User login
Study: Stick with TMP-SMX for posttransplant PJP prophylaxis
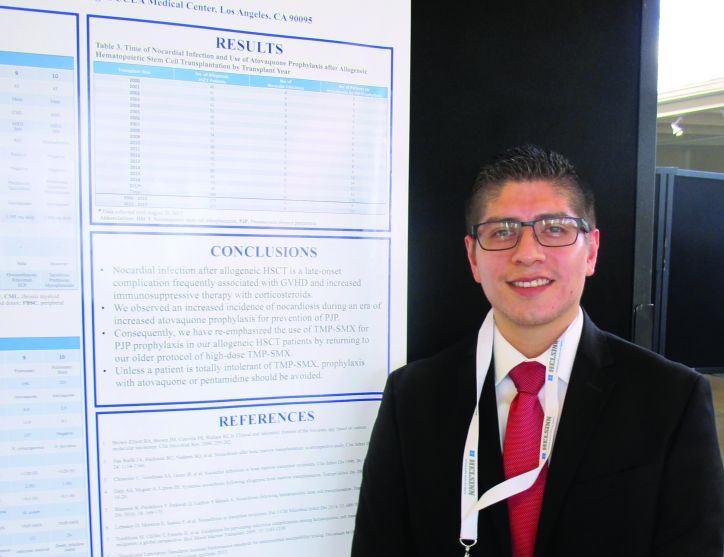
NEWPORT BEACH, CALIF. – Use of atovaquone or pentamidine for Pneumocystis jiroveci pneumonia (PJP) prophylaxis was associated with an increased incidence of nocardiosis in allogeneic hematopoietic stem call transplant (HSCT) recipients at the University of California, Los Angeles, according to a review of patient records.
Of 10 cases of late-onset nocardiosis identified among patients who received HSCT between Jan. 1, 2000, and Aug. 30, 2017, 9 cases occurred in 411 patients (2.2%) treated between 2012 and 2017 – a period of increased use of atovaquone prophylaxis, compared with only 1 in 575 patients (0.17%) treated in the prior 12 years when trimethoprim-sulfamethoxazole (TMP-SMX) was used for prophylaxis, Alfonso Molina reported in a poster at the Acute Leukemia Forum of Hemedicus.
None of the 575 patients treated between 2000 and 2012, versus 119 of the 411 treated after 2012, received atovaquone, he reported.
To assess the potential relationship between the use of atovaquone and the increased incidence of nocardiosis, he and his colleagues reviewed patient medical records and UCLA Clinical Microbiology Laboratory culture results.
Nocardiosis occurred mainly in patients on high doses of corticosteroids for graft-versus-host disease, and 8 of the 10 affected patients were not receiving TMP-SMX for PJP prophylaxis; 7 were on atovaquone, and 1 was on intravenous pentamidine, Mr. Molina said.
The findings suggest that TMP-SMX should remain the agent of choice for PJP prophylaxis in HSCT recipients and have prompted a return to the older protocol of high-dose TMP-SMX for this purpose at UCLA, he said.
“Unless a patient is totally intolerant of TMP-SMX, prophylaxis with atovaquone or pentamidine should be avoided,” he concluded.
Mr. Molina reported having no financial disclosures. The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Molina A et al., ALF 2018, Poster Session.
NEWPORT BEACH, CALIF. – Use of atovaquone or pentamidine for Pneumocystis jiroveci pneumonia (PJP) prophylaxis was associated with an increased incidence of nocardiosis in allogeneic hematopoietic stem call transplant (HSCT) recipients at the University of California, Los Angeles, according to a review of patient records.
Of 10 cases of late-onset nocardiosis identified among patients who received HSCT between Jan. 1, 2000, and Aug. 30, 2017, 9 cases occurred in 411 patients (2.2%) treated between 2012 and 2017 – a period of increased use of atovaquone prophylaxis, compared with only 1 in 575 patients (0.17%) treated in the prior 12 years when trimethoprim-sulfamethoxazole (TMP-SMX) was used for prophylaxis, Alfonso Molina reported in a poster at the Acute Leukemia Forum of Hemedicus.
None of the 575 patients treated between 2000 and 2012, versus 119 of the 411 treated after 2012, received atovaquone, he reported.
To assess the potential relationship between the use of atovaquone and the increased incidence of nocardiosis, he and his colleagues reviewed patient medical records and UCLA Clinical Microbiology Laboratory culture results.
Nocardiosis occurred mainly in patients on high doses of corticosteroids for graft-versus-host disease, and 8 of the 10 affected patients were not receiving TMP-SMX for PJP prophylaxis; 7 were on atovaquone, and 1 was on intravenous pentamidine, Mr. Molina said.
The findings suggest that TMP-SMX should remain the agent of choice for PJP prophylaxis in HSCT recipients and have prompted a return to the older protocol of high-dose TMP-SMX for this purpose at UCLA, he said.
“Unless a patient is totally intolerant of TMP-SMX, prophylaxis with atovaquone or pentamidine should be avoided,” he concluded.
Mr. Molina reported having no financial disclosures. The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Molina A et al., ALF 2018, Poster Session.
NEWPORT BEACH, CALIF. – Use of atovaquone or pentamidine for Pneumocystis jiroveci pneumonia (PJP) prophylaxis was associated with an increased incidence of nocardiosis in allogeneic hematopoietic stem call transplant (HSCT) recipients at the University of California, Los Angeles, according to a review of patient records.
Of 10 cases of late-onset nocardiosis identified among patients who received HSCT between Jan. 1, 2000, and Aug. 30, 2017, 9 cases occurred in 411 patients (2.2%) treated between 2012 and 2017 – a period of increased use of atovaquone prophylaxis, compared with only 1 in 575 patients (0.17%) treated in the prior 12 years when trimethoprim-sulfamethoxazole (TMP-SMX) was used for prophylaxis, Alfonso Molina reported in a poster at the Acute Leukemia Forum of Hemedicus.
None of the 575 patients treated between 2000 and 2012, versus 119 of the 411 treated after 2012, received atovaquone, he reported.
To assess the potential relationship between the use of atovaquone and the increased incidence of nocardiosis, he and his colleagues reviewed patient medical records and UCLA Clinical Microbiology Laboratory culture results.
Nocardiosis occurred mainly in patients on high doses of corticosteroids for graft-versus-host disease, and 8 of the 10 affected patients were not receiving TMP-SMX for PJP prophylaxis; 7 were on atovaquone, and 1 was on intravenous pentamidine, Mr. Molina said.
The findings suggest that TMP-SMX should remain the agent of choice for PJP prophylaxis in HSCT recipients and have prompted a return to the older protocol of high-dose TMP-SMX for this purpose at UCLA, he said.
“Unless a patient is totally intolerant of TMP-SMX, prophylaxis with atovaquone or pentamidine should be avoided,” he concluded.
Mr. Molina reported having no financial disclosures. The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Molina A et al., ALF 2018, Poster Session.
REPORTING FROM ALF 2018
Key clinical point:
Major finding: The incidence of nocardiosis was 2.2% during atovaquone use versus 0.17% prior to its use.
Study details: A retrospective review of records for 986 patients.
Disclosures: Mr. Molina reported having no financial disclosures.
Source: Molina A et al. ALF 2018, Poster Session.
VIDEO: Screening ECG patch boosts AF diagnoses ninefold
ORLANDO – An ECG patch worn twice for a total of about 24 days produced a nearly ninefold increase in the number of high-risk people diagnosed with atrial fibrillation, compared with those followed with usual care in a randomized trial with 2,655 people.
During 4 months of follow-up, 1,364 high-risk people assigned to ECG patch screening had a 5.1% rate of new atrial fibrillation (AF) diagnoses, compared with a 0.6% rate among 1,291 controls who wore the patch but were identified with new-onset AF using standard follow-up that did not take the patch data into account. This was a statistically significant difference for the study’s primary endpoint, Steven R. Steinhubl, MD, said at the annual meeting of the American College of Cardiology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
In addition to proving that the ECG patch can better identify asymptomatic people who have AF than conventional means – usually waiting until a stroke occurs or for symptoms to appear – the noninvasive and relatively low-cost patch also gives researchers a new way to try to address the more fundamental medical question created by this line of investigation: How clinically important are relatively brief, asymptomatic episodes of atrial fibrillation, and are patient outcomes improved by treatments begun in this early phase?
The study results “show we can look beyond implantable devices with a less expensive, noninvasive way” to identify patients with asymptomatic AF and determine its natural history and need for intervention, Dr. Steinhubl said in a video interview.
The mSToP (mHealth Screening to Prevent Strokes) trial ran at Scripps and began by identifying more than 359,000 U.S. residents with Aetna health insurance who met the study’s definition of having high AF risk, either by being at least 75 years old, or at least 55 years old and male or at least 65 years old and female. To qualify as high risk those younger than 75 years also had to have at least one clinical risk factor, which could include a prior cerebrovascular event, heart failure, hypertension plus diabetes, obstructive sleep apnea, or any of six other comorbidities. The researchers also excluded potential participants because of several factors, including a history of atrial fibrillation or flutter, current treatment with an anticoagulant, end-stage renal disease, and patients with an implanted pacemaker or defibrillator.
They invited more than 100,000 of these qualifying Aetna beneficiaries to participate, and 2,655 agreed and received by mail a pair of ECG measurement patches (Zio) with instructions to wear one for 2 weeks at the start of the study and to wear the second during the final 2 weeks of the 4-month study period. The participants averaged 73 years of age, and their average CHA2DS2-VASc score was 3.
All patients in the study were told to wear their patches and mail them in, but the researchers used the collected ECG data for diagnosing AF in only the 1,364 patients randomized to the active arm. The ECG findings for the 1,291 controls wasn’t provided to their physicians, and so any new-onset AF had to be found either by symptom onset or incidentally. About one-third of the people assigned to each of the study arms never wore their patches. Those who wore their patches did so for an average of nearly 12 days each. Diagnosis of new-onset AF was based on finding either at least one AF episode recorded by the patches that lasted at least 30 seconds or an AF diagnosis appearing in the patient’s record. The average AF burden – the percentage of time a person with incident AF had an abnormal sinus rhythm – was 0.9%.
Even though many patients did not use their patches, the investigators assessed the primary endpoint of new AF diagnoses during the 4-month study period on an intention-to-treat basis. Their analysis showed an 8.8-fold higher rate of new AF diagnoses among people in the intervention arm whose patch data were used for immediate diagnosis, reported Dr. Steinhubl, an interventional cardiologist and director of digital medicine at the Scripps Translational Science Institute in La Jolla, Ca.
As a secondary endpoint, the researchers merged the entire group of 1,738 participants who had sent in patches with ECG data and compared their 1-year incidence of diagnosed AF against 3,476 matched controls from the Aetna database. After 1 year, the rate of new AF diagnoses was 6.3% in those with patch information and 2.3% among the controls, a threefold difference in diagnosis rates after adjustment for potential confounders.
“The clinical significance of the short AF episodes” manifested by many patch users identified with AF “requires greater clarity, especially in terms of stroke risk,” Dr. Steinhubl said. But he added, “I like to think that, as we learn more, we can look at more than just anticoagulation” as intervention options. For example, if a morbidly obese patient has asymptomatic AF found by patch screening, it might strengthen the case for bariatric surgery if it’s eventually shown that weight loss after bariatric surgery slows AF progression. The same holds true for more aggressive sleep apnea intervention in patients with sleep apnea and asymptomatic AF, as well as for patients with asymptomatic AF and another type of associated comorbidity.
SOURCE: Steinhubl S. ACC 18, Abstract 402-19.
Results from several studies have now shown that some kind of monitoring for AF in asymptomatic, at-risk people results in an increased diagnosis of subclinical AF. Study results also suggest that, in general, people diagnosed with subclinical AF are at a lower risk of stroke than patients with symptomatic AF. As of now, no prospective study has evaluated the efficacy of anticoagulant therapy in people diagnosed with subclinical AF, although such studies are now in progress. Until we have these results, the question of how to manage patients with subclinical AF remains unanswered.
N.A. Mark Estes, MD , is professor of medicine and director of the New England Cardiac Arrhythmia Center at Tufts Medical Center in Boston. He has been a consultant to Boston Scientific, Medtronic, and St. Jude. He made these comments as designated discussant for the mSToPS report.
Results from several studies have now shown that some kind of monitoring for AF in asymptomatic, at-risk people results in an increased diagnosis of subclinical AF. Study results also suggest that, in general, people diagnosed with subclinical AF are at a lower risk of stroke than patients with symptomatic AF. As of now, no prospective study has evaluated the efficacy of anticoagulant therapy in people diagnosed with subclinical AF, although such studies are now in progress. Until we have these results, the question of how to manage patients with subclinical AF remains unanswered.
N.A. Mark Estes, MD , is professor of medicine and director of the New England Cardiac Arrhythmia Center at Tufts Medical Center in Boston. He has been a consultant to Boston Scientific, Medtronic, and St. Jude. He made these comments as designated discussant for the mSToPS report.
Results from several studies have now shown that some kind of monitoring for AF in asymptomatic, at-risk people results in an increased diagnosis of subclinical AF. Study results also suggest that, in general, people diagnosed with subclinical AF are at a lower risk of stroke than patients with symptomatic AF. As of now, no prospective study has evaluated the efficacy of anticoagulant therapy in people diagnosed with subclinical AF, although such studies are now in progress. Until we have these results, the question of how to manage patients with subclinical AF remains unanswered.
N.A. Mark Estes, MD , is professor of medicine and director of the New England Cardiac Arrhythmia Center at Tufts Medical Center in Boston. He has been a consultant to Boston Scientific, Medtronic, and St. Jude. He made these comments as designated discussant for the mSToPS report.
ORLANDO – An ECG patch worn twice for a total of about 24 days produced a nearly ninefold increase in the number of high-risk people diagnosed with atrial fibrillation, compared with those followed with usual care in a randomized trial with 2,655 people.
During 4 months of follow-up, 1,364 high-risk people assigned to ECG patch screening had a 5.1% rate of new atrial fibrillation (AF) diagnoses, compared with a 0.6% rate among 1,291 controls who wore the patch but were identified with new-onset AF using standard follow-up that did not take the patch data into account. This was a statistically significant difference for the study’s primary endpoint, Steven R. Steinhubl, MD, said at the annual meeting of the American College of Cardiology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
In addition to proving that the ECG patch can better identify asymptomatic people who have AF than conventional means – usually waiting until a stroke occurs or for symptoms to appear – the noninvasive and relatively low-cost patch also gives researchers a new way to try to address the more fundamental medical question created by this line of investigation: How clinically important are relatively brief, asymptomatic episodes of atrial fibrillation, and are patient outcomes improved by treatments begun in this early phase?
The study results “show we can look beyond implantable devices with a less expensive, noninvasive way” to identify patients with asymptomatic AF and determine its natural history and need for intervention, Dr. Steinhubl said in a video interview.
The mSToP (mHealth Screening to Prevent Strokes) trial ran at Scripps and began by identifying more than 359,000 U.S. residents with Aetna health insurance who met the study’s definition of having high AF risk, either by being at least 75 years old, or at least 55 years old and male or at least 65 years old and female. To qualify as high risk those younger than 75 years also had to have at least one clinical risk factor, which could include a prior cerebrovascular event, heart failure, hypertension plus diabetes, obstructive sleep apnea, or any of six other comorbidities. The researchers also excluded potential participants because of several factors, including a history of atrial fibrillation or flutter, current treatment with an anticoagulant, end-stage renal disease, and patients with an implanted pacemaker or defibrillator.
They invited more than 100,000 of these qualifying Aetna beneficiaries to participate, and 2,655 agreed and received by mail a pair of ECG measurement patches (Zio) with instructions to wear one for 2 weeks at the start of the study and to wear the second during the final 2 weeks of the 4-month study period. The participants averaged 73 years of age, and their average CHA2DS2-VASc score was 3.
All patients in the study were told to wear their patches and mail them in, but the researchers used the collected ECG data for diagnosing AF in only the 1,364 patients randomized to the active arm. The ECG findings for the 1,291 controls wasn’t provided to their physicians, and so any new-onset AF had to be found either by symptom onset or incidentally. About one-third of the people assigned to each of the study arms never wore their patches. Those who wore their patches did so for an average of nearly 12 days each. Diagnosis of new-onset AF was based on finding either at least one AF episode recorded by the patches that lasted at least 30 seconds or an AF diagnosis appearing in the patient’s record. The average AF burden – the percentage of time a person with incident AF had an abnormal sinus rhythm – was 0.9%.
Even though many patients did not use their patches, the investigators assessed the primary endpoint of new AF diagnoses during the 4-month study period on an intention-to-treat basis. Their analysis showed an 8.8-fold higher rate of new AF diagnoses among people in the intervention arm whose patch data were used for immediate diagnosis, reported Dr. Steinhubl, an interventional cardiologist and director of digital medicine at the Scripps Translational Science Institute in La Jolla, Ca.
As a secondary endpoint, the researchers merged the entire group of 1,738 participants who had sent in patches with ECG data and compared their 1-year incidence of diagnosed AF against 3,476 matched controls from the Aetna database. After 1 year, the rate of new AF diagnoses was 6.3% in those with patch information and 2.3% among the controls, a threefold difference in diagnosis rates after adjustment for potential confounders.
“The clinical significance of the short AF episodes” manifested by many patch users identified with AF “requires greater clarity, especially in terms of stroke risk,” Dr. Steinhubl said. But he added, “I like to think that, as we learn more, we can look at more than just anticoagulation” as intervention options. For example, if a morbidly obese patient has asymptomatic AF found by patch screening, it might strengthen the case for bariatric surgery if it’s eventually shown that weight loss after bariatric surgery slows AF progression. The same holds true for more aggressive sleep apnea intervention in patients with sleep apnea and asymptomatic AF, as well as for patients with asymptomatic AF and another type of associated comorbidity.
SOURCE: Steinhubl S. ACC 18, Abstract 402-19.
ORLANDO – An ECG patch worn twice for a total of about 24 days produced a nearly ninefold increase in the number of high-risk people diagnosed with atrial fibrillation, compared with those followed with usual care in a randomized trial with 2,655 people.
During 4 months of follow-up, 1,364 high-risk people assigned to ECG patch screening had a 5.1% rate of new atrial fibrillation (AF) diagnoses, compared with a 0.6% rate among 1,291 controls who wore the patch but were identified with new-onset AF using standard follow-up that did not take the patch data into account. This was a statistically significant difference for the study’s primary endpoint, Steven R. Steinhubl, MD, said at the annual meeting of the American College of Cardiology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
In addition to proving that the ECG patch can better identify asymptomatic people who have AF than conventional means – usually waiting until a stroke occurs or for symptoms to appear – the noninvasive and relatively low-cost patch also gives researchers a new way to try to address the more fundamental medical question created by this line of investigation: How clinically important are relatively brief, asymptomatic episodes of atrial fibrillation, and are patient outcomes improved by treatments begun in this early phase?
The study results “show we can look beyond implantable devices with a less expensive, noninvasive way” to identify patients with asymptomatic AF and determine its natural history and need for intervention, Dr. Steinhubl said in a video interview.
The mSToP (mHealth Screening to Prevent Strokes) trial ran at Scripps and began by identifying more than 359,000 U.S. residents with Aetna health insurance who met the study’s definition of having high AF risk, either by being at least 75 years old, or at least 55 years old and male or at least 65 years old and female. To qualify as high risk those younger than 75 years also had to have at least one clinical risk factor, which could include a prior cerebrovascular event, heart failure, hypertension plus diabetes, obstructive sleep apnea, or any of six other comorbidities. The researchers also excluded potential participants because of several factors, including a history of atrial fibrillation or flutter, current treatment with an anticoagulant, end-stage renal disease, and patients with an implanted pacemaker or defibrillator.
They invited more than 100,000 of these qualifying Aetna beneficiaries to participate, and 2,655 agreed and received by mail a pair of ECG measurement patches (Zio) with instructions to wear one for 2 weeks at the start of the study and to wear the second during the final 2 weeks of the 4-month study period. The participants averaged 73 years of age, and their average CHA2DS2-VASc score was 3.
All patients in the study were told to wear their patches and mail them in, but the researchers used the collected ECG data for diagnosing AF in only the 1,364 patients randomized to the active arm. The ECG findings for the 1,291 controls wasn’t provided to their physicians, and so any new-onset AF had to be found either by symptom onset or incidentally. About one-third of the people assigned to each of the study arms never wore their patches. Those who wore their patches did so for an average of nearly 12 days each. Diagnosis of new-onset AF was based on finding either at least one AF episode recorded by the patches that lasted at least 30 seconds or an AF diagnosis appearing in the patient’s record. The average AF burden – the percentage of time a person with incident AF had an abnormal sinus rhythm – was 0.9%.
Even though many patients did not use their patches, the investigators assessed the primary endpoint of new AF diagnoses during the 4-month study period on an intention-to-treat basis. Their analysis showed an 8.8-fold higher rate of new AF diagnoses among people in the intervention arm whose patch data were used for immediate diagnosis, reported Dr. Steinhubl, an interventional cardiologist and director of digital medicine at the Scripps Translational Science Institute in La Jolla, Ca.
As a secondary endpoint, the researchers merged the entire group of 1,738 participants who had sent in patches with ECG data and compared their 1-year incidence of diagnosed AF against 3,476 matched controls from the Aetna database. After 1 year, the rate of new AF diagnoses was 6.3% in those with patch information and 2.3% among the controls, a threefold difference in diagnosis rates after adjustment for potential confounders.
“The clinical significance of the short AF episodes” manifested by many patch users identified with AF “requires greater clarity, especially in terms of stroke risk,” Dr. Steinhubl said. But he added, “I like to think that, as we learn more, we can look at more than just anticoagulation” as intervention options. For example, if a morbidly obese patient has asymptomatic AF found by patch screening, it might strengthen the case for bariatric surgery if it’s eventually shown that weight loss after bariatric surgery slows AF progression. The same holds true for more aggressive sleep apnea intervention in patients with sleep apnea and asymptomatic AF, as well as for patients with asymptomatic AF and another type of associated comorbidity.
SOURCE: Steinhubl S. ACC 18, Abstract 402-19.
REPORTING FROM ACC 18
Key clinical point: .
Major finding: After 4 months, new AF diagnoses occurred in 5.1% of patch users and 0.6% of usual-care controls.
Study details: mSToPS, a single-center, randomized study with 2,655 people at high risk for developing AF.
Disclosures: mSToPS received support from Aetna, Janssen, and iRhythm. Dr. Steinhubl has been an advisor to Airstrip, DynoSense, EasyG, FocusMotion, LifeWatch, MyoKardia, Novartis, and Spry Health, he serves on the board of Celes Health, and he has received research support from Janssen and Novartis.
Source: Steinhubl S. ACC 18, Abstract 402-19.
Erenumab found beneficial to migraine patients with unsuccessful preventive treatment history
Results from the phase 3b LIBERTY trial of the investigational migraine-prevention drug erenumab indicate its potential effectiveness in patients with episodic migraine attacks who have unsuccessfully tried other migraine-prevention drugs to reduce the frequency of migraine days.
Erenumab, a fully human monoclonal antibody that is designed to block the calcitonin gene-related peptide (CGRP) receptor, reduced the average number of monthly migraine headaches by half or more for 30% of study participants, which is a level of improvement that “can greatly improve a person’s quality of life,” first author Uwe Reuter, MD, of Charité–University Medicine Berlin said in a press release. Dr. Reuter will present the full results of the study during the Emerging Science Platform Session at the annual meeting of the American Academy of Neurology in Los Angeles on April 24.
At 3 months, patients treated with erenumab significantly more often met the study’s primary endpoint of the proportion of patients achieving a 50% or greater reduction in mean monthly migraine days (MMDs) during weeks 9-12: At week 12, 30% on erenumab vs. 14% on placebo (odds ratio, 2.73; 95% confidence interval, 1.43-5.19) met the endpoint.
Those treated with erenumab also had a greater average reduction in MMDs in several secondary endpoints. For those on erenumab, there was an overall mean difference of –1.61 MMDs, compared with placebo. Erenumab-treated patients also had an overall mean difference of –1.73 acute medication days, compared with placebo.
The authors reported that erenumab had safety and tolerability comparable to placebo, and none of the patients taking erenumab discontinued because of adverse events.
Dr. Reuter cautioned that additional studies will need to be conducted to determine if the effects last longer than 3 months and to identify patients most likely to respond.
The study was funded by Novartis, which is developing erenumab.
SOURCE: Reuter E et al. AAN 2018, Emerging Science Abstract 009.
Results from the phase 3b LIBERTY trial of the investigational migraine-prevention drug erenumab indicate its potential effectiveness in patients with episodic migraine attacks who have unsuccessfully tried other migraine-prevention drugs to reduce the frequency of migraine days.
Erenumab, a fully human monoclonal antibody that is designed to block the calcitonin gene-related peptide (CGRP) receptor, reduced the average number of monthly migraine headaches by half or more for 30% of study participants, which is a level of improvement that “can greatly improve a person’s quality of life,” first author Uwe Reuter, MD, of Charité–University Medicine Berlin said in a press release. Dr. Reuter will present the full results of the study during the Emerging Science Platform Session at the annual meeting of the American Academy of Neurology in Los Angeles on April 24.
At 3 months, patients treated with erenumab significantly more often met the study’s primary endpoint of the proportion of patients achieving a 50% or greater reduction in mean monthly migraine days (MMDs) during weeks 9-12: At week 12, 30% on erenumab vs. 14% on placebo (odds ratio, 2.73; 95% confidence interval, 1.43-5.19) met the endpoint.
Those treated with erenumab also had a greater average reduction in MMDs in several secondary endpoints. For those on erenumab, there was an overall mean difference of –1.61 MMDs, compared with placebo. Erenumab-treated patients also had an overall mean difference of –1.73 acute medication days, compared with placebo.
The authors reported that erenumab had safety and tolerability comparable to placebo, and none of the patients taking erenumab discontinued because of adverse events.
Dr. Reuter cautioned that additional studies will need to be conducted to determine if the effects last longer than 3 months and to identify patients most likely to respond.
The study was funded by Novartis, which is developing erenumab.
SOURCE: Reuter E et al. AAN 2018, Emerging Science Abstract 009.
Results from the phase 3b LIBERTY trial of the investigational migraine-prevention drug erenumab indicate its potential effectiveness in patients with episodic migraine attacks who have unsuccessfully tried other migraine-prevention drugs to reduce the frequency of migraine days.
Erenumab, a fully human monoclonal antibody that is designed to block the calcitonin gene-related peptide (CGRP) receptor, reduced the average number of monthly migraine headaches by half or more for 30% of study participants, which is a level of improvement that “can greatly improve a person’s quality of life,” first author Uwe Reuter, MD, of Charité–University Medicine Berlin said in a press release. Dr. Reuter will present the full results of the study during the Emerging Science Platform Session at the annual meeting of the American Academy of Neurology in Los Angeles on April 24.
At 3 months, patients treated with erenumab significantly more often met the study’s primary endpoint of the proportion of patients achieving a 50% or greater reduction in mean monthly migraine days (MMDs) during weeks 9-12: At week 12, 30% on erenumab vs. 14% on placebo (odds ratio, 2.73; 95% confidence interval, 1.43-5.19) met the endpoint.
Those treated with erenumab also had a greater average reduction in MMDs in several secondary endpoints. For those on erenumab, there was an overall mean difference of –1.61 MMDs, compared with placebo. Erenumab-treated patients also had an overall mean difference of –1.73 acute medication days, compared with placebo.
The authors reported that erenumab had safety and tolerability comparable to placebo, and none of the patients taking erenumab discontinued because of adverse events.
Dr. Reuter cautioned that additional studies will need to be conducted to determine if the effects last longer than 3 months and to identify patients most likely to respond.
The study was funded by Novartis, which is developing erenumab.
SOURCE: Reuter E et al. AAN 2018, Emerging Science Abstract 009.
FROM AAN 2018
Key clinical point:
Major finding: Patients treated with erenumab significantly more often achieved a 50% or greater reduction in mean monthly migraine days during weeks 9-12: At week 12, 30% with erenumab vs. 14% with placebo met the endpoint.
Study details: A 12-week, double-blind study of 246 patients with episodic migraine randomized to receive erenumab 140 mg or placebo.
Disclosures: The study was funded by Novartis, which is developing erenumab.
Source: Reuter E et al. AAN 2018, Emerging Science Abstract 009.
Statin plus chemo yields encouraging results in poor-risk AML
Patients with poor-risk acute myelogenous leukemia (AML) had promising rates of response and survival following treatment with a statin added to standard chemotherapy, researchers reported.
Pravastatin in combination with idarubicin and cytarabine had a 30% response rate in poor-risk AML patients, according to Anjali S. Advani, MD, of the Taussig Cancer Institute at the Cleveland Clinic, and her coauthors.
Although that response rate did not meet a prespecified threshold for statistical significance, results of the phase 2 study were nevertheless “encouraging” for a group of patients with unfavorable cytogenetics and poor-risk molecular mutations, the researchers wrote. The study was published in Leukemia Research.
The estimated median overall survival was 4.1 months in the phase 2 trial, known as SWOG S0919. About one-quarter of the patients were able to proceed to allogeneic hematopoietic stem cell transplant, and for that group, median overall survival was 27.1 months.
These findings appear to provide further support for the hypothesis that targeting the cholesterol pathway may be a promising approach in patients with AML.
Some previous investigations suggested that AML blasts overexpress genes for lipoprotein receptors and regulatory enzymes, while others showed that these cells import and synthesize cholesterol at levels higher than what is seen in normal progenitor cells. In addition, some AML patients have hypocholesterolemia that usually resolves when they achieve a complete remission.
“These observations suggest that AML cells may require high levels of cholesterol for their survival and that abnormalities in cholesterol homeostasis are necessary for AML cell survival,” the researchers wrote.
This led to a phase 1 trial of pravastatin plus idarubicin/cytarabine, followed by the phase 2 SWOG S0919 trial, which demonstrated a 75% rate of complete response (CR) or complete response with incomplete count recovery (CRi) for the regimen.
The SWOG S0919 study was amended to include the poor-risk AML patients described in the present study. That cohort of 46 patients had a CR/CRi of less than 6 months after their last induction regimen or refractory disease. Many had poor-risk cytogenetics (43%) or one of a number of poor-risk mutations, according to the study report.
Pravastatin, in addition to working on the cholesterol pathway in AML, may also have a therapeutic advantage in patients with FLT3 mutations. Three out of six patients with FLT3 mutations achieved CR/CRi, corroborating earlier preclinical studies and suggesting further study of this specific patient population would be worthwhile, the researchers noted.
The study was supported in part by the National Institutes of Health and Bristol-Myers Squibb. Dr. Advani reported having no financial disclosures but other study authors reported relationships with various pharmaceutical companies.
SOURCE: Advani AS et al. Leuk Res. 2018 Apr;67:17-20.
Patients with poor-risk acute myelogenous leukemia (AML) had promising rates of response and survival following treatment with a statin added to standard chemotherapy, researchers reported.
Pravastatin in combination with idarubicin and cytarabine had a 30% response rate in poor-risk AML patients, according to Anjali S. Advani, MD, of the Taussig Cancer Institute at the Cleveland Clinic, and her coauthors.
Although that response rate did not meet a prespecified threshold for statistical significance, results of the phase 2 study were nevertheless “encouraging” for a group of patients with unfavorable cytogenetics and poor-risk molecular mutations, the researchers wrote. The study was published in Leukemia Research.
The estimated median overall survival was 4.1 months in the phase 2 trial, known as SWOG S0919. About one-quarter of the patients were able to proceed to allogeneic hematopoietic stem cell transplant, and for that group, median overall survival was 27.1 months.
These findings appear to provide further support for the hypothesis that targeting the cholesterol pathway may be a promising approach in patients with AML.
Some previous investigations suggested that AML blasts overexpress genes for lipoprotein receptors and regulatory enzymes, while others showed that these cells import and synthesize cholesterol at levels higher than what is seen in normal progenitor cells. In addition, some AML patients have hypocholesterolemia that usually resolves when they achieve a complete remission.
“These observations suggest that AML cells may require high levels of cholesterol for their survival and that abnormalities in cholesterol homeostasis are necessary for AML cell survival,” the researchers wrote.
This led to a phase 1 trial of pravastatin plus idarubicin/cytarabine, followed by the phase 2 SWOG S0919 trial, which demonstrated a 75% rate of complete response (CR) or complete response with incomplete count recovery (CRi) for the regimen.
The SWOG S0919 study was amended to include the poor-risk AML patients described in the present study. That cohort of 46 patients had a CR/CRi of less than 6 months after their last induction regimen or refractory disease. Many had poor-risk cytogenetics (43%) or one of a number of poor-risk mutations, according to the study report.
Pravastatin, in addition to working on the cholesterol pathway in AML, may also have a therapeutic advantage in patients with FLT3 mutations. Three out of six patients with FLT3 mutations achieved CR/CRi, corroborating earlier preclinical studies and suggesting further study of this specific patient population would be worthwhile, the researchers noted.
The study was supported in part by the National Institutes of Health and Bristol-Myers Squibb. Dr. Advani reported having no financial disclosures but other study authors reported relationships with various pharmaceutical companies.
SOURCE: Advani AS et al. Leuk Res. 2018 Apr;67:17-20.
Patients with poor-risk acute myelogenous leukemia (AML) had promising rates of response and survival following treatment with a statin added to standard chemotherapy, researchers reported.
Pravastatin in combination with idarubicin and cytarabine had a 30% response rate in poor-risk AML patients, according to Anjali S. Advani, MD, of the Taussig Cancer Institute at the Cleveland Clinic, and her coauthors.
Although that response rate did not meet a prespecified threshold for statistical significance, results of the phase 2 study were nevertheless “encouraging” for a group of patients with unfavorable cytogenetics and poor-risk molecular mutations, the researchers wrote. The study was published in Leukemia Research.
The estimated median overall survival was 4.1 months in the phase 2 trial, known as SWOG S0919. About one-quarter of the patients were able to proceed to allogeneic hematopoietic stem cell transplant, and for that group, median overall survival was 27.1 months.
These findings appear to provide further support for the hypothesis that targeting the cholesterol pathway may be a promising approach in patients with AML.
Some previous investigations suggested that AML blasts overexpress genes for lipoprotein receptors and regulatory enzymes, while others showed that these cells import and synthesize cholesterol at levels higher than what is seen in normal progenitor cells. In addition, some AML patients have hypocholesterolemia that usually resolves when they achieve a complete remission.
“These observations suggest that AML cells may require high levels of cholesterol for their survival and that abnormalities in cholesterol homeostasis are necessary for AML cell survival,” the researchers wrote.
This led to a phase 1 trial of pravastatin plus idarubicin/cytarabine, followed by the phase 2 SWOG S0919 trial, which demonstrated a 75% rate of complete response (CR) or complete response with incomplete count recovery (CRi) for the regimen.
The SWOG S0919 study was amended to include the poor-risk AML patients described in the present study. That cohort of 46 patients had a CR/CRi of less than 6 months after their last induction regimen or refractory disease. Many had poor-risk cytogenetics (43%) or one of a number of poor-risk mutations, according to the study report.
Pravastatin, in addition to working on the cholesterol pathway in AML, may also have a therapeutic advantage in patients with FLT3 mutations. Three out of six patients with FLT3 mutations achieved CR/CRi, corroborating earlier preclinical studies and suggesting further study of this specific patient population would be worthwhile, the researchers noted.
The study was supported in part by the National Institutes of Health and Bristol-Myers Squibb. Dr. Advani reported having no financial disclosures but other study authors reported relationships with various pharmaceutical companies.
SOURCE: Advani AS et al. Leuk Res. 2018 Apr;67:17-20.
FROM LEUKEMIA RESEARCH
Key clinical point:
Major finding: Pravastatin in combination with idarubicin and cytarabine had a 30% response rate in poor risk AML patients.
Study details: Results from the poor-risk cohort (n = 46) in SWOG S0919, a phase 2 study.
Disclosures: The research was supported in part by the National Institutes of Health and Bristol-Myers Squibb. Dr. Advani reported having no financial disclosures but other study authors reported relationships with various pharmaceutical companies.
Source: Advani AS et al. Leuk Res. 2018 Apr;67:17-20.
Do hospitalists improve inpatient outcomes?
Long continues the debate on what impact hospitalists have on inpatient outcomes. This issue has been playing out in the medical literature for 20 years, since the coining of the term in 1997. In a recent iteration of the debate, a study was published in JAMA Internal Medicine entitled “Comparison of Hospital Resource Use and Outcomes Among Hospitalists, Primary Care Physicians, and Other Generalists.”
The study retrospectively evaluated health care resources and outcomes from over a half-million Medicare beneficiaries hospitalized in 2013 for 20 common diagnosis-related groups, by type of physician provider (hospitalist, their primary care physician, or other generalist). The study found that nonhospitalists used more consultations and had longer lengths of stays, compared with hospitalists. In addition, relative to hospitalists, PCPs were more likely to discharge patients to home, had similar readmission rates, and lower 30-day mortality rates, but generalists were less likely to discharge patients home, had higher readmission rates, and higher mortality rates.
As hospitalists, we need to understand and acknowledge that most of our patients are “brand new” to us, and it is paramount that we use all available resources to gain a deep understanding of the patient in as short a time as possible. For example, ensuring all medical records available are reviewed, at least as much as possible, including a medical list (including a medication reconciliation). Interviewing family members or caregivers is also obviously a “best practice.” As well, having the insight of the PCP in these patients’ care is unquestionably good for us, for the PCP, and for the patient.
With good communication processes and an eye for excellence in care transitions, hospitalists can and should achieve the best outcomes for all of their patients. I look forward to more research in this arena, including a better understanding of the mechanisms by which we can all reliably produce excellent outcomes for the patients we serve.
Read the full post at hospitalleader.org.
Also on The Hospital Leader …
• Locums vs. F/T Hospitalists: Do Temps Stack Up? by Brad Flansbaum, DO, MPH, MHM
• Rounds: Are We Spinning Our Wheels? by Vineet Arora, MD, MPP, MHM
• Up Your Game in APP Integration by Tracy Cardin, ACNP-BC, SFHM
Long continues the debate on what impact hospitalists have on inpatient outcomes. This issue has been playing out in the medical literature for 20 years, since the coining of the term in 1997. In a recent iteration of the debate, a study was published in JAMA Internal Medicine entitled “Comparison of Hospital Resource Use and Outcomes Among Hospitalists, Primary Care Physicians, and Other Generalists.”
The study retrospectively evaluated health care resources and outcomes from over a half-million Medicare beneficiaries hospitalized in 2013 for 20 common diagnosis-related groups, by type of physician provider (hospitalist, their primary care physician, or other generalist). The study found that nonhospitalists used more consultations and had longer lengths of stays, compared with hospitalists. In addition, relative to hospitalists, PCPs were more likely to discharge patients to home, had similar readmission rates, and lower 30-day mortality rates, but generalists were less likely to discharge patients home, had higher readmission rates, and higher mortality rates.
As hospitalists, we need to understand and acknowledge that most of our patients are “brand new” to us, and it is paramount that we use all available resources to gain a deep understanding of the patient in as short a time as possible. For example, ensuring all medical records available are reviewed, at least as much as possible, including a medical list (including a medication reconciliation). Interviewing family members or caregivers is also obviously a “best practice.” As well, having the insight of the PCP in these patients’ care is unquestionably good for us, for the PCP, and for the patient.
With good communication processes and an eye for excellence in care transitions, hospitalists can and should achieve the best outcomes for all of their patients. I look forward to more research in this arena, including a better understanding of the mechanisms by which we can all reliably produce excellent outcomes for the patients we serve.
Read the full post at hospitalleader.org.
Also on The Hospital Leader …
• Locums vs. F/T Hospitalists: Do Temps Stack Up? by Brad Flansbaum, DO, MPH, MHM
• Rounds: Are We Spinning Our Wheels? by Vineet Arora, MD, MPP, MHM
• Up Your Game in APP Integration by Tracy Cardin, ACNP-BC, SFHM
Long continues the debate on what impact hospitalists have on inpatient outcomes. This issue has been playing out in the medical literature for 20 years, since the coining of the term in 1997. In a recent iteration of the debate, a study was published in JAMA Internal Medicine entitled “Comparison of Hospital Resource Use and Outcomes Among Hospitalists, Primary Care Physicians, and Other Generalists.”
The study retrospectively evaluated health care resources and outcomes from over a half-million Medicare beneficiaries hospitalized in 2013 for 20 common diagnosis-related groups, by type of physician provider (hospitalist, their primary care physician, or other generalist). The study found that nonhospitalists used more consultations and had longer lengths of stays, compared with hospitalists. In addition, relative to hospitalists, PCPs were more likely to discharge patients to home, had similar readmission rates, and lower 30-day mortality rates, but generalists were less likely to discharge patients home, had higher readmission rates, and higher mortality rates.
As hospitalists, we need to understand and acknowledge that most of our patients are “brand new” to us, and it is paramount that we use all available resources to gain a deep understanding of the patient in as short a time as possible. For example, ensuring all medical records available are reviewed, at least as much as possible, including a medical list (including a medication reconciliation). Interviewing family members or caregivers is also obviously a “best practice.” As well, having the insight of the PCP in these patients’ care is unquestionably good for us, for the PCP, and for the patient.
With good communication processes and an eye for excellence in care transitions, hospitalists can and should achieve the best outcomes for all of their patients. I look forward to more research in this arena, including a better understanding of the mechanisms by which we can all reliably produce excellent outcomes for the patients we serve.
Read the full post at hospitalleader.org.
Also on The Hospital Leader …
• Locums vs. F/T Hospitalists: Do Temps Stack Up? by Brad Flansbaum, DO, MPH, MHM
• Rounds: Are We Spinning Our Wheels? by Vineet Arora, MD, MPP, MHM
• Up Your Game in APP Integration by Tracy Cardin, ACNP-BC, SFHM
Skin rollers
, but only a few actually have any scientific data or clinical studies supporting their claims. In general, these rollers promise to increase collagen, depuff the skin, lift and firm, increase circulation, increase oxygenation, and decrease inflammation. But no clinically significant results have been reported with most of these over-the-counter devices. Furthermore, not every roller is meant for every skin type – and some should stay within the hands of an experienced professional.
Ice rollers have been used for many years and are very effective to cool the skin for in-office procedures. They are drum-shaped stainless steel rollers that are left in the freezer and cool the epidermis upon application. At-home ice rollers cause immediate vasoconstriction and are a quick fix for periorbital edema or skin erythema. Three-dimensional roller face massagers are simply a massage tool and can be used on any skin type to increase facial circulation; they do not provide any visible clinical benefits. Nanocurrent or vibrating rollers use nanocurrents and vibration alongside a conductor gel to glide across the skin; they massage the skin and help topically applied agents penetrate into the stratum corneum.
Dr. Talakoub and Dr. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Orentreich DS et al. Dermatol Surg. 1995;21(6):543-9.
Aust MC et al. Plast Reconstr Surg. 2008;21(4):1421-9.Fernandes D et al. Clin Dermatol. 2008 Mar-Apr;26(2):192-9.
Nair PA et al. GMJ. 2014;69:24-7.
, but only a few actually have any scientific data or clinical studies supporting their claims. In general, these rollers promise to increase collagen, depuff the skin, lift and firm, increase circulation, increase oxygenation, and decrease inflammation. But no clinically significant results have been reported with most of these over-the-counter devices. Furthermore, not every roller is meant for every skin type – and some should stay within the hands of an experienced professional.
Ice rollers have been used for many years and are very effective to cool the skin for in-office procedures. They are drum-shaped stainless steel rollers that are left in the freezer and cool the epidermis upon application. At-home ice rollers cause immediate vasoconstriction and are a quick fix for periorbital edema or skin erythema. Three-dimensional roller face massagers are simply a massage tool and can be used on any skin type to increase facial circulation; they do not provide any visible clinical benefits. Nanocurrent or vibrating rollers use nanocurrents and vibration alongside a conductor gel to glide across the skin; they massage the skin and help topically applied agents penetrate into the stratum corneum.
Dr. Talakoub and Dr. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Orentreich DS et al. Dermatol Surg. 1995;21(6):543-9.
Aust MC et al. Plast Reconstr Surg. 2008;21(4):1421-9.Fernandes D et al. Clin Dermatol. 2008 Mar-Apr;26(2):192-9.
Nair PA et al. GMJ. 2014;69:24-7.
, but only a few actually have any scientific data or clinical studies supporting their claims. In general, these rollers promise to increase collagen, depuff the skin, lift and firm, increase circulation, increase oxygenation, and decrease inflammation. But no clinically significant results have been reported with most of these over-the-counter devices. Furthermore, not every roller is meant for every skin type – and some should stay within the hands of an experienced professional.
Ice rollers have been used for many years and are very effective to cool the skin for in-office procedures. They are drum-shaped stainless steel rollers that are left in the freezer and cool the epidermis upon application. At-home ice rollers cause immediate vasoconstriction and are a quick fix for periorbital edema or skin erythema. Three-dimensional roller face massagers are simply a massage tool and can be used on any skin type to increase facial circulation; they do not provide any visible clinical benefits. Nanocurrent or vibrating rollers use nanocurrents and vibration alongside a conductor gel to glide across the skin; they massage the skin and help topically applied agents penetrate into the stratum corneum.
Dr. Talakoub and Dr. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Orentreich DS et al. Dermatol Surg. 1995;21(6):543-9.
Aust MC et al. Plast Reconstr Surg. 2008;21(4):1421-9.Fernandes D et al. Clin Dermatol. 2008 Mar-Apr;26(2):192-9.
Nair PA et al. GMJ. 2014;69:24-7.
‘Fast food swamps’ linked to type 1 diabetes
Areas with a high density of fast food outlets are associated with a greater prevalence of type 1 diabetes but not type 2 diabetes, according to new research.
These findings come from an analysis of emergency claims data for 5 million adults and 1.6 million children in New York who visited an emergency department at least once during 2009-2013. Researchers also looked at sociodemographic data for the area from community surveys and used local authorities’ inspection data to characterize local restaurant and retail food environments.
But when the analysis was adjusted to account for a range of factors, including age, sex, ethnicity, household income, and employment rates, the association between fast food swamps and diabetes was significant for pediatric type 1 diabetes only.
“Given the rising prevalence of type 1 diabetes, there has been increasing belief that certain environmental influences are contributing sharply to these increases,” wrote David C. Lee, MD, New York University Langone Health, and his coauthors. “There is some emerging literature which suggests that pregnant women in adverse food environments may have a higher likelihood of gestational diabetes, which some believe may affect health outcomes in their offspring.”
The study also failed to find an influence of retail food swamps – areas with more bodegas or small convenience stores within a 1-mile radius – on the prevalence of either type 1 or type 2 diabetes, in either adults or children. When researchers extended this to a 2-mile radius, they did find a significantly higher prevalence of pediatric type 1 diabetes associated with retail food swamps but a significantly lower prevalence of adult type 1 diabetes.
“This result may suggest that the retail food environment does not have a strong association with local diabetes prevalence or may be due to how we measured the retail food environment,” they wrote.
In general, the study found that the prevalence of adult and pediatric type 1 diabetes was significantly lower in most black neighborhoods, while the prevalence of adult type 1 diabetes was significantly lower in most Hispanic neighborhoods. Higher-income neighborhoods showed a significantly higher prevalence of pediatric type 1 diabetes.
The prevalence of type 2 diabetes in adults was significantly higher in low-income neighborhoods and those with more elderly residents, while the highest rates of pediatric type 2 diabetes were found in black neighborhoods.
The authors commented that they were surprised that their data did not show a higher prevalence of adult type 2 diabetes in black neighborhoods.
“In our multivariate analysis, older age and lower income were the only demographic or socioeconomic factors associated with higher adult type 2 diabetes prevalence,” they wrote.
Their use of ED surveillance data may have skewed the findings toward individuals more likely to visit those departments, namely Medicaid patients. But they suggested this would be balanced by the fact that the analysis was based on small geographic areas.
“Overall, our results may suggest that the physical food environment may not play as strong a role in characterizing the risk of type 2 diabetes among children and that other factors such as genetics, health behaviors, environmental exposures, or family influences may play more important roles.”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the Juvenile Diabetes Research Foundation. No conflicts of interest were declared.
SOURCE: Lee DC et al. J Endocr Soc. 2018. Apr 17. doi: 10.1210/js.2018-00001.
Areas with a high density of fast food outlets are associated with a greater prevalence of type 1 diabetes but not type 2 diabetes, according to new research.
These findings come from an analysis of emergency claims data for 5 million adults and 1.6 million children in New York who visited an emergency department at least once during 2009-2013. Researchers also looked at sociodemographic data for the area from community surveys and used local authorities’ inspection data to characterize local restaurant and retail food environments.
But when the analysis was adjusted to account for a range of factors, including age, sex, ethnicity, household income, and employment rates, the association between fast food swamps and diabetes was significant for pediatric type 1 diabetes only.
“Given the rising prevalence of type 1 diabetes, there has been increasing belief that certain environmental influences are contributing sharply to these increases,” wrote David C. Lee, MD, New York University Langone Health, and his coauthors. “There is some emerging literature which suggests that pregnant women in adverse food environments may have a higher likelihood of gestational diabetes, which some believe may affect health outcomes in their offspring.”
The study also failed to find an influence of retail food swamps – areas with more bodegas or small convenience stores within a 1-mile radius – on the prevalence of either type 1 or type 2 diabetes, in either adults or children. When researchers extended this to a 2-mile radius, they did find a significantly higher prevalence of pediatric type 1 diabetes associated with retail food swamps but a significantly lower prevalence of adult type 1 diabetes.
“This result may suggest that the retail food environment does not have a strong association with local diabetes prevalence or may be due to how we measured the retail food environment,” they wrote.
In general, the study found that the prevalence of adult and pediatric type 1 diabetes was significantly lower in most black neighborhoods, while the prevalence of adult type 1 diabetes was significantly lower in most Hispanic neighborhoods. Higher-income neighborhoods showed a significantly higher prevalence of pediatric type 1 diabetes.
The prevalence of type 2 diabetes in adults was significantly higher in low-income neighborhoods and those with more elderly residents, while the highest rates of pediatric type 2 diabetes were found in black neighborhoods.
The authors commented that they were surprised that their data did not show a higher prevalence of adult type 2 diabetes in black neighborhoods.
“In our multivariate analysis, older age and lower income were the only demographic or socioeconomic factors associated with higher adult type 2 diabetes prevalence,” they wrote.
Their use of ED surveillance data may have skewed the findings toward individuals more likely to visit those departments, namely Medicaid patients. But they suggested this would be balanced by the fact that the analysis was based on small geographic areas.
“Overall, our results may suggest that the physical food environment may not play as strong a role in characterizing the risk of type 2 diabetes among children and that other factors such as genetics, health behaviors, environmental exposures, or family influences may play more important roles.”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the Juvenile Diabetes Research Foundation. No conflicts of interest were declared.
SOURCE: Lee DC et al. J Endocr Soc. 2018. Apr 17. doi: 10.1210/js.2018-00001.
Areas with a high density of fast food outlets are associated with a greater prevalence of type 1 diabetes but not type 2 diabetes, according to new research.
These findings come from an analysis of emergency claims data for 5 million adults and 1.6 million children in New York who visited an emergency department at least once during 2009-2013. Researchers also looked at sociodemographic data for the area from community surveys and used local authorities’ inspection data to characterize local restaurant and retail food environments.
But when the analysis was adjusted to account for a range of factors, including age, sex, ethnicity, household income, and employment rates, the association between fast food swamps and diabetes was significant for pediatric type 1 diabetes only.
“Given the rising prevalence of type 1 diabetes, there has been increasing belief that certain environmental influences are contributing sharply to these increases,” wrote David C. Lee, MD, New York University Langone Health, and his coauthors. “There is some emerging literature which suggests that pregnant women in adverse food environments may have a higher likelihood of gestational diabetes, which some believe may affect health outcomes in their offspring.”
The study also failed to find an influence of retail food swamps – areas with more bodegas or small convenience stores within a 1-mile radius – on the prevalence of either type 1 or type 2 diabetes, in either adults or children. When researchers extended this to a 2-mile radius, they did find a significantly higher prevalence of pediatric type 1 diabetes associated with retail food swamps but a significantly lower prevalence of adult type 1 diabetes.
“This result may suggest that the retail food environment does not have a strong association with local diabetes prevalence or may be due to how we measured the retail food environment,” they wrote.
In general, the study found that the prevalence of adult and pediatric type 1 diabetes was significantly lower in most black neighborhoods, while the prevalence of adult type 1 diabetes was significantly lower in most Hispanic neighborhoods. Higher-income neighborhoods showed a significantly higher prevalence of pediatric type 1 diabetes.
The prevalence of type 2 diabetes in adults was significantly higher in low-income neighborhoods and those with more elderly residents, while the highest rates of pediatric type 2 diabetes were found in black neighborhoods.
The authors commented that they were surprised that their data did not show a higher prevalence of adult type 2 diabetes in black neighborhoods.
“In our multivariate analysis, older age and lower income were the only demographic or socioeconomic factors associated with higher adult type 2 diabetes prevalence,” they wrote.
Their use of ED surveillance data may have skewed the findings toward individuals more likely to visit those departments, namely Medicaid patients. But they suggested this would be balanced by the fact that the analysis was based on small geographic areas.
“Overall, our results may suggest that the physical food environment may not play as strong a role in characterizing the risk of type 2 diabetes among children and that other factors such as genetics, health behaviors, environmental exposures, or family influences may play more important roles.”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the Juvenile Diabetes Research Foundation. No conflicts of interest were declared.
SOURCE: Lee DC et al. J Endocr Soc. 2018. Apr 17. doi: 10.1210/js.2018-00001.
FROM JOURNAL OF THE ENDOCRINE SOCIETY
Key clinical point: Neighborhoods with higher numbers of fast food restaurants are linked to a higher prevalence of type 1, not type 2, diabetes.
Major finding: Fast food swamps are associated with a higher prevalence of pediatric type 1 diabetes.
Study details: Retrospective analysis of emergency claims data for 5 million adults and 1.6 million children.
Disclosures: The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the Juvenile Diabetes Research Foundation. No conflicts of interest were declared.
Source: Lee DC et al. J Endocr Soc. 2018. Apr 17. doi: 10.1210/js.2018-00001.
Nivolumab plus ipilimumab boosts PFS in advanced NSCLC with high tumor mutational burden
CHICAGO – The combination of nivolumab plus ipilimumab prolonged progression-free survival (PFS), in comparison with platinum based chemotherapy, as initial treatment for advanced non–small cell lung cancer (NSCLC) patients with a high tumor mutation burden (TMB), regardless of PDL-1 status, according to the first analysis of Checkmate 227.
Median PFS was 7.2 months for patients receiving the immunotherapy combination (95% confidence interval, 5.5-13.2) versus 5.5 months (95% CI, 4.4-5.8) for those receiving platinum-based chemotherapy (hazard ratio for disease progression or death, 0.58; 97.5% CI, 0.41-0.81; P less than .001).
The trial results validate the benefit of nivolumab plus ipilimumab in NSCLC and the role of tumor mutational burden as a biomarker for patient selection, Matthew D. Hellmann, MD, said at the annual meeting of the American Association for Cancer Research.
“Checkmate 227 is the pivotal phase 3 study to validate TMB as an important and independent biomarker to be routinely tested in treatment-naive advanced NSCLC,” he said.
Overall survival data with the combination versus chemotherapy was “encouraging” but not yet complete in patients with high TMB, Dr. Hellmann said.
Results from this first analysis (part 1) of Checkmate 227, a multipart trial, were simultaneously published in the New England Journal of Medicine.
The trial was designed prior to emerging data about TMB. The study was later amended prior to initial analysis to include a second coprimary endpoint evaluating PFS with nivolumab plus ipilimumab versus chemotherapy among patients with a tumor mutational burden of at least 10 mutations per megabase (mut/Mb), irrespective of PD-L1 expression level.
For part 1 of the trial, patients were randomized 1:1:1 to nivolumab 3 mg/kg every 2 weeks plus low-dose ipilimumab 1 mg/kg every 6 weeks; histology-based platinum-doublet chemotherapy every 3 weeks for up to four cycles; and nivolumab 240 mg every 2 weeks or nivolumab 360 mg plus histology-based platinum-doublet chemotherapy every 3 weeks for up to four cycles, followed by nivolumab monotherapy.
Of all randomized patients in part 1 (n=1,739), 1,004 (58%) were evaluable for TMB analyses. Of all TMB-evaluable patients, 444 (44%) had TMB greater than or equal to 10 mut/Mb, including 139 patients randomized to nivolumab plus ipilimumab and 160 patients randomized to chemotherapy. TMB was assessed using the validated assay, FoundationOne CDx.
One-year PFS was higher with nivolumab plus ipilimumab than with chemotherapy among all randomized patients in part 1 (30.9% vs. 17.0%; HR for disease progression or death, 0.83; 95% CI, 0.72-0.96).
The PFS was significantly prolonged with the combination, compared with chemotherapy among patients with a high TMB; the 1-year PFS rate was 42.6% versus 13.2%, respectively, and the median PFS was 7.2 months (95% CI, 5.5-13.2) versus 5.5 months (95% CI, 4.4-5.8) respectively (HR for disease progression or death, 0.58; 97.5% CI, 0.41-0.81; P less than .001). In a subgroup analysis, PFS was longer with nivolumab plus ipilimumab versus chemotherapy for patients with a programmed death ligand 1 expression level of at least 1% and those with a level of less than 1%, reported Dr. Hellmann of Memorial Sloan Kettering Cancer Center, New York.
Safety was manageable and consistent with previous reports of nivolumab plus low-dose ipilimumab in NSCLC. Grade 3-4 treatment-related adverse events with the combination were skin reactions (34%), endocrine (23%), gastrointestinal (18%), hepatic (15%), pulmonary (8%), hypersensitivity (4%), and renal (4%) events. Overall, treatment-related deaths occurred in 1% of patients treated in both the combination and chemotherapy arms.
Results from Checkmate 227 may introduce two new standards of care for the first-line treatment of NSCLC, Dr. Hellmann said. The immunotherapy combination is introduced as a new option for the first-line treatment of NSCLC with a high TMB, sparing first-line chemotherapy, and it validates TMB as an “important and independent biomarker to be routinely tested in treatment-naive, advanced NSCLC,” he concluded.
Dr. Hellmann disclosed relationships with Genentech, Bristol-Myers Squibb, Merck, AstraZeneca, Novartis, Janssen, Mirati, and Shattuck Labs.
SOURCE: Hellmann MD et al. AACR Annual Meeting, Abstract CT077.
CHICAGO – The combination of nivolumab plus ipilimumab prolonged progression-free survival (PFS), in comparison with platinum based chemotherapy, as initial treatment for advanced non–small cell lung cancer (NSCLC) patients with a high tumor mutation burden (TMB), regardless of PDL-1 status, according to the first analysis of Checkmate 227.
Median PFS was 7.2 months for patients receiving the immunotherapy combination (95% confidence interval, 5.5-13.2) versus 5.5 months (95% CI, 4.4-5.8) for those receiving platinum-based chemotherapy (hazard ratio for disease progression or death, 0.58; 97.5% CI, 0.41-0.81; P less than .001).
The trial results validate the benefit of nivolumab plus ipilimumab in NSCLC and the role of tumor mutational burden as a biomarker for patient selection, Matthew D. Hellmann, MD, said at the annual meeting of the American Association for Cancer Research.
“Checkmate 227 is the pivotal phase 3 study to validate TMB as an important and independent biomarker to be routinely tested in treatment-naive advanced NSCLC,” he said.
Overall survival data with the combination versus chemotherapy was “encouraging” but not yet complete in patients with high TMB, Dr. Hellmann said.
Results from this first analysis (part 1) of Checkmate 227, a multipart trial, were simultaneously published in the New England Journal of Medicine.
The trial was designed prior to emerging data about TMB. The study was later amended prior to initial analysis to include a second coprimary endpoint evaluating PFS with nivolumab plus ipilimumab versus chemotherapy among patients with a tumor mutational burden of at least 10 mutations per megabase (mut/Mb), irrespective of PD-L1 expression level.
For part 1 of the trial, patients were randomized 1:1:1 to nivolumab 3 mg/kg every 2 weeks plus low-dose ipilimumab 1 mg/kg every 6 weeks; histology-based platinum-doublet chemotherapy every 3 weeks for up to four cycles; and nivolumab 240 mg every 2 weeks or nivolumab 360 mg plus histology-based platinum-doublet chemotherapy every 3 weeks for up to four cycles, followed by nivolumab monotherapy.
Of all randomized patients in part 1 (n=1,739), 1,004 (58%) were evaluable for TMB analyses. Of all TMB-evaluable patients, 444 (44%) had TMB greater than or equal to 10 mut/Mb, including 139 patients randomized to nivolumab plus ipilimumab and 160 patients randomized to chemotherapy. TMB was assessed using the validated assay, FoundationOne CDx.
One-year PFS was higher with nivolumab plus ipilimumab than with chemotherapy among all randomized patients in part 1 (30.9% vs. 17.0%; HR for disease progression or death, 0.83; 95% CI, 0.72-0.96).
The PFS was significantly prolonged with the combination, compared with chemotherapy among patients with a high TMB; the 1-year PFS rate was 42.6% versus 13.2%, respectively, and the median PFS was 7.2 months (95% CI, 5.5-13.2) versus 5.5 months (95% CI, 4.4-5.8) respectively (HR for disease progression or death, 0.58; 97.5% CI, 0.41-0.81; P less than .001). In a subgroup analysis, PFS was longer with nivolumab plus ipilimumab versus chemotherapy for patients with a programmed death ligand 1 expression level of at least 1% and those with a level of less than 1%, reported Dr. Hellmann of Memorial Sloan Kettering Cancer Center, New York.
Safety was manageable and consistent with previous reports of nivolumab plus low-dose ipilimumab in NSCLC. Grade 3-4 treatment-related adverse events with the combination were skin reactions (34%), endocrine (23%), gastrointestinal (18%), hepatic (15%), pulmonary (8%), hypersensitivity (4%), and renal (4%) events. Overall, treatment-related deaths occurred in 1% of patients treated in both the combination and chemotherapy arms.
Results from Checkmate 227 may introduce two new standards of care for the first-line treatment of NSCLC, Dr. Hellmann said. The immunotherapy combination is introduced as a new option for the first-line treatment of NSCLC with a high TMB, sparing first-line chemotherapy, and it validates TMB as an “important and independent biomarker to be routinely tested in treatment-naive, advanced NSCLC,” he concluded.
Dr. Hellmann disclosed relationships with Genentech, Bristol-Myers Squibb, Merck, AstraZeneca, Novartis, Janssen, Mirati, and Shattuck Labs.
SOURCE: Hellmann MD et al. AACR Annual Meeting, Abstract CT077.
CHICAGO – The combination of nivolumab plus ipilimumab prolonged progression-free survival (PFS), in comparison with platinum based chemotherapy, as initial treatment for advanced non–small cell lung cancer (NSCLC) patients with a high tumor mutation burden (TMB), regardless of PDL-1 status, according to the first analysis of Checkmate 227.
Median PFS was 7.2 months for patients receiving the immunotherapy combination (95% confidence interval, 5.5-13.2) versus 5.5 months (95% CI, 4.4-5.8) for those receiving platinum-based chemotherapy (hazard ratio for disease progression or death, 0.58; 97.5% CI, 0.41-0.81; P less than .001).
The trial results validate the benefit of nivolumab plus ipilimumab in NSCLC and the role of tumor mutational burden as a biomarker for patient selection, Matthew D. Hellmann, MD, said at the annual meeting of the American Association for Cancer Research.
“Checkmate 227 is the pivotal phase 3 study to validate TMB as an important and independent biomarker to be routinely tested in treatment-naive advanced NSCLC,” he said.
Overall survival data with the combination versus chemotherapy was “encouraging” but not yet complete in patients with high TMB, Dr. Hellmann said.
Results from this first analysis (part 1) of Checkmate 227, a multipart trial, were simultaneously published in the New England Journal of Medicine.
The trial was designed prior to emerging data about TMB. The study was later amended prior to initial analysis to include a second coprimary endpoint evaluating PFS with nivolumab plus ipilimumab versus chemotherapy among patients with a tumor mutational burden of at least 10 mutations per megabase (mut/Mb), irrespective of PD-L1 expression level.
For part 1 of the trial, patients were randomized 1:1:1 to nivolumab 3 mg/kg every 2 weeks plus low-dose ipilimumab 1 mg/kg every 6 weeks; histology-based platinum-doublet chemotherapy every 3 weeks for up to four cycles; and nivolumab 240 mg every 2 weeks or nivolumab 360 mg plus histology-based platinum-doublet chemotherapy every 3 weeks for up to four cycles, followed by nivolumab monotherapy.
Of all randomized patients in part 1 (n=1,739), 1,004 (58%) were evaluable for TMB analyses. Of all TMB-evaluable patients, 444 (44%) had TMB greater than or equal to 10 mut/Mb, including 139 patients randomized to nivolumab plus ipilimumab and 160 patients randomized to chemotherapy. TMB was assessed using the validated assay, FoundationOne CDx.
One-year PFS was higher with nivolumab plus ipilimumab than with chemotherapy among all randomized patients in part 1 (30.9% vs. 17.0%; HR for disease progression or death, 0.83; 95% CI, 0.72-0.96).
The PFS was significantly prolonged with the combination, compared with chemotherapy among patients with a high TMB; the 1-year PFS rate was 42.6% versus 13.2%, respectively, and the median PFS was 7.2 months (95% CI, 5.5-13.2) versus 5.5 months (95% CI, 4.4-5.8) respectively (HR for disease progression or death, 0.58; 97.5% CI, 0.41-0.81; P less than .001). In a subgroup analysis, PFS was longer with nivolumab plus ipilimumab versus chemotherapy for patients with a programmed death ligand 1 expression level of at least 1% and those with a level of less than 1%, reported Dr. Hellmann of Memorial Sloan Kettering Cancer Center, New York.
Safety was manageable and consistent with previous reports of nivolumab plus low-dose ipilimumab in NSCLC. Grade 3-4 treatment-related adverse events with the combination were skin reactions (34%), endocrine (23%), gastrointestinal (18%), hepatic (15%), pulmonary (8%), hypersensitivity (4%), and renal (4%) events. Overall, treatment-related deaths occurred in 1% of patients treated in both the combination and chemotherapy arms.
Results from Checkmate 227 may introduce two new standards of care for the first-line treatment of NSCLC, Dr. Hellmann said. The immunotherapy combination is introduced as a new option for the first-line treatment of NSCLC with a high TMB, sparing first-line chemotherapy, and it validates TMB as an “important and independent biomarker to be routinely tested in treatment-naive, advanced NSCLC,” he concluded.
Dr. Hellmann disclosed relationships with Genentech, Bristol-Myers Squibb, Merck, AstraZeneca, Novartis, Janssen, Mirati, and Shattuck Labs.
SOURCE: Hellmann MD et al. AACR Annual Meeting, Abstract CT077.
REPORTING FROM THE AACR ANNUAL MEETING
Key clinical point: PFS was prolonged with the immunotherapy combination of nivolumab plus low-dose ipilimumab versus chemotherapy in first-line advanced NSCLC patients with high tumor mutational burden, independent of PD-L1 expression or tumor histology.
Major finding: Median progression-free survival was 7.2 months (95% CI, 5.5-13.2) for the immunotherapy combination versus 5.5 months (95% CI, 4.4-5.8) for chemotherapy (HR, 0.58; 97.5% CI, 0.41-0.81; P less than .001).
Study details: CheckMate-227 is a multipart open-label phase 3 trial evaluating nivolumab-based combinations versus platinum-doublet chemotherapy in patients with first-line advanced non–small cell lung cancer across nonsquamous and squamous tumor histology.
Disclosures: Dr. Hellmann disclosed relationships with Genentech, Bristol-Myers Squibb, Merck, AstraZeneca, Novartis, Janssen, Mirati, and Shattuck Labs.
Source: Hellmann MD et al. AACR Annual Meeting, Abstract CT077.
Clopidogrel flunks platelet reactivity control test in TAVI
WASHINGTON – For antithrombotic therapy after transcatheter aortic valve implantation (TAVI), ticagrelor plus aspirin may be a better strategy than clopidogrel plus aspirin even though the latter combination is guideline recommended, according to a late-breaking, randomized study presented at CRT 2018 sponsored by the Cardiovascular Research Institute at Washington Hospital Center.
Unlike the ticagrelor regimen, which did deliver the goal antiplatelet effect for all 3 months of the study, “clopidogrel did not achieve adequate platelet inhibition before or after TAVI in most patients,” reported Victor A. Jimenez Diaz, MD, a cardiologist at University Hospital, Vigo, Spain.
The current American Heart Association/American College of Cardiology guidelines label the clopidogrel/aspirin combination for the first 6 months after TAVI “reasonable,” but Dr. Jimenez Diaz said that the value of this combination over other antiplatelet strategies has not been supported by a randomized clinical trial. The known variability in response to clopidogrel is among the reasons such data are needed.
Thrombotic and hemorrhagic complications are frequent after TAVI, making choice of antithrombotic treatment an important consideration for improving outcomes, according to Dr. Jimenez Diaz. The aim of the REAC TAVI trial was to evaluate whether ticagrelor provides a more consistent antiplatelet effect than clopidogrel for TAVI patients, which was undertaken at seven participating centers in Spain.
A total of 65 candidates for TAVI were enrolled in this study. The key exclusion criterion was chronic oral anticoagulation therapy. In a baseline assessment, patients in the study, all of whom were on 75 mg clopidogrel plus aspirin, were evaluated for high on-treatment platelet reactivity (HTPR), defined as a score of at least 208 platelet reaction units (PRU) on a standard assay.
The 46 (71%) patients found to have HTPR were randomized to 90 mg ticagrelor twice daily plus aspirin or to remain on the clopidogrel/aspirin combination. Unlike those with HTPR, in whom the mean PRU was 274 units, all of the patients without HTPR, who had a mean PRU of 134 units, remained on the baseline dual antiplatelet therapy. The study was open label.
The primary endpoint was adequate platelet antiaggregation, defined as absence of HTPR (less than 208 PRU), which was greater in the ticagrelor-treated group than the clopidogrel-treated group at 6 hours (91% vs. 4%), 5 days (100% vs. 10%), and 3 months (100% vs. 21%). In the patients without HTPR, the proportion with adequate platelet antiaggregation at these three time points were 73%, 64%, and 78%, respectively.
“The net difference in the randomized arms over the course of the study was 79%,” reported Dr. Jimenez Diaz, emphasizing that the study verified the hypothesis that ticagrelor would provide a more consistent antiplatelet effect than clopidogrel.
Although in-hospital bleeding complications were numerically higher in the clopidogrel-treated group (25% vs. 4%), this difference did not reach significance, and there were no significant differences in bleeding complications at any other time points or overall. There were two deaths in the clopidogrel-treated group, two deaths in the group without baseline HTPR, but no deaths in the ticagrelor-treated group.
While acknowledging that this study was small and not powered to show a difference in clinical events, Dr. Jimenez Diaz said it is important to emphasize that two-thirds of patients had HTPR at baseline. The high rate of HTPR among TAVI patients on clopidogrel and aspirin at baseline was identified as an important message from this study. However, a study is now needed to determine whether a ticagrelor strategy improves clinical outcomes when compared with a clopidogrel strategy.
A panel of experts at the CRT late-breaker session where these results were presented offered mixed reactions. While Jeffrey Popma, MD, director of interventional cardiology at Beth Israel Deaconess Hospital, Boston, called the results both “intriguing” and “provocative,” Ron Waksman, MD, associate director of the division of cardiology at the Medstar Health Institute, Washington, offered a note of caution, commenting that this application of ticagrelor “is off label, and then you would have to be concerned about the bleeding risk.”
However, all agreed that the optimal antithrombotic therapy for TAVI remains poorly defined and that randomized trials are needed to explore this issue.
This investigator-initiated study had no commercial sponsor. Dr. Jimenez Diaz reported no relevant financial relationships.
SOURCE: Jimenez Diaz VA. CRT 2018, Abstract LBT-10.
WASHINGTON – For antithrombotic therapy after transcatheter aortic valve implantation (TAVI), ticagrelor plus aspirin may be a better strategy than clopidogrel plus aspirin even though the latter combination is guideline recommended, according to a late-breaking, randomized study presented at CRT 2018 sponsored by the Cardiovascular Research Institute at Washington Hospital Center.
Unlike the ticagrelor regimen, which did deliver the goal antiplatelet effect for all 3 months of the study, “clopidogrel did not achieve adequate platelet inhibition before or after TAVI in most patients,” reported Victor A. Jimenez Diaz, MD, a cardiologist at University Hospital, Vigo, Spain.
The current American Heart Association/American College of Cardiology guidelines label the clopidogrel/aspirin combination for the first 6 months after TAVI “reasonable,” but Dr. Jimenez Diaz said that the value of this combination over other antiplatelet strategies has not been supported by a randomized clinical trial. The known variability in response to clopidogrel is among the reasons such data are needed.
Thrombotic and hemorrhagic complications are frequent after TAVI, making choice of antithrombotic treatment an important consideration for improving outcomes, according to Dr. Jimenez Diaz. The aim of the REAC TAVI trial was to evaluate whether ticagrelor provides a more consistent antiplatelet effect than clopidogrel for TAVI patients, which was undertaken at seven participating centers in Spain.
A total of 65 candidates for TAVI were enrolled in this study. The key exclusion criterion was chronic oral anticoagulation therapy. In a baseline assessment, patients in the study, all of whom were on 75 mg clopidogrel plus aspirin, were evaluated for high on-treatment platelet reactivity (HTPR), defined as a score of at least 208 platelet reaction units (PRU) on a standard assay.
The 46 (71%) patients found to have HTPR were randomized to 90 mg ticagrelor twice daily plus aspirin or to remain on the clopidogrel/aspirin combination. Unlike those with HTPR, in whom the mean PRU was 274 units, all of the patients without HTPR, who had a mean PRU of 134 units, remained on the baseline dual antiplatelet therapy. The study was open label.
The primary endpoint was adequate platelet antiaggregation, defined as absence of HTPR (less than 208 PRU), which was greater in the ticagrelor-treated group than the clopidogrel-treated group at 6 hours (91% vs. 4%), 5 days (100% vs. 10%), and 3 months (100% vs. 21%). In the patients without HTPR, the proportion with adequate platelet antiaggregation at these three time points were 73%, 64%, and 78%, respectively.
“The net difference in the randomized arms over the course of the study was 79%,” reported Dr. Jimenez Diaz, emphasizing that the study verified the hypothesis that ticagrelor would provide a more consistent antiplatelet effect than clopidogrel.
Although in-hospital bleeding complications were numerically higher in the clopidogrel-treated group (25% vs. 4%), this difference did not reach significance, and there were no significant differences in bleeding complications at any other time points or overall. There were two deaths in the clopidogrel-treated group, two deaths in the group without baseline HTPR, but no deaths in the ticagrelor-treated group.
While acknowledging that this study was small and not powered to show a difference in clinical events, Dr. Jimenez Diaz said it is important to emphasize that two-thirds of patients had HTPR at baseline. The high rate of HTPR among TAVI patients on clopidogrel and aspirin at baseline was identified as an important message from this study. However, a study is now needed to determine whether a ticagrelor strategy improves clinical outcomes when compared with a clopidogrel strategy.
A panel of experts at the CRT late-breaker session where these results were presented offered mixed reactions. While Jeffrey Popma, MD, director of interventional cardiology at Beth Israel Deaconess Hospital, Boston, called the results both “intriguing” and “provocative,” Ron Waksman, MD, associate director of the division of cardiology at the Medstar Health Institute, Washington, offered a note of caution, commenting that this application of ticagrelor “is off label, and then you would have to be concerned about the bleeding risk.”
However, all agreed that the optimal antithrombotic therapy for TAVI remains poorly defined and that randomized trials are needed to explore this issue.
This investigator-initiated study had no commercial sponsor. Dr. Jimenez Diaz reported no relevant financial relationships.
SOURCE: Jimenez Diaz VA. CRT 2018, Abstract LBT-10.
WASHINGTON – For antithrombotic therapy after transcatheter aortic valve implantation (TAVI), ticagrelor plus aspirin may be a better strategy than clopidogrel plus aspirin even though the latter combination is guideline recommended, according to a late-breaking, randomized study presented at CRT 2018 sponsored by the Cardiovascular Research Institute at Washington Hospital Center.
Unlike the ticagrelor regimen, which did deliver the goal antiplatelet effect for all 3 months of the study, “clopidogrel did not achieve adequate platelet inhibition before or after TAVI in most patients,” reported Victor A. Jimenez Diaz, MD, a cardiologist at University Hospital, Vigo, Spain.
The current American Heart Association/American College of Cardiology guidelines label the clopidogrel/aspirin combination for the first 6 months after TAVI “reasonable,” but Dr. Jimenez Diaz said that the value of this combination over other antiplatelet strategies has not been supported by a randomized clinical trial. The known variability in response to clopidogrel is among the reasons such data are needed.
Thrombotic and hemorrhagic complications are frequent after TAVI, making choice of antithrombotic treatment an important consideration for improving outcomes, according to Dr. Jimenez Diaz. The aim of the REAC TAVI trial was to evaluate whether ticagrelor provides a more consistent antiplatelet effect than clopidogrel for TAVI patients, which was undertaken at seven participating centers in Spain.
A total of 65 candidates for TAVI were enrolled in this study. The key exclusion criterion was chronic oral anticoagulation therapy. In a baseline assessment, patients in the study, all of whom were on 75 mg clopidogrel plus aspirin, were evaluated for high on-treatment platelet reactivity (HTPR), defined as a score of at least 208 platelet reaction units (PRU) on a standard assay.
The 46 (71%) patients found to have HTPR were randomized to 90 mg ticagrelor twice daily plus aspirin or to remain on the clopidogrel/aspirin combination. Unlike those with HTPR, in whom the mean PRU was 274 units, all of the patients without HTPR, who had a mean PRU of 134 units, remained on the baseline dual antiplatelet therapy. The study was open label.
The primary endpoint was adequate platelet antiaggregation, defined as absence of HTPR (less than 208 PRU), which was greater in the ticagrelor-treated group than the clopidogrel-treated group at 6 hours (91% vs. 4%), 5 days (100% vs. 10%), and 3 months (100% vs. 21%). In the patients without HTPR, the proportion with adequate platelet antiaggregation at these three time points were 73%, 64%, and 78%, respectively.
“The net difference in the randomized arms over the course of the study was 79%,” reported Dr. Jimenez Diaz, emphasizing that the study verified the hypothesis that ticagrelor would provide a more consistent antiplatelet effect than clopidogrel.
Although in-hospital bleeding complications were numerically higher in the clopidogrel-treated group (25% vs. 4%), this difference did not reach significance, and there were no significant differences in bleeding complications at any other time points or overall. There were two deaths in the clopidogrel-treated group, two deaths in the group without baseline HTPR, but no deaths in the ticagrelor-treated group.
While acknowledging that this study was small and not powered to show a difference in clinical events, Dr. Jimenez Diaz said it is important to emphasize that two-thirds of patients had HTPR at baseline. The high rate of HTPR among TAVI patients on clopidogrel and aspirin at baseline was identified as an important message from this study. However, a study is now needed to determine whether a ticagrelor strategy improves clinical outcomes when compared with a clopidogrel strategy.
A panel of experts at the CRT late-breaker session where these results were presented offered mixed reactions. While Jeffrey Popma, MD, director of interventional cardiology at Beth Israel Deaconess Hospital, Boston, called the results both “intriguing” and “provocative,” Ron Waksman, MD, associate director of the division of cardiology at the Medstar Health Institute, Washington, offered a note of caution, commenting that this application of ticagrelor “is off label, and then you would have to be concerned about the bleeding risk.”
However, all agreed that the optimal antithrombotic therapy for TAVI remains poorly defined and that randomized trials are needed to explore this issue.
This investigator-initiated study had no commercial sponsor. Dr. Jimenez Diaz reported no relevant financial relationships.
SOURCE: Jimenez Diaz VA. CRT 2018, Abstract LBT-10.
REPORTING FROM CRT 2018
Key clinical point: For platelet reactivity after transcatheter aortic valve implantation (TAVI), ticagrelor is more effective than clopidogrel.
Major finding:
Study details: A multicenter, randomized trial with 65 patients.
Disclosures: This investigator-initiated study had no commercial sponsor. Dr. Jimenez Diaz reported no relevant financial relationships.
Source: Jimenez Diaz VA. CRT 2018, Abstract LBT-10.
Don’t use cannabis to treat OSA, AASM recommends
, according to a position statement published in the Journal of Clinical Sleep Medicine’s April issue.
In the statement, the professional society recommends that state legislators, regulators, and health departments exclude obstructive sleep apnea (OSA) as an indication for medical cannabis programs.
The “unreliable delivery methods and insufficient evidence of treatment effectiveness, tolerability, and safety” of medical cannabis and its synthetic extracts are among the reasons the AASM gave for making its recommendations. “Further research is needed to better understand the mechanistic actions of medical cannabis and its synthetic extracts, the long-term role of these synthetic extracts on OSA treatment, and harms and benefits,” the AASM concluded in its statement, authored by Kannan Ramar, MD, and other members of a panel of experts on sleep medicine.
Dronabinol is the only cannabis product that has been tested on patients with OSA for the treatment of this disorder. While some synthetic cannabis products are approved by the Food and Drug Administration for other medical indications, the synthetic-based cannabis product dronabinol has not received FDA approval for the treatment of OSA.
Researchers have examined dronabinol’s use for treating OSA in small pilot and proof-of-concept studies and most patients in these studies reported experiencing treatment-related side effects, such as somnolence, wrote Dr. Ramar, of the division of pulmonary and critical care medicine at the Center for Sleep Medicine, Mayo Clinic, Rochester Minn., and his colleagues.
These trials involved patients having taken dronabinol pills in strengths ranging from 2.5 mg to 10 mg. One such study (Front Psychiatry. 2013 Jan 22. doi: 10.3389/fpsyt.2013.00001), authored by Bharati Prasad of the University of Illinois, Chicago, and colleagues, showed a significant improvement in apnea-hypopnea index (AHI) of 32%, after 17 patients used dronabinol for 3 weeks, when compared with baseline AHIs (–14.1; P = .007).
A placebo-controlled randomized study of 73 adults with moderate or severe OSA similarly found a 33% decline in AHI in patients following 6 weeks of treatment with 10-mg doses of dronabinol (Sleep. 2018 Jan 1. doi: 10.1093/sleep/zsx184).
In the placebo-controlled study, 73 patients were randomized to receive 2.5 mg of dronabinol or 10 mg of dronabinol daily for up to 6 weeks, or placebo. At the end of treatment, researchers saw significant increases in the AHI among the patients on placebo, while those who received dronabinol showed decreases in the number of apnea and hypopnea events per hour. Patients given the 2.5-mg dose of dronabinol had a mean decrease of 10.7 events per hour, and those on the 10-mg dose had a mean decrease of 12.9 events per hour compared with placebo. The difference between the placebo and treatment arms was significant for both dosages, and the AHI decreases were similar between the two dosages of dronabinol.
These effects were largely due to reductions in apnea events; the largest reduction was seen in the REM apnea index in patients treated with the 10-mg dose of dronabinol. However, there were few effects on the expression of hypopneas, except in the higher-dose group.
After adjustment for age, race, ethnicity, and baseline AHI, the increases seen in the placebo group were no longer significant, but the decreases from baseline seen in the treatment arms were greater. Dronabinol treatment also was associated with significant decreases, compared with placebo, in non-REM AHI and REM AHI.
Overall, nearly 90% of patients in this trial reported at least one adverse event, with the rates having not differed significantly between the treatment and placebo arms. The most frequently reported adverse events were “sleepiness/drowsiness” (n = 25; 8% of total adverse events reported), headache (n = 24; 8%), “nausea/vomiting” (n = 23; 8%), and “dizziness/lightheadedness” (n = 12; 4%). In addition, one patient experienced diarrhea and vomiting that required admission to a hospital, which was judged as possibly related to the study medication. There were six other withdrawals due to adverse events, including dizziness and vision changes, vertigo, ECG arrhythmias, and headache with dizziness and vomiting.
“Synthetic medical cannabis may have differential side effects, with variable efficacy and side effects in the treatment of OSA. Therefore, it is the position of the American Academy of Sleep Medicine that medical cannabis and/or its synthetic extracts should not be used for the treatment of OSA,” Dr. Ramar and his associates wrote.
, according to a position statement published in the Journal of Clinical Sleep Medicine’s April issue.
In the statement, the professional society recommends that state legislators, regulators, and health departments exclude obstructive sleep apnea (OSA) as an indication for medical cannabis programs.
The “unreliable delivery methods and insufficient evidence of treatment effectiveness, tolerability, and safety” of medical cannabis and its synthetic extracts are among the reasons the AASM gave for making its recommendations. “Further research is needed to better understand the mechanistic actions of medical cannabis and its synthetic extracts, the long-term role of these synthetic extracts on OSA treatment, and harms and benefits,” the AASM concluded in its statement, authored by Kannan Ramar, MD, and other members of a panel of experts on sleep medicine.
Dronabinol is the only cannabis product that has been tested on patients with OSA for the treatment of this disorder. While some synthetic cannabis products are approved by the Food and Drug Administration for other medical indications, the synthetic-based cannabis product dronabinol has not received FDA approval for the treatment of OSA.
Researchers have examined dronabinol’s use for treating OSA in small pilot and proof-of-concept studies and most patients in these studies reported experiencing treatment-related side effects, such as somnolence, wrote Dr. Ramar, of the division of pulmonary and critical care medicine at the Center for Sleep Medicine, Mayo Clinic, Rochester Minn., and his colleagues.
These trials involved patients having taken dronabinol pills in strengths ranging from 2.5 mg to 10 mg. One such study (Front Psychiatry. 2013 Jan 22. doi: 10.3389/fpsyt.2013.00001), authored by Bharati Prasad of the University of Illinois, Chicago, and colleagues, showed a significant improvement in apnea-hypopnea index (AHI) of 32%, after 17 patients used dronabinol for 3 weeks, when compared with baseline AHIs (–14.1; P = .007).
A placebo-controlled randomized study of 73 adults with moderate or severe OSA similarly found a 33% decline in AHI in patients following 6 weeks of treatment with 10-mg doses of dronabinol (Sleep. 2018 Jan 1. doi: 10.1093/sleep/zsx184).
In the placebo-controlled study, 73 patients were randomized to receive 2.5 mg of dronabinol or 10 mg of dronabinol daily for up to 6 weeks, or placebo. At the end of treatment, researchers saw significant increases in the AHI among the patients on placebo, while those who received dronabinol showed decreases in the number of apnea and hypopnea events per hour. Patients given the 2.5-mg dose of dronabinol had a mean decrease of 10.7 events per hour, and those on the 10-mg dose had a mean decrease of 12.9 events per hour compared with placebo. The difference between the placebo and treatment arms was significant for both dosages, and the AHI decreases were similar between the two dosages of dronabinol.
These effects were largely due to reductions in apnea events; the largest reduction was seen in the REM apnea index in patients treated with the 10-mg dose of dronabinol. However, there were few effects on the expression of hypopneas, except in the higher-dose group.
After adjustment for age, race, ethnicity, and baseline AHI, the increases seen in the placebo group were no longer significant, but the decreases from baseline seen in the treatment arms were greater. Dronabinol treatment also was associated with significant decreases, compared with placebo, in non-REM AHI and REM AHI.
Overall, nearly 90% of patients in this trial reported at least one adverse event, with the rates having not differed significantly between the treatment and placebo arms. The most frequently reported adverse events were “sleepiness/drowsiness” (n = 25; 8% of total adverse events reported), headache (n = 24; 8%), “nausea/vomiting” (n = 23; 8%), and “dizziness/lightheadedness” (n = 12; 4%). In addition, one patient experienced diarrhea and vomiting that required admission to a hospital, which was judged as possibly related to the study medication. There were six other withdrawals due to adverse events, including dizziness and vision changes, vertigo, ECG arrhythmias, and headache with dizziness and vomiting.
“Synthetic medical cannabis may have differential side effects, with variable efficacy and side effects in the treatment of OSA. Therefore, it is the position of the American Academy of Sleep Medicine that medical cannabis and/or its synthetic extracts should not be used for the treatment of OSA,” Dr. Ramar and his associates wrote.
, according to a position statement published in the Journal of Clinical Sleep Medicine’s April issue.
In the statement, the professional society recommends that state legislators, regulators, and health departments exclude obstructive sleep apnea (OSA) as an indication for medical cannabis programs.
The “unreliable delivery methods and insufficient evidence of treatment effectiveness, tolerability, and safety” of medical cannabis and its synthetic extracts are among the reasons the AASM gave for making its recommendations. “Further research is needed to better understand the mechanistic actions of medical cannabis and its synthetic extracts, the long-term role of these synthetic extracts on OSA treatment, and harms and benefits,” the AASM concluded in its statement, authored by Kannan Ramar, MD, and other members of a panel of experts on sleep medicine.
Dronabinol is the only cannabis product that has been tested on patients with OSA for the treatment of this disorder. While some synthetic cannabis products are approved by the Food and Drug Administration for other medical indications, the synthetic-based cannabis product dronabinol has not received FDA approval for the treatment of OSA.
Researchers have examined dronabinol’s use for treating OSA in small pilot and proof-of-concept studies and most patients in these studies reported experiencing treatment-related side effects, such as somnolence, wrote Dr. Ramar, of the division of pulmonary and critical care medicine at the Center for Sleep Medicine, Mayo Clinic, Rochester Minn., and his colleagues.
These trials involved patients having taken dronabinol pills in strengths ranging from 2.5 mg to 10 mg. One such study (Front Psychiatry. 2013 Jan 22. doi: 10.3389/fpsyt.2013.00001), authored by Bharati Prasad of the University of Illinois, Chicago, and colleagues, showed a significant improvement in apnea-hypopnea index (AHI) of 32%, after 17 patients used dronabinol for 3 weeks, when compared with baseline AHIs (–14.1; P = .007).
A placebo-controlled randomized study of 73 adults with moderate or severe OSA similarly found a 33% decline in AHI in patients following 6 weeks of treatment with 10-mg doses of dronabinol (Sleep. 2018 Jan 1. doi: 10.1093/sleep/zsx184).
In the placebo-controlled study, 73 patients were randomized to receive 2.5 mg of dronabinol or 10 mg of dronabinol daily for up to 6 weeks, or placebo. At the end of treatment, researchers saw significant increases in the AHI among the patients on placebo, while those who received dronabinol showed decreases in the number of apnea and hypopnea events per hour. Patients given the 2.5-mg dose of dronabinol had a mean decrease of 10.7 events per hour, and those on the 10-mg dose had a mean decrease of 12.9 events per hour compared with placebo. The difference between the placebo and treatment arms was significant for both dosages, and the AHI decreases were similar between the two dosages of dronabinol.
These effects were largely due to reductions in apnea events; the largest reduction was seen in the REM apnea index in patients treated with the 10-mg dose of dronabinol. However, there were few effects on the expression of hypopneas, except in the higher-dose group.
After adjustment for age, race, ethnicity, and baseline AHI, the increases seen in the placebo group were no longer significant, but the decreases from baseline seen in the treatment arms were greater. Dronabinol treatment also was associated with significant decreases, compared with placebo, in non-REM AHI and REM AHI.
Overall, nearly 90% of patients in this trial reported at least one adverse event, with the rates having not differed significantly between the treatment and placebo arms. The most frequently reported adverse events were “sleepiness/drowsiness” (n = 25; 8% of total adverse events reported), headache (n = 24; 8%), “nausea/vomiting” (n = 23; 8%), and “dizziness/lightheadedness” (n = 12; 4%). In addition, one patient experienced diarrhea and vomiting that required admission to a hospital, which was judged as possibly related to the study medication. There were six other withdrawals due to adverse events, including dizziness and vision changes, vertigo, ECG arrhythmias, and headache with dizziness and vomiting.
“Synthetic medical cannabis may have differential side effects, with variable efficacy and side effects in the treatment of OSA. Therefore, it is the position of the American Academy of Sleep Medicine that medical cannabis and/or its synthetic extracts should not be used for the treatment of OSA,” Dr. Ramar and his associates wrote.
FROM THE JOURNAL OF CLINICAL SLEEP MEDICINE