User login
VIDEO: Pioglitazone benefited NASH patients with and without T2DM
Pioglitazone therapy given for 18 months benefited patients with nonalcoholic steatohepatitis (NASH) similarly regardless of whether they had type 2 diabetes mellitus or prediabetes, according to the results of a randomized prospective trial.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
The primary outcome, at least a 2-point reduction in nonalcoholic fatty liver disease activity score compared with placebo, without worsening fibrosis, was met by 48% of NASH patients with T2DM and by 46% of those with prediabetes, reported Fernando Bril, MD, of the division of endocrinology, diabetes, and metabolism at the University of Florida, Gainesville, and his associates. The report was published in Clinical Gastroenterology and Hepatology.
NASH resolved completely in 44% with T2DM and 26% of patients without it, respectively, perhaps indicating that pioglitazone acts slightly differently when patients with NASH have T2DM, according to the investigators. “Although the effects on fibrosis appear to be similar in both groups, pioglitazone may contribute to halting [its] rapid progression [in T2DM],” they wrote. “These differences will deserve further exploration in larger clinical trials.”
The trial (NCT00994682) enrolled 101 patients with biopsy-confirmed NASH, of whom 52 had T2DM and 49 had prediabetes based on clinical history, baseline fasting plasma glucose, hemoglobin A1c, and an oral glucose tolerance test, as per American Diabetes Association guidelines. After a 4-week run-in period, patients were randomly assigned to receive either pioglitazone (45 mg per day) or placebo for 18 months. All patients received lifestyle counseling and a hypocaloric (500-kcal reduced) diet.
Compared with placebo, pioglitazone improved most secondary outcomes similarly regardless of whether patients were T2DM or prediabetes. The two exceptions were fibrosis and insulin sensitivity of adipose tissue. Patients with T2DM only experienced improved fibrosis in the setting of pioglitazone therapy (P = .035 vs. baseline). In prediabetic patients, fibrosis lessened moderately over time, regardless of whether they received pioglitazone or placebo. Insulin sensitivity of adipose tissue improved much more markedly with treatment in patients with T2DM (P less than .001 vs. baseline) than in those with prediabetes (P = .002 for T2DM vs. prediabetes).
Compared with placebo, pioglitazone improved hepatic and skeletal muscle insulin sensitivity similarly, regardless of diabetes status. Likewise, intrahepatic triglyceride content, as measured by proton magnetic resonance spectroscopy, fell by 11% in pioglitazone recipients with T2DM and by 9% of those with prediabetes, a nonsignificant difference. Pioglitazone also led to a statistically similar decrease in plasma alanine aminotransferase level regardless of whether patients had T2DM (50 U/L) or were prediabetic (36 U/L).
This trial’s key takeaway is that pioglitazone improves liver histology in NASH whether or not patients are diabetic, said the researchers. “We believed that it was essential to compare its efficacy in patients with [and] without T2DM because of the vast number of patients with prediabetes and NASH and given the significant metabolic and cardioprotective effects of pioglitazone among patients without T2DM,” they wrote. The natural history of NASH is worse in the presence of T2DM, which might explain pioglitazone’s superior effects on fibrosis and insulin sensitivity of adipose tissue in this population, they added.
The Burroughs Wellcome Fund, the American Diabetes Association, and the Veteran’s Affairs Merit Award supported the work. Senior author Kenneth Cusi, MD, disclosed nonfinancial support from Takeda Pharmaceuticals, grants from Novartis and Janssen Research and Development, and consulting relationships with Eli Lilly, Tobira Therapeutics, and Pfizer. The other authors had no conflicts.
Source: Bril F, et al. Clin Gastroenterol Hepatol. 2018 Feb 24. doi: 10.1016/j.cgh.2017.12.001.
Pioglitazone therapy given for 18 months benefited patients with nonalcoholic steatohepatitis (NASH) similarly regardless of whether they had type 2 diabetes mellitus or prediabetes, according to the results of a randomized prospective trial.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
The primary outcome, at least a 2-point reduction in nonalcoholic fatty liver disease activity score compared with placebo, without worsening fibrosis, was met by 48% of NASH patients with T2DM and by 46% of those with prediabetes, reported Fernando Bril, MD, of the division of endocrinology, diabetes, and metabolism at the University of Florida, Gainesville, and his associates. The report was published in Clinical Gastroenterology and Hepatology.
NASH resolved completely in 44% with T2DM and 26% of patients without it, respectively, perhaps indicating that pioglitazone acts slightly differently when patients with NASH have T2DM, according to the investigators. “Although the effects on fibrosis appear to be similar in both groups, pioglitazone may contribute to halting [its] rapid progression [in T2DM],” they wrote. “These differences will deserve further exploration in larger clinical trials.”
The trial (NCT00994682) enrolled 101 patients with biopsy-confirmed NASH, of whom 52 had T2DM and 49 had prediabetes based on clinical history, baseline fasting plasma glucose, hemoglobin A1c, and an oral glucose tolerance test, as per American Diabetes Association guidelines. After a 4-week run-in period, patients were randomly assigned to receive either pioglitazone (45 mg per day) or placebo for 18 months. All patients received lifestyle counseling and a hypocaloric (500-kcal reduced) diet.
Compared with placebo, pioglitazone improved most secondary outcomes similarly regardless of whether patients were T2DM or prediabetes. The two exceptions were fibrosis and insulin sensitivity of adipose tissue. Patients with T2DM only experienced improved fibrosis in the setting of pioglitazone therapy (P = .035 vs. baseline). In prediabetic patients, fibrosis lessened moderately over time, regardless of whether they received pioglitazone or placebo. Insulin sensitivity of adipose tissue improved much more markedly with treatment in patients with T2DM (P less than .001 vs. baseline) than in those with prediabetes (P = .002 for T2DM vs. prediabetes).
Compared with placebo, pioglitazone improved hepatic and skeletal muscle insulin sensitivity similarly, regardless of diabetes status. Likewise, intrahepatic triglyceride content, as measured by proton magnetic resonance spectroscopy, fell by 11% in pioglitazone recipients with T2DM and by 9% of those with prediabetes, a nonsignificant difference. Pioglitazone also led to a statistically similar decrease in plasma alanine aminotransferase level regardless of whether patients had T2DM (50 U/L) or were prediabetic (36 U/L).
This trial’s key takeaway is that pioglitazone improves liver histology in NASH whether or not patients are diabetic, said the researchers. “We believed that it was essential to compare its efficacy in patients with [and] without T2DM because of the vast number of patients with prediabetes and NASH and given the significant metabolic and cardioprotective effects of pioglitazone among patients without T2DM,” they wrote. The natural history of NASH is worse in the presence of T2DM, which might explain pioglitazone’s superior effects on fibrosis and insulin sensitivity of adipose tissue in this population, they added.
The Burroughs Wellcome Fund, the American Diabetes Association, and the Veteran’s Affairs Merit Award supported the work. Senior author Kenneth Cusi, MD, disclosed nonfinancial support from Takeda Pharmaceuticals, grants from Novartis and Janssen Research and Development, and consulting relationships with Eli Lilly, Tobira Therapeutics, and Pfizer. The other authors had no conflicts.
Source: Bril F, et al. Clin Gastroenterol Hepatol. 2018 Feb 24. doi: 10.1016/j.cgh.2017.12.001.
Pioglitazone therapy given for 18 months benefited patients with nonalcoholic steatohepatitis (NASH) similarly regardless of whether they had type 2 diabetes mellitus or prediabetes, according to the results of a randomized prospective trial.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
The primary outcome, at least a 2-point reduction in nonalcoholic fatty liver disease activity score compared with placebo, without worsening fibrosis, was met by 48% of NASH patients with T2DM and by 46% of those with prediabetes, reported Fernando Bril, MD, of the division of endocrinology, diabetes, and metabolism at the University of Florida, Gainesville, and his associates. The report was published in Clinical Gastroenterology and Hepatology.
NASH resolved completely in 44% with T2DM and 26% of patients without it, respectively, perhaps indicating that pioglitazone acts slightly differently when patients with NASH have T2DM, according to the investigators. “Although the effects on fibrosis appear to be similar in both groups, pioglitazone may contribute to halting [its] rapid progression [in T2DM],” they wrote. “These differences will deserve further exploration in larger clinical trials.”
The trial (NCT00994682) enrolled 101 patients with biopsy-confirmed NASH, of whom 52 had T2DM and 49 had prediabetes based on clinical history, baseline fasting plasma glucose, hemoglobin A1c, and an oral glucose tolerance test, as per American Diabetes Association guidelines. After a 4-week run-in period, patients were randomly assigned to receive either pioglitazone (45 mg per day) or placebo for 18 months. All patients received lifestyle counseling and a hypocaloric (500-kcal reduced) diet.
Compared with placebo, pioglitazone improved most secondary outcomes similarly regardless of whether patients were T2DM or prediabetes. The two exceptions were fibrosis and insulin sensitivity of adipose tissue. Patients with T2DM only experienced improved fibrosis in the setting of pioglitazone therapy (P = .035 vs. baseline). In prediabetic patients, fibrosis lessened moderately over time, regardless of whether they received pioglitazone or placebo. Insulin sensitivity of adipose tissue improved much more markedly with treatment in patients with T2DM (P less than .001 vs. baseline) than in those with prediabetes (P = .002 for T2DM vs. prediabetes).
Compared with placebo, pioglitazone improved hepatic and skeletal muscle insulin sensitivity similarly, regardless of diabetes status. Likewise, intrahepatic triglyceride content, as measured by proton magnetic resonance spectroscopy, fell by 11% in pioglitazone recipients with T2DM and by 9% of those with prediabetes, a nonsignificant difference. Pioglitazone also led to a statistically similar decrease in plasma alanine aminotransferase level regardless of whether patients had T2DM (50 U/L) or were prediabetic (36 U/L).
This trial’s key takeaway is that pioglitazone improves liver histology in NASH whether or not patients are diabetic, said the researchers. “We believed that it was essential to compare its efficacy in patients with [and] without T2DM because of the vast number of patients with prediabetes and NASH and given the significant metabolic and cardioprotective effects of pioglitazone among patients without T2DM,” they wrote. The natural history of NASH is worse in the presence of T2DM, which might explain pioglitazone’s superior effects on fibrosis and insulin sensitivity of adipose tissue in this population, they added.
The Burroughs Wellcome Fund, the American Diabetes Association, and the Veteran’s Affairs Merit Award supported the work. Senior author Kenneth Cusi, MD, disclosed nonfinancial support from Takeda Pharmaceuticals, grants from Novartis and Janssen Research and Development, and consulting relationships with Eli Lilly, Tobira Therapeutics, and Pfizer. The other authors had no conflicts.
Source: Bril F, et al. Clin Gastroenterol Hepatol. 2018 Feb 24. doi: 10.1016/j.cgh.2017.12.001.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Pioglitazone improved liver measures in patients with nonalcoholic steatohepatitis whether or not they were diabetic.
Major finding: Nonalcoholic fatty liver disease activity score fell by at least 2 points, without worsening fibrosis, in 48% of T2DM patients and 46% of patients with prediabetes.
Data source: A prospective study of 101 patients with NASH, of whom 52 had type 2 diabetes and 49 had prediabetes.
Disclosures: The Burroughs Wellcome Fund, the American Diabetes Association, and the Veteran’s Affairs Merit Award supported the work. Senior author Kenneth Cusi, MD, disclosed nonfinancial support from Takeda Pharmaceuticals, grants from Novartis and Janssen Research and Development, and consulting relationships with Eli Lilly and Company, Tobira Therapeutics, and Pfizer. The other authors had no conflicts.
Source: Bril F et al. Clin Gastroenterol Hepatol. 2018 Feb 24. doi: 10.1016/j.cgh.2017.12.001.
Most patients off transfusions after gene therapy for thalassemia
SALT LAKE CITY – Lentiviral delivery of BB305 gene therapy via autologous hematopoietic stem cell transplant (HSCT) was safe and effective for individuals with transfusion dependent beta thalassemia, according to results of a phase 1/2 study.
None of the study participants died, and the majority of patients are now transfusion independent.
The Northstar study is an international, multicenter open-label, single-arm study of adolescents and adults with transfusion dependent beta thalassemia (TDT). A total of 18 patients at a median 21 years of age – 15 young adults aged 18-35 years and three adolescents aged 12-17 years – have now been treated, Mark Walters, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
Of these, 11 are now transfusion independent, with most patients stopping transfusions within 6 months of receiving gene therapy, said Dr. Walters, director of the blood and marrow transplantation program at the University of California, San Francisco’s Benioff Children’s Hospital, Oakland.
Eight patients had the beta0/beta0 genotype, and had essentially been transfusion dependent from infancy. Six other patients were betaE/beta0, and had become transfusion dependent over time. Four patients had other thalassemia genotypes.
Patients who enrolled in the Northstar study first had peripheral stem cell collection via apheresis after mobilization with granulocyte-colony stimulating factor and plerixafor. Then they received myeloablative conditioning with busulfan. At the same time, selected CD34+ cells were tranduced with the BB305 lentiviral vector and cryopreserved. Patients were infused with the transduced cells and managed through the engraftment process.
As a measure of annualized pre-procedure transfusion requirements, patients had received a median 163.6 mL/kg/year of packed red blood cells, Dr. Walters said. Not unexpectedly, liver iron concentration was a median 5.7 mg/g, though with a wide range among participants (0.4-26.4 mg/g). However, participants did not show signs of cardiac tissue iron on T2* magnetic resonance imaging . Six patients had undergone a splenectomy.
The median vector copy number was 0.7 (range, 0.3-1.5), with a median 31.5 CD34+ cells transduced (range, 17.0-58.0). The final cell dose delivered was a median 8.1 x 106 CD34+ cells/kg (range, 5.2-18.1).
“All 18 patients have had at least 18 months of follow-up,” said Dr. Walters, and data from 10 patients has been analyzed out to 2 years. Three patients have a full 3 years of follow-up, he said.
The self-inactivating lentiviral vector has behaved as expected; no replication-competent lentivirus has been found, with investigators conducting assessments at months 3, 6, and 12, and then annually through year 5.
The study protocol also calls for integration site analysis every 6 months for 5 years, and additional analyses at years 7, 10, and 15. Thus far, all samples have shown a polyclonal vector integration profile without clonal dominance, Dr. Walter said.
The median time to neutrophil engraftment was study day 18.5 (range, 14-30), while platelet engraftment was more variable, and overall slower, with engraftment at a median of study day 39.5 (range, 19-191).
Dr. Walters said that he and his colleagues examined characteristics of the four patients who still had platelet counts at or less than 100,000/microliters at 12 months after HSCT. They found that two of these patients had had splenectomies, but saw no clear relationship between speed of platelet engraftment and platelet count at 12 months. Three of the four patients had drug product cell doses less than the median.
However, two patients had no bleeding events after neutrophil engraftment, and bleeding events were all grade 1 or 2 in the other two patients. The slower-than-expected platelet engraftment rate was likely attributable to the ex vivo manipulation of the stem cells, Dr. Walters noted.
Looking at safety data from the point of neutrophil engraftment to the last follow-up, there have been no graft failures; six patients have had serious adverse events. Two events of veno-occlusive disease were assessed as grade 3 and attributed to the transplant. Two of these three patients had an extended hospital stay. Other grade 3 events including intracardiac thrombus, central catheter thrombosis, and cellulitis, as well as hyperglycemia and infectious diseases.
No grade 4 or 5 infections were reported, and the researchers saw no viral reactivations or opportunistic infections.
The safety profile for autologous HSCT with LentiGlobin was overall as expected for a myeloablative regimen that used single-agent busulfan, Dr. Walters said.
Most patients (11/18) with transfusion dependent beta thalassemia were able to stop transfusions, and the remaining patients had reduced transfusion requirements. Participants’ clinical status has stayed consistent through up to 3 years of follow-up, he said.
Of the patients who were able to stop transfusions, just two had the beta0/beta0 genotype. Among all transfusion independent participants, hemoglobin levels at the last study visit ranged from 8.4-13.7 g/dL. Beta0/beta0 genotype patients still receiving transfusions have seen a 60% median reduction in transfusion volume and a similar reduction in number of transfusions.
In response to an attendee question, Dr. Walters said that an analysis not included in the presentation has shown a fairly direct relationship between vector copy numbers and transfusion independence.
Currently, he said, vector copy numbers are higher, at around 3. With a higher vector copy number, more CD34+ cells will be transduced and infused, so there may be less concern about the dilutional effect of incomplete myeloablation.
“There may be an opportunity in the future to lessen the intensity of the conditioning regimen,” Dr. Walters said.
The study was funded by bluebird bio. Dr. Walters also reported several consulting relationships with pharmaceutical companies and laboratories.
SOURCE: Walters, M et al. 2018 BMT Tandem Meetings, Abstract 62.
SALT LAKE CITY – Lentiviral delivery of BB305 gene therapy via autologous hematopoietic stem cell transplant (HSCT) was safe and effective for individuals with transfusion dependent beta thalassemia, according to results of a phase 1/2 study.
None of the study participants died, and the majority of patients are now transfusion independent.
The Northstar study is an international, multicenter open-label, single-arm study of adolescents and adults with transfusion dependent beta thalassemia (TDT). A total of 18 patients at a median 21 years of age – 15 young adults aged 18-35 years and three adolescents aged 12-17 years – have now been treated, Mark Walters, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
Of these, 11 are now transfusion independent, with most patients stopping transfusions within 6 months of receiving gene therapy, said Dr. Walters, director of the blood and marrow transplantation program at the University of California, San Francisco’s Benioff Children’s Hospital, Oakland.
Eight patients had the beta0/beta0 genotype, and had essentially been transfusion dependent from infancy. Six other patients were betaE/beta0, and had become transfusion dependent over time. Four patients had other thalassemia genotypes.
Patients who enrolled in the Northstar study first had peripheral stem cell collection via apheresis after mobilization with granulocyte-colony stimulating factor and plerixafor. Then they received myeloablative conditioning with busulfan. At the same time, selected CD34+ cells were tranduced with the BB305 lentiviral vector and cryopreserved. Patients were infused with the transduced cells and managed through the engraftment process.
As a measure of annualized pre-procedure transfusion requirements, patients had received a median 163.6 mL/kg/year of packed red blood cells, Dr. Walters said. Not unexpectedly, liver iron concentration was a median 5.7 mg/g, though with a wide range among participants (0.4-26.4 mg/g). However, participants did not show signs of cardiac tissue iron on T2* magnetic resonance imaging . Six patients had undergone a splenectomy.
The median vector copy number was 0.7 (range, 0.3-1.5), with a median 31.5 CD34+ cells transduced (range, 17.0-58.0). The final cell dose delivered was a median 8.1 x 106 CD34+ cells/kg (range, 5.2-18.1).
“All 18 patients have had at least 18 months of follow-up,” said Dr. Walters, and data from 10 patients has been analyzed out to 2 years. Three patients have a full 3 years of follow-up, he said.
The self-inactivating lentiviral vector has behaved as expected; no replication-competent lentivirus has been found, with investigators conducting assessments at months 3, 6, and 12, and then annually through year 5.
The study protocol also calls for integration site analysis every 6 months for 5 years, and additional analyses at years 7, 10, and 15. Thus far, all samples have shown a polyclonal vector integration profile without clonal dominance, Dr. Walter said.
The median time to neutrophil engraftment was study day 18.5 (range, 14-30), while platelet engraftment was more variable, and overall slower, with engraftment at a median of study day 39.5 (range, 19-191).
Dr. Walters said that he and his colleagues examined characteristics of the four patients who still had platelet counts at or less than 100,000/microliters at 12 months after HSCT. They found that two of these patients had had splenectomies, but saw no clear relationship between speed of platelet engraftment and platelet count at 12 months. Three of the four patients had drug product cell doses less than the median.
However, two patients had no bleeding events after neutrophil engraftment, and bleeding events were all grade 1 or 2 in the other two patients. The slower-than-expected platelet engraftment rate was likely attributable to the ex vivo manipulation of the stem cells, Dr. Walters noted.
Looking at safety data from the point of neutrophil engraftment to the last follow-up, there have been no graft failures; six patients have had serious adverse events. Two events of veno-occlusive disease were assessed as grade 3 and attributed to the transplant. Two of these three patients had an extended hospital stay. Other grade 3 events including intracardiac thrombus, central catheter thrombosis, and cellulitis, as well as hyperglycemia and infectious diseases.
No grade 4 or 5 infections were reported, and the researchers saw no viral reactivations or opportunistic infections.
The safety profile for autologous HSCT with LentiGlobin was overall as expected for a myeloablative regimen that used single-agent busulfan, Dr. Walters said.
Most patients (11/18) with transfusion dependent beta thalassemia were able to stop transfusions, and the remaining patients had reduced transfusion requirements. Participants’ clinical status has stayed consistent through up to 3 years of follow-up, he said.
Of the patients who were able to stop transfusions, just two had the beta0/beta0 genotype. Among all transfusion independent participants, hemoglobin levels at the last study visit ranged from 8.4-13.7 g/dL. Beta0/beta0 genotype patients still receiving transfusions have seen a 60% median reduction in transfusion volume and a similar reduction in number of transfusions.
In response to an attendee question, Dr. Walters said that an analysis not included in the presentation has shown a fairly direct relationship between vector copy numbers and transfusion independence.
Currently, he said, vector copy numbers are higher, at around 3. With a higher vector copy number, more CD34+ cells will be transduced and infused, so there may be less concern about the dilutional effect of incomplete myeloablation.
“There may be an opportunity in the future to lessen the intensity of the conditioning regimen,” Dr. Walters said.
The study was funded by bluebird bio. Dr. Walters also reported several consulting relationships with pharmaceutical companies and laboratories.
SOURCE: Walters, M et al. 2018 BMT Tandem Meetings, Abstract 62.
SALT LAKE CITY – Lentiviral delivery of BB305 gene therapy via autologous hematopoietic stem cell transplant (HSCT) was safe and effective for individuals with transfusion dependent beta thalassemia, according to results of a phase 1/2 study.
None of the study participants died, and the majority of patients are now transfusion independent.
The Northstar study is an international, multicenter open-label, single-arm study of adolescents and adults with transfusion dependent beta thalassemia (TDT). A total of 18 patients at a median 21 years of age – 15 young adults aged 18-35 years and three adolescents aged 12-17 years – have now been treated, Mark Walters, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
Of these, 11 are now transfusion independent, with most patients stopping transfusions within 6 months of receiving gene therapy, said Dr. Walters, director of the blood and marrow transplantation program at the University of California, San Francisco’s Benioff Children’s Hospital, Oakland.
Eight patients had the beta0/beta0 genotype, and had essentially been transfusion dependent from infancy. Six other patients were betaE/beta0, and had become transfusion dependent over time. Four patients had other thalassemia genotypes.
Patients who enrolled in the Northstar study first had peripheral stem cell collection via apheresis after mobilization with granulocyte-colony stimulating factor and plerixafor. Then they received myeloablative conditioning with busulfan. At the same time, selected CD34+ cells were tranduced with the BB305 lentiviral vector and cryopreserved. Patients were infused with the transduced cells and managed through the engraftment process.
As a measure of annualized pre-procedure transfusion requirements, patients had received a median 163.6 mL/kg/year of packed red blood cells, Dr. Walters said. Not unexpectedly, liver iron concentration was a median 5.7 mg/g, though with a wide range among participants (0.4-26.4 mg/g). However, participants did not show signs of cardiac tissue iron on T2* magnetic resonance imaging . Six patients had undergone a splenectomy.
The median vector copy number was 0.7 (range, 0.3-1.5), with a median 31.5 CD34+ cells transduced (range, 17.0-58.0). The final cell dose delivered was a median 8.1 x 106 CD34+ cells/kg (range, 5.2-18.1).
“All 18 patients have had at least 18 months of follow-up,” said Dr. Walters, and data from 10 patients has been analyzed out to 2 years. Three patients have a full 3 years of follow-up, he said.
The self-inactivating lentiviral vector has behaved as expected; no replication-competent lentivirus has been found, with investigators conducting assessments at months 3, 6, and 12, and then annually through year 5.
The study protocol also calls for integration site analysis every 6 months for 5 years, and additional analyses at years 7, 10, and 15. Thus far, all samples have shown a polyclonal vector integration profile without clonal dominance, Dr. Walter said.
The median time to neutrophil engraftment was study day 18.5 (range, 14-30), while platelet engraftment was more variable, and overall slower, with engraftment at a median of study day 39.5 (range, 19-191).
Dr. Walters said that he and his colleagues examined characteristics of the four patients who still had platelet counts at or less than 100,000/microliters at 12 months after HSCT. They found that two of these patients had had splenectomies, but saw no clear relationship between speed of platelet engraftment and platelet count at 12 months. Three of the four patients had drug product cell doses less than the median.
However, two patients had no bleeding events after neutrophil engraftment, and bleeding events were all grade 1 or 2 in the other two patients. The slower-than-expected platelet engraftment rate was likely attributable to the ex vivo manipulation of the stem cells, Dr. Walters noted.
Looking at safety data from the point of neutrophil engraftment to the last follow-up, there have been no graft failures; six patients have had serious adverse events. Two events of veno-occlusive disease were assessed as grade 3 and attributed to the transplant. Two of these three patients had an extended hospital stay. Other grade 3 events including intracardiac thrombus, central catheter thrombosis, and cellulitis, as well as hyperglycemia and infectious diseases.
No grade 4 or 5 infections were reported, and the researchers saw no viral reactivations or opportunistic infections.
The safety profile for autologous HSCT with LentiGlobin was overall as expected for a myeloablative regimen that used single-agent busulfan, Dr. Walters said.
Most patients (11/18) with transfusion dependent beta thalassemia were able to stop transfusions, and the remaining patients had reduced transfusion requirements. Participants’ clinical status has stayed consistent through up to 3 years of follow-up, he said.
Of the patients who were able to stop transfusions, just two had the beta0/beta0 genotype. Among all transfusion independent participants, hemoglobin levels at the last study visit ranged from 8.4-13.7 g/dL. Beta0/beta0 genotype patients still receiving transfusions have seen a 60% median reduction in transfusion volume and a similar reduction in number of transfusions.
In response to an attendee question, Dr. Walters said that an analysis not included in the presentation has shown a fairly direct relationship between vector copy numbers and transfusion independence.
Currently, he said, vector copy numbers are higher, at around 3. With a higher vector copy number, more CD34+ cells will be transduced and infused, so there may be less concern about the dilutional effect of incomplete myeloablation.
“There may be an opportunity in the future to lessen the intensity of the conditioning regimen,” Dr. Walters said.
The study was funded by bluebird bio. Dr. Walters also reported several consulting relationships with pharmaceutical companies and laboratories.
SOURCE: Walters, M et al. 2018 BMT Tandem Meetings, Abstract 62.
REPORTING FROM THE 2018 BMT TANDEM MEETINGS
Key clinical point: Major finding: Eleven of 18 patients became transfusion independent, and transfusions were reduced for the remainder of patients.
Study details: Open label, international, single-arm phase 1/2 study of 20 patients with transfusion-dependent beta thalassemia.
Disclosures: The study was funded by bluebird bio. Dr. Walters also reported consulting agreements with several pharmaceutical companies and laboratories.
Source: Walters, M et al. 2018 BMT Tandem Meetings, Abstract 62.
AGA Clinical Practice Update: Incorporating psychological care in the management of chronic digestive diseases
This burden includes digestive symptoms and disease severity, as well as patients’ ability to cope with them. Chronic digestive diseases, such as irritable bowel syndrome, gastroesophageal reflux disease, and inflammatory bowel diseases, cannot be disentangled from their psychosocial context. In this regard, the role of gastroenterologists in promoting best practices for the assessment and referral of patients across the spectrum of disease to brain-gut psychotherapies is crucial.
A review by Laurie Keefer, PhD, AGAF, and her coauthors, published in the April issue of Gastroenterology, provided a clinical update on the structure and efficacy of two major classes of psychogastroenterology – cognitive-behavioral therapy (CBT) and gut-directed hypnotherapy (HYP). The review discussed the effects of these therapies on GI symptoms and the patients’ ability to improve coping, resilience, and self-regulation. The review also provided a framework to understand the scientific rationale and best practices associated with incorporating brain-gut psychotherapies into routine GI care. Furthermore, it presented recommendations on how to address psychological issues and make effective referrals in routine practice.
Previous studies had highlighted that the burden of chronic digestive diseases is amplified by psychosocial factors, including poor coping, depression, and poor social support. Mental health professionals specializing in psychogastroenterology integrate the use of brain-gut psychotherapies into GI practice settings, which may help reduce health care utilization and symptom burden.
The article contains best practice advice based on a review of the literature, including existing systematic reviews and expert opinions. These best practices include the following:
- Gastroenterologists routinely should assess health-related quality of life, symptom-specific anxieties, early-life adversity, and functional impairment related to a patient’s digestive complaints.
- Gastroenterologists should master patient-friendly language to help explain the brain-gut pathway and how this pathway can become dysregulated by any number of factors, the psychosocial risks perpetuating and maintaining factors of GI diseases, and why the gastroenterologist is referring a patient to a mental health provider.
- Gastroenterologists should know the structure and core features of the most effective brain-gut psychotherapies.
- Gastroenterologists should establish a direct referral and ongoing communication pathway with one or two qualified mental health providers and assure patients that he/she will remain a part of the care team.
- Gastroenterologists should familiarize themselves with one or two neuromodulators that can be used to augment behavioral therapies when necessary.
Patient education about the referral to a mental health provider is difficult and requires attention to detail and fostering a good physician-patient relationship. It is important to help patients understand why they are being referred to a psychologist for a gastrointestinal complaint and that their physical symptoms are not being discounted. Failure to properly explain the reason for referral may lead to poor follow-through and even lead the patient to seek care with another provider.
In order to foster widespread integration of these services, research and clinical gaps need to be addressed. Research gaps include the lack of prospective trials that compare the relative effectiveness of brain-gut psychotherapies with each other and/or with that of psychotropic medications. Other promising brain-gut therapies, such as mindfulness meditation or acceptance-based approaches, lack sufficient research to be included in clinical practice. Limited evidence supports the effect of psychotherapies have in accelerating or enhancing the efficacy of pharmacologic therapies and on improving disease course or inflammation in conditions such as Crohn’s and ulcerative colitis.
Clinical gaps include the need for better coverage for these therapies by insurance – many providers are out of network or do not accept insurance, although Medicare and commercial insurance plans often cover the cost of services in network. Health psychologists can be reimbursed for health and behavior codes for treating these conditions (CPTs 96150/96152), but there are restrictions on which other types of professionals can use them. Ongoing research is focusing on the cost-effectiveness of these therapies, although some highly effective therapies may be short term and have a one-time total cost of $1,000-$2,000 paid out of pocket. There is a growing need to expand remote, online, or digitally based brain-gut therapies with more trained health care providers that could offset overhead and other therapy costs.
SOURCE: Keefer L et al. Gastroenterology. doi: 10.1053/j.gastro.2018.01.045.
This burden includes digestive symptoms and disease severity, as well as patients’ ability to cope with them. Chronic digestive diseases, such as irritable bowel syndrome, gastroesophageal reflux disease, and inflammatory bowel diseases, cannot be disentangled from their psychosocial context. In this regard, the role of gastroenterologists in promoting best practices for the assessment and referral of patients across the spectrum of disease to brain-gut psychotherapies is crucial.
A review by Laurie Keefer, PhD, AGAF, and her coauthors, published in the April issue of Gastroenterology, provided a clinical update on the structure and efficacy of two major classes of psychogastroenterology – cognitive-behavioral therapy (CBT) and gut-directed hypnotherapy (HYP). The review discussed the effects of these therapies on GI symptoms and the patients’ ability to improve coping, resilience, and self-regulation. The review also provided a framework to understand the scientific rationale and best practices associated with incorporating brain-gut psychotherapies into routine GI care. Furthermore, it presented recommendations on how to address psychological issues and make effective referrals in routine practice.
Previous studies had highlighted that the burden of chronic digestive diseases is amplified by psychosocial factors, including poor coping, depression, and poor social support. Mental health professionals specializing in psychogastroenterology integrate the use of brain-gut psychotherapies into GI practice settings, which may help reduce health care utilization and symptom burden.
The article contains best practice advice based on a review of the literature, including existing systematic reviews and expert opinions. These best practices include the following:
- Gastroenterologists routinely should assess health-related quality of life, symptom-specific anxieties, early-life adversity, and functional impairment related to a patient’s digestive complaints.
- Gastroenterologists should master patient-friendly language to help explain the brain-gut pathway and how this pathway can become dysregulated by any number of factors, the psychosocial risks perpetuating and maintaining factors of GI diseases, and why the gastroenterologist is referring a patient to a mental health provider.
- Gastroenterologists should know the structure and core features of the most effective brain-gut psychotherapies.
- Gastroenterologists should establish a direct referral and ongoing communication pathway with one or two qualified mental health providers and assure patients that he/she will remain a part of the care team.
- Gastroenterologists should familiarize themselves with one or two neuromodulators that can be used to augment behavioral therapies when necessary.
Patient education about the referral to a mental health provider is difficult and requires attention to detail and fostering a good physician-patient relationship. It is important to help patients understand why they are being referred to a psychologist for a gastrointestinal complaint and that their physical symptoms are not being discounted. Failure to properly explain the reason for referral may lead to poor follow-through and even lead the patient to seek care with another provider.
In order to foster widespread integration of these services, research and clinical gaps need to be addressed. Research gaps include the lack of prospective trials that compare the relative effectiveness of brain-gut psychotherapies with each other and/or with that of psychotropic medications. Other promising brain-gut therapies, such as mindfulness meditation or acceptance-based approaches, lack sufficient research to be included in clinical practice. Limited evidence supports the effect of psychotherapies have in accelerating or enhancing the efficacy of pharmacologic therapies and on improving disease course or inflammation in conditions such as Crohn’s and ulcerative colitis.
Clinical gaps include the need for better coverage for these therapies by insurance – many providers are out of network or do not accept insurance, although Medicare and commercial insurance plans often cover the cost of services in network. Health psychologists can be reimbursed for health and behavior codes for treating these conditions (CPTs 96150/96152), but there are restrictions on which other types of professionals can use them. Ongoing research is focusing on the cost-effectiveness of these therapies, although some highly effective therapies may be short term and have a one-time total cost of $1,000-$2,000 paid out of pocket. There is a growing need to expand remote, online, or digitally based brain-gut therapies with more trained health care providers that could offset overhead and other therapy costs.
SOURCE: Keefer L et al. Gastroenterology. doi: 10.1053/j.gastro.2018.01.045.
This burden includes digestive symptoms and disease severity, as well as patients’ ability to cope with them. Chronic digestive diseases, such as irritable bowel syndrome, gastroesophageal reflux disease, and inflammatory bowel diseases, cannot be disentangled from their psychosocial context. In this regard, the role of gastroenterologists in promoting best practices for the assessment and referral of patients across the spectrum of disease to brain-gut psychotherapies is crucial.
A review by Laurie Keefer, PhD, AGAF, and her coauthors, published in the April issue of Gastroenterology, provided a clinical update on the structure and efficacy of two major classes of psychogastroenterology – cognitive-behavioral therapy (CBT) and gut-directed hypnotherapy (HYP). The review discussed the effects of these therapies on GI symptoms and the patients’ ability to improve coping, resilience, and self-regulation. The review also provided a framework to understand the scientific rationale and best practices associated with incorporating brain-gut psychotherapies into routine GI care. Furthermore, it presented recommendations on how to address psychological issues and make effective referrals in routine practice.
Previous studies had highlighted that the burden of chronic digestive diseases is amplified by psychosocial factors, including poor coping, depression, and poor social support. Mental health professionals specializing in psychogastroenterology integrate the use of brain-gut psychotherapies into GI practice settings, which may help reduce health care utilization and symptom burden.
The article contains best practice advice based on a review of the literature, including existing systematic reviews and expert opinions. These best practices include the following:
- Gastroenterologists routinely should assess health-related quality of life, symptom-specific anxieties, early-life adversity, and functional impairment related to a patient’s digestive complaints.
- Gastroenterologists should master patient-friendly language to help explain the brain-gut pathway and how this pathway can become dysregulated by any number of factors, the psychosocial risks perpetuating and maintaining factors of GI diseases, and why the gastroenterologist is referring a patient to a mental health provider.
- Gastroenterologists should know the structure and core features of the most effective brain-gut psychotherapies.
- Gastroenterologists should establish a direct referral and ongoing communication pathway with one or two qualified mental health providers and assure patients that he/she will remain a part of the care team.
- Gastroenterologists should familiarize themselves with one or two neuromodulators that can be used to augment behavioral therapies when necessary.
Patient education about the referral to a mental health provider is difficult and requires attention to detail and fostering a good physician-patient relationship. It is important to help patients understand why they are being referred to a psychologist for a gastrointestinal complaint and that their physical symptoms are not being discounted. Failure to properly explain the reason for referral may lead to poor follow-through and even lead the patient to seek care with another provider.
In order to foster widespread integration of these services, research and clinical gaps need to be addressed. Research gaps include the lack of prospective trials that compare the relative effectiveness of brain-gut psychotherapies with each other and/or with that of psychotropic medications. Other promising brain-gut therapies, such as mindfulness meditation or acceptance-based approaches, lack sufficient research to be included in clinical practice. Limited evidence supports the effect of psychotherapies have in accelerating or enhancing the efficacy of pharmacologic therapies and on improving disease course or inflammation in conditions such as Crohn’s and ulcerative colitis.
Clinical gaps include the need for better coverage for these therapies by insurance – many providers are out of network or do not accept insurance, although Medicare and commercial insurance plans often cover the cost of services in network. Health psychologists can be reimbursed for health and behavior codes for treating these conditions (CPTs 96150/96152), but there are restrictions on which other types of professionals can use them. Ongoing research is focusing on the cost-effectiveness of these therapies, although some highly effective therapies may be short term and have a one-time total cost of $1,000-$2,000 paid out of pocket. There is a growing need to expand remote, online, or digitally based brain-gut therapies with more trained health care providers that could offset overhead and other therapy costs.
SOURCE: Keefer L et al. Gastroenterology. doi: 10.1053/j.gastro.2018.01.045.
FROM GASTROENTEROLOGY
New IDSA guidelines for managing infectious diarrhea
Clinical question: What is the best management of acute or persistent infectious diarrhea in adults and children?
Background: The last set of guidelines from the Infectious Diseases Society of America (IDSA) regarding acute or persistent infectious diarrhea in adults and children was published in 2001. This provides a comprehensive evidence-based update.
Setting: Expert panel assembled by IDSA.
Synopsis: A panel of experts convened by IDSA reviewed studies through December 2013, focusing on acute or persistent infectious diarrhea in infants, children, adolescents, and adults in the United States. Using GRADE criteria, the panel generated 60 recommendations. Recommendations of interest to hospitalists include those for testing and treating acute diarrhea. Testing stool for bacterial pathogens is recommended for patients with diarrhea and fever, bloody or mucoid stools, severe abdominal cramping or tenderness, or sepsis (additional testing is recommended in immunocompromised patients). Blood cultures are recommended for those who are less than 3 months of age, septic, or at risk for enteric fever. Antibiotics are not recommended for immunocompetent adults or children with either watery or bloody diarrhea, unless sepsis is present or the patient is less than 3 months of age with a presumed bacterial etiology in the latter. Recommendations regarding Clostridium difficile infections are not included in these guidelines.
Bottom line: These updated guidelines provide evidence-based recommendations for the management of acute or persistent diarrhea in infants, children, adolescents, and adults.
Citation: Shane AL et al. 2017 Infectious Diseases Society of America clinical practice guidelines for the diagnosis and management of infectious diarrhea. Clin Infect Dis. 2017 Nov 29; 65(12):1963-73. doi: 10.1093/cid/cix959.
Dr. Bonsall is associate professor of medicine in the division of hospital medicine, Emory University, Atlanta.
Clinical question: What is the best management of acute or persistent infectious diarrhea in adults and children?
Background: The last set of guidelines from the Infectious Diseases Society of America (IDSA) regarding acute or persistent infectious diarrhea in adults and children was published in 2001. This provides a comprehensive evidence-based update.
Setting: Expert panel assembled by IDSA.
Synopsis: A panel of experts convened by IDSA reviewed studies through December 2013, focusing on acute or persistent infectious diarrhea in infants, children, adolescents, and adults in the United States. Using GRADE criteria, the panel generated 60 recommendations. Recommendations of interest to hospitalists include those for testing and treating acute diarrhea. Testing stool for bacterial pathogens is recommended for patients with diarrhea and fever, bloody or mucoid stools, severe abdominal cramping or tenderness, or sepsis (additional testing is recommended in immunocompromised patients). Blood cultures are recommended for those who are less than 3 months of age, septic, or at risk for enteric fever. Antibiotics are not recommended for immunocompetent adults or children with either watery or bloody diarrhea, unless sepsis is present or the patient is less than 3 months of age with a presumed bacterial etiology in the latter. Recommendations regarding Clostridium difficile infections are not included in these guidelines.
Bottom line: These updated guidelines provide evidence-based recommendations for the management of acute or persistent diarrhea in infants, children, adolescents, and adults.
Citation: Shane AL et al. 2017 Infectious Diseases Society of America clinical practice guidelines for the diagnosis and management of infectious diarrhea. Clin Infect Dis. 2017 Nov 29; 65(12):1963-73. doi: 10.1093/cid/cix959.
Dr. Bonsall is associate professor of medicine in the division of hospital medicine, Emory University, Atlanta.
Clinical question: What is the best management of acute or persistent infectious diarrhea in adults and children?
Background: The last set of guidelines from the Infectious Diseases Society of America (IDSA) regarding acute or persistent infectious diarrhea in adults and children was published in 2001. This provides a comprehensive evidence-based update.
Setting: Expert panel assembled by IDSA.
Synopsis: A panel of experts convened by IDSA reviewed studies through December 2013, focusing on acute or persistent infectious diarrhea in infants, children, adolescents, and adults in the United States. Using GRADE criteria, the panel generated 60 recommendations. Recommendations of interest to hospitalists include those for testing and treating acute diarrhea. Testing stool for bacterial pathogens is recommended for patients with diarrhea and fever, bloody or mucoid stools, severe abdominal cramping or tenderness, or sepsis (additional testing is recommended in immunocompromised patients). Blood cultures are recommended for those who are less than 3 months of age, septic, or at risk for enteric fever. Antibiotics are not recommended for immunocompetent adults or children with either watery or bloody diarrhea, unless sepsis is present or the patient is less than 3 months of age with a presumed bacterial etiology in the latter. Recommendations regarding Clostridium difficile infections are not included in these guidelines.
Bottom line: These updated guidelines provide evidence-based recommendations for the management of acute or persistent diarrhea in infants, children, adolescents, and adults.
Citation: Shane AL et al. 2017 Infectious Diseases Society of America clinical practice guidelines for the diagnosis and management of infectious diarrhea. Clin Infect Dis. 2017 Nov 29; 65(12):1963-73. doi: 10.1093/cid/cix959.
Dr. Bonsall is associate professor of medicine in the division of hospital medicine, Emory University, Atlanta.
Opioids linked to mortality in IBD
Among patients with inflammatory bowel disease (IBD), opioid prescriptions tripled during a recent 20-year period, and heavy use of strong opioids was a significant predictor of all-cause mortality, according to a large cohort study reported in the April issue of Clinical Gastroenterology and Hepatology.
Because this study was retrospective, it could not establish causality, said Nicholas E. Burr, MD, of the University of Leeds (England) and his associates. But “[de]signing and conducting a large-scale randomized controlled trial may not be feasible,” they wrote. “Despite the limitations of observational data, population data sets may be the best method to investigate a potential effect.”
The gastrointestinal side effects of many analgesics complicate pain management for patients with IBD, who not only live with chronic abdominal pain but also can develop arthropathy-related musculoskeletal pain, chronic widespread pain, and fibromyalgia. In addition to the risk of narcotic bowel associated with opioid use in IBD, opioids can mask flares in IBD or can cause toxic dilatation if administered during acute flares, the researchers noted. Because few studies had examined opioid use in IBD, the investigators retrospectively studied 3,517 individuals with Crohn’s disease and 5,349 patients with ulcerative colitis from ResearchOne, a primary care electronic health records database that covers about 10% of patients in England. The data set excluded patients with indeterminate colitis or who underwent colectomy for ulcerative colitis.
From 1990 through 1993, only 10% of patients with IBD were prescribed opioids, vs. 30% from 2010 through 2013 (P less than .005). After the investigators controlled for numerous demographic and clinical variables, being prescribed a strong opioid (morphine, oxycodone, fentanyl, buprenorphine, methadone, hydromorphone, or pethidine) more than three times per year significantly correlated with all-cause mortality in both Crohn’s disease (hazard ratio, 2.2; 95% confidence interval, 1.2-4.0) and ulcerative colitis (HR, 3.3; 95% CI, 1.8-6.2), the researchers reported.Among patients with ulcerative colitis, more moderate use of strong opioids (one to three prescriptions annually) also significantly correlated with all-cause mortality (HR, 2.4; 95% CI, 1.2-5.2), as did heavy use of codeine (HR, 1.8; 95% CI, 1.1-3.1), but these associations did not reach statistical significance among patients with Crohn’s disease. Tramadol was not linked to mortality in either IBD subtype when used alone or in combination with codeine.
Dr. Burr and his associates said they could not control for several important potential confounders, including fistulating disease, quality of life, mental illness, substance abuse, and history of abuse, all of which have been linked to opioid use in IBD. Nonetheless, they found dose-dependent correlations with mortality that highlight a need for pharmacovigilance of opioids in IBD, particularly given dramatic increases in prescriptions, they said. These were primary care data, which tend to accurately reflect long-term medication use, they noted.
Crohn’s and Colitis U.K. and the Leeds Teaching Hospitals NHS Trust Charitable Foundation provided funding. The investigators reported having no conflicts of interest.
SOURCE: Burr NE et al. Clin Gastroenterol Hepatol. doi: 10.1016/j.cgh.2017.10.022.
Balancing control of pain and prevention of opioid-related morbidity and mortality remains a major challenge for health care providers, particularly in IBD. This study by Burr et al. highlights the potential dangers of opiate use among patients with IBD with the finding that opioid prescriptions at least three times per year were associated with a two- to threefold increase in mortality. Another important observation from this study was that the prevalence of opioid use among IBD patients increased from 10% to 30% during 1990-2013. One would like to believe that, with better treatment modalities for IBD, fewer patients would require chronic opioid medications over time; however, this observation suggests that there has been a shift in the perception and acceptance of opioids for IBD patients.
Studying opioid use among IBD patients remains challenging as even well-controlled retrospective studies are unable to fully separate whether opioid use is merely associated with more aggressive IBD courses and hence worse outcomes, or whether opioid use directly results in increased mortality. As clinicians, we are left with the difficult balance of addressing true symptoms of pain with the potential harm from opioids; we often counsel against the use of nonsteroidal anti-inflammatory medications in IBD, and yet there is growing concern about use of opioids in this same population. Further research is needed to address patients with pain not directly tied to inflammation or complications of IBD, as well as nonmedical, behavioral approaches to pain management.
Jason K. Hou, MD, MS, is an investigator in the clinical epidemiology and outcomes program, Center for Innovations in Quality, Effectiveness and Safety at the Michael E. DeBakey VA Medical Center, Houston; assistant professor, department of medicine, section of gastroenterology & hepatology, Baylor College of Medicine, Houston; and codirector of Inflammatory Bowel Disease Center at the VA Medical Center at Baylor. He has no conflicts of interest.
Balancing control of pain and prevention of opioid-related morbidity and mortality remains a major challenge for health care providers, particularly in IBD. This study by Burr et al. highlights the potential dangers of opiate use among patients with IBD with the finding that opioid prescriptions at least three times per year were associated with a two- to threefold increase in mortality. Another important observation from this study was that the prevalence of opioid use among IBD patients increased from 10% to 30% during 1990-2013. One would like to believe that, with better treatment modalities for IBD, fewer patients would require chronic opioid medications over time; however, this observation suggests that there has been a shift in the perception and acceptance of opioids for IBD patients.
Studying opioid use among IBD patients remains challenging as even well-controlled retrospective studies are unable to fully separate whether opioid use is merely associated with more aggressive IBD courses and hence worse outcomes, or whether opioid use directly results in increased mortality. As clinicians, we are left with the difficult balance of addressing true symptoms of pain with the potential harm from opioids; we often counsel against the use of nonsteroidal anti-inflammatory medications in IBD, and yet there is growing concern about use of opioids in this same population. Further research is needed to address patients with pain not directly tied to inflammation or complications of IBD, as well as nonmedical, behavioral approaches to pain management.
Jason K. Hou, MD, MS, is an investigator in the clinical epidemiology and outcomes program, Center for Innovations in Quality, Effectiveness and Safety at the Michael E. DeBakey VA Medical Center, Houston; assistant professor, department of medicine, section of gastroenterology & hepatology, Baylor College of Medicine, Houston; and codirector of Inflammatory Bowel Disease Center at the VA Medical Center at Baylor. He has no conflicts of interest.
Balancing control of pain and prevention of opioid-related morbidity and mortality remains a major challenge for health care providers, particularly in IBD. This study by Burr et al. highlights the potential dangers of opiate use among patients with IBD with the finding that opioid prescriptions at least three times per year were associated with a two- to threefold increase in mortality. Another important observation from this study was that the prevalence of opioid use among IBD patients increased from 10% to 30% during 1990-2013. One would like to believe that, with better treatment modalities for IBD, fewer patients would require chronic opioid medications over time; however, this observation suggests that there has been a shift in the perception and acceptance of opioids for IBD patients.
Studying opioid use among IBD patients remains challenging as even well-controlled retrospective studies are unable to fully separate whether opioid use is merely associated with more aggressive IBD courses and hence worse outcomes, or whether opioid use directly results in increased mortality. As clinicians, we are left with the difficult balance of addressing true symptoms of pain with the potential harm from opioids; we often counsel against the use of nonsteroidal anti-inflammatory medications in IBD, and yet there is growing concern about use of opioids in this same population. Further research is needed to address patients with pain not directly tied to inflammation or complications of IBD, as well as nonmedical, behavioral approaches to pain management.
Jason K. Hou, MD, MS, is an investigator in the clinical epidemiology and outcomes program, Center for Innovations in Quality, Effectiveness and Safety at the Michael E. DeBakey VA Medical Center, Houston; assistant professor, department of medicine, section of gastroenterology & hepatology, Baylor College of Medicine, Houston; and codirector of Inflammatory Bowel Disease Center at the VA Medical Center at Baylor. He has no conflicts of interest.
Among patients with inflammatory bowel disease (IBD), opioid prescriptions tripled during a recent 20-year period, and heavy use of strong opioids was a significant predictor of all-cause mortality, according to a large cohort study reported in the April issue of Clinical Gastroenterology and Hepatology.
Because this study was retrospective, it could not establish causality, said Nicholas E. Burr, MD, of the University of Leeds (England) and his associates. But “[de]signing and conducting a large-scale randomized controlled trial may not be feasible,” they wrote. “Despite the limitations of observational data, population data sets may be the best method to investigate a potential effect.”
The gastrointestinal side effects of many analgesics complicate pain management for patients with IBD, who not only live with chronic abdominal pain but also can develop arthropathy-related musculoskeletal pain, chronic widespread pain, and fibromyalgia. In addition to the risk of narcotic bowel associated with opioid use in IBD, opioids can mask flares in IBD or can cause toxic dilatation if administered during acute flares, the researchers noted. Because few studies had examined opioid use in IBD, the investigators retrospectively studied 3,517 individuals with Crohn’s disease and 5,349 patients with ulcerative colitis from ResearchOne, a primary care electronic health records database that covers about 10% of patients in England. The data set excluded patients with indeterminate colitis or who underwent colectomy for ulcerative colitis.
From 1990 through 1993, only 10% of patients with IBD were prescribed opioids, vs. 30% from 2010 through 2013 (P less than .005). After the investigators controlled for numerous demographic and clinical variables, being prescribed a strong opioid (morphine, oxycodone, fentanyl, buprenorphine, methadone, hydromorphone, or pethidine) more than three times per year significantly correlated with all-cause mortality in both Crohn’s disease (hazard ratio, 2.2; 95% confidence interval, 1.2-4.0) and ulcerative colitis (HR, 3.3; 95% CI, 1.8-6.2), the researchers reported.Among patients with ulcerative colitis, more moderate use of strong opioids (one to three prescriptions annually) also significantly correlated with all-cause mortality (HR, 2.4; 95% CI, 1.2-5.2), as did heavy use of codeine (HR, 1.8; 95% CI, 1.1-3.1), but these associations did not reach statistical significance among patients with Crohn’s disease. Tramadol was not linked to mortality in either IBD subtype when used alone or in combination with codeine.
Dr. Burr and his associates said they could not control for several important potential confounders, including fistulating disease, quality of life, mental illness, substance abuse, and history of abuse, all of which have been linked to opioid use in IBD. Nonetheless, they found dose-dependent correlations with mortality that highlight a need for pharmacovigilance of opioids in IBD, particularly given dramatic increases in prescriptions, they said. These were primary care data, which tend to accurately reflect long-term medication use, they noted.
Crohn’s and Colitis U.K. and the Leeds Teaching Hospitals NHS Trust Charitable Foundation provided funding. The investigators reported having no conflicts of interest.
SOURCE: Burr NE et al. Clin Gastroenterol Hepatol. doi: 10.1016/j.cgh.2017.10.022.
Among patients with inflammatory bowel disease (IBD), opioid prescriptions tripled during a recent 20-year period, and heavy use of strong opioids was a significant predictor of all-cause mortality, according to a large cohort study reported in the April issue of Clinical Gastroenterology and Hepatology.
Because this study was retrospective, it could not establish causality, said Nicholas E. Burr, MD, of the University of Leeds (England) and his associates. But “[de]signing and conducting a large-scale randomized controlled trial may not be feasible,” they wrote. “Despite the limitations of observational data, population data sets may be the best method to investigate a potential effect.”
The gastrointestinal side effects of many analgesics complicate pain management for patients with IBD, who not only live with chronic abdominal pain but also can develop arthropathy-related musculoskeletal pain, chronic widespread pain, and fibromyalgia. In addition to the risk of narcotic bowel associated with opioid use in IBD, opioids can mask flares in IBD or can cause toxic dilatation if administered during acute flares, the researchers noted. Because few studies had examined opioid use in IBD, the investigators retrospectively studied 3,517 individuals with Crohn’s disease and 5,349 patients with ulcerative colitis from ResearchOne, a primary care electronic health records database that covers about 10% of patients in England. The data set excluded patients with indeterminate colitis or who underwent colectomy for ulcerative colitis.
From 1990 through 1993, only 10% of patients with IBD were prescribed opioids, vs. 30% from 2010 through 2013 (P less than .005). After the investigators controlled for numerous demographic and clinical variables, being prescribed a strong opioid (morphine, oxycodone, fentanyl, buprenorphine, methadone, hydromorphone, or pethidine) more than three times per year significantly correlated with all-cause mortality in both Crohn’s disease (hazard ratio, 2.2; 95% confidence interval, 1.2-4.0) and ulcerative colitis (HR, 3.3; 95% CI, 1.8-6.2), the researchers reported.Among patients with ulcerative colitis, more moderate use of strong opioids (one to three prescriptions annually) also significantly correlated with all-cause mortality (HR, 2.4; 95% CI, 1.2-5.2), as did heavy use of codeine (HR, 1.8; 95% CI, 1.1-3.1), but these associations did not reach statistical significance among patients with Crohn’s disease. Tramadol was not linked to mortality in either IBD subtype when used alone or in combination with codeine.
Dr. Burr and his associates said they could not control for several important potential confounders, including fistulating disease, quality of life, mental illness, substance abuse, and history of abuse, all of which have been linked to opioid use in IBD. Nonetheless, they found dose-dependent correlations with mortality that highlight a need for pharmacovigilance of opioids in IBD, particularly given dramatic increases in prescriptions, they said. These were primary care data, which tend to accurately reflect long-term medication use, they noted.
Crohn’s and Colitis U.K. and the Leeds Teaching Hospitals NHS Trust Charitable Foundation provided funding. The investigators reported having no conflicts of interest.
SOURCE: Burr NE et al. Clin Gastroenterol Hepatol. doi: 10.1016/j.cgh.2017.10.022.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point:
Major finding: Thirty percent of patients were prescribed opioids in 2010-2013 vs. only 10% in 1990-1993 (P less than .005 for trend). Heavy use of strong opioids significantly correlated with all-cause mortality in both Crohn’s disease (hazard ratio, 2.2; 95% confidence interval, 1.2-4.0) and ulcerative colitis (HR, 3.3; 95% CI, 1.8- 6.2).
Study details: A retrospective cohort study of 3,517 individuals with Crohn’s disease and 5,349 individuals with ulcerative colitis.
Disclosures: Crohn’s and Colitis U.K. and the Leeds Teaching Hospitals NHS Trust Charitable Foundation provided funding. The investigators reported having no conflicts.
Source: Burr NE et al. Clin Gastroenterol Hepatol. doi: 10.1016/j.cgh.2017.10.022.
Prior bariatric surgery may lead to IBD
.
“A past history of bariatric surgery, but not recent surgery, was associated with both new-onset” Crohn’s disease and ulcerative colitis, wrote Ryan Ungaro, MD, assistant professor of medicine at the Icahn School of Medicine at Mount Sinai, New York. “Analyses further classifying recent bariatric surgery as preserved or altered intestinal anatomy showed no significant difference in risk … when compared to patients without a history of bariatric surgery.”
IBD and more specific conditions like ulcerative colitis (UC) and Crohn’s disease (CD) are on the rise. One environmental factor that can increase the likelihood of these disorders is surgery. To investigate how IBD may develop in response to bariatric surgery, Dr. Ungaro and his colleagues compiled descriptive case studies from six (three New York, three European) medical centers, then conducted a case-control study with a sample of patients from a large health claims database (Symphony Health Solutions Integrated Dataverse) to assess the association between prior bariatric surgery and risk of new-onset IBD. Using the information from the Symphony database, a database focusing exclusively on IBD patients was developed.
From the case studies included in the study, Dr. Ungaro and his colleagues identified 15 patients with IBD who had a prior history of bariatric surgery: 10 patients had CD, 4 had UC, and 1 had an unclassified form of IBD. Most of the patients had undergone Roux-en-Y gastroenterostomy. The average time between surgery and diagnosis of IBD was 5.7 years. Most of the cases (67%) were mild or moderate in severity and over half (53.3%) of the cases were mildly active. Only about a quarter of these patients required immunosuppressant therapy.
The database portion of the study also revealed some interesting associations between bariatric surgery and IBD. The researchers identified 8,980 patients with IBD and 43,059 controls. Ultimately, Dr. Ungaro and his colleagues found that any type of bariatric surgery increased the odds of developing IBD (adjusted odds ratio, 1.45; 95% confidence interval, 1.08-1.94). Interestingly, only past history of bariatric surgery was associated with an almost twofold increase in onset of IBD. The study also revealed that bariatric surgeries prior to 2008 were associated with an increase chance of developing IBD.
Bariatric surgery was not limited to increasing the risk of IBD, but also increased the specific risks for CD and UC. A past history of bariatric surgery was heavily associated with an increase of both CD (aOR,1.86; 95% CI,1.10-3.15; P = .066) and UC (aOR, 2.12; 95% CI, 1.26-3.57; P = .015).
The size of the sample and utilization of a large, national database strengthen the results of the study, but the use of retrospective data is a potential limitation. The deidentified nature of the data also makes it difficult to validate cases and determine whether new cases of IBD were definitely incident cases.
Regardless, there is still no clear-cut explanation why bariatric surgery would cause IBD. One of the proposed mechanisms is vitamin D deficiency caused by malabsorption, a common consequence of the Roux-en-Y procedure. Vitamin D deficiency is often linked with an increased risk of developing IBD. Additionally, bariatric surgery may alter bile acid composition, which can have inflammatory effects.
Because no direct mechanism has been identified, Dr. Ungaro stated that further research needs to be done.
“The potential association between prior bariatric surgery and new IBD highlights the need to perform a thorough work-up and have a broad differential diagnosis in postbariatric surgery patients with new gastrointestinal symptoms,” Dr. Ungaro and his colleagues wrote. “However, given the nature of administrative database studies, we cannot draw causative conclusions and further prospective studies are needed to confirm this association and delineate if certain types of bariatric surgeries have differential effects on risk of IBD.”
Multiple authors who worked on this study have worked as consultants for pharmaceutical companies. Dr. Ungaro is supported by a Crohn’s and Colitis Foundation career development award and a KL2 Scholar award.
SOURCE: Ungaro R et al. Aliment Pharmacol Ther. 2018 Mar 7;47[8]:1126-34: doi: 10.1111/apt.14569.
.
“A past history of bariatric surgery, but not recent surgery, was associated with both new-onset” Crohn’s disease and ulcerative colitis, wrote Ryan Ungaro, MD, assistant professor of medicine at the Icahn School of Medicine at Mount Sinai, New York. “Analyses further classifying recent bariatric surgery as preserved or altered intestinal anatomy showed no significant difference in risk … when compared to patients without a history of bariatric surgery.”
IBD and more specific conditions like ulcerative colitis (UC) and Crohn’s disease (CD) are on the rise. One environmental factor that can increase the likelihood of these disorders is surgery. To investigate how IBD may develop in response to bariatric surgery, Dr. Ungaro and his colleagues compiled descriptive case studies from six (three New York, three European) medical centers, then conducted a case-control study with a sample of patients from a large health claims database (Symphony Health Solutions Integrated Dataverse) to assess the association between prior bariatric surgery and risk of new-onset IBD. Using the information from the Symphony database, a database focusing exclusively on IBD patients was developed.
From the case studies included in the study, Dr. Ungaro and his colleagues identified 15 patients with IBD who had a prior history of bariatric surgery: 10 patients had CD, 4 had UC, and 1 had an unclassified form of IBD. Most of the patients had undergone Roux-en-Y gastroenterostomy. The average time between surgery and diagnosis of IBD was 5.7 years. Most of the cases (67%) were mild or moderate in severity and over half (53.3%) of the cases were mildly active. Only about a quarter of these patients required immunosuppressant therapy.
The database portion of the study also revealed some interesting associations between bariatric surgery and IBD. The researchers identified 8,980 patients with IBD and 43,059 controls. Ultimately, Dr. Ungaro and his colleagues found that any type of bariatric surgery increased the odds of developing IBD (adjusted odds ratio, 1.45; 95% confidence interval, 1.08-1.94). Interestingly, only past history of bariatric surgery was associated with an almost twofold increase in onset of IBD. The study also revealed that bariatric surgeries prior to 2008 were associated with an increase chance of developing IBD.
Bariatric surgery was not limited to increasing the risk of IBD, but also increased the specific risks for CD and UC. A past history of bariatric surgery was heavily associated with an increase of both CD (aOR,1.86; 95% CI,1.10-3.15; P = .066) and UC (aOR, 2.12; 95% CI, 1.26-3.57; P = .015).
The size of the sample and utilization of a large, national database strengthen the results of the study, but the use of retrospective data is a potential limitation. The deidentified nature of the data also makes it difficult to validate cases and determine whether new cases of IBD were definitely incident cases.
Regardless, there is still no clear-cut explanation why bariatric surgery would cause IBD. One of the proposed mechanisms is vitamin D deficiency caused by malabsorption, a common consequence of the Roux-en-Y procedure. Vitamin D deficiency is often linked with an increased risk of developing IBD. Additionally, bariatric surgery may alter bile acid composition, which can have inflammatory effects.
Because no direct mechanism has been identified, Dr. Ungaro stated that further research needs to be done.
“The potential association between prior bariatric surgery and new IBD highlights the need to perform a thorough work-up and have a broad differential diagnosis in postbariatric surgery patients with new gastrointestinal symptoms,” Dr. Ungaro and his colleagues wrote. “However, given the nature of administrative database studies, we cannot draw causative conclusions and further prospective studies are needed to confirm this association and delineate if certain types of bariatric surgeries have differential effects on risk of IBD.”
Multiple authors who worked on this study have worked as consultants for pharmaceutical companies. Dr. Ungaro is supported by a Crohn’s and Colitis Foundation career development award and a KL2 Scholar award.
SOURCE: Ungaro R et al. Aliment Pharmacol Ther. 2018 Mar 7;47[8]:1126-34: doi: 10.1111/apt.14569.
.
“A past history of bariatric surgery, but not recent surgery, was associated with both new-onset” Crohn’s disease and ulcerative colitis, wrote Ryan Ungaro, MD, assistant professor of medicine at the Icahn School of Medicine at Mount Sinai, New York. “Analyses further classifying recent bariatric surgery as preserved or altered intestinal anatomy showed no significant difference in risk … when compared to patients without a history of bariatric surgery.”
IBD and more specific conditions like ulcerative colitis (UC) and Crohn’s disease (CD) are on the rise. One environmental factor that can increase the likelihood of these disorders is surgery. To investigate how IBD may develop in response to bariatric surgery, Dr. Ungaro and his colleagues compiled descriptive case studies from six (three New York, three European) medical centers, then conducted a case-control study with a sample of patients from a large health claims database (Symphony Health Solutions Integrated Dataverse) to assess the association between prior bariatric surgery and risk of new-onset IBD. Using the information from the Symphony database, a database focusing exclusively on IBD patients was developed.
From the case studies included in the study, Dr. Ungaro and his colleagues identified 15 patients with IBD who had a prior history of bariatric surgery: 10 patients had CD, 4 had UC, and 1 had an unclassified form of IBD. Most of the patients had undergone Roux-en-Y gastroenterostomy. The average time between surgery and diagnosis of IBD was 5.7 years. Most of the cases (67%) were mild or moderate in severity and over half (53.3%) of the cases were mildly active. Only about a quarter of these patients required immunosuppressant therapy.
The database portion of the study also revealed some interesting associations between bariatric surgery and IBD. The researchers identified 8,980 patients with IBD and 43,059 controls. Ultimately, Dr. Ungaro and his colleagues found that any type of bariatric surgery increased the odds of developing IBD (adjusted odds ratio, 1.45; 95% confidence interval, 1.08-1.94). Interestingly, only past history of bariatric surgery was associated with an almost twofold increase in onset of IBD. The study also revealed that bariatric surgeries prior to 2008 were associated with an increase chance of developing IBD.
Bariatric surgery was not limited to increasing the risk of IBD, but also increased the specific risks for CD and UC. A past history of bariatric surgery was heavily associated with an increase of both CD (aOR,1.86; 95% CI,1.10-3.15; P = .066) and UC (aOR, 2.12; 95% CI, 1.26-3.57; P = .015).
The size of the sample and utilization of a large, national database strengthen the results of the study, but the use of retrospective data is a potential limitation. The deidentified nature of the data also makes it difficult to validate cases and determine whether new cases of IBD were definitely incident cases.
Regardless, there is still no clear-cut explanation why bariatric surgery would cause IBD. One of the proposed mechanisms is vitamin D deficiency caused by malabsorption, a common consequence of the Roux-en-Y procedure. Vitamin D deficiency is often linked with an increased risk of developing IBD. Additionally, bariatric surgery may alter bile acid composition, which can have inflammatory effects.
Because no direct mechanism has been identified, Dr. Ungaro stated that further research needs to be done.
“The potential association between prior bariatric surgery and new IBD highlights the need to perform a thorough work-up and have a broad differential diagnosis in postbariatric surgery patients with new gastrointestinal symptoms,” Dr. Ungaro and his colleagues wrote. “However, given the nature of administrative database studies, we cannot draw causative conclusions and further prospective studies are needed to confirm this association and delineate if certain types of bariatric surgeries have differential effects on risk of IBD.”
Multiple authors who worked on this study have worked as consultants for pharmaceutical companies. Dr. Ungaro is supported by a Crohn’s and Colitis Foundation career development award and a KL2 Scholar award.
SOURCE: Ungaro R et al. Aliment Pharmacol Ther. 2018 Mar 7;47[8]:1126-34: doi: 10.1111/apt.14569.
FROM ALIMENTARY PHARMACOLOGY AND THERAPEUTICS
Key clinical point: Bariatric surgery is associated with an increase of bowel disorders.
Major finding: Any type of bariatric surgery increased the odds of developing IBD (aOR 1.45; 95% CI, 1.08-1.94).
Study details: A multicenter case study analysis and a case-control study using a medical claims database from 2008 to 2012.
Disclosures: Multiple authors who worked on this study have worked as consultants for pharmaceutical companies.
Source: Ungaro R et al. Aliment Pharmacol Ther. 2018 Mar 7;47[8]:1126-34. doi: 10.1111/apt.14569.
Understanding the new CMS bundle model
Hospitalists have been among the highest-volume participants in Medicare’s Bundled Payments for Care Improvement (BPCI) demonstration model, initiating over 200,000 episodes representing $4.7 billion in spending since the model began.1 On Jan. 9, the Centers for Medicare & Medicaid Services announced BPCI’s follow-on model, “BPCI Advanced.”2
BPCI launched in October 2013 and sunsets at the end of Q3 2018. BPCI Advanced starts immediately upon conclusion of BPCI (Q4 2018) and is slated to finish at year-end 2023.
CMS intends for the program to qualify as an Advanced Alternative Payment Model (APM). As BPCI Advanced focuses on episodes of care involving an inpatient stay (It also includes three outpatient episodes.) and the subsequent 90-day recovery period, it represents the first large-scale opportunity for hospitalists to meet criteria for Advanced APM participation. Qualifying for the Advanced APM track of the Quality Payment Program – which involves meeting patient volume or payment thresholds3 – comes with a 5% lump-sum bonus based on Medicare Part B fees and avoids exposure to penalties and reporting requirements of the Merit-based Incentive Payment System (MIPS).
Key program features
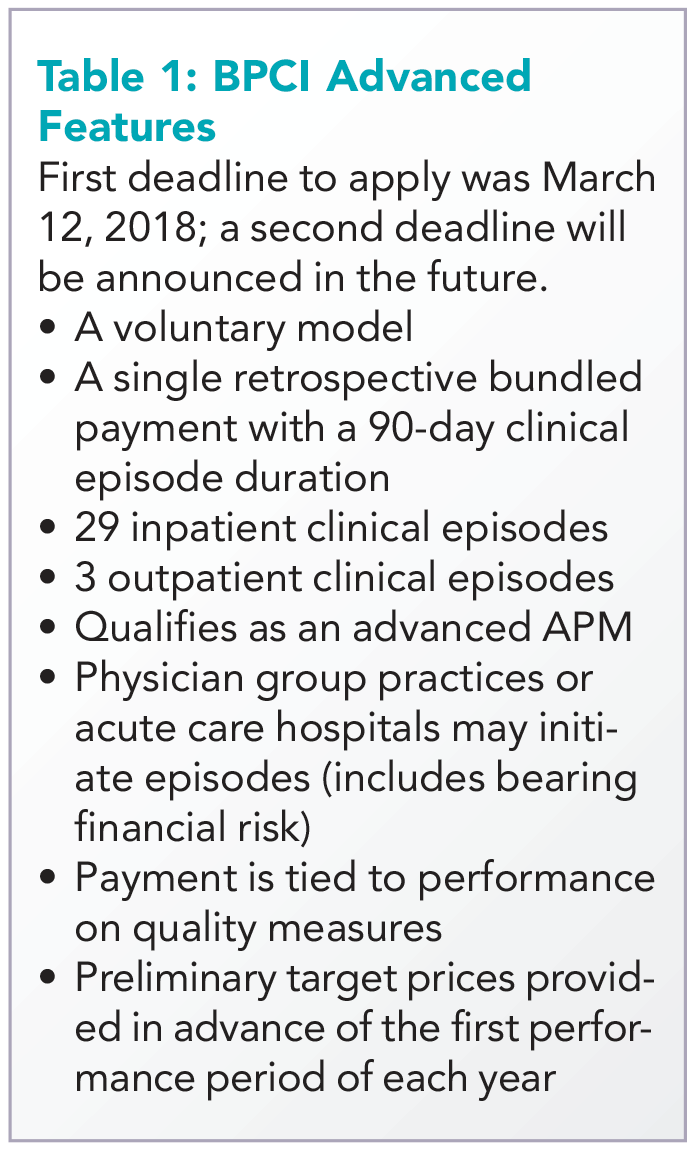
Acute care hospitals and physician groups may initiate episodes under BPCI Advanced, assuming financial risk under the model. Similar to its predecessor, BPCI Advanced assigns a target price based on past claims payments associated with the “episode initiator.”
During the performance period, if the initiator can beat the price in the aggregate for its bundles, it can keep the difference, and if it comes in over the price, it must pay the difference back to Medicare. Medicare discounts the target price by 3%, effectively paying itself that amount. After that, there is no sharing of savings with Medicare, as opposed to the permanent ACO programs, where there is sharing after the ACO meets the minimum savings rate.
The program allows physician groups and hospital initiators to go it alone or to work with a “convener,” which may share risk and reward with initiators, and may provide software, analytics, networks of high-performing providers like nursing facilities, and knowledge of specific care redesign approaches to enable program success. See Table 1 for a listing of other notable features of BPCI Advanced.
Quality measures
BPCI Advanced qualifies as an Advanced APM in part because payment is tied to performance on a set of quality measures (see Table 2). There are two measures applied to all episodes: all-cause hospital readmissions and advance care plan. These are notable because hospitalists may be especially focused on improvement activities in these areas.
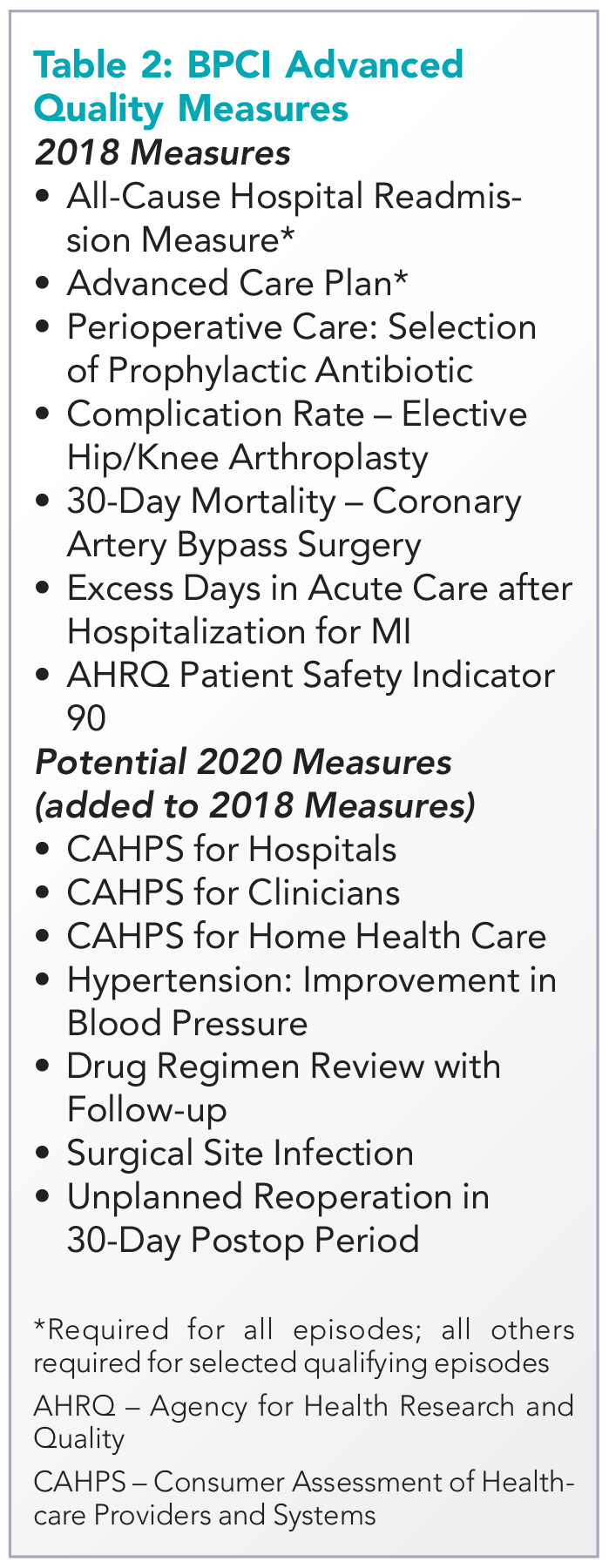
While the advance care plan measure refers to a process reflected by record documentation and is therefore directly under the control of hospitalists, readmissions – and most of the other measures – require a team approach. Because the outcome measures are risk adjusted, accurate and complete clinical documentation is crucial, as it drives how risk is adjusted. Of note, all the 2018 measures, collected directly through claims, will place no additional administrative burden for collection on providers.
Two ways for hospitalists to participate
Hospitalist groups – whether independent or employed – may be episode initiators in BPCI Advanced. In this case, any episodes in which the group participates that carry the name of a member of the hospitalist group in the “Attending Provider” field on the hospital bill claim form to Medicare (and the associated carrier claim) are attributed to that member’s physician group.
For example, if the group has chosen heart failure as an episode in which to participate at the program’s outset, a hospitalization is assigned the heart failure DRG (diagnosis-related group) and a group member is the Attending Provider on the claim form (and submits a claim for the physician services), then the episode is attributed to that group. This means that the group is responsible for payments represented by Medicare Part A and Part B claims (with a few exclusions like trauma and cancer) against the target price for the initial hospitalization and subsequent 90-day period. In practice, hospitalists are rewarded for actions aimed at optimizing location after discharge,4 avoiding readmissions, choosing efficient nursing facilities, and helping patients to maximize functional status.
The other way hospitalists may participate is through an agreement to share in savings with a hospital or physician group episode initiator. This requires hospitalist individuals or groups to enter into a contract with the initiator that meets certain program requirements – for example, report quality measures, engage in care redesign, use certified EHR technology (hospital-based clinicians automatically fulfill this criterion).
If there is broad participation, BPCI Advanced could represent a key milestone for hospitalists, as they seek to be recognized for the value they confer to the system as a whole instead of simply their professional billings. While there are legitimate concerns about the effect MIPS may have on health care value and the complexity of participation in APMs, barring a repeal of the law that created them, hospitalists now have the chance to extend their influence within and outside the hospital’s four walls and be more fairly rewarded for it.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of the Society of Hospital Medicine. Contact him at [email protected]. Disclosure: The author’s employer, Remedy Partners, is an Awardee Convener for the BPCI initiative and intends to apply as a Convener in BPCI Advanced.
References
1. Based on BPCI awardee convener Remedy Partners claims analysis.
2. https://innovation.cms.gov/initiatives/bpci-advanced.
3. https://qpp.cms.gov/apms/overview.
4. Whitcomb W. Choosing location after discharge wisely. The-hospitalist.org. 2018 Jan 3. Digital edition. Accessed Jan 13, 2018.
Hospitalists have been among the highest-volume participants in Medicare’s Bundled Payments for Care Improvement (BPCI) demonstration model, initiating over 200,000 episodes representing $4.7 billion in spending since the model began.1 On Jan. 9, the Centers for Medicare & Medicaid Services announced BPCI’s follow-on model, “BPCI Advanced.”2
BPCI launched in October 2013 and sunsets at the end of Q3 2018. BPCI Advanced starts immediately upon conclusion of BPCI (Q4 2018) and is slated to finish at year-end 2023.
CMS intends for the program to qualify as an Advanced Alternative Payment Model (APM). As BPCI Advanced focuses on episodes of care involving an inpatient stay (It also includes three outpatient episodes.) and the subsequent 90-day recovery period, it represents the first large-scale opportunity for hospitalists to meet criteria for Advanced APM participation. Qualifying for the Advanced APM track of the Quality Payment Program – which involves meeting patient volume or payment thresholds3 – comes with a 5% lump-sum bonus based on Medicare Part B fees and avoids exposure to penalties and reporting requirements of the Merit-based Incentive Payment System (MIPS).
Key program features
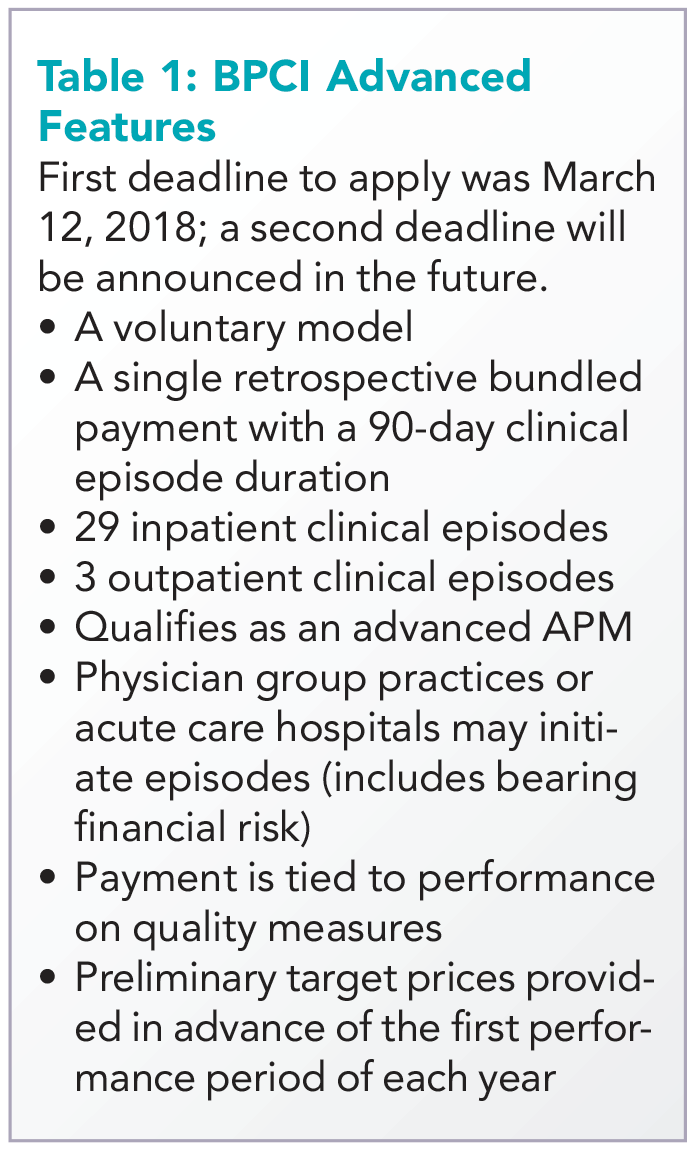
Acute care hospitals and physician groups may initiate episodes under BPCI Advanced, assuming financial risk under the model. Similar to its predecessor, BPCI Advanced assigns a target price based on past claims payments associated with the “episode initiator.”
During the performance period, if the initiator can beat the price in the aggregate for its bundles, it can keep the difference, and if it comes in over the price, it must pay the difference back to Medicare. Medicare discounts the target price by 3%, effectively paying itself that amount. After that, there is no sharing of savings with Medicare, as opposed to the permanent ACO programs, where there is sharing after the ACO meets the minimum savings rate.
The program allows physician groups and hospital initiators to go it alone or to work with a “convener,” which may share risk and reward with initiators, and may provide software, analytics, networks of high-performing providers like nursing facilities, and knowledge of specific care redesign approaches to enable program success. See Table 1 for a listing of other notable features of BPCI Advanced.
Quality measures
BPCI Advanced qualifies as an Advanced APM in part because payment is tied to performance on a set of quality measures (see Table 2). There are two measures applied to all episodes: all-cause hospital readmissions and advance care plan. These are notable because hospitalists may be especially focused on improvement activities in these areas.
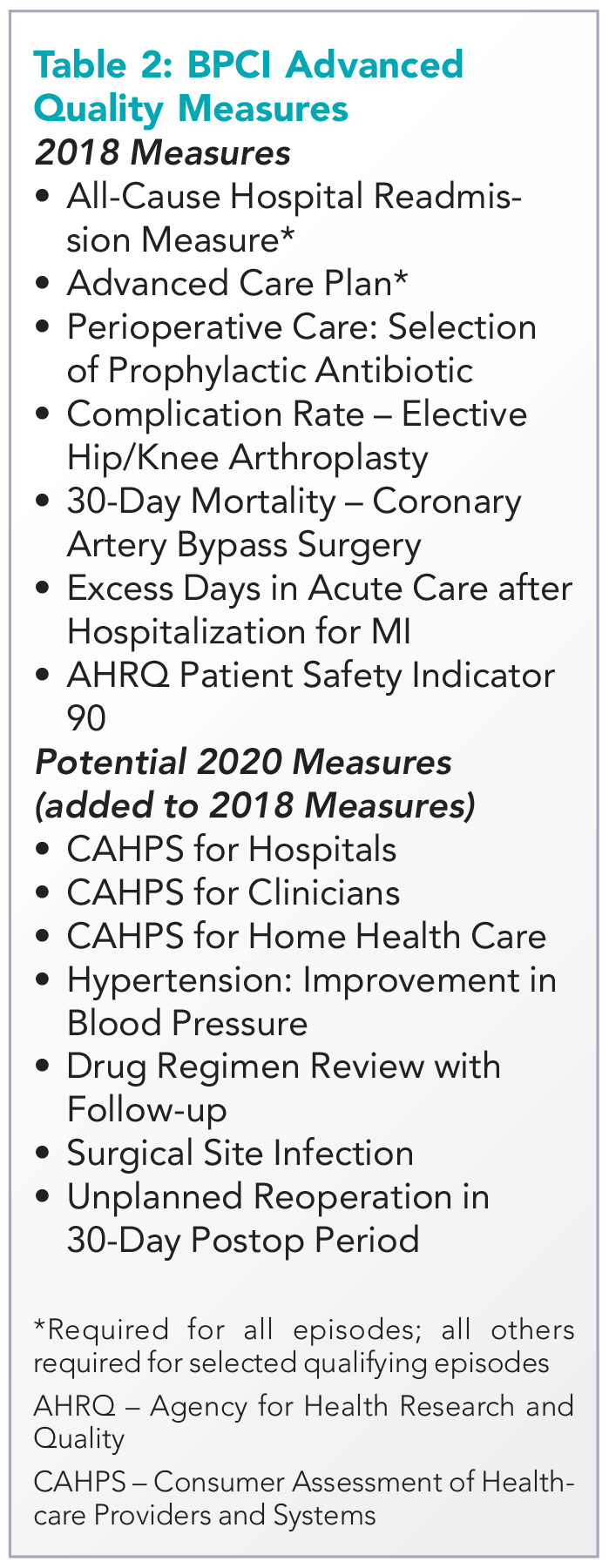
While the advance care plan measure refers to a process reflected by record documentation and is therefore directly under the control of hospitalists, readmissions – and most of the other measures – require a team approach. Because the outcome measures are risk adjusted, accurate and complete clinical documentation is crucial, as it drives how risk is adjusted. Of note, all the 2018 measures, collected directly through claims, will place no additional administrative burden for collection on providers.
Two ways for hospitalists to participate
Hospitalist groups – whether independent or employed – may be episode initiators in BPCI Advanced. In this case, any episodes in which the group participates that carry the name of a member of the hospitalist group in the “Attending Provider” field on the hospital bill claim form to Medicare (and the associated carrier claim) are attributed to that member’s physician group.
For example, if the group has chosen heart failure as an episode in which to participate at the program’s outset, a hospitalization is assigned the heart failure DRG (diagnosis-related group) and a group member is the Attending Provider on the claim form (and submits a claim for the physician services), then the episode is attributed to that group. This means that the group is responsible for payments represented by Medicare Part A and Part B claims (with a few exclusions like trauma and cancer) against the target price for the initial hospitalization and subsequent 90-day period. In practice, hospitalists are rewarded for actions aimed at optimizing location after discharge,4 avoiding readmissions, choosing efficient nursing facilities, and helping patients to maximize functional status.
The other way hospitalists may participate is through an agreement to share in savings with a hospital or physician group episode initiator. This requires hospitalist individuals or groups to enter into a contract with the initiator that meets certain program requirements – for example, report quality measures, engage in care redesign, use certified EHR technology (hospital-based clinicians automatically fulfill this criterion).
If there is broad participation, BPCI Advanced could represent a key milestone for hospitalists, as they seek to be recognized for the value they confer to the system as a whole instead of simply their professional billings. While there are legitimate concerns about the effect MIPS may have on health care value and the complexity of participation in APMs, barring a repeal of the law that created them, hospitalists now have the chance to extend their influence within and outside the hospital’s four walls and be more fairly rewarded for it.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of the Society of Hospital Medicine. Contact him at [email protected]. Disclosure: The author’s employer, Remedy Partners, is an Awardee Convener for the BPCI initiative and intends to apply as a Convener in BPCI Advanced.
References
1. Based on BPCI awardee convener Remedy Partners claims analysis.
2. https://innovation.cms.gov/initiatives/bpci-advanced.
3. https://qpp.cms.gov/apms/overview.
4. Whitcomb W. Choosing location after discharge wisely. The-hospitalist.org. 2018 Jan 3. Digital edition. Accessed Jan 13, 2018.
Hospitalists have been among the highest-volume participants in Medicare’s Bundled Payments for Care Improvement (BPCI) demonstration model, initiating over 200,000 episodes representing $4.7 billion in spending since the model began.1 On Jan. 9, the Centers for Medicare & Medicaid Services announced BPCI’s follow-on model, “BPCI Advanced.”2
BPCI launched in October 2013 and sunsets at the end of Q3 2018. BPCI Advanced starts immediately upon conclusion of BPCI (Q4 2018) and is slated to finish at year-end 2023.
CMS intends for the program to qualify as an Advanced Alternative Payment Model (APM). As BPCI Advanced focuses on episodes of care involving an inpatient stay (It also includes three outpatient episodes.) and the subsequent 90-day recovery period, it represents the first large-scale opportunity for hospitalists to meet criteria for Advanced APM participation. Qualifying for the Advanced APM track of the Quality Payment Program – which involves meeting patient volume or payment thresholds3 – comes with a 5% lump-sum bonus based on Medicare Part B fees and avoids exposure to penalties and reporting requirements of the Merit-based Incentive Payment System (MIPS).
Key program features
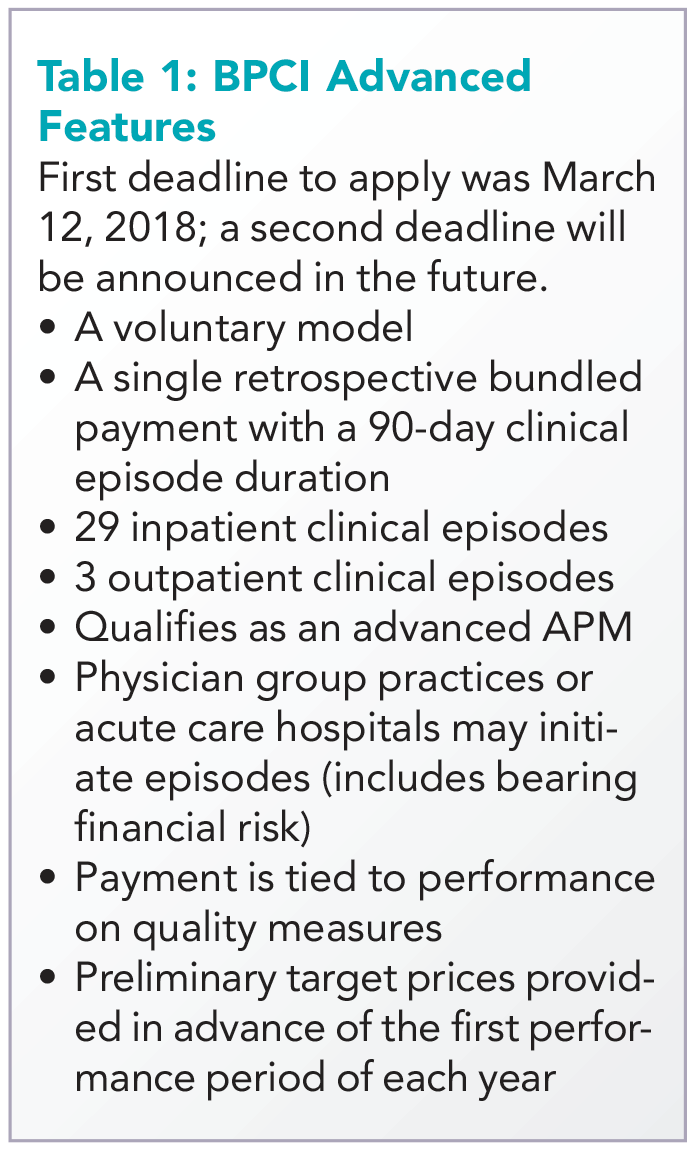
Acute care hospitals and physician groups may initiate episodes under BPCI Advanced, assuming financial risk under the model. Similar to its predecessor, BPCI Advanced assigns a target price based on past claims payments associated with the “episode initiator.”
During the performance period, if the initiator can beat the price in the aggregate for its bundles, it can keep the difference, and if it comes in over the price, it must pay the difference back to Medicare. Medicare discounts the target price by 3%, effectively paying itself that amount. After that, there is no sharing of savings with Medicare, as opposed to the permanent ACO programs, where there is sharing after the ACO meets the minimum savings rate.
The program allows physician groups and hospital initiators to go it alone or to work with a “convener,” which may share risk and reward with initiators, and may provide software, analytics, networks of high-performing providers like nursing facilities, and knowledge of specific care redesign approaches to enable program success. See Table 1 for a listing of other notable features of BPCI Advanced.
Quality measures
BPCI Advanced qualifies as an Advanced APM in part because payment is tied to performance on a set of quality measures (see Table 2). There are two measures applied to all episodes: all-cause hospital readmissions and advance care plan. These are notable because hospitalists may be especially focused on improvement activities in these areas.
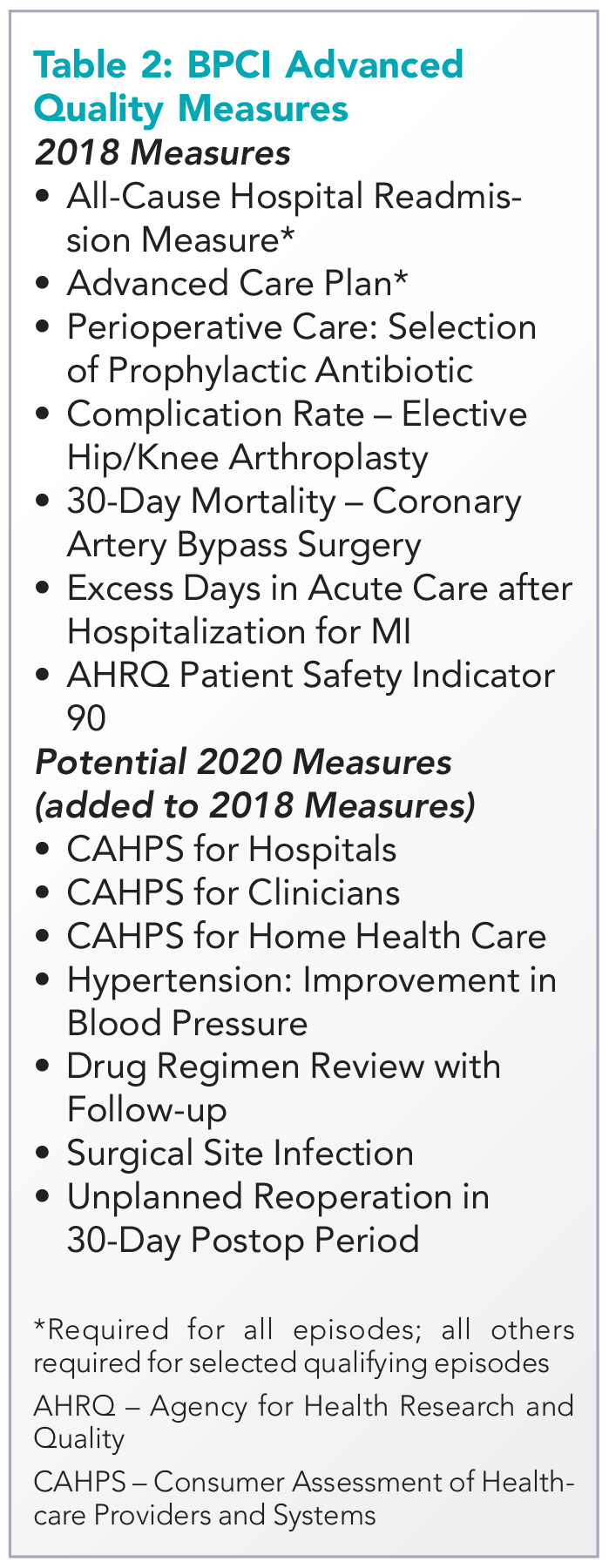
While the advance care plan measure refers to a process reflected by record documentation and is therefore directly under the control of hospitalists, readmissions – and most of the other measures – require a team approach. Because the outcome measures are risk adjusted, accurate and complete clinical documentation is crucial, as it drives how risk is adjusted. Of note, all the 2018 measures, collected directly through claims, will place no additional administrative burden for collection on providers.
Two ways for hospitalists to participate
Hospitalist groups – whether independent or employed – may be episode initiators in BPCI Advanced. In this case, any episodes in which the group participates that carry the name of a member of the hospitalist group in the “Attending Provider” field on the hospital bill claim form to Medicare (and the associated carrier claim) are attributed to that member’s physician group.
For example, if the group has chosen heart failure as an episode in which to participate at the program’s outset, a hospitalization is assigned the heart failure DRG (diagnosis-related group) and a group member is the Attending Provider on the claim form (and submits a claim for the physician services), then the episode is attributed to that group. This means that the group is responsible for payments represented by Medicare Part A and Part B claims (with a few exclusions like trauma and cancer) against the target price for the initial hospitalization and subsequent 90-day period. In practice, hospitalists are rewarded for actions aimed at optimizing location after discharge,4 avoiding readmissions, choosing efficient nursing facilities, and helping patients to maximize functional status.
The other way hospitalists may participate is through an agreement to share in savings with a hospital or physician group episode initiator. This requires hospitalist individuals or groups to enter into a contract with the initiator that meets certain program requirements – for example, report quality measures, engage in care redesign, use certified EHR technology (hospital-based clinicians automatically fulfill this criterion).
If there is broad participation, BPCI Advanced could represent a key milestone for hospitalists, as they seek to be recognized for the value they confer to the system as a whole instead of simply their professional billings. While there are legitimate concerns about the effect MIPS may have on health care value and the complexity of participation in APMs, barring a repeal of the law that created them, hospitalists now have the chance to extend their influence within and outside the hospital’s four walls and be more fairly rewarded for it.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of the Society of Hospital Medicine. Contact him at [email protected]. Disclosure: The author’s employer, Remedy Partners, is an Awardee Convener for the BPCI initiative and intends to apply as a Convener in BPCI Advanced.
References
1. Based on BPCI awardee convener Remedy Partners claims analysis.
2. https://innovation.cms.gov/initiatives/bpci-advanced.
3. https://qpp.cms.gov/apms/overview.
4. Whitcomb W. Choosing location after discharge wisely. The-hospitalist.org. 2018 Jan 3. Digital edition. Accessed Jan 13, 2018.
Federal budget grants $1.8 billion to Alzheimer’s and dementia research
Congress has appropriated an additional $414 million for research into Alzheimer’s disease and other dementias – the full increase requested by the National Institutes of Health for fiscal year 2018. The boost brings the total AD funding available this year to $1.8 billion.
Bolstered by the mandate of the National Plan to Address Alzheimer’s Disease, to prevent or treat AD by 2025, the NIH is aiming higher still. Its draft FY2019 AD appropriation asks for another $597 million; if passed, nearly $2.4 billion could be available for AD research as soon as next October.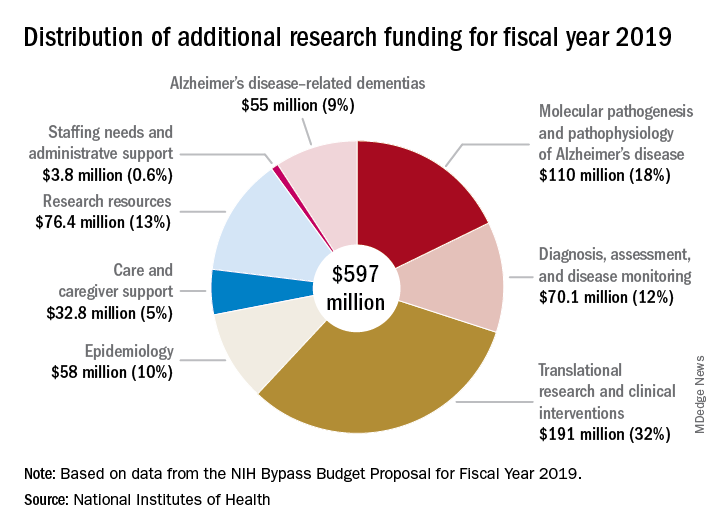
“For the third consecutive fiscal year, Congress has approved the Alzheimer’s Association’s appeal for a historic funding increase for Alzheimer’s and dementia research at the NIH,” Alzheimer’s Association president Harry Johns said in a press statement. “This decision demonstrates that Congress is deeply committed to providing the Alzheimer’s and dementia science community with the resources needed to move research forward.”
Several members of Congress championed the AD funding request, including Roy Blunt (R-Mo.), Patty Murray (D-Wash.), Nita Lowey (D-N.Y.), and Tom Cole (R-Okla.).
The forward momentum is on pace to continue into FY2019, according to Robert Egge, chief public policy officer and executive vice president of governmental affairs for the association. The NIH Bypass Budget, an estimate of how much additional funding is necessary to reach the 2025 goal, contains an additional $597 million appropriation for AD and other dementias.
“This is what we need to fund scientific projects that are meritorious and ready to go,” Mr. Egge said in an interview. “Congress has the assurance that this request is scientifically driven and that NIH is already thinking about how the money will be used.”
While a record-setting amount in the AD research world, this year’s $1.8 billion appropriation is a fraction of what other costly diseases receive. By comparison, the budget granted the National Cancer Institute $5.7 billion for its research programs.
“Compared to what the cost of the disease brings to Americans in terms of Medicare, Medicaid, and out of pocket expenses, it’s not that much,” Mr. Egge said. “But we have the opportunity to use this money to change these huge numbers that we’re facing.”
A 2013 report by the Rand Corporation found that, although Alzheimer’s affects fewer people than cancer or heart disease, the cost of treating and caring for those patients far outstrips spending in either of those other categories. The conclusions were perhaps even more startling, considering that it looked only at costs related solely to Alzheimer’s, not the cost of treating comorbid illnesses.
Long-term care was a key driver of the total cost in 2013, and remains the bulk of expenses today, Mr. Egge said. Transitions – going from home to nursing home to hospital – are terribly expensive, he noted. And although the Rand report didn’t include it, managing comorbid illnesses in Alzheimer’s is an enormous money drain. “Diabetes is just one example. It costs 80% more to manage diabetes in a patient with AD than in one without AD.”
The Facts and Figures report notes that the average 2017 per-person payout for Medicare beneficiaries was more than three times higher in AD patients than in those without the disease ($48,028 vs. $13,705). These are the kinds of numbers it takes to put partisan bickering on hold and grapple with tough decisions, Mr. Egge said.
“The fiscal argument is one thing that really impressed Congress. They do know how worried Americans are about this disease and how tough it is on families, but the growing fiscal impact has really focused them on addressing it.”
Congress has appropriated an additional $414 million for research into Alzheimer’s disease and other dementias – the full increase requested by the National Institutes of Health for fiscal year 2018. The boost brings the total AD funding available this year to $1.8 billion.
Bolstered by the mandate of the National Plan to Address Alzheimer’s Disease, to prevent or treat AD by 2025, the NIH is aiming higher still. Its draft FY2019 AD appropriation asks for another $597 million; if passed, nearly $2.4 billion could be available for AD research as soon as next October.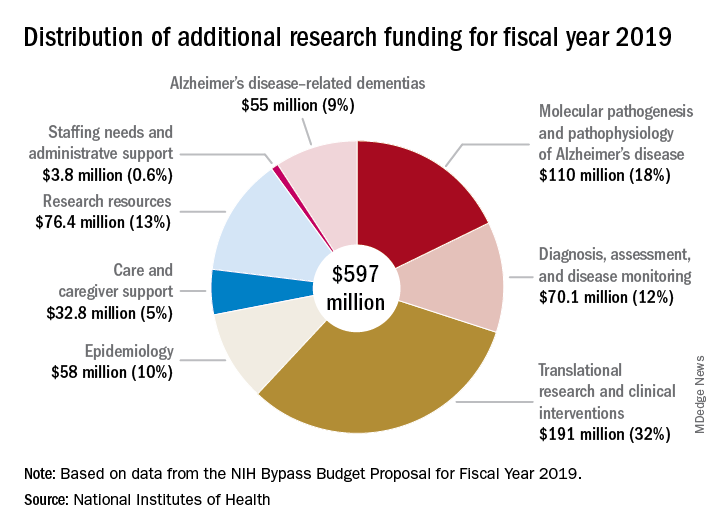
“For the third consecutive fiscal year, Congress has approved the Alzheimer’s Association’s appeal for a historic funding increase for Alzheimer’s and dementia research at the NIH,” Alzheimer’s Association president Harry Johns said in a press statement. “This decision demonstrates that Congress is deeply committed to providing the Alzheimer’s and dementia science community with the resources needed to move research forward.”
Several members of Congress championed the AD funding request, including Roy Blunt (R-Mo.), Patty Murray (D-Wash.), Nita Lowey (D-N.Y.), and Tom Cole (R-Okla.).
The forward momentum is on pace to continue into FY2019, according to Robert Egge, chief public policy officer and executive vice president of governmental affairs for the association. The NIH Bypass Budget, an estimate of how much additional funding is necessary to reach the 2025 goal, contains an additional $597 million appropriation for AD and other dementias.
“This is what we need to fund scientific projects that are meritorious and ready to go,” Mr. Egge said in an interview. “Congress has the assurance that this request is scientifically driven and that NIH is already thinking about how the money will be used.”
While a record-setting amount in the AD research world, this year’s $1.8 billion appropriation is a fraction of what other costly diseases receive. By comparison, the budget granted the National Cancer Institute $5.7 billion for its research programs.
“Compared to what the cost of the disease brings to Americans in terms of Medicare, Medicaid, and out of pocket expenses, it’s not that much,” Mr. Egge said. “But we have the opportunity to use this money to change these huge numbers that we’re facing.”
A 2013 report by the Rand Corporation found that, although Alzheimer’s affects fewer people than cancer or heart disease, the cost of treating and caring for those patients far outstrips spending in either of those other categories. The conclusions were perhaps even more startling, considering that it looked only at costs related solely to Alzheimer’s, not the cost of treating comorbid illnesses.
Long-term care was a key driver of the total cost in 2013, and remains the bulk of expenses today, Mr. Egge said. Transitions – going from home to nursing home to hospital – are terribly expensive, he noted. And although the Rand report didn’t include it, managing comorbid illnesses in Alzheimer’s is an enormous money drain. “Diabetes is just one example. It costs 80% more to manage diabetes in a patient with AD than in one without AD.”
The Facts and Figures report notes that the average 2017 per-person payout for Medicare beneficiaries was more than three times higher in AD patients than in those without the disease ($48,028 vs. $13,705). These are the kinds of numbers it takes to put partisan bickering on hold and grapple with tough decisions, Mr. Egge said.
“The fiscal argument is one thing that really impressed Congress. They do know how worried Americans are about this disease and how tough it is on families, but the growing fiscal impact has really focused them on addressing it.”
Congress has appropriated an additional $414 million for research into Alzheimer’s disease and other dementias – the full increase requested by the National Institutes of Health for fiscal year 2018. The boost brings the total AD funding available this year to $1.8 billion.
Bolstered by the mandate of the National Plan to Address Alzheimer’s Disease, to prevent or treat AD by 2025, the NIH is aiming higher still. Its draft FY2019 AD appropriation asks for another $597 million; if passed, nearly $2.4 billion could be available for AD research as soon as next October.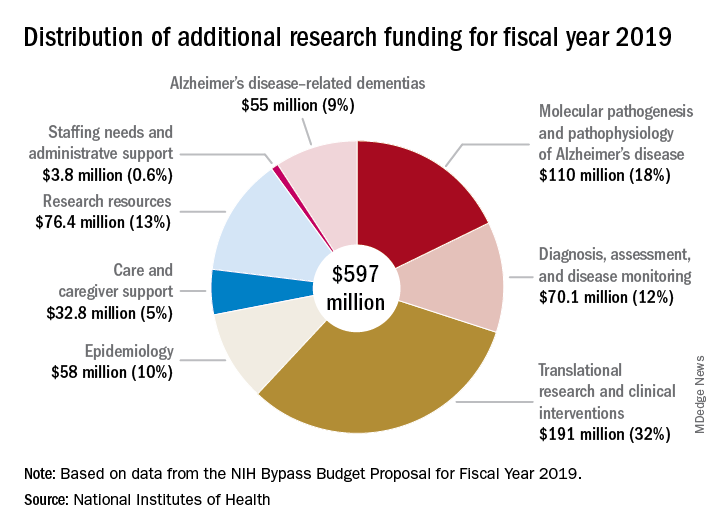
“For the third consecutive fiscal year, Congress has approved the Alzheimer’s Association’s appeal for a historic funding increase for Alzheimer’s and dementia research at the NIH,” Alzheimer’s Association president Harry Johns said in a press statement. “This decision demonstrates that Congress is deeply committed to providing the Alzheimer’s and dementia science community with the resources needed to move research forward.”
Several members of Congress championed the AD funding request, including Roy Blunt (R-Mo.), Patty Murray (D-Wash.), Nita Lowey (D-N.Y.), and Tom Cole (R-Okla.).
The forward momentum is on pace to continue into FY2019, according to Robert Egge, chief public policy officer and executive vice president of governmental affairs for the association. The NIH Bypass Budget, an estimate of how much additional funding is necessary to reach the 2025 goal, contains an additional $597 million appropriation for AD and other dementias.
“This is what we need to fund scientific projects that are meritorious and ready to go,” Mr. Egge said in an interview. “Congress has the assurance that this request is scientifically driven and that NIH is already thinking about how the money will be used.”
While a record-setting amount in the AD research world, this year’s $1.8 billion appropriation is a fraction of what other costly diseases receive. By comparison, the budget granted the National Cancer Institute $5.7 billion for its research programs.
“Compared to what the cost of the disease brings to Americans in terms of Medicare, Medicaid, and out of pocket expenses, it’s not that much,” Mr. Egge said. “But we have the opportunity to use this money to change these huge numbers that we’re facing.”
A 2013 report by the Rand Corporation found that, although Alzheimer’s affects fewer people than cancer or heart disease, the cost of treating and caring for those patients far outstrips spending in either of those other categories. The conclusions were perhaps even more startling, considering that it looked only at costs related solely to Alzheimer’s, not the cost of treating comorbid illnesses.
Long-term care was a key driver of the total cost in 2013, and remains the bulk of expenses today, Mr. Egge said. Transitions – going from home to nursing home to hospital – are terribly expensive, he noted. And although the Rand report didn’t include it, managing comorbid illnesses in Alzheimer’s is an enormous money drain. “Diabetes is just one example. It costs 80% more to manage diabetes in a patient with AD than in one without AD.”
The Facts and Figures report notes that the average 2017 per-person payout for Medicare beneficiaries was more than three times higher in AD patients than in those without the disease ($48,028 vs. $13,705). These are the kinds of numbers it takes to put partisan bickering on hold and grapple with tough decisions, Mr. Egge said.
“The fiscal argument is one thing that really impressed Congress. They do know how worried Americans are about this disease and how tough it is on families, but the growing fiscal impact has really focused them on addressing it.”
Fetal pathology exam performed without consent: $500,000 verdict
Fetal pathology exam performed without consent: $500,000 verdict
At 12 to 15 weeks' gestation, a fetus was found to have died. An ObGyn stimulated uterine contractions with misoprostol and the fetus was delivered.
The parents requested chromosomal testing to determine the cause of death. The ObGyn took samples of the baby's skin near the umbilical cord and from the placenta. He told the parents that the tests might come back as inconclusive, and that it may be necessary to take further samples. The couple was also told that, under hospital policy, the fetus must go to the pathology department before being taken to a funeral home. The parents told the ObGyn that they did not want further samples taken for any reason, and that nothing else should be done to their child before funeral preparations. The placenta, umbilical cord, and fetus were placed in 2 separate containers. The container with the placenta and umbilical cord had an anatomic pathology requisition form, indicating that a surgical pathology exam was to be performed. The container with the fetus did not have a requisition form. When the father accompanied the nurse who carried the containers to the pathology department, he told a general technologist that no additional tissue samples were to be taken from the fetus.
The next day, the pathologist made an incision on the fetus' left side and took a sample to create a slide for microscopic analysis. The parents discovered the incision at the funeral home.
PARENTS' CLAIM: The parents sued the hospital and pathologist. The pathologist was negligent in performing a surgical pathology examination without consent. The hospital had a duty to communicate the parents' desires to the pathologist.
According to hospital protocol, the nurse who attended the delivery was to fill out the proper forms and ensure that they were available to the pathologist. The container with the fetus should have had its own requisition form that instructed the pathologist to not perform any further testing. Every specimen that goes to pathology should have a requisition form, per guidelines from the College of American Pathologists (CAP). Without a form, the pathologist should not do anything with the sample.
The parents' verbal instructions not to take additional samples from the fetus were never relayed to the pathologist.
DEFENDANTS' DEFENSE: The hospital and pathologist denied negligence. A single requisition form was appropriate; the containers' labeling and the form made it clear that the placenta, umbilical cord, and fetus were from the same patient. CAP guidelines do not require separate forms. The remains were in the gross room at pathology, which is where specimens are taken for review and analysis. Therefore, the pathologist assumed he was to perform a standard pathology exam on both containers. The technologist with whom the father had spoken met the accepted standard of care.
VERDICT: A $500,000 Maine verdict was returned. The pathologist (through insurance) and the hospital equally shared payment of the award.
When should delivery have occurred? $4M verdict
Concerned that her fetus had stopped moving, a mother presented to the ED. Results of fetal heart-rate (FHR) monitoring ordered by the attending ObGyn (Dr. A) were nonreassuring. A second ObGyn (Dr. B) ordered a fetal biophysical profile (BPP); the score was 2 points. Although a low score usually results in immediate delivery, Dr. B consulted a maternal-fetal medicine (MFM) specialist. After another fetal BPP scored 8 points, the mother was discharged.
The next day, the mother called her ObGyn (Dr. C), who told her to immediately come to his office. A fetal BPP scored 4 points, with nonreassuring fetal heart sounds.
The mother was transported to the hospital for emergency cesarean delivery. At birth, the baby was blue, not breathing, and had meconium in his lungs. After 6 minutes' resuscitation, he began breathing. The child has an hypoxic brain injury.
PARENTS' CLAIM: Based on the nonreassuring FHR readings when the mother first reported lack of fetal movement, and a BPP of 2 points, an immediate cesarean delivery should have been performed. If the child had been delivered in a timely manner, he would have escaped a brain injury. At the very least, the mother should have been kept in the hospital for monitoring.
DEFENDANTS' DEFENSE: Drs. A and B and the hospital claimed that the child did not have a hypoxic injury; he had gastroschisis.
VERDICT: A $4,098,266 New York verdict was returned.
Second twin's birth delayed; brain damage: $1.5M settlement
A 35-year-old woman was 30 weeks' pregnant with twins when she was admitted to a hospital at high risk. At 36 weeks' gestation, she went into labor. A resident called the ObGyn to report that the patient was ready to deliver and waiting to push. The ObGyn advised that he was tied up in another procedure and for the mother to wait until he could get there.
Forty minutes later, the ObGyn arrived and the mother was allowed to push. A first-year resident delivered the first twin without incident. The second twin shifted from a cephalic presentation to a double foot- ling breech presentation and his FHR reflected severe bradycardia. Under the supervision of the ObGyn, a fourth-year resident managed the delivery, which took 28 minutes. The second twin's Apgar scores were low. He was intubated and transferred to a children's hospital for brain cooling.
PARENTS' CLAIM: Although excellent care following the birth reduced the degree of brain damage, the delay caused by the ObGyn's late arrival was responsible for the child's injuries.
PHYSICIAN'S DEFENSE: In pretrial findings, a panel of physicians reported that the child did not have a qualifying injury. However, the case settled before the trial began.
VERDICT: A $1.5 million Virginia settlement was reached.
Pregnant mother prepares for child's congenital heart disorder
A mother was told that her fetus had tricuspid atresia, a congenital defect. The mother and pediatric cardiologist developed a treatment plan to perform a balloon heart procedure at birth then transfer the baby to a specialized hospital.
After birth at a local hospital, the child was also found to have a lung disorder. He was promptly placed on a respirator. The hospital's pediatric cardiologist decided that the baby was too fragile to undergo the balloon procedure, and that the procedure could wait until the child was more stable. The baby died on his third day of life.
The neonatologists involved in treating the baby determined that the cause of death was tricuspid atresia. A pathologist reported that the death was due to a combination of congenital heart and lung disorders.
ESTATE'S CLAIM: The hospital team was sued for not following the prenatal plan. The baby's condition was serious but survivable if treated properly.
DEFENDANTS' DEFENSE: The hospital team made the correct decision to stabilize the baby's lung conditions before performing the balloon repair. The baby died because both his heart and lungs were compromised. The child's chance of survival was very small.
VERDICT: A Mississippi defense verdict was returned.
Severe uterine atony and PPH: hysterectomy
A 35-year-old woman at 41 weeks' gestation was admitted to the hospital in active labor at 5:45 am on July 26. At 2:45 pm, an ObGyn noted that she was 8+ cm dilated, 90% effaced, and that the baby's head was at -1 station. At 6:00 pm, the membranes were artificially ruptured. At 7:45 pm, examination revealed no change in her cervix. The ObGyn reviewed the options with the mother, including offering an epidural and cesarean delivery. At 8:30 pm, an intrauterine pressure catheter was placed. The ObGyn noted an inadequate labor pattern and ordered augmentation with oxytocin. On July 27 at 12:50 am, examination revealed that the cervix was completely dilated and the baby's head was at +1 station. At 2:30 am, oxytocin was infusing at 12 mU/m. At 2:30 am, the patient began to push. By 4:30 am, oxytocin was running at 14 mU/m and the patient continued to push. At 5:00 am, the ObGyn noted no further progression of labor and recommended a cesarean delivery, but the mother wanted to push a little longer. At 6:00 am, with no further progress, the decision was made to perform cesarean delivery. At 6:40 am, the patient was transferred to the operating room and delivery occurred at 7:08 am. The baby weighed 9.5 lb.
The mother's uterus was closed and hemostasis was reached. However, uterine atony was persistent and did not respond to multiple doses of medication or uterine massage. Persistent atony led to postpartum hemorrhaging (PPH). The ObGyn used conservative methods to control the hemorrhage, including medications and sutures. He then called for assistance from another ObGyn, and performed ligation of the utero-ovarian ligaments and additional suturing, which had no effect on the bleeding. They attempted an ovarian artery ligation and placed additional sutures, but the PPH continued. The ObGyn recommended a hysterectomy to the patient and her husband, who agreed. A supracervical hysterectomy was performed. During the procedure, the left ovary tore and was removed.
PARENTS' CLAIM: The patient and her husband spoke at trial of their intention to have more than one child. They sued the ObGyn, her practice, and the hospital. The ObGyn was negligent in allowing labor to continue for too long, for using oxytocin to stimulate contractions, and for allowing the patient to push for several hours, given that the baby was large. Oxytocin stimulation for so many hours without labor progression created an unacceptably high risk of uterine atony. This led to a nonreversible atonic state after delivery, which caused the patient to lose her uterus, left ovary, and her ability to reproduce.
DEFENDANTS' DEFENSE: The ObGyn was not negligent. The ObGyn met the standard of care in the management of labor and delivery. She was attentive, present at appropriate intervals, and there was no point at which a different decision should have been made. The ObGyn allowed the patient to have input in the decision-making process, as long as the ObGyn was comfortable that the decision was not compromising the safety of mother and baby. The length of labor and size of the fetus increased the risk of atony. However, in most cases, this does not occur; it can occur without those risk factors. PPH is a serious but frequently unavoidable complication of childbirth. The ObGyn's management was appropriate and prevented the patient's death.
VERDICT: A Pennsylvania defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Fetal pathology exam performed without consent: $500,000 verdict
At 12 to 15 weeks' gestation, a fetus was found to have died. An ObGyn stimulated uterine contractions with misoprostol and the fetus was delivered.
The parents requested chromosomal testing to determine the cause of death. The ObGyn took samples of the baby's skin near the umbilical cord and from the placenta. He told the parents that the tests might come back as inconclusive, and that it may be necessary to take further samples. The couple was also told that, under hospital policy, the fetus must go to the pathology department before being taken to a funeral home. The parents told the ObGyn that they did not want further samples taken for any reason, and that nothing else should be done to their child before funeral preparations. The placenta, umbilical cord, and fetus were placed in 2 separate containers. The container with the placenta and umbilical cord had an anatomic pathology requisition form, indicating that a surgical pathology exam was to be performed. The container with the fetus did not have a requisition form. When the father accompanied the nurse who carried the containers to the pathology department, he told a general technologist that no additional tissue samples were to be taken from the fetus.
The next day, the pathologist made an incision on the fetus' left side and took a sample to create a slide for microscopic analysis. The parents discovered the incision at the funeral home.
PARENTS' CLAIM: The parents sued the hospital and pathologist. The pathologist was negligent in performing a surgical pathology examination without consent. The hospital had a duty to communicate the parents' desires to the pathologist.
According to hospital protocol, the nurse who attended the delivery was to fill out the proper forms and ensure that they were available to the pathologist. The container with the fetus should have had its own requisition form that instructed the pathologist to not perform any further testing. Every specimen that goes to pathology should have a requisition form, per guidelines from the College of American Pathologists (CAP). Without a form, the pathologist should not do anything with the sample.
The parents' verbal instructions not to take additional samples from the fetus were never relayed to the pathologist.
DEFENDANTS' DEFENSE: The hospital and pathologist denied negligence. A single requisition form was appropriate; the containers' labeling and the form made it clear that the placenta, umbilical cord, and fetus were from the same patient. CAP guidelines do not require separate forms. The remains were in the gross room at pathology, which is where specimens are taken for review and analysis. Therefore, the pathologist assumed he was to perform a standard pathology exam on both containers. The technologist with whom the father had spoken met the accepted standard of care.
VERDICT: A $500,000 Maine verdict was returned. The pathologist (through insurance) and the hospital equally shared payment of the award.
When should delivery have occurred? $4M verdict
Concerned that her fetus had stopped moving, a mother presented to the ED. Results of fetal heart-rate (FHR) monitoring ordered by the attending ObGyn (Dr. A) were nonreassuring. A second ObGyn (Dr. B) ordered a fetal biophysical profile (BPP); the score was 2 points. Although a low score usually results in immediate delivery, Dr. B consulted a maternal-fetal medicine (MFM) specialist. After another fetal BPP scored 8 points, the mother was discharged.
The next day, the mother called her ObGyn (Dr. C), who told her to immediately come to his office. A fetal BPP scored 4 points, with nonreassuring fetal heart sounds.
The mother was transported to the hospital for emergency cesarean delivery. At birth, the baby was blue, not breathing, and had meconium in his lungs. After 6 minutes' resuscitation, he began breathing. The child has an hypoxic brain injury.
PARENTS' CLAIM: Based on the nonreassuring FHR readings when the mother first reported lack of fetal movement, and a BPP of 2 points, an immediate cesarean delivery should have been performed. If the child had been delivered in a timely manner, he would have escaped a brain injury. At the very least, the mother should have been kept in the hospital for monitoring.
DEFENDANTS' DEFENSE: Drs. A and B and the hospital claimed that the child did not have a hypoxic injury; he had gastroschisis.
VERDICT: A $4,098,266 New York verdict was returned.
Second twin's birth delayed; brain damage: $1.5M settlement
A 35-year-old woman was 30 weeks' pregnant with twins when she was admitted to a hospital at high risk. At 36 weeks' gestation, she went into labor. A resident called the ObGyn to report that the patient was ready to deliver and waiting to push. The ObGyn advised that he was tied up in another procedure and for the mother to wait until he could get there.
Forty minutes later, the ObGyn arrived and the mother was allowed to push. A first-year resident delivered the first twin without incident. The second twin shifted from a cephalic presentation to a double foot- ling breech presentation and his FHR reflected severe bradycardia. Under the supervision of the ObGyn, a fourth-year resident managed the delivery, which took 28 minutes. The second twin's Apgar scores were low. He was intubated and transferred to a children's hospital for brain cooling.
PARENTS' CLAIM: Although excellent care following the birth reduced the degree of brain damage, the delay caused by the ObGyn's late arrival was responsible for the child's injuries.
PHYSICIAN'S DEFENSE: In pretrial findings, a panel of physicians reported that the child did not have a qualifying injury. However, the case settled before the trial began.
VERDICT: A $1.5 million Virginia settlement was reached.
Pregnant mother prepares for child's congenital heart disorder
A mother was told that her fetus had tricuspid atresia, a congenital defect. The mother and pediatric cardiologist developed a treatment plan to perform a balloon heart procedure at birth then transfer the baby to a specialized hospital.
After birth at a local hospital, the child was also found to have a lung disorder. He was promptly placed on a respirator. The hospital's pediatric cardiologist decided that the baby was too fragile to undergo the balloon procedure, and that the procedure could wait until the child was more stable. The baby died on his third day of life.
The neonatologists involved in treating the baby determined that the cause of death was tricuspid atresia. A pathologist reported that the death was due to a combination of congenital heart and lung disorders.
ESTATE'S CLAIM: The hospital team was sued for not following the prenatal plan. The baby's condition was serious but survivable if treated properly.
DEFENDANTS' DEFENSE: The hospital team made the correct decision to stabilize the baby's lung conditions before performing the balloon repair. The baby died because both his heart and lungs were compromised. The child's chance of survival was very small.
VERDICT: A Mississippi defense verdict was returned.
Severe uterine atony and PPH: hysterectomy
A 35-year-old woman at 41 weeks' gestation was admitted to the hospital in active labor at 5:45 am on July 26. At 2:45 pm, an ObGyn noted that she was 8+ cm dilated, 90% effaced, and that the baby's head was at -1 station. At 6:00 pm, the membranes were artificially ruptured. At 7:45 pm, examination revealed no change in her cervix. The ObGyn reviewed the options with the mother, including offering an epidural and cesarean delivery. At 8:30 pm, an intrauterine pressure catheter was placed. The ObGyn noted an inadequate labor pattern and ordered augmentation with oxytocin. On July 27 at 12:50 am, examination revealed that the cervix was completely dilated and the baby's head was at +1 station. At 2:30 am, oxytocin was infusing at 12 mU/m. At 2:30 am, the patient began to push. By 4:30 am, oxytocin was running at 14 mU/m and the patient continued to push. At 5:00 am, the ObGyn noted no further progression of labor and recommended a cesarean delivery, but the mother wanted to push a little longer. At 6:00 am, with no further progress, the decision was made to perform cesarean delivery. At 6:40 am, the patient was transferred to the operating room and delivery occurred at 7:08 am. The baby weighed 9.5 lb.
The mother's uterus was closed and hemostasis was reached. However, uterine atony was persistent and did not respond to multiple doses of medication or uterine massage. Persistent atony led to postpartum hemorrhaging (PPH). The ObGyn used conservative methods to control the hemorrhage, including medications and sutures. He then called for assistance from another ObGyn, and performed ligation of the utero-ovarian ligaments and additional suturing, which had no effect on the bleeding. They attempted an ovarian artery ligation and placed additional sutures, but the PPH continued. The ObGyn recommended a hysterectomy to the patient and her husband, who agreed. A supracervical hysterectomy was performed. During the procedure, the left ovary tore and was removed.
PARENTS' CLAIM: The patient and her husband spoke at trial of their intention to have more than one child. They sued the ObGyn, her practice, and the hospital. The ObGyn was negligent in allowing labor to continue for too long, for using oxytocin to stimulate contractions, and for allowing the patient to push for several hours, given that the baby was large. Oxytocin stimulation for so many hours without labor progression created an unacceptably high risk of uterine atony. This led to a nonreversible atonic state after delivery, which caused the patient to lose her uterus, left ovary, and her ability to reproduce.
DEFENDANTS' DEFENSE: The ObGyn was not negligent. The ObGyn met the standard of care in the management of labor and delivery. She was attentive, present at appropriate intervals, and there was no point at which a different decision should have been made. The ObGyn allowed the patient to have input in the decision-making process, as long as the ObGyn was comfortable that the decision was not compromising the safety of mother and baby. The length of labor and size of the fetus increased the risk of atony. However, in most cases, this does not occur; it can occur without those risk factors. PPH is a serious but frequently unavoidable complication of childbirth. The ObGyn's management was appropriate and prevented the patient's death.
VERDICT: A Pennsylvania defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Fetal pathology exam performed without consent: $500,000 verdict
At 12 to 15 weeks' gestation, a fetus was found to have died. An ObGyn stimulated uterine contractions with misoprostol and the fetus was delivered.
The parents requested chromosomal testing to determine the cause of death. The ObGyn took samples of the baby's skin near the umbilical cord and from the placenta. He told the parents that the tests might come back as inconclusive, and that it may be necessary to take further samples. The couple was also told that, under hospital policy, the fetus must go to the pathology department before being taken to a funeral home. The parents told the ObGyn that they did not want further samples taken for any reason, and that nothing else should be done to their child before funeral preparations. The placenta, umbilical cord, and fetus were placed in 2 separate containers. The container with the placenta and umbilical cord had an anatomic pathology requisition form, indicating that a surgical pathology exam was to be performed. The container with the fetus did not have a requisition form. When the father accompanied the nurse who carried the containers to the pathology department, he told a general technologist that no additional tissue samples were to be taken from the fetus.
The next day, the pathologist made an incision on the fetus' left side and took a sample to create a slide for microscopic analysis. The parents discovered the incision at the funeral home.
PARENTS' CLAIM: The parents sued the hospital and pathologist. The pathologist was negligent in performing a surgical pathology examination without consent. The hospital had a duty to communicate the parents' desires to the pathologist.
According to hospital protocol, the nurse who attended the delivery was to fill out the proper forms and ensure that they were available to the pathologist. The container with the fetus should have had its own requisition form that instructed the pathologist to not perform any further testing. Every specimen that goes to pathology should have a requisition form, per guidelines from the College of American Pathologists (CAP). Without a form, the pathologist should not do anything with the sample.
The parents' verbal instructions not to take additional samples from the fetus were never relayed to the pathologist.
DEFENDANTS' DEFENSE: The hospital and pathologist denied negligence. A single requisition form was appropriate; the containers' labeling and the form made it clear that the placenta, umbilical cord, and fetus were from the same patient. CAP guidelines do not require separate forms. The remains were in the gross room at pathology, which is where specimens are taken for review and analysis. Therefore, the pathologist assumed he was to perform a standard pathology exam on both containers. The technologist with whom the father had spoken met the accepted standard of care.
VERDICT: A $500,000 Maine verdict was returned. The pathologist (through insurance) and the hospital equally shared payment of the award.
When should delivery have occurred? $4M verdict
Concerned that her fetus had stopped moving, a mother presented to the ED. Results of fetal heart-rate (FHR) monitoring ordered by the attending ObGyn (Dr. A) were nonreassuring. A second ObGyn (Dr. B) ordered a fetal biophysical profile (BPP); the score was 2 points. Although a low score usually results in immediate delivery, Dr. B consulted a maternal-fetal medicine (MFM) specialist. After another fetal BPP scored 8 points, the mother was discharged.
The next day, the mother called her ObGyn (Dr. C), who told her to immediately come to his office. A fetal BPP scored 4 points, with nonreassuring fetal heart sounds.
The mother was transported to the hospital for emergency cesarean delivery. At birth, the baby was blue, not breathing, and had meconium in his lungs. After 6 minutes' resuscitation, he began breathing. The child has an hypoxic brain injury.
PARENTS' CLAIM: Based on the nonreassuring FHR readings when the mother first reported lack of fetal movement, and a BPP of 2 points, an immediate cesarean delivery should have been performed. If the child had been delivered in a timely manner, he would have escaped a brain injury. At the very least, the mother should have been kept in the hospital for monitoring.
DEFENDANTS' DEFENSE: Drs. A and B and the hospital claimed that the child did not have a hypoxic injury; he had gastroschisis.
VERDICT: A $4,098,266 New York verdict was returned.
Second twin's birth delayed; brain damage: $1.5M settlement
A 35-year-old woman was 30 weeks' pregnant with twins when she was admitted to a hospital at high risk. At 36 weeks' gestation, she went into labor. A resident called the ObGyn to report that the patient was ready to deliver and waiting to push. The ObGyn advised that he was tied up in another procedure and for the mother to wait until he could get there.
Forty minutes later, the ObGyn arrived and the mother was allowed to push. A first-year resident delivered the first twin without incident. The second twin shifted from a cephalic presentation to a double foot- ling breech presentation and his FHR reflected severe bradycardia. Under the supervision of the ObGyn, a fourth-year resident managed the delivery, which took 28 minutes. The second twin's Apgar scores were low. He was intubated and transferred to a children's hospital for brain cooling.
PARENTS' CLAIM: Although excellent care following the birth reduced the degree of brain damage, the delay caused by the ObGyn's late arrival was responsible for the child's injuries.
PHYSICIAN'S DEFENSE: In pretrial findings, a panel of physicians reported that the child did not have a qualifying injury. However, the case settled before the trial began.
VERDICT: A $1.5 million Virginia settlement was reached.
Pregnant mother prepares for child's congenital heart disorder
A mother was told that her fetus had tricuspid atresia, a congenital defect. The mother and pediatric cardiologist developed a treatment plan to perform a balloon heart procedure at birth then transfer the baby to a specialized hospital.
After birth at a local hospital, the child was also found to have a lung disorder. He was promptly placed on a respirator. The hospital's pediatric cardiologist decided that the baby was too fragile to undergo the balloon procedure, and that the procedure could wait until the child was more stable. The baby died on his third day of life.
The neonatologists involved in treating the baby determined that the cause of death was tricuspid atresia. A pathologist reported that the death was due to a combination of congenital heart and lung disorders.
ESTATE'S CLAIM: The hospital team was sued for not following the prenatal plan. The baby's condition was serious but survivable if treated properly.
DEFENDANTS' DEFENSE: The hospital team made the correct decision to stabilize the baby's lung conditions before performing the balloon repair. The baby died because both his heart and lungs were compromised. The child's chance of survival was very small.
VERDICT: A Mississippi defense verdict was returned.
Severe uterine atony and PPH: hysterectomy
A 35-year-old woman at 41 weeks' gestation was admitted to the hospital in active labor at 5:45 am on July 26. At 2:45 pm, an ObGyn noted that she was 8+ cm dilated, 90% effaced, and that the baby's head was at -1 station. At 6:00 pm, the membranes were artificially ruptured. At 7:45 pm, examination revealed no change in her cervix. The ObGyn reviewed the options with the mother, including offering an epidural and cesarean delivery. At 8:30 pm, an intrauterine pressure catheter was placed. The ObGyn noted an inadequate labor pattern and ordered augmentation with oxytocin. On July 27 at 12:50 am, examination revealed that the cervix was completely dilated and the baby's head was at +1 station. At 2:30 am, oxytocin was infusing at 12 mU/m. At 2:30 am, the patient began to push. By 4:30 am, oxytocin was running at 14 mU/m and the patient continued to push. At 5:00 am, the ObGyn noted no further progression of labor and recommended a cesarean delivery, but the mother wanted to push a little longer. At 6:00 am, with no further progress, the decision was made to perform cesarean delivery. At 6:40 am, the patient was transferred to the operating room and delivery occurred at 7:08 am. The baby weighed 9.5 lb.
The mother's uterus was closed and hemostasis was reached. However, uterine atony was persistent and did not respond to multiple doses of medication or uterine massage. Persistent atony led to postpartum hemorrhaging (PPH). The ObGyn used conservative methods to control the hemorrhage, including medications and sutures. He then called for assistance from another ObGyn, and performed ligation of the utero-ovarian ligaments and additional suturing, which had no effect on the bleeding. They attempted an ovarian artery ligation and placed additional sutures, but the PPH continued. The ObGyn recommended a hysterectomy to the patient and her husband, who agreed. A supracervical hysterectomy was performed. During the procedure, the left ovary tore and was removed.
PARENTS' CLAIM: The patient and her husband spoke at trial of their intention to have more than one child. They sued the ObGyn, her practice, and the hospital. The ObGyn was negligent in allowing labor to continue for too long, for using oxytocin to stimulate contractions, and for allowing the patient to push for several hours, given that the baby was large. Oxytocin stimulation for so many hours without labor progression created an unacceptably high risk of uterine atony. This led to a nonreversible atonic state after delivery, which caused the patient to lose her uterus, left ovary, and her ability to reproduce.
DEFENDANTS' DEFENSE: The ObGyn was not negligent. The ObGyn met the standard of care in the management of labor and delivery. She was attentive, present at appropriate intervals, and there was no point at which a different decision should have been made. The ObGyn allowed the patient to have input in the decision-making process, as long as the ObGyn was comfortable that the decision was not compromising the safety of mother and baby. The length of labor and size of the fetus increased the risk of atony. However, in most cases, this does not occur; it can occur without those risk factors. PPH is a serious but frequently unavoidable complication of childbirth. The ObGyn's management was appropriate and prevented the patient's death.
VERDICT: A Pennsylvania defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
From the Editors: “Okay” is not good enough
Keeping up with refinements in old procedures and adopting new procedures throughout one’s surgical career has always been a challenge.
That challenge has grown as advancements in technology have become ever more disruptive, requiring the learning of radically different skills. Surgeons are highly motivated to learn new procedures, lest they become extinct like professional “dodo birds.” But doing so requires a considerable expenditure of time and money to attend courses and then a period of being proctored in the new procedure once it has been learned.
The acquisition of technical skill in surgery is well recognized as a primary responsibility of surgical residency training programs. Surgical meetings and surgical journals have recently given a lot of space to the question of whether training programs are imparting adequate surgical skill to their learners and whether new graduates have achieved surgical competence at graduation. Some highly cited articles, having surveyed surgical teachers, maintain that a significant percentage of the new graduates have not achieved the needed skills to practice independently.1,2 Many place the blame at the feet of the much-maligned restriction in the resident work week to 80 hours, a limitation imposed by the Accreditation Council of Graduate Medical Education in 2003.
The reasons for the perceived decline in competence are many, including an increase in the number and complexity of surgical procedures, as well as institutional expectations for increased involvement of attendings in procedures. Recommended solutions include lengthening training, encouraging increased and earlier specialization, and proctoring by senior surgeons in the first year of a surgeon’s practice. Less frequently mentioned is the fact that, although the work hours are shorter and the surgery more complex, we have not compensated for these factors by appreciably changing the methods used to teach surgical technique. In many programs, faculty are performing an increasing proportion of procedures: doing more and teaching less.
Mandated surgical skills labs may be helpful to teach a basic level of skill. Simulation can be helpful in imparting the ability to perform more complex procedures and quickly adapt to unexpected intraoperative findings or occurrences. Virtual reality simulators are available, but they’re very expensive and often beyond the budgets of most residency programs. While simulation can help, it is not the whole solution to learning surgical skills.
It is now long past due for surgical training programs to rethink the process of teaching surgical skill in a more deliberate way to residents. One way to accomplish this might be through utilizing “master teachers” or “coaches” who are trained specifically to impart not only skill in performing a given procedure but also an understanding of how to critically assess one’s own performance in practice and learn how to improve that performance through self-reflection and self-assessment. Some very thoughtful and compelling studies have described how coaching might aid performance improvement of both residents and of surgeons already in practice.3,4,5
The process involves a review of videotaped procedures by both the operating surgeon (or surgical resident) and the coach to recognize points at which performance was subpar and to have a discussion about steps needed for improvement. Through further reviews of videotapes of subsequent procedures, the surgeon or resident learns to internalize the techniques of performance improvement.
While ideal in a perfect world, such a schema is far from universally feasible in our current surgical culture. Although master classes and coaching are accepted as the norm in other fields that also require technical excellence, such as classical music and athletics, our surgical culture does not readily accept that our surgical technique might be less than perfect. We tend to downplay the notion that we (and our patients) might benefit from improving our surgical skills beyond mere competence to the point of mastery. A culture change in this regard will not occur overnight and most likely must begin by making coaching a standard and accepted part of surgical training programs, both for the residents and for the teachers themselves.
We make the tacit assumption that attending surgeons are teachers, but we rarely teach them how to teach. The fact that many attendings don’t know how to give effective feedback to residents may be a reason that they fail to give specific coaching on how their learners might improve and why these attendings take over an increasing portion of the procedures themselves. In order for faculty to improve the quality of their teaching, they need training of their own. The training should be a mandatory, “protected” part of their day or it will not occur, and the “teaching the teachers” must be done by master teachers who are respected for their skill not only as a surgeons but also as a surgical educators. This role is an appropriate one for Associate Members of the new ACS Academy of Master Surgeon Educators to assume (see https://www.facs.org/education/academy/membership).
Coaching by master surgeons should become a professional norm. It is only after surgical education and coaching are incorporated all along the training continuum – from novice to competent to master during residency training – that surgeons already in practice will accept it as a regular part of their work. Refinements in procedures and new procedures would be met by continued professional improvement that would be enhanced by master surgeon coaching. We owe it to ourselves and our patients to achieve excellence, not mere competence. “Okay” is not good enough.
Dr. Deveney is a professor of surgery and the vice chair of education in the department of surgery at Oregon Health & Science University, Portland. She is the coeditor of ACS Surgery News.
1. Mattar SG et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg. 2013;258(3):440-9.
2. Damewood RB et al. “Taking training to the next level”: The American College of Surgeons Committee on residency training survey. J Surg Educ. 2017;74(6):e95-e105.
3. Gawande A. Coaching a surgeon: What makes top performers better? The New Yorker, Oct. 3, 2011.
4. Bonrath EM et al. Comprehensive surgical coaching enhances surgical skill in the operating room: a randomized controlled trial. Ann Surg. 2015;262:205-12.
5. Greenberg CC et al. Surgical coaching for individual performance improvement. Ann Surg. 2015;261(1):32-4.
Keeping up with refinements in old procedures and adopting new procedures throughout one’s surgical career has always been a challenge.
That challenge has grown as advancements in technology have become ever more disruptive, requiring the learning of radically different skills. Surgeons are highly motivated to learn new procedures, lest they become extinct like professional “dodo birds.” But doing so requires a considerable expenditure of time and money to attend courses and then a period of being proctored in the new procedure once it has been learned.
The acquisition of technical skill in surgery is well recognized as a primary responsibility of surgical residency training programs. Surgical meetings and surgical journals have recently given a lot of space to the question of whether training programs are imparting adequate surgical skill to their learners and whether new graduates have achieved surgical competence at graduation. Some highly cited articles, having surveyed surgical teachers, maintain that a significant percentage of the new graduates have not achieved the needed skills to practice independently.1,2 Many place the blame at the feet of the much-maligned restriction in the resident work week to 80 hours, a limitation imposed by the Accreditation Council of Graduate Medical Education in 2003.
The reasons for the perceived decline in competence are many, including an increase in the number and complexity of surgical procedures, as well as institutional expectations for increased involvement of attendings in procedures. Recommended solutions include lengthening training, encouraging increased and earlier specialization, and proctoring by senior surgeons in the first year of a surgeon’s practice. Less frequently mentioned is the fact that, although the work hours are shorter and the surgery more complex, we have not compensated for these factors by appreciably changing the methods used to teach surgical technique. In many programs, faculty are performing an increasing proportion of procedures: doing more and teaching less.
Mandated surgical skills labs may be helpful to teach a basic level of skill. Simulation can be helpful in imparting the ability to perform more complex procedures and quickly adapt to unexpected intraoperative findings or occurrences. Virtual reality simulators are available, but they’re very expensive and often beyond the budgets of most residency programs. While simulation can help, it is not the whole solution to learning surgical skills.
It is now long past due for surgical training programs to rethink the process of teaching surgical skill in a more deliberate way to residents. One way to accomplish this might be through utilizing “master teachers” or “coaches” who are trained specifically to impart not only skill in performing a given procedure but also an understanding of how to critically assess one’s own performance in practice and learn how to improve that performance through self-reflection and self-assessment. Some very thoughtful and compelling studies have described how coaching might aid performance improvement of both residents and of surgeons already in practice.3,4,5
The process involves a review of videotaped procedures by both the operating surgeon (or surgical resident) and the coach to recognize points at which performance was subpar and to have a discussion about steps needed for improvement. Through further reviews of videotapes of subsequent procedures, the surgeon or resident learns to internalize the techniques of performance improvement.
While ideal in a perfect world, such a schema is far from universally feasible in our current surgical culture. Although master classes and coaching are accepted as the norm in other fields that also require technical excellence, such as classical music and athletics, our surgical culture does not readily accept that our surgical technique might be less than perfect. We tend to downplay the notion that we (and our patients) might benefit from improving our surgical skills beyond mere competence to the point of mastery. A culture change in this regard will not occur overnight and most likely must begin by making coaching a standard and accepted part of surgical training programs, both for the residents and for the teachers themselves.
We make the tacit assumption that attending surgeons are teachers, but we rarely teach them how to teach. The fact that many attendings don’t know how to give effective feedback to residents may be a reason that they fail to give specific coaching on how their learners might improve and why these attendings take over an increasing portion of the procedures themselves. In order for faculty to improve the quality of their teaching, they need training of their own. The training should be a mandatory, “protected” part of their day or it will not occur, and the “teaching the teachers” must be done by master teachers who are respected for their skill not only as a surgeons but also as a surgical educators. This role is an appropriate one for Associate Members of the new ACS Academy of Master Surgeon Educators to assume (see https://www.facs.org/education/academy/membership).
Coaching by master surgeons should become a professional norm. It is only after surgical education and coaching are incorporated all along the training continuum – from novice to competent to master during residency training – that surgeons already in practice will accept it as a regular part of their work. Refinements in procedures and new procedures would be met by continued professional improvement that would be enhanced by master surgeon coaching. We owe it to ourselves and our patients to achieve excellence, not mere competence. “Okay” is not good enough.
Dr. Deveney is a professor of surgery and the vice chair of education in the department of surgery at Oregon Health & Science University, Portland. She is the coeditor of ACS Surgery News.
Keeping up with refinements in old procedures and adopting new procedures throughout one’s surgical career has always been a challenge.
That challenge has grown as advancements in technology have become ever more disruptive, requiring the learning of radically different skills. Surgeons are highly motivated to learn new procedures, lest they become extinct like professional “dodo birds.” But doing so requires a considerable expenditure of time and money to attend courses and then a period of being proctored in the new procedure once it has been learned.
The acquisition of technical skill in surgery is well recognized as a primary responsibility of surgical residency training programs. Surgical meetings and surgical journals have recently given a lot of space to the question of whether training programs are imparting adequate surgical skill to their learners and whether new graduates have achieved surgical competence at graduation. Some highly cited articles, having surveyed surgical teachers, maintain that a significant percentage of the new graduates have not achieved the needed skills to practice independently.1,2 Many place the blame at the feet of the much-maligned restriction in the resident work week to 80 hours, a limitation imposed by the Accreditation Council of Graduate Medical Education in 2003.
The reasons for the perceived decline in competence are many, including an increase in the number and complexity of surgical procedures, as well as institutional expectations for increased involvement of attendings in procedures. Recommended solutions include lengthening training, encouraging increased and earlier specialization, and proctoring by senior surgeons in the first year of a surgeon’s practice. Less frequently mentioned is the fact that, although the work hours are shorter and the surgery more complex, we have not compensated for these factors by appreciably changing the methods used to teach surgical technique. In many programs, faculty are performing an increasing proportion of procedures: doing more and teaching less.
Mandated surgical skills labs may be helpful to teach a basic level of skill. Simulation can be helpful in imparting the ability to perform more complex procedures and quickly adapt to unexpected intraoperative findings or occurrences. Virtual reality simulators are available, but they’re very expensive and often beyond the budgets of most residency programs. While simulation can help, it is not the whole solution to learning surgical skills.
It is now long past due for surgical training programs to rethink the process of teaching surgical skill in a more deliberate way to residents. One way to accomplish this might be through utilizing “master teachers” or “coaches” who are trained specifically to impart not only skill in performing a given procedure but also an understanding of how to critically assess one’s own performance in practice and learn how to improve that performance through self-reflection and self-assessment. Some very thoughtful and compelling studies have described how coaching might aid performance improvement of both residents and of surgeons already in practice.3,4,5
The process involves a review of videotaped procedures by both the operating surgeon (or surgical resident) and the coach to recognize points at which performance was subpar and to have a discussion about steps needed for improvement. Through further reviews of videotapes of subsequent procedures, the surgeon or resident learns to internalize the techniques of performance improvement.
While ideal in a perfect world, such a schema is far from universally feasible in our current surgical culture. Although master classes and coaching are accepted as the norm in other fields that also require technical excellence, such as classical music and athletics, our surgical culture does not readily accept that our surgical technique might be less than perfect. We tend to downplay the notion that we (and our patients) might benefit from improving our surgical skills beyond mere competence to the point of mastery. A culture change in this regard will not occur overnight and most likely must begin by making coaching a standard and accepted part of surgical training programs, both for the residents and for the teachers themselves.
We make the tacit assumption that attending surgeons are teachers, but we rarely teach them how to teach. The fact that many attendings don’t know how to give effective feedback to residents may be a reason that they fail to give specific coaching on how their learners might improve and why these attendings take over an increasing portion of the procedures themselves. In order for faculty to improve the quality of their teaching, they need training of their own. The training should be a mandatory, “protected” part of their day or it will not occur, and the “teaching the teachers” must be done by master teachers who are respected for their skill not only as a surgeons but also as a surgical educators. This role is an appropriate one for Associate Members of the new ACS Academy of Master Surgeon Educators to assume (see https://www.facs.org/education/academy/membership).
Coaching by master surgeons should become a professional norm. It is only after surgical education and coaching are incorporated all along the training continuum – from novice to competent to master during residency training – that surgeons already in practice will accept it as a regular part of their work. Refinements in procedures and new procedures would be met by continued professional improvement that would be enhanced by master surgeon coaching. We owe it to ourselves and our patients to achieve excellence, not mere competence. “Okay” is not good enough.
Dr. Deveney is a professor of surgery and the vice chair of education in the department of surgery at Oregon Health & Science University, Portland. She is the coeditor of ACS Surgery News.
1. Mattar SG et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg. 2013;258(3):440-9.
2. Damewood RB et al. “Taking training to the next level”: The American College of Surgeons Committee on residency training survey. J Surg Educ. 2017;74(6):e95-e105.
3. Gawande A. Coaching a surgeon: What makes top performers better? The New Yorker, Oct. 3, 2011.
4. Bonrath EM et al. Comprehensive surgical coaching enhances surgical skill in the operating room: a randomized controlled trial. Ann Surg. 2015;262:205-12.
5. Greenberg CC et al. Surgical coaching for individual performance improvement. Ann Surg. 2015;261(1):32-4.
1. Mattar SG et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg. 2013;258(3):440-9.
2. Damewood RB et al. “Taking training to the next level”: The American College of Surgeons Committee on residency training survey. J Surg Educ. 2017;74(6):e95-e105.
3. Gawande A. Coaching a surgeon: What makes top performers better? The New Yorker, Oct. 3, 2011.
4. Bonrath EM et al. Comprehensive surgical coaching enhances surgical skill in the operating room: a randomized controlled trial. Ann Surg. 2015;262:205-12.
5. Greenberg CC et al. Surgical coaching for individual performance improvement. Ann Surg. 2015;261(1):32-4.