User login
Effectiveness of an Employee Skin Cancer Screening Program for Secondary Prevention
The incidence of skin cancer, along with its effects on patients and the economy, has continued to increase and therefore requires particular attention from dermatologists. UV light has been shown to be of etiopathologic importance in the development of various types of skin cancer.1-3 Studies have shown that there is a direct correlation between the incidence of skin cancer and average annual amounts of UV radiation exposure.3 Accordingly, in 2009 the International Agency for Research on Cancer classified UV light as carcinogenic to humans.4 Therefore, the general public must be made aware of the danger of exposure to UV radiation.
In Australia, government initiatives to educate the population on causes of skin cancer development and its relationship to UV radiation have already caused the public to change their way of thinking and to deal with sunlight in a conscious and responsible manner.5 A large proportion of the Australian population with light skin is at a particularly high risk for developing skin cancer due to intense exposure to UV radiation. Numerous campaigns in Germany and other countries have attempted to sensitize the public to this issue by emphasizing a reduction in UV exposure (primary prevention) or highlighting the importance of early diagnosis (secondary prevention).6,7
For a good prognosis, it is crucial that skin cancer, particularly melanoma, is discovered at an early or precancerous stage.8 For this reason, self-examination of the skin and skin cancer screening are important factors that can contribute to ensuring early and curative treatment.9-11 Since July 1, 2008, skin cancer screenings have been included in the preventative health care program by statutory health insurance providers in Germany. As part of this program, the cost of screening once every 2 years for individuals 35 years and older is covered by statutory health insurance.12 Several studies have shown a decline in the melanoma mortality rate since the introduction of skin cancer screening programs in Germany.11,13,14
Employee skin cancer screening programs are an important method of examining high numbers of individuals quickly and effectively. These programs have been carried out in Germany and other countries.15,16 Studies have shown that skin cancer screening carried out selectively on defined groups can be an effective form of secondary prevention, particularly for those who work outdoors.17
An employee skin cancer screening program was carried out as part of this study. The findings are interpreted and discussed in relation to other employee screening programs that have been reported as well as those introduced by statutory health insurance providers in Germany. The aim of this study was to determine the importance and effectiveness of employee skin cancer screening programs and the role they play in secondary prevention of skin cancer.
Methods
Study Population
Employees of a technical company in Bavaria, Germany, were offered a skin cancer screening program by the employer’s occupational health service and health insurance provider in collaboration with the Department of Dermatology at the University Hospital Erlangen (Erlangen, Germany). Skin examinations were performed exclusively by 5 trained dermatologists. Only direct employees of the company at 3 of its locations in the Erlangen area were eligible to participate. The total number of employees varied by location (1072–5126 employees). The majority of employees had a university education or had completed technical training. Family members and other individuals who were not members of the company were excluded. There were no further inclusion or exclusion criteria. Over a period of 13 days, 783 of 7823 total employees (10.0%) were examined and included in the study. The study was approved by the Responsible Ethics Commission of the Faculty of Medicine at Friedrich-Alexander-University Erlangen-Nürnberg, Germany.
Study Design
Employees signed a consent form for participation in the study and completed a standardized questionnaire. The questionnaire was based on surveys used in a prior study18 and collected information on current and prior skin lesions, prior dermatological screening, personal and family history of skin tumors, frequency of UV exposure, and type of UV protection used. For the question on measures taken for protection from UV radiation, possible answers included with sunscreen cream, with suitable sun-protective clothing, and by staying in the shade, or no measures were taken. In contrast to the other questions, multiple answers were accepted for this question. Answering no automatically excluded other possible answers. Participants also were asked to assess their own Fitzpatrick skin type19; the questionnaire included explanations of each skin type (I–IV).
The participants were then called in for examination by the dermatologist at 15-minute intervals. All clothing was removed and the skin was examined. Dermatoscopes were used for closer examination of suspicious skin lesions. The clinical results of the examinations were recorded on a standardized form.
An estimation of the number of melanocytic nevi—≤20, 21–49, or ≥50—was recorded for each patient. Suspicious skin lesions were assigned to one of the following categories: nevus requiring future checkup (Nc), nevus requiring excision (Ne), suspected malignant melanoma (MM), suspected squamous cell carcinoma, suspected basal cell carcinoma (BCC), suspected other skin tumor, and precancerous lesion. Fitzpatrick skin type also was assessed for all participants and recorded by the dermatologist carrying out the examination. Each participant was assigned to a risk group—low, moderate, or high risk—based on their individual risk for developing a skin tumor. Factors that were considered when determining participants’ risk for developing skin cancer included Fitzpatrick skin type, number of melanocytic nevi, personal and family history, leisure activities, UV protection used, and current clinical diagnosis of skin lesions.
After the skin examination, participants were informed of recommended treatment but were not given any additional dermatologic advice. Participants could arrange an appointment at the Department of Dermatology, University Hospital Erlangen, for the excision and histological analysis of the skin lesions. All recorded data were collected in a computerized spreadsheet program. When evaluating the questionnaires, questions that were not answered or were answered incorrectly (participant chose more than 1 answer) were ignored.
Statistical Analysis
Statistical analysis was carried out using SPSS software version 16.0. The majority of the data were nominal or ordinal. Metric data were checked for normal distribution using the Shapiro-Wilk test before carrying out parametric tests. Statistical tests were carried out using the χ2 test and the t test for independent samples. Non-nominal distributed data were checked using the Mann-Whitney U test. P<.05 was considered statistically significant in the exploratory data analysis.
Results
Of 783 employees included in the study, 288 (36.8%) were female and 495 (63.2%) were male (Table 1). In comparison with the total workforce, a significantly higher proportion of women than men took part in the cross-sectional study (P<.01). The average age (SD) was 42.3 (9.5) years (range, 18–64 years). Female participants (average age [SD], 39.8 [10.2] years) were significantly younger than male participants (average age [SD], 43.8 [8.8] years; P<.01). Forty-one percent of participants had a prior skin cancer screening. One percent of participants had a personal history of skin cancer, with 1 participant reporting a history of MM; 6.5% had a family history of skin cancer, of which 39.2% had a family history of MM.
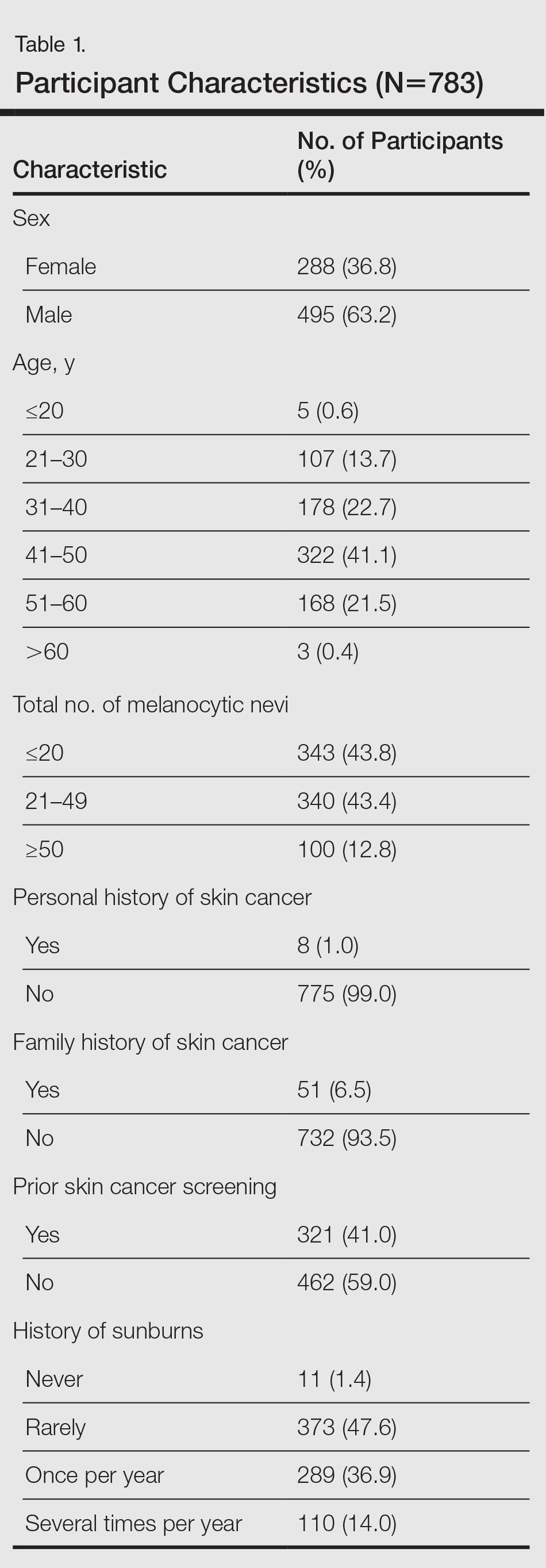
The results of the clinical examinations showed that 43.8% of participants had 20 or fewer melanocytic nevi, 43.4% had 21 to 49 melanocytic nevi, and 12.8% had 50 or more melanocytic nevi. Significantly more women than men had 20 or fewer melanocytic nevi (P<.05).
Approximately 92% of participants assessed themselves as having Fitzpatrick skin types II (35.2%) or III (56.7%), while only approximately 3.6% and 4.5% assessed themselves as having skin types I and IV, respectively. The results of the Fitzpatrick skin type assessments made by dermatologists were similar: 96.9% of participants were assessed as having Fitzpatrick skin types II (43.0%) and III (53.8%); approximately 1.9% and 1.3% were assessed as having Fitzpatrick skin types I and IV, respectively. Results showed that 80.2% of all participants assessed their skin type in the same way as the dermatologist; 13.5% assessed their skin type as darker and 6.3% (49/783) assessed it as lighter. A quantitative analysis of Fitzpatrick skin type and sex showed that significantly more male participants than female participants assessed their Fitzpatrick skin type darker than their actual skin type (P<.01).
Overall, 47.6% of participants reported having had sunburn rarely in the past, while 36.9% and 14.0% had experienced sunburn once per year and several times per year, respectively. Approximately 1.4% of participants reported never having a sunburn. More of the male participants made use of comprehensive sun protection using all methods listed (34.5%; P<.05) or a combination of sunscreen and sun-protective clothing (14.9%; P<.01) than the female participants who relied more frequently on sunscreen alone (29.5%; P<.01) or a combination of sunscreen and staying in the shade (29.5%; P<.01)
In general it was clear that sunscreen, either alone or in combination with other sun-protection methods, was used most frequently (88.0%); 58.0% protected themselves by staying in the shade, while 48.0% used suitable sun-protective clothing. Only 3.6% of participants did not protect themselves using any of the suggested methods.
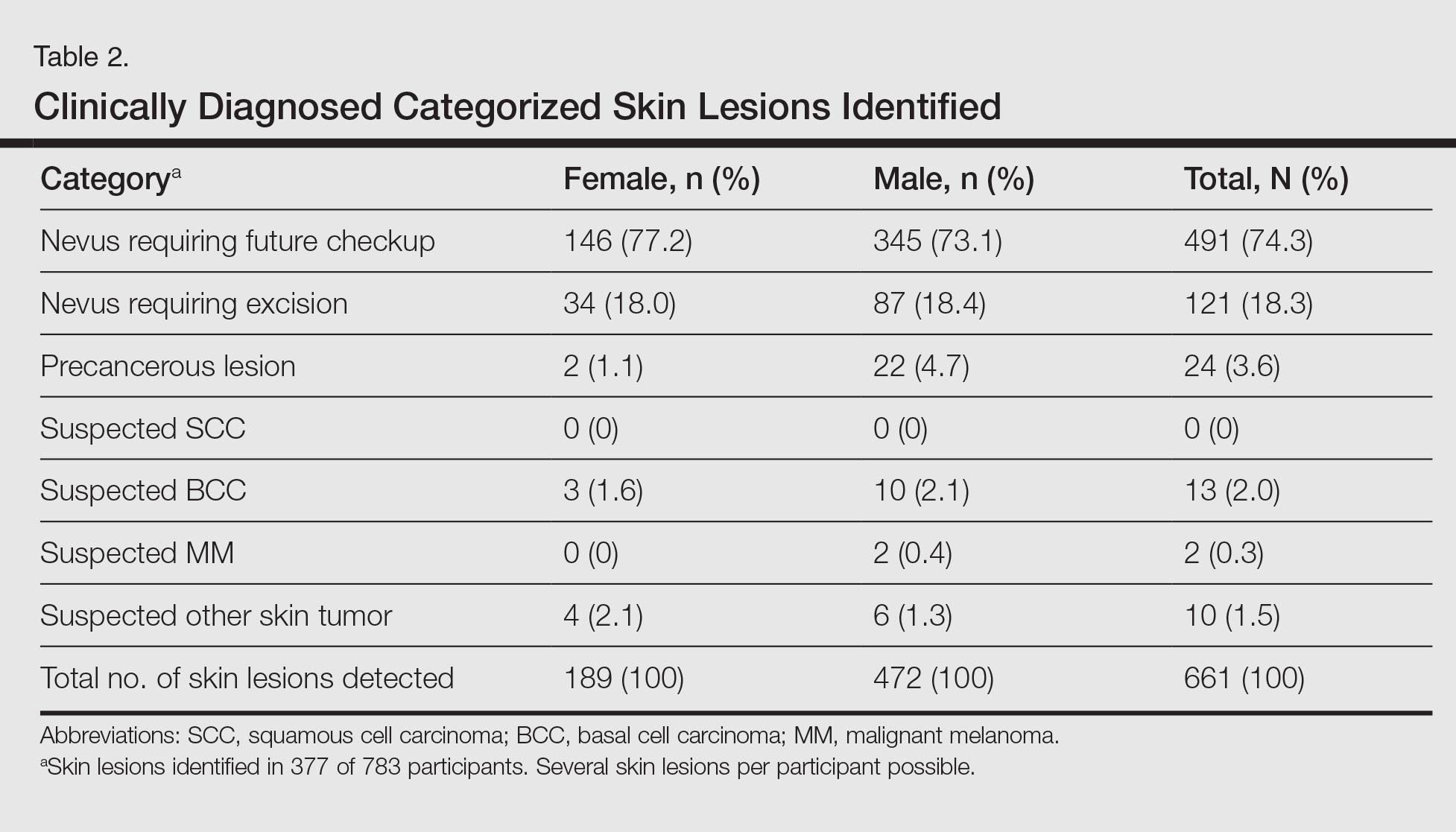
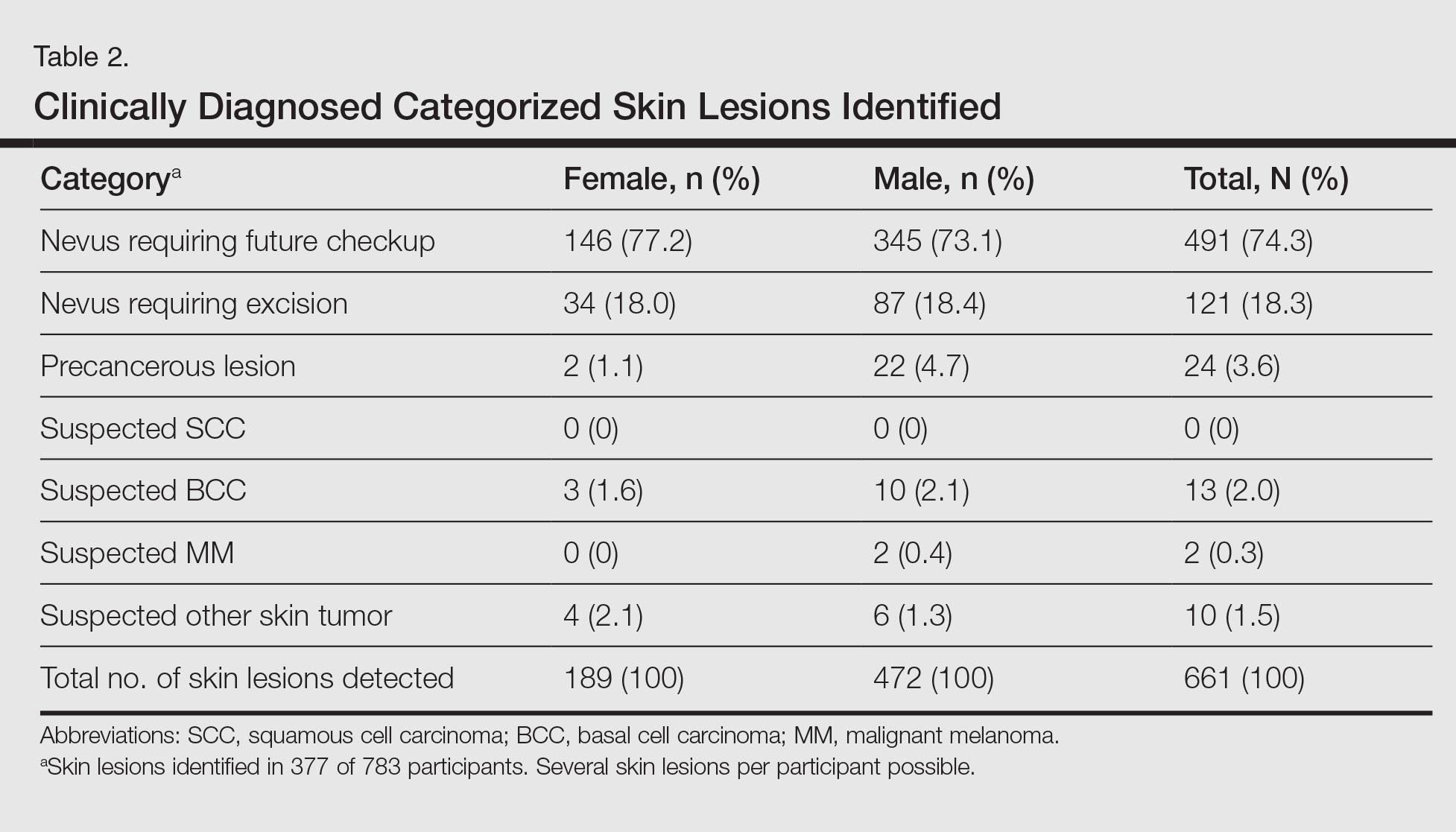
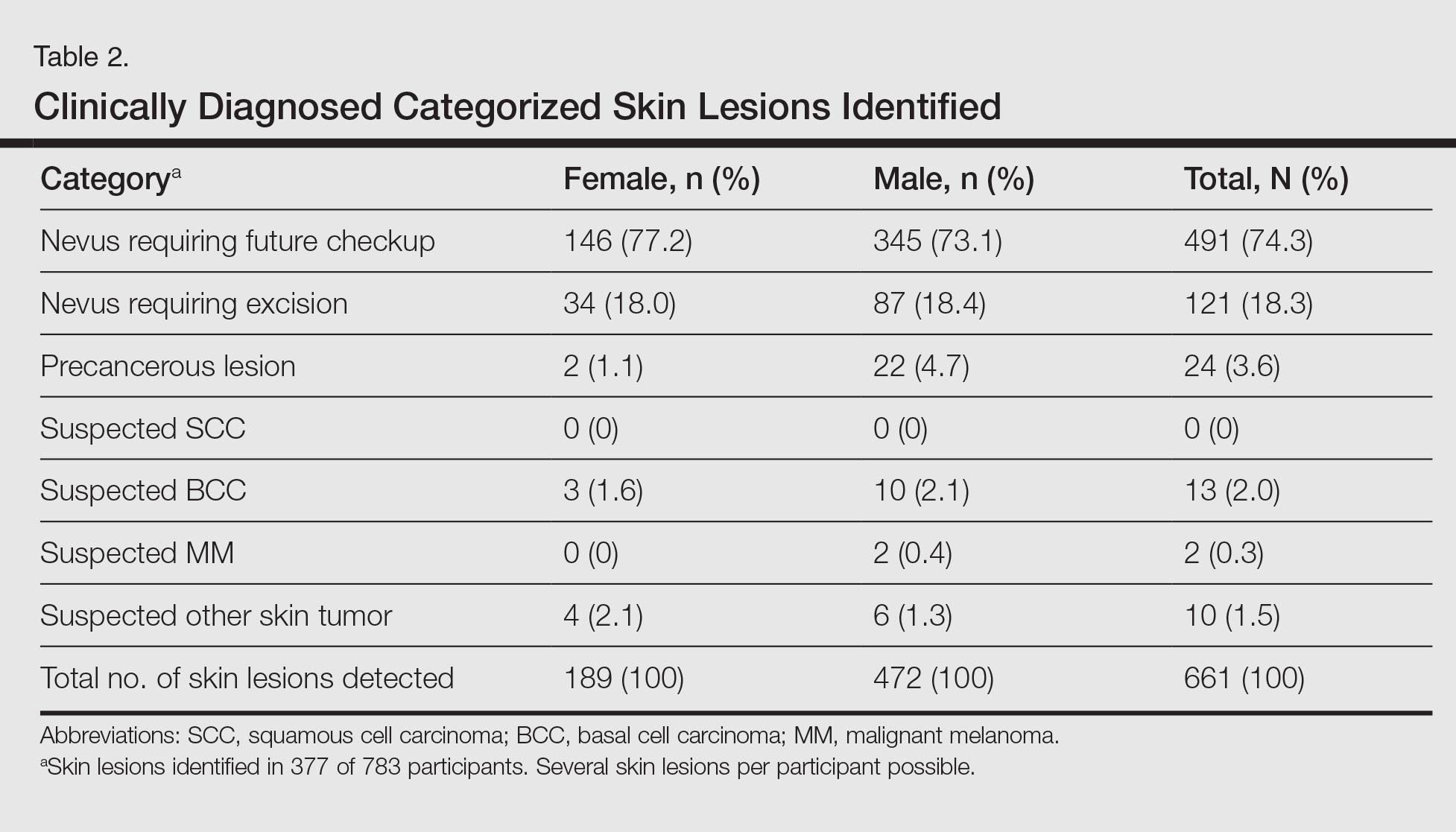
A total of 661 categorized skin lesions were found in 377 participants. Of these lesions, 491 were Nc and 121 were Ne. Twenty-four of the skin lesions were suspected precancerous lesions, 13 were suspected BCC, 2 were suspected MM, and 10 were suspected other skin tumor (Table 2). Overall, male participants who were diagnosed with at least 1 skin lesion (average age, 44.0 years) were significantly older than the women (average age, 39.3 years)(P<.01). Similar findings were observed in participants with at least 1 Nc (men, 43.3 years; women, 38.7 years; P<.01) and at least 1 Ne (men, 44.2 years; women, 38.0 years; P<.05). With regard to the individual risk for developing skin cancer, 32.6% of participants were considered to be at low risk, 64.9% were at moderate risk, and 2.6% were at high risk.
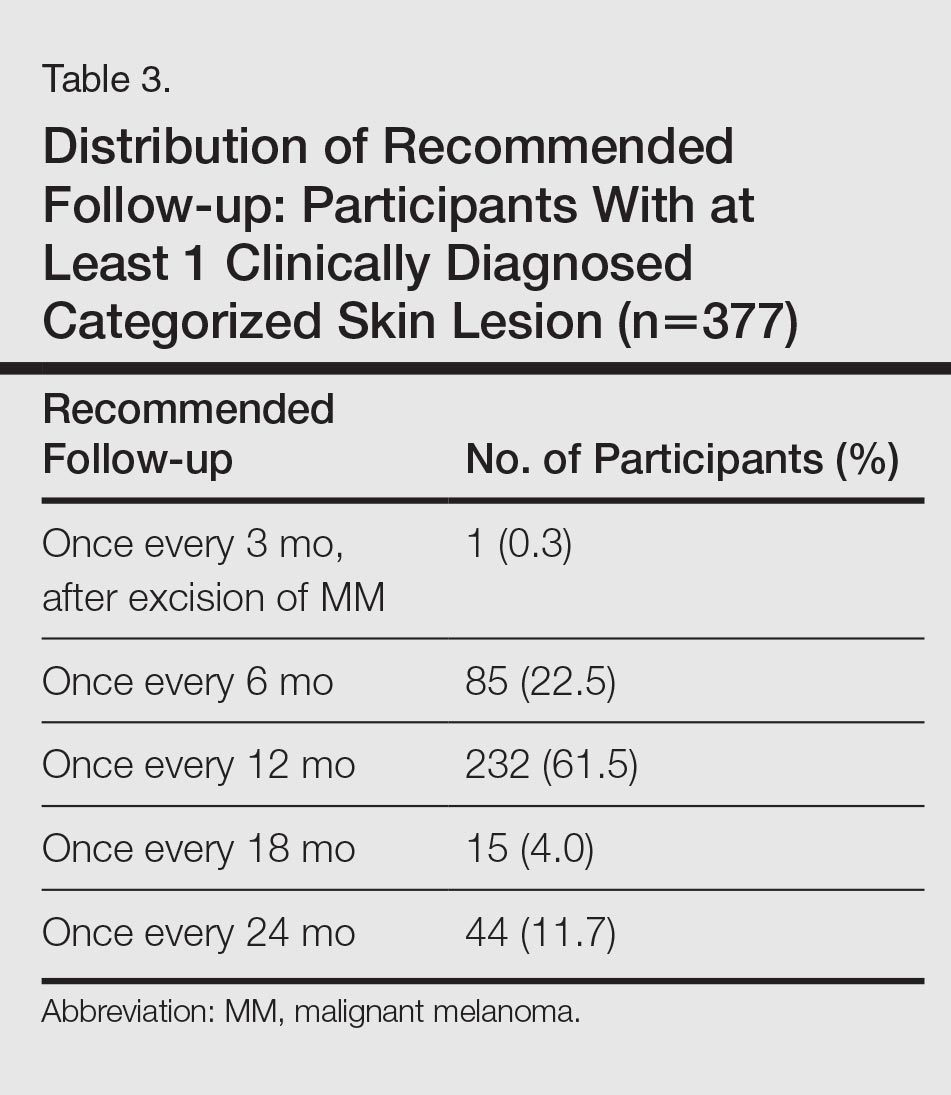
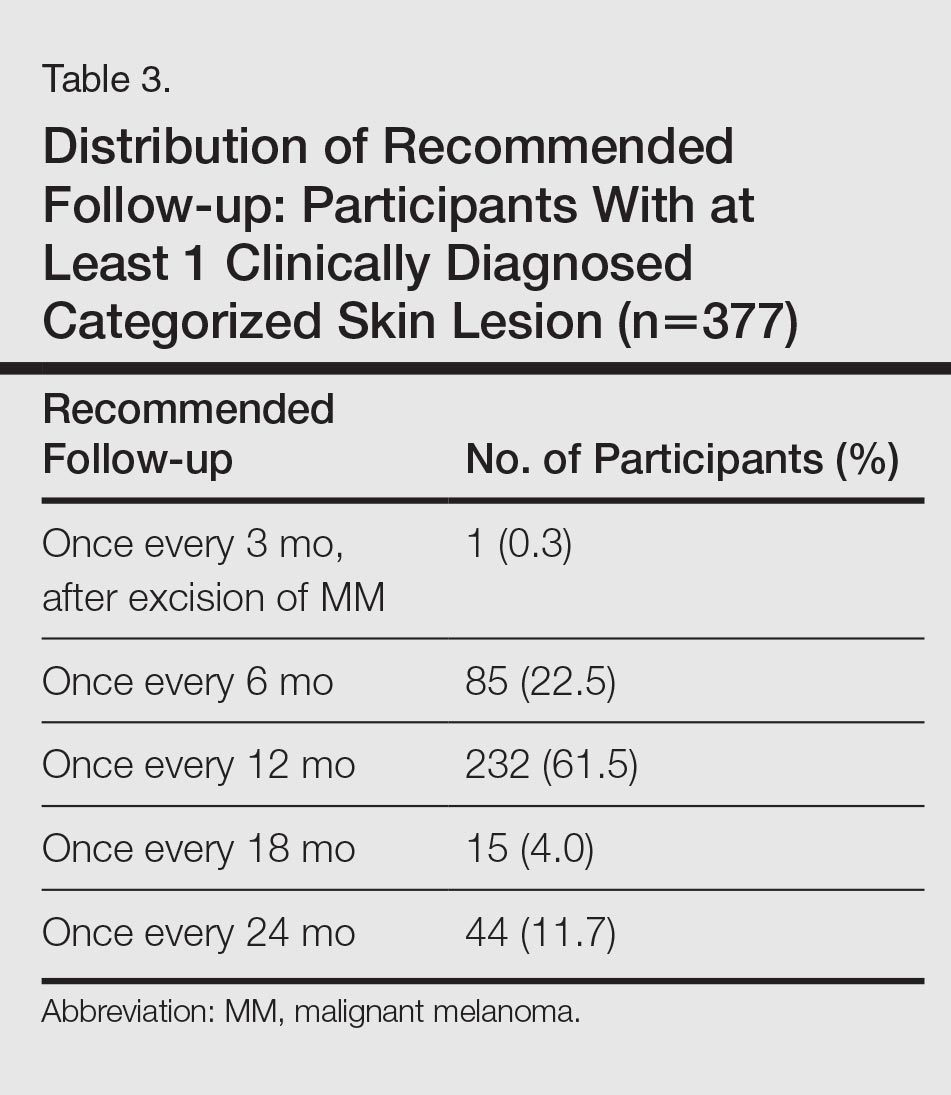
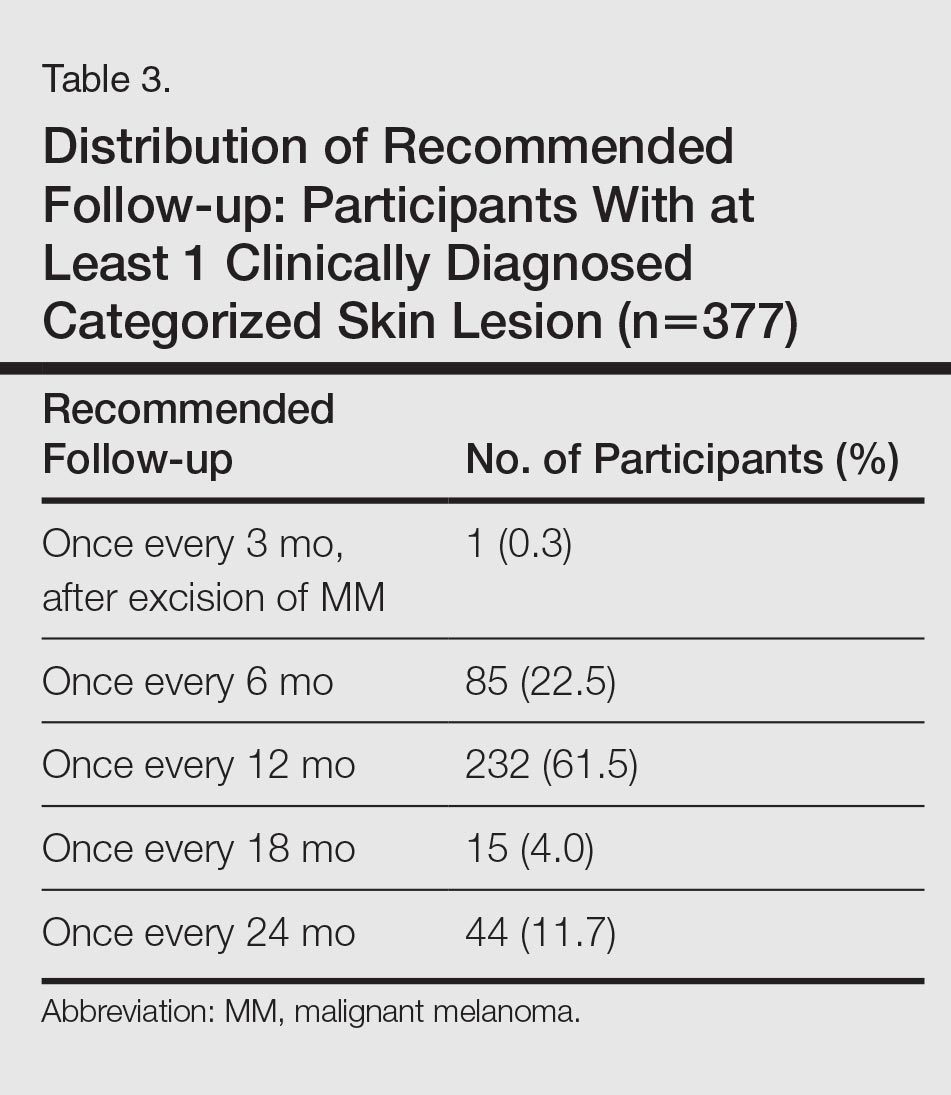
Approximately 61.5% of 377 participants who were diagnosed with at least 1 categorized skin lesion were advised to have a specific skin lesion checked by a dermatologist or to have a full examination for skin cancer once every 12 months. Furthermore, 22.5% were advised to follow-up biannually and 11.7% were advised to follow-up once every 2 years. Of the remaining participants who were advised to have follow-ups, 0.3% were advised to have a skin examination once every 3 months after having had MM, and 4.0% were advised to have follow-up once every 18 months. Overall, follow-up was recommended within 1 year in 84.4% of cases and within 1 to 2 years in 15.6% (Table 3).
Subsequent histological analysis of the excised tissue resulted in a diagnosis of only 21 clinically significant skin conditions. One case of Bowen disease and 1 case of BCC was confirmed. Histological analysis identified the remaining 19 excised skin lesions, which included the 2 suspected MMs, as dysplastic nevi.
Comment
The aim of this cross-sectional study was to examine the importance and effectiveness of employee skin cancer screening programs. In comparison with the total workforce, significantly more women took part than men. Female participants were significantly younger than male participants, which mirrors the findings of prior studies showing that screening programs reach women more frequently than men and that women who participate in screenings are also younger on average in comparison to men.7-13 Men and older individuals usually are underrepresented.7,13 The average age of participants in our study was 42.3 years, which is lower than in the SCREEN (Skin Cancer Research to Provide Evidence for Effectiveness of Screening in Northern Germany) study (average age, 49.7 years).13 The average age in our study also is likely to be lower than patients who undergo skin cancer screenings offered by statutory health insurance providers in Germany, which has a minimum age restriction of 35 years; however, it is comparable to the average age of participants in other employee screening programs and therefore represents the average age of individuals employed in Germany.15,16
The employee skin cancer screening program in this study generated a high level of interest, indicated by the fact that all available appointments had been booked just 36 hours after the screening was announced. Furthermore, there was a waiting list of approximately 300 employees who were not able to undergo a skin examination. For logistical reasons, the number of participants was limited to 10% of the workforce. The high level of interest is an indication of increased awareness of the importance of recognizing skin tumors early and the associated need for information as well as the need to undergo screening for skin cancer as a precaution. This observation also can be made with regard to the skin cancer screening introduced by statutory health insurance providers in Germany. Studies published by Augustin et al20 and Kornek et al21,22 confirm that skin cancer screenings have gained wide acceptance in Germany because they were introduced by statutory health insurance providers in 2008. The number of skin cancer screenings carried out by dermatologists in Germany also is increasing.20-22 Although approximately 19% of those eligible to participate took part in the SCREEN pilot project,13 approximately 31% of individuals who were eligible to participate took part in skin cancer screenings offered by statutory health insurance providers in Germany in 2012, and the percentage is rising.23 Two important factors affecting the high level of interest in the employee screening program used in our study were undoubtedly the advantages of the examination taking place during working hours and being held on the occupational health services’ premises in the workplace, which helped participants avoid the cost of travel and wait times associated with visiting a medical practice.
Of 783 participants included in this study, 377 displayed at least 1 categorized skin lesion; the majority were suspicious melanocytic nevi. This high incidence rate suggested that regular skin cancer screenings are useful, as it has been shown that there is a correlation between higher numbers of melanocytic nevi and increased risk for developing melanoma.24
In a study by Winkler et al,25 a skin cancer screening of 1658 bank and insurance employees found that 33.8% of those examined displayed at least 1 atypical melanocytic nevus and 27.2% displayed more than 50 melanocytic nevi (compared to 12.8% with ≥50 melanocytic nevi in the current study). The risk for developing skin cancer was classified as intermediate or high in 54.5% (compared to 67.5% at moderate or high risk in the current study).25 Therefore, the rate of suspicious skin lesions was lower in the population of the study by Winkler et al25 in comparison to the population of the current study. As the overall number of melanocytic nevi and the individual risk for skin cancer, however, was underestimated by the majority of the bank and insurance employees,25 employee skin cancer screening programs can be used as a potentially effective tool to make employees aware of the issue and sensitizing them to it. Employee screening in addition to a final diagnosis can contribute to ensuring suitable treatment is started. For example, in the large-scale employee screening published by Schaefer et al15 and Augustin et al,16 48,665 and 90,880 employees, respectively, were screened for inflammatory and noninflammatory skin diseases, and 19% and 27% of participants, respectively, were diagnosed with skin lesions that required treatment.
Participants in the current study were given no further treatment or advice. Recommendations were made that participants monitor suspicious skin lesions or have them removed. With regard to future screening, 84.4% of participants with at least 1 categorized skin lesion were advised to have a regular follow-up within 1 year, while 15.6% were advised to follow-up within 1 to 2 years. Therefore, a period of 2 years before the next checkup, the period between screenings offered by statutory health insurance providers in Germany,12 was considered too long for the majority of participants, according to the dermatologists involved with our study.
Conclusion
The high rate of suspicious skin lesions diagnosed demonstrated the effectiveness of skin cancer screenings organized in the workplace, which should be recommended for all employees, not only those who are at high risk for developing skin cancer due to the nature of their work, such as those who work outdoors. It should be noted that the study group examined in the current study was a homogeneous group of employees of a technical company only and is therefore relatively selective. Nevertheless, despite the comparatively selective and young participant group, these examinations provide evidence of the importance of skin cancer screening programs for a wider population.
Acknowledgments
The authors thank Heidi Seybold, MD; Petra Wörl, MD; Sybille Thoma-Uszynski, MD; and Jens Bussmann, MD (all from Erlangen, Germany), for their support and active assistance in the practical implementation of this study.
- Boniol M, Autier P, Boyle P, et al. Cutaneous melanoma attributable to sunbed use: systematic review and meta-analysis. BMJ. 2012;345:e4757.
- Gilchrest BA, Eller MS, Geller AC, et al. The pathogenesis of melanoma induced by ultraviolet radiation. N Engl J Med. 1999;340:1341-1348.
- Rigel DS. Cutaneous ultraviolet exposure and its relationship to the development of skin cancer. J Am Acad Dermatol. 2008;58:129-132.
- El Ghissassi F, Baan R, Straif K, et al; WHO International Agency for Research on Cancer Monograph Working Group. A review of human carcinogens—part D: radiation. Lancet Oncol. 2009;10:751-752.
- MacLennan R, Green AC, McLeod GR, et al. Increasing incidence of cutaneous melanoma in Queensland, Australia. J Natl Cancer Inst. 1992;84:1427-1432.
- Heinzerling LM, Dummer R, Panizzon RG, et al. Prevention campaign against skin cancer. Dermatology. 2002;205:229-233.
- Stratigos A, Nikolaou V, Kedicoglou S, et al. Melanoma/skin cancer screening in a Mediterranean country: results of the Euromelanoma Screening Day Campaign in Greece. J Eur Acad Dermatol Venereol. 2007;21:56-62.
- Garbe C, Hauschild A, Volkenandt M, et al. Evidence and interdisciplinary consense-based German guidelines: diagnosis and surveillance of melanoma. Melanoma Res. 2007;17:393-399.
- Choudhury K, Volkmer B, Greinert R, et al. Effectiveness of skin cancer screening programmes. Br J Dermatol. 2012;167:94-98.
- Eisemann N, Waldmann A, Geller AC, et al. Non-melanoma skin cancer incidence and impact of skin cancer screening on incidence. J Invest Dermatol. 2014;134:43-50.
- Katalinic A, Waldmann A, Weinstock MA, et al. Does skin cancer screening save lives? an observational study comparing trends in melanoma mortality in regions with and without screening. Cancer. 2012;118:5395-5402.
- Bekanntmachung (1430 A) eines Beschlusses des Gemeinsamen Bundeausschusses über eine Änderung der Krebsfrüherkennungs-Richtlinien: Hautkrebs-Screening [press release]. Berlin, Germany: Bundesministerium für Gesundheit (Federal Ministry of Health, Germany); vom 15. November 2007.
- Breitbart EW, Waldmann A, Nolte S, et al. Systematic skin cancer screening in Northern Germany. J Am Acad Dermatol. 2012;66:201-211.
- Waldmann A, Nolte S, Weinstock MA, et al. Skin cancer screening participation and impact on melanoma incidence in Germany—an observational study on incidence trends in regions with and without population-based screening. Br J Cancer. 2012;106:970-974.
- Schaefer I, Rustenbach SJ, Zimmer L, et al. Prevalence of skin diseases in a cohort of 48,665 employees in Germany. Dermatology. 2008;217:169-172.
- Augustin M, Herberger K, Hintzen S, et al. Prevalence of skin lesions and need for treatment in a cohort of 90880 workers. Br J Dermatol. 2011;165:865-873.
- LeBlanc WG, Vidal L, Kirsner RS, et al. Reported skin cancer screening of US adult workers. J Am Acad Dermatol. 2008;59:55-63.
- Harbauer A, Binder M, Pehamberger H, et al. Validity of an unsupervised self-administered questionnaire for self-assessment of melanoma risk. Melanoma Res. 2003;13:537-542.
- Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869-871.
- Augustin M, Stadler R, Reusch M, et al. Skin cancer screening in Germany—perception by the public. J Dtsch Dermatol Ges. 2012;10:42-49.
- Kornek T, Augustin M. Skin cancer prevention. J Dtsch Dermatol Ges. 2013;11:283-296.
- Kornek T, Schäfer I, Reusch M, et al. Routine skin cancer screening in Germany: four years of experience from the dermatologists’ perspective. Dermatology. 2012;225:289-293.
- Barmer GEK Arztreport 2014 [press release]. Berlin, Germany: Barmer GEK; February 4, 2014.
- Bauer J, Garbe C. Acquired melanocytic nevi as riskfactor for melanoma development. a comprehensive review of epidemiological data. Pigment Cell Res. 2003;16:297-306.
- Winkler A, Plugfelder A, Weide B, et al. Screening for skin cancer in bank and insurance employees: risk profile and correlation of self and physician’s assessment. Int J Dermatol. 2015;54:419-423.
The incidence of skin cancer, along with its effects on patients and the economy, has continued to increase and therefore requires particular attention from dermatologists. UV light has been shown to be of etiopathologic importance in the development of various types of skin cancer.1-3 Studies have shown that there is a direct correlation between the incidence of skin cancer and average annual amounts of UV radiation exposure.3 Accordingly, in 2009 the International Agency for Research on Cancer classified UV light as carcinogenic to humans.4 Therefore, the general public must be made aware of the danger of exposure to UV radiation.
In Australia, government initiatives to educate the population on causes of skin cancer development and its relationship to UV radiation have already caused the public to change their way of thinking and to deal with sunlight in a conscious and responsible manner.5 A large proportion of the Australian population with light skin is at a particularly high risk for developing skin cancer due to intense exposure to UV radiation. Numerous campaigns in Germany and other countries have attempted to sensitize the public to this issue by emphasizing a reduction in UV exposure (primary prevention) or highlighting the importance of early diagnosis (secondary prevention).6,7
For a good prognosis, it is crucial that skin cancer, particularly melanoma, is discovered at an early or precancerous stage.8 For this reason, self-examination of the skin and skin cancer screening are important factors that can contribute to ensuring early and curative treatment.9-11 Since July 1, 2008, skin cancer screenings have been included in the preventative health care program by statutory health insurance providers in Germany. As part of this program, the cost of screening once every 2 years for individuals 35 years and older is covered by statutory health insurance.12 Several studies have shown a decline in the melanoma mortality rate since the introduction of skin cancer screening programs in Germany.11,13,14
Employee skin cancer screening programs are an important method of examining high numbers of individuals quickly and effectively. These programs have been carried out in Germany and other countries.15,16 Studies have shown that skin cancer screening carried out selectively on defined groups can be an effective form of secondary prevention, particularly for those who work outdoors.17
An employee skin cancer screening program was carried out as part of this study. The findings are interpreted and discussed in relation to other employee screening programs that have been reported as well as those introduced by statutory health insurance providers in Germany. The aim of this study was to determine the importance and effectiveness of employee skin cancer screening programs and the role they play in secondary prevention of skin cancer.
Methods
Study Population
Employees of a technical company in Bavaria, Germany, were offered a skin cancer screening program by the employer’s occupational health service and health insurance provider in collaboration with the Department of Dermatology at the University Hospital Erlangen (Erlangen, Germany). Skin examinations were performed exclusively by 5 trained dermatologists. Only direct employees of the company at 3 of its locations in the Erlangen area were eligible to participate. The total number of employees varied by location (1072–5126 employees). The majority of employees had a university education or had completed technical training. Family members and other individuals who were not members of the company were excluded. There were no further inclusion or exclusion criteria. Over a period of 13 days, 783 of 7823 total employees (10.0%) were examined and included in the study. The study was approved by the Responsible Ethics Commission of the Faculty of Medicine at Friedrich-Alexander-University Erlangen-Nürnberg, Germany.
Study Design
Employees signed a consent form for participation in the study and completed a standardized questionnaire. The questionnaire was based on surveys used in a prior study18 and collected information on current and prior skin lesions, prior dermatological screening, personal and family history of skin tumors, frequency of UV exposure, and type of UV protection used. For the question on measures taken for protection from UV radiation, possible answers included with sunscreen cream, with suitable sun-protective clothing, and by staying in the shade, or no measures were taken. In contrast to the other questions, multiple answers were accepted for this question. Answering no automatically excluded other possible answers. Participants also were asked to assess their own Fitzpatrick skin type19; the questionnaire included explanations of each skin type (I–IV).
The participants were then called in for examination by the dermatologist at 15-minute intervals. All clothing was removed and the skin was examined. Dermatoscopes were used for closer examination of suspicious skin lesions. The clinical results of the examinations were recorded on a standardized form.
An estimation of the number of melanocytic nevi—≤20, 21–49, or ≥50—was recorded for each patient. Suspicious skin lesions were assigned to one of the following categories: nevus requiring future checkup (Nc), nevus requiring excision (Ne), suspected malignant melanoma (MM), suspected squamous cell carcinoma, suspected basal cell carcinoma (BCC), suspected other skin tumor, and precancerous lesion. Fitzpatrick skin type also was assessed for all participants and recorded by the dermatologist carrying out the examination. Each participant was assigned to a risk group—low, moderate, or high risk—based on their individual risk for developing a skin tumor. Factors that were considered when determining participants’ risk for developing skin cancer included Fitzpatrick skin type, number of melanocytic nevi, personal and family history, leisure activities, UV protection used, and current clinical diagnosis of skin lesions.
After the skin examination, participants were informed of recommended treatment but were not given any additional dermatologic advice. Participants could arrange an appointment at the Department of Dermatology, University Hospital Erlangen, for the excision and histological analysis of the skin lesions. All recorded data were collected in a computerized spreadsheet program. When evaluating the questionnaires, questions that were not answered or were answered incorrectly (participant chose more than 1 answer) were ignored.
Statistical Analysis
Statistical analysis was carried out using SPSS software version 16.0. The majority of the data were nominal or ordinal. Metric data were checked for normal distribution using the Shapiro-Wilk test before carrying out parametric tests. Statistical tests were carried out using the χ2 test and the t test for independent samples. Non-nominal distributed data were checked using the Mann-Whitney U test. P<.05 was considered statistically significant in the exploratory data analysis.
Results
Of 783 employees included in the study, 288 (36.8%) were female and 495 (63.2%) were male (Table 1). In comparison with the total workforce, a significantly higher proportion of women than men took part in the cross-sectional study (P<.01). The average age (SD) was 42.3 (9.5) years (range, 18–64 years). Female participants (average age [SD], 39.8 [10.2] years) were significantly younger than male participants (average age [SD], 43.8 [8.8] years; P<.01). Forty-one percent of participants had a prior skin cancer screening. One percent of participants had a personal history of skin cancer, with 1 participant reporting a history of MM; 6.5% had a family history of skin cancer, of which 39.2% had a family history of MM.
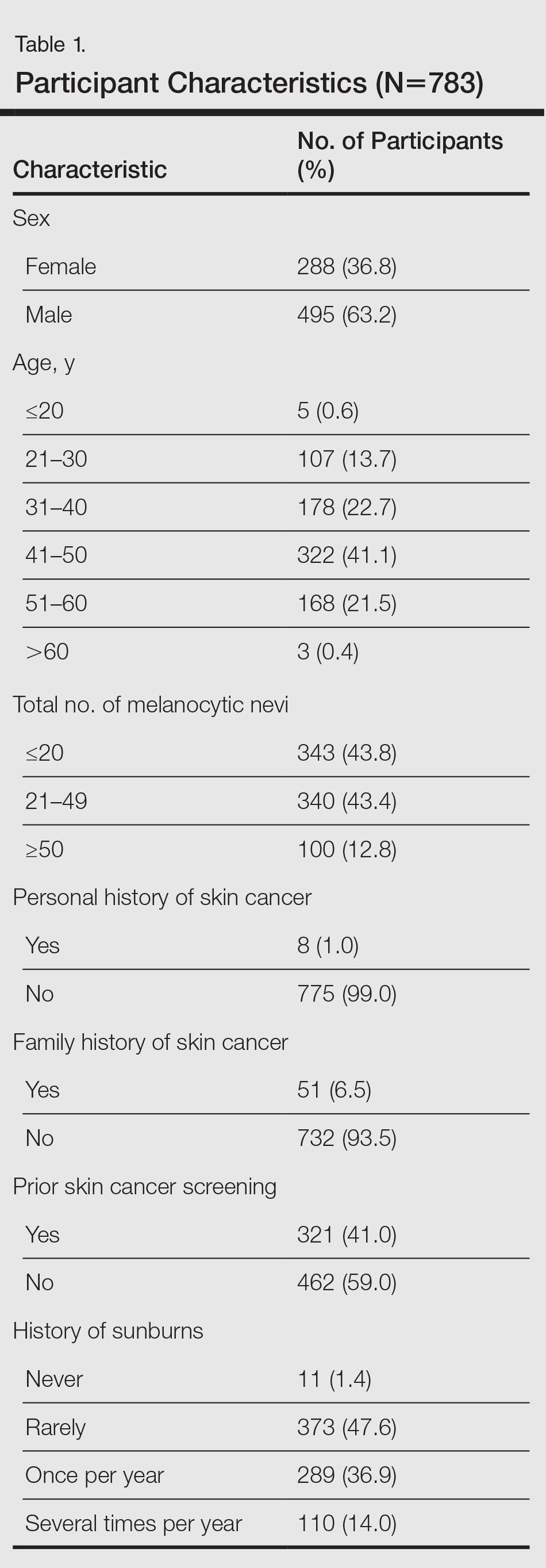
The results of the clinical examinations showed that 43.8% of participants had 20 or fewer melanocytic nevi, 43.4% had 21 to 49 melanocytic nevi, and 12.8% had 50 or more melanocytic nevi. Significantly more women than men had 20 or fewer melanocytic nevi (P<.05).
Approximately 92% of participants assessed themselves as having Fitzpatrick skin types II (35.2%) or III (56.7%), while only approximately 3.6% and 4.5% assessed themselves as having skin types I and IV, respectively. The results of the Fitzpatrick skin type assessments made by dermatologists were similar: 96.9% of participants were assessed as having Fitzpatrick skin types II (43.0%) and III (53.8%); approximately 1.9% and 1.3% were assessed as having Fitzpatrick skin types I and IV, respectively. Results showed that 80.2% of all participants assessed their skin type in the same way as the dermatologist; 13.5% assessed their skin type as darker and 6.3% (49/783) assessed it as lighter. A quantitative analysis of Fitzpatrick skin type and sex showed that significantly more male participants than female participants assessed their Fitzpatrick skin type darker than their actual skin type (P<.01).
Overall, 47.6% of participants reported having had sunburn rarely in the past, while 36.9% and 14.0% had experienced sunburn once per year and several times per year, respectively. Approximately 1.4% of participants reported never having a sunburn. More of the male participants made use of comprehensive sun protection using all methods listed (34.5%; P<.05) or a combination of sunscreen and sun-protective clothing (14.9%; P<.01) than the female participants who relied more frequently on sunscreen alone (29.5%; P<.01) or a combination of sunscreen and staying in the shade (29.5%; P<.01)
In general it was clear that sunscreen, either alone or in combination with other sun-protection methods, was used most frequently (88.0%); 58.0% protected themselves by staying in the shade, while 48.0% used suitable sun-protective clothing. Only 3.6% of participants did not protect themselves using any of the suggested methods.
A total of 661 categorized skin lesions were found in 377 participants. Of these lesions, 491 were Nc and 121 were Ne. Twenty-four of the skin lesions were suspected precancerous lesions, 13 were suspected BCC, 2 were suspected MM, and 10 were suspected other skin tumor (Table 2). Overall, male participants who were diagnosed with at least 1 skin lesion (average age, 44.0 years) were significantly older than the women (average age, 39.3 years)(P<.01). Similar findings were observed in participants with at least 1 Nc (men, 43.3 years; women, 38.7 years; P<.01) and at least 1 Ne (men, 44.2 years; women, 38.0 years; P<.05). With regard to the individual risk for developing skin cancer, 32.6% of participants were considered to be at low risk, 64.9% were at moderate risk, and 2.6% were at high risk.
Approximately 61.5% of 377 participants who were diagnosed with at least 1 categorized skin lesion were advised to have a specific skin lesion checked by a dermatologist or to have a full examination for skin cancer once every 12 months. Furthermore, 22.5% were advised to follow-up biannually and 11.7% were advised to follow-up once every 2 years. Of the remaining participants who were advised to have follow-ups, 0.3% were advised to have a skin examination once every 3 months after having had MM, and 4.0% were advised to have follow-up once every 18 months. Overall, follow-up was recommended within 1 year in 84.4% of cases and within 1 to 2 years in 15.6% (Table 3).
Subsequent histological analysis of the excised tissue resulted in a diagnosis of only 21 clinically significant skin conditions. One case of Bowen disease and 1 case of BCC was confirmed. Histological analysis identified the remaining 19 excised skin lesions, which included the 2 suspected MMs, as dysplastic nevi.
Comment
The aim of this cross-sectional study was to examine the importance and effectiveness of employee skin cancer screening programs. In comparison with the total workforce, significantly more women took part than men. Female participants were significantly younger than male participants, which mirrors the findings of prior studies showing that screening programs reach women more frequently than men and that women who participate in screenings are also younger on average in comparison to men.7-13 Men and older individuals usually are underrepresented.7,13 The average age of participants in our study was 42.3 years, which is lower than in the SCREEN (Skin Cancer Research to Provide Evidence for Effectiveness of Screening in Northern Germany) study (average age, 49.7 years).13 The average age in our study also is likely to be lower than patients who undergo skin cancer screenings offered by statutory health insurance providers in Germany, which has a minimum age restriction of 35 years; however, it is comparable to the average age of participants in other employee screening programs and therefore represents the average age of individuals employed in Germany.15,16
The employee skin cancer screening program in this study generated a high level of interest, indicated by the fact that all available appointments had been booked just 36 hours after the screening was announced. Furthermore, there was a waiting list of approximately 300 employees who were not able to undergo a skin examination. For logistical reasons, the number of participants was limited to 10% of the workforce. The high level of interest is an indication of increased awareness of the importance of recognizing skin tumors early and the associated need for information as well as the need to undergo screening for skin cancer as a precaution. This observation also can be made with regard to the skin cancer screening introduced by statutory health insurance providers in Germany. Studies published by Augustin et al20 and Kornek et al21,22 confirm that skin cancer screenings have gained wide acceptance in Germany because they were introduced by statutory health insurance providers in 2008. The number of skin cancer screenings carried out by dermatologists in Germany also is increasing.20-22 Although approximately 19% of those eligible to participate took part in the SCREEN pilot project,13 approximately 31% of individuals who were eligible to participate took part in skin cancer screenings offered by statutory health insurance providers in Germany in 2012, and the percentage is rising.23 Two important factors affecting the high level of interest in the employee screening program used in our study were undoubtedly the advantages of the examination taking place during working hours and being held on the occupational health services’ premises in the workplace, which helped participants avoid the cost of travel and wait times associated with visiting a medical practice.
Of 783 participants included in this study, 377 displayed at least 1 categorized skin lesion; the majority were suspicious melanocytic nevi. This high incidence rate suggested that regular skin cancer screenings are useful, as it has been shown that there is a correlation between higher numbers of melanocytic nevi and increased risk for developing melanoma.24
In a study by Winkler et al,25 a skin cancer screening of 1658 bank and insurance employees found that 33.8% of those examined displayed at least 1 atypical melanocytic nevus and 27.2% displayed more than 50 melanocytic nevi (compared to 12.8% with ≥50 melanocytic nevi in the current study). The risk for developing skin cancer was classified as intermediate or high in 54.5% (compared to 67.5% at moderate or high risk in the current study).25 Therefore, the rate of suspicious skin lesions was lower in the population of the study by Winkler et al25 in comparison to the population of the current study. As the overall number of melanocytic nevi and the individual risk for skin cancer, however, was underestimated by the majority of the bank and insurance employees,25 employee skin cancer screening programs can be used as a potentially effective tool to make employees aware of the issue and sensitizing them to it. Employee screening in addition to a final diagnosis can contribute to ensuring suitable treatment is started. For example, in the large-scale employee screening published by Schaefer et al15 and Augustin et al,16 48,665 and 90,880 employees, respectively, were screened for inflammatory and noninflammatory skin diseases, and 19% and 27% of participants, respectively, were diagnosed with skin lesions that required treatment.
Participants in the current study were given no further treatment or advice. Recommendations were made that participants monitor suspicious skin lesions or have them removed. With regard to future screening, 84.4% of participants with at least 1 categorized skin lesion were advised to have a regular follow-up within 1 year, while 15.6% were advised to follow-up within 1 to 2 years. Therefore, a period of 2 years before the next checkup, the period between screenings offered by statutory health insurance providers in Germany,12 was considered too long for the majority of participants, according to the dermatologists involved with our study.
Conclusion
The high rate of suspicious skin lesions diagnosed demonstrated the effectiveness of skin cancer screenings organized in the workplace, which should be recommended for all employees, not only those who are at high risk for developing skin cancer due to the nature of their work, such as those who work outdoors. It should be noted that the study group examined in the current study was a homogeneous group of employees of a technical company only and is therefore relatively selective. Nevertheless, despite the comparatively selective and young participant group, these examinations provide evidence of the importance of skin cancer screening programs for a wider population.
Acknowledgments
The authors thank Heidi Seybold, MD; Petra Wörl, MD; Sybille Thoma-Uszynski, MD; and Jens Bussmann, MD (all from Erlangen, Germany), for their support and active assistance in the practical implementation of this study.
The incidence of skin cancer, along with its effects on patients and the economy, has continued to increase and therefore requires particular attention from dermatologists. UV light has been shown to be of etiopathologic importance in the development of various types of skin cancer.1-3 Studies have shown that there is a direct correlation between the incidence of skin cancer and average annual amounts of UV radiation exposure.3 Accordingly, in 2009 the International Agency for Research on Cancer classified UV light as carcinogenic to humans.4 Therefore, the general public must be made aware of the danger of exposure to UV radiation.
In Australia, government initiatives to educate the population on causes of skin cancer development and its relationship to UV radiation have already caused the public to change their way of thinking and to deal with sunlight in a conscious and responsible manner.5 A large proportion of the Australian population with light skin is at a particularly high risk for developing skin cancer due to intense exposure to UV radiation. Numerous campaigns in Germany and other countries have attempted to sensitize the public to this issue by emphasizing a reduction in UV exposure (primary prevention) or highlighting the importance of early diagnosis (secondary prevention).6,7
For a good prognosis, it is crucial that skin cancer, particularly melanoma, is discovered at an early or precancerous stage.8 For this reason, self-examination of the skin and skin cancer screening are important factors that can contribute to ensuring early and curative treatment.9-11 Since July 1, 2008, skin cancer screenings have been included in the preventative health care program by statutory health insurance providers in Germany. As part of this program, the cost of screening once every 2 years for individuals 35 years and older is covered by statutory health insurance.12 Several studies have shown a decline in the melanoma mortality rate since the introduction of skin cancer screening programs in Germany.11,13,14
Employee skin cancer screening programs are an important method of examining high numbers of individuals quickly and effectively. These programs have been carried out in Germany and other countries.15,16 Studies have shown that skin cancer screening carried out selectively on defined groups can be an effective form of secondary prevention, particularly for those who work outdoors.17
An employee skin cancer screening program was carried out as part of this study. The findings are interpreted and discussed in relation to other employee screening programs that have been reported as well as those introduced by statutory health insurance providers in Germany. The aim of this study was to determine the importance and effectiveness of employee skin cancer screening programs and the role they play in secondary prevention of skin cancer.
Methods
Study Population
Employees of a technical company in Bavaria, Germany, were offered a skin cancer screening program by the employer’s occupational health service and health insurance provider in collaboration with the Department of Dermatology at the University Hospital Erlangen (Erlangen, Germany). Skin examinations were performed exclusively by 5 trained dermatologists. Only direct employees of the company at 3 of its locations in the Erlangen area were eligible to participate. The total number of employees varied by location (1072–5126 employees). The majority of employees had a university education or had completed technical training. Family members and other individuals who were not members of the company were excluded. There were no further inclusion or exclusion criteria. Over a period of 13 days, 783 of 7823 total employees (10.0%) were examined and included in the study. The study was approved by the Responsible Ethics Commission of the Faculty of Medicine at Friedrich-Alexander-University Erlangen-Nürnberg, Germany.
Study Design
Employees signed a consent form for participation in the study and completed a standardized questionnaire. The questionnaire was based on surveys used in a prior study18 and collected information on current and prior skin lesions, prior dermatological screening, personal and family history of skin tumors, frequency of UV exposure, and type of UV protection used. For the question on measures taken for protection from UV radiation, possible answers included with sunscreen cream, with suitable sun-protective clothing, and by staying in the shade, or no measures were taken. In contrast to the other questions, multiple answers were accepted for this question. Answering no automatically excluded other possible answers. Participants also were asked to assess their own Fitzpatrick skin type19; the questionnaire included explanations of each skin type (I–IV).
The participants were then called in for examination by the dermatologist at 15-minute intervals. All clothing was removed and the skin was examined. Dermatoscopes were used for closer examination of suspicious skin lesions. The clinical results of the examinations were recorded on a standardized form.
An estimation of the number of melanocytic nevi—≤20, 21–49, or ≥50—was recorded for each patient. Suspicious skin lesions were assigned to one of the following categories: nevus requiring future checkup (Nc), nevus requiring excision (Ne), suspected malignant melanoma (MM), suspected squamous cell carcinoma, suspected basal cell carcinoma (BCC), suspected other skin tumor, and precancerous lesion. Fitzpatrick skin type also was assessed for all participants and recorded by the dermatologist carrying out the examination. Each participant was assigned to a risk group—low, moderate, or high risk—based on their individual risk for developing a skin tumor. Factors that were considered when determining participants’ risk for developing skin cancer included Fitzpatrick skin type, number of melanocytic nevi, personal and family history, leisure activities, UV protection used, and current clinical diagnosis of skin lesions.
After the skin examination, participants were informed of recommended treatment but were not given any additional dermatologic advice. Participants could arrange an appointment at the Department of Dermatology, University Hospital Erlangen, for the excision and histological analysis of the skin lesions. All recorded data were collected in a computerized spreadsheet program. When evaluating the questionnaires, questions that were not answered or were answered incorrectly (participant chose more than 1 answer) were ignored.
Statistical Analysis
Statistical analysis was carried out using SPSS software version 16.0. The majority of the data were nominal or ordinal. Metric data were checked for normal distribution using the Shapiro-Wilk test before carrying out parametric tests. Statistical tests were carried out using the χ2 test and the t test for independent samples. Non-nominal distributed data were checked using the Mann-Whitney U test. P<.05 was considered statistically significant in the exploratory data analysis.
Results
Of 783 employees included in the study, 288 (36.8%) were female and 495 (63.2%) were male (Table 1). In comparison with the total workforce, a significantly higher proportion of women than men took part in the cross-sectional study (P<.01). The average age (SD) was 42.3 (9.5) years (range, 18–64 years). Female participants (average age [SD], 39.8 [10.2] years) were significantly younger than male participants (average age [SD], 43.8 [8.8] years; P<.01). Forty-one percent of participants had a prior skin cancer screening. One percent of participants had a personal history of skin cancer, with 1 participant reporting a history of MM; 6.5% had a family history of skin cancer, of which 39.2% had a family history of MM.
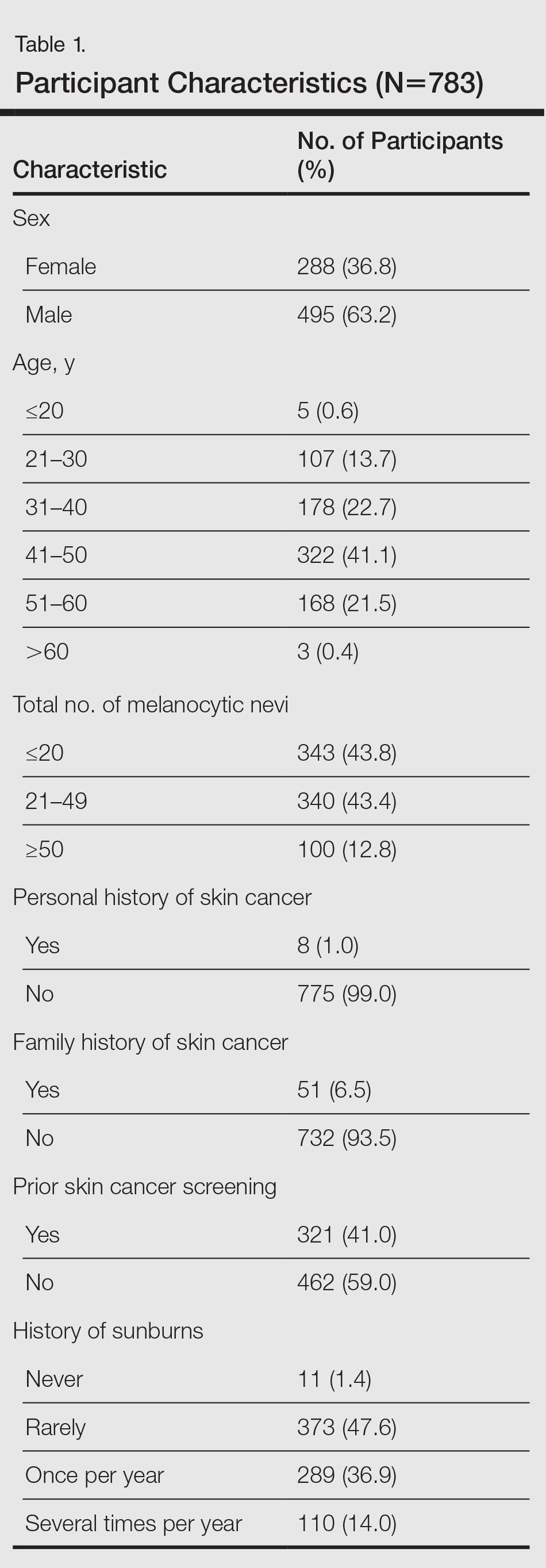
The results of the clinical examinations showed that 43.8% of participants had 20 or fewer melanocytic nevi, 43.4% had 21 to 49 melanocytic nevi, and 12.8% had 50 or more melanocytic nevi. Significantly more women than men had 20 or fewer melanocytic nevi (P<.05).
Approximately 92% of participants assessed themselves as having Fitzpatrick skin types II (35.2%) or III (56.7%), while only approximately 3.6% and 4.5% assessed themselves as having skin types I and IV, respectively. The results of the Fitzpatrick skin type assessments made by dermatologists were similar: 96.9% of participants were assessed as having Fitzpatrick skin types II (43.0%) and III (53.8%); approximately 1.9% and 1.3% were assessed as having Fitzpatrick skin types I and IV, respectively. Results showed that 80.2% of all participants assessed their skin type in the same way as the dermatologist; 13.5% assessed their skin type as darker and 6.3% (49/783) assessed it as lighter. A quantitative analysis of Fitzpatrick skin type and sex showed that significantly more male participants than female participants assessed their Fitzpatrick skin type darker than their actual skin type (P<.01).
Overall, 47.6% of participants reported having had sunburn rarely in the past, while 36.9% and 14.0% had experienced sunburn once per year and several times per year, respectively. Approximately 1.4% of participants reported never having a sunburn. More of the male participants made use of comprehensive sun protection using all methods listed (34.5%; P<.05) or a combination of sunscreen and sun-protective clothing (14.9%; P<.01) than the female participants who relied more frequently on sunscreen alone (29.5%; P<.01) or a combination of sunscreen and staying in the shade (29.5%; P<.01)
In general it was clear that sunscreen, either alone or in combination with other sun-protection methods, was used most frequently (88.0%); 58.0% protected themselves by staying in the shade, while 48.0% used suitable sun-protective clothing. Only 3.6% of participants did not protect themselves using any of the suggested methods.
A total of 661 categorized skin lesions were found in 377 participants. Of these lesions, 491 were Nc and 121 were Ne. Twenty-four of the skin lesions were suspected precancerous lesions, 13 were suspected BCC, 2 were suspected MM, and 10 were suspected other skin tumor (Table 2). Overall, male participants who were diagnosed with at least 1 skin lesion (average age, 44.0 years) were significantly older than the women (average age, 39.3 years)(P<.01). Similar findings were observed in participants with at least 1 Nc (men, 43.3 years; women, 38.7 years; P<.01) and at least 1 Ne (men, 44.2 years; women, 38.0 years; P<.05). With regard to the individual risk for developing skin cancer, 32.6% of participants were considered to be at low risk, 64.9% were at moderate risk, and 2.6% were at high risk.
Approximately 61.5% of 377 participants who were diagnosed with at least 1 categorized skin lesion were advised to have a specific skin lesion checked by a dermatologist or to have a full examination for skin cancer once every 12 months. Furthermore, 22.5% were advised to follow-up biannually and 11.7% were advised to follow-up once every 2 years. Of the remaining participants who were advised to have follow-ups, 0.3% were advised to have a skin examination once every 3 months after having had MM, and 4.0% were advised to have follow-up once every 18 months. Overall, follow-up was recommended within 1 year in 84.4% of cases and within 1 to 2 years in 15.6% (Table 3).
Subsequent histological analysis of the excised tissue resulted in a diagnosis of only 21 clinically significant skin conditions. One case of Bowen disease and 1 case of BCC was confirmed. Histological analysis identified the remaining 19 excised skin lesions, which included the 2 suspected MMs, as dysplastic nevi.
Comment
The aim of this cross-sectional study was to examine the importance and effectiveness of employee skin cancer screening programs. In comparison with the total workforce, significantly more women took part than men. Female participants were significantly younger than male participants, which mirrors the findings of prior studies showing that screening programs reach women more frequently than men and that women who participate in screenings are also younger on average in comparison to men.7-13 Men and older individuals usually are underrepresented.7,13 The average age of participants in our study was 42.3 years, which is lower than in the SCREEN (Skin Cancer Research to Provide Evidence for Effectiveness of Screening in Northern Germany) study (average age, 49.7 years).13 The average age in our study also is likely to be lower than patients who undergo skin cancer screenings offered by statutory health insurance providers in Germany, which has a minimum age restriction of 35 years; however, it is comparable to the average age of participants in other employee screening programs and therefore represents the average age of individuals employed in Germany.15,16
The employee skin cancer screening program in this study generated a high level of interest, indicated by the fact that all available appointments had been booked just 36 hours after the screening was announced. Furthermore, there was a waiting list of approximately 300 employees who were not able to undergo a skin examination. For logistical reasons, the number of participants was limited to 10% of the workforce. The high level of interest is an indication of increased awareness of the importance of recognizing skin tumors early and the associated need for information as well as the need to undergo screening for skin cancer as a precaution. This observation also can be made with regard to the skin cancer screening introduced by statutory health insurance providers in Germany. Studies published by Augustin et al20 and Kornek et al21,22 confirm that skin cancer screenings have gained wide acceptance in Germany because they were introduced by statutory health insurance providers in 2008. The number of skin cancer screenings carried out by dermatologists in Germany also is increasing.20-22 Although approximately 19% of those eligible to participate took part in the SCREEN pilot project,13 approximately 31% of individuals who were eligible to participate took part in skin cancer screenings offered by statutory health insurance providers in Germany in 2012, and the percentage is rising.23 Two important factors affecting the high level of interest in the employee screening program used in our study were undoubtedly the advantages of the examination taking place during working hours and being held on the occupational health services’ premises in the workplace, which helped participants avoid the cost of travel and wait times associated with visiting a medical practice.
Of 783 participants included in this study, 377 displayed at least 1 categorized skin lesion; the majority were suspicious melanocytic nevi. This high incidence rate suggested that regular skin cancer screenings are useful, as it has been shown that there is a correlation between higher numbers of melanocytic nevi and increased risk for developing melanoma.24
In a study by Winkler et al,25 a skin cancer screening of 1658 bank and insurance employees found that 33.8% of those examined displayed at least 1 atypical melanocytic nevus and 27.2% displayed more than 50 melanocytic nevi (compared to 12.8% with ≥50 melanocytic nevi in the current study). The risk for developing skin cancer was classified as intermediate or high in 54.5% (compared to 67.5% at moderate or high risk in the current study).25 Therefore, the rate of suspicious skin lesions was lower in the population of the study by Winkler et al25 in comparison to the population of the current study. As the overall number of melanocytic nevi and the individual risk for skin cancer, however, was underestimated by the majority of the bank and insurance employees,25 employee skin cancer screening programs can be used as a potentially effective tool to make employees aware of the issue and sensitizing them to it. Employee screening in addition to a final diagnosis can contribute to ensuring suitable treatment is started. For example, in the large-scale employee screening published by Schaefer et al15 and Augustin et al,16 48,665 and 90,880 employees, respectively, were screened for inflammatory and noninflammatory skin diseases, and 19% and 27% of participants, respectively, were diagnosed with skin lesions that required treatment.
Participants in the current study were given no further treatment or advice. Recommendations were made that participants monitor suspicious skin lesions or have them removed. With regard to future screening, 84.4% of participants with at least 1 categorized skin lesion were advised to have a regular follow-up within 1 year, while 15.6% were advised to follow-up within 1 to 2 years. Therefore, a period of 2 years before the next checkup, the period between screenings offered by statutory health insurance providers in Germany,12 was considered too long for the majority of participants, according to the dermatologists involved with our study.
Conclusion
The high rate of suspicious skin lesions diagnosed demonstrated the effectiveness of skin cancer screenings organized in the workplace, which should be recommended for all employees, not only those who are at high risk for developing skin cancer due to the nature of their work, such as those who work outdoors. It should be noted that the study group examined in the current study was a homogeneous group of employees of a technical company only and is therefore relatively selective. Nevertheless, despite the comparatively selective and young participant group, these examinations provide evidence of the importance of skin cancer screening programs for a wider population.
Acknowledgments
The authors thank Heidi Seybold, MD; Petra Wörl, MD; Sybille Thoma-Uszynski, MD; and Jens Bussmann, MD (all from Erlangen, Germany), for their support and active assistance in the practical implementation of this study.
- Boniol M, Autier P, Boyle P, et al. Cutaneous melanoma attributable to sunbed use: systematic review and meta-analysis. BMJ. 2012;345:e4757.
- Gilchrest BA, Eller MS, Geller AC, et al. The pathogenesis of melanoma induced by ultraviolet radiation. N Engl J Med. 1999;340:1341-1348.
- Rigel DS. Cutaneous ultraviolet exposure and its relationship to the development of skin cancer. J Am Acad Dermatol. 2008;58:129-132.
- El Ghissassi F, Baan R, Straif K, et al; WHO International Agency for Research on Cancer Monograph Working Group. A review of human carcinogens—part D: radiation. Lancet Oncol. 2009;10:751-752.
- MacLennan R, Green AC, McLeod GR, et al. Increasing incidence of cutaneous melanoma in Queensland, Australia. J Natl Cancer Inst. 1992;84:1427-1432.
- Heinzerling LM, Dummer R, Panizzon RG, et al. Prevention campaign against skin cancer. Dermatology. 2002;205:229-233.
- Stratigos A, Nikolaou V, Kedicoglou S, et al. Melanoma/skin cancer screening in a Mediterranean country: results of the Euromelanoma Screening Day Campaign in Greece. J Eur Acad Dermatol Venereol. 2007;21:56-62.
- Garbe C, Hauschild A, Volkenandt M, et al. Evidence and interdisciplinary consense-based German guidelines: diagnosis and surveillance of melanoma. Melanoma Res. 2007;17:393-399.
- Choudhury K, Volkmer B, Greinert R, et al. Effectiveness of skin cancer screening programmes. Br J Dermatol. 2012;167:94-98.
- Eisemann N, Waldmann A, Geller AC, et al. Non-melanoma skin cancer incidence and impact of skin cancer screening on incidence. J Invest Dermatol. 2014;134:43-50.
- Katalinic A, Waldmann A, Weinstock MA, et al. Does skin cancer screening save lives? an observational study comparing trends in melanoma mortality in regions with and without screening. Cancer. 2012;118:5395-5402.
- Bekanntmachung (1430 A) eines Beschlusses des Gemeinsamen Bundeausschusses über eine Änderung der Krebsfrüherkennungs-Richtlinien: Hautkrebs-Screening [press release]. Berlin, Germany: Bundesministerium für Gesundheit (Federal Ministry of Health, Germany); vom 15. November 2007.
- Breitbart EW, Waldmann A, Nolte S, et al. Systematic skin cancer screening in Northern Germany. J Am Acad Dermatol. 2012;66:201-211.
- Waldmann A, Nolte S, Weinstock MA, et al. Skin cancer screening participation and impact on melanoma incidence in Germany—an observational study on incidence trends in regions with and without population-based screening. Br J Cancer. 2012;106:970-974.
- Schaefer I, Rustenbach SJ, Zimmer L, et al. Prevalence of skin diseases in a cohort of 48,665 employees in Germany. Dermatology. 2008;217:169-172.
- Augustin M, Herberger K, Hintzen S, et al. Prevalence of skin lesions and need for treatment in a cohort of 90880 workers. Br J Dermatol. 2011;165:865-873.
- LeBlanc WG, Vidal L, Kirsner RS, et al. Reported skin cancer screening of US adult workers. J Am Acad Dermatol. 2008;59:55-63.
- Harbauer A, Binder M, Pehamberger H, et al. Validity of an unsupervised self-administered questionnaire for self-assessment of melanoma risk. Melanoma Res. 2003;13:537-542.
- Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869-871.
- Augustin M, Stadler R, Reusch M, et al. Skin cancer screening in Germany—perception by the public. J Dtsch Dermatol Ges. 2012;10:42-49.
- Kornek T, Augustin M. Skin cancer prevention. J Dtsch Dermatol Ges. 2013;11:283-296.
- Kornek T, Schäfer I, Reusch M, et al. Routine skin cancer screening in Germany: four years of experience from the dermatologists’ perspective. Dermatology. 2012;225:289-293.
- Barmer GEK Arztreport 2014 [press release]. Berlin, Germany: Barmer GEK; February 4, 2014.
- Bauer J, Garbe C. Acquired melanocytic nevi as riskfactor for melanoma development. a comprehensive review of epidemiological data. Pigment Cell Res. 2003;16:297-306.
- Winkler A, Plugfelder A, Weide B, et al. Screening for skin cancer in bank and insurance employees: risk profile and correlation of self and physician’s assessment. Int J Dermatol. 2015;54:419-423.
- Boniol M, Autier P, Boyle P, et al. Cutaneous melanoma attributable to sunbed use: systematic review and meta-analysis. BMJ. 2012;345:e4757.
- Gilchrest BA, Eller MS, Geller AC, et al. The pathogenesis of melanoma induced by ultraviolet radiation. N Engl J Med. 1999;340:1341-1348.
- Rigel DS. Cutaneous ultraviolet exposure and its relationship to the development of skin cancer. J Am Acad Dermatol. 2008;58:129-132.
- El Ghissassi F, Baan R, Straif K, et al; WHO International Agency for Research on Cancer Monograph Working Group. A review of human carcinogens—part D: radiation. Lancet Oncol. 2009;10:751-752.
- MacLennan R, Green AC, McLeod GR, et al. Increasing incidence of cutaneous melanoma in Queensland, Australia. J Natl Cancer Inst. 1992;84:1427-1432.
- Heinzerling LM, Dummer R, Panizzon RG, et al. Prevention campaign against skin cancer. Dermatology. 2002;205:229-233.
- Stratigos A, Nikolaou V, Kedicoglou S, et al. Melanoma/skin cancer screening in a Mediterranean country: results of the Euromelanoma Screening Day Campaign in Greece. J Eur Acad Dermatol Venereol. 2007;21:56-62.
- Garbe C, Hauschild A, Volkenandt M, et al. Evidence and interdisciplinary consense-based German guidelines: diagnosis and surveillance of melanoma. Melanoma Res. 2007;17:393-399.
- Choudhury K, Volkmer B, Greinert R, et al. Effectiveness of skin cancer screening programmes. Br J Dermatol. 2012;167:94-98.
- Eisemann N, Waldmann A, Geller AC, et al. Non-melanoma skin cancer incidence and impact of skin cancer screening on incidence. J Invest Dermatol. 2014;134:43-50.
- Katalinic A, Waldmann A, Weinstock MA, et al. Does skin cancer screening save lives? an observational study comparing trends in melanoma mortality in regions with and without screening. Cancer. 2012;118:5395-5402.
- Bekanntmachung (1430 A) eines Beschlusses des Gemeinsamen Bundeausschusses über eine Änderung der Krebsfrüherkennungs-Richtlinien: Hautkrebs-Screening [press release]. Berlin, Germany: Bundesministerium für Gesundheit (Federal Ministry of Health, Germany); vom 15. November 2007.
- Breitbart EW, Waldmann A, Nolte S, et al. Systematic skin cancer screening in Northern Germany. J Am Acad Dermatol. 2012;66:201-211.
- Waldmann A, Nolte S, Weinstock MA, et al. Skin cancer screening participation and impact on melanoma incidence in Germany—an observational study on incidence trends in regions with and without population-based screening. Br J Cancer. 2012;106:970-974.
- Schaefer I, Rustenbach SJ, Zimmer L, et al. Prevalence of skin diseases in a cohort of 48,665 employees in Germany. Dermatology. 2008;217:169-172.
- Augustin M, Herberger K, Hintzen S, et al. Prevalence of skin lesions and need for treatment in a cohort of 90880 workers. Br J Dermatol. 2011;165:865-873.
- LeBlanc WG, Vidal L, Kirsner RS, et al. Reported skin cancer screening of US adult workers. J Am Acad Dermatol. 2008;59:55-63.
- Harbauer A, Binder M, Pehamberger H, et al. Validity of an unsupervised self-administered questionnaire for self-assessment of melanoma risk. Melanoma Res. 2003;13:537-542.
- Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869-871.
- Augustin M, Stadler R, Reusch M, et al. Skin cancer screening in Germany—perception by the public. J Dtsch Dermatol Ges. 2012;10:42-49.
- Kornek T, Augustin M. Skin cancer prevention. J Dtsch Dermatol Ges. 2013;11:283-296.
- Kornek T, Schäfer I, Reusch M, et al. Routine skin cancer screening in Germany: four years of experience from the dermatologists’ perspective. Dermatology. 2012;225:289-293.
- Barmer GEK Arztreport 2014 [press release]. Berlin, Germany: Barmer GEK; February 4, 2014.
- Bauer J, Garbe C. Acquired melanocytic nevi as riskfactor for melanoma development. a comprehensive review of epidemiological data. Pigment Cell Res. 2003;16:297-306.
- Winkler A, Plugfelder A, Weide B, et al. Screening for skin cancer in bank and insurance employees: risk profile and correlation of self and physician’s assessment. Int J Dermatol. 2015;54:419-423.
Practice Points
- Employee skin cancer screening programs are an important method of examining high numbers of individuals quickly and efficiently and should be used as an important tool for secondary skin cancer prevention.
- The high rate of suspicious skin lesions diagnosed in this study demonstrates the effectiveness of skin cancer screenings organized in the workplace and provides evidence of the importance of skin cancer screening programs for a wider population.
- Employee skin cancer screening programs should be recommended for all employees, not only those who are at high risk for developing skin cancer due to the nature of their work, such as those who work outdoors.
Subungual Onycholemmal Cyst of the Toenail Mimicking Subungual Melanoma
Case Report
A 23-year-old woman presented with a horizontal split along the midline of the right great toenail associated with some tenderness of 2 to 3 months’ duration. Approximately 5 years prior, she noticed a bluish-colored area under the nail that had been steadily increasing in size. She denied a history of trauma, drainage, or bleeding. There was no history of other nail abnormalities. Her medications and personal, family, and social history were noncontributory.
Physical examination of the right great toenail revealed a horizontal split of the nail plate with a bluish hue visible under the nail plate (Figure 1A). The remaining toenails and fingernails were normal. A punch biopsy of the nail bed was performed with a presumptive clinical diagnosis of subungual melanoma versus melanocytic nevus versus cyst (Figure 1B). Nail plate avulsion revealed a blackened nail bed dotted with areas of bluish color and a red friable nodule present focally. Upon further inspection, extension was apparent into the distal matrix.

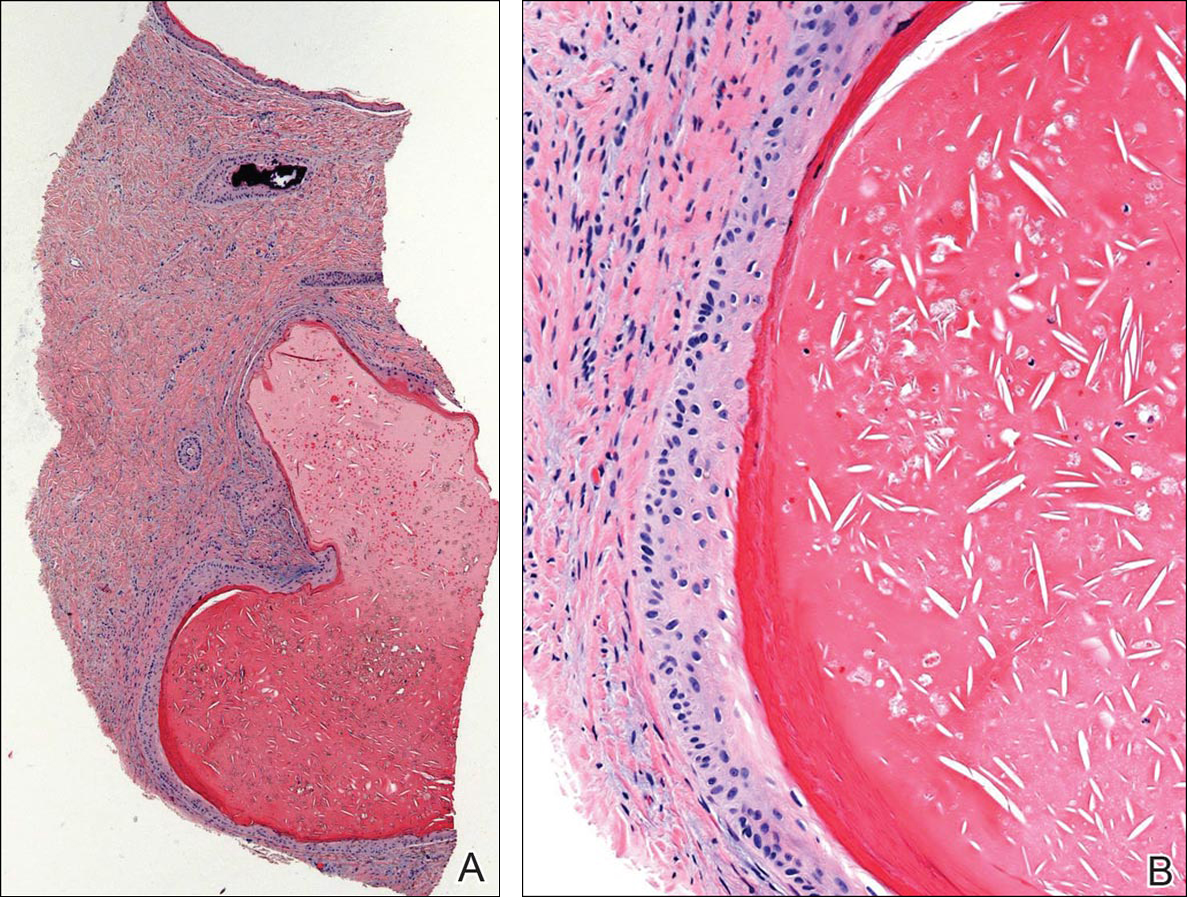
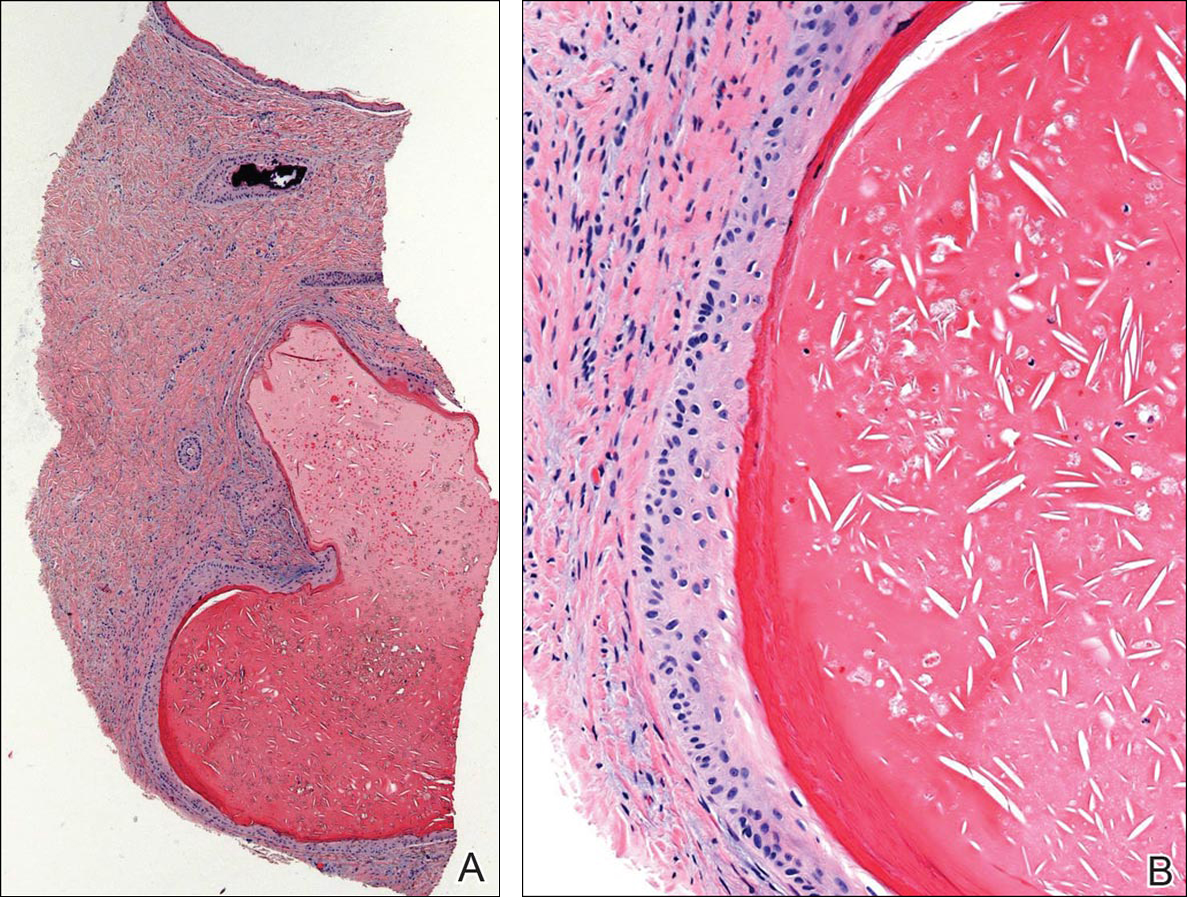
Histopathologic examination revealed a cystic structure with an epithelial lining mostly reminiscent of an isthmus catagen cyst admixed with the presence of both an intermittent focal granular layer and an eosinophilic cuticle surrounding pink laminated keratin, most consistent with a diagnosis of subungual onycholemmal cyst (SOC)(Figure 2). A reexcision was performed with removal of half of the nail bed, including a portion of the distal matrix extending inferiorly to the bone. Variably sized, epithelium-lined, keratin-filled cystic structures emanated from the nail bed epithelium. There were foci of hemorrhage and granulation tissue secondary to cyst rupture (Figure 3). The defect healed by secondary intention. No clinical evidence of recurrence was seen at 6-month follow-up.

Subungual onycholemmal cysts, also known as subungual epidermoid cysts or subungual epidermoid inclusions, are rare and distinctive nail abnormalities occurring in the dermis of the nail bed. We present a case of an SOC in a toenail mimicking subungual malignant melanoma.
Originally described by Samman1 in 1959, SOCs were attributed to trauma to the nail with resultant implantation of the epidermis into the deeper tissue. Lewin2,3 examined 90 postmortem fingernail and nail bed samples and found 8 subungual epidermoid cysts associated with clubbing of the fingernails. He postulated that the early pathogenesis of clubbing involved dermal fibroblast proliferation in the nail bed, leading to sequestration of nail bed epithelium into the dermis with resultant cyst formation. Microscopic subungual cysts also were identified in normal-appearing nails without evidence of trauma, thought to have arisen from the tips of the nail bed rete ridges by a process of bulbous proliferation rather than sequestration. These findings in normal nails suggest that SOCs may represent a more common entity than previously recognized.
It is imperative to recognize the presence of nail unit tumors early because of the risk for permanent nail plate dystrophy and the possibility of a malignant tumor.4,5 Subungual onycholemmal cysts may present with a wide spectrum of clinical findings including marked subungual hyperkeratosis, onychodystrophy, ridging, nail bed pigmentation, clubbing, thickening, or less often a normal-appearing nail. Based on reported cases, several trends are evident. Although nail dystrophy is most often asymptomatic, pain is not uncommon.5,6 It most commonly involves single digits, predominantly thumbs and great toenails.7,8 This predilection suggests that trauma or other local factors may be involved in its pathogenesis. Of note, trauma to the nail may occur years before the development of the lesions or it may not be recalled at all.
Diagnosis requires a degree of clinical suspicion and a nail bed biopsy with partial or total nail plate avulsion to visualize the pathologic portion of the nail bed. Because surgical intervention may lead to the implantation of epithelium, recurrences after nail biopsy or excision may occur.
In contrast to epidermal inclusion cysts arising in the skin, most SOCs do not have a granular layer.9 Hair and nails represent analogous differentiation products of the ectoderm. The nail matrix is homologous to portions of the hair matrix, while the nail bed epithelium is comparable to the outer root sheath of the hair follicle.7 Subungual onycholemmal cysts originate from the nail bed epithelium, which keratinizes in the absence of a granular layer, similar to the follicular isthmus outer root sheath. Thus, SOCs are comparable to the outer root sheath–derived isthmus-catagen cysts because of their abrupt central keratinization.8
Subungual onycholemmal cysts also must be distinguished from slowly growing malignant tumors of the nail bed epithelium, referred to as onycholemmal carcinomas by Alessi et al.10 This entity characteristically presents in elderly patients as a slowly growing, circumscribed, subungual discoloration that may ulcerate, destroying the nail apparatus and penetrating the phalangeal bone. On histopathology, it is characterized by small cysts filled with eosinophilic keratin devoid of a granular layer and lined by atypical squamous epithelium accompanied by solid nests and strands of atypical keratinocytes within the dermis.11 When a cystic component and clear cells predominate, the designation of malignant proliferating onycholemmal cyst has been applied. Its infiltrative growth pattern with destruction of the underlying bone makes it an important entity to exclude when considering the differential diagnosis of tumors of the nail bed.
Subungual melanomas comprise only 1% to 3% of malignant melanomas and 85% are initially misdiagnosed due to their rarity and nonspecific variable presentation. Aside from clinical evidence of Hutchinson sign in the early stages in almost all cases, accurate diagnosis of subungual melanoma and differentiation from SOCs relies on histopathology. A biopsy is necessary to make the diagnosis, but even microscopic findings may be nonspecific during the early stages.
Conclusion
We report a case of a 23-year-old woman with horizontal ridging and tenderness of the right great toenail associated with pigmentation of 5 years’ duration due to an SOC. The etiology of these subungual cysts, with or without nail abnormalities, still remains unclear. Its predilection for the thumbs and great toenails suggests that trauma or other local factors may be involved in its pathogenesis. Because of the rarity of this entity, there are no guidelines for surgical treatment. Subungual onycholemmal cysts may be an underrecognized and more common entity that must be considered when discussing tumors of the nail unit.
- Samman PD. The human toe nail. its genesis and blood supply. Br J Dermatol. 1959;71:296-302.
- Lewin K. The normal fingernail. Br J Dermatol. 1965;77:421-430.
- Lewin K. Subungual epidermoid inclusions. Br J Dermatol. 1969;81:671-675.
- Dominguez-Cherit J, Chanussot-Deprez C, Maria-Sarti H, et al. Nail unit tumors: a study of 234 patients in the dermatology department of the “Dr. Manuel Gea González” General Hospital in Mexico City. Dermatol Surg. 2008;34:1363-1371.
- Sáez-de-Ocariz MM, Domínguez-Cherit J, García-Corona C. Subungual epidermoid cysts. Int J Dermatol. 2001;40:524-526.
- Molly DO, Herbert K. Subungual epidermoid cyst. J Hand Surg Br. 2006;31:345.
- Telang GH, Jellinek N. Multiple calcified subungual epidermoid inclusions. J Am Acad Dermatol. 2007;56:336-339.
- Fanti PA, Tosti A. Subungual epidermoid inclusions: report of 8 cases. Dermatologica. 1989;178:209-212.
- Takiyoshi N, Nakano H, Matsuzaki T, et al. An eclipse in the subungual space: a diagnostic sign for a subungual epidermal cyst? Br J Dermatol. 2009;161:962-963.
- Alessi E, Coggi A, Gianotti R, et al. Onycholemmal carcinoma. Am J Dermatopathol. 2004;26:397-402.
- Inaoki M, Makino E, Adachi M, et al. Onycholemmal carcinoma. J Cutan Pathol. 2006;33:577-580.
Case Report
A 23-year-old woman presented with a horizontal split along the midline of the right great toenail associated with some tenderness of 2 to 3 months’ duration. Approximately 5 years prior, she noticed a bluish-colored area under the nail that had been steadily increasing in size. She denied a history of trauma, drainage, or bleeding. There was no history of other nail abnormalities. Her medications and personal, family, and social history were noncontributory.
Physical examination of the right great toenail revealed a horizontal split of the nail plate with a bluish hue visible under the nail plate (Figure 1A). The remaining toenails and fingernails were normal. A punch biopsy of the nail bed was performed with a presumptive clinical diagnosis of subungual melanoma versus melanocytic nevus versus cyst (Figure 1B). Nail plate avulsion revealed a blackened nail bed dotted with areas of bluish color and a red friable nodule present focally. Upon further inspection, extension was apparent into the distal matrix.

Histopathologic examination revealed a cystic structure with an epithelial lining mostly reminiscent of an isthmus catagen cyst admixed with the presence of both an intermittent focal granular layer and an eosinophilic cuticle surrounding pink laminated keratin, most consistent with a diagnosis of subungual onycholemmal cyst (SOC)(Figure 2). A reexcision was performed with removal of half of the nail bed, including a portion of the distal matrix extending inferiorly to the bone. Variably sized, epithelium-lined, keratin-filled cystic structures emanated from the nail bed epithelium. There were foci of hemorrhage and granulation tissue secondary to cyst rupture (Figure 3). The defect healed by secondary intention. No clinical evidence of recurrence was seen at 6-month follow-up.

Subungual onycholemmal cysts, also known as subungual epidermoid cysts or subungual epidermoid inclusions, are rare and distinctive nail abnormalities occurring in the dermis of the nail bed. We present a case of an SOC in a toenail mimicking subungual malignant melanoma.
Originally described by Samman1 in 1959, SOCs were attributed to trauma to the nail with resultant implantation of the epidermis into the deeper tissue. Lewin2,3 examined 90 postmortem fingernail and nail bed samples and found 8 subungual epidermoid cysts associated with clubbing of the fingernails. He postulated that the early pathogenesis of clubbing involved dermal fibroblast proliferation in the nail bed, leading to sequestration of nail bed epithelium into the dermis with resultant cyst formation. Microscopic subungual cysts also were identified in normal-appearing nails without evidence of trauma, thought to have arisen from the tips of the nail bed rete ridges by a process of bulbous proliferation rather than sequestration. These findings in normal nails suggest that SOCs may represent a more common entity than previously recognized.
It is imperative to recognize the presence of nail unit tumors early because of the risk for permanent nail plate dystrophy and the possibility of a malignant tumor.4,5 Subungual onycholemmal cysts may present with a wide spectrum of clinical findings including marked subungual hyperkeratosis, onychodystrophy, ridging, nail bed pigmentation, clubbing, thickening, or less often a normal-appearing nail. Based on reported cases, several trends are evident. Although nail dystrophy is most often asymptomatic, pain is not uncommon.5,6 It most commonly involves single digits, predominantly thumbs and great toenails.7,8 This predilection suggests that trauma or other local factors may be involved in its pathogenesis. Of note, trauma to the nail may occur years before the development of the lesions or it may not be recalled at all.
Diagnosis requires a degree of clinical suspicion and a nail bed biopsy with partial or total nail plate avulsion to visualize the pathologic portion of the nail bed. Because surgical intervention may lead to the implantation of epithelium, recurrences after nail biopsy or excision may occur.
In contrast to epidermal inclusion cysts arising in the skin, most SOCs do not have a granular layer.9 Hair and nails represent analogous differentiation products of the ectoderm. The nail matrix is homologous to portions of the hair matrix, while the nail bed epithelium is comparable to the outer root sheath of the hair follicle.7 Subungual onycholemmal cysts originate from the nail bed epithelium, which keratinizes in the absence of a granular layer, similar to the follicular isthmus outer root sheath. Thus, SOCs are comparable to the outer root sheath–derived isthmus-catagen cysts because of their abrupt central keratinization.8
Subungual onycholemmal cysts also must be distinguished from slowly growing malignant tumors of the nail bed epithelium, referred to as onycholemmal carcinomas by Alessi et al.10 This entity characteristically presents in elderly patients as a slowly growing, circumscribed, subungual discoloration that may ulcerate, destroying the nail apparatus and penetrating the phalangeal bone. On histopathology, it is characterized by small cysts filled with eosinophilic keratin devoid of a granular layer and lined by atypical squamous epithelium accompanied by solid nests and strands of atypical keratinocytes within the dermis.11 When a cystic component and clear cells predominate, the designation of malignant proliferating onycholemmal cyst has been applied. Its infiltrative growth pattern with destruction of the underlying bone makes it an important entity to exclude when considering the differential diagnosis of tumors of the nail bed.
Subungual melanomas comprise only 1% to 3% of malignant melanomas and 85% are initially misdiagnosed due to their rarity and nonspecific variable presentation. Aside from clinical evidence of Hutchinson sign in the early stages in almost all cases, accurate diagnosis of subungual melanoma and differentiation from SOCs relies on histopathology. A biopsy is necessary to make the diagnosis, but even microscopic findings may be nonspecific during the early stages.
Conclusion
We report a case of a 23-year-old woman with horizontal ridging and tenderness of the right great toenail associated with pigmentation of 5 years’ duration due to an SOC. The etiology of these subungual cysts, with or without nail abnormalities, still remains unclear. Its predilection for the thumbs and great toenails suggests that trauma or other local factors may be involved in its pathogenesis. Because of the rarity of this entity, there are no guidelines for surgical treatment. Subungual onycholemmal cysts may be an underrecognized and more common entity that must be considered when discussing tumors of the nail unit.
Case Report
A 23-year-old woman presented with a horizontal split along the midline of the right great toenail associated with some tenderness of 2 to 3 months’ duration. Approximately 5 years prior, she noticed a bluish-colored area under the nail that had been steadily increasing in size. She denied a history of trauma, drainage, or bleeding. There was no history of other nail abnormalities. Her medications and personal, family, and social history were noncontributory.
Physical examination of the right great toenail revealed a horizontal split of the nail plate with a bluish hue visible under the nail plate (Figure 1A). The remaining toenails and fingernails were normal. A punch biopsy of the nail bed was performed with a presumptive clinical diagnosis of subungual melanoma versus melanocytic nevus versus cyst (Figure 1B). Nail plate avulsion revealed a blackened nail bed dotted with areas of bluish color and a red friable nodule present focally. Upon further inspection, extension was apparent into the distal matrix.

Histopathologic examination revealed a cystic structure with an epithelial lining mostly reminiscent of an isthmus catagen cyst admixed with the presence of both an intermittent focal granular layer and an eosinophilic cuticle surrounding pink laminated keratin, most consistent with a diagnosis of subungual onycholemmal cyst (SOC)(Figure 2). A reexcision was performed with removal of half of the nail bed, including a portion of the distal matrix extending inferiorly to the bone. Variably sized, epithelium-lined, keratin-filled cystic structures emanated from the nail bed epithelium. There were foci of hemorrhage and granulation tissue secondary to cyst rupture (Figure 3). The defect healed by secondary intention. No clinical evidence of recurrence was seen at 6-month follow-up.
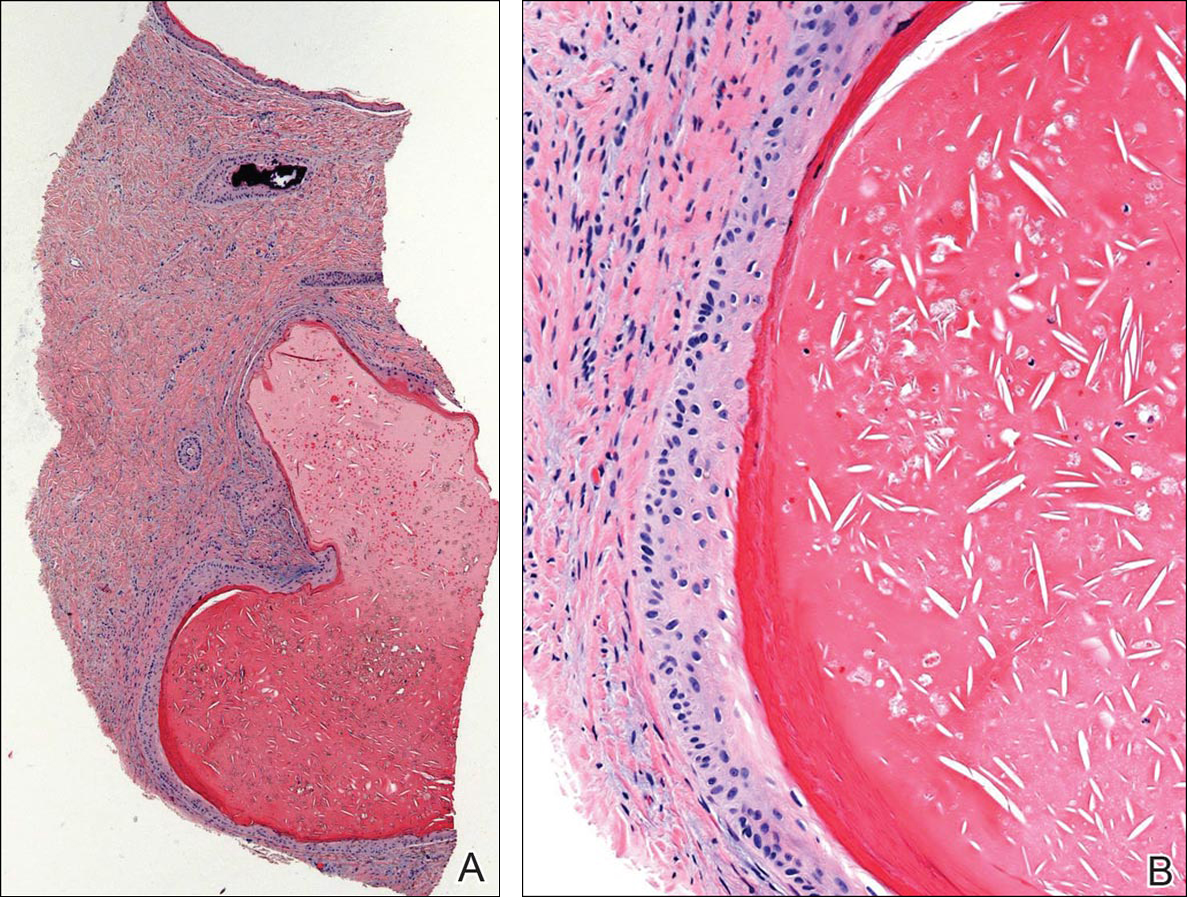

Subungual onycholemmal cysts, also known as subungual epidermoid cysts or subungual epidermoid inclusions, are rare and distinctive nail abnormalities occurring in the dermis of the nail bed. We present a case of an SOC in a toenail mimicking subungual malignant melanoma.
Originally described by Samman1 in 1959, SOCs were attributed to trauma to the nail with resultant implantation of the epidermis into the deeper tissue. Lewin2,3 examined 90 postmortem fingernail and nail bed samples and found 8 subungual epidermoid cysts associated with clubbing of the fingernails. He postulated that the early pathogenesis of clubbing involved dermal fibroblast proliferation in the nail bed, leading to sequestration of nail bed epithelium into the dermis with resultant cyst formation. Microscopic subungual cysts also were identified in normal-appearing nails without evidence of trauma, thought to have arisen from the tips of the nail bed rete ridges by a process of bulbous proliferation rather than sequestration. These findings in normal nails suggest that SOCs may represent a more common entity than previously recognized.
It is imperative to recognize the presence of nail unit tumors early because of the risk for permanent nail plate dystrophy and the possibility of a malignant tumor.4,5 Subungual onycholemmal cysts may present with a wide spectrum of clinical findings including marked subungual hyperkeratosis, onychodystrophy, ridging, nail bed pigmentation, clubbing, thickening, or less often a normal-appearing nail. Based on reported cases, several trends are evident. Although nail dystrophy is most often asymptomatic, pain is not uncommon.5,6 It most commonly involves single digits, predominantly thumbs and great toenails.7,8 This predilection suggests that trauma or other local factors may be involved in its pathogenesis. Of note, trauma to the nail may occur years before the development of the lesions or it may not be recalled at all.
Diagnosis requires a degree of clinical suspicion and a nail bed biopsy with partial or total nail plate avulsion to visualize the pathologic portion of the nail bed. Because surgical intervention may lead to the implantation of epithelium, recurrences after nail biopsy or excision may occur.
In contrast to epidermal inclusion cysts arising in the skin, most SOCs do not have a granular layer.9 Hair and nails represent analogous differentiation products of the ectoderm. The nail matrix is homologous to portions of the hair matrix, while the nail bed epithelium is comparable to the outer root sheath of the hair follicle.7 Subungual onycholemmal cysts originate from the nail bed epithelium, which keratinizes in the absence of a granular layer, similar to the follicular isthmus outer root sheath. Thus, SOCs are comparable to the outer root sheath–derived isthmus-catagen cysts because of their abrupt central keratinization.8
Subungual onycholemmal cysts also must be distinguished from slowly growing malignant tumors of the nail bed epithelium, referred to as onycholemmal carcinomas by Alessi et al.10 This entity characteristically presents in elderly patients as a slowly growing, circumscribed, subungual discoloration that may ulcerate, destroying the nail apparatus and penetrating the phalangeal bone. On histopathology, it is characterized by small cysts filled with eosinophilic keratin devoid of a granular layer and lined by atypical squamous epithelium accompanied by solid nests and strands of atypical keratinocytes within the dermis.11 When a cystic component and clear cells predominate, the designation of malignant proliferating onycholemmal cyst has been applied. Its infiltrative growth pattern with destruction of the underlying bone makes it an important entity to exclude when considering the differential diagnosis of tumors of the nail bed.
Subungual melanomas comprise only 1% to 3% of malignant melanomas and 85% are initially misdiagnosed due to their rarity and nonspecific variable presentation. Aside from clinical evidence of Hutchinson sign in the early stages in almost all cases, accurate diagnosis of subungual melanoma and differentiation from SOCs relies on histopathology. A biopsy is necessary to make the diagnosis, but even microscopic findings may be nonspecific during the early stages.
Conclusion
We report a case of a 23-year-old woman with horizontal ridging and tenderness of the right great toenail associated with pigmentation of 5 years’ duration due to an SOC. The etiology of these subungual cysts, with or without nail abnormalities, still remains unclear. Its predilection for the thumbs and great toenails suggests that trauma or other local factors may be involved in its pathogenesis. Because of the rarity of this entity, there are no guidelines for surgical treatment. Subungual onycholemmal cysts may be an underrecognized and more common entity that must be considered when discussing tumors of the nail unit.
- Samman PD. The human toe nail. its genesis and blood supply. Br J Dermatol. 1959;71:296-302.
- Lewin K. The normal fingernail. Br J Dermatol. 1965;77:421-430.
- Lewin K. Subungual epidermoid inclusions. Br J Dermatol. 1969;81:671-675.
- Dominguez-Cherit J, Chanussot-Deprez C, Maria-Sarti H, et al. Nail unit tumors: a study of 234 patients in the dermatology department of the “Dr. Manuel Gea González” General Hospital in Mexico City. Dermatol Surg. 2008;34:1363-1371.
- Sáez-de-Ocariz MM, Domínguez-Cherit J, García-Corona C. Subungual epidermoid cysts. Int J Dermatol. 2001;40:524-526.
- Molly DO, Herbert K. Subungual epidermoid cyst. J Hand Surg Br. 2006;31:345.
- Telang GH, Jellinek N. Multiple calcified subungual epidermoid inclusions. J Am Acad Dermatol. 2007;56:336-339.
- Fanti PA, Tosti A. Subungual epidermoid inclusions: report of 8 cases. Dermatologica. 1989;178:209-212.
- Takiyoshi N, Nakano H, Matsuzaki T, et al. An eclipse in the subungual space: a diagnostic sign for a subungual epidermal cyst? Br J Dermatol. 2009;161:962-963.
- Alessi E, Coggi A, Gianotti R, et al. Onycholemmal carcinoma. Am J Dermatopathol. 2004;26:397-402.
- Inaoki M, Makino E, Adachi M, et al. Onycholemmal carcinoma. J Cutan Pathol. 2006;33:577-580.
- Samman PD. The human toe nail. its genesis and blood supply. Br J Dermatol. 1959;71:296-302.
- Lewin K. The normal fingernail. Br J Dermatol. 1965;77:421-430.
- Lewin K. Subungual epidermoid inclusions. Br J Dermatol. 1969;81:671-675.
- Dominguez-Cherit J, Chanussot-Deprez C, Maria-Sarti H, et al. Nail unit tumors: a study of 234 patients in the dermatology department of the “Dr. Manuel Gea González” General Hospital in Mexico City. Dermatol Surg. 2008;34:1363-1371.
- Sáez-de-Ocariz MM, Domínguez-Cherit J, García-Corona C. Subungual epidermoid cysts. Int J Dermatol. 2001;40:524-526.
- Molly DO, Herbert K. Subungual epidermoid cyst. J Hand Surg Br. 2006;31:345.
- Telang GH, Jellinek N. Multiple calcified subungual epidermoid inclusions. J Am Acad Dermatol. 2007;56:336-339.
- Fanti PA, Tosti A. Subungual epidermoid inclusions: report of 8 cases. Dermatologica. 1989;178:209-212.
- Takiyoshi N, Nakano H, Matsuzaki T, et al. An eclipse in the subungual space: a diagnostic sign for a subungual epidermal cyst? Br J Dermatol. 2009;161:962-963.
- Alessi E, Coggi A, Gianotti R, et al. Onycholemmal carcinoma. Am J Dermatopathol. 2004;26:397-402.
- Inaoki M, Makino E, Adachi M, et al. Onycholemmal carcinoma. J Cutan Pathol. 2006;33:577-580.
Practice Points
- Trauma to the nail may occur years before the development of subungual onycholemmal cysts or it may not be recalled at all.
- Diagnosis requires a degree of clinical suspicion and a nail bed biopsy.
- Subungual onycholemmal cysts must be distinguished from slowly growing malignant tumors of the nail bed epithelium.
HIV research update: Early August 2016
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
Text message reminders are a promising intervention that can be used to increase HIV care compliance when logistically feasible, according to a meta-analysis published in AIDS Care.
A study published in AIDS found that people living with HIV who are older than age 65years are at higher risk of comorbidities than are other fee-for-service Medicare beneficiaries.
A study in Thailand found a marked divergence of HIV DNA values between untreated and treated groups that occurred within the first 2 weeks of antiretroviral therapy (ART) and increased with time. The authors conclude that very-early ART offers the opportunity to significantly reduce the frequency of cells harboring HIV DNA.
An independent source of HIV RNA contributes to viral rebound within the cerebrospinal fluid after treatment interruption, according to a study in Virus Evolution. The most likely source of compartmentalized HIV RNA is a CNS reservoir that would need to be targeted to achieve complete HIV eradication, investigators said.
A recent six-site U.S. study discovered that 36% of nondrinking persons living with HIV in routine clinical care had a prior alcohol use disorder.
A study in HIV Medicine found that treatment of patients infected with hepatitis C virus and coinfected with HCV/HIV with all-oral direct-acting antiviral combinations, under real-life conditions, led to high and similar rates of sustained virologic response 12 weeks after the end of therapy.
A first-of-its-kind study in Tanzania demonstrated a significantly increased risk of acquiring HIV for lymphatic filariasis-infected individuals.
A clinical trial of HIV-infected adults treated with efavirenz-based antiretroviral therapy found that the late virologic failure rate was very low after successful suppression. The authors said virologic monitoring, if achievable in routine clinical practice, involving infrequent measurements might be considered.
The introduction of a low viral load threshold provides crucial improvements in recent infection testing algorithms, according to a study in AIDS. However, the authors said it does not eliminate non-zero “false-recent” rates, and mean durations of “recent” infection must be consistently estimated.
The risk of virologic failure in a population of HIV-infected patients on antiretroviral therapy, who achieved viral suppression at less than 20 copies/mL, was no different for patients who remained fully suppressed, compared with those who experienced subsequent episodes of very low level viremia.
A British study found that HIV self-testing among men who have sex with men represents an opportunity to reduce barriers to HIV testing and enhance prevention and access to care.
Hepatitis B virus coinfection was the most important risk factor for liver fibrosis and cirrhosis in HIV patients, and should be diagnosed early in HIV care to optimize treatment outcomes, according to a report in Tropical Medicine & International Health.
A recent study found that higher HIV RNA and wasting before antiretroviral therapy were independent risk factors for pneumonia in early ART-treated HIV-infected infants.
New information increases concerns about the association between the hormonal contraceptive depot medroxyprogesterone acetate and HIV acquisition risk in women, researchers said in a recent study. If the association is causal, the magnitude of effect is likely a hazard ratio of 1.5, although investigators said data for other hormonal contraceptive methods are largely reassuring.
A study of virally suppressed HIV-infected men with extensive antiretroviral exposure found no consistent associations between use of specific ART drugs and both subclinical coronary plaque presence and extent. Investigators said the findings support the hypothesis that, among virally suppressed persons, type of ART used is not in general a major determinant of subclinical coronary plaque risk.
More cost-effective and impactful HIV-prevention investments could be achieved across sub-Saharan Africa if domestic and international funders were to align strategically to build an aggregate funding pattern guided by the emerging understanding of local dynamics and epidemic drivers, a Lancet HIV study found.
A cross-sectional cohort study found evidence of endothelial dysfunction in HIV infection and in untreated compared to treated HIV infection, although asymmetric dimethylarginine (a marker of endothelial dysfunction) was not associated with subclinical atherosclerosis.
A modeling study in the journal AIDS concluded that, in mature HIV epidemics, between 3%-6% of transmission events are attributable to acute HIV infection among people who inject drugs.
The HIV epidemic serves as an amplifier of TB outbreaks by providing a reservoir of susceptible hosts, a study in eLife found, but HIV coinfection is not a direct driver for the emergence and transmission of drug-resistant strains.
A recent study of HIV-infected patients coinfected with hepatitis B and C viruses found that, despite increasing use of antiretrovirals, no clear reduction in end-stage liver disease risk was observed. The authors said treatment with direct acting antivirals for HCV and wider use of tenofovir-based regimens for HBV should be prioritized for coinfected patients.
HIV incidence, prevalence, and undiagnosed infections can be estimated using HIV case surveillance data and information on first CD4 test result after diagnosis, according to analysis published in JAIDS.
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
Text message reminders are a promising intervention that can be used to increase HIV care compliance when logistically feasible, according to a meta-analysis published in AIDS Care.
A study published in AIDS found that people living with HIV who are older than age 65years are at higher risk of comorbidities than are other fee-for-service Medicare beneficiaries.
A study in Thailand found a marked divergence of HIV DNA values between untreated and treated groups that occurred within the first 2 weeks of antiretroviral therapy (ART) and increased with time. The authors conclude that very-early ART offers the opportunity to significantly reduce the frequency of cells harboring HIV DNA.
An independent source of HIV RNA contributes to viral rebound within the cerebrospinal fluid after treatment interruption, according to a study in Virus Evolution. The most likely source of compartmentalized HIV RNA is a CNS reservoir that would need to be targeted to achieve complete HIV eradication, investigators said.
A recent six-site U.S. study discovered that 36% of nondrinking persons living with HIV in routine clinical care had a prior alcohol use disorder.
A study in HIV Medicine found that treatment of patients infected with hepatitis C virus and coinfected with HCV/HIV with all-oral direct-acting antiviral combinations, under real-life conditions, led to high and similar rates of sustained virologic response 12 weeks after the end of therapy.
A first-of-its-kind study in Tanzania demonstrated a significantly increased risk of acquiring HIV for lymphatic filariasis-infected individuals.
A clinical trial of HIV-infected adults treated with efavirenz-based antiretroviral therapy found that the late virologic failure rate was very low after successful suppression. The authors said virologic monitoring, if achievable in routine clinical practice, involving infrequent measurements might be considered.
The introduction of a low viral load threshold provides crucial improvements in recent infection testing algorithms, according to a study in AIDS. However, the authors said it does not eliminate non-zero “false-recent” rates, and mean durations of “recent” infection must be consistently estimated.
The risk of virologic failure in a population of HIV-infected patients on antiretroviral therapy, who achieved viral suppression at less than 20 copies/mL, was no different for patients who remained fully suppressed, compared with those who experienced subsequent episodes of very low level viremia.
A British study found that HIV self-testing among men who have sex with men represents an opportunity to reduce barriers to HIV testing and enhance prevention and access to care.
Hepatitis B virus coinfection was the most important risk factor for liver fibrosis and cirrhosis in HIV patients, and should be diagnosed early in HIV care to optimize treatment outcomes, according to a report in Tropical Medicine & International Health.
A recent study found that higher HIV RNA and wasting before antiretroviral therapy were independent risk factors for pneumonia in early ART-treated HIV-infected infants.
New information increases concerns about the association between the hormonal contraceptive depot medroxyprogesterone acetate and HIV acquisition risk in women, researchers said in a recent study. If the association is causal, the magnitude of effect is likely a hazard ratio of 1.5, although investigators said data for other hormonal contraceptive methods are largely reassuring.
A study of virally suppressed HIV-infected men with extensive antiretroviral exposure found no consistent associations between use of specific ART drugs and both subclinical coronary plaque presence and extent. Investigators said the findings support the hypothesis that, among virally suppressed persons, type of ART used is not in general a major determinant of subclinical coronary plaque risk.
More cost-effective and impactful HIV-prevention investments could be achieved across sub-Saharan Africa if domestic and international funders were to align strategically to build an aggregate funding pattern guided by the emerging understanding of local dynamics and epidemic drivers, a Lancet HIV study found.
A cross-sectional cohort study found evidence of endothelial dysfunction in HIV infection and in untreated compared to treated HIV infection, although asymmetric dimethylarginine (a marker of endothelial dysfunction) was not associated with subclinical atherosclerosis.
A modeling study in the journal AIDS concluded that, in mature HIV epidemics, between 3%-6% of transmission events are attributable to acute HIV infection among people who inject drugs.
The HIV epidemic serves as an amplifier of TB outbreaks by providing a reservoir of susceptible hosts, a study in eLife found, but HIV coinfection is not a direct driver for the emergence and transmission of drug-resistant strains.
A recent study of HIV-infected patients coinfected with hepatitis B and C viruses found that, despite increasing use of antiretrovirals, no clear reduction in end-stage liver disease risk was observed. The authors said treatment with direct acting antivirals for HCV and wider use of tenofovir-based regimens for HBV should be prioritized for coinfected patients.
HIV incidence, prevalence, and undiagnosed infections can be estimated using HIV case surveillance data and information on first CD4 test result after diagnosis, according to analysis published in JAIDS.
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
Text message reminders are a promising intervention that can be used to increase HIV care compliance when logistically feasible, according to a meta-analysis published in AIDS Care.
A study published in AIDS found that people living with HIV who are older than age 65years are at higher risk of comorbidities than are other fee-for-service Medicare beneficiaries.
A study in Thailand found a marked divergence of HIV DNA values between untreated and treated groups that occurred within the first 2 weeks of antiretroviral therapy (ART) and increased with time. The authors conclude that very-early ART offers the opportunity to significantly reduce the frequency of cells harboring HIV DNA.
An independent source of HIV RNA contributes to viral rebound within the cerebrospinal fluid after treatment interruption, according to a study in Virus Evolution. The most likely source of compartmentalized HIV RNA is a CNS reservoir that would need to be targeted to achieve complete HIV eradication, investigators said.
A recent six-site U.S. study discovered that 36% of nondrinking persons living with HIV in routine clinical care had a prior alcohol use disorder.
A study in HIV Medicine found that treatment of patients infected with hepatitis C virus and coinfected with HCV/HIV with all-oral direct-acting antiviral combinations, under real-life conditions, led to high and similar rates of sustained virologic response 12 weeks after the end of therapy.
A first-of-its-kind study in Tanzania demonstrated a significantly increased risk of acquiring HIV for lymphatic filariasis-infected individuals.
A clinical trial of HIV-infected adults treated with efavirenz-based antiretroviral therapy found that the late virologic failure rate was very low after successful suppression. The authors said virologic monitoring, if achievable in routine clinical practice, involving infrequent measurements might be considered.
The introduction of a low viral load threshold provides crucial improvements in recent infection testing algorithms, according to a study in AIDS. However, the authors said it does not eliminate non-zero “false-recent” rates, and mean durations of “recent” infection must be consistently estimated.
The risk of virologic failure in a population of HIV-infected patients on antiretroviral therapy, who achieved viral suppression at less than 20 copies/mL, was no different for patients who remained fully suppressed, compared with those who experienced subsequent episodes of very low level viremia.
A British study found that HIV self-testing among men who have sex with men represents an opportunity to reduce barriers to HIV testing and enhance prevention and access to care.
Hepatitis B virus coinfection was the most important risk factor for liver fibrosis and cirrhosis in HIV patients, and should be diagnosed early in HIV care to optimize treatment outcomes, according to a report in Tropical Medicine & International Health.
A recent study found that higher HIV RNA and wasting before antiretroviral therapy were independent risk factors for pneumonia in early ART-treated HIV-infected infants.
New information increases concerns about the association between the hormonal contraceptive depot medroxyprogesterone acetate and HIV acquisition risk in women, researchers said in a recent study. If the association is causal, the magnitude of effect is likely a hazard ratio of 1.5, although investigators said data for other hormonal contraceptive methods are largely reassuring.
A study of virally suppressed HIV-infected men with extensive antiretroviral exposure found no consistent associations between use of specific ART drugs and both subclinical coronary plaque presence and extent. Investigators said the findings support the hypothesis that, among virally suppressed persons, type of ART used is not in general a major determinant of subclinical coronary plaque risk.
More cost-effective and impactful HIV-prevention investments could be achieved across sub-Saharan Africa if domestic and international funders were to align strategically to build an aggregate funding pattern guided by the emerging understanding of local dynamics and epidemic drivers, a Lancet HIV study found.
A cross-sectional cohort study found evidence of endothelial dysfunction in HIV infection and in untreated compared to treated HIV infection, although asymmetric dimethylarginine (a marker of endothelial dysfunction) was not associated with subclinical atherosclerosis.
A modeling study in the journal AIDS concluded that, in mature HIV epidemics, between 3%-6% of transmission events are attributable to acute HIV infection among people who inject drugs.
The HIV epidemic serves as an amplifier of TB outbreaks by providing a reservoir of susceptible hosts, a study in eLife found, but HIV coinfection is not a direct driver for the emergence and transmission of drug-resistant strains.
A recent study of HIV-infected patients coinfected with hepatitis B and C viruses found that, despite increasing use of antiretrovirals, no clear reduction in end-stage liver disease risk was observed. The authors said treatment with direct acting antivirals for HCV and wider use of tenofovir-based regimens for HBV should be prioritized for coinfected patients.
HIV incidence, prevalence, and undiagnosed infections can be estimated using HIV case surveillance data and information on first CD4 test result after diagnosis, according to analysis published in JAIDS.
On Twitter @richpizzi
Predicting outcomes in relapsed BCP-ALL

Image by Vashi Donsk
Screening for genetic abnormalities can provide a more accurate prediction of outcomes in children with relapsed B-cell precursor acute lymphoblastic leukemia (BCP-ALL), according to a study published in Blood.
Researchers found that mutations or deletions in TP53, NR3C1, BTG1, and NRAS were associated with inferior outcomes in relapsed BCP-ALL.
And screening for these abnormalities could improve upon the predictive accuracy of clinical risk factors.
“Current methods used to guide treatment for relapsed leukemia are not accurate enough, with some children believed to have a good chance of survival actually responding very poorly to chemotherapy,” said study author Anthony Moorman, PhD, of Newcastle University in Newcastle upon Tyne, UK.
“Screening patients at relapse for key genetic abnormalities that influence outcome will ensure that treatment can be personalized, thereby improving their chances of survival.”
For this study, Dr Moorman and his colleagues analyzed cytogenetic data from 427 children with relapsed BCP-ALL and screened 238 patients with a marrow relapse for certain copy number alterations and mutations.
According to univariate analysis, alterations in TP53, NR3C1 deletions, and BTG1 deletions were significantly associated with patient outcomes.
Patients with TP53 alterations had a higher risk of progression (hazard ratio [HR]=2.36, P<0.001) and death (HR=2.56, P<0.001), as did patients with deletions in NR3C1 and BTG1.
Because both NR3C1 and BTG1 are implicated in resistance to glucocorticoids and the deletions are mutually exclusive, the researchers considered the effect of the deletions together. So for patients with NR3C1 and BTG1 deletions, the HR for progression was 2.15 (P=0.002), and the HR for death was 1.91 (P=0.015).
Patients with NRAS mutations had an increased risk of progression and death as well, but this did not reach statistical significance.
The researchers also found that patients who were standard risk according to clinical characteristics but, at the time of relapse, had one or more high-risk genetic abnormalities had poorer outcomes.
Standard-risk patients with a TP53 alteration had an increased risk of death (HR=2.56, P<0.001), as did standard-risk patients with NR3C1 and BTG1 deletions (HR=1.91, P=0.015).
Standard-risk patients with NRAS mutations and high hyperdiploidy had an increased risk of progression (HR=3.17, P=0.026) and death (HR=3.41, P=0.032).
The researchers concluded that the outcomes of clinical standard-risk patients with high-risk cytogenetics were equivalent to outcomes of clinical high-risk patients.
The team therefore believes that screening BCP-ALL patients for the aforementioned genetic abnormalities at relapse will improve patient stratification and outcomes. ![]()

Image by Vashi Donsk
Screening for genetic abnormalities can provide a more accurate prediction of outcomes in children with relapsed B-cell precursor acute lymphoblastic leukemia (BCP-ALL), according to a study published in Blood.
Researchers found that mutations or deletions in TP53, NR3C1, BTG1, and NRAS were associated with inferior outcomes in relapsed BCP-ALL.
And screening for these abnormalities could improve upon the predictive accuracy of clinical risk factors.
“Current methods used to guide treatment for relapsed leukemia are not accurate enough, with some children believed to have a good chance of survival actually responding very poorly to chemotherapy,” said study author Anthony Moorman, PhD, of Newcastle University in Newcastle upon Tyne, UK.
“Screening patients at relapse for key genetic abnormalities that influence outcome will ensure that treatment can be personalized, thereby improving their chances of survival.”
For this study, Dr Moorman and his colleagues analyzed cytogenetic data from 427 children with relapsed BCP-ALL and screened 238 patients with a marrow relapse for certain copy number alterations and mutations.
According to univariate analysis, alterations in TP53, NR3C1 deletions, and BTG1 deletions were significantly associated with patient outcomes.
Patients with TP53 alterations had a higher risk of progression (hazard ratio [HR]=2.36, P<0.001) and death (HR=2.56, P<0.001), as did patients with deletions in NR3C1 and BTG1.
Because both NR3C1 and BTG1 are implicated in resistance to glucocorticoids and the deletions are mutually exclusive, the researchers considered the effect of the deletions together. So for patients with NR3C1 and BTG1 deletions, the HR for progression was 2.15 (P=0.002), and the HR for death was 1.91 (P=0.015).
Patients with NRAS mutations had an increased risk of progression and death as well, but this did not reach statistical significance.
The researchers also found that patients who were standard risk according to clinical characteristics but, at the time of relapse, had one or more high-risk genetic abnormalities had poorer outcomes.
Standard-risk patients with a TP53 alteration had an increased risk of death (HR=2.56, P<0.001), as did standard-risk patients with NR3C1 and BTG1 deletions (HR=1.91, P=0.015).
Standard-risk patients with NRAS mutations and high hyperdiploidy had an increased risk of progression (HR=3.17, P=0.026) and death (HR=3.41, P=0.032).
The researchers concluded that the outcomes of clinical standard-risk patients with high-risk cytogenetics were equivalent to outcomes of clinical high-risk patients.
The team therefore believes that screening BCP-ALL patients for the aforementioned genetic abnormalities at relapse will improve patient stratification and outcomes. ![]()

Image by Vashi Donsk
Screening for genetic abnormalities can provide a more accurate prediction of outcomes in children with relapsed B-cell precursor acute lymphoblastic leukemia (BCP-ALL), according to a study published in Blood.
Researchers found that mutations or deletions in TP53, NR3C1, BTG1, and NRAS were associated with inferior outcomes in relapsed BCP-ALL.
And screening for these abnormalities could improve upon the predictive accuracy of clinical risk factors.
“Current methods used to guide treatment for relapsed leukemia are not accurate enough, with some children believed to have a good chance of survival actually responding very poorly to chemotherapy,” said study author Anthony Moorman, PhD, of Newcastle University in Newcastle upon Tyne, UK.
“Screening patients at relapse for key genetic abnormalities that influence outcome will ensure that treatment can be personalized, thereby improving their chances of survival.”
For this study, Dr Moorman and his colleagues analyzed cytogenetic data from 427 children with relapsed BCP-ALL and screened 238 patients with a marrow relapse for certain copy number alterations and mutations.
According to univariate analysis, alterations in TP53, NR3C1 deletions, and BTG1 deletions were significantly associated with patient outcomes.
Patients with TP53 alterations had a higher risk of progression (hazard ratio [HR]=2.36, P<0.001) and death (HR=2.56, P<0.001), as did patients with deletions in NR3C1 and BTG1.
Because both NR3C1 and BTG1 are implicated in resistance to glucocorticoids and the deletions are mutually exclusive, the researchers considered the effect of the deletions together. So for patients with NR3C1 and BTG1 deletions, the HR for progression was 2.15 (P=0.002), and the HR for death was 1.91 (P=0.015).
Patients with NRAS mutations had an increased risk of progression and death as well, but this did not reach statistical significance.
The researchers also found that patients who were standard risk according to clinical characteristics but, at the time of relapse, had one or more high-risk genetic abnormalities had poorer outcomes.
Standard-risk patients with a TP53 alteration had an increased risk of death (HR=2.56, P<0.001), as did standard-risk patients with NR3C1 and BTG1 deletions (HR=1.91, P=0.015).
Standard-risk patients with NRAS mutations and high hyperdiploidy had an increased risk of progression (HR=3.17, P=0.026) and death (HR=3.41, P=0.032).
The researchers concluded that the outcomes of clinical standard-risk patients with high-risk cytogenetics were equivalent to outcomes of clinical high-risk patients.
The team therefore believes that screening BCP-ALL patients for the aforementioned genetic abnormalities at relapse will improve patient stratification and outcomes. ![]()
Preorder 2016 State of Hospital Medicine Report
The State of Hospital Medicine Report (SoHM) is the most comprehensive survey of hospital medicine in the country and provides current data on hospitalist compensation and productivity, plus covers practice demographics, staffing levels, staff growth, and compensation models.
Don’t miss out on getting your copy when it becomes available. Order now at www.hospitalmedicine.org/survey and be notified directly when the report is released.
The State of Hospital Medicine Report (SoHM) is the most comprehensive survey of hospital medicine in the country and provides current data on hospitalist compensation and productivity, plus covers practice demographics, staffing levels, staff growth, and compensation models.
Don’t miss out on getting your copy when it becomes available. Order now at www.hospitalmedicine.org/survey and be notified directly when the report is released.
The State of Hospital Medicine Report (SoHM) is the most comprehensive survey of hospital medicine in the country and provides current data on hospitalist compensation and productivity, plus covers practice demographics, staffing levels, staff growth, and compensation models.
Don’t miss out on getting your copy when it becomes available. Order now at www.hospitalmedicine.org/survey and be notified directly when the report is released.
Last Call to Participate in SHM’s Engagement Benchmarking Survey
One of the most important questions for leaders of hospital medicine groups is, “How can I measure the level of engagement of my hospitalists?” Measuring hospitalist engagement can be difficult, and many leaders are not satisfied with the tools they currently have at their disposal.
SHM developed an Engagement Benchmarking Service that evaluates care quality, autonomy, effective motivation, burnout risk, and more. You can see your standardization scores ranked against national benchmarks to help you determine what’s working well and what needs improvement.
Recruiting ends at the end of September, so register now for the next cohort at www.hospitalmedicine.org/pmad3.
One of the most important questions for leaders of hospital medicine groups is, “How can I measure the level of engagement of my hospitalists?” Measuring hospitalist engagement can be difficult, and many leaders are not satisfied with the tools they currently have at their disposal.
SHM developed an Engagement Benchmarking Service that evaluates care quality, autonomy, effective motivation, burnout risk, and more. You can see your standardization scores ranked against national benchmarks to help you determine what’s working well and what needs improvement.
Recruiting ends at the end of September, so register now for the next cohort at www.hospitalmedicine.org/pmad3.
One of the most important questions for leaders of hospital medicine groups is, “How can I measure the level of engagement of my hospitalists?” Measuring hospitalist engagement can be difficult, and many leaders are not satisfied with the tools they currently have at their disposal.
SHM developed an Engagement Benchmarking Service that evaluates care quality, autonomy, effective motivation, burnout risk, and more. You can see your standardization scores ranked against national benchmarks to help you determine what’s working well and what needs improvement.
Recruiting ends at the end of September, so register now for the next cohort at www.hospitalmedicine.org/pmad3.
Apparent Zika transmission via platelet transfusion

Photo from Flickr
Researchers have reported 2 cases in which the Zika virus seems to have been transmitted via platelet transfusion.
Brazilian health officials previously announced 2 cases of Zika virus—in a liver transplant recipient and a gunshot victim—that likely resulted from blood transfusions performed in 2015.
Now, researchers have reported possible transmission via transfusion in 2 more Brazilians—a patient with primary myelofibrosis (PMF) and one with acute myeloid leukemia (AML).
The researchers described these cases in a letter to NEJM.
An individual who donated platelets via apheresis on January 16, 2016, later tested positive for the Zika virus.
On January 19, platelets from that donor were transfused into a 54-year-old woman with PMF and a 14-year-old girl with AML who had also received a haploidentical bone marrow transplant on January 6.
The platelet donor called the blood bank on January 21 to report worrying symptoms—a cutaneous rash, retro-orbital pain, and pain in both knees—that had developed on January 18.
Subsequent testing revealed that the donor was negative for chikungunya and dengue virus. However, both plasma and urine samples tested positive for Zika virus.
Pre-transfusion samples collected from both of the recipients were negative for chikungunya, dengue, and Zika. However, samples collected after the transfusions—6 days after for the woman with PMF and 23 to 51 days after for the girl with AML—tested positive for Zika.
Researchers performed molecular sequencing and phylogenetic analysis of Zika virus RNA isolated from the donor and the recipients. Isolates from all 3 parties had nucleotide changes in the envelope gene (codons 11 and 186) that were not observed among other available isolates from Brazil.
The researchers said these results suggest the platelet transfusions were the source of Zika virus infection in the PMF patient and the AML patient.
Although both patients could have been exposed to Zika-carrying mosquitoes, both the RNA results and the timing of Zika infection suggest the transfusions were the cause. ![]()

Photo from Flickr
Researchers have reported 2 cases in which the Zika virus seems to have been transmitted via platelet transfusion.
Brazilian health officials previously announced 2 cases of Zika virus—in a liver transplant recipient and a gunshot victim—that likely resulted from blood transfusions performed in 2015.
Now, researchers have reported possible transmission via transfusion in 2 more Brazilians—a patient with primary myelofibrosis (PMF) and one with acute myeloid leukemia (AML).
The researchers described these cases in a letter to NEJM.
An individual who donated platelets via apheresis on January 16, 2016, later tested positive for the Zika virus.
On January 19, platelets from that donor were transfused into a 54-year-old woman with PMF and a 14-year-old girl with AML who had also received a haploidentical bone marrow transplant on January 6.
The platelet donor called the blood bank on January 21 to report worrying symptoms—a cutaneous rash, retro-orbital pain, and pain in both knees—that had developed on January 18.
Subsequent testing revealed that the donor was negative for chikungunya and dengue virus. However, both plasma and urine samples tested positive for Zika virus.
Pre-transfusion samples collected from both of the recipients were negative for chikungunya, dengue, and Zika. However, samples collected after the transfusions—6 days after for the woman with PMF and 23 to 51 days after for the girl with AML—tested positive for Zika.
Researchers performed molecular sequencing and phylogenetic analysis of Zika virus RNA isolated from the donor and the recipients. Isolates from all 3 parties had nucleotide changes in the envelope gene (codons 11 and 186) that were not observed among other available isolates from Brazil.
The researchers said these results suggest the platelet transfusions were the source of Zika virus infection in the PMF patient and the AML patient.
Although both patients could have been exposed to Zika-carrying mosquitoes, both the RNA results and the timing of Zika infection suggest the transfusions were the cause. ![]()

Photo from Flickr
Researchers have reported 2 cases in which the Zika virus seems to have been transmitted via platelet transfusion.
Brazilian health officials previously announced 2 cases of Zika virus—in a liver transplant recipient and a gunshot victim—that likely resulted from blood transfusions performed in 2015.
Now, researchers have reported possible transmission via transfusion in 2 more Brazilians—a patient with primary myelofibrosis (PMF) and one with acute myeloid leukemia (AML).
The researchers described these cases in a letter to NEJM.
An individual who donated platelets via apheresis on January 16, 2016, later tested positive for the Zika virus.
On January 19, platelets from that donor were transfused into a 54-year-old woman with PMF and a 14-year-old girl with AML who had also received a haploidentical bone marrow transplant on January 6.
The platelet donor called the blood bank on January 21 to report worrying symptoms—a cutaneous rash, retro-orbital pain, and pain in both knees—that had developed on January 18.
Subsequent testing revealed that the donor was negative for chikungunya and dengue virus. However, both plasma and urine samples tested positive for Zika virus.
Pre-transfusion samples collected from both of the recipients were negative for chikungunya, dengue, and Zika. However, samples collected after the transfusions—6 days after for the woman with PMF and 23 to 51 days after for the girl with AML—tested positive for Zika.
Researchers performed molecular sequencing and phylogenetic analysis of Zika virus RNA isolated from the donor and the recipients. Isolates from all 3 parties had nucleotide changes in the envelope gene (codons 11 and 186) that were not observed among other available isolates from Brazil.
The researchers said these results suggest the platelet transfusions were the source of Zika virus infection in the PMF patient and the AML patient.
Although both patients could have been exposed to Zika-carrying mosquitoes, both the RNA results and the timing of Zika infection suggest the transfusions were the cause. ![]()
Study supports expanded prenatal genetic testing

Photo by Nina Matthews
New research suggests expanded prenatal genetic testing may increase the detection of carrier status for potentially serious genetic conditions, including hemoglobinopathies.
Researchers analyzed nearly 350,000 adults of diverse racial and ethnic backgrounds and found evidence to suggest that expanded screening for up to 94 conditions can increase the detection of carrier status when compared with current genetic testing recommendations from professional societies.
Imran S. Haque, PhD, of Counsyl in San Francisco, California, and his colleagues reported these findings in JAMA. The study was funded by Counsyl, a laboratory providing expanded carrier screening.
Genetic testing of prospective parents to detect carriers of specific inherited recessive diseases is part of routine obstetrical practice. The current recommendations are to test for a limited number of individual diseases, in part based on self-reported racial/ethnic background.
Dr Haque and his colleagues wanted to determine if recent advances in genetic testing could facilitate screening for an expanded number of conditions independent of racial/ethnic background.
The researchers analyzed results from expanded carrier screening in 346,790 reproductive-aged individuals, primarily from the US, without known indication for specific genetic testing.
The individuals were tested for carrier status for up to 94 conditions. Tests were offered by clinicians providing reproductive care.
Risk was defined as the probability that a hypothetical fetus created from a random pairing of individuals (within or across 15 self-reported racial/ethnic categories) would be homozygous or compound heterozygous for 2 mutations presumed to cause severe or profound disease.
Severe conditions were defined as those that, if left untreated, cause intellectual disability or a substantially shortened lifespan. Profound conditions were those causing both intellectual disability and a shortened lifespan.
The researchers found that, in most racial/ethnic categories, expanded carrier screening modeled more hypothetical fetuses at risk for severe or profound conditions than did screening based on current professional guidelines.
Overall, relative to expanded carrier screening, guideline-based screening ranged from identifying 6% of hypothetical fetuses affected for East Asian couples to 87% for African or African American couples.
Though this study suggests expanded screening could be beneficial, the researchers said their findings should be confirmed with prospective studies comparing current carrier screening with expanded screening in at-risk populations. ![]()

Photo by Nina Matthews
New research suggests expanded prenatal genetic testing may increase the detection of carrier status for potentially serious genetic conditions, including hemoglobinopathies.
Researchers analyzed nearly 350,000 adults of diverse racial and ethnic backgrounds and found evidence to suggest that expanded screening for up to 94 conditions can increase the detection of carrier status when compared with current genetic testing recommendations from professional societies.
Imran S. Haque, PhD, of Counsyl in San Francisco, California, and his colleagues reported these findings in JAMA. The study was funded by Counsyl, a laboratory providing expanded carrier screening.
Genetic testing of prospective parents to detect carriers of specific inherited recessive diseases is part of routine obstetrical practice. The current recommendations are to test for a limited number of individual diseases, in part based on self-reported racial/ethnic background.
Dr Haque and his colleagues wanted to determine if recent advances in genetic testing could facilitate screening for an expanded number of conditions independent of racial/ethnic background.
The researchers analyzed results from expanded carrier screening in 346,790 reproductive-aged individuals, primarily from the US, without known indication for specific genetic testing.
The individuals were tested for carrier status for up to 94 conditions. Tests were offered by clinicians providing reproductive care.
Risk was defined as the probability that a hypothetical fetus created from a random pairing of individuals (within or across 15 self-reported racial/ethnic categories) would be homozygous or compound heterozygous for 2 mutations presumed to cause severe or profound disease.
Severe conditions were defined as those that, if left untreated, cause intellectual disability or a substantially shortened lifespan. Profound conditions were those causing both intellectual disability and a shortened lifespan.
The researchers found that, in most racial/ethnic categories, expanded carrier screening modeled more hypothetical fetuses at risk for severe or profound conditions than did screening based on current professional guidelines.
Overall, relative to expanded carrier screening, guideline-based screening ranged from identifying 6% of hypothetical fetuses affected for East Asian couples to 87% for African or African American couples.
Though this study suggests expanded screening could be beneficial, the researchers said their findings should be confirmed with prospective studies comparing current carrier screening with expanded screening in at-risk populations. ![]()

Photo by Nina Matthews
New research suggests expanded prenatal genetic testing may increase the detection of carrier status for potentially serious genetic conditions, including hemoglobinopathies.
Researchers analyzed nearly 350,000 adults of diverse racial and ethnic backgrounds and found evidence to suggest that expanded screening for up to 94 conditions can increase the detection of carrier status when compared with current genetic testing recommendations from professional societies.
Imran S. Haque, PhD, of Counsyl in San Francisco, California, and his colleagues reported these findings in JAMA. The study was funded by Counsyl, a laboratory providing expanded carrier screening.
Genetic testing of prospective parents to detect carriers of specific inherited recessive diseases is part of routine obstetrical practice. The current recommendations are to test for a limited number of individual diseases, in part based on self-reported racial/ethnic background.
Dr Haque and his colleagues wanted to determine if recent advances in genetic testing could facilitate screening for an expanded number of conditions independent of racial/ethnic background.
The researchers analyzed results from expanded carrier screening in 346,790 reproductive-aged individuals, primarily from the US, without known indication for specific genetic testing.
The individuals were tested for carrier status for up to 94 conditions. Tests were offered by clinicians providing reproductive care.
Risk was defined as the probability that a hypothetical fetus created from a random pairing of individuals (within or across 15 self-reported racial/ethnic categories) would be homozygous or compound heterozygous for 2 mutations presumed to cause severe or profound disease.
Severe conditions were defined as those that, if left untreated, cause intellectual disability or a substantially shortened lifespan. Profound conditions were those causing both intellectual disability and a shortened lifespan.
The researchers found that, in most racial/ethnic categories, expanded carrier screening modeled more hypothetical fetuses at risk for severe or profound conditions than did screening based on current professional guidelines.
Overall, relative to expanded carrier screening, guideline-based screening ranged from identifying 6% of hypothetical fetuses affected for East Asian couples to 87% for African or African American couples.
Though this study suggests expanded screening could be beneficial, the researchers said their findings should be confirmed with prospective studies comparing current carrier screening with expanded screening in at-risk populations. ![]()
Immunogene therapy granted conditional authorization

Image by NIAID
The European Commission (EC) has granted conditional marketing authorization for an immunogene therapy known as Zalmoxis.
This means Zalmoxis can be marketed in the European Economic Area as an adjunctive therapy to aid immune reconstitution and help treat graft-versus-host disease (GVHD) in adults with high-risk hematologic malignancies who are receiving a haploidentical hematopoietic stem cell transplant (haplo-HSCT).
Zalmoxis consists of allogeneic T cells genetically modified to express both a truncated form of the human low-affinity nerve growth factor receptor (ΔLNGFR), as a cell-surface selectable marker, and the suicide gene herpes simplex I virus thymidine kinase (HSV-TK Mut2).
The modified T cells are given to haplo-HSCT recipients to help fight off infection, enhance the success of the transplant, and support long-lasting anticancer effects.
Because the T cells can also cause GVHD, they are equipped with the suicide gene, which makes them susceptible to treatment with ganciclovir or valganciclovir. So if a patient develops GVHD, he or she can receive ganciclovir/valganciclovir, which should kill the modified T cells and prevent further development of the disease.
Zalmoxis is being developed by MolMed S.p.A. The company said the treatment should become available in the first European market during the first half of 2017.
About conditional marketing authorization
Conditional marketing authorization represents an expedited path for approval. The EC grants this type of authorization before pivotal registration studies are completed.
Conditional marketing authorization is granted to products whose benefits are thought to outweigh their risks, products that address unmet needs, and products that are expected to provide a significant public health benefit.
Under the provisions of the conditional marketing authorization for Zalmoxis, MolMed will be required to complete a post-marketing study aimed at confirming the clinical benefit of the treatment.
The European Medicines Agency’s Committee for Medicinal Products for Human Use has accepted the ongoing phase 3 TK008 trial as a post-marketing confirmatory study.
Trials of Zalmoxis
The EC’s decision to grant Zalmoxis conditional marketing authorization was based on cumulative efficacy and safety data collected from patients enrolled in a phase 1/2 trial (TK007) and an ongoing phase 3 trial (TK008).
The Zalmoxis group comprised 30 patients from the TK007 trial and 15 patients from the experimental arm of the TK008 trial. The TK007 trial included haplo-HSCT recipients with various high-risk hematologic malignancies, and the TK008 trial is enrolling haplo-HSCT recipients with high-risk acute leukemia.
The data thus far have indicated that Zalmoxis can provide rapid immune reconstitution, an anti-leukemia effect, and complete control of GVHD, in the absence of any post-transplant immunosuppression.
Overall, these effects led to a clinically meaningful increase in survival rates in Zalmoxis-treated patients, when compared to historical controls from the European Society for Blood and Marrow Transplantation (EBMT) database.
The only adverse event related to Zalmoxis treatment was GVHD, which was fully resolved by the activation of the suicide gene system with ganciclovir treatment, without any GVHD-related death.
Detailed results of this analysis are set to be presented during the MolMed-sponsored symposium “A new era of haplo-transplantation” at the EBMT International Transplant Course, which is scheduled to take place September 9-11 in Barcelona, Spain. ![]()

Image by NIAID
The European Commission (EC) has granted conditional marketing authorization for an immunogene therapy known as Zalmoxis.
This means Zalmoxis can be marketed in the European Economic Area as an adjunctive therapy to aid immune reconstitution and help treat graft-versus-host disease (GVHD) in adults with high-risk hematologic malignancies who are receiving a haploidentical hematopoietic stem cell transplant (haplo-HSCT).
Zalmoxis consists of allogeneic T cells genetically modified to express both a truncated form of the human low-affinity nerve growth factor receptor (ΔLNGFR), as a cell-surface selectable marker, and the suicide gene herpes simplex I virus thymidine kinase (HSV-TK Mut2).
The modified T cells are given to haplo-HSCT recipients to help fight off infection, enhance the success of the transplant, and support long-lasting anticancer effects.
Because the T cells can also cause GVHD, they are equipped with the suicide gene, which makes them susceptible to treatment with ganciclovir or valganciclovir. So if a patient develops GVHD, he or she can receive ganciclovir/valganciclovir, which should kill the modified T cells and prevent further development of the disease.
Zalmoxis is being developed by MolMed S.p.A. The company said the treatment should become available in the first European market during the first half of 2017.
About conditional marketing authorization
Conditional marketing authorization represents an expedited path for approval. The EC grants this type of authorization before pivotal registration studies are completed.
Conditional marketing authorization is granted to products whose benefits are thought to outweigh their risks, products that address unmet needs, and products that are expected to provide a significant public health benefit.
Under the provisions of the conditional marketing authorization for Zalmoxis, MolMed will be required to complete a post-marketing study aimed at confirming the clinical benefit of the treatment.
The European Medicines Agency’s Committee for Medicinal Products for Human Use has accepted the ongoing phase 3 TK008 trial as a post-marketing confirmatory study.
Trials of Zalmoxis
The EC’s decision to grant Zalmoxis conditional marketing authorization was based on cumulative efficacy and safety data collected from patients enrolled in a phase 1/2 trial (TK007) and an ongoing phase 3 trial (TK008).
The Zalmoxis group comprised 30 patients from the TK007 trial and 15 patients from the experimental arm of the TK008 trial. The TK007 trial included haplo-HSCT recipients with various high-risk hematologic malignancies, and the TK008 trial is enrolling haplo-HSCT recipients with high-risk acute leukemia.
The data thus far have indicated that Zalmoxis can provide rapid immune reconstitution, an anti-leukemia effect, and complete control of GVHD, in the absence of any post-transplant immunosuppression.
Overall, these effects led to a clinically meaningful increase in survival rates in Zalmoxis-treated patients, when compared to historical controls from the European Society for Blood and Marrow Transplantation (EBMT) database.
The only adverse event related to Zalmoxis treatment was GVHD, which was fully resolved by the activation of the suicide gene system with ganciclovir treatment, without any GVHD-related death.
Detailed results of this analysis are set to be presented during the MolMed-sponsored symposium “A new era of haplo-transplantation” at the EBMT International Transplant Course, which is scheduled to take place September 9-11 in Barcelona, Spain. ![]()

Image by NIAID
The European Commission (EC) has granted conditional marketing authorization for an immunogene therapy known as Zalmoxis.
This means Zalmoxis can be marketed in the European Economic Area as an adjunctive therapy to aid immune reconstitution and help treat graft-versus-host disease (GVHD) in adults with high-risk hematologic malignancies who are receiving a haploidentical hematopoietic stem cell transplant (haplo-HSCT).
Zalmoxis consists of allogeneic T cells genetically modified to express both a truncated form of the human low-affinity nerve growth factor receptor (ΔLNGFR), as a cell-surface selectable marker, and the suicide gene herpes simplex I virus thymidine kinase (HSV-TK Mut2).
The modified T cells are given to haplo-HSCT recipients to help fight off infection, enhance the success of the transplant, and support long-lasting anticancer effects.
Because the T cells can also cause GVHD, they are equipped with the suicide gene, which makes them susceptible to treatment with ganciclovir or valganciclovir. So if a patient develops GVHD, he or she can receive ganciclovir/valganciclovir, which should kill the modified T cells and prevent further development of the disease.
Zalmoxis is being developed by MolMed S.p.A. The company said the treatment should become available in the first European market during the first half of 2017.
About conditional marketing authorization
Conditional marketing authorization represents an expedited path for approval. The EC grants this type of authorization before pivotal registration studies are completed.
Conditional marketing authorization is granted to products whose benefits are thought to outweigh their risks, products that address unmet needs, and products that are expected to provide a significant public health benefit.
Under the provisions of the conditional marketing authorization for Zalmoxis, MolMed will be required to complete a post-marketing study aimed at confirming the clinical benefit of the treatment.
The European Medicines Agency’s Committee for Medicinal Products for Human Use has accepted the ongoing phase 3 TK008 trial as a post-marketing confirmatory study.
Trials of Zalmoxis
The EC’s decision to grant Zalmoxis conditional marketing authorization was based on cumulative efficacy and safety data collected from patients enrolled in a phase 1/2 trial (TK007) and an ongoing phase 3 trial (TK008).
The Zalmoxis group comprised 30 patients from the TK007 trial and 15 patients from the experimental arm of the TK008 trial. The TK007 trial included haplo-HSCT recipients with various high-risk hematologic malignancies, and the TK008 trial is enrolling haplo-HSCT recipients with high-risk acute leukemia.
The data thus far have indicated that Zalmoxis can provide rapid immune reconstitution, an anti-leukemia effect, and complete control of GVHD, in the absence of any post-transplant immunosuppression.
Overall, these effects led to a clinically meaningful increase in survival rates in Zalmoxis-treated patients, when compared to historical controls from the European Society for Blood and Marrow Transplantation (EBMT) database.
The only adverse event related to Zalmoxis treatment was GVHD, which was fully resolved by the activation of the suicide gene system with ganciclovir treatment, without any GVHD-related death.
Detailed results of this analysis are set to be presented during the MolMed-sponsored symposium “A new era of haplo-transplantation” at the EBMT International Transplant Course, which is scheduled to take place September 9-11 in Barcelona, Spain. ![]()
Healthy donor stool safe, effective for recurrent CDI
For patients with recurrent Clostridium difficile infection (CDI), donor stool administered via colonoscopy seemed safe and achieved clinical cure significantly more often than autologous fecal microbiota transplantation (FMT), based on a small trial reported online in Annals of Internal Medicine.
In all, 20 of 22 patients (91%) achieved cure with donor FMT, compared with 63% of patients who received their own markedly dysbiotic stool (P = .04), reported Colleen Kelly, MD, of The Miriam Hospital, Providence, R.I., together with her associates. “Differences in efficacy between sites suggest that some patients with lower risk for CDI recurrence may not benefit from FMT. Further research may help determine the best candidates,” the researchers wrote.
FMT corrects the dysbiosis associated with CDI and is recommended in the event of failed antibiotic therapy leading to a third episode of infection. But this advice is based mainly on case series and open-label trials, the researchers noted. Their dual-center, randomized, controlled, double-blinded study included 46 patients with at least three recurrences of CDI who had completed a course of vancomycin during their most recent episode of infection. Patients older than age 75 years or who were immunocompromised were excluded (Ann Intern Med. 2016 Aug 22. doi: 10.7326/M16-0271).
The overall clinical cure rates reflected the literature, the researchers reported, and all nine patients who developed CDI after autologous FMT were subsequently cured by donor FMT. Indeed, donor FMT “restored normal microbial community structure, with reductions in Proteobacteria and Verrucomicrobia and increases in Bacteroidetes and Firmicutes. In contrast, microbial diversity did not improve after autologous FMT.”
Notably, however, 90% of autologous FMT patients at the center in New York achieved clinical cure, compared with 43% of patients at the center in Rhode Island. Further analyses revealed differences between patients and fecal microbiota at the two sites, the investigators said. Patients in New York typically had CDI for longer, with more recurrences and up to 148 weeks of vancomycin and other antibiotics. Thus, they might have been cured before enrollment. But “autologous FMT patients at the New York site [also] had greater abundances of Clostridia, raising the possibility of emergence of microbial community assemblages inhibitory to C. difficile via competitive niche exclusion, or possibly by emergence of nontoxigenic organisms,” the researchers wrote.
There were no serious adverse effects associated with either type of FMT, they noted.
Dr. Kelly disclosed ties to Seres Health outside the submitted work. Two coauthors had patents or patents pending for “compositions and methods for transplantation of colon microbiota.” A third coauthor disclosed ties to OpenBiome and personal fees from CIPAC/Crestovo outside the submitted work. The remaining coauthors had no conflicts of interest.
Kelly and her colleagues demonstrate that rigorous controlled trials are valuable even when we think we know the answer. Their results prompt us to ask again whether microbial manipulation has any as-yet unappreciated health benefits or risks and whether there are preferred microbiomes for specific human populations or locales.
Careful review of reported adverse events in the current trial is instructive. One participant reported a 9.1-kg weight gain (donor details were not provided), a problem previously described in a separate case report. There is great interest in understanding whether the microbiome can be manipulated to modify weight in humans, as has been clearly shown in mice. In addition, patients receiving donor stool more frequently reported chills. In my own practice, I have rarely observed transient fever after healthy donor FMT delivered orally in encapsulated form, and I hypothesize that this may be due to an immune reaction to a new microbial ecosystem. Patients considering FMT should be informed of both of these possible adverse events.
Elizabeth L. Hohmann, MD, is at Massachusetts General Hospital, Boston. She reported grant support and personal fees from Seres Therapeutics outside the submitted work. These comments are from an editorial accompanying the article (Ann Intern Med. 2016 Aug 22. doi: 10.7326/M16-1784).
AGA Resource
The AGA Center for Gut Microbiome Research and Education was created to serve as a virtual ‘home’ for AGA activities related to the gut microbiome with a mission to advance research and education on the gut microbiome with the goal of improving human health. Learn more at www.gastro.org/microbiome.
Kelly and her colleagues demonstrate that rigorous controlled trials are valuable even when we think we know the answer. Their results prompt us to ask again whether microbial manipulation has any as-yet unappreciated health benefits or risks and whether there are preferred microbiomes for specific human populations or locales.
Careful review of reported adverse events in the current trial is instructive. One participant reported a 9.1-kg weight gain (donor details were not provided), a problem previously described in a separate case report. There is great interest in understanding whether the microbiome can be manipulated to modify weight in humans, as has been clearly shown in mice. In addition, patients receiving donor stool more frequently reported chills. In my own practice, I have rarely observed transient fever after healthy donor FMT delivered orally in encapsulated form, and I hypothesize that this may be due to an immune reaction to a new microbial ecosystem. Patients considering FMT should be informed of both of these possible adverse events.
Elizabeth L. Hohmann, MD, is at Massachusetts General Hospital, Boston. She reported grant support and personal fees from Seres Therapeutics outside the submitted work. These comments are from an editorial accompanying the article (Ann Intern Med. 2016 Aug 22. doi: 10.7326/M16-1784).
AGA Resource
The AGA Center for Gut Microbiome Research and Education was created to serve as a virtual ‘home’ for AGA activities related to the gut microbiome with a mission to advance research and education on the gut microbiome with the goal of improving human health. Learn more at www.gastro.org/microbiome.
Kelly and her colleagues demonstrate that rigorous controlled trials are valuable even when we think we know the answer. Their results prompt us to ask again whether microbial manipulation has any as-yet unappreciated health benefits or risks and whether there are preferred microbiomes for specific human populations or locales.
Careful review of reported adverse events in the current trial is instructive. One participant reported a 9.1-kg weight gain (donor details were not provided), a problem previously described in a separate case report. There is great interest in understanding whether the microbiome can be manipulated to modify weight in humans, as has been clearly shown in mice. In addition, patients receiving donor stool more frequently reported chills. In my own practice, I have rarely observed transient fever after healthy donor FMT delivered orally in encapsulated form, and I hypothesize that this may be due to an immune reaction to a new microbial ecosystem. Patients considering FMT should be informed of both of these possible adverse events.
Elizabeth L. Hohmann, MD, is at Massachusetts General Hospital, Boston. She reported grant support and personal fees from Seres Therapeutics outside the submitted work. These comments are from an editorial accompanying the article (Ann Intern Med. 2016 Aug 22. doi: 10.7326/M16-1784).
AGA Resource
The AGA Center for Gut Microbiome Research and Education was created to serve as a virtual ‘home’ for AGA activities related to the gut microbiome with a mission to advance research and education on the gut microbiome with the goal of improving human health. Learn more at www.gastro.org/microbiome.
For patients with recurrent Clostridium difficile infection (CDI), donor stool administered via colonoscopy seemed safe and achieved clinical cure significantly more often than autologous fecal microbiota transplantation (FMT), based on a small trial reported online in Annals of Internal Medicine.
In all, 20 of 22 patients (91%) achieved cure with donor FMT, compared with 63% of patients who received their own markedly dysbiotic stool (P = .04), reported Colleen Kelly, MD, of The Miriam Hospital, Providence, R.I., together with her associates. “Differences in efficacy between sites suggest that some patients with lower risk for CDI recurrence may not benefit from FMT. Further research may help determine the best candidates,” the researchers wrote.
FMT corrects the dysbiosis associated with CDI and is recommended in the event of failed antibiotic therapy leading to a third episode of infection. But this advice is based mainly on case series and open-label trials, the researchers noted. Their dual-center, randomized, controlled, double-blinded study included 46 patients with at least three recurrences of CDI who had completed a course of vancomycin during their most recent episode of infection. Patients older than age 75 years or who were immunocompromised were excluded (Ann Intern Med. 2016 Aug 22. doi: 10.7326/M16-0271).
The overall clinical cure rates reflected the literature, the researchers reported, and all nine patients who developed CDI after autologous FMT were subsequently cured by donor FMT. Indeed, donor FMT “restored normal microbial community structure, with reductions in Proteobacteria and Verrucomicrobia and increases in Bacteroidetes and Firmicutes. In contrast, microbial diversity did not improve after autologous FMT.”
Notably, however, 90% of autologous FMT patients at the center in New York achieved clinical cure, compared with 43% of patients at the center in Rhode Island. Further analyses revealed differences between patients and fecal microbiota at the two sites, the investigators said. Patients in New York typically had CDI for longer, with more recurrences and up to 148 weeks of vancomycin and other antibiotics. Thus, they might have been cured before enrollment. But “autologous FMT patients at the New York site [also] had greater abundances of Clostridia, raising the possibility of emergence of microbial community assemblages inhibitory to C. difficile via competitive niche exclusion, or possibly by emergence of nontoxigenic organisms,” the researchers wrote.
There were no serious adverse effects associated with either type of FMT, they noted.
Dr. Kelly disclosed ties to Seres Health outside the submitted work. Two coauthors had patents or patents pending for “compositions and methods for transplantation of colon microbiota.” A third coauthor disclosed ties to OpenBiome and personal fees from CIPAC/Crestovo outside the submitted work. The remaining coauthors had no conflicts of interest.
For patients with recurrent Clostridium difficile infection (CDI), donor stool administered via colonoscopy seemed safe and achieved clinical cure significantly more often than autologous fecal microbiota transplantation (FMT), based on a small trial reported online in Annals of Internal Medicine.
In all, 20 of 22 patients (91%) achieved cure with donor FMT, compared with 63% of patients who received their own markedly dysbiotic stool (P = .04), reported Colleen Kelly, MD, of The Miriam Hospital, Providence, R.I., together with her associates. “Differences in efficacy between sites suggest that some patients with lower risk for CDI recurrence may not benefit from FMT. Further research may help determine the best candidates,” the researchers wrote.
FMT corrects the dysbiosis associated with CDI and is recommended in the event of failed antibiotic therapy leading to a third episode of infection. But this advice is based mainly on case series and open-label trials, the researchers noted. Their dual-center, randomized, controlled, double-blinded study included 46 patients with at least three recurrences of CDI who had completed a course of vancomycin during their most recent episode of infection. Patients older than age 75 years or who were immunocompromised were excluded (Ann Intern Med. 2016 Aug 22. doi: 10.7326/M16-0271).
The overall clinical cure rates reflected the literature, the researchers reported, and all nine patients who developed CDI after autologous FMT were subsequently cured by donor FMT. Indeed, donor FMT “restored normal microbial community structure, with reductions in Proteobacteria and Verrucomicrobia and increases in Bacteroidetes and Firmicutes. In contrast, microbial diversity did not improve after autologous FMT.”
Notably, however, 90% of autologous FMT patients at the center in New York achieved clinical cure, compared with 43% of patients at the center in Rhode Island. Further analyses revealed differences between patients and fecal microbiota at the two sites, the investigators said. Patients in New York typically had CDI for longer, with more recurrences and up to 148 weeks of vancomycin and other antibiotics. Thus, they might have been cured before enrollment. But “autologous FMT patients at the New York site [also] had greater abundances of Clostridia, raising the possibility of emergence of microbial community assemblages inhibitory to C. difficile via competitive niche exclusion, or possibly by emergence of nontoxigenic organisms,” the researchers wrote.
There were no serious adverse effects associated with either type of FMT, they noted.
Dr. Kelly disclosed ties to Seres Health outside the submitted work. Two coauthors had patents or patents pending for “compositions and methods for transplantation of colon microbiota.” A third coauthor disclosed ties to OpenBiome and personal fees from CIPAC/Crestovo outside the submitted work. The remaining coauthors had no conflicts of interest.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Donor stool administered via colonoscopy seemed safe and achieved clinical cure significantly more often than autologous fecal microbiota transplantation (FMT) in patients with recurrent Clostridium difficile infection (CDI).
Major finding: In all, 91% of donor FMT patients and 63% of autologous FMT patients achieved clinical cure stool (P = .04).
Data source: A prospective, double-blind, randomized trial of 46 patients with at least three episodes of CDI, who had completed a full course of vancomycin during the most recent episode.
Disclosures: Dr. Kelly disclosed ties to Seres Health outside the submitted work. Two coauthors had patents or patents pending for “compositions and methods for transplantation of colon microbiota.” A third coauthor disclosed ties to OpenBiome and personal fees from CIPAC/Crestovo outside the submitted work. The remaining coauthors had no conflicts of interest.