User login
Tips Toward Better Clinical Summaries
“I recently discharged a complex patient from the hospital, and I was shocked to see the poor quality of his clinical summary,” says Erin Sarzynski, MD, MS, of Michigan State University’s Department of Family Medicine. This observation drove the research underlying the paper she co-wrote titled “Opportunities to Improve Clinical Summaries for Patients at Hospital Discharge,” published in BMJ Quality & Safety.
The problem, the paper lays out, is that, “presently, it is unclear whether clinical summaries include relevant content or whether healthcare organizations configure their EHRs to generate content in a way that promotes patient self-management after hospital discharge.”
As a first step toward improving these documents, Dr. Sarzynski worked with a team to evaluate 100 clinical summaries generated at two Michigan hospitals based on content, organization, and understandability. They became aware of systemic problems.
“Clinical summaries are produced from templates, but physicians’ workflows do not prompt them to preview the document before the nurse prints it to review with the patient,” Dr. Sarzynski says. “Clinical summaries are lengthy yet omit key discharge information. They are poorly organized, written at the 8th- to 12th-grade reading level, and score poorly on assessments of understandability and actionability.
“Medication lists illustrate a key safety issue resulting from poor-quality clinical summaries; for example, we routinely send patients home without parameters for sliding-scale insulin.”
The study highlights opportunities to improve clinical summaries for guiding patients’ post-discharge care.
“We developed an audit tool based on the Meaningful Use view-download-transmit objective and the SHM Discharge Checklist (content); the Institute of Medicine recommendations for distributing easy-to-understand print material (organization); and five readability formulas and the Patient Education Materials Assessment Tool,” the authors write.
“If possible, hospitalists should preview their patients’ clinical summaries before printing—it’s an opportunity to ensure key discharge information is correct and appropriately emphasized,” Dr. Sarzynski says.
Reference
- Sarzynski E, Hashmi H, Subramanian J, et al. Opportunities to improve clinical summaries for patients at hospital discharge. BMJ Qual Saf. doi:10.1136/bmjqs-2015-005201.
“I recently discharged a complex patient from the hospital, and I was shocked to see the poor quality of his clinical summary,” says Erin Sarzynski, MD, MS, of Michigan State University’s Department of Family Medicine. This observation drove the research underlying the paper she co-wrote titled “Opportunities to Improve Clinical Summaries for Patients at Hospital Discharge,” published in BMJ Quality & Safety.
The problem, the paper lays out, is that, “presently, it is unclear whether clinical summaries include relevant content or whether healthcare organizations configure their EHRs to generate content in a way that promotes patient self-management after hospital discharge.”
As a first step toward improving these documents, Dr. Sarzynski worked with a team to evaluate 100 clinical summaries generated at two Michigan hospitals based on content, organization, and understandability. They became aware of systemic problems.
“Clinical summaries are produced from templates, but physicians’ workflows do not prompt them to preview the document before the nurse prints it to review with the patient,” Dr. Sarzynski says. “Clinical summaries are lengthy yet omit key discharge information. They are poorly organized, written at the 8th- to 12th-grade reading level, and score poorly on assessments of understandability and actionability.
“Medication lists illustrate a key safety issue resulting from poor-quality clinical summaries; for example, we routinely send patients home without parameters for sliding-scale insulin.”
The study highlights opportunities to improve clinical summaries for guiding patients’ post-discharge care.
“We developed an audit tool based on the Meaningful Use view-download-transmit objective and the SHM Discharge Checklist (content); the Institute of Medicine recommendations for distributing easy-to-understand print material (organization); and five readability formulas and the Patient Education Materials Assessment Tool,” the authors write.
“If possible, hospitalists should preview their patients’ clinical summaries before printing—it’s an opportunity to ensure key discharge information is correct and appropriately emphasized,” Dr. Sarzynski says.
Reference
- Sarzynski E, Hashmi H, Subramanian J, et al. Opportunities to improve clinical summaries for patients at hospital discharge. BMJ Qual Saf. doi:10.1136/bmjqs-2015-005201.
“I recently discharged a complex patient from the hospital, and I was shocked to see the poor quality of his clinical summary,” says Erin Sarzynski, MD, MS, of Michigan State University’s Department of Family Medicine. This observation drove the research underlying the paper she co-wrote titled “Opportunities to Improve Clinical Summaries for Patients at Hospital Discharge,” published in BMJ Quality & Safety.
The problem, the paper lays out, is that, “presently, it is unclear whether clinical summaries include relevant content or whether healthcare organizations configure their EHRs to generate content in a way that promotes patient self-management after hospital discharge.”
As a first step toward improving these documents, Dr. Sarzynski worked with a team to evaluate 100 clinical summaries generated at two Michigan hospitals based on content, organization, and understandability. They became aware of systemic problems.
“Clinical summaries are produced from templates, but physicians’ workflows do not prompt them to preview the document before the nurse prints it to review with the patient,” Dr. Sarzynski says. “Clinical summaries are lengthy yet omit key discharge information. They are poorly organized, written at the 8th- to 12th-grade reading level, and score poorly on assessments of understandability and actionability.
“Medication lists illustrate a key safety issue resulting from poor-quality clinical summaries; for example, we routinely send patients home without parameters for sliding-scale insulin.”
The study highlights opportunities to improve clinical summaries for guiding patients’ post-discharge care.
“We developed an audit tool based on the Meaningful Use view-download-transmit objective and the SHM Discharge Checklist (content); the Institute of Medicine recommendations for distributing easy-to-understand print material (organization); and five readability formulas and the Patient Education Materials Assessment Tool,” the authors write.
“If possible, hospitalists should preview their patients’ clinical summaries before printing—it’s an opportunity to ensure key discharge information is correct and appropriately emphasized,” Dr. Sarzynski says.
Reference
- Sarzynski E, Hashmi H, Subramanian J, et al. Opportunities to improve clinical summaries for patients at hospital discharge. BMJ Qual Saf. doi:10.1136/bmjqs-2015-005201.
CHMP rejects ofatumumab as maintenance

Photo courtesy of GSK
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended against expanding the approved indication for ofatumumab (Arzerra).
Novartis, which is developing ofatumumab in cooperation with Genmab, had submitted an application requesting that ofatumumab be authorized as maintenance therapy for patients with relapsed chronic lymphocytic leukemia (CLL).
But the CHMP has advised the European Commission (EC) not to grant this authorization.
The CHMP noted that, in the phase 3 PROLONG trial, ofatumumab maintenance improved progression-free survival (PFS) in CLL patients.
However, the committee said the importance of this improvement is not clear because the PFS results were not supported by other measures, such as overall survival or a significant improvement in patients’ quality of life.
The CHMP also said the use of ofatumumab for maintenance treatment should be seen in the context of its side effects. Common side effects of ofatumumab in the PROLONG trial were infusion reactions, neutropenia, and upper respiratory tract infections.
In the end, the CHMP decided that the PROLONG data were not sufficient to conclude that maintenance treatment with ofatumumab is of more benefit than no treatment. So the committee recommended against expanding the drug’s marketing authorization.
This decision does not have any impact on ongoing clinical trials with ofatumumab.
About ofatumumab
Ofatumumab has been authorized for use in the European Union since April 2010.
The EC first granted ofatumumab conditional approval to treat CLL patients who are refractory to fludarabine and alemtuzumab.
Then, in 2014, the EC granted ofatumumab conditional approval for use in combination with chlorambucil or bendamustine in CLL patients who have not received prior therapy and are not eligible for fludarabine-based therapy.
Ofatumumab received conditional approval because the drug’s benefits appear to outweigh the risks it poses in the aforementioned indications. Ofatumumab will not receive full approval until the drug’s developers submit results of additional research to the EC.
About the PROLONG trial
The PROLONG trial was designed to compare ofatumumab maintenance to no further treatment in patients with a complete or partial response after second- or third-line treatment for CLL. Interim results of the study were presented at ASH 2014.
These results—in 474 patients—suggested that ofatumumab can significantly improve PFS. The median PFS was about 29 months in patients who received ofatumumab and about 15 months for patients who did not receive maintenance therapy (P<0.0001).
There was no significant difference in the median overall survival, which was not reached in either treatment arm.
The researchers said there were no unexpected safety findings. The most common adverse events (≥10%) were infusion reactions, neutropenia, and upper respiratory tract infection. ![]()

Photo courtesy of GSK
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended against expanding the approved indication for ofatumumab (Arzerra).
Novartis, which is developing ofatumumab in cooperation with Genmab, had submitted an application requesting that ofatumumab be authorized as maintenance therapy for patients with relapsed chronic lymphocytic leukemia (CLL).
But the CHMP has advised the European Commission (EC) not to grant this authorization.
The CHMP noted that, in the phase 3 PROLONG trial, ofatumumab maintenance improved progression-free survival (PFS) in CLL patients.
However, the committee said the importance of this improvement is not clear because the PFS results were not supported by other measures, such as overall survival or a significant improvement in patients’ quality of life.
The CHMP also said the use of ofatumumab for maintenance treatment should be seen in the context of its side effects. Common side effects of ofatumumab in the PROLONG trial were infusion reactions, neutropenia, and upper respiratory tract infections.
In the end, the CHMP decided that the PROLONG data were not sufficient to conclude that maintenance treatment with ofatumumab is of more benefit than no treatment. So the committee recommended against expanding the drug’s marketing authorization.
This decision does not have any impact on ongoing clinical trials with ofatumumab.
About ofatumumab
Ofatumumab has been authorized for use in the European Union since April 2010.
The EC first granted ofatumumab conditional approval to treat CLL patients who are refractory to fludarabine and alemtuzumab.
Then, in 2014, the EC granted ofatumumab conditional approval for use in combination with chlorambucil or bendamustine in CLL patients who have not received prior therapy and are not eligible for fludarabine-based therapy.
Ofatumumab received conditional approval because the drug’s benefits appear to outweigh the risks it poses in the aforementioned indications. Ofatumumab will not receive full approval until the drug’s developers submit results of additional research to the EC.
About the PROLONG trial
The PROLONG trial was designed to compare ofatumumab maintenance to no further treatment in patients with a complete or partial response after second- or third-line treatment for CLL. Interim results of the study were presented at ASH 2014.
These results—in 474 patients—suggested that ofatumumab can significantly improve PFS. The median PFS was about 29 months in patients who received ofatumumab and about 15 months for patients who did not receive maintenance therapy (P<0.0001).
There was no significant difference in the median overall survival, which was not reached in either treatment arm.
The researchers said there were no unexpected safety findings. The most common adverse events (≥10%) were infusion reactions, neutropenia, and upper respiratory tract infection. ![]()

Photo courtesy of GSK
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended against expanding the approved indication for ofatumumab (Arzerra).
Novartis, which is developing ofatumumab in cooperation with Genmab, had submitted an application requesting that ofatumumab be authorized as maintenance therapy for patients with relapsed chronic lymphocytic leukemia (CLL).
But the CHMP has advised the European Commission (EC) not to grant this authorization.
The CHMP noted that, in the phase 3 PROLONG trial, ofatumumab maintenance improved progression-free survival (PFS) in CLL patients.
However, the committee said the importance of this improvement is not clear because the PFS results were not supported by other measures, such as overall survival or a significant improvement in patients’ quality of life.
The CHMP also said the use of ofatumumab for maintenance treatment should be seen in the context of its side effects. Common side effects of ofatumumab in the PROLONG trial were infusion reactions, neutropenia, and upper respiratory tract infections.
In the end, the CHMP decided that the PROLONG data were not sufficient to conclude that maintenance treatment with ofatumumab is of more benefit than no treatment. So the committee recommended against expanding the drug’s marketing authorization.
This decision does not have any impact on ongoing clinical trials with ofatumumab.
About ofatumumab
Ofatumumab has been authorized for use in the European Union since April 2010.
The EC first granted ofatumumab conditional approval to treat CLL patients who are refractory to fludarabine and alemtuzumab.
Then, in 2014, the EC granted ofatumumab conditional approval for use in combination with chlorambucil or bendamustine in CLL patients who have not received prior therapy and are not eligible for fludarabine-based therapy.
Ofatumumab received conditional approval because the drug’s benefits appear to outweigh the risks it poses in the aforementioned indications. Ofatumumab will not receive full approval until the drug’s developers submit results of additional research to the EC.
About the PROLONG trial
The PROLONG trial was designed to compare ofatumumab maintenance to no further treatment in patients with a complete or partial response after second- or third-line treatment for CLL. Interim results of the study were presented at ASH 2014.
These results—in 474 patients—suggested that ofatumumab can significantly improve PFS. The median PFS was about 29 months in patients who received ofatumumab and about 15 months for patients who did not receive maintenance therapy (P<0.0001).
There was no significant difference in the median overall survival, which was not reached in either treatment arm.
The researchers said there were no unexpected safety findings. The most common adverse events (≥10%) were infusion reactions, neutropenia, and upper respiratory tract infection. ![]()
Endoscopic, laparoscopic pseudocyst drainage comparable if necrotic debris minimal
SAN DIEGO – Endoscopic and laparoscopic drainage worked about equally well for pancreatic pseudocysts and walled off necrosis in a small randomized trial from India, the first to compare the two options.
Both are in common use, but until now it wasn’t clear if one was better than the other. The findings mean that “in general, one could do either; the choice of treatment depends [largely] on the expertise available. As an endoscopist, I prefer endoscopic drainage,” said gastroenterologist Pramod Garg, of the All India Institute of Medical Sciences, New Delhi.
Laparoscopic drainage was a technical success in 23 of the 30 patients (76.6%) randomized to it, six of whom (20%) had symptomatic pseudocysts larger than 6 cm for more than 6 weeks; the rest had walled off necrosis (WON) containing less than 30% necrotic debris. Five of the other patients were converted to open surgery, and two underwent percutaneous drainage. One of the 30 patients required endoscopic lavage and necrosectomy for secondary infection.
Endoscopic drainage, meanwhile, was technically successful in 22 of 30 patients (73.3%) with similar distributions of pseudocysts and WON. Most of the other patients needed subsequent endoscopic lavage and necrosectomy for secondary infection.
Clinical success – defined as resolution by week 4 – was 100% in the laparoscopic and 97% (29/30) in the endoscopic groups; one endoscopic patient had a splenic artery pseudoaneurysm that required further surgery. The differences in technical and clinical success rates were not statistically significant. There were no recurrences and no deaths in either group after an average follow-up of 22 months.
Although it seems okay to opt for either approach, “it’s very important for us to assess the amount of necrotic debris. If the amount is sizable, say 50% or more of the volume, one should hesitate before doing purely endoscopic drainage.” As seen in the study, “the chances of developing an infection are pretty high, especially if,” like the investigators, “you place only a plastic stent,” Dr. Garg said at the annual Digestive Disease Week.
Laparoscopic drainage would probably be better when there’s a lot of necrotic tissue, and certainly so if patients need their gallbladder removed, because it can be taken out at the same time. If endoscopy is still the choice, “you should be prepared to do repeat procedures for endoscopic lavage and necrosectomy. The chance of infection may be less if you use a metal stent with a wide diameter,” Dr. Garg said. Before tackling WON with endoscopy, he suggested getting input from a radiologist and surgeon.
Laparoscopic cystogastrostomy was done in the usual manner, with an endostapler to create a wide cystogastrostomy, necrotic debris suction, and concomitant cholecystectomies as needed.
Endoscopic drainage was performed under endosonographic guidance in the 13 patients without bulging cysts, and directly in the 17 patients whose cysts bulged. A balloon was used to dilate the cystogastrostomy tract to 12-15 mm, and a 10 F double pigtail plastic stent placed to keep it open.
Patients in both groups received perioperative antibiotics. The demographic, clinical, and laboratory parameters and etiology of acute pancreatitis were comparable between the two groups. Patients tended to be in their mid-30s, and about 75% in both groups were women. Over a third in each group had gallstone disease. The median hospital stay in both groups was about a week. Fever was more common following endoscopic drainage, probably because of the higher incidence of secondary infection.
Patients with complicated pseudocysts, coagulopathies, or organ failure were excluded from the investigation, as well as those otherwise unfit for surgery.
There was no industry funding for the work, and Dr. Garg had no disclosures.
SAN DIEGO – Endoscopic and laparoscopic drainage worked about equally well for pancreatic pseudocysts and walled off necrosis in a small randomized trial from India, the first to compare the two options.
Both are in common use, but until now it wasn’t clear if one was better than the other. The findings mean that “in general, one could do either; the choice of treatment depends [largely] on the expertise available. As an endoscopist, I prefer endoscopic drainage,” said gastroenterologist Pramod Garg, of the All India Institute of Medical Sciences, New Delhi.
Laparoscopic drainage was a technical success in 23 of the 30 patients (76.6%) randomized to it, six of whom (20%) had symptomatic pseudocysts larger than 6 cm for more than 6 weeks; the rest had walled off necrosis (WON) containing less than 30% necrotic debris. Five of the other patients were converted to open surgery, and two underwent percutaneous drainage. One of the 30 patients required endoscopic lavage and necrosectomy for secondary infection.
Endoscopic drainage, meanwhile, was technically successful in 22 of 30 patients (73.3%) with similar distributions of pseudocysts and WON. Most of the other patients needed subsequent endoscopic lavage and necrosectomy for secondary infection.
Clinical success – defined as resolution by week 4 – was 100% in the laparoscopic and 97% (29/30) in the endoscopic groups; one endoscopic patient had a splenic artery pseudoaneurysm that required further surgery. The differences in technical and clinical success rates were not statistically significant. There were no recurrences and no deaths in either group after an average follow-up of 22 months.
Although it seems okay to opt for either approach, “it’s very important for us to assess the amount of necrotic debris. If the amount is sizable, say 50% or more of the volume, one should hesitate before doing purely endoscopic drainage.” As seen in the study, “the chances of developing an infection are pretty high, especially if,” like the investigators, “you place only a plastic stent,” Dr. Garg said at the annual Digestive Disease Week.
Laparoscopic drainage would probably be better when there’s a lot of necrotic tissue, and certainly so if patients need their gallbladder removed, because it can be taken out at the same time. If endoscopy is still the choice, “you should be prepared to do repeat procedures for endoscopic lavage and necrosectomy. The chance of infection may be less if you use a metal stent with a wide diameter,” Dr. Garg said. Before tackling WON with endoscopy, he suggested getting input from a radiologist and surgeon.
Laparoscopic cystogastrostomy was done in the usual manner, with an endostapler to create a wide cystogastrostomy, necrotic debris suction, and concomitant cholecystectomies as needed.
Endoscopic drainage was performed under endosonographic guidance in the 13 patients without bulging cysts, and directly in the 17 patients whose cysts bulged. A balloon was used to dilate the cystogastrostomy tract to 12-15 mm, and a 10 F double pigtail plastic stent placed to keep it open.
Patients in both groups received perioperative antibiotics. The demographic, clinical, and laboratory parameters and etiology of acute pancreatitis were comparable between the two groups. Patients tended to be in their mid-30s, and about 75% in both groups were women. Over a third in each group had gallstone disease. The median hospital stay in both groups was about a week. Fever was more common following endoscopic drainage, probably because of the higher incidence of secondary infection.
Patients with complicated pseudocysts, coagulopathies, or organ failure were excluded from the investigation, as well as those otherwise unfit for surgery.
There was no industry funding for the work, and Dr. Garg had no disclosures.
SAN DIEGO – Endoscopic and laparoscopic drainage worked about equally well for pancreatic pseudocysts and walled off necrosis in a small randomized trial from India, the first to compare the two options.
Both are in common use, but until now it wasn’t clear if one was better than the other. The findings mean that “in general, one could do either; the choice of treatment depends [largely] on the expertise available. As an endoscopist, I prefer endoscopic drainage,” said gastroenterologist Pramod Garg, of the All India Institute of Medical Sciences, New Delhi.
Laparoscopic drainage was a technical success in 23 of the 30 patients (76.6%) randomized to it, six of whom (20%) had symptomatic pseudocysts larger than 6 cm for more than 6 weeks; the rest had walled off necrosis (WON) containing less than 30% necrotic debris. Five of the other patients were converted to open surgery, and two underwent percutaneous drainage. One of the 30 patients required endoscopic lavage and necrosectomy for secondary infection.
Endoscopic drainage, meanwhile, was technically successful in 22 of 30 patients (73.3%) with similar distributions of pseudocysts and WON. Most of the other patients needed subsequent endoscopic lavage and necrosectomy for secondary infection.
Clinical success – defined as resolution by week 4 – was 100% in the laparoscopic and 97% (29/30) in the endoscopic groups; one endoscopic patient had a splenic artery pseudoaneurysm that required further surgery. The differences in technical and clinical success rates were not statistically significant. There were no recurrences and no deaths in either group after an average follow-up of 22 months.
Although it seems okay to opt for either approach, “it’s very important for us to assess the amount of necrotic debris. If the amount is sizable, say 50% or more of the volume, one should hesitate before doing purely endoscopic drainage.” As seen in the study, “the chances of developing an infection are pretty high, especially if,” like the investigators, “you place only a plastic stent,” Dr. Garg said at the annual Digestive Disease Week.
Laparoscopic drainage would probably be better when there’s a lot of necrotic tissue, and certainly so if patients need their gallbladder removed, because it can be taken out at the same time. If endoscopy is still the choice, “you should be prepared to do repeat procedures for endoscopic lavage and necrosectomy. The chance of infection may be less if you use a metal stent with a wide diameter,” Dr. Garg said. Before tackling WON with endoscopy, he suggested getting input from a radiologist and surgeon.
Laparoscopic cystogastrostomy was done in the usual manner, with an endostapler to create a wide cystogastrostomy, necrotic debris suction, and concomitant cholecystectomies as needed.
Endoscopic drainage was performed under endosonographic guidance in the 13 patients without bulging cysts, and directly in the 17 patients whose cysts bulged. A balloon was used to dilate the cystogastrostomy tract to 12-15 mm, and a 10 F double pigtail plastic stent placed to keep it open.
Patients in both groups received perioperative antibiotics. The demographic, clinical, and laboratory parameters and etiology of acute pancreatitis were comparable between the two groups. Patients tended to be in their mid-30s, and about 75% in both groups were women. Over a third in each group had gallstone disease. The median hospital stay in both groups was about a week. Fever was more common following endoscopic drainage, probably because of the higher incidence of secondary infection.
Patients with complicated pseudocysts, coagulopathies, or organ failure were excluded from the investigation, as well as those otherwise unfit for surgery.
There was no industry funding for the work, and Dr. Garg had no disclosures.
AT DDW 2016
Key clinical point: Choosing between endoscopic and laparoscopic drainage for pancreatic pseudocysts comes down to local expertise and the amount of necrotic tissue that needs to be removed.
Major finding: Clinical success – defined as resolution by week 4 – was 100% in the laparoscopic and 97% (29/30) in the endoscopic groups.
Data source: Randomized trial with 60 patients.
Disclosures: There was no industry funding for the work, and the presenter had no disclosures.
Obesity may attenuate anti-TNF response in psoriatic arthritis
LONDON – Patients with psoriatic arthritis appear less likely to achieve a good response to their first anti–tumor necrosis factor (anti-TNF) therapy if they are obese, according to data taken from two Nordic registries.
In a large observational cohort study, obese individuals with psoriatic arthritis (PsA) were significantly less likely than their nonobese counterparts to achieve a European League Against Rheumatism (EULAR) good or moderate response at 6 months (55% vs. 65%, P = .02). The overall odds ratio for achieving a good or moderate response was 0.47 when comparing obese with nonobese individuals.
The findings are potentially important because, with the exception of infliximab, anti-TNF therapy is not currently adjusted according to body weight, said presenting study author Pil Højgaard in an interview at the European Congress of Rheumatology.
Ms. Højgaard, who is an M.D. Ph.D. student at the department of rheumatology, Copenhagen University Hospital Gentofte, Rigshospitalet and the Parker Institute in Copenhagen, noted that obesity was a frequent comorbid condition in patients with PsA and that it is a known proinflammatory condition. As such, obesity could potentially affect immunologic processes, the pharmacokinetics of treatments, and ultimately patient outcomes.
Since TNF-alpha inhibitor (TNFi) treatment fails in around half of all patients with PsA treated in routine care, Ms. Højgaard noted that the aim of the cohort study was to investigate whether obesity could be having any influence on this.
Data on baseline characteristics, EULAR response rates, and drug adherence were obtained for 1,943 patients with PsA prescribed their anti-TNF therapy from two nationwide registries of disease-modifying therapies being used to treat rheumatic conditions in Denmark and Iceland, DANBIO (Rheumatology. 2011;50:69–77) and ICEBIO, respectively.
At baseline, body mass index (BMI) data were available for 1,271 patients and 408 (32%) of these had a BMI of 30 kg/m2 or more and were classed as being obese. The majority (39%) had received a first prescription for adalimumab, with around a quarter each prescribed etanercept (26%) or infliximab (24%), and the remainder prescribed golimumab (7%) and certolizumab (4%).
Compared to the 863 (68%) nonobese individuals, the obese patients were older (47 vs. 49 years, P = .01), less likely to smoke (30% vs. 23%, P = .01), and had higher disease activity measured on the Disease Activity Score 28 (DAS28) (4.4 vs. 4.6, P = .01). Health Assessment Questionnaire scores were also higher in obese than in nonobese individuals (1.1 vs. 0.9, P less than .01), and there were higher tender joint counts (6 vs. 5, P = .01), and higher pain levels assessed on a visual analog scale (VAS). Obese patients also had higher scores on a VAS patient global scale. The median follow-up time was 1.5 years.
Patients who were obese were found to adhere to TNFi treatment for shorter periods of time than nonobese patients, with median durations of 1.76 and 3.08 years, respectively (P less than .001). This discrepancy was most pronounced among men, a finding that may account for the fact that they were less likely to achieve a good EULAR response than their nonobese counterparts (OR = 0.5).
Being obese versus not being obese independently predicted TNFi withdrawal overall (hazard ratio, 1.6), especially in men (HR, 1.8; HR, 1.5 in women). TNFi withdrawal was more likely in obese than in nonobese patients even when individual treatments were considered; adalimumab: HR, 1.6; etanercept: HR, 2.0; infliximab: HR, 1.6.
An association between obesity and reduced response to anti-TNF therapy has also been observed in patients with rheumatoid arthritis, Ms. Højgaard acknowledged. There have also been a few studies of PsA and psoriasis “but to my knowledge, I think in the field of psoriatic arthritis, we are one of the few that have been looking at long-time drug survival,” she said. “We also include quite a lot of patients.”
“Of course this is not a randomized clinical study, so there could be residual confounding factors,” Ms. Højgaard cautioned. “It is always a bit difficult to say something about causality when it is a database study,” she added. “I think what we can see here is that there is an association, but in order to recommend weight loss we need some prospective studies.”
She noted that there was one published clinical study (Ann Rheum Dis. 2014;73:1157–62) that had looked at the benefit of a weight reduction program started at the same time as TNFi initiation in patients with PsA. This found there was a benefit of weight loss on response to TNFis, regardless of the type of diet.
DANBIO is supported by unrestricted grants from Abbott, Pfizer, MSD, Bristol-Myers Squibb, Roche, and UCB-Nordic. The sponsors have had no influence on data collection, analysis, or publication. ICEBIO is part of the electronic medical record system held by the University of Reykjavik and receives no industrial funding. Ms. Højgaard has received speaking fees from Celgene and UCB not related to this work.
LONDON – Patients with psoriatic arthritis appear less likely to achieve a good response to their first anti–tumor necrosis factor (anti-TNF) therapy if they are obese, according to data taken from two Nordic registries.
In a large observational cohort study, obese individuals with psoriatic arthritis (PsA) were significantly less likely than their nonobese counterparts to achieve a European League Against Rheumatism (EULAR) good or moderate response at 6 months (55% vs. 65%, P = .02). The overall odds ratio for achieving a good or moderate response was 0.47 when comparing obese with nonobese individuals.
The findings are potentially important because, with the exception of infliximab, anti-TNF therapy is not currently adjusted according to body weight, said presenting study author Pil Højgaard in an interview at the European Congress of Rheumatology.
Ms. Højgaard, who is an M.D. Ph.D. student at the department of rheumatology, Copenhagen University Hospital Gentofte, Rigshospitalet and the Parker Institute in Copenhagen, noted that obesity was a frequent comorbid condition in patients with PsA and that it is a known proinflammatory condition. As such, obesity could potentially affect immunologic processes, the pharmacokinetics of treatments, and ultimately patient outcomes.
Since TNF-alpha inhibitor (TNFi) treatment fails in around half of all patients with PsA treated in routine care, Ms. Højgaard noted that the aim of the cohort study was to investigate whether obesity could be having any influence on this.
Data on baseline characteristics, EULAR response rates, and drug adherence were obtained for 1,943 patients with PsA prescribed their anti-TNF therapy from two nationwide registries of disease-modifying therapies being used to treat rheumatic conditions in Denmark and Iceland, DANBIO (Rheumatology. 2011;50:69–77) and ICEBIO, respectively.
At baseline, body mass index (BMI) data were available for 1,271 patients and 408 (32%) of these had a BMI of 30 kg/m2 or more and were classed as being obese. The majority (39%) had received a first prescription for adalimumab, with around a quarter each prescribed etanercept (26%) or infliximab (24%), and the remainder prescribed golimumab (7%) and certolizumab (4%).
Compared to the 863 (68%) nonobese individuals, the obese patients were older (47 vs. 49 years, P = .01), less likely to smoke (30% vs. 23%, P = .01), and had higher disease activity measured on the Disease Activity Score 28 (DAS28) (4.4 vs. 4.6, P = .01). Health Assessment Questionnaire scores were also higher in obese than in nonobese individuals (1.1 vs. 0.9, P less than .01), and there were higher tender joint counts (6 vs. 5, P = .01), and higher pain levels assessed on a visual analog scale (VAS). Obese patients also had higher scores on a VAS patient global scale. The median follow-up time was 1.5 years.
Patients who were obese were found to adhere to TNFi treatment for shorter periods of time than nonobese patients, with median durations of 1.76 and 3.08 years, respectively (P less than .001). This discrepancy was most pronounced among men, a finding that may account for the fact that they were less likely to achieve a good EULAR response than their nonobese counterparts (OR = 0.5).
Being obese versus not being obese independently predicted TNFi withdrawal overall (hazard ratio, 1.6), especially in men (HR, 1.8; HR, 1.5 in women). TNFi withdrawal was more likely in obese than in nonobese patients even when individual treatments were considered; adalimumab: HR, 1.6; etanercept: HR, 2.0; infliximab: HR, 1.6.
An association between obesity and reduced response to anti-TNF therapy has also been observed in patients with rheumatoid arthritis, Ms. Højgaard acknowledged. There have also been a few studies of PsA and psoriasis “but to my knowledge, I think in the field of psoriatic arthritis, we are one of the few that have been looking at long-time drug survival,” she said. “We also include quite a lot of patients.”
“Of course this is not a randomized clinical study, so there could be residual confounding factors,” Ms. Højgaard cautioned. “It is always a bit difficult to say something about causality when it is a database study,” she added. “I think what we can see here is that there is an association, but in order to recommend weight loss we need some prospective studies.”
She noted that there was one published clinical study (Ann Rheum Dis. 2014;73:1157–62) that had looked at the benefit of a weight reduction program started at the same time as TNFi initiation in patients with PsA. This found there was a benefit of weight loss on response to TNFis, regardless of the type of diet.
DANBIO is supported by unrestricted grants from Abbott, Pfizer, MSD, Bristol-Myers Squibb, Roche, and UCB-Nordic. The sponsors have had no influence on data collection, analysis, or publication. ICEBIO is part of the electronic medical record system held by the University of Reykjavik and receives no industrial funding. Ms. Højgaard has received speaking fees from Celgene and UCB not related to this work.
LONDON – Patients with psoriatic arthritis appear less likely to achieve a good response to their first anti–tumor necrosis factor (anti-TNF) therapy if they are obese, according to data taken from two Nordic registries.
In a large observational cohort study, obese individuals with psoriatic arthritis (PsA) were significantly less likely than their nonobese counterparts to achieve a European League Against Rheumatism (EULAR) good or moderate response at 6 months (55% vs. 65%, P = .02). The overall odds ratio for achieving a good or moderate response was 0.47 when comparing obese with nonobese individuals.
The findings are potentially important because, with the exception of infliximab, anti-TNF therapy is not currently adjusted according to body weight, said presenting study author Pil Højgaard in an interview at the European Congress of Rheumatology.
Ms. Højgaard, who is an M.D. Ph.D. student at the department of rheumatology, Copenhagen University Hospital Gentofte, Rigshospitalet and the Parker Institute in Copenhagen, noted that obesity was a frequent comorbid condition in patients with PsA and that it is a known proinflammatory condition. As such, obesity could potentially affect immunologic processes, the pharmacokinetics of treatments, and ultimately patient outcomes.
Since TNF-alpha inhibitor (TNFi) treatment fails in around half of all patients with PsA treated in routine care, Ms. Højgaard noted that the aim of the cohort study was to investigate whether obesity could be having any influence on this.
Data on baseline characteristics, EULAR response rates, and drug adherence were obtained for 1,943 patients with PsA prescribed their anti-TNF therapy from two nationwide registries of disease-modifying therapies being used to treat rheumatic conditions in Denmark and Iceland, DANBIO (Rheumatology. 2011;50:69–77) and ICEBIO, respectively.
At baseline, body mass index (BMI) data were available for 1,271 patients and 408 (32%) of these had a BMI of 30 kg/m2 or more and were classed as being obese. The majority (39%) had received a first prescription for adalimumab, with around a quarter each prescribed etanercept (26%) or infliximab (24%), and the remainder prescribed golimumab (7%) and certolizumab (4%).
Compared to the 863 (68%) nonobese individuals, the obese patients were older (47 vs. 49 years, P = .01), less likely to smoke (30% vs. 23%, P = .01), and had higher disease activity measured on the Disease Activity Score 28 (DAS28) (4.4 vs. 4.6, P = .01). Health Assessment Questionnaire scores were also higher in obese than in nonobese individuals (1.1 vs. 0.9, P less than .01), and there were higher tender joint counts (6 vs. 5, P = .01), and higher pain levels assessed on a visual analog scale (VAS). Obese patients also had higher scores on a VAS patient global scale. The median follow-up time was 1.5 years.
Patients who were obese were found to adhere to TNFi treatment for shorter periods of time than nonobese patients, with median durations of 1.76 and 3.08 years, respectively (P less than .001). This discrepancy was most pronounced among men, a finding that may account for the fact that they were less likely to achieve a good EULAR response than their nonobese counterparts (OR = 0.5).
Being obese versus not being obese independently predicted TNFi withdrawal overall (hazard ratio, 1.6), especially in men (HR, 1.8; HR, 1.5 in women). TNFi withdrawal was more likely in obese than in nonobese patients even when individual treatments were considered; adalimumab: HR, 1.6; etanercept: HR, 2.0; infliximab: HR, 1.6.
An association between obesity and reduced response to anti-TNF therapy has also been observed in patients with rheumatoid arthritis, Ms. Højgaard acknowledged. There have also been a few studies of PsA and psoriasis “but to my knowledge, I think in the field of psoriatic arthritis, we are one of the few that have been looking at long-time drug survival,” she said. “We also include quite a lot of patients.”
“Of course this is not a randomized clinical study, so there could be residual confounding factors,” Ms. Højgaard cautioned. “It is always a bit difficult to say something about causality when it is a database study,” she added. “I think what we can see here is that there is an association, but in order to recommend weight loss we need some prospective studies.”
She noted that there was one published clinical study (Ann Rheum Dis. 2014;73:1157–62) that had looked at the benefit of a weight reduction program started at the same time as TNFi initiation in patients with PsA. This found there was a benefit of weight loss on response to TNFis, regardless of the type of diet.
DANBIO is supported by unrestricted grants from Abbott, Pfizer, MSD, Bristol-Myers Squibb, Roche, and UCB-Nordic. The sponsors have had no influence on data collection, analysis, or publication. ICEBIO is part of the electronic medical record system held by the University of Reykjavik and receives no industrial funding. Ms. Højgaard has received speaking fees from Celgene and UCB not related to this work.
Key clinical point: Obesity may reduce response and adherence to tumor necrosis factor–inhibitor therapy in patients with psoriatic arthritis.
Major finding: The EULAR good or moderate response rate at 6 months was 55% in obese vs. 65% in nonobese patients (P = .02).
Data source: Observational cohort study based on two Nordic registries of 1,943 patients with PsA prescribed their first TNFi.
Disclosures: DANBIO is supported by unrestricted grants from Abbott, Pfizer, MSD, Bristol-Myers Squibb, Roche, and UCB-Nordic. The sponsors have had no influence on data collection, analysis, or publication. ICEBIO is part of the electronic medical record system held by the University of Reykjavik and receives no industrial funding. Ms. Højgaard has received speaking fees from Celgene and UCB not related to this work.
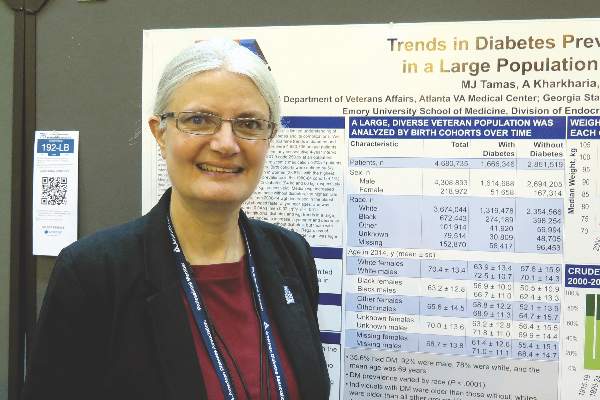
Body weight of U.S. veterans increased significantly from 2000 to 2014
NEW ORLEANS – United States veterans born since 1950 have gained weight faster than a comparable cohort of older veterans, results from a large analysis demonstrated. In fact, they’re starting out about 10 kg heavier than previous generations.
“There is a tremendous need for an intervention to prevent or reverse weight gain in this population to prevent the development of diabetes,” lead author Margery J. Tamas said in an interview at the annual scientific sessions of the American Diabetes Association.
In an effort to examine age-related trends in body weight and diabetes prevalence in the U.S. Veterans Health Administration system, Ms. Tamas and her associates used the VA Informatics and Computing Infrastructure to examine trends in diabetes among 4,680,735 patients born between 1915 and 1984 who had at least one outpatient visit per year within any consecutive 4-year interval between 2000 and 2014. More than one-third (36%) had diabetes, 92% were male, 78% were white, and their mean age was 69 years. The researchers defined the birth cohorts by 5-year intervals.
Ms. Tamas, who conducted the research as part of her master’s thesis at the Georgia State University School of Public Health, Atlanta, reported that diabetes was more prevalent among men, compared with women (38% vs. 24%, respectively). Diabetes prevalence was highest among patients born between 1940 and 1944 (44%) and lowest among those born between 1980 and 1984 (4%).
The assessment of weight also revealed that the median baseline weight was higher in men and women with diabetes (94 kg and 86 kg, respectively), compared with their counterparts who did not have diabetes (84 kg and 73 kg, respectively). The researchers observed that median weight increased significantly between 2000 and 2014 (P less than .001), with the greatest increase among patients without diabetes. The highest rate of weight increase occurred in women without diabetes (an increase of 0.39 kg per year). However, between 2000 and 2014 weight decreased in the oldest patient cohorts and increased in the youngest cohorts. “Weight changed faster at younger ages, and was highest in those with diabetes and in women,” Ms. Tamas said. “This kind of pattern where young people are gaining weight faster than older people has also been seen in the Global Burden of Disease Study.”
She acknowledged certain limitations of the analysis, including the fact that the data do not correct for survival bias. The study was based on work supported by the Department of Veterans Affairs. Ms. Tamas reported having no financial disclosures relevant to this research.
NEW ORLEANS – United States veterans born since 1950 have gained weight faster than a comparable cohort of older veterans, results from a large analysis demonstrated. In fact, they’re starting out about 10 kg heavier than previous generations.
“There is a tremendous need for an intervention to prevent or reverse weight gain in this population to prevent the development of diabetes,” lead author Margery J. Tamas said in an interview at the annual scientific sessions of the American Diabetes Association.
In an effort to examine age-related trends in body weight and diabetes prevalence in the U.S. Veterans Health Administration system, Ms. Tamas and her associates used the VA Informatics and Computing Infrastructure to examine trends in diabetes among 4,680,735 patients born between 1915 and 1984 who had at least one outpatient visit per year within any consecutive 4-year interval between 2000 and 2014. More than one-third (36%) had diabetes, 92% were male, 78% were white, and their mean age was 69 years. The researchers defined the birth cohorts by 5-year intervals.
Ms. Tamas, who conducted the research as part of her master’s thesis at the Georgia State University School of Public Health, Atlanta, reported that diabetes was more prevalent among men, compared with women (38% vs. 24%, respectively). Diabetes prevalence was highest among patients born between 1940 and 1944 (44%) and lowest among those born between 1980 and 1984 (4%).
The assessment of weight also revealed that the median baseline weight was higher in men and women with diabetes (94 kg and 86 kg, respectively), compared with their counterparts who did not have diabetes (84 kg and 73 kg, respectively). The researchers observed that median weight increased significantly between 2000 and 2014 (P less than .001), with the greatest increase among patients without diabetes. The highest rate of weight increase occurred in women without diabetes (an increase of 0.39 kg per year). However, between 2000 and 2014 weight decreased in the oldest patient cohorts and increased in the youngest cohorts. “Weight changed faster at younger ages, and was highest in those with diabetes and in women,” Ms. Tamas said. “This kind of pattern where young people are gaining weight faster than older people has also been seen in the Global Burden of Disease Study.”
She acknowledged certain limitations of the analysis, including the fact that the data do not correct for survival bias. The study was based on work supported by the Department of Veterans Affairs. Ms. Tamas reported having no financial disclosures relevant to this research.
NEW ORLEANS – United States veterans born since 1950 have gained weight faster than a comparable cohort of older veterans, results from a large analysis demonstrated. In fact, they’re starting out about 10 kg heavier than previous generations.
“There is a tremendous need for an intervention to prevent or reverse weight gain in this population to prevent the development of diabetes,” lead author Margery J. Tamas said in an interview at the annual scientific sessions of the American Diabetes Association.
In an effort to examine age-related trends in body weight and diabetes prevalence in the U.S. Veterans Health Administration system, Ms. Tamas and her associates used the VA Informatics and Computing Infrastructure to examine trends in diabetes among 4,680,735 patients born between 1915 and 1984 who had at least one outpatient visit per year within any consecutive 4-year interval between 2000 and 2014. More than one-third (36%) had diabetes, 92% were male, 78% were white, and their mean age was 69 years. The researchers defined the birth cohorts by 5-year intervals.
Ms. Tamas, who conducted the research as part of her master’s thesis at the Georgia State University School of Public Health, Atlanta, reported that diabetes was more prevalent among men, compared with women (38% vs. 24%, respectively). Diabetes prevalence was highest among patients born between 1940 and 1944 (44%) and lowest among those born between 1980 and 1984 (4%).
The assessment of weight also revealed that the median baseline weight was higher in men and women with diabetes (94 kg and 86 kg, respectively), compared with their counterparts who did not have diabetes (84 kg and 73 kg, respectively). The researchers observed that median weight increased significantly between 2000 and 2014 (P less than .001), with the greatest increase among patients without diabetes. The highest rate of weight increase occurred in women without diabetes (an increase of 0.39 kg per year). However, between 2000 and 2014 weight decreased in the oldest patient cohorts and increased in the youngest cohorts. “Weight changed faster at younger ages, and was highest in those with diabetes and in women,” Ms. Tamas said. “This kind of pattern where young people are gaining weight faster than older people has also been seen in the Global Burden of Disease Study.”
She acknowledged certain limitations of the analysis, including the fact that the data do not correct for survival bias. The study was based on work supported by the Department of Veterans Affairs. Ms. Tamas reported having no financial disclosures relevant to this research.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: The body weight of U.S. veterans increased significantly between 2000 and 2014.
Major finding: The median weight of U.S. veterans increased significantly between 2000 and 2014 (P less than .001), with the greatest increase among patients without diabetes.
Data source: An analysis of data from 4,680,735 VA patients born between 1915 and 1984 who had at least one outpatient visit per year within any consecutive 4-year interval between 2000 and 2014.
Disclosures: The study was based on work supported by the Department of Veterans Affairs. Ms. Tamas reported having no financial disclosures relevant to this research.
There’s still a place for HA fillers in fine facial lines
NEWPORT BEACH, CALIF. – Despite all the technical advances in aesthetic medicine, there’s still a place for treating fine facial lines with thin hyaluronic acid fillers, according to Dr. Mark G. Rubin, a dermatologist at the Lasky Skin Center in Beverly Hills, Calif.
“In the last couple of years, with all the volumizing products, a lot of people say they don’t treat wrinkles anymore. The idea is if you just put some volume in [a patient’s] nasojugal groove, you inflate the cheek, pull the skin tight, and the nasolabial fold will miraculously disappear. I don’t think that’s really true,” he said at the meeting held by Global Academy for Medical Education.
When patients don’t have good skin elasticity and tightness – and most older patients worried about fine lines don’t – volumizing will improve skin contour but not do much for atrophic lines.
That’s a good time to turn to fillers. “Basically, you are putting putty into a dent. Different wrinkles need different depths of material. We have fillers that are thin like sand, medium like pebbles, or thick like boulders.” Shallow lines need thinner material; deeper folds need volumizing boulders for lift. In some patients, “you need to layer them, boulders first then more superficial fillers to smooth out the surface,” Dr. Rubin said. “There are a lot of medium and deep fillers, but for really fine lines and superficial filling, there’s only Restylane Silk and Belotero.”
However, even superficial fillers need to be diluted sometimes with saline or lidocaine. “There isn’t a perfect filler; you need to create the one that works by changing its characteristics,” he said.
“With Restylane, if you dilute it too much, it turns into water, and you get no lift at all. You can dilute Juvederm down pretty well, but in some patients it still leaves ridges. You can dilute Belotero a lot without losing its ability to create lift, but I think in a lot of patients, Restylane Silk has a little better persistence than Belotero,” he said.
Staying in the dermis is important for superficial lines. “You need to come in at a very acute angle, and you have to see drug coming back at you through the pores. If you are not seeing that, you are definitely too deep. You also need to overcorrect, and see the area blanch a little bit,” he said.
Dr. Rubin warns patients that they might have what looks like a string of pearls under their skin after injection. “We massage [the beads] down with a Q-tip,” rolling it back and forth over the bulges, and they melt over time. A part of the reaction is histamine-related, so antihistamines like loratadine (Claritin) can help.
There can be more serious swelling as well, especially after perioral injections, and “it’s more common with Silk than with regular Restylane. Some patients have erythema that stays a long time, and some have a burning sensation. If it’s not horrific, you wait and see. If it’s still there in 10 days or 2 weeks, my inclination is to dissolve it out and switch drugs,” he said.
Dr. Rubin is a consultant for Merz, maker of Belotero, Radiesse, and other products. Global Academy and this news organization are owned by the same company.
NEWPORT BEACH, CALIF. – Despite all the technical advances in aesthetic medicine, there’s still a place for treating fine facial lines with thin hyaluronic acid fillers, according to Dr. Mark G. Rubin, a dermatologist at the Lasky Skin Center in Beverly Hills, Calif.
“In the last couple of years, with all the volumizing products, a lot of people say they don’t treat wrinkles anymore. The idea is if you just put some volume in [a patient’s] nasojugal groove, you inflate the cheek, pull the skin tight, and the nasolabial fold will miraculously disappear. I don’t think that’s really true,” he said at the meeting held by Global Academy for Medical Education.
When patients don’t have good skin elasticity and tightness – and most older patients worried about fine lines don’t – volumizing will improve skin contour but not do much for atrophic lines.
That’s a good time to turn to fillers. “Basically, you are putting putty into a dent. Different wrinkles need different depths of material. We have fillers that are thin like sand, medium like pebbles, or thick like boulders.” Shallow lines need thinner material; deeper folds need volumizing boulders for lift. In some patients, “you need to layer them, boulders first then more superficial fillers to smooth out the surface,” Dr. Rubin said. “There are a lot of medium and deep fillers, but for really fine lines and superficial filling, there’s only Restylane Silk and Belotero.”
However, even superficial fillers need to be diluted sometimes with saline or lidocaine. “There isn’t a perfect filler; you need to create the one that works by changing its characteristics,” he said.
“With Restylane, if you dilute it too much, it turns into water, and you get no lift at all. You can dilute Juvederm down pretty well, but in some patients it still leaves ridges. You can dilute Belotero a lot without losing its ability to create lift, but I think in a lot of patients, Restylane Silk has a little better persistence than Belotero,” he said.
Staying in the dermis is important for superficial lines. “You need to come in at a very acute angle, and you have to see drug coming back at you through the pores. If you are not seeing that, you are definitely too deep. You also need to overcorrect, and see the area blanch a little bit,” he said.
Dr. Rubin warns patients that they might have what looks like a string of pearls under their skin after injection. “We massage [the beads] down with a Q-tip,” rolling it back and forth over the bulges, and they melt over time. A part of the reaction is histamine-related, so antihistamines like loratadine (Claritin) can help.
There can be more serious swelling as well, especially after perioral injections, and “it’s more common with Silk than with regular Restylane. Some patients have erythema that stays a long time, and some have a burning sensation. If it’s not horrific, you wait and see. If it’s still there in 10 days or 2 weeks, my inclination is to dissolve it out and switch drugs,” he said.
Dr. Rubin is a consultant for Merz, maker of Belotero, Radiesse, and other products. Global Academy and this news organization are owned by the same company.
NEWPORT BEACH, CALIF. – Despite all the technical advances in aesthetic medicine, there’s still a place for treating fine facial lines with thin hyaluronic acid fillers, according to Dr. Mark G. Rubin, a dermatologist at the Lasky Skin Center in Beverly Hills, Calif.
“In the last couple of years, with all the volumizing products, a lot of people say they don’t treat wrinkles anymore. The idea is if you just put some volume in [a patient’s] nasojugal groove, you inflate the cheek, pull the skin tight, and the nasolabial fold will miraculously disappear. I don’t think that’s really true,” he said at the meeting held by Global Academy for Medical Education.
When patients don’t have good skin elasticity and tightness – and most older patients worried about fine lines don’t – volumizing will improve skin contour but not do much for atrophic lines.
That’s a good time to turn to fillers. “Basically, you are putting putty into a dent. Different wrinkles need different depths of material. We have fillers that are thin like sand, medium like pebbles, or thick like boulders.” Shallow lines need thinner material; deeper folds need volumizing boulders for lift. In some patients, “you need to layer them, boulders first then more superficial fillers to smooth out the surface,” Dr. Rubin said. “There are a lot of medium and deep fillers, but for really fine lines and superficial filling, there’s only Restylane Silk and Belotero.”
However, even superficial fillers need to be diluted sometimes with saline or lidocaine. “There isn’t a perfect filler; you need to create the one that works by changing its characteristics,” he said.
“With Restylane, if you dilute it too much, it turns into water, and you get no lift at all. You can dilute Juvederm down pretty well, but in some patients it still leaves ridges. You can dilute Belotero a lot without losing its ability to create lift, but I think in a lot of patients, Restylane Silk has a little better persistence than Belotero,” he said.
Staying in the dermis is important for superficial lines. “You need to come in at a very acute angle, and you have to see drug coming back at you through the pores. If you are not seeing that, you are definitely too deep. You also need to overcorrect, and see the area blanch a little bit,” he said.
Dr. Rubin warns patients that they might have what looks like a string of pearls under their skin after injection. “We massage [the beads] down with a Q-tip,” rolling it back and forth over the bulges, and they melt over time. A part of the reaction is histamine-related, so antihistamines like loratadine (Claritin) can help.
There can be more serious swelling as well, especially after perioral injections, and “it’s more common with Silk than with regular Restylane. Some patients have erythema that stays a long time, and some have a burning sensation. If it’s not horrific, you wait and see. If it’s still there in 10 days or 2 weeks, my inclination is to dissolve it out and switch drugs,” he said.
Dr. Rubin is a consultant for Merz, maker of Belotero, Radiesse, and other products. Global Academy and this news organization are owned by the same company.
EXPERT ANALYSIS FROM THE SUMMIT IN AESTHETIC MEDICINE
American Diet Improving, but Not Yet Healthy
Americans are adding more whole grains,nuts and seeds to their diets and cutting back on sodas and sugary drinks, a U.S. study suggests.
While these changes point to some improvements in U.S.eating habits over the past decade, many people still consume too much sugar and processed food and not enough whole fruits and vegetables, the study scheduled for online publication June 21 in JAMA found.
"The overall diet is still far from optimal - less than one-third of American adults meet guidelines for most foods," said senior study author Dr. Dariush Mozaffarian, dean of the Tufts Friedman School of Nutrition Science and Policy in Boston.
"The single biggest focus should be on reducing highly processed foods rich in refined grains, starch, added sugars and salt; and increasing minimally processed healthful foods such as fruits, non-starchy vegetables, nuts, seeds, beans, fish and yogurt," Mozaffarian added by email.
Researchers looked at trends in eating habits for almost 34,000 adults aged 20 or older who participated in seven nationally representative surveys from 1999 to 2012.
The study team scored diets based, among other things, on how well people followed recommendations from the American Heart Association (AHA) that are designed to help prevent chronic health problems like cardiovascular disease.
Under these guidelines, a healthy diet includes at least 4.5 cups a day of fruits and vegetables, at least three ounces a day of fiber-rich whole grains and at least seven ounces a week of fish. It also caps sodium intake at 1,500 mg a day, the amount in three quarters of a teaspoon (3.75 g) of salt, and limits sodas and sugary juices at 36 ounces (1 liter) a week.
Overall, the percentage of Americans with poor diets based on these AHA standards dropped from 56 percent to 46 percent during the study period. The proportion of people with ideal diets was low but inched up to 1.5 percent from less than 1 percent.
Racial disparities in eating habits persisted throughout the study period. The proportion of white people with poor diets declined, while remaining little changed among black and Hispanic adults.
More affluent adults saw greater improvements in diet than lower-income people, the study also found.
For some eating patterns - including consumption of total vegetables, whole grains, unprocessed red meat and milk - trends over time were similar regardless of race, ethnicity, income or education levels. Intake of these things was consistently higher for more affluent people and white people and lower for poor people and black and Hispanic adults.
At the same time, salt intake was unchanged for white people but increased for black and Hispanic people during the study period.
Refined grain consumption dropped for white and black adults while increasing for Hispanics.
Limitations of the study include its reliance on survey participants to accurately recall and report what they ate and drank, as well as the potential for diet fads or food trends in popular culture to influence how people described their diets, the authors note.
Even so, the findings suggest that doctors need to do a better job educating patients about how to eat and how food choices influence their health, Dr. Margo Denke, a former researcher at the University of Texas Southwestern Medical Center in Dallas noted in an accompanying editorial.
Physicians also have to recognize that improving diets may be not be just a question of education, but of access and affordability, Denke added by email. While it's possible some people are confused about what to eat, the bigger problem is that they aren't sure what to do when fresh produce isn't at their local store.
"The import of less expensive fruits and vegetables I believe drove improved intake among those who have higher incomes," Denke said. "How can we pass this on to those who are financially struggling?"
SOURCE: http://bit.ly/28LE2ye JAMA 2016.
Americans are adding more whole grains,nuts and seeds to their diets and cutting back on sodas and sugary drinks, a U.S. study suggests.
While these changes point to some improvements in U.S.eating habits over the past decade, many people still consume too much sugar and processed food and not enough whole fruits and vegetables, the study scheduled for online publication June 21 in JAMA found.
"The overall diet is still far from optimal - less than one-third of American adults meet guidelines for most foods," said senior study author Dr. Dariush Mozaffarian, dean of the Tufts Friedman School of Nutrition Science and Policy in Boston.
"The single biggest focus should be on reducing highly processed foods rich in refined grains, starch, added sugars and salt; and increasing minimally processed healthful foods such as fruits, non-starchy vegetables, nuts, seeds, beans, fish and yogurt," Mozaffarian added by email.
Researchers looked at trends in eating habits for almost 34,000 adults aged 20 or older who participated in seven nationally representative surveys from 1999 to 2012.
The study team scored diets based, among other things, on how well people followed recommendations from the American Heart Association (AHA) that are designed to help prevent chronic health problems like cardiovascular disease.
Under these guidelines, a healthy diet includes at least 4.5 cups a day of fruits and vegetables, at least three ounces a day of fiber-rich whole grains and at least seven ounces a week of fish. It also caps sodium intake at 1,500 mg a day, the amount in three quarters of a teaspoon (3.75 g) of salt, and limits sodas and sugary juices at 36 ounces (1 liter) a week.
Overall, the percentage of Americans with poor diets based on these AHA standards dropped from 56 percent to 46 percent during the study period. The proportion of people with ideal diets was low but inched up to 1.5 percent from less than 1 percent.
Racial disparities in eating habits persisted throughout the study period. The proportion of white people with poor diets declined, while remaining little changed among black and Hispanic adults.
More affluent adults saw greater improvements in diet than lower-income people, the study also found.
For some eating patterns - including consumption of total vegetables, whole grains, unprocessed red meat and milk - trends over time were similar regardless of race, ethnicity, income or education levels. Intake of these things was consistently higher for more affluent people and white people and lower for poor people and black and Hispanic adults.
At the same time, salt intake was unchanged for white people but increased for black and Hispanic people during the study period.
Refined grain consumption dropped for white and black adults while increasing for Hispanics.
Limitations of the study include its reliance on survey participants to accurately recall and report what they ate and drank, as well as the potential for diet fads or food trends in popular culture to influence how people described their diets, the authors note.
Even so, the findings suggest that doctors need to do a better job educating patients about how to eat and how food choices influence their health, Dr. Margo Denke, a former researcher at the University of Texas Southwestern Medical Center in Dallas noted in an accompanying editorial.
Physicians also have to recognize that improving diets may be not be just a question of education, but of access and affordability, Denke added by email. While it's possible some people are confused about what to eat, the bigger problem is that they aren't sure what to do when fresh produce isn't at their local store.
"The import of less expensive fruits and vegetables I believe drove improved intake among those who have higher incomes," Denke said. "How can we pass this on to those who are financially struggling?"
SOURCE: http://bit.ly/28LE2ye JAMA 2016.
Americans are adding more whole grains,nuts and seeds to their diets and cutting back on sodas and sugary drinks, a U.S. study suggests.
While these changes point to some improvements in U.S.eating habits over the past decade, many people still consume too much sugar and processed food and not enough whole fruits and vegetables, the study scheduled for online publication June 21 in JAMA found.
"The overall diet is still far from optimal - less than one-third of American adults meet guidelines for most foods," said senior study author Dr. Dariush Mozaffarian, dean of the Tufts Friedman School of Nutrition Science and Policy in Boston.
"The single biggest focus should be on reducing highly processed foods rich in refined grains, starch, added sugars and salt; and increasing minimally processed healthful foods such as fruits, non-starchy vegetables, nuts, seeds, beans, fish and yogurt," Mozaffarian added by email.
Researchers looked at trends in eating habits for almost 34,000 adults aged 20 or older who participated in seven nationally representative surveys from 1999 to 2012.
The study team scored diets based, among other things, on how well people followed recommendations from the American Heart Association (AHA) that are designed to help prevent chronic health problems like cardiovascular disease.
Under these guidelines, a healthy diet includes at least 4.5 cups a day of fruits and vegetables, at least three ounces a day of fiber-rich whole grains and at least seven ounces a week of fish. It also caps sodium intake at 1,500 mg a day, the amount in three quarters of a teaspoon (3.75 g) of salt, and limits sodas and sugary juices at 36 ounces (1 liter) a week.
Overall, the percentage of Americans with poor diets based on these AHA standards dropped from 56 percent to 46 percent during the study period. The proportion of people with ideal diets was low but inched up to 1.5 percent from less than 1 percent.
Racial disparities in eating habits persisted throughout the study period. The proportion of white people with poor diets declined, while remaining little changed among black and Hispanic adults.
More affluent adults saw greater improvements in diet than lower-income people, the study also found.
For some eating patterns - including consumption of total vegetables, whole grains, unprocessed red meat and milk - trends over time were similar regardless of race, ethnicity, income or education levels. Intake of these things was consistently higher for more affluent people and white people and lower for poor people and black and Hispanic adults.
At the same time, salt intake was unchanged for white people but increased for black and Hispanic people during the study period.
Refined grain consumption dropped for white and black adults while increasing for Hispanics.
Limitations of the study include its reliance on survey participants to accurately recall and report what they ate and drank, as well as the potential for diet fads or food trends in popular culture to influence how people described their diets, the authors note.
Even so, the findings suggest that doctors need to do a better job educating patients about how to eat and how food choices influence their health, Dr. Margo Denke, a former researcher at the University of Texas Southwestern Medical Center in Dallas noted in an accompanying editorial.
Physicians also have to recognize that improving diets may be not be just a question of education, but of access and affordability, Denke added by email. While it's possible some people are confused about what to eat, the bigger problem is that they aren't sure what to do when fresh produce isn't at their local store.
"The import of less expensive fruits and vegetables I believe drove improved intake among those who have higher incomes," Denke said. "How can we pass this on to those who are financially struggling?"
SOURCE: http://bit.ly/28LE2ye JAMA 2016.
European ANCA-associated vasculitis guidance gets first makeover since 2009
LONDON – Updated management recommendations for patients with antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis from the European League Against Rheumatism and the European Renal Association-European Dialysis and Transplant Association aim to provide clinicians with reliable guidance on the best approach to treatment.
The update, presented at the European Congress of Rheumatology and recently published online in Annals of the Rheumatic Diseases (Ann Rheum Dis. 2016 Jun 23. doi:10.1136/annrheumdis-2016-209133), reassessed items in the 2009 recommendations for the management of primary systemic vasculitis and focused only on the management of ANCA-associated vasculitis (AAV), according to recommendations task force member Dr. Max Yates.
“In the past 5 years, 1,691 papers have been published on primary systemic vasculitis in internal medicine, rheumatology, and nephrology journals. Together with the licensing of rituximab for AAV, it was an opportune time to update the recommendations with an AAV focus,” Dr. Yates explained. The revised guidance is based on a systematic literature review from January 2007 to February 2015, focusing in particular on specific items that needed updating, such as the importance of ANCA testing and biopsy in diagnosis and follow-up, disease staging at diagnosis, the choices for remission-induction and remission-maintenance therapies, and the drug choices for relapsing and refractory disease. The task force considered for the first time the choice of immunosuppressive drugs and biologic agents (principally rituximab) and immunologic monitoring. They identified patient education as another priority.
“These updated recommendations provide a framework of practice and should apply to the majority of patients with AAV,” added Dr. Yates, who is a clinical fellow at Norwich Medical School at the University of East Anglia and works in the department of rheumatology at the Norfolk and Norwich (England) University Hospital.
The 22-member task force included rheumatologists, internists, nephrologists, a clinical immunologist, an otorhinolaryngologist, a chest physician, an ophthalmologist, a vasculitis nurse, and a patient with vasculitis from 11 countries in Europe and the United States. The task force was convened by rheumatologist Dr. Chetan Mukhtyar of the Norfolk and Norwich University Hospital on behalf of EULAR and by vasculitis and renal specialist Dr. David Jayne of Addenbrooke’s Hospital in Cambridge (England) on behalf of the European Renal Association-European Dialysis and Transplant Association.
The recommendations now contain one single, simple overarching principle, Dr. Mukhtyar said at the congress. That is, the need for shared decision making between the patient and the clinician. This principle is also included as the first point in many of the other recently updated EULAR recommendations on the management of rheumatic diseases.
Both previous and updated versions of the vasculitis recommendations contain 15 recommendations, with some changed and others combined. One key recommendation is about who should treat patients with AAV; it states that patients “should be managed in close collaboration with, or at, centers of expertise,” Dr. Mukhtyar said.“Patients with ANCA-associated vasculitis have often very complex presentations that involve several different specialties, and it is always worthwhile that these patients are looked after by people who commonly see them, because these are rare conditions,” he observed.
Deciding when to perform a biopsy is also covered, with the recommendation being that it can be used to establish a new diagnosis and to further evaluate cases of suspected relapsing vasculitis. “When do you do a biopsy?” Dr. Mukhtyar asked. “Well, every time you can, every time it is clinically feasible,” he suggested.
As for treatment, there are different recommendations depending on whether the aim is to induce or maintain remission and whether there has been a major relapse. In patients with organ- or life-threatening disease, for example, the advice is to use glucocorticoids and either cyclophosphamide or rituximab to induce remission, Dr. Mukhtyar said. The specific dosing or administration of glucocorticoids is not specified as this will depend on the clinical situation, but the advice is to taper down when possible, somewhere between month 3 and 5.
For remission induction in less severe (non–organ threatening) disease, the recommendation is to use glucocorticoids plus either methotrexate or mycophenolate mofetil. Situations when methotrexate or mycophenolate mofetil should and should not be used are specified, notably when cyclophosphamide or rituximab are not available or are contraindicated.
For maintenance of remission, the task force advised using low-dose glucocorticoids plus azathioprine, rituximab, methotrexate, or mycophenolate mofetil.
Guidance on when to use plasma exchange is given for patients with severe disease and options following failure of remission-induction therapy, and when to switch therapy is also covered.
There are also several follow-up recommendations, such as the periodic assessment of cardiovascular risk, and patient-focused recommendations on awareness of the nature, benefits, and risks of therapy.
The recommendations should provide clinicians with reliable guidance on the best approach to treating AAV, according to Dr. Yates. “From the patients’ point of view, these recommendations should provide useful insight into which treatments they are likely to be offered and when. They also emphasize that as a patient, you should have a voice in your treatment and if you have any questions or concerns, be sure to speak with your specialist.”
Dr. Yates and Dr. Mukhtyar did not report having any relevant disclosures.
The prior 2009 EULAR recommendations were very much in need of updating given the plethora of studies in the past 7 years addressing ANCA-associated vasculitis (AAV). The emergence of rituximab as an effective therapy in AAV had to be considered and included in these newer guidelines. Its potential role in both remission induction, as well as remission maintenance of AAV, is addressed.
The recommendations are somewhat complicated, particularly as eosinophilic granulomatosis with polyangiitis (EGPA, previously referred to as Churg-Strauss syndrome) has been included, but most of the well-done prospective clinical trials addressing remission induction and remission maintenance in AAV were limited to patients with granulomatosis with polyangiitis or microscopic polyangiitis and did not include patients with EGPA. The role of plasma exchange is also discussed, but the results of the PEXIVAS trial, which will address that more definitively, are not yet forthcoming. Those results are anticipated in the not too distant future and will much better define that component of management in those most severely ill patients with AAV.

|
| Dr. Robert Spiera |
These recommendations serve as a framework for helping clinicians understand what is widely accepted as standard of care for these diseases but in no way can define individual treatment decisions as the authors acknowledge. Such decisions must become very personalized in relation to details of the patient’s individual comorbidities and other features of their medical and even socioeconomic status. For example, when choosing between rituximab and cyclophosphamide for remission induction in a young woman (or man, for that matter), future fertility concerns (which cyclophosphamide could potentially compromise) are very relevant. Moreover, the costs of rituximab are substantial, and the lack of superiority of rituximab over cyclophosphamide in many situations, particularly in patients with new severe disease, could be an important factor to consider when choosing which immunosuppressive will be used.
Many of the unanswered questions await results of ongoing or upcoming trials, including some addressing the relative efficacy of various remission maintenance regimens (rituximab vs. azathioprine) or the role of plasmapheresis. Many questions in AAV are not easily addressable in clinical trials, such as whether there are some groups of patients in whom remission maintenance therapy should never be withdrawn. However, such questions may be addressed through observational studies of the well-defined patient cohorts and registries that have been developed in the United States and Europe.
Robert F. Spiera, MD, is director of the Scleroderma, Vasculitis, & Myositis Center at the Hospital for Special Surgery, N.Y. He is also professor of clinical medicine at Cornell University, N.Y. He has received research funding and consulting fees from Roche/Genentech, which markets rituximab.
The prior 2009 EULAR recommendations were very much in need of updating given the plethora of studies in the past 7 years addressing ANCA-associated vasculitis (AAV). The emergence of rituximab as an effective therapy in AAV had to be considered and included in these newer guidelines. Its potential role in both remission induction, as well as remission maintenance of AAV, is addressed.
The recommendations are somewhat complicated, particularly as eosinophilic granulomatosis with polyangiitis (EGPA, previously referred to as Churg-Strauss syndrome) has been included, but most of the well-done prospective clinical trials addressing remission induction and remission maintenance in AAV were limited to patients with granulomatosis with polyangiitis or microscopic polyangiitis and did not include patients with EGPA. The role of plasma exchange is also discussed, but the results of the PEXIVAS trial, which will address that more definitively, are not yet forthcoming. Those results are anticipated in the not too distant future and will much better define that component of management in those most severely ill patients with AAV.

|
| Dr. Robert Spiera |
These recommendations serve as a framework for helping clinicians understand what is widely accepted as standard of care for these diseases but in no way can define individual treatment decisions as the authors acknowledge. Such decisions must become very personalized in relation to details of the patient’s individual comorbidities and other features of their medical and even socioeconomic status. For example, when choosing between rituximab and cyclophosphamide for remission induction in a young woman (or man, for that matter), future fertility concerns (which cyclophosphamide could potentially compromise) are very relevant. Moreover, the costs of rituximab are substantial, and the lack of superiority of rituximab over cyclophosphamide in many situations, particularly in patients with new severe disease, could be an important factor to consider when choosing which immunosuppressive will be used.
Many of the unanswered questions await results of ongoing or upcoming trials, including some addressing the relative efficacy of various remission maintenance regimens (rituximab vs. azathioprine) or the role of plasmapheresis. Many questions in AAV are not easily addressable in clinical trials, such as whether there are some groups of patients in whom remission maintenance therapy should never be withdrawn. However, such questions may be addressed through observational studies of the well-defined patient cohorts and registries that have been developed in the United States and Europe.
Robert F. Spiera, MD, is director of the Scleroderma, Vasculitis, & Myositis Center at the Hospital for Special Surgery, N.Y. He is also professor of clinical medicine at Cornell University, N.Y. He has received research funding and consulting fees from Roche/Genentech, which markets rituximab.
The prior 2009 EULAR recommendations were very much in need of updating given the plethora of studies in the past 7 years addressing ANCA-associated vasculitis (AAV). The emergence of rituximab as an effective therapy in AAV had to be considered and included in these newer guidelines. Its potential role in both remission induction, as well as remission maintenance of AAV, is addressed.
The recommendations are somewhat complicated, particularly as eosinophilic granulomatosis with polyangiitis (EGPA, previously referred to as Churg-Strauss syndrome) has been included, but most of the well-done prospective clinical trials addressing remission induction and remission maintenance in AAV were limited to patients with granulomatosis with polyangiitis or microscopic polyangiitis and did not include patients with EGPA. The role of plasma exchange is also discussed, but the results of the PEXIVAS trial, which will address that more definitively, are not yet forthcoming. Those results are anticipated in the not too distant future and will much better define that component of management in those most severely ill patients with AAV.

|
| Dr. Robert Spiera |
These recommendations serve as a framework for helping clinicians understand what is widely accepted as standard of care for these diseases but in no way can define individual treatment decisions as the authors acknowledge. Such decisions must become very personalized in relation to details of the patient’s individual comorbidities and other features of their medical and even socioeconomic status. For example, when choosing between rituximab and cyclophosphamide for remission induction in a young woman (or man, for that matter), future fertility concerns (which cyclophosphamide could potentially compromise) are very relevant. Moreover, the costs of rituximab are substantial, and the lack of superiority of rituximab over cyclophosphamide in many situations, particularly in patients with new severe disease, could be an important factor to consider when choosing which immunosuppressive will be used.
Many of the unanswered questions await results of ongoing or upcoming trials, including some addressing the relative efficacy of various remission maintenance regimens (rituximab vs. azathioprine) or the role of plasmapheresis. Many questions in AAV are not easily addressable in clinical trials, such as whether there are some groups of patients in whom remission maintenance therapy should never be withdrawn. However, such questions may be addressed through observational studies of the well-defined patient cohorts and registries that have been developed in the United States and Europe.
Robert F. Spiera, MD, is director of the Scleroderma, Vasculitis, & Myositis Center at the Hospital for Special Surgery, N.Y. He is also professor of clinical medicine at Cornell University, N.Y. He has received research funding and consulting fees from Roche/Genentech, which markets rituximab.
LONDON – Updated management recommendations for patients with antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis from the European League Against Rheumatism and the European Renal Association-European Dialysis and Transplant Association aim to provide clinicians with reliable guidance on the best approach to treatment.
The update, presented at the European Congress of Rheumatology and recently published online in Annals of the Rheumatic Diseases (Ann Rheum Dis. 2016 Jun 23. doi:10.1136/annrheumdis-2016-209133), reassessed items in the 2009 recommendations for the management of primary systemic vasculitis and focused only on the management of ANCA-associated vasculitis (AAV), according to recommendations task force member Dr. Max Yates.
“In the past 5 years, 1,691 papers have been published on primary systemic vasculitis in internal medicine, rheumatology, and nephrology journals. Together with the licensing of rituximab for AAV, it was an opportune time to update the recommendations with an AAV focus,” Dr. Yates explained. The revised guidance is based on a systematic literature review from January 2007 to February 2015, focusing in particular on specific items that needed updating, such as the importance of ANCA testing and biopsy in diagnosis and follow-up, disease staging at diagnosis, the choices for remission-induction and remission-maintenance therapies, and the drug choices for relapsing and refractory disease. The task force considered for the first time the choice of immunosuppressive drugs and biologic agents (principally rituximab) and immunologic monitoring. They identified patient education as another priority.
“These updated recommendations provide a framework of practice and should apply to the majority of patients with AAV,” added Dr. Yates, who is a clinical fellow at Norwich Medical School at the University of East Anglia and works in the department of rheumatology at the Norfolk and Norwich (England) University Hospital.
The 22-member task force included rheumatologists, internists, nephrologists, a clinical immunologist, an otorhinolaryngologist, a chest physician, an ophthalmologist, a vasculitis nurse, and a patient with vasculitis from 11 countries in Europe and the United States. The task force was convened by rheumatologist Dr. Chetan Mukhtyar of the Norfolk and Norwich University Hospital on behalf of EULAR and by vasculitis and renal specialist Dr. David Jayne of Addenbrooke’s Hospital in Cambridge (England) on behalf of the European Renal Association-European Dialysis and Transplant Association.
The recommendations now contain one single, simple overarching principle, Dr. Mukhtyar said at the congress. That is, the need for shared decision making between the patient and the clinician. This principle is also included as the first point in many of the other recently updated EULAR recommendations on the management of rheumatic diseases.
Both previous and updated versions of the vasculitis recommendations contain 15 recommendations, with some changed and others combined. One key recommendation is about who should treat patients with AAV; it states that patients “should be managed in close collaboration with, or at, centers of expertise,” Dr. Mukhtyar said.“Patients with ANCA-associated vasculitis have often very complex presentations that involve several different specialties, and it is always worthwhile that these patients are looked after by people who commonly see them, because these are rare conditions,” he observed.
Deciding when to perform a biopsy is also covered, with the recommendation being that it can be used to establish a new diagnosis and to further evaluate cases of suspected relapsing vasculitis. “When do you do a biopsy?” Dr. Mukhtyar asked. “Well, every time you can, every time it is clinically feasible,” he suggested.
As for treatment, there are different recommendations depending on whether the aim is to induce or maintain remission and whether there has been a major relapse. In patients with organ- or life-threatening disease, for example, the advice is to use glucocorticoids and either cyclophosphamide or rituximab to induce remission, Dr. Mukhtyar said. The specific dosing or administration of glucocorticoids is not specified as this will depend on the clinical situation, but the advice is to taper down when possible, somewhere between month 3 and 5.
For remission induction in less severe (non–organ threatening) disease, the recommendation is to use glucocorticoids plus either methotrexate or mycophenolate mofetil. Situations when methotrexate or mycophenolate mofetil should and should not be used are specified, notably when cyclophosphamide or rituximab are not available or are contraindicated.
For maintenance of remission, the task force advised using low-dose glucocorticoids plus azathioprine, rituximab, methotrexate, or mycophenolate mofetil.
Guidance on when to use plasma exchange is given for patients with severe disease and options following failure of remission-induction therapy, and when to switch therapy is also covered.
There are also several follow-up recommendations, such as the periodic assessment of cardiovascular risk, and patient-focused recommendations on awareness of the nature, benefits, and risks of therapy.
The recommendations should provide clinicians with reliable guidance on the best approach to treating AAV, according to Dr. Yates. “From the patients’ point of view, these recommendations should provide useful insight into which treatments they are likely to be offered and when. They also emphasize that as a patient, you should have a voice in your treatment and if you have any questions or concerns, be sure to speak with your specialist.”
Dr. Yates and Dr. Mukhtyar did not report having any relevant disclosures.
LONDON – Updated management recommendations for patients with antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis from the European League Against Rheumatism and the European Renal Association-European Dialysis and Transplant Association aim to provide clinicians with reliable guidance on the best approach to treatment.
The update, presented at the European Congress of Rheumatology and recently published online in Annals of the Rheumatic Diseases (Ann Rheum Dis. 2016 Jun 23. doi:10.1136/annrheumdis-2016-209133), reassessed items in the 2009 recommendations for the management of primary systemic vasculitis and focused only on the management of ANCA-associated vasculitis (AAV), according to recommendations task force member Dr. Max Yates.
“In the past 5 years, 1,691 papers have been published on primary systemic vasculitis in internal medicine, rheumatology, and nephrology journals. Together with the licensing of rituximab for AAV, it was an opportune time to update the recommendations with an AAV focus,” Dr. Yates explained. The revised guidance is based on a systematic literature review from January 2007 to February 2015, focusing in particular on specific items that needed updating, such as the importance of ANCA testing and biopsy in diagnosis and follow-up, disease staging at diagnosis, the choices for remission-induction and remission-maintenance therapies, and the drug choices for relapsing and refractory disease. The task force considered for the first time the choice of immunosuppressive drugs and biologic agents (principally rituximab) and immunologic monitoring. They identified patient education as another priority.
“These updated recommendations provide a framework of practice and should apply to the majority of patients with AAV,” added Dr. Yates, who is a clinical fellow at Norwich Medical School at the University of East Anglia and works in the department of rheumatology at the Norfolk and Norwich (England) University Hospital.
The 22-member task force included rheumatologists, internists, nephrologists, a clinical immunologist, an otorhinolaryngologist, a chest physician, an ophthalmologist, a vasculitis nurse, and a patient with vasculitis from 11 countries in Europe and the United States. The task force was convened by rheumatologist Dr. Chetan Mukhtyar of the Norfolk and Norwich University Hospital on behalf of EULAR and by vasculitis and renal specialist Dr. David Jayne of Addenbrooke’s Hospital in Cambridge (England) on behalf of the European Renal Association-European Dialysis and Transplant Association.
The recommendations now contain one single, simple overarching principle, Dr. Mukhtyar said at the congress. That is, the need for shared decision making between the patient and the clinician. This principle is also included as the first point in many of the other recently updated EULAR recommendations on the management of rheumatic diseases.
Both previous and updated versions of the vasculitis recommendations contain 15 recommendations, with some changed and others combined. One key recommendation is about who should treat patients with AAV; it states that patients “should be managed in close collaboration with, or at, centers of expertise,” Dr. Mukhtyar said.“Patients with ANCA-associated vasculitis have often very complex presentations that involve several different specialties, and it is always worthwhile that these patients are looked after by people who commonly see them, because these are rare conditions,” he observed.
Deciding when to perform a biopsy is also covered, with the recommendation being that it can be used to establish a new diagnosis and to further evaluate cases of suspected relapsing vasculitis. “When do you do a biopsy?” Dr. Mukhtyar asked. “Well, every time you can, every time it is clinically feasible,” he suggested.
As for treatment, there are different recommendations depending on whether the aim is to induce or maintain remission and whether there has been a major relapse. In patients with organ- or life-threatening disease, for example, the advice is to use glucocorticoids and either cyclophosphamide or rituximab to induce remission, Dr. Mukhtyar said. The specific dosing or administration of glucocorticoids is not specified as this will depend on the clinical situation, but the advice is to taper down when possible, somewhere between month 3 and 5.
For remission induction in less severe (non–organ threatening) disease, the recommendation is to use glucocorticoids plus either methotrexate or mycophenolate mofetil. Situations when methotrexate or mycophenolate mofetil should and should not be used are specified, notably when cyclophosphamide or rituximab are not available or are contraindicated.
For maintenance of remission, the task force advised using low-dose glucocorticoids plus azathioprine, rituximab, methotrexate, or mycophenolate mofetil.
Guidance on when to use plasma exchange is given for patients with severe disease and options following failure of remission-induction therapy, and when to switch therapy is also covered.
There are also several follow-up recommendations, such as the periodic assessment of cardiovascular risk, and patient-focused recommendations on awareness of the nature, benefits, and risks of therapy.
The recommendations should provide clinicians with reliable guidance on the best approach to treating AAV, according to Dr. Yates. “From the patients’ point of view, these recommendations should provide useful insight into which treatments they are likely to be offered and when. They also emphasize that as a patient, you should have a voice in your treatment and if you have any questions or concerns, be sure to speak with your specialist.”
Dr. Yates and Dr. Mukhtyar did not report having any relevant disclosures.
AT THE EULAR 2016 CONGRESS
As Summer—and Interns—Roll In, Try a Little Empathy on Your Patients, Colleagues
It’s July, the month that marks the annual rite of passage for both newly minted physicians starting their internships and somewhat-less-fresh trainees completing their residencies and moving on to the next stage of their professional journey. I would imagine that many of you, like me, spend at least a fleeting moment this time of year thinking back to your first days as interns and, hopefully, extend at least a little empathy to those anxious souls who are being called upon to serve as “doctors” for the very first time.
When I reflect a little further, I am also reminded of the immense power and influence of role models over the course of our training. Although internal medicine was certainly interesting to me, even during medical school, I will candidly also say that the residents and attendings who I served with on teams during medical school at the University of Pennsylvania had at least as much if not more to do with my choice to match in internal medicine. I remember many of their names to this day. While I am not in touch with them, I will always be grateful for the way they demonstrated enthusiasm for medicine; compassion for their patients; partnership with nurses, therapists, and the many other members of our teams; and a genuine love for teaching and conveying a sense of mission in what they did.
I had many great teachers in other areas (particularly, I have to admit, surgery, where some of us students were so enamored of the clinical clerkship director that we memorialized him in a sendup of Forrest Gump in our annual comedy show). However, the consistency of this enthusiasm in the medicine teams was incomparable. In short, these were physicians who I wanted to be like, to emulate. They were role models.
Likewise, during residency, it was those attendings who were among the earliest of academic hospitalists who demonstrated those same skills. I will always remember an encounter with one of my chief residents at the Veterans Affairs early in my internship, when I was struggling with a particular issue. Perhaps it was a foreshadowing of my ultimate career choice, but I was disappointed with my ambulatory clinic experience. As a chief resident, he could have dismissed my frustration or told me to suck it up. He didn’t. He empathized, acknowledging my exasperation and assuring me that I wasn’t alone in how I felt. He also helped me frame the experience to find positive learning aspects—after all, it wasn’t a problem he could just fix and make go away.
Most important, he listened and didn’t judge.
Long before we started thinking of empathy as a teachable communication skill, I experienced it firsthand, and it turned my entire experience around. To this day, I try to emulate that empathy when frustrated physicians or employees come to me with issues.
As hospitalists and physicians, the spotlight is on us almost every minute of every day. We are watched (yes, we are judged) all the time by nurses, pharmacists, case managers, and our patients to see if we live the values of teamwork, collaboration, and emotional intelligence that we claim to embody as system thinkers and system reformers.
But no one watches us more closely than those who we are charged with training. From the very earliest medical student to the most seasoned resident and fellow, how we act is how they will act. When we demonstrate that the bar is highest for us in terms of professionalism, collegiality, and empathy, we imprint upon our trainees those same behaviors and the values that they reflect.
We also show trainees a way of practicing medicine that has the ability to be profoundly satisfying to not only ourselves but also to those who collaborate with us and the patients who benefit from that teamwork. And, hopefully, by doing so we are guiding students, interns, and residents to become hospitalists like us.
So, this July, I call upon all of us in the hospitalist teaching community to reach out and welcome the new trainees in your institution and to remember what it was like to be where they are now. Appreciate the profound impact that you have on them by not only the medicine you teach but the way you practice and communicate and your body language and attitude.
As we think about the continuous need to focus on building up the pipeline of future hospital-based practitioners, there is no better way to develop that bench strength than by using our presence as role models to positively influence our new trainees.
Happy July, everyone! TH
It’s July, the month that marks the annual rite of passage for both newly minted physicians starting their internships and somewhat-less-fresh trainees completing their residencies and moving on to the next stage of their professional journey. I would imagine that many of you, like me, spend at least a fleeting moment this time of year thinking back to your first days as interns and, hopefully, extend at least a little empathy to those anxious souls who are being called upon to serve as “doctors” for the very first time.
When I reflect a little further, I am also reminded of the immense power and influence of role models over the course of our training. Although internal medicine was certainly interesting to me, even during medical school, I will candidly also say that the residents and attendings who I served with on teams during medical school at the University of Pennsylvania had at least as much if not more to do with my choice to match in internal medicine. I remember many of their names to this day. While I am not in touch with them, I will always be grateful for the way they demonstrated enthusiasm for medicine; compassion for their patients; partnership with nurses, therapists, and the many other members of our teams; and a genuine love for teaching and conveying a sense of mission in what they did.
I had many great teachers in other areas (particularly, I have to admit, surgery, where some of us students were so enamored of the clinical clerkship director that we memorialized him in a sendup of Forrest Gump in our annual comedy show). However, the consistency of this enthusiasm in the medicine teams was incomparable. In short, these were physicians who I wanted to be like, to emulate. They were role models.
Likewise, during residency, it was those attendings who were among the earliest of academic hospitalists who demonstrated those same skills. I will always remember an encounter with one of my chief residents at the Veterans Affairs early in my internship, when I was struggling with a particular issue. Perhaps it was a foreshadowing of my ultimate career choice, but I was disappointed with my ambulatory clinic experience. As a chief resident, he could have dismissed my frustration or told me to suck it up. He didn’t. He empathized, acknowledging my exasperation and assuring me that I wasn’t alone in how I felt. He also helped me frame the experience to find positive learning aspects—after all, it wasn’t a problem he could just fix and make go away.
Most important, he listened and didn’t judge.
Long before we started thinking of empathy as a teachable communication skill, I experienced it firsthand, and it turned my entire experience around. To this day, I try to emulate that empathy when frustrated physicians or employees come to me with issues.
As hospitalists and physicians, the spotlight is on us almost every minute of every day. We are watched (yes, we are judged) all the time by nurses, pharmacists, case managers, and our patients to see if we live the values of teamwork, collaboration, and emotional intelligence that we claim to embody as system thinkers and system reformers.
But no one watches us more closely than those who we are charged with training. From the very earliest medical student to the most seasoned resident and fellow, how we act is how they will act. When we demonstrate that the bar is highest for us in terms of professionalism, collegiality, and empathy, we imprint upon our trainees those same behaviors and the values that they reflect.
We also show trainees a way of practicing medicine that has the ability to be profoundly satisfying to not only ourselves but also to those who collaborate with us and the patients who benefit from that teamwork. And, hopefully, by doing so we are guiding students, interns, and residents to become hospitalists like us.
So, this July, I call upon all of us in the hospitalist teaching community to reach out and welcome the new trainees in your institution and to remember what it was like to be where they are now. Appreciate the profound impact that you have on them by not only the medicine you teach but the way you practice and communicate and your body language and attitude.
As we think about the continuous need to focus on building up the pipeline of future hospital-based practitioners, there is no better way to develop that bench strength than by using our presence as role models to positively influence our new trainees.
Happy July, everyone! TH
It’s July, the month that marks the annual rite of passage for both newly minted physicians starting their internships and somewhat-less-fresh trainees completing their residencies and moving on to the next stage of their professional journey. I would imagine that many of you, like me, spend at least a fleeting moment this time of year thinking back to your first days as interns and, hopefully, extend at least a little empathy to those anxious souls who are being called upon to serve as “doctors” for the very first time.
When I reflect a little further, I am also reminded of the immense power and influence of role models over the course of our training. Although internal medicine was certainly interesting to me, even during medical school, I will candidly also say that the residents and attendings who I served with on teams during medical school at the University of Pennsylvania had at least as much if not more to do with my choice to match in internal medicine. I remember many of their names to this day. While I am not in touch with them, I will always be grateful for the way they demonstrated enthusiasm for medicine; compassion for their patients; partnership with nurses, therapists, and the many other members of our teams; and a genuine love for teaching and conveying a sense of mission in what they did.
I had many great teachers in other areas (particularly, I have to admit, surgery, where some of us students were so enamored of the clinical clerkship director that we memorialized him in a sendup of Forrest Gump in our annual comedy show). However, the consistency of this enthusiasm in the medicine teams was incomparable. In short, these were physicians who I wanted to be like, to emulate. They were role models.
Likewise, during residency, it was those attendings who were among the earliest of academic hospitalists who demonstrated those same skills. I will always remember an encounter with one of my chief residents at the Veterans Affairs early in my internship, when I was struggling with a particular issue. Perhaps it was a foreshadowing of my ultimate career choice, but I was disappointed with my ambulatory clinic experience. As a chief resident, he could have dismissed my frustration or told me to suck it up. He didn’t. He empathized, acknowledging my exasperation and assuring me that I wasn’t alone in how I felt. He also helped me frame the experience to find positive learning aspects—after all, it wasn’t a problem he could just fix and make go away.
Most important, he listened and didn’t judge.
Long before we started thinking of empathy as a teachable communication skill, I experienced it firsthand, and it turned my entire experience around. To this day, I try to emulate that empathy when frustrated physicians or employees come to me with issues.
As hospitalists and physicians, the spotlight is on us almost every minute of every day. We are watched (yes, we are judged) all the time by nurses, pharmacists, case managers, and our patients to see if we live the values of teamwork, collaboration, and emotional intelligence that we claim to embody as system thinkers and system reformers.
But no one watches us more closely than those who we are charged with training. From the very earliest medical student to the most seasoned resident and fellow, how we act is how they will act. When we demonstrate that the bar is highest for us in terms of professionalism, collegiality, and empathy, we imprint upon our trainees those same behaviors and the values that they reflect.
We also show trainees a way of practicing medicine that has the ability to be profoundly satisfying to not only ourselves but also to those who collaborate with us and the patients who benefit from that teamwork. And, hopefully, by doing so we are guiding students, interns, and residents to become hospitalists like us.
So, this July, I call upon all of us in the hospitalist teaching community to reach out and welcome the new trainees in your institution and to remember what it was like to be where they are now. Appreciate the profound impact that you have on them by not only the medicine you teach but the way you practice and communicate and your body language and attitude.
As we think about the continuous need to focus on building up the pipeline of future hospital-based practitioners, there is no better way to develop that bench strength than by using our presence as role models to positively influence our new trainees.
Happy July, everyone! TH
HCPs may underestimate cancer risk from CT scans

Photo by Angela Mary Butler
Healthcare professionals (HCPs) may not be fully aware of a CT scan’s effect on lifetime malignancy risk, according to a study published in the Journal of Medical Imaging and Radiation Sciences.
Researchers surveyed a group of HCPs on radiation exposure from CT.
And although most of the respondents recognized that CT scans confer an increased risk of cancer, many underestimated the actual dose of radiation a person receives from a CT scan.
The survey was given to 308 HCPs—including physicians, radiologists, and technologists—in Saskatchewan, Canada.
Seventy-three percent of physicians, 97% of radiologists, and 76% of technologists correctly reported that there is an increased cancer risk from one abdominal-pelvic CT.
However, only 18% of physicians, 28% of radiologists, and 22% of technologists were able to correctly identify the dose in relation to chest X-rays.
In fact, 14% of physicians and 12% of technologists (but 0% of radiologists) “vastly” underestimated the dose as less than 10 chest X-ray equivalents, according to researchers.
The average radiation dose from an abdominal-pelvic CT is 10 millisieverts (mSv), compared to 0.02 mSv to 0.2 mSv from one chest X-ray, meaning that a radiation dose from a CT scan is equivalent to the dose from 100 to 250 chest radiographs.
“Underestimating radiation dose from a CT scan is more concerning than knowing the exact dose level, particularly when it is a vast underestimation, as this may lead to minimization of the risk estimate when considering a test,” said study author David Leswick, MD, of the University of Saskatchewan in Saskatoon.
“Although [cancer] risk from radiation dose levels in the range of medical imaging procedures is small, it is real, as evidenced from atomic bomb survivors and nuclear industry workers showing significantly increased risk of malignancy after exposure to doses in the range of diagnostic CT.”
“The risk of fatal malignancy may be as high as 1 in 1000 for a 10-mSv exposure. This risk is significant on a population basis, with up to 2% of cancers in the United States population possibly attributable to CT.”
Another aspect highlighted by the survey was some confusion regarding radiation exposure from MRIs and ultrasounds.
MRIs and ultrasounds do not employ ionizing radiation. However, 20% of physicians, 6% of radiologists, and 7% of technologists attributed radiation exposure to MRIs. Eleven percent of physicians, 0% of radiologists, and 7% of technologists believed an ultrasound used radiation.
“Belief that ionizing radiation is utilized by ultrasound and MRI is troubling, as it may result in underutilization of these imaging modalities because of unfounded radiation concerns,” Dr Leswick said.
“It is important for healthcare professionals (including referring physicians, radiologists, and technologists) to be aware of radiation dose levels and risks from imaging tests for several reasons, including the ability to weigh the risks and benefits of tests, counsel patients on relevant risks, optimize protocols to minimize radiation dose, and select appropriate protocols to minimize radiation dose.” ![]()

Photo by Angela Mary Butler
Healthcare professionals (HCPs) may not be fully aware of a CT scan’s effect on lifetime malignancy risk, according to a study published in the Journal of Medical Imaging and Radiation Sciences.
Researchers surveyed a group of HCPs on radiation exposure from CT.
And although most of the respondents recognized that CT scans confer an increased risk of cancer, many underestimated the actual dose of radiation a person receives from a CT scan.
The survey was given to 308 HCPs—including physicians, radiologists, and technologists—in Saskatchewan, Canada.
Seventy-three percent of physicians, 97% of radiologists, and 76% of technologists correctly reported that there is an increased cancer risk from one abdominal-pelvic CT.
However, only 18% of physicians, 28% of radiologists, and 22% of technologists were able to correctly identify the dose in relation to chest X-rays.
In fact, 14% of physicians and 12% of technologists (but 0% of radiologists) “vastly” underestimated the dose as less than 10 chest X-ray equivalents, according to researchers.
The average radiation dose from an abdominal-pelvic CT is 10 millisieverts (mSv), compared to 0.02 mSv to 0.2 mSv from one chest X-ray, meaning that a radiation dose from a CT scan is equivalent to the dose from 100 to 250 chest radiographs.
“Underestimating radiation dose from a CT scan is more concerning than knowing the exact dose level, particularly when it is a vast underestimation, as this may lead to minimization of the risk estimate when considering a test,” said study author David Leswick, MD, of the University of Saskatchewan in Saskatoon.
“Although [cancer] risk from radiation dose levels in the range of medical imaging procedures is small, it is real, as evidenced from atomic bomb survivors and nuclear industry workers showing significantly increased risk of malignancy after exposure to doses in the range of diagnostic CT.”
“The risk of fatal malignancy may be as high as 1 in 1000 for a 10-mSv exposure. This risk is significant on a population basis, with up to 2% of cancers in the United States population possibly attributable to CT.”
Another aspect highlighted by the survey was some confusion regarding radiation exposure from MRIs and ultrasounds.
MRIs and ultrasounds do not employ ionizing radiation. However, 20% of physicians, 6% of radiologists, and 7% of technologists attributed radiation exposure to MRIs. Eleven percent of physicians, 0% of radiologists, and 7% of technologists believed an ultrasound used radiation.
“Belief that ionizing radiation is utilized by ultrasound and MRI is troubling, as it may result in underutilization of these imaging modalities because of unfounded radiation concerns,” Dr Leswick said.
“It is important for healthcare professionals (including referring physicians, radiologists, and technologists) to be aware of radiation dose levels and risks from imaging tests for several reasons, including the ability to weigh the risks and benefits of tests, counsel patients on relevant risks, optimize protocols to minimize radiation dose, and select appropriate protocols to minimize radiation dose.” ![]()

Photo by Angela Mary Butler
Healthcare professionals (HCPs) may not be fully aware of a CT scan’s effect on lifetime malignancy risk, according to a study published in the Journal of Medical Imaging and Radiation Sciences.
Researchers surveyed a group of HCPs on radiation exposure from CT.
And although most of the respondents recognized that CT scans confer an increased risk of cancer, many underestimated the actual dose of radiation a person receives from a CT scan.
The survey was given to 308 HCPs—including physicians, radiologists, and technologists—in Saskatchewan, Canada.
Seventy-three percent of physicians, 97% of radiologists, and 76% of technologists correctly reported that there is an increased cancer risk from one abdominal-pelvic CT.
However, only 18% of physicians, 28% of radiologists, and 22% of technologists were able to correctly identify the dose in relation to chest X-rays.
In fact, 14% of physicians and 12% of technologists (but 0% of radiologists) “vastly” underestimated the dose as less than 10 chest X-ray equivalents, according to researchers.
The average radiation dose from an abdominal-pelvic CT is 10 millisieverts (mSv), compared to 0.02 mSv to 0.2 mSv from one chest X-ray, meaning that a radiation dose from a CT scan is equivalent to the dose from 100 to 250 chest radiographs.
“Underestimating radiation dose from a CT scan is more concerning than knowing the exact dose level, particularly when it is a vast underestimation, as this may lead to minimization of the risk estimate when considering a test,” said study author David Leswick, MD, of the University of Saskatchewan in Saskatoon.
“Although [cancer] risk from radiation dose levels in the range of medical imaging procedures is small, it is real, as evidenced from atomic bomb survivors and nuclear industry workers showing significantly increased risk of malignancy after exposure to doses in the range of diagnostic CT.”
“The risk of fatal malignancy may be as high as 1 in 1000 for a 10-mSv exposure. This risk is significant on a population basis, with up to 2% of cancers in the United States population possibly attributable to CT.”
Another aspect highlighted by the survey was some confusion regarding radiation exposure from MRIs and ultrasounds.
MRIs and ultrasounds do not employ ionizing radiation. However, 20% of physicians, 6% of radiologists, and 7% of technologists attributed radiation exposure to MRIs. Eleven percent of physicians, 0% of radiologists, and 7% of technologists believed an ultrasound used radiation.
“Belief that ionizing radiation is utilized by ultrasound and MRI is troubling, as it may result in underutilization of these imaging modalities because of unfounded radiation concerns,” Dr Leswick said.
“It is important for healthcare professionals (including referring physicians, radiologists, and technologists) to be aware of radiation dose levels and risks from imaging tests for several reasons, including the ability to weigh the risks and benefits of tests, counsel patients on relevant risks, optimize protocols to minimize radiation dose, and select appropriate protocols to minimize radiation dose.” ![]()