User login
Prices impacting insulin use
. Also today, methotrexate fails to cut cardiovascular events, a single-item scale is effective for assessing sleep quality, and deaths from opioid overdose for inpatients with sickle cell disease do not match those of general inpatients.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
. Also today, methotrexate fails to cut cardiovascular events, a single-item scale is effective for assessing sleep quality, and deaths from opioid overdose for inpatients with sickle cell disease do not match those of general inpatients.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
. Also today, methotrexate fails to cut cardiovascular events, a single-item scale is effective for assessing sleep quality, and deaths from opioid overdose for inpatients with sickle cell disease do not match those of general inpatients.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Overemphasizing Communities in the National Strategy for Preventing Veteran Suicide Could Undercut VA Successes
In June 2018, the US Department of Veterans Affairs (VA) issued its National Strategy for Preventing Veteran Suicide, 2018-2028. Its 14 goals—many highly innovative—are “to provide a framework for identifying priorities, organizing efforts, and contributing to a national focus on Veteran suicide prevention.”1
The National Strategy recognizes that suicide prevention requires a 3-pronged approach that includes universal, selective, and targeted strategies because “suicide cannot be prevented by any single strategy.”1 Even so, the National Strategy does not heed this core tenet. It focuses exclusively on universal, non-VA community-based priorities and efforts. That focus causes a problem because it neglects the other strategies. It also is precarious because in the current era of VA zero sum budgets, increases in 1 domain come from decreases in another. Thus, sole prioritizing of universal community components could divert funds from extant effective VA suicide prevention programs.
Community-based engagement is unquestionably necessary to prevent suicide among all veterans. Even so, a 10-year prospective strategy should build up, not compromise, VA initiatives. The plan would be improved by explicitly bolstering VA programs that are making a vital difference.
Undercutting VA Suicide Prevention
As my recent review in Federal Practitioner documented, VA’s multiple levels of evidenced-based suicide prevention practices are pre-eminent in the field.2 The VA’s innovative use of predictive analytics to identify and intervene with at-risk individuals is more advanced than anything available in the community. For older veterans who constitute the majority of veterans and the majority of veteran suicides, the VA has more comprehensive and integrated mental health care services than those found in community-based care systems. The embedding of suicide prevention coordinators at every VA facility is unparalleled.
But one would never know about such quality from the National Strategy document: The VA is barely mentioned. The report never advocates for strengthening—or even maintaining—VA’s resources, programs, and efforts. It never recommends that eligible veterans be connected to VA mental health services.
The strategy observes that employment and housing are keys that protect against suicide risk. It does not, however, call for boosting and resourcing VA’s integrated approach that wraps in social services better than does any other program. Similarly, it acknowledges the role of family involvement in mitigating risk but does not propose expanding VA treatments to improve relationship well-being, leaving these services to the private sector.
The National Strategy expands on the recent suicide prevention executive order (EO) for supporting veterans during their transition from military to civilian life. Yet the EO has no funding allocated to this critical initiative. The National Strategy has the same shortcoming. In failing to advocate for more funds to pay for vastly enhanced outreach and intervention, the plan could drain the VA of existing resources needed to maintain its high-quality, suicide prevention services.
First Step: Define the Problem
The National Strategy wisely specifies that the initial step in any suicide prevention effort should be to “define the problem. This involves collecting data to determine the ‘who,’ ‘what,’ ‘where,’ ‘when,’ and ‘how’ of suicide deaths.” Then, “identify risk and protective factors.”
Yet the report doesn’t follow its own advice. Although little is known about the 14 of 20 veterans who die by suicide daily who are not recent users of VA health services, the National Strategy foregoes the necessity of first ascertaining crucial factors, including whether those veterans were (a) eligible for VA care; (b) receiving any mental health or substance use treatment; and (c) going through life crises, etc. What’s needed before reallocating funds to community-based programs is for Congress to finance a post-suicide, case-by-case study of these veteran decedents who did not use VA.
Proceeding in this manner has 2 benefits. First, it would allow initiatives to be targeted. Second, it could preserve funds for successful VA programs that otherwise might be cut to pay for private sector programs.
A Positive Starting Point
There are many positive components of the National Strategy for Preventing Veteran Suicide that will make a difference. That said, they fall short of their potential. The following are suggestions that could strengthen the VA’s plan.
First, given the overwhelming use of firearms by veterans who die by suicide, the National Strategy acknowledges that an effective prevention policy must attend to this factor. It prudently calls for expansion of firearm safety/suicide prevention collaboration with firearm owners, firearm dealers, shooting clubs, and gun/hunting organizations. This will help ensure that lethal means safety counseling is culturally relevant, comes from a trusted source, and has no antifirearm bias.
Nothing would be more useful in diminishing suicide than correcting the false belief among many veterans that “the VA wants to take away our guns.” If that misperception were replaced with an accurate message, not only would more at-risk veterans seek out VA mental health care, more veterans/families/friends would adopt a new cultural norm akin to buddies talk to vets in crisis about safely storing guns. Establishing a workgroup with gun constituency collaborators could spearhead such a shift.
Second, although, the National Strategy emphasizes the benefits of using peer supports, peers currently express qualms that they have too little expertise intervening with this vulnerable population. Peers could be given extensive training and continued supervision in suicide prevention techniques.
Third, the National Strategy calls for expanded use of big data predictive analytics, whose initial implementation has shown great promise. However, it fails to mention that this approach depends on linked electronic health records and therefore best succeeds for at-risk veterans within VA but not in insulated community care.
Fourth, the National Strategy recognizes that reshaping media and entertainment portrayals could help prevent veteran suicide. Yet it ignores the importance of correcting the sullied narrative about the VA. The disproportionate negative image contributes to veterans’ reticence to seek VA health care. One simple solution would be to require that service members readying to transition to civilian life be informed about the superior nature of VA mental health care. Another is to provide the media with positive VA stories more routinely.
Fifth, the National Strategy suggests that enhanced community care guidelines be developed, but it never recommends that community partners should equal VA’s standards. Those providers should be mandated to conduct the same root cause analyses and comprehensive documentation of suicide risk assessments that VA does.
Conclusion
With zero sum department budgets, the National Strategy’s exclusive priority on public health, community-based initiatives could undercut VA successes. An amended plan that explicitly supports and further strengthens successful VA suicide prevention programs is warranted.
1. US Department of Veterans Affairs. National Strategy for Preventing Veteran Suicide, 2018-2028. https://www.mentalhealth.va.gov/suicide_prevention/docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-Veterans-Suicide.pdf Published June 2018. Accessed November 6, 2018.
2. Lemle RB. Choice program expansion jeopardizes high-quality VHA mental health Services. Fed Pract. 2018;35(3):18-24.
In June 2018, the US Department of Veterans Affairs (VA) issued its National Strategy for Preventing Veteran Suicide, 2018-2028. Its 14 goals—many highly innovative—are “to provide a framework for identifying priorities, organizing efforts, and contributing to a national focus on Veteran suicide prevention.”1
The National Strategy recognizes that suicide prevention requires a 3-pronged approach that includes universal, selective, and targeted strategies because “suicide cannot be prevented by any single strategy.”1 Even so, the National Strategy does not heed this core tenet. It focuses exclusively on universal, non-VA community-based priorities and efforts. That focus causes a problem because it neglects the other strategies. It also is precarious because in the current era of VA zero sum budgets, increases in 1 domain come from decreases in another. Thus, sole prioritizing of universal community components could divert funds from extant effective VA suicide prevention programs.
Community-based engagement is unquestionably necessary to prevent suicide among all veterans. Even so, a 10-year prospective strategy should build up, not compromise, VA initiatives. The plan would be improved by explicitly bolstering VA programs that are making a vital difference.
Undercutting VA Suicide Prevention
As my recent review in Federal Practitioner documented, VA’s multiple levels of evidenced-based suicide prevention practices are pre-eminent in the field.2 The VA’s innovative use of predictive analytics to identify and intervene with at-risk individuals is more advanced than anything available in the community. For older veterans who constitute the majority of veterans and the majority of veteran suicides, the VA has more comprehensive and integrated mental health care services than those found in community-based care systems. The embedding of suicide prevention coordinators at every VA facility is unparalleled.
But one would never know about such quality from the National Strategy document: The VA is barely mentioned. The report never advocates for strengthening—or even maintaining—VA’s resources, programs, and efforts. It never recommends that eligible veterans be connected to VA mental health services.
The strategy observes that employment and housing are keys that protect against suicide risk. It does not, however, call for boosting and resourcing VA’s integrated approach that wraps in social services better than does any other program. Similarly, it acknowledges the role of family involvement in mitigating risk but does not propose expanding VA treatments to improve relationship well-being, leaving these services to the private sector.
The National Strategy expands on the recent suicide prevention executive order (EO) for supporting veterans during their transition from military to civilian life. Yet the EO has no funding allocated to this critical initiative. The National Strategy has the same shortcoming. In failing to advocate for more funds to pay for vastly enhanced outreach and intervention, the plan could drain the VA of existing resources needed to maintain its high-quality, suicide prevention services.
First Step: Define the Problem
The National Strategy wisely specifies that the initial step in any suicide prevention effort should be to “define the problem. This involves collecting data to determine the ‘who,’ ‘what,’ ‘where,’ ‘when,’ and ‘how’ of suicide deaths.” Then, “identify risk and protective factors.”
Yet the report doesn’t follow its own advice. Although little is known about the 14 of 20 veterans who die by suicide daily who are not recent users of VA health services, the National Strategy foregoes the necessity of first ascertaining crucial factors, including whether those veterans were (a) eligible for VA care; (b) receiving any mental health or substance use treatment; and (c) going through life crises, etc. What’s needed before reallocating funds to community-based programs is for Congress to finance a post-suicide, case-by-case study of these veteran decedents who did not use VA.
Proceeding in this manner has 2 benefits. First, it would allow initiatives to be targeted. Second, it could preserve funds for successful VA programs that otherwise might be cut to pay for private sector programs.
A Positive Starting Point
There are many positive components of the National Strategy for Preventing Veteran Suicide that will make a difference. That said, they fall short of their potential. The following are suggestions that could strengthen the VA’s plan.
First, given the overwhelming use of firearms by veterans who die by suicide, the National Strategy acknowledges that an effective prevention policy must attend to this factor. It prudently calls for expansion of firearm safety/suicide prevention collaboration with firearm owners, firearm dealers, shooting clubs, and gun/hunting organizations. This will help ensure that lethal means safety counseling is culturally relevant, comes from a trusted source, and has no antifirearm bias.
Nothing would be more useful in diminishing suicide than correcting the false belief among many veterans that “the VA wants to take away our guns.” If that misperception were replaced with an accurate message, not only would more at-risk veterans seek out VA mental health care, more veterans/families/friends would adopt a new cultural norm akin to buddies talk to vets in crisis about safely storing guns. Establishing a workgroup with gun constituency collaborators could spearhead such a shift.
Second, although, the National Strategy emphasizes the benefits of using peer supports, peers currently express qualms that they have too little expertise intervening with this vulnerable population. Peers could be given extensive training and continued supervision in suicide prevention techniques.
Third, the National Strategy calls for expanded use of big data predictive analytics, whose initial implementation has shown great promise. However, it fails to mention that this approach depends on linked electronic health records and therefore best succeeds for at-risk veterans within VA but not in insulated community care.
Fourth, the National Strategy recognizes that reshaping media and entertainment portrayals could help prevent veteran suicide. Yet it ignores the importance of correcting the sullied narrative about the VA. The disproportionate negative image contributes to veterans’ reticence to seek VA health care. One simple solution would be to require that service members readying to transition to civilian life be informed about the superior nature of VA mental health care. Another is to provide the media with positive VA stories more routinely.
Fifth, the National Strategy suggests that enhanced community care guidelines be developed, but it never recommends that community partners should equal VA’s standards. Those providers should be mandated to conduct the same root cause analyses and comprehensive documentation of suicide risk assessments that VA does.
Conclusion
With zero sum department budgets, the National Strategy’s exclusive priority on public health, community-based initiatives could undercut VA successes. An amended plan that explicitly supports and further strengthens successful VA suicide prevention programs is warranted.
In June 2018, the US Department of Veterans Affairs (VA) issued its National Strategy for Preventing Veteran Suicide, 2018-2028. Its 14 goals—many highly innovative—are “to provide a framework for identifying priorities, organizing efforts, and contributing to a national focus on Veteran suicide prevention.”1
The National Strategy recognizes that suicide prevention requires a 3-pronged approach that includes universal, selective, and targeted strategies because “suicide cannot be prevented by any single strategy.”1 Even so, the National Strategy does not heed this core tenet. It focuses exclusively on universal, non-VA community-based priorities and efforts. That focus causes a problem because it neglects the other strategies. It also is precarious because in the current era of VA zero sum budgets, increases in 1 domain come from decreases in another. Thus, sole prioritizing of universal community components could divert funds from extant effective VA suicide prevention programs.
Community-based engagement is unquestionably necessary to prevent suicide among all veterans. Even so, a 10-year prospective strategy should build up, not compromise, VA initiatives. The plan would be improved by explicitly bolstering VA programs that are making a vital difference.
Undercutting VA Suicide Prevention
As my recent review in Federal Practitioner documented, VA’s multiple levels of evidenced-based suicide prevention practices are pre-eminent in the field.2 The VA’s innovative use of predictive analytics to identify and intervene with at-risk individuals is more advanced than anything available in the community. For older veterans who constitute the majority of veterans and the majority of veteran suicides, the VA has more comprehensive and integrated mental health care services than those found in community-based care systems. The embedding of suicide prevention coordinators at every VA facility is unparalleled.
But one would never know about such quality from the National Strategy document: The VA is barely mentioned. The report never advocates for strengthening—or even maintaining—VA’s resources, programs, and efforts. It never recommends that eligible veterans be connected to VA mental health services.
The strategy observes that employment and housing are keys that protect against suicide risk. It does not, however, call for boosting and resourcing VA’s integrated approach that wraps in social services better than does any other program. Similarly, it acknowledges the role of family involvement in mitigating risk but does not propose expanding VA treatments to improve relationship well-being, leaving these services to the private sector.
The National Strategy expands on the recent suicide prevention executive order (EO) for supporting veterans during their transition from military to civilian life. Yet the EO has no funding allocated to this critical initiative. The National Strategy has the same shortcoming. In failing to advocate for more funds to pay for vastly enhanced outreach and intervention, the plan could drain the VA of existing resources needed to maintain its high-quality, suicide prevention services.
First Step: Define the Problem
The National Strategy wisely specifies that the initial step in any suicide prevention effort should be to “define the problem. This involves collecting data to determine the ‘who,’ ‘what,’ ‘where,’ ‘when,’ and ‘how’ of suicide deaths.” Then, “identify risk and protective factors.”
Yet the report doesn’t follow its own advice. Although little is known about the 14 of 20 veterans who die by suicide daily who are not recent users of VA health services, the National Strategy foregoes the necessity of first ascertaining crucial factors, including whether those veterans were (a) eligible for VA care; (b) receiving any mental health or substance use treatment; and (c) going through life crises, etc. What’s needed before reallocating funds to community-based programs is for Congress to finance a post-suicide, case-by-case study of these veteran decedents who did not use VA.
Proceeding in this manner has 2 benefits. First, it would allow initiatives to be targeted. Second, it could preserve funds for successful VA programs that otherwise might be cut to pay for private sector programs.
A Positive Starting Point
There are many positive components of the National Strategy for Preventing Veteran Suicide that will make a difference. That said, they fall short of their potential. The following are suggestions that could strengthen the VA’s plan.
First, given the overwhelming use of firearms by veterans who die by suicide, the National Strategy acknowledges that an effective prevention policy must attend to this factor. It prudently calls for expansion of firearm safety/suicide prevention collaboration with firearm owners, firearm dealers, shooting clubs, and gun/hunting organizations. This will help ensure that lethal means safety counseling is culturally relevant, comes from a trusted source, and has no antifirearm bias.
Nothing would be more useful in diminishing suicide than correcting the false belief among many veterans that “the VA wants to take away our guns.” If that misperception were replaced with an accurate message, not only would more at-risk veterans seek out VA mental health care, more veterans/families/friends would adopt a new cultural norm akin to buddies talk to vets in crisis about safely storing guns. Establishing a workgroup with gun constituency collaborators could spearhead such a shift.
Second, although, the National Strategy emphasizes the benefits of using peer supports, peers currently express qualms that they have too little expertise intervening with this vulnerable population. Peers could be given extensive training and continued supervision in suicide prevention techniques.
Third, the National Strategy calls for expanded use of big data predictive analytics, whose initial implementation has shown great promise. However, it fails to mention that this approach depends on linked electronic health records and therefore best succeeds for at-risk veterans within VA but not in insulated community care.
Fourth, the National Strategy recognizes that reshaping media and entertainment portrayals could help prevent veteran suicide. Yet it ignores the importance of correcting the sullied narrative about the VA. The disproportionate negative image contributes to veterans’ reticence to seek VA health care. One simple solution would be to require that service members readying to transition to civilian life be informed about the superior nature of VA mental health care. Another is to provide the media with positive VA stories more routinely.
Fifth, the National Strategy suggests that enhanced community care guidelines be developed, but it never recommends that community partners should equal VA’s standards. Those providers should be mandated to conduct the same root cause analyses and comprehensive documentation of suicide risk assessments that VA does.
Conclusion
With zero sum department budgets, the National Strategy’s exclusive priority on public health, community-based initiatives could undercut VA successes. An amended plan that explicitly supports and further strengthens successful VA suicide prevention programs is warranted.
1. US Department of Veterans Affairs. National Strategy for Preventing Veteran Suicide, 2018-2028. https://www.mentalhealth.va.gov/suicide_prevention/docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-Veterans-Suicide.pdf Published June 2018. Accessed November 6, 2018.
2. Lemle RB. Choice program expansion jeopardizes high-quality VHA mental health Services. Fed Pract. 2018;35(3):18-24.
1. US Department of Veterans Affairs. National Strategy for Preventing Veteran Suicide, 2018-2028. https://www.mentalhealth.va.gov/suicide_prevention/docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-Veterans-Suicide.pdf Published June 2018. Accessed November 6, 2018.
2. Lemle RB. Choice program expansion jeopardizes high-quality VHA mental health Services. Fed Pract. 2018;35(3):18-24.
ALL regimens clear disease in kids with MPAL
SAN DIEGO—Pediatric patients with mixed phenotype acute leukemia (MPAL) can achieve minimal residual disease (MRD) negativity with acute lymphoblastic leukemia (ALL)-directed chemotherapy, according to new research.
In a retrospective study, most pediatric MPAL patients who received ALL-directed chemotherapy achieved an MRD-negative complete response (CR).
Ninety-three percent of patients achieved a CR at the end of induction with an ALL regimen, 70% were MRD-negative at the end of induction, and 86% were MRD-negative at the end of induction or consolidation.
Etan Orgel, MD, of the University of Southern California, Los Angeles, presented these findings at the ASH 2018 Annual Meeting (abstract 558*).
The study included 94 patients aged 1-21 years who met World Health Organization MPAL criteria and were treated between 2008 and 2016 at one of six U.S. institutions.
Most patients had B/Myeloid phenotype (89%, n=84), 10% (n=9) had T/Myeloid, and 1% (n=1) had B/T phenotype.
Eighty-seven patients (93%) received ALL induction, and 83 (89%) continued on ALL therapy after induction.
Ninety-three percent (81/87) of patients treated with an ALL induction regimen had a CR at the end of induction. One patient died during induction, and six had induction failures, defined as either disease progression (n=2) or MRD of 5% or greater (n=4).
The MRD-negative rates, defined as MRD less than 0.01%, were 70% (59/84) at the end of induction and 86% (68/79) at the end of induction or consolidation.
Twelve of 14 patients (86%) who were MRD-positive at the end of induction and continued on ALL therapy achieved MRD negativity at the end of consolidation.
Survival
The researchers assessed 5-year survival in patients who received an ALL regimen but did not go on to transplant.
In these patients, the 5-year event-free survival (EFS) was 75%, and the 5-year overall survival (OS) was 89%, “thus demonstrating that, for a majority of patients, transplant in first remission may not be necessary,” Dr. Orgel said.
“[T]his is very different from the approach used at many adult centers and many of the adult recommendations,” he added.
The 5-year EFS rate was 80% in patients who were MRD-negative at the end of induction and 52% in patients who were MRD-positive at the end of induction. Five-year OS rates were 91% and 84%, respectively.
The 5-year EFS rate was 77% in patients who were MRD-negative at the end of consolidation and was unavailable in the three patients who were MRD-positive. The 5-year OS rates were 89% and not available, respectively.
In a multivariable analysis, MRD was the strongest predictor of EFS (hazard ratio [HR]=3.5) and OS (HR=4.6).
There was a trend toward earlier failure and worse OS (HR=4.49, P=0.074) for T-lineage-containing MPAL.
“That indicates that this might be a group that needs careful scrutiny of which form of ALL therapy they receive,” Dr. Orgel said.
In closing, he said this research suggests that ALL therapy without transplant may be sufficient to treat most patients with pediatric MPAL. However, he noted that clinical trials are necessary to prospectively validate MRD thresholds at end of induction and consolidation and to establish the threshold for favorable survival.
“Future research should explore either intensification of therapy or different therapies for patients with persistent MRD,” Dr. Orgel said.
He disclosed no conflicts of interest.
* Data in the presentation differ from the abstract.
SAN DIEGO—Pediatric patients with mixed phenotype acute leukemia (MPAL) can achieve minimal residual disease (MRD) negativity with acute lymphoblastic leukemia (ALL)-directed chemotherapy, according to new research.
In a retrospective study, most pediatric MPAL patients who received ALL-directed chemotherapy achieved an MRD-negative complete response (CR).
Ninety-three percent of patients achieved a CR at the end of induction with an ALL regimen, 70% were MRD-negative at the end of induction, and 86% were MRD-negative at the end of induction or consolidation.
Etan Orgel, MD, of the University of Southern California, Los Angeles, presented these findings at the ASH 2018 Annual Meeting (abstract 558*).
The study included 94 patients aged 1-21 years who met World Health Organization MPAL criteria and were treated between 2008 and 2016 at one of six U.S. institutions.
Most patients had B/Myeloid phenotype (89%, n=84), 10% (n=9) had T/Myeloid, and 1% (n=1) had B/T phenotype.
Eighty-seven patients (93%) received ALL induction, and 83 (89%) continued on ALL therapy after induction.
Ninety-three percent (81/87) of patients treated with an ALL induction regimen had a CR at the end of induction. One patient died during induction, and six had induction failures, defined as either disease progression (n=2) or MRD of 5% or greater (n=4).
The MRD-negative rates, defined as MRD less than 0.01%, were 70% (59/84) at the end of induction and 86% (68/79) at the end of induction or consolidation.
Twelve of 14 patients (86%) who were MRD-positive at the end of induction and continued on ALL therapy achieved MRD negativity at the end of consolidation.
Survival
The researchers assessed 5-year survival in patients who received an ALL regimen but did not go on to transplant.
In these patients, the 5-year event-free survival (EFS) was 75%, and the 5-year overall survival (OS) was 89%, “thus demonstrating that, for a majority of patients, transplant in first remission may not be necessary,” Dr. Orgel said.
“[T]his is very different from the approach used at many adult centers and many of the adult recommendations,” he added.
The 5-year EFS rate was 80% in patients who were MRD-negative at the end of induction and 52% in patients who were MRD-positive at the end of induction. Five-year OS rates were 91% and 84%, respectively.
The 5-year EFS rate was 77% in patients who were MRD-negative at the end of consolidation and was unavailable in the three patients who were MRD-positive. The 5-year OS rates were 89% and not available, respectively.
In a multivariable analysis, MRD was the strongest predictor of EFS (hazard ratio [HR]=3.5) and OS (HR=4.6).
There was a trend toward earlier failure and worse OS (HR=4.49, P=0.074) for T-lineage-containing MPAL.
“That indicates that this might be a group that needs careful scrutiny of which form of ALL therapy they receive,” Dr. Orgel said.
In closing, he said this research suggests that ALL therapy without transplant may be sufficient to treat most patients with pediatric MPAL. However, he noted that clinical trials are necessary to prospectively validate MRD thresholds at end of induction and consolidation and to establish the threshold for favorable survival.
“Future research should explore either intensification of therapy or different therapies for patients with persistent MRD,” Dr. Orgel said.
He disclosed no conflicts of interest.
* Data in the presentation differ from the abstract.
SAN DIEGO—Pediatric patients with mixed phenotype acute leukemia (MPAL) can achieve minimal residual disease (MRD) negativity with acute lymphoblastic leukemia (ALL)-directed chemotherapy, according to new research.
In a retrospective study, most pediatric MPAL patients who received ALL-directed chemotherapy achieved an MRD-negative complete response (CR).
Ninety-three percent of patients achieved a CR at the end of induction with an ALL regimen, 70% were MRD-negative at the end of induction, and 86% were MRD-negative at the end of induction or consolidation.
Etan Orgel, MD, of the University of Southern California, Los Angeles, presented these findings at the ASH 2018 Annual Meeting (abstract 558*).
The study included 94 patients aged 1-21 years who met World Health Organization MPAL criteria and were treated between 2008 and 2016 at one of six U.S. institutions.
Most patients had B/Myeloid phenotype (89%, n=84), 10% (n=9) had T/Myeloid, and 1% (n=1) had B/T phenotype.
Eighty-seven patients (93%) received ALL induction, and 83 (89%) continued on ALL therapy after induction.
Ninety-three percent (81/87) of patients treated with an ALL induction regimen had a CR at the end of induction. One patient died during induction, and six had induction failures, defined as either disease progression (n=2) or MRD of 5% or greater (n=4).
The MRD-negative rates, defined as MRD less than 0.01%, were 70% (59/84) at the end of induction and 86% (68/79) at the end of induction or consolidation.
Twelve of 14 patients (86%) who were MRD-positive at the end of induction and continued on ALL therapy achieved MRD negativity at the end of consolidation.
Survival
The researchers assessed 5-year survival in patients who received an ALL regimen but did not go on to transplant.
In these patients, the 5-year event-free survival (EFS) was 75%, and the 5-year overall survival (OS) was 89%, “thus demonstrating that, for a majority of patients, transplant in first remission may not be necessary,” Dr. Orgel said.
“[T]his is very different from the approach used at many adult centers and many of the adult recommendations,” he added.
The 5-year EFS rate was 80% in patients who were MRD-negative at the end of induction and 52% in patients who were MRD-positive at the end of induction. Five-year OS rates were 91% and 84%, respectively.
The 5-year EFS rate was 77% in patients who were MRD-negative at the end of consolidation and was unavailable in the three patients who were MRD-positive. The 5-year OS rates were 89% and not available, respectively.
In a multivariable analysis, MRD was the strongest predictor of EFS (hazard ratio [HR]=3.5) and OS (HR=4.6).
There was a trend toward earlier failure and worse OS (HR=4.49, P=0.074) for T-lineage-containing MPAL.
“That indicates that this might be a group that needs careful scrutiny of which form of ALL therapy they receive,” Dr. Orgel said.
In closing, he said this research suggests that ALL therapy without transplant may be sufficient to treat most patients with pediatric MPAL. However, he noted that clinical trials are necessary to prospectively validate MRD thresholds at end of induction and consolidation and to establish the threshold for favorable survival.
“Future research should explore either intensification of therapy or different therapies for patients with persistent MRD,” Dr. Orgel said.
He disclosed no conflicts of interest.
* Data in the presentation differ from the abstract.
Data support apixaban for cancer-associated VTE, doc says
SAN DIEGO—Apixaban is as safe as, and more effective than, dalteparin for patients with cancer-associated venous thromboembolism (VTE), according to the ADAM VTE trial.
Patients who received apixaban in this trial had similar rates of major bleeding and clinically relevant non-major bleeding as patients who received dalteparin.
However, the rate of VTE recurrence was significantly lower with apixaban than with dalteparin.
“[A]pixaban was associated with very low bleeding rates and venous thrombosis recurrence rates compared to dalteparin,” said Robert D. McBane, MD, of the Mayo Clinic in Rochester, Minnesota.
Dr. McBane presented these results at the 2018 ASH Annual Meeting (abstract 421*).
ADAM VTE (NCT02585713) included 300 adults (age 18 and older) with active cancer and acute VTE who were randomized to receive apixaban (n=150) or dalteparin (n=150).
The dose and schedule for oral apixaban was 10 mg twice daily for 7 days, followed by 5 mg twice daily for 6 months. Dalteparin was given subcutaneously at 200 IU/kg per day for 1 month, followed by 150 IU/kg daily for 6 months.
One hundred and forty-five patients in the apixaban arm and 142 in the dalteparin arm ultimately received their assigned treatment.
Every month, patients completed an anticoagulation satisfaction survey and bruise survey (a modification of the Duke Anticoagulation Satisfaction Scale). They also underwent lab testing (complete blood count, liver and renal function testing) and were assessed for outcomes, medication reconciliation, drug compliance, and ECOG status on a monthly basis.
Patient characteristics
Baseline characteristics were similar between the treatment arms. The mean age was 64 in both arms, and roughly half of patients in both arms were female.
Nine percent of patients in the apixaban arm and 11% in the dalteparin arm had hematologic malignancies. Other cancers included colorectal, lung, pancreatic/hepatobiliary, gynecologic, breast, genitourinary, upper gastrointestinal, and brain cancers.
Sixty-five percent of patients in the apixaban arm and 66% in the dalteparin arm had distant metastasis. Seventy-four percent of patients in both arms were receiving chemotherapy while on study.
Patients had the following qualifying thrombotic events:
- Any pulmonary embolism (PE)—55% of patients in the apixaban arm and 51% in the dalteparin arm
- Any deep vein thrombosis (DVT)—48% and 47%, respectively
- PE only—44% and 39%, respectively
- PE with DVT—12% in both arms
- DVT only—37% and 35%, respectively
- Lower extremity DVT—31% and 34%, respectively
- Upper extremity DVT—17% and 14%, respectively
- Cerebral venous thrombosis (VT)—1% and 0%, respectively
- Splanchnic VT—8% and 18%, respectively.
Bleeding, thrombosis, and death
The study’s primary endpoint was major bleeding, which did not occur in any of the apixaban-treated patients. However, major bleeding did occur in two (1.4%) patients in the dalteparin arm (P=0.14).
A secondary endpoint was major bleeding plus clinically relevant nonmajor bleeding. This occurred in nine (6.2%) patients in the apixaban arm and nine (6.3%) in the dalteparin arm (P=0.88).
The researchers also assessed VTE recurrence. One patient in the apixaban arm (0.7%) and nine in the dalteparin arm (6.3%) had VTE recurrence (P=0.03).
The patient in the apixaban arm experienced cerebral VT, and the patients with recurrence in the dalteparin arm had leg (n=4) or arm (n=2) VTE, PE (n=1), or splanchnic VT (n=2).
One patient in each arm (0.7%) had arterial thrombosis.
There was no significant difference in cumulative mortality between the treatment arms (hazard ratio=1.40; P=0.3078).
Satisfaction and discontinuation
Overall, apixaban fared better than dalteparin in the monthly patient satisfaction surveys. At various time points, apixaban-treated patients were significantly less likely to:
- Be concerned about excessive bruising
- Find anticoagulant treatment a burden or difficult to carry out
- Say anticoagulant treatment added stress to their lives, negatively impacted their quality of life, or caused them “a great deal” of worry, irritation, or frustration.
However, apixaban-treated patients were also less likely than dalteparin recipients to have confidence that their drug protected them from VTE recurrence.
Still, the apixaban recipients were more likely than the dalteparin group to report overall satisfaction with their treatment.
In addition, premature treatment discontinuation was more common in the dalteparin group than in the apixaban group—15% and 4%, respectively (P=0.0012).
“Apixaban was well tolerated with superior patient safety satisfaction as well as significantly fewer study drug discontinuations compared to dalteparin,” Dr. McBane said. “I believe that these data support the use of apixaban for the acute treatment of cancer-associated venous thromboembolism.”
This study was funded by BMS/Pfizer Alliance. Dr. McBane declared no other conflicts of interest.
*Data in the presentation differ from the abstract.
SAN DIEGO—Apixaban is as safe as, and more effective than, dalteparin for patients with cancer-associated venous thromboembolism (VTE), according to the ADAM VTE trial.
Patients who received apixaban in this trial had similar rates of major bleeding and clinically relevant non-major bleeding as patients who received dalteparin.
However, the rate of VTE recurrence was significantly lower with apixaban than with dalteparin.
“[A]pixaban was associated with very low bleeding rates and venous thrombosis recurrence rates compared to dalteparin,” said Robert D. McBane, MD, of the Mayo Clinic in Rochester, Minnesota.
Dr. McBane presented these results at the 2018 ASH Annual Meeting (abstract 421*).
ADAM VTE (NCT02585713) included 300 adults (age 18 and older) with active cancer and acute VTE who were randomized to receive apixaban (n=150) or dalteparin (n=150).
The dose and schedule for oral apixaban was 10 mg twice daily for 7 days, followed by 5 mg twice daily for 6 months. Dalteparin was given subcutaneously at 200 IU/kg per day for 1 month, followed by 150 IU/kg daily for 6 months.
One hundred and forty-five patients in the apixaban arm and 142 in the dalteparin arm ultimately received their assigned treatment.
Every month, patients completed an anticoagulation satisfaction survey and bruise survey (a modification of the Duke Anticoagulation Satisfaction Scale). They also underwent lab testing (complete blood count, liver and renal function testing) and were assessed for outcomes, medication reconciliation, drug compliance, and ECOG status on a monthly basis.
Patient characteristics
Baseline characteristics were similar between the treatment arms. The mean age was 64 in both arms, and roughly half of patients in both arms were female.
Nine percent of patients in the apixaban arm and 11% in the dalteparin arm had hematologic malignancies. Other cancers included colorectal, lung, pancreatic/hepatobiliary, gynecologic, breast, genitourinary, upper gastrointestinal, and brain cancers.
Sixty-five percent of patients in the apixaban arm and 66% in the dalteparin arm had distant metastasis. Seventy-four percent of patients in both arms were receiving chemotherapy while on study.
Patients had the following qualifying thrombotic events:
- Any pulmonary embolism (PE)—55% of patients in the apixaban arm and 51% in the dalteparin arm
- Any deep vein thrombosis (DVT)—48% and 47%, respectively
- PE only—44% and 39%, respectively
- PE with DVT—12% in both arms
- DVT only—37% and 35%, respectively
- Lower extremity DVT—31% and 34%, respectively
- Upper extremity DVT—17% and 14%, respectively
- Cerebral venous thrombosis (VT)—1% and 0%, respectively
- Splanchnic VT—8% and 18%, respectively.
Bleeding, thrombosis, and death
The study’s primary endpoint was major bleeding, which did not occur in any of the apixaban-treated patients. However, major bleeding did occur in two (1.4%) patients in the dalteparin arm (P=0.14).
A secondary endpoint was major bleeding plus clinically relevant nonmajor bleeding. This occurred in nine (6.2%) patients in the apixaban arm and nine (6.3%) in the dalteparin arm (P=0.88).
The researchers also assessed VTE recurrence. One patient in the apixaban arm (0.7%) and nine in the dalteparin arm (6.3%) had VTE recurrence (P=0.03).
The patient in the apixaban arm experienced cerebral VT, and the patients with recurrence in the dalteparin arm had leg (n=4) or arm (n=2) VTE, PE (n=1), or splanchnic VT (n=2).
One patient in each arm (0.7%) had arterial thrombosis.
There was no significant difference in cumulative mortality between the treatment arms (hazard ratio=1.40; P=0.3078).
Satisfaction and discontinuation
Overall, apixaban fared better than dalteparin in the monthly patient satisfaction surveys. At various time points, apixaban-treated patients were significantly less likely to:
- Be concerned about excessive bruising
- Find anticoagulant treatment a burden or difficult to carry out
- Say anticoagulant treatment added stress to their lives, negatively impacted their quality of life, or caused them “a great deal” of worry, irritation, or frustration.
However, apixaban-treated patients were also less likely than dalteparin recipients to have confidence that their drug protected them from VTE recurrence.
Still, the apixaban recipients were more likely than the dalteparin group to report overall satisfaction with their treatment.
In addition, premature treatment discontinuation was more common in the dalteparin group than in the apixaban group—15% and 4%, respectively (P=0.0012).
“Apixaban was well tolerated with superior patient safety satisfaction as well as significantly fewer study drug discontinuations compared to dalteparin,” Dr. McBane said. “I believe that these data support the use of apixaban for the acute treatment of cancer-associated venous thromboembolism.”
This study was funded by BMS/Pfizer Alliance. Dr. McBane declared no other conflicts of interest.
*Data in the presentation differ from the abstract.
SAN DIEGO—Apixaban is as safe as, and more effective than, dalteparin for patients with cancer-associated venous thromboembolism (VTE), according to the ADAM VTE trial.
Patients who received apixaban in this trial had similar rates of major bleeding and clinically relevant non-major bleeding as patients who received dalteparin.
However, the rate of VTE recurrence was significantly lower with apixaban than with dalteparin.
“[A]pixaban was associated with very low bleeding rates and venous thrombosis recurrence rates compared to dalteparin,” said Robert D. McBane, MD, of the Mayo Clinic in Rochester, Minnesota.
Dr. McBane presented these results at the 2018 ASH Annual Meeting (abstract 421*).
ADAM VTE (NCT02585713) included 300 adults (age 18 and older) with active cancer and acute VTE who were randomized to receive apixaban (n=150) or dalteparin (n=150).
The dose and schedule for oral apixaban was 10 mg twice daily for 7 days, followed by 5 mg twice daily for 6 months. Dalteparin was given subcutaneously at 200 IU/kg per day for 1 month, followed by 150 IU/kg daily for 6 months.
One hundred and forty-five patients in the apixaban arm and 142 in the dalteparin arm ultimately received their assigned treatment.
Every month, patients completed an anticoagulation satisfaction survey and bruise survey (a modification of the Duke Anticoagulation Satisfaction Scale). They also underwent lab testing (complete blood count, liver and renal function testing) and were assessed for outcomes, medication reconciliation, drug compliance, and ECOG status on a monthly basis.
Patient characteristics
Baseline characteristics were similar between the treatment arms. The mean age was 64 in both arms, and roughly half of patients in both arms were female.
Nine percent of patients in the apixaban arm and 11% in the dalteparin arm had hematologic malignancies. Other cancers included colorectal, lung, pancreatic/hepatobiliary, gynecologic, breast, genitourinary, upper gastrointestinal, and brain cancers.
Sixty-five percent of patients in the apixaban arm and 66% in the dalteparin arm had distant metastasis. Seventy-four percent of patients in both arms were receiving chemotherapy while on study.
Patients had the following qualifying thrombotic events:
- Any pulmonary embolism (PE)—55% of patients in the apixaban arm and 51% in the dalteparin arm
- Any deep vein thrombosis (DVT)—48% and 47%, respectively
- PE only—44% and 39%, respectively
- PE with DVT—12% in both arms
- DVT only—37% and 35%, respectively
- Lower extremity DVT—31% and 34%, respectively
- Upper extremity DVT—17% and 14%, respectively
- Cerebral venous thrombosis (VT)—1% and 0%, respectively
- Splanchnic VT—8% and 18%, respectively.
Bleeding, thrombosis, and death
The study’s primary endpoint was major bleeding, which did not occur in any of the apixaban-treated patients. However, major bleeding did occur in two (1.4%) patients in the dalteparin arm (P=0.14).
A secondary endpoint was major bleeding plus clinically relevant nonmajor bleeding. This occurred in nine (6.2%) patients in the apixaban arm and nine (6.3%) in the dalteparin arm (P=0.88).
The researchers also assessed VTE recurrence. One patient in the apixaban arm (0.7%) and nine in the dalteparin arm (6.3%) had VTE recurrence (P=0.03).
The patient in the apixaban arm experienced cerebral VT, and the patients with recurrence in the dalteparin arm had leg (n=4) or arm (n=2) VTE, PE (n=1), or splanchnic VT (n=2).
One patient in each arm (0.7%) had arterial thrombosis.
There was no significant difference in cumulative mortality between the treatment arms (hazard ratio=1.40; P=0.3078).
Satisfaction and discontinuation
Overall, apixaban fared better than dalteparin in the monthly patient satisfaction surveys. At various time points, apixaban-treated patients were significantly less likely to:
- Be concerned about excessive bruising
- Find anticoagulant treatment a burden or difficult to carry out
- Say anticoagulant treatment added stress to their lives, negatively impacted their quality of life, or caused them “a great deal” of worry, irritation, or frustration.
However, apixaban-treated patients were also less likely than dalteparin recipients to have confidence that their drug protected them from VTE recurrence.
Still, the apixaban recipients were more likely than the dalteparin group to report overall satisfaction with their treatment.
In addition, premature treatment discontinuation was more common in the dalteparin group than in the apixaban group—15% and 4%, respectively (P=0.0012).
“Apixaban was well tolerated with superior patient safety satisfaction as well as significantly fewer study drug discontinuations compared to dalteparin,” Dr. McBane said. “I believe that these data support the use of apixaban for the acute treatment of cancer-associated venous thromboembolism.”
This study was funded by BMS/Pfizer Alliance. Dr. McBane declared no other conflicts of interest.
*Data in the presentation differ from the abstract.
Shorter R-CHOP regimen noninferior in certain DLBCL patients
SAN DIEGO—A shortened regimen of four cycles of rituximab (R) plus cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) chemotherapy was noninferior in efficacy to the standard six cycles of R-CHOP in younger patients with favorable-risk diffuse large B-cell lymphoma (DLBCL), according to investigators of the FLYER trial.
In addition, the truncated regimen was associated with about a one-third reduction in non-hematologic adverse events.
Viola Poeschel, MD, of Saarland University Medical School in Homburg/Saar, Germany, reported results of this study on behalf of the German High-Grade Non-Hodgkin’s Lymphoma Study Group/German Lymphoma Alliance at the 2018 ASH Annual Meeting (abstract 781).
Among 588 evaluable patients younger than 60 with favorable-prognosis DLBCL, there were no significant differences in progression-free survival (PFS), event-free survival (EFS), or overall survival (OS) between patients who received four cycles of R-CHOP and those who received six cycles, Dr. Poeschel reported.
“Six cycles of R-CHOP led to a higher toxicity with respect to leukocytopenia and anemia, both of any grade and also of grades 3 to 4, compared to four cycles of R-CHOP,” she said.
The findings suggest that, for younger patients with favorable-prognosis DLBCL—defined as an age-adjusted International Prognostic Index score of 0 and low tumor burden (less than 7.5 cm)—four cycles of R-CHOP can be a new standard of care, Dr. Poeschel said.
The investigators were prompted to look at the question of a shorter R-CHOP regimen by results of the MInT trial, in which a subpopulation of favorable-prognosis DLBCL patients had a 3-year PFS rate of 89%.
The FLYER trial (NCT00278421) was designed as a non-inferiority study to see whether, in a similar group of patients, reducing the number of R-CHOP cycles could maintain efficacy while reducing toxicity.
At a median follow-up of 66 months, the PFS rate, the primary endpoint, was 94% in the six-cycle group and 96% for the four-cycle group.
“As the lower limit of the 95% confidence interval of our experimental arm was 94%, it is shown that it is definitely non-inferior to the standard arm, six cycles of R-CHOP,” Dr. Poeschel said.
Similarly, the rate of 3-year OS was 98% in the six-cycle group, compared with 99% in the four-cycle group, and the survival curves were virtually superimposable out to more than 10 years of follow-up.
Treatment with six cycles was associated with more frequent hematologic adverse events than four cycles. Leukopenia of any grade occurred in 237 and 171 patients, respectively. Grade 3-4 leukopenia occurred in 110 and 80 patients, respectively.
Any-grade anemia occurred in 172 patients assigned to six cycles and 107 assigned to four cycles. Rates of grade 3-4 anemia were similar between the groups, as were rates of thrombocytopenia of any grade or grade 3-4.
Non-hematologic adverse events of any grade or grade 3-4 that were more frequent with six cycles included parasthesia, nausea, infection, vomiting, and mucositis.
The total number of non-hematologic adverse events was reduced by about one-third.
“We are certainly always looking for ways to make treatments easier for our patients to reduce adverse effects, and, certainly, for this subgroup of patients, it appears that we can make their treatment shorter and have less burden but equivalent efficacy,” said David Steensma, MD, of the Dana-Farber Cancer Institute/Harvard Cancer Center in Boston, Massachusetts.
Drs. Steensma and Poeschel both cautioned that the results of this study pertain only to those patients with DLBCL who are younger and have favorable-prognosis disease.
“We can’t extend it to other subtypes of large-cell lymphoma, but that’s always a laudable goal, so I think this will immediately influence clinical practice,” Dr. Steensma said.
The study was supported by Deutsche Krebshilfe. Dr. Poeschel disclosed travel grants from Roche and Amgen. Dr. Steensma had no disclosures relevant to the study.
SAN DIEGO—A shortened regimen of four cycles of rituximab (R) plus cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) chemotherapy was noninferior in efficacy to the standard six cycles of R-CHOP in younger patients with favorable-risk diffuse large B-cell lymphoma (DLBCL), according to investigators of the FLYER trial.
In addition, the truncated regimen was associated with about a one-third reduction in non-hematologic adverse events.
Viola Poeschel, MD, of Saarland University Medical School in Homburg/Saar, Germany, reported results of this study on behalf of the German High-Grade Non-Hodgkin’s Lymphoma Study Group/German Lymphoma Alliance at the 2018 ASH Annual Meeting (abstract 781).
Among 588 evaluable patients younger than 60 with favorable-prognosis DLBCL, there were no significant differences in progression-free survival (PFS), event-free survival (EFS), or overall survival (OS) between patients who received four cycles of R-CHOP and those who received six cycles, Dr. Poeschel reported.
“Six cycles of R-CHOP led to a higher toxicity with respect to leukocytopenia and anemia, both of any grade and also of grades 3 to 4, compared to four cycles of R-CHOP,” she said.
The findings suggest that, for younger patients with favorable-prognosis DLBCL—defined as an age-adjusted International Prognostic Index score of 0 and low tumor burden (less than 7.5 cm)—four cycles of R-CHOP can be a new standard of care, Dr. Poeschel said.
The investigators were prompted to look at the question of a shorter R-CHOP regimen by results of the MInT trial, in which a subpopulation of favorable-prognosis DLBCL patients had a 3-year PFS rate of 89%.
The FLYER trial (NCT00278421) was designed as a non-inferiority study to see whether, in a similar group of patients, reducing the number of R-CHOP cycles could maintain efficacy while reducing toxicity.
At a median follow-up of 66 months, the PFS rate, the primary endpoint, was 94% in the six-cycle group and 96% for the four-cycle group.
“As the lower limit of the 95% confidence interval of our experimental arm was 94%, it is shown that it is definitely non-inferior to the standard arm, six cycles of R-CHOP,” Dr. Poeschel said.
Similarly, the rate of 3-year OS was 98% in the six-cycle group, compared with 99% in the four-cycle group, and the survival curves were virtually superimposable out to more than 10 years of follow-up.
Treatment with six cycles was associated with more frequent hematologic adverse events than four cycles. Leukopenia of any grade occurred in 237 and 171 patients, respectively. Grade 3-4 leukopenia occurred in 110 and 80 patients, respectively.
Any-grade anemia occurred in 172 patients assigned to six cycles and 107 assigned to four cycles. Rates of grade 3-4 anemia were similar between the groups, as were rates of thrombocytopenia of any grade or grade 3-4.
Non-hematologic adverse events of any grade or grade 3-4 that were more frequent with six cycles included parasthesia, nausea, infection, vomiting, and mucositis.
The total number of non-hematologic adverse events was reduced by about one-third.
“We are certainly always looking for ways to make treatments easier for our patients to reduce adverse effects, and, certainly, for this subgroup of patients, it appears that we can make their treatment shorter and have less burden but equivalent efficacy,” said David Steensma, MD, of the Dana-Farber Cancer Institute/Harvard Cancer Center in Boston, Massachusetts.
Drs. Steensma and Poeschel both cautioned that the results of this study pertain only to those patients with DLBCL who are younger and have favorable-prognosis disease.
“We can’t extend it to other subtypes of large-cell lymphoma, but that’s always a laudable goal, so I think this will immediately influence clinical practice,” Dr. Steensma said.
The study was supported by Deutsche Krebshilfe. Dr. Poeschel disclosed travel grants from Roche and Amgen. Dr. Steensma had no disclosures relevant to the study.
SAN DIEGO—A shortened regimen of four cycles of rituximab (R) plus cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) chemotherapy was noninferior in efficacy to the standard six cycles of R-CHOP in younger patients with favorable-risk diffuse large B-cell lymphoma (DLBCL), according to investigators of the FLYER trial.
In addition, the truncated regimen was associated with about a one-third reduction in non-hematologic adverse events.
Viola Poeschel, MD, of Saarland University Medical School in Homburg/Saar, Germany, reported results of this study on behalf of the German High-Grade Non-Hodgkin’s Lymphoma Study Group/German Lymphoma Alliance at the 2018 ASH Annual Meeting (abstract 781).
Among 588 evaluable patients younger than 60 with favorable-prognosis DLBCL, there were no significant differences in progression-free survival (PFS), event-free survival (EFS), or overall survival (OS) between patients who received four cycles of R-CHOP and those who received six cycles, Dr. Poeschel reported.
“Six cycles of R-CHOP led to a higher toxicity with respect to leukocytopenia and anemia, both of any grade and also of grades 3 to 4, compared to four cycles of R-CHOP,” she said.
The findings suggest that, for younger patients with favorable-prognosis DLBCL—defined as an age-adjusted International Prognostic Index score of 0 and low tumor burden (less than 7.5 cm)—four cycles of R-CHOP can be a new standard of care, Dr. Poeschel said.
The investigators were prompted to look at the question of a shorter R-CHOP regimen by results of the MInT trial, in which a subpopulation of favorable-prognosis DLBCL patients had a 3-year PFS rate of 89%.
The FLYER trial (NCT00278421) was designed as a non-inferiority study to see whether, in a similar group of patients, reducing the number of R-CHOP cycles could maintain efficacy while reducing toxicity.
At a median follow-up of 66 months, the PFS rate, the primary endpoint, was 94% in the six-cycle group and 96% for the four-cycle group.
“As the lower limit of the 95% confidence interval of our experimental arm was 94%, it is shown that it is definitely non-inferior to the standard arm, six cycles of R-CHOP,” Dr. Poeschel said.
Similarly, the rate of 3-year OS was 98% in the six-cycle group, compared with 99% in the four-cycle group, and the survival curves were virtually superimposable out to more than 10 years of follow-up.
Treatment with six cycles was associated with more frequent hematologic adverse events than four cycles. Leukopenia of any grade occurred in 237 and 171 patients, respectively. Grade 3-4 leukopenia occurred in 110 and 80 patients, respectively.
Any-grade anemia occurred in 172 patients assigned to six cycles and 107 assigned to four cycles. Rates of grade 3-4 anemia were similar between the groups, as were rates of thrombocytopenia of any grade or grade 3-4.
Non-hematologic adverse events of any grade or grade 3-4 that were more frequent with six cycles included parasthesia, nausea, infection, vomiting, and mucositis.
The total number of non-hematologic adverse events was reduced by about one-third.
“We are certainly always looking for ways to make treatments easier for our patients to reduce adverse effects, and, certainly, for this subgroup of patients, it appears that we can make their treatment shorter and have less burden but equivalent efficacy,” said David Steensma, MD, of the Dana-Farber Cancer Institute/Harvard Cancer Center in Boston, Massachusetts.
Drs. Steensma and Poeschel both cautioned that the results of this study pertain only to those patients with DLBCL who are younger and have favorable-prognosis disease.
“We can’t extend it to other subtypes of large-cell lymphoma, but that’s always a laudable goal, so I think this will immediately influence clinical practice,” Dr. Steensma said.
The study was supported by Deutsche Krebshilfe. Dr. Poeschel disclosed travel grants from Roche and Amgen. Dr. Steensma had no disclosures relevant to the study.
Early caffeine therapy linked to improved neurologic outcomes in premature babies
Premature babies may benefit more if caffeine therapy is given within 2 days of birth, based on a retrospective observational cohort study of more than 2,000 newborns.
When caffeine was given within the first 2 days of birth, neonates had an adjusted odds ratio of significant neurodevelopmental impairment of 0.68, compared with neonates who received caffeine after 2 or more days. Further, the early-caffeine group had a 0.67 adjusted odds ratio for having cognitive scores of less than 85 on the Bayley Scales of Infant and Toddler Development, Third Edition, compared with the late-caffeine group. After researchers corrected for small-for-gestational-age status and other risk factors, however, early-caffeine therapy was associated with lower odds of cerebral palsy and hearing impairment only, according to the study published online in Pediatrics.
Caffeine administration should be a priority once extremely preterm neonates are stabilized, Abhay Lodha, MD, of the University of Calgary (Alta.), and his coauthors wrote. “It is rather easy to organize the administration of caffeine as early as possible for Level 3 nurseries, and many units have already accomplished this. However, certain Level 2 nurseries may not have facilities available for such early administration. We do not have data that indicate the earliest that caffeine would have to be given to get maximum benefit, and thus, it should not be counted as an emergency medication yet,” they wrote.
The study examined data from 2,108 neonates born before 29 weeks of gestational age and given caffeine to treat or prevent apnea; 1,545 received the caffeine within 2 days of birth and the remaining 563 were treated with caffeine after 2 days. Data were adjusted for gestational age, sex, antenatal steroids, and SNAP-II (Score of Neonatal Acute Physiology-II) score.
The early-caffeine group had a significantly reduced odds of hearing impairment and cerebral palsy, bronchopulmonary dysplasia, patent ductus arteriosus, and severe neurologic injury. When the data were further analyzed using propensity-matched groups – which also accounted for small-for-gestational-age status – the difference in outcomes was a nonsignificant trend in favor of early caffeine.
The authors noted that the late-caffeine group contained a higher proportion of infants born at or before 24 weeks’ gestational age, and a lower proportion of infants born at 25-28 weeks’ gestational age, compared with the early-caffeine group. The infants in the early-caffeine group also had higher Apgar scores, higher median birth weight, and lower SNAP-II scores, and received a longer median duration of caffeine treatment.
Dr. Lodha and his coauthors said the reason for the differences between the early- and late-caffeine groups was unclear. “However, it could be attributable to an increased growth of dendrites and spines in neurons that is initiated by the especially prolonged use of caffeine in the early-caffeine group,” they wrote. “The other speculation is that caffeine improves cardiac output and blood pressure in infants who are relatively stable.”
No funding or conflicts of interest were declared.
SOURCE: Lodha A et al. Pediatrics. 2018 Dec. 5. doi. org/10.1542/peds.2018-1348.
Premature babies may benefit more if caffeine therapy is given within 2 days of birth, based on a retrospective observational cohort study of more than 2,000 newborns.
When caffeine was given within the first 2 days of birth, neonates had an adjusted odds ratio of significant neurodevelopmental impairment of 0.68, compared with neonates who received caffeine after 2 or more days. Further, the early-caffeine group had a 0.67 adjusted odds ratio for having cognitive scores of less than 85 on the Bayley Scales of Infant and Toddler Development, Third Edition, compared with the late-caffeine group. After researchers corrected for small-for-gestational-age status and other risk factors, however, early-caffeine therapy was associated with lower odds of cerebral palsy and hearing impairment only, according to the study published online in Pediatrics.
Caffeine administration should be a priority once extremely preterm neonates are stabilized, Abhay Lodha, MD, of the University of Calgary (Alta.), and his coauthors wrote. “It is rather easy to organize the administration of caffeine as early as possible for Level 3 nurseries, and many units have already accomplished this. However, certain Level 2 nurseries may not have facilities available for such early administration. We do not have data that indicate the earliest that caffeine would have to be given to get maximum benefit, and thus, it should not be counted as an emergency medication yet,” they wrote.
The study examined data from 2,108 neonates born before 29 weeks of gestational age and given caffeine to treat or prevent apnea; 1,545 received the caffeine within 2 days of birth and the remaining 563 were treated with caffeine after 2 days. Data were adjusted for gestational age, sex, antenatal steroids, and SNAP-II (Score of Neonatal Acute Physiology-II) score.
The early-caffeine group had a significantly reduced odds of hearing impairment and cerebral palsy, bronchopulmonary dysplasia, patent ductus arteriosus, and severe neurologic injury. When the data were further analyzed using propensity-matched groups – which also accounted for small-for-gestational-age status – the difference in outcomes was a nonsignificant trend in favor of early caffeine.
The authors noted that the late-caffeine group contained a higher proportion of infants born at or before 24 weeks’ gestational age, and a lower proportion of infants born at 25-28 weeks’ gestational age, compared with the early-caffeine group. The infants in the early-caffeine group also had higher Apgar scores, higher median birth weight, and lower SNAP-II scores, and received a longer median duration of caffeine treatment.
Dr. Lodha and his coauthors said the reason for the differences between the early- and late-caffeine groups was unclear. “However, it could be attributable to an increased growth of dendrites and spines in neurons that is initiated by the especially prolonged use of caffeine in the early-caffeine group,” they wrote. “The other speculation is that caffeine improves cardiac output and blood pressure in infants who are relatively stable.”
No funding or conflicts of interest were declared.
SOURCE: Lodha A et al. Pediatrics. 2018 Dec. 5. doi. org/10.1542/peds.2018-1348.
Premature babies may benefit more if caffeine therapy is given within 2 days of birth, based on a retrospective observational cohort study of more than 2,000 newborns.
When caffeine was given within the first 2 days of birth, neonates had an adjusted odds ratio of significant neurodevelopmental impairment of 0.68, compared with neonates who received caffeine after 2 or more days. Further, the early-caffeine group had a 0.67 adjusted odds ratio for having cognitive scores of less than 85 on the Bayley Scales of Infant and Toddler Development, Third Edition, compared with the late-caffeine group. After researchers corrected for small-for-gestational-age status and other risk factors, however, early-caffeine therapy was associated with lower odds of cerebral palsy and hearing impairment only, according to the study published online in Pediatrics.
Caffeine administration should be a priority once extremely preterm neonates are stabilized, Abhay Lodha, MD, of the University of Calgary (Alta.), and his coauthors wrote. “It is rather easy to organize the administration of caffeine as early as possible for Level 3 nurseries, and many units have already accomplished this. However, certain Level 2 nurseries may not have facilities available for such early administration. We do not have data that indicate the earliest that caffeine would have to be given to get maximum benefit, and thus, it should not be counted as an emergency medication yet,” they wrote.
The study examined data from 2,108 neonates born before 29 weeks of gestational age and given caffeine to treat or prevent apnea; 1,545 received the caffeine within 2 days of birth and the remaining 563 were treated with caffeine after 2 days. Data were adjusted for gestational age, sex, antenatal steroids, and SNAP-II (Score of Neonatal Acute Physiology-II) score.
The early-caffeine group had a significantly reduced odds of hearing impairment and cerebral palsy, bronchopulmonary dysplasia, patent ductus arteriosus, and severe neurologic injury. When the data were further analyzed using propensity-matched groups – which also accounted for small-for-gestational-age status – the difference in outcomes was a nonsignificant trend in favor of early caffeine.
The authors noted that the late-caffeine group contained a higher proportion of infants born at or before 24 weeks’ gestational age, and a lower proportion of infants born at 25-28 weeks’ gestational age, compared with the early-caffeine group. The infants in the early-caffeine group also had higher Apgar scores, higher median birth weight, and lower SNAP-II scores, and received a longer median duration of caffeine treatment.
Dr. Lodha and his coauthors said the reason for the differences between the early- and late-caffeine groups was unclear. “However, it could be attributable to an increased growth of dendrites and spines in neurons that is initiated by the especially prolonged use of caffeine in the early-caffeine group,” they wrote. “The other speculation is that caffeine improves cardiac output and blood pressure in infants who are relatively stable.”
No funding or conflicts of interest were declared.
SOURCE: Lodha A et al. Pediatrics. 2018 Dec. 5. doi. org/10.1542/peds.2018-1348.
FROM PEDIATRICS
Key clinical point: Earlier caffeine treatment for premature infants may improve neurologic outcomes.
Major finding: Preterm neonates treated with caffeine within 2 days of birth have a significantly lower risk of hearing impairment and cerebral palsy.
Study details: A retrospective observational cohort study in 2,108 preterm neonates.
Disclosures: No funding or conflicts of interest were declared.
Source: Lodha A et al. Pediatrics. 2018 Dec. 5. doi. org/10.1542/peds.2018-1348.
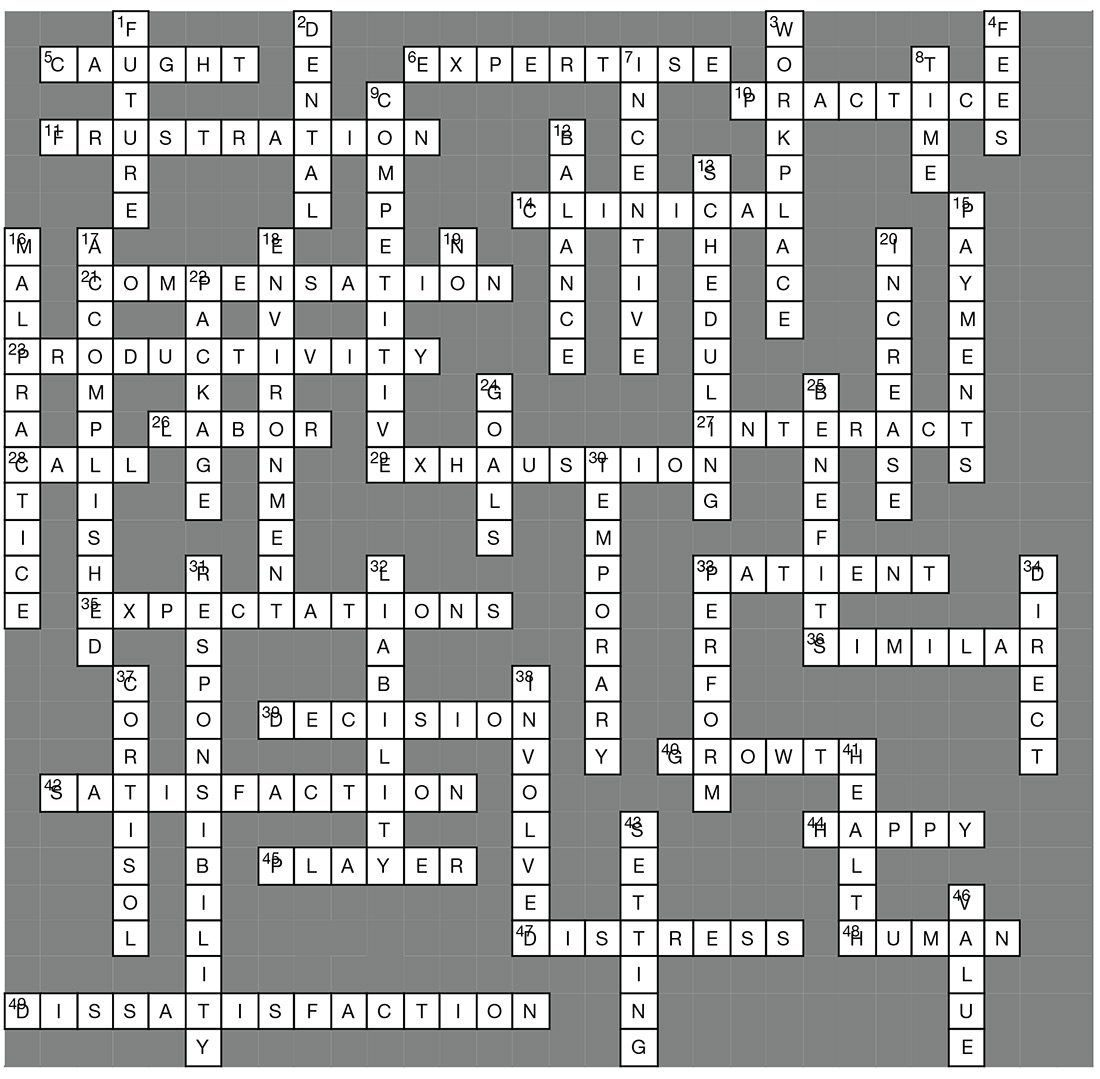
Job Satisfaction & Burnout
ACROSS
5. Some feel _____ in an unattainable quest.
6. Area of _____.
10. Focus on attributes of an advanced _____ career.
11. Discuss key _____ points with management.
14. High stress nature of _____ environments.
21. Negotiating a ____ package can cause anxiety.
23. Individual _____ compensation.
26. Bureau of _____ Statistics.
27. Inadequate time to _____ with patients.
28. Base pay rates and on-_____ pay.
29. Burn out characterized by emotional _____.
33. Direct _____ care.
35. Poor management with unclear _____.
36. NPs and PAs are more statistically _____ than different.
39. Having no say in ____ making is frustrating.
40. Opportunities for professional _____.
42. Long wait times impede patient _____.
44. Both professions are _____ about their career choice.
45. Feeling you are not a team _____.
47. Bad stress or “___” can cause health problems.
48. Stress is a part of _____ nature.
49. Not satisfied.
DOWN
1. Making decisions about your _____.
2. Health and _____ insurance.
3. Mitigating _____ stress is a challenge.
4. Licensing _____.
7. Good benefits provide _____ to do a better job.
8. NPs and PAs spend their _____ similarly.
9. Low attrition rates and _____ wages.
12. Issues related to work/life _____.
13. Patient _____ can affect job satisfaction.
15. Incentive _____ improve job satisfaction.
16. Threat of _____ lawsuits.
17. Focus on what you have _____.
18. Don’t suppress concerns about the work __.
19. Learn to say “_____.”
20. Employment opportunities are expected to ___.
22. The non-cash portion of a compensation ____.
24. Set realistic _____ for your day.
25. A great _____ package will improve your work climate.
30. ____ stress can be beneficial.
31. A heavy workload or too much _____ causes stress.
32. Professional _____ insurance
33. Stress can motivate people to _____.
34. Increased satisfaction in those who sped more time in _____ patient care.
37. Stress causes _____ release and weight gain.
38. Look for ways to become more _____.
41. Managing stress is key to good _____.
43. Goal _____ provides purposeful direction.
46. The _____ your employer places on you affects attitude.
Answer key on next page...
ACROSS
5. Some feel _____ in an unattainable quest.
6. Area of _____.
10. Focus on attributes of an advanced _____ career.
11. Discuss key _____ points with management.
14. High stress nature of _____ environments.
21. Negotiating a ____ package can cause anxiety.
23. Individual _____ compensation.
26. Bureau of _____ Statistics.
27. Inadequate time to _____ with patients.
28. Base pay rates and on-_____ pay.
29. Burn out characterized by emotional _____.
33. Direct _____ care.
35. Poor management with unclear _____.
36. NPs and PAs are more statistically _____ than different.
39. Having no say in ____ making is frustrating.
40. Opportunities for professional _____.
42. Long wait times impede patient _____.
44. Both professions are _____ about their career choice.
45. Feeling you are not a team _____.
47. Bad stress or “___” can cause health problems.
48. Stress is a part of _____ nature.
49. Not satisfied.
DOWN
1. Making decisions about your _____.
2. Health and _____ insurance.
3. Mitigating _____ stress is a challenge.
4. Licensing _____.
7. Good benefits provide _____ to do a better job.
8. NPs and PAs spend their _____ similarly.
9. Low attrition rates and _____ wages.
12. Issues related to work/life _____.
13. Patient _____ can affect job satisfaction.
15. Incentive _____ improve job satisfaction.
16. Threat of _____ lawsuits.
17. Focus on what you have _____.
18. Don’t suppress concerns about the work __.
19. Learn to say “_____.”
20. Employment opportunities are expected to ___.
22. The non-cash portion of a compensation ____.
24. Set realistic _____ for your day.
25. A great _____ package will improve your work climate.
30. ____ stress can be beneficial.
31. A heavy workload or too much _____ causes stress.
32. Professional _____ insurance
33. Stress can motivate people to _____.
34. Increased satisfaction in those who sped more time in _____ patient care.
37. Stress causes _____ release and weight gain.
38. Look for ways to become more _____.
41. Managing stress is key to good _____.
43. Goal _____ provides purposeful direction.
46. The _____ your employer places on you affects attitude.
Answer key on next page...
ACROSS
5. Some feel _____ in an unattainable quest.
6. Area of _____.
10. Focus on attributes of an advanced _____ career.
11. Discuss key _____ points with management.
14. High stress nature of _____ environments.
21. Negotiating a ____ package can cause anxiety.
23. Individual _____ compensation.
26. Bureau of _____ Statistics.
27. Inadequate time to _____ with patients.
28. Base pay rates and on-_____ pay.
29. Burn out characterized by emotional _____.
33. Direct _____ care.
35. Poor management with unclear _____.
36. NPs and PAs are more statistically _____ than different.
39. Having no say in ____ making is frustrating.
40. Opportunities for professional _____.
42. Long wait times impede patient _____.
44. Both professions are _____ about their career choice.
45. Feeling you are not a team _____.
47. Bad stress or “___” can cause health problems.
48. Stress is a part of _____ nature.
49. Not satisfied.
DOWN
1. Making decisions about your _____.
2. Health and _____ insurance.
3. Mitigating _____ stress is a challenge.
4. Licensing _____.
7. Good benefits provide _____ to do a better job.
8. NPs and PAs spend their _____ similarly.
9. Low attrition rates and _____ wages.
12. Issues related to work/life _____.
13. Patient _____ can affect job satisfaction.
15. Incentive _____ improve job satisfaction.
16. Threat of _____ lawsuits.
17. Focus on what you have _____.
18. Don’t suppress concerns about the work __.
19. Learn to say “_____.”
20. Employment opportunities are expected to ___.
22. The non-cash portion of a compensation ____.
24. Set realistic _____ for your day.
25. A great _____ package will improve your work climate.
30. ____ stress can be beneficial.
31. A heavy workload or too much _____ causes stress.
32. Professional _____ insurance
33. Stress can motivate people to _____.
34. Increased satisfaction in those who sped more time in _____ patient care.
37. Stress causes _____ release and weight gain.
38. Look for ways to become more _____.
41. Managing stress is key to good _____.
43. Goal _____ provides purposeful direction.
46. The _____ your employer places on you affects attitude.
Answer key on next page...
Tidying up a motley crew
It probably is buried in a box in your parents’ basement, but try to remember your soccer or football or track team picture from when you were in eighth grade. Tragically but predictably, most of your peers who were chubby in third grade are nowhere to be seen in the photo. But still it was a pretty motley crew. Some of you weren’t even up to the armpits of your taller teammates. Some guys were shaving. Others had little boys’ voices. Half the girls had reached menarche. Another third were still waiting impatiently for a breast bud.
The precocious and the late bloomers, you were all on the team. But it was pretty clear that those who had matured first generally were the more talented and successful athletes. By the time you were juniors in high school, many of those who matured late had quit the sport or been cut from the team, unable to catch up. Others may have been forced to give up the sport by their parents, who were concerned about the risk of injury when bodies of disparate size collide. A few of the early bloomers may have become depressed, older adolescents who had failed to match the hype and expectations that came when they were a head taller than their grade school teammates.
These natural consequences of biological variation are not small potatoes for the fragile egos of adolescents and preadolescents. The lead article in the November 2018 Pediatrics offers a partial solution for the issue of sports participation in a population with widely discrepant states of maturity (“Biobanding: A New Paradigm for Youth Sports and Training,” Pediatrics. 2018 Nov;142[5]:e20180423). The authors describe a system they call biobanding, in which “the percentage of predicted adult stature attained at the time of observation as the indicator of maturity status” is used to create groups or bands of participants with similar levels of maturity. They argue that this method is easy to use and report and that has been used with some success in Great Britain.
At first blush, biobanding sounds appealing, particularly for large communities. However, as someone who grew up in and practiced in a small town, I’m not sure how successfully it could be scaled down. There have been years when I could easily have disqualified a third of the high school football team were I to take into consideration the size and maturity of the competition they would be facing. But I didn’t. The fading interest in football in Maine has prompted some schools to consider moving to less-than-11-player competition or even to flag football. To some extent, the problem is taking care of itself.
How much tinkering should we be doing with something that is arguably a distorted natural selection process? With thoughtfully crafted rules, diligent supervision, and officiating, most of the issues of safety that one might attribute to discrepancies in maturity can be minimized. There always will be children who become discouraged and quit when they see the handwriting on the wall that reads “those who mature early win.” I’m certainly not wild about parents holding their children out of school to give them a jump on their peers. It can spiral out of control.
A more appealing solution is to do a better job of advertising the many successful late bloomers in professional sports ... and making sure that late-blooming children are given an abundance of active and competitive (if they wish) alternatives to sports dominated by their early maturing peers.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
It probably is buried in a box in your parents’ basement, but try to remember your soccer or football or track team picture from when you were in eighth grade. Tragically but predictably, most of your peers who were chubby in third grade are nowhere to be seen in the photo. But still it was a pretty motley crew. Some of you weren’t even up to the armpits of your taller teammates. Some guys were shaving. Others had little boys’ voices. Half the girls had reached menarche. Another third were still waiting impatiently for a breast bud.
The precocious and the late bloomers, you were all on the team. But it was pretty clear that those who had matured first generally were the more talented and successful athletes. By the time you were juniors in high school, many of those who matured late had quit the sport or been cut from the team, unable to catch up. Others may have been forced to give up the sport by their parents, who were concerned about the risk of injury when bodies of disparate size collide. A few of the early bloomers may have become depressed, older adolescents who had failed to match the hype and expectations that came when they were a head taller than their grade school teammates.
These natural consequences of biological variation are not small potatoes for the fragile egos of adolescents and preadolescents. The lead article in the November 2018 Pediatrics offers a partial solution for the issue of sports participation in a population with widely discrepant states of maturity (“Biobanding: A New Paradigm for Youth Sports and Training,” Pediatrics. 2018 Nov;142[5]:e20180423). The authors describe a system they call biobanding, in which “the percentage of predicted adult stature attained at the time of observation as the indicator of maturity status” is used to create groups or bands of participants with similar levels of maturity. They argue that this method is easy to use and report and that has been used with some success in Great Britain.
At first blush, biobanding sounds appealing, particularly for large communities. However, as someone who grew up in and practiced in a small town, I’m not sure how successfully it could be scaled down. There have been years when I could easily have disqualified a third of the high school football team were I to take into consideration the size and maturity of the competition they would be facing. But I didn’t. The fading interest in football in Maine has prompted some schools to consider moving to less-than-11-player competition or even to flag football. To some extent, the problem is taking care of itself.
How much tinkering should we be doing with something that is arguably a distorted natural selection process? With thoughtfully crafted rules, diligent supervision, and officiating, most of the issues of safety that one might attribute to discrepancies in maturity can be minimized. There always will be children who become discouraged and quit when they see the handwriting on the wall that reads “those who mature early win.” I’m certainly not wild about parents holding their children out of school to give them a jump on their peers. It can spiral out of control.
A more appealing solution is to do a better job of advertising the many successful late bloomers in professional sports ... and making sure that late-blooming children are given an abundance of active and competitive (if they wish) alternatives to sports dominated by their early maturing peers.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
It probably is buried in a box in your parents’ basement, but try to remember your soccer or football or track team picture from when you were in eighth grade. Tragically but predictably, most of your peers who were chubby in third grade are nowhere to be seen in the photo. But still it was a pretty motley crew. Some of you weren’t even up to the armpits of your taller teammates. Some guys were shaving. Others had little boys’ voices. Half the girls had reached menarche. Another third were still waiting impatiently for a breast bud.
The precocious and the late bloomers, you were all on the team. But it was pretty clear that those who had matured first generally were the more talented and successful athletes. By the time you were juniors in high school, many of those who matured late had quit the sport or been cut from the team, unable to catch up. Others may have been forced to give up the sport by their parents, who were concerned about the risk of injury when bodies of disparate size collide. A few of the early bloomers may have become depressed, older adolescents who had failed to match the hype and expectations that came when they were a head taller than their grade school teammates.
These natural consequences of biological variation are not small potatoes for the fragile egos of adolescents and preadolescents. The lead article in the November 2018 Pediatrics offers a partial solution for the issue of sports participation in a population with widely discrepant states of maturity (“Biobanding: A New Paradigm for Youth Sports and Training,” Pediatrics. 2018 Nov;142[5]:e20180423). The authors describe a system they call biobanding, in which “the percentage of predicted adult stature attained at the time of observation as the indicator of maturity status” is used to create groups or bands of participants with similar levels of maturity. They argue that this method is easy to use and report and that has been used with some success in Great Britain.
At first blush, biobanding sounds appealing, particularly for large communities. However, as someone who grew up in and practiced in a small town, I’m not sure how successfully it could be scaled down. There have been years when I could easily have disqualified a third of the high school football team were I to take into consideration the size and maturity of the competition they would be facing. But I didn’t. The fading interest in football in Maine has prompted some schools to consider moving to less-than-11-player competition or even to flag football. To some extent, the problem is taking care of itself.
How much tinkering should we be doing with something that is arguably a distorted natural selection process? With thoughtfully crafted rules, diligent supervision, and officiating, most of the issues of safety that one might attribute to discrepancies in maturity can be minimized. There always will be children who become discouraged and quit when they see the handwriting on the wall that reads “those who mature early win.” I’m certainly not wild about parents holding their children out of school to give them a jump on their peers. It can spiral out of control.
A more appealing solution is to do a better job of advertising the many successful late bloomers in professional sports ... and making sure that late-blooming children are given an abundance of active and competitive (if they wish) alternatives to sports dominated by their early maturing peers.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Phase 3 study of novel pemphigus treatment is initiated
and will enroll about 120 patients with moderate to severe disease, according to Principia Biopharma, which is developing the drug.
In a press release, the company said that the randomized, double-blind PEGASYS study will compare PRN1008 with placebo, in about 120 patients with newly diagnosed or relapsing moderate to severe pemphigus.
The company also reported the results of an open label phase 2 study of patients with newly diagnosed or relapsing mild or moderate pemphigus, including pemphigus vulgaris and pemphigus foliaceus, which found that control of disease activity within 4 weeks of starting treatment – the primary efficacy endpoint – was achieved by more than 50% of patients taking PRN1008. Principia has extended the trial’s active treatment period from 12 to 24 weeks. The results also led the company to initiate the phase 3 trial.
PRN1008 is an inhibitor of BTK, an enzyme that “is present in the signaling pathways of most types of white blood cells except for T cells and plasma cells,” according to the company’s press release.
and will enroll about 120 patients with moderate to severe disease, according to Principia Biopharma, which is developing the drug.
In a press release, the company said that the randomized, double-blind PEGASYS study will compare PRN1008 with placebo, in about 120 patients with newly diagnosed or relapsing moderate to severe pemphigus.
The company also reported the results of an open label phase 2 study of patients with newly diagnosed or relapsing mild or moderate pemphigus, including pemphigus vulgaris and pemphigus foliaceus, which found that control of disease activity within 4 weeks of starting treatment – the primary efficacy endpoint – was achieved by more than 50% of patients taking PRN1008. Principia has extended the trial’s active treatment period from 12 to 24 weeks. The results also led the company to initiate the phase 3 trial.
PRN1008 is an inhibitor of BTK, an enzyme that “is present in the signaling pathways of most types of white blood cells except for T cells and plasma cells,” according to the company’s press release.
and will enroll about 120 patients with moderate to severe disease, according to Principia Biopharma, which is developing the drug.
In a press release, the company said that the randomized, double-blind PEGASYS study will compare PRN1008 with placebo, in about 120 patients with newly diagnosed or relapsing moderate to severe pemphigus.
The company also reported the results of an open label phase 2 study of patients with newly diagnosed or relapsing mild or moderate pemphigus, including pemphigus vulgaris and pemphigus foliaceus, which found that control of disease activity within 4 weeks of starting treatment – the primary efficacy endpoint – was achieved by more than 50% of patients taking PRN1008. Principia has extended the trial’s active treatment period from 12 to 24 weeks. The results also led the company to initiate the phase 3 trial.
PRN1008 is an inhibitor of BTK, an enzyme that “is present in the signaling pathways of most types of white blood cells except for T cells and plasma cells,” according to the company’s press release.
hTERT expression predicts RCC survival, tumor aggressiveness
Human telomerase reverse transcriptase (hTERT) protein expression is associated with clear cell renal carcinoma (ccRCC) tumor aggressiveness and disease-specific survival (DSS), according to investigators.
Associations between hTERT expression and clinicopathologic features and outcomes were less robust or nonexistent in papillary and chromophobe subtypes, reported Leili Saeednejad Zanjani, MD, of the Oncopathology Research Center at Iran University of Medical Sciences in Tehran, and colleagues.
“Evidence shows that telomerase is expressed in 85% of malignancies, and the level of its activity is higher in advanced and metastatic tumors,” the authors wrote in Pathology.
“A number of clinical studies have been performed to evaluate the association between telomerase activity and clinicopathological parameters in renal cancer showing that telomerase activity level correlates with progression of RCC,” Dr. Zanjani and associates wrote. As none of these specifically evaluated hTERT protein expression, the investigators conducted a study to learn more.
The investigators analyzed hTERT expression level in 176 cases of RCC, requiring that each tumor had three core biopsies because of concerns of heterogeneity. The population consisted of 113 clear cell, 12 type I papillary, 20 type II papillary, and 31 chromophobe subtypes. Patient and clinicopathologic features were compared with survival and hTERT expression. Median follow-up time was 42 months.
Correlations between hTERT expression and disease characteristics were pronounced in cases of ccRCC, compared with other subtypes. In ccRCC, hTERT expression was significantly associated with tumor stage, nucleolar grade, tumor size, microvascular invasion, lymph node invasion, renal pelvis involvement, renal sinus fat involvement, Gerota fascia invasion, and distant metastasis. Survival analysis showed that DSS of ccRCC patients with high hTERT expression was 58 months, compared with 68 months for those with low hTERT expression (P =.012). Other parameters associated with survival were nucleolar grade, tumor stage, and tumor size.
For type I and II papillary subtypes, associations were found between hTERT expression and tumor stage and distant metastasis. In contrast, chromophobe RCC revealed no such relationships. No associations were found between hTERT expression and survival in any of these three latter subtypes, for slightly different reasons; no patients with type I disease died of renal cancer, disallowing creation of a Kaplan-Meier survival curve, whereas type II and chromophobe survival curves revealed insignificant relationships with hTERT expression. Along the same lines, no clinicopathologic characteristics of these subtypes were tied with survival.
“From these findings we are able to conclude that hTERT protein expression may be a novel prognostic indicator of worse outcome in tumor biopsies of patients with ccRCC, if follow up time is more prolonged,” the authors wrote. They noted that “telomerase is an attractive and ideal target for therapy due to overexpression in the majority of malignancies and low or nonexpression in most somatic cells.”
The study was funded by the Iran National Science Foundation. The authors declared no conflicts of interest.
SOURCE: Zanjani LS et al. Pathology. 2018 Nov 19. doi: 10.1016/j.pathol.2018.08.019.
Human telomerase reverse transcriptase (hTERT) protein expression is associated with clear cell renal carcinoma (ccRCC) tumor aggressiveness and disease-specific survival (DSS), according to investigators.
Associations between hTERT expression and clinicopathologic features and outcomes were less robust or nonexistent in papillary and chromophobe subtypes, reported Leili Saeednejad Zanjani, MD, of the Oncopathology Research Center at Iran University of Medical Sciences in Tehran, and colleagues.
“Evidence shows that telomerase is expressed in 85% of malignancies, and the level of its activity is higher in advanced and metastatic tumors,” the authors wrote in Pathology.
“A number of clinical studies have been performed to evaluate the association between telomerase activity and clinicopathological parameters in renal cancer showing that telomerase activity level correlates with progression of RCC,” Dr. Zanjani and associates wrote. As none of these specifically evaluated hTERT protein expression, the investigators conducted a study to learn more.
The investigators analyzed hTERT expression level in 176 cases of RCC, requiring that each tumor had three core biopsies because of concerns of heterogeneity. The population consisted of 113 clear cell, 12 type I papillary, 20 type II papillary, and 31 chromophobe subtypes. Patient and clinicopathologic features were compared with survival and hTERT expression. Median follow-up time was 42 months.
Correlations between hTERT expression and disease characteristics were pronounced in cases of ccRCC, compared with other subtypes. In ccRCC, hTERT expression was significantly associated with tumor stage, nucleolar grade, tumor size, microvascular invasion, lymph node invasion, renal pelvis involvement, renal sinus fat involvement, Gerota fascia invasion, and distant metastasis. Survival analysis showed that DSS of ccRCC patients with high hTERT expression was 58 months, compared with 68 months for those with low hTERT expression (P =.012). Other parameters associated with survival were nucleolar grade, tumor stage, and tumor size.
For type I and II papillary subtypes, associations were found between hTERT expression and tumor stage and distant metastasis. In contrast, chromophobe RCC revealed no such relationships. No associations were found between hTERT expression and survival in any of these three latter subtypes, for slightly different reasons; no patients with type I disease died of renal cancer, disallowing creation of a Kaplan-Meier survival curve, whereas type II and chromophobe survival curves revealed insignificant relationships with hTERT expression. Along the same lines, no clinicopathologic characteristics of these subtypes were tied with survival.
“From these findings we are able to conclude that hTERT protein expression may be a novel prognostic indicator of worse outcome in tumor biopsies of patients with ccRCC, if follow up time is more prolonged,” the authors wrote. They noted that “telomerase is an attractive and ideal target for therapy due to overexpression in the majority of malignancies and low or nonexpression in most somatic cells.”
The study was funded by the Iran National Science Foundation. The authors declared no conflicts of interest.
SOURCE: Zanjani LS et al. Pathology. 2018 Nov 19. doi: 10.1016/j.pathol.2018.08.019.
Human telomerase reverse transcriptase (hTERT) protein expression is associated with clear cell renal carcinoma (ccRCC) tumor aggressiveness and disease-specific survival (DSS), according to investigators.
Associations between hTERT expression and clinicopathologic features and outcomes were less robust or nonexistent in papillary and chromophobe subtypes, reported Leili Saeednejad Zanjani, MD, of the Oncopathology Research Center at Iran University of Medical Sciences in Tehran, and colleagues.
“Evidence shows that telomerase is expressed in 85% of malignancies, and the level of its activity is higher in advanced and metastatic tumors,” the authors wrote in Pathology.
“A number of clinical studies have been performed to evaluate the association between telomerase activity and clinicopathological parameters in renal cancer showing that telomerase activity level correlates with progression of RCC,” Dr. Zanjani and associates wrote. As none of these specifically evaluated hTERT protein expression, the investigators conducted a study to learn more.
The investigators analyzed hTERT expression level in 176 cases of RCC, requiring that each tumor had three core biopsies because of concerns of heterogeneity. The population consisted of 113 clear cell, 12 type I papillary, 20 type II papillary, and 31 chromophobe subtypes. Patient and clinicopathologic features were compared with survival and hTERT expression. Median follow-up time was 42 months.
Correlations between hTERT expression and disease characteristics were pronounced in cases of ccRCC, compared with other subtypes. In ccRCC, hTERT expression was significantly associated with tumor stage, nucleolar grade, tumor size, microvascular invasion, lymph node invasion, renal pelvis involvement, renal sinus fat involvement, Gerota fascia invasion, and distant metastasis. Survival analysis showed that DSS of ccRCC patients with high hTERT expression was 58 months, compared with 68 months for those with low hTERT expression (P =.012). Other parameters associated with survival were nucleolar grade, tumor stage, and tumor size.
For type I and II papillary subtypes, associations were found between hTERT expression and tumor stage and distant metastasis. In contrast, chromophobe RCC revealed no such relationships. No associations were found between hTERT expression and survival in any of these three latter subtypes, for slightly different reasons; no patients with type I disease died of renal cancer, disallowing creation of a Kaplan-Meier survival curve, whereas type II and chromophobe survival curves revealed insignificant relationships with hTERT expression. Along the same lines, no clinicopathologic characteristics of these subtypes were tied with survival.
“From these findings we are able to conclude that hTERT protein expression may be a novel prognostic indicator of worse outcome in tumor biopsies of patients with ccRCC, if follow up time is more prolonged,” the authors wrote. They noted that “telomerase is an attractive and ideal target for therapy due to overexpression in the majority of malignancies and low or nonexpression in most somatic cells.”
The study was funded by the Iran National Science Foundation. The authors declared no conflicts of interest.
SOURCE: Zanjani LS et al. Pathology. 2018 Nov 19. doi: 10.1016/j.pathol.2018.08.019.
FROM PATHOLOGY
Key clinical point: Human telomerase reverse transcriptase (hTERT) protein expression is associated with clear cell renal carcinoma (ccRCC) tumor aggressiveness and disease-specific survival (DSS).
Major finding: DSS of ccRCC patients with high hTERT expression was 58 months, compared with 68 months for those with low hTERT expression (P equal to .012).
Study details: An analysis of hTERT protein expression and disease characteristics in 176 patients with RCC. The subtype population consisted of 113 clear cell, 12 type I papillary, 20 type II papillary, and 31 chromophobe cases.
Disclosures: The study was funded by the Iran National Science Foundation. The authors declared no conflicts of interest.
Source: Zanjani LS et al. Pathology. 2018 Nov 19. doi: 10.1016/j.pathol.2018.08.019.