User login
Racial Differences in Adherence to Prescribed Analgesia in Cancer Patients: An Integrated Review of Quantitative Research
From the University of Pennsylvania School of Nursing, Philadelphia, PA.
Abstract
- Background: Racial/ethnic disparities in analgesic treatment for pain have been widely documented in the United States. However, the connection between race/ethnicity and adherence to prescribed analgesics has not been described.
- Objectives: To review and synthesize quantitative research documenting racial/ethnic differences in adherence to prescribed analgesia in cancer patients.
- Methods: We performed a systematic search of quantitative, primary studies in Scopus, CINAHL, PubMed, Ovid, PsychInfo, and EMBASE. The title and abstract of each article was reviewed for relevance and whether inclusion criteria were met. Evidence was examined for relevant outcomes, data collection methods, variables studied in relation to adherence, and the magnitude of association between race/ethnicity and adherence.
- Results: Seven studies met inclusion criteria. Reported rates of adherence varied in studies among Hispanic/Latinos, African Americans, Asians, and whites based on variation in measurement tools, research questions, populations from which participants were recruited, and predictive variables analyzed. Most existing studies of analgesic adherence used self-report to measure adherence. Only 1 study used a validated, real-time electronic instrument to monitor prescribed opioid adherence and had a longitudinal study design.
- Conclusion: Limited research has examined relationships between adherence to prescribed analgesic regimens and racial disparities. Existing studies point to the clinical and socioeconomic factors that may interact with race/ethnicity in explaining analgesic and opioid adherence outcomes in cancer patients.
Key words: race, ethnicity, adherence, opiates, analgesics, pain management, cancer, pain treatment disparities.
The ongoing opioid epidemic and recent development of the Centers for Disease Control and Prevention (CDC) guidelines for chronic pain management have shaped a national conversation on opioid prescription and utilization [1]. The CDC delineates provider recommendations for opioid prescription. This focus on prescribed medication regimens is inadequate without an understanding of how patients take or adhere to prescribed medications. Cancer patients are a unique group. Moderate to severe pain in cancer patients is usually treated with opioids, and adherence to analgesia has been conceptualized a key mediator of cancer pain outcomes. For instance, a recent study found that patterns of analgesic adherence, specifically, inconsistent adherence to strong opioids (World Health Organization step 3), is one of the strongest predictors of health care utilization among outpatients with cancer pain [2]. Approximately 67% to 77% of cancer patients experience pain that requires management with analgesia [3], especially in the absence of access to nonpharmacologic pain treatments [2]. Thus, barriers in relation to adequate pain management can result in poor pain treatment outcomes and impaired quality of life for cancer patients.
Insufficient pain management has been found to have a negative impact on the quality of life and physical and mental functions of patients with cancer [4]. Patients who experience severe cancer pain are significantly more likely to experience multiple other symptoms such as depression, fatigue, and insomnia, resulting in diminished physical function [5], social role function [6], and greater out of pocket cost of managing pain and asso-ciated symptoms [7]. Minority populations, however, disproportionately carry the burden of undertreated pain [4,8–11,13–16]. Evidence suggests that blacks/African Americans are more likely to experience unrelieved cancer pain [4,8–11,13–16]. They are also less likely than their white counterparts to receive analgesic treatment for cancer pain [8–11,13,15,16]. Little is known, however, about racial disparities in relation to adherence to analgesia for cancer pain when providers prescribe analgesics.
The purpose of this paper is to review the published literature that has addressed the associations between disparities and adherence to analgesia among cancer patients. Evidence was examined for outcomes studied, data collection methods, variables studied in relation to adherence, and the magnitude of association based on race and adherence.
Methods
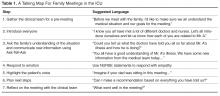
We performed a systematic search of studies published between 1990 and the present in Scopus, CINAHL, PubMed, Ovid, PsychInfo, and the EMBASE databases. The inclusion criteria consisted of published articles in the aforementioned databases that were (1) set in the United States, (2) primary studies, (3) employed quantitative design, (4) assessed adherence or compliance to analgesics or adequacy of pain management using the Pain Management Index (PMI), (5) sample was exclusively minority or may have had a comparative group. The title and abstract of each article in the the search results was reviewed for relevance to study aims and inclusion and exclusion criteria, and any duplicates were eliminated. A total of 6 studies were found using this method (Table 1), and an additional study was found in the reference list of 1 of these 6.
Results
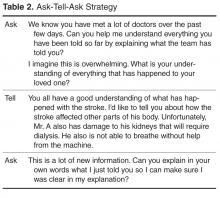
The 7 included studies were observational in nature; 4 were cross-sectional [4,12,15,16], 2 were retrospective [3,14], and 1 was prospective and used objective measures of analgesic adherence [13] (Table 2).
Defining and Operationalizing Adherence
Meghani and Bruner [16] point out that analgesic adherence is a “heterogeneous construct that lends itself to varied results and interpretations depending on the measurements used or dimensions studied.” Adherence to analgesia was explicitly defined in all 7 studies (Table 3). One study reported an adherence rate that was the total dose over 24 hours divided by the dose prescribed then multiplied by 100 [4]. The total dose over 24 hours was used in another study but was converted to an equianalgesic calculation [12]. Another set of studies used a similar definition but specified percentages based on medication or type of prescription, such as an around-the-clock(ATC) regimen [13,15,16]. In 2 studies, adherence was measured based on chart review of yes/no questions posed about whether or not patients had taken medications as prescribed [3,15].
The measurements of adherence differed between studies. Four studies [4,12,14,16] used adherence as a primary outcome and the rest employed adherence as a facet of pain management [3,13,15]. The most frequent measure of adherence was self-report. The widely validated Morisky Medication Adherence Scale (MMAS) instrument was used in 3 of 7 studies [12,13,15]. Meghani and Bruner [15] utilized the modified MMAS plus a previously validated visual analog scale for doses of medication to assess adherence over week- and month-long intervals. One study used patient interviews to capture self-reporting of opioid prescription and opioid use. Additionally, the study used MMAS to further characterize the adherence measurements [12]. Using a more objective method, Meghani et al [13] employed a microprocessor in the medication cap to determine the percentage of the total number of prescribed doses that were actually taken [13]. The processor sensed when the bottle was open, which served as a proxy for taking medications at appropriate times.
Analgesic Adherence Rate
To report the analgesic adherence rates, 6 studies presented a percentage [3,4,12,13,15] and all but 1 highlighted the barriers associated with poor adherence [3,4,12,13,15,16].
The results of a pilot study exploring intentional and unintentional adherence revealed that 85.5% of patients took the prescribed medications in the previous week. Further analysis using visual analogue scale for dose adherence found that that 51% took up to 60% of the prescribed medications [15]. In an exclusively African-American sample, the adherence rate was reported as 46% [4]. Another study by Meghani et al compared adherence to prescribed ATC analgesics between African Americans and whites with cancer-related pain using an electronic monitoring system [13]. The overall adherence rate for African Americans was 53% and 74% for whites [13]. The authors concluded that there was a significant difference between the analgesic adherence rates between African Americans and whites in this study. On sub-analysis, analgesic adherence rates for African Americans were much lower for weak opioids (34%) and higher for long-acting opioids (63%).
In a study of individuals from an outpatient supportive care center with a majority white sample (74% Caucasian), overall 9.6% of patients deviated from the opioid regimen, while approximately 90% reported high adherence [12]. It is important to note that a convenience sample was used here. Of the total 19 patients that deviated from the regimen, 11 used less opioids than prescribed and 8 used higher doses. Upon analysis, the opioid deviation was more frequent in males and non-whites. However, statistical analyses of the magnitude of deviation from prescribed dose and non-white racial/ethnic background were not reported. Within the “non-whites” category, the race/ethnicity is defined as African American (16%, n = 32) and “other” (9%, n = 18). The authors contend that this strong adherence resulted from a strong understanding of the regimen as evidenced by a high agreement between the prescribed dose and the patient reported prescription [12]. Nguyen et al [12] argue that the literature shows that lower adherence rates for minority patients may be explained by the presence of comorbidities and lack of insurance.
Two other studies reported adherence rates for separate insurance cohorts [3,14]. The Medicaid cohort was younger and had a higher percentage of African-American individuals. However, in the self-pay/charity care group, the majority was Hispanic [3]. In the pilot study, the differences between the groups on adherence with prescribed medication regimens did not achieve statistical significance. The data were summarized to suggest that nonadherence was more likely in the self-pay/charity care group and more follow-up visits occurred after discharge [3]. During the larger retrospective study there was no difference in number of patients adhering to the regimen at each follow-up visit in each benefit group. The study concluded that the long-acting opiate adherence was influenced only by the benefits of use and that race/ethnicity was not a statistically significant predictor [14].
Factors Associated with Adherence
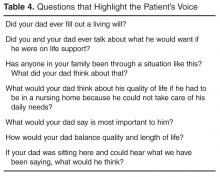
Multiple studies investigated factors underlying reported analgesic adherence rates for the ethnic and racial groups studied. Both clinical and sociodemographic variables were associated with analgesic adherence (Table 4). These included cancer type and disease stage [3,4,13,14], pain intensity [3,4,13–16], side effects [13,15], type of analgesic prescribed [3,4,13–16], income/socioeconomic status [3,13,14], behavioral history [3,12,13], gender [3,4,12–16], and perceived barriers [3,4,13,15,16].
Cancer Type and Stage
Most studies did not find significant associations between analgesic adherence rates and cancer type and stage [3,12,14]. However, 1 study that sought to identify unique factors underlying analgesic adherence for African Americans and whites found that whites reported higher analgesic adherence in relation to “time since cancer diagnosis,” possibly indicating disease severity and progression [13]. In another study that involved a majority of African-American patients, individuals with colon and rectal cancer had lower adherence rates [4]. In this study, patients with colon and rectal cancer had more analgesic prescriptions (2.5 +/– 2.3 analgesics) compared to patients with other cancer diagnoses. The authors concluded that an increased medication burden might have contributed to a decreased adherence rate. Overall, other cancer types did not correlate with adherence rates [4].
Pain Intensity
Six studies examined pain intensity and duration [3,4,13–16]. Three studies found a difference in reported pain intensity between racial/ethnic groups [3,13,16], 1 found no correlation between pain intensity and race/ethnicity [14], and 3 concluded that pain intensity was a significant predictor of adherence rates [3,13,15].
Meghani and Bruner’s pilot study explored possible correlates associated with intentional and unintentional nonadherence [15]. Overall, individuals were more likely to report forgetfulness (unintentional nonadherence) and to stop taking pain medicine when feeling “worse” (intentional nonadherence) if they believed that it was easier to deal with pain than with the side effects of analgesia [15]. Further, forgetfulness was negatively associated with the need for “stronger” pain medication. Concern about using too much pain medication was positively correlated with both forgetfulness and carelessness. The need for stronger pain medication was also correlated with significantly higher pain levels and lower pain relief [15].
In a comparative study of African Americans and whites, African Americans reported greater cancer pain and lower pain relief on the Brief Pain Inventory (BPI) and had a negative PMI. The PMI measure is a simple index linking the usual severity of cancer pain with the category of medication prescribed to treat it. PMI is calculated by subtracting patient’s pain levels (“pain worst” score from the BPI coded as mild, moderate, or severe) from the most potent analgesia prescribed. A negative PMI implies inadequate analgesic prescription relative to the reported pain level. Pain intensity was a significant factor related to increased adherence in whites but not African Americans. For African Americans, analgesic adherence was predicted by socioeconomic status, provider communication factors, and side effects. Similarly, in another study that compared African Americans and Hispanics, African Americans were more likely to have a negative PMI than Hispanics and were less likely to report that pain medication relieved pain [16]. In a pilot study that compared Medicaid recipients to self-pay/charity care patients, African-American participants had lower reported pain scores than Hispanics and Caucasians [3]. In the larger follow-up study, however, ethnicity did not prove a significant predictor for pain levels [14].
In a study with exclusively African-American patients, a significant correlation was found between pain intensity and adherence; specifically, as intensity increased, adherence increased [4]. Results for the entire African-American cohort indicated that 90% of patients had analgesic prescriptions for cancer-related pain, but 86% continued to report having moderate to severe worst pain [4]. A study that compared African Americans and whites showed that lower pain relief with analgesics was associated with lower adherence to analgesia for cancer pain among whites [13]. For every unit increase in “least pain” scores (indicating lower pain relief) on the BPI item, dose adherence decreased by 2.88%. Pain levels and relief did not explain adherence rates among African Americans. Whites were also more likely to make decisions on analgesic use based on the amount of relief anticipated from the use of analgesics [13] whereas African Americans were more likely to make analgesic use decisions based on analgesic side effects.
Side Effects
In a pilot study that explored the intricacies of adherence, some individuals felt it was easier to deal with pain than with the side effects of pain medications. These individuals were also more likely to report forgetfulness and to stop taking medications if feeling “worse” [15]. One study, which included African-American and white cohorts, found that an increase in the severity of side effects was associated with lower adherence to analgesia for African Americans but not whites. Furthermore, African Americans reported a greater number of analgesic side effects at baseline. African Americans were also more likely to make analgesic decisions based on side effects in comparison to whites participants, who made decisions based on expectation of pain relief [13]. In a study with exclusively African-American patients, patients with concerns about pain medication possibly causing confusion were more likely to have poor adherence [4].
Type of Analgesic Prescribed
In the analyses, 3 studies found a difference between analgesic prescriptions among ethnic groups [12,13,16], 3 found that there was a statistical significance between type of prescription and adherence [4,13,16], and 2 studies [3,14] found no statistical correlation between type of analgesic prescribed and adherence.
In a study of African Americans and Hispanics, both groups took analgesics on an “as-needed” basis despite the guidelines for cancer pain management [16]. However, African Americans reported taking analgesics less than twice daily. Overall, only a small percentage of patients took sustained-release analgesics that require fewer doses per day [16]. Similarly, in another study that compared adherence between African Americans and whites, the overall analgesic adherence rate was different on sub-analysis for specific analgesic prescriptions. The analgesic adherence rates for African Americans ranged from 34% for weak opioids to 63% for long-acting opioids. In comparison, the analgesic adherence rates for whites ranged from 55% for weak opioids to 78% for long-acting opioids [13]. In conclusion, patients on long-acting opioids were more likely to have higher adherence. Adherence rates for African Americans were found in another study. The adherence rate for adjuvant analgesics was highest at 65%, step 2 opioids at 44% and step 3 opioids at 43% [4].
In a study with exclusively African-American patients, poor adherence was significantly correlated with step 3 opioids [4]. Another study that explored the correlation between type of analgesic and adherence found that intentional nonadherence was less likely in individuals that were prescribed step 3 opioids [15]. Specifically, individuals with this behavior were also more likely to report lower pain levels and chose to stop the use of analgesics when feeling better [15].
Within a pilot study that compared benefit programs and payor groups, the differences in the prescription of long-acting opiates did not reach statistical significance [3]. However, in the larger, definitive study, the comparison revealed that patients in the self-pay/charity care group were less likely to receive a prescription for long-acting opiates. The data further revealed that Hispanic and Asian patients were prescribed long-acting opiates at a lower rate compared to the larger sample. Further, African Americans and Caucasians were prescribed long-acting opiates at a higher rate than the larger sample. In another analysis, with benefits and race/ethnicity, benefits were the only statistically significant predictor. While statistically controlling for race/ethnicity, Medicaid patients were 2.4 times more likely to receive a prescription for long-acting opioids than the self-pay/charity care patients [14].
Income/Socioeconomic Status
Three studies in this analysis [3,13,14] found that income and socioeconomic status were significant predictors of analgesic adherence for cancer pain. In a comparison between African Americans and whites, income was the strongest predictor of analgesic adherence for cancer pain in African Americans [13]; specifically, individuals with a household income of less than $10,000 a year had a 41.83% lower percentage of dose adherence. Among whites, income did not have a significant correlation with analgesic rates [13].
A pilot study and larger definitive study [3,14] were conducted to compare the effects of prescription benefits. The prescription benefits included were Medicaid and self-pay/charity care. Through comparison, none of the Medicaid patients reported financial barriers but the self-pay/charity care patients were more likely to report financial barriers to adherence [3]. In the larger study, the findings indicated that there was significant association of adherence by benefits and race/ethnicity. As mentioned above, benefits were a dominant predictor of long acting opiate use and further adherence [14].
Gender
Apart from ethnicity or race as a variable associated with adherence, association of analgesic adherence and gender were observed in 4 studies [3,13–15] and evaluated in 2 studies. One study [4] found that a patient’s gender and education level did not correlate with adherence rates. However, in another study [12] men were more likely to deviate from the prescribed dose. Overall, within the entire cohort [12] men and minority patients were most likely to deviate from the prescribed dosing regimen in comparison to all other patient demographic factors.
Attitudes and Barriers
Five of the 7 studies investigated perceived barriers to analgesic adherence [3,4,13,15,16]. Four used the Barriers Questionnaire II (BQ-II) [18] to further understand patients’ beliefs about cancer pain management [3,12,13,15]. Using this validated tool, 1 study found that non-white individuals had higher scores on the BQ-II than white patients [12]. Within the non-white group in the above study, the mean score on the BQ-II for African Americans was 1.76 (± 0.81) and the mean score for “other” was 2.16 (± 0.93) [12]. Further, low MMAS scores were significantly associated with higher BQ-II scores. Similarly, higher BQ-II scores correlated with opioid deviation toward higher than prescribed dose [12].
Another study with a primarily African-American cohort did not use the BQ-II but asked specific questions in regards to perceived barriers to analgesics. Within the cohort, 87% reported a fear of addiction to pain medicine. Further, 77% had a fear of injection, 75% were concerned about a tolerance for analgesics, and side effects were a major concern. Overall, nausea was the greatest reported concern followed by potential for confusion, which was negatively associated with taking analgesics. Distracting the doctor from curing their illness was a predictor of improved adherence; however, individuals were more likely to take Tylenol for pain relief. Similarly, no significant barrier items affected adherence to NSAIDs. In relation to step 2 opioids, patients who felt it was important to be strong by not talking about pain were more likely to have better adherence [4]. Similar results with African Americans were identified in another study [13]. In the comparison between African Americans and whites, African Americans had more subjective barriers compared to whites. Particularly for African Americans, each unit increase in concern about distracting the doctor from curing the disease, the percentage of dose adherence decreased by 7.44 [13].
In a study that compared payer groups, a questionnaire elicited reasons for nonadherence [3]. Similar reasons for nonadherence emerged including financial, fear of addiction or increased medication use, and running out medication.
Behavioral History
Only 1 study used CAGE (Cut down, Annoyed, Guilty, and Eye-opener), an alcohol-screening questionnaire, to determine a possible relationship with analgesic adherence. In this study, there were 19 cases of opioid deviation, 16% of which were CAGE positive and had severe deviation toward less than the prescribed doses [12]. In further analysis, no association was found between CAGE positively and opioid deviation to higher intake [12]. Two other studies gathered data on history of depression, substance use, and alcohol use but no significant correlation was found [3,13].
Discussion
Previous literature has reported overall analgesic adherence rates among oncology patients ranging from 62% to 72% [23]. Factors at the provider and system level have been considered in past research, but the patient perspective is poorly represented in the literature [13]. A majority of studies on analgesic adherence have been completed with cohorts made up predominantly of white individuals [13,23,24], while others focus on racially homogenous and/or ethnically different populations in other countries [21,25,26].
This review confirms that there is a paucity of well-designed studies that describe the associations between racial and ethnic disparities and adherence to opioids among patients with cancer pain. This is despite the fact that moderate to severe cancer pain in the U.S. is managed mainly with analgesics and specifically with opioids [19]. In addition, cancer patients with health insurance have both more pharmacy claims as well as more claims for higher doses of opioids [20] compared to noncancer patients. The lack of attention to analgesic and opioid adherence among cancer patients is surprising in the light of the recent high-profile initiatives to reduce opioid misuse [31].
Multiple studies highlighted the importance of pain management education and adequate pain assessment for effective analgesic use [4,16]. In the study in the palliative care setting, the authors concluded that patients who are educated, counseled, and monitored by a palliative or supportive care team have less episodes of opioid deviation and trends toward lower opioid use [12]. A systematic review and meta-analysis confirmed findings that educational interventions for patients improved knowledge about cancer pain management, however, most did not improve reported adherence to analgesics [27,28]. These findings emphasize the need for further research on interventions to improve racial/ethnic disparities in analgesic adherence for cancer pain.
Limitations
The findings of this review should be evaluated in the context of the following limitations. First, adherence to a prescribed regimen is a difficult outcome to measure and a majority of studies in this review used subjective measures to assess analgesic adherence for cancer pain. Of note, self-report was the primary measurement employed. Studies in non–cancer pain settings that have evaluated various methodological approaches to adherence measurement found that patients are likely to over-report adherence when using self-report or a diary format in comparison to an electronic monitoring system. Only 1 study in this review used an objective measure of adherence [13]. Some previous studies contend that self-report in comparison to other, objective measurements of medication adherence are accurate [23]. Further research is needed to determine the most accurate measurement of analgesic adherence in cancer patients.
Also, invariably the studies employed an English-speaking sample, which excludes an understanding of analgesic adherence for cancer pain in linguistically diverse Americans. In addition, most studies included patients who were either white Americans or African Americans and some studies lumped several racial ethnic minority subgroups as “nonwhites” or “other.”
A majority of studies were cross-sectional [4,12,15,16]. For instance, studies used a 24-hour time period to assess ATC medication as well as as-needed regimens, which may not capture the information needed to understand adherence to as-needed regimens [4]. With longitudinal studies, a greater understanding of adherence can be determined. However, there is potential bias with studies that track patients primarily at follow-up appointments. Individuals who are compliant with follow-up appointments may present with different analgesic adherence compared to those who do not attend follow-up appointments. This potential bias should be evaluated in longitudinal studies with various sensitivity analyses or using tools that identify healthy user bias.
Most studies recruited patients from outpatient oncology clinics, however, 1 study was conducted with a sample from an outpatient supportive care center managed by a palliative care team [12]. Due to the goals of palliative care, which include specialized treatment for individuals with serious illness and a focus on symptom management and relief, patients in this setting may have a different attitude toward using opioids.
Conclusion
Although data remain limited, our review suggests that while overuse of opioids has been a well-cited concern in patients with chronic non-cancer pain [21,33], cancer patients demonstrate considerable underuse and inconsistent use of prescribed analgesics. This is important as a recent study found that inconsistent adherence to prescribed around-the-clock analgesics, specifically the interaction of strong opioids and inconsistent adherence, is a strong risk factor for hospitalization among cancer outpatients who are prescribed analgesics for pain [1]. Of note, adherence to opioids in patients with cancer may be driven by a unique set of factors and these factors may differ for minorities and non-minority patients. For instance, studies in this review indicate that income is a strong predictor of analgesic adherence for African Americans but not for whites. This is because race and socioeconomic status frequently overlap in the United States [29]. In addition, like cancer pain, analgesic side effects may also be poorly managed among African Americans and other minorities. For example, in 1 study, Meghani et al used a trade-off analysis technique (conjoint analysis) to understand trade-offs African Americans and whites employ in using analgesics for cancer pain [30]. The authors found that African Americans were more likely to make analgesic adherence decisions based on side effects whereas whites were more likely to make adherence decisions based on pain relief [30]. In subsequent analysis, these authors showed that the race effect found in their previous studies was mediated by the type of analgesics prescribed to African Americans vs. whites [31]. African Americans with cancer pain were prescribed analgesics that had a worse side effect profile after statistically adjusting for insurance type and clinical risks such as renal insufficiency [31].
Together, the available evidence indicates that both patients’ socioeconomic status and clinician treatment bias contributes to racial and ethnic disparities in analgesic adherence for cancer pain and subsequent cancer pain outcomes. Thus, future research should investigate interventions for improving analgesic adherence among low-income minorities. Also, there is a need for clinician-level interventions focusing on cognitive bias modification related to cancer pain and side effects management, which appears to relate to analgesic nonadherence among racial/ethnic minorities. In addition, further research is needed to (1) rigorously describe analgesic and opioid adherence for cancer pain, (2) elucidate racial/ethnic and other socioeconomic and clinical disparities in analgesic and opioid adherence for cancer pain; (3) and clarify the role of analgesic and opioid adherence for cancer patients including outcomes for the patients and the health care system.
Corresponding author: Salimah H. Meghani, PhD, MBE, RN, University of Pennsylvania School of Nursing, Room 337, Fagin Hall, 418 Curie Blvd, Philadelphia, PA 19104, [email protected].
Financial disclosures: None.
1. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain - United States, 2016. JAMA 2016;315:1624–45.
2. Meghani SH, Knafl GJ. Patterns of analgesic adherence predict health care utilization among outpatients with cancer pain. Patient Prefer Adher 2016;10:81–98.
3. Bryan M, De La Rosa N, Hill AM, et al. Influence of prescription benefits on reported pain in cancer patients. Pain Med 2008;9:1148–57.
4. Rhee YO, Kim E, Kim B. Assessment of pain and analgesic use in African American cancer patients: Factors related to adherence to analgesics. J Immigr Minor Health 2012;14:1045–51.
5. Laird BJ, Scott AC, Colvin LA, et al. Pain, depression, and fatigue as a symptom cluster in advanced cancer. J Pain Symptom Manage 2011;42:1–11.
6. Ferreira KA, Kimura M, Teixeira MJ, et al. Impact of cancer-related symptom synergisms on health-related quality of life and performance status. J Pain Symptom Manage 2008;35:604–16.
7. Craig BM, Strassels SA. Out-of-pocket prices of opioid analgesics in the United States, 1999-2004. Pain Med 2010;11:240–47.
8. Institute of Medicine: Relieving pain in america: a blueprint for transforming prevention, care, education, and research. Washington, DC: National Academies Press; 2011.
9. Institutes of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003.
10. Meghani SH, Byun E, Gallagher RM. Time to take stock: A meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med 2012;13:150–74.
11. Cleeland CS, Gonin R, Baez L, Loehrer P, Pandya KJ. Pain and treatment of pain in minority patients with cancer. The Eastern Cooperative Oncology Group Minority Outpatient Pain Study. Ann Intern Med 1997;127:813–6.
12. Nguyen LMT, Rhondali W, De la Cruz M, et al. Frequency and predictors of patient deviation from prescribed opioids and barriers to opioid pain management in patients with advanced cancer. J Pain Symptom Manage 2013;45:506–16.
13. Meghani SH, Thompson AML, Chittams J, et al. Adherence to analgesics for cancer pain: A comparative study of African Americans and whites using an electronic monitoring device. J Pain 2015;16:825–35.
14. Weider R, DeLaRosa N, Bryan M, et al. Prescription coverage in indigent patients affects the use of long acting opioids in management of cancer pain. Pain Med 2014;15:42–51.
15. Meghani SH, Brune DW. A pilot study to identify correlates of intentional versus unintentional nonadherence. Pain Manag Nurs 2013;14:e22-30.
16. Anderson KO, Mendoza TR, Valero V, et al. Minority cancer patients and their providers: pain management attitudes and practice. Cancer 2000;88:1929–38.
17. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52:377–84.
18. Ward SE, Goldberg N, Miller-McCauley V, et al. Patient-related barriers to management of cancer pain. Pain 1993;52:319–24.
19. Glare PA, Davies PS, Finlay E, et al. Pain in cancer survivors. J Clin Oncol 2014;32:1739–47.
20. van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, et al. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol 2007;18:1437–49.
21. Jacobsen R, Samsanaviciene J, Liubarskiene Z, et al. Barriers to cancer pain management in Danish and Lithuanian patients treated in pain and palliative care units. Pain Manag Nurs 2014; 15:51–8.
22. National Institutes of Health. Pathways to prevention: the role of opioids in the treatment of chronic pain. September 29–30, 2014. Executive summary: final report. Accessed 10 Sep 2015 at https://prevention.nih.gov/docs/programs/p2p/ODPPainPanelStatementFinal_10-02-14.pdf.
23. Miaskowski C, Dodd MJ, West C, et al. Lack of adherence with the analgesic regimen: A significant barrier to effective cancer pain management. J Clin Oncol 2001;19:4275–79.
24. Yoong J, Traeger LN, Gallagher ER, et al. A pilot study to investigate adherence to long-acting opioids among patients with advanced lung cancer. J Palliat Med 2013;16:391–6.
25. Lai YH, Keefe FJ, Sun WZ, et al. Relationship between pain-specific beliefs and adherence to analgesic regimens in Taiwanese cancer patients: A preliminary study. J Pain Symptom Manage 2002;24:415–22.
26. Cohen MZ, Musgrave CF, McGuire DB, et al. The cancer pain experience of Israeli adults 65 years and older: the influence of pain interference, symptom severity, and knowledge and attitudes on pain and pain control. Support Care Cancer 2005;13:708–14.
27. Bennett MI, Bagnall AM, Jose Closs S. How effective are patient-based educational interventions in the management of cancer pain? Systematic review and meta analysis. Pain 2009;143:192–9.
28. Oldenmenger WH, Sillevis Smitt PA, van Dooren S, et al. A systematic review on barriers hindering adequate cancer pain management and interventions to reduce them: a critical appraisal. Eur J Cancer 2009;45:1370–80.
29. Meghani SH, Chittams J. Controlling for socioeconomic status in pain disparities research: all-else-equal analysis when “all else” is not equal. Pain Med 2015;16:2222–5.
30. Meghani SH, Chittams J, Hanlon A, Curry J. Measuring preferences for analgesic treatment for cancer pain: how do African Americans and whites perform on choice-based conjoint analysis experiments? BMC Med Inform Decis Mak 2013;13:118.
31. Meghani SH, Kang Y, Chittams J, et al. African Americans with cancer pain are more likely to receive an analgesic with toxic metabolite despite clinical risks: a mediation analysis study. J Clin Oncol 2014;32:2773–9.
32. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids forchronic pain - United States, 2016. MMWR Recomm Rep 2016 Mar 18;65:1–49.
33. Chapman CR, Lipschitz DL, Angst MS, et al. Opioid pharmacotherapy for chronic non-cancer pain in the United States: a research guideline for developing an evidence-base. J Pain 2010;11:807–29.
From the University of Pennsylvania School of Nursing, Philadelphia, PA.
Abstract
- Background: Racial/ethnic disparities in analgesic treatment for pain have been widely documented in the United States. However, the connection between race/ethnicity and adherence to prescribed analgesics has not been described.
- Objectives: To review and synthesize quantitative research documenting racial/ethnic differences in adherence to prescribed analgesia in cancer patients.
- Methods: We performed a systematic search of quantitative, primary studies in Scopus, CINAHL, PubMed, Ovid, PsychInfo, and EMBASE. The title and abstract of each article was reviewed for relevance and whether inclusion criteria were met. Evidence was examined for relevant outcomes, data collection methods, variables studied in relation to adherence, and the magnitude of association between race/ethnicity and adherence.
- Results: Seven studies met inclusion criteria. Reported rates of adherence varied in studies among Hispanic/Latinos, African Americans, Asians, and whites based on variation in measurement tools, research questions, populations from which participants were recruited, and predictive variables analyzed. Most existing studies of analgesic adherence used self-report to measure adherence. Only 1 study used a validated, real-time electronic instrument to monitor prescribed opioid adherence and had a longitudinal study design.
- Conclusion: Limited research has examined relationships between adherence to prescribed analgesic regimens and racial disparities. Existing studies point to the clinical and socioeconomic factors that may interact with race/ethnicity in explaining analgesic and opioid adherence outcomes in cancer patients.
Key words: race, ethnicity, adherence, opiates, analgesics, pain management, cancer, pain treatment disparities.
The ongoing opioid epidemic and recent development of the Centers for Disease Control and Prevention (CDC) guidelines for chronic pain management have shaped a national conversation on opioid prescription and utilization [1]. The CDC delineates provider recommendations for opioid prescription. This focus on prescribed medication regimens is inadequate without an understanding of how patients take or adhere to prescribed medications. Cancer patients are a unique group. Moderate to severe pain in cancer patients is usually treated with opioids, and adherence to analgesia has been conceptualized a key mediator of cancer pain outcomes. For instance, a recent study found that patterns of analgesic adherence, specifically, inconsistent adherence to strong opioids (World Health Organization step 3), is one of the strongest predictors of health care utilization among outpatients with cancer pain [2]. Approximately 67% to 77% of cancer patients experience pain that requires management with analgesia [3], especially in the absence of access to nonpharmacologic pain treatments [2]. Thus, barriers in relation to adequate pain management can result in poor pain treatment outcomes and impaired quality of life for cancer patients.
Insufficient pain management has been found to have a negative impact on the quality of life and physical and mental functions of patients with cancer [4]. Patients who experience severe cancer pain are significantly more likely to experience multiple other symptoms such as depression, fatigue, and insomnia, resulting in diminished physical function [5], social role function [6], and greater out of pocket cost of managing pain and asso-ciated symptoms [7]. Minority populations, however, disproportionately carry the burden of undertreated pain [4,8–11,13–16]. Evidence suggests that blacks/African Americans are more likely to experience unrelieved cancer pain [4,8–11,13–16]. They are also less likely than their white counterparts to receive analgesic treatment for cancer pain [8–11,13,15,16]. Little is known, however, about racial disparities in relation to adherence to analgesia for cancer pain when providers prescribe analgesics.
The purpose of this paper is to review the published literature that has addressed the associations between disparities and adherence to analgesia among cancer patients. Evidence was examined for outcomes studied, data collection methods, variables studied in relation to adherence, and the magnitude of association based on race and adherence.
Methods
We performed a systematic search of studies published between 1990 and the present in Scopus, CINAHL, PubMed, Ovid, PsychInfo, and the EMBASE databases. The inclusion criteria consisted of published articles in the aforementioned databases that were (1) set in the United States, (2) primary studies, (3) employed quantitative design, (4) assessed adherence or compliance to analgesics or adequacy of pain management using the Pain Management Index (PMI), (5) sample was exclusively minority or may have had a comparative group. The title and abstract of each article in the the search results was reviewed for relevance to study aims and inclusion and exclusion criteria, and any duplicates were eliminated. A total of 6 studies were found using this method (Table 1), and an additional study was found in the reference list of 1 of these 6.
Results
The 7 included studies were observational in nature; 4 were cross-sectional [4,12,15,16], 2 were retrospective [3,14], and 1 was prospective and used objective measures of analgesic adherence [13] (Table 2).
Defining and Operationalizing Adherence
Meghani and Bruner [16] point out that analgesic adherence is a “heterogeneous construct that lends itself to varied results and interpretations depending on the measurements used or dimensions studied.” Adherence to analgesia was explicitly defined in all 7 studies (Table 3). One study reported an adherence rate that was the total dose over 24 hours divided by the dose prescribed then multiplied by 100 [4]. The total dose over 24 hours was used in another study but was converted to an equianalgesic calculation [12]. Another set of studies used a similar definition but specified percentages based on medication or type of prescription, such as an around-the-clock(ATC) regimen [13,15,16]. In 2 studies, adherence was measured based on chart review of yes/no questions posed about whether or not patients had taken medications as prescribed [3,15].
The measurements of adherence differed between studies. Four studies [4,12,14,16] used adherence as a primary outcome and the rest employed adherence as a facet of pain management [3,13,15]. The most frequent measure of adherence was self-report. The widely validated Morisky Medication Adherence Scale (MMAS) instrument was used in 3 of 7 studies [12,13,15]. Meghani and Bruner [15] utilized the modified MMAS plus a previously validated visual analog scale for doses of medication to assess adherence over week- and month-long intervals. One study used patient interviews to capture self-reporting of opioid prescription and opioid use. Additionally, the study used MMAS to further characterize the adherence measurements [12]. Using a more objective method, Meghani et al [13] employed a microprocessor in the medication cap to determine the percentage of the total number of prescribed doses that were actually taken [13]. The processor sensed when the bottle was open, which served as a proxy for taking medications at appropriate times.
Analgesic Adherence Rate
To report the analgesic adherence rates, 6 studies presented a percentage [3,4,12,13,15] and all but 1 highlighted the barriers associated with poor adherence [3,4,12,13,15,16].
The results of a pilot study exploring intentional and unintentional adherence revealed that 85.5% of patients took the prescribed medications in the previous week. Further analysis using visual analogue scale for dose adherence found that that 51% took up to 60% of the prescribed medications [15]. In an exclusively African-American sample, the adherence rate was reported as 46% [4]. Another study by Meghani et al compared adherence to prescribed ATC analgesics between African Americans and whites with cancer-related pain using an electronic monitoring system [13]. The overall adherence rate for African Americans was 53% and 74% for whites [13]. The authors concluded that there was a significant difference between the analgesic adherence rates between African Americans and whites in this study. On sub-analysis, analgesic adherence rates for African Americans were much lower for weak opioids (34%) and higher for long-acting opioids (63%).
In a study of individuals from an outpatient supportive care center with a majority white sample (74% Caucasian), overall 9.6% of patients deviated from the opioid regimen, while approximately 90% reported high adherence [12]. It is important to note that a convenience sample was used here. Of the total 19 patients that deviated from the regimen, 11 used less opioids than prescribed and 8 used higher doses. Upon analysis, the opioid deviation was more frequent in males and non-whites. However, statistical analyses of the magnitude of deviation from prescribed dose and non-white racial/ethnic background were not reported. Within the “non-whites” category, the race/ethnicity is defined as African American (16%, n = 32) and “other” (9%, n = 18). The authors contend that this strong adherence resulted from a strong understanding of the regimen as evidenced by a high agreement between the prescribed dose and the patient reported prescription [12]. Nguyen et al [12] argue that the literature shows that lower adherence rates for minority patients may be explained by the presence of comorbidities and lack of insurance.
Two other studies reported adherence rates for separate insurance cohorts [3,14]. The Medicaid cohort was younger and had a higher percentage of African-American individuals. However, in the self-pay/charity care group, the majority was Hispanic [3]. In the pilot study, the differences between the groups on adherence with prescribed medication regimens did not achieve statistical significance. The data were summarized to suggest that nonadherence was more likely in the self-pay/charity care group and more follow-up visits occurred after discharge [3]. During the larger retrospective study there was no difference in number of patients adhering to the regimen at each follow-up visit in each benefit group. The study concluded that the long-acting opiate adherence was influenced only by the benefits of use and that race/ethnicity was not a statistically significant predictor [14].
Factors Associated with Adherence
Multiple studies investigated factors underlying reported analgesic adherence rates for the ethnic and racial groups studied. Both clinical and sociodemographic variables were associated with analgesic adherence (Table 4). These included cancer type and disease stage [3,4,13,14], pain intensity [3,4,13–16], side effects [13,15], type of analgesic prescribed [3,4,13–16], income/socioeconomic status [3,13,14], behavioral history [3,12,13], gender [3,4,12–16], and perceived barriers [3,4,13,15,16].
Cancer Type and Stage
Most studies did not find significant associations between analgesic adherence rates and cancer type and stage [3,12,14]. However, 1 study that sought to identify unique factors underlying analgesic adherence for African Americans and whites found that whites reported higher analgesic adherence in relation to “time since cancer diagnosis,” possibly indicating disease severity and progression [13]. In another study that involved a majority of African-American patients, individuals with colon and rectal cancer had lower adherence rates [4]. In this study, patients with colon and rectal cancer had more analgesic prescriptions (2.5 +/– 2.3 analgesics) compared to patients with other cancer diagnoses. The authors concluded that an increased medication burden might have contributed to a decreased adherence rate. Overall, other cancer types did not correlate with adherence rates [4].
Pain Intensity
Six studies examined pain intensity and duration [3,4,13–16]. Three studies found a difference in reported pain intensity between racial/ethnic groups [3,13,16], 1 found no correlation between pain intensity and race/ethnicity [14], and 3 concluded that pain intensity was a significant predictor of adherence rates [3,13,15].
Meghani and Bruner’s pilot study explored possible correlates associated with intentional and unintentional nonadherence [15]. Overall, individuals were more likely to report forgetfulness (unintentional nonadherence) and to stop taking pain medicine when feeling “worse” (intentional nonadherence) if they believed that it was easier to deal with pain than with the side effects of analgesia [15]. Further, forgetfulness was negatively associated with the need for “stronger” pain medication. Concern about using too much pain medication was positively correlated with both forgetfulness and carelessness. The need for stronger pain medication was also correlated with significantly higher pain levels and lower pain relief [15].
In a comparative study of African Americans and whites, African Americans reported greater cancer pain and lower pain relief on the Brief Pain Inventory (BPI) and had a negative PMI. The PMI measure is a simple index linking the usual severity of cancer pain with the category of medication prescribed to treat it. PMI is calculated by subtracting patient’s pain levels (“pain worst” score from the BPI coded as mild, moderate, or severe) from the most potent analgesia prescribed. A negative PMI implies inadequate analgesic prescription relative to the reported pain level. Pain intensity was a significant factor related to increased adherence in whites but not African Americans. For African Americans, analgesic adherence was predicted by socioeconomic status, provider communication factors, and side effects. Similarly, in another study that compared African Americans and Hispanics, African Americans were more likely to have a negative PMI than Hispanics and were less likely to report that pain medication relieved pain [16]. In a pilot study that compared Medicaid recipients to self-pay/charity care patients, African-American participants had lower reported pain scores than Hispanics and Caucasians [3]. In the larger follow-up study, however, ethnicity did not prove a significant predictor for pain levels [14].
In a study with exclusively African-American patients, a significant correlation was found between pain intensity and adherence; specifically, as intensity increased, adherence increased [4]. Results for the entire African-American cohort indicated that 90% of patients had analgesic prescriptions for cancer-related pain, but 86% continued to report having moderate to severe worst pain [4]. A study that compared African Americans and whites showed that lower pain relief with analgesics was associated with lower adherence to analgesia for cancer pain among whites [13]. For every unit increase in “least pain” scores (indicating lower pain relief) on the BPI item, dose adherence decreased by 2.88%. Pain levels and relief did not explain adherence rates among African Americans. Whites were also more likely to make decisions on analgesic use based on the amount of relief anticipated from the use of analgesics [13] whereas African Americans were more likely to make analgesic use decisions based on analgesic side effects.
Side Effects
In a pilot study that explored the intricacies of adherence, some individuals felt it was easier to deal with pain than with the side effects of pain medications. These individuals were also more likely to report forgetfulness and to stop taking medications if feeling “worse” [15]. One study, which included African-American and white cohorts, found that an increase in the severity of side effects was associated with lower adherence to analgesia for African Americans but not whites. Furthermore, African Americans reported a greater number of analgesic side effects at baseline. African Americans were also more likely to make analgesic decisions based on side effects in comparison to whites participants, who made decisions based on expectation of pain relief [13]. In a study with exclusively African-American patients, patients with concerns about pain medication possibly causing confusion were more likely to have poor adherence [4].
Type of Analgesic Prescribed
In the analyses, 3 studies found a difference between analgesic prescriptions among ethnic groups [12,13,16], 3 found that there was a statistical significance between type of prescription and adherence [4,13,16], and 2 studies [3,14] found no statistical correlation between type of analgesic prescribed and adherence.
In a study of African Americans and Hispanics, both groups took analgesics on an “as-needed” basis despite the guidelines for cancer pain management [16]. However, African Americans reported taking analgesics less than twice daily. Overall, only a small percentage of patients took sustained-release analgesics that require fewer doses per day [16]. Similarly, in another study that compared adherence between African Americans and whites, the overall analgesic adherence rate was different on sub-analysis for specific analgesic prescriptions. The analgesic adherence rates for African Americans ranged from 34% for weak opioids to 63% for long-acting opioids. In comparison, the analgesic adherence rates for whites ranged from 55% for weak opioids to 78% for long-acting opioids [13]. In conclusion, patients on long-acting opioids were more likely to have higher adherence. Adherence rates for African Americans were found in another study. The adherence rate for adjuvant analgesics was highest at 65%, step 2 opioids at 44% and step 3 opioids at 43% [4].
In a study with exclusively African-American patients, poor adherence was significantly correlated with step 3 opioids [4]. Another study that explored the correlation between type of analgesic and adherence found that intentional nonadherence was less likely in individuals that were prescribed step 3 opioids [15]. Specifically, individuals with this behavior were also more likely to report lower pain levels and chose to stop the use of analgesics when feeling better [15].
Within a pilot study that compared benefit programs and payor groups, the differences in the prescription of long-acting opiates did not reach statistical significance [3]. However, in the larger, definitive study, the comparison revealed that patients in the self-pay/charity care group were less likely to receive a prescription for long-acting opiates. The data further revealed that Hispanic and Asian patients were prescribed long-acting opiates at a lower rate compared to the larger sample. Further, African Americans and Caucasians were prescribed long-acting opiates at a higher rate than the larger sample. In another analysis, with benefits and race/ethnicity, benefits were the only statistically significant predictor. While statistically controlling for race/ethnicity, Medicaid patients were 2.4 times more likely to receive a prescription for long-acting opioids than the self-pay/charity care patients [14].
Income/Socioeconomic Status
Three studies in this analysis [3,13,14] found that income and socioeconomic status were significant predictors of analgesic adherence for cancer pain. In a comparison between African Americans and whites, income was the strongest predictor of analgesic adherence for cancer pain in African Americans [13]; specifically, individuals with a household income of less than $10,000 a year had a 41.83% lower percentage of dose adherence. Among whites, income did not have a significant correlation with analgesic rates [13].
A pilot study and larger definitive study [3,14] were conducted to compare the effects of prescription benefits. The prescription benefits included were Medicaid and self-pay/charity care. Through comparison, none of the Medicaid patients reported financial barriers but the self-pay/charity care patients were more likely to report financial barriers to adherence [3]. In the larger study, the findings indicated that there was significant association of adherence by benefits and race/ethnicity. As mentioned above, benefits were a dominant predictor of long acting opiate use and further adherence [14].
Gender
Apart from ethnicity or race as a variable associated with adherence, association of analgesic adherence and gender were observed in 4 studies [3,13–15] and evaluated in 2 studies. One study [4] found that a patient’s gender and education level did not correlate with adherence rates. However, in another study [12] men were more likely to deviate from the prescribed dose. Overall, within the entire cohort [12] men and minority patients were most likely to deviate from the prescribed dosing regimen in comparison to all other patient demographic factors.
Attitudes and Barriers
Five of the 7 studies investigated perceived barriers to analgesic adherence [3,4,13,15,16]. Four used the Barriers Questionnaire II (BQ-II) [18] to further understand patients’ beliefs about cancer pain management [3,12,13,15]. Using this validated tool, 1 study found that non-white individuals had higher scores on the BQ-II than white patients [12]. Within the non-white group in the above study, the mean score on the BQ-II for African Americans was 1.76 (± 0.81) and the mean score for “other” was 2.16 (± 0.93) [12]. Further, low MMAS scores were significantly associated with higher BQ-II scores. Similarly, higher BQ-II scores correlated with opioid deviation toward higher than prescribed dose [12].
Another study with a primarily African-American cohort did not use the BQ-II but asked specific questions in regards to perceived barriers to analgesics. Within the cohort, 87% reported a fear of addiction to pain medicine. Further, 77% had a fear of injection, 75% were concerned about a tolerance for analgesics, and side effects were a major concern. Overall, nausea was the greatest reported concern followed by potential for confusion, which was negatively associated with taking analgesics. Distracting the doctor from curing their illness was a predictor of improved adherence; however, individuals were more likely to take Tylenol for pain relief. Similarly, no significant barrier items affected adherence to NSAIDs. In relation to step 2 opioids, patients who felt it was important to be strong by not talking about pain were more likely to have better adherence [4]. Similar results with African Americans were identified in another study [13]. In the comparison between African Americans and whites, African Americans had more subjective barriers compared to whites. Particularly for African Americans, each unit increase in concern about distracting the doctor from curing the disease, the percentage of dose adherence decreased by 7.44 [13].
In a study that compared payer groups, a questionnaire elicited reasons for nonadherence [3]. Similar reasons for nonadherence emerged including financial, fear of addiction or increased medication use, and running out medication.
Behavioral History
Only 1 study used CAGE (Cut down, Annoyed, Guilty, and Eye-opener), an alcohol-screening questionnaire, to determine a possible relationship with analgesic adherence. In this study, there were 19 cases of opioid deviation, 16% of which were CAGE positive and had severe deviation toward less than the prescribed doses [12]. In further analysis, no association was found between CAGE positively and opioid deviation to higher intake [12]. Two other studies gathered data on history of depression, substance use, and alcohol use but no significant correlation was found [3,13].
Discussion
Previous literature has reported overall analgesic adherence rates among oncology patients ranging from 62% to 72% [23]. Factors at the provider and system level have been considered in past research, but the patient perspective is poorly represented in the literature [13]. A majority of studies on analgesic adherence have been completed with cohorts made up predominantly of white individuals [13,23,24], while others focus on racially homogenous and/or ethnically different populations in other countries [21,25,26].
This review confirms that there is a paucity of well-designed studies that describe the associations between racial and ethnic disparities and adherence to opioids among patients with cancer pain. This is despite the fact that moderate to severe cancer pain in the U.S. is managed mainly with analgesics and specifically with opioids [19]. In addition, cancer patients with health insurance have both more pharmacy claims as well as more claims for higher doses of opioids [20] compared to noncancer patients. The lack of attention to analgesic and opioid adherence among cancer patients is surprising in the light of the recent high-profile initiatives to reduce opioid misuse [31].
Multiple studies highlighted the importance of pain management education and adequate pain assessment for effective analgesic use [4,16]. In the study in the palliative care setting, the authors concluded that patients who are educated, counseled, and monitored by a palliative or supportive care team have less episodes of opioid deviation and trends toward lower opioid use [12]. A systematic review and meta-analysis confirmed findings that educational interventions for patients improved knowledge about cancer pain management, however, most did not improve reported adherence to analgesics [27,28]. These findings emphasize the need for further research on interventions to improve racial/ethnic disparities in analgesic adherence for cancer pain.
Limitations
The findings of this review should be evaluated in the context of the following limitations. First, adherence to a prescribed regimen is a difficult outcome to measure and a majority of studies in this review used subjective measures to assess analgesic adherence for cancer pain. Of note, self-report was the primary measurement employed. Studies in non–cancer pain settings that have evaluated various methodological approaches to adherence measurement found that patients are likely to over-report adherence when using self-report or a diary format in comparison to an electronic monitoring system. Only 1 study in this review used an objective measure of adherence [13]. Some previous studies contend that self-report in comparison to other, objective measurements of medication adherence are accurate [23]. Further research is needed to determine the most accurate measurement of analgesic adherence in cancer patients.
Also, invariably the studies employed an English-speaking sample, which excludes an understanding of analgesic adherence for cancer pain in linguistically diverse Americans. In addition, most studies included patients who were either white Americans or African Americans and some studies lumped several racial ethnic minority subgroups as “nonwhites” or “other.”
A majority of studies were cross-sectional [4,12,15,16]. For instance, studies used a 24-hour time period to assess ATC medication as well as as-needed regimens, which may not capture the information needed to understand adherence to as-needed regimens [4]. With longitudinal studies, a greater understanding of adherence can be determined. However, there is potential bias with studies that track patients primarily at follow-up appointments. Individuals who are compliant with follow-up appointments may present with different analgesic adherence compared to those who do not attend follow-up appointments. This potential bias should be evaluated in longitudinal studies with various sensitivity analyses or using tools that identify healthy user bias.
Most studies recruited patients from outpatient oncology clinics, however, 1 study was conducted with a sample from an outpatient supportive care center managed by a palliative care team [12]. Due to the goals of palliative care, which include specialized treatment for individuals with serious illness and a focus on symptom management and relief, patients in this setting may have a different attitude toward using opioids.
Conclusion
Although data remain limited, our review suggests that while overuse of opioids has been a well-cited concern in patients with chronic non-cancer pain [21,33], cancer patients demonstrate considerable underuse and inconsistent use of prescribed analgesics. This is important as a recent study found that inconsistent adherence to prescribed around-the-clock analgesics, specifically the interaction of strong opioids and inconsistent adherence, is a strong risk factor for hospitalization among cancer outpatients who are prescribed analgesics for pain [1]. Of note, adherence to opioids in patients with cancer may be driven by a unique set of factors and these factors may differ for minorities and non-minority patients. For instance, studies in this review indicate that income is a strong predictor of analgesic adherence for African Americans but not for whites. This is because race and socioeconomic status frequently overlap in the United States [29]. In addition, like cancer pain, analgesic side effects may also be poorly managed among African Americans and other minorities. For example, in 1 study, Meghani et al used a trade-off analysis technique (conjoint analysis) to understand trade-offs African Americans and whites employ in using analgesics for cancer pain [30]. The authors found that African Americans were more likely to make analgesic adherence decisions based on side effects whereas whites were more likely to make adherence decisions based on pain relief [30]. In subsequent analysis, these authors showed that the race effect found in their previous studies was mediated by the type of analgesics prescribed to African Americans vs. whites [31]. African Americans with cancer pain were prescribed analgesics that had a worse side effect profile after statistically adjusting for insurance type and clinical risks such as renal insufficiency [31].
Together, the available evidence indicates that both patients’ socioeconomic status and clinician treatment bias contributes to racial and ethnic disparities in analgesic adherence for cancer pain and subsequent cancer pain outcomes. Thus, future research should investigate interventions for improving analgesic adherence among low-income minorities. Also, there is a need for clinician-level interventions focusing on cognitive bias modification related to cancer pain and side effects management, which appears to relate to analgesic nonadherence among racial/ethnic minorities. In addition, further research is needed to (1) rigorously describe analgesic and opioid adherence for cancer pain, (2) elucidate racial/ethnic and other socioeconomic and clinical disparities in analgesic and opioid adherence for cancer pain; (3) and clarify the role of analgesic and opioid adherence for cancer patients including outcomes for the patients and the health care system.
Corresponding author: Salimah H. Meghani, PhD, MBE, RN, University of Pennsylvania School of Nursing, Room 337, Fagin Hall, 418 Curie Blvd, Philadelphia, PA 19104, [email protected].
Financial disclosures: None.
From the University of Pennsylvania School of Nursing, Philadelphia, PA.
Abstract
- Background: Racial/ethnic disparities in analgesic treatment for pain have been widely documented in the United States. However, the connection between race/ethnicity and adherence to prescribed analgesics has not been described.
- Objectives: To review and synthesize quantitative research documenting racial/ethnic differences in adherence to prescribed analgesia in cancer patients.
- Methods: We performed a systematic search of quantitative, primary studies in Scopus, CINAHL, PubMed, Ovid, PsychInfo, and EMBASE. The title and abstract of each article was reviewed for relevance and whether inclusion criteria were met. Evidence was examined for relevant outcomes, data collection methods, variables studied in relation to adherence, and the magnitude of association between race/ethnicity and adherence.
- Results: Seven studies met inclusion criteria. Reported rates of adherence varied in studies among Hispanic/Latinos, African Americans, Asians, and whites based on variation in measurement tools, research questions, populations from which participants were recruited, and predictive variables analyzed. Most existing studies of analgesic adherence used self-report to measure adherence. Only 1 study used a validated, real-time electronic instrument to monitor prescribed opioid adherence and had a longitudinal study design.
- Conclusion: Limited research has examined relationships between adherence to prescribed analgesic regimens and racial disparities. Existing studies point to the clinical and socioeconomic factors that may interact with race/ethnicity in explaining analgesic and opioid adherence outcomes in cancer patients.
Key words: race, ethnicity, adherence, opiates, analgesics, pain management, cancer, pain treatment disparities.
The ongoing opioid epidemic and recent development of the Centers for Disease Control and Prevention (CDC) guidelines for chronic pain management have shaped a national conversation on opioid prescription and utilization [1]. The CDC delineates provider recommendations for opioid prescription. This focus on prescribed medication regimens is inadequate without an understanding of how patients take or adhere to prescribed medications. Cancer patients are a unique group. Moderate to severe pain in cancer patients is usually treated with opioids, and adherence to analgesia has been conceptualized a key mediator of cancer pain outcomes. For instance, a recent study found that patterns of analgesic adherence, specifically, inconsistent adherence to strong opioids (World Health Organization step 3), is one of the strongest predictors of health care utilization among outpatients with cancer pain [2]. Approximately 67% to 77% of cancer patients experience pain that requires management with analgesia [3], especially in the absence of access to nonpharmacologic pain treatments [2]. Thus, barriers in relation to adequate pain management can result in poor pain treatment outcomes and impaired quality of life for cancer patients.
Insufficient pain management has been found to have a negative impact on the quality of life and physical and mental functions of patients with cancer [4]. Patients who experience severe cancer pain are significantly more likely to experience multiple other symptoms such as depression, fatigue, and insomnia, resulting in diminished physical function [5], social role function [6], and greater out of pocket cost of managing pain and asso-ciated symptoms [7]. Minority populations, however, disproportionately carry the burden of undertreated pain [4,8–11,13–16]. Evidence suggests that blacks/African Americans are more likely to experience unrelieved cancer pain [4,8–11,13–16]. They are also less likely than their white counterparts to receive analgesic treatment for cancer pain [8–11,13,15,16]. Little is known, however, about racial disparities in relation to adherence to analgesia for cancer pain when providers prescribe analgesics.
The purpose of this paper is to review the published literature that has addressed the associations between disparities and adherence to analgesia among cancer patients. Evidence was examined for outcomes studied, data collection methods, variables studied in relation to adherence, and the magnitude of association based on race and adherence.
Methods
We performed a systematic search of studies published between 1990 and the present in Scopus, CINAHL, PubMed, Ovid, PsychInfo, and the EMBASE databases. The inclusion criteria consisted of published articles in the aforementioned databases that were (1) set in the United States, (2) primary studies, (3) employed quantitative design, (4) assessed adherence or compliance to analgesics or adequacy of pain management using the Pain Management Index (PMI), (5) sample was exclusively minority or may have had a comparative group. The title and abstract of each article in the the search results was reviewed for relevance to study aims and inclusion and exclusion criteria, and any duplicates were eliminated. A total of 6 studies were found using this method (Table 1), and an additional study was found in the reference list of 1 of these 6.
Results
The 7 included studies were observational in nature; 4 were cross-sectional [4,12,15,16], 2 were retrospective [3,14], and 1 was prospective and used objective measures of analgesic adherence [13] (Table 2).
Defining and Operationalizing Adherence
Meghani and Bruner [16] point out that analgesic adherence is a “heterogeneous construct that lends itself to varied results and interpretations depending on the measurements used or dimensions studied.” Adherence to analgesia was explicitly defined in all 7 studies (Table 3). One study reported an adherence rate that was the total dose over 24 hours divided by the dose prescribed then multiplied by 100 [4]. The total dose over 24 hours was used in another study but was converted to an equianalgesic calculation [12]. Another set of studies used a similar definition but specified percentages based on medication or type of prescription, such as an around-the-clock(ATC) regimen [13,15,16]. In 2 studies, adherence was measured based on chart review of yes/no questions posed about whether or not patients had taken medications as prescribed [3,15].
The measurements of adherence differed between studies. Four studies [4,12,14,16] used adherence as a primary outcome and the rest employed adherence as a facet of pain management [3,13,15]. The most frequent measure of adherence was self-report. The widely validated Morisky Medication Adherence Scale (MMAS) instrument was used in 3 of 7 studies [12,13,15]. Meghani and Bruner [15] utilized the modified MMAS plus a previously validated visual analog scale for doses of medication to assess adherence over week- and month-long intervals. One study used patient interviews to capture self-reporting of opioid prescription and opioid use. Additionally, the study used MMAS to further characterize the adherence measurements [12]. Using a more objective method, Meghani et al [13] employed a microprocessor in the medication cap to determine the percentage of the total number of prescribed doses that were actually taken [13]. The processor sensed when the bottle was open, which served as a proxy for taking medications at appropriate times.
Analgesic Adherence Rate
To report the analgesic adherence rates, 6 studies presented a percentage [3,4,12,13,15] and all but 1 highlighted the barriers associated with poor adherence [3,4,12,13,15,16].
The results of a pilot study exploring intentional and unintentional adherence revealed that 85.5% of patients took the prescribed medications in the previous week. Further analysis using visual analogue scale for dose adherence found that that 51% took up to 60% of the prescribed medications [15]. In an exclusively African-American sample, the adherence rate was reported as 46% [4]. Another study by Meghani et al compared adherence to prescribed ATC analgesics between African Americans and whites with cancer-related pain using an electronic monitoring system [13]. The overall adherence rate for African Americans was 53% and 74% for whites [13]. The authors concluded that there was a significant difference between the analgesic adherence rates between African Americans and whites in this study. On sub-analysis, analgesic adherence rates for African Americans were much lower for weak opioids (34%) and higher for long-acting opioids (63%).
In a study of individuals from an outpatient supportive care center with a majority white sample (74% Caucasian), overall 9.6% of patients deviated from the opioid regimen, while approximately 90% reported high adherence [12]. It is important to note that a convenience sample was used here. Of the total 19 patients that deviated from the regimen, 11 used less opioids than prescribed and 8 used higher doses. Upon analysis, the opioid deviation was more frequent in males and non-whites. However, statistical analyses of the magnitude of deviation from prescribed dose and non-white racial/ethnic background were not reported. Within the “non-whites” category, the race/ethnicity is defined as African American (16%, n = 32) and “other” (9%, n = 18). The authors contend that this strong adherence resulted from a strong understanding of the regimen as evidenced by a high agreement between the prescribed dose and the patient reported prescription [12]. Nguyen et al [12] argue that the literature shows that lower adherence rates for minority patients may be explained by the presence of comorbidities and lack of insurance.
Two other studies reported adherence rates for separate insurance cohorts [3,14]. The Medicaid cohort was younger and had a higher percentage of African-American individuals. However, in the self-pay/charity care group, the majority was Hispanic [3]. In the pilot study, the differences between the groups on adherence with prescribed medication regimens did not achieve statistical significance. The data were summarized to suggest that nonadherence was more likely in the self-pay/charity care group and more follow-up visits occurred after discharge [3]. During the larger retrospective study there was no difference in number of patients adhering to the regimen at each follow-up visit in each benefit group. The study concluded that the long-acting opiate adherence was influenced only by the benefits of use and that race/ethnicity was not a statistically significant predictor [14].
Factors Associated with Adherence
Multiple studies investigated factors underlying reported analgesic adherence rates for the ethnic and racial groups studied. Both clinical and sociodemographic variables were associated with analgesic adherence (Table 4). These included cancer type and disease stage [3,4,13,14], pain intensity [3,4,13–16], side effects [13,15], type of analgesic prescribed [3,4,13–16], income/socioeconomic status [3,13,14], behavioral history [3,12,13], gender [3,4,12–16], and perceived barriers [3,4,13,15,16].
Cancer Type and Stage
Most studies did not find significant associations between analgesic adherence rates and cancer type and stage [3,12,14]. However, 1 study that sought to identify unique factors underlying analgesic adherence for African Americans and whites found that whites reported higher analgesic adherence in relation to “time since cancer diagnosis,” possibly indicating disease severity and progression [13]. In another study that involved a majority of African-American patients, individuals with colon and rectal cancer had lower adherence rates [4]. In this study, patients with colon and rectal cancer had more analgesic prescriptions (2.5 +/– 2.3 analgesics) compared to patients with other cancer diagnoses. The authors concluded that an increased medication burden might have contributed to a decreased adherence rate. Overall, other cancer types did not correlate with adherence rates [4].
Pain Intensity
Six studies examined pain intensity and duration [3,4,13–16]. Three studies found a difference in reported pain intensity between racial/ethnic groups [3,13,16], 1 found no correlation between pain intensity and race/ethnicity [14], and 3 concluded that pain intensity was a significant predictor of adherence rates [3,13,15].
Meghani and Bruner’s pilot study explored possible correlates associated with intentional and unintentional nonadherence [15]. Overall, individuals were more likely to report forgetfulness (unintentional nonadherence) and to stop taking pain medicine when feeling “worse” (intentional nonadherence) if they believed that it was easier to deal with pain than with the side effects of analgesia [15]. Further, forgetfulness was negatively associated with the need for “stronger” pain medication. Concern about using too much pain medication was positively correlated with both forgetfulness and carelessness. The need for stronger pain medication was also correlated with significantly higher pain levels and lower pain relief [15].
In a comparative study of African Americans and whites, African Americans reported greater cancer pain and lower pain relief on the Brief Pain Inventory (BPI) and had a negative PMI. The PMI measure is a simple index linking the usual severity of cancer pain with the category of medication prescribed to treat it. PMI is calculated by subtracting patient’s pain levels (“pain worst” score from the BPI coded as mild, moderate, or severe) from the most potent analgesia prescribed. A negative PMI implies inadequate analgesic prescription relative to the reported pain level. Pain intensity was a significant factor related to increased adherence in whites but not African Americans. For African Americans, analgesic adherence was predicted by socioeconomic status, provider communication factors, and side effects. Similarly, in another study that compared African Americans and Hispanics, African Americans were more likely to have a negative PMI than Hispanics and were less likely to report that pain medication relieved pain [16]. In a pilot study that compared Medicaid recipients to self-pay/charity care patients, African-American participants had lower reported pain scores than Hispanics and Caucasians [3]. In the larger follow-up study, however, ethnicity did not prove a significant predictor for pain levels [14].
In a study with exclusively African-American patients, a significant correlation was found between pain intensity and adherence; specifically, as intensity increased, adherence increased [4]. Results for the entire African-American cohort indicated that 90% of patients had analgesic prescriptions for cancer-related pain, but 86% continued to report having moderate to severe worst pain [4]. A study that compared African Americans and whites showed that lower pain relief with analgesics was associated with lower adherence to analgesia for cancer pain among whites [13]. For every unit increase in “least pain” scores (indicating lower pain relief) on the BPI item, dose adherence decreased by 2.88%. Pain levels and relief did not explain adherence rates among African Americans. Whites were also more likely to make decisions on analgesic use based on the amount of relief anticipated from the use of analgesics [13] whereas African Americans were more likely to make analgesic use decisions based on analgesic side effects.
Side Effects
In a pilot study that explored the intricacies of adherence, some individuals felt it was easier to deal with pain than with the side effects of pain medications. These individuals were also more likely to report forgetfulness and to stop taking medications if feeling “worse” [15]. One study, which included African-American and white cohorts, found that an increase in the severity of side effects was associated with lower adherence to analgesia for African Americans but not whites. Furthermore, African Americans reported a greater number of analgesic side effects at baseline. African Americans were also more likely to make analgesic decisions based on side effects in comparison to whites participants, who made decisions based on expectation of pain relief [13]. In a study with exclusively African-American patients, patients with concerns about pain medication possibly causing confusion were more likely to have poor adherence [4].
Type of Analgesic Prescribed
In the analyses, 3 studies found a difference between analgesic prescriptions among ethnic groups [12,13,16], 3 found that there was a statistical significance between type of prescription and adherence [4,13,16], and 2 studies [3,14] found no statistical correlation between type of analgesic prescribed and adherence.
In a study of African Americans and Hispanics, both groups took analgesics on an “as-needed” basis despite the guidelines for cancer pain management [16]. However, African Americans reported taking analgesics less than twice daily. Overall, only a small percentage of patients took sustained-release analgesics that require fewer doses per day [16]. Similarly, in another study that compared adherence between African Americans and whites, the overall analgesic adherence rate was different on sub-analysis for specific analgesic prescriptions. The analgesic adherence rates for African Americans ranged from 34% for weak opioids to 63% for long-acting opioids. In comparison, the analgesic adherence rates for whites ranged from 55% for weak opioids to 78% for long-acting opioids [13]. In conclusion, patients on long-acting opioids were more likely to have higher adherence. Adherence rates for African Americans were found in another study. The adherence rate for adjuvant analgesics was highest at 65%, step 2 opioids at 44% and step 3 opioids at 43% [4].
In a study with exclusively African-American patients, poor adherence was significantly correlated with step 3 opioids [4]. Another study that explored the correlation between type of analgesic and adherence found that intentional nonadherence was less likely in individuals that were prescribed step 3 opioids [15]. Specifically, individuals with this behavior were also more likely to report lower pain levels and chose to stop the use of analgesics when feeling better [15].
Within a pilot study that compared benefit programs and payor groups, the differences in the prescription of long-acting opiates did not reach statistical significance [3]. However, in the larger, definitive study, the comparison revealed that patients in the self-pay/charity care group were less likely to receive a prescription for long-acting opiates. The data further revealed that Hispanic and Asian patients were prescribed long-acting opiates at a lower rate compared to the larger sample. Further, African Americans and Caucasians were prescribed long-acting opiates at a higher rate than the larger sample. In another analysis, with benefits and race/ethnicity, benefits were the only statistically significant predictor. While statistically controlling for race/ethnicity, Medicaid patients were 2.4 times more likely to receive a prescription for long-acting opioids than the self-pay/charity care patients [14].
Income/Socioeconomic Status
Three studies in this analysis [3,13,14] found that income and socioeconomic status were significant predictors of analgesic adherence for cancer pain. In a comparison between African Americans and whites, income was the strongest predictor of analgesic adherence for cancer pain in African Americans [13]; specifically, individuals with a household income of less than $10,000 a year had a 41.83% lower percentage of dose adherence. Among whites, income did not have a significant correlation with analgesic rates [13].
A pilot study and larger definitive study [3,14] were conducted to compare the effects of prescription benefits. The prescription benefits included were Medicaid and self-pay/charity care. Through comparison, none of the Medicaid patients reported financial barriers but the self-pay/charity care patients were more likely to report financial barriers to adherence [3]. In the larger study, the findings indicated that there was significant association of adherence by benefits and race/ethnicity. As mentioned above, benefits were a dominant predictor of long acting opiate use and further adherence [14].
Gender
Apart from ethnicity or race as a variable associated with adherence, association of analgesic adherence and gender were observed in 4 studies [3,13–15] and evaluated in 2 studies. One study [4] found that a patient’s gender and education level did not correlate with adherence rates. However, in another study [12] men were more likely to deviate from the prescribed dose. Overall, within the entire cohort [12] men and minority patients were most likely to deviate from the prescribed dosing regimen in comparison to all other patient demographic factors.
Attitudes and Barriers
Five of the 7 studies investigated perceived barriers to analgesic adherence [3,4,13,15,16]. Four used the Barriers Questionnaire II (BQ-II) [18] to further understand patients’ beliefs about cancer pain management [3,12,13,15]. Using this validated tool, 1 study found that non-white individuals had higher scores on the BQ-II than white patients [12]. Within the non-white group in the above study, the mean score on the BQ-II for African Americans was 1.76 (± 0.81) and the mean score for “other” was 2.16 (± 0.93) [12]. Further, low MMAS scores were significantly associated with higher BQ-II scores. Similarly, higher BQ-II scores correlated with opioid deviation toward higher than prescribed dose [12].
Another study with a primarily African-American cohort did not use the BQ-II but asked specific questions in regards to perceived barriers to analgesics. Within the cohort, 87% reported a fear of addiction to pain medicine. Further, 77% had a fear of injection, 75% were concerned about a tolerance for analgesics, and side effects were a major concern. Overall, nausea was the greatest reported concern followed by potential for confusion, which was negatively associated with taking analgesics. Distracting the doctor from curing their illness was a predictor of improved adherence; however, individuals were more likely to take Tylenol for pain relief. Similarly, no significant barrier items affected adherence to NSAIDs. In relation to step 2 opioids, patients who felt it was important to be strong by not talking about pain were more likely to have better adherence [4]. Similar results with African Americans were identified in another study [13]. In the comparison between African Americans and whites, African Americans had more subjective barriers compared to whites. Particularly for African Americans, each unit increase in concern about distracting the doctor from curing the disease, the percentage of dose adherence decreased by 7.44 [13].
In a study that compared payer groups, a questionnaire elicited reasons for nonadherence [3]. Similar reasons for nonadherence emerged including financial, fear of addiction or increased medication use, and running out medication.
Behavioral History
Only 1 study used CAGE (Cut down, Annoyed, Guilty, and Eye-opener), an alcohol-screening questionnaire, to determine a possible relationship with analgesic adherence. In this study, there were 19 cases of opioid deviation, 16% of which were CAGE positive and had severe deviation toward less than the prescribed doses [12]. In further analysis, no association was found between CAGE positively and opioid deviation to higher intake [12]. Two other studies gathered data on history of depression, substance use, and alcohol use but no significant correlation was found [3,13].
Discussion
Previous literature has reported overall analgesic adherence rates among oncology patients ranging from 62% to 72% [23]. Factors at the provider and system level have been considered in past research, but the patient perspective is poorly represented in the literature [13]. A majority of studies on analgesic adherence have been completed with cohorts made up predominantly of white individuals [13,23,24], while others focus on racially homogenous and/or ethnically different populations in other countries [21,25,26].
This review confirms that there is a paucity of well-designed studies that describe the associations between racial and ethnic disparities and adherence to opioids among patients with cancer pain. This is despite the fact that moderate to severe cancer pain in the U.S. is managed mainly with analgesics and specifically with opioids [19]. In addition, cancer patients with health insurance have both more pharmacy claims as well as more claims for higher doses of opioids [20] compared to noncancer patients. The lack of attention to analgesic and opioid adherence among cancer patients is surprising in the light of the recent high-profile initiatives to reduce opioid misuse [31].
Multiple studies highlighted the importance of pain management education and adequate pain assessment for effective analgesic use [4,16]. In the study in the palliative care setting, the authors concluded that patients who are educated, counseled, and monitored by a palliative or supportive care team have less episodes of opioid deviation and trends toward lower opioid use [12]. A systematic review and meta-analysis confirmed findings that educational interventions for patients improved knowledge about cancer pain management, however, most did not improve reported adherence to analgesics [27,28]. These findings emphasize the need for further research on interventions to improve racial/ethnic disparities in analgesic adherence for cancer pain.
Limitations
The findings of this review should be evaluated in the context of the following limitations. First, adherence to a prescribed regimen is a difficult outcome to measure and a majority of studies in this review used subjective measures to assess analgesic adherence for cancer pain. Of note, self-report was the primary measurement employed. Studies in non–cancer pain settings that have evaluated various methodological approaches to adherence measurement found that patients are likely to over-report adherence when using self-report or a diary format in comparison to an electronic monitoring system. Only 1 study in this review used an objective measure of adherence [13]. Some previous studies contend that self-report in comparison to other, objective measurements of medication adherence are accurate [23]. Further research is needed to determine the most accurate measurement of analgesic adherence in cancer patients.
Also, invariably the studies employed an English-speaking sample, which excludes an understanding of analgesic adherence for cancer pain in linguistically diverse Americans. In addition, most studies included patients who were either white Americans or African Americans and some studies lumped several racial ethnic minority subgroups as “nonwhites” or “other.”
A majority of studies were cross-sectional [4,12,15,16]. For instance, studies used a 24-hour time period to assess ATC medication as well as as-needed regimens, which may not capture the information needed to understand adherence to as-needed regimens [4]. With longitudinal studies, a greater understanding of adherence can be determined. However, there is potential bias with studies that track patients primarily at follow-up appointments. Individuals who are compliant with follow-up appointments may present with different analgesic adherence compared to those who do not attend follow-up appointments. This potential bias should be evaluated in longitudinal studies with various sensitivity analyses or using tools that identify healthy user bias.
Most studies recruited patients from outpatient oncology clinics, however, 1 study was conducted with a sample from an outpatient supportive care center managed by a palliative care team [12]. Due to the goals of palliative care, which include specialized treatment for individuals with serious illness and a focus on symptom management and relief, patients in this setting may have a different attitude toward using opioids.
Conclusion
Although data remain limited, our review suggests that while overuse of opioids has been a well-cited concern in patients with chronic non-cancer pain [21,33], cancer patients demonstrate considerable underuse and inconsistent use of prescribed analgesics. This is important as a recent study found that inconsistent adherence to prescribed around-the-clock analgesics, specifically the interaction of strong opioids and inconsistent adherence, is a strong risk factor for hospitalization among cancer outpatients who are prescribed analgesics for pain [1]. Of note, adherence to opioids in patients with cancer may be driven by a unique set of factors and these factors may differ for minorities and non-minority patients. For instance, studies in this review indicate that income is a strong predictor of analgesic adherence for African Americans but not for whites. This is because race and socioeconomic status frequently overlap in the United States [29]. In addition, like cancer pain, analgesic side effects may also be poorly managed among African Americans and other minorities. For example, in 1 study, Meghani et al used a trade-off analysis technique (conjoint analysis) to understand trade-offs African Americans and whites employ in using analgesics for cancer pain [30]. The authors found that African Americans were more likely to make analgesic adherence decisions based on side effects whereas whites were more likely to make adherence decisions based on pain relief [30]. In subsequent analysis, these authors showed that the race effect found in their previous studies was mediated by the type of analgesics prescribed to African Americans vs. whites [31]. African Americans with cancer pain were prescribed analgesics that had a worse side effect profile after statistically adjusting for insurance type and clinical risks such as renal insufficiency [31].
Together, the available evidence indicates that both patients’ socioeconomic status and clinician treatment bias contributes to racial and ethnic disparities in analgesic adherence for cancer pain and subsequent cancer pain outcomes. Thus, future research should investigate interventions for improving analgesic adherence among low-income minorities. Also, there is a need for clinician-level interventions focusing on cognitive bias modification related to cancer pain and side effects management, which appears to relate to analgesic nonadherence among racial/ethnic minorities. In addition, further research is needed to (1) rigorously describe analgesic and opioid adherence for cancer pain, (2) elucidate racial/ethnic and other socioeconomic and clinical disparities in analgesic and opioid adherence for cancer pain; (3) and clarify the role of analgesic and opioid adherence for cancer patients including outcomes for the patients and the health care system.
Corresponding author: Salimah H. Meghani, PhD, MBE, RN, University of Pennsylvania School of Nursing, Room 337, Fagin Hall, 418 Curie Blvd, Philadelphia, PA 19104, [email protected].
Financial disclosures: None.
1. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain - United States, 2016. JAMA 2016;315:1624–45.
2. Meghani SH, Knafl GJ. Patterns of analgesic adherence predict health care utilization among outpatients with cancer pain. Patient Prefer Adher 2016;10:81–98.
3. Bryan M, De La Rosa N, Hill AM, et al. Influence of prescription benefits on reported pain in cancer patients. Pain Med 2008;9:1148–57.
4. Rhee YO, Kim E, Kim B. Assessment of pain and analgesic use in African American cancer patients: Factors related to adherence to analgesics. J Immigr Minor Health 2012;14:1045–51.
5. Laird BJ, Scott AC, Colvin LA, et al. Pain, depression, and fatigue as a symptom cluster in advanced cancer. J Pain Symptom Manage 2011;42:1–11.
6. Ferreira KA, Kimura M, Teixeira MJ, et al. Impact of cancer-related symptom synergisms on health-related quality of life and performance status. J Pain Symptom Manage 2008;35:604–16.
7. Craig BM, Strassels SA. Out-of-pocket prices of opioid analgesics in the United States, 1999-2004. Pain Med 2010;11:240–47.
8. Institute of Medicine: Relieving pain in america: a blueprint for transforming prevention, care, education, and research. Washington, DC: National Academies Press; 2011.
9. Institutes of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003.
10. Meghani SH, Byun E, Gallagher RM. Time to take stock: A meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med 2012;13:150–74.
11. Cleeland CS, Gonin R, Baez L, Loehrer P, Pandya KJ. Pain and treatment of pain in minority patients with cancer. The Eastern Cooperative Oncology Group Minority Outpatient Pain Study. Ann Intern Med 1997;127:813–6.
12. Nguyen LMT, Rhondali W, De la Cruz M, et al. Frequency and predictors of patient deviation from prescribed opioids and barriers to opioid pain management in patients with advanced cancer. J Pain Symptom Manage 2013;45:506–16.
13. Meghani SH, Thompson AML, Chittams J, et al. Adherence to analgesics for cancer pain: A comparative study of African Americans and whites using an electronic monitoring device. J Pain 2015;16:825–35.
14. Weider R, DeLaRosa N, Bryan M, et al. Prescription coverage in indigent patients affects the use of long acting opioids in management of cancer pain. Pain Med 2014;15:42–51.
15. Meghani SH, Brune DW. A pilot study to identify correlates of intentional versus unintentional nonadherence. Pain Manag Nurs 2013;14:e22-30.
16. Anderson KO, Mendoza TR, Valero V, et al. Minority cancer patients and their providers: pain management attitudes and practice. Cancer 2000;88:1929–38.
17. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52:377–84.
18. Ward SE, Goldberg N, Miller-McCauley V, et al. Patient-related barriers to management of cancer pain. Pain 1993;52:319–24.
19. Glare PA, Davies PS, Finlay E, et al. Pain in cancer survivors. J Clin Oncol 2014;32:1739–47.
20. van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, et al. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol 2007;18:1437–49.
21. Jacobsen R, Samsanaviciene J, Liubarskiene Z, et al. Barriers to cancer pain management in Danish and Lithuanian patients treated in pain and palliative care units. Pain Manag Nurs 2014; 15:51–8.
22. National Institutes of Health. Pathways to prevention: the role of opioids in the treatment of chronic pain. September 29–30, 2014. Executive summary: final report. Accessed 10 Sep 2015 at https://prevention.nih.gov/docs/programs/p2p/ODPPainPanelStatementFinal_10-02-14.pdf.
23. Miaskowski C, Dodd MJ, West C, et al. Lack of adherence with the analgesic regimen: A significant barrier to effective cancer pain management. J Clin Oncol 2001;19:4275–79.
24. Yoong J, Traeger LN, Gallagher ER, et al. A pilot study to investigate adherence to long-acting opioids among patients with advanced lung cancer. J Palliat Med 2013;16:391–6.
25. Lai YH, Keefe FJ, Sun WZ, et al. Relationship between pain-specific beliefs and adherence to analgesic regimens in Taiwanese cancer patients: A preliminary study. J Pain Symptom Manage 2002;24:415–22.
26. Cohen MZ, Musgrave CF, McGuire DB, et al. The cancer pain experience of Israeli adults 65 years and older: the influence of pain interference, symptom severity, and knowledge and attitudes on pain and pain control. Support Care Cancer 2005;13:708–14.
27. Bennett MI, Bagnall AM, Jose Closs S. How effective are patient-based educational interventions in the management of cancer pain? Systematic review and meta analysis. Pain 2009;143:192–9.
28. Oldenmenger WH, Sillevis Smitt PA, van Dooren S, et al. A systematic review on barriers hindering adequate cancer pain management and interventions to reduce them: a critical appraisal. Eur J Cancer 2009;45:1370–80.
29. Meghani SH, Chittams J. Controlling for socioeconomic status in pain disparities research: all-else-equal analysis when “all else” is not equal. Pain Med 2015;16:2222–5.
30. Meghani SH, Chittams J, Hanlon A, Curry J. Measuring preferences for analgesic treatment for cancer pain: how do African Americans and whites perform on choice-based conjoint analysis experiments? BMC Med Inform Decis Mak 2013;13:118.
31. Meghani SH, Kang Y, Chittams J, et al. African Americans with cancer pain are more likely to receive an analgesic with toxic metabolite despite clinical risks: a mediation analysis study. J Clin Oncol 2014;32:2773–9.
32. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids forchronic pain - United States, 2016. MMWR Recomm Rep 2016 Mar 18;65:1–49.
33. Chapman CR, Lipschitz DL, Angst MS, et al. Opioid pharmacotherapy for chronic non-cancer pain in the United States: a research guideline for developing an evidence-base. J Pain 2010;11:807–29.
1. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain - United States, 2016. JAMA 2016;315:1624–45.
2. Meghani SH, Knafl GJ. Patterns of analgesic adherence predict health care utilization among outpatients with cancer pain. Patient Prefer Adher 2016;10:81–98.
3. Bryan M, De La Rosa N, Hill AM, et al. Influence of prescription benefits on reported pain in cancer patients. Pain Med 2008;9:1148–57.
4. Rhee YO, Kim E, Kim B. Assessment of pain and analgesic use in African American cancer patients: Factors related to adherence to analgesics. J Immigr Minor Health 2012;14:1045–51.
5. Laird BJ, Scott AC, Colvin LA, et al. Pain, depression, and fatigue as a symptom cluster in advanced cancer. J Pain Symptom Manage 2011;42:1–11.
6. Ferreira KA, Kimura M, Teixeira MJ, et al. Impact of cancer-related symptom synergisms on health-related quality of life and performance status. J Pain Symptom Manage 2008;35:604–16.
7. Craig BM, Strassels SA. Out-of-pocket prices of opioid analgesics in the United States, 1999-2004. Pain Med 2010;11:240–47.
8. Institute of Medicine: Relieving pain in america: a blueprint for transforming prevention, care, education, and research. Washington, DC: National Academies Press; 2011.
9. Institutes of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003.
10. Meghani SH, Byun E, Gallagher RM. Time to take stock: A meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med 2012;13:150–74.
11. Cleeland CS, Gonin R, Baez L, Loehrer P, Pandya KJ. Pain and treatment of pain in minority patients with cancer. The Eastern Cooperative Oncology Group Minority Outpatient Pain Study. Ann Intern Med 1997;127:813–6.
12. Nguyen LMT, Rhondali W, De la Cruz M, et al. Frequency and predictors of patient deviation from prescribed opioids and barriers to opioid pain management in patients with advanced cancer. J Pain Symptom Manage 2013;45:506–16.
13. Meghani SH, Thompson AML, Chittams J, et al. Adherence to analgesics for cancer pain: A comparative study of African Americans and whites using an electronic monitoring device. J Pain 2015;16:825–35.
14. Weider R, DeLaRosa N, Bryan M, et al. Prescription coverage in indigent patients affects the use of long acting opioids in management of cancer pain. Pain Med 2014;15:42–51.
15. Meghani SH, Brune DW. A pilot study to identify correlates of intentional versus unintentional nonadherence. Pain Manag Nurs 2013;14:e22-30.
16. Anderson KO, Mendoza TR, Valero V, et al. Minority cancer patients and their providers: pain management attitudes and practice. Cancer 2000;88:1929–38.
17. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52:377–84.
18. Ward SE, Goldberg N, Miller-McCauley V, et al. Patient-related barriers to management of cancer pain. Pain 1993;52:319–24.
19. Glare PA, Davies PS, Finlay E, et al. Pain in cancer survivors. J Clin Oncol 2014;32:1739–47.
20. van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, et al. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol 2007;18:1437–49.
21. Jacobsen R, Samsanaviciene J, Liubarskiene Z, et al. Barriers to cancer pain management in Danish and Lithuanian patients treated in pain and palliative care units. Pain Manag Nurs 2014; 15:51–8.
22. National Institutes of Health. Pathways to prevention: the role of opioids in the treatment of chronic pain. September 29–30, 2014. Executive summary: final report. Accessed 10 Sep 2015 at https://prevention.nih.gov/docs/programs/p2p/ODPPainPanelStatementFinal_10-02-14.pdf.
23. Miaskowski C, Dodd MJ, West C, et al. Lack of adherence with the analgesic regimen: A significant barrier to effective cancer pain management. J Clin Oncol 2001;19:4275–79.
24. Yoong J, Traeger LN, Gallagher ER, et al. A pilot study to investigate adherence to long-acting opioids among patients with advanced lung cancer. J Palliat Med 2013;16:391–6.
25. Lai YH, Keefe FJ, Sun WZ, et al. Relationship between pain-specific beliefs and adherence to analgesic regimens in Taiwanese cancer patients: A preliminary study. J Pain Symptom Manage 2002;24:415–22.
26. Cohen MZ, Musgrave CF, McGuire DB, et al. The cancer pain experience of Israeli adults 65 years and older: the influence of pain interference, symptom severity, and knowledge and attitudes on pain and pain control. Support Care Cancer 2005;13:708–14.
27. Bennett MI, Bagnall AM, Jose Closs S. How effective are patient-based educational interventions in the management of cancer pain? Systematic review and meta analysis. Pain 2009;143:192–9.
28. Oldenmenger WH, Sillevis Smitt PA, van Dooren S, et al. A systematic review on barriers hindering adequate cancer pain management and interventions to reduce them: a critical appraisal. Eur J Cancer 2009;45:1370–80.
29. Meghani SH, Chittams J. Controlling for socioeconomic status in pain disparities research: all-else-equal analysis when “all else” is not equal. Pain Med 2015;16:2222–5.
30. Meghani SH, Chittams J, Hanlon A, Curry J. Measuring preferences for analgesic treatment for cancer pain: how do African Americans and whites perform on choice-based conjoint analysis experiments? BMC Med Inform Decis Mak 2013;13:118.
31. Meghani SH, Kang Y, Chittams J, et al. African Americans with cancer pain are more likely to receive an analgesic with toxic metabolite despite clinical risks: a mediation analysis study. J Clin Oncol 2014;32:2773–9.
32. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids forchronic pain - United States, 2016. MMWR Recomm Rep 2016 Mar 18;65:1–49.
33. Chapman CR, Lipschitz DL, Angst MS, et al. Opioid pharmacotherapy for chronic non-cancer pain in the United States: a research guideline for developing an evidence-base. J Pain 2010;11:807–29.
A Talking Map for Family Meetings in the Intensive Care Unit
From the Department of Neurology, Duke University Medical Center, Durham, NC (Dr. McFarlin), the Department of Psychosocial Oncology and Palliative Care, Dana-Farber Cancer Institute, Boston, MA (Dr. Tulsky), Harborview Medical Center, University of Washington, Seattle, WA (Dr. Back), and Department of Medicine, University of Pittsburgh, Pittsburgh, PA (Dr. Arnold).
Abstract
- Objective: To describe the use of a cognitive map for navigating family meetings with surrogate decision makers of patients in an intensive care unit.
- Methods: Descriptive report and discussion using an illustrative case to outline the steps in the cognitive map.
- Results: The use of cognitive maps has improved the ability of physicians to efficiently perform a specific communication skill. During a “goals of care” conversation, the cognitive map follows these steps: (1) Gather the clinical team for a pre-meeting, (2) Introduce everyone, (3) Use the “ask-tell-ask” strategy to communicate information, (4) Respond to emotion, (5) Highlight the patient’s voice, (6) Plan next steps, (7) Reflect on the meeting with the team. Providing this map of key communication skills will help faculty teach learners the core components of a family meeting.
- Conclusion: Practicing the behaviors demonstrated in the cognitive map may increase clinician skill during difficult conversations. Improving communication with surrogate decision makers will increase the support we offer to critically ill patients and their loved ones.
Key words: intensive care unit; communication; family meeting; critical illness; decision making; end of life care.
Family members of patients in the ICU value high-quality communication with the medical team. In fact, family members report that physicians’ communication skills are often more important than their medical skills [1]. Multiple professional societies, including the American Thoracic Society and the Society of Critical Care Medicine, define communication with families as a key component of high-quality critical care. Effective physician-patient communication improves measureable outcomes including decreased ICU length of stay [2] and may reduce distress amongst patients’ families [3]. The American College of Chest Physicians position statement on Palliative and End-of-Life Care for Patients with Cardiopulmonary Diseases urges physicians to develop curricula that incorporate interpersonal communication skills into training [4].
Unfortunately, such high-quality communication is not the norm. Surrogate decision makers are often displeased with the frequency of communication, the limited availability of attending physicians, and report feeling excluded from discussions [5]. When family meetings do occur, surrogate decision makers report inadequate understanding of diagnosis, prognosis, and treatment plans [6].
Physicians also find family meetings difficult. Intensivists worry that high-quality family meetings are time consuming and difficult to do in a busy ICU [7]. Critical care fellows report not feeling adequately trained to conduct family meetings [8]. It makes sense that untrained clinicians would want to avoid a conversation that is emotionally charged, particularly if one is unsure how to respond effectively.
The Case of Mr. A
Thomas A. is a 79-year-old man admitted to the medical intensive care unit 7 days earlier with a large left middle cerebral artery territory infarction. Given his decreased mental status, on admission he was intubated for airway protection. He is awake but aphasic and unable to follow any commands or move his right side. The neurology consultants do not feel this will improve. He has significant secretions and episodes of hypoxia. He has also developed acute on chronic kidney injury and may need to start dialysis. The social worker explains that his need for dialysis limits his placement options and that he will not be able to be discharged to home. Given his lack of improvement the team is concerned he will need a tracheostomy and feeding tube placed in order to safely continue this level of care. A family meeting is arranged to understand Mr. A’s goals of care.
Talking Map Basics
Before each step is discussed in detail, some definitions are needed. “Family” can be defined as anyone important enough, biologically related or not, to be present at a conversation with a clinician [10]. Second, a “family meeting” is a planned event between the family and interdisciplinary members of the ICU team as well as any other health care providers who have been involved in the patient’s care. The meeting takes place in a private space and at a time that is scheduled with the families’ needs in mind. Thus it is different from having families present on rounds or one-off meetings with particular clinicians.
Goals of care meetings are typically held when, in the clinicians’ view, the current treatments are not achieving the previously stated goals. Thus, the meeting has 2 purposes: first, to give the family the bad news that the current plan is not working and second, to develop a new plan based on the patient’s values. The family’s job, as surrogate decision maker, is to provide information about what would be most important to the patient. The clinician’s job is to suggest treatment plans that have the best probability of matching the patient’s values.
Not all of these tasks need be done at once. Some families will not be able to move from hearing bad news to making a decision without having time to first reflect and grieve. Others will need to confer with other family members privately before deciding on a plan. In many cases, a time-limited trial may be the right option with a plan for subsequent meetings. Given this, we recommend checking in with the family between each step to ensure that they feel safe moving ahead. For example, one might ask “Is it OK if we talk about what happens next?”
Talking Map Steps in Detail
1. Gather the Clinical Team for a Pre-Meeting
ICU care involves a large interdisciplinary care team. A “meeting before the meeting” with the entire clinical team is an opportunity to reach consensus on prognosis and therapeutic options, share prior interactions with family, and determine goals for the family meeting. It is also helpful to clarify team members’ roles at the meeting and to choose a primary facilitator. All of this helps to ensure that the family receives a consistent message during the meeting. The pre-meeting is also an opportunity to ask a team member to observe the communication skills of the facilitator and be prepared to give feedback after the meeting.
At this time, the team should also create the proper environment for the family meeting. This includes a quiet room free of interruptions with ample seating, available tissues, and transferred pagers and cell phones.
The intensivist and bedside nurse should always be present at the family meeting, and it is best when the same attending can be at subsequent family meetings Their consistent dual presence provides the uniform communication from the team, can reduce anxiety in family members and the collaboration reduces ICU nurse and physician burnout [11]. For illnesses that involve a specific disease or organ system, it is important to have the specialist at the meeting who can provide the appropriate expertise.
The Pre-Meeting
A family meeting was scheduled in the family meeting room for 3 pm, after morning rounds. Thirty minutes prior to the meeting the medical team, including the MICU intensivist, the bedside nurse, the neurology attending who has been involved in the care, the case manager and 2 residents sat to discuss Mr. A’s care. The neurology team confirmed that this stroke was considered very large and would result in a level of disability that could only be cared for in a nursing home and would require both a tracheostomy and feeding tube for safe care. The bedside nurse relayed that the family had asked if Mr. A. would ever recover enough to get back to his home. The neurology team shared they did not expect much improvement at all. Given the worsening renal failure and need for dialysis the case manager reminded the team that Mr. A’s nursing home placements were limited. The team decided that the intensivist would lead the meeting as she had updated various family members on rounds for the past 4 days and would be on service for another week. The team decided that their goal for the meeting was to make sure the family understands that Mr. A’s several medical illnesses portend a poor prognosis. They recognized this may be breaking bad news to the family. They also wanted to better understand what Mr. A would have thought given this situation. The residents were asked to watch for the family’s responses when the team delivered the news.
2. Introduce Everyone
Each meeting should start with formal introductions. Even if most providers know most family members it is a polite way to start the meeting. Introducing each family member present and how they know the patient provides insight into how the family is constructed and makes decisions. For example, the entire family may defer to the daughter who introduces herself as a nurse. In other situations, although there is one legal decision maker, the family may explain that they make decisions by consensus.
Each member of the treating team should also introduce themselves. Even if the clinician has been working with the family, it is polite to be formal and give your name and role. Given the number of people the family sees every day, one should not assume that the family remembers all of the clinicians.
In teaching hospitals, providers should also help the family understand their level of training. Surrogates do not always understand the different roles or level of training between students, residents and fellows, advanced practice providers, consultants and their attending physicians. Uncertainty about the roles can lead to family members feeling as though they are receiving contradictory information. Family satisfaction decreases when multiple attending physicians are involved in a patient’s care [12]. When possible, a consistent presence among providers at family meetings is always best.
3. Ask the Family's Understanding of the Situation (Ask-Tell-Ask)
Asking the family to explain the situation in their own language reveals how well they understand the medical facts and helps the medical team determine what information will be most helpful to the family. An opening statement might be “We have all seen your dad and talked to many of his providers. It would help us all be on the same page if you can you tell me what the doctors are telling you?” Starting with the family’s understanding builds trust with the medical team as it creates an opportunity for the family to lead the meeting and indicates that the team is available to listen to their concerns. Asking surrogates for their understanding allows them to tell their story and not hear a reiteration of things they already know. Providing time for the family to share their perspective of the care elicits family’s concerns.
In a large meeting, ensure that all members of the family have an opportunity to communicate their concerns. Does a particular person do all of the talking? Are there individuals that do not speak at all? One way to further understand unspoken concerns during the meeting is to ask “I notice you have been quiet, what questions do you have that I can answer?” There may be several rounds of “asking” in order to ensure all the family members’ concerns are heard. Letting the family tell what they have heard helps the clinicians get a better idea of their health literacy. Do they explain information using technical data or jargon? Finally, as the family talks the clinicians can determine how surprising the “serious news” will be to them. For example, if the family says they know their dad is doing much worse and may die, the information to be delivered can be truncated. However if family incorrectly thinks their dad is doing better or is uncertain they will be much more surprised by the serious news.
After providing time for the family to express their understanding, tell them the information the team needs to communicate. When delivering serious news it is important to focus on the key 1 to 2 points you want the family to take away from the meeting. Typically when health care professionals talk to each other, they talk about every medical detail. Families find this amount of information overwhelming and are not sure what is most important, asking “So what does that mean?” Focusing on the “headline” helps the family focus on what you think the most important piece of information is. Studies suggest that what families most want to know is what the information means for the patient’s future and what treatments are possible. After delivering the new information, stop to allow the family space to think about what you said. If you are giving serious news, you will know they have heard what you said as they will get emotional (see next step).
Checking for understanding is the final “ask” in Ask-Tell-Ask. Begin by asking “What questions do you have?” Data in primary care has shown that patients are more likely to ask questions if you ask “what questions do you have” rather than “do you have any questions?” It is important to continue to ask this question until the family has asked all their questions. Often the family’s tough questions do not come until they get more comfortable and confident in the health care team. In cases where one family member is dominant it might also help to say “What questions do others have?” Next, using techniques like the “teach back” model the physician should check in to see what the family is taking away from the conversation. If a family understands, they can “teach back” the information accurately. This “ask” can be done in a way that does not make the family feel they are being tested: “I am not always clear when I communicate. Do you mind telling me back in your own words what you thought I said so I know we are on the same page?” This also provides an opportunity to answer any new questions that arise. Hearing the information directly from the family can allow the team to clarify any misconceptions and give insight into any emotional responses that the family might have.
4. Respond to Emotion
Discussing serious news in the ICU setting naturally leads to an emotional reaction. The clinician’s ability to notice emotional cues and respond with empathy is a key communication skill in family meetings [13]. Emotional reactions impede individual’s ability to process cognitive information and make it hard to think cognitively about what should be done next.
Physicians miss opportunities to respond to emotion in family meetings [14]. Missed opportunities lead to decreased family satisfaction and may lead to treatment decisions not consistent with the wishes of their loved ones. Empathic responses improve the family-clinician relationship and helps build trust and rapport [15]. Well- placed empathic statements may help surrogates disclose concerns that help the physician better understand the goals and values of the family and patient. Families also can more fully process cognitive information when their emotional responses have been attended to.
Physicians can develop the capacity to recognize and respond to the emotional cues family members are delivering. Intensivists should actively look for the emotions, the empathic opportunity, that are displayed by the family. This emotion is the “data” that will help lead to an empathic response. A family that just received bad news typically responds by showing emotion. Clues that emotions are present include: the family asking the same questions multiple times; using emotional words such as “sad” or “frustrated;” existential questions that do not have a cognitive answer such as “Why did God let this happen?;” or non-verbal cues like tears and hand wringing.
Sometimes the emotional responses are more difficult to recognize. Families may continue to ask for more cognitive information after hearing bad news. Someone keeps asking “Why did his kidney function worsen?” or “I thought the team said the chest x-ray looked better.” It is tempting to start answering these questions with more medical facts. However, if the question comes after bad news, it is usually an expression of frustration or sadness rather than a request for more information. Rather than giving information, it might help to acknowledge this by saying “I imagine this new is overwhelming.”
5. Highlight the Patient’s Voice
Family meetings are often used to develop new treatment plans (given that the old plans are not working). In these situations, it is essential to understand what the incapacitated patient would say if they were part of the family meeting. The surrogate’s primary role is to represent the patient’s voice. To do this, surrogates need assistance in applying their critically ill loved one’s thoughts and values to complex, possibly life limiting, situations. Surrogate decision makers struggle with the decisions’ emotional impact, as well as how to reconcile their desires with their loved one’s wishes [18]. This can lead them to make decisions that conflict with the loved one’s values [19] as well as emotional sequelae such as PTSD and depression [20].
As families reflect on their loved one’s values, conflicting desires will arise. For example, someone may have wanted to live as long as possible and also values independence. Or someone may value their ability to think clearly more than being physically well but would not want to be physically dependent on artificial life support. Exploring which values would be more important can help resolve these conflicts.
Clinicians should check for understanding while family members are identifying the values of their loved ones. Providing the family with a summary of what you have heard will help ensure a more accurate understanding of these crucial issues. A summary statement might be, “It sounds like you are saying your dad really valued his independence. He enjoyed being able to take care of his loved ones and himself. Is that right?”
6. Plan Next Steps
The family meeting serves to attend to family emotion and allow space to elicit patients’ values. Following a family meeting surrogate decision makers may be able to begin to consider the next steps in their loved one’s care. If bad news was delivered they may need space to adjust to a different future than they expected. Using an empathic statement of support “We will continue to make sure we communicate with you as we work together to plan next steps” will reassure a family that they have time and space to plan for the future.
Families vary regarding how much physician input they desire in planning next steps [21]. You can explicitly ask how the team can best help the family with decisions: “Some families like to hear the options for next steps from the team and make a decision, other families like to hear a recommendation from the team. What would be the most helpful for you?” Throughout the course of an illness a surrogate’s preference for decision making may change and clinicians should be responsive to those changing needs.
If the surrogate wants a clinician’s recommendation, 3 points are worth stressing. First, the recommendation should be personalized to this patient and his values. The goal is to reveal how the understanding of the patient’s values led to the treatment plan offered. Second, the recommendation should focus primarily on what will be done to achieve the patient’s values. Focusing on what the clinicians will do may help the family feel that the clinicians are still “trying” and not abandoning their loved one. In this case, the team will continue medical care that will help the patient regain/maintain independence. Only after talking about what will be done should the clinician point out that certain interventions will not achieve the patient’s goals and thus will not be done:
“It sounds like your father really valued his independence and that this illness has really taken that away. Knowing this, would it be helpful for me to make a recommendation for next steps?” “I think we should continue providing excellent medical care for your father in hopes he can get better and go home. One the other hand, if he gets worse, we should not use therapies such as CPR or dialysis that are unlikely to help him regain his independence.”
Finally, be concrete when planning next steps. If a time-limited trial of a therapy is proposed, make sure the family understands what a successful and unsuccessful trial will look like. Make plans to meet again on a specific date in order to ensure the family understands the progress being made. If a transition to comfort care is agreed upon, ensure support of the entire family during the next hours to days and offer services such as chaplaincy or child life specialists.
A family may not agree with the recommendation and back and forth discussion can help create a plan that is in line with their understanding of the illness. Rather than convincing, a clinician should keep an open mind about why they and the surrogate disagree. Do they have different views about the patient’s future? Did the medical team misunderstand the patient’s values? Are there emotional factors that inhibit the surrogate’s ability to attend to the discussion? It is only by learning where the disagreement is that a clinician can move the conversation forward.
A surrogate may ask about a therapy that is not beneficial or may increase distress to the patient. The use of “I wish” or “I worry” statements can be helpful at these points. These specific phrases recognize the surrogate’s desire to do more but also imply that the therapies are not helpful.
“I wish that his ability to communicate and tell you what he wants would get better with a little more time as well.”
“I worry that waiting 2 more weeks for improvement will actually cause complications to occur.”
7. Reflect
Family meetings have an impact on both the family and the medical team. Following the meeting, a short debriefing with the clinical team can be helpful. Summarizing the events of the meeting ensures clarity about the treatment plan going forward. It provides team members a chance to discuss conflicts that may have arisen. It allows the participants in the meeting to reflect on what communication skills they used and how they can improve their skills going forward.
Conclusion
Family meetings with surrogate decision makers must navigate multiple agendas of the family and providers. The goal of excellent communication with surrogates in an ICU should be to understand the patient’s goals and values and seek to make treatment plans that align with their perspective. This talking map provides a conceptual framework for physicians to guide a family through these conversations. The framework creates an opportunity to focus on the patient’s values and preferences for care while allowing space to attend to emotional responses to reduce the distress inherent in surrogate decision-making. Practicing the behaviors demonstrated in the talking map may increase clinician skill during difficult conversations. Improving communication with surrogate decision makers will increase the support we offer to critically ill patients and their loved ones.
Corresponding author: Jessica McFarlin, MD, [email protected].
Funding/support: Dr. Arnold receives support though the Leo H. Criep Chair in Patient Care.
Financial disclosures: None.
1. Hickey M. What are the needs of families of critically ill patients? A review of the literature since 1976. Heart Lung 1990;19:401–15.
2. Mosenthal AC, Murphy PA, Barker LK, et al. Changing culture around end-of-life care in the trauma intensive care unit. J Trauma 2008;64:1587–93.
3. Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 2007;356:469–78.
4. Selecky PA, Eliasson AH, Hall RI, et al. Palliative and end-of-life care for patients with cardiopulmonary diseases. Chest 2005;128:3599–610.
5. Henrich NJ, Dodek P, Heyland D, et al. Qualitative analysis of an intensive care unit family satisfaction survey. Crit Care Med 2011;39:1000–5.
6. Azoulet E, Chevret S, Leleu G, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med 2000;28:3044–9.
7. Curtis JR. Communicating about end-of-life care with patients and families in the intensive care unit. Crit Care Clin 2004;20:363–80.
8. Hope AA, Hsieh SJ, Howes JM, et al. Let’s talk critical. Development and evaluation of a communication skills training program for critical care fellows. Ann Am Thorac Soc 2015;12:505–11.
9. Back AL, Arnold RM, Baile WF, et al. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 2007;167:453–60.
10. Vital Talk. Conduct a family conference. Accessed 27 June 2016 at www.vitaltalk.org/clinicians/family.
11. Kramer M, Schmalenberg C. Securing “good” nurse/physician relationships. Nurs Manage 2003;34:34–8.
12. Johnson D, Wilson M, Cavanaugh B, et al. Measuring the ability to meet family needs in an intensive care unit. Crit Care Med 1998;26:266–71.
13. Back AL, Arnold RM. “Isn’t there anything more you can do?’’: when empathic statements work, and when they don’t. J Palliat Med 2013;16:1429–32.
14. Curtis JR, Engelberg RA, Wenrich MD. Missed opportunities during family conferences about end-of-life care in the intensive care unit. Am J Respir Crit Care Med 2005;171:844–9.
15. Pollak KI, Arnold RM, Jeffreys AS, et al. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol 2007;36:5748–52.
16. Back AL, Arnold RM, Tulsky JA. Mastering communication with seriously ill patients: balancing honesty with empathy and hope. Cambridge: Cambridge University Press; 2009.
17. Back AL, Arnold RM, Baile WF, et al. Approaching difficult communication tasks in oncology. CA Cancer J Clin 2005;55:164–77.
18. Schenker Y, White D, Crowley-Matoka M, et al. “It hurts to know…and it helps”: exploring how surrogates in the ICU cope with prognostic information. J Palliat Med 2013;16:243–9.
19. Scheunemann LP, Arnold RM, White DB. The facilitated values history: helping surrogates make authentic decisions for incapacitated patients with advanced illness. Am J Respir Crit Care Med 2012;186:480–6.
20. Azoulay E, Pochard F, Kentish-Barnes N, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 2005;171:987–94.
21. White DB, Braddock CH, Bereknyei et al. Toward shared decision making at the end of life in intensive care units: opportunities for improvement. Arch Intern Med 2007;167:461–7.
From the Department of Neurology, Duke University Medical Center, Durham, NC (Dr. McFarlin), the Department of Psychosocial Oncology and Palliative Care, Dana-Farber Cancer Institute, Boston, MA (Dr. Tulsky), Harborview Medical Center, University of Washington, Seattle, WA (Dr. Back), and Department of Medicine, University of Pittsburgh, Pittsburgh, PA (Dr. Arnold).
Abstract
- Objective: To describe the use of a cognitive map for navigating family meetings with surrogate decision makers of patients in an intensive care unit.
- Methods: Descriptive report and discussion using an illustrative case to outline the steps in the cognitive map.
- Results: The use of cognitive maps has improved the ability of physicians to efficiently perform a specific communication skill. During a “goals of care” conversation, the cognitive map follows these steps: (1) Gather the clinical team for a pre-meeting, (2) Introduce everyone, (3) Use the “ask-tell-ask” strategy to communicate information, (4) Respond to emotion, (5) Highlight the patient’s voice, (6) Plan next steps, (7) Reflect on the meeting with the team. Providing this map of key communication skills will help faculty teach learners the core components of a family meeting.
- Conclusion: Practicing the behaviors demonstrated in the cognitive map may increase clinician skill during difficult conversations. Improving communication with surrogate decision makers will increase the support we offer to critically ill patients and their loved ones.
Key words: intensive care unit; communication; family meeting; critical illness; decision making; end of life care.
Family members of patients in the ICU value high-quality communication with the medical team. In fact, family members report that physicians’ communication skills are often more important than their medical skills [1]. Multiple professional societies, including the American Thoracic Society and the Society of Critical Care Medicine, define communication with families as a key component of high-quality critical care. Effective physician-patient communication improves measureable outcomes including decreased ICU length of stay [2] and may reduce distress amongst patients’ families [3]. The American College of Chest Physicians position statement on Palliative and End-of-Life Care for Patients with Cardiopulmonary Diseases urges physicians to develop curricula that incorporate interpersonal communication skills into training [4].
Unfortunately, such high-quality communication is not the norm. Surrogate decision makers are often displeased with the frequency of communication, the limited availability of attending physicians, and report feeling excluded from discussions [5]. When family meetings do occur, surrogate decision makers report inadequate understanding of diagnosis, prognosis, and treatment plans [6].
Physicians also find family meetings difficult. Intensivists worry that high-quality family meetings are time consuming and difficult to do in a busy ICU [7]. Critical care fellows report not feeling adequately trained to conduct family meetings [8]. It makes sense that untrained clinicians would want to avoid a conversation that is emotionally charged, particularly if one is unsure how to respond effectively.
The Case of Mr. A
Thomas A. is a 79-year-old man admitted to the medical intensive care unit 7 days earlier with a large left middle cerebral artery territory infarction. Given his decreased mental status, on admission he was intubated for airway protection. He is awake but aphasic and unable to follow any commands or move his right side. The neurology consultants do not feel this will improve. He has significant secretions and episodes of hypoxia. He has also developed acute on chronic kidney injury and may need to start dialysis. The social worker explains that his need for dialysis limits his placement options and that he will not be able to be discharged to home. Given his lack of improvement the team is concerned he will need a tracheostomy and feeding tube placed in order to safely continue this level of care. A family meeting is arranged to understand Mr. A’s goals of care.
Talking Map Basics
Before each step is discussed in detail, some definitions are needed. “Family” can be defined as anyone important enough, biologically related or not, to be present at a conversation with a clinician [10]. Second, a “family meeting” is a planned event between the family and interdisciplinary members of the ICU team as well as any other health care providers who have been involved in the patient’s care. The meeting takes place in a private space and at a time that is scheduled with the families’ needs in mind. Thus it is different from having families present on rounds or one-off meetings with particular clinicians.
Goals of care meetings are typically held when, in the clinicians’ view, the current treatments are not achieving the previously stated goals. Thus, the meeting has 2 purposes: first, to give the family the bad news that the current plan is not working and second, to develop a new plan based on the patient’s values. The family’s job, as surrogate decision maker, is to provide information about what would be most important to the patient. The clinician’s job is to suggest treatment plans that have the best probability of matching the patient’s values.
Not all of these tasks need be done at once. Some families will not be able to move from hearing bad news to making a decision without having time to first reflect and grieve. Others will need to confer with other family members privately before deciding on a plan. In many cases, a time-limited trial may be the right option with a plan for subsequent meetings. Given this, we recommend checking in with the family between each step to ensure that they feel safe moving ahead. For example, one might ask “Is it OK if we talk about what happens next?”
Talking Map Steps in Detail
1. Gather the Clinical Team for a Pre-Meeting
ICU care involves a large interdisciplinary care team. A “meeting before the meeting” with the entire clinical team is an opportunity to reach consensus on prognosis and therapeutic options, share prior interactions with family, and determine goals for the family meeting. It is also helpful to clarify team members’ roles at the meeting and to choose a primary facilitator. All of this helps to ensure that the family receives a consistent message during the meeting. The pre-meeting is also an opportunity to ask a team member to observe the communication skills of the facilitator and be prepared to give feedback after the meeting.
At this time, the team should also create the proper environment for the family meeting. This includes a quiet room free of interruptions with ample seating, available tissues, and transferred pagers and cell phones.
The intensivist and bedside nurse should always be present at the family meeting, and it is best when the same attending can be at subsequent family meetings Their consistent dual presence provides the uniform communication from the team, can reduce anxiety in family members and the collaboration reduces ICU nurse and physician burnout [11]. For illnesses that involve a specific disease or organ system, it is important to have the specialist at the meeting who can provide the appropriate expertise.
The Pre-Meeting
A family meeting was scheduled in the family meeting room for 3 pm, after morning rounds. Thirty minutes prior to the meeting the medical team, including the MICU intensivist, the bedside nurse, the neurology attending who has been involved in the care, the case manager and 2 residents sat to discuss Mr. A’s care. The neurology team confirmed that this stroke was considered very large and would result in a level of disability that could only be cared for in a nursing home and would require both a tracheostomy and feeding tube for safe care. The bedside nurse relayed that the family had asked if Mr. A. would ever recover enough to get back to his home. The neurology team shared they did not expect much improvement at all. Given the worsening renal failure and need for dialysis the case manager reminded the team that Mr. A’s nursing home placements were limited. The team decided that the intensivist would lead the meeting as she had updated various family members on rounds for the past 4 days and would be on service for another week. The team decided that their goal for the meeting was to make sure the family understands that Mr. A’s several medical illnesses portend a poor prognosis. They recognized this may be breaking bad news to the family. They also wanted to better understand what Mr. A would have thought given this situation. The residents were asked to watch for the family’s responses when the team delivered the news.
2. Introduce Everyone
Each meeting should start with formal introductions. Even if most providers know most family members it is a polite way to start the meeting. Introducing each family member present and how they know the patient provides insight into how the family is constructed and makes decisions. For example, the entire family may defer to the daughter who introduces herself as a nurse. In other situations, although there is one legal decision maker, the family may explain that they make decisions by consensus.
Each member of the treating team should also introduce themselves. Even if the clinician has been working with the family, it is polite to be formal and give your name and role. Given the number of people the family sees every day, one should not assume that the family remembers all of the clinicians.
In teaching hospitals, providers should also help the family understand their level of training. Surrogates do not always understand the different roles or level of training between students, residents and fellows, advanced practice providers, consultants and their attending physicians. Uncertainty about the roles can lead to family members feeling as though they are receiving contradictory information. Family satisfaction decreases when multiple attending physicians are involved in a patient’s care [12]. When possible, a consistent presence among providers at family meetings is always best.
3. Ask the Family's Understanding of the Situation (Ask-Tell-Ask)
Asking the family to explain the situation in their own language reveals how well they understand the medical facts and helps the medical team determine what information will be most helpful to the family. An opening statement might be “We have all seen your dad and talked to many of his providers. It would help us all be on the same page if you can you tell me what the doctors are telling you?” Starting with the family’s understanding builds trust with the medical team as it creates an opportunity for the family to lead the meeting and indicates that the team is available to listen to their concerns. Asking surrogates for their understanding allows them to tell their story and not hear a reiteration of things they already know. Providing time for the family to share their perspective of the care elicits family’s concerns.
In a large meeting, ensure that all members of the family have an opportunity to communicate their concerns. Does a particular person do all of the talking? Are there individuals that do not speak at all? One way to further understand unspoken concerns during the meeting is to ask “I notice you have been quiet, what questions do you have that I can answer?” There may be several rounds of “asking” in order to ensure all the family members’ concerns are heard. Letting the family tell what they have heard helps the clinicians get a better idea of their health literacy. Do they explain information using technical data or jargon? Finally, as the family talks the clinicians can determine how surprising the “serious news” will be to them. For example, if the family says they know their dad is doing much worse and may die, the information to be delivered can be truncated. However if family incorrectly thinks their dad is doing better or is uncertain they will be much more surprised by the serious news.
After providing time for the family to express their understanding, tell them the information the team needs to communicate. When delivering serious news it is important to focus on the key 1 to 2 points you want the family to take away from the meeting. Typically when health care professionals talk to each other, they talk about every medical detail. Families find this amount of information overwhelming and are not sure what is most important, asking “So what does that mean?” Focusing on the “headline” helps the family focus on what you think the most important piece of information is. Studies suggest that what families most want to know is what the information means for the patient’s future and what treatments are possible. After delivering the new information, stop to allow the family space to think about what you said. If you are giving serious news, you will know they have heard what you said as they will get emotional (see next step).
Checking for understanding is the final “ask” in Ask-Tell-Ask. Begin by asking “What questions do you have?” Data in primary care has shown that patients are more likely to ask questions if you ask “what questions do you have” rather than “do you have any questions?” It is important to continue to ask this question until the family has asked all their questions. Often the family’s tough questions do not come until they get more comfortable and confident in the health care team. In cases where one family member is dominant it might also help to say “What questions do others have?” Next, using techniques like the “teach back” model the physician should check in to see what the family is taking away from the conversation. If a family understands, they can “teach back” the information accurately. This “ask” can be done in a way that does not make the family feel they are being tested: “I am not always clear when I communicate. Do you mind telling me back in your own words what you thought I said so I know we are on the same page?” This also provides an opportunity to answer any new questions that arise. Hearing the information directly from the family can allow the team to clarify any misconceptions and give insight into any emotional responses that the family might have.
4. Respond to Emotion
Discussing serious news in the ICU setting naturally leads to an emotional reaction. The clinician’s ability to notice emotional cues and respond with empathy is a key communication skill in family meetings [13]. Emotional reactions impede individual’s ability to process cognitive information and make it hard to think cognitively about what should be done next.
Physicians miss opportunities to respond to emotion in family meetings [14]. Missed opportunities lead to decreased family satisfaction and may lead to treatment decisions not consistent with the wishes of their loved ones. Empathic responses improve the family-clinician relationship and helps build trust and rapport [15]. Well- placed empathic statements may help surrogates disclose concerns that help the physician better understand the goals and values of the family and patient. Families also can more fully process cognitive information when their emotional responses have been attended to.
Physicians can develop the capacity to recognize and respond to the emotional cues family members are delivering. Intensivists should actively look for the emotions, the empathic opportunity, that are displayed by the family. This emotion is the “data” that will help lead to an empathic response. A family that just received bad news typically responds by showing emotion. Clues that emotions are present include: the family asking the same questions multiple times; using emotional words such as “sad” or “frustrated;” existential questions that do not have a cognitive answer such as “Why did God let this happen?;” or non-verbal cues like tears and hand wringing.
Sometimes the emotional responses are more difficult to recognize. Families may continue to ask for more cognitive information after hearing bad news. Someone keeps asking “Why did his kidney function worsen?” or “I thought the team said the chest x-ray looked better.” It is tempting to start answering these questions with more medical facts. However, if the question comes after bad news, it is usually an expression of frustration or sadness rather than a request for more information. Rather than giving information, it might help to acknowledge this by saying “I imagine this new is overwhelming.”
5. Highlight the Patient’s Voice
Family meetings are often used to develop new treatment plans (given that the old plans are not working). In these situations, it is essential to understand what the incapacitated patient would say if they were part of the family meeting. The surrogate’s primary role is to represent the patient’s voice. To do this, surrogates need assistance in applying their critically ill loved one’s thoughts and values to complex, possibly life limiting, situations. Surrogate decision makers struggle with the decisions’ emotional impact, as well as how to reconcile their desires with their loved one’s wishes [18]. This can lead them to make decisions that conflict with the loved one’s values [19] as well as emotional sequelae such as PTSD and depression [20].
As families reflect on their loved one’s values, conflicting desires will arise. For example, someone may have wanted to live as long as possible and also values independence. Or someone may value their ability to think clearly more than being physically well but would not want to be physically dependent on artificial life support. Exploring which values would be more important can help resolve these conflicts.
Clinicians should check for understanding while family members are identifying the values of their loved ones. Providing the family with a summary of what you have heard will help ensure a more accurate understanding of these crucial issues. A summary statement might be, “It sounds like you are saying your dad really valued his independence. He enjoyed being able to take care of his loved ones and himself. Is that right?”
6. Plan Next Steps
The family meeting serves to attend to family emotion and allow space to elicit patients’ values. Following a family meeting surrogate decision makers may be able to begin to consider the next steps in their loved one’s care. If bad news was delivered they may need space to adjust to a different future than they expected. Using an empathic statement of support “We will continue to make sure we communicate with you as we work together to plan next steps” will reassure a family that they have time and space to plan for the future.
Families vary regarding how much physician input they desire in planning next steps [21]. You can explicitly ask how the team can best help the family with decisions: “Some families like to hear the options for next steps from the team and make a decision, other families like to hear a recommendation from the team. What would be the most helpful for you?” Throughout the course of an illness a surrogate’s preference for decision making may change and clinicians should be responsive to those changing needs.
If the surrogate wants a clinician’s recommendation, 3 points are worth stressing. First, the recommendation should be personalized to this patient and his values. The goal is to reveal how the understanding of the patient’s values led to the treatment plan offered. Second, the recommendation should focus primarily on what will be done to achieve the patient’s values. Focusing on what the clinicians will do may help the family feel that the clinicians are still “trying” and not abandoning their loved one. In this case, the team will continue medical care that will help the patient regain/maintain independence. Only after talking about what will be done should the clinician point out that certain interventions will not achieve the patient’s goals and thus will not be done:
“It sounds like your father really valued his independence and that this illness has really taken that away. Knowing this, would it be helpful for me to make a recommendation for next steps?” “I think we should continue providing excellent medical care for your father in hopes he can get better and go home. One the other hand, if he gets worse, we should not use therapies such as CPR or dialysis that are unlikely to help him regain his independence.”
Finally, be concrete when planning next steps. If a time-limited trial of a therapy is proposed, make sure the family understands what a successful and unsuccessful trial will look like. Make plans to meet again on a specific date in order to ensure the family understands the progress being made. If a transition to comfort care is agreed upon, ensure support of the entire family during the next hours to days and offer services such as chaplaincy or child life specialists.
A family may not agree with the recommendation and back and forth discussion can help create a plan that is in line with their understanding of the illness. Rather than convincing, a clinician should keep an open mind about why they and the surrogate disagree. Do they have different views about the patient’s future? Did the medical team misunderstand the patient’s values? Are there emotional factors that inhibit the surrogate’s ability to attend to the discussion? It is only by learning where the disagreement is that a clinician can move the conversation forward.
A surrogate may ask about a therapy that is not beneficial or may increase distress to the patient. The use of “I wish” or “I worry” statements can be helpful at these points. These specific phrases recognize the surrogate’s desire to do more but also imply that the therapies are not helpful.
“I wish that his ability to communicate and tell you what he wants would get better with a little more time as well.”
“I worry that waiting 2 more weeks for improvement will actually cause complications to occur.”
7. Reflect
Family meetings have an impact on both the family and the medical team. Following the meeting, a short debriefing with the clinical team can be helpful. Summarizing the events of the meeting ensures clarity about the treatment plan going forward. It provides team members a chance to discuss conflicts that may have arisen. It allows the participants in the meeting to reflect on what communication skills they used and how they can improve their skills going forward.
Conclusion
Family meetings with surrogate decision makers must navigate multiple agendas of the family and providers. The goal of excellent communication with surrogates in an ICU should be to understand the patient’s goals and values and seek to make treatment plans that align with their perspective. This talking map provides a conceptual framework for physicians to guide a family through these conversations. The framework creates an opportunity to focus on the patient’s values and preferences for care while allowing space to attend to emotional responses to reduce the distress inherent in surrogate decision-making. Practicing the behaviors demonstrated in the talking map may increase clinician skill during difficult conversations. Improving communication with surrogate decision makers will increase the support we offer to critically ill patients and their loved ones.
Corresponding author: Jessica McFarlin, MD, [email protected].
Funding/support: Dr. Arnold receives support though the Leo H. Criep Chair in Patient Care.
Financial disclosures: None.
From the Department of Neurology, Duke University Medical Center, Durham, NC (Dr. McFarlin), the Department of Psychosocial Oncology and Palliative Care, Dana-Farber Cancer Institute, Boston, MA (Dr. Tulsky), Harborview Medical Center, University of Washington, Seattle, WA (Dr. Back), and Department of Medicine, University of Pittsburgh, Pittsburgh, PA (Dr. Arnold).
Abstract
- Objective: To describe the use of a cognitive map for navigating family meetings with surrogate decision makers of patients in an intensive care unit.
- Methods: Descriptive report and discussion using an illustrative case to outline the steps in the cognitive map.
- Results: The use of cognitive maps has improved the ability of physicians to efficiently perform a specific communication skill. During a “goals of care” conversation, the cognitive map follows these steps: (1) Gather the clinical team for a pre-meeting, (2) Introduce everyone, (3) Use the “ask-tell-ask” strategy to communicate information, (4) Respond to emotion, (5) Highlight the patient’s voice, (6) Plan next steps, (7) Reflect on the meeting with the team. Providing this map of key communication skills will help faculty teach learners the core components of a family meeting.
- Conclusion: Practicing the behaviors demonstrated in the cognitive map may increase clinician skill during difficult conversations. Improving communication with surrogate decision makers will increase the support we offer to critically ill patients and their loved ones.
Key words: intensive care unit; communication; family meeting; critical illness; decision making; end of life care.
Family members of patients in the ICU value high-quality communication with the medical team. In fact, family members report that physicians’ communication skills are often more important than their medical skills [1]. Multiple professional societies, including the American Thoracic Society and the Society of Critical Care Medicine, define communication with families as a key component of high-quality critical care. Effective physician-patient communication improves measureable outcomes including decreased ICU length of stay [2] and may reduce distress amongst patients’ families [3]. The American College of Chest Physicians position statement on Palliative and End-of-Life Care for Patients with Cardiopulmonary Diseases urges physicians to develop curricula that incorporate interpersonal communication skills into training [4].
Unfortunately, such high-quality communication is not the norm. Surrogate decision makers are often displeased with the frequency of communication, the limited availability of attending physicians, and report feeling excluded from discussions [5]. When family meetings do occur, surrogate decision makers report inadequate understanding of diagnosis, prognosis, and treatment plans [6].
Physicians also find family meetings difficult. Intensivists worry that high-quality family meetings are time consuming and difficult to do in a busy ICU [7]. Critical care fellows report not feeling adequately trained to conduct family meetings [8]. It makes sense that untrained clinicians would want to avoid a conversation that is emotionally charged, particularly if one is unsure how to respond effectively.
The Case of Mr. A
Thomas A. is a 79-year-old man admitted to the medical intensive care unit 7 days earlier with a large left middle cerebral artery territory infarction. Given his decreased mental status, on admission he was intubated for airway protection. He is awake but aphasic and unable to follow any commands or move his right side. The neurology consultants do not feel this will improve. He has significant secretions and episodes of hypoxia. He has also developed acute on chronic kidney injury and may need to start dialysis. The social worker explains that his need for dialysis limits his placement options and that he will not be able to be discharged to home. Given his lack of improvement the team is concerned he will need a tracheostomy and feeding tube placed in order to safely continue this level of care. A family meeting is arranged to understand Mr. A’s goals of care.
Talking Map Basics
Before each step is discussed in detail, some definitions are needed. “Family” can be defined as anyone important enough, biologically related or not, to be present at a conversation with a clinician [10]. Second, a “family meeting” is a planned event between the family and interdisciplinary members of the ICU team as well as any other health care providers who have been involved in the patient’s care. The meeting takes place in a private space and at a time that is scheduled with the families’ needs in mind. Thus it is different from having families present on rounds or one-off meetings with particular clinicians.
Goals of care meetings are typically held when, in the clinicians’ view, the current treatments are not achieving the previously stated goals. Thus, the meeting has 2 purposes: first, to give the family the bad news that the current plan is not working and second, to develop a new plan based on the patient’s values. The family’s job, as surrogate decision maker, is to provide information about what would be most important to the patient. The clinician’s job is to suggest treatment plans that have the best probability of matching the patient’s values.
Not all of these tasks need be done at once. Some families will not be able to move from hearing bad news to making a decision without having time to first reflect and grieve. Others will need to confer with other family members privately before deciding on a plan. In many cases, a time-limited trial may be the right option with a plan for subsequent meetings. Given this, we recommend checking in with the family between each step to ensure that they feel safe moving ahead. For example, one might ask “Is it OK if we talk about what happens next?”
Talking Map Steps in Detail
1. Gather the Clinical Team for a Pre-Meeting
ICU care involves a large interdisciplinary care team. A “meeting before the meeting” with the entire clinical team is an opportunity to reach consensus on prognosis and therapeutic options, share prior interactions with family, and determine goals for the family meeting. It is also helpful to clarify team members’ roles at the meeting and to choose a primary facilitator. All of this helps to ensure that the family receives a consistent message during the meeting. The pre-meeting is also an opportunity to ask a team member to observe the communication skills of the facilitator and be prepared to give feedback after the meeting.
At this time, the team should also create the proper environment for the family meeting. This includes a quiet room free of interruptions with ample seating, available tissues, and transferred pagers and cell phones.
The intensivist and bedside nurse should always be present at the family meeting, and it is best when the same attending can be at subsequent family meetings Their consistent dual presence provides the uniform communication from the team, can reduce anxiety in family members and the collaboration reduces ICU nurse and physician burnout [11]. For illnesses that involve a specific disease or organ system, it is important to have the specialist at the meeting who can provide the appropriate expertise.
The Pre-Meeting
A family meeting was scheduled in the family meeting room for 3 pm, after morning rounds. Thirty minutes prior to the meeting the medical team, including the MICU intensivist, the bedside nurse, the neurology attending who has been involved in the care, the case manager and 2 residents sat to discuss Mr. A’s care. The neurology team confirmed that this stroke was considered very large and would result in a level of disability that could only be cared for in a nursing home and would require both a tracheostomy and feeding tube for safe care. The bedside nurse relayed that the family had asked if Mr. A. would ever recover enough to get back to his home. The neurology team shared they did not expect much improvement at all. Given the worsening renal failure and need for dialysis the case manager reminded the team that Mr. A’s nursing home placements were limited. The team decided that the intensivist would lead the meeting as she had updated various family members on rounds for the past 4 days and would be on service for another week. The team decided that their goal for the meeting was to make sure the family understands that Mr. A’s several medical illnesses portend a poor prognosis. They recognized this may be breaking bad news to the family. They also wanted to better understand what Mr. A would have thought given this situation. The residents were asked to watch for the family’s responses when the team delivered the news.
2. Introduce Everyone
Each meeting should start with formal introductions. Even if most providers know most family members it is a polite way to start the meeting. Introducing each family member present and how they know the patient provides insight into how the family is constructed and makes decisions. For example, the entire family may defer to the daughter who introduces herself as a nurse. In other situations, although there is one legal decision maker, the family may explain that they make decisions by consensus.
Each member of the treating team should also introduce themselves. Even if the clinician has been working with the family, it is polite to be formal and give your name and role. Given the number of people the family sees every day, one should not assume that the family remembers all of the clinicians.
In teaching hospitals, providers should also help the family understand their level of training. Surrogates do not always understand the different roles or level of training between students, residents and fellows, advanced practice providers, consultants and their attending physicians. Uncertainty about the roles can lead to family members feeling as though they are receiving contradictory information. Family satisfaction decreases when multiple attending physicians are involved in a patient’s care [12]. When possible, a consistent presence among providers at family meetings is always best.
3. Ask the Family's Understanding of the Situation (Ask-Tell-Ask)
Asking the family to explain the situation in their own language reveals how well they understand the medical facts and helps the medical team determine what information will be most helpful to the family. An opening statement might be “We have all seen your dad and talked to many of his providers. It would help us all be on the same page if you can you tell me what the doctors are telling you?” Starting with the family’s understanding builds trust with the medical team as it creates an opportunity for the family to lead the meeting and indicates that the team is available to listen to their concerns. Asking surrogates for their understanding allows them to tell their story and not hear a reiteration of things they already know. Providing time for the family to share their perspective of the care elicits family’s concerns.
In a large meeting, ensure that all members of the family have an opportunity to communicate their concerns. Does a particular person do all of the talking? Are there individuals that do not speak at all? One way to further understand unspoken concerns during the meeting is to ask “I notice you have been quiet, what questions do you have that I can answer?” There may be several rounds of “asking” in order to ensure all the family members’ concerns are heard. Letting the family tell what they have heard helps the clinicians get a better idea of their health literacy. Do they explain information using technical data or jargon? Finally, as the family talks the clinicians can determine how surprising the “serious news” will be to them. For example, if the family says they know their dad is doing much worse and may die, the information to be delivered can be truncated. However if family incorrectly thinks their dad is doing better or is uncertain they will be much more surprised by the serious news.
After providing time for the family to express their understanding, tell them the information the team needs to communicate. When delivering serious news it is important to focus on the key 1 to 2 points you want the family to take away from the meeting. Typically when health care professionals talk to each other, they talk about every medical detail. Families find this amount of information overwhelming and are not sure what is most important, asking “So what does that mean?” Focusing on the “headline” helps the family focus on what you think the most important piece of information is. Studies suggest that what families most want to know is what the information means for the patient’s future and what treatments are possible. After delivering the new information, stop to allow the family space to think about what you said. If you are giving serious news, you will know they have heard what you said as they will get emotional (see next step).
Checking for understanding is the final “ask” in Ask-Tell-Ask. Begin by asking “What questions do you have?” Data in primary care has shown that patients are more likely to ask questions if you ask “what questions do you have” rather than “do you have any questions?” It is important to continue to ask this question until the family has asked all their questions. Often the family’s tough questions do not come until they get more comfortable and confident in the health care team. In cases where one family member is dominant it might also help to say “What questions do others have?” Next, using techniques like the “teach back” model the physician should check in to see what the family is taking away from the conversation. If a family understands, they can “teach back” the information accurately. This “ask” can be done in a way that does not make the family feel they are being tested: “I am not always clear when I communicate. Do you mind telling me back in your own words what you thought I said so I know we are on the same page?” This also provides an opportunity to answer any new questions that arise. Hearing the information directly from the family can allow the team to clarify any misconceptions and give insight into any emotional responses that the family might have.
4. Respond to Emotion
Discussing serious news in the ICU setting naturally leads to an emotional reaction. The clinician’s ability to notice emotional cues and respond with empathy is a key communication skill in family meetings [13]. Emotional reactions impede individual’s ability to process cognitive information and make it hard to think cognitively about what should be done next.
Physicians miss opportunities to respond to emotion in family meetings [14]. Missed opportunities lead to decreased family satisfaction and may lead to treatment decisions not consistent with the wishes of their loved ones. Empathic responses improve the family-clinician relationship and helps build trust and rapport [15]. Well- placed empathic statements may help surrogates disclose concerns that help the physician better understand the goals and values of the family and patient. Families also can more fully process cognitive information when their emotional responses have been attended to.
Physicians can develop the capacity to recognize and respond to the emotional cues family members are delivering. Intensivists should actively look for the emotions, the empathic opportunity, that are displayed by the family. This emotion is the “data” that will help lead to an empathic response. A family that just received bad news typically responds by showing emotion. Clues that emotions are present include: the family asking the same questions multiple times; using emotional words such as “sad” or “frustrated;” existential questions that do not have a cognitive answer such as “Why did God let this happen?;” or non-verbal cues like tears and hand wringing.
Sometimes the emotional responses are more difficult to recognize. Families may continue to ask for more cognitive information after hearing bad news. Someone keeps asking “Why did his kidney function worsen?” or “I thought the team said the chest x-ray looked better.” It is tempting to start answering these questions with more medical facts. However, if the question comes after bad news, it is usually an expression of frustration or sadness rather than a request for more information. Rather than giving information, it might help to acknowledge this by saying “I imagine this new is overwhelming.”
5. Highlight the Patient’s Voice
Family meetings are often used to develop new treatment plans (given that the old plans are not working). In these situations, it is essential to understand what the incapacitated patient would say if they were part of the family meeting. The surrogate’s primary role is to represent the patient’s voice. To do this, surrogates need assistance in applying their critically ill loved one’s thoughts and values to complex, possibly life limiting, situations. Surrogate decision makers struggle with the decisions’ emotional impact, as well as how to reconcile their desires with their loved one’s wishes [18]. This can lead them to make decisions that conflict with the loved one’s values [19] as well as emotional sequelae such as PTSD and depression [20].
As families reflect on their loved one’s values, conflicting desires will arise. For example, someone may have wanted to live as long as possible and also values independence. Or someone may value their ability to think clearly more than being physically well but would not want to be physically dependent on artificial life support. Exploring which values would be more important can help resolve these conflicts.
Clinicians should check for understanding while family members are identifying the values of their loved ones. Providing the family with a summary of what you have heard will help ensure a more accurate understanding of these crucial issues. A summary statement might be, “It sounds like you are saying your dad really valued his independence. He enjoyed being able to take care of his loved ones and himself. Is that right?”
6. Plan Next Steps
The family meeting serves to attend to family emotion and allow space to elicit patients’ values. Following a family meeting surrogate decision makers may be able to begin to consider the next steps in their loved one’s care. If bad news was delivered they may need space to adjust to a different future than they expected. Using an empathic statement of support “We will continue to make sure we communicate with you as we work together to plan next steps” will reassure a family that they have time and space to plan for the future.
Families vary regarding how much physician input they desire in planning next steps [21]. You can explicitly ask how the team can best help the family with decisions: “Some families like to hear the options for next steps from the team and make a decision, other families like to hear a recommendation from the team. What would be the most helpful for you?” Throughout the course of an illness a surrogate’s preference for decision making may change and clinicians should be responsive to those changing needs.
If the surrogate wants a clinician’s recommendation, 3 points are worth stressing. First, the recommendation should be personalized to this patient and his values. The goal is to reveal how the understanding of the patient’s values led to the treatment plan offered. Second, the recommendation should focus primarily on what will be done to achieve the patient’s values. Focusing on what the clinicians will do may help the family feel that the clinicians are still “trying” and not abandoning their loved one. In this case, the team will continue medical care that will help the patient regain/maintain independence. Only after talking about what will be done should the clinician point out that certain interventions will not achieve the patient’s goals and thus will not be done:
“It sounds like your father really valued his independence and that this illness has really taken that away. Knowing this, would it be helpful for me to make a recommendation for next steps?” “I think we should continue providing excellent medical care for your father in hopes he can get better and go home. One the other hand, if he gets worse, we should not use therapies such as CPR or dialysis that are unlikely to help him regain his independence.”
Finally, be concrete when planning next steps. If a time-limited trial of a therapy is proposed, make sure the family understands what a successful and unsuccessful trial will look like. Make plans to meet again on a specific date in order to ensure the family understands the progress being made. If a transition to comfort care is agreed upon, ensure support of the entire family during the next hours to days and offer services such as chaplaincy or child life specialists.
A family may not agree with the recommendation and back and forth discussion can help create a plan that is in line with their understanding of the illness. Rather than convincing, a clinician should keep an open mind about why they and the surrogate disagree. Do they have different views about the patient’s future? Did the medical team misunderstand the patient’s values? Are there emotional factors that inhibit the surrogate’s ability to attend to the discussion? It is only by learning where the disagreement is that a clinician can move the conversation forward.
A surrogate may ask about a therapy that is not beneficial or may increase distress to the patient. The use of “I wish” or “I worry” statements can be helpful at these points. These specific phrases recognize the surrogate’s desire to do more but also imply that the therapies are not helpful.
“I wish that his ability to communicate and tell you what he wants would get better with a little more time as well.”
“I worry that waiting 2 more weeks for improvement will actually cause complications to occur.”
7. Reflect
Family meetings have an impact on both the family and the medical team. Following the meeting, a short debriefing with the clinical team can be helpful. Summarizing the events of the meeting ensures clarity about the treatment plan going forward. It provides team members a chance to discuss conflicts that may have arisen. It allows the participants in the meeting to reflect on what communication skills they used and how they can improve their skills going forward.
Conclusion
Family meetings with surrogate decision makers must navigate multiple agendas of the family and providers. The goal of excellent communication with surrogates in an ICU should be to understand the patient’s goals and values and seek to make treatment plans that align with their perspective. This talking map provides a conceptual framework for physicians to guide a family through these conversations. The framework creates an opportunity to focus on the patient’s values and preferences for care while allowing space to attend to emotional responses to reduce the distress inherent in surrogate decision-making. Practicing the behaviors demonstrated in the talking map may increase clinician skill during difficult conversations. Improving communication with surrogate decision makers will increase the support we offer to critically ill patients and their loved ones.
Corresponding author: Jessica McFarlin, MD, [email protected].
Funding/support: Dr. Arnold receives support though the Leo H. Criep Chair in Patient Care.
Financial disclosures: None.
1. Hickey M. What are the needs of families of critically ill patients? A review of the literature since 1976. Heart Lung 1990;19:401–15.
2. Mosenthal AC, Murphy PA, Barker LK, et al. Changing culture around end-of-life care in the trauma intensive care unit. J Trauma 2008;64:1587–93.
3. Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 2007;356:469–78.
4. Selecky PA, Eliasson AH, Hall RI, et al. Palliative and end-of-life care for patients with cardiopulmonary diseases. Chest 2005;128:3599–610.
5. Henrich NJ, Dodek P, Heyland D, et al. Qualitative analysis of an intensive care unit family satisfaction survey. Crit Care Med 2011;39:1000–5.
6. Azoulet E, Chevret S, Leleu G, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med 2000;28:3044–9.
7. Curtis JR. Communicating about end-of-life care with patients and families in the intensive care unit. Crit Care Clin 2004;20:363–80.
8. Hope AA, Hsieh SJ, Howes JM, et al. Let’s talk critical. Development and evaluation of a communication skills training program for critical care fellows. Ann Am Thorac Soc 2015;12:505–11.
9. Back AL, Arnold RM, Baile WF, et al. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 2007;167:453–60.
10. Vital Talk. Conduct a family conference. Accessed 27 June 2016 at www.vitaltalk.org/clinicians/family.
11. Kramer M, Schmalenberg C. Securing “good” nurse/physician relationships. Nurs Manage 2003;34:34–8.
12. Johnson D, Wilson M, Cavanaugh B, et al. Measuring the ability to meet family needs in an intensive care unit. Crit Care Med 1998;26:266–71.
13. Back AL, Arnold RM. “Isn’t there anything more you can do?’’: when empathic statements work, and when they don’t. J Palliat Med 2013;16:1429–32.
14. Curtis JR, Engelberg RA, Wenrich MD. Missed opportunities during family conferences about end-of-life care in the intensive care unit. Am J Respir Crit Care Med 2005;171:844–9.
15. Pollak KI, Arnold RM, Jeffreys AS, et al. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol 2007;36:5748–52.
16. Back AL, Arnold RM, Tulsky JA. Mastering communication with seriously ill patients: balancing honesty with empathy and hope. Cambridge: Cambridge University Press; 2009.
17. Back AL, Arnold RM, Baile WF, et al. Approaching difficult communication tasks in oncology. CA Cancer J Clin 2005;55:164–77.
18. Schenker Y, White D, Crowley-Matoka M, et al. “It hurts to know…and it helps”: exploring how surrogates in the ICU cope with prognostic information. J Palliat Med 2013;16:243–9.
19. Scheunemann LP, Arnold RM, White DB. The facilitated values history: helping surrogates make authentic decisions for incapacitated patients with advanced illness. Am J Respir Crit Care Med 2012;186:480–6.
20. Azoulay E, Pochard F, Kentish-Barnes N, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 2005;171:987–94.
21. White DB, Braddock CH, Bereknyei et al. Toward shared decision making at the end of life in intensive care units: opportunities for improvement. Arch Intern Med 2007;167:461–7.
1. Hickey M. What are the needs of families of critically ill patients? A review of the literature since 1976. Heart Lung 1990;19:401–15.
2. Mosenthal AC, Murphy PA, Barker LK, et al. Changing culture around end-of-life care in the trauma intensive care unit. J Trauma 2008;64:1587–93.
3. Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 2007;356:469–78.
4. Selecky PA, Eliasson AH, Hall RI, et al. Palliative and end-of-life care for patients with cardiopulmonary diseases. Chest 2005;128:3599–610.
5. Henrich NJ, Dodek P, Heyland D, et al. Qualitative analysis of an intensive care unit family satisfaction survey. Crit Care Med 2011;39:1000–5.
6. Azoulet E, Chevret S, Leleu G, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med 2000;28:3044–9.
7. Curtis JR. Communicating about end-of-life care with patients and families in the intensive care unit. Crit Care Clin 2004;20:363–80.
8. Hope AA, Hsieh SJ, Howes JM, et al. Let’s talk critical. Development and evaluation of a communication skills training program for critical care fellows. Ann Am Thorac Soc 2015;12:505–11.
9. Back AL, Arnold RM, Baile WF, et al. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 2007;167:453–60.
10. Vital Talk. Conduct a family conference. Accessed 27 June 2016 at www.vitaltalk.org/clinicians/family.
11. Kramer M, Schmalenberg C. Securing “good” nurse/physician relationships. Nurs Manage 2003;34:34–8.
12. Johnson D, Wilson M, Cavanaugh B, et al. Measuring the ability to meet family needs in an intensive care unit. Crit Care Med 1998;26:266–71.
13. Back AL, Arnold RM. “Isn’t there anything more you can do?’’: when empathic statements work, and when they don’t. J Palliat Med 2013;16:1429–32.
14. Curtis JR, Engelberg RA, Wenrich MD. Missed opportunities during family conferences about end-of-life care in the intensive care unit. Am J Respir Crit Care Med 2005;171:844–9.
15. Pollak KI, Arnold RM, Jeffreys AS, et al. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol 2007;36:5748–52.
16. Back AL, Arnold RM, Tulsky JA. Mastering communication with seriously ill patients: balancing honesty with empathy and hope. Cambridge: Cambridge University Press; 2009.
17. Back AL, Arnold RM, Baile WF, et al. Approaching difficult communication tasks in oncology. CA Cancer J Clin 2005;55:164–77.
18. Schenker Y, White D, Crowley-Matoka M, et al. “It hurts to know…and it helps”: exploring how surrogates in the ICU cope with prognostic information. J Palliat Med 2013;16:243–9.
19. Scheunemann LP, Arnold RM, White DB. The facilitated values history: helping surrogates make authentic decisions for incapacitated patients with advanced illness. Am J Respir Crit Care Med 2012;186:480–6.
20. Azoulay E, Pochard F, Kentish-Barnes N, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 2005;171:987–94.
21. White DB, Braddock CH, Bereknyei et al. Toward shared decision making at the end of life in intensive care units: opportunities for improvement. Arch Intern Med 2007;167:461–7.
Should the DASH Diet Be Recommended for Gout Patients?
Study Overview
Objective. To determine if the Dietary Approaches to Stop Hypertension (DASH) diet is effective for lowering serum uric acid (SUA) levels, and if lower sodium intake as part of the diet would have an effect on SUA.
Design. Ancillary study of a randomized, crossover feeding trial.
Setting and participants. The original DASH study was an National Institute of Health (NIH)–funded, investigator-initiated trial conducted at 4 university centers in the United States from 1997 to 1999. Participants aged 22 years or older who did not have preexisting renal insufficiency, heart disease, uncontrolled dyslipidemia, or diabetes were recruited. Those on antihypertensives, insulin, or with alcohol intake exceeding daily recommended limits for men (> 14 drinks per week) were excluded. For the current secondary analysis, only subjects from 1 center, where SUA was measured, were studied. Participants were randomized to a consume a diet consistent with the typical American diet (control diet) or a diet in line with the principles of the DASH diet. For the first 2 weeks, all groups ate the high-sodium control diet. After this 2-week run-in period, the patients in the study then ate the diet they were assigned to for 30 days. After this 30-day period, participants ate their usual home diet for 5 days. The groups were then crossed over.
Intervention. The DASH diet emphasizes fruits, vegetables, and low-fat dairy foods; includes whole grains, poultry, fish, and nuts; and contains smaller amounts of red meat, sweets, and sugar-containing beverages than the typical US diet. It also contains smaller amounts of total and saturated fat and cholesterol and larger amounts of potassium, calcium, magnesium, dietary fiber, and protein than the typical diet. Both diets contained the same number of calories overall. The diets were similar in mg/day of sodium, however, each arm was subdivided to intake either a high (4400 mg/day), intermediate (3000 mg/day), or low (1400 mg/day) level of sodium. During the study period, all food was provided for participants, including meals and snacks, and was donated by various food vendors in the United States.
Main outcome measure. SUA levels, which were measured after each change in diet and at baseline. Other measures were blood pressure, body mass index, renal function, and fasting glucose and lipids.
Main results. There were 103 participants with an average blood pressure of 139/87 mm Hg at baseline. Mean age was 51 years and about half of the patients were women. The majority of patients were overweight (mean BMI, 29.5 kg/m2) and African American (74.8%), with an average SUA level of 5.0 mg/dL. There were 8 participants with a SUA level > 7 mg/dL at baseline. Daily alcohol intake, fasting glucose and triglycerides, renal function, and blood pressure did not differ significantly between the groups. The DASH diet was effective in lowering SUA levels overall by an average of 0.35 mg/dL (P = 0.02). The sodium content had an effect on SUA levels regardless of the diet. The intermediate sodium subset of both the DASH and the control diets resulted in an overall decrease in SUA by 0.34 mg/dL, P < 0.001 (0.35 mg/dL for the DASH diet, P = 0.04; 0.33 mg/dL for the control diet, P < 0.001). There was no difference in SUA between the low- and high-sodium groups. Those participants with the highest SUA at the start of the study had the greatest reduction in SUA. For those with levels > 7 mg/dL, there was a decrease in SUA by 1.29 mg/dL. If the SUA at the start of the trial was lower, reductions were more modest. SUA was reduced by 0.76 mg/dL when the starting level was between 6 and 7 mg/dL. When the participants had a SUA between 4 and 5 mg/dL, the effect of the diet was nonexistent. Other variables such as hypertension and obesity were found not to be confounders.
Conclusion. For participants with SUA levels > 7, an average reduction in serum uric acid of 1.29 mg/dL can reasonably be expected from implementation of a DASH-type diet.
Commentary
SUA is considered an important etiologic factor in gout, but there has been little evidence for success in controlling uric acid with diet. Dietary recommendations for gout patients from the American College of Rheumatology include avoiding organ meats, high-fructose corn syrup, and alcohol in excess, and suggest that beef, lamb, pork, shellfish and sugary beverages should be limited while vegetables and nonfat dairy be encouraged [1].
The DASH diet, promoted by the National Heart, Lung, and Blood Institute to prevent and control hypertension, has been widely disseminated in the popular press and is well known to many Americans. Clinical evidence supporting DASH as first-line nonpharmacologic treatment for high blood pressure is based mainly on the results of 3 trials: DASH Trial[2], DASH-Sodium Trial [3], and PREMIER clinical trial [4]. The DASH diet, while it overlaps with the ACR recommendations of encouraging intake of vegetables and non-fat dairy and discouraging added sugars, recommends as a primary calorie source whole grains, followed by vegetables, fruits, and lean meats, poultry, or fish. One to 2 servings of nuts, seeds, or legumes is also encouraged as well as healthful fats and oils.
The authors’ hypothesis, that the DASH diet would lower uric acid levels as compared with the control diet, was affirmed, with the greater effect seen in patients with higher SUA at baseline. The authors also hypothesized that reducing sodium intake would lower uric acid levels, given its association with high blood pressure. In this study, higher levels of sodium were found to be associated with a decrease in uric acid. The reason for this is unclear and the authors speculate as to why this could be physiologically. The relationship between sodium intake and SUA level is controversial and the authors do not recommend advising anincrease in sodium in the diet to lower SUA levels based on their findings.
Long-term dietary change is not easy. It is encouraging that, according to the authors, most of the participants in the study found the DASH diet to be preferable to the typical Western control diet provided and expressed a desire to maintain the DASH style of eating. This is important to consider, as any lifestyle change must be sustained to see continued benefit. The study participants maintained a constant weight, which eliminates this potentially confounding variable as weight reduction alone leads to a reduction in SUA.
While this study showed a positive effect of implementing the DASH diet in those with elevated SUA levels, it excluded those with comorbidities often found in patients with gout, such as cardiovascular disease, diabetes, and renal impairment. This limits generalizability, as does excluding those who consume alcohol beyond the daily recommended quantities—a known risk factor for hyperuricemia. As with any dietary study, it is difficult to know for certain that participants did not eat any foods outside of the study protocol even when the food was provided.
Patients with gout and hyperuricemia are at an increased risk for cardiovascular disease and the metabolic syndrome, making lifestyle interventions and dietary counselling crucial to the global wellbeing of the patient. Overall, this randomized crossover study provides compelling evidence that the DASH diet should be recommended to patients with hyperuricemia.
Applications for Clinical Practice
For patients with borderline-high SUA (between 6–7 mg/dL), it is reasonable to encourage implementation of the DASH diet with the expectation that SUA will be lowered by about 1.29 mg/dL, getting the patient to goal SUA. As a greater benefit was seen in patients with higher levels of SUA at baseline, it is also reasonable to attempt to lower SUA with a DASH-style diet prior to pharmacologic intervention for higher SUA level if the patient is amenable to trying this tactic.
—Christina Downey, MD, Geisinger Medical Center, Danville, PA
1. Khanna D, Fitzgerald JD, Khanna PP, et al; American College of Rheumatology. 2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res (Hoboken) 2012;64:1431–46.
2. Sacks FM, Svetkey LP, Vollmer WM, et al; DASH-Sodium Collaborative Research Group.. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001;344:3–10.
3. Svetkey LP, Sacks FM, Obarzanek E, et al. The DASH Diet, Sodium Intake and Blood Pressure Trial (DASH-sodium):rationale and design. DASH-Sodium Collaborative Research Group. J Am Diet Assoc 1999;99(8 Suppl):S96–104.
4. Appel LJ, Champagne CM, Harsha DW, et al; Writing Group of the PREMIER Collaborative Research Group. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA 2003;289:2083–93.
Study Overview
Objective. To determine if the Dietary Approaches to Stop Hypertension (DASH) diet is effective for lowering serum uric acid (SUA) levels, and if lower sodium intake as part of the diet would have an effect on SUA.
Design. Ancillary study of a randomized, crossover feeding trial.
Setting and participants. The original DASH study was an National Institute of Health (NIH)–funded, investigator-initiated trial conducted at 4 university centers in the United States from 1997 to 1999. Participants aged 22 years or older who did not have preexisting renal insufficiency, heart disease, uncontrolled dyslipidemia, or diabetes were recruited. Those on antihypertensives, insulin, or with alcohol intake exceeding daily recommended limits for men (> 14 drinks per week) were excluded. For the current secondary analysis, only subjects from 1 center, where SUA was measured, were studied. Participants were randomized to a consume a diet consistent with the typical American diet (control diet) or a diet in line with the principles of the DASH diet. For the first 2 weeks, all groups ate the high-sodium control diet. After this 2-week run-in period, the patients in the study then ate the diet they were assigned to for 30 days. After this 30-day period, participants ate their usual home diet for 5 days. The groups were then crossed over.
Intervention. The DASH diet emphasizes fruits, vegetables, and low-fat dairy foods; includes whole grains, poultry, fish, and nuts; and contains smaller amounts of red meat, sweets, and sugar-containing beverages than the typical US diet. It also contains smaller amounts of total and saturated fat and cholesterol and larger amounts of potassium, calcium, magnesium, dietary fiber, and protein than the typical diet. Both diets contained the same number of calories overall. The diets were similar in mg/day of sodium, however, each arm was subdivided to intake either a high (4400 mg/day), intermediate (3000 mg/day), or low (1400 mg/day) level of sodium. During the study period, all food was provided for participants, including meals and snacks, and was donated by various food vendors in the United States.
Main outcome measure. SUA levels, which were measured after each change in diet and at baseline. Other measures were blood pressure, body mass index, renal function, and fasting glucose and lipids.
Main results. There were 103 participants with an average blood pressure of 139/87 mm Hg at baseline. Mean age was 51 years and about half of the patients were women. The majority of patients were overweight (mean BMI, 29.5 kg/m2) and African American (74.8%), with an average SUA level of 5.0 mg/dL. There were 8 participants with a SUA level > 7 mg/dL at baseline. Daily alcohol intake, fasting glucose and triglycerides, renal function, and blood pressure did not differ significantly between the groups. The DASH diet was effective in lowering SUA levels overall by an average of 0.35 mg/dL (P = 0.02). The sodium content had an effect on SUA levels regardless of the diet. The intermediate sodium subset of both the DASH and the control diets resulted in an overall decrease in SUA by 0.34 mg/dL, P < 0.001 (0.35 mg/dL for the DASH diet, P = 0.04; 0.33 mg/dL for the control diet, P < 0.001). There was no difference in SUA between the low- and high-sodium groups. Those participants with the highest SUA at the start of the study had the greatest reduction in SUA. For those with levels > 7 mg/dL, there was a decrease in SUA by 1.29 mg/dL. If the SUA at the start of the trial was lower, reductions were more modest. SUA was reduced by 0.76 mg/dL when the starting level was between 6 and 7 mg/dL. When the participants had a SUA between 4 and 5 mg/dL, the effect of the diet was nonexistent. Other variables such as hypertension and obesity were found not to be confounders.
Conclusion. For participants with SUA levels > 7, an average reduction in serum uric acid of 1.29 mg/dL can reasonably be expected from implementation of a DASH-type diet.
Commentary
SUA is considered an important etiologic factor in gout, but there has been little evidence for success in controlling uric acid with diet. Dietary recommendations for gout patients from the American College of Rheumatology include avoiding organ meats, high-fructose corn syrup, and alcohol in excess, and suggest that beef, lamb, pork, shellfish and sugary beverages should be limited while vegetables and nonfat dairy be encouraged [1].
The DASH diet, promoted by the National Heart, Lung, and Blood Institute to prevent and control hypertension, has been widely disseminated in the popular press and is well known to many Americans. Clinical evidence supporting DASH as first-line nonpharmacologic treatment for high blood pressure is based mainly on the results of 3 trials: DASH Trial[2], DASH-Sodium Trial [3], and PREMIER clinical trial [4]. The DASH diet, while it overlaps with the ACR recommendations of encouraging intake of vegetables and non-fat dairy and discouraging added sugars, recommends as a primary calorie source whole grains, followed by vegetables, fruits, and lean meats, poultry, or fish. One to 2 servings of nuts, seeds, or legumes is also encouraged as well as healthful fats and oils.
The authors’ hypothesis, that the DASH diet would lower uric acid levels as compared with the control diet, was affirmed, with the greater effect seen in patients with higher SUA at baseline. The authors also hypothesized that reducing sodium intake would lower uric acid levels, given its association with high blood pressure. In this study, higher levels of sodium were found to be associated with a decrease in uric acid. The reason for this is unclear and the authors speculate as to why this could be physiologically. The relationship between sodium intake and SUA level is controversial and the authors do not recommend advising anincrease in sodium in the diet to lower SUA levels based on their findings.
Long-term dietary change is not easy. It is encouraging that, according to the authors, most of the participants in the study found the DASH diet to be preferable to the typical Western control diet provided and expressed a desire to maintain the DASH style of eating. This is important to consider, as any lifestyle change must be sustained to see continued benefit. The study participants maintained a constant weight, which eliminates this potentially confounding variable as weight reduction alone leads to a reduction in SUA.
While this study showed a positive effect of implementing the DASH diet in those with elevated SUA levels, it excluded those with comorbidities often found in patients with gout, such as cardiovascular disease, diabetes, and renal impairment. This limits generalizability, as does excluding those who consume alcohol beyond the daily recommended quantities—a known risk factor for hyperuricemia. As with any dietary study, it is difficult to know for certain that participants did not eat any foods outside of the study protocol even when the food was provided.
Patients with gout and hyperuricemia are at an increased risk for cardiovascular disease and the metabolic syndrome, making lifestyle interventions and dietary counselling crucial to the global wellbeing of the patient. Overall, this randomized crossover study provides compelling evidence that the DASH diet should be recommended to patients with hyperuricemia.
Applications for Clinical Practice
For patients with borderline-high SUA (between 6–7 mg/dL), it is reasonable to encourage implementation of the DASH diet with the expectation that SUA will be lowered by about 1.29 mg/dL, getting the patient to goal SUA. As a greater benefit was seen in patients with higher levels of SUA at baseline, it is also reasonable to attempt to lower SUA with a DASH-style diet prior to pharmacologic intervention for higher SUA level if the patient is amenable to trying this tactic.
—Christina Downey, MD, Geisinger Medical Center, Danville, PA
Study Overview
Objective. To determine if the Dietary Approaches to Stop Hypertension (DASH) diet is effective for lowering serum uric acid (SUA) levels, and if lower sodium intake as part of the diet would have an effect on SUA.
Design. Ancillary study of a randomized, crossover feeding trial.
Setting and participants. The original DASH study was an National Institute of Health (NIH)–funded, investigator-initiated trial conducted at 4 university centers in the United States from 1997 to 1999. Participants aged 22 years or older who did not have preexisting renal insufficiency, heart disease, uncontrolled dyslipidemia, or diabetes were recruited. Those on antihypertensives, insulin, or with alcohol intake exceeding daily recommended limits for men (> 14 drinks per week) were excluded. For the current secondary analysis, only subjects from 1 center, where SUA was measured, were studied. Participants were randomized to a consume a diet consistent with the typical American diet (control diet) or a diet in line with the principles of the DASH diet. For the first 2 weeks, all groups ate the high-sodium control diet. After this 2-week run-in period, the patients in the study then ate the diet they were assigned to for 30 days. After this 30-day period, participants ate their usual home diet for 5 days. The groups were then crossed over.
Intervention. The DASH diet emphasizes fruits, vegetables, and low-fat dairy foods; includes whole grains, poultry, fish, and nuts; and contains smaller amounts of red meat, sweets, and sugar-containing beverages than the typical US diet. It also contains smaller amounts of total and saturated fat and cholesterol and larger amounts of potassium, calcium, magnesium, dietary fiber, and protein than the typical diet. Both diets contained the same number of calories overall. The diets were similar in mg/day of sodium, however, each arm was subdivided to intake either a high (4400 mg/day), intermediate (3000 mg/day), or low (1400 mg/day) level of sodium. During the study period, all food was provided for participants, including meals and snacks, and was donated by various food vendors in the United States.
Main outcome measure. SUA levels, which were measured after each change in diet and at baseline. Other measures were blood pressure, body mass index, renal function, and fasting glucose and lipids.
Main results. There were 103 participants with an average blood pressure of 139/87 mm Hg at baseline. Mean age was 51 years and about half of the patients were women. The majority of patients were overweight (mean BMI, 29.5 kg/m2) and African American (74.8%), with an average SUA level of 5.0 mg/dL. There were 8 participants with a SUA level > 7 mg/dL at baseline. Daily alcohol intake, fasting glucose and triglycerides, renal function, and blood pressure did not differ significantly between the groups. The DASH diet was effective in lowering SUA levels overall by an average of 0.35 mg/dL (P = 0.02). The sodium content had an effect on SUA levels regardless of the diet. The intermediate sodium subset of both the DASH and the control diets resulted in an overall decrease in SUA by 0.34 mg/dL, P < 0.001 (0.35 mg/dL for the DASH diet, P = 0.04; 0.33 mg/dL for the control diet, P < 0.001). There was no difference in SUA between the low- and high-sodium groups. Those participants with the highest SUA at the start of the study had the greatest reduction in SUA. For those with levels > 7 mg/dL, there was a decrease in SUA by 1.29 mg/dL. If the SUA at the start of the trial was lower, reductions were more modest. SUA was reduced by 0.76 mg/dL when the starting level was between 6 and 7 mg/dL. When the participants had a SUA between 4 and 5 mg/dL, the effect of the diet was nonexistent. Other variables such as hypertension and obesity were found not to be confounders.
Conclusion. For participants with SUA levels > 7, an average reduction in serum uric acid of 1.29 mg/dL can reasonably be expected from implementation of a DASH-type diet.
Commentary
SUA is considered an important etiologic factor in gout, but there has been little evidence for success in controlling uric acid with diet. Dietary recommendations for gout patients from the American College of Rheumatology include avoiding organ meats, high-fructose corn syrup, and alcohol in excess, and suggest that beef, lamb, pork, shellfish and sugary beverages should be limited while vegetables and nonfat dairy be encouraged [1].
The DASH diet, promoted by the National Heart, Lung, and Blood Institute to prevent and control hypertension, has been widely disseminated in the popular press and is well known to many Americans. Clinical evidence supporting DASH as first-line nonpharmacologic treatment for high blood pressure is based mainly on the results of 3 trials: DASH Trial[2], DASH-Sodium Trial [3], and PREMIER clinical trial [4]. The DASH diet, while it overlaps with the ACR recommendations of encouraging intake of vegetables and non-fat dairy and discouraging added sugars, recommends as a primary calorie source whole grains, followed by vegetables, fruits, and lean meats, poultry, or fish. One to 2 servings of nuts, seeds, or legumes is also encouraged as well as healthful fats and oils.
The authors’ hypothesis, that the DASH diet would lower uric acid levels as compared with the control diet, was affirmed, with the greater effect seen in patients with higher SUA at baseline. The authors also hypothesized that reducing sodium intake would lower uric acid levels, given its association with high blood pressure. In this study, higher levels of sodium were found to be associated with a decrease in uric acid. The reason for this is unclear and the authors speculate as to why this could be physiologically. The relationship between sodium intake and SUA level is controversial and the authors do not recommend advising anincrease in sodium in the diet to lower SUA levels based on their findings.
Long-term dietary change is not easy. It is encouraging that, according to the authors, most of the participants in the study found the DASH diet to be preferable to the typical Western control diet provided and expressed a desire to maintain the DASH style of eating. This is important to consider, as any lifestyle change must be sustained to see continued benefit. The study participants maintained a constant weight, which eliminates this potentially confounding variable as weight reduction alone leads to a reduction in SUA.
While this study showed a positive effect of implementing the DASH diet in those with elevated SUA levels, it excluded those with comorbidities often found in patients with gout, such as cardiovascular disease, diabetes, and renal impairment. This limits generalizability, as does excluding those who consume alcohol beyond the daily recommended quantities—a known risk factor for hyperuricemia. As with any dietary study, it is difficult to know for certain that participants did not eat any foods outside of the study protocol even when the food was provided.
Patients with gout and hyperuricemia are at an increased risk for cardiovascular disease and the metabolic syndrome, making lifestyle interventions and dietary counselling crucial to the global wellbeing of the patient. Overall, this randomized crossover study provides compelling evidence that the DASH diet should be recommended to patients with hyperuricemia.
Applications for Clinical Practice
For patients with borderline-high SUA (between 6–7 mg/dL), it is reasonable to encourage implementation of the DASH diet with the expectation that SUA will be lowered by about 1.29 mg/dL, getting the patient to goal SUA. As a greater benefit was seen in patients with higher levels of SUA at baseline, it is also reasonable to attempt to lower SUA with a DASH-style diet prior to pharmacologic intervention for higher SUA level if the patient is amenable to trying this tactic.
—Christina Downey, MD, Geisinger Medical Center, Danville, PA
1. Khanna D, Fitzgerald JD, Khanna PP, et al; American College of Rheumatology. 2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res (Hoboken) 2012;64:1431–46.
2. Sacks FM, Svetkey LP, Vollmer WM, et al; DASH-Sodium Collaborative Research Group.. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001;344:3–10.
3. Svetkey LP, Sacks FM, Obarzanek E, et al. The DASH Diet, Sodium Intake and Blood Pressure Trial (DASH-sodium):rationale and design. DASH-Sodium Collaborative Research Group. J Am Diet Assoc 1999;99(8 Suppl):S96–104.
4. Appel LJ, Champagne CM, Harsha DW, et al; Writing Group of the PREMIER Collaborative Research Group. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA 2003;289:2083–93.
1. Khanna D, Fitzgerald JD, Khanna PP, et al; American College of Rheumatology. 2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res (Hoboken) 2012;64:1431–46.
2. Sacks FM, Svetkey LP, Vollmer WM, et al; DASH-Sodium Collaborative Research Group.. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001;344:3–10.
3. Svetkey LP, Sacks FM, Obarzanek E, et al. The DASH Diet, Sodium Intake and Blood Pressure Trial (DASH-sodium):rationale and design. DASH-Sodium Collaborative Research Group. J Am Diet Assoc 1999;99(8 Suppl):S96–104.
4. Appel LJ, Champagne CM, Harsha DW, et al; Writing Group of the PREMIER Collaborative Research Group. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA 2003;289:2083–93.
Multiple Myeloma and Stroke: What’s the Risk?
Related: Treating Patients With Multiple Myeloma in the VA
Patients were enrolled in Total Therapy protocols (TT2, TT3a, and TT3b), which tested varying combinations of thalidomide, bortezomib, lenalidomide, and dexamethasone. Of 1,148 patients, 46 (4%) had strokes, usually ischemic stroke (33 patients, or 72%). Hypercoagulability, atrial fibrillation and small-vessel occlusion were common mechanisms. Whereas other research has found a higher risk of arterial thrombosis from activated prothrombotic factors, especially during the early period of chemotherapy, in this study vascular events occurred months later.
Seven patients died in the hospital (15% compared with a national average of 5%). Although 6 of those deaths were stroke related, 36 patients were discharged home or to a rehabilitation facility; 2 were discharged to a long-term nursing facility. During a median follow-up of 10 years, 6 patients had another stroke. The cumulative risk of recurrent stroke was 15% compared with 5% for the general population.
Related: Link Found Between Agent Orange Exposure and Multiple Myeloma
Stage I and II cancers and renal insufficiency independently predicted stroke. Also noteworthy, according to the researchers: Patients with MM who developed renal insufficiency had worse clinical outcomes despite improvement in their renal function or lack of significant difference in their baseline renal functions between various treatment protocols. Thus, the increased risk of stroke, recurrent stroke, and mortality could partly be due to renal disease, which may or may not have resulted from myeloma.
Use of combination chemotherapy has “markedly improved” clinical outcomes for MM patients, the researchers say, but those drugs have also been associated with an increased risk of VTE, especially during the first months of chemotherapy. Thalidomide alone did not increase the risk of VTE, nor did lenalinomide on its own. However, thalidomide combined with multiagent chemotherapy increased VTE risk as much as 34% in newly diagnosed patients, and lenalinomide with dexamethasone boosted risk as high as 75%.
The researchers found no significant relationship between mortality and use of thalidomide. Median survival was 103 months for a thalidomide-based regimen and 78 months for a regimen without thalidomide.
Related: Multiple Myeloma: Updates on Diagnosis and Management
The researchers noted that the patients developed strokes despite a trend toward coagulopathy, to the extent that half were ineligible for immediate use of antiplatelet agents. The study findings “heightened our awareness,” the researchers say, that aggressive preventive measures can help reduce the incidence of stroke in patients with renal insufficiency.
Source:
Hinduja A, Limaye K, Ravilla R, et al. PLoS One. 2016;11(11): e0166627.
doi: 10.1371/journal.pone.0166627.
Related: Treating Patients With Multiple Myeloma in the VA
Patients were enrolled in Total Therapy protocols (TT2, TT3a, and TT3b), which tested varying combinations of thalidomide, bortezomib, lenalidomide, and dexamethasone. Of 1,148 patients, 46 (4%) had strokes, usually ischemic stroke (33 patients, or 72%). Hypercoagulability, atrial fibrillation and small-vessel occlusion were common mechanisms. Whereas other research has found a higher risk of arterial thrombosis from activated prothrombotic factors, especially during the early period of chemotherapy, in this study vascular events occurred months later.
Seven patients died in the hospital (15% compared with a national average of 5%). Although 6 of those deaths were stroke related, 36 patients were discharged home or to a rehabilitation facility; 2 were discharged to a long-term nursing facility. During a median follow-up of 10 years, 6 patients had another stroke. The cumulative risk of recurrent stroke was 15% compared with 5% for the general population.
Related: Link Found Between Agent Orange Exposure and Multiple Myeloma
Stage I and II cancers and renal insufficiency independently predicted stroke. Also noteworthy, according to the researchers: Patients with MM who developed renal insufficiency had worse clinical outcomes despite improvement in their renal function or lack of significant difference in their baseline renal functions between various treatment protocols. Thus, the increased risk of stroke, recurrent stroke, and mortality could partly be due to renal disease, which may or may not have resulted from myeloma.
Use of combination chemotherapy has “markedly improved” clinical outcomes for MM patients, the researchers say, but those drugs have also been associated with an increased risk of VTE, especially during the first months of chemotherapy. Thalidomide alone did not increase the risk of VTE, nor did lenalinomide on its own. However, thalidomide combined with multiagent chemotherapy increased VTE risk as much as 34% in newly diagnosed patients, and lenalinomide with dexamethasone boosted risk as high as 75%.
The researchers found no significant relationship between mortality and use of thalidomide. Median survival was 103 months for a thalidomide-based regimen and 78 months for a regimen without thalidomide.
Related: Multiple Myeloma: Updates on Diagnosis and Management
The researchers noted that the patients developed strokes despite a trend toward coagulopathy, to the extent that half were ineligible for immediate use of antiplatelet agents. The study findings “heightened our awareness,” the researchers say, that aggressive preventive measures can help reduce the incidence of stroke in patients with renal insufficiency.
Source:
Hinduja A, Limaye K, Ravilla R, et al. PLoS One. 2016;11(11): e0166627.
doi: 10.1371/journal.pone.0166627.
Related: Treating Patients With Multiple Myeloma in the VA
Patients were enrolled in Total Therapy protocols (TT2, TT3a, and TT3b), which tested varying combinations of thalidomide, bortezomib, lenalidomide, and dexamethasone. Of 1,148 patients, 46 (4%) had strokes, usually ischemic stroke (33 patients, or 72%). Hypercoagulability, atrial fibrillation and small-vessel occlusion were common mechanisms. Whereas other research has found a higher risk of arterial thrombosis from activated prothrombotic factors, especially during the early period of chemotherapy, in this study vascular events occurred months later.
Seven patients died in the hospital (15% compared with a national average of 5%). Although 6 of those deaths were stroke related, 36 patients were discharged home or to a rehabilitation facility; 2 were discharged to a long-term nursing facility. During a median follow-up of 10 years, 6 patients had another stroke. The cumulative risk of recurrent stroke was 15% compared with 5% for the general population.
Related: Link Found Between Agent Orange Exposure and Multiple Myeloma
Stage I and II cancers and renal insufficiency independently predicted stroke. Also noteworthy, according to the researchers: Patients with MM who developed renal insufficiency had worse clinical outcomes despite improvement in their renal function or lack of significant difference in their baseline renal functions between various treatment protocols. Thus, the increased risk of stroke, recurrent stroke, and mortality could partly be due to renal disease, which may or may not have resulted from myeloma.
Use of combination chemotherapy has “markedly improved” clinical outcomes for MM patients, the researchers say, but those drugs have also been associated with an increased risk of VTE, especially during the first months of chemotherapy. Thalidomide alone did not increase the risk of VTE, nor did lenalinomide on its own. However, thalidomide combined with multiagent chemotherapy increased VTE risk as much as 34% in newly diagnosed patients, and lenalinomide with dexamethasone boosted risk as high as 75%.
The researchers found no significant relationship between mortality and use of thalidomide. Median survival was 103 months for a thalidomide-based regimen and 78 months for a regimen without thalidomide.
Related: Multiple Myeloma: Updates on Diagnosis and Management
The researchers noted that the patients developed strokes despite a trend toward coagulopathy, to the extent that half were ineligible for immediate use of antiplatelet agents. The study findings “heightened our awareness,” the researchers say, that aggressive preventive measures can help reduce the incidence of stroke in patients with renal insufficiency.
Source:
Hinduja A, Limaye K, Ravilla R, et al. PLoS One. 2016;11(11): e0166627.
doi: 10.1371/journal.pone.0166627.
Combo granted orphan designation for CLL

The US Food and Drug Administration (FDA) has granted orphan drug designation for the combination of TG-1101 (ublituximab) and TGR-1202 for the treatment of patients with chronic lymphocytic leukemia (CLL).
Ublituximab is a glycoengineered anti-CD20 monoclonal antibody, and TGR-1202 is a next-generation PI3K delta inhibitor. Both drugs are being developed by TG Therapeutics, Inc.
Researchers have evaluated ublituximab and TGR-1202 in combination in a phase 1 trial of patients with relapsed or refractory CLL/small lymphocytic lymphoma (SLL) and non-Hodgkin lymphomas (NHLs).
Results were presented at the 2015 ASH Annual Meeting.
There was a 3+3 dose-escalation portion of the study and a dose-expansion phase. The patients received TGR-1202 at doses ranging from 400 mg to 1200 mg and 2 different doses of ublituximab—900 mg for patients with NHL and 600 mg or 900 mg for patients with CLL/SLL.
As of ASH, there were 58 patients evaluable for efficacy and 71 evaluable for safety.
There were 10 CLL/SLL patients exposed to higher doses of TGR-1202. Among these patients, the overall response rate was 80%. Seven patients achieved a partial response, 1 achieved a complete response, and the remaining 2 patients had stable disease.
For the entire safety population, the most common adverse events were nausea (46%), diarrhea (44%), fatigue (41%), neutropenia (30%), and infusion-related reactions (25%).
Grade 3/4 adverse events included neutropenia (25%), diarrhea (3%), fatigue (3%), dyspnea (3%), pyrexia (3%), nausea (1%), infusion-related reactions (1%), sinusitis (1%), anemia (1%), hypophosphatemia (1%), and peripheral edema (1%).
Now, the combination of ublituximab and TGR-1202 is being evaluated in the UNITY-CLL phase 3 trial for patients with previously treated or untreated CLL.
“[W]ith enrollment into our UNITY-CLL phase 3 trial currently exceeding our expectations, we expect to be able to commence a regulatory filing for the combination in 2018, and having orphan drug designation will provide certain cost-saving advantages for us during the regulatory approval process,” said Michael S. Weiss, executive chairman and chief executive officer of TG Therapeutics.
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()

The US Food and Drug Administration (FDA) has granted orphan drug designation for the combination of TG-1101 (ublituximab) and TGR-1202 for the treatment of patients with chronic lymphocytic leukemia (CLL).
Ublituximab is a glycoengineered anti-CD20 monoclonal antibody, and TGR-1202 is a next-generation PI3K delta inhibitor. Both drugs are being developed by TG Therapeutics, Inc.
Researchers have evaluated ublituximab and TGR-1202 in combination in a phase 1 trial of patients with relapsed or refractory CLL/small lymphocytic lymphoma (SLL) and non-Hodgkin lymphomas (NHLs).
Results were presented at the 2015 ASH Annual Meeting.
There was a 3+3 dose-escalation portion of the study and a dose-expansion phase. The patients received TGR-1202 at doses ranging from 400 mg to 1200 mg and 2 different doses of ublituximab—900 mg for patients with NHL and 600 mg or 900 mg for patients with CLL/SLL.
As of ASH, there were 58 patients evaluable for efficacy and 71 evaluable for safety.
There were 10 CLL/SLL patients exposed to higher doses of TGR-1202. Among these patients, the overall response rate was 80%. Seven patients achieved a partial response, 1 achieved a complete response, and the remaining 2 patients had stable disease.
For the entire safety population, the most common adverse events were nausea (46%), diarrhea (44%), fatigue (41%), neutropenia (30%), and infusion-related reactions (25%).
Grade 3/4 adverse events included neutropenia (25%), diarrhea (3%), fatigue (3%), dyspnea (3%), pyrexia (3%), nausea (1%), infusion-related reactions (1%), sinusitis (1%), anemia (1%), hypophosphatemia (1%), and peripheral edema (1%).
Now, the combination of ublituximab and TGR-1202 is being evaluated in the UNITY-CLL phase 3 trial for patients with previously treated or untreated CLL.
“[W]ith enrollment into our UNITY-CLL phase 3 trial currently exceeding our expectations, we expect to be able to commence a regulatory filing for the combination in 2018, and having orphan drug designation will provide certain cost-saving advantages for us during the regulatory approval process,” said Michael S. Weiss, executive chairman and chief executive officer of TG Therapeutics.
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()

The US Food and Drug Administration (FDA) has granted orphan drug designation for the combination of TG-1101 (ublituximab) and TGR-1202 for the treatment of patients with chronic lymphocytic leukemia (CLL).
Ublituximab is a glycoengineered anti-CD20 monoclonal antibody, and TGR-1202 is a next-generation PI3K delta inhibitor. Both drugs are being developed by TG Therapeutics, Inc.
Researchers have evaluated ublituximab and TGR-1202 in combination in a phase 1 trial of patients with relapsed or refractory CLL/small lymphocytic lymphoma (SLL) and non-Hodgkin lymphomas (NHLs).
Results were presented at the 2015 ASH Annual Meeting.
There was a 3+3 dose-escalation portion of the study and a dose-expansion phase. The patients received TGR-1202 at doses ranging from 400 mg to 1200 mg and 2 different doses of ublituximab—900 mg for patients with NHL and 600 mg or 900 mg for patients with CLL/SLL.
As of ASH, there were 58 patients evaluable for efficacy and 71 evaluable for safety.
There were 10 CLL/SLL patients exposed to higher doses of TGR-1202. Among these patients, the overall response rate was 80%. Seven patients achieved a partial response, 1 achieved a complete response, and the remaining 2 patients had stable disease.
For the entire safety population, the most common adverse events were nausea (46%), diarrhea (44%), fatigue (41%), neutropenia (30%), and infusion-related reactions (25%).
Grade 3/4 adverse events included neutropenia (25%), diarrhea (3%), fatigue (3%), dyspnea (3%), pyrexia (3%), nausea (1%), infusion-related reactions (1%), sinusitis (1%), anemia (1%), hypophosphatemia (1%), and peripheral edema (1%).
Now, the combination of ublituximab and TGR-1202 is being evaluated in the UNITY-CLL phase 3 trial for patients with previously treated or untreated CLL.
“[W]ith enrollment into our UNITY-CLL phase 3 trial currently exceeding our expectations, we expect to be able to commence a regulatory filing for the combination in 2018, and having orphan drug designation will provide certain cost-saving advantages for us during the regulatory approval process,” said Michael S. Weiss, executive chairman and chief executive officer of TG Therapeutics.
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
Consortium to undertake longitudinal study of acquired TTP

Image by Erhabor Osaro
SAN DIEGO—The US Thrombotic Microangiopathies (USTMA) Consortium is planning a longitudinal study to identify biomarkers of relapse and neurocognitive dysfunction in acquired thrombotic thrombocytopenic purpura (TTP).
Earlier studies suggested that ADAMTS13 activity during remission has
limited utility in estimating relapse risk, and cognitive dysfunction
observed in TTP appears to be progressive and independent of relapses.
However, these studies were small with minimal longitudinal data.
Now, the USTMA Consortium, with 13 large referral centers for thrombotic microangiopathies (TMAs) in the US, is providing “the infrastructure for larger US studies in TTP with the goal of improving outcomes in TMAs,” said Marshall A. Mazepa, MD, of the University of Minnesota in Minneapolis.
He described the efforts of the consortium and its plans to conduct a long-term study at the first TTP-TMA Workshop, which took place immediately before the 2016 ASH Annual Meeting.
Dr Mazepa said the objective of the study is to identify biomarkers that
predict the danger period for neurocognitive dysfunction and relapse.
“Hematologists usually do not realize the
neurocognitive dysfunction among patients with TTP, and it is important
that they [hematologists] talk to neurologists,” said Spero Cataland, MD, an organizer of the TTP-TMA Workshop from The Ohio State University in
Columbus.
“This study will be crucial in
improving our understanding of this issue.”
The consortium plans to study 100 TTP patients in remission for 3 years.
Every
3 months, patients will complete neuropsychologic testing, and
investigators will evaluate patients’ end-organ ischemic biomarkers,
ADAMTS13 activity, ultra-large von Willebrand factor levels, and
complement activation biomarkers.
In addition to this study, the USTMA Consortium is participating in the phase 3 HERCULES study of caplacizumab for acquired TTP.
Caplacizumab, which is being developed by Ablynx, was previously evaluated for acquired TTP in the phase 2 TITAN study.
The phase 3 study is a double-blind, placebo-controlled trial designed to determine whether neurocognitive function can be preserved with caplacizumab intervention.
Investigators intend to enroll 92 patients at clinical sites in 17 countries. Recruitment is expected to be complete by the end of 2017.
In closing, Dr Mazepa invited interested clinicians to join the USTMA Consortium by contacting him ([email protected]) or Dr Cataland ([email protected]). ![]()

Image by Erhabor Osaro
SAN DIEGO—The US Thrombotic Microangiopathies (USTMA) Consortium is planning a longitudinal study to identify biomarkers of relapse and neurocognitive dysfunction in acquired thrombotic thrombocytopenic purpura (TTP).
Earlier studies suggested that ADAMTS13 activity during remission has
limited utility in estimating relapse risk, and cognitive dysfunction
observed in TTP appears to be progressive and independent of relapses.
However, these studies were small with minimal longitudinal data.
Now, the USTMA Consortium, with 13 large referral centers for thrombotic microangiopathies (TMAs) in the US, is providing “the infrastructure for larger US studies in TTP with the goal of improving outcomes in TMAs,” said Marshall A. Mazepa, MD, of the University of Minnesota in Minneapolis.
He described the efforts of the consortium and its plans to conduct a long-term study at the first TTP-TMA Workshop, which took place immediately before the 2016 ASH Annual Meeting.
Dr Mazepa said the objective of the study is to identify biomarkers that
predict the danger period for neurocognitive dysfunction and relapse.
“Hematologists usually do not realize the
neurocognitive dysfunction among patients with TTP, and it is important
that they [hematologists] talk to neurologists,” said Spero Cataland, MD, an organizer of the TTP-TMA Workshop from The Ohio State University in
Columbus.
“This study will be crucial in
improving our understanding of this issue.”
The consortium plans to study 100 TTP patients in remission for 3 years.
Every
3 months, patients will complete neuropsychologic testing, and
investigators will evaluate patients’ end-organ ischemic biomarkers,
ADAMTS13 activity, ultra-large von Willebrand factor levels, and
complement activation biomarkers.
In addition to this study, the USTMA Consortium is participating in the phase 3 HERCULES study of caplacizumab for acquired TTP.
Caplacizumab, which is being developed by Ablynx, was previously evaluated for acquired TTP in the phase 2 TITAN study.
The phase 3 study is a double-blind, placebo-controlled trial designed to determine whether neurocognitive function can be preserved with caplacizumab intervention.
Investigators intend to enroll 92 patients at clinical sites in 17 countries. Recruitment is expected to be complete by the end of 2017.
In closing, Dr Mazepa invited interested clinicians to join the USTMA Consortium by contacting him ([email protected]) or Dr Cataland ([email protected]). ![]()

Image by Erhabor Osaro
SAN DIEGO—The US Thrombotic Microangiopathies (USTMA) Consortium is planning a longitudinal study to identify biomarkers of relapse and neurocognitive dysfunction in acquired thrombotic thrombocytopenic purpura (TTP).
Earlier studies suggested that ADAMTS13 activity during remission has
limited utility in estimating relapse risk, and cognitive dysfunction
observed in TTP appears to be progressive and independent of relapses.
However, these studies were small with minimal longitudinal data.
Now, the USTMA Consortium, with 13 large referral centers for thrombotic microangiopathies (TMAs) in the US, is providing “the infrastructure for larger US studies in TTP with the goal of improving outcomes in TMAs,” said Marshall A. Mazepa, MD, of the University of Minnesota in Minneapolis.
He described the efforts of the consortium and its plans to conduct a long-term study at the first TTP-TMA Workshop, which took place immediately before the 2016 ASH Annual Meeting.
Dr Mazepa said the objective of the study is to identify biomarkers that
predict the danger period for neurocognitive dysfunction and relapse.
“Hematologists usually do not realize the
neurocognitive dysfunction among patients with TTP, and it is important
that they [hematologists] talk to neurologists,” said Spero Cataland, MD, an organizer of the TTP-TMA Workshop from The Ohio State University in
Columbus.
“This study will be crucial in
improving our understanding of this issue.”
The consortium plans to study 100 TTP patients in remission for 3 years.
Every
3 months, patients will complete neuropsychologic testing, and
investigators will evaluate patients’ end-organ ischemic biomarkers,
ADAMTS13 activity, ultra-large von Willebrand factor levels, and
complement activation biomarkers.
In addition to this study, the USTMA Consortium is participating in the phase 3 HERCULES study of caplacizumab for acquired TTP.
Caplacizumab, which is being developed by Ablynx, was previously evaluated for acquired TTP in the phase 2 TITAN study.
The phase 3 study is a double-blind, placebo-controlled trial designed to determine whether neurocognitive function can be preserved with caplacizumab intervention.
Investigators intend to enroll 92 patients at clinical sites in 17 countries. Recruitment is expected to be complete by the end of 2017.
In closing, Dr Mazepa invited interested clinicians to join the USTMA Consortium by contacting him ([email protected]) or Dr Cataland ([email protected]). ![]()
Iron deficiency anemia protects kids from malaria better than sickle cell trait
Photo by Aurimas Rimsa
New research suggests that, for young children, iron deficiency anemia offers a
greater protective effect against malaria than sickle cell trait.
The
study indicates that iron deficiency anemia can protect children age 2 and
younger from the blood stage of Plasmodium falciparum malaria, and
treating the anemia with iron supplementation removes this protective
effect.
The researchers reported these findings in EBioMedicine.
“This study is elegant in its simplicity yet remains one of the most
substantial and systematic attempts to unveil the cellular-level
relationship between anemia, iron supplementation, and malaria risk,”
said study author Carla Cerami, MD, PhD, of the Medical Research Council
Unit The Gambia in Banjul, Gambia.
For this study, she and her colleagues analyzed the red blood cells of 135 anemic children who were participating in an iron supplementation trial.
The children ranged in age from 6 months to 24 months and lived in a malaria-endemic region of The Gambia where sickle cell trait was also common.
The children received iron (12 mg/day) through micronutrient powder for 84 days, and the researchers analyzed the children’s red blood cells at baseline, day 49, and day 84.
The team conducted in vitro growth and invasion assays with P falciparum laboratory and field strains. The study’s primary endpoint was in vitro parasite growth in the children’s RBCs.
The researchers found that “anemia substantially reduced the invasion and growth of both laboratory and field strains of P falciparum.” The team noted a roughly 10% growth reduction per standard deviation shift in hemoglobin.
On a population-wide basis, anemia reduced the blood stage of malaria by 15.9%, while the sickle cell trait reduced it by 3.5%.
“Our finding that anemia offers greater natural protection against blood-stage malaria infection than sickle cell trait has led us to formulate the interesting hypothesis that the widespread prevalence of anemia in people of African descent is a genetic signature of malaria,” said study author Morgan Goheen, PhD, of University of North Carolina in Chapel Hill.
The researchers also found that deficits in invasion and growth for blood-stage P falciparum were reversed when anemic children had received 7 weeks of iron supplementation. Parasite growth was 2.4-fold higher after supplementation than it was at baseline (P<0.001).
Prior work by the same research group suggested the increased invasion and growth rates following iron supplementation are caused by the parasites’ strong preference for young red blood cells.
The researchers said these new field results consolidate the evidence that iron supplementation increases the risk of P falciparum malaria and provide support for the use of malaria prophylaxis in
conjunction with iron supplementation, especially during the early
phases of erythroid recovery. ![]()
Photo by Aurimas Rimsa
New research suggests that, for young children, iron deficiency anemia offers a
greater protective effect against malaria than sickle cell trait.
The
study indicates that iron deficiency anemia can protect children age 2 and
younger from the blood stage of Plasmodium falciparum malaria, and
treating the anemia with iron supplementation removes this protective
effect.
The researchers reported these findings in EBioMedicine.
“This study is elegant in its simplicity yet remains one of the most
substantial and systematic attempts to unveil the cellular-level
relationship between anemia, iron supplementation, and malaria risk,”
said study author Carla Cerami, MD, PhD, of the Medical Research Council
Unit The Gambia in Banjul, Gambia.
For this study, she and her colleagues analyzed the red blood cells of 135 anemic children who were participating in an iron supplementation trial.
The children ranged in age from 6 months to 24 months and lived in a malaria-endemic region of The Gambia where sickle cell trait was also common.
The children received iron (12 mg/day) through micronutrient powder for 84 days, and the researchers analyzed the children’s red blood cells at baseline, day 49, and day 84.
The team conducted in vitro growth and invasion assays with P falciparum laboratory and field strains. The study’s primary endpoint was in vitro parasite growth in the children’s RBCs.
The researchers found that “anemia substantially reduced the invasion and growth of both laboratory and field strains of P falciparum.” The team noted a roughly 10% growth reduction per standard deviation shift in hemoglobin.
On a population-wide basis, anemia reduced the blood stage of malaria by 15.9%, while the sickle cell trait reduced it by 3.5%.
“Our finding that anemia offers greater natural protection against blood-stage malaria infection than sickle cell trait has led us to formulate the interesting hypothesis that the widespread prevalence of anemia in people of African descent is a genetic signature of malaria,” said study author Morgan Goheen, PhD, of University of North Carolina in Chapel Hill.
The researchers also found that deficits in invasion and growth for blood-stage P falciparum were reversed when anemic children had received 7 weeks of iron supplementation. Parasite growth was 2.4-fold higher after supplementation than it was at baseline (P<0.001).
Prior work by the same research group suggested the increased invasion and growth rates following iron supplementation are caused by the parasites’ strong preference for young red blood cells.
The researchers said these new field results consolidate the evidence that iron supplementation increases the risk of P falciparum malaria and provide support for the use of malaria prophylaxis in
conjunction with iron supplementation, especially during the early
phases of erythroid recovery. ![]()
Photo by Aurimas Rimsa
New research suggests that, for young children, iron deficiency anemia offers a
greater protective effect against malaria than sickle cell trait.
The
study indicates that iron deficiency anemia can protect children age 2 and
younger from the blood stage of Plasmodium falciparum malaria, and
treating the anemia with iron supplementation removes this protective
effect.
The researchers reported these findings in EBioMedicine.
“This study is elegant in its simplicity yet remains one of the most
substantial and systematic attempts to unveil the cellular-level
relationship between anemia, iron supplementation, and malaria risk,”
said study author Carla Cerami, MD, PhD, of the Medical Research Council
Unit The Gambia in Banjul, Gambia.
For this study, she and her colleagues analyzed the red blood cells of 135 anemic children who were participating in an iron supplementation trial.
The children ranged in age from 6 months to 24 months and lived in a malaria-endemic region of The Gambia where sickle cell trait was also common.
The children received iron (12 mg/day) through micronutrient powder for 84 days, and the researchers analyzed the children’s red blood cells at baseline, day 49, and day 84.
The team conducted in vitro growth and invasion assays with P falciparum laboratory and field strains. The study’s primary endpoint was in vitro parasite growth in the children’s RBCs.
The researchers found that “anemia substantially reduced the invasion and growth of both laboratory and field strains of P falciparum.” The team noted a roughly 10% growth reduction per standard deviation shift in hemoglobin.
On a population-wide basis, anemia reduced the blood stage of malaria by 15.9%, while the sickle cell trait reduced it by 3.5%.
“Our finding that anemia offers greater natural protection against blood-stage malaria infection than sickle cell trait has led us to formulate the interesting hypothesis that the widespread prevalence of anemia in people of African descent is a genetic signature of malaria,” said study author Morgan Goheen, PhD, of University of North Carolina in Chapel Hill.
The researchers also found that deficits in invasion and growth for blood-stage P falciparum were reversed when anemic children had received 7 weeks of iron supplementation. Parasite growth was 2.4-fold higher after supplementation than it was at baseline (P<0.001).
Prior work by the same research group suggested the increased invasion and growth rates following iron supplementation are caused by the parasites’ strong preference for young red blood cells.
The researchers said these new field results consolidate the evidence that iron supplementation increases the risk of P falciparum malaria and provide support for the use of malaria prophylaxis in
conjunction with iron supplementation, especially during the early
phases of erythroid recovery. ![]()
Hemophilia A drug approved in Europe

The European Commission has granted marketing authorization for lonoctocog alfa (Afstyla), a recombinant factor VIII (FVIII) single-chain therapy.
Lonoctocog alfa is indicated for the treatment and prophylaxis of bleeding in hemophilia A patients of all ages.
Lonoctocog alfa is the first and only single-chain recombinant FVIII therapy for hemophilia A specifically designed to provide long-lasting protection from bleeds with 2- to 3-times weekly dosing, according to CSL Behring, the company developing the product.
The company says lonoctocog alfa uses a covalent bond that forms one structural entity—a single polypeptide chain—to improve the stability of FVIII and provide FVIII activity with the option of twice-weekly dosing.
According to CSL Behring, lonoctocog alfa will be launched in European markets in the coming months, as market access is obtained.
Lonoctocog alfa is also approved for use in the US and Canada.
Regulatory submissions for lonoctocog alfa are based on results from the AFFINITY clinical development program, which includes a trial of children (n=84) and a trial of adolescents and adults (n=175).
Among patients who received lonoctocog alfa prophylactically in these trials, the median annualized bleeding rate was 1.14 in the adults/adolescents and 3.69 in children younger than 12.
In all, there were 1195 bleeding events—848 in the adults/adolescents and 347 in the children.
Ninety-four percent of bleeds in adults/adolescents and 96% of bleeds in pediatric patients were effectively controlled with no more than 2 infusions of lonoctocog alfa weekly.
Eighty-one percent of bleeds in adults/adolescents and 86% of bleeds in pediatric patients were controlled by a single infusion.
Researchers assessed safety in 258 patients from both studies. Adverse reactions occurred in 14 patients and included hypersensitivity (n=4), dizziness (n=2), paresthesia (n=1), rash (n=1), erythema (n=1), pruritus (n=1), pyrexia (n=1), injection-site pain (n=1), chills (n=1), and feeling hot (n=1).
One patient withdrew from treatment due to hypersensitivity.
None of the patients developed neutralizing antibodies to FVIII or antibodies to host cell proteins. There were no reports of anaphylaxis or thrombosis.
Results from the trial of adolescents/adults were published in Blood in August 2016. Results from the trial of children were presented at the World Federation of Hemophilia 2016 World Congress in July 2016.* ![]()
*Stasyshyn
O et al; rVIII-SingleChain, results of the pivotal efficacy data from a
phase III PK, efficacy and safety clinical study in children less than
12 years of age with severe hemophilia A; WFH 2016 World Congress, July
2016.

The European Commission has granted marketing authorization for lonoctocog alfa (Afstyla), a recombinant factor VIII (FVIII) single-chain therapy.
Lonoctocog alfa is indicated for the treatment and prophylaxis of bleeding in hemophilia A patients of all ages.
Lonoctocog alfa is the first and only single-chain recombinant FVIII therapy for hemophilia A specifically designed to provide long-lasting protection from bleeds with 2- to 3-times weekly dosing, according to CSL Behring, the company developing the product.
The company says lonoctocog alfa uses a covalent bond that forms one structural entity—a single polypeptide chain—to improve the stability of FVIII and provide FVIII activity with the option of twice-weekly dosing.
According to CSL Behring, lonoctocog alfa will be launched in European markets in the coming months, as market access is obtained.
Lonoctocog alfa is also approved for use in the US and Canada.
Regulatory submissions for lonoctocog alfa are based on results from the AFFINITY clinical development program, which includes a trial of children (n=84) and a trial of adolescents and adults (n=175).
Among patients who received lonoctocog alfa prophylactically in these trials, the median annualized bleeding rate was 1.14 in the adults/adolescents and 3.69 in children younger than 12.
In all, there were 1195 bleeding events—848 in the adults/adolescents and 347 in the children.
Ninety-four percent of bleeds in adults/adolescents and 96% of bleeds in pediatric patients were effectively controlled with no more than 2 infusions of lonoctocog alfa weekly.
Eighty-one percent of bleeds in adults/adolescents and 86% of bleeds in pediatric patients were controlled by a single infusion.
Researchers assessed safety in 258 patients from both studies. Adverse reactions occurred in 14 patients and included hypersensitivity (n=4), dizziness (n=2), paresthesia (n=1), rash (n=1), erythema (n=1), pruritus (n=1), pyrexia (n=1), injection-site pain (n=1), chills (n=1), and feeling hot (n=1).
One patient withdrew from treatment due to hypersensitivity.
None of the patients developed neutralizing antibodies to FVIII or antibodies to host cell proteins. There were no reports of anaphylaxis or thrombosis.
Results from the trial of adolescents/adults were published in Blood in August 2016. Results from the trial of children were presented at the World Federation of Hemophilia 2016 World Congress in July 2016.* ![]()
*Stasyshyn
O et al; rVIII-SingleChain, results of the pivotal efficacy data from a
phase III PK, efficacy and safety clinical study in children less than
12 years of age with severe hemophilia A; WFH 2016 World Congress, July
2016.

The European Commission has granted marketing authorization for lonoctocog alfa (Afstyla), a recombinant factor VIII (FVIII) single-chain therapy.
Lonoctocog alfa is indicated for the treatment and prophylaxis of bleeding in hemophilia A patients of all ages.
Lonoctocog alfa is the first and only single-chain recombinant FVIII therapy for hemophilia A specifically designed to provide long-lasting protection from bleeds with 2- to 3-times weekly dosing, according to CSL Behring, the company developing the product.
The company says lonoctocog alfa uses a covalent bond that forms one structural entity—a single polypeptide chain—to improve the stability of FVIII and provide FVIII activity with the option of twice-weekly dosing.
According to CSL Behring, lonoctocog alfa will be launched in European markets in the coming months, as market access is obtained.
Lonoctocog alfa is also approved for use in the US and Canada.
Regulatory submissions for lonoctocog alfa are based on results from the AFFINITY clinical development program, which includes a trial of children (n=84) and a trial of adolescents and adults (n=175).
Among patients who received lonoctocog alfa prophylactically in these trials, the median annualized bleeding rate was 1.14 in the adults/adolescents and 3.69 in children younger than 12.
In all, there were 1195 bleeding events—848 in the adults/adolescents and 347 in the children.
Ninety-four percent of bleeds in adults/adolescents and 96% of bleeds in pediatric patients were effectively controlled with no more than 2 infusions of lonoctocog alfa weekly.
Eighty-one percent of bleeds in adults/adolescents and 86% of bleeds in pediatric patients were controlled by a single infusion.
Researchers assessed safety in 258 patients from both studies. Adverse reactions occurred in 14 patients and included hypersensitivity (n=4), dizziness (n=2), paresthesia (n=1), rash (n=1), erythema (n=1), pruritus (n=1), pyrexia (n=1), injection-site pain (n=1), chills (n=1), and feeling hot (n=1).
One patient withdrew from treatment due to hypersensitivity.
None of the patients developed neutralizing antibodies to FVIII or antibodies to host cell proteins. There were no reports of anaphylaxis or thrombosis.
Results from the trial of adolescents/adults were published in Blood in August 2016. Results from the trial of children were presented at the World Federation of Hemophilia 2016 World Congress in July 2016.* ![]()
*Stasyshyn
O et al; rVIII-SingleChain, results of the pivotal efficacy data from a
phase III PK, efficacy and safety clinical study in children less than
12 years of age with severe hemophilia A; WFH 2016 World Congress, July
2016.
Kidney Disease Progression: How to Attenuate Risk
Q)I overheard a conversation at the hospital in which one of the nephrologists told an internist that allopurinol is better than other medications for treating gout because it slows the progression of chronic kidney disease (CKD). What does the data say?
CKD is a growing problem in America; the number of adults with CKD doubled from 2000 to 2008.1 Gout is considered an independent risk factor for CKD progression.2 Some randomized contr
A recent large retrospective review of Medicare charts assessed the correlation between use and dose of allopurinol and incidence of renal failure in patients older than 65.1 The researchers found that, compared with lower doses, allopurinol doses of 200 to 299 mg/d and > 300 mg/d were associated with a significantly lower hazard ratio for kidney failure, in a multivariate-adjusted model. The findings therefore suggest that doses > 199 mg may slow progression to kidney failure in the elderly.
Despite the strengths of this study, it is worth noting that it did not consider stage of kidney disease, nor did it distinguish comorbidities of the patients. The retrospective chart review format did not allow for identification of concurrent medication use (including OTC and herbal products).
The National Institute of Diabetes and Digestive and Kidney Diseases is currently conducting an RCT to investigate the renoprotective effects of allopurinol versus placebo in diabetic patients. (Clinical Trials.gov identifier: NCT02017171). Enrollment was completed in 2014, and results are expected in June 2019.
One important proviso about allopurinol: While it is inexpensive and generally well tolerated, prescribers should be aware of rare sensitivity reactions, particularly Stevens-Johnson syndrome. —MRS
Mary Rogers Sorey, MSN
Division of Nephrology and Hypertension at Vanderbilt University Medical Center, Nashville
1. Singh JA, Yu S. Are allopurinol dose and duration of use nephroprotective in the elderly? A Medicare claims study of allopurinol use and incident renal failure. Ann Rheum Dis. 2016 Jun 13. [Epub ahead of print]
2. Roughley MJ, Belcher J, Mallen CD, Roddy E. Gout and risk of chronic kidney disease and nephrolithiasis: meta-analysis of observational studies. Arthritis Res Ther. 2015;17:90.
3. Kanbay M, Huddam B, Azak A, et al. A randomized study of allopurinol on endothelial function and estimated glomerular filtration rate in asymptomatic hyperuricemic subjects with normal renal function. Clin J Am Soc Nephrol. 2011;6(8):1887-1894.
Q)I overheard a conversation at the hospital in which one of the nephrologists told an internist that allopurinol is better than other medications for treating gout because it slows the progression of chronic kidney disease (CKD). What does the data say?
CKD is a growing problem in America; the number of adults with CKD doubled from 2000 to 2008.1 Gout is considered an independent risk factor for CKD progression.2 Some randomized contr
A recent large retrospective review of Medicare charts assessed the correlation between use and dose of allopurinol and incidence of renal failure in patients older than 65.1 The researchers found that, compared with lower doses, allopurinol doses of 200 to 299 mg/d and > 300 mg/d were associated with a significantly lower hazard ratio for kidney failure, in a multivariate-adjusted model. The findings therefore suggest that doses > 199 mg may slow progression to kidney failure in the elderly.
Despite the strengths of this study, it is worth noting that it did not consider stage of kidney disease, nor did it distinguish comorbidities of the patients. The retrospective chart review format did not allow for identification of concurrent medication use (including OTC and herbal products).
The National Institute of Diabetes and Digestive and Kidney Diseases is currently conducting an RCT to investigate the renoprotective effects of allopurinol versus placebo in diabetic patients. (Clinical Trials.gov identifier: NCT02017171). Enrollment was completed in 2014, and results are expected in June 2019.
One important proviso about allopurinol: While it is inexpensive and generally well tolerated, prescribers should be aware of rare sensitivity reactions, particularly Stevens-Johnson syndrome. —MRS
Mary Rogers Sorey, MSN
Division of Nephrology and Hypertension at Vanderbilt University Medical Center, Nashville
Q)I overheard a conversation at the hospital in which one of the nephrologists told an internist that allopurinol is better than other medications for treating gout because it slows the progression of chronic kidney disease (CKD). What does the data say?
CKD is a growing problem in America; the number of adults with CKD doubled from 2000 to 2008.1 Gout is considered an independent risk factor for CKD progression.2 Some randomized contr
A recent large retrospective review of Medicare charts assessed the correlation between use and dose of allopurinol and incidence of renal failure in patients older than 65.1 The researchers found that, compared with lower doses, allopurinol doses of 200 to 299 mg/d and > 300 mg/d were associated with a significantly lower hazard ratio for kidney failure, in a multivariate-adjusted model. The findings therefore suggest that doses > 199 mg may slow progression to kidney failure in the elderly.
Despite the strengths of this study, it is worth noting that it did not consider stage of kidney disease, nor did it distinguish comorbidities of the patients. The retrospective chart review format did not allow for identification of concurrent medication use (including OTC and herbal products).
The National Institute of Diabetes and Digestive and Kidney Diseases is currently conducting an RCT to investigate the renoprotective effects of allopurinol versus placebo in diabetic patients. (Clinical Trials.gov identifier: NCT02017171). Enrollment was completed in 2014, and results are expected in June 2019.
One important proviso about allopurinol: While it is inexpensive and generally well tolerated, prescribers should be aware of rare sensitivity reactions, particularly Stevens-Johnson syndrome. —MRS
Mary Rogers Sorey, MSN
Division of Nephrology and Hypertension at Vanderbilt University Medical Center, Nashville
1. Singh JA, Yu S. Are allopurinol dose and duration of use nephroprotective in the elderly? A Medicare claims study of allopurinol use and incident renal failure. Ann Rheum Dis. 2016 Jun 13. [Epub ahead of print]
2. Roughley MJ, Belcher J, Mallen CD, Roddy E. Gout and risk of chronic kidney disease and nephrolithiasis: meta-analysis of observational studies. Arthritis Res Ther. 2015;17:90.
3. Kanbay M, Huddam B, Azak A, et al. A randomized study of allopurinol on endothelial function and estimated glomerular filtration rate in asymptomatic hyperuricemic subjects with normal renal function. Clin J Am Soc Nephrol. 2011;6(8):1887-1894.
1. Singh JA, Yu S. Are allopurinol dose and duration of use nephroprotective in the elderly? A Medicare claims study of allopurinol use and incident renal failure. Ann Rheum Dis. 2016 Jun 13. [Epub ahead of print]
2. Roughley MJ, Belcher J, Mallen CD, Roddy E. Gout and risk of chronic kidney disease and nephrolithiasis: meta-analysis of observational studies. Arthritis Res Ther. 2015;17:90.
3. Kanbay M, Huddam B, Azak A, et al. A randomized study of allopurinol on endothelial function and estimated glomerular filtration rate in asymptomatic hyperuricemic subjects with normal renal function. Clin J Am Soc Nephrol. 2011;6(8):1887-1894.
Longer follow-up needed to track mesh explantation trends
Explantation of mesh used in ventral hernia repair occurs in approximately 1 of every 1,000 surgeries, but it’s a “hidden” morbidity because it almost always happens well after the 30- to 90-day window in which postoperative complications are typically reported in most registries and surveillance systems, according to a report in the Journal of the American College of Surgeons.
Mesh explantation usually occurs 1-3 years after implantation and triples the operative costs of the original ventral hernia repair. The rate of 1 per 1,000 surgeries and the massive increase in cost are comparable with those of occult injury of the common bile duct during cholecystectomy that later requires biliary reconstruction. But mesh explantation doesn’t generate the “profound attention” accorded to bile duct injury, perhaps because it develops much later in the postoperative course.
“It is surprising that mesh complications have not yet prompted similar concern,” said Kristy Kummerow Broman, MD, of the department of surgery, Vanderbilt University Medical Center, Nashville, Tenn., and her associates.
Until now, the frequency and cost of mesh explantation after ventral hernia repair in the general population have not been known. To make a reasonable estimate, the investigators constructed a cohort of 619,751 patients using information from inpatient and surgery databases for New York, California, and Florida between 2005 and 2011. Most of these were open procedures (91%), while 9% were laparoscopic.
During a mean follow-up of 3 years, 438 patients (0.7 per 1,000) underwent mesh explantation. This is a clinically significant incidence, and is likely an underestimate because ICD-9 and CPT coding for mesh removal is highly variable, Dr. Broman and her associates said.
This rate, for just three states during 3 years of follow-up, is nearly twice as high as the rate of mesh-related complications voluntarily reported to the FDA in post-marketing surveillance for the entire country during a 7-year period, they noted (J Am Coll Surg. 2017 Jan;224:35-42).
“It is paramount” that surgeons, manufacturers, and regulatory groups advocate mandatory reporting and “extend the surveillance for at least 1-3 years after implantation of a mesh device,” Dr. Broman and her associates said.
In this study, the median time to explantation was approximately 1 year (range, 2 days to 6 years), and 80% of explantations occurred within 2 years.
The median cumulative operative cost – excluding physician fees, nonsurgical medical costs, and the costs of patient disability and lost productivity – were $21,889 for patients requiring mesh explantation, compared with only $6,579 for those who did not. This finding highlights “the profound long-term implications of implantable devices in abdominal wall reconstruction,” they noted.
To put their findings in context, the investigators reviewed the literature regarding major bile duct injury during cholecystectomy. One large study on cases from 2001 to 2011 found that the rate of biliary reconstruction was comparable with that of explantation, at 0.8 to 1.1 per 1,000. Similarly, reoperation for bile duct injury approximately tripled the operative costs ($9,061 for patients who required biliary reconstruction vs $2,689 for those who didn’t). However, the $21,000 for mesh reoperation far exceeds the $9,000 for biliary reoperation.
This study was supported by the Department of Veterans Affairs, the VA Tennessee Valley Healthcare System, and the Americas Hernia Society Quality Collaborative. Dr. Broman reported having no relevant financial disclosures; her associates reported ties to Intuitive Surgical Solutions, Bard Davol, Ariste Medical, and Pfizer.
Explantation of mesh used in ventral hernia repair occurs in approximately 1 of every 1,000 surgeries, but it’s a “hidden” morbidity because it almost always happens well after the 30- to 90-day window in which postoperative complications are typically reported in most registries and surveillance systems, according to a report in the Journal of the American College of Surgeons.
Mesh explantation usually occurs 1-3 years after implantation and triples the operative costs of the original ventral hernia repair. The rate of 1 per 1,000 surgeries and the massive increase in cost are comparable with those of occult injury of the common bile duct during cholecystectomy that later requires biliary reconstruction. But mesh explantation doesn’t generate the “profound attention” accorded to bile duct injury, perhaps because it develops much later in the postoperative course.
“It is surprising that mesh complications have not yet prompted similar concern,” said Kristy Kummerow Broman, MD, of the department of surgery, Vanderbilt University Medical Center, Nashville, Tenn., and her associates.
Until now, the frequency and cost of mesh explantation after ventral hernia repair in the general population have not been known. To make a reasonable estimate, the investigators constructed a cohort of 619,751 patients using information from inpatient and surgery databases for New York, California, and Florida between 2005 and 2011. Most of these were open procedures (91%), while 9% were laparoscopic.
During a mean follow-up of 3 years, 438 patients (0.7 per 1,000) underwent mesh explantation. This is a clinically significant incidence, and is likely an underestimate because ICD-9 and CPT coding for mesh removal is highly variable, Dr. Broman and her associates said.
This rate, for just three states during 3 years of follow-up, is nearly twice as high as the rate of mesh-related complications voluntarily reported to the FDA in post-marketing surveillance for the entire country during a 7-year period, they noted (J Am Coll Surg. 2017 Jan;224:35-42).
“It is paramount” that surgeons, manufacturers, and regulatory groups advocate mandatory reporting and “extend the surveillance for at least 1-3 years after implantation of a mesh device,” Dr. Broman and her associates said.
In this study, the median time to explantation was approximately 1 year (range, 2 days to 6 years), and 80% of explantations occurred within 2 years.
The median cumulative operative cost – excluding physician fees, nonsurgical medical costs, and the costs of patient disability and lost productivity – were $21,889 for patients requiring mesh explantation, compared with only $6,579 for those who did not. This finding highlights “the profound long-term implications of implantable devices in abdominal wall reconstruction,” they noted.
To put their findings in context, the investigators reviewed the literature regarding major bile duct injury during cholecystectomy. One large study on cases from 2001 to 2011 found that the rate of biliary reconstruction was comparable with that of explantation, at 0.8 to 1.1 per 1,000. Similarly, reoperation for bile duct injury approximately tripled the operative costs ($9,061 for patients who required biliary reconstruction vs $2,689 for those who didn’t). However, the $21,000 for mesh reoperation far exceeds the $9,000 for biliary reoperation.
This study was supported by the Department of Veterans Affairs, the VA Tennessee Valley Healthcare System, and the Americas Hernia Society Quality Collaborative. Dr. Broman reported having no relevant financial disclosures; her associates reported ties to Intuitive Surgical Solutions, Bard Davol, Ariste Medical, and Pfizer.
Explantation of mesh used in ventral hernia repair occurs in approximately 1 of every 1,000 surgeries, but it’s a “hidden” morbidity because it almost always happens well after the 30- to 90-day window in which postoperative complications are typically reported in most registries and surveillance systems, according to a report in the Journal of the American College of Surgeons.
Mesh explantation usually occurs 1-3 years after implantation and triples the operative costs of the original ventral hernia repair. The rate of 1 per 1,000 surgeries and the massive increase in cost are comparable with those of occult injury of the common bile duct during cholecystectomy that later requires biliary reconstruction. But mesh explantation doesn’t generate the “profound attention” accorded to bile duct injury, perhaps because it develops much later in the postoperative course.
“It is surprising that mesh complications have not yet prompted similar concern,” said Kristy Kummerow Broman, MD, of the department of surgery, Vanderbilt University Medical Center, Nashville, Tenn., and her associates.
Until now, the frequency and cost of mesh explantation after ventral hernia repair in the general population have not been known. To make a reasonable estimate, the investigators constructed a cohort of 619,751 patients using information from inpatient and surgery databases for New York, California, and Florida between 2005 and 2011. Most of these were open procedures (91%), while 9% were laparoscopic.
During a mean follow-up of 3 years, 438 patients (0.7 per 1,000) underwent mesh explantation. This is a clinically significant incidence, and is likely an underestimate because ICD-9 and CPT coding for mesh removal is highly variable, Dr. Broman and her associates said.
This rate, for just three states during 3 years of follow-up, is nearly twice as high as the rate of mesh-related complications voluntarily reported to the FDA in post-marketing surveillance for the entire country during a 7-year period, they noted (J Am Coll Surg. 2017 Jan;224:35-42).
“It is paramount” that surgeons, manufacturers, and regulatory groups advocate mandatory reporting and “extend the surveillance for at least 1-3 years after implantation of a mesh device,” Dr. Broman and her associates said.
In this study, the median time to explantation was approximately 1 year (range, 2 days to 6 years), and 80% of explantations occurred within 2 years.
The median cumulative operative cost – excluding physician fees, nonsurgical medical costs, and the costs of patient disability and lost productivity – were $21,889 for patients requiring mesh explantation, compared with only $6,579 for those who did not. This finding highlights “the profound long-term implications of implantable devices in abdominal wall reconstruction,” they noted.
To put their findings in context, the investigators reviewed the literature regarding major bile duct injury during cholecystectomy. One large study on cases from 2001 to 2011 found that the rate of biliary reconstruction was comparable with that of explantation, at 0.8 to 1.1 per 1,000. Similarly, reoperation for bile duct injury approximately tripled the operative costs ($9,061 for patients who required biliary reconstruction vs $2,689 for those who didn’t). However, the $21,000 for mesh reoperation far exceeds the $9,000 for biliary reoperation.
This study was supported by the Department of Veterans Affairs, the VA Tennessee Valley Healthcare System, and the Americas Hernia Society Quality Collaborative. Dr. Broman reported having no relevant financial disclosures; her associates reported ties to Intuitive Surgical Solutions, Bard Davol, Ariste Medical, and Pfizer.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Explantation of mesh used in ventral hernia repair occurs in approximately 1 of every 1,000 surgeries, but it’s a “hidden” morbidity because it almost always happens well after the 30- to 90-day window in which postoperative complications are typically reported in most registries and surveillance systems.
Major finding: The 1/1,000 rate of mesh explantation, for three states during 3 years of follow-up, is nearly twice as high as the rate voluntarily reported to the Food and Drug Administration in post-marketing surveillance for the entire country during a 7-year period.
Data source: A longitudinal cohort study involving 619,751 adults undergoing ventral hernia repair in New York, California, and Florida who were followed for up to 6 years for mesh explantation.
Disclosures: This study was supported by the Department of Veterans Affairs, the VA Tennessee Valley Healthcare System, and the Americas Hernia Society Quality Collaborative. Dr. Broman reported having no relevant financial disclosures; her associates reported ties to Intuitive Surgical Solutions, Bard Davol, Ariste Medical, and Pfizer.