User login
Tool aids analysis of genomic data

Credit: Christoph Bock
Computer scientists have developed a web-based tool that allows researchers to visualize and compare large amounts of genomic information from high-throughput sequencing experiments.
The group described the tool, called Epiviz, in Nature Methods.
“Prior tools limited visualization to presentation and dissemination, rather than a hybrid tool integrating interactive visualization with algorithmic analysis,” said Héctor Corrada Bravo, PhD, of the University of Maryland in College Park.
Dr Corrada Bravo and his colleagues developed Epiviz, a web-based genome browser that integrates with the widely used, open-source Bioconductor analysis software through its Epivizr Bioconductor package.
Epiviz supports many popular next-generation sequencing techniques, such as ChIP-seq, RNA-seq, and DNA methylation analyses.
The tool also implements multiple visualization methods for location-based data (such as genomic regions of interest) and feature-based data (such as gene expression).
For example, because display objects are mapped directly to data elements, Epiviz links data across different visualizations, giving users visual insights of the spatial relationships of multiple data sets. The tool is designed to allow biomedical scientists to easily incorporate their own visualizations.
In the Nature Methods paper, Dr Corrada Bravo and his colleagues describe how they used Epiviz to visualize and analyze DNA methylation and gene expression data in colon cancer.
Using Epiviz and Bioconductor, the team found consistent regions of DNA methylation changes in colon cancer samples generated by the Cancer Genome Atlas project and similar gene expression in these regions of DNA methylation changes in other cancer types.
The results were in agreement with previous experiments showing DNA methylation changes across large regions in the colon cancer genome. ![]()

Credit: Christoph Bock
Computer scientists have developed a web-based tool that allows researchers to visualize and compare large amounts of genomic information from high-throughput sequencing experiments.
The group described the tool, called Epiviz, in Nature Methods.
“Prior tools limited visualization to presentation and dissemination, rather than a hybrid tool integrating interactive visualization with algorithmic analysis,” said Héctor Corrada Bravo, PhD, of the University of Maryland in College Park.
Dr Corrada Bravo and his colleagues developed Epiviz, a web-based genome browser that integrates with the widely used, open-source Bioconductor analysis software through its Epivizr Bioconductor package.
Epiviz supports many popular next-generation sequencing techniques, such as ChIP-seq, RNA-seq, and DNA methylation analyses.
The tool also implements multiple visualization methods for location-based data (such as genomic regions of interest) and feature-based data (such as gene expression).
For example, because display objects are mapped directly to data elements, Epiviz links data across different visualizations, giving users visual insights of the spatial relationships of multiple data sets. The tool is designed to allow biomedical scientists to easily incorporate their own visualizations.
In the Nature Methods paper, Dr Corrada Bravo and his colleagues describe how they used Epiviz to visualize and analyze DNA methylation and gene expression data in colon cancer.
Using Epiviz and Bioconductor, the team found consistent regions of DNA methylation changes in colon cancer samples generated by the Cancer Genome Atlas project and similar gene expression in these regions of DNA methylation changes in other cancer types.
The results were in agreement with previous experiments showing DNA methylation changes across large regions in the colon cancer genome. ![]()

Credit: Christoph Bock
Computer scientists have developed a web-based tool that allows researchers to visualize and compare large amounts of genomic information from high-throughput sequencing experiments.
The group described the tool, called Epiviz, in Nature Methods.
“Prior tools limited visualization to presentation and dissemination, rather than a hybrid tool integrating interactive visualization with algorithmic analysis,” said Héctor Corrada Bravo, PhD, of the University of Maryland in College Park.
Dr Corrada Bravo and his colleagues developed Epiviz, a web-based genome browser that integrates with the widely used, open-source Bioconductor analysis software through its Epivizr Bioconductor package.
Epiviz supports many popular next-generation sequencing techniques, such as ChIP-seq, RNA-seq, and DNA methylation analyses.
The tool also implements multiple visualization methods for location-based data (such as genomic regions of interest) and feature-based data (such as gene expression).
For example, because display objects are mapped directly to data elements, Epiviz links data across different visualizations, giving users visual insights of the spatial relationships of multiple data sets. The tool is designed to allow biomedical scientists to easily incorporate their own visualizations.
In the Nature Methods paper, Dr Corrada Bravo and his colleagues describe how they used Epiviz to visualize and analyze DNA methylation and gene expression data in colon cancer.
Using Epiviz and Bioconductor, the team found consistent regions of DNA methylation changes in colon cancer samples generated by the Cancer Genome Atlas project and similar gene expression in these regions of DNA methylation changes in other cancer types.
The results were in agreement with previous experiments showing DNA methylation changes across large regions in the colon cancer genome. ![]()
System simplifies complex pipetting protocols

Credit: John Correa
Researchers say they’ve developed a simple system that can help scientists perform complex pipetting protocols efficiently and accurately.
The system, called iPipet, allows users to track the transfer of samples and reagents by illuminating well plates on a computer tablet.
In tests, iPipet proved more efficient than a liquid-handling robot.
The researchers have made information on iPipet available online so scientists can use the system in their own labs.
The team also described iPipet in a letter to Nature Methods.
They noted that experiments frequently rely on high-throughput methods that combine large numbers of samples with large-scale, complex pipetting designs. And pipetting errors can lead to experimental failure.
Although liquid-handling robots would seem to be a logical choice for such work, they are also extremely expensive, difficult to program, and require trained personnel. Moreover, they can be plagued by technical snafus, ranging from bent or clogged tips to an inability to capture liquids lying close to the bottoms of individual wells.
“We needed an alternative to costly robots that would allow us to execute complex pipetting protocols,” said Yaniv Erlich, PhD, of the Whitehead Institute in Cambridge, Massachusetts.
So Dr Erlich and his colleagues developed iPipet. The system illuminates individual wells of standard 96- or 384-well plates placed on top of a tablet screen, guiding users through the transfer of samples or reagents from source to destination plates according to specific designs.
Users create their own protocols in Microsoft Excel files in comma-separated format and upload them to the iPipet website, which generates a downloadable link for execution on a tablet computer. Included on the iPipet site are a variety of demos and an instructional video.
In a test of the tool against a liquid-handling robot, iPipet enabled nearly 3000 fixed-volume pipetting steps in approximately 7 hours. After significant time spent on calibration, the robot accomplished only half that number of steps in the same allotted time.
To date, one of the only challenges lab users have encountered is keeping well plates in a fixed position on the tablet screen. For that, Dr Erlich’s team provides a solution: a 3D printed plastic adaptor that users can create with a file accessible via the iPipet website.
“The entire iPipet system is open source,” Dr Erlich said. “We want to maximize the benefit for the community and allow them to further develop this new man-machine interface for biological experiments.” ![]()

Credit: John Correa
Researchers say they’ve developed a simple system that can help scientists perform complex pipetting protocols efficiently and accurately.
The system, called iPipet, allows users to track the transfer of samples and reagents by illuminating well plates on a computer tablet.
In tests, iPipet proved more efficient than a liquid-handling robot.
The researchers have made information on iPipet available online so scientists can use the system in their own labs.
The team also described iPipet in a letter to Nature Methods.
They noted that experiments frequently rely on high-throughput methods that combine large numbers of samples with large-scale, complex pipetting designs. And pipetting errors can lead to experimental failure.
Although liquid-handling robots would seem to be a logical choice for such work, they are also extremely expensive, difficult to program, and require trained personnel. Moreover, they can be plagued by technical snafus, ranging from bent or clogged tips to an inability to capture liquids lying close to the bottoms of individual wells.
“We needed an alternative to costly robots that would allow us to execute complex pipetting protocols,” said Yaniv Erlich, PhD, of the Whitehead Institute in Cambridge, Massachusetts.
So Dr Erlich and his colleagues developed iPipet. The system illuminates individual wells of standard 96- or 384-well plates placed on top of a tablet screen, guiding users through the transfer of samples or reagents from source to destination plates according to specific designs.
Users create their own protocols in Microsoft Excel files in comma-separated format and upload them to the iPipet website, which generates a downloadable link for execution on a tablet computer. Included on the iPipet site are a variety of demos and an instructional video.
In a test of the tool against a liquid-handling robot, iPipet enabled nearly 3000 fixed-volume pipetting steps in approximately 7 hours. After significant time spent on calibration, the robot accomplished only half that number of steps in the same allotted time.
To date, one of the only challenges lab users have encountered is keeping well plates in a fixed position on the tablet screen. For that, Dr Erlich’s team provides a solution: a 3D printed plastic adaptor that users can create with a file accessible via the iPipet website.
“The entire iPipet system is open source,” Dr Erlich said. “We want to maximize the benefit for the community and allow them to further develop this new man-machine interface for biological experiments.” ![]()

Credit: John Correa
Researchers say they’ve developed a simple system that can help scientists perform complex pipetting protocols efficiently and accurately.
The system, called iPipet, allows users to track the transfer of samples and reagents by illuminating well plates on a computer tablet.
In tests, iPipet proved more efficient than a liquid-handling robot.
The researchers have made information on iPipet available online so scientists can use the system in their own labs.
The team also described iPipet in a letter to Nature Methods.
They noted that experiments frequently rely on high-throughput methods that combine large numbers of samples with large-scale, complex pipetting designs. And pipetting errors can lead to experimental failure.
Although liquid-handling robots would seem to be a logical choice for such work, they are also extremely expensive, difficult to program, and require trained personnel. Moreover, they can be plagued by technical snafus, ranging from bent or clogged tips to an inability to capture liquids lying close to the bottoms of individual wells.
“We needed an alternative to costly robots that would allow us to execute complex pipetting protocols,” said Yaniv Erlich, PhD, of the Whitehead Institute in Cambridge, Massachusetts.
So Dr Erlich and his colleagues developed iPipet. The system illuminates individual wells of standard 96- or 384-well plates placed on top of a tablet screen, guiding users through the transfer of samples or reagents from source to destination plates according to specific designs.
Users create their own protocols in Microsoft Excel files in comma-separated format and upload them to the iPipet website, which generates a downloadable link for execution on a tablet computer. Included on the iPipet site are a variety of demos and an instructional video.
In a test of the tool against a liquid-handling robot, iPipet enabled nearly 3000 fixed-volume pipetting steps in approximately 7 hours. After significant time spent on calibration, the robot accomplished only half that number of steps in the same allotted time.
To date, one of the only challenges lab users have encountered is keeping well plates in a fixed position on the tablet screen. For that, Dr Erlich’s team provides a solution: a 3D printed plastic adaptor that users can create with a file accessible via the iPipet website.
“The entire iPipet system is open source,” Dr Erlich said. “We want to maximize the benefit for the community and allow them to further develop this new man-machine interface for biological experiments.” ![]()
LISTEN NOW: Highlights of the August 2014 issue of The Hospitalist newsmagazine
Highlights from The Hospitalist this month include an interview with SHM President Dr. Burke Kealey about his series of President's Desk columns. Dr. Kealey talks about how the hospital medicine movement arose and expands on the transformational nature of hospital medicine. Also in this issue, we provide a comprehensive look at medical decision making, focused on the ins and outs of turning decisions into the right codes for billing and ongoing. Dr. Christopher Moreland, a deaf teaching hospitalist at University Hospital at the University of Texas is profiled on our cover, and Team Hospitalist member Dr. Julie Fedderson tells us what drew her to the specialty. In addition, we offer a progress report of SHM’s performance assessment tool for hospital medicine groups. Our Key Clinical Question this month addresses hypontremia treatment and managment, and our In The Literature section features the latest in clinical literature.
Highlights from The Hospitalist this month include an interview with SHM President Dr. Burke Kealey about his series of President's Desk columns. Dr. Kealey talks about how the hospital medicine movement arose and expands on the transformational nature of hospital medicine. Also in this issue, we provide a comprehensive look at medical decision making, focused on the ins and outs of turning decisions into the right codes for billing and ongoing. Dr. Christopher Moreland, a deaf teaching hospitalist at University Hospital at the University of Texas is profiled on our cover, and Team Hospitalist member Dr. Julie Fedderson tells us what drew her to the specialty. In addition, we offer a progress report of SHM’s performance assessment tool for hospital medicine groups. Our Key Clinical Question this month addresses hypontremia treatment and managment, and our In The Literature section features the latest in clinical literature.
Highlights from The Hospitalist this month include an interview with SHM President Dr. Burke Kealey about his series of President's Desk columns. Dr. Kealey talks about how the hospital medicine movement arose and expands on the transformational nature of hospital medicine. Also in this issue, we provide a comprehensive look at medical decision making, focused on the ins and outs of turning decisions into the right codes for billing and ongoing. Dr. Christopher Moreland, a deaf teaching hospitalist at University Hospital at the University of Texas is profiled on our cover, and Team Hospitalist member Dr. Julie Fedderson tells us what drew her to the specialty. In addition, we offer a progress report of SHM’s performance assessment tool for hospital medicine groups. Our Key Clinical Question this month addresses hypontremia treatment and managment, and our In The Literature section features the latest in clinical literature.
Biliary pain, no gallstones—remove the gallbladder, anyway?
CASE 1 › A 28-year-old woman (G0P0) came to our office with recurrent episodes of postprandial epigastric and right upper quadrant pain. Upper and lower endoscopy, sonography, body imaging, and laboratory tests were normal. A biliary nuclear scan showed an ejection fraction (EF) of 95%; normal is >35%. We made a diagnosis of biliary dyskinesia (BD) and recommended a laparoscopic cholecystectomy. The patient underwent this procedure and her pain was relieved. She has been much improved for 2 years, although she has since been diagnosed with an autoimmune disorder.
CASE 2 › A 21-year-old woman with right upper quadrant, postprandial, colicky pain presented to the emergency department. The episode lasted approximately 30 minutes and was followed by residual soreness. This episode was one of several that had been increasing in frequency and intensity. A sonogram showed a normal gallbladder and common duct. All laboratory tests were normal. She improved and was discharged. Outpatient evaluation included body imaging and endoscopy, which were negative. A hepatobiliary (HIDA) scan revealed an EF of 90%, and the scan reproduced her symptoms.
We diagnosed BD in this patient. After reviewing the risks and benefits of cholecystectomy, the patient consented to the procedure. She has been asymptomatic for 2 years.
Family physicians often are the first to evaluate patients with recurrent biliary colic. Biliary colic without gallstones—also known as BD or acalculous cholecystitis—is a functional disorder of the gallbladder or bile duct. Approximately 8% of men and 21% of women with biliary pain do not have gallstones.1-5
BD has been successfully treated with cholecystectomy. Physicians typically have viewed cholecystectomy as being effective primarily for patients with biliary pain who have a low EF (<35%).2-4 However, recent studies and our experience with cholecystectomy in these 2 patients with high EFs suggest that EF is only one of several factors to consider when deciding whether cholecystectomy might be appropriate for a given patient.
Which patients are most likely to benefit from cholecystectomy?
BD is a diagnosis of exclusion, considered when other upper abdominal disorders are eliminated. To receive a diagnosis of BD, patients must meet the Rome III criteria (TABLE).2
Before the advent of oral cholecystography in the 1920s, biliary disease was a clinical diagnosis confirmed by examination of the excised gallbladder.6 In 2 large studies conducted before cholecystography was in common use, researchers noted improvement in 75% to 85% of BD patients after cholecystectomy.7,8 Several years later, with the benefit, of cholecystography, Mackey9 reported similar improvement rates among patients with BD who underwent cholecystectomy.
Cholecystography has largely been replaced with HIDA scanning, which provides an objective measure of EF. Although some studies have suggested low EFs may predict which patients will benefit from cholecystectomy, others have suggested this value doesn’t tell the whole story.2,4,10,11 In some studies, patients who had biliary symptoms and a low EF (<35%) were found to be most likely to experience relief after cholecystectomy.2,4 More recently, in a chart review, DuCoin et al10 found that of 19 BD patients with an EF >35% who underwent cholecystectomy, 17 had complete symptom resolution, one had partial resolution, and one was unchanged. Only one abstract of a study of cholecystectomy for BD patients with a high EF (>80%) has been published.11 Of 28 patients who received cholecystectomy, 22 were asymptomatic after cholecystectomy and 5 others improved.11
Other tests to consider. A cholecystokinin infusion without a scan has been used to reproduce biliary colic; some physicians consider this to be diagnostic of BD and sufficient for cholecystectomy.12 Others have advocated endoscopic injection of botulinum into the sphincter of Oddi to differentiate pain arising from the sphincter of Oddi from pain in the gallbladder.5,13 If symptoms are relieved by this injection, an endoscopic biliary sphincterotomy—cutting of the biliary sphincter—is done. Cholecystectomy is reserved for patients whose pain is not relieved by botulinum. In an initial report, 25 BD patients received botulinum injections into the sphincter of Oddi; of the 11 whose pain was relieved by this injection, 10 underwent endoscopic biliary sphincterotomy, and pain resolved for all of these patients.13
Why we chose cholecystectomy for our patients
Despite a plethora of tests available to visualize and assess gallbladder and bile duct function, clinical assessment of BD by experienced physicians may be sufficient to determine which BD patients will benefit from cholecystectomy. In the cases we report on here, each patient had a high EF, but both met Rome III criteria and were experiencing clinically significant pain. Also, for both patients, a cholecystokinin infusion administered to calculate EF reproduced their pain. This clinical picture led us to recommend laparoscopic cholecystectomy, which ultimately relieved their symptoms.
CORRESPONDENCE
Mazen Iskandar, MD, The Pancreas and Biliary Center of New York, Beth Israel Medical Center, 350 East 17th Street, 16 Baird Hall, New York, NY 10010; [email protected]
1. Drossman DA, Dumitrascu DL. Rome III: new standard for functional gastrointestinal disorders. J Gastrointest Liver Dis. 2006;15:237-241.
2. Hansel SL, DiBaise JK. Functional gallbladder disorder: gallbladder dyskinesia. Gastroenterol Clin North Am. 2010;39:369-379.
3. Francis G, Baillie J. Gallbladder dyskinesia: fact or fiction? Curr Gastroenterol Rep. 2011;13:188-192.
4. Yap L, Wycherley AG, Morphett AD, et al. Acalculous biliary pain; cholecystectomy alleviates symptoms in patients with abnormal cholescintigraphy. Gastroenterology. 1991;101:786-793.
5. Behar J, Corazziari E, Guelrud M, et al. Functional gallbladder and sphincter of oddi disorders. Gastroenterology. 2006;130: 1498-1509.
6. Graham EA, Cole WH. Roentgenologic examination of the gallbladder: preliminary report of a new method utilizing the intravenous injection of tetrabromophenolphthalein. JAMA. 1924;82:613-614.
7. Blalock A. A study of eight hundred and eighty-eight cases of biliary tract disease. Johns Hopkins Hosp Bull. 1924;35:391-409.
8. Whipple AO. Surgical criteria for cholecystectomy. Bull N Y Acad Med. 1926;2:302-306.
9. Mackey WA. Cholecystitis without stone an investigation of 264 operated cases from the clinical, radiological, and pathological aspects. An attempt to determine the factors of service in estimating prognosis. Br J Surg. 1934;22:274-295.
10. DuCoin C, Faber R, Ilagan M, et al. Normokinetic biliary dyskinesia: a novel diagnosis. Surg Endosc. 2012;26:3088-3093.
11. Holes-Lewis KA, Hakim S, Rehman F, al. CCK-induced gall bladder hyperkinesia: An indication for cholecystectomy and brain-GI connectivity research. J Nucl Med. 2009;50(suppl 2):1312.
12. Carr JA, Walls J, Bryan LJ, et al. The treatment of gallbladder dyskinesia based upon symptoms: results of a 2-year, prospective, nonrandomized, concurrent cohort study. Surg Laparosc Endosc Percutan Tech. 2009;19:222-226.
13. Murray WR. Botulinum toxin-induced relaxation of the sphincter of Oddi may select patients with acalculous biliary pain who will benefit from cholecystectomy. Surg Endosc. 2011;25:813-816.
CASE 1 › A 28-year-old woman (G0P0) came to our office with recurrent episodes of postprandial epigastric and right upper quadrant pain. Upper and lower endoscopy, sonography, body imaging, and laboratory tests were normal. A biliary nuclear scan showed an ejection fraction (EF) of 95%; normal is >35%. We made a diagnosis of biliary dyskinesia (BD) and recommended a laparoscopic cholecystectomy. The patient underwent this procedure and her pain was relieved. She has been much improved for 2 years, although she has since been diagnosed with an autoimmune disorder.
CASE 2 › A 21-year-old woman with right upper quadrant, postprandial, colicky pain presented to the emergency department. The episode lasted approximately 30 minutes and was followed by residual soreness. This episode was one of several that had been increasing in frequency and intensity. A sonogram showed a normal gallbladder and common duct. All laboratory tests were normal. She improved and was discharged. Outpatient evaluation included body imaging and endoscopy, which were negative. A hepatobiliary (HIDA) scan revealed an EF of 90%, and the scan reproduced her symptoms.
We diagnosed BD in this patient. After reviewing the risks and benefits of cholecystectomy, the patient consented to the procedure. She has been asymptomatic for 2 years.
Family physicians often are the first to evaluate patients with recurrent biliary colic. Biliary colic without gallstones—also known as BD or acalculous cholecystitis—is a functional disorder of the gallbladder or bile duct. Approximately 8% of men and 21% of women with biliary pain do not have gallstones.1-5
BD has been successfully treated with cholecystectomy. Physicians typically have viewed cholecystectomy as being effective primarily for patients with biliary pain who have a low EF (<35%).2-4 However, recent studies and our experience with cholecystectomy in these 2 patients with high EFs suggest that EF is only one of several factors to consider when deciding whether cholecystectomy might be appropriate for a given patient.
Which patients are most likely to benefit from cholecystectomy?
BD is a diagnosis of exclusion, considered when other upper abdominal disorders are eliminated. To receive a diagnosis of BD, patients must meet the Rome III criteria (TABLE).2
Before the advent of oral cholecystography in the 1920s, biliary disease was a clinical diagnosis confirmed by examination of the excised gallbladder.6 In 2 large studies conducted before cholecystography was in common use, researchers noted improvement in 75% to 85% of BD patients after cholecystectomy.7,8 Several years later, with the benefit, of cholecystography, Mackey9 reported similar improvement rates among patients with BD who underwent cholecystectomy.
Cholecystography has largely been replaced with HIDA scanning, which provides an objective measure of EF. Although some studies have suggested low EFs may predict which patients will benefit from cholecystectomy, others have suggested this value doesn’t tell the whole story.2,4,10,11 In some studies, patients who had biliary symptoms and a low EF (<35%) were found to be most likely to experience relief after cholecystectomy.2,4 More recently, in a chart review, DuCoin et al10 found that of 19 BD patients with an EF >35% who underwent cholecystectomy, 17 had complete symptom resolution, one had partial resolution, and one was unchanged. Only one abstract of a study of cholecystectomy for BD patients with a high EF (>80%) has been published.11 Of 28 patients who received cholecystectomy, 22 were asymptomatic after cholecystectomy and 5 others improved.11
Other tests to consider. A cholecystokinin infusion without a scan has been used to reproduce biliary colic; some physicians consider this to be diagnostic of BD and sufficient for cholecystectomy.12 Others have advocated endoscopic injection of botulinum into the sphincter of Oddi to differentiate pain arising from the sphincter of Oddi from pain in the gallbladder.5,13 If symptoms are relieved by this injection, an endoscopic biliary sphincterotomy—cutting of the biliary sphincter—is done. Cholecystectomy is reserved for patients whose pain is not relieved by botulinum. In an initial report, 25 BD patients received botulinum injections into the sphincter of Oddi; of the 11 whose pain was relieved by this injection, 10 underwent endoscopic biliary sphincterotomy, and pain resolved for all of these patients.13
Why we chose cholecystectomy for our patients
Despite a plethora of tests available to visualize and assess gallbladder and bile duct function, clinical assessment of BD by experienced physicians may be sufficient to determine which BD patients will benefit from cholecystectomy. In the cases we report on here, each patient had a high EF, but both met Rome III criteria and were experiencing clinically significant pain. Also, for both patients, a cholecystokinin infusion administered to calculate EF reproduced their pain. This clinical picture led us to recommend laparoscopic cholecystectomy, which ultimately relieved their symptoms.
CORRESPONDENCE
Mazen Iskandar, MD, The Pancreas and Biliary Center of New York, Beth Israel Medical Center, 350 East 17th Street, 16 Baird Hall, New York, NY 10010; [email protected]
CASE 1 › A 28-year-old woman (G0P0) came to our office with recurrent episodes of postprandial epigastric and right upper quadrant pain. Upper and lower endoscopy, sonography, body imaging, and laboratory tests were normal. A biliary nuclear scan showed an ejection fraction (EF) of 95%; normal is >35%. We made a diagnosis of biliary dyskinesia (BD) and recommended a laparoscopic cholecystectomy. The patient underwent this procedure and her pain was relieved. She has been much improved for 2 years, although she has since been diagnosed with an autoimmune disorder.
CASE 2 › A 21-year-old woman with right upper quadrant, postprandial, colicky pain presented to the emergency department. The episode lasted approximately 30 minutes and was followed by residual soreness. This episode was one of several that had been increasing in frequency and intensity. A sonogram showed a normal gallbladder and common duct. All laboratory tests were normal. She improved and was discharged. Outpatient evaluation included body imaging and endoscopy, which were negative. A hepatobiliary (HIDA) scan revealed an EF of 90%, and the scan reproduced her symptoms.
We diagnosed BD in this patient. After reviewing the risks and benefits of cholecystectomy, the patient consented to the procedure. She has been asymptomatic for 2 years.
Family physicians often are the first to evaluate patients with recurrent biliary colic. Biliary colic without gallstones—also known as BD or acalculous cholecystitis—is a functional disorder of the gallbladder or bile duct. Approximately 8% of men and 21% of women with biliary pain do not have gallstones.1-5
BD has been successfully treated with cholecystectomy. Physicians typically have viewed cholecystectomy as being effective primarily for patients with biliary pain who have a low EF (<35%).2-4 However, recent studies and our experience with cholecystectomy in these 2 patients with high EFs suggest that EF is only one of several factors to consider when deciding whether cholecystectomy might be appropriate for a given patient.
Which patients are most likely to benefit from cholecystectomy?
BD is a diagnosis of exclusion, considered when other upper abdominal disorders are eliminated. To receive a diagnosis of BD, patients must meet the Rome III criteria (TABLE).2
Before the advent of oral cholecystography in the 1920s, biliary disease was a clinical diagnosis confirmed by examination of the excised gallbladder.6 In 2 large studies conducted before cholecystography was in common use, researchers noted improvement in 75% to 85% of BD patients after cholecystectomy.7,8 Several years later, with the benefit, of cholecystography, Mackey9 reported similar improvement rates among patients with BD who underwent cholecystectomy.
Cholecystography has largely been replaced with HIDA scanning, which provides an objective measure of EF. Although some studies have suggested low EFs may predict which patients will benefit from cholecystectomy, others have suggested this value doesn’t tell the whole story.2,4,10,11 In some studies, patients who had biliary symptoms and a low EF (<35%) were found to be most likely to experience relief after cholecystectomy.2,4 More recently, in a chart review, DuCoin et al10 found that of 19 BD patients with an EF >35% who underwent cholecystectomy, 17 had complete symptom resolution, one had partial resolution, and one was unchanged. Only one abstract of a study of cholecystectomy for BD patients with a high EF (>80%) has been published.11 Of 28 patients who received cholecystectomy, 22 were asymptomatic after cholecystectomy and 5 others improved.11
Other tests to consider. A cholecystokinin infusion without a scan has been used to reproduce biliary colic; some physicians consider this to be diagnostic of BD and sufficient for cholecystectomy.12 Others have advocated endoscopic injection of botulinum into the sphincter of Oddi to differentiate pain arising from the sphincter of Oddi from pain in the gallbladder.5,13 If symptoms are relieved by this injection, an endoscopic biliary sphincterotomy—cutting of the biliary sphincter—is done. Cholecystectomy is reserved for patients whose pain is not relieved by botulinum. In an initial report, 25 BD patients received botulinum injections into the sphincter of Oddi; of the 11 whose pain was relieved by this injection, 10 underwent endoscopic biliary sphincterotomy, and pain resolved for all of these patients.13
Why we chose cholecystectomy for our patients
Despite a plethora of tests available to visualize and assess gallbladder and bile duct function, clinical assessment of BD by experienced physicians may be sufficient to determine which BD patients will benefit from cholecystectomy. In the cases we report on here, each patient had a high EF, but both met Rome III criteria and were experiencing clinically significant pain. Also, for both patients, a cholecystokinin infusion administered to calculate EF reproduced their pain. This clinical picture led us to recommend laparoscopic cholecystectomy, which ultimately relieved their symptoms.
CORRESPONDENCE
Mazen Iskandar, MD, The Pancreas and Biliary Center of New York, Beth Israel Medical Center, 350 East 17th Street, 16 Baird Hall, New York, NY 10010; [email protected]
1. Drossman DA, Dumitrascu DL. Rome III: new standard for functional gastrointestinal disorders. J Gastrointest Liver Dis. 2006;15:237-241.
2. Hansel SL, DiBaise JK. Functional gallbladder disorder: gallbladder dyskinesia. Gastroenterol Clin North Am. 2010;39:369-379.
3. Francis G, Baillie J. Gallbladder dyskinesia: fact or fiction? Curr Gastroenterol Rep. 2011;13:188-192.
4. Yap L, Wycherley AG, Morphett AD, et al. Acalculous biliary pain; cholecystectomy alleviates symptoms in patients with abnormal cholescintigraphy. Gastroenterology. 1991;101:786-793.
5. Behar J, Corazziari E, Guelrud M, et al. Functional gallbladder and sphincter of oddi disorders. Gastroenterology. 2006;130: 1498-1509.
6. Graham EA, Cole WH. Roentgenologic examination of the gallbladder: preliminary report of a new method utilizing the intravenous injection of tetrabromophenolphthalein. JAMA. 1924;82:613-614.
7. Blalock A. A study of eight hundred and eighty-eight cases of biliary tract disease. Johns Hopkins Hosp Bull. 1924;35:391-409.
8. Whipple AO. Surgical criteria for cholecystectomy. Bull N Y Acad Med. 1926;2:302-306.
9. Mackey WA. Cholecystitis without stone an investigation of 264 operated cases from the clinical, radiological, and pathological aspects. An attempt to determine the factors of service in estimating prognosis. Br J Surg. 1934;22:274-295.
10. DuCoin C, Faber R, Ilagan M, et al. Normokinetic biliary dyskinesia: a novel diagnosis. Surg Endosc. 2012;26:3088-3093.
11. Holes-Lewis KA, Hakim S, Rehman F, al. CCK-induced gall bladder hyperkinesia: An indication for cholecystectomy and brain-GI connectivity research. J Nucl Med. 2009;50(suppl 2):1312.
12. Carr JA, Walls J, Bryan LJ, et al. The treatment of gallbladder dyskinesia based upon symptoms: results of a 2-year, prospective, nonrandomized, concurrent cohort study. Surg Laparosc Endosc Percutan Tech. 2009;19:222-226.
13. Murray WR. Botulinum toxin-induced relaxation of the sphincter of Oddi may select patients with acalculous biliary pain who will benefit from cholecystectomy. Surg Endosc. 2011;25:813-816.
1. Drossman DA, Dumitrascu DL. Rome III: new standard for functional gastrointestinal disorders. J Gastrointest Liver Dis. 2006;15:237-241.
2. Hansel SL, DiBaise JK. Functional gallbladder disorder: gallbladder dyskinesia. Gastroenterol Clin North Am. 2010;39:369-379.
3. Francis G, Baillie J. Gallbladder dyskinesia: fact or fiction? Curr Gastroenterol Rep. 2011;13:188-192.
4. Yap L, Wycherley AG, Morphett AD, et al. Acalculous biliary pain; cholecystectomy alleviates symptoms in patients with abnormal cholescintigraphy. Gastroenterology. 1991;101:786-793.
5. Behar J, Corazziari E, Guelrud M, et al. Functional gallbladder and sphincter of oddi disorders. Gastroenterology. 2006;130: 1498-1509.
6. Graham EA, Cole WH. Roentgenologic examination of the gallbladder: preliminary report of a new method utilizing the intravenous injection of tetrabromophenolphthalein. JAMA. 1924;82:613-614.
7. Blalock A. A study of eight hundred and eighty-eight cases of biliary tract disease. Johns Hopkins Hosp Bull. 1924;35:391-409.
8. Whipple AO. Surgical criteria for cholecystectomy. Bull N Y Acad Med. 1926;2:302-306.
9. Mackey WA. Cholecystitis without stone an investigation of 264 operated cases from the clinical, radiological, and pathological aspects. An attempt to determine the factors of service in estimating prognosis. Br J Surg. 1934;22:274-295.
10. DuCoin C, Faber R, Ilagan M, et al. Normokinetic biliary dyskinesia: a novel diagnosis. Surg Endosc. 2012;26:3088-3093.
11. Holes-Lewis KA, Hakim S, Rehman F, al. CCK-induced gall bladder hyperkinesia: An indication for cholecystectomy and brain-GI connectivity research. J Nucl Med. 2009;50(suppl 2):1312.
12. Carr JA, Walls J, Bryan LJ, et al. The treatment of gallbladder dyskinesia based upon symptoms: results of a 2-year, prospective, nonrandomized, concurrent cohort study. Surg Laparosc Endosc Percutan Tech. 2009;19:222-226.
13. Murray WR. Botulinum toxin-induced relaxation of the sphincter of Oddi may select patients with acalculous biliary pain who will benefit from cholecystectomy. Surg Endosc. 2011;25:813-816.
Failure to spot CHF leads to heart transplant
Failure to spot CHF leads to heart transplant
A 49-YEAR-OLD MAN SOUGHT TREATMENT AT AN URGENT CARE FACILITY after having shortness of breath every morning for 2 weeks. His heart rate was 119 beats/min, his blood pressure was 170/101 mm Hg, and he did not have chest pain. An electrocardiogram (EKG) was abnormal and chest x-ray showed fluid in the lung. The patient was diagnosed with pneumonia, prescribed antibiotics, and told to follow up with his physician. A follow-up chest x-ray 2 weeks later showed an enlarged heart and more fluid in the lung. A computed tomography scan indicated congestive heart failure and an EKG showed signs of a heart attack. The patient underwent a heart transplant and requires immunosuppressants.
PLAINTIFF'S CLAIM If the physician at the urgent care facility had noticed the patient’s enlarged heart, there would have been less heart damage, and the patient might have required a bypass, rather than a transplant.
THE DEFENSE No information about the defense is available.
VERDICT $1 million New Jersey verdict.
COMMENT When evaluating shortness of breath, always think lungs and heart until you have a definite diagnosis. Remember that neurological disease can present with shortness of breath, too. Consider amyotrophic lateral sclerosis, Guillain-Barré syndrome, and myasthenia gravis.
Infant suffers brain injury after delayed lab results
PARENTS BROUGHT THEIR 2-WEEK-OLD DAUGHTER TO THE EMERGENCY DEPARTMENT (ED) after she had missed several feedings and was short of breath. The ED physician ordered blood tests, but discharged the patient before receiving the results and told the parents to follow up with the infant’s pediatrician. Blood work subsequently revealed that the child had a Group B streptococcus infection, but by the time these results were communicated to the parents and treatment had begun, the infant had developed meningitis. She suffered brain injury, and was diagnosed with cerebral palsy.
PLAINTIFF'S CLAIM There was a delay in the diagnosis and treatment of the infant. Blood test results showing a bacterial infection were available the morning after discharge, but instead of notifying the parents, an additional blood culture was ordered to determine the type of bacteria present. The parents were then contacted 6 hours after the bacteria was identified as Group B streptococcus.
THE DEFENSE The defendants denied any negligence, although a nurse who cared for the infant claimed she had expressed concerns about the decision to discharge the patient.
VERDICT $7.15 million Maryland verdict.
COMMENT In newborns, the differential diagnosis for shortness of breath widens to include infection. In this case, I suspect the problem was a lack of tight follow-up, which can lead to bad outcomes—especially in newborns.
Failure to spot CHF leads to heart transplant
A 49-YEAR-OLD MAN SOUGHT TREATMENT AT AN URGENT CARE FACILITY after having shortness of breath every morning for 2 weeks. His heart rate was 119 beats/min, his blood pressure was 170/101 mm Hg, and he did not have chest pain. An electrocardiogram (EKG) was abnormal and chest x-ray showed fluid in the lung. The patient was diagnosed with pneumonia, prescribed antibiotics, and told to follow up with his physician. A follow-up chest x-ray 2 weeks later showed an enlarged heart and more fluid in the lung. A computed tomography scan indicated congestive heart failure and an EKG showed signs of a heart attack. The patient underwent a heart transplant and requires immunosuppressants.
PLAINTIFF'S CLAIM If the physician at the urgent care facility had noticed the patient’s enlarged heart, there would have been less heart damage, and the patient might have required a bypass, rather than a transplant.
THE DEFENSE No information about the defense is available.
VERDICT $1 million New Jersey verdict.
COMMENT When evaluating shortness of breath, always think lungs and heart until you have a definite diagnosis. Remember that neurological disease can present with shortness of breath, too. Consider amyotrophic lateral sclerosis, Guillain-Barré syndrome, and myasthenia gravis.
Infant suffers brain injury after delayed lab results
PARENTS BROUGHT THEIR 2-WEEK-OLD DAUGHTER TO THE EMERGENCY DEPARTMENT (ED) after she had missed several feedings and was short of breath. The ED physician ordered blood tests, but discharged the patient before receiving the results and told the parents to follow up with the infant’s pediatrician. Blood work subsequently revealed that the child had a Group B streptococcus infection, but by the time these results were communicated to the parents and treatment had begun, the infant had developed meningitis. She suffered brain injury, and was diagnosed with cerebral palsy.
PLAINTIFF'S CLAIM There was a delay in the diagnosis and treatment of the infant. Blood test results showing a bacterial infection were available the morning after discharge, but instead of notifying the parents, an additional blood culture was ordered to determine the type of bacteria present. The parents were then contacted 6 hours after the bacteria was identified as Group B streptococcus.
THE DEFENSE The defendants denied any negligence, although a nurse who cared for the infant claimed she had expressed concerns about the decision to discharge the patient.
VERDICT $7.15 million Maryland verdict.
COMMENT In newborns, the differential diagnosis for shortness of breath widens to include infection. In this case, I suspect the problem was a lack of tight follow-up, which can lead to bad outcomes—especially in newborns.
Failure to spot CHF leads to heart transplant
A 49-YEAR-OLD MAN SOUGHT TREATMENT AT AN URGENT CARE FACILITY after having shortness of breath every morning for 2 weeks. His heart rate was 119 beats/min, his blood pressure was 170/101 mm Hg, and he did not have chest pain. An electrocardiogram (EKG) was abnormal and chest x-ray showed fluid in the lung. The patient was diagnosed with pneumonia, prescribed antibiotics, and told to follow up with his physician. A follow-up chest x-ray 2 weeks later showed an enlarged heart and more fluid in the lung. A computed tomography scan indicated congestive heart failure and an EKG showed signs of a heart attack. The patient underwent a heart transplant and requires immunosuppressants.
PLAINTIFF'S CLAIM If the physician at the urgent care facility had noticed the patient’s enlarged heart, there would have been less heart damage, and the patient might have required a bypass, rather than a transplant.
THE DEFENSE No information about the defense is available.
VERDICT $1 million New Jersey verdict.
COMMENT When evaluating shortness of breath, always think lungs and heart until you have a definite diagnosis. Remember that neurological disease can present with shortness of breath, too. Consider amyotrophic lateral sclerosis, Guillain-Barré syndrome, and myasthenia gravis.
Infant suffers brain injury after delayed lab results
PARENTS BROUGHT THEIR 2-WEEK-OLD DAUGHTER TO THE EMERGENCY DEPARTMENT (ED) after she had missed several feedings and was short of breath. The ED physician ordered blood tests, but discharged the patient before receiving the results and told the parents to follow up with the infant’s pediatrician. Blood work subsequently revealed that the child had a Group B streptococcus infection, but by the time these results were communicated to the parents and treatment had begun, the infant had developed meningitis. She suffered brain injury, and was diagnosed with cerebral palsy.
PLAINTIFF'S CLAIM There was a delay in the diagnosis and treatment of the infant. Blood test results showing a bacterial infection were available the morning after discharge, but instead of notifying the parents, an additional blood culture was ordered to determine the type of bacteria present. The parents were then contacted 6 hours after the bacteria was identified as Group B streptococcus.
THE DEFENSE The defendants denied any negligence, although a nurse who cared for the infant claimed she had expressed concerns about the decision to discharge the patient.
VERDICT $7.15 million Maryland verdict.
COMMENT In newborns, the differential diagnosis for shortness of breath widens to include infection. In this case, I suspect the problem was a lack of tight follow-up, which can lead to bad outcomes—especially in newborns.
How well do physician and patient visit priorities align?
ABSTRACT
Purpose We undertook this study to explore the factors associated with differences between patients’ stated main reasons for outpatient visits and physicians’ main concerns at those same visits.
Methods This cross-sectional, mixed-methods study examined 192 outpatient visits with 4 physicians at 4 diverse primary care practices. During each visit, participating physicians elicited the patient’s main reason for the visit. Immediately after each visit, physicians documented 1) their understanding of the patient’s stated reason and 2) their main concern for the patient during that visit, and 3) assessed the extent of their alignment with the patient’s reason for visit. We assessed bivariate and multivariable associations of patient and visit characteristics with alignment, and further examined cases with unaligned physician-patient priorities to identify patterns.
Results In 69% of visits, the patient’s stated reason for the visit was completely aligned with the physician’s main concern. In 12% of visits, we observed totally unaligned priorities; 19% were only partially aligned. Uninsured or publicly-insured patients and visits with more problems addressed were less likely to be fully aligned. In many visits with unaligned priorities, patients’ stated reason for the visit was a self-limiting, symptomatic concern while physicians prioritized potentially dangerous asymptomatic conditions or ill-managed chronic conditions.
Conclusions In diverse family medicine practices, lack of alignment between physician and patient visit priorities reflects differing prioritization processes. Patients presenting with concerns unaligned with their physician’s priorities may require more time or different approaches to ensure the relevance and patient-centeredness of their care. These findings may inform the design of systems of care that promote mindful attention to patients’ priorities while addressing medically urgent or preventive services delivery.
T oday’s family physicians must balance patient’s acute concerns with chronic disease management, health promotion, and disease prevention. It’s not easy. As the content of outpatient visits expands and available time contracts,1 patients’, clinicians’, and payers’ agendas compete for attention. From a patient experience perspective, the health care encounter may seem diminished when guideline-driven agendas championing chronic disease management and preventive service delivery appear to take precedence over their personal concerns.2-4
In the matter of physician-patient alignment of visit priorities, prior research5,6 inadequately reflects current practice realities such as increased time pressure,7 greater chronic disease prevalence,8 growing expectations for preventive care,1 and increasing physician proactivity in longitudinal care.9-12 With so much to do and so little time and mounting pressure to deliver patient-centered care and patient satisfaction, it would be helpful to have a better understanding of how often and with whom physicians choose to depart from a patient’s explicitly stated reasons for a visit and instead prioritize other concerns.
We sought to examine alignment between patients’ stated main reasons for a visit as understood by the physician and the physician’s main concern during that same visit. Using a diverse sample of family physician-researchers to serve as data collectors and analysts, this study aimed to identify patient and visit characteristics associated with differing physician-patient visit priorities.
METHODS
Study design and sample
Four family physicians participating in a research fellowship undertook this cross- sectional descriptive study of a sample of their outpatient encounters. Each physician’s practice was unique: a free clinic, an inner city family practice within a teaching hospital, a geriatric home visit practice, and a suburban pediatric practice. Using the card study method pioneered by the Ambulatory Sentinel Practice Network,13,14 physicians collected observational and reflective data on a sample of 50 consecutive patients seen at his or her primary care practice. The University Hospitals Case Medical Center Institutional Review Board approved the study protocol.
Measures
Immediately following each patient visit, physicians recorded on a standardized data card the patient’s characteristics, visit characteristics, the reason for the visit provided to the office staff, the reason for visit reported by the patient at the beginning of the visit, and the physician’s own main concern for the patient during the visit. Patient characteristics included gender, age, race, type of insurance, and number of chronic conditions on the problem list. Visit characteristics included the total number of problems addressed, whether a second person (eg, family member, caregiver) was present in the exam room during the visit, and visit duration. To elicit the patient’s reason for the visit, physicians systematically asked, “How can I help you today?” If more than one problem was elicited from this prompt, the concern expressed as most important by the patient was noted.
In completing the data card, physicians also reflected on the extent to which the patient’s stated reason for the visit aligned with their own main concern for the patient during the visit, rating the relationship between their respective priorities as fully aligned, partially aligned, or totally unaligned. Visits were considered fully aligned if the patient’s reason for the visit and the physician’s concern were the same, or if the patient’s expressed concern was determined to be a symptom related to the physician’s main concern. Partial alignment occurred when the patient’s concern was shared by the physician but was not the physician’s main concern. Visit priorities were rated as totally unaligned if patient and physician concerns were different and determined not to be medically related.
Data analysis
We computed descriptive statistics and performed bivariate tests of association between physician-patient alignment of priorities and patient/visit characteristics, using chi-square statistics for categorical variables and analysis of variance (ANOVA) for continuous variables. We used logistic regression analysis to identify characteristics independently associated with either partially aligned or totally unaligned visit priorities, vs fully aligned priorities.
To better understand the unaligned cases, the study team examined all of the data cards identified as either only partially aligned or totally unaligned and categorized the nature of the disparate prioritization in each case. Study team members (PT, AW, MR, and PDG) individually reviewed and sorted the cards into similar observed patterns and wrote brief descriptions of those patterns. The group refined the preliminary descriptions of the overarching patterns and selected several cases to represent the patterns.
RESULTS
Quantitative findings
We collected data on 192 patients (TABLE 1). Median patient age was 47. Median number of prescription medications and chronic medical conditions were 3 and 2, respectively. Most patients (80%) primarily spoke English, 58% were female, and 59% were Caucasian. Insurance status was equally distributed among patients: 33% held private insurance, 33% had public insurance, and 34% were uninsured.
The majority of cases showed physician- patient priorities that were fully aligned (69%); only 12% were totally unaligned. TABLE 1 shows the associations between level of alignment and patient and visit characteristics. Patients whose expressed reason for their visit was less than fully aligned with their physicians’ primary concern were more likely to be older, with more chronic conditions, of Hispanic ethnicity, and either publicly insured or uninsured. Patients with some degree of unaligned concerns also tended to have greater numbers of prescribed medications and had a primary language other than English. Unaligned visit priorities were also observed more often when greater numbers of problems were addressed during the visit. Patients familiar to the physician were also more likely to express a reason for their visit that differed in some way from the primary concern of their family physician.
Multivariable logistic regression analyses showed that having more problems addressed during a visit and being publicly insured or uninsured (compared with having private insurance) were each independently associated with less than fully aligned visit priorities (indicated by § in TABLE 1).
Qualitative findings
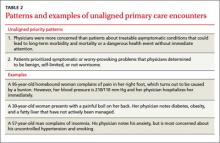
Cases classified as partially or totally unaligned showed 2 main patterns that reflect differences in the ways that patients and physicians prioritize problems. First, when physician priorities were unaligned with the patient’s stated reason for a visit, physicians typically focused on treatable, asymptomatic conditions that could lead to long-term morbidity and mortality or, absent immediate attention, to a dangerous event. Examples include chronic disease management (eg, hypertension, diabetes, asthma) and disease prevention (eg, smoking cessation, cholesterol level monitoring, cardiac disease risk reduction). Second, in those visits that were unaligned, patients tended to show more initial concern about symptomatic problems (eg, skin rash, upper respiratory infection) that would likely resolve with minimal or no medical intervention. Most of these conditions were determined by the physician to be benign, self-limited, or not worrisome (TABLE 2).
DISCUSSION
This study examined the alignment between a patient’s stated reason for a visit and the physician’s main concern. Physician-patient alignment was common, with 69% of visits showing full alignment between the patient’s reason for the visit and the physician’s main concern. While this rate is higher than that seen in prior studies,5 our method for data collection uniquely reflected how information actually is elicited and received during outpatient encounters, which likely yielded more accurate results. Also, in contrast to past approaches, our study equated patients’ symptoms to the underlying diagnosis for purposes of determining alignment.
Similar to previous studies, alignment between patient and physician concerns was less likely when the number of items addressed during the visit increased.5,6 Interestingly, physician-perceived time pressure during the visit and lack of an established patient-physician relationship were not observed to influence alignment. When time is limited, physicians may choose to prioritize the patient’s verbalized concern to avoid more complex negotiations about the agenda. In addition, during an encounter with an unfamiliar patient, prevention and chronic illness care may be deferred until the relationship becomes established.15-18
Patient insurance status was also observed to influence alignment. This finding could reflect socioeconomic or access issues among uninsured or publicly-insured patients that contribute to more complex visits.19-21 To shed further light on this finding, further research is needed that includes indicators of education or income and that separately examines Medicaid vs Medicare enrollees.
Possible study weaknesses. A potential weakness of this study is that alignment was rated by the physicians who elicited and recorded their patients’ reasons for the visit. It is possible that the central role of the physician as observer and analyst may have introduced bias and that an outside observer may have come to different conclusions about the extent to which priorities were aligned. However, by placing the physician-researcher at the center of both data collection and analysis, our study method reflects the realistic constraints of limited information on the processes of clinical discovery and sense-making that physicians regularly undertake with their patients, which we believe to be a strength of this study. While the inclusion of pediatric visits in the sample is another possible weakness, we believe that the diverse clinical settings and diverse patient populations potentially strengthen the findings. Replication with different samples of clinicians and patients is needed to assess the robustness of the findings.
Root differences in physician and patient perspectives. Collectively, these findings suggest that patients’ and physicians’ differing approaches to prioritization may limit alignment. In general, physicians tend to evaluate the full scope of the patient’s health and risk factors for future disease, while patients more often focus on symptomatically troublesome—though often self-limiting— conditions. Physicians have the knowledge and clinical experience to prioritize or deprioritize patient concerns based on an assessment of long-term risks of morbidity and mortality, yet the future-orientation of treatments and surveillance for insensible conditions (like hypertension) is less likely to align with the immediately painful or worrisome symptoms of patients. This highlights the importance of patient education on chronic disease management and disease prevention, and cooperative agenda-setting. Further work needs to be done to examine the differences in patients’ and physicians’ cognitive processes of prioritization, with the ultimate goal of providing patient-centered care through shared decision-making.
Take-home messages for all stakeholders. Amidst growing time pressures and guideline-driven protocols for care, it is important to attend to the intersecting and diverging patient, physician, and payer agendas that drive the content of the visit. Patients who are less likely to share the physician’s prioritization of their concerns—including individuals with no insurance or public insurance and those with multiple medical problems—may require more time and additional effort on the part of the physician to create a mutually acceptable agenda for the visit. Attempts at pay-for-performance should consider patients’ priorities and preferences for care, particularly when those preferences differ from the priorities of physicians or health insurance plans. A more thorough understanding of patient and physician prioritization during primary care visits could potentially guide the organization of outpatient care and inform the mindful physician’s patient-centered practice to maximize patient benefit.
CORRESPONDENCE
Susan A. Flocke, PhD, Family Medicine Research Division, Case Western Reserve University, 11000 Cedar Avenue, Suite 402, Cleveland, OH 44106; [email protected]
ACKNOWLEDGEMENTS
This study was completed as part of the culture of inquiry fellowship, supported by Academic Administrative Units in primary care Grant #D54HP05444 from the Health Resources and Services Administration, US Department of Health and Human Services. Dr. Stange’s time is supported in part by a clinical research professorship from the American Cancer Society.
1. Yarnall KS, Pollak KI, Østbye T, et al. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635-641.
2. Weyer SM, Bobiak S, Stange KC. Possible unintended consequences of a focus on performance: insights over time from the research association of practices network. Qual Manag Health Care. 2008;17:47-52.
3. Campbell SM, McDonald R, Lester H. The experience of pay for performance in English family practice: a qualitative study. Ann Fam Med. 2008;6:228-234.
4. Casalino LP. The unintended consequences of measuring quality on the quality of medical care. N Engl J Med. 1999;341:1147-1150.
5. Friedin RB, Goldman L, Cecil RR. Patient-physician concordance in problem identification in the primary care setting. Ann Intern Med. 1980;93:490-493.
6. Boland BJ, Scheitel SM, Wollan PC, et al. Patient-physician agreement on reasons for ambulatory general medical examinations. Mayo Clin Proc. 1998;73:109-117.
7. Abbo ED, Zhang Q, Zelder M, et al. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med. 2008;23:2058-2065.
8. Østbye T, Yarnall KS, Krause KM, et al. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3:209-214.
9. Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511-544.
10. Wagner EH, Austin BT, Von Korff M. Improving outcomes in chronic illness. Manag Care Q. 1996;4:12-25.
11. Glasgow RE, Orleans CT, Wagner EH. Does the chronic care model serve also as a template for improving prevention? Milbank Q. 2001;79:579-612,iv-v.
12. Wagner EH, Bennett SM, Austin BT, et al. Finding common ground: patient-centeredness and evidence-based chronic illness care. J Altern Complement Med. 2005;11(suppl 1):S7-S15.
13. Green LA. The weekly return as a practical instrument for data collection in office based research. Fam Med. 1988;20:182-184.
14. Green LA, Reed FM, Miller RS, et al. Verification of data reported by practices for a study of spontaneous abortion. Fam Med. 1988;20:189-191.
15. Ettner SL. The relationship between continuity of care and the health behaviors of patients: Does having a usual physician make a difference? Med Care. 1999;37:547-555.
16. Parchman ML, Burge SK. The patient-physician relationship, primary care attributes, and preventive services. Fam Med. 2004;36:22-27.
17. Blewett LA, Johnson PJ, Lee B, et al. When a usual source of care and usual provider matter: adult prevention and screening services. J Gen Intern Med. 2008;23:1354-1360.
18. Flocke SA, Stange KC, Zyzanski SJ. The association of attributes of primary care with the delivery of clinical preventive services. Med Care. 1998;36(8 suppl):AS21-AS30.
19. Ayanian JZ, Weissman JS, Schneider EC, et al. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061-2069.
20. Fiscella K, Williams DR. Health disparities based on socioeconomic inequities: implications for urban health care. Acad Med. 2004;79:1139-1147.
21. McWilliams JM. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q. 2009;87:443-494.
ABSTRACT
Purpose We undertook this study to explore the factors associated with differences between patients’ stated main reasons for outpatient visits and physicians’ main concerns at those same visits.
Methods This cross-sectional, mixed-methods study examined 192 outpatient visits with 4 physicians at 4 diverse primary care practices. During each visit, participating physicians elicited the patient’s main reason for the visit. Immediately after each visit, physicians documented 1) their understanding of the patient’s stated reason and 2) their main concern for the patient during that visit, and 3) assessed the extent of their alignment with the patient’s reason for visit. We assessed bivariate and multivariable associations of patient and visit characteristics with alignment, and further examined cases with unaligned physician-patient priorities to identify patterns.
Results In 69% of visits, the patient’s stated reason for the visit was completely aligned with the physician’s main concern. In 12% of visits, we observed totally unaligned priorities; 19% were only partially aligned. Uninsured or publicly-insured patients and visits with more problems addressed were less likely to be fully aligned. In many visits with unaligned priorities, patients’ stated reason for the visit was a self-limiting, symptomatic concern while physicians prioritized potentially dangerous asymptomatic conditions or ill-managed chronic conditions.
Conclusions In diverse family medicine practices, lack of alignment between physician and patient visit priorities reflects differing prioritization processes. Patients presenting with concerns unaligned with their physician’s priorities may require more time or different approaches to ensure the relevance and patient-centeredness of their care. These findings may inform the design of systems of care that promote mindful attention to patients’ priorities while addressing medically urgent or preventive services delivery.
T oday’s family physicians must balance patient’s acute concerns with chronic disease management, health promotion, and disease prevention. It’s not easy. As the content of outpatient visits expands and available time contracts,1 patients’, clinicians’, and payers’ agendas compete for attention. From a patient experience perspective, the health care encounter may seem diminished when guideline-driven agendas championing chronic disease management and preventive service delivery appear to take precedence over their personal concerns.2-4
In the matter of physician-patient alignment of visit priorities, prior research5,6 inadequately reflects current practice realities such as increased time pressure,7 greater chronic disease prevalence,8 growing expectations for preventive care,1 and increasing physician proactivity in longitudinal care.9-12 With so much to do and so little time and mounting pressure to deliver patient-centered care and patient satisfaction, it would be helpful to have a better understanding of how often and with whom physicians choose to depart from a patient’s explicitly stated reasons for a visit and instead prioritize other concerns.
We sought to examine alignment between patients’ stated main reasons for a visit as understood by the physician and the physician’s main concern during that same visit. Using a diverse sample of family physician-researchers to serve as data collectors and analysts, this study aimed to identify patient and visit characteristics associated with differing physician-patient visit priorities.
METHODS
Study design and sample
Four family physicians participating in a research fellowship undertook this cross- sectional descriptive study of a sample of their outpatient encounters. Each physician’s practice was unique: a free clinic, an inner city family practice within a teaching hospital, a geriatric home visit practice, and a suburban pediatric practice. Using the card study method pioneered by the Ambulatory Sentinel Practice Network,13,14 physicians collected observational and reflective data on a sample of 50 consecutive patients seen at his or her primary care practice. The University Hospitals Case Medical Center Institutional Review Board approved the study protocol.
Measures
Immediately following each patient visit, physicians recorded on a standardized data card the patient’s characteristics, visit characteristics, the reason for the visit provided to the office staff, the reason for visit reported by the patient at the beginning of the visit, and the physician’s own main concern for the patient during the visit. Patient characteristics included gender, age, race, type of insurance, and number of chronic conditions on the problem list. Visit characteristics included the total number of problems addressed, whether a second person (eg, family member, caregiver) was present in the exam room during the visit, and visit duration. To elicit the patient’s reason for the visit, physicians systematically asked, “How can I help you today?” If more than one problem was elicited from this prompt, the concern expressed as most important by the patient was noted.
In completing the data card, physicians also reflected on the extent to which the patient’s stated reason for the visit aligned with their own main concern for the patient during the visit, rating the relationship between their respective priorities as fully aligned, partially aligned, or totally unaligned. Visits were considered fully aligned if the patient’s reason for the visit and the physician’s concern were the same, or if the patient’s expressed concern was determined to be a symptom related to the physician’s main concern. Partial alignment occurred when the patient’s concern was shared by the physician but was not the physician’s main concern. Visit priorities were rated as totally unaligned if patient and physician concerns were different and determined not to be medically related.
Data analysis
We computed descriptive statistics and performed bivariate tests of association between physician-patient alignment of priorities and patient/visit characteristics, using chi-square statistics for categorical variables and analysis of variance (ANOVA) for continuous variables. We used logistic regression analysis to identify characteristics independently associated with either partially aligned or totally unaligned visit priorities, vs fully aligned priorities.
To better understand the unaligned cases, the study team examined all of the data cards identified as either only partially aligned or totally unaligned and categorized the nature of the disparate prioritization in each case. Study team members (PT, AW, MR, and PDG) individually reviewed and sorted the cards into similar observed patterns and wrote brief descriptions of those patterns. The group refined the preliminary descriptions of the overarching patterns and selected several cases to represent the patterns.
RESULTS
Quantitative findings
We collected data on 192 patients (TABLE 1). Median patient age was 47. Median number of prescription medications and chronic medical conditions were 3 and 2, respectively. Most patients (80%) primarily spoke English, 58% were female, and 59% were Caucasian. Insurance status was equally distributed among patients: 33% held private insurance, 33% had public insurance, and 34% were uninsured.
The majority of cases showed physician- patient priorities that were fully aligned (69%); only 12% were totally unaligned. TABLE 1 shows the associations between level of alignment and patient and visit characteristics. Patients whose expressed reason for their visit was less than fully aligned with their physicians’ primary concern were more likely to be older, with more chronic conditions, of Hispanic ethnicity, and either publicly insured or uninsured. Patients with some degree of unaligned concerns also tended to have greater numbers of prescribed medications and had a primary language other than English. Unaligned visit priorities were also observed more often when greater numbers of problems were addressed during the visit. Patients familiar to the physician were also more likely to express a reason for their visit that differed in some way from the primary concern of their family physician.
Multivariable logistic regression analyses showed that having more problems addressed during a visit and being publicly insured or uninsured (compared with having private insurance) were each independently associated with less than fully aligned visit priorities (indicated by § in TABLE 1).
Qualitative findings
Cases classified as partially or totally unaligned showed 2 main patterns that reflect differences in the ways that patients and physicians prioritize problems. First, when physician priorities were unaligned with the patient’s stated reason for a visit, physicians typically focused on treatable, asymptomatic conditions that could lead to long-term morbidity and mortality or, absent immediate attention, to a dangerous event. Examples include chronic disease management (eg, hypertension, diabetes, asthma) and disease prevention (eg, smoking cessation, cholesterol level monitoring, cardiac disease risk reduction). Second, in those visits that were unaligned, patients tended to show more initial concern about symptomatic problems (eg, skin rash, upper respiratory infection) that would likely resolve with minimal or no medical intervention. Most of these conditions were determined by the physician to be benign, self-limited, or not worrisome (TABLE 2).
DISCUSSION
This study examined the alignment between a patient’s stated reason for a visit and the physician’s main concern. Physician-patient alignment was common, with 69% of visits showing full alignment between the patient’s reason for the visit and the physician’s main concern. While this rate is higher than that seen in prior studies,5 our method for data collection uniquely reflected how information actually is elicited and received during outpatient encounters, which likely yielded more accurate results. Also, in contrast to past approaches, our study equated patients’ symptoms to the underlying diagnosis for purposes of determining alignment.
Similar to previous studies, alignment between patient and physician concerns was less likely when the number of items addressed during the visit increased.5,6 Interestingly, physician-perceived time pressure during the visit and lack of an established patient-physician relationship were not observed to influence alignment. When time is limited, physicians may choose to prioritize the patient’s verbalized concern to avoid more complex negotiations about the agenda. In addition, during an encounter with an unfamiliar patient, prevention and chronic illness care may be deferred until the relationship becomes established.15-18
Patient insurance status was also observed to influence alignment. This finding could reflect socioeconomic or access issues among uninsured or publicly-insured patients that contribute to more complex visits.19-21 To shed further light on this finding, further research is needed that includes indicators of education or income and that separately examines Medicaid vs Medicare enrollees.
Possible study weaknesses. A potential weakness of this study is that alignment was rated by the physicians who elicited and recorded their patients’ reasons for the visit. It is possible that the central role of the physician as observer and analyst may have introduced bias and that an outside observer may have come to different conclusions about the extent to which priorities were aligned. However, by placing the physician-researcher at the center of both data collection and analysis, our study method reflects the realistic constraints of limited information on the processes of clinical discovery and sense-making that physicians regularly undertake with their patients, which we believe to be a strength of this study. While the inclusion of pediatric visits in the sample is another possible weakness, we believe that the diverse clinical settings and diverse patient populations potentially strengthen the findings. Replication with different samples of clinicians and patients is needed to assess the robustness of the findings.
Root differences in physician and patient perspectives. Collectively, these findings suggest that patients’ and physicians’ differing approaches to prioritization may limit alignment. In general, physicians tend to evaluate the full scope of the patient’s health and risk factors for future disease, while patients more often focus on symptomatically troublesome—though often self-limiting— conditions. Physicians have the knowledge and clinical experience to prioritize or deprioritize patient concerns based on an assessment of long-term risks of morbidity and mortality, yet the future-orientation of treatments and surveillance for insensible conditions (like hypertension) is less likely to align with the immediately painful or worrisome symptoms of patients. This highlights the importance of patient education on chronic disease management and disease prevention, and cooperative agenda-setting. Further work needs to be done to examine the differences in patients’ and physicians’ cognitive processes of prioritization, with the ultimate goal of providing patient-centered care through shared decision-making.
Take-home messages for all stakeholders. Amidst growing time pressures and guideline-driven protocols for care, it is important to attend to the intersecting and diverging patient, physician, and payer agendas that drive the content of the visit. Patients who are less likely to share the physician’s prioritization of their concerns—including individuals with no insurance or public insurance and those with multiple medical problems—may require more time and additional effort on the part of the physician to create a mutually acceptable agenda for the visit. Attempts at pay-for-performance should consider patients’ priorities and preferences for care, particularly when those preferences differ from the priorities of physicians or health insurance plans. A more thorough understanding of patient and physician prioritization during primary care visits could potentially guide the organization of outpatient care and inform the mindful physician’s patient-centered practice to maximize patient benefit.
CORRESPONDENCE
Susan A. Flocke, PhD, Family Medicine Research Division, Case Western Reserve University, 11000 Cedar Avenue, Suite 402, Cleveland, OH 44106; [email protected]
ACKNOWLEDGEMENTS
This study was completed as part of the culture of inquiry fellowship, supported by Academic Administrative Units in primary care Grant #D54HP05444 from the Health Resources and Services Administration, US Department of Health and Human Services. Dr. Stange’s time is supported in part by a clinical research professorship from the American Cancer Society.
ABSTRACT
Purpose We undertook this study to explore the factors associated with differences between patients’ stated main reasons for outpatient visits and physicians’ main concerns at those same visits.
Methods This cross-sectional, mixed-methods study examined 192 outpatient visits with 4 physicians at 4 diverse primary care practices. During each visit, participating physicians elicited the patient’s main reason for the visit. Immediately after each visit, physicians documented 1) their understanding of the patient’s stated reason and 2) their main concern for the patient during that visit, and 3) assessed the extent of their alignment with the patient’s reason for visit. We assessed bivariate and multivariable associations of patient and visit characteristics with alignment, and further examined cases with unaligned physician-patient priorities to identify patterns.
Results In 69% of visits, the patient’s stated reason for the visit was completely aligned with the physician’s main concern. In 12% of visits, we observed totally unaligned priorities; 19% were only partially aligned. Uninsured or publicly-insured patients and visits with more problems addressed were less likely to be fully aligned. In many visits with unaligned priorities, patients’ stated reason for the visit was a self-limiting, symptomatic concern while physicians prioritized potentially dangerous asymptomatic conditions or ill-managed chronic conditions.
Conclusions In diverse family medicine practices, lack of alignment between physician and patient visit priorities reflects differing prioritization processes. Patients presenting with concerns unaligned with their physician’s priorities may require more time or different approaches to ensure the relevance and patient-centeredness of their care. These findings may inform the design of systems of care that promote mindful attention to patients’ priorities while addressing medically urgent or preventive services delivery.
T oday’s family physicians must balance patient’s acute concerns with chronic disease management, health promotion, and disease prevention. It’s not easy. As the content of outpatient visits expands and available time contracts,1 patients’, clinicians’, and payers’ agendas compete for attention. From a patient experience perspective, the health care encounter may seem diminished when guideline-driven agendas championing chronic disease management and preventive service delivery appear to take precedence over their personal concerns.2-4
In the matter of physician-patient alignment of visit priorities, prior research5,6 inadequately reflects current practice realities such as increased time pressure,7 greater chronic disease prevalence,8 growing expectations for preventive care,1 and increasing physician proactivity in longitudinal care.9-12 With so much to do and so little time and mounting pressure to deliver patient-centered care and patient satisfaction, it would be helpful to have a better understanding of how often and with whom physicians choose to depart from a patient’s explicitly stated reasons for a visit and instead prioritize other concerns.
We sought to examine alignment between patients’ stated main reasons for a visit as understood by the physician and the physician’s main concern during that same visit. Using a diverse sample of family physician-researchers to serve as data collectors and analysts, this study aimed to identify patient and visit characteristics associated with differing physician-patient visit priorities.
METHODS
Study design and sample
Four family physicians participating in a research fellowship undertook this cross- sectional descriptive study of a sample of their outpatient encounters. Each physician’s practice was unique: a free clinic, an inner city family practice within a teaching hospital, a geriatric home visit practice, and a suburban pediatric practice. Using the card study method pioneered by the Ambulatory Sentinel Practice Network,13,14 physicians collected observational and reflective data on a sample of 50 consecutive patients seen at his or her primary care practice. The University Hospitals Case Medical Center Institutional Review Board approved the study protocol.
Measures
Immediately following each patient visit, physicians recorded on a standardized data card the patient’s characteristics, visit characteristics, the reason for the visit provided to the office staff, the reason for visit reported by the patient at the beginning of the visit, and the physician’s own main concern for the patient during the visit. Patient characteristics included gender, age, race, type of insurance, and number of chronic conditions on the problem list. Visit characteristics included the total number of problems addressed, whether a second person (eg, family member, caregiver) was present in the exam room during the visit, and visit duration. To elicit the patient’s reason for the visit, physicians systematically asked, “How can I help you today?” If more than one problem was elicited from this prompt, the concern expressed as most important by the patient was noted.
In completing the data card, physicians also reflected on the extent to which the patient’s stated reason for the visit aligned with their own main concern for the patient during the visit, rating the relationship between their respective priorities as fully aligned, partially aligned, or totally unaligned. Visits were considered fully aligned if the patient’s reason for the visit and the physician’s concern were the same, or if the patient’s expressed concern was determined to be a symptom related to the physician’s main concern. Partial alignment occurred when the patient’s concern was shared by the physician but was not the physician’s main concern. Visit priorities were rated as totally unaligned if patient and physician concerns were different and determined not to be medically related.
Data analysis
We computed descriptive statistics and performed bivariate tests of association between physician-patient alignment of priorities and patient/visit characteristics, using chi-square statistics for categorical variables and analysis of variance (ANOVA) for continuous variables. We used logistic regression analysis to identify characteristics independently associated with either partially aligned or totally unaligned visit priorities, vs fully aligned priorities.
To better understand the unaligned cases, the study team examined all of the data cards identified as either only partially aligned or totally unaligned and categorized the nature of the disparate prioritization in each case. Study team members (PT, AW, MR, and PDG) individually reviewed and sorted the cards into similar observed patterns and wrote brief descriptions of those patterns. The group refined the preliminary descriptions of the overarching patterns and selected several cases to represent the patterns.
RESULTS
Quantitative findings
We collected data on 192 patients (TABLE 1). Median patient age was 47. Median number of prescription medications and chronic medical conditions were 3 and 2, respectively. Most patients (80%) primarily spoke English, 58% were female, and 59% were Caucasian. Insurance status was equally distributed among patients: 33% held private insurance, 33% had public insurance, and 34% were uninsured.
The majority of cases showed physician- patient priorities that were fully aligned (69%); only 12% were totally unaligned. TABLE 1 shows the associations between level of alignment and patient and visit characteristics. Patients whose expressed reason for their visit was less than fully aligned with their physicians’ primary concern were more likely to be older, with more chronic conditions, of Hispanic ethnicity, and either publicly insured or uninsured. Patients with some degree of unaligned concerns also tended to have greater numbers of prescribed medications and had a primary language other than English. Unaligned visit priorities were also observed more often when greater numbers of problems were addressed during the visit. Patients familiar to the physician were also more likely to express a reason for their visit that differed in some way from the primary concern of their family physician.
Multivariable logistic regression analyses showed that having more problems addressed during a visit and being publicly insured or uninsured (compared with having private insurance) were each independently associated with less than fully aligned visit priorities (indicated by § in TABLE 1).
Qualitative findings
Cases classified as partially or totally unaligned showed 2 main patterns that reflect differences in the ways that patients and physicians prioritize problems. First, when physician priorities were unaligned with the patient’s stated reason for a visit, physicians typically focused on treatable, asymptomatic conditions that could lead to long-term morbidity and mortality or, absent immediate attention, to a dangerous event. Examples include chronic disease management (eg, hypertension, diabetes, asthma) and disease prevention (eg, smoking cessation, cholesterol level monitoring, cardiac disease risk reduction). Second, in those visits that were unaligned, patients tended to show more initial concern about symptomatic problems (eg, skin rash, upper respiratory infection) that would likely resolve with minimal or no medical intervention. Most of these conditions were determined by the physician to be benign, self-limited, or not worrisome (TABLE 2).
DISCUSSION
This study examined the alignment between a patient’s stated reason for a visit and the physician’s main concern. Physician-patient alignment was common, with 69% of visits showing full alignment between the patient’s reason for the visit and the physician’s main concern. While this rate is higher than that seen in prior studies,5 our method for data collection uniquely reflected how information actually is elicited and received during outpatient encounters, which likely yielded more accurate results. Also, in contrast to past approaches, our study equated patients’ symptoms to the underlying diagnosis for purposes of determining alignment.
Similar to previous studies, alignment between patient and physician concerns was less likely when the number of items addressed during the visit increased.5,6 Interestingly, physician-perceived time pressure during the visit and lack of an established patient-physician relationship were not observed to influence alignment. When time is limited, physicians may choose to prioritize the patient’s verbalized concern to avoid more complex negotiations about the agenda. In addition, during an encounter with an unfamiliar patient, prevention and chronic illness care may be deferred until the relationship becomes established.15-18
Patient insurance status was also observed to influence alignment. This finding could reflect socioeconomic or access issues among uninsured or publicly-insured patients that contribute to more complex visits.19-21 To shed further light on this finding, further research is needed that includes indicators of education or income and that separately examines Medicaid vs Medicare enrollees.
Possible study weaknesses. A potential weakness of this study is that alignment was rated by the physicians who elicited and recorded their patients’ reasons for the visit. It is possible that the central role of the physician as observer and analyst may have introduced bias and that an outside observer may have come to different conclusions about the extent to which priorities were aligned. However, by placing the physician-researcher at the center of both data collection and analysis, our study method reflects the realistic constraints of limited information on the processes of clinical discovery and sense-making that physicians regularly undertake with their patients, which we believe to be a strength of this study. While the inclusion of pediatric visits in the sample is another possible weakness, we believe that the diverse clinical settings and diverse patient populations potentially strengthen the findings. Replication with different samples of clinicians and patients is needed to assess the robustness of the findings.
Root differences in physician and patient perspectives. Collectively, these findings suggest that patients’ and physicians’ differing approaches to prioritization may limit alignment. In general, physicians tend to evaluate the full scope of the patient’s health and risk factors for future disease, while patients more often focus on symptomatically troublesome—though often self-limiting— conditions. Physicians have the knowledge and clinical experience to prioritize or deprioritize patient concerns based on an assessment of long-term risks of morbidity and mortality, yet the future-orientation of treatments and surveillance for insensible conditions (like hypertension) is less likely to align with the immediately painful or worrisome symptoms of patients. This highlights the importance of patient education on chronic disease management and disease prevention, and cooperative agenda-setting. Further work needs to be done to examine the differences in patients’ and physicians’ cognitive processes of prioritization, with the ultimate goal of providing patient-centered care through shared decision-making.
Take-home messages for all stakeholders. Amidst growing time pressures and guideline-driven protocols for care, it is important to attend to the intersecting and diverging patient, physician, and payer agendas that drive the content of the visit. Patients who are less likely to share the physician’s prioritization of their concerns—including individuals with no insurance or public insurance and those with multiple medical problems—may require more time and additional effort on the part of the physician to create a mutually acceptable agenda for the visit. Attempts at pay-for-performance should consider patients’ priorities and preferences for care, particularly when those preferences differ from the priorities of physicians or health insurance plans. A more thorough understanding of patient and physician prioritization during primary care visits could potentially guide the organization of outpatient care and inform the mindful physician’s patient-centered practice to maximize patient benefit.
CORRESPONDENCE
Susan A. Flocke, PhD, Family Medicine Research Division, Case Western Reserve University, 11000 Cedar Avenue, Suite 402, Cleveland, OH 44106; [email protected]
ACKNOWLEDGEMENTS
This study was completed as part of the culture of inquiry fellowship, supported by Academic Administrative Units in primary care Grant #D54HP05444 from the Health Resources and Services Administration, US Department of Health and Human Services. Dr. Stange’s time is supported in part by a clinical research professorship from the American Cancer Society.
1. Yarnall KS, Pollak KI, Østbye T, et al. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635-641.
2. Weyer SM, Bobiak S, Stange KC. Possible unintended consequences of a focus on performance: insights over time from the research association of practices network. Qual Manag Health Care. 2008;17:47-52.
3. Campbell SM, McDonald R, Lester H. The experience of pay for performance in English family practice: a qualitative study. Ann Fam Med. 2008;6:228-234.
4. Casalino LP. The unintended consequences of measuring quality on the quality of medical care. N Engl J Med. 1999;341:1147-1150.
5. Friedin RB, Goldman L, Cecil RR. Patient-physician concordance in problem identification in the primary care setting. Ann Intern Med. 1980;93:490-493.
6. Boland BJ, Scheitel SM, Wollan PC, et al. Patient-physician agreement on reasons for ambulatory general medical examinations. Mayo Clin Proc. 1998;73:109-117.
7. Abbo ED, Zhang Q, Zelder M, et al. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med. 2008;23:2058-2065.
8. Østbye T, Yarnall KS, Krause KM, et al. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3:209-214.
9. Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511-544.
10. Wagner EH, Austin BT, Von Korff M. Improving outcomes in chronic illness. Manag Care Q. 1996;4:12-25.
11. Glasgow RE, Orleans CT, Wagner EH. Does the chronic care model serve also as a template for improving prevention? Milbank Q. 2001;79:579-612,iv-v.
12. Wagner EH, Bennett SM, Austin BT, et al. Finding common ground: patient-centeredness and evidence-based chronic illness care. J Altern Complement Med. 2005;11(suppl 1):S7-S15.
13. Green LA. The weekly return as a practical instrument for data collection in office based research. Fam Med. 1988;20:182-184.
14. Green LA, Reed FM, Miller RS, et al. Verification of data reported by practices for a study of spontaneous abortion. Fam Med. 1988;20:189-191.
15. Ettner SL. The relationship between continuity of care and the health behaviors of patients: Does having a usual physician make a difference? Med Care. 1999;37:547-555.
16. Parchman ML, Burge SK. The patient-physician relationship, primary care attributes, and preventive services. Fam Med. 2004;36:22-27.
17. Blewett LA, Johnson PJ, Lee B, et al. When a usual source of care and usual provider matter: adult prevention and screening services. J Gen Intern Med. 2008;23:1354-1360.
18. Flocke SA, Stange KC, Zyzanski SJ. The association of attributes of primary care with the delivery of clinical preventive services. Med Care. 1998;36(8 suppl):AS21-AS30.
19. Ayanian JZ, Weissman JS, Schneider EC, et al. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061-2069.
20. Fiscella K, Williams DR. Health disparities based on socioeconomic inequities: implications for urban health care. Acad Med. 2004;79:1139-1147.
21. McWilliams JM. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q. 2009;87:443-494.
1. Yarnall KS, Pollak KI, Østbye T, et al. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635-641.
2. Weyer SM, Bobiak S, Stange KC. Possible unintended consequences of a focus on performance: insights over time from the research association of practices network. Qual Manag Health Care. 2008;17:47-52.
3. Campbell SM, McDonald R, Lester H. The experience of pay for performance in English family practice: a qualitative study. Ann Fam Med. 2008;6:228-234.
4. Casalino LP. The unintended consequences of measuring quality on the quality of medical care. N Engl J Med. 1999;341:1147-1150.
5. Friedin RB, Goldman L, Cecil RR. Patient-physician concordance in problem identification in the primary care setting. Ann Intern Med. 1980;93:490-493.
6. Boland BJ, Scheitel SM, Wollan PC, et al. Patient-physician agreement on reasons for ambulatory general medical examinations. Mayo Clin Proc. 1998;73:109-117.
7. Abbo ED, Zhang Q, Zelder M, et al. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med. 2008;23:2058-2065.
8. Østbye T, Yarnall KS, Krause KM, et al. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3:209-214.
9. Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511-544.
10. Wagner EH, Austin BT, Von Korff M. Improving outcomes in chronic illness. Manag Care Q. 1996;4:12-25.
11. Glasgow RE, Orleans CT, Wagner EH. Does the chronic care model serve also as a template for improving prevention? Milbank Q. 2001;79:579-612,iv-v.
12. Wagner EH, Bennett SM, Austin BT, et al. Finding common ground: patient-centeredness and evidence-based chronic illness care. J Altern Complement Med. 2005;11(suppl 1):S7-S15.
13. Green LA. The weekly return as a practical instrument for data collection in office based research. Fam Med. 1988;20:182-184.
14. Green LA, Reed FM, Miller RS, et al. Verification of data reported by practices for a study of spontaneous abortion. Fam Med. 1988;20:189-191.
15. Ettner SL. The relationship between continuity of care and the health behaviors of patients: Does having a usual physician make a difference? Med Care. 1999;37:547-555.
16. Parchman ML, Burge SK. The patient-physician relationship, primary care attributes, and preventive services. Fam Med. 2004;36:22-27.
17. Blewett LA, Johnson PJ, Lee B, et al. When a usual source of care and usual provider matter: adult prevention and screening services. J Gen Intern Med. 2008;23:1354-1360.
18. Flocke SA, Stange KC, Zyzanski SJ. The association of attributes of primary care with the delivery of clinical preventive services. Med Care. 1998;36(8 suppl):AS21-AS30.
19. Ayanian JZ, Weissman JS, Schneider EC, et al. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061-2069.
20. Fiscella K, Williams DR. Health disparities based on socioeconomic inequities: implications for urban health care. Acad Med. 2004;79:1139-1147.
21. McWilliams JM. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q. 2009;87:443-494.
What is the best nonsurgical therapy for pelvic organ prolapse?
Pelvic floor muscle training (PFMT) and pessaries are equally effective in treating symptoms of pelvic organ prolapse (POP). PFMT transiently improves patient satisfaction and reduces urinary incontinence more than pessaries do (strength of recommendation [SOR]: B, a randomized controlled trial [RCT]).
PFMT moderately improves prolapse symptoms and severity, especially following 6 months of supervised intervention (SOR: B, a systematic review of randomized trials with some methodologic flaws).
Two pessaries (ring with support and Gellhorn) reduce symptoms in as many as 60% of patients (SOR: B, a systematic review of randomized trials).
Untreated postmenopausal women with mild grades of uterine prolapse are unlikely to develop more severe prolapse; 25% to 50% improve spontaneously (SOR: C, a prospective cohort study with methodologic flaws).
EVIDENCE SUMMARY
A 2010 multicenter RCT with 445 women (mean age 49.8 years) compared PFMT, pessary use, and combined treatment.1 Investigators used the Patient Global Impression of Improvement and the stress incontinence subscale of the Pelvic Floor Distress Inventory to measure patient satisfaction and urinary incontinence symptoms.
At 3 months, equivalent numbers of women using PFMT and a pessary (49% and 40%, respectively; P=.09) reported they were “much better” or “very much better.” More women in the PFMT cohort than women using a pessary reported resolution of incontinence symptoms at 3 months (49% vs 33%; P=.006), and satisfaction with treatment (75% vs 63%; P=.02), but these differences disappeared at 12 months. Combination therapy wasn’t superior to PFMT alone.
Pelvic floor muscle training improves symptoms, especially with perseverance
A 2011 Cochrane review that compared women receiving PFMT with a control group (observed but not treated) found that PFMT moderately improved prolapse symptoms and severity, especially following 6 months of supervised intervention.2 Investigators evalu-ated 4 trials, (N=857), including 3 with fewer than 25 women per arm.
Three studies found that PFMT improved symptom severity and manometric measures. Although the authors couldn’t pool the data because of different symptom scoring instruments, typical improvements ranged from 20% to 30%. Two trials found that PFMT increased the chance of improvement in POP stage by 17% (pooled data, relative risk=.83; 95% confidence interval [CI], .71-.96). PFMT also improved urinary outcomes (approximately 30% reduction in urinary frequency and stress incontinence symptoms) in 2 of 3 trials and improved bowel symptoms in one trial (approximately 25% to 30% reduction).
Pessaries also relieve symptoms
A 2013 Cochrane Review seeking to determine the effectiveness of pessaries in POP, identified one RCT (crossover, 3 month, multicenter, United States) that compared symptom relief and change in life impact over baseline for 134 women (parous, mean age 61 years, range 30-89 years) with POP stage II or greater who were treated with ring with support or Gellhorn pessaries.3 Sixty percent of patients who completed the study (the dropout rate was 37%) reported symptom relief with both types of pessary. Outcomes were measured by multiple questionnaires and Likert scales.
Patients reported improved symptoms on both the Pelvic Organ Prolapse Distress Inventory (POPDI) and Pelvic Organ Prolapse Impact Questionnaire (POPIQ) scales (P<.05 for difference from baseline on each scale, actual scores not reported). The ring with support and Gellhorn pessaries didn’t produce different scores on either scale (POPDI, P=.99; POPIQ, P=.29).
Untreated mild prolapse postmenopause usually doesn’t progress and may regress
A cohort of 412 postmenopausal women (ages ≥50 years) with POP who were observed, but not treated, found that mild POP was unlikely to progress and sometimes improved spontaneously.4 Over a mean follow-up of 5.7 years, few women with grade 1 POP (prolapsed pelvic organs remaining within the vagina) progressed to grade 2 or 3 (probability of progression for women with cystoceles=.095, 95% CI, .07-.13; women with rectoceles=.135, 95% CI, .09-.19; and women with uterine prolapse=.019, 95% CI, .0005-.099).
Some women with grade 1 POP regressed to grade 0 (probability of regression for women with cystoceles=.235, 95% CI, .19- .28; women with rectoceles=.22, 95% CI, .16-.28; and women with uterine prolapse=.48, 95% CI, 0.34-.62). Women with grades 2 and 3 POP were less likely to regress to grade 0 (probability of regression for women with cystoceles=.093, 95% CI, .05-.14; women with rectoceles=.033, 95% CI, .011-.075; and women with uterine prolapse=0, 95% CI, 0-.37).
One flaw of this study was that the women received hormone replacement therapy, which the investigators didn’t evaluate independently. However, a 2010 Cochrane review (2 small trials, one meta-analysis) found insufficient data to determine whether hormone replacement therapy alters POP.5
RECOMMENDATIONS
The American College of Obstetricians and Gynecologists Practice Bulletin on POP recommends the following:6
- Pessaries can be fitted in most women with prolapse, regardless of prolapse stage (equivalent to grade) or site of predominant prolapse.
- Pessary use should be considered before surgical intervention in women with symptomatic prolapse.
- Women with prolapse who are asymptomatic or mildly symptomatic can be observed at regular intervals, unless new bothersome symptoms develop.
1. Richter HE, Burgio KL, Brubaker L, et al;Pelvic Floor Disorders Network. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010;115:609-617.
2. Hagen S, Stark D. Conservative prevention and management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2011;12:CD003882.
3. Bugge C, Adams EJ, Gopinath D, et al. Pessaries (mechanical devices) for pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;2:CD004010.
4. Handa VL, Garrett E, Hendrix S, et al. Progression and remission of pelvic organ prolapse: a longitudinal study of menopausal women. Am J Obstet Gynecol. 2004;190:27-32.
5. Ismail SI, Bain C, Hagen S. Oestrogens for treatment or prevention of pelvic organ prolapse in postmenopausal women. Cochrane Database Syst Rev. 2010;9:CD007063.
6. ACOG Committee on Practice Bulletins—Gynecology. ACOG Practice Bulletin No. 85: Pelvic organ prolapse. Obstet Gynecol. 2007;110:717-729.
Pelvic floor muscle training (PFMT) and pessaries are equally effective in treating symptoms of pelvic organ prolapse (POP). PFMT transiently improves patient satisfaction and reduces urinary incontinence more than pessaries do (strength of recommendation [SOR]: B, a randomized controlled trial [RCT]).
PFMT moderately improves prolapse symptoms and severity, especially following 6 months of supervised intervention (SOR: B, a systematic review of randomized trials with some methodologic flaws).
Two pessaries (ring with support and Gellhorn) reduce symptoms in as many as 60% of patients (SOR: B, a systematic review of randomized trials).
Untreated postmenopausal women with mild grades of uterine prolapse are unlikely to develop more severe prolapse; 25% to 50% improve spontaneously (SOR: C, a prospective cohort study with methodologic flaws).
EVIDENCE SUMMARY
A 2010 multicenter RCT with 445 women (mean age 49.8 years) compared PFMT, pessary use, and combined treatment.1 Investigators used the Patient Global Impression of Improvement and the stress incontinence subscale of the Pelvic Floor Distress Inventory to measure patient satisfaction and urinary incontinence symptoms.
At 3 months, equivalent numbers of women using PFMT and a pessary (49% and 40%, respectively; P=.09) reported they were “much better” or “very much better.” More women in the PFMT cohort than women using a pessary reported resolution of incontinence symptoms at 3 months (49% vs 33%; P=.006), and satisfaction with treatment (75% vs 63%; P=.02), but these differences disappeared at 12 months. Combination therapy wasn’t superior to PFMT alone.
Pelvic floor muscle training improves symptoms, especially with perseverance
A 2011 Cochrane review that compared women receiving PFMT with a control group (observed but not treated) found that PFMT moderately improved prolapse symptoms and severity, especially following 6 months of supervised intervention.2 Investigators evalu-ated 4 trials, (N=857), including 3 with fewer than 25 women per arm.
Three studies found that PFMT improved symptom severity and manometric measures. Although the authors couldn’t pool the data because of different symptom scoring instruments, typical improvements ranged from 20% to 30%. Two trials found that PFMT increased the chance of improvement in POP stage by 17% (pooled data, relative risk=.83; 95% confidence interval [CI], .71-.96). PFMT also improved urinary outcomes (approximately 30% reduction in urinary frequency and stress incontinence symptoms) in 2 of 3 trials and improved bowel symptoms in one trial (approximately 25% to 30% reduction).
Pessaries also relieve symptoms
A 2013 Cochrane Review seeking to determine the effectiveness of pessaries in POP, identified one RCT (crossover, 3 month, multicenter, United States) that compared symptom relief and change in life impact over baseline for 134 women (parous, mean age 61 years, range 30-89 years) with POP stage II or greater who were treated with ring with support or Gellhorn pessaries.3 Sixty percent of patients who completed the study (the dropout rate was 37%) reported symptom relief with both types of pessary. Outcomes were measured by multiple questionnaires and Likert scales.
Patients reported improved symptoms on both the Pelvic Organ Prolapse Distress Inventory (POPDI) and Pelvic Organ Prolapse Impact Questionnaire (POPIQ) scales (P<.05 for difference from baseline on each scale, actual scores not reported). The ring with support and Gellhorn pessaries didn’t produce different scores on either scale (POPDI, P=.99; POPIQ, P=.29).
Untreated mild prolapse postmenopause usually doesn’t progress and may regress
A cohort of 412 postmenopausal women (ages ≥50 years) with POP who were observed, but not treated, found that mild POP was unlikely to progress and sometimes improved spontaneously.4 Over a mean follow-up of 5.7 years, few women with grade 1 POP (prolapsed pelvic organs remaining within the vagina) progressed to grade 2 or 3 (probability of progression for women with cystoceles=.095, 95% CI, .07-.13; women with rectoceles=.135, 95% CI, .09-.19; and women with uterine prolapse=.019, 95% CI, .0005-.099).
Some women with grade 1 POP regressed to grade 0 (probability of regression for women with cystoceles=.235, 95% CI, .19- .28; women with rectoceles=.22, 95% CI, .16-.28; and women with uterine prolapse=.48, 95% CI, 0.34-.62). Women with grades 2 and 3 POP were less likely to regress to grade 0 (probability of regression for women with cystoceles=.093, 95% CI, .05-.14; women with rectoceles=.033, 95% CI, .011-.075; and women with uterine prolapse=0, 95% CI, 0-.37).
One flaw of this study was that the women received hormone replacement therapy, which the investigators didn’t evaluate independently. However, a 2010 Cochrane review (2 small trials, one meta-analysis) found insufficient data to determine whether hormone replacement therapy alters POP.5
RECOMMENDATIONS
The American College of Obstetricians and Gynecologists Practice Bulletin on POP recommends the following:6
- Pessaries can be fitted in most women with prolapse, regardless of prolapse stage (equivalent to grade) or site of predominant prolapse.
- Pessary use should be considered before surgical intervention in women with symptomatic prolapse.
- Women with prolapse who are asymptomatic or mildly symptomatic can be observed at regular intervals, unless new bothersome symptoms develop.
Pelvic floor muscle training (PFMT) and pessaries are equally effective in treating symptoms of pelvic organ prolapse (POP). PFMT transiently improves patient satisfaction and reduces urinary incontinence more than pessaries do (strength of recommendation [SOR]: B, a randomized controlled trial [RCT]).
PFMT moderately improves prolapse symptoms and severity, especially following 6 months of supervised intervention (SOR: B, a systematic review of randomized trials with some methodologic flaws).
Two pessaries (ring with support and Gellhorn) reduce symptoms in as many as 60% of patients (SOR: B, a systematic review of randomized trials).
Untreated postmenopausal women with mild grades of uterine prolapse are unlikely to develop more severe prolapse; 25% to 50% improve spontaneously (SOR: C, a prospective cohort study with methodologic flaws).
EVIDENCE SUMMARY
A 2010 multicenter RCT with 445 women (mean age 49.8 years) compared PFMT, pessary use, and combined treatment.1 Investigators used the Patient Global Impression of Improvement and the stress incontinence subscale of the Pelvic Floor Distress Inventory to measure patient satisfaction and urinary incontinence symptoms.
At 3 months, equivalent numbers of women using PFMT and a pessary (49% and 40%, respectively; P=.09) reported they were “much better” or “very much better.” More women in the PFMT cohort than women using a pessary reported resolution of incontinence symptoms at 3 months (49% vs 33%; P=.006), and satisfaction with treatment (75% vs 63%; P=.02), but these differences disappeared at 12 months. Combination therapy wasn’t superior to PFMT alone.
Pelvic floor muscle training improves symptoms, especially with perseverance
A 2011 Cochrane review that compared women receiving PFMT with a control group (observed but not treated) found that PFMT moderately improved prolapse symptoms and severity, especially following 6 months of supervised intervention.2 Investigators evalu-ated 4 trials, (N=857), including 3 with fewer than 25 women per arm.
Three studies found that PFMT improved symptom severity and manometric measures. Although the authors couldn’t pool the data because of different symptom scoring instruments, typical improvements ranged from 20% to 30%. Two trials found that PFMT increased the chance of improvement in POP stage by 17% (pooled data, relative risk=.83; 95% confidence interval [CI], .71-.96). PFMT also improved urinary outcomes (approximately 30% reduction in urinary frequency and stress incontinence symptoms) in 2 of 3 trials and improved bowel symptoms in one trial (approximately 25% to 30% reduction).
Pessaries also relieve symptoms
A 2013 Cochrane Review seeking to determine the effectiveness of pessaries in POP, identified one RCT (crossover, 3 month, multicenter, United States) that compared symptom relief and change in life impact over baseline for 134 women (parous, mean age 61 years, range 30-89 years) with POP stage II or greater who were treated with ring with support or Gellhorn pessaries.3 Sixty percent of patients who completed the study (the dropout rate was 37%) reported symptom relief with both types of pessary. Outcomes were measured by multiple questionnaires and Likert scales.
Patients reported improved symptoms on both the Pelvic Organ Prolapse Distress Inventory (POPDI) and Pelvic Organ Prolapse Impact Questionnaire (POPIQ) scales (P<.05 for difference from baseline on each scale, actual scores not reported). The ring with support and Gellhorn pessaries didn’t produce different scores on either scale (POPDI, P=.99; POPIQ, P=.29).
Untreated mild prolapse postmenopause usually doesn’t progress and may regress
A cohort of 412 postmenopausal women (ages ≥50 years) with POP who were observed, but not treated, found that mild POP was unlikely to progress and sometimes improved spontaneously.4 Over a mean follow-up of 5.7 years, few women with grade 1 POP (prolapsed pelvic organs remaining within the vagina) progressed to grade 2 or 3 (probability of progression for women with cystoceles=.095, 95% CI, .07-.13; women with rectoceles=.135, 95% CI, .09-.19; and women with uterine prolapse=.019, 95% CI, .0005-.099).
Some women with grade 1 POP regressed to grade 0 (probability of regression for women with cystoceles=.235, 95% CI, .19- .28; women with rectoceles=.22, 95% CI, .16-.28; and women with uterine prolapse=.48, 95% CI, 0.34-.62). Women with grades 2 and 3 POP were less likely to regress to grade 0 (probability of regression for women with cystoceles=.093, 95% CI, .05-.14; women with rectoceles=.033, 95% CI, .011-.075; and women with uterine prolapse=0, 95% CI, 0-.37).
One flaw of this study was that the women received hormone replacement therapy, which the investigators didn’t evaluate independently. However, a 2010 Cochrane review (2 small trials, one meta-analysis) found insufficient data to determine whether hormone replacement therapy alters POP.5
RECOMMENDATIONS
The American College of Obstetricians and Gynecologists Practice Bulletin on POP recommends the following:6
- Pessaries can be fitted in most women with prolapse, regardless of prolapse stage (equivalent to grade) or site of predominant prolapse.
- Pessary use should be considered before surgical intervention in women with symptomatic prolapse.
- Women with prolapse who are asymptomatic or mildly symptomatic can be observed at regular intervals, unless new bothersome symptoms develop.
1. Richter HE, Burgio KL, Brubaker L, et al;Pelvic Floor Disorders Network. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010;115:609-617.
2. Hagen S, Stark D. Conservative prevention and management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2011;12:CD003882.
3. Bugge C, Adams EJ, Gopinath D, et al. Pessaries (mechanical devices) for pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;2:CD004010.
4. Handa VL, Garrett E, Hendrix S, et al. Progression and remission of pelvic organ prolapse: a longitudinal study of menopausal women. Am J Obstet Gynecol. 2004;190:27-32.
5. Ismail SI, Bain C, Hagen S. Oestrogens for treatment or prevention of pelvic organ prolapse in postmenopausal women. Cochrane Database Syst Rev. 2010;9:CD007063.
6. ACOG Committee on Practice Bulletins—Gynecology. ACOG Practice Bulletin No. 85: Pelvic organ prolapse. Obstet Gynecol. 2007;110:717-729.
1. Richter HE, Burgio KL, Brubaker L, et al;Pelvic Floor Disorders Network. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010;115:609-617.
2. Hagen S, Stark D. Conservative prevention and management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2011;12:CD003882.
3. Bugge C, Adams EJ, Gopinath D, et al. Pessaries (mechanical devices) for pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;2:CD004010.
4. Handa VL, Garrett E, Hendrix S, et al. Progression and remission of pelvic organ prolapse: a longitudinal study of menopausal women. Am J Obstet Gynecol. 2004;190:27-32.
5. Ismail SI, Bain C, Hagen S. Oestrogens for treatment or prevention of pelvic organ prolapse in postmenopausal women. Cochrane Database Syst Rev. 2010;9:CD007063.
6. ACOG Committee on Practice Bulletins—Gynecology. ACOG Practice Bulletin No. 85: Pelvic organ prolapse. Obstet Gynecol. 2007;110:717-729.
Evidence-based answers from the Family Physicians Inquiries Network
Medicare Billing Practices More Transparent as CMS Cracks Down on Overchargers
The U.S. Department of Health and Human Services (HHS) is putting forth stricter interventions and penalties aimed at curbing acts of careless billing by physicians it refers to as “recalcitrant providers.” Webster’s defines recalcitrant as “obstinately defiant of authority or restraint…difficult to manage or operate.” According to Medicare, these “recalcitrants” are providers who routinely and repeatedly overcharge for services billed through Medicare, despite proper training on how to bill appropriately for these services.1
Medicare has long battled the issue of finding and curbing overcharging and overpayment. CMS estimates that such defiance accounts for up to $6 billion a year in unnecessary Medicare costs, which makes up about 10% of all physician fee payments, given the fact that total Medicare Part B payments are about $65 billion a year.2
Medicare has systems in place to prevent, detect, and/or mitigate improper payments, whether they result from mistakes or from intentional fraud. In 2011, CMS’ Center for Program Integrity implemented sophisticated technology, called the Fraud Prevention System (FPS), which uses predictive analytics to detect provider irregularities warranting further inspection. According to their 2012 report, the FPS generated 536 new investigations, assisted in providing additional information for 511 active investigations, and initiated thousands of verification interviews of beneficiaries and providers to validate the legitimate receipt of services and items. The center estimates that in the first year of this program, FPS prevented about $115 million in payments.3
So what is Medicare’s response to providers who are identified as outliers? For overpayments from mistakes, CMS generally aims to recover the overpayments and educate the providers. Tactics range from educational letters and phone calls to on-site reviews and “prepayment medical reviews.” For fraud, on the other hand, Medicare (obviously) pursues more disciplinary sanctions, including criminal or civil penalties.
A New Paradigm
Now CMS is stepping up its expectations of provider accountability, adding heftier penalties for infractions, including higher financial penalties and even expulsion from Medicare, Medicaid, and other federal programs. In addition to these disciplinary actions, the agency plans to utilize recently changed laws to maximize public transparency around provider billing practices.
As of March 2014, Medicare will be able to publicly report all federal payments that have been paid out to individual providers. Although it has not yet disclosed how or when these will be reported, CMS now has the authority, for the first time since 1979, to display this information publicly. The history on this topic is that a federal district judge in Florida in 1979 prohibited the disclosure of individual payments to physicians, based on the contention that such disclosure would be an invasion of physician privacy. This longstanding mandate, which was reversed in May 2012, now allows Medicare to weigh the risks and benefits of individual requests for information on charges/payments by individual physicians. According to a New York Times article, Medicare is now being pressured by advocacy groups (insurers, employers, consumers) to release as much of the data as possible, to aid in data dissection and analysis and prompt early identification of abusive providers.4
Understandably, many physician advocacy groups, such as the American Medical Association, are concerned that such unfiltered access to this raw data may lead to inaccurate and unnecessary conclusions about physician practice and billing patterns.
The good news is that the federal government currently estimates that the recalcitrant provider list comprises a relatively small group of providers, roughly 300 or so. Some of these providers have received up to $3 million in Medicare payments a year. They estimate that, overall, about 2% of total Medicare licensed providers charged 25% of total payments, and that the total volume of these high-charging outliers increased by 78% between the years 2008 to 2011. A 2009 audit found that more than half of these recalcitrants were internists; other “high offenders” were ophthalmology and radiation oncology.
The list of these particular high-outlier offenders will be turned over to the Office of the Inspector General (OIG) at HHS to impose the appropriate degree of penalty. Then the federal government will determine an appropriate process of “screening” for providers that may meet the criteria for penalties and will start with those at the highest levels of cumulative payments. The OIG acknowledges that high payments do not necessarily imply fraud or abuse but believes it is reasonable to start there when analyzing and investigating potential areas of fraud or abuse.
Transparency Is Coming
So, while it is not exactly clear when or how the data will be released, what is clear is that the federal government has been granted the authority to dissect and release the data as it sees fit, opening up a new era of transparency in pricing, cost, charges, billing, and payments.
This change should affect all types of providers that bill Medicare part B, including hospitalists and other physicians, as well as nurse practitioners and physical therapists.5 While this is likely to cause some degree of discomfort and generate many questions from the public, hospitalists should be willing to embrace such transparency and engage in the dialogue needed to help the lay public understand the data. Most hospitalists work in practices that routinely share their data about billing, at least among the group, if not with a larger audience.
This is just one of many examples of how transparency can and should identify those providers considered “recalcitrant” in a number of realms, including patient satisfaction, quality, utilization, or cost. And, similar to other publicly reported “metrics,” release of this data will likely generate more questions than answers in the short run. In the long run, we should all be prepared for the release of data that is coming, one that will usher us into a whole new era of transparency.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
- Department of Health and Human Services. Centers for Medicare and Medicaid Services. CMS Manual System. Pub 100-08 Medicare program integrity. December 13, 2013. Available at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R495PI.pdf. Accessed April 6, 2014.
- Levinson DR. Department of Health and Human Services. Office of Inspector General. Reviews of clinicians associated with high cumulative payments could improve Medicare program integrity efforts. December 2013. Available at: http://oig.hhs.gov/oas/reports/region1/11100511.pdf. Accessed April 6, 2014.
- Department of Health and Human Services. Centers for Medicare and Medicaid Services. Report to Congress: fraud prevention system—first implementation year, 2012. Available at: http://www.stopmedicarefraud.gov/fraud-rtc12142012.pdf. Accessed April 6, 2014.
- Pear R. Doctors abusing Medicare face fines and expulsion. January 25, 2014. The New York Times website. Available at: http://www.nytimes.com/2014/01/26/us/doctors-abusing-medicare-to-face-fines.html. Accessed April 6, 2014.
- Steinbrook R. Public disclosure of Medicare payments to individual physicians. The Journal of the American Medical Association website. April 2, 2014. Available at: http://jama.jamanetwork.com/article.aspx?articleID=1832217&utm_source=Silverchair%20Information%20Systems&utm_medium=email&utm_campaign=JAMA%3AOnlineFirst02%2F17%2F2014. Accessed April 6,
2014.
The U.S. Department of Health and Human Services (HHS) is putting forth stricter interventions and penalties aimed at curbing acts of careless billing by physicians it refers to as “recalcitrant providers.” Webster’s defines recalcitrant as “obstinately defiant of authority or restraint…difficult to manage or operate.” According to Medicare, these “recalcitrants” are providers who routinely and repeatedly overcharge for services billed through Medicare, despite proper training on how to bill appropriately for these services.1
Medicare has long battled the issue of finding and curbing overcharging and overpayment. CMS estimates that such defiance accounts for up to $6 billion a year in unnecessary Medicare costs, which makes up about 10% of all physician fee payments, given the fact that total Medicare Part B payments are about $65 billion a year.2
Medicare has systems in place to prevent, detect, and/or mitigate improper payments, whether they result from mistakes or from intentional fraud. In 2011, CMS’ Center for Program Integrity implemented sophisticated technology, called the Fraud Prevention System (FPS), which uses predictive analytics to detect provider irregularities warranting further inspection. According to their 2012 report, the FPS generated 536 new investigations, assisted in providing additional information for 511 active investigations, and initiated thousands of verification interviews of beneficiaries and providers to validate the legitimate receipt of services and items. The center estimates that in the first year of this program, FPS prevented about $115 million in payments.3
So what is Medicare’s response to providers who are identified as outliers? For overpayments from mistakes, CMS generally aims to recover the overpayments and educate the providers. Tactics range from educational letters and phone calls to on-site reviews and “prepayment medical reviews.” For fraud, on the other hand, Medicare (obviously) pursues more disciplinary sanctions, including criminal or civil penalties.
A New Paradigm
Now CMS is stepping up its expectations of provider accountability, adding heftier penalties for infractions, including higher financial penalties and even expulsion from Medicare, Medicaid, and other federal programs. In addition to these disciplinary actions, the agency plans to utilize recently changed laws to maximize public transparency around provider billing practices.
As of March 2014, Medicare will be able to publicly report all federal payments that have been paid out to individual providers. Although it has not yet disclosed how or when these will be reported, CMS now has the authority, for the first time since 1979, to display this information publicly. The history on this topic is that a federal district judge in Florida in 1979 prohibited the disclosure of individual payments to physicians, based on the contention that such disclosure would be an invasion of physician privacy. This longstanding mandate, which was reversed in May 2012, now allows Medicare to weigh the risks and benefits of individual requests for information on charges/payments by individual physicians. According to a New York Times article, Medicare is now being pressured by advocacy groups (insurers, employers, consumers) to release as much of the data as possible, to aid in data dissection and analysis and prompt early identification of abusive providers.4
Understandably, many physician advocacy groups, such as the American Medical Association, are concerned that such unfiltered access to this raw data may lead to inaccurate and unnecessary conclusions about physician practice and billing patterns.
The good news is that the federal government currently estimates that the recalcitrant provider list comprises a relatively small group of providers, roughly 300 or so. Some of these providers have received up to $3 million in Medicare payments a year. They estimate that, overall, about 2% of total Medicare licensed providers charged 25% of total payments, and that the total volume of these high-charging outliers increased by 78% between the years 2008 to 2011. A 2009 audit found that more than half of these recalcitrants were internists; other “high offenders” were ophthalmology and radiation oncology.
The list of these particular high-outlier offenders will be turned over to the Office of the Inspector General (OIG) at HHS to impose the appropriate degree of penalty. Then the federal government will determine an appropriate process of “screening” for providers that may meet the criteria for penalties and will start with those at the highest levels of cumulative payments. The OIG acknowledges that high payments do not necessarily imply fraud or abuse but believes it is reasonable to start there when analyzing and investigating potential areas of fraud or abuse.
Transparency Is Coming
So, while it is not exactly clear when or how the data will be released, what is clear is that the federal government has been granted the authority to dissect and release the data as it sees fit, opening up a new era of transparency in pricing, cost, charges, billing, and payments.
This change should affect all types of providers that bill Medicare part B, including hospitalists and other physicians, as well as nurse practitioners and physical therapists.5 While this is likely to cause some degree of discomfort and generate many questions from the public, hospitalists should be willing to embrace such transparency and engage in the dialogue needed to help the lay public understand the data. Most hospitalists work in practices that routinely share their data about billing, at least among the group, if not with a larger audience.
This is just one of many examples of how transparency can and should identify those providers considered “recalcitrant” in a number of realms, including patient satisfaction, quality, utilization, or cost. And, similar to other publicly reported “metrics,” release of this data will likely generate more questions than answers in the short run. In the long run, we should all be prepared for the release of data that is coming, one that will usher us into a whole new era of transparency.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
- Department of Health and Human Services. Centers for Medicare and Medicaid Services. CMS Manual System. Pub 100-08 Medicare program integrity. December 13, 2013. Available at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R495PI.pdf. Accessed April 6, 2014.
- Levinson DR. Department of Health and Human Services. Office of Inspector General. Reviews of clinicians associated with high cumulative payments could improve Medicare program integrity efforts. December 2013. Available at: http://oig.hhs.gov/oas/reports/region1/11100511.pdf. Accessed April 6, 2014.
- Department of Health and Human Services. Centers for Medicare and Medicaid Services. Report to Congress: fraud prevention system—first implementation year, 2012. Available at: http://www.stopmedicarefraud.gov/fraud-rtc12142012.pdf. Accessed April 6, 2014.
- Pear R. Doctors abusing Medicare face fines and expulsion. January 25, 2014. The New York Times website. Available at: http://www.nytimes.com/2014/01/26/us/doctors-abusing-medicare-to-face-fines.html. Accessed April 6, 2014.
- Steinbrook R. Public disclosure of Medicare payments to individual physicians. The Journal of the American Medical Association website. April 2, 2014. Available at: http://jama.jamanetwork.com/article.aspx?articleID=1832217&utm_source=Silverchair%20Information%20Systems&utm_medium=email&utm_campaign=JAMA%3AOnlineFirst02%2F17%2F2014. Accessed April 6,
2014.
The U.S. Department of Health and Human Services (HHS) is putting forth stricter interventions and penalties aimed at curbing acts of careless billing by physicians it refers to as “recalcitrant providers.” Webster’s defines recalcitrant as “obstinately defiant of authority or restraint…difficult to manage or operate.” According to Medicare, these “recalcitrants” are providers who routinely and repeatedly overcharge for services billed through Medicare, despite proper training on how to bill appropriately for these services.1
Medicare has long battled the issue of finding and curbing overcharging and overpayment. CMS estimates that such defiance accounts for up to $6 billion a year in unnecessary Medicare costs, which makes up about 10% of all physician fee payments, given the fact that total Medicare Part B payments are about $65 billion a year.2
Medicare has systems in place to prevent, detect, and/or mitigate improper payments, whether they result from mistakes or from intentional fraud. In 2011, CMS’ Center for Program Integrity implemented sophisticated technology, called the Fraud Prevention System (FPS), which uses predictive analytics to detect provider irregularities warranting further inspection. According to their 2012 report, the FPS generated 536 new investigations, assisted in providing additional information for 511 active investigations, and initiated thousands of verification interviews of beneficiaries and providers to validate the legitimate receipt of services and items. The center estimates that in the first year of this program, FPS prevented about $115 million in payments.3
So what is Medicare’s response to providers who are identified as outliers? For overpayments from mistakes, CMS generally aims to recover the overpayments and educate the providers. Tactics range from educational letters and phone calls to on-site reviews and “prepayment medical reviews.” For fraud, on the other hand, Medicare (obviously) pursues more disciplinary sanctions, including criminal or civil penalties.
A New Paradigm
Now CMS is stepping up its expectations of provider accountability, adding heftier penalties for infractions, including higher financial penalties and even expulsion from Medicare, Medicaid, and other federal programs. In addition to these disciplinary actions, the agency plans to utilize recently changed laws to maximize public transparency around provider billing practices.
As of March 2014, Medicare will be able to publicly report all federal payments that have been paid out to individual providers. Although it has not yet disclosed how or when these will be reported, CMS now has the authority, for the first time since 1979, to display this information publicly. The history on this topic is that a federal district judge in Florida in 1979 prohibited the disclosure of individual payments to physicians, based on the contention that such disclosure would be an invasion of physician privacy. This longstanding mandate, which was reversed in May 2012, now allows Medicare to weigh the risks and benefits of individual requests for information on charges/payments by individual physicians. According to a New York Times article, Medicare is now being pressured by advocacy groups (insurers, employers, consumers) to release as much of the data as possible, to aid in data dissection and analysis and prompt early identification of abusive providers.4
Understandably, many physician advocacy groups, such as the American Medical Association, are concerned that such unfiltered access to this raw data may lead to inaccurate and unnecessary conclusions about physician practice and billing patterns.
The good news is that the federal government currently estimates that the recalcitrant provider list comprises a relatively small group of providers, roughly 300 or so. Some of these providers have received up to $3 million in Medicare payments a year. They estimate that, overall, about 2% of total Medicare licensed providers charged 25% of total payments, and that the total volume of these high-charging outliers increased by 78% between the years 2008 to 2011. A 2009 audit found that more than half of these recalcitrants were internists; other “high offenders” were ophthalmology and radiation oncology.
The list of these particular high-outlier offenders will be turned over to the Office of the Inspector General (OIG) at HHS to impose the appropriate degree of penalty. Then the federal government will determine an appropriate process of “screening” for providers that may meet the criteria for penalties and will start with those at the highest levels of cumulative payments. The OIG acknowledges that high payments do not necessarily imply fraud or abuse but believes it is reasonable to start there when analyzing and investigating potential areas of fraud or abuse.
Transparency Is Coming
So, while it is not exactly clear when or how the data will be released, what is clear is that the federal government has been granted the authority to dissect and release the data as it sees fit, opening up a new era of transparency in pricing, cost, charges, billing, and payments.
This change should affect all types of providers that bill Medicare part B, including hospitalists and other physicians, as well as nurse practitioners and physical therapists.5 While this is likely to cause some degree of discomfort and generate many questions from the public, hospitalists should be willing to embrace such transparency and engage in the dialogue needed to help the lay public understand the data. Most hospitalists work in practices that routinely share their data about billing, at least among the group, if not with a larger audience.
This is just one of many examples of how transparency can and should identify those providers considered “recalcitrant” in a number of realms, including patient satisfaction, quality, utilization, or cost. And, similar to other publicly reported “metrics,” release of this data will likely generate more questions than answers in the short run. In the long run, we should all be prepared for the release of data that is coming, one that will usher us into a whole new era of transparency.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
- Department of Health and Human Services. Centers for Medicare and Medicaid Services. CMS Manual System. Pub 100-08 Medicare program integrity. December 13, 2013. Available at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R495PI.pdf. Accessed April 6, 2014.
- Levinson DR. Department of Health and Human Services. Office of Inspector General. Reviews of clinicians associated with high cumulative payments could improve Medicare program integrity efforts. December 2013. Available at: http://oig.hhs.gov/oas/reports/region1/11100511.pdf. Accessed April 6, 2014.
- Department of Health and Human Services. Centers for Medicare and Medicaid Services. Report to Congress: fraud prevention system—first implementation year, 2012. Available at: http://www.stopmedicarefraud.gov/fraud-rtc12142012.pdf. Accessed April 6, 2014.
- Pear R. Doctors abusing Medicare face fines and expulsion. January 25, 2014. The New York Times website. Available at: http://www.nytimes.com/2014/01/26/us/doctors-abusing-medicare-to-face-fines.html. Accessed April 6, 2014.
- Steinbrook R. Public disclosure of Medicare payments to individual physicians. The Journal of the American Medical Association website. April 2, 2014. Available at: http://jama.jamanetwork.com/article.aspx?articleID=1832217&utm_source=Silverchair%20Information%20Systems&utm_medium=email&utm_campaign=JAMA%3AOnlineFirst02%2F17%2F2014. Accessed April 6,
2014.
Hospital Patient Safety, Quality Movement Helped Propel Hospitalists
Hippocrates, Epidemics.“The Physician must be able to do good or to do no harm.”
This is part three of my ongoing series on the journey of hospital medicine and how we are poised for greater things yet. In part one, “Tinder and Spark,” macro changes in the American healthcare landscape pressured primary care physicians to get creative with new ways to practice, the most prominent result being the creation of hospitalist practices. Wachter and Goldman provided the spark that gave the field its name and cohesiveness. In part two, “Fuel,” the Baby Boomers shaped the field, setting the stage for the Generation X physicians who fueled HM’s early growth.
But the field might have stagnated there, the fire attenuated, if not for the rise of something new, something that stoked our growth to new heights.
Orlando, Fla., December 2006.
SHM President-Elect Rusty Holman, MD, MHM, was on stage representing hospitalists at the annual Institute for Healthcare Improvement (IHI) National Forum in front of more than 5,000 enthusiastic attendees representing every discipline of clinical care from hundreds of healthcare organizations across the country and internationally. This was a special event. Two years earlier, IHI President Don Berwick, MD, MPP, had launched an audacious campaign, called the 100,000 Lives Campaign, that aimed to prevent the deaths of 100,000 patients in our nation’s hospitals in the following 18 months, not by utilizing some great new technological advance but by changing the culture around safety and quality in our nation’s hospitals and enacting proven safety methods and processes.1 Out of this plan came widespread use of terms and programs that weren’t widely adopted then but are familiar to all of us now: rapid response teams, medicine reconciliation, surgical site infection prevention, and ventilator-acquired pneumonia.
That program estimated that it saved 122,000 lives.1
IHI was looking to build on the safety and quality infrastructure that had been built up to make the 100,000 Lives Campaign a success and to launch an even bigger program. The 5 Million Lives Campaign’s goal was to reduce incidents of harm in five million patients over the next two years. For this campaign, IHI understood that success could only be achieved with partners. SHM and the field of hospital medicine, which had grown in size and influence, was seen as a critical and influential partner in achieving the goal of reducing harm in our nation’s hospitals. Thus, Dr. Holman was standing on that stage for SHM at the launch of the biggest safety and quality initiative in our nation’s history. SHM was among seven partner organizations, including the American Nurses Association, the Centers for Medicare and Medicaid Services (CMS), the American Heart Association, and the CDC. SHM was the only medical society represented. Pretty heady stuff for a field barely 10 years old. How did we get there? For that story, we need to go back a few years.
In 1984, Libby Zion, an 18-year-old college student, died from serotonin syndrome. A contributing factor was felt to be overworked residents not getting enough sleep. In his landmark 1990 article, “Human Factors in Hazardous Situations,” James Reason, PhD, introduced the world to some key concepts: active versus latent errors and the Swiss cheese model of errors.2 These concepts influence our thinking to this day. In 1994, Betsy Lehman, a health reporter for the Boston Globe, died from a massive chemotherapy overdose. That same year Lucian Leape, MD, a Harvard pediatric surgeon, published his influential article in JAMA, “Errors in Medicine,” which called for a systems approach to improving patient safety.3
These key moments in safety and quality, all of which occurred in the years leading up to hospitalists gaining their identity, were but a prelude to the widespread patient safety and quality movement. Like our own social movement, “Patient Safety and Quality” was born with an influential publication. This was the 1999 release of the Institute of Medicine’s “To Err is Human,” a report that reiterated claims that up to 98,000 U.S. patients per year were dying from medical errors.4 It also supported Dr. Leape’s earlier work calling for systems changes. In 2001, the Institute of Medicine published a second report, “Crossing the Quality Chasm: A New Health System for the 21st Century,” which introduced the six aims for healthcare improvement: safe, timely, effective, efficient, equitable, and patient-centered.5
Before 1999, hospitalists were just getting their feet on the ground. Groups were experimenting with practice models and recruiting young talent, mostly with a pitch for a new way to practice with freedom to design their day and often an interesting work schedule.
After the publication of “To Err is Human” in 1999, changes in patient safety and quality began to accelerate. Taking one of the recommendations from “To Err is Human,” which suggested that employers should use their market power to improve quality and safety, the Leapfrog Group, a consortium of large employers, organized in 2000. Leapfrog began rewarding and recognizing hospitals that put accepted safety measures in place.6 Suddenly, hospital CEOs began to see tangible rewards for improving quality in their hospitals.
Here is where the hospitalist movement and the patient safety and quality movement began to intersect.
Shift to Quality and Safety
In 2001, the same year “Crossing the Quality Chasm” was published, Congress created the Center for Quality Improvement and Patient Safety within the Agency for Healthcare Research and Quality. Significant funding was suddenly available for quality and safety research, and a more organized reporting mechanism for quality would soon be available.
In 2002, the Joint Commission released its first set of National Patient Safety Goals. There were seven, and key goals for hospitalists included improving the effectiveness of communication among caregivers, reducing the risk of healthcare-acquired infections, and reconciling medications.
And, lastly, as if that weren’t enough activity in the patient safety and quality world, the Joint Commission and CMS released in 2003 the first joint, aligned set of core measures, with which we are all now very familiar, around acute myocardial infarction, congestive heart failure, and pneumonia.
Hospital executives were trying to get a handle on the meaning of this flurry of activity for their hospitals. It certainly meant new regulatory requirements. It probably meant greater visibility to the public around what happened behind the walls of their facilities. No doubt dollars on the line wouldn’t be too far behind. They needed help, and they needed it fast.
No longer were hospitalists a small group of young docs roaming the halls; now, instead of just taking care of one patient at a time, they were reaching the threshold of size—and even status in some organizations—where they could leverage their working knowledge of the system and presence on site to affect the various facets of quality now being measured and incented. Additionally, as the information technology (IT) revolution rolled out, hospitalists, mostly tech-savvy Gen X’ers, looked to ease the transition into the new world of EHRs, which promised to serve as a new base for improving quality.
As the C-suite continued making value calculations in their heads, they saw that, in addition to helping them manage the many facets of the transition of primary care and specialty teaching attendings out of the hospital, hospitalists could now be a powerful weapon in helping them stay competitive in the looming patient safety and quality revolution. They pulled out their checkbooks.
When SHM first started gathering data to explore this gap, we discovered that in 2003 the reported median support per FTE of an adult hospitalist in this country was $60,000.7 With an estimated 11,000 hospitalists in the country at that time, C-suite funders paid out over $600 million to help overcome the deficit between hospitalist professional billings and salary and benefits. By the time SHM partnered with IHI on the 5 Million Lives Campaign in 2006, the figure stood at well over $2 billion. The 2011 SHM/Medical Group Management Association survey data showed $139,090 support per FTE. With 31,000 U.S. hospitalists estimated at the time, that figure had doubled to over $4 billion in just five years’ time.
The new generation of doctors had come along in the late 1990s looking for a practice that fit their wants and needs. HM gave them what they were looking for: autonomy, the promise of work-life balance, and the ability to help patients in their most vulnerable time. The traditional E&M [evaluation and management]-based funding mechanisms simply weren’t designed to account for physicians who spend all of their time doing the critical cognitive and coordinating clinical work. To account for this, hospitals and medical groups, seeing the value to their organizations in this new specialty, anteed up to cover the difference. That gave us a great beginning.
But it was the convergence of the early hospitalist movement and the emergent patient safety and quality movement that created a synergy that propelled both movements forward. Boosted by the influx of funding directly and indirectly related to patient safety and quality, hospitalists grew in number from an estimated 5,000 physicians at the 1999 publication of “To Err is Human” to north of 40,000 today.
The synergy was evident when SHM President-Elect Dr. Holman, representing our fledgling specialty and society, faced that cheering throng in Orlando alongside Dr. Don Berwick, the face of the patient safety and quality movement.
But that’s not quite the end of the story.
To get us up to the present and on to our bright future, there will be a few more additions to the quality story and an all-new generation arriving on the scene to shake things up.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
References
- Institute for Healthcare Improvement. Overview of the 100,000 Lives Campaign. Available at: http://www.ihi.org/Engage/Initiatives/Completed/5MillionLivesCampaign/Documents/Overview%20of%20the%20100K%20Campaign.pdf. Accessed July 6, 2014.
- Broadbent DE, Reason J, Baddeley A, eds. Human Factors in Hazardous Situations: Proceedings of a Royal Society Discussion Meeting Held on 28 and 29 June 1989. Gloucestershire, England: Clarendon Press; 1990:475-484.
- Leape LL. Error in medicine JAMA.1994;272(23):1851-1857.
- Institute of Medicine. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, D.C.: The National Academy Press; 2000.
- Institute of Medicine. Committee on Quality of Healthcare in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: The National Academy Press; 2001.
- The Leapfrog Group. About Leapfrog. Available at: http://www.leapfroggroup.org/about_leapfrog. Accessed July 6, 2014.
- Society of Hospital Medicine. SHM’s State of Hospital Medicine Surveys 2003-2012. Available at: www.hospitalmedicine.org/survey. Accessed July 3, 2014.
Hippocrates, Epidemics.“The Physician must be able to do good or to do no harm.”
This is part three of my ongoing series on the journey of hospital medicine and how we are poised for greater things yet. In part one, “Tinder and Spark,” macro changes in the American healthcare landscape pressured primary care physicians to get creative with new ways to practice, the most prominent result being the creation of hospitalist practices. Wachter and Goldman provided the spark that gave the field its name and cohesiveness. In part two, “Fuel,” the Baby Boomers shaped the field, setting the stage for the Generation X physicians who fueled HM’s early growth.
But the field might have stagnated there, the fire attenuated, if not for the rise of something new, something that stoked our growth to new heights.
Orlando, Fla., December 2006.
SHM President-Elect Rusty Holman, MD, MHM, was on stage representing hospitalists at the annual Institute for Healthcare Improvement (IHI) National Forum in front of more than 5,000 enthusiastic attendees representing every discipline of clinical care from hundreds of healthcare organizations across the country and internationally. This was a special event. Two years earlier, IHI President Don Berwick, MD, MPP, had launched an audacious campaign, called the 100,000 Lives Campaign, that aimed to prevent the deaths of 100,000 patients in our nation’s hospitals in the following 18 months, not by utilizing some great new technological advance but by changing the culture around safety and quality in our nation’s hospitals and enacting proven safety methods and processes.1 Out of this plan came widespread use of terms and programs that weren’t widely adopted then but are familiar to all of us now: rapid response teams, medicine reconciliation, surgical site infection prevention, and ventilator-acquired pneumonia.
That program estimated that it saved 122,000 lives.1
IHI was looking to build on the safety and quality infrastructure that had been built up to make the 100,000 Lives Campaign a success and to launch an even bigger program. The 5 Million Lives Campaign’s goal was to reduce incidents of harm in five million patients over the next two years. For this campaign, IHI understood that success could only be achieved with partners. SHM and the field of hospital medicine, which had grown in size and influence, was seen as a critical and influential partner in achieving the goal of reducing harm in our nation’s hospitals. Thus, Dr. Holman was standing on that stage for SHM at the launch of the biggest safety and quality initiative in our nation’s history. SHM was among seven partner organizations, including the American Nurses Association, the Centers for Medicare and Medicaid Services (CMS), the American Heart Association, and the CDC. SHM was the only medical society represented. Pretty heady stuff for a field barely 10 years old. How did we get there? For that story, we need to go back a few years.
In 1984, Libby Zion, an 18-year-old college student, died from serotonin syndrome. A contributing factor was felt to be overworked residents not getting enough sleep. In his landmark 1990 article, “Human Factors in Hazardous Situations,” James Reason, PhD, introduced the world to some key concepts: active versus latent errors and the Swiss cheese model of errors.2 These concepts influence our thinking to this day. In 1994, Betsy Lehman, a health reporter for the Boston Globe, died from a massive chemotherapy overdose. That same year Lucian Leape, MD, a Harvard pediatric surgeon, published his influential article in JAMA, “Errors in Medicine,” which called for a systems approach to improving patient safety.3
These key moments in safety and quality, all of which occurred in the years leading up to hospitalists gaining their identity, were but a prelude to the widespread patient safety and quality movement. Like our own social movement, “Patient Safety and Quality” was born with an influential publication. This was the 1999 release of the Institute of Medicine’s “To Err is Human,” a report that reiterated claims that up to 98,000 U.S. patients per year were dying from medical errors.4 It also supported Dr. Leape’s earlier work calling for systems changes. In 2001, the Institute of Medicine published a second report, “Crossing the Quality Chasm: A New Health System for the 21st Century,” which introduced the six aims for healthcare improvement: safe, timely, effective, efficient, equitable, and patient-centered.5
Before 1999, hospitalists were just getting their feet on the ground. Groups were experimenting with practice models and recruiting young talent, mostly with a pitch for a new way to practice with freedom to design their day and often an interesting work schedule.
After the publication of “To Err is Human” in 1999, changes in patient safety and quality began to accelerate. Taking one of the recommendations from “To Err is Human,” which suggested that employers should use their market power to improve quality and safety, the Leapfrog Group, a consortium of large employers, organized in 2000. Leapfrog began rewarding and recognizing hospitals that put accepted safety measures in place.6 Suddenly, hospital CEOs began to see tangible rewards for improving quality in their hospitals.
Here is where the hospitalist movement and the patient safety and quality movement began to intersect.
Shift to Quality and Safety
In 2001, the same year “Crossing the Quality Chasm” was published, Congress created the Center for Quality Improvement and Patient Safety within the Agency for Healthcare Research and Quality. Significant funding was suddenly available for quality and safety research, and a more organized reporting mechanism for quality would soon be available.
In 2002, the Joint Commission released its first set of National Patient Safety Goals. There were seven, and key goals for hospitalists included improving the effectiveness of communication among caregivers, reducing the risk of healthcare-acquired infections, and reconciling medications.
And, lastly, as if that weren’t enough activity in the patient safety and quality world, the Joint Commission and CMS released in 2003 the first joint, aligned set of core measures, with which we are all now very familiar, around acute myocardial infarction, congestive heart failure, and pneumonia.
Hospital executives were trying to get a handle on the meaning of this flurry of activity for their hospitals. It certainly meant new regulatory requirements. It probably meant greater visibility to the public around what happened behind the walls of their facilities. No doubt dollars on the line wouldn’t be too far behind. They needed help, and they needed it fast.
No longer were hospitalists a small group of young docs roaming the halls; now, instead of just taking care of one patient at a time, they were reaching the threshold of size—and even status in some organizations—where they could leverage their working knowledge of the system and presence on site to affect the various facets of quality now being measured and incented. Additionally, as the information technology (IT) revolution rolled out, hospitalists, mostly tech-savvy Gen X’ers, looked to ease the transition into the new world of EHRs, which promised to serve as a new base for improving quality.
As the C-suite continued making value calculations in their heads, they saw that, in addition to helping them manage the many facets of the transition of primary care and specialty teaching attendings out of the hospital, hospitalists could now be a powerful weapon in helping them stay competitive in the looming patient safety and quality revolution. They pulled out their checkbooks.
When SHM first started gathering data to explore this gap, we discovered that in 2003 the reported median support per FTE of an adult hospitalist in this country was $60,000.7 With an estimated 11,000 hospitalists in the country at that time, C-suite funders paid out over $600 million to help overcome the deficit between hospitalist professional billings and salary and benefits. By the time SHM partnered with IHI on the 5 Million Lives Campaign in 2006, the figure stood at well over $2 billion. The 2011 SHM/Medical Group Management Association survey data showed $139,090 support per FTE. With 31,000 U.S. hospitalists estimated at the time, that figure had doubled to over $4 billion in just five years’ time.
The new generation of doctors had come along in the late 1990s looking for a practice that fit their wants and needs. HM gave them what they were looking for: autonomy, the promise of work-life balance, and the ability to help patients in their most vulnerable time. The traditional E&M [evaluation and management]-based funding mechanisms simply weren’t designed to account for physicians who spend all of their time doing the critical cognitive and coordinating clinical work. To account for this, hospitals and medical groups, seeing the value to their organizations in this new specialty, anteed up to cover the difference. That gave us a great beginning.
But it was the convergence of the early hospitalist movement and the emergent patient safety and quality movement that created a synergy that propelled both movements forward. Boosted by the influx of funding directly and indirectly related to patient safety and quality, hospitalists grew in number from an estimated 5,000 physicians at the 1999 publication of “To Err is Human” to north of 40,000 today.
The synergy was evident when SHM President-Elect Dr. Holman, representing our fledgling specialty and society, faced that cheering throng in Orlando alongside Dr. Don Berwick, the face of the patient safety and quality movement.
But that’s not quite the end of the story.
To get us up to the present and on to our bright future, there will be a few more additions to the quality story and an all-new generation arriving on the scene to shake things up.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
References
- Institute for Healthcare Improvement. Overview of the 100,000 Lives Campaign. Available at: http://www.ihi.org/Engage/Initiatives/Completed/5MillionLivesCampaign/Documents/Overview%20of%20the%20100K%20Campaign.pdf. Accessed July 6, 2014.
- Broadbent DE, Reason J, Baddeley A, eds. Human Factors in Hazardous Situations: Proceedings of a Royal Society Discussion Meeting Held on 28 and 29 June 1989. Gloucestershire, England: Clarendon Press; 1990:475-484.
- Leape LL. Error in medicine JAMA.1994;272(23):1851-1857.
- Institute of Medicine. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, D.C.: The National Academy Press; 2000.
- Institute of Medicine. Committee on Quality of Healthcare in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: The National Academy Press; 2001.
- The Leapfrog Group. About Leapfrog. Available at: http://www.leapfroggroup.org/about_leapfrog. Accessed July 6, 2014.
- Society of Hospital Medicine. SHM’s State of Hospital Medicine Surveys 2003-2012. Available at: www.hospitalmedicine.org/survey. Accessed July 3, 2014.
Hippocrates, Epidemics.“The Physician must be able to do good or to do no harm.”
This is part three of my ongoing series on the journey of hospital medicine and how we are poised for greater things yet. In part one, “Tinder and Spark,” macro changes in the American healthcare landscape pressured primary care physicians to get creative with new ways to practice, the most prominent result being the creation of hospitalist practices. Wachter and Goldman provided the spark that gave the field its name and cohesiveness. In part two, “Fuel,” the Baby Boomers shaped the field, setting the stage for the Generation X physicians who fueled HM’s early growth.
But the field might have stagnated there, the fire attenuated, if not for the rise of something new, something that stoked our growth to new heights.
Orlando, Fla., December 2006.
SHM President-Elect Rusty Holman, MD, MHM, was on stage representing hospitalists at the annual Institute for Healthcare Improvement (IHI) National Forum in front of more than 5,000 enthusiastic attendees representing every discipline of clinical care from hundreds of healthcare organizations across the country and internationally. This was a special event. Two years earlier, IHI President Don Berwick, MD, MPP, had launched an audacious campaign, called the 100,000 Lives Campaign, that aimed to prevent the deaths of 100,000 patients in our nation’s hospitals in the following 18 months, not by utilizing some great new technological advance but by changing the culture around safety and quality in our nation’s hospitals and enacting proven safety methods and processes.1 Out of this plan came widespread use of terms and programs that weren’t widely adopted then but are familiar to all of us now: rapid response teams, medicine reconciliation, surgical site infection prevention, and ventilator-acquired pneumonia.
That program estimated that it saved 122,000 lives.1
IHI was looking to build on the safety and quality infrastructure that had been built up to make the 100,000 Lives Campaign a success and to launch an even bigger program. The 5 Million Lives Campaign’s goal was to reduce incidents of harm in five million patients over the next two years. For this campaign, IHI understood that success could only be achieved with partners. SHM and the field of hospital medicine, which had grown in size and influence, was seen as a critical and influential partner in achieving the goal of reducing harm in our nation’s hospitals. Thus, Dr. Holman was standing on that stage for SHM at the launch of the biggest safety and quality initiative in our nation’s history. SHM was among seven partner organizations, including the American Nurses Association, the Centers for Medicare and Medicaid Services (CMS), the American Heart Association, and the CDC. SHM was the only medical society represented. Pretty heady stuff for a field barely 10 years old. How did we get there? For that story, we need to go back a few years.
In 1984, Libby Zion, an 18-year-old college student, died from serotonin syndrome. A contributing factor was felt to be overworked residents not getting enough sleep. In his landmark 1990 article, “Human Factors in Hazardous Situations,” James Reason, PhD, introduced the world to some key concepts: active versus latent errors and the Swiss cheese model of errors.2 These concepts influence our thinking to this day. In 1994, Betsy Lehman, a health reporter for the Boston Globe, died from a massive chemotherapy overdose. That same year Lucian Leape, MD, a Harvard pediatric surgeon, published his influential article in JAMA, “Errors in Medicine,” which called for a systems approach to improving patient safety.3
These key moments in safety and quality, all of which occurred in the years leading up to hospitalists gaining their identity, were but a prelude to the widespread patient safety and quality movement. Like our own social movement, “Patient Safety and Quality” was born with an influential publication. This was the 1999 release of the Institute of Medicine’s “To Err is Human,” a report that reiterated claims that up to 98,000 U.S. patients per year were dying from medical errors.4 It also supported Dr. Leape’s earlier work calling for systems changes. In 2001, the Institute of Medicine published a second report, “Crossing the Quality Chasm: A New Health System for the 21st Century,” which introduced the six aims for healthcare improvement: safe, timely, effective, efficient, equitable, and patient-centered.5
Before 1999, hospitalists were just getting their feet on the ground. Groups were experimenting with practice models and recruiting young talent, mostly with a pitch for a new way to practice with freedom to design their day and often an interesting work schedule.
After the publication of “To Err is Human” in 1999, changes in patient safety and quality began to accelerate. Taking one of the recommendations from “To Err is Human,” which suggested that employers should use their market power to improve quality and safety, the Leapfrog Group, a consortium of large employers, organized in 2000. Leapfrog began rewarding and recognizing hospitals that put accepted safety measures in place.6 Suddenly, hospital CEOs began to see tangible rewards for improving quality in their hospitals.
Here is where the hospitalist movement and the patient safety and quality movement began to intersect.
Shift to Quality and Safety
In 2001, the same year “Crossing the Quality Chasm” was published, Congress created the Center for Quality Improvement and Patient Safety within the Agency for Healthcare Research and Quality. Significant funding was suddenly available for quality and safety research, and a more organized reporting mechanism for quality would soon be available.
In 2002, the Joint Commission released its first set of National Patient Safety Goals. There were seven, and key goals for hospitalists included improving the effectiveness of communication among caregivers, reducing the risk of healthcare-acquired infections, and reconciling medications.
And, lastly, as if that weren’t enough activity in the patient safety and quality world, the Joint Commission and CMS released in 2003 the first joint, aligned set of core measures, with which we are all now very familiar, around acute myocardial infarction, congestive heart failure, and pneumonia.
Hospital executives were trying to get a handle on the meaning of this flurry of activity for their hospitals. It certainly meant new regulatory requirements. It probably meant greater visibility to the public around what happened behind the walls of their facilities. No doubt dollars on the line wouldn’t be too far behind. They needed help, and they needed it fast.
No longer were hospitalists a small group of young docs roaming the halls; now, instead of just taking care of one patient at a time, they were reaching the threshold of size—and even status in some organizations—where they could leverage their working knowledge of the system and presence on site to affect the various facets of quality now being measured and incented. Additionally, as the information technology (IT) revolution rolled out, hospitalists, mostly tech-savvy Gen X’ers, looked to ease the transition into the new world of EHRs, which promised to serve as a new base for improving quality.
As the C-suite continued making value calculations in their heads, they saw that, in addition to helping them manage the many facets of the transition of primary care and specialty teaching attendings out of the hospital, hospitalists could now be a powerful weapon in helping them stay competitive in the looming patient safety and quality revolution. They pulled out their checkbooks.
When SHM first started gathering data to explore this gap, we discovered that in 2003 the reported median support per FTE of an adult hospitalist in this country was $60,000.7 With an estimated 11,000 hospitalists in the country at that time, C-suite funders paid out over $600 million to help overcome the deficit between hospitalist professional billings and salary and benefits. By the time SHM partnered with IHI on the 5 Million Lives Campaign in 2006, the figure stood at well over $2 billion. The 2011 SHM/Medical Group Management Association survey data showed $139,090 support per FTE. With 31,000 U.S. hospitalists estimated at the time, that figure had doubled to over $4 billion in just five years’ time.
The new generation of doctors had come along in the late 1990s looking for a practice that fit their wants and needs. HM gave them what they were looking for: autonomy, the promise of work-life balance, and the ability to help patients in their most vulnerable time. The traditional E&M [evaluation and management]-based funding mechanisms simply weren’t designed to account for physicians who spend all of their time doing the critical cognitive and coordinating clinical work. To account for this, hospitals and medical groups, seeing the value to their organizations in this new specialty, anteed up to cover the difference. That gave us a great beginning.
But it was the convergence of the early hospitalist movement and the emergent patient safety and quality movement that created a synergy that propelled both movements forward. Boosted by the influx of funding directly and indirectly related to patient safety and quality, hospitalists grew in number from an estimated 5,000 physicians at the 1999 publication of “To Err is Human” to north of 40,000 today.
The synergy was evident when SHM President-Elect Dr. Holman, representing our fledgling specialty and society, faced that cheering throng in Orlando alongside Dr. Don Berwick, the face of the patient safety and quality movement.
But that’s not quite the end of the story.
To get us up to the present and on to our bright future, there will be a few more additions to the quality story and an all-new generation arriving on the scene to shake things up.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
References
- Institute for Healthcare Improvement. Overview of the 100,000 Lives Campaign. Available at: http://www.ihi.org/Engage/Initiatives/Completed/5MillionLivesCampaign/Documents/Overview%20of%20the%20100K%20Campaign.pdf. Accessed July 6, 2014.
- Broadbent DE, Reason J, Baddeley A, eds. Human Factors in Hazardous Situations: Proceedings of a Royal Society Discussion Meeting Held on 28 and 29 June 1989. Gloucestershire, England: Clarendon Press; 1990:475-484.
- Leape LL. Error in medicine JAMA.1994;272(23):1851-1857.
- Institute of Medicine. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, D.C.: The National Academy Press; 2000.
- Institute of Medicine. Committee on Quality of Healthcare in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: The National Academy Press; 2001.
- The Leapfrog Group. About Leapfrog. Available at: http://www.leapfroggroup.org/about_leapfrog. Accessed July 6, 2014.
- Society of Hospital Medicine. SHM’s State of Hospital Medicine Surveys 2003-2012. Available at: www.hospitalmedicine.org/survey. Accessed July 3, 2014.
Hospitalist Julie Fedderson, MD, Driven by Dedication to Patient Care
Growing up in America’s heartland, Julie Fedderson, MD, realized at an early age that something wasn’t right with the U.S. healthcare system. Her grandmother, a “headstrong” immigrant from the Czech Republic, died of colon cancer when Dr. Fedderson was young, and that experience—watching a loved one “reduced to tears” trying to navigate a complicated and impersonal healthcare system in rural Nebraska—made her realize “how important having dedicated physicians is.”
“It may sound naïve, but I really wanted to help people,” says Dr. Fedderson, who grew up and went to high school in a small town two hours from an urban center. She eventually attended college in what she saw as the big city—Lincoln, Nebraska. After attending the University of Nebraska, Dr. Fedderson went to medical school at the University of Nebraska Medical School (UNMC) in Omaha. She did her residency at Baylor College of Medicine in Houston, then returned to Nebraska.
Since 2003, she has worked as a hospitalist and is currently an assistant professor in the department of internal medicine at the UNMC. Her story, practicing as a “traditional” internist for several years before making the switch to HM, is similar to many in hospital medicine.
“I wanted to make an impact on the seamless transition of in-house care to outpatient care,” says one of the newest members of Team Hospitalist, the volunteer editorial advisory board of The Hospitalist. “The two are so intricately intertwined, yet so siloed, and many times the patient—who is the least capable of navigating our complex systems—is the one who is left with the responsibility to do it. I wanted to improve that.”
Dr. Fedderson is working toward her master’s degree from the University of Colorado’s Executive MBA Program. She is the resident supervisor for UNMC’s Physicians Midtown Clinic, serves as the Nebraska Medical Center’s enterprise chief quality and outcomes officer, and is on the board of directors of Nebraska Health Partners. She is also a member of the department of internal medicine’s executive committee.
Question: What do you like most about working as a hospitalist?
Answer: The ability to implement rapid change of process in a controlled environment.
Q: What do you dislike most?
A: The regulatory ties placed on hospitals that may not be quality oriented [and] the difficulty of handling the outpatient care of uninsured or underinsured patients.
Q: What’s the best advice you ever received?
A: For life: Shut up and listen. From one of my attendings during my residency: Piss, pus, and hostility all must come out eventually.
Q: What’s the biggest change you’ve seen in hospital medicine in your career?
A: The shift to technology as a basis of care. When done well, it is phenomenal. When done without appropriate thought, it can be disastrous for patients and providers alike.
Q: Why is it important for you, as a hospitalist group leader, to continue seeing patients?
A: How do you implement change if you have no skin in the game? I stay current and see patients to see the system work firsthand and to provide innovative—but practical—solutions.
Q: Outside of patient care, what are your career interests?
A: I am currently our new chief quality and outcomes officer at The Nebraska Medical Center Enterprise. I am also involved as a physician champion for our electronic health record [EHR] implementation and in clinical documentation improvement at all levels.
Q: What is your biggest professional challenge?
A: There are a lot of daunting things coming from entities that don’t necessarily have a patient’s best interests at heart. Keeping sane doing the “regulatory” quality while still providing good quality care is a challenge. Sometimes it feels like a game—but obviously a game with serious consequences.
Q: What is your biggest professional reward?
A: Frankly, [it is] when one of my colleagues relates to me a success story with a new process or plan. I hear so many of my medical friends so dissatisfied with healthcare’s trajectory—they’re burned out, telling their kids to not go into medicine. When I see someone get that spark back for their career and their reason for choosing it, that makes me feel fantastic.
Q: When you aren’t working, what is important to you?
A: I have two boys, and they hung the moon. We hang out as much as possible. I am also into physical fitness, so I try to run, do yoga, and hike as much as I can.
Q: Where do you see yourself in 10 years?
A: I would like to continue to be a chief quality officer, potentially for an entire healthcare system.
Q: If you weren’t a doctor, what would you be doing right now?
A: Writing romance novels.
Q: What’s the best book you’ve read recently? Why?
A: “Mountains Beyond Mountains” by Tracy Kidder. It’s about Dr. Paul Farmer’s work in Haiti. Really exemplifies that one person can change lives.
Q: How many Apple products (phones, iPods, tablets, iTunes, etc.) do you interface with in a given week?
A: I’ve been infiltrated with Apples. My iPhone seldom leaves my hand. I use an iPad for notes and to chart. I run three miles a day with my iPod. I own two Macs.
Q: What’s next in your Netflix queue?
A: I have a six- and a seven-year-old, so anything with animation. Last great movie I saw was “Silver Linings Playbook.”
Richard Quinn is a freelance writer in New Jersey.
Growing up in America’s heartland, Julie Fedderson, MD, realized at an early age that something wasn’t right with the U.S. healthcare system. Her grandmother, a “headstrong” immigrant from the Czech Republic, died of colon cancer when Dr. Fedderson was young, and that experience—watching a loved one “reduced to tears” trying to navigate a complicated and impersonal healthcare system in rural Nebraska—made her realize “how important having dedicated physicians is.”
“It may sound naïve, but I really wanted to help people,” says Dr. Fedderson, who grew up and went to high school in a small town two hours from an urban center. She eventually attended college in what she saw as the big city—Lincoln, Nebraska. After attending the University of Nebraska, Dr. Fedderson went to medical school at the University of Nebraska Medical School (UNMC) in Omaha. She did her residency at Baylor College of Medicine in Houston, then returned to Nebraska.
Since 2003, she has worked as a hospitalist and is currently an assistant professor in the department of internal medicine at the UNMC. Her story, practicing as a “traditional” internist for several years before making the switch to HM, is similar to many in hospital medicine.
“I wanted to make an impact on the seamless transition of in-house care to outpatient care,” says one of the newest members of Team Hospitalist, the volunteer editorial advisory board of The Hospitalist. “The two are so intricately intertwined, yet so siloed, and many times the patient—who is the least capable of navigating our complex systems—is the one who is left with the responsibility to do it. I wanted to improve that.”
Dr. Fedderson is working toward her master’s degree from the University of Colorado’s Executive MBA Program. She is the resident supervisor for UNMC’s Physicians Midtown Clinic, serves as the Nebraska Medical Center’s enterprise chief quality and outcomes officer, and is on the board of directors of Nebraska Health Partners. She is also a member of the department of internal medicine’s executive committee.
Question: What do you like most about working as a hospitalist?
Answer: The ability to implement rapid change of process in a controlled environment.
Q: What do you dislike most?
A: The regulatory ties placed on hospitals that may not be quality oriented [and] the difficulty of handling the outpatient care of uninsured or underinsured patients.
Q: What’s the best advice you ever received?
A: For life: Shut up and listen. From one of my attendings during my residency: Piss, pus, and hostility all must come out eventually.
Q: What’s the biggest change you’ve seen in hospital medicine in your career?
A: The shift to technology as a basis of care. When done well, it is phenomenal. When done without appropriate thought, it can be disastrous for patients and providers alike.
Q: Why is it important for you, as a hospitalist group leader, to continue seeing patients?
A: How do you implement change if you have no skin in the game? I stay current and see patients to see the system work firsthand and to provide innovative—but practical—solutions.
Q: Outside of patient care, what are your career interests?
A: I am currently our new chief quality and outcomes officer at The Nebraska Medical Center Enterprise. I am also involved as a physician champion for our electronic health record [EHR] implementation and in clinical documentation improvement at all levels.
Q: What is your biggest professional challenge?
A: There are a lot of daunting things coming from entities that don’t necessarily have a patient’s best interests at heart. Keeping sane doing the “regulatory” quality while still providing good quality care is a challenge. Sometimes it feels like a game—but obviously a game with serious consequences.
Q: What is your biggest professional reward?
A: Frankly, [it is] when one of my colleagues relates to me a success story with a new process or plan. I hear so many of my medical friends so dissatisfied with healthcare’s trajectory—they’re burned out, telling their kids to not go into medicine. When I see someone get that spark back for their career and their reason for choosing it, that makes me feel fantastic.
Q: When you aren’t working, what is important to you?
A: I have two boys, and they hung the moon. We hang out as much as possible. I am also into physical fitness, so I try to run, do yoga, and hike as much as I can.
Q: Where do you see yourself in 10 years?
A: I would like to continue to be a chief quality officer, potentially for an entire healthcare system.
Q: If you weren’t a doctor, what would you be doing right now?
A: Writing romance novels.
Q: What’s the best book you’ve read recently? Why?
A: “Mountains Beyond Mountains” by Tracy Kidder. It’s about Dr. Paul Farmer’s work in Haiti. Really exemplifies that one person can change lives.
Q: How many Apple products (phones, iPods, tablets, iTunes, etc.) do you interface with in a given week?
A: I’ve been infiltrated with Apples. My iPhone seldom leaves my hand. I use an iPad for notes and to chart. I run three miles a day with my iPod. I own two Macs.
Q: What’s next in your Netflix queue?
A: I have a six- and a seven-year-old, so anything with animation. Last great movie I saw was “Silver Linings Playbook.”
Richard Quinn is a freelance writer in New Jersey.
Growing up in America’s heartland, Julie Fedderson, MD, realized at an early age that something wasn’t right with the U.S. healthcare system. Her grandmother, a “headstrong” immigrant from the Czech Republic, died of colon cancer when Dr. Fedderson was young, and that experience—watching a loved one “reduced to tears” trying to navigate a complicated and impersonal healthcare system in rural Nebraska—made her realize “how important having dedicated physicians is.”
“It may sound naïve, but I really wanted to help people,” says Dr. Fedderson, who grew up and went to high school in a small town two hours from an urban center. She eventually attended college in what she saw as the big city—Lincoln, Nebraska. After attending the University of Nebraska, Dr. Fedderson went to medical school at the University of Nebraska Medical School (UNMC) in Omaha. She did her residency at Baylor College of Medicine in Houston, then returned to Nebraska.
Since 2003, she has worked as a hospitalist and is currently an assistant professor in the department of internal medicine at the UNMC. Her story, practicing as a “traditional” internist for several years before making the switch to HM, is similar to many in hospital medicine.
“I wanted to make an impact on the seamless transition of in-house care to outpatient care,” says one of the newest members of Team Hospitalist, the volunteer editorial advisory board of The Hospitalist. “The two are so intricately intertwined, yet so siloed, and many times the patient—who is the least capable of navigating our complex systems—is the one who is left with the responsibility to do it. I wanted to improve that.”
Dr. Fedderson is working toward her master’s degree from the University of Colorado’s Executive MBA Program. She is the resident supervisor for UNMC’s Physicians Midtown Clinic, serves as the Nebraska Medical Center’s enterprise chief quality and outcomes officer, and is on the board of directors of Nebraska Health Partners. She is also a member of the department of internal medicine’s executive committee.
Question: What do you like most about working as a hospitalist?
Answer: The ability to implement rapid change of process in a controlled environment.
Q: What do you dislike most?
A: The regulatory ties placed on hospitals that may not be quality oriented [and] the difficulty of handling the outpatient care of uninsured or underinsured patients.
Q: What’s the best advice you ever received?
A: For life: Shut up and listen. From one of my attendings during my residency: Piss, pus, and hostility all must come out eventually.
Q: What’s the biggest change you’ve seen in hospital medicine in your career?
A: The shift to technology as a basis of care. When done well, it is phenomenal. When done without appropriate thought, it can be disastrous for patients and providers alike.
Q: Why is it important for you, as a hospitalist group leader, to continue seeing patients?
A: How do you implement change if you have no skin in the game? I stay current and see patients to see the system work firsthand and to provide innovative—but practical—solutions.
Q: Outside of patient care, what are your career interests?
A: I am currently our new chief quality and outcomes officer at The Nebraska Medical Center Enterprise. I am also involved as a physician champion for our electronic health record [EHR] implementation and in clinical documentation improvement at all levels.
Q: What is your biggest professional challenge?
A: There are a lot of daunting things coming from entities that don’t necessarily have a patient’s best interests at heart. Keeping sane doing the “regulatory” quality while still providing good quality care is a challenge. Sometimes it feels like a game—but obviously a game with serious consequences.
Q: What is your biggest professional reward?
A: Frankly, [it is] when one of my colleagues relates to me a success story with a new process or plan. I hear so many of my medical friends so dissatisfied with healthcare’s trajectory—they’re burned out, telling their kids to not go into medicine. When I see someone get that spark back for their career and their reason for choosing it, that makes me feel fantastic.
Q: When you aren’t working, what is important to you?
A: I have two boys, and they hung the moon. We hang out as much as possible. I am also into physical fitness, so I try to run, do yoga, and hike as much as I can.
Q: Where do you see yourself in 10 years?
A: I would like to continue to be a chief quality officer, potentially for an entire healthcare system.
Q: If you weren’t a doctor, what would you be doing right now?
A: Writing romance novels.
Q: What’s the best book you’ve read recently? Why?
A: “Mountains Beyond Mountains” by Tracy Kidder. It’s about Dr. Paul Farmer’s work in Haiti. Really exemplifies that one person can change lives.
Q: How many Apple products (phones, iPods, tablets, iTunes, etc.) do you interface with in a given week?
A: I’ve been infiltrated with Apples. My iPhone seldom leaves my hand. I use an iPad for notes and to chart. I run three miles a day with my iPod. I own two Macs.
Q: What’s next in your Netflix queue?
A: I have a six- and a seven-year-old, so anything with animation. Last great movie I saw was “Silver Linings Playbook.”
Richard Quinn is a freelance writer in New Jersey.