User login
Findings question value of pessary for pelvic organ prolapse
The standard nonsurgical treatment for pelvic organ prolapse does not appear to work as well as surgery to correct the problem, Dutch researchers have found.
Pelvic organ prolapse is an uncomfortable condition, causing a troublesome vaginal bulge, often accompanied by urinary, bowel, or sexual dysfunction. Between 3% and 6% of women develop symptomatic prolapse, with the highest incidence in women aged 60-69 years – a fast-growing demographic.
Although many women choose surgical treatment, the American College of Obstetricians and Gynecologists recommends that women be offered a vaginal pessary as a noninvasive alternative, despite inconsistent data from observational studies on their effectiveness.
Lisa van der Vaart, MD, a doctoral student in ob.gyn. at the University of Amsterdam and the lead author of the new study, published in JAMA, said that differences in outcome measures, small sample size, and lack of long-term follow-up have bedeviled previous comparisons of the two techniques.
“We thought it was very important to perform a randomized control trial on this subject to improve counseling to women who suffer from symptomatic pelvic organ prolapse,” Dr. van der Vaart said.
She and her colleagues conducted a noninferiority randomized clinical trial that recruited 1,605 women with stage II or higher prolapse who were referred to specialty care at 21 hospitals in the Netherlands between 2015 and 2019. Of the 440 women who agreed to participate in the trial, 218 received a pessary, a device inserted into the vagina that provides support to tissues displaced by prolapse, and 222 underwent surgery.
The primary outcome was subjective improvement using a standardized questionnaire at 24 months; women were asked to rank their symptoms on a seven-point scale, and subjective improvement was defined as a response of much better or very much better.
“We saw a substantial amount of improvement in both groups,” Dr. van der Vaart said in an interview.
After 24 months of follow-up, outcome data were available for 173 women in the pessary group and 162 in the surgery group. For this intention-to treat population, 76.3% in the pessary group and 81.5% in the surgery group reported improvement.
Results were similar for the smaller group of participants who completed the study per protocol, without crossing over to a treatment to which they had not been allocated.
However, neither the intention-to-treat nor per-protocol analysis met the prespecified criteria for noninferiority, suggesting that use of a vaginal pessary is not equivalent to surgery.
The study also found differences in adverse events. Among women randomly assigned to surgery, 9% suffered a postoperative urinary tract infection, and 5.4% underwent additional therapy, such as pessary or repeat operation.
But use of a pessary also had downsides. The most common adverse event was discomfort (42.7%), and by 24 months, 60% of the participants in the pessary group had discontinued use.
Dr. van der Vaart said that she was surprised by the high number of women assigned to the pessary group who later elected to undergo surgery. “Women should be told that their chance of crossing over to a surgical intervention is quite high – more than 50% do eventually end up having surgery.”
Cheryl Iglesia, MD, director of the National Center for Advanced Pelvic Surgery at MedStar Health and professor of obstetrics and gynecology and urology at Georgetown University, both in Washington, was also struck by the high crossover rate. “We’ve had the same pessaries probably for the last 100 years,” she said. “We need to get better.”
Dr. Iglesia welcomed new approaches to making vaginal pessaries that are custom designed for each woman’s unique anatomy using 3D printing and pointed to promising initial clinical trials of disposable pessaries. With the aging of the population and demand for treatment of prolapse increasing, she cited a need for better nonsurgical alternatives: “We have a work-force issue and may not have enough adequately trained urogynecologists to meet the demand for prolapse repairs as our population ages.”
The study was funded by a grant from ZonMW, a Dutch governmental health care organization. Dr. van der Vaart reported grants from ZonMW during the conduct of the study.
A version of this article first appeared on Medscape.com.
The standard nonsurgical treatment for pelvic organ prolapse does not appear to work as well as surgery to correct the problem, Dutch researchers have found.
Pelvic organ prolapse is an uncomfortable condition, causing a troublesome vaginal bulge, often accompanied by urinary, bowel, or sexual dysfunction. Between 3% and 6% of women develop symptomatic prolapse, with the highest incidence in women aged 60-69 years – a fast-growing demographic.
Although many women choose surgical treatment, the American College of Obstetricians and Gynecologists recommends that women be offered a vaginal pessary as a noninvasive alternative, despite inconsistent data from observational studies on their effectiveness.
Lisa van der Vaart, MD, a doctoral student in ob.gyn. at the University of Amsterdam and the lead author of the new study, published in JAMA, said that differences in outcome measures, small sample size, and lack of long-term follow-up have bedeviled previous comparisons of the two techniques.
“We thought it was very important to perform a randomized control trial on this subject to improve counseling to women who suffer from symptomatic pelvic organ prolapse,” Dr. van der Vaart said.
She and her colleagues conducted a noninferiority randomized clinical trial that recruited 1,605 women with stage II or higher prolapse who were referred to specialty care at 21 hospitals in the Netherlands between 2015 and 2019. Of the 440 women who agreed to participate in the trial, 218 received a pessary, a device inserted into the vagina that provides support to tissues displaced by prolapse, and 222 underwent surgery.
The primary outcome was subjective improvement using a standardized questionnaire at 24 months; women were asked to rank their symptoms on a seven-point scale, and subjective improvement was defined as a response of much better or very much better.
“We saw a substantial amount of improvement in both groups,” Dr. van der Vaart said in an interview.
After 24 months of follow-up, outcome data were available for 173 women in the pessary group and 162 in the surgery group. For this intention-to treat population, 76.3% in the pessary group and 81.5% in the surgery group reported improvement.
Results were similar for the smaller group of participants who completed the study per protocol, without crossing over to a treatment to which they had not been allocated.
However, neither the intention-to-treat nor per-protocol analysis met the prespecified criteria for noninferiority, suggesting that use of a vaginal pessary is not equivalent to surgery.
The study also found differences in adverse events. Among women randomly assigned to surgery, 9% suffered a postoperative urinary tract infection, and 5.4% underwent additional therapy, such as pessary or repeat operation.
But use of a pessary also had downsides. The most common adverse event was discomfort (42.7%), and by 24 months, 60% of the participants in the pessary group had discontinued use.
Dr. van der Vaart said that she was surprised by the high number of women assigned to the pessary group who later elected to undergo surgery. “Women should be told that their chance of crossing over to a surgical intervention is quite high – more than 50% do eventually end up having surgery.”
Cheryl Iglesia, MD, director of the National Center for Advanced Pelvic Surgery at MedStar Health and professor of obstetrics and gynecology and urology at Georgetown University, both in Washington, was also struck by the high crossover rate. “We’ve had the same pessaries probably for the last 100 years,” she said. “We need to get better.”
Dr. Iglesia welcomed new approaches to making vaginal pessaries that are custom designed for each woman’s unique anatomy using 3D printing and pointed to promising initial clinical trials of disposable pessaries. With the aging of the population and demand for treatment of prolapse increasing, she cited a need for better nonsurgical alternatives: “We have a work-force issue and may not have enough adequately trained urogynecologists to meet the demand for prolapse repairs as our population ages.”
The study was funded by a grant from ZonMW, a Dutch governmental health care organization. Dr. van der Vaart reported grants from ZonMW during the conduct of the study.
A version of this article first appeared on Medscape.com.
The standard nonsurgical treatment for pelvic organ prolapse does not appear to work as well as surgery to correct the problem, Dutch researchers have found.
Pelvic organ prolapse is an uncomfortable condition, causing a troublesome vaginal bulge, often accompanied by urinary, bowel, or sexual dysfunction. Between 3% and 6% of women develop symptomatic prolapse, with the highest incidence in women aged 60-69 years – a fast-growing demographic.
Although many women choose surgical treatment, the American College of Obstetricians and Gynecologists recommends that women be offered a vaginal pessary as a noninvasive alternative, despite inconsistent data from observational studies on their effectiveness.
Lisa van der Vaart, MD, a doctoral student in ob.gyn. at the University of Amsterdam and the lead author of the new study, published in JAMA, said that differences in outcome measures, small sample size, and lack of long-term follow-up have bedeviled previous comparisons of the two techniques.
“We thought it was very important to perform a randomized control trial on this subject to improve counseling to women who suffer from symptomatic pelvic organ prolapse,” Dr. van der Vaart said.
She and her colleagues conducted a noninferiority randomized clinical trial that recruited 1,605 women with stage II or higher prolapse who were referred to specialty care at 21 hospitals in the Netherlands between 2015 and 2019. Of the 440 women who agreed to participate in the trial, 218 received a pessary, a device inserted into the vagina that provides support to tissues displaced by prolapse, and 222 underwent surgery.
The primary outcome was subjective improvement using a standardized questionnaire at 24 months; women were asked to rank their symptoms on a seven-point scale, and subjective improvement was defined as a response of much better or very much better.
“We saw a substantial amount of improvement in both groups,” Dr. van der Vaart said in an interview.
After 24 months of follow-up, outcome data were available for 173 women in the pessary group and 162 in the surgery group. For this intention-to treat population, 76.3% in the pessary group and 81.5% in the surgery group reported improvement.
Results were similar for the smaller group of participants who completed the study per protocol, without crossing over to a treatment to which they had not been allocated.
However, neither the intention-to-treat nor per-protocol analysis met the prespecified criteria for noninferiority, suggesting that use of a vaginal pessary is not equivalent to surgery.
The study also found differences in adverse events. Among women randomly assigned to surgery, 9% suffered a postoperative urinary tract infection, and 5.4% underwent additional therapy, such as pessary or repeat operation.
But use of a pessary also had downsides. The most common adverse event was discomfort (42.7%), and by 24 months, 60% of the participants in the pessary group had discontinued use.
Dr. van der Vaart said that she was surprised by the high number of women assigned to the pessary group who later elected to undergo surgery. “Women should be told that their chance of crossing over to a surgical intervention is quite high – more than 50% do eventually end up having surgery.”
Cheryl Iglesia, MD, director of the National Center for Advanced Pelvic Surgery at MedStar Health and professor of obstetrics and gynecology and urology at Georgetown University, both in Washington, was also struck by the high crossover rate. “We’ve had the same pessaries probably for the last 100 years,” she said. “We need to get better.”
Dr. Iglesia welcomed new approaches to making vaginal pessaries that are custom designed for each woman’s unique anatomy using 3D printing and pointed to promising initial clinical trials of disposable pessaries. With the aging of the population and demand for treatment of prolapse increasing, she cited a need for better nonsurgical alternatives: “We have a work-force issue and may not have enough adequately trained urogynecologists to meet the demand for prolapse repairs as our population ages.”
The study was funded by a grant from ZonMW, a Dutch governmental health care organization. Dr. van der Vaart reported grants from ZonMW during the conduct of the study.
A version of this article first appeared on Medscape.com.
FROM JAMA
Medical practice gave 8,000 patients cancer for Christmas
We wish you a merry Christmas and a happy heart failure
Does anyone really like it when places of business send out cards or messages for the holidays? A card from a truly small family business is one thing, but when you start getting emails from multibillion dollar corporations, it feels a bit dishonest. And that’s not even mentioning the potential blowback when things go wrong.
Now, you may wonder how a company could possibly mess up something so simple. “We wish you a merry Christmas and a happy New Year.” Not that difficult. Unless you’re Askern Medical Practice in Doncaster, England. Instead of expressing a simple expression of joy for the holiday season, Askern informed all 8,000 of its patients that they had aggressive lung cancer with metastases and they needed to fill out a DS1500 form, which entitles terminal patients to certain benefits.
It only took an hour for Askern to recognize its mistake and send a second text apologizing and adding in the appropriate season’s greetings, but obviously the damage was done. Presumably patients who were last at the doctor to have their cold treated were able to shrug off the text, or simply didn’t see it before the correction came through, but obviously many patients had concerns directly related to cancer and panicked. They called in but were by and large unable to reach anyone at the practice. Some patients close by even went to center itself to clear things up.
One patient, Mr. Carl Chegwin, raised an excellent point about the debacle: “What if that message was meant for someone, and then they are told it’s a Christmas message, then again told, ‘Oh no, that was actually meant for you?’ ” The old double backtrack into yes, you actually do have cancer has got to be a candidate for worst Christmas gift of all. Yes, even worse than socks.
Genes know it: You are when you eat
There’s been a lot of recent research on intermittent fasting and what it can and can’t do for one’s health. Much of it has focused on participants’ metabolic rates, but a study just published in Cell Metabolism shows how time-restricted feeding (TRF) has an impact on gene expression, the process through which genes are activated and respond to their environment by creating proteins.
The research conducted by Satchidananda Panda, PhD, of the Salk Institute and his team involved two groups of mice, one with free access to food and the other with a daily 9-hour feeding window. Analysis of tissue samples collected from 22 organ groups revealed that nearly 80% of mouse genes responded to TRF. Interestingly, 40% of the genes in the hypothalamus, adrenal gland, and pancreas, which handle hormone regulation, were affected, suggesting that TRF could potentially aid in diabetes and stress disorder management, the investigators said in a written statement.
The researchers also found that TRF aligned the circadian rhythms of multiple organs of the body, which brings sleep into the picture. “Time-restricted eating synchronized the circadian rhythms to have two major waves: one during fasting, and another just after eating. We suspect this allows the body to coordinate different processes,” said Dr. Panda, whose previous research looked at TRF in firefighters, who typically work on shift schedules.
Time-restricted eating, it appears, affects gene expression throughout the body and allows interconnected organ systems to work smoothly. It’s not just about eating. Go figure.
This group practice reduced stress for everyone
It’s been awhile since we checked in on the good folks at Maharishi International University in Fairfield, Iowa – fictional home of the Fighting Transcendentalists [MAHARISHI RULES!] – but we just have to mention their long-term effort to reduce the national stress.
Way back in the year 2000, a group from MIU began practicing transcendental meditation. The size of the group increased over the next few years and eventually reached 1,725 in 2006. That number is important because it represents the square root of 1% of the U.S. population. When that “transition threshold was achieved,” the university explained in a written statement, “all stress indicators immediately started decreasing.”
By stress indicators they mean the U.S. stress index, the mean of eight variables – murder, rape, assault, robbery, infant mortality, drug deaths, vehicle fatalities, and child deaths by injuries – that the study investigators used to track the effectiveness of the meditation program, they said in the World Journal of Social Science.
After 2011, “when the size of the group size began to decline the rate of decrease in stress slowed and then it reversed and began to increase,” MIU reported.
Coauthor Dr. Kenneth Cavanaugh of MIU explained the process: “This study used state-of-the-art methods of time series regression analysis for eliminating potential alternative explanations due to intrinsic preexisting trends and fluctuations in the data. We carefully studied potential alternative explanations in terms of changes in economic conditions, political leadership, population demographics, and policing strategies. None of these factors could account for the results.”
Since we here at LOTME are serious professional journalists, the use of quotes means we are not making this up. Here’s one more thing in quotes: “A grant for 75 million dollars from the Howard and Alice Settle Foundation provided stipends for participants to be in the group and provided funding to bring several hundred visiting [meditation] experts from India to further augment the MIU group.”
Who needs to make up stuff? Not us.
We wish you a merry Christmas and a happy heart failure
Does anyone really like it when places of business send out cards or messages for the holidays? A card from a truly small family business is one thing, but when you start getting emails from multibillion dollar corporations, it feels a bit dishonest. And that’s not even mentioning the potential blowback when things go wrong.
Now, you may wonder how a company could possibly mess up something so simple. “We wish you a merry Christmas and a happy New Year.” Not that difficult. Unless you’re Askern Medical Practice in Doncaster, England. Instead of expressing a simple expression of joy for the holiday season, Askern informed all 8,000 of its patients that they had aggressive lung cancer with metastases and they needed to fill out a DS1500 form, which entitles terminal patients to certain benefits.
It only took an hour for Askern to recognize its mistake and send a second text apologizing and adding in the appropriate season’s greetings, but obviously the damage was done. Presumably patients who were last at the doctor to have their cold treated were able to shrug off the text, or simply didn’t see it before the correction came through, but obviously many patients had concerns directly related to cancer and panicked. They called in but were by and large unable to reach anyone at the practice. Some patients close by even went to center itself to clear things up.
One patient, Mr. Carl Chegwin, raised an excellent point about the debacle: “What if that message was meant for someone, and then they are told it’s a Christmas message, then again told, ‘Oh no, that was actually meant for you?’ ” The old double backtrack into yes, you actually do have cancer has got to be a candidate for worst Christmas gift of all. Yes, even worse than socks.
Genes know it: You are when you eat
There’s been a lot of recent research on intermittent fasting and what it can and can’t do for one’s health. Much of it has focused on participants’ metabolic rates, but a study just published in Cell Metabolism shows how time-restricted feeding (TRF) has an impact on gene expression, the process through which genes are activated and respond to their environment by creating proteins.
The research conducted by Satchidananda Panda, PhD, of the Salk Institute and his team involved two groups of mice, one with free access to food and the other with a daily 9-hour feeding window. Analysis of tissue samples collected from 22 organ groups revealed that nearly 80% of mouse genes responded to TRF. Interestingly, 40% of the genes in the hypothalamus, adrenal gland, and pancreas, which handle hormone regulation, were affected, suggesting that TRF could potentially aid in diabetes and stress disorder management, the investigators said in a written statement.
The researchers also found that TRF aligned the circadian rhythms of multiple organs of the body, which brings sleep into the picture. “Time-restricted eating synchronized the circadian rhythms to have two major waves: one during fasting, and another just after eating. We suspect this allows the body to coordinate different processes,” said Dr. Panda, whose previous research looked at TRF in firefighters, who typically work on shift schedules.
Time-restricted eating, it appears, affects gene expression throughout the body and allows interconnected organ systems to work smoothly. It’s not just about eating. Go figure.
This group practice reduced stress for everyone
It’s been awhile since we checked in on the good folks at Maharishi International University in Fairfield, Iowa – fictional home of the Fighting Transcendentalists [MAHARISHI RULES!] – but we just have to mention their long-term effort to reduce the national stress.
Way back in the year 2000, a group from MIU began practicing transcendental meditation. The size of the group increased over the next few years and eventually reached 1,725 in 2006. That number is important because it represents the square root of 1% of the U.S. population. When that “transition threshold was achieved,” the university explained in a written statement, “all stress indicators immediately started decreasing.”
By stress indicators they mean the U.S. stress index, the mean of eight variables – murder, rape, assault, robbery, infant mortality, drug deaths, vehicle fatalities, and child deaths by injuries – that the study investigators used to track the effectiveness of the meditation program, they said in the World Journal of Social Science.
After 2011, “when the size of the group size began to decline the rate of decrease in stress slowed and then it reversed and began to increase,” MIU reported.
Coauthor Dr. Kenneth Cavanaugh of MIU explained the process: “This study used state-of-the-art methods of time series regression analysis for eliminating potential alternative explanations due to intrinsic preexisting trends and fluctuations in the data. We carefully studied potential alternative explanations in terms of changes in economic conditions, political leadership, population demographics, and policing strategies. None of these factors could account for the results.”
Since we here at LOTME are serious professional journalists, the use of quotes means we are not making this up. Here’s one more thing in quotes: “A grant for 75 million dollars from the Howard and Alice Settle Foundation provided stipends for participants to be in the group and provided funding to bring several hundred visiting [meditation] experts from India to further augment the MIU group.”
Who needs to make up stuff? Not us.
We wish you a merry Christmas and a happy heart failure
Does anyone really like it when places of business send out cards or messages for the holidays? A card from a truly small family business is one thing, but when you start getting emails from multibillion dollar corporations, it feels a bit dishonest. And that’s not even mentioning the potential blowback when things go wrong.
Now, you may wonder how a company could possibly mess up something so simple. “We wish you a merry Christmas and a happy New Year.” Not that difficult. Unless you’re Askern Medical Practice in Doncaster, England. Instead of expressing a simple expression of joy for the holiday season, Askern informed all 8,000 of its patients that they had aggressive lung cancer with metastases and they needed to fill out a DS1500 form, which entitles terminal patients to certain benefits.
It only took an hour for Askern to recognize its mistake and send a second text apologizing and adding in the appropriate season’s greetings, but obviously the damage was done. Presumably patients who were last at the doctor to have their cold treated were able to shrug off the text, or simply didn’t see it before the correction came through, but obviously many patients had concerns directly related to cancer and panicked. They called in but were by and large unable to reach anyone at the practice. Some patients close by even went to center itself to clear things up.
One patient, Mr. Carl Chegwin, raised an excellent point about the debacle: “What if that message was meant for someone, and then they are told it’s a Christmas message, then again told, ‘Oh no, that was actually meant for you?’ ” The old double backtrack into yes, you actually do have cancer has got to be a candidate for worst Christmas gift of all. Yes, even worse than socks.
Genes know it: You are when you eat
There’s been a lot of recent research on intermittent fasting and what it can and can’t do for one’s health. Much of it has focused on participants’ metabolic rates, but a study just published in Cell Metabolism shows how time-restricted feeding (TRF) has an impact on gene expression, the process through which genes are activated and respond to their environment by creating proteins.
The research conducted by Satchidananda Panda, PhD, of the Salk Institute and his team involved two groups of mice, one with free access to food and the other with a daily 9-hour feeding window. Analysis of tissue samples collected from 22 organ groups revealed that nearly 80% of mouse genes responded to TRF. Interestingly, 40% of the genes in the hypothalamus, adrenal gland, and pancreas, which handle hormone regulation, were affected, suggesting that TRF could potentially aid in diabetes and stress disorder management, the investigators said in a written statement.
The researchers also found that TRF aligned the circadian rhythms of multiple organs of the body, which brings sleep into the picture. “Time-restricted eating synchronized the circadian rhythms to have two major waves: one during fasting, and another just after eating. We suspect this allows the body to coordinate different processes,” said Dr. Panda, whose previous research looked at TRF in firefighters, who typically work on shift schedules.
Time-restricted eating, it appears, affects gene expression throughout the body and allows interconnected organ systems to work smoothly. It’s not just about eating. Go figure.
This group practice reduced stress for everyone
It’s been awhile since we checked in on the good folks at Maharishi International University in Fairfield, Iowa – fictional home of the Fighting Transcendentalists [MAHARISHI RULES!] – but we just have to mention their long-term effort to reduce the national stress.
Way back in the year 2000, a group from MIU began practicing transcendental meditation. The size of the group increased over the next few years and eventually reached 1,725 in 2006. That number is important because it represents the square root of 1% of the U.S. population. When that “transition threshold was achieved,” the university explained in a written statement, “all stress indicators immediately started decreasing.”
By stress indicators they mean the U.S. stress index, the mean of eight variables – murder, rape, assault, robbery, infant mortality, drug deaths, vehicle fatalities, and child deaths by injuries – that the study investigators used to track the effectiveness of the meditation program, they said in the World Journal of Social Science.
After 2011, “when the size of the group size began to decline the rate of decrease in stress slowed and then it reversed and began to increase,” MIU reported.
Coauthor Dr. Kenneth Cavanaugh of MIU explained the process: “This study used state-of-the-art methods of time series regression analysis for eliminating potential alternative explanations due to intrinsic preexisting trends and fluctuations in the data. We carefully studied potential alternative explanations in terms of changes in economic conditions, political leadership, population demographics, and policing strategies. None of these factors could account for the results.”
Since we here at LOTME are serious professional journalists, the use of quotes means we are not making this up. Here’s one more thing in quotes: “A grant for 75 million dollars from the Howard and Alice Settle Foundation provided stipends for participants to be in the group and provided funding to bring several hundred visiting [meditation] experts from India to further augment the MIU group.”
Who needs to make up stuff? Not us.
Oral Propranolol Used as Adjunct Therapy in Cutaneous Angiosarcoma
To the Editor:
Angiosarcoma is a malignancy of the vascular endothelium that most commonly presents on the skin.1 Patients diagnosed with cutaneous angiosarcoma, which is a rare and aggressive malignancy, have a 5-year survival rate of approximately 30%.2,3 Angiosarcoma can be seen in the setting of chronic lymphedema; radiation therapy; and sporadically in elderly patients, where it is commonly seen on the head and neck. Presentation on the head and neck has been associated with worse outcomes, with a projected overall 10-year survival rate of 13.8%; the survival rate is lower if the tumor is surgically unresectable or larger in size. Metastasis can occur via both lymphatic and hematogenous routes, with pulmonary and hepatic metastases most frequently observed.1 Prognostications of poor outcomes for patients with head and neck cutaneous angiosarcoma via a 5-year survival rate were identified in a meta-analysis and included the following: patient age older than 70 years, larger tumors, tumor location of scalp vs face, nonsurgical treatments, and lack of clear margins on histology.2
Treatment of angiosarcoma historically has encompassed both surgical resection and adjuvant radiation therapy with suboptimal success. Evidence supporting various treatment regimens remains sparse due to the low incidence of the neoplasm. Although surgical resection is the only documented curative treatment, cutaneous angiosarcomas frequently are found to have positive surgical margins and require adjuvant radiation. Use of high-dose radiation (>50 Gy) with application over a wide treatment area such as total scalp irradiation is recommended.4 Although radiation has been found to diminish local recurrence rates, it has not substantially affected rates of distant disease recurrence.1 Cytotoxic chemotherapy has clinical utility in minimizing progression, but standard regimens afford a progression-free survival of only months.3 Adjuvant treatment with paclitaxel has been shown to have improved efficacy in scalp angiosarcoma vs other visceral sites, showing a nonprogression rate of 42% at 4 months after treatment.5 More recently, targeted chemotherapeutics, including the vascular endothelial growth factor inhibitor bevacizumab and tyrosine kinase inhibitor sorafenib, have shown some survival benefit, but it is unclear if these agents are superior to traditional cytotoxic agents.4,6-10 A phase 2 study of paclitaxel administered weekly with or without bevacizumab showed similar progression-free survival and overall survival, albeit at the expense of added toxicity experienced by participants in the combined group.10
The addition of the nonselective β-adrenergic blocker propranolol to the treatment armamentarium, which was pursued due to its utility in the treatment of benign infantile hemangioma and demonstrated ability to limit the expression of adrenergic receptors in angiosarcoma, has gained clinical attention for possible augmentation of cutaneous angiosarcoma therapy.11-14 Propranolol has been shown to reduce metastasis in other neoplasms—both vascular and nonvascular—and may play a role as an adjuvant treatment to current therapies in angiosarcoma.15-20 We report a patient with cutaneous angiosarcoma (T2 classification) with disease-free survival of nearly 6 years without evidence of recurrence in the setting of continuous propranolol use supplementary to chemotherapy and radiation.
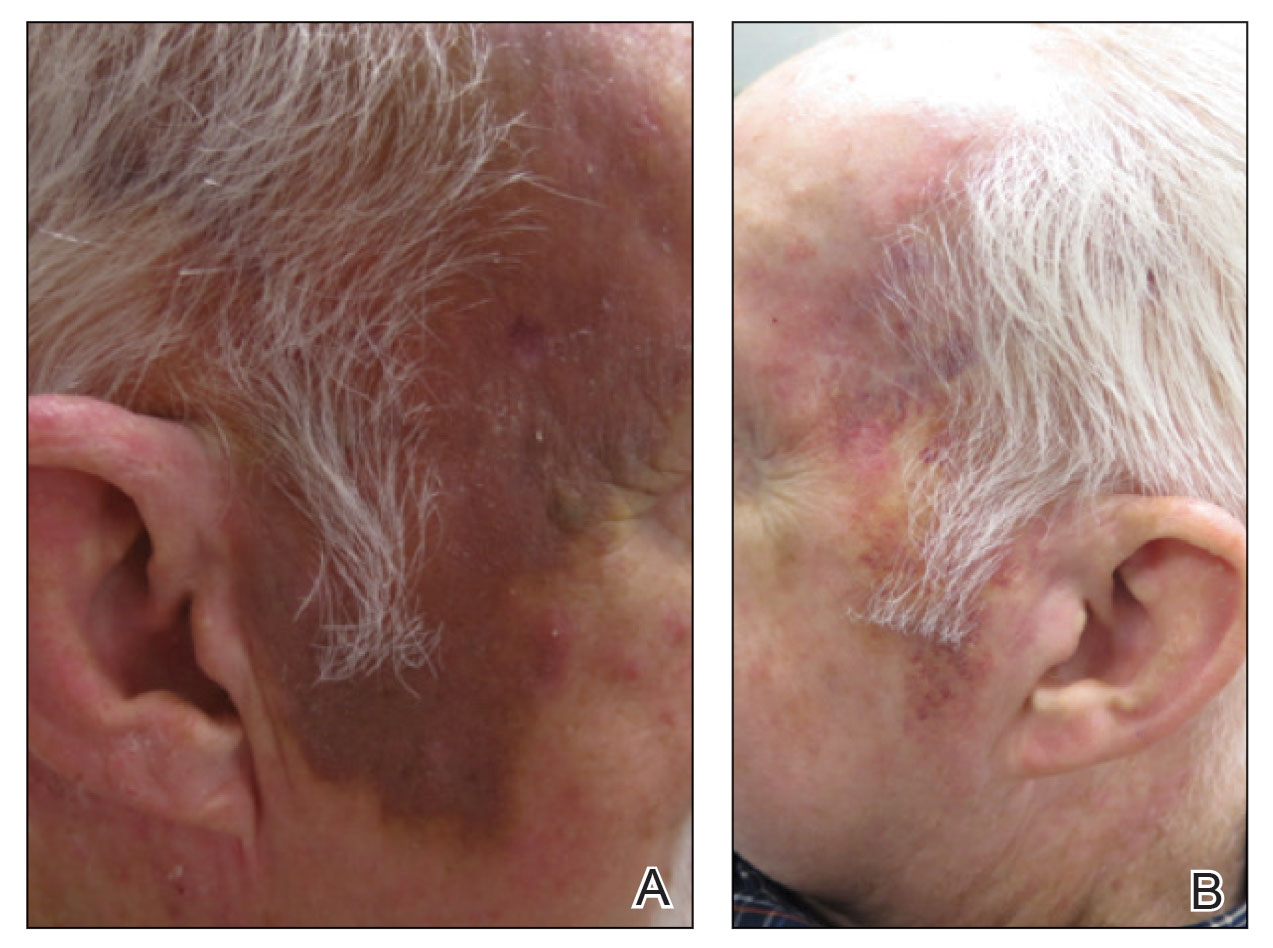
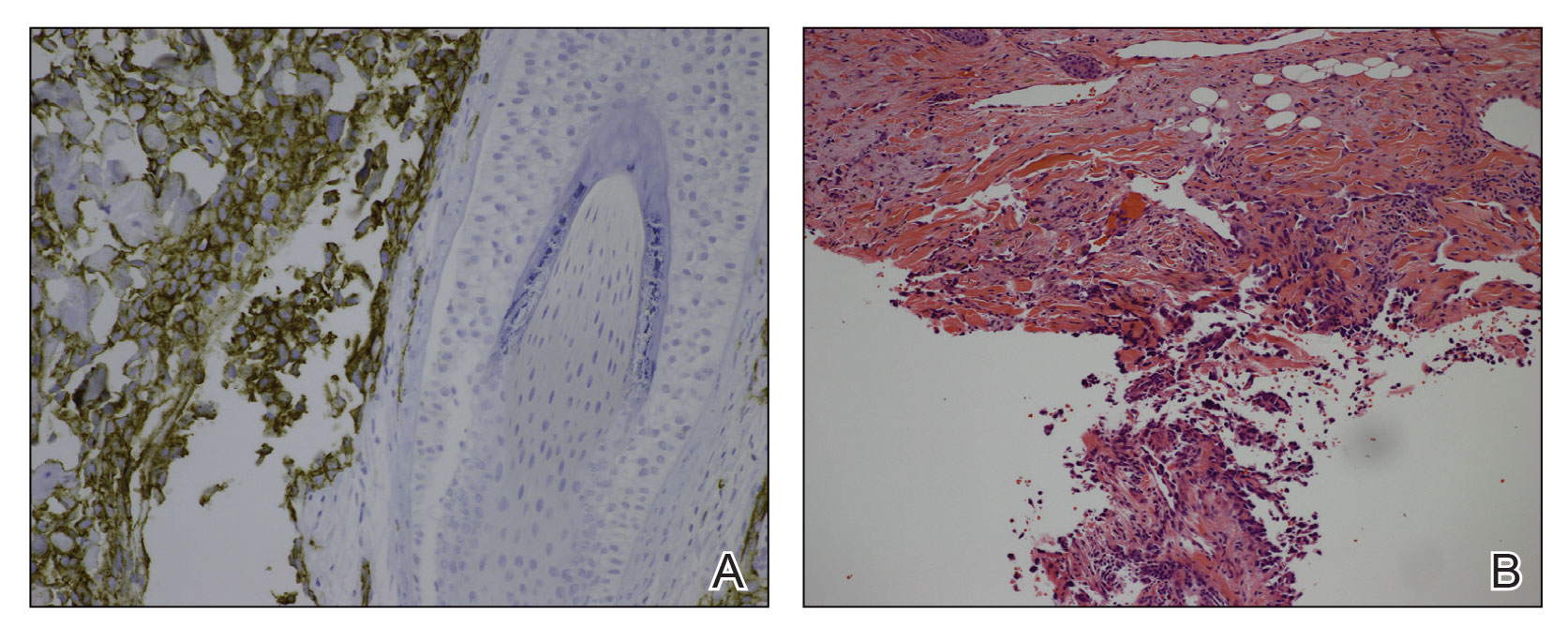
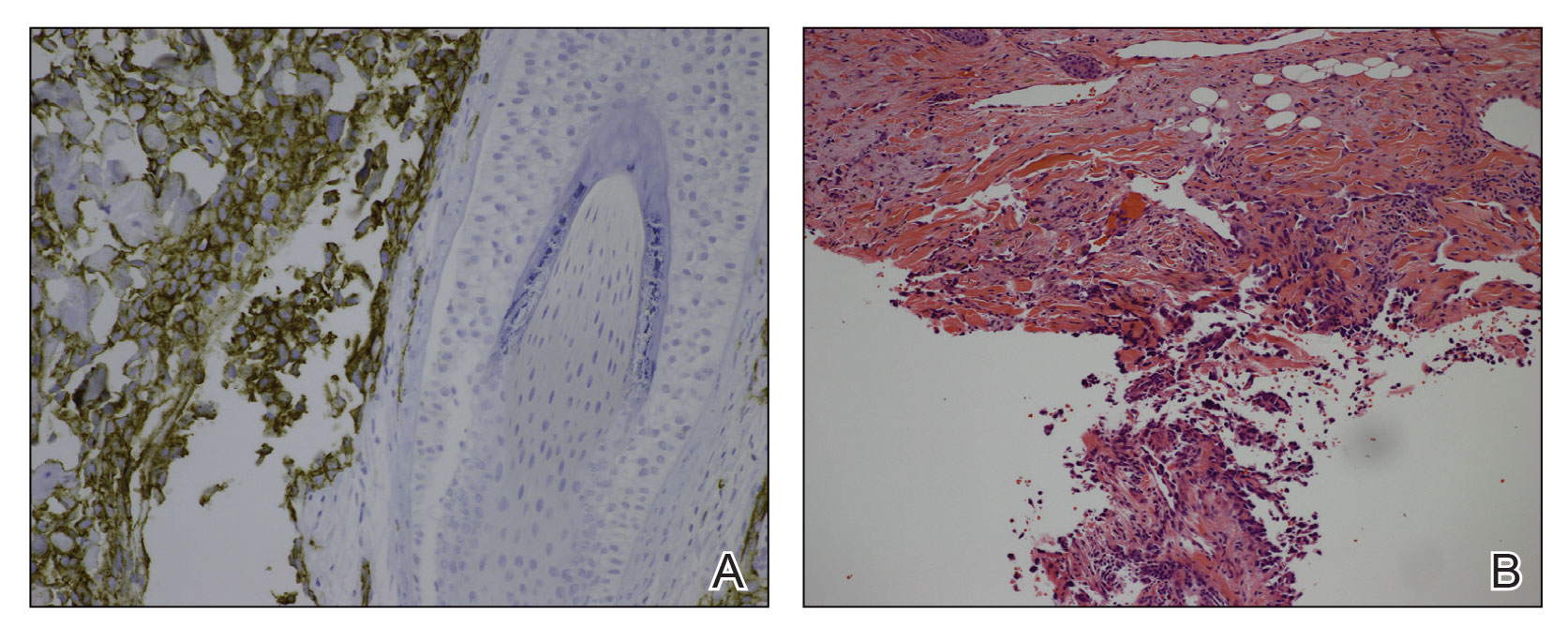
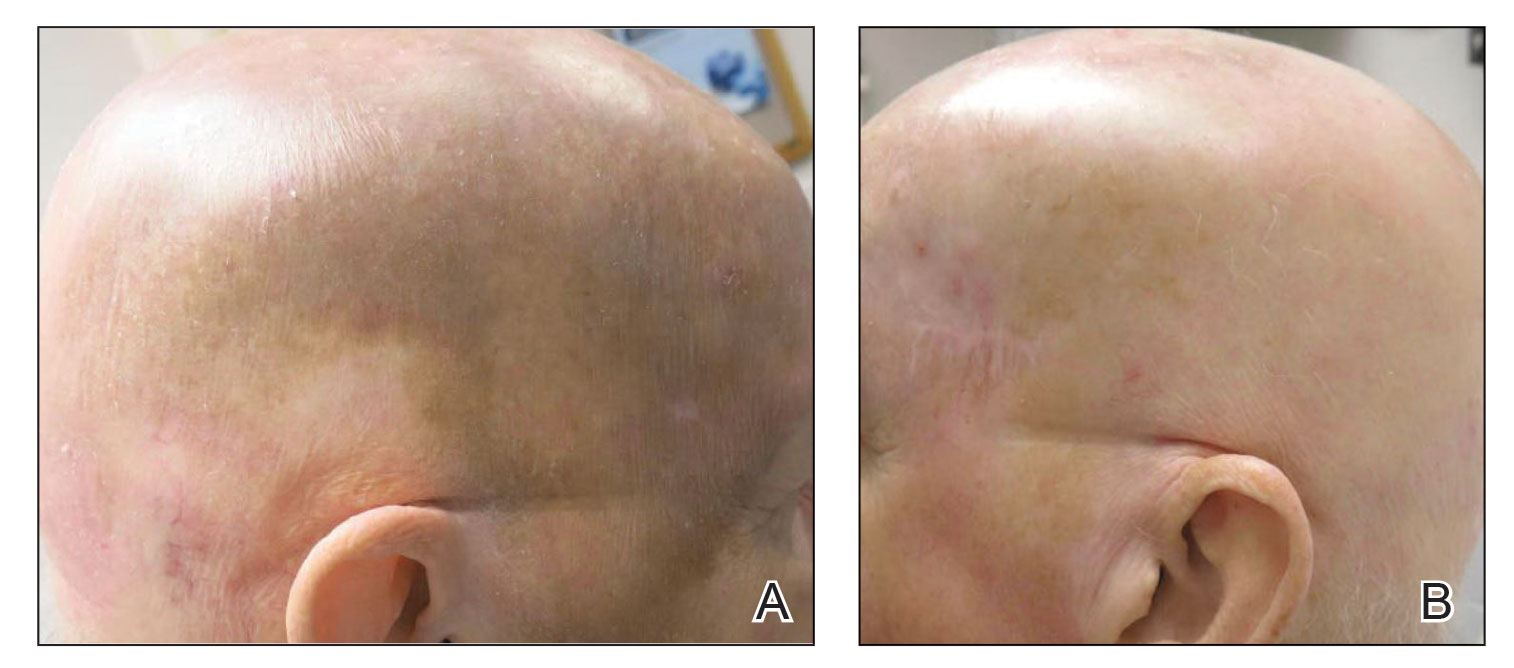
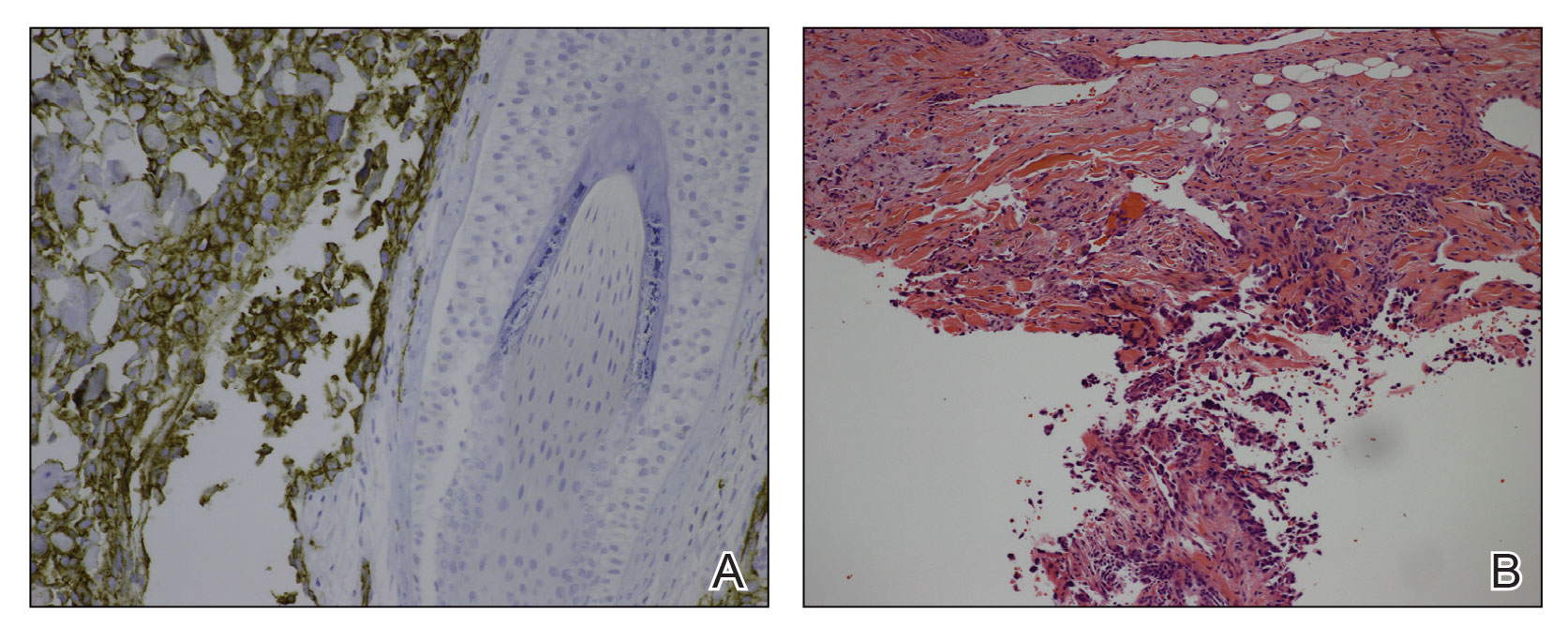
A 78-year-old man with a history of multiple basal cell carcinomas, hypertension, and remote smoking history presented to the dermatology clinic with an enlarging red-brown plaque on the scalp of 2 months’ duration. The lesion had grown rapidly to involve the forehead, right temple, preauricular region, and parietal scalp. At presentation, the tumor measured more than 20 cm in diameter at its greatest point (Figure 1). Physical examination revealed a 6-mm purple nodule within the lesion on the patient’s right parietal scalp. No clinical lymphadenopathy was appreciated at the time of diagnosis. Punch biopsies of the right parietal scalp nodule and right temple patch showed findings consistent with angiosarcoma with diffuse cytoplasmic staining of CD31 in atypical endothelial cells and no staining for human herpesvirus 8 (Figure 2). Concurrent computed tomography of the head showed thickening of the right epidermis, dermis, and deeper scalp tissues, but there was no evidence of skull involvement. Computed tomography of the thorax, abdomen, and pelvis showed no evidence of metastatic disease. After a diagnostic workup, the patient was diagnosed with T2bN0M0 angiosarcoma.
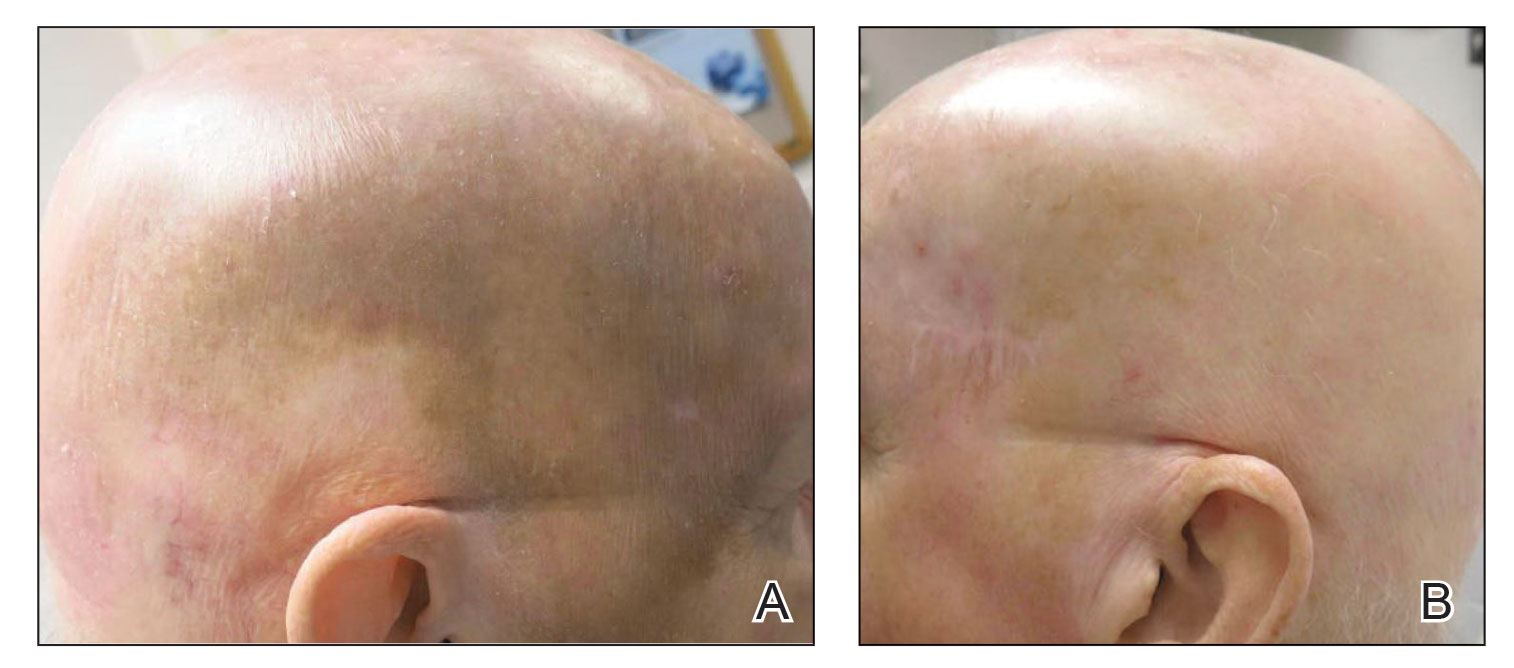
The lesion was determined to be nonresectable due to the extent of the patient’s cutaneous disease. The patient was started on a regimen of paclitaxel, scalp radiation, and oral propranolol. Propranolol 40 mg twice daily was initiated at the time of diagnosis with a plan to continue indefinitely. Starting 1 month after staging, the patient completed 10 weekly cycles of paclitaxel, and he was treated with 60 Gy of scalp radiation in 30 fractions, starting with the second cycle of paclitaxel. He tolerated both well with no reported adverse events. Repeat computed tomography performed 1 month after completion of chemotherapy and radiation showed no evidence of a mass or fluid collection in subcutaneous scalp tissues and no evidence of metastatic disease. This correlated with an observed clinical regression at 1 month and complete clinical response at 5 months with residual hemosiderin and radiation changes. The area of prior disease involvement subsequently evolved from violet to dusky gray in appearance to an eventual complete resolution 26 months after diagnosis, accompanied by atrophic radiation-induced sequelae (Figure 3).
The patient’s postchemotherapy course was complicated by hospitalization for a suspected malignant pleural effusion. Analysis revealed growing ground-glass opacities and nodules in the right lower lung lobe. A thoracentesis with cytology studies was negative for malignancy. Continued monitoring over 19 months demonstrated eventual resolution of those findings. He experienced notable complication from local radiation therapy to the scalp with chronic cutaneous ulceration refractory to wound care and surgical intervention. The patient did not exhibit additional signs or symptoms concerning for recurrence or metastasis and was followed by dermatology and oncology until he died nearly 5 years after initial diagnosis due to complications from acute hypoxic respiratory failure secondary to COVID-19. The last imaging obtained showed no convincing evidence of metastasis, though spinal imaging within a month of his death showed lesions favored to represent benign angiomatous growths. His survival after diagnosis ultimately reached 57 months without confirmed disease recurrence and cause of death unrelated to malignancy history, which is a markedly long documented survival for this extent of disease.
Cutaneous angiosarcoma is an aggressive yet rare malignancy without effective treatments for prolonging survival or eradicating disease. Cutaneous angiosarcoma of the head and neck has a reported 10-year survival rate of 13.8%.1 Although angiosarcoma in any location holds a bleak prognosis, cutaneous angiosarcoma of the scalp with a T2 classification has a 2-year survival rate of 0%. Moreover, even if remission is achieved, disease is highly recurrent, typically within months with the current standard of care.3,21,22
Emerging evidence for the possible role of β-adrenergic receptor blockade in the treatment of malignant vascular neoplasms is promising. Microarrays from a host of vascular growths have demonstrated expression of β-adrenergic receptors in 77% of sampled angiosarcoma specimens in addition to strong expression in infantile hemangiomas, hemangiomas, hemangioendotheliomas, and vascular malformations.19 Research findings have further verified the validity of this approach with the demonstration of b1-, b2-, and b3- adrenergic receptor expression by angiosarcoma cell lines. Propranolol subsequently was shown to effectively target proliferation of these cells and induce apoptosis in a dose-dependent manner and moreover be synergistic in effect with other chemotherapies.15 Several genes have exhibited differential expression between control tumor cells and propranolol-treated cells. Specifically, target genes including AXL (a receptor tyrosine kinase associated with cell adhesion, proliferation, and apoptosis and found to upregulated in melanoma and leukemia) and ERBB receptor feedback inhibitor 1 (receptor tyrosine kinase, with ERBB family members commonly overexpressed or mutated in the setting malignancy) have been posited as possible explanatory factors in the observed angiosarcoma response to propranolol.23
Several cases describing propranolol use as an adjunctive therapy for angiosarcoma suggest a beneficial role in clinical medicine. One case report described propranolol monotherapy for lesion to our patient, with a resultant reduction in Ki-67 as a measure of proliferative index within 1 week of initiating propranolol therapy.13 Propranolol also has been shown to halt or slow progression of metastatic disease in visceral and metastatic angiosarcomas.12-14 In combination with oral etoposide and cyclophosphamide, maintenance propranolol therapy in 7 cases of advanced cutaneous angiosarcoma resulted in 1 complete response and 3 very good partial responses, with a median progression-free survival of 11 months.11 Larger-scale studies have not been published, but the growing number of case reports and case series warrants further investigation of the utility of propranolol as an adjunct to current therapies in advanced angiosarcoma.
- Abraham JA, Hornicek FJ, Kaufman AM, et al. Treatment and outcome of 82 patients with angiosarcoma. Ann Surg Oncol. 2007;14:1953-1967.
- Shin JY, Roh SG, Lee NH, et al. Predisposing factors for poor prognosis of angiosarcoma of the scalp and face: systematic review and meta-analysis. Head Neck. 2017;39:380-386.
- Fury MG, Antonescu CR, Zee KJV, et al. A 14-year retrospective review of angiosarcoma: clinical characteristics, prognostic factors, and treatment outcomes with surgery and chemotherapy. Cancer. 2005;11:241-247.
- Dossett LA, Harrington M, Cruse CW, et al. Cutaneous angiosarcoma. Curr Probl Cancer. 2015;39:258-263.
- Penel N, Bui BN, Bay JO, et al. Phase II trial of weekly paclitaxel for unresectable angiosarcoma: the ANGIOTAX study. J Clin Oncol. 2008;26:5269-5274.
- Agulnik M, Yarber JL, Okuno SH, et al. An open-label, multicenter, phase II study of bevacizumab for the treatment of angiosarcoma and epithelioid hemangioendotheliomas. Ann Oncol. 2013;24:257-263.
- Maki RG, D’Adamo DR, Keohan ML, et al. Phase II study of sorafenib in patients with metastatic or recurrent sarcomas. J Clin Oncol. 2009;27:3133-3140.
- Ishida Y, Otsuka A, Kabashima K. Cutaneous angiosarcoma: update on biology and latest treatment. Curr Opin Oncol. 2018;30:107-112.
- Ray-Coquard I, Italiano A, Bompas E, et al. Sorafenib for patients with advanced angiosarcoma: a phase II trial from the French Sarcoma Group (GSF/GETO). Oncologist. 2012;17:260-266.
- Ray-Coquard IL, Domont J, Tresch-Bruneel E, et al. Paclitaxel given once per week with or without bevacizumab in patients with advanced angiosarcoma: a randomized phase II trial. J Clin Oncol. 2015;33:2797-2802.
- Pasquier E, Andre N, Street J, et al. Effective management of advanced angiosarcoma by the synergistic combination of propranolol and vinblastine-based metronomic chemotherapy: a bench to bedside study. EBioMedicine. 2016;6:87-95.
- Banavali S, Pasquier E, Andre N. Targeted therapy with propranolol and metronomic chemotherapy combination: sustained complete response of a relapsing metastatic angiosarcoma. Ecancermedicalscience. 2015;9:499.
- Chow W, Amaya CN, Rains S, et al. Growth attenuation of cutaneous angiosarcoma with propranolol-mediated beta-blockade. JAMA Dermatol. 2015;151:1226-1229.
- Daguze J, Saint-Jean M, Peuvrel L, et al. Visceral metastatic angiosarcoma treated effectively with oral cyclophosphamide combined with propranolol. JAAD Case Rep. 2016;2:497-499.
- Stiles JM, Amaya C, Rains S, et al. Targeting of beta adrenergic receptors results in therapeutic efficacy against models of hemangioendothelioma and angiosarcoma. PLoS One. 2013;8:e60021.
- Chang PY, Chung CH, Chang WC, et al. The effect of propranolol on the prognosis of hepatocellular carcinoma: a nationwide population-based study. PLoS One. 2019;14:e0216828.
- De Giorgi V, Grazzini M, Benemei S, et al. Propranolol for off-label treatment of patients with melanoma: results from a cohort study. JAMA Oncol. 2018;4:e172908.
- Rico M, Baglioni M, Bondarenko M, et al. Metformin and propranolol combination prevents cancer progression and metastasis in different breast cancer models. Oncotarget. 2017;8:2874-2889.
- Chisholm KM, Chang KW, Truong MT, et al. β-Adrenergic receptor expression in vascular tumors. Mod Pathol. 2012;25:1446-1451.
- Leaute-Labreze C, Dumas de la Roque E, Hubiche T, et al. Propranolol for severe hemangiomas of infancy. N Engl J Med. 2008;358:2649-2651.
- Maddox JC, Evans HL. Angiosarcoma of skin and soft tissue: a study of forty-four cases. Cancer. 1981;48:1907-1921.
- Morgan MB, Swann M, Somach S, et al. Cutaneous angiosarcoma: a case series with prognostic correlation. J Am Acad Dermatol. 2004;50:867-874.
- Zhou S, Liu P, Jiang W, et al. Identification of potential target genes associated with the effect of propranolol on angiosarcoma via microarray analysis. Oncol Lett. 2017;13:4267-4275.
To the Editor:
Angiosarcoma is a malignancy of the vascular endothelium that most commonly presents on the skin.1 Patients diagnosed with cutaneous angiosarcoma, which is a rare and aggressive malignancy, have a 5-year survival rate of approximately 30%.2,3 Angiosarcoma can be seen in the setting of chronic lymphedema; radiation therapy; and sporadically in elderly patients, where it is commonly seen on the head and neck. Presentation on the head and neck has been associated with worse outcomes, with a projected overall 10-year survival rate of 13.8%; the survival rate is lower if the tumor is surgically unresectable or larger in size. Metastasis can occur via both lymphatic and hematogenous routes, with pulmonary and hepatic metastases most frequently observed.1 Prognostications of poor outcomes for patients with head and neck cutaneous angiosarcoma via a 5-year survival rate were identified in a meta-analysis and included the following: patient age older than 70 years, larger tumors, tumor location of scalp vs face, nonsurgical treatments, and lack of clear margins on histology.2
Treatment of angiosarcoma historically has encompassed both surgical resection and adjuvant radiation therapy with suboptimal success. Evidence supporting various treatment regimens remains sparse due to the low incidence of the neoplasm. Although surgical resection is the only documented curative treatment, cutaneous angiosarcomas frequently are found to have positive surgical margins and require adjuvant radiation. Use of high-dose radiation (>50 Gy) with application over a wide treatment area such as total scalp irradiation is recommended.4 Although radiation has been found to diminish local recurrence rates, it has not substantially affected rates of distant disease recurrence.1 Cytotoxic chemotherapy has clinical utility in minimizing progression, but standard regimens afford a progression-free survival of only months.3 Adjuvant treatment with paclitaxel has been shown to have improved efficacy in scalp angiosarcoma vs other visceral sites, showing a nonprogression rate of 42% at 4 months after treatment.5 More recently, targeted chemotherapeutics, including the vascular endothelial growth factor inhibitor bevacizumab and tyrosine kinase inhibitor sorafenib, have shown some survival benefit, but it is unclear if these agents are superior to traditional cytotoxic agents.4,6-10 A phase 2 study of paclitaxel administered weekly with or without bevacizumab showed similar progression-free survival and overall survival, albeit at the expense of added toxicity experienced by participants in the combined group.10
The addition of the nonselective β-adrenergic blocker propranolol to the treatment armamentarium, which was pursued due to its utility in the treatment of benign infantile hemangioma and demonstrated ability to limit the expression of adrenergic receptors in angiosarcoma, has gained clinical attention for possible augmentation of cutaneous angiosarcoma therapy.11-14 Propranolol has been shown to reduce metastasis in other neoplasms—both vascular and nonvascular—and may play a role as an adjuvant treatment to current therapies in angiosarcoma.15-20 We report a patient with cutaneous angiosarcoma (T2 classification) with disease-free survival of nearly 6 years without evidence of recurrence in the setting of continuous propranolol use supplementary to chemotherapy and radiation.
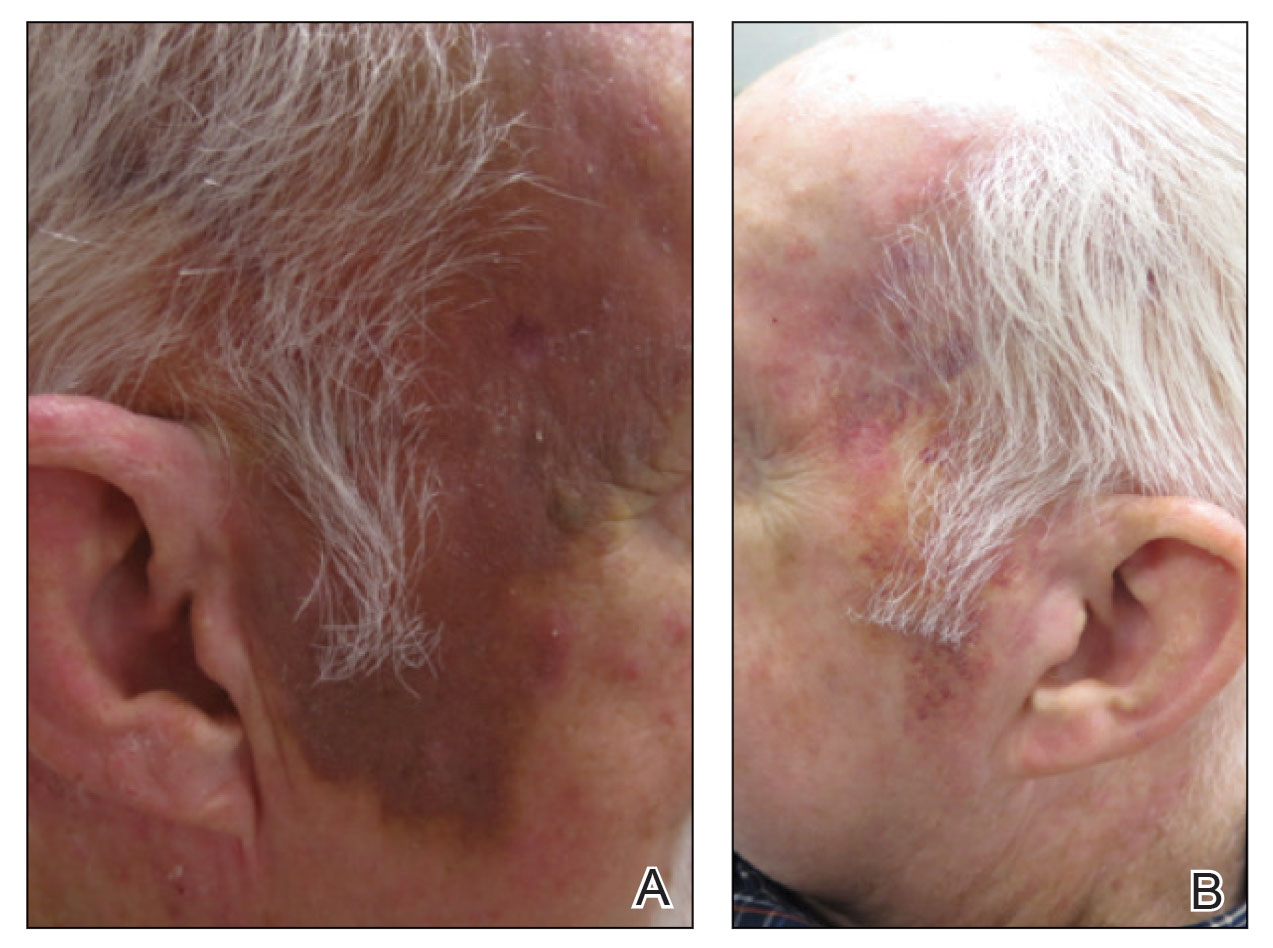
A 78-year-old man with a history of multiple basal cell carcinomas, hypertension, and remote smoking history presented to the dermatology clinic with an enlarging red-brown plaque on the scalp of 2 months’ duration. The lesion had grown rapidly to involve the forehead, right temple, preauricular region, and parietal scalp. At presentation, the tumor measured more than 20 cm in diameter at its greatest point (Figure 1). Physical examination revealed a 6-mm purple nodule within the lesion on the patient’s right parietal scalp. No clinical lymphadenopathy was appreciated at the time of diagnosis. Punch biopsies of the right parietal scalp nodule and right temple patch showed findings consistent with angiosarcoma with diffuse cytoplasmic staining of CD31 in atypical endothelial cells and no staining for human herpesvirus 8 (Figure 2). Concurrent computed tomography of the head showed thickening of the right epidermis, dermis, and deeper scalp tissues, but there was no evidence of skull involvement. Computed tomography of the thorax, abdomen, and pelvis showed no evidence of metastatic disease. After a diagnostic workup, the patient was diagnosed with T2bN0M0 angiosarcoma.
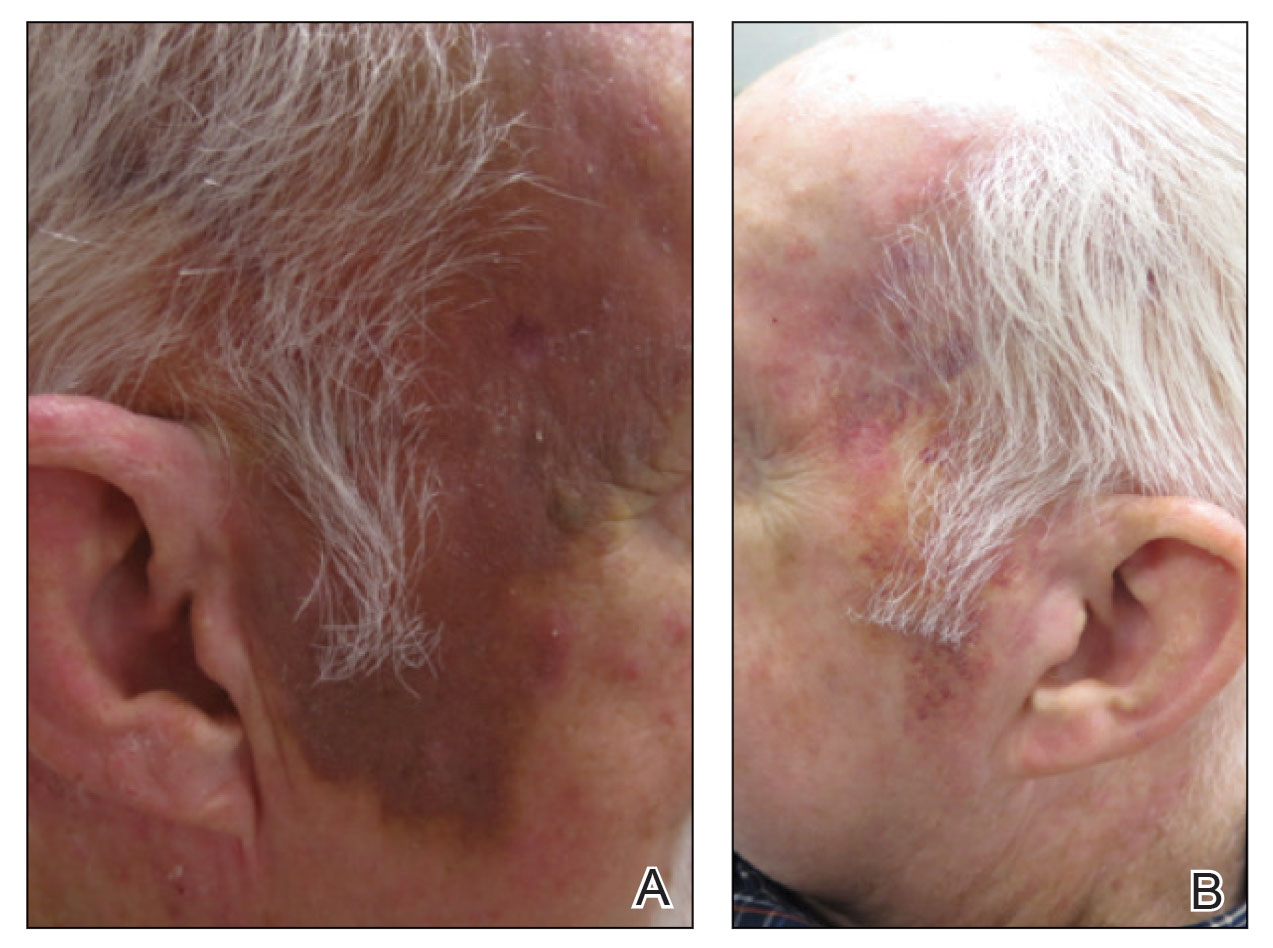
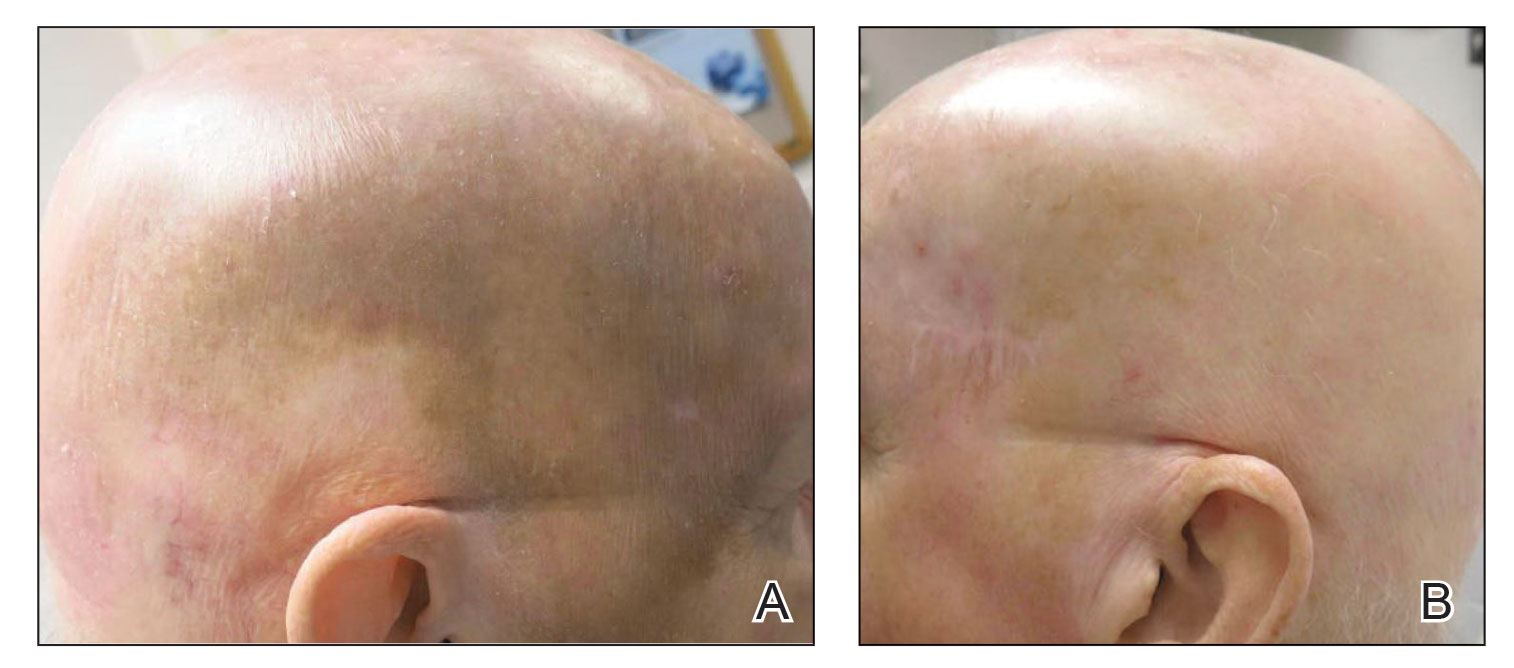
The lesion was determined to be nonresectable due to the extent of the patient’s cutaneous disease. The patient was started on a regimen of paclitaxel, scalp radiation, and oral propranolol. Propranolol 40 mg twice daily was initiated at the time of diagnosis with a plan to continue indefinitely. Starting 1 month after staging, the patient completed 10 weekly cycles of paclitaxel, and he was treated with 60 Gy of scalp radiation in 30 fractions, starting with the second cycle of paclitaxel. He tolerated both well with no reported adverse events. Repeat computed tomography performed 1 month after completion of chemotherapy and radiation showed no evidence of a mass or fluid collection in subcutaneous scalp tissues and no evidence of metastatic disease. This correlated with an observed clinical regression at 1 month and complete clinical response at 5 months with residual hemosiderin and radiation changes. The area of prior disease involvement subsequently evolved from violet to dusky gray in appearance to an eventual complete resolution 26 months after diagnosis, accompanied by atrophic radiation-induced sequelae (Figure 3).
The patient’s postchemotherapy course was complicated by hospitalization for a suspected malignant pleural effusion. Analysis revealed growing ground-glass opacities and nodules in the right lower lung lobe. A thoracentesis with cytology studies was negative for malignancy. Continued monitoring over 19 months demonstrated eventual resolution of those findings. He experienced notable complication from local radiation therapy to the scalp with chronic cutaneous ulceration refractory to wound care and surgical intervention. The patient did not exhibit additional signs or symptoms concerning for recurrence or metastasis and was followed by dermatology and oncology until he died nearly 5 years after initial diagnosis due to complications from acute hypoxic respiratory failure secondary to COVID-19. The last imaging obtained showed no convincing evidence of metastasis, though spinal imaging within a month of his death showed lesions favored to represent benign angiomatous growths. His survival after diagnosis ultimately reached 57 months without confirmed disease recurrence and cause of death unrelated to malignancy history, which is a markedly long documented survival for this extent of disease.
Cutaneous angiosarcoma is an aggressive yet rare malignancy without effective treatments for prolonging survival or eradicating disease. Cutaneous angiosarcoma of the head and neck has a reported 10-year survival rate of 13.8%.1 Although angiosarcoma in any location holds a bleak prognosis, cutaneous angiosarcoma of the scalp with a T2 classification has a 2-year survival rate of 0%. Moreover, even if remission is achieved, disease is highly recurrent, typically within months with the current standard of care.3,21,22
Emerging evidence for the possible role of β-adrenergic receptor blockade in the treatment of malignant vascular neoplasms is promising. Microarrays from a host of vascular growths have demonstrated expression of β-adrenergic receptors in 77% of sampled angiosarcoma specimens in addition to strong expression in infantile hemangiomas, hemangiomas, hemangioendotheliomas, and vascular malformations.19 Research findings have further verified the validity of this approach with the demonstration of b1-, b2-, and b3- adrenergic receptor expression by angiosarcoma cell lines. Propranolol subsequently was shown to effectively target proliferation of these cells and induce apoptosis in a dose-dependent manner and moreover be synergistic in effect with other chemotherapies.15 Several genes have exhibited differential expression between control tumor cells and propranolol-treated cells. Specifically, target genes including AXL (a receptor tyrosine kinase associated with cell adhesion, proliferation, and apoptosis and found to upregulated in melanoma and leukemia) and ERBB receptor feedback inhibitor 1 (receptor tyrosine kinase, with ERBB family members commonly overexpressed or mutated in the setting malignancy) have been posited as possible explanatory factors in the observed angiosarcoma response to propranolol.23
Several cases describing propranolol use as an adjunctive therapy for angiosarcoma suggest a beneficial role in clinical medicine. One case report described propranolol monotherapy for lesion to our patient, with a resultant reduction in Ki-67 as a measure of proliferative index within 1 week of initiating propranolol therapy.13 Propranolol also has been shown to halt or slow progression of metastatic disease in visceral and metastatic angiosarcomas.12-14 In combination with oral etoposide and cyclophosphamide, maintenance propranolol therapy in 7 cases of advanced cutaneous angiosarcoma resulted in 1 complete response and 3 very good partial responses, with a median progression-free survival of 11 months.11 Larger-scale studies have not been published, but the growing number of case reports and case series warrants further investigation of the utility of propranolol as an adjunct to current therapies in advanced angiosarcoma.
To the Editor:
Angiosarcoma is a malignancy of the vascular endothelium that most commonly presents on the skin.1 Patients diagnosed with cutaneous angiosarcoma, which is a rare and aggressive malignancy, have a 5-year survival rate of approximately 30%.2,3 Angiosarcoma can be seen in the setting of chronic lymphedema; radiation therapy; and sporadically in elderly patients, where it is commonly seen on the head and neck. Presentation on the head and neck has been associated with worse outcomes, with a projected overall 10-year survival rate of 13.8%; the survival rate is lower if the tumor is surgically unresectable or larger in size. Metastasis can occur via both lymphatic and hematogenous routes, with pulmonary and hepatic metastases most frequently observed.1 Prognostications of poor outcomes for patients with head and neck cutaneous angiosarcoma via a 5-year survival rate were identified in a meta-analysis and included the following: patient age older than 70 years, larger tumors, tumor location of scalp vs face, nonsurgical treatments, and lack of clear margins on histology.2
Treatment of angiosarcoma historically has encompassed both surgical resection and adjuvant radiation therapy with suboptimal success. Evidence supporting various treatment regimens remains sparse due to the low incidence of the neoplasm. Although surgical resection is the only documented curative treatment, cutaneous angiosarcomas frequently are found to have positive surgical margins and require adjuvant radiation. Use of high-dose radiation (>50 Gy) with application over a wide treatment area such as total scalp irradiation is recommended.4 Although radiation has been found to diminish local recurrence rates, it has not substantially affected rates of distant disease recurrence.1 Cytotoxic chemotherapy has clinical utility in minimizing progression, but standard regimens afford a progression-free survival of only months.3 Adjuvant treatment with paclitaxel has been shown to have improved efficacy in scalp angiosarcoma vs other visceral sites, showing a nonprogression rate of 42% at 4 months after treatment.5 More recently, targeted chemotherapeutics, including the vascular endothelial growth factor inhibitor bevacizumab and tyrosine kinase inhibitor sorafenib, have shown some survival benefit, but it is unclear if these agents are superior to traditional cytotoxic agents.4,6-10 A phase 2 study of paclitaxel administered weekly with or without bevacizumab showed similar progression-free survival and overall survival, albeit at the expense of added toxicity experienced by participants in the combined group.10
The addition of the nonselective β-adrenergic blocker propranolol to the treatment armamentarium, which was pursued due to its utility in the treatment of benign infantile hemangioma and demonstrated ability to limit the expression of adrenergic receptors in angiosarcoma, has gained clinical attention for possible augmentation of cutaneous angiosarcoma therapy.11-14 Propranolol has been shown to reduce metastasis in other neoplasms—both vascular and nonvascular—and may play a role as an adjuvant treatment to current therapies in angiosarcoma.15-20 We report a patient with cutaneous angiosarcoma (T2 classification) with disease-free survival of nearly 6 years without evidence of recurrence in the setting of continuous propranolol use supplementary to chemotherapy and radiation.
A 78-year-old man with a history of multiple basal cell carcinomas, hypertension, and remote smoking history presented to the dermatology clinic with an enlarging red-brown plaque on the scalp of 2 months’ duration. The lesion had grown rapidly to involve the forehead, right temple, preauricular region, and parietal scalp. At presentation, the tumor measured more than 20 cm in diameter at its greatest point (Figure 1). Physical examination revealed a 6-mm purple nodule within the lesion on the patient’s right parietal scalp. No clinical lymphadenopathy was appreciated at the time of diagnosis. Punch biopsies of the right parietal scalp nodule and right temple patch showed findings consistent with angiosarcoma with diffuse cytoplasmic staining of CD31 in atypical endothelial cells and no staining for human herpesvirus 8 (Figure 2). Concurrent computed tomography of the head showed thickening of the right epidermis, dermis, and deeper scalp tissues, but there was no evidence of skull involvement. Computed tomography of the thorax, abdomen, and pelvis showed no evidence of metastatic disease. After a diagnostic workup, the patient was diagnosed with T2bN0M0 angiosarcoma.
The lesion was determined to be nonresectable due to the extent of the patient’s cutaneous disease. The patient was started on a regimen of paclitaxel, scalp radiation, and oral propranolol. Propranolol 40 mg twice daily was initiated at the time of diagnosis with a plan to continue indefinitely. Starting 1 month after staging, the patient completed 10 weekly cycles of paclitaxel, and he was treated with 60 Gy of scalp radiation in 30 fractions, starting with the second cycle of paclitaxel. He tolerated both well with no reported adverse events. Repeat computed tomography performed 1 month after completion of chemotherapy and radiation showed no evidence of a mass or fluid collection in subcutaneous scalp tissues and no evidence of metastatic disease. This correlated with an observed clinical regression at 1 month and complete clinical response at 5 months with residual hemosiderin and radiation changes. The area of prior disease involvement subsequently evolved from violet to dusky gray in appearance to an eventual complete resolution 26 months after diagnosis, accompanied by atrophic radiation-induced sequelae (Figure 3).
The patient’s postchemotherapy course was complicated by hospitalization for a suspected malignant pleural effusion. Analysis revealed growing ground-glass opacities and nodules in the right lower lung lobe. A thoracentesis with cytology studies was negative for malignancy. Continued monitoring over 19 months demonstrated eventual resolution of those findings. He experienced notable complication from local radiation therapy to the scalp with chronic cutaneous ulceration refractory to wound care and surgical intervention. The patient did not exhibit additional signs or symptoms concerning for recurrence or metastasis and was followed by dermatology and oncology until he died nearly 5 years after initial diagnosis due to complications from acute hypoxic respiratory failure secondary to COVID-19. The last imaging obtained showed no convincing evidence of metastasis, though spinal imaging within a month of his death showed lesions favored to represent benign angiomatous growths. His survival after diagnosis ultimately reached 57 months without confirmed disease recurrence and cause of death unrelated to malignancy history, which is a markedly long documented survival for this extent of disease.
Cutaneous angiosarcoma is an aggressive yet rare malignancy without effective treatments for prolonging survival or eradicating disease. Cutaneous angiosarcoma of the head and neck has a reported 10-year survival rate of 13.8%.1 Although angiosarcoma in any location holds a bleak prognosis, cutaneous angiosarcoma of the scalp with a T2 classification has a 2-year survival rate of 0%. Moreover, even if remission is achieved, disease is highly recurrent, typically within months with the current standard of care.3,21,22
Emerging evidence for the possible role of β-adrenergic receptor blockade in the treatment of malignant vascular neoplasms is promising. Microarrays from a host of vascular growths have demonstrated expression of β-adrenergic receptors in 77% of sampled angiosarcoma specimens in addition to strong expression in infantile hemangiomas, hemangiomas, hemangioendotheliomas, and vascular malformations.19 Research findings have further verified the validity of this approach with the demonstration of b1-, b2-, and b3- adrenergic receptor expression by angiosarcoma cell lines. Propranolol subsequently was shown to effectively target proliferation of these cells and induce apoptosis in a dose-dependent manner and moreover be synergistic in effect with other chemotherapies.15 Several genes have exhibited differential expression between control tumor cells and propranolol-treated cells. Specifically, target genes including AXL (a receptor tyrosine kinase associated with cell adhesion, proliferation, and apoptosis and found to upregulated in melanoma and leukemia) and ERBB receptor feedback inhibitor 1 (receptor tyrosine kinase, with ERBB family members commonly overexpressed or mutated in the setting malignancy) have been posited as possible explanatory factors in the observed angiosarcoma response to propranolol.23
Several cases describing propranolol use as an adjunctive therapy for angiosarcoma suggest a beneficial role in clinical medicine. One case report described propranolol monotherapy for lesion to our patient, with a resultant reduction in Ki-67 as a measure of proliferative index within 1 week of initiating propranolol therapy.13 Propranolol also has been shown to halt or slow progression of metastatic disease in visceral and metastatic angiosarcomas.12-14 In combination with oral etoposide and cyclophosphamide, maintenance propranolol therapy in 7 cases of advanced cutaneous angiosarcoma resulted in 1 complete response and 3 very good partial responses, with a median progression-free survival of 11 months.11 Larger-scale studies have not been published, but the growing number of case reports and case series warrants further investigation of the utility of propranolol as an adjunct to current therapies in advanced angiosarcoma.
- Abraham JA, Hornicek FJ, Kaufman AM, et al. Treatment and outcome of 82 patients with angiosarcoma. Ann Surg Oncol. 2007;14:1953-1967.
- Shin JY, Roh SG, Lee NH, et al. Predisposing factors for poor prognosis of angiosarcoma of the scalp and face: systematic review and meta-analysis. Head Neck. 2017;39:380-386.
- Fury MG, Antonescu CR, Zee KJV, et al. A 14-year retrospective review of angiosarcoma: clinical characteristics, prognostic factors, and treatment outcomes with surgery and chemotherapy. Cancer. 2005;11:241-247.
- Dossett LA, Harrington M, Cruse CW, et al. Cutaneous angiosarcoma. Curr Probl Cancer. 2015;39:258-263.
- Penel N, Bui BN, Bay JO, et al. Phase II trial of weekly paclitaxel for unresectable angiosarcoma: the ANGIOTAX study. J Clin Oncol. 2008;26:5269-5274.
- Agulnik M, Yarber JL, Okuno SH, et al. An open-label, multicenter, phase II study of bevacizumab for the treatment of angiosarcoma and epithelioid hemangioendotheliomas. Ann Oncol. 2013;24:257-263.
- Maki RG, D’Adamo DR, Keohan ML, et al. Phase II study of sorafenib in patients with metastatic or recurrent sarcomas. J Clin Oncol. 2009;27:3133-3140.
- Ishida Y, Otsuka A, Kabashima K. Cutaneous angiosarcoma: update on biology and latest treatment. Curr Opin Oncol. 2018;30:107-112.
- Ray-Coquard I, Italiano A, Bompas E, et al. Sorafenib for patients with advanced angiosarcoma: a phase II trial from the French Sarcoma Group (GSF/GETO). Oncologist. 2012;17:260-266.
- Ray-Coquard IL, Domont J, Tresch-Bruneel E, et al. Paclitaxel given once per week with or without bevacizumab in patients with advanced angiosarcoma: a randomized phase II trial. J Clin Oncol. 2015;33:2797-2802.
- Pasquier E, Andre N, Street J, et al. Effective management of advanced angiosarcoma by the synergistic combination of propranolol and vinblastine-based metronomic chemotherapy: a bench to bedside study. EBioMedicine. 2016;6:87-95.
- Banavali S, Pasquier E, Andre N. Targeted therapy with propranolol and metronomic chemotherapy combination: sustained complete response of a relapsing metastatic angiosarcoma. Ecancermedicalscience. 2015;9:499.
- Chow W, Amaya CN, Rains S, et al. Growth attenuation of cutaneous angiosarcoma with propranolol-mediated beta-blockade. JAMA Dermatol. 2015;151:1226-1229.
- Daguze J, Saint-Jean M, Peuvrel L, et al. Visceral metastatic angiosarcoma treated effectively with oral cyclophosphamide combined with propranolol. JAAD Case Rep. 2016;2:497-499.
- Stiles JM, Amaya C, Rains S, et al. Targeting of beta adrenergic receptors results in therapeutic efficacy against models of hemangioendothelioma and angiosarcoma. PLoS One. 2013;8:e60021.
- Chang PY, Chung CH, Chang WC, et al. The effect of propranolol on the prognosis of hepatocellular carcinoma: a nationwide population-based study. PLoS One. 2019;14:e0216828.
- De Giorgi V, Grazzini M, Benemei S, et al. Propranolol for off-label treatment of patients with melanoma: results from a cohort study. JAMA Oncol. 2018;4:e172908.
- Rico M, Baglioni M, Bondarenko M, et al. Metformin and propranolol combination prevents cancer progression and metastasis in different breast cancer models. Oncotarget. 2017;8:2874-2889.
- Chisholm KM, Chang KW, Truong MT, et al. β-Adrenergic receptor expression in vascular tumors. Mod Pathol. 2012;25:1446-1451.
- Leaute-Labreze C, Dumas de la Roque E, Hubiche T, et al. Propranolol for severe hemangiomas of infancy. N Engl J Med. 2008;358:2649-2651.
- Maddox JC, Evans HL. Angiosarcoma of skin and soft tissue: a study of forty-four cases. Cancer. 1981;48:1907-1921.
- Morgan MB, Swann M, Somach S, et al. Cutaneous angiosarcoma: a case series with prognostic correlation. J Am Acad Dermatol. 2004;50:867-874.
- Zhou S, Liu P, Jiang W, et al. Identification of potential target genes associated with the effect of propranolol on angiosarcoma via microarray analysis. Oncol Lett. 2017;13:4267-4275.
- Abraham JA, Hornicek FJ, Kaufman AM, et al. Treatment and outcome of 82 patients with angiosarcoma. Ann Surg Oncol. 2007;14:1953-1967.
- Shin JY, Roh SG, Lee NH, et al. Predisposing factors for poor prognosis of angiosarcoma of the scalp and face: systematic review and meta-analysis. Head Neck. 2017;39:380-386.
- Fury MG, Antonescu CR, Zee KJV, et al. A 14-year retrospective review of angiosarcoma: clinical characteristics, prognostic factors, and treatment outcomes with surgery and chemotherapy. Cancer. 2005;11:241-247.
- Dossett LA, Harrington M, Cruse CW, et al. Cutaneous angiosarcoma. Curr Probl Cancer. 2015;39:258-263.
- Penel N, Bui BN, Bay JO, et al. Phase II trial of weekly paclitaxel for unresectable angiosarcoma: the ANGIOTAX study. J Clin Oncol. 2008;26:5269-5274.
- Agulnik M, Yarber JL, Okuno SH, et al. An open-label, multicenter, phase II study of bevacizumab for the treatment of angiosarcoma and epithelioid hemangioendotheliomas. Ann Oncol. 2013;24:257-263.
- Maki RG, D’Adamo DR, Keohan ML, et al. Phase II study of sorafenib in patients with metastatic or recurrent sarcomas. J Clin Oncol. 2009;27:3133-3140.
- Ishida Y, Otsuka A, Kabashima K. Cutaneous angiosarcoma: update on biology and latest treatment. Curr Opin Oncol. 2018;30:107-112.
- Ray-Coquard I, Italiano A, Bompas E, et al. Sorafenib for patients with advanced angiosarcoma: a phase II trial from the French Sarcoma Group (GSF/GETO). Oncologist. 2012;17:260-266.
- Ray-Coquard IL, Domont J, Tresch-Bruneel E, et al. Paclitaxel given once per week with or without bevacizumab in patients with advanced angiosarcoma: a randomized phase II trial. J Clin Oncol. 2015;33:2797-2802.
- Pasquier E, Andre N, Street J, et al. Effective management of advanced angiosarcoma by the synergistic combination of propranolol and vinblastine-based metronomic chemotherapy: a bench to bedside study. EBioMedicine. 2016;6:87-95.
- Banavali S, Pasquier E, Andre N. Targeted therapy with propranolol and metronomic chemotherapy combination: sustained complete response of a relapsing metastatic angiosarcoma. Ecancermedicalscience. 2015;9:499.
- Chow W, Amaya CN, Rains S, et al. Growth attenuation of cutaneous angiosarcoma with propranolol-mediated beta-blockade. JAMA Dermatol. 2015;151:1226-1229.
- Daguze J, Saint-Jean M, Peuvrel L, et al. Visceral metastatic angiosarcoma treated effectively with oral cyclophosphamide combined with propranolol. JAAD Case Rep. 2016;2:497-499.
- Stiles JM, Amaya C, Rains S, et al. Targeting of beta adrenergic receptors results in therapeutic efficacy against models of hemangioendothelioma and angiosarcoma. PLoS One. 2013;8:e60021.
- Chang PY, Chung CH, Chang WC, et al. The effect of propranolol on the prognosis of hepatocellular carcinoma: a nationwide population-based study. PLoS One. 2019;14:e0216828.
- De Giorgi V, Grazzini M, Benemei S, et al. Propranolol for off-label treatment of patients with melanoma: results from a cohort study. JAMA Oncol. 2018;4:e172908.
- Rico M, Baglioni M, Bondarenko M, et al. Metformin and propranolol combination prevents cancer progression and metastasis in different breast cancer models. Oncotarget. 2017;8:2874-2889.
- Chisholm KM, Chang KW, Truong MT, et al. β-Adrenergic receptor expression in vascular tumors. Mod Pathol. 2012;25:1446-1451.
- Leaute-Labreze C, Dumas de la Roque E, Hubiche T, et al. Propranolol for severe hemangiomas of infancy. N Engl J Med. 2008;358:2649-2651.
- Maddox JC, Evans HL. Angiosarcoma of skin and soft tissue: a study of forty-four cases. Cancer. 1981;48:1907-1921.
- Morgan MB, Swann M, Somach S, et al. Cutaneous angiosarcoma: a case series with prognostic correlation. J Am Acad Dermatol. 2004;50:867-874.
- Zhou S, Liu P, Jiang W, et al. Identification of potential target genes associated with the effect of propranolol on angiosarcoma via microarray analysis. Oncol Lett. 2017;13:4267-4275.
PRACTICE POINTS
- In one classic presentation, cutaneous angiosarcoma characteristically appears as a bruiselike patch on the head and neck of an elderly gentleman.
- Although cutaneous angiosarcoma typically portends a poor prognosis at the time of diagnosis, adjunctive oral propranolol may be a promising and relatively benign therapy, posited to afford benefit in a manner similar to its efficacy in the treatment of infantile hemangiomas.
Use of Dupilumab in Severe, Multifactorial, Chronic Itch for Geriatric Patients
To the Editor:
Today’s geriatric population is the fastest growing in history. The National Institutes of Health predicts there will be over 1.5 billion individuals aged 65 years and older by the year 2050: 17% of the world’s population.1 Pruritus—either acute or chronic (>6 weeks)—is defined as a sensory perception that leads to an intense desire to scratch.2 Chronic pruritus is an increasing health concern that impacts quality of life within the geriatric population. Elderly patients have various risk factors for developing chronic itch, including aging skin, polypharmacy, and increased systemic comorbidities.3-7
Although the therapeutic armamentarium for chronic itch continues to grow, health care providers often are hesitant to prescribe medications for geriatric patients because of comorbidities and potential drug-drug interactions. Novel biologic therapies now provide alternatives for this complex population. Dupilumab is a fully humanized, monoclonal antibody approved for treatment-resistant atopic dermatitis. This biologic prevents helper T-cell (TH2) signaling, IL-4 and IL-13 release, and subsequent effector cell (eg, mast cell, eosinophil) activity.8-10 The combined efficacy and safety of this medication has changed the treatment landscape of resistant atopic dermatitis. We present the use of dupilumab in a geriatric patient with severe and recalcitrant itch resistant to numerous topical and oral medications.
An 81-year-old man presented to the clinic with a long history of generalized pruritic rash. His medical history was significant for insulin-dependent type 2 diabetes mellitus (T2DM), hypertension, and renal cancer following a right nephrectomy. Laboratory results approximately 14 months prior to the visit revealed a blood urea nitrogen level of 31 mg/dL (reference range, 7–20 mg/dL), creatinine level of 2.20 mg/dL (reference range, 0.7–1.3 mg/dL), and glomerular filtration rate of 29 mL/min (reference range, 90–120 mL/min). Physical examination revealed numerous pink excoriated papules on the face, neck, trunk, and extremities. Lichenified plaques were present on both arms and legs. The patient received the diagnosis of severe atopic dermatitis with greater than 10% body surface area involvement. The investigator global assessment score was 4/4, indicating severe disease burden, and biopsy results reported spongiotic dermatitis. He proceeded to trial various topical corticosteroids, including hydrocortisone ointment 2.5%, betamethasone valerate ointment 0.01%, fluocinonide ointment 0.05%, and mupirocin ointment without benefit. Three subsequent courses of oral steroids failed to provide durable relief. At this point, the peak pruritus numerical rating scale (NRS) score was 7/10, indicating severe pruritus, with a negative impact on the patient’s quality of life and sleep.
Therapy was switched to tacrolimus acetonide ointment 0.1%, betamethasone dipropionate ointment 0.05%, and triamcinolone acetonide ointment 0.1%. Eleven days later, the patient denied experiencing any response to the topical regimen and sought alternative therapy for the itch and associated poor sleep; the NRS score was 10/10, indicating very severe pruritus. Prednisone 20 mg and doxepin 10 mg were initiated for symptom management until the intended transition to dupilumab. The patient began dupilumab with a loading dose of 600 mg, then 300 mg every other week thereafter. At 2- and 4-month follow-up, the patient reported notable relief in symptoms. The rash had improved, and the NRS score decreased from 10/10 to 3/10. He endorsed improved sleep and quality of life.
Pruritus may arise from a series of age-related mechanisms such as structural and chemical changes within the epidermis, underlying neuropathy, medication side effects, infection, malignancy, thyroid dysregulation, liver disease, and chronic kidney disease (CKD).5,6,11 Identifying the underlying etiology often is difficult and involves a complete history and physical examination as well as an appropriate contextualized laboratory workup.
Our patient’s comorbid T2DM and renal disease may have contributed to the pruritus. Type 2 diabetes mellitus can cause diabetic neuropathy, a sequela known to lead to various complications, including pruritus. One study identified a 4-fold increase in pruritus in those with diabetic polyneuropathy compared with age-matched nondiabetics.12,13 An additional study found that pruritus was present in 70% of patients with small fiber neuropathy.14 We needed to consider the role of our patient’s insulin-dependent T2DM and potential underlying neuropathy when addressing the pruritic symptoms.
Furthermore, our patient’s stage IV CKD and elevated urea level also may factor into the pruritus. The pathophysiology of CKD-associated pruritus (also referred to as uremic pruritus) remains poorly understood. Suggested mechanisms include immune-mediated neural inflammation and erroneous nociceptive-receptor activity.15,16 Although uremic pruritus is appreciated primarily in late dialysis-dependent disease, research shows that a notable portion of those with lesser disease, similar to our patient, also experience a significant itch burden.17 Diminishing pruritus is difficult and often aided by management of the underlying renal disease.18
In addition to disease management, symptomatic treatment incorporates the use of emollients, corticosteroids, and antihistamines. Unfortunately, the clinical response in the elderly population to such regimens often is poor.19 Dupilumab is an optimistic therapeutic option for chronic pruritus. By inhibiting the IL-4α receptor found on helper T cells, this biologic inhibits TH2 differentiation and subsequent inflammatory activity. One report identified an optimistic response to dupilumab in the management of uremic pruritus.20 The remarkable improvement and absence of adverse effects in our patient confirmed the utility and safety of dupilumab in complex cases such as elderly patients with multiple comorbidities. Such relief may result from inhibition of proinflammatory cytokine activity as well as decreased afferent spinal cord itch stimuli.10 The positive results from this case cast a favorable outlook on the treatment of chronic itch in the complex geriatric population.
- World’s older population grows dramatically. News release. National Institute on Aging. Published March 28, 2016. Accessed December 23, 2022. http://www.nih.gov/news-events/news-releases/worlds-older-population-grows-dramatically
- Grundmann S, Ständer S. Chronic pruritus: clinics and treatment. Ann Dermatol. 2011;23:1-11.
- Berger TG, Shive M, Harper GM. Pruritus in the older patient: a clinical review. JAMA. 2013;310:2443-2450. doi:10.1001/jama.2013.282023
- Valdes-Rodriguez, R, Mollanazar NK, González-Muro J, et al. Itch prevalence and characteristics in a Hispanic geriatric population: a comprehensive study using a standardized itch questionnaire. Acta Derm Venereol. 2015;95:417-421. doi:10.2340/00015555-1968
- Li J, Tang H, Hu X, et al. Aquaporin-3 gene and protein expression in sun-protected human skin decreases with skin ageing. Australas J Dermatol. 2010;51:106-112.
- Choi EH, Man MQ, Xu P, et al. Stratum corneum acidification is impaired in moderately aged human and murine skin. J Invest Dermatol. 2007;127:2847-2856.
- Fenske NA, Lober CW. Structural and functional changes of normal aging skin. J Am Acad Dermatol. 1986;15(4 pt 1):571-585.
- Paller AS, Kabashima K, Bieber T. Therapeutic pipeline for atopic dermatitis: end of the drought? J Allergy Clin Immunol. 2017;140:633-643. doi:10.1016/j.jaci.2017.07.006
- Kabashima K. New concept of the pathogenesis of atopic dermatitis: interplay among the barrier, allergy, and pruritus as a trinity. J Dermatol Sci. 2013;70:3-11.
- Feld M, Garcia R, Buddenkotte J, et al. The pruritus- and TH2-associated cytokine IL-31 promotes growth of sensory nerves. J Allergy Clin Immunol. 2016;138:500-508.
- Valdes-Rodriguez R, Stull C, Yosipovitch G. Chronic pruritus in the elderly: pathophysiology, diagnosis and management. Drugs Aging. 2015;32:201-215. doi:10.1007/s40266-015-0246-0
- Misery L, Brenaut E, Le Garrec R, et al. Neuropathic pruritus. Nat Rev Neurol. 2014;10:408-416.
- Yamaoka H, Sasaki H, Yamasaki H, et al. Truncal pruritus of unknown origin may be a symptom of diabetic polyneuropathy. Diabetes Care. 2010;33:150-155.
- Brenaut E, Marcorelles P, Genestet S, et al. Pruritus: an underrecognized symptom of small-fiber neuropathies. J Am Acad Dermatol. 2015;72:328-332.
- Adigun M, Badu LA, Berner NM, et al. Uremic pruritus review. US Pharm. 2015;40:HS12-HS15.
- Simonsen E, Komenda P, Lerner B, et al. Treatment of uremic pruritus: a systematic review. Am J Kidney Dis. 2017;70:638-655.
- Carstens E, Akiyama T, eds. Itch: Mechanisms and Treatment. CRC Press/Taylor & Francis; 2014.
- Shirazian S, Aina O, Park Y, et al. Chronic kidney disease-associated pruritus: impact on quality of life and current management challenges. Int J Nephrol Renovasc Dis. 2017;10:11-26.
- Brummer GC, Wang LT, Sontheimer RD. A possible role for dupilumab (Dupixent) in the management of idiopathic chronic eczematous eruption of aging. Dermatol Online J. 2018;24:13030/qt55z1f6xh.
- Silverberg JI, Brieva J. A successful case of dupilumab treatment for severe uremic pruritus. JAAD Case Rep. 2019;5:339-341.
To the Editor:
Today’s geriatric population is the fastest growing in history. The National Institutes of Health predicts there will be over 1.5 billion individuals aged 65 years and older by the year 2050: 17% of the world’s population.1 Pruritus—either acute or chronic (>6 weeks)—is defined as a sensory perception that leads to an intense desire to scratch.2 Chronic pruritus is an increasing health concern that impacts quality of life within the geriatric population. Elderly patients have various risk factors for developing chronic itch, including aging skin, polypharmacy, and increased systemic comorbidities.3-7
Although the therapeutic armamentarium for chronic itch continues to grow, health care providers often are hesitant to prescribe medications for geriatric patients because of comorbidities and potential drug-drug interactions. Novel biologic therapies now provide alternatives for this complex population. Dupilumab is a fully humanized, monoclonal antibody approved for treatment-resistant atopic dermatitis. This biologic prevents helper T-cell (TH2) signaling, IL-4 and IL-13 release, and subsequent effector cell (eg, mast cell, eosinophil) activity.8-10 The combined efficacy and safety of this medication has changed the treatment landscape of resistant atopic dermatitis. We present the use of dupilumab in a geriatric patient with severe and recalcitrant itch resistant to numerous topical and oral medications.
An 81-year-old man presented to the clinic with a long history of generalized pruritic rash. His medical history was significant for insulin-dependent type 2 diabetes mellitus (T2DM), hypertension, and renal cancer following a right nephrectomy. Laboratory results approximately 14 months prior to the visit revealed a blood urea nitrogen level of 31 mg/dL (reference range, 7–20 mg/dL), creatinine level of 2.20 mg/dL (reference range, 0.7–1.3 mg/dL), and glomerular filtration rate of 29 mL/min (reference range, 90–120 mL/min). Physical examination revealed numerous pink excoriated papules on the face, neck, trunk, and extremities. Lichenified plaques were present on both arms and legs. The patient received the diagnosis of severe atopic dermatitis with greater than 10% body surface area involvement. The investigator global assessment score was 4/4, indicating severe disease burden, and biopsy results reported spongiotic dermatitis. He proceeded to trial various topical corticosteroids, including hydrocortisone ointment 2.5%, betamethasone valerate ointment 0.01%, fluocinonide ointment 0.05%, and mupirocin ointment without benefit. Three subsequent courses of oral steroids failed to provide durable relief. At this point, the peak pruritus numerical rating scale (NRS) score was 7/10, indicating severe pruritus, with a negative impact on the patient’s quality of life and sleep.
Therapy was switched to tacrolimus acetonide ointment 0.1%, betamethasone dipropionate ointment 0.05%, and triamcinolone acetonide ointment 0.1%. Eleven days later, the patient denied experiencing any response to the topical regimen and sought alternative therapy for the itch and associated poor sleep; the NRS score was 10/10, indicating very severe pruritus. Prednisone 20 mg and doxepin 10 mg were initiated for symptom management until the intended transition to dupilumab. The patient began dupilumab with a loading dose of 600 mg, then 300 mg every other week thereafter. At 2- and 4-month follow-up, the patient reported notable relief in symptoms. The rash had improved, and the NRS score decreased from 10/10 to 3/10. He endorsed improved sleep and quality of life.
Pruritus may arise from a series of age-related mechanisms such as structural and chemical changes within the epidermis, underlying neuropathy, medication side effects, infection, malignancy, thyroid dysregulation, liver disease, and chronic kidney disease (CKD).5,6,11 Identifying the underlying etiology often is difficult and involves a complete history and physical examination as well as an appropriate contextualized laboratory workup.
Our patient’s comorbid T2DM and renal disease may have contributed to the pruritus. Type 2 diabetes mellitus can cause diabetic neuropathy, a sequela known to lead to various complications, including pruritus. One study identified a 4-fold increase in pruritus in those with diabetic polyneuropathy compared with age-matched nondiabetics.12,13 An additional study found that pruritus was present in 70% of patients with small fiber neuropathy.14 We needed to consider the role of our patient’s insulin-dependent T2DM and potential underlying neuropathy when addressing the pruritic symptoms.
Furthermore, our patient’s stage IV CKD and elevated urea level also may factor into the pruritus. The pathophysiology of CKD-associated pruritus (also referred to as uremic pruritus) remains poorly understood. Suggested mechanisms include immune-mediated neural inflammation and erroneous nociceptive-receptor activity.15,16 Although uremic pruritus is appreciated primarily in late dialysis-dependent disease, research shows that a notable portion of those with lesser disease, similar to our patient, also experience a significant itch burden.17 Diminishing pruritus is difficult and often aided by management of the underlying renal disease.18
In addition to disease management, symptomatic treatment incorporates the use of emollients, corticosteroids, and antihistamines. Unfortunately, the clinical response in the elderly population to such regimens often is poor.19 Dupilumab is an optimistic therapeutic option for chronic pruritus. By inhibiting the IL-4α receptor found on helper T cells, this biologic inhibits TH2 differentiation and subsequent inflammatory activity. One report identified an optimistic response to dupilumab in the management of uremic pruritus.20 The remarkable improvement and absence of adverse effects in our patient confirmed the utility and safety of dupilumab in complex cases such as elderly patients with multiple comorbidities. Such relief may result from inhibition of proinflammatory cytokine activity as well as decreased afferent spinal cord itch stimuli.10 The positive results from this case cast a favorable outlook on the treatment of chronic itch in the complex geriatric population.
To the Editor:
Today’s geriatric population is the fastest growing in history. The National Institutes of Health predicts there will be over 1.5 billion individuals aged 65 years and older by the year 2050: 17% of the world’s population.1 Pruritus—either acute or chronic (>6 weeks)—is defined as a sensory perception that leads to an intense desire to scratch.2 Chronic pruritus is an increasing health concern that impacts quality of life within the geriatric population. Elderly patients have various risk factors for developing chronic itch, including aging skin, polypharmacy, and increased systemic comorbidities.3-7
Although the therapeutic armamentarium for chronic itch continues to grow, health care providers often are hesitant to prescribe medications for geriatric patients because of comorbidities and potential drug-drug interactions. Novel biologic therapies now provide alternatives for this complex population. Dupilumab is a fully humanized, monoclonal antibody approved for treatment-resistant atopic dermatitis. This biologic prevents helper T-cell (TH2) signaling, IL-4 and IL-13 release, and subsequent effector cell (eg, mast cell, eosinophil) activity.8-10 The combined efficacy and safety of this medication has changed the treatment landscape of resistant atopic dermatitis. We present the use of dupilumab in a geriatric patient with severe and recalcitrant itch resistant to numerous topical and oral medications.
An 81-year-old man presented to the clinic with a long history of generalized pruritic rash. His medical history was significant for insulin-dependent type 2 diabetes mellitus (T2DM), hypertension, and renal cancer following a right nephrectomy. Laboratory results approximately 14 months prior to the visit revealed a blood urea nitrogen level of 31 mg/dL (reference range, 7–20 mg/dL), creatinine level of 2.20 mg/dL (reference range, 0.7–1.3 mg/dL), and glomerular filtration rate of 29 mL/min (reference range, 90–120 mL/min). Physical examination revealed numerous pink excoriated papules on the face, neck, trunk, and extremities. Lichenified plaques were present on both arms and legs. The patient received the diagnosis of severe atopic dermatitis with greater than 10% body surface area involvement. The investigator global assessment score was 4/4, indicating severe disease burden, and biopsy results reported spongiotic dermatitis. He proceeded to trial various topical corticosteroids, including hydrocortisone ointment 2.5%, betamethasone valerate ointment 0.01%, fluocinonide ointment 0.05%, and mupirocin ointment without benefit. Three subsequent courses of oral steroids failed to provide durable relief. At this point, the peak pruritus numerical rating scale (NRS) score was 7/10, indicating severe pruritus, with a negative impact on the patient’s quality of life and sleep.
Therapy was switched to tacrolimus acetonide ointment 0.1%, betamethasone dipropionate ointment 0.05%, and triamcinolone acetonide ointment 0.1%. Eleven days later, the patient denied experiencing any response to the topical regimen and sought alternative therapy for the itch and associated poor sleep; the NRS score was 10/10, indicating very severe pruritus. Prednisone 20 mg and doxepin 10 mg were initiated for symptom management until the intended transition to dupilumab. The patient began dupilumab with a loading dose of 600 mg, then 300 mg every other week thereafter. At 2- and 4-month follow-up, the patient reported notable relief in symptoms. The rash had improved, and the NRS score decreased from 10/10 to 3/10. He endorsed improved sleep and quality of life.
Pruritus may arise from a series of age-related mechanisms such as structural and chemical changes within the epidermis, underlying neuropathy, medication side effects, infection, malignancy, thyroid dysregulation, liver disease, and chronic kidney disease (CKD).5,6,11 Identifying the underlying etiology often is difficult and involves a complete history and physical examination as well as an appropriate contextualized laboratory workup.
Our patient’s comorbid T2DM and renal disease may have contributed to the pruritus. Type 2 diabetes mellitus can cause diabetic neuropathy, a sequela known to lead to various complications, including pruritus. One study identified a 4-fold increase in pruritus in those with diabetic polyneuropathy compared with age-matched nondiabetics.12,13 An additional study found that pruritus was present in 70% of patients with small fiber neuropathy.14 We needed to consider the role of our patient’s insulin-dependent T2DM and potential underlying neuropathy when addressing the pruritic symptoms.
Furthermore, our patient’s stage IV CKD and elevated urea level also may factor into the pruritus. The pathophysiology of CKD-associated pruritus (also referred to as uremic pruritus) remains poorly understood. Suggested mechanisms include immune-mediated neural inflammation and erroneous nociceptive-receptor activity.15,16 Although uremic pruritus is appreciated primarily in late dialysis-dependent disease, research shows that a notable portion of those with lesser disease, similar to our patient, also experience a significant itch burden.17 Diminishing pruritus is difficult and often aided by management of the underlying renal disease.18
In addition to disease management, symptomatic treatment incorporates the use of emollients, corticosteroids, and antihistamines. Unfortunately, the clinical response in the elderly population to such regimens often is poor.19 Dupilumab is an optimistic therapeutic option for chronic pruritus. By inhibiting the IL-4α receptor found on helper T cells, this biologic inhibits TH2 differentiation and subsequent inflammatory activity. One report identified an optimistic response to dupilumab in the management of uremic pruritus.20 The remarkable improvement and absence of adverse effects in our patient confirmed the utility and safety of dupilumab in complex cases such as elderly patients with multiple comorbidities. Such relief may result from inhibition of proinflammatory cytokine activity as well as decreased afferent spinal cord itch stimuli.10 The positive results from this case cast a favorable outlook on the treatment of chronic itch in the complex geriatric population.
- World’s older population grows dramatically. News release. National Institute on Aging. Published March 28, 2016. Accessed December 23, 2022. http://www.nih.gov/news-events/news-releases/worlds-older-population-grows-dramatically
- Grundmann S, Ständer S. Chronic pruritus: clinics and treatment. Ann Dermatol. 2011;23:1-11.
- Berger TG, Shive M, Harper GM. Pruritus in the older patient: a clinical review. JAMA. 2013;310:2443-2450. doi:10.1001/jama.2013.282023
- Valdes-Rodriguez, R, Mollanazar NK, González-Muro J, et al. Itch prevalence and characteristics in a Hispanic geriatric population: a comprehensive study using a standardized itch questionnaire. Acta Derm Venereol. 2015;95:417-421. doi:10.2340/00015555-1968
- Li J, Tang H, Hu X, et al. Aquaporin-3 gene and protein expression in sun-protected human skin decreases with skin ageing. Australas J Dermatol. 2010;51:106-112.
- Choi EH, Man MQ, Xu P, et al. Stratum corneum acidification is impaired in moderately aged human and murine skin. J Invest Dermatol. 2007;127:2847-2856.
- Fenske NA, Lober CW. Structural and functional changes of normal aging skin. J Am Acad Dermatol. 1986;15(4 pt 1):571-585.
- Paller AS, Kabashima K, Bieber T. Therapeutic pipeline for atopic dermatitis: end of the drought? J Allergy Clin Immunol. 2017;140:633-643. doi:10.1016/j.jaci.2017.07.006
- Kabashima K. New concept of the pathogenesis of atopic dermatitis: interplay among the barrier, allergy, and pruritus as a trinity. J Dermatol Sci. 2013;70:3-11.
- Feld M, Garcia R, Buddenkotte J, et al. The pruritus- and TH2-associated cytokine IL-31 promotes growth of sensory nerves. J Allergy Clin Immunol. 2016;138:500-508.
- Valdes-Rodriguez R, Stull C, Yosipovitch G. Chronic pruritus in the elderly: pathophysiology, diagnosis and management. Drugs Aging. 2015;32:201-215. doi:10.1007/s40266-015-0246-0
- Misery L, Brenaut E, Le Garrec R, et al. Neuropathic pruritus. Nat Rev Neurol. 2014;10:408-416.
- Yamaoka H, Sasaki H, Yamasaki H, et al. Truncal pruritus of unknown origin may be a symptom of diabetic polyneuropathy. Diabetes Care. 2010;33:150-155.
- Brenaut E, Marcorelles P, Genestet S, et al. Pruritus: an underrecognized symptom of small-fiber neuropathies. J Am Acad Dermatol. 2015;72:328-332.
- Adigun M, Badu LA, Berner NM, et al. Uremic pruritus review. US Pharm. 2015;40:HS12-HS15.
- Simonsen E, Komenda P, Lerner B, et al. Treatment of uremic pruritus: a systematic review. Am J Kidney Dis. 2017;70:638-655.
- Carstens E, Akiyama T, eds. Itch: Mechanisms and Treatment. CRC Press/Taylor & Francis; 2014.
- Shirazian S, Aina O, Park Y, et al. Chronic kidney disease-associated pruritus: impact on quality of life and current management challenges. Int J Nephrol Renovasc Dis. 2017;10:11-26.
- Brummer GC, Wang LT, Sontheimer RD. A possible role for dupilumab (Dupixent) in the management of idiopathic chronic eczematous eruption of aging. Dermatol Online J. 2018;24:13030/qt55z1f6xh.
- Silverberg JI, Brieva J. A successful case of dupilumab treatment for severe uremic pruritus. JAAD Case Rep. 2019;5:339-341.
- World’s older population grows dramatically. News release. National Institute on Aging. Published March 28, 2016. Accessed December 23, 2022. http://www.nih.gov/news-events/news-releases/worlds-older-population-grows-dramatically
- Grundmann S, Ständer S. Chronic pruritus: clinics and treatment. Ann Dermatol. 2011;23:1-11.
- Berger TG, Shive M, Harper GM. Pruritus in the older patient: a clinical review. JAMA. 2013;310:2443-2450. doi:10.1001/jama.2013.282023
- Valdes-Rodriguez, R, Mollanazar NK, González-Muro J, et al. Itch prevalence and characteristics in a Hispanic geriatric population: a comprehensive study using a standardized itch questionnaire. Acta Derm Venereol. 2015;95:417-421. doi:10.2340/00015555-1968
- Li J, Tang H, Hu X, et al. Aquaporin-3 gene and protein expression in sun-protected human skin decreases with skin ageing. Australas J Dermatol. 2010;51:106-112.
- Choi EH, Man MQ, Xu P, et al. Stratum corneum acidification is impaired in moderately aged human and murine skin. J Invest Dermatol. 2007;127:2847-2856.
- Fenske NA, Lober CW. Structural and functional changes of normal aging skin. J Am Acad Dermatol. 1986;15(4 pt 1):571-585.
- Paller AS, Kabashima K, Bieber T. Therapeutic pipeline for atopic dermatitis: end of the drought? J Allergy Clin Immunol. 2017;140:633-643. doi:10.1016/j.jaci.2017.07.006
- Kabashima K. New concept of the pathogenesis of atopic dermatitis: interplay among the barrier, allergy, and pruritus as a trinity. J Dermatol Sci. 2013;70:3-11.
- Feld M, Garcia R, Buddenkotte J, et al. The pruritus- and TH2-associated cytokine IL-31 promotes growth of sensory nerves. J Allergy Clin Immunol. 2016;138:500-508.
- Valdes-Rodriguez R, Stull C, Yosipovitch G. Chronic pruritus in the elderly: pathophysiology, diagnosis and management. Drugs Aging. 2015;32:201-215. doi:10.1007/s40266-015-0246-0
- Misery L, Brenaut E, Le Garrec R, et al. Neuropathic pruritus. Nat Rev Neurol. 2014;10:408-416.
- Yamaoka H, Sasaki H, Yamasaki H, et al. Truncal pruritus of unknown origin may be a symptom of diabetic polyneuropathy. Diabetes Care. 2010;33:150-155.
- Brenaut E, Marcorelles P, Genestet S, et al. Pruritus: an underrecognized symptom of small-fiber neuropathies. J Am Acad Dermatol. 2015;72:328-332.
- Adigun M, Badu LA, Berner NM, et al. Uremic pruritus review. US Pharm. 2015;40:HS12-HS15.
- Simonsen E, Komenda P, Lerner B, et al. Treatment of uremic pruritus: a systematic review. Am J Kidney Dis. 2017;70:638-655.
- Carstens E, Akiyama T, eds. Itch: Mechanisms and Treatment. CRC Press/Taylor & Francis; 2014.
- Shirazian S, Aina O, Park Y, et al. Chronic kidney disease-associated pruritus: impact on quality of life and current management challenges. Int J Nephrol Renovasc Dis. 2017;10:11-26.
- Brummer GC, Wang LT, Sontheimer RD. A possible role for dupilumab (Dupixent) in the management of idiopathic chronic eczematous eruption of aging. Dermatol Online J. 2018;24:13030/qt55z1f6xh.
- Silverberg JI, Brieva J. A successful case of dupilumab treatment for severe uremic pruritus. JAAD Case Rep. 2019;5:339-341.
PRACTICE POINTS
- A series of age-related mechanisms within the epidermis, underlying neuropathy, medication side effects, infection, malignancy, thyroid dysregulation, liver disease, and chronic kidney disease may contribute to pruritus in elderly patients.
- Patients with mild kidney disease may still experience a recalcitrant and notable itch burden.
- Dupilumab is efficacious and safe in the management of chronic pruritus, even in complex cases such as elderly patients with multiple comorbidities.
Abortion laws link to state-level mortality
States that have moderate state abortion laws had lower rates of maternal, fetal, and infant mortality, but not lower all-cause mortality, in reproductive-aged females compared with states that have restrictive laws, new research using 2000-2019 data indicates.
Additionally, having a higher number of laws that restrict abortion in a state was linked with higher maternal and infant mortality in the state, the study states.
Mortality increases with number of laws
“Each additional abortion regulation was associated with an increase in maternal mortality (1.09/100,000 live births; 95% confidence interval, 0.36-1.82) and infant mortality (0.20/1,000 live births; 95% CI, 0.12-0.26),” the authors write.
Lorie M. Harper, MD, MSCI, with the department of women’s health, University of Texas at Austin, led a team that simultaneously studied four categories of mortality: all-cause mortality in females ages 15-49 years; maternal mortality; infant mortality; and fetal mortality.
Her team did a retrospective cohort study using the Centers for Disease Control and Prevention’s WONDER (Wide-ranging ONline Data for Epidemiologic Research) database. WONDER collects publicly available data with information on mortality by state.
Data were available from 2000 to 2019 for all-cause, maternal, and infant mortality. Fetal mortality data were available from 2005 to 2019.
Findings were published ahead of print in February’s Obstetrics & Gynecology.
Though the study was done before the Supreme Court decision overturning Roe v. Wade in June 2022, its findings may shed light on potential trends depending on states’ decisions.
In the wake of the Dobbs v. Jackson Women’s Health Organization, an estimated 33 million U.S. women will live in states without available abortion services, the authors note.
State abortion laws changed dramatically in the study period
The authors chose the 2-decade time frame because data could be accessed for both maternal and infant mortality for all the years and because state level abortion laws changed dramatically in that time.
The Guttmacher Institute has analyzed each state’s abortion policy landscape and scored states as restrictive, moderate, or supportive. Certain types of abortion laws were associated with higher rates of all-cause mortality in reproductive-age females.
Those laws included trigger laws (the laws that automatically outlaw abortion in a state when federal law is overturned), laws that limit access to medication abortion, and parental consent laws, according to the paper.
Additionally, states that restrict access to abortion have higher rates of maternal and infant death, even after accounting for the general health of the population.
Trigger-law states have strong mortality association
Blair G. Darney, PhD, MPH, with the department of obstetrics and gynecology, Oregon Health & Science University and the OHSU-PSU School of Public Health in Portland, and two OHSU coauthors note in an accompanying editorial that having a trigger law in place was associated with elevations in all four mortality measures. However, trigger laws had not yet been enacted during the study.
The existence of trigger laws is likely a proxy for other factors, they write.
“[T]he relationship between trigger laws and increased mortality may more likely be explained by other factors that were not considered in the analysis than by laws that were not enacted at the time of the study,” the editorialists write.
Those factors may include lack of Medicaid expansion, socioeconomic inequities, and other policies.
The editorialists also caution that just because some types of abortion restrictions don’t appear to increase mortality, it doesn’t mean they aren’t harmful.
“For example, laws prohibiting private or Medicaid insurance coverage for abortions were not associated with maternal mortality, but these laws may simply shift the burden of payment to the individual seeking an abortion or be mitigated by funds that support an individual’s out-of-pocket cost for care. The lack of an association may therefore reflect women’s resilience and their ability to obtain needed health care in the face of financial challenges,” they write.
They point out that, conversely, Targeted Regulation of Abortion Providers (TRAP) laws, which supporters say protect women, have been associated instead with increases in maternal mortality.
Dr. Harper and study coauthors, noting that the relationship between abortion laws and mortality is complex, urge states with restrictive abortion laws to consider proven countermeasures to offset the rates, including Medicaid expansion.
One coauthor served on a medical advisory board, was a site primary investigator for several clinical trials, and received royalties from UpToDate for two topics related to trial of labor after cesarean. The other authors did not report any potential conflicts of interest. Dr. Darney’s institution receives research funding from Organon and the Office of Population Affairs on which she is the primary investigator, and she is a member of the board of directors of the Society of Family Planning and a deputy editor at Contraception. She has received an honorarium from ACOG for committee work. The other editorialists did not report any potential conflicts of interest.
States that have moderate state abortion laws had lower rates of maternal, fetal, and infant mortality, but not lower all-cause mortality, in reproductive-aged females compared with states that have restrictive laws, new research using 2000-2019 data indicates.
Additionally, having a higher number of laws that restrict abortion in a state was linked with higher maternal and infant mortality in the state, the study states.
Mortality increases with number of laws
“Each additional abortion regulation was associated with an increase in maternal mortality (1.09/100,000 live births; 95% confidence interval, 0.36-1.82) and infant mortality (0.20/1,000 live births; 95% CI, 0.12-0.26),” the authors write.
Lorie M. Harper, MD, MSCI, with the department of women’s health, University of Texas at Austin, led a team that simultaneously studied four categories of mortality: all-cause mortality in females ages 15-49 years; maternal mortality; infant mortality; and fetal mortality.
Her team did a retrospective cohort study using the Centers for Disease Control and Prevention’s WONDER (Wide-ranging ONline Data for Epidemiologic Research) database. WONDER collects publicly available data with information on mortality by state.
Data were available from 2000 to 2019 for all-cause, maternal, and infant mortality. Fetal mortality data were available from 2005 to 2019.
Findings were published ahead of print in February’s Obstetrics & Gynecology.
Though the study was done before the Supreme Court decision overturning Roe v. Wade in June 2022, its findings may shed light on potential trends depending on states’ decisions.
In the wake of the Dobbs v. Jackson Women’s Health Organization, an estimated 33 million U.S. women will live in states without available abortion services, the authors note.
State abortion laws changed dramatically in the study period
The authors chose the 2-decade time frame because data could be accessed for both maternal and infant mortality for all the years and because state level abortion laws changed dramatically in that time.
The Guttmacher Institute has analyzed each state’s abortion policy landscape and scored states as restrictive, moderate, or supportive. Certain types of abortion laws were associated with higher rates of all-cause mortality in reproductive-age females.
Those laws included trigger laws (the laws that automatically outlaw abortion in a state when federal law is overturned), laws that limit access to medication abortion, and parental consent laws, according to the paper.
Additionally, states that restrict access to abortion have higher rates of maternal and infant death, even after accounting for the general health of the population.
Trigger-law states have strong mortality association
Blair G. Darney, PhD, MPH, with the department of obstetrics and gynecology, Oregon Health & Science University and the OHSU-PSU School of Public Health in Portland, and two OHSU coauthors note in an accompanying editorial that having a trigger law in place was associated with elevations in all four mortality measures. However, trigger laws had not yet been enacted during the study.
The existence of trigger laws is likely a proxy for other factors, they write.
“[T]he relationship between trigger laws and increased mortality may more likely be explained by other factors that were not considered in the analysis than by laws that were not enacted at the time of the study,” the editorialists write.
Those factors may include lack of Medicaid expansion, socioeconomic inequities, and other policies.
The editorialists also caution that just because some types of abortion restrictions don’t appear to increase mortality, it doesn’t mean they aren’t harmful.
“For example, laws prohibiting private or Medicaid insurance coverage for abortions were not associated with maternal mortality, but these laws may simply shift the burden of payment to the individual seeking an abortion or be mitigated by funds that support an individual’s out-of-pocket cost for care. The lack of an association may therefore reflect women’s resilience and their ability to obtain needed health care in the face of financial challenges,” they write.
They point out that, conversely, Targeted Regulation of Abortion Providers (TRAP) laws, which supporters say protect women, have been associated instead with increases in maternal mortality.
Dr. Harper and study coauthors, noting that the relationship between abortion laws and mortality is complex, urge states with restrictive abortion laws to consider proven countermeasures to offset the rates, including Medicaid expansion.
One coauthor served on a medical advisory board, was a site primary investigator for several clinical trials, and received royalties from UpToDate for two topics related to trial of labor after cesarean. The other authors did not report any potential conflicts of interest. Dr. Darney’s institution receives research funding from Organon and the Office of Population Affairs on which she is the primary investigator, and she is a member of the board of directors of the Society of Family Planning and a deputy editor at Contraception. She has received an honorarium from ACOG for committee work. The other editorialists did not report any potential conflicts of interest.
States that have moderate state abortion laws had lower rates of maternal, fetal, and infant mortality, but not lower all-cause mortality, in reproductive-aged females compared with states that have restrictive laws, new research using 2000-2019 data indicates.
Additionally, having a higher number of laws that restrict abortion in a state was linked with higher maternal and infant mortality in the state, the study states.
Mortality increases with number of laws
“Each additional abortion regulation was associated with an increase in maternal mortality (1.09/100,000 live births; 95% confidence interval, 0.36-1.82) and infant mortality (0.20/1,000 live births; 95% CI, 0.12-0.26),” the authors write.
Lorie M. Harper, MD, MSCI, with the department of women’s health, University of Texas at Austin, led a team that simultaneously studied four categories of mortality: all-cause mortality in females ages 15-49 years; maternal mortality; infant mortality; and fetal mortality.
Her team did a retrospective cohort study using the Centers for Disease Control and Prevention’s WONDER (Wide-ranging ONline Data for Epidemiologic Research) database. WONDER collects publicly available data with information on mortality by state.
Data were available from 2000 to 2019 for all-cause, maternal, and infant mortality. Fetal mortality data were available from 2005 to 2019.
Findings were published ahead of print in February’s Obstetrics & Gynecology.
Though the study was done before the Supreme Court decision overturning Roe v. Wade in June 2022, its findings may shed light on potential trends depending on states’ decisions.
In the wake of the Dobbs v. Jackson Women’s Health Organization, an estimated 33 million U.S. women will live in states without available abortion services, the authors note.
State abortion laws changed dramatically in the study period
The authors chose the 2-decade time frame because data could be accessed for both maternal and infant mortality for all the years and because state level abortion laws changed dramatically in that time.
The Guttmacher Institute has analyzed each state’s abortion policy landscape and scored states as restrictive, moderate, or supportive. Certain types of abortion laws were associated with higher rates of all-cause mortality in reproductive-age females.
Those laws included trigger laws (the laws that automatically outlaw abortion in a state when federal law is overturned), laws that limit access to medication abortion, and parental consent laws, according to the paper.
Additionally, states that restrict access to abortion have higher rates of maternal and infant death, even after accounting for the general health of the population.
Trigger-law states have strong mortality association
Blair G. Darney, PhD, MPH, with the department of obstetrics and gynecology, Oregon Health & Science University and the OHSU-PSU School of Public Health in Portland, and two OHSU coauthors note in an accompanying editorial that having a trigger law in place was associated with elevations in all four mortality measures. However, trigger laws had not yet been enacted during the study.
The existence of trigger laws is likely a proxy for other factors, they write.
“[T]he relationship between trigger laws and increased mortality may more likely be explained by other factors that were not considered in the analysis than by laws that were not enacted at the time of the study,” the editorialists write.
Those factors may include lack of Medicaid expansion, socioeconomic inequities, and other policies.
The editorialists also caution that just because some types of abortion restrictions don’t appear to increase mortality, it doesn’t mean they aren’t harmful.
“For example, laws prohibiting private or Medicaid insurance coverage for abortions were not associated with maternal mortality, but these laws may simply shift the burden of payment to the individual seeking an abortion or be mitigated by funds that support an individual’s out-of-pocket cost for care. The lack of an association may therefore reflect women’s resilience and their ability to obtain needed health care in the face of financial challenges,” they write.
They point out that, conversely, Targeted Regulation of Abortion Providers (TRAP) laws, which supporters say protect women, have been associated instead with increases in maternal mortality.
Dr. Harper and study coauthors, noting that the relationship between abortion laws and mortality is complex, urge states with restrictive abortion laws to consider proven countermeasures to offset the rates, including Medicaid expansion.
One coauthor served on a medical advisory board, was a site primary investigator for several clinical trials, and received royalties from UpToDate for two topics related to trial of labor after cesarean. The other authors did not report any potential conflicts of interest. Dr. Darney’s institution receives research funding from Organon and the Office of Population Affairs on which she is the primary investigator, and she is a member of the board of directors of the Society of Family Planning and a deputy editor at Contraception. She has received an honorarium from ACOG for committee work. The other editorialists did not report any potential conflicts of interest.
FROM OBSTETRICS & GYNECOLOGY
Year in Review: How Targeted Drug Therapies Have Expanded Breast Cancer Treatment Options in 2022
Breast cancer (BC) is the most diagnosed cancer and the second leading cause of cancer deaths in women. In 2022, more than 275,000 women were diagnosed with BC, and at least 43,000 of these cases resulted in death. With targeted drug therapy for treating BC now approved by the US Food and Drug Administration (FDA) and available (or in the late phases of clinical trials and pending availability and FDA approval), clinicians are beginning to be able to move away from a “one-size-fits-all” treatment approach that has been used in the past, enhancing prognosis and survival rates in their patients living with BC.
The new targeted drug therapies available are more precise and individualized. They treat patients more effectively because they are based on the patient’s own biology. These therapies open the possibility of having more valuable treatment options, which can be beneficial for the outcome of many patients diagnosed with BC—especially the highly aggressive forms that were previously difficult to treat.
In March 2022, the FDA approved the drug olaparib to treat HER2-, high-risk, early breast cancer (EBC). The approval was made after the conclusion of the phase 3 OlympiA trial. The clinical trial results showed a statistically significant improvement in overall survival rates (by 32%) with adjuvant olaparib compared with placebo for germline BRCA1/2-mutated EBC.
In August 2022, the FDA approved the antibody drug conjugate fam-trastuzumab deruxtecan-nxki (or T-DXd), which is the first FDA-approved therapy targeted to treat patients who have the HER2-low BC subtype. It is also approved for patients with unresectable or metastatic HER2+ breast cancer who have already been treated with 2 or more prior anti-HER2–based therapies in the metastatic setting. The approval of T-DXd was given on the basis of DESTINY-Breast04, a randomized, multicenter, open-label clinical trial that was published in June 2022. T-DXd had been previously approved in HER2+ metastatic breast cancer.
The results from the phase 3 CAPItello-291 clinical trial of capivasertib in combination with fulvestrant suggests the combination could become a new treatment option for patients with hormone receptor–positive, HER2-low, locally advanced or metastatic BC following recurrence or progression after treatment with endocrine therapy and a CDK4/6 inhibitor. Capivasertib is a novel, selective, ATP-competitive, pan-AKT kinase inhibitor. In clinical trials, the drug was shown to successfully block activity of the cancer-driving protein molecule AKT. This research was presented at the 2022 San Antonio Breast Cancer Symposium, and the findings demonstrated a significant improvement in the overall population, as well as the subgroup of patients with PI3K pathway–altered tumors.
The year 2022 was full of exciting discoveries in the field of targeted drug therapies for treating BC, expanding patients’ treatment options and giving hope to people who have been diagnosed with breast cancer and their loved ones. In addition, emerging technologies such as immunotherapy and new antibody-drug conjugates continue to be evaluated as potential treatment options for treating breast cancer in the near future.
Breast cancer (BC) is the most diagnosed cancer and the second leading cause of cancer deaths in women. In 2022, more than 275,000 women were diagnosed with BC, and at least 43,000 of these cases resulted in death. With targeted drug therapy for treating BC now approved by the US Food and Drug Administration (FDA) and available (or in the late phases of clinical trials and pending availability and FDA approval), clinicians are beginning to be able to move away from a “one-size-fits-all” treatment approach that has been used in the past, enhancing prognosis and survival rates in their patients living with BC.
The new targeted drug therapies available are more precise and individualized. They treat patients more effectively because they are based on the patient’s own biology. These therapies open the possibility of having more valuable treatment options, which can be beneficial for the outcome of many patients diagnosed with BC—especially the highly aggressive forms that were previously difficult to treat.
In March 2022, the FDA approved the drug olaparib to treat HER2-, high-risk, early breast cancer (EBC). The approval was made after the conclusion of the phase 3 OlympiA trial. The clinical trial results showed a statistically significant improvement in overall survival rates (by 32%) with adjuvant olaparib compared with placebo for germline BRCA1/2-mutated EBC.
In August 2022, the FDA approved the antibody drug conjugate fam-trastuzumab deruxtecan-nxki (or T-DXd), which is the first FDA-approved therapy targeted to treat patients who have the HER2-low BC subtype. It is also approved for patients with unresectable or metastatic HER2+ breast cancer who have already been treated with 2 or more prior anti-HER2–based therapies in the metastatic setting. The approval of T-DXd was given on the basis of DESTINY-Breast04, a randomized, multicenter, open-label clinical trial that was published in June 2022. T-DXd had been previously approved in HER2+ metastatic breast cancer.
The results from the phase 3 CAPItello-291 clinical trial of capivasertib in combination with fulvestrant suggests the combination could become a new treatment option for patients with hormone receptor–positive, HER2-low, locally advanced or metastatic BC following recurrence or progression after treatment with endocrine therapy and a CDK4/6 inhibitor. Capivasertib is a novel, selective, ATP-competitive, pan-AKT kinase inhibitor. In clinical trials, the drug was shown to successfully block activity of the cancer-driving protein molecule AKT. This research was presented at the 2022 San Antonio Breast Cancer Symposium, and the findings demonstrated a significant improvement in the overall population, as well as the subgroup of patients with PI3K pathway–altered tumors.
The year 2022 was full of exciting discoveries in the field of targeted drug therapies for treating BC, expanding patients’ treatment options and giving hope to people who have been diagnosed with breast cancer and their loved ones. In addition, emerging technologies such as immunotherapy and new antibody-drug conjugates continue to be evaluated as potential treatment options for treating breast cancer in the near future.
Breast cancer (BC) is the most diagnosed cancer and the second leading cause of cancer deaths in women. In 2022, more than 275,000 women were diagnosed with BC, and at least 43,000 of these cases resulted in death. With targeted drug therapy for treating BC now approved by the US Food and Drug Administration (FDA) and available (or in the late phases of clinical trials and pending availability and FDA approval), clinicians are beginning to be able to move away from a “one-size-fits-all” treatment approach that has been used in the past, enhancing prognosis and survival rates in their patients living with BC.
The new targeted drug therapies available are more precise and individualized. They treat patients more effectively because they are based on the patient’s own biology. These therapies open the possibility of having more valuable treatment options, which can be beneficial for the outcome of many patients diagnosed with BC—especially the highly aggressive forms that were previously difficult to treat.
In March 2022, the FDA approved the drug olaparib to treat HER2-, high-risk, early breast cancer (EBC). The approval was made after the conclusion of the phase 3 OlympiA trial. The clinical trial results showed a statistically significant improvement in overall survival rates (by 32%) with adjuvant olaparib compared with placebo for germline BRCA1/2-mutated EBC.
In August 2022, the FDA approved the antibody drug conjugate fam-trastuzumab deruxtecan-nxki (or T-DXd), which is the first FDA-approved therapy targeted to treat patients who have the HER2-low BC subtype. It is also approved for patients with unresectable or metastatic HER2+ breast cancer who have already been treated with 2 or more prior anti-HER2–based therapies in the metastatic setting. The approval of T-DXd was given on the basis of DESTINY-Breast04, a randomized, multicenter, open-label clinical trial that was published in June 2022. T-DXd had been previously approved in HER2+ metastatic breast cancer.
The results from the phase 3 CAPItello-291 clinical trial of capivasertib in combination with fulvestrant suggests the combination could become a new treatment option for patients with hormone receptor–positive, HER2-low, locally advanced or metastatic BC following recurrence or progression after treatment with endocrine therapy and a CDK4/6 inhibitor. Capivasertib is a novel, selective, ATP-competitive, pan-AKT kinase inhibitor. In clinical trials, the drug was shown to successfully block activity of the cancer-driving protein molecule AKT. This research was presented at the 2022 San Antonio Breast Cancer Symposium, and the findings demonstrated a significant improvement in the overall population, as well as the subgroup of patients with PI3K pathway–altered tumors.
The year 2022 was full of exciting discoveries in the field of targeted drug therapies for treating BC, expanding patients’ treatment options and giving hope to people who have been diagnosed with breast cancer and their loved ones. In addition, emerging technologies such as immunotherapy and new antibody-drug conjugates continue to be evaluated as potential treatment options for treating breast cancer in the near future.
We Have the Tools to Prevent Cervical Cancer— So Why Are Rates Increasing?
Cervical cancer screening is often hailed as the most successful screening program ever implemented. Despite these past successes, cervical cancer incidence is no longer decreasing and is actually rising significantly in younger women within the United States. In a country with a well-established screening program, effective screening tools, and HPV vaccination, it seems unfathomable that we are witnessing an increase in cervical cancers. This alarming trend should be cause for concern among all healthcare professionals.
Cervical cancer screening is often hailed as the most successful screening program ever implemented. Despite these past successes, cervical cancer incidence is no longer decreasing and is actually rising significantly in younger women within the United States. In a country with a well-established screening program, effective screening tools, and HPV vaccination, it seems unfathomable that we are witnessing an increase in cervical cancers. This alarming trend should be cause for concern among all healthcare professionals.
Cervical cancer screening is often hailed as the most successful screening program ever implemented. Despite these past successes, cervical cancer incidence is no longer decreasing and is actually rising significantly in younger women within the United States. In a country with a well-established screening program, effective screening tools, and HPV vaccination, it seems unfathomable that we are witnessing an increase in cervical cancers. This alarming trend should be cause for concern among all healthcare professionals.
The anecdote as antidote: Psychiatric paradigms in Disney films
A common refrain in psychiatry is that the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, (DSM-5-TR), published in 2022, is the best we can do.
Since the DSM-III was released in 1980, the American Psychiatric Association, which publishes the manual, has espoused the position that we should list symptoms, in a manner that is reminiscent of a checklist. For example, having a depressed mood on most days for a 2-week period, or a loss of interest in pleasurable things, as well as 4 additional symptoms – among them changes in appetite, changes in sleep, changes in psychomotor activity, fatigue, worthlessness, poor concentration, or thoughts of death – can lead to a diagnosis of a major depressive episode as part of a major depressive disorder.
Criticisms of this approach can be apparent. Patients subjected to such checklists, including being repeatedly asked to complete the Patient Health Questionnaire 9 (PHQ-9), which closely follows those criteria, can feel lost and even alienated by their providers. After all, one can ask all those questions and make a diagnosis of depression without even knowing about the patient’s stressors, their history, or their social context.
The DSM permits the diagnosis of psychiatric disorders without an understanding of the narrative of the patient. In its defense, the DSM is not a textbook of psychiatry, it is a guide on how to diagnose individuals. The DSM does not demand that psychiatrists only ask about the symptoms on the checklists; it is the providers who can choose to dismiss asking about the important facets of one’s life.
Yet every time we attend a lecture that starts by enumerating the DSM symptoms of the disorder being discussed, we are left with the dissatisfying impression that a specialist of this disorder should have a more nuanced and interesting description of their disorder of study. This feeling of discontent is compounded when we see a movie that encompasses so much of what is missing in today’s psychiatric parlance, and even more so if that movie is ostensibly made for children. Movies, by design, are particularly adept at encapsulating the narrative of someone’s life in a way that psychiatry can learn from.
Other than the embarrassment of not knowing a patient outside the checklist, the importance of narrative cannot be understated. Dr. Erik Erikson rightfully suggested that the point of life is “the acceptance of one’s one and only life cycle”1 or rather to know it was okay to have been oneself without additions or substitutions. Therefore, one must know what it has meant to be themselves to reconcile this question and achieve Ego Integrity rather than disgust and despair. Narrative is the way in which we understand who we are and what it has meant to be ourselves. An understanding of our personal narrative presents a unique opportunity in expressing what is missing in the DSM. Below, we provide two of our favorite examples in Disney films, among many.
‘Ratatouille’ (2007)
One of the missing features of the DSM is its inability to explain to patients the intrapsychic processes that guide us. One of these processes is how our values can lead us to a deep sense of guilt, shame, and the resulting feelings of alienation. It is extremely common for patients to enter our clinical practice feeling shackled by beliefs that they should accomplish more and be more than they are.
The animated film “Ratatouille” does an excellent job at addressing this feeling. The film follows Remy, the protagonist rat, and his adventures as he explores his passion for cooking. Remy teams up with the inept but good-natured human Alfredo Linguini and guides him through cooking while hiding under his chef’s hat. The primary antagonist, Anton Ego, is a particularly harsh food critic. His presence and appearance are somber. He exudes disdain. His trim physique and scarf suggest a man that will break and react to anything, and his skull-shaped typewriter in his coffin-shaped office informs the viewer that he is out to kill with his cruel words. Anton Ego serves as our projected super-ego. He is not an external judge but the judgment deep inside ourselves, goading us to be better with such severity that we are ultimately left feeling condemned.
Remy is the younger of two siblings. He is less physically adept but more intellectual than his older brother, who does not understand why Remy isn’t content eating scraps from the garbage like the rest of their rat clan. Remy is the creative part within us that wants to challenge the status quo and try something new. Remy also represents our shame and guilt for leaving our home. On one hand, we want to dare greatly, in this case at being an extraordinary chef, but on the other we are shy and cook in secret, hiding within the hat of another person. Remy struggles with the deep feeling that we do not deserve our success, that our family will leave us for being who we are, and that we are better off isolating and segregating from our challenges.
The movie concludes that through talent and hard work, our critics will accept us. Furthermore, once accepted for what we do, we can be further accepted for who we are. The movie ends with Remy cooking the eponymous dish ratatouille. He prepares it so remarkably well, the dish transports Anton Ego back to a sublime experience of eating ratatouille as a child, a touching moment which not only underscores food’s evocative link to memory but gives a glimpse at Anton Ego’s own narrative.
Ego is first won over by the dish, and only afterward learns of Remy’s true identity. Remy’s talent is undeniable though, and even the stuffy Ego must accept the film’s theme that “Anyone can cook,” even a rat – the rat that we all sometimes feel we are deep inside, rotten to the core but trying so hard to be accepted by others, and ultimately by ourselves. In the end, we overcome the disgust inherent in the imagery of a rat in a kitchen and instead embrace our hero’s achievement of ego integrity as he combines his identities as a member of a clan of rats, and one of Paris’s finest chefs.
While modern psychiatry can favor looking at people through the lens of biology rather than narrative, “Ratatouille” can serve as a reminder of the powerful unconscious forces that guide our lives. “Ratatouille” is not a successful movie only because of the compelling narrative, but also because the narrative matches the important psychic paradigms that psychiatry once embraced.
‘Inside Out’ (2015)
Another missing feature of the DSM is its inability to explain how symptoms feel and manifest psychologically. One such feeling is that of control – whether one is in control of one’s life, feelings, and action or rather a victim of external forces. It is extremely common for patients to enter our clinical practice feeling traumatized by the life they’ve lived and powerless to produce any change. Part of our role is to guide them through this journey from the object of their lives to the subject of their lives.
In the animated feature “Inside Out,” Riley, a preteen girl, goes through the tribulation of growing up and learning about herself. This seemingly happy child, content playing hockey with her best friend, Meg, on the picturesque frozen lakes of Minnesota, reaches her inevitable conflict. Her parents uproot her life, moving the family to San Francisco. By doing so, they disconnect her from her school, her friends, and her hobbies. While all this is happening, we spend time inside Riley’s psyche with the personified characters of Riley’s emotions as they affect her decisions and daily actions amidst the backdrop of her core memories and islands of personality.
During the move, her parents seemingly change and ultimately destroy every facet of Riley’s sense of self, which is animated as the collapse of her personality islands. Her best friend engages Riley in a video call just to inform her that she has a new friend who plays hockey equally well. Her parents do not hear Riley’s concerns and are portrayed as distracted by their adult problems. Riley feels ridiculed in her new school and unable to share her feelings with her parents, who ask her to still be their “happy girl” and indirectly ask her to fake pleasure to alleviate their own anxiety.
The climax of the movie is when Riley decides to run away from San Francisco and her parents, to return to her perceived true home, Minnesota. The climax is resolved when Riley realizes that her parents’ love, representing the connection we have to others, transcends her need for control. To some degree, we are all powerless in the face of the tremendous forces of life and share the difficult task of accepting the cards we were dealt, thus making the story of Riley so compelling.
Additionally, the climax is further resolved by another argument that psychiatry (and the DSM) should consider embracing. Emotions are not all symptoms and living without negative emotion is not the goal of life. Riley grows from preteen to teenager, and from object to subject of her life, by realizing that her symptoms/feelings are not just nuisances to avoid and hide, but the key to meaning. Our anger drives us to try hard. Our fear protects us from harm. Our sadness attracts the warmth and care of others. Our disgust protects us physically from noxious material (symbolized as a dreaded broccoli floret for preteen Riley) and socially by encouraging us to share societal norms. Similarly, patients and people in general would benefit by being taught that, while symptoms may permit the better assessment of psychiatric conditions using the DSM, life is much more than that.
It is unfair to blame the DSM for things it was not designed to do. The DSM doesn’t advertise itself as a guidebook of all behaviors, at all times. However, for a variety of reasons, it has become the main way psychiatry describes people. While we commend the APA for its effort and do not know that we could make it any better, we are frequently happily reminded that in about 90 minutes, filmmakers are able to display an empathic understanding of personal narratives that biologic psychiatry can miss.
Dr. Pulido is a psychiatry resident at the University of California, San Diego. She is interested in women’s mental health, medical education, and outpatient psychiatry. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. Erikson, EH. Childhood and society (New York: WW Norton, 1950).
A common refrain in psychiatry is that the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, (DSM-5-TR), published in 2022, is the best we can do.
Since the DSM-III was released in 1980, the American Psychiatric Association, which publishes the manual, has espoused the position that we should list symptoms, in a manner that is reminiscent of a checklist. For example, having a depressed mood on most days for a 2-week period, or a loss of interest in pleasurable things, as well as 4 additional symptoms – among them changes in appetite, changes in sleep, changes in psychomotor activity, fatigue, worthlessness, poor concentration, or thoughts of death – can lead to a diagnosis of a major depressive episode as part of a major depressive disorder.
Criticisms of this approach can be apparent. Patients subjected to such checklists, including being repeatedly asked to complete the Patient Health Questionnaire 9 (PHQ-9), which closely follows those criteria, can feel lost and even alienated by their providers. After all, one can ask all those questions and make a diagnosis of depression without even knowing about the patient’s stressors, their history, or their social context.
The DSM permits the diagnosis of psychiatric disorders without an understanding of the narrative of the patient. In its defense, the DSM is not a textbook of psychiatry, it is a guide on how to diagnose individuals. The DSM does not demand that psychiatrists only ask about the symptoms on the checklists; it is the providers who can choose to dismiss asking about the important facets of one’s life.
Yet every time we attend a lecture that starts by enumerating the DSM symptoms of the disorder being discussed, we are left with the dissatisfying impression that a specialist of this disorder should have a more nuanced and interesting description of their disorder of study. This feeling of discontent is compounded when we see a movie that encompasses so much of what is missing in today’s psychiatric parlance, and even more so if that movie is ostensibly made for children. Movies, by design, are particularly adept at encapsulating the narrative of someone’s life in a way that psychiatry can learn from.
Other than the embarrassment of not knowing a patient outside the checklist, the importance of narrative cannot be understated. Dr. Erik Erikson rightfully suggested that the point of life is “the acceptance of one’s one and only life cycle”1 or rather to know it was okay to have been oneself without additions or substitutions. Therefore, one must know what it has meant to be themselves to reconcile this question and achieve Ego Integrity rather than disgust and despair. Narrative is the way in which we understand who we are and what it has meant to be ourselves. An understanding of our personal narrative presents a unique opportunity in expressing what is missing in the DSM. Below, we provide two of our favorite examples in Disney films, among many.
‘Ratatouille’ (2007)
One of the missing features of the DSM is its inability to explain to patients the intrapsychic processes that guide us. One of these processes is how our values can lead us to a deep sense of guilt, shame, and the resulting feelings of alienation. It is extremely common for patients to enter our clinical practice feeling shackled by beliefs that they should accomplish more and be more than they are.
The animated film “Ratatouille” does an excellent job at addressing this feeling. The film follows Remy, the protagonist rat, and his adventures as he explores his passion for cooking. Remy teams up with the inept but good-natured human Alfredo Linguini and guides him through cooking while hiding under his chef’s hat. The primary antagonist, Anton Ego, is a particularly harsh food critic. His presence and appearance are somber. He exudes disdain. His trim physique and scarf suggest a man that will break and react to anything, and his skull-shaped typewriter in his coffin-shaped office informs the viewer that he is out to kill with his cruel words. Anton Ego serves as our projected super-ego. He is not an external judge but the judgment deep inside ourselves, goading us to be better with such severity that we are ultimately left feeling condemned.
Remy is the younger of two siblings. He is less physically adept but more intellectual than his older brother, who does not understand why Remy isn’t content eating scraps from the garbage like the rest of their rat clan. Remy is the creative part within us that wants to challenge the status quo and try something new. Remy also represents our shame and guilt for leaving our home. On one hand, we want to dare greatly, in this case at being an extraordinary chef, but on the other we are shy and cook in secret, hiding within the hat of another person. Remy struggles with the deep feeling that we do not deserve our success, that our family will leave us for being who we are, and that we are better off isolating and segregating from our challenges.
The movie concludes that through talent and hard work, our critics will accept us. Furthermore, once accepted for what we do, we can be further accepted for who we are. The movie ends with Remy cooking the eponymous dish ratatouille. He prepares it so remarkably well, the dish transports Anton Ego back to a sublime experience of eating ratatouille as a child, a touching moment which not only underscores food’s evocative link to memory but gives a glimpse at Anton Ego’s own narrative.
Ego is first won over by the dish, and only afterward learns of Remy’s true identity. Remy’s talent is undeniable though, and even the stuffy Ego must accept the film’s theme that “Anyone can cook,” even a rat – the rat that we all sometimes feel we are deep inside, rotten to the core but trying so hard to be accepted by others, and ultimately by ourselves. In the end, we overcome the disgust inherent in the imagery of a rat in a kitchen and instead embrace our hero’s achievement of ego integrity as he combines his identities as a member of a clan of rats, and one of Paris’s finest chefs.
While modern psychiatry can favor looking at people through the lens of biology rather than narrative, “Ratatouille” can serve as a reminder of the powerful unconscious forces that guide our lives. “Ratatouille” is not a successful movie only because of the compelling narrative, but also because the narrative matches the important psychic paradigms that psychiatry once embraced.
‘Inside Out’ (2015)
Another missing feature of the DSM is its inability to explain how symptoms feel and manifest psychologically. One such feeling is that of control – whether one is in control of one’s life, feelings, and action or rather a victim of external forces. It is extremely common for patients to enter our clinical practice feeling traumatized by the life they’ve lived and powerless to produce any change. Part of our role is to guide them through this journey from the object of their lives to the subject of their lives.
In the animated feature “Inside Out,” Riley, a preteen girl, goes through the tribulation of growing up and learning about herself. This seemingly happy child, content playing hockey with her best friend, Meg, on the picturesque frozen lakes of Minnesota, reaches her inevitable conflict. Her parents uproot her life, moving the family to San Francisco. By doing so, they disconnect her from her school, her friends, and her hobbies. While all this is happening, we spend time inside Riley’s psyche with the personified characters of Riley’s emotions as they affect her decisions and daily actions amidst the backdrop of her core memories and islands of personality.
During the move, her parents seemingly change and ultimately destroy every facet of Riley’s sense of self, which is animated as the collapse of her personality islands. Her best friend engages Riley in a video call just to inform her that she has a new friend who plays hockey equally well. Her parents do not hear Riley’s concerns and are portrayed as distracted by their adult problems. Riley feels ridiculed in her new school and unable to share her feelings with her parents, who ask her to still be their “happy girl” and indirectly ask her to fake pleasure to alleviate their own anxiety.
The climax of the movie is when Riley decides to run away from San Francisco and her parents, to return to her perceived true home, Minnesota. The climax is resolved when Riley realizes that her parents’ love, representing the connection we have to others, transcends her need for control. To some degree, we are all powerless in the face of the tremendous forces of life and share the difficult task of accepting the cards we were dealt, thus making the story of Riley so compelling.
Additionally, the climax is further resolved by another argument that psychiatry (and the DSM) should consider embracing. Emotions are not all symptoms and living without negative emotion is not the goal of life. Riley grows from preteen to teenager, and from object to subject of her life, by realizing that her symptoms/feelings are not just nuisances to avoid and hide, but the key to meaning. Our anger drives us to try hard. Our fear protects us from harm. Our sadness attracts the warmth and care of others. Our disgust protects us physically from noxious material (symbolized as a dreaded broccoli floret for preteen Riley) and socially by encouraging us to share societal norms. Similarly, patients and people in general would benefit by being taught that, while symptoms may permit the better assessment of psychiatric conditions using the DSM, life is much more than that.
It is unfair to blame the DSM for things it was not designed to do. The DSM doesn’t advertise itself as a guidebook of all behaviors, at all times. However, for a variety of reasons, it has become the main way psychiatry describes people. While we commend the APA for its effort and do not know that we could make it any better, we are frequently happily reminded that in about 90 minutes, filmmakers are able to display an empathic understanding of personal narratives that biologic psychiatry can miss.
Dr. Pulido is a psychiatry resident at the University of California, San Diego. She is interested in women’s mental health, medical education, and outpatient psychiatry. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. Erikson, EH. Childhood and society (New York: WW Norton, 1950).
A common refrain in psychiatry is that the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, (DSM-5-TR), published in 2022, is the best we can do.
Since the DSM-III was released in 1980, the American Psychiatric Association, which publishes the manual, has espoused the position that we should list symptoms, in a manner that is reminiscent of a checklist. For example, having a depressed mood on most days for a 2-week period, or a loss of interest in pleasurable things, as well as 4 additional symptoms – among them changes in appetite, changes in sleep, changes in psychomotor activity, fatigue, worthlessness, poor concentration, or thoughts of death – can lead to a diagnosis of a major depressive episode as part of a major depressive disorder.
Criticisms of this approach can be apparent. Patients subjected to such checklists, including being repeatedly asked to complete the Patient Health Questionnaire 9 (PHQ-9), which closely follows those criteria, can feel lost and even alienated by their providers. After all, one can ask all those questions and make a diagnosis of depression without even knowing about the patient’s stressors, their history, or their social context.
The DSM permits the diagnosis of psychiatric disorders without an understanding of the narrative of the patient. In its defense, the DSM is not a textbook of psychiatry, it is a guide on how to diagnose individuals. The DSM does not demand that psychiatrists only ask about the symptoms on the checklists; it is the providers who can choose to dismiss asking about the important facets of one’s life.
Yet every time we attend a lecture that starts by enumerating the DSM symptoms of the disorder being discussed, we are left with the dissatisfying impression that a specialist of this disorder should have a more nuanced and interesting description of their disorder of study. This feeling of discontent is compounded when we see a movie that encompasses so much of what is missing in today’s psychiatric parlance, and even more so if that movie is ostensibly made for children. Movies, by design, are particularly adept at encapsulating the narrative of someone’s life in a way that psychiatry can learn from.
Other than the embarrassment of not knowing a patient outside the checklist, the importance of narrative cannot be understated. Dr. Erik Erikson rightfully suggested that the point of life is “the acceptance of one’s one and only life cycle”1 or rather to know it was okay to have been oneself without additions or substitutions. Therefore, one must know what it has meant to be themselves to reconcile this question and achieve Ego Integrity rather than disgust and despair. Narrative is the way in which we understand who we are and what it has meant to be ourselves. An understanding of our personal narrative presents a unique opportunity in expressing what is missing in the DSM. Below, we provide two of our favorite examples in Disney films, among many.
‘Ratatouille’ (2007)
One of the missing features of the DSM is its inability to explain to patients the intrapsychic processes that guide us. One of these processes is how our values can lead us to a deep sense of guilt, shame, and the resulting feelings of alienation. It is extremely common for patients to enter our clinical practice feeling shackled by beliefs that they should accomplish more and be more than they are.
The animated film “Ratatouille” does an excellent job at addressing this feeling. The film follows Remy, the protagonist rat, and his adventures as he explores his passion for cooking. Remy teams up with the inept but good-natured human Alfredo Linguini and guides him through cooking while hiding under his chef’s hat. The primary antagonist, Anton Ego, is a particularly harsh food critic. His presence and appearance are somber. He exudes disdain. His trim physique and scarf suggest a man that will break and react to anything, and his skull-shaped typewriter in his coffin-shaped office informs the viewer that he is out to kill with his cruel words. Anton Ego serves as our projected super-ego. He is not an external judge but the judgment deep inside ourselves, goading us to be better with such severity that we are ultimately left feeling condemned.
Remy is the younger of two siblings. He is less physically adept but more intellectual than his older brother, who does not understand why Remy isn’t content eating scraps from the garbage like the rest of their rat clan. Remy is the creative part within us that wants to challenge the status quo and try something new. Remy also represents our shame and guilt for leaving our home. On one hand, we want to dare greatly, in this case at being an extraordinary chef, but on the other we are shy and cook in secret, hiding within the hat of another person. Remy struggles with the deep feeling that we do not deserve our success, that our family will leave us for being who we are, and that we are better off isolating and segregating from our challenges.
The movie concludes that through talent and hard work, our critics will accept us. Furthermore, once accepted for what we do, we can be further accepted for who we are. The movie ends with Remy cooking the eponymous dish ratatouille. He prepares it so remarkably well, the dish transports Anton Ego back to a sublime experience of eating ratatouille as a child, a touching moment which not only underscores food’s evocative link to memory but gives a glimpse at Anton Ego’s own narrative.
Ego is first won over by the dish, and only afterward learns of Remy’s true identity. Remy’s talent is undeniable though, and even the stuffy Ego must accept the film’s theme that “Anyone can cook,” even a rat – the rat that we all sometimes feel we are deep inside, rotten to the core but trying so hard to be accepted by others, and ultimately by ourselves. In the end, we overcome the disgust inherent in the imagery of a rat in a kitchen and instead embrace our hero’s achievement of ego integrity as he combines his identities as a member of a clan of rats, and one of Paris’s finest chefs.
While modern psychiatry can favor looking at people through the lens of biology rather than narrative, “Ratatouille” can serve as a reminder of the powerful unconscious forces that guide our lives. “Ratatouille” is not a successful movie only because of the compelling narrative, but also because the narrative matches the important psychic paradigms that psychiatry once embraced.
‘Inside Out’ (2015)
Another missing feature of the DSM is its inability to explain how symptoms feel and manifest psychologically. One such feeling is that of control – whether one is in control of one’s life, feelings, and action or rather a victim of external forces. It is extremely common for patients to enter our clinical practice feeling traumatized by the life they’ve lived and powerless to produce any change. Part of our role is to guide them through this journey from the object of their lives to the subject of their lives.
In the animated feature “Inside Out,” Riley, a preteen girl, goes through the tribulation of growing up and learning about herself. This seemingly happy child, content playing hockey with her best friend, Meg, on the picturesque frozen lakes of Minnesota, reaches her inevitable conflict. Her parents uproot her life, moving the family to San Francisco. By doing so, they disconnect her from her school, her friends, and her hobbies. While all this is happening, we spend time inside Riley’s psyche with the personified characters of Riley’s emotions as they affect her decisions and daily actions amidst the backdrop of her core memories and islands of personality.
During the move, her parents seemingly change and ultimately destroy every facet of Riley’s sense of self, which is animated as the collapse of her personality islands. Her best friend engages Riley in a video call just to inform her that she has a new friend who plays hockey equally well. Her parents do not hear Riley’s concerns and are portrayed as distracted by their adult problems. Riley feels ridiculed in her new school and unable to share her feelings with her parents, who ask her to still be their “happy girl” and indirectly ask her to fake pleasure to alleviate their own anxiety.
The climax of the movie is when Riley decides to run away from San Francisco and her parents, to return to her perceived true home, Minnesota. The climax is resolved when Riley realizes that her parents’ love, representing the connection we have to others, transcends her need for control. To some degree, we are all powerless in the face of the tremendous forces of life and share the difficult task of accepting the cards we were dealt, thus making the story of Riley so compelling.
Additionally, the climax is further resolved by another argument that psychiatry (and the DSM) should consider embracing. Emotions are not all symptoms and living without negative emotion is not the goal of life. Riley grows from preteen to teenager, and from object to subject of her life, by realizing that her symptoms/feelings are not just nuisances to avoid and hide, but the key to meaning. Our anger drives us to try hard. Our fear protects us from harm. Our sadness attracts the warmth and care of others. Our disgust protects us physically from noxious material (symbolized as a dreaded broccoli floret for preteen Riley) and socially by encouraging us to share societal norms. Similarly, patients and people in general would benefit by being taught that, while symptoms may permit the better assessment of psychiatric conditions using the DSM, life is much more than that.
It is unfair to blame the DSM for things it was not designed to do. The DSM doesn’t advertise itself as a guidebook of all behaviors, at all times. However, for a variety of reasons, it has become the main way psychiatry describes people. While we commend the APA for its effort and do not know that we could make it any better, we are frequently happily reminded that in about 90 minutes, filmmakers are able to display an empathic understanding of personal narratives that biologic psychiatry can miss.
Dr. Pulido is a psychiatry resident at the University of California, San Diego. She is interested in women’s mental health, medical education, and outpatient psychiatry. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. Erikson, EH. Childhood and society (New York: WW Norton, 1950).
IBD patients have limited protection against Omicron with third vaccine dose
For people with inflammatory bowel disease (IBD) taking immunosuppressive medication, a third dose of a COVID-19 mRNA vaccine significantly increases neutralizing antibodies against the original SARS-CoV-2 strain, but the picture is more complicated for protection against the Omicron variant, according to a research letter published in Gastroenterology.
“As further mutations in the viral genome accumulate over time, with the attendant risk of immune evasion, it remains important to continue to reappraise vaccination strategy, including the implementation of personalized approaches for some patients, such as those treated with anti-TNF drugs and JAK inhibitors,” wrote Zhigang Liu, PhD, a research associate in the department of metabolism, digestion, and reproduction at Imperial College London, and his colleagues. “Preferential use of bivalent vaccines may be especially valuable in IBD patients taking anti-TNF agents or JAK inhibitors,” they wrote. Their study did not assess neutralizing antibodies resulting from use of the bivalent vaccine, however.
The researchers tracked 268 participants, including 49 healthy participants serving as controls, from May 2021 through March 2022. The other participants had IBD and included 51 patients taking thiopurines, 36 patients taking infliximab, 39 taking both infliximab and thiopurines, 39 taking ustekinumab, 38 taking vedolizumab, and 16 taking tofacitinib. The IBD patients were all enrolled in the SARS-CoV-2 Vaccination Immunogenicity in Immunosuppressed Inflammatory Bowel Disease Patients (VIP) cohort.
None of the participants had evidence of a SARS-CoV-2 infection at baseline. All had received two doses of an mRNA COVID-19 vaccine (all received Pfizer, except two controls who received Moderna) or two doses of the AstraZeneca vaccine as their primary vaccination. All received an mRNA vaccine for their third dose. Among the IBD patients, 137 received the AstraZeneca in their primary two-dose series, and 82 received Pfizer.
First the researchers assessed the participants’ humoral response to the vaccine against the original SARS-CoV-2 strain and against the Omicron BA.1 variant. Neutralizing antibody titers rose significantly against both strains after the third vaccine dose for all participants.
“However, 50% neutralization titer (NT50) values were significantly lower against Omicron than against the ancestral strain in all study groups, irrespective of the immunosuppressive treatment regimen,” the authors reported. NT50 values are a measure that reflect a vaccine-induced humoral immunity against SARS-CoV-2 after vaccination.
Compared to the healthy controls, individuals receiving infliximab, tofacitinib, or infliximab/thiopurine combination therapy showed significantly lower responses after the second and third vaccine doses. Thirteen patients did not generate NT50 against Omicron after the second vaccine dose, and 7 of them were on infliximab monotherapy. They represented nearly 20% of all infliximab monotherapy participants.
Next the researchers assessed the risk of a breakthrough infection according to neutralizing titer thresholds. Individuals with an NT50 less than 500 had 1.6 times greater odds of a breakthrough infection than those with an NT50 above 500, they noted. After two vaccine doses, 46% of participants with IBD had an NT50 above 500 for the ancestral strain, which rose to 85% of those with IBD after a third dose.
In the healthy control group, 35% had an NT50 under 500 after two doses, and 14% of them had a breakthrough infection, all of which were mild and none of which required hospitalization. The NT50 in healthy controls, however, was not significantly associated with risk of breakthrough infection.
“In this study, neutralizing titers elicited against the omicron variant were generally poor for all individuals and were substantially lower in recipients of infliximab, infliximab/thiopurine combination, or tofacitinib therapy,” the authors concluded. “This raises concerns about whether currently available vaccines will be sufficient to protect against continually evolving SARS-CoV-2 variants, especially in patients established on certain immunosuppressive drugs.”
The small population sizes for each subgroup based on medication was one of the study’s limitations. Another was the fact that it was underpowered to conclusively determine whether an increased risk of breakthrough infection exists in IBD patients who have lower titers of neutralizing antibodies. A limitation for generalization to U.S. patients is that just 64% of the IBD patients received the AstraZeneca vaccine, which is not offered in the United States, for their first two doses before receiving the third mRNA (Pfizer) dose.
The study was funded by Pfizer in an independent research grant and by the NIHR Biomedical Research Centres in Imperial College London and Imperial College Healthcare NHS Trust and Cambridge, and the NIHR Clinical Research Facility Cambridge.
Dr. Liu and one other author had no disclosures. The other 18 authors have a range of disclosures related to various pharmaceutical companies, including Pfizer.
Understanding how inflammatory bowel disease (IBD) impacts COVID-19 infection risk and how IBD medications influence this risk remains an ever-evolving discussion, particularly with the emergence of new SARS-CoV-2 variants and booster vaccines. In this study, Liu et al. further shape this conversation: They show that a third mRNA COVID-19 vaccine dose increases neutralizing antibody levels against the Omicron variant in IBD patients compared to the level following a second vaccine dose, but that infliximab and tofacitinib significantly attenuate this response. They additionally suggest that IBD patients achieve lower neutralizing antibody levels after a third COVID-19 vaccine and may have a higher breakthrough infection risk compared to healthy controls without IBD.
Whether to change booster vaccination recommendations specifically for IBD patients on tofacitinib or infliximab, however, remains an unanswered question. The small sample of patients on tofacitinib precludes definitive conclusions regarding tofacitinib’s impact on vaccine response. Moreover, this humoral antibody-based study tells only half the story: We need analyses of the cell-mediated booster vaccine response to truly understand vaccine efficacy during immunosuppressant use. Lastly, future studies including the bivalent booster will provide the most up-to-date information on protecting our IBD patients from the Omicron variant.
Dr. Erica J. Brenner MD, MSCR is an Assistant Professor, Department of Pediatrics, Division of Pediatric Gastroenterology, University of North Carolina School of Medicine; and a cofounder of the Surveillance Epidemiology of Coronavirus Under Research Exclusion for Inflammatory Bowel Disease (SECURE-IBD) Registry. She has no relevant financial conflicts of interest.
Understanding how inflammatory bowel disease (IBD) impacts COVID-19 infection risk and how IBD medications influence this risk remains an ever-evolving discussion, particularly with the emergence of new SARS-CoV-2 variants and booster vaccines. In this study, Liu et al. further shape this conversation: They show that a third mRNA COVID-19 vaccine dose increases neutralizing antibody levels against the Omicron variant in IBD patients compared to the level following a second vaccine dose, but that infliximab and tofacitinib significantly attenuate this response. They additionally suggest that IBD patients achieve lower neutralizing antibody levels after a third COVID-19 vaccine and may have a higher breakthrough infection risk compared to healthy controls without IBD.
Whether to change booster vaccination recommendations specifically for IBD patients on tofacitinib or infliximab, however, remains an unanswered question. The small sample of patients on tofacitinib precludes definitive conclusions regarding tofacitinib’s impact on vaccine response. Moreover, this humoral antibody-based study tells only half the story: We need analyses of the cell-mediated booster vaccine response to truly understand vaccine efficacy during immunosuppressant use. Lastly, future studies including the bivalent booster will provide the most up-to-date information on protecting our IBD patients from the Omicron variant.
Dr. Erica J. Brenner MD, MSCR is an Assistant Professor, Department of Pediatrics, Division of Pediatric Gastroenterology, University of North Carolina School of Medicine; and a cofounder of the Surveillance Epidemiology of Coronavirus Under Research Exclusion for Inflammatory Bowel Disease (SECURE-IBD) Registry. She has no relevant financial conflicts of interest.
Understanding how inflammatory bowel disease (IBD) impacts COVID-19 infection risk and how IBD medications influence this risk remains an ever-evolving discussion, particularly with the emergence of new SARS-CoV-2 variants and booster vaccines. In this study, Liu et al. further shape this conversation: They show that a third mRNA COVID-19 vaccine dose increases neutralizing antibody levels against the Omicron variant in IBD patients compared to the level following a second vaccine dose, but that infliximab and tofacitinib significantly attenuate this response. They additionally suggest that IBD patients achieve lower neutralizing antibody levels after a third COVID-19 vaccine and may have a higher breakthrough infection risk compared to healthy controls without IBD.
Whether to change booster vaccination recommendations specifically for IBD patients on tofacitinib or infliximab, however, remains an unanswered question. The small sample of patients on tofacitinib precludes definitive conclusions regarding tofacitinib’s impact on vaccine response. Moreover, this humoral antibody-based study tells only half the story: We need analyses of the cell-mediated booster vaccine response to truly understand vaccine efficacy during immunosuppressant use. Lastly, future studies including the bivalent booster will provide the most up-to-date information on protecting our IBD patients from the Omicron variant.
Dr. Erica J. Brenner MD, MSCR is an Assistant Professor, Department of Pediatrics, Division of Pediatric Gastroenterology, University of North Carolina School of Medicine; and a cofounder of the Surveillance Epidemiology of Coronavirus Under Research Exclusion for Inflammatory Bowel Disease (SECURE-IBD) Registry. She has no relevant financial conflicts of interest.
For people with inflammatory bowel disease (IBD) taking immunosuppressive medication, a third dose of a COVID-19 mRNA vaccine significantly increases neutralizing antibodies against the original SARS-CoV-2 strain, but the picture is more complicated for protection against the Omicron variant, according to a research letter published in Gastroenterology.
“As further mutations in the viral genome accumulate over time, with the attendant risk of immune evasion, it remains important to continue to reappraise vaccination strategy, including the implementation of personalized approaches for some patients, such as those treated with anti-TNF drugs and JAK inhibitors,” wrote Zhigang Liu, PhD, a research associate in the department of metabolism, digestion, and reproduction at Imperial College London, and his colleagues. “Preferential use of bivalent vaccines may be especially valuable in IBD patients taking anti-TNF agents or JAK inhibitors,” they wrote. Their study did not assess neutralizing antibodies resulting from use of the bivalent vaccine, however.
The researchers tracked 268 participants, including 49 healthy participants serving as controls, from May 2021 through March 2022. The other participants had IBD and included 51 patients taking thiopurines, 36 patients taking infliximab, 39 taking both infliximab and thiopurines, 39 taking ustekinumab, 38 taking vedolizumab, and 16 taking tofacitinib. The IBD patients were all enrolled in the SARS-CoV-2 Vaccination Immunogenicity in Immunosuppressed Inflammatory Bowel Disease Patients (VIP) cohort.
None of the participants had evidence of a SARS-CoV-2 infection at baseline. All had received two doses of an mRNA COVID-19 vaccine (all received Pfizer, except two controls who received Moderna) or two doses of the AstraZeneca vaccine as their primary vaccination. All received an mRNA vaccine for their third dose. Among the IBD patients, 137 received the AstraZeneca in their primary two-dose series, and 82 received Pfizer.
First the researchers assessed the participants’ humoral response to the vaccine against the original SARS-CoV-2 strain and against the Omicron BA.1 variant. Neutralizing antibody titers rose significantly against both strains after the third vaccine dose for all participants.
“However, 50% neutralization titer (NT50) values were significantly lower against Omicron than against the ancestral strain in all study groups, irrespective of the immunosuppressive treatment regimen,” the authors reported. NT50 values are a measure that reflect a vaccine-induced humoral immunity against SARS-CoV-2 after vaccination.
Compared to the healthy controls, individuals receiving infliximab, tofacitinib, or infliximab/thiopurine combination therapy showed significantly lower responses after the second and third vaccine doses. Thirteen patients did not generate NT50 against Omicron after the second vaccine dose, and 7 of them were on infliximab monotherapy. They represented nearly 20% of all infliximab monotherapy participants.
Next the researchers assessed the risk of a breakthrough infection according to neutralizing titer thresholds. Individuals with an NT50 less than 500 had 1.6 times greater odds of a breakthrough infection than those with an NT50 above 500, they noted. After two vaccine doses, 46% of participants with IBD had an NT50 above 500 for the ancestral strain, which rose to 85% of those with IBD after a third dose.
In the healthy control group, 35% had an NT50 under 500 after two doses, and 14% of them had a breakthrough infection, all of which were mild and none of which required hospitalization. The NT50 in healthy controls, however, was not significantly associated with risk of breakthrough infection.
“In this study, neutralizing titers elicited against the omicron variant were generally poor for all individuals and were substantially lower in recipients of infliximab, infliximab/thiopurine combination, or tofacitinib therapy,” the authors concluded. “This raises concerns about whether currently available vaccines will be sufficient to protect against continually evolving SARS-CoV-2 variants, especially in patients established on certain immunosuppressive drugs.”
The small population sizes for each subgroup based on medication was one of the study’s limitations. Another was the fact that it was underpowered to conclusively determine whether an increased risk of breakthrough infection exists in IBD patients who have lower titers of neutralizing antibodies. A limitation for generalization to U.S. patients is that just 64% of the IBD patients received the AstraZeneca vaccine, which is not offered in the United States, for their first two doses before receiving the third mRNA (Pfizer) dose.
The study was funded by Pfizer in an independent research grant and by the NIHR Biomedical Research Centres in Imperial College London and Imperial College Healthcare NHS Trust and Cambridge, and the NIHR Clinical Research Facility Cambridge.
Dr. Liu and one other author had no disclosures. The other 18 authors have a range of disclosures related to various pharmaceutical companies, including Pfizer.
For people with inflammatory bowel disease (IBD) taking immunosuppressive medication, a third dose of a COVID-19 mRNA vaccine significantly increases neutralizing antibodies against the original SARS-CoV-2 strain, but the picture is more complicated for protection against the Omicron variant, according to a research letter published in Gastroenterology.
“As further mutations in the viral genome accumulate over time, with the attendant risk of immune evasion, it remains important to continue to reappraise vaccination strategy, including the implementation of personalized approaches for some patients, such as those treated with anti-TNF drugs and JAK inhibitors,” wrote Zhigang Liu, PhD, a research associate in the department of metabolism, digestion, and reproduction at Imperial College London, and his colleagues. “Preferential use of bivalent vaccines may be especially valuable in IBD patients taking anti-TNF agents or JAK inhibitors,” they wrote. Their study did not assess neutralizing antibodies resulting from use of the bivalent vaccine, however.
The researchers tracked 268 participants, including 49 healthy participants serving as controls, from May 2021 through March 2022. The other participants had IBD and included 51 patients taking thiopurines, 36 patients taking infliximab, 39 taking both infliximab and thiopurines, 39 taking ustekinumab, 38 taking vedolizumab, and 16 taking tofacitinib. The IBD patients were all enrolled in the SARS-CoV-2 Vaccination Immunogenicity in Immunosuppressed Inflammatory Bowel Disease Patients (VIP) cohort.
None of the participants had evidence of a SARS-CoV-2 infection at baseline. All had received two doses of an mRNA COVID-19 vaccine (all received Pfizer, except two controls who received Moderna) or two doses of the AstraZeneca vaccine as their primary vaccination. All received an mRNA vaccine for their third dose. Among the IBD patients, 137 received the AstraZeneca in their primary two-dose series, and 82 received Pfizer.
First the researchers assessed the participants’ humoral response to the vaccine against the original SARS-CoV-2 strain and against the Omicron BA.1 variant. Neutralizing antibody titers rose significantly against both strains after the third vaccine dose for all participants.
“However, 50% neutralization titer (NT50) values were significantly lower against Omicron than against the ancestral strain in all study groups, irrespective of the immunosuppressive treatment regimen,” the authors reported. NT50 values are a measure that reflect a vaccine-induced humoral immunity against SARS-CoV-2 after vaccination.
Compared to the healthy controls, individuals receiving infliximab, tofacitinib, or infliximab/thiopurine combination therapy showed significantly lower responses after the second and third vaccine doses. Thirteen patients did not generate NT50 against Omicron after the second vaccine dose, and 7 of them were on infliximab monotherapy. They represented nearly 20% of all infliximab monotherapy participants.
Next the researchers assessed the risk of a breakthrough infection according to neutralizing titer thresholds. Individuals with an NT50 less than 500 had 1.6 times greater odds of a breakthrough infection than those with an NT50 above 500, they noted. After two vaccine doses, 46% of participants with IBD had an NT50 above 500 for the ancestral strain, which rose to 85% of those with IBD after a third dose.
In the healthy control group, 35% had an NT50 under 500 after two doses, and 14% of them had a breakthrough infection, all of which were mild and none of which required hospitalization. The NT50 in healthy controls, however, was not significantly associated with risk of breakthrough infection.
“In this study, neutralizing titers elicited against the omicron variant were generally poor for all individuals and were substantially lower in recipients of infliximab, infliximab/thiopurine combination, or tofacitinib therapy,” the authors concluded. “This raises concerns about whether currently available vaccines will be sufficient to protect against continually evolving SARS-CoV-2 variants, especially in patients established on certain immunosuppressive drugs.”
The small population sizes for each subgroup based on medication was one of the study’s limitations. Another was the fact that it was underpowered to conclusively determine whether an increased risk of breakthrough infection exists in IBD patients who have lower titers of neutralizing antibodies. A limitation for generalization to U.S. patients is that just 64% of the IBD patients received the AstraZeneca vaccine, which is not offered in the United States, for their first two doses before receiving the third mRNA (Pfizer) dose.
The study was funded by Pfizer in an independent research grant and by the NIHR Biomedical Research Centres in Imperial College London and Imperial College Healthcare NHS Trust and Cambridge, and the NIHR Clinical Research Facility Cambridge.
Dr. Liu and one other author had no disclosures. The other 18 authors have a range of disclosures related to various pharmaceutical companies, including Pfizer.
FROM GASTROENTEROLOGY
CHEST simulation courses support learning for every career stage
One mark of an excellent clinician is their commitment to lifelong learning, and CHEST’s hands-on simulation courses offer the chance for practitioners of all experience levels to enhance their knowledge.
A variety of interactive courses are offered at CHEST’s state-of-the-art Innovation, Simulation, and Training Center in Glenview, Illinois, covering topics like ultrasonography, bronchoscopy, and mechanical ventilation. And this year, our simulation schedule will offer several new sessions on advances in invasive and noninvasive ventilation, critical care transesophageal echocardiography, master-level EBUS practice, and mechanical circulatory support.
Each course is led by expert instructors and includes attendees from a full range of career stages, from trainees and mid-career clinicians to long-time CHEST faculty members.
At a fall 2022 session of the Ultrasonography: Essentials in Critical Care course, Adil Ahmed, MD, an intern at the University of Texas Health Science Center at San Antonio, shared his perspective attending as a resident.
“CHEST has lots of specialized resources and renowned faculty members, and they’re doing an exceptional job,” he said. “A lot of the things I’ve learned in the first workshop alone are completely brand new to me. I think more programs should start sending residents to these courses.”
Trainees don’t just attend simulation courses – they teach them, too. Carmen Mei, MD, a pulmonary and critical care fellow at Rutgers University, was a faculty member at the recent ultrasound course. She taught attendees representing a wide array of ages.
“It’s a learning environment. Everybody’s very engaged, no matter where they are in their career,” she said.
As a mid-career clinician, Yonatan Y. Greenstein, MD, FCCP – who serves as a co-chair of the ultrasonography course – appreciates the diversity of experiences among attendees.
“Over the years, we’ve found that the wide breadth enhances the course because learners appreciate the questions that are brought up from different angles,” he said.
For experienced clinicians like CHEST Immediate Past President David Schulman, MD, MPH, FCCP, the interactive courses provide an opportunity to continue expanding his expertise. At the ultrasound course, Dr. Schulman said he enjoyed the chance to extend and refine his skillset alongside clinicians with a broad range of experience levels.
“Ultrasound is one of those skills that many clinicians, even in their forties and older, have never trained in. It’s great to see how the more junior learners approach this with a very excited mindset, and they’re learning right beside mid-career faculty who didn’t have the exposure to ultrasound when they were young,” he said.
To find the simulation course that’s the best fit for your practice, visit chestnet.org/simulation.
One mark of an excellent clinician is their commitment to lifelong learning, and CHEST’s hands-on simulation courses offer the chance for practitioners of all experience levels to enhance their knowledge.
A variety of interactive courses are offered at CHEST’s state-of-the-art Innovation, Simulation, and Training Center in Glenview, Illinois, covering topics like ultrasonography, bronchoscopy, and mechanical ventilation. And this year, our simulation schedule will offer several new sessions on advances in invasive and noninvasive ventilation, critical care transesophageal echocardiography, master-level EBUS practice, and mechanical circulatory support.
Each course is led by expert instructors and includes attendees from a full range of career stages, from trainees and mid-career clinicians to long-time CHEST faculty members.
At a fall 2022 session of the Ultrasonography: Essentials in Critical Care course, Adil Ahmed, MD, an intern at the University of Texas Health Science Center at San Antonio, shared his perspective attending as a resident.
“CHEST has lots of specialized resources and renowned faculty members, and they’re doing an exceptional job,” he said. “A lot of the things I’ve learned in the first workshop alone are completely brand new to me. I think more programs should start sending residents to these courses.”
Trainees don’t just attend simulation courses – they teach them, too. Carmen Mei, MD, a pulmonary and critical care fellow at Rutgers University, was a faculty member at the recent ultrasound course. She taught attendees representing a wide array of ages.
“It’s a learning environment. Everybody’s very engaged, no matter where they are in their career,” she said.
As a mid-career clinician, Yonatan Y. Greenstein, MD, FCCP – who serves as a co-chair of the ultrasonography course – appreciates the diversity of experiences among attendees.
“Over the years, we’ve found that the wide breadth enhances the course because learners appreciate the questions that are brought up from different angles,” he said.
For experienced clinicians like CHEST Immediate Past President David Schulman, MD, MPH, FCCP, the interactive courses provide an opportunity to continue expanding his expertise. At the ultrasound course, Dr. Schulman said he enjoyed the chance to extend and refine his skillset alongside clinicians with a broad range of experience levels.
“Ultrasound is one of those skills that many clinicians, even in their forties and older, have never trained in. It’s great to see how the more junior learners approach this with a very excited mindset, and they’re learning right beside mid-career faculty who didn’t have the exposure to ultrasound when they were young,” he said.
To find the simulation course that’s the best fit for your practice, visit chestnet.org/simulation.
One mark of an excellent clinician is their commitment to lifelong learning, and CHEST’s hands-on simulation courses offer the chance for practitioners of all experience levels to enhance their knowledge.
A variety of interactive courses are offered at CHEST’s state-of-the-art Innovation, Simulation, and Training Center in Glenview, Illinois, covering topics like ultrasonography, bronchoscopy, and mechanical ventilation. And this year, our simulation schedule will offer several new sessions on advances in invasive and noninvasive ventilation, critical care transesophageal echocardiography, master-level EBUS practice, and mechanical circulatory support.
Each course is led by expert instructors and includes attendees from a full range of career stages, from trainees and mid-career clinicians to long-time CHEST faculty members.
At a fall 2022 session of the Ultrasonography: Essentials in Critical Care course, Adil Ahmed, MD, an intern at the University of Texas Health Science Center at San Antonio, shared his perspective attending as a resident.
“CHEST has lots of specialized resources and renowned faculty members, and they’re doing an exceptional job,” he said. “A lot of the things I’ve learned in the first workshop alone are completely brand new to me. I think more programs should start sending residents to these courses.”
Trainees don’t just attend simulation courses – they teach them, too. Carmen Mei, MD, a pulmonary and critical care fellow at Rutgers University, was a faculty member at the recent ultrasound course. She taught attendees representing a wide array of ages.
“It’s a learning environment. Everybody’s very engaged, no matter where they are in their career,” she said.
As a mid-career clinician, Yonatan Y. Greenstein, MD, FCCP – who serves as a co-chair of the ultrasonography course – appreciates the diversity of experiences among attendees.
“Over the years, we’ve found that the wide breadth enhances the course because learners appreciate the questions that are brought up from different angles,” he said.
For experienced clinicians like CHEST Immediate Past President David Schulman, MD, MPH, FCCP, the interactive courses provide an opportunity to continue expanding his expertise. At the ultrasound course, Dr. Schulman said he enjoyed the chance to extend and refine his skillset alongside clinicians with a broad range of experience levels.
“Ultrasound is one of those skills that many clinicians, even in their forties and older, have never trained in. It’s great to see how the more junior learners approach this with a very excited mindset, and they’re learning right beside mid-career faculty who didn’t have the exposure to ultrasound when they were young,” he said.
To find the simulation course that’s the best fit for your practice, visit chestnet.org/simulation.











