User login
FDA lifts hold on trials of universal CAR T-cell therapy
The US Food and Drug Administration (FDA) has lifted the full clinical hold on 2 phase 1 studies of UCART123, an allogeneic chimeric antigen receptor (CAR) T-cell therapy targeting CD123.
One of these studies was designed for patients with acute myeloid leukemia (AML), and the other was designed for patients with blastic plasmacytoid dendritic cell neoplasm (BPDCN).
The hold meant no new subjects could be enrolled in either trial, and there could be no further dosing of subjects who were already enrolled.
The hold was placed in September because the first patient treated in the BPDCN trial died. The patient developed grade 2 cytokine release syndrome (CRS) and a grade 3 lung infection. This was followed by grade 4 capillary leak syndrome and grade 5 CRS.
The first patient treated in the AML trial also developed grade 4 capillary leak syndrome and grade 3 CRS, but both resolved.
Now, the FDA has lifted the hold on the trials because Cellectis, the company developing UCART123, agreed to implement the following main revisions to phase 1 UCART123 protocols:
- Decrease the cohort dose level to 6.25 x 104 UCART123 cells/kg
- Decrease the cyclophosphamide dose of the lymphodepleting regimen to 750 mg/m²/day over 3 days, with a maximum daily dose of 1.33 grams
- Include specific criteria at Day 0, the day of UCART123 infusion, such as no new uncontrolled infection after receipt of lymphodepletion, afebrile, off all but replacement dose of corticosteroids, and no organ dysfunction since eligibility screening
- Ensure the next 3 patients to be treated in each protocol will be under the age of 65
- Ensure that enrollment will be staggered across the UCART123 protocols; at least 28 days should elapse between the enrollments of 2 patients across the 2 studies.
Cellectis is currently working with investigators and clinical sites to obtain internal review board approval on the revised protocols and resume patient enrollment. ![]()
The US Food and Drug Administration (FDA) has lifted the full clinical hold on 2 phase 1 studies of UCART123, an allogeneic chimeric antigen receptor (CAR) T-cell therapy targeting CD123.
One of these studies was designed for patients with acute myeloid leukemia (AML), and the other was designed for patients with blastic plasmacytoid dendritic cell neoplasm (BPDCN).
The hold meant no new subjects could be enrolled in either trial, and there could be no further dosing of subjects who were already enrolled.
The hold was placed in September because the first patient treated in the BPDCN trial died. The patient developed grade 2 cytokine release syndrome (CRS) and a grade 3 lung infection. This was followed by grade 4 capillary leak syndrome and grade 5 CRS.
The first patient treated in the AML trial also developed grade 4 capillary leak syndrome and grade 3 CRS, but both resolved.
Now, the FDA has lifted the hold on the trials because Cellectis, the company developing UCART123, agreed to implement the following main revisions to phase 1 UCART123 protocols:
- Decrease the cohort dose level to 6.25 x 104 UCART123 cells/kg
- Decrease the cyclophosphamide dose of the lymphodepleting regimen to 750 mg/m²/day over 3 days, with a maximum daily dose of 1.33 grams
- Include specific criteria at Day 0, the day of UCART123 infusion, such as no new uncontrolled infection after receipt of lymphodepletion, afebrile, off all but replacement dose of corticosteroids, and no organ dysfunction since eligibility screening
- Ensure the next 3 patients to be treated in each protocol will be under the age of 65
- Ensure that enrollment will be staggered across the UCART123 protocols; at least 28 days should elapse between the enrollments of 2 patients across the 2 studies.
Cellectis is currently working with investigators and clinical sites to obtain internal review board approval on the revised protocols and resume patient enrollment. ![]()
The US Food and Drug Administration (FDA) has lifted the full clinical hold on 2 phase 1 studies of UCART123, an allogeneic chimeric antigen receptor (CAR) T-cell therapy targeting CD123.
One of these studies was designed for patients with acute myeloid leukemia (AML), and the other was designed for patients with blastic plasmacytoid dendritic cell neoplasm (BPDCN).
The hold meant no new subjects could be enrolled in either trial, and there could be no further dosing of subjects who were already enrolled.
The hold was placed in September because the first patient treated in the BPDCN trial died. The patient developed grade 2 cytokine release syndrome (CRS) and a grade 3 lung infection. This was followed by grade 4 capillary leak syndrome and grade 5 CRS.
The first patient treated in the AML trial also developed grade 4 capillary leak syndrome and grade 3 CRS, but both resolved.
Now, the FDA has lifted the hold on the trials because Cellectis, the company developing UCART123, agreed to implement the following main revisions to phase 1 UCART123 protocols:
- Decrease the cohort dose level to 6.25 x 104 UCART123 cells/kg
- Decrease the cyclophosphamide dose of the lymphodepleting regimen to 750 mg/m²/day over 3 days, with a maximum daily dose of 1.33 grams
- Include specific criteria at Day 0, the day of UCART123 infusion, such as no new uncontrolled infection after receipt of lymphodepletion, afebrile, off all but replacement dose of corticosteroids, and no organ dysfunction since eligibility screening
- Ensure the next 3 patients to be treated in each protocol will be under the age of 65
- Ensure that enrollment will be staggered across the UCART123 protocols; at least 28 days should elapse between the enrollments of 2 patients across the 2 studies.
Cellectis is currently working with investigators and clinical sites to obtain internal review board approval on the revised protocols and resume patient enrollment. ![]()
From 5K to … the End of the Driveway
ANSWER
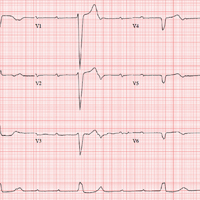
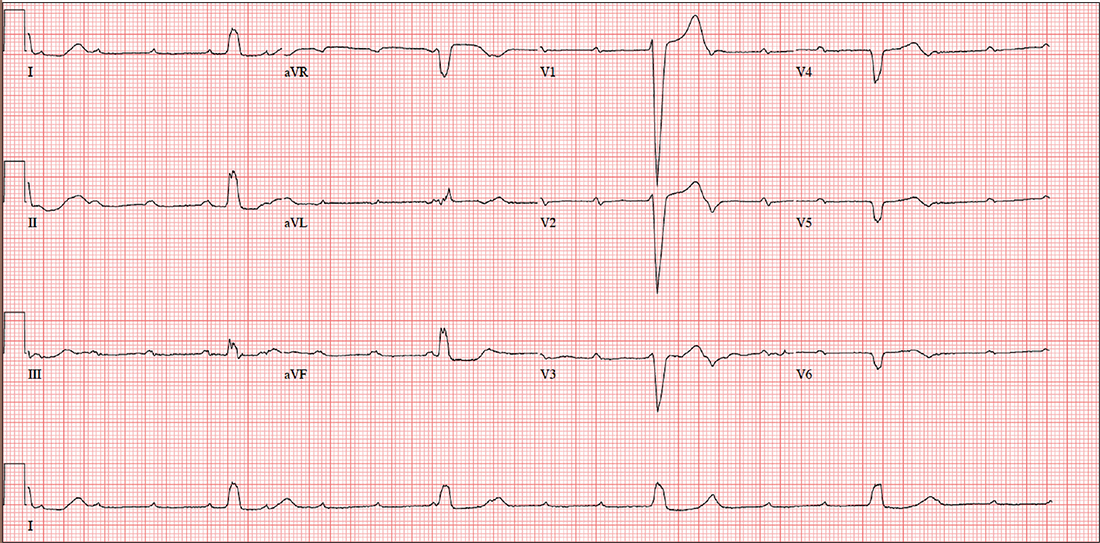
The correct interpretation includes sinus tachycardia with complete heart block and an idioventricular rhythm. Careful review of this ECG confirms complete atrioventricular dissociation, which is indicative of complete heart block.
Sinus tachycardia is indicated by a consistent P-P interval at a rate of 110 beats/min, idioventricular rhythm with a regular (but not normal) rate, and prolonged QRS interval of 148 ms. In this patient’s case, the tachycardia was presumed to be due to his upper respiratory infection. He underwent permanent pacemaker placement and resumed his normal activities without restriction.
ANSWER
The correct interpretation includes sinus tachycardia with complete heart block and an idioventricular rhythm. Careful review of this ECG confirms complete atrioventricular dissociation, which is indicative of complete heart block.
Sinus tachycardia is indicated by a consistent P-P interval at a rate of 110 beats/min, idioventricular rhythm with a regular (but not normal) rate, and prolonged QRS interval of 148 ms. In this patient’s case, the tachycardia was presumed to be due to his upper respiratory infection. He underwent permanent pacemaker placement and resumed his normal activities without restriction.
ANSWER
The correct interpretation includes sinus tachycardia with complete heart block and an idioventricular rhythm. Careful review of this ECG confirms complete atrioventricular dissociation, which is indicative of complete heart block.
Sinus tachycardia is indicated by a consistent P-P interval at a rate of 110 beats/min, idioventricular rhythm with a regular (but not normal) rate, and prolonged QRS interval of 148 ms. In this patient’s case, the tachycardia was presumed to be due to his upper respiratory infection. He underwent permanent pacemaker placement and resumed his normal activities without restriction.
Until three weeks ago, this 74-year-old man walked three miles every day without difficulty. But now, shortness of breath forces him to stop walking before he even reaches the end of his driveway. He denies chest pain (at rest or on exertion), palpitations, dyspnea at rest, and paroxysmal nocturnal dyspnea. There have been no recent weight changes.
Four years ago, he was diagnosed with coronary artery disease after experiencing chest pain at rest. A coronary angiography revealed stenosis in the proximal right coronary artery and the second obtuse marginal branch of his circumflex coronary artery; drug-eluting stents were placed, and he has had no further symptoms. An echocardiogram performed at a routine clinic visit six months ago showed mild aortic valve sclerosis, a left ventricular ejection fraction of 64%, and no regional wall motion abnormalities.
Surgical history is also remarkable for an open reduction and stabilization of a right high ankle fracture 10 years ago. Medical history includes type 2 diabetes and hyperlipidemia; treatment has normalized his A1C and his lipid panel.
His current medication list includes metoprolol, isosorbide dinitrate, metformin, and atorvastatin. He has no known drug allergies. He is unaware of any medical issues with his parents or grandparents.
The patient has two adult sons who live abroad and visit once a year. He was married for 53 years but lost his wife to lung cancer three years ago; her diagnosis prompted him to quit his long-term smoking habit. He consumes alcohol socially, having “one or two beers with friends on the weekends,” but denies current or previous use of marijuana or nonprescribed medications.
Review of systems is remarkable for a three-day history of upper respiratory infection with cough and rhinitis. He denies any change in bowel or bladder function.
Vital signs include a blood pressure of 104/54 mm Hg; pulse, 30 beats/min; respiratory rate, 16 breaths/min-1; and temperature, 99.4°F. His weight is 169 lb and his height, 70 in.
On physical exam, you note a thin, healthy-looking male in no acute distress. Pertinent findings include internally inflamed nares and oropharynx, a few scattered rales in both lower lung fields that clear with coughing, and no wheezing. There are no palpable lymph nodes in the head or neck.
Cardiac exam reveals a regular rhythm of 30 beats/min with no murmurs, rubs, or extra heart sounds. The abdomen is soft and nontender. Peripheral pulses are strong and palpable in both upper and lower extremities, and there is no peripheral edema. The neurologic exam is intact, without evidence of diabetic neuropathy.
Given the slow heart rate observed on physical exam, an ECG is ordered. It shows a ventricular rate of 29 beats/min; no discernable PR interval; QRS duration, 148 ms; QT/QTc interval, 584/405 ms; P axis, 64°; R axis, 55°; and T axis, 83°. What is your interpretation?
Apple pie and ...
How do you feel about apple pie? Is it a concept that evokes a positive feeling for you? Even if you prefer pumpkin or blueberry? Although your attitude toward apple pie may be relevant as we approach the holidays, is it a topic worthy of discussion in a publication devoted to pediatrics?
Certainly not, but what about motherhood? How do you feel about motherhood? As someone who is devoting his or her professional energies to the health of children, you must have formed some opinions about motherhood. Although your patients are children, it is their parents – and more often their mothers – with whom you communicate, particularly in the first several years of life.
You may never have been asked that question in exactly that way before, but I suspect you have thought about it both professionally and personally. You may have considered the answer as you were deciding if, when, and how you were going to return to work after maternity leave. Or you may have been forced to consider the question in formulating an opinion in a case of contested child custody.
An opinion piece in the Wall Street Journal (“The Politicization of Motherhood,” by James Taranto, Oct. 27, 2017) suggests that how you answer my question about the biological necessity of motherhood will determine your position on one of our nation’s political divides. The article focuses on Erica Komisar, who has written a book in which she lays out evidence from the fields of neuroscience, psychology, and epigenetics supporting her view that a mother is biologically equipped to provide for the emotional development of her child (“Being There: Why Prioritizing Motherhood in the First Three Years Matters,” New York: TarcherPerigee, 2017).
I haven’t read Ms. Komisar’s book, nor am I aware of the studies she cites, but reading the article prompted me to think a bit more deeply regarding how I feel about motherhood. I guess I always have felt that there is something special that a mother can provide her children, particularly during the first 3 years of life. I don’t know whether there is a neurobiological basis for this special something, but if it is missing, the child’s emotional development can suffer. Are there situations where another person(s) can provide a substitute for this special maternal sauce? Of course, but it doesn’t always work as well as the real thing. And not every mother has an adequate amount of that certain maternal something.
As pediatricians, we are faced with two challenges. The first is to help families cope with situations in which that special maternal ingredient is absent or in short supply. Our second challenge is to help mothers who believe there is something special they can offer their children but feel guilty because, for whatever reason, they can’t be there to provide it.
I am interested to hear how you feel about motherhood ... and apple pie.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
Email him at [email protected].
How do you feel about apple pie? Is it a concept that evokes a positive feeling for you? Even if you prefer pumpkin or blueberry? Although your attitude toward apple pie may be relevant as we approach the holidays, is it a topic worthy of discussion in a publication devoted to pediatrics?
Certainly not, but what about motherhood? How do you feel about motherhood? As someone who is devoting his or her professional energies to the health of children, you must have formed some opinions about motherhood. Although your patients are children, it is their parents – and more often their mothers – with whom you communicate, particularly in the first several years of life.
You may never have been asked that question in exactly that way before, but I suspect you have thought about it both professionally and personally. You may have considered the answer as you were deciding if, when, and how you were going to return to work after maternity leave. Or you may have been forced to consider the question in formulating an opinion in a case of contested child custody.
An opinion piece in the Wall Street Journal (“The Politicization of Motherhood,” by James Taranto, Oct. 27, 2017) suggests that how you answer my question about the biological necessity of motherhood will determine your position on one of our nation’s political divides. The article focuses on Erica Komisar, who has written a book in which she lays out evidence from the fields of neuroscience, psychology, and epigenetics supporting her view that a mother is biologically equipped to provide for the emotional development of her child (“Being There: Why Prioritizing Motherhood in the First Three Years Matters,” New York: TarcherPerigee, 2017).
I haven’t read Ms. Komisar’s book, nor am I aware of the studies she cites, but reading the article prompted me to think a bit more deeply regarding how I feel about motherhood. I guess I always have felt that there is something special that a mother can provide her children, particularly during the first 3 years of life. I don’t know whether there is a neurobiological basis for this special something, but if it is missing, the child’s emotional development can suffer. Are there situations where another person(s) can provide a substitute for this special maternal sauce? Of course, but it doesn’t always work as well as the real thing. And not every mother has an adequate amount of that certain maternal something.
As pediatricians, we are faced with two challenges. The first is to help families cope with situations in which that special maternal ingredient is absent or in short supply. Our second challenge is to help mothers who believe there is something special they can offer their children but feel guilty because, for whatever reason, they can’t be there to provide it.
I am interested to hear how you feel about motherhood ... and apple pie.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
Email him at [email protected].
How do you feel about apple pie? Is it a concept that evokes a positive feeling for you? Even if you prefer pumpkin or blueberry? Although your attitude toward apple pie may be relevant as we approach the holidays, is it a topic worthy of discussion in a publication devoted to pediatrics?
Certainly not, but what about motherhood? How do you feel about motherhood? As someone who is devoting his or her professional energies to the health of children, you must have formed some opinions about motherhood. Although your patients are children, it is their parents – and more often their mothers – with whom you communicate, particularly in the first several years of life.
You may never have been asked that question in exactly that way before, but I suspect you have thought about it both professionally and personally. You may have considered the answer as you were deciding if, when, and how you were going to return to work after maternity leave. Or you may have been forced to consider the question in formulating an opinion in a case of contested child custody.
An opinion piece in the Wall Street Journal (“The Politicization of Motherhood,” by James Taranto, Oct. 27, 2017) suggests that how you answer my question about the biological necessity of motherhood will determine your position on one of our nation’s political divides. The article focuses on Erica Komisar, who has written a book in which she lays out evidence from the fields of neuroscience, psychology, and epigenetics supporting her view that a mother is biologically equipped to provide for the emotional development of her child (“Being There: Why Prioritizing Motherhood in the First Three Years Matters,” New York: TarcherPerigee, 2017).
I haven’t read Ms. Komisar’s book, nor am I aware of the studies she cites, but reading the article prompted me to think a bit more deeply regarding how I feel about motherhood. I guess I always have felt that there is something special that a mother can provide her children, particularly during the first 3 years of life. I don’t know whether there is a neurobiological basis for this special something, but if it is missing, the child’s emotional development can suffer. Are there situations where another person(s) can provide a substitute for this special maternal sauce? Of course, but it doesn’t always work as well as the real thing. And not every mother has an adequate amount of that certain maternal something.
As pediatricians, we are faced with two challenges. The first is to help families cope with situations in which that special maternal ingredient is absent or in short supply. Our second challenge is to help mothers who believe there is something special they can offer their children but feel guilty because, for whatever reason, they can’t be there to provide it.
I am interested to hear how you feel about motherhood ... and apple pie.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
Email him at [email protected].
Use of opioids, SSRIs linked to increased fracture risk in RA
SAN DIEGO – The use of selective serotonin reuptake inhibitors and opioids was associated with an increased osteoporotic fracture risk in patients with rheumatoid arthritis, results from an analysis of national data showed.
“Osteoporotic fractures are one of the important causes of disability, health-related costs, and mortality in RA, with substantially higher complication and mortality rates than the general population,” study author Gulsen Ozen, MD, said in an interview prior to the annual meeting of the American College of Rheumatology. “Given the burden of osteoporotic fractures and the suboptimal osteoporosis care, identifying the factors associated with fracture risk in RA patients is of paramount importance.”
During a median follow-up of nearly 6 years, 863 patients (7.8%) sustained osteoporotic fractures. Compared with patients who did not develop fractures, those who did were significantly older, had higher disease duration and activity, glucocorticoid use, comorbidity and FRAX, a fracture risk assessment tool, scores at baseline. After adjusting for sociodemographics, comorbidities, body mass index, fracture risk by FRAX, and RA severity measures, the researchers found a significant risk of osteoporotic fractures with use of opioids of any strength (weak agents, hazard ratio, 1.45; strong agents, HR, 1.79; P less than .001 for both), SSRI use (HR, 1.35; P = .003), and glucocorticoid use of 3 months or longer at a dose of at least 7.5 mg per day (HR, 1.74; P less than .05). Osteoporotic fracture risk increase started even after 1-30 days of opioid use (HR, 1.96; P less than .001), whereas SSRI-associated risk increase started after 3 months of use (HR, 1.42; P = .054). No significant association with fracture risk was observed with the use of other disease-modifying antirheumatic drugs, statins, antidepressants, proton pump inhibitors, NSAIDs, anticonvulsants, and antipsychotics.
“One of the first surprising findings was that almost 40% of the RA patients older than 40 years of age were at least once exposed to opioid analgesics,” said Dr. Ozen, who is a research fellow in the division of immunology and rheumatology at the medical center. “Another surprising finding was that even very short-term (1-30 days) use of opioids was associated with increased fracture risk.” She went on to note that careful and regular reviewing of patient medications “is an essential part of the RA patient care, as the use of medications not indicated anymore brings harm rather than a benefit. The most well-known example for this is glucocorticoid use. This is valid for all medications, too. Therefore, we hope that our findings provide more awareness about osteoporotic fractures and associated risk factors in RA patients.”
She acknowledged certain limitations of the study, including its observational design. “Additionally, fracture and the level of the trauma in our cohort were reported by patients,” she said. “Therefore, there might be some misclassification of fractures as osteoporotic fractures. Lastly, we did not have detailed data regarding fall risk, which might explain the associations we observed with opioids and potentially, SSRIs.”
Dr. Ozen reported having no disclosures.
SAN DIEGO – The use of selective serotonin reuptake inhibitors and opioids was associated with an increased osteoporotic fracture risk in patients with rheumatoid arthritis, results from an analysis of national data showed.
“Osteoporotic fractures are one of the important causes of disability, health-related costs, and mortality in RA, with substantially higher complication and mortality rates than the general population,” study author Gulsen Ozen, MD, said in an interview prior to the annual meeting of the American College of Rheumatology. “Given the burden of osteoporotic fractures and the suboptimal osteoporosis care, identifying the factors associated with fracture risk in RA patients is of paramount importance.”
During a median follow-up of nearly 6 years, 863 patients (7.8%) sustained osteoporotic fractures. Compared with patients who did not develop fractures, those who did were significantly older, had higher disease duration and activity, glucocorticoid use, comorbidity and FRAX, a fracture risk assessment tool, scores at baseline. After adjusting for sociodemographics, comorbidities, body mass index, fracture risk by FRAX, and RA severity measures, the researchers found a significant risk of osteoporotic fractures with use of opioids of any strength (weak agents, hazard ratio, 1.45; strong agents, HR, 1.79; P less than .001 for both), SSRI use (HR, 1.35; P = .003), and glucocorticoid use of 3 months or longer at a dose of at least 7.5 mg per day (HR, 1.74; P less than .05). Osteoporotic fracture risk increase started even after 1-30 days of opioid use (HR, 1.96; P less than .001), whereas SSRI-associated risk increase started after 3 months of use (HR, 1.42; P = .054). No significant association with fracture risk was observed with the use of other disease-modifying antirheumatic drugs, statins, antidepressants, proton pump inhibitors, NSAIDs, anticonvulsants, and antipsychotics.
“One of the first surprising findings was that almost 40% of the RA patients older than 40 years of age were at least once exposed to opioid analgesics,” said Dr. Ozen, who is a research fellow in the division of immunology and rheumatology at the medical center. “Another surprising finding was that even very short-term (1-30 days) use of opioids was associated with increased fracture risk.” She went on to note that careful and regular reviewing of patient medications “is an essential part of the RA patient care, as the use of medications not indicated anymore brings harm rather than a benefit. The most well-known example for this is glucocorticoid use. This is valid for all medications, too. Therefore, we hope that our findings provide more awareness about osteoporotic fractures and associated risk factors in RA patients.”
She acknowledged certain limitations of the study, including its observational design. “Additionally, fracture and the level of the trauma in our cohort were reported by patients,” she said. “Therefore, there might be some misclassification of fractures as osteoporotic fractures. Lastly, we did not have detailed data regarding fall risk, which might explain the associations we observed with opioids and potentially, SSRIs.”
Dr. Ozen reported having no disclosures.
SAN DIEGO – The use of selective serotonin reuptake inhibitors and opioids was associated with an increased osteoporotic fracture risk in patients with rheumatoid arthritis, results from an analysis of national data showed.
“Osteoporotic fractures are one of the important causes of disability, health-related costs, and mortality in RA, with substantially higher complication and mortality rates than the general population,” study author Gulsen Ozen, MD, said in an interview prior to the annual meeting of the American College of Rheumatology. “Given the burden of osteoporotic fractures and the suboptimal osteoporosis care, identifying the factors associated with fracture risk in RA patients is of paramount importance.”
During a median follow-up of nearly 6 years, 863 patients (7.8%) sustained osteoporotic fractures. Compared with patients who did not develop fractures, those who did were significantly older, had higher disease duration and activity, glucocorticoid use, comorbidity and FRAX, a fracture risk assessment tool, scores at baseline. After adjusting for sociodemographics, comorbidities, body mass index, fracture risk by FRAX, and RA severity measures, the researchers found a significant risk of osteoporotic fractures with use of opioids of any strength (weak agents, hazard ratio, 1.45; strong agents, HR, 1.79; P less than .001 for both), SSRI use (HR, 1.35; P = .003), and glucocorticoid use of 3 months or longer at a dose of at least 7.5 mg per day (HR, 1.74; P less than .05). Osteoporotic fracture risk increase started even after 1-30 days of opioid use (HR, 1.96; P less than .001), whereas SSRI-associated risk increase started after 3 months of use (HR, 1.42; P = .054). No significant association with fracture risk was observed with the use of other disease-modifying antirheumatic drugs, statins, antidepressants, proton pump inhibitors, NSAIDs, anticonvulsants, and antipsychotics.
“One of the first surprising findings was that almost 40% of the RA patients older than 40 years of age were at least once exposed to opioid analgesics,” said Dr. Ozen, who is a research fellow in the division of immunology and rheumatology at the medical center. “Another surprising finding was that even very short-term (1-30 days) use of opioids was associated with increased fracture risk.” She went on to note that careful and regular reviewing of patient medications “is an essential part of the RA patient care, as the use of medications not indicated anymore brings harm rather than a benefit. The most well-known example for this is glucocorticoid use. This is valid for all medications, too. Therefore, we hope that our findings provide more awareness about osteoporotic fractures and associated risk factors in RA patients.”
She acknowledged certain limitations of the study, including its observational design. “Additionally, fracture and the level of the trauma in our cohort were reported by patients,” she said. “Therefore, there might be some misclassification of fractures as osteoporotic fractures. Lastly, we did not have detailed data regarding fall risk, which might explain the associations we observed with opioids and potentially, SSRIs.”
Dr. Ozen reported having no disclosures.
AT ACR 2017
Key clinical point: When managing with opioids, even in the short-term, clinicians should be aware of the fracture risk.
Major finding: In patients with RA, concomitant use of selective serotonin reuptake inhibitors was associated with an increased risk of osteoporotic fracture (HR, 1.35; P = .003), as was opioid use (HR, 1.45 and HR, 1.79) for weak and strong agents, respectively; P less than .001 for both).
Study details: An observational study of 11,049 patients from the National Data Bank for Rheumatic Diseases.
Disclosures: Dr. Ozen reported having no disclosures.
Clinical and Radiographic Outcomes of Total Shoulder Arthroplasty With a Hybrid Dual-Radii Glenoid Component
Take-Home Points
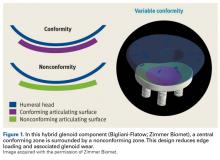
- The authors have developed a total shoulder glenoid prosthesis that conforms with the humeral head in its center and is nonconforming on its peripheral edge.
- All clinical survey and range of motion parameters demonstrated statistically significant improvements at final follow-up.
- Only 3 shoulders (1.7%) required revision surgery.
- Eighty-six (63%) of 136 shoulders demonstrated no radiographic evidence of glenoid loosening.
- This is the first and largest study that evaluates the clinical and radiographic outcomes of this hybrid shoulder prosthesis.
Fixation of the glenoid component is the limiting factor in modern total shoulder arthroplasty (TSA). Glenoid loosening, the most common long-term complication, necessitates revision in up to 12% of patients.1-4 By contrast, humeral component loosening is relatively uncommon, affecting as few as 0.34% of patients.5 Multiple long-term studies have found consistently high rates (45%-93%) of radiolucencies around the glenoid component.3,6,7 Although their clinical significance has been debated, radiolucencies around the glenoid component raise concern about progressive loss of fixation.
Since TSA was introduced in the 1970s, complications with the glenoid component have been addressed with 2 different designs: conforming (congruent) and nonconforming. In a congruent articulation, the radii of curvature of the glenoid and humeral head components are identical, whereas they differ in a nonconforming model. Joint conformity is inversely related to glenohumeral translation.8 Neer’s original TSA was made congruent in order to limit translation and maximize the contact area. However, this design results in edge loading and a so-called rocking-horse phenomenon, which may lead to glenoid loosening.9-13 Surgeons therefore have increasingly turned to nonconforming implants. In the nonconforming design, the radius of curvature of the humeral head is smaller than that of the glenoid. Although this design may reduce edge loading,14 it allows more translation and reduces the relative contact area of the glenohumeral joint. As a result, more contact stress is transmitted to the glenoid component, leading to polyethylene deformation and wear.15,16
Dual radii of curvature are designed to augment joint stability without increasing component wear. Biomechanical data have indicated that edge loading is not increased by having a central conforming region added to a nonconforming model.17 The clinical value of this prosthesis, however, has not been determined. Therefore, we conducted a study to describe the intermediate-term clinical and radiographic outcomes of TSAs that use a novel hybrid glenoid component.
Materials and Methods
This study was approved (protocol AAAD3473) by the Institutional Review Board of Columbia University and was conducted in compliance with Health Insurance Portability and Accountability Act (HIPAA) regulations.
Patient Selection
At Columbia University Medical Center, Dr. Bigliani performed 196 TSAs with a hybrid glenoid component (Bigliani-Flatow; Zimmer Biomet) in 169 patients between September 1998 and November 2007. All patients had received a diagnosis of primary glenohumeral arthritis as defined by Neer.18 Patients with previous surgery such as rotator cuff repair or subacromial decompression were included in our review, and patients with a nonprimary form of arthritis, such as rheumatoid, posttraumatic, or post-capsulorrhaphy arthritis, were excluded.
Operative Technique
For all surgeries, Dr. Bigliani performed a subscapularis tenotomy with regional anesthesia and a standard deltopectoral approach. A partial anterior capsulectomy was performed to increase the glenoid’s visibility. The inferior labrum was removed with a needle-tip bovie while the axillary nerve was being protected with a metal finger or narrow Darrach retractor. After reaming and trialing, the final glenoid component was cemented into place. Cement was placed only in the peg or keel holes and pressurized twice before final implantation. Of the 196 glenoid components, 168 (86%) were pegged and 28 (14%) keeled; in addition,190 of these components were all-polyethylene, whereas 6 had trabecular-metal backing. All glenoid components incorporated the hybrid design of dual radii of curvature. After the glenoid was cemented, the final humeral component was placed in 30° of retroversion. Whenever posterior wear was found, retroversion was reduced by 5° to 10°. The humeral prosthesis was cemented in cases (104/196, 53%) of poor bone quality or a large canal.
After surgery, the patient’s sling was fitted with an abduction pillow and a swathe, to be worn the first 24 hours, and the arm was passively ranged. Patients typically were discharged on postoperative day 2. Then, for 2 weeks, they followed an assisted passive range of motion (ROM) protocol, with limited external rotation, for promotion of subscapularis healing.
Clinical Outcomes
Dr. Bigliani assessed preoperative ROM in all planes. During initial evaluation, patients completed a questionnaire that consisted of the 36-Item Short Form Health Survey19,20 (SF-36) and the American Shoulder and Elbow Surgeons21 (ASES) and Simple Shoulder Test22 (SST) surveys. Postoperative clinical data were collected from office follow-up visits, survey questionnaires, or both. Postoperative office data included ROM, subscapularis integrity testing (belly-press or lift-off), and any complications. Patients with <1 year of office follow-up were excluded. In addition, the same survey questionnaire that was used before surgery was mailed to all patients after surgery; then, for anyone who did not respond by mail, we attempted contact by telephone. Neer criteria were based on patients’ subjective assessment of each arm on a 3-point Likert scale (1 = very satisfied, 2 = satisfied, 3 = dissatisfied). Patients were also asked about any specific complications or revision operations since their index procedure.
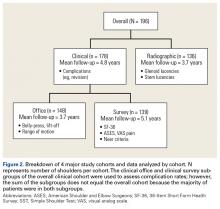
Physical examination and office follow-up data were obtained for 129 patients (148/196 shoulders, 76% follow-up) at a mean of 3.7 years (range 1.0-10.2 years) after surgery. Surveys were completed by 117 patients (139/196 shoulders, 71% follow-up) at a mean of 5.1 years (range, 1.6-11.2 years) after surgery. Only 15 patients had neither 1 year of office follow-up nor a completed questionnaire. The remaining 154 patients (178/196 shoulders, 91% follow-up) had clinical follow-up with office, mail, or telephone questionnaire at a mean of 4.8 years (range, 1.0-11.2 years) after surgery. This cohort of patients was used to determine rates of surgical revisions, subscapularis tears, dislocations, and other complications.
Radiographic Outcomes
Patients were included in the radiographic analysis if they had a shoulder radiograph at least 1 year after surgery. One hundred nineteen patients (136/196 shoulders, 69% follow-up) had radiographic follow-up at a mean of 3.7 years (range, 1.0-9.4 years) after surgery.
Statistical Analysis
Statistical analysis was performed with Stata Version 10.0. Paired t tests were used to compare preoperative and postoperative numerical data, including ROM and survey scores. We calculated 95% confidence intervals (CIs) and set statistical significance at P < .05. For qualitative measures, the Fisher exact test was used. Survivorship analysis was performed according to the Kaplan-Meier method, with right-censored data for no event or missing data.25
Results
Clinical Analysis of Demographics
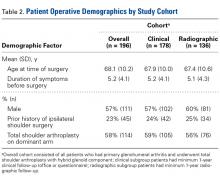
In demographics, the clinical and radiographic patient subgroups were similar to each other and to the overall study population (Table 2). Of 196 patients overall, 16 (8%) had a concomitant rotator cuff repair, and 27 (14%) underwent staged bilateral shoulder arthroplasties.
Clinical Analysis of ROM and Survey Scores
Operative shoulder ROM in forward elevation, external rotation at side, external rotation in abduction, and internal rotation all showed statistically significant (P < .001) improvement from before surgery to after surgery. Over 3.7 years, mean (SD) forward elevation improved from 107.3° (34.8°) to 159.0° (29.4°), external rotation at side improved from 20.4° (16.7°) to 49.4° (11.3°), and external rotation in abduction improved from 53.7° (24.3°) to 84.7° (9.1°). Internal rotation improved from a mean (SD) vertebral level of S1 (6.0 levels) to T9 (3.7 levels).
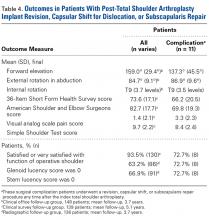
All validated survey scores also showed statistically significant (P < .001) improvement from before surgery to after surgery. Over 5.1 years, mean (SD) SF-36 scores improved from 64.9 (13.4) to 73.6 (17.1), ASES scores improved from 41.1 (22.5) to 82.7 (17.7), SST scores improved from 3.9 (2.8) to 9.7 (2.2), and visual analog scale pain scores improved from 5.6 (3.2) to 1.4 (2.1). Of 139 patients with follow-up, 130 (93.5%) were either satisfied or very satisfied with their TSA, and only 119 (86%) were either satisfied or very satisfied with the nonoperative shoulder.
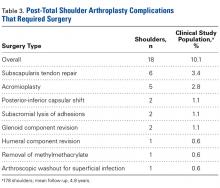
Clinical Analysis of Postoperative Complications
Of the 178 shoulders evaluated for complications, 3 (1.7%) underwent revision surgery. Mean time to revision was 2.3 years (range, 1.5-3.9 years). Two revisions involved the glenoid component, and the third involved the humerus. In one of the glenoid cases, a 77-year-old woman fell and sustained a fracture at the base of the trabecular metal glenoid pegs; her component was revised to an all-polyethylene component, and she had no further complications. In the other glenoid case, a 73-year-old man’s all-polyethylene component loosened after 2 years and was revised to a trabecular metal implant, which loosened as well and was later converted to a hemiarthroplasty. In the humeral case, a 33-year-old man had his 4-year-old index TSA revised to a cemented stem and had no further complications.
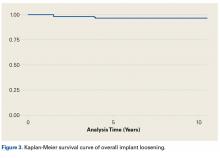
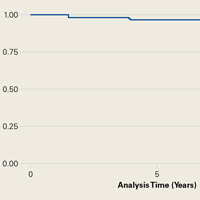
Table 4 compares the clinical and radiographic outcomes of patients who required subscapularis repair, capsular shift, or implant revision with the outcomes of all other study patients, and Figure 3 shows Kaplan-Meier survivorship.
Postoperative Radiographic Analysis
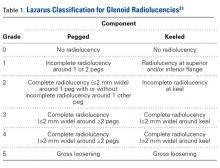
Glenoid Component. At a mean of 3.7 years (minimum, 1 year) after surgery, 86 (63%) of 136 radiographically evaluated shoulders showed no glenoid lucencies; the other 50 (37%) showed ≥1 lucency. Of the 136 shoulders, 33 (24%) had a Lazarus score of 1, 15 (11%) had a score of 2, and only 2 (2%) had a score of 3. None of the shoulders had a score of 4 or 5.
Humeral Component. Of the 136 shoulders, 91 (67%) showed no lucencies in any of the 8 humeral stem zones; the other 45 (33%) showed 1 to 3 lucencies. Thirty (22%) of the 136 shoulders had 1 stem lucency zone, 8 (6%) had 2, and 3 (2%) had 3. None of the shoulders had >3 periprosthetic zones with lucent lines.
Discussion
In this article, we describe a hybrid glenoid TSA component with dual radii of curvature. Its central portion is congruent with the humeral head, and its peripheral portion is noncongruent and larger. The most significant finding of our study is the low rate (1.1%) of glenoid component revision 4.8 years after surgery. This rate is the lowest that has been reported in a study of ≥100 patients. Overall implant survival appeared as an almost flat Kaplan-Meir curve. We attribute this low revision rate to improved biomechanics with the hybrid glenoid design.
Symptomatic glenoid component loosening is the most common TSA complication.1,26-28 In a review of 73 Neer TSAs, Cofield7 found glenoid radiolucencies in 71% of patients 3.8 years after surgery. Radiographic evidence of loosening, defined as component migration, or tilt, or a circumferential lucency 1.5 mm thick, was present in another 11% of patients, and 4.1% developed symptomatic loosening that required glenoid revision. In a study with 12.2-year follow-up, Torchia and colleagues3 found rates of 84% for glenoid radiolucencies, 44% for radiographic loosening, and 5.6% for symptomatic loosening that required revision. In a systematic review of studies with follow-up of ≥10 years, Bohsali and colleagues27 found similar lucency and radiographic loosening rates and a 7% glenoid revision rate. These data suggest glenoid radiolucencies may progress to component loosening.
Degree of joint congruence is a key factor in glenoid loosening. Neer’s congruent design increases the contact area with concentric loading and reduces glenohumeral translation, which leads to reduced polyethylene wear and improved joint stability. In extreme arm positions, however, humeral head subluxation results in edge loading and a glenoid rocking-horse effect.9-13,17,29-31 Conversely, nonconforming implants allow increased glenohumeral translation without edge loading,14 though they also reduce the relative glenohumeral contact area and thus transmit more contact stress to the glenoid.16,17 A hybrid glenoid component with central conforming and peripheral nonconforming zones may reduce the rocking-horse effect while maximizing ROM and joint stability. Wang and colleagues32 studied the biomechanical properties of this glenoid design and found that the addition of a central conforming region did not increase edge loading.
Additional results from our study support the efficacy of a hybrid glenoid component. Patients’ clinical outcomes improved significantly. At 5.1 years after surgery, 93.5% of patients were satisfied or very satisfied with their procedure and reported less satisfaction (86%) with the nonoperative shoulder. Also significant was the reduced number of radiolucencies. At 3.7 years after surgery, the overall percentage of shoulders with ≥1 glenoid radiolucency was 37%, considerably lower than the 82% reported by Cofield7 and the rates in more recent studies.3,16,33-36 Of the 178 shoulders in our study, 10 (5.6%) had subscapularis tears, and 6 (3.4%) of 178 had these tears surgically repaired. This 3.4% compares favorably with the 5.9% (of 119 patients) found by Miller and colleagues37 28 months after surgery. Of our 178 shoulders, 27 (15.2%) had clinically significant postoperative complications; 18 (10.1%) of the 178 had these complications surgically treated, and 9 (5.1%) had them managed nonoperatively. Bohsali and colleagues27 systematically reviewed 33 TSA studies and found a slightly higher complication rate (16.3%) 5.3 years after surgery. Furthermore, in our study, the 11 patients who underwent revision, capsular shift, or subscapularis repair had final outcomes comparable to those of the rest of our study population.
Our study had several potential weaknesses. First, its minimum clinical and radiographic follow-up was 1 year, whereas most long-term TSA series set a minimum of 2 years. We used 1 year because this was the first clinical study of the hybrid glenoid component design, and we wanted to maximize its sample size by reporting on intermediate-length outcomes. Even so, 93% (166/178) of our clinical patients and 83% (113/136) of our radiographic patients have had ≥2 years of follow-up, and we continue to follow all study patients for long-term outcomes. Another weakness of the study was its lack of a uniform group of patients with all the office, survey, complications, and radiographic data. Our retrospective study design made it difficult to obtain such a group without significantly reducing the sample size, so we divided patients into 4 data groups. A third potential weakness was the study’s variable method for collecting complications data. Rates of complications in the 178 shoulders were calculated from either office evaluation or patient self-report by mail or telephone. This data collection method is subject to recall bias, but mail and telephone contact was needed so the study would capture the large number of patients who had traveled to our institution for their surgery or had since moved away. Fourth, belly-press and lift-off tests were used in part to assess subscapularis function, but recent literature suggests post-TSA subscapularis assessment can be unreliable.38 These tests may be positive in up to two-thirds of patients after 2 years.39 Fifth, the generalizability of our findings to diagnoses such as rheumatoid and posttraumatic arthritis is limited. We had to restrict the study to patients with primary glenohumeral arthritis in order to minimize confounders.
This study’s main strength is its description of the clinical and radiographic outcomes of using a single prosthetic system in operations performed by a single surgeon in a large number of patients. This was the first and largest study evaluating the clinical and radiographic outcomes of this hybrid glenoid implant. Excluding patients with nonprimary arthritis allowed us to minimize potential confounding factors that affect patient outcomes. In conclusion, our study results showed the favorable clinical and radiographic outcomes of TSAs that have a hybrid glenoid component with dual radii of curvature. At a mean of 3.7 years after surgery, 63% of patients had no glenoid lucencies, and, at a mean of 4.8 years, only 1.7% of patients required revision. We continue to follow these patients to obtain long-term results of this innovative prosthesis.
1. Rodosky MW, Bigliani LU. Indications for glenoid resurfacing in shoulder arthroplasty. J Shoulder Elbow Surg. 1996;5(3):231-248.
2. Boyd AD Jr, Thomas WH, Scott RD, Sledge CB, Thornhill TS. Total shoulder arthroplasty versus hemiarthroplasty. Indications for glenoid resurfacing. J Arthroplasty. 1990;5(4):329-336.
3. Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Shoulder Elbow Surg. 1997;6(6):495-505.
4. Iannotti JP, Norris TR. Influence of preoperative factors on outcome of shoulder arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 2003;85(2):251-258.
5. Cofield RH. Degenerative and arthritic problems of the glenohumeral joint. In: Rockwood CA, Matsen FA, eds. The Shoulder. Philadelphia, PA: Saunders; 1990:740-745.
6. Neer CS 2nd, Watson KC, Stanton FJ. Recent experience in total shoulder replacement. J Bone Joint Surg Am. 1982;64(3):319-337.
7. Cofield RH. Total shoulder arthroplasty with the Neer prosthesis. J Bone Joint Surg Am. 1984;66(6):899-906.
8. Karduna AR, Williams GR, Williams JL, Iannotti JP. Kinematics of the glenohumeral joint: influences of muscle forces, ligamentous constraints, and articular geometry. J Orthop Res. 1996;14(6):986-993.
9. Karduna AR, Williams GR, Iannotti JP, Williams JL. Total shoulder arthroplasty biomechanics: a study of the forces and strains at the glenoid component. J Biomech Eng. 1998;120(1):92-99.
10. Karduna AR, Williams GR, Williams JL, Iannotti JP. Glenohumeral joint translations before and after total shoulder arthroplasty. A study in cadavera. J Bone Joint Surg Am. 1997;79(8):1166-1174.
11. Matsen FA 3rd, Clinton J, Lynch J, Bertelsen A, Richardson ML. Glenoid component failure in total shoulder arthroplasty. J Bone Joint Surg Am. 2008;90(4):885-896.
12. Franklin JL, Barrett WP, Jackins SE, Matsen FA 3rd. Glenoid loosening in total shoulder arthroplasty. Association with rotator cuff deficiency. J Arthroplasty. 1988;3(1):39-46.
13. Barrett WP, Franklin JL, Jackins SE, Wyss CR, Matsen FA 3rd. Total shoulder arthroplasty. J Bone Joint Surg Am. 1987;69(6):865-872.
14. Harryman DT, Sidles JA, Harris SL, Lippitt SB, Matsen FA 3rd. The effect of articular conformity and the size of the humeral head component on laxity and motion after glenohumeral arthroplasty. A study in cadavera. J Bone Joint Surg Am. 1995;77(4):555-563.
15. Flatow EL. Prosthetic design considerations in total shoulder arthroplasty. Semin Arthroplasty. 1995;6(4):233-244.
16. Klimkiewicz JJ, Iannotti JP, Rubash HE, Shanbhag AS. Aseptic loosening of the humeral component in total shoulder arthroplasty. J Shoulder Elbow Surg. 1998;7(4):422-426.
17. Wang VM, Krishnan R, Ugwonali OF, Flatow EL, Bigliani LU, Ateshian GA. Biomechanical evaluation of a novel glenoid design in total shoulder arthroplasty. J Shoulder Elbow Surg. 2005;14(1 suppl S):129S-140S.
18. Neer CS 2nd. Replacement arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 1974;56(1):1-13.
19. Boorman RS, Kopjar B, Fehringer E, Churchill RS, Smith K, Matsen FA 3rd. The effect of total shoulder arthroplasty on self-assessed health status is comparable to that of total hip arthroplasty and coronary artery bypass grafting. J Shoulder Elbow Surg. 2003;12(2):158-163.
20. Patel AA, Donegan D, Albert T. The 36-Item Short Form. J Am Acad Orthop Surg. 2007;15(2):126-134.
21. Richards RR, An KN, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3(6):347-352.
22. Wright RW, Baumgarten KM. Shoulder outcomes measures. J Am Acad Orthop Surg. 2010;18(7):436-444.
23. Lazarus MD, Jensen KL, Southworth C, Matsen FA 3rd. The radiographic evaluation of keeled and pegged glenoid component insertion. J Bone Joint Surg Am. 2002;84(7):1174-1182.
24. Sperling JW, Cofield RH, O’Driscoll SW, Torchia ME, Rowland CM. Radiographic assessment of ingrowth total shoulder arthroplasty. J Shoulder Elbow Surg. 2000;9(6):507-513.
25. Dinse GE, Lagakos SW. Nonparametric estimation of lifetime and disease onset distributions from incomplete observations. Biometrics. 1982;38(4):921-932.
26. Baumgarten KM, Lashgari CJ, Yamaguchi K. Glenoid resurfacing in shoulder arthroplasty: indications and contraindications. Instr Course Lect. 2004;53:3-11.
27. Bohsali KI, Wirth MA, Rockwood CA Jr. Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006;88(10):2279-2292.
28. Wirth MA, Rockwood CA Jr. Complications of total shoulder-replacement arthroplasty. J Bone Joint Surg Am. 1996;78(4):603-616.
29. Poppen NK, Walker PS. Normal and abnormal motion of the shoulder. J Bone Joint Surg Am. 1976;58(2):195-201.
30. Cotton RE, Rideout DF. Tears of the humeral rotator cuff; a radiological and pathological necropsy survey. J Bone Joint Surg Br. 1964;46:314-328.
31. Bigliani LU, Kelkar R, Flatow EL, Pollock RG, Mow VC. Glenohumeral stability. Biomechanical properties of passive and active stabilizers. Clin Orthop Relat Res. 1996;(330):13-30.
32. Wang VM, Sugalski MT, Levine WN, Pawluk RJ, Mow VC, Bigliani LU. Comparison of glenohumeral mechanics following a capsular shift and anterior tightening. J Bone Joint Surg Am. 2005;87(6):1312-1322.
33. Young A, Walch G, Boileau P, et al. A multicentre study of the long-term results of using a flat-back polyethylene glenoid component in shoulder replacement for primary osteoarthritis. J Bone Joint Surg Br. 2011;93(2):210-216.
34. Khan A, Bunker TD, Kitson JB. Clinical and radiological follow-up of the Aequalis third-generation cemented total shoulder replacement: a minimum ten-year study. J Bone Joint Surg Br. 2009;91(12):1594-1600.
35. Walch G, Edwards TB, Boulahia A, Boileau P, Mole D, Adeleine P. The influence of glenohumeral prosthetic mismatch on glenoid radiolucent lines: results of a multicenter study. J Bone Joint Surg Am. 2002;84(12):2186-2191.
36. Bartelt R, Sperling JW, Schleck CD, Cofield RH. Shoulder arthroplasty in patients aged fifty-five years or younger with osteoarthritis. J Shoulder Elbow Surg. 2011;20(1):123-130.
37. Miller BS, Joseph TA, Noonan TJ, Horan MP, Hawkins RJ. Rupture of the subscapularis tendon after shoulder arthroplasty: diagnosis, treatment, and outcome. J Shoulder Elbow Surg. 2005;14(5):492-496.
38. Armstrong A, Lashgari C, Teefey S, Menendez J, Yamaguchi K, Galatz LM. Ultrasound evaluation and clinical correlation of subscapularis repair after total shoulder arthroplasty. J Shoulder Elbow Surg. 2006;15(5):541-548.
39. Miller SL, Hazrati Y, Klepps S, Chiang A, Flatow EL. Loss of subscapularis function after total shoulder replacement: a seldom recognized problem. J Shoulder Elbow Surg. 2003;12(1):29-34.
Take-Home Points
- The authors have developed a total shoulder glenoid prosthesis that conforms with the humeral head in its center and is nonconforming on its peripheral edge.
- All clinical survey and range of motion parameters demonstrated statistically significant improvements at final follow-up.
- Only 3 shoulders (1.7%) required revision surgery.
- Eighty-six (63%) of 136 shoulders demonstrated no radiographic evidence of glenoid loosening.
- This is the first and largest study that evaluates the clinical and radiographic outcomes of this hybrid shoulder prosthesis.
Fixation of the glenoid component is the limiting factor in modern total shoulder arthroplasty (TSA). Glenoid loosening, the most common long-term complication, necessitates revision in up to 12% of patients.1-4 By contrast, humeral component loosening is relatively uncommon, affecting as few as 0.34% of patients.5 Multiple long-term studies have found consistently high rates (45%-93%) of radiolucencies around the glenoid component.3,6,7 Although their clinical significance has been debated, radiolucencies around the glenoid component raise concern about progressive loss of fixation.
Since TSA was introduced in the 1970s, complications with the glenoid component have been addressed with 2 different designs: conforming (congruent) and nonconforming. In a congruent articulation, the radii of curvature of the glenoid and humeral head components are identical, whereas they differ in a nonconforming model. Joint conformity is inversely related to glenohumeral translation.8 Neer’s original TSA was made congruent in order to limit translation and maximize the contact area. However, this design results in edge loading and a so-called rocking-horse phenomenon, which may lead to glenoid loosening.9-13 Surgeons therefore have increasingly turned to nonconforming implants. In the nonconforming design, the radius of curvature of the humeral head is smaller than that of the glenoid. Although this design may reduce edge loading,14 it allows more translation and reduces the relative contact area of the glenohumeral joint. As a result, more contact stress is transmitted to the glenoid component, leading to polyethylene deformation and wear.15,16
Dual radii of curvature are designed to augment joint stability without increasing component wear. Biomechanical data have indicated that edge loading is not increased by having a central conforming region added to a nonconforming model.17 The clinical value of this prosthesis, however, has not been determined. Therefore, we conducted a study to describe the intermediate-term clinical and radiographic outcomes of TSAs that use a novel hybrid glenoid component.
Materials and Methods
This study was approved (protocol AAAD3473) by the Institutional Review Board of Columbia University and was conducted in compliance with Health Insurance Portability and Accountability Act (HIPAA) regulations.
Patient Selection
At Columbia University Medical Center, Dr. Bigliani performed 196 TSAs with a hybrid glenoid component (Bigliani-Flatow; Zimmer Biomet) in 169 patients between September 1998 and November 2007. All patients had received a diagnosis of primary glenohumeral arthritis as defined by Neer.18 Patients with previous surgery such as rotator cuff repair or subacromial decompression were included in our review, and patients with a nonprimary form of arthritis, such as rheumatoid, posttraumatic, or post-capsulorrhaphy arthritis, were excluded.
Operative Technique
For all surgeries, Dr. Bigliani performed a subscapularis tenotomy with regional anesthesia and a standard deltopectoral approach. A partial anterior capsulectomy was performed to increase the glenoid’s visibility. The inferior labrum was removed with a needle-tip bovie while the axillary nerve was being protected with a metal finger or narrow Darrach retractor. After reaming and trialing, the final glenoid component was cemented into place. Cement was placed only in the peg or keel holes and pressurized twice before final implantation. Of the 196 glenoid components, 168 (86%) were pegged and 28 (14%) keeled; in addition,190 of these components were all-polyethylene, whereas 6 had trabecular-metal backing. All glenoid components incorporated the hybrid design of dual radii of curvature. After the glenoid was cemented, the final humeral component was placed in 30° of retroversion. Whenever posterior wear was found, retroversion was reduced by 5° to 10°. The humeral prosthesis was cemented in cases (104/196, 53%) of poor bone quality or a large canal.
After surgery, the patient’s sling was fitted with an abduction pillow and a swathe, to be worn the first 24 hours, and the arm was passively ranged. Patients typically were discharged on postoperative day 2. Then, for 2 weeks, they followed an assisted passive range of motion (ROM) protocol, with limited external rotation, for promotion of subscapularis healing.
Clinical Outcomes
Dr. Bigliani assessed preoperative ROM in all planes. During initial evaluation, patients completed a questionnaire that consisted of the 36-Item Short Form Health Survey19,20 (SF-36) and the American Shoulder and Elbow Surgeons21 (ASES) and Simple Shoulder Test22 (SST) surveys. Postoperative clinical data were collected from office follow-up visits, survey questionnaires, or both. Postoperative office data included ROM, subscapularis integrity testing (belly-press or lift-off), and any complications. Patients with <1 year of office follow-up were excluded. In addition, the same survey questionnaire that was used before surgery was mailed to all patients after surgery; then, for anyone who did not respond by mail, we attempted contact by telephone. Neer criteria were based on patients’ subjective assessment of each arm on a 3-point Likert scale (1 = very satisfied, 2 = satisfied, 3 = dissatisfied). Patients were also asked about any specific complications or revision operations since their index procedure.
Physical examination and office follow-up data were obtained for 129 patients (148/196 shoulders, 76% follow-up) at a mean of 3.7 years (range 1.0-10.2 years) after surgery. Surveys were completed by 117 patients (139/196 shoulders, 71% follow-up) at a mean of 5.1 years (range, 1.6-11.2 years) after surgery. Only 15 patients had neither 1 year of office follow-up nor a completed questionnaire. The remaining 154 patients (178/196 shoulders, 91% follow-up) had clinical follow-up with office, mail, or telephone questionnaire at a mean of 4.8 years (range, 1.0-11.2 years) after surgery. This cohort of patients was used to determine rates of surgical revisions, subscapularis tears, dislocations, and other complications.
Radiographic Outcomes
Patients were included in the radiographic analysis if they had a shoulder radiograph at least 1 year after surgery. One hundred nineteen patients (136/196 shoulders, 69% follow-up) had radiographic follow-up at a mean of 3.7 years (range, 1.0-9.4 years) after surgery.
Statistical Analysis
Statistical analysis was performed with Stata Version 10.0. Paired t tests were used to compare preoperative and postoperative numerical data, including ROM and survey scores. We calculated 95% confidence intervals (CIs) and set statistical significance at P < .05. For qualitative measures, the Fisher exact test was used. Survivorship analysis was performed according to the Kaplan-Meier method, with right-censored data for no event or missing data.25
Results
Clinical Analysis of Demographics
In demographics, the clinical and radiographic patient subgroups were similar to each other and to the overall study population (Table 2). Of 196 patients overall, 16 (8%) had a concomitant rotator cuff repair, and 27 (14%) underwent staged bilateral shoulder arthroplasties.
Clinical Analysis of ROM and Survey Scores
Operative shoulder ROM in forward elevation, external rotation at side, external rotation in abduction, and internal rotation all showed statistically significant (P < .001) improvement from before surgery to after surgery. Over 3.7 years, mean (SD) forward elevation improved from 107.3° (34.8°) to 159.0° (29.4°), external rotation at side improved from 20.4° (16.7°) to 49.4° (11.3°), and external rotation in abduction improved from 53.7° (24.3°) to 84.7° (9.1°). Internal rotation improved from a mean (SD) vertebral level of S1 (6.0 levels) to T9 (3.7 levels).
All validated survey scores also showed statistically significant (P < .001) improvement from before surgery to after surgery. Over 5.1 years, mean (SD) SF-36 scores improved from 64.9 (13.4) to 73.6 (17.1), ASES scores improved from 41.1 (22.5) to 82.7 (17.7), SST scores improved from 3.9 (2.8) to 9.7 (2.2), and visual analog scale pain scores improved from 5.6 (3.2) to 1.4 (2.1). Of 139 patients with follow-up, 130 (93.5%) were either satisfied or very satisfied with their TSA, and only 119 (86%) were either satisfied or very satisfied with the nonoperative shoulder.
Clinical Analysis of Postoperative Complications
Of the 178 shoulders evaluated for complications, 3 (1.7%) underwent revision surgery. Mean time to revision was 2.3 years (range, 1.5-3.9 years). Two revisions involved the glenoid component, and the third involved the humerus. In one of the glenoid cases, a 77-year-old woman fell and sustained a fracture at the base of the trabecular metal glenoid pegs; her component was revised to an all-polyethylene component, and she had no further complications. In the other glenoid case, a 73-year-old man’s all-polyethylene component loosened after 2 years and was revised to a trabecular metal implant, which loosened as well and was later converted to a hemiarthroplasty. In the humeral case, a 33-year-old man had his 4-year-old index TSA revised to a cemented stem and had no further complications.
Table 4 compares the clinical and radiographic outcomes of patients who required subscapularis repair, capsular shift, or implant revision with the outcomes of all other study patients, and Figure 3 shows Kaplan-Meier survivorship.
Postoperative Radiographic Analysis
Glenoid Component. At a mean of 3.7 years (minimum, 1 year) after surgery, 86 (63%) of 136 radiographically evaluated shoulders showed no glenoid lucencies; the other 50 (37%) showed ≥1 lucency. Of the 136 shoulders, 33 (24%) had a Lazarus score of 1, 15 (11%) had a score of 2, and only 2 (2%) had a score of 3. None of the shoulders had a score of 4 or 5.
Humeral Component. Of the 136 shoulders, 91 (67%) showed no lucencies in any of the 8 humeral stem zones; the other 45 (33%) showed 1 to 3 lucencies. Thirty (22%) of the 136 shoulders had 1 stem lucency zone, 8 (6%) had 2, and 3 (2%) had 3. None of the shoulders had >3 periprosthetic zones with lucent lines.
Discussion
In this article, we describe a hybrid glenoid TSA component with dual radii of curvature. Its central portion is congruent with the humeral head, and its peripheral portion is noncongruent and larger. The most significant finding of our study is the low rate (1.1%) of glenoid component revision 4.8 years after surgery. This rate is the lowest that has been reported in a study of ≥100 patients. Overall implant survival appeared as an almost flat Kaplan-Meir curve. We attribute this low revision rate to improved biomechanics with the hybrid glenoid design.
Symptomatic glenoid component loosening is the most common TSA complication.1,26-28 In a review of 73 Neer TSAs, Cofield7 found glenoid radiolucencies in 71% of patients 3.8 years after surgery. Radiographic evidence of loosening, defined as component migration, or tilt, or a circumferential lucency 1.5 mm thick, was present in another 11% of patients, and 4.1% developed symptomatic loosening that required glenoid revision. In a study with 12.2-year follow-up, Torchia and colleagues3 found rates of 84% for glenoid radiolucencies, 44% for radiographic loosening, and 5.6% for symptomatic loosening that required revision. In a systematic review of studies with follow-up of ≥10 years, Bohsali and colleagues27 found similar lucency and radiographic loosening rates and a 7% glenoid revision rate. These data suggest glenoid radiolucencies may progress to component loosening.
Degree of joint congruence is a key factor in glenoid loosening. Neer’s congruent design increases the contact area with concentric loading and reduces glenohumeral translation, which leads to reduced polyethylene wear and improved joint stability. In extreme arm positions, however, humeral head subluxation results in edge loading and a glenoid rocking-horse effect.9-13,17,29-31 Conversely, nonconforming implants allow increased glenohumeral translation without edge loading,14 though they also reduce the relative glenohumeral contact area and thus transmit more contact stress to the glenoid.16,17 A hybrid glenoid component with central conforming and peripheral nonconforming zones may reduce the rocking-horse effect while maximizing ROM and joint stability. Wang and colleagues32 studied the biomechanical properties of this glenoid design and found that the addition of a central conforming region did not increase edge loading.
Additional results from our study support the efficacy of a hybrid glenoid component. Patients’ clinical outcomes improved significantly. At 5.1 years after surgery, 93.5% of patients were satisfied or very satisfied with their procedure and reported less satisfaction (86%) with the nonoperative shoulder. Also significant was the reduced number of radiolucencies. At 3.7 years after surgery, the overall percentage of shoulders with ≥1 glenoid radiolucency was 37%, considerably lower than the 82% reported by Cofield7 and the rates in more recent studies.3,16,33-36 Of the 178 shoulders in our study, 10 (5.6%) had subscapularis tears, and 6 (3.4%) of 178 had these tears surgically repaired. This 3.4% compares favorably with the 5.9% (of 119 patients) found by Miller and colleagues37 28 months after surgery. Of our 178 shoulders, 27 (15.2%) had clinically significant postoperative complications; 18 (10.1%) of the 178 had these complications surgically treated, and 9 (5.1%) had them managed nonoperatively. Bohsali and colleagues27 systematically reviewed 33 TSA studies and found a slightly higher complication rate (16.3%) 5.3 years after surgery. Furthermore, in our study, the 11 patients who underwent revision, capsular shift, or subscapularis repair had final outcomes comparable to those of the rest of our study population.
Our study had several potential weaknesses. First, its minimum clinical and radiographic follow-up was 1 year, whereas most long-term TSA series set a minimum of 2 years. We used 1 year because this was the first clinical study of the hybrid glenoid component design, and we wanted to maximize its sample size by reporting on intermediate-length outcomes. Even so, 93% (166/178) of our clinical patients and 83% (113/136) of our radiographic patients have had ≥2 years of follow-up, and we continue to follow all study patients for long-term outcomes. Another weakness of the study was its lack of a uniform group of patients with all the office, survey, complications, and radiographic data. Our retrospective study design made it difficult to obtain such a group without significantly reducing the sample size, so we divided patients into 4 data groups. A third potential weakness was the study’s variable method for collecting complications data. Rates of complications in the 178 shoulders were calculated from either office evaluation or patient self-report by mail or telephone. This data collection method is subject to recall bias, but mail and telephone contact was needed so the study would capture the large number of patients who had traveled to our institution for their surgery or had since moved away. Fourth, belly-press and lift-off tests were used in part to assess subscapularis function, but recent literature suggests post-TSA subscapularis assessment can be unreliable.38 These tests may be positive in up to two-thirds of patients after 2 years.39 Fifth, the generalizability of our findings to diagnoses such as rheumatoid and posttraumatic arthritis is limited. We had to restrict the study to patients with primary glenohumeral arthritis in order to minimize confounders.
This study’s main strength is its description of the clinical and radiographic outcomes of using a single prosthetic system in operations performed by a single surgeon in a large number of patients. This was the first and largest study evaluating the clinical and radiographic outcomes of this hybrid glenoid implant. Excluding patients with nonprimary arthritis allowed us to minimize potential confounding factors that affect patient outcomes. In conclusion, our study results showed the favorable clinical and radiographic outcomes of TSAs that have a hybrid glenoid component with dual radii of curvature. At a mean of 3.7 years after surgery, 63% of patients had no glenoid lucencies, and, at a mean of 4.8 years, only 1.7% of patients required revision. We continue to follow these patients to obtain long-term results of this innovative prosthesis.
Take-Home Points
- The authors have developed a total shoulder glenoid prosthesis that conforms with the humeral head in its center and is nonconforming on its peripheral edge.
- All clinical survey and range of motion parameters demonstrated statistically significant improvements at final follow-up.
- Only 3 shoulders (1.7%) required revision surgery.
- Eighty-six (63%) of 136 shoulders demonstrated no radiographic evidence of glenoid loosening.
- This is the first and largest study that evaluates the clinical and radiographic outcomes of this hybrid shoulder prosthesis.
Fixation of the glenoid component is the limiting factor in modern total shoulder arthroplasty (TSA). Glenoid loosening, the most common long-term complication, necessitates revision in up to 12% of patients.1-4 By contrast, humeral component loosening is relatively uncommon, affecting as few as 0.34% of patients.5 Multiple long-term studies have found consistently high rates (45%-93%) of radiolucencies around the glenoid component.3,6,7 Although their clinical significance has been debated, radiolucencies around the glenoid component raise concern about progressive loss of fixation.
Since TSA was introduced in the 1970s, complications with the glenoid component have been addressed with 2 different designs: conforming (congruent) and nonconforming. In a congruent articulation, the radii of curvature of the glenoid and humeral head components are identical, whereas they differ in a nonconforming model. Joint conformity is inversely related to glenohumeral translation.8 Neer’s original TSA was made congruent in order to limit translation and maximize the contact area. However, this design results in edge loading and a so-called rocking-horse phenomenon, which may lead to glenoid loosening.9-13 Surgeons therefore have increasingly turned to nonconforming implants. In the nonconforming design, the radius of curvature of the humeral head is smaller than that of the glenoid. Although this design may reduce edge loading,14 it allows more translation and reduces the relative contact area of the glenohumeral joint. As a result, more contact stress is transmitted to the glenoid component, leading to polyethylene deformation and wear.15,16
Dual radii of curvature are designed to augment joint stability without increasing component wear. Biomechanical data have indicated that edge loading is not increased by having a central conforming region added to a nonconforming model.17 The clinical value of this prosthesis, however, has not been determined. Therefore, we conducted a study to describe the intermediate-term clinical and radiographic outcomes of TSAs that use a novel hybrid glenoid component.
Materials and Methods
This study was approved (protocol AAAD3473) by the Institutional Review Board of Columbia University and was conducted in compliance with Health Insurance Portability and Accountability Act (HIPAA) regulations.
Patient Selection
At Columbia University Medical Center, Dr. Bigliani performed 196 TSAs with a hybrid glenoid component (Bigliani-Flatow; Zimmer Biomet) in 169 patients between September 1998 and November 2007. All patients had received a diagnosis of primary glenohumeral arthritis as defined by Neer.18 Patients with previous surgery such as rotator cuff repair or subacromial decompression were included in our review, and patients with a nonprimary form of arthritis, such as rheumatoid, posttraumatic, or post-capsulorrhaphy arthritis, were excluded.
Operative Technique
For all surgeries, Dr. Bigliani performed a subscapularis tenotomy with regional anesthesia and a standard deltopectoral approach. A partial anterior capsulectomy was performed to increase the glenoid’s visibility. The inferior labrum was removed with a needle-tip bovie while the axillary nerve was being protected with a metal finger or narrow Darrach retractor. After reaming and trialing, the final glenoid component was cemented into place. Cement was placed only in the peg or keel holes and pressurized twice before final implantation. Of the 196 glenoid components, 168 (86%) were pegged and 28 (14%) keeled; in addition,190 of these components were all-polyethylene, whereas 6 had trabecular-metal backing. All glenoid components incorporated the hybrid design of dual radii of curvature. After the glenoid was cemented, the final humeral component was placed in 30° of retroversion. Whenever posterior wear was found, retroversion was reduced by 5° to 10°. The humeral prosthesis was cemented in cases (104/196, 53%) of poor bone quality or a large canal.
After surgery, the patient’s sling was fitted with an abduction pillow and a swathe, to be worn the first 24 hours, and the arm was passively ranged. Patients typically were discharged on postoperative day 2. Then, for 2 weeks, they followed an assisted passive range of motion (ROM) protocol, with limited external rotation, for promotion of subscapularis healing.
Clinical Outcomes
Dr. Bigliani assessed preoperative ROM in all planes. During initial evaluation, patients completed a questionnaire that consisted of the 36-Item Short Form Health Survey19,20 (SF-36) and the American Shoulder and Elbow Surgeons21 (ASES) and Simple Shoulder Test22 (SST) surveys. Postoperative clinical data were collected from office follow-up visits, survey questionnaires, or both. Postoperative office data included ROM, subscapularis integrity testing (belly-press or lift-off), and any complications. Patients with <1 year of office follow-up were excluded. In addition, the same survey questionnaire that was used before surgery was mailed to all patients after surgery; then, for anyone who did not respond by mail, we attempted contact by telephone. Neer criteria were based on patients’ subjective assessment of each arm on a 3-point Likert scale (1 = very satisfied, 2 = satisfied, 3 = dissatisfied). Patients were also asked about any specific complications or revision operations since their index procedure.
Physical examination and office follow-up data were obtained for 129 patients (148/196 shoulders, 76% follow-up) at a mean of 3.7 years (range 1.0-10.2 years) after surgery. Surveys were completed by 117 patients (139/196 shoulders, 71% follow-up) at a mean of 5.1 years (range, 1.6-11.2 years) after surgery. Only 15 patients had neither 1 year of office follow-up nor a completed questionnaire. The remaining 154 patients (178/196 shoulders, 91% follow-up) had clinical follow-up with office, mail, or telephone questionnaire at a mean of 4.8 years (range, 1.0-11.2 years) after surgery. This cohort of patients was used to determine rates of surgical revisions, subscapularis tears, dislocations, and other complications.
Radiographic Outcomes
Patients were included in the radiographic analysis if they had a shoulder radiograph at least 1 year after surgery. One hundred nineteen patients (136/196 shoulders, 69% follow-up) had radiographic follow-up at a mean of 3.7 years (range, 1.0-9.4 years) after surgery.
Statistical Analysis
Statistical analysis was performed with Stata Version 10.0. Paired t tests were used to compare preoperative and postoperative numerical data, including ROM and survey scores. We calculated 95% confidence intervals (CIs) and set statistical significance at P < .05. For qualitative measures, the Fisher exact test was used. Survivorship analysis was performed according to the Kaplan-Meier method, with right-censored data for no event or missing data.25
Results
Clinical Analysis of Demographics
In demographics, the clinical and radiographic patient subgroups were similar to each other and to the overall study population (Table 2). Of 196 patients overall, 16 (8%) had a concomitant rotator cuff repair, and 27 (14%) underwent staged bilateral shoulder arthroplasties.
Clinical Analysis of ROM and Survey Scores
Operative shoulder ROM in forward elevation, external rotation at side, external rotation in abduction, and internal rotation all showed statistically significant (P < .001) improvement from before surgery to after surgery. Over 3.7 years, mean (SD) forward elevation improved from 107.3° (34.8°) to 159.0° (29.4°), external rotation at side improved from 20.4° (16.7°) to 49.4° (11.3°), and external rotation in abduction improved from 53.7° (24.3°) to 84.7° (9.1°). Internal rotation improved from a mean (SD) vertebral level of S1 (6.0 levels) to T9 (3.7 levels).
All validated survey scores also showed statistically significant (P < .001) improvement from before surgery to after surgery. Over 5.1 years, mean (SD) SF-36 scores improved from 64.9 (13.4) to 73.6 (17.1), ASES scores improved from 41.1 (22.5) to 82.7 (17.7), SST scores improved from 3.9 (2.8) to 9.7 (2.2), and visual analog scale pain scores improved from 5.6 (3.2) to 1.4 (2.1). Of 139 patients with follow-up, 130 (93.5%) were either satisfied or very satisfied with their TSA, and only 119 (86%) were either satisfied or very satisfied with the nonoperative shoulder.
Clinical Analysis of Postoperative Complications
Of the 178 shoulders evaluated for complications, 3 (1.7%) underwent revision surgery. Mean time to revision was 2.3 years (range, 1.5-3.9 years). Two revisions involved the glenoid component, and the third involved the humerus. In one of the glenoid cases, a 77-year-old woman fell and sustained a fracture at the base of the trabecular metal glenoid pegs; her component was revised to an all-polyethylene component, and she had no further complications. In the other glenoid case, a 73-year-old man’s all-polyethylene component loosened after 2 years and was revised to a trabecular metal implant, which loosened as well and was later converted to a hemiarthroplasty. In the humeral case, a 33-year-old man had his 4-year-old index TSA revised to a cemented stem and had no further complications.
Table 4 compares the clinical and radiographic outcomes of patients who required subscapularis repair, capsular shift, or implant revision with the outcomes of all other study patients, and Figure 3 shows Kaplan-Meier survivorship.
Postoperative Radiographic Analysis
Glenoid Component. At a mean of 3.7 years (minimum, 1 year) after surgery, 86 (63%) of 136 radiographically evaluated shoulders showed no glenoid lucencies; the other 50 (37%) showed ≥1 lucency. Of the 136 shoulders, 33 (24%) had a Lazarus score of 1, 15 (11%) had a score of 2, and only 2 (2%) had a score of 3. None of the shoulders had a score of 4 or 5.
Humeral Component. Of the 136 shoulders, 91 (67%) showed no lucencies in any of the 8 humeral stem zones; the other 45 (33%) showed 1 to 3 lucencies. Thirty (22%) of the 136 shoulders had 1 stem lucency zone, 8 (6%) had 2, and 3 (2%) had 3. None of the shoulders had >3 periprosthetic zones with lucent lines.
Discussion
In this article, we describe a hybrid glenoid TSA component with dual radii of curvature. Its central portion is congruent with the humeral head, and its peripheral portion is noncongruent and larger. The most significant finding of our study is the low rate (1.1%) of glenoid component revision 4.8 years after surgery. This rate is the lowest that has been reported in a study of ≥100 patients. Overall implant survival appeared as an almost flat Kaplan-Meir curve. We attribute this low revision rate to improved biomechanics with the hybrid glenoid design.
Symptomatic glenoid component loosening is the most common TSA complication.1,26-28 In a review of 73 Neer TSAs, Cofield7 found glenoid radiolucencies in 71% of patients 3.8 years after surgery. Radiographic evidence of loosening, defined as component migration, or tilt, or a circumferential lucency 1.5 mm thick, was present in another 11% of patients, and 4.1% developed symptomatic loosening that required glenoid revision. In a study with 12.2-year follow-up, Torchia and colleagues3 found rates of 84% for glenoid radiolucencies, 44% for radiographic loosening, and 5.6% for symptomatic loosening that required revision. In a systematic review of studies with follow-up of ≥10 years, Bohsali and colleagues27 found similar lucency and radiographic loosening rates and a 7% glenoid revision rate. These data suggest glenoid radiolucencies may progress to component loosening.
Degree of joint congruence is a key factor in glenoid loosening. Neer’s congruent design increases the contact area with concentric loading and reduces glenohumeral translation, which leads to reduced polyethylene wear and improved joint stability. In extreme arm positions, however, humeral head subluxation results in edge loading and a glenoid rocking-horse effect.9-13,17,29-31 Conversely, nonconforming implants allow increased glenohumeral translation without edge loading,14 though they also reduce the relative glenohumeral contact area and thus transmit more contact stress to the glenoid.16,17 A hybrid glenoid component with central conforming and peripheral nonconforming zones may reduce the rocking-horse effect while maximizing ROM and joint stability. Wang and colleagues32 studied the biomechanical properties of this glenoid design and found that the addition of a central conforming region did not increase edge loading.
Additional results from our study support the efficacy of a hybrid glenoid component. Patients’ clinical outcomes improved significantly. At 5.1 years after surgery, 93.5% of patients were satisfied or very satisfied with their procedure and reported less satisfaction (86%) with the nonoperative shoulder. Also significant was the reduced number of radiolucencies. At 3.7 years after surgery, the overall percentage of shoulders with ≥1 glenoid radiolucency was 37%, considerably lower than the 82% reported by Cofield7 and the rates in more recent studies.3,16,33-36 Of the 178 shoulders in our study, 10 (5.6%) had subscapularis tears, and 6 (3.4%) of 178 had these tears surgically repaired. This 3.4% compares favorably with the 5.9% (of 119 patients) found by Miller and colleagues37 28 months after surgery. Of our 178 shoulders, 27 (15.2%) had clinically significant postoperative complications; 18 (10.1%) of the 178 had these complications surgically treated, and 9 (5.1%) had them managed nonoperatively. Bohsali and colleagues27 systematically reviewed 33 TSA studies and found a slightly higher complication rate (16.3%) 5.3 years after surgery. Furthermore, in our study, the 11 patients who underwent revision, capsular shift, or subscapularis repair had final outcomes comparable to those of the rest of our study population.
Our study had several potential weaknesses. First, its minimum clinical and radiographic follow-up was 1 year, whereas most long-term TSA series set a minimum of 2 years. We used 1 year because this was the first clinical study of the hybrid glenoid component design, and we wanted to maximize its sample size by reporting on intermediate-length outcomes. Even so, 93% (166/178) of our clinical patients and 83% (113/136) of our radiographic patients have had ≥2 years of follow-up, and we continue to follow all study patients for long-term outcomes. Another weakness of the study was its lack of a uniform group of patients with all the office, survey, complications, and radiographic data. Our retrospective study design made it difficult to obtain such a group without significantly reducing the sample size, so we divided patients into 4 data groups. A third potential weakness was the study’s variable method for collecting complications data. Rates of complications in the 178 shoulders were calculated from either office evaluation or patient self-report by mail or telephone. This data collection method is subject to recall bias, but mail and telephone contact was needed so the study would capture the large number of patients who had traveled to our institution for their surgery or had since moved away. Fourth, belly-press and lift-off tests were used in part to assess subscapularis function, but recent literature suggests post-TSA subscapularis assessment can be unreliable.38 These tests may be positive in up to two-thirds of patients after 2 years.39 Fifth, the generalizability of our findings to diagnoses such as rheumatoid and posttraumatic arthritis is limited. We had to restrict the study to patients with primary glenohumeral arthritis in order to minimize confounders.
This study’s main strength is its description of the clinical and radiographic outcomes of using a single prosthetic system in operations performed by a single surgeon in a large number of patients. This was the first and largest study evaluating the clinical and radiographic outcomes of this hybrid glenoid implant. Excluding patients with nonprimary arthritis allowed us to minimize potential confounding factors that affect patient outcomes. In conclusion, our study results showed the favorable clinical and radiographic outcomes of TSAs that have a hybrid glenoid component with dual radii of curvature. At a mean of 3.7 years after surgery, 63% of patients had no glenoid lucencies, and, at a mean of 4.8 years, only 1.7% of patients required revision. We continue to follow these patients to obtain long-term results of this innovative prosthesis.
1. Rodosky MW, Bigliani LU. Indications for glenoid resurfacing in shoulder arthroplasty. J Shoulder Elbow Surg. 1996;5(3):231-248.
2. Boyd AD Jr, Thomas WH, Scott RD, Sledge CB, Thornhill TS. Total shoulder arthroplasty versus hemiarthroplasty. Indications for glenoid resurfacing. J Arthroplasty. 1990;5(4):329-336.
3. Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Shoulder Elbow Surg. 1997;6(6):495-505.
4. Iannotti JP, Norris TR. Influence of preoperative factors on outcome of shoulder arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 2003;85(2):251-258.
5. Cofield RH. Degenerative and arthritic problems of the glenohumeral joint. In: Rockwood CA, Matsen FA, eds. The Shoulder. Philadelphia, PA: Saunders; 1990:740-745.
6. Neer CS 2nd, Watson KC, Stanton FJ. Recent experience in total shoulder replacement. J Bone Joint Surg Am. 1982;64(3):319-337.
7. Cofield RH. Total shoulder arthroplasty with the Neer prosthesis. J Bone Joint Surg Am. 1984;66(6):899-906.
8. Karduna AR, Williams GR, Williams JL, Iannotti JP. Kinematics of the glenohumeral joint: influences of muscle forces, ligamentous constraints, and articular geometry. J Orthop Res. 1996;14(6):986-993.
9. Karduna AR, Williams GR, Iannotti JP, Williams JL. Total shoulder arthroplasty biomechanics: a study of the forces and strains at the glenoid component. J Biomech Eng. 1998;120(1):92-99.
10. Karduna AR, Williams GR, Williams JL, Iannotti JP. Glenohumeral joint translations before and after total shoulder arthroplasty. A study in cadavera. J Bone Joint Surg Am. 1997;79(8):1166-1174.
11. Matsen FA 3rd, Clinton J, Lynch J, Bertelsen A, Richardson ML. Glenoid component failure in total shoulder arthroplasty. J Bone Joint Surg Am. 2008;90(4):885-896.
12. Franklin JL, Barrett WP, Jackins SE, Matsen FA 3rd. Glenoid loosening in total shoulder arthroplasty. Association with rotator cuff deficiency. J Arthroplasty. 1988;3(1):39-46.
13. Barrett WP, Franklin JL, Jackins SE, Wyss CR, Matsen FA 3rd. Total shoulder arthroplasty. J Bone Joint Surg Am. 1987;69(6):865-872.
14. Harryman DT, Sidles JA, Harris SL, Lippitt SB, Matsen FA 3rd. The effect of articular conformity and the size of the humeral head component on laxity and motion after glenohumeral arthroplasty. A study in cadavera. J Bone Joint Surg Am. 1995;77(4):555-563.
15. Flatow EL. Prosthetic design considerations in total shoulder arthroplasty. Semin Arthroplasty. 1995;6(4):233-244.
16. Klimkiewicz JJ, Iannotti JP, Rubash HE, Shanbhag AS. Aseptic loosening of the humeral component in total shoulder arthroplasty. J Shoulder Elbow Surg. 1998;7(4):422-426.
17. Wang VM, Krishnan R, Ugwonali OF, Flatow EL, Bigliani LU, Ateshian GA. Biomechanical evaluation of a novel glenoid design in total shoulder arthroplasty. J Shoulder Elbow Surg. 2005;14(1 suppl S):129S-140S.
18. Neer CS 2nd. Replacement arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 1974;56(1):1-13.
19. Boorman RS, Kopjar B, Fehringer E, Churchill RS, Smith K, Matsen FA 3rd. The effect of total shoulder arthroplasty on self-assessed health status is comparable to that of total hip arthroplasty and coronary artery bypass grafting. J Shoulder Elbow Surg. 2003;12(2):158-163.
20. Patel AA, Donegan D, Albert T. The 36-Item Short Form. J Am Acad Orthop Surg. 2007;15(2):126-134.
21. Richards RR, An KN, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3(6):347-352.
22. Wright RW, Baumgarten KM. Shoulder outcomes measures. J Am Acad Orthop Surg. 2010;18(7):436-444.
23. Lazarus MD, Jensen KL, Southworth C, Matsen FA 3rd. The radiographic evaluation of keeled and pegged glenoid component insertion. J Bone Joint Surg Am. 2002;84(7):1174-1182.
24. Sperling JW, Cofield RH, O’Driscoll SW, Torchia ME, Rowland CM. Radiographic assessment of ingrowth total shoulder arthroplasty. J Shoulder Elbow Surg. 2000;9(6):507-513.
25. Dinse GE, Lagakos SW. Nonparametric estimation of lifetime and disease onset distributions from incomplete observations. Biometrics. 1982;38(4):921-932.
26. Baumgarten KM, Lashgari CJ, Yamaguchi K. Glenoid resurfacing in shoulder arthroplasty: indications and contraindications. Instr Course Lect. 2004;53:3-11.
27. Bohsali KI, Wirth MA, Rockwood CA Jr. Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006;88(10):2279-2292.
28. Wirth MA, Rockwood CA Jr. Complications of total shoulder-replacement arthroplasty. J Bone Joint Surg Am. 1996;78(4):603-616.
29. Poppen NK, Walker PS. Normal and abnormal motion of the shoulder. J Bone Joint Surg Am. 1976;58(2):195-201.
30. Cotton RE, Rideout DF. Tears of the humeral rotator cuff; a radiological and pathological necropsy survey. J Bone Joint Surg Br. 1964;46:314-328.
31. Bigliani LU, Kelkar R, Flatow EL, Pollock RG, Mow VC. Glenohumeral stability. Biomechanical properties of passive and active stabilizers. Clin Orthop Relat Res. 1996;(330):13-30.
32. Wang VM, Sugalski MT, Levine WN, Pawluk RJ, Mow VC, Bigliani LU. Comparison of glenohumeral mechanics following a capsular shift and anterior tightening. J Bone Joint Surg Am. 2005;87(6):1312-1322.
33. Young A, Walch G, Boileau P, et al. A multicentre study of the long-term results of using a flat-back polyethylene glenoid component in shoulder replacement for primary osteoarthritis. J Bone Joint Surg Br. 2011;93(2):210-216.
34. Khan A, Bunker TD, Kitson JB. Clinical and radiological follow-up of the Aequalis third-generation cemented total shoulder replacement: a minimum ten-year study. J Bone Joint Surg Br. 2009;91(12):1594-1600.
35. Walch G, Edwards TB, Boulahia A, Boileau P, Mole D, Adeleine P. The influence of glenohumeral prosthetic mismatch on glenoid radiolucent lines: results of a multicenter study. J Bone Joint Surg Am. 2002;84(12):2186-2191.
36. Bartelt R, Sperling JW, Schleck CD, Cofield RH. Shoulder arthroplasty in patients aged fifty-five years or younger with osteoarthritis. J Shoulder Elbow Surg. 2011;20(1):123-130.
37. Miller BS, Joseph TA, Noonan TJ, Horan MP, Hawkins RJ. Rupture of the subscapularis tendon after shoulder arthroplasty: diagnosis, treatment, and outcome. J Shoulder Elbow Surg. 2005;14(5):492-496.
38. Armstrong A, Lashgari C, Teefey S, Menendez J, Yamaguchi K, Galatz LM. Ultrasound evaluation and clinical correlation of subscapularis repair after total shoulder arthroplasty. J Shoulder Elbow Surg. 2006;15(5):541-548.
39. Miller SL, Hazrati Y, Klepps S, Chiang A, Flatow EL. Loss of subscapularis function after total shoulder replacement: a seldom recognized problem. J Shoulder Elbow Surg. 2003;12(1):29-34.
1. Rodosky MW, Bigliani LU. Indications for glenoid resurfacing in shoulder arthroplasty. J Shoulder Elbow Surg. 1996;5(3):231-248.
2. Boyd AD Jr, Thomas WH, Scott RD, Sledge CB, Thornhill TS. Total shoulder arthroplasty versus hemiarthroplasty. Indications for glenoid resurfacing. J Arthroplasty. 1990;5(4):329-336.
3. Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Shoulder Elbow Surg. 1997;6(6):495-505.
4. Iannotti JP, Norris TR. Influence of preoperative factors on outcome of shoulder arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 2003;85(2):251-258.
5. Cofield RH. Degenerative and arthritic problems of the glenohumeral joint. In: Rockwood CA, Matsen FA, eds. The Shoulder. Philadelphia, PA: Saunders; 1990:740-745.
6. Neer CS 2nd, Watson KC, Stanton FJ. Recent experience in total shoulder replacement. J Bone Joint Surg Am. 1982;64(3):319-337.
7. Cofield RH. Total shoulder arthroplasty with the Neer prosthesis. J Bone Joint Surg Am. 1984;66(6):899-906.
8. Karduna AR, Williams GR, Williams JL, Iannotti JP. Kinematics of the glenohumeral joint: influences of muscle forces, ligamentous constraints, and articular geometry. J Orthop Res. 1996;14(6):986-993.
9. Karduna AR, Williams GR, Iannotti JP, Williams JL. Total shoulder arthroplasty biomechanics: a study of the forces and strains at the glenoid component. J Biomech Eng. 1998;120(1):92-99.
10. Karduna AR, Williams GR, Williams JL, Iannotti JP. Glenohumeral joint translations before and after total shoulder arthroplasty. A study in cadavera. J Bone Joint Surg Am. 1997;79(8):1166-1174.
11. Matsen FA 3rd, Clinton J, Lynch J, Bertelsen A, Richardson ML. Glenoid component failure in total shoulder arthroplasty. J Bone Joint Surg Am. 2008;90(4):885-896.
12. Franklin JL, Barrett WP, Jackins SE, Matsen FA 3rd. Glenoid loosening in total shoulder arthroplasty. Association with rotator cuff deficiency. J Arthroplasty. 1988;3(1):39-46.
13. Barrett WP, Franklin JL, Jackins SE, Wyss CR, Matsen FA 3rd. Total shoulder arthroplasty. J Bone Joint Surg Am. 1987;69(6):865-872.
14. Harryman DT, Sidles JA, Harris SL, Lippitt SB, Matsen FA 3rd. The effect of articular conformity and the size of the humeral head component on laxity and motion after glenohumeral arthroplasty. A study in cadavera. J Bone Joint Surg Am. 1995;77(4):555-563.
15. Flatow EL. Prosthetic design considerations in total shoulder arthroplasty. Semin Arthroplasty. 1995;6(4):233-244.
16. Klimkiewicz JJ, Iannotti JP, Rubash HE, Shanbhag AS. Aseptic loosening of the humeral component in total shoulder arthroplasty. J Shoulder Elbow Surg. 1998;7(4):422-426.
17. Wang VM, Krishnan R, Ugwonali OF, Flatow EL, Bigliani LU, Ateshian GA. Biomechanical evaluation of a novel glenoid design in total shoulder arthroplasty. J Shoulder Elbow Surg. 2005;14(1 suppl S):129S-140S.
18. Neer CS 2nd. Replacement arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 1974;56(1):1-13.
19. Boorman RS, Kopjar B, Fehringer E, Churchill RS, Smith K, Matsen FA 3rd. The effect of total shoulder arthroplasty on self-assessed health status is comparable to that of total hip arthroplasty and coronary artery bypass grafting. J Shoulder Elbow Surg. 2003;12(2):158-163.
20. Patel AA, Donegan D, Albert T. The 36-Item Short Form. J Am Acad Orthop Surg. 2007;15(2):126-134.
21. Richards RR, An KN, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3(6):347-352.
22. Wright RW, Baumgarten KM. Shoulder outcomes measures. J Am Acad Orthop Surg. 2010;18(7):436-444.
23. Lazarus MD, Jensen KL, Southworth C, Matsen FA 3rd. The radiographic evaluation of keeled and pegged glenoid component insertion. J Bone Joint Surg Am. 2002;84(7):1174-1182.
24. Sperling JW, Cofield RH, O’Driscoll SW, Torchia ME, Rowland CM. Radiographic assessment of ingrowth total shoulder arthroplasty. J Shoulder Elbow Surg. 2000;9(6):507-513.
25. Dinse GE, Lagakos SW. Nonparametric estimation of lifetime and disease onset distributions from incomplete observations. Biometrics. 1982;38(4):921-932.
26. Baumgarten KM, Lashgari CJ, Yamaguchi K. Glenoid resurfacing in shoulder arthroplasty: indications and contraindications. Instr Course Lect. 2004;53:3-11.
27. Bohsali KI, Wirth MA, Rockwood CA Jr. Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006;88(10):2279-2292.
28. Wirth MA, Rockwood CA Jr. Complications of total shoulder-replacement arthroplasty. J Bone Joint Surg Am. 1996;78(4):603-616.
29. Poppen NK, Walker PS. Normal and abnormal motion of the shoulder. J Bone Joint Surg Am. 1976;58(2):195-201.
30. Cotton RE, Rideout DF. Tears of the humeral rotator cuff; a radiological and pathological necropsy survey. J Bone Joint Surg Br. 1964;46:314-328.
31. Bigliani LU, Kelkar R, Flatow EL, Pollock RG, Mow VC. Glenohumeral stability. Biomechanical properties of passive and active stabilizers. Clin Orthop Relat Res. 1996;(330):13-30.
32. Wang VM, Sugalski MT, Levine WN, Pawluk RJ, Mow VC, Bigliani LU. Comparison of glenohumeral mechanics following a capsular shift and anterior tightening. J Bone Joint Surg Am. 2005;87(6):1312-1322.
33. Young A, Walch G, Boileau P, et al. A multicentre study of the long-term results of using a flat-back polyethylene glenoid component in shoulder replacement for primary osteoarthritis. J Bone Joint Surg Br. 2011;93(2):210-216.
34. Khan A, Bunker TD, Kitson JB. Clinical and radiological follow-up of the Aequalis third-generation cemented total shoulder replacement: a minimum ten-year study. J Bone Joint Surg Br. 2009;91(12):1594-1600.
35. Walch G, Edwards TB, Boulahia A, Boileau P, Mole D, Adeleine P. The influence of glenohumeral prosthetic mismatch on glenoid radiolucent lines: results of a multicenter study. J Bone Joint Surg Am. 2002;84(12):2186-2191.
36. Bartelt R, Sperling JW, Schleck CD, Cofield RH. Shoulder arthroplasty in patients aged fifty-five years or younger with osteoarthritis. J Shoulder Elbow Surg. 2011;20(1):123-130.
37. Miller BS, Joseph TA, Noonan TJ, Horan MP, Hawkins RJ. Rupture of the subscapularis tendon after shoulder arthroplasty: diagnosis, treatment, and outcome. J Shoulder Elbow Surg. 2005;14(5):492-496.
38. Armstrong A, Lashgari C, Teefey S, Menendez J, Yamaguchi K, Galatz LM. Ultrasound evaluation and clinical correlation of subscapularis repair after total shoulder arthroplasty. J Shoulder Elbow Surg. 2006;15(5):541-548.
39. Miller SL, Hazrati Y, Klepps S, Chiang A, Flatow EL. Loss of subscapularis function after total shoulder replacement: a seldom recognized problem. J Shoulder Elbow Surg. 2003;12(1):29-34.
Immunization information systems show progress over recent years
From 2013 to 2016, all U.S. immunization information systems showed progress in bidirectional information exchange with EHRs, said Neil Murthy, MD, and his associates at the National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta.
Across all 55 jurisdictions in 49 states and six cities in the United States using immunization information systems (IIS), 106% of U.S. births were registered in IIS in 2016, which is an increase from 102% in 2013; percentages may exceed 100%, because a child who is born in one state but who lives in a different state might be recorded in both IISs.
Bidirectional exchange of data with EHRs is an important part of an IIS. In 2016, 91% of jurisdictions had an IIS that used a platform-independent messaging system that received vaccination histories from providers and returned acknowledgment messages, compared with 87% in 2013, the investigators said.
“Clinical Decision Support (CDS) functionalities enable providers to evaluate the validity of vaccine doses administered to patients and forecast future vaccines that will be needed, based on recommendations developed by the Advisory Committee on Immunization Practices,” Dr. Murthy and his associates said. In 2016, 58% of the 55 jurisdictions sent a vaccine forecast to another system, compared with 31% in 2013.
In 2016, 95% of the 55 jurisdictions gave a “predefined, automatic report on immunization coverage by provider site,” compared with 89% of jurisdictions in 2013.
“IISs are integral components of routine clinical practice and public health surveillance for immunization,” Dr. Murthy and his associates said. “Availability of more complete IIS data also offers many benefits to health care providers and public health practitioners, including consolidating patients’ vaccination histories, identifying undervaccinated subgroups, and forecasting the needs of individual patients for recommended vaccines.”
Read more in Morbidity and Mortality Weekly Report (2017 Nov 3;66[43]:1178-81).
From 2013 to 2016, all U.S. immunization information systems showed progress in bidirectional information exchange with EHRs, said Neil Murthy, MD, and his associates at the National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta.
Across all 55 jurisdictions in 49 states and six cities in the United States using immunization information systems (IIS), 106% of U.S. births were registered in IIS in 2016, which is an increase from 102% in 2013; percentages may exceed 100%, because a child who is born in one state but who lives in a different state might be recorded in both IISs.
Bidirectional exchange of data with EHRs is an important part of an IIS. In 2016, 91% of jurisdictions had an IIS that used a platform-independent messaging system that received vaccination histories from providers and returned acknowledgment messages, compared with 87% in 2013, the investigators said.
“Clinical Decision Support (CDS) functionalities enable providers to evaluate the validity of vaccine doses administered to patients and forecast future vaccines that will be needed, based on recommendations developed by the Advisory Committee on Immunization Practices,” Dr. Murthy and his associates said. In 2016, 58% of the 55 jurisdictions sent a vaccine forecast to another system, compared with 31% in 2013.
In 2016, 95% of the 55 jurisdictions gave a “predefined, automatic report on immunization coverage by provider site,” compared with 89% of jurisdictions in 2013.
“IISs are integral components of routine clinical practice and public health surveillance for immunization,” Dr. Murthy and his associates said. “Availability of more complete IIS data also offers many benefits to health care providers and public health practitioners, including consolidating patients’ vaccination histories, identifying undervaccinated subgroups, and forecasting the needs of individual patients for recommended vaccines.”
Read more in Morbidity and Mortality Weekly Report (2017 Nov 3;66[43]:1178-81).
From 2013 to 2016, all U.S. immunization information systems showed progress in bidirectional information exchange with EHRs, said Neil Murthy, MD, and his associates at the National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta.
Across all 55 jurisdictions in 49 states and six cities in the United States using immunization information systems (IIS), 106% of U.S. births were registered in IIS in 2016, which is an increase from 102% in 2013; percentages may exceed 100%, because a child who is born in one state but who lives in a different state might be recorded in both IISs.
Bidirectional exchange of data with EHRs is an important part of an IIS. In 2016, 91% of jurisdictions had an IIS that used a platform-independent messaging system that received vaccination histories from providers and returned acknowledgment messages, compared with 87% in 2013, the investigators said.
“Clinical Decision Support (CDS) functionalities enable providers to evaluate the validity of vaccine doses administered to patients and forecast future vaccines that will be needed, based on recommendations developed by the Advisory Committee on Immunization Practices,” Dr. Murthy and his associates said. In 2016, 58% of the 55 jurisdictions sent a vaccine forecast to another system, compared with 31% in 2013.
In 2016, 95% of the 55 jurisdictions gave a “predefined, automatic report on immunization coverage by provider site,” compared with 89% of jurisdictions in 2013.
“IISs are integral components of routine clinical practice and public health surveillance for immunization,” Dr. Murthy and his associates said. “Availability of more complete IIS data also offers many benefits to health care providers and public health practitioners, including consolidating patients’ vaccination histories, identifying undervaccinated subgroups, and forecasting the needs of individual patients for recommended vaccines.”
Read more in Morbidity and Mortality Weekly Report (2017 Nov 3;66[43]:1178-81).
FROM MMWR
Seven days of opioids adequate for most hernia and other general surgery procedures
A 7-day limit on the initial opioid prescription may be sufficient for many common general surgery procedures, including hernia surgery and gynecologic procedures, findings of a large retrospective study suggest.
Rebecca E. Scully, MD, of the Center for Surgery and Public Health at Brigham and Women’s Hospital in Boston, and her associates examined opioid pain medication prescriptions and refills from records of the Military Health System Data Repository and the TRICARE insurance program of 215,140 opioid-naive patients. These patients were aged 18-64 years who underwent either cholecystectomy, appendectomy, inguinal hernia repair, anterior cruciate ligament reconstruction, rotator cuff tear repair, discectomy, mastectomy, or hysterectomy (JAMA Surg. 2017. doi: 10.1001/jamasurg.2017.3132). Only 20% of the covered individuals are active members of the U.S. military. The mean age was 40 years; 50% were male, and 60% were white.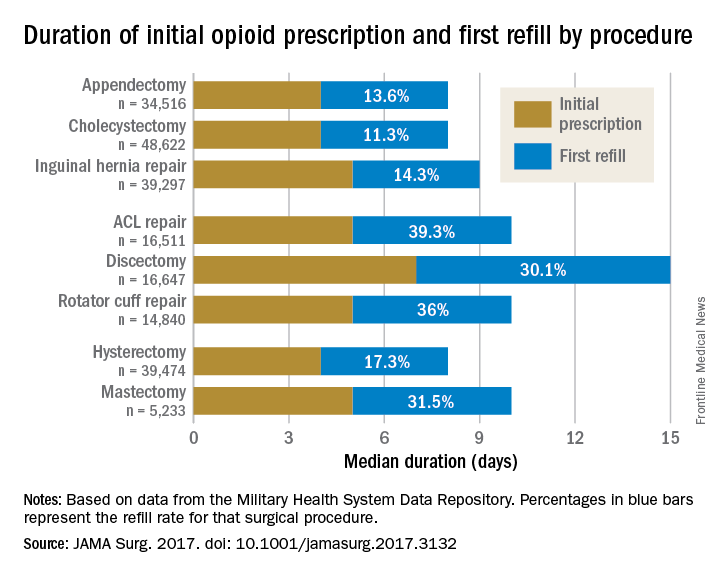
For appendectomy, cholecystectomy, and hysterectomy, the prescription was a median 4 days. For inguinal hernia repair, anterior cruciate ligament repair, rotator cuff repair, and mastectomy, the initial prescription was for 5 days. For discectomy, the median was 7 days.
Refill rates were the least at 11.3% for cholecystectomy and the most at 39.3% after anterior cruciate ligament repair. The time after the initial prescription until a refill was a median 6 days for appendectomy, cholecystectomy, and inguinal hernia repair, compared with a median 10 days for discectomy. The median duration of a refill prescription was 4 days for appendectomy, cholecystectomy, hernia repair, and hysterectomy versus 8 days for discectomy.
“Although 7 days appears to be more than adequate for many patients undergoing common general surgery and gynecologic procedures, prescription lengths likely should be extended to 10 days, particularly after common neurosurgical and musculoskeletal procedures, recognizing that as many as 40% of patients may still require one refill at a 7-day limit,” Dr. Scully and her associates said.
Although this study did not include rates of unused prescriptions or use of nonopioid pain relievers such as acetaminophen or NSAIDs, it did include a large population considered to be nationally representative “in many respects,” and it included a variety of procedures for which patients are commonly discharged to home, the researchers said.
The study was funded in part by the Department of Defense/Henry M. Jackson Foundation. The investigators had no conflict of interests. Adil H. Haider, MD, MPH, is deputy editor of JAMA Surgery, but he was not involved in any of the decisions regarding review of the manuscript or its acceptance.
A 7-day limit on the initial opioid prescription may be sufficient for many common general surgery procedures, including hernia surgery and gynecologic procedures, findings of a large retrospective study suggest.
Rebecca E. Scully, MD, of the Center for Surgery and Public Health at Brigham and Women’s Hospital in Boston, and her associates examined opioid pain medication prescriptions and refills from records of the Military Health System Data Repository and the TRICARE insurance program of 215,140 opioid-naive patients. These patients were aged 18-64 years who underwent either cholecystectomy, appendectomy, inguinal hernia repair, anterior cruciate ligament reconstruction, rotator cuff tear repair, discectomy, mastectomy, or hysterectomy (JAMA Surg. 2017. doi: 10.1001/jamasurg.2017.3132). Only 20% of the covered individuals are active members of the U.S. military. The mean age was 40 years; 50% were male, and 60% were white.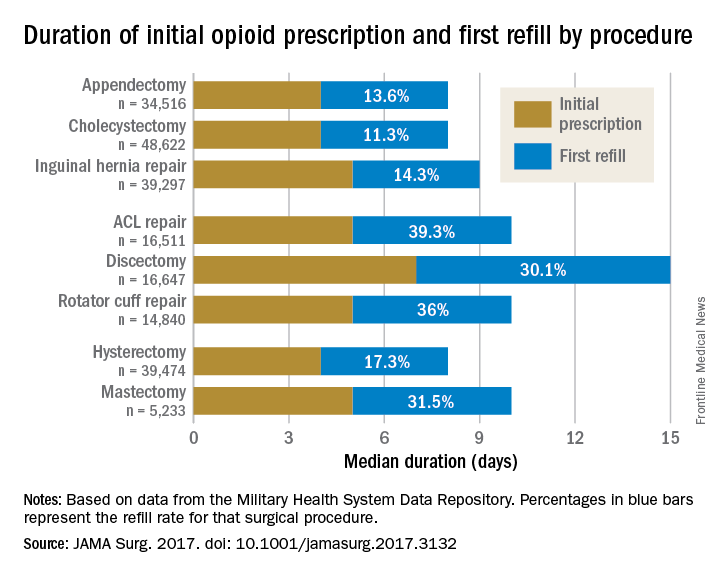
For appendectomy, cholecystectomy, and hysterectomy, the prescription was a median 4 days. For inguinal hernia repair, anterior cruciate ligament repair, rotator cuff repair, and mastectomy, the initial prescription was for 5 days. For discectomy, the median was 7 days.
Refill rates were the least at 11.3% for cholecystectomy and the most at 39.3% after anterior cruciate ligament repair. The time after the initial prescription until a refill was a median 6 days for appendectomy, cholecystectomy, and inguinal hernia repair, compared with a median 10 days for discectomy. The median duration of a refill prescription was 4 days for appendectomy, cholecystectomy, hernia repair, and hysterectomy versus 8 days for discectomy.
“Although 7 days appears to be more than adequate for many patients undergoing common general surgery and gynecologic procedures, prescription lengths likely should be extended to 10 days, particularly after common neurosurgical and musculoskeletal procedures, recognizing that as many as 40% of patients may still require one refill at a 7-day limit,” Dr. Scully and her associates said.
Although this study did not include rates of unused prescriptions or use of nonopioid pain relievers such as acetaminophen or NSAIDs, it did include a large population considered to be nationally representative “in many respects,” and it included a variety of procedures for which patients are commonly discharged to home, the researchers said.
The study was funded in part by the Department of Defense/Henry M. Jackson Foundation. The investigators had no conflict of interests. Adil H. Haider, MD, MPH, is deputy editor of JAMA Surgery, but he was not involved in any of the decisions regarding review of the manuscript or its acceptance.
A 7-day limit on the initial opioid prescription may be sufficient for many common general surgery procedures, including hernia surgery and gynecologic procedures, findings of a large retrospective study suggest.
Rebecca E. Scully, MD, of the Center for Surgery and Public Health at Brigham and Women’s Hospital in Boston, and her associates examined opioid pain medication prescriptions and refills from records of the Military Health System Data Repository and the TRICARE insurance program of 215,140 opioid-naive patients. These patients were aged 18-64 years who underwent either cholecystectomy, appendectomy, inguinal hernia repair, anterior cruciate ligament reconstruction, rotator cuff tear repair, discectomy, mastectomy, or hysterectomy (JAMA Surg. 2017. doi: 10.1001/jamasurg.2017.3132). Only 20% of the covered individuals are active members of the U.S. military. The mean age was 40 years; 50% were male, and 60% were white.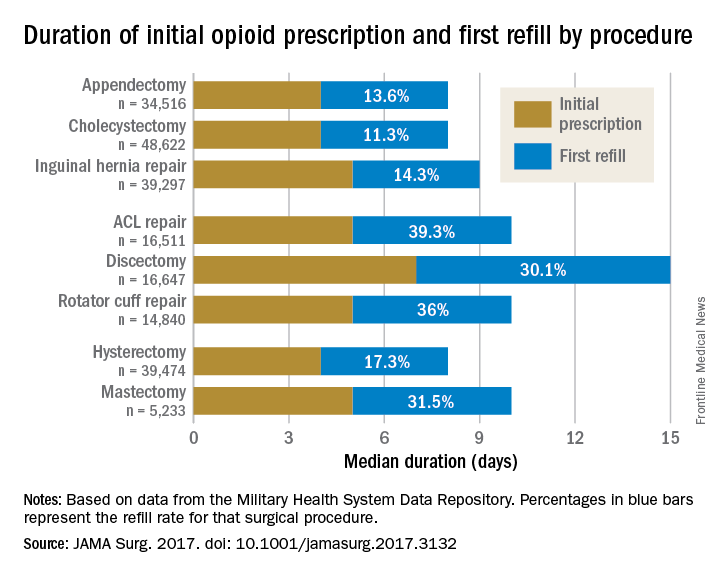
For appendectomy, cholecystectomy, and hysterectomy, the prescription was a median 4 days. For inguinal hernia repair, anterior cruciate ligament repair, rotator cuff repair, and mastectomy, the initial prescription was for 5 days. For discectomy, the median was 7 days.
Refill rates were the least at 11.3% for cholecystectomy and the most at 39.3% after anterior cruciate ligament repair. The time after the initial prescription until a refill was a median 6 days for appendectomy, cholecystectomy, and inguinal hernia repair, compared with a median 10 days for discectomy. The median duration of a refill prescription was 4 days for appendectomy, cholecystectomy, hernia repair, and hysterectomy versus 8 days for discectomy.
“Although 7 days appears to be more than adequate for many patients undergoing common general surgery and gynecologic procedures, prescription lengths likely should be extended to 10 days, particularly after common neurosurgical and musculoskeletal procedures, recognizing that as many as 40% of patients may still require one refill at a 7-day limit,” Dr. Scully and her associates said.
Although this study did not include rates of unused prescriptions or use of nonopioid pain relievers such as acetaminophen or NSAIDs, it did include a large population considered to be nationally representative “in many respects,” and it included a variety of procedures for which patients are commonly discharged to home, the researchers said.
The study was funded in part by the Department of Defense/Henry M. Jackson Foundation. The investigators had no conflict of interests. Adil H. Haider, MD, MPH, is deputy editor of JAMA Surgery, but he was not involved in any of the decisions regarding review of the manuscript or its acceptance.
FROM JAMA SURGERY
Key clinical point:
Major finding: The initial opioid prescription was a median 4 days for appendectomy and cholecystectomy, a median 5 days for inguinal hernia repair and anterior cruciate ligament and rotator cuff repair, and a median 7 days for discectomy.
Data source: A study of opioid prescriptions in 215,140 surgery patients aged 18-64 years.
Disclosures: The study was funded in part by the Department of Defense/Henry M. Jackson Foundation. The investigators had no conflict of interests. Adil H. Haider, MD, MPH, is deputy editor of JAMA Surgery, but he was not involved in any of the decisions regarding review of the manuscript or its acceptance.
Clinical hepatology debrief wraps up 2017 Liver Meeting
WASHINGTON – Research into alcoholic liver disease, drug-induced liver injury, the complications of chronic liver disease, and cholestatic liver diseases were among the clinical hepatology highlights presented at the annual meeting of the American Association for the Study of Liver Diseases.
This year’s debrief was given by Kris V. Kowdley, MD, of Swedish Medical Center in Seattle.
Over a median of 1.6 years of follow-up, 27% of patients resumed alcohol consumption post transplant with a median time to alcohol of 160 days, according to Brian Lee, MD, of the University of California, San Francisco. Younger age and lack of complete acceptance of their alcoholic hepatitis diagnosis were significant predictors of alcohol use post transplant while factors such as length of abstinence, race/ethnicity, insurance status, history of illicit drug use, and history of failed rehab attempts were not. Further, heavy drinking at presentation (more than 10 drinks per day), any alcohol use post transplant, and sustained alcohol use post transplant were significant predictors of posttransplant death.
Alcoholic hepatitis now “appears to be affecting more and more younger women, who present with a higher level of acuity,” Dr. Kowdley noted. He added that, while recent advances have decreased the absolute number of hepatitis C patients with decompensated liver disease who are listed for liver transplant, “the number is increasing rapidly in alcoholic liver disease, approaching the rate of patients being listed for hepatitis C.”
Unknown ingredients in herbal and dietary supplements continue to be of concern, Dr. Kowdley noted, as highlighted by Victor J. Navarro, MD, of Einstein Healthcare Network, Philadelphia, and his colleagues at the Drug-Induced Liver Injury Network (DILIN).
Investigators collected herbal and dietary supplements from patients enrolled in the DILIN prospective study and had chemical analysis performed by an outside laboratory. Labeled contents could not be verified in over half of the supplements collected and several unlabeled hepatotoxic ingredients were identified, Dr. Navarro and colleagues found (abstract 264).
“Even though we collect the supplements and review them with the patients, it’s not clear that we even know what it is that they are taking,” Dr. Kowdley commented.
Another DILIN study, this one presented by Jawad Ahmad, MD, of the Icahn School of Medicine at Mount Sinai, New York, “provided an opportunity for pause,” Dr. Kowdley said.
Dr. Ahmad and colleagues looked at hepatitis C virus (HCV) testing in DILIN patients and were able to correlate anti-HCV test results with HCV RNA tests results in more than 95% of 1,500 patients (abstract 16). About 7% of patients were HCV positive, and 23 cases of acute hepatitis were identified (16 with anti-HCV antibodies and HCV RNA, 7 with HCV RNA alone, and none with anti-HCV antibodies alone).
“So the take-home message here for me is, even if we think the patient has drug-induced liver injury, if they have not been tested for hepatitis C, especially if in the hospitalized setting … it is important to check not only the antibody test but also the RNA test,” Dr. Kowdley said.
Finally, in children, minocycline and valproate were the most commonly indicated agents in pediatric drug-induced liver injury, according to Frank DiPaola, MD, of the University of Michigan, and colleagues, on behalf of DILIN (abstract 13).
Dr. Kowdley also highlighted a couple of studies that addressed the complications of chronic liver disease.
The ADAPT-1 and ADAPT-2 trials (abstract 217) studied the use of avatrombopag, a thrombopoietin (TPO)–receptor agonist, to reduce severe thrombocytopenia in patients with chronic liver disease. Platelet transfusion is the current standard of care to reduce the risk of bleeding during invasive procedures in these patients; currently there are no drugs approved for this indication, Dr. Kowdley said.
Avatrombopag is an oral, small molecule TPO-receptor agonist, he said. “Because it binds to a different site on the TPO receptor than endogenous TPO, the effects are additive.”
In the phase 3 ADAPT-1 and ADAPT-2, the proportion of patients who did not require platelet transfusion or any rescue procedure for bleeding was significantly less in avatrombopag-treated patients than those receiving placebo. The effect was the same for patients with a low baseline platelet count (less than 40,000 platelets per mcL) as well as those with a high baseline platelet count (between 40,000/mcL and 50,000/mcL). Further, the proportion of patients who by procedure day achieved platelet count of at least 50,000/mcL was significantly higher in patients on the study drug.
Data on lusutrombopag, another TPO-receptor agonist, was presented as a late-breaker at the meeting, with very similar results in avoiding platelet transfusion, Dr. Kowdley noted.Two abstracts (502 and 219) focused on reducing ammonia levels in hospitalized cirrhosis patients with hepatic encephalitis.
Patients in the STOP-HE trial were randomized to either physician’s choice for standard of care or standard of care plus continuous infusion of ornithine phenylacetate for up to 5 days. Patients were assigned to one of three dosing groups (20 g, 15 g, or 10 g), based on severity of underlying liver disease; those with the most severe disease received the lowest dose.
Reduction in plasma ammonia levels correlated significantly with clinical improvement. At 48 hours, meaningful clinical improvement occurred in 84% of patients on ornithine phenylacetate, compared with 58% of placebo patients, according to Robert S. Rahimi, MD, of Baylor University, Dallas, and his colleagues.
“So, this may be an option for our hepatic encephalopathy patients who are admitted to the hospital and need acute treatment,” Dr. Kowdley said.
Dr. Kowdley finished up with two studies on primary biliary cholangitis (PBC).
Carla Murillo Perez, MD, of Toronto General Hospital and her colleagues in the Global PBC Study Group investigated the role of serum bilirubin in predicting transplant-free survival in patients with PBC (abstract 70).
When serum bilirubin levels from a previous study were input into a Cox regression analysis as a cubic spline function, then adjusted for factors such as age, sex, treatment with ursodeoxycholic acid, and year of diagnosis, the investigators found that patients with serum bilirubin levels of 0.7 times the upper limit of normal had a significantly increased risk of liver transplantation or death.
“We may want to be more sensitive in looking at bilirubin levels,” Dr. Kowdley said.
Another small but notable study presented by Gideon M. Hirschfield, MD, of the University of Birmingham (England), looked into whether a lower dose of seladelpar would safely and effectively lower alkaline phosphatase (AP) levels in PBC patients. A previous study of seladelpar at 50 mg and 200 mg doses indicated the drug’s effectiveness; however, the study was stopped because of the development of grade 3 alanine aminotransferase increases in a number of patients (Lancet Gastroenterol Hepatol. 2017;2;716-26).
Dr. Hirschfield and colleagues enrolled 24 patients and randomized 12 to seladelpar 5 mg and another 12 to 10 mg. The study cohort was mostly female, with an average age of 58 years. Most were either intolerant of or inadequately treated by ursodeoxycholic acid. AP levels were reduced significantly over time in both groups; however, differences between the groups were not significant, the investigators noted.
The Liver Meeting will be held in San Francisco in 2018, taking place Nov. 9-13. Many investigators in these trials reported relevant conflicts of interest; information is available (open access) in a supplement to Hepatology.
[email protected]
On Twitter @denisefulton
WASHINGTON – Research into alcoholic liver disease, drug-induced liver injury, the complications of chronic liver disease, and cholestatic liver diseases were among the clinical hepatology highlights presented at the annual meeting of the American Association for the Study of Liver Diseases.
This year’s debrief was given by Kris V. Kowdley, MD, of Swedish Medical Center in Seattle.
Over a median of 1.6 years of follow-up, 27% of patients resumed alcohol consumption post transplant with a median time to alcohol of 160 days, according to Brian Lee, MD, of the University of California, San Francisco. Younger age and lack of complete acceptance of their alcoholic hepatitis diagnosis were significant predictors of alcohol use post transplant while factors such as length of abstinence, race/ethnicity, insurance status, history of illicit drug use, and history of failed rehab attempts were not. Further, heavy drinking at presentation (more than 10 drinks per day), any alcohol use post transplant, and sustained alcohol use post transplant were significant predictors of posttransplant death.
Alcoholic hepatitis now “appears to be affecting more and more younger women, who present with a higher level of acuity,” Dr. Kowdley noted. He added that, while recent advances have decreased the absolute number of hepatitis C patients with decompensated liver disease who are listed for liver transplant, “the number is increasing rapidly in alcoholic liver disease, approaching the rate of patients being listed for hepatitis C.”
Unknown ingredients in herbal and dietary supplements continue to be of concern, Dr. Kowdley noted, as highlighted by Victor J. Navarro, MD, of Einstein Healthcare Network, Philadelphia, and his colleagues at the Drug-Induced Liver Injury Network (DILIN).
Investigators collected herbal and dietary supplements from patients enrolled in the DILIN prospective study and had chemical analysis performed by an outside laboratory. Labeled contents could not be verified in over half of the supplements collected and several unlabeled hepatotoxic ingredients were identified, Dr. Navarro and colleagues found (abstract 264).
“Even though we collect the supplements and review them with the patients, it’s not clear that we even know what it is that they are taking,” Dr. Kowdley commented.
Another DILIN study, this one presented by Jawad Ahmad, MD, of the Icahn School of Medicine at Mount Sinai, New York, “provided an opportunity for pause,” Dr. Kowdley said.
Dr. Ahmad and colleagues looked at hepatitis C virus (HCV) testing in DILIN patients and were able to correlate anti-HCV test results with HCV RNA tests results in more than 95% of 1,500 patients (abstract 16). About 7% of patients were HCV positive, and 23 cases of acute hepatitis were identified (16 with anti-HCV antibodies and HCV RNA, 7 with HCV RNA alone, and none with anti-HCV antibodies alone).
“So the take-home message here for me is, even if we think the patient has drug-induced liver injury, if they have not been tested for hepatitis C, especially if in the hospitalized setting … it is important to check not only the antibody test but also the RNA test,” Dr. Kowdley said.
Finally, in children, minocycline and valproate were the most commonly indicated agents in pediatric drug-induced liver injury, according to Frank DiPaola, MD, of the University of Michigan, and colleagues, on behalf of DILIN (abstract 13).
Dr. Kowdley also highlighted a couple of studies that addressed the complications of chronic liver disease.
The ADAPT-1 and ADAPT-2 trials (abstract 217) studied the use of avatrombopag, a thrombopoietin (TPO)–receptor agonist, to reduce severe thrombocytopenia in patients with chronic liver disease. Platelet transfusion is the current standard of care to reduce the risk of bleeding during invasive procedures in these patients; currently there are no drugs approved for this indication, Dr. Kowdley said.
Avatrombopag is an oral, small molecule TPO-receptor agonist, he said. “Because it binds to a different site on the TPO receptor than endogenous TPO, the effects are additive.”
In the phase 3 ADAPT-1 and ADAPT-2, the proportion of patients who did not require platelet transfusion or any rescue procedure for bleeding was significantly less in avatrombopag-treated patients than those receiving placebo. The effect was the same for patients with a low baseline platelet count (less than 40,000 platelets per mcL) as well as those with a high baseline platelet count (between 40,000/mcL and 50,000/mcL). Further, the proportion of patients who by procedure day achieved platelet count of at least 50,000/mcL was significantly higher in patients on the study drug.
Data on lusutrombopag, another TPO-receptor agonist, was presented as a late-breaker at the meeting, with very similar results in avoiding platelet transfusion, Dr. Kowdley noted.Two abstracts (502 and 219) focused on reducing ammonia levels in hospitalized cirrhosis patients with hepatic encephalitis.
Patients in the STOP-HE trial were randomized to either physician’s choice for standard of care or standard of care plus continuous infusion of ornithine phenylacetate for up to 5 days. Patients were assigned to one of three dosing groups (20 g, 15 g, or 10 g), based on severity of underlying liver disease; those with the most severe disease received the lowest dose.
Reduction in plasma ammonia levels correlated significantly with clinical improvement. At 48 hours, meaningful clinical improvement occurred in 84% of patients on ornithine phenylacetate, compared with 58% of placebo patients, according to Robert S. Rahimi, MD, of Baylor University, Dallas, and his colleagues.
“So, this may be an option for our hepatic encephalopathy patients who are admitted to the hospital and need acute treatment,” Dr. Kowdley said.
Dr. Kowdley finished up with two studies on primary biliary cholangitis (PBC).
Carla Murillo Perez, MD, of Toronto General Hospital and her colleagues in the Global PBC Study Group investigated the role of serum bilirubin in predicting transplant-free survival in patients with PBC (abstract 70).
When serum bilirubin levels from a previous study were input into a Cox regression analysis as a cubic spline function, then adjusted for factors such as age, sex, treatment with ursodeoxycholic acid, and year of diagnosis, the investigators found that patients with serum bilirubin levels of 0.7 times the upper limit of normal had a significantly increased risk of liver transplantation or death.
“We may want to be more sensitive in looking at bilirubin levels,” Dr. Kowdley said.
Another small but notable study presented by Gideon M. Hirschfield, MD, of the University of Birmingham (England), looked into whether a lower dose of seladelpar would safely and effectively lower alkaline phosphatase (AP) levels in PBC patients. A previous study of seladelpar at 50 mg and 200 mg doses indicated the drug’s effectiveness; however, the study was stopped because of the development of grade 3 alanine aminotransferase increases in a number of patients (Lancet Gastroenterol Hepatol. 2017;2;716-26).
Dr. Hirschfield and colleagues enrolled 24 patients and randomized 12 to seladelpar 5 mg and another 12 to 10 mg. The study cohort was mostly female, with an average age of 58 years. Most were either intolerant of or inadequately treated by ursodeoxycholic acid. AP levels were reduced significantly over time in both groups; however, differences between the groups were not significant, the investigators noted.
The Liver Meeting will be held in San Francisco in 2018, taking place Nov. 9-13. Many investigators in these trials reported relevant conflicts of interest; information is available (open access) in a supplement to Hepatology.
[email protected]
On Twitter @denisefulton
WASHINGTON – Research into alcoholic liver disease, drug-induced liver injury, the complications of chronic liver disease, and cholestatic liver diseases were among the clinical hepatology highlights presented at the annual meeting of the American Association for the Study of Liver Diseases.
This year’s debrief was given by Kris V. Kowdley, MD, of Swedish Medical Center in Seattle.
Over a median of 1.6 years of follow-up, 27% of patients resumed alcohol consumption post transplant with a median time to alcohol of 160 days, according to Brian Lee, MD, of the University of California, San Francisco. Younger age and lack of complete acceptance of their alcoholic hepatitis diagnosis were significant predictors of alcohol use post transplant while factors such as length of abstinence, race/ethnicity, insurance status, history of illicit drug use, and history of failed rehab attempts were not. Further, heavy drinking at presentation (more than 10 drinks per day), any alcohol use post transplant, and sustained alcohol use post transplant were significant predictors of posttransplant death.
Alcoholic hepatitis now “appears to be affecting more and more younger women, who present with a higher level of acuity,” Dr. Kowdley noted. He added that, while recent advances have decreased the absolute number of hepatitis C patients with decompensated liver disease who are listed for liver transplant, “the number is increasing rapidly in alcoholic liver disease, approaching the rate of patients being listed for hepatitis C.”
Unknown ingredients in herbal and dietary supplements continue to be of concern, Dr. Kowdley noted, as highlighted by Victor J. Navarro, MD, of Einstein Healthcare Network, Philadelphia, and his colleagues at the Drug-Induced Liver Injury Network (DILIN).
Investigators collected herbal and dietary supplements from patients enrolled in the DILIN prospective study and had chemical analysis performed by an outside laboratory. Labeled contents could not be verified in over half of the supplements collected and several unlabeled hepatotoxic ingredients were identified, Dr. Navarro and colleagues found (abstract 264).
“Even though we collect the supplements and review them with the patients, it’s not clear that we even know what it is that they are taking,” Dr. Kowdley commented.
Another DILIN study, this one presented by Jawad Ahmad, MD, of the Icahn School of Medicine at Mount Sinai, New York, “provided an opportunity for pause,” Dr. Kowdley said.
Dr. Ahmad and colleagues looked at hepatitis C virus (HCV) testing in DILIN patients and were able to correlate anti-HCV test results with HCV RNA tests results in more than 95% of 1,500 patients (abstract 16). About 7% of patients were HCV positive, and 23 cases of acute hepatitis were identified (16 with anti-HCV antibodies and HCV RNA, 7 with HCV RNA alone, and none with anti-HCV antibodies alone).
“So the take-home message here for me is, even if we think the patient has drug-induced liver injury, if they have not been tested for hepatitis C, especially if in the hospitalized setting … it is important to check not only the antibody test but also the RNA test,” Dr. Kowdley said.
Finally, in children, minocycline and valproate were the most commonly indicated agents in pediatric drug-induced liver injury, according to Frank DiPaola, MD, of the University of Michigan, and colleagues, on behalf of DILIN (abstract 13).
Dr. Kowdley also highlighted a couple of studies that addressed the complications of chronic liver disease.
The ADAPT-1 and ADAPT-2 trials (abstract 217) studied the use of avatrombopag, a thrombopoietin (TPO)–receptor agonist, to reduce severe thrombocytopenia in patients with chronic liver disease. Platelet transfusion is the current standard of care to reduce the risk of bleeding during invasive procedures in these patients; currently there are no drugs approved for this indication, Dr. Kowdley said.
Avatrombopag is an oral, small molecule TPO-receptor agonist, he said. “Because it binds to a different site on the TPO receptor than endogenous TPO, the effects are additive.”
In the phase 3 ADAPT-1 and ADAPT-2, the proportion of patients who did not require platelet transfusion or any rescue procedure for bleeding was significantly less in avatrombopag-treated patients than those receiving placebo. The effect was the same for patients with a low baseline platelet count (less than 40,000 platelets per mcL) as well as those with a high baseline platelet count (between 40,000/mcL and 50,000/mcL). Further, the proportion of patients who by procedure day achieved platelet count of at least 50,000/mcL was significantly higher in patients on the study drug.
Data on lusutrombopag, another TPO-receptor agonist, was presented as a late-breaker at the meeting, with very similar results in avoiding platelet transfusion, Dr. Kowdley noted.Two abstracts (502 and 219) focused on reducing ammonia levels in hospitalized cirrhosis patients with hepatic encephalitis.
Patients in the STOP-HE trial were randomized to either physician’s choice for standard of care or standard of care plus continuous infusion of ornithine phenylacetate for up to 5 days. Patients were assigned to one of three dosing groups (20 g, 15 g, or 10 g), based on severity of underlying liver disease; those with the most severe disease received the lowest dose.
Reduction in plasma ammonia levels correlated significantly with clinical improvement. At 48 hours, meaningful clinical improvement occurred in 84% of patients on ornithine phenylacetate, compared with 58% of placebo patients, according to Robert S. Rahimi, MD, of Baylor University, Dallas, and his colleagues.
“So, this may be an option for our hepatic encephalopathy patients who are admitted to the hospital and need acute treatment,” Dr. Kowdley said.
Dr. Kowdley finished up with two studies on primary biliary cholangitis (PBC).
Carla Murillo Perez, MD, of Toronto General Hospital and her colleagues in the Global PBC Study Group investigated the role of serum bilirubin in predicting transplant-free survival in patients with PBC (abstract 70).
When serum bilirubin levels from a previous study were input into a Cox regression analysis as a cubic spline function, then adjusted for factors such as age, sex, treatment with ursodeoxycholic acid, and year of diagnosis, the investigators found that patients with serum bilirubin levels of 0.7 times the upper limit of normal had a significantly increased risk of liver transplantation or death.
“We may want to be more sensitive in looking at bilirubin levels,” Dr. Kowdley said.
Another small but notable study presented by Gideon M. Hirschfield, MD, of the University of Birmingham (England), looked into whether a lower dose of seladelpar would safely and effectively lower alkaline phosphatase (AP) levels in PBC patients. A previous study of seladelpar at 50 mg and 200 mg doses indicated the drug’s effectiveness; however, the study was stopped because of the development of grade 3 alanine aminotransferase increases in a number of patients (Lancet Gastroenterol Hepatol. 2017;2;716-26).
Dr. Hirschfield and colleagues enrolled 24 patients and randomized 12 to seladelpar 5 mg and another 12 to 10 mg. The study cohort was mostly female, with an average age of 58 years. Most were either intolerant of or inadequately treated by ursodeoxycholic acid. AP levels were reduced significantly over time in both groups; however, differences between the groups were not significant, the investigators noted.
The Liver Meeting will be held in San Francisco in 2018, taking place Nov. 9-13. Many investigators in these trials reported relevant conflicts of interest; information is available (open access) in a supplement to Hepatology.
[email protected]
On Twitter @denisefulton
AT THE LIVER MEETING 2017
Legislative landscape affecting rheumatology has potential wins but many challenges
SAN DIEGO – , but ongoing efforts to advocate for the specialty and patients are showing signs of paying off in some areas, Angus Worthing, MD, said at the annual meeting of the American College of Rheumatology.
Dr. Worthing, who is chair of the ACR’s Government Affairs Committee and a practicing rheumatologist in the Washington area, encouraged rheumatologists to become involved in advocacy efforts and asked members of the audience at the meeting to visit the ACR’s advocacy website to learn how to help.
The ACR supports a group of bills that have been introduced in either the House or Senate that should have an effect on alleviating the projected shortage of rheumatologists across the United States through 2030. These bills will help, although much of the effort to address the shortage and maldistribution of rheumatologists across the United States will “probably be solved at the local level. It’s not going to be a federal solution. It will be relationships and treatment programs between primary care and rheumatology care that are very local,” Dr. Worthing said.
The Conrad State 30 and Physician Access Reauthorization Act (H.R. 2141, S. 898) aims to streamline visas for foreign physicians to practice in underserved areas.
The Resident Physician Shortage Reduction Act of 2017 (H.R. 2267) would increase for the first time since 1997 the number of graduate medical education residency slots in the United States.
The Ensuring Children’s Access to Specialty Care Act of 2017 (S. 989) allows pediatric subspecialists, including pediatric rheumatologists, to get access to the National Health Service Corps loan repayment program when they work in underserved areas.
More recently, in spring 2017 the American Medical Association played a big role in getting the Trump administration to reverse its stance on not allowing premium processing of H1-B visas for professionals such as physicians. If this had gone into effect, all the rheumatology fellows in training who were going to be practicing – some in underserved areas – might have been forced to return to their home country because of a lack of time to get their H1-B visa processed before finishing their fellowship, Dr. Worthing said.
Affordable Care Act (ACA)
- Provide sufficient, affordable, continuous coverage that encourages access to high-quality care for all.
- Prohibit exclusions based on preexisting conditions.
- Allow children to remain on parent’s insurance until age 26 years.
- Remove excessive administrative burdens that take focus away from patient care.
- Cap annual out-of-pocket costs and ban lifetime limits.
- Have affordable premiums, deductibles, and cost sharing.
- Continue the 10 essential health benefits that are required for ACA marketplace plans.
Alliance for Transparent & Affordable Prescriptions (ATAP)
The ACR convened this alliance along with the Coalition of State Rheumatology Organizations, the Global Healthy Living Foundation, the Association of Women in Rheumatology, the Rheumatology Nurses Society, and others to try to bring transparency to how pharmacy benefit managers (PBMs) operate in getting certain drugs on the formularies of payers. The ATAP recently had some success in making lawmakers aware of the PBM’s role in influencing drug prices via rebates to drug manufacturers. At a Congressional hearing in Oct. 2017, after many visits from rheumatologists and members of ATAP, the members of the Senate Committee on Health, Education, Labor, and Pensions “held the feet of these PBMs to the fire a little bit asking them about these rebates,” Dr. Worthing said, where at one point committee chair Sen. Lamar Alexander (R-Tenn.) asked, “ ‘Do we really need these rebates?’ ”
National Institutes of Health budget
After the National Institutes of Health received a $2 billion increase in funding for fiscal year 2017, the Trump administration proposed last summer to cut the NIH budget by 22%. Since then, however, bills to increase the NIH budget by $1.1 billion from the House and by $2 billion from the Senate have made their way through committees. But a budget must be passed by Congress and then signed by the president to make a potential budget increase a reality. Otherwise, a continuing resolution would leave the current level of funding in place through fiscal year 2018, Dr. Worthing noted.
Patients’ Access to Treatments Act of 2017 (H.R. 2999)
This bill has been raised for a fourth time after not making it past committees in previous Congresses, but the prospects for it passing appear somewhat better this time around, Dr. Worthing said. It would prevent insurance companies from putting drugs in specialty tiers that require patients to pay increasingly higher rates of coinsurance for the drugs on different tiers.
“It has been gathering momentum. We hope to get it across the finish line. And if we don’t get this across, then we’ll join with the coalition that rheumatology has formed around this issue of access to specialty treatments some other way, because this is a burning issue for us and our patients,” he said.
Medicare Access to Rehabilitation Services Act of 2017 (H.R. 807 and S. 253)
This bill would repeal the annual cap that was placed on rehabilitation services for patients covered by Medicare in 1997. The bill has bipartisan, majority support and has been gaining momentum for the past 4 years, Dr. Worthing said. It was advanced from both Senate and House committees in Oct. 2017.
SAN DIEGO – , but ongoing efforts to advocate for the specialty and patients are showing signs of paying off in some areas, Angus Worthing, MD, said at the annual meeting of the American College of Rheumatology.
Dr. Worthing, who is chair of the ACR’s Government Affairs Committee and a practicing rheumatologist in the Washington area, encouraged rheumatologists to become involved in advocacy efforts and asked members of the audience at the meeting to visit the ACR’s advocacy website to learn how to help.
The ACR supports a group of bills that have been introduced in either the House or Senate that should have an effect on alleviating the projected shortage of rheumatologists across the United States through 2030. These bills will help, although much of the effort to address the shortage and maldistribution of rheumatologists across the United States will “probably be solved at the local level. It’s not going to be a federal solution. It will be relationships and treatment programs between primary care and rheumatology care that are very local,” Dr. Worthing said.
The Conrad State 30 and Physician Access Reauthorization Act (H.R. 2141, S. 898) aims to streamline visas for foreign physicians to practice in underserved areas.
The Resident Physician Shortage Reduction Act of 2017 (H.R. 2267) would increase for the first time since 1997 the number of graduate medical education residency slots in the United States.
The Ensuring Children’s Access to Specialty Care Act of 2017 (S. 989) allows pediatric subspecialists, including pediatric rheumatologists, to get access to the National Health Service Corps loan repayment program when they work in underserved areas.
More recently, in spring 2017 the American Medical Association played a big role in getting the Trump administration to reverse its stance on not allowing premium processing of H1-B visas for professionals such as physicians. If this had gone into effect, all the rheumatology fellows in training who were going to be practicing – some in underserved areas – might have been forced to return to their home country because of a lack of time to get their H1-B visa processed before finishing their fellowship, Dr. Worthing said.
Affordable Care Act (ACA)
- Provide sufficient, affordable, continuous coverage that encourages access to high-quality care for all.
- Prohibit exclusions based on preexisting conditions.
- Allow children to remain on parent’s insurance until age 26 years.
- Remove excessive administrative burdens that take focus away from patient care.
- Cap annual out-of-pocket costs and ban lifetime limits.
- Have affordable premiums, deductibles, and cost sharing.
- Continue the 10 essential health benefits that are required for ACA marketplace plans.
Alliance for Transparent & Affordable Prescriptions (ATAP)
The ACR convened this alliance along with the Coalition of State Rheumatology Organizations, the Global Healthy Living Foundation, the Association of Women in Rheumatology, the Rheumatology Nurses Society, and others to try to bring transparency to how pharmacy benefit managers (PBMs) operate in getting certain drugs on the formularies of payers. The ATAP recently had some success in making lawmakers aware of the PBM’s role in influencing drug prices via rebates to drug manufacturers. At a Congressional hearing in Oct. 2017, after many visits from rheumatologists and members of ATAP, the members of the Senate Committee on Health, Education, Labor, and Pensions “held the feet of these PBMs to the fire a little bit asking them about these rebates,” Dr. Worthing said, where at one point committee chair Sen. Lamar Alexander (R-Tenn.) asked, “ ‘Do we really need these rebates?’ ”
National Institutes of Health budget
After the National Institutes of Health received a $2 billion increase in funding for fiscal year 2017, the Trump administration proposed last summer to cut the NIH budget by 22%. Since then, however, bills to increase the NIH budget by $1.1 billion from the House and by $2 billion from the Senate have made their way through committees. But a budget must be passed by Congress and then signed by the president to make a potential budget increase a reality. Otherwise, a continuing resolution would leave the current level of funding in place through fiscal year 2018, Dr. Worthing noted.
Patients’ Access to Treatments Act of 2017 (H.R. 2999)
This bill has been raised for a fourth time after not making it past committees in previous Congresses, but the prospects for it passing appear somewhat better this time around, Dr. Worthing said. It would prevent insurance companies from putting drugs in specialty tiers that require patients to pay increasingly higher rates of coinsurance for the drugs on different tiers.
“It has been gathering momentum. We hope to get it across the finish line. And if we don’t get this across, then we’ll join with the coalition that rheumatology has formed around this issue of access to specialty treatments some other way, because this is a burning issue for us and our patients,” he said.
Medicare Access to Rehabilitation Services Act of 2017 (H.R. 807 and S. 253)
This bill would repeal the annual cap that was placed on rehabilitation services for patients covered by Medicare in 1997. The bill has bipartisan, majority support and has been gaining momentum for the past 4 years, Dr. Worthing said. It was advanced from both Senate and House committees in Oct. 2017.
SAN DIEGO – , but ongoing efforts to advocate for the specialty and patients are showing signs of paying off in some areas, Angus Worthing, MD, said at the annual meeting of the American College of Rheumatology.
Dr. Worthing, who is chair of the ACR’s Government Affairs Committee and a practicing rheumatologist in the Washington area, encouraged rheumatologists to become involved in advocacy efforts and asked members of the audience at the meeting to visit the ACR’s advocacy website to learn how to help.
The ACR supports a group of bills that have been introduced in either the House or Senate that should have an effect on alleviating the projected shortage of rheumatologists across the United States through 2030. These bills will help, although much of the effort to address the shortage and maldistribution of rheumatologists across the United States will “probably be solved at the local level. It’s not going to be a federal solution. It will be relationships and treatment programs between primary care and rheumatology care that are very local,” Dr. Worthing said.
The Conrad State 30 and Physician Access Reauthorization Act (H.R. 2141, S. 898) aims to streamline visas for foreign physicians to practice in underserved areas.
The Resident Physician Shortage Reduction Act of 2017 (H.R. 2267) would increase for the first time since 1997 the number of graduate medical education residency slots in the United States.
The Ensuring Children’s Access to Specialty Care Act of 2017 (S. 989) allows pediatric subspecialists, including pediatric rheumatologists, to get access to the National Health Service Corps loan repayment program when they work in underserved areas.
More recently, in spring 2017 the American Medical Association played a big role in getting the Trump administration to reverse its stance on not allowing premium processing of H1-B visas for professionals such as physicians. If this had gone into effect, all the rheumatology fellows in training who were going to be practicing – some in underserved areas – might have been forced to return to their home country because of a lack of time to get their H1-B visa processed before finishing their fellowship, Dr. Worthing said.
Affordable Care Act (ACA)
- Provide sufficient, affordable, continuous coverage that encourages access to high-quality care for all.
- Prohibit exclusions based on preexisting conditions.
- Allow children to remain on parent’s insurance until age 26 years.
- Remove excessive administrative burdens that take focus away from patient care.
- Cap annual out-of-pocket costs and ban lifetime limits.
- Have affordable premiums, deductibles, and cost sharing.
- Continue the 10 essential health benefits that are required for ACA marketplace plans.
Alliance for Transparent & Affordable Prescriptions (ATAP)
The ACR convened this alliance along with the Coalition of State Rheumatology Organizations, the Global Healthy Living Foundation, the Association of Women in Rheumatology, the Rheumatology Nurses Society, and others to try to bring transparency to how pharmacy benefit managers (PBMs) operate in getting certain drugs on the formularies of payers. The ATAP recently had some success in making lawmakers aware of the PBM’s role in influencing drug prices via rebates to drug manufacturers. At a Congressional hearing in Oct. 2017, after many visits from rheumatologists and members of ATAP, the members of the Senate Committee on Health, Education, Labor, and Pensions “held the feet of these PBMs to the fire a little bit asking them about these rebates,” Dr. Worthing said, where at one point committee chair Sen. Lamar Alexander (R-Tenn.) asked, “ ‘Do we really need these rebates?’ ”
National Institutes of Health budget
After the National Institutes of Health received a $2 billion increase in funding for fiscal year 2017, the Trump administration proposed last summer to cut the NIH budget by 22%. Since then, however, bills to increase the NIH budget by $1.1 billion from the House and by $2 billion from the Senate have made their way through committees. But a budget must be passed by Congress and then signed by the president to make a potential budget increase a reality. Otherwise, a continuing resolution would leave the current level of funding in place through fiscal year 2018, Dr. Worthing noted.
Patients’ Access to Treatments Act of 2017 (H.R. 2999)
This bill has been raised for a fourth time after not making it past committees in previous Congresses, but the prospects for it passing appear somewhat better this time around, Dr. Worthing said. It would prevent insurance companies from putting drugs in specialty tiers that require patients to pay increasingly higher rates of coinsurance for the drugs on different tiers.
“It has been gathering momentum. We hope to get it across the finish line. And if we don’t get this across, then we’ll join with the coalition that rheumatology has formed around this issue of access to specialty treatments some other way, because this is a burning issue for us and our patients,” he said.
Medicare Access to Rehabilitation Services Act of 2017 (H.R. 807 and S. 253)
This bill would repeal the annual cap that was placed on rehabilitation services for patients covered by Medicare in 1997. The bill has bipartisan, majority support and has been gaining momentum for the past 4 years, Dr. Worthing said. It was advanced from both Senate and House committees in Oct. 2017.
AT ACR 2017
Obesity linked to RA disease activity, disability
SAN DIEGO – In what may be the largest study of its kind, British researchers have linked obesity to significantly higher odds of rheumatoid arthritis disease activity and disability.
“This study emphasizes that obesity can have a profound effect on treatment goals in rheumatoid arthritis,” says Elena Nikiphorou, MD, of King’s College London, who presented the study findings at the annual meeting of the American College of Rheumatology. “Obesity reduced the odds of achieving remission or low disease activity by around 30%. And the odds of having disability were increased by 63%. This confirms what’s been shown in other, smaller studies.”
Despite obesity having been tied to decreased joint damage in established RA, Eric L. Matteson, MD, noted in an interview, that“the biomechanical effect of [being] overweight, especially on the weight-bearing joints” is one of the two “especially important” mechanisms explaining the link between RA and obesity. “The other is that fat cells produce inflammatory proteins, which contribute to the disease process and make it more difficult to treat,” said Dr. Matteson, a rheumatologist at the Mayo Clinic, Rochester, Minn.
“In my view the mechanical risk to the joint outweighs any possible ‘protective’ effect of RA,” Dr. Matteson added in an interview.
For the new study, Dr. Nikiphorou and colleagues compiled statistics from two consecutive United Kingdom RA inception cohorts. One tracked 1,465 patients for up to 25 years (median follow-up, 10 years), and the other tracked 1,236 patients for as many as 10 years (median follow-up, 6 years).
At baseline, 37.2% of 2,420 patients (90% of total) were overweight, and 21.3% were obese. Average body mass index (BMI) rose between the two consecutive studies from 25.5 to 27.6.
The researchers found that obesity was linked to lower likelihoods of remission and low disease activity status (odds ratio, 0.71; 95% confidence interval, 0.55-0.93 and OR, 0.69; 95% CI, 0.55-0.87, respectively.) After controlling for factors such as age and gender, they also saw slightly lower odds of remission in those with higher BMI (OR, 0.97; 95% CI, 0.95-0.99). But there was no statistically significant link between higher BMI and low disease activity status.
The study also connected obesity to higher odds of disability (OR, 1.63; 95% CI, 1.20-2.23). Furthermore, higher BMI was linked to higher odds of disability (OR, 1.04; 95% CI, 1.01-1.06).
Study lead author Dr. Nikiphorou, who spoke in an interview and in comments at an ACR press conference, said “this study emphasizes that obesity can have a profound effect on treatment goals in rheumatoid arthritis. It creates a strong case for addressing BMI and addressing obesity, flagging it up to primary care.”
She added that rheumatologists too often focus on only rheumatoid conditions. “We place so much evidence on disease activity scores,” she said. “How often do we really address the patient in terms of other things going on, including obesity? What we can do is include discussion of BMI, exercise, nutrition.”
Dr. Nikiphorou and Dr. Matteson report no relevant disclosures. No specific study funding is reported.
This article was updated 11/10/17.
SAN DIEGO – In what may be the largest study of its kind, British researchers have linked obesity to significantly higher odds of rheumatoid arthritis disease activity and disability.
“This study emphasizes that obesity can have a profound effect on treatment goals in rheumatoid arthritis,” says Elena Nikiphorou, MD, of King’s College London, who presented the study findings at the annual meeting of the American College of Rheumatology. “Obesity reduced the odds of achieving remission or low disease activity by around 30%. And the odds of having disability were increased by 63%. This confirms what’s been shown in other, smaller studies.”
Despite obesity having been tied to decreased joint damage in established RA, Eric L. Matteson, MD, noted in an interview, that“the biomechanical effect of [being] overweight, especially on the weight-bearing joints” is one of the two “especially important” mechanisms explaining the link between RA and obesity. “The other is that fat cells produce inflammatory proteins, which contribute to the disease process and make it more difficult to treat,” said Dr. Matteson, a rheumatologist at the Mayo Clinic, Rochester, Minn.
“In my view the mechanical risk to the joint outweighs any possible ‘protective’ effect of RA,” Dr. Matteson added in an interview.
For the new study, Dr. Nikiphorou and colleagues compiled statistics from two consecutive United Kingdom RA inception cohorts. One tracked 1,465 patients for up to 25 years (median follow-up, 10 years), and the other tracked 1,236 patients for as many as 10 years (median follow-up, 6 years).
At baseline, 37.2% of 2,420 patients (90% of total) were overweight, and 21.3% were obese. Average body mass index (BMI) rose between the two consecutive studies from 25.5 to 27.6.
The researchers found that obesity was linked to lower likelihoods of remission and low disease activity status (odds ratio, 0.71; 95% confidence interval, 0.55-0.93 and OR, 0.69; 95% CI, 0.55-0.87, respectively.) After controlling for factors such as age and gender, they also saw slightly lower odds of remission in those with higher BMI (OR, 0.97; 95% CI, 0.95-0.99). But there was no statistically significant link between higher BMI and low disease activity status.
The study also connected obesity to higher odds of disability (OR, 1.63; 95% CI, 1.20-2.23). Furthermore, higher BMI was linked to higher odds of disability (OR, 1.04; 95% CI, 1.01-1.06).
Study lead author Dr. Nikiphorou, who spoke in an interview and in comments at an ACR press conference, said “this study emphasizes that obesity can have a profound effect on treatment goals in rheumatoid arthritis. It creates a strong case for addressing BMI and addressing obesity, flagging it up to primary care.”
She added that rheumatologists too often focus on only rheumatoid conditions. “We place so much evidence on disease activity scores,” she said. “How often do we really address the patient in terms of other things going on, including obesity? What we can do is include discussion of BMI, exercise, nutrition.”
Dr. Nikiphorou and Dr. Matteson report no relevant disclosures. No specific study funding is reported.
This article was updated 11/10/17.
SAN DIEGO – In what may be the largest study of its kind, British researchers have linked obesity to significantly higher odds of rheumatoid arthritis disease activity and disability.
“This study emphasizes that obesity can have a profound effect on treatment goals in rheumatoid arthritis,” says Elena Nikiphorou, MD, of King’s College London, who presented the study findings at the annual meeting of the American College of Rheumatology. “Obesity reduced the odds of achieving remission or low disease activity by around 30%. And the odds of having disability were increased by 63%. This confirms what’s been shown in other, smaller studies.”
Despite obesity having been tied to decreased joint damage in established RA, Eric L. Matteson, MD, noted in an interview, that“the biomechanical effect of [being] overweight, especially on the weight-bearing joints” is one of the two “especially important” mechanisms explaining the link between RA and obesity. “The other is that fat cells produce inflammatory proteins, which contribute to the disease process and make it more difficult to treat,” said Dr. Matteson, a rheumatologist at the Mayo Clinic, Rochester, Minn.
“In my view the mechanical risk to the joint outweighs any possible ‘protective’ effect of RA,” Dr. Matteson added in an interview.
For the new study, Dr. Nikiphorou and colleagues compiled statistics from two consecutive United Kingdom RA inception cohorts. One tracked 1,465 patients for up to 25 years (median follow-up, 10 years), and the other tracked 1,236 patients for as many as 10 years (median follow-up, 6 years).
At baseline, 37.2% of 2,420 patients (90% of total) were overweight, and 21.3% were obese. Average body mass index (BMI) rose between the two consecutive studies from 25.5 to 27.6.
The researchers found that obesity was linked to lower likelihoods of remission and low disease activity status (odds ratio, 0.71; 95% confidence interval, 0.55-0.93 and OR, 0.69; 95% CI, 0.55-0.87, respectively.) After controlling for factors such as age and gender, they also saw slightly lower odds of remission in those with higher BMI (OR, 0.97; 95% CI, 0.95-0.99). But there was no statistically significant link between higher BMI and low disease activity status.
The study also connected obesity to higher odds of disability (OR, 1.63; 95% CI, 1.20-2.23). Furthermore, higher BMI was linked to higher odds of disability (OR, 1.04; 95% CI, 1.01-1.06).
Study lead author Dr. Nikiphorou, who spoke in an interview and in comments at an ACR press conference, said “this study emphasizes that obesity can have a profound effect on treatment goals in rheumatoid arthritis. It creates a strong case for addressing BMI and addressing obesity, flagging it up to primary care.”
She added that rheumatologists too often focus on only rheumatoid conditions. “We place so much evidence on disease activity scores,” she said. “How often do we really address the patient in terms of other things going on, including obesity? What we can do is include discussion of BMI, exercise, nutrition.”
Dr. Nikiphorou and Dr. Matteson report no relevant disclosures. No specific study funding is reported.
This article was updated 11/10/17.
AT ACR 2017
Key clinical point: Obesity may worsen the risk of disease activity and disability in rheumatoid arthritis.
Major finding: In an adjusted analysis, obese patients with RA were less likely to reach remission and low disease activity status (OR, 0.71; 95% CI, 0.55-0.93 and OR, 0.69; 95% CI, 0.55-0.87, respectively).
Data source: Two consecutive inception cohorts with a total of 1,236 RA patients followed for up to 25 years.
Disclosures: The lead study author reports no disclosures, and no other disclosures are reported. No specific study funding is reported.