User login
How to avoid 3 common errors in dementia screening
› Use age- and education-corrected normative data when using dementia screening tools. C
› Use verbatim instructions and the same size stimuli and response pages provided in a test’s manual. C
› Ensure that norms used for comparisons are current. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Treatment options for dementia are expanding and improving, giving extra impetus to detecting this progressive disease as early as possible. For example, research on the cholinesterase inhibitor donepezil has shown it can delay cognitive decline by 6 months or more compared with controls1,2 and possibly postpone institutionalization. With the number of elderly individuals and cases of dementia projected to grow significantly over the next 20 years,3 primary care physicians will increasingly be screening for cognitive impairment. Given the time constraints and patient loads in today’s practices, it’s not surprising that physicians tend to use evaluation tools that are brief and simple to administer. However, there are also serious pitfalls in the use of these tools.
When to screen. Many health-related organizations address screening for dementia4,5 and offer screening criteria (eg, the Alzheimer’s Association,6 the US Preventive Services Task Force7). Our experience suggests that specific behavioral changes are reasonable indicators of suspected dementia that should prompt cognitive screening. Using the Kingston Standardized Behavioural Assessment,8 we demonstrated a consistent pattern of earliest behavior change in a community-dwelling group with dementia.9 Meaningful clues are a decreased ability to engage in specific functional activities (including participation in favorite pastimes, ability to eat properly if left to prepare one’s own food, handling of personal finances, word finding, and reading) and unsteadiness. These specific behavioral changes reported by family or a caregiver suggest the need for cognitive screening.
Pitfalls associated with common screening tools, if not taken into account, can seriously limit the usefulness of information gained during assessment and potentially lead to a wrong conclusion. Screening tools are just that: a means of detecting the possible existence of a condition. Results are based on probability and subject to error. Therefore, a single test score is insufficient to render a diagnosis of dementia, and is one variable in a set of diagnostic criteria.
The purpose of this article is to review some of the most commonly used tools and procedures for dementia screening, identify procedural or interpretive errors made in everyday clinical practice, and suggest practical yet simple strategies to address these problems and improve the accuracy of assessments. We illustrate key points with clinical examples and vignettes using the Mini-Mental State Examination (MMSE),10 an Animal Naming Task, and the Trail Making Test.11
Common error #1: Reliance on simple, single cutoff scores
There are a number of important considerations to keep in mind when trying to make sense of scores from the many available cognitive tests.
The range of normal test results is wide. The normal range for most physiologic measures, such as glucose levels or hemoglobin counts, is relatively narrow. However, human cognitive functions can naturally differ from person to person, and the range of normal can be extremely large.
A single, all-purpose cutoff score ignores critical factors. Very often, clinicians have dealt with the issue of wide variance in cognition scores by establishing a general cutoff point to serve as a pass-fail mark. But this practice can result in both under- and overidentification of dementia, and it ignores the 2 components that chiefly determine how individuals differ cognitively: age and intelligence.
Practical fix: Use age-, intelligence-corrected normative data
Level of cognitive performance can be revealing when adjustments are made for age and intelligence. Not taking these factors into account can lead to many errors in clinical decision making.
Age matters. Many cognitive capacities decline as part of normal aging even in otherwise healthy individuals (eg, reaction time, spatial abilities, flexibility in novel problem solving).12 With this in mind, psychologists often have made the distinction between “hold” tests (remaining stable or even improving with age) and “no-hold” tests (declining with age).13 Therefore it is critical to ask, “What is normal, given a particular patient’s age?” If normative data corrected for age are available for a given test, use them.
Intelligence is a factor, too. Intelligence, like most human qualities, is distributed along a bell-shaped curve of normal distribution, wherein most people fall somewhere in the middle and a smaller number will be at the lower and higher tails of the curve. Not all of us fall into the average range of intelligence; indeed, psychometrically, only half of us do. The other half are found somewhere in the more extreme ends. In evaluating a person for dementia, it is critical to compare test results with those found in the appropriate intellectual group. But how does the physician looking for a brief assessment strategy determine a patient’s premorbid level of intellectual functioning?
A widely used and accepted heuristic for gauging intelligence is “years of education.” Of course, education is not perfectly correlated with intelligence, particularly as those who are now elderly may have been denied the opportunity to attend school due to the Great Depression, war, or other life events. Nevertheless, with these limitations in mind, level of education is a reasonable approximation of intelligence. In practical application, premorbid intellectual level is determined by using education-corrected normative data.
Typically with cognitive tests, cutoff scores and score ranges are defined for general levels of education (eg, less than grade 12 or more than grade 12; elementary school, high school, post-secondary, etc). Adjusted norms for age and education are usually determined by taking large samples of subjects and stratifying the distribution by subgroups—eg, 5-year age groups; levels of education such as elementary school or high school—and then statistically analyzing each group and noting the relative differences between them.
Illustration: MMSE. Although not designed for the overall measurement of cognitive impairment in dementia, the MMSE10 has become widely used for that purpose. It is fairly insensitive to cognitive changes associated with earlier stages of dementia,14 and is intended only as a means of identifying patients in need of more comprehensive assessment. However, the MMSE is increasingly used to make a diagnosis of dementia.15 In some areas (eg, Ontario, Canada), it is used to justify paying for treatment with cognitive enhancers.
The universal cutoff score proves inadequate. Although several dementia cutoff scores for the MMSE have been proposed, it is common practice to use an MMSE score ≥24 to rule out dementia.16 In our clinical practice, however, many patients who ultimately are diagnosed with early dementia often perform well on the MMSE, although rather poorly on other dementia screens, such as the Kingston Standardized Cognitive Assessment-Revised (KSCAr)17 or the mini-KSCAr.18
Recently, we reviewed cases of >70 individuals from our outpatient clinic who were given the MMSE and were also diagnosed as having dementia by both DSM-IV (Diagnostic and Statistical Manual of Mental Disorders)19 and the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association20 criteria. Over three-quarters (78%) of these cases had an MMSE score of ≥24. Based on MMSE scores alone, these individuals would have been declared “not demented.”17
Correcting for age and intelligence increases accuracy. Published age and education norms are available for the MMSE.21 In applying these norms to our sample described above, the number of misidentified patients drops to approximately one-third (35.7%). This means that instead of misidentifying 2 out of 3 cases, the age and education corrections reduced this to about one out of 3, thereby increasing sensitivity and specificity. While this is still an unacceptably high rate of false negatives, it shows the considerable value of using age and education corrections.
The challenge of optimizing sensitivity and specificity of dementia screening tools is ongoing. As a matter of interest, we include TABLE 1,4,18,22-24 which shows calculated sensitivities and specificities of some commonly used screening tests.
Another practical fix: Use distributions and percentile-based normative data
Instead of simple cutoff scores, test scores can be, and often are, translated into percentiles to provide a meaningful context for evaluation and to make it easier to compare scores between patients. Someone with a score at the 70th percentile has performed as well as or better than 70% of others in the group who have taken the test. Usually, the average range of a normal population is defined as being between the 25th to 75th percentiles, encompassing 50% of that population. In general, percentiles make interpreting performance easier. Percentile-based test norms can also help determine with increased accuracy if there has been a decline over time.
Illustration: Animal naming task. In a common version of this task, patients are asked to name as many animals as they can in 60 seconds. This task has its roots in neuro- psychological tests of verbal fluency, such as the Controlled Oral Word Association Task.25 Verbal fluency tasks such as naming animals tap verbal generativity/problem-solving and self-monitoring, but are also highly dependent on vocabulary (word knowledge), a cognitive ability that is quite stable and even improves as one ages until individuals are well into their 80s.26
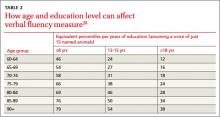
It is common practice with this procedure to consider a cutoff score of 15 as a minimally acceptable level of performance.27 Here again, there are potentially great differences in expected performance based on age and intelligence. TABLE 2 shows the effect of age and education on verbal fluency, expressed as percentiles, using a raw score of 15.28 For an individual in their early 60s who has a university degree, naming just 15 animals puts their performance at the 12th percentile (below average). The same performance for someone in their 90s who has only 8 years of education puts them in the 79th percentile (above the average range of 25th-75th percentiles). This performance would indicate impairment for the 60-year-old university-educated individual, but strong cognitive function for the 90-year-old.
Common error #2: Deviating from standardized procedures
While clinicians specifically trained in cognitive measurement are familiar with the rigor by which tests are constructed, those with less training are often unaware that even seemingly minor deviations in procedure can contaminate results as surely as using nonsterile containers in biologic testing, leading to inaccurate interpretations of cognition.
Practical fix: Administer tests using verbatim instructions
Failing to follow instructions can significantly bias acquired data, particularly when using performance tests that are timed.
Illustration: Trail Making Test. Trail Making is an old 2-part test developed for the United States Army in the 1940s,11 and used in the Halstead-Reitan neuropsychological battery. Part A is a timed measure of an individual’s ability to join up a series of numbered circles in ascending order. Part B measures the ability to alternately switch between 2 related tasks: namely, alternately joining numbered and lettered circles, in ascending order. This is considered a measure of complex attention, which is often disrupted in early dementia.29
The test uses a specific standardized set of instructions, and Part B’s interpretation depends on having first administered Part A. Anecdotally, we have increasingly seen clinician reports using only Part B. Eliminating Part A removes a significant opportunity for patients to become familiar with the task’s demands, placing them at a considerable disadvantage on Part B and thereby invalidating the normative data.
In addition, follow the exact phrasing of the instructions and use stimuli and response pages that are the same size as those provided in the manual. If a patient errs at any point, it’s important that the test administrator reads, verbatim, the provided correction statements because these statements influence the amount of time spent correcting an error and therefore the final score.
Common error #3: Using outdated normative data
Neglecting to use updated norms that reflect current cohort differences can compromise screening accuracy.
Practical fix: Ensure current norms are used for comparisons
Societal influences—computers and other technologies, nutrition, etc—have led to steady improvements in cognitive and physical abilities. In basic psychology, this pattern of improving cognition, documented as an approximate increase of 3 IQ points per decade, is referred to as the Flynn effect.30 Therefore, not only do age and education need to be controlled for, but normative data must be current.
Cognitive screening tools are usually published with norms compiled at the time of the test’s development. However, scores are periodically “re-normed” to reflect current levels of ability. These updated norms are readily available in published journal articles or online. (Current norms for each of the tests used as examples in this article are provided in the references).21,28,31
Illustration: Trail Making Test. The normative data for this test are not only age- and education-sensitive, but are also highly sensitive to cohort effects. Early norms such as those of Davies,32 while often still quoted in literature and even in some training initiatives, are now seriously outdated and should not be used for interpretation. TABLE 3 shows how an average individual (ie, 50th percentile) in the 1960s, in one of 2 age groups, would compare in speed to an individual of similar age today.31 A time score that was at the 50th percentile in 1968 is now at or below the 1st percentile. More recent norms are also usually corrected for education, as are those provided by Tombaugh.31
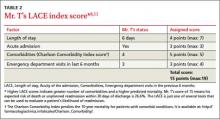
In “A 'case' for using optimal procedures” (below), TABLE 4 shows the results of using outdated Trail Making norms vs current Trail Making norms.
George is a 77-year-old retired school teacher with >15 years of education who was referred to us for complaints of memory loss and suspicion of progressive cognitive deficits. On cognitive screening he scored 26/30 on the Mini-Mental State Examination, generated 16 animal names in 60 seconds, and completed Parts A and B of the Trail Making test in 80 seconds and 196 seconds, respectively. TABLE 4 summarizes test scores and interpretation with and without appropriate corrections.
George’s case dramatically illustrates the clinical impact of using (or not using) optimal interpretive procedures—ie, age and education corrections and current (not outdated) norms. Using the basic cutoff scores without corrections, George’s performance is within acceptable limits on all 3 screening tests, and he is sent home with the comforting news that his performance was within normal limits. However, by using appropriate comparative data, the same scores on all 3 screens indicate impairment. A likely next step would be referral for specialized testing. Monitoring for progressive deterioration is advisable, and perhaps initiation of medication.
TABLE 4
Trail Making: Outdated norms vs current norms
| Version 1 – No corrections for age or education for MMSE or COWAT; outdated Trail Making norms | |||
| Test | Score | Results | Suggests dementia |
| MMSE | 26 | ≥24 within normal limits10 | No |
| COWAT | 16 | >15 within normal limits25 | No |
| Trail Making A | 80 secs | 50th percentile32 | No |
| Trail Making B | 196 secs | 50th percentile32 | No |
| Decision: Negative for dementia | |||
|
|
|
|
|
| Version 2 – Applied age and education corrections for MMSE and COWAT; current Trail Making norms | |||
| Test | Score | Results | Suggests dementia |
| MMSE | 26 | Expected = 2822 | Yes |
| COWAT | 16 | 38th percentile28 | Yes |
| Trail Making A | 80 secs | <1st percentile31 | Yes |
| Trail Making B | 196 secs | <2nd percentile31 | Yes |
| Decision: Positive for dementia | |||
COWAT, Controlled Oral Word Association Task; MMSE, Mini-Mental State Examination.
Patients deserve an accurate assessment
A diagnosis of dementia profoundly affects patients and families. Progressive dementia such as Alzheimer’s disease means an individual will spend the rest of his or her life (usually 8-10 years) with decreasing cognitive capacity and quality of life.33-35 It also means families will spend years providing or arranging for care, and watching their family member deteriorate. Early detection can afford affected individuals and families the opportunity to make plans for fulfilling wishes and dreams before increased impairment makes such plans unattainable. The importance of rigor in assessment is therefore essential.
Optimizing accuracy in screening for dementia also can enable physicians to reasonably reassure patients that they likely do not suffer from a dementia at the present time, or to at least recommend that they be further assessed by a specialist. Without rigor, time and resources are wasted and the important question that triggered the referral is neither satisfactorily—nor accurately—addressed. Thus, there is a need to use not just simple cutoff scores but to apply the most current age and education normative data, and adhere to administrative instructions verbatim.
CORRESPONDENCE
Lindy A. Kilik, PhD, Geriatric Psychiatry Program, Providence Care Mental Health Services, PO Bag 603, Kingston, Ontario, Canada K7L 4X3; [email protected]
1. Loveman E, Green C, Kirby J, et al. The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease. Health Technol Assess. 2006;10:iii-iv,ix- xi,1-160.
2. Medical Care Corporation. Delaying the onset and progression of Alzheimer’s disease. Prevent AD Web site. Available at: http://www.preventad.com/pdf/support/article/DelayingADProgression.pdf. Accessed June 18, 2014.
3. Hopkins RW. Dementia projections for the counties, regional municipalities and districts of Ontario. Geriatric Psychiatry Unit Clinical/Research Bulletin, No. 16. Providence Care Web site. Available at: http://www.providencecare.ca/clinical-tools/Documents/Ontario-Dementia-Projections-2010.pdf. Accessed June 18, 2014.
4. Simmons BB, Hartmann B, Dejoseph D. Evaluation of suspected dementia. Am Fam Physician. 2011;84:895-902.
5. McCarten JR, Borson S. Should family physicians routinely screen patients for cognitive impairment? Yes: screening is the first step toward improving care. Am Fam Physician. 2014;89: 861-862.
6. Alzheimer’s Association. Health Care Professionals and Alzheimer’s. Alzheimer’s Association Web site. Available at: http://www.alz.org/health-care-professionals/cognitive-tests-patient-assessment.asp. Accessed June 18, 2014.
7. US Preventive Services Task Force. Screening for cognitive impairment in older adults. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsdeme.htm. Accessed June 18, 2014.
8. Hopkins RW, Kilik LA, Day D, et al. Kingston Standardized Behavioural Assessment. Am J Alzheimers Dis Other Demen. 2006;21:339-346.
9. Kilik LA, Hopkins RW, Day D, et al. The progression of behaviour in dementia: an in-office guide for clinicians. Am J Alzheimers Dis Other Demen. 2008;23:242-249.
10. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189-198.
11. Army Individual Test Battery. Manual of Directions and Scoring. Washington, DC: War Department, Adjutant General’s Office; 1944.
12. Wechsler D. The Measurement and Appraisal of Adult Intelligence. 4th ed. The Williams & Wilkins Company: Baltimore, MD; 1958.
13. Larrabee GJ, Largen JW, Levin HS. Sensitivity of age-decline resistant (“hold”) WAIS subtests to Alzheimer’s disease. J Clin Exp Neuropsychol. 1985;7:497-504.
14. Herndon RM. Assessment of the elderly with dementia. In: Handbook of Neurologic Rating Scales. 2nd ed. Demos Medical Publishing LLC: New York, NY; 2006:199.
15. Brugnolo A, Nobili F, Barbieri MP, et al. The factorial structure of the mini mental state examination (MMSE) in Alzheimer’s disease. Arch Gerontol Geriatr. 2009;49:180-185.
16. Folstein M, Anthony JC, Parhad I, et al. The meaning of cognitive impairment in the elderly. J Am Geriatr Soc. 1985;33:228-235.
17. Hopkins RW, Kilik LA, Day DJ, et al. The Revised Kingston Standardized Cognitive Assessment. Int J Geriatr Psychiatry. 2004;19:320-326.
18. Hopkins R, Kilik L. The mini-Kingston Standardized Cognitive Assessment. Kingston Scales Web site. Available at: http://www.kingstonscales.org. Accessed June 18, 2014.
19. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994.
20. McKhann G, Drachman D, Folstein M, et al. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34: 939-944.
21. Crum RM, Anthony JC, Bassett SS, et al. Population-based norms for the Mini-Mental State Examination by age and educational level. JAMA. 1993;269:2386-2391.
22. O’Bryant SE, Humphreys JD, Smith GE, et al. Detecting dementia with the mini-mental state examination in highly educated individuals. Arch Neurol. 2008;65:963-967.
23. O’Sullivan M, Morris RG, Markus HS. Brief cognitive assessment for patients with cerebral small vessel disease. J Neurol Neurosurg Psychiatry. 2005;76:1140-1145.
24. Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment (MoCA): a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695-699.
25. Benton AL, Hamsher K. Multilingual Aphasia Examination. 2nd ed. Iowa City, OA: AJA Associates, Inc; 1976.
26. Wechsler D. WAIS-III Administration and Scoring Manual. San Antonio, TX: The Psychological Corporation; 1997.
27. Morris JC, Heyman A, Mohs RC, et al. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part I. Clinical and neuropsychological assesment of Alzheimer’s disease. Neurology. 1989;39:1159-1165.
28. Gladsjo JA, Miller SW, Heaton RK. Norms for Letter and Category Fluency: Demographic Corrections for Age, Education and Ethnicity. Odessa, FL: Psychological Assessment Resources; 1999.
29. Perry R, Hodges J. Attention and executive deficits in Alzheimer’s disease. A critical review. Brain. 1999;122(pt 3):383-404.
30. Flynn JR. The mean IQ of Americans: Massive gains 1932 to 1978. Psychol Bull. 1984;95:29-51.
31. Tombaugh TN. Trail Making Test A and B: normative data stratified by age and education. Arch Clin Neuropsychol. 2004;19: 203-214.
32. Davies A. The influence of age on trail making test performance. J Clin Psychol. 1968;24:96-98.
33. Bianchetti A, Trabucch M. Clinical aspects of Alzheimer’s disease. Aging (Milano). 2001;13:221-230.
34. Kay D, Forster DP, Newens AJ. Long-term survival, place of death, and death certification in clinically diagnosed pre-senile dementia in northern England. Follow-up after 8-12 years. Br J Psychiatry. 2000;177:156-162.
35. Chaussalet T, Thompson WA. Data requirements in a model of the natural history of Alzheimer’s disease. Health Care Manag Sci. 2001;4:13-19.
› Use age- and education-corrected normative data when using dementia screening tools. C
› Use verbatim instructions and the same size stimuli and response pages provided in a test’s manual. C
› Ensure that norms used for comparisons are current. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Treatment options for dementia are expanding and improving, giving extra impetus to detecting this progressive disease as early as possible. For example, research on the cholinesterase inhibitor donepezil has shown it can delay cognitive decline by 6 months or more compared with controls1,2 and possibly postpone institutionalization. With the number of elderly individuals and cases of dementia projected to grow significantly over the next 20 years,3 primary care physicians will increasingly be screening for cognitive impairment. Given the time constraints and patient loads in today’s practices, it’s not surprising that physicians tend to use evaluation tools that are brief and simple to administer. However, there are also serious pitfalls in the use of these tools.
When to screen. Many health-related organizations address screening for dementia4,5 and offer screening criteria (eg, the Alzheimer’s Association,6 the US Preventive Services Task Force7). Our experience suggests that specific behavioral changes are reasonable indicators of suspected dementia that should prompt cognitive screening. Using the Kingston Standardized Behavioural Assessment,8 we demonstrated a consistent pattern of earliest behavior change in a community-dwelling group with dementia.9 Meaningful clues are a decreased ability to engage in specific functional activities (including participation in favorite pastimes, ability to eat properly if left to prepare one’s own food, handling of personal finances, word finding, and reading) and unsteadiness. These specific behavioral changes reported by family or a caregiver suggest the need for cognitive screening.
Pitfalls associated with common screening tools, if not taken into account, can seriously limit the usefulness of information gained during assessment and potentially lead to a wrong conclusion. Screening tools are just that: a means of detecting the possible existence of a condition. Results are based on probability and subject to error. Therefore, a single test score is insufficient to render a diagnosis of dementia, and is one variable in a set of diagnostic criteria.
The purpose of this article is to review some of the most commonly used tools and procedures for dementia screening, identify procedural or interpretive errors made in everyday clinical practice, and suggest practical yet simple strategies to address these problems and improve the accuracy of assessments. We illustrate key points with clinical examples and vignettes using the Mini-Mental State Examination (MMSE),10 an Animal Naming Task, and the Trail Making Test.11
Common error #1: Reliance on simple, single cutoff scores
There are a number of important considerations to keep in mind when trying to make sense of scores from the many available cognitive tests.
The range of normal test results is wide. The normal range for most physiologic measures, such as glucose levels or hemoglobin counts, is relatively narrow. However, human cognitive functions can naturally differ from person to person, and the range of normal can be extremely large.
A single, all-purpose cutoff score ignores critical factors. Very often, clinicians have dealt with the issue of wide variance in cognition scores by establishing a general cutoff point to serve as a pass-fail mark. But this practice can result in both under- and overidentification of dementia, and it ignores the 2 components that chiefly determine how individuals differ cognitively: age and intelligence.
Practical fix: Use age-, intelligence-corrected normative data
Level of cognitive performance can be revealing when adjustments are made for age and intelligence. Not taking these factors into account can lead to many errors in clinical decision making.
Age matters. Many cognitive capacities decline as part of normal aging even in otherwise healthy individuals (eg, reaction time, spatial abilities, flexibility in novel problem solving).12 With this in mind, psychologists often have made the distinction between “hold” tests (remaining stable or even improving with age) and “no-hold” tests (declining with age).13 Therefore it is critical to ask, “What is normal, given a particular patient’s age?” If normative data corrected for age are available for a given test, use them.
Intelligence is a factor, too. Intelligence, like most human qualities, is distributed along a bell-shaped curve of normal distribution, wherein most people fall somewhere in the middle and a smaller number will be at the lower and higher tails of the curve. Not all of us fall into the average range of intelligence; indeed, psychometrically, only half of us do. The other half are found somewhere in the more extreme ends. In evaluating a person for dementia, it is critical to compare test results with those found in the appropriate intellectual group. But how does the physician looking for a brief assessment strategy determine a patient’s premorbid level of intellectual functioning?
A widely used and accepted heuristic for gauging intelligence is “years of education.” Of course, education is not perfectly correlated with intelligence, particularly as those who are now elderly may have been denied the opportunity to attend school due to the Great Depression, war, or other life events. Nevertheless, with these limitations in mind, level of education is a reasonable approximation of intelligence. In practical application, premorbid intellectual level is determined by using education-corrected normative data.
Typically with cognitive tests, cutoff scores and score ranges are defined for general levels of education (eg, less than grade 12 or more than grade 12; elementary school, high school, post-secondary, etc). Adjusted norms for age and education are usually determined by taking large samples of subjects and stratifying the distribution by subgroups—eg, 5-year age groups; levels of education such as elementary school or high school—and then statistically analyzing each group and noting the relative differences between them.
Illustration: MMSE. Although not designed for the overall measurement of cognitive impairment in dementia, the MMSE10 has become widely used for that purpose. It is fairly insensitive to cognitive changes associated with earlier stages of dementia,14 and is intended only as a means of identifying patients in need of more comprehensive assessment. However, the MMSE is increasingly used to make a diagnosis of dementia.15 In some areas (eg, Ontario, Canada), it is used to justify paying for treatment with cognitive enhancers.
The universal cutoff score proves inadequate. Although several dementia cutoff scores for the MMSE have been proposed, it is common practice to use an MMSE score ≥24 to rule out dementia.16 In our clinical practice, however, many patients who ultimately are diagnosed with early dementia often perform well on the MMSE, although rather poorly on other dementia screens, such as the Kingston Standardized Cognitive Assessment-Revised (KSCAr)17 or the mini-KSCAr.18
Recently, we reviewed cases of >70 individuals from our outpatient clinic who were given the MMSE and were also diagnosed as having dementia by both DSM-IV (Diagnostic and Statistical Manual of Mental Disorders)19 and the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association20 criteria. Over three-quarters (78%) of these cases had an MMSE score of ≥24. Based on MMSE scores alone, these individuals would have been declared “not demented.”17
Correcting for age and intelligence increases accuracy. Published age and education norms are available for the MMSE.21 In applying these norms to our sample described above, the number of misidentified patients drops to approximately one-third (35.7%). This means that instead of misidentifying 2 out of 3 cases, the age and education corrections reduced this to about one out of 3, thereby increasing sensitivity and specificity. While this is still an unacceptably high rate of false negatives, it shows the considerable value of using age and education corrections.
The challenge of optimizing sensitivity and specificity of dementia screening tools is ongoing. As a matter of interest, we include TABLE 1,4,18,22-24 which shows calculated sensitivities and specificities of some commonly used screening tests.
Another practical fix: Use distributions and percentile-based normative data
Instead of simple cutoff scores, test scores can be, and often are, translated into percentiles to provide a meaningful context for evaluation and to make it easier to compare scores between patients. Someone with a score at the 70th percentile has performed as well as or better than 70% of others in the group who have taken the test. Usually, the average range of a normal population is defined as being between the 25th to 75th percentiles, encompassing 50% of that population. In general, percentiles make interpreting performance easier. Percentile-based test norms can also help determine with increased accuracy if there has been a decline over time.
Illustration: Animal naming task. In a common version of this task, patients are asked to name as many animals as they can in 60 seconds. This task has its roots in neuro- psychological tests of verbal fluency, such as the Controlled Oral Word Association Task.25 Verbal fluency tasks such as naming animals tap verbal generativity/problem-solving and self-monitoring, but are also highly dependent on vocabulary (word knowledge), a cognitive ability that is quite stable and even improves as one ages until individuals are well into their 80s.26
It is common practice with this procedure to consider a cutoff score of 15 as a minimally acceptable level of performance.27 Here again, there are potentially great differences in expected performance based on age and intelligence. TABLE 2 shows the effect of age and education on verbal fluency, expressed as percentiles, using a raw score of 15.28 For an individual in their early 60s who has a university degree, naming just 15 animals puts their performance at the 12th percentile (below average). The same performance for someone in their 90s who has only 8 years of education puts them in the 79th percentile (above the average range of 25th-75th percentiles). This performance would indicate impairment for the 60-year-old university-educated individual, but strong cognitive function for the 90-year-old.
Common error #2: Deviating from standardized procedures
While clinicians specifically trained in cognitive measurement are familiar with the rigor by which tests are constructed, those with less training are often unaware that even seemingly minor deviations in procedure can contaminate results as surely as using nonsterile containers in biologic testing, leading to inaccurate interpretations of cognition.
Practical fix: Administer tests using verbatim instructions
Failing to follow instructions can significantly bias acquired data, particularly when using performance tests that are timed.
Illustration: Trail Making Test. Trail Making is an old 2-part test developed for the United States Army in the 1940s,11 and used in the Halstead-Reitan neuropsychological battery. Part A is a timed measure of an individual’s ability to join up a series of numbered circles in ascending order. Part B measures the ability to alternately switch between 2 related tasks: namely, alternately joining numbered and lettered circles, in ascending order. This is considered a measure of complex attention, which is often disrupted in early dementia.29
The test uses a specific standardized set of instructions, and Part B’s interpretation depends on having first administered Part A. Anecdotally, we have increasingly seen clinician reports using only Part B. Eliminating Part A removes a significant opportunity for patients to become familiar with the task’s demands, placing them at a considerable disadvantage on Part B and thereby invalidating the normative data.
In addition, follow the exact phrasing of the instructions and use stimuli and response pages that are the same size as those provided in the manual. If a patient errs at any point, it’s important that the test administrator reads, verbatim, the provided correction statements because these statements influence the amount of time spent correcting an error and therefore the final score.
Common error #3: Using outdated normative data
Neglecting to use updated norms that reflect current cohort differences can compromise screening accuracy.
Practical fix: Ensure current norms are used for comparisons
Societal influences—computers and other technologies, nutrition, etc—have led to steady improvements in cognitive and physical abilities. In basic psychology, this pattern of improving cognition, documented as an approximate increase of 3 IQ points per decade, is referred to as the Flynn effect.30 Therefore, not only do age and education need to be controlled for, but normative data must be current.
Cognitive screening tools are usually published with norms compiled at the time of the test’s development. However, scores are periodically “re-normed” to reflect current levels of ability. These updated norms are readily available in published journal articles or online. (Current norms for each of the tests used as examples in this article are provided in the references).21,28,31
Illustration: Trail Making Test. The normative data for this test are not only age- and education-sensitive, but are also highly sensitive to cohort effects. Early norms such as those of Davies,32 while often still quoted in literature and even in some training initiatives, are now seriously outdated and should not be used for interpretation. TABLE 3 shows how an average individual (ie, 50th percentile) in the 1960s, in one of 2 age groups, would compare in speed to an individual of similar age today.31 A time score that was at the 50th percentile in 1968 is now at or below the 1st percentile. More recent norms are also usually corrected for education, as are those provided by Tombaugh.31
In “A 'case' for using optimal procedures” (below), TABLE 4 shows the results of using outdated Trail Making norms vs current Trail Making norms.
George is a 77-year-old retired school teacher with >15 years of education who was referred to us for complaints of memory loss and suspicion of progressive cognitive deficits. On cognitive screening he scored 26/30 on the Mini-Mental State Examination, generated 16 animal names in 60 seconds, and completed Parts A and B of the Trail Making test in 80 seconds and 196 seconds, respectively. TABLE 4 summarizes test scores and interpretation with and without appropriate corrections.
George’s case dramatically illustrates the clinical impact of using (or not using) optimal interpretive procedures—ie, age and education corrections and current (not outdated) norms. Using the basic cutoff scores without corrections, George’s performance is within acceptable limits on all 3 screening tests, and he is sent home with the comforting news that his performance was within normal limits. However, by using appropriate comparative data, the same scores on all 3 screens indicate impairment. A likely next step would be referral for specialized testing. Monitoring for progressive deterioration is advisable, and perhaps initiation of medication.
TABLE 4
Trail Making: Outdated norms vs current norms
| Version 1 – No corrections for age or education for MMSE or COWAT; outdated Trail Making norms | |||
| Test | Score | Results | Suggests dementia |
| MMSE | 26 | ≥24 within normal limits10 | No |
| COWAT | 16 | >15 within normal limits25 | No |
| Trail Making A | 80 secs | 50th percentile32 | No |
| Trail Making B | 196 secs | 50th percentile32 | No |
| Decision: Negative for dementia | |||
|
|
|
|
|
| Version 2 – Applied age and education corrections for MMSE and COWAT; current Trail Making norms | |||
| Test | Score | Results | Suggests dementia |
| MMSE | 26 | Expected = 2822 | Yes |
| COWAT | 16 | 38th percentile28 | Yes |
| Trail Making A | 80 secs | <1st percentile31 | Yes |
| Trail Making B | 196 secs | <2nd percentile31 | Yes |
| Decision: Positive for dementia | |||
COWAT, Controlled Oral Word Association Task; MMSE, Mini-Mental State Examination.
Patients deserve an accurate assessment
A diagnosis of dementia profoundly affects patients and families. Progressive dementia such as Alzheimer’s disease means an individual will spend the rest of his or her life (usually 8-10 years) with decreasing cognitive capacity and quality of life.33-35 It also means families will spend years providing or arranging for care, and watching their family member deteriorate. Early detection can afford affected individuals and families the opportunity to make plans for fulfilling wishes and dreams before increased impairment makes such plans unattainable. The importance of rigor in assessment is therefore essential.
Optimizing accuracy in screening for dementia also can enable physicians to reasonably reassure patients that they likely do not suffer from a dementia at the present time, or to at least recommend that they be further assessed by a specialist. Without rigor, time and resources are wasted and the important question that triggered the referral is neither satisfactorily—nor accurately—addressed. Thus, there is a need to use not just simple cutoff scores but to apply the most current age and education normative data, and adhere to administrative instructions verbatim.
CORRESPONDENCE
Lindy A. Kilik, PhD, Geriatric Psychiatry Program, Providence Care Mental Health Services, PO Bag 603, Kingston, Ontario, Canada K7L 4X3; [email protected]
› Use age- and education-corrected normative data when using dementia screening tools. C
› Use verbatim instructions and the same size stimuli and response pages provided in a test’s manual. C
› Ensure that norms used for comparisons are current. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Treatment options for dementia are expanding and improving, giving extra impetus to detecting this progressive disease as early as possible. For example, research on the cholinesterase inhibitor donepezil has shown it can delay cognitive decline by 6 months or more compared with controls1,2 and possibly postpone institutionalization. With the number of elderly individuals and cases of dementia projected to grow significantly over the next 20 years,3 primary care physicians will increasingly be screening for cognitive impairment. Given the time constraints and patient loads in today’s practices, it’s not surprising that physicians tend to use evaluation tools that are brief and simple to administer. However, there are also serious pitfalls in the use of these tools.
When to screen. Many health-related organizations address screening for dementia4,5 and offer screening criteria (eg, the Alzheimer’s Association,6 the US Preventive Services Task Force7). Our experience suggests that specific behavioral changes are reasonable indicators of suspected dementia that should prompt cognitive screening. Using the Kingston Standardized Behavioural Assessment,8 we demonstrated a consistent pattern of earliest behavior change in a community-dwelling group with dementia.9 Meaningful clues are a decreased ability to engage in specific functional activities (including participation in favorite pastimes, ability to eat properly if left to prepare one’s own food, handling of personal finances, word finding, and reading) and unsteadiness. These specific behavioral changes reported by family or a caregiver suggest the need for cognitive screening.
Pitfalls associated with common screening tools, if not taken into account, can seriously limit the usefulness of information gained during assessment and potentially lead to a wrong conclusion. Screening tools are just that: a means of detecting the possible existence of a condition. Results are based on probability and subject to error. Therefore, a single test score is insufficient to render a diagnosis of dementia, and is one variable in a set of diagnostic criteria.
The purpose of this article is to review some of the most commonly used tools and procedures for dementia screening, identify procedural or interpretive errors made in everyday clinical practice, and suggest practical yet simple strategies to address these problems and improve the accuracy of assessments. We illustrate key points with clinical examples and vignettes using the Mini-Mental State Examination (MMSE),10 an Animal Naming Task, and the Trail Making Test.11
Common error #1: Reliance on simple, single cutoff scores
There are a number of important considerations to keep in mind when trying to make sense of scores from the many available cognitive tests.
The range of normal test results is wide. The normal range for most physiologic measures, such as glucose levels or hemoglobin counts, is relatively narrow. However, human cognitive functions can naturally differ from person to person, and the range of normal can be extremely large.
A single, all-purpose cutoff score ignores critical factors. Very often, clinicians have dealt with the issue of wide variance in cognition scores by establishing a general cutoff point to serve as a pass-fail mark. But this practice can result in both under- and overidentification of dementia, and it ignores the 2 components that chiefly determine how individuals differ cognitively: age and intelligence.
Practical fix: Use age-, intelligence-corrected normative data
Level of cognitive performance can be revealing when adjustments are made for age and intelligence. Not taking these factors into account can lead to many errors in clinical decision making.
Age matters. Many cognitive capacities decline as part of normal aging even in otherwise healthy individuals (eg, reaction time, spatial abilities, flexibility in novel problem solving).12 With this in mind, psychologists often have made the distinction between “hold” tests (remaining stable or even improving with age) and “no-hold” tests (declining with age).13 Therefore it is critical to ask, “What is normal, given a particular patient’s age?” If normative data corrected for age are available for a given test, use them.
Intelligence is a factor, too. Intelligence, like most human qualities, is distributed along a bell-shaped curve of normal distribution, wherein most people fall somewhere in the middle and a smaller number will be at the lower and higher tails of the curve. Not all of us fall into the average range of intelligence; indeed, psychometrically, only half of us do. The other half are found somewhere in the more extreme ends. In evaluating a person for dementia, it is critical to compare test results with those found in the appropriate intellectual group. But how does the physician looking for a brief assessment strategy determine a patient’s premorbid level of intellectual functioning?
A widely used and accepted heuristic for gauging intelligence is “years of education.” Of course, education is not perfectly correlated with intelligence, particularly as those who are now elderly may have been denied the opportunity to attend school due to the Great Depression, war, or other life events. Nevertheless, with these limitations in mind, level of education is a reasonable approximation of intelligence. In practical application, premorbid intellectual level is determined by using education-corrected normative data.
Typically with cognitive tests, cutoff scores and score ranges are defined for general levels of education (eg, less than grade 12 or more than grade 12; elementary school, high school, post-secondary, etc). Adjusted norms for age and education are usually determined by taking large samples of subjects and stratifying the distribution by subgroups—eg, 5-year age groups; levels of education such as elementary school or high school—and then statistically analyzing each group and noting the relative differences between them.
Illustration: MMSE. Although not designed for the overall measurement of cognitive impairment in dementia, the MMSE10 has become widely used for that purpose. It is fairly insensitive to cognitive changes associated with earlier stages of dementia,14 and is intended only as a means of identifying patients in need of more comprehensive assessment. However, the MMSE is increasingly used to make a diagnosis of dementia.15 In some areas (eg, Ontario, Canada), it is used to justify paying for treatment with cognitive enhancers.
The universal cutoff score proves inadequate. Although several dementia cutoff scores for the MMSE have been proposed, it is common practice to use an MMSE score ≥24 to rule out dementia.16 In our clinical practice, however, many patients who ultimately are diagnosed with early dementia often perform well on the MMSE, although rather poorly on other dementia screens, such as the Kingston Standardized Cognitive Assessment-Revised (KSCAr)17 or the mini-KSCAr.18
Recently, we reviewed cases of >70 individuals from our outpatient clinic who were given the MMSE and were also diagnosed as having dementia by both DSM-IV (Diagnostic and Statistical Manual of Mental Disorders)19 and the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association20 criteria. Over three-quarters (78%) of these cases had an MMSE score of ≥24. Based on MMSE scores alone, these individuals would have been declared “not demented.”17
Correcting for age and intelligence increases accuracy. Published age and education norms are available for the MMSE.21 In applying these norms to our sample described above, the number of misidentified patients drops to approximately one-third (35.7%). This means that instead of misidentifying 2 out of 3 cases, the age and education corrections reduced this to about one out of 3, thereby increasing sensitivity and specificity. While this is still an unacceptably high rate of false negatives, it shows the considerable value of using age and education corrections.
The challenge of optimizing sensitivity and specificity of dementia screening tools is ongoing. As a matter of interest, we include TABLE 1,4,18,22-24 which shows calculated sensitivities and specificities of some commonly used screening tests.
Another practical fix: Use distributions and percentile-based normative data
Instead of simple cutoff scores, test scores can be, and often are, translated into percentiles to provide a meaningful context for evaluation and to make it easier to compare scores between patients. Someone with a score at the 70th percentile has performed as well as or better than 70% of others in the group who have taken the test. Usually, the average range of a normal population is defined as being between the 25th to 75th percentiles, encompassing 50% of that population. In general, percentiles make interpreting performance easier. Percentile-based test norms can also help determine with increased accuracy if there has been a decline over time.
Illustration: Animal naming task. In a common version of this task, patients are asked to name as many animals as they can in 60 seconds. This task has its roots in neuro- psychological tests of verbal fluency, such as the Controlled Oral Word Association Task.25 Verbal fluency tasks such as naming animals tap verbal generativity/problem-solving and self-monitoring, but are also highly dependent on vocabulary (word knowledge), a cognitive ability that is quite stable and even improves as one ages until individuals are well into their 80s.26
It is common practice with this procedure to consider a cutoff score of 15 as a minimally acceptable level of performance.27 Here again, there are potentially great differences in expected performance based on age and intelligence. TABLE 2 shows the effect of age and education on verbal fluency, expressed as percentiles, using a raw score of 15.28 For an individual in their early 60s who has a university degree, naming just 15 animals puts their performance at the 12th percentile (below average). The same performance for someone in their 90s who has only 8 years of education puts them in the 79th percentile (above the average range of 25th-75th percentiles). This performance would indicate impairment for the 60-year-old university-educated individual, but strong cognitive function for the 90-year-old.
Common error #2: Deviating from standardized procedures
While clinicians specifically trained in cognitive measurement are familiar with the rigor by which tests are constructed, those with less training are often unaware that even seemingly minor deviations in procedure can contaminate results as surely as using nonsterile containers in biologic testing, leading to inaccurate interpretations of cognition.
Practical fix: Administer tests using verbatim instructions
Failing to follow instructions can significantly bias acquired data, particularly when using performance tests that are timed.
Illustration: Trail Making Test. Trail Making is an old 2-part test developed for the United States Army in the 1940s,11 and used in the Halstead-Reitan neuropsychological battery. Part A is a timed measure of an individual’s ability to join up a series of numbered circles in ascending order. Part B measures the ability to alternately switch between 2 related tasks: namely, alternately joining numbered and lettered circles, in ascending order. This is considered a measure of complex attention, which is often disrupted in early dementia.29
The test uses a specific standardized set of instructions, and Part B’s interpretation depends on having first administered Part A. Anecdotally, we have increasingly seen clinician reports using only Part B. Eliminating Part A removes a significant opportunity for patients to become familiar with the task’s demands, placing them at a considerable disadvantage on Part B and thereby invalidating the normative data.
In addition, follow the exact phrasing of the instructions and use stimuli and response pages that are the same size as those provided in the manual. If a patient errs at any point, it’s important that the test administrator reads, verbatim, the provided correction statements because these statements influence the amount of time spent correcting an error and therefore the final score.
Common error #3: Using outdated normative data
Neglecting to use updated norms that reflect current cohort differences can compromise screening accuracy.
Practical fix: Ensure current norms are used for comparisons
Societal influences—computers and other technologies, nutrition, etc—have led to steady improvements in cognitive and physical abilities. In basic psychology, this pattern of improving cognition, documented as an approximate increase of 3 IQ points per decade, is referred to as the Flynn effect.30 Therefore, not only do age and education need to be controlled for, but normative data must be current.
Cognitive screening tools are usually published with norms compiled at the time of the test’s development. However, scores are periodically “re-normed” to reflect current levels of ability. These updated norms are readily available in published journal articles or online. (Current norms for each of the tests used as examples in this article are provided in the references).21,28,31
Illustration: Trail Making Test. The normative data for this test are not only age- and education-sensitive, but are also highly sensitive to cohort effects. Early norms such as those of Davies,32 while often still quoted in literature and even in some training initiatives, are now seriously outdated and should not be used for interpretation. TABLE 3 shows how an average individual (ie, 50th percentile) in the 1960s, in one of 2 age groups, would compare in speed to an individual of similar age today.31 A time score that was at the 50th percentile in 1968 is now at or below the 1st percentile. More recent norms are also usually corrected for education, as are those provided by Tombaugh.31
In “A 'case' for using optimal procedures” (below), TABLE 4 shows the results of using outdated Trail Making norms vs current Trail Making norms.
George is a 77-year-old retired school teacher with >15 years of education who was referred to us for complaints of memory loss and suspicion of progressive cognitive deficits. On cognitive screening he scored 26/30 on the Mini-Mental State Examination, generated 16 animal names in 60 seconds, and completed Parts A and B of the Trail Making test in 80 seconds and 196 seconds, respectively. TABLE 4 summarizes test scores and interpretation with and without appropriate corrections.
George’s case dramatically illustrates the clinical impact of using (or not using) optimal interpretive procedures—ie, age and education corrections and current (not outdated) norms. Using the basic cutoff scores without corrections, George’s performance is within acceptable limits on all 3 screening tests, and he is sent home with the comforting news that his performance was within normal limits. However, by using appropriate comparative data, the same scores on all 3 screens indicate impairment. A likely next step would be referral for specialized testing. Monitoring for progressive deterioration is advisable, and perhaps initiation of medication.
TABLE 4
Trail Making: Outdated norms vs current norms
| Version 1 – No corrections for age or education for MMSE or COWAT; outdated Trail Making norms | |||
| Test | Score | Results | Suggests dementia |
| MMSE | 26 | ≥24 within normal limits10 | No |
| COWAT | 16 | >15 within normal limits25 | No |
| Trail Making A | 80 secs | 50th percentile32 | No |
| Trail Making B | 196 secs | 50th percentile32 | No |
| Decision: Negative for dementia | |||
|
|
|
|
|
| Version 2 – Applied age and education corrections for MMSE and COWAT; current Trail Making norms | |||
| Test | Score | Results | Suggests dementia |
| MMSE | 26 | Expected = 2822 | Yes |
| COWAT | 16 | 38th percentile28 | Yes |
| Trail Making A | 80 secs | <1st percentile31 | Yes |
| Trail Making B | 196 secs | <2nd percentile31 | Yes |
| Decision: Positive for dementia | |||
COWAT, Controlled Oral Word Association Task; MMSE, Mini-Mental State Examination.
Patients deserve an accurate assessment
A diagnosis of dementia profoundly affects patients and families. Progressive dementia such as Alzheimer’s disease means an individual will spend the rest of his or her life (usually 8-10 years) with decreasing cognitive capacity and quality of life.33-35 It also means families will spend years providing or arranging for care, and watching their family member deteriorate. Early detection can afford affected individuals and families the opportunity to make plans for fulfilling wishes and dreams before increased impairment makes such plans unattainable. The importance of rigor in assessment is therefore essential.
Optimizing accuracy in screening for dementia also can enable physicians to reasonably reassure patients that they likely do not suffer from a dementia at the present time, or to at least recommend that they be further assessed by a specialist. Without rigor, time and resources are wasted and the important question that triggered the referral is neither satisfactorily—nor accurately—addressed. Thus, there is a need to use not just simple cutoff scores but to apply the most current age and education normative data, and adhere to administrative instructions verbatim.
CORRESPONDENCE
Lindy A. Kilik, PhD, Geriatric Psychiatry Program, Providence Care Mental Health Services, PO Bag 603, Kingston, Ontario, Canada K7L 4X3; [email protected]
1. Loveman E, Green C, Kirby J, et al. The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease. Health Technol Assess. 2006;10:iii-iv,ix- xi,1-160.
2. Medical Care Corporation. Delaying the onset and progression of Alzheimer’s disease. Prevent AD Web site. Available at: http://www.preventad.com/pdf/support/article/DelayingADProgression.pdf. Accessed June 18, 2014.
3. Hopkins RW. Dementia projections for the counties, regional municipalities and districts of Ontario. Geriatric Psychiatry Unit Clinical/Research Bulletin, No. 16. Providence Care Web site. Available at: http://www.providencecare.ca/clinical-tools/Documents/Ontario-Dementia-Projections-2010.pdf. Accessed June 18, 2014.
4. Simmons BB, Hartmann B, Dejoseph D. Evaluation of suspected dementia. Am Fam Physician. 2011;84:895-902.
5. McCarten JR, Borson S. Should family physicians routinely screen patients for cognitive impairment? Yes: screening is the first step toward improving care. Am Fam Physician. 2014;89: 861-862.
6. Alzheimer’s Association. Health Care Professionals and Alzheimer’s. Alzheimer’s Association Web site. Available at: http://www.alz.org/health-care-professionals/cognitive-tests-patient-assessment.asp. Accessed June 18, 2014.
7. US Preventive Services Task Force. Screening for cognitive impairment in older adults. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsdeme.htm. Accessed June 18, 2014.
8. Hopkins RW, Kilik LA, Day D, et al. Kingston Standardized Behavioural Assessment. Am J Alzheimers Dis Other Demen. 2006;21:339-346.
9. Kilik LA, Hopkins RW, Day D, et al. The progression of behaviour in dementia: an in-office guide for clinicians. Am J Alzheimers Dis Other Demen. 2008;23:242-249.
10. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189-198.
11. Army Individual Test Battery. Manual of Directions and Scoring. Washington, DC: War Department, Adjutant General’s Office; 1944.
12. Wechsler D. The Measurement and Appraisal of Adult Intelligence. 4th ed. The Williams & Wilkins Company: Baltimore, MD; 1958.
13. Larrabee GJ, Largen JW, Levin HS. Sensitivity of age-decline resistant (“hold”) WAIS subtests to Alzheimer’s disease. J Clin Exp Neuropsychol. 1985;7:497-504.
14. Herndon RM. Assessment of the elderly with dementia. In: Handbook of Neurologic Rating Scales. 2nd ed. Demos Medical Publishing LLC: New York, NY; 2006:199.
15. Brugnolo A, Nobili F, Barbieri MP, et al. The factorial structure of the mini mental state examination (MMSE) in Alzheimer’s disease. Arch Gerontol Geriatr. 2009;49:180-185.
16. Folstein M, Anthony JC, Parhad I, et al. The meaning of cognitive impairment in the elderly. J Am Geriatr Soc. 1985;33:228-235.
17. Hopkins RW, Kilik LA, Day DJ, et al. The Revised Kingston Standardized Cognitive Assessment. Int J Geriatr Psychiatry. 2004;19:320-326.
18. Hopkins R, Kilik L. The mini-Kingston Standardized Cognitive Assessment. Kingston Scales Web site. Available at: http://www.kingstonscales.org. Accessed June 18, 2014.
19. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994.
20. McKhann G, Drachman D, Folstein M, et al. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34: 939-944.
21. Crum RM, Anthony JC, Bassett SS, et al. Population-based norms for the Mini-Mental State Examination by age and educational level. JAMA. 1993;269:2386-2391.
22. O’Bryant SE, Humphreys JD, Smith GE, et al. Detecting dementia with the mini-mental state examination in highly educated individuals. Arch Neurol. 2008;65:963-967.
23. O’Sullivan M, Morris RG, Markus HS. Brief cognitive assessment for patients with cerebral small vessel disease. J Neurol Neurosurg Psychiatry. 2005;76:1140-1145.
24. Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment (MoCA): a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695-699.
25. Benton AL, Hamsher K. Multilingual Aphasia Examination. 2nd ed. Iowa City, OA: AJA Associates, Inc; 1976.
26. Wechsler D. WAIS-III Administration and Scoring Manual. San Antonio, TX: The Psychological Corporation; 1997.
27. Morris JC, Heyman A, Mohs RC, et al. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part I. Clinical and neuropsychological assesment of Alzheimer’s disease. Neurology. 1989;39:1159-1165.
28. Gladsjo JA, Miller SW, Heaton RK. Norms for Letter and Category Fluency: Demographic Corrections for Age, Education and Ethnicity. Odessa, FL: Psychological Assessment Resources; 1999.
29. Perry R, Hodges J. Attention and executive deficits in Alzheimer’s disease. A critical review. Brain. 1999;122(pt 3):383-404.
30. Flynn JR. The mean IQ of Americans: Massive gains 1932 to 1978. Psychol Bull. 1984;95:29-51.
31. Tombaugh TN. Trail Making Test A and B: normative data stratified by age and education. Arch Clin Neuropsychol. 2004;19: 203-214.
32. Davies A. The influence of age on trail making test performance. J Clin Psychol. 1968;24:96-98.
33. Bianchetti A, Trabucch M. Clinical aspects of Alzheimer’s disease. Aging (Milano). 2001;13:221-230.
34. Kay D, Forster DP, Newens AJ. Long-term survival, place of death, and death certification in clinically diagnosed pre-senile dementia in northern England. Follow-up after 8-12 years. Br J Psychiatry. 2000;177:156-162.
35. Chaussalet T, Thompson WA. Data requirements in a model of the natural history of Alzheimer’s disease. Health Care Manag Sci. 2001;4:13-19.
1. Loveman E, Green C, Kirby J, et al. The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease. Health Technol Assess. 2006;10:iii-iv,ix- xi,1-160.
2. Medical Care Corporation. Delaying the onset and progression of Alzheimer’s disease. Prevent AD Web site. Available at: http://www.preventad.com/pdf/support/article/DelayingADProgression.pdf. Accessed June 18, 2014.
3. Hopkins RW. Dementia projections for the counties, regional municipalities and districts of Ontario. Geriatric Psychiatry Unit Clinical/Research Bulletin, No. 16. Providence Care Web site. Available at: http://www.providencecare.ca/clinical-tools/Documents/Ontario-Dementia-Projections-2010.pdf. Accessed June 18, 2014.
4. Simmons BB, Hartmann B, Dejoseph D. Evaluation of suspected dementia. Am Fam Physician. 2011;84:895-902.
5. McCarten JR, Borson S. Should family physicians routinely screen patients for cognitive impairment? Yes: screening is the first step toward improving care. Am Fam Physician. 2014;89: 861-862.
6. Alzheimer’s Association. Health Care Professionals and Alzheimer’s. Alzheimer’s Association Web site. Available at: http://www.alz.org/health-care-professionals/cognitive-tests-patient-assessment.asp. Accessed June 18, 2014.
7. US Preventive Services Task Force. Screening for cognitive impairment in older adults. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsdeme.htm. Accessed June 18, 2014.
8. Hopkins RW, Kilik LA, Day D, et al. Kingston Standardized Behavioural Assessment. Am J Alzheimers Dis Other Demen. 2006;21:339-346.
9. Kilik LA, Hopkins RW, Day D, et al. The progression of behaviour in dementia: an in-office guide for clinicians. Am J Alzheimers Dis Other Demen. 2008;23:242-249.
10. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189-198.
11. Army Individual Test Battery. Manual of Directions and Scoring. Washington, DC: War Department, Adjutant General’s Office; 1944.
12. Wechsler D. The Measurement and Appraisal of Adult Intelligence. 4th ed. The Williams & Wilkins Company: Baltimore, MD; 1958.
13. Larrabee GJ, Largen JW, Levin HS. Sensitivity of age-decline resistant (“hold”) WAIS subtests to Alzheimer’s disease. J Clin Exp Neuropsychol. 1985;7:497-504.
14. Herndon RM. Assessment of the elderly with dementia. In: Handbook of Neurologic Rating Scales. 2nd ed. Demos Medical Publishing LLC: New York, NY; 2006:199.
15. Brugnolo A, Nobili F, Barbieri MP, et al. The factorial structure of the mini mental state examination (MMSE) in Alzheimer’s disease. Arch Gerontol Geriatr. 2009;49:180-185.
16. Folstein M, Anthony JC, Parhad I, et al. The meaning of cognitive impairment in the elderly. J Am Geriatr Soc. 1985;33:228-235.
17. Hopkins RW, Kilik LA, Day DJ, et al. The Revised Kingston Standardized Cognitive Assessment. Int J Geriatr Psychiatry. 2004;19:320-326.
18. Hopkins R, Kilik L. The mini-Kingston Standardized Cognitive Assessment. Kingston Scales Web site. Available at: http://www.kingstonscales.org. Accessed June 18, 2014.
19. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994.
20. McKhann G, Drachman D, Folstein M, et al. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34: 939-944.
21. Crum RM, Anthony JC, Bassett SS, et al. Population-based norms for the Mini-Mental State Examination by age and educational level. JAMA. 1993;269:2386-2391.
22. O’Bryant SE, Humphreys JD, Smith GE, et al. Detecting dementia with the mini-mental state examination in highly educated individuals. Arch Neurol. 2008;65:963-967.
23. O’Sullivan M, Morris RG, Markus HS. Brief cognitive assessment for patients with cerebral small vessel disease. J Neurol Neurosurg Psychiatry. 2005;76:1140-1145.
24. Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment (MoCA): a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695-699.
25. Benton AL, Hamsher K. Multilingual Aphasia Examination. 2nd ed. Iowa City, OA: AJA Associates, Inc; 1976.
26. Wechsler D. WAIS-III Administration and Scoring Manual. San Antonio, TX: The Psychological Corporation; 1997.
27. Morris JC, Heyman A, Mohs RC, et al. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part I. Clinical and neuropsychological assesment of Alzheimer’s disease. Neurology. 1989;39:1159-1165.
28. Gladsjo JA, Miller SW, Heaton RK. Norms for Letter and Category Fluency: Demographic Corrections for Age, Education and Ethnicity. Odessa, FL: Psychological Assessment Resources; 1999.
29. Perry R, Hodges J. Attention and executive deficits in Alzheimer’s disease. A critical review. Brain. 1999;122(pt 3):383-404.
30. Flynn JR. The mean IQ of Americans: Massive gains 1932 to 1978. Psychol Bull. 1984;95:29-51.
31. Tombaugh TN. Trail Making Test A and B: normative data stratified by age and education. Arch Clin Neuropsychol. 2004;19: 203-214.
32. Davies A. The influence of age on trail making test performance. J Clin Psychol. 1968;24:96-98.
33. Bianchetti A, Trabucch M. Clinical aspects of Alzheimer’s disease. Aging (Milano). 2001;13:221-230.
34. Kay D, Forster DP, Newens AJ. Long-term survival, place of death, and death certification in clinically diagnosed pre-senile dementia in northern England. Follow-up after 8-12 years. Br J Psychiatry. 2000;177:156-162.
35. Chaussalet T, Thompson WA. Data requirements in a model of the natural history of Alzheimer’s disease. Health Care Manag Sci. 2001;4:13-19.
Deaf Hospitalist Focuses on Teaching, Co-Management, Patient-Centered Care
"What’s the bigger picture here?” Hospitalist Christopher Moreland, MD, MPH, FACP, drops his question neatly into the pause in resident Adrienne Victor, MD’s presentation of patient status and lab results.
We’re on the bustling 9th floor of University Hospital at the University of Texas Health Science Center (UTHSCSA) in San Antonio during fast-paced morning rounds. As attending physician, Dr. Moreland is focusing intently on Dr. Victor’s face, simultaneously monitoring the American Sign Language (ASL) interpretation of Todd Agan, CI/CT, BEI Master Interpreter. Immediately after his question to Dr. Victor, the discussion—conducted in both ASL and spoken English—shifts to the patient’s psychosocial issues and whether a palliative care consult would be advisable.
It’s clear that for Dr. Moreland, the work, not his lack of hearing, is the main point here. A hospitalist with the UTHSCSA team since 2010, Dr. Moreland quickly established himself not only as a valuable HM team member and educator, but also as a leader in other domains. For example, in addition to his academic appointment as assistant clinical professor of medicine, he previously was co-director of the medicine consult and co-management service at University Hospital and now serves as UTHSCSA’s associate program director for the internal medicine residency program.
Dr. Moreland’s question this morning is typical of his teaching, says Bret Simon, PhD, an educational development specialist and assistant professor with the division of hospital medicine at UTHSCSA.

–Christopher Moreland, MD, MPH, FACP
“He’s very good at using questions to teach, promoting reflection rather than simply telling the student what to do,” Dr. Simon explains.
Why Medicine?
Chris Moreland’s parents discovered their son was deaf at age two, by which time he had acquired very few spoken words. After multiple visits to healthcare professionals, a physician finally identified his deafness. The family then embarked on a bimodal approach to his education, using both signed and spoken English. He learned ASL in college. As a result, he communicates through a variety of channels: ASL with interpreters Agan and Keri Richardson, speech reading, and spoken English. When examining patients, he uses an electronic stethoscope that interfaces with his cochlear implant.
Medicine was not Dr. Moreland’s first academic choice.
“I went into college thinking I wanted to do computer science,” he says, speaking of his undergraduate studies at the University of Texas in Austin. When he realized computers were not for him, he switched his major to theater arts, continuing an interest he had had in high school. After that, research seemed appealing, and he became a research assistant in a lab in the Department of Anthropology. Finally, after shadowing a number of physicians, his interest in medical science was stimulated.
“Medicine,” he says, “became a nice culmination of everything I was interested in doing.” From computer science, he learned to appreciate an understanding of algorithms; from theater arts came the ability to understand where people are coming from; and from his link with research in linguistics and anthropology came the contribution of problem solving and methodology.
Fearless Communicator
Dr. Moreland says his deafness presents no impediments to his practice of medicine. “I grew up working with interpreters, so I’m used to that process,” he says. “It forces you to become less inhibited about what you’re doing. People have questions [‘who is that other person in the room?’], and you learn how to handle those questions quickly, without interfering with communication in order to advance the work.”
When Dr. Moreland started his clinical rotations as a third-year medical student, he grappled with the best way to introduce himself and his interpreter to patients. His first attempt at explaining the interpretive process “went on for quite a while” and was too much information. “It ended up overwhelming the patient,” he says.
The next time he chose not to introduce the interpreter but to simply address the patient directly. “That didn’t work either, because the patient’s eyes kept wandering to that other person in the room.”
Finally, “I realized that it wasn’t about me,” he says. “It was about the patient.” So he simply shortened the introduction to himself and the interpreter and asked the patients how they were doing.
“Once I became more professional about the situation, the more positive and patient-centered it became, and it went well.” He says he’s had no negative experiences since then, at least not related to his deafness. He approaches each new patient interaction proactively, and he and his interpreters become part of the flow of care.
Teaching’s Missing Pieces
As illustrated with his first question, Dr. Moreland intends for his trainees to learn to think globally about their patients.
“Although rote information has its role,” he explains later in the conference room, “I’m always afraid of overemphasizing it. When I trained in medical school, we didn’t learn that much about communication skills and teamwork. We talked a lot about information we use as physicians—the mechanism of disease, the drugs we use.
“What I try to emphasize with trainees is, what skills in communication, teamwork, and self-education can we develop so that we can use those skills continuously throughout our practice?”
Dr. Moreland takes setting resident-generated learning goals seriously, says Dr. Simon, for which he and trainees give him high marks.
“He is very supportive and encourages us to make our own management decisions,” Dr. Victor says. “Though, of course, he will let us know if something is likely the wrong choice, usually by discussing it first.”
Patrick S. Romano, MD, MPH, professor of general medicine and pediatrics and former director of the Primary Care Outcomes Research (PCOR) faculty development program at the University of California Davis, where Dr. Moreland was a resident and then a fellow, found his trainee was always “very thoughtful and conscientious, presenting different ways of looking at problems and asking the right questions. And, of course, that’s what we look for in teachers: people who know how to ask the right questions, because, then, of course, they are able to answer students’ questions.”
Transformational and Inspirational
For many of Dr. Moreland’s colleagues and trainees, working with him has been their first exposure to a hearing-impaired physician. Richard L. Kravitz, MD, MSPH, professor and co-vice chair of research in the department of medicine at UC Davis, supervised Dr. Moreland during his residency and later during his PCOR fellowship. The American Disabilities Act-mandated interpreter for Dr. Moreland introduced a “change in standard operating procedure,” Dr. Kravitz notes. “None of us knew what to expect when he came onboard the residency program. But, very quickly, any unease was put to rest because he was just so talented.”
For visitors, Dr. Moreland seamlessly addresses his hearing impairment and makes sure that everyone on the team is following the discussion. Luci K. Leykum, MD, MBA, MSc, hospital medicine division chief and associate dean for clinical affairs at UTHSCSA, says that Dr. Moreland has brought “a lot of positive energy to the group—and in ways I would not have expected.” She praised his talents as both a clinician and teacher.
John G. Rees, DBA, RN, patient care coordinator in the 5th Acute Care Unit, says that Dr. Moreland immediately “blended” with the staff on his service. “The rapport was perfect,” he adds.
Robert L. Talbert, PharmD, the SmithKline Centennial Professor of Pharmacy at the College of Pharmacy at the University of Texas at Austin, often participates in teaching rounds. Dr. Moreland, he says, “has an excellent fund of knowledge; he’s very rational and evidence-based in decisions he makes. He’s exactly what a physician should be.”
Watching interpreters Agan and Richardson during group meetings, Dr. Leykum believes, has influenced their group dynamics. “On a subtle level, having Chris in the group has made us more aware of how we interact with each other.”
Nilam Soni, MD, FHM associate professor in the department of medicine and leader of ultrasound education, has noticed that he has become attuned to Dr. Moreland’s way of communicating and often does not need the interpreters to decipher the conversation between them. Working with Dr. Moreland has given Dr. Soni “a better understanding of how to communicate effectively with patients that have difficulty hearing.”
After working with Dr. Moreland at UC Davis, Dr. Kravitz observed that employing physicians with hearing impairment or other disabilities brings additional benefits to the institution. Dr. Moreland’s presence “probably raised the level of understanding of the entire internal medicine staff, because it demonstrated that a disability is what you make of it,” he says. “One recognizes how porous the barriers are, provided that people with disabilities are supported appropriately. In that way, Chris was inspiring, and may have changed the way some of us look at this specific disability that he had, but also other disabilities.”
A bigger picture, indeed.
Gretchen Henkel is a freelance writer in California.
Reference
"What’s the bigger picture here?” Hospitalist Christopher Moreland, MD, MPH, FACP, drops his question neatly into the pause in resident Adrienne Victor, MD’s presentation of patient status and lab results.
We’re on the bustling 9th floor of University Hospital at the University of Texas Health Science Center (UTHSCSA) in San Antonio during fast-paced morning rounds. As attending physician, Dr. Moreland is focusing intently on Dr. Victor’s face, simultaneously monitoring the American Sign Language (ASL) interpretation of Todd Agan, CI/CT, BEI Master Interpreter. Immediately after his question to Dr. Victor, the discussion—conducted in both ASL and spoken English—shifts to the patient’s psychosocial issues and whether a palliative care consult would be advisable.
It’s clear that for Dr. Moreland, the work, not his lack of hearing, is the main point here. A hospitalist with the UTHSCSA team since 2010, Dr. Moreland quickly established himself not only as a valuable HM team member and educator, but also as a leader in other domains. For example, in addition to his academic appointment as assistant clinical professor of medicine, he previously was co-director of the medicine consult and co-management service at University Hospital and now serves as UTHSCSA’s associate program director for the internal medicine residency program.
Dr. Moreland’s question this morning is typical of his teaching, says Bret Simon, PhD, an educational development specialist and assistant professor with the division of hospital medicine at UTHSCSA.

–Christopher Moreland, MD, MPH, FACP
“He’s very good at using questions to teach, promoting reflection rather than simply telling the student what to do,” Dr. Simon explains.
Why Medicine?
Chris Moreland’s parents discovered their son was deaf at age two, by which time he had acquired very few spoken words. After multiple visits to healthcare professionals, a physician finally identified his deafness. The family then embarked on a bimodal approach to his education, using both signed and spoken English. He learned ASL in college. As a result, he communicates through a variety of channels: ASL with interpreters Agan and Keri Richardson, speech reading, and spoken English. When examining patients, he uses an electronic stethoscope that interfaces with his cochlear implant.
Medicine was not Dr. Moreland’s first academic choice.
“I went into college thinking I wanted to do computer science,” he says, speaking of his undergraduate studies at the University of Texas in Austin. When he realized computers were not for him, he switched his major to theater arts, continuing an interest he had had in high school. After that, research seemed appealing, and he became a research assistant in a lab in the Department of Anthropology. Finally, after shadowing a number of physicians, his interest in medical science was stimulated.
“Medicine,” he says, “became a nice culmination of everything I was interested in doing.” From computer science, he learned to appreciate an understanding of algorithms; from theater arts came the ability to understand where people are coming from; and from his link with research in linguistics and anthropology came the contribution of problem solving and methodology.
Fearless Communicator
Dr. Moreland says his deafness presents no impediments to his practice of medicine. “I grew up working with interpreters, so I’m used to that process,” he says. “It forces you to become less inhibited about what you’re doing. People have questions [‘who is that other person in the room?’], and you learn how to handle those questions quickly, without interfering with communication in order to advance the work.”
When Dr. Moreland started his clinical rotations as a third-year medical student, he grappled with the best way to introduce himself and his interpreter to patients. His first attempt at explaining the interpretive process “went on for quite a while” and was too much information. “It ended up overwhelming the patient,” he says.
The next time he chose not to introduce the interpreter but to simply address the patient directly. “That didn’t work either, because the patient’s eyes kept wandering to that other person in the room.”
Finally, “I realized that it wasn’t about me,” he says. “It was about the patient.” So he simply shortened the introduction to himself and the interpreter and asked the patients how they were doing.
“Once I became more professional about the situation, the more positive and patient-centered it became, and it went well.” He says he’s had no negative experiences since then, at least not related to his deafness. He approaches each new patient interaction proactively, and he and his interpreters become part of the flow of care.
Teaching’s Missing Pieces
As illustrated with his first question, Dr. Moreland intends for his trainees to learn to think globally about their patients.
“Although rote information has its role,” he explains later in the conference room, “I’m always afraid of overemphasizing it. When I trained in medical school, we didn’t learn that much about communication skills and teamwork. We talked a lot about information we use as physicians—the mechanism of disease, the drugs we use.
“What I try to emphasize with trainees is, what skills in communication, teamwork, and self-education can we develop so that we can use those skills continuously throughout our practice?”
Dr. Moreland takes setting resident-generated learning goals seriously, says Dr. Simon, for which he and trainees give him high marks.
“He is very supportive and encourages us to make our own management decisions,” Dr. Victor says. “Though, of course, he will let us know if something is likely the wrong choice, usually by discussing it first.”
Patrick S. Romano, MD, MPH, professor of general medicine and pediatrics and former director of the Primary Care Outcomes Research (PCOR) faculty development program at the University of California Davis, where Dr. Moreland was a resident and then a fellow, found his trainee was always “very thoughtful and conscientious, presenting different ways of looking at problems and asking the right questions. And, of course, that’s what we look for in teachers: people who know how to ask the right questions, because, then, of course, they are able to answer students’ questions.”
Transformational and Inspirational
For many of Dr. Moreland’s colleagues and trainees, working with him has been their first exposure to a hearing-impaired physician. Richard L. Kravitz, MD, MSPH, professor and co-vice chair of research in the department of medicine at UC Davis, supervised Dr. Moreland during his residency and later during his PCOR fellowship. The American Disabilities Act-mandated interpreter for Dr. Moreland introduced a “change in standard operating procedure,” Dr. Kravitz notes. “None of us knew what to expect when he came onboard the residency program. But, very quickly, any unease was put to rest because he was just so talented.”
For visitors, Dr. Moreland seamlessly addresses his hearing impairment and makes sure that everyone on the team is following the discussion. Luci K. Leykum, MD, MBA, MSc, hospital medicine division chief and associate dean for clinical affairs at UTHSCSA, says that Dr. Moreland has brought “a lot of positive energy to the group—and in ways I would not have expected.” She praised his talents as both a clinician and teacher.
John G. Rees, DBA, RN, patient care coordinator in the 5th Acute Care Unit, says that Dr. Moreland immediately “blended” with the staff on his service. “The rapport was perfect,” he adds.
Robert L. Talbert, PharmD, the SmithKline Centennial Professor of Pharmacy at the College of Pharmacy at the University of Texas at Austin, often participates in teaching rounds. Dr. Moreland, he says, “has an excellent fund of knowledge; he’s very rational and evidence-based in decisions he makes. He’s exactly what a physician should be.”
Watching interpreters Agan and Richardson during group meetings, Dr. Leykum believes, has influenced their group dynamics. “On a subtle level, having Chris in the group has made us more aware of how we interact with each other.”
Nilam Soni, MD, FHM associate professor in the department of medicine and leader of ultrasound education, has noticed that he has become attuned to Dr. Moreland’s way of communicating and often does not need the interpreters to decipher the conversation between them. Working with Dr. Moreland has given Dr. Soni “a better understanding of how to communicate effectively with patients that have difficulty hearing.”
After working with Dr. Moreland at UC Davis, Dr. Kravitz observed that employing physicians with hearing impairment or other disabilities brings additional benefits to the institution. Dr. Moreland’s presence “probably raised the level of understanding of the entire internal medicine staff, because it demonstrated that a disability is what you make of it,” he says. “One recognizes how porous the barriers are, provided that people with disabilities are supported appropriately. In that way, Chris was inspiring, and may have changed the way some of us look at this specific disability that he had, but also other disabilities.”
A bigger picture, indeed.
Gretchen Henkel is a freelance writer in California.
Reference
"What’s the bigger picture here?” Hospitalist Christopher Moreland, MD, MPH, FACP, drops his question neatly into the pause in resident Adrienne Victor, MD’s presentation of patient status and lab results.
We’re on the bustling 9th floor of University Hospital at the University of Texas Health Science Center (UTHSCSA) in San Antonio during fast-paced morning rounds. As attending physician, Dr. Moreland is focusing intently on Dr. Victor’s face, simultaneously monitoring the American Sign Language (ASL) interpretation of Todd Agan, CI/CT, BEI Master Interpreter. Immediately after his question to Dr. Victor, the discussion—conducted in both ASL and spoken English—shifts to the patient’s psychosocial issues and whether a palliative care consult would be advisable.
It’s clear that for Dr. Moreland, the work, not his lack of hearing, is the main point here. A hospitalist with the UTHSCSA team since 2010, Dr. Moreland quickly established himself not only as a valuable HM team member and educator, but also as a leader in other domains. For example, in addition to his academic appointment as assistant clinical professor of medicine, he previously was co-director of the medicine consult and co-management service at University Hospital and now serves as UTHSCSA’s associate program director for the internal medicine residency program.
Dr. Moreland’s question this morning is typical of his teaching, says Bret Simon, PhD, an educational development specialist and assistant professor with the division of hospital medicine at UTHSCSA.

–Christopher Moreland, MD, MPH, FACP
“He’s very good at using questions to teach, promoting reflection rather than simply telling the student what to do,” Dr. Simon explains.
Why Medicine?
Chris Moreland’s parents discovered their son was deaf at age two, by which time he had acquired very few spoken words. After multiple visits to healthcare professionals, a physician finally identified his deafness. The family then embarked on a bimodal approach to his education, using both signed and spoken English. He learned ASL in college. As a result, he communicates through a variety of channels: ASL with interpreters Agan and Keri Richardson, speech reading, and spoken English. When examining patients, he uses an electronic stethoscope that interfaces with his cochlear implant.
Medicine was not Dr. Moreland’s first academic choice.
“I went into college thinking I wanted to do computer science,” he says, speaking of his undergraduate studies at the University of Texas in Austin. When he realized computers were not for him, he switched his major to theater arts, continuing an interest he had had in high school. After that, research seemed appealing, and he became a research assistant in a lab in the Department of Anthropology. Finally, after shadowing a number of physicians, his interest in medical science was stimulated.
“Medicine,” he says, “became a nice culmination of everything I was interested in doing.” From computer science, he learned to appreciate an understanding of algorithms; from theater arts came the ability to understand where people are coming from; and from his link with research in linguistics and anthropology came the contribution of problem solving and methodology.
Fearless Communicator
Dr. Moreland says his deafness presents no impediments to his practice of medicine. “I grew up working with interpreters, so I’m used to that process,” he says. “It forces you to become less inhibited about what you’re doing. People have questions [‘who is that other person in the room?’], and you learn how to handle those questions quickly, without interfering with communication in order to advance the work.”
When Dr. Moreland started his clinical rotations as a third-year medical student, he grappled with the best way to introduce himself and his interpreter to patients. His first attempt at explaining the interpretive process “went on for quite a while” and was too much information. “It ended up overwhelming the patient,” he says.
The next time he chose not to introduce the interpreter but to simply address the patient directly. “That didn’t work either, because the patient’s eyes kept wandering to that other person in the room.”
Finally, “I realized that it wasn’t about me,” he says. “It was about the patient.” So he simply shortened the introduction to himself and the interpreter and asked the patients how they were doing.
“Once I became more professional about the situation, the more positive and patient-centered it became, and it went well.” He says he’s had no negative experiences since then, at least not related to his deafness. He approaches each new patient interaction proactively, and he and his interpreters become part of the flow of care.
Teaching’s Missing Pieces
As illustrated with his first question, Dr. Moreland intends for his trainees to learn to think globally about their patients.
“Although rote information has its role,” he explains later in the conference room, “I’m always afraid of overemphasizing it. When I trained in medical school, we didn’t learn that much about communication skills and teamwork. We talked a lot about information we use as physicians—the mechanism of disease, the drugs we use.
“What I try to emphasize with trainees is, what skills in communication, teamwork, and self-education can we develop so that we can use those skills continuously throughout our practice?”
Dr. Moreland takes setting resident-generated learning goals seriously, says Dr. Simon, for which he and trainees give him high marks.
“He is very supportive and encourages us to make our own management decisions,” Dr. Victor says. “Though, of course, he will let us know if something is likely the wrong choice, usually by discussing it first.”
Patrick S. Romano, MD, MPH, professor of general medicine and pediatrics and former director of the Primary Care Outcomes Research (PCOR) faculty development program at the University of California Davis, where Dr. Moreland was a resident and then a fellow, found his trainee was always “very thoughtful and conscientious, presenting different ways of looking at problems and asking the right questions. And, of course, that’s what we look for in teachers: people who know how to ask the right questions, because, then, of course, they are able to answer students’ questions.”
Transformational and Inspirational
For many of Dr. Moreland’s colleagues and trainees, working with him has been their first exposure to a hearing-impaired physician. Richard L. Kravitz, MD, MSPH, professor and co-vice chair of research in the department of medicine at UC Davis, supervised Dr. Moreland during his residency and later during his PCOR fellowship. The American Disabilities Act-mandated interpreter for Dr. Moreland introduced a “change in standard operating procedure,” Dr. Kravitz notes. “None of us knew what to expect when he came onboard the residency program. But, very quickly, any unease was put to rest because he was just so talented.”
For visitors, Dr. Moreland seamlessly addresses his hearing impairment and makes sure that everyone on the team is following the discussion. Luci K. Leykum, MD, MBA, MSc, hospital medicine division chief and associate dean for clinical affairs at UTHSCSA, says that Dr. Moreland has brought “a lot of positive energy to the group—and in ways I would not have expected.” She praised his talents as both a clinician and teacher.
John G. Rees, DBA, RN, patient care coordinator in the 5th Acute Care Unit, says that Dr. Moreland immediately “blended” with the staff on his service. “The rapport was perfect,” he adds.
Robert L. Talbert, PharmD, the SmithKline Centennial Professor of Pharmacy at the College of Pharmacy at the University of Texas at Austin, often participates in teaching rounds. Dr. Moreland, he says, “has an excellent fund of knowledge; he’s very rational and evidence-based in decisions he makes. He’s exactly what a physician should be.”
Watching interpreters Agan and Richardson during group meetings, Dr. Leykum believes, has influenced their group dynamics. “On a subtle level, having Chris in the group has made us more aware of how we interact with each other.”
Nilam Soni, MD, FHM associate professor in the department of medicine and leader of ultrasound education, has noticed that he has become attuned to Dr. Moreland’s way of communicating and often does not need the interpreters to decipher the conversation between them. Working with Dr. Moreland has given Dr. Soni “a better understanding of how to communicate effectively with patients that have difficulty hearing.”
After working with Dr. Moreland at UC Davis, Dr. Kravitz observed that employing physicians with hearing impairment or other disabilities brings additional benefits to the institution. Dr. Moreland’s presence “probably raised the level of understanding of the entire internal medicine staff, because it demonstrated that a disability is what you make of it,” he says. “One recognizes how porous the barriers are, provided that people with disabilities are supported appropriately. In that way, Chris was inspiring, and may have changed the way some of us look at this specific disability that he had, but also other disabilities.”
A bigger picture, indeed.
Gretchen Henkel is a freelance writer in California.
Reference
SUPPLEMENTS
Enter text here
Enter text here
Enter text here
Gout exacerbation, weakness, hypotension—Dx?
THE CASE
A 58-year-old female came to the emergency department (ED) because she had progressive weakness, hypotension, and altered mental status. In the ED she had a heart rate of 107 beats per minute; blood pressure, 96/68 mm Hg; respiratory rate, 20 breaths per minute; oxygen saturation, 96%; and a 96.7°F temperature that spiked to 101.6°F. The absolute neutrophil count (ANC) was 1500 cells/mm3, hemoglobin was 13 g/dL, and platelet count was 95 × 109/L. Her serum creatinine was 2.5 mg/dL (baseline of 1.0) and cyclosporine concentration was <25 ng/mL.
Our patient had a history of renal transplant, gout, and chronic kidney disease. Her medications included bumetanide, clonazepam, colchicine .6 mg BID, a therapeutic dose of cyclosporine, flurazepam, gabapentin, levothyroxine, mirtazapine, oxycodone, prednisone, and premarin. Three days before she came to the ED, she experienced a gout exacerbation and took six .6 mg doses (3.6 mg total) of colchicine that resulted in severe diarrhea. The next day, she took 3 mg of colchicine and had more severe diarrhea and a fever. Our patient took another 1.2 mg of colchicine the next day and developed the progressive weakness, hypotension, and altered mental status that led her to seek care in the ED.
THE DIAGNOSIS
Our patient was admitted to the hospital with a diagnosis of pancytopenia and presumed sepsis and intravenous broad-spectrum antibiotics were administered. Blood, urine, and sputum cultures, stool studies, and chest x-ray were negative for pneumonia. A peripheral blood smear revealed dysplastic-appearing neutrophils with vacuolization, which is characteristic of colchicine toxicity, myelodysplastic syndromes, or acute leukemia. However, the absence of blast cells in the peripheral blood smear and the normal appearance of the liver and spleen on a subsequent abdominal ultrasound refuted a primary hematologic disorder. Thus, based on the patient’s recent colchicine use and subsequent progressive pancytopenia and sepsis, we diagnosed colchicine toxicity in this patient.
DISCUSSION
Colchicine is a potent anti-inflammatory drug that has a narrow therapeutic index. Indicated for treating gout and familial Mediterranean fever, it inhibits mitosis by interfering with microtubule formation and arresting cell division. Colchicine is rapidly absorbed in the gastrointestinal (GI) tract and undergoes first-pass hepatic metabolism with enterohepatic recirculation of metabolites prior to excretion via the biliary tract.1 Ten percent to 20% of colchicine is excreted by the kidneys.2
Colchicine toxicity begins with GI symptoms, such as diarrhea, is followed by falling peripheral blood cell counts and altered mental status. A late sign of colchicine toxicity is alopecia. If the toxicity is left unchecked, multi-organ dysfunction that mimics severe sepsis will occur, resulting in death.3
Toxicity typically occurs at doses of .5 mg/kg/d. Fatal overdose from colchicine has been described in patients taking as little as 7 mg; however, survival from a 60-mg overdose has been reported.1 In a review of 150 patients who overdosed on colchicine, a single dose of .8 mg/kg was universally fatal.4 Therapeutic doses of colchicine have resulted in severe toxicity in patients with hepatic or renal dysfunction.5,6
Toxicity risk is increased in patients taking immunosuppressants
Colchicine toxicity from therapeutic doses may occur in patients taking concomitant immunosuppressive drugs, particularly cyclosporine. In case series, patients taking stable doses of cyclosporine and prophylactic doses of colchicine exhibited toxicity when they took therapeutic doses of colchicine for gout exacerbations.7,8 Another case series described 2 post-renal transplant patients, immunosuppressed with azathioprine and prednisone, who had comorbid familial Mediterranean fever and were maintained on colchicine prophylaxis.9 When they converted to cyclosporine for immunosuppression, each patient began to demonstrate GI and muscular symptoms of colchicine toxicity. Upon discontinuing cyclosporine, the GI and muscular symptoms rapidly resolved.9
How cyclosporine interacts with colchicine. Cyclosporine is a potent CYP3A4 and P-glycoprotein inhibitor, and colchicine is a CYP3A4 and P-glycoprotein substrate. In vivo studies have demonstrated that cyclosporine inhibits hepatic and renal clearance of colchicine, thus increasing serum colchicine levels, further lowering the toxic colchicine dose.10,11
Our patient. The prophylactic dosage of colchicine our patient had been taking before her recent gout flare (.6 mg BID) was higher than the adjusted dose recommended to treat gout flares for patients taking cyclosporine (a single .6 mg dose to be repeated no earlier than 3 days).4 The dosages she took to treat her flare far exceeded this recommendation.
As a result, our patient developed severe colchicine toxicity. During her hospitalization, our patient’s cell counts continued to fall, requiring blood and platelet transfusions; her ANC nadir was 14 cells/mm3. She continued to have progressive multi-organ failure and developed alopecia. Management revolved around supportive measures for all of the end-organ effects.
Our patient died on hospital Day 7. Contributing factors included premorbid immunosuppression, renal insufficiency, and concomitant P-glycoprotein and CYP3A4 inhibition.
THE TAKEAWAY
Colchicine toxicity from therapeutic doses may occur in patients taking concomitant immunosuppressive drugs. Physicians who prescribe colchicine should be aware of these additional risks and adjust dosages accordingly. Activated charcoal can be given for acute overdose.
1. Maxwell MJ, Muthu P, Pritty PE. Accidental colchicine overdose. A case report and literature review. Emerg Med J. 2002;19:265-267.
2. Gruberg L, Har-Zahav Y, Agranat O, et al. Acute myopathy induced by colchicine in a cyclosporine treated heart transplant recipient: possible role of the multidrug resistance transporter. Transplant Proc. 1999;31:2157-2158.
3. Colchicine: serious interactions. Prescrire Int. 2008;17:151-153.
4. Colcrys [package insert]. Deerfield, IL: Takeda Pharmaceuticals America, Inc; 2012.
5. Dickinson M, Juneja S. Haematological toxicity of colchicine. Br J Haematol. 2009;146:465.
6. Lee KY, Kim do Y, Chang JY, et al. Two cases of acute leukopenia induced by colchicine with concurrent immunosuppressants use in Behçet’s disease. Yonsei Med J. 2008;49:171-173.
7. Rieger EH, Halasz NA, Wahlstrom HE. Colchicine neuromyopathy after renal transplantation. Transplantation. 1990;49:1196-1198.
8. Minetti E, Minetti L. Multiple organ failure in a kidney transplant patient receiving both colchicine and cyclosporine. J Nephrol. 2003;16:421-425.
9. Yussim A, Bar-Nathan N, Lustig S, et al. Gastrointestinal, hepatorenal, and neuromuscular toxicity caused by cyclosporine-colchicine interaction in renal transplantation. Transplant Proc. 1994;26:2825-2826.
10. Speeg KV, Maldonado AL, Liaci J, et al. Effect of cyclosporine on colchicine secretion by the kidney multidrug transporter studied in vivo. J Pharmacol Exp Ther. 1992;261:50-55.
11. Speeg KV, Maldonado AL, Liaci J, et al. Effect of cyclosporine on colchicine secretion by a liver canalicular transporter studied in vivo. Hepatology. 1992;15:899-903.
THE CASE
A 58-year-old female came to the emergency department (ED) because she had progressive weakness, hypotension, and altered mental status. In the ED she had a heart rate of 107 beats per minute; blood pressure, 96/68 mm Hg; respiratory rate, 20 breaths per minute; oxygen saturation, 96%; and a 96.7°F temperature that spiked to 101.6°F. The absolute neutrophil count (ANC) was 1500 cells/mm3, hemoglobin was 13 g/dL, and platelet count was 95 × 109/L. Her serum creatinine was 2.5 mg/dL (baseline of 1.0) and cyclosporine concentration was <25 ng/mL.
Our patient had a history of renal transplant, gout, and chronic kidney disease. Her medications included bumetanide, clonazepam, colchicine .6 mg BID, a therapeutic dose of cyclosporine, flurazepam, gabapentin, levothyroxine, mirtazapine, oxycodone, prednisone, and premarin. Three days before she came to the ED, she experienced a gout exacerbation and took six .6 mg doses (3.6 mg total) of colchicine that resulted in severe diarrhea. The next day, she took 3 mg of colchicine and had more severe diarrhea and a fever. Our patient took another 1.2 mg of colchicine the next day and developed the progressive weakness, hypotension, and altered mental status that led her to seek care in the ED.
THE DIAGNOSIS
Our patient was admitted to the hospital with a diagnosis of pancytopenia and presumed sepsis and intravenous broad-spectrum antibiotics were administered. Blood, urine, and sputum cultures, stool studies, and chest x-ray were negative for pneumonia. A peripheral blood smear revealed dysplastic-appearing neutrophils with vacuolization, which is characteristic of colchicine toxicity, myelodysplastic syndromes, or acute leukemia. However, the absence of blast cells in the peripheral blood smear and the normal appearance of the liver and spleen on a subsequent abdominal ultrasound refuted a primary hematologic disorder. Thus, based on the patient’s recent colchicine use and subsequent progressive pancytopenia and sepsis, we diagnosed colchicine toxicity in this patient.
DISCUSSION
Colchicine is a potent anti-inflammatory drug that has a narrow therapeutic index. Indicated for treating gout and familial Mediterranean fever, it inhibits mitosis by interfering with microtubule formation and arresting cell division. Colchicine is rapidly absorbed in the gastrointestinal (GI) tract and undergoes first-pass hepatic metabolism with enterohepatic recirculation of metabolites prior to excretion via the biliary tract.1 Ten percent to 20% of colchicine is excreted by the kidneys.2
Colchicine toxicity begins with GI symptoms, such as diarrhea, is followed by falling peripheral blood cell counts and altered mental status. A late sign of colchicine toxicity is alopecia. If the toxicity is left unchecked, multi-organ dysfunction that mimics severe sepsis will occur, resulting in death.3
Toxicity typically occurs at doses of .5 mg/kg/d. Fatal overdose from colchicine has been described in patients taking as little as 7 mg; however, survival from a 60-mg overdose has been reported.1 In a review of 150 patients who overdosed on colchicine, a single dose of .8 mg/kg was universally fatal.4 Therapeutic doses of colchicine have resulted in severe toxicity in patients with hepatic or renal dysfunction.5,6
Toxicity risk is increased in patients taking immunosuppressants
Colchicine toxicity from therapeutic doses may occur in patients taking concomitant immunosuppressive drugs, particularly cyclosporine. In case series, patients taking stable doses of cyclosporine and prophylactic doses of colchicine exhibited toxicity when they took therapeutic doses of colchicine for gout exacerbations.7,8 Another case series described 2 post-renal transplant patients, immunosuppressed with azathioprine and prednisone, who had comorbid familial Mediterranean fever and were maintained on colchicine prophylaxis.9 When they converted to cyclosporine for immunosuppression, each patient began to demonstrate GI and muscular symptoms of colchicine toxicity. Upon discontinuing cyclosporine, the GI and muscular symptoms rapidly resolved.9
How cyclosporine interacts with colchicine. Cyclosporine is a potent CYP3A4 and P-glycoprotein inhibitor, and colchicine is a CYP3A4 and P-glycoprotein substrate. In vivo studies have demonstrated that cyclosporine inhibits hepatic and renal clearance of colchicine, thus increasing serum colchicine levels, further lowering the toxic colchicine dose.10,11
Our patient. The prophylactic dosage of colchicine our patient had been taking before her recent gout flare (.6 mg BID) was higher than the adjusted dose recommended to treat gout flares for patients taking cyclosporine (a single .6 mg dose to be repeated no earlier than 3 days).4 The dosages she took to treat her flare far exceeded this recommendation.
As a result, our patient developed severe colchicine toxicity. During her hospitalization, our patient’s cell counts continued to fall, requiring blood and platelet transfusions; her ANC nadir was 14 cells/mm3. She continued to have progressive multi-organ failure and developed alopecia. Management revolved around supportive measures for all of the end-organ effects.
Our patient died on hospital Day 7. Contributing factors included premorbid immunosuppression, renal insufficiency, and concomitant P-glycoprotein and CYP3A4 inhibition.
THE TAKEAWAY
Colchicine toxicity from therapeutic doses may occur in patients taking concomitant immunosuppressive drugs. Physicians who prescribe colchicine should be aware of these additional risks and adjust dosages accordingly. Activated charcoal can be given for acute overdose.
THE CASE
A 58-year-old female came to the emergency department (ED) because she had progressive weakness, hypotension, and altered mental status. In the ED she had a heart rate of 107 beats per minute; blood pressure, 96/68 mm Hg; respiratory rate, 20 breaths per minute; oxygen saturation, 96%; and a 96.7°F temperature that spiked to 101.6°F. The absolute neutrophil count (ANC) was 1500 cells/mm3, hemoglobin was 13 g/dL, and platelet count was 95 × 109/L. Her serum creatinine was 2.5 mg/dL (baseline of 1.0) and cyclosporine concentration was <25 ng/mL.
Our patient had a history of renal transplant, gout, and chronic kidney disease. Her medications included bumetanide, clonazepam, colchicine .6 mg BID, a therapeutic dose of cyclosporine, flurazepam, gabapentin, levothyroxine, mirtazapine, oxycodone, prednisone, and premarin. Three days before she came to the ED, she experienced a gout exacerbation and took six .6 mg doses (3.6 mg total) of colchicine that resulted in severe diarrhea. The next day, she took 3 mg of colchicine and had more severe diarrhea and a fever. Our patient took another 1.2 mg of colchicine the next day and developed the progressive weakness, hypotension, and altered mental status that led her to seek care in the ED.
THE DIAGNOSIS
Our patient was admitted to the hospital with a diagnosis of pancytopenia and presumed sepsis and intravenous broad-spectrum antibiotics were administered. Blood, urine, and sputum cultures, stool studies, and chest x-ray were negative for pneumonia. A peripheral blood smear revealed dysplastic-appearing neutrophils with vacuolization, which is characteristic of colchicine toxicity, myelodysplastic syndromes, or acute leukemia. However, the absence of blast cells in the peripheral blood smear and the normal appearance of the liver and spleen on a subsequent abdominal ultrasound refuted a primary hematologic disorder. Thus, based on the patient’s recent colchicine use and subsequent progressive pancytopenia and sepsis, we diagnosed colchicine toxicity in this patient.
DISCUSSION
Colchicine is a potent anti-inflammatory drug that has a narrow therapeutic index. Indicated for treating gout and familial Mediterranean fever, it inhibits mitosis by interfering with microtubule formation and arresting cell division. Colchicine is rapidly absorbed in the gastrointestinal (GI) tract and undergoes first-pass hepatic metabolism with enterohepatic recirculation of metabolites prior to excretion via the biliary tract.1 Ten percent to 20% of colchicine is excreted by the kidneys.2
Colchicine toxicity begins with GI symptoms, such as diarrhea, is followed by falling peripheral blood cell counts and altered mental status. A late sign of colchicine toxicity is alopecia. If the toxicity is left unchecked, multi-organ dysfunction that mimics severe sepsis will occur, resulting in death.3
Toxicity typically occurs at doses of .5 mg/kg/d. Fatal overdose from colchicine has been described in patients taking as little as 7 mg; however, survival from a 60-mg overdose has been reported.1 In a review of 150 patients who overdosed on colchicine, a single dose of .8 mg/kg was universally fatal.4 Therapeutic doses of colchicine have resulted in severe toxicity in patients with hepatic or renal dysfunction.5,6
Toxicity risk is increased in patients taking immunosuppressants
Colchicine toxicity from therapeutic doses may occur in patients taking concomitant immunosuppressive drugs, particularly cyclosporine. In case series, patients taking stable doses of cyclosporine and prophylactic doses of colchicine exhibited toxicity when they took therapeutic doses of colchicine for gout exacerbations.7,8 Another case series described 2 post-renal transplant patients, immunosuppressed with azathioprine and prednisone, who had comorbid familial Mediterranean fever and were maintained on colchicine prophylaxis.9 When they converted to cyclosporine for immunosuppression, each patient began to demonstrate GI and muscular symptoms of colchicine toxicity. Upon discontinuing cyclosporine, the GI and muscular symptoms rapidly resolved.9
How cyclosporine interacts with colchicine. Cyclosporine is a potent CYP3A4 and P-glycoprotein inhibitor, and colchicine is a CYP3A4 and P-glycoprotein substrate. In vivo studies have demonstrated that cyclosporine inhibits hepatic and renal clearance of colchicine, thus increasing serum colchicine levels, further lowering the toxic colchicine dose.10,11
Our patient. The prophylactic dosage of colchicine our patient had been taking before her recent gout flare (.6 mg BID) was higher than the adjusted dose recommended to treat gout flares for patients taking cyclosporine (a single .6 mg dose to be repeated no earlier than 3 days).4 The dosages she took to treat her flare far exceeded this recommendation.
As a result, our patient developed severe colchicine toxicity. During her hospitalization, our patient’s cell counts continued to fall, requiring blood and platelet transfusions; her ANC nadir was 14 cells/mm3. She continued to have progressive multi-organ failure and developed alopecia. Management revolved around supportive measures for all of the end-organ effects.
Our patient died on hospital Day 7. Contributing factors included premorbid immunosuppression, renal insufficiency, and concomitant P-glycoprotein and CYP3A4 inhibition.
THE TAKEAWAY
Colchicine toxicity from therapeutic doses may occur in patients taking concomitant immunosuppressive drugs. Physicians who prescribe colchicine should be aware of these additional risks and adjust dosages accordingly. Activated charcoal can be given for acute overdose.
1. Maxwell MJ, Muthu P, Pritty PE. Accidental colchicine overdose. A case report and literature review. Emerg Med J. 2002;19:265-267.
2. Gruberg L, Har-Zahav Y, Agranat O, et al. Acute myopathy induced by colchicine in a cyclosporine treated heart transplant recipient: possible role of the multidrug resistance transporter. Transplant Proc. 1999;31:2157-2158.
3. Colchicine: serious interactions. Prescrire Int. 2008;17:151-153.
4. Colcrys [package insert]. Deerfield, IL: Takeda Pharmaceuticals America, Inc; 2012.
5. Dickinson M, Juneja S. Haematological toxicity of colchicine. Br J Haematol. 2009;146:465.
6. Lee KY, Kim do Y, Chang JY, et al. Two cases of acute leukopenia induced by colchicine with concurrent immunosuppressants use in Behçet’s disease. Yonsei Med J. 2008;49:171-173.
7. Rieger EH, Halasz NA, Wahlstrom HE. Colchicine neuromyopathy after renal transplantation. Transplantation. 1990;49:1196-1198.
8. Minetti E, Minetti L. Multiple organ failure in a kidney transplant patient receiving both colchicine and cyclosporine. J Nephrol. 2003;16:421-425.
9. Yussim A, Bar-Nathan N, Lustig S, et al. Gastrointestinal, hepatorenal, and neuromuscular toxicity caused by cyclosporine-colchicine interaction in renal transplantation. Transplant Proc. 1994;26:2825-2826.
10. Speeg KV, Maldonado AL, Liaci J, et al. Effect of cyclosporine on colchicine secretion by the kidney multidrug transporter studied in vivo. J Pharmacol Exp Ther. 1992;261:50-55.
11. Speeg KV, Maldonado AL, Liaci J, et al. Effect of cyclosporine on colchicine secretion by a liver canalicular transporter studied in vivo. Hepatology. 1992;15:899-903.
1. Maxwell MJ, Muthu P, Pritty PE. Accidental colchicine overdose. A case report and literature review. Emerg Med J. 2002;19:265-267.
2. Gruberg L, Har-Zahav Y, Agranat O, et al. Acute myopathy induced by colchicine in a cyclosporine treated heart transplant recipient: possible role of the multidrug resistance transporter. Transplant Proc. 1999;31:2157-2158.
3. Colchicine: serious interactions. Prescrire Int. 2008;17:151-153.
4. Colcrys [package insert]. Deerfield, IL: Takeda Pharmaceuticals America, Inc; 2012.
5. Dickinson M, Juneja S. Haematological toxicity of colchicine. Br J Haematol. 2009;146:465.
6. Lee KY, Kim do Y, Chang JY, et al. Two cases of acute leukopenia induced by colchicine with concurrent immunosuppressants use in Behçet’s disease. Yonsei Med J. 2008;49:171-173.
7. Rieger EH, Halasz NA, Wahlstrom HE. Colchicine neuromyopathy after renal transplantation. Transplantation. 1990;49:1196-1198.
8. Minetti E, Minetti L. Multiple organ failure in a kidney transplant patient receiving both colchicine and cyclosporine. J Nephrol. 2003;16:421-425.
9. Yussim A, Bar-Nathan N, Lustig S, et al. Gastrointestinal, hepatorenal, and neuromuscular toxicity caused by cyclosporine-colchicine interaction in renal transplantation. Transplant Proc. 1994;26:2825-2826.
10. Speeg KV, Maldonado AL, Liaci J, et al. Effect of cyclosporine on colchicine secretion by the kidney multidrug transporter studied in vivo. J Pharmacol Exp Ther. 1992;261:50-55.
11. Speeg KV, Maldonado AL, Liaci J, et al. Effect of cyclosporine on colchicine secretion by a liver canalicular transporter studied in vivo. Hepatology. 1992;15:899-903.
Diet, exercise, and CVD: When counseling makes the most sense
In the past 2 years, the US Preventive Services Task Force (USPSTF) has released 2 recommendations on the primary prevention of cardiovascular disease (CVD). And it is proposing a third. The first recommendation, released in 2012, covered behavioral counseling on diet and physical activity to prevent CVD in individuals without documented CVD risks.1 The second recommendation, released earlier this year, covered the use of vitamins and mineral supplements to prevent CVD.2 A draft of the proposed third recommendation, which was posted for public review until early June, covers behavioral counseling to help adults with known CVD risk factors improve their diet and physical activity (TABLE).1-3
Counseling can influence behavior, but does it affect outcomes?
CVD is the leading cause of death in the United States, accounting for >596,000 deaths per year with an age-adjusted rate of 191.4 per 100,000.4 Age-adjusted CVD mortality has been declining for decades thanks to improved medical care and a reduction in smoking and other risk factors. It is well documented that adults who follow national recommendations for a healthy diet and levels of physical activity have lower rates of CVD and CVD mortality.1 The USPSTF agrees with the American Heart Association (AHA) and the American College of Cardiology (ACC) that everyone would benefit from a healthier diet and more exercise.5 However, the Task Force reviewed the evidence on behavioral counseling in the primary care setting and found that, for adults who do not have known CVD, hypertension, hyperlipidemia, or diabetes, even high-intensity behavioral counseling resulted in only a small benefit in intermediate outcomes, which would translate into very small population-wide improvements.
In the evidence report prepared by the Task Force, the intensity of counseling intervention was defined as low, medium, or high if it lasted, respectively, 1 to 30 minutes, 31 to 360 minutes, or ≥361 minutes. Low-intensity interventions involved brief counseling sessions performed by primary care clinicians or mailing educational materials to patients or both. Medium- and high-intensity interventions usually were conducted by health educators, nutritionists, or other professionals instead of primary care clinicians. These interventions improved patients’ consumption of a healthier diet and participation in physical activity, but yielded only modest reductions in body mass index (BMI), blood pressure (BP), and lipid levels. Moreover, no direct evidence exists for improved CVD outcomes with these interventions.
The recent AHA/ACC guideline on lifestyle modifications recommends that clinicians advise all adults on healthy dietary choices and exercise, based on the known benefits of these behaviors. The guideline developers recognized that the evidence for benefits appears in the highest risk groups, and they did not assess the evidence for effectiveness of behavioral counseling itself.6
The Task Force rationale for recommending counseling
In the draft of its third recommendation addressing those at highest risk for CVD, the Task Force does advise high-intensity behavioral counseling for those who are overweight or obese and who have other CVD risk factors such as hypertension, hyperlipidemia, or impaired fasting glucose levels. This proposed new recommendation replaces one from 2003 that advised intensive dietary counseling for those with CVD risks including hyperlipidemia. The draft focuses attention in primary care on those who are overweight or obese. It complements another Task Force recommendation to provide or to refer patients for intensive multicomponent behavioral interventions if they are obese, defined as a BMI ≥30 kg/m2.7
The Task Force cited 2 examples of behavioral interventions that can improve outcomes in those with CVD risks—the Diabetes Prevention Program and PREMIER, a set of interventions to lower BP.8,9 These programs have improved intermediate outcomes after 12 to 24 months, decreasing total cholesterol by 3 to 6 mg/dL and low-density lipoprotein cholesterol by 1.5 to 5 mg/dL; systolic and diastolic BP by 1 to 3 mm Hg and 1 to 2 mm Hg, respectively; fasting glucose by 1 to 3 mg/dL; and weight by approximately 3 kg. The Task Force felt that while hard evidence is lacking for reducing CVD with counseling, epidemiologic studies demonstrate that, in those at high risk, reductions in CVD rates generally reflect the magnitude of improvement in intermediate measures.
Half of all adults in the United States have at least one documented CVD risk factor. But the potential benefit of behavioral counseling for those without documented CVD risks is relatively small. Rather than expending effort for only modest gain in the lower risk group, the Task Force recommends focusing on those with highest CVD risk. Thus the non-high risk group received a “C” recommendation, while the group of overweight and obese patients with other CVD risks received a “B” recommendation for essentially the same interventions. (For more on the grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.)
In addition to counseling...
The Task Force also recommends other interventions for the primary prevention of CVD:
- screening for and treating hypertension
- selectively screening for hyperlipidemia
- using aspirin to prevent CVD in those at high risk
- intensive counseling on weight management for those who are obese
- advising children and adolescents to avoid tobacco, and using brief interventions for tobacco cessation for smokers.
The recent Task Force recommendation on the use of vitamins, minerals, and multivitamins2 states that, while many adults take vitamin and mineral supplements in the belief that they prevent both heart disease and cancer, there is no evidence to support that belief. And there is good evidence that both β-carotene and vitamin E do not prevent disease. For other vitamins and minerals, singly or in combination, there is insufficient evidence to recommend for or against their use.2
The Community Preventive Services Task Force—a separate expert panel established by the US Department of Health and Human Services to complement the USPSTF—makes recommendations on population-level interventions and has a series of recommendations on ways to improve the population’s nutrition and physical activity.10 These community-based interventions, if widely implemented, would probably yield greater improvements in healthy eating and increased activity levels than resource-intense clinical interventions based on individual patients with low risk.
1. USPSTF. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsphys.htm. Accessed May 21, 2014.
2. USPSTF. Vitamin, mineral, and multivitamin supplements for the primary prevention of cardiovascular disease and cancer. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf14/vitasupp/vitasuppfinalrs.htm. Accessed May 21, 2014.
3. USPSTF. Behavioral counseling to promote a healthy diet and physical activity for cardiovascular disease prevention in adults with known risk factors: US Preventive Services Task Force Recommendation Statement (Draft). US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf13/cvdhighrisk/cvdhighriskdraftrec.htm. Accessed July 22, 2014.
4. Centers for Disease Control and Prevention. Hoyert DL, Xu J. Deaths: preliminary data for 2011. Natl Vital Stat Report. 2012;61:1-51.
5. Eckel RH, Jakicic JM, Ard, JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Nov 12. [Epub ahead of print].
6. Stone NJ, Robinson JG, Lichtenstein AH, et al; 2013 ACC/AHA Cholesterol Guideline Panel. Treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: synopsis of the 2013 American College of Cardiology/American Heart Association cholesterol guideline. Ann Intern Med. 2014;160:339-343.
7. USPSTF. Screening for and management of obesity in adults. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsobes.htm. Accessed May 21, 2014.
8. Knowler WC, Barrett-Connor E, Fowler SE, et al; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403.
9. Elmer PJ, Obarzanek E, Vollmer WM, et al; PREMIER Collaborative Research Group. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med. 2006;144:485-495.
10. USPSTF. The Guide to Community Preventive Services. Community Preventive Services Task Force Web site. Available at: http://www.thecommunityguide.org/index.html. Accessed May 21, 2014.
In the past 2 years, the US Preventive Services Task Force (USPSTF) has released 2 recommendations on the primary prevention of cardiovascular disease (CVD). And it is proposing a third. The first recommendation, released in 2012, covered behavioral counseling on diet and physical activity to prevent CVD in individuals without documented CVD risks.1 The second recommendation, released earlier this year, covered the use of vitamins and mineral supplements to prevent CVD.2 A draft of the proposed third recommendation, which was posted for public review until early June, covers behavioral counseling to help adults with known CVD risk factors improve their diet and physical activity (TABLE).1-3
Counseling can influence behavior, but does it affect outcomes?
CVD is the leading cause of death in the United States, accounting for >596,000 deaths per year with an age-adjusted rate of 191.4 per 100,000.4 Age-adjusted CVD mortality has been declining for decades thanks to improved medical care and a reduction in smoking and other risk factors. It is well documented that adults who follow national recommendations for a healthy diet and levels of physical activity have lower rates of CVD and CVD mortality.1 The USPSTF agrees with the American Heart Association (AHA) and the American College of Cardiology (ACC) that everyone would benefit from a healthier diet and more exercise.5 However, the Task Force reviewed the evidence on behavioral counseling in the primary care setting and found that, for adults who do not have known CVD, hypertension, hyperlipidemia, or diabetes, even high-intensity behavioral counseling resulted in only a small benefit in intermediate outcomes, which would translate into very small population-wide improvements.
In the evidence report prepared by the Task Force, the intensity of counseling intervention was defined as low, medium, or high if it lasted, respectively, 1 to 30 minutes, 31 to 360 minutes, or ≥361 minutes. Low-intensity interventions involved brief counseling sessions performed by primary care clinicians or mailing educational materials to patients or both. Medium- and high-intensity interventions usually were conducted by health educators, nutritionists, or other professionals instead of primary care clinicians. These interventions improved patients’ consumption of a healthier diet and participation in physical activity, but yielded only modest reductions in body mass index (BMI), blood pressure (BP), and lipid levels. Moreover, no direct evidence exists for improved CVD outcomes with these interventions.
The recent AHA/ACC guideline on lifestyle modifications recommends that clinicians advise all adults on healthy dietary choices and exercise, based on the known benefits of these behaviors. The guideline developers recognized that the evidence for benefits appears in the highest risk groups, and they did not assess the evidence for effectiveness of behavioral counseling itself.6
The Task Force rationale for recommending counseling
In the draft of its third recommendation addressing those at highest risk for CVD, the Task Force does advise high-intensity behavioral counseling for those who are overweight or obese and who have other CVD risk factors such as hypertension, hyperlipidemia, or impaired fasting glucose levels. This proposed new recommendation replaces one from 2003 that advised intensive dietary counseling for those with CVD risks including hyperlipidemia. The draft focuses attention in primary care on those who are overweight or obese. It complements another Task Force recommendation to provide or to refer patients for intensive multicomponent behavioral interventions if they are obese, defined as a BMI ≥30 kg/m2.7
The Task Force cited 2 examples of behavioral interventions that can improve outcomes in those with CVD risks—the Diabetes Prevention Program and PREMIER, a set of interventions to lower BP.8,9 These programs have improved intermediate outcomes after 12 to 24 months, decreasing total cholesterol by 3 to 6 mg/dL and low-density lipoprotein cholesterol by 1.5 to 5 mg/dL; systolic and diastolic BP by 1 to 3 mm Hg and 1 to 2 mm Hg, respectively; fasting glucose by 1 to 3 mg/dL; and weight by approximately 3 kg. The Task Force felt that while hard evidence is lacking for reducing CVD with counseling, epidemiologic studies demonstrate that, in those at high risk, reductions in CVD rates generally reflect the magnitude of improvement in intermediate measures.
Half of all adults in the United States have at least one documented CVD risk factor. But the potential benefit of behavioral counseling for those without documented CVD risks is relatively small. Rather than expending effort for only modest gain in the lower risk group, the Task Force recommends focusing on those with highest CVD risk. Thus the non-high risk group received a “C” recommendation, while the group of overweight and obese patients with other CVD risks received a “B” recommendation for essentially the same interventions. (For more on the grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.)
In addition to counseling...
The Task Force also recommends other interventions for the primary prevention of CVD:
- screening for and treating hypertension
- selectively screening for hyperlipidemia
- using aspirin to prevent CVD in those at high risk
- intensive counseling on weight management for those who are obese
- advising children and adolescents to avoid tobacco, and using brief interventions for tobacco cessation for smokers.
The recent Task Force recommendation on the use of vitamins, minerals, and multivitamins2 states that, while many adults take vitamin and mineral supplements in the belief that they prevent both heart disease and cancer, there is no evidence to support that belief. And there is good evidence that both β-carotene and vitamin E do not prevent disease. For other vitamins and minerals, singly or in combination, there is insufficient evidence to recommend for or against their use.2
The Community Preventive Services Task Force—a separate expert panel established by the US Department of Health and Human Services to complement the USPSTF—makes recommendations on population-level interventions and has a series of recommendations on ways to improve the population’s nutrition and physical activity.10 These community-based interventions, if widely implemented, would probably yield greater improvements in healthy eating and increased activity levels than resource-intense clinical interventions based on individual patients with low risk.
In the past 2 years, the US Preventive Services Task Force (USPSTF) has released 2 recommendations on the primary prevention of cardiovascular disease (CVD). And it is proposing a third. The first recommendation, released in 2012, covered behavioral counseling on diet and physical activity to prevent CVD in individuals without documented CVD risks.1 The second recommendation, released earlier this year, covered the use of vitamins and mineral supplements to prevent CVD.2 A draft of the proposed third recommendation, which was posted for public review until early June, covers behavioral counseling to help adults with known CVD risk factors improve their diet and physical activity (TABLE).1-3
Counseling can influence behavior, but does it affect outcomes?
CVD is the leading cause of death in the United States, accounting for >596,000 deaths per year with an age-adjusted rate of 191.4 per 100,000.4 Age-adjusted CVD mortality has been declining for decades thanks to improved medical care and a reduction in smoking and other risk factors. It is well documented that adults who follow national recommendations for a healthy diet and levels of physical activity have lower rates of CVD and CVD mortality.1 The USPSTF agrees with the American Heart Association (AHA) and the American College of Cardiology (ACC) that everyone would benefit from a healthier diet and more exercise.5 However, the Task Force reviewed the evidence on behavioral counseling in the primary care setting and found that, for adults who do not have known CVD, hypertension, hyperlipidemia, or diabetes, even high-intensity behavioral counseling resulted in only a small benefit in intermediate outcomes, which would translate into very small population-wide improvements.
In the evidence report prepared by the Task Force, the intensity of counseling intervention was defined as low, medium, or high if it lasted, respectively, 1 to 30 minutes, 31 to 360 minutes, or ≥361 minutes. Low-intensity interventions involved brief counseling sessions performed by primary care clinicians or mailing educational materials to patients or both. Medium- and high-intensity interventions usually were conducted by health educators, nutritionists, or other professionals instead of primary care clinicians. These interventions improved patients’ consumption of a healthier diet and participation in physical activity, but yielded only modest reductions in body mass index (BMI), blood pressure (BP), and lipid levels. Moreover, no direct evidence exists for improved CVD outcomes with these interventions.
The recent AHA/ACC guideline on lifestyle modifications recommends that clinicians advise all adults on healthy dietary choices and exercise, based on the known benefits of these behaviors. The guideline developers recognized that the evidence for benefits appears in the highest risk groups, and they did not assess the evidence for effectiveness of behavioral counseling itself.6
The Task Force rationale for recommending counseling
In the draft of its third recommendation addressing those at highest risk for CVD, the Task Force does advise high-intensity behavioral counseling for those who are overweight or obese and who have other CVD risk factors such as hypertension, hyperlipidemia, or impaired fasting glucose levels. This proposed new recommendation replaces one from 2003 that advised intensive dietary counseling for those with CVD risks including hyperlipidemia. The draft focuses attention in primary care on those who are overweight or obese. It complements another Task Force recommendation to provide or to refer patients for intensive multicomponent behavioral interventions if they are obese, defined as a BMI ≥30 kg/m2.7
The Task Force cited 2 examples of behavioral interventions that can improve outcomes in those with CVD risks—the Diabetes Prevention Program and PREMIER, a set of interventions to lower BP.8,9 These programs have improved intermediate outcomes after 12 to 24 months, decreasing total cholesterol by 3 to 6 mg/dL and low-density lipoprotein cholesterol by 1.5 to 5 mg/dL; systolic and diastolic BP by 1 to 3 mm Hg and 1 to 2 mm Hg, respectively; fasting glucose by 1 to 3 mg/dL; and weight by approximately 3 kg. The Task Force felt that while hard evidence is lacking for reducing CVD with counseling, epidemiologic studies demonstrate that, in those at high risk, reductions in CVD rates generally reflect the magnitude of improvement in intermediate measures.
Half of all adults in the United States have at least one documented CVD risk factor. But the potential benefit of behavioral counseling for those without documented CVD risks is relatively small. Rather than expending effort for only modest gain in the lower risk group, the Task Force recommends focusing on those with highest CVD risk. Thus the non-high risk group received a “C” recommendation, while the group of overweight and obese patients with other CVD risks received a “B” recommendation for essentially the same interventions. (For more on the grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.)
In addition to counseling...
The Task Force also recommends other interventions for the primary prevention of CVD:
- screening for and treating hypertension
- selectively screening for hyperlipidemia
- using aspirin to prevent CVD in those at high risk
- intensive counseling on weight management for those who are obese
- advising children and adolescents to avoid tobacco, and using brief interventions for tobacco cessation for smokers.
The recent Task Force recommendation on the use of vitamins, minerals, and multivitamins2 states that, while many adults take vitamin and mineral supplements in the belief that they prevent both heart disease and cancer, there is no evidence to support that belief. And there is good evidence that both β-carotene and vitamin E do not prevent disease. For other vitamins and minerals, singly or in combination, there is insufficient evidence to recommend for or against their use.2
The Community Preventive Services Task Force—a separate expert panel established by the US Department of Health and Human Services to complement the USPSTF—makes recommendations on population-level interventions and has a series of recommendations on ways to improve the population’s nutrition and physical activity.10 These community-based interventions, if widely implemented, would probably yield greater improvements in healthy eating and increased activity levels than resource-intense clinical interventions based on individual patients with low risk.
1. USPSTF. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsphys.htm. Accessed May 21, 2014.
2. USPSTF. Vitamin, mineral, and multivitamin supplements for the primary prevention of cardiovascular disease and cancer. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf14/vitasupp/vitasuppfinalrs.htm. Accessed May 21, 2014.
3. USPSTF. Behavioral counseling to promote a healthy diet and physical activity for cardiovascular disease prevention in adults with known risk factors: US Preventive Services Task Force Recommendation Statement (Draft). US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf13/cvdhighrisk/cvdhighriskdraftrec.htm. Accessed July 22, 2014.
4. Centers for Disease Control and Prevention. Hoyert DL, Xu J. Deaths: preliminary data for 2011. Natl Vital Stat Report. 2012;61:1-51.
5. Eckel RH, Jakicic JM, Ard, JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Nov 12. [Epub ahead of print].
6. Stone NJ, Robinson JG, Lichtenstein AH, et al; 2013 ACC/AHA Cholesterol Guideline Panel. Treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: synopsis of the 2013 American College of Cardiology/American Heart Association cholesterol guideline. Ann Intern Med. 2014;160:339-343.
7. USPSTF. Screening for and management of obesity in adults. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsobes.htm. Accessed May 21, 2014.
8. Knowler WC, Barrett-Connor E, Fowler SE, et al; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403.
9. Elmer PJ, Obarzanek E, Vollmer WM, et al; PREMIER Collaborative Research Group. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med. 2006;144:485-495.
10. USPSTF. The Guide to Community Preventive Services. Community Preventive Services Task Force Web site. Available at: http://www.thecommunityguide.org/index.html. Accessed May 21, 2014.
1. USPSTF. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsphys.htm. Accessed May 21, 2014.
2. USPSTF. Vitamin, mineral, and multivitamin supplements for the primary prevention of cardiovascular disease and cancer. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf14/vitasupp/vitasuppfinalrs.htm. Accessed May 21, 2014.
3. USPSTF. Behavioral counseling to promote a healthy diet and physical activity for cardiovascular disease prevention in adults with known risk factors: US Preventive Services Task Force Recommendation Statement (Draft). US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf13/cvdhighrisk/cvdhighriskdraftrec.htm. Accessed July 22, 2014.
4. Centers for Disease Control and Prevention. Hoyert DL, Xu J. Deaths: preliminary data for 2011. Natl Vital Stat Report. 2012;61:1-51.
5. Eckel RH, Jakicic JM, Ard, JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Nov 12. [Epub ahead of print].
6. Stone NJ, Robinson JG, Lichtenstein AH, et al; 2013 ACC/AHA Cholesterol Guideline Panel. Treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: synopsis of the 2013 American College of Cardiology/American Heart Association cholesterol guideline. Ann Intern Med. 2014;160:339-343.
7. USPSTF. Screening for and management of obesity in adults. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsobes.htm. Accessed May 21, 2014.
8. Knowler WC, Barrett-Connor E, Fowler SE, et al; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403.
9. Elmer PJ, Obarzanek E, Vollmer WM, et al; PREMIER Collaborative Research Group. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med. 2006;144:485-495.
10. USPSTF. The Guide to Community Preventive Services. Community Preventive Services Task Force Web site. Available at: http://www.thecommunityguide.org/index.html. Accessed May 21, 2014.
Strategies to help reduce hospital readmissions
› Use risk stratification methods such as the Probability of Repeated Admission (Pra) or the LACE index to identify patients at high risk for readmission. B
› Take steps to ensure that follow-up appointments are made within the first one to 2 weeks of discharge, depending on the patient’s risk of readmission. C
› Reconcile preadmission and postdischarge medications to identify discrepancies and possible interactions. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Charles T, age 74, has a 3-year history of myocardial infarction (MI) and congestive heart failure (CHF) and a 10-year his-tory of type 2 diabetes with retinopathy. You have cared for him in the outpatient setting for 8 years. You are notified that he is in the emergency department (ED) and being admitted to the hospital, again. This is his third ED visit in the past 3 months; he was hospitalized for 6 days during his last admission 3 weeks ago.
What should you do with this information? How can you best communicate with the admitting team?
Hospital readmissions are widespread, costly, and often avoidable. Nearly 20% of Medicare beneficiaries discharged from hospitals are rehospitalized within 30 days, and 34% are rehospitalized within 90 days.1 For patients with conditions like CHF, the rate of readmission within 30 days approaches 25%.2 The estimated cost to Medicare for unplanned rehospitalizations in 2004 was $17.4 billion.1 The Centers for Medicare and Medicaid Services penalizes hospitals for high rates of readmission within 30 days of discharge for patients with CHF, MI, and pneumonia.
“Avoidable” hospitalizations are those that may be prevented by effective outpatient management and improved care coordination. Although efforts to reduce readmissions have focused on improving the discharge process, family physicians (FPs) can play a central role in reducing readmissions. This article describes key approaches that FPs can take to address this important issue. Because patients ages ≥65 years consistently have the highest rate of hospital readmissions,1 we will focus on this population.
Multiple complex factors are associated with hospital readmissions
Characteristics of the patient, physician, and health care setting contribute to potentially avoidable readmissions (TABLE 1).3,4
Medical conditions and comorbidities associated with high rates of rehospitalization include CHF, acute MI, pneumonia, diabetes, and chronic obstructive pulmonary disease. However, a recent study found that a diverse range of conditions, frequently differing from the index cause of hospitalization, were responsible for 30-day readmissions of Medicare patients.5
Identifying those at high risk: Why and how
Determining which patients are at highest risk for readmission enables health care teams to match the intensity of interventions to the individual’s likelihood of readmission. However, current readmission risk prediction models remain a work in progress6 and few models have been tested in the outpatient setting. Despite numerous limitations, it’s still important to focus resources more efficiently. Thus, we recommend using risk stratification tools to identify patients at high risk for readmission.
Many risk stratification methods use data from electronic medical records (EMRs) and administrative databases or self-reported data from patients.7 Risk prediction tools that are relatively simple and easy to administer or generate through EMRs—such as the Probability of Repeated Admission (Pra),8 the LACE (Length of stay, acuity of the admission, comorbidities, ED visits in the previous 6 months) index,9 or the Community Assessment Risk Screen (CARS)10—may be best for use in the primary care setting. These tools generally identify key risk factors, such as prior health care utilization, presence of specific conditions such as heart disease or cognitive impairment, self-reported health status, absence of a caregiver, and/or need for assistance with daily routines.
Many of these tools have been used to identify high-risk older adults and may not be appropriate for patients who are likely to be readmitted for different reasons, such as mental illness, substance abuse, or chronic pain. Therefore, it is important to use a risk stratification method that captures the issues most likely to cause readmissions in your patient population, or to consider using a variety of methods.
The American Academy of Family Physicians (AAFP) offers resources to help FPs design methods for determining a patient’s health risk status and linking higher levels of risk to increasing care management at http://www.aafp.org/practice-management/pcmh/initiatives/cpci/rscm.html.
CASE › Mr. T has been admitted to the hospital 3 times in the past 3 months, so you use the lace index to evaluate his risk. You determine that Mr. T’s score is 15, which means his expected risk of death or unplanned readmission is 26.6% (TABLE 2).8,11 What are your next steps?
Foster communication between the hospital and outpatient office
Patients are particularly vulnerable during the transition from hospital to home. Delayed or inaccurate information adversely affects continuity of care, patient safety and satisfaction, and efficient use of resources.12 Discharge summaries are the main method of communication between providers, but their content, timeliness, availability, and quality frequently are lacking.13 Discharge summaries are available at only 12% to 34% of first postdischarge visits, and these summaries often lack important information such as diagnostic test results (33%-63%) or discharge medications (2%-40%).12 Although researchers have not consistently found that transferring a discharge summary to an outpatient physician reduces readmission rates, it is likely that direct communication can improve the handoff process independent of its effects on readmissions.12,14
Timely follow-up appointments are essential
Many factors influence the need for rapid follow-up, including disease severity, management complexity, ability of the patient to provide sufficient self-care, and adequacy of social supports.15,16 Studies have found that discharged patients who receive timely outpatient follow-up are less likely to be readmitted.1,17 While the optimal time interval between discharge and the first follow-up appointment is unknown, some literature supports follow-up within 4 weeks.15,18 However, because readmissions often cluster in the first several days or week following discharge,18 follow-up within the first 2 weeks (and within the first week for higher-risk patients) may be appropriate.19 Ideally, follow-up appointments should be scheduled before the patient is discharged. Patients who schedule a follow-up appointment before they are discharged are more likely to make their follow-up visit than those who are asked to call after discharge and schedule their own appointment.12
Employ outpatient follow-up alternatives
Follow-up telephone calls to patients after discharge help patients understand and adhere to discharge instructions and troubleshoot problems. Clinicians who use scripted telephone calls can evaluate symptoms related to the index hospitalization, provide patient education, schedule relevant appointments or testing, and, most importantly, initiate medication reconciliation, which is described at right.20 The FIGURE includes the script we use at our practice.
Home visits may be appropriate for certain patients, including the frail elderly. Home visits allow clinicians to evaluate the patient’s environmental safety, social sup port, and medication adherence.12 Preventive home visits generally have not been found to reduce hospital readmissions, but do enhance patient satisfaction with care.21
Bundled interventions, such as alternating home visits and follow-up telephone calls, may be more effective than individual interventions in reducing readmission.22
Reconciling medications may have far-reaching benefits
Medication discrepancies are observed in up to 70% of all patients at admission or discharge and are associated with adverse drug events (ADEs).23 To prevent ADEs and possibly readmission, take the following steps to reconcile a patient’s medications23:
Obtain a complete list of current medications. Information on all of the patient’s prescription and nonprescription medications should be collected from the patient/caregiver, the discharge summary, prescription bottles, home visits, and pharmacies.12,24
Reconcile preadmission and postdischarge medications. Clarify any discrepancies, review all medications for safety and appropriateness, and, when appropriate, resume any held medications and/or discontinue unnecessary ones.
Research shows that patients who received a phone call from a pharmacist within 3 to 7 days of discharge had lower readmission rates.Enlist pharmacy support. Pharmacists are uniquely positioned to review indications as well as potential duplication and interactions of a patient’s medications. Inpatient studies have demonstrated that partnering with pharmacists results in fewer ADEs.12,25 One study showed that patients at high risk for readmission who received a phone call from a pharmacist 3 to 7 days after discharge had lower readmission rates.26 The pharmacist reconciled the patients’ medications and ensured that patients had a clear understanding of each medication, its common safety concerns, and how often they were supposed to take it.26
Make medication adherence as easy as possible
As many as half of all patients don’t take their medications as prescribed.27 There is limited data on health outcomes associated with medication nonadherence, and existing data frequently are contradictory—some studies have found that as many as 11% of hospital admissions are attributed to nonadherence, while others show no association.28
Factors that affect adherence include psychiatric or cognitive impairment, limited insight into disease process or lack of belief in benefit of treatment, medication cost or adverse effect profile, poor provider-patient relationship, limited access to care or medication, or complexity of treatment.29 To promote medication adherence, consider the following educational and behavioral strategies30:
Identify patients at risk for nonadherence. This includes those with complex regimens and/or uncontrolled disease states or symptoms.
Increase patient communication and counseling. Patient education, particularly on the importance of adherence, is one of the few solo interventions that can improve compliance.31 Involving caregivers and using both verbal and written materials provides additional benefit.31,32
Simplify dosing schedules. Simple, convenient medication regimens may im- prove adherence. For example, adjusting dosing from 3 times a day to once a day can increase adherence from 59% to 83%.33 Aids such as pillboxes to organize medications may be of benefit.29,32
Ensure consistent follow-up. Patients who miss appointments are more likely to be nonadherent. They may benefit from easy access, help with scheduling, and frequent visits.32
Be mindful of patients’ out-of-pocket expenses. Reducing copayments improves adherence rates.30
Minimize polypharmacy. Polypharmacy has been independently associated with nonadherence and increased risk for ADEs.34
Identify patients who have limited health literacy. Limited health literacy may be linked to increased medication errors and nonadherence.12,35 Patients with low health literacy may be unable to identify medications recorded in their medical record. TABLE W336-41 outlines strategies for identifying patients with low health literacy and improving communication with them.
CASE › By speaking with hospital staff before Mr. T is discharged, you are able to confirm that he has scheduled a follow-up visit with you for one week after discharge, and that a discharge summary will be available for him to bring to that visit. Mr. T brings his discharge summary with him to your office, and you reconcile his medication list. Because he is your last patient of the day, you have some time to sit with him and his wife to explore his goals of care.
Improve care—and possibly reduce readmissions—through goal setting
Goal setting is an important element of postdischarge follow-up, particularly for elderly patients and those with progressive or end-stage diseases. Goal setting can improve patient care by linking care plans with desired outcomes and keeping diagnostic and therapeutic interventions relevant to the patient.42 A patient who understands the purpose of a recommendation—especially when directly linked to a patient-derived goal—may be more likely to adhere to the plan of care.
Asking patients to articulate their goals of care using “Ask-Tell-Ask” framework described in TABLE W336-41 will allow you to deliver the prognosis, reinforce treatment options to achieve patient-specific goals, empower patients to assert their preferences, and develop a follow-up plan to see if treatment is successful.
Empowering patients
Consider using both verbal and written approaches when educating patients about self-care behaviors such as monitoring symptoms and adhering to dietary/behavior restrictions and medication instructions. One study showed that a brief one-on-one patient education session decreased readmissions in patients with heart failure,43 although another study found that patient education alone yielded a nonsignificant decrease.44
Providing caregivers with education and support is a critical and perhaps overlooked opportunity to reduce readmissions.45 Involving key family members in discharge planning, preparation, follow-up, and ongoing management is essential in caring for patients with functional deficits and/or complex care needs. Educating caregivers can help them feel more prepared and effective in their roles.
Establish an “action plan.” For patients with chronic, periodically symptomatic diseases such as asthma and heart failure, action planning can be useful. Action plans should include information that reinforces patients’ daily self-care behaviors and instructions for what to do if symptoms get worse. Action planning also might include simple if-then plans (“if x happens, then I will do y”), which can help with problem solving for common scenarios. Action plans have been shown to reduce admissions for children with asthma46 and adults with heart failure when coupled with home monitoring or telephone support from a registered nurse.16,47
Generate an individualized care plan for each patient, taking into account your patient’s health literacy, goals of care, and level of social support. This care plan may include educational and behavioral interventions, action planning, and follow-up plans. Most successful approaches to reducing readmissions have included both system-level and patient-level interventions that use an interdisciplinary team of providers.48
Make the most of follow-up visits. The traditional 15-minute FP visit can make it challenging to provide the level of care necessary for recently discharged patients. Multiple models of team-based care have been proposed to improve this situation, including using the “teamlet” model, which may include a clinician and one or 2 health coaches.49 During each visit, the health coaches—often medical assistants trained in chronic disease self-management skills—see patients before and after the physician. They also contact patients be- tween visits to facilitate action planning and to promote self-management.
Palliative care programs: A resource for FPs
The growth of palliative care programs in US hospitals has helped increase the emphasis on establishing goals of care. Inpatient-based palliative care consultation programs work with patients and families to establish goals. However, after discharge, many of these goals and plans begin to unravel due to gaps in the current health care model, including lack of follow-up and support.50 Outpatient palliative care programs have begun to address these gaps in care.50 Comprehensive palliative care programs are quickly becoming an important resource for FPs to help address transitional care issues.
CASE › When you ask Mr. and Mrs. T about his goals for treatment, they say are getting tired of the “back and forth” to the hospital. After discussing his lengthy history of worsening CHF and diabetes, you raise the idea of palliative care, including hospice, with the couple. They acknowledge that they have had family members get hospice care, and they are open to it—just not yet. The 3 of you craft an “if-then” plan of care to use at home. You schedule a 2-week follow-up visit and remind Mr. T and his wife of your office’s 24-hour on-call service.
CORRESPONDENCE
Danielle Snyderman, MD, Department of Family and Community Medicine, Jefferson University, 1015 Walnut Street, Suite 401, Philadelphia, Pa 19107; [email protected]
1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418-1428
2. O’Connor CM, Miller AB, Blair JE, et al; Efficacy of Vasopressin Antagonism in heart Failure Outcome Study with Tolvaptan (EVEREST) investigators. Causes of death and rehospitalization in patients hospitalized with worsening heart failure and reduce left ventricular ejection fraction; results from EVEREST program. Am Heart J. 2010;159:841-849.e1.
3. Garrison GM, Mansukhani MP, Bohn B. Predictors of thirty-day readmission among hospitalized family medicine patients. J Am Board Fam Med. 2013;26:71-77.
4. Boult C, Dowd B, McCaffrey D, et al. Screening elders for risk of hospital admission. J Am Geriatr Soc. 1993;41:811-817.
5. Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355-363.
6. Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688-1698.
7. Haas LR, Takahashi PY, Shah ND, et al. Risk-stratification methods for identifying patients for care coordination. Am J Manag Care. 2013;19:725-732.
8. Wallace E, Hinchey T, Dimitrov BD, et al. A systematic review of the probability of repeated admission score in community-dwelling adults. J Am Geriatr Soc. 2013;61:357-364.
9. Cotter PE, Bhalla VK, Wallis SJ, et al. Predicting readmissions: poor performance of the LACE index in an older UK population. Age Ageing. 2012;41:784-789.
10. Shelton P, Sager MA, Schraeder C. The community assessment risk screen (CARS): identifying elderly persons at risk for hospitalization or emergency department visit. Am J Manag Care. 2000;6:925-933.
11. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373-383.
12. Kripalani S, Jackson AT, Schnipper JL, et al. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2:314-323.
13. Kim CS, Flanders SA. In the clinic. Transitions of care. Ann Intern Med. 2013;158(5 pt 1):ITC3-1.
14. Hansen LO, Strater A, Smith L, et al. Hospital discharge documentation and risk of rehospitalisation. BMJ Qual Saf. 2011;20:773-778.
15. Vaduganathan M, Bonow RO, Gheorghiade M. Thirty-day readmissions: the clock is ticking. JAMA. 2013;309:345-346.
16. Hansen LO, Young RS, Hinami K, et al. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520-528.
17. Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5:392-397.
18. van Walraven C, Jennings A, Taljaard M, et al. Incidence of potentially avoidable urgent readmissions and their relation to all-cause urgent readmissions. CMAJ. 2011;183:E1067-E1072.
19. Tang, N. A primary care physician’s ideal transitions of care—where’s the evidence? J Hosp Med. 2013;8:472-477.
20. Crocker JB, Crocker JT, Greenwald JL. Telephone follow-up as a primary care intervention for postdischarge outcomes improvement: a systematic review. Am J Med. 2012;125:915-921.
21. Wong FK, Chow S, Chung L, et al. Can home visits help reduce hospital readmissions? Randomized controlled trial. J Adv Nurs. 2008;62:585-595.
22. Wong FK, Chow SK, Chan TM, et al. Comparison of effects between home visits with telephone calls and telephone calls only for transitional discharge support: a randomised controlled trial. Age Ageing. 2014;43:91-97.
23. Mueller SK, Sponsler KC, Kripalani S, et al. Hospital-based medication reconciliation practices: a systematic review. Arch Intern Med. 2012;172:1057-1069.
24. Glintborg B, Andersen SE, Dalhoff K. Insufficient communication about medication use at the interface between hospital and primary care. Qual Saf Health Care. 2007;16:34-39.
25. Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166:565-571.
26. Kilcup M, Schultz D, Carlson J, et al. Postdischarge pharmacist medication reconciliation: impact on readmission rates and financial savings. J Am Pharm Assoc (2003). 2013;53:78-84.
27. Vermeire E, Hearnshaw H, Van Royen P, et al. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26:331-342.
28. Vik SA, Maxwell CJ, Hogan DB. Measurement, correlates, and health outcomes of medication adherence among seniors. Ann Pharmacother. 2004;38:303-312.
29. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487-497.
30. Viswanathan M, Golin CE, Jones CD, et al. Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Ann Intern Med. 2012;157:785-795.
31. McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA. 2002;288:2868-2879.
32. Kripalani S, Yao X, Haynes RB. Interventions to enhance medication adherence in chronic medical conditions: a systematic review. Arch Intern Med. 2007;167:540-550.
33. Eisen SA, Miller DK, Woodward RS, et al. The effect of prescribed daily dose frequency on patient medication compliance. Arch Intern Med. 1990;150:1881-1884.
34. Field TS, Gurwitz JH, Avorn J, et al. Risk factors for adverse drug events among nursing home residents. Arch Intern Med. 2001;161:1629-1634.
35. Persell SD, Osborn CY, Richard R, et al. Limited health literacy is a barrier to medication reconciliation in ambulatory care. J Gen Intern Med. 2007;22:1523-1526.
36. Weiss BD. Health Literacy and Patient Safety: Help Patients Understand. Manual for Clinicians. Chicago, IL: American Medical Association Foundation; 2007.
37. Chew LD, Bradley KA, Bokyo EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588-594.
38. Wallace LS, Rogers ES, Roskos SE, et al. Brief report: screening items to identify patients with limited health literacy skills. J Gen Intern Med. 2006;21:874-877.
39. Doak CC, Doak LG, Root JH. Teaching Patients with Low Literacy Skills. 2nd ed. Philadelphia, PA: JB Lippincott Company; 1996.
40. Back AL, Arnold RM, Baile WF, et al. Approaching difficult communication tasks in oncology. CA Cancer J Clin. 2005;55: 164-177.
41. Doak LG, Doak CC, eds. Pfizer Principles for Clear Health Communication: A Handbook for Creating Patient Education Materials that Enhance Understanding and Promote Health Outcomes. 2nd ed. New York, NY: Pfizer; 2004.
42. Bradley EH, Bogardus ST Jr, Tinetti M, et al. Goal-setting in clinical medicine. Soc Sci Med. 1999;49:267-278.
43. Koelling TM, Johnson ML, Cody RJ, et al. Discharge education improves clinical outcomes in patients with chronic heart failure. Circulation. 2005;111:179-185.
44. Krumholz HM, Amatruda J, Smith GL, et al. Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. J Am Coll Cardiol. 2002;39:83-89.
45. Burke RE, Coleman EA. Interventions to decrease hospital readmissions: keys for cost-effectiveness. JAMA Intern Med. 2013;173:695-698.
46. Kessler KR. Relationship between the use of asthma action plans and asthma exacerbations in children with asthma: A systematic review. J Asthma Allergy Educators. 2011;2:11-21.
47. Maric B, Kaan A, Ignaszewski A, et al. A systematic review of telemonitoring technologies in heart failure. Eur J Heart Fail. 2009;11:506-517.
48. Boutwell A, Hwu S. Effective Interventions to Reduce Rehospitalizations: A Survey of the Published Evidence. Cambridge, MA: Institute for Healthcare Improvement; 2009.
49. Bodenheimer T, Laing BY. The teamlet model of primary care. Ann Fam Med. 2007;5:457-461.
50. Meier D, Beresford L. Outpatient clinics are a new frontier for palliative care. J Pall Med. 2008;11:823-828.
› Use risk stratification methods such as the Probability of Repeated Admission (Pra) or the LACE index to identify patients at high risk for readmission. B
› Take steps to ensure that follow-up appointments are made within the first one to 2 weeks of discharge, depending on the patient’s risk of readmission. C
› Reconcile preadmission and postdischarge medications to identify discrepancies and possible interactions. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Charles T, age 74, has a 3-year history of myocardial infarction (MI) and congestive heart failure (CHF) and a 10-year his-tory of type 2 diabetes with retinopathy. You have cared for him in the outpatient setting for 8 years. You are notified that he is in the emergency department (ED) and being admitted to the hospital, again. This is his third ED visit in the past 3 months; he was hospitalized for 6 days during his last admission 3 weeks ago.
What should you do with this information? How can you best communicate with the admitting team?
Hospital readmissions are widespread, costly, and often avoidable. Nearly 20% of Medicare beneficiaries discharged from hospitals are rehospitalized within 30 days, and 34% are rehospitalized within 90 days.1 For patients with conditions like CHF, the rate of readmission within 30 days approaches 25%.2 The estimated cost to Medicare for unplanned rehospitalizations in 2004 was $17.4 billion.1 The Centers for Medicare and Medicaid Services penalizes hospitals for high rates of readmission within 30 days of discharge for patients with CHF, MI, and pneumonia.
“Avoidable” hospitalizations are those that may be prevented by effective outpatient management and improved care coordination. Although efforts to reduce readmissions have focused on improving the discharge process, family physicians (FPs) can play a central role in reducing readmissions. This article describes key approaches that FPs can take to address this important issue. Because patients ages ≥65 years consistently have the highest rate of hospital readmissions,1 we will focus on this population.
Multiple complex factors are associated with hospital readmissions
Characteristics of the patient, physician, and health care setting contribute to potentially avoidable readmissions (TABLE 1).3,4
Medical conditions and comorbidities associated with high rates of rehospitalization include CHF, acute MI, pneumonia, diabetes, and chronic obstructive pulmonary disease. However, a recent study found that a diverse range of conditions, frequently differing from the index cause of hospitalization, were responsible for 30-day readmissions of Medicare patients.5
Identifying those at high risk: Why and how
Determining which patients are at highest risk for readmission enables health care teams to match the intensity of interventions to the individual’s likelihood of readmission. However, current readmission risk prediction models remain a work in progress6 and few models have been tested in the outpatient setting. Despite numerous limitations, it’s still important to focus resources more efficiently. Thus, we recommend using risk stratification tools to identify patients at high risk for readmission.
Many risk stratification methods use data from electronic medical records (EMRs) and administrative databases or self-reported data from patients.7 Risk prediction tools that are relatively simple and easy to administer or generate through EMRs—such as the Probability of Repeated Admission (Pra),8 the LACE (Length of stay, acuity of the admission, comorbidities, ED visits in the previous 6 months) index,9 or the Community Assessment Risk Screen (CARS)10—may be best for use in the primary care setting. These tools generally identify key risk factors, such as prior health care utilization, presence of specific conditions such as heart disease or cognitive impairment, self-reported health status, absence of a caregiver, and/or need for assistance with daily routines.
Many of these tools have been used to identify high-risk older adults and may not be appropriate for patients who are likely to be readmitted for different reasons, such as mental illness, substance abuse, or chronic pain. Therefore, it is important to use a risk stratification method that captures the issues most likely to cause readmissions in your patient population, or to consider using a variety of methods.
The American Academy of Family Physicians (AAFP) offers resources to help FPs design methods for determining a patient’s health risk status and linking higher levels of risk to increasing care management at http://www.aafp.org/practice-management/pcmh/initiatives/cpci/rscm.html.
CASE › Mr. T has been admitted to the hospital 3 times in the past 3 months, so you use the lace index to evaluate his risk. You determine that Mr. T’s score is 15, which means his expected risk of death or unplanned readmission is 26.6% (TABLE 2).8,11 What are your next steps?
Foster communication between the hospital and outpatient office
Patients are particularly vulnerable during the transition from hospital to home. Delayed or inaccurate information adversely affects continuity of care, patient safety and satisfaction, and efficient use of resources.12 Discharge summaries are the main method of communication between providers, but their content, timeliness, availability, and quality frequently are lacking.13 Discharge summaries are available at only 12% to 34% of first postdischarge visits, and these summaries often lack important information such as diagnostic test results (33%-63%) or discharge medications (2%-40%).12 Although researchers have not consistently found that transferring a discharge summary to an outpatient physician reduces readmission rates, it is likely that direct communication can improve the handoff process independent of its effects on readmissions.12,14
Timely follow-up appointments are essential
Many factors influence the need for rapid follow-up, including disease severity, management complexity, ability of the patient to provide sufficient self-care, and adequacy of social supports.15,16 Studies have found that discharged patients who receive timely outpatient follow-up are less likely to be readmitted.1,17 While the optimal time interval between discharge and the first follow-up appointment is unknown, some literature supports follow-up within 4 weeks.15,18 However, because readmissions often cluster in the first several days or week following discharge,18 follow-up within the first 2 weeks (and within the first week for higher-risk patients) may be appropriate.19 Ideally, follow-up appointments should be scheduled before the patient is discharged. Patients who schedule a follow-up appointment before they are discharged are more likely to make their follow-up visit than those who are asked to call after discharge and schedule their own appointment.12
Employ outpatient follow-up alternatives
Follow-up telephone calls to patients after discharge help patients understand and adhere to discharge instructions and troubleshoot problems. Clinicians who use scripted telephone calls can evaluate symptoms related to the index hospitalization, provide patient education, schedule relevant appointments or testing, and, most importantly, initiate medication reconciliation, which is described at right.20 The FIGURE includes the script we use at our practice.
Home visits may be appropriate for certain patients, including the frail elderly. Home visits allow clinicians to evaluate the patient’s environmental safety, social sup port, and medication adherence.12 Preventive home visits generally have not been found to reduce hospital readmissions, but do enhance patient satisfaction with care.21
Bundled interventions, such as alternating home visits and follow-up telephone calls, may be more effective than individual interventions in reducing readmission.22
Reconciling medications may have far-reaching benefits
Medication discrepancies are observed in up to 70% of all patients at admission or discharge and are associated with adverse drug events (ADEs).23 To prevent ADEs and possibly readmission, take the following steps to reconcile a patient’s medications23:
Obtain a complete list of current medications. Information on all of the patient’s prescription and nonprescription medications should be collected from the patient/caregiver, the discharge summary, prescription bottles, home visits, and pharmacies.12,24
Reconcile preadmission and postdischarge medications. Clarify any discrepancies, review all medications for safety and appropriateness, and, when appropriate, resume any held medications and/or discontinue unnecessary ones.
Research shows that patients who received a phone call from a pharmacist within 3 to 7 days of discharge had lower readmission rates.Enlist pharmacy support. Pharmacists are uniquely positioned to review indications as well as potential duplication and interactions of a patient’s medications. Inpatient studies have demonstrated that partnering with pharmacists results in fewer ADEs.12,25 One study showed that patients at high risk for readmission who received a phone call from a pharmacist 3 to 7 days after discharge had lower readmission rates.26 The pharmacist reconciled the patients’ medications and ensured that patients had a clear understanding of each medication, its common safety concerns, and how often they were supposed to take it.26
Make medication adherence as easy as possible
As many as half of all patients don’t take their medications as prescribed.27 There is limited data on health outcomes associated with medication nonadherence, and existing data frequently are contradictory—some studies have found that as many as 11% of hospital admissions are attributed to nonadherence, while others show no association.28
Factors that affect adherence include psychiatric or cognitive impairment, limited insight into disease process or lack of belief in benefit of treatment, medication cost or adverse effect profile, poor provider-patient relationship, limited access to care or medication, or complexity of treatment.29 To promote medication adherence, consider the following educational and behavioral strategies30:
Identify patients at risk for nonadherence. This includes those with complex regimens and/or uncontrolled disease states or symptoms.
Increase patient communication and counseling. Patient education, particularly on the importance of adherence, is one of the few solo interventions that can improve compliance.31 Involving caregivers and using both verbal and written materials provides additional benefit.31,32
Simplify dosing schedules. Simple, convenient medication regimens may im- prove adherence. For example, adjusting dosing from 3 times a day to once a day can increase adherence from 59% to 83%.33 Aids such as pillboxes to organize medications may be of benefit.29,32
Ensure consistent follow-up. Patients who miss appointments are more likely to be nonadherent. They may benefit from easy access, help with scheduling, and frequent visits.32
Be mindful of patients’ out-of-pocket expenses. Reducing copayments improves adherence rates.30
Minimize polypharmacy. Polypharmacy has been independently associated with nonadherence and increased risk for ADEs.34
Identify patients who have limited health literacy. Limited health literacy may be linked to increased medication errors and nonadherence.12,35 Patients with low health literacy may be unable to identify medications recorded in their medical record. TABLE W336-41 outlines strategies for identifying patients with low health literacy and improving communication with them.
CASE › By speaking with hospital staff before Mr. T is discharged, you are able to confirm that he has scheduled a follow-up visit with you for one week after discharge, and that a discharge summary will be available for him to bring to that visit. Mr. T brings his discharge summary with him to your office, and you reconcile his medication list. Because he is your last patient of the day, you have some time to sit with him and his wife to explore his goals of care.
Improve care—and possibly reduce readmissions—through goal setting
Goal setting is an important element of postdischarge follow-up, particularly for elderly patients and those with progressive or end-stage diseases. Goal setting can improve patient care by linking care plans with desired outcomes and keeping diagnostic and therapeutic interventions relevant to the patient.42 A patient who understands the purpose of a recommendation—especially when directly linked to a patient-derived goal—may be more likely to adhere to the plan of care.
Asking patients to articulate their goals of care using “Ask-Tell-Ask” framework described in TABLE W336-41 will allow you to deliver the prognosis, reinforce treatment options to achieve patient-specific goals, empower patients to assert their preferences, and develop a follow-up plan to see if treatment is successful.
Empowering patients
Consider using both verbal and written approaches when educating patients about self-care behaviors such as monitoring symptoms and adhering to dietary/behavior restrictions and medication instructions. One study showed that a brief one-on-one patient education session decreased readmissions in patients with heart failure,43 although another study found that patient education alone yielded a nonsignificant decrease.44
Providing caregivers with education and support is a critical and perhaps overlooked opportunity to reduce readmissions.45 Involving key family members in discharge planning, preparation, follow-up, and ongoing management is essential in caring for patients with functional deficits and/or complex care needs. Educating caregivers can help them feel more prepared and effective in their roles.
Establish an “action plan.” For patients with chronic, periodically symptomatic diseases such as asthma and heart failure, action planning can be useful. Action plans should include information that reinforces patients’ daily self-care behaviors and instructions for what to do if symptoms get worse. Action planning also might include simple if-then plans (“if x happens, then I will do y”), which can help with problem solving for common scenarios. Action plans have been shown to reduce admissions for children with asthma46 and adults with heart failure when coupled with home monitoring or telephone support from a registered nurse.16,47
Generate an individualized care plan for each patient, taking into account your patient’s health literacy, goals of care, and level of social support. This care plan may include educational and behavioral interventions, action planning, and follow-up plans. Most successful approaches to reducing readmissions have included both system-level and patient-level interventions that use an interdisciplinary team of providers.48
Make the most of follow-up visits. The traditional 15-minute FP visit can make it challenging to provide the level of care necessary for recently discharged patients. Multiple models of team-based care have been proposed to improve this situation, including using the “teamlet” model, which may include a clinician and one or 2 health coaches.49 During each visit, the health coaches—often medical assistants trained in chronic disease self-management skills—see patients before and after the physician. They also contact patients be- tween visits to facilitate action planning and to promote self-management.
Palliative care programs: A resource for FPs
The growth of palliative care programs in US hospitals has helped increase the emphasis on establishing goals of care. Inpatient-based palliative care consultation programs work with patients and families to establish goals. However, after discharge, many of these goals and plans begin to unravel due to gaps in the current health care model, including lack of follow-up and support.50 Outpatient palliative care programs have begun to address these gaps in care.50 Comprehensive palliative care programs are quickly becoming an important resource for FPs to help address transitional care issues.
CASE › When you ask Mr. and Mrs. T about his goals for treatment, they say are getting tired of the “back and forth” to the hospital. After discussing his lengthy history of worsening CHF and diabetes, you raise the idea of palliative care, including hospice, with the couple. They acknowledge that they have had family members get hospice care, and they are open to it—just not yet. The 3 of you craft an “if-then” plan of care to use at home. You schedule a 2-week follow-up visit and remind Mr. T and his wife of your office’s 24-hour on-call service.
CORRESPONDENCE
Danielle Snyderman, MD, Department of Family and Community Medicine, Jefferson University, 1015 Walnut Street, Suite 401, Philadelphia, Pa 19107; [email protected]
› Use risk stratification methods such as the Probability of Repeated Admission (Pra) or the LACE index to identify patients at high risk for readmission. B
› Take steps to ensure that follow-up appointments are made within the first one to 2 weeks of discharge, depending on the patient’s risk of readmission. C
› Reconcile preadmission and postdischarge medications to identify discrepancies and possible interactions. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Charles T, age 74, has a 3-year history of myocardial infarction (MI) and congestive heart failure (CHF) and a 10-year his-tory of type 2 diabetes with retinopathy. You have cared for him in the outpatient setting for 8 years. You are notified that he is in the emergency department (ED) and being admitted to the hospital, again. This is his third ED visit in the past 3 months; he was hospitalized for 6 days during his last admission 3 weeks ago.
What should you do with this information? How can you best communicate with the admitting team?
Hospital readmissions are widespread, costly, and often avoidable. Nearly 20% of Medicare beneficiaries discharged from hospitals are rehospitalized within 30 days, and 34% are rehospitalized within 90 days.1 For patients with conditions like CHF, the rate of readmission within 30 days approaches 25%.2 The estimated cost to Medicare for unplanned rehospitalizations in 2004 was $17.4 billion.1 The Centers for Medicare and Medicaid Services penalizes hospitals for high rates of readmission within 30 days of discharge for patients with CHF, MI, and pneumonia.
“Avoidable” hospitalizations are those that may be prevented by effective outpatient management and improved care coordination. Although efforts to reduce readmissions have focused on improving the discharge process, family physicians (FPs) can play a central role in reducing readmissions. This article describes key approaches that FPs can take to address this important issue. Because patients ages ≥65 years consistently have the highest rate of hospital readmissions,1 we will focus on this population.
Multiple complex factors are associated with hospital readmissions
Characteristics of the patient, physician, and health care setting contribute to potentially avoidable readmissions (TABLE 1).3,4
Medical conditions and comorbidities associated with high rates of rehospitalization include CHF, acute MI, pneumonia, diabetes, and chronic obstructive pulmonary disease. However, a recent study found that a diverse range of conditions, frequently differing from the index cause of hospitalization, were responsible for 30-day readmissions of Medicare patients.5
Identifying those at high risk: Why and how
Determining which patients are at highest risk for readmission enables health care teams to match the intensity of interventions to the individual’s likelihood of readmission. However, current readmission risk prediction models remain a work in progress6 and few models have been tested in the outpatient setting. Despite numerous limitations, it’s still important to focus resources more efficiently. Thus, we recommend using risk stratification tools to identify patients at high risk for readmission.
Many risk stratification methods use data from electronic medical records (EMRs) and administrative databases or self-reported data from patients.7 Risk prediction tools that are relatively simple and easy to administer or generate through EMRs—such as the Probability of Repeated Admission (Pra),8 the LACE (Length of stay, acuity of the admission, comorbidities, ED visits in the previous 6 months) index,9 or the Community Assessment Risk Screen (CARS)10—may be best for use in the primary care setting. These tools generally identify key risk factors, such as prior health care utilization, presence of specific conditions such as heart disease or cognitive impairment, self-reported health status, absence of a caregiver, and/or need for assistance with daily routines.
Many of these tools have been used to identify high-risk older adults and may not be appropriate for patients who are likely to be readmitted for different reasons, such as mental illness, substance abuse, or chronic pain. Therefore, it is important to use a risk stratification method that captures the issues most likely to cause readmissions in your patient population, or to consider using a variety of methods.
The American Academy of Family Physicians (AAFP) offers resources to help FPs design methods for determining a patient’s health risk status and linking higher levels of risk to increasing care management at http://www.aafp.org/practice-management/pcmh/initiatives/cpci/rscm.html.
CASE › Mr. T has been admitted to the hospital 3 times in the past 3 months, so you use the lace index to evaluate his risk. You determine that Mr. T’s score is 15, which means his expected risk of death or unplanned readmission is 26.6% (TABLE 2).8,11 What are your next steps?
Foster communication between the hospital and outpatient office
Patients are particularly vulnerable during the transition from hospital to home. Delayed or inaccurate information adversely affects continuity of care, patient safety and satisfaction, and efficient use of resources.12 Discharge summaries are the main method of communication between providers, but their content, timeliness, availability, and quality frequently are lacking.13 Discharge summaries are available at only 12% to 34% of first postdischarge visits, and these summaries often lack important information such as diagnostic test results (33%-63%) or discharge medications (2%-40%).12 Although researchers have not consistently found that transferring a discharge summary to an outpatient physician reduces readmission rates, it is likely that direct communication can improve the handoff process independent of its effects on readmissions.12,14
Timely follow-up appointments are essential
Many factors influence the need for rapid follow-up, including disease severity, management complexity, ability of the patient to provide sufficient self-care, and adequacy of social supports.15,16 Studies have found that discharged patients who receive timely outpatient follow-up are less likely to be readmitted.1,17 While the optimal time interval between discharge and the first follow-up appointment is unknown, some literature supports follow-up within 4 weeks.15,18 However, because readmissions often cluster in the first several days or week following discharge,18 follow-up within the first 2 weeks (and within the first week for higher-risk patients) may be appropriate.19 Ideally, follow-up appointments should be scheduled before the patient is discharged. Patients who schedule a follow-up appointment before they are discharged are more likely to make their follow-up visit than those who are asked to call after discharge and schedule their own appointment.12
Employ outpatient follow-up alternatives
Follow-up telephone calls to patients after discharge help patients understand and adhere to discharge instructions and troubleshoot problems. Clinicians who use scripted telephone calls can evaluate symptoms related to the index hospitalization, provide patient education, schedule relevant appointments or testing, and, most importantly, initiate medication reconciliation, which is described at right.20 The FIGURE includes the script we use at our practice.
Home visits may be appropriate for certain patients, including the frail elderly. Home visits allow clinicians to evaluate the patient’s environmental safety, social sup port, and medication adherence.12 Preventive home visits generally have not been found to reduce hospital readmissions, but do enhance patient satisfaction with care.21
Bundled interventions, such as alternating home visits and follow-up telephone calls, may be more effective than individual interventions in reducing readmission.22
Reconciling medications may have far-reaching benefits
Medication discrepancies are observed in up to 70% of all patients at admission or discharge and are associated with adverse drug events (ADEs).23 To prevent ADEs and possibly readmission, take the following steps to reconcile a patient’s medications23:
Obtain a complete list of current medications. Information on all of the patient’s prescription and nonprescription medications should be collected from the patient/caregiver, the discharge summary, prescription bottles, home visits, and pharmacies.12,24
Reconcile preadmission and postdischarge medications. Clarify any discrepancies, review all medications for safety and appropriateness, and, when appropriate, resume any held medications and/or discontinue unnecessary ones.
Research shows that patients who received a phone call from a pharmacist within 3 to 7 days of discharge had lower readmission rates.Enlist pharmacy support. Pharmacists are uniquely positioned to review indications as well as potential duplication and interactions of a patient’s medications. Inpatient studies have demonstrated that partnering with pharmacists results in fewer ADEs.12,25 One study showed that patients at high risk for readmission who received a phone call from a pharmacist 3 to 7 days after discharge had lower readmission rates.26 The pharmacist reconciled the patients’ medications and ensured that patients had a clear understanding of each medication, its common safety concerns, and how often they were supposed to take it.26
Make medication adherence as easy as possible
As many as half of all patients don’t take their medications as prescribed.27 There is limited data on health outcomes associated with medication nonadherence, and existing data frequently are contradictory—some studies have found that as many as 11% of hospital admissions are attributed to nonadherence, while others show no association.28
Factors that affect adherence include psychiatric or cognitive impairment, limited insight into disease process or lack of belief in benefit of treatment, medication cost or adverse effect profile, poor provider-patient relationship, limited access to care or medication, or complexity of treatment.29 To promote medication adherence, consider the following educational and behavioral strategies30:
Identify patients at risk for nonadherence. This includes those with complex regimens and/or uncontrolled disease states or symptoms.
Increase patient communication and counseling. Patient education, particularly on the importance of adherence, is one of the few solo interventions that can improve compliance.31 Involving caregivers and using both verbal and written materials provides additional benefit.31,32
Simplify dosing schedules. Simple, convenient medication regimens may im- prove adherence. For example, adjusting dosing from 3 times a day to once a day can increase adherence from 59% to 83%.33 Aids such as pillboxes to organize medications may be of benefit.29,32
Ensure consistent follow-up. Patients who miss appointments are more likely to be nonadherent. They may benefit from easy access, help with scheduling, and frequent visits.32
Be mindful of patients’ out-of-pocket expenses. Reducing copayments improves adherence rates.30
Minimize polypharmacy. Polypharmacy has been independently associated with nonadherence and increased risk for ADEs.34
Identify patients who have limited health literacy. Limited health literacy may be linked to increased medication errors and nonadherence.12,35 Patients with low health literacy may be unable to identify medications recorded in their medical record. TABLE W336-41 outlines strategies for identifying patients with low health literacy and improving communication with them.
CASE › By speaking with hospital staff before Mr. T is discharged, you are able to confirm that he has scheduled a follow-up visit with you for one week after discharge, and that a discharge summary will be available for him to bring to that visit. Mr. T brings his discharge summary with him to your office, and you reconcile his medication list. Because he is your last patient of the day, you have some time to sit with him and his wife to explore his goals of care.
Improve care—and possibly reduce readmissions—through goal setting
Goal setting is an important element of postdischarge follow-up, particularly for elderly patients and those with progressive or end-stage diseases. Goal setting can improve patient care by linking care plans with desired outcomes and keeping diagnostic and therapeutic interventions relevant to the patient.42 A patient who understands the purpose of a recommendation—especially when directly linked to a patient-derived goal—may be more likely to adhere to the plan of care.
Asking patients to articulate their goals of care using “Ask-Tell-Ask” framework described in TABLE W336-41 will allow you to deliver the prognosis, reinforce treatment options to achieve patient-specific goals, empower patients to assert their preferences, and develop a follow-up plan to see if treatment is successful.
Empowering patients
Consider using both verbal and written approaches when educating patients about self-care behaviors such as monitoring symptoms and adhering to dietary/behavior restrictions and medication instructions. One study showed that a brief one-on-one patient education session decreased readmissions in patients with heart failure,43 although another study found that patient education alone yielded a nonsignificant decrease.44
Providing caregivers with education and support is a critical and perhaps overlooked opportunity to reduce readmissions.45 Involving key family members in discharge planning, preparation, follow-up, and ongoing management is essential in caring for patients with functional deficits and/or complex care needs. Educating caregivers can help them feel more prepared and effective in their roles.
Establish an “action plan.” For patients with chronic, periodically symptomatic diseases such as asthma and heart failure, action planning can be useful. Action plans should include information that reinforces patients’ daily self-care behaviors and instructions for what to do if symptoms get worse. Action planning also might include simple if-then plans (“if x happens, then I will do y”), which can help with problem solving for common scenarios. Action plans have been shown to reduce admissions for children with asthma46 and adults with heart failure when coupled with home monitoring or telephone support from a registered nurse.16,47
Generate an individualized care plan for each patient, taking into account your patient’s health literacy, goals of care, and level of social support. This care plan may include educational and behavioral interventions, action planning, and follow-up plans. Most successful approaches to reducing readmissions have included both system-level and patient-level interventions that use an interdisciplinary team of providers.48
Make the most of follow-up visits. The traditional 15-minute FP visit can make it challenging to provide the level of care necessary for recently discharged patients. Multiple models of team-based care have been proposed to improve this situation, including using the “teamlet” model, which may include a clinician and one or 2 health coaches.49 During each visit, the health coaches—often medical assistants trained in chronic disease self-management skills—see patients before and after the physician. They also contact patients be- tween visits to facilitate action planning and to promote self-management.
Palliative care programs: A resource for FPs
The growth of palliative care programs in US hospitals has helped increase the emphasis on establishing goals of care. Inpatient-based palliative care consultation programs work with patients and families to establish goals. However, after discharge, many of these goals and plans begin to unravel due to gaps in the current health care model, including lack of follow-up and support.50 Outpatient palliative care programs have begun to address these gaps in care.50 Comprehensive palliative care programs are quickly becoming an important resource for FPs to help address transitional care issues.
CASE › When you ask Mr. and Mrs. T about his goals for treatment, they say are getting tired of the “back and forth” to the hospital. After discussing his lengthy history of worsening CHF and diabetes, you raise the idea of palliative care, including hospice, with the couple. They acknowledge that they have had family members get hospice care, and they are open to it—just not yet. The 3 of you craft an “if-then” plan of care to use at home. You schedule a 2-week follow-up visit and remind Mr. T and his wife of your office’s 24-hour on-call service.
CORRESPONDENCE
Danielle Snyderman, MD, Department of Family and Community Medicine, Jefferson University, 1015 Walnut Street, Suite 401, Philadelphia, Pa 19107; [email protected]
1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418-1428
2. O’Connor CM, Miller AB, Blair JE, et al; Efficacy of Vasopressin Antagonism in heart Failure Outcome Study with Tolvaptan (EVEREST) investigators. Causes of death and rehospitalization in patients hospitalized with worsening heart failure and reduce left ventricular ejection fraction; results from EVEREST program. Am Heart J. 2010;159:841-849.e1.
3. Garrison GM, Mansukhani MP, Bohn B. Predictors of thirty-day readmission among hospitalized family medicine patients. J Am Board Fam Med. 2013;26:71-77.
4. Boult C, Dowd B, McCaffrey D, et al. Screening elders for risk of hospital admission. J Am Geriatr Soc. 1993;41:811-817.
5. Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355-363.
6. Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688-1698.
7. Haas LR, Takahashi PY, Shah ND, et al. Risk-stratification methods for identifying patients for care coordination. Am J Manag Care. 2013;19:725-732.
8. Wallace E, Hinchey T, Dimitrov BD, et al. A systematic review of the probability of repeated admission score in community-dwelling adults. J Am Geriatr Soc. 2013;61:357-364.
9. Cotter PE, Bhalla VK, Wallis SJ, et al. Predicting readmissions: poor performance of the LACE index in an older UK population. Age Ageing. 2012;41:784-789.
10. Shelton P, Sager MA, Schraeder C. The community assessment risk screen (CARS): identifying elderly persons at risk for hospitalization or emergency department visit. Am J Manag Care. 2000;6:925-933.
11. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373-383.
12. Kripalani S, Jackson AT, Schnipper JL, et al. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2:314-323.
13. Kim CS, Flanders SA. In the clinic. Transitions of care. Ann Intern Med. 2013;158(5 pt 1):ITC3-1.
14. Hansen LO, Strater A, Smith L, et al. Hospital discharge documentation and risk of rehospitalisation. BMJ Qual Saf. 2011;20:773-778.
15. Vaduganathan M, Bonow RO, Gheorghiade M. Thirty-day readmissions: the clock is ticking. JAMA. 2013;309:345-346.
16. Hansen LO, Young RS, Hinami K, et al. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520-528.
17. Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5:392-397.
18. van Walraven C, Jennings A, Taljaard M, et al. Incidence of potentially avoidable urgent readmissions and their relation to all-cause urgent readmissions. CMAJ. 2011;183:E1067-E1072.
19. Tang, N. A primary care physician’s ideal transitions of care—where’s the evidence? J Hosp Med. 2013;8:472-477.
20. Crocker JB, Crocker JT, Greenwald JL. Telephone follow-up as a primary care intervention for postdischarge outcomes improvement: a systematic review. Am J Med. 2012;125:915-921.
21. Wong FK, Chow S, Chung L, et al. Can home visits help reduce hospital readmissions? Randomized controlled trial. J Adv Nurs. 2008;62:585-595.
22. Wong FK, Chow SK, Chan TM, et al. Comparison of effects between home visits with telephone calls and telephone calls only for transitional discharge support: a randomised controlled trial. Age Ageing. 2014;43:91-97.
23. Mueller SK, Sponsler KC, Kripalani S, et al. Hospital-based medication reconciliation practices: a systematic review. Arch Intern Med. 2012;172:1057-1069.
24. Glintborg B, Andersen SE, Dalhoff K. Insufficient communication about medication use at the interface between hospital and primary care. Qual Saf Health Care. 2007;16:34-39.
25. Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166:565-571.
26. Kilcup M, Schultz D, Carlson J, et al. Postdischarge pharmacist medication reconciliation: impact on readmission rates and financial savings. J Am Pharm Assoc (2003). 2013;53:78-84.
27. Vermeire E, Hearnshaw H, Van Royen P, et al. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26:331-342.
28. Vik SA, Maxwell CJ, Hogan DB. Measurement, correlates, and health outcomes of medication adherence among seniors. Ann Pharmacother. 2004;38:303-312.
29. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487-497.
30. Viswanathan M, Golin CE, Jones CD, et al. Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Ann Intern Med. 2012;157:785-795.
31. McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA. 2002;288:2868-2879.
32. Kripalani S, Yao X, Haynes RB. Interventions to enhance medication adherence in chronic medical conditions: a systematic review. Arch Intern Med. 2007;167:540-550.
33. Eisen SA, Miller DK, Woodward RS, et al. The effect of prescribed daily dose frequency on patient medication compliance. Arch Intern Med. 1990;150:1881-1884.
34. Field TS, Gurwitz JH, Avorn J, et al. Risk factors for adverse drug events among nursing home residents. Arch Intern Med. 2001;161:1629-1634.
35. Persell SD, Osborn CY, Richard R, et al. Limited health literacy is a barrier to medication reconciliation in ambulatory care. J Gen Intern Med. 2007;22:1523-1526.
36. Weiss BD. Health Literacy and Patient Safety: Help Patients Understand. Manual for Clinicians. Chicago, IL: American Medical Association Foundation; 2007.
37. Chew LD, Bradley KA, Bokyo EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588-594.
38. Wallace LS, Rogers ES, Roskos SE, et al. Brief report: screening items to identify patients with limited health literacy skills. J Gen Intern Med. 2006;21:874-877.
39. Doak CC, Doak LG, Root JH. Teaching Patients with Low Literacy Skills. 2nd ed. Philadelphia, PA: JB Lippincott Company; 1996.
40. Back AL, Arnold RM, Baile WF, et al. Approaching difficult communication tasks in oncology. CA Cancer J Clin. 2005;55: 164-177.
41. Doak LG, Doak CC, eds. Pfizer Principles for Clear Health Communication: A Handbook for Creating Patient Education Materials that Enhance Understanding and Promote Health Outcomes. 2nd ed. New York, NY: Pfizer; 2004.
42. Bradley EH, Bogardus ST Jr, Tinetti M, et al. Goal-setting in clinical medicine. Soc Sci Med. 1999;49:267-278.
43. Koelling TM, Johnson ML, Cody RJ, et al. Discharge education improves clinical outcomes in patients with chronic heart failure. Circulation. 2005;111:179-185.
44. Krumholz HM, Amatruda J, Smith GL, et al. Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. J Am Coll Cardiol. 2002;39:83-89.
45. Burke RE, Coleman EA. Interventions to decrease hospital readmissions: keys for cost-effectiveness. JAMA Intern Med. 2013;173:695-698.
46. Kessler KR. Relationship between the use of asthma action plans and asthma exacerbations in children with asthma: A systematic review. J Asthma Allergy Educators. 2011;2:11-21.
47. Maric B, Kaan A, Ignaszewski A, et al. A systematic review of telemonitoring technologies in heart failure. Eur J Heart Fail. 2009;11:506-517.
48. Boutwell A, Hwu S. Effective Interventions to Reduce Rehospitalizations: A Survey of the Published Evidence. Cambridge, MA: Institute for Healthcare Improvement; 2009.
49. Bodenheimer T, Laing BY. The teamlet model of primary care. Ann Fam Med. 2007;5:457-461.
50. Meier D, Beresford L. Outpatient clinics are a new frontier for palliative care. J Pall Med. 2008;11:823-828.
1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418-1428
2. O’Connor CM, Miller AB, Blair JE, et al; Efficacy of Vasopressin Antagonism in heart Failure Outcome Study with Tolvaptan (EVEREST) investigators. Causes of death and rehospitalization in patients hospitalized with worsening heart failure and reduce left ventricular ejection fraction; results from EVEREST program. Am Heart J. 2010;159:841-849.e1.
3. Garrison GM, Mansukhani MP, Bohn B. Predictors of thirty-day readmission among hospitalized family medicine patients. J Am Board Fam Med. 2013;26:71-77.
4. Boult C, Dowd B, McCaffrey D, et al. Screening elders for risk of hospital admission. J Am Geriatr Soc. 1993;41:811-817.
5. Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355-363.
6. Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688-1698.
7. Haas LR, Takahashi PY, Shah ND, et al. Risk-stratification methods for identifying patients for care coordination. Am J Manag Care. 2013;19:725-732.
8. Wallace E, Hinchey T, Dimitrov BD, et al. A systematic review of the probability of repeated admission score in community-dwelling adults. J Am Geriatr Soc. 2013;61:357-364.
9. Cotter PE, Bhalla VK, Wallis SJ, et al. Predicting readmissions: poor performance of the LACE index in an older UK population. Age Ageing. 2012;41:784-789.
10. Shelton P, Sager MA, Schraeder C. The community assessment risk screen (CARS): identifying elderly persons at risk for hospitalization or emergency department visit. Am J Manag Care. 2000;6:925-933.
11. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373-383.
12. Kripalani S, Jackson AT, Schnipper JL, et al. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2:314-323.
13. Kim CS, Flanders SA. In the clinic. Transitions of care. Ann Intern Med. 2013;158(5 pt 1):ITC3-1.
14. Hansen LO, Strater A, Smith L, et al. Hospital discharge documentation and risk of rehospitalisation. BMJ Qual Saf. 2011;20:773-778.
15. Vaduganathan M, Bonow RO, Gheorghiade M. Thirty-day readmissions: the clock is ticking. JAMA. 2013;309:345-346.
16. Hansen LO, Young RS, Hinami K, et al. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520-528.
17. Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5:392-397.
18. van Walraven C, Jennings A, Taljaard M, et al. Incidence of potentially avoidable urgent readmissions and their relation to all-cause urgent readmissions. CMAJ. 2011;183:E1067-E1072.
19. Tang, N. A primary care physician’s ideal transitions of care—where’s the evidence? J Hosp Med. 2013;8:472-477.
20. Crocker JB, Crocker JT, Greenwald JL. Telephone follow-up as a primary care intervention for postdischarge outcomes improvement: a systematic review. Am J Med. 2012;125:915-921.
21. Wong FK, Chow S, Chung L, et al. Can home visits help reduce hospital readmissions? Randomized controlled trial. J Adv Nurs. 2008;62:585-595.
22. Wong FK, Chow SK, Chan TM, et al. Comparison of effects between home visits with telephone calls and telephone calls only for transitional discharge support: a randomised controlled trial. Age Ageing. 2014;43:91-97.
23. Mueller SK, Sponsler KC, Kripalani S, et al. Hospital-based medication reconciliation practices: a systematic review. Arch Intern Med. 2012;172:1057-1069.
24. Glintborg B, Andersen SE, Dalhoff K. Insufficient communication about medication use at the interface between hospital and primary care. Qual Saf Health Care. 2007;16:34-39.
25. Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166:565-571.
26. Kilcup M, Schultz D, Carlson J, et al. Postdischarge pharmacist medication reconciliation: impact on readmission rates and financial savings. J Am Pharm Assoc (2003). 2013;53:78-84.
27. Vermeire E, Hearnshaw H, Van Royen P, et al. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26:331-342.
28. Vik SA, Maxwell CJ, Hogan DB. Measurement, correlates, and health outcomes of medication adherence among seniors. Ann Pharmacother. 2004;38:303-312.
29. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487-497.
30. Viswanathan M, Golin CE, Jones CD, et al. Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Ann Intern Med. 2012;157:785-795.
31. McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA. 2002;288:2868-2879.
32. Kripalani S, Yao X, Haynes RB. Interventions to enhance medication adherence in chronic medical conditions: a systematic review. Arch Intern Med. 2007;167:540-550.
33. Eisen SA, Miller DK, Woodward RS, et al. The effect of prescribed daily dose frequency on patient medication compliance. Arch Intern Med. 1990;150:1881-1884.
34. Field TS, Gurwitz JH, Avorn J, et al. Risk factors for adverse drug events among nursing home residents. Arch Intern Med. 2001;161:1629-1634.
35. Persell SD, Osborn CY, Richard R, et al. Limited health literacy is a barrier to medication reconciliation in ambulatory care. J Gen Intern Med. 2007;22:1523-1526.
36. Weiss BD. Health Literacy and Patient Safety: Help Patients Understand. Manual for Clinicians. Chicago, IL: American Medical Association Foundation; 2007.
37. Chew LD, Bradley KA, Bokyo EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588-594.
38. Wallace LS, Rogers ES, Roskos SE, et al. Brief report: screening items to identify patients with limited health literacy skills. J Gen Intern Med. 2006;21:874-877.
39. Doak CC, Doak LG, Root JH. Teaching Patients with Low Literacy Skills. 2nd ed. Philadelphia, PA: JB Lippincott Company; 1996.
40. Back AL, Arnold RM, Baile WF, et al. Approaching difficult communication tasks in oncology. CA Cancer J Clin. 2005;55: 164-177.
41. Doak LG, Doak CC, eds. Pfizer Principles for Clear Health Communication: A Handbook for Creating Patient Education Materials that Enhance Understanding and Promote Health Outcomes. 2nd ed. New York, NY: Pfizer; 2004.
42. Bradley EH, Bogardus ST Jr, Tinetti M, et al. Goal-setting in clinical medicine. Soc Sci Med. 1999;49:267-278.
43. Koelling TM, Johnson ML, Cody RJ, et al. Discharge education improves clinical outcomes in patients with chronic heart failure. Circulation. 2005;111:179-185.
44. Krumholz HM, Amatruda J, Smith GL, et al. Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. J Am Coll Cardiol. 2002;39:83-89.
45. Burke RE, Coleman EA. Interventions to decrease hospital readmissions: keys for cost-effectiveness. JAMA Intern Med. 2013;173:695-698.
46. Kessler KR. Relationship between the use of asthma action plans and asthma exacerbations in children with asthma: A systematic review. J Asthma Allergy Educators. 2011;2:11-21.
47. Maric B, Kaan A, Ignaszewski A, et al. A systematic review of telemonitoring technologies in heart failure. Eur J Heart Fail. 2009;11:506-517.
48. Boutwell A, Hwu S. Effective Interventions to Reduce Rehospitalizations: A Survey of the Published Evidence. Cambridge, MA: Institute for Healthcare Improvement; 2009.
49. Bodenheimer T, Laing BY. The teamlet model of primary care. Ann Fam Med. 2007;5:457-461.
50. Meier D, Beresford L. Outpatient clinics are a new frontier for palliative care. J Pall Med. 2008;11:823-828.
Learn how to get reimbursed for postdischarge care
Team pinpoints possible target for T-ALL

Researchers have discovered a potential therapeutic target for T-cell acute lymphoblastic leukemia (T-ALL), according to a paper published in Cell.
The team first identified long, non-coding strands of RNA (lncRNA) that were active in T cells from patients with T-ALL but not in the healthy T cells of subjects without the disease.
Further analysis revealed that inhibiting 1 of these lncRNAs, LUNAR1 (leukemia-induced non-coding activator RNA-1), stalled T-ALL growth in vitro and in vivo.
The study offers preliminary evidence that drugs targeting LUNAR1 could treat T-ALL, and LUNAR1 could aid in diagnosing the disease, said Iannis Aifantis, PhD, of NYU Langone Medical Center in New York.
“Our study shows that LUNAR1 is highly specific for T-cell acute lymphoblastic leukemia and plays a key role in how this cancer develops,” he noted, adding that overproduction of LUNAR1 was recorded in almost all (90%) of the leukemia patients analyzed.
To make these discoveries, Dr Aifantis and his colleagues performed ultra-high-depth RNA sequencing of human T-ALL cell lines and primary leukemia samples.
They used the resulting data to generate the most comprehensive T-ALL transcriptome assembly to date and then isolated putative lncRNA genes. This revealed 6023 lncRNAs that are active in T-ALL, 60% of which had not been identified before.
The researchers zeroed in on LUNAR1 by pinpointing the lncRNAs that were active in the NOTCH1 pathway, which is active in at least half of T-ALL patients. LUNAR1 stood out right away, the team said, as the most highly expressed lncRNA.
The researchers also found that LUNAR1 does not produce cancerous proteins on its own. However, its production proved essential to the cell-to-cell signaling action of another protein, IGF-1R (insulin-like growth factor 1 receptor), which is tied to many cancers, including leukemia.
Additional experiments showed that the gene coding for LUNAR1 is near the gene for IGF-1R and located toward the end of the chromosome. When activated, LUNAR1’s position allows it to chemically loop back and, in turn, bind to and activate IGF-1R.
According to Dr Aifantis, this research shows that T-ALL could simply be described as a condition of “too much errant signaling.” He noted that, in normal T cells, lncRNAs such as LUNAR1 are not transcribed, NOTCH1 is inactive, and there is no looping back of LUNAR1 to activate IGF-1R.
To confirm their findings, the researchers also transplanted human leukemia T cells into mice and inhibited LUNAR1 in some of the animals. Tumor growth stalled only in those mice in which LUNAR1 was inactivated.
The researchers said their next step is to develop a more effective inhibitor of LUNAR1, preferably something that would precisely target 1 or more of its 200-plus component nucleotides. ![]()

Researchers have discovered a potential therapeutic target for T-cell acute lymphoblastic leukemia (T-ALL), according to a paper published in Cell.
The team first identified long, non-coding strands of RNA (lncRNA) that were active in T cells from patients with T-ALL but not in the healthy T cells of subjects without the disease.
Further analysis revealed that inhibiting 1 of these lncRNAs, LUNAR1 (leukemia-induced non-coding activator RNA-1), stalled T-ALL growth in vitro and in vivo.
The study offers preliminary evidence that drugs targeting LUNAR1 could treat T-ALL, and LUNAR1 could aid in diagnosing the disease, said Iannis Aifantis, PhD, of NYU Langone Medical Center in New York.
“Our study shows that LUNAR1 is highly specific for T-cell acute lymphoblastic leukemia and plays a key role in how this cancer develops,” he noted, adding that overproduction of LUNAR1 was recorded in almost all (90%) of the leukemia patients analyzed.
To make these discoveries, Dr Aifantis and his colleagues performed ultra-high-depth RNA sequencing of human T-ALL cell lines and primary leukemia samples.
They used the resulting data to generate the most comprehensive T-ALL transcriptome assembly to date and then isolated putative lncRNA genes. This revealed 6023 lncRNAs that are active in T-ALL, 60% of which had not been identified before.
The researchers zeroed in on LUNAR1 by pinpointing the lncRNAs that were active in the NOTCH1 pathway, which is active in at least half of T-ALL patients. LUNAR1 stood out right away, the team said, as the most highly expressed lncRNA.
The researchers also found that LUNAR1 does not produce cancerous proteins on its own. However, its production proved essential to the cell-to-cell signaling action of another protein, IGF-1R (insulin-like growth factor 1 receptor), which is tied to many cancers, including leukemia.
Additional experiments showed that the gene coding for LUNAR1 is near the gene for IGF-1R and located toward the end of the chromosome. When activated, LUNAR1’s position allows it to chemically loop back and, in turn, bind to and activate IGF-1R.
According to Dr Aifantis, this research shows that T-ALL could simply be described as a condition of “too much errant signaling.” He noted that, in normal T cells, lncRNAs such as LUNAR1 are not transcribed, NOTCH1 is inactive, and there is no looping back of LUNAR1 to activate IGF-1R.
To confirm their findings, the researchers also transplanted human leukemia T cells into mice and inhibited LUNAR1 in some of the animals. Tumor growth stalled only in those mice in which LUNAR1 was inactivated.
The researchers said their next step is to develop a more effective inhibitor of LUNAR1, preferably something that would precisely target 1 or more of its 200-plus component nucleotides. ![]()

Researchers have discovered a potential therapeutic target for T-cell acute lymphoblastic leukemia (T-ALL), according to a paper published in Cell.
The team first identified long, non-coding strands of RNA (lncRNA) that were active in T cells from patients with T-ALL but not in the healthy T cells of subjects without the disease.
Further analysis revealed that inhibiting 1 of these lncRNAs, LUNAR1 (leukemia-induced non-coding activator RNA-1), stalled T-ALL growth in vitro and in vivo.
The study offers preliminary evidence that drugs targeting LUNAR1 could treat T-ALL, and LUNAR1 could aid in diagnosing the disease, said Iannis Aifantis, PhD, of NYU Langone Medical Center in New York.
“Our study shows that LUNAR1 is highly specific for T-cell acute lymphoblastic leukemia and plays a key role in how this cancer develops,” he noted, adding that overproduction of LUNAR1 was recorded in almost all (90%) of the leukemia patients analyzed.
To make these discoveries, Dr Aifantis and his colleagues performed ultra-high-depth RNA sequencing of human T-ALL cell lines and primary leukemia samples.
They used the resulting data to generate the most comprehensive T-ALL transcriptome assembly to date and then isolated putative lncRNA genes. This revealed 6023 lncRNAs that are active in T-ALL, 60% of which had not been identified before.
The researchers zeroed in on LUNAR1 by pinpointing the lncRNAs that were active in the NOTCH1 pathway, which is active in at least half of T-ALL patients. LUNAR1 stood out right away, the team said, as the most highly expressed lncRNA.
The researchers also found that LUNAR1 does not produce cancerous proteins on its own. However, its production proved essential to the cell-to-cell signaling action of another protein, IGF-1R (insulin-like growth factor 1 receptor), which is tied to many cancers, including leukemia.
Additional experiments showed that the gene coding for LUNAR1 is near the gene for IGF-1R and located toward the end of the chromosome. When activated, LUNAR1’s position allows it to chemically loop back and, in turn, bind to and activate IGF-1R.
According to Dr Aifantis, this research shows that T-ALL could simply be described as a condition of “too much errant signaling.” He noted that, in normal T cells, lncRNAs such as LUNAR1 are not transcribed, NOTCH1 is inactive, and there is no looping back of LUNAR1 to activate IGF-1R.
To confirm their findings, the researchers also transplanted human leukemia T cells into mice and inhibited LUNAR1 in some of the animals. Tumor growth stalled only in those mice in which LUNAR1 was inactivated.
The researchers said their next step is to develop a more effective inhibitor of LUNAR1, preferably something that would precisely target 1 or more of its 200-plus component nucleotides. ![]()
Approach could improve treatment of lymphoma, other cancers

Credit: NIH
Targeting a molecule in endothelial cells could make cancer therapies significantly more effective, preclinical research suggests.
The researchers found that a molecule called focal adhesion kinase (FAK) can help protect cancer cells from the damaging effects of chemotherapy and radiotherapy.
But deleting FAK can enhance the effects of treatment directed against melanoma, lung cancer, and lymphoma.
The team recounted these findings in Nature.
“This work shows that sensitivity to cancer treatment is related to our own body mistakenly trying to shield the cancer from cell-killing effects caused by radiotherapy and chemotherapy,” said study author Bernardo Tavora, PhD, of Rockefeller University in New York.
“Although taking out FAK from blood vessels won’t destroy the cancer by itself, it can remove the barrier cancer uses to protect itself from treatment.”
Dr Tavora and his colleagues removed FAK from endothelial cells in mouse models of melanoma, lung cancer, and lymphoma. This had no effect on tumor growth in untreated mice.
However, the loss of endothelial-cell FAK did aid the effects of doxorubicin and radiotherapy. It increased apoptosis and decreased proliferation within perivascular tumor-cell compartments, thereby extending survival in the mice.
The researchers also studied samples from lymphoma patients. And they found that patients with low levels of FAK were more likely to achieve a complete remission after treatment.
Investigation into the mechanism behind these effects revealed that endothelial-cell FAK is required for the production of cytokines and for NF-κB activation induced by DNA damage.
So the loss of endothelial-cell FAK reduces DNA-damage-induced cytokine production, thereby increasing cancer cells’ sensitivity to DNA-damaging therapies in vitro and in vivo.
Taken together, these results suggest that developing drugs to target FAK could help improve the efficacy of cancer treatments and potentially prevent relapse in a number of malignancies. ![]()

Credit: NIH
Targeting a molecule in endothelial cells could make cancer therapies significantly more effective, preclinical research suggests.
The researchers found that a molecule called focal adhesion kinase (FAK) can help protect cancer cells from the damaging effects of chemotherapy and radiotherapy.
But deleting FAK can enhance the effects of treatment directed against melanoma, lung cancer, and lymphoma.
The team recounted these findings in Nature.
“This work shows that sensitivity to cancer treatment is related to our own body mistakenly trying to shield the cancer from cell-killing effects caused by radiotherapy and chemotherapy,” said study author Bernardo Tavora, PhD, of Rockefeller University in New York.
“Although taking out FAK from blood vessels won’t destroy the cancer by itself, it can remove the barrier cancer uses to protect itself from treatment.”
Dr Tavora and his colleagues removed FAK from endothelial cells in mouse models of melanoma, lung cancer, and lymphoma. This had no effect on tumor growth in untreated mice.
However, the loss of endothelial-cell FAK did aid the effects of doxorubicin and radiotherapy. It increased apoptosis and decreased proliferation within perivascular tumor-cell compartments, thereby extending survival in the mice.
The researchers also studied samples from lymphoma patients. And they found that patients with low levels of FAK were more likely to achieve a complete remission after treatment.
Investigation into the mechanism behind these effects revealed that endothelial-cell FAK is required for the production of cytokines and for NF-κB activation induced by DNA damage.
So the loss of endothelial-cell FAK reduces DNA-damage-induced cytokine production, thereby increasing cancer cells’ sensitivity to DNA-damaging therapies in vitro and in vivo.
Taken together, these results suggest that developing drugs to target FAK could help improve the efficacy of cancer treatments and potentially prevent relapse in a number of malignancies. ![]()

Credit: NIH
Targeting a molecule in endothelial cells could make cancer therapies significantly more effective, preclinical research suggests.
The researchers found that a molecule called focal adhesion kinase (FAK) can help protect cancer cells from the damaging effects of chemotherapy and radiotherapy.
But deleting FAK can enhance the effects of treatment directed against melanoma, lung cancer, and lymphoma.
The team recounted these findings in Nature.
“This work shows that sensitivity to cancer treatment is related to our own body mistakenly trying to shield the cancer from cell-killing effects caused by radiotherapy and chemotherapy,” said study author Bernardo Tavora, PhD, of Rockefeller University in New York.
“Although taking out FAK from blood vessels won’t destroy the cancer by itself, it can remove the barrier cancer uses to protect itself from treatment.”
Dr Tavora and his colleagues removed FAK from endothelial cells in mouse models of melanoma, lung cancer, and lymphoma. This had no effect on tumor growth in untreated mice.
However, the loss of endothelial-cell FAK did aid the effects of doxorubicin and radiotherapy. It increased apoptosis and decreased proliferation within perivascular tumor-cell compartments, thereby extending survival in the mice.
The researchers also studied samples from lymphoma patients. And they found that patients with low levels of FAK were more likely to achieve a complete remission after treatment.
Investigation into the mechanism behind these effects revealed that endothelial-cell FAK is required for the production of cytokines and for NF-κB activation induced by DNA damage.
So the loss of endothelial-cell FAK reduces DNA-damage-induced cytokine production, thereby increasing cancer cells’ sensitivity to DNA-damaging therapies in vitro and in vivo.
Taken together, these results suggest that developing drugs to target FAK could help improve the efficacy of cancer treatments and potentially prevent relapse in a number of malignancies. ![]()
Early HSCT best for infants with SCID, study shows

Credit: Chad McNeeley
Children with severe combined immune deficiency (SCID) have a good chance of survival if they undergo hematopoietic stem cell transplant (HSCT) within 3.5 months of birth, a new analysis suggests.
The risk of death is also lower if patients are free of infection at transplant and have a matched sibling donor.
“Survival is much, much better if infants undergo transplant before they turn 3.5 months old and before they contract any SCID-related infections,” said Sung-Yun Pai, MD, of the Dana-Farber Cancer Institute in Boston.
This underlines the importance of screening newborns for SCID, she added.
Dr Pai and her colleagues expressed this viewpoint, and detailed the research to support it, in The New England Journal of Medicine.
The team analyzed data on 240 children with SCID who were transplanted at 25 centers across North America between January 1, 2000, and December 31, 2009, (before the US Department of Health and Human Services recommended newborn screening for SCID in 2010).
The researchers assessed the patients’ outcomes according to age, infection status, donor source, and conditioning regimen.
Results revealed that children who underwent transplant before 3.5 months of age had excellent survival, regardless of donor source or infection status, as did patients with a matched sibling donor.
Children transplanted after 3.5 months also had a high survival rate regardless of donor source, as long as they did not have an active infection at the time of transplant.
Overall, 74% of patients survived at least 5 years. The 5-year survival rate was 97% in patients with a matched sibling donor, 94% among patients transplanted within 3.5 months of birth, 90% among patients who never had an infection, and 82% in patients whose infection resolved before transplant.
Survival was low—50%—among patients who were older than 3.5 months and had active infections at the time of transplant.
Actively infected infants who did not have a matched sibling donor and received immunosuppressive therapy or chemotherapy before transplant had particularly poor survival as well, ranging from 39% to 53%.
“This study accomplishes several things,” Dr Pai said. “First, it creates a baseline with which to compare patient outcomes since the advent of newborn screening for SCID. Second, it provides guidance for clinicians regarding the use of chemotherapy conditioning before transplantation.”
“Third, it highlights the relative impacts of infection status and patient age on transplant success. Lastly, it establishes the importance of early detection and transplantation, which points to the benefit of expanding newborn screening for SCID as broadly as possible.” ![]()

Credit: Chad McNeeley
Children with severe combined immune deficiency (SCID) have a good chance of survival if they undergo hematopoietic stem cell transplant (HSCT) within 3.5 months of birth, a new analysis suggests.
The risk of death is also lower if patients are free of infection at transplant and have a matched sibling donor.
“Survival is much, much better if infants undergo transplant before they turn 3.5 months old and before they contract any SCID-related infections,” said Sung-Yun Pai, MD, of the Dana-Farber Cancer Institute in Boston.
This underlines the importance of screening newborns for SCID, she added.
Dr Pai and her colleagues expressed this viewpoint, and detailed the research to support it, in The New England Journal of Medicine.
The team analyzed data on 240 children with SCID who were transplanted at 25 centers across North America between January 1, 2000, and December 31, 2009, (before the US Department of Health and Human Services recommended newborn screening for SCID in 2010).
The researchers assessed the patients’ outcomes according to age, infection status, donor source, and conditioning regimen.
Results revealed that children who underwent transplant before 3.5 months of age had excellent survival, regardless of donor source or infection status, as did patients with a matched sibling donor.
Children transplanted after 3.5 months also had a high survival rate regardless of donor source, as long as they did not have an active infection at the time of transplant.
Overall, 74% of patients survived at least 5 years. The 5-year survival rate was 97% in patients with a matched sibling donor, 94% among patients transplanted within 3.5 months of birth, 90% among patients who never had an infection, and 82% in patients whose infection resolved before transplant.
Survival was low—50%—among patients who were older than 3.5 months and had active infections at the time of transplant.
Actively infected infants who did not have a matched sibling donor and received immunosuppressive therapy or chemotherapy before transplant had particularly poor survival as well, ranging from 39% to 53%.
“This study accomplishes several things,” Dr Pai said. “First, it creates a baseline with which to compare patient outcomes since the advent of newborn screening for SCID. Second, it provides guidance for clinicians regarding the use of chemotherapy conditioning before transplantation.”
“Third, it highlights the relative impacts of infection status and patient age on transplant success. Lastly, it establishes the importance of early detection and transplantation, which points to the benefit of expanding newborn screening for SCID as broadly as possible.” ![]()

Credit: Chad McNeeley
Children with severe combined immune deficiency (SCID) have a good chance of survival if they undergo hematopoietic stem cell transplant (HSCT) within 3.5 months of birth, a new analysis suggests.
The risk of death is also lower if patients are free of infection at transplant and have a matched sibling donor.
“Survival is much, much better if infants undergo transplant before they turn 3.5 months old and before they contract any SCID-related infections,” said Sung-Yun Pai, MD, of the Dana-Farber Cancer Institute in Boston.
This underlines the importance of screening newborns for SCID, she added.
Dr Pai and her colleagues expressed this viewpoint, and detailed the research to support it, in The New England Journal of Medicine.
The team analyzed data on 240 children with SCID who were transplanted at 25 centers across North America between January 1, 2000, and December 31, 2009, (before the US Department of Health and Human Services recommended newborn screening for SCID in 2010).
The researchers assessed the patients’ outcomes according to age, infection status, donor source, and conditioning regimen.
Results revealed that children who underwent transplant before 3.5 months of age had excellent survival, regardless of donor source or infection status, as did patients with a matched sibling donor.
Children transplanted after 3.5 months also had a high survival rate regardless of donor source, as long as they did not have an active infection at the time of transplant.
Overall, 74% of patients survived at least 5 years. The 5-year survival rate was 97% in patients with a matched sibling donor, 94% among patients transplanted within 3.5 months of birth, 90% among patients who never had an infection, and 82% in patients whose infection resolved before transplant.
Survival was low—50%—among patients who were older than 3.5 months and had active infections at the time of transplant.
Actively infected infants who did not have a matched sibling donor and received immunosuppressive therapy or chemotherapy before transplant had particularly poor survival as well, ranging from 39% to 53%.
“This study accomplishes several things,” Dr Pai said. “First, it creates a baseline with which to compare patient outcomes since the advent of newborn screening for SCID. Second, it provides guidance for clinicians regarding the use of chemotherapy conditioning before transplantation.”
“Third, it highlights the relative impacts of infection status and patient age on transplant success. Lastly, it establishes the importance of early detection and transplantation, which points to the benefit of expanding newborn screening for SCID as broadly as possible.” ![]()