User login
Welcome to Orlando and HM18
Welcome to HM18 and Orlando! This is the annual conference’s first time in Orlando, a city dubbed “the happiest place on earth,” which conjures up magic and curiosity and brings out the kid in everyone. As Walt Disney noted, “Adults are only kids, grown up.” So we hope you have brought your sense of adventure and curiosity, as we have a lot planned for you!
Over the next 3 days, we invite you to network with nearly 5,000 hospitalist colleagues from around the “small world.” Introduce yourself to total strangers and discover you have a lot in common. This conference provides a wonderful opportunity to share best practices and discuss ideas.
Please have fun taking advantage of the wide array of learning opportunities the Annual Conference Committee developed for HM18. We hope the topics will grab your interest and pique your curiosity. We encourage you (and your inner kid) to try on new ideas, attend lectures that catch your eye, and roll up your sleeves to dive into interactive workshops. For extra fun, the committee created catchy Orlando-themed titles for many of the talks. We hope they make you smile!
The Annual Conference Committee members will be wearing large buttons to identify themselves. We welcome any feedback about the meeting. Please take the time to share your thoughts with us, and we are happy to help in any way. The committee members worked hard to create a pre-course day and meeting with something for everyone, knowing there is great diversity under the hospitalist tent. We also strove to make it relevant and timely. The driving force behind the content was “What do practicing hospitalists need and want to know now?”
HM18 contains an abundance of clinical content. Enjoy the 2 days of Clinical Update talks to hear the latest evidence from a diversity of fields. New this year is Updates in Addiction Medicine, given the large opioid crisis that affecting health care. There are 3 days of Rapid Fire talks to answer the clinical questions we all have while caring for patients. The Perioperative/Co-Management track is back with is unique and useful content. We even repeat some of the most popular talks on Tuesday, so you will be able to attend all the “can’t miss” sessions.
New this year is a focus on careers and how to make yours enjoyable and sustainable. Hospital medicine is more than 20 years old, and there are increasing numbers of mid-career hospitalists. The Career Development track offers a series of topics in case you want to spice up your current role, change your schedule, or plan for retirement. Accompanying this are career development workshops that provide practical skills to do just that.
We have also added a new NP/PA track, a palliative care track, and The Great Debate track. Come watch two entertaining speakers have a “smackdown” on a clinical topic. You’ll learn something while laughing.
We’ve also brought back your favorites: practice management, quality, high value care, diagnostic reasoning, academic/research, pediatrics, medical education, and health policy tracks. Don’t forget to check out our interactive workshops. Nearly 150 workshop ideas were submitted, and we are proud to feature 18 of the best.
Of course, you must attend the highly anticipated Updates in Hospital Medicine talk and Plenary Sessions, and be sure to catch the Research, Innovations, and Clinical Vignettes (RIV) Poster Competition. Check out the Exhibit Hall and join a Special Interest Forum! Remember to download the SHM events app, and make sure you get your MOC credit from 34 different lectures.
This conference would not be possible without the tireless effort of SHM staff and leadership, our amazing speakers and faculty, and the committee members. We are excited you are here, and we hope this conference nurtures your curiosity, expands your career, and provides you with valuable educational and networking opportunities.
We sincerely thank you for attending HM18! Enjoy Orlando.
Dr. Finn is an assistant professor of medicine at Harvard Medical School, Boston, and course director of HM18.
Welcome to HM18 and Orlando! This is the annual conference’s first time in Orlando, a city dubbed “the happiest place on earth,” which conjures up magic and curiosity and brings out the kid in everyone. As Walt Disney noted, “Adults are only kids, grown up.” So we hope you have brought your sense of adventure and curiosity, as we have a lot planned for you!
Over the next 3 days, we invite you to network with nearly 5,000 hospitalist colleagues from around the “small world.” Introduce yourself to total strangers and discover you have a lot in common. This conference provides a wonderful opportunity to share best practices and discuss ideas.
Please have fun taking advantage of the wide array of learning opportunities the Annual Conference Committee developed for HM18. We hope the topics will grab your interest and pique your curiosity. We encourage you (and your inner kid) to try on new ideas, attend lectures that catch your eye, and roll up your sleeves to dive into interactive workshops. For extra fun, the committee created catchy Orlando-themed titles for many of the talks. We hope they make you smile!
The Annual Conference Committee members will be wearing large buttons to identify themselves. We welcome any feedback about the meeting. Please take the time to share your thoughts with us, and we are happy to help in any way. The committee members worked hard to create a pre-course day and meeting with something for everyone, knowing there is great diversity under the hospitalist tent. We also strove to make it relevant and timely. The driving force behind the content was “What do practicing hospitalists need and want to know now?”
HM18 contains an abundance of clinical content. Enjoy the 2 days of Clinical Update talks to hear the latest evidence from a diversity of fields. New this year is Updates in Addiction Medicine, given the large opioid crisis that affecting health care. There are 3 days of Rapid Fire talks to answer the clinical questions we all have while caring for patients. The Perioperative/Co-Management track is back with is unique and useful content. We even repeat some of the most popular talks on Tuesday, so you will be able to attend all the “can’t miss” sessions.
New this year is a focus on careers and how to make yours enjoyable and sustainable. Hospital medicine is more than 20 years old, and there are increasing numbers of mid-career hospitalists. The Career Development track offers a series of topics in case you want to spice up your current role, change your schedule, or plan for retirement. Accompanying this are career development workshops that provide practical skills to do just that.
We have also added a new NP/PA track, a palliative care track, and The Great Debate track. Come watch two entertaining speakers have a “smackdown” on a clinical topic. You’ll learn something while laughing.
We’ve also brought back your favorites: practice management, quality, high value care, diagnostic reasoning, academic/research, pediatrics, medical education, and health policy tracks. Don’t forget to check out our interactive workshops. Nearly 150 workshop ideas were submitted, and we are proud to feature 18 of the best.
Of course, you must attend the highly anticipated Updates in Hospital Medicine talk and Plenary Sessions, and be sure to catch the Research, Innovations, and Clinical Vignettes (RIV) Poster Competition. Check out the Exhibit Hall and join a Special Interest Forum! Remember to download the SHM events app, and make sure you get your MOC credit from 34 different lectures.
This conference would not be possible without the tireless effort of SHM staff and leadership, our amazing speakers and faculty, and the committee members. We are excited you are here, and we hope this conference nurtures your curiosity, expands your career, and provides you with valuable educational and networking opportunities.
We sincerely thank you for attending HM18! Enjoy Orlando.
Dr. Finn is an assistant professor of medicine at Harvard Medical School, Boston, and course director of HM18.
Welcome to HM18 and Orlando! This is the annual conference’s first time in Orlando, a city dubbed “the happiest place on earth,” which conjures up magic and curiosity and brings out the kid in everyone. As Walt Disney noted, “Adults are only kids, grown up.” So we hope you have brought your sense of adventure and curiosity, as we have a lot planned for you!
Over the next 3 days, we invite you to network with nearly 5,000 hospitalist colleagues from around the “small world.” Introduce yourself to total strangers and discover you have a lot in common. This conference provides a wonderful opportunity to share best practices and discuss ideas.
Please have fun taking advantage of the wide array of learning opportunities the Annual Conference Committee developed for HM18. We hope the topics will grab your interest and pique your curiosity. We encourage you (and your inner kid) to try on new ideas, attend lectures that catch your eye, and roll up your sleeves to dive into interactive workshops. For extra fun, the committee created catchy Orlando-themed titles for many of the talks. We hope they make you smile!
The Annual Conference Committee members will be wearing large buttons to identify themselves. We welcome any feedback about the meeting. Please take the time to share your thoughts with us, and we are happy to help in any way. The committee members worked hard to create a pre-course day and meeting with something for everyone, knowing there is great diversity under the hospitalist tent. We also strove to make it relevant and timely. The driving force behind the content was “What do practicing hospitalists need and want to know now?”
HM18 contains an abundance of clinical content. Enjoy the 2 days of Clinical Update talks to hear the latest evidence from a diversity of fields. New this year is Updates in Addiction Medicine, given the large opioid crisis that affecting health care. There are 3 days of Rapid Fire talks to answer the clinical questions we all have while caring for patients. The Perioperative/Co-Management track is back with is unique and useful content. We even repeat some of the most popular talks on Tuesday, so you will be able to attend all the “can’t miss” sessions.
New this year is a focus on careers and how to make yours enjoyable and sustainable. Hospital medicine is more than 20 years old, and there are increasing numbers of mid-career hospitalists. The Career Development track offers a series of topics in case you want to spice up your current role, change your schedule, or plan for retirement. Accompanying this are career development workshops that provide practical skills to do just that.
We have also added a new NP/PA track, a palliative care track, and The Great Debate track. Come watch two entertaining speakers have a “smackdown” on a clinical topic. You’ll learn something while laughing.
We’ve also brought back your favorites: practice management, quality, high value care, diagnostic reasoning, academic/research, pediatrics, medical education, and health policy tracks. Don’t forget to check out our interactive workshops. Nearly 150 workshop ideas were submitted, and we are proud to feature 18 of the best.
Of course, you must attend the highly anticipated Updates in Hospital Medicine talk and Plenary Sessions, and be sure to catch the Research, Innovations, and Clinical Vignettes (RIV) Poster Competition. Check out the Exhibit Hall and join a Special Interest Forum! Remember to download the SHM events app, and make sure you get your MOC credit from 34 different lectures.
This conference would not be possible without the tireless effort of SHM staff and leadership, our amazing speakers and faculty, and the committee members. We are excited you are here, and we hope this conference nurtures your curiosity, expands your career, and provides you with valuable educational and networking opportunities.
We sincerely thank you for attending HM18! Enjoy Orlando.
Dr. Finn is an assistant professor of medicine at Harvard Medical School, Boston, and course director of HM18.
Global attendees: Visit the International Lounge
Over the past several years, the Society of Hospital Medicine has become more involved in developing global relationships in an attempt to become a resource for hospital medicine movements in other countries. As part of this initiative, HM18 will host an International Lounge on Tuesday, April 10, from 10 a.m. to 3 p.m. in the Anaheim Room at the Orlando Marriott World Center.
“SHM has been taking a more deliberate approach to cultivating international relationships,” said Ethan Gray, CAE, vice president of membership for the society. “Although we are still in the beginning phases of establishing a global footprint that will provide enduring resources that respond to the needs of international members similar to those we provide to our U.S. members, we are making efforts toward that end.”
The International Lounge at HM18 is one such effort. Its purpose is to provide worldwide attendees with enhanced networking opportunities, information on how to launch an SHM chapter, and the opportunity to interact with SHM staff and board leaders.
“On Monday, HM18 will be hosting an International Special Interest Forum, which will allow global participants to share their experiences and interact with thought leaders from the United States and abroad, including SHM board members,” continued Mr. Gray. “The International Lounge is an extension of our global outreach at the annual meeting.”
The International Lounge will offer informal networking. As the SHM staff liaison, Mr. Gray will be on hand to answer any questions from and interact with global attendees. SHM board members also will be available on a rotating schedule throughout the day to network, dialogue, and share their knowledge and expertise.
As SHM expands its international activities, it is dedicating staff resources at its Philadelphia headquarters to international chapter development, including facilitating virtual communities on its Hospital Medical Exchange (HMX).
“Those visiting the lounge will be able to pick up a written fact sheet on the elements needed to create an SHM chapter,” stated Mr. Gray. “And, I will be available to discuss chapter launch requisites and any other questions they might have.”
Items covered in the fact sheet will include criteria for establishing an SHM international chapter, definition of a potential chapter’s geographic area, and the requirements for demonstrating necessary interest and leadership at the local level. It also will describe the SHM resources that will be available to international chapters – dedicated staff and physician leader liaisons, data support and management, creation of a chapter-specific HMX community to facilitate virtual networking and communications, meeting support, and counsel on how to build and maintain chapter audience and membership.
In addition, the lounge will have a global map that identifies geographic concentrations of international attendees and photos from recent international chapter meetings.
SHM has been surveying the field beyond U.S. borders through the initiation of conversations with organizations abroad. These efforts allow the society to learn from and support hospital medicine leaders and health systems around the world.
“The hospital medicine movement is in various stages of development outside the United States,” explained Mr. Gray. “Many factors influence the rate at which a hospital medicine model can become implemented, including the structure of the health system, education and training curricula, existing scope of practice and care-delivery constructs, fluidity of government and systems, and other factors.
“We urge participants from abroad to visit the International Lounge to meet and share information with their counterparts from other countries, learn more about SHM and what it has to offer, find out about the potential for launching an SHM chapter, and interact with SHM staff and board members,” concluded Mr. Gray. “We have so much to learn from each other.”
International Lounge
Tuesday, April 10, 10 a.m.-3 p.m.
Anaheim Room
Over the past several years, the Society of Hospital Medicine has become more involved in developing global relationships in an attempt to become a resource for hospital medicine movements in other countries. As part of this initiative, HM18 will host an International Lounge on Tuesday, April 10, from 10 a.m. to 3 p.m. in the Anaheim Room at the Orlando Marriott World Center.
“SHM has been taking a more deliberate approach to cultivating international relationships,” said Ethan Gray, CAE, vice president of membership for the society. “Although we are still in the beginning phases of establishing a global footprint that will provide enduring resources that respond to the needs of international members similar to those we provide to our U.S. members, we are making efforts toward that end.”
The International Lounge at HM18 is one such effort. Its purpose is to provide worldwide attendees with enhanced networking opportunities, information on how to launch an SHM chapter, and the opportunity to interact with SHM staff and board leaders.
“On Monday, HM18 will be hosting an International Special Interest Forum, which will allow global participants to share their experiences and interact with thought leaders from the United States and abroad, including SHM board members,” continued Mr. Gray. “The International Lounge is an extension of our global outreach at the annual meeting.”
The International Lounge will offer informal networking. As the SHM staff liaison, Mr. Gray will be on hand to answer any questions from and interact with global attendees. SHM board members also will be available on a rotating schedule throughout the day to network, dialogue, and share their knowledge and expertise.
As SHM expands its international activities, it is dedicating staff resources at its Philadelphia headquarters to international chapter development, including facilitating virtual communities on its Hospital Medical Exchange (HMX).
“Those visiting the lounge will be able to pick up a written fact sheet on the elements needed to create an SHM chapter,” stated Mr. Gray. “And, I will be available to discuss chapter launch requisites and any other questions they might have.”
Items covered in the fact sheet will include criteria for establishing an SHM international chapter, definition of a potential chapter’s geographic area, and the requirements for demonstrating necessary interest and leadership at the local level. It also will describe the SHM resources that will be available to international chapters – dedicated staff and physician leader liaisons, data support and management, creation of a chapter-specific HMX community to facilitate virtual networking and communications, meeting support, and counsel on how to build and maintain chapter audience and membership.
In addition, the lounge will have a global map that identifies geographic concentrations of international attendees and photos from recent international chapter meetings.
SHM has been surveying the field beyond U.S. borders through the initiation of conversations with organizations abroad. These efforts allow the society to learn from and support hospital medicine leaders and health systems around the world.
“The hospital medicine movement is in various stages of development outside the United States,” explained Mr. Gray. “Many factors influence the rate at which a hospital medicine model can become implemented, including the structure of the health system, education and training curricula, existing scope of practice and care-delivery constructs, fluidity of government and systems, and other factors.
“We urge participants from abroad to visit the International Lounge to meet and share information with their counterparts from other countries, learn more about SHM and what it has to offer, find out about the potential for launching an SHM chapter, and interact with SHM staff and board members,” concluded Mr. Gray. “We have so much to learn from each other.”
International Lounge
Tuesday, April 10, 10 a.m.-3 p.m.
Anaheim Room
Over the past several years, the Society of Hospital Medicine has become more involved in developing global relationships in an attempt to become a resource for hospital medicine movements in other countries. As part of this initiative, HM18 will host an International Lounge on Tuesday, April 10, from 10 a.m. to 3 p.m. in the Anaheim Room at the Orlando Marriott World Center.
“SHM has been taking a more deliberate approach to cultivating international relationships,” said Ethan Gray, CAE, vice president of membership for the society. “Although we are still in the beginning phases of establishing a global footprint that will provide enduring resources that respond to the needs of international members similar to those we provide to our U.S. members, we are making efforts toward that end.”
The International Lounge at HM18 is one such effort. Its purpose is to provide worldwide attendees with enhanced networking opportunities, information on how to launch an SHM chapter, and the opportunity to interact with SHM staff and board leaders.
“On Monday, HM18 will be hosting an International Special Interest Forum, which will allow global participants to share their experiences and interact with thought leaders from the United States and abroad, including SHM board members,” continued Mr. Gray. “The International Lounge is an extension of our global outreach at the annual meeting.”
The International Lounge will offer informal networking. As the SHM staff liaison, Mr. Gray will be on hand to answer any questions from and interact with global attendees. SHM board members also will be available on a rotating schedule throughout the day to network, dialogue, and share their knowledge and expertise.
As SHM expands its international activities, it is dedicating staff resources at its Philadelphia headquarters to international chapter development, including facilitating virtual communities on its Hospital Medical Exchange (HMX).
“Those visiting the lounge will be able to pick up a written fact sheet on the elements needed to create an SHM chapter,” stated Mr. Gray. “And, I will be available to discuss chapter launch requisites and any other questions they might have.”
Items covered in the fact sheet will include criteria for establishing an SHM international chapter, definition of a potential chapter’s geographic area, and the requirements for demonstrating necessary interest and leadership at the local level. It also will describe the SHM resources that will be available to international chapters – dedicated staff and physician leader liaisons, data support and management, creation of a chapter-specific HMX community to facilitate virtual networking and communications, meeting support, and counsel on how to build and maintain chapter audience and membership.
In addition, the lounge will have a global map that identifies geographic concentrations of international attendees and photos from recent international chapter meetings.
SHM has been surveying the field beyond U.S. borders through the initiation of conversations with organizations abroad. These efforts allow the society to learn from and support hospital medicine leaders and health systems around the world.
“The hospital medicine movement is in various stages of development outside the United States,” explained Mr. Gray. “Many factors influence the rate at which a hospital medicine model can become implemented, including the structure of the health system, education and training curricula, existing scope of practice and care-delivery constructs, fluidity of government and systems, and other factors.
“We urge participants from abroad to visit the International Lounge to meet and share information with their counterparts from other countries, learn more about SHM and what it has to offer, find out about the potential for launching an SHM chapter, and interact with SHM staff and board members,” concluded Mr. Gray. “We have so much to learn from each other.”
International Lounge
Tuesday, April 10, 10 a.m.-3 p.m.
Anaheim Room
The Resident and Student Luncheon exposes future hospitalists to professional possibilities
“Trainees can ask hospitalists who are administrative leaders, QI gurus, medical educators, global health hospitalists, pediatricians, and researchers about their day-to-day life and what they love about their careers,” stated Darlene B. Tad-y, MD, SFHM, who is an associate professor and hospitalist at the University of Colorado Hospital, Denver. “It’s a great way for trainees to build their network in hospital medicine in addition to learning about the diverse careers available in our field.”
The luncheon is structured in such a way to maximizes attendees’ exposure and interaction with experienced hospitalists. Brian Kwan, MD, FHM, an associate professor of health science at the University of California, San Diego, and a hospitalist, elaborated on the sessions design.
“Each round table features a speaker that will highlight a different topic, including but not limited to medical education, executive leadership, global and rural health, quality improvement, advocacy, and informatics,” said Dr. Kwan.
But the session is not limited to a one-way presentation. “Conversations are facilitated by members of the SHM Physicians in Training (PIT) Committee,” he said. To maximize their exposure, “attendees will have an opportunity to select one table for the main meal and a different one for dessert, so that they have the opportunity to hear from more than one speaker.”
Dr. Kwan and Dr. Tad-y said they believe that this type of exposure is important in the professional development of medical students and residents.
“We believe it is critical for students and residents to be exposed to hospitalists working at the forefront of our field who inspire and can provide a glimpse at different HM career paths and practices. Invited speakers are selected by the PIT Committee, and the luncheon serves as a launching point for networking and potential mentorship. Engaging residents and students is critical to sustaining our pipeline for future hospitalist leaders,” Dr. Kwan said.
Dr. Tad-y stated that this could be a defining professional moment for many of the attendees. “The resident or student may even meet their next project or career mentor, as well as potential peers or project partners.”
Resident and Student Luncheon
April 9, Monday, 12-1 p.m.
New York/New Orleans Room
“Trainees can ask hospitalists who are administrative leaders, QI gurus, medical educators, global health hospitalists, pediatricians, and researchers about their day-to-day life and what they love about their careers,” stated Darlene B. Tad-y, MD, SFHM, who is an associate professor and hospitalist at the University of Colorado Hospital, Denver. “It’s a great way for trainees to build their network in hospital medicine in addition to learning about the diverse careers available in our field.”
The luncheon is structured in such a way to maximizes attendees’ exposure and interaction with experienced hospitalists. Brian Kwan, MD, FHM, an associate professor of health science at the University of California, San Diego, and a hospitalist, elaborated on the sessions design.
“Each round table features a speaker that will highlight a different topic, including but not limited to medical education, executive leadership, global and rural health, quality improvement, advocacy, and informatics,” said Dr. Kwan.
But the session is not limited to a one-way presentation. “Conversations are facilitated by members of the SHM Physicians in Training (PIT) Committee,” he said. To maximize their exposure, “attendees will have an opportunity to select one table for the main meal and a different one for dessert, so that they have the opportunity to hear from more than one speaker.”
Dr. Kwan and Dr. Tad-y said they believe that this type of exposure is important in the professional development of medical students and residents.
“We believe it is critical for students and residents to be exposed to hospitalists working at the forefront of our field who inspire and can provide a glimpse at different HM career paths and practices. Invited speakers are selected by the PIT Committee, and the luncheon serves as a launching point for networking and potential mentorship. Engaging residents and students is critical to sustaining our pipeline for future hospitalist leaders,” Dr. Kwan said.
Dr. Tad-y stated that this could be a defining professional moment for many of the attendees. “The resident or student may even meet their next project or career mentor, as well as potential peers or project partners.”
Resident and Student Luncheon
April 9, Monday, 12-1 p.m.
New York/New Orleans Room
“Trainees can ask hospitalists who are administrative leaders, QI gurus, medical educators, global health hospitalists, pediatricians, and researchers about their day-to-day life and what they love about their careers,” stated Darlene B. Tad-y, MD, SFHM, who is an associate professor and hospitalist at the University of Colorado Hospital, Denver. “It’s a great way for trainees to build their network in hospital medicine in addition to learning about the diverse careers available in our field.”
The luncheon is structured in such a way to maximizes attendees’ exposure and interaction with experienced hospitalists. Brian Kwan, MD, FHM, an associate professor of health science at the University of California, San Diego, and a hospitalist, elaborated on the sessions design.
“Each round table features a speaker that will highlight a different topic, including but not limited to medical education, executive leadership, global and rural health, quality improvement, advocacy, and informatics,” said Dr. Kwan.
But the session is not limited to a one-way presentation. “Conversations are facilitated by members of the SHM Physicians in Training (PIT) Committee,” he said. To maximize their exposure, “attendees will have an opportunity to select one table for the main meal and a different one for dessert, so that they have the opportunity to hear from more than one speaker.”
Dr. Kwan and Dr. Tad-y said they believe that this type of exposure is important in the professional development of medical students and residents.
“We believe it is critical for students and residents to be exposed to hospitalists working at the forefront of our field who inspire and can provide a glimpse at different HM career paths and practices. Invited speakers are selected by the PIT Committee, and the luncheon serves as a launching point for networking and potential mentorship. Engaging residents and students is critical to sustaining our pipeline for future hospitalist leaders,” Dr. Kwan said.
Dr. Tad-y stated that this could be a defining professional moment for many of the attendees. “The resident or student may even meet their next project or career mentor, as well as potential peers or project partners.”
Resident and Student Luncheon
April 9, Monday, 12-1 p.m.
New York/New Orleans Room
Fun in the Florida sun
Chris Harrington knows that not all the benefits of attending the Society of Hospital Medicine’s annual meetings come from the lectures and courses; there is the formation of friendships that endure.
“I am very grateful to SHM for allowing me the opportunity to accompany Bob to their annual conferences and leadership academies over the years,” said Mrs. Harrington, spouse of former SHM president Robert Harrington Jr., MD, SFHM in an interview.
“It truly has been a rewarding experience for me both as a spouse to travel with my husband and spend time with our friends, and as a health care professional to witness the tremendous growth of SHM membership and the educational and networking opportunities it provides to its members. Watching SHM become even more innovative in universally improving patient care has been an amazing experience as well.
“It is through many SHM conferences that Bob and I have met some wonderful people and have formed many lasting friendships that we will be forever grateful for,” she said.
Mrs. Harrington has some suggestions for activities in Orlando, starting with the Walt Disney World Resort theme parks, which are convenient to the meeting headquarters at the Orlando World Center Marriott. Other popular spots for those with kids (or the young at heart) include SeaWorld Orlando, Legoland Florida, and Universal’s Islands of Adventure, notably the Harry Potter and the Forbidden Journey and the Jurassic Park River Adventure attractions.
Within the Orlando World Center Marriott, families can check out the pool complex with its waterslides and slide tower, as well as the kids’ activity center, interactive game room, and table tennis. The resort also offers full-day (10 a.m. to 5 p.m.) or half-day (10 a.m. to 1:30 p.m. or 1:30 p.m. to 5 p.m.) Kid’s World programs and evening Kid’s Night Out programs (6-10 p.m.) for children aged 4-12, so parents get some time to themselves.
For the fitness enthusiasts, “bring your golf clubs, tennis rackets, and running shoes,” Mrs. Harrington said. The resort offers eight tennis courts, volleyball courts, swimming pools for laps, and Hawk’s Landing, a championship golf course that includes a Jack Nicklaus Academy of Golf, should the urge for instruction strike.
Runners, set your alarms for the 5K SHM Fun Run at 6 a.m. on April 10. The Harringtons said they will sign up and be at the start line after a quick visit to the resort’s in-house Starbucks.
“If you want to unwind after a day of meetings and workshops or rejuvenate after a workout, make an appointment (as soon as possible) at the resort’s full service spa,” Mrs. Harrington advised. Spa services include manicures/pedicures, facials, and even couple’s massages, she noted.
Other activities for individuals and families include ZE Segway Tours, the nearby town of Celebration, and the Basilica of the National Shrine of Mary, Queen of the Universe.
Spouses seeking some shopping during meeting time may enjoy nearby outlet malls, the Florida Mall, and the high-end shops of the Mall at Millenia, Mrs Harrington said. One of her favorite “hidden gems” for out-of-town shopping is Park Avenue in Winter Park, which has many boutiques and restaurants. Mount Dora, a small town once known as the Antiques Capital of Florida, includes a wide variety of specialty shops, she noted, and foodies should explore the East End Market, an Orlando neighborhood market and cultural food hub inspired by Central Florida’s local farmers and food artisans.
When it’s time for dining out in Orlando, Mrs. Harrington recommended the Big Fin Seafood Kitchen, a family-owned upscale casual restaurant serving lobster, snow crabs, fresh raw oysters, sushi rolls, steaks, and pasta with an option for outdoor dining on a covered balcony. Christini’s Ristorante Italiano, the most-awarded fine dining Italian restaurant in Orlando for more than 30 years, is consistently popular, and Vines Grille and Wine Bar, “a gem on Orlando’s Restaurant Row,” Mrs. Harrington said, is a great choice for happy hour and features jazz and blues in the evenings starting about 7 p.m.
Finally, “I would recommend meeting some SHM staff members either at registration or between meetings,” Mrs. Harrington advised. “They have been so welcoming to me over the years and have been a great resource and support system. Also, be open to meeting other spouses at group outings, dinners, or networking events whenever you have the opportunity, as they might become a treasured friend,” she said.
Chris Harrington knows that not all the benefits of attending the Society of Hospital Medicine’s annual meetings come from the lectures and courses; there is the formation of friendships that endure.
“I am very grateful to SHM for allowing me the opportunity to accompany Bob to their annual conferences and leadership academies over the years,” said Mrs. Harrington, spouse of former SHM president Robert Harrington Jr., MD, SFHM in an interview.
“It truly has been a rewarding experience for me both as a spouse to travel with my husband and spend time with our friends, and as a health care professional to witness the tremendous growth of SHM membership and the educational and networking opportunities it provides to its members. Watching SHM become even more innovative in universally improving patient care has been an amazing experience as well.
“It is through many SHM conferences that Bob and I have met some wonderful people and have formed many lasting friendships that we will be forever grateful for,” she said.
Mrs. Harrington has some suggestions for activities in Orlando, starting with the Walt Disney World Resort theme parks, which are convenient to the meeting headquarters at the Orlando World Center Marriott. Other popular spots for those with kids (or the young at heart) include SeaWorld Orlando, Legoland Florida, and Universal’s Islands of Adventure, notably the Harry Potter and the Forbidden Journey and the Jurassic Park River Adventure attractions.
Within the Orlando World Center Marriott, families can check out the pool complex with its waterslides and slide tower, as well as the kids’ activity center, interactive game room, and table tennis. The resort also offers full-day (10 a.m. to 5 p.m.) or half-day (10 a.m. to 1:30 p.m. or 1:30 p.m. to 5 p.m.) Kid’s World programs and evening Kid’s Night Out programs (6-10 p.m.) for children aged 4-12, so parents get some time to themselves.
For the fitness enthusiasts, “bring your golf clubs, tennis rackets, and running shoes,” Mrs. Harrington said. The resort offers eight tennis courts, volleyball courts, swimming pools for laps, and Hawk’s Landing, a championship golf course that includes a Jack Nicklaus Academy of Golf, should the urge for instruction strike.
Runners, set your alarms for the 5K SHM Fun Run at 6 a.m. on April 10. The Harringtons said they will sign up and be at the start line after a quick visit to the resort’s in-house Starbucks.
“If you want to unwind after a day of meetings and workshops or rejuvenate after a workout, make an appointment (as soon as possible) at the resort’s full service spa,” Mrs. Harrington advised. Spa services include manicures/pedicures, facials, and even couple’s massages, she noted.
Other activities for individuals and families include ZE Segway Tours, the nearby town of Celebration, and the Basilica of the National Shrine of Mary, Queen of the Universe.
Spouses seeking some shopping during meeting time may enjoy nearby outlet malls, the Florida Mall, and the high-end shops of the Mall at Millenia, Mrs Harrington said. One of her favorite “hidden gems” for out-of-town shopping is Park Avenue in Winter Park, which has many boutiques and restaurants. Mount Dora, a small town once known as the Antiques Capital of Florida, includes a wide variety of specialty shops, she noted, and foodies should explore the East End Market, an Orlando neighborhood market and cultural food hub inspired by Central Florida’s local farmers and food artisans.
When it’s time for dining out in Orlando, Mrs. Harrington recommended the Big Fin Seafood Kitchen, a family-owned upscale casual restaurant serving lobster, snow crabs, fresh raw oysters, sushi rolls, steaks, and pasta with an option for outdoor dining on a covered balcony. Christini’s Ristorante Italiano, the most-awarded fine dining Italian restaurant in Orlando for more than 30 years, is consistently popular, and Vines Grille and Wine Bar, “a gem on Orlando’s Restaurant Row,” Mrs. Harrington said, is a great choice for happy hour and features jazz and blues in the evenings starting about 7 p.m.
Finally, “I would recommend meeting some SHM staff members either at registration or between meetings,” Mrs. Harrington advised. “They have been so welcoming to me over the years and have been a great resource and support system. Also, be open to meeting other spouses at group outings, dinners, or networking events whenever you have the opportunity, as they might become a treasured friend,” she said.
Chris Harrington knows that not all the benefits of attending the Society of Hospital Medicine’s annual meetings come from the lectures and courses; there is the formation of friendships that endure.
“I am very grateful to SHM for allowing me the opportunity to accompany Bob to their annual conferences and leadership academies over the years,” said Mrs. Harrington, spouse of former SHM president Robert Harrington Jr., MD, SFHM in an interview.
“It truly has been a rewarding experience for me both as a spouse to travel with my husband and spend time with our friends, and as a health care professional to witness the tremendous growth of SHM membership and the educational and networking opportunities it provides to its members. Watching SHM become even more innovative in universally improving patient care has been an amazing experience as well.
“It is through many SHM conferences that Bob and I have met some wonderful people and have formed many lasting friendships that we will be forever grateful for,” she said.
Mrs. Harrington has some suggestions for activities in Orlando, starting with the Walt Disney World Resort theme parks, which are convenient to the meeting headquarters at the Orlando World Center Marriott. Other popular spots for those with kids (or the young at heart) include SeaWorld Orlando, Legoland Florida, and Universal’s Islands of Adventure, notably the Harry Potter and the Forbidden Journey and the Jurassic Park River Adventure attractions.
Within the Orlando World Center Marriott, families can check out the pool complex with its waterslides and slide tower, as well as the kids’ activity center, interactive game room, and table tennis. The resort also offers full-day (10 a.m. to 5 p.m.) or half-day (10 a.m. to 1:30 p.m. or 1:30 p.m. to 5 p.m.) Kid’s World programs and evening Kid’s Night Out programs (6-10 p.m.) for children aged 4-12, so parents get some time to themselves.
For the fitness enthusiasts, “bring your golf clubs, tennis rackets, and running shoes,” Mrs. Harrington said. The resort offers eight tennis courts, volleyball courts, swimming pools for laps, and Hawk’s Landing, a championship golf course that includes a Jack Nicklaus Academy of Golf, should the urge for instruction strike.
Runners, set your alarms for the 5K SHM Fun Run at 6 a.m. on April 10. The Harringtons said they will sign up and be at the start line after a quick visit to the resort’s in-house Starbucks.
“If you want to unwind after a day of meetings and workshops or rejuvenate after a workout, make an appointment (as soon as possible) at the resort’s full service spa,” Mrs. Harrington advised. Spa services include manicures/pedicures, facials, and even couple’s massages, she noted.
Other activities for individuals and families include ZE Segway Tours, the nearby town of Celebration, and the Basilica of the National Shrine of Mary, Queen of the Universe.
Spouses seeking some shopping during meeting time may enjoy nearby outlet malls, the Florida Mall, and the high-end shops of the Mall at Millenia, Mrs Harrington said. One of her favorite “hidden gems” for out-of-town shopping is Park Avenue in Winter Park, which has many boutiques and restaurants. Mount Dora, a small town once known as the Antiques Capital of Florida, includes a wide variety of specialty shops, she noted, and foodies should explore the East End Market, an Orlando neighborhood market and cultural food hub inspired by Central Florida’s local farmers and food artisans.
When it’s time for dining out in Orlando, Mrs. Harrington recommended the Big Fin Seafood Kitchen, a family-owned upscale casual restaurant serving lobster, snow crabs, fresh raw oysters, sushi rolls, steaks, and pasta with an option for outdoor dining on a covered balcony. Christini’s Ristorante Italiano, the most-awarded fine dining Italian restaurant in Orlando for more than 30 years, is consistently popular, and Vines Grille and Wine Bar, “a gem on Orlando’s Restaurant Row,” Mrs. Harrington said, is a great choice for happy hour and features jazz and blues in the evenings starting about 7 p.m.
Finally, “I would recommend meeting some SHM staff members either at registration or between meetings,” Mrs. Harrington advised. “They have been so welcoming to me over the years and have been a great resource and support system. Also, be open to meeting other spouses at group outings, dinners, or networking events whenever you have the opportunity, as they might become a treasured friend,” she said.
Oncologist-led BRCA mutation testing and counseling may reduce wait times for women with ovarian cancer
For women with ovarian cancer, an oncologist-led BRCA1/2 (BRCAm) counseling process is associated with favorable waiting times for test results and high levels of satisfaction, according to results of a prospective observational study.
The median turnaround time from initial counseling to receiving a test result was 9.1 weeks, investigators reported in the Journal of Clinical Oncology.
“Following a pathway similar to the one used in this study could allow faster treatment decisions and better use of resources in the management of patients with ovarian cancer,” said lead author Nicoletta Colombo, MD, of European Institute of Oncology, University of Milan-Bicocca, Italy, and her associates.
Establishing an ovarian cancer patient’s BRCAm status provides useful prognostic information and helps identify patients most likely to benefit from therapy with poly(ADP-ribose) polymerase (PARP) inhibitors, Dr. Colombo and her colleagues wrote.
However, despite guideline recommendations, many patients with an ovarian cancer diagnosis are currently not receiving BRCAm testing, they added.
“Given the high volume of BRCAm tests now being ordered, a new, more streamlined testing approach is needed to shorten testing turnaround times and to ease the pressure on genetic counselors,” the authors said.
In a pilot study from the United Kingdom, a streamlined, oncologist-led BRCAm testing model reduced a 20-week average turnaround time by fourfold, Dr. Colombo and her colleagues said.
Accordingly, the prospective, observational ENGAGE study sought to evaluate a streamlined oncologist-led BRCAm testing pathway in 700 patients with ovarian cancer at 26 sites in the United States, Spain, and Italy.
Oncologists and oncology nurses involved in the study received training on pretest genetic counseling techniques and on how to discuss the role of BRCAm testing with patients, according to the study description. Patients with a positive test were recommended for an appointment with a geneticist or genetic counselor.
The median time from initial counseling to receiving a test result was 9.1 weeks, the investigators reported. For patients in the United States, that median turnaround time was 4.1 weeks, while turnaround times in Spain and Italy were 12.0 and 20.4 weeks, respectively.
“BRCAm testing usually occurred shortly after the initial oncology team counseling, whereas the average time from patient consent to BRCAm testing was expected to be more than 1 month in approximately 25% of patients using standard procedures,” the investigators said in their report.
More than 99% of patients expressed satisfaction with the oncologist-led testing pathway, Dr. Colombo and her associates said. In addition, more than 80% of oncologists said the testing worked well and that counseling was an efficient use of their time.
Geneticists and genetic counselors showed less enthusiasm for the oncologist-led approach, according to investigators.
Less than half of surveyed geneticists or genetic counselors felt that patients received accurate information about the BRCAm test in the pretest counseling session, according to the report.
“It should be noted that the purpose of the oncologist-led pretest counseling was to provide enough information on why the patient should have the test, rather than full genetic counseling, which is appropriate once the test result is known,” investigators said in the report.
The study was supported by AstraZeneca. Dr. Colombo and her associates reported potential conflicts of interest related to AstraZeneca, Genentech, PharmaMar, Amgen, Clovis Oncology, Pfizer, MSD, Tesaro, and others.
SOURCE: Colombo N et al. J Clin Oncol. 2018 Mar 20. doi: 10.1200/JCO.2017.76.278.
For women with ovarian cancer, an oncologist-led BRCA1/2 (BRCAm) counseling process is associated with favorable waiting times for test results and high levels of satisfaction, according to results of a prospective observational study.
The median turnaround time from initial counseling to receiving a test result was 9.1 weeks, investigators reported in the Journal of Clinical Oncology.
“Following a pathway similar to the one used in this study could allow faster treatment decisions and better use of resources in the management of patients with ovarian cancer,” said lead author Nicoletta Colombo, MD, of European Institute of Oncology, University of Milan-Bicocca, Italy, and her associates.
Establishing an ovarian cancer patient’s BRCAm status provides useful prognostic information and helps identify patients most likely to benefit from therapy with poly(ADP-ribose) polymerase (PARP) inhibitors, Dr. Colombo and her colleagues wrote.
However, despite guideline recommendations, many patients with an ovarian cancer diagnosis are currently not receiving BRCAm testing, they added.
“Given the high volume of BRCAm tests now being ordered, a new, more streamlined testing approach is needed to shorten testing turnaround times and to ease the pressure on genetic counselors,” the authors said.
In a pilot study from the United Kingdom, a streamlined, oncologist-led BRCAm testing model reduced a 20-week average turnaround time by fourfold, Dr. Colombo and her colleagues said.
Accordingly, the prospective, observational ENGAGE study sought to evaluate a streamlined oncologist-led BRCAm testing pathway in 700 patients with ovarian cancer at 26 sites in the United States, Spain, and Italy.
Oncologists and oncology nurses involved in the study received training on pretest genetic counseling techniques and on how to discuss the role of BRCAm testing with patients, according to the study description. Patients with a positive test were recommended for an appointment with a geneticist or genetic counselor.
The median time from initial counseling to receiving a test result was 9.1 weeks, the investigators reported. For patients in the United States, that median turnaround time was 4.1 weeks, while turnaround times in Spain and Italy were 12.0 and 20.4 weeks, respectively.
“BRCAm testing usually occurred shortly after the initial oncology team counseling, whereas the average time from patient consent to BRCAm testing was expected to be more than 1 month in approximately 25% of patients using standard procedures,” the investigators said in their report.
More than 99% of patients expressed satisfaction with the oncologist-led testing pathway, Dr. Colombo and her associates said. In addition, more than 80% of oncologists said the testing worked well and that counseling was an efficient use of their time.
Geneticists and genetic counselors showed less enthusiasm for the oncologist-led approach, according to investigators.
Less than half of surveyed geneticists or genetic counselors felt that patients received accurate information about the BRCAm test in the pretest counseling session, according to the report.
“It should be noted that the purpose of the oncologist-led pretest counseling was to provide enough information on why the patient should have the test, rather than full genetic counseling, which is appropriate once the test result is known,” investigators said in the report.
The study was supported by AstraZeneca. Dr. Colombo and her associates reported potential conflicts of interest related to AstraZeneca, Genentech, PharmaMar, Amgen, Clovis Oncology, Pfizer, MSD, Tesaro, and others.
SOURCE: Colombo N et al. J Clin Oncol. 2018 Mar 20. doi: 10.1200/JCO.2017.76.278.
For women with ovarian cancer, an oncologist-led BRCA1/2 (BRCAm) counseling process is associated with favorable waiting times for test results and high levels of satisfaction, according to results of a prospective observational study.
The median turnaround time from initial counseling to receiving a test result was 9.1 weeks, investigators reported in the Journal of Clinical Oncology.
“Following a pathway similar to the one used in this study could allow faster treatment decisions and better use of resources in the management of patients with ovarian cancer,” said lead author Nicoletta Colombo, MD, of European Institute of Oncology, University of Milan-Bicocca, Italy, and her associates.
Establishing an ovarian cancer patient’s BRCAm status provides useful prognostic information and helps identify patients most likely to benefit from therapy with poly(ADP-ribose) polymerase (PARP) inhibitors, Dr. Colombo and her colleagues wrote.
However, despite guideline recommendations, many patients with an ovarian cancer diagnosis are currently not receiving BRCAm testing, they added.
“Given the high volume of BRCAm tests now being ordered, a new, more streamlined testing approach is needed to shorten testing turnaround times and to ease the pressure on genetic counselors,” the authors said.
In a pilot study from the United Kingdom, a streamlined, oncologist-led BRCAm testing model reduced a 20-week average turnaround time by fourfold, Dr. Colombo and her colleagues said.
Accordingly, the prospective, observational ENGAGE study sought to evaluate a streamlined oncologist-led BRCAm testing pathway in 700 patients with ovarian cancer at 26 sites in the United States, Spain, and Italy.
Oncologists and oncology nurses involved in the study received training on pretest genetic counseling techniques and on how to discuss the role of BRCAm testing with patients, according to the study description. Patients with a positive test were recommended for an appointment with a geneticist or genetic counselor.
The median time from initial counseling to receiving a test result was 9.1 weeks, the investigators reported. For patients in the United States, that median turnaround time was 4.1 weeks, while turnaround times in Spain and Italy were 12.0 and 20.4 weeks, respectively.
“BRCAm testing usually occurred shortly after the initial oncology team counseling, whereas the average time from patient consent to BRCAm testing was expected to be more than 1 month in approximately 25% of patients using standard procedures,” the investigators said in their report.
More than 99% of patients expressed satisfaction with the oncologist-led testing pathway, Dr. Colombo and her associates said. In addition, more than 80% of oncologists said the testing worked well and that counseling was an efficient use of their time.
Geneticists and genetic counselors showed less enthusiasm for the oncologist-led approach, according to investigators.
Less than half of surveyed geneticists or genetic counselors felt that patients received accurate information about the BRCAm test in the pretest counseling session, according to the report.
“It should be noted that the purpose of the oncologist-led pretest counseling was to provide enough information on why the patient should have the test, rather than full genetic counseling, which is appropriate once the test result is known,” investigators said in the report.
The study was supported by AstraZeneca. Dr. Colombo and her associates reported potential conflicts of interest related to AstraZeneca, Genentech, PharmaMar, Amgen, Clovis Oncology, Pfizer, MSD, Tesaro, and others.
SOURCE: Colombo N et al. J Clin Oncol. 2018 Mar 20. doi: 10.1200/JCO.2017.76.278.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: An oncologist-led BRCA1/2 (BRCAm) counseling process is associated with favorable waiting times for test results and high levels of satisfaction among women with ovarian cancer.
Major finding: The median turnaround time from initial counseling to receiving a test result was 9.1 weeks.
Study details: The prospective, observational ENGAGE study evaluating a streamlined oncologist-led BRCAm testing pathway in 700 patients with ovarian cancer at 26 sites in the United States, Spain, and Italy.
Disclosures: The study was supported by AstraZeneca. Study authors reported potential conflicts of interest related to AstraZeneca, Genentech, PharmaMar, Amgen, Clovis Oncology, Pfizer, MSD, Tesaro, and others.
Source: Colombo N et al. J Clin Oncol. 2018 Mar 20. doi: 10.1200/JCO.2017.76.278.
Ibrutinib plus venetoclax is active in mantle cell lymphoma
In mantle cell lymphoma (MCL), ibrutinib plus venetoclax significantly improved the complete response rate, compared with what has been previously reported for ibrutinib alone, according to results of a phase 2 study.
Clinical outcomes with the combination seem superior to previously reported results for either treatment alone, said lead investigator Constantine S. Tam, MBBS, MD, of the Peter MacCallum Cancer Centre, Melbourne, and his coinvestigators.
“The results of our study, which used a historical cohort as a control, are consistent with the notion that the combination of ibrutinib and venetoclax is highly effective in mantle-cell lymphoma,” the investigators wrote in the New England Journal of Medicine.
The BTK inhibitor ibrutinib and the BCL2 inhibitor venetoclax are two of the most active agents for this B-cell cancer, investigators reported. The rationale for combining the agents is “compelling” because they affect different critical pathways in the malignant B cell.
Both agents have demonstrated complete response rates of 21% in previous studies of relapsed or refractory MCL, and preclinical studies suggest the combination of ibrutinib and venetoclax would be synergistic.
In the present single-group, phase 2 study, 24 patients with MCL (23 relapsed or refractory, 1 previously untreated) started ibrutinib 560 mg daily; at 4 weeks, venetoclax was started at a low dose and increased to 400 mg daily.
The study primary end point – complete response rate at week 16 assessed by CT – was 42%, compared with 9% for ibrutinib monotherapy in the phase 2 PCYC-1104-CA study (P less than .001).
Computed tomography assessment was used for the primary end point to allow comparison to the ibrutinib monotherapy study, which did not use positron emission tomography for restaging. “Our study was designed to have 80% power to reject a complete response rate of 9% (at a one-sided alpha level of 0.05) if the rate of complete response was at least 30%,” the investigators noted.
Complete response rate assessed by positron emission tomography at week 16 was 62%, and was 71% overall.
In all, 67% of patients had absence of minimal residual disease by flow cytometry. At 15 months, 78% of the responses were ongoing, and at 18 months, 57% of patients were alive and progression free.
“Such outcomes appear to be substantially better than those that have been reported for ibrutinib or venetoclax monotherapy,” the investigators wrote.
The combination had side effects that are “acceptable to both patients and physicians,” investigators wrote. Side effects, usually low grade, included diarrhea in 83% of patients, fatigue in 75%, and nausea or vomiting in 71%. Tumor lysis syndrome was seen in two patients.
Whether ibrutinib plus venetoclax is superior to ibrutinib alone is being formally evaluated in an ongoing phase 3 study.
Janssen and AbbVie partially funded the current phase 2 study. Dr. Tam reported financial ties to Janssen, AbbVie, and Pharmacyclics. Other study authors reported financial ties to various pharmaceutical companies.
SOURCE: Tam C et al. N Engl J Med. 2018;378:1211-23.
In mantle cell lymphoma (MCL), ibrutinib plus venetoclax significantly improved the complete response rate, compared with what has been previously reported for ibrutinib alone, according to results of a phase 2 study.
Clinical outcomes with the combination seem superior to previously reported results for either treatment alone, said lead investigator Constantine S. Tam, MBBS, MD, of the Peter MacCallum Cancer Centre, Melbourne, and his coinvestigators.
“The results of our study, which used a historical cohort as a control, are consistent with the notion that the combination of ibrutinib and venetoclax is highly effective in mantle-cell lymphoma,” the investigators wrote in the New England Journal of Medicine.
The BTK inhibitor ibrutinib and the BCL2 inhibitor venetoclax are two of the most active agents for this B-cell cancer, investigators reported. The rationale for combining the agents is “compelling” because they affect different critical pathways in the malignant B cell.
Both agents have demonstrated complete response rates of 21% in previous studies of relapsed or refractory MCL, and preclinical studies suggest the combination of ibrutinib and venetoclax would be synergistic.
In the present single-group, phase 2 study, 24 patients with MCL (23 relapsed or refractory, 1 previously untreated) started ibrutinib 560 mg daily; at 4 weeks, venetoclax was started at a low dose and increased to 400 mg daily.
The study primary end point – complete response rate at week 16 assessed by CT – was 42%, compared with 9% for ibrutinib monotherapy in the phase 2 PCYC-1104-CA study (P less than .001).
Computed tomography assessment was used for the primary end point to allow comparison to the ibrutinib monotherapy study, which did not use positron emission tomography for restaging. “Our study was designed to have 80% power to reject a complete response rate of 9% (at a one-sided alpha level of 0.05) if the rate of complete response was at least 30%,” the investigators noted.
Complete response rate assessed by positron emission tomography at week 16 was 62%, and was 71% overall.
In all, 67% of patients had absence of minimal residual disease by flow cytometry. At 15 months, 78% of the responses were ongoing, and at 18 months, 57% of patients were alive and progression free.
“Such outcomes appear to be substantially better than those that have been reported for ibrutinib or venetoclax monotherapy,” the investigators wrote.
The combination had side effects that are “acceptable to both patients and physicians,” investigators wrote. Side effects, usually low grade, included diarrhea in 83% of patients, fatigue in 75%, and nausea or vomiting in 71%. Tumor lysis syndrome was seen in two patients.
Whether ibrutinib plus venetoclax is superior to ibrutinib alone is being formally evaluated in an ongoing phase 3 study.
Janssen and AbbVie partially funded the current phase 2 study. Dr. Tam reported financial ties to Janssen, AbbVie, and Pharmacyclics. Other study authors reported financial ties to various pharmaceutical companies.
SOURCE: Tam C et al. N Engl J Med. 2018;378:1211-23.
In mantle cell lymphoma (MCL), ibrutinib plus venetoclax significantly improved the complete response rate, compared with what has been previously reported for ibrutinib alone, according to results of a phase 2 study.
Clinical outcomes with the combination seem superior to previously reported results for either treatment alone, said lead investigator Constantine S. Tam, MBBS, MD, of the Peter MacCallum Cancer Centre, Melbourne, and his coinvestigators.
“The results of our study, which used a historical cohort as a control, are consistent with the notion that the combination of ibrutinib and venetoclax is highly effective in mantle-cell lymphoma,” the investigators wrote in the New England Journal of Medicine.
The BTK inhibitor ibrutinib and the BCL2 inhibitor venetoclax are two of the most active agents for this B-cell cancer, investigators reported. The rationale for combining the agents is “compelling” because they affect different critical pathways in the malignant B cell.
Both agents have demonstrated complete response rates of 21% in previous studies of relapsed or refractory MCL, and preclinical studies suggest the combination of ibrutinib and venetoclax would be synergistic.
In the present single-group, phase 2 study, 24 patients with MCL (23 relapsed or refractory, 1 previously untreated) started ibrutinib 560 mg daily; at 4 weeks, venetoclax was started at a low dose and increased to 400 mg daily.
The study primary end point – complete response rate at week 16 assessed by CT – was 42%, compared with 9% for ibrutinib monotherapy in the phase 2 PCYC-1104-CA study (P less than .001).
Computed tomography assessment was used for the primary end point to allow comparison to the ibrutinib monotherapy study, which did not use positron emission tomography for restaging. “Our study was designed to have 80% power to reject a complete response rate of 9% (at a one-sided alpha level of 0.05) if the rate of complete response was at least 30%,” the investigators noted.
Complete response rate assessed by positron emission tomography at week 16 was 62%, and was 71% overall.
In all, 67% of patients had absence of minimal residual disease by flow cytometry. At 15 months, 78% of the responses were ongoing, and at 18 months, 57% of patients were alive and progression free.
“Such outcomes appear to be substantially better than those that have been reported for ibrutinib or venetoclax monotherapy,” the investigators wrote.
The combination had side effects that are “acceptable to both patients and physicians,” investigators wrote. Side effects, usually low grade, included diarrhea in 83% of patients, fatigue in 75%, and nausea or vomiting in 71%. Tumor lysis syndrome was seen in two patients.
Whether ibrutinib plus venetoclax is superior to ibrutinib alone is being formally evaluated in an ongoing phase 3 study.
Janssen and AbbVie partially funded the current phase 2 study. Dr. Tam reported financial ties to Janssen, AbbVie, and Pharmacyclics. Other study authors reported financial ties to various pharmaceutical companies.
SOURCE: Tam C et al. N Engl J Med. 2018;378:1211-23.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Dual targeting of BTK and BCL2 with ibrutinib and venetoclax may improve complete response rate versus ibrutinib alone in patients with mantle cell lymphoma.
Major finding: Complete response rate at week 16 as assessed by CT was 42%, compared with 9% with ibrutinib monotherapy in a previous study (P less than .001).
Study details: A single-group phase 2 study of daily oral ibrutinib and venetoclax in 24 patients with mantle cell lymphoma (23 relapsed or refractory, 1 previously untreated), as compared with historical controls.
Disclosures: Janssen and AbbVie partially funded the study. Dr. Tam reported financial ties to Janssen, Abbvie, and Pharmacyclics. Other study authors reported financial ties to various pharmaceutical companies.
Source: Tam C et al. N Engl J Med. 2018;378:1211-23.
Arm teachers with mental health providers
The gun control bill passed recently in Florida is a promising step forward in helping to protect children from deadly violence in schools. While various attempts to minimize gun violence have been stalled in state legislatures, in some cases for decades, this bill, which includes funding to expand mental health services for students, highlights a simple, sustainable, and nonpolitical solution: mental health providers.
School-based health centers arm educators with the powerful combination of on-site medical, mental health, and community health services that could address and aid in preventing violence through education, screening, ongoing care, crisis management, and advocacy.
At Montefiore Health System in the Bronx, our school health program plays a crucial role in keeping kids safe and healthy, and sometimes even saving lives. This past fall a potential tragedy was averted when a student disclosed to one of our on-site mental health providers a plan to murder a classmate after school. The child was fully assessed, resulting in a brief hospitalization. The child is back in school, receiving on-site services and being carefully monitored.
Our dedicated staff works closely with teachers and school staff to identify children in need of services. Barriers to care are eliminated as services are provided directly in the school in collaboration with teachers and school administrators. Coordination with the school and family allows for comprehensive, high-quality treatment that cannot be provided in any other setting.
School-based health centers offer protection and support on many levels. Mental health professionals can train teachers and other school staff to recognize red flags in students. They can collaborate with educators to carry out regular school-wide screenings to identify students who need immediate follow-up. And primary care providers in the clinic also screen for troubling behaviors and refer students for treatment within the clinic.
We know mental health providers make a difference. But we also must acknowledge that accessing these services often is a challenge. Estimates suggest that only half of children aged 8-15 years who need mental services actually get them. This is why having school-based health centers and mental health providers located where children spend most of their day is so vital. Often, school-based mental health providers have a chance to reach kids who are the least likely to receive care in the community.
Mental health professionals and school based clinics are invaluable resources; they are on the front lines of recognizing and treating worrisome student behaviors. Funding and providing these services is essential.
Dr. Appel is director of the Montefiore School Health Program, which makes primary care, mental health, dental and vision services available to almost 40,000 K-12 students in 26 school-based health centers throughout the Bronx.
*This article was updated 3/29/2018.
The gun control bill passed recently in Florida is a promising step forward in helping to protect children from deadly violence in schools. While various attempts to minimize gun violence have been stalled in state legislatures, in some cases for decades, this bill, which includes funding to expand mental health services for students, highlights a simple, sustainable, and nonpolitical solution: mental health providers.
School-based health centers arm educators with the powerful combination of on-site medical, mental health, and community health services that could address and aid in preventing violence through education, screening, ongoing care, crisis management, and advocacy.
At Montefiore Health System in the Bronx, our school health program plays a crucial role in keeping kids safe and healthy, and sometimes even saving lives. This past fall a potential tragedy was averted when a student disclosed to one of our on-site mental health providers a plan to murder a classmate after school. The child was fully assessed, resulting in a brief hospitalization. The child is back in school, receiving on-site services and being carefully monitored.
Our dedicated staff works closely with teachers and school staff to identify children in need of services. Barriers to care are eliminated as services are provided directly in the school in collaboration with teachers and school administrators. Coordination with the school and family allows for comprehensive, high-quality treatment that cannot be provided in any other setting.
School-based health centers offer protection and support on many levels. Mental health professionals can train teachers and other school staff to recognize red flags in students. They can collaborate with educators to carry out regular school-wide screenings to identify students who need immediate follow-up. And primary care providers in the clinic also screen for troubling behaviors and refer students for treatment within the clinic.
We know mental health providers make a difference. But we also must acknowledge that accessing these services often is a challenge. Estimates suggest that only half of children aged 8-15 years who need mental services actually get them. This is why having school-based health centers and mental health providers located where children spend most of their day is so vital. Often, school-based mental health providers have a chance to reach kids who are the least likely to receive care in the community.
Mental health professionals and school based clinics are invaluable resources; they are on the front lines of recognizing and treating worrisome student behaviors. Funding and providing these services is essential.
Dr. Appel is director of the Montefiore School Health Program, which makes primary care, mental health, dental and vision services available to almost 40,000 K-12 students in 26 school-based health centers throughout the Bronx.
*This article was updated 3/29/2018.
The gun control bill passed recently in Florida is a promising step forward in helping to protect children from deadly violence in schools. While various attempts to minimize gun violence have been stalled in state legislatures, in some cases for decades, this bill, which includes funding to expand mental health services for students, highlights a simple, sustainable, and nonpolitical solution: mental health providers.
School-based health centers arm educators with the powerful combination of on-site medical, mental health, and community health services that could address and aid in preventing violence through education, screening, ongoing care, crisis management, and advocacy.
At Montefiore Health System in the Bronx, our school health program plays a crucial role in keeping kids safe and healthy, and sometimes even saving lives. This past fall a potential tragedy was averted when a student disclosed to one of our on-site mental health providers a plan to murder a classmate after school. The child was fully assessed, resulting in a brief hospitalization. The child is back in school, receiving on-site services and being carefully monitored.
Our dedicated staff works closely with teachers and school staff to identify children in need of services. Barriers to care are eliminated as services are provided directly in the school in collaboration with teachers and school administrators. Coordination with the school and family allows for comprehensive, high-quality treatment that cannot be provided in any other setting.
School-based health centers offer protection and support on many levels. Mental health professionals can train teachers and other school staff to recognize red flags in students. They can collaborate with educators to carry out regular school-wide screenings to identify students who need immediate follow-up. And primary care providers in the clinic also screen for troubling behaviors and refer students for treatment within the clinic.
We know mental health providers make a difference. But we also must acknowledge that accessing these services often is a challenge. Estimates suggest that only half of children aged 8-15 years who need mental services actually get them. This is why having school-based health centers and mental health providers located where children spend most of their day is so vital. Often, school-based mental health providers have a chance to reach kids who are the least likely to receive care in the community.
Mental health professionals and school based clinics are invaluable resources; they are on the front lines of recognizing and treating worrisome student behaviors. Funding and providing these services is essential.
Dr. Appel is director of the Montefiore School Health Program, which makes primary care, mental health, dental and vision services available to almost 40,000 K-12 students in 26 school-based health centers throughout the Bronx.
*This article was updated 3/29/2018.
Incredible edibles … Guilty as charged
“We should not consider marijuana ‘innocent until proven guilty,’ given what we already know about the harms to adolescents,”1 Sharon Levy, MD, chair of the American Academy of Pediatrics Committee on Substance Abuse, said in an AAP press release, speaking of the legalization of marijuana in Washington and Colorado. The press release was issued in 2015 when the AAP updated its policy on the impact of marijuana policies on youth (Pediatrics. 2015. doi: 10.1542/peds.2014-4146), reaffirming its opposition to legalization of marijuana because it contended that limited studies had been done on “medical marijuana” in adults, and that there were no published studies either on the form of marijuana or other preparations that involved children.
Marijuana is a schedule I controlled substance, so the Food and Drug Administration does not regulate marijuana edibles, resulting in poor labeling and unregulated formulations.2
Edibles are marijuana-infused foods. Extraction of the cannabinoid THC, the major psychoactive ingredient, from the cannabis plant involves heating the flowers from the female plant in an oil base liquid. As it is heated, the inactive tetrahydrocannabinoid acid (THCA) is converted to THC and dissolves into the oil base liquids, and it is this additive that is used in food products to create the edible. A safe “serving size,” was determined to be 10 mg of THC,3 but an edible may contain 100 mg of THC if consumed in its entirety.
Many prefer ingesting edibles, compared with smoking, because there are no toxic effects from the inhalation of smoke, no odors, it’s more potent, and its duration of action is longer.3 The downside is the onset of action is slower, compared with smoking, so many will consume more before the “high” begins, and therefore there is a greater risk for intoxication. For example, a chocolate bar may contain 100 mg of THC, and despite the “serving size” stated as one square, a person might consume the entire bar before the onset of the high begins. Improved labeling and warning of intoxication now are required on packaging, but this does little to reduce the risk.3
Edibles also are made in way that is attractive to children. Commonly, they come in packaging and forms that resemble candy, such as gummies and chocolate bars. Although laws have been put in place to require them to be sold in childproof containers, 3,4 As feared, once cannabis oil is obtained legally, there is little control over what it is put in.
As for medicinal purposes, edibles have a great advantage for children when used for that purpose. Ease of administration, long duration of action, and a great taste are all positive attributes. As with all good things, there is a downside when used inappropriately.
Marijuana overdoses can result in cognitive and motor impairment, extreme sedation, agitation, anxiety, cardiac stress, and vomiting. High quantities of THC have been reported to cause transient psychotic symptoms such as hallucinations, delusions, and anxiety.3
As pediatricians, it is essential to educate teens and their families on the harmful effects of marijuana and dispel the myth that is benign. They need to be informed of the negative impact of marijuana, which leads to impairment of memory and executive function, on the developing brain. Parents also need to be aware of the current trends of use and formulations, so they can be aware of potential exposures.5
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. “American Academy of Pediatrics Reaffirms Opposition to Legalizing Marijuana for Recreational or Medical Use,” AAP press release on Jan. 26, 2015.
2. N Engl J Med. 2015;372:989-91.
3. Methods Rep RTI Press. 2016 Nov. doi: 10.3768/rtipress.2016.op.0035.1611.
4. JAMA. 2015;313(3):241-2.
5. Pediatrics. 2017 Mar;139(3):e20164069.
“We should not consider marijuana ‘innocent until proven guilty,’ given what we already know about the harms to adolescents,”1 Sharon Levy, MD, chair of the American Academy of Pediatrics Committee on Substance Abuse, said in an AAP press release, speaking of the legalization of marijuana in Washington and Colorado. The press release was issued in 2015 when the AAP updated its policy on the impact of marijuana policies on youth (Pediatrics. 2015. doi: 10.1542/peds.2014-4146), reaffirming its opposition to legalization of marijuana because it contended that limited studies had been done on “medical marijuana” in adults, and that there were no published studies either on the form of marijuana or other preparations that involved children.
Marijuana is a schedule I controlled substance, so the Food and Drug Administration does not regulate marijuana edibles, resulting in poor labeling and unregulated formulations.2
Edibles are marijuana-infused foods. Extraction of the cannabinoid THC, the major psychoactive ingredient, from the cannabis plant involves heating the flowers from the female plant in an oil base liquid. As it is heated, the inactive tetrahydrocannabinoid acid (THCA) is converted to THC and dissolves into the oil base liquids, and it is this additive that is used in food products to create the edible. A safe “serving size,” was determined to be 10 mg of THC,3 but an edible may contain 100 mg of THC if consumed in its entirety.
Many prefer ingesting edibles, compared with smoking, because there are no toxic effects from the inhalation of smoke, no odors, it’s more potent, and its duration of action is longer.3 The downside is the onset of action is slower, compared with smoking, so many will consume more before the “high” begins, and therefore there is a greater risk for intoxication. For example, a chocolate bar may contain 100 mg of THC, and despite the “serving size” stated as one square, a person might consume the entire bar before the onset of the high begins. Improved labeling and warning of intoxication now are required on packaging, but this does little to reduce the risk.3
Edibles also are made in way that is attractive to children. Commonly, they come in packaging and forms that resemble candy, such as gummies and chocolate bars. Although laws have been put in place to require them to be sold in childproof containers, 3,4 As feared, once cannabis oil is obtained legally, there is little control over what it is put in.
As for medicinal purposes, edibles have a great advantage for children when used for that purpose. Ease of administration, long duration of action, and a great taste are all positive attributes. As with all good things, there is a downside when used inappropriately.
Marijuana overdoses can result in cognitive and motor impairment, extreme sedation, agitation, anxiety, cardiac stress, and vomiting. High quantities of THC have been reported to cause transient psychotic symptoms such as hallucinations, delusions, and anxiety.3
As pediatricians, it is essential to educate teens and their families on the harmful effects of marijuana and dispel the myth that is benign. They need to be informed of the negative impact of marijuana, which leads to impairment of memory and executive function, on the developing brain. Parents also need to be aware of the current trends of use and formulations, so they can be aware of potential exposures.5
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. “American Academy of Pediatrics Reaffirms Opposition to Legalizing Marijuana for Recreational or Medical Use,” AAP press release on Jan. 26, 2015.
2. N Engl J Med. 2015;372:989-91.
3. Methods Rep RTI Press. 2016 Nov. doi: 10.3768/rtipress.2016.op.0035.1611.
4. JAMA. 2015;313(3):241-2.
5. Pediatrics. 2017 Mar;139(3):e20164069.
“We should not consider marijuana ‘innocent until proven guilty,’ given what we already know about the harms to adolescents,”1 Sharon Levy, MD, chair of the American Academy of Pediatrics Committee on Substance Abuse, said in an AAP press release, speaking of the legalization of marijuana in Washington and Colorado. The press release was issued in 2015 when the AAP updated its policy on the impact of marijuana policies on youth (Pediatrics. 2015. doi: 10.1542/peds.2014-4146), reaffirming its opposition to legalization of marijuana because it contended that limited studies had been done on “medical marijuana” in adults, and that there were no published studies either on the form of marijuana or other preparations that involved children.
Marijuana is a schedule I controlled substance, so the Food and Drug Administration does not regulate marijuana edibles, resulting in poor labeling and unregulated formulations.2
Edibles are marijuana-infused foods. Extraction of the cannabinoid THC, the major psychoactive ingredient, from the cannabis plant involves heating the flowers from the female plant in an oil base liquid. As it is heated, the inactive tetrahydrocannabinoid acid (THCA) is converted to THC and dissolves into the oil base liquids, and it is this additive that is used in food products to create the edible. A safe “serving size,” was determined to be 10 mg of THC,3 but an edible may contain 100 mg of THC if consumed in its entirety.
Many prefer ingesting edibles, compared with smoking, because there are no toxic effects from the inhalation of smoke, no odors, it’s more potent, and its duration of action is longer.3 The downside is the onset of action is slower, compared with smoking, so many will consume more before the “high” begins, and therefore there is a greater risk for intoxication. For example, a chocolate bar may contain 100 mg of THC, and despite the “serving size” stated as one square, a person might consume the entire bar before the onset of the high begins. Improved labeling and warning of intoxication now are required on packaging, but this does little to reduce the risk.3
Edibles also are made in way that is attractive to children. Commonly, they come in packaging and forms that resemble candy, such as gummies and chocolate bars. Although laws have been put in place to require them to be sold in childproof containers, 3,4 As feared, once cannabis oil is obtained legally, there is little control over what it is put in.
As for medicinal purposes, edibles have a great advantage for children when used for that purpose. Ease of administration, long duration of action, and a great taste are all positive attributes. As with all good things, there is a downside when used inappropriately.
Marijuana overdoses can result in cognitive and motor impairment, extreme sedation, agitation, anxiety, cardiac stress, and vomiting. High quantities of THC have been reported to cause transient psychotic symptoms such as hallucinations, delusions, and anxiety.3
As pediatricians, it is essential to educate teens and their families on the harmful effects of marijuana and dispel the myth that is benign. They need to be informed of the negative impact of marijuana, which leads to impairment of memory and executive function, on the developing brain. Parents also need to be aware of the current trends of use and formulations, so they can be aware of potential exposures.5
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. “American Academy of Pediatrics Reaffirms Opposition to Legalizing Marijuana for Recreational or Medical Use,” AAP press release on Jan. 26, 2015.
2. N Engl J Med. 2015;372:989-91.
3. Methods Rep RTI Press. 2016 Nov. doi: 10.3768/rtipress.2016.op.0035.1611.
4. JAMA. 2015;313(3):241-2.
5. Pediatrics. 2017 Mar;139(3):e20164069.
Time to HIV rebound in infants off ART linked to birth health
BOSTON – For infants with HIV infection, baseline immune function and birth health appear to influence viral control after the discontinuation of antiretroviral therapy (ART), an analysis of data from the landmark CHER trial shows.
Among 183 children diagnosed with HIV between 6 and 12 weeks of age who were started on early, time-limited ART, longer time to viral rebound after treatment discontinuation was associated with higher baseline CD4 percentages, higher birth weight, and with achievement of viral suppression within 40 weeks of starting on ART, reported Man Chan, PhD, of the Medical Research Council clinical trials unit at University College London.
The CHER trial compared South African infants with HIV on either 40 or 96 weeks of immediate ART with those on deferred ART. The results showed that early time-limited ART was associated with better clinical and immunologic outcomes than was deferred ART and influenced a change in treatment guidelines (Lancet 2013 Nov 9;382[9904]:1555-63).
In the current analysis, investigators examined viral control after treatment interruption in early-treated children and looked for factors that could influence time to viral rebound after ART cessation.
They measured viral load from stored samples at 1.8 weeks after ART interruption and then every 12 weeks thereafter. They defined viral rebound as two consecutive samples with 400 or more copies/mL.
Of the 183 children in the sample, 177 had a rebound; the remaining six children were censored from the analysis, five because they had restarted ART, and one child who remained in viral suppression with an undetectable viral load and was asymptomatic for 8.5 years off ART.
The estimated cumulative probability of rebound was 70% at 2 months following ART interruption, 80% at 4 months, 94% at 6 months, and 99% at 8 months.
In multivariable analysis, factors significantly associated with longer time to viral rebound included higher baseline CD4 counts (P = .03), higher birth weight (P = .032), and viral suppression within 40 weeks of starting on ART (P = .028)
In contrast, there were no significant associations with other factors in the multivariate model, including sex, baseline viral load, baseline CD8 percentage, HIV stage, status of therapy to prevent mother-to-child transmission, age at ART initiation, length of therapy, or treatment center.
Sensitivity analyses of a few cases in which there was a 4-7 month gap between rebound and the last viral load below 400 copies/mL before rebound showed similar results, Dr. Chan noted.
The study was the U.S. National Institutes of Health. Dr. Chan reported having nothing to disclose.
SOURCE: Violari A et al. CROI 2018, Abstract 137
BOSTON – For infants with HIV infection, baseline immune function and birth health appear to influence viral control after the discontinuation of antiretroviral therapy (ART), an analysis of data from the landmark CHER trial shows.
Among 183 children diagnosed with HIV between 6 and 12 weeks of age who were started on early, time-limited ART, longer time to viral rebound after treatment discontinuation was associated with higher baseline CD4 percentages, higher birth weight, and with achievement of viral suppression within 40 weeks of starting on ART, reported Man Chan, PhD, of the Medical Research Council clinical trials unit at University College London.
The CHER trial compared South African infants with HIV on either 40 or 96 weeks of immediate ART with those on deferred ART. The results showed that early time-limited ART was associated with better clinical and immunologic outcomes than was deferred ART and influenced a change in treatment guidelines (Lancet 2013 Nov 9;382[9904]:1555-63).
In the current analysis, investigators examined viral control after treatment interruption in early-treated children and looked for factors that could influence time to viral rebound after ART cessation.
They measured viral load from stored samples at 1.8 weeks after ART interruption and then every 12 weeks thereafter. They defined viral rebound as two consecutive samples with 400 or more copies/mL.
Of the 183 children in the sample, 177 had a rebound; the remaining six children were censored from the analysis, five because they had restarted ART, and one child who remained in viral suppression with an undetectable viral load and was asymptomatic for 8.5 years off ART.
The estimated cumulative probability of rebound was 70% at 2 months following ART interruption, 80% at 4 months, 94% at 6 months, and 99% at 8 months.
In multivariable analysis, factors significantly associated with longer time to viral rebound included higher baseline CD4 counts (P = .03), higher birth weight (P = .032), and viral suppression within 40 weeks of starting on ART (P = .028)
In contrast, there were no significant associations with other factors in the multivariate model, including sex, baseline viral load, baseline CD8 percentage, HIV stage, status of therapy to prevent mother-to-child transmission, age at ART initiation, length of therapy, or treatment center.
Sensitivity analyses of a few cases in which there was a 4-7 month gap between rebound and the last viral load below 400 copies/mL before rebound showed similar results, Dr. Chan noted.
The study was the U.S. National Institutes of Health. Dr. Chan reported having nothing to disclose.
SOURCE: Violari A et al. CROI 2018, Abstract 137
BOSTON – For infants with HIV infection, baseline immune function and birth health appear to influence viral control after the discontinuation of antiretroviral therapy (ART), an analysis of data from the landmark CHER trial shows.
Among 183 children diagnosed with HIV between 6 and 12 weeks of age who were started on early, time-limited ART, longer time to viral rebound after treatment discontinuation was associated with higher baseline CD4 percentages, higher birth weight, and with achievement of viral suppression within 40 weeks of starting on ART, reported Man Chan, PhD, of the Medical Research Council clinical trials unit at University College London.
The CHER trial compared South African infants with HIV on either 40 or 96 weeks of immediate ART with those on deferred ART. The results showed that early time-limited ART was associated with better clinical and immunologic outcomes than was deferred ART and influenced a change in treatment guidelines (Lancet 2013 Nov 9;382[9904]:1555-63).
In the current analysis, investigators examined viral control after treatment interruption in early-treated children and looked for factors that could influence time to viral rebound after ART cessation.
They measured viral load from stored samples at 1.8 weeks after ART interruption and then every 12 weeks thereafter. They defined viral rebound as two consecutive samples with 400 or more copies/mL.
Of the 183 children in the sample, 177 had a rebound; the remaining six children were censored from the analysis, five because they had restarted ART, and one child who remained in viral suppression with an undetectable viral load and was asymptomatic for 8.5 years off ART.
The estimated cumulative probability of rebound was 70% at 2 months following ART interruption, 80% at 4 months, 94% at 6 months, and 99% at 8 months.
In multivariable analysis, factors significantly associated with longer time to viral rebound included higher baseline CD4 counts (P = .03), higher birth weight (P = .032), and viral suppression within 40 weeks of starting on ART (P = .028)
In contrast, there were no significant associations with other factors in the multivariate model, including sex, baseline viral load, baseline CD8 percentage, HIV stage, status of therapy to prevent mother-to-child transmission, age at ART initiation, length of therapy, or treatment center.
Sensitivity analyses of a few cases in which there was a 4-7 month gap between rebound and the last viral load below 400 copies/mL before rebound showed similar results, Dr. Chan noted.
The study was the U.S. National Institutes of Health. Dr. Chan reported having nothing to disclose.
SOURCE: Violari A et al. CROI 2018, Abstract 137
FROM CROI 2018
Key clinical point: Early initiation of antiretroviral therapy in infants is associated with better outcomes.
Major finding: Longer time to viral rebound was associated with higher baseline CD4, higher birth weight, and viral suppression within 40 weeks of starting ART.
Study details: Analysis of outcomes in 183 infants with HIV infection in the CHER trial.
Disclosures: The study was funded by the U.S. National Institutes of Health. Dr. Chan reported having nothing to disclose.
Source: Violari A et al. CROI 2018, Abstract 137.
Implant Survivorship and Complication Rates After Total Knee Arthroplasty With a Third-Generation Cemented System: 15-Year Follow-Up
ABSTRACT
This work is a retrospective cohort study evaluating patients who had undergone third-generation cemented total knee arthroplasty (TKA) with prostheses (NexGen, Zimmer Biomet) utilizing posterior-stabilized (PS) and cruciate-retaining (CR) designs at a single center at their 15-year follow-up.
The purpose of this study is to determine the functional knee scores, reoperations, and long-term survivorship for patients with the NexGen Zimmer Biomet Knee system at the 15-year follow-up. In total, 99 patients who had undergone primary TKA were followed for 15 years.
At the 15-year follow-up, survivorship in both study groups was similar: 98% for PS TKAs and 100% for CR TKAs. The 2 groups also showed similar functionality: 80% of the PS implants and 89% of the CR implants were associated with no or mild pain (P = .40). Reoperation rates were 2% for the PS group and 0% for the CR group (P = .38). No differences in any of the outcomes analyzed were observed between patients who had CR TKA and those who had undergone PS TKA.
Our study found no significant differences in functional outcomes between PS and CR NexGen knee implants. Patients treated by both methods showed excellent longevity and survivorship at the 15-year follow-up.
Continue to: Total knee arthroplasty...
Total knee arthroplasty (TKA) is an orthopedic procedure with increasing demand.1 Over the past 2 decades, a surge in TKA implants has been observed. Of the available prosthetic designs, only a few implants with long-term follow-up have been reported.2-9 The NexGen TKA system (Zimmer Biomet) has been shown to have excellent clinical and radiographic results at an intermediate follow-up term of 8 years.10 This system is a third-generation prosthetic design that was developed to improve problems seen with its predecessors, such as the Miller-Galante II system (Zimmer Biomet), the Insall-Burstein II system (Zimmer Biomet), and the Constrained Condylar Knee (Zimmer Biomet), which were mainly for patellar maltracking.11-17 The NexGen TKA system is a fixed-bearing system designed to include an anatomic femoral trochlea with the option of cruciate-retaining (CR), posterior-stabilized (PS), or more constrained implants. This study evaluates the long-term success of the CR and PS NexGen TKA systems. Outcomes measured include functional knee scores and reoperation rates at the 15-year follow-up. Based on the measured outcomes, potential differences between the PS and CR implants from this system are cited.
MATERIAL AND METHODS
Between July 1995 and July 1997, 334 consecutive primary TKAs were performed on 287 patients at our institution. In total, 167 patients (186 knees) underwent posterior CR TKAs with the NexGen CR prosthesis (Zimmer Biomet), and 120 patients (148 knees) underwent PS TKAs using the NexGen Legacy PS prosthesis (Zimmer Biomet). This retrospective double cohort study was reviewed and approved by our Institutional Review Board. At the 15-year postoperative follow-up, 99 patients were available (Figure 1).
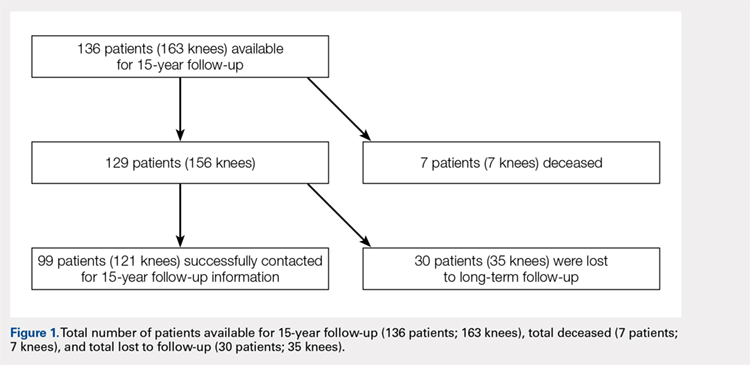
The CR and PS implants were used with similar frequencies by the surgeons who performed the procedures. Patients were not randomized into either the PS- or CR-implant teams; the final decision on implant selection was left to the operating surgeon’s discretion. However, in addition to standard indications for TKA (pain and disability associated with severe arthritic change seen on radiographs and refractory to conservative measures), absolute contraindications to the CR implant included severe combined deformity (flexion contraction >30° combined with a varus or valgus deformity >20°) or posterior cruciate ligament insufficiency (often associated with inflammatory arthritis).
The surgical technique for the CR and PS designs was identical, and included a median parapatellar approach, femoral rotational alignment perpendicular to the transepicondylar axis, measured resection of the flexion and extension gaps, intramedullary femoral alignment, and extramedullary tibial alignment. All components were cemented, and the patella of each patient was resurfaced. All patients received preoperative antibiotics that were continued for 48 hours postoperatively, and 4 weeks of anticoagulation with dose-adjusted warfarin to maintain an international normalized ratio of 1.5 to 2.0.
Patients were observed postoperatively at the 5- to 8-year and 15-year time points. The 5-year data were previously published in 2005 by Bozic and colleagues.10 Patients available for follow-up at the 15-year time-point were evaluated using the 100-point Hospital for Special Surgery (HSS) knee scoring system, which assigns up to 30 points for pain, 22 points for function, 18 points for range of motion, and 10 points each for quadricep strength, deformity, and instability. In addition, common medical conditions limiting patient activity were assessed; these included joint replacement; arthritis in another joint, the back, or spine; weakness or fatigue; breathing or heart ailments; and others.
Continue to: At the 15-year follow-up...
At the 15-year follow-up, patients were contacted via telephone to obtain their HSS knee scores. If patients were unavailable/unable to answer the questions asked, knee score information was collected from a first-degree relative or caretaker. Patients that could not be contacted by phone were sent a HSS knee score survey to their last known address. The online Social Security Death Index was queried for confirmation of death. If deceased, a first-degree relative was contacted for confirmation.
Survivorship was evaluated using revision for any reason and revision for aseptic loosening as separate endpoints via the Kaplan-Meier product-limit method, and the CR and PS TKA groups were compared using the log-rank test. The power of the study for detecting differences between the TKA groups was determined to be 80%, based on a moderate hazard ratio of 1.5, using the log-rank test. Differences between PS and CR TKAs were assessed using the Pearson chi-square test for knee pain and functional outcomes, Fisher’s exact test for patient limitations, such as joint replacement, and the non-parametric Mann Whitney U-test for median pain scores (Table 1). Spearman correlations between the patients’ self-reported knee scores (as a percentage of normal) and physician-based knee scores were performed to assess whether self-reported knee scores were significantly correlated with physician-based knee scores. Kaplan-Meier analysis was performed to evaluate time-related freedom from reoperation at 95% confidence intervals. Statistical analysis was conducted using IBM SPSS Statistics (version 21.0, IBM). Two-tailed P < .05 was considered statistically significant.
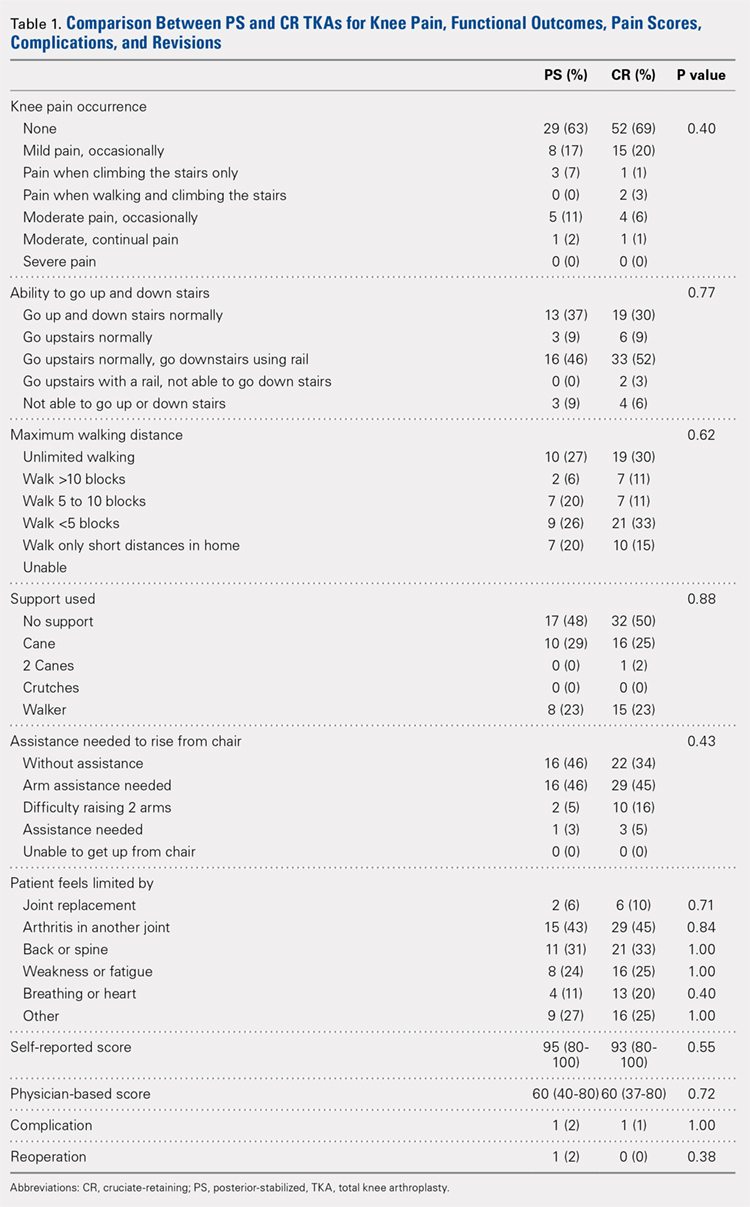
RESULTS
Of the 287 patients (334 knees) who had primary TKAs, 99 patients (121 knees; 75 CR and 46 PS) were available at the 15-year follow-up. A total of 155 patients (171 knees) died before the 15-year follow-up, and 33 (42 knees) were lost to follow-up (Figure 1). The functional status of the knees of patients who were lost to follow-up or who had died since the previous follow-up data were published is unknown.
Demographic and outcome data for the cohort of 121 TKAs (99 patients) are summarized in Table 2. The median age at surgery was 64 years, and 71% of the cohort was female.
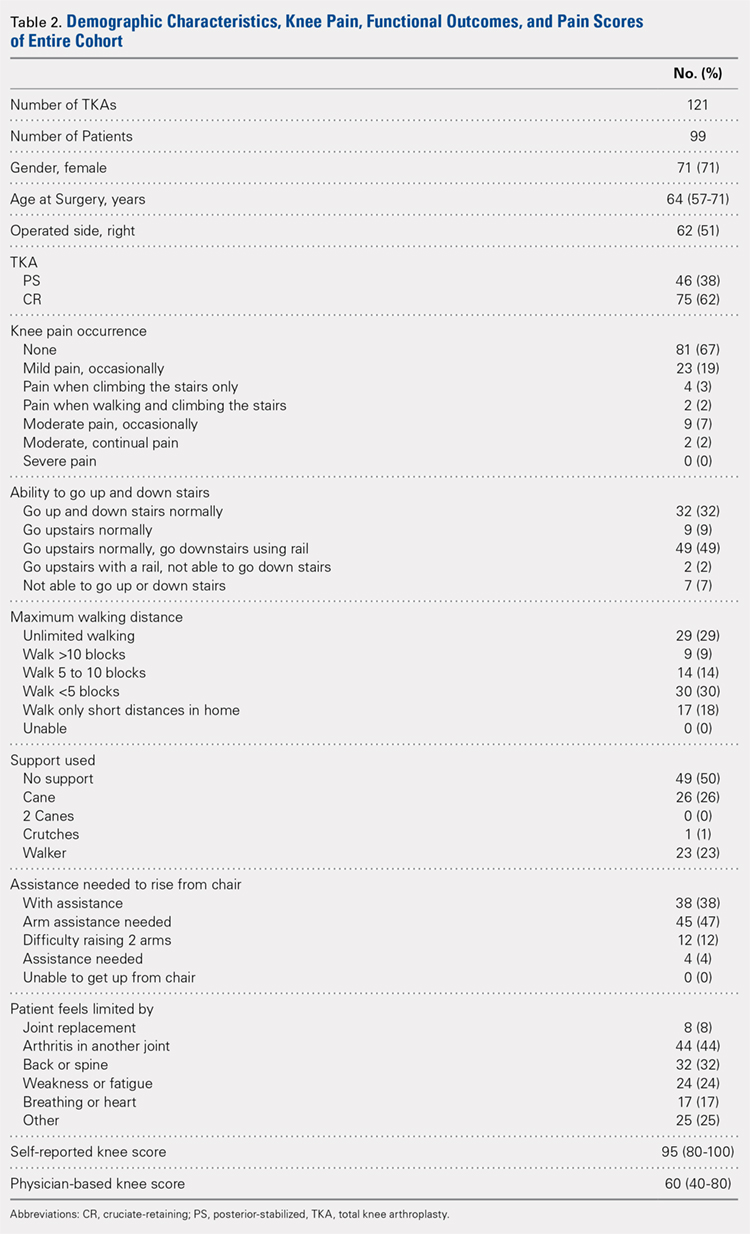
At the 15-year follow-up, survivorship in both groups was similar: 98% for PS TKAs and 100% for CR TKAs. The 2 groups were also similar functionally: 80% of the PS implants and 89% of the CR implants were associated with no or mild pain (P = .40). Approximately half of the patients in both groups (52% PS; 50% CR; P = .88) required walking support (canes or walkers) and nearly half of both groups (46% PS; 48% CR; P = .62) could walk <5 blocks or only short distances in their homes. In addition, 46% of the patients in both groups reported needing arm assistance to functionally rise from a chair (P = .43); 91% of the patients in both groups could also walk up and down stairs (P = .77). No statistical difference in the medical conditions limiting the patients in the 2 groups was found: joint replacement (2% PS; 6% CR; P = .71), arthritis in another joint (43% PS; 45% CR; P = .84), back or spine arthritis (31% PS; 33% CR; P = 1.00), weakness or fatigue (24% PS; 25% CR; P = 1.00), breathing or heart ailments (11% PS; 20% CR; P = .40), and other reasons (27% PS; 25% CR; P = 1.00). In addition, median self-reported knee scores were 95 and 93 points for the PS and CR groups, respectively (P = .55).
Continue to: Patients reported 2 complications...
Patients reported 2 complications since the previous 5- to 8-year follow-up, 1 in each group. The first case underwent a PS TKA that required open reduction internal fixation for a bilateral supracondylar peri-prosthesis femur fracture following a fall, which was subsequently complicated with infection and ultimately led to above-the-knee amputation. In the second case, a CR TKA patient experienced persistent swelling and knee instability. The patient followed up with a local orthopaedist, but to date, no reoperations on the knee have been reported.
Spearman correlations between the patients’ self-reported knee scores (as a percentage of normal) and physician-based knee scores were moderately correlated with physician-based knee scores (rs = 0.42; P < .001).
Reoperation rates were 2% for PS and 0% for CR (P = .38). Kaplan-Meier analysis was performed to evaluate time-related freedom from reoperation and no significance difference between the PS and CR groups was revealed (log-rank test = 1.40, P = .24, Figure 2).
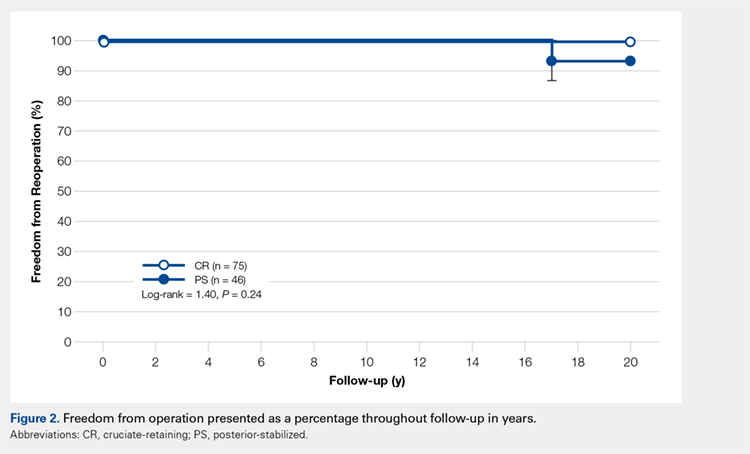
DISCUSSION
The success of TKA in pain relief and restoration of function has led to increased demands for this surgery.1 Such demand has enabled the introduction of a new joint replacement prosthesis to the market.18 Considering the increased incidence of osteoarthritis in the younger population (<55 years of age), critically reviewing the longevity and durability of TKA implant designs is of great importance. Compared with other TKA implant designs, the NexGen Zimmer Biomet Knee system has shown excellent longevity at the 15-year follow-up.5,6,9,11-15 Our study began with 136 patients, and, after eliminating the deceased, those lost to follow-up, and non-responders, a total of 99 patients were available for the 15-year follow-up. At this time-point, 80% of the PS implants and 89% of the CR implants were associated with no or mild pain. Survivorship at the 15-year follow-up was similar in both groups: 98% for PS TKAs and 100% for CR TKAs. The reoperation rate was low in both groups, and no evidence of aseptic loosening was found. Based on our results, the NexGen Zimmer Biomet Knee system can be concluded to show excellent longevity and functional outcomes at the 15-year follow-up.
Our study includes several limiting factors that were taken into consideration during the analysis of the results. One of the main limitations of this work is that it required a 15-year follow-up of predominantly elderly patients; many of the participants may be expected to be deceased at this time-point. In our study, a total of 7 patients were confirmed to be deceased by a first-degree relative or the Social Security Death Index. In addition, unlike Bozic and colleagues’10 previous 5-year follow-up study, radiographic imaging data were not collected at the 15-year follow-up. However, given that this study aimed to assess the functional knee scores and reoperation rates of the PS and CR NexGen Zimmer Biomet Knee system, radiographic information did not appear to be necessary.
CONCLUSION
This study found no significant differences in functional outcomes between the PS and CR NexGen knee implants. Patients who received these implants showed excellent longevity and survivorship at their 15-year follow-up.
1. Lützner J, Hübel U, Kirschner S, Günther KP, Krummenauer F. Langzeitergebnisse in der Knieendoprothetik. Chirurg. 2011;82(7):618-624. doi:10.1007/s00104-010-2001-8.
2. Font-Rodriguez DE, Scuderi GR, Insall J. Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res. 1997;345:79-86.
3. Rodriguez JA, Bhende H, Ranawat CS. Total condylar knee replacement: a 20-year followup study. Clin Orthop Relat Res. 2001;388:10-17.
4. Van Loon CJM, Wisse MA, de Waal Malefijt MC, Jansen RH, Veth RPH. The kinematic total knee arthroplasty. Arch Orth Traum Surg. 2000;120(1-2):48-52. doi:10.1007/PL00021215.
5. Buechel FFS. Long-term followup after mobile-bearing total knee replacement. Clin Orthop Relat Res. 2002;404:40-50.
6. Ito J, Koshino T, Okamoto R, Saito T. 15-year follow-up study of total knee arthroplasty in patients with rheumatoid arthritis. J Arthroplasty. 2003;18(8):984-992. doi:10.1016/S0883-5403(03)00262-6.
7. Dixon MC, Brown RR, Parsch D, Scott RD. Modular fixed-bearing total knee arthroplasty with retention of the posterior cruciate ligament. J Bone Joint Surg. 2005;87(3):598-603. doi:10.2106/JBJS.C.00591.
8. Duffy GP, Crowder AR, Trousdale RR, Berry DJ. Cemented total knee arthroplasty using a modern prosthesis in young patients with osteoarthritis. J Arthroplasty. 2007;22(6 Suppl 2):67-70. doi:10.1016/j.arth.2007.05.001.
9. Baker PN, Khaw FM, Kirk LMG, Esler CNA, Gregg PJ. A randomised controlled trial of cemented versus cementless press-fit condylar total knee replacement: 15-year survival analysis. J Bone Joint Surg. 2007;89-B(12):1608-1614. doi:10.1302/0301-620x.89b12.19363.
10. Bozic KJ, Kinder J, Menegini M, Zurakowski D, Rosenberg AG, Galante JO. Implant survivorship and complication rates after total knee arthroplasty with a third-generation cemented system: 5 to 8 years followup. Clin Orthop Relat Res. 2005;430:117-124. doi:10.1097/01.blo.0000146539.23869.14.
11. Effenberger H, Berka J, Hilzensauer G, Ramsauer T, Dorn U, Kißlinger E. Miller-Galante total knee arthroplasty: the importance of material and design on the revision rate. Int Orthop. 2001;25(6):378-381. doi:10.1007/s002640100294.
12. Kirk PG, Rorabeck CH, Bourne RB. Clinical comparison of the Miller Galante I and AMK total knee systems. J Arthroplasty. 1994;9(2):131-136. doi:10.1016/0883-5403(94)90061-2.
13. Kobori M, Kamisato S, Yoshida M, Kobori K. Revision of failed metal-backed patellar component of Miller/Galante-I total knee prosthesis. J Orthop Sci. 2000;5(5):436-438. doi:10.1007/s007760070020.
14. Larson CM, Lachiewicz PF. Patellofemoral complications with the insall-burstein II posterior-stabilized total knee arthroplasty. J Arthroplasty. 1999;14(3):288-292. doi:http://dx.doi.org/10.1016/S0883-5403(99)90053-0.
15. Matsuda S, Miura H, Nagamine R, Urabe K, Hirata G, Iwamoto Y. Effect of femoral and tibial component position on patellar tracking following total knee arthroplasty: 10-year follow-up of Miller-Galante I knees. Am J Knee Surg. 2001;14(3):152-156.
16. Miyagi T, Matsuda S, Miura H, Nagamine R, Urabe K. Changes in patellar tracking after total knee arthroplasty: 10-year follow-up of Miller-Balante I knees. Orthopedics. 2002;25(8):811-813. doi:10.3928/0147-7447-20020801-10.
17. Rao AR, Engh GA, Collier MB, Lounici S. Tibial interface wear in retrieved total knee components and correlations with modular insert motion. J Bone Joint Surg. 2002;84(10):1849-1855.
18. Anand R, Graves SE, de Steiger RN, et al. What is the benefit of introducing new hip and knee prostheses? J Bone Joint Surg. 2011;93(3):51-54. doi:10.2106/JBJS.K.00867.
ABSTRACT
This work is a retrospective cohort study evaluating patients who had undergone third-generation cemented total knee arthroplasty (TKA) with prostheses (NexGen, Zimmer Biomet) utilizing posterior-stabilized (PS) and cruciate-retaining (CR) designs at a single center at their 15-year follow-up.
The purpose of this study is to determine the functional knee scores, reoperations, and long-term survivorship for patients with the NexGen Zimmer Biomet Knee system at the 15-year follow-up. In total, 99 patients who had undergone primary TKA were followed for 15 years.
At the 15-year follow-up, survivorship in both study groups was similar: 98% for PS TKAs and 100% for CR TKAs. The 2 groups also showed similar functionality: 80% of the PS implants and 89% of the CR implants were associated with no or mild pain (P = .40). Reoperation rates were 2% for the PS group and 0% for the CR group (P = .38). No differences in any of the outcomes analyzed were observed between patients who had CR TKA and those who had undergone PS TKA.
Our study found no significant differences in functional outcomes between PS and CR NexGen knee implants. Patients treated by both methods showed excellent longevity and survivorship at the 15-year follow-up.
Continue to: Total knee arthroplasty...
Total knee arthroplasty (TKA) is an orthopedic procedure with increasing demand.1 Over the past 2 decades, a surge in TKA implants has been observed. Of the available prosthetic designs, only a few implants with long-term follow-up have been reported.2-9 The NexGen TKA system (Zimmer Biomet) has been shown to have excellent clinical and radiographic results at an intermediate follow-up term of 8 years.10 This system is a third-generation prosthetic design that was developed to improve problems seen with its predecessors, such as the Miller-Galante II system (Zimmer Biomet), the Insall-Burstein II system (Zimmer Biomet), and the Constrained Condylar Knee (Zimmer Biomet), which were mainly for patellar maltracking.11-17 The NexGen TKA system is a fixed-bearing system designed to include an anatomic femoral trochlea with the option of cruciate-retaining (CR), posterior-stabilized (PS), or more constrained implants. This study evaluates the long-term success of the CR and PS NexGen TKA systems. Outcomes measured include functional knee scores and reoperation rates at the 15-year follow-up. Based on the measured outcomes, potential differences between the PS and CR implants from this system are cited.
MATERIAL AND METHODS
Between July 1995 and July 1997, 334 consecutive primary TKAs were performed on 287 patients at our institution. In total, 167 patients (186 knees) underwent posterior CR TKAs with the NexGen CR prosthesis (Zimmer Biomet), and 120 patients (148 knees) underwent PS TKAs using the NexGen Legacy PS prosthesis (Zimmer Biomet). This retrospective double cohort study was reviewed and approved by our Institutional Review Board. At the 15-year postoperative follow-up, 99 patients were available (Figure 1).
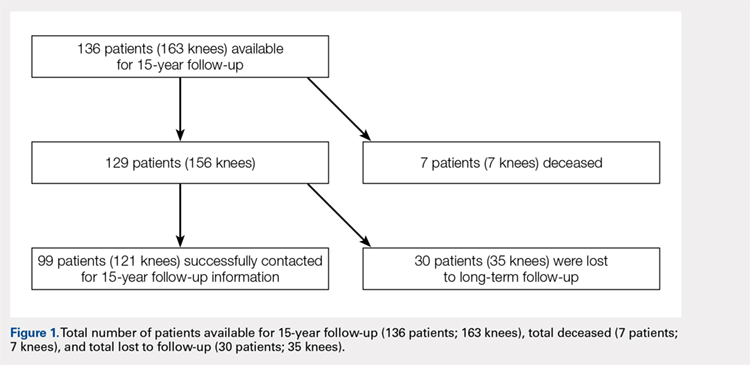
The CR and PS implants were used with similar frequencies by the surgeons who performed the procedures. Patients were not randomized into either the PS- or CR-implant teams; the final decision on implant selection was left to the operating surgeon’s discretion. However, in addition to standard indications for TKA (pain and disability associated with severe arthritic change seen on radiographs and refractory to conservative measures), absolute contraindications to the CR implant included severe combined deformity (flexion contraction >30° combined with a varus or valgus deformity >20°) or posterior cruciate ligament insufficiency (often associated with inflammatory arthritis).
The surgical technique for the CR and PS designs was identical, and included a median parapatellar approach, femoral rotational alignment perpendicular to the transepicondylar axis, measured resection of the flexion and extension gaps, intramedullary femoral alignment, and extramedullary tibial alignment. All components were cemented, and the patella of each patient was resurfaced. All patients received preoperative antibiotics that were continued for 48 hours postoperatively, and 4 weeks of anticoagulation with dose-adjusted warfarin to maintain an international normalized ratio of 1.5 to 2.0.
Patients were observed postoperatively at the 5- to 8-year and 15-year time points. The 5-year data were previously published in 2005 by Bozic and colleagues.10 Patients available for follow-up at the 15-year time-point were evaluated using the 100-point Hospital for Special Surgery (HSS) knee scoring system, which assigns up to 30 points for pain, 22 points for function, 18 points for range of motion, and 10 points each for quadricep strength, deformity, and instability. In addition, common medical conditions limiting patient activity were assessed; these included joint replacement; arthritis in another joint, the back, or spine; weakness or fatigue; breathing or heart ailments; and others.
Continue to: At the 15-year follow-up...
At the 15-year follow-up, patients were contacted via telephone to obtain their HSS knee scores. If patients were unavailable/unable to answer the questions asked, knee score information was collected from a first-degree relative or caretaker. Patients that could not be contacted by phone were sent a HSS knee score survey to their last known address. The online Social Security Death Index was queried for confirmation of death. If deceased, a first-degree relative was contacted for confirmation.
Survivorship was evaluated using revision for any reason and revision for aseptic loosening as separate endpoints via the Kaplan-Meier product-limit method, and the CR and PS TKA groups were compared using the log-rank test. The power of the study for detecting differences between the TKA groups was determined to be 80%, based on a moderate hazard ratio of 1.5, using the log-rank test. Differences between PS and CR TKAs were assessed using the Pearson chi-square test for knee pain and functional outcomes, Fisher’s exact test for patient limitations, such as joint replacement, and the non-parametric Mann Whitney U-test for median pain scores (Table 1). Spearman correlations between the patients’ self-reported knee scores (as a percentage of normal) and physician-based knee scores were performed to assess whether self-reported knee scores were significantly correlated with physician-based knee scores. Kaplan-Meier analysis was performed to evaluate time-related freedom from reoperation at 95% confidence intervals. Statistical analysis was conducted using IBM SPSS Statistics (version 21.0, IBM). Two-tailed P < .05 was considered statistically significant.
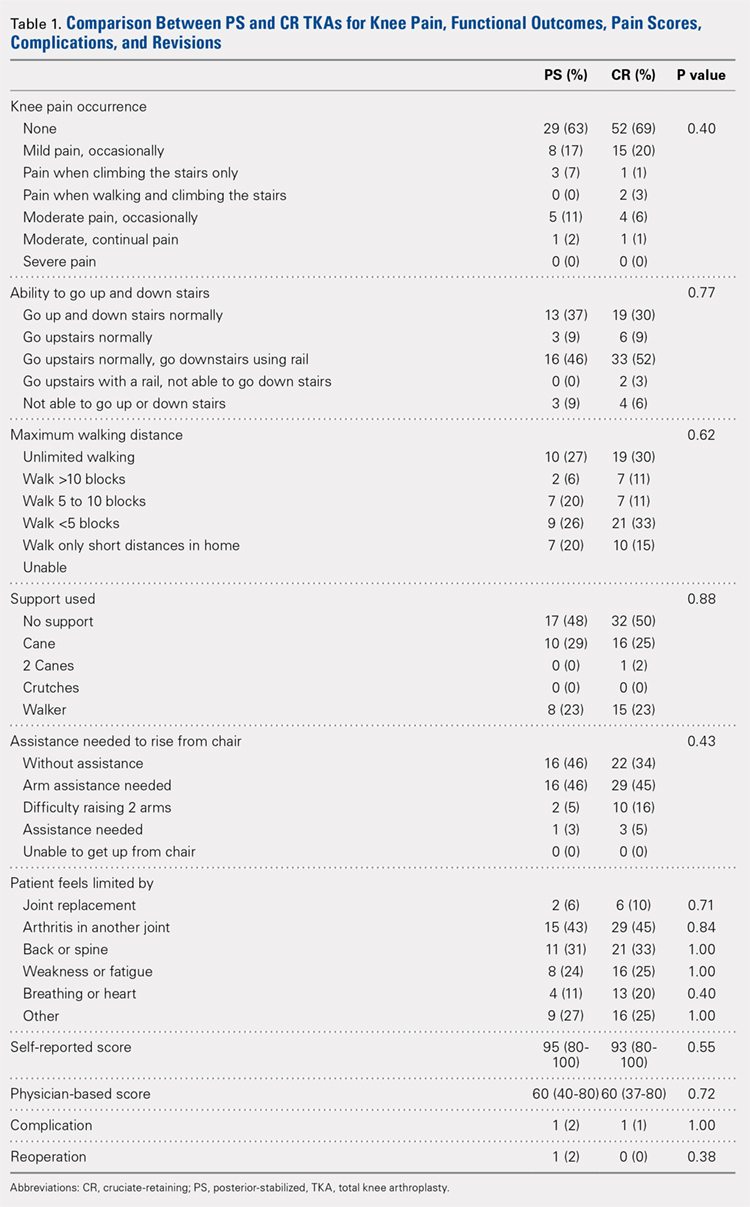
RESULTS
Of the 287 patients (334 knees) who had primary TKAs, 99 patients (121 knees; 75 CR and 46 PS) were available at the 15-year follow-up. A total of 155 patients (171 knees) died before the 15-year follow-up, and 33 (42 knees) were lost to follow-up (Figure 1). The functional status of the knees of patients who were lost to follow-up or who had died since the previous follow-up data were published is unknown.
Demographic and outcome data for the cohort of 121 TKAs (99 patients) are summarized in Table 2. The median age at surgery was 64 years, and 71% of the cohort was female.
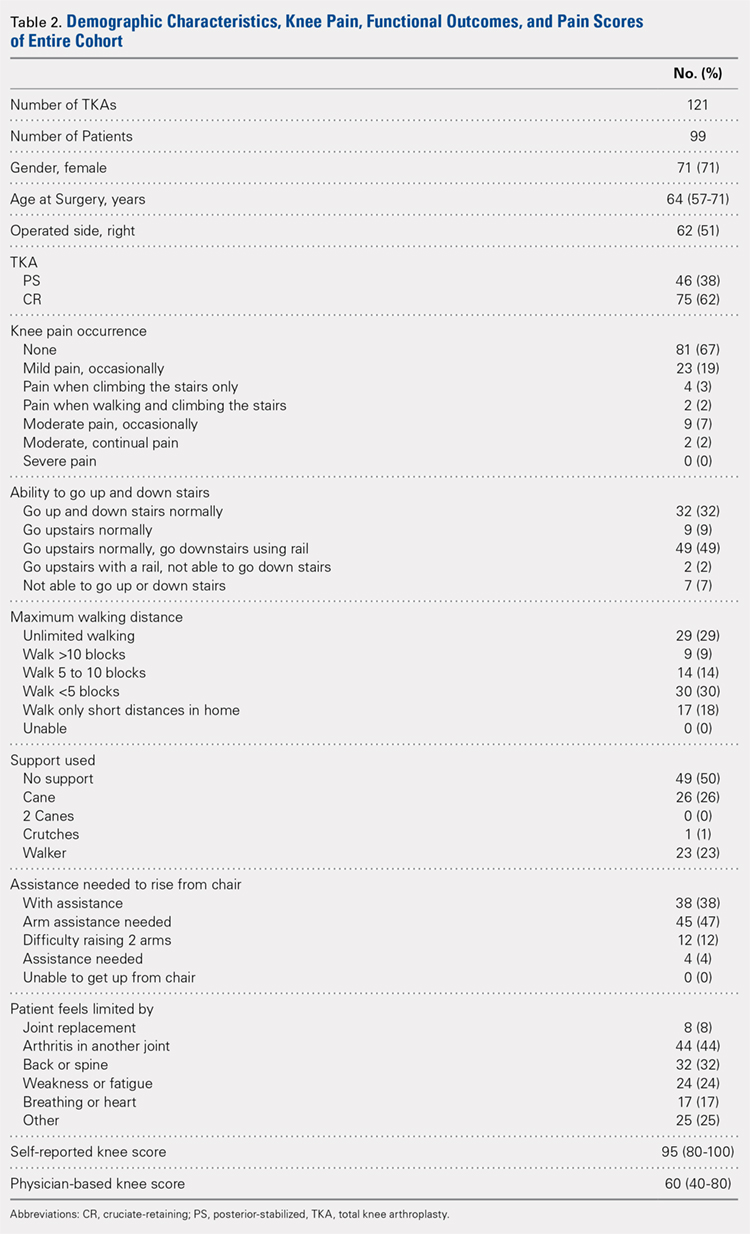
At the 15-year follow-up, survivorship in both groups was similar: 98% for PS TKAs and 100% for CR TKAs. The 2 groups were also similar functionally: 80% of the PS implants and 89% of the CR implants were associated with no or mild pain (P = .40). Approximately half of the patients in both groups (52% PS; 50% CR; P = .88) required walking support (canes or walkers) and nearly half of both groups (46% PS; 48% CR; P = .62) could walk <5 blocks or only short distances in their homes. In addition, 46% of the patients in both groups reported needing arm assistance to functionally rise from a chair (P = .43); 91% of the patients in both groups could also walk up and down stairs (P = .77). No statistical difference in the medical conditions limiting the patients in the 2 groups was found: joint replacement (2% PS; 6% CR; P = .71), arthritis in another joint (43% PS; 45% CR; P = .84), back or spine arthritis (31% PS; 33% CR; P = 1.00), weakness or fatigue (24% PS; 25% CR; P = 1.00), breathing or heart ailments (11% PS; 20% CR; P = .40), and other reasons (27% PS; 25% CR; P = 1.00). In addition, median self-reported knee scores were 95 and 93 points for the PS and CR groups, respectively (P = .55).
Continue to: Patients reported 2 complications...
Patients reported 2 complications since the previous 5- to 8-year follow-up, 1 in each group. The first case underwent a PS TKA that required open reduction internal fixation for a bilateral supracondylar peri-prosthesis femur fracture following a fall, which was subsequently complicated with infection and ultimately led to above-the-knee amputation. In the second case, a CR TKA patient experienced persistent swelling and knee instability. The patient followed up with a local orthopaedist, but to date, no reoperations on the knee have been reported.
Spearman correlations between the patients’ self-reported knee scores (as a percentage of normal) and physician-based knee scores were moderately correlated with physician-based knee scores (rs = 0.42; P < .001).
Reoperation rates were 2% for PS and 0% for CR (P = .38). Kaplan-Meier analysis was performed to evaluate time-related freedom from reoperation and no significance difference between the PS and CR groups was revealed (log-rank test = 1.40, P = .24, Figure 2).
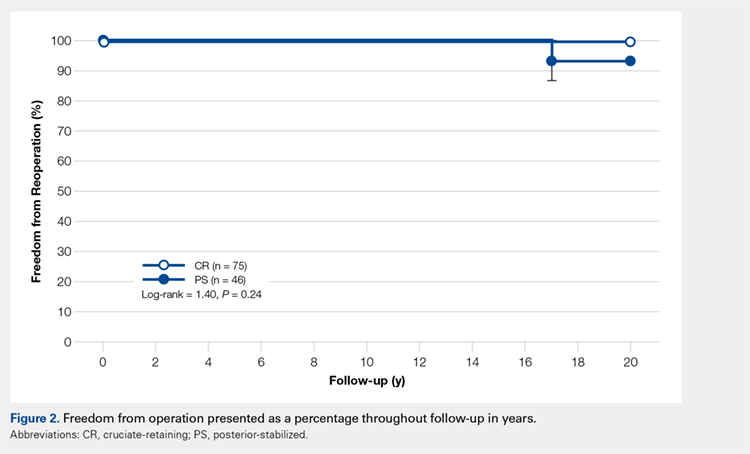
DISCUSSION
The success of TKA in pain relief and restoration of function has led to increased demands for this surgery.1 Such demand has enabled the introduction of a new joint replacement prosthesis to the market.18 Considering the increased incidence of osteoarthritis in the younger population (<55 years of age), critically reviewing the longevity and durability of TKA implant designs is of great importance. Compared with other TKA implant designs, the NexGen Zimmer Biomet Knee system has shown excellent longevity at the 15-year follow-up.5,6,9,11-15 Our study began with 136 patients, and, after eliminating the deceased, those lost to follow-up, and non-responders, a total of 99 patients were available for the 15-year follow-up. At this time-point, 80% of the PS implants and 89% of the CR implants were associated with no or mild pain. Survivorship at the 15-year follow-up was similar in both groups: 98% for PS TKAs and 100% for CR TKAs. The reoperation rate was low in both groups, and no evidence of aseptic loosening was found. Based on our results, the NexGen Zimmer Biomet Knee system can be concluded to show excellent longevity and functional outcomes at the 15-year follow-up.
Our study includes several limiting factors that were taken into consideration during the analysis of the results. One of the main limitations of this work is that it required a 15-year follow-up of predominantly elderly patients; many of the participants may be expected to be deceased at this time-point. In our study, a total of 7 patients were confirmed to be deceased by a first-degree relative or the Social Security Death Index. In addition, unlike Bozic and colleagues’10 previous 5-year follow-up study, radiographic imaging data were not collected at the 15-year follow-up. However, given that this study aimed to assess the functional knee scores and reoperation rates of the PS and CR NexGen Zimmer Biomet Knee system, radiographic information did not appear to be necessary.
CONCLUSION
This study found no significant differences in functional outcomes between the PS and CR NexGen knee implants. Patients who received these implants showed excellent longevity and survivorship at their 15-year follow-up.
ABSTRACT
This work is a retrospective cohort study evaluating patients who had undergone third-generation cemented total knee arthroplasty (TKA) with prostheses (NexGen, Zimmer Biomet) utilizing posterior-stabilized (PS) and cruciate-retaining (CR) designs at a single center at their 15-year follow-up.
The purpose of this study is to determine the functional knee scores, reoperations, and long-term survivorship for patients with the NexGen Zimmer Biomet Knee system at the 15-year follow-up. In total, 99 patients who had undergone primary TKA were followed for 15 years.
At the 15-year follow-up, survivorship in both study groups was similar: 98% for PS TKAs and 100% for CR TKAs. The 2 groups also showed similar functionality: 80% of the PS implants and 89% of the CR implants were associated with no or mild pain (P = .40). Reoperation rates were 2% for the PS group and 0% for the CR group (P = .38). No differences in any of the outcomes analyzed were observed between patients who had CR TKA and those who had undergone PS TKA.
Our study found no significant differences in functional outcomes between PS and CR NexGen knee implants. Patients treated by both methods showed excellent longevity and survivorship at the 15-year follow-up.
Continue to: Total knee arthroplasty...
Total knee arthroplasty (TKA) is an orthopedic procedure with increasing demand.1 Over the past 2 decades, a surge in TKA implants has been observed. Of the available prosthetic designs, only a few implants with long-term follow-up have been reported.2-9 The NexGen TKA system (Zimmer Biomet) has been shown to have excellent clinical and radiographic results at an intermediate follow-up term of 8 years.10 This system is a third-generation prosthetic design that was developed to improve problems seen with its predecessors, such as the Miller-Galante II system (Zimmer Biomet), the Insall-Burstein II system (Zimmer Biomet), and the Constrained Condylar Knee (Zimmer Biomet), which were mainly for patellar maltracking.11-17 The NexGen TKA system is a fixed-bearing system designed to include an anatomic femoral trochlea with the option of cruciate-retaining (CR), posterior-stabilized (PS), or more constrained implants. This study evaluates the long-term success of the CR and PS NexGen TKA systems. Outcomes measured include functional knee scores and reoperation rates at the 15-year follow-up. Based on the measured outcomes, potential differences between the PS and CR implants from this system are cited.
MATERIAL AND METHODS
Between July 1995 and July 1997, 334 consecutive primary TKAs were performed on 287 patients at our institution. In total, 167 patients (186 knees) underwent posterior CR TKAs with the NexGen CR prosthesis (Zimmer Biomet), and 120 patients (148 knees) underwent PS TKAs using the NexGen Legacy PS prosthesis (Zimmer Biomet). This retrospective double cohort study was reviewed and approved by our Institutional Review Board. At the 15-year postoperative follow-up, 99 patients were available (Figure 1).
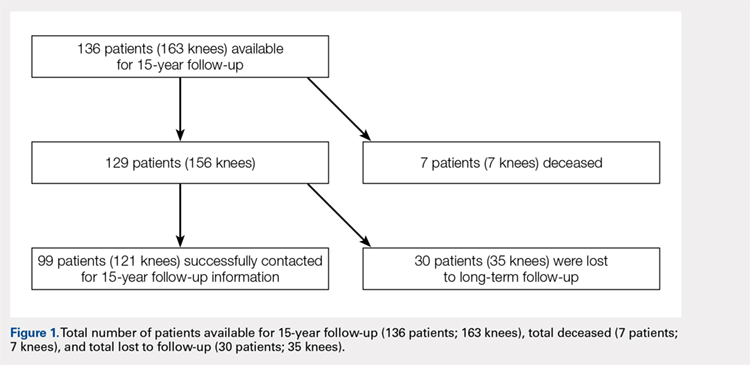
The CR and PS implants were used with similar frequencies by the surgeons who performed the procedures. Patients were not randomized into either the PS- or CR-implant teams; the final decision on implant selection was left to the operating surgeon’s discretion. However, in addition to standard indications for TKA (pain and disability associated with severe arthritic change seen on radiographs and refractory to conservative measures), absolute contraindications to the CR implant included severe combined deformity (flexion contraction >30° combined with a varus or valgus deformity >20°) or posterior cruciate ligament insufficiency (often associated with inflammatory arthritis).
The surgical technique for the CR and PS designs was identical, and included a median parapatellar approach, femoral rotational alignment perpendicular to the transepicondylar axis, measured resection of the flexion and extension gaps, intramedullary femoral alignment, and extramedullary tibial alignment. All components were cemented, and the patella of each patient was resurfaced. All patients received preoperative antibiotics that were continued for 48 hours postoperatively, and 4 weeks of anticoagulation with dose-adjusted warfarin to maintain an international normalized ratio of 1.5 to 2.0.
Patients were observed postoperatively at the 5- to 8-year and 15-year time points. The 5-year data were previously published in 2005 by Bozic and colleagues.10 Patients available for follow-up at the 15-year time-point were evaluated using the 100-point Hospital for Special Surgery (HSS) knee scoring system, which assigns up to 30 points for pain, 22 points for function, 18 points for range of motion, and 10 points each for quadricep strength, deformity, and instability. In addition, common medical conditions limiting patient activity were assessed; these included joint replacement; arthritis in another joint, the back, or spine; weakness or fatigue; breathing or heart ailments; and others.
Continue to: At the 15-year follow-up...
At the 15-year follow-up, patients were contacted via telephone to obtain their HSS knee scores. If patients were unavailable/unable to answer the questions asked, knee score information was collected from a first-degree relative or caretaker. Patients that could not be contacted by phone were sent a HSS knee score survey to their last known address. The online Social Security Death Index was queried for confirmation of death. If deceased, a first-degree relative was contacted for confirmation.
Survivorship was evaluated using revision for any reason and revision for aseptic loosening as separate endpoints via the Kaplan-Meier product-limit method, and the CR and PS TKA groups were compared using the log-rank test. The power of the study for detecting differences between the TKA groups was determined to be 80%, based on a moderate hazard ratio of 1.5, using the log-rank test. Differences between PS and CR TKAs were assessed using the Pearson chi-square test for knee pain and functional outcomes, Fisher’s exact test for patient limitations, such as joint replacement, and the non-parametric Mann Whitney U-test for median pain scores (Table 1). Spearman correlations between the patients’ self-reported knee scores (as a percentage of normal) and physician-based knee scores were performed to assess whether self-reported knee scores were significantly correlated with physician-based knee scores. Kaplan-Meier analysis was performed to evaluate time-related freedom from reoperation at 95% confidence intervals. Statistical analysis was conducted using IBM SPSS Statistics (version 21.0, IBM). Two-tailed P < .05 was considered statistically significant.
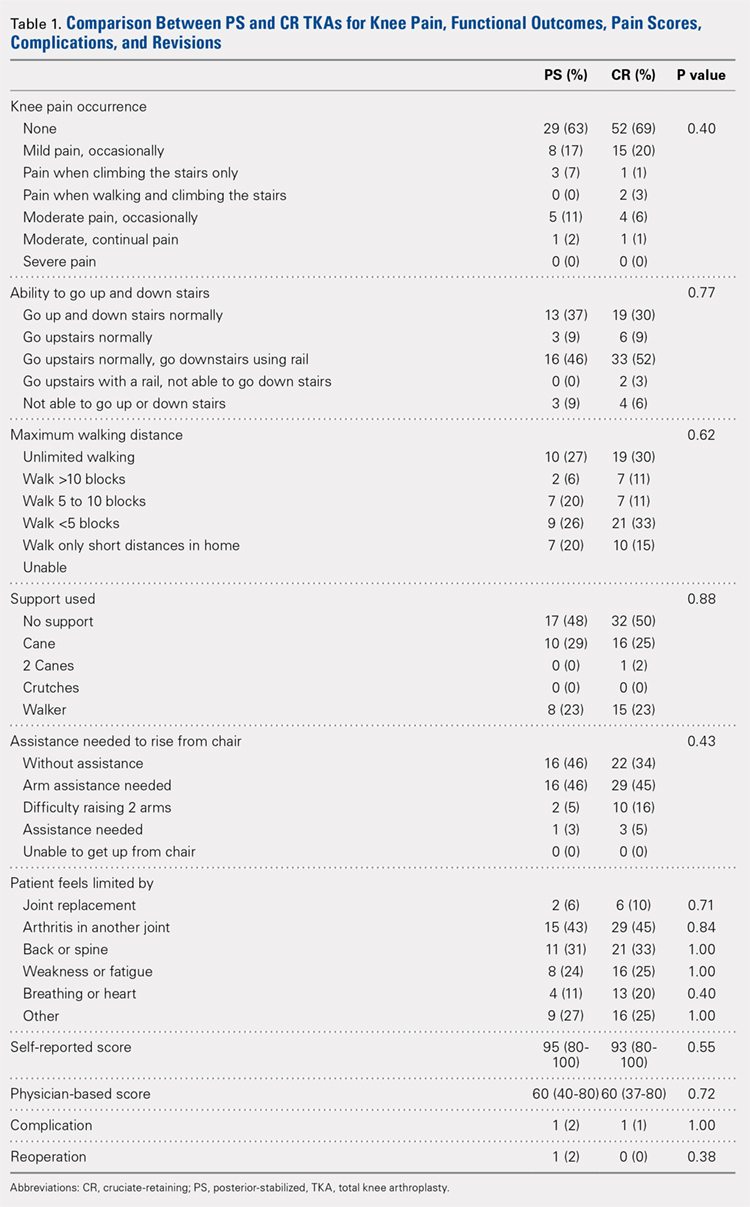
RESULTS
Of the 287 patients (334 knees) who had primary TKAs, 99 patients (121 knees; 75 CR and 46 PS) were available at the 15-year follow-up. A total of 155 patients (171 knees) died before the 15-year follow-up, and 33 (42 knees) were lost to follow-up (Figure 1). The functional status of the knees of patients who were lost to follow-up or who had died since the previous follow-up data were published is unknown.
Demographic and outcome data for the cohort of 121 TKAs (99 patients) are summarized in Table 2. The median age at surgery was 64 years, and 71% of the cohort was female.
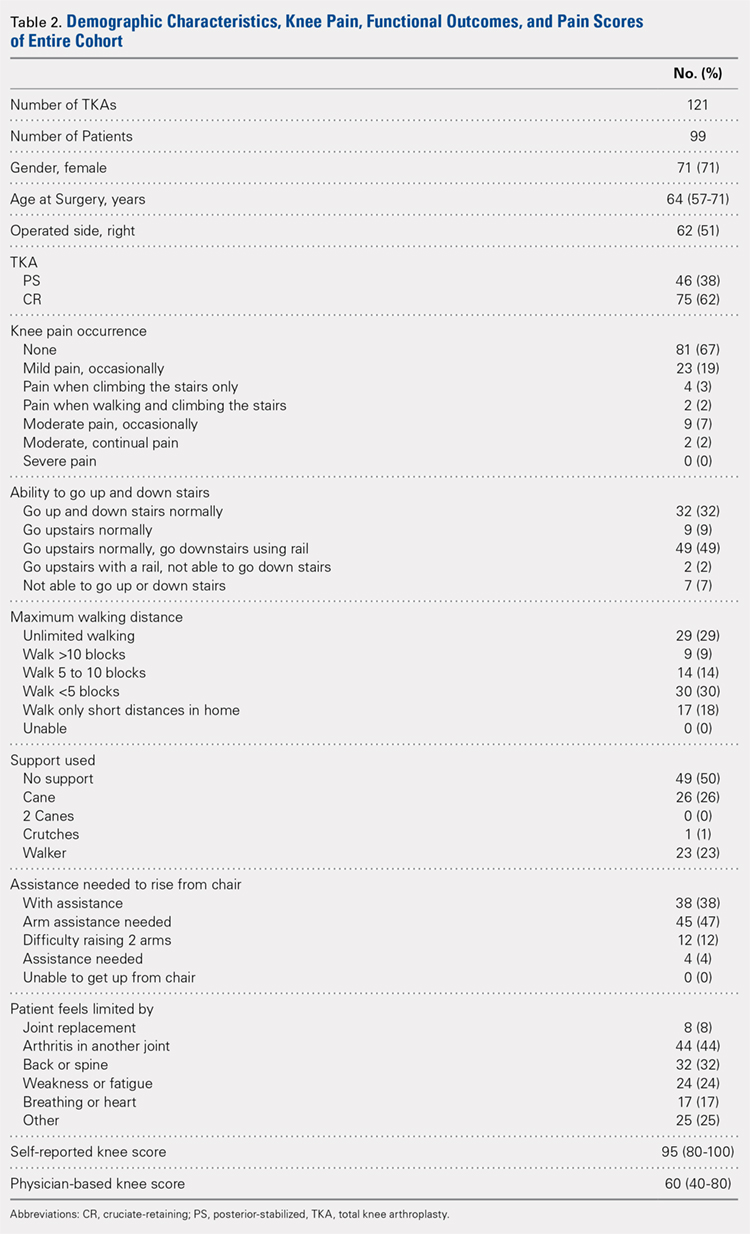
At the 15-year follow-up, survivorship in both groups was similar: 98% for PS TKAs and 100% for CR TKAs. The 2 groups were also similar functionally: 80% of the PS implants and 89% of the CR implants were associated with no or mild pain (P = .40). Approximately half of the patients in both groups (52% PS; 50% CR; P = .88) required walking support (canes or walkers) and nearly half of both groups (46% PS; 48% CR; P = .62) could walk <5 blocks or only short distances in their homes. In addition, 46% of the patients in both groups reported needing arm assistance to functionally rise from a chair (P = .43); 91% of the patients in both groups could also walk up and down stairs (P = .77). No statistical difference in the medical conditions limiting the patients in the 2 groups was found: joint replacement (2% PS; 6% CR; P = .71), arthritis in another joint (43% PS; 45% CR; P = .84), back or spine arthritis (31% PS; 33% CR; P = 1.00), weakness or fatigue (24% PS; 25% CR; P = 1.00), breathing or heart ailments (11% PS; 20% CR; P = .40), and other reasons (27% PS; 25% CR; P = 1.00). In addition, median self-reported knee scores were 95 and 93 points for the PS and CR groups, respectively (P = .55).
Continue to: Patients reported 2 complications...
Patients reported 2 complications since the previous 5- to 8-year follow-up, 1 in each group. The first case underwent a PS TKA that required open reduction internal fixation for a bilateral supracondylar peri-prosthesis femur fracture following a fall, which was subsequently complicated with infection and ultimately led to above-the-knee amputation. In the second case, a CR TKA patient experienced persistent swelling and knee instability. The patient followed up with a local orthopaedist, but to date, no reoperations on the knee have been reported.
Spearman correlations between the patients’ self-reported knee scores (as a percentage of normal) and physician-based knee scores were moderately correlated with physician-based knee scores (rs = 0.42; P < .001).
Reoperation rates were 2% for PS and 0% for CR (P = .38). Kaplan-Meier analysis was performed to evaluate time-related freedom from reoperation and no significance difference between the PS and CR groups was revealed (log-rank test = 1.40, P = .24, Figure 2).
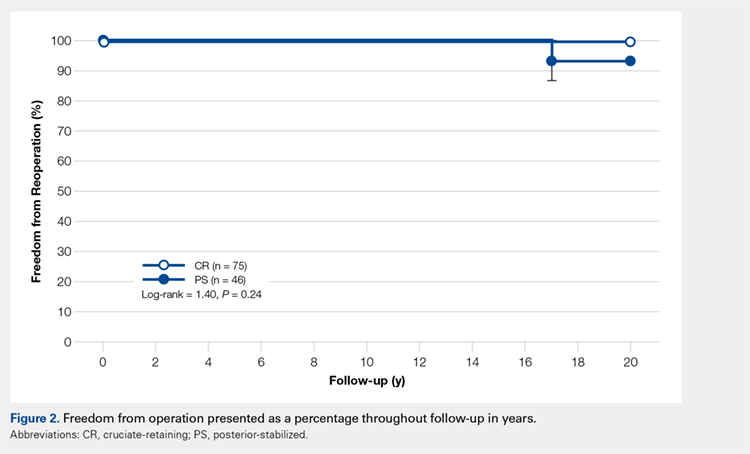
DISCUSSION
The success of TKA in pain relief and restoration of function has led to increased demands for this surgery.1 Such demand has enabled the introduction of a new joint replacement prosthesis to the market.18 Considering the increased incidence of osteoarthritis in the younger population (<55 years of age), critically reviewing the longevity and durability of TKA implant designs is of great importance. Compared with other TKA implant designs, the NexGen Zimmer Biomet Knee system has shown excellent longevity at the 15-year follow-up.5,6,9,11-15 Our study began with 136 patients, and, after eliminating the deceased, those lost to follow-up, and non-responders, a total of 99 patients were available for the 15-year follow-up. At this time-point, 80% of the PS implants and 89% of the CR implants were associated with no or mild pain. Survivorship at the 15-year follow-up was similar in both groups: 98% for PS TKAs and 100% for CR TKAs. The reoperation rate was low in both groups, and no evidence of aseptic loosening was found. Based on our results, the NexGen Zimmer Biomet Knee system can be concluded to show excellent longevity and functional outcomes at the 15-year follow-up.
Our study includes several limiting factors that were taken into consideration during the analysis of the results. One of the main limitations of this work is that it required a 15-year follow-up of predominantly elderly patients; many of the participants may be expected to be deceased at this time-point. In our study, a total of 7 patients were confirmed to be deceased by a first-degree relative or the Social Security Death Index. In addition, unlike Bozic and colleagues’10 previous 5-year follow-up study, radiographic imaging data were not collected at the 15-year follow-up. However, given that this study aimed to assess the functional knee scores and reoperation rates of the PS and CR NexGen Zimmer Biomet Knee system, radiographic information did not appear to be necessary.
CONCLUSION
This study found no significant differences in functional outcomes between the PS and CR NexGen knee implants. Patients who received these implants showed excellent longevity and survivorship at their 15-year follow-up.
1. Lützner J, Hübel U, Kirschner S, Günther KP, Krummenauer F. Langzeitergebnisse in der Knieendoprothetik. Chirurg. 2011;82(7):618-624. doi:10.1007/s00104-010-2001-8.
2. Font-Rodriguez DE, Scuderi GR, Insall J. Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res. 1997;345:79-86.
3. Rodriguez JA, Bhende H, Ranawat CS. Total condylar knee replacement: a 20-year followup study. Clin Orthop Relat Res. 2001;388:10-17.
4. Van Loon CJM, Wisse MA, de Waal Malefijt MC, Jansen RH, Veth RPH. The kinematic total knee arthroplasty. Arch Orth Traum Surg. 2000;120(1-2):48-52. doi:10.1007/PL00021215.
5. Buechel FFS. Long-term followup after mobile-bearing total knee replacement. Clin Orthop Relat Res. 2002;404:40-50.
6. Ito J, Koshino T, Okamoto R, Saito T. 15-year follow-up study of total knee arthroplasty in patients with rheumatoid arthritis. J Arthroplasty. 2003;18(8):984-992. doi:10.1016/S0883-5403(03)00262-6.
7. Dixon MC, Brown RR, Parsch D, Scott RD. Modular fixed-bearing total knee arthroplasty with retention of the posterior cruciate ligament. J Bone Joint Surg. 2005;87(3):598-603. doi:10.2106/JBJS.C.00591.
8. Duffy GP, Crowder AR, Trousdale RR, Berry DJ. Cemented total knee arthroplasty using a modern prosthesis in young patients with osteoarthritis. J Arthroplasty. 2007;22(6 Suppl 2):67-70. doi:10.1016/j.arth.2007.05.001.
9. Baker PN, Khaw FM, Kirk LMG, Esler CNA, Gregg PJ. A randomised controlled trial of cemented versus cementless press-fit condylar total knee replacement: 15-year survival analysis. J Bone Joint Surg. 2007;89-B(12):1608-1614. doi:10.1302/0301-620x.89b12.19363.
10. Bozic KJ, Kinder J, Menegini M, Zurakowski D, Rosenberg AG, Galante JO. Implant survivorship and complication rates after total knee arthroplasty with a third-generation cemented system: 5 to 8 years followup. Clin Orthop Relat Res. 2005;430:117-124. doi:10.1097/01.blo.0000146539.23869.14.
11. Effenberger H, Berka J, Hilzensauer G, Ramsauer T, Dorn U, Kißlinger E. Miller-Galante total knee arthroplasty: the importance of material and design on the revision rate. Int Orthop. 2001;25(6):378-381. doi:10.1007/s002640100294.
12. Kirk PG, Rorabeck CH, Bourne RB. Clinical comparison of the Miller Galante I and AMK total knee systems. J Arthroplasty. 1994;9(2):131-136. doi:10.1016/0883-5403(94)90061-2.
13. Kobori M, Kamisato S, Yoshida M, Kobori K. Revision of failed metal-backed patellar component of Miller/Galante-I total knee prosthesis. J Orthop Sci. 2000;5(5):436-438. doi:10.1007/s007760070020.
14. Larson CM, Lachiewicz PF. Patellofemoral complications with the insall-burstein II posterior-stabilized total knee arthroplasty. J Arthroplasty. 1999;14(3):288-292. doi:http://dx.doi.org/10.1016/S0883-5403(99)90053-0.
15. Matsuda S, Miura H, Nagamine R, Urabe K, Hirata G, Iwamoto Y. Effect of femoral and tibial component position on patellar tracking following total knee arthroplasty: 10-year follow-up of Miller-Galante I knees. Am J Knee Surg. 2001;14(3):152-156.
16. Miyagi T, Matsuda S, Miura H, Nagamine R, Urabe K. Changes in patellar tracking after total knee arthroplasty: 10-year follow-up of Miller-Balante I knees. Orthopedics. 2002;25(8):811-813. doi:10.3928/0147-7447-20020801-10.
17. Rao AR, Engh GA, Collier MB, Lounici S. Tibial interface wear in retrieved total knee components and correlations with modular insert motion. J Bone Joint Surg. 2002;84(10):1849-1855.
18. Anand R, Graves SE, de Steiger RN, et al. What is the benefit of introducing new hip and knee prostheses? J Bone Joint Surg. 2011;93(3):51-54. doi:10.2106/JBJS.K.00867.
1. Lützner J, Hübel U, Kirschner S, Günther KP, Krummenauer F. Langzeitergebnisse in der Knieendoprothetik. Chirurg. 2011;82(7):618-624. doi:10.1007/s00104-010-2001-8.
2. Font-Rodriguez DE, Scuderi GR, Insall J. Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res. 1997;345:79-86.
3. Rodriguez JA, Bhende H, Ranawat CS. Total condylar knee replacement: a 20-year followup study. Clin Orthop Relat Res. 2001;388:10-17.
4. Van Loon CJM, Wisse MA, de Waal Malefijt MC, Jansen RH, Veth RPH. The kinematic total knee arthroplasty. Arch Orth Traum Surg. 2000;120(1-2):48-52. doi:10.1007/PL00021215.
5. Buechel FFS. Long-term followup after mobile-bearing total knee replacement. Clin Orthop Relat Res. 2002;404:40-50.
6. Ito J, Koshino T, Okamoto R, Saito T. 15-year follow-up study of total knee arthroplasty in patients with rheumatoid arthritis. J Arthroplasty. 2003;18(8):984-992. doi:10.1016/S0883-5403(03)00262-6.
7. Dixon MC, Brown RR, Parsch D, Scott RD. Modular fixed-bearing total knee arthroplasty with retention of the posterior cruciate ligament. J Bone Joint Surg. 2005;87(3):598-603. doi:10.2106/JBJS.C.00591.
8. Duffy GP, Crowder AR, Trousdale RR, Berry DJ. Cemented total knee arthroplasty using a modern prosthesis in young patients with osteoarthritis. J Arthroplasty. 2007;22(6 Suppl 2):67-70. doi:10.1016/j.arth.2007.05.001.
9. Baker PN, Khaw FM, Kirk LMG, Esler CNA, Gregg PJ. A randomised controlled trial of cemented versus cementless press-fit condylar total knee replacement: 15-year survival analysis. J Bone Joint Surg. 2007;89-B(12):1608-1614. doi:10.1302/0301-620x.89b12.19363.
10. Bozic KJ, Kinder J, Menegini M, Zurakowski D, Rosenberg AG, Galante JO. Implant survivorship and complication rates after total knee arthroplasty with a third-generation cemented system: 5 to 8 years followup. Clin Orthop Relat Res. 2005;430:117-124. doi:10.1097/01.blo.0000146539.23869.14.
11. Effenberger H, Berka J, Hilzensauer G, Ramsauer T, Dorn U, Kißlinger E. Miller-Galante total knee arthroplasty: the importance of material and design on the revision rate. Int Orthop. 2001;25(6):378-381. doi:10.1007/s002640100294.
12. Kirk PG, Rorabeck CH, Bourne RB. Clinical comparison of the Miller Galante I and AMK total knee systems. J Arthroplasty. 1994;9(2):131-136. doi:10.1016/0883-5403(94)90061-2.
13. Kobori M, Kamisato S, Yoshida M, Kobori K. Revision of failed metal-backed patellar component of Miller/Galante-I total knee prosthesis. J Orthop Sci. 2000;5(5):436-438. doi:10.1007/s007760070020.
14. Larson CM, Lachiewicz PF. Patellofemoral complications with the insall-burstein II posterior-stabilized total knee arthroplasty. J Arthroplasty. 1999;14(3):288-292. doi:http://dx.doi.org/10.1016/S0883-5403(99)90053-0.
15. Matsuda S, Miura H, Nagamine R, Urabe K, Hirata G, Iwamoto Y. Effect of femoral and tibial component position on patellar tracking following total knee arthroplasty: 10-year follow-up of Miller-Galante I knees. Am J Knee Surg. 2001;14(3):152-156.
16. Miyagi T, Matsuda S, Miura H, Nagamine R, Urabe K. Changes in patellar tracking after total knee arthroplasty: 10-year follow-up of Miller-Balante I knees. Orthopedics. 2002;25(8):811-813. doi:10.3928/0147-7447-20020801-10.
17. Rao AR, Engh GA, Collier MB, Lounici S. Tibial interface wear in retrieved total knee components and correlations with modular insert motion. J Bone Joint Surg. 2002;84(10):1849-1855.
18. Anand R, Graves SE, de Steiger RN, et al. What is the benefit of introducing new hip and knee prostheses? J Bone Joint Surg. 2011;93(3):51-54. doi:10.2106/JBJS.K.00867.
TAKE-HOME POINTS
- TKA has a high success rate in pain relief and restoration of function in patients with severe osteoarthritis.
- NexGen (Zimmer Biomet) knee implants showed excellent functional outcomes at 15 years.
- There are no significant differences in functional outcomes between the PS and CR knee systems.
- NexGen knee implants showed excellent longevity and survivorship at 15-year follow-up with no evidence of aseptic loosening.
- There is an increased incidence of knee osteoarthritis in the younger population (<55 years of age).