User login
Emapalumab safe, effective in pediatric primary hemophagocytic lymphohistiocytosis
, according to Franco Locatelli, MD, of the department of pediatric hematology and oncology at Ospedale Pediatrico Bambino Gesù, Rome.
The recently approved agent should be considered a new therapeutic option for this rare and life-threatening syndrome because of its targeted mode of action, Dr. Locatelli and his coinvestigators reported at the annual meeting of the American Society of Hematology.
Multiple lines of evidence have pointed to interferon gamma as a “rational target” in this disease, and elevated levels of interferon gamma are consistently observed in patients with HLH, Dr. Locatelli said in a press conference at the meeting.
Emapalumab binds to its target with high affinity, recognizing both free and receptor-bound interferon gamma, he added.
Primary HLH is a rare, life-threatening syndrome of hyperinflammation, characterized by prolonged fever, cytopenias, and splenomegaly and hepatomegaly, among other clinical manifestations, Dr. Locatelli said.
In the open-label, single-arm, pivotal study, 34 children with primary HLH were treated: 7 who were treatment naive and 27 who had failed conventional HLH therapy.
The patients received emapalumab intravenously with concomitant dexamethasone for up to 8 weeks, or extended to the point of allogeneic hematopoietic stem cell transplantation (HSCT), if needed.
The study met its primary endpoint of overall response rate higher than 40%, Dr. Locatelli reported. The overall response rate was 64.7% for all 34 treated patients (95% confidence interval, 46% to 80%; P = .0031), and 63% for the 27 patients who had failed prior therapy (95% CI, 42% to 81%; P = .0134), reported data show.
Response was rapid, occurring at a median of 8 days after starting emapalumab, and patients were in response for a median of 75% of days during treatment, Dr. Locatelli said.
Common adverse events in the study included infections, infusion-related reactions, pyrexia, and hypertension, while one patient had disseminated histoplasmosis that resolved with appropriate treatment, according to investigators.
In light of these results, the Food and Drug Administration approved emapalumab on Nov. 20, 2018, for the treatment of pediatric and adult patients with primary HLH with refractory, recurrent or progressive disease, or intolerance to conventional HLH treatments.
There is “certainly room for enlarging the indication” to first-line treatment of HLH once a sufficient number of previously untreated patients have been treated with the monoclonal antibody, Dr. Locatelli said.
However, a randomized trial would not be feasible, he said. “It’s a very rare disease, and it would be almost impossible to run a prospective, randomized trial in a reasonable period of time.”
The study described by Dr. Locatelli was sponsored by Novimmune. Study authors provided disclosures related to Sobi, Novimmune, Rocket Pharmaceuticals, Inc., AB2Bio, Novartis, Eli Lilly, Sanofi, UCB, Pfizer, and Abbvie. Two authors reported employment with Novimmune.
SOURCE: Locatelli F et al. ASH 2018; Abstract LBA-6.
, according to Franco Locatelli, MD, of the department of pediatric hematology and oncology at Ospedale Pediatrico Bambino Gesù, Rome.
The recently approved agent should be considered a new therapeutic option for this rare and life-threatening syndrome because of its targeted mode of action, Dr. Locatelli and his coinvestigators reported at the annual meeting of the American Society of Hematology.
Multiple lines of evidence have pointed to interferon gamma as a “rational target” in this disease, and elevated levels of interferon gamma are consistently observed in patients with HLH, Dr. Locatelli said in a press conference at the meeting.
Emapalumab binds to its target with high affinity, recognizing both free and receptor-bound interferon gamma, he added.
Primary HLH is a rare, life-threatening syndrome of hyperinflammation, characterized by prolonged fever, cytopenias, and splenomegaly and hepatomegaly, among other clinical manifestations, Dr. Locatelli said.
In the open-label, single-arm, pivotal study, 34 children with primary HLH were treated: 7 who were treatment naive and 27 who had failed conventional HLH therapy.
The patients received emapalumab intravenously with concomitant dexamethasone for up to 8 weeks, or extended to the point of allogeneic hematopoietic stem cell transplantation (HSCT), if needed.
The study met its primary endpoint of overall response rate higher than 40%, Dr. Locatelli reported. The overall response rate was 64.7% for all 34 treated patients (95% confidence interval, 46% to 80%; P = .0031), and 63% for the 27 patients who had failed prior therapy (95% CI, 42% to 81%; P = .0134), reported data show.
Response was rapid, occurring at a median of 8 days after starting emapalumab, and patients were in response for a median of 75% of days during treatment, Dr. Locatelli said.
Common adverse events in the study included infections, infusion-related reactions, pyrexia, and hypertension, while one patient had disseminated histoplasmosis that resolved with appropriate treatment, according to investigators.
In light of these results, the Food and Drug Administration approved emapalumab on Nov. 20, 2018, for the treatment of pediatric and adult patients with primary HLH with refractory, recurrent or progressive disease, or intolerance to conventional HLH treatments.
There is “certainly room for enlarging the indication” to first-line treatment of HLH once a sufficient number of previously untreated patients have been treated with the monoclonal antibody, Dr. Locatelli said.
However, a randomized trial would not be feasible, he said. “It’s a very rare disease, and it would be almost impossible to run a prospective, randomized trial in a reasonable period of time.”
The study described by Dr. Locatelli was sponsored by Novimmune. Study authors provided disclosures related to Sobi, Novimmune, Rocket Pharmaceuticals, Inc., AB2Bio, Novartis, Eli Lilly, Sanofi, UCB, Pfizer, and Abbvie. Two authors reported employment with Novimmune.
SOURCE: Locatelli F et al. ASH 2018; Abstract LBA-6.
, according to Franco Locatelli, MD, of the department of pediatric hematology and oncology at Ospedale Pediatrico Bambino Gesù, Rome.
The recently approved agent should be considered a new therapeutic option for this rare and life-threatening syndrome because of its targeted mode of action, Dr. Locatelli and his coinvestigators reported at the annual meeting of the American Society of Hematology.
Multiple lines of evidence have pointed to interferon gamma as a “rational target” in this disease, and elevated levels of interferon gamma are consistently observed in patients with HLH, Dr. Locatelli said in a press conference at the meeting.
Emapalumab binds to its target with high affinity, recognizing both free and receptor-bound interferon gamma, he added.
Primary HLH is a rare, life-threatening syndrome of hyperinflammation, characterized by prolonged fever, cytopenias, and splenomegaly and hepatomegaly, among other clinical manifestations, Dr. Locatelli said.
In the open-label, single-arm, pivotal study, 34 children with primary HLH were treated: 7 who were treatment naive and 27 who had failed conventional HLH therapy.
The patients received emapalumab intravenously with concomitant dexamethasone for up to 8 weeks, or extended to the point of allogeneic hematopoietic stem cell transplantation (HSCT), if needed.
The study met its primary endpoint of overall response rate higher than 40%, Dr. Locatelli reported. The overall response rate was 64.7% for all 34 treated patients (95% confidence interval, 46% to 80%; P = .0031), and 63% for the 27 patients who had failed prior therapy (95% CI, 42% to 81%; P = .0134), reported data show.
Response was rapid, occurring at a median of 8 days after starting emapalumab, and patients were in response for a median of 75% of days during treatment, Dr. Locatelli said.
Common adverse events in the study included infections, infusion-related reactions, pyrexia, and hypertension, while one patient had disseminated histoplasmosis that resolved with appropriate treatment, according to investigators.
In light of these results, the Food and Drug Administration approved emapalumab on Nov. 20, 2018, for the treatment of pediatric and adult patients with primary HLH with refractory, recurrent or progressive disease, or intolerance to conventional HLH treatments.
There is “certainly room for enlarging the indication” to first-line treatment of HLH once a sufficient number of previously untreated patients have been treated with the monoclonal antibody, Dr. Locatelli said.
However, a randomized trial would not be feasible, he said. “It’s a very rare disease, and it would be almost impossible to run a prospective, randomized trial in a reasonable period of time.”
The study described by Dr. Locatelli was sponsored by Novimmune. Study authors provided disclosures related to Sobi, Novimmune, Rocket Pharmaceuticals, Inc., AB2Bio, Novartis, Eli Lilly, Sanofi, UCB, Pfizer, and Abbvie. Two authors reported employment with Novimmune.
SOURCE: Locatelli F et al. ASH 2018; Abstract LBA-6.
FROM ASH 2018
Key clinical point: Emapalumab, an interferon gamma-blocking antibody, controls disease activity and has a favorable safety profile in patients with primary hemophagocytic lymphohistiocytosis.
Major finding: The overall response rate was 64.7% for all 34 treated patients (95% CI, 46%-80%; P = .0031), and 63% for the 27 patients who had failed prior therapy (95% CI, 42%-81%; P = .0134).
Study details: In the open-label, single-arm, pivotal study, 34 children with primary HLH were treated: 7 who were treatment naive and 27 who had failed conventional HLH therapy.
Disclosures: The study described by Dr. Locatelli was sponsored by Novimmune. Study authors provided disclosures related to Sobi, Novimmune, Rocket Pharmaceuticals, AB2Bio, Novartis, Eli Lilly, Sanofi, UCB, Pfizer, and Abbvie. Two authors reported employment with Novimmune.
Source: Locatelli F et al. ASH 2018; Abstract LBA-6.
Prenatal, postnatal neuroimaging IDs most Zika-related brain injuries
Prenatal ultrasound can identify most abnormalities in fetuses exposed to Zika virus during pregnancy, and neuroimaging after birth can detect infant exposure in cases that appeared normal on prenatal ultrasound, according to research published in JAMA Pediatrics.
“Absence of prolonged maternal viremia did not have predictive associations with normal fetal or neonatal brain imaging,” Sarah B. Mulkey, MD, PhD, from the division of fetal and transitional medicine at Children’s National Health System, in Washington, and her colleagues wrote. “Postnatal imaging can detect changes not seen on fetal imaging, supporting the current CDC [Centers for Disease Control and Prevention] recommendation for postnatal cranial [ultrasound].”
Dr. Mulkey and her colleagues performed a prospective cohort analysis of 82 pregnant women from Colombia and the United States who had clinical evidence of probable exposure to the Zika virus through travel (U.S. cases, 2 patients), physician referral, or community cases during June 2016-June 2017. Pregnant women underwent fetal MRI or ultrasound during the second or third trimesters between 4 weeks and 10 weeks after symptom onset, with infants undergoing brain MRI and cranial ultrasound after birth.
Of those 82 pregnancies, there were 80 live births, 1 case of termination because of severe fetal brain abnormalities, and 1 near-term fetal death of unknown cause. There was one death 3 days after birth and one instance of neurosurgical intervention from encephalocele. The researchers found 3 of 82 cases (4%) displayed fetal abnormalities from MRI, which consisted of 2 cases of heterotopias and malformations in cortical development and 1 case with parietal encephalocele, Chiari II malformation, and microcephaly. One infant had a normal ultrasound despite abnormalities displayed on fetal MRI.
After birth, of the 79 infants with normal ultrasound results, 53 infants underwent a postnatal brain MRI and Dr. Mulkey and her associates found 7 cases with mild abnormalities (13%). There were 57 infants who underwent cranial ultrasound, which yielded 21 cases of lenticulostriate vasculopathy, choroid plexus cysts, germinolytic/subependymal cysts, and/or calcification; these were poorly characterized by MRI.
“Normal fetal imaging had predictive associations with normal postnatal imaging or mild postnatal imaging findings unlikely to be of significant clinical consequence,” they said.
Nonetheless, “there is a need for long-term follow-up to assess the neurodevelopmental significance of these early neuroimaging findings, both normal and abnormal; such studies are in progress,” Dr. Mulkey and her colleagues said.
The researchers noted the timing of maternal infections and symptoms as well as the Zika testing, ultrasound, and MRI performance, technique during fetal MRI, and incomplete prenatal testing in the cohort as limitations in the study.
This study was funded in part by Children’s National Health System and by a philanthropic gift from the Ikaria Healthcare Fund. Dr. Mulkey received research support from the Thrasher Research Fund and is supported by awards from the National Institutes of Health National Center for Advancing Translational Sciences. The other authors reported no relevant conflicts of interest.
SOURCE: Mulkey SB et al. JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4138.
While the study by Mulkey et al. adds to the body of evidence of prenatal and postnatal brain abnormalities, there are still many unanswered questions about the Zika virus and how to handle its unique diagnostic and clinical challenges, Margaret A. Honein, PhD, MPH, and Denise J. Jamieson, MD, MPH, wrote in a related editorial.
For example, Centers for Disease Control and Prevention recommendations state that infants with possible Zika exposure should receive an ophthalmologic and ultrasonographic examination at 1 month, and if the hearing test used otoacoustic emissions methods only, an automated auditory brainstem response test should be administered. While Mulkey et al. examined brain abnormalities in utero and in infants, it is not clear whether all CDC guidelines were followed in these cases.
In addition, because there is no reliable way to determine whether infants acquired Zika virus through the mother or through vertical transmission, assessing the proportion of congenitally infected infants or vertical-transmission infected infants who have neurodevelopmental disabilities and defects is not possible, they said. More longitudinal studies are needed to study the effects of the Zika virus and to prepare for the next outbreak.
“Zika was affecting pregnant women and their infants years before its teratogenic effect was recognized, and Zika will remain a serious risk to pregnant women and their infants until we have a safe vaccine that can fully prevent Zika virus infection during pregnancy,” they said. “Until then, ongoing public health efforts are essential to protect mothers and babies from this threat and ensure all disabilities associated with Zika virus infection are promptly identified, so that timely interventions can be provided.”
Dr. Honein is from the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention, and Dr. Jamieson is from the department of gynecology & obstetrics at Emory University School of Medicine, Atlanta. These comments summarize their editorial in response to Mulkey et al. (JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4164). They reported no relevant conflicts of interest.
While the study by Mulkey et al. adds to the body of evidence of prenatal and postnatal brain abnormalities, there are still many unanswered questions about the Zika virus and how to handle its unique diagnostic and clinical challenges, Margaret A. Honein, PhD, MPH, and Denise J. Jamieson, MD, MPH, wrote in a related editorial.
For example, Centers for Disease Control and Prevention recommendations state that infants with possible Zika exposure should receive an ophthalmologic and ultrasonographic examination at 1 month, and if the hearing test used otoacoustic emissions methods only, an automated auditory brainstem response test should be administered. While Mulkey et al. examined brain abnormalities in utero and in infants, it is not clear whether all CDC guidelines were followed in these cases.
In addition, because there is no reliable way to determine whether infants acquired Zika virus through the mother or through vertical transmission, assessing the proportion of congenitally infected infants or vertical-transmission infected infants who have neurodevelopmental disabilities and defects is not possible, they said. More longitudinal studies are needed to study the effects of the Zika virus and to prepare for the next outbreak.
“Zika was affecting pregnant women and their infants years before its teratogenic effect was recognized, and Zika will remain a serious risk to pregnant women and their infants until we have a safe vaccine that can fully prevent Zika virus infection during pregnancy,” they said. “Until then, ongoing public health efforts are essential to protect mothers and babies from this threat and ensure all disabilities associated with Zika virus infection are promptly identified, so that timely interventions can be provided.”
Dr. Honein is from the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention, and Dr. Jamieson is from the department of gynecology & obstetrics at Emory University School of Medicine, Atlanta. These comments summarize their editorial in response to Mulkey et al. (JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4164). They reported no relevant conflicts of interest.
While the study by Mulkey et al. adds to the body of evidence of prenatal and postnatal brain abnormalities, there are still many unanswered questions about the Zika virus and how to handle its unique diagnostic and clinical challenges, Margaret A. Honein, PhD, MPH, and Denise J. Jamieson, MD, MPH, wrote in a related editorial.
For example, Centers for Disease Control and Prevention recommendations state that infants with possible Zika exposure should receive an ophthalmologic and ultrasonographic examination at 1 month, and if the hearing test used otoacoustic emissions methods only, an automated auditory brainstem response test should be administered. While Mulkey et al. examined brain abnormalities in utero and in infants, it is not clear whether all CDC guidelines were followed in these cases.
In addition, because there is no reliable way to determine whether infants acquired Zika virus through the mother or through vertical transmission, assessing the proportion of congenitally infected infants or vertical-transmission infected infants who have neurodevelopmental disabilities and defects is not possible, they said. More longitudinal studies are needed to study the effects of the Zika virus and to prepare for the next outbreak.
“Zika was affecting pregnant women and their infants years before its teratogenic effect was recognized, and Zika will remain a serious risk to pregnant women and their infants until we have a safe vaccine that can fully prevent Zika virus infection during pregnancy,” they said. “Until then, ongoing public health efforts are essential to protect mothers and babies from this threat and ensure all disabilities associated with Zika virus infection are promptly identified, so that timely interventions can be provided.”
Dr. Honein is from the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention, and Dr. Jamieson is from the department of gynecology & obstetrics at Emory University School of Medicine, Atlanta. These comments summarize their editorial in response to Mulkey et al. (JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4164). They reported no relevant conflicts of interest.
Prenatal ultrasound can identify most abnormalities in fetuses exposed to Zika virus during pregnancy, and neuroimaging after birth can detect infant exposure in cases that appeared normal on prenatal ultrasound, according to research published in JAMA Pediatrics.
“Absence of prolonged maternal viremia did not have predictive associations with normal fetal or neonatal brain imaging,” Sarah B. Mulkey, MD, PhD, from the division of fetal and transitional medicine at Children’s National Health System, in Washington, and her colleagues wrote. “Postnatal imaging can detect changes not seen on fetal imaging, supporting the current CDC [Centers for Disease Control and Prevention] recommendation for postnatal cranial [ultrasound].”
Dr. Mulkey and her colleagues performed a prospective cohort analysis of 82 pregnant women from Colombia and the United States who had clinical evidence of probable exposure to the Zika virus through travel (U.S. cases, 2 patients), physician referral, or community cases during June 2016-June 2017. Pregnant women underwent fetal MRI or ultrasound during the second or third trimesters between 4 weeks and 10 weeks after symptom onset, with infants undergoing brain MRI and cranial ultrasound after birth.
Of those 82 pregnancies, there were 80 live births, 1 case of termination because of severe fetal brain abnormalities, and 1 near-term fetal death of unknown cause. There was one death 3 days after birth and one instance of neurosurgical intervention from encephalocele. The researchers found 3 of 82 cases (4%) displayed fetal abnormalities from MRI, which consisted of 2 cases of heterotopias and malformations in cortical development and 1 case with parietal encephalocele, Chiari II malformation, and microcephaly. One infant had a normal ultrasound despite abnormalities displayed on fetal MRI.
After birth, of the 79 infants with normal ultrasound results, 53 infants underwent a postnatal brain MRI and Dr. Mulkey and her associates found 7 cases with mild abnormalities (13%). There were 57 infants who underwent cranial ultrasound, which yielded 21 cases of lenticulostriate vasculopathy, choroid plexus cysts, germinolytic/subependymal cysts, and/or calcification; these were poorly characterized by MRI.
“Normal fetal imaging had predictive associations with normal postnatal imaging or mild postnatal imaging findings unlikely to be of significant clinical consequence,” they said.
Nonetheless, “there is a need for long-term follow-up to assess the neurodevelopmental significance of these early neuroimaging findings, both normal and abnormal; such studies are in progress,” Dr. Mulkey and her colleagues said.
The researchers noted the timing of maternal infections and symptoms as well as the Zika testing, ultrasound, and MRI performance, technique during fetal MRI, and incomplete prenatal testing in the cohort as limitations in the study.
This study was funded in part by Children’s National Health System and by a philanthropic gift from the Ikaria Healthcare Fund. Dr. Mulkey received research support from the Thrasher Research Fund and is supported by awards from the National Institutes of Health National Center for Advancing Translational Sciences. The other authors reported no relevant conflicts of interest.
SOURCE: Mulkey SB et al. JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4138.
Prenatal ultrasound can identify most abnormalities in fetuses exposed to Zika virus during pregnancy, and neuroimaging after birth can detect infant exposure in cases that appeared normal on prenatal ultrasound, according to research published in JAMA Pediatrics.
“Absence of prolonged maternal viremia did not have predictive associations with normal fetal or neonatal brain imaging,” Sarah B. Mulkey, MD, PhD, from the division of fetal and transitional medicine at Children’s National Health System, in Washington, and her colleagues wrote. “Postnatal imaging can detect changes not seen on fetal imaging, supporting the current CDC [Centers for Disease Control and Prevention] recommendation for postnatal cranial [ultrasound].”
Dr. Mulkey and her colleagues performed a prospective cohort analysis of 82 pregnant women from Colombia and the United States who had clinical evidence of probable exposure to the Zika virus through travel (U.S. cases, 2 patients), physician referral, or community cases during June 2016-June 2017. Pregnant women underwent fetal MRI or ultrasound during the second or third trimesters between 4 weeks and 10 weeks after symptom onset, with infants undergoing brain MRI and cranial ultrasound after birth.
Of those 82 pregnancies, there were 80 live births, 1 case of termination because of severe fetal brain abnormalities, and 1 near-term fetal death of unknown cause. There was one death 3 days after birth and one instance of neurosurgical intervention from encephalocele. The researchers found 3 of 82 cases (4%) displayed fetal abnormalities from MRI, which consisted of 2 cases of heterotopias and malformations in cortical development and 1 case with parietal encephalocele, Chiari II malformation, and microcephaly. One infant had a normal ultrasound despite abnormalities displayed on fetal MRI.
After birth, of the 79 infants with normal ultrasound results, 53 infants underwent a postnatal brain MRI and Dr. Mulkey and her associates found 7 cases with mild abnormalities (13%). There were 57 infants who underwent cranial ultrasound, which yielded 21 cases of lenticulostriate vasculopathy, choroid plexus cysts, germinolytic/subependymal cysts, and/or calcification; these were poorly characterized by MRI.
“Normal fetal imaging had predictive associations with normal postnatal imaging or mild postnatal imaging findings unlikely to be of significant clinical consequence,” they said.
Nonetheless, “there is a need for long-term follow-up to assess the neurodevelopmental significance of these early neuroimaging findings, both normal and abnormal; such studies are in progress,” Dr. Mulkey and her colleagues said.
The researchers noted the timing of maternal infections and symptoms as well as the Zika testing, ultrasound, and MRI performance, technique during fetal MRI, and incomplete prenatal testing in the cohort as limitations in the study.
This study was funded in part by Children’s National Health System and by a philanthropic gift from the Ikaria Healthcare Fund. Dr. Mulkey received research support from the Thrasher Research Fund and is supported by awards from the National Institutes of Health National Center for Advancing Translational Sciences. The other authors reported no relevant conflicts of interest.
SOURCE: Mulkey SB et al. JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4138.
FROM JAMA PEDIATRICS
Key clinical point:
Major finding: In 82 pregnant women, prenatal neuroimaging identified fetal abnormalities in 3 cases, while postnatal neuroimaging in 53 of the remaining 79 cases yielded an additional 7 cases with mild abnormalities.
Study details: A prospective longitudinal cohort study of 82 pregnant women with clinical evidence of probable Zika infection in Colombia and the United States.
Disclosures: This study was funded in part by Children’s National Health System and by a philanthropic gift from the Ikaria Healthcare Fund. Dr Mulkey received research support from the Thrasher Research Fund and is supported by awards from the National Institutes of Health National Center for Advancing Translational Sciences. The other authors reported no relevant conflicts of interest.
Source: Mulkey SB et al. JAMA Pediatr. 2018 Nov. 26; doi: 10.1001/jamapediatrics.2018.4138.
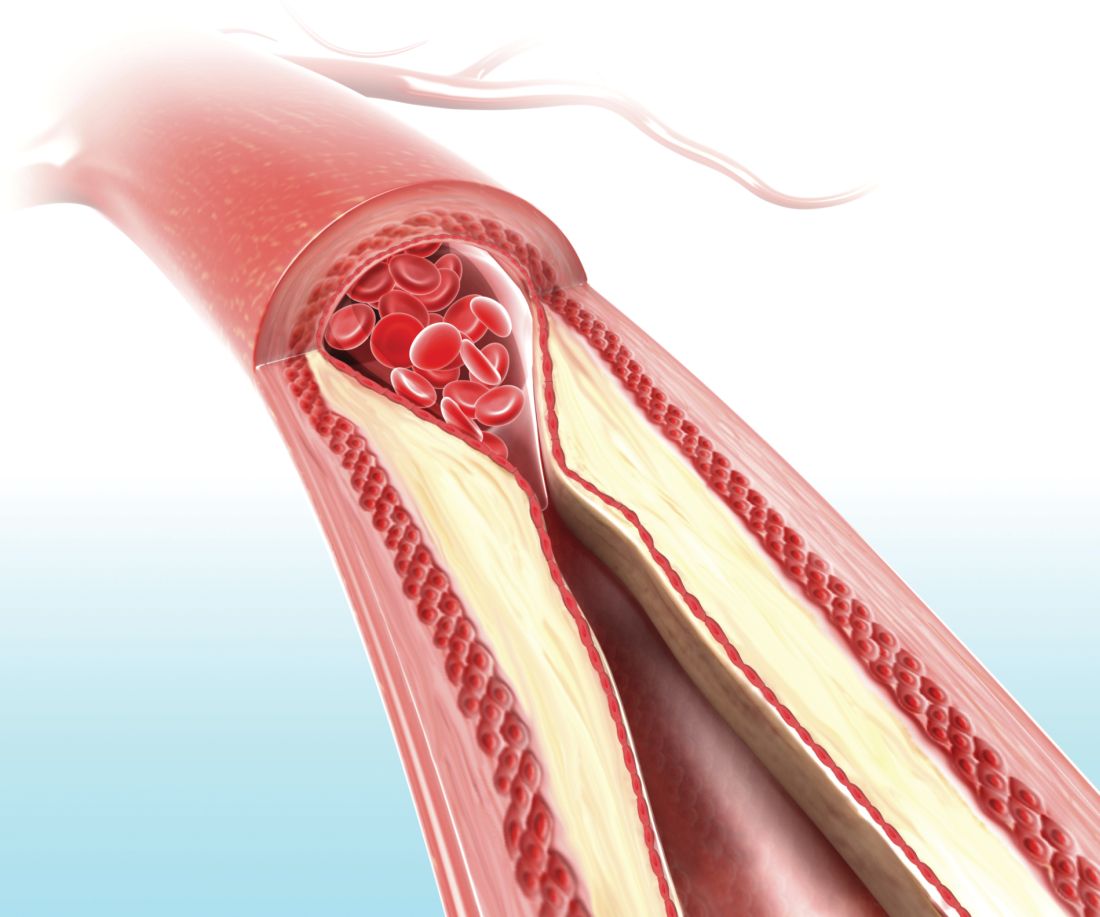
EARLY: Angiography within 2 hours of acute non-ST event cut recurrent ischemic events
CHICAGO – Coronary angiography within 2 hours of a diagnosis of non–ST-segment elevation acute coronary syndrome (NSTE-ACS) significantly reduced the risk of recurrent ischemic events as compared to angiography delayed for 12 hours or more, based on the results of the EARLY trial presented at the American Heart Association scientific sessions.
EARLY examined the impacts of not pretreating with a P2Y12-ADP antagonist and of delay before coronary angiography; all study participants received the loading dose of a P2Y12-ADP antagonist at the time of intervention. The early group received angiography within 2 hours, and a delayed group received angiography 12 or more hours after NSTE-ACS.
“Regarding the primary endpoint at 30 days, which is a composite of cardiovascular death and recurrent ischemic event, there is a fivefold lower rate of MACE [major adverse cardiovascular events] in the very-early [group as] compared to the control group,” said Laurent Bonello, MD, PhD, of University Hospital North in Marseilles, France.
The MACE rate was 4.4% in the early group and 21.3% in the delayed group. However, the reduction in MACE was largely because of a reduction in recurrent ischemic events; death rates were similar in the two groups.
The EARLY trial randomized 740 patients at 16 hospitals in France with NSTE-ACS to one of two timing strategies for intervention: within 2 hours of diagnosis, the early-intervention group, and between 12 and 72 hours after diagnosis, the delayed group. Intermediate- and high-risk patients did not receive pretreatment with a P2Y12-ADP antagonist such as clopidogrel before angiography; they received the loading dose at the time of the intervention.
On average, angiography was done within 1 hour in the early group and at 18 hours in the delayed group. Percutaneous coronary intervention (PCI) was performed on 75% of the study population; 3% underwent coronary artery bypass grafting; and 20% received medical therapy.
Dr. Bonello said the purpose of the trial was to settle some uncertainties over the management of NSTE-ACS patients regarding the benefit of pretreatment with P2Y12-ADP antagonists – namely, to evaluate the impact of the lack of pretreatment on the optimal timing of the intervention. “There are no randomized clinical trials available on this specific group of non-ST elevation acute coronary syndrome patients not pretreated for the timing of the invasive strategy,” he said.
Both groups had similar baseline characteristics, such as history of MI, PCI, and aspirin and P2Y12-ADP use, although the delayed group had a higher rate of diabetes (35% vs. 28.3%).
Regarding secondary endpoints, rates of recurrent ischemic events were 2.9% for the early group and 19.8% for the delayed group during hospitalization, and 4.1% vs. 20.7% at 30 days.
Dr. Bonello noted that rates of cardiovascular death were similar for both groups: 0.3% and 0.8% in-hospital deaths, and 0.6% and 1.1% deaths at 30 days.
The disparity in MACE between all subgroups paralleled that of the overall results with two exceptions, Dr. Bonello said: The positive effect of early intervention was less pronounced in women, and there were no differences in MACE rates among those who had interventions other than PCI.
In his discussion of the trial, Gilles Montalescot, MD, PhD, of the Institute of Cardiology at Pitié-Salpêtrière Hospital in Paris, said the EARLY trial with no P2Y12-ADP pretreatment confirms findings of studies before the ACCOAST trial (N Engl J Med. 2013;369:999-1010), that early angiography has no benefit on survival, recurrent MI, revascularization, or bleeding. While the ACCOAST trial, of which Dr. Montalescot was a principal investigator, found no benefit of pretreatment with prasugrel in patients with NTSE-ASC, the EARLY trial extends those findings to other P2Y12-ADP antagonists. “With the immediate angiography strategy, there is a trivial benefit on recurrent ischemia and length of stay, like in the previous studies, thus not related to pretreatment,” he said.
Dr. Montalescot cautioned against embracing this early-intervention strategy with no P2Y12-ADP pretreatment in all situations.
“If you have a conservative strategy for managing the NTSE-ASC patient or if you are in a center far away from a cath lab and your patients have to wait days for a test, yes, you should consider administration of the P2Y12-ADP antagonist,” Dr. Montalescot said.
Dr. Montalescot disclosed receiving grants or honoraria from ADIR, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Beth Israel Deaconess Medical, and Action Coeur Academic Research Organization.
Dr. Bonello reported financial relationships with AstraZeneca, Boston Scientific, Abbott, and Biotronik. The EARLY trial received funding from the French Ministry of Health.
SOURCE: Bonello B et al. AHA scientific sessions, Session LBS.04 19343.
CHICAGO – Coronary angiography within 2 hours of a diagnosis of non–ST-segment elevation acute coronary syndrome (NSTE-ACS) significantly reduced the risk of recurrent ischemic events as compared to angiography delayed for 12 hours or more, based on the results of the EARLY trial presented at the American Heart Association scientific sessions.
EARLY examined the impacts of not pretreating with a P2Y12-ADP antagonist and of delay before coronary angiography; all study participants received the loading dose of a P2Y12-ADP antagonist at the time of intervention. The early group received angiography within 2 hours, and a delayed group received angiography 12 or more hours after NSTE-ACS.
“Regarding the primary endpoint at 30 days, which is a composite of cardiovascular death and recurrent ischemic event, there is a fivefold lower rate of MACE [major adverse cardiovascular events] in the very-early [group as] compared to the control group,” said Laurent Bonello, MD, PhD, of University Hospital North in Marseilles, France.
The MACE rate was 4.4% in the early group and 21.3% in the delayed group. However, the reduction in MACE was largely because of a reduction in recurrent ischemic events; death rates were similar in the two groups.
The EARLY trial randomized 740 patients at 16 hospitals in France with NSTE-ACS to one of two timing strategies for intervention: within 2 hours of diagnosis, the early-intervention group, and between 12 and 72 hours after diagnosis, the delayed group. Intermediate- and high-risk patients did not receive pretreatment with a P2Y12-ADP antagonist such as clopidogrel before angiography; they received the loading dose at the time of the intervention.
On average, angiography was done within 1 hour in the early group and at 18 hours in the delayed group. Percutaneous coronary intervention (PCI) was performed on 75% of the study population; 3% underwent coronary artery bypass grafting; and 20% received medical therapy.
Dr. Bonello said the purpose of the trial was to settle some uncertainties over the management of NSTE-ACS patients regarding the benefit of pretreatment with P2Y12-ADP antagonists – namely, to evaluate the impact of the lack of pretreatment on the optimal timing of the intervention. “There are no randomized clinical trials available on this specific group of non-ST elevation acute coronary syndrome patients not pretreated for the timing of the invasive strategy,” he said.
Both groups had similar baseline characteristics, such as history of MI, PCI, and aspirin and P2Y12-ADP use, although the delayed group had a higher rate of diabetes (35% vs. 28.3%).
Regarding secondary endpoints, rates of recurrent ischemic events were 2.9% for the early group and 19.8% for the delayed group during hospitalization, and 4.1% vs. 20.7% at 30 days.
Dr. Bonello noted that rates of cardiovascular death were similar for both groups: 0.3% and 0.8% in-hospital deaths, and 0.6% and 1.1% deaths at 30 days.
The disparity in MACE between all subgroups paralleled that of the overall results with two exceptions, Dr. Bonello said: The positive effect of early intervention was less pronounced in women, and there were no differences in MACE rates among those who had interventions other than PCI.
In his discussion of the trial, Gilles Montalescot, MD, PhD, of the Institute of Cardiology at Pitié-Salpêtrière Hospital in Paris, said the EARLY trial with no P2Y12-ADP pretreatment confirms findings of studies before the ACCOAST trial (N Engl J Med. 2013;369:999-1010), that early angiography has no benefit on survival, recurrent MI, revascularization, or bleeding. While the ACCOAST trial, of which Dr. Montalescot was a principal investigator, found no benefit of pretreatment with prasugrel in patients with NTSE-ASC, the EARLY trial extends those findings to other P2Y12-ADP antagonists. “With the immediate angiography strategy, there is a trivial benefit on recurrent ischemia and length of stay, like in the previous studies, thus not related to pretreatment,” he said.
Dr. Montalescot cautioned against embracing this early-intervention strategy with no P2Y12-ADP pretreatment in all situations.
“If you have a conservative strategy for managing the NTSE-ASC patient or if you are in a center far away from a cath lab and your patients have to wait days for a test, yes, you should consider administration of the P2Y12-ADP antagonist,” Dr. Montalescot said.
Dr. Montalescot disclosed receiving grants or honoraria from ADIR, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Beth Israel Deaconess Medical, and Action Coeur Academic Research Organization.
Dr. Bonello reported financial relationships with AstraZeneca, Boston Scientific, Abbott, and Biotronik. The EARLY trial received funding from the French Ministry of Health.
SOURCE: Bonello B et al. AHA scientific sessions, Session LBS.04 19343.
CHICAGO – Coronary angiography within 2 hours of a diagnosis of non–ST-segment elevation acute coronary syndrome (NSTE-ACS) significantly reduced the risk of recurrent ischemic events as compared to angiography delayed for 12 hours or more, based on the results of the EARLY trial presented at the American Heart Association scientific sessions.
EARLY examined the impacts of not pretreating with a P2Y12-ADP antagonist and of delay before coronary angiography; all study participants received the loading dose of a P2Y12-ADP antagonist at the time of intervention. The early group received angiography within 2 hours, and a delayed group received angiography 12 or more hours after NSTE-ACS.
“Regarding the primary endpoint at 30 days, which is a composite of cardiovascular death and recurrent ischemic event, there is a fivefold lower rate of MACE [major adverse cardiovascular events] in the very-early [group as] compared to the control group,” said Laurent Bonello, MD, PhD, of University Hospital North in Marseilles, France.
The MACE rate was 4.4% in the early group and 21.3% in the delayed group. However, the reduction in MACE was largely because of a reduction in recurrent ischemic events; death rates were similar in the two groups.
The EARLY trial randomized 740 patients at 16 hospitals in France with NSTE-ACS to one of two timing strategies for intervention: within 2 hours of diagnosis, the early-intervention group, and between 12 and 72 hours after diagnosis, the delayed group. Intermediate- and high-risk patients did not receive pretreatment with a P2Y12-ADP antagonist such as clopidogrel before angiography; they received the loading dose at the time of the intervention.
On average, angiography was done within 1 hour in the early group and at 18 hours in the delayed group. Percutaneous coronary intervention (PCI) was performed on 75% of the study population; 3% underwent coronary artery bypass grafting; and 20% received medical therapy.
Dr. Bonello said the purpose of the trial was to settle some uncertainties over the management of NSTE-ACS patients regarding the benefit of pretreatment with P2Y12-ADP antagonists – namely, to evaluate the impact of the lack of pretreatment on the optimal timing of the intervention. “There are no randomized clinical trials available on this specific group of non-ST elevation acute coronary syndrome patients not pretreated for the timing of the invasive strategy,” he said.
Both groups had similar baseline characteristics, such as history of MI, PCI, and aspirin and P2Y12-ADP use, although the delayed group had a higher rate of diabetes (35% vs. 28.3%).
Regarding secondary endpoints, rates of recurrent ischemic events were 2.9% for the early group and 19.8% for the delayed group during hospitalization, and 4.1% vs. 20.7% at 30 days.
Dr. Bonello noted that rates of cardiovascular death were similar for both groups: 0.3% and 0.8% in-hospital deaths, and 0.6% and 1.1% deaths at 30 days.
The disparity in MACE between all subgroups paralleled that of the overall results with two exceptions, Dr. Bonello said: The positive effect of early intervention was less pronounced in women, and there were no differences in MACE rates among those who had interventions other than PCI.
In his discussion of the trial, Gilles Montalescot, MD, PhD, of the Institute of Cardiology at Pitié-Salpêtrière Hospital in Paris, said the EARLY trial with no P2Y12-ADP pretreatment confirms findings of studies before the ACCOAST trial (N Engl J Med. 2013;369:999-1010), that early angiography has no benefit on survival, recurrent MI, revascularization, or bleeding. While the ACCOAST trial, of which Dr. Montalescot was a principal investigator, found no benefit of pretreatment with prasugrel in patients with NTSE-ASC, the EARLY trial extends those findings to other P2Y12-ADP antagonists. “With the immediate angiography strategy, there is a trivial benefit on recurrent ischemia and length of stay, like in the previous studies, thus not related to pretreatment,” he said.
Dr. Montalescot cautioned against embracing this early-intervention strategy with no P2Y12-ADP pretreatment in all situations.
“If you have a conservative strategy for managing the NTSE-ASC patient or if you are in a center far away from a cath lab and your patients have to wait days for a test, yes, you should consider administration of the P2Y12-ADP antagonist,” Dr. Montalescot said.
Dr. Montalescot disclosed receiving grants or honoraria from ADIR, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Beth Israel Deaconess Medical, and Action Coeur Academic Research Organization.
Dr. Bonello reported financial relationships with AstraZeneca, Boston Scientific, Abbott, and Biotronik. The EARLY trial received funding from the French Ministry of Health.
SOURCE: Bonello B et al. AHA scientific sessions, Session LBS.04 19343.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: Coronary angiography within 2 hours of non–ST-segment elevation acute coronary syndrome yielded improved outcomes.
Major finding: Rates of major cardiovascular events were 4.4% with early intervention and 21.3% with delayed intervention.
Study details: Prospective, multicenter, randomized clinical trial of 709 patients.
Disclosures: Dr. Bonello reported financial relationships with AstraZeneca, Boston Scientific, Abbott, and Biotronik. The trial received funding from the French Ministry of Health.
Source: Bonello B et al. AHA scientific sessions, Session LBS.04 19343.
People with HIV still at increased cardiovascular risk
CHICAGO – HIV infection remained linked with an increased risk for developing a cardiovascular disease event among U.S. patients, even in a recent era of antiretroviral therapy.
U.S. health insurance beneficiaries diagnosed with an HIV infection and likely put on antiretroviral therapy sometime during 2011-2015 had a statistically significant, 21% increased risk for the combination of MIs, coronary revascularizations, stroke, and lower-extremity peripheral artery disease (PAD) in a case-control, retrospective analysis, Robert S. Rosenson, MD, said in a poster he presented at the American Heart Association scientific sessions.
“We looked at a contemporary population of people with HIV treated with antiretroviral therapy, and we looked at stroke and lower-extremity PAD [peripheral artery disease] as well as MI, while most prior studies only looked at MIs,” noted Dr. Rosenson, a professor of medicine and director of cardiometabolic disorders at the Icahn School of Medicine at Mount Sinai Medical Center in New York.
The analysis found no significant differences in outcomes that linked with the specific type of antiretroviral therapy patients received. The most commonly used antiretroviral drug was a non–nucleoside reverse transcriptase inhibitor, taken by about 80% of the HIV-infected patients, Dr. Rosenson said. The 2011-2015 period examined in the study largely predated the more recent era, when integrase strand transfer inhibitor drugs have increasingly become the core agent for treating HIV infection.
Another key finding in the study was that a scant 19% of the people infected with HIV received statin treatment, and only 4% were on a high-intensity dosage. The 2018 guideline on cholesterol management identifies HIV infection as one of several “risk enhancers” that boost a person’s cardiovascular disease (CVD) risk and intensify their need for statin treatment (Circulation. 2018 Nov 10. doi: 10.1161/CIR.0000000000000625).
“Hopefully use of statins will increase in people with HIV, but of course we need evidence because so far the evidence does not show benefit,” he noted. In the data Dr. Rosenson reported, the HIV-infected patients who received a statin had roughly the same elevated risk for a CVD event as did HIV-infected patients who did not get a statin.
His study used data from a U.S. commercial database that combined Medicare patients with patients covered by commercial insurers. The analysis identified 82,426 people presumed recently infected by HIV based on either a hospitalization discharge with a diagnostic code for HIV or after filling at least two prescriptions for an antiretroviral drug during January 2011–June 2015. The researchers matched these cases on a 4:1 basis with 329,704 controls from the database matched by age, sex, and year for their index date. The total study cohort averaged about 45 years old, but the people infected by HIV averaged a couple of years older and also had at baseline an increased prevalence of several CVD risk factors and comorbidities. The people with HIV had a more than threefold higher rate of tobacco use, chronic kidney disease, and liver disease, and double the rate of diagnosed depression.
In a multivariate analysis that controlled for many demographic, social, and clinical variables, the results showed that the HIV-infected people had statistically significant higher rates of every individual element in the CVD composite. They had a 26% higher rate of MIs, a 17% higher rate of MIs plus coronary revascularization, a 30% higher rate of stroke, and a doubled rate of lower-extremity PAD.
SOURCE: Rosenson RS et al. Circulation. 2018 Nov 6;138[suppl 1]:A14410.
CHICAGO – HIV infection remained linked with an increased risk for developing a cardiovascular disease event among U.S. patients, even in a recent era of antiretroviral therapy.
U.S. health insurance beneficiaries diagnosed with an HIV infection and likely put on antiretroviral therapy sometime during 2011-2015 had a statistically significant, 21% increased risk for the combination of MIs, coronary revascularizations, stroke, and lower-extremity peripheral artery disease (PAD) in a case-control, retrospective analysis, Robert S. Rosenson, MD, said in a poster he presented at the American Heart Association scientific sessions.
“We looked at a contemporary population of people with HIV treated with antiretroviral therapy, and we looked at stroke and lower-extremity PAD [peripheral artery disease] as well as MI, while most prior studies only looked at MIs,” noted Dr. Rosenson, a professor of medicine and director of cardiometabolic disorders at the Icahn School of Medicine at Mount Sinai Medical Center in New York.
The analysis found no significant differences in outcomes that linked with the specific type of antiretroviral therapy patients received. The most commonly used antiretroviral drug was a non–nucleoside reverse transcriptase inhibitor, taken by about 80% of the HIV-infected patients, Dr. Rosenson said. The 2011-2015 period examined in the study largely predated the more recent era, when integrase strand transfer inhibitor drugs have increasingly become the core agent for treating HIV infection.
Another key finding in the study was that a scant 19% of the people infected with HIV received statin treatment, and only 4% were on a high-intensity dosage. The 2018 guideline on cholesterol management identifies HIV infection as one of several “risk enhancers” that boost a person’s cardiovascular disease (CVD) risk and intensify their need for statin treatment (Circulation. 2018 Nov 10. doi: 10.1161/CIR.0000000000000625).
“Hopefully use of statins will increase in people with HIV, but of course we need evidence because so far the evidence does not show benefit,” he noted. In the data Dr. Rosenson reported, the HIV-infected patients who received a statin had roughly the same elevated risk for a CVD event as did HIV-infected patients who did not get a statin.
His study used data from a U.S. commercial database that combined Medicare patients with patients covered by commercial insurers. The analysis identified 82,426 people presumed recently infected by HIV based on either a hospitalization discharge with a diagnostic code for HIV or after filling at least two prescriptions for an antiretroviral drug during January 2011–June 2015. The researchers matched these cases on a 4:1 basis with 329,704 controls from the database matched by age, sex, and year for their index date. The total study cohort averaged about 45 years old, but the people infected by HIV averaged a couple of years older and also had at baseline an increased prevalence of several CVD risk factors and comorbidities. The people with HIV had a more than threefold higher rate of tobacco use, chronic kidney disease, and liver disease, and double the rate of diagnosed depression.
In a multivariate analysis that controlled for many demographic, social, and clinical variables, the results showed that the HIV-infected people had statistically significant higher rates of every individual element in the CVD composite. They had a 26% higher rate of MIs, a 17% higher rate of MIs plus coronary revascularization, a 30% higher rate of stroke, and a doubled rate of lower-extremity PAD.
SOURCE: Rosenson RS et al. Circulation. 2018 Nov 6;138[suppl 1]:A14410.
CHICAGO – HIV infection remained linked with an increased risk for developing a cardiovascular disease event among U.S. patients, even in a recent era of antiretroviral therapy.
U.S. health insurance beneficiaries diagnosed with an HIV infection and likely put on antiretroviral therapy sometime during 2011-2015 had a statistically significant, 21% increased risk for the combination of MIs, coronary revascularizations, stroke, and lower-extremity peripheral artery disease (PAD) in a case-control, retrospective analysis, Robert S. Rosenson, MD, said in a poster he presented at the American Heart Association scientific sessions.
“We looked at a contemporary population of people with HIV treated with antiretroviral therapy, and we looked at stroke and lower-extremity PAD [peripheral artery disease] as well as MI, while most prior studies only looked at MIs,” noted Dr. Rosenson, a professor of medicine and director of cardiometabolic disorders at the Icahn School of Medicine at Mount Sinai Medical Center in New York.
The analysis found no significant differences in outcomes that linked with the specific type of antiretroviral therapy patients received. The most commonly used antiretroviral drug was a non–nucleoside reverse transcriptase inhibitor, taken by about 80% of the HIV-infected patients, Dr. Rosenson said. The 2011-2015 period examined in the study largely predated the more recent era, when integrase strand transfer inhibitor drugs have increasingly become the core agent for treating HIV infection.
Another key finding in the study was that a scant 19% of the people infected with HIV received statin treatment, and only 4% were on a high-intensity dosage. The 2018 guideline on cholesterol management identifies HIV infection as one of several “risk enhancers” that boost a person’s cardiovascular disease (CVD) risk and intensify their need for statin treatment (Circulation. 2018 Nov 10. doi: 10.1161/CIR.0000000000000625).
“Hopefully use of statins will increase in people with HIV, but of course we need evidence because so far the evidence does not show benefit,” he noted. In the data Dr. Rosenson reported, the HIV-infected patients who received a statin had roughly the same elevated risk for a CVD event as did HIV-infected patients who did not get a statin.
His study used data from a U.S. commercial database that combined Medicare patients with patients covered by commercial insurers. The analysis identified 82,426 people presumed recently infected by HIV based on either a hospitalization discharge with a diagnostic code for HIV or after filling at least two prescriptions for an antiretroviral drug during January 2011–June 2015. The researchers matched these cases on a 4:1 basis with 329,704 controls from the database matched by age, sex, and year for their index date. The total study cohort averaged about 45 years old, but the people infected by HIV averaged a couple of years older and also had at baseline an increased prevalence of several CVD risk factors and comorbidities. The people with HIV had a more than threefold higher rate of tobacco use, chronic kidney disease, and liver disease, and double the rate of diagnosed depression.
In a multivariate analysis that controlled for many demographic, social, and clinical variables, the results showed that the HIV-infected people had statistically significant higher rates of every individual element in the CVD composite. They had a 26% higher rate of MIs, a 17% higher rate of MIs plus coronary revascularization, a 30% higher rate of stroke, and a doubled rate of lower-extremity PAD.
SOURCE: Rosenson RS et al. Circulation. 2018 Nov 6;138[suppl 1]:A14410.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: U.S. insurance beneficiaries newly diagnosed with HIV had a significantly higher rate of CVD events than people without HIV.
Major finding: The adjusted rate of cardiovascular disease events was 21% higher in people infected with HIV, compared with matched, uninfected people.
Study details: A retrospective, case control study of 412,130 U.S. health insurance beneficiaries.
Disclosures: The study received partial funding from Amgen. Dr. Rosenson has received honoraria from Amgen, Akcaa, and Kowa; he has been an advisor to Amgen, Regeneron, and Sanofi; and he has received research funding from Amgen, Akcaa, AstraZeneca, and The Medicines Company.
Source: Rosenson RS et al. Circulation. 2018 Nov 6;138[suppl 1]:A14410.
Cure for Sickle Cell?
Apixaban edges other direct acting anticoagulants for octogenarians, heavy menstrual bleeding in teens is often linked to bleeding disorders, and tanning use disorder should be added to the diagnostic and statistical manual of mental disorders.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Apixaban edges other direct acting anticoagulants for octogenarians, heavy menstrual bleeding in teens is often linked to bleeding disorders, and tanning use disorder should be added to the diagnostic and statistical manual of mental disorders.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Apixaban edges other direct acting anticoagulants for octogenarians, heavy menstrual bleeding in teens is often linked to bleeding disorders, and tanning use disorder should be added to the diagnostic and statistical manual of mental disorders.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Regimen provides survival benefit in PTCL
SAN DIEGO—A newly approved treatment regimen provides a survival benefit over standard therapy for patients with CD30-positive peripheral T-cell lymphomas (PTCLs), according to a presentation at the 2018 ASH Annual Meeting.
In the ECHELON-2 trial, patients who received brentuximab vedotin (BV) plus cyclophosphamide, doxorubicin, and prednisone (CHP) had superior progression-free survival (PFS) and overall survival (OS) compared to patients who received standard treatment with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP).
These results supported the recent U.S. approval of BV in combination with CHP for adults with previously untreated, systemic anaplastic large-cell lymphoma or other CD30-expressing PTCLs, including angioimmunoblastic T-cell lymphoma and PTCL not otherwise specified.
“ECHELON-2 is the first prospective trial in peripheral T-cell lymphoma to show an overall survival benefit over CHOP,” said Steven M. Horwitz, MD, of Memorial Sloan Kettering Cancer Center in Basking Ridge, New Jersey.
Dr. Horwitz presented results from this trial at ASH as abstract 997. Results were simultaneously published in The Lancet.
Patients and treatment
ECHELON-2 (NCT01777152) enrolled 452 patients with previously untreated, CD30-positive PTCL. Subtypes included ALK-positive (n=98) or -negative (n=218) systemic anaplastic large-cell lymphoma, PTCL not otherwise specified (n=72), angioimmunoblastic T-cell lymphoma (n=54), enteropathy-associated T-cell lymphoma (n=7), and adult T-cell leukemia/lymphoma (n=3).
Patients were randomized to receive BV-CHP plus placebo (n=226) or CHOP plus placebo (n=226) every 3 weeks for six to eight cycles.
At baseline, the median age was 58 in both the BV-CHP arm (range, 18-85) and the CHOP arm (range, 18-83). The majority of patients were male—59% in the BV-CHP arm and 67% in the CHOP arm—and most patients had stage III/IV disease—81% and 80%, respectively.
Eighty-nine percent of patients in the BV-CHP arm and 81% in the CHOP arm completed six or more cycles of their assigned treatment.
Twenty-seven percent of patients in the BV-CHP arm and 19% in the CHOP arm received consolidation consisting of radiotherapy (6% and 3%, respectively) and/or stem cell transplant (22% and 17%).
Twenty-six percent of patients in the BV-CHP arm and 42% in the CHOP arm received systemic therapy for residual or progressive disease, and 4% of patients in each arm received palliative radiation.
Efficacy
The overall response rate was 83% in the BV-CHP arm and 72% in the CHOP arm (P=0.0032). The complete response rates were 68% and 56%, respectively (P=0.0066).
At a median follow-up of 36.2 months, the median PFS was 48.2 months in the BV-CHP arm and 20.8 months in the CHOP arm. The rate of death or progression was 42% in the BV-CHP arm and 55% in the CHOP arm (hazard ratio=0.71, P=0.011).
At a median follow-up of 42.1 months, the median OS was not reached in either treatment arm. The rate of death was 23% in the BV-CHP arm and 32% in the CHOP arm (hazard ratio=0.66, P=0.0244).
Dr. Horwitz noted that this study was not powered to determine differences in OS or PFS according to PTCL subtypes.
Safety
BV-CHP had a comparable safety profile to CHOP, Dr. Horwitz said.
The rate of adverse events (AEs) was 99% in the BV-CHP arm and 98% in the CHOP arm. Grade 3 or higher AEs occurred in 66% and 65% of patients, respectively. Serious AEs occurred in 39% and 38%, respectively.
Three percent of patients in the BV-CHP arm and 4% of those in the CHOP arm had fatal AEs.
The most common AEs of any grade occurring in at least 20% of patients (in the BV-CHP and CHOP arms, respectively) were:
- Nausea (46% and 38%)
- Peripheral sensory neuropathy (45% and 41%)
- Neutropenia (38% for both)
- Diarrhea (38% and 20%)
- Constipation (29% and 30%)
- Alopecia (26% and 25%)
- Pyrexia (26% and 19%)
- Vomiting (26% and 17%)
- Fatigue (24% and 20%)
- Anemia (21% and 16%).
This research was funded by Seattle Genetics Inc. and Millennium Pharmaceuticals Inc., a wholly owned subsidiary of Takeda Pharmaceutical Company Limited.
Dr. Horwitz disclosed relationships with Seattle Genetics, Aileron Therapeutics, Innate Pharma, Millennium/Takeda, Forty Seven, Corvus, Mundipharma, ADC Therapeutics, Trillium, Celgene, Portola, Infinity/Verastem, Spectrum, and Kyowa-Hakka-Kirin.
SAN DIEGO—A newly approved treatment regimen provides a survival benefit over standard therapy for patients with CD30-positive peripheral T-cell lymphomas (PTCLs), according to a presentation at the 2018 ASH Annual Meeting.
In the ECHELON-2 trial, patients who received brentuximab vedotin (BV) plus cyclophosphamide, doxorubicin, and prednisone (CHP) had superior progression-free survival (PFS) and overall survival (OS) compared to patients who received standard treatment with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP).
These results supported the recent U.S. approval of BV in combination with CHP for adults with previously untreated, systemic anaplastic large-cell lymphoma or other CD30-expressing PTCLs, including angioimmunoblastic T-cell lymphoma and PTCL not otherwise specified.
“ECHELON-2 is the first prospective trial in peripheral T-cell lymphoma to show an overall survival benefit over CHOP,” said Steven M. Horwitz, MD, of Memorial Sloan Kettering Cancer Center in Basking Ridge, New Jersey.
Dr. Horwitz presented results from this trial at ASH as abstract 997. Results were simultaneously published in The Lancet.
Patients and treatment
ECHELON-2 (NCT01777152) enrolled 452 patients with previously untreated, CD30-positive PTCL. Subtypes included ALK-positive (n=98) or -negative (n=218) systemic anaplastic large-cell lymphoma, PTCL not otherwise specified (n=72), angioimmunoblastic T-cell lymphoma (n=54), enteropathy-associated T-cell lymphoma (n=7), and adult T-cell leukemia/lymphoma (n=3).
Patients were randomized to receive BV-CHP plus placebo (n=226) or CHOP plus placebo (n=226) every 3 weeks for six to eight cycles.
At baseline, the median age was 58 in both the BV-CHP arm (range, 18-85) and the CHOP arm (range, 18-83). The majority of patients were male—59% in the BV-CHP arm and 67% in the CHOP arm—and most patients had stage III/IV disease—81% and 80%, respectively.
Eighty-nine percent of patients in the BV-CHP arm and 81% in the CHOP arm completed six or more cycles of their assigned treatment.
Twenty-seven percent of patients in the BV-CHP arm and 19% in the CHOP arm received consolidation consisting of radiotherapy (6% and 3%, respectively) and/or stem cell transplant (22% and 17%).
Twenty-six percent of patients in the BV-CHP arm and 42% in the CHOP arm received systemic therapy for residual or progressive disease, and 4% of patients in each arm received palliative radiation.
Efficacy
The overall response rate was 83% in the BV-CHP arm and 72% in the CHOP arm (P=0.0032). The complete response rates were 68% and 56%, respectively (P=0.0066).
At a median follow-up of 36.2 months, the median PFS was 48.2 months in the BV-CHP arm and 20.8 months in the CHOP arm. The rate of death or progression was 42% in the BV-CHP arm and 55% in the CHOP arm (hazard ratio=0.71, P=0.011).
At a median follow-up of 42.1 months, the median OS was not reached in either treatment arm. The rate of death was 23% in the BV-CHP arm and 32% in the CHOP arm (hazard ratio=0.66, P=0.0244).
Dr. Horwitz noted that this study was not powered to determine differences in OS or PFS according to PTCL subtypes.
Safety
BV-CHP had a comparable safety profile to CHOP, Dr. Horwitz said.
The rate of adverse events (AEs) was 99% in the BV-CHP arm and 98% in the CHOP arm. Grade 3 or higher AEs occurred in 66% and 65% of patients, respectively. Serious AEs occurred in 39% and 38%, respectively.
Three percent of patients in the BV-CHP arm and 4% of those in the CHOP arm had fatal AEs.
The most common AEs of any grade occurring in at least 20% of patients (in the BV-CHP and CHOP arms, respectively) were:
- Nausea (46% and 38%)
- Peripheral sensory neuropathy (45% and 41%)
- Neutropenia (38% for both)
- Diarrhea (38% and 20%)
- Constipation (29% and 30%)
- Alopecia (26% and 25%)
- Pyrexia (26% and 19%)
- Vomiting (26% and 17%)
- Fatigue (24% and 20%)
- Anemia (21% and 16%).
This research was funded by Seattle Genetics Inc. and Millennium Pharmaceuticals Inc., a wholly owned subsidiary of Takeda Pharmaceutical Company Limited.
Dr. Horwitz disclosed relationships with Seattle Genetics, Aileron Therapeutics, Innate Pharma, Millennium/Takeda, Forty Seven, Corvus, Mundipharma, ADC Therapeutics, Trillium, Celgene, Portola, Infinity/Verastem, Spectrum, and Kyowa-Hakka-Kirin.
SAN DIEGO—A newly approved treatment regimen provides a survival benefit over standard therapy for patients with CD30-positive peripheral T-cell lymphomas (PTCLs), according to a presentation at the 2018 ASH Annual Meeting.
In the ECHELON-2 trial, patients who received brentuximab vedotin (BV) plus cyclophosphamide, doxorubicin, and prednisone (CHP) had superior progression-free survival (PFS) and overall survival (OS) compared to patients who received standard treatment with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP).
These results supported the recent U.S. approval of BV in combination with CHP for adults with previously untreated, systemic anaplastic large-cell lymphoma or other CD30-expressing PTCLs, including angioimmunoblastic T-cell lymphoma and PTCL not otherwise specified.
“ECHELON-2 is the first prospective trial in peripheral T-cell lymphoma to show an overall survival benefit over CHOP,” said Steven M. Horwitz, MD, of Memorial Sloan Kettering Cancer Center in Basking Ridge, New Jersey.
Dr. Horwitz presented results from this trial at ASH as abstract 997. Results were simultaneously published in The Lancet.
Patients and treatment
ECHELON-2 (NCT01777152) enrolled 452 patients with previously untreated, CD30-positive PTCL. Subtypes included ALK-positive (n=98) or -negative (n=218) systemic anaplastic large-cell lymphoma, PTCL not otherwise specified (n=72), angioimmunoblastic T-cell lymphoma (n=54), enteropathy-associated T-cell lymphoma (n=7), and adult T-cell leukemia/lymphoma (n=3).
Patients were randomized to receive BV-CHP plus placebo (n=226) or CHOP plus placebo (n=226) every 3 weeks for six to eight cycles.
At baseline, the median age was 58 in both the BV-CHP arm (range, 18-85) and the CHOP arm (range, 18-83). The majority of patients were male—59% in the BV-CHP arm and 67% in the CHOP arm—and most patients had stage III/IV disease—81% and 80%, respectively.
Eighty-nine percent of patients in the BV-CHP arm and 81% in the CHOP arm completed six or more cycles of their assigned treatment.
Twenty-seven percent of patients in the BV-CHP arm and 19% in the CHOP arm received consolidation consisting of radiotherapy (6% and 3%, respectively) and/or stem cell transplant (22% and 17%).
Twenty-six percent of patients in the BV-CHP arm and 42% in the CHOP arm received systemic therapy for residual or progressive disease, and 4% of patients in each arm received palliative radiation.
Efficacy
The overall response rate was 83% in the BV-CHP arm and 72% in the CHOP arm (P=0.0032). The complete response rates were 68% and 56%, respectively (P=0.0066).
At a median follow-up of 36.2 months, the median PFS was 48.2 months in the BV-CHP arm and 20.8 months in the CHOP arm. The rate of death or progression was 42% in the BV-CHP arm and 55% in the CHOP arm (hazard ratio=0.71, P=0.011).
At a median follow-up of 42.1 months, the median OS was not reached in either treatment arm. The rate of death was 23% in the BV-CHP arm and 32% in the CHOP arm (hazard ratio=0.66, P=0.0244).
Dr. Horwitz noted that this study was not powered to determine differences in OS or PFS according to PTCL subtypes.
Safety
BV-CHP had a comparable safety profile to CHOP, Dr. Horwitz said.
The rate of adverse events (AEs) was 99% in the BV-CHP arm and 98% in the CHOP arm. Grade 3 or higher AEs occurred in 66% and 65% of patients, respectively. Serious AEs occurred in 39% and 38%, respectively.
Three percent of patients in the BV-CHP arm and 4% of those in the CHOP arm had fatal AEs.
The most common AEs of any grade occurring in at least 20% of patients (in the BV-CHP and CHOP arms, respectively) were:
- Nausea (46% and 38%)
- Peripheral sensory neuropathy (45% and 41%)
- Neutropenia (38% for both)
- Diarrhea (38% and 20%)
- Constipation (29% and 30%)
- Alopecia (26% and 25%)
- Pyrexia (26% and 19%)
- Vomiting (26% and 17%)
- Fatigue (24% and 20%)
- Anemia (21% and 16%).
This research was funded by Seattle Genetics Inc. and Millennium Pharmaceuticals Inc., a wholly owned subsidiary of Takeda Pharmaceutical Company Limited.
Dr. Horwitz disclosed relationships with Seattle Genetics, Aileron Therapeutics, Innate Pharma, Millennium/Takeda, Forty Seven, Corvus, Mundipharma, ADC Therapeutics, Trillium, Celgene, Portola, Infinity/Verastem, Spectrum, and Kyowa-Hakka-Kirin.
Ixazomib improves PFS after ASCT in MM
SAN DIEGO—Ixazomib improved progression-free survival (PFS) following autologous stem cell transplant (ASCT) in patients with newly diagnosed multiple myeloma (MM) in the TOURMALINE-MM3 trial.
The oral proteasome inhibitor improved PFS by 39% compared to placebo.
In addition, treatment with ixazomib was well tolerated, and there was a low discontinuation rate.
TOURMALINE-MM3 is the first-ever randomized, double-blind, placebo-controlled study of a proteasome inhibitor used as maintenance after ASCT, according to Meletios A. Dimopoulos, MD, of the National and Kapodistrian University of Athens in Greece.
Dr. Dimopoulos presented results from the trial at the 2018 ASH Annual Meeting (abstract 301).
He said the results suggest ixazomib represents a new treatment option for maintenance after ASCT in MM.
“Proteasome inhibitors have a different mechanism of action and may provide an alternative to lenalidomide,” Dr. Dimopoulos said.
He noted that ixazomib has a manageable toxicity profile and “convenient” weekly oral dosing, making it “well suited” for maintenance.
The TOURMALINE-MM3 study (NCT02181413) included 656 MM patients randomized post-ASCT to receive weekly ixazomib or placebo for up to 2 years.
The median PFS was 26.5 months for ixazomib and 21.3 months for placebo (hazard ratio=0.720; 95% confidence interval, 0.582-0.890; P=0.002).
At a median follow-up of 31 months, the median overall survival has not been reached in either treatment arm.
The discontinuation rate due to adverse events was 7% for ixazomib and 5% for placebo.
Ixazomib was associated with “low toxicity,” Dr Dimopoulos said, and there was no difference in the rates of new primary malignancies, at 3% in both arms.
When asked by an attendee whether ixazomib would become the standard of care for younger MM patients in this setting, Dr. Dimopoulos said the results show that ixazomib “is an option for patients, especially for those where a physician may believe that a proteasome inhibitor may be indicated.”
However, when pressed to comment on how ixazomib compares with lenalidomide for maintenance, Dr. Dimopoulos remarked that current maintenance studies are moving in the direction of combining therapies.
“I think that instead of saying, ‘Is ixazomib better than lenalidomide or vice-versa,’ it is better to see how one may combine those drugs in subsets of patients or even combine these drugs with other agents,” he said.
A manuscript describing results of the TOURMALINE-MM3 study is in press at The Lancet, with an expected online publication date of December 10, Dr. Dimopoulos said.
TOURMALINE-MM3 is sponsored by Takeda (Millennium), the maker of ixazomib.
Dr. Dimopoulos reported honoraria and consultancy with Janssen, Takeda Pharmaceuticals, Amgen, Bristol-Myers Squibb, and Celgene.
SAN DIEGO—Ixazomib improved progression-free survival (PFS) following autologous stem cell transplant (ASCT) in patients with newly diagnosed multiple myeloma (MM) in the TOURMALINE-MM3 trial.
The oral proteasome inhibitor improved PFS by 39% compared to placebo.
In addition, treatment with ixazomib was well tolerated, and there was a low discontinuation rate.
TOURMALINE-MM3 is the first-ever randomized, double-blind, placebo-controlled study of a proteasome inhibitor used as maintenance after ASCT, according to Meletios A. Dimopoulos, MD, of the National and Kapodistrian University of Athens in Greece.
Dr. Dimopoulos presented results from the trial at the 2018 ASH Annual Meeting (abstract 301).
He said the results suggest ixazomib represents a new treatment option for maintenance after ASCT in MM.
“Proteasome inhibitors have a different mechanism of action and may provide an alternative to lenalidomide,” Dr. Dimopoulos said.
He noted that ixazomib has a manageable toxicity profile and “convenient” weekly oral dosing, making it “well suited” for maintenance.
The TOURMALINE-MM3 study (NCT02181413) included 656 MM patients randomized post-ASCT to receive weekly ixazomib or placebo for up to 2 years.
The median PFS was 26.5 months for ixazomib and 21.3 months for placebo (hazard ratio=0.720; 95% confidence interval, 0.582-0.890; P=0.002).
At a median follow-up of 31 months, the median overall survival has not been reached in either treatment arm.
The discontinuation rate due to adverse events was 7% for ixazomib and 5% for placebo.
Ixazomib was associated with “low toxicity,” Dr Dimopoulos said, and there was no difference in the rates of new primary malignancies, at 3% in both arms.
When asked by an attendee whether ixazomib would become the standard of care for younger MM patients in this setting, Dr. Dimopoulos said the results show that ixazomib “is an option for patients, especially for those where a physician may believe that a proteasome inhibitor may be indicated.”
However, when pressed to comment on how ixazomib compares with lenalidomide for maintenance, Dr. Dimopoulos remarked that current maintenance studies are moving in the direction of combining therapies.
“I think that instead of saying, ‘Is ixazomib better than lenalidomide or vice-versa,’ it is better to see how one may combine those drugs in subsets of patients or even combine these drugs with other agents,” he said.
A manuscript describing results of the TOURMALINE-MM3 study is in press at The Lancet, with an expected online publication date of December 10, Dr. Dimopoulos said.
TOURMALINE-MM3 is sponsored by Takeda (Millennium), the maker of ixazomib.
Dr. Dimopoulos reported honoraria and consultancy with Janssen, Takeda Pharmaceuticals, Amgen, Bristol-Myers Squibb, and Celgene.
SAN DIEGO—Ixazomib improved progression-free survival (PFS) following autologous stem cell transplant (ASCT) in patients with newly diagnosed multiple myeloma (MM) in the TOURMALINE-MM3 trial.
The oral proteasome inhibitor improved PFS by 39% compared to placebo.
In addition, treatment with ixazomib was well tolerated, and there was a low discontinuation rate.
TOURMALINE-MM3 is the first-ever randomized, double-blind, placebo-controlled study of a proteasome inhibitor used as maintenance after ASCT, according to Meletios A. Dimopoulos, MD, of the National and Kapodistrian University of Athens in Greece.
Dr. Dimopoulos presented results from the trial at the 2018 ASH Annual Meeting (abstract 301).
He said the results suggest ixazomib represents a new treatment option for maintenance after ASCT in MM.
“Proteasome inhibitors have a different mechanism of action and may provide an alternative to lenalidomide,” Dr. Dimopoulos said.
He noted that ixazomib has a manageable toxicity profile and “convenient” weekly oral dosing, making it “well suited” for maintenance.
The TOURMALINE-MM3 study (NCT02181413) included 656 MM patients randomized post-ASCT to receive weekly ixazomib or placebo for up to 2 years.
The median PFS was 26.5 months for ixazomib and 21.3 months for placebo (hazard ratio=0.720; 95% confidence interval, 0.582-0.890; P=0.002).
At a median follow-up of 31 months, the median overall survival has not been reached in either treatment arm.
The discontinuation rate due to adverse events was 7% for ixazomib and 5% for placebo.
Ixazomib was associated with “low toxicity,” Dr Dimopoulos said, and there was no difference in the rates of new primary malignancies, at 3% in both arms.
When asked by an attendee whether ixazomib would become the standard of care for younger MM patients in this setting, Dr. Dimopoulos said the results show that ixazomib “is an option for patients, especially for those where a physician may believe that a proteasome inhibitor may be indicated.”
However, when pressed to comment on how ixazomib compares with lenalidomide for maintenance, Dr. Dimopoulos remarked that current maintenance studies are moving in the direction of combining therapies.
“I think that instead of saying, ‘Is ixazomib better than lenalidomide or vice-versa,’ it is better to see how one may combine those drugs in subsets of patients or even combine these drugs with other agents,” he said.
A manuscript describing results of the TOURMALINE-MM3 study is in press at The Lancet, with an expected online publication date of December 10, Dr. Dimopoulos said.
TOURMALINE-MM3 is sponsored by Takeda (Millennium), the maker of ixazomib.
Dr. Dimopoulos reported honoraria and consultancy with Janssen, Takeda Pharmaceuticals, Amgen, Bristol-Myers Squibb, and Celgene.
Update shows durable responses in rel/ref DLBCL
SAN DIEGO—An updated analysis of the JULIET trial showed that tisagenlecleucel produced a high rate of durable responses in adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL).
After a median follow-up of 19 months, two-thirds of adults with relapsed/refractory DLBCL who had early responses to the chimeric antigen receptor (CAR) T-cell therapy remained in remission with no evidence of minimal residual disease.
“Since the previous report, no new deaths have been reported due to any cause other than patient disease progression, no treatment-related mortality was seen throughout the study, and there were three early deaths, all related to lymphoma that progressed,” said study investigator Richard Thomas Maziarz, MD, of Oregon Health & Science University’s Knight Cancer Institute in Portland.
Dr. Maziarz and his colleagues reported the updated study results at the 2018 ASH Annual Meeting (abstract 1684). Results were published simultaneously in The New England Journal of Medicine. Data reported here are based on the ASH data.
JULIET then
In the phase 2, single-arm trial, investigators enrolled adults with DLBCL who had relapsed or were refractory after two or more prior lines of therapy and who were either ineligible for hematopoietic stem cell transplant (HSCT) or who experienced disease progression after HSCT.
Interim results of the study were previously reported at the 22nd Congress of the European Hematology Association in 2017.
At that meeting, Gilles Salles, MD, PhD, of the University of Lyon in France, presented results of an analysis of available efficacy data on 51 patients with at least 3 months of follow-up.
In this population, the best overall response rate (ORR) was 59%. Three-month ORR was 45%, consisting of 37% complete responses (CR) and 8% partial responses (PR).
Relapse-free survival at 6 months was 79%, and all patients who had responses at 3 months continued to have responses at the time of data cutoff.
JULIET now
The current analysis was completed after a median time from infusion to data cutoff of 19 months as of May 21, 2018. The analysis included 115 patients who received CAR T-cell infusions, 99 of whom were evaluable for efficacy.
As reported at ASH, the best ORR, the primary endpoint, was 54%, comprised of 40% CR and 13% PR.
Fifty-four percent of patients who had achieved PR converted to CR.
The response rates were consistent across all subgroups, regardless of age, sex, previous response status, International Prognostic Index score at enrollment, prior therapy, molecular subtype, and other factors.
Estimated relapse-free survival 12 months after documentation of an initial response was 64%.
The median duration of response had not been reached at the time of data cutoff, and the median overall survival had not been reached for patients with a CR.
Median overall survival in this heavily pretreated population as a whole (all patients who received CAR T-cell infusions) was 11.1 months and not reached for patients in CR.
Adverse events of special interest included grade 3 or 4 cytokine release syndrome (CRS) in 23% of patients, prolonged cytopenia in 34%, infections in 19%, neurologic events in 11%, febrile neutropenia in 15%, and tumor lysis syndrome in 2%.
There were no deaths attributable to the treatment, CRS, or to cerebral edema, a complication of CAR T-cell therapy that appears to be related to the costimulatory molecule used in various constructs.
The JULIET trial is supported by Novartis. Dr. Maziarz disclosed honoraria, consultancy fees, and/or research funding from Novartis, Incyte, Juno Therapeutics, and Kite Therapeutics as well as patents/royalties from Athersys, Inc.
SAN DIEGO—An updated analysis of the JULIET trial showed that tisagenlecleucel produced a high rate of durable responses in adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL).
After a median follow-up of 19 months, two-thirds of adults with relapsed/refractory DLBCL who had early responses to the chimeric antigen receptor (CAR) T-cell therapy remained in remission with no evidence of minimal residual disease.
“Since the previous report, no new deaths have been reported due to any cause other than patient disease progression, no treatment-related mortality was seen throughout the study, and there were three early deaths, all related to lymphoma that progressed,” said study investigator Richard Thomas Maziarz, MD, of Oregon Health & Science University’s Knight Cancer Institute in Portland.
Dr. Maziarz and his colleagues reported the updated study results at the 2018 ASH Annual Meeting (abstract 1684). Results were published simultaneously in The New England Journal of Medicine. Data reported here are based on the ASH data.
JULIET then
In the phase 2, single-arm trial, investigators enrolled adults with DLBCL who had relapsed or were refractory after two or more prior lines of therapy and who were either ineligible for hematopoietic stem cell transplant (HSCT) or who experienced disease progression after HSCT.
Interim results of the study were previously reported at the 22nd Congress of the European Hematology Association in 2017.
At that meeting, Gilles Salles, MD, PhD, of the University of Lyon in France, presented results of an analysis of available efficacy data on 51 patients with at least 3 months of follow-up.
In this population, the best overall response rate (ORR) was 59%. Three-month ORR was 45%, consisting of 37% complete responses (CR) and 8% partial responses (PR).
Relapse-free survival at 6 months was 79%, and all patients who had responses at 3 months continued to have responses at the time of data cutoff.
JULIET now
The current analysis was completed after a median time from infusion to data cutoff of 19 months as of May 21, 2018. The analysis included 115 patients who received CAR T-cell infusions, 99 of whom were evaluable for efficacy.
As reported at ASH, the best ORR, the primary endpoint, was 54%, comprised of 40% CR and 13% PR.
Fifty-four percent of patients who had achieved PR converted to CR.
The response rates were consistent across all subgroups, regardless of age, sex, previous response status, International Prognostic Index score at enrollment, prior therapy, molecular subtype, and other factors.
Estimated relapse-free survival 12 months after documentation of an initial response was 64%.
The median duration of response had not been reached at the time of data cutoff, and the median overall survival had not been reached for patients with a CR.
Median overall survival in this heavily pretreated population as a whole (all patients who received CAR T-cell infusions) was 11.1 months and not reached for patients in CR.
Adverse events of special interest included grade 3 or 4 cytokine release syndrome (CRS) in 23% of patients, prolonged cytopenia in 34%, infections in 19%, neurologic events in 11%, febrile neutropenia in 15%, and tumor lysis syndrome in 2%.
There were no deaths attributable to the treatment, CRS, or to cerebral edema, a complication of CAR T-cell therapy that appears to be related to the costimulatory molecule used in various constructs.
The JULIET trial is supported by Novartis. Dr. Maziarz disclosed honoraria, consultancy fees, and/or research funding from Novartis, Incyte, Juno Therapeutics, and Kite Therapeutics as well as patents/royalties from Athersys, Inc.
SAN DIEGO—An updated analysis of the JULIET trial showed that tisagenlecleucel produced a high rate of durable responses in adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL).
After a median follow-up of 19 months, two-thirds of adults with relapsed/refractory DLBCL who had early responses to the chimeric antigen receptor (CAR) T-cell therapy remained in remission with no evidence of minimal residual disease.
“Since the previous report, no new deaths have been reported due to any cause other than patient disease progression, no treatment-related mortality was seen throughout the study, and there were three early deaths, all related to lymphoma that progressed,” said study investigator Richard Thomas Maziarz, MD, of Oregon Health & Science University’s Knight Cancer Institute in Portland.
Dr. Maziarz and his colleagues reported the updated study results at the 2018 ASH Annual Meeting (abstract 1684). Results were published simultaneously in The New England Journal of Medicine. Data reported here are based on the ASH data.
JULIET then
In the phase 2, single-arm trial, investigators enrolled adults with DLBCL who had relapsed or were refractory after two or more prior lines of therapy and who were either ineligible for hematopoietic stem cell transplant (HSCT) or who experienced disease progression after HSCT.
Interim results of the study were previously reported at the 22nd Congress of the European Hematology Association in 2017.
At that meeting, Gilles Salles, MD, PhD, of the University of Lyon in France, presented results of an analysis of available efficacy data on 51 patients with at least 3 months of follow-up.
In this population, the best overall response rate (ORR) was 59%. Three-month ORR was 45%, consisting of 37% complete responses (CR) and 8% partial responses (PR).
Relapse-free survival at 6 months was 79%, and all patients who had responses at 3 months continued to have responses at the time of data cutoff.
JULIET now
The current analysis was completed after a median time from infusion to data cutoff of 19 months as of May 21, 2018. The analysis included 115 patients who received CAR T-cell infusions, 99 of whom were evaluable for efficacy.
As reported at ASH, the best ORR, the primary endpoint, was 54%, comprised of 40% CR and 13% PR.
Fifty-four percent of patients who had achieved PR converted to CR.
The response rates were consistent across all subgroups, regardless of age, sex, previous response status, International Prognostic Index score at enrollment, prior therapy, molecular subtype, and other factors.
Estimated relapse-free survival 12 months after documentation of an initial response was 64%.
The median duration of response had not been reached at the time of data cutoff, and the median overall survival had not been reached for patients with a CR.
Median overall survival in this heavily pretreated population as a whole (all patients who received CAR T-cell infusions) was 11.1 months and not reached for patients in CR.
Adverse events of special interest included grade 3 or 4 cytokine release syndrome (CRS) in 23% of patients, prolonged cytopenia in 34%, infections in 19%, neurologic events in 11%, febrile neutropenia in 15%, and tumor lysis syndrome in 2%.
There were no deaths attributable to the treatment, CRS, or to cerebral edema, a complication of CAR T-cell therapy that appears to be related to the costimulatory molecule used in various constructs.
The JULIET trial is supported by Novartis. Dr. Maziarz disclosed honoraria, consultancy fees, and/or research funding from Novartis, Incyte, Juno Therapeutics, and Kite Therapeutics as well as patents/royalties from Athersys, Inc.
5 Important Lessons I’ve Learned in Practice
Health care is a constantly changing field, thanks to innovative research and technological advancements. And with optimal team practice and full practice authority, PAs and NPs are poised to drive further improvements to patient care. But while we all recognize the need to keep learning, some of the greatest lessons I’ve learned in my career have little to do with the “latest and greatest” tools—they are fundamentals of being a good person and effective health care provider. I would like to share some of them with you.
1 It’s OK to make a mistake, but be sure to own it and learn from it.
You can’t grow as a person or a provider if you can’t acknowledge failure and vow to improve. Don’t become complacent; a little bit of fear keeps us on our toes and hopefully out of trouble.
It always seems to be Friday at 4:45
But while many providers would stop there, assuming that they have solved the problem, I would advocate for calling the patient directly and addressing the issue head-on. The patient may be thinking, “What an idiot, she missed that in my chart.” Clearly, there was a breakdown in the process, but you are the one who is ultimately responsible.
A phone call to verify the allergy and the type of reaction is very valuable. It proves to the patient that you take patient care seriously and that you recognize that the system needs to be improved.
2 Find one thing in common with each patient, even if it is something small.
Maybe you grew up in the same town, or like the same sports team, or enjoy the same type of food. It isn’t difficult to find a commonality; a note in the patient’s chart ensures you’ll remember. That personal touch demonstrates that you care and increases the patient’s comfort with you.
This technique can make a huge difference with a “difficult” patient. One day, a new patient presented to my office for a change in bowel habits. He was clearly anxious and angry with his wife (who accompanied him) for “making me come here.”
Continue to: During the social history...
During the social history, I learned that he owned a trucking business. I asked what kind of trucks. He said, “Big ones!” I was more specific in my next attempt, asking, “Volvo, Peterbilt, International, or Kenworth?” He looked puzzled and said, “I see you know something about trucks.” I explained that my husband is a diesel mechanic and that we play “identify the truck” when travelling with our young sons. It turned out that my husband had worked on the patient’s truck the week before.
The dynamic of our encounter changed immediately, and we were able to schedule him for a much-needed colonoscopy. He was diagnosed with a large precancerous colon polyp, and I was relieved that our “connection” smoothed the way to getting him the care he needed.
3 Always remember that people are watching.
Nothing is truly private anymore. Social media can be a great forum for exchanging information and knowledge, but you could become the latest YouTube sensation (not necessarily in a positive way) at any time.
When a patient asks if he can record our visit to share with family, I wonder how many have done so without permission. The bottom line is that we, as health care professionals, have a high standard to live up to.
This was brought home to me in my work as a volunteer firefighter and EMT. One night I had barely finished loading a patient from a serious motor vehicle collision into a helicopter to be transferred to definitive care when my phone started buzzing. A photographer from the local newspaper—whom I didn’t even know was on scene—had snapped a picture of me in action and posted it to his online news site and social media accounts. Within 5 minutes, several coworkers had seen it and texted me. My surname across the bottom of my jacket provided a clear indication of where I was and what I was doing. I was absolutely shocked at how quickly news spread, and although nothing untoward or inappropriate was documented, it was unsettling to realize that I was “in the public eye” while I was focused on doing my job.
Continue to: That photo is now the screensaver...
That photo is now the screensaver on my computer. It’s a daily reminder that someone is always watching and I must conduct myself accordingly.
4 Don’t be afraid to speak up.
Don’t be a tattletale, but do stand up for what you know is right. When presented with a choice, always do the right thing, even if it is more difficult.
This is harder than it sounds; I know how tough it was for me to find my voice. But I did during the case of a middle-aged woman with a significant upper GI bleed. She had been in her normal state of health until she experienced a sudden onset of nausea and vomiting; her husband called EMS when she began vomiting large amounts of bright red blood. Her care plan involved multiple members of our GI service, as well as colleagues from an affiliated tertiary care hospital, and I spent hours coordinating care and obtaining the necessary consults. When the patient subsequently developed abdominal compartment syndrome and required bedside surgical intervention, the attending surgeon proceeded to dress me down in front of the entire ICU team, screaming, “Why isn’t Dr. So-and-so here caring for this patient? Why aren’t you doing anything to care for this woman?”
In the old days, I would have walked away without saying anything—that’s what was expected. But, my own hurt feelings aside, I couldn’t stop thinking, “What if he treats others like that? If I don’t speak up, I’m an accomplice to his bad behavior.” So I waited for his team to perform the urgent procedure and then politely asked if I could speak with him. I was shaking in my shoes when I began by asking if he had read my notes in the patient’s chart. He grudgingly said, “No.” I listed the physicians who had been consulted about this patient and documented the time the team had spent developing a safe treatment plan for her. I ended by saying that it was unfair and unprofessional for him to yell at me, particularly in front of our colleagues, and I asked how he would have felt if treated the same way. He apologized and agreed to approach me privately if he had concerns in future. I can honestly say that encounter changed our working relationship in a very positive manner. One of the most difficult experiences of my entire career helped me to grow as a professional.
Continue to: Each and every one of us is an educator...
5 Each and every one of us is an educator, even if we don’t consciously choose to be.
You can be an educator without being employed as a teacher. Educators go above and beyond to make sure that learning is student centered and that knowledge is received and understood. Every day, we educate patients, families, friends, neighbors, and other members of the health care team.
A few months ago, I began a new paramedic job at a different agency. During training, one of my coworkers made an offhand comment: “It’s your fault that I’m here.” At my puzzled expression, he continued, “You don’t remember, do you? When you did my last firefighter physical, we talked about the best way to get a full-time job as a firefighter. You recommended that I consider a job in EMS to gain additional experience and interface with the fire departments, so here I am and I love it.” At that point, I did recall our conversation—but what I had seen as simple small talk with a patient had really been an educational moment. I had a smile on my face the whole drive home as I thought about how my casual conversation had a positive effect on him and his career path.
PAs and NPs are educators even when they are not presenting in the classroom or serving as a clinical preceptor. It doesn’t matter if you are new to the profession or have been working for many years—you have valuable experience that can help someone else. Please remember that even small moments can make a large impact. Strive to be a good educator at all times.
Health care is a constantly changing field, thanks to innovative research and technological advancements. And with optimal team practice and full practice authority, PAs and NPs are poised to drive further improvements to patient care. But while we all recognize the need to keep learning, some of the greatest lessons I’ve learned in my career have little to do with the “latest and greatest” tools—they are fundamentals of being a good person and effective health care provider. I would like to share some of them with you.
1 It’s OK to make a mistake, but be sure to own it and learn from it.
You can’t grow as a person or a provider if you can’t acknowledge failure and vow to improve. Don’t become complacent; a little bit of fear keeps us on our toes and hopefully out of trouble.
It always seems to be Friday at 4:45
But while many providers would stop there, assuming that they have solved the problem, I would advocate for calling the patient directly and addressing the issue head-on. The patient may be thinking, “What an idiot, she missed that in my chart.” Clearly, there was a breakdown in the process, but you are the one who is ultimately responsible.
A phone call to verify the allergy and the type of reaction is very valuable. It proves to the patient that you take patient care seriously and that you recognize that the system needs to be improved.
2 Find one thing in common with each patient, even if it is something small.
Maybe you grew up in the same town, or like the same sports team, or enjoy the same type of food. It isn’t difficult to find a commonality; a note in the patient’s chart ensures you’ll remember. That personal touch demonstrates that you care and increases the patient’s comfort with you.
This technique can make a huge difference with a “difficult” patient. One day, a new patient presented to my office for a change in bowel habits. He was clearly anxious and angry with his wife (who accompanied him) for “making me come here.”
Continue to: During the social history...
During the social history, I learned that he owned a trucking business. I asked what kind of trucks. He said, “Big ones!” I was more specific in my next attempt, asking, “Volvo, Peterbilt, International, or Kenworth?” He looked puzzled and said, “I see you know something about trucks.” I explained that my husband is a diesel mechanic and that we play “identify the truck” when travelling with our young sons. It turned out that my husband had worked on the patient’s truck the week before.
The dynamic of our encounter changed immediately, and we were able to schedule him for a much-needed colonoscopy. He was diagnosed with a large precancerous colon polyp, and I was relieved that our “connection” smoothed the way to getting him the care he needed.
3 Always remember that people are watching.
Nothing is truly private anymore. Social media can be a great forum for exchanging information and knowledge, but you could become the latest YouTube sensation (not necessarily in a positive way) at any time.
When a patient asks if he can record our visit to share with family, I wonder how many have done so without permission. The bottom line is that we, as health care professionals, have a high standard to live up to.
This was brought home to me in my work as a volunteer firefighter and EMT. One night I had barely finished loading a patient from a serious motor vehicle collision into a helicopter to be transferred to definitive care when my phone started buzzing. A photographer from the local newspaper—whom I didn’t even know was on scene—had snapped a picture of me in action and posted it to his online news site and social media accounts. Within 5 minutes, several coworkers had seen it and texted me. My surname across the bottom of my jacket provided a clear indication of where I was and what I was doing. I was absolutely shocked at how quickly news spread, and although nothing untoward or inappropriate was documented, it was unsettling to realize that I was “in the public eye” while I was focused on doing my job.
Continue to: That photo is now the screensaver...
That photo is now the screensaver on my computer. It’s a daily reminder that someone is always watching and I must conduct myself accordingly.
4 Don’t be afraid to speak up.
Don’t be a tattletale, but do stand up for what you know is right. When presented with a choice, always do the right thing, even if it is more difficult.
This is harder than it sounds; I know how tough it was for me to find my voice. But I did during the case of a middle-aged woman with a significant upper GI bleed. She had been in her normal state of health until she experienced a sudden onset of nausea and vomiting; her husband called EMS when she began vomiting large amounts of bright red blood. Her care plan involved multiple members of our GI service, as well as colleagues from an affiliated tertiary care hospital, and I spent hours coordinating care and obtaining the necessary consults. When the patient subsequently developed abdominal compartment syndrome and required bedside surgical intervention, the attending surgeon proceeded to dress me down in front of the entire ICU team, screaming, “Why isn’t Dr. So-and-so here caring for this patient? Why aren’t you doing anything to care for this woman?”
In the old days, I would have walked away without saying anything—that’s what was expected. But, my own hurt feelings aside, I couldn’t stop thinking, “What if he treats others like that? If I don’t speak up, I’m an accomplice to his bad behavior.” So I waited for his team to perform the urgent procedure and then politely asked if I could speak with him. I was shaking in my shoes when I began by asking if he had read my notes in the patient’s chart. He grudgingly said, “No.” I listed the physicians who had been consulted about this patient and documented the time the team had spent developing a safe treatment plan for her. I ended by saying that it was unfair and unprofessional for him to yell at me, particularly in front of our colleagues, and I asked how he would have felt if treated the same way. He apologized and agreed to approach me privately if he had concerns in future. I can honestly say that encounter changed our working relationship in a very positive manner. One of the most difficult experiences of my entire career helped me to grow as a professional.
Continue to: Each and every one of us is an educator...
5 Each and every one of us is an educator, even if we don’t consciously choose to be.
You can be an educator without being employed as a teacher. Educators go above and beyond to make sure that learning is student centered and that knowledge is received and understood. Every day, we educate patients, families, friends, neighbors, and other members of the health care team.
A few months ago, I began a new paramedic job at a different agency. During training, one of my coworkers made an offhand comment: “It’s your fault that I’m here.” At my puzzled expression, he continued, “You don’t remember, do you? When you did my last firefighter physical, we talked about the best way to get a full-time job as a firefighter. You recommended that I consider a job in EMS to gain additional experience and interface with the fire departments, so here I am and I love it.” At that point, I did recall our conversation—but what I had seen as simple small talk with a patient had really been an educational moment. I had a smile on my face the whole drive home as I thought about how my casual conversation had a positive effect on him and his career path.
PAs and NPs are educators even when they are not presenting in the classroom or serving as a clinical preceptor. It doesn’t matter if you are new to the profession or have been working for many years—you have valuable experience that can help someone else. Please remember that even small moments can make a large impact. Strive to be a good educator at all times.
Health care is a constantly changing field, thanks to innovative research and technological advancements. And with optimal team practice and full practice authority, PAs and NPs are poised to drive further improvements to patient care. But while we all recognize the need to keep learning, some of the greatest lessons I’ve learned in my career have little to do with the “latest and greatest” tools—they are fundamentals of being a good person and effective health care provider. I would like to share some of them with you.
1 It’s OK to make a mistake, but be sure to own it and learn from it.
You can’t grow as a person or a provider if you can’t acknowledge failure and vow to improve. Don’t become complacent; a little bit of fear keeps us on our toes and hopefully out of trouble.
It always seems to be Friday at 4:45
But while many providers would stop there, assuming that they have solved the problem, I would advocate for calling the patient directly and addressing the issue head-on. The patient may be thinking, “What an idiot, she missed that in my chart.” Clearly, there was a breakdown in the process, but you are the one who is ultimately responsible.
A phone call to verify the allergy and the type of reaction is very valuable. It proves to the patient that you take patient care seriously and that you recognize that the system needs to be improved.
2 Find one thing in common with each patient, even if it is something small.
Maybe you grew up in the same town, or like the same sports team, or enjoy the same type of food. It isn’t difficult to find a commonality; a note in the patient’s chart ensures you’ll remember. That personal touch demonstrates that you care and increases the patient’s comfort with you.
This technique can make a huge difference with a “difficult” patient. One day, a new patient presented to my office for a change in bowel habits. He was clearly anxious and angry with his wife (who accompanied him) for “making me come here.”
Continue to: During the social history...
During the social history, I learned that he owned a trucking business. I asked what kind of trucks. He said, “Big ones!” I was more specific in my next attempt, asking, “Volvo, Peterbilt, International, or Kenworth?” He looked puzzled and said, “I see you know something about trucks.” I explained that my husband is a diesel mechanic and that we play “identify the truck” when travelling with our young sons. It turned out that my husband had worked on the patient’s truck the week before.
The dynamic of our encounter changed immediately, and we were able to schedule him for a much-needed colonoscopy. He was diagnosed with a large precancerous colon polyp, and I was relieved that our “connection” smoothed the way to getting him the care he needed.
3 Always remember that people are watching.
Nothing is truly private anymore. Social media can be a great forum for exchanging information and knowledge, but you could become the latest YouTube sensation (not necessarily in a positive way) at any time.
When a patient asks if he can record our visit to share with family, I wonder how many have done so without permission. The bottom line is that we, as health care professionals, have a high standard to live up to.
This was brought home to me in my work as a volunteer firefighter and EMT. One night I had barely finished loading a patient from a serious motor vehicle collision into a helicopter to be transferred to definitive care when my phone started buzzing. A photographer from the local newspaper—whom I didn’t even know was on scene—had snapped a picture of me in action and posted it to his online news site and social media accounts. Within 5 minutes, several coworkers had seen it and texted me. My surname across the bottom of my jacket provided a clear indication of where I was and what I was doing. I was absolutely shocked at how quickly news spread, and although nothing untoward or inappropriate was documented, it was unsettling to realize that I was “in the public eye” while I was focused on doing my job.
Continue to: That photo is now the screensaver...
That photo is now the screensaver on my computer. It’s a daily reminder that someone is always watching and I must conduct myself accordingly.
4 Don’t be afraid to speak up.
Don’t be a tattletale, but do stand up for what you know is right. When presented with a choice, always do the right thing, even if it is more difficult.
This is harder than it sounds; I know how tough it was for me to find my voice. But I did during the case of a middle-aged woman with a significant upper GI bleed. She had been in her normal state of health until she experienced a sudden onset of nausea and vomiting; her husband called EMS when she began vomiting large amounts of bright red blood. Her care plan involved multiple members of our GI service, as well as colleagues from an affiliated tertiary care hospital, and I spent hours coordinating care and obtaining the necessary consults. When the patient subsequently developed abdominal compartment syndrome and required bedside surgical intervention, the attending surgeon proceeded to dress me down in front of the entire ICU team, screaming, “Why isn’t Dr. So-and-so here caring for this patient? Why aren’t you doing anything to care for this woman?”
In the old days, I would have walked away without saying anything—that’s what was expected. But, my own hurt feelings aside, I couldn’t stop thinking, “What if he treats others like that? If I don’t speak up, I’m an accomplice to his bad behavior.” So I waited for his team to perform the urgent procedure and then politely asked if I could speak with him. I was shaking in my shoes when I began by asking if he had read my notes in the patient’s chart. He grudgingly said, “No.” I listed the physicians who had been consulted about this patient and documented the time the team had spent developing a safe treatment plan for her. I ended by saying that it was unfair and unprofessional for him to yell at me, particularly in front of our colleagues, and I asked how he would have felt if treated the same way. He apologized and agreed to approach me privately if he had concerns in future. I can honestly say that encounter changed our working relationship in a very positive manner. One of the most difficult experiences of my entire career helped me to grow as a professional.
Continue to: Each and every one of us is an educator...
5 Each and every one of us is an educator, even if we don’t consciously choose to be.
You can be an educator without being employed as a teacher. Educators go above and beyond to make sure that learning is student centered and that knowledge is received and understood. Every day, we educate patients, families, friends, neighbors, and other members of the health care team.
A few months ago, I began a new paramedic job at a different agency. During training, one of my coworkers made an offhand comment: “It’s your fault that I’m here.” At my puzzled expression, he continued, “You don’t remember, do you? When you did my last firefighter physical, we talked about the best way to get a full-time job as a firefighter. You recommended that I consider a job in EMS to gain additional experience and interface with the fire departments, so here I am and I love it.” At that point, I did recall our conversation—but what I had seen as simple small talk with a patient had really been an educational moment. I had a smile on my face the whole drive home as I thought about how my casual conversation had a positive effect on him and his career path.
PAs and NPs are educators even when they are not presenting in the classroom or serving as a clinical preceptor. It doesn’t matter if you are new to the profession or have been working for many years—you have valuable experience that can help someone else. Please remember that even small moments can make a large impact. Strive to be a good educator at all times.
Visual representation of atherosclerosis helps reduce cardiovascular risk
A pictorial representation of carotid ultrasound coupled with a follow-up phone call from a nurse led to reduced cardiovascular disease risk at 1-year follow-up, according to a randomized, controlled study of northern Sweden residents at risk of cardiovascular disease.
“Our study supports further attempts to solve the major problem of prevention failure because of low adherence, despite effective, cost-effective, and evidence-based medications and methods for a healthier lifestyle,” wrote lead author Ulf Näslund, of Umeå (Sweden) University, and his coauthors. The study was published online in the Lancet.
In this trial of 3,532 individuals who were aged 40-60 years with one or more conventional cardiovascular risk factors, the intervention group (1,749) received pictorial information of atherosclerosis as an add-on to normal care. Their primary care physician received the same information, and these participants also received a follow-up phone call from a nurse 2-4 weeks later. The other participants (1,783) received standard care but neither the presentation nor the phone call.
Both the Framingham risk score (FRS) and European Systematic Coronary Risk Evaluation (SCORE) were both used to assess outcomes; at 1-year follow-up, the intervention group had an FRS that decreased from baseline (–0.58; 95% confidence interval, –0.86 to –0.30), compared with an increase in the control group (0.35; 95% CI, 0.08-0.63). SCORE values increased twice as much in the control group (0.27; 95% CI, 0.23-0.30), compared with the intervention group (0.13; 95% CI, 0.09-0.18). The authors also observed no differential responses for education level, surmising that “this type of risk communication might contribute to reduction of the social gap in health.”
The authors shared their study’s limitations, including notable differences between dropouts and participants at 1-year follow-up with regard to metabolic risk factors and such fast-developing imaging technologies as CT and MRI out-dating ultrasound findings. They also acknowledged that more research needs to be undertaken to prove that these outcomes are genuine.
This study was funded by Västerbotten County Council, the Swedish Research Council, the Heart and Lung Foundation, and the Swedish Society of Medicine. No conflicts of interest were reported.
SOURCE: Näslund U et al. Lancet. 2018 Dec 3. doi: 10.1016/S0140-6736(18)32818-6.
Though improving adherence and outcomes has long eluded clinicians and researchers, this study by Näslund and colleagues provides optimism that cardiovascular risk can be mitigated through educational and motivational factors, according to Richard Kones, MD, of the Cardiometabolic Research Institute in Houston; Umme Rumana, MBBS, of the University of Texas at Houston and the New York Institute of Technology in Old Westbury; and Alberto Morales-Salinas, MD, of the Cardiocentro Ernesto Che Guevara in Villa Clara, Cuba.
The three authors underlined the struggles that low- and middle-income countries go through in terms of “poor adherence and uneven availability and access” for those with high cardiovascular risk; even richer countries like the United States still suffer through a high percentage of hospital admissions that stem from nonadherence to medication. As such, the work of Näslund and colleagues displays the potential of image-based information plus follow-up reinforcement in a manner not often utilized.
“The strengths of the study include size, detail, and the pragmatic, randomized, controlled trial design,” they noted, adding that few other analyses in this area are even comparable. At the same time, lack of resources — including access to transportation and medication — may limit the effectiveness of motivation, especially since the United States differs in prices and health disparities as compared to the study’s Swedish populace.
Coronary heart disease remains one of the world’s leading causes of deaths, and higher adherence will likely lead to “drastic improvements in cardiovascular outcomes.” Yet the three authors state that more research needs to be done to quantify the exact impact of adherence in regard to medication, physical activity, or any reliever of cardiovascular risk: “Whether the results are sustainable and will reduce subsequent major adverse cardiac and cerebrovascular events requires longer follow-up.”
These comments are adapted from an accompanying editorial (Lancet. 2018 Dec 3. doi: 10.1016/S0140-6736[18]33079-4 ). The authors declared no conflict of interest.
Though improving adherence and outcomes has long eluded clinicians and researchers, this study by Näslund and colleagues provides optimism that cardiovascular risk can be mitigated through educational and motivational factors, according to Richard Kones, MD, of the Cardiometabolic Research Institute in Houston; Umme Rumana, MBBS, of the University of Texas at Houston and the New York Institute of Technology in Old Westbury; and Alberto Morales-Salinas, MD, of the Cardiocentro Ernesto Che Guevara in Villa Clara, Cuba.
The three authors underlined the struggles that low- and middle-income countries go through in terms of “poor adherence and uneven availability and access” for those with high cardiovascular risk; even richer countries like the United States still suffer through a high percentage of hospital admissions that stem from nonadherence to medication. As such, the work of Näslund and colleagues displays the potential of image-based information plus follow-up reinforcement in a manner not often utilized.
“The strengths of the study include size, detail, and the pragmatic, randomized, controlled trial design,” they noted, adding that few other analyses in this area are even comparable. At the same time, lack of resources — including access to transportation and medication — may limit the effectiveness of motivation, especially since the United States differs in prices and health disparities as compared to the study’s Swedish populace.
Coronary heart disease remains one of the world’s leading causes of deaths, and higher adherence will likely lead to “drastic improvements in cardiovascular outcomes.” Yet the three authors state that more research needs to be done to quantify the exact impact of adherence in regard to medication, physical activity, or any reliever of cardiovascular risk: “Whether the results are sustainable and will reduce subsequent major adverse cardiac and cerebrovascular events requires longer follow-up.”
These comments are adapted from an accompanying editorial (Lancet. 2018 Dec 3. doi: 10.1016/S0140-6736[18]33079-4 ). The authors declared no conflict of interest.
Though improving adherence and outcomes has long eluded clinicians and researchers, this study by Näslund and colleagues provides optimism that cardiovascular risk can be mitigated through educational and motivational factors, according to Richard Kones, MD, of the Cardiometabolic Research Institute in Houston; Umme Rumana, MBBS, of the University of Texas at Houston and the New York Institute of Technology in Old Westbury; and Alberto Morales-Salinas, MD, of the Cardiocentro Ernesto Che Guevara in Villa Clara, Cuba.
The three authors underlined the struggles that low- and middle-income countries go through in terms of “poor adherence and uneven availability and access” for those with high cardiovascular risk; even richer countries like the United States still suffer through a high percentage of hospital admissions that stem from nonadherence to medication. As such, the work of Näslund and colleagues displays the potential of image-based information plus follow-up reinforcement in a manner not often utilized.
“The strengths of the study include size, detail, and the pragmatic, randomized, controlled trial design,” they noted, adding that few other analyses in this area are even comparable. At the same time, lack of resources — including access to transportation and medication — may limit the effectiveness of motivation, especially since the United States differs in prices and health disparities as compared to the study’s Swedish populace.
Coronary heart disease remains one of the world’s leading causes of deaths, and higher adherence will likely lead to “drastic improvements in cardiovascular outcomes.” Yet the three authors state that more research needs to be done to quantify the exact impact of adherence in regard to medication, physical activity, or any reliever of cardiovascular risk: “Whether the results are sustainable and will reduce subsequent major adverse cardiac and cerebrovascular events requires longer follow-up.”
These comments are adapted from an accompanying editorial (Lancet. 2018 Dec 3. doi: 10.1016/S0140-6736[18]33079-4 ). The authors declared no conflict of interest.
A pictorial representation of carotid ultrasound coupled with a follow-up phone call from a nurse led to reduced cardiovascular disease risk at 1-year follow-up, according to a randomized, controlled study of northern Sweden residents at risk of cardiovascular disease.
“Our study supports further attempts to solve the major problem of prevention failure because of low adherence, despite effective, cost-effective, and evidence-based medications and methods for a healthier lifestyle,” wrote lead author Ulf Näslund, of Umeå (Sweden) University, and his coauthors. The study was published online in the Lancet.
In this trial of 3,532 individuals who were aged 40-60 years with one or more conventional cardiovascular risk factors, the intervention group (1,749) received pictorial information of atherosclerosis as an add-on to normal care. Their primary care physician received the same information, and these participants also received a follow-up phone call from a nurse 2-4 weeks later. The other participants (1,783) received standard care but neither the presentation nor the phone call.
Both the Framingham risk score (FRS) and European Systematic Coronary Risk Evaluation (SCORE) were both used to assess outcomes; at 1-year follow-up, the intervention group had an FRS that decreased from baseline (–0.58; 95% confidence interval, –0.86 to –0.30), compared with an increase in the control group (0.35; 95% CI, 0.08-0.63). SCORE values increased twice as much in the control group (0.27; 95% CI, 0.23-0.30), compared with the intervention group (0.13; 95% CI, 0.09-0.18). The authors also observed no differential responses for education level, surmising that “this type of risk communication might contribute to reduction of the social gap in health.”
The authors shared their study’s limitations, including notable differences between dropouts and participants at 1-year follow-up with regard to metabolic risk factors and such fast-developing imaging technologies as CT and MRI out-dating ultrasound findings. They also acknowledged that more research needs to be undertaken to prove that these outcomes are genuine.
This study was funded by Västerbotten County Council, the Swedish Research Council, the Heart and Lung Foundation, and the Swedish Society of Medicine. No conflicts of interest were reported.
SOURCE: Näslund U et al. Lancet. 2018 Dec 3. doi: 10.1016/S0140-6736(18)32818-6.
A pictorial representation of carotid ultrasound coupled with a follow-up phone call from a nurse led to reduced cardiovascular disease risk at 1-year follow-up, according to a randomized, controlled study of northern Sweden residents at risk of cardiovascular disease.
“Our study supports further attempts to solve the major problem of prevention failure because of low adherence, despite effective, cost-effective, and evidence-based medications and methods for a healthier lifestyle,” wrote lead author Ulf Näslund, of Umeå (Sweden) University, and his coauthors. The study was published online in the Lancet.
In this trial of 3,532 individuals who were aged 40-60 years with one or more conventional cardiovascular risk factors, the intervention group (1,749) received pictorial information of atherosclerosis as an add-on to normal care. Their primary care physician received the same information, and these participants also received a follow-up phone call from a nurse 2-4 weeks later. The other participants (1,783) received standard care but neither the presentation nor the phone call.
Both the Framingham risk score (FRS) and European Systematic Coronary Risk Evaluation (SCORE) were both used to assess outcomes; at 1-year follow-up, the intervention group had an FRS that decreased from baseline (–0.58; 95% confidence interval, –0.86 to –0.30), compared with an increase in the control group (0.35; 95% CI, 0.08-0.63). SCORE values increased twice as much in the control group (0.27; 95% CI, 0.23-0.30), compared with the intervention group (0.13; 95% CI, 0.09-0.18). The authors also observed no differential responses for education level, surmising that “this type of risk communication might contribute to reduction of the social gap in health.”
The authors shared their study’s limitations, including notable differences between dropouts and participants at 1-year follow-up with regard to metabolic risk factors and such fast-developing imaging technologies as CT and MRI out-dating ultrasound findings. They also acknowledged that more research needs to be undertaken to prove that these outcomes are genuine.
This study was funded by Västerbotten County Council, the Swedish Research Council, the Heart and Lung Foundation, and the Swedish Society of Medicine. No conflicts of interest were reported.
SOURCE: Näslund U et al. Lancet. 2018 Dec 3. doi: 10.1016/S0140-6736(18)32818-6.
FROM THE LANCET
Key clinical point: Patients who received a pictorial representation of atherosclerosis, plus a nurse-led follow-up phone call, saw reduced cardiovascular disease risk after 1 year.
Major finding: At 1-year follow-up, the intervention group had a Framingham risk score that decreased from baseline (–0.58; 95% confidence interval, –0.86 to –0.30) while the control group saw an increase (0.35; 95% CI, 0.08-0.63).
Study details: A randomized controlled trial of 3,532 participants in a cardiovascular disease prevention program in northern Sweden.
Disclosures: This study was funded by Västerbotten County Council, the Swedish Research Council, the Heart and Lung Foundation, and the Swedish Society of Medicine. No conflicts of interest were reported.
Source: Näslund U et al. Lancet. 2018 Dec 3. doi: 10.1016/S0140-6736(18)32818-6.