User login
Cold packs help reduce pain after laparoscopic hysterectomy
LAS VEGAS – Patients like cold packs for pain control after laparoscopic hysterectomy, according to a small trial from Cleveland Clinic Florida (Weston).
Cold packs have been shown to reduce pain in other types of surgery, so investigators at the clinic wanted to try them out for the procedure, said study lead Pamela Frazzini Padilla, MD, an ob.gyn. at the clinic.
Twenty-eight women were randomized to get packs right after surgery, and told to use them – before turning to oxycodone tabs – every 6 hours for 72 hours – and then as needed. Twenty-eight other women were randomized to the control group. Surgery was for benign indications, most often uterine bleeding secondary to fibroids. Besides the cold packs, there were no differences between the groups in analgesia protocols.
The differences in pain control, assessed on a 10-point scale over the phone, weren’t statistically significant, but they di move in the right direction. At 24 hours, women who were cold pack users reported a median pain score of 4, versus 4.5 among controls. At 72 hours, they reported a median score of 2, versus 2.5 in the control group.
At 2 weeks postoperatively, women who were cold pack users had used a mean of 4 oxycodone pills, versus 7 among the controls, which translated into a mean of 13 IV morphine equivalents versus 24 in favor of cold packs (P = .143).
While not significantly different, overall numbers of opioid tabs consumed and morphine equivalents “demonstrated lower use in the study group,” Dr. Frazzini Padilla noted at the meeting sponsored by AAGL.
Also, 89% of women said that cold packs helped reduce their pain, and 92% said they’d use them again after an operation. “In a day when everything is driven by patient satisfaction, patients’ perception of their recovery” is important. Because cold packs are cheap, harmless, and seemed to help with patient perceptions, “we do recommend that people use” them. “It’s just another added measure that we give” at Cleveland Clinic Florida, she said.
The study team also found that 86% of the women in the trial used 10 or fewer oxycodone tabs after surgery. Across the country, women are prescribed about 25 tabs after a laparoscopic hysterectomy; the study suggests it’s overkill, as an audience member noted, especially given the current climate.
The two arms of the study were well balanced. The mean age was 46 years, and mean body mass index 30.4 kg/m2.
There was no outside funding, and the investigators didn’t have any disclosures.
SOURCE: Frazzini Padilla P et al. 2018 AAGL Global Congress, Abstract 21.
LAS VEGAS – Patients like cold packs for pain control after laparoscopic hysterectomy, according to a small trial from Cleveland Clinic Florida (Weston).
Cold packs have been shown to reduce pain in other types of surgery, so investigators at the clinic wanted to try them out for the procedure, said study lead Pamela Frazzini Padilla, MD, an ob.gyn. at the clinic.
Twenty-eight women were randomized to get packs right after surgery, and told to use them – before turning to oxycodone tabs – every 6 hours for 72 hours – and then as needed. Twenty-eight other women were randomized to the control group. Surgery was for benign indications, most often uterine bleeding secondary to fibroids. Besides the cold packs, there were no differences between the groups in analgesia protocols.
The differences in pain control, assessed on a 10-point scale over the phone, weren’t statistically significant, but they di move in the right direction. At 24 hours, women who were cold pack users reported a median pain score of 4, versus 4.5 among controls. At 72 hours, they reported a median score of 2, versus 2.5 in the control group.
At 2 weeks postoperatively, women who were cold pack users had used a mean of 4 oxycodone pills, versus 7 among the controls, which translated into a mean of 13 IV morphine equivalents versus 24 in favor of cold packs (P = .143).
While not significantly different, overall numbers of opioid tabs consumed and morphine equivalents “demonstrated lower use in the study group,” Dr. Frazzini Padilla noted at the meeting sponsored by AAGL.
Also, 89% of women said that cold packs helped reduce their pain, and 92% said they’d use them again after an operation. “In a day when everything is driven by patient satisfaction, patients’ perception of their recovery” is important. Because cold packs are cheap, harmless, and seemed to help with patient perceptions, “we do recommend that people use” them. “It’s just another added measure that we give” at Cleveland Clinic Florida, she said.
The study team also found that 86% of the women in the trial used 10 or fewer oxycodone tabs after surgery. Across the country, women are prescribed about 25 tabs after a laparoscopic hysterectomy; the study suggests it’s overkill, as an audience member noted, especially given the current climate.
The two arms of the study were well balanced. The mean age was 46 years, and mean body mass index 30.4 kg/m2.
There was no outside funding, and the investigators didn’t have any disclosures.
SOURCE: Frazzini Padilla P et al. 2018 AAGL Global Congress, Abstract 21.
LAS VEGAS – Patients like cold packs for pain control after laparoscopic hysterectomy, according to a small trial from Cleveland Clinic Florida (Weston).
Cold packs have been shown to reduce pain in other types of surgery, so investigators at the clinic wanted to try them out for the procedure, said study lead Pamela Frazzini Padilla, MD, an ob.gyn. at the clinic.
Twenty-eight women were randomized to get packs right after surgery, and told to use them – before turning to oxycodone tabs – every 6 hours for 72 hours – and then as needed. Twenty-eight other women were randomized to the control group. Surgery was for benign indications, most often uterine bleeding secondary to fibroids. Besides the cold packs, there were no differences between the groups in analgesia protocols.
The differences in pain control, assessed on a 10-point scale over the phone, weren’t statistically significant, but they di move in the right direction. At 24 hours, women who were cold pack users reported a median pain score of 4, versus 4.5 among controls. At 72 hours, they reported a median score of 2, versus 2.5 in the control group.
At 2 weeks postoperatively, women who were cold pack users had used a mean of 4 oxycodone pills, versus 7 among the controls, which translated into a mean of 13 IV morphine equivalents versus 24 in favor of cold packs (P = .143).
While not significantly different, overall numbers of opioid tabs consumed and morphine equivalents “demonstrated lower use in the study group,” Dr. Frazzini Padilla noted at the meeting sponsored by AAGL.
Also, 89% of women said that cold packs helped reduce their pain, and 92% said they’d use them again after an operation. “In a day when everything is driven by patient satisfaction, patients’ perception of their recovery” is important. Because cold packs are cheap, harmless, and seemed to help with patient perceptions, “we do recommend that people use” them. “It’s just another added measure that we give” at Cleveland Clinic Florida, she said.
The study team also found that 86% of the women in the trial used 10 or fewer oxycodone tabs after surgery. Across the country, women are prescribed about 25 tabs after a laparoscopic hysterectomy; the study suggests it’s overkill, as an audience member noted, especially given the current climate.
The two arms of the study were well balanced. The mean age was 46 years, and mean body mass index 30.4 kg/m2.
There was no outside funding, and the investigators didn’t have any disclosures.
SOURCE: Frazzini Padilla P et al. 2018 AAGL Global Congress, Abstract 21.
REPORTING FROM AAGL GLOBAL CONGRESS
Key clinical point:
Major finding: Cold pack women at 2 weeks used a mean of 4 oxycodone pills, versus 7 among the controls, which translated into a mean of 13 IV morphine equivalents versus 24 in favor of cold packs (P = 0.143)
Study details: A study of 28 women using cold packs and 28 controls.
Disclosures: There was no outside funding, and the investigators didn’t have any disclosures.
Source: Frazzini Padilla P et al. 2018 AAGL Global Congress, Abstract 21.
Methotrexate fails to cut CVD events in a large RCT
CHICAGO – Both methotrexate and canakinumab are anti-inflammatory drugs, but only canakinumab cut the incidence of cardiovascular disease events in a major clinical trial, CANTOS. A second big trial designed to parallel CANTOS tested methotrexate in roughly the same way and found it produced no cardiovascular disease benefit among high-risk patients.
The CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study) results with canakinumab and the new results with methotrexate “demonstrate that inflammation inhibition [with canakinumab] can significantly reduce cardiovascular event rates independent of lipid lowering and blood pressure reduction,” Paul M. Ridker, MD, said at the American Heart Association scientific sessions. But, “inhibition of the IL [interleukin]–1 beta to IL-6 to CRP [C-reactive protein] pathway of innate immunity appears to be important for atheroprotection,” and was something methotrexate couldn’t deliver, concluded Dr. Ridker, a professor of medicine at Harvard Medical School and director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital in Boston.
The new results he reported showed that weekly treatment with a single, oral, 15- to 20-mg dose of methotrexate not only had no effect on cardiovascular events but also had no discernible impact on serum levels of IL-1beta (IL-1B), IL-6, or high sensitivity (hs) CRP, in contrast to canakinumab, which Dr. Ridker took as evidence that this inflammatory pathway links to the pathophysiology of atherosclerotic cardiovascular disease.
CIRT (Cardiovascular Inflammation Reduction Trial) randomized 4,786 patients at 417 centers in the United States or Canada. Enrolled patients had to have a history of an MI or documented multivessel coronary disease, and also had to have type 2 diabetes, metabolic syndrome, or both. All patients were maintained on optimized dosages of a statin, aspirin, a beta-blocker, and an angiotensin-converting enzyme inhibitor or angiotensin-receptor blocker. All patients also received 1 mg folate daily. Randomization assigned patients to either receive 15-20 mg methotrexate orally once a week or placebo.
CIRT stopped prematurely because of futility after a median follow-up of 2.3 years. At that time, the incidence of one of two primary endpoints, the combination of cardiovascular death, nonfatal MI, and nonfatal stroke was 3.46/100 person-years with methotrexate treatment and 3.43/100 person-years with placebo, a difference that was not statistically significant. The incidence of the second primary endpoint, which combined the first three types of events plus hospitalization for unstable angina that led to urgent coronary revascularization, occurred in 4.13/100 person-years with methotrexate and 4.31/100 person years with placebo, also a difference that was not statistically significant. Concurrently with this report, the results were published online (N Engl J Med. 2018 Nov 10. doi: 10.1056/NEJMoa1809798).
Analysis of inflammatory markers in the blood after 8 months on treatment showed that methotrexate had no effect on levels of IL-1B, IL-6, and hsCRP. Methotrexate’s lack of an effect on these markers as well as the absence of an effect on cardiovascular disease events contrasted sharply with results that Dr. Ridker and his associates reported a little more than a year earlier in CANTOS. The study’s investigators randomized 10,061 patients with a history of an MI and an elevated serum level of hsCRP, at least 2.0 mg/L. After a median follow-up of 3.7 years, treatment with 150 mg of canakinumab injected subcutaneously once every 3 months produced a 15% relative risk reduction in the combined rate of cardiovascular death, nonfatal MI, and nonfatal stroke, compared with patients treated with placebo, a statistically significant between-group difference (N Engl J Med. 2017 Sep 21;377[12]:1119-31). Canakinumab had no impact on LDL cholesterol levels, but lowered hsCRP levels by more than a third. Dr. Ridker and his associates designed the CIRT and CANTOS trials “in parallel,” he said, and the CIRT results using methotrexate provided a “neutral control” to complement the positive results from canakinumab in CANTOS,
Given its high cost, canakinumab (Ilaris) is not an obviously practical option for treating patients similar to those enrolled in CANTOS, so other candidate agents that inhibit the IL-1B, IL-6, CRP inflammatory pathway are now under study, Dr. Ridker said in an interview. The mechanism of methotrexate’s inhibition of inflammation is unknown, but clearly does not involve this pathway; it may be mediated by adenosine, Dr. Ridker suggested. Canakinumab has Food and Drug Administration approval for treating systemic juvenile idiopathic arthritis and a handful of additional, low-prevalence diseases. Novartis, the company that markets canakinumab, made a submission to the Food and Drug Administration seeking an indication for prevention of cardiovascular disease based on the CANTOS results, and the company said in October 2018 that the FDA denied this request.
The CIRT results also showed a previously unseen signal of a possible safety issue with the tested methotrexate regimen. The incidence of non–basal cell skin cancer was 0.65/100 person-years with methotrexate, compared with 0.24/100 person-years with placebo, a statistically significant difference. Until now, no one had reported a link like this and it requires further analysis, Dr. Ridker said.
CIRT received no commercial funding. Dr. Ridker has been a consultant to Corvidia, Inflazome, and Novartis; he has received research funding from Kowa and Novartis; and his work led to a patent held by Brigham and Women’s Hospital for inflammatory biomarkers licensed to Siemens and AstraZeneca.
SOURCE: Ridker P et al. AHA scientific sessions, Abstract 17778.
CIRT is an important study. Considering the results from CIRT, which used methotrexate, along with the results from CANTOS, which used canakinumab, provides helpful mechanistic observations about selective drug effects when targeting inflammation. Two additional trials that are now in progress using colchicine in a clinical setting similar to CIRT and CANTOS should give us even more insight into the relationships between inflammation and atherosclerotic cardiovascular disease and possible new approaches to treatment.
Despite these differences between the two trials, the results from CIRT clearly showed that, in the enrolled patients, the dosage of methotrexate used had no apparent impact on levels of hsCRP, IL-1B, and IL-6.
Sidney C. Smith Jr., MD, is a cardiologist and professor of medicine at the University of North Carolina at Chapel Hill. He made these comments as the designated discussant for the CIRT trial. He had no disclosures.
CIRT is an important study. Considering the results from CIRT, which used methotrexate, along with the results from CANTOS, which used canakinumab, provides helpful mechanistic observations about selective drug effects when targeting inflammation. Two additional trials that are now in progress using colchicine in a clinical setting similar to CIRT and CANTOS should give us even more insight into the relationships between inflammation and atherosclerotic cardiovascular disease and possible new approaches to treatment.
Despite these differences between the two trials, the results from CIRT clearly showed that, in the enrolled patients, the dosage of methotrexate used had no apparent impact on levels of hsCRP, IL-1B, and IL-6.
Sidney C. Smith Jr., MD, is a cardiologist and professor of medicine at the University of North Carolina at Chapel Hill. He made these comments as the designated discussant for the CIRT trial. He had no disclosures.
CIRT is an important study. Considering the results from CIRT, which used methotrexate, along with the results from CANTOS, which used canakinumab, provides helpful mechanistic observations about selective drug effects when targeting inflammation. Two additional trials that are now in progress using colchicine in a clinical setting similar to CIRT and CANTOS should give us even more insight into the relationships between inflammation and atherosclerotic cardiovascular disease and possible new approaches to treatment.
Despite these differences between the two trials, the results from CIRT clearly showed that, in the enrolled patients, the dosage of methotrexate used had no apparent impact on levels of hsCRP, IL-1B, and IL-6.
Sidney C. Smith Jr., MD, is a cardiologist and professor of medicine at the University of North Carolina at Chapel Hill. He made these comments as the designated discussant for the CIRT trial. He had no disclosures.
CHICAGO – Both methotrexate and canakinumab are anti-inflammatory drugs, but only canakinumab cut the incidence of cardiovascular disease events in a major clinical trial, CANTOS. A second big trial designed to parallel CANTOS tested methotrexate in roughly the same way and found it produced no cardiovascular disease benefit among high-risk patients.
The CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study) results with canakinumab and the new results with methotrexate “demonstrate that inflammation inhibition [with canakinumab] can significantly reduce cardiovascular event rates independent of lipid lowering and blood pressure reduction,” Paul M. Ridker, MD, said at the American Heart Association scientific sessions. But, “inhibition of the IL [interleukin]–1 beta to IL-6 to CRP [C-reactive protein] pathway of innate immunity appears to be important for atheroprotection,” and was something methotrexate couldn’t deliver, concluded Dr. Ridker, a professor of medicine at Harvard Medical School and director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital in Boston.
The new results he reported showed that weekly treatment with a single, oral, 15- to 20-mg dose of methotrexate not only had no effect on cardiovascular events but also had no discernible impact on serum levels of IL-1beta (IL-1B), IL-6, or high sensitivity (hs) CRP, in contrast to canakinumab, which Dr. Ridker took as evidence that this inflammatory pathway links to the pathophysiology of atherosclerotic cardiovascular disease.
CIRT (Cardiovascular Inflammation Reduction Trial) randomized 4,786 patients at 417 centers in the United States or Canada. Enrolled patients had to have a history of an MI or documented multivessel coronary disease, and also had to have type 2 diabetes, metabolic syndrome, or both. All patients were maintained on optimized dosages of a statin, aspirin, a beta-blocker, and an angiotensin-converting enzyme inhibitor or angiotensin-receptor blocker. All patients also received 1 mg folate daily. Randomization assigned patients to either receive 15-20 mg methotrexate orally once a week or placebo.
CIRT stopped prematurely because of futility after a median follow-up of 2.3 years. At that time, the incidence of one of two primary endpoints, the combination of cardiovascular death, nonfatal MI, and nonfatal stroke was 3.46/100 person-years with methotrexate treatment and 3.43/100 person-years with placebo, a difference that was not statistically significant. The incidence of the second primary endpoint, which combined the first three types of events plus hospitalization for unstable angina that led to urgent coronary revascularization, occurred in 4.13/100 person-years with methotrexate and 4.31/100 person years with placebo, also a difference that was not statistically significant. Concurrently with this report, the results were published online (N Engl J Med. 2018 Nov 10. doi: 10.1056/NEJMoa1809798).
Analysis of inflammatory markers in the blood after 8 months on treatment showed that methotrexate had no effect on levels of IL-1B, IL-6, and hsCRP. Methotrexate’s lack of an effect on these markers as well as the absence of an effect on cardiovascular disease events contrasted sharply with results that Dr. Ridker and his associates reported a little more than a year earlier in CANTOS. The study’s investigators randomized 10,061 patients with a history of an MI and an elevated serum level of hsCRP, at least 2.0 mg/L. After a median follow-up of 3.7 years, treatment with 150 mg of canakinumab injected subcutaneously once every 3 months produced a 15% relative risk reduction in the combined rate of cardiovascular death, nonfatal MI, and nonfatal stroke, compared with patients treated with placebo, a statistically significant between-group difference (N Engl J Med. 2017 Sep 21;377[12]:1119-31). Canakinumab had no impact on LDL cholesterol levels, but lowered hsCRP levels by more than a third. Dr. Ridker and his associates designed the CIRT and CANTOS trials “in parallel,” he said, and the CIRT results using methotrexate provided a “neutral control” to complement the positive results from canakinumab in CANTOS,
Given its high cost, canakinumab (Ilaris) is not an obviously practical option for treating patients similar to those enrolled in CANTOS, so other candidate agents that inhibit the IL-1B, IL-6, CRP inflammatory pathway are now under study, Dr. Ridker said in an interview. The mechanism of methotrexate’s inhibition of inflammation is unknown, but clearly does not involve this pathway; it may be mediated by adenosine, Dr. Ridker suggested. Canakinumab has Food and Drug Administration approval for treating systemic juvenile idiopathic arthritis and a handful of additional, low-prevalence diseases. Novartis, the company that markets canakinumab, made a submission to the Food and Drug Administration seeking an indication for prevention of cardiovascular disease based on the CANTOS results, and the company said in October 2018 that the FDA denied this request.
The CIRT results also showed a previously unseen signal of a possible safety issue with the tested methotrexate regimen. The incidence of non–basal cell skin cancer was 0.65/100 person-years with methotrexate, compared with 0.24/100 person-years with placebo, a statistically significant difference. Until now, no one had reported a link like this and it requires further analysis, Dr. Ridker said.
CIRT received no commercial funding. Dr. Ridker has been a consultant to Corvidia, Inflazome, and Novartis; he has received research funding from Kowa and Novartis; and his work led to a patent held by Brigham and Women’s Hospital for inflammatory biomarkers licensed to Siemens and AstraZeneca.
SOURCE: Ridker P et al. AHA scientific sessions, Abstract 17778.
CHICAGO – Both methotrexate and canakinumab are anti-inflammatory drugs, but only canakinumab cut the incidence of cardiovascular disease events in a major clinical trial, CANTOS. A second big trial designed to parallel CANTOS tested methotrexate in roughly the same way and found it produced no cardiovascular disease benefit among high-risk patients.
The CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study) results with canakinumab and the new results with methotrexate “demonstrate that inflammation inhibition [with canakinumab] can significantly reduce cardiovascular event rates independent of lipid lowering and blood pressure reduction,” Paul M. Ridker, MD, said at the American Heart Association scientific sessions. But, “inhibition of the IL [interleukin]–1 beta to IL-6 to CRP [C-reactive protein] pathway of innate immunity appears to be important for atheroprotection,” and was something methotrexate couldn’t deliver, concluded Dr. Ridker, a professor of medicine at Harvard Medical School and director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital in Boston.
The new results he reported showed that weekly treatment with a single, oral, 15- to 20-mg dose of methotrexate not only had no effect on cardiovascular events but also had no discernible impact on serum levels of IL-1beta (IL-1B), IL-6, or high sensitivity (hs) CRP, in contrast to canakinumab, which Dr. Ridker took as evidence that this inflammatory pathway links to the pathophysiology of atherosclerotic cardiovascular disease.
CIRT (Cardiovascular Inflammation Reduction Trial) randomized 4,786 patients at 417 centers in the United States or Canada. Enrolled patients had to have a history of an MI or documented multivessel coronary disease, and also had to have type 2 diabetes, metabolic syndrome, or both. All patients were maintained on optimized dosages of a statin, aspirin, a beta-blocker, and an angiotensin-converting enzyme inhibitor or angiotensin-receptor blocker. All patients also received 1 mg folate daily. Randomization assigned patients to either receive 15-20 mg methotrexate orally once a week or placebo.
CIRT stopped prematurely because of futility after a median follow-up of 2.3 years. At that time, the incidence of one of two primary endpoints, the combination of cardiovascular death, nonfatal MI, and nonfatal stroke was 3.46/100 person-years with methotrexate treatment and 3.43/100 person-years with placebo, a difference that was not statistically significant. The incidence of the second primary endpoint, which combined the first three types of events plus hospitalization for unstable angina that led to urgent coronary revascularization, occurred in 4.13/100 person-years with methotrexate and 4.31/100 person years with placebo, also a difference that was not statistically significant. Concurrently with this report, the results were published online (N Engl J Med. 2018 Nov 10. doi: 10.1056/NEJMoa1809798).
Analysis of inflammatory markers in the blood after 8 months on treatment showed that methotrexate had no effect on levels of IL-1B, IL-6, and hsCRP. Methotrexate’s lack of an effect on these markers as well as the absence of an effect on cardiovascular disease events contrasted sharply with results that Dr. Ridker and his associates reported a little more than a year earlier in CANTOS. The study’s investigators randomized 10,061 patients with a history of an MI and an elevated serum level of hsCRP, at least 2.0 mg/L. After a median follow-up of 3.7 years, treatment with 150 mg of canakinumab injected subcutaneously once every 3 months produced a 15% relative risk reduction in the combined rate of cardiovascular death, nonfatal MI, and nonfatal stroke, compared with patients treated with placebo, a statistically significant between-group difference (N Engl J Med. 2017 Sep 21;377[12]:1119-31). Canakinumab had no impact on LDL cholesterol levels, but lowered hsCRP levels by more than a third. Dr. Ridker and his associates designed the CIRT and CANTOS trials “in parallel,” he said, and the CIRT results using methotrexate provided a “neutral control” to complement the positive results from canakinumab in CANTOS,
Given its high cost, canakinumab (Ilaris) is not an obviously practical option for treating patients similar to those enrolled in CANTOS, so other candidate agents that inhibit the IL-1B, IL-6, CRP inflammatory pathway are now under study, Dr. Ridker said in an interview. The mechanism of methotrexate’s inhibition of inflammation is unknown, but clearly does not involve this pathway; it may be mediated by adenosine, Dr. Ridker suggested. Canakinumab has Food and Drug Administration approval for treating systemic juvenile idiopathic arthritis and a handful of additional, low-prevalence diseases. Novartis, the company that markets canakinumab, made a submission to the Food and Drug Administration seeking an indication for prevention of cardiovascular disease based on the CANTOS results, and the company said in October 2018 that the FDA denied this request.
The CIRT results also showed a previously unseen signal of a possible safety issue with the tested methotrexate regimen. The incidence of non–basal cell skin cancer was 0.65/100 person-years with methotrexate, compared with 0.24/100 person-years with placebo, a statistically significant difference. Until now, no one had reported a link like this and it requires further analysis, Dr. Ridker said.
CIRT received no commercial funding. Dr. Ridker has been a consultant to Corvidia, Inflazome, and Novartis; he has received research funding from Kowa and Novartis; and his work led to a patent held by Brigham and Women’s Hospital for inflammatory biomarkers licensed to Siemens and AstraZeneca.
SOURCE: Ridker P et al. AHA scientific sessions, Abstract 17778.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: The combined rate of CVD events was 3.46/100 person-years on methotrexate and 3.43/100 on placebo.
Study details: CIRT, a multicenter, randomized trial with 4,786 high-risk patients.
Disclosures: CIRT received no commercial funding. Dr. Ridker has been a consultant to Corvidia, Inflazome, and Novartis; he has received research funding from Kowa and Novartis; and his work led to a patent held by Brigham and Women’s Hospital for inflammatory biomarkers licensed to Seimens and AstraZeneca.
Source: Ridker P et al. AHA scientific sessions, Abstract 17778.
Filgotinib shows efficacy, safety in RA phase 3 and PsA phase 2 trials
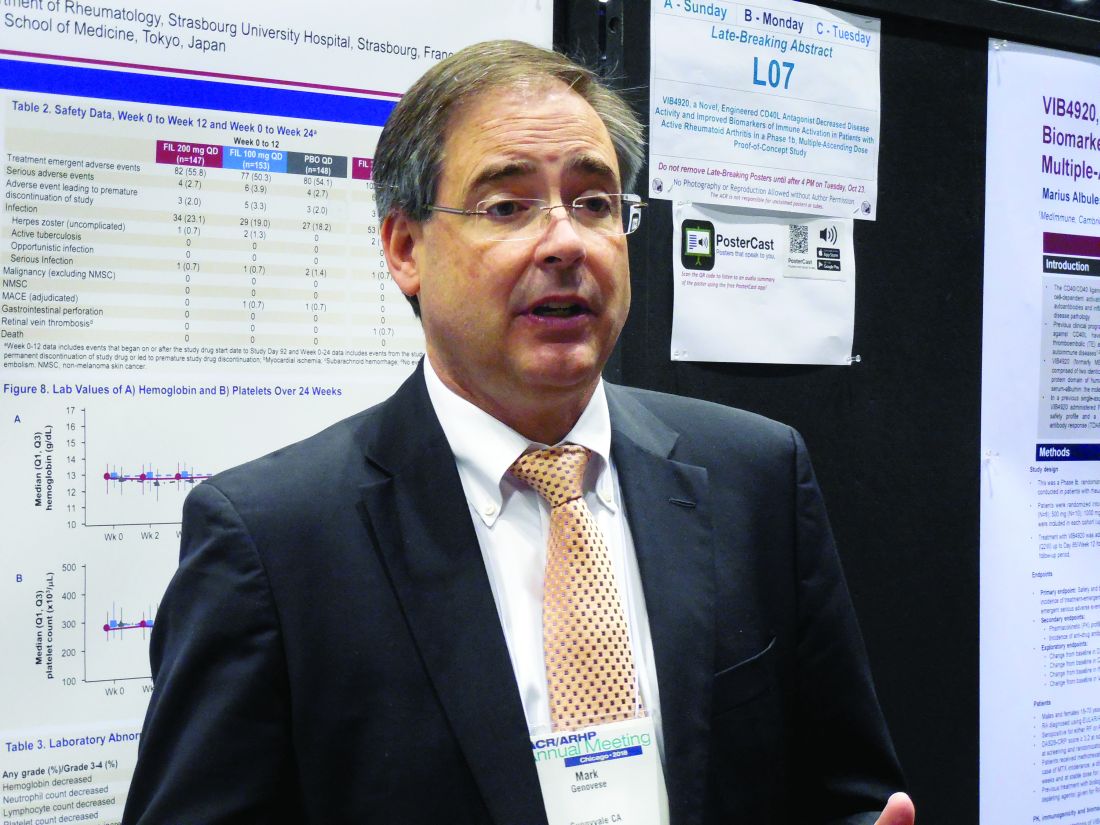
CHICAGO – The selective Janus kinase 1 inhibitor filgotinib showed efficacy and safety for patients with rheumatoid arthritis in a phase 3 trial, and efficacy and safety for treating patients with psoriatic arthritis in results from a phase 2 study in two separate reports at the annual meeting of the American College of Rheumatology.
In the phase 3 study, treatment with filgotinib at an oral dosage of 200 mg once daily led to a 66% incidence of American College of Rheumatology 20 (ACR20) responses after 16 weeks of treatment in 147 patients with moderately to severely active rheumatoid arthritis (RA), compared with a 31% rate among 148 patients randomized to receive placebo, a statistically significant improvement for the study’s primary efficacy endpoint, Mark C. Genovese, MD, reported in a poster at the meeting. The rate of ACR20 responses among the 153 RA patients who received 100 mg/day filgotinib was 58%, reported Dr. Genovese, professor of medicine and director of the rheumatology clinic at Stanford (Calif.) University.
After 24 weeks of daily treatment, the longest duration studied in the trial, ACR20 rates were 69%, 55%, and 35% in the 200-mg, 100-mg, and placebo patients, respectively. Dr. Genovese also reported that after 24 weeks on treatment, the rates of patients achieving low disease activity measured by their disease activity score based on 28 joints and C-reactive protein level (DAS28-CRP) were 48%, 38%, and 21%, respectively, and the percentages of patients achieving complete remission at 24 weeks based on their DAS28-CRP scores were 31%, 26%, and 12%, respectively.
“We were incredibly fortunate to see such positive results. The drug worked very well in very-challenging-to-treat patients,” Dr. Genovese said in an interview. All of the RA patients enrolled in the study had not previously responded to or were intolerant of prior treatment with at least one biologic disease-modifying antirheumatic drug (DMARD), and almost a quarter of enrolled patients had failed prior treatment with at least three different biologic DMARDs. The number of biologic DMARDs a patient had previously received showed no relationship to how well patients responded to filgotinib, he noted.
Dr. Genovese also highlighted the relatively high percentage of patients who achieved low disease activity and remission. The 48% and 31% rates, respectively, of low disease activity and remission among patients treated with the higher filgotinib dosage for 24 weeks “is fairly impressive in patients who did not previously respond to a biologic DMARD,” the researcher said. These findings are similar to data previously reported for upadacitinib, another Janus kinase (JAK) inhibitor that, like filgotinib, is selective for the JAK1 receptor, noted Dr. Genovese, who also was the lead investigator for a phase 3 study of upadacitinib in RA patients (Lancet. 2018 June 23;391[10139]:2513-24).
The filgotinib data he presented came from the FINCH 2 (Filgotinib Versus Placebo in Adults With Active Rheumatoid Arthritis Who Have an Inadequate Response to Biologic Disease-Modifying Anti-Rheumatic Drug[s] Treatment) trial, which was run at 104 sites in 15 countries, including the United States. The results also showed a “favorable safety profile and stable laboratory parameters,” Dr. Genovese reported. Results from two additional phase 3 trials in RA patients are expected in 2019, he said.
Filgotinib studied in psoriatic arthritis
The separate, phase 2 study of filgotinib in patients with psoriatic arthritis (PsA) reported during the meeting showed safety “in line with previous reports without new safety signals” in a multicenter trial with 131 patients randomized to receive oral filgotinib 200 mg daily for 16 weeks or placebo, Philip J. Mease, MD, reported in a talk at the meeting. For the primary endpoint of achievement of ACR20 response after 16 weeks, the rate was 80% of the filgotinib-treated patients and 33% of patients in the placebo group, a statistically significant difference, said Dr. Mease, a rheumatologist at Swedish Medical Center in Seattle.
EQUATOR (A Study to Assess Efficacy and Safety of Filgotinib in Active Psoriatic Arthritis) enrolled patients at sites in seven European countries who had “very active” PsA and either a history of or current plaque psoriasis. All patients had to have a history of either insufficient response to or intolerance of at least one conventional synthetic DMARD. The enrollment criteria had no specifications for prior use of an anti–tumor necrosis factor drug, and about 15% of patients had used least one of these drugs. At entry, about three-quarters of patients were on treatment with a conventional synthetic DMARD and about a quarter received treatment with a glucocorticoid.
The results showed statistically significant benefits from filgotinib, compared with placebo, for several other measures of arthritis activity, as well as measures of psoriasis, enthesitis, and pain, Dr. Mease reported. He also highlighted a “lack of meaningful changes in hemoglobin” or other laboratory measures that, along with the efficacy findings, make filgotinib “a promising first step” for patients with PsA. Dr. Mease also noted that roughly concurrently with his report, a separate group of researchers published results from a phase 2 study of filgotinib in patients with ankylosing spondylitis that also found evidence for efficacy and safety during 12 weeks of treating 116 randomized patients (Lancet. 2018 Oct 22. doi: 10.1016/S0140-6736[18]32463-2).
FINCH 2 was sponsored by Galapagos and Gilead, the two companies developing filgotinib. Dr. Genovese has had financial relationships with Galapagos and Gilead and also with AbbVie, Lilly, and Pfizer. Dr. Mease has had financial relationships with Galapagos and Gilead and a dozen other companies.
SOURCES: Genovese M et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract L06; Mease P et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 1821.
CHICAGO – The selective Janus kinase 1 inhibitor filgotinib showed efficacy and safety for patients with rheumatoid arthritis in a phase 3 trial, and efficacy and safety for treating patients with psoriatic arthritis in results from a phase 2 study in two separate reports at the annual meeting of the American College of Rheumatology.
In the phase 3 study, treatment with filgotinib at an oral dosage of 200 mg once daily led to a 66% incidence of American College of Rheumatology 20 (ACR20) responses after 16 weeks of treatment in 147 patients with moderately to severely active rheumatoid arthritis (RA), compared with a 31% rate among 148 patients randomized to receive placebo, a statistically significant improvement for the study’s primary efficacy endpoint, Mark C. Genovese, MD, reported in a poster at the meeting. The rate of ACR20 responses among the 153 RA patients who received 100 mg/day filgotinib was 58%, reported Dr. Genovese, professor of medicine and director of the rheumatology clinic at Stanford (Calif.) University.
After 24 weeks of daily treatment, the longest duration studied in the trial, ACR20 rates were 69%, 55%, and 35% in the 200-mg, 100-mg, and placebo patients, respectively. Dr. Genovese also reported that after 24 weeks on treatment, the rates of patients achieving low disease activity measured by their disease activity score based on 28 joints and C-reactive protein level (DAS28-CRP) were 48%, 38%, and 21%, respectively, and the percentages of patients achieving complete remission at 24 weeks based on their DAS28-CRP scores were 31%, 26%, and 12%, respectively.
“We were incredibly fortunate to see such positive results. The drug worked very well in very-challenging-to-treat patients,” Dr. Genovese said in an interview. All of the RA patients enrolled in the study had not previously responded to or were intolerant of prior treatment with at least one biologic disease-modifying antirheumatic drug (DMARD), and almost a quarter of enrolled patients had failed prior treatment with at least three different biologic DMARDs. The number of biologic DMARDs a patient had previously received showed no relationship to how well patients responded to filgotinib, he noted.
Dr. Genovese also highlighted the relatively high percentage of patients who achieved low disease activity and remission. The 48% and 31% rates, respectively, of low disease activity and remission among patients treated with the higher filgotinib dosage for 24 weeks “is fairly impressive in patients who did not previously respond to a biologic DMARD,” the researcher said. These findings are similar to data previously reported for upadacitinib, another Janus kinase (JAK) inhibitor that, like filgotinib, is selective for the JAK1 receptor, noted Dr. Genovese, who also was the lead investigator for a phase 3 study of upadacitinib in RA patients (Lancet. 2018 June 23;391[10139]:2513-24).
The filgotinib data he presented came from the FINCH 2 (Filgotinib Versus Placebo in Adults With Active Rheumatoid Arthritis Who Have an Inadequate Response to Biologic Disease-Modifying Anti-Rheumatic Drug[s] Treatment) trial, which was run at 104 sites in 15 countries, including the United States. The results also showed a “favorable safety profile and stable laboratory parameters,” Dr. Genovese reported. Results from two additional phase 3 trials in RA patients are expected in 2019, he said.
Filgotinib studied in psoriatic arthritis
The separate, phase 2 study of filgotinib in patients with psoriatic arthritis (PsA) reported during the meeting showed safety “in line with previous reports without new safety signals” in a multicenter trial with 131 patients randomized to receive oral filgotinib 200 mg daily for 16 weeks or placebo, Philip J. Mease, MD, reported in a talk at the meeting. For the primary endpoint of achievement of ACR20 response after 16 weeks, the rate was 80% of the filgotinib-treated patients and 33% of patients in the placebo group, a statistically significant difference, said Dr. Mease, a rheumatologist at Swedish Medical Center in Seattle.
EQUATOR (A Study to Assess Efficacy and Safety of Filgotinib in Active Psoriatic Arthritis) enrolled patients at sites in seven European countries who had “very active” PsA and either a history of or current plaque psoriasis. All patients had to have a history of either insufficient response to or intolerance of at least one conventional synthetic DMARD. The enrollment criteria had no specifications for prior use of an anti–tumor necrosis factor drug, and about 15% of patients had used least one of these drugs. At entry, about three-quarters of patients were on treatment with a conventional synthetic DMARD and about a quarter received treatment with a glucocorticoid.
The results showed statistically significant benefits from filgotinib, compared with placebo, for several other measures of arthritis activity, as well as measures of psoriasis, enthesitis, and pain, Dr. Mease reported. He also highlighted a “lack of meaningful changes in hemoglobin” or other laboratory measures that, along with the efficacy findings, make filgotinib “a promising first step” for patients with PsA. Dr. Mease also noted that roughly concurrently with his report, a separate group of researchers published results from a phase 2 study of filgotinib in patients with ankylosing spondylitis that also found evidence for efficacy and safety during 12 weeks of treating 116 randomized patients (Lancet. 2018 Oct 22. doi: 10.1016/S0140-6736[18]32463-2).
FINCH 2 was sponsored by Galapagos and Gilead, the two companies developing filgotinib. Dr. Genovese has had financial relationships with Galapagos and Gilead and also with AbbVie, Lilly, and Pfizer. Dr. Mease has had financial relationships with Galapagos and Gilead and a dozen other companies.
SOURCES: Genovese M et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract L06; Mease P et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 1821.
CHICAGO – The selective Janus kinase 1 inhibitor filgotinib showed efficacy and safety for patients with rheumatoid arthritis in a phase 3 trial, and efficacy and safety for treating patients with psoriatic arthritis in results from a phase 2 study in two separate reports at the annual meeting of the American College of Rheumatology.
In the phase 3 study, treatment with filgotinib at an oral dosage of 200 mg once daily led to a 66% incidence of American College of Rheumatology 20 (ACR20) responses after 16 weeks of treatment in 147 patients with moderately to severely active rheumatoid arthritis (RA), compared with a 31% rate among 148 patients randomized to receive placebo, a statistically significant improvement for the study’s primary efficacy endpoint, Mark C. Genovese, MD, reported in a poster at the meeting. The rate of ACR20 responses among the 153 RA patients who received 100 mg/day filgotinib was 58%, reported Dr. Genovese, professor of medicine and director of the rheumatology clinic at Stanford (Calif.) University.
After 24 weeks of daily treatment, the longest duration studied in the trial, ACR20 rates were 69%, 55%, and 35% in the 200-mg, 100-mg, and placebo patients, respectively. Dr. Genovese also reported that after 24 weeks on treatment, the rates of patients achieving low disease activity measured by their disease activity score based on 28 joints and C-reactive protein level (DAS28-CRP) were 48%, 38%, and 21%, respectively, and the percentages of patients achieving complete remission at 24 weeks based on their DAS28-CRP scores were 31%, 26%, and 12%, respectively.
“We were incredibly fortunate to see such positive results. The drug worked very well in very-challenging-to-treat patients,” Dr. Genovese said in an interview. All of the RA patients enrolled in the study had not previously responded to or were intolerant of prior treatment with at least one biologic disease-modifying antirheumatic drug (DMARD), and almost a quarter of enrolled patients had failed prior treatment with at least three different biologic DMARDs. The number of biologic DMARDs a patient had previously received showed no relationship to how well patients responded to filgotinib, he noted.
Dr. Genovese also highlighted the relatively high percentage of patients who achieved low disease activity and remission. The 48% and 31% rates, respectively, of low disease activity and remission among patients treated with the higher filgotinib dosage for 24 weeks “is fairly impressive in patients who did not previously respond to a biologic DMARD,” the researcher said. These findings are similar to data previously reported for upadacitinib, another Janus kinase (JAK) inhibitor that, like filgotinib, is selective for the JAK1 receptor, noted Dr. Genovese, who also was the lead investigator for a phase 3 study of upadacitinib in RA patients (Lancet. 2018 June 23;391[10139]:2513-24).
The filgotinib data he presented came from the FINCH 2 (Filgotinib Versus Placebo in Adults With Active Rheumatoid Arthritis Who Have an Inadequate Response to Biologic Disease-Modifying Anti-Rheumatic Drug[s] Treatment) trial, which was run at 104 sites in 15 countries, including the United States. The results also showed a “favorable safety profile and stable laboratory parameters,” Dr. Genovese reported. Results from two additional phase 3 trials in RA patients are expected in 2019, he said.
Filgotinib studied in psoriatic arthritis
The separate, phase 2 study of filgotinib in patients with psoriatic arthritis (PsA) reported during the meeting showed safety “in line with previous reports without new safety signals” in a multicenter trial with 131 patients randomized to receive oral filgotinib 200 mg daily for 16 weeks or placebo, Philip J. Mease, MD, reported in a talk at the meeting. For the primary endpoint of achievement of ACR20 response after 16 weeks, the rate was 80% of the filgotinib-treated patients and 33% of patients in the placebo group, a statistically significant difference, said Dr. Mease, a rheumatologist at Swedish Medical Center in Seattle.
EQUATOR (A Study to Assess Efficacy and Safety of Filgotinib in Active Psoriatic Arthritis) enrolled patients at sites in seven European countries who had “very active” PsA and either a history of or current plaque psoriasis. All patients had to have a history of either insufficient response to or intolerance of at least one conventional synthetic DMARD. The enrollment criteria had no specifications for prior use of an anti–tumor necrosis factor drug, and about 15% of patients had used least one of these drugs. At entry, about three-quarters of patients were on treatment with a conventional synthetic DMARD and about a quarter received treatment with a glucocorticoid.
The results showed statistically significant benefits from filgotinib, compared with placebo, for several other measures of arthritis activity, as well as measures of psoriasis, enthesitis, and pain, Dr. Mease reported. He also highlighted a “lack of meaningful changes in hemoglobin” or other laboratory measures that, along with the efficacy findings, make filgotinib “a promising first step” for patients with PsA. Dr. Mease also noted that roughly concurrently with his report, a separate group of researchers published results from a phase 2 study of filgotinib in patients with ankylosing spondylitis that also found evidence for efficacy and safety during 12 weeks of treating 116 randomized patients (Lancet. 2018 Oct 22. doi: 10.1016/S0140-6736[18]32463-2).
FINCH 2 was sponsored by Galapagos and Gilead, the two companies developing filgotinib. Dr. Genovese has had financial relationships with Galapagos and Gilead and also with AbbVie, Lilly, and Pfizer. Dr. Mease has had financial relationships with Galapagos and Gilead and a dozen other companies.
SOURCES: Genovese M et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract L06; Mease P et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 1821.
REPORTING FROM THE ACR ANNUAL MEETING
Clinical trial: Assessment of Ventilatory Management During General Anesthesia for Robotic Surgery
The trial will assess the incidence of postoperative pulmonary complications in patients who receive mechanical ventilation while under general anesthesia during robotic surgery to characterize current ventilation practices and evaluate any association between ventilator parameters and postoperative pulmonary complications.
Patients will be included if they are at least 18 years old and had their robotic surgical procedure done under general anesthesia. Exclusion criteria include being pregnant during surgery and having their procedure done outside an operating room.
The primary outcome measure is incidence of postoperative pulmonary complications within 5 days of the procedure or hospital discharge. Secondary outcomes include intraoperative mechanical ventilation practice, mechanical ventilation practice, and postoperative pulmonary complications within 5 days of the procedure or hospital discharge, intraoperative surgical positioning and ventilation, preoperative risk for postoperative pulmonary complications, and intraoperative mechanical ventilation practice and complications.
The estimated primary completion date is March 1, 2019, and the estimated study completion date is May 1, 2019. About 500 patients are estimated to be enrolled.
Find more information on the study at Clinicaltrials.gov.
The trial will assess the incidence of postoperative pulmonary complications in patients who receive mechanical ventilation while under general anesthesia during robotic surgery to characterize current ventilation practices and evaluate any association between ventilator parameters and postoperative pulmonary complications.
Patients will be included if they are at least 18 years old and had their robotic surgical procedure done under general anesthesia. Exclusion criteria include being pregnant during surgery and having their procedure done outside an operating room.
The primary outcome measure is incidence of postoperative pulmonary complications within 5 days of the procedure or hospital discharge. Secondary outcomes include intraoperative mechanical ventilation practice, mechanical ventilation practice, and postoperative pulmonary complications within 5 days of the procedure or hospital discharge, intraoperative surgical positioning and ventilation, preoperative risk for postoperative pulmonary complications, and intraoperative mechanical ventilation practice and complications.
The estimated primary completion date is March 1, 2019, and the estimated study completion date is May 1, 2019. About 500 patients are estimated to be enrolled.
Find more information on the study at Clinicaltrials.gov.
The trial will assess the incidence of postoperative pulmonary complications in patients who receive mechanical ventilation while under general anesthesia during robotic surgery to characterize current ventilation practices and evaluate any association between ventilator parameters and postoperative pulmonary complications.
Patients will be included if they are at least 18 years old and had their robotic surgical procedure done under general anesthesia. Exclusion criteria include being pregnant during surgery and having their procedure done outside an operating room.
The primary outcome measure is incidence of postoperative pulmonary complications within 5 days of the procedure or hospital discharge. Secondary outcomes include intraoperative mechanical ventilation practice, mechanical ventilation practice, and postoperative pulmonary complications within 5 days of the procedure or hospital discharge, intraoperative surgical positioning and ventilation, preoperative risk for postoperative pulmonary complications, and intraoperative mechanical ventilation practice and complications.
The estimated primary completion date is March 1, 2019, and the estimated study completion date is May 1, 2019. About 500 patients are estimated to be enrolled.
Find more information on the study at Clinicaltrials.gov.
Clinical trial: Treating Sleep Apnea in Female Veterans
The Treating Sleep Apnea in Women Veterans study is an interventional, randomized, controlled trial for woman veterans recently diagnosed with sleep apnea and prescribed positive airway pressure (PAP) treatment with at least one risk factor for sleep-disordered breathing (SDB).
The trial will compare the efficacy of two different programs combining patient education with behavioral techniques to improve adherence to PAP therapy in women veterans. The recommended first-line treatment for SDB is PAP therapy, but women have been shown to have lower adherence to men, especially in woman veterans, who experience significant sleep disturbance and other consequences of sleep disorders. No study has tested possible interventions to increase PAP adherence in this population.
Among inclusion criteria are being a woman veteran aged at least 18 years, having received care from a Veterans Affairs facility, and having been diagnosed with sleep apnea with an apnea-hypopnea index of 5 or greater. Patients will be excluded if they are currently using a sleep apnea treatment, are pregnant, are an active substance user or started recovery in the past 90 days, are too ill to participate, do not have transportation, cannot self-consent, have unstable housing, have another sleep disorder that accounts for sleep disturbance, or have no sleep complaints or symptoms.
The primary outcome measures are PAP adherence 3 months post PAP initiation and sleep quality by patient-reported sleep questionnaire 3 months after randomizations. In addition, remote PAP usage data will be collected for 12 months post PAP initiation.
The estimated primary completion date is Dec. 21, 2021, and the estimated study completion date is Jan. 31, 2022. About 300 patients are estimated to be recruited.
Find more information on the study page at Clinicaltrials.gov.
The Treating Sleep Apnea in Women Veterans study is an interventional, randomized, controlled trial for woman veterans recently diagnosed with sleep apnea and prescribed positive airway pressure (PAP) treatment with at least one risk factor for sleep-disordered breathing (SDB).
The trial will compare the efficacy of two different programs combining patient education with behavioral techniques to improve adherence to PAP therapy in women veterans. The recommended first-line treatment for SDB is PAP therapy, but women have been shown to have lower adherence to men, especially in woman veterans, who experience significant sleep disturbance and other consequences of sleep disorders. No study has tested possible interventions to increase PAP adherence in this population.
Among inclusion criteria are being a woman veteran aged at least 18 years, having received care from a Veterans Affairs facility, and having been diagnosed with sleep apnea with an apnea-hypopnea index of 5 or greater. Patients will be excluded if they are currently using a sleep apnea treatment, are pregnant, are an active substance user or started recovery in the past 90 days, are too ill to participate, do not have transportation, cannot self-consent, have unstable housing, have another sleep disorder that accounts for sleep disturbance, or have no sleep complaints or symptoms.
The primary outcome measures are PAP adherence 3 months post PAP initiation and sleep quality by patient-reported sleep questionnaire 3 months after randomizations. In addition, remote PAP usage data will be collected for 12 months post PAP initiation.
The estimated primary completion date is Dec. 21, 2021, and the estimated study completion date is Jan. 31, 2022. About 300 patients are estimated to be recruited.
Find more information on the study page at Clinicaltrials.gov.
The Treating Sleep Apnea in Women Veterans study is an interventional, randomized, controlled trial for woman veterans recently diagnosed with sleep apnea and prescribed positive airway pressure (PAP) treatment with at least one risk factor for sleep-disordered breathing (SDB).
The trial will compare the efficacy of two different programs combining patient education with behavioral techniques to improve adherence to PAP therapy in women veterans. The recommended first-line treatment for SDB is PAP therapy, but women have been shown to have lower adherence to men, especially in woman veterans, who experience significant sleep disturbance and other consequences of sleep disorders. No study has tested possible interventions to increase PAP adherence in this population.
Among inclusion criteria are being a woman veteran aged at least 18 years, having received care from a Veterans Affairs facility, and having been diagnosed with sleep apnea with an apnea-hypopnea index of 5 or greater. Patients will be excluded if they are currently using a sleep apnea treatment, are pregnant, are an active substance user or started recovery in the past 90 days, are too ill to participate, do not have transportation, cannot self-consent, have unstable housing, have another sleep disorder that accounts for sleep disturbance, or have no sleep complaints or symptoms.
The primary outcome measures are PAP adherence 3 months post PAP initiation and sleep quality by patient-reported sleep questionnaire 3 months after randomizations. In addition, remote PAP usage data will be collected for 12 months post PAP initiation.
The estimated primary completion date is Dec. 21, 2021, and the estimated study completion date is Jan. 31, 2022. About 300 patients are estimated to be recruited.
Find more information on the study page at Clinicaltrials.gov.
Clinical trial: Magnetic Resonance Imaging in Obstructive Sleep Apnea
The Magnetic Resonance Imaging in Obstructive Sleep Apnea trial is an observational cohort study recruiting adults with obstructive sleep apnea undergoing surgery.
The trial will compare drug-induced sleep endoscopy and upper airway MRI in order to determine which is the better predictor of success in patients who cannot tolerate nonsurgical solutions. Upper airway MRI is a more complete evaluation during wakefulness and is cheaper than drug-induced sleep endoscopy, but no studies have thus far utilized MRI as a surgical evaluation tool.
Patients will be included if they are at least 21 years old, have moderate to severe obstructive sleep apnea, and have a body mass index less than 40 kg/m2. Exclusion criteria include prior surgery for obstructive sleep apnea; known neurologic, cardiac, pulmonary, renal, or hepatic disorders; psychiatric problems except for treated depression or mild anxiety; a coexisting sleep disorder; or another contraindication to drug-induced sleep endoscopy or MRI, such as propofol allergy.
The primary outcome measure is surgical results after 6 months, which will be measured using sleep studies. Secondary outcomes include sleep-related quality of life after 6 months and daytime sleepiness after 6 months.
The estimated primary completion date is June 2020, and the estimated study completion date is July 2020. About 40 patients are expected to be recruited.
Find more information on the study page at Clinicaltrials.gov.
The Magnetic Resonance Imaging in Obstructive Sleep Apnea trial is an observational cohort study recruiting adults with obstructive sleep apnea undergoing surgery.
The trial will compare drug-induced sleep endoscopy and upper airway MRI in order to determine which is the better predictor of success in patients who cannot tolerate nonsurgical solutions. Upper airway MRI is a more complete evaluation during wakefulness and is cheaper than drug-induced sleep endoscopy, but no studies have thus far utilized MRI as a surgical evaluation tool.
Patients will be included if they are at least 21 years old, have moderate to severe obstructive sleep apnea, and have a body mass index less than 40 kg/m2. Exclusion criteria include prior surgery for obstructive sleep apnea; known neurologic, cardiac, pulmonary, renal, or hepatic disorders; psychiatric problems except for treated depression or mild anxiety; a coexisting sleep disorder; or another contraindication to drug-induced sleep endoscopy or MRI, such as propofol allergy.
The primary outcome measure is surgical results after 6 months, which will be measured using sleep studies. Secondary outcomes include sleep-related quality of life after 6 months and daytime sleepiness after 6 months.
The estimated primary completion date is June 2020, and the estimated study completion date is July 2020. About 40 patients are expected to be recruited.
Find more information on the study page at Clinicaltrials.gov.
The Magnetic Resonance Imaging in Obstructive Sleep Apnea trial is an observational cohort study recruiting adults with obstructive sleep apnea undergoing surgery.
The trial will compare drug-induced sleep endoscopy and upper airway MRI in order to determine which is the better predictor of success in patients who cannot tolerate nonsurgical solutions. Upper airway MRI is a more complete evaluation during wakefulness and is cheaper than drug-induced sleep endoscopy, but no studies have thus far utilized MRI as a surgical evaluation tool.
Patients will be included if they are at least 21 years old, have moderate to severe obstructive sleep apnea, and have a body mass index less than 40 kg/m2. Exclusion criteria include prior surgery for obstructive sleep apnea; known neurologic, cardiac, pulmonary, renal, or hepatic disorders; psychiatric problems except for treated depression or mild anxiety; a coexisting sleep disorder; or another contraindication to drug-induced sleep endoscopy or MRI, such as propofol allergy.
The primary outcome measure is surgical results after 6 months, which will be measured using sleep studies. Secondary outcomes include sleep-related quality of life after 6 months and daytime sleepiness after 6 months.
The estimated primary completion date is June 2020, and the estimated study completion date is July 2020. About 40 patients are expected to be recruited.
Find more information on the study page at Clinicaltrials.gov.
Building on diversity
Maryland SHM chapter follows expansive vision
Nidhi Goel, MD, MHS, is a Med-Peds hospitalist and assistant professor of internal medicine and pediatrics at the University of Maryland, Baltimore. Since August 2017, she has been the president of the Maryland chapter of SHM.
The Hospitalist recently sat down with her to discuss some of the initiatives that the large and active Maryland chapter is focused on.
Can you talk about your background and how you became interested in hospital medicine?
I grew up in the Baltimore area, and I went to medical school at the University of Maryland in Baltimore. I trained in internal medicine and pediatrics, also at the University of Maryland. Then I joined the faculty after I finished residency in 2014. I practiced as a hospitalist in internal medicine and pediatrics and was also a teaching hospitalist.
Early in my residency, I worked with teaching hospitalists. I rotated on the hospitalist teams, and I was inspired by their perspective on taking care of patients through a lens of quality and safety. I gained a greater appreciation for the risks associated with taking care of a patient in the hospital setting, and the opportunities to mitigate those risks and provide really high quality patient care. It made me realize that was what I wanted to do – and also to teach residents and students how to do the same.
So it was a philosophical attraction to the hospitalist approach?
Yes, and intellectually I’d say that I liked taking care of really complicated, very sick patients. I found that to be interesting – and rewarding when they got better.
Tell us more about what kind of research you do.
I work primarily on projects centered on quality and safety; they involve both adult internal medicine and pediatric patients. Currently on the adult medicine side, we have a project looking at improving outcomes for sepsis in the hospital setting. On the pediatric side, I’ve done a lot of work related to throughput – trying to increase the efficiency of our admissions – and especially our discharge process. Moving patients through the system efficiently has become a significant quality issue, especially during the winter months when our volumes pick up.
How long have you been involved in the Maryland SHM chapter, and what are the rewards of participation?
Early in my residency, I got involved in the chapter because some of the hospitalist faculty I worked with were chapter officers. They believed that the chapter was a good place for residents to be exposed to research and to other hospitalists for networking and camaraderie. So they began inviting us to Maryland chapter meetings, and I found those meetings to be very enlightening – from the practical and research content related to hospital medicine, and to networking with other hospitalists.
I was invited to be part of the Maryland chapter advisory board when I was still a resident, so that I might present trainee perspectives on how the chapter could continue to grow and target some of their activities for the benefit of residents. I stayed involved with the chapter after I finished residency, and when the opportunity presented itself to become an officer, and I decided to take it. I thought serving as a chapter officer would be a really interesting chance to meet more people in the field and to continue to innovate within the chapter setting.
Tell us more about the Maryland chapter.
We are a large chapter and we’re very, very active. Around 7 or 8 years ago, the Maryland chapter reached a significant turning point because the officers that were in place at that time had a vision for building the chapter. That was a major inflexion point in how active the chapter became, leading to the kinds of activities that we do now, and the variety of memberships.
One thing that I’m super proud of our chapter for is that we’ve really tried to continue building on the diversity that is represented in our membership. We have members stretching geographically all through the Baltimore and the Washington corridor, as well as out to western Maryland and the Eastern shore. The Maryland chapter has been able to attract members from different organizations throughout the state and from a diversity of practice settings. We have active members who are not just physicians, but also a nurse practitioners, physician assistants, and clinical pharmacists. We have members from throughout the health care delivery process, which really enriches the discussion and the value of the chapter as a whole.
What kind of initiatives and programs is the chapter working on?
Every year we have an abstracts competition at our fall meeting. Whoever wins that competition is allowed to present at the national SHM conference, which is a great opportunity. We’re really pushing that competition to make it an even more robust experience.
One thing that we had heard from some of our members, and that we recognized as a need as well, was to make our career guidance a little bit more robust. To that end, we’re creating a separate job fair that is almost like an employment workshop – to help people to buff up their CVs, to talk about interviewing skills, contracts, salary negotiations, as well as exposing job candidates to various hospital groups from throughout the area. That’s something that we’re really excited about. It’s going to take a lot of work, but I think it could be a really high-yield event for our members.
We’re also encouraging our nonphysician members to take more active leadership roles in the chapter; several of our nonphysician members on our chapter advisory board, including pharmacists and physician assistants, and we are trying to make sure that we’re also liaising with some of the professional organizations that represent our nonphysician members. So, for example, the clinical pharmacist who’s on our advisory board also is president of the Maryland chapter of the Society for Hospital Pharmacists. She brings a lot of really great ideas and interesting perspectives, and she’s brought a lot of exposure of our SHM chapter to the clinical pharmacy community as well.
What about more long-term goals for your chapter? What’s on the horizon?
We’re targeting early-career hospitalists and helping them to develop their career goals in whatever fashion they see as appropriate.
So, as someone who’s in academics, obviously research and publications are very important for me, but they’re not necessarily as important for other hospitalists. I think our early-career hospitalists are increasingly looking to incorporate things into their practice aside from direct patient care. Our members have interests in various elements of hospital medicine, including patient safety and quality improvement initiatives, clinical informatics, advocacy (especially related to the myriad aspects of health care reform), and strategies surrounding billing and denials. I think having our chapter help our members to realize some of those opportunities and develop their skills in a way that’s personally meaningful to them, as well as good for their marketability as they build their careers, would be a really positive step.
The ultimate goal of the chapter is to service members, so whatever long-term goals we have right now could definitely be fluid as time goes on.
What are some concerns of the chapter?
One area of significant discussion among hospitalists in Maryland has been global budgets. Our system of reimbursement is unique in the nation. It’s a system that aims to emphasize high-value care: the idea is to prioritize quality over quantity.
This system requires that hospitals rethink how we provide care in the inpatient setting, and how we create a continuum of care to the post-acute setting. It poses a lot of challenges, but also a lot of opportunities. Hospitalists are positioned perfectly to play a substantial role in implementing solutions.
Why might readers want to consider getting involved in their local SHM chapters?
I think it’s really beneficial to have the exposure that being involved with an SHM chapter brings – to people, to perspectives, to knowledge. There’s not really a downside to being involved with a chapter. You can take as little or as much as you want out of it, but I think most of our members find it to be a very enriching experience. Being involved in a chapter means you can have a voice, so that the chapter ends up serving you and your needs as well.
Maryland SHM chapter follows expansive vision
Maryland SHM chapter follows expansive vision
Nidhi Goel, MD, MHS, is a Med-Peds hospitalist and assistant professor of internal medicine and pediatrics at the University of Maryland, Baltimore. Since August 2017, she has been the president of the Maryland chapter of SHM.
The Hospitalist recently sat down with her to discuss some of the initiatives that the large and active Maryland chapter is focused on.
Can you talk about your background and how you became interested in hospital medicine?
I grew up in the Baltimore area, and I went to medical school at the University of Maryland in Baltimore. I trained in internal medicine and pediatrics, also at the University of Maryland. Then I joined the faculty after I finished residency in 2014. I practiced as a hospitalist in internal medicine and pediatrics and was also a teaching hospitalist.
Early in my residency, I worked with teaching hospitalists. I rotated on the hospitalist teams, and I was inspired by their perspective on taking care of patients through a lens of quality and safety. I gained a greater appreciation for the risks associated with taking care of a patient in the hospital setting, and the opportunities to mitigate those risks and provide really high quality patient care. It made me realize that was what I wanted to do – and also to teach residents and students how to do the same.
So it was a philosophical attraction to the hospitalist approach?
Yes, and intellectually I’d say that I liked taking care of really complicated, very sick patients. I found that to be interesting – and rewarding when they got better.
Tell us more about what kind of research you do.
I work primarily on projects centered on quality and safety; they involve both adult internal medicine and pediatric patients. Currently on the adult medicine side, we have a project looking at improving outcomes for sepsis in the hospital setting. On the pediatric side, I’ve done a lot of work related to throughput – trying to increase the efficiency of our admissions – and especially our discharge process. Moving patients through the system efficiently has become a significant quality issue, especially during the winter months when our volumes pick up.
How long have you been involved in the Maryland SHM chapter, and what are the rewards of participation?
Early in my residency, I got involved in the chapter because some of the hospitalist faculty I worked with were chapter officers. They believed that the chapter was a good place for residents to be exposed to research and to other hospitalists for networking and camaraderie. So they began inviting us to Maryland chapter meetings, and I found those meetings to be very enlightening – from the practical and research content related to hospital medicine, and to networking with other hospitalists.
I was invited to be part of the Maryland chapter advisory board when I was still a resident, so that I might present trainee perspectives on how the chapter could continue to grow and target some of their activities for the benefit of residents. I stayed involved with the chapter after I finished residency, and when the opportunity presented itself to become an officer, and I decided to take it. I thought serving as a chapter officer would be a really interesting chance to meet more people in the field and to continue to innovate within the chapter setting.
Tell us more about the Maryland chapter.
We are a large chapter and we’re very, very active. Around 7 or 8 years ago, the Maryland chapter reached a significant turning point because the officers that were in place at that time had a vision for building the chapter. That was a major inflexion point in how active the chapter became, leading to the kinds of activities that we do now, and the variety of memberships.
One thing that I’m super proud of our chapter for is that we’ve really tried to continue building on the diversity that is represented in our membership. We have members stretching geographically all through the Baltimore and the Washington corridor, as well as out to western Maryland and the Eastern shore. The Maryland chapter has been able to attract members from different organizations throughout the state and from a diversity of practice settings. We have active members who are not just physicians, but also a nurse practitioners, physician assistants, and clinical pharmacists. We have members from throughout the health care delivery process, which really enriches the discussion and the value of the chapter as a whole.
What kind of initiatives and programs is the chapter working on?
Every year we have an abstracts competition at our fall meeting. Whoever wins that competition is allowed to present at the national SHM conference, which is a great opportunity. We’re really pushing that competition to make it an even more robust experience.
One thing that we had heard from some of our members, and that we recognized as a need as well, was to make our career guidance a little bit more robust. To that end, we’re creating a separate job fair that is almost like an employment workshop – to help people to buff up their CVs, to talk about interviewing skills, contracts, salary negotiations, as well as exposing job candidates to various hospital groups from throughout the area. That’s something that we’re really excited about. It’s going to take a lot of work, but I think it could be a really high-yield event for our members.
We’re also encouraging our nonphysician members to take more active leadership roles in the chapter; several of our nonphysician members on our chapter advisory board, including pharmacists and physician assistants, and we are trying to make sure that we’re also liaising with some of the professional organizations that represent our nonphysician members. So, for example, the clinical pharmacist who’s on our advisory board also is president of the Maryland chapter of the Society for Hospital Pharmacists. She brings a lot of really great ideas and interesting perspectives, and she’s brought a lot of exposure of our SHM chapter to the clinical pharmacy community as well.
What about more long-term goals for your chapter? What’s on the horizon?
We’re targeting early-career hospitalists and helping them to develop their career goals in whatever fashion they see as appropriate.
So, as someone who’s in academics, obviously research and publications are very important for me, but they’re not necessarily as important for other hospitalists. I think our early-career hospitalists are increasingly looking to incorporate things into their practice aside from direct patient care. Our members have interests in various elements of hospital medicine, including patient safety and quality improvement initiatives, clinical informatics, advocacy (especially related to the myriad aspects of health care reform), and strategies surrounding billing and denials. I think having our chapter help our members to realize some of those opportunities and develop their skills in a way that’s personally meaningful to them, as well as good for their marketability as they build their careers, would be a really positive step.
The ultimate goal of the chapter is to service members, so whatever long-term goals we have right now could definitely be fluid as time goes on.
What are some concerns of the chapter?
One area of significant discussion among hospitalists in Maryland has been global budgets. Our system of reimbursement is unique in the nation. It’s a system that aims to emphasize high-value care: the idea is to prioritize quality over quantity.
This system requires that hospitals rethink how we provide care in the inpatient setting, and how we create a continuum of care to the post-acute setting. It poses a lot of challenges, but also a lot of opportunities. Hospitalists are positioned perfectly to play a substantial role in implementing solutions.
Why might readers want to consider getting involved in their local SHM chapters?
I think it’s really beneficial to have the exposure that being involved with an SHM chapter brings – to people, to perspectives, to knowledge. There’s not really a downside to being involved with a chapter. You can take as little or as much as you want out of it, but I think most of our members find it to be a very enriching experience. Being involved in a chapter means you can have a voice, so that the chapter ends up serving you and your needs as well.
Nidhi Goel, MD, MHS, is a Med-Peds hospitalist and assistant professor of internal medicine and pediatrics at the University of Maryland, Baltimore. Since August 2017, she has been the president of the Maryland chapter of SHM.
The Hospitalist recently sat down with her to discuss some of the initiatives that the large and active Maryland chapter is focused on.
Can you talk about your background and how you became interested in hospital medicine?
I grew up in the Baltimore area, and I went to medical school at the University of Maryland in Baltimore. I trained in internal medicine and pediatrics, also at the University of Maryland. Then I joined the faculty after I finished residency in 2014. I practiced as a hospitalist in internal medicine and pediatrics and was also a teaching hospitalist.
Early in my residency, I worked with teaching hospitalists. I rotated on the hospitalist teams, and I was inspired by their perspective on taking care of patients through a lens of quality and safety. I gained a greater appreciation for the risks associated with taking care of a patient in the hospital setting, and the opportunities to mitigate those risks and provide really high quality patient care. It made me realize that was what I wanted to do – and also to teach residents and students how to do the same.
So it was a philosophical attraction to the hospitalist approach?
Yes, and intellectually I’d say that I liked taking care of really complicated, very sick patients. I found that to be interesting – and rewarding when they got better.
Tell us more about what kind of research you do.
I work primarily on projects centered on quality and safety; they involve both adult internal medicine and pediatric patients. Currently on the adult medicine side, we have a project looking at improving outcomes for sepsis in the hospital setting. On the pediatric side, I’ve done a lot of work related to throughput – trying to increase the efficiency of our admissions – and especially our discharge process. Moving patients through the system efficiently has become a significant quality issue, especially during the winter months when our volumes pick up.
How long have you been involved in the Maryland SHM chapter, and what are the rewards of participation?
Early in my residency, I got involved in the chapter because some of the hospitalist faculty I worked with were chapter officers. They believed that the chapter was a good place for residents to be exposed to research and to other hospitalists for networking and camaraderie. So they began inviting us to Maryland chapter meetings, and I found those meetings to be very enlightening – from the practical and research content related to hospital medicine, and to networking with other hospitalists.
I was invited to be part of the Maryland chapter advisory board when I was still a resident, so that I might present trainee perspectives on how the chapter could continue to grow and target some of their activities for the benefit of residents. I stayed involved with the chapter after I finished residency, and when the opportunity presented itself to become an officer, and I decided to take it. I thought serving as a chapter officer would be a really interesting chance to meet more people in the field and to continue to innovate within the chapter setting.
Tell us more about the Maryland chapter.
We are a large chapter and we’re very, very active. Around 7 or 8 years ago, the Maryland chapter reached a significant turning point because the officers that were in place at that time had a vision for building the chapter. That was a major inflexion point in how active the chapter became, leading to the kinds of activities that we do now, and the variety of memberships.
One thing that I’m super proud of our chapter for is that we’ve really tried to continue building on the diversity that is represented in our membership. We have members stretching geographically all through the Baltimore and the Washington corridor, as well as out to western Maryland and the Eastern shore. The Maryland chapter has been able to attract members from different organizations throughout the state and from a diversity of practice settings. We have active members who are not just physicians, but also a nurse practitioners, physician assistants, and clinical pharmacists. We have members from throughout the health care delivery process, which really enriches the discussion and the value of the chapter as a whole.
What kind of initiatives and programs is the chapter working on?
Every year we have an abstracts competition at our fall meeting. Whoever wins that competition is allowed to present at the national SHM conference, which is a great opportunity. We’re really pushing that competition to make it an even more robust experience.
One thing that we had heard from some of our members, and that we recognized as a need as well, was to make our career guidance a little bit more robust. To that end, we’re creating a separate job fair that is almost like an employment workshop – to help people to buff up their CVs, to talk about interviewing skills, contracts, salary negotiations, as well as exposing job candidates to various hospital groups from throughout the area. That’s something that we’re really excited about. It’s going to take a lot of work, but I think it could be a really high-yield event for our members.
We’re also encouraging our nonphysician members to take more active leadership roles in the chapter; several of our nonphysician members on our chapter advisory board, including pharmacists and physician assistants, and we are trying to make sure that we’re also liaising with some of the professional organizations that represent our nonphysician members. So, for example, the clinical pharmacist who’s on our advisory board also is president of the Maryland chapter of the Society for Hospital Pharmacists. She brings a lot of really great ideas and interesting perspectives, and she’s brought a lot of exposure of our SHM chapter to the clinical pharmacy community as well.
What about more long-term goals for your chapter? What’s on the horizon?
We’re targeting early-career hospitalists and helping them to develop their career goals in whatever fashion they see as appropriate.
So, as someone who’s in academics, obviously research and publications are very important for me, but they’re not necessarily as important for other hospitalists. I think our early-career hospitalists are increasingly looking to incorporate things into their practice aside from direct patient care. Our members have interests in various elements of hospital medicine, including patient safety and quality improvement initiatives, clinical informatics, advocacy (especially related to the myriad aspects of health care reform), and strategies surrounding billing and denials. I think having our chapter help our members to realize some of those opportunities and develop their skills in a way that’s personally meaningful to them, as well as good for their marketability as they build their careers, would be a really positive step.
The ultimate goal of the chapter is to service members, so whatever long-term goals we have right now could definitely be fluid as time goes on.
What are some concerns of the chapter?
One area of significant discussion among hospitalists in Maryland has been global budgets. Our system of reimbursement is unique in the nation. It’s a system that aims to emphasize high-value care: the idea is to prioritize quality over quantity.
This system requires that hospitals rethink how we provide care in the inpatient setting, and how we create a continuum of care to the post-acute setting. It poses a lot of challenges, but also a lot of opportunities. Hospitalists are positioned perfectly to play a substantial role in implementing solutions.
Why might readers want to consider getting involved in their local SHM chapters?
I think it’s really beneficial to have the exposure that being involved with an SHM chapter brings – to people, to perspectives, to knowledge. There’s not really a downside to being involved with a chapter. You can take as little or as much as you want out of it, but I think most of our members find it to be a very enriching experience. Being involved in a chapter means you can have a voice, so that the chapter ends up serving you and your needs as well.
Laparoscope doubles as cystoscope in robotic hysterectomy
LAS VEGAS – to check for injuries, according to a review from St. Joseph’s University Medical Center, in Paterson, N.J.
Postoperative urinary tract infections (UTIs) are the big worry with using the same scope, but they really weren’t a problem at St. Joe’s; in a study of 45 women, there was just one UTI, confirmed by culture, at the 2-week postoperative visit, yielding a rate (2.2%) that is actually better the 5%-10% reported for stand-alone cystoscopy, said lead investigator and ob.gyn. resident Nikki Amirlatifi, MD.
“This is a safe alternative to traditional cystoscopy. We had no problems with visualization, and it doesn’t increase the rate of UTIs. Of course, it’s not only cost saving but time saving, as well,” she said.
The cases all were routine, however. For tougher ones, “where we need a more in-depth look at the bladder, we would [still] do cystoscopy,” she said at the meeting sponsored by AAGL.
There’s some debate about routine cystoscopy during laparoscopic hysterectomy, but Dr. Amirlatifi noted that it’s been reported to detect up to 89% of ureter injuries and up to 95% of bladder injuries. Using the same scope for both procedures makes it easier.
After the uterus was taken out, the bladder was backfilled with 180 mL of sterile water, then the Foley catheter was pulled. The previously used 5 mm laparoscope, which had been used for abdominal entry at 0 degrees, was introduced into the bladder. Efflux from both ureteral orifices was visualized, then the catheter reinserted until the end of surgery.
The women were an average of 44 years old, with an average body mass index of 32 kg/m2. Abnormal uterine bleeding, pelvic pain, and fibroids were the main indications for surgery. No ureteral or bladder injuries were detected.
Everyone was questioned about UTI symptoms and gave a clean-catch urine sample at the first postoperative visit. Cultures were performed on the seven women who reported symptoms or had white cells in their sample, and they were treated empirically with antibiotics. Only one culture grew out despite a high prevalence of UTI risk factors, including diabetes (13%), obesity (42%), and smoking (11%).
All the women had preoperative antibiotics and phenazopyridine. Most went home on the day of surgery.
There was no outside funding for the work, and the investigators didn’t have any relevant financial disclosures.
SOURCE: J Minim. Invasive Gynecol. 2018 Nov-Dec;25[7]:S46-47.
LAS VEGAS – to check for injuries, according to a review from St. Joseph’s University Medical Center, in Paterson, N.J.
Postoperative urinary tract infections (UTIs) are the big worry with using the same scope, but they really weren’t a problem at St. Joe’s; in a study of 45 women, there was just one UTI, confirmed by culture, at the 2-week postoperative visit, yielding a rate (2.2%) that is actually better the 5%-10% reported for stand-alone cystoscopy, said lead investigator and ob.gyn. resident Nikki Amirlatifi, MD.
“This is a safe alternative to traditional cystoscopy. We had no problems with visualization, and it doesn’t increase the rate of UTIs. Of course, it’s not only cost saving but time saving, as well,” she said.
The cases all were routine, however. For tougher ones, “where we need a more in-depth look at the bladder, we would [still] do cystoscopy,” she said at the meeting sponsored by AAGL.
There’s some debate about routine cystoscopy during laparoscopic hysterectomy, but Dr. Amirlatifi noted that it’s been reported to detect up to 89% of ureter injuries and up to 95% of bladder injuries. Using the same scope for both procedures makes it easier.
After the uterus was taken out, the bladder was backfilled with 180 mL of sterile water, then the Foley catheter was pulled. The previously used 5 mm laparoscope, which had been used for abdominal entry at 0 degrees, was introduced into the bladder. Efflux from both ureteral orifices was visualized, then the catheter reinserted until the end of surgery.
The women were an average of 44 years old, with an average body mass index of 32 kg/m2. Abnormal uterine bleeding, pelvic pain, and fibroids were the main indications for surgery. No ureteral or bladder injuries were detected.
Everyone was questioned about UTI symptoms and gave a clean-catch urine sample at the first postoperative visit. Cultures were performed on the seven women who reported symptoms or had white cells in their sample, and they were treated empirically with antibiotics. Only one culture grew out despite a high prevalence of UTI risk factors, including diabetes (13%), obesity (42%), and smoking (11%).
All the women had preoperative antibiotics and phenazopyridine. Most went home on the day of surgery.
There was no outside funding for the work, and the investigators didn’t have any relevant financial disclosures.
SOURCE: J Minim. Invasive Gynecol. 2018 Nov-Dec;25[7]:S46-47.
LAS VEGAS – to check for injuries, according to a review from St. Joseph’s University Medical Center, in Paterson, N.J.
Postoperative urinary tract infections (UTIs) are the big worry with using the same scope, but they really weren’t a problem at St. Joe’s; in a study of 45 women, there was just one UTI, confirmed by culture, at the 2-week postoperative visit, yielding a rate (2.2%) that is actually better the 5%-10% reported for stand-alone cystoscopy, said lead investigator and ob.gyn. resident Nikki Amirlatifi, MD.
“This is a safe alternative to traditional cystoscopy. We had no problems with visualization, and it doesn’t increase the rate of UTIs. Of course, it’s not only cost saving but time saving, as well,” she said.
The cases all were routine, however. For tougher ones, “where we need a more in-depth look at the bladder, we would [still] do cystoscopy,” she said at the meeting sponsored by AAGL.
There’s some debate about routine cystoscopy during laparoscopic hysterectomy, but Dr. Amirlatifi noted that it’s been reported to detect up to 89% of ureter injuries and up to 95% of bladder injuries. Using the same scope for both procedures makes it easier.
After the uterus was taken out, the bladder was backfilled with 180 mL of sterile water, then the Foley catheter was pulled. The previously used 5 mm laparoscope, which had been used for abdominal entry at 0 degrees, was introduced into the bladder. Efflux from both ureteral orifices was visualized, then the catheter reinserted until the end of surgery.
The women were an average of 44 years old, with an average body mass index of 32 kg/m2. Abnormal uterine bleeding, pelvic pain, and fibroids were the main indications for surgery. No ureteral or bladder injuries were detected.
Everyone was questioned about UTI symptoms and gave a clean-catch urine sample at the first postoperative visit. Cultures were performed on the seven women who reported symptoms or had white cells in their sample, and they were treated empirically with antibiotics. Only one culture grew out despite a high prevalence of UTI risk factors, including diabetes (13%), obesity (42%), and smoking (11%).
All the women had preoperative antibiotics and phenazopyridine. Most went home on the day of surgery.
There was no outside funding for the work, and the investigators didn’t have any relevant financial disclosures.
SOURCE: J Minim. Invasive Gynecol. 2018 Nov-Dec;25[7]:S46-47.
REPORTING FROM AAGL GLOBAL CONGRESS
Key clinical point: It is just as safe to look inside the bladder with the laparoscope after robotic hysterectomy in routine cases as to use a separate cystoscopy setup.
Major finding: Only 2.2% of women had a UTI, and there were no ureteral or bladder injuries detected using the laparoscope.
Study details: This was a prospective study of 45 women who underwent robotic hysterectomy whose bladder was inspected with the laparoscope at the end of surgery.
Disclosures: There was no outside funding for the work, and the investigators didn’t have any relevant financial disclosures.
Huntington’s research returns to Latin America, as scientists tread with care
BARRANQUILLA, COLOMBIA – “We don’t like to call them brigades. That sounds militant,” said neuropsychologist Johan Acosta-López, PhD.
Dr. Acosta-López, the head of cognitive neurosciences at Simón Bolivar University in this city on Colombia’s Atlantic coast, was among five Colombian clinicians – neurologists, psychiatrists, and neuropsychologists – stuffed into a car on their way to a conference hotel in July 2018.

The following day they would be joined by clinicians and researchers from North America, other Latin American countries, and Europe for a first-of-its kind meeting on Huntington’s disease (HD) in the region, sponsored by Factor-H, an HD charity working in Latin America.
Once the talks wrapped up, the researchers – clinicians and basic scientists – were invited to see patients at a hospital in a town an hour inland with a large concentration of HD families, most of them extremely poor. For some, the Factor-H–sponsored “brigade” would be their first hands-on experience with HD patients in a developing country.
There was some debate in the car about what to call such events: brigades, “integrated health days,” or clinics. Around here – where HD abounded but patients were weary of researchers – terminology mattered.
“We’ve had so many investigators arrive in this area – foreigners and Colombians – telling people ‘we’ve got this huge, great project that you’ll benefit from.’ And they take blood samples and never return,” Dr. Acosta-López said.

Even as a local investigator, Dr. Acosta-López has faced challenges getting a new study off the ground. Dr. Acosta-López and his colleagues are working under a grant from the Colombian government to recruit 241 presymptomatic subjects with confirmed genetic markers for HD, and evaluate them for cognitive and neurologic changes preceding disease onset.
It’s a cross-sectional study, and such studies are usually funded for a year. But the investigators knew it would take much more than a year to recruit patients here, and planned their study for 3 years. As of July, the team had been engaging with the community for 6 months but still didn’t have a single blood sample.
“We’ve had to convince everyone that this time is different,” he said, “and that means focusing on the social aspect” – setting up a legal-assistance program through the university to help families claim health benefits and a job-training program sponsored by local businesses.
It’s unusual for researchers to find themselves playing such extensive roles in coordinating social and economic support for their subjects. But with HD, it’s happening across Latin America, where researchers speak frequently of a “debt” owed to HD families in this region.
Huntington’s disease is a neurodegenerative disease caused by a genetic mutation in the huntingtin (HTT) gene, changing the normal protein it expresses in the body to a toxic form that damages cortical and basal ganglia neurons. It affects between 0.5 to 1 in 10,000 people worldwide, with higher prevalence in the United States, Europe, and Australia.
HD is inherited in an autosomal dominant pattern; a child of a parent with the mutation has a 50% chance of developing the disease. Patients develop cognitive symptoms that progress to dementia, along with the debilitating involuntary, dancelike movements that gave the disease the name by which it was formerly known: Huntington’s chorea.
In the 1980s and 1990s, several generations of Latin American HD families provided data that allowed for some of the greatest research advances in the disease – and they may represent a large share of the world’s HD cases. Yet, they continue to live in extreme poverty and have benefited little from the findings of the past 3 decades.
Without recognizing this and working to improve the families’ well-being, the researchers at the conference said it’s unlikely that promising therapies in the pipeline will ever reach the populations that need them the most.
Discovery in Venezuela
Some 8 hours by car from Barranquilla sits Lake Maracaibo, Venezuela, home to the largest known clusters of HD patients worldwide. The disease is believed to have come to the shores of Lake Maracaibo with a lone European immigrant – a Spanish sailor, many claim – at the end of the 18th century. Cases were first described in the 1950s by a young Venezuelan physician named Américo Negrette, MD.
Dr. Negrette’s findings were ignored by health officials in Venezuela and went unnoticed in the international research community until 1972, when a student of Dr. Negrette’s presented at an HD conference in Ohio. There he drew the attention of the American neuropsychologist Nancy S. Wexler, PhD. Dr. Wexler’s own mother had died of HD, and her father Milton, a noted psychoanalyst, founded the first research foundation dedicated to the disease.

While prevalence of HD in North America, Australia, and Europe is about 1 in 10,000, the region around Lake Maracaibo saw 70 times that rate at the time, thanks to high birth rates, geographic isolation, and extensive intermarriage within a handful of families. The families comprised mostly poor fishermen who lived in makeshift homes in towns ringing the lake.
In 1979, Dr. Wexler, with funding from the U.S. National Institutes of Health, began making annual research visits to Lake Maracaibo, and in 1983, the research group she coordinated, using data from blood and tissue samples donated by affected families, identified the location of the huntingtin gene on chromosome 4 (Nature. 1983 Nov 17;306[5940]:234-8). A decade later, the researchers isolated the mutant version of the gene and found it to be a triplet (CAG) expansion mutation, with more CAG repetitions associated with earlier age at disease onset (Cell. 1993 Mar 26;72[6]:971-83). Dr. Wexler and her colleagues’ findings led to the first genetic tests for HD.

Nationalist policies in Venezuela ended Dr. Wexler and her colleagues’ annual visits to Lake Maracaibo in 2002, along with the food, clothing, and medicines that the group routinely distributed to the families when they came.
Over 23 years, the researchers obtained data from some 18,000 individuals, but the families did not benefit in any durable way from the research. Local investigators with whom Dr. Wexler’s group collaborated lacked the resources and training to continue independently.
Access to medications is limited in Venezuela, and there is no institutional support for hundreds of HD patients living in extreme poverty, many of them descendants of the patients who contributed to the research and generation of these samples. The families’ biological material was sent to labs abroad, where investigators continue to derive findings from it today. Though genetic testing was performed on thousands at risk for the disease, few received access to their results through genetic counseling. A hospice established by Dr. Wexler’s foundation limped along until 2014, when it was finally shuttered.
Rebuilding bridges
A handful of families from the Lake Maracaibo towns attended the conference in Barranquilla. Their travel costs were picked up by Factor-H, which sponsored the event.
Ignacio Muñoz-Sanjuán, PhD, Factor-H’s founder and president, knew the families personally. He’s visited them regularly for years. In 2017, Dr. Muñoz-Sanjuán, a molecular biologist known affectionately in the HD community as “Nacho,” invited several to Rome for a meeting with Pope Francis, as part of an effort to raise awareness of HD and to request support from the Catholic Church for the Latin American families.
Humanitarian work is relatively new to Dr. Muñoz-Sanjuán, who’s spent his career in drug development. In addition to his unpaid work with Factor-H, he is vice president of biology with the CHDI Foundation, a Los Angeles–based nonprofit that funds drug research in HD. CHDI is reported to have about $100 million in annual funding – about triple the NIH budget in recent years for HD research. Its major donors are a group of investors who for years have remained anonymous and do not publicly discuss their philanthropy.
The Spanish-born Dr. Muñoz-Sanjuán had little direct experience with HD populations in Latin America until a few years ago, he said.
At a CHDI meeting in Brazil, he said, “I was talking with physicians and patient advocates from Latin America, telling them they had to be willing to be involved, that these communities with high prevalence had a lot to offer science,” Dr. Muñoz-Sanjuán said in an interview. “I was told that it was me who needed to understand the conditions in which HD patients lived. It completely put me on the spot.”
HD tends to strike during the most productive years of a person’s life, from the late 30s onward, keeping them from working and obliging family members to stop working to care for them. In a poor community, it can condemn a family to a state of extreme poverty for generations. Tetrabenazine (Xenazine), a medication to quiet chorea symptoms, is costly enough that many patients must do without it. Ensuring adequate calorie intake is difficult in HD patients, whose constant movements cause them to lose weight.
Dr. Muñoz-Sanjuán traveled to Colombia, Venezuela, and Brazil, meeting HD families and doctors like neurologist Gustavo Barrios, MD, of Hospital Occidente de Kennedy in Bogotá, Colombia. In a talk at the Barranquilla conference, Dr. Barrios related the experience of his first visit to El Dificil, a community in northern Colombia where some large HD families are forced to survive on the equivalent of $5 a day. “I had to confront not only the fact that these families were living with a terrible disease but in conditions of extreme deprivation,” he said. “My life as a doctor changed that day.”
Dr. Muñoz-Sanjuán helped form a Latin American HD network to involve clinicians like Dr. Barrios who worked with HD clusters, most of them poorly studied. “These are all neglected communities that share similar features,” Dr. Muñoz-Sanjuán said.
On Colombia’s Caribbean coast, for example, HD had been documented since the early 1990s, but genotyping was not performed until recently. Prevalence data are “virtually nonexistent” in Colombia, said Sonia Moreno, PhD, a neuropsychologist at the University of Antioquia in Medellin. In a pilot study presented this year at the CHDI Foundation’s Enroll-HD Congress, Dr. Moreno and her colleagues mined Colombian public health data for likely HD cases, and argued for the creation of a national registry.
In 2012, Dr. Muñoz-Sanjuán founded Factor-H with the aim of improving living conditions for Latin American communities with HD.

Factor-H does not receive funds from CHDI Foundation and instead relies on donations from individuals and companies; its annual budget is less than $200,000. But through contracts with local nongovernmental organizations, it has sponsored health clinics and ongoing food assistance, delivered shipments of medicines and clothing, and started a sponsorship program for young people in HD families, whose studies often are interrupted caring for sick parents. It hopes to build permanent support centers in Colombia and Venezuela where HD families can get their food and medical needs met.
“The traditional thinking in the HD research community is that we’re helping people by doing the legwork to make medicine – and that’s not necessarily enough. You need a more holistic approach,” Dr. Muñoz-Sanjuán said.
Lennie Pineda, MSc, who recently retired as a geneticist with the University of Zulia in Maracaibo, Venezuela, said that Dr. Muñoz-Sanjuán was viewed skeptically when he first visited, in part because of his biomedical research background.
Ms. Pineda, who worked with the region’s HD families her whole career, has been wary of past research efforts in Venezuela. In 2010, she published a paper critical of Dr. Wexler’s and his colleagues’ approach (Revista Redbioética/UNESCO. 2010;1[2]:50-61), particularly regarding issues of informed consent.
“I was very cold to Nacho,” she laughed. “We all looked at him suspiciously.”
Ms. Pineda said Dr. Muñoz-Sanjuán won her over with his interest and creativity in finding concrete ways improve the lives of families in the Lake Maracaibo towns.
In a talk at the conference, Edison Soto, a young man from San Luis, a town on Lake Maracaibo that is a key cluster of HD, said Dr. Muñoz-Sanjuán’s visits had reawakened hope among the families there. “For years, no one thought about us, and because of the situation in the country it’s been hard, really hard,” he said.
“Nacho’s smart,” Ms. Pineda said. “He’s not coming to build a research cohort, he’s coming with genuine intention to help. But if one day conditions are adequate to support investigation, and the people here are well informed and volunteer for a study with full consent, well, all the better,” she said.
Dr. Muñoz-Sanjuán acknowledged that his humanitarian work could be perceived as preparing the ground for future clinical trials.
“I’m not doing anything research oriented with Latin America,” he said. “I would never approach these communities and recommend they take part in a study or give samples, unless their conditions change significantly. But the idea of cross-contamination is a problem I might need to fix. There may come a day where I need to depersonalize Factor-H from me.”
A research platform, a novel agent
Though HD research in Latin America remains rife with challenges, a number of investigators at the conference talked optimistically about planned and ongoing HD studies in Latin America.
The biggest of these is ENROLL-HD, a long-term global observational study of families with HD that uses a standardized approach to data collection. The platform, launched in 2013, aims to enroll 20,000 participants for yearly (or more frequent) assessment. Data from ENROLL-HD will support a diverse range of studies on everything from biomarkers to genetic modifiers to quality of life measures in HD.
ENROLL-HD has opened study sites in Argentina, Chile, and Colombia, and plans to launch a site near Lima, Peru, that is home to an HD cluster. Venezuela is considered out of reach, at least for now.
In Barranquilla, Claudia Perandones, MD, PhD, a genetics researcher in Argentina who manages ENROLL-HD for Latin America and is a cofounder of Factor-H, explained why the kind of clusters seen in Latin America are so valuable scientifically.
The extended family groups share a disease haplotype, eat the same foods, and live in similar environments, Dr. Perandones noted. Because not all the variation in HD can be explained by the number of CAG repeats a patient has, having a large sample with a common haplotype would help researchers pinpoint other environmental and genetic factors that can modify the onset or progress of the disease.
Another key goal of ENROLL-HD, investigators say, is to speed recruitment into clinical trials as they arise. And for the first time in history, potentially game-changing therapies are being developed specifically for HD.
For the past 5 years the Swiss pharmaceutical giant Roche has worked with a smaller biotech firm, Ionis Pharmaceuticals, on an agent called RG6042, which was known until recently as IONIS-HTTRx. CHDI was extensively involved in the agent’s preclinical development, contributing some $10 million to get it off the ground.
RG6042 is an antisense oligonucleotide, delivered by spinal injection, which works by interrupting an mRNA signaling pathway to suppress production of mutant HTT (mHTT) protein in the brain. Antisense oligonucleotides, sometimes called gene silencing therapies, are a new and promising approach in neurodegenerative diseases. Two have received FDA approval to treat spinal muscular atrophy and Duchenne muscular dystrophy.
In April 2018, Roche announced positive results from phase 1/2a study in 46 HD patients in Europe and North America. Patients in that 13-week study saw significant (up to 60%) dose-dependent reductions of the mHTT in their cerebrospinal fluid; a post hoc analysis also found some evidence of functional improvement (Neurology. 2018;90[15 Supplement]:CT.002).
These encouraging findings led to Roche’s announcement of a global phase 3 randomized, controlled trial that is scheduled to begin enrolling in 2019. Roche hopes to randomize 660 patients with mild HD across 15 countries for the 2-year trial, called GENERATION-HD1.
Sites in Latin America are expected to include Argentina, Chile, and Colombia.
At the Barranquilla meeting, Daniel Ciriano, MD, Roche’s Argentina-based medical director for Latin America, extolled the company’s commitment to ethics and social welfare in the region. In recent years, Roche has increased its humanitarian commitments across Latin America, including helping rebuild a Chilean village after an earthquake and offering free breast cancer and kidney disease treatments.
RG6042 is only one of a number of promising approaches to HD. Other therapies in the pipeline include gene silencing delivered by viral vectors instead of repeated spinal injections, an oral drug that interrupts mHTT production, immunotherapies, and even CRISPR gene–editing techniques.
Little was said at the conference, however, about how Latin American HD communities might be able to afford RG6042 or any other therapy that emerges from the pipeline.
Dr. Muñoz-Sanjuán called the issue “a theme for future discussion.”
“This is an area that has to be handled carefully and not one we are heavily invested in yet, although it’s very important,” he said.
On the ground
Several of the European and North American scientists who presented in Barranquilla took pains to express their concern with the well-being of HD patients in Latin America and to demonstrate goodwill toward the local researchers and clinicians.
Hilal A. Lashuel, PhD, a molecular biologist working on the structure and behavior of the HTT protein, said his participation in the Factor-H event at the Vatican the year before had awakened him to “the real human part of HD,” and changed the way he does science.
Normally, Dr. Lashuel said, “we do research disconnected from the realities of the diseases we work with.”
“We need to not just to do research but [to ensure] that research is done right,” he said, which means also focusing on improving patients’ standard of living.
The room broke out in applause when Dr. Lashuel announced new internships for investigators from developing countries. He also presented a parting video from his research team at the École Polytechnique Fédérale de Lausanne (Switzerland), complete with music and affectionate messages in Spanish.
Pharmacologist Elena Cattaneo, PhD, a stem cell researcher long active in the HD community, and also a senator in Italy’s parliament, delivered a similarly warm, carefully choreographed video message from her laboratory at the University of Milan.
Just days later in the town of Juan de Acosta, an hour inland of Barranquilla, the same researchers sat down with patients and families who crowded the waiting room of the town’s only hospital, as the sun beat in through the windows and as mule carts, stray dogs, and buses passed by on the main drag outside.
The event had been titled a “brigade” after all, but the HD families did not seem to mind – and indeed so many showed up that a sign had to be placed on the door saying that no one who arrived after noon could be seen. Consults were not limited to HD-related matters, so families could be seen for any complaint.
HD was first documented in this town in the early 1990s, but much remains to be understood about the size of the cluster, the haplotype, and its relation to other clusters in Colombia or Venezuela. The families here share a handful of last names and likely share a common ancestor. In the early 19th century, the Barranquilla region was flooded with European migrants who reached the city by ship. (HD clusters in Latin America tend to be concentrated in coastal regions, possibly because of migration patterns.)
The waiting room of the hospital was loud with chatter. Small children played as their relatives waited for consults. Some showed the characteristic restless movements and emaciated bodies of people with advanced HD.
The foreign scientists were barred from taking any patient data out of the hospital or asking for samples. Even picture taking was prohibited. Instead they performed genetic counseling and neuropsychological tests; they sorted out differential diagnoses and advised on medications. Visiting Colombian and Venezuelan physicians did the same, while their assistants met with families in the waiting room, taking medical histories and sketching out basic genealogies.
Some of the foreign researchers reported fruitful interactions with patients, while others seemed perplexed by what they’d experienced. Alba di Pardo, PhD, a genetic epidemiologist at the Istituto Neurologico Mediterraneo Pozzilli (Italy), said she’d spent the morning doing genetic counseling with families and going over genealogies to assess risk. Yet, despite the fact that anyone with an HD parent has a 50% chance of developing the disease, some family members acted uninterested, she said.
Dr. di Pardo’s colleague at the Istituto, biologist Vittorio Maglione, PhD, reported having a similar experience. As he was counseling a young woman about her risk for HD, she scrolled indifferently through Facebook posts on her phone, he said.
On some level, Dr. Maglione said, he could understand patients’ reluctance to engage noting that, while there were many potential HD therapies to try, any new treatment paradigm for HD was many years away from a place like this – and potentially very costly. Dr. Maglione – along with Dr. di Pardo – is researching the SP1 axis, a sphingolipid pathway implicated in neurodegenerative such diseases as HD and which has potential as a drug target (Trends Pharmacol Sci. 2018;39[5]:468-80).
Psychologist Pedro Puentes Rozo of Simón Bolivar University, who is working with Dr. Acosta-López on the local cohort study of presymptomatic HD patients, said that, for most of the families in the clinic that day, any seeming indifference probably masked deeper fears. People already were well aware of their risk. “They’ve known about it forever, said Dr. Puentes Rozo, who has been working with this HD population for a decade. “But this is a catastrophic illness and can generate a lot of anxiety.”
Dr. Puentes Rozo said the group’s planned study, unlike studies in the past, would be conducted under strict “international ethical norms and standards.” Subjects would receive ongoing psychological support, and the researchers were working to establish a genetic counseling center so that people who want to know their status “can be prepared,” he said, and plan for their lives and families.
By fall 2018, the cohort study was underway. The group had sponsored several more hospital brigades – or “integrated health days” as they preferred to call them, at the hospital in Juan de Acosta, giving them a chance to work face to face with families.
They drew no blood during the clinics, as investigators in the past had done. Instead, they explained the study to patients, performed the initial screenings, and invited them to designated study appointments at the university. Legal assistance was up and running, and the jobs program would start in 2019.
Enrollment was climbing. And the group was steadily accumulating data.
BARRANQUILLA, COLOMBIA – “We don’t like to call them brigades. That sounds militant,” said neuropsychologist Johan Acosta-López, PhD.
Dr. Acosta-López, the head of cognitive neurosciences at Simón Bolivar University in this city on Colombia’s Atlantic coast, was among five Colombian clinicians – neurologists, psychiatrists, and neuropsychologists – stuffed into a car on their way to a conference hotel in July 2018.

The following day they would be joined by clinicians and researchers from North America, other Latin American countries, and Europe for a first-of-its kind meeting on Huntington’s disease (HD) in the region, sponsored by Factor-H, an HD charity working in Latin America.
Once the talks wrapped up, the researchers – clinicians and basic scientists – were invited to see patients at a hospital in a town an hour inland with a large concentration of HD families, most of them extremely poor. For some, the Factor-H–sponsored “brigade” would be their first hands-on experience with HD patients in a developing country.
There was some debate in the car about what to call such events: brigades, “integrated health days,” or clinics. Around here – where HD abounded but patients were weary of researchers – terminology mattered.
“We’ve had so many investigators arrive in this area – foreigners and Colombians – telling people ‘we’ve got this huge, great project that you’ll benefit from.’ And they take blood samples and never return,” Dr. Acosta-López said.

Even as a local investigator, Dr. Acosta-López has faced challenges getting a new study off the ground. Dr. Acosta-López and his colleagues are working under a grant from the Colombian government to recruit 241 presymptomatic subjects with confirmed genetic markers for HD, and evaluate them for cognitive and neurologic changes preceding disease onset.
It’s a cross-sectional study, and such studies are usually funded for a year. But the investigators knew it would take much more than a year to recruit patients here, and planned their study for 3 years. As of July, the team had been engaging with the community for 6 months but still didn’t have a single blood sample.
“We’ve had to convince everyone that this time is different,” he said, “and that means focusing on the social aspect” – setting up a legal-assistance program through the university to help families claim health benefits and a job-training program sponsored by local businesses.
It’s unusual for researchers to find themselves playing such extensive roles in coordinating social and economic support for their subjects. But with HD, it’s happening across Latin America, where researchers speak frequently of a “debt” owed to HD families in this region.
Huntington’s disease is a neurodegenerative disease caused by a genetic mutation in the huntingtin (HTT) gene, changing the normal protein it expresses in the body to a toxic form that damages cortical and basal ganglia neurons. It affects between 0.5 to 1 in 10,000 people worldwide, with higher prevalence in the United States, Europe, and Australia.
HD is inherited in an autosomal dominant pattern; a child of a parent with the mutation has a 50% chance of developing the disease. Patients develop cognitive symptoms that progress to dementia, along with the debilitating involuntary, dancelike movements that gave the disease the name by which it was formerly known: Huntington’s chorea.
In the 1980s and 1990s, several generations of Latin American HD families provided data that allowed for some of the greatest research advances in the disease – and they may represent a large share of the world’s HD cases. Yet, they continue to live in extreme poverty and have benefited little from the findings of the past 3 decades.
Without recognizing this and working to improve the families’ well-being, the researchers at the conference said it’s unlikely that promising therapies in the pipeline will ever reach the populations that need them the most.
Discovery in Venezuela
Some 8 hours by car from Barranquilla sits Lake Maracaibo, Venezuela, home to the largest known clusters of HD patients worldwide. The disease is believed to have come to the shores of Lake Maracaibo with a lone European immigrant – a Spanish sailor, many claim – at the end of the 18th century. Cases were first described in the 1950s by a young Venezuelan physician named Américo Negrette, MD.
Dr. Negrette’s findings were ignored by health officials in Venezuela and went unnoticed in the international research community until 1972, when a student of Dr. Negrette’s presented at an HD conference in Ohio. There he drew the attention of the American neuropsychologist Nancy S. Wexler, PhD. Dr. Wexler’s own mother had died of HD, and her father Milton, a noted psychoanalyst, founded the first research foundation dedicated to the disease.

While prevalence of HD in North America, Australia, and Europe is about 1 in 10,000, the region around Lake Maracaibo saw 70 times that rate at the time, thanks to high birth rates, geographic isolation, and extensive intermarriage within a handful of families. The families comprised mostly poor fishermen who lived in makeshift homes in towns ringing the lake.
In 1979, Dr. Wexler, with funding from the U.S. National Institutes of Health, began making annual research visits to Lake Maracaibo, and in 1983, the research group she coordinated, using data from blood and tissue samples donated by affected families, identified the location of the huntingtin gene on chromosome 4 (Nature. 1983 Nov 17;306[5940]:234-8). A decade later, the researchers isolated the mutant version of the gene and found it to be a triplet (CAG) expansion mutation, with more CAG repetitions associated with earlier age at disease onset (Cell. 1993 Mar 26;72[6]:971-83). Dr. Wexler and her colleagues’ findings led to the first genetic tests for HD.

Nationalist policies in Venezuela ended Dr. Wexler and her colleagues’ annual visits to Lake Maracaibo in 2002, along with the food, clothing, and medicines that the group routinely distributed to the families when they came.
Over 23 years, the researchers obtained data from some 18,000 individuals, but the families did not benefit in any durable way from the research. Local investigators with whom Dr. Wexler’s group collaborated lacked the resources and training to continue independently.
Access to medications is limited in Venezuela, and there is no institutional support for hundreds of HD patients living in extreme poverty, many of them descendants of the patients who contributed to the research and generation of these samples. The families’ biological material was sent to labs abroad, where investigators continue to derive findings from it today. Though genetic testing was performed on thousands at risk for the disease, few received access to their results through genetic counseling. A hospice established by Dr. Wexler’s foundation limped along until 2014, when it was finally shuttered.
Rebuilding bridges
A handful of families from the Lake Maracaibo towns attended the conference in Barranquilla. Their travel costs were picked up by Factor-H, which sponsored the event.
Ignacio Muñoz-Sanjuán, PhD, Factor-H’s founder and president, knew the families personally. He’s visited them regularly for years. In 2017, Dr. Muñoz-Sanjuán, a molecular biologist known affectionately in the HD community as “Nacho,” invited several to Rome for a meeting with Pope Francis, as part of an effort to raise awareness of HD and to request support from the Catholic Church for the Latin American families.
Humanitarian work is relatively new to Dr. Muñoz-Sanjuán, who’s spent his career in drug development. In addition to his unpaid work with Factor-H, he is vice president of biology with the CHDI Foundation, a Los Angeles–based nonprofit that funds drug research in HD. CHDI is reported to have about $100 million in annual funding – about triple the NIH budget in recent years for HD research. Its major donors are a group of investors who for years have remained anonymous and do not publicly discuss their philanthropy.
The Spanish-born Dr. Muñoz-Sanjuán had little direct experience with HD populations in Latin America until a few years ago, he said.
At a CHDI meeting in Brazil, he said, “I was talking with physicians and patient advocates from Latin America, telling them they had to be willing to be involved, that these communities with high prevalence had a lot to offer science,” Dr. Muñoz-Sanjuán said in an interview. “I was told that it was me who needed to understand the conditions in which HD patients lived. It completely put me on the spot.”
HD tends to strike during the most productive years of a person’s life, from the late 30s onward, keeping them from working and obliging family members to stop working to care for them. In a poor community, it can condemn a family to a state of extreme poverty for generations. Tetrabenazine (Xenazine), a medication to quiet chorea symptoms, is costly enough that many patients must do without it. Ensuring adequate calorie intake is difficult in HD patients, whose constant movements cause them to lose weight.
Dr. Muñoz-Sanjuán traveled to Colombia, Venezuela, and Brazil, meeting HD families and doctors like neurologist Gustavo Barrios, MD, of Hospital Occidente de Kennedy in Bogotá, Colombia. In a talk at the Barranquilla conference, Dr. Barrios related the experience of his first visit to El Dificil, a community in northern Colombia where some large HD families are forced to survive on the equivalent of $5 a day. “I had to confront not only the fact that these families were living with a terrible disease but in conditions of extreme deprivation,” he said. “My life as a doctor changed that day.”
Dr. Muñoz-Sanjuán helped form a Latin American HD network to involve clinicians like Dr. Barrios who worked with HD clusters, most of them poorly studied. “These are all neglected communities that share similar features,” Dr. Muñoz-Sanjuán said.
On Colombia’s Caribbean coast, for example, HD had been documented since the early 1990s, but genotyping was not performed until recently. Prevalence data are “virtually nonexistent” in Colombia, said Sonia Moreno, PhD, a neuropsychologist at the University of Antioquia in Medellin. In a pilot study presented this year at the CHDI Foundation’s Enroll-HD Congress, Dr. Moreno and her colleagues mined Colombian public health data for likely HD cases, and argued for the creation of a national registry.
In 2012, Dr. Muñoz-Sanjuán founded Factor-H with the aim of improving living conditions for Latin American communities with HD.

Factor-H does not receive funds from CHDI Foundation and instead relies on donations from individuals and companies; its annual budget is less than $200,000. But through contracts with local nongovernmental organizations, it has sponsored health clinics and ongoing food assistance, delivered shipments of medicines and clothing, and started a sponsorship program for young people in HD families, whose studies often are interrupted caring for sick parents. It hopes to build permanent support centers in Colombia and Venezuela where HD families can get their food and medical needs met.
“The traditional thinking in the HD research community is that we’re helping people by doing the legwork to make medicine – and that’s not necessarily enough. You need a more holistic approach,” Dr. Muñoz-Sanjuán said.
Lennie Pineda, MSc, who recently retired as a geneticist with the University of Zulia in Maracaibo, Venezuela, said that Dr. Muñoz-Sanjuán was viewed skeptically when he first visited, in part because of his biomedical research background.
Ms. Pineda, who worked with the region’s HD families her whole career, has been wary of past research efforts in Venezuela. In 2010, she published a paper critical of Dr. Wexler’s and his colleagues’ approach (Revista Redbioética/UNESCO. 2010;1[2]:50-61), particularly regarding issues of informed consent.
“I was very cold to Nacho,” she laughed. “We all looked at him suspiciously.”
Ms. Pineda said Dr. Muñoz-Sanjuán won her over with his interest and creativity in finding concrete ways improve the lives of families in the Lake Maracaibo towns.
In a talk at the conference, Edison Soto, a young man from San Luis, a town on Lake Maracaibo that is a key cluster of HD, said Dr. Muñoz-Sanjuán’s visits had reawakened hope among the families there. “For years, no one thought about us, and because of the situation in the country it’s been hard, really hard,” he said.
“Nacho’s smart,” Ms. Pineda said. “He’s not coming to build a research cohort, he’s coming with genuine intention to help. But if one day conditions are adequate to support investigation, and the people here are well informed and volunteer for a study with full consent, well, all the better,” she said.
Dr. Muñoz-Sanjuán acknowledged that his humanitarian work could be perceived as preparing the ground for future clinical trials.
“I’m not doing anything research oriented with Latin America,” he said. “I would never approach these communities and recommend they take part in a study or give samples, unless their conditions change significantly. But the idea of cross-contamination is a problem I might need to fix. There may come a day where I need to depersonalize Factor-H from me.”
A research platform, a novel agent
Though HD research in Latin America remains rife with challenges, a number of investigators at the conference talked optimistically about planned and ongoing HD studies in Latin America.
The biggest of these is ENROLL-HD, a long-term global observational study of families with HD that uses a standardized approach to data collection. The platform, launched in 2013, aims to enroll 20,000 participants for yearly (or more frequent) assessment. Data from ENROLL-HD will support a diverse range of studies on everything from biomarkers to genetic modifiers to quality of life measures in HD.
ENROLL-HD has opened study sites in Argentina, Chile, and Colombia, and plans to launch a site near Lima, Peru, that is home to an HD cluster. Venezuela is considered out of reach, at least for now.
In Barranquilla, Claudia Perandones, MD, PhD, a genetics researcher in Argentina who manages ENROLL-HD for Latin America and is a cofounder of Factor-H, explained why the kind of clusters seen in Latin America are so valuable scientifically.
The extended family groups share a disease haplotype, eat the same foods, and live in similar environments, Dr. Perandones noted. Because not all the variation in HD can be explained by the number of CAG repeats a patient has, having a large sample with a common haplotype would help researchers pinpoint other environmental and genetic factors that can modify the onset or progress of the disease.
Another key goal of ENROLL-HD, investigators say, is to speed recruitment into clinical trials as they arise. And for the first time in history, potentially game-changing therapies are being developed specifically for HD.
For the past 5 years the Swiss pharmaceutical giant Roche has worked with a smaller biotech firm, Ionis Pharmaceuticals, on an agent called RG6042, which was known until recently as IONIS-HTTRx. CHDI was extensively involved in the agent’s preclinical development, contributing some $10 million to get it off the ground.
RG6042 is an antisense oligonucleotide, delivered by spinal injection, which works by interrupting an mRNA signaling pathway to suppress production of mutant HTT (mHTT) protein in the brain. Antisense oligonucleotides, sometimes called gene silencing therapies, are a new and promising approach in neurodegenerative diseases. Two have received FDA approval to treat spinal muscular atrophy and Duchenne muscular dystrophy.
In April 2018, Roche announced positive results from phase 1/2a study in 46 HD patients in Europe and North America. Patients in that 13-week study saw significant (up to 60%) dose-dependent reductions of the mHTT in their cerebrospinal fluid; a post hoc analysis also found some evidence of functional improvement (Neurology. 2018;90[15 Supplement]:CT.002).
These encouraging findings led to Roche’s announcement of a global phase 3 randomized, controlled trial that is scheduled to begin enrolling in 2019. Roche hopes to randomize 660 patients with mild HD across 15 countries for the 2-year trial, called GENERATION-HD1.
Sites in Latin America are expected to include Argentina, Chile, and Colombia.
At the Barranquilla meeting, Daniel Ciriano, MD, Roche’s Argentina-based medical director for Latin America, extolled the company’s commitment to ethics and social welfare in the region. In recent years, Roche has increased its humanitarian commitments across Latin America, including helping rebuild a Chilean village after an earthquake and offering free breast cancer and kidney disease treatments.
RG6042 is only one of a number of promising approaches to HD. Other therapies in the pipeline include gene silencing delivered by viral vectors instead of repeated spinal injections, an oral drug that interrupts mHTT production, immunotherapies, and even CRISPR gene–editing techniques.
Little was said at the conference, however, about how Latin American HD communities might be able to afford RG6042 or any other therapy that emerges from the pipeline.
Dr. Muñoz-Sanjuán called the issue “a theme for future discussion.”
“This is an area that has to be handled carefully and not one we are heavily invested in yet, although it’s very important,” he said.
On the ground
Several of the European and North American scientists who presented in Barranquilla took pains to express their concern with the well-being of HD patients in Latin America and to demonstrate goodwill toward the local researchers and clinicians.
Hilal A. Lashuel, PhD, a molecular biologist working on the structure and behavior of the HTT protein, said his participation in the Factor-H event at the Vatican the year before had awakened him to “the real human part of HD,” and changed the way he does science.
Normally, Dr. Lashuel said, “we do research disconnected from the realities of the diseases we work with.”
“We need to not just to do research but [to ensure] that research is done right,” he said, which means also focusing on improving patients’ standard of living.
The room broke out in applause when Dr. Lashuel announced new internships for investigators from developing countries. He also presented a parting video from his research team at the École Polytechnique Fédérale de Lausanne (Switzerland), complete with music and affectionate messages in Spanish.
Pharmacologist Elena Cattaneo, PhD, a stem cell researcher long active in the HD community, and also a senator in Italy’s parliament, delivered a similarly warm, carefully choreographed video message from her laboratory at the University of Milan.
Just days later in the town of Juan de Acosta, an hour inland of Barranquilla, the same researchers sat down with patients and families who crowded the waiting room of the town’s only hospital, as the sun beat in through the windows and as mule carts, stray dogs, and buses passed by on the main drag outside.
The event had been titled a “brigade” after all, but the HD families did not seem to mind – and indeed so many showed up that a sign had to be placed on the door saying that no one who arrived after noon could be seen. Consults were not limited to HD-related matters, so families could be seen for any complaint.
HD was first documented in this town in the early 1990s, but much remains to be understood about the size of the cluster, the haplotype, and its relation to other clusters in Colombia or Venezuela. The families here share a handful of last names and likely share a common ancestor. In the early 19th century, the Barranquilla region was flooded with European migrants who reached the city by ship. (HD clusters in Latin America tend to be concentrated in coastal regions, possibly because of migration patterns.)
The waiting room of the hospital was loud with chatter. Small children played as their relatives waited for consults. Some showed the characteristic restless movements and emaciated bodies of people with advanced HD.
The foreign scientists were barred from taking any patient data out of the hospital or asking for samples. Even picture taking was prohibited. Instead they performed genetic counseling and neuropsychological tests; they sorted out differential diagnoses and advised on medications. Visiting Colombian and Venezuelan physicians did the same, while their assistants met with families in the waiting room, taking medical histories and sketching out basic genealogies.
Some of the foreign researchers reported fruitful interactions with patients, while others seemed perplexed by what they’d experienced. Alba di Pardo, PhD, a genetic epidemiologist at the Istituto Neurologico Mediterraneo Pozzilli (Italy), said she’d spent the morning doing genetic counseling with families and going over genealogies to assess risk. Yet, despite the fact that anyone with an HD parent has a 50% chance of developing the disease, some family members acted uninterested, she said.
Dr. di Pardo’s colleague at the Istituto, biologist Vittorio Maglione, PhD, reported having a similar experience. As he was counseling a young woman about her risk for HD, she scrolled indifferently through Facebook posts on her phone, he said.
On some level, Dr. Maglione said, he could understand patients’ reluctance to engage noting that, while there were many potential HD therapies to try, any new treatment paradigm for HD was many years away from a place like this – and potentially very costly. Dr. Maglione – along with Dr. di Pardo – is researching the SP1 axis, a sphingolipid pathway implicated in neurodegenerative such diseases as HD and which has potential as a drug target (Trends Pharmacol Sci. 2018;39[5]:468-80).
Psychologist Pedro Puentes Rozo of Simón Bolivar University, who is working with Dr. Acosta-López on the local cohort study of presymptomatic HD patients, said that, for most of the families in the clinic that day, any seeming indifference probably masked deeper fears. People already were well aware of their risk. “They’ve known about it forever, said Dr. Puentes Rozo, who has been working with this HD population for a decade. “But this is a catastrophic illness and can generate a lot of anxiety.”
Dr. Puentes Rozo said the group’s planned study, unlike studies in the past, would be conducted under strict “international ethical norms and standards.” Subjects would receive ongoing psychological support, and the researchers were working to establish a genetic counseling center so that people who want to know their status “can be prepared,” he said, and plan for their lives and families.
By fall 2018, the cohort study was underway. The group had sponsored several more hospital brigades – or “integrated health days” as they preferred to call them, at the hospital in Juan de Acosta, giving them a chance to work face to face with families.
They drew no blood during the clinics, as investigators in the past had done. Instead, they explained the study to patients, performed the initial screenings, and invited them to designated study appointments at the university. Legal assistance was up and running, and the jobs program would start in 2019.
Enrollment was climbing. And the group was steadily accumulating data.
BARRANQUILLA, COLOMBIA – “We don’t like to call them brigades. That sounds militant,” said neuropsychologist Johan Acosta-López, PhD.
Dr. Acosta-López, the head of cognitive neurosciences at Simón Bolivar University in this city on Colombia’s Atlantic coast, was among five Colombian clinicians – neurologists, psychiatrists, and neuropsychologists – stuffed into a car on their way to a conference hotel in July 2018.

The following day they would be joined by clinicians and researchers from North America, other Latin American countries, and Europe for a first-of-its kind meeting on Huntington’s disease (HD) in the region, sponsored by Factor-H, an HD charity working in Latin America.
Once the talks wrapped up, the researchers – clinicians and basic scientists – were invited to see patients at a hospital in a town an hour inland with a large concentration of HD families, most of them extremely poor. For some, the Factor-H–sponsored “brigade” would be their first hands-on experience with HD patients in a developing country.
There was some debate in the car about what to call such events: brigades, “integrated health days,” or clinics. Around here – where HD abounded but patients were weary of researchers – terminology mattered.
“We’ve had so many investigators arrive in this area – foreigners and Colombians – telling people ‘we’ve got this huge, great project that you’ll benefit from.’ And they take blood samples and never return,” Dr. Acosta-López said.

Even as a local investigator, Dr. Acosta-López has faced challenges getting a new study off the ground. Dr. Acosta-López and his colleagues are working under a grant from the Colombian government to recruit 241 presymptomatic subjects with confirmed genetic markers for HD, and evaluate them for cognitive and neurologic changes preceding disease onset.
It’s a cross-sectional study, and such studies are usually funded for a year. But the investigators knew it would take much more than a year to recruit patients here, and planned their study for 3 years. As of July, the team had been engaging with the community for 6 months but still didn’t have a single blood sample.
“We’ve had to convince everyone that this time is different,” he said, “and that means focusing on the social aspect” – setting up a legal-assistance program through the university to help families claim health benefits and a job-training program sponsored by local businesses.
It’s unusual for researchers to find themselves playing such extensive roles in coordinating social and economic support for their subjects. But with HD, it’s happening across Latin America, where researchers speak frequently of a “debt” owed to HD families in this region.
Huntington’s disease is a neurodegenerative disease caused by a genetic mutation in the huntingtin (HTT) gene, changing the normal protein it expresses in the body to a toxic form that damages cortical and basal ganglia neurons. It affects between 0.5 to 1 in 10,000 people worldwide, with higher prevalence in the United States, Europe, and Australia.
HD is inherited in an autosomal dominant pattern; a child of a parent with the mutation has a 50% chance of developing the disease. Patients develop cognitive symptoms that progress to dementia, along with the debilitating involuntary, dancelike movements that gave the disease the name by which it was formerly known: Huntington’s chorea.
In the 1980s and 1990s, several generations of Latin American HD families provided data that allowed for some of the greatest research advances in the disease – and they may represent a large share of the world’s HD cases. Yet, they continue to live in extreme poverty and have benefited little from the findings of the past 3 decades.
Without recognizing this and working to improve the families’ well-being, the researchers at the conference said it’s unlikely that promising therapies in the pipeline will ever reach the populations that need them the most.
Discovery in Venezuela
Some 8 hours by car from Barranquilla sits Lake Maracaibo, Venezuela, home to the largest known clusters of HD patients worldwide. The disease is believed to have come to the shores of Lake Maracaibo with a lone European immigrant – a Spanish sailor, many claim – at the end of the 18th century. Cases were first described in the 1950s by a young Venezuelan physician named Américo Negrette, MD.
Dr. Negrette’s findings were ignored by health officials in Venezuela and went unnoticed in the international research community until 1972, when a student of Dr. Negrette’s presented at an HD conference in Ohio. There he drew the attention of the American neuropsychologist Nancy S. Wexler, PhD. Dr. Wexler’s own mother had died of HD, and her father Milton, a noted psychoanalyst, founded the first research foundation dedicated to the disease.

While prevalence of HD in North America, Australia, and Europe is about 1 in 10,000, the region around Lake Maracaibo saw 70 times that rate at the time, thanks to high birth rates, geographic isolation, and extensive intermarriage within a handful of families. The families comprised mostly poor fishermen who lived in makeshift homes in towns ringing the lake.
In 1979, Dr. Wexler, with funding from the U.S. National Institutes of Health, began making annual research visits to Lake Maracaibo, and in 1983, the research group she coordinated, using data from blood and tissue samples donated by affected families, identified the location of the huntingtin gene on chromosome 4 (Nature. 1983 Nov 17;306[5940]:234-8). A decade later, the researchers isolated the mutant version of the gene and found it to be a triplet (CAG) expansion mutation, with more CAG repetitions associated with earlier age at disease onset (Cell. 1993 Mar 26;72[6]:971-83). Dr. Wexler and her colleagues’ findings led to the first genetic tests for HD.

Nationalist policies in Venezuela ended Dr. Wexler and her colleagues’ annual visits to Lake Maracaibo in 2002, along with the food, clothing, and medicines that the group routinely distributed to the families when they came.
Over 23 years, the researchers obtained data from some 18,000 individuals, but the families did not benefit in any durable way from the research. Local investigators with whom Dr. Wexler’s group collaborated lacked the resources and training to continue independently.
Access to medications is limited in Venezuela, and there is no institutional support for hundreds of HD patients living in extreme poverty, many of them descendants of the patients who contributed to the research and generation of these samples. The families’ biological material was sent to labs abroad, where investigators continue to derive findings from it today. Though genetic testing was performed on thousands at risk for the disease, few received access to their results through genetic counseling. A hospice established by Dr. Wexler’s foundation limped along until 2014, when it was finally shuttered.
Rebuilding bridges
A handful of families from the Lake Maracaibo towns attended the conference in Barranquilla. Their travel costs were picked up by Factor-H, which sponsored the event.
Ignacio Muñoz-Sanjuán, PhD, Factor-H’s founder and president, knew the families personally. He’s visited them regularly for years. In 2017, Dr. Muñoz-Sanjuán, a molecular biologist known affectionately in the HD community as “Nacho,” invited several to Rome for a meeting with Pope Francis, as part of an effort to raise awareness of HD and to request support from the Catholic Church for the Latin American families.
Humanitarian work is relatively new to Dr. Muñoz-Sanjuán, who’s spent his career in drug development. In addition to his unpaid work with Factor-H, he is vice president of biology with the CHDI Foundation, a Los Angeles–based nonprofit that funds drug research in HD. CHDI is reported to have about $100 million in annual funding – about triple the NIH budget in recent years for HD research. Its major donors are a group of investors who for years have remained anonymous and do not publicly discuss their philanthropy.
The Spanish-born Dr. Muñoz-Sanjuán had little direct experience with HD populations in Latin America until a few years ago, he said.
At a CHDI meeting in Brazil, he said, “I was talking with physicians and patient advocates from Latin America, telling them they had to be willing to be involved, that these communities with high prevalence had a lot to offer science,” Dr. Muñoz-Sanjuán said in an interview. “I was told that it was me who needed to understand the conditions in which HD patients lived. It completely put me on the spot.”
HD tends to strike during the most productive years of a person’s life, from the late 30s onward, keeping them from working and obliging family members to stop working to care for them. In a poor community, it can condemn a family to a state of extreme poverty for generations. Tetrabenazine (Xenazine), a medication to quiet chorea symptoms, is costly enough that many patients must do without it. Ensuring adequate calorie intake is difficult in HD patients, whose constant movements cause them to lose weight.
Dr. Muñoz-Sanjuán traveled to Colombia, Venezuela, and Brazil, meeting HD families and doctors like neurologist Gustavo Barrios, MD, of Hospital Occidente de Kennedy in Bogotá, Colombia. In a talk at the Barranquilla conference, Dr. Barrios related the experience of his first visit to El Dificil, a community in northern Colombia where some large HD families are forced to survive on the equivalent of $5 a day. “I had to confront not only the fact that these families were living with a terrible disease but in conditions of extreme deprivation,” he said. “My life as a doctor changed that day.”
Dr. Muñoz-Sanjuán helped form a Latin American HD network to involve clinicians like Dr. Barrios who worked with HD clusters, most of them poorly studied. “These are all neglected communities that share similar features,” Dr. Muñoz-Sanjuán said.
On Colombia’s Caribbean coast, for example, HD had been documented since the early 1990s, but genotyping was not performed until recently. Prevalence data are “virtually nonexistent” in Colombia, said Sonia Moreno, PhD, a neuropsychologist at the University of Antioquia in Medellin. In a pilot study presented this year at the CHDI Foundation’s Enroll-HD Congress, Dr. Moreno and her colleagues mined Colombian public health data for likely HD cases, and argued for the creation of a national registry.
In 2012, Dr. Muñoz-Sanjuán founded Factor-H with the aim of improving living conditions for Latin American communities with HD.

Factor-H does not receive funds from CHDI Foundation and instead relies on donations from individuals and companies; its annual budget is less than $200,000. But through contracts with local nongovernmental organizations, it has sponsored health clinics and ongoing food assistance, delivered shipments of medicines and clothing, and started a sponsorship program for young people in HD families, whose studies often are interrupted caring for sick parents. It hopes to build permanent support centers in Colombia and Venezuela where HD families can get their food and medical needs met.
“The traditional thinking in the HD research community is that we’re helping people by doing the legwork to make medicine – and that’s not necessarily enough. You need a more holistic approach,” Dr. Muñoz-Sanjuán said.
Lennie Pineda, MSc, who recently retired as a geneticist with the University of Zulia in Maracaibo, Venezuela, said that Dr. Muñoz-Sanjuán was viewed skeptically when he first visited, in part because of his biomedical research background.
Ms. Pineda, who worked with the region’s HD families her whole career, has been wary of past research efforts in Venezuela. In 2010, she published a paper critical of Dr. Wexler’s and his colleagues’ approach (Revista Redbioética/UNESCO. 2010;1[2]:50-61), particularly regarding issues of informed consent.
“I was very cold to Nacho,” she laughed. “We all looked at him suspiciously.”
Ms. Pineda said Dr. Muñoz-Sanjuán won her over with his interest and creativity in finding concrete ways improve the lives of families in the Lake Maracaibo towns.
In a talk at the conference, Edison Soto, a young man from San Luis, a town on Lake Maracaibo that is a key cluster of HD, said Dr. Muñoz-Sanjuán’s visits had reawakened hope among the families there. “For years, no one thought about us, and because of the situation in the country it’s been hard, really hard,” he said.
“Nacho’s smart,” Ms. Pineda said. “He’s not coming to build a research cohort, he’s coming with genuine intention to help. But if one day conditions are adequate to support investigation, and the people here are well informed and volunteer for a study with full consent, well, all the better,” she said.
Dr. Muñoz-Sanjuán acknowledged that his humanitarian work could be perceived as preparing the ground for future clinical trials.
“I’m not doing anything research oriented with Latin America,” he said. “I would never approach these communities and recommend they take part in a study or give samples, unless their conditions change significantly. But the idea of cross-contamination is a problem I might need to fix. There may come a day where I need to depersonalize Factor-H from me.”
A research platform, a novel agent
Though HD research in Latin America remains rife with challenges, a number of investigators at the conference talked optimistically about planned and ongoing HD studies in Latin America.
The biggest of these is ENROLL-HD, a long-term global observational study of families with HD that uses a standardized approach to data collection. The platform, launched in 2013, aims to enroll 20,000 participants for yearly (or more frequent) assessment. Data from ENROLL-HD will support a diverse range of studies on everything from biomarkers to genetic modifiers to quality of life measures in HD.
ENROLL-HD has opened study sites in Argentina, Chile, and Colombia, and plans to launch a site near Lima, Peru, that is home to an HD cluster. Venezuela is considered out of reach, at least for now.
In Barranquilla, Claudia Perandones, MD, PhD, a genetics researcher in Argentina who manages ENROLL-HD for Latin America and is a cofounder of Factor-H, explained why the kind of clusters seen in Latin America are so valuable scientifically.
The extended family groups share a disease haplotype, eat the same foods, and live in similar environments, Dr. Perandones noted. Because not all the variation in HD can be explained by the number of CAG repeats a patient has, having a large sample with a common haplotype would help researchers pinpoint other environmental and genetic factors that can modify the onset or progress of the disease.
Another key goal of ENROLL-HD, investigators say, is to speed recruitment into clinical trials as they arise. And for the first time in history, potentially game-changing therapies are being developed specifically for HD.
For the past 5 years the Swiss pharmaceutical giant Roche has worked with a smaller biotech firm, Ionis Pharmaceuticals, on an agent called RG6042, which was known until recently as IONIS-HTTRx. CHDI was extensively involved in the agent’s preclinical development, contributing some $10 million to get it off the ground.
RG6042 is an antisense oligonucleotide, delivered by spinal injection, which works by interrupting an mRNA signaling pathway to suppress production of mutant HTT (mHTT) protein in the brain. Antisense oligonucleotides, sometimes called gene silencing therapies, are a new and promising approach in neurodegenerative diseases. Two have received FDA approval to treat spinal muscular atrophy and Duchenne muscular dystrophy.
In April 2018, Roche announced positive results from phase 1/2a study in 46 HD patients in Europe and North America. Patients in that 13-week study saw significant (up to 60%) dose-dependent reductions of the mHTT in their cerebrospinal fluid; a post hoc analysis also found some evidence of functional improvement (Neurology. 2018;90[15 Supplement]:CT.002).
These encouraging findings led to Roche’s announcement of a global phase 3 randomized, controlled trial that is scheduled to begin enrolling in 2019. Roche hopes to randomize 660 patients with mild HD across 15 countries for the 2-year trial, called GENERATION-HD1.
Sites in Latin America are expected to include Argentina, Chile, and Colombia.
At the Barranquilla meeting, Daniel Ciriano, MD, Roche’s Argentina-based medical director for Latin America, extolled the company’s commitment to ethics and social welfare in the region. In recent years, Roche has increased its humanitarian commitments across Latin America, including helping rebuild a Chilean village after an earthquake and offering free breast cancer and kidney disease treatments.
RG6042 is only one of a number of promising approaches to HD. Other therapies in the pipeline include gene silencing delivered by viral vectors instead of repeated spinal injections, an oral drug that interrupts mHTT production, immunotherapies, and even CRISPR gene–editing techniques.
Little was said at the conference, however, about how Latin American HD communities might be able to afford RG6042 or any other therapy that emerges from the pipeline.
Dr. Muñoz-Sanjuán called the issue “a theme for future discussion.”
“This is an area that has to be handled carefully and not one we are heavily invested in yet, although it’s very important,” he said.
On the ground
Several of the European and North American scientists who presented in Barranquilla took pains to express their concern with the well-being of HD patients in Latin America and to demonstrate goodwill toward the local researchers and clinicians.
Hilal A. Lashuel, PhD, a molecular biologist working on the structure and behavior of the HTT protein, said his participation in the Factor-H event at the Vatican the year before had awakened him to “the real human part of HD,” and changed the way he does science.
Normally, Dr. Lashuel said, “we do research disconnected from the realities of the diseases we work with.”
“We need to not just to do research but [to ensure] that research is done right,” he said, which means also focusing on improving patients’ standard of living.
The room broke out in applause when Dr. Lashuel announced new internships for investigators from developing countries. He also presented a parting video from his research team at the École Polytechnique Fédérale de Lausanne (Switzerland), complete with music and affectionate messages in Spanish.
Pharmacologist Elena Cattaneo, PhD, a stem cell researcher long active in the HD community, and also a senator in Italy’s parliament, delivered a similarly warm, carefully choreographed video message from her laboratory at the University of Milan.
Just days later in the town of Juan de Acosta, an hour inland of Barranquilla, the same researchers sat down with patients and families who crowded the waiting room of the town’s only hospital, as the sun beat in through the windows and as mule carts, stray dogs, and buses passed by on the main drag outside.
The event had been titled a “brigade” after all, but the HD families did not seem to mind – and indeed so many showed up that a sign had to be placed on the door saying that no one who arrived after noon could be seen. Consults were not limited to HD-related matters, so families could be seen for any complaint.
HD was first documented in this town in the early 1990s, but much remains to be understood about the size of the cluster, the haplotype, and its relation to other clusters in Colombia or Venezuela. The families here share a handful of last names and likely share a common ancestor. In the early 19th century, the Barranquilla region was flooded with European migrants who reached the city by ship. (HD clusters in Latin America tend to be concentrated in coastal regions, possibly because of migration patterns.)
The waiting room of the hospital was loud with chatter. Small children played as their relatives waited for consults. Some showed the characteristic restless movements and emaciated bodies of people with advanced HD.
The foreign scientists were barred from taking any patient data out of the hospital or asking for samples. Even picture taking was prohibited. Instead they performed genetic counseling and neuropsychological tests; they sorted out differential diagnoses and advised on medications. Visiting Colombian and Venezuelan physicians did the same, while their assistants met with families in the waiting room, taking medical histories and sketching out basic genealogies.
Some of the foreign researchers reported fruitful interactions with patients, while others seemed perplexed by what they’d experienced. Alba di Pardo, PhD, a genetic epidemiologist at the Istituto Neurologico Mediterraneo Pozzilli (Italy), said she’d spent the morning doing genetic counseling with families and going over genealogies to assess risk. Yet, despite the fact that anyone with an HD parent has a 50% chance of developing the disease, some family members acted uninterested, she said.
Dr. di Pardo’s colleague at the Istituto, biologist Vittorio Maglione, PhD, reported having a similar experience. As he was counseling a young woman about her risk for HD, she scrolled indifferently through Facebook posts on her phone, he said.
On some level, Dr. Maglione said, he could understand patients’ reluctance to engage noting that, while there were many potential HD therapies to try, any new treatment paradigm for HD was many years away from a place like this – and potentially very costly. Dr. Maglione – along with Dr. di Pardo – is researching the SP1 axis, a sphingolipid pathway implicated in neurodegenerative such diseases as HD and which has potential as a drug target (Trends Pharmacol Sci. 2018;39[5]:468-80).
Psychologist Pedro Puentes Rozo of Simón Bolivar University, who is working with Dr. Acosta-López on the local cohort study of presymptomatic HD patients, said that, for most of the families in the clinic that day, any seeming indifference probably masked deeper fears. People already were well aware of their risk. “They’ve known about it forever, said Dr. Puentes Rozo, who has been working with this HD population for a decade. “But this is a catastrophic illness and can generate a lot of anxiety.”
Dr. Puentes Rozo said the group’s planned study, unlike studies in the past, would be conducted under strict “international ethical norms and standards.” Subjects would receive ongoing psychological support, and the researchers were working to establish a genetic counseling center so that people who want to know their status “can be prepared,” he said, and plan for their lives and families.
By fall 2018, the cohort study was underway. The group had sponsored several more hospital brigades – or “integrated health days” as they preferred to call them, at the hospital in Juan de Acosta, giving them a chance to work face to face with families.
They drew no blood during the clinics, as investigators in the past had done. Instead, they explained the study to patients, performed the initial screenings, and invited them to designated study appointments at the university. Legal assistance was up and running, and the jobs program would start in 2019.
Enrollment was climbing. And the group was steadily accumulating data.
High prices driving insulin underuse
One in four patients at an urban diabetes center reported underusing insulin because of concerns about cost, according to a survey of patients with type 1 or type 2 diabetes mellitus who were recently prescribed the drug.
“These results highlight an urgent need to address affordability of insulin,” lead author Darby Herkert of Yale College in New Haven, Conn., and her coauthors wrote in a study published online in JAMA Internal Medicine.
In the survey of 199 diabetes patients who had an outpatient visit at the Yale Diabetes Center between June and August 2017, 25.5% reported cost-related insulin underuse. Only 60.8% of those patients discussed the prohibitive costs with their clinician, and 29.4% changed insulin types because of high prices. Patients who reported insulin underuse were also more likely to have poorer glycemic control than patients who did not, at a rate of 43.1% versus 28.1% (odds ratio, 2.96; 95% confidence interval, 1.14-8.16; P = .03).
The authors noted potential limitations in their study, including focusing on patients of just one treatment center and the inability to establish a causal relationship between cost-related underuse and poor glycemic control. Nonetheless, they strongly encouraged asking diabetes patients about potential cost issues; they also stressed the need for larger forces to step in and guarantee insulin’s availability. “Insulin is a life-saving, essential medicine, and most patients cannot act as price-sensitive buyers. Regulators and the medical community need to intervene to ensure that insulin is affordable to patients who need it,” they wrote.
This study was supported by the Global Health Field Experiences Award, the Yale College Fellowship for Research in Global Health Studies, and the Global Health Field Experiences Seed Funding Award. The corresponding author reported receiving funding from the Centers of Medicare and Medicaid Services to develop publicly reported quality measures. Another author reported receiving support from Health Action International and Alosa Health. No other disclosures were reported.
SOURCE: Herkert D et al. JAMA Internal Medicine. 2018 Dec 3. doi: 10.1001/jamainternmed.2018.5008.
This study by Herkert and colleagues reinforces that American drug makers, device manufacturers, and insurers are willing to sacrifice human lives in their quest for profit, according to Elisabeth Rosenthal, MD, of Kaiser Health News.
Diabetes is a disease that starts in childhood, she noted, which means young Americans who are often low-earning and uninsured must start managing it with insulin before they are financially stable. And if drug prices keep going up – and if competitors are sued out of the market – then that means people with chronic disease will suffer, including the 25.5% that Herkert et al. found underuse insulin because of cost.
“As drug costs have generally increased in the United States, we know that many patients are skimping on medicines, taking less than prescribed, and cutting pills in half to make every fill last longer. This is terrible, but for many diseases, it is not catastrophic,” she wrote.
“But skimping on insulin,” she added, “can be rapidly deadly in people whose bodies make none of their own and can result in a life-threatening metabolic disturbance.”
Dr. Rosenthal shared the story of a 29-year-old diabetes patient in Missouri who would consider only doctoral programs outside the United States. “My one goal in life has been to move to Europe so I don’t have to pay these staggering prices just to survive,” the patient revealed.
But others – that 25% – will quietly skimp on their insulin, taking less than they need but more, perhaps, than they can really afford. Some of them will die.
Dr. Rosenthal is the author of “An American Sickness: How Healthcare Became Big Business and How You Can Take It Back.” These comments are adapted from an accompanying editorial (JAMA Internal Med. 2018 Dec 3. doi: 10.1001/jamainternmed.2018.5007).
This study by Herkert and colleagues reinforces that American drug makers, device manufacturers, and insurers are willing to sacrifice human lives in their quest for profit, according to Elisabeth Rosenthal, MD, of Kaiser Health News.
Diabetes is a disease that starts in childhood, she noted, which means young Americans who are often low-earning and uninsured must start managing it with insulin before they are financially stable. And if drug prices keep going up – and if competitors are sued out of the market – then that means people with chronic disease will suffer, including the 25.5% that Herkert et al. found underuse insulin because of cost.
“As drug costs have generally increased in the United States, we know that many patients are skimping on medicines, taking less than prescribed, and cutting pills in half to make every fill last longer. This is terrible, but for many diseases, it is not catastrophic,” she wrote.
“But skimping on insulin,” she added, “can be rapidly deadly in people whose bodies make none of their own and can result in a life-threatening metabolic disturbance.”
Dr. Rosenthal shared the story of a 29-year-old diabetes patient in Missouri who would consider only doctoral programs outside the United States. “My one goal in life has been to move to Europe so I don’t have to pay these staggering prices just to survive,” the patient revealed.
But others – that 25% – will quietly skimp on their insulin, taking less than they need but more, perhaps, than they can really afford. Some of them will die.
Dr. Rosenthal is the author of “An American Sickness: How Healthcare Became Big Business and How You Can Take It Back.” These comments are adapted from an accompanying editorial (JAMA Internal Med. 2018 Dec 3. doi: 10.1001/jamainternmed.2018.5007).
This study by Herkert and colleagues reinforces that American drug makers, device manufacturers, and insurers are willing to sacrifice human lives in their quest for profit, according to Elisabeth Rosenthal, MD, of Kaiser Health News.
Diabetes is a disease that starts in childhood, she noted, which means young Americans who are often low-earning and uninsured must start managing it with insulin before they are financially stable. And if drug prices keep going up – and if competitors are sued out of the market – then that means people with chronic disease will suffer, including the 25.5% that Herkert et al. found underuse insulin because of cost.
“As drug costs have generally increased in the United States, we know that many patients are skimping on medicines, taking less than prescribed, and cutting pills in half to make every fill last longer. This is terrible, but for many diseases, it is not catastrophic,” she wrote.
“But skimping on insulin,” she added, “can be rapidly deadly in people whose bodies make none of their own and can result in a life-threatening metabolic disturbance.”
Dr. Rosenthal shared the story of a 29-year-old diabetes patient in Missouri who would consider only doctoral programs outside the United States. “My one goal in life has been to move to Europe so I don’t have to pay these staggering prices just to survive,” the patient revealed.
But others – that 25% – will quietly skimp on their insulin, taking less than they need but more, perhaps, than they can really afford. Some of them will die.
Dr. Rosenthal is the author of “An American Sickness: How Healthcare Became Big Business and How You Can Take It Back.” These comments are adapted from an accompanying editorial (JAMA Internal Med. 2018 Dec 3. doi: 10.1001/jamainternmed.2018.5007).
One in four patients at an urban diabetes center reported underusing insulin because of concerns about cost, according to a survey of patients with type 1 or type 2 diabetes mellitus who were recently prescribed the drug.
“These results highlight an urgent need to address affordability of insulin,” lead author Darby Herkert of Yale College in New Haven, Conn., and her coauthors wrote in a study published online in JAMA Internal Medicine.
In the survey of 199 diabetes patients who had an outpatient visit at the Yale Diabetes Center between June and August 2017, 25.5% reported cost-related insulin underuse. Only 60.8% of those patients discussed the prohibitive costs with their clinician, and 29.4% changed insulin types because of high prices. Patients who reported insulin underuse were also more likely to have poorer glycemic control than patients who did not, at a rate of 43.1% versus 28.1% (odds ratio, 2.96; 95% confidence interval, 1.14-8.16; P = .03).
The authors noted potential limitations in their study, including focusing on patients of just one treatment center and the inability to establish a causal relationship between cost-related underuse and poor glycemic control. Nonetheless, they strongly encouraged asking diabetes patients about potential cost issues; they also stressed the need for larger forces to step in and guarantee insulin’s availability. “Insulin is a life-saving, essential medicine, and most patients cannot act as price-sensitive buyers. Regulators and the medical community need to intervene to ensure that insulin is affordable to patients who need it,” they wrote.
This study was supported by the Global Health Field Experiences Award, the Yale College Fellowship for Research in Global Health Studies, and the Global Health Field Experiences Seed Funding Award. The corresponding author reported receiving funding from the Centers of Medicare and Medicaid Services to develop publicly reported quality measures. Another author reported receiving support from Health Action International and Alosa Health. No other disclosures were reported.
SOURCE: Herkert D et al. JAMA Internal Medicine. 2018 Dec 3. doi: 10.1001/jamainternmed.2018.5008.
One in four patients at an urban diabetes center reported underusing insulin because of concerns about cost, according to a survey of patients with type 1 or type 2 diabetes mellitus who were recently prescribed the drug.
“These results highlight an urgent need to address affordability of insulin,” lead author Darby Herkert of Yale College in New Haven, Conn., and her coauthors wrote in a study published online in JAMA Internal Medicine.
In the survey of 199 diabetes patients who had an outpatient visit at the Yale Diabetes Center between June and August 2017, 25.5% reported cost-related insulin underuse. Only 60.8% of those patients discussed the prohibitive costs with their clinician, and 29.4% changed insulin types because of high prices. Patients who reported insulin underuse were also more likely to have poorer glycemic control than patients who did not, at a rate of 43.1% versus 28.1% (odds ratio, 2.96; 95% confidence interval, 1.14-8.16; P = .03).
The authors noted potential limitations in their study, including focusing on patients of just one treatment center and the inability to establish a causal relationship between cost-related underuse and poor glycemic control. Nonetheless, they strongly encouraged asking diabetes patients about potential cost issues; they also stressed the need for larger forces to step in and guarantee insulin’s availability. “Insulin is a life-saving, essential medicine, and most patients cannot act as price-sensitive buyers. Regulators and the medical community need to intervene to ensure that insulin is affordable to patients who need it,” they wrote.
This study was supported by the Global Health Field Experiences Award, the Yale College Fellowship for Research in Global Health Studies, and the Global Health Field Experiences Seed Funding Award. The corresponding author reported receiving funding from the Centers of Medicare and Medicaid Services to develop publicly reported quality measures. Another author reported receiving support from Health Action International and Alosa Health. No other disclosures were reported.
SOURCE: Herkert D et al. JAMA Internal Medicine. 2018 Dec 3. doi: 10.1001/jamainternmed.2018.5008.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Patients who reported cost-related insulin underuse were more likely to have poorer glycemic control than those who were able to afford the drug.
Major finding: Insulin cost accounted for its underuse by 25.5% of diabetic patients surveyed.
Study details: A survey of 199 patients with type 1 or type 2 diabetes mellitus who were prescribed insulin in the last 6 months and had an outpatient visit at the Yale Diabetes Center between June and August 2017.
Disclosures: This study was supported by the Global Health Field Experiences Award, the Yale College Fellowship for Research in Global Health Studies, and the Global Health Field Experiences Seed Funding Award. The corresponding author reported receiving funding from the Centers of Medicare and Medicaid Services to develop publicly reported quality measures. Another author reported receiving support from Health Action International and Alosa Health. No other disclosures were reported.
Source: Herkert D et al. JAMA Inter Med. 2018 Dec 3. doi: 10.1001/jamainternmed.2018.5008.