User login
Avoid presumptions with LGBTQ+ patients
More than 11 million individuals in the United States identify as LGBTQ+, and data show that this population has a shorter life expectancy and increased rates of suicide, violence, and cardiovascular disease, according to Keshav Khanijow, MD, of Northwestern University, Chicago, and Nicole Rosendale, MD, of the University of California, San Francisco.
More than half of these individuals report experiencing discrimination, and one in three transgendered individuals have reported prejudice when visiting a doctor or health clinic, they said in a presentation at SHM Converge, the annual conference of the Society of Hospital Medicine.
“It is impossible to know how someone identifies by gender just by looking at them,” Dr. Rosendale emphasized.
However, attention to terminology, use of affirming language and documentation, and attention to clinical considerations can help LGBTQ+ patients feel comfortable in the health care setting.
Ask, don’t assume
Do ask patients how they identify themselves, Dr. Khanijow said. It is important to ask about sexual orientation as part of a social history. One big “Don’t” in terminology is to avoid the use of the term “homosexual,” he added. Although the description “homosexual” began as a scientific term, it has become associated with pathology, rather than identity, and is often used by hate groups. Also, do not assume sexual orientation based on a patient’s partner.
Always ask about sexual orientation before assuming it, and include that information in documentation. Dr. Khanijow used an example of a “one-liner” case of a 45-year-old male who self-identifies as “queer” and presents with a migraine. The most appropriate version would be “45yoM who identifies as queer with PMHx Migraines presents with Headache,” Dr. Khanijow said. However, as a clinician, consider why you are including sexual orientation in the one-liner. If there isn’t any real reason to include it (such as stress related to coming out, increased risk for other conditions) it may not be necessary in all visits.
Transgender considerations
Dr. Khanijow shared some specific considerations for the transgender/nonbinary population.
In terms of gender, “it is most respectful to identify the patient as they would like to be identified,” he said.
Ask how they identify their gender, including their preferred pronouns, and be sure to note this identification in their documents, he said. Be vigilant in addressing a transgender patient correctly. Mistakes happen, and when they do, correct yourself, apologize succinctly and move on.
Clinical challenges
Research on LGBTQ+ health is limited, and these individuals are often grouped into a single category despite diverse experiences, Dr. Rosendale said. Another limitation in LGBTQ+ research is that some studies assess based on identity (such as gay, lesbian, bisexual) while others assess behavior (studies of men who have sex with men).
Dr. Rosendale went on to highlight several important clinical concerns for the LGBTQ+ population. Compared with the general population, lesbian women are at higher risk for breast cancer, and gay men are at increased risk for prostate, colon, and testicular cancers. Potential heart disease risk factors of physical inactivity, obesity, and smoking are more prevalent among lesbian women, and tobacco and alcohol use are more prevalent among gay men, and men who have sex with men are at increased risk for STIs.
Clinicians also should be aware that “bisexual individuals face worse health outcomes than their lesbian, gay, and heterosexual counterparts,” Dr. Rosendale said.
LGBTQ+ patients often use hormone therapy, so clinicians should be aware of some potential adverse effects, Dr. Rosendale said. For example, trans women on gender-affirming estrogen therapy may have increased cardiovascular risks including incident MI, ischemic stroke, and cardiovascular mortality, compared with cisgender women.
In trans men, testosterone use has not been definitively linked to cardiovascular risk, although patients may show small changes in systolic blood pressure, lipid profiles, and blood glucose, Dr. Rosendale noted.
In-hospital issues
Inpatient and critical care of transgender and LGBTQ+ patients may have unique psychosocial considerations in hospital care, Dr. Rosendale said. To provide some guidance, a document on “Transgender-Affirming Hospital Policies” has been developed jointly by Lamda Legal, the Human Rights Campaign, the law firm of Hogan Lovells, and the New York City Bar.
Best practices noted in the document include rooming transgender individuals according to their identity, and recognizing that these patients may experience additional stress while an inpatient if personal clothing or other means of gender expression are replaced during the hospital stay, Dr. Rosendale noted.
Finally, clinicians seeing LGBTQ+ patients in an acute care setting should keep in mind that socioeconomic disparities may limit access to outpatient care, and that this population has higher rates of unemployment, exacerbated by the ongoing COVID-19 pandemic, Dr. Rosendale said. In addition, she advised clinicians to be aware that LGBTQ+ people may experience discrimination in rehabilitation centers, and their surrogate decision makers may be individuals other than family members.
Dr. Khanijow and Dr. Rosendale had no financial conflicts to disclose.
More than 11 million individuals in the United States identify as LGBTQ+, and data show that this population has a shorter life expectancy and increased rates of suicide, violence, and cardiovascular disease, according to Keshav Khanijow, MD, of Northwestern University, Chicago, and Nicole Rosendale, MD, of the University of California, San Francisco.
More than half of these individuals report experiencing discrimination, and one in three transgendered individuals have reported prejudice when visiting a doctor or health clinic, they said in a presentation at SHM Converge, the annual conference of the Society of Hospital Medicine.
“It is impossible to know how someone identifies by gender just by looking at them,” Dr. Rosendale emphasized.
However, attention to terminology, use of affirming language and documentation, and attention to clinical considerations can help LGBTQ+ patients feel comfortable in the health care setting.
Ask, don’t assume
Do ask patients how they identify themselves, Dr. Khanijow said. It is important to ask about sexual orientation as part of a social history. One big “Don’t” in terminology is to avoid the use of the term “homosexual,” he added. Although the description “homosexual” began as a scientific term, it has become associated with pathology, rather than identity, and is often used by hate groups. Also, do not assume sexual orientation based on a patient’s partner.
Always ask about sexual orientation before assuming it, and include that information in documentation. Dr. Khanijow used an example of a “one-liner” case of a 45-year-old male who self-identifies as “queer” and presents with a migraine. The most appropriate version would be “45yoM who identifies as queer with PMHx Migraines presents with Headache,” Dr. Khanijow said. However, as a clinician, consider why you are including sexual orientation in the one-liner. If there isn’t any real reason to include it (such as stress related to coming out, increased risk for other conditions) it may not be necessary in all visits.
Transgender considerations
Dr. Khanijow shared some specific considerations for the transgender/nonbinary population.
In terms of gender, “it is most respectful to identify the patient as they would like to be identified,” he said.
Ask how they identify their gender, including their preferred pronouns, and be sure to note this identification in their documents, he said. Be vigilant in addressing a transgender patient correctly. Mistakes happen, and when they do, correct yourself, apologize succinctly and move on.
Clinical challenges
Research on LGBTQ+ health is limited, and these individuals are often grouped into a single category despite diverse experiences, Dr. Rosendale said. Another limitation in LGBTQ+ research is that some studies assess based on identity (such as gay, lesbian, bisexual) while others assess behavior (studies of men who have sex with men).
Dr. Rosendale went on to highlight several important clinical concerns for the LGBTQ+ population. Compared with the general population, lesbian women are at higher risk for breast cancer, and gay men are at increased risk for prostate, colon, and testicular cancers. Potential heart disease risk factors of physical inactivity, obesity, and smoking are more prevalent among lesbian women, and tobacco and alcohol use are more prevalent among gay men, and men who have sex with men are at increased risk for STIs.
Clinicians also should be aware that “bisexual individuals face worse health outcomes than their lesbian, gay, and heterosexual counterparts,” Dr. Rosendale said.
LGBTQ+ patients often use hormone therapy, so clinicians should be aware of some potential adverse effects, Dr. Rosendale said. For example, trans women on gender-affirming estrogen therapy may have increased cardiovascular risks including incident MI, ischemic stroke, and cardiovascular mortality, compared with cisgender women.
In trans men, testosterone use has not been definitively linked to cardiovascular risk, although patients may show small changes in systolic blood pressure, lipid profiles, and blood glucose, Dr. Rosendale noted.
In-hospital issues
Inpatient and critical care of transgender and LGBTQ+ patients may have unique psychosocial considerations in hospital care, Dr. Rosendale said. To provide some guidance, a document on “Transgender-Affirming Hospital Policies” has been developed jointly by Lamda Legal, the Human Rights Campaign, the law firm of Hogan Lovells, and the New York City Bar.
Best practices noted in the document include rooming transgender individuals according to their identity, and recognizing that these patients may experience additional stress while an inpatient if personal clothing or other means of gender expression are replaced during the hospital stay, Dr. Rosendale noted.
Finally, clinicians seeing LGBTQ+ patients in an acute care setting should keep in mind that socioeconomic disparities may limit access to outpatient care, and that this population has higher rates of unemployment, exacerbated by the ongoing COVID-19 pandemic, Dr. Rosendale said. In addition, she advised clinicians to be aware that LGBTQ+ people may experience discrimination in rehabilitation centers, and their surrogate decision makers may be individuals other than family members.
Dr. Khanijow and Dr. Rosendale had no financial conflicts to disclose.
More than 11 million individuals in the United States identify as LGBTQ+, and data show that this population has a shorter life expectancy and increased rates of suicide, violence, and cardiovascular disease, according to Keshav Khanijow, MD, of Northwestern University, Chicago, and Nicole Rosendale, MD, of the University of California, San Francisco.
More than half of these individuals report experiencing discrimination, and one in three transgendered individuals have reported prejudice when visiting a doctor or health clinic, they said in a presentation at SHM Converge, the annual conference of the Society of Hospital Medicine.
“It is impossible to know how someone identifies by gender just by looking at them,” Dr. Rosendale emphasized.
However, attention to terminology, use of affirming language and documentation, and attention to clinical considerations can help LGBTQ+ patients feel comfortable in the health care setting.
Ask, don’t assume
Do ask patients how they identify themselves, Dr. Khanijow said. It is important to ask about sexual orientation as part of a social history. One big “Don’t” in terminology is to avoid the use of the term “homosexual,” he added. Although the description “homosexual” began as a scientific term, it has become associated with pathology, rather than identity, and is often used by hate groups. Also, do not assume sexual orientation based on a patient’s partner.
Always ask about sexual orientation before assuming it, and include that information in documentation. Dr. Khanijow used an example of a “one-liner” case of a 45-year-old male who self-identifies as “queer” and presents with a migraine. The most appropriate version would be “45yoM who identifies as queer with PMHx Migraines presents with Headache,” Dr. Khanijow said. However, as a clinician, consider why you are including sexual orientation in the one-liner. If there isn’t any real reason to include it (such as stress related to coming out, increased risk for other conditions) it may not be necessary in all visits.
Transgender considerations
Dr. Khanijow shared some specific considerations for the transgender/nonbinary population.
In terms of gender, “it is most respectful to identify the patient as they would like to be identified,” he said.
Ask how they identify their gender, including their preferred pronouns, and be sure to note this identification in their documents, he said. Be vigilant in addressing a transgender patient correctly. Mistakes happen, and when they do, correct yourself, apologize succinctly and move on.
Clinical challenges
Research on LGBTQ+ health is limited, and these individuals are often grouped into a single category despite diverse experiences, Dr. Rosendale said. Another limitation in LGBTQ+ research is that some studies assess based on identity (such as gay, lesbian, bisexual) while others assess behavior (studies of men who have sex with men).
Dr. Rosendale went on to highlight several important clinical concerns for the LGBTQ+ population. Compared with the general population, lesbian women are at higher risk for breast cancer, and gay men are at increased risk for prostate, colon, and testicular cancers. Potential heart disease risk factors of physical inactivity, obesity, and smoking are more prevalent among lesbian women, and tobacco and alcohol use are more prevalent among gay men, and men who have sex with men are at increased risk for STIs.
Clinicians also should be aware that “bisexual individuals face worse health outcomes than their lesbian, gay, and heterosexual counterparts,” Dr. Rosendale said.
LGBTQ+ patients often use hormone therapy, so clinicians should be aware of some potential adverse effects, Dr. Rosendale said. For example, trans women on gender-affirming estrogen therapy may have increased cardiovascular risks including incident MI, ischemic stroke, and cardiovascular mortality, compared with cisgender women.
In trans men, testosterone use has not been definitively linked to cardiovascular risk, although patients may show small changes in systolic blood pressure, lipid profiles, and blood glucose, Dr. Rosendale noted.
In-hospital issues
Inpatient and critical care of transgender and LGBTQ+ patients may have unique psychosocial considerations in hospital care, Dr. Rosendale said. To provide some guidance, a document on “Transgender-Affirming Hospital Policies” has been developed jointly by Lamda Legal, the Human Rights Campaign, the law firm of Hogan Lovells, and the New York City Bar.
Best practices noted in the document include rooming transgender individuals according to their identity, and recognizing that these patients may experience additional stress while an inpatient if personal clothing or other means of gender expression are replaced during the hospital stay, Dr. Rosendale noted.
Finally, clinicians seeing LGBTQ+ patients in an acute care setting should keep in mind that socioeconomic disparities may limit access to outpatient care, and that this population has higher rates of unemployment, exacerbated by the ongoing COVID-19 pandemic, Dr. Rosendale said. In addition, she advised clinicians to be aware that LGBTQ+ people may experience discrimination in rehabilitation centers, and their surrogate decision makers may be individuals other than family members.
Dr. Khanijow and Dr. Rosendale had no financial conflicts to disclose.
FROM SHM CONVERGE 2021
Moderna announces first data showing efficacy of COVID-19 vaccine booster in development
among people already vaccinated for COVID-19, according to first results released May 5.
Furthermore, data from the company’s ongoing phase 2 study show the variant-specific booster, known as mRNA-1273.351, achieved higher antibody titers against the B.1.351 variant than did a booster with the original Moderna vaccine.
“We are encouraged by these new data, which reinforce our confidence that our booster strategy should be protective against these newly detected variants. The strong and rapid boost in titers to levels above primary vaccination also clearly demonstrates the ability of mRNA-1273 to induce immune memory,” Stéphane Bancel, chief executive officer of Moderna, said in a statement.
The phase 2 study researchers also are evaluating a multivariant booster that is a 50/50 mix of mRNA-1273.351 and mRNA-1273, the initial vaccine given Food and Drug Administration emergency use authorization, in a single vial.
Unlike the two-dose regimen with the original vaccine, the boosters are administered as a single dose immunization.
The trial participants received a booster 6-8 months after primary vaccination. Titers to the wild-type SARS-CoV-2 virus remained high and detectable in 37 out of 40 participants. However, prior to the booster, titers against the two variants of concern, B.1.351 and P.1, were lower, with about half of participants showing undetectable levels.
In contrast, 2 weeks after a booster with the original vaccine or the B.1.351 strain-specific product, pseudovirus neutralizing titers were boosted in all participants and all variants tested.
“Following [the] boost, geometric mean titers against the wild-type, B.1.351, and P.1 variants increased to levels similar to or higher than the previously reported peak titers against the ancestral (D614G) strain following primary vaccination,” the company stated.
Both mRNA-1273.351 and mRNA-1273 booster doses were generally well tolerated, the company reported. Safety and tolerability were generally comparable to those reported after the second dose of the original vaccine. Most adverse events were mild to moderate, with injection site pain most common in both groups. Participants also reported fatigue, headache, myalgia, and arthralgia.
The company plans to release data shortly on the booster efficacy at additional time points beyond 2 weeks for mRNA-1273.351, a lower-dose booster with mRNA-1272/351, as well as data on the multivariant mRNA vaccine booster.
In addition to the company’s phase 2 study, the National Institute of Allergy and Infectious Diseases is conducting a separate phase 1 study of mRNA-1273.351.
A version of this article first appeared on Medscape.com.
among people already vaccinated for COVID-19, according to first results released May 5.
Furthermore, data from the company’s ongoing phase 2 study show the variant-specific booster, known as mRNA-1273.351, achieved higher antibody titers against the B.1.351 variant than did a booster with the original Moderna vaccine.
“We are encouraged by these new data, which reinforce our confidence that our booster strategy should be protective against these newly detected variants. The strong and rapid boost in titers to levels above primary vaccination also clearly demonstrates the ability of mRNA-1273 to induce immune memory,” Stéphane Bancel, chief executive officer of Moderna, said in a statement.
The phase 2 study researchers also are evaluating a multivariant booster that is a 50/50 mix of mRNA-1273.351 and mRNA-1273, the initial vaccine given Food and Drug Administration emergency use authorization, in a single vial.
Unlike the two-dose regimen with the original vaccine, the boosters are administered as a single dose immunization.
The trial participants received a booster 6-8 months after primary vaccination. Titers to the wild-type SARS-CoV-2 virus remained high and detectable in 37 out of 40 participants. However, prior to the booster, titers against the two variants of concern, B.1.351 and P.1, were lower, with about half of participants showing undetectable levels.
In contrast, 2 weeks after a booster with the original vaccine or the B.1.351 strain-specific product, pseudovirus neutralizing titers were boosted in all participants and all variants tested.
“Following [the] boost, geometric mean titers against the wild-type, B.1.351, and P.1 variants increased to levels similar to or higher than the previously reported peak titers against the ancestral (D614G) strain following primary vaccination,” the company stated.
Both mRNA-1273.351 and mRNA-1273 booster doses were generally well tolerated, the company reported. Safety and tolerability were generally comparable to those reported after the second dose of the original vaccine. Most adverse events were mild to moderate, with injection site pain most common in both groups. Participants also reported fatigue, headache, myalgia, and arthralgia.
The company plans to release data shortly on the booster efficacy at additional time points beyond 2 weeks for mRNA-1273.351, a lower-dose booster with mRNA-1272/351, as well as data on the multivariant mRNA vaccine booster.
In addition to the company’s phase 2 study, the National Institute of Allergy and Infectious Diseases is conducting a separate phase 1 study of mRNA-1273.351.
A version of this article first appeared on Medscape.com.
among people already vaccinated for COVID-19, according to first results released May 5.
Furthermore, data from the company’s ongoing phase 2 study show the variant-specific booster, known as mRNA-1273.351, achieved higher antibody titers against the B.1.351 variant than did a booster with the original Moderna vaccine.
“We are encouraged by these new data, which reinforce our confidence that our booster strategy should be protective against these newly detected variants. The strong and rapid boost in titers to levels above primary vaccination also clearly demonstrates the ability of mRNA-1273 to induce immune memory,” Stéphane Bancel, chief executive officer of Moderna, said in a statement.
The phase 2 study researchers also are evaluating a multivariant booster that is a 50/50 mix of mRNA-1273.351 and mRNA-1273, the initial vaccine given Food and Drug Administration emergency use authorization, in a single vial.
Unlike the two-dose regimen with the original vaccine, the boosters are administered as a single dose immunization.
The trial participants received a booster 6-8 months after primary vaccination. Titers to the wild-type SARS-CoV-2 virus remained high and detectable in 37 out of 40 participants. However, prior to the booster, titers against the two variants of concern, B.1.351 and P.1, were lower, with about half of participants showing undetectable levels.
In contrast, 2 weeks after a booster with the original vaccine or the B.1.351 strain-specific product, pseudovirus neutralizing titers were boosted in all participants and all variants tested.
“Following [the] boost, geometric mean titers against the wild-type, B.1.351, and P.1 variants increased to levels similar to or higher than the previously reported peak titers against the ancestral (D614G) strain following primary vaccination,” the company stated.
Both mRNA-1273.351 and mRNA-1273 booster doses were generally well tolerated, the company reported. Safety and tolerability were generally comparable to those reported after the second dose of the original vaccine. Most adverse events were mild to moderate, with injection site pain most common in both groups. Participants also reported fatigue, headache, myalgia, and arthralgia.
The company plans to release data shortly on the booster efficacy at additional time points beyond 2 weeks for mRNA-1273.351, a lower-dose booster with mRNA-1272/351, as well as data on the multivariant mRNA vaccine booster.
In addition to the company’s phase 2 study, the National Institute of Allergy and Infectious Diseases is conducting a separate phase 1 study of mRNA-1273.351.
A version of this article first appeared on Medscape.com.
Hypertension worsened by commonly used prescription meds
Nearly half of these American adults had hypertension, and in this subgroup, 18.5% reported using a prescription drug known to increase blood pressure. The most widely used class of agents with this effect was antidepressants, used by 8.7%; followed by nonsteroidal anti-inflammatory drugs (NSAIDs), used by 6.5%; steroids, 1.9%; estrogens, 1.7%; and several other agents each used by fewer than 1% of the study cohort, John Vitarello, MD, said during a press briefing on reports from the upcoming annual scientific sessions of the American College of Cardiology.
He and his associates estimated that this use of prescription drugs known to raise blood pressure could be what stands in the way of some 560,000-2.2 million Americans from having their hypertension under control, depending on the exact blood pressure impact that various pressure-increasing drugs have and presuming that half of those on blood pressure increasing agents could stop them and switch to alternative agents, said Dr. Vitarello, a researcher at Beth Israel Deaconess Medical Center in Boston.
He also highlighted that the study assessed only prescription drugs and did not examine OTC drug use, which may be especially relevant for the many people who regularly take NSAIDs.
“Clinicians should review the prescription and OTC drug use of patients with hypertension and consider stopping drugs that increase blood pressure or switching the patient to alternatives” that are blood pressure neutral, Dr. Vitarello said during the briefing. He cautioned that maintaining hypertensive patients on agents that raise their blood pressure can result in “prescribing cascades” where taking drugs that boost blood pressure results in need for intensified antihypertensive treatment.
An opportunity for NSAID alternatives
“This study hopefully raises awareness that there is a very high use of medications that increase blood pressure, and use of OTC agents could increase the rate even higher” said Eugene Yang, MD, a cardiologist and codirector of the Cardiovascular Wellness and Prevention Program of the University of Washington, Seattle. Substituting for certain antidepressant agents may often not be realistic, but an opportunity exists for reducing NSAID use, a class also linked with an increased risk for bleeding and other adverse effects, Dr. Yang said during the briefing. Minimizing use of NSAIDs including ibuprofen and naproxen use “is something to think about,” he suggested.
“The effect of NSAIDs on blood pressure is not well studied and can vary from person to person” noted Dr. Vitarello, who added that higher NSAID dosages and more prolonged use likely increase the risk for an adverse effect on blood pressure. One reasonable option is to encourage patients to use an alternative class of pain reliever such as acetaminophen.
It remains “a challenge” to discern differences in adverse blood pressure effects, and in all adverse cardiovascular effects among different NSAIDs, said Dr. Yang. Results from “some studies show that certain NSAIDs may be safer, but other studies did not. We need to be very careful using NSAIDs because, on average, they increase blood pressure by about 3 mm Hg. We need to be mindful to try to prescribe alternative agents, like acetaminophen.”
A decade of data from NHANES
The analysis run by Dr. Vitarello and associates used data from 27,599 American adults included in the NHANES during 2009-2018, and focused on the 44% who either had an average blood pressure measurement of at least 130/80 mm Hg or reported having ever been told by a clinician that they had hypertension. The NHANES assessments included the prescription medications taken by each participant. The prevalence of using at least one prescription drug known to raise blood pressure was 24% among women and 14% among men, and 4% of those with hypertension were on two or more pressure-increasing agents.
The researchers based their identification of pressure-increasing prescription drugs on the list included in the 2017 guideline for managing high blood pressure from the American College of Cardiology and American Heart Association. This list specifies that the antidepressants that raise blood pressure are the monoamine oxidase inhibitors, serotonin norepinephrine reuptake inhibitors, and tricyclic antidepressants.
Dr. Vitarello and Dr. Yang had no disclosures.
Nearly half of these American adults had hypertension, and in this subgroup, 18.5% reported using a prescription drug known to increase blood pressure. The most widely used class of agents with this effect was antidepressants, used by 8.7%; followed by nonsteroidal anti-inflammatory drugs (NSAIDs), used by 6.5%; steroids, 1.9%; estrogens, 1.7%; and several other agents each used by fewer than 1% of the study cohort, John Vitarello, MD, said during a press briefing on reports from the upcoming annual scientific sessions of the American College of Cardiology.
He and his associates estimated that this use of prescription drugs known to raise blood pressure could be what stands in the way of some 560,000-2.2 million Americans from having their hypertension under control, depending on the exact blood pressure impact that various pressure-increasing drugs have and presuming that half of those on blood pressure increasing agents could stop them and switch to alternative agents, said Dr. Vitarello, a researcher at Beth Israel Deaconess Medical Center in Boston.
He also highlighted that the study assessed only prescription drugs and did not examine OTC drug use, which may be especially relevant for the many people who regularly take NSAIDs.
“Clinicians should review the prescription and OTC drug use of patients with hypertension and consider stopping drugs that increase blood pressure or switching the patient to alternatives” that are blood pressure neutral, Dr. Vitarello said during the briefing. He cautioned that maintaining hypertensive patients on agents that raise their blood pressure can result in “prescribing cascades” where taking drugs that boost blood pressure results in need for intensified antihypertensive treatment.
An opportunity for NSAID alternatives
“This study hopefully raises awareness that there is a very high use of medications that increase blood pressure, and use of OTC agents could increase the rate even higher” said Eugene Yang, MD, a cardiologist and codirector of the Cardiovascular Wellness and Prevention Program of the University of Washington, Seattle. Substituting for certain antidepressant agents may often not be realistic, but an opportunity exists for reducing NSAID use, a class also linked with an increased risk for bleeding and other adverse effects, Dr. Yang said during the briefing. Minimizing use of NSAIDs including ibuprofen and naproxen use “is something to think about,” he suggested.
“The effect of NSAIDs on blood pressure is not well studied and can vary from person to person” noted Dr. Vitarello, who added that higher NSAID dosages and more prolonged use likely increase the risk for an adverse effect on blood pressure. One reasonable option is to encourage patients to use an alternative class of pain reliever such as acetaminophen.
It remains “a challenge” to discern differences in adverse blood pressure effects, and in all adverse cardiovascular effects among different NSAIDs, said Dr. Yang. Results from “some studies show that certain NSAIDs may be safer, but other studies did not. We need to be very careful using NSAIDs because, on average, they increase blood pressure by about 3 mm Hg. We need to be mindful to try to prescribe alternative agents, like acetaminophen.”
A decade of data from NHANES
The analysis run by Dr. Vitarello and associates used data from 27,599 American adults included in the NHANES during 2009-2018, and focused on the 44% who either had an average blood pressure measurement of at least 130/80 mm Hg or reported having ever been told by a clinician that they had hypertension. The NHANES assessments included the prescription medications taken by each participant. The prevalence of using at least one prescription drug known to raise blood pressure was 24% among women and 14% among men, and 4% of those with hypertension were on two or more pressure-increasing agents.
The researchers based their identification of pressure-increasing prescription drugs on the list included in the 2017 guideline for managing high blood pressure from the American College of Cardiology and American Heart Association. This list specifies that the antidepressants that raise blood pressure are the monoamine oxidase inhibitors, serotonin norepinephrine reuptake inhibitors, and tricyclic antidepressants.
Dr. Vitarello and Dr. Yang had no disclosures.
Nearly half of these American adults had hypertension, and in this subgroup, 18.5% reported using a prescription drug known to increase blood pressure. The most widely used class of agents with this effect was antidepressants, used by 8.7%; followed by nonsteroidal anti-inflammatory drugs (NSAIDs), used by 6.5%; steroids, 1.9%; estrogens, 1.7%; and several other agents each used by fewer than 1% of the study cohort, John Vitarello, MD, said during a press briefing on reports from the upcoming annual scientific sessions of the American College of Cardiology.
He and his associates estimated that this use of prescription drugs known to raise blood pressure could be what stands in the way of some 560,000-2.2 million Americans from having their hypertension under control, depending on the exact blood pressure impact that various pressure-increasing drugs have and presuming that half of those on blood pressure increasing agents could stop them and switch to alternative agents, said Dr. Vitarello, a researcher at Beth Israel Deaconess Medical Center in Boston.
He also highlighted that the study assessed only prescription drugs and did not examine OTC drug use, which may be especially relevant for the many people who regularly take NSAIDs.
“Clinicians should review the prescription and OTC drug use of patients with hypertension and consider stopping drugs that increase blood pressure or switching the patient to alternatives” that are blood pressure neutral, Dr. Vitarello said during the briefing. He cautioned that maintaining hypertensive patients on agents that raise their blood pressure can result in “prescribing cascades” where taking drugs that boost blood pressure results in need for intensified antihypertensive treatment.
An opportunity for NSAID alternatives
“This study hopefully raises awareness that there is a very high use of medications that increase blood pressure, and use of OTC agents could increase the rate even higher” said Eugene Yang, MD, a cardiologist and codirector of the Cardiovascular Wellness and Prevention Program of the University of Washington, Seattle. Substituting for certain antidepressant agents may often not be realistic, but an opportunity exists for reducing NSAID use, a class also linked with an increased risk for bleeding and other adverse effects, Dr. Yang said during the briefing. Minimizing use of NSAIDs including ibuprofen and naproxen use “is something to think about,” he suggested.
“The effect of NSAIDs on blood pressure is not well studied and can vary from person to person” noted Dr. Vitarello, who added that higher NSAID dosages and more prolonged use likely increase the risk for an adverse effect on blood pressure. One reasonable option is to encourage patients to use an alternative class of pain reliever such as acetaminophen.
It remains “a challenge” to discern differences in adverse blood pressure effects, and in all adverse cardiovascular effects among different NSAIDs, said Dr. Yang. Results from “some studies show that certain NSAIDs may be safer, but other studies did not. We need to be very careful using NSAIDs because, on average, they increase blood pressure by about 3 mm Hg. We need to be mindful to try to prescribe alternative agents, like acetaminophen.”
A decade of data from NHANES
The analysis run by Dr. Vitarello and associates used data from 27,599 American adults included in the NHANES during 2009-2018, and focused on the 44% who either had an average blood pressure measurement of at least 130/80 mm Hg or reported having ever been told by a clinician that they had hypertension. The NHANES assessments included the prescription medications taken by each participant. The prevalence of using at least one prescription drug known to raise blood pressure was 24% among women and 14% among men, and 4% of those with hypertension were on two or more pressure-increasing agents.
The researchers based their identification of pressure-increasing prescription drugs on the list included in the 2017 guideline for managing high blood pressure from the American College of Cardiology and American Heart Association. This list specifies that the antidepressants that raise blood pressure are the monoamine oxidase inhibitors, serotonin norepinephrine reuptake inhibitors, and tricyclic antidepressants.
Dr. Vitarello and Dr. Yang had no disclosures.
FROM ACC 2021
Exercise plus liraglutide better for maintaining weight loss than either strategy alone
For persons with obesity who lost a substantial amount of weight on a low-calorie diet, the combination of exercise and medication significantly improved weight-loss maintenance, and more so than either strategy alone, according to results of a randomized, head-to-head trial.
A year after starting moderate to vigorous exercise coupled with liraglutide treatment, study participants had a weight loss 9.5 kg more than those who received placebo and usual activity, study results show.
Reductions in both weight and fat loss seen with exercise and liraglutide was roughly twice as much as what was achieved at 1 year with the strategies of liraglutide or exercise alone, according to authors of the study, which appears in the New England Journal of Medicine .
Although the findings may not apply to those who can’t or won’t perform moderate to vigorous exercise, the intervention in this study was nevertheless feasible in this group of persons with obesity who had a very low level of fitness, according to the authors.
Hope for healthy weight loss maintenance
Investigator Signe S. Torekov, PhD, said in an interview that these results provide hope that more-intensive exercise regimens, with or without medication, can be useful and well accepted among individuals struggling with obesity.
“When we started our study, we were told, ‘you are never going to have people with obesity exercising that much, and for that long’ – but people were actually very happy about the exercise,” said Dr. Torekov, a professor in the department of biomedical sciences at the University of Copenhagen.
“If you actually set up a program where people are monitored and you have a feedback system, then exercise is an excellent component in obesity treatment that should be much more actively used – not only for its weight-lowering component, but also for improving health and quality of life,” she said in an interview.
Weight-management specialist John D. Clark, MD, PhD, said results of this study can be used to help inform patients about how successful different strategies incorporating exercise and medication may be following initial weight loss.
“When patients plateau on a consistent, calorie-restricted dietary plan, we can educate them and manage expectations about what options may be available to them after their initial weight loss,” said Dr. Clark, of the University of Texas, Dallas.
“If the patient’s goal specifically is weight loss at all costs, then I may suggest, ‘let’s consider liraglutide or liraglutide in combination with exercise,’ ” he said in an interview. “Exercise improves body composition, even if it may not on its own be as successful in the next phase of their weight-loss journey, as shown in this study.”
Obesity and weight-loss challenges
Although it’s not uncommon for obese patients to lose a large amount of weight, keeping the weight off is frequently a challenge unless the patient follows a structured weight maintenance program, according to Dr. Torekov and coauthors.
The rapid weight regain seen in many obese patients could be a result of reductions in total energy expenditure or increased appetite. Exercise is one strategy to sustain weight loss, though according to the authors, very few studies have looked at exercise in isolation to quantify its contribution to maintenance.
Accordingly, the present study sought to determine whether exercise, medication, or the combination thereof works best to keep weight off.
The study incorporated liraglutide, a GLP-1 receptor agonist indicated for chronic weight management, along with a reduced-calorie diet and increased physical activity, in adults with elevated body mass index and at least one weight-related comorbidity.
The investigator-initiated phase 3 trial included 215 adults with a body mass index of 32-43. Individuals with type 2 diabetes were excluded. All participants followed an 8-week, low-calorie diet comprising 800 calories per day.
Participants who lost 5% or more of their body weight were then randomized to 1 year of exercise plus liraglutide, exercise plus placebo, usual activity plus liraglutide, or usual activity plus placebo.
The exercise program – which was structured but flexible, according to investigators – included group exercise sessions that incorporated 30 minutes of indoor cycling and 15 minutes of circuit training 2 days each week. Participants wore heart rate monitors during exercise to make sure they reached targets for moderate to vigorous intensity.
Instructors trained in exercise physiology planned and monitored individualized exercise programs for each participant in the exercise-medication or exercise-only arms of the study.
Participants in all groups attended 12 one-on-one consultations where body weight was measured and dietetic support was provided.
Weight loss with exercise and medication
Out of 215 individuals enrolled in the study, 195 lost at least 5% of body weight and continued on to the randomized portion, the investigators reported. During the diet phase, they lost a mean of 13.1 kg, translating into a 12% mean reduction in body weight.
The mean frequency of exercise was 2.4 times per week in the exercise-plus-medication group and 2.5 times per week in the exercise-only group. About one-third of the exercise took place in the group sessions, and there was no difference in relative intensity between group and individual exercise regimens, the investigators said.
Individuals in the exercise plus medication group continued to lose more weight, such that, at the end of 1 year, the weight loss decreased even further, by a mean of –3.4 kg. By contrast, weight increased by a mean of 6.1 kg for the placebo group, adding up to a treatment difference of –9.5 kg (95% confidence interval, –13.1 to –5.9; P < .001), according to the report.
That treatment effect was also seen, but more muted, in the exercise- and liraglutide-only groups, at –4.1 kg and –6.8 kg, respectively.
A significant treatment effect was observed for exercise plus liraglutide, compared with exercise alone, at –5.4 kg (P = .004), while the treatment effect for the combination versus liraglutide alone was not significant at –2.7 kg (P = .13), the data show.
Body-fat reduction at 52 weeks was –3.9 percentage points for exercise plus liraglutide as compared with placebo, or roughly twice the reductions seen in the exercise- and liraglutide-alone groups, the investigators said, adding that the combination preserved lean mass.
Reductions in hemoglobin A1c, which are generally thought to reduce diabetes risk, were reduced in both the liraglutide and liraglutide-exercise combination group, according to their report.
The research was supported in part by grants from the Novo Nordisk Foundation.
For persons with obesity who lost a substantial amount of weight on a low-calorie diet, the combination of exercise and medication significantly improved weight-loss maintenance, and more so than either strategy alone, according to results of a randomized, head-to-head trial.
A year after starting moderate to vigorous exercise coupled with liraglutide treatment, study participants had a weight loss 9.5 kg more than those who received placebo and usual activity, study results show.
Reductions in both weight and fat loss seen with exercise and liraglutide was roughly twice as much as what was achieved at 1 year with the strategies of liraglutide or exercise alone, according to authors of the study, which appears in the New England Journal of Medicine .
Although the findings may not apply to those who can’t or won’t perform moderate to vigorous exercise, the intervention in this study was nevertheless feasible in this group of persons with obesity who had a very low level of fitness, according to the authors.
Hope for healthy weight loss maintenance
Investigator Signe S. Torekov, PhD, said in an interview that these results provide hope that more-intensive exercise regimens, with or without medication, can be useful and well accepted among individuals struggling with obesity.
“When we started our study, we were told, ‘you are never going to have people with obesity exercising that much, and for that long’ – but people were actually very happy about the exercise,” said Dr. Torekov, a professor in the department of biomedical sciences at the University of Copenhagen.
“If you actually set up a program where people are monitored and you have a feedback system, then exercise is an excellent component in obesity treatment that should be much more actively used – not only for its weight-lowering component, but also for improving health and quality of life,” she said in an interview.
Weight-management specialist John D. Clark, MD, PhD, said results of this study can be used to help inform patients about how successful different strategies incorporating exercise and medication may be following initial weight loss.
“When patients plateau on a consistent, calorie-restricted dietary plan, we can educate them and manage expectations about what options may be available to them after their initial weight loss,” said Dr. Clark, of the University of Texas, Dallas.
“If the patient’s goal specifically is weight loss at all costs, then I may suggest, ‘let’s consider liraglutide or liraglutide in combination with exercise,’ ” he said in an interview. “Exercise improves body composition, even if it may not on its own be as successful in the next phase of their weight-loss journey, as shown in this study.”
Obesity and weight-loss challenges
Although it’s not uncommon for obese patients to lose a large amount of weight, keeping the weight off is frequently a challenge unless the patient follows a structured weight maintenance program, according to Dr. Torekov and coauthors.
The rapid weight regain seen in many obese patients could be a result of reductions in total energy expenditure or increased appetite. Exercise is one strategy to sustain weight loss, though according to the authors, very few studies have looked at exercise in isolation to quantify its contribution to maintenance.
Accordingly, the present study sought to determine whether exercise, medication, or the combination thereof works best to keep weight off.
The study incorporated liraglutide, a GLP-1 receptor agonist indicated for chronic weight management, along with a reduced-calorie diet and increased physical activity, in adults with elevated body mass index and at least one weight-related comorbidity.
The investigator-initiated phase 3 trial included 215 adults with a body mass index of 32-43. Individuals with type 2 diabetes were excluded. All participants followed an 8-week, low-calorie diet comprising 800 calories per day.
Participants who lost 5% or more of their body weight were then randomized to 1 year of exercise plus liraglutide, exercise plus placebo, usual activity plus liraglutide, or usual activity plus placebo.
The exercise program – which was structured but flexible, according to investigators – included group exercise sessions that incorporated 30 minutes of indoor cycling and 15 minutes of circuit training 2 days each week. Participants wore heart rate monitors during exercise to make sure they reached targets for moderate to vigorous intensity.
Instructors trained in exercise physiology planned and monitored individualized exercise programs for each participant in the exercise-medication or exercise-only arms of the study.
Participants in all groups attended 12 one-on-one consultations where body weight was measured and dietetic support was provided.
Weight loss with exercise and medication
Out of 215 individuals enrolled in the study, 195 lost at least 5% of body weight and continued on to the randomized portion, the investigators reported. During the diet phase, they lost a mean of 13.1 kg, translating into a 12% mean reduction in body weight.
The mean frequency of exercise was 2.4 times per week in the exercise-plus-medication group and 2.5 times per week in the exercise-only group. About one-third of the exercise took place in the group sessions, and there was no difference in relative intensity between group and individual exercise regimens, the investigators said.
Individuals in the exercise plus medication group continued to lose more weight, such that, at the end of 1 year, the weight loss decreased even further, by a mean of –3.4 kg. By contrast, weight increased by a mean of 6.1 kg for the placebo group, adding up to a treatment difference of –9.5 kg (95% confidence interval, –13.1 to –5.9; P < .001), according to the report.
That treatment effect was also seen, but more muted, in the exercise- and liraglutide-only groups, at –4.1 kg and –6.8 kg, respectively.
A significant treatment effect was observed for exercise plus liraglutide, compared with exercise alone, at –5.4 kg (P = .004), while the treatment effect for the combination versus liraglutide alone was not significant at –2.7 kg (P = .13), the data show.
Body-fat reduction at 52 weeks was –3.9 percentage points for exercise plus liraglutide as compared with placebo, or roughly twice the reductions seen in the exercise- and liraglutide-alone groups, the investigators said, adding that the combination preserved lean mass.
Reductions in hemoglobin A1c, which are generally thought to reduce diabetes risk, were reduced in both the liraglutide and liraglutide-exercise combination group, according to their report.
The research was supported in part by grants from the Novo Nordisk Foundation.
For persons with obesity who lost a substantial amount of weight on a low-calorie diet, the combination of exercise and medication significantly improved weight-loss maintenance, and more so than either strategy alone, according to results of a randomized, head-to-head trial.
A year after starting moderate to vigorous exercise coupled with liraglutide treatment, study participants had a weight loss 9.5 kg more than those who received placebo and usual activity, study results show.
Reductions in both weight and fat loss seen with exercise and liraglutide was roughly twice as much as what was achieved at 1 year with the strategies of liraglutide or exercise alone, according to authors of the study, which appears in the New England Journal of Medicine .
Although the findings may not apply to those who can’t or won’t perform moderate to vigorous exercise, the intervention in this study was nevertheless feasible in this group of persons with obesity who had a very low level of fitness, according to the authors.
Hope for healthy weight loss maintenance
Investigator Signe S. Torekov, PhD, said in an interview that these results provide hope that more-intensive exercise regimens, with or without medication, can be useful and well accepted among individuals struggling with obesity.
“When we started our study, we were told, ‘you are never going to have people with obesity exercising that much, and for that long’ – but people were actually very happy about the exercise,” said Dr. Torekov, a professor in the department of biomedical sciences at the University of Copenhagen.
“If you actually set up a program where people are monitored and you have a feedback system, then exercise is an excellent component in obesity treatment that should be much more actively used – not only for its weight-lowering component, but also for improving health and quality of life,” she said in an interview.
Weight-management specialist John D. Clark, MD, PhD, said results of this study can be used to help inform patients about how successful different strategies incorporating exercise and medication may be following initial weight loss.
“When patients plateau on a consistent, calorie-restricted dietary plan, we can educate them and manage expectations about what options may be available to them after their initial weight loss,” said Dr. Clark, of the University of Texas, Dallas.
“If the patient’s goal specifically is weight loss at all costs, then I may suggest, ‘let’s consider liraglutide or liraglutide in combination with exercise,’ ” he said in an interview. “Exercise improves body composition, even if it may not on its own be as successful in the next phase of their weight-loss journey, as shown in this study.”
Obesity and weight-loss challenges
Although it’s not uncommon for obese patients to lose a large amount of weight, keeping the weight off is frequently a challenge unless the patient follows a structured weight maintenance program, according to Dr. Torekov and coauthors.
The rapid weight regain seen in many obese patients could be a result of reductions in total energy expenditure or increased appetite. Exercise is one strategy to sustain weight loss, though according to the authors, very few studies have looked at exercise in isolation to quantify its contribution to maintenance.
Accordingly, the present study sought to determine whether exercise, medication, or the combination thereof works best to keep weight off.
The study incorporated liraglutide, a GLP-1 receptor agonist indicated for chronic weight management, along with a reduced-calorie diet and increased physical activity, in adults with elevated body mass index and at least one weight-related comorbidity.
The investigator-initiated phase 3 trial included 215 adults with a body mass index of 32-43. Individuals with type 2 diabetes were excluded. All participants followed an 8-week, low-calorie diet comprising 800 calories per day.
Participants who lost 5% or more of their body weight were then randomized to 1 year of exercise plus liraglutide, exercise plus placebo, usual activity plus liraglutide, or usual activity plus placebo.
The exercise program – which was structured but flexible, according to investigators – included group exercise sessions that incorporated 30 minutes of indoor cycling and 15 minutes of circuit training 2 days each week. Participants wore heart rate monitors during exercise to make sure they reached targets for moderate to vigorous intensity.
Instructors trained in exercise physiology planned and monitored individualized exercise programs for each participant in the exercise-medication or exercise-only arms of the study.
Participants in all groups attended 12 one-on-one consultations where body weight was measured and dietetic support was provided.
Weight loss with exercise and medication
Out of 215 individuals enrolled in the study, 195 lost at least 5% of body weight and continued on to the randomized portion, the investigators reported. During the diet phase, they lost a mean of 13.1 kg, translating into a 12% mean reduction in body weight.
The mean frequency of exercise was 2.4 times per week in the exercise-plus-medication group and 2.5 times per week in the exercise-only group. About one-third of the exercise took place in the group sessions, and there was no difference in relative intensity between group and individual exercise regimens, the investigators said.
Individuals in the exercise plus medication group continued to lose more weight, such that, at the end of 1 year, the weight loss decreased even further, by a mean of –3.4 kg. By contrast, weight increased by a mean of 6.1 kg for the placebo group, adding up to a treatment difference of –9.5 kg (95% confidence interval, –13.1 to –5.9; P < .001), according to the report.
That treatment effect was also seen, but more muted, in the exercise- and liraglutide-only groups, at –4.1 kg and –6.8 kg, respectively.
A significant treatment effect was observed for exercise plus liraglutide, compared with exercise alone, at –5.4 kg (P = .004), while the treatment effect for the combination versus liraglutide alone was not significant at –2.7 kg (P = .13), the data show.
Body-fat reduction at 52 weeks was –3.9 percentage points for exercise plus liraglutide as compared with placebo, or roughly twice the reductions seen in the exercise- and liraglutide-alone groups, the investigators said, adding that the combination preserved lean mass.
Reductions in hemoglobin A1c, which are generally thought to reduce diabetes risk, were reduced in both the liraglutide and liraglutide-exercise combination group, according to their report.
The research was supported in part by grants from the Novo Nordisk Foundation.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Only a third of adults with diabetes receive ADA-recommended care
In 2017-2018, only one in three U.S. adults with diabetes received five basic elements of care recommended by the American Diabetes Association, new research indicates.
The proportions of patients who visited a physician for diabetes care and received hemoglobin A1c testing, foot and eye exams, and cholesterol testing increased from 2005 to 2018. However, this increase was primarily among those aged 65 years and older, and therefore eligible for Medicare.
“Our study suggests that providing affordable health care coverage can help ensure people with diabetes get recommended care. We also found that patients who were not receiving recommended care were more likely to be younger, newly diagnosed with diabetes, and not on diabetes medication. Clinicians can pay more attention to these patient populations to improve recommended care delivery and prevent diabetes-related complications,” lead author Jung-Im Shin, MD, said in an interview.
The data predate the COVID-19 pandemic, which has also had major effects on delivery of diabetes care, added Dr. Shin of Johns Hopkins University, Baltimore.
“Routine visits to the doctor and important screenings for retinopathy or foot examination have been postponed. People with diabetes have had to reschedule or cancel nonurgent visits, some have lost ... insurance following unemployment, and many have avoided health care facilities out of fear. We are only just beginning to understand the consequences of the pandemic on the health of people with diabetes,” Dr. Shin noted.
Overall improvements seen only in those aged 65 and older
The data, from 4,069 adults aged 20 years and older from the 2005-2018 National Health and Nutrition and Examination Survey (NHANES), were published online April 16, 2021, in Diabetes Care.
Dr. Shin and colleagues defined receipt of diabetes care as meeting all of the following five criteria in the past 12 months, based on the ADA Standards of Care and NHANES data availability: seeing a primary doctor for diabetes care, receiving A1c testing, receiving a foot examination, receiving an eye examination, and receiving cholesterol testing.
Over the entire 13-year period, 29.2% of respondents reported having received all five components.
That proportion increased significantly over time, from 25.0% in 2005-2006 to 34.1% in 2017-2018 (P = .004). However, among the individual components, only receiving A1c testing increased significantly over time, from 64.4% to 85.3%, in all age groups (P < .001).
Moreover, when stratified by age, receipt of all five components only increased significantly among participants aged 65 and older, from 29.3% in 2005-2006 to 44.2% in 2017-2018 (P = .001).
The proportion remained unchanged among those aged 40-64 (25.2% to 25.8%; P = .457) and showed a nonsignificant increase in those aged 20-39 (9.9% to 26.0%; P = .401).
In adjusted analyses, older age, higher income and education, health insurance, longer duration of diabetes, use of diabetes medications, and hypercholesterolemia were significantly associated with receipt of ADA guideline–recommended diabetes care.
Factors not found to be associated with care receipt included sex, race/ethnicity, body mass index, smoking status, A1c, hypertension, cardiovascular disease, chronic kidney disease, and depressive symptoms.
Participants who received ADA guideline–recommended care were significantly more likely to achieve A1c below 7.5% (adjusted odds ratio, 1.52), blood pressure less than 140/90 mm Hg (aOR, 1.47), and LDL cholesterol below 100 mg/dL (aOR, 1.47), and to receive cholesterol-lowering medication (aOR, 1.79).
Dr. Shin said that it will be “important to study the impact of COVID-19 on diabetes care when new data are available.”
The project was supported by a research grant from Merck to Johns Hopkins University. Shin has reported receiving a grant from the National Institute of Diabetes and Digestive and Kidney Diseases. Two coauthors are Merck employees.
A version of this article first appeared on Medscape.com.
In 2017-2018, only one in three U.S. adults with diabetes received five basic elements of care recommended by the American Diabetes Association, new research indicates.
The proportions of patients who visited a physician for diabetes care and received hemoglobin A1c testing, foot and eye exams, and cholesterol testing increased from 2005 to 2018. However, this increase was primarily among those aged 65 years and older, and therefore eligible for Medicare.
“Our study suggests that providing affordable health care coverage can help ensure people with diabetes get recommended care. We also found that patients who were not receiving recommended care were more likely to be younger, newly diagnosed with diabetes, and not on diabetes medication. Clinicians can pay more attention to these patient populations to improve recommended care delivery and prevent diabetes-related complications,” lead author Jung-Im Shin, MD, said in an interview.
The data predate the COVID-19 pandemic, which has also had major effects on delivery of diabetes care, added Dr. Shin of Johns Hopkins University, Baltimore.
“Routine visits to the doctor and important screenings for retinopathy or foot examination have been postponed. People with diabetes have had to reschedule or cancel nonurgent visits, some have lost ... insurance following unemployment, and many have avoided health care facilities out of fear. We are only just beginning to understand the consequences of the pandemic on the health of people with diabetes,” Dr. Shin noted.
Overall improvements seen only in those aged 65 and older
The data, from 4,069 adults aged 20 years and older from the 2005-2018 National Health and Nutrition and Examination Survey (NHANES), were published online April 16, 2021, in Diabetes Care.
Dr. Shin and colleagues defined receipt of diabetes care as meeting all of the following five criteria in the past 12 months, based on the ADA Standards of Care and NHANES data availability: seeing a primary doctor for diabetes care, receiving A1c testing, receiving a foot examination, receiving an eye examination, and receiving cholesterol testing.
Over the entire 13-year period, 29.2% of respondents reported having received all five components.
That proportion increased significantly over time, from 25.0% in 2005-2006 to 34.1% in 2017-2018 (P = .004). However, among the individual components, only receiving A1c testing increased significantly over time, from 64.4% to 85.3%, in all age groups (P < .001).
Moreover, when stratified by age, receipt of all five components only increased significantly among participants aged 65 and older, from 29.3% in 2005-2006 to 44.2% in 2017-2018 (P = .001).
The proportion remained unchanged among those aged 40-64 (25.2% to 25.8%; P = .457) and showed a nonsignificant increase in those aged 20-39 (9.9% to 26.0%; P = .401).
In adjusted analyses, older age, higher income and education, health insurance, longer duration of diabetes, use of diabetes medications, and hypercholesterolemia were significantly associated with receipt of ADA guideline–recommended diabetes care.
Factors not found to be associated with care receipt included sex, race/ethnicity, body mass index, smoking status, A1c, hypertension, cardiovascular disease, chronic kidney disease, and depressive symptoms.
Participants who received ADA guideline–recommended care were significantly more likely to achieve A1c below 7.5% (adjusted odds ratio, 1.52), blood pressure less than 140/90 mm Hg (aOR, 1.47), and LDL cholesterol below 100 mg/dL (aOR, 1.47), and to receive cholesterol-lowering medication (aOR, 1.79).
Dr. Shin said that it will be “important to study the impact of COVID-19 on diabetes care when new data are available.”
The project was supported by a research grant from Merck to Johns Hopkins University. Shin has reported receiving a grant from the National Institute of Diabetes and Digestive and Kidney Diseases. Two coauthors are Merck employees.
A version of this article first appeared on Medscape.com.
In 2017-2018, only one in three U.S. adults with diabetes received five basic elements of care recommended by the American Diabetes Association, new research indicates.
The proportions of patients who visited a physician for diabetes care and received hemoglobin A1c testing, foot and eye exams, and cholesterol testing increased from 2005 to 2018. However, this increase was primarily among those aged 65 years and older, and therefore eligible for Medicare.
“Our study suggests that providing affordable health care coverage can help ensure people with diabetes get recommended care. We also found that patients who were not receiving recommended care were more likely to be younger, newly diagnosed with diabetes, and not on diabetes medication. Clinicians can pay more attention to these patient populations to improve recommended care delivery and prevent diabetes-related complications,” lead author Jung-Im Shin, MD, said in an interview.
The data predate the COVID-19 pandemic, which has also had major effects on delivery of diabetes care, added Dr. Shin of Johns Hopkins University, Baltimore.
“Routine visits to the doctor and important screenings for retinopathy or foot examination have been postponed. People with diabetes have had to reschedule or cancel nonurgent visits, some have lost ... insurance following unemployment, and many have avoided health care facilities out of fear. We are only just beginning to understand the consequences of the pandemic on the health of people with diabetes,” Dr. Shin noted.
Overall improvements seen only in those aged 65 and older
The data, from 4,069 adults aged 20 years and older from the 2005-2018 National Health and Nutrition and Examination Survey (NHANES), were published online April 16, 2021, in Diabetes Care.
Dr. Shin and colleagues defined receipt of diabetes care as meeting all of the following five criteria in the past 12 months, based on the ADA Standards of Care and NHANES data availability: seeing a primary doctor for diabetes care, receiving A1c testing, receiving a foot examination, receiving an eye examination, and receiving cholesterol testing.
Over the entire 13-year period, 29.2% of respondents reported having received all five components.
That proportion increased significantly over time, from 25.0% in 2005-2006 to 34.1% in 2017-2018 (P = .004). However, among the individual components, only receiving A1c testing increased significantly over time, from 64.4% to 85.3%, in all age groups (P < .001).
Moreover, when stratified by age, receipt of all five components only increased significantly among participants aged 65 and older, from 29.3% in 2005-2006 to 44.2% in 2017-2018 (P = .001).
The proportion remained unchanged among those aged 40-64 (25.2% to 25.8%; P = .457) and showed a nonsignificant increase in those aged 20-39 (9.9% to 26.0%; P = .401).
In adjusted analyses, older age, higher income and education, health insurance, longer duration of diabetes, use of diabetes medications, and hypercholesterolemia were significantly associated with receipt of ADA guideline–recommended diabetes care.
Factors not found to be associated with care receipt included sex, race/ethnicity, body mass index, smoking status, A1c, hypertension, cardiovascular disease, chronic kidney disease, and depressive symptoms.
Participants who received ADA guideline–recommended care were significantly more likely to achieve A1c below 7.5% (adjusted odds ratio, 1.52), blood pressure less than 140/90 mm Hg (aOR, 1.47), and LDL cholesterol below 100 mg/dL (aOR, 1.47), and to receive cholesterol-lowering medication (aOR, 1.79).
Dr. Shin said that it will be “important to study the impact of COVID-19 on diabetes care when new data are available.”
The project was supported by a research grant from Merck to Johns Hopkins University. Shin has reported receiving a grant from the National Institute of Diabetes and Digestive and Kidney Diseases. Two coauthors are Merck employees.
A version of this article first appeared on Medscape.com.
Increasing salt intake proves beneficial in POTS
For patients with postural tachycardia syndrome (POTS), dietary sodium intake can be increased more confidently, suggests the first study to yield solid evidence to support this treatment strategy.
The results showed that high dietary sodium intake can lower plasma norepinephrine levels and ameliorate standing and orthostatic tachycardia for patients with POTS.
“These results suggest that increasing dietary salt is a good rationale for treatment of this condition, and this study gives reassurance we are doing the right thing for POTS patients by increasing their sodium intake,” senior author Satish R. Raj, MD, said in an interview.
The study, with lead author Emily M. Garland, PhD, was published online April 26, 2021, in the Journal of the American College of Cardiology.
Dr. Raj, who is professor of cardiac science at the University of Calgary (Alta.), explained that POTS includes a spectrum of disorders that affect the automatic nervous system, which regulates heart rate and blood pressure.
“It is a disorder of orthostatic intolerance – patients feel better when they lie down. It differs from orthostatic hypotension in that, when a POTS patient stands up, the blood pressure does not necessarily drop, but the heart rate increases excessively.”
Although it is normal for the heart rate to increase somewhat on standing, among patients with POTS, the heart rate increases excessively. The condition is defined as an orthostatic heart rate increase of at least 30 beats/min (or 40 beats/min among individuals aged 12-19 years ) in the absence of orthostatic hypotension.
The disorder is characterized by a range of symptoms, including lightheadedness, shortness of breath, palpitations, and exertional intolerance, that are worse when in an upright position. Patients also experience chronic fatigue and perceived cognitive impairment, Dr. Raj noted.
The typical demographic for POTS is young women; the condition often starts during the teenage years.
Patients often have low blood volume, so one approach to treatment is to increase the intake of salt and water so as to increase blood volume.
“This is one of the mainstays of treatment, but it has never really been properly studied,” Dr. Raj commented. Increasing salt intake “is an unusual message from a cardiologist, and there have been concerns that we are making recommendations against traditional advice, so we urgently need evidence to support this recommendation.”
The current crossover study enrolled 14 patients with POTS and 13 healthy control persons who, over a period of 6 days, underwent treatment with a low-sodium diet (10 mEq sodium per day) or a high-sodium diet (300 mEq sodium per day).
Supine and standing heart rate, blood pressure, serum aldosterone level, plasma renin activity, blood volume, and plasma norepinephrine and epinephrine levels were measured.
Results showed that, among the POTS patients, the high-sodium diet reduced upright heart rate and the change in heart rate on standing, compared with the low-sodium diet.
Heart rate increased by 46 beats/min with the high-sodium diet versus 60 beats/min with the low-sodium diet.
Total blood volume and plasma volume increased, and standing norepinephrine levels decreased with the high-sodium diet, compared with the low-sodium diet.
However, upright heart rate, change in heart rate, and upright norepinephrine levels remained higher among POTS patients than among control persons receiving the high-sodium diet.
There was a nonsignificant trend for a lower symptom burden score among the POTS patients who received the high-sodium diet in comparison with those taking the low-sodium diet. Scores for mental confusion, palpitations, lightheadedness, and headache trending downward on the high-sodium diet.
“We found that high levels of dietary salt did what we hoped, with increased blood volume and reduced norepinephrine levels on standing and reduced excessive increase in heart rate. While it didn’t completely normalize heart rate, this was reduced significantly,” Dr. Raj said.
Another observation from the study was that the increased salt intake seemed to be beneficial across the whole spectrum of patients.
“There are some patients who have very high levels of sympathetic activation, and there have been anecdotal reports that increasing salt may not work so well in this group,” he said. “In this study, we didn’t differentiate, but average norepinephrine levels were very high, and many patients would be considered to be hyperadrenergic. Our results suggest this treatment will help these patients too.”
He noted that sodium intake was increased in this study just through diet. “We had a special metabolic kitchen. In clinical practice, we advise patients to add regular table salt to their food, and we only use salt tablets when they cannot tolerate so much salt in their diet.”
Recognizing that there may be concerns about hypertension with long-term use of such a treatment, Dr. Raj said there were no signs of an increase in blood pressure in this study. “But this should be considered a short-term therapy for the time being, and patients need to be reassessed every few years as their physiology changes.”
The authors estimated that POTS affects up to 1% of the population. Because there is no diagnostic code for the condition at present, all incidence data are estimates.
Dr. Raj pointed out that potentially a lot of people are affected, but there is little recognition of the condition among patients and physicians.
“Many family doctors are unaware of POTS,” he noted. “Patients often have to research their symptoms themselves and inform their doctor of the condition. Many patients wait years and often see many different doctors before getting a correct diagnosis.”
He explained that patients with POTS are often diagnosed as having a psychiatric illness. “They are mainly young women with palpitations, heart pounding, shakiness, which is often labeled as anxiety.”
Dr. Raj urged clinicians to consider POTS if patients have symptoms that are worse when standing up. The diagnosis is confirmed if their blood pressure doesn’t fall when standing up but their heart rate increases by at least 30 beats/min.
He noted that not enough specialists treat this condition, so family doctors need to be able to diagnose and initiate treatment. If more aggressive treatment is required, patients can be referred to a specialist.
“One of the problems is that this condition pans across different medical specialties. No one field owns it, so it tends to get ignored. But there are clinicians who are interested in POTS, and the key is finding one of these,” he said.
“We have finally established that this high-sodium diet works as treatment for POTS,” he concluded. “We have been using it for some time, but now we have evidence for its use across the whole spectrum of patients.”
In an accompanying editorial (J Am Coll Cardiol. 2021 May 4;77[17]:2185-2186), Blair P. Grubb, MD, University of Toledo (Ohio) Medical Center, wrote that this “superb study by Garland et al. helps better establish our understanding of the pathophysiologic process taking place in POTS while at the same time providing good evidence for the augmentation of dietary sodium as one of the cornerstones of treatment.”
He added that the field needs more such studies “in our quest to better understand POTS and to elaborate therapeutic modalities to help those suffering from this debilitating illness.”
The study was supported in part by the National Heart, Lung, and Blood Institute; the National Center for Advancing Translational Sciences; and the Vanderbilt Hormone and Analytical Services Core. Dr. Raj has served as a consultant for Lundbeck NA and Theravance; has served as chair of the data safety and monitoring board for Arena Pharmaceuticals and as Cardiac Arrhythmia Network of Canada network investigator; and has served on the medical advisory board of Dysautonomia International and PoTS UK, both without financial compensation.
A version of this article first appeared on Medscape.com.
For patients with postural tachycardia syndrome (POTS), dietary sodium intake can be increased more confidently, suggests the first study to yield solid evidence to support this treatment strategy.
The results showed that high dietary sodium intake can lower plasma norepinephrine levels and ameliorate standing and orthostatic tachycardia for patients with POTS.
“These results suggest that increasing dietary salt is a good rationale for treatment of this condition, and this study gives reassurance we are doing the right thing for POTS patients by increasing their sodium intake,” senior author Satish R. Raj, MD, said in an interview.
The study, with lead author Emily M. Garland, PhD, was published online April 26, 2021, in the Journal of the American College of Cardiology.
Dr. Raj, who is professor of cardiac science at the University of Calgary (Alta.), explained that POTS includes a spectrum of disorders that affect the automatic nervous system, which regulates heart rate and blood pressure.
“It is a disorder of orthostatic intolerance – patients feel better when they lie down. It differs from orthostatic hypotension in that, when a POTS patient stands up, the blood pressure does not necessarily drop, but the heart rate increases excessively.”
Although it is normal for the heart rate to increase somewhat on standing, among patients with POTS, the heart rate increases excessively. The condition is defined as an orthostatic heart rate increase of at least 30 beats/min (or 40 beats/min among individuals aged 12-19 years ) in the absence of orthostatic hypotension.
The disorder is characterized by a range of symptoms, including lightheadedness, shortness of breath, palpitations, and exertional intolerance, that are worse when in an upright position. Patients also experience chronic fatigue and perceived cognitive impairment, Dr. Raj noted.
The typical demographic for POTS is young women; the condition often starts during the teenage years.
Patients often have low blood volume, so one approach to treatment is to increase the intake of salt and water so as to increase blood volume.
“This is one of the mainstays of treatment, but it has never really been properly studied,” Dr. Raj commented. Increasing salt intake “is an unusual message from a cardiologist, and there have been concerns that we are making recommendations against traditional advice, so we urgently need evidence to support this recommendation.”
The current crossover study enrolled 14 patients with POTS and 13 healthy control persons who, over a period of 6 days, underwent treatment with a low-sodium diet (10 mEq sodium per day) or a high-sodium diet (300 mEq sodium per day).
Supine and standing heart rate, blood pressure, serum aldosterone level, plasma renin activity, blood volume, and plasma norepinephrine and epinephrine levels were measured.
Results showed that, among the POTS patients, the high-sodium diet reduced upright heart rate and the change in heart rate on standing, compared with the low-sodium diet.
Heart rate increased by 46 beats/min with the high-sodium diet versus 60 beats/min with the low-sodium diet.
Total blood volume and plasma volume increased, and standing norepinephrine levels decreased with the high-sodium diet, compared with the low-sodium diet.
However, upright heart rate, change in heart rate, and upright norepinephrine levels remained higher among POTS patients than among control persons receiving the high-sodium diet.
There was a nonsignificant trend for a lower symptom burden score among the POTS patients who received the high-sodium diet in comparison with those taking the low-sodium diet. Scores for mental confusion, palpitations, lightheadedness, and headache trending downward on the high-sodium diet.
“We found that high levels of dietary salt did what we hoped, with increased blood volume and reduced norepinephrine levels on standing and reduced excessive increase in heart rate. While it didn’t completely normalize heart rate, this was reduced significantly,” Dr. Raj said.
Another observation from the study was that the increased salt intake seemed to be beneficial across the whole spectrum of patients.
“There are some patients who have very high levels of sympathetic activation, and there have been anecdotal reports that increasing salt may not work so well in this group,” he said. “In this study, we didn’t differentiate, but average norepinephrine levels were very high, and many patients would be considered to be hyperadrenergic. Our results suggest this treatment will help these patients too.”
He noted that sodium intake was increased in this study just through diet. “We had a special metabolic kitchen. In clinical practice, we advise patients to add regular table salt to their food, and we only use salt tablets when they cannot tolerate so much salt in their diet.”
Recognizing that there may be concerns about hypertension with long-term use of such a treatment, Dr. Raj said there were no signs of an increase in blood pressure in this study. “But this should be considered a short-term therapy for the time being, and patients need to be reassessed every few years as their physiology changes.”
The authors estimated that POTS affects up to 1% of the population. Because there is no diagnostic code for the condition at present, all incidence data are estimates.
Dr. Raj pointed out that potentially a lot of people are affected, but there is little recognition of the condition among patients and physicians.
“Many family doctors are unaware of POTS,” he noted. “Patients often have to research their symptoms themselves and inform their doctor of the condition. Many patients wait years and often see many different doctors before getting a correct diagnosis.”
He explained that patients with POTS are often diagnosed as having a psychiatric illness. “They are mainly young women with palpitations, heart pounding, shakiness, which is often labeled as anxiety.”
Dr. Raj urged clinicians to consider POTS if patients have symptoms that are worse when standing up. The diagnosis is confirmed if their blood pressure doesn’t fall when standing up but their heart rate increases by at least 30 beats/min.
He noted that not enough specialists treat this condition, so family doctors need to be able to diagnose and initiate treatment. If more aggressive treatment is required, patients can be referred to a specialist.
“One of the problems is that this condition pans across different medical specialties. No one field owns it, so it tends to get ignored. But there are clinicians who are interested in POTS, and the key is finding one of these,” he said.
“We have finally established that this high-sodium diet works as treatment for POTS,” he concluded. “We have been using it for some time, but now we have evidence for its use across the whole spectrum of patients.”
In an accompanying editorial (J Am Coll Cardiol. 2021 May 4;77[17]:2185-2186), Blair P. Grubb, MD, University of Toledo (Ohio) Medical Center, wrote that this “superb study by Garland et al. helps better establish our understanding of the pathophysiologic process taking place in POTS while at the same time providing good evidence for the augmentation of dietary sodium as one of the cornerstones of treatment.”
He added that the field needs more such studies “in our quest to better understand POTS and to elaborate therapeutic modalities to help those suffering from this debilitating illness.”
The study was supported in part by the National Heart, Lung, and Blood Institute; the National Center for Advancing Translational Sciences; and the Vanderbilt Hormone and Analytical Services Core. Dr. Raj has served as a consultant for Lundbeck NA and Theravance; has served as chair of the data safety and monitoring board for Arena Pharmaceuticals and as Cardiac Arrhythmia Network of Canada network investigator; and has served on the medical advisory board of Dysautonomia International and PoTS UK, both without financial compensation.
A version of this article first appeared on Medscape.com.
For patients with postural tachycardia syndrome (POTS), dietary sodium intake can be increased more confidently, suggests the first study to yield solid evidence to support this treatment strategy.
The results showed that high dietary sodium intake can lower plasma norepinephrine levels and ameliorate standing and orthostatic tachycardia for patients with POTS.
“These results suggest that increasing dietary salt is a good rationale for treatment of this condition, and this study gives reassurance we are doing the right thing for POTS patients by increasing their sodium intake,” senior author Satish R. Raj, MD, said in an interview.
The study, with lead author Emily M. Garland, PhD, was published online April 26, 2021, in the Journal of the American College of Cardiology.
Dr. Raj, who is professor of cardiac science at the University of Calgary (Alta.), explained that POTS includes a spectrum of disorders that affect the automatic nervous system, which regulates heart rate and blood pressure.
“It is a disorder of orthostatic intolerance – patients feel better when they lie down. It differs from orthostatic hypotension in that, when a POTS patient stands up, the blood pressure does not necessarily drop, but the heart rate increases excessively.”
Although it is normal for the heart rate to increase somewhat on standing, among patients with POTS, the heart rate increases excessively. The condition is defined as an orthostatic heart rate increase of at least 30 beats/min (or 40 beats/min among individuals aged 12-19 years ) in the absence of orthostatic hypotension.
The disorder is characterized by a range of symptoms, including lightheadedness, shortness of breath, palpitations, and exertional intolerance, that are worse when in an upright position. Patients also experience chronic fatigue and perceived cognitive impairment, Dr. Raj noted.
The typical demographic for POTS is young women; the condition often starts during the teenage years.
Patients often have low blood volume, so one approach to treatment is to increase the intake of salt and water so as to increase blood volume.
“This is one of the mainstays of treatment, but it has never really been properly studied,” Dr. Raj commented. Increasing salt intake “is an unusual message from a cardiologist, and there have been concerns that we are making recommendations against traditional advice, so we urgently need evidence to support this recommendation.”
The current crossover study enrolled 14 patients with POTS and 13 healthy control persons who, over a period of 6 days, underwent treatment with a low-sodium diet (10 mEq sodium per day) or a high-sodium diet (300 mEq sodium per day).
Supine and standing heart rate, blood pressure, serum aldosterone level, plasma renin activity, blood volume, and plasma norepinephrine and epinephrine levels were measured.
Results showed that, among the POTS patients, the high-sodium diet reduced upright heart rate and the change in heart rate on standing, compared with the low-sodium diet.
Heart rate increased by 46 beats/min with the high-sodium diet versus 60 beats/min with the low-sodium diet.
Total blood volume and plasma volume increased, and standing norepinephrine levels decreased with the high-sodium diet, compared with the low-sodium diet.
However, upright heart rate, change in heart rate, and upright norepinephrine levels remained higher among POTS patients than among control persons receiving the high-sodium diet.
There was a nonsignificant trend for a lower symptom burden score among the POTS patients who received the high-sodium diet in comparison with those taking the low-sodium diet. Scores for mental confusion, palpitations, lightheadedness, and headache trending downward on the high-sodium diet.
“We found that high levels of dietary salt did what we hoped, with increased blood volume and reduced norepinephrine levels on standing and reduced excessive increase in heart rate. While it didn’t completely normalize heart rate, this was reduced significantly,” Dr. Raj said.
Another observation from the study was that the increased salt intake seemed to be beneficial across the whole spectrum of patients.
“There are some patients who have very high levels of sympathetic activation, and there have been anecdotal reports that increasing salt may not work so well in this group,” he said. “In this study, we didn’t differentiate, but average norepinephrine levels were very high, and many patients would be considered to be hyperadrenergic. Our results suggest this treatment will help these patients too.”
He noted that sodium intake was increased in this study just through diet. “We had a special metabolic kitchen. In clinical practice, we advise patients to add regular table salt to their food, and we only use salt tablets when they cannot tolerate so much salt in their diet.”
Recognizing that there may be concerns about hypertension with long-term use of such a treatment, Dr. Raj said there were no signs of an increase in blood pressure in this study. “But this should be considered a short-term therapy for the time being, and patients need to be reassessed every few years as their physiology changes.”
The authors estimated that POTS affects up to 1% of the population. Because there is no diagnostic code for the condition at present, all incidence data are estimates.
Dr. Raj pointed out that potentially a lot of people are affected, but there is little recognition of the condition among patients and physicians.
“Many family doctors are unaware of POTS,” he noted. “Patients often have to research their symptoms themselves and inform their doctor of the condition. Many patients wait years and often see many different doctors before getting a correct diagnosis.”
He explained that patients with POTS are often diagnosed as having a psychiatric illness. “They are mainly young women with palpitations, heart pounding, shakiness, which is often labeled as anxiety.”
Dr. Raj urged clinicians to consider POTS if patients have symptoms that are worse when standing up. The diagnosis is confirmed if their blood pressure doesn’t fall when standing up but their heart rate increases by at least 30 beats/min.
He noted that not enough specialists treat this condition, so family doctors need to be able to diagnose and initiate treatment. If more aggressive treatment is required, patients can be referred to a specialist.
“One of the problems is that this condition pans across different medical specialties. No one field owns it, so it tends to get ignored. But there are clinicians who are interested in POTS, and the key is finding one of these,” he said.
“We have finally established that this high-sodium diet works as treatment for POTS,” he concluded. “We have been using it for some time, but now we have evidence for its use across the whole spectrum of patients.”
In an accompanying editorial (J Am Coll Cardiol. 2021 May 4;77[17]:2185-2186), Blair P. Grubb, MD, University of Toledo (Ohio) Medical Center, wrote that this “superb study by Garland et al. helps better establish our understanding of the pathophysiologic process taking place in POTS while at the same time providing good evidence for the augmentation of dietary sodium as one of the cornerstones of treatment.”
He added that the field needs more such studies “in our quest to better understand POTS and to elaborate therapeutic modalities to help those suffering from this debilitating illness.”
The study was supported in part by the National Heart, Lung, and Blood Institute; the National Center for Advancing Translational Sciences; and the Vanderbilt Hormone and Analytical Services Core. Dr. Raj has served as a consultant for Lundbeck NA and Theravance; has served as chair of the data safety and monitoring board for Arena Pharmaceuticals and as Cardiac Arrhythmia Network of Canada network investigator; and has served on the medical advisory board of Dysautonomia International and PoTS UK, both without financial compensation.
A version of this article first appeared on Medscape.com.
Brown plaque on the arm

Due to its size, 2 shave biopsies targeting the most concerning portions of the lesion were performed; the results were consistent with a lichenoid keratosis (LK), also known as lichen planus-like keratosis.
LK is a benign solitary lesion that mimics basal cell carcinoma, squamous cell carcinoma, and superficial spreading or amelanotic melanoma.1 One theory suggests that LK is a solar lentigo or actinic keratosis undergoing attack from the immune system. Lesions most often manifest as a pink, gray, or brown macule to thin papule on the trunk or extremities. Itching or mild pain may be present. Dermoscopy can help distinguish an LK from malignancy but overlapping features of fine dark regression structures (called peppering, as seen in this case) should prompt further evaluation.
LKs are great mimics and biopsy is key to distinguishing them from cancer. In this case, shave biopsies were performed in the thickest and most characteristic portions of the lesion. Punch or incisional biopsies also would have been appropriate, but any result would have been a partial result. If the result had come back as an atypical melanocytic lesion, a complete excision would have been necessary to make sure the pathology reflected the entirety of the lesion.
Armed with the knowledge that the LK was benign, the patient in this case was scheduled for a follow-up visit for cryotherapy to remove the residual lesion.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
1. Maor D, Ondhia C, Yu LL, et al. Lichenoid keratosis is frequently misdiagnosed as basal cell carcinoma. Clin Exp Dermatol. 2017;42:663-666. doi: 10.1111/ced.13178

Due to its size, 2 shave biopsies targeting the most concerning portions of the lesion were performed; the results were consistent with a lichenoid keratosis (LK), also known as lichen planus-like keratosis.
LK is a benign solitary lesion that mimics basal cell carcinoma, squamous cell carcinoma, and superficial spreading or amelanotic melanoma.1 One theory suggests that LK is a solar lentigo or actinic keratosis undergoing attack from the immune system. Lesions most often manifest as a pink, gray, or brown macule to thin papule on the trunk or extremities. Itching or mild pain may be present. Dermoscopy can help distinguish an LK from malignancy but overlapping features of fine dark regression structures (called peppering, as seen in this case) should prompt further evaluation.
LKs are great mimics and biopsy is key to distinguishing them from cancer. In this case, shave biopsies were performed in the thickest and most characteristic portions of the lesion. Punch or incisional biopsies also would have been appropriate, but any result would have been a partial result. If the result had come back as an atypical melanocytic lesion, a complete excision would have been necessary to make sure the pathology reflected the entirety of the lesion.
Armed with the knowledge that the LK was benign, the patient in this case was scheduled for a follow-up visit for cryotherapy to remove the residual lesion.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).

Due to its size, 2 shave biopsies targeting the most concerning portions of the lesion were performed; the results were consistent with a lichenoid keratosis (LK), also known as lichen planus-like keratosis.
LK is a benign solitary lesion that mimics basal cell carcinoma, squamous cell carcinoma, and superficial spreading or amelanotic melanoma.1 One theory suggests that LK is a solar lentigo or actinic keratosis undergoing attack from the immune system. Lesions most often manifest as a pink, gray, or brown macule to thin papule on the trunk or extremities. Itching or mild pain may be present. Dermoscopy can help distinguish an LK from malignancy but overlapping features of fine dark regression structures (called peppering, as seen in this case) should prompt further evaluation.
LKs are great mimics and biopsy is key to distinguishing them from cancer. In this case, shave biopsies were performed in the thickest and most characteristic portions of the lesion. Punch or incisional biopsies also would have been appropriate, but any result would have been a partial result. If the result had come back as an atypical melanocytic lesion, a complete excision would have been necessary to make sure the pathology reflected the entirety of the lesion.
Armed with the knowledge that the LK was benign, the patient in this case was scheduled for a follow-up visit for cryotherapy to remove the residual lesion.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
1. Maor D, Ondhia C, Yu LL, et al. Lichenoid keratosis is frequently misdiagnosed as basal cell carcinoma. Clin Exp Dermatol. 2017;42:663-666. doi: 10.1111/ced.13178
1. Maor D, Ondhia C, Yu LL, et al. Lichenoid keratosis is frequently misdiagnosed as basal cell carcinoma. Clin Exp Dermatol. 2017;42:663-666. doi: 10.1111/ced.13178
Prioritize goals of older patients with multimorbidities, gerontologist says
said Mary Tinetti, MD, Gladys Phillips Crofoot Professor of Medicine and Public Health and chief of geriatrics at Yale University, New Haven, Conn.
During a virtual presentation at the American College of Physicians annual Internal Medicine meeting, the gerontologist noted that primary care providers face a number of challenges when managing elderly patients with multimorbidity. These challenges include a lack of representative data in clinical trials, conflicting guideline recommendations, patient nonadherence, and decreased benefit from therapies due to competing conditions, she said.
“Trying to follow multiple guidelines can result in unintentional harms to these people with multiple conditions,” Dr. Tinetti said. She gave examples of the wide-ranging goals patients can have.
“Some [patients] will maximize the focus on function, regardless of how long they are likely to live,” Dr. Tinetti said. “Others will say symptom burden management is most important to them. And others will say they want to live as long as possible, and survival is most important, even if that means a reduction in their function. These individuals also vary in the care they are willing and able to receive to achieve the outcomes that matter most to them.”
For these reasons, Dr. Tinetti recommended patient priorities care, which she and her colleagues have been developing and implementing over the past 5-6 years.
“If the benefits and harms of addressing each condition in isolation is of uncertain benefit and potentially burdensome to both clinician and patient, and we know that patients vary in their health priorities ... then what else would you want to focus on in your 20-minute visit ... except each patient’s priorities?” Dr. Tinetti asked. “This is one solution to the challenge.”
What is patient priorities care?
Patient priorities care is a multidisciplinary, cyclical approach to clinical decision-making composed of three steps, Dr. Tinetti explained. First, a clinician identifies the patient’s health priorities. Second, this information is transmitted to comanaging providers, who decide which of their respective treatments are consistent with the patient’s priorities. And third, those decisions are disseminated to everyone involved in the patient’s care, both within and outside of the health care system, allowing all care providers to align with the patient’s priorities, she noted.
“Each person does that from their own expertise,” Dr. Tinetti said. “The social worker will do something different than the cardiologist, the physical therapist, the endocrinologist – but everybody is aiming at the same outcome – the patient’s priorities.”
In 2019, Dr. Tinetti led a nonrandomized clinical trial to test the feasibility of patient priorities care. The study involved 366 older adults with multimorbidity, among whom 203 received usual care, while 163 received this type of care. Patients in the latter group were twice as likely to have medications stopped, and significantly less likely to have self-management tasks added and diagnostic tests ordered.
How electronic health records can help
In an interview, Dr. Tinetti suggested that comanaging physicians communicate through electronic health records (EHRs), first to ensure that all care providers understand a patient’s goals, then to determine if recommended therapies align with those goals.
“It would be a little bit of a culture change to do that,” Dr. Tinetti said, “but the technology is there and it isn’t too terribly time consuming.”
She went on to suggest that primary care providers are typically best suited to coordinate this process; however, if a patient receives the majority of their care from a particular specialist, then that clinician may be the most suitable coordinator.
Systemic obstacles and solutions
According to Cynthia Boyd, MD, interim director of the division of geriatric medicine and gerontology, Johns Hopkins University, Baltimore, clinicians may encounter obstacles when implementing patient priorities care.
“Our health care system doesn’t always make it easy to do this,” Dr. Boyd said. “It’s important to acknowledge this because it can be hard to do. There’s no question,” Dr. Boyd said in an interview.
Among the headwinds that clinicians may face are clinical practice guidelines, the structure of electronic health records, and quality metrics focused on specific conditions, she explained.
“There’s a lot of things that push us – in primary care and other parts of medicine – away from the approach that’s best for people with multiple chronic conditions,” Dr. Boyd said.
Dr. Tinetti said a challenge to providing this care that she expects is for clinicians, regardless of specialty, “to feel uneasy” about transitioning away from a conventional approach.
Among Dr. Tinetti’s arguments in favor of providing patient priorities care is that “it’s going to bring more joy in practice because you’re really addressing what matters to that individual while also providing good care.”
To get the most out of patient priorities care, Dr. Boyd recommended that clinicians focus on ‘the 4 M’s’: what matters most, mentation, mobility, and medications.
In an effort to address the last of these on a broad scale, Dr. Boyd is co-leading the US Deprescribing Research Network(USDeN), which aims to “improve medication use among older adults and the outcomes that are important to them,” according to the USDeN website.
To encourage deprescribing on a day-to-day level, Dr. Boyd called for strong communication between co–managing providers.
In an ideal world, there would be a better way to communicate than largely via electronic health records, she said.
“We need more than the EHR to connect us. That’s why it’s really important for primary care providers and specialists to be able to have time to actually talk to each other. This gets into how we reimburse and organize the communication and cognitive aspects of care,” Dr. Boyd noted.
Dr. Tinetti disclosed support from the John A. Hartford Foundation, the Donaghue Foundation, the National Institute on Aging, and the Institute for Healthcare Improvement. Dr. Boyd disclosed a relationship with UpToDate, for which she coauthored a chapter on multimorbidity.
said Mary Tinetti, MD, Gladys Phillips Crofoot Professor of Medicine and Public Health and chief of geriatrics at Yale University, New Haven, Conn.
During a virtual presentation at the American College of Physicians annual Internal Medicine meeting, the gerontologist noted that primary care providers face a number of challenges when managing elderly patients with multimorbidity. These challenges include a lack of representative data in clinical trials, conflicting guideline recommendations, patient nonadherence, and decreased benefit from therapies due to competing conditions, she said.
“Trying to follow multiple guidelines can result in unintentional harms to these people with multiple conditions,” Dr. Tinetti said. She gave examples of the wide-ranging goals patients can have.
“Some [patients] will maximize the focus on function, regardless of how long they are likely to live,” Dr. Tinetti said. “Others will say symptom burden management is most important to them. And others will say they want to live as long as possible, and survival is most important, even if that means a reduction in their function. These individuals also vary in the care they are willing and able to receive to achieve the outcomes that matter most to them.”
For these reasons, Dr. Tinetti recommended patient priorities care, which she and her colleagues have been developing and implementing over the past 5-6 years.
“If the benefits and harms of addressing each condition in isolation is of uncertain benefit and potentially burdensome to both clinician and patient, and we know that patients vary in their health priorities ... then what else would you want to focus on in your 20-minute visit ... except each patient’s priorities?” Dr. Tinetti asked. “This is one solution to the challenge.”
What is patient priorities care?
Patient priorities care is a multidisciplinary, cyclical approach to clinical decision-making composed of three steps, Dr. Tinetti explained. First, a clinician identifies the patient’s health priorities. Second, this information is transmitted to comanaging providers, who decide which of their respective treatments are consistent with the patient’s priorities. And third, those decisions are disseminated to everyone involved in the patient’s care, both within and outside of the health care system, allowing all care providers to align with the patient’s priorities, she noted.
“Each person does that from their own expertise,” Dr. Tinetti said. “The social worker will do something different than the cardiologist, the physical therapist, the endocrinologist – but everybody is aiming at the same outcome – the patient’s priorities.”
In 2019, Dr. Tinetti led a nonrandomized clinical trial to test the feasibility of patient priorities care. The study involved 366 older adults with multimorbidity, among whom 203 received usual care, while 163 received this type of care. Patients in the latter group were twice as likely to have medications stopped, and significantly less likely to have self-management tasks added and diagnostic tests ordered.
How electronic health records can help
In an interview, Dr. Tinetti suggested that comanaging physicians communicate through electronic health records (EHRs), first to ensure that all care providers understand a patient’s goals, then to determine if recommended therapies align with those goals.
“It would be a little bit of a culture change to do that,” Dr. Tinetti said, “but the technology is there and it isn’t too terribly time consuming.”
She went on to suggest that primary care providers are typically best suited to coordinate this process; however, if a patient receives the majority of their care from a particular specialist, then that clinician may be the most suitable coordinator.
Systemic obstacles and solutions
According to Cynthia Boyd, MD, interim director of the division of geriatric medicine and gerontology, Johns Hopkins University, Baltimore, clinicians may encounter obstacles when implementing patient priorities care.
“Our health care system doesn’t always make it easy to do this,” Dr. Boyd said. “It’s important to acknowledge this because it can be hard to do. There’s no question,” Dr. Boyd said in an interview.
Among the headwinds that clinicians may face are clinical practice guidelines, the structure of electronic health records, and quality metrics focused on specific conditions, she explained.
“There’s a lot of things that push us – in primary care and other parts of medicine – away from the approach that’s best for people with multiple chronic conditions,” Dr. Boyd said.
Dr. Tinetti said a challenge to providing this care that she expects is for clinicians, regardless of specialty, “to feel uneasy” about transitioning away from a conventional approach.
Among Dr. Tinetti’s arguments in favor of providing patient priorities care is that “it’s going to bring more joy in practice because you’re really addressing what matters to that individual while also providing good care.”
To get the most out of patient priorities care, Dr. Boyd recommended that clinicians focus on ‘the 4 M’s’: what matters most, mentation, mobility, and medications.
In an effort to address the last of these on a broad scale, Dr. Boyd is co-leading the US Deprescribing Research Network(USDeN), which aims to “improve medication use among older adults and the outcomes that are important to them,” according to the USDeN website.
To encourage deprescribing on a day-to-day level, Dr. Boyd called for strong communication between co–managing providers.
In an ideal world, there would be a better way to communicate than largely via electronic health records, she said.
“We need more than the EHR to connect us. That’s why it’s really important for primary care providers and specialists to be able to have time to actually talk to each other. This gets into how we reimburse and organize the communication and cognitive aspects of care,” Dr. Boyd noted.
Dr. Tinetti disclosed support from the John A. Hartford Foundation, the Donaghue Foundation, the National Institute on Aging, and the Institute for Healthcare Improvement. Dr. Boyd disclosed a relationship with UpToDate, for which she coauthored a chapter on multimorbidity.
said Mary Tinetti, MD, Gladys Phillips Crofoot Professor of Medicine and Public Health and chief of geriatrics at Yale University, New Haven, Conn.
During a virtual presentation at the American College of Physicians annual Internal Medicine meeting, the gerontologist noted that primary care providers face a number of challenges when managing elderly patients with multimorbidity. These challenges include a lack of representative data in clinical trials, conflicting guideline recommendations, patient nonadherence, and decreased benefit from therapies due to competing conditions, she said.
“Trying to follow multiple guidelines can result in unintentional harms to these people with multiple conditions,” Dr. Tinetti said. She gave examples of the wide-ranging goals patients can have.
“Some [patients] will maximize the focus on function, regardless of how long they are likely to live,” Dr. Tinetti said. “Others will say symptom burden management is most important to them. And others will say they want to live as long as possible, and survival is most important, even if that means a reduction in their function. These individuals also vary in the care they are willing and able to receive to achieve the outcomes that matter most to them.”
For these reasons, Dr. Tinetti recommended patient priorities care, which she and her colleagues have been developing and implementing over the past 5-6 years.
“If the benefits and harms of addressing each condition in isolation is of uncertain benefit and potentially burdensome to both clinician and patient, and we know that patients vary in their health priorities ... then what else would you want to focus on in your 20-minute visit ... except each patient’s priorities?” Dr. Tinetti asked. “This is one solution to the challenge.”
What is patient priorities care?
Patient priorities care is a multidisciplinary, cyclical approach to clinical decision-making composed of three steps, Dr. Tinetti explained. First, a clinician identifies the patient’s health priorities. Second, this information is transmitted to comanaging providers, who decide which of their respective treatments are consistent with the patient’s priorities. And third, those decisions are disseminated to everyone involved in the patient’s care, both within and outside of the health care system, allowing all care providers to align with the patient’s priorities, she noted.
“Each person does that from their own expertise,” Dr. Tinetti said. “The social worker will do something different than the cardiologist, the physical therapist, the endocrinologist – but everybody is aiming at the same outcome – the patient’s priorities.”
In 2019, Dr. Tinetti led a nonrandomized clinical trial to test the feasibility of patient priorities care. The study involved 366 older adults with multimorbidity, among whom 203 received usual care, while 163 received this type of care. Patients in the latter group were twice as likely to have medications stopped, and significantly less likely to have self-management tasks added and diagnostic tests ordered.
How electronic health records can help
In an interview, Dr. Tinetti suggested that comanaging physicians communicate through electronic health records (EHRs), first to ensure that all care providers understand a patient’s goals, then to determine if recommended therapies align with those goals.
“It would be a little bit of a culture change to do that,” Dr. Tinetti said, “but the technology is there and it isn’t too terribly time consuming.”
She went on to suggest that primary care providers are typically best suited to coordinate this process; however, if a patient receives the majority of their care from a particular specialist, then that clinician may be the most suitable coordinator.
Systemic obstacles and solutions
According to Cynthia Boyd, MD, interim director of the division of geriatric medicine and gerontology, Johns Hopkins University, Baltimore, clinicians may encounter obstacles when implementing patient priorities care.
“Our health care system doesn’t always make it easy to do this,” Dr. Boyd said. “It’s important to acknowledge this because it can be hard to do. There’s no question,” Dr. Boyd said in an interview.
Among the headwinds that clinicians may face are clinical practice guidelines, the structure of electronic health records, and quality metrics focused on specific conditions, she explained.
“There’s a lot of things that push us – in primary care and other parts of medicine – away from the approach that’s best for people with multiple chronic conditions,” Dr. Boyd said.
Dr. Tinetti said a challenge to providing this care that she expects is for clinicians, regardless of specialty, “to feel uneasy” about transitioning away from a conventional approach.
Among Dr. Tinetti’s arguments in favor of providing patient priorities care is that “it’s going to bring more joy in practice because you’re really addressing what matters to that individual while also providing good care.”
To get the most out of patient priorities care, Dr. Boyd recommended that clinicians focus on ‘the 4 M’s’: what matters most, mentation, mobility, and medications.
In an effort to address the last of these on a broad scale, Dr. Boyd is co-leading the US Deprescribing Research Network(USDeN), which aims to “improve medication use among older adults and the outcomes that are important to them,” according to the USDeN website.
To encourage deprescribing on a day-to-day level, Dr. Boyd called for strong communication between co–managing providers.
In an ideal world, there would be a better way to communicate than largely via electronic health records, she said.
“We need more than the EHR to connect us. That’s why it’s really important for primary care providers and specialists to be able to have time to actually talk to each other. This gets into how we reimburse and organize the communication and cognitive aspects of care,” Dr. Boyd noted.
Dr. Tinetti disclosed support from the John A. Hartford Foundation, the Donaghue Foundation, the National Institute on Aging, and the Institute for Healthcare Improvement. Dr. Boyd disclosed a relationship with UpToDate, for which she coauthored a chapter on multimorbidity.
FROM INTERNAL MEDICINE 2021
SHM Converge Daily News -- Day 2
Click here for the Thursday issue of the SHM Converge Daily News newsletter.
Click here for the Thursday issue of the SHM Converge Daily News newsletter.
Click here for the Thursday issue of the SHM Converge Daily News newsletter.
Home Treatment of Presumed Melanocytic Nevus With Frankincense
To the Editor:
Melanocytic nevi are ubiquitous, and although they are benign, patients often desire to have them removed. We report a patient who presented to our clinic after attempting home removal of a concerning mole on the back with frankincense, a remedy that she found online.
A 43-year-old woman presented with a worrisome mole on the back. She had no personal history of skin cancer, but her father had a history of melanoma in situ in his 60s. The patient reported that she had the mole for years, but approximately 1 month prior to her visit she noticed that it began to bleed and crust, causing concern for melanoma. She read online that the lesion could be removed with topical application of the essential oil frankincense; she applied it directly to the lesion on the back. Within hours she developed a burn where it was applied with associated blistering.
Clinically, the lesion appeared as a darkly pigmented, well-circumscribed papule with hemorrhagic crust overlying a well-demarcated pink plaque (Figure 1). Dermatoscopically, the lesion lacked a pigment network and demonstrated 2 distinct pink papules with peripheral telangiectasia and a pink background with white streaks (Figure 2). A shave biopsy of the lesion demonstrated a nodular basal cell carcinoma extending to the base and margin.

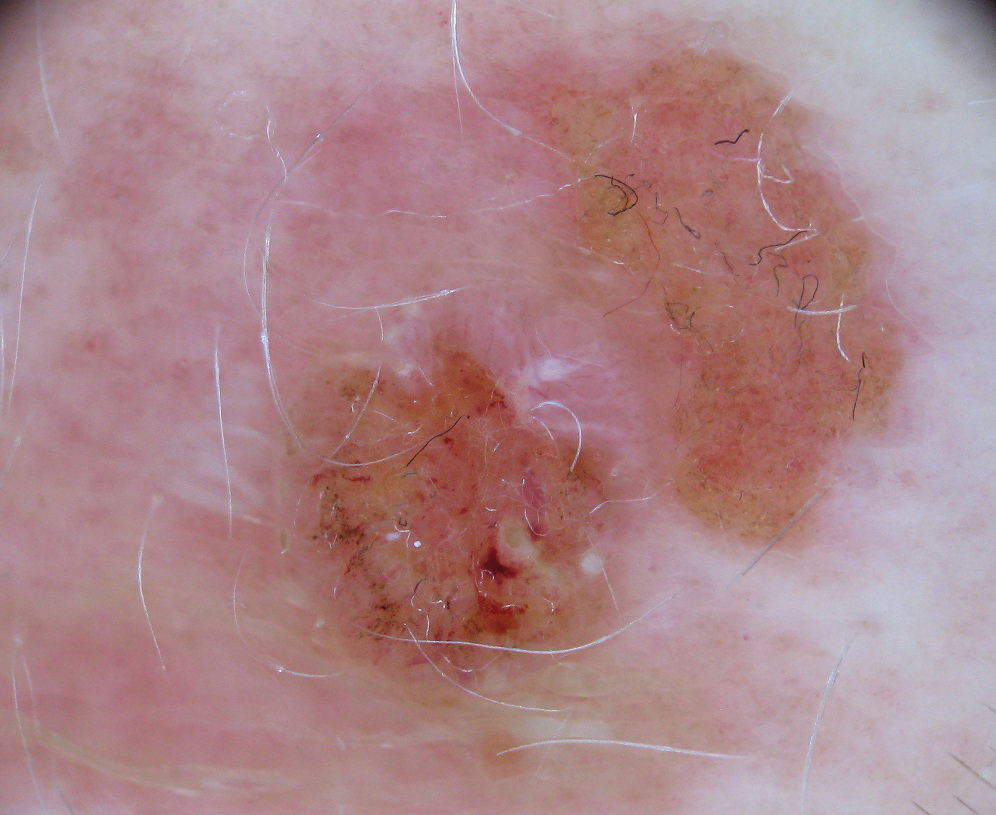
Frankincense is the common name given to oleo-gum-resins of Boswellia species.1 It has been studied extensively for anti-inflammatory and antitumoral properties. It has been demonstrated that high concentrations of its active component, boswellic acid, can have a cytotoxic or cytostatic effect on certain malignant cell lines, such as melanoma, in vitro.2,3 It also has been shown to be antitumoral in mouse models.4 There are limited in vivo studies in the literature assessing the effects of boswellic acid or frankincense on cutaneous melanocytic lesions or other cutaneous malignancies, such as basal cell carcinoma.
A Google search of home remedy mole removal yielded more than 1,000,000 results. At the time of submission, the top 5 results all listed frankincense as a potential treatment along with garlic, iodine, castor oil, onion juice, pineapple juice, banana peels, honey, and aloe vera. None of the results cited evidence for their treatments. Although all recommended dilution of the frankincense prior to application, none warned of potential risks or side effects of its use.
Natural methods of home mole removal have long been sought after. Escharotics are most commonly utilized, including bloodroot (Sanguinaria canadensis), zinc chloride, Chelidonium majus, and Solanum sodomaeum. Many formulations are commercially available online, despite the fact that they can be mutilating and potentially dangerous when used without appropriate supervision.5 This case and an online search demonstrated that these agents are not only potentially harmful home remedies but also are currently falsely advertised as effective therapeutic management for melanocytic nevi.
Approximately 6 million individuals in the United States search the internet for health information daily, and as many as 41% of those do so to learn about alternative medicine.5,6 Although information gleaned from search engines can be useful, it is unregulated and often can be inaccurate. Clinicians generally are unaware of the erroneous material presented online and, therefore, cannot appropriately combat patient misinformation. Our case demonstrates the need to maintain an awareness of common online fallacies to better answer patient questions and guide them to more accurate sources of dermatologic information and appropriate treatment.
- Du Z, Liu Z, Ning Z, et al. Prospects of boswellic acids as potential pharmaceutics. Planta Med. 2015;81:259-271.
- Eichhorn T, Greten HJ, Efferth T. Molecular determinants of the response of tumor cells to boswellic acids. Pharmaceuticals (Basel). 2011;4:1171-1182.
- Zhao W, Entschladen F, Liu H, et al. Boswellic acid acetate induces differentiation and apoptosis in highly metastatic melanoma and fibrosarcoma cell. Cancer Detect Prev. 2003;27:67-75.
- Huang MT, Badmaev V, Ding Y, et al. Anti-tumor and anti-carcinogenic activities of triterpenoid, beta-boswellic acid. Biofactors. 2000;13:225-230.
- Adler BL, Friedman AJ. Safety & efficacy of agents used for home mole removal and skin cancer treatment in the internet age, and analysis of cases. J Drugs Dermatol. 2013;12:1058-1063.
- Kanthawala S, Vermeesch A, Given B, et al. Answers to health questions: internet search results versus online health community responses. J Med Internet Res. 2016;18:E95.
To the Editor:
Melanocytic nevi are ubiquitous, and although they are benign, patients often desire to have them removed. We report a patient who presented to our clinic after attempting home removal of a concerning mole on the back with frankincense, a remedy that she found online.
A 43-year-old woman presented with a worrisome mole on the back. She had no personal history of skin cancer, but her father had a history of melanoma in situ in his 60s. The patient reported that she had the mole for years, but approximately 1 month prior to her visit she noticed that it began to bleed and crust, causing concern for melanoma. She read online that the lesion could be removed with topical application of the essential oil frankincense; she applied it directly to the lesion on the back. Within hours she developed a burn where it was applied with associated blistering.
Clinically, the lesion appeared as a darkly pigmented, well-circumscribed papule with hemorrhagic crust overlying a well-demarcated pink plaque (Figure 1). Dermatoscopically, the lesion lacked a pigment network and demonstrated 2 distinct pink papules with peripheral telangiectasia and a pink background with white streaks (Figure 2). A shave biopsy of the lesion demonstrated a nodular basal cell carcinoma extending to the base and margin.

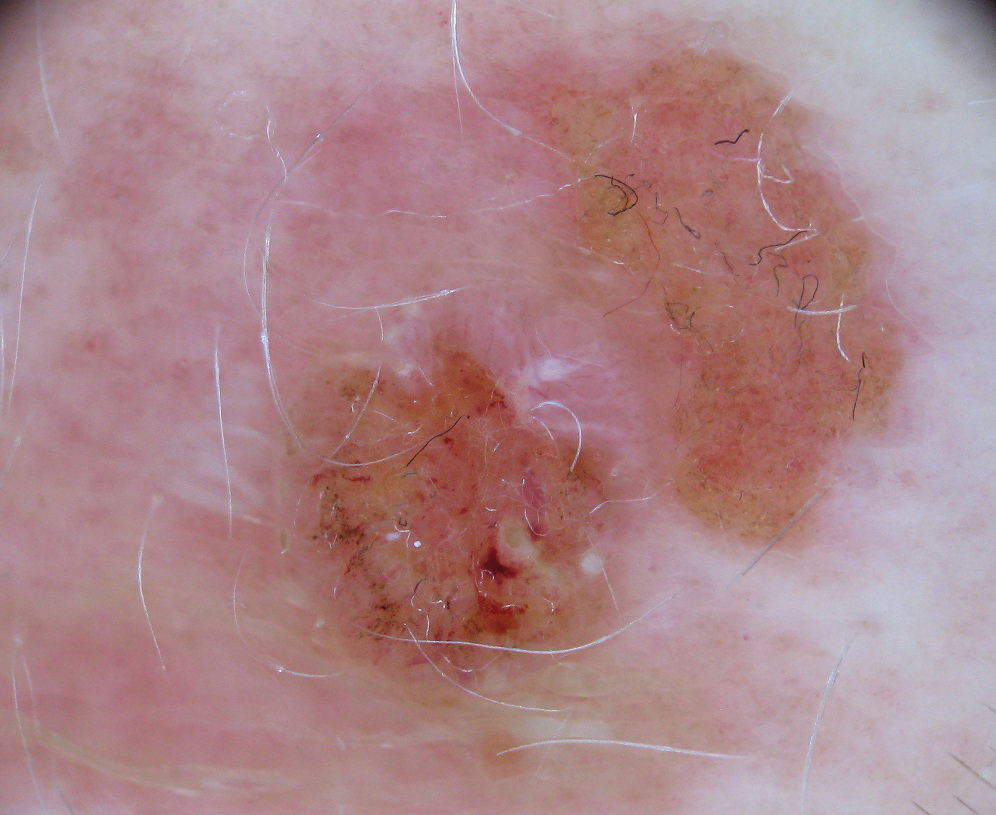
Frankincense is the common name given to oleo-gum-resins of Boswellia species.1 It has been studied extensively for anti-inflammatory and antitumoral properties. It has been demonstrated that high concentrations of its active component, boswellic acid, can have a cytotoxic or cytostatic effect on certain malignant cell lines, such as melanoma, in vitro.2,3 It also has been shown to be antitumoral in mouse models.4 There are limited in vivo studies in the literature assessing the effects of boswellic acid or frankincense on cutaneous melanocytic lesions or other cutaneous malignancies, such as basal cell carcinoma.
A Google search of home remedy mole removal yielded more than 1,000,000 results. At the time of submission, the top 5 results all listed frankincense as a potential treatment along with garlic, iodine, castor oil, onion juice, pineapple juice, banana peels, honey, and aloe vera. None of the results cited evidence for their treatments. Although all recommended dilution of the frankincense prior to application, none warned of potential risks or side effects of its use.
Natural methods of home mole removal have long been sought after. Escharotics are most commonly utilized, including bloodroot (Sanguinaria canadensis), zinc chloride, Chelidonium majus, and Solanum sodomaeum. Many formulations are commercially available online, despite the fact that they can be mutilating and potentially dangerous when used without appropriate supervision.5 This case and an online search demonstrated that these agents are not only potentially harmful home remedies but also are currently falsely advertised as effective therapeutic management for melanocytic nevi.
Approximately 6 million individuals in the United States search the internet for health information daily, and as many as 41% of those do so to learn about alternative medicine.5,6 Although information gleaned from search engines can be useful, it is unregulated and often can be inaccurate. Clinicians generally are unaware of the erroneous material presented online and, therefore, cannot appropriately combat patient misinformation. Our case demonstrates the need to maintain an awareness of common online fallacies to better answer patient questions and guide them to more accurate sources of dermatologic information and appropriate treatment.
To the Editor:
Melanocytic nevi are ubiquitous, and although they are benign, patients often desire to have them removed. We report a patient who presented to our clinic after attempting home removal of a concerning mole on the back with frankincense, a remedy that she found online.
A 43-year-old woman presented with a worrisome mole on the back. She had no personal history of skin cancer, but her father had a history of melanoma in situ in his 60s. The patient reported that she had the mole for years, but approximately 1 month prior to her visit she noticed that it began to bleed and crust, causing concern for melanoma. She read online that the lesion could be removed with topical application of the essential oil frankincense; she applied it directly to the lesion on the back. Within hours she developed a burn where it was applied with associated blistering.
Clinically, the lesion appeared as a darkly pigmented, well-circumscribed papule with hemorrhagic crust overlying a well-demarcated pink plaque (Figure 1). Dermatoscopically, the lesion lacked a pigment network and demonstrated 2 distinct pink papules with peripheral telangiectasia and a pink background with white streaks (Figure 2). A shave biopsy of the lesion demonstrated a nodular basal cell carcinoma extending to the base and margin.

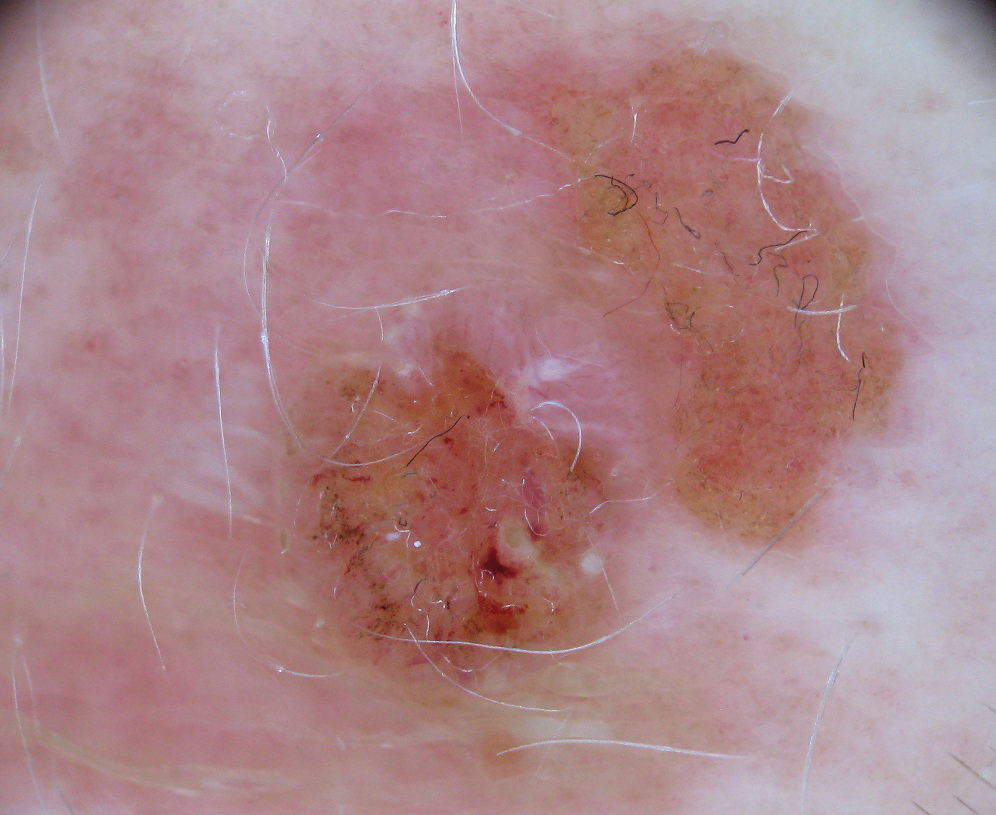
Frankincense is the common name given to oleo-gum-resins of Boswellia species.1 It has been studied extensively for anti-inflammatory and antitumoral properties. It has been demonstrated that high concentrations of its active component, boswellic acid, can have a cytotoxic or cytostatic effect on certain malignant cell lines, such as melanoma, in vitro.2,3 It also has been shown to be antitumoral in mouse models.4 There are limited in vivo studies in the literature assessing the effects of boswellic acid or frankincense on cutaneous melanocytic lesions or other cutaneous malignancies, such as basal cell carcinoma.
A Google search of home remedy mole removal yielded more than 1,000,000 results. At the time of submission, the top 5 results all listed frankincense as a potential treatment along with garlic, iodine, castor oil, onion juice, pineapple juice, banana peels, honey, and aloe vera. None of the results cited evidence for their treatments. Although all recommended dilution of the frankincense prior to application, none warned of potential risks or side effects of its use.
Natural methods of home mole removal have long been sought after. Escharotics are most commonly utilized, including bloodroot (Sanguinaria canadensis), zinc chloride, Chelidonium majus, and Solanum sodomaeum. Many formulations are commercially available online, despite the fact that they can be mutilating and potentially dangerous when used without appropriate supervision.5 This case and an online search demonstrated that these agents are not only potentially harmful home remedies but also are currently falsely advertised as effective therapeutic management for melanocytic nevi.
Approximately 6 million individuals in the United States search the internet for health information daily, and as many as 41% of those do so to learn about alternative medicine.5,6 Although information gleaned from search engines can be useful, it is unregulated and often can be inaccurate. Clinicians generally are unaware of the erroneous material presented online and, therefore, cannot appropriately combat patient misinformation. Our case demonstrates the need to maintain an awareness of common online fallacies to better answer patient questions and guide them to more accurate sources of dermatologic information and appropriate treatment.
- Du Z, Liu Z, Ning Z, et al. Prospects of boswellic acids as potential pharmaceutics. Planta Med. 2015;81:259-271.
- Eichhorn T, Greten HJ, Efferth T. Molecular determinants of the response of tumor cells to boswellic acids. Pharmaceuticals (Basel). 2011;4:1171-1182.
- Zhao W, Entschladen F, Liu H, et al. Boswellic acid acetate induces differentiation and apoptosis in highly metastatic melanoma and fibrosarcoma cell. Cancer Detect Prev. 2003;27:67-75.
- Huang MT, Badmaev V, Ding Y, et al. Anti-tumor and anti-carcinogenic activities of triterpenoid, beta-boswellic acid. Biofactors. 2000;13:225-230.
- Adler BL, Friedman AJ. Safety & efficacy of agents used for home mole removal and skin cancer treatment in the internet age, and analysis of cases. J Drugs Dermatol. 2013;12:1058-1063.
- Kanthawala S, Vermeesch A, Given B, et al. Answers to health questions: internet search results versus online health community responses. J Med Internet Res. 2016;18:E95.
- Du Z, Liu Z, Ning Z, et al. Prospects of boswellic acids as potential pharmaceutics. Planta Med. 2015;81:259-271.
- Eichhorn T, Greten HJ, Efferth T. Molecular determinants of the response of tumor cells to boswellic acids. Pharmaceuticals (Basel). 2011;4:1171-1182.
- Zhao W, Entschladen F, Liu H, et al. Boswellic acid acetate induces differentiation and apoptosis in highly metastatic melanoma and fibrosarcoma cell. Cancer Detect Prev. 2003;27:67-75.
- Huang MT, Badmaev V, Ding Y, et al. Anti-tumor and anti-carcinogenic activities of triterpenoid, beta-boswellic acid. Biofactors. 2000;13:225-230.
- Adler BL, Friedman AJ. Safety & efficacy of agents used for home mole removal and skin cancer treatment in the internet age, and analysis of cases. J Drugs Dermatol. 2013;12:1058-1063.
- Kanthawala S, Vermeesch A, Given B, et al. Answers to health questions: internet search results versus online health community responses. J Med Internet Res. 2016;18:E95.
Practice Points
- Many patients seek natural methods of home mole removal online, including topical application of essential oils such as frankincense.
- These agents often are unregulated and can be potentially harmful when used without appropriate supervision.
- Dermatologists should be aware of common online fallacies to better answer patient questions and guide them to more accurate sources of dermatologic information and appropriate treatment.














