User login
Evolving strategies in sequencing for HER2+ MBC therapy
The landscape for therapies targeting HER2-positive metastatic breast cancer (MBC) has evolved rapidly in the past few years. In a 12-month window, the U.S. Food and Drug Administration approved four agents targeting human epidermal growth factor 2 (HER2)–positive MBC, starting with trastuzumab deruxtecan in December 2019, followed by neratinib and tucatinib a few months later, and margetuximab last December.
Although first-line therapy for the majority of patients continues to be the CLEOPATRA regimen — the monoclonal antibodies trastuzumab and pertuzumab plus a taxane, such as docetaxel or paclitaxel — .
“We have been really fortunate to see a number of highly effective new therapies approved for HER2-positive MBC in the past year, and this has given us even more options to offer our patients,” remarked Rita Nanda, MD, director of the Breast Oncology Program and associate professor of medicine at University of Chicago Medicine.
What considerations do experts weigh when sequencing HER2-positive MBC?
For Kelly McCann, MD, PhD, the order largely depends on balancing two factors: regimens that will provide the best efficacy in terms of patient survival and quality of life. “In the metastatic setting, I know I’m going to end up using all of the available medications one after the other, so the order that allows patients to continue living their best life for as long as possible is essential,” commented Dr. McCann, a hematologist/oncologist in the department of medicine at the David Geffen School of Medicine, University of California, Los Angeles.
A new second-line option?
Before the wave of drug approvals for metastatic HER2-positive disease last year, oncologists routinely looked to trastuzumab emtansine (T-DM1) as second-line therapy.
But tucatinib may also now be considered in the second-line setting, after results from the HER2CLIMB trial. The decision between tucatinib and T-DM1 largely comes down to the presence or absence of brain metastases.
“T-DM1 is well-tolerated, so it’s still my go-to in the second-line setting unless my patient has a brain metastasis, in which case I opt for tucatinib,” Dr. McCann noted, adding that the HER2-specific oral tyrosine kinase inhibitor (TKI) not only crosses the blood-brain barrier but is also effective in patients with untreated brain metastases.
In HER2CLIMB, tucatinib exhibited strong efficacy in patients with advanced HER2-positive disease, including those with previously treated or untreated brain metastases. The randomized controlled trial, which paired tucatinib with trastuzumab and capecitabine, showed median progression-free survival of 7.8 months in 410 patients with HER2-positive MBC compared with 5.6 months in the 202 patients receiving the placebo regimen. The tucatinib cohort showed an overall survival advantage compared with the placebo group (21.9 vs 17.4 months).
Perhaps the most notable finding occurred in patients with brain or central nervous system (CNS) involvement, which develops in as many as half of patients with HER-positive MBC and is associated with shorter survival. In the HER2CLIMB trial, median progression-free survival was 7.6 months in patients with brain metastases compared with 5.4 months in the placebo group.
A follow-up exploratory analysis, which focused on 291 patients with brain metastases, found that adding tucatinib reduced the risk for intracranial progression by two thirds and death by almost half. In patients with active brain metastases, median progression-free survival reached 9.5 months vs 4.1 months in the placebo group. Those with stable metastases also benefited from tucatinib, with median progression-free survival of 13.9 vs 5.6 months in the placebo group.
On the basis of the results, the authors concluded that this randomized trial was the first to demonstrate improvements in both CNS progression–free survival and overall survival in patients with HER2-positive MBC and brain metastases.
Evolving options in the third-line setting and after
For third-line therapy and beyond, oncologists have an array of newer agents to choose from alongside longer-standing options — which include trastuzumab plus lapatinib, trastuzumab or lapatinib plus capecitabine, as well as T-DM1, if not given as second-line therapy.
According to Dr. McCann, the antibody-drug conjugate trastuzumab deruxtecan has been a particularly exciting addition to third-line treatment. In the phase 2 DESTINY-01 trial, more than 60% of a heavily pretreated population showed an objective response to trastuzumab deruxtecan, with a median response duration of almost 15 months and a median progression-free survival of 16.4 months. Longer-term follow-up results, presented in December at the 2020 San Antonio Breast Cancer Symposium, revealed progression-free survival of 19.4 months and preliminary median overall survival of 24.6 months.
Neratinib, the second TKI to bridge the blood-brain barrier in HER2-positive disease, was also approved for third-line use; however, Sayeh Lavasani, MD, MS, said she is more likely to consider this agent later in the sequence, potentially in the fourth-line setting and beyond, given the more robust outcomes observed in the HER2CLIMB tucatinib trial.
“Neratinib improved progression-free survival and time to intervention for CNS metastasis but, unlike tucatinib, did not demonstrate an overall survival benefit,” remarked Dr. Lavasani, a medical oncologist at City of Hope, a comprehensive cancer center in Los Angeles County.
More specifically, the phase 3 NALA trial, which randomly assigned patients to receive neratinib plus capecitabine or lapatinib plus capecitabine, reported progression-free survival of 8.8 months in the neratinib group compared with 6.6 months in the control arm but no significant gains in overall survival (hazard ratio, 0.88; P = .2098).
The fourth recently approved drug, margetuximab, has not yet made a significant mark on sequencing decisions for Dr. McCann.
“Margetuximab could have been a potential game changer, but clinical trial results were underwhelming,” she said.
In the phase 3 randomized clinical SOPHIA trial, margetuximab plus chemotherapy prolonged median progression-free survival by just over 1 month compared with trastuzumab plus chemotherapy. Preliminary overall survival data showed a slight, but not significant, benefit in the margetuximab group (21.6 vs 19.8 months).
For Dr. Lavasani, the presence of brain metastases is the most important consideration when weighing sequencing options. “For some of my patients with HER2-positive MBC, it’s ultimately disease progression in the brain that takes their life,” she said.
Aside from CNS metastases, specific sequencing choices may vary on the basis of drug-related tolerance as well as patient preferences. “It is critical to get a patient’s input in treatment selection,” Dr. Nanda remarked. “Given the number of effective treatments for HER2-positive MBC and the lack of data to guide how to sequence these regimens, it is important to ask patients what their preferences are.”
Dr. McCann agreed, noting that “a patient with HER2-positive MBC typically has a life expectancy measured in years, which is also why sequencing should be influenced by quality of life considerations.”
Convenience, side-effect profile, and financial toxicity should factor into clinical decision-making, according to Dr. Nanda. Some patients may, for instance, prefer a combination of tucatinib, capecitabine, and trastuzumab over trastuzumab deruxtecan to avoid hair loss and the risk for interstitial lung disease, which has been reported in more than 13% of patients, whereas others may prefer trastuzumab deruxtecan to avoid the possibility of diarrhea.
Taxanes come with a high risk for infusion reactions — which occur in about 30% of patients — and can cause neuropathy as well as hair loss and severe gastrointestinal side effects. In first-line care, Dr. McCann typically stops the taxane at some point for toxicity reasons and continues with trastuzumab plus pertuzumab until disease progression.
Even with an array of new options for treating metastatic HER2-positive disease, ultimately drug resistance does occur, Dr. Lavasani cautioned. Several ongoing trials are exploring new combinations of existing drugs to see whether those variations move the needle on survival outcomes. The HER2CLIMB-04 trial, for instance, is pairing tucatinib with trastuzumab deruxtecan, whereas HER2CLIMB-02 is pairing tucatinib with T-DM1.
But given progress in drug development in just the past few years, Lisa A. Carey, MD, deputy director of Clinical Sciences at the University of North Carolina Lineberger Comprehensive Cancer Center in Chapel Hill, sees a promising future for treating metastatic HER2-positive disease. “There is so much going on in the HER2-positive MBC therapeutics space that almost every 6 months, oncologists have to regroup and reevaluate treatment and sequencing, which is a great position to be in,” Dr. Carey noted.
A version of this article first appeared on Medscape.com .
The landscape for therapies targeting HER2-positive metastatic breast cancer (MBC) has evolved rapidly in the past few years. In a 12-month window, the U.S. Food and Drug Administration approved four agents targeting human epidermal growth factor 2 (HER2)–positive MBC, starting with trastuzumab deruxtecan in December 2019, followed by neratinib and tucatinib a few months later, and margetuximab last December.
Although first-line therapy for the majority of patients continues to be the CLEOPATRA regimen — the monoclonal antibodies trastuzumab and pertuzumab plus a taxane, such as docetaxel or paclitaxel — .
“We have been really fortunate to see a number of highly effective new therapies approved for HER2-positive MBC in the past year, and this has given us even more options to offer our patients,” remarked Rita Nanda, MD, director of the Breast Oncology Program and associate professor of medicine at University of Chicago Medicine.
What considerations do experts weigh when sequencing HER2-positive MBC?
For Kelly McCann, MD, PhD, the order largely depends on balancing two factors: regimens that will provide the best efficacy in terms of patient survival and quality of life. “In the metastatic setting, I know I’m going to end up using all of the available medications one after the other, so the order that allows patients to continue living their best life for as long as possible is essential,” commented Dr. McCann, a hematologist/oncologist in the department of medicine at the David Geffen School of Medicine, University of California, Los Angeles.
A new second-line option?
Before the wave of drug approvals for metastatic HER2-positive disease last year, oncologists routinely looked to trastuzumab emtansine (T-DM1) as second-line therapy.
But tucatinib may also now be considered in the second-line setting, after results from the HER2CLIMB trial. The decision between tucatinib and T-DM1 largely comes down to the presence or absence of brain metastases.
“T-DM1 is well-tolerated, so it’s still my go-to in the second-line setting unless my patient has a brain metastasis, in which case I opt for tucatinib,” Dr. McCann noted, adding that the HER2-specific oral tyrosine kinase inhibitor (TKI) not only crosses the blood-brain barrier but is also effective in patients with untreated brain metastases.
In HER2CLIMB, tucatinib exhibited strong efficacy in patients with advanced HER2-positive disease, including those with previously treated or untreated brain metastases. The randomized controlled trial, which paired tucatinib with trastuzumab and capecitabine, showed median progression-free survival of 7.8 months in 410 patients with HER2-positive MBC compared with 5.6 months in the 202 patients receiving the placebo regimen. The tucatinib cohort showed an overall survival advantage compared with the placebo group (21.9 vs 17.4 months).
Perhaps the most notable finding occurred in patients with brain or central nervous system (CNS) involvement, which develops in as many as half of patients with HER-positive MBC and is associated with shorter survival. In the HER2CLIMB trial, median progression-free survival was 7.6 months in patients with brain metastases compared with 5.4 months in the placebo group.
A follow-up exploratory analysis, which focused on 291 patients with brain metastases, found that adding tucatinib reduced the risk for intracranial progression by two thirds and death by almost half. In patients with active brain metastases, median progression-free survival reached 9.5 months vs 4.1 months in the placebo group. Those with stable metastases also benefited from tucatinib, with median progression-free survival of 13.9 vs 5.6 months in the placebo group.
On the basis of the results, the authors concluded that this randomized trial was the first to demonstrate improvements in both CNS progression–free survival and overall survival in patients with HER2-positive MBC and brain metastases.
Evolving options in the third-line setting and after
For third-line therapy and beyond, oncologists have an array of newer agents to choose from alongside longer-standing options — which include trastuzumab plus lapatinib, trastuzumab or lapatinib plus capecitabine, as well as T-DM1, if not given as second-line therapy.
According to Dr. McCann, the antibody-drug conjugate trastuzumab deruxtecan has been a particularly exciting addition to third-line treatment. In the phase 2 DESTINY-01 trial, more than 60% of a heavily pretreated population showed an objective response to trastuzumab deruxtecan, with a median response duration of almost 15 months and a median progression-free survival of 16.4 months. Longer-term follow-up results, presented in December at the 2020 San Antonio Breast Cancer Symposium, revealed progression-free survival of 19.4 months and preliminary median overall survival of 24.6 months.
Neratinib, the second TKI to bridge the blood-brain barrier in HER2-positive disease, was also approved for third-line use; however, Sayeh Lavasani, MD, MS, said she is more likely to consider this agent later in the sequence, potentially in the fourth-line setting and beyond, given the more robust outcomes observed in the HER2CLIMB tucatinib trial.
“Neratinib improved progression-free survival and time to intervention for CNS metastasis but, unlike tucatinib, did not demonstrate an overall survival benefit,” remarked Dr. Lavasani, a medical oncologist at City of Hope, a comprehensive cancer center in Los Angeles County.
More specifically, the phase 3 NALA trial, which randomly assigned patients to receive neratinib plus capecitabine or lapatinib plus capecitabine, reported progression-free survival of 8.8 months in the neratinib group compared with 6.6 months in the control arm but no significant gains in overall survival (hazard ratio, 0.88; P = .2098).
The fourth recently approved drug, margetuximab, has not yet made a significant mark on sequencing decisions for Dr. McCann.
“Margetuximab could have been a potential game changer, but clinical trial results were underwhelming,” she said.
In the phase 3 randomized clinical SOPHIA trial, margetuximab plus chemotherapy prolonged median progression-free survival by just over 1 month compared with trastuzumab plus chemotherapy. Preliminary overall survival data showed a slight, but not significant, benefit in the margetuximab group (21.6 vs 19.8 months).
For Dr. Lavasani, the presence of brain metastases is the most important consideration when weighing sequencing options. “For some of my patients with HER2-positive MBC, it’s ultimately disease progression in the brain that takes their life,” she said.
Aside from CNS metastases, specific sequencing choices may vary on the basis of drug-related tolerance as well as patient preferences. “It is critical to get a patient’s input in treatment selection,” Dr. Nanda remarked. “Given the number of effective treatments for HER2-positive MBC and the lack of data to guide how to sequence these regimens, it is important to ask patients what their preferences are.”
Dr. McCann agreed, noting that “a patient with HER2-positive MBC typically has a life expectancy measured in years, which is also why sequencing should be influenced by quality of life considerations.”
Convenience, side-effect profile, and financial toxicity should factor into clinical decision-making, according to Dr. Nanda. Some patients may, for instance, prefer a combination of tucatinib, capecitabine, and trastuzumab over trastuzumab deruxtecan to avoid hair loss and the risk for interstitial lung disease, which has been reported in more than 13% of patients, whereas others may prefer trastuzumab deruxtecan to avoid the possibility of diarrhea.
Taxanes come with a high risk for infusion reactions — which occur in about 30% of patients — and can cause neuropathy as well as hair loss and severe gastrointestinal side effects. In first-line care, Dr. McCann typically stops the taxane at some point for toxicity reasons and continues with trastuzumab plus pertuzumab until disease progression.
Even with an array of new options for treating metastatic HER2-positive disease, ultimately drug resistance does occur, Dr. Lavasani cautioned. Several ongoing trials are exploring new combinations of existing drugs to see whether those variations move the needle on survival outcomes. The HER2CLIMB-04 trial, for instance, is pairing tucatinib with trastuzumab deruxtecan, whereas HER2CLIMB-02 is pairing tucatinib with T-DM1.
But given progress in drug development in just the past few years, Lisa A. Carey, MD, deputy director of Clinical Sciences at the University of North Carolina Lineberger Comprehensive Cancer Center in Chapel Hill, sees a promising future for treating metastatic HER2-positive disease. “There is so much going on in the HER2-positive MBC therapeutics space that almost every 6 months, oncologists have to regroup and reevaluate treatment and sequencing, which is a great position to be in,” Dr. Carey noted.
A version of this article first appeared on Medscape.com .
The landscape for therapies targeting HER2-positive metastatic breast cancer (MBC) has evolved rapidly in the past few years. In a 12-month window, the U.S. Food and Drug Administration approved four agents targeting human epidermal growth factor 2 (HER2)–positive MBC, starting with trastuzumab deruxtecan in December 2019, followed by neratinib and tucatinib a few months later, and margetuximab last December.
Although first-line therapy for the majority of patients continues to be the CLEOPATRA regimen — the monoclonal antibodies trastuzumab and pertuzumab plus a taxane, such as docetaxel or paclitaxel — .
“We have been really fortunate to see a number of highly effective new therapies approved for HER2-positive MBC in the past year, and this has given us even more options to offer our patients,” remarked Rita Nanda, MD, director of the Breast Oncology Program and associate professor of medicine at University of Chicago Medicine.
What considerations do experts weigh when sequencing HER2-positive MBC?
For Kelly McCann, MD, PhD, the order largely depends on balancing two factors: regimens that will provide the best efficacy in terms of patient survival and quality of life. “In the metastatic setting, I know I’m going to end up using all of the available medications one after the other, so the order that allows patients to continue living their best life for as long as possible is essential,” commented Dr. McCann, a hematologist/oncologist in the department of medicine at the David Geffen School of Medicine, University of California, Los Angeles.
A new second-line option?
Before the wave of drug approvals for metastatic HER2-positive disease last year, oncologists routinely looked to trastuzumab emtansine (T-DM1) as second-line therapy.
But tucatinib may also now be considered in the second-line setting, after results from the HER2CLIMB trial. The decision between tucatinib and T-DM1 largely comes down to the presence or absence of brain metastases.
“T-DM1 is well-tolerated, so it’s still my go-to in the second-line setting unless my patient has a brain metastasis, in which case I opt for tucatinib,” Dr. McCann noted, adding that the HER2-specific oral tyrosine kinase inhibitor (TKI) not only crosses the blood-brain barrier but is also effective in patients with untreated brain metastases.
In HER2CLIMB, tucatinib exhibited strong efficacy in patients with advanced HER2-positive disease, including those with previously treated or untreated brain metastases. The randomized controlled trial, which paired tucatinib with trastuzumab and capecitabine, showed median progression-free survival of 7.8 months in 410 patients with HER2-positive MBC compared with 5.6 months in the 202 patients receiving the placebo regimen. The tucatinib cohort showed an overall survival advantage compared with the placebo group (21.9 vs 17.4 months).
Perhaps the most notable finding occurred in patients with brain or central nervous system (CNS) involvement, which develops in as many as half of patients with HER-positive MBC and is associated with shorter survival. In the HER2CLIMB trial, median progression-free survival was 7.6 months in patients with brain metastases compared with 5.4 months in the placebo group.
A follow-up exploratory analysis, which focused on 291 patients with brain metastases, found that adding tucatinib reduced the risk for intracranial progression by two thirds and death by almost half. In patients with active brain metastases, median progression-free survival reached 9.5 months vs 4.1 months in the placebo group. Those with stable metastases also benefited from tucatinib, with median progression-free survival of 13.9 vs 5.6 months in the placebo group.
On the basis of the results, the authors concluded that this randomized trial was the first to demonstrate improvements in both CNS progression–free survival and overall survival in patients with HER2-positive MBC and brain metastases.
Evolving options in the third-line setting and after
For third-line therapy and beyond, oncologists have an array of newer agents to choose from alongside longer-standing options — which include trastuzumab plus lapatinib, trastuzumab or lapatinib plus capecitabine, as well as T-DM1, if not given as second-line therapy.
According to Dr. McCann, the antibody-drug conjugate trastuzumab deruxtecan has been a particularly exciting addition to third-line treatment. In the phase 2 DESTINY-01 trial, more than 60% of a heavily pretreated population showed an objective response to trastuzumab deruxtecan, with a median response duration of almost 15 months and a median progression-free survival of 16.4 months. Longer-term follow-up results, presented in December at the 2020 San Antonio Breast Cancer Symposium, revealed progression-free survival of 19.4 months and preliminary median overall survival of 24.6 months.
Neratinib, the second TKI to bridge the blood-brain barrier in HER2-positive disease, was also approved for third-line use; however, Sayeh Lavasani, MD, MS, said she is more likely to consider this agent later in the sequence, potentially in the fourth-line setting and beyond, given the more robust outcomes observed in the HER2CLIMB tucatinib trial.
“Neratinib improved progression-free survival and time to intervention for CNS metastasis but, unlike tucatinib, did not demonstrate an overall survival benefit,” remarked Dr. Lavasani, a medical oncologist at City of Hope, a comprehensive cancer center in Los Angeles County.
More specifically, the phase 3 NALA trial, which randomly assigned patients to receive neratinib plus capecitabine or lapatinib plus capecitabine, reported progression-free survival of 8.8 months in the neratinib group compared with 6.6 months in the control arm but no significant gains in overall survival (hazard ratio, 0.88; P = .2098).
The fourth recently approved drug, margetuximab, has not yet made a significant mark on sequencing decisions for Dr. McCann.
“Margetuximab could have been a potential game changer, but clinical trial results were underwhelming,” she said.
In the phase 3 randomized clinical SOPHIA trial, margetuximab plus chemotherapy prolonged median progression-free survival by just over 1 month compared with trastuzumab plus chemotherapy. Preliminary overall survival data showed a slight, but not significant, benefit in the margetuximab group (21.6 vs 19.8 months).
For Dr. Lavasani, the presence of brain metastases is the most important consideration when weighing sequencing options. “For some of my patients with HER2-positive MBC, it’s ultimately disease progression in the brain that takes their life,” she said.
Aside from CNS metastases, specific sequencing choices may vary on the basis of drug-related tolerance as well as patient preferences. “It is critical to get a patient’s input in treatment selection,” Dr. Nanda remarked. “Given the number of effective treatments for HER2-positive MBC and the lack of data to guide how to sequence these regimens, it is important to ask patients what their preferences are.”
Dr. McCann agreed, noting that “a patient with HER2-positive MBC typically has a life expectancy measured in years, which is also why sequencing should be influenced by quality of life considerations.”
Convenience, side-effect profile, and financial toxicity should factor into clinical decision-making, according to Dr. Nanda. Some patients may, for instance, prefer a combination of tucatinib, capecitabine, and trastuzumab over trastuzumab deruxtecan to avoid hair loss and the risk for interstitial lung disease, which has been reported in more than 13% of patients, whereas others may prefer trastuzumab deruxtecan to avoid the possibility of diarrhea.
Taxanes come with a high risk for infusion reactions — which occur in about 30% of patients — and can cause neuropathy as well as hair loss and severe gastrointestinal side effects. In first-line care, Dr. McCann typically stops the taxane at some point for toxicity reasons and continues with trastuzumab plus pertuzumab until disease progression.
Even with an array of new options for treating metastatic HER2-positive disease, ultimately drug resistance does occur, Dr. Lavasani cautioned. Several ongoing trials are exploring new combinations of existing drugs to see whether those variations move the needle on survival outcomes. The HER2CLIMB-04 trial, for instance, is pairing tucatinib with trastuzumab deruxtecan, whereas HER2CLIMB-02 is pairing tucatinib with T-DM1.
But given progress in drug development in just the past few years, Lisa A. Carey, MD, deputy director of Clinical Sciences at the University of North Carolina Lineberger Comprehensive Cancer Center in Chapel Hill, sees a promising future for treating metastatic HER2-positive disease. “There is so much going on in the HER2-positive MBC therapeutics space that almost every 6 months, oncologists have to regroup and reevaluate treatment and sequencing, which is a great position to be in,” Dr. Carey noted.
A version of this article first appeared on Medscape.com .
Patients with moderate COPD also benefit from triple therapy
The benefits of a triple fixed-dose inhaled corticosteroid, long-acting muscarinic antagonist, and long-acting beta2 agonist combination extend to patients with moderate as well as severe chronic obstructive pulmonary disease (COPD).
That’s according to investigators in the ETHOS (Efficacy and Safety of Triple Therapy in Obstructive Lung Disease) trial (NCT02465567).
In a subanalysis of data on patients with moderate COPD who were enrolled in the comparison trial, the single-inhaler combination of the inhaled corticosteroid (ICS) budesonide, the long-acting muscarinic antagonist (LAMA) glycopyrrolate, and the long-acting beta2 agonist (LABA) formoterol fumarate (BGF) showed benefits in terms of COPD exacerbations, lung function, symptoms, and quality-of-life compared with either of two dual therapy combinations (glycopyrrolate or budesonide with formoterol [GFF/BFF]).
“A moderate benefit:risk ratio was demonstrated in patients with moderate COPD, consistent with the results of the overall ETHOS population, indicating the results of the ETHOS study were not driven by patients with severe or very severe COPD,” wrote Gary T. Ferguson, MD, from the Pulmonary Research Institute of Southeast Michigan in Farmington Hills, and colleagues. Their poster was presented during the American Thoracic Society’s virtual international conference. (Abstract A2244).
As reported at ATS 2020, in the overall ETHOS population of 8,509 patients with moderate to very severe COPD the annual rate of moderate or severe COPD exacerbations was 1.08 and 1.07 for the triple combinations with 320-mcg and 160-mcg doses of budesonide, respectively, compared with 1.42 for glycopyrrolate-formoterol, and 1.24 for budesonide-formoterol.
, Klaus F. Rabe, MD, PhD, of LungenClinic Grosshansdorf and Christian-Albrechts University Kiel (Germany), and colleagues found.
Subanalysis details
At the 2021 iteration of ATS, ETHOS investigator Dr. Ferguson and colleagues reported results for 613 patients with moderate COPD assigned to BGF 320 mcg, 604 assigned to BGF 160 mcg, 596 assigned to GFF, and 614 randomized to BFF.
Baseline demographic and clinical characteristics were similar among the groups, including age, sex, smoking status, mean COPD Assessment Test (CAT) score, mean blood eosinophil count, ICS use at screening, exacerbations in the previous year, mean postbronchodilator forced expiratory volume in 1 second (FEV1) percentage of predicted, and mean postbronchodilator percentage reversibility.
A modified intention-to-treat (ITT) analysis showed that the rate of moderate or severe exacerbations over 52 weeks with BGF 320 mcg was 21% lower than with GFF (P = .0123), but only 4% lower than with BFF, a difference that was not statistically significant.
The BGF 160-mg dose was associated with a 30% reduction in exacerbations vs. GFF (P = .0002), and with a nonsignificant reduction of 15% compared with BFF.
There was a numerical but not statistically significant improvement from baseline at week 24 in morning pre-dose trough FEV1 between the BGF 320-mcg dose and GFF (difference 47 mL), and a significant improvement (90 mL) with BGF compared with BFF (P = .0006). The BGF 160-mcg dose was associated with a larger improvement (89 mL) compared with BFF (P = .0004) but not with GFF.
The FEV1 area under the curve (AUC) of receiver operating characteristics from 0 to 4 hours was superior with BGF at both doses compared with both GFF and BFF.
Patients who used BGF 320 mcg also used significantly less rescue medication over 24 weeks compared with patients who used GFF (P < .0001) or BFF (P = .0001). There were no significant differences in rescue medication use between the BGF 160-mg dose and either of the dual therapy combinations.
Time to clinically important deterioration – defined as a greater than 100 mL decrease in trough FEV1, or a 4 units increase in St. George’s Respiratory Questionnaire total score, or a treatment-emergent moderate/severe COPD exacerbation occurring up to week 52 – was significantly longer with the 320-mcg but not 160-mcg BGF dose compared with GFF (P = .0295) or BFF (P = .0172).
Safety
Treatment-emergent adverse events (TEAEs) occurred in about two-thirds of patients in each trial arm, although TEAEs related to study treatment were more common with the two triple-therapy combinations and with BFF than with GFF.
TEAEs leading to study discontinuation occurred in 5.5% of patients on BGF 320 mcg, 4% on BGF 160 mcg, 4.5% on GFF, and 3.2% on BFF.
Confirmed major adverse cardiovascular events occurred in 0.8% and 1.5% in the BGF 320- and 160-mcg groups, respectively, in 1.8% of patients in the GFF arm, and 1.5% in the BFF arm.
Confirmed pneumonia was seen in 2.6% of patients in each BGF arm, 2.2% in the GFF arm, and 3.6% in the BFF arm.
Selected population
In a comment, David Mannino, MD, medical director of the COPD Foundation, who was not involved in the study, noted that the enrollment criteria for ETHOS tended to skew the population toward patients with severe disease.
In the trial, all patients were receiving at least two inhaled maintenance therapies at the time of screening, and had a postbronchodilator ratio of FEV1 to forced vital capacity of less than 0.7, with a postbronchodilator FEV1 of 25%-65% of the predicted normal value. The patients all had a smoking history of at least 10 pack-years and a documented history of at least one moderate or severe COPD exacerbation in the year before screening.
“The question was whether they would see the same results in people with more moderate impairment, and the answer in this subanalysis is ‘yes.’ The findings weren’t identical between patients with severe and moderate disease, but there were similarities with what was seen in the overall ETHOS study,” he said.
The ETHOS Trial was supported by Pearl Therapeutics. Dr. Ferguson reported grants, personal fees, and nonfinancial support from AstraZeneca during the conduct of the study; and grants, fees, and nonfinancial support from Pearl and others. Dr. Mannino reports recruitment to an advisory board for AstraZeneca.
The benefits of a triple fixed-dose inhaled corticosteroid, long-acting muscarinic antagonist, and long-acting beta2 agonist combination extend to patients with moderate as well as severe chronic obstructive pulmonary disease (COPD).
That’s according to investigators in the ETHOS (Efficacy and Safety of Triple Therapy in Obstructive Lung Disease) trial (NCT02465567).
In a subanalysis of data on patients with moderate COPD who were enrolled in the comparison trial, the single-inhaler combination of the inhaled corticosteroid (ICS) budesonide, the long-acting muscarinic antagonist (LAMA) glycopyrrolate, and the long-acting beta2 agonist (LABA) formoterol fumarate (BGF) showed benefits in terms of COPD exacerbations, lung function, symptoms, and quality-of-life compared with either of two dual therapy combinations (glycopyrrolate or budesonide with formoterol [GFF/BFF]).
“A moderate benefit:risk ratio was demonstrated in patients with moderate COPD, consistent with the results of the overall ETHOS population, indicating the results of the ETHOS study were not driven by patients with severe or very severe COPD,” wrote Gary T. Ferguson, MD, from the Pulmonary Research Institute of Southeast Michigan in Farmington Hills, and colleagues. Their poster was presented during the American Thoracic Society’s virtual international conference. (Abstract A2244).
As reported at ATS 2020, in the overall ETHOS population of 8,509 patients with moderate to very severe COPD the annual rate of moderate or severe COPD exacerbations was 1.08 and 1.07 for the triple combinations with 320-mcg and 160-mcg doses of budesonide, respectively, compared with 1.42 for glycopyrrolate-formoterol, and 1.24 for budesonide-formoterol.
, Klaus F. Rabe, MD, PhD, of LungenClinic Grosshansdorf and Christian-Albrechts University Kiel (Germany), and colleagues found.
Subanalysis details
At the 2021 iteration of ATS, ETHOS investigator Dr. Ferguson and colleagues reported results for 613 patients with moderate COPD assigned to BGF 320 mcg, 604 assigned to BGF 160 mcg, 596 assigned to GFF, and 614 randomized to BFF.
Baseline demographic and clinical characteristics were similar among the groups, including age, sex, smoking status, mean COPD Assessment Test (CAT) score, mean blood eosinophil count, ICS use at screening, exacerbations in the previous year, mean postbronchodilator forced expiratory volume in 1 second (FEV1) percentage of predicted, and mean postbronchodilator percentage reversibility.
A modified intention-to-treat (ITT) analysis showed that the rate of moderate or severe exacerbations over 52 weeks with BGF 320 mcg was 21% lower than with GFF (P = .0123), but only 4% lower than with BFF, a difference that was not statistically significant.
The BGF 160-mg dose was associated with a 30% reduction in exacerbations vs. GFF (P = .0002), and with a nonsignificant reduction of 15% compared with BFF.
There was a numerical but not statistically significant improvement from baseline at week 24 in morning pre-dose trough FEV1 between the BGF 320-mcg dose and GFF (difference 47 mL), and a significant improvement (90 mL) with BGF compared with BFF (P = .0006). The BGF 160-mcg dose was associated with a larger improvement (89 mL) compared with BFF (P = .0004) but not with GFF.
The FEV1 area under the curve (AUC) of receiver operating characteristics from 0 to 4 hours was superior with BGF at both doses compared with both GFF and BFF.
Patients who used BGF 320 mcg also used significantly less rescue medication over 24 weeks compared with patients who used GFF (P < .0001) or BFF (P = .0001). There were no significant differences in rescue medication use between the BGF 160-mg dose and either of the dual therapy combinations.
Time to clinically important deterioration – defined as a greater than 100 mL decrease in trough FEV1, or a 4 units increase in St. George’s Respiratory Questionnaire total score, or a treatment-emergent moderate/severe COPD exacerbation occurring up to week 52 – was significantly longer with the 320-mcg but not 160-mcg BGF dose compared with GFF (P = .0295) or BFF (P = .0172).
Safety
Treatment-emergent adverse events (TEAEs) occurred in about two-thirds of patients in each trial arm, although TEAEs related to study treatment were more common with the two triple-therapy combinations and with BFF than with GFF.
TEAEs leading to study discontinuation occurred in 5.5% of patients on BGF 320 mcg, 4% on BGF 160 mcg, 4.5% on GFF, and 3.2% on BFF.
Confirmed major adverse cardiovascular events occurred in 0.8% and 1.5% in the BGF 320- and 160-mcg groups, respectively, in 1.8% of patients in the GFF arm, and 1.5% in the BFF arm.
Confirmed pneumonia was seen in 2.6% of patients in each BGF arm, 2.2% in the GFF arm, and 3.6% in the BFF arm.
Selected population
In a comment, David Mannino, MD, medical director of the COPD Foundation, who was not involved in the study, noted that the enrollment criteria for ETHOS tended to skew the population toward patients with severe disease.
In the trial, all patients were receiving at least two inhaled maintenance therapies at the time of screening, and had a postbronchodilator ratio of FEV1 to forced vital capacity of less than 0.7, with a postbronchodilator FEV1 of 25%-65% of the predicted normal value. The patients all had a smoking history of at least 10 pack-years and a documented history of at least one moderate or severe COPD exacerbation in the year before screening.
“The question was whether they would see the same results in people with more moderate impairment, and the answer in this subanalysis is ‘yes.’ The findings weren’t identical between patients with severe and moderate disease, but there were similarities with what was seen in the overall ETHOS study,” he said.
The ETHOS Trial was supported by Pearl Therapeutics. Dr. Ferguson reported grants, personal fees, and nonfinancial support from AstraZeneca during the conduct of the study; and grants, fees, and nonfinancial support from Pearl and others. Dr. Mannino reports recruitment to an advisory board for AstraZeneca.
The benefits of a triple fixed-dose inhaled corticosteroid, long-acting muscarinic antagonist, and long-acting beta2 agonist combination extend to patients with moderate as well as severe chronic obstructive pulmonary disease (COPD).
That’s according to investigators in the ETHOS (Efficacy and Safety of Triple Therapy in Obstructive Lung Disease) trial (NCT02465567).
In a subanalysis of data on patients with moderate COPD who were enrolled in the comparison trial, the single-inhaler combination of the inhaled corticosteroid (ICS) budesonide, the long-acting muscarinic antagonist (LAMA) glycopyrrolate, and the long-acting beta2 agonist (LABA) formoterol fumarate (BGF) showed benefits in terms of COPD exacerbations, lung function, symptoms, and quality-of-life compared with either of two dual therapy combinations (glycopyrrolate or budesonide with formoterol [GFF/BFF]).
“A moderate benefit:risk ratio was demonstrated in patients with moderate COPD, consistent with the results of the overall ETHOS population, indicating the results of the ETHOS study were not driven by patients with severe or very severe COPD,” wrote Gary T. Ferguson, MD, from the Pulmonary Research Institute of Southeast Michigan in Farmington Hills, and colleagues. Their poster was presented during the American Thoracic Society’s virtual international conference. (Abstract A2244).
As reported at ATS 2020, in the overall ETHOS population of 8,509 patients with moderate to very severe COPD the annual rate of moderate or severe COPD exacerbations was 1.08 and 1.07 for the triple combinations with 320-mcg and 160-mcg doses of budesonide, respectively, compared with 1.42 for glycopyrrolate-formoterol, and 1.24 for budesonide-formoterol.
, Klaus F. Rabe, MD, PhD, of LungenClinic Grosshansdorf and Christian-Albrechts University Kiel (Germany), and colleagues found.
Subanalysis details
At the 2021 iteration of ATS, ETHOS investigator Dr. Ferguson and colleagues reported results for 613 patients with moderate COPD assigned to BGF 320 mcg, 604 assigned to BGF 160 mcg, 596 assigned to GFF, and 614 randomized to BFF.
Baseline demographic and clinical characteristics were similar among the groups, including age, sex, smoking status, mean COPD Assessment Test (CAT) score, mean blood eosinophil count, ICS use at screening, exacerbations in the previous year, mean postbronchodilator forced expiratory volume in 1 second (FEV1) percentage of predicted, and mean postbronchodilator percentage reversibility.
A modified intention-to-treat (ITT) analysis showed that the rate of moderate or severe exacerbations over 52 weeks with BGF 320 mcg was 21% lower than with GFF (P = .0123), but only 4% lower than with BFF, a difference that was not statistically significant.
The BGF 160-mg dose was associated with a 30% reduction in exacerbations vs. GFF (P = .0002), and with a nonsignificant reduction of 15% compared with BFF.
There was a numerical but not statistically significant improvement from baseline at week 24 in morning pre-dose trough FEV1 between the BGF 320-mcg dose and GFF (difference 47 mL), and a significant improvement (90 mL) with BGF compared with BFF (P = .0006). The BGF 160-mcg dose was associated with a larger improvement (89 mL) compared with BFF (P = .0004) but not with GFF.
The FEV1 area under the curve (AUC) of receiver operating characteristics from 0 to 4 hours was superior with BGF at both doses compared with both GFF and BFF.
Patients who used BGF 320 mcg also used significantly less rescue medication over 24 weeks compared with patients who used GFF (P < .0001) or BFF (P = .0001). There were no significant differences in rescue medication use between the BGF 160-mg dose and either of the dual therapy combinations.
Time to clinically important deterioration – defined as a greater than 100 mL decrease in trough FEV1, or a 4 units increase in St. George’s Respiratory Questionnaire total score, or a treatment-emergent moderate/severe COPD exacerbation occurring up to week 52 – was significantly longer with the 320-mcg but not 160-mcg BGF dose compared with GFF (P = .0295) or BFF (P = .0172).
Safety
Treatment-emergent adverse events (TEAEs) occurred in about two-thirds of patients in each trial arm, although TEAEs related to study treatment were more common with the two triple-therapy combinations and with BFF than with GFF.
TEAEs leading to study discontinuation occurred in 5.5% of patients on BGF 320 mcg, 4% on BGF 160 mcg, 4.5% on GFF, and 3.2% on BFF.
Confirmed major adverse cardiovascular events occurred in 0.8% and 1.5% in the BGF 320- and 160-mcg groups, respectively, in 1.8% of patients in the GFF arm, and 1.5% in the BFF arm.
Confirmed pneumonia was seen in 2.6% of patients in each BGF arm, 2.2% in the GFF arm, and 3.6% in the BFF arm.
Selected population
In a comment, David Mannino, MD, medical director of the COPD Foundation, who was not involved in the study, noted that the enrollment criteria for ETHOS tended to skew the population toward patients with severe disease.
In the trial, all patients were receiving at least two inhaled maintenance therapies at the time of screening, and had a postbronchodilator ratio of FEV1 to forced vital capacity of less than 0.7, with a postbronchodilator FEV1 of 25%-65% of the predicted normal value. The patients all had a smoking history of at least 10 pack-years and a documented history of at least one moderate or severe COPD exacerbation in the year before screening.
“The question was whether they would see the same results in people with more moderate impairment, and the answer in this subanalysis is ‘yes.’ The findings weren’t identical between patients with severe and moderate disease, but there were similarities with what was seen in the overall ETHOS study,” he said.
The ETHOS Trial was supported by Pearl Therapeutics. Dr. Ferguson reported grants, personal fees, and nonfinancial support from AstraZeneca during the conduct of the study; and grants, fees, and nonfinancial support from Pearl and others. Dr. Mannino reports recruitment to an advisory board for AstraZeneca.
FROM ATS 2021
Benefit from cooling temps for cardiac arrest does not differ in randomized trial
The first randomized controlled trial to compare specific temperatures for therapeutic hypothermia in comatose survivors of out-of-hospital cardiac arrest showed no differences in major outcomes, according to a single-center, double-blind study.
In the CAPITAL-CHILL trial, cooling temperatures of 31° C and 34° C were compared to explore the hypothesis that a lower temperature would improve major outcomes, explained Michel Le May, MD.
No differences for the primary composite outcome of all-cause mortality or poor neurologic outcome at 180 days were observed, he reported at the annual scientific sessions of the American College of Cardiology.
The study was completed over a period of almost 7 years in patients presumed to have had an out-of-hospital cardiac arrest and who were unconscious when they reached a center affiliated with the Ottawa Heart Institute, where Dr. Le May directs the regional STEMI (ST-elevation myocardial infarction) program. The initial rhythm at the time of the cardiac arrest was not an entry criterion.
Of 389 patients enrolled, the intention-to-treat analysis included 184 randomized to a cooling temperature of 31° C group and 183 to a temperature of 34° C. The assigned target temperature, reached with an endovascular device, was known only by the managing nurses.
31° C and 34° C are equivalent
There was a small numerical disadvantage for the lower temperature assignment, but none reached statistical significance. This was true of the primary outcome (48.4% vs. 45.4% for the higher temperature) and its components of mortality (43.5% vs. 41.0%) and poor neurologic outcome (4.9% vs. 4.4%). Poor neurologic outcome was defined as a Disability Rating Scale score of greater than 5.
Deaths were most common in the early part of the 180-day follow-up in both arms. On a Kaplan-Meier survival graph, Dr. Le May showed curves that he characterized as “almost superimposable.”
There were no significant differences for any subgroup stratifications, such as age 75 years or older versus younger, males versus females, presence versus absence or an initial shockable rhythm, percutaneous coronary intervention (PCI) within 24 hours versus later, and STEMI versus non-STEMI. In these analyses, the higher temperature was associated with a potential trend for benefit among females and those with a shockable rhythm.
There was no signal for a difference in neurologic outcomes on the Disability Rating Scale or the Modified Rankin Scale. On the latter, for example, 46% of those in the 31° C group and 44% of these in the 34° C group had a score of four or greater at the end of follow-up.
The baseline characteristics of the two groups were similar. About 80% were male; the average age was roughly 62 years. More than 80% of the cardiac arrests were witnessed with CPR being administered by bystanders in nearly 70%. Nearly 40% had a STEMI.
Interventions were similar. Almost all patients underwent coronary angiography, of which nearly 60% received a percutaneous coronary intervention. More than 50% received a stent. The time from arrest to randomization was slightly longer in the 31° C group (228 vs. 204 minutes). The time to balloon inflation from arrival at the cardiac center was also slightly longer (73 vs. 60 minutes).
There was a trend for an increased rate of seizures in the 31° C group (12.5% vs. 7.1%; P = .08), but other secondary outcomes, including pneumonia (67.8% vs. 63.4%), renal replacement therapy (9.2% vs. 9.3%), and stroke (4.4% vs. 1.6%), were similar in the 31° C and 34° C groups, respectively.
Bleeding, whether measured by transfusion (19.6% vs. 22.4%) or TIMI major bleed (23.4% vs. 19.7%) were similar in the 31° C and 34° C groups, respectively. Thrombosis, whether measured by stent thrombosis (1.2% vs. 2.2%) or deep venous thrombosis (11.4% vs. 10.9%) were similar in these two groups, respectively.
The length of stay in the cardiac intensive care unit was significantly greater in the 31° C group (10 vs. 7 days; P = .004). Some of this increased length of stay can be attributed to the longer rewarming process required for the greater cooling, according to Dr. Le May, but he acknowledged that it is not clear this provides a full explanation.
More trials like CAPITAL-CHILL needed
The validity of these findings is supported by several strengths of the methodology, according to Jeanne E. Poole, MD, director of the arrhythmia service and electrophysiology laboratory, University of Washington, Seattle. This includes the reliance of an endovascular device, which can accelerate the time to the target temperature and assure the precision with which it is reached and maintained.
Dr. Poole did note that many of the primary and secondary measures, including the rates of stroke, seizures, and major bleeds, even though not significantly different, favored the higher temperature. The slightly longer door-to-balloon times might have been a factor. For the higher rate of pneumonia in the 31° C group, she questioned whether the longer period of ventilation linked to a longer period of rewarming might have been a factor.
However, Dr. Poole praised the CAPITAL-CHILL trial for drawing attention to a group of patients for whom survival rates remain “dismally low.” She indicated that these types of high-level trials are needed to look for strategies to improve outcomes.
Dr. Le May and Dr. Poole report no potential conflicts of interest.
The first randomized controlled trial to compare specific temperatures for therapeutic hypothermia in comatose survivors of out-of-hospital cardiac arrest showed no differences in major outcomes, according to a single-center, double-blind study.
In the CAPITAL-CHILL trial, cooling temperatures of 31° C and 34° C were compared to explore the hypothesis that a lower temperature would improve major outcomes, explained Michel Le May, MD.
No differences for the primary composite outcome of all-cause mortality or poor neurologic outcome at 180 days were observed, he reported at the annual scientific sessions of the American College of Cardiology.
The study was completed over a period of almost 7 years in patients presumed to have had an out-of-hospital cardiac arrest and who were unconscious when they reached a center affiliated with the Ottawa Heart Institute, where Dr. Le May directs the regional STEMI (ST-elevation myocardial infarction) program. The initial rhythm at the time of the cardiac arrest was not an entry criterion.
Of 389 patients enrolled, the intention-to-treat analysis included 184 randomized to a cooling temperature of 31° C group and 183 to a temperature of 34° C. The assigned target temperature, reached with an endovascular device, was known only by the managing nurses.
31° C and 34° C are equivalent
There was a small numerical disadvantage for the lower temperature assignment, but none reached statistical significance. This was true of the primary outcome (48.4% vs. 45.4% for the higher temperature) and its components of mortality (43.5% vs. 41.0%) and poor neurologic outcome (4.9% vs. 4.4%). Poor neurologic outcome was defined as a Disability Rating Scale score of greater than 5.
Deaths were most common in the early part of the 180-day follow-up in both arms. On a Kaplan-Meier survival graph, Dr. Le May showed curves that he characterized as “almost superimposable.”
There were no significant differences for any subgroup stratifications, such as age 75 years or older versus younger, males versus females, presence versus absence or an initial shockable rhythm, percutaneous coronary intervention (PCI) within 24 hours versus later, and STEMI versus non-STEMI. In these analyses, the higher temperature was associated with a potential trend for benefit among females and those with a shockable rhythm.
There was no signal for a difference in neurologic outcomes on the Disability Rating Scale or the Modified Rankin Scale. On the latter, for example, 46% of those in the 31° C group and 44% of these in the 34° C group had a score of four or greater at the end of follow-up.
The baseline characteristics of the two groups were similar. About 80% were male; the average age was roughly 62 years. More than 80% of the cardiac arrests were witnessed with CPR being administered by bystanders in nearly 70%. Nearly 40% had a STEMI.
Interventions were similar. Almost all patients underwent coronary angiography, of which nearly 60% received a percutaneous coronary intervention. More than 50% received a stent. The time from arrest to randomization was slightly longer in the 31° C group (228 vs. 204 minutes). The time to balloon inflation from arrival at the cardiac center was also slightly longer (73 vs. 60 minutes).
There was a trend for an increased rate of seizures in the 31° C group (12.5% vs. 7.1%; P = .08), but other secondary outcomes, including pneumonia (67.8% vs. 63.4%), renal replacement therapy (9.2% vs. 9.3%), and stroke (4.4% vs. 1.6%), were similar in the 31° C and 34° C groups, respectively.
Bleeding, whether measured by transfusion (19.6% vs. 22.4%) or TIMI major bleed (23.4% vs. 19.7%) were similar in the 31° C and 34° C groups, respectively. Thrombosis, whether measured by stent thrombosis (1.2% vs. 2.2%) or deep venous thrombosis (11.4% vs. 10.9%) were similar in these two groups, respectively.
The length of stay in the cardiac intensive care unit was significantly greater in the 31° C group (10 vs. 7 days; P = .004). Some of this increased length of stay can be attributed to the longer rewarming process required for the greater cooling, according to Dr. Le May, but he acknowledged that it is not clear this provides a full explanation.
More trials like CAPITAL-CHILL needed
The validity of these findings is supported by several strengths of the methodology, according to Jeanne E. Poole, MD, director of the arrhythmia service and electrophysiology laboratory, University of Washington, Seattle. This includes the reliance of an endovascular device, which can accelerate the time to the target temperature and assure the precision with which it is reached and maintained.
Dr. Poole did note that many of the primary and secondary measures, including the rates of stroke, seizures, and major bleeds, even though not significantly different, favored the higher temperature. The slightly longer door-to-balloon times might have been a factor. For the higher rate of pneumonia in the 31° C group, she questioned whether the longer period of ventilation linked to a longer period of rewarming might have been a factor.
However, Dr. Poole praised the CAPITAL-CHILL trial for drawing attention to a group of patients for whom survival rates remain “dismally low.” She indicated that these types of high-level trials are needed to look for strategies to improve outcomes.
Dr. Le May and Dr. Poole report no potential conflicts of interest.
The first randomized controlled trial to compare specific temperatures for therapeutic hypothermia in comatose survivors of out-of-hospital cardiac arrest showed no differences in major outcomes, according to a single-center, double-blind study.
In the CAPITAL-CHILL trial, cooling temperatures of 31° C and 34° C were compared to explore the hypothesis that a lower temperature would improve major outcomes, explained Michel Le May, MD.
No differences for the primary composite outcome of all-cause mortality or poor neurologic outcome at 180 days were observed, he reported at the annual scientific sessions of the American College of Cardiology.
The study was completed over a period of almost 7 years in patients presumed to have had an out-of-hospital cardiac arrest and who were unconscious when they reached a center affiliated with the Ottawa Heart Institute, where Dr. Le May directs the regional STEMI (ST-elevation myocardial infarction) program. The initial rhythm at the time of the cardiac arrest was not an entry criterion.
Of 389 patients enrolled, the intention-to-treat analysis included 184 randomized to a cooling temperature of 31° C group and 183 to a temperature of 34° C. The assigned target temperature, reached with an endovascular device, was known only by the managing nurses.
31° C and 34° C are equivalent
There was a small numerical disadvantage for the lower temperature assignment, but none reached statistical significance. This was true of the primary outcome (48.4% vs. 45.4% for the higher temperature) and its components of mortality (43.5% vs. 41.0%) and poor neurologic outcome (4.9% vs. 4.4%). Poor neurologic outcome was defined as a Disability Rating Scale score of greater than 5.
Deaths were most common in the early part of the 180-day follow-up in both arms. On a Kaplan-Meier survival graph, Dr. Le May showed curves that he characterized as “almost superimposable.”
There were no significant differences for any subgroup stratifications, such as age 75 years or older versus younger, males versus females, presence versus absence or an initial shockable rhythm, percutaneous coronary intervention (PCI) within 24 hours versus later, and STEMI versus non-STEMI. In these analyses, the higher temperature was associated with a potential trend for benefit among females and those with a shockable rhythm.
There was no signal for a difference in neurologic outcomes on the Disability Rating Scale or the Modified Rankin Scale. On the latter, for example, 46% of those in the 31° C group and 44% of these in the 34° C group had a score of four or greater at the end of follow-up.
The baseline characteristics of the two groups were similar. About 80% were male; the average age was roughly 62 years. More than 80% of the cardiac arrests were witnessed with CPR being administered by bystanders in nearly 70%. Nearly 40% had a STEMI.
Interventions were similar. Almost all patients underwent coronary angiography, of which nearly 60% received a percutaneous coronary intervention. More than 50% received a stent. The time from arrest to randomization was slightly longer in the 31° C group (228 vs. 204 minutes). The time to balloon inflation from arrival at the cardiac center was also slightly longer (73 vs. 60 minutes).
There was a trend for an increased rate of seizures in the 31° C group (12.5% vs. 7.1%; P = .08), but other secondary outcomes, including pneumonia (67.8% vs. 63.4%), renal replacement therapy (9.2% vs. 9.3%), and stroke (4.4% vs. 1.6%), were similar in the 31° C and 34° C groups, respectively.
Bleeding, whether measured by transfusion (19.6% vs. 22.4%) or TIMI major bleed (23.4% vs. 19.7%) were similar in the 31° C and 34° C groups, respectively. Thrombosis, whether measured by stent thrombosis (1.2% vs. 2.2%) or deep venous thrombosis (11.4% vs. 10.9%) were similar in these two groups, respectively.
The length of stay in the cardiac intensive care unit was significantly greater in the 31° C group (10 vs. 7 days; P = .004). Some of this increased length of stay can be attributed to the longer rewarming process required for the greater cooling, according to Dr. Le May, but he acknowledged that it is not clear this provides a full explanation.
More trials like CAPITAL-CHILL needed
The validity of these findings is supported by several strengths of the methodology, according to Jeanne E. Poole, MD, director of the arrhythmia service and electrophysiology laboratory, University of Washington, Seattle. This includes the reliance of an endovascular device, which can accelerate the time to the target temperature and assure the precision with which it is reached and maintained.
Dr. Poole did note that many of the primary and secondary measures, including the rates of stroke, seizures, and major bleeds, even though not significantly different, favored the higher temperature. The slightly longer door-to-balloon times might have been a factor. For the higher rate of pneumonia in the 31° C group, she questioned whether the longer period of ventilation linked to a longer period of rewarming might have been a factor.
However, Dr. Poole praised the CAPITAL-CHILL trial for drawing attention to a group of patients for whom survival rates remain “dismally low.” She indicated that these types of high-level trials are needed to look for strategies to improve outcomes.
Dr. Le May and Dr. Poole report no potential conflicts of interest.
FROM ACC 2021
The end of happy hour? No safe level of alcohol for the brain
There is no safe amount of alcohol consumption for the brain; even moderate drinking adversely affects brain structure and function, according a British study of more 25,000 adults.
“This is one of the largest studies of alcohol and brain health to date,” Anya Topiwala, DPhil, University of Oxford (England), told this news organization.
“There have been previous claims the relationship between alcohol and brain health are J-shaped (ie., small amounts are protective), but we formally tested this and did not find it to be the case. In fact, we found that any level of alcohol was associated with poorer brain health, compared to no alcohol,” Dr. Topiwala added.
The study, which has not yet been peer reviewed, was published online May 12 in MedRxiv.
Global impact on the brain
Participants provided detailed information on their alcohol intake. The cohort included 691 never-drinkers, 617 former drinkers, and 24,069 current drinkers.
Median alcohol intake was 13.5 units (102 g) weekly. Almost half of the sample (48.2%) were drinking above current UK low-risk guidelines (14 units, 112 g weekly), but few were heavy drinkers (>50 units, 400 g weekly).
After adjusting for all known potential confounders and multiple comparisons, a higher volume of alcohol consumed per week was associated with lower gray matter in “almost all areas of the brain,” Dr. Topiwala said in an interview.
Alcohol consumption accounted for up to 0.8% of gray matter volume variance. “The size of the effect is small, albeit greater than any other modifiable risk factor. These brain changes have been previously linked to aging, poorer performance on memory changes, and dementia,” Dr. Topiwala said.
Widespread negative associations were also found between drinking alcohol and all the measures of white matter integrity that were assessed. There was a significant positive association between alcohol consumption and resting-state functional connectivity.
Higher blood pressure and body mass index “steepened” the negative associations between alcohol and brain health, and binge drinking had additive negative effects on brain structure beyond the absolute volume consumed.
There was no evidence that the risk for alcohol-related brain harm differs according to the type of alcohol consumed (wine, beer, or spirits).
A key limitation of the study is that the study population from the UK Biobank represents a sample that is healthier, better educated, and less deprived and is characterized by less ethnic diversity than the general population. “As with any observational study, we cannot infer causality from association,” the authors note.
What remains unclear, they say, is the duration of drinking needed to cause an effect on the brain. It may be that vulnerability is increased during periods of life in which dynamic brain changes occur, such as adolescence and older age.
They also note that some studies of alcohol-dependent individuals have suggested that at least some brain damage is reversible upon abstinence. Whether that is true for moderate drinkers is unknown.
On the basis of their findings, there is “no safe dose of alcohol for the brain,” Dr. Topiwala and colleagues conclude. They suggest that current low-risk drinking guidelines be revisited to take account of brain effects.
Experts weigh in
Several experts weighed in on the study in a statement from the nonprofit UK Science Media Center.
Paul Matthews, MD, head of the department of brain sciences, Imperial College London, noted that this “carefully performed preliminary report extends our earlier UK Dementia Research Institute study of a smaller group from same UK Biobank population also showing that even moderate drinking is associated with greater atrophy of the brain, as well as injury to the heart and liver.”
Dr. Matthews said the investigators’ conclusion that there is no safe threshold below which alcohol consumption has no toxic effects “echoes our own. We join with them in suggesting that current public health guidelines concerning alcohol consumption may need to be revisited.”
Rebecca Dewey, PhD, research fellow in neuroimaging, University of Nottingham (England), cautioned that “the degree to which very small changes in brain volume are harmful” is unknown.
“While there was no threshold under which alcohol consumption did not cause changes in the brain, there may a degree of brain volume difference that is irrelevant to brain health. We don’t know what these people’s brains looked like before they drank alcohol, so the brain may have learned to cope/compensate,” Dewey said.
Sadie Boniface, PhD, head of research at the Institute of Alcohol Studies and visiting researcher at King’s College London, said, “While we can’t yet say for sure whether there is ‘no safe level’ of alcohol regarding brain health at the moment, it has been known for decades that heavy drinking is bad for brain health.
“We also shouldn’t forget alcohol affects all parts of the body and there are multiple health risks. For example, it is already known there is ‘no safe level’ of alcohol consumption for the seven types of cancer caused by alcohol, as identified by the UK chief medical officers,” Dr. Boniface said.
The study was supported in part by the Wellcome Trust, Li Ka Shing Center for Health Information and Discovery, the National Institutes of Health, and the UK Medical Research Council. Dr. Topiwala, Dr. Boniface, Dr. Dewey, and Dr. Matthews have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
There is no safe amount of alcohol consumption for the brain; even moderate drinking adversely affects brain structure and function, according a British study of more 25,000 adults.
“This is one of the largest studies of alcohol and brain health to date,” Anya Topiwala, DPhil, University of Oxford (England), told this news organization.
“There have been previous claims the relationship between alcohol and brain health are J-shaped (ie., small amounts are protective), but we formally tested this and did not find it to be the case. In fact, we found that any level of alcohol was associated with poorer brain health, compared to no alcohol,” Dr. Topiwala added.
The study, which has not yet been peer reviewed, was published online May 12 in MedRxiv.
Global impact on the brain
Participants provided detailed information on their alcohol intake. The cohort included 691 never-drinkers, 617 former drinkers, and 24,069 current drinkers.
Median alcohol intake was 13.5 units (102 g) weekly. Almost half of the sample (48.2%) were drinking above current UK low-risk guidelines (14 units, 112 g weekly), but few were heavy drinkers (>50 units, 400 g weekly).
After adjusting for all known potential confounders and multiple comparisons, a higher volume of alcohol consumed per week was associated with lower gray matter in “almost all areas of the brain,” Dr. Topiwala said in an interview.
Alcohol consumption accounted for up to 0.8% of gray matter volume variance. “The size of the effect is small, albeit greater than any other modifiable risk factor. These brain changes have been previously linked to aging, poorer performance on memory changes, and dementia,” Dr. Topiwala said.
Widespread negative associations were also found between drinking alcohol and all the measures of white matter integrity that were assessed. There was a significant positive association between alcohol consumption and resting-state functional connectivity.
Higher blood pressure and body mass index “steepened” the negative associations between alcohol and brain health, and binge drinking had additive negative effects on brain structure beyond the absolute volume consumed.
There was no evidence that the risk for alcohol-related brain harm differs according to the type of alcohol consumed (wine, beer, or spirits).
A key limitation of the study is that the study population from the UK Biobank represents a sample that is healthier, better educated, and less deprived and is characterized by less ethnic diversity than the general population. “As with any observational study, we cannot infer causality from association,” the authors note.
What remains unclear, they say, is the duration of drinking needed to cause an effect on the brain. It may be that vulnerability is increased during periods of life in which dynamic brain changes occur, such as adolescence and older age.
They also note that some studies of alcohol-dependent individuals have suggested that at least some brain damage is reversible upon abstinence. Whether that is true for moderate drinkers is unknown.
On the basis of their findings, there is “no safe dose of alcohol for the brain,” Dr. Topiwala and colleagues conclude. They suggest that current low-risk drinking guidelines be revisited to take account of brain effects.
Experts weigh in
Several experts weighed in on the study in a statement from the nonprofit UK Science Media Center.
Paul Matthews, MD, head of the department of brain sciences, Imperial College London, noted that this “carefully performed preliminary report extends our earlier UK Dementia Research Institute study of a smaller group from same UK Biobank population also showing that even moderate drinking is associated with greater atrophy of the brain, as well as injury to the heart and liver.”
Dr. Matthews said the investigators’ conclusion that there is no safe threshold below which alcohol consumption has no toxic effects “echoes our own. We join with them in suggesting that current public health guidelines concerning alcohol consumption may need to be revisited.”
Rebecca Dewey, PhD, research fellow in neuroimaging, University of Nottingham (England), cautioned that “the degree to which very small changes in brain volume are harmful” is unknown.
“While there was no threshold under which alcohol consumption did not cause changes in the brain, there may a degree of brain volume difference that is irrelevant to brain health. We don’t know what these people’s brains looked like before they drank alcohol, so the brain may have learned to cope/compensate,” Dewey said.
Sadie Boniface, PhD, head of research at the Institute of Alcohol Studies and visiting researcher at King’s College London, said, “While we can’t yet say for sure whether there is ‘no safe level’ of alcohol regarding brain health at the moment, it has been known for decades that heavy drinking is bad for brain health.
“We also shouldn’t forget alcohol affects all parts of the body and there are multiple health risks. For example, it is already known there is ‘no safe level’ of alcohol consumption for the seven types of cancer caused by alcohol, as identified by the UK chief medical officers,” Dr. Boniface said.
The study was supported in part by the Wellcome Trust, Li Ka Shing Center for Health Information and Discovery, the National Institutes of Health, and the UK Medical Research Council. Dr. Topiwala, Dr. Boniface, Dr. Dewey, and Dr. Matthews have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
There is no safe amount of alcohol consumption for the brain; even moderate drinking adversely affects brain structure and function, according a British study of more 25,000 adults.
“This is one of the largest studies of alcohol and brain health to date,” Anya Topiwala, DPhil, University of Oxford (England), told this news organization.
“There have been previous claims the relationship between alcohol and brain health are J-shaped (ie., small amounts are protective), but we formally tested this and did not find it to be the case. In fact, we found that any level of alcohol was associated with poorer brain health, compared to no alcohol,” Dr. Topiwala added.
The study, which has not yet been peer reviewed, was published online May 12 in MedRxiv.
Global impact on the brain
Participants provided detailed information on their alcohol intake. The cohort included 691 never-drinkers, 617 former drinkers, and 24,069 current drinkers.
Median alcohol intake was 13.5 units (102 g) weekly. Almost half of the sample (48.2%) were drinking above current UK low-risk guidelines (14 units, 112 g weekly), but few were heavy drinkers (>50 units, 400 g weekly).
After adjusting for all known potential confounders and multiple comparisons, a higher volume of alcohol consumed per week was associated with lower gray matter in “almost all areas of the brain,” Dr. Topiwala said in an interview.
Alcohol consumption accounted for up to 0.8% of gray matter volume variance. “The size of the effect is small, albeit greater than any other modifiable risk factor. These brain changes have been previously linked to aging, poorer performance on memory changes, and dementia,” Dr. Topiwala said.
Widespread negative associations were also found between drinking alcohol and all the measures of white matter integrity that were assessed. There was a significant positive association between alcohol consumption and resting-state functional connectivity.
Higher blood pressure and body mass index “steepened” the negative associations between alcohol and brain health, and binge drinking had additive negative effects on brain structure beyond the absolute volume consumed.
There was no evidence that the risk for alcohol-related brain harm differs according to the type of alcohol consumed (wine, beer, or spirits).
A key limitation of the study is that the study population from the UK Biobank represents a sample that is healthier, better educated, and less deprived and is characterized by less ethnic diversity than the general population. “As with any observational study, we cannot infer causality from association,” the authors note.
What remains unclear, they say, is the duration of drinking needed to cause an effect on the brain. It may be that vulnerability is increased during periods of life in which dynamic brain changes occur, such as adolescence and older age.
They also note that some studies of alcohol-dependent individuals have suggested that at least some brain damage is reversible upon abstinence. Whether that is true for moderate drinkers is unknown.
On the basis of their findings, there is “no safe dose of alcohol for the brain,” Dr. Topiwala and colleagues conclude. They suggest that current low-risk drinking guidelines be revisited to take account of brain effects.
Experts weigh in
Several experts weighed in on the study in a statement from the nonprofit UK Science Media Center.
Paul Matthews, MD, head of the department of brain sciences, Imperial College London, noted that this “carefully performed preliminary report extends our earlier UK Dementia Research Institute study of a smaller group from same UK Biobank population also showing that even moderate drinking is associated with greater atrophy of the brain, as well as injury to the heart and liver.”
Dr. Matthews said the investigators’ conclusion that there is no safe threshold below which alcohol consumption has no toxic effects “echoes our own. We join with them in suggesting that current public health guidelines concerning alcohol consumption may need to be revisited.”
Rebecca Dewey, PhD, research fellow in neuroimaging, University of Nottingham (England), cautioned that “the degree to which very small changes in brain volume are harmful” is unknown.
“While there was no threshold under which alcohol consumption did not cause changes in the brain, there may a degree of brain volume difference that is irrelevant to brain health. We don’t know what these people’s brains looked like before they drank alcohol, so the brain may have learned to cope/compensate,” Dewey said.
Sadie Boniface, PhD, head of research at the Institute of Alcohol Studies and visiting researcher at King’s College London, said, “While we can’t yet say for sure whether there is ‘no safe level’ of alcohol regarding brain health at the moment, it has been known for decades that heavy drinking is bad for brain health.
“We also shouldn’t forget alcohol affects all parts of the body and there are multiple health risks. For example, it is already known there is ‘no safe level’ of alcohol consumption for the seven types of cancer caused by alcohol, as identified by the UK chief medical officers,” Dr. Boniface said.
The study was supported in part by the Wellcome Trust, Li Ka Shing Center for Health Information and Discovery, the National Institutes of Health, and the UK Medical Research Council. Dr. Topiwala, Dr. Boniface, Dr. Dewey, and Dr. Matthews have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Hospital at Home: Delivering hospital-level care without the hospital
How to implement a new model of care
The United States spends one-third of the nation’s health dollars on hospital care, amounting to $1.2 trillion in 2018.1 U.S. hospital beds are prevalent2, and expensive to build and operate, with most hospital services costs related to buildings, equipment, salaried labor, and overhead.3
Despite their mission to heal, hospitals can be harmful, especially for frail and elderly patients. A study completed by the Office of the Inspector General (OIG) found that 13.5% of hospitalized Medicare patients experienced an adverse event that resulted in a prolonged hospital stay, permanent harm, a life-sustaining intervention or death.4 In addition, there is growing concern about acquired post-hospitalization syndrome caused by the physiological stress that patients experience in the hospital, leaving them vulnerable to clinical adverse events such as falls and infections.5
In the mid-1990s, driven by a goal to “avoid the harm of inpatient care and honor the wishes of older adults who refused to go to the hospital”, Dr. Bruce Leff, director of the Center for Transformative Geriatric Research and professor of medicine at Johns Hopkins University in Baltimore, and his team set out to develop and test Hospital at Home (HaH) – an innovative model for delivering hospital-level care to selected patients in the safety of their homes.
More than 20 years later, despite extensive evidence supporting HaH safety and efficacy, and its successful rollout in other countries, the model has not been widely adopted in the U.S. However, the COVID-19 pandemic amplified interest in HaH by creating an urgent need for flexible hospital bed capacity and heightening concerns about hospital care safety, especially for vulnerable adults.
In this article, we will introduce HaH history and efficacy, and then discuss what it takes to successfully implement HaH.
Hospital at Home: History, efficacy, and early adoption
The earliest HaH study, a 17-patient pilot conducted by Dr. Leff’s team from 1996 to 1998, proved that HaH was feasible, safe, highly satisfactory and cost-effective for selected acutely ill older patients with community-acquired pneumonia, chronic heart failure, chronic obstructive pulmonary disease or cellulitis.6 In 2000 to 2002, a National Demonstration and Evaluation Study of 455 patients across three sites determined that patients treated in Hospital at Home had statistically significant shorter length of stay (3.2 vs 4.9 days), lower cost ($5,081 vs. $7,480) and complications.7 Equipped with evidence, Dr. Leff and his team focused on HaH dissemination and implementation across several health care systems.8
Presbyterian Healthcare Services in Albuquerque, N.M., was one of the earliest adopters of HaH and launched the program in 2008. The integrated system serves one-third of New Mexicans and includes nine hospitals, more than 100 clinics and the state’s largest health plan. According to Nancy Guinn, MD, a medical director of Presbyterian Healthcare at Home, “Innovation is key to survive in a lean environment like New Mexico, which has the lowest percentage of residents with insurance from their employer and a high rate of government payers.”
Presbyterian selected nine diagnoses for HaH focus: congestive heart failure, chronic obstructive pulmonary disease, community-acquired pneumonia, cellulitis, deep venous thrombosis, pulmonary embolism, complicated urinary tract infection or urosepsis, nausea and vomiting, and dehydration. The HaH care, including physician services, is reimbursed via a partial DRG (diagnosis-related group) payment that was negotiated internally between the health system and Presbyterian Health Plan.
The results demonstrated that, compared to hospitalized patients with similar conditions, patients in HaH had a lower rate of falls (0% vs. .8%), lower mortality (.93% vs. 3.4%), higher satisfaction (mean score 90.7 vs. 83.9) and 19% lower cost.9 According to Dr. Guinn, more recent results showed even larger cost savings of 42%.10 After starting the HaH model, Presbyterian has launched other programs that work closely with HaH to provide a seamless experience for patients. That includes the Complete Care Program, which offers home-based primary, urgent, and acute care to members covered through Presbyterian Health Plan and has a daily census of 600-700 patients.
Another important milestone came in 2014 when Icahn School of Medicine at Mount Sinai in New York was awarded $9.6 million by the Center for Medicare and Medicaid Innovation (CMMI) to test the HaH model during acute illness and for 30 days after admission. A case study of 507 patients enrolled in the program in 2014 through 2017 revealed that HaH patients had statistically significant shorter length of stay (3.2 days vs. 5.5 days), and lower rates of all-cause 30-day hospital readmissions (8.6% vs. 15.6%), 30-day ED revisits (5.8% vs. 11.7%), and SNF admissions (1.7% vs. 10.4%), and were also more likely to rate their hospital care highly (68.8% vs. 45.3%).11
In 2017, using data from their CMMI study, Mount Sinai submitted an application to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to implement Hospital at Home as an alternative payment model that bundles the acute episode with 30 days of post‐acute transitional care. The PTAC unanimously approved the proposal and submitted their recommendations to the Secretary of Health and Human Services (HHS) to implement HaH as an alternative payment model that included two parts:
1. A bundled payment equal to a percentage of the prospective DRG (diagnosis-related group) payment that would have been paid to a hospital.
2. A performance-based payment (shared savings/losses) based on (a) total spending during the acute care phase and 30 days afterward relative to a target price, and (b) performance on quality measures.12
In June 2018, the HHS secretary announced that he was not approving the proposal as written, citing, among other things, concerns about proposed payment methodology and patient safety.13
Hospital at Home: Present state
Despite additional evidence of HaH’s impact on lowering cost, decreasing 30-day readmissions, improving patient satisfaction and functional outcomes without an adverse effect on mortality,14, 15 the model has not been widely adopted, largely due to lack of fee-for-service reimbursement from the public payers (Medicare and Medicaid) and complex logistics to implement it.
However, the COVID-19 pandemic created an urgent need for flexible hospital bed capacity and amplified concerns about hospital care safety for vulnerable populations. In response, the Centers for Medicare and Medicaid Services (CMS) introduced its Hospitals without Walls initiative that allowed hospitals to provide services in other health care facilities and sites that are not part of the existing hospital.16 On November 25, 2020, CMS announced expansion of the Hospital without Walls initiatives to include a Hospital Care at Home program that allows eligible hospitals to treat eligible patients at home.17
With significant evidence supporting HaH’s safety and efficacy, and long overdue support from CMS, it’s now a matter of how to successfully implement it. Let’s explore what it takes to select and enroll patients, deliver acute care at home, and ensure a smooth post-acute transition within the HaH model.
Successfully implementing Hospital at Home
HaH implementation requires five key components – people, processes, technology, supply chain, and analytics – to select and enroll patients, deliver acute care at home, and ensure a smooth postacute transition. Let’s discuss each of them in more detail below.
Selecting and enrolling patients
Patients eligible for HaH are identified based on their insurance, as well as clinical and social criteria. Despite a lack of public payer support, several commercial payers embraced the model for selected patients who consented to receive acute hospital care at home. The patients must meet criteria for an inpatient admission, be medically stable and have a low level of diagnostic uncertainty. Advances in home monitoring technology expanded clinical criteria to include acutely ill patients with multiple comorbidities, including cancer. It is important that patients reside in a safe home environment and live within a reasonable distance from the hospital.
CareMore Health, an integrated health care delivery system serving more than 180,000 Medicare Advantage and Medicaid patients across nine states and Washington D.C., launched Hospital at Home in December 2018, and rapidly scaled from a few referrals to averaging more than 20 new patients per week.
Sashidaran Moodley, MD, medical director at CareMore Health and Aspire Health, in Cerritos, Calif., shared a valuable lesson regarding launching the program: “Do not presume that if you build it, they will come. This is a new model of care that requires physicians to change their behavior and health systems to modify their traditional admission work flows. Program designers should not limit their thinking around sourcing patients just from the emergency department.”
Dr. Moodley recommends moving upstream and bring awareness to the program to drive additional referrals from primary care providers, case managers, and remote patient monitoring programs (for example, heart failure).
Linda DeCherrie, MD, clinical director of Mount Sinai at Home, based in New York, says that “educating and involving hospitalists is key.” At Mount Sinai, patients eligible for HaH are initially evaluated by hospitalists in the ED who write initial orders and then transfer care to HaH hospitalists.
HaH also can enroll eligible patients who still require hospital-level care to complete the last few days of acute hospitalization at home. Early discharge programs have been implemented at CareMore, Presbyterian Healthcare Services in Albuquerque, N.M., and Mount Sinai. At Mount Sinai, a program called Completing Hospitalization at Home initially started with non-COVID patients and expanded to include COVID-19 early discharges, helping to free up much-needed hospital beds.
Delivering acute care at home
HaH requires a well-coordinated multidisciplinary team. Patient care is directed by a team of physicians and nurse practitioners who provide daily in-person or virtual visits. To enable provider work flow, an ambulatory version of electronic medical records (for example, Epic) must be customized to include specialized order sets that mimic inpatient orders and diagnoses-specific care delivery protocols. HaH physicians and nurse practitioners are available 24/7 to address acute patient issues.
In addition, patients receive at least daily visits from registered nurses (RNs) who carry out orders, administer medications, draw labs, and provide clinical assessment and patient education. Some organizations employ HaH nurses, while others contract with home health agencies.
Typically, patients are provided with a tablet to enable telehealth visits, as well as a blood pressure monitor, thermometer, pulse oximeter, and, if needed, scale and glucometer, that allow on-demand or continuous remote monitoring. Recent technology advances in home monitoring enhanced HaH’s capability to care for complex, high-acuity patients, and increased the potential volume of patients that can be safely treated at home.
Providence St. Joseph Health, a not-for-profit health care system operating 51 hospitals and 1,085 clinics across seven states, launched their HaH program earlier this year. Per Danielsson, MD, executive medical director for hospital medicine at Swedish Medical Center in Seattle, describes it as a “high-touch, high-tech program anchored by hospitalists.” The Providence HaH team utilizes a wearable medical device for patients that enables at-home continuous monitoring of vital signs such as temperature, blood pressure, heart rate, respirations, and pulse oximetry. Single-lead EKG monitoring is available for selected patients. Individual patient data is transmitted to a central command center, where a team of nurses and physicians remotely monitor HaH patients. According to Todd Czartoski, MD, chief medical technology officer at Providence, “Hospital at Home improves quality and access, and can substitute for 20%-30% of hospital admissions.”
In addition to patient monitoring and 24/7 provider access, some HaH programs partner with community paramedics for emergency responses. At Mount Sinai, HaH providers can trigger paramedic response, if needed. Paramedics can set up a video link with a doctor and, under the direction of a physician, will provide treatment at home or transport patients to the hospital.
HaH would be impossible without a partnership with local ancillary service providers that can promptly deliver services and goods to patient homes. Raphael Rakowski, CEO of Medically Home, a Boston-based company that partners with health care providers to build virtual hospitals at home, calls it an “acute rapid response supply chain.” The services, both clinical and nonclinical, consist of infusions; x-rays; bedside ultrasound; laboratory; transportation; and skilled physical, occupational, and speech therapy. If patients require services that are not available at home (for example, a CT scan), patients can be transported to and from a diagnostic center. Medical and nonmedical goods include medications, oxygen, durable medical equipment, and even meals.
Delivery of hospital-level services at home requires a seamless coordination between clinical teams and suppliers that relies on nursing care coordinators and supporting nonclinical staff, and is enabled by a secure text messaging platform to communicate within the care team, with suppliers, and with other providers (for example, primary care providers and specialists).
Ensuring smooth postacute transition
Thirty days after hospital discharge is the most critical period, especially for elderly patients. According to one study, 19% of patients experienced adverse events within 3 weeks after hospital discharge.18 Adverse drug events were the most common postdischarge complication, followed by procedural complications and hospital-acquired infections. Furthermore, 30-day all-cause hospital readmissions is a common occurrence. Per the Healthcare Cost and Utilization Project database, 17.1% of Medicare and 13.9% of all-payers patients were readmitted to the hospital within 30 days in 2016.19
It is not surprising that some organizations offer ongoing home care during the postacute period. At Mount Sinai, patients discharged from HaH continue to have access to the HaH team around the clock for 30 days to address emergencies and health concerns. Recovery Care Coordinators and social workers monitor patient health status, develop a follow-up plan, coordinate care, and answer questions. Medically Home provides 24/7 care to HaH patients for the entire duration of the acute care episode (34 days) to ensure maximum access to care and no gaps in care and communication. At Presbyterian, most HaH patients are transitioned into a Home Health episode of care to ensure continued high-quality care.
In addition to people, processes, technology, and the supply chain, HaH implementation requires capabilities to collect and analyze quality and cost data to measure program efficacy and, in some arrangements with payers, to reconcile clams data to determine shared savings or losses.
Partnering with third parties
Considering the resources and capabilities required for HaH program development and implementation, it is not surprising that health care providers are choosing to partner with third parties. For example, Mount Sinai partnered with Contessa Health, a Nashville, Tenn.–based company that offers hospitals a turn-key Home Recovery Care program, to assist with supply chain contracting and management, and claims data reconciliation.
Medically Home has partnered with seven health care systems, including the Mayo Clinic, Tufts Medical Center in Boston, and Adventist Health in southern California, to create virtual beds, and is expected to launch the program with 15 health care systems by the end of 2020.
Medically Home offers the following services to its partners to enable care for high-acuity patients at home:
- Assistance with hiring and training of clinical staff.
- Proprietary EMR-integrated orders, notes, and clinical protocols.
- Technology for patient monitoring by the 24/7 central command center; tablets that provide health status updates and daily schedules, and enable televisits; a video platform for video communication; and secure texting.
- Selection, contracting and monitoring the performance of supply chain vendors.
- Analytics.
The future of Hospital at Home
There is no question that HaH can offer a safe, high-quality, and lower-cost alternative to hospitalizations for select patients, which is aligned with the Centers for Medicare and Medicaid Services’ triple aim of better care for individuals, better health for populations, and lower cost.20
The future of HaH depends on development of a common payment model that will be adopted beyond the pandemic by government and commercial payers. Current payment models vary and include capitated agreements, discounted diagnosis-related group payments for the acute episode, and discounted DRG payments plus shared losses or savings.
The COVID-19 pandemic has created, arguably, the biggest crisis that U.S. health care has ever experienced, and it is far from over. Short term, Hospital at Home offers a solution to create flexible hospital bed capacity and deliver safe hospital-level care for vulnerable populations. Long term, it may be the solution that helps achieve better care for individuals, better health for populations and lower health care costs.
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of the Hospitalist’s editorial advisory board.
References
1. Source: www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf
2. Source: www.aha.org/statistics/fast-facts-us-hospitals
3. Roberts RR, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999 Feb;281(7):644-9.
4. Levinson DR; US Department of Health and Human Services; HHS; Office of the Inspector General; OIG.
5. Krumholz HM. Post-Hospital Syndrome – An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013 Jan;368:100-102.
6. Leff B, et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999 Jun;47(6):697-702.
7. Leff B, et al. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec;143(11):798-808.
8. Source: www.johnshopkinssolutions.com/solution/hospital-at-home/
9. Cryer L, et al. Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs. 2012 Jun;31(6):1237–43.
10. Personal communication with Presbyterian Health Services. May 20, 2020.
11. Federman A, et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018 Aug;178(8):1033–40.
12. Source: aspe.hhs.gov/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf
13. Source: aspe.hhs.gov/system/files/pdf/255906/Secretarial_Responses_June_13_2018.508.pdf
14. Shepperd S, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):CD007491. DOI:10.1002/14651858.CD007491.pub2.
15. Levine DM, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020 Jan;172(2);77-85.
16. Source: www.cms.gov/files/document/covid-hospitals.pdf
17. Centers for Medicare & Medicaid Services. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 2020 Nov 20.
18. Forster AJ et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Mar;138(3):161-7. doi: 10.7326/0003-4819-138-3-200302040-00007.
19. Bailey MK et al. Characteristics of 30-Day All-Cause Hospital Readmissions, 2010-2016. Statistical Brief 248. Agency for Healthcare Research and Quality. 2019 Feb 12. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb248-Hospital-Readmissions-2010-2016.jsp.
20. Centers for Medicare & Medicaid Services. What are the value-based programs? 2020 Jan 6. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs.
How to implement a new model of care
How to implement a new model of care
The United States spends one-third of the nation’s health dollars on hospital care, amounting to $1.2 trillion in 2018.1 U.S. hospital beds are prevalent2, and expensive to build and operate, with most hospital services costs related to buildings, equipment, salaried labor, and overhead.3
Despite their mission to heal, hospitals can be harmful, especially for frail and elderly patients. A study completed by the Office of the Inspector General (OIG) found that 13.5% of hospitalized Medicare patients experienced an adverse event that resulted in a prolonged hospital stay, permanent harm, a life-sustaining intervention or death.4 In addition, there is growing concern about acquired post-hospitalization syndrome caused by the physiological stress that patients experience in the hospital, leaving them vulnerable to clinical adverse events such as falls and infections.5
In the mid-1990s, driven by a goal to “avoid the harm of inpatient care and honor the wishes of older adults who refused to go to the hospital”, Dr. Bruce Leff, director of the Center for Transformative Geriatric Research and professor of medicine at Johns Hopkins University in Baltimore, and his team set out to develop and test Hospital at Home (HaH) – an innovative model for delivering hospital-level care to selected patients in the safety of their homes.
More than 20 years later, despite extensive evidence supporting HaH safety and efficacy, and its successful rollout in other countries, the model has not been widely adopted in the U.S. However, the COVID-19 pandemic amplified interest in HaH by creating an urgent need for flexible hospital bed capacity and heightening concerns about hospital care safety, especially for vulnerable adults.
In this article, we will introduce HaH history and efficacy, and then discuss what it takes to successfully implement HaH.
Hospital at Home: History, efficacy, and early adoption
The earliest HaH study, a 17-patient pilot conducted by Dr. Leff’s team from 1996 to 1998, proved that HaH was feasible, safe, highly satisfactory and cost-effective for selected acutely ill older patients with community-acquired pneumonia, chronic heart failure, chronic obstructive pulmonary disease or cellulitis.6 In 2000 to 2002, a National Demonstration and Evaluation Study of 455 patients across three sites determined that patients treated in Hospital at Home had statistically significant shorter length of stay (3.2 vs 4.9 days), lower cost ($5,081 vs. $7,480) and complications.7 Equipped with evidence, Dr. Leff and his team focused on HaH dissemination and implementation across several health care systems.8
Presbyterian Healthcare Services in Albuquerque, N.M., was one of the earliest adopters of HaH and launched the program in 2008. The integrated system serves one-third of New Mexicans and includes nine hospitals, more than 100 clinics and the state’s largest health plan. According to Nancy Guinn, MD, a medical director of Presbyterian Healthcare at Home, “Innovation is key to survive in a lean environment like New Mexico, which has the lowest percentage of residents with insurance from their employer and a high rate of government payers.”
Presbyterian selected nine diagnoses for HaH focus: congestive heart failure, chronic obstructive pulmonary disease, community-acquired pneumonia, cellulitis, deep venous thrombosis, pulmonary embolism, complicated urinary tract infection or urosepsis, nausea and vomiting, and dehydration. The HaH care, including physician services, is reimbursed via a partial DRG (diagnosis-related group) payment that was negotiated internally between the health system and Presbyterian Health Plan.
The results demonstrated that, compared to hospitalized patients with similar conditions, patients in HaH had a lower rate of falls (0% vs. .8%), lower mortality (.93% vs. 3.4%), higher satisfaction (mean score 90.7 vs. 83.9) and 19% lower cost.9 According to Dr. Guinn, more recent results showed even larger cost savings of 42%.10 After starting the HaH model, Presbyterian has launched other programs that work closely with HaH to provide a seamless experience for patients. That includes the Complete Care Program, which offers home-based primary, urgent, and acute care to members covered through Presbyterian Health Plan and has a daily census of 600-700 patients.
Another important milestone came in 2014 when Icahn School of Medicine at Mount Sinai in New York was awarded $9.6 million by the Center for Medicare and Medicaid Innovation (CMMI) to test the HaH model during acute illness and for 30 days after admission. A case study of 507 patients enrolled in the program in 2014 through 2017 revealed that HaH patients had statistically significant shorter length of stay (3.2 days vs. 5.5 days), and lower rates of all-cause 30-day hospital readmissions (8.6% vs. 15.6%), 30-day ED revisits (5.8% vs. 11.7%), and SNF admissions (1.7% vs. 10.4%), and were also more likely to rate their hospital care highly (68.8% vs. 45.3%).11
In 2017, using data from their CMMI study, Mount Sinai submitted an application to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to implement Hospital at Home as an alternative payment model that bundles the acute episode with 30 days of post‐acute transitional care. The PTAC unanimously approved the proposal and submitted their recommendations to the Secretary of Health and Human Services (HHS) to implement HaH as an alternative payment model that included two parts:
1. A bundled payment equal to a percentage of the prospective DRG (diagnosis-related group) payment that would have been paid to a hospital.
2. A performance-based payment (shared savings/losses) based on (a) total spending during the acute care phase and 30 days afterward relative to a target price, and (b) performance on quality measures.12
In June 2018, the HHS secretary announced that he was not approving the proposal as written, citing, among other things, concerns about proposed payment methodology and patient safety.13
Hospital at Home: Present state
Despite additional evidence of HaH’s impact on lowering cost, decreasing 30-day readmissions, improving patient satisfaction and functional outcomes without an adverse effect on mortality,14, 15 the model has not been widely adopted, largely due to lack of fee-for-service reimbursement from the public payers (Medicare and Medicaid) and complex logistics to implement it.
However, the COVID-19 pandemic created an urgent need for flexible hospital bed capacity and amplified concerns about hospital care safety for vulnerable populations. In response, the Centers for Medicare and Medicaid Services (CMS) introduced its Hospitals without Walls initiative that allowed hospitals to provide services in other health care facilities and sites that are not part of the existing hospital.16 On November 25, 2020, CMS announced expansion of the Hospital without Walls initiatives to include a Hospital Care at Home program that allows eligible hospitals to treat eligible patients at home.17
With significant evidence supporting HaH’s safety and efficacy, and long overdue support from CMS, it’s now a matter of how to successfully implement it. Let’s explore what it takes to select and enroll patients, deliver acute care at home, and ensure a smooth post-acute transition within the HaH model.
Successfully implementing Hospital at Home
HaH implementation requires five key components – people, processes, technology, supply chain, and analytics – to select and enroll patients, deliver acute care at home, and ensure a smooth postacute transition. Let’s discuss each of them in more detail below.
Selecting and enrolling patients
Patients eligible for HaH are identified based on their insurance, as well as clinical and social criteria. Despite a lack of public payer support, several commercial payers embraced the model for selected patients who consented to receive acute hospital care at home. The patients must meet criteria for an inpatient admission, be medically stable and have a low level of diagnostic uncertainty. Advances in home monitoring technology expanded clinical criteria to include acutely ill patients with multiple comorbidities, including cancer. It is important that patients reside in a safe home environment and live within a reasonable distance from the hospital.
CareMore Health, an integrated health care delivery system serving more than 180,000 Medicare Advantage and Medicaid patients across nine states and Washington D.C., launched Hospital at Home in December 2018, and rapidly scaled from a few referrals to averaging more than 20 new patients per week.
Sashidaran Moodley, MD, medical director at CareMore Health and Aspire Health, in Cerritos, Calif., shared a valuable lesson regarding launching the program: “Do not presume that if you build it, they will come. This is a new model of care that requires physicians to change their behavior and health systems to modify their traditional admission work flows. Program designers should not limit their thinking around sourcing patients just from the emergency department.”
Dr. Moodley recommends moving upstream and bring awareness to the program to drive additional referrals from primary care providers, case managers, and remote patient monitoring programs (for example, heart failure).
Linda DeCherrie, MD, clinical director of Mount Sinai at Home, based in New York, says that “educating and involving hospitalists is key.” At Mount Sinai, patients eligible for HaH are initially evaluated by hospitalists in the ED who write initial orders and then transfer care to HaH hospitalists.
HaH also can enroll eligible patients who still require hospital-level care to complete the last few days of acute hospitalization at home. Early discharge programs have been implemented at CareMore, Presbyterian Healthcare Services in Albuquerque, N.M., and Mount Sinai. At Mount Sinai, a program called Completing Hospitalization at Home initially started with non-COVID patients and expanded to include COVID-19 early discharges, helping to free up much-needed hospital beds.
Delivering acute care at home
HaH requires a well-coordinated multidisciplinary team. Patient care is directed by a team of physicians and nurse practitioners who provide daily in-person or virtual visits. To enable provider work flow, an ambulatory version of electronic medical records (for example, Epic) must be customized to include specialized order sets that mimic inpatient orders and diagnoses-specific care delivery protocols. HaH physicians and nurse practitioners are available 24/7 to address acute patient issues.
In addition, patients receive at least daily visits from registered nurses (RNs) who carry out orders, administer medications, draw labs, and provide clinical assessment and patient education. Some organizations employ HaH nurses, while others contract with home health agencies.
Typically, patients are provided with a tablet to enable telehealth visits, as well as a blood pressure monitor, thermometer, pulse oximeter, and, if needed, scale and glucometer, that allow on-demand or continuous remote monitoring. Recent technology advances in home monitoring enhanced HaH’s capability to care for complex, high-acuity patients, and increased the potential volume of patients that can be safely treated at home.
Providence St. Joseph Health, a not-for-profit health care system operating 51 hospitals and 1,085 clinics across seven states, launched their HaH program earlier this year. Per Danielsson, MD, executive medical director for hospital medicine at Swedish Medical Center in Seattle, describes it as a “high-touch, high-tech program anchored by hospitalists.” The Providence HaH team utilizes a wearable medical device for patients that enables at-home continuous monitoring of vital signs such as temperature, blood pressure, heart rate, respirations, and pulse oximetry. Single-lead EKG monitoring is available for selected patients. Individual patient data is transmitted to a central command center, where a team of nurses and physicians remotely monitor HaH patients. According to Todd Czartoski, MD, chief medical technology officer at Providence, “Hospital at Home improves quality and access, and can substitute for 20%-30% of hospital admissions.”
In addition to patient monitoring and 24/7 provider access, some HaH programs partner with community paramedics for emergency responses. At Mount Sinai, HaH providers can trigger paramedic response, if needed. Paramedics can set up a video link with a doctor and, under the direction of a physician, will provide treatment at home or transport patients to the hospital.
HaH would be impossible without a partnership with local ancillary service providers that can promptly deliver services and goods to patient homes. Raphael Rakowski, CEO of Medically Home, a Boston-based company that partners with health care providers to build virtual hospitals at home, calls it an “acute rapid response supply chain.” The services, both clinical and nonclinical, consist of infusions; x-rays; bedside ultrasound; laboratory; transportation; and skilled physical, occupational, and speech therapy. If patients require services that are not available at home (for example, a CT scan), patients can be transported to and from a diagnostic center. Medical and nonmedical goods include medications, oxygen, durable medical equipment, and even meals.
Delivery of hospital-level services at home requires a seamless coordination between clinical teams and suppliers that relies on nursing care coordinators and supporting nonclinical staff, and is enabled by a secure text messaging platform to communicate within the care team, with suppliers, and with other providers (for example, primary care providers and specialists).
Ensuring smooth postacute transition
Thirty days after hospital discharge is the most critical period, especially for elderly patients. According to one study, 19% of patients experienced adverse events within 3 weeks after hospital discharge.18 Adverse drug events were the most common postdischarge complication, followed by procedural complications and hospital-acquired infections. Furthermore, 30-day all-cause hospital readmissions is a common occurrence. Per the Healthcare Cost and Utilization Project database, 17.1% of Medicare and 13.9% of all-payers patients were readmitted to the hospital within 30 days in 2016.19
It is not surprising that some organizations offer ongoing home care during the postacute period. At Mount Sinai, patients discharged from HaH continue to have access to the HaH team around the clock for 30 days to address emergencies and health concerns. Recovery Care Coordinators and social workers monitor patient health status, develop a follow-up plan, coordinate care, and answer questions. Medically Home provides 24/7 care to HaH patients for the entire duration of the acute care episode (34 days) to ensure maximum access to care and no gaps in care and communication. At Presbyterian, most HaH patients are transitioned into a Home Health episode of care to ensure continued high-quality care.
In addition to people, processes, technology, and the supply chain, HaH implementation requires capabilities to collect and analyze quality and cost data to measure program efficacy and, in some arrangements with payers, to reconcile clams data to determine shared savings or losses.
Partnering with third parties
Considering the resources and capabilities required for HaH program development and implementation, it is not surprising that health care providers are choosing to partner with third parties. For example, Mount Sinai partnered with Contessa Health, a Nashville, Tenn.–based company that offers hospitals a turn-key Home Recovery Care program, to assist with supply chain contracting and management, and claims data reconciliation.
Medically Home has partnered with seven health care systems, including the Mayo Clinic, Tufts Medical Center in Boston, and Adventist Health in southern California, to create virtual beds, and is expected to launch the program with 15 health care systems by the end of 2020.
Medically Home offers the following services to its partners to enable care for high-acuity patients at home:
- Assistance with hiring and training of clinical staff.
- Proprietary EMR-integrated orders, notes, and clinical protocols.
- Technology for patient monitoring by the 24/7 central command center; tablets that provide health status updates and daily schedules, and enable televisits; a video platform for video communication; and secure texting.
- Selection, contracting and monitoring the performance of supply chain vendors.
- Analytics.
The future of Hospital at Home
There is no question that HaH can offer a safe, high-quality, and lower-cost alternative to hospitalizations for select patients, which is aligned with the Centers for Medicare and Medicaid Services’ triple aim of better care for individuals, better health for populations, and lower cost.20
The future of HaH depends on development of a common payment model that will be adopted beyond the pandemic by government and commercial payers. Current payment models vary and include capitated agreements, discounted diagnosis-related group payments for the acute episode, and discounted DRG payments plus shared losses or savings.
The COVID-19 pandemic has created, arguably, the biggest crisis that U.S. health care has ever experienced, and it is far from over. Short term, Hospital at Home offers a solution to create flexible hospital bed capacity and deliver safe hospital-level care for vulnerable populations. Long term, it may be the solution that helps achieve better care for individuals, better health for populations and lower health care costs.
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of the Hospitalist’s editorial advisory board.
References
1. Source: www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf
2. Source: www.aha.org/statistics/fast-facts-us-hospitals
3. Roberts RR, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999 Feb;281(7):644-9.
4. Levinson DR; US Department of Health and Human Services; HHS; Office of the Inspector General; OIG.
5. Krumholz HM. Post-Hospital Syndrome – An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013 Jan;368:100-102.
6. Leff B, et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999 Jun;47(6):697-702.
7. Leff B, et al. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec;143(11):798-808.
8. Source: www.johnshopkinssolutions.com/solution/hospital-at-home/
9. Cryer L, et al. Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs. 2012 Jun;31(6):1237–43.
10. Personal communication with Presbyterian Health Services. May 20, 2020.
11. Federman A, et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018 Aug;178(8):1033–40.
12. Source: aspe.hhs.gov/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf
13. Source: aspe.hhs.gov/system/files/pdf/255906/Secretarial_Responses_June_13_2018.508.pdf
14. Shepperd S, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):CD007491. DOI:10.1002/14651858.CD007491.pub2.
15. Levine DM, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020 Jan;172(2);77-85.
16. Source: www.cms.gov/files/document/covid-hospitals.pdf
17. Centers for Medicare & Medicaid Services. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 2020 Nov 20.
18. Forster AJ et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Mar;138(3):161-7. doi: 10.7326/0003-4819-138-3-200302040-00007.
19. Bailey MK et al. Characteristics of 30-Day All-Cause Hospital Readmissions, 2010-2016. Statistical Brief 248. Agency for Healthcare Research and Quality. 2019 Feb 12. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb248-Hospital-Readmissions-2010-2016.jsp.
20. Centers for Medicare & Medicaid Services. What are the value-based programs? 2020 Jan 6. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs.
The United States spends one-third of the nation’s health dollars on hospital care, amounting to $1.2 trillion in 2018.1 U.S. hospital beds are prevalent2, and expensive to build and operate, with most hospital services costs related to buildings, equipment, salaried labor, and overhead.3
Despite their mission to heal, hospitals can be harmful, especially for frail and elderly patients. A study completed by the Office of the Inspector General (OIG) found that 13.5% of hospitalized Medicare patients experienced an adverse event that resulted in a prolonged hospital stay, permanent harm, a life-sustaining intervention or death.4 In addition, there is growing concern about acquired post-hospitalization syndrome caused by the physiological stress that patients experience in the hospital, leaving them vulnerable to clinical adverse events such as falls and infections.5
In the mid-1990s, driven by a goal to “avoid the harm of inpatient care and honor the wishes of older adults who refused to go to the hospital”, Dr. Bruce Leff, director of the Center for Transformative Geriatric Research and professor of medicine at Johns Hopkins University in Baltimore, and his team set out to develop and test Hospital at Home (HaH) – an innovative model for delivering hospital-level care to selected patients in the safety of their homes.
More than 20 years later, despite extensive evidence supporting HaH safety and efficacy, and its successful rollout in other countries, the model has not been widely adopted in the U.S. However, the COVID-19 pandemic amplified interest in HaH by creating an urgent need for flexible hospital bed capacity and heightening concerns about hospital care safety, especially for vulnerable adults.
In this article, we will introduce HaH history and efficacy, and then discuss what it takes to successfully implement HaH.
Hospital at Home: History, efficacy, and early adoption
The earliest HaH study, a 17-patient pilot conducted by Dr. Leff’s team from 1996 to 1998, proved that HaH was feasible, safe, highly satisfactory and cost-effective for selected acutely ill older patients with community-acquired pneumonia, chronic heart failure, chronic obstructive pulmonary disease or cellulitis.6 In 2000 to 2002, a National Demonstration and Evaluation Study of 455 patients across three sites determined that patients treated in Hospital at Home had statistically significant shorter length of stay (3.2 vs 4.9 days), lower cost ($5,081 vs. $7,480) and complications.7 Equipped with evidence, Dr. Leff and his team focused on HaH dissemination and implementation across several health care systems.8
Presbyterian Healthcare Services in Albuquerque, N.M., was one of the earliest adopters of HaH and launched the program in 2008. The integrated system serves one-third of New Mexicans and includes nine hospitals, more than 100 clinics and the state’s largest health plan. According to Nancy Guinn, MD, a medical director of Presbyterian Healthcare at Home, “Innovation is key to survive in a lean environment like New Mexico, which has the lowest percentage of residents with insurance from their employer and a high rate of government payers.”
Presbyterian selected nine diagnoses for HaH focus: congestive heart failure, chronic obstructive pulmonary disease, community-acquired pneumonia, cellulitis, deep venous thrombosis, pulmonary embolism, complicated urinary tract infection or urosepsis, nausea and vomiting, and dehydration. The HaH care, including physician services, is reimbursed via a partial DRG (diagnosis-related group) payment that was negotiated internally between the health system and Presbyterian Health Plan.
The results demonstrated that, compared to hospitalized patients with similar conditions, patients in HaH had a lower rate of falls (0% vs. .8%), lower mortality (.93% vs. 3.4%), higher satisfaction (mean score 90.7 vs. 83.9) and 19% lower cost.9 According to Dr. Guinn, more recent results showed even larger cost savings of 42%.10 After starting the HaH model, Presbyterian has launched other programs that work closely with HaH to provide a seamless experience for patients. That includes the Complete Care Program, which offers home-based primary, urgent, and acute care to members covered through Presbyterian Health Plan and has a daily census of 600-700 patients.
Another important milestone came in 2014 when Icahn School of Medicine at Mount Sinai in New York was awarded $9.6 million by the Center for Medicare and Medicaid Innovation (CMMI) to test the HaH model during acute illness and for 30 days after admission. A case study of 507 patients enrolled in the program in 2014 through 2017 revealed that HaH patients had statistically significant shorter length of stay (3.2 days vs. 5.5 days), and lower rates of all-cause 30-day hospital readmissions (8.6% vs. 15.6%), 30-day ED revisits (5.8% vs. 11.7%), and SNF admissions (1.7% vs. 10.4%), and were also more likely to rate their hospital care highly (68.8% vs. 45.3%).11
In 2017, using data from their CMMI study, Mount Sinai submitted an application to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to implement Hospital at Home as an alternative payment model that bundles the acute episode with 30 days of post‐acute transitional care. The PTAC unanimously approved the proposal and submitted their recommendations to the Secretary of Health and Human Services (HHS) to implement HaH as an alternative payment model that included two parts:
1. A bundled payment equal to a percentage of the prospective DRG (diagnosis-related group) payment that would have been paid to a hospital.
2. A performance-based payment (shared savings/losses) based on (a) total spending during the acute care phase and 30 days afterward relative to a target price, and (b) performance on quality measures.12
In June 2018, the HHS secretary announced that he was not approving the proposal as written, citing, among other things, concerns about proposed payment methodology and patient safety.13
Hospital at Home: Present state
Despite additional evidence of HaH’s impact on lowering cost, decreasing 30-day readmissions, improving patient satisfaction and functional outcomes without an adverse effect on mortality,14, 15 the model has not been widely adopted, largely due to lack of fee-for-service reimbursement from the public payers (Medicare and Medicaid) and complex logistics to implement it.
However, the COVID-19 pandemic created an urgent need for flexible hospital bed capacity and amplified concerns about hospital care safety for vulnerable populations. In response, the Centers for Medicare and Medicaid Services (CMS) introduced its Hospitals without Walls initiative that allowed hospitals to provide services in other health care facilities and sites that are not part of the existing hospital.16 On November 25, 2020, CMS announced expansion of the Hospital without Walls initiatives to include a Hospital Care at Home program that allows eligible hospitals to treat eligible patients at home.17
With significant evidence supporting HaH’s safety and efficacy, and long overdue support from CMS, it’s now a matter of how to successfully implement it. Let’s explore what it takes to select and enroll patients, deliver acute care at home, and ensure a smooth post-acute transition within the HaH model.
Successfully implementing Hospital at Home
HaH implementation requires five key components – people, processes, technology, supply chain, and analytics – to select and enroll patients, deliver acute care at home, and ensure a smooth postacute transition. Let’s discuss each of them in more detail below.
Selecting and enrolling patients
Patients eligible for HaH are identified based on their insurance, as well as clinical and social criteria. Despite a lack of public payer support, several commercial payers embraced the model for selected patients who consented to receive acute hospital care at home. The patients must meet criteria for an inpatient admission, be medically stable and have a low level of diagnostic uncertainty. Advances in home monitoring technology expanded clinical criteria to include acutely ill patients with multiple comorbidities, including cancer. It is important that patients reside in a safe home environment and live within a reasonable distance from the hospital.
CareMore Health, an integrated health care delivery system serving more than 180,000 Medicare Advantage and Medicaid patients across nine states and Washington D.C., launched Hospital at Home in December 2018, and rapidly scaled from a few referrals to averaging more than 20 new patients per week.
Sashidaran Moodley, MD, medical director at CareMore Health and Aspire Health, in Cerritos, Calif., shared a valuable lesson regarding launching the program: “Do not presume that if you build it, they will come. This is a new model of care that requires physicians to change their behavior and health systems to modify their traditional admission work flows. Program designers should not limit their thinking around sourcing patients just from the emergency department.”
Dr. Moodley recommends moving upstream and bring awareness to the program to drive additional referrals from primary care providers, case managers, and remote patient monitoring programs (for example, heart failure).
Linda DeCherrie, MD, clinical director of Mount Sinai at Home, based in New York, says that “educating and involving hospitalists is key.” At Mount Sinai, patients eligible for HaH are initially evaluated by hospitalists in the ED who write initial orders and then transfer care to HaH hospitalists.
HaH also can enroll eligible patients who still require hospital-level care to complete the last few days of acute hospitalization at home. Early discharge programs have been implemented at CareMore, Presbyterian Healthcare Services in Albuquerque, N.M., and Mount Sinai. At Mount Sinai, a program called Completing Hospitalization at Home initially started with non-COVID patients and expanded to include COVID-19 early discharges, helping to free up much-needed hospital beds.
Delivering acute care at home
HaH requires a well-coordinated multidisciplinary team. Patient care is directed by a team of physicians and nurse practitioners who provide daily in-person or virtual visits. To enable provider work flow, an ambulatory version of electronic medical records (for example, Epic) must be customized to include specialized order sets that mimic inpatient orders and diagnoses-specific care delivery protocols. HaH physicians and nurse practitioners are available 24/7 to address acute patient issues.
In addition, patients receive at least daily visits from registered nurses (RNs) who carry out orders, administer medications, draw labs, and provide clinical assessment and patient education. Some organizations employ HaH nurses, while others contract with home health agencies.
Typically, patients are provided with a tablet to enable telehealth visits, as well as a blood pressure monitor, thermometer, pulse oximeter, and, if needed, scale and glucometer, that allow on-demand or continuous remote monitoring. Recent technology advances in home monitoring enhanced HaH’s capability to care for complex, high-acuity patients, and increased the potential volume of patients that can be safely treated at home.
Providence St. Joseph Health, a not-for-profit health care system operating 51 hospitals and 1,085 clinics across seven states, launched their HaH program earlier this year. Per Danielsson, MD, executive medical director for hospital medicine at Swedish Medical Center in Seattle, describes it as a “high-touch, high-tech program anchored by hospitalists.” The Providence HaH team utilizes a wearable medical device for patients that enables at-home continuous monitoring of vital signs such as temperature, blood pressure, heart rate, respirations, and pulse oximetry. Single-lead EKG monitoring is available for selected patients. Individual patient data is transmitted to a central command center, where a team of nurses and physicians remotely monitor HaH patients. According to Todd Czartoski, MD, chief medical technology officer at Providence, “Hospital at Home improves quality and access, and can substitute for 20%-30% of hospital admissions.”
In addition to patient monitoring and 24/7 provider access, some HaH programs partner with community paramedics for emergency responses. At Mount Sinai, HaH providers can trigger paramedic response, if needed. Paramedics can set up a video link with a doctor and, under the direction of a physician, will provide treatment at home or transport patients to the hospital.
HaH would be impossible without a partnership with local ancillary service providers that can promptly deliver services and goods to patient homes. Raphael Rakowski, CEO of Medically Home, a Boston-based company that partners with health care providers to build virtual hospitals at home, calls it an “acute rapid response supply chain.” The services, both clinical and nonclinical, consist of infusions; x-rays; bedside ultrasound; laboratory; transportation; and skilled physical, occupational, and speech therapy. If patients require services that are not available at home (for example, a CT scan), patients can be transported to and from a diagnostic center. Medical and nonmedical goods include medications, oxygen, durable medical equipment, and even meals.
Delivery of hospital-level services at home requires a seamless coordination between clinical teams and suppliers that relies on nursing care coordinators and supporting nonclinical staff, and is enabled by a secure text messaging platform to communicate within the care team, with suppliers, and with other providers (for example, primary care providers and specialists).
Ensuring smooth postacute transition
Thirty days after hospital discharge is the most critical period, especially for elderly patients. According to one study, 19% of patients experienced adverse events within 3 weeks after hospital discharge.18 Adverse drug events were the most common postdischarge complication, followed by procedural complications and hospital-acquired infections. Furthermore, 30-day all-cause hospital readmissions is a common occurrence. Per the Healthcare Cost and Utilization Project database, 17.1% of Medicare and 13.9% of all-payers patients were readmitted to the hospital within 30 days in 2016.19
It is not surprising that some organizations offer ongoing home care during the postacute period. At Mount Sinai, patients discharged from HaH continue to have access to the HaH team around the clock for 30 days to address emergencies and health concerns. Recovery Care Coordinators and social workers monitor patient health status, develop a follow-up plan, coordinate care, and answer questions. Medically Home provides 24/7 care to HaH patients for the entire duration of the acute care episode (34 days) to ensure maximum access to care and no gaps in care and communication. At Presbyterian, most HaH patients are transitioned into a Home Health episode of care to ensure continued high-quality care.
In addition to people, processes, technology, and the supply chain, HaH implementation requires capabilities to collect and analyze quality and cost data to measure program efficacy and, in some arrangements with payers, to reconcile clams data to determine shared savings or losses.
Partnering with third parties
Considering the resources and capabilities required for HaH program development and implementation, it is not surprising that health care providers are choosing to partner with third parties. For example, Mount Sinai partnered with Contessa Health, a Nashville, Tenn.–based company that offers hospitals a turn-key Home Recovery Care program, to assist with supply chain contracting and management, and claims data reconciliation.
Medically Home has partnered with seven health care systems, including the Mayo Clinic, Tufts Medical Center in Boston, and Adventist Health in southern California, to create virtual beds, and is expected to launch the program with 15 health care systems by the end of 2020.
Medically Home offers the following services to its partners to enable care for high-acuity patients at home:
- Assistance with hiring and training of clinical staff.
- Proprietary EMR-integrated orders, notes, and clinical protocols.
- Technology for patient monitoring by the 24/7 central command center; tablets that provide health status updates and daily schedules, and enable televisits; a video platform for video communication; and secure texting.
- Selection, contracting and monitoring the performance of supply chain vendors.
- Analytics.
The future of Hospital at Home
There is no question that HaH can offer a safe, high-quality, and lower-cost alternative to hospitalizations for select patients, which is aligned with the Centers for Medicare and Medicaid Services’ triple aim of better care for individuals, better health for populations, and lower cost.20
The future of HaH depends on development of a common payment model that will be adopted beyond the pandemic by government and commercial payers. Current payment models vary and include capitated agreements, discounted diagnosis-related group payments for the acute episode, and discounted DRG payments plus shared losses or savings.
The COVID-19 pandemic has created, arguably, the biggest crisis that U.S. health care has ever experienced, and it is far from over. Short term, Hospital at Home offers a solution to create flexible hospital bed capacity and deliver safe hospital-level care for vulnerable populations. Long term, it may be the solution that helps achieve better care for individuals, better health for populations and lower health care costs.
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of the Hospitalist’s editorial advisory board.
References
1. Source: www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf
2. Source: www.aha.org/statistics/fast-facts-us-hospitals
3. Roberts RR, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999 Feb;281(7):644-9.
4. Levinson DR; US Department of Health and Human Services; HHS; Office of the Inspector General; OIG.
5. Krumholz HM. Post-Hospital Syndrome – An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013 Jan;368:100-102.
6. Leff B, et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999 Jun;47(6):697-702.
7. Leff B, et al. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec;143(11):798-808.
8. Source: www.johnshopkinssolutions.com/solution/hospital-at-home/
9. Cryer L, et al. Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs. 2012 Jun;31(6):1237–43.
10. Personal communication with Presbyterian Health Services. May 20, 2020.
11. Federman A, et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018 Aug;178(8):1033–40.
12. Source: aspe.hhs.gov/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf
13. Source: aspe.hhs.gov/system/files/pdf/255906/Secretarial_Responses_June_13_2018.508.pdf
14. Shepperd S, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):CD007491. DOI:10.1002/14651858.CD007491.pub2.
15. Levine DM, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020 Jan;172(2);77-85.
16. Source: www.cms.gov/files/document/covid-hospitals.pdf
17. Centers for Medicare & Medicaid Services. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 2020 Nov 20.
18. Forster AJ et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Mar;138(3):161-7. doi: 10.7326/0003-4819-138-3-200302040-00007.
19. Bailey MK et al. Characteristics of 30-Day All-Cause Hospital Readmissions, 2010-2016. Statistical Brief 248. Agency for Healthcare Research and Quality. 2019 Feb 12. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb248-Hospital-Readmissions-2010-2016.jsp.
20. Centers for Medicare & Medicaid Services. What are the value-based programs? 2020 Jan 6. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs.
AHA reassures myocarditis rare after COVID vaccination, benefits overwhelm risks
The benefits of COVID-19 vaccination “enormously outweigh” the rare possible risk for heart-related complications, including myocarditis, the American Heart Association/American Stroke Association (ASA) says in new statement.
The message follows a Centers for Disease Control and Prevention report that the agency is monitoring the Vaccine Adverse Events Reporting System (VAERS) and the Vaccine Safety Datalink (VSD) for cases of myocarditis that have been associated with the mRNA vaccines against SARS-CoV-2 from Pfizer and Moderna.
The “relatively few” reported cases myocarditis in adolescents or young adults have involved males more often than females, more often followed the second dose rather than the first, and were usually seen in the 4 days after vaccination, the CDC’s COVID-19 Vaccine Safety Technical Work Group (VaST) found.
“Most cases appear to be mild, and follow-up of cases is ongoing,” the CDC says. “Within CDC safety monitoring systems, rates of myocarditis reports in the window following COVID-19 vaccination have not differed from expected baseline rates.”
In their statement, the AHA/ASA “strongly urge” all adults and children 12 years and older to receive a COVID-19 vaccine as soon as possible.
“The evidence continues to indicate that the COVID-19 vaccines are nearly 100% effective at preventing death and hospitalization due to COVID-19 infection,” the groups say.
Although the investigation of cases of myocarditis related to COVID-19 vaccination is ongoing, the AHA/ASA notes that myocarditis is typically the result of an actual viral infection, “and it is yet to be determined if these cases have any correlation to receiving a COVID-19 vaccine.”
“We’ve lost hundreds of children, and there have been thousands who have been hospitalized, thousands who developed an inflammatory syndrome, and one of the pieces of that can be myocarditis,” Richard Besser, MD, president and CEO of the Robert Wood Johnson Foundation (RWJF), said today on ABC’s Good Morning America.
Still, “from my perspective, the risk of COVID is so much greater than any theoretical risk from the vaccine,” said Dr. Besser, former acting director of the CDC.
The symptoms that can occur after COVID-19 vaccination include tiredness, headache, muscle pain, chills, fever, and nausea, reminds the AHA/ASA statement. Such symptoms would “typically appear within 24-48 hours and usually pass within 36-48 hours after receiving the vaccine.”
All health care providers should be aware of the “very rare” adverse events that could be related to a COVID-19 vaccine, including myocarditis, blood clots, low platelets, and symptoms of severe inflammation, it says.
“Health care professionals should strongly consider inquiring about the timing of any recent COVID vaccination among patients presenting with these conditions, as needed, in order to provide appropriate treatment quickly,” the statement advises.
A version of this article first appeared on Medscape.com.
The benefits of COVID-19 vaccination “enormously outweigh” the rare possible risk for heart-related complications, including myocarditis, the American Heart Association/American Stroke Association (ASA) says in new statement.
The message follows a Centers for Disease Control and Prevention report that the agency is monitoring the Vaccine Adverse Events Reporting System (VAERS) and the Vaccine Safety Datalink (VSD) for cases of myocarditis that have been associated with the mRNA vaccines against SARS-CoV-2 from Pfizer and Moderna.
The “relatively few” reported cases myocarditis in adolescents or young adults have involved males more often than females, more often followed the second dose rather than the first, and were usually seen in the 4 days after vaccination, the CDC’s COVID-19 Vaccine Safety Technical Work Group (VaST) found.
“Most cases appear to be mild, and follow-up of cases is ongoing,” the CDC says. “Within CDC safety monitoring systems, rates of myocarditis reports in the window following COVID-19 vaccination have not differed from expected baseline rates.”
In their statement, the AHA/ASA “strongly urge” all adults and children 12 years and older to receive a COVID-19 vaccine as soon as possible.
“The evidence continues to indicate that the COVID-19 vaccines are nearly 100% effective at preventing death and hospitalization due to COVID-19 infection,” the groups say.
Although the investigation of cases of myocarditis related to COVID-19 vaccination is ongoing, the AHA/ASA notes that myocarditis is typically the result of an actual viral infection, “and it is yet to be determined if these cases have any correlation to receiving a COVID-19 vaccine.”
“We’ve lost hundreds of children, and there have been thousands who have been hospitalized, thousands who developed an inflammatory syndrome, and one of the pieces of that can be myocarditis,” Richard Besser, MD, president and CEO of the Robert Wood Johnson Foundation (RWJF), said today on ABC’s Good Morning America.
Still, “from my perspective, the risk of COVID is so much greater than any theoretical risk from the vaccine,” said Dr. Besser, former acting director of the CDC.
The symptoms that can occur after COVID-19 vaccination include tiredness, headache, muscle pain, chills, fever, and nausea, reminds the AHA/ASA statement. Such symptoms would “typically appear within 24-48 hours and usually pass within 36-48 hours after receiving the vaccine.”
All health care providers should be aware of the “very rare” adverse events that could be related to a COVID-19 vaccine, including myocarditis, blood clots, low platelets, and symptoms of severe inflammation, it says.
“Health care professionals should strongly consider inquiring about the timing of any recent COVID vaccination among patients presenting with these conditions, as needed, in order to provide appropriate treatment quickly,” the statement advises.
A version of this article first appeared on Medscape.com.
The benefits of COVID-19 vaccination “enormously outweigh” the rare possible risk for heart-related complications, including myocarditis, the American Heart Association/American Stroke Association (ASA) says in new statement.
The message follows a Centers for Disease Control and Prevention report that the agency is monitoring the Vaccine Adverse Events Reporting System (VAERS) and the Vaccine Safety Datalink (VSD) for cases of myocarditis that have been associated with the mRNA vaccines against SARS-CoV-2 from Pfizer and Moderna.
The “relatively few” reported cases myocarditis in adolescents or young adults have involved males more often than females, more often followed the second dose rather than the first, and were usually seen in the 4 days after vaccination, the CDC’s COVID-19 Vaccine Safety Technical Work Group (VaST) found.
“Most cases appear to be mild, and follow-up of cases is ongoing,” the CDC says. “Within CDC safety monitoring systems, rates of myocarditis reports in the window following COVID-19 vaccination have not differed from expected baseline rates.”
In their statement, the AHA/ASA “strongly urge” all adults and children 12 years and older to receive a COVID-19 vaccine as soon as possible.
“The evidence continues to indicate that the COVID-19 vaccines are nearly 100% effective at preventing death and hospitalization due to COVID-19 infection,” the groups say.
Although the investigation of cases of myocarditis related to COVID-19 vaccination is ongoing, the AHA/ASA notes that myocarditis is typically the result of an actual viral infection, “and it is yet to be determined if these cases have any correlation to receiving a COVID-19 vaccine.”
“We’ve lost hundreds of children, and there have been thousands who have been hospitalized, thousands who developed an inflammatory syndrome, and one of the pieces of that can be myocarditis,” Richard Besser, MD, president and CEO of the Robert Wood Johnson Foundation (RWJF), said today on ABC’s Good Morning America.
Still, “from my perspective, the risk of COVID is so much greater than any theoretical risk from the vaccine,” said Dr. Besser, former acting director of the CDC.
The symptoms that can occur after COVID-19 vaccination include tiredness, headache, muscle pain, chills, fever, and nausea, reminds the AHA/ASA statement. Such symptoms would “typically appear within 24-48 hours and usually pass within 36-48 hours after receiving the vaccine.”
All health care providers should be aware of the “very rare” adverse events that could be related to a COVID-19 vaccine, including myocarditis, blood clots, low platelets, and symptoms of severe inflammation, it says.
“Health care professionals should strongly consider inquiring about the timing of any recent COVID vaccination among patients presenting with these conditions, as needed, in order to provide appropriate treatment quickly,” the statement advises.
A version of this article first appeared on Medscape.com.
Novel drug approvals of 2020
In 2020, the Food and Drug Administration approved 53 new drugs for humans. One of these agents, Annovera (segesterone and ethinyl estradiol), is a vaginal ring to prevent pregnancy and is not relevant in this article. A second drug, Asparlas (calaspargase pegol), indicated to treat acute lymphoblastic leukemia, has not yet been released by its manufacturer. Orgovyx (relugolix) is used for prostate cancer and Lampit (nifurtimox) is drug used in children – neither of these two agents will be covered. The remaining 49 are covered below. The agents with molecular weights less than 1,000 probably cross the placenta in the first half of pregnancy, but nearly all, regardless of MW, will cross in the second half of pregnancy.
No human pregnancy data for these agents has been found, but there are five drugs included in pregnancy registries. It will take some time before the outcomes of these drugs are published. The routine absence of pregnancy data for most drugs was pointed out in an article that I coauthored, “Should pregnant women be included in phase 4 clinical drug trials?”. The article makes a strong argument for including some pregnant women in these trials.
Anti-infectives
Artesunate (384)
The drug appears low risk when used in the second and third trimesters. There is inadequate information regarding its use in the first trimester, so the safest course for the embryo appears to be avoiding its use during this period. A single intravenous dose given to rats early in gestation resulted in embryolethality.
Ebanga (ansuvimab) (147,000)
Studies on its use in pregnant animals have not been conducted.
Inmazeb (atoltivimab, maftivimab, odesivimab) (144,000-146,000)
Inmazeb is a combination of the three agents. Studies on its use in pregnant animals have not been conducted.
Veklury (remdesivir) (603)
Veklury is indicated for the treatment of pregnant women hospitalized with COVID-19 who are at risk for serious morbidity and mortality. The drug should be used during pregnancy only if the potential benefit justifies the potential risk for the mother and the fetus.
Antineoplastics
Ayvakit (avapritinib) (499)
The drug may cause fetal harm. The drug was teratogenic in animals.
Blenrep (belantamab mafodotin-blmf) (152,000)
A B-cell maturation antigen, it is indicated for the treatment of multiple myeloma. No human or animal pregnancy data have been located.
Danyelza (naxitamab-gqgk) (144,000)
This agent is used for the treatment of neuroblastoma. Based on its mechanism of action it may cause fetal harm if used in pregnancy.
Gavreto (pralsetinib) (534)
Gavreto is indicated for the treatment of small cell lung cancer. It may cause embryo-fetal harm if used in pregnancy.
Inqovi (cedazuridine + decitabine) (268,228)
The drug combination can cause fetal harm in human pregnancy. It is toxic in pregnant animals.
Margenza (margetuximab-cmkb) (149,000)
Although there are no data on the use of this drug in human pregnancy, the findings in animals and mechanism of action suggest that it will cause fetal harm.
Monjuvi (tafasitamab-cxix) (150,000)
This drug is a cytolytic antibody that is indicated in combination with lenalidomide. The combination may cause fetal harm.
Pemazyre (pemigatinib) (488)
It is indicated for the treatment of cholangiocarcinoma. In an animal study, the drug caused fetal defects, fetal growth retardation, and embryo-fetal death at maternal exposures lower than the human exposure.
Qinlock (ripretinib) (510)
This drug is used for the treatment of patients with advanced gastrointestinal stromal tumor. The drug was teratogenic in pregnant animals.
Retevmo (selpercatinib) (526)
This is a kinase inhibitor used for the treatment of small cell lung cancer. The drug is teratogenic in animals.
Sarclisa (isatuximab-irfc) (148,000)This drug is used in combination with pomalidomide and dexamethasone. The combination would probably cause major toxicity in an embryo or fetus.
Tabrecta (capmatinib) (412 – free base)Capmatinib is a kinase inhibitor used for the treatment of metastatic non–small cell lung cancer. It is teratogenic in animals.
Tazverik (tazemetostat) (654)Tazemetostat is indicated for the treatment of epithelioid sarcoma and follicular lymphoma, The drug is teratogenic in animals.
Trodelvy (sacituzumab govitecan-hziy) (1,602)This agent is used for the treatment of breast cancer. The drug has not been tested in pregnant animals. However, according to the manufacturer, there is a high possibility of human teratogenicity if it is given to a pregnant woman.
Tukysa (tucatinib) (481)
Tukysa is a tyrosine kinase inhibitor that is used in combination with trastuzumab and capecitabine for the treatment of breast cancer. The drug is teratogenic in animals.
Zeposia (ozanimod) (441)
Zeposia is indicated for the treatment of multiple sclerosis. The drug takes about 3 months to eliminate from the body. The drug is teratogenic in animals.
Zepzelca (lurbinectedin) (785)
This agent is used for the treatment of metastatic small cell lung cancer. The drug is teratogenic in animals.
Antiemetics
Barhemsys (amisulpride) (369)
This agent is Indicated to prevent nausea and vomiting. Animal data suggest low risk of embryo/fetal birth defects.
Antimigraine
Nurtec (rimegepant) (611)
Nurtec is indicated for acute treatment of migraine. Development toxicity was not observed in animals given doses similar to those used in humans.
Vyepti (eptinezumab-jjmr) (143,000)
A humanized monoclonal antibody that is given every 3 months to prevent migraine. There was no embryo-fetal harm in animals given the drug.
CNS
Byfavo (remimazolam) (493 – free base)
This drug is indicated for procedural sedation in adults undergoing procedures lasting 30 minutes or less. No defects were observed in animals.
Diagnostics
Cerianna (fluoroestradiol F 18) (289)
It is indicated for use with PET for characterization of estrogen receptor status in patients with ER-positive breast cancer. It has the potential to cause fetal harm depending on the fetal stage of development and the magnitude of radiation dose. There are no data on its use in pregnant women or animals.
Detectnet (copper CU-64 dotatate) (1,497)
All radiopharmaceuticals have the potential to cause fetal harm depending on the fetal stage of development and the magnitude of the radiation dose. There are no pregnancy data in humans or animals
Miscellaneous
Dojolvi (triheptanoin) (429)
This agent is indicated as a source of calories and fatty acids for the treatment of pediatric and adult patients with molecularly confirmed long-chain fatty acid oxidation disorders. Advise patients that there is a pregnancy safety study that collects pregnancy outcome data in women taking Dojolvi during pregnancy. Pregnant patients can enroll in the study by calling 1-888-756-8657.
Enspryng (satralizumab-mwge) (143,000)
It is indicated for the treatment of neuromyelitis optica spectrum disorder in adult patients who are anti–aquaporin-4 (AQP4) antibody positive. No information is available on the risks, if any, in pregnancy. No adverse effects on maternal or fetal development were observed in pregnant monkeys and their offspring.
Evrysdi (risdiplam) (401)
This is a prescription medicine used to treat spinal muscular atrophy in adults and children aged 2 months and older. In pregnant animals the drug caused adverse effects on fetal development.
Gemtesa (vibegron) (445)
Gemtesa is used in adults to treat the symptoms of overactive bladder. The drug had no adverse effects on pregnant animals.
Imcivree (setmelanotide) (1,117)
This drug is indicated for chronic weight management in adult and pediatric patients aged 6 years and older with obesity because of proopiomelanocortin, proprotein convertase subtilisin/kexin type 1, or leptin receptor deficiency. The drug was not embryo toxic in animals.
Isturisa (osilodrostat) (325)
Isturisa is a cortisol synthesis inhibitor indicated for the treatment of adult patients with Cushing’s disease. No adverse fetal effects were observed in pregnant animals.
Klisyri (tirbanibulin) (431)
Tirbanibulin ointment is a microtubule inhibitor that is used to treat actinic keratosis. Information on its effects in pregnancy is not available.
Koselugo (selumetinib) (556)
This is a kinase inhibitor indicated for the treatment of pediatric patients aged 2 years and older. The drug is toxic in pregnant animals but its effects in human pregnancy are not known.
Nexletol (bempedoic acid) (344)
Nexletol is indicated as an adjunct to diet and maximally tolerated statin therapy for the treatment of adults with heterozygous familial hypercholesterolemia or established atherosclerotic cardiovascular disease who require additional lowering of LDL cholesterol. The drug was not teratogenic in animals. Discontinue Nexletol when pregnancy is recognized unless the benefits of therapy outweigh the potential risks to the fetus.
Olinvyk (oliceridine) (503)
Olinvyk injection is indicated in adults for the management of acute pain severe enough to require an intravenous opioid analgesic. Prolonged use of Olinvyk during pregnancy can result in neonatal opioid withdrawal syndrome. The drug was not teratogenic in animals.
Ongentys (opicapone) (413)
Ongentys is indicated as adjunctive treatment to levodopa/carbidopa in patients with Parkinson’s disease experiencing “off” episodes. The drug was teratogenic in rabbits but not in rats.
Orladeyo (berotralstat) (635)
This drug is a plasma kallikrein inhibitor indicated for prophylaxis to prevent attacks of hereditary angioedema. It was not teratogenic in animals.
Oxlumo (lumasiran) (17,286)
Oxlumo is a HAO1-directed small interfering ribonucleic acid indicated for the treatment of primary hyperoxaluria type 1 to lower urinary oxalate levels. No adverse effects on pregnancy or embryo-fetal development related to the drug were observed in animals.
Pizensy (lactitol) (344)
Lactitol is minimally absorbed systemically following oral administration. It is unknown whether maternal use will result in fetal exposure to the drug. No effects on embryo-fetal development were observed in animals at doses much higher than the maximum recommended human dosage.
Rukobia (fostemsavir) (705; 584 for free acid)
This drug is an HIV-1–directed attachment inhibitor, in combination with other antiretrovirals. There is a pregnancy exposure registry that monitors pregnancy outcomes in individuals exposed to the drug during pregnancy. Health care providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry at 1-800-258-4263.
Sogroya (somapacitan-beco) (23,305)
This is a human growth hormone analog indicated for replacement of endogenous growth hormone in adults with growth hormone deficiency. The drug was not teratogenic in animals.
Tepezza (teprotumumab-trbw) (148,000)
Drug is indicated for the treatment of thyroid eye disease. The drug was teratogenic in cynomolgus monkeys. The manufacturer states that because of the risk, the drug should not be used in pregnancy.
Tauvid (flortaucipir F-18) (262)
This drug is indicated for use with PET imaging of the brain to evaluate for Alzheimer’s disease. It is a radioactive drug and should not be used in pregnant women.
Uplizna (inebilizumab-cdon) (149,000)
Uplizna is indicated for the treatment of neuromyelitis optica spectrum disorder in adult patients who are anti-AQP4 antibody positive. It is a humanized IgG1 monoclonal antibody and immunoglobulins are known to cross the placental barrier. Based on animal data, the drug can cause fetal harm because of B-cell lymphopenia and reduce antibody response in offspring exposed to the drug. Women of childbearing potential should use contraception while receiving Uplizna and for 6 months after the last dose.
Winlevi (clascoterone) (403)
This cream is an androgen receptor inhibitor that is indicated for the topical treatment of acne vulgaris in patients aged 12 years and older. Subcutaneous use in animals was associated with fetal defects.
Xeglyze (abametapir) (1,840)
Xeglyze is indicated for the topical treatment of head lice infestation in patients aged 6 months and older. The drug was not teratogenic in animals.
Zokinvy (lonafarnib) (639)
Zokinvy is indicated in patients 12 months or older to reduce the risk of mortality in several conditions. Animal studies have found embryo-fetal harm.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
In 2020, the Food and Drug Administration approved 53 new drugs for humans. One of these agents, Annovera (segesterone and ethinyl estradiol), is a vaginal ring to prevent pregnancy and is not relevant in this article. A second drug, Asparlas (calaspargase pegol), indicated to treat acute lymphoblastic leukemia, has not yet been released by its manufacturer. Orgovyx (relugolix) is used for prostate cancer and Lampit (nifurtimox) is drug used in children – neither of these two agents will be covered. The remaining 49 are covered below. The agents with molecular weights less than 1,000 probably cross the placenta in the first half of pregnancy, but nearly all, regardless of MW, will cross in the second half of pregnancy.
No human pregnancy data for these agents has been found, but there are five drugs included in pregnancy registries. It will take some time before the outcomes of these drugs are published. The routine absence of pregnancy data for most drugs was pointed out in an article that I coauthored, “Should pregnant women be included in phase 4 clinical drug trials?”. The article makes a strong argument for including some pregnant women in these trials.
Anti-infectives
Artesunate (384)
The drug appears low risk when used in the second and third trimesters. There is inadequate information regarding its use in the first trimester, so the safest course for the embryo appears to be avoiding its use during this period. A single intravenous dose given to rats early in gestation resulted in embryolethality.
Ebanga (ansuvimab) (147,000)
Studies on its use in pregnant animals have not been conducted.
Inmazeb (atoltivimab, maftivimab, odesivimab) (144,000-146,000)
Inmazeb is a combination of the three agents. Studies on its use in pregnant animals have not been conducted.
Veklury (remdesivir) (603)
Veklury is indicated for the treatment of pregnant women hospitalized with COVID-19 who are at risk for serious morbidity and mortality. The drug should be used during pregnancy only if the potential benefit justifies the potential risk for the mother and the fetus.
Antineoplastics
Ayvakit (avapritinib) (499)
The drug may cause fetal harm. The drug was teratogenic in animals.
Blenrep (belantamab mafodotin-blmf) (152,000)
A B-cell maturation antigen, it is indicated for the treatment of multiple myeloma. No human or animal pregnancy data have been located.
Danyelza (naxitamab-gqgk) (144,000)
This agent is used for the treatment of neuroblastoma. Based on its mechanism of action it may cause fetal harm if used in pregnancy.
Gavreto (pralsetinib) (534)
Gavreto is indicated for the treatment of small cell lung cancer. It may cause embryo-fetal harm if used in pregnancy.
Inqovi (cedazuridine + decitabine) (268,228)
The drug combination can cause fetal harm in human pregnancy. It is toxic in pregnant animals.
Margenza (margetuximab-cmkb) (149,000)
Although there are no data on the use of this drug in human pregnancy, the findings in animals and mechanism of action suggest that it will cause fetal harm.
Monjuvi (tafasitamab-cxix) (150,000)
This drug is a cytolytic antibody that is indicated in combination with lenalidomide. The combination may cause fetal harm.
Pemazyre (pemigatinib) (488)
It is indicated for the treatment of cholangiocarcinoma. In an animal study, the drug caused fetal defects, fetal growth retardation, and embryo-fetal death at maternal exposures lower than the human exposure.
Qinlock (ripretinib) (510)
This drug is used for the treatment of patients with advanced gastrointestinal stromal tumor. The drug was teratogenic in pregnant animals.
Retevmo (selpercatinib) (526)
This is a kinase inhibitor used for the treatment of small cell lung cancer. The drug is teratogenic in animals.
Sarclisa (isatuximab-irfc) (148,000)This drug is used in combination with pomalidomide and dexamethasone. The combination would probably cause major toxicity in an embryo or fetus.
Tabrecta (capmatinib) (412 – free base)Capmatinib is a kinase inhibitor used for the treatment of metastatic non–small cell lung cancer. It is teratogenic in animals.
Tazverik (tazemetostat) (654)Tazemetostat is indicated for the treatment of epithelioid sarcoma and follicular lymphoma, The drug is teratogenic in animals.
Trodelvy (sacituzumab govitecan-hziy) (1,602)This agent is used for the treatment of breast cancer. The drug has not been tested in pregnant animals. However, according to the manufacturer, there is a high possibility of human teratogenicity if it is given to a pregnant woman.
Tukysa (tucatinib) (481)
Tukysa is a tyrosine kinase inhibitor that is used in combination with trastuzumab and capecitabine for the treatment of breast cancer. The drug is teratogenic in animals.
Zeposia (ozanimod) (441)
Zeposia is indicated for the treatment of multiple sclerosis. The drug takes about 3 months to eliminate from the body. The drug is teratogenic in animals.
Zepzelca (lurbinectedin) (785)
This agent is used for the treatment of metastatic small cell lung cancer. The drug is teratogenic in animals.
Antiemetics
Barhemsys (amisulpride) (369)
This agent is Indicated to prevent nausea and vomiting. Animal data suggest low risk of embryo/fetal birth defects.
Antimigraine
Nurtec (rimegepant) (611)
Nurtec is indicated for acute treatment of migraine. Development toxicity was not observed in animals given doses similar to those used in humans.
Vyepti (eptinezumab-jjmr) (143,000)
A humanized monoclonal antibody that is given every 3 months to prevent migraine. There was no embryo-fetal harm in animals given the drug.
CNS
Byfavo (remimazolam) (493 – free base)
This drug is indicated for procedural sedation in adults undergoing procedures lasting 30 minutes or less. No defects were observed in animals.
Diagnostics
Cerianna (fluoroestradiol F 18) (289)
It is indicated for use with PET for characterization of estrogen receptor status in patients with ER-positive breast cancer. It has the potential to cause fetal harm depending on the fetal stage of development and the magnitude of radiation dose. There are no data on its use in pregnant women or animals.
Detectnet (copper CU-64 dotatate) (1,497)
All radiopharmaceuticals have the potential to cause fetal harm depending on the fetal stage of development and the magnitude of the radiation dose. There are no pregnancy data in humans or animals
Miscellaneous
Dojolvi (triheptanoin) (429)
This agent is indicated as a source of calories and fatty acids for the treatment of pediatric and adult patients with molecularly confirmed long-chain fatty acid oxidation disorders. Advise patients that there is a pregnancy safety study that collects pregnancy outcome data in women taking Dojolvi during pregnancy. Pregnant patients can enroll in the study by calling 1-888-756-8657.
Enspryng (satralizumab-mwge) (143,000)
It is indicated for the treatment of neuromyelitis optica spectrum disorder in adult patients who are anti–aquaporin-4 (AQP4) antibody positive. No information is available on the risks, if any, in pregnancy. No adverse effects on maternal or fetal development were observed in pregnant monkeys and their offspring.
Evrysdi (risdiplam) (401)
This is a prescription medicine used to treat spinal muscular atrophy in adults and children aged 2 months and older. In pregnant animals the drug caused adverse effects on fetal development.
Gemtesa (vibegron) (445)
Gemtesa is used in adults to treat the symptoms of overactive bladder. The drug had no adverse effects on pregnant animals.
Imcivree (setmelanotide) (1,117)
This drug is indicated for chronic weight management in adult and pediatric patients aged 6 years and older with obesity because of proopiomelanocortin, proprotein convertase subtilisin/kexin type 1, or leptin receptor deficiency. The drug was not embryo toxic in animals.
Isturisa (osilodrostat) (325)
Isturisa is a cortisol synthesis inhibitor indicated for the treatment of adult patients with Cushing’s disease. No adverse fetal effects were observed in pregnant animals.
Klisyri (tirbanibulin) (431)
Tirbanibulin ointment is a microtubule inhibitor that is used to treat actinic keratosis. Information on its effects in pregnancy is not available.
Koselugo (selumetinib) (556)
This is a kinase inhibitor indicated for the treatment of pediatric patients aged 2 years and older. The drug is toxic in pregnant animals but its effects in human pregnancy are not known.
Nexletol (bempedoic acid) (344)
Nexletol is indicated as an adjunct to diet and maximally tolerated statin therapy for the treatment of adults with heterozygous familial hypercholesterolemia or established atherosclerotic cardiovascular disease who require additional lowering of LDL cholesterol. The drug was not teratogenic in animals. Discontinue Nexletol when pregnancy is recognized unless the benefits of therapy outweigh the potential risks to the fetus.
Olinvyk (oliceridine) (503)
Olinvyk injection is indicated in adults for the management of acute pain severe enough to require an intravenous opioid analgesic. Prolonged use of Olinvyk during pregnancy can result in neonatal opioid withdrawal syndrome. The drug was not teratogenic in animals.
Ongentys (opicapone) (413)
Ongentys is indicated as adjunctive treatment to levodopa/carbidopa in patients with Parkinson’s disease experiencing “off” episodes. The drug was teratogenic in rabbits but not in rats.
Orladeyo (berotralstat) (635)
This drug is a plasma kallikrein inhibitor indicated for prophylaxis to prevent attacks of hereditary angioedema. It was not teratogenic in animals.
Oxlumo (lumasiran) (17,286)
Oxlumo is a HAO1-directed small interfering ribonucleic acid indicated for the treatment of primary hyperoxaluria type 1 to lower urinary oxalate levels. No adverse effects on pregnancy or embryo-fetal development related to the drug were observed in animals.
Pizensy (lactitol) (344)
Lactitol is minimally absorbed systemically following oral administration. It is unknown whether maternal use will result in fetal exposure to the drug. No effects on embryo-fetal development were observed in animals at doses much higher than the maximum recommended human dosage.
Rukobia (fostemsavir) (705; 584 for free acid)
This drug is an HIV-1–directed attachment inhibitor, in combination with other antiretrovirals. There is a pregnancy exposure registry that monitors pregnancy outcomes in individuals exposed to the drug during pregnancy. Health care providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry at 1-800-258-4263.
Sogroya (somapacitan-beco) (23,305)
This is a human growth hormone analog indicated for replacement of endogenous growth hormone in adults with growth hormone deficiency. The drug was not teratogenic in animals.
Tepezza (teprotumumab-trbw) (148,000)
Drug is indicated for the treatment of thyroid eye disease. The drug was teratogenic in cynomolgus monkeys. The manufacturer states that because of the risk, the drug should not be used in pregnancy.
Tauvid (flortaucipir F-18) (262)
This drug is indicated for use with PET imaging of the brain to evaluate for Alzheimer’s disease. It is a radioactive drug and should not be used in pregnant women.
Uplizna (inebilizumab-cdon) (149,000)
Uplizna is indicated for the treatment of neuromyelitis optica spectrum disorder in adult patients who are anti-AQP4 antibody positive. It is a humanized IgG1 monoclonal antibody and immunoglobulins are known to cross the placental barrier. Based on animal data, the drug can cause fetal harm because of B-cell lymphopenia and reduce antibody response in offspring exposed to the drug. Women of childbearing potential should use contraception while receiving Uplizna and for 6 months after the last dose.
Winlevi (clascoterone) (403)
This cream is an androgen receptor inhibitor that is indicated for the topical treatment of acne vulgaris in patients aged 12 years and older. Subcutaneous use in animals was associated with fetal defects.
Xeglyze (abametapir) (1,840)
Xeglyze is indicated for the topical treatment of head lice infestation in patients aged 6 months and older. The drug was not teratogenic in animals.
Zokinvy (lonafarnib) (639)
Zokinvy is indicated in patients 12 months or older to reduce the risk of mortality in several conditions. Animal studies have found embryo-fetal harm.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
In 2020, the Food and Drug Administration approved 53 new drugs for humans. One of these agents, Annovera (segesterone and ethinyl estradiol), is a vaginal ring to prevent pregnancy and is not relevant in this article. A second drug, Asparlas (calaspargase pegol), indicated to treat acute lymphoblastic leukemia, has not yet been released by its manufacturer. Orgovyx (relugolix) is used for prostate cancer and Lampit (nifurtimox) is drug used in children – neither of these two agents will be covered. The remaining 49 are covered below. The agents with molecular weights less than 1,000 probably cross the placenta in the first half of pregnancy, but nearly all, regardless of MW, will cross in the second half of pregnancy.
No human pregnancy data for these agents has been found, but there are five drugs included in pregnancy registries. It will take some time before the outcomes of these drugs are published. The routine absence of pregnancy data for most drugs was pointed out in an article that I coauthored, “Should pregnant women be included in phase 4 clinical drug trials?”. The article makes a strong argument for including some pregnant women in these trials.
Anti-infectives
Artesunate (384)
The drug appears low risk when used in the second and third trimesters. There is inadequate information regarding its use in the first trimester, so the safest course for the embryo appears to be avoiding its use during this period. A single intravenous dose given to rats early in gestation resulted in embryolethality.
Ebanga (ansuvimab) (147,000)
Studies on its use in pregnant animals have not been conducted.
Inmazeb (atoltivimab, maftivimab, odesivimab) (144,000-146,000)
Inmazeb is a combination of the three agents. Studies on its use in pregnant animals have not been conducted.
Veklury (remdesivir) (603)
Veklury is indicated for the treatment of pregnant women hospitalized with COVID-19 who are at risk for serious morbidity and mortality. The drug should be used during pregnancy only if the potential benefit justifies the potential risk for the mother and the fetus.
Antineoplastics
Ayvakit (avapritinib) (499)
The drug may cause fetal harm. The drug was teratogenic in animals.
Blenrep (belantamab mafodotin-blmf) (152,000)
A B-cell maturation antigen, it is indicated for the treatment of multiple myeloma. No human or animal pregnancy data have been located.
Danyelza (naxitamab-gqgk) (144,000)
This agent is used for the treatment of neuroblastoma. Based on its mechanism of action it may cause fetal harm if used in pregnancy.
Gavreto (pralsetinib) (534)
Gavreto is indicated for the treatment of small cell lung cancer. It may cause embryo-fetal harm if used in pregnancy.
Inqovi (cedazuridine + decitabine) (268,228)
The drug combination can cause fetal harm in human pregnancy. It is toxic in pregnant animals.
Margenza (margetuximab-cmkb) (149,000)
Although there are no data on the use of this drug in human pregnancy, the findings in animals and mechanism of action suggest that it will cause fetal harm.
Monjuvi (tafasitamab-cxix) (150,000)
This drug is a cytolytic antibody that is indicated in combination with lenalidomide. The combination may cause fetal harm.
Pemazyre (pemigatinib) (488)
It is indicated for the treatment of cholangiocarcinoma. In an animal study, the drug caused fetal defects, fetal growth retardation, and embryo-fetal death at maternal exposures lower than the human exposure.
Qinlock (ripretinib) (510)
This drug is used for the treatment of patients with advanced gastrointestinal stromal tumor. The drug was teratogenic in pregnant animals.
Retevmo (selpercatinib) (526)
This is a kinase inhibitor used for the treatment of small cell lung cancer. The drug is teratogenic in animals.
Sarclisa (isatuximab-irfc) (148,000)This drug is used in combination with pomalidomide and dexamethasone. The combination would probably cause major toxicity in an embryo or fetus.
Tabrecta (capmatinib) (412 – free base)Capmatinib is a kinase inhibitor used for the treatment of metastatic non–small cell lung cancer. It is teratogenic in animals.
Tazverik (tazemetostat) (654)Tazemetostat is indicated for the treatment of epithelioid sarcoma and follicular lymphoma, The drug is teratogenic in animals.
Trodelvy (sacituzumab govitecan-hziy) (1,602)This agent is used for the treatment of breast cancer. The drug has not been tested in pregnant animals. However, according to the manufacturer, there is a high possibility of human teratogenicity if it is given to a pregnant woman.
Tukysa (tucatinib) (481)
Tukysa is a tyrosine kinase inhibitor that is used in combination with trastuzumab and capecitabine for the treatment of breast cancer. The drug is teratogenic in animals.
Zeposia (ozanimod) (441)
Zeposia is indicated for the treatment of multiple sclerosis. The drug takes about 3 months to eliminate from the body. The drug is teratogenic in animals.
Zepzelca (lurbinectedin) (785)
This agent is used for the treatment of metastatic small cell lung cancer. The drug is teratogenic in animals.
Antiemetics
Barhemsys (amisulpride) (369)
This agent is Indicated to prevent nausea and vomiting. Animal data suggest low risk of embryo/fetal birth defects.
Antimigraine
Nurtec (rimegepant) (611)
Nurtec is indicated for acute treatment of migraine. Development toxicity was not observed in animals given doses similar to those used in humans.
Vyepti (eptinezumab-jjmr) (143,000)
A humanized monoclonal antibody that is given every 3 months to prevent migraine. There was no embryo-fetal harm in animals given the drug.
CNS
Byfavo (remimazolam) (493 – free base)
This drug is indicated for procedural sedation in adults undergoing procedures lasting 30 minutes or less. No defects were observed in animals.
Diagnostics
Cerianna (fluoroestradiol F 18) (289)
It is indicated for use with PET for characterization of estrogen receptor status in patients with ER-positive breast cancer. It has the potential to cause fetal harm depending on the fetal stage of development and the magnitude of radiation dose. There are no data on its use in pregnant women or animals.
Detectnet (copper CU-64 dotatate) (1,497)
All radiopharmaceuticals have the potential to cause fetal harm depending on the fetal stage of development and the magnitude of the radiation dose. There are no pregnancy data in humans or animals
Miscellaneous
Dojolvi (triheptanoin) (429)
This agent is indicated as a source of calories and fatty acids for the treatment of pediatric and adult patients with molecularly confirmed long-chain fatty acid oxidation disorders. Advise patients that there is a pregnancy safety study that collects pregnancy outcome data in women taking Dojolvi during pregnancy. Pregnant patients can enroll in the study by calling 1-888-756-8657.
Enspryng (satralizumab-mwge) (143,000)
It is indicated for the treatment of neuromyelitis optica spectrum disorder in adult patients who are anti–aquaporin-4 (AQP4) antibody positive. No information is available on the risks, if any, in pregnancy. No adverse effects on maternal or fetal development were observed in pregnant monkeys and their offspring.
Evrysdi (risdiplam) (401)
This is a prescription medicine used to treat spinal muscular atrophy in adults and children aged 2 months and older. In pregnant animals the drug caused adverse effects on fetal development.
Gemtesa (vibegron) (445)
Gemtesa is used in adults to treat the symptoms of overactive bladder. The drug had no adverse effects on pregnant animals.
Imcivree (setmelanotide) (1,117)
This drug is indicated for chronic weight management in adult and pediatric patients aged 6 years and older with obesity because of proopiomelanocortin, proprotein convertase subtilisin/kexin type 1, or leptin receptor deficiency. The drug was not embryo toxic in animals.
Isturisa (osilodrostat) (325)
Isturisa is a cortisol synthesis inhibitor indicated for the treatment of adult patients with Cushing’s disease. No adverse fetal effects were observed in pregnant animals.
Klisyri (tirbanibulin) (431)
Tirbanibulin ointment is a microtubule inhibitor that is used to treat actinic keratosis. Information on its effects in pregnancy is not available.
Koselugo (selumetinib) (556)
This is a kinase inhibitor indicated for the treatment of pediatric patients aged 2 years and older. The drug is toxic in pregnant animals but its effects in human pregnancy are not known.
Nexletol (bempedoic acid) (344)
Nexletol is indicated as an adjunct to diet and maximally tolerated statin therapy for the treatment of adults with heterozygous familial hypercholesterolemia or established atherosclerotic cardiovascular disease who require additional lowering of LDL cholesterol. The drug was not teratogenic in animals. Discontinue Nexletol when pregnancy is recognized unless the benefits of therapy outweigh the potential risks to the fetus.
Olinvyk (oliceridine) (503)
Olinvyk injection is indicated in adults for the management of acute pain severe enough to require an intravenous opioid analgesic. Prolonged use of Olinvyk during pregnancy can result in neonatal opioid withdrawal syndrome. The drug was not teratogenic in animals.
Ongentys (opicapone) (413)
Ongentys is indicated as adjunctive treatment to levodopa/carbidopa in patients with Parkinson’s disease experiencing “off” episodes. The drug was teratogenic in rabbits but not in rats.
Orladeyo (berotralstat) (635)
This drug is a plasma kallikrein inhibitor indicated for prophylaxis to prevent attacks of hereditary angioedema. It was not teratogenic in animals.
Oxlumo (lumasiran) (17,286)
Oxlumo is a HAO1-directed small interfering ribonucleic acid indicated for the treatment of primary hyperoxaluria type 1 to lower urinary oxalate levels. No adverse effects on pregnancy or embryo-fetal development related to the drug were observed in animals.
Pizensy (lactitol) (344)
Lactitol is minimally absorbed systemically following oral administration. It is unknown whether maternal use will result in fetal exposure to the drug. No effects on embryo-fetal development were observed in animals at doses much higher than the maximum recommended human dosage.
Rukobia (fostemsavir) (705; 584 for free acid)
This drug is an HIV-1–directed attachment inhibitor, in combination with other antiretrovirals. There is a pregnancy exposure registry that monitors pregnancy outcomes in individuals exposed to the drug during pregnancy. Health care providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry at 1-800-258-4263.
Sogroya (somapacitan-beco) (23,305)
This is a human growth hormone analog indicated for replacement of endogenous growth hormone in adults with growth hormone deficiency. The drug was not teratogenic in animals.
Tepezza (teprotumumab-trbw) (148,000)
Drug is indicated for the treatment of thyroid eye disease. The drug was teratogenic in cynomolgus monkeys. The manufacturer states that because of the risk, the drug should not be used in pregnancy.
Tauvid (flortaucipir F-18) (262)
This drug is indicated for use with PET imaging of the brain to evaluate for Alzheimer’s disease. It is a radioactive drug and should not be used in pregnant women.
Uplizna (inebilizumab-cdon) (149,000)
Uplizna is indicated for the treatment of neuromyelitis optica spectrum disorder in adult patients who are anti-AQP4 antibody positive. It is a humanized IgG1 monoclonal antibody and immunoglobulins are known to cross the placental barrier. Based on animal data, the drug can cause fetal harm because of B-cell lymphopenia and reduce antibody response in offspring exposed to the drug. Women of childbearing potential should use contraception while receiving Uplizna and for 6 months after the last dose.
Winlevi (clascoterone) (403)
This cream is an androgen receptor inhibitor that is indicated for the topical treatment of acne vulgaris in patients aged 12 years and older. Subcutaneous use in animals was associated with fetal defects.
Xeglyze (abametapir) (1,840)
Xeglyze is indicated for the topical treatment of head lice infestation in patients aged 6 months and older. The drug was not teratogenic in animals.
Zokinvy (lonafarnib) (639)
Zokinvy is indicated in patients 12 months or older to reduce the risk of mortality in several conditions. Animal studies have found embryo-fetal harm.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
Bullous Pemphigoid Triggered by Liraglutide
To the Editor:
Bullous pemphigoid (BP) is an autoimmune blistering disease that typically affects the elderly, with an incidence of approximately 7 new cases per million.1 The pathogenesis of BP involves autoantibodies to BP antigens 180 and 230 at the dermoepidermal junction. Bullous pemphigoid has been associated with the use of multiple medications; vaccines; and physical damage to the skin, including trauma, radiation, and surgery.2
Several classes of medications may cause BP; one study described an association of BP with loop diuretics,3 while others found higher incidences of BP in patients taking aldosterone antagonists and neuroleptics.4 We describe a case of drug-triggered BP to liraglutide, a glucagonlike peptide 1 (GLP-1) receptor agonist.
A 75-year-old man presented to dermatology for evaluation of a vesicular eruption on the head, neck, trunk, and arms of 6 months’ duration. The eruption developed 2 weeks after starting liraglutide 1.2 mg subcutaneously daily for diabetes mellitus. The patient had a medical history of type 2 diabetes mellitus, hypertension, stroke, and prostate cancer treated with prostatectomy, and he also was taking insulin. Liraglutide was discontinued shortly after the onset of the eruption.
Physical examination revealed annular plaques on the head, neck, trunk, and arms with central hypopigmentation and hyperpigmented borders (Figure 1). Two tense bullae were evident on the left flank (Figure 2). Histopathology revealed a subepidermal blister, mixed perivascular infiltrate with numerous eosinophils, and pigment incontinence (Figure 3). Direct immunofluorescence showed linear deposition of IgG and C3 along the basement membrane zone that was localized to the roof of the blister on salt-split analysis. No microorganisms were identified on periodic acid–Schiff, Grocott-Gomori methenamine-silver, acid-fast bacilli, and Fite stains. The patient initially was treated with clobetasol ointment 0.05%, leading to marginal improvement. He declined treatment with prednisone or dapsone, and he was started on doxycycline. Seven months after stopping liraglutide and starting doxycycline, the patient had no blisters, but residual pigmentary changes remained.


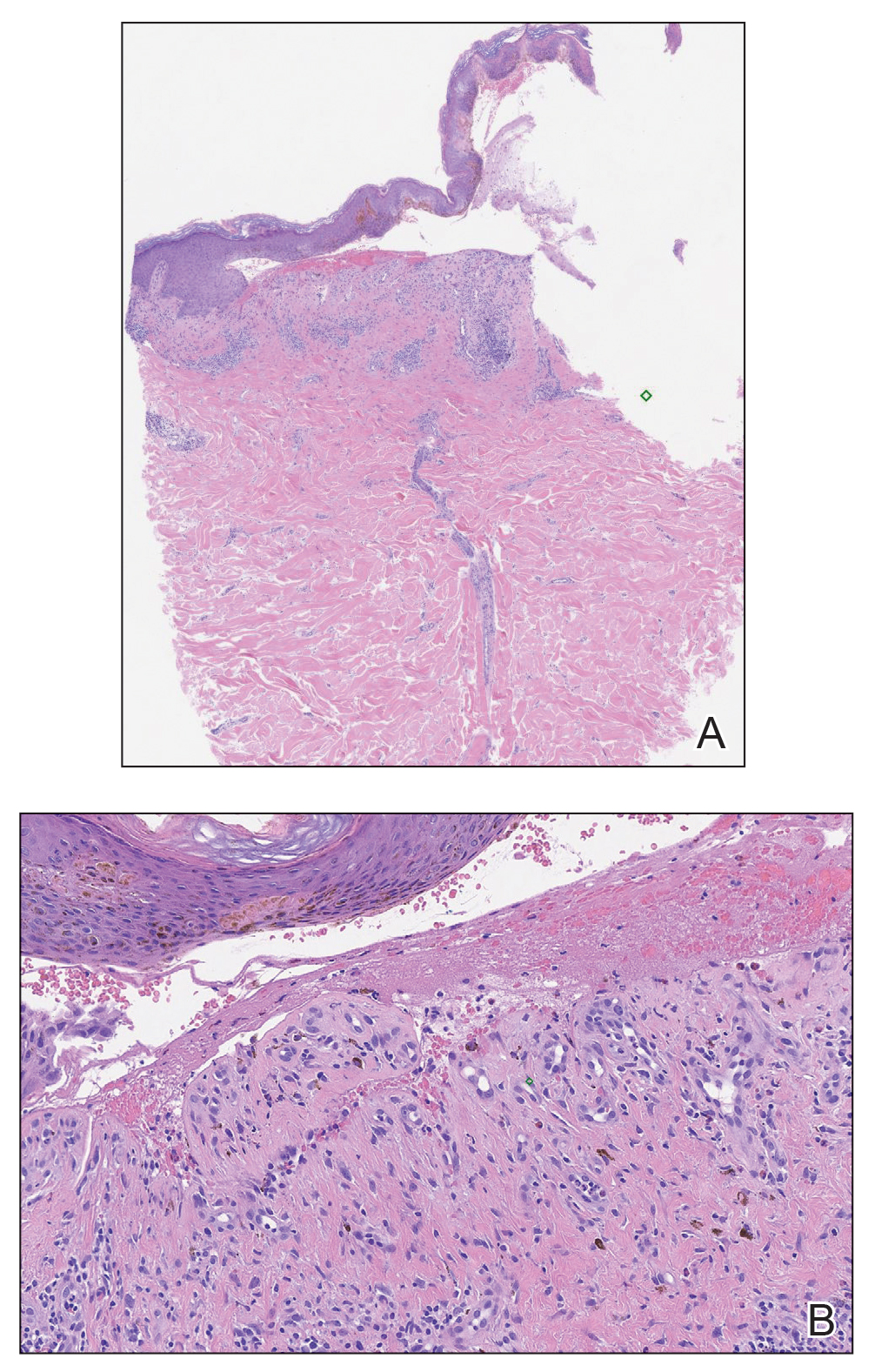
Two types of BP have been described in response to medications: drug-induced BP and drug-triggered BP. Drug-induced BP presents as an acute, self-limited eruption that typically resolves after withdrawal of the offending agent. It tends to involve a younger population and may present with mucosal involvement and target lesions on the palms and soles. Direct immunofluorescence shows linear IgG and C3 deposition at the basement membrane zone. Patients tend to respond quickly to systemic corticosteroids and have low recurrence rates. Drug-triggered BP is a chronic form of BP that is caused by a medication and is not resolved with removal of the offending agent.5 Therefore, drug-triggered BP is more difficult to detect, especially in patients taking multiple medications.
Our patient represents a case of drug-triggered BP to liraglutide. Liraglutide is a GLP-1 receptor agonist that is US Food and Drug Administration approved for the treatment of type 2 diabetes mellitus. Glucagonlike peptide 1 is an incretin hormone that is secreted by the intestine during digestion. It binds to the GLP-1 receptor leading to an increase in glucose-dependent insulin secretion and a decrease in glucagon secretion.6 Glucagonlike peptide 1 agonists also affect the immune system; liraglutide has been shown to modestly improve psoriasis, reduce the number of dermal gamma delta T cells, and decrease IL-17 expression.7 Glucagonlike peptide 1 agonists also produce anti-inflammatory effects on multiple organs including the liver, brain, vasculature, kidney, and skin.8
Dipeptidyl peptidase 4 (DPP-4) inhibitors that function to inhibit the degradation of GLP-1 and other peptides also have been reported to cause BP. In several patients, the DPP-4 inhibitors vildagliptin and sitagliptin caused drug-induced BP that resolved with discontinuation of the medication.9 Dipeptidyl peptidase 4 is expressed in various organ systems including the skin, and inhibition of DPP-4 enhances eosinophil mobilization in the blood and recruitment to the skin in animal models.10
Although the pathogenesis of BP involves autoantibodies to BP antigens 180 and 230, these antibodies are not sufficient to cause disease, as antibasement antibodies have been detected in patients without clinically evident BP. These patients, however, may be more susceptible to developing medication-induced BP. Several hypotheses regarding the pathogenesis of medication-induced BP have been proposed, including immune dysregulation, molecular mimicry, and cross-reactivity to a prior sensitizing agent.5 Liraglutide and the DPP-4 inhibitors affect the immune system, supporting the hypothesis of immune dysregulation; however, the exact mechanism of how immune modulating medications such as GLP-1 agonists and DPP-4 inhibitors cause BP remains unclear.
The effects of liraglutide and the DPP-4 inhibitors on the immune system may play a role in the pathogenesis of drug-triggered BP and drug-induced BP, respectively. Additional studies of the immunomodulatory effects of GLP-1 agonists and DPP-4 inhibitors may help elucidate the pathogenesis of drug-triggered or drug-induced BP.
- Serwin AB, Musialkowska E, Piascik M. Incidence and mortality of bullous pemphigoid in north-east Poland (Podlaskie Province), 1999-2012: a retrospective bicentric cohort study. Int J Dermatol. 2014;53:E432-E437.
- Danescu S, Chiorean R, Macovei V, et al. Role of physical factors in the pathogenesis of bullous pemphigoid: case report series and a comprehensive review of the published work. J Dermatol. 2016;43:134-130.
- Lloyd-Lavery A, Chi CC, Wojnarowska F, et al. The associations between bullous pemphigoid and drug use: a UK case-control study. JAMA Dermatol. 2013;149:58-62.
- Bastuji-Garin S, Joly P, Picard-Dahan C, et al. Drugs associated with bullous pemphigoid. a case-control study. Arch Dermatol. 1996;132:272-276.
- Stavropoulos PG, Soura E, Antoniou C. Drug-induced pemphigoid: a review of the literature. J Eur Acad Dermatol Venereol. 2014;28:1133-1140.
- Triplitt C, Solis-Herrera C. GLP-1 receptor agonists: practical considerations for clinical practice. Diabetes Educ. 2015;41(suppl 1):32S-46S.
- Buysschaert M, Baeck M, Preumont V, et al. Improvement of psoriasis during glucagon-like peptide-1 analogue therapy in type 2 diabetes is associated with decreasing dermal gammadelta T-cell number: a prospective case-series study. Br J Dermatol. 2014;171:155-161.
- Lee YS, Jun HS. Anti-inflammatory effects of GLP-1-based therapies beyond glucose control. Mediators Inflamm. 2016;2016:3094642.
- Skandalis K, Spirova M, Gaitanis G, et al Drug-induced bullous pemphigoid in diabetes mellitus patients receiving dipeptidyl peptidase-IV inhibitors plus metformin. J Eur Acad Dermatol Venereol. 2012;26:249-253.
- Forssmann U, Stoetzer C, Stephan M, et al. Inhibition of CD26/dipeptidyl peptidase IV enhances CCL11/eotaxin-mediated recruitment of eosinophils in vivo. J Immunol. 2008;181:1120-1127.
To the Editor:
Bullous pemphigoid (BP) is an autoimmune blistering disease that typically affects the elderly, with an incidence of approximately 7 new cases per million.1 The pathogenesis of BP involves autoantibodies to BP antigens 180 and 230 at the dermoepidermal junction. Bullous pemphigoid has been associated with the use of multiple medications; vaccines; and physical damage to the skin, including trauma, radiation, and surgery.2
Several classes of medications may cause BP; one study described an association of BP with loop diuretics,3 while others found higher incidences of BP in patients taking aldosterone antagonists and neuroleptics.4 We describe a case of drug-triggered BP to liraglutide, a glucagonlike peptide 1 (GLP-1) receptor agonist.
A 75-year-old man presented to dermatology for evaluation of a vesicular eruption on the head, neck, trunk, and arms of 6 months’ duration. The eruption developed 2 weeks after starting liraglutide 1.2 mg subcutaneously daily for diabetes mellitus. The patient had a medical history of type 2 diabetes mellitus, hypertension, stroke, and prostate cancer treated with prostatectomy, and he also was taking insulin. Liraglutide was discontinued shortly after the onset of the eruption.
Physical examination revealed annular plaques on the head, neck, trunk, and arms with central hypopigmentation and hyperpigmented borders (Figure 1). Two tense bullae were evident on the left flank (Figure 2). Histopathology revealed a subepidermal blister, mixed perivascular infiltrate with numerous eosinophils, and pigment incontinence (Figure 3). Direct immunofluorescence showed linear deposition of IgG and C3 along the basement membrane zone that was localized to the roof of the blister on salt-split analysis. No microorganisms were identified on periodic acid–Schiff, Grocott-Gomori methenamine-silver, acid-fast bacilli, and Fite stains. The patient initially was treated with clobetasol ointment 0.05%, leading to marginal improvement. He declined treatment with prednisone or dapsone, and he was started on doxycycline. Seven months after stopping liraglutide and starting doxycycline, the patient had no blisters, but residual pigmentary changes remained.


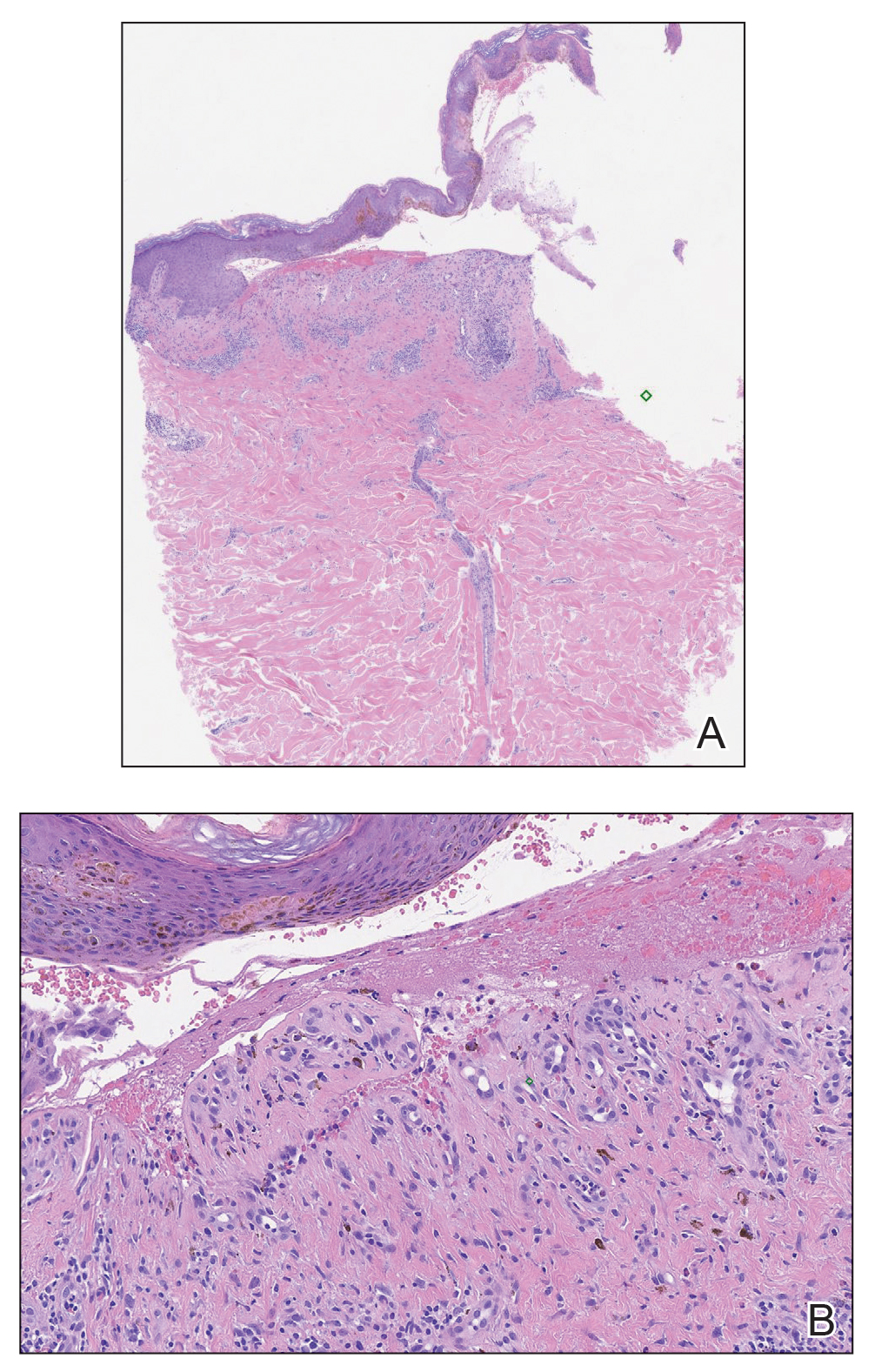
Two types of BP have been described in response to medications: drug-induced BP and drug-triggered BP. Drug-induced BP presents as an acute, self-limited eruption that typically resolves after withdrawal of the offending agent. It tends to involve a younger population and may present with mucosal involvement and target lesions on the palms and soles. Direct immunofluorescence shows linear IgG and C3 deposition at the basement membrane zone. Patients tend to respond quickly to systemic corticosteroids and have low recurrence rates. Drug-triggered BP is a chronic form of BP that is caused by a medication and is not resolved with removal of the offending agent.5 Therefore, drug-triggered BP is more difficult to detect, especially in patients taking multiple medications.
Our patient represents a case of drug-triggered BP to liraglutide. Liraglutide is a GLP-1 receptor agonist that is US Food and Drug Administration approved for the treatment of type 2 diabetes mellitus. Glucagonlike peptide 1 is an incretin hormone that is secreted by the intestine during digestion. It binds to the GLP-1 receptor leading to an increase in glucose-dependent insulin secretion and a decrease in glucagon secretion.6 Glucagonlike peptide 1 agonists also affect the immune system; liraglutide has been shown to modestly improve psoriasis, reduce the number of dermal gamma delta T cells, and decrease IL-17 expression.7 Glucagonlike peptide 1 agonists also produce anti-inflammatory effects on multiple organs including the liver, brain, vasculature, kidney, and skin.8
Dipeptidyl peptidase 4 (DPP-4) inhibitors that function to inhibit the degradation of GLP-1 and other peptides also have been reported to cause BP. In several patients, the DPP-4 inhibitors vildagliptin and sitagliptin caused drug-induced BP that resolved with discontinuation of the medication.9 Dipeptidyl peptidase 4 is expressed in various organ systems including the skin, and inhibition of DPP-4 enhances eosinophil mobilization in the blood and recruitment to the skin in animal models.10
Although the pathogenesis of BP involves autoantibodies to BP antigens 180 and 230, these antibodies are not sufficient to cause disease, as antibasement antibodies have been detected in patients without clinically evident BP. These patients, however, may be more susceptible to developing medication-induced BP. Several hypotheses regarding the pathogenesis of medication-induced BP have been proposed, including immune dysregulation, molecular mimicry, and cross-reactivity to a prior sensitizing agent.5 Liraglutide and the DPP-4 inhibitors affect the immune system, supporting the hypothesis of immune dysregulation; however, the exact mechanism of how immune modulating medications such as GLP-1 agonists and DPP-4 inhibitors cause BP remains unclear.
The effects of liraglutide and the DPP-4 inhibitors on the immune system may play a role in the pathogenesis of drug-triggered BP and drug-induced BP, respectively. Additional studies of the immunomodulatory effects of GLP-1 agonists and DPP-4 inhibitors may help elucidate the pathogenesis of drug-triggered or drug-induced BP.
To the Editor:
Bullous pemphigoid (BP) is an autoimmune blistering disease that typically affects the elderly, with an incidence of approximately 7 new cases per million.1 The pathogenesis of BP involves autoantibodies to BP antigens 180 and 230 at the dermoepidermal junction. Bullous pemphigoid has been associated with the use of multiple medications; vaccines; and physical damage to the skin, including trauma, radiation, and surgery.2
Several classes of medications may cause BP; one study described an association of BP with loop diuretics,3 while others found higher incidences of BP in patients taking aldosterone antagonists and neuroleptics.4 We describe a case of drug-triggered BP to liraglutide, a glucagonlike peptide 1 (GLP-1) receptor agonist.
A 75-year-old man presented to dermatology for evaluation of a vesicular eruption on the head, neck, trunk, and arms of 6 months’ duration. The eruption developed 2 weeks after starting liraglutide 1.2 mg subcutaneously daily for diabetes mellitus. The patient had a medical history of type 2 diabetes mellitus, hypertension, stroke, and prostate cancer treated with prostatectomy, and he also was taking insulin. Liraglutide was discontinued shortly after the onset of the eruption.
Physical examination revealed annular plaques on the head, neck, trunk, and arms with central hypopigmentation and hyperpigmented borders (Figure 1). Two tense bullae were evident on the left flank (Figure 2). Histopathology revealed a subepidermal blister, mixed perivascular infiltrate with numerous eosinophils, and pigment incontinence (Figure 3). Direct immunofluorescence showed linear deposition of IgG and C3 along the basement membrane zone that was localized to the roof of the blister on salt-split analysis. No microorganisms were identified on periodic acid–Schiff, Grocott-Gomori methenamine-silver, acid-fast bacilli, and Fite stains. The patient initially was treated with clobetasol ointment 0.05%, leading to marginal improvement. He declined treatment with prednisone or dapsone, and he was started on doxycycline. Seven months after stopping liraglutide and starting doxycycline, the patient had no blisters, but residual pigmentary changes remained.


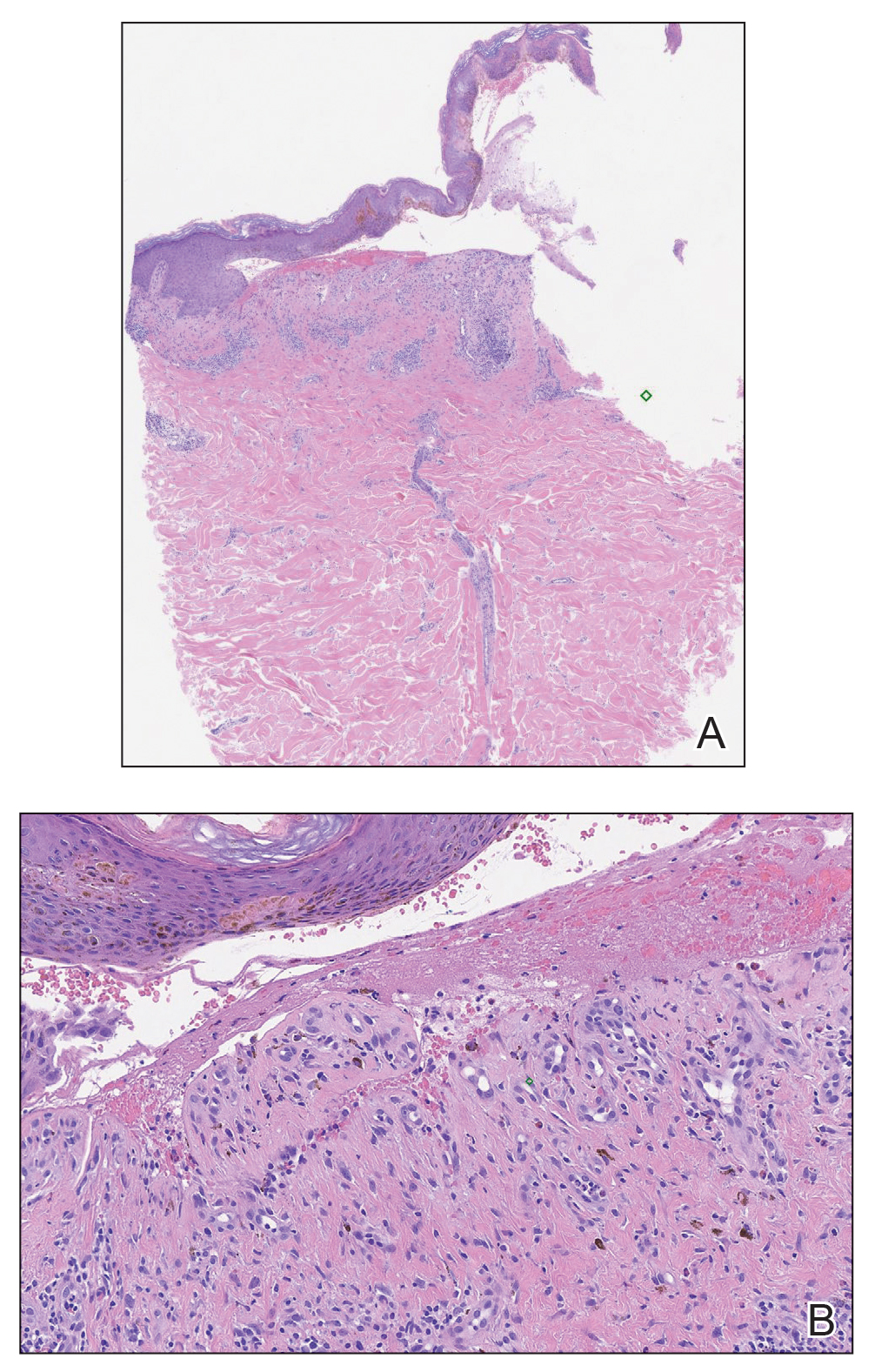
Two types of BP have been described in response to medications: drug-induced BP and drug-triggered BP. Drug-induced BP presents as an acute, self-limited eruption that typically resolves after withdrawal of the offending agent. It tends to involve a younger population and may present with mucosal involvement and target lesions on the palms and soles. Direct immunofluorescence shows linear IgG and C3 deposition at the basement membrane zone. Patients tend to respond quickly to systemic corticosteroids and have low recurrence rates. Drug-triggered BP is a chronic form of BP that is caused by a medication and is not resolved with removal of the offending agent.5 Therefore, drug-triggered BP is more difficult to detect, especially in patients taking multiple medications.
Our patient represents a case of drug-triggered BP to liraglutide. Liraglutide is a GLP-1 receptor agonist that is US Food and Drug Administration approved for the treatment of type 2 diabetes mellitus. Glucagonlike peptide 1 is an incretin hormone that is secreted by the intestine during digestion. It binds to the GLP-1 receptor leading to an increase in glucose-dependent insulin secretion and a decrease in glucagon secretion.6 Glucagonlike peptide 1 agonists also affect the immune system; liraglutide has been shown to modestly improve psoriasis, reduce the number of dermal gamma delta T cells, and decrease IL-17 expression.7 Glucagonlike peptide 1 agonists also produce anti-inflammatory effects on multiple organs including the liver, brain, vasculature, kidney, and skin.8
Dipeptidyl peptidase 4 (DPP-4) inhibitors that function to inhibit the degradation of GLP-1 and other peptides also have been reported to cause BP. In several patients, the DPP-4 inhibitors vildagliptin and sitagliptin caused drug-induced BP that resolved with discontinuation of the medication.9 Dipeptidyl peptidase 4 is expressed in various organ systems including the skin, and inhibition of DPP-4 enhances eosinophil mobilization in the blood and recruitment to the skin in animal models.10
Although the pathogenesis of BP involves autoantibodies to BP antigens 180 and 230, these antibodies are not sufficient to cause disease, as antibasement antibodies have been detected in patients without clinically evident BP. These patients, however, may be more susceptible to developing medication-induced BP. Several hypotheses regarding the pathogenesis of medication-induced BP have been proposed, including immune dysregulation, molecular mimicry, and cross-reactivity to a prior sensitizing agent.5 Liraglutide and the DPP-4 inhibitors affect the immune system, supporting the hypothesis of immune dysregulation; however, the exact mechanism of how immune modulating medications such as GLP-1 agonists and DPP-4 inhibitors cause BP remains unclear.
The effects of liraglutide and the DPP-4 inhibitors on the immune system may play a role in the pathogenesis of drug-triggered BP and drug-induced BP, respectively. Additional studies of the immunomodulatory effects of GLP-1 agonists and DPP-4 inhibitors may help elucidate the pathogenesis of drug-triggered or drug-induced BP.
- Serwin AB, Musialkowska E, Piascik M. Incidence and mortality of bullous pemphigoid in north-east Poland (Podlaskie Province), 1999-2012: a retrospective bicentric cohort study. Int J Dermatol. 2014;53:E432-E437.
- Danescu S, Chiorean R, Macovei V, et al. Role of physical factors in the pathogenesis of bullous pemphigoid: case report series and a comprehensive review of the published work. J Dermatol. 2016;43:134-130.
- Lloyd-Lavery A, Chi CC, Wojnarowska F, et al. The associations between bullous pemphigoid and drug use: a UK case-control study. JAMA Dermatol. 2013;149:58-62.
- Bastuji-Garin S, Joly P, Picard-Dahan C, et al. Drugs associated with bullous pemphigoid. a case-control study. Arch Dermatol. 1996;132:272-276.
- Stavropoulos PG, Soura E, Antoniou C. Drug-induced pemphigoid: a review of the literature. J Eur Acad Dermatol Venereol. 2014;28:1133-1140.
- Triplitt C, Solis-Herrera C. GLP-1 receptor agonists: practical considerations for clinical practice. Diabetes Educ. 2015;41(suppl 1):32S-46S.
- Buysschaert M, Baeck M, Preumont V, et al. Improvement of psoriasis during glucagon-like peptide-1 analogue therapy in type 2 diabetes is associated with decreasing dermal gammadelta T-cell number: a prospective case-series study. Br J Dermatol. 2014;171:155-161.
- Lee YS, Jun HS. Anti-inflammatory effects of GLP-1-based therapies beyond glucose control. Mediators Inflamm. 2016;2016:3094642.
- Skandalis K, Spirova M, Gaitanis G, et al Drug-induced bullous pemphigoid in diabetes mellitus patients receiving dipeptidyl peptidase-IV inhibitors plus metformin. J Eur Acad Dermatol Venereol. 2012;26:249-253.
- Forssmann U, Stoetzer C, Stephan M, et al. Inhibition of CD26/dipeptidyl peptidase IV enhances CCL11/eotaxin-mediated recruitment of eosinophils in vivo. J Immunol. 2008;181:1120-1127.
- Serwin AB, Musialkowska E, Piascik M. Incidence and mortality of bullous pemphigoid in north-east Poland (Podlaskie Province), 1999-2012: a retrospective bicentric cohort study. Int J Dermatol. 2014;53:E432-E437.
- Danescu S, Chiorean R, Macovei V, et al. Role of physical factors in the pathogenesis of bullous pemphigoid: case report series and a comprehensive review of the published work. J Dermatol. 2016;43:134-130.
- Lloyd-Lavery A, Chi CC, Wojnarowska F, et al. The associations between bullous pemphigoid and drug use: a UK case-control study. JAMA Dermatol. 2013;149:58-62.
- Bastuji-Garin S, Joly P, Picard-Dahan C, et al. Drugs associated with bullous pemphigoid. a case-control study. Arch Dermatol. 1996;132:272-276.
- Stavropoulos PG, Soura E, Antoniou C. Drug-induced pemphigoid: a review of the literature. J Eur Acad Dermatol Venereol. 2014;28:1133-1140.
- Triplitt C, Solis-Herrera C. GLP-1 receptor agonists: practical considerations for clinical practice. Diabetes Educ. 2015;41(suppl 1):32S-46S.
- Buysschaert M, Baeck M, Preumont V, et al. Improvement of psoriasis during glucagon-like peptide-1 analogue therapy in type 2 diabetes is associated with decreasing dermal gammadelta T-cell number: a prospective case-series study. Br J Dermatol. 2014;171:155-161.
- Lee YS, Jun HS. Anti-inflammatory effects of GLP-1-based therapies beyond glucose control. Mediators Inflamm. 2016;2016:3094642.
- Skandalis K, Spirova M, Gaitanis G, et al Drug-induced bullous pemphigoid in diabetes mellitus patients receiving dipeptidyl peptidase-IV inhibitors plus metformin. J Eur Acad Dermatol Venereol. 2012;26:249-253.
- Forssmann U, Stoetzer C, Stephan M, et al. Inhibition of CD26/dipeptidyl peptidase IV enhances CCL11/eotaxin-mediated recruitment of eosinophils in vivo. J Immunol. 2008;181:1120-1127.
Practice Points
- Liraglutide and dipeptidyl peptidase 4 inhibitors, medications used in the treatment of diabetes mellitus, may be linked to the development of bullous pemphigoid (BP).
- Further study of the mechanism of action of these medications may lead to improved understanding of the pathogenesis of BP.