User login
FDA chief calls for release of all data tracking problems with medical devices
Food and Drug Administration Commissioner Scott Gottlieb, MD, announced in a tweet Wednesday that the agency plans to
“We’re now prioritizing making ALL of this data available,” Dr. Gottlieb tweeted.
A recent Kaiser Health News investigation revealed the scope of a hidden reporting pathway for device makers, with the agency accepting more than 1.1 million such reports since the start of 2016.
Device makers for nearly 20 years were able to quietly seek an “exemption” from standard, public harm-reporting rules. Devices with such exemptions have included surgical staplers and balloon pumps used in the vessels of heart-surgery patients.
Dr. Gottlieb’s tweet also referenced the challenge in opening the database, saying it “wasn’t easily accessible electronically owing to the system’s age. But it’s imperative that all safety information be available to the public.”
The agency made changes to the “alternative summary reporting” program in mid-2017 to require a public report summarizing data filed within the FDA. But nearly two decades of data remained cordoned off from doctors, patients, and device-safety researchers who say they could use it to detect problems.
Dr. Gottlieb’s announcement was welcomed by Madris Tomes, who has testified to FDA device-review panels about the importance of making summary data on patient harm open to the public.
“That’s the best news I’ve heard in years,” said Ms. Tomes, president of Device Events, which makes the FDA device-harm data more user-friendly. “I’m really happy that they’re taking notice and realizing that physicians who couldn’t see this data before were using devices that they wouldn’t have used if they had this data in front of them.”
Since September, KHN has filed Freedom of Information Act requests for parts or all of the “alternative summary reporting” database and for other special “exemption” reports, to little effect. A request to expedite delivery of those records was denied, and the FDA cited the lack of “compelling need” for the public to have the information. Officials noted that it might take up to 2 years to get such records through the FOIA process.
As recently as March 22, though, the agency began publishing previously undisclosed reports of harm, suddenly updating the numbers of breast implant malfunctions or injuries submitted over the years. The new data was presented to an FDA advisory panel, which is reviewing the safety of such devices. The panel, which met March 25 and 26, saw a chart showing hundreds of thousands more accounts of harm or malfunctions than had previously been acknowledged.
Michael Carome, MD, director of Public Citizen’s health research group, said his initial reaction to the news is “better late than never.”
“If [Dr. Gottlieb] follows through with his pledge to make all this data public, then that’s certainly a positive development,” he said. “But this is safety information that should have been made available years ago.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Food and Drug Administration Commissioner Scott Gottlieb, MD, announced in a tweet Wednesday that the agency plans to
“We’re now prioritizing making ALL of this data available,” Dr. Gottlieb tweeted.
A recent Kaiser Health News investigation revealed the scope of a hidden reporting pathway for device makers, with the agency accepting more than 1.1 million such reports since the start of 2016.
Device makers for nearly 20 years were able to quietly seek an “exemption” from standard, public harm-reporting rules. Devices with such exemptions have included surgical staplers and balloon pumps used in the vessels of heart-surgery patients.
Dr. Gottlieb’s tweet also referenced the challenge in opening the database, saying it “wasn’t easily accessible electronically owing to the system’s age. But it’s imperative that all safety information be available to the public.”
The agency made changes to the “alternative summary reporting” program in mid-2017 to require a public report summarizing data filed within the FDA. But nearly two decades of data remained cordoned off from doctors, patients, and device-safety researchers who say they could use it to detect problems.
Dr. Gottlieb’s announcement was welcomed by Madris Tomes, who has testified to FDA device-review panels about the importance of making summary data on patient harm open to the public.
“That’s the best news I’ve heard in years,” said Ms. Tomes, president of Device Events, which makes the FDA device-harm data more user-friendly. “I’m really happy that they’re taking notice and realizing that physicians who couldn’t see this data before were using devices that they wouldn’t have used if they had this data in front of them.”
Since September, KHN has filed Freedom of Information Act requests for parts or all of the “alternative summary reporting” database and for other special “exemption” reports, to little effect. A request to expedite delivery of those records was denied, and the FDA cited the lack of “compelling need” for the public to have the information. Officials noted that it might take up to 2 years to get such records through the FOIA process.
As recently as March 22, though, the agency began publishing previously undisclosed reports of harm, suddenly updating the numbers of breast implant malfunctions or injuries submitted over the years. The new data was presented to an FDA advisory panel, which is reviewing the safety of such devices. The panel, which met March 25 and 26, saw a chart showing hundreds of thousands more accounts of harm or malfunctions than had previously been acknowledged.
Michael Carome, MD, director of Public Citizen’s health research group, said his initial reaction to the news is “better late than never.”
“If [Dr. Gottlieb] follows through with his pledge to make all this data public, then that’s certainly a positive development,” he said. “But this is safety information that should have been made available years ago.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Food and Drug Administration Commissioner Scott Gottlieb, MD, announced in a tweet Wednesday that the agency plans to
“We’re now prioritizing making ALL of this data available,” Dr. Gottlieb tweeted.
A recent Kaiser Health News investigation revealed the scope of a hidden reporting pathway for device makers, with the agency accepting more than 1.1 million such reports since the start of 2016.
Device makers for nearly 20 years were able to quietly seek an “exemption” from standard, public harm-reporting rules. Devices with such exemptions have included surgical staplers and balloon pumps used in the vessels of heart-surgery patients.
Dr. Gottlieb’s tweet also referenced the challenge in opening the database, saying it “wasn’t easily accessible electronically owing to the system’s age. But it’s imperative that all safety information be available to the public.”
The agency made changes to the “alternative summary reporting” program in mid-2017 to require a public report summarizing data filed within the FDA. But nearly two decades of data remained cordoned off from doctors, patients, and device-safety researchers who say they could use it to detect problems.
Dr. Gottlieb’s announcement was welcomed by Madris Tomes, who has testified to FDA device-review panels about the importance of making summary data on patient harm open to the public.
“That’s the best news I’ve heard in years,” said Ms. Tomes, president of Device Events, which makes the FDA device-harm data more user-friendly. “I’m really happy that they’re taking notice and realizing that physicians who couldn’t see this data before were using devices that they wouldn’t have used if they had this data in front of them.”
Since September, KHN has filed Freedom of Information Act requests for parts or all of the “alternative summary reporting” database and for other special “exemption” reports, to little effect. A request to expedite delivery of those records was denied, and the FDA cited the lack of “compelling need” for the public to have the information. Officials noted that it might take up to 2 years to get such records through the FOIA process.
As recently as March 22, though, the agency began publishing previously undisclosed reports of harm, suddenly updating the numbers of breast implant malfunctions or injuries submitted over the years. The new data was presented to an FDA advisory panel, which is reviewing the safety of such devices. The panel, which met March 25 and 26, saw a chart showing hundreds of thousands more accounts of harm or malfunctions than had previously been acknowledged.
Michael Carome, MD, director of Public Citizen’s health research group, said his initial reaction to the news is “better late than never.”
“If [Dr. Gottlieb] follows through with his pledge to make all this data public, then that’s certainly a positive development,” he said. “But this is safety information that should have been made available years ago.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Cimzia becomes first FDA-approved treatment for nonradiographic axial spondyloarthritis
, with objective evidence of inflammation, making it the first treatment approved by the agency for the condition.
The FDA approved the tumor necrosis factor inhibitor based on results from a randomized clinical trial in 317 adult patients with nonradiographic axial spondyloarthritis (nr-axSpA) who had elevated C-reactive protein levels and/or sacroiliitis (inflammation of the sacroiliac joints) on MRI.
The trial entailed 52 weeks of double-blind therapy with certolizumab at a starting dose of 400 mg on weeks 0, 2, and 4 followed by 200 mg every 2 weeks, or placebo. The Ankylosing Spondylitis Disease Activity Score Major Improvement rate, defined as at least a 2-point improvement from baseline, was 47% in the active treatment arm, compared with 7% on placebo. The Assessment in Ankylosing Spondylitis International Society 40% response rate, a more patient-reported outcome measure, was 57% in the certolizumab group and 16% in controls (Arthritis Rheumatol. 2019 March 8. doi: 10.1002/art.40866).
The overall safety profile observed in the Cimzia treatment group was consistent with the known safety profile of certolizumab.
Cimzia was first approved in 2008 and has FDA-approved indications for adult patients with Crohn’s disease, moderate to severe rheumatoid arthritis, active ankylosing spondylitis and moderate to severe plaque psoriasis who are candidates for systemic therapy or phototherapy.
, with objective evidence of inflammation, making it the first treatment approved by the agency for the condition.
The FDA approved the tumor necrosis factor inhibitor based on results from a randomized clinical trial in 317 adult patients with nonradiographic axial spondyloarthritis (nr-axSpA) who had elevated C-reactive protein levels and/or sacroiliitis (inflammation of the sacroiliac joints) on MRI.
The trial entailed 52 weeks of double-blind therapy with certolizumab at a starting dose of 400 mg on weeks 0, 2, and 4 followed by 200 mg every 2 weeks, or placebo. The Ankylosing Spondylitis Disease Activity Score Major Improvement rate, defined as at least a 2-point improvement from baseline, was 47% in the active treatment arm, compared with 7% on placebo. The Assessment in Ankylosing Spondylitis International Society 40% response rate, a more patient-reported outcome measure, was 57% in the certolizumab group and 16% in controls (Arthritis Rheumatol. 2019 March 8. doi: 10.1002/art.40866).
The overall safety profile observed in the Cimzia treatment group was consistent with the known safety profile of certolizumab.
Cimzia was first approved in 2008 and has FDA-approved indications for adult patients with Crohn’s disease, moderate to severe rheumatoid arthritis, active ankylosing spondylitis and moderate to severe plaque psoriasis who are candidates for systemic therapy or phototherapy.
, with objective evidence of inflammation, making it the first treatment approved by the agency for the condition.
The FDA approved the tumor necrosis factor inhibitor based on results from a randomized clinical trial in 317 adult patients with nonradiographic axial spondyloarthritis (nr-axSpA) who had elevated C-reactive protein levels and/or sacroiliitis (inflammation of the sacroiliac joints) on MRI.
The trial entailed 52 weeks of double-blind therapy with certolizumab at a starting dose of 400 mg on weeks 0, 2, and 4 followed by 200 mg every 2 weeks, or placebo. The Ankylosing Spondylitis Disease Activity Score Major Improvement rate, defined as at least a 2-point improvement from baseline, was 47% in the active treatment arm, compared with 7% on placebo. The Assessment in Ankylosing Spondylitis International Society 40% response rate, a more patient-reported outcome measure, was 57% in the certolizumab group and 16% in controls (Arthritis Rheumatol. 2019 March 8. doi: 10.1002/art.40866).
The overall safety profile observed in the Cimzia treatment group was consistent with the known safety profile of certolizumab.
Cimzia was first approved in 2008 and has FDA-approved indications for adult patients with Crohn’s disease, moderate to severe rheumatoid arthritis, active ankylosing spondylitis and moderate to severe plaque psoriasis who are candidates for systemic therapy or phototherapy.
Four biomarkers could distinguish psoriatic arthritis from osteoarthritis
A panel of four biomarkers of cartilage metabolism, metabolic syndrome, and inflammation could help physicians to distinguish between osteoarthritis and psoriatic arthritis, new research suggests.
Such a test for distinguishing between the two conditions, which have “similarities in the distribution of joints involved,” could offer a way to make earlier diagnoses and avoid inappropriate treatment, according to Vinod Chandran, MD, PhD, of the department of medicine at the University of Toronto and Toronto Western Hospital and his colleagues. Dr. Chandran was first author on a study published online in Annals of the Rheumatic Diseases that analyzed serum samples from the University of Toronto Psoriatic Arthritis Program and University Health Network Arthritis Program for differences in certain biomarkers from 201 individuals with osteoarthritis, 77 with psoriatic arthritis, and 76 healthy controls.
The samples were tested for 15 biomarkers, including those related to cartilage metabolism (cartilage oligomeric matrix protein and hyaluronan), to metabolic syndrome (adiponectin, adipsin, resistin, hepatocyte growth factor, insulin, and leptin), and to inflammation (C-reactive protein, interleukin-1-beta, interleukin-6, interleukin-8, tumor necrosis factor alpha, monocyte chemoattractant protein–1, and nerve growth factor).
Researchers found that levels of 12 of these markers were different in patients with psoriatic arthritis, osteoarthritis, or controls, and 9 markers showed altered expression in psoriatic arthritis, compared with osteoarthritis.
Further analysis showed that levels of cartilage oligomeric matrix protein, resistin, monocyte chemoattractant protein–1, and nerve growth factor were significantly different between patients with psoriatic arthritis and those with osteoarthritis. The ROC curve for a model based on these four biomarkers that also incorporated age and sex had an area under the curve of 0.9984.
Researchers then validated the four biomarkers in an independent set of 75 patients with osteoarthritis and 73 with psoriatic arthritis and found these biomarkers were able to discriminate between the two conditions beyond what would be achieved based on age and sex alone.
The authors noted that previous research has observed high expression of monocyte chemoattractant protein–1 and resistin in patients with psoriatic arthritis when compared with those with osteoarthritis.
Nerve growth factor has been seen at elevated levels in the synovial fluid of individuals with osteoarthritis and is known to play a role in the chronic pain associated with that disease.
Similarly, higher cartilage oligomeric matrix protein levels are associated with a higher risk of knee osteoarthritis.
However, the authors noted that individuals with osteoarthritis in the study were all undergoing joint replacement surgery and therefore may not be typical of patients presenting to family practices or rheumatology clinics.
The University of Toronto Psoriatic Arthritis Program is supported by the Krembil Foundation. No conflicts of interest were declared.
SOURCE: Chandran V et al. Ann Rheum Dis. 2019 Mar 25. doi: 10.1136/annrheumdis-2018-214737.
A panel of four biomarkers of cartilage metabolism, metabolic syndrome, and inflammation could help physicians to distinguish between osteoarthritis and psoriatic arthritis, new research suggests.
Such a test for distinguishing between the two conditions, which have “similarities in the distribution of joints involved,” could offer a way to make earlier diagnoses and avoid inappropriate treatment, according to Vinod Chandran, MD, PhD, of the department of medicine at the University of Toronto and Toronto Western Hospital and his colleagues. Dr. Chandran was first author on a study published online in Annals of the Rheumatic Diseases that analyzed serum samples from the University of Toronto Psoriatic Arthritis Program and University Health Network Arthritis Program for differences in certain biomarkers from 201 individuals with osteoarthritis, 77 with psoriatic arthritis, and 76 healthy controls.
The samples were tested for 15 biomarkers, including those related to cartilage metabolism (cartilage oligomeric matrix protein and hyaluronan), to metabolic syndrome (adiponectin, adipsin, resistin, hepatocyte growth factor, insulin, and leptin), and to inflammation (C-reactive protein, interleukin-1-beta, interleukin-6, interleukin-8, tumor necrosis factor alpha, monocyte chemoattractant protein–1, and nerve growth factor).
Researchers found that levels of 12 of these markers were different in patients with psoriatic arthritis, osteoarthritis, or controls, and 9 markers showed altered expression in psoriatic arthritis, compared with osteoarthritis.
Further analysis showed that levels of cartilage oligomeric matrix protein, resistin, monocyte chemoattractant protein–1, and nerve growth factor were significantly different between patients with psoriatic arthritis and those with osteoarthritis. The ROC curve for a model based on these four biomarkers that also incorporated age and sex had an area under the curve of 0.9984.
Researchers then validated the four biomarkers in an independent set of 75 patients with osteoarthritis and 73 with psoriatic arthritis and found these biomarkers were able to discriminate between the two conditions beyond what would be achieved based on age and sex alone.
The authors noted that previous research has observed high expression of monocyte chemoattractant protein–1 and resistin in patients with psoriatic arthritis when compared with those with osteoarthritis.
Nerve growth factor has been seen at elevated levels in the synovial fluid of individuals with osteoarthritis and is known to play a role in the chronic pain associated with that disease.
Similarly, higher cartilage oligomeric matrix protein levels are associated with a higher risk of knee osteoarthritis.
However, the authors noted that individuals with osteoarthritis in the study were all undergoing joint replacement surgery and therefore may not be typical of patients presenting to family practices or rheumatology clinics.
The University of Toronto Psoriatic Arthritis Program is supported by the Krembil Foundation. No conflicts of interest were declared.
SOURCE: Chandran V et al. Ann Rheum Dis. 2019 Mar 25. doi: 10.1136/annrheumdis-2018-214737.
A panel of four biomarkers of cartilage metabolism, metabolic syndrome, and inflammation could help physicians to distinguish between osteoarthritis and psoriatic arthritis, new research suggests.
Such a test for distinguishing between the two conditions, which have “similarities in the distribution of joints involved,” could offer a way to make earlier diagnoses and avoid inappropriate treatment, according to Vinod Chandran, MD, PhD, of the department of medicine at the University of Toronto and Toronto Western Hospital and his colleagues. Dr. Chandran was first author on a study published online in Annals of the Rheumatic Diseases that analyzed serum samples from the University of Toronto Psoriatic Arthritis Program and University Health Network Arthritis Program for differences in certain biomarkers from 201 individuals with osteoarthritis, 77 with psoriatic arthritis, and 76 healthy controls.
The samples were tested for 15 biomarkers, including those related to cartilage metabolism (cartilage oligomeric matrix protein and hyaluronan), to metabolic syndrome (adiponectin, adipsin, resistin, hepatocyte growth factor, insulin, and leptin), and to inflammation (C-reactive protein, interleukin-1-beta, interleukin-6, interleukin-8, tumor necrosis factor alpha, monocyte chemoattractant protein–1, and nerve growth factor).
Researchers found that levels of 12 of these markers were different in patients with psoriatic arthritis, osteoarthritis, or controls, and 9 markers showed altered expression in psoriatic arthritis, compared with osteoarthritis.
Further analysis showed that levels of cartilage oligomeric matrix protein, resistin, monocyte chemoattractant protein–1, and nerve growth factor were significantly different between patients with psoriatic arthritis and those with osteoarthritis. The ROC curve for a model based on these four biomarkers that also incorporated age and sex had an area under the curve of 0.9984.
Researchers then validated the four biomarkers in an independent set of 75 patients with osteoarthritis and 73 with psoriatic arthritis and found these biomarkers were able to discriminate between the two conditions beyond what would be achieved based on age and sex alone.
The authors noted that previous research has observed high expression of monocyte chemoattractant protein–1 and resistin in patients with psoriatic arthritis when compared with those with osteoarthritis.
Nerve growth factor has been seen at elevated levels in the synovial fluid of individuals with osteoarthritis and is known to play a role in the chronic pain associated with that disease.
Similarly, higher cartilage oligomeric matrix protein levels are associated with a higher risk of knee osteoarthritis.
However, the authors noted that individuals with osteoarthritis in the study were all undergoing joint replacement surgery and therefore may not be typical of patients presenting to family practices or rheumatology clinics.
The University of Toronto Psoriatic Arthritis Program is supported by the Krembil Foundation. No conflicts of interest were declared.
SOURCE: Chandran V et al. Ann Rheum Dis. 2019 Mar 25. doi: 10.1136/annrheumdis-2018-214737.
FROM ANNALS OF THE RHEUMATIC DISEASES
The paclitaxel paradox
As medical editor of Vascular Specialist, it has always been my hope to use our excellent reporters and rapid production schedule to keep readers abreast of the latest news in vascular surgery. While my colleagues at the Journal of Vascular Surgery publish studies that will drive treatment, my goal is to drive discussion.
With topics like burnout, workforce shortages, and electronic medical records, I feel we have been successful. The downside of staying current is we sometimes find ourselves publishing contradictory stories. This has been the case with paclitaxel. Let’s take a break from the fray and review where we are, and where we might go from here.
In 2012, the Zilver PTX became the first drug-eluting stent (DES) to gain Food and Drug Administration approval for the treatment of peripheral vascular disease. Two years later, the FDA approved the Lutonix 035 as the first drug-coated balloon (DCB) for use in the femoral-popliteal arteries. The Lutonix would also gain a second indication for failing dialysis fistulas. Medtronic and Spectranetics received authorizations for their DCBs in 2015 and 2017, respectively.
While the safety of paclitaxel-coated devices in the coronary system had previously been called into question, the drug was generally considered safe and effective in the peripheral arterial system. The controversy began in December 2018, when Katsanos et al.1 published a meta-analysis of 28 randomized, controlled trials (RCTs) investigating paclitaxel-coated devices in the femoral-popliteal arteries. While all-cause patient mortality was similar at 1 year between paclitaxel-coated devices and controls (2.3% in each), at 2 years the risk of death was significantly higher in those treated with paclitaxel (7.2% vs. 3.8%). The 5-year data were available for three trials where there was a continued significantly increased risk of mortality with paclitaxel (14.7% vs. 8.1%).
Opposition to these findings was prompt from both physicians and industry. Weaknesses of the analysis, both perceived and real, were hammered. The meta-analysis did not include individual patient data, and the actual cause of death was unknown in most of the included trials. The study was not adequately powered to eliminate the risk of type 1 error when comparing mortality after 2 years. Individuals assigned to the control group may have received paclitaxel treatment at some point in their follow-up. The DCB and DES treatment groups were combined. The methods employed by the authors, however, stood up reasonably well to scrutiny.
On Jan. 17, 2019, the FDA issued their first response stating, “the FDA believes that the benefits continue to outweigh the risks for approved paclitaxel-coated balloons and paclitaxel-eluting stents when used in accordance with their indications for use.”2
Later that month, Peter Schneider, MD, and associates published a patient-level meta-analysis in the Journal of the American College of Cardiology.3 The study included 1,980 patients and found no statistically significant difference in all-cause mortality between DCB (9.3%) and percutaneous transluminal angioplasty (PTA) (11.2%) through 5 years. Shortly after that, however, a correction was issued.
On Feb. 15, 2019, Medtronic reported an error in the 2- and 3-year follow-up periods for the IN.PACT Global postmarket study. The company stated, “Due to a programming error, mortality data were inadvertently omitted from the summary tables included in the statistical analysis.” The mortality in the DCB cohort was corrected from 9.30% to 15.12%. The authors stated that this new mortality rate was still not significantly higher than the PTA group (P = .09).4
Less than 1 week later, another device company issued a correction. And once again, the error had been made in favor of the paclitaxel-treated group. In 2016, the 5-year data from Cook Medical’s Zilver PTX trial were published in Circulation. The study reported a mortality of 10.2% in the DES group and 16.9% in the PTA cohort. Regrettably, these numbers were reversed and significantly higher in the paclitaxel-treated group (16.9% vs. 10.2%, P = .03).5
On Feb. 12, 2019, another response to the Katsanos meta-analysis was published in JAMA Cardiology.6 In this study, Secemsky et al. analyzed patient-level data from a Medicare database. The authors reported finding no evidence of paclitaxel- related deaths in 16,560 patients. Unfortunately, the mean follow-up time was only 389 days, which may have been insufficient to detect the late mortality reported in the Katsanos meta-analysis.
On March 15, 2019, the FDA issued a second statement, this time with a much stronger tone.7 The agency reported an ongoing analysis of the long-term survival data from the pivotal randomized trials. In the three studies with 5-year data available, each showed a significantly higher mortality in the paclitaxel group.
When pooled, there were 975 patients, and the risk of death was 20.1% in the paclitaxel group versus 13.4 % in the controls. The FDA recommended discussing the increased risk of mortality with all patients receiving paclitaxel therapy as part of the informed consent process. They also stated that for most patients alternative options should generally be used until additional analysis of the mortality risk is performed.
Industry bristled at this new, strongly worded statement. Becton Dickinson, makers of the Lutonix balloon, asserted that the FDA recommendation was based on “a limited review of data from less than 1,000 patients.”8 The company noted that its LEVANT 2 trial did not see a signal of increased mortality at 5 years. Although they did acknowledge that, among the randomized patients, there was a significantly higher mortality at 5 years for those treated with paclitaxel.
How do we make sense of this? Pac-litaxel is a cytotoxic drug. Its pharmacokinetics vary significantly based on the preparation and administration. The FDA label for the injectable form (Taxol) warns of anaphylaxis and severe hypersensitivity reactions, but there is no mention of long-term mortality. In the coronary vessels, paclitaxel-coated devices have been associated with myocardial infarction and death. Obviously it is easy to comprehend how local vessel effects in the coronary system can lead to increased mortality. The pathway is less clear with femoral-popliteal interventions. If the association of paclitaxel with death is truly causation there must be some systemic effects. The dose delivered with femoral- popliteal interventions is much higher than that seen with coronary devices.
The mortality may be associated with the platform used or even the formulation (crystalline formularies have a longer half-life). Could it be something more benign? Paclitaxel-treated patients see less recurrence of their femoral-popliteal disease. Are the control group patients with more recurrences seeing their interventionalist more often and therefore receiving more frequent reminders to comply with medical therapy?
At this point, we have few answers. After an all-day town hall at the recent Cardiovascular Research Technologies conference,9 one moderator said, “I came in with uncertainty and now I’m going away with uncertainty, but we made tremendous progress.” His comoderator added, “I know I don’t know.” Well then, glad we cleared that up!
In any event, changes are coming. The BASIL-3 trial has suspended recruitment. Physicians using paclitaxel-coated devices are now advised by the FDA to inform patients of the increased risk of death and to use alternatives in most cases. Therefore, if you employ these devices routinely in the femoral-popliteal vessels you are seemingly doing so in opposition to the recommendations of the FDA. Legal peril may follow.
The time for nitpicking the Katsanos analysis has ended. Our industry partners must be compelled to supply the data and finances needed to settle this issue. The signal seems real and it is time to find answers. Research initiatives are underway through the SVS, the VIVA group, the UK Medicines and Healthcare Products Regulatory Agency, and the FDA.
Going forward, the SVS has formed a Paclitaxel Safety Task Force under the leadership of President-elect Kim Hodgson. Their mission is to facilitate the performance and interpretation of an Individual Patient Data meta-analysis using patient-level RCT data from industry partners. The task force states: “We remain troubled by the recent reports of reanalysis of existing datasets, pooled analyses of RCTs, and other ‘series’, as we believe that the findings of these statistically inferior analyses bring no additional clarity, cannot be relied upon for guidance, and distract us from the analysis that needs to be performed.”
References
1. J Am Heart Assoc. 2018 Dec 18;7(24):e011245.
2. www.fda.gov/medicaldevices/safety/letterstohealthcareproviders/ucm629589.htm.
3. J Am Coll Cardiol. Jan 2019. doi: 10.1016/j.jacc.2019.01.013.
4. Circulation. 2019;139:e42.
5. https://evtoday.com/2019/02/20/zilver-ptx-trial-5-year-mortality-data-corrected-in-circulation.
6. JAMA Cardiol. 2019 Feb 12. doi:10.1001/jamacardio.2019.0325.
7. www.fda.gov/MedicalDevices/Safety/LetterstoHealthCareProviders/ucm633614.htm.
8. www.med-technews.com/news/bud-defends-safety-of-drug-coated-device-following-fda-warnin/.
9. www.crtonline.org/news-detail/paclitaxel-device-safety-thoroughly-discussed-at-c.
As medical editor of Vascular Specialist, it has always been my hope to use our excellent reporters and rapid production schedule to keep readers abreast of the latest news in vascular surgery. While my colleagues at the Journal of Vascular Surgery publish studies that will drive treatment, my goal is to drive discussion.
With topics like burnout, workforce shortages, and electronic medical records, I feel we have been successful. The downside of staying current is we sometimes find ourselves publishing contradictory stories. This has been the case with paclitaxel. Let’s take a break from the fray and review where we are, and where we might go from here.
In 2012, the Zilver PTX became the first drug-eluting stent (DES) to gain Food and Drug Administration approval for the treatment of peripheral vascular disease. Two years later, the FDA approved the Lutonix 035 as the first drug-coated balloon (DCB) for use in the femoral-popliteal arteries. The Lutonix would also gain a second indication for failing dialysis fistulas. Medtronic and Spectranetics received authorizations for their DCBs in 2015 and 2017, respectively.
While the safety of paclitaxel-coated devices in the coronary system had previously been called into question, the drug was generally considered safe and effective in the peripheral arterial system. The controversy began in December 2018, when Katsanos et al.1 published a meta-analysis of 28 randomized, controlled trials (RCTs) investigating paclitaxel-coated devices in the femoral-popliteal arteries. While all-cause patient mortality was similar at 1 year between paclitaxel-coated devices and controls (2.3% in each), at 2 years the risk of death was significantly higher in those treated with paclitaxel (7.2% vs. 3.8%). The 5-year data were available for three trials where there was a continued significantly increased risk of mortality with paclitaxel (14.7% vs. 8.1%).
Opposition to these findings was prompt from both physicians and industry. Weaknesses of the analysis, both perceived and real, were hammered. The meta-analysis did not include individual patient data, and the actual cause of death was unknown in most of the included trials. The study was not adequately powered to eliminate the risk of type 1 error when comparing mortality after 2 years. Individuals assigned to the control group may have received paclitaxel treatment at some point in their follow-up. The DCB and DES treatment groups were combined. The methods employed by the authors, however, stood up reasonably well to scrutiny.
On Jan. 17, 2019, the FDA issued their first response stating, “the FDA believes that the benefits continue to outweigh the risks for approved paclitaxel-coated balloons and paclitaxel-eluting stents when used in accordance with their indications for use.”2
Later that month, Peter Schneider, MD, and associates published a patient-level meta-analysis in the Journal of the American College of Cardiology.3 The study included 1,980 patients and found no statistically significant difference in all-cause mortality between DCB (9.3%) and percutaneous transluminal angioplasty (PTA) (11.2%) through 5 years. Shortly after that, however, a correction was issued.
On Feb. 15, 2019, Medtronic reported an error in the 2- and 3-year follow-up periods for the IN.PACT Global postmarket study. The company stated, “Due to a programming error, mortality data were inadvertently omitted from the summary tables included in the statistical analysis.” The mortality in the DCB cohort was corrected from 9.30% to 15.12%. The authors stated that this new mortality rate was still not significantly higher than the PTA group (P = .09).4
Less than 1 week later, another device company issued a correction. And once again, the error had been made in favor of the paclitaxel-treated group. In 2016, the 5-year data from Cook Medical’s Zilver PTX trial were published in Circulation. The study reported a mortality of 10.2% in the DES group and 16.9% in the PTA cohort. Regrettably, these numbers were reversed and significantly higher in the paclitaxel-treated group (16.9% vs. 10.2%, P = .03).5
On Feb. 12, 2019, another response to the Katsanos meta-analysis was published in JAMA Cardiology.6 In this study, Secemsky et al. analyzed patient-level data from a Medicare database. The authors reported finding no evidence of paclitaxel- related deaths in 16,560 patients. Unfortunately, the mean follow-up time was only 389 days, which may have been insufficient to detect the late mortality reported in the Katsanos meta-analysis.
On March 15, 2019, the FDA issued a second statement, this time with a much stronger tone.7 The agency reported an ongoing analysis of the long-term survival data from the pivotal randomized trials. In the three studies with 5-year data available, each showed a significantly higher mortality in the paclitaxel group.
When pooled, there were 975 patients, and the risk of death was 20.1% in the paclitaxel group versus 13.4 % in the controls. The FDA recommended discussing the increased risk of mortality with all patients receiving paclitaxel therapy as part of the informed consent process. They also stated that for most patients alternative options should generally be used until additional analysis of the mortality risk is performed.
Industry bristled at this new, strongly worded statement. Becton Dickinson, makers of the Lutonix balloon, asserted that the FDA recommendation was based on “a limited review of data from less than 1,000 patients.”8 The company noted that its LEVANT 2 trial did not see a signal of increased mortality at 5 years. Although they did acknowledge that, among the randomized patients, there was a significantly higher mortality at 5 years for those treated with paclitaxel.
How do we make sense of this? Pac-litaxel is a cytotoxic drug. Its pharmacokinetics vary significantly based on the preparation and administration. The FDA label for the injectable form (Taxol) warns of anaphylaxis and severe hypersensitivity reactions, but there is no mention of long-term mortality. In the coronary vessels, paclitaxel-coated devices have been associated with myocardial infarction and death. Obviously it is easy to comprehend how local vessel effects in the coronary system can lead to increased mortality. The pathway is less clear with femoral-popliteal interventions. If the association of paclitaxel with death is truly causation there must be some systemic effects. The dose delivered with femoral- popliteal interventions is much higher than that seen with coronary devices.
The mortality may be associated with the platform used or even the formulation (crystalline formularies have a longer half-life). Could it be something more benign? Paclitaxel-treated patients see less recurrence of their femoral-popliteal disease. Are the control group patients with more recurrences seeing their interventionalist more often and therefore receiving more frequent reminders to comply with medical therapy?
At this point, we have few answers. After an all-day town hall at the recent Cardiovascular Research Technologies conference,9 one moderator said, “I came in with uncertainty and now I’m going away with uncertainty, but we made tremendous progress.” His comoderator added, “I know I don’t know.” Well then, glad we cleared that up!
In any event, changes are coming. The BASIL-3 trial has suspended recruitment. Physicians using paclitaxel-coated devices are now advised by the FDA to inform patients of the increased risk of death and to use alternatives in most cases. Therefore, if you employ these devices routinely in the femoral-popliteal vessels you are seemingly doing so in opposition to the recommendations of the FDA. Legal peril may follow.
The time for nitpicking the Katsanos analysis has ended. Our industry partners must be compelled to supply the data and finances needed to settle this issue. The signal seems real and it is time to find answers. Research initiatives are underway through the SVS, the VIVA group, the UK Medicines and Healthcare Products Regulatory Agency, and the FDA.
Going forward, the SVS has formed a Paclitaxel Safety Task Force under the leadership of President-elect Kim Hodgson. Their mission is to facilitate the performance and interpretation of an Individual Patient Data meta-analysis using patient-level RCT data from industry partners. The task force states: “We remain troubled by the recent reports of reanalysis of existing datasets, pooled analyses of RCTs, and other ‘series’, as we believe that the findings of these statistically inferior analyses bring no additional clarity, cannot be relied upon for guidance, and distract us from the analysis that needs to be performed.”
References
1. J Am Heart Assoc. 2018 Dec 18;7(24):e011245.
2. www.fda.gov/medicaldevices/safety/letterstohealthcareproviders/ucm629589.htm.
3. J Am Coll Cardiol. Jan 2019. doi: 10.1016/j.jacc.2019.01.013.
4. Circulation. 2019;139:e42.
5. https://evtoday.com/2019/02/20/zilver-ptx-trial-5-year-mortality-data-corrected-in-circulation.
6. JAMA Cardiol. 2019 Feb 12. doi:10.1001/jamacardio.2019.0325.
7. www.fda.gov/MedicalDevices/Safety/LetterstoHealthCareProviders/ucm633614.htm.
8. www.med-technews.com/news/bud-defends-safety-of-drug-coated-device-following-fda-warnin/.
9. www.crtonline.org/news-detail/paclitaxel-device-safety-thoroughly-discussed-at-c.
As medical editor of Vascular Specialist, it has always been my hope to use our excellent reporters and rapid production schedule to keep readers abreast of the latest news in vascular surgery. While my colleagues at the Journal of Vascular Surgery publish studies that will drive treatment, my goal is to drive discussion.
With topics like burnout, workforce shortages, and electronic medical records, I feel we have been successful. The downside of staying current is we sometimes find ourselves publishing contradictory stories. This has been the case with paclitaxel. Let’s take a break from the fray and review where we are, and where we might go from here.
In 2012, the Zilver PTX became the first drug-eluting stent (DES) to gain Food and Drug Administration approval for the treatment of peripheral vascular disease. Two years later, the FDA approved the Lutonix 035 as the first drug-coated balloon (DCB) for use in the femoral-popliteal arteries. The Lutonix would also gain a second indication for failing dialysis fistulas. Medtronic and Spectranetics received authorizations for their DCBs in 2015 and 2017, respectively.
While the safety of paclitaxel-coated devices in the coronary system had previously been called into question, the drug was generally considered safe and effective in the peripheral arterial system. The controversy began in December 2018, when Katsanos et al.1 published a meta-analysis of 28 randomized, controlled trials (RCTs) investigating paclitaxel-coated devices in the femoral-popliteal arteries. While all-cause patient mortality was similar at 1 year between paclitaxel-coated devices and controls (2.3% in each), at 2 years the risk of death was significantly higher in those treated with paclitaxel (7.2% vs. 3.8%). The 5-year data were available for three trials where there was a continued significantly increased risk of mortality with paclitaxel (14.7% vs. 8.1%).
Opposition to these findings was prompt from both physicians and industry. Weaknesses of the analysis, both perceived and real, were hammered. The meta-analysis did not include individual patient data, and the actual cause of death was unknown in most of the included trials. The study was not adequately powered to eliminate the risk of type 1 error when comparing mortality after 2 years. Individuals assigned to the control group may have received paclitaxel treatment at some point in their follow-up. The DCB and DES treatment groups were combined. The methods employed by the authors, however, stood up reasonably well to scrutiny.
On Jan. 17, 2019, the FDA issued their first response stating, “the FDA believes that the benefits continue to outweigh the risks for approved paclitaxel-coated balloons and paclitaxel-eluting stents when used in accordance with their indications for use.”2
Later that month, Peter Schneider, MD, and associates published a patient-level meta-analysis in the Journal of the American College of Cardiology.3 The study included 1,980 patients and found no statistically significant difference in all-cause mortality between DCB (9.3%) and percutaneous transluminal angioplasty (PTA) (11.2%) through 5 years. Shortly after that, however, a correction was issued.
On Feb. 15, 2019, Medtronic reported an error in the 2- and 3-year follow-up periods for the IN.PACT Global postmarket study. The company stated, “Due to a programming error, mortality data were inadvertently omitted from the summary tables included in the statistical analysis.” The mortality in the DCB cohort was corrected from 9.30% to 15.12%. The authors stated that this new mortality rate was still not significantly higher than the PTA group (P = .09).4
Less than 1 week later, another device company issued a correction. And once again, the error had been made in favor of the paclitaxel-treated group. In 2016, the 5-year data from Cook Medical’s Zilver PTX trial were published in Circulation. The study reported a mortality of 10.2% in the DES group and 16.9% in the PTA cohort. Regrettably, these numbers were reversed and significantly higher in the paclitaxel-treated group (16.9% vs. 10.2%, P = .03).5
On Feb. 12, 2019, another response to the Katsanos meta-analysis was published in JAMA Cardiology.6 In this study, Secemsky et al. analyzed patient-level data from a Medicare database. The authors reported finding no evidence of paclitaxel- related deaths in 16,560 patients. Unfortunately, the mean follow-up time was only 389 days, which may have been insufficient to detect the late mortality reported in the Katsanos meta-analysis.
On March 15, 2019, the FDA issued a second statement, this time with a much stronger tone.7 The agency reported an ongoing analysis of the long-term survival data from the pivotal randomized trials. In the three studies with 5-year data available, each showed a significantly higher mortality in the paclitaxel group.
When pooled, there were 975 patients, and the risk of death was 20.1% in the paclitaxel group versus 13.4 % in the controls. The FDA recommended discussing the increased risk of mortality with all patients receiving paclitaxel therapy as part of the informed consent process. They also stated that for most patients alternative options should generally be used until additional analysis of the mortality risk is performed.
Industry bristled at this new, strongly worded statement. Becton Dickinson, makers of the Lutonix balloon, asserted that the FDA recommendation was based on “a limited review of data from less than 1,000 patients.”8 The company noted that its LEVANT 2 trial did not see a signal of increased mortality at 5 years. Although they did acknowledge that, among the randomized patients, there was a significantly higher mortality at 5 years for those treated with paclitaxel.
How do we make sense of this? Pac-litaxel is a cytotoxic drug. Its pharmacokinetics vary significantly based on the preparation and administration. The FDA label for the injectable form (Taxol) warns of anaphylaxis and severe hypersensitivity reactions, but there is no mention of long-term mortality. In the coronary vessels, paclitaxel-coated devices have been associated with myocardial infarction and death. Obviously it is easy to comprehend how local vessel effects in the coronary system can lead to increased mortality. The pathway is less clear with femoral-popliteal interventions. If the association of paclitaxel with death is truly causation there must be some systemic effects. The dose delivered with femoral- popliteal interventions is much higher than that seen with coronary devices.
The mortality may be associated with the platform used or even the formulation (crystalline formularies have a longer half-life). Could it be something more benign? Paclitaxel-treated patients see less recurrence of their femoral-popliteal disease. Are the control group patients with more recurrences seeing their interventionalist more often and therefore receiving more frequent reminders to comply with medical therapy?
At this point, we have few answers. After an all-day town hall at the recent Cardiovascular Research Technologies conference,9 one moderator said, “I came in with uncertainty and now I’m going away with uncertainty, but we made tremendous progress.” His comoderator added, “I know I don’t know.” Well then, glad we cleared that up!
In any event, changes are coming. The BASIL-3 trial has suspended recruitment. Physicians using paclitaxel-coated devices are now advised by the FDA to inform patients of the increased risk of death and to use alternatives in most cases. Therefore, if you employ these devices routinely in the femoral-popliteal vessels you are seemingly doing so in opposition to the recommendations of the FDA. Legal peril may follow.
The time for nitpicking the Katsanos analysis has ended. Our industry partners must be compelled to supply the data and finances needed to settle this issue. The signal seems real and it is time to find answers. Research initiatives are underway through the SVS, the VIVA group, the UK Medicines and Healthcare Products Regulatory Agency, and the FDA.
Going forward, the SVS has formed a Paclitaxel Safety Task Force under the leadership of President-elect Kim Hodgson. Their mission is to facilitate the performance and interpretation of an Individual Patient Data meta-analysis using patient-level RCT data from industry partners. The task force states: “We remain troubled by the recent reports of reanalysis of existing datasets, pooled analyses of RCTs, and other ‘series’, as we believe that the findings of these statistically inferior analyses bring no additional clarity, cannot be relied upon for guidance, and distract us from the analysis that needs to be performed.”
References
1. J Am Heart Assoc. 2018 Dec 18;7(24):e011245.
2. www.fda.gov/medicaldevices/safety/letterstohealthcareproviders/ucm629589.htm.
3. J Am Coll Cardiol. Jan 2019. doi: 10.1016/j.jacc.2019.01.013.
4. Circulation. 2019;139:e42.
5. https://evtoday.com/2019/02/20/zilver-ptx-trial-5-year-mortality-data-corrected-in-circulation.
6. JAMA Cardiol. 2019 Feb 12. doi:10.1001/jamacardio.2019.0325.
7. www.fda.gov/MedicalDevices/Safety/LetterstoHealthCareProviders/ucm633614.htm.
8. www.med-technews.com/news/bud-defends-safety-of-drug-coated-device-following-fda-warnin/.
9. www.crtonline.org/news-detail/paclitaxel-device-safety-thoroughly-discussed-at-c.
Ticagrelor reversal agent looks promising
NEW ORLEANS – A novel targeted ticagrelor reversal agent demonstrated rapid and sustained reversal of the potent antiplatelet agent in a phase 1 proof-of-concept study, Deepak L. Bhatt, MD, reported at the annual meeting of the American College of Cardiology.
“Hopefully the FDA will view this as something that really is a breakthrough,” commented Dr. Bhatt, executive director of interventional cardiology programs at Brigham and Women’s Hospital and professor of medicine at Harvard University, both in Boston.
Why a breakthrough? Because despite recent major advances in the ability to reverse the action of the direct-acting oral anticoagulants and thereby greatly improve their safety margin, there have been no parallel developments with regard to the potent antiplatelet agents ticagrelor (Brilinta), prasugrel (Effient), and clopidogrel. The effects of these antiplatelet drugs take 3-5 days to dissipate after they’ve been stopped, which is highly problematic when they’ve induced catastrophic bleeding or a patient requires emergent or urgent surgery, the cardiologist explained.
“The ability to reverse tigracelor’s antiplatelet effects rapidly could distinguish it from other antiplatelet agents such as prasugrel or even generic clopidogrel and, for that matter, even aspirin,” Dr. Bhatt said.
The ticagrelor reversal agent, known for now as PB2452, is an intravenously administered recombinant human immunoglobulin G1 monoclonal antibody antigen-binding fragment. It binds specifically and with high affinity to ticagrelor and its active metabolite. In the phase 1, placebo-controlled, double-blind study conducted in 64 healthy volunteers pretreated with ticagrelor for 48 hours, it reversed oral ticagrelor’s antiplatelet effects within 5 minutes and, with prolonged infusion, showed sustained effect for at least 20 hours.
The only adverse events observed in blinded assessment were minor injection site issues.
PB2452 is specific to ticagrelor and will not reverse the activity of other potent antiplatelet agents. Indeed, because of their chemical structure, neither prasugrel nor clopidogrel is reversible, according to Dr. Bhatt.
He said the developmental game plan for the ticagrelor reversal agent is initially to get it approved by the Food and Drug Administration for ticagrelor-related catastrophic bleeding, such as intracranial hemorrhage, since there is a recognized major unmet need in such situations. But as shown in the phase 1 study, BP2452 is potentially titratable by varying the size of the initial bolus dose and the dosing and duration of the subsequent infusion. So after initial approval for catastrophic bleeding, it makes sense to branch out and conduct further studies establishing the reversal agent’s value for prevention of bleeding complications caused by ticagrelor. An example might be a patient on ticagrelor because she recently received a stent in her left main coronary artery who falls and breaks her hip, and her surgeon says she needs surgery right away.
“If someone on ticagrelor came in with an intracranial hemorrhage, you’d want rapid reversal and have it sustained for as many days as the neurologist advises, whereas maybe if someone came in on ticagrelor after placement of a left main stent and you needed to do a lumbar puncture, you’d want to reverse the antiplatelet effect for the LP, and then if things go smoothly you’d want to get the ticagrelor back on board so the stent doesn’t thrombose. But that type of more precise dosing will require further work,” according to the cardiologist.
Discussant Barbara S. Wiggins, PharmD, commented, “We’ve been fortunate to have reversal agents come out for oral anticoagulants, but in terms of antiplatelet activity we’ve not been able to be successful with platelet transfusions. So having a reversal agent added to our armamentarium certainly is something that’s desirable.”
The phase 1 study of PB2452 indicates the monoclonal antibody checks the key boxes one looks for in a reversal agent: quick onset, long duration of effect, lack of a rebound in platelet activity after drug cessation, and potential for tailored titration. Of course, data on efficacy outcomes will also be necessary, noted Dr. Wiggins, a clinical pharmacologist at the Medical University of South Carolina, Charleston.
She added that she was favorably impressed that Dr. Bhatt and his coinvestigators went to the trouble of convincingly demonstrating reversal of ticagrelor’s antiplatelet effects using three different assays: light transmission aggregometry, which is considered the standard, as well as the point-of-care VerifyNow P2Y12 assay and the modified CY-QUANT assay.
The phase 1 study was funded by PhaseBio Pharmaceuticals. Dr. Bhatt reported the company provided a research grant directly to Brigham and Women’s Hospital.
Simultaneous with Dr. Bhatt’s presentation, the study results were published online (N Engl J Med. 2019 Mar 17. doi: 10.1056/NEJMoa1901778).
NEW ORLEANS – A novel targeted ticagrelor reversal agent demonstrated rapid and sustained reversal of the potent antiplatelet agent in a phase 1 proof-of-concept study, Deepak L. Bhatt, MD, reported at the annual meeting of the American College of Cardiology.
“Hopefully the FDA will view this as something that really is a breakthrough,” commented Dr. Bhatt, executive director of interventional cardiology programs at Brigham and Women’s Hospital and professor of medicine at Harvard University, both in Boston.
Why a breakthrough? Because despite recent major advances in the ability to reverse the action of the direct-acting oral anticoagulants and thereby greatly improve their safety margin, there have been no parallel developments with regard to the potent antiplatelet agents ticagrelor (Brilinta), prasugrel (Effient), and clopidogrel. The effects of these antiplatelet drugs take 3-5 days to dissipate after they’ve been stopped, which is highly problematic when they’ve induced catastrophic bleeding or a patient requires emergent or urgent surgery, the cardiologist explained.
“The ability to reverse tigracelor’s antiplatelet effects rapidly could distinguish it from other antiplatelet agents such as prasugrel or even generic clopidogrel and, for that matter, even aspirin,” Dr. Bhatt said.
The ticagrelor reversal agent, known for now as PB2452, is an intravenously administered recombinant human immunoglobulin G1 monoclonal antibody antigen-binding fragment. It binds specifically and with high affinity to ticagrelor and its active metabolite. In the phase 1, placebo-controlled, double-blind study conducted in 64 healthy volunteers pretreated with ticagrelor for 48 hours, it reversed oral ticagrelor’s antiplatelet effects within 5 minutes and, with prolonged infusion, showed sustained effect for at least 20 hours.
The only adverse events observed in blinded assessment were minor injection site issues.
PB2452 is specific to ticagrelor and will not reverse the activity of other potent antiplatelet agents. Indeed, because of their chemical structure, neither prasugrel nor clopidogrel is reversible, according to Dr. Bhatt.
He said the developmental game plan for the ticagrelor reversal agent is initially to get it approved by the Food and Drug Administration for ticagrelor-related catastrophic bleeding, such as intracranial hemorrhage, since there is a recognized major unmet need in such situations. But as shown in the phase 1 study, BP2452 is potentially titratable by varying the size of the initial bolus dose and the dosing and duration of the subsequent infusion. So after initial approval for catastrophic bleeding, it makes sense to branch out and conduct further studies establishing the reversal agent’s value for prevention of bleeding complications caused by ticagrelor. An example might be a patient on ticagrelor because she recently received a stent in her left main coronary artery who falls and breaks her hip, and her surgeon says she needs surgery right away.
“If someone on ticagrelor came in with an intracranial hemorrhage, you’d want rapid reversal and have it sustained for as many days as the neurologist advises, whereas maybe if someone came in on ticagrelor after placement of a left main stent and you needed to do a lumbar puncture, you’d want to reverse the antiplatelet effect for the LP, and then if things go smoothly you’d want to get the ticagrelor back on board so the stent doesn’t thrombose. But that type of more precise dosing will require further work,” according to the cardiologist.
Discussant Barbara S. Wiggins, PharmD, commented, “We’ve been fortunate to have reversal agents come out for oral anticoagulants, but in terms of antiplatelet activity we’ve not been able to be successful with platelet transfusions. So having a reversal agent added to our armamentarium certainly is something that’s desirable.”
The phase 1 study of PB2452 indicates the monoclonal antibody checks the key boxes one looks for in a reversal agent: quick onset, long duration of effect, lack of a rebound in platelet activity after drug cessation, and potential for tailored titration. Of course, data on efficacy outcomes will also be necessary, noted Dr. Wiggins, a clinical pharmacologist at the Medical University of South Carolina, Charleston.
She added that she was favorably impressed that Dr. Bhatt and his coinvestigators went to the trouble of convincingly demonstrating reversal of ticagrelor’s antiplatelet effects using three different assays: light transmission aggregometry, which is considered the standard, as well as the point-of-care VerifyNow P2Y12 assay and the modified CY-QUANT assay.
The phase 1 study was funded by PhaseBio Pharmaceuticals. Dr. Bhatt reported the company provided a research grant directly to Brigham and Women’s Hospital.
Simultaneous with Dr. Bhatt’s presentation, the study results were published online (N Engl J Med. 2019 Mar 17. doi: 10.1056/NEJMoa1901778).
NEW ORLEANS – A novel targeted ticagrelor reversal agent demonstrated rapid and sustained reversal of the potent antiplatelet agent in a phase 1 proof-of-concept study, Deepak L. Bhatt, MD, reported at the annual meeting of the American College of Cardiology.
“Hopefully the FDA will view this as something that really is a breakthrough,” commented Dr. Bhatt, executive director of interventional cardiology programs at Brigham and Women’s Hospital and professor of medicine at Harvard University, both in Boston.
Why a breakthrough? Because despite recent major advances in the ability to reverse the action of the direct-acting oral anticoagulants and thereby greatly improve their safety margin, there have been no parallel developments with regard to the potent antiplatelet agents ticagrelor (Brilinta), prasugrel (Effient), and clopidogrel. The effects of these antiplatelet drugs take 3-5 days to dissipate after they’ve been stopped, which is highly problematic when they’ve induced catastrophic bleeding or a patient requires emergent or urgent surgery, the cardiologist explained.
“The ability to reverse tigracelor’s antiplatelet effects rapidly could distinguish it from other antiplatelet agents such as prasugrel or even generic clopidogrel and, for that matter, even aspirin,” Dr. Bhatt said.
The ticagrelor reversal agent, known for now as PB2452, is an intravenously administered recombinant human immunoglobulin G1 monoclonal antibody antigen-binding fragment. It binds specifically and with high affinity to ticagrelor and its active metabolite. In the phase 1, placebo-controlled, double-blind study conducted in 64 healthy volunteers pretreated with ticagrelor for 48 hours, it reversed oral ticagrelor’s antiplatelet effects within 5 minutes and, with prolonged infusion, showed sustained effect for at least 20 hours.
The only adverse events observed in blinded assessment were minor injection site issues.
PB2452 is specific to ticagrelor and will not reverse the activity of other potent antiplatelet agents. Indeed, because of their chemical structure, neither prasugrel nor clopidogrel is reversible, according to Dr. Bhatt.
He said the developmental game plan for the ticagrelor reversal agent is initially to get it approved by the Food and Drug Administration for ticagrelor-related catastrophic bleeding, such as intracranial hemorrhage, since there is a recognized major unmet need in such situations. But as shown in the phase 1 study, BP2452 is potentially titratable by varying the size of the initial bolus dose and the dosing and duration of the subsequent infusion. So after initial approval for catastrophic bleeding, it makes sense to branch out and conduct further studies establishing the reversal agent’s value for prevention of bleeding complications caused by ticagrelor. An example might be a patient on ticagrelor because she recently received a stent in her left main coronary artery who falls and breaks her hip, and her surgeon says she needs surgery right away.
“If someone on ticagrelor came in with an intracranial hemorrhage, you’d want rapid reversal and have it sustained for as many days as the neurologist advises, whereas maybe if someone came in on ticagrelor after placement of a left main stent and you needed to do a lumbar puncture, you’d want to reverse the antiplatelet effect for the LP, and then if things go smoothly you’d want to get the ticagrelor back on board so the stent doesn’t thrombose. But that type of more precise dosing will require further work,” according to the cardiologist.
Discussant Barbara S. Wiggins, PharmD, commented, “We’ve been fortunate to have reversal agents come out for oral anticoagulants, but in terms of antiplatelet activity we’ve not been able to be successful with platelet transfusions. So having a reversal agent added to our armamentarium certainly is something that’s desirable.”
The phase 1 study of PB2452 indicates the monoclonal antibody checks the key boxes one looks for in a reversal agent: quick onset, long duration of effect, lack of a rebound in platelet activity after drug cessation, and potential for tailored titration. Of course, data on efficacy outcomes will also be necessary, noted Dr. Wiggins, a clinical pharmacologist at the Medical University of South Carolina, Charleston.
She added that she was favorably impressed that Dr. Bhatt and his coinvestigators went to the trouble of convincingly demonstrating reversal of ticagrelor’s antiplatelet effects using three different assays: light transmission aggregometry, which is considered the standard, as well as the point-of-care VerifyNow P2Y12 assay and the modified CY-QUANT assay.
The phase 1 study was funded by PhaseBio Pharmaceuticals. Dr. Bhatt reported the company provided a research grant directly to Brigham and Women’s Hospital.
Simultaneous with Dr. Bhatt’s presentation, the study results were published online (N Engl J Med. 2019 Mar 17. doi: 10.1056/NEJMoa1901778).
REPORTING FROM ACC 19
Key clinical point: Oral ticagrelor’s antiplatelet effect was reversed within 5 minutes by a novel targeted monoclonal antibody.
Major finding: A novel targeted monoclonal antibody reversed oral ticagrelor’s antiplatelet effects within 5 minutes and, with prolonged infusion, showed sustained effect for at least 20 hours.
Study details: This phase 1 study included 64 healthy subjects pretreated with 48 hours of ticagrelor before receiving various doses of the reversal agent or placebo.
Disclosures: The study was funded by PhaseBio Pharmaceuticals, which provided a research grant directly to Brigham and Women’s Hospital.
FDA proposes updates to mammography regulations
Proposed changes to federal mammography regulations aim to provide more information for doctors and patients, as well as standardize patient information on breast density’s impact on screening.
The Food and Drug Administration posted a new proposed rule online March 27 that would “expand the information mammography facilities must provide to patients and health care professionals, allowing for more informed medical decision making,” the agency said in a statement. “It would also modernize mammography quality standards and better position the FDA to enforce regulations that apply to the safety and quality of mammography services.”
Key among the proposed changes is the addition of breast density information to the summary letter provided to patients and to the medical report provided to referring health care professionals.
“The FDA is proposing specific language that would explain how breast density can influence the accuracy of mammography and would recommend patients with dense breasts talk to their health care provider about high breast density and how it relates to breast cancer risk and their individual situation,” the agency said in a statement.
Laurie Margolies, MD, section chief of breast imaging at Mount Sinai Health System in New York, said the regulations would bring some uniformity to the communication process.
“It builds on the experience of the 37 states and the District of Columbia, all of whom have passed dense breast notification laws, and can serve to unify those disparate regulations into one that would be uniform throughout the country to give one clear message to women and health care providers,” Dr. Margolies said in an interview.
She noted that dense breasts are very common and communicating issues that are related to them, including the potential need for supplemental screening, are important.
“Almost half of American women have dense breasts and why that is significant is because the dense breast issue not only increases one’s risk of getting breast cancer, but it also can hide small breast cancers on the mammogram,” she said.
If you take 1,000 women with dense breasts and then do a breast ultrasound as a supplemental screening measure, “you will find three more small node-negative breast cancers that would not have come to light if you didn’t do the extra supplemental screening,” underscoring the importance of communicating dense breast information, she continued.
FDA also is seeking to enhance information provided to health care professionals by codifying three additional categories for mammogram assessments, including the addition of the “known biopsy proven malignancy” category, which the agency says would help identify which scans were being used to evaluate treatment of already diagnosed cancers.
Both patients and health care professionals would receive more detailed information about the mammography facility under the proposed rule.
FDA is proposing modernization of quality standards to help the agency enforce regulations, including giving the agency the authority to notify patients and health care professionals directly if a mammography facility does not meet quality standards and that a reevaluation or repeat of the exam at a different facility may be needed. The proposed amendments also include requiring that only digital accessory components specifically FDA approved or cleared for mammography be used or that facilities use components that otherwise meet the requirements, and stronger record-keeping requirements.
Dr. Margolies did note one potential deficiency in the proposed rule – the lack of any information on health insurance coverage of supplemental screening for women with dense breasts, though she noted this may not fall under the FDA’s authority.
“It would do the most good if everybody could get the supplemental screening without regards to their ability to pay for it out of pocket,” she said.
The proposal amends regulations issued under the Mammography Quality Standards Act of 1992, which gives FDA oversight authority over mammography facilities, including accreditation, certification, annual inspection, and enforcement of standards.
Comments on the proposal are due 90 days after the proposed rule is published in the Federal Register, which is scheduled for March 28.
Proposed changes to federal mammography regulations aim to provide more information for doctors and patients, as well as standardize patient information on breast density’s impact on screening.
The Food and Drug Administration posted a new proposed rule online March 27 that would “expand the information mammography facilities must provide to patients and health care professionals, allowing for more informed medical decision making,” the agency said in a statement. “It would also modernize mammography quality standards and better position the FDA to enforce regulations that apply to the safety and quality of mammography services.”
Key among the proposed changes is the addition of breast density information to the summary letter provided to patients and to the medical report provided to referring health care professionals.
“The FDA is proposing specific language that would explain how breast density can influence the accuracy of mammography and would recommend patients with dense breasts talk to their health care provider about high breast density and how it relates to breast cancer risk and their individual situation,” the agency said in a statement.
Laurie Margolies, MD, section chief of breast imaging at Mount Sinai Health System in New York, said the regulations would bring some uniformity to the communication process.
“It builds on the experience of the 37 states and the District of Columbia, all of whom have passed dense breast notification laws, and can serve to unify those disparate regulations into one that would be uniform throughout the country to give one clear message to women and health care providers,” Dr. Margolies said in an interview.
She noted that dense breasts are very common and communicating issues that are related to them, including the potential need for supplemental screening, are important.
“Almost half of American women have dense breasts and why that is significant is because the dense breast issue not only increases one’s risk of getting breast cancer, but it also can hide small breast cancers on the mammogram,” she said.
If you take 1,000 women with dense breasts and then do a breast ultrasound as a supplemental screening measure, “you will find three more small node-negative breast cancers that would not have come to light if you didn’t do the extra supplemental screening,” underscoring the importance of communicating dense breast information, she continued.
FDA also is seeking to enhance information provided to health care professionals by codifying three additional categories for mammogram assessments, including the addition of the “known biopsy proven malignancy” category, which the agency says would help identify which scans were being used to evaluate treatment of already diagnosed cancers.
Both patients and health care professionals would receive more detailed information about the mammography facility under the proposed rule.
FDA is proposing modernization of quality standards to help the agency enforce regulations, including giving the agency the authority to notify patients and health care professionals directly if a mammography facility does not meet quality standards and that a reevaluation or repeat of the exam at a different facility may be needed. The proposed amendments also include requiring that only digital accessory components specifically FDA approved or cleared for mammography be used or that facilities use components that otherwise meet the requirements, and stronger record-keeping requirements.
Dr. Margolies did note one potential deficiency in the proposed rule – the lack of any information on health insurance coverage of supplemental screening for women with dense breasts, though she noted this may not fall under the FDA’s authority.
“It would do the most good if everybody could get the supplemental screening without regards to their ability to pay for it out of pocket,” she said.
The proposal amends regulations issued under the Mammography Quality Standards Act of 1992, which gives FDA oversight authority over mammography facilities, including accreditation, certification, annual inspection, and enforcement of standards.
Comments on the proposal are due 90 days after the proposed rule is published in the Federal Register, which is scheduled for March 28.
Proposed changes to federal mammography regulations aim to provide more information for doctors and patients, as well as standardize patient information on breast density’s impact on screening.
The Food and Drug Administration posted a new proposed rule online March 27 that would “expand the information mammography facilities must provide to patients and health care professionals, allowing for more informed medical decision making,” the agency said in a statement. “It would also modernize mammography quality standards and better position the FDA to enforce regulations that apply to the safety and quality of mammography services.”
Key among the proposed changes is the addition of breast density information to the summary letter provided to patients and to the medical report provided to referring health care professionals.
“The FDA is proposing specific language that would explain how breast density can influence the accuracy of mammography and would recommend patients with dense breasts talk to their health care provider about high breast density and how it relates to breast cancer risk and their individual situation,” the agency said in a statement.
Laurie Margolies, MD, section chief of breast imaging at Mount Sinai Health System in New York, said the regulations would bring some uniformity to the communication process.
“It builds on the experience of the 37 states and the District of Columbia, all of whom have passed dense breast notification laws, and can serve to unify those disparate regulations into one that would be uniform throughout the country to give one clear message to women and health care providers,” Dr. Margolies said in an interview.
She noted that dense breasts are very common and communicating issues that are related to them, including the potential need for supplemental screening, are important.
“Almost half of American women have dense breasts and why that is significant is because the dense breast issue not only increases one’s risk of getting breast cancer, but it also can hide small breast cancers on the mammogram,” she said.
If you take 1,000 women with dense breasts and then do a breast ultrasound as a supplemental screening measure, “you will find three more small node-negative breast cancers that would not have come to light if you didn’t do the extra supplemental screening,” underscoring the importance of communicating dense breast information, she continued.
FDA also is seeking to enhance information provided to health care professionals by codifying three additional categories for mammogram assessments, including the addition of the “known biopsy proven malignancy” category, which the agency says would help identify which scans were being used to evaluate treatment of already diagnosed cancers.
Both patients and health care professionals would receive more detailed information about the mammography facility under the proposed rule.
FDA is proposing modernization of quality standards to help the agency enforce regulations, including giving the agency the authority to notify patients and health care professionals directly if a mammography facility does not meet quality standards and that a reevaluation or repeat of the exam at a different facility may be needed. The proposed amendments also include requiring that only digital accessory components specifically FDA approved or cleared for mammography be used or that facilities use components that otherwise meet the requirements, and stronger record-keeping requirements.
Dr. Margolies did note one potential deficiency in the proposed rule – the lack of any information on health insurance coverage of supplemental screening for women with dense breasts, though she noted this may not fall under the FDA’s authority.
“It would do the most good if everybody could get the supplemental screening without regards to their ability to pay for it out of pocket,” she said.
The proposal amends regulations issued under the Mammography Quality Standards Act of 1992, which gives FDA oversight authority over mammography facilities, including accreditation, certification, annual inspection, and enforcement of standards.
Comments on the proposal are due 90 days after the proposed rule is published in the Federal Register, which is scheduled for March 28.
Montana named ‘best state to practice medicine’ in 2019
This year’s race for “best state to practice medicine” came down to the proverbial photo finish, with Montana edging out Wisconsin by 0.02 points, according to personal finance website WalletHub.
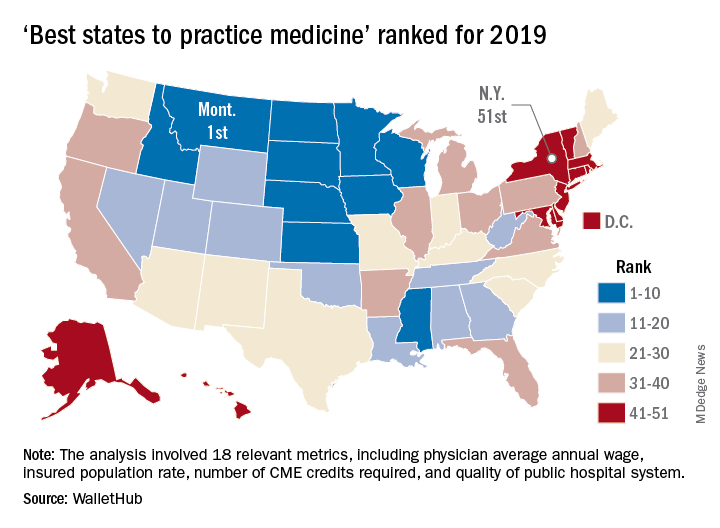
Montana had a total score of 69.15 out of 100 in the ranking of the best and worst states for doctors for 2019, with Wisconsin coming in at 69.13. The small degree of separation didn’t stop there, though, as third-place Idaho (68.55) and fourth-place Minnesota (68.32) both finished within a single point of the top, with Iowa a bit further behind at 67.58, WalletHub reported. In last year’s ranking, South Dakota won by more than 5 points over Nebraska, and in 2017 Iowa finished more than 2 points ahead of Minnesota.
The lowest-ranked state in 2019 was New York, with a score of 34.01 that was well below the 41.55 earned by 50th-place Washington, D.C. The rest of the bottom five was occupied by Rhode Island, New Jersey, and Connecticut, WalletHub said. New Jersey was the worst state in which to practice medicine in 2018, and New York finished last in 2017.
The rankings are based on 18 metrics across two broad categories: “opportunity and competition” (11 metrics worth 70 points) and “medical environment” (7 metrics worth 30 points). One metric in the opportunity and competition category, physicians’ average annual wage (adjusted for cost of living), was given double weight; other metrics included employer-based insurance rate, projected share of elderly population, punitiveness of state medical board, and malpractice award payout amount per capita.
Montana posted top-five scores in such areas as average physician monthly starting salary, share of medical residents retained, and presence of nationally accredited health departments. New York took big hits with bottom-five scores in adjusted average annual wage, projected competition, and annual cost of malpractice insurance, according to WalletHub.
This year’s race for “best state to practice medicine” came down to the proverbial photo finish, with Montana edging out Wisconsin by 0.02 points, according to personal finance website WalletHub.
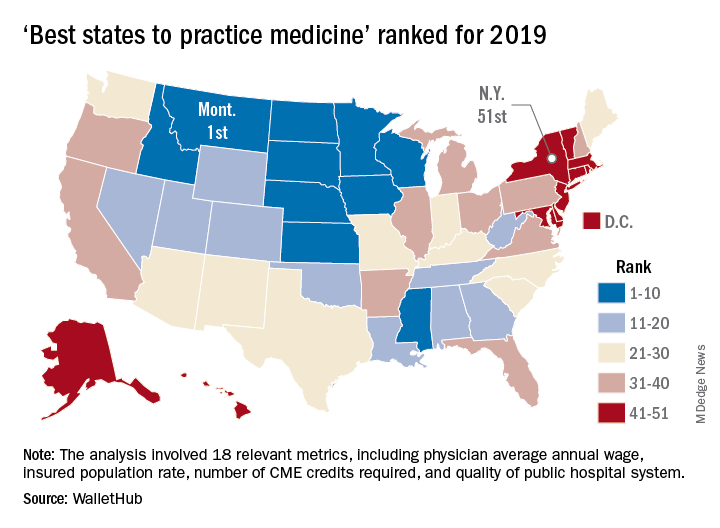
Montana had a total score of 69.15 out of 100 in the ranking of the best and worst states for doctors for 2019, with Wisconsin coming in at 69.13. The small degree of separation didn’t stop there, though, as third-place Idaho (68.55) and fourth-place Minnesota (68.32) both finished within a single point of the top, with Iowa a bit further behind at 67.58, WalletHub reported. In last year’s ranking, South Dakota won by more than 5 points over Nebraska, and in 2017 Iowa finished more than 2 points ahead of Minnesota.
The lowest-ranked state in 2019 was New York, with a score of 34.01 that was well below the 41.55 earned by 50th-place Washington, D.C. The rest of the bottom five was occupied by Rhode Island, New Jersey, and Connecticut, WalletHub said. New Jersey was the worst state in which to practice medicine in 2018, and New York finished last in 2017.
The rankings are based on 18 metrics across two broad categories: “opportunity and competition” (11 metrics worth 70 points) and “medical environment” (7 metrics worth 30 points). One metric in the opportunity and competition category, physicians’ average annual wage (adjusted for cost of living), was given double weight; other metrics included employer-based insurance rate, projected share of elderly population, punitiveness of state medical board, and malpractice award payout amount per capita.
Montana posted top-five scores in such areas as average physician monthly starting salary, share of medical residents retained, and presence of nationally accredited health departments. New York took big hits with bottom-five scores in adjusted average annual wage, projected competition, and annual cost of malpractice insurance, according to WalletHub.
This year’s race for “best state to practice medicine” came down to the proverbial photo finish, with Montana edging out Wisconsin by 0.02 points, according to personal finance website WalletHub.
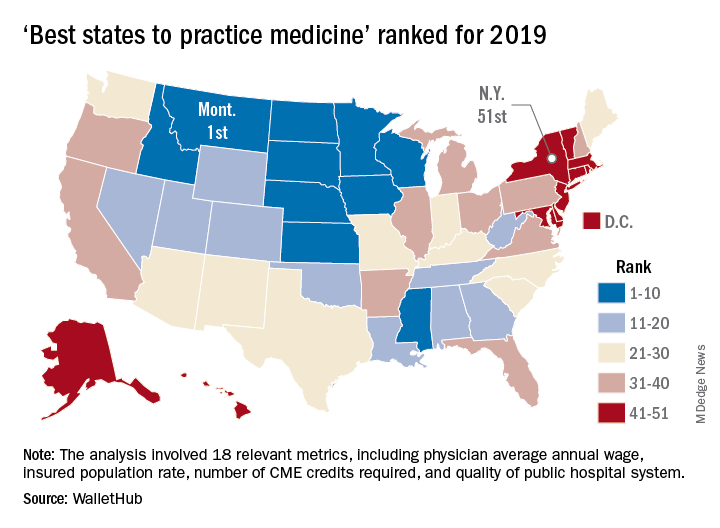
Montana had a total score of 69.15 out of 100 in the ranking of the best and worst states for doctors for 2019, with Wisconsin coming in at 69.13. The small degree of separation didn’t stop there, though, as third-place Idaho (68.55) and fourth-place Minnesota (68.32) both finished within a single point of the top, with Iowa a bit further behind at 67.58, WalletHub reported. In last year’s ranking, South Dakota won by more than 5 points over Nebraska, and in 2017 Iowa finished more than 2 points ahead of Minnesota.
The lowest-ranked state in 2019 was New York, with a score of 34.01 that was well below the 41.55 earned by 50th-place Washington, D.C. The rest of the bottom five was occupied by Rhode Island, New Jersey, and Connecticut, WalletHub said. New Jersey was the worst state in which to practice medicine in 2018, and New York finished last in 2017.
The rankings are based on 18 metrics across two broad categories: “opportunity and competition” (11 metrics worth 70 points) and “medical environment” (7 metrics worth 30 points). One metric in the opportunity and competition category, physicians’ average annual wage (adjusted for cost of living), was given double weight; other metrics included employer-based insurance rate, projected share of elderly population, punitiveness of state medical board, and malpractice award payout amount per capita.
Montana posted top-five scores in such areas as average physician monthly starting salary, share of medical residents retained, and presence of nationally accredited health departments. New York took big hits with bottom-five scores in adjusted average annual wage, projected competition, and annual cost of malpractice insurance, according to WalletHub.
One HCV infection leads to another in HIV+ MSM
SEATTLE – Once HIV positive men who have sex with men contract the hepatitis C virus, they are more likely to get it again, according a study of 305 men in New York.
Overall, 38 men (12%) picked up another HCV infection a median of 1.9 years after clearance of their first, yielding a reinfection rate was 4.4/100 person-years, “a solid seven times higher than the primary infection rate” among HIV-positive men who have sex with men (MSM), said senior investigator Daniel Fierer, MD, an associate professor of infectious diseases at Mount Sinai Hospital, New York.
Thirty-three men cleared their second infection. Of those, six picked up a third infection at a median of 1.1 years, yielding an overall third infection incidence of 8.7/100 person-years.
The results held no matter how the men cleared HCV, whether spontaneously, as in about 10%, or by interferon before 2013, and direct-acting antivirals (DAAs) after.
Most reinfections occurred within 2 years of initial clearance, but some occurred more than a decade later.
The results suggest that there’s a particular need for HCV prevention efforts among men who have previously cleared the infection. For those patients, testing for HCV at an annual HIV checkup might not be frequent enough, Dr. Fierer said at the Conference on Retroviruses and Opportunistic Infections.
“Long-term surveillance is warranted for all HIV-infected MSM after clearance of HCV infection. Further, strategies to reduce HCV reinfections are needed to meet the goal of eliminating HCV in these men,” he said.
Also, “the large difference between primary” and secondary infection “rates suggests HCV risk is not distributed evenly between HIV-infected MSM, but concentrated among a small subpopulation. By definition, this subpopulation would have a higher prevalence” of risky behavior, such as condomless receptive anal sex and sexualized injection methamphetamine use, he said.
The high reinfection rate “tells us basically that we have not done a good job of” preventing infection and reinfection among at risk, HIV-positive men. There’s an “inadequate level of HCV treatment ... we need to eliminate restrictions on DAA” access, Dr. Fierer said.
As far as prevention goes, “I believe we just don’t know what to do. I tell all of my patients about the body fluids that have HCV in them,” which is a good start, he said.
The median age at first clearance was about 45 years, 82% of the men were white, and there was about a 50-50 split between people with private and public insurance.
The work was funded by Gilead. Dr. Fierer did not mention any disclosures.
SOURCE: Carollo JR et al. CROI 2019, Abstract 86
SEATTLE – Once HIV positive men who have sex with men contract the hepatitis C virus, they are more likely to get it again, according a study of 305 men in New York.
Overall, 38 men (12%) picked up another HCV infection a median of 1.9 years after clearance of their first, yielding a reinfection rate was 4.4/100 person-years, “a solid seven times higher than the primary infection rate” among HIV-positive men who have sex with men (MSM), said senior investigator Daniel Fierer, MD, an associate professor of infectious diseases at Mount Sinai Hospital, New York.
Thirty-three men cleared their second infection. Of those, six picked up a third infection at a median of 1.1 years, yielding an overall third infection incidence of 8.7/100 person-years.
The results held no matter how the men cleared HCV, whether spontaneously, as in about 10%, or by interferon before 2013, and direct-acting antivirals (DAAs) after.
Most reinfections occurred within 2 years of initial clearance, but some occurred more than a decade later.
The results suggest that there’s a particular need for HCV prevention efforts among men who have previously cleared the infection. For those patients, testing for HCV at an annual HIV checkup might not be frequent enough, Dr. Fierer said at the Conference on Retroviruses and Opportunistic Infections.
“Long-term surveillance is warranted for all HIV-infected MSM after clearance of HCV infection. Further, strategies to reduce HCV reinfections are needed to meet the goal of eliminating HCV in these men,” he said.
Also, “the large difference between primary” and secondary infection “rates suggests HCV risk is not distributed evenly between HIV-infected MSM, but concentrated among a small subpopulation. By definition, this subpopulation would have a higher prevalence” of risky behavior, such as condomless receptive anal sex and sexualized injection methamphetamine use, he said.
The high reinfection rate “tells us basically that we have not done a good job of” preventing infection and reinfection among at risk, HIV-positive men. There’s an “inadequate level of HCV treatment ... we need to eliminate restrictions on DAA” access, Dr. Fierer said.
As far as prevention goes, “I believe we just don’t know what to do. I tell all of my patients about the body fluids that have HCV in them,” which is a good start, he said.
The median age at first clearance was about 45 years, 82% of the men were white, and there was about a 50-50 split between people with private and public insurance.
The work was funded by Gilead. Dr. Fierer did not mention any disclosures.
SOURCE: Carollo JR et al. CROI 2019, Abstract 86
SEATTLE – Once HIV positive men who have sex with men contract the hepatitis C virus, they are more likely to get it again, according a study of 305 men in New York.
Overall, 38 men (12%) picked up another HCV infection a median of 1.9 years after clearance of their first, yielding a reinfection rate was 4.4/100 person-years, “a solid seven times higher than the primary infection rate” among HIV-positive men who have sex with men (MSM), said senior investigator Daniel Fierer, MD, an associate professor of infectious diseases at Mount Sinai Hospital, New York.
Thirty-three men cleared their second infection. Of those, six picked up a third infection at a median of 1.1 years, yielding an overall third infection incidence of 8.7/100 person-years.
The results held no matter how the men cleared HCV, whether spontaneously, as in about 10%, or by interferon before 2013, and direct-acting antivirals (DAAs) after.
Most reinfections occurred within 2 years of initial clearance, but some occurred more than a decade later.
The results suggest that there’s a particular need for HCV prevention efforts among men who have previously cleared the infection. For those patients, testing for HCV at an annual HIV checkup might not be frequent enough, Dr. Fierer said at the Conference on Retroviruses and Opportunistic Infections.
“Long-term surveillance is warranted for all HIV-infected MSM after clearance of HCV infection. Further, strategies to reduce HCV reinfections are needed to meet the goal of eliminating HCV in these men,” he said.
Also, “the large difference between primary” and secondary infection “rates suggests HCV risk is not distributed evenly between HIV-infected MSM, but concentrated among a small subpopulation. By definition, this subpopulation would have a higher prevalence” of risky behavior, such as condomless receptive anal sex and sexualized injection methamphetamine use, he said.
The high reinfection rate “tells us basically that we have not done a good job of” preventing infection and reinfection among at risk, HIV-positive men. There’s an “inadequate level of HCV treatment ... we need to eliminate restrictions on DAA” access, Dr. Fierer said.
As far as prevention goes, “I believe we just don’t know what to do. I tell all of my patients about the body fluids that have HCV in them,” which is a good start, he said.
The median age at first clearance was about 45 years, 82% of the men were white, and there was about a 50-50 split between people with private and public insurance.
The work was funded by Gilead. Dr. Fierer did not mention any disclosures.
SOURCE: Carollo JR et al. CROI 2019, Abstract 86
REPORTING FROM CROI 2019
Do Collaborative Models Work for Mental Health in a General Clinical Setting?
Collaborative chronic care models (CCMs) are effective in serious mental illnesses, which has been shown in extensive randomized clinical trials. Much of their effectiveness comes from the emphasis on flexibility: They are implemented according to local needs, capabilities, and priorities. Collaborative chronic care models also provide support: for redesigned work roles that promote “anticipatory” continuous care, for self-management, and for clinical decision making at a local level.
In 2013, the VA Office of Mental Health and Suicide Prevention (OMHSP) began an initiative to enhance care coordination in general mental health clinics with mixed-diagnosis populations. It established interdisciplinary teams in each VA medical center throughout the US. Although providing centrally developed guidance, VAOMHSP gave facilities “broad latitude” to develop their team processes. In 2015, VAOMHSP adopted the CCM.
But most of the data on how well CCMs work for mental health conditions come from depression treatment in primary care—and the effects seem to be inconsistent. So researchers from Veterans Affairs Boston Healthcare System and others partnered with VAOMHSP to find out whether the CCM model would be effective in a general clinical setting.
They recruited 9 VA facilities for a 2-year study conducted in 3 waves. The implementation strategy was based on the premise that “health care is a complex adaptive system rather than a highly controlled machine.” That is, it would work best if local solutions for local challenges could be developed in accordance with evidence-based guidance. The multifaceted approach included an external facilitator who provided guidance and quality improvement expertise and an on-site internal facilitator to direct the implementation.
In the study, 5,596 veterans treated by outpatient general mental health teams were included in hospitalization analyses. A randomly selected sample of 1,050 (including 210 women) was identified for health status interviews.
The researchers found a “robust” and sustained reduction in mental health hospitalization. However, the effects on self-reported health outcomes were “limited,” the researchers say. The mental component score (the primary intervention outcome) did not change statistically significantly with implementation support in adjusted or unadjusted models, nor did other interview measures. The researchers say they saw no difference in the way veterans were treated between higher and lower implementing teams.
In post hoc analyses, though, patients with more complex problems, defined as receiving treatment for ≥ 3 mental health diagnoses in the previous year, did show statistically significant improvements in the facilitation year (by a magnitude of 0.31 SD). By contrast, those with ≤ 2 diagnoses declined nonsignificantly during the same time. The researchers note that other studies have found that CCM-based teams in patient-centered medical homes have also shown more benefit among higher morbidity patients.
Overall, the model was shown to be effectively implemented with “practical, scalable support” for clinicians. Another benefit was that teams performed better, the researchers found. They assessed team function at baseline and during the second 6 months on measures, including communication, cohesion, role clarity, and team primacy (prioritizing team over individual goals). The subscales showed high ratings for cohesion and communication at baseline, which did not change with implementation support. However, role clarity and team primacy improved significantly. The researchers conclude that under typical practice conditions CCMs can help the clinicians help the sickest patients.
Collaborative chronic care models (CCMs) are effective in serious mental illnesses, which has been shown in extensive randomized clinical trials. Much of their effectiveness comes from the emphasis on flexibility: They are implemented according to local needs, capabilities, and priorities. Collaborative chronic care models also provide support: for redesigned work roles that promote “anticipatory” continuous care, for self-management, and for clinical decision making at a local level.
In 2013, the VA Office of Mental Health and Suicide Prevention (OMHSP) began an initiative to enhance care coordination in general mental health clinics with mixed-diagnosis populations. It established interdisciplinary teams in each VA medical center throughout the US. Although providing centrally developed guidance, VAOMHSP gave facilities “broad latitude” to develop their team processes. In 2015, VAOMHSP adopted the CCM.
But most of the data on how well CCMs work for mental health conditions come from depression treatment in primary care—and the effects seem to be inconsistent. So researchers from Veterans Affairs Boston Healthcare System and others partnered with VAOMHSP to find out whether the CCM model would be effective in a general clinical setting.
They recruited 9 VA facilities for a 2-year study conducted in 3 waves. The implementation strategy was based on the premise that “health care is a complex adaptive system rather than a highly controlled machine.” That is, it would work best if local solutions for local challenges could be developed in accordance with evidence-based guidance. The multifaceted approach included an external facilitator who provided guidance and quality improvement expertise and an on-site internal facilitator to direct the implementation.
In the study, 5,596 veterans treated by outpatient general mental health teams were included in hospitalization analyses. A randomly selected sample of 1,050 (including 210 women) was identified for health status interviews.
The researchers found a “robust” and sustained reduction in mental health hospitalization. However, the effects on self-reported health outcomes were “limited,” the researchers say. The mental component score (the primary intervention outcome) did not change statistically significantly with implementation support in adjusted or unadjusted models, nor did other interview measures. The researchers say they saw no difference in the way veterans were treated between higher and lower implementing teams.
In post hoc analyses, though, patients with more complex problems, defined as receiving treatment for ≥ 3 mental health diagnoses in the previous year, did show statistically significant improvements in the facilitation year (by a magnitude of 0.31 SD). By contrast, those with ≤ 2 diagnoses declined nonsignificantly during the same time. The researchers note that other studies have found that CCM-based teams in patient-centered medical homes have also shown more benefit among higher morbidity patients.
Overall, the model was shown to be effectively implemented with “practical, scalable support” for clinicians. Another benefit was that teams performed better, the researchers found. They assessed team function at baseline and during the second 6 months on measures, including communication, cohesion, role clarity, and team primacy (prioritizing team over individual goals). The subscales showed high ratings for cohesion and communication at baseline, which did not change with implementation support. However, role clarity and team primacy improved significantly. The researchers conclude that under typical practice conditions CCMs can help the clinicians help the sickest patients.
Collaborative chronic care models (CCMs) are effective in serious mental illnesses, which has been shown in extensive randomized clinical trials. Much of their effectiveness comes from the emphasis on flexibility: They are implemented according to local needs, capabilities, and priorities. Collaborative chronic care models also provide support: for redesigned work roles that promote “anticipatory” continuous care, for self-management, and for clinical decision making at a local level.
In 2013, the VA Office of Mental Health and Suicide Prevention (OMHSP) began an initiative to enhance care coordination in general mental health clinics with mixed-diagnosis populations. It established interdisciplinary teams in each VA medical center throughout the US. Although providing centrally developed guidance, VAOMHSP gave facilities “broad latitude” to develop their team processes. In 2015, VAOMHSP adopted the CCM.
But most of the data on how well CCMs work for mental health conditions come from depression treatment in primary care—and the effects seem to be inconsistent. So researchers from Veterans Affairs Boston Healthcare System and others partnered with VAOMHSP to find out whether the CCM model would be effective in a general clinical setting.
They recruited 9 VA facilities for a 2-year study conducted in 3 waves. The implementation strategy was based on the premise that “health care is a complex adaptive system rather than a highly controlled machine.” That is, it would work best if local solutions for local challenges could be developed in accordance with evidence-based guidance. The multifaceted approach included an external facilitator who provided guidance and quality improvement expertise and an on-site internal facilitator to direct the implementation.
In the study, 5,596 veterans treated by outpatient general mental health teams were included in hospitalization analyses. A randomly selected sample of 1,050 (including 210 women) was identified for health status interviews.
The researchers found a “robust” and sustained reduction in mental health hospitalization. However, the effects on self-reported health outcomes were “limited,” the researchers say. The mental component score (the primary intervention outcome) did not change statistically significantly with implementation support in adjusted or unadjusted models, nor did other interview measures. The researchers say they saw no difference in the way veterans were treated between higher and lower implementing teams.
In post hoc analyses, though, patients with more complex problems, defined as receiving treatment for ≥ 3 mental health diagnoses in the previous year, did show statistically significant improvements in the facilitation year (by a magnitude of 0.31 SD). By contrast, those with ≤ 2 diagnoses declined nonsignificantly during the same time. The researchers note that other studies have found that CCM-based teams in patient-centered medical homes have also shown more benefit among higher morbidity patients.
Overall, the model was shown to be effectively implemented with “practical, scalable support” for clinicians. Another benefit was that teams performed better, the researchers found. They assessed team function at baseline and during the second 6 months on measures, including communication, cohesion, role clarity, and team primacy (prioritizing team over individual goals). The subscales showed high ratings for cohesion and communication at baseline, which did not change with implementation support. However, role clarity and team primacy improved significantly. The researchers conclude that under typical practice conditions CCMs can help the clinicians help the sickest patients.
Imaging mass cytometry sheds light on inflammation, demyelination in MS
DALLAS – Imaging mass cytometry is helping researchers to better understand how meningeal inflammation relates to cortical pathology in a subset of multiple sclerosis patients.
This technique for examining multiple proteins within intact tissue and distinguishing cell types based on complex combinations of markers has helped to spot evidence of meningeal inflammation in areas of patient brain samples with cortical gray matter lesions, confirming demyelination and meningeal inflammation observed in experimental allergic encephalomyelitis mouse models.
Imaging mass cytometry “allows us to potentially discriminate microglia from macrophages within brain lesions,” Jennifer Gommerman, PhD, said at a meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “We can look at lymphocytes as well. There’s a lot of potential with this technique, and we’re excited to apply it to the meningeal inflammatory sections of the brain.”
Dr. Gommerman, professor of immunology at the University of Toronto, noted that multiple sclerosis (MS) begins often with a relapsing form of the disease, which tracks with deep white matter lesions that clinicians can image with MRI. “But as the disease progresses, we know that pathology can change, and we can see more pathology in the cortex, including varied bands of demyelination that are adjacent to the meninges,” she said. “This phase of the disease is not effectively treated by therapeutics.”
In this later phase of the disease, she continued, “it’s thought perhaps that the immune system isn’t playing such a big role, but there has been a fair bit of evidence in the literature in recent years that there are in fact immune cells in the brains of people with progressive MS. You can find them in the meninges. They can form clusters of cells within the meninges and they tend to be adjacent to areas of cortical demyelination, suggesting they might be involved in this pathology.”
Dr. Gommerman and her colleagues developed an animal model to evaluate meningeal inflammation in an effort to determine if they can model cortical injury and disease progression. They used an adoptive transfer form of experimental allergic encephalomyelitis in which they prime T cells in SJL mice, remove them, polarize them toward a Th17 phenotype, and transfer them into naive recipients. “When we do this we can see clusters of immune cells forming in the meninges,” Dr. Gommerman said. “They start with T cells but then become overwhelmingly populated by B cells.” Adjacent to these clusters they noted disruption of the glia limitans and demyelination in the cortex. “There’s clearly something going on in the cortex of these animals.”
Mindful that age is one of the most significant predictors of disease progression, the researchers transferred young T cells into mice that were 6-8 months old in addition to animals that were 6-8 weeks old. “Upon sacrifice, the younger mice that got the young T cells had largely resolved their cortical pathology, while the old mice that got the young T cells still showed evidence of demyelination, very angry microglia, and a continual disruption of the glial limitans,” Dr. Gommerman said. “We were able to see axonal stress in comparison to the young mice. We also saw some evidence of synapse loss. It seems that these animals not only have demyelination in the cortex, but there are problems with the axons and the synapses.”
To apply this model in humans, she and her colleagues collaborated with Netherlands Brain Bank in order to obtain brain samples for analysis with imaging mass cytometry, which provides a time-of-flight mass spectrometry readout of the staining pattern of heavy metal ion–tagged antibodies on a single slide-mounted tissue section.
“We really have to be careful which [brain] samples we choose, because not all samples from progressive MS patients have evidence of meningeal inflammation,” she noted. So far, they have observed that meningeal inflammation is associated with gray matter lesions, rather than with normal-appearing gray matter.
“We also need to look at appropriate controls, so our plan is to look at patients who have meningeal inflammation but do not have MS,” she said.
Dr. Gommerman reported having received grants from Novartis, Roche, and Merck, as well as a consulting agreement with Roche.
DALLAS – Imaging mass cytometry is helping researchers to better understand how meningeal inflammation relates to cortical pathology in a subset of multiple sclerosis patients.
This technique for examining multiple proteins within intact tissue and distinguishing cell types based on complex combinations of markers has helped to spot evidence of meningeal inflammation in areas of patient brain samples with cortical gray matter lesions, confirming demyelination and meningeal inflammation observed in experimental allergic encephalomyelitis mouse models.
Imaging mass cytometry “allows us to potentially discriminate microglia from macrophages within brain lesions,” Jennifer Gommerman, PhD, said at a meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “We can look at lymphocytes as well. There’s a lot of potential with this technique, and we’re excited to apply it to the meningeal inflammatory sections of the brain.”
Dr. Gommerman, professor of immunology at the University of Toronto, noted that multiple sclerosis (MS) begins often with a relapsing form of the disease, which tracks with deep white matter lesions that clinicians can image with MRI. “But as the disease progresses, we know that pathology can change, and we can see more pathology in the cortex, including varied bands of demyelination that are adjacent to the meninges,” she said. “This phase of the disease is not effectively treated by therapeutics.”
In this later phase of the disease, she continued, “it’s thought perhaps that the immune system isn’t playing such a big role, but there has been a fair bit of evidence in the literature in recent years that there are in fact immune cells in the brains of people with progressive MS. You can find them in the meninges. They can form clusters of cells within the meninges and they tend to be adjacent to areas of cortical demyelination, suggesting they might be involved in this pathology.”
Dr. Gommerman and her colleagues developed an animal model to evaluate meningeal inflammation in an effort to determine if they can model cortical injury and disease progression. They used an adoptive transfer form of experimental allergic encephalomyelitis in which they prime T cells in SJL mice, remove them, polarize them toward a Th17 phenotype, and transfer them into naive recipients. “When we do this we can see clusters of immune cells forming in the meninges,” Dr. Gommerman said. “They start with T cells but then become overwhelmingly populated by B cells.” Adjacent to these clusters they noted disruption of the glia limitans and demyelination in the cortex. “There’s clearly something going on in the cortex of these animals.”
Mindful that age is one of the most significant predictors of disease progression, the researchers transferred young T cells into mice that were 6-8 months old in addition to animals that were 6-8 weeks old. “Upon sacrifice, the younger mice that got the young T cells had largely resolved their cortical pathology, while the old mice that got the young T cells still showed evidence of demyelination, very angry microglia, and a continual disruption of the glial limitans,” Dr. Gommerman said. “We were able to see axonal stress in comparison to the young mice. We also saw some evidence of synapse loss. It seems that these animals not only have demyelination in the cortex, but there are problems with the axons and the synapses.”
To apply this model in humans, she and her colleagues collaborated with Netherlands Brain Bank in order to obtain brain samples for analysis with imaging mass cytometry, which provides a time-of-flight mass spectrometry readout of the staining pattern of heavy metal ion–tagged antibodies on a single slide-mounted tissue section.
“We really have to be careful which [brain] samples we choose, because not all samples from progressive MS patients have evidence of meningeal inflammation,” she noted. So far, they have observed that meningeal inflammation is associated with gray matter lesions, rather than with normal-appearing gray matter.
“We also need to look at appropriate controls, so our plan is to look at patients who have meningeal inflammation but do not have MS,” she said.
Dr. Gommerman reported having received grants from Novartis, Roche, and Merck, as well as a consulting agreement with Roche.
DALLAS – Imaging mass cytometry is helping researchers to better understand how meningeal inflammation relates to cortical pathology in a subset of multiple sclerosis patients.
This technique for examining multiple proteins within intact tissue and distinguishing cell types based on complex combinations of markers has helped to spot evidence of meningeal inflammation in areas of patient brain samples with cortical gray matter lesions, confirming demyelination and meningeal inflammation observed in experimental allergic encephalomyelitis mouse models.
Imaging mass cytometry “allows us to potentially discriminate microglia from macrophages within brain lesions,” Jennifer Gommerman, PhD, said at a meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “We can look at lymphocytes as well. There’s a lot of potential with this technique, and we’re excited to apply it to the meningeal inflammatory sections of the brain.”
Dr. Gommerman, professor of immunology at the University of Toronto, noted that multiple sclerosis (MS) begins often with a relapsing form of the disease, which tracks with deep white matter lesions that clinicians can image with MRI. “But as the disease progresses, we know that pathology can change, and we can see more pathology in the cortex, including varied bands of demyelination that are adjacent to the meninges,” she said. “This phase of the disease is not effectively treated by therapeutics.”
In this later phase of the disease, she continued, “it’s thought perhaps that the immune system isn’t playing such a big role, but there has been a fair bit of evidence in the literature in recent years that there are in fact immune cells in the brains of people with progressive MS. You can find them in the meninges. They can form clusters of cells within the meninges and they tend to be adjacent to areas of cortical demyelination, suggesting they might be involved in this pathology.”
Dr. Gommerman and her colleagues developed an animal model to evaluate meningeal inflammation in an effort to determine if they can model cortical injury and disease progression. They used an adoptive transfer form of experimental allergic encephalomyelitis in which they prime T cells in SJL mice, remove them, polarize them toward a Th17 phenotype, and transfer them into naive recipients. “When we do this we can see clusters of immune cells forming in the meninges,” Dr. Gommerman said. “They start with T cells but then become overwhelmingly populated by B cells.” Adjacent to these clusters they noted disruption of the glia limitans and demyelination in the cortex. “There’s clearly something going on in the cortex of these animals.”
Mindful that age is one of the most significant predictors of disease progression, the researchers transferred young T cells into mice that were 6-8 months old in addition to animals that were 6-8 weeks old. “Upon sacrifice, the younger mice that got the young T cells had largely resolved their cortical pathology, while the old mice that got the young T cells still showed evidence of demyelination, very angry microglia, and a continual disruption of the glial limitans,” Dr. Gommerman said. “We were able to see axonal stress in comparison to the young mice. We also saw some evidence of synapse loss. It seems that these animals not only have demyelination in the cortex, but there are problems with the axons and the synapses.”
To apply this model in humans, she and her colleagues collaborated with Netherlands Brain Bank in order to obtain brain samples for analysis with imaging mass cytometry, which provides a time-of-flight mass spectrometry readout of the staining pattern of heavy metal ion–tagged antibodies on a single slide-mounted tissue section.
“We really have to be careful which [brain] samples we choose, because not all samples from progressive MS patients have evidence of meningeal inflammation,” she noted. So far, they have observed that meningeal inflammation is associated with gray matter lesions, rather than with normal-appearing gray matter.
“We also need to look at appropriate controls, so our plan is to look at patients who have meningeal inflammation but do not have MS,” she said.
Dr. Gommerman reported having received grants from Novartis, Roche, and Merck, as well as a consulting agreement with Roche.
EXPERT ANALYSIS FROM ACTRIMS FORUM 2019