine at Harvard Medical School in Boston. A lot of his colleagues were surprised and said, “It’s just one trial.”
“Now we have three trials,” with the addition of the CANVAS trial for canagliflozin (N Engl J Med. 2017 Aug 17;377[7]:644-57) and the DECLARE-TIMI 58 trial (N Engl J Med. 2018 Nov 10. doi:10.1056/NEJMoa1812389) for dapagliflozin reported at the AHA meeting in November.
“We are in the midst of two pandemics: heart failure and type 2 diabetes. As cardiologists, we have to learn how to deal with this,” said Dr. Braunwald, and the evidence now clearly shows that these drugs can help with that.
As another speaker at the meeting, Javed Butler, MD, a heart failure specialist, observed in a separate talk at the meeting, “Heart failure is one of the most common, if not the most common complication, of patients with diabetes.” This tight link between heart failure and diabetes helps make cardiovascular mortality “the number one cause of death” in patients with diabetes, said Dr. Butler, professor and chairman of medicine at the University of Mississippi in Jackson.
“Thanks to the cardiovascular outcome trials, we now have a much broader and deeper appreciation of heart failure and renal disease as integral components of the cardiovascular-renal spectrum in people with diabetes,” said Subodh Verma, MD, a professor at the University of Toronto and cardiac surgeon at St. Michael’s Hospital in Toronto. Dr. Braunwald spelled out in his talk some of the interrelationships of diabetes, heart failure, and renal dysfunction that together produce a downward-spiraling vicious circle for patients, a pathophysiological process that clinicians can now short-circuit by treatment with a SGLT2 inhibitor.
Cardiovascular outcome trials show the way
In the context of antihyperglycemic drugs, the “cardiovascular outcome trials” refers to a series of large trials mandated by the Food and Drug Administration in 2008 to assess the cardiovascular disease effects of new agents coming onto the U.S. market to treat type 2 diabetes mellitus (T2DM). By the time Dr. Verma spoke at the AHA meeting, he could cite reported results from 12 of these trials: 5 different drugs in the GLP-1 RA class, 4 drugs in the dipeptidyl peptidase-4 (DPP-4) inhibitor class, and 3 drugs from the SGLT2 inhibitor class. Dr. Verma summed what the findings have shown.
The four tested DDP-4 inhibitors (alogliptin, linagliptin, saxagliptin, and sitagliptin) consistently showed neutrality for the primary outcome of major adverse cardiovascular disease events (MACE), constituted by cardiovascular disease death, MI, or stroke.
The five tested GLP-1 RAs (albiglutide, exenatide, liraglutide, lixisenatide, and semaglutide) showed a mixed pattern of MACE results that seemed to be linked with the subclass the drug fell into. The two exedin-4–based drugs, exenatide and lixisenatide, each showed a statistically neutral effect for MACE, as well as collectively in a combined analysis. In contrast, three human GLP-1–based drugs, albiglutide, liraglutide, and semaglutide, each showed a consistent, statistically-significant MACE reduction in their respective outcome trials, and collectively they showed a highly significant 18% reduction in MACE, compared with placebo, Dr. Verma said. Further, recent analysis by Dr. Verma that used data from liraglutide treatment in the LEADER trial showed the MACE benefit occurred only among enrolled patients treated with liraglutide who had established atherosclerotic cardiovascular disease (ASCVD). Patients enrolled in the trial with only multiple risk factors (in addition to having T2DM) but without established ASCVD showed no significant benefit from liraglutide treatment for the MACE endpoint, compared with control patients.
Recently a press-release announcement of results from a sixth GLP-1 RA, dulaglutide, in the REWIND trial of MACE outcomes suggested that a drug in this class could have broader effect. The majority, 69%, of the 9,901 patients with T2DM enrolled in REWIND had risk factors but not established ASCVD at enrollment. A Nov. 5, 2018, statement from the company developing this drug, Lilly, reported that the study overall produced a statistically significant reduction in MACE, although it provided no additional details. As the released noted, this made REWIND the first trial to show a MACE benefit from a drug in the GLP-1 RA class in patients without established ASCVD.
The MACE outcome results from the three SGLT2 inhibitor trials showed a similar pattern as liraglutide: In patients with established ASCVD, the drugs individually each produced a MACE reduction, although dapagliflozin just missed having a statistically significant reduction. Collectively, the three drugs showed a statistically significant, 14% relative risk reduction for MACE, compared with control patients. But among patients with multiple risk factors only, but without established ASCVD, included in two of the three trials (CANVAS and DECLARE-TIMI 58), the results showed both individually and collectively a neutral MACE effect.
But unlike the other antihyperglycemic drugs tested in the cardiovascular outcome trials, the SGLT2 inhibitors have shown two additional, highly important secondary outcomes: a consistent reduction in hospitalization for heart failure and a consistent reduction in renal-disease progression.
A meta-analysis of the three SGLT2 inhibitor trials published coincident with the release of the DECLARE-TIMI 58 results showed that, for the outcome of either cardiovascular death or hospitalization for heart failure, the SGLT2 inhibitors collectively showed a significant 29% relative decrease in this incidence among patients with a history of heart failure, and a significant 21% relative decrease among patients without history of heart failure (Lancet. 2018 Nov 10. doi: 10.1016/S0140-6736(18)32590-X). Among the subset of patients with established ASCVD, treatment with a SGLT2 inhibitor across all three trials showed a significant 16% relative risk reduction, and in the subset with multiple risk factors but no established ASCVD, the two SGLT2 inhibitors collectively produced a 16% relative cut in cardiovascular death or heart failure hospitalization with a P value of .06. Finally, the Lancet meta-analysis showed that, for a combined endpoint that reflected renal worsening, the SGLT2 inhibitors showed a significant relative reduction of about 45% in both the subgroup of patients with established ASCVD and in the subgroup of those with just risk factors.
“This is a big step forward for patients with multiple risk factors and diabetes but without ASCVD, that both renal disease and hospitalization for heart failure are sensitive” to the SGLT2 inhibitors, Dr. Verma noted. “We see renal protection and reduction of heart failure hospitalization across both primary and secondary prevention patients, with no need to distinguish them based on ASCVD.” In contrast, he noted, the MACE benefit from the SGLT2 inhibitors seems limited to patients with ASCVD. The day before making this point in a talk during the meeting, Dr. Verma had published the same message in a commentary (Lancet. 2018 Nov 10. doi: 10.1016/S0140-6736(18)32824-1).
Although the “nomenclature of primary versus secondary prevention is appropriate for atherosclerotic outcomes, it is likely to be inappropriate for a person with type 2 diabetes who is at risk of hospitalization for heart failure and renal disease,” Dr. Verma wrote with his associates in the commentary.
What it means for clinicians
The upshot of all of these cardiovascular outcome trial results that came out over the past 3 years has been a new appreciation of how antihyperglycemic drugs can have cardiovascular and renal benefits that transcend their effects on glycemia. The evidence has put the SGLT2 inhibitors and GLP-1 RAs on track to challenge, and potentially displace, metformin as the top drug to prescribe for patients with T2DM.
Clinicians should realize that they should prescribe SGLT2 inhibitors and selected GLP-1 RAs “as early as metformin in patients with established ASCVD,” said Dr. Verma. “For patients with recalcitrant atherosclerotic disease and a history of MI and ischemia, I’d primarily treat with a GLP-1 RA. In a patient with left ventricular dysfunction or evidence of heart failure, I’d use an SGLT2 inhibitor. But it’s not a fight between these two. You could treat a patients with type 2 diabetes with both classes,” although the practicality of this approach is limited by the high cost of these drugs.
The SGLT2 inhibitors “should now be considered as first-line therapy after metformin in most people with type 2 diabetes, irrespective of whether or not they have established atherosclerotic vascular disease, chronic kidney disease, or heart failure,” he and his associates wrote in their recent commentary.
“What I struggle with the most is how we prioritize and individualize secondary-prevention therapies based on risk for ischemia and heart failure. Some therapies [the SGLT2 inhibitors] are predominantly for heart failure prevention, and some [the GLP-1 RAs] are primarily for ischemia. How do we choose when a patient cannot afford to take both? Does a combination of a SGLT2 inhibitor and a GLP-1 RA offer the greatest CVD benefit? We need to test this in a trial. And will metformin be displaced as first-line treatment?” Dr. Verma asked.
“The day will probably come when, for maximal protection, you treat with both classes. But right now we’re forced to choose because of the cost,” said John McMurray, MD, professor of cardiology at the University of Glasgow, in a talk during the meeting.
As to specifically which SGLT2 inhibitor to prescribe, “they all look pretty much the same” in the newly published meta-analysis, Dr. McMurray said, although he noted that safety differences among agents in the class remain possible.
“For patients similar to those studied in the three SGLT2 inhibitor trials, clinicians should use one of these drugs to reduce the risk for incident heart failure, irrespective of their effect on MACE,” said Dr. Butler. Reducing the risk for incident heart failure and of progressive renal dysfunction are two new goals for antihyperglycemic therapy that now overlay the long-standing goals of controlling glycemia and reducing cardiovascular disease risk and the more recent goals of cutting cardiovascular disease mortality and cutting the risk for a MACE event.
A current limitation for practice is that the none of the three drug companies that market the tested SGLT2 inhibitor drugs has sought regulatory approval for an indication of reducing the risk for heart failure hospitalization. Despite that, “these drugs should be used for renal protection and reducing heart failure hospitalizations,” Dr. Butler said. “We need to start thinking about this and not get lost thinking about only their MACE effect because, when you focus on MACE, there is a competition between the SGLT2 inhibitors and the GLP-1 RA. If we think of GLP-1 RAs as drugs to prevent MACE, and SGLT2 inhibitors as drugs that primarily prevent heart failure and renal dysfunction, then there is no competition. Perhaps combined treatment is where we need to go,” he said in an interview.
But the enthusiasm that experts like Dr. Butler, Dr. McMurray, and Dr. Verma have for wider use of both classes of drugs in appropriate patients is not necessarily matched right now among many community physicians. Cardiologist David J. Becker, MD, is an example of the clinicians who appreciate the growing evidence that supports wider use of these antihyperglycemic drugs but remain uneasy about applying this evidence in their practice.
Dr. Becker, associate director of the Preventive and Integrative Heart Health Program of the Temple Heart and Vascular Institute in Philadelphia, writes a column for the Philadelphia Inquirer on medical care. In a December 2018 piece, he said “like most cardiologists, I ‘don’t do diabetes’ – because it’s not my expertise. The new drugs, however, mean I need to learn more” about treating these patients. “The problem: There are so many of these medications that they present a bewildering choice for patients and doctors.”
Dr. Becker cited several barriers he sees for himself and his nonendocrinologist colleagues to prescribe these drugs – and for patients to take them:
- High cost, with prices that run close to $20/day for each medication.
- A thicket of names and choices that “lead to confusion and paralysis,” which has been exacerbated by “advertising wars” among competing drug companies.
- Cardiologists and primary care physicians usually defer to endocrinologists to prescribe these drugs, but most patients with T2DM aren’t seen by endocrinologists. The result: “Few doctors prescribe them.”
The cardiovascular disease benefits of these drugs have not been adequately promoted. Until that changes, “cardiologists like me will not realize their importance,” Dr. Becker concluded.
While christening the new diabetocardiology subspecialty, Dr. Braunwald placed the onus for managing this emerging facet of diabetes largely outside the scope of endocrinology.
“We can’t call in a consultant every time we have a patient with diabetes; it would bankrupt the system,” he said. Training of cardiologists now needs to include several months of treating patients with diabetes, Dr. Braunwald advised, just like 30 or so years ago when cardiologists like himself had to become more familiar with blood clotting to better manage thrombotic disease.
Dr. Braunwald has been a consultant to Cardurion, Myokardia, and Sanofi; an advisor to Endcardia; and has received research funding from AstraZeneca, Daiishi Sankyo, and Novartis. Dr. Butler has been a consultant or advisor to AstraZeneca, Amgen, Bayer, Boehringer Ingelheim, Janssen, Merck, Novartis, Novo Nordisk, and Sanofi. Dr. Verma has received honoraria and research funding from Abbott, Amgen, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Janssen, Merck, Novartis, NovoNordisk, Sanofi, and Valeant. Dr. McMurray has received research funding from 12 companies. Dr. Becker had no disclosures.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Hospital Readmissions Reduction Program may be doing more harm than good
A Medicare program aimed at lowering readmissions to hospitals could be having an adverse effect on mortality.
Results from a retrospective cohort study of hospitalizations for heart failure, acute myocardial infarction, and pneumonia among Medicare beneficiaries aged 65 years and older between April 1, 2005 and March 31, 2015 (covering the period before and after the Medicare Hospital Readmissions Reduction Program was announced in April 2010 and implemented in October 2012) found a significant increase in 30-day post discharge mortality among heart failure and pneumonia patients.
“Most concerning, however, is the possibility that the relationship between the HRRP and postdischarge mortality for heart failure and pneumonia is causal, indicating that the HRRP led to changes in quality of care that adversely affected patients,” Rishi Wadhera, MD, Harvard Medical School, Boston, and his colleagues wrote in a report published Dec. 25, 2018, in JAMA.
They looked at 8.3 million hospitalizations for heart failure, acute MI, and pneumonia, among whom 7.9 million were alive at the time of discharge. There were roughly 270,000 deaths within 30 days of discharge for heart failure; 128,000 for acute MI; and 246,000 for pneumonia.
To examine trends, the timing was divided into four periods: two prior to the announcement of the HRRP (April 2005–September 2007 and October 2007–March 2010); a third covering the time when the HRRP was announced (April 2010–September 2012); and the fourth when HRRP was implemented (October 2012–March 2015).
They found that among patients discharged with heart failure, 30-day mortality was rising even before the announcement of the HRRP, by 0.27% from the first period to the second period. That baseline trend continued when the HRRP was announced, by 0.49%, from second period to third. The difference in change between those periods was 0.22%. After implementation, 30-day mortality increased by 0.52%, with a difference in change from the third period of 0.25%. Both changes were statistically significant.
Among pneumonia patients, postdischarge mortality was stable before HRRP, but significantly increased after HRRP announcement, by 0.26%, with a difference in change from the second period to the third period of 0.22%. After implementation, the 30-day postdischarge mortality was 0.44%, with a significant difference in change of 0.40%.
Acute MI was a different story. Postdischarge mortality decreased significantly after the implementation of the HRRP, by 0.22%. The difference in change was –0.26%.
The authors suggested that “some hospitals may have focused more resources and efforts on reducing or avoiding readmissions than on prioritizing survival.” They add that the increases in heart failure morbidity could be related to patients with more severe heart conditions.
They noted that “although hospitals that reduce readmissions also appear to reduce mortality, this hospital-level concordance does not reflect the change in readmissions and mortality at the level of the patient population, which is arguably of greater importance to individual patients and to public health.”
Further research is needed to understand whether the increase in 30-day postdischarge mortality is a result of the HRRP, the authors concluded.
SOURCE: Wadhera R et al. JAMA. 2018 Dec 25. doi: 10.1001/jama.2018.19232.
Evidence in this study shows that while the Hospital Readmissions Reduction Program my be succeeding in reducing hospital admissions, little evidence is available to show that it is having a positive effect on patient outcomes.
The Centers for Medicare & Medicaid Services needs to reexamine the program and find alternative methods that are both effective at reducing hospital readmissions while at the same time protect patients from unintentional harm, including death.
Gregg C. Fonarow, MD , University of California Medical Center, Los Angeles, in an editorial published in JAMA, Dec. 25, 2018. doi:10.1001/jama.2018.19325 .
Evidence in this study shows that while the Hospital Readmissions Reduction Program my be succeeding in reducing hospital admissions, little evidence is available to show that it is having a positive effect on patient outcomes.
The Centers for Medicare & Medicaid Services needs to reexamine the program and find alternative methods that are both effective at reducing hospital readmissions while at the same time protect patients from unintentional harm, including death.
Gregg C. Fonarow, MD , University of California Medical Center, Los Angeles, in an editorial published in JAMA, Dec. 25, 2018. doi:10.1001/jama.2018.19325 .
Evidence in this study shows that while the Hospital Readmissions Reduction Program my be succeeding in reducing hospital admissions, little evidence is available to show that it is having a positive effect on patient outcomes.
The Centers for Medicare & Medicaid Services needs to reexamine the program and find alternative methods that are both effective at reducing hospital readmissions while at the same time protect patients from unintentional harm, including death.
Gregg C. Fonarow, MD , University of California Medical Center, Los Angeles, in an editorial published in JAMA, Dec. 25, 2018. doi:10.1001/jama.2018.19325 .
A Medicare program aimed at lowering readmissions to hospitals could be having an adverse effect on mortality.
Results from a retrospective cohort study of hospitalizations for heart failure, acute myocardial infarction, and pneumonia among Medicare beneficiaries aged 65 years and older between April 1, 2005 and March 31, 2015 (covering the period before and after the Medicare Hospital Readmissions Reduction Program was announced in April 2010 and implemented in October 2012) found a significant increase in 30-day post discharge mortality among heart failure and pneumonia patients.
“Most concerning, however, is the possibility that the relationship between the HRRP and postdischarge mortality for heart failure and pneumonia is causal, indicating that the HRRP led to changes in quality of care that adversely affected patients,” Rishi Wadhera, MD, Harvard Medical School, Boston, and his colleagues wrote in a report published Dec. 25, 2018, in JAMA.
They looked at 8.3 million hospitalizations for heart failure, acute MI, and pneumonia, among whom 7.9 million were alive at the time of discharge. There were roughly 270,000 deaths within 30 days of discharge for heart failure; 128,000 for acute MI; and 246,000 for pneumonia.
To examine trends, the timing was divided into four periods: two prior to the announcement of the HRRP (April 2005–September 2007 and October 2007–March 2010); a third covering the time when the HRRP was announced (April 2010–September 2012); and the fourth when HRRP was implemented (October 2012–March 2015).
They found that among patients discharged with heart failure, 30-day mortality was rising even before the announcement of the HRRP, by 0.27% from the first period to the second period. That baseline trend continued when the HRRP was announced, by 0.49%, from second period to third. The difference in change between those periods was 0.22%. After implementation, 30-day mortality increased by 0.52%, with a difference in change from the third period of 0.25%. Both changes were statistically significant.
Among pneumonia patients, postdischarge mortality was stable before HRRP, but significantly increased after HRRP announcement, by 0.26%, with a difference in change from the second period to the third period of 0.22%. After implementation, the 30-day postdischarge mortality was 0.44%, with a significant difference in change of 0.40%.
Acute MI was a different story. Postdischarge mortality decreased significantly after the implementation of the HRRP, by 0.22%. The difference in change was –0.26%.
The authors suggested that “some hospitals may have focused more resources and efforts on reducing or avoiding readmissions than on prioritizing survival.” They add that the increases in heart failure morbidity could be related to patients with more severe heart conditions.
They noted that “although hospitals that reduce readmissions also appear to reduce mortality, this hospital-level concordance does not reflect the change in readmissions and mortality at the level of the patient population, which is arguably of greater importance to individual patients and to public health.”
Further research is needed to understand whether the increase in 30-day postdischarge mortality is a result of the HRRP, the authors concluded.
SOURCE: Wadhera R et al. JAMA. 2018 Dec 25. doi: 10.1001/jama.2018.19232.
A Medicare program aimed at lowering readmissions to hospitals could be having an adverse effect on mortality.
Results from a retrospective cohort study of hospitalizations for heart failure, acute myocardial infarction, and pneumonia among Medicare beneficiaries aged 65 years and older between April 1, 2005 and March 31, 2015 (covering the period before and after the Medicare Hospital Readmissions Reduction Program was announced in April 2010 and implemented in October 2012) found a significant increase in 30-day post discharge mortality among heart failure and pneumonia patients.
“Most concerning, however, is the possibility that the relationship between the HRRP and postdischarge mortality for heart failure and pneumonia is causal, indicating that the HRRP led to changes in quality of care that adversely affected patients,” Rishi Wadhera, MD, Harvard Medical School, Boston, and his colleagues wrote in a report published Dec. 25, 2018, in JAMA.
They looked at 8.3 million hospitalizations for heart failure, acute MI, and pneumonia, among whom 7.9 million were alive at the time of discharge. There were roughly 270,000 deaths within 30 days of discharge for heart failure; 128,000 for acute MI; and 246,000 for pneumonia.
To examine trends, the timing was divided into four periods: two prior to the announcement of the HRRP (April 2005–September 2007 and October 2007–March 2010); a third covering the time when the HRRP was announced (April 2010–September 2012); and the fourth when HRRP was implemented (October 2012–March 2015).
They found that among patients discharged with heart failure, 30-day mortality was rising even before the announcement of the HRRP, by 0.27% from the first period to the second period. That baseline trend continued when the HRRP was announced, by 0.49%, from second period to third. The difference in change between those periods was 0.22%. After implementation, 30-day mortality increased by 0.52%, with a difference in change from the third period of 0.25%. Both changes were statistically significant.
Among pneumonia patients, postdischarge mortality was stable before HRRP, but significantly increased after HRRP announcement, by 0.26%, with a difference in change from the second period to the third period of 0.22%. After implementation, the 30-day postdischarge mortality was 0.44%, with a significant difference in change of 0.40%.
Acute MI was a different story. Postdischarge mortality decreased significantly after the implementation of the HRRP, by 0.22%. The difference in change was –0.26%.
The authors suggested that “some hospitals may have focused more resources and efforts on reducing or avoiding readmissions than on prioritizing survival.” They add that the increases in heart failure morbidity could be related to patients with more severe heart conditions.
They noted that “although hospitals that reduce readmissions also appear to reduce mortality, this hospital-level concordance does not reflect the change in readmissions and mortality at the level of the patient population, which is arguably of greater importance to individual patients and to public health.”
Further research is needed to understand whether the increase in 30-day postdischarge mortality is a result of the HRRP, the authors concluded.
SOURCE: Wadhera R et al. JAMA. 2018 Dec 25. doi: 10.1001/jama.2018.19232.
FROM JAMA
Key clinical point:
Major finding: Heart failure patients saw mortality increase 0.52% after HRRP launched.
Study details: A retrospective cohort study across 10 years, including time before and after the implementation of the HRRP.
Disclosures: The Richard A. and Susan F. Smith Center for Outcomes Research in Cardiology funded the study. No relevant conflicts of interest were disclosed.
Source: Wadhera R et al. JAMA 2018 Dec 25. doi: 10.1001/jama.2018.19232.
Synthetic opioids drive spike in U.S. fatal drug overdoses
New federal statistics suggest that the opioid epidemic in the United States is evolving as physicians crack down on the use of prescription painkillers: Fatal drug overdose deaths rose by 12% from 2016 to 2017, boosted by a wave of fatalities linked to illicit synthetic opioids like fentanyl that are now linked to an estimated 60% of opioid-related deaths.
“Overall, the overdose epidemic continues to worsen, and it has grown increasingly complex by coinvolvement of prescription and illicit drugs,” Lawrence Scholl, PhD, MPH, and his associates at the Centers for Disease Control & Prevention wrote in the Morbidity and Mortality Weekly Report.
The new statistics provide more evidence that 2017 marked “a sharp increase in what has characterized as the third wave of the opioid epidemic,” said drug and health policy researcher Stephen Crystal, PhD, of Rutgers University, New Brunswick, N.J., in an interview. He was referring to a wave that experts believe started in 2013 amid a spike in U.S. overdose deaths from fentanyl and other synthetic opioids.
The new report analyzes fatal drug overdose data from 2013 to 2017. According to the findings, the total number of those overdoses rose to 70,237 in 2017, up from 63,632 in 2016. The highest drug overdose death rates in 2017 were in West Virginia, followed by Ohio, Pennsylvania, and the District of Columbia.
Some statistics did not change much from 2016 to 2017: About two-thirds of the drug overdose deaths were linked to opioids in both years, and the death rate of cases linked to prescription drugs and heroin remained steady. (Death rates in the report were age adjusted.)
However, the percentage of fatal overdose cases linked to synthetic opioids grew 45% from 2016 to 2017. Overall, 60% of opioid-related fatal overdoses in 2017 involved synthetic opioids.
The report identifies increases in several areas from 2016 to 2017. Opioid-related drug overdose deaths among black people rose by 25%, and an analysis of data from 34 states and the District of Columbia found the highest increases in death rates in North Carolina (29%), Ohio (19%), and Maine (19%).
In regard to deaths linked to synthetic opioids specifically, the highest death rates in 2017 were in West Virginia (37 per 100,000), Ohio (32 per 100,000), and New Hampshire (30 per 100,000).
“Part of what we’re seeing in these increased numbers are individuals who have pain, can’t get prescribed opioids, and turn to street drugs,” Dr. Crystal said, adding that “abruptly cutting patients off is not good, and leaving patients with a lot of untreated pain is not good. If people are going to be discontinued [from opioids] or have their doses reduced, the taper needs to be done very slowly and carefully.”
Synthetic opioids were not the only drugs that are driving up fatal overdoses, as the death rates of cases linked to cocaine and psychostimulants (such as methamphetamine) jumped by more than a third in 2017.
“The most important thing these numbers are telling me is that it’s becoming more and more attractive to drug dealers to put fentanyl in the heroin, cocaine, and other drugs they sell,” Dr. Crystal said. “When that happens, dependence on street drugs becomes much more deadly. It’s almost impossible to get the dose right. Every time you shoot up, you’re taking a chance that you’ll overdose.”
The report had limitations, including the fact that details about drug use were missing from 12% (2016) and 15% (2017) of death certificates in fatal overdose cases. By state, the percentages of those death certificates that included drug information ranged from as little as 55% to 99%.
There’s some possible positive news: The report points to preliminary data from 2018 suggesting that the number of annual drug overdose deaths may be leveling off – although it says more analysis is needed to confirm the trend.
Dr. Crystal, however, is not celebrating. “I don’t see this as a good news story, really,” he said, adding that there’s “a little too much of people patting themselves on the back” because they’re proud of cutbacks in opioid prescriptions.
“This doesn’t have to do with the huge number of people who got started with opioids years ago” and are now at risk of using street drugs, he said. “We haven’t engaged that population at the rate we need to. And flattening out at 70,000 drug overdoses a year is not a good news story.”
Dr. Crystal reported no relevant disclosures.
SOURCE: Scholl L et al. MMWR. 2019 Jan 4;67(5152):1419-27.
New federal statistics suggest that the opioid epidemic in the United States is evolving as physicians crack down on the use of prescription painkillers: Fatal drug overdose deaths rose by 12% from 2016 to 2017, boosted by a wave of fatalities linked to illicit synthetic opioids like fentanyl that are now linked to an estimated 60% of opioid-related deaths.
“Overall, the overdose epidemic continues to worsen, and it has grown increasingly complex by coinvolvement of prescription and illicit drugs,” Lawrence Scholl, PhD, MPH, and his associates at the Centers for Disease Control & Prevention wrote in the Morbidity and Mortality Weekly Report.
The new statistics provide more evidence that 2017 marked “a sharp increase in what has characterized as the third wave of the opioid epidemic,” said drug and health policy researcher Stephen Crystal, PhD, of Rutgers University, New Brunswick, N.J., in an interview. He was referring to a wave that experts believe started in 2013 amid a spike in U.S. overdose deaths from fentanyl and other synthetic opioids.
The new report analyzes fatal drug overdose data from 2013 to 2017. According to the findings, the total number of those overdoses rose to 70,237 in 2017, up from 63,632 in 2016. The highest drug overdose death rates in 2017 were in West Virginia, followed by Ohio, Pennsylvania, and the District of Columbia.
Some statistics did not change much from 2016 to 2017: About two-thirds of the drug overdose deaths were linked to opioids in both years, and the death rate of cases linked to prescription drugs and heroin remained steady. (Death rates in the report were age adjusted.)
However, the percentage of fatal overdose cases linked to synthetic opioids grew 45% from 2016 to 2017. Overall, 60% of opioid-related fatal overdoses in 2017 involved synthetic opioids.
The report identifies increases in several areas from 2016 to 2017. Opioid-related drug overdose deaths among black people rose by 25%, and an analysis of data from 34 states and the District of Columbia found the highest increases in death rates in North Carolina (29%), Ohio (19%), and Maine (19%).
In regard to deaths linked to synthetic opioids specifically, the highest death rates in 2017 were in West Virginia (37 per 100,000), Ohio (32 per 100,000), and New Hampshire (30 per 100,000).
“Part of what we’re seeing in these increased numbers are individuals who have pain, can’t get prescribed opioids, and turn to street drugs,” Dr. Crystal said, adding that “abruptly cutting patients off is not good, and leaving patients with a lot of untreated pain is not good. If people are going to be discontinued [from opioids] or have their doses reduced, the taper needs to be done very slowly and carefully.”
Synthetic opioids were not the only drugs that are driving up fatal overdoses, as the death rates of cases linked to cocaine and psychostimulants (such as methamphetamine) jumped by more than a third in 2017.
“The most important thing these numbers are telling me is that it’s becoming more and more attractive to drug dealers to put fentanyl in the heroin, cocaine, and other drugs they sell,” Dr. Crystal said. “When that happens, dependence on street drugs becomes much more deadly. It’s almost impossible to get the dose right. Every time you shoot up, you’re taking a chance that you’ll overdose.”
The report had limitations, including the fact that details about drug use were missing from 12% (2016) and 15% (2017) of death certificates in fatal overdose cases. By state, the percentages of those death certificates that included drug information ranged from as little as 55% to 99%.
There’s some possible positive news: The report points to preliminary data from 2018 suggesting that the number of annual drug overdose deaths may be leveling off – although it says more analysis is needed to confirm the trend.
Dr. Crystal, however, is not celebrating. “I don’t see this as a good news story, really,” he said, adding that there’s “a little too much of people patting themselves on the back” because they’re proud of cutbacks in opioid prescriptions.
“This doesn’t have to do with the huge number of people who got started with opioids years ago” and are now at risk of using street drugs, he said. “We haven’t engaged that population at the rate we need to. And flattening out at 70,000 drug overdoses a year is not a good news story.”
Dr. Crystal reported no relevant disclosures.
SOURCE: Scholl L et al. MMWR. 2019 Jan 4;67(5152):1419-27.
New federal statistics suggest that the opioid epidemic in the United States is evolving as physicians crack down on the use of prescription painkillers: Fatal drug overdose deaths rose by 12% from 2016 to 2017, boosted by a wave of fatalities linked to illicit synthetic opioids like fentanyl that are now linked to an estimated 60% of opioid-related deaths.
“Overall, the overdose epidemic continues to worsen, and it has grown increasingly complex by coinvolvement of prescription and illicit drugs,” Lawrence Scholl, PhD, MPH, and his associates at the Centers for Disease Control & Prevention wrote in the Morbidity and Mortality Weekly Report.
The new statistics provide more evidence that 2017 marked “a sharp increase in what has characterized as the third wave of the opioid epidemic,” said drug and health policy researcher Stephen Crystal, PhD, of Rutgers University, New Brunswick, N.J., in an interview. He was referring to a wave that experts believe started in 2013 amid a spike in U.S. overdose deaths from fentanyl and other synthetic opioids.
The new report analyzes fatal drug overdose data from 2013 to 2017. According to the findings, the total number of those overdoses rose to 70,237 in 2017, up from 63,632 in 2016. The highest drug overdose death rates in 2017 were in West Virginia, followed by Ohio, Pennsylvania, and the District of Columbia.
Some statistics did not change much from 2016 to 2017: About two-thirds of the drug overdose deaths were linked to opioids in both years, and the death rate of cases linked to prescription drugs and heroin remained steady. (Death rates in the report were age adjusted.)
However, the percentage of fatal overdose cases linked to synthetic opioids grew 45% from 2016 to 2017. Overall, 60% of opioid-related fatal overdoses in 2017 involved synthetic opioids.
The report identifies increases in several areas from 2016 to 2017. Opioid-related drug overdose deaths among black people rose by 25%, and an analysis of data from 34 states and the District of Columbia found the highest increases in death rates in North Carolina (29%), Ohio (19%), and Maine (19%).
In regard to deaths linked to synthetic opioids specifically, the highest death rates in 2017 were in West Virginia (37 per 100,000), Ohio (32 per 100,000), and New Hampshire (30 per 100,000).
“Part of what we’re seeing in these increased numbers are individuals who have pain, can’t get prescribed opioids, and turn to street drugs,” Dr. Crystal said, adding that “abruptly cutting patients off is not good, and leaving patients with a lot of untreated pain is not good. If people are going to be discontinued [from opioids] or have their doses reduced, the taper needs to be done very slowly and carefully.”
Synthetic opioids were not the only drugs that are driving up fatal overdoses, as the death rates of cases linked to cocaine and psychostimulants (such as methamphetamine) jumped by more than a third in 2017.
“The most important thing these numbers are telling me is that it’s becoming more and more attractive to drug dealers to put fentanyl in the heroin, cocaine, and other drugs they sell,” Dr. Crystal said. “When that happens, dependence on street drugs becomes much more deadly. It’s almost impossible to get the dose right. Every time you shoot up, you’re taking a chance that you’ll overdose.”
The report had limitations, including the fact that details about drug use were missing from 12% (2016) and 15% (2017) of death certificates in fatal overdose cases. By state, the percentages of those death certificates that included drug information ranged from as little as 55% to 99%.
There’s some possible positive news: The report points to preliminary data from 2018 suggesting that the number of annual drug overdose deaths may be leveling off – although it says more analysis is needed to confirm the trend.
Dr. Crystal, however, is not celebrating. “I don’t see this as a good news story, really,” he said, adding that there’s “a little too much of people patting themselves on the back” because they’re proud of cutbacks in opioid prescriptions.
“This doesn’t have to do with the huge number of people who got started with opioids years ago” and are now at risk of using street drugs, he said. “We haven’t engaged that population at the rate we need to. And flattening out at 70,000 drug overdoses a year is not a good news story.”
Dr. Crystal reported no relevant disclosures.
SOURCE: Scholl L et al. MMWR. 2019 Jan 4;67(5152):1419-27.
FROM MMWR
HIPAA compliance: Three cases to learn from
Data security experts say three HIPAA violations that resulted in significant fines by the Office for Civil Rights (OCR) in 2018 hold important lessons for health professionals about safeguarding records and training staff in HIPAA compliance.
Read on to learn how the cases unfolded and what knowledge practices can gain from the common HIPAA mistakes.
Who? Allergy Associates of Hartford, Conn.
What happened? A patient contacted a local television station to complain about a dispute between herself and a physician at Allergy Associates in Hartford, Conn. The disagreement stemmed from the office turning away the patient because she allegedly brought her service animal, according to a Nov. 26 announcement by the Department of Health & Human Services. The reporter contacted the doctor in question for a news story and, in responding, the physician disclosed protected patient information to the reporter.
What else? An OCR investigation determined that a privacy officer with Allergy Associates had instructed the physician not to respond to the media about the complaint or to respond with “no comment”; that advice was disregarded. The practice then failed to discipline the physician or take any corrective action following the disclosure, according to the OCR.
How much? The OCR imposed a $125,000 fine on the practice and a corrective action plan that includes 2 years of OCR monitoring.
Lessons learned: Had the practice disciplined the physician or taken corrective action after the disclosure, the OCR may not have penalized the group so severely, according to Jennifer Mitchell, a Cincinnati-based health law attorney and vice chair of the American Bar Association eHealth, Privacy, & Security Interest Group.
“In my opinion, the government levied these penalties because the provider did not sanction the doctor,” Ms. Mitchell said in an interview. “Health care entities need to take proper steps to remediate and, at a minimum, hold their workforce responsible for their behavior and ensure that it won’t happen again.”
The case emphasizes the need to train team members on media protocols and to ensure that protected health information is not mistakenly released. In addition to implementing policies and procedures, practices must also be willing to discipline health professionals when violations occur.
“A health care provider’s natural inclination is to defend themselves if they are being accused by a patient,” she said. “However, under the HIPAA rules, health care providers have to understand that they are prohibited from making such public statements about any patient.”
Who? Advanced Care Hospitalists of Lakeland, Fla.
What happened? Advanced Care Hospitalists (ACH) received billing services from an individual who represented himself to be affiliated with a Florida-based company named Doctor’s First Choice Billing. A local hospital later notified ACH that patient information, including names and Social Security numbers, were viewable on the First Choice website. ACH identified at least 400 patients affected by the breach and reported the breach to the OCR. However, ACH later determined that an additional 8,855 patients may have been affected and revised its OCR notification.
What else? During its investigation, the OCR found that the hospitalist group had never entered into a business associate agreement for billing services with First Choice, as required by HIPAA, and that the practice also failed to adopt any policies regarding business associate agreements until 2014, according to a Dec. 4 announcement from HHS.
How much? The OCR fined the practice $500,000 and also imposed a robust corrective action plan that includes an enterprise-wide risk analysis and the adoption of business associate agreements. Roger Severino, OCR director, called the case especially troubling because “the practice allowed the names and Social Security numbers of thousands of patients to be exposed on the Internet after it failed to follow basic security requirements under HIPAA.”
Lessons learned: The case illustrates the importance of having a business associate agreement in place for all third parties that may have access to protected health information, said Clinton Mikel, a Farmington Hills, Mich., health law attorney specializing in HIPAA compliance.
Under HIPAA, a business associate is defined as a person or entity, other than a member of the workforce of a covered entity, who “performs functions or activities on behalf of, or provides certain services to, a covered entity that involve access by the business associate to protected health information.”
HIPAA requires that covered entities enter into contracts with business associates to ensure appropriate safeguarding of protected health information.
“If your business associate has a breach, your practice must report the breach to OCR and your patients,” Mr. Mikel said in an interview. “The OCR will then investigate your practice and your relationship with the business associate. Just because the breach and fault clearly happened elsewhere, you will still be investigated, and could face a penalty if HIPAA requirements weren’t met.”
Who? Filefax of Northbrook, Ill.
What happened? The OCR opened an investigation after receiving an anonymous complaint that medical records obtained from Filefax, a company that provided storage, maintenance, and delivery of medical records for health professionals, were left unmonitored at a shredding and recycling facility. OCR’s investigation revealed that a person left the records of 2,150 patients at the recycling plant and that the records contained protected health information, according to an HHS announcement. It is unclear if the person worked for Filefax.
What else? The OCR discovered that, in a related incident, an individual who obtained medical records from Filefax left them unattended in an unlocked truck in the Filefax parking lot.
How much? The OCR imposed a $100,000 fine on Filefax. The company is no longer in business; however, a court-appointed liquidator has agreed to properly store and dispose of the remaining records.
Lessons learned: Although the case did not involve a health provider, the circumstances are applicable to physicians, particularly when practices move or close, Mr. Mikel said. In some cases, a former patient may contact a shuttered practice only to learn their record cannot be located, or worse, that a breach has occurred.
“[Such a case is] ripe for a patient to complain to OCR,” he said. “OCR doesn’t care if you’re closed or retired, they’re going to look.”
HIPAA requires thatcovered entities apply appropriate administrative, technical, and physical safeguards to protect the privacy of protected health information in any form when moving or closing. The safeguards must prevent prohibited uses and disclosures of protected health information in connection with the disposal of such information, according to the rule. The HHS provides guidance for the disposing of medical records; further, the American Academy of Family Physicians has created a checklist on closing a practice that addresses the transferring of medical records.
Without taking the correct measures, doctors may end up drawing scrutiny from OCR and face a potential fine if violations are found, experts said.
“Covered entities and business associates need to be aware that OCR is committed to enforcing HIPAA regardless of whether a covered entity is opening its doors or closing them,” Mr. Severino of the OCR said in a statement. “HIPAA still applies.”
Data security experts say three HIPAA violations that resulted in significant fines by the Office for Civil Rights (OCR) in 2018 hold important lessons for health professionals about safeguarding records and training staff in HIPAA compliance.
Read on to learn how the cases unfolded and what knowledge practices can gain from the common HIPAA mistakes.
Who? Allergy Associates of Hartford, Conn.
What happened? A patient contacted a local television station to complain about a dispute between herself and a physician at Allergy Associates in Hartford, Conn. The disagreement stemmed from the office turning away the patient because she allegedly brought her service animal, according to a Nov. 26 announcement by the Department of Health & Human Services. The reporter contacted the doctor in question for a news story and, in responding, the physician disclosed protected patient information to the reporter.
What else? An OCR investigation determined that a privacy officer with Allergy Associates had instructed the physician not to respond to the media about the complaint or to respond with “no comment”; that advice was disregarded. The practice then failed to discipline the physician or take any corrective action following the disclosure, according to the OCR.
How much? The OCR imposed a $125,000 fine on the practice and a corrective action plan that includes 2 years of OCR monitoring.
Lessons learned: Had the practice disciplined the physician or taken corrective action after the disclosure, the OCR may not have penalized the group so severely, according to Jennifer Mitchell, a Cincinnati-based health law attorney and vice chair of the American Bar Association eHealth, Privacy, & Security Interest Group.
“In my opinion, the government levied these penalties because the provider did not sanction the doctor,” Ms. Mitchell said in an interview. “Health care entities need to take proper steps to remediate and, at a minimum, hold their workforce responsible for their behavior and ensure that it won’t happen again.”
The case emphasizes the need to train team members on media protocols and to ensure that protected health information is not mistakenly released. In addition to implementing policies and procedures, practices must also be willing to discipline health professionals when violations occur.
“A health care provider’s natural inclination is to defend themselves if they are being accused by a patient,” she said. “However, under the HIPAA rules, health care providers have to understand that they are prohibited from making such public statements about any patient.”
Who? Advanced Care Hospitalists of Lakeland, Fla.
What happened? Advanced Care Hospitalists (ACH) received billing services from an individual who represented himself to be affiliated with a Florida-based company named Doctor’s First Choice Billing. A local hospital later notified ACH that patient information, including names and Social Security numbers, were viewable on the First Choice website. ACH identified at least 400 patients affected by the breach and reported the breach to the OCR. However, ACH later determined that an additional 8,855 patients may have been affected and revised its OCR notification.
What else? During its investigation, the OCR found that the hospitalist group had never entered into a business associate agreement for billing services with First Choice, as required by HIPAA, and that the practice also failed to adopt any policies regarding business associate agreements until 2014, according to a Dec. 4 announcement from HHS.
How much? The OCR fined the practice $500,000 and also imposed a robust corrective action plan that includes an enterprise-wide risk analysis and the adoption of business associate agreements. Roger Severino, OCR director, called the case especially troubling because “the practice allowed the names and Social Security numbers of thousands of patients to be exposed on the Internet after it failed to follow basic security requirements under HIPAA.”
Lessons learned: The case illustrates the importance of having a business associate agreement in place for all third parties that may have access to protected health information, said Clinton Mikel, a Farmington Hills, Mich., health law attorney specializing in HIPAA compliance.
Under HIPAA, a business associate is defined as a person or entity, other than a member of the workforce of a covered entity, who “performs functions or activities on behalf of, or provides certain services to, a covered entity that involve access by the business associate to protected health information.”
HIPAA requires that covered entities enter into contracts with business associates to ensure appropriate safeguarding of protected health information.
“If your business associate has a breach, your practice must report the breach to OCR and your patients,” Mr. Mikel said in an interview. “The OCR will then investigate your practice and your relationship with the business associate. Just because the breach and fault clearly happened elsewhere, you will still be investigated, and could face a penalty if HIPAA requirements weren’t met.”
Who? Filefax of Northbrook, Ill.
What happened? The OCR opened an investigation after receiving an anonymous complaint that medical records obtained from Filefax, a company that provided storage, maintenance, and delivery of medical records for health professionals, were left unmonitored at a shredding and recycling facility. OCR’s investigation revealed that a person left the records of 2,150 patients at the recycling plant and that the records contained protected health information, according to an HHS announcement. It is unclear if the person worked for Filefax.
What else? The OCR discovered that, in a related incident, an individual who obtained medical records from Filefax left them unattended in an unlocked truck in the Filefax parking lot.
How much? The OCR imposed a $100,000 fine on Filefax. The company is no longer in business; however, a court-appointed liquidator has agreed to properly store and dispose of the remaining records.
Lessons learned: Although the case did not involve a health provider, the circumstances are applicable to physicians, particularly when practices move or close, Mr. Mikel said. In some cases, a former patient may contact a shuttered practice only to learn their record cannot be located, or worse, that a breach has occurred.
“[Such a case is] ripe for a patient to complain to OCR,” he said. “OCR doesn’t care if you’re closed or retired, they’re going to look.”
HIPAA requires thatcovered entities apply appropriate administrative, technical, and physical safeguards to protect the privacy of protected health information in any form when moving or closing. The safeguards must prevent prohibited uses and disclosures of protected health information in connection with the disposal of such information, according to the rule. The HHS provides guidance for the disposing of medical records; further, the American Academy of Family Physicians has created a checklist on closing a practice that addresses the transferring of medical records.
Without taking the correct measures, doctors may end up drawing scrutiny from OCR and face a potential fine if violations are found, experts said.
“Covered entities and business associates need to be aware that OCR is committed to enforcing HIPAA regardless of whether a covered entity is opening its doors or closing them,” Mr. Severino of the OCR said in a statement. “HIPAA still applies.”
Data security experts say three HIPAA violations that resulted in significant fines by the Office for Civil Rights (OCR) in 2018 hold important lessons for health professionals about safeguarding records and training staff in HIPAA compliance.
Read on to learn how the cases unfolded and what knowledge practices can gain from the common HIPAA mistakes.
Who? Allergy Associates of Hartford, Conn.
What happened? A patient contacted a local television station to complain about a dispute between herself and a physician at Allergy Associates in Hartford, Conn. The disagreement stemmed from the office turning away the patient because she allegedly brought her service animal, according to a Nov. 26 announcement by the Department of Health & Human Services. The reporter contacted the doctor in question for a news story and, in responding, the physician disclosed protected patient information to the reporter.
What else? An OCR investigation determined that a privacy officer with Allergy Associates had instructed the physician not to respond to the media about the complaint or to respond with “no comment”; that advice was disregarded. The practice then failed to discipline the physician or take any corrective action following the disclosure, according to the OCR.
How much? The OCR imposed a $125,000 fine on the practice and a corrective action plan that includes 2 years of OCR monitoring.
Lessons learned: Had the practice disciplined the physician or taken corrective action after the disclosure, the OCR may not have penalized the group so severely, according to Jennifer Mitchell, a Cincinnati-based health law attorney and vice chair of the American Bar Association eHealth, Privacy, & Security Interest Group.
“In my opinion, the government levied these penalties because the provider did not sanction the doctor,” Ms. Mitchell said in an interview. “Health care entities need to take proper steps to remediate and, at a minimum, hold their workforce responsible for their behavior and ensure that it won’t happen again.”
The case emphasizes the need to train team members on media protocols and to ensure that protected health information is not mistakenly released. In addition to implementing policies and procedures, practices must also be willing to discipline health professionals when violations occur.
“A health care provider’s natural inclination is to defend themselves if they are being accused by a patient,” she said. “However, under the HIPAA rules, health care providers have to understand that they are prohibited from making such public statements about any patient.”
Who? Advanced Care Hospitalists of Lakeland, Fla.
What happened? Advanced Care Hospitalists (ACH) received billing services from an individual who represented himself to be affiliated with a Florida-based company named Doctor’s First Choice Billing. A local hospital later notified ACH that patient information, including names and Social Security numbers, were viewable on the First Choice website. ACH identified at least 400 patients affected by the breach and reported the breach to the OCR. However, ACH later determined that an additional 8,855 patients may have been affected and revised its OCR notification.
What else? During its investigation, the OCR found that the hospitalist group had never entered into a business associate agreement for billing services with First Choice, as required by HIPAA, and that the practice also failed to adopt any policies regarding business associate agreements until 2014, according to a Dec. 4 announcement from HHS.
How much? The OCR fined the practice $500,000 and also imposed a robust corrective action plan that includes an enterprise-wide risk analysis and the adoption of business associate agreements. Roger Severino, OCR director, called the case especially troubling because “the practice allowed the names and Social Security numbers of thousands of patients to be exposed on the Internet after it failed to follow basic security requirements under HIPAA.”
Lessons learned: The case illustrates the importance of having a business associate agreement in place for all third parties that may have access to protected health information, said Clinton Mikel, a Farmington Hills, Mich., health law attorney specializing in HIPAA compliance.
Under HIPAA, a business associate is defined as a person or entity, other than a member of the workforce of a covered entity, who “performs functions or activities on behalf of, or provides certain services to, a covered entity that involve access by the business associate to protected health information.”
HIPAA requires that covered entities enter into contracts with business associates to ensure appropriate safeguarding of protected health information.
“If your business associate has a breach, your practice must report the breach to OCR and your patients,” Mr. Mikel said in an interview. “The OCR will then investigate your practice and your relationship with the business associate. Just because the breach and fault clearly happened elsewhere, you will still be investigated, and could face a penalty if HIPAA requirements weren’t met.”
Who? Filefax of Northbrook, Ill.
What happened? The OCR opened an investigation after receiving an anonymous complaint that medical records obtained from Filefax, a company that provided storage, maintenance, and delivery of medical records for health professionals, were left unmonitored at a shredding and recycling facility. OCR’s investigation revealed that a person left the records of 2,150 patients at the recycling plant and that the records contained protected health information, according to an HHS announcement. It is unclear if the person worked for Filefax.
What else? The OCR discovered that, in a related incident, an individual who obtained medical records from Filefax left them unattended in an unlocked truck in the Filefax parking lot.
How much? The OCR imposed a $100,000 fine on Filefax. The company is no longer in business; however, a court-appointed liquidator has agreed to properly store and dispose of the remaining records.
Lessons learned: Although the case did not involve a health provider, the circumstances are applicable to physicians, particularly when practices move or close, Mr. Mikel said. In some cases, a former patient may contact a shuttered practice only to learn their record cannot be located, or worse, that a breach has occurred.
“[Such a case is] ripe for a patient to complain to OCR,” he said. “OCR doesn’t care if you’re closed or retired, they’re going to look.”
HIPAA requires thatcovered entities apply appropriate administrative, technical, and physical safeguards to protect the privacy of protected health information in any form when moving or closing. The safeguards must prevent prohibited uses and disclosures of protected health information in connection with the disposal of such information, according to the rule. The HHS provides guidance for the disposing of medical records; further, the American Academy of Family Physicians has created a checklist on closing a practice that addresses the transferring of medical records.
Without taking the correct measures, doctors may end up drawing scrutiny from OCR and face a potential fine if violations are found, experts said.
“Covered entities and business associates need to be aware that OCR is committed to enforcing HIPAA regardless of whether a covered entity is opening its doors or closing them,” Mr. Severino of the OCR said in a statement. “HIPAA still applies.”
How can I improve opioid safety at my hospital?
Quality improvement is essential
Case
A 67-year-old opioid-naive male with a history of obstructive sleep apnea and chronic kidney disease became unresponsive 2 days after hip replacement. Physical exam revealed a respiratory rate of 6 breaths/minute and oxygen saturation of 82%. He had received 6 doses of 6-mg IV morphine within the past 7 hours. How can I improve opioid safety at my hospital?
Background
Opioids are the most commonly prescribed class of medication in the hospital and the second–most common class causing adverse drug events (ADEs), the most serious being respiratory depression and death.1
Opioid ADEs and side effects can cause prolonged length of stay and patient suffering. These vary from potentially life-threatening events such as serotonin syndrome and adrenal insufficiency to more manageable problems still requiring intervention such as constipation, urinary retention, cognitive impairment, nausea, and vomiting. Treatment of side effects can lead to complications, including side effects from antiemetics and urinary tract infections from catheters.
A 4-year review found 700 deaths in the United States attributed to patient-controlled analgesia (PCA) use.2 Another study revealed that one out of every 200 patients has postoperative respiratory depression attributable to opioids.3
It is estimated that 2 million patients a year become chronic opioid users. Inpatient opioid prescribing contributes to this problem;4 for instance, 5.9% of patients after minor surgery and 6.5% after major surgery become chronic opioid users if discharged with an opioid.5 Calcaterra et al. found 25% of opioid-naive medical patients received an opioid at discharge from a medical service.6 Those patients had an odds ratio of 4.90 for becoming a chronic opioid user that year.6
Most hospitals have incomplete or outdated policies and procedures for safe opioid prescribing and administration.7 The Joint Commission on Accreditation of Healthcare Organizations has specific pain standards for pain assessment, pain management, and safe opioid prescribing for hospitals. Additions and revisions were developed to go into effect Jan. 1, 2018. (Table 1)8
Quality improvement
Quality improvement (QI) is an effective way to improve opioid safety. The Society of Hospital Medicine has developed a QI guide, “Reducing adverse drug events related to opioids” or “RADEO,” to increase safety and decrease serious ADEs attributable to opioids.7
The steps in the RADEO program are as follows:
1. Assemble your team
It is critical to identify and include stakeholders from multiple disciplines on your project team. This team will be essential to develop a practical project, identify barriers, create solutions, and gain buy-in from medical staff and administrative leadership.
Front-line staff will have invaluable insight and need to be team members. The majority of interventions are performed by nurses; therefore, nursing leadership and input is essential. Representatives from pharmacy, information technology, and the quality department will be extremely valuable team members to guide you through the correct approach to a successful QI project.
A project champion can keep a high profile for the project and build and lead the team.
Identify an “executive sponsor” such as your CEO, CMO, or CNO. This leader will focus the team on issues critical to your organization, such as accreditation from governmental agencies, and help you obtain dedicated time and resources. Aligning with hospital goals will make your project a priority.
Coordinate with existing opioid initiative teams in the hospital to integrate efforts. This will keep the work of different departments aligned and allow you to learn from pitfalls and barriers the other groups experienced.
Patients/families contribute a unique and valuable perspective. Consider including a member of your hospital’s patient and family advisory council on your team.
2. Perform a needs assessment
Determine the current state of your hospital including: opioid prescribers; opioids prescribed; areas with increased ADEs or naloxone use; formulary restrictions, policies, or guidelines for monitoring, prescribing, and administering opioids; order sets; safety alerts; provider education; or patient education.
Your risk management or quality department may be able to a share root cause analysis of ADEs related to opioids. Joint Commission and CMS recommendations as well as other regulatory requirements may shape your QI interventions.8
Most importantly, review all of the concerns and priorities of your diverse team, which will identify areas of most pressing need and provide insight regarding needs you have not considered.
3. Develop SMART aims
Frame your QI project into a series of well-defined, clear SMART aims.9
Specific: Who will carry out the intervention? Who is your target population? What will be improved? In what way will it be improved?
Measurable: What will be measured? How it will be measured? Does it measure the outcome that needs to be improved?
Attainable/achievable: Ensure you have the resources and time to achieve the aim.
Relevant: Ensure each aim moves your team toward the project vision.
Timely: The aim should be achieved within a realistic time frame, long enough to meet goals but not so long that interest is lost.
An example of a poor aim is “Clinicians will improve knowledge of opioids.”
An example of a SMART aim is “75% of inpatient opioid prescribers including MDs, NPs, and PAs will complete and pass the opioid safety training module by July 1, 2018.”
4. Choose metrics
Outcome metrics measure if the intervention has improved patient safety, for example, measuring a decrease in opioid related ADEs. Structure metrics are the physical and organizational properties of the health care delivery setting, for example, the presence of EMR opioid safety. Processes are communication and practice patterns, for example, adherence to policy by examining nursing documentation of pain assessments.
5. Development and implementation 7,10
Use PDSA for development and implementation of the QI intervention.
Plan: Determine the intervention group such as a specific unit, number of units, and if there will be a control group. Determine who will collect the data, if baseline data will be collected, and who will analyze the data. Your information technology department will be essential to determine if the data can be collected via the EMR and how. Input from your multidisciplinary team is critical to anticipate unintended consequences, such as limiting opioid prescribing at discharge inadvertently increasing emergency department visits for pain control.
Do: Start as a small pilot study to make it as easy as possible to implement the project and begin data collection. A small-scale intervention will be more manageable and allow rapid responses to unanticipated problems.
Study: Analyze the data early to determine if the intervention is improving opioid safety and if alterations are needed. At this stage both process metrics (are processes being followed?) and outcome metrics (is the process leading to a desired outcome?) are important.
Act: Based on data analysis, refine the intervention as necessary. You may have to repeat cycles of PDSA to develop the final intervention. Then implement the final intervention to the entire hospital.
The Joint Commission recommendations for opioid QI
The Joint Commission recommends7 the following to reduce opioid-related respiratory depression:
- Effective processes which include processes such as tracking and analyzing ADEs related to opioids.
- Safe technology which includes using technology such as the EMR to monitor opioid prescribing of greater than 90 morphine milligram equivalents.
- Effective tools which include valid and reliable tools to improve opioid safety, such as the Pasero Opioid Induced Sedation Scale (POSS).
- Opioid education and training which includes provider and patient education such as patient discharge education.
Education
Develop educational interventions to ensure medical and hospital staff are aware of new processes, with an emphasis on “why.”7 If possible, use web-based programs that provide CME. Improve education interventions by using multiple live, interactive, and multimedia exposures.
Principles for successful interventions
- Keep it simple for the end user. This makes it more likely that the intervention is performed. Minimize complex tasks such as calculations and if possible design automated processes.
- Build your process into current work flow. If possible simplify or streamline work flow. A project that competes with staff’s other tasks and competing priorities is doomed to fail. It is critical to have input from those performing the intervention to develop a user-friendly and less disruptive intervention.
- Design reliability into the process. Make your intervention the default action. Build prompts into the work flow. Standardize the intervention into the work flow. And, consider having the intervention at scheduled intervals.7
Opioid safety QI interventions
Interventions for improving opioid safety and reducing opioid -elated ADEs may be generalized into areas including risk screening and assessment, pain treatment, opioid administration, pain assessment, post opioid administration monitoring, and patient and provider education (Table 2).7
Back to the case
The patient received naloxone. His respiratory rate and oxygen saturation returned to normal. His dose of morphine was reduced and his interval increased. A multimodal approach was implemented including low-dose scheduled acetaminophen. There were no further ADEs while maintaining good pain control.
A multidisciplinary opioid task force was created and performed a hospital-wide review of opioid ADEs. Opportunities for improvement were identified and new procedures implemented. The Pasero opioid sedation scale (POSS) was added to the nursing work flow to monitor patients who received an opioid for sedation. An algorithm was developed for opioid-naive patients including guidance for opioid selection, dosing, and frequency. Multiple pain control modalities were added to pain control order sets. Annual training was developed for opioid prescribers, pharmacists, and nurses regarding safe and responsible use of opioids.
And, lastly, in-hospital and discharge patient education was developed for patients and families to be well-informed of opioid risk and benefit including how to identify and respond to ADEs.
Bottom line
Quality improvement is an effective method to improve patient safety and reduce serious adverse events related to opioids in the hospital setting.
Dr. Holmes-Maybank, is codirector, Fundamentals of Patient Care Year 1 and Internship 101, and chair, Clinical Competency Examination Committee, division of hospital medicine, Medical University of South Carolina. Dr. Frederickson is medical director, Hospital Medicine and Palliative Care at CHI Health, Omaha, Neb., and assistant professor at Creighton University School of Medicine, Omaha.
References
1. Davies EC et al. Adverse drug reactions in hospital inpatients: a prospective analysis of 3695 patient-episodes. PLoS One. 2009;4(2):e4439. doi: 10.1371/journal.pone.0004439. Epub 2009 Feb 11.
2. Association for the Advancement of Medical Instrumentation. Infusing patients safely: Priority issues from the AAMI/FDA Infusion Device Summit. 2010;1-39.
3. Dahan Aet al. Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology. 2010;112:226-238. doi: 10.1097/ALN.0b013e3181c38c25.
4. Estimate about opioid users.
5. Brummett CM et al. New persistent opioid use after minor and major surgical procedures in U.S. adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504.
6. Calcaterra SL et al. Opioid prescribing at hospital discharge contributes to chronic opioid use. J Gen Intern Med. 2016;31(5):478-85. doi: 10.1007/s11606-015-3539-4.
7. Frederickson TW et al. Reducing adverse drug events related to opioids implementation guide. Philadelphia: Society of Hospital Medicine, 2015.
8. Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
9. Minnesota Department of Health. SMART objectives.
10. Agency for Healthcare Research and Quality. Health Literacy Universal Precautions Toolkit, 2nd Edition.
Plan-Do-Study-Act (PDSA) Directions and Examples.
Recommended reading
Dowell D et al. CDC guideline for prescribing opioids for chronic pain – United States, 2016. Recommendations and Reports. 2016 Mar 18;65(1):1-49.
Frederickson TW et al. Using the 2018 guidelines from the Joint Commission to kickstart your hospital’s program to reduce opioid-induced ventilatory impairment. Anesthesia Patient Safety Foundation Newsletter. 2018;33(1):1-32.
Herzig SJ et al. Safe opioid prescribing for acute noncancer pain in hospitalized adults: a systematic review of existing guidelines. J Hosp Med. 2018 Apr;13(4):256-62. doi: 10.12788/jhm.2979.
Herzig SJ et al. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med. 2018 Apr;13(4):263-71. doi: 10.12788/jhm.2980.
Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
Key points
- Quality improvement is required by the Joint Commission and is an effective method to improve opioid safety in the hospital setting.
- It is critical to the success of a QI project to develop a multidisciplinary team.
- Input from frontline users of the intervention is essential to produce an effective intervention.
- Executive sponsorship and aligning the goals of your QI project with those of your institution will prioritize your project and increase resource availability.
Quiz
1. Based on a needs assessment at your hospital you assemble a multidisciplinary team to improve education for patients discharged on opioids. You recognize the importance of multidisciplinary input to develop a successful intervention for discharge education. Essential team members include all EXCEPT the following:
a. Executive sponsor
b. Patient representative
c. Nursing
d. Medical student representative ---- CORRECT
Explanation: The assembly of a multidisciplinary team is critical to the success of a QI intervention. An executive sponsor may assist you in aligning your goals with that of the hospital and provide resources for its development and implementation. Patient input would help determine how to best deliver the education. Lastly, the individuals carrying out the intervention are essential to develop an intervention that will easy for the end user and increase the likelihood of being used, in this case nursing.
2. You performed a review of naloxone use at your hospital and find that it is greater than similar hospitals. Prior to starting the QI project, you review SHM’s “Reducing adverse events related to opioids implementation guide” and learn that keys to success for QI implementation include:
a. A team of primarily hospitalists
b. Implementing the intervention hospital wide
c. Information technology input for data collection ---- CORRECT
d. No team – it is more effective to work alone
Explanation: Successful implementation of a QI project involves a multidisciplinary team. It is critical to involve information technology early in the development of the project to determine how and if the data can be collected from the EMR. It is best to pilot the intervention on one or two units to make alterations as needed rapidly and perfect the final intervention prior to rolling it out to the entire hospital.
3. You have assembled a multidisciplinary team to respond to the newly revised JCAHO pain standards. An example of a requirement from the new and revised JCAHO standards for pain assessment and management includes:
a. Programs for physician wellness
b. No opioids for chronic pain
c. No more than 5 days of opioids for acute pain
d. Nonpharmacologic pain management options ---- CORRECT
Explanation: JCAHO released new and revised requirements for pain assessment and management including offering nonpharmacologic pain management options. (See Table 1)
4. Your multidisciplinary QI team decides to develop a project to reduce respiratory depression in patients receiving opioids by monitoring for sedation with the Pasero Opioid Induced Sedation Scale. Principles for successful QI interventions include:
a. Complex tasks
b. Make the intervention a default action ---- CORRECT
c. Avoid EMR prompts
d. Competing with other hospital priorities
Explanation: Principles for successful QI interventions include keeping tasks simple, ensuring the intervention does not compete with other priorities, making the intervention the default action, installing prompts in the EMR, and standardizing the intervention into the work flow.
Quality improvement is essential
Quality improvement is essential
Case
A 67-year-old opioid-naive male with a history of obstructive sleep apnea and chronic kidney disease became unresponsive 2 days after hip replacement. Physical exam revealed a respiratory rate of 6 breaths/minute and oxygen saturation of 82%. He had received 6 doses of 6-mg IV morphine within the past 7 hours. How can I improve opioid safety at my hospital?
Background
Opioids are the most commonly prescribed class of medication in the hospital and the second–most common class causing adverse drug events (ADEs), the most serious being respiratory depression and death.1
Opioid ADEs and side effects can cause prolonged length of stay and patient suffering. These vary from potentially life-threatening events such as serotonin syndrome and adrenal insufficiency to more manageable problems still requiring intervention such as constipation, urinary retention, cognitive impairment, nausea, and vomiting. Treatment of side effects can lead to complications, including side effects from antiemetics and urinary tract infections from catheters.
A 4-year review found 700 deaths in the United States attributed to patient-controlled analgesia (PCA) use.2 Another study revealed that one out of every 200 patients has postoperative respiratory depression attributable to opioids.3
It is estimated that 2 million patients a year become chronic opioid users. Inpatient opioid prescribing contributes to this problem;4 for instance, 5.9% of patients after minor surgery and 6.5% after major surgery become chronic opioid users if discharged with an opioid.5 Calcaterra et al. found 25% of opioid-naive medical patients received an opioid at discharge from a medical service.6 Those patients had an odds ratio of 4.90 for becoming a chronic opioid user that year.6
Most hospitals have incomplete or outdated policies and procedures for safe opioid prescribing and administration.7 The Joint Commission on Accreditation of Healthcare Organizations has specific pain standards for pain assessment, pain management, and safe opioid prescribing for hospitals. Additions and revisions were developed to go into effect Jan. 1, 2018. (Table 1)8
Quality improvement
Quality improvement (QI) is an effective way to improve opioid safety. The Society of Hospital Medicine has developed a QI guide, “Reducing adverse drug events related to opioids” or “RADEO,” to increase safety and decrease serious ADEs attributable to opioids.7
The steps in the RADEO program are as follows:
1. Assemble your team
It is critical to identify and include stakeholders from multiple disciplines on your project team. This team will be essential to develop a practical project, identify barriers, create solutions, and gain buy-in from medical staff and administrative leadership.
Front-line staff will have invaluable insight and need to be team members. The majority of interventions are performed by nurses; therefore, nursing leadership and input is essential. Representatives from pharmacy, information technology, and the quality department will be extremely valuable team members to guide you through the correct approach to a successful QI project.
A project champion can keep a high profile for the project and build and lead the team.
Identify an “executive sponsor” such as your CEO, CMO, or CNO. This leader will focus the team on issues critical to your organization, such as accreditation from governmental agencies, and help you obtain dedicated time and resources. Aligning with hospital goals will make your project a priority.
Coordinate with existing opioid initiative teams in the hospital to integrate efforts. This will keep the work of different departments aligned and allow you to learn from pitfalls and barriers the other groups experienced.
Patients/families contribute a unique and valuable perspective. Consider including a member of your hospital’s patient and family advisory council on your team.
2. Perform a needs assessment
Determine the current state of your hospital including: opioid prescribers; opioids prescribed; areas with increased ADEs or naloxone use; formulary restrictions, policies, or guidelines for monitoring, prescribing, and administering opioids; order sets; safety alerts; provider education; or patient education.
Your risk management or quality department may be able to a share root cause analysis of ADEs related to opioids. Joint Commission and CMS recommendations as well as other regulatory requirements may shape your QI interventions.8
Most importantly, review all of the concerns and priorities of your diverse team, which will identify areas of most pressing need and provide insight regarding needs you have not considered.
3. Develop SMART aims
Frame your QI project into a series of well-defined, clear SMART aims.9
Specific: Who will carry out the intervention? Who is your target population? What will be improved? In what way will it be improved?
Measurable: What will be measured? How it will be measured? Does it measure the outcome that needs to be improved?
Attainable/achievable: Ensure you have the resources and time to achieve the aim.
Relevant: Ensure each aim moves your team toward the project vision.
Timely: The aim should be achieved within a realistic time frame, long enough to meet goals but not so long that interest is lost.
An example of a poor aim is “Clinicians will improve knowledge of opioids.”
An example of a SMART aim is “75% of inpatient opioid prescribers including MDs, NPs, and PAs will complete and pass the opioid safety training module by July 1, 2018.”
4. Choose metrics
Outcome metrics measure if the intervention has improved patient safety, for example, measuring a decrease in opioid related ADEs. Structure metrics are the physical and organizational properties of the health care delivery setting, for example, the presence of EMR opioid safety. Processes are communication and practice patterns, for example, adherence to policy by examining nursing documentation of pain assessments.
5. Development and implementation 7,10
Use PDSA for development and implementation of the QI intervention.
Plan: Determine the intervention group such as a specific unit, number of units, and if there will be a control group. Determine who will collect the data, if baseline data will be collected, and who will analyze the data. Your information technology department will be essential to determine if the data can be collected via the EMR and how. Input from your multidisciplinary team is critical to anticipate unintended consequences, such as limiting opioid prescribing at discharge inadvertently increasing emergency department visits for pain control.
Do: Start as a small pilot study to make it as easy as possible to implement the project and begin data collection. A small-scale intervention will be more manageable and allow rapid responses to unanticipated problems.
Study: Analyze the data early to determine if the intervention is improving opioid safety and if alterations are needed. At this stage both process metrics (are processes being followed?) and outcome metrics (is the process leading to a desired outcome?) are important.
Act: Based on data analysis, refine the intervention as necessary. You may have to repeat cycles of PDSA to develop the final intervention. Then implement the final intervention to the entire hospital.
The Joint Commission recommendations for opioid QI
The Joint Commission recommends7 the following to reduce opioid-related respiratory depression:
- Effective processes which include processes such as tracking and analyzing ADEs related to opioids.
- Safe technology which includes using technology such as the EMR to monitor opioid prescribing of greater than 90 morphine milligram equivalents.
- Effective tools which include valid and reliable tools to improve opioid safety, such as the Pasero Opioid Induced Sedation Scale (POSS).
- Opioid education and training which includes provider and patient education such as patient discharge education.
Education
Develop educational interventions to ensure medical and hospital staff are aware of new processes, with an emphasis on “why.”7 If possible, use web-based programs that provide CME. Improve education interventions by using multiple live, interactive, and multimedia exposures.
Principles for successful interventions
- Keep it simple for the end user. This makes it more likely that the intervention is performed. Minimize complex tasks such as calculations and if possible design automated processes.
- Build your process into current work flow. If possible simplify or streamline work flow. A project that competes with staff’s other tasks and competing priorities is doomed to fail. It is critical to have input from those performing the intervention to develop a user-friendly and less disruptive intervention.
- Design reliability into the process. Make your intervention the default action. Build prompts into the work flow. Standardize the intervention into the work flow. And, consider having the intervention at scheduled intervals.7
Opioid safety QI interventions
Interventions for improving opioid safety and reducing opioid -elated ADEs may be generalized into areas including risk screening and assessment, pain treatment, opioid administration, pain assessment, post opioid administration monitoring, and patient and provider education (Table 2).7
Back to the case
The patient received naloxone. His respiratory rate and oxygen saturation returned to normal. His dose of morphine was reduced and his interval increased. A multimodal approach was implemented including low-dose scheduled acetaminophen. There were no further ADEs while maintaining good pain control.
A multidisciplinary opioid task force was created and performed a hospital-wide review of opioid ADEs. Opportunities for improvement were identified and new procedures implemented. The Pasero opioid sedation scale (POSS) was added to the nursing work flow to monitor patients who received an opioid for sedation. An algorithm was developed for opioid-naive patients including guidance for opioid selection, dosing, and frequency. Multiple pain control modalities were added to pain control order sets. Annual training was developed for opioid prescribers, pharmacists, and nurses regarding safe and responsible use of opioids.
And, lastly, in-hospital and discharge patient education was developed for patients and families to be well-informed of opioid risk and benefit including how to identify and respond to ADEs.
Bottom line
Quality improvement is an effective method to improve patient safety and reduce serious adverse events related to opioids in the hospital setting.
Dr. Holmes-Maybank, is codirector, Fundamentals of Patient Care Year 1 and Internship 101, and chair, Clinical Competency Examination Committee, division of hospital medicine, Medical University of South Carolina. Dr. Frederickson is medical director, Hospital Medicine and Palliative Care at CHI Health, Omaha, Neb., and assistant professor at Creighton University School of Medicine, Omaha.
References
1. Davies EC et al. Adverse drug reactions in hospital inpatients: a prospective analysis of 3695 patient-episodes. PLoS One. 2009;4(2):e4439. doi: 10.1371/journal.pone.0004439. Epub 2009 Feb 11.
2. Association for the Advancement of Medical Instrumentation. Infusing patients safely: Priority issues from the AAMI/FDA Infusion Device Summit. 2010;1-39.
3. Dahan Aet al. Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology. 2010;112:226-238. doi: 10.1097/ALN.0b013e3181c38c25.
4. Estimate about opioid users.
5. Brummett CM et al. New persistent opioid use after minor and major surgical procedures in U.S. adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504.
6. Calcaterra SL et al. Opioid prescribing at hospital discharge contributes to chronic opioid use. J Gen Intern Med. 2016;31(5):478-85. doi: 10.1007/s11606-015-3539-4.
7. Frederickson TW et al. Reducing adverse drug events related to opioids implementation guide. Philadelphia: Society of Hospital Medicine, 2015.
8. Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
9. Minnesota Department of Health. SMART objectives.
10. Agency for Healthcare Research and Quality. Health Literacy Universal Precautions Toolkit, 2nd Edition.
Plan-Do-Study-Act (PDSA) Directions and Examples.
Recommended reading
Dowell D et al. CDC guideline for prescribing opioids for chronic pain – United States, 2016. Recommendations and Reports. 2016 Mar 18;65(1):1-49.
Frederickson TW et al. Using the 2018 guidelines from the Joint Commission to kickstart your hospital’s program to reduce opioid-induced ventilatory impairment. Anesthesia Patient Safety Foundation Newsletter. 2018;33(1):1-32.
Herzig SJ et al. Safe opioid prescribing for acute noncancer pain in hospitalized adults: a systematic review of existing guidelines. J Hosp Med. 2018 Apr;13(4):256-62. doi: 10.12788/jhm.2979.
Herzig SJ et al. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med. 2018 Apr;13(4):263-71. doi: 10.12788/jhm.2980.
Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
Key points
- Quality improvement is required by the Joint Commission and is an effective method to improve opioid safety in the hospital setting.
- It is critical to the success of a QI project to develop a multidisciplinary team.
- Input from frontline users of the intervention is essential to produce an effective intervention.
- Executive sponsorship and aligning the goals of your QI project with those of your institution will prioritize your project and increase resource availability.
Quiz
1. Based on a needs assessment at your hospital you assemble a multidisciplinary team to improve education for patients discharged on opioids. You recognize the importance of multidisciplinary input to develop a successful intervention for discharge education. Essential team members include all EXCEPT the following:
a. Executive sponsor
b. Patient representative
c. Nursing
d. Medical student representative ---- CORRECT
Explanation: The assembly of a multidisciplinary team is critical to the success of a QI intervention. An executive sponsor may assist you in aligning your goals with that of the hospital and provide resources for its development and implementation. Patient input would help determine how to best deliver the education. Lastly, the individuals carrying out the intervention are essential to develop an intervention that will easy for the end user and increase the likelihood of being used, in this case nursing.
2. You performed a review of naloxone use at your hospital and find that it is greater than similar hospitals. Prior to starting the QI project, you review SHM’s “Reducing adverse events related to opioids implementation guide” and learn that keys to success for QI implementation include:
a. A team of primarily hospitalists
b. Implementing the intervention hospital wide
c. Information technology input for data collection ---- CORRECT
d. No team – it is more effective to work alone
Explanation: Successful implementation of a QI project involves a multidisciplinary team. It is critical to involve information technology early in the development of the project to determine how and if the data can be collected from the EMR. It is best to pilot the intervention on one or two units to make alterations as needed rapidly and perfect the final intervention prior to rolling it out to the entire hospital.
3. You have assembled a multidisciplinary team to respond to the newly revised JCAHO pain standards. An example of a requirement from the new and revised JCAHO standards for pain assessment and management includes:
a. Programs for physician wellness
b. No opioids for chronic pain
c. No more than 5 days of opioids for acute pain
d. Nonpharmacologic pain management options ---- CORRECT
Explanation: JCAHO released new and revised requirements for pain assessment and management including offering nonpharmacologic pain management options. (See Table 1)
4. Your multidisciplinary QI team decides to develop a project to reduce respiratory depression in patients receiving opioids by monitoring for sedation with the Pasero Opioid Induced Sedation Scale. Principles for successful QI interventions include:
a. Complex tasks
b. Make the intervention a default action ---- CORRECT
c. Avoid EMR prompts
d. Competing with other hospital priorities
Explanation: Principles for successful QI interventions include keeping tasks simple, ensuring the intervention does not compete with other priorities, making the intervention the default action, installing prompts in the EMR, and standardizing the intervention into the work flow.
Case
A 67-year-old opioid-naive male with a history of obstructive sleep apnea and chronic kidney disease became unresponsive 2 days after hip replacement. Physical exam revealed a respiratory rate of 6 breaths/minute and oxygen saturation of 82%. He had received 6 doses of 6-mg IV morphine within the past 7 hours. How can I improve opioid safety at my hospital?
Background
Opioids are the most commonly prescribed class of medication in the hospital and the second–most common class causing adverse drug events (ADEs), the most serious being respiratory depression and death.1
Opioid ADEs and side effects can cause prolonged length of stay and patient suffering. These vary from potentially life-threatening events such as serotonin syndrome and adrenal insufficiency to more manageable problems still requiring intervention such as constipation, urinary retention, cognitive impairment, nausea, and vomiting. Treatment of side effects can lead to complications, including side effects from antiemetics and urinary tract infections from catheters.
A 4-year review found 700 deaths in the United States attributed to patient-controlled analgesia (PCA) use.2 Another study revealed that one out of every 200 patients has postoperative respiratory depression attributable to opioids.3
It is estimated that 2 million patients a year become chronic opioid users. Inpatient opioid prescribing contributes to this problem;4 for instance, 5.9% of patients after minor surgery and 6.5% after major surgery become chronic opioid users if discharged with an opioid.5 Calcaterra et al. found 25% of opioid-naive medical patients received an opioid at discharge from a medical service.6 Those patients had an odds ratio of 4.90 for becoming a chronic opioid user that year.6
Most hospitals have incomplete or outdated policies and procedures for safe opioid prescribing and administration.7 The Joint Commission on Accreditation of Healthcare Organizations has specific pain standards for pain assessment, pain management, and safe opioid prescribing for hospitals. Additions and revisions were developed to go into effect Jan. 1, 2018. (Table 1)8
Quality improvement
Quality improvement (QI) is an effective way to improve opioid safety. The Society of Hospital Medicine has developed a QI guide, “Reducing adverse drug events related to opioids” or “RADEO,” to increase safety and decrease serious ADEs attributable to opioids.7
The steps in the RADEO program are as follows:
1. Assemble your team
It is critical to identify and include stakeholders from multiple disciplines on your project team. This team will be essential to develop a practical project, identify barriers, create solutions, and gain buy-in from medical staff and administrative leadership.
Front-line staff will have invaluable insight and need to be team members. The majority of interventions are performed by nurses; therefore, nursing leadership and input is essential. Representatives from pharmacy, information technology, and the quality department will be extremely valuable team members to guide you through the correct approach to a successful QI project.
A project champion can keep a high profile for the project and build and lead the team.
Identify an “executive sponsor” such as your CEO, CMO, or CNO. This leader will focus the team on issues critical to your organization, such as accreditation from governmental agencies, and help you obtain dedicated time and resources. Aligning with hospital goals will make your project a priority.
Coordinate with existing opioid initiative teams in the hospital to integrate efforts. This will keep the work of different departments aligned and allow you to learn from pitfalls and barriers the other groups experienced.
Patients/families contribute a unique and valuable perspective. Consider including a member of your hospital’s patient and family advisory council on your team.
2. Perform a needs assessment
Determine the current state of your hospital including: opioid prescribers; opioids prescribed; areas with increased ADEs or naloxone use; formulary restrictions, policies, or guidelines for monitoring, prescribing, and administering opioids; order sets; safety alerts; provider education; or patient education.
Your risk management or quality department may be able to a share root cause analysis of ADEs related to opioids. Joint Commission and CMS recommendations as well as other regulatory requirements may shape your QI interventions.8
Most importantly, review all of the concerns and priorities of your diverse team, which will identify areas of most pressing need and provide insight regarding needs you have not considered.
3. Develop SMART aims
Frame your QI project into a series of well-defined, clear SMART aims.9
Specific: Who will carry out the intervention? Who is your target population? What will be improved? In what way will it be improved?
Measurable: What will be measured? How it will be measured? Does it measure the outcome that needs to be improved?
Attainable/achievable: Ensure you have the resources and time to achieve the aim.
Relevant: Ensure each aim moves your team toward the project vision.
Timely: The aim should be achieved within a realistic time frame, long enough to meet goals but not so long that interest is lost.
An example of a poor aim is “Clinicians will improve knowledge of opioids.”
An example of a SMART aim is “75% of inpatient opioid prescribers including MDs, NPs, and PAs will complete and pass the opioid safety training module by July 1, 2018.”
4. Choose metrics
Outcome metrics measure if the intervention has improved patient safety, for example, measuring a decrease in opioid related ADEs. Structure metrics are the physical and organizational properties of the health care delivery setting, for example, the presence of EMR opioid safety. Processes are communication and practice patterns, for example, adherence to policy by examining nursing documentation of pain assessments.
5. Development and implementation 7,10
Use PDSA for development and implementation of the QI intervention.
Plan: Determine the intervention group such as a specific unit, number of units, and if there will be a control group. Determine who will collect the data, if baseline data will be collected, and who will analyze the data. Your information technology department will be essential to determine if the data can be collected via the EMR and how. Input from your multidisciplinary team is critical to anticipate unintended consequences, such as limiting opioid prescribing at discharge inadvertently increasing emergency department visits for pain control.
Do: Start as a small pilot study to make it as easy as possible to implement the project and begin data collection. A small-scale intervention will be more manageable and allow rapid responses to unanticipated problems.
Study: Analyze the data early to determine if the intervention is improving opioid safety and if alterations are needed. At this stage both process metrics (are processes being followed?) and outcome metrics (is the process leading to a desired outcome?) are important.
Act: Based on data analysis, refine the intervention as necessary. You may have to repeat cycles of PDSA to develop the final intervention. Then implement the final intervention to the entire hospital.
The Joint Commission recommendations for opioid QI
The Joint Commission recommends7 the following to reduce opioid-related respiratory depression:
- Effective processes which include processes such as tracking and analyzing ADEs related to opioids.
- Safe technology which includes using technology such as the EMR to monitor opioid prescribing of greater than 90 morphine milligram equivalents.
- Effective tools which include valid and reliable tools to improve opioid safety, such as the Pasero Opioid Induced Sedation Scale (POSS).
- Opioid education and training which includes provider and patient education such as patient discharge education.
Education
Develop educational interventions to ensure medical and hospital staff are aware of new processes, with an emphasis on “why.”7 If possible, use web-based programs that provide CME. Improve education interventions by using multiple live, interactive, and multimedia exposures.
Principles for successful interventions
- Keep it simple for the end user. This makes it more likely that the intervention is performed. Minimize complex tasks such as calculations and if possible design automated processes.
- Build your process into current work flow. If possible simplify or streamline work flow. A project that competes with staff’s other tasks and competing priorities is doomed to fail. It is critical to have input from those performing the intervention to develop a user-friendly and less disruptive intervention.
- Design reliability into the process. Make your intervention the default action. Build prompts into the work flow. Standardize the intervention into the work flow. And, consider having the intervention at scheduled intervals.7
Opioid safety QI interventions
Interventions for improving opioid safety and reducing opioid -elated ADEs may be generalized into areas including risk screening and assessment, pain treatment, opioid administration, pain assessment, post opioid administration monitoring, and patient and provider education (Table 2).7
Back to the case
The patient received naloxone. His respiratory rate and oxygen saturation returned to normal. His dose of morphine was reduced and his interval increased. A multimodal approach was implemented including low-dose scheduled acetaminophen. There were no further ADEs while maintaining good pain control.
A multidisciplinary opioid task force was created and performed a hospital-wide review of opioid ADEs. Opportunities for improvement were identified and new procedures implemented. The Pasero opioid sedation scale (POSS) was added to the nursing work flow to monitor patients who received an opioid for sedation. An algorithm was developed for opioid-naive patients including guidance for opioid selection, dosing, and frequency. Multiple pain control modalities were added to pain control order sets. Annual training was developed for opioid prescribers, pharmacists, and nurses regarding safe and responsible use of opioids.
And, lastly, in-hospital and discharge patient education was developed for patients and families to be well-informed of opioid risk and benefit including how to identify and respond to ADEs.
Bottom line
Quality improvement is an effective method to improve patient safety and reduce serious adverse events related to opioids in the hospital setting.
Dr. Holmes-Maybank, is codirector, Fundamentals of Patient Care Year 1 and Internship 101, and chair, Clinical Competency Examination Committee, division of hospital medicine, Medical University of South Carolina. Dr. Frederickson is medical director, Hospital Medicine and Palliative Care at CHI Health, Omaha, Neb., and assistant professor at Creighton University School of Medicine, Omaha.
References
1. Davies EC et al. Adverse drug reactions in hospital inpatients: a prospective analysis of 3695 patient-episodes. PLoS One. 2009;4(2):e4439. doi: 10.1371/journal.pone.0004439. Epub 2009 Feb 11.
2. Association for the Advancement of Medical Instrumentation. Infusing patients safely: Priority issues from the AAMI/FDA Infusion Device Summit. 2010;1-39.
3. Dahan Aet al. Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology. 2010;112:226-238. doi: 10.1097/ALN.0b013e3181c38c25.
4. Estimate about opioid users.
5. Brummett CM et al. New persistent opioid use after minor and major surgical procedures in U.S. adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504.
6. Calcaterra SL et al. Opioid prescribing at hospital discharge contributes to chronic opioid use. J Gen Intern Med. 2016;31(5):478-85. doi: 10.1007/s11606-015-3539-4.
7. Frederickson TW et al. Reducing adverse drug events related to opioids implementation guide. Philadelphia: Society of Hospital Medicine, 2015.
8. Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
9. Minnesota Department of Health. SMART objectives.
10. Agency for Healthcare Research and Quality. Health Literacy Universal Precautions Toolkit, 2nd Edition.
Plan-Do-Study-Act (PDSA) Directions and Examples.
Recommended reading
Dowell D et al. CDC guideline for prescribing opioids for chronic pain – United States, 2016. Recommendations and Reports. 2016 Mar 18;65(1):1-49.
Frederickson TW et al. Using the 2018 guidelines from the Joint Commission to kickstart your hospital’s program to reduce opioid-induced ventilatory impairment. Anesthesia Patient Safety Foundation Newsletter. 2018;33(1):1-32.
Herzig SJ et al. Safe opioid prescribing for acute noncancer pain in hospitalized adults: a systematic review of existing guidelines. J Hosp Med. 2018 Apr;13(4):256-62. doi: 10.12788/jhm.2979.
Herzig SJ et al. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med. 2018 Apr;13(4):263-71. doi: 10.12788/jhm.2980.
Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
Key points
- Quality improvement is required by the Joint Commission and is an effective method to improve opioid safety in the hospital setting.
- It is critical to the success of a QI project to develop a multidisciplinary team.
- Input from frontline users of the intervention is essential to produce an effective intervention.
- Executive sponsorship and aligning the goals of your QI project with those of your institution will prioritize your project and increase resource availability.
Quiz
1. Based on a needs assessment at your hospital you assemble a multidisciplinary team to improve education for patients discharged on opioids. You recognize the importance of multidisciplinary input to develop a successful intervention for discharge education. Essential team members include all EXCEPT the following:
a. Executive sponsor
b. Patient representative
c. Nursing
d. Medical student representative ---- CORRECT
Explanation: The assembly of a multidisciplinary team is critical to the success of a QI intervention. An executive sponsor may assist you in aligning your goals with that of the hospital and provide resources for its development and implementation. Patient input would help determine how to best deliver the education. Lastly, the individuals carrying out the intervention are essential to develop an intervention that will easy for the end user and increase the likelihood of being used, in this case nursing.
2. You performed a review of naloxone use at your hospital and find that it is greater than similar hospitals. Prior to starting the QI project, you review SHM’s “Reducing adverse events related to opioids implementation guide” and learn that keys to success for QI implementation include:
a. A team of primarily hospitalists
b. Implementing the intervention hospital wide
c. Information technology input for data collection ---- CORRECT
d. No team – it is more effective to work alone
Explanation: Successful implementation of a QI project involves a multidisciplinary team. It is critical to involve information technology early in the development of the project to determine how and if the data can be collected from the EMR. It is best to pilot the intervention on one or two units to make alterations as needed rapidly and perfect the final intervention prior to rolling it out to the entire hospital.
3. You have assembled a multidisciplinary team to respond to the newly revised JCAHO pain standards. An example of a requirement from the new and revised JCAHO standards for pain assessment and management includes:
a. Programs for physician wellness
b. No opioids for chronic pain
c. No more than 5 days of opioids for acute pain
d. Nonpharmacologic pain management options ---- CORRECT
Explanation: JCAHO released new and revised requirements for pain assessment and management including offering nonpharmacologic pain management options. (See Table 1)
4. Your multidisciplinary QI team decides to develop a project to reduce respiratory depression in patients receiving opioids by monitoring for sedation with the Pasero Opioid Induced Sedation Scale. Principles for successful QI interventions include:
a. Complex tasks
b. Make the intervention a default action ---- CORRECT
c. Avoid EMR prompts
d. Competing with other hospital priorities
Explanation: Principles for successful QI interventions include keeping tasks simple, ensuring the intervention does not compete with other priorities, making the intervention the default action, installing prompts in the EMR, and standardizing the intervention into the work flow.
Topical antibiotic decolonizes S. aureus in NICU infants
Application of the topical antibiotic mupirocin to multiple body sites was reported to be safe and efficacious in eradicating Staphylococcus aureus (SA) colonization on infants in the neonatal intensive care unit (NICU), according to researchers at the University of Maryland, Baltimore.
Karen L. Kotloff, MD, and her colleagues conducted a phase 2 multicenter, open-label, randomized trial to assess the safety and efficacy of intranasal plus topical mupirocin in eradicating SA colonization in critically ill infants between April 2014 and May 2016.
“Staph aureus is a leading cause of sepsis in young children admitted to the NICU. Sepsis, which is systemic infection, can be fatal in infants. Thus, preventing these infections is very important in managing risk for babies in the NICU who are fragile and struggling with multiple medical problems,” said Dr. Kotloff in a university interview.
The researchers examined infants in the NICU at eight study centers who were less than 24 months old who underwent serial screening for nasal SA. Infants colonized with SA and were randomly assigned to receive 5 days of mupirocin versus no mupirocin to the intranasal, periumbilical, and perianal areas. Treatment effects were assessed on day 8 (primary decolonization) and day 22 (persistent decolonization) for all three body areas (Pediatrics. 2019 Jan 1. doi: 10.1542/peds.2018-1565).
Primary decolonization occurred in 62/66 (93.9%) of treated infants and 3/64 (4.7%) of the control infants (P less than .001). Persistent decolonization was seen in 21/46 (45.7%) of treated infants compared with 1/48 (2.1%) of the controls (P less than .001).
“This multicenter trial supervised by Dr. Kotloff provides strong support for a safe strategy to minimize Staphylococcus aureus infections in some of the most at-risk patients in any hospital, premature babies,” E. Albert Reece, MD, dean of the University of Maryland School of Medicine, said in a university press release commenting on the study.
Application of the topical antibiotic mupirocin to multiple body sites was reported to be safe and efficacious in eradicating Staphylococcus aureus (SA) colonization on infants in the neonatal intensive care unit (NICU), according to researchers at the University of Maryland, Baltimore.
Karen L. Kotloff, MD, and her colleagues conducted a phase 2 multicenter, open-label, randomized trial to assess the safety and efficacy of intranasal plus topical mupirocin in eradicating SA colonization in critically ill infants between April 2014 and May 2016.
“Staph aureus is a leading cause of sepsis in young children admitted to the NICU. Sepsis, which is systemic infection, can be fatal in infants. Thus, preventing these infections is very important in managing risk for babies in the NICU who are fragile and struggling with multiple medical problems,” said Dr. Kotloff in a university interview.
The researchers examined infants in the NICU at eight study centers who were less than 24 months old who underwent serial screening for nasal SA. Infants colonized with SA and were randomly assigned to receive 5 days of mupirocin versus no mupirocin to the intranasal, periumbilical, and perianal areas. Treatment effects were assessed on day 8 (primary decolonization) and day 22 (persistent decolonization) for all three body areas (Pediatrics. 2019 Jan 1. doi: 10.1542/peds.2018-1565).
Primary decolonization occurred in 62/66 (93.9%) of treated infants and 3/64 (4.7%) of the control infants (P less than .001). Persistent decolonization was seen in 21/46 (45.7%) of treated infants compared with 1/48 (2.1%) of the controls (P less than .001).
“This multicenter trial supervised by Dr. Kotloff provides strong support for a safe strategy to minimize Staphylococcus aureus infections in some of the most at-risk patients in any hospital, premature babies,” E. Albert Reece, MD, dean of the University of Maryland School of Medicine, said in a university press release commenting on the study.
Application of the topical antibiotic mupirocin to multiple body sites was reported to be safe and efficacious in eradicating Staphylococcus aureus (SA) colonization on infants in the neonatal intensive care unit (NICU), according to researchers at the University of Maryland, Baltimore.
Karen L. Kotloff, MD, and her colleagues conducted a phase 2 multicenter, open-label, randomized trial to assess the safety and efficacy of intranasal plus topical mupirocin in eradicating SA colonization in critically ill infants between April 2014 and May 2016.
“Staph aureus is a leading cause of sepsis in young children admitted to the NICU. Sepsis, which is systemic infection, can be fatal in infants. Thus, preventing these infections is very important in managing risk for babies in the NICU who are fragile and struggling with multiple medical problems,” said Dr. Kotloff in a university interview.
The researchers examined infants in the NICU at eight study centers who were less than 24 months old who underwent serial screening for nasal SA. Infants colonized with SA and were randomly assigned to receive 5 days of mupirocin versus no mupirocin to the intranasal, periumbilical, and perianal areas. Treatment effects were assessed on day 8 (primary decolonization) and day 22 (persistent decolonization) for all three body areas (Pediatrics. 2019 Jan 1. doi: 10.1542/peds.2018-1565).
Primary decolonization occurred in 62/66 (93.9%) of treated infants and 3/64 (4.7%) of the control infants (P less than .001). Persistent decolonization was seen in 21/46 (45.7%) of treated infants compared with 1/48 (2.1%) of the controls (P less than .001).
“This multicenter trial supervised by Dr. Kotloff provides strong support for a safe strategy to minimize Staphylococcus aureus infections in some of the most at-risk patients in any hospital, premature babies,” E. Albert Reece, MD, dean of the University of Maryland School of Medicine, said in a university press release commenting on the study.
FROM PEDIATRICS
Meal programs for dual eligibles
Do food delivery programs reduce the use of costly health services and decrease medical spending in a population of patients dually eligible for Medicare and Medicaid?
Researchers in Massachusetts wanted to determine whether home meal delivery of either medically tailored food or nontailored food reduces the use of selected health care services and medical spending in a sample of adult “dual eligibles.”
“Compared with matched nonparticipants, participants had fewer emergency department visits in both the medically tailored meal program and the nontailored food program,” the investigators found. “Participants in the medically tailored meal program also had fewer inpatient admissions and lower medical spending. Participation in the nontailored food program was not associated with fewer inpatient admissions but was associated with lower medical spending.”
Reference
Berkowitz SA et al. Meal delivery programs reduce the use of costly health care in dually eligible Medicare and Medicaid beneficiaries. Health Aff (Millwood). 2018 Apr;37(4):535-42.
Do food delivery programs reduce the use of costly health services and decrease medical spending in a population of patients dually eligible for Medicare and Medicaid?
Researchers in Massachusetts wanted to determine whether home meal delivery of either medically tailored food or nontailored food reduces the use of selected health care services and medical spending in a sample of adult “dual eligibles.”
“Compared with matched nonparticipants, participants had fewer emergency department visits in both the medically tailored meal program and the nontailored food program,” the investigators found. “Participants in the medically tailored meal program also had fewer inpatient admissions and lower medical spending. Participation in the nontailored food program was not associated with fewer inpatient admissions but was associated with lower medical spending.”
Reference
Berkowitz SA et al. Meal delivery programs reduce the use of costly health care in dually eligible Medicare and Medicaid beneficiaries. Health Aff (Millwood). 2018 Apr;37(4):535-42.
Do food delivery programs reduce the use of costly health services and decrease medical spending in a population of patients dually eligible for Medicare and Medicaid?
Researchers in Massachusetts wanted to determine whether home meal delivery of either medically tailored food or nontailored food reduces the use of selected health care services and medical spending in a sample of adult “dual eligibles.”
“Compared with matched nonparticipants, participants had fewer emergency department visits in both the medically tailored meal program and the nontailored food program,” the investigators found. “Participants in the medically tailored meal program also had fewer inpatient admissions and lower medical spending. Participation in the nontailored food program was not associated with fewer inpatient admissions but was associated with lower medical spending.”
Reference
Berkowitz SA et al. Meal delivery programs reduce the use of costly health care in dually eligible Medicare and Medicaid beneficiaries. Health Aff (Millwood). 2018 Apr;37(4):535-42.