User login
Skip routine probiotics for preemies, AAP says
The American Academy of Pediatrics now recommends against the routine administration of probiotics to preterm infants, particularly the most vulnerable (those whose birth weight is <1,000 g), for the treatment or prevention of necrotizing enterocolitis (NEC) and late-onset sepsis.
Although probiotics are increasingly given to preterm infants, the AAP notes that the data on their safety and efficacy are inconsistent. In addition, the supplements are not subject to approval by the Food and Drug Administration.
Therefore, the academy advises clinicians to use extreme caution in selecting preterm neonates to receive these microorganisms and recommends obtaining informed consent from parents after carefully discussing the risks. It also recommends that centers using probiotics conduct surveillance, inasmuch as probiotics can alter a center’s flora, potentially affecting all patients. Such centers should also carefully document outcomes, adverse events, and safety.
The AAP’s clinical report, published online May 24 in Pediatrics, highlights wide differences between commercially available formulations and a lack of regulatory standards in this country.
Absent FDA-approved drug labeling, these nutritional supplements cannot be marketed as treatment or prophylaxis, but that has scarcely stopped their use. “Despite lack of availability of a pharmaceutical-grade product, the number of preterm infants receiving probiotics in the United States and Canada is steadily increasing,” wrote Brenda Poindexter, MD, FAAP, chief of neonatology at Children’s Healthcare of Atlanta, and members of the AAP’s Committee on Fetus and Newborn.
Analyses of U.S. collaborative databases indicate that approximately 10% of neonates of extremely low gestational age receive a probiotic preparation in the neonatal intensive care unit (NICU). The use of these preparations varies widely across institutions.
“NEC is a devastating morbidity of prematurity, and it’s multifactorial. Some babies only given mother’s milk still get NEC, and the decision to use these products is a very nuanced one,” Dr. Poindexter said in an interview. “I suspect some people will disagree with the report, and we tried to give folks some wiggle room.”
Evidence from other countries suggests that probiotics can be protective against NEC, she added, “so not to have a reliable product in this country is very frustrating.”
Dr. Poindexter and colleagues pointed to a 2015 study that found that only 1 of 16 commercial products tested contained the exact organisms listed on their labels. One product contained none of the species listed on the label.
In light of increasing use, the AAP emphasizes the need for development of pharmaceutical-grade probiotics that would be rigorously evaluated for safety and efficacy.
The infant microbiome
Over the past decade, the gut microbiome has been increasingly recognized as a factor relevant to health and disease in preterm infants, the authors noted. Differences in the intestinal microbiota between full-term and preterm infants are substantial. The microbiome of preterm infants tends to include fewer bacterial species and greater proportions of potentially pathogenic strains.
Evidence of benefit from probiotics has been mixed. Some studies and pooled systematic analyses suggest a significant benefit. However, Dr. Poindexter and colleagues noted that some researchers express concerns about the study methods used, such as pooling results from trials that tested different probiotic strains or that had few infants in the highest risk category.
Whereas the potential for probiotic-related infection appears low, there does seem to be some risk for sepsis associated with colonization by a strain in a given product or from contamination with a pathogen during manufacturing, the report explains.
At least one trial found that a third of infants randomly assigned to receive placebo showed evidence of the probiotic strain.
“However, it may be difficult to distinguish the change in the infant from the change in the resident flora of the NICU,” the AAP panel wrote.
In addition, there have recently been several recalls of dietary supplement–grade probiotics for contamination, which have raised concerns. Pathogens include Salmonella, Rhizopus, and Penicillium species. Fatal gastrointestinal mucormycosis has also been reported in a preterm infant who received ABC Dophilus powder that was contaminated with the microfungus Rhizopus oryzae.
Other safety considerations, according to the authors, are the unknown longer-term effect of probiotics on preterm infants and the unknown impact of microorganisms on the microbiome over time.
Last year, the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition published a position paper with a conditional recommendation for selected probiotics to reduce NEC rates. “These guidelines would be applicable in the U.S. if we had products manufactured in a way that could guarantee that what’s on the label is in the bottle,” Dr. Poindexter said.
Asked for her perspective on the AAP clinical report, Erica Wymore, MD, assistant professor of neonatal and perinatal medicine at the University of Colorado at Denver, Aurora, called it “an excellent review of the current literature” that shows the inadequacy of data on the composition, dosage, timing, duration, and use of single-strain vs. multiple-strain probiotics to reduce NEC. Her clinical center, Children’s Hospital Colorado, does not administer probiotics to preterm babies.
Although guidelines can improve outcomes, said Dr. Wymore, who was not involved in the AAP report, improvement observed with probiotics results from more stringent care in centers that experience high NEC rates. “It’s hard to know if it’s due to the probiotics if they already have a high rate of NEC,” Dr. Wymore said.
She echoed the AAP’s position and stressed the need for extreme caution in giving these products to vulnerable infants with immature immune systems. Before that can be safely done, she said, “we need more FDA oversight of product composition [and] pharmaceutical-grade products, and more studies to determine efficacy.”
Added Dr. Poindexter: “Hopefully, this report will inform clinicians of the risks of using non–pharmaceutical-grade products and encourage industry to actually develop probiotics for neonates that we can feel comfortable using.”
The report received no external funding. Dr. Poindexter and Dr. Wymore have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The American Academy of Pediatrics now recommends against the routine administration of probiotics to preterm infants, particularly the most vulnerable (those whose birth weight is <1,000 g), for the treatment or prevention of necrotizing enterocolitis (NEC) and late-onset sepsis.
Although probiotics are increasingly given to preterm infants, the AAP notes that the data on their safety and efficacy are inconsistent. In addition, the supplements are not subject to approval by the Food and Drug Administration.
Therefore, the academy advises clinicians to use extreme caution in selecting preterm neonates to receive these microorganisms and recommends obtaining informed consent from parents after carefully discussing the risks. It also recommends that centers using probiotics conduct surveillance, inasmuch as probiotics can alter a center’s flora, potentially affecting all patients. Such centers should also carefully document outcomes, adverse events, and safety.
The AAP’s clinical report, published online May 24 in Pediatrics, highlights wide differences between commercially available formulations and a lack of regulatory standards in this country.
Absent FDA-approved drug labeling, these nutritional supplements cannot be marketed as treatment or prophylaxis, but that has scarcely stopped their use. “Despite lack of availability of a pharmaceutical-grade product, the number of preterm infants receiving probiotics in the United States and Canada is steadily increasing,” wrote Brenda Poindexter, MD, FAAP, chief of neonatology at Children’s Healthcare of Atlanta, and members of the AAP’s Committee on Fetus and Newborn.
Analyses of U.S. collaborative databases indicate that approximately 10% of neonates of extremely low gestational age receive a probiotic preparation in the neonatal intensive care unit (NICU). The use of these preparations varies widely across institutions.
“NEC is a devastating morbidity of prematurity, and it’s multifactorial. Some babies only given mother’s milk still get NEC, and the decision to use these products is a very nuanced one,” Dr. Poindexter said in an interview. “I suspect some people will disagree with the report, and we tried to give folks some wiggle room.”
Evidence from other countries suggests that probiotics can be protective against NEC, she added, “so not to have a reliable product in this country is very frustrating.”
Dr. Poindexter and colleagues pointed to a 2015 study that found that only 1 of 16 commercial products tested contained the exact organisms listed on their labels. One product contained none of the species listed on the label.
In light of increasing use, the AAP emphasizes the need for development of pharmaceutical-grade probiotics that would be rigorously evaluated for safety and efficacy.
The infant microbiome
Over the past decade, the gut microbiome has been increasingly recognized as a factor relevant to health and disease in preterm infants, the authors noted. Differences in the intestinal microbiota between full-term and preterm infants are substantial. The microbiome of preterm infants tends to include fewer bacterial species and greater proportions of potentially pathogenic strains.
Evidence of benefit from probiotics has been mixed. Some studies and pooled systematic analyses suggest a significant benefit. However, Dr. Poindexter and colleagues noted that some researchers express concerns about the study methods used, such as pooling results from trials that tested different probiotic strains or that had few infants in the highest risk category.
Whereas the potential for probiotic-related infection appears low, there does seem to be some risk for sepsis associated with colonization by a strain in a given product or from contamination with a pathogen during manufacturing, the report explains.
At least one trial found that a third of infants randomly assigned to receive placebo showed evidence of the probiotic strain.
“However, it may be difficult to distinguish the change in the infant from the change in the resident flora of the NICU,” the AAP panel wrote.
In addition, there have recently been several recalls of dietary supplement–grade probiotics for contamination, which have raised concerns. Pathogens include Salmonella, Rhizopus, and Penicillium species. Fatal gastrointestinal mucormycosis has also been reported in a preterm infant who received ABC Dophilus powder that was contaminated with the microfungus Rhizopus oryzae.
Other safety considerations, according to the authors, are the unknown longer-term effect of probiotics on preterm infants and the unknown impact of microorganisms on the microbiome over time.
Last year, the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition published a position paper with a conditional recommendation for selected probiotics to reduce NEC rates. “These guidelines would be applicable in the U.S. if we had products manufactured in a way that could guarantee that what’s on the label is in the bottle,” Dr. Poindexter said.
Asked for her perspective on the AAP clinical report, Erica Wymore, MD, assistant professor of neonatal and perinatal medicine at the University of Colorado at Denver, Aurora, called it “an excellent review of the current literature” that shows the inadequacy of data on the composition, dosage, timing, duration, and use of single-strain vs. multiple-strain probiotics to reduce NEC. Her clinical center, Children’s Hospital Colorado, does not administer probiotics to preterm babies.
Although guidelines can improve outcomes, said Dr. Wymore, who was not involved in the AAP report, improvement observed with probiotics results from more stringent care in centers that experience high NEC rates. “It’s hard to know if it’s due to the probiotics if they already have a high rate of NEC,” Dr. Wymore said.
She echoed the AAP’s position and stressed the need for extreme caution in giving these products to vulnerable infants with immature immune systems. Before that can be safely done, she said, “we need more FDA oversight of product composition [and] pharmaceutical-grade products, and more studies to determine efficacy.”
Added Dr. Poindexter: “Hopefully, this report will inform clinicians of the risks of using non–pharmaceutical-grade products and encourage industry to actually develop probiotics for neonates that we can feel comfortable using.”
The report received no external funding. Dr. Poindexter and Dr. Wymore have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The American Academy of Pediatrics now recommends against the routine administration of probiotics to preterm infants, particularly the most vulnerable (those whose birth weight is <1,000 g), for the treatment or prevention of necrotizing enterocolitis (NEC) and late-onset sepsis.
Although probiotics are increasingly given to preterm infants, the AAP notes that the data on their safety and efficacy are inconsistent. In addition, the supplements are not subject to approval by the Food and Drug Administration.
Therefore, the academy advises clinicians to use extreme caution in selecting preterm neonates to receive these microorganisms and recommends obtaining informed consent from parents after carefully discussing the risks. It also recommends that centers using probiotics conduct surveillance, inasmuch as probiotics can alter a center’s flora, potentially affecting all patients. Such centers should also carefully document outcomes, adverse events, and safety.
The AAP’s clinical report, published online May 24 in Pediatrics, highlights wide differences between commercially available formulations and a lack of regulatory standards in this country.
Absent FDA-approved drug labeling, these nutritional supplements cannot be marketed as treatment or prophylaxis, but that has scarcely stopped their use. “Despite lack of availability of a pharmaceutical-grade product, the number of preterm infants receiving probiotics in the United States and Canada is steadily increasing,” wrote Brenda Poindexter, MD, FAAP, chief of neonatology at Children’s Healthcare of Atlanta, and members of the AAP’s Committee on Fetus and Newborn.
Analyses of U.S. collaborative databases indicate that approximately 10% of neonates of extremely low gestational age receive a probiotic preparation in the neonatal intensive care unit (NICU). The use of these preparations varies widely across institutions.
“NEC is a devastating morbidity of prematurity, and it’s multifactorial. Some babies only given mother’s milk still get NEC, and the decision to use these products is a very nuanced one,” Dr. Poindexter said in an interview. “I suspect some people will disagree with the report, and we tried to give folks some wiggle room.”
Evidence from other countries suggests that probiotics can be protective against NEC, she added, “so not to have a reliable product in this country is very frustrating.”
Dr. Poindexter and colleagues pointed to a 2015 study that found that only 1 of 16 commercial products tested contained the exact organisms listed on their labels. One product contained none of the species listed on the label.
In light of increasing use, the AAP emphasizes the need for development of pharmaceutical-grade probiotics that would be rigorously evaluated for safety and efficacy.
The infant microbiome
Over the past decade, the gut microbiome has been increasingly recognized as a factor relevant to health and disease in preterm infants, the authors noted. Differences in the intestinal microbiota between full-term and preterm infants are substantial. The microbiome of preterm infants tends to include fewer bacterial species and greater proportions of potentially pathogenic strains.
Evidence of benefit from probiotics has been mixed. Some studies and pooled systematic analyses suggest a significant benefit. However, Dr. Poindexter and colleagues noted that some researchers express concerns about the study methods used, such as pooling results from trials that tested different probiotic strains or that had few infants in the highest risk category.
Whereas the potential for probiotic-related infection appears low, there does seem to be some risk for sepsis associated with colonization by a strain in a given product or from contamination with a pathogen during manufacturing, the report explains.
At least one trial found that a third of infants randomly assigned to receive placebo showed evidence of the probiotic strain.
“However, it may be difficult to distinguish the change in the infant from the change in the resident flora of the NICU,” the AAP panel wrote.
In addition, there have recently been several recalls of dietary supplement–grade probiotics for contamination, which have raised concerns. Pathogens include Salmonella, Rhizopus, and Penicillium species. Fatal gastrointestinal mucormycosis has also been reported in a preterm infant who received ABC Dophilus powder that was contaminated with the microfungus Rhizopus oryzae.
Other safety considerations, according to the authors, are the unknown longer-term effect of probiotics on preterm infants and the unknown impact of microorganisms on the microbiome over time.
Last year, the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition published a position paper with a conditional recommendation for selected probiotics to reduce NEC rates. “These guidelines would be applicable in the U.S. if we had products manufactured in a way that could guarantee that what’s on the label is in the bottle,” Dr. Poindexter said.
Asked for her perspective on the AAP clinical report, Erica Wymore, MD, assistant professor of neonatal and perinatal medicine at the University of Colorado at Denver, Aurora, called it “an excellent review of the current literature” that shows the inadequacy of data on the composition, dosage, timing, duration, and use of single-strain vs. multiple-strain probiotics to reduce NEC. Her clinical center, Children’s Hospital Colorado, does not administer probiotics to preterm babies.
Although guidelines can improve outcomes, said Dr. Wymore, who was not involved in the AAP report, improvement observed with probiotics results from more stringent care in centers that experience high NEC rates. “It’s hard to know if it’s due to the probiotics if they already have a high rate of NEC,” Dr. Wymore said.
She echoed the AAP’s position and stressed the need for extreme caution in giving these products to vulnerable infants with immature immune systems. Before that can be safely done, she said, “we need more FDA oversight of product composition [and] pharmaceutical-grade products, and more studies to determine efficacy.”
Added Dr. Poindexter: “Hopefully, this report will inform clinicians of the risks of using non–pharmaceutical-grade products and encourage industry to actually develop probiotics for neonates that we can feel comfortable using.”
The report received no external funding. Dr. Poindexter and Dr. Wymore have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Dengue may double the risk of symptomatic COVID-19
In a surprising study from the Amazon rain forest, Brazilian scientists found that symptomatic COVID-19 infections were twice as likely to occur in people who had prior dengue.
The study, led by Marcelo Urbano Ferreira, MD, PhD, of the University of São Paulo Biomedical Sciences Institute, was conducted in Mâncio Lima, a town in the Amazon region of Brazil, and published May 6, 2021, in Clinical Infectious Diseases.
In the study, supported by the São Paulo Research Foundation, Ferreira’s team looked at sequential blood samples from 1,285 residents of Mâncio Lima.
An earlier study by Miguel Nicolelis, MD, PhD, and colleagues (published as a preprint) had analyzed data from the first COVID-19 wave in Brazil in 2020. It was an “ecological study” and examined dengue cases in different geographic regions of Brazil. That study concluded that dengue actually seemed to protect people from later developing COVID-19.
Dr. Ferreira anticipated finding a similar effect. Instead, he found the opposite effect. Although dengue did not increase the risk of subsequent COVID-19 infection, symptomatic COVID-19 became twice as likely in people with prior dengue. His study was longitudinal, following a single group of patients in Mâncio Lima over time.
Dr. Ferreira explained that ecological studies are inherently less accurate, as they look at populations in different places. “All the older cases are diagnosed on clinical grounds ... Because most infections are either asymptomatic or symptoms can be easily confused with” other diseases, many cases are missed. So, during the dengue transmission season, “We have some overestimation of the actual number of cases, and outside the transmission season, we have underestimation of the cases.”
On the apparent discrepancy with the earlier study by Dr. Nicolelis, Dr. Ferreira commented, “It’s a wonderful study because it’s something you can do quickly and test a hypothesis [in a] very, very timely [manner], but the problem is if your diagnosis is not very reliable.”
Dr. Ferreira had another advantage: Knowing from sequential blood samples that his patients were exposed to dengue within the past 5 years. He also could tell serologically when they became infected with the SARS-CoV-2 virus, which causes COVID-19.
Dr. Ferreira told this news organization that very few of their patients became seriously ill or required hospitalization. Because their sample size was too small, he could not say if prior dengue made the COVID-19 infection worse.
The type of interaction between two infections like dengue and COVID-19 is called a “syndemic,” which the CDC defines as “synergistically interacting epidemics.” Dr. Ferreira hypothesized about some of the factors that might be at play but does not yet have enough data. For example, he speculated about a biologic basis, such as a link to autoimmunity or vasculitis from prior dengue, but “has no real data to either support or reject these things.”
Dr. Ferreira added that perhaps there are social factors that put certain people at higher risk of infection; for example, maybe some people are “more exposed to high viral loads.”
In Brazil’s first wave of COVID-19, Dr. Ferreira’s team calculated dengue seroconversion as about 10%; many cases of dengue were asymptomatic. Ferreira expects they will “have a very different clinical spectrum during the second wave,” with young people becoming much more ill from the P1 variant of concern.
Scott O’Neill, PhD, founder and director of the World Mosquito Program, told this news organization that, while he found the Brazil results intriguing, at present they are not sufficient to say that there’s a causal relationship between dengue and COVID-19. He expressed concern that the results seem counterintuitive and doubts there’s a biological or mechanistic cause. Instead, Dr. O’Neill wondered if “there could be something about social or economic conditions or living conditions” that might account for the correlation. For example, perhaps poverty increases exposure to both dengue and COVID-19.
Furthermore, Dr. O’Neill said in an interview that he suspects that, with the COVID-19 lockdowns, “You might expect to see more dengue.” This is because “most transmission occurs around the house, and so [with] having more people confined to houses, you might expect to see more dengue.” Such appears to be the case in Singapore.
In an article in the Journal of Infectious Diseases, Jue Tao Lim and colleagues described increased dengue in Singapore during COVID-19. They noted that most employees in Singapore work in air-conditioned settings. With social distancing enforced to try to reduce COVID-19, people stayed at home. The mosquito that transmits dengue, Aedes aegypti, gathers in wet spots in residential areas and bites during the daytime. The authors hypothesized that the spike in dengue was because of this change in habits, which shifted people’s exposure.
The syndemic in Brazil is complicated, with malaria and multiple arboviral diseases (chikungunya, dengue, Zika) overlapping with COVID-19 in areas of high population density, poverty, and poor sanitation, among other social ills. Such overlapping factors make it harder to distinguish correlations from causations. Prospective longitudinal studies might be needed to provide definitive answers.
Dr. Ferreira and Dr. O’Neill have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a surprising study from the Amazon rain forest, Brazilian scientists found that symptomatic COVID-19 infections were twice as likely to occur in people who had prior dengue.
The study, led by Marcelo Urbano Ferreira, MD, PhD, of the University of São Paulo Biomedical Sciences Institute, was conducted in Mâncio Lima, a town in the Amazon region of Brazil, and published May 6, 2021, in Clinical Infectious Diseases.
In the study, supported by the São Paulo Research Foundation, Ferreira’s team looked at sequential blood samples from 1,285 residents of Mâncio Lima.
An earlier study by Miguel Nicolelis, MD, PhD, and colleagues (published as a preprint) had analyzed data from the first COVID-19 wave in Brazil in 2020. It was an “ecological study” and examined dengue cases in different geographic regions of Brazil. That study concluded that dengue actually seemed to protect people from later developing COVID-19.
Dr. Ferreira anticipated finding a similar effect. Instead, he found the opposite effect. Although dengue did not increase the risk of subsequent COVID-19 infection, symptomatic COVID-19 became twice as likely in people with prior dengue. His study was longitudinal, following a single group of patients in Mâncio Lima over time.
Dr. Ferreira explained that ecological studies are inherently less accurate, as they look at populations in different places. “All the older cases are diagnosed on clinical grounds ... Because most infections are either asymptomatic or symptoms can be easily confused with” other diseases, many cases are missed. So, during the dengue transmission season, “We have some overestimation of the actual number of cases, and outside the transmission season, we have underestimation of the cases.”
On the apparent discrepancy with the earlier study by Dr. Nicolelis, Dr. Ferreira commented, “It’s a wonderful study because it’s something you can do quickly and test a hypothesis [in a] very, very timely [manner], but the problem is if your diagnosis is not very reliable.”
Dr. Ferreira had another advantage: Knowing from sequential blood samples that his patients were exposed to dengue within the past 5 years. He also could tell serologically when they became infected with the SARS-CoV-2 virus, which causes COVID-19.
Dr. Ferreira told this news organization that very few of their patients became seriously ill or required hospitalization. Because their sample size was too small, he could not say if prior dengue made the COVID-19 infection worse.
The type of interaction between two infections like dengue and COVID-19 is called a “syndemic,” which the CDC defines as “synergistically interacting epidemics.” Dr. Ferreira hypothesized about some of the factors that might be at play but does not yet have enough data. For example, he speculated about a biologic basis, such as a link to autoimmunity or vasculitis from prior dengue, but “has no real data to either support or reject these things.”
Dr. Ferreira added that perhaps there are social factors that put certain people at higher risk of infection; for example, maybe some people are “more exposed to high viral loads.”
In Brazil’s first wave of COVID-19, Dr. Ferreira’s team calculated dengue seroconversion as about 10%; many cases of dengue were asymptomatic. Ferreira expects they will “have a very different clinical spectrum during the second wave,” with young people becoming much more ill from the P1 variant of concern.
Scott O’Neill, PhD, founder and director of the World Mosquito Program, told this news organization that, while he found the Brazil results intriguing, at present they are not sufficient to say that there’s a causal relationship between dengue and COVID-19. He expressed concern that the results seem counterintuitive and doubts there’s a biological or mechanistic cause. Instead, Dr. O’Neill wondered if “there could be something about social or economic conditions or living conditions” that might account for the correlation. For example, perhaps poverty increases exposure to both dengue and COVID-19.
Furthermore, Dr. O’Neill said in an interview that he suspects that, with the COVID-19 lockdowns, “You might expect to see more dengue.” This is because “most transmission occurs around the house, and so [with] having more people confined to houses, you might expect to see more dengue.” Such appears to be the case in Singapore.
In an article in the Journal of Infectious Diseases, Jue Tao Lim and colleagues described increased dengue in Singapore during COVID-19. They noted that most employees in Singapore work in air-conditioned settings. With social distancing enforced to try to reduce COVID-19, people stayed at home. The mosquito that transmits dengue, Aedes aegypti, gathers in wet spots in residential areas and bites during the daytime. The authors hypothesized that the spike in dengue was because of this change in habits, which shifted people’s exposure.
The syndemic in Brazil is complicated, with malaria and multiple arboviral diseases (chikungunya, dengue, Zika) overlapping with COVID-19 in areas of high population density, poverty, and poor sanitation, among other social ills. Such overlapping factors make it harder to distinguish correlations from causations. Prospective longitudinal studies might be needed to provide definitive answers.
Dr. Ferreira and Dr. O’Neill have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a surprising study from the Amazon rain forest, Brazilian scientists found that symptomatic COVID-19 infections were twice as likely to occur in people who had prior dengue.
The study, led by Marcelo Urbano Ferreira, MD, PhD, of the University of São Paulo Biomedical Sciences Institute, was conducted in Mâncio Lima, a town in the Amazon region of Brazil, and published May 6, 2021, in Clinical Infectious Diseases.
In the study, supported by the São Paulo Research Foundation, Ferreira’s team looked at sequential blood samples from 1,285 residents of Mâncio Lima.
An earlier study by Miguel Nicolelis, MD, PhD, and colleagues (published as a preprint) had analyzed data from the first COVID-19 wave in Brazil in 2020. It was an “ecological study” and examined dengue cases in different geographic regions of Brazil. That study concluded that dengue actually seemed to protect people from later developing COVID-19.
Dr. Ferreira anticipated finding a similar effect. Instead, he found the opposite effect. Although dengue did not increase the risk of subsequent COVID-19 infection, symptomatic COVID-19 became twice as likely in people with prior dengue. His study was longitudinal, following a single group of patients in Mâncio Lima over time.
Dr. Ferreira explained that ecological studies are inherently less accurate, as they look at populations in different places. “All the older cases are diagnosed on clinical grounds ... Because most infections are either asymptomatic or symptoms can be easily confused with” other diseases, many cases are missed. So, during the dengue transmission season, “We have some overestimation of the actual number of cases, and outside the transmission season, we have underestimation of the cases.”
On the apparent discrepancy with the earlier study by Dr. Nicolelis, Dr. Ferreira commented, “It’s a wonderful study because it’s something you can do quickly and test a hypothesis [in a] very, very timely [manner], but the problem is if your diagnosis is not very reliable.”
Dr. Ferreira had another advantage: Knowing from sequential blood samples that his patients were exposed to dengue within the past 5 years. He also could tell serologically when they became infected with the SARS-CoV-2 virus, which causes COVID-19.
Dr. Ferreira told this news organization that very few of their patients became seriously ill or required hospitalization. Because their sample size was too small, he could not say if prior dengue made the COVID-19 infection worse.
The type of interaction between two infections like dengue and COVID-19 is called a “syndemic,” which the CDC defines as “synergistically interacting epidemics.” Dr. Ferreira hypothesized about some of the factors that might be at play but does not yet have enough data. For example, he speculated about a biologic basis, such as a link to autoimmunity or vasculitis from prior dengue, but “has no real data to either support or reject these things.”
Dr. Ferreira added that perhaps there are social factors that put certain people at higher risk of infection; for example, maybe some people are “more exposed to high viral loads.”
In Brazil’s first wave of COVID-19, Dr. Ferreira’s team calculated dengue seroconversion as about 10%; many cases of dengue were asymptomatic. Ferreira expects they will “have a very different clinical spectrum during the second wave,” with young people becoming much more ill from the P1 variant of concern.
Scott O’Neill, PhD, founder and director of the World Mosquito Program, told this news organization that, while he found the Brazil results intriguing, at present they are not sufficient to say that there’s a causal relationship between dengue and COVID-19. He expressed concern that the results seem counterintuitive and doubts there’s a biological or mechanistic cause. Instead, Dr. O’Neill wondered if “there could be something about social or economic conditions or living conditions” that might account for the correlation. For example, perhaps poverty increases exposure to both dengue and COVID-19.
Furthermore, Dr. O’Neill said in an interview that he suspects that, with the COVID-19 lockdowns, “You might expect to see more dengue.” This is because “most transmission occurs around the house, and so [with] having more people confined to houses, you might expect to see more dengue.” Such appears to be the case in Singapore.
In an article in the Journal of Infectious Diseases, Jue Tao Lim and colleagues described increased dengue in Singapore during COVID-19. They noted that most employees in Singapore work in air-conditioned settings. With social distancing enforced to try to reduce COVID-19, people stayed at home. The mosquito that transmits dengue, Aedes aegypti, gathers in wet spots in residential areas and bites during the daytime. The authors hypothesized that the spike in dengue was because of this change in habits, which shifted people’s exposure.
The syndemic in Brazil is complicated, with malaria and multiple arboviral diseases (chikungunya, dengue, Zika) overlapping with COVID-19 in areas of high population density, poverty, and poor sanitation, among other social ills. Such overlapping factors make it harder to distinguish correlations from causations. Prospective longitudinal studies might be needed to provide definitive answers.
Dr. Ferreira and Dr. O’Neill have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
USPSTF final recommendation on CRC screening: 45 is the new 50
Screening for colorectal cancer (CRC) should now begin at the age of 45 and not 50 for average-risk individuals in the United States, notes the final recommendation from the U.S. Preventive Services Task Force.
The recommendation finalizes draft guidelines issued in October 2020 and mandates insurance coverage to ensure equal access to CRC screening regardless of a patient’s insurance status.
The USPSTF’s final recommendations also now align with those of the American Cancer Society, which lowered the age for initiation of CRC screening to 45 years in 2018.
“New statistics project an alarming rise in the incidence of young-onset colorectal cancer, projected to be the leading cause of cancer death in patients aged 20-49 by 2040,” commented Kimmie Ng, MD, MPH, director, Young-Onset Colorectal Cancer Center, Dana-Farber Cancer Institute, Boston, and lead author of a JAMA editorial about the new guideline.
“We must take bold steps to translate the lowered age of beginning screening into meaningful decreases in CRC incidence and mortality,” she emphasized.
The USPSTF recommendations and substantial evidence supporting them were published online May 18, 2021, in JAMA.
Risk factors for CRC
As the USPSTF authors noted, age is one of the most important risk factors for CRC, with nearly 94% of all new cases of CRC occurring in adults 45 years of age and older. Justification for the lower age of CRC screening initiation was based on simulation models showing that initiation of screening at the age of 45 was associated with an estimated additional 22-27 life-years gained, compared with starting at the age of 50.
The USPSTF continues to recommend screening for CRC in all adults aged between 50 and 75 years, lowering the age for screening to 45 years in recognition of the fact that, in 2020, 11% of colon cancers and 15% of rectal cancers occurred in patients under the age of 50.
The USPSTF also continues to conclude that there is a “small net benefit” of screening for CRC in adults aged between 76 and 85 years who have been previously screened.
However, the decision to screen patients in this age group should be based on individual risk factors for CRC, a patient’s overall health status, and personal preference. Perhaps self-evidently, adults in this age group who have never been screened for CRC are more likely to benefit from CRC screening than those who have been previously screened.
Similar to the previous guidelines released in 2016, the updated USPSTF recommendations continue to offer a menu of screening strategies, although the frequency of screening for each of the screening strategies varies. Recommended screening strategies include:
- High-sensitivity guaiac fecal occult blood test or fecal immunochemical test (FIT) every year
- Stool DNA-FIT every 1-3 years
- CT colonography every 5 years
- every 5 years
- Flexible sigmoidoscopy every 10 years plus annual FIT
- screening every 10 years
“Based on the evidence, there are many tests available that can effectively screen for colorectal cancer and the right test is the one that gets done,” USPSTF member Martha Kubik, PhD, RN, said in a statement.
“To encourage screening and help patients select the best test for them, we urge primary care clinicians to talk about the pros and cons of the various recommended options with their patients,” she added.
An accompanying review of the effectiveness, accuracy, and potential harms of CRC screening methods underscores how different screening tests have different levels of evidence demonstrating their ability to detect cancer, precursor lesions, or both, as well as their ability to reduce mortality from cancer.
Eligible patients
Currently, fewer than 70% of eligible patients in the United States undergo CRC screening, Dr. Ng pointed out in the editorial. In addition, CRC disproportionately affects African American patients, who are about 20% more likely to get CRC and about 40% more likely to die from it, compared with other patient groups. Modeling studies published along with the USPSTF recommendations showed equal benefit for screening regardless of race and gender, underscoring the importance of screening adherence, especially in patient populations disproportionately affected by CRC.
“Far too many people in the U.S. are not receiving this lifesaving preventive service,” USPSTF vice chair Michael Barry, MD, said in a statement.
“We hope that this new recommendation to screen people ages 45-49, coupled with our long-standing recommendation to screen people 50-75, will prevent more people from dying from colorectal cancer,” he added.
Dr. Ng echoed this sentiment in her editorial: “The USPSTF recommendation for beginning colorectal cancer screening for average-risk adults at age 45 years has moved the field one step forward and indicates that ‘45 is the new 50,’ ” she observed.
“Lowering the recommended age to initiate screening will make colorectal cancer screening available to millions more people in the United States and, hopefully, many more lives will be saved by catching colorectal cancer earlier as well as by preventing colorectal cancer,” Dr. Ng affirmed.
All members of the USPSTF received travel reimbursement and an honorarium for participating in USPSTF meetings.
Dr. Ng reported receiving nonfinancial support from Pharmavite as well as grants from the Evergrande Group, Janssen, Revolution Medicines, Genentech, and Gilead Sciences. She has also reported receiving personal fees from Seattle Genetics, Array Biopharma, BiomX, and X-Biotix Therapeutics.
A version of this article first appeared on Medscape.com.
Screening for colorectal cancer (CRC) should now begin at the age of 45 and not 50 for average-risk individuals in the United States, notes the final recommendation from the U.S. Preventive Services Task Force.
The recommendation finalizes draft guidelines issued in October 2020 and mandates insurance coverage to ensure equal access to CRC screening regardless of a patient’s insurance status.
The USPSTF’s final recommendations also now align with those of the American Cancer Society, which lowered the age for initiation of CRC screening to 45 years in 2018.
“New statistics project an alarming rise in the incidence of young-onset colorectal cancer, projected to be the leading cause of cancer death in patients aged 20-49 by 2040,” commented Kimmie Ng, MD, MPH, director, Young-Onset Colorectal Cancer Center, Dana-Farber Cancer Institute, Boston, and lead author of a JAMA editorial about the new guideline.
“We must take bold steps to translate the lowered age of beginning screening into meaningful decreases in CRC incidence and mortality,” she emphasized.
The USPSTF recommendations and substantial evidence supporting them were published online May 18, 2021, in JAMA.
Risk factors for CRC
As the USPSTF authors noted, age is one of the most important risk factors for CRC, with nearly 94% of all new cases of CRC occurring in adults 45 years of age and older. Justification for the lower age of CRC screening initiation was based on simulation models showing that initiation of screening at the age of 45 was associated with an estimated additional 22-27 life-years gained, compared with starting at the age of 50.
The USPSTF continues to recommend screening for CRC in all adults aged between 50 and 75 years, lowering the age for screening to 45 years in recognition of the fact that, in 2020, 11% of colon cancers and 15% of rectal cancers occurred in patients under the age of 50.
The USPSTF also continues to conclude that there is a “small net benefit” of screening for CRC in adults aged between 76 and 85 years who have been previously screened.
However, the decision to screen patients in this age group should be based on individual risk factors for CRC, a patient’s overall health status, and personal preference. Perhaps self-evidently, adults in this age group who have never been screened for CRC are more likely to benefit from CRC screening than those who have been previously screened.
Similar to the previous guidelines released in 2016, the updated USPSTF recommendations continue to offer a menu of screening strategies, although the frequency of screening for each of the screening strategies varies. Recommended screening strategies include:
- High-sensitivity guaiac fecal occult blood test or fecal immunochemical test (FIT) every year
- Stool DNA-FIT every 1-3 years
- CT colonography every 5 years
- every 5 years
- Flexible sigmoidoscopy every 10 years plus annual FIT
- screening every 10 years
“Based on the evidence, there are many tests available that can effectively screen for colorectal cancer and the right test is the one that gets done,” USPSTF member Martha Kubik, PhD, RN, said in a statement.
“To encourage screening and help patients select the best test for them, we urge primary care clinicians to talk about the pros and cons of the various recommended options with their patients,” she added.
An accompanying review of the effectiveness, accuracy, and potential harms of CRC screening methods underscores how different screening tests have different levels of evidence demonstrating their ability to detect cancer, precursor lesions, or both, as well as their ability to reduce mortality from cancer.
Eligible patients
Currently, fewer than 70% of eligible patients in the United States undergo CRC screening, Dr. Ng pointed out in the editorial. In addition, CRC disproportionately affects African American patients, who are about 20% more likely to get CRC and about 40% more likely to die from it, compared with other patient groups. Modeling studies published along with the USPSTF recommendations showed equal benefit for screening regardless of race and gender, underscoring the importance of screening adherence, especially in patient populations disproportionately affected by CRC.
“Far too many people in the U.S. are not receiving this lifesaving preventive service,” USPSTF vice chair Michael Barry, MD, said in a statement.
“We hope that this new recommendation to screen people ages 45-49, coupled with our long-standing recommendation to screen people 50-75, will prevent more people from dying from colorectal cancer,” he added.
Dr. Ng echoed this sentiment in her editorial: “The USPSTF recommendation for beginning colorectal cancer screening for average-risk adults at age 45 years has moved the field one step forward and indicates that ‘45 is the new 50,’ ” she observed.
“Lowering the recommended age to initiate screening will make colorectal cancer screening available to millions more people in the United States and, hopefully, many more lives will be saved by catching colorectal cancer earlier as well as by preventing colorectal cancer,” Dr. Ng affirmed.
All members of the USPSTF received travel reimbursement and an honorarium for participating in USPSTF meetings.
Dr. Ng reported receiving nonfinancial support from Pharmavite as well as grants from the Evergrande Group, Janssen, Revolution Medicines, Genentech, and Gilead Sciences. She has also reported receiving personal fees from Seattle Genetics, Array Biopharma, BiomX, and X-Biotix Therapeutics.
A version of this article first appeared on Medscape.com.
Screening for colorectal cancer (CRC) should now begin at the age of 45 and not 50 for average-risk individuals in the United States, notes the final recommendation from the U.S. Preventive Services Task Force.
The recommendation finalizes draft guidelines issued in October 2020 and mandates insurance coverage to ensure equal access to CRC screening regardless of a patient’s insurance status.
The USPSTF’s final recommendations also now align with those of the American Cancer Society, which lowered the age for initiation of CRC screening to 45 years in 2018.
“New statistics project an alarming rise in the incidence of young-onset colorectal cancer, projected to be the leading cause of cancer death in patients aged 20-49 by 2040,” commented Kimmie Ng, MD, MPH, director, Young-Onset Colorectal Cancer Center, Dana-Farber Cancer Institute, Boston, and lead author of a JAMA editorial about the new guideline.
“We must take bold steps to translate the lowered age of beginning screening into meaningful decreases in CRC incidence and mortality,” she emphasized.
The USPSTF recommendations and substantial evidence supporting them were published online May 18, 2021, in JAMA.
Risk factors for CRC
As the USPSTF authors noted, age is one of the most important risk factors for CRC, with nearly 94% of all new cases of CRC occurring in adults 45 years of age and older. Justification for the lower age of CRC screening initiation was based on simulation models showing that initiation of screening at the age of 45 was associated with an estimated additional 22-27 life-years gained, compared with starting at the age of 50.
The USPSTF continues to recommend screening for CRC in all adults aged between 50 and 75 years, lowering the age for screening to 45 years in recognition of the fact that, in 2020, 11% of colon cancers and 15% of rectal cancers occurred in patients under the age of 50.
The USPSTF also continues to conclude that there is a “small net benefit” of screening for CRC in adults aged between 76 and 85 years who have been previously screened.
However, the decision to screen patients in this age group should be based on individual risk factors for CRC, a patient’s overall health status, and personal preference. Perhaps self-evidently, adults in this age group who have never been screened for CRC are more likely to benefit from CRC screening than those who have been previously screened.
Similar to the previous guidelines released in 2016, the updated USPSTF recommendations continue to offer a menu of screening strategies, although the frequency of screening for each of the screening strategies varies. Recommended screening strategies include:
- High-sensitivity guaiac fecal occult blood test or fecal immunochemical test (FIT) every year
- Stool DNA-FIT every 1-3 years
- CT colonography every 5 years
- every 5 years
- Flexible sigmoidoscopy every 10 years plus annual FIT
- screening every 10 years
“Based on the evidence, there are many tests available that can effectively screen for colorectal cancer and the right test is the one that gets done,” USPSTF member Martha Kubik, PhD, RN, said in a statement.
“To encourage screening and help patients select the best test for them, we urge primary care clinicians to talk about the pros and cons of the various recommended options with their patients,” she added.
An accompanying review of the effectiveness, accuracy, and potential harms of CRC screening methods underscores how different screening tests have different levels of evidence demonstrating their ability to detect cancer, precursor lesions, or both, as well as their ability to reduce mortality from cancer.
Eligible patients
Currently, fewer than 70% of eligible patients in the United States undergo CRC screening, Dr. Ng pointed out in the editorial. In addition, CRC disproportionately affects African American patients, who are about 20% more likely to get CRC and about 40% more likely to die from it, compared with other patient groups. Modeling studies published along with the USPSTF recommendations showed equal benefit for screening regardless of race and gender, underscoring the importance of screening adherence, especially in patient populations disproportionately affected by CRC.
“Far too many people in the U.S. are not receiving this lifesaving preventive service,” USPSTF vice chair Michael Barry, MD, said in a statement.
“We hope that this new recommendation to screen people ages 45-49, coupled with our long-standing recommendation to screen people 50-75, will prevent more people from dying from colorectal cancer,” he added.
Dr. Ng echoed this sentiment in her editorial: “The USPSTF recommendation for beginning colorectal cancer screening for average-risk adults at age 45 years has moved the field one step forward and indicates that ‘45 is the new 50,’ ” she observed.
“Lowering the recommended age to initiate screening will make colorectal cancer screening available to millions more people in the United States and, hopefully, many more lives will be saved by catching colorectal cancer earlier as well as by preventing colorectal cancer,” Dr. Ng affirmed.
All members of the USPSTF received travel reimbursement and an honorarium for participating in USPSTF meetings.
Dr. Ng reported receiving nonfinancial support from Pharmavite as well as grants from the Evergrande Group, Janssen, Revolution Medicines, Genentech, and Gilead Sciences. She has also reported receiving personal fees from Seattle Genetics, Array Biopharma, BiomX, and X-Biotix Therapeutics.
A version of this article first appeared on Medscape.com.
How to help vaccinated patients navigate FOGO (fear of going out)
Remember FOMO (fear of missing out)? The pandemic cured most of us of that! In its place, many are suffering from a new syndrome that has been coined “FOGO” (fear of going out). As the COVID-19 vaccines roll out, restrictions lessen, and cases decline, we face new challenges. The pandemic showed us that “we are all in it together.” Now our patients, family, friends – and even we, ourselves – may face similar anxieties as we transition back.
Our brains love routines. They save energy as we transverse the same pathway with ease. We created new patterns in the first 30 days of quarantine, and we spent more than a year engraining them. Many people are feeling even more anxiety as restrictions are lifting and expectations are rising. Those with preexisting anxiety disorders may have an even more difficult time resuming routine activities.
Since the virus is still among us, we need to maintain caution, so some degree of FOGO is wise. But when we limit our activities too much, we create a whole new host of issues. The pandemic gave us all a taste of the agoraphobic lifestyle. It is difficult to know where exactly to draw the line right now between healthy anxiety and anxiety that becomes the disease for ourselves, our families and friends – and our patients.
Recommendations for FOGO
- Talk to your families, friends, and patients about what activities you recommend, which they might resume and which they should continue to avoid. People should make plans to optimize their physical and mental health while continuing to protect themselves from COVID-19. If anxiety is becoming the main problem, psychotherapy or medication may be necessary to treat their symptoms.
- Continue to encourage those with FOGO to practice techniques to be calm. Suggest that they take deep breaths with long exhales. This breathing pattern activates the parasympathetic nervous system and will help them feel calmer. We have all been under chronic stress, and our sympathetic nervous system has been in overdrive. We need to be calm to make the best decisions so our frontal lobe can be in charge rather than our primitive, fear-based brain that has been running the show for more a year. Encourage calming activities, such as yoga, meditation, warm baths, spending time in nature, hugging a pet, and more.
- Advise sufferers to start slowly. They should resume activities where they feel the safest. Walking outside with a friend is a good way to start. We now know that transmission is remarkably low or nonexistent if both parties are vaccinated. Exercise is a great way to combat many psychological issues, including FOGO.
- FOGO sufferers should build confidence gradually. Recommend taking one day at a time and trying to find ways to enjoy new ventures out. Soon, our brains will adapt to the new routines and the days of COVID-19 will recede from our thoughts.
- Respect whatever feelings emerge. The closer we and our patients were to trauma, the more challenging it may be to recover. If you or your patients suffered from COVID-19 or had a close family member or friend who did, be prepared to reemerge more slowly. Don’t feel pressured by what others are doing. Go at your own pace. Only you can decide what is the right way to move forward in these times.
- Look for signs of substance overuse or misuse. FOGO sufferers may turn to drugs or alcohol to mask their anxiety. This is a common pothole and should be avoided. Be alert for this problem and discuss it with patients, friends, or family members who may be making unhealthy choices.
Time is a great healer, and remind others that “this too shall pass.” FOGO will give rise to another yet-to-be named syndrome. We seem to be moving in a very positive direction at a remarkable pace. As Alexander Pope so wisely wrote, “Hope springs eternal.” Better times are ahead.
Dr. Ritvo, who has almost 30 years’ experience in psychiatry, practices in Miami Beach, Fla. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa. Momosa Publishing, 2018). Dr. Ritvo has no disclosures.
Remember FOMO (fear of missing out)? The pandemic cured most of us of that! In its place, many are suffering from a new syndrome that has been coined “FOGO” (fear of going out). As the COVID-19 vaccines roll out, restrictions lessen, and cases decline, we face new challenges. The pandemic showed us that “we are all in it together.” Now our patients, family, friends – and even we, ourselves – may face similar anxieties as we transition back.
Our brains love routines. They save energy as we transverse the same pathway with ease. We created new patterns in the first 30 days of quarantine, and we spent more than a year engraining them. Many people are feeling even more anxiety as restrictions are lifting and expectations are rising. Those with preexisting anxiety disorders may have an even more difficult time resuming routine activities.
Since the virus is still among us, we need to maintain caution, so some degree of FOGO is wise. But when we limit our activities too much, we create a whole new host of issues. The pandemic gave us all a taste of the agoraphobic lifestyle. It is difficult to know where exactly to draw the line right now between healthy anxiety and anxiety that becomes the disease for ourselves, our families and friends – and our patients.
Recommendations for FOGO
- Talk to your families, friends, and patients about what activities you recommend, which they might resume and which they should continue to avoid. People should make plans to optimize their physical and mental health while continuing to protect themselves from COVID-19. If anxiety is becoming the main problem, psychotherapy or medication may be necessary to treat their symptoms.
- Continue to encourage those with FOGO to practice techniques to be calm. Suggest that they take deep breaths with long exhales. This breathing pattern activates the parasympathetic nervous system and will help them feel calmer. We have all been under chronic stress, and our sympathetic nervous system has been in overdrive. We need to be calm to make the best decisions so our frontal lobe can be in charge rather than our primitive, fear-based brain that has been running the show for more a year. Encourage calming activities, such as yoga, meditation, warm baths, spending time in nature, hugging a pet, and more.
- Advise sufferers to start slowly. They should resume activities where they feel the safest. Walking outside with a friend is a good way to start. We now know that transmission is remarkably low or nonexistent if both parties are vaccinated. Exercise is a great way to combat many psychological issues, including FOGO.
- FOGO sufferers should build confidence gradually. Recommend taking one day at a time and trying to find ways to enjoy new ventures out. Soon, our brains will adapt to the new routines and the days of COVID-19 will recede from our thoughts.
- Respect whatever feelings emerge. The closer we and our patients were to trauma, the more challenging it may be to recover. If you or your patients suffered from COVID-19 or had a close family member or friend who did, be prepared to reemerge more slowly. Don’t feel pressured by what others are doing. Go at your own pace. Only you can decide what is the right way to move forward in these times.
- Look for signs of substance overuse or misuse. FOGO sufferers may turn to drugs or alcohol to mask their anxiety. This is a common pothole and should be avoided. Be alert for this problem and discuss it with patients, friends, or family members who may be making unhealthy choices.
Time is a great healer, and remind others that “this too shall pass.” FOGO will give rise to another yet-to-be named syndrome. We seem to be moving in a very positive direction at a remarkable pace. As Alexander Pope so wisely wrote, “Hope springs eternal.” Better times are ahead.
Dr. Ritvo, who has almost 30 years’ experience in psychiatry, practices in Miami Beach, Fla. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa. Momosa Publishing, 2018). Dr. Ritvo has no disclosures.
Remember FOMO (fear of missing out)? The pandemic cured most of us of that! In its place, many are suffering from a new syndrome that has been coined “FOGO” (fear of going out). As the COVID-19 vaccines roll out, restrictions lessen, and cases decline, we face new challenges. The pandemic showed us that “we are all in it together.” Now our patients, family, friends – and even we, ourselves – may face similar anxieties as we transition back.
Our brains love routines. They save energy as we transverse the same pathway with ease. We created new patterns in the first 30 days of quarantine, and we spent more than a year engraining them. Many people are feeling even more anxiety as restrictions are lifting and expectations are rising. Those with preexisting anxiety disorders may have an even more difficult time resuming routine activities.
Since the virus is still among us, we need to maintain caution, so some degree of FOGO is wise. But when we limit our activities too much, we create a whole new host of issues. The pandemic gave us all a taste of the agoraphobic lifestyle. It is difficult to know where exactly to draw the line right now between healthy anxiety and anxiety that becomes the disease for ourselves, our families and friends – and our patients.
Recommendations for FOGO
- Talk to your families, friends, and patients about what activities you recommend, which they might resume and which they should continue to avoid. People should make plans to optimize their physical and mental health while continuing to protect themselves from COVID-19. If anxiety is becoming the main problem, psychotherapy or medication may be necessary to treat their symptoms.
- Continue to encourage those with FOGO to practice techniques to be calm. Suggest that they take deep breaths with long exhales. This breathing pattern activates the parasympathetic nervous system and will help them feel calmer. We have all been under chronic stress, and our sympathetic nervous system has been in overdrive. We need to be calm to make the best decisions so our frontal lobe can be in charge rather than our primitive, fear-based brain that has been running the show for more a year. Encourage calming activities, such as yoga, meditation, warm baths, spending time in nature, hugging a pet, and more.
- Advise sufferers to start slowly. They should resume activities where they feel the safest. Walking outside with a friend is a good way to start. We now know that transmission is remarkably low or nonexistent if both parties are vaccinated. Exercise is a great way to combat many psychological issues, including FOGO.
- FOGO sufferers should build confidence gradually. Recommend taking one day at a time and trying to find ways to enjoy new ventures out. Soon, our brains will adapt to the new routines and the days of COVID-19 will recede from our thoughts.
- Respect whatever feelings emerge. The closer we and our patients were to trauma, the more challenging it may be to recover. If you or your patients suffered from COVID-19 or had a close family member or friend who did, be prepared to reemerge more slowly. Don’t feel pressured by what others are doing. Go at your own pace. Only you can decide what is the right way to move forward in these times.
- Look for signs of substance overuse or misuse. FOGO sufferers may turn to drugs or alcohol to mask their anxiety. This is a common pothole and should be avoided. Be alert for this problem and discuss it with patients, friends, or family members who may be making unhealthy choices.
Time is a great healer, and remind others that “this too shall pass.” FOGO will give rise to another yet-to-be named syndrome. We seem to be moving in a very positive direction at a remarkable pace. As Alexander Pope so wisely wrote, “Hope springs eternal.” Better times are ahead.
Dr. Ritvo, who has almost 30 years’ experience in psychiatry, practices in Miami Beach, Fla. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa. Momosa Publishing, 2018). Dr. Ritvo has no disclosures.
Cardiologists’ pay increases, despite COVID-19 impacts
Despite the huge challenges of COVID-19, including a drop in patient visits, cardiologists reported an average increase in income in 2020 and remain among the top earners in medicine, according to the 2021 Medscape Cardiologist Compensation Report.
Although 46% of cardiologists reported some decline in compensation, average cardiologist income was $459,000 in 2020 – up from $438,000 in 2019.
Cardiologist pay is the third highest of all specialties in the overall 2021 Medscape Physician Compensation Report, which covers U.S. physicians as a whole and almost 18,000 physicians in 29 specialties.
Only plastic surgeons ($526,000) and orthopedists ($511,000) earned more than cardiologists in 2020.
On average among cardiologists, self-employment yields a somewhat higher paycheck than does being employed ($477,000 vs. $450,000).
Just like in last year’s report, nearly two-thirds (61%) of cardiologists overall say they feel fairly compensated.
The average incentive bonus payment for cardiologists in 2020 was 14% of total salary, about the same as last year. Two-thirds of cardiologists who earn an incentive bonus achieve more than three-quarters of their potential annual payment, up from 55% the prior year.
COVID challenges and the road back
The vast majority (92%) of cardiologists who saw a drop in income last year cited COVID-related issues such as job loss, working fewer hours, and seeing fewer patients.
Close to half (48%) of cardiologists who suffered financial or practice-related ill effects as a result of the pandemic expect their income to return to normal this year; 38% believe it will take 2 to 3 years. Notably, 45% of physicians overall said the pandemic did not cause them financial or practice-related harm.
Physician work hours generally declined for at least some time during the pandemic – and some physicians were furloughed – but most are now working about the same number of hours they did prior to COVID-19.
Cardiologists are back working an average of 57 hours per week. Perhaps not surprising, intensivists, infectious disease physicians, and public health/preventive medicine physicians are pulling longer hours now, about 6 or 7 more per week than before.
Although working about the same number of hours per week now as they did before the pandemic, physicians overall are typically seeing fewer patients because of time spent on medical office safety protocols, answering COVID-19–related questions and other factors.
Cardiologists are seeing an average decline in weekly patient visits of about 6% – from 77 to 72 patients. Pediatricians are experiencing the largest average declines – from 78 patients per week prior to 64 now, an 18% drop.
Among self-employed cardiologists, 43% believe that a drop in patient volume of up to one-quarter is permanent.
Most cardiologists remain happy at work
Despite COVID-19 and other professional challenges, most cardiologists (and physicians overall) continue to find their work rewarding.
Cardiologists say the most rewarding aspect of their profession is “being good at what I do/finding answers and diagnoses” (27%), followed by relationships with and gratitude from patients (26%), making the world a better place (23%) and making good money at a job they like (12%). A few cited pride in their profession (6%) and teaching (2%). These figures are in line with last year’s responses.
The most challenging part of practicing cardiology is having so many rules and regulations (22%), followed by having to work long hours (16%), working with electronic health records (13%), trouble getting fair reimbursement (11%), danger/risk associated with treating COVID-19 patients (11%), dealing with difficult patients (8%) and worry about being sued (7%).
Bureaucratic tasks continue to be a burden for physicians in all specialties. On average, cardiologists spend 17.4 hours per week on paperwork and administration, similar to last year (16.9 hours per week) and to physicians overall (16.3 hours).
Despite the challenges, 86% of cardiologists said they would choose medicine again, and 92% would choose cardiology again, about the same as last year.
Most cardiologists (83%) plan to keep Medicare and/or Medicaid patients; only 1% say they won’t take new Medicare or Medicaid patients; and 16% are undecided.
Thirty-nine percent of cardiologists plan to participate in the Merit-based Incentive Payment System (MIPS) in 2021.
“The stakes of the Quality Payment Program – the program that incorporates MIPS – are high, with a 9% penalty applied to all Medicare reimbursement for failure to participate,” said Elizabeth Woodcock, MBA, CPC, president of physician practice consulting firm Woodcock & Associates, Atlanta.
“With margins already slim, most physicians can’t afford this massive penalty. It makes sense to protect your revenue by complying with at least the bare minimum,” she noted.
A version of this article first appeared on Medscape.com.
Despite the huge challenges of COVID-19, including a drop in patient visits, cardiologists reported an average increase in income in 2020 and remain among the top earners in medicine, according to the 2021 Medscape Cardiologist Compensation Report.
Although 46% of cardiologists reported some decline in compensation, average cardiologist income was $459,000 in 2020 – up from $438,000 in 2019.
Cardiologist pay is the third highest of all specialties in the overall 2021 Medscape Physician Compensation Report, which covers U.S. physicians as a whole and almost 18,000 physicians in 29 specialties.
Only plastic surgeons ($526,000) and orthopedists ($511,000) earned more than cardiologists in 2020.
On average among cardiologists, self-employment yields a somewhat higher paycheck than does being employed ($477,000 vs. $450,000).
Just like in last year’s report, nearly two-thirds (61%) of cardiologists overall say they feel fairly compensated.
The average incentive bonus payment for cardiologists in 2020 was 14% of total salary, about the same as last year. Two-thirds of cardiologists who earn an incentive bonus achieve more than three-quarters of their potential annual payment, up from 55% the prior year.
COVID challenges and the road back
The vast majority (92%) of cardiologists who saw a drop in income last year cited COVID-related issues such as job loss, working fewer hours, and seeing fewer patients.
Close to half (48%) of cardiologists who suffered financial or practice-related ill effects as a result of the pandemic expect their income to return to normal this year; 38% believe it will take 2 to 3 years. Notably, 45% of physicians overall said the pandemic did not cause them financial or practice-related harm.
Physician work hours generally declined for at least some time during the pandemic – and some physicians were furloughed – but most are now working about the same number of hours they did prior to COVID-19.
Cardiologists are back working an average of 57 hours per week. Perhaps not surprising, intensivists, infectious disease physicians, and public health/preventive medicine physicians are pulling longer hours now, about 6 or 7 more per week than before.
Although working about the same number of hours per week now as they did before the pandemic, physicians overall are typically seeing fewer patients because of time spent on medical office safety protocols, answering COVID-19–related questions and other factors.
Cardiologists are seeing an average decline in weekly patient visits of about 6% – from 77 to 72 patients. Pediatricians are experiencing the largest average declines – from 78 patients per week prior to 64 now, an 18% drop.
Among self-employed cardiologists, 43% believe that a drop in patient volume of up to one-quarter is permanent.
Most cardiologists remain happy at work
Despite COVID-19 and other professional challenges, most cardiologists (and physicians overall) continue to find their work rewarding.
Cardiologists say the most rewarding aspect of their profession is “being good at what I do/finding answers and diagnoses” (27%), followed by relationships with and gratitude from patients (26%), making the world a better place (23%) and making good money at a job they like (12%). A few cited pride in their profession (6%) and teaching (2%). These figures are in line with last year’s responses.
The most challenging part of practicing cardiology is having so many rules and regulations (22%), followed by having to work long hours (16%), working with electronic health records (13%), trouble getting fair reimbursement (11%), danger/risk associated with treating COVID-19 patients (11%), dealing with difficult patients (8%) and worry about being sued (7%).
Bureaucratic tasks continue to be a burden for physicians in all specialties. On average, cardiologists spend 17.4 hours per week on paperwork and administration, similar to last year (16.9 hours per week) and to physicians overall (16.3 hours).
Despite the challenges, 86% of cardiologists said they would choose medicine again, and 92% would choose cardiology again, about the same as last year.
Most cardiologists (83%) plan to keep Medicare and/or Medicaid patients; only 1% say they won’t take new Medicare or Medicaid patients; and 16% are undecided.
Thirty-nine percent of cardiologists plan to participate in the Merit-based Incentive Payment System (MIPS) in 2021.
“The stakes of the Quality Payment Program – the program that incorporates MIPS – are high, with a 9% penalty applied to all Medicare reimbursement for failure to participate,” said Elizabeth Woodcock, MBA, CPC, president of physician practice consulting firm Woodcock & Associates, Atlanta.
“With margins already slim, most physicians can’t afford this massive penalty. It makes sense to protect your revenue by complying with at least the bare minimum,” she noted.
A version of this article first appeared on Medscape.com.
Despite the huge challenges of COVID-19, including a drop in patient visits, cardiologists reported an average increase in income in 2020 and remain among the top earners in medicine, according to the 2021 Medscape Cardiologist Compensation Report.
Although 46% of cardiologists reported some decline in compensation, average cardiologist income was $459,000 in 2020 – up from $438,000 in 2019.
Cardiologist pay is the third highest of all specialties in the overall 2021 Medscape Physician Compensation Report, which covers U.S. physicians as a whole and almost 18,000 physicians in 29 specialties.
Only plastic surgeons ($526,000) and orthopedists ($511,000) earned more than cardiologists in 2020.
On average among cardiologists, self-employment yields a somewhat higher paycheck than does being employed ($477,000 vs. $450,000).
Just like in last year’s report, nearly two-thirds (61%) of cardiologists overall say they feel fairly compensated.
The average incentive bonus payment for cardiologists in 2020 was 14% of total salary, about the same as last year. Two-thirds of cardiologists who earn an incentive bonus achieve more than three-quarters of their potential annual payment, up from 55% the prior year.
COVID challenges and the road back
The vast majority (92%) of cardiologists who saw a drop in income last year cited COVID-related issues such as job loss, working fewer hours, and seeing fewer patients.
Close to half (48%) of cardiologists who suffered financial or practice-related ill effects as a result of the pandemic expect their income to return to normal this year; 38% believe it will take 2 to 3 years. Notably, 45% of physicians overall said the pandemic did not cause them financial or practice-related harm.
Physician work hours generally declined for at least some time during the pandemic – and some physicians were furloughed – but most are now working about the same number of hours they did prior to COVID-19.
Cardiologists are back working an average of 57 hours per week. Perhaps not surprising, intensivists, infectious disease physicians, and public health/preventive medicine physicians are pulling longer hours now, about 6 or 7 more per week than before.
Although working about the same number of hours per week now as they did before the pandemic, physicians overall are typically seeing fewer patients because of time spent on medical office safety protocols, answering COVID-19–related questions and other factors.
Cardiologists are seeing an average decline in weekly patient visits of about 6% – from 77 to 72 patients. Pediatricians are experiencing the largest average declines – from 78 patients per week prior to 64 now, an 18% drop.
Among self-employed cardiologists, 43% believe that a drop in patient volume of up to one-quarter is permanent.
Most cardiologists remain happy at work
Despite COVID-19 and other professional challenges, most cardiologists (and physicians overall) continue to find their work rewarding.
Cardiologists say the most rewarding aspect of their profession is “being good at what I do/finding answers and diagnoses” (27%), followed by relationships with and gratitude from patients (26%), making the world a better place (23%) and making good money at a job they like (12%). A few cited pride in their profession (6%) and teaching (2%). These figures are in line with last year’s responses.
The most challenging part of practicing cardiology is having so many rules and regulations (22%), followed by having to work long hours (16%), working with electronic health records (13%), trouble getting fair reimbursement (11%), danger/risk associated with treating COVID-19 patients (11%), dealing with difficult patients (8%) and worry about being sued (7%).
Bureaucratic tasks continue to be a burden for physicians in all specialties. On average, cardiologists spend 17.4 hours per week on paperwork and administration, similar to last year (16.9 hours per week) and to physicians overall (16.3 hours).
Despite the challenges, 86% of cardiologists said they would choose medicine again, and 92% would choose cardiology again, about the same as last year.
Most cardiologists (83%) plan to keep Medicare and/or Medicaid patients; only 1% say they won’t take new Medicare or Medicaid patients; and 16% are undecided.
Thirty-nine percent of cardiologists plan to participate in the Merit-based Incentive Payment System (MIPS) in 2021.
“The stakes of the Quality Payment Program – the program that incorporates MIPS – are high, with a 9% penalty applied to all Medicare reimbursement for failure to participate,” said Elizabeth Woodcock, MBA, CPC, president of physician practice consulting firm Woodcock & Associates, Atlanta.
“With margins already slim, most physicians can’t afford this massive penalty. It makes sense to protect your revenue by complying with at least the bare minimum,” she noted.
A version of this article first appeared on Medscape.com.
USPSTF recommends clinicians counsel pregnant patients to limit gestational weight gain
The U.S. Preventive Services Task Force has recommended clinicians counsel their adolescent and adult pregnant patients in primary care settings to use interventions to limit excess gestational weight gain.
Counseling pregnant persons on gestational weight gain (GWG) carries a B recommendation from the U.S. Preventive Services Task Force (USPSTF), meaning there is “moderate certainty that behavioral counseling interventions aimed at promoting healthy weight gain and preventing excess GWG in pregnancy have a moderate net benefit for pregnant persons,” the task force said in its recommendation statement, which was published in JAMA on May 25.
While the USPSTF has made other recommendations on screening for obesity in adults and gestational diabetes, this is the first recommendation from the task force on behavioral counseling interventions for pregnant persons to promote a healthy weight and limit GWG. The recommendation is important, the USPSTF said, because half of individuals entered pregnancy while either overweight (24%) or obese (24%) in 2015, with the prevalence of prepregnancy obesity higher among Alaska Native/American Indian (36.4%), Black (34.7%), and Hispanic (27.3%) women.
To define gestational weight gain, the USPSTF used National Academy of Medicine recommendations of weight change of 28-40 pounds in the underweight category (body mass index [BMI], < 18.5 kg/m2), 25-35 pounds in the normal-weight category (BMI, 18.5-24.9 kg/m2), 15-25 pounds in the overweight category (BMI, 25-29.9 kg/m2), and 11-20 pounds in the obese category (≥ 30 kg/m2).
Implementations of this recommendation include content with a focus on nutrition, physical activity, lifestyle change, or behavioral change. The counseling should be performed at the end of the first trimester or start of the second trimester and should stop shortly before delivery. “The most common types of behavioral counseling interventions included active or supervised exercise or counseling about diet and physical activity,” the USPSTF said.
The average duration of counseling sessions was between 15 and 120 minutes, varying from less than 2 contacts to more than 12 contacts involved in the intervention. Primary care clinicians can deliver these interventions themselves or refer the patient out to an intervention in another setting. “Effective behavioral counseling interventions often referred participants to various interventionists in different settings,” such as a local community fitness center, the authors wrote. “Participants were counseled on healthy diet and exercise through individual or group education sessions. Some interventions provided medically supervised group exercise classes with or without counseling.”
In their evidence report for the USPSTF recommendation, Amy G. Cantor, MD, of the Pacific Northwest Evidence-Based Practice Center, department of medical informatics and clinical epidemiology at Oregon Health & Science University in Portland, and colleagues performed a systematic review of 68 studies in the Ovid MEDLINE, Cochrane Central Register of Controlled Trials, and Cochrane Database of Systematic Reviews evaluating the effect of diet, exercise, and/or behavioral counseling interventions for 25,789 pregnant patients with GWG. The results were current up to February 2021 when the last search was performed. The mean ages of patients across all studies were 18.6 to 33.8 years, and 41% of studies contained patients from “diverse backgrounds.”
The results of the systematic review showed use of an intervention to limit GWG decreased the risk of gestational diabetes compared with a control group in 43 trials (relative risk, 0.87; 95% confidence interval, 0.79-0.95), emergency cesarean delivery in 14 trials (RR, 0.85; 95% CI, 0.74-0.96), macrosomia in 25 trials (RR, 0.77; 95% CI, 0.65-0.92), and large for gestational age infants in 26 trials (RR, 0.89; 95% CI, 0.80-0.99). There was not an association between GWG interventions and reduced gestational hypertension in 28 trials (RR, 0.87; 95% CI, 0.70-1.04), preeclampsia in 27 trials (RR, 0.98; 95% CI, 0.84-1.13), and lower risk of preterm birth in 33 trials (RR, 0.93; 95% CI, 0.81-1.07), as well as other outcomes such as respiratory distress syndrome, shoulder dystocia, neonatal intensive care unit admission, neonatal death, or infant growth during the first year.
In terms of the types of interventions used, Dr. Canton and colleagues found the greatest impact on GWG occurred when a high-intensity intervention with 12 or more sessions was used in 28 trials (−1.47 kg; 95% CI, −1.78 to −1.22) than in moderate-intensity interventions in 18 trials (−0.32 kg; 95% CI, −0.71 to −0.04) and low-intensity interventions in 9 trials (−0.64 kg; 94% CI, −1.44 to 0.02).
Implementing these interventions could be challenging
D. Yvette LaCoursiere, MD, of the department of obstetrics, gynecology, and reproductive sciences at the University of California, San Diego, in La Jolla, Calif., wrote in an accompanying editorial that the USPSTF recommendation supports the recommendation of the American College of Obstetricians and Gynecologists (ACOG) of offering nutritional and exercise-based support for patients with “excessive GWG,” but noted that leaving implementation of behavioral counseling interventions to the clinicians “is where challenges lie.”
“The USPSTF recommendations will require lengthening already time-constrained prenatal visits or relying on adjunctive professionals,” she said.
Dr. LaCoursiere highlighted the amount of time the behavioral counseling interventions took to implement, with the shortest intervention lasting 15 minutes. “With the exception of those in group prenatal care practices, clinicians conducting the standard prenatal visit will find it difficult to accommodate moderate- or high-intensity interventions. On a similar note, the topics included in many of the interventions are broad and not necessarily in the purview of clinicians who provide prenatal care,” she said.
In addition, behavioral counseling interventions may not be covered by some patients’ insurance plans, Dr. LaCoursiere explained. “While it is a federal requirement for states to provide pregnant Medicaid enrollees smoking cessation counseling and prescription drugs, there is no such mandate for nutrition or physical activity counseling. Neither is it required that states provide these services to nonpregnant enrollees,” she said. “These are not insurmountable challenges, but more groundwork is necessary to ensure an effective and efficient implementation.”
Commenting on how a clinician could fit a behavioral counseling intervention into the prenatal care model, Dr. LaCoursiere said creativity may be needed. Some researchers in the systematic review used Internet or telehealth-based programs for dietary education, exercise support, health information, and goal setting, for example, which could help with continuity of care during the COVID-19 pandemic. “These types of interventions may help overcome the obstacle of insufficient clinic time by separating the primary implementation phase from the traditional clinical setting,” she said.
While the evidence supports the implementation of these interventions, “additional work remains for clinicians and researchers to identify high-yield components and determine best practices for the delivery of GWG interventions,” she said.
“The success of this intervention will depend on improving resources for clinicians to facilitate provision of direct counseling or to refer patients to skilled professionals and explore novel alternatives. Promising innovative approaches such as the use of telehealth, technology-based delivery systems, and group prenatal care are under investigation and may expand the ability to successfully implement these recommendations and ultimately improve outcomes for pregnant persons and their infants,” Dr. LaCoursiere concluded.
This research was funded by contracts from the Agency for Healthcare Research and Quality and U.S. Department of Health and Human Services. The authors report no relevant conflict of interest.
The U.S. Preventive Services Task Force has recommended clinicians counsel their adolescent and adult pregnant patients in primary care settings to use interventions to limit excess gestational weight gain.
Counseling pregnant persons on gestational weight gain (GWG) carries a B recommendation from the U.S. Preventive Services Task Force (USPSTF), meaning there is “moderate certainty that behavioral counseling interventions aimed at promoting healthy weight gain and preventing excess GWG in pregnancy have a moderate net benefit for pregnant persons,” the task force said in its recommendation statement, which was published in JAMA on May 25.
While the USPSTF has made other recommendations on screening for obesity in adults and gestational diabetes, this is the first recommendation from the task force on behavioral counseling interventions for pregnant persons to promote a healthy weight and limit GWG. The recommendation is important, the USPSTF said, because half of individuals entered pregnancy while either overweight (24%) or obese (24%) in 2015, with the prevalence of prepregnancy obesity higher among Alaska Native/American Indian (36.4%), Black (34.7%), and Hispanic (27.3%) women.
To define gestational weight gain, the USPSTF used National Academy of Medicine recommendations of weight change of 28-40 pounds in the underweight category (body mass index [BMI], < 18.5 kg/m2), 25-35 pounds in the normal-weight category (BMI, 18.5-24.9 kg/m2), 15-25 pounds in the overweight category (BMI, 25-29.9 kg/m2), and 11-20 pounds in the obese category (≥ 30 kg/m2).
Implementations of this recommendation include content with a focus on nutrition, physical activity, lifestyle change, or behavioral change. The counseling should be performed at the end of the first trimester or start of the second trimester and should stop shortly before delivery. “The most common types of behavioral counseling interventions included active or supervised exercise or counseling about diet and physical activity,” the USPSTF said.
The average duration of counseling sessions was between 15 and 120 minutes, varying from less than 2 contacts to more than 12 contacts involved in the intervention. Primary care clinicians can deliver these interventions themselves or refer the patient out to an intervention in another setting. “Effective behavioral counseling interventions often referred participants to various interventionists in different settings,” such as a local community fitness center, the authors wrote. “Participants were counseled on healthy diet and exercise through individual or group education sessions. Some interventions provided medically supervised group exercise classes with or without counseling.”
In their evidence report for the USPSTF recommendation, Amy G. Cantor, MD, of the Pacific Northwest Evidence-Based Practice Center, department of medical informatics and clinical epidemiology at Oregon Health & Science University in Portland, and colleagues performed a systematic review of 68 studies in the Ovid MEDLINE, Cochrane Central Register of Controlled Trials, and Cochrane Database of Systematic Reviews evaluating the effect of diet, exercise, and/or behavioral counseling interventions for 25,789 pregnant patients with GWG. The results were current up to February 2021 when the last search was performed. The mean ages of patients across all studies were 18.6 to 33.8 years, and 41% of studies contained patients from “diverse backgrounds.”
The results of the systematic review showed use of an intervention to limit GWG decreased the risk of gestational diabetes compared with a control group in 43 trials (relative risk, 0.87; 95% confidence interval, 0.79-0.95), emergency cesarean delivery in 14 trials (RR, 0.85; 95% CI, 0.74-0.96), macrosomia in 25 trials (RR, 0.77; 95% CI, 0.65-0.92), and large for gestational age infants in 26 trials (RR, 0.89; 95% CI, 0.80-0.99). There was not an association between GWG interventions and reduced gestational hypertension in 28 trials (RR, 0.87; 95% CI, 0.70-1.04), preeclampsia in 27 trials (RR, 0.98; 95% CI, 0.84-1.13), and lower risk of preterm birth in 33 trials (RR, 0.93; 95% CI, 0.81-1.07), as well as other outcomes such as respiratory distress syndrome, shoulder dystocia, neonatal intensive care unit admission, neonatal death, or infant growth during the first year.
In terms of the types of interventions used, Dr. Canton and colleagues found the greatest impact on GWG occurred when a high-intensity intervention with 12 or more sessions was used in 28 trials (−1.47 kg; 95% CI, −1.78 to −1.22) than in moderate-intensity interventions in 18 trials (−0.32 kg; 95% CI, −0.71 to −0.04) and low-intensity interventions in 9 trials (−0.64 kg; 94% CI, −1.44 to 0.02).
Implementing these interventions could be challenging
D. Yvette LaCoursiere, MD, of the department of obstetrics, gynecology, and reproductive sciences at the University of California, San Diego, in La Jolla, Calif., wrote in an accompanying editorial that the USPSTF recommendation supports the recommendation of the American College of Obstetricians and Gynecologists (ACOG) of offering nutritional and exercise-based support for patients with “excessive GWG,” but noted that leaving implementation of behavioral counseling interventions to the clinicians “is where challenges lie.”
“The USPSTF recommendations will require lengthening already time-constrained prenatal visits or relying on adjunctive professionals,” she said.
Dr. LaCoursiere highlighted the amount of time the behavioral counseling interventions took to implement, with the shortest intervention lasting 15 minutes. “With the exception of those in group prenatal care practices, clinicians conducting the standard prenatal visit will find it difficult to accommodate moderate- or high-intensity interventions. On a similar note, the topics included in many of the interventions are broad and not necessarily in the purview of clinicians who provide prenatal care,” she said.
In addition, behavioral counseling interventions may not be covered by some patients’ insurance plans, Dr. LaCoursiere explained. “While it is a federal requirement for states to provide pregnant Medicaid enrollees smoking cessation counseling and prescription drugs, there is no such mandate for nutrition or physical activity counseling. Neither is it required that states provide these services to nonpregnant enrollees,” she said. “These are not insurmountable challenges, but more groundwork is necessary to ensure an effective and efficient implementation.”
Commenting on how a clinician could fit a behavioral counseling intervention into the prenatal care model, Dr. LaCoursiere said creativity may be needed. Some researchers in the systematic review used Internet or telehealth-based programs for dietary education, exercise support, health information, and goal setting, for example, which could help with continuity of care during the COVID-19 pandemic. “These types of interventions may help overcome the obstacle of insufficient clinic time by separating the primary implementation phase from the traditional clinical setting,” she said.
While the evidence supports the implementation of these interventions, “additional work remains for clinicians and researchers to identify high-yield components and determine best practices for the delivery of GWG interventions,” she said.
“The success of this intervention will depend on improving resources for clinicians to facilitate provision of direct counseling or to refer patients to skilled professionals and explore novel alternatives. Promising innovative approaches such as the use of telehealth, technology-based delivery systems, and group prenatal care are under investigation and may expand the ability to successfully implement these recommendations and ultimately improve outcomes for pregnant persons and their infants,” Dr. LaCoursiere concluded.
This research was funded by contracts from the Agency for Healthcare Research and Quality and U.S. Department of Health and Human Services. The authors report no relevant conflict of interest.
The U.S. Preventive Services Task Force has recommended clinicians counsel their adolescent and adult pregnant patients in primary care settings to use interventions to limit excess gestational weight gain.
Counseling pregnant persons on gestational weight gain (GWG) carries a B recommendation from the U.S. Preventive Services Task Force (USPSTF), meaning there is “moderate certainty that behavioral counseling interventions aimed at promoting healthy weight gain and preventing excess GWG in pregnancy have a moderate net benefit for pregnant persons,” the task force said in its recommendation statement, which was published in JAMA on May 25.
While the USPSTF has made other recommendations on screening for obesity in adults and gestational diabetes, this is the first recommendation from the task force on behavioral counseling interventions for pregnant persons to promote a healthy weight and limit GWG. The recommendation is important, the USPSTF said, because half of individuals entered pregnancy while either overweight (24%) or obese (24%) in 2015, with the prevalence of prepregnancy obesity higher among Alaska Native/American Indian (36.4%), Black (34.7%), and Hispanic (27.3%) women.
To define gestational weight gain, the USPSTF used National Academy of Medicine recommendations of weight change of 28-40 pounds in the underweight category (body mass index [BMI], < 18.5 kg/m2), 25-35 pounds in the normal-weight category (BMI, 18.5-24.9 kg/m2), 15-25 pounds in the overweight category (BMI, 25-29.9 kg/m2), and 11-20 pounds in the obese category (≥ 30 kg/m2).
Implementations of this recommendation include content with a focus on nutrition, physical activity, lifestyle change, or behavioral change. The counseling should be performed at the end of the first trimester or start of the second trimester and should stop shortly before delivery. “The most common types of behavioral counseling interventions included active or supervised exercise or counseling about diet and physical activity,” the USPSTF said.
The average duration of counseling sessions was between 15 and 120 minutes, varying from less than 2 contacts to more than 12 contacts involved in the intervention. Primary care clinicians can deliver these interventions themselves or refer the patient out to an intervention in another setting. “Effective behavioral counseling interventions often referred participants to various interventionists in different settings,” such as a local community fitness center, the authors wrote. “Participants were counseled on healthy diet and exercise through individual or group education sessions. Some interventions provided medically supervised group exercise classes with or without counseling.”
In their evidence report for the USPSTF recommendation, Amy G. Cantor, MD, of the Pacific Northwest Evidence-Based Practice Center, department of medical informatics and clinical epidemiology at Oregon Health & Science University in Portland, and colleagues performed a systematic review of 68 studies in the Ovid MEDLINE, Cochrane Central Register of Controlled Trials, and Cochrane Database of Systematic Reviews evaluating the effect of diet, exercise, and/or behavioral counseling interventions for 25,789 pregnant patients with GWG. The results were current up to February 2021 when the last search was performed. The mean ages of patients across all studies were 18.6 to 33.8 years, and 41% of studies contained patients from “diverse backgrounds.”
The results of the systematic review showed use of an intervention to limit GWG decreased the risk of gestational diabetes compared with a control group in 43 trials (relative risk, 0.87; 95% confidence interval, 0.79-0.95), emergency cesarean delivery in 14 trials (RR, 0.85; 95% CI, 0.74-0.96), macrosomia in 25 trials (RR, 0.77; 95% CI, 0.65-0.92), and large for gestational age infants in 26 trials (RR, 0.89; 95% CI, 0.80-0.99). There was not an association between GWG interventions and reduced gestational hypertension in 28 trials (RR, 0.87; 95% CI, 0.70-1.04), preeclampsia in 27 trials (RR, 0.98; 95% CI, 0.84-1.13), and lower risk of preterm birth in 33 trials (RR, 0.93; 95% CI, 0.81-1.07), as well as other outcomes such as respiratory distress syndrome, shoulder dystocia, neonatal intensive care unit admission, neonatal death, or infant growth during the first year.
In terms of the types of interventions used, Dr. Canton and colleagues found the greatest impact on GWG occurred when a high-intensity intervention with 12 or more sessions was used in 28 trials (−1.47 kg; 95% CI, −1.78 to −1.22) than in moderate-intensity interventions in 18 trials (−0.32 kg; 95% CI, −0.71 to −0.04) and low-intensity interventions in 9 trials (−0.64 kg; 94% CI, −1.44 to 0.02).
Implementing these interventions could be challenging
D. Yvette LaCoursiere, MD, of the department of obstetrics, gynecology, and reproductive sciences at the University of California, San Diego, in La Jolla, Calif., wrote in an accompanying editorial that the USPSTF recommendation supports the recommendation of the American College of Obstetricians and Gynecologists (ACOG) of offering nutritional and exercise-based support for patients with “excessive GWG,” but noted that leaving implementation of behavioral counseling interventions to the clinicians “is where challenges lie.”
“The USPSTF recommendations will require lengthening already time-constrained prenatal visits or relying on adjunctive professionals,” she said.
Dr. LaCoursiere highlighted the amount of time the behavioral counseling interventions took to implement, with the shortest intervention lasting 15 minutes. “With the exception of those in group prenatal care practices, clinicians conducting the standard prenatal visit will find it difficult to accommodate moderate- or high-intensity interventions. On a similar note, the topics included in many of the interventions are broad and not necessarily in the purview of clinicians who provide prenatal care,” she said.
In addition, behavioral counseling interventions may not be covered by some patients’ insurance plans, Dr. LaCoursiere explained. “While it is a federal requirement for states to provide pregnant Medicaid enrollees smoking cessation counseling and prescription drugs, there is no such mandate for nutrition or physical activity counseling. Neither is it required that states provide these services to nonpregnant enrollees,” she said. “These are not insurmountable challenges, but more groundwork is necessary to ensure an effective and efficient implementation.”
Commenting on how a clinician could fit a behavioral counseling intervention into the prenatal care model, Dr. LaCoursiere said creativity may be needed. Some researchers in the systematic review used Internet or telehealth-based programs for dietary education, exercise support, health information, and goal setting, for example, which could help with continuity of care during the COVID-19 pandemic. “These types of interventions may help overcome the obstacle of insufficient clinic time by separating the primary implementation phase from the traditional clinical setting,” she said.
While the evidence supports the implementation of these interventions, “additional work remains for clinicians and researchers to identify high-yield components and determine best practices for the delivery of GWG interventions,” she said.
“The success of this intervention will depend on improving resources for clinicians to facilitate provision of direct counseling or to refer patients to skilled professionals and explore novel alternatives. Promising innovative approaches such as the use of telehealth, technology-based delivery systems, and group prenatal care are under investigation and may expand the ability to successfully implement these recommendations and ultimately improve outcomes for pregnant persons and their infants,” Dr. LaCoursiere concluded.
This research was funded by contracts from the Agency for Healthcare Research and Quality and U.S. Department of Health and Human Services. The authors report no relevant conflict of interest.
FROM JAMA
The more drinking, the higher the risk of heart disease, especially in those genetically predisposed
Cardiovascular disease risk is associated with alcohol intake in general, but variations in risk exist with levels of intake, based on data from a genetic-based assessment of more than 300,000 individuals.
Previous studies have identified the “J-shaped model” of alcohol intake and cardiovascular disease, Kiran J. Biddinger of the Broad Institute, Cambridge, Mass., and colleagues said. The J-shaped model suggests that light alcohol intake, defined as one to two drinks per day, appears to reduce cardiovascular disease risk, while heavy alcohol intake, defined as about five drinks per day, increases cardiovascular disease risk, Mr. Biddenger said. However, most studies of the association between alcohol and cardiovascular disease risk are observational, and subject to confounders such as the impact of healthy lifestyle behaviors.
To better assess causality, the researchers used a genetics technique known as Mendelian randomization.
“Some individuals are genetically predisposed to drink more alcohol than others, based on the random allocation of alleles,” he explained. This genetic risk should not be associated with confounding variables such as vegetable consumption or physical activity.
In a study presented at the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health meeting, sponsored by the American Heart Association, the researchers analyzed genetic and lifestyle data from 371,463 participants in the U.K. Biobank, a population-based study of more than 500,000 individuals in the United Kingdom. The researchers used traditional and nonlinear genetic approaches to assess causality between alcohol consumption and cardiovascular disease.
Overall, study participants averaged 9.2 drinks per week. A total of 121,708 (32.8%) had hypertension, and 27,667 (7.5%) had coronary artery disease. The researchers found that individuals who consumed light to moderate amounts of alcohol also lived healthier lifestyles, and had a lower body mass index and higher levels of physical activity than did those who abstained from alcohol. Light to moderate drinkers also had higher vegetable consumption, lower red meat consumption, were less likely to smoke, and had higher self-reported overall health ratings, compared with abstainers.
The researchers then applied Mendelian randomization analyses, creating a genetic proxy and finding that individuals who were predisposed to drink more alcohol had a higher risk of cardiovascular disease.
Traditional and nonlinear Mendelian randomization using quadratic associations showed consistently increased risk of cardiovascular disease with increased alcohol consumption, and this risk increased dramatically for the heaviest drinkers. Compared with individuals who abstained, alcohol consumption of 7, 14, 21, and 28 drinks per week was associated, respectively, with 1.2-, 1.7-, 3.4-, and 8.9-fold odds of hypertension, and 1.2-, 2.3-, 6.2-, and 25.9-fold odds of coronary artery disease.
Notably, an increase of one standard deviation in genetic predisposition for alcohol consumption was associated with a 1.28-fold increase in hypertension, as well as significantly increased risk of coronary artery disease (odds ratio, 1.38), MI (OR, 1.37), stroke (OR, 1.26), heart failure (OR, 1.34), and atrial fibrillation (OR, 1.24).
The study findings were limited by several factors, including the inability to detect specific benefits associated with moderate alcohol consumption. However, the results suggest that, although all amounts of alcohol intake convey some increase in cardiovascular disease risk, “recommendations around alcohol use should reflect this nuanced relationship,” Mr. Biddinger said.
Distinctive study design supports association
Studies examining the association of alcohol consumption with cardiovascular (CVD) outcomes have been mostly observational in nature because of ethical considerations, Anna Kucharska-Newton, PhD, of the University of North Carolina at Chapel Hill, said in an interview. “Results of those studies have not been conclusive, and more research is needed. This study takes advantage of the ‘natural experiment’ of the randomized distribution of genetic variants associated with alcohol consumption,” said Dr. Kucharska-Newton, who served as moderator for the session at the meeting when the study was presented. “This method is similar to a randomized clinical trial and as such is less subject to confounding and potential reverse causality than an observational study..
“The findings confirm data from previous studies, including published data based on the UK Biobank study and the FinnGen registry of genetic data,” said Dr. Kucharska-Newton. “Findings from that study are largely supportive, suggesting that alcohol intake is associated with increased risk of coronary artery disease, an association that is sustained following adjustment for smoking.
“What the present study adds is an elegant presentation of the nonlinearity in that association. However, in contrast to the earlier study that included participants who reported drinking 1-2 drinks per week, Mr. Biddinger and colleagues examined effects among those drinking 7-28 drinks per week, making generalization to light to moderate drinkers [the majority] difficult,” she noted.
As for clinical implications, “assessment of habitual drinking is an important element in routine clinical care.” Dr. Kucharska-Newton noted. “Alcohol intake of seven or more drinks per week is associated exponentially with increased risk of coronary artery disease and, as other data suggest, increased levels of CVD risk factors. Therefore, CVD risk factor control is of particular importance in this population.
“Additional research in populations of ancestry other than White European is very much needed,” Dr. Kucharska-Newton emphasized. “Replication of the analyses presented by Mr. Biddinger and colleagues in different cohorts would strengthen inferences from this study. Extension of study findings to clinically manifest CVD would provide more relevant take-home messages. However, prior studies, based on Mendelian randomization protocols, suggest that adjustment for lifestyle factors attenuates the association of alcohol intake with adverse clinical CVD outcomes.”
Mr. Biddinger had no financial conflicts to disclose, but several coauthors disclosed relationships with companies including Novartis, Regeneron, Bayer, Quest Diagnostics, Corvidia, Pfizer, Verve Therapeutics, and Medgenome. Dr. Kucharska-Newton had no financial conflicts to disclose.
Cardiovascular disease risk is associated with alcohol intake in general, but variations in risk exist with levels of intake, based on data from a genetic-based assessment of more than 300,000 individuals.
Previous studies have identified the “J-shaped model” of alcohol intake and cardiovascular disease, Kiran J. Biddinger of the Broad Institute, Cambridge, Mass., and colleagues said. The J-shaped model suggests that light alcohol intake, defined as one to two drinks per day, appears to reduce cardiovascular disease risk, while heavy alcohol intake, defined as about five drinks per day, increases cardiovascular disease risk, Mr. Biddenger said. However, most studies of the association between alcohol and cardiovascular disease risk are observational, and subject to confounders such as the impact of healthy lifestyle behaviors.
To better assess causality, the researchers used a genetics technique known as Mendelian randomization.
“Some individuals are genetically predisposed to drink more alcohol than others, based on the random allocation of alleles,” he explained. This genetic risk should not be associated with confounding variables such as vegetable consumption or physical activity.
In a study presented at the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health meeting, sponsored by the American Heart Association, the researchers analyzed genetic and lifestyle data from 371,463 participants in the U.K. Biobank, a population-based study of more than 500,000 individuals in the United Kingdom. The researchers used traditional and nonlinear genetic approaches to assess causality between alcohol consumption and cardiovascular disease.
Overall, study participants averaged 9.2 drinks per week. A total of 121,708 (32.8%) had hypertension, and 27,667 (7.5%) had coronary artery disease. The researchers found that individuals who consumed light to moderate amounts of alcohol also lived healthier lifestyles, and had a lower body mass index and higher levels of physical activity than did those who abstained from alcohol. Light to moderate drinkers also had higher vegetable consumption, lower red meat consumption, were less likely to smoke, and had higher self-reported overall health ratings, compared with abstainers.
The researchers then applied Mendelian randomization analyses, creating a genetic proxy and finding that individuals who were predisposed to drink more alcohol had a higher risk of cardiovascular disease.
Traditional and nonlinear Mendelian randomization using quadratic associations showed consistently increased risk of cardiovascular disease with increased alcohol consumption, and this risk increased dramatically for the heaviest drinkers. Compared with individuals who abstained, alcohol consumption of 7, 14, 21, and 28 drinks per week was associated, respectively, with 1.2-, 1.7-, 3.4-, and 8.9-fold odds of hypertension, and 1.2-, 2.3-, 6.2-, and 25.9-fold odds of coronary artery disease.
Notably, an increase of one standard deviation in genetic predisposition for alcohol consumption was associated with a 1.28-fold increase in hypertension, as well as significantly increased risk of coronary artery disease (odds ratio, 1.38), MI (OR, 1.37), stroke (OR, 1.26), heart failure (OR, 1.34), and atrial fibrillation (OR, 1.24).
The study findings were limited by several factors, including the inability to detect specific benefits associated with moderate alcohol consumption. However, the results suggest that, although all amounts of alcohol intake convey some increase in cardiovascular disease risk, “recommendations around alcohol use should reflect this nuanced relationship,” Mr. Biddinger said.
Distinctive study design supports association
Studies examining the association of alcohol consumption with cardiovascular (CVD) outcomes have been mostly observational in nature because of ethical considerations, Anna Kucharska-Newton, PhD, of the University of North Carolina at Chapel Hill, said in an interview. “Results of those studies have not been conclusive, and more research is needed. This study takes advantage of the ‘natural experiment’ of the randomized distribution of genetic variants associated with alcohol consumption,” said Dr. Kucharska-Newton, who served as moderator for the session at the meeting when the study was presented. “This method is similar to a randomized clinical trial and as such is less subject to confounding and potential reverse causality than an observational study..
“The findings confirm data from previous studies, including published data based on the UK Biobank study and the FinnGen registry of genetic data,” said Dr. Kucharska-Newton. “Findings from that study are largely supportive, suggesting that alcohol intake is associated with increased risk of coronary artery disease, an association that is sustained following adjustment for smoking.
“What the present study adds is an elegant presentation of the nonlinearity in that association. However, in contrast to the earlier study that included participants who reported drinking 1-2 drinks per week, Mr. Biddinger and colleagues examined effects among those drinking 7-28 drinks per week, making generalization to light to moderate drinkers [the majority] difficult,” she noted.
As for clinical implications, “assessment of habitual drinking is an important element in routine clinical care.” Dr. Kucharska-Newton noted. “Alcohol intake of seven or more drinks per week is associated exponentially with increased risk of coronary artery disease and, as other data suggest, increased levels of CVD risk factors. Therefore, CVD risk factor control is of particular importance in this population.
“Additional research in populations of ancestry other than White European is very much needed,” Dr. Kucharska-Newton emphasized. “Replication of the analyses presented by Mr. Biddinger and colleagues in different cohorts would strengthen inferences from this study. Extension of study findings to clinically manifest CVD would provide more relevant take-home messages. However, prior studies, based on Mendelian randomization protocols, suggest that adjustment for lifestyle factors attenuates the association of alcohol intake with adverse clinical CVD outcomes.”
Mr. Biddinger had no financial conflicts to disclose, but several coauthors disclosed relationships with companies including Novartis, Regeneron, Bayer, Quest Diagnostics, Corvidia, Pfizer, Verve Therapeutics, and Medgenome. Dr. Kucharska-Newton had no financial conflicts to disclose.
Cardiovascular disease risk is associated with alcohol intake in general, but variations in risk exist with levels of intake, based on data from a genetic-based assessment of more than 300,000 individuals.
Previous studies have identified the “J-shaped model” of alcohol intake and cardiovascular disease, Kiran J. Biddinger of the Broad Institute, Cambridge, Mass., and colleagues said. The J-shaped model suggests that light alcohol intake, defined as one to two drinks per day, appears to reduce cardiovascular disease risk, while heavy alcohol intake, defined as about five drinks per day, increases cardiovascular disease risk, Mr. Biddenger said. However, most studies of the association between alcohol and cardiovascular disease risk are observational, and subject to confounders such as the impact of healthy lifestyle behaviors.
To better assess causality, the researchers used a genetics technique known as Mendelian randomization.
“Some individuals are genetically predisposed to drink more alcohol than others, based on the random allocation of alleles,” he explained. This genetic risk should not be associated with confounding variables such as vegetable consumption or physical activity.
In a study presented at the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health meeting, sponsored by the American Heart Association, the researchers analyzed genetic and lifestyle data from 371,463 participants in the U.K. Biobank, a population-based study of more than 500,000 individuals in the United Kingdom. The researchers used traditional and nonlinear genetic approaches to assess causality between alcohol consumption and cardiovascular disease.
Overall, study participants averaged 9.2 drinks per week. A total of 121,708 (32.8%) had hypertension, and 27,667 (7.5%) had coronary artery disease. The researchers found that individuals who consumed light to moderate amounts of alcohol also lived healthier lifestyles, and had a lower body mass index and higher levels of physical activity than did those who abstained from alcohol. Light to moderate drinkers also had higher vegetable consumption, lower red meat consumption, were less likely to smoke, and had higher self-reported overall health ratings, compared with abstainers.
The researchers then applied Mendelian randomization analyses, creating a genetic proxy and finding that individuals who were predisposed to drink more alcohol had a higher risk of cardiovascular disease.
Traditional and nonlinear Mendelian randomization using quadratic associations showed consistently increased risk of cardiovascular disease with increased alcohol consumption, and this risk increased dramatically for the heaviest drinkers. Compared with individuals who abstained, alcohol consumption of 7, 14, 21, and 28 drinks per week was associated, respectively, with 1.2-, 1.7-, 3.4-, and 8.9-fold odds of hypertension, and 1.2-, 2.3-, 6.2-, and 25.9-fold odds of coronary artery disease.
Notably, an increase of one standard deviation in genetic predisposition for alcohol consumption was associated with a 1.28-fold increase in hypertension, as well as significantly increased risk of coronary artery disease (odds ratio, 1.38), MI (OR, 1.37), stroke (OR, 1.26), heart failure (OR, 1.34), and atrial fibrillation (OR, 1.24).
The study findings were limited by several factors, including the inability to detect specific benefits associated with moderate alcohol consumption. However, the results suggest that, although all amounts of alcohol intake convey some increase in cardiovascular disease risk, “recommendations around alcohol use should reflect this nuanced relationship,” Mr. Biddinger said.
Distinctive study design supports association
Studies examining the association of alcohol consumption with cardiovascular (CVD) outcomes have been mostly observational in nature because of ethical considerations, Anna Kucharska-Newton, PhD, of the University of North Carolina at Chapel Hill, said in an interview. “Results of those studies have not been conclusive, and more research is needed. This study takes advantage of the ‘natural experiment’ of the randomized distribution of genetic variants associated with alcohol consumption,” said Dr. Kucharska-Newton, who served as moderator for the session at the meeting when the study was presented. “This method is similar to a randomized clinical trial and as such is less subject to confounding and potential reverse causality than an observational study..
“The findings confirm data from previous studies, including published data based on the UK Biobank study and the FinnGen registry of genetic data,” said Dr. Kucharska-Newton. “Findings from that study are largely supportive, suggesting that alcohol intake is associated with increased risk of coronary artery disease, an association that is sustained following adjustment for smoking.
“What the present study adds is an elegant presentation of the nonlinearity in that association. However, in contrast to the earlier study that included participants who reported drinking 1-2 drinks per week, Mr. Biddinger and colleagues examined effects among those drinking 7-28 drinks per week, making generalization to light to moderate drinkers [the majority] difficult,” she noted.
As for clinical implications, “assessment of habitual drinking is an important element in routine clinical care.” Dr. Kucharska-Newton noted. “Alcohol intake of seven or more drinks per week is associated exponentially with increased risk of coronary artery disease and, as other data suggest, increased levels of CVD risk factors. Therefore, CVD risk factor control is of particular importance in this population.
“Additional research in populations of ancestry other than White European is very much needed,” Dr. Kucharska-Newton emphasized. “Replication of the analyses presented by Mr. Biddinger and colleagues in different cohorts would strengthen inferences from this study. Extension of study findings to clinically manifest CVD would provide more relevant take-home messages. However, prior studies, based on Mendelian randomization protocols, suggest that adjustment for lifestyle factors attenuates the association of alcohol intake with adverse clinical CVD outcomes.”
Mr. Biddinger had no financial conflicts to disclose, but several coauthors disclosed relationships with companies including Novartis, Regeneron, Bayer, Quest Diagnostics, Corvidia, Pfizer, Verve Therapeutics, and Medgenome. Dr. Kucharska-Newton had no financial conflicts to disclose.
FROM EPI LIFESTYLE
Decision making regarding LEEP versus cone biopsy for excision of cervical dysplasia
Loop electrosurgical excision procedure (LEEP) or cold knife conization of the cervix (CKC) is the standard of care approach for women with cervical intra-epithelial neoplasia (CIN 3) because it achieves both disease control and diagnostic evaluation to rule out invasive carcinoma. While both techniques are associated with equivalent efficacy in disease control, each has its virtues and advantages, and clinical judgment is necessary when choosing a technique.1
LEEP, or large loop electrosurgical excision of the transformation zone (LLETZ) involves use of electrosurgical current directed through wire loops to excise pieces of cervical tissue. The equipment for this technique is widely available and this procedure can most often be performed safely and comfortably in an outpatient office setting, making it a cost-effective strategy. Its ease of access means that it can be employed in “see-and-treat” programs where there is concern regarding follow-up. The loop from the device has a tendency to take more shallow pieces of tissue, preserving more cervical stroma. This may be why LEEP has been associated with decreased risk for obstetric complications associated with cervical insufficiency when compared with CKC.2,3
The shallowness and standardized, preset shapes of the loops present challenges with this technique. It can be more difficult to tailor the shape of the excision for particular lesions, and surgeons may need to add a second “top hat” endocervical LEEP after the first ectocervical excision to adequately excise the endocervical canal. If the “coagulation” setting is used instead of “blend” or “cut,” excessive drag and resistance can develop during the procedure, which can result in the specimen’s being amputated, fragmented, or interrupted mid-sweep. This can severely limit pathologic interpretation of the specimen. Orienting these multiple fragments for pathology to specify margin status can be limited or impossible. Electrosurgical effect (“thermal effect”) at the margins of the specimen can limit accurate interpretation of adequacy of the excision.
CKC of the cervix is a procedure in which a narrow scalpel (typically an 11-blade) is used to excise the ecto- and endocervical tissues in a cone-shaped specimen that ensures maximal inclusion of ectocervical and endocervical mucosa but minimization of stromal excision. Absence of electrosurgery in the primary excision means that pathologists have clean edges to evaluate for margin status. Because the shape of the incision is unique for each patient, the surgeon can tailor the shape and extent of the cone to focus on known or suspected areas of disease. It is particularly useful when there is an endocervical lesion, such as in cases of adenocarcinoma in situ and in postmenopausal women whose transformation zone is frequently within the canal. In cases of a distorted, atrophic cervix, or one that is flush with the vagina, a conization procedure in the operating room affords surgeons greater control and precision. Major limitations of this procedure are that it is typically performed in an operating room setting because of the potential for intraoperative bleeding, and its increased risk for early and late complications. The conization procedure is associated with increased obstetric risk in later pregnancies, possibly because of more significant disturbance of cervical stroma.2,3
As mentioned earlier, both procedures are associated with equivalent outcomes with respect to control of disease.1 CKC procedures are associated with more complications, including bleeding (intraoperatively and postoperatively) than are LEEPs. Traditionally, adenocarcinoma in situ (AIS) has been preferentially treated with CKC because of the propensity of this lesion to reside within the endocervical canal, a region more readily and extensively sampled with the CKC. However, provided that the LEEP specimen achieves negative margin status, there is no specific benefit of CKC over LEEP. Guidelines recommend that AIS is excised as a single specimen (without a “top hat”) to achieve accurate pathology regarding margins in the endocervical canal.4 Considering that a specimen depth between 10 and 20 mm is ideal in the setting of AIS, it may be difficult to achieve this depth with a single-pass LEEP depending upon the dimensions of the cervix. It is due to these technical challenges associated with LEEP that CKC is typically preferred in the treatment of AIS.
Ultimately, the decision regarding when to choose LEEP versus CKC is nuanced and should be tailored for each patient. Factors to consider include the patient’s ease of follow-up, financial limitations, preexisting distortion of anatomy, and the need to minimize obstetrics risks or achieve wider margins. For example, a young, nulliparous patient with an ectocervical lesion of squamous dysplasia would likely best be served by a LEEP, which preserves her cervical stroma and affords her easy access and affordability of the procedure. A patient with a bleeding diathesis including iatrogenic anticoagulant therapy may also benefit from a LEEP to achieve better hemostasis and lower risk of bleeding complications.
A postmenopausal woman with a narrow upper vagina and cervix flush with the vagina from prior excisional procedures may benefit from a conization in the operating room where adequate retraction and exposure can minimize the risk of damage to adjacent structures, and the shape and size of the excision can be tailored to the long, narrow segment that is indicated. The table highlights some of the factors to consider when choosing these options. 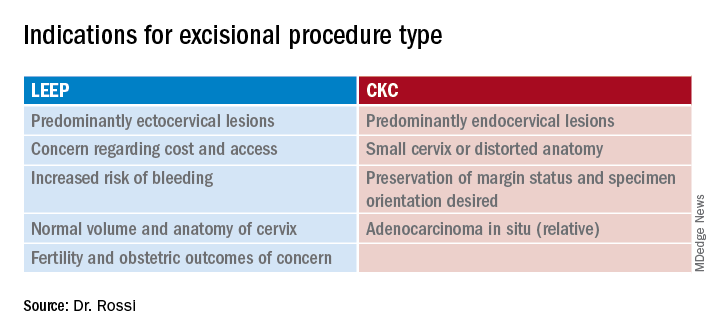
In summary, LEEP and CKC are both highly effective excisional procedures that can be considered for all patients with cervical dysplasia. Decisions regarding which is preferred for patients are nuanced and should consider individualized anatomic, pathologic, functional and financial implications.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest. Contact her at [email protected].
References
1. Martin-Hirsch PL et al. Cochrane Database Syst Rev 2000;(2):CD001318.
2. Arbyn M et al. BMJ. 2008;337:a1284.
3. Jin G et al. Arch Gynecol Obstet. 2014 Jan;289(1):85-99.
4. Perkins RB et al. J Low Genit Tract Dis. 2020;24(2):102.
Loop electrosurgical excision procedure (LEEP) or cold knife conization of the cervix (CKC) is the standard of care approach for women with cervical intra-epithelial neoplasia (CIN 3) because it achieves both disease control and diagnostic evaluation to rule out invasive carcinoma. While both techniques are associated with equivalent efficacy in disease control, each has its virtues and advantages, and clinical judgment is necessary when choosing a technique.1
LEEP, or large loop electrosurgical excision of the transformation zone (LLETZ) involves use of electrosurgical current directed through wire loops to excise pieces of cervical tissue. The equipment for this technique is widely available and this procedure can most often be performed safely and comfortably in an outpatient office setting, making it a cost-effective strategy. Its ease of access means that it can be employed in “see-and-treat” programs where there is concern regarding follow-up. The loop from the device has a tendency to take more shallow pieces of tissue, preserving more cervical stroma. This may be why LEEP has been associated with decreased risk for obstetric complications associated with cervical insufficiency when compared with CKC.2,3
The shallowness and standardized, preset shapes of the loops present challenges with this technique. It can be more difficult to tailor the shape of the excision for particular lesions, and surgeons may need to add a second “top hat” endocervical LEEP after the first ectocervical excision to adequately excise the endocervical canal. If the “coagulation” setting is used instead of “blend” or “cut,” excessive drag and resistance can develop during the procedure, which can result in the specimen’s being amputated, fragmented, or interrupted mid-sweep. This can severely limit pathologic interpretation of the specimen. Orienting these multiple fragments for pathology to specify margin status can be limited or impossible. Electrosurgical effect (“thermal effect”) at the margins of the specimen can limit accurate interpretation of adequacy of the excision.
CKC of the cervix is a procedure in which a narrow scalpel (typically an 11-blade) is used to excise the ecto- and endocervical tissues in a cone-shaped specimen that ensures maximal inclusion of ectocervical and endocervical mucosa but minimization of stromal excision. Absence of electrosurgery in the primary excision means that pathologists have clean edges to evaluate for margin status. Because the shape of the incision is unique for each patient, the surgeon can tailor the shape and extent of the cone to focus on known or suspected areas of disease. It is particularly useful when there is an endocervical lesion, such as in cases of adenocarcinoma in situ and in postmenopausal women whose transformation zone is frequently within the canal. In cases of a distorted, atrophic cervix, or one that is flush with the vagina, a conization procedure in the operating room affords surgeons greater control and precision. Major limitations of this procedure are that it is typically performed in an operating room setting because of the potential for intraoperative bleeding, and its increased risk for early and late complications. The conization procedure is associated with increased obstetric risk in later pregnancies, possibly because of more significant disturbance of cervical stroma.2,3
As mentioned earlier, both procedures are associated with equivalent outcomes with respect to control of disease.1 CKC procedures are associated with more complications, including bleeding (intraoperatively and postoperatively) than are LEEPs. Traditionally, adenocarcinoma in situ (AIS) has been preferentially treated with CKC because of the propensity of this lesion to reside within the endocervical canal, a region more readily and extensively sampled with the CKC. However, provided that the LEEP specimen achieves negative margin status, there is no specific benefit of CKC over LEEP. Guidelines recommend that AIS is excised as a single specimen (without a “top hat”) to achieve accurate pathology regarding margins in the endocervical canal.4 Considering that a specimen depth between 10 and 20 mm is ideal in the setting of AIS, it may be difficult to achieve this depth with a single-pass LEEP depending upon the dimensions of the cervix. It is due to these technical challenges associated with LEEP that CKC is typically preferred in the treatment of AIS.
Ultimately, the decision regarding when to choose LEEP versus CKC is nuanced and should be tailored for each patient. Factors to consider include the patient’s ease of follow-up, financial limitations, preexisting distortion of anatomy, and the need to minimize obstetrics risks or achieve wider margins. For example, a young, nulliparous patient with an ectocervical lesion of squamous dysplasia would likely best be served by a LEEP, which preserves her cervical stroma and affords her easy access and affordability of the procedure. A patient with a bleeding diathesis including iatrogenic anticoagulant therapy may also benefit from a LEEP to achieve better hemostasis and lower risk of bleeding complications.
A postmenopausal woman with a narrow upper vagina and cervix flush with the vagina from prior excisional procedures may benefit from a conization in the operating room where adequate retraction and exposure can minimize the risk of damage to adjacent structures, and the shape and size of the excision can be tailored to the long, narrow segment that is indicated. The table highlights some of the factors to consider when choosing these options. 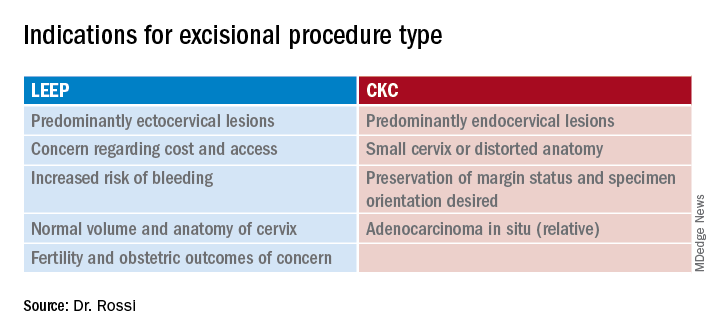
In summary, LEEP and CKC are both highly effective excisional procedures that can be considered for all patients with cervical dysplasia. Decisions regarding which is preferred for patients are nuanced and should consider individualized anatomic, pathologic, functional and financial implications.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest. Contact her at [email protected].
References
1. Martin-Hirsch PL et al. Cochrane Database Syst Rev 2000;(2):CD001318.
2. Arbyn M et al. BMJ. 2008;337:a1284.
3. Jin G et al. Arch Gynecol Obstet. 2014 Jan;289(1):85-99.
4. Perkins RB et al. J Low Genit Tract Dis. 2020;24(2):102.
Loop electrosurgical excision procedure (LEEP) or cold knife conization of the cervix (CKC) is the standard of care approach for women with cervical intra-epithelial neoplasia (CIN 3) because it achieves both disease control and diagnostic evaluation to rule out invasive carcinoma. While both techniques are associated with equivalent efficacy in disease control, each has its virtues and advantages, and clinical judgment is necessary when choosing a technique.1
LEEP, or large loop electrosurgical excision of the transformation zone (LLETZ) involves use of electrosurgical current directed through wire loops to excise pieces of cervical tissue. The equipment for this technique is widely available and this procedure can most often be performed safely and comfortably in an outpatient office setting, making it a cost-effective strategy. Its ease of access means that it can be employed in “see-and-treat” programs where there is concern regarding follow-up. The loop from the device has a tendency to take more shallow pieces of tissue, preserving more cervical stroma. This may be why LEEP has been associated with decreased risk for obstetric complications associated with cervical insufficiency when compared with CKC.2,3
The shallowness and standardized, preset shapes of the loops present challenges with this technique. It can be more difficult to tailor the shape of the excision for particular lesions, and surgeons may need to add a second “top hat” endocervical LEEP after the first ectocervical excision to adequately excise the endocervical canal. If the “coagulation” setting is used instead of “blend” or “cut,” excessive drag and resistance can develop during the procedure, which can result in the specimen’s being amputated, fragmented, or interrupted mid-sweep. This can severely limit pathologic interpretation of the specimen. Orienting these multiple fragments for pathology to specify margin status can be limited or impossible. Electrosurgical effect (“thermal effect”) at the margins of the specimen can limit accurate interpretation of adequacy of the excision.
CKC of the cervix is a procedure in which a narrow scalpel (typically an 11-blade) is used to excise the ecto- and endocervical tissues in a cone-shaped specimen that ensures maximal inclusion of ectocervical and endocervical mucosa but minimization of stromal excision. Absence of electrosurgery in the primary excision means that pathologists have clean edges to evaluate for margin status. Because the shape of the incision is unique for each patient, the surgeon can tailor the shape and extent of the cone to focus on known or suspected areas of disease. It is particularly useful when there is an endocervical lesion, such as in cases of adenocarcinoma in situ and in postmenopausal women whose transformation zone is frequently within the canal. In cases of a distorted, atrophic cervix, or one that is flush with the vagina, a conization procedure in the operating room affords surgeons greater control and precision. Major limitations of this procedure are that it is typically performed in an operating room setting because of the potential for intraoperative bleeding, and its increased risk for early and late complications. The conization procedure is associated with increased obstetric risk in later pregnancies, possibly because of more significant disturbance of cervical stroma.2,3
As mentioned earlier, both procedures are associated with equivalent outcomes with respect to control of disease.1 CKC procedures are associated with more complications, including bleeding (intraoperatively and postoperatively) than are LEEPs. Traditionally, adenocarcinoma in situ (AIS) has been preferentially treated with CKC because of the propensity of this lesion to reside within the endocervical canal, a region more readily and extensively sampled with the CKC. However, provided that the LEEP specimen achieves negative margin status, there is no specific benefit of CKC over LEEP. Guidelines recommend that AIS is excised as a single specimen (without a “top hat”) to achieve accurate pathology regarding margins in the endocervical canal.4 Considering that a specimen depth between 10 and 20 mm is ideal in the setting of AIS, it may be difficult to achieve this depth with a single-pass LEEP depending upon the dimensions of the cervix. It is due to these technical challenges associated with LEEP that CKC is typically preferred in the treatment of AIS.
Ultimately, the decision regarding when to choose LEEP versus CKC is nuanced and should be tailored for each patient. Factors to consider include the patient’s ease of follow-up, financial limitations, preexisting distortion of anatomy, and the need to minimize obstetrics risks or achieve wider margins. For example, a young, nulliparous patient with an ectocervical lesion of squamous dysplasia would likely best be served by a LEEP, which preserves her cervical stroma and affords her easy access and affordability of the procedure. A patient with a bleeding diathesis including iatrogenic anticoagulant therapy may also benefit from a LEEP to achieve better hemostasis and lower risk of bleeding complications.
A postmenopausal woman with a narrow upper vagina and cervix flush with the vagina from prior excisional procedures may benefit from a conization in the operating room where adequate retraction and exposure can minimize the risk of damage to adjacent structures, and the shape and size of the excision can be tailored to the long, narrow segment that is indicated. The table highlights some of the factors to consider when choosing these options. 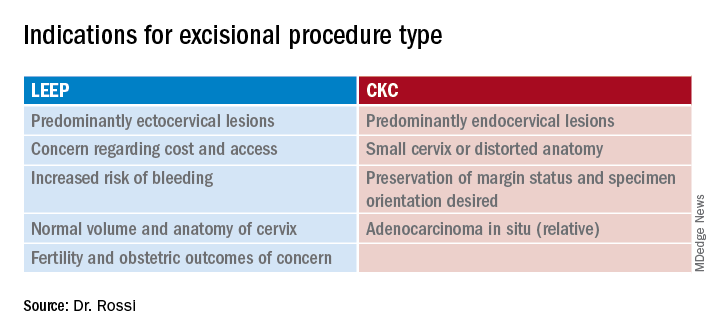
In summary, LEEP and CKC are both highly effective excisional procedures that can be considered for all patients with cervical dysplasia. Decisions regarding which is preferred for patients are nuanced and should consider individualized anatomic, pathologic, functional and financial implications.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest. Contact her at [email protected].
References
1. Martin-Hirsch PL et al. Cochrane Database Syst Rev 2000;(2):CD001318.
2. Arbyn M et al. BMJ. 2008;337:a1284.
3. Jin G et al. Arch Gynecol Obstet. 2014 Jan;289(1):85-99.
4. Perkins RB et al. J Low Genit Tract Dis. 2020;24(2):102.
Adversity accelerates aging at early ages, now measurable in real-time
Adversity in early life – whether preterm birth or socioeconomic disadvantage in childhood – accelerates aging, according to two recent studies, but underlying mechanisms remain unclear, and methods of investigation continue to evolve.
While one study used an established epigenetic clock to measure biological age among adults with extremely low birth weight, the other showcased a relatively new tool to measure pace of biological aging in disadvantaged children, suggesting that the metric may one day serve as a real-time measure of interventional efficacy.
These findings build upon previous studies that have demonstrated a correlation between biological age, also known as methylation age, and an increased risk of health problems later in life, according to Daniel A. Notterman, MD, professor of molecular biology at Princeton (N.J.) University.
“Finding that a person’s methylation age is greater than their chronological age has been taken as evidence of increased ‘biological age’ and perhaps a tendency to greater future morbidity,” Dr. Notterman wrote in a Pediatrics editorial. “Indeed, methylation age is advanced in association with a number of childhood and midlife adversities as well as morbidities such as atherosclerosis, cancer, and obesity.”
Extremely low birth weight associated with faster aging in men
For some individuals, accelerated biological aging begins at birth, or even in utero, according to Ryan J. Van Lieshout, MD, PhD, Canada Research Chair in the Perinatal Programming of Mental Disorders and the Albert Einstein/Irving Zucker Chair in Neuroscience at McMaster University, Hamilton, Ont., and colleagues.
The investigators conducted a study involving 45 extremely low birth weight (ELBW) survivors and 49 individuals born at normal birth weight. All participants were drawn from a longitudinal study conducted between 1977 and 1982 that assessed advances in neonatal intensive care. Controls were recruited at 8 years of age and matched with ELBW survivors based on family socioeconomic status, sex, and age. Follow-up continued through adulthood, allowing for the present trial to compare data from ages 8, 30, and 35.
Using samples of buccal epithelial cells, the investigators measured biological age with the Horvath epigenetic clock, the most commonly used tool of its kind, which measures cytosine-5 methylation at 353 cytosine-phosphate-guanine sites. Results were adjusted for a variety of covariates, such as smoking status, body mass index, number of chronic health conditions, and others.
Between groups, ELBW survivors trended toward older biological age, compared with adults born at normal birth weight (29.0 vs. 27.9 years), a difference that was not statistically significant. Further analysis, however, showed a significant sex-based difference between groups: Male survivors of ELBW, in adulthood, were almost 5 years biologically older than men born at normal birth weight (31.4 vs. 26.9 years; P = .01).
“[W]e provide preliminary evidence of a new link between ELBW and accelerated biological aging among men,” the investigators concluded.
In an accompanying editorial, Pam Factor-Litvak, PhD, vice chair of epidemiology at Columbia University, New York, wrote, “The findings are intriguing and open many questions for further study.”
Dr. Factor-Litvak noted that it remains unclear whether differences in biological aging were present at birth.
“[D]ifferences would provide evidence that accelerated aging begins during the in utero period, perhaps because of maternal undernutrition, stress, or another exposure,” Dr. Factor-Litvak wrote. “[R]eductions in chronic stress levels, which may begin for neonates with ELBW in utero and in the first hours of life, may provide an opportunity for interventions,” she added.
According to Calvin J. Hobel, MD, professor of pediatrics at Cedars-Sinai and professor of obstetrics and gynecology at University of California, Los Angeles, who has been studying preterm birth for more than 40 years, interventions may need to begin even earlier.
“The only way to prevent preterm birth is to do it before women get pregnant,” Dr. Hobel said in an interview. “The reason for preterm birth and poor fetal growth is the fact that the mother has early cardiovascular disease – unrecognized.”
Compared with women who give birth to full-term infants, women who give birth to preterm infants typically have increased blood pressure, Dr. Hobel said. Although these elevations in blood pressure are generally asymptomatic and not high enough to be classified as hypertensive, they impact umbilical artery vascular resistance starting at 28 weeks of gestation.
“In utero, [preterm infants] are programmed for increased vascular resistance and increased risk of cardiovascular disease,” Dr. Hobel said.
Regarding the effects of ELBW in men versus women, Dr. Hobel suggested that dissimilar neuroendocrine systems between sexes may protect females from adverse outcomes, although exact mechanisms remain elusive.
Measuring the impact of socioeconomic status on biological aging, now in real-time
A second study, by Laurel Raffington, PhD, of the University of Texas at Austin, and colleagues, evaluated the relationship between socioeconomic disadvantage in childhood and pace of biological aging.
To do so, they used the DunedinPoAm DNA methylation algorithm, a relatively new tool that was developed by analyzing changes in organ system integrity over time among adults with the same chronological age.
“Whereas epigenetic clocks quantify the amount of aging that has already occurred up to the time of measurement, DunedinPoAm quantifies how fast an individual is aging,” Dr. Raffington and colleagues wrote. “In other words, whereas epigenetic clocks tell you what time it is, pace-of-aging measures tell you how fast the clock is ticking.”
The investigators measured pace of aging in 600 children and adolescents (8-18 years of age) from the Texas Twin Project, “an ongoing longitudinal study that includes the collection of salivary samples.” The final dataset included 457 participants who identified as White, 77 who identified as Latinx, and 61 who identified as both White and Latinx.
The investigators evaluated pace of aging compared with family-level and neighborhood-level socioeconomic status, and tested for confounding by tobacco exposure, BMI, and pubertal development.
This analysis revealed that children experiencing socioeconomic disadvantage were aging more quickly than their peers, in terms of both family-level and neighborhood-level inequity (both levels, r = 0.18; P = .001).
Children who identified as Latinx aged faster than did those who identified as White only or White and Latinx, “consistent with higher levels of disadvantage in this group,” the investigators wrote. “Thus, our findings are consistent with observations that racial and/or ethnic socioeconomic disparities are an important contributor to racial and/or ethnic disparities in health.”
Higher BMI, greater tobacco exposure, and more advanced pubertal development were also associated with more rapid aging. After adjustment for these covariates, however, the significant correlation between socioeconomic disadvantage and rapid aging remained, the investigators noted.
“Our results suggest that salivary DNA methylation measures of pace of aging may provide a surrogate or intermediate endpoint for understanding the health impacts of [childhood] interventions,” the investigators concluded. “Such applications may prove particularly useful for evaluating the effectiveness of health-promoting interventions in at-risk groups.”
Still, more work is needed to understand exactly how socioeconomic disadvantage is associated with accelerated aging.
“Ultimately, not only longitudinal repeated-measures studies but also natural experiment studies and randomized controlled trials of social programs are needed to establish causal effects of social disadvantage on DunedinPoAm-measured pace of aging and to establish DunedinPoAm as a mediator of the process through which childhood disadvantage leads to aging-related health conditions,” the investigators wrote.
In his editorial, Dr. Notterman emphasized this point.
“[I]t is worth remembering that associations with either methylation age or pace of aging and health or longevity may represent the effect of an exposure on both the measure and the outcome of interest rather than a causal pathway that runs from the exposure (low socioeconomic status, adversity) to health outcome (i.e., cancer, vascular disease),” he wrote.
Paul Chung, MD, professor and chair of health systems science at Kaiser Permanente Bernard J. Tyson School of Medicine, Pasadena, Calif., and adjunct professor at the University of California, Los Angeles, called the findings “preliminary,” but noted that confirmation through further research could “fill in some really important gaps.
“Right now, to some degree, we’re at a little bit of an impasse,” Dr. Chung said.
Adverse childhood experiences are “associated very strongly” with mental and physical health issues, Dr. Chung said, “but we don’t know exactly why, and because of that, it’s really hard to come up with social policy solutions that aren’t anything but extremely sort of blunt-ended. We just say, ‘Well, I guess you gotta fix everything.’ And it’s a hard place to be, I think, in the field.”
Although the present study doesn’t resolve this issue, Dr. Chung suggested that the findings “really open the door to a lot of really exciting research that could have a lot of impacts on practice and policy.”
“Sometimes the only way to get people to pay attention enough to generate the level of excitement that would allow you to even do these sorts of studies ... is to generate some initial exploratory data that makes people perk up their ears, and makes people go, ‘Hey, wow, maybe we should be looking into this.’ ”
The study by Dr. Raffington and colleagues was funded by the National Institutes of Health and the Jacobs Foundation, with additional support from the German Research Foundation, Russell Sage Foundation Biology and Social Science Grant, the Canadian Institute for Advanced Research Child and Brain Development Network, and others. The study by Dr. Lieshout and colleagues was supported by Canadian Institutes of Health Research. Dr. Factor-Litvak and Dr. Notterman reported funding from the National Institutes of Health. All of the investigators and interviewees reported no conflicts of interest.
Adversity in early life – whether preterm birth or socioeconomic disadvantage in childhood – accelerates aging, according to two recent studies, but underlying mechanisms remain unclear, and methods of investigation continue to evolve.
While one study used an established epigenetic clock to measure biological age among adults with extremely low birth weight, the other showcased a relatively new tool to measure pace of biological aging in disadvantaged children, suggesting that the metric may one day serve as a real-time measure of interventional efficacy.
These findings build upon previous studies that have demonstrated a correlation between biological age, also known as methylation age, and an increased risk of health problems later in life, according to Daniel A. Notterman, MD, professor of molecular biology at Princeton (N.J.) University.
“Finding that a person’s methylation age is greater than their chronological age has been taken as evidence of increased ‘biological age’ and perhaps a tendency to greater future morbidity,” Dr. Notterman wrote in a Pediatrics editorial. “Indeed, methylation age is advanced in association with a number of childhood and midlife adversities as well as morbidities such as atherosclerosis, cancer, and obesity.”
Extremely low birth weight associated with faster aging in men
For some individuals, accelerated biological aging begins at birth, or even in utero, according to Ryan J. Van Lieshout, MD, PhD, Canada Research Chair in the Perinatal Programming of Mental Disorders and the Albert Einstein/Irving Zucker Chair in Neuroscience at McMaster University, Hamilton, Ont., and colleagues.
The investigators conducted a study involving 45 extremely low birth weight (ELBW) survivors and 49 individuals born at normal birth weight. All participants were drawn from a longitudinal study conducted between 1977 and 1982 that assessed advances in neonatal intensive care. Controls were recruited at 8 years of age and matched with ELBW survivors based on family socioeconomic status, sex, and age. Follow-up continued through adulthood, allowing for the present trial to compare data from ages 8, 30, and 35.
Using samples of buccal epithelial cells, the investigators measured biological age with the Horvath epigenetic clock, the most commonly used tool of its kind, which measures cytosine-5 methylation at 353 cytosine-phosphate-guanine sites. Results were adjusted for a variety of covariates, such as smoking status, body mass index, number of chronic health conditions, and others.
Between groups, ELBW survivors trended toward older biological age, compared with adults born at normal birth weight (29.0 vs. 27.9 years), a difference that was not statistically significant. Further analysis, however, showed a significant sex-based difference between groups: Male survivors of ELBW, in adulthood, were almost 5 years biologically older than men born at normal birth weight (31.4 vs. 26.9 years; P = .01).
“[W]e provide preliminary evidence of a new link between ELBW and accelerated biological aging among men,” the investigators concluded.
In an accompanying editorial, Pam Factor-Litvak, PhD, vice chair of epidemiology at Columbia University, New York, wrote, “The findings are intriguing and open many questions for further study.”
Dr. Factor-Litvak noted that it remains unclear whether differences in biological aging were present at birth.
“[D]ifferences would provide evidence that accelerated aging begins during the in utero period, perhaps because of maternal undernutrition, stress, or another exposure,” Dr. Factor-Litvak wrote. “[R]eductions in chronic stress levels, which may begin for neonates with ELBW in utero and in the first hours of life, may provide an opportunity for interventions,” she added.
According to Calvin J. Hobel, MD, professor of pediatrics at Cedars-Sinai and professor of obstetrics and gynecology at University of California, Los Angeles, who has been studying preterm birth for more than 40 years, interventions may need to begin even earlier.
“The only way to prevent preterm birth is to do it before women get pregnant,” Dr. Hobel said in an interview. “The reason for preterm birth and poor fetal growth is the fact that the mother has early cardiovascular disease – unrecognized.”
Compared with women who give birth to full-term infants, women who give birth to preterm infants typically have increased blood pressure, Dr. Hobel said. Although these elevations in blood pressure are generally asymptomatic and not high enough to be classified as hypertensive, they impact umbilical artery vascular resistance starting at 28 weeks of gestation.
“In utero, [preterm infants] are programmed for increased vascular resistance and increased risk of cardiovascular disease,” Dr. Hobel said.
Regarding the effects of ELBW in men versus women, Dr. Hobel suggested that dissimilar neuroendocrine systems between sexes may protect females from adverse outcomes, although exact mechanisms remain elusive.
Measuring the impact of socioeconomic status on biological aging, now in real-time
A second study, by Laurel Raffington, PhD, of the University of Texas at Austin, and colleagues, evaluated the relationship between socioeconomic disadvantage in childhood and pace of biological aging.
To do so, they used the DunedinPoAm DNA methylation algorithm, a relatively new tool that was developed by analyzing changes in organ system integrity over time among adults with the same chronological age.
“Whereas epigenetic clocks quantify the amount of aging that has already occurred up to the time of measurement, DunedinPoAm quantifies how fast an individual is aging,” Dr. Raffington and colleagues wrote. “In other words, whereas epigenetic clocks tell you what time it is, pace-of-aging measures tell you how fast the clock is ticking.”
The investigators measured pace of aging in 600 children and adolescents (8-18 years of age) from the Texas Twin Project, “an ongoing longitudinal study that includes the collection of salivary samples.” The final dataset included 457 participants who identified as White, 77 who identified as Latinx, and 61 who identified as both White and Latinx.
The investigators evaluated pace of aging compared with family-level and neighborhood-level socioeconomic status, and tested for confounding by tobacco exposure, BMI, and pubertal development.
This analysis revealed that children experiencing socioeconomic disadvantage were aging more quickly than their peers, in terms of both family-level and neighborhood-level inequity (both levels, r = 0.18; P = .001).
Children who identified as Latinx aged faster than did those who identified as White only or White and Latinx, “consistent with higher levels of disadvantage in this group,” the investigators wrote. “Thus, our findings are consistent with observations that racial and/or ethnic socioeconomic disparities are an important contributor to racial and/or ethnic disparities in health.”
Higher BMI, greater tobacco exposure, and more advanced pubertal development were also associated with more rapid aging. After adjustment for these covariates, however, the significant correlation between socioeconomic disadvantage and rapid aging remained, the investigators noted.
“Our results suggest that salivary DNA methylation measures of pace of aging may provide a surrogate or intermediate endpoint for understanding the health impacts of [childhood] interventions,” the investigators concluded. “Such applications may prove particularly useful for evaluating the effectiveness of health-promoting interventions in at-risk groups.”
Still, more work is needed to understand exactly how socioeconomic disadvantage is associated with accelerated aging.
“Ultimately, not only longitudinal repeated-measures studies but also natural experiment studies and randomized controlled trials of social programs are needed to establish causal effects of social disadvantage on DunedinPoAm-measured pace of aging and to establish DunedinPoAm as a mediator of the process through which childhood disadvantage leads to aging-related health conditions,” the investigators wrote.
In his editorial, Dr. Notterman emphasized this point.
“[I]t is worth remembering that associations with either methylation age or pace of aging and health or longevity may represent the effect of an exposure on both the measure and the outcome of interest rather than a causal pathway that runs from the exposure (low socioeconomic status, adversity) to health outcome (i.e., cancer, vascular disease),” he wrote.
Paul Chung, MD, professor and chair of health systems science at Kaiser Permanente Bernard J. Tyson School of Medicine, Pasadena, Calif., and adjunct professor at the University of California, Los Angeles, called the findings “preliminary,” but noted that confirmation through further research could “fill in some really important gaps.
“Right now, to some degree, we’re at a little bit of an impasse,” Dr. Chung said.
Adverse childhood experiences are “associated very strongly” with mental and physical health issues, Dr. Chung said, “but we don’t know exactly why, and because of that, it’s really hard to come up with social policy solutions that aren’t anything but extremely sort of blunt-ended. We just say, ‘Well, I guess you gotta fix everything.’ And it’s a hard place to be, I think, in the field.”
Although the present study doesn’t resolve this issue, Dr. Chung suggested that the findings “really open the door to a lot of really exciting research that could have a lot of impacts on practice and policy.”
“Sometimes the only way to get people to pay attention enough to generate the level of excitement that would allow you to even do these sorts of studies ... is to generate some initial exploratory data that makes people perk up their ears, and makes people go, ‘Hey, wow, maybe we should be looking into this.’ ”
The study by Dr. Raffington and colleagues was funded by the National Institutes of Health and the Jacobs Foundation, with additional support from the German Research Foundation, Russell Sage Foundation Biology and Social Science Grant, the Canadian Institute for Advanced Research Child and Brain Development Network, and others. The study by Dr. Lieshout and colleagues was supported by Canadian Institutes of Health Research. Dr. Factor-Litvak and Dr. Notterman reported funding from the National Institutes of Health. All of the investigators and interviewees reported no conflicts of interest.
Adversity in early life – whether preterm birth or socioeconomic disadvantage in childhood – accelerates aging, according to two recent studies, but underlying mechanisms remain unclear, and methods of investigation continue to evolve.
While one study used an established epigenetic clock to measure biological age among adults with extremely low birth weight, the other showcased a relatively new tool to measure pace of biological aging in disadvantaged children, suggesting that the metric may one day serve as a real-time measure of interventional efficacy.
These findings build upon previous studies that have demonstrated a correlation between biological age, also known as methylation age, and an increased risk of health problems later in life, according to Daniel A. Notterman, MD, professor of molecular biology at Princeton (N.J.) University.
“Finding that a person’s methylation age is greater than their chronological age has been taken as evidence of increased ‘biological age’ and perhaps a tendency to greater future morbidity,” Dr. Notterman wrote in a Pediatrics editorial. “Indeed, methylation age is advanced in association with a number of childhood and midlife adversities as well as morbidities such as atherosclerosis, cancer, and obesity.”
Extremely low birth weight associated with faster aging in men
For some individuals, accelerated biological aging begins at birth, or even in utero, according to Ryan J. Van Lieshout, MD, PhD, Canada Research Chair in the Perinatal Programming of Mental Disorders and the Albert Einstein/Irving Zucker Chair in Neuroscience at McMaster University, Hamilton, Ont., and colleagues.
The investigators conducted a study involving 45 extremely low birth weight (ELBW) survivors and 49 individuals born at normal birth weight. All participants were drawn from a longitudinal study conducted between 1977 and 1982 that assessed advances in neonatal intensive care. Controls were recruited at 8 years of age and matched with ELBW survivors based on family socioeconomic status, sex, and age. Follow-up continued through adulthood, allowing for the present trial to compare data from ages 8, 30, and 35.
Using samples of buccal epithelial cells, the investigators measured biological age with the Horvath epigenetic clock, the most commonly used tool of its kind, which measures cytosine-5 methylation at 353 cytosine-phosphate-guanine sites. Results were adjusted for a variety of covariates, such as smoking status, body mass index, number of chronic health conditions, and others.
Between groups, ELBW survivors trended toward older biological age, compared with adults born at normal birth weight (29.0 vs. 27.9 years), a difference that was not statistically significant. Further analysis, however, showed a significant sex-based difference between groups: Male survivors of ELBW, in adulthood, were almost 5 years biologically older than men born at normal birth weight (31.4 vs. 26.9 years; P = .01).
“[W]e provide preliminary evidence of a new link between ELBW and accelerated biological aging among men,” the investigators concluded.
In an accompanying editorial, Pam Factor-Litvak, PhD, vice chair of epidemiology at Columbia University, New York, wrote, “The findings are intriguing and open many questions for further study.”
Dr. Factor-Litvak noted that it remains unclear whether differences in biological aging were present at birth.
“[D]ifferences would provide evidence that accelerated aging begins during the in utero period, perhaps because of maternal undernutrition, stress, or another exposure,” Dr. Factor-Litvak wrote. “[R]eductions in chronic stress levels, which may begin for neonates with ELBW in utero and in the first hours of life, may provide an opportunity for interventions,” she added.
According to Calvin J. Hobel, MD, professor of pediatrics at Cedars-Sinai and professor of obstetrics and gynecology at University of California, Los Angeles, who has been studying preterm birth for more than 40 years, interventions may need to begin even earlier.
“The only way to prevent preterm birth is to do it before women get pregnant,” Dr. Hobel said in an interview. “The reason for preterm birth and poor fetal growth is the fact that the mother has early cardiovascular disease – unrecognized.”
Compared with women who give birth to full-term infants, women who give birth to preterm infants typically have increased blood pressure, Dr. Hobel said. Although these elevations in blood pressure are generally asymptomatic and not high enough to be classified as hypertensive, they impact umbilical artery vascular resistance starting at 28 weeks of gestation.
“In utero, [preterm infants] are programmed for increased vascular resistance and increased risk of cardiovascular disease,” Dr. Hobel said.
Regarding the effects of ELBW in men versus women, Dr. Hobel suggested that dissimilar neuroendocrine systems between sexes may protect females from adverse outcomes, although exact mechanisms remain elusive.
Measuring the impact of socioeconomic status on biological aging, now in real-time
A second study, by Laurel Raffington, PhD, of the University of Texas at Austin, and colleagues, evaluated the relationship between socioeconomic disadvantage in childhood and pace of biological aging.
To do so, they used the DunedinPoAm DNA methylation algorithm, a relatively new tool that was developed by analyzing changes in organ system integrity over time among adults with the same chronological age.
“Whereas epigenetic clocks quantify the amount of aging that has already occurred up to the time of measurement, DunedinPoAm quantifies how fast an individual is aging,” Dr. Raffington and colleagues wrote. “In other words, whereas epigenetic clocks tell you what time it is, pace-of-aging measures tell you how fast the clock is ticking.”
The investigators measured pace of aging in 600 children and adolescents (8-18 years of age) from the Texas Twin Project, “an ongoing longitudinal study that includes the collection of salivary samples.” The final dataset included 457 participants who identified as White, 77 who identified as Latinx, and 61 who identified as both White and Latinx.
The investigators evaluated pace of aging compared with family-level and neighborhood-level socioeconomic status, and tested for confounding by tobacco exposure, BMI, and pubertal development.
This analysis revealed that children experiencing socioeconomic disadvantage were aging more quickly than their peers, in terms of both family-level and neighborhood-level inequity (both levels, r = 0.18; P = .001).
Children who identified as Latinx aged faster than did those who identified as White only or White and Latinx, “consistent with higher levels of disadvantage in this group,” the investigators wrote. “Thus, our findings are consistent with observations that racial and/or ethnic socioeconomic disparities are an important contributor to racial and/or ethnic disparities in health.”
Higher BMI, greater tobacco exposure, and more advanced pubertal development were also associated with more rapid aging. After adjustment for these covariates, however, the significant correlation between socioeconomic disadvantage and rapid aging remained, the investigators noted.
“Our results suggest that salivary DNA methylation measures of pace of aging may provide a surrogate or intermediate endpoint for understanding the health impacts of [childhood] interventions,” the investigators concluded. “Such applications may prove particularly useful for evaluating the effectiveness of health-promoting interventions in at-risk groups.”
Still, more work is needed to understand exactly how socioeconomic disadvantage is associated with accelerated aging.
“Ultimately, not only longitudinal repeated-measures studies but also natural experiment studies and randomized controlled trials of social programs are needed to establish causal effects of social disadvantage on DunedinPoAm-measured pace of aging and to establish DunedinPoAm as a mediator of the process through which childhood disadvantage leads to aging-related health conditions,” the investigators wrote.
In his editorial, Dr. Notterman emphasized this point.
“[I]t is worth remembering that associations with either methylation age or pace of aging and health or longevity may represent the effect of an exposure on both the measure and the outcome of interest rather than a causal pathway that runs from the exposure (low socioeconomic status, adversity) to health outcome (i.e., cancer, vascular disease),” he wrote.
Paul Chung, MD, professor and chair of health systems science at Kaiser Permanente Bernard J. Tyson School of Medicine, Pasadena, Calif., and adjunct professor at the University of California, Los Angeles, called the findings “preliminary,” but noted that confirmation through further research could “fill in some really important gaps.
“Right now, to some degree, we’re at a little bit of an impasse,” Dr. Chung said.
Adverse childhood experiences are “associated very strongly” with mental and physical health issues, Dr. Chung said, “but we don’t know exactly why, and because of that, it’s really hard to come up with social policy solutions that aren’t anything but extremely sort of blunt-ended. We just say, ‘Well, I guess you gotta fix everything.’ And it’s a hard place to be, I think, in the field.”
Although the present study doesn’t resolve this issue, Dr. Chung suggested that the findings “really open the door to a lot of really exciting research that could have a lot of impacts on practice and policy.”
“Sometimes the only way to get people to pay attention enough to generate the level of excitement that would allow you to even do these sorts of studies ... is to generate some initial exploratory data that makes people perk up their ears, and makes people go, ‘Hey, wow, maybe we should be looking into this.’ ”
The study by Dr. Raffington and colleagues was funded by the National Institutes of Health and the Jacobs Foundation, with additional support from the German Research Foundation, Russell Sage Foundation Biology and Social Science Grant, the Canadian Institute for Advanced Research Child and Brain Development Network, and others. The study by Dr. Lieshout and colleagues was supported by Canadian Institutes of Health Research. Dr. Factor-Litvak and Dr. Notterman reported funding from the National Institutes of Health. All of the investigators and interviewees reported no conflicts of interest.
FROM PEDIATRICS
COPD in younger adults deadlier than expected
Adults in their 30s, 40s and 50s with chronic obstructive pulmonary disease (COPD) experience significant morbidity and excess mortality from the disease, results of a population-based study show.
Among adults aged 35-55 years with COPD in Ontario in a longitudinal population cohort study, the overall mortality rate was fivefold higher, compared with other adults in the same age range without COPD.
In contrast, the mortality rate among adults 65 years and older with COPD was 2.5-fold higher than that of their peers without COPD, reported Alina J. Blazer, MSc, MD, a clinical and research fellow at the University of Toronto.
“Overall, our study has shown that younger adults with COPD experience significant morbidity, as evidence by their elevated rates of health care use and excess mortality from their disease. This study provides further evidence that so-called ‘early’ COPD is not a benign disease, and suggests that we should focus clinical efforts on identifying COPD in younger patients, in the hopes that earlier intervention may improve their current health, reduce resource utilization, and prevent further disease progression,” she said during a minisymposium at the American Thoracic Society’s virtual international conference (Abstract A1131).
COPD is widely regarded as a disease affecting only older adults, but it can also occur in those younger than 65, and although it is commonly assumed that COPD diagnosed earlier in life will be milder in severity, this assumption has not been fully explored in real-world settings, Dr. Blazer said.
She and her colleagues conducted a study to examine disease burden as measured by health services utilization and mortality among younger adults with COPD, and compared the rates with those of older adults with COPD.
The sample for this study included 194,759 adults with COPD aged 35-55 years in Ontario in 2016. COPD was identified from health administrative data for three or more outpatient claims or one or more hospitalization claims for COPD over a 2-year period.
For context, the data were compared with those for 496,2113 COPD patients aged 65 years and older.
They found that, compared with their peers without the disease, younger adults had a 3.1-fold higher rate of hospitalization for any cause, a 2.2-fold higher rate of all-cause ED visits, and a 1.7-fold higher rate of outpatient visits for any cause.
In contrast, the comparative rates for seniors with versus without COPD were 2.1-fold, 1.8-fold, and 1.4-fold, respectively.
As noted before, the mortality rate for younger adults with COPD was 5-fold higher than for those without COPD, compared with 2.5-fold among older adults with COPD versus those without.
Earlier diagnosis, follow-up
“A very important talk,” commented session comoderator Valerie Press, MD, MPH, from the University of Chicago. “I know that there’s a lot of work to be done in earlier diagnosis in general, and I think starting with the younger population is a really important area.”
She asked Dr. Blazer about the possibility of asthma codiagnosis or misdiagnosis in the younger patients.
“We use a very specific, validated case definition in the study that our group has used before, and the specificity is over 96% for physician-diagnosed COPD, at the expense of sensitivity, so if anything we probably underestimated the rate of COPD in our study,” Dr. Blazer said.
Audience member Sherry Rogers, MD, an allergist and immunologist in private practice in Syracuse, N.Y., asked whether the investigators could determine what proportion of the excess mortality they saw was attributable to COPD.
“This was looking at all-cause mortality, so we don’t know that it’s necessarily all attributable to COPD per se but perhaps also to COPD-attributable comorbidities,” Dr. Blazer said. “It would be important to piece out the actual causes of mortality that are contributing to that elevated [morality] in that population.”
She added that the next step could include examining rates of specialty referrals and pharmacotherapy to see whether younger patients with COPD are receiving appropriate care, and to ascertain how they are being followed.
The study was supported by the University of Toronto and Sunnybrook Research Institute. Dr. Blazer reported no conflicts of interest to disclose.
Adults in their 30s, 40s and 50s with chronic obstructive pulmonary disease (COPD) experience significant morbidity and excess mortality from the disease, results of a population-based study show.
Among adults aged 35-55 years with COPD in Ontario in a longitudinal population cohort study, the overall mortality rate was fivefold higher, compared with other adults in the same age range without COPD.
In contrast, the mortality rate among adults 65 years and older with COPD was 2.5-fold higher than that of their peers without COPD, reported Alina J. Blazer, MSc, MD, a clinical and research fellow at the University of Toronto.
“Overall, our study has shown that younger adults with COPD experience significant morbidity, as evidence by their elevated rates of health care use and excess mortality from their disease. This study provides further evidence that so-called ‘early’ COPD is not a benign disease, and suggests that we should focus clinical efforts on identifying COPD in younger patients, in the hopes that earlier intervention may improve their current health, reduce resource utilization, and prevent further disease progression,” she said during a minisymposium at the American Thoracic Society’s virtual international conference (Abstract A1131).
COPD is widely regarded as a disease affecting only older adults, but it can also occur in those younger than 65, and although it is commonly assumed that COPD diagnosed earlier in life will be milder in severity, this assumption has not been fully explored in real-world settings, Dr. Blazer said.
She and her colleagues conducted a study to examine disease burden as measured by health services utilization and mortality among younger adults with COPD, and compared the rates with those of older adults with COPD.
The sample for this study included 194,759 adults with COPD aged 35-55 years in Ontario in 2016. COPD was identified from health administrative data for three or more outpatient claims or one or more hospitalization claims for COPD over a 2-year period.
For context, the data were compared with those for 496,2113 COPD patients aged 65 years and older.
They found that, compared with their peers without the disease, younger adults had a 3.1-fold higher rate of hospitalization for any cause, a 2.2-fold higher rate of all-cause ED visits, and a 1.7-fold higher rate of outpatient visits for any cause.
In contrast, the comparative rates for seniors with versus without COPD were 2.1-fold, 1.8-fold, and 1.4-fold, respectively.
As noted before, the mortality rate for younger adults with COPD was 5-fold higher than for those without COPD, compared with 2.5-fold among older adults with COPD versus those without.
Earlier diagnosis, follow-up
“A very important talk,” commented session comoderator Valerie Press, MD, MPH, from the University of Chicago. “I know that there’s a lot of work to be done in earlier diagnosis in general, and I think starting with the younger population is a really important area.”
She asked Dr. Blazer about the possibility of asthma codiagnosis or misdiagnosis in the younger patients.
“We use a very specific, validated case definition in the study that our group has used before, and the specificity is over 96% for physician-diagnosed COPD, at the expense of sensitivity, so if anything we probably underestimated the rate of COPD in our study,” Dr. Blazer said.
Audience member Sherry Rogers, MD, an allergist and immunologist in private practice in Syracuse, N.Y., asked whether the investigators could determine what proportion of the excess mortality they saw was attributable to COPD.
“This was looking at all-cause mortality, so we don’t know that it’s necessarily all attributable to COPD per se but perhaps also to COPD-attributable comorbidities,” Dr. Blazer said. “It would be important to piece out the actual causes of mortality that are contributing to that elevated [morality] in that population.”
She added that the next step could include examining rates of specialty referrals and pharmacotherapy to see whether younger patients with COPD are receiving appropriate care, and to ascertain how they are being followed.
The study was supported by the University of Toronto and Sunnybrook Research Institute. Dr. Blazer reported no conflicts of interest to disclose.
Adults in their 30s, 40s and 50s with chronic obstructive pulmonary disease (COPD) experience significant morbidity and excess mortality from the disease, results of a population-based study show.
Among adults aged 35-55 years with COPD in Ontario in a longitudinal population cohort study, the overall mortality rate was fivefold higher, compared with other adults in the same age range without COPD.
In contrast, the mortality rate among adults 65 years and older with COPD was 2.5-fold higher than that of their peers without COPD, reported Alina J. Blazer, MSc, MD, a clinical and research fellow at the University of Toronto.
“Overall, our study has shown that younger adults with COPD experience significant morbidity, as evidence by their elevated rates of health care use and excess mortality from their disease. This study provides further evidence that so-called ‘early’ COPD is not a benign disease, and suggests that we should focus clinical efforts on identifying COPD in younger patients, in the hopes that earlier intervention may improve their current health, reduce resource utilization, and prevent further disease progression,” she said during a minisymposium at the American Thoracic Society’s virtual international conference (Abstract A1131).
COPD is widely regarded as a disease affecting only older adults, but it can also occur in those younger than 65, and although it is commonly assumed that COPD diagnosed earlier in life will be milder in severity, this assumption has not been fully explored in real-world settings, Dr. Blazer said.
She and her colleagues conducted a study to examine disease burden as measured by health services utilization and mortality among younger adults with COPD, and compared the rates with those of older adults with COPD.
The sample for this study included 194,759 adults with COPD aged 35-55 years in Ontario in 2016. COPD was identified from health administrative data for three or more outpatient claims or one or more hospitalization claims for COPD over a 2-year period.
For context, the data were compared with those for 496,2113 COPD patients aged 65 years and older.
They found that, compared with their peers without the disease, younger adults had a 3.1-fold higher rate of hospitalization for any cause, a 2.2-fold higher rate of all-cause ED visits, and a 1.7-fold higher rate of outpatient visits for any cause.
In contrast, the comparative rates for seniors with versus without COPD were 2.1-fold, 1.8-fold, and 1.4-fold, respectively.
As noted before, the mortality rate for younger adults with COPD was 5-fold higher than for those without COPD, compared with 2.5-fold among older adults with COPD versus those without.
Earlier diagnosis, follow-up
“A very important talk,” commented session comoderator Valerie Press, MD, MPH, from the University of Chicago. “I know that there’s a lot of work to be done in earlier diagnosis in general, and I think starting with the younger population is a really important area.”
She asked Dr. Blazer about the possibility of asthma codiagnosis or misdiagnosis in the younger patients.
“We use a very specific, validated case definition in the study that our group has used before, and the specificity is over 96% for physician-diagnosed COPD, at the expense of sensitivity, so if anything we probably underestimated the rate of COPD in our study,” Dr. Blazer said.
Audience member Sherry Rogers, MD, an allergist and immunologist in private practice in Syracuse, N.Y., asked whether the investigators could determine what proportion of the excess mortality they saw was attributable to COPD.
“This was looking at all-cause mortality, so we don’t know that it’s necessarily all attributable to COPD per se but perhaps also to COPD-attributable comorbidities,” Dr. Blazer said. “It would be important to piece out the actual causes of mortality that are contributing to that elevated [morality] in that population.”
She added that the next step could include examining rates of specialty referrals and pharmacotherapy to see whether younger patients with COPD are receiving appropriate care, and to ascertain how they are being followed.
The study was supported by the University of Toronto and Sunnybrook Research Institute. Dr. Blazer reported no conflicts of interest to disclose.
FROM ATS 2021