User login
Drug Abuse Follows a Broken Heart
ANSWER
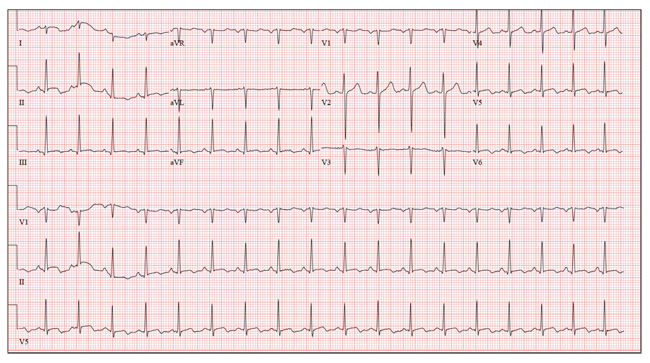
This ECG shows sinus tachycardia at a rate of 110 beats/min, evidenced by the presence of a P wave for every QRS complex with regular R-R intervals. Left atrial enlargement is evident from the presence of P waves ≥ 110 ms (admittedly difficult to see in this example) and a terminal negativity of the P wave in lead V1 ≥ 1 mm2. A rightward axis is evidenced by the presence of an R-wave axis of 96°; however, it does not meet criteria for a true right-axis deviation
(≥ 105°). Nonspecific T-wave abnormalities are observed in leads V5 and V6.
The most intriguing aspect of this ECG is observed in lead V3. Note the abrupt disruption of R-wave progression between leads V2 and V4. This was due to incorrect placement of the ECG electrode for V3, which occurred in the haste to obtain the ECG prior to the CT scan. This illustrates the importance of correct electrode placement for an accurate tracing.
ANSWER
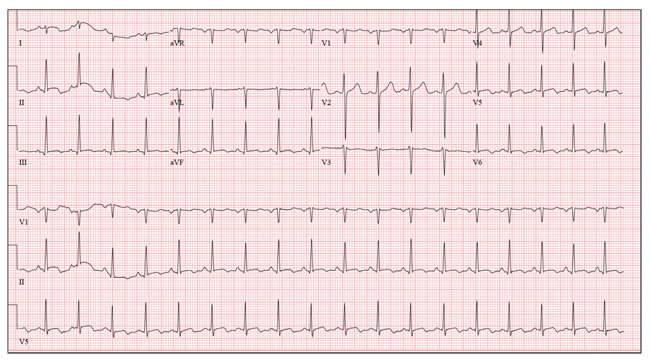
This ECG shows sinus tachycardia at a rate of 110 beats/min, evidenced by the presence of a P wave for every QRS complex with regular R-R intervals. Left atrial enlargement is evident from the presence of P waves ≥ 110 ms (admittedly difficult to see in this example) and a terminal negativity of the P wave in lead V1 ≥ 1 mm2. A rightward axis is evidenced by the presence of an R-wave axis of 96°; however, it does not meet criteria for a true right-axis deviation
(≥ 105°). Nonspecific T-wave abnormalities are observed in leads V5 and V6.
The most intriguing aspect of this ECG is observed in lead V3. Note the abrupt disruption of R-wave progression between leads V2 and V4. This was due to incorrect placement of the ECG electrode for V3, which occurred in the haste to obtain the ECG prior to the CT scan. This illustrates the importance of correct electrode placement for an accurate tracing.
ANSWER
This ECG shows sinus tachycardia at a rate of 110 beats/min, evidenced by the presence of a P wave for every QRS complex with regular R-R intervals. Left atrial enlargement is evident from the presence of P waves ≥ 110 ms (admittedly difficult to see in this example) and a terminal negativity of the P wave in lead V1 ≥ 1 mm2. A rightward axis is evidenced by the presence of an R-wave axis of 96°; however, it does not meet criteria for a true right-axis deviation
(≥ 105°). Nonspecific T-wave abnormalities are observed in leads V5 and V6.
The most intriguing aspect of this ECG is observed in lead V3. Note the abrupt disruption of R-wave progression between leads V2 and V4. This was due to incorrect placement of the ECG electrode for V3, which occurred in the haste to obtain the ECG prior to the CT scan. This illustrates the importance of correct electrode placement for an accurate tracing.
A 26-year-old man is brought to the emergency department (ED) by three friends who hadn’t seen him for two days and went to his apartment to check on him. They found him unconscious on the floor with four empty syringes on the coffee table beside him. The patient was aroused with difficulty but remained incoherent. Rather than call 911, they carried him to their car and brought him to the ED. According to his friends, he has been an IV drug abuser since breaking up with his girlfriend two years ago. He has been increasingly despondent over the past few days after seeing her with anoth-er man. The friends state that they know he has used heroin, cocaine, marijuana, and methamphet-amines in the past, but do not know what he used on this occasion. He has not had any prior illnesses, surgical procedures, or medical conditions that they are aware of. They do not know whether the patient is taking any prescription medications, nor whether he is aller-gic to any medications. According to one of the friends, the patient works with him as a welder at a local factory. He states the patient has been absent from work since last seeing his ex-girlfriend. You are unable to obtain a review of systems. A cursory examination reveals a thin, disheveled male who is unconscious but arousable. Blood pressure is 102/62 mm Hg, and pulse, 110 beats/min. Res-pirations are shallow at a rate of 20 breaths/min-1. Examination of the skin is remarkable for multiple recent and mature needle tracks in both upper ex-tremities, as well as multiple excoriations and shallow ulcers on both lower extremities. The EENT exam is remarkable for constricted pupils that react to light. Corneal reflexes are intact. The teeth are in poor repair with multiple caries and missing teeth. The neck veins are not distended, the thyroid is normal, and there are palpable lymph nodes in the left anterior cervical chain. The lungs have diffuse, scattered dry rales. The cardiac exam reveals a regular rate at 110 beats/min with a soft, early systolic murmur best heard at the left upper sternal border. A rub is also present. Peripheral pulses are equal bilaterally in both upper and lower extremities. The abdomen is soft and nontender. The liver edge is palpable 2 cm below the right costal margin, and a firm spleen is palpable on the left. The neurologic exam reveals hyperactive deep tendon re-flexes in all four extremities. Laboratory samples are drawn; results are positive for cocaine, cannabis, and methamphetamine. Stat blood cultures are positive for Staphylococcus aureus, and the white blood count is 21,000/μL. A bedside echocardiogram performed in the ED shows evidence of a pericardial effusion and a perivalvular abscess on the septal side of the mitral valve, consistent with endocarditis. Prior to the patient’s transport to radiology for a CT scan, a quick ECG is performed. It reveals a ven-tricular rate of 110 beats/min; PR interval, 130 ms; QRS duration, 76 ms; QT/QTc interval, 352/476 ms; P axis, 59°; R axis, 96°; and T axis, 106°. What is your interpretation of this ECG?
Wife Wants Husband’s “Zits” Gone!
ANSWER
The correct answer is dilated pore of Winer (choice “b”), a hair structure anomaly discussed below. Sebaceous cysts (choice “a”) often present with a surface punctum, but the depth and appearance of this pore are not consistent with a simple punctum. The same could be said of the other two choices: ice-pick scar secondary to acne (choice “c”) and ingrown hair (choice “d”).
DISCUSSION
Dilated pore of Winer is actually a tumor of the intraepidermal follicle and related infundibulum of the pilosebaceous apparatus, a fact confirmed by immunohistochemical studies. It has no implication for health, but its appearance is occasionally distressing. Unfortunately, this patient has matching dilated pores on either side of his nose.
These scar-like pits are most commonly seen on the face, especially the maxillae. Even though they resemble one another, dilated pore of Winer differs significantly from a simple comedone: The former is considerably deeper, as well as markedly different in structure.
TREATMENT
The only effective treatment for dilated pore of Winer is surgical excision, which is easily accomplished under local anesthesia. A 4- to 5-mm punch biopsy tool is introduced into the skin at the same angle as the course of the pore, then taken down to adipose tissue, which ensures complete removal. Two interrupted skin sutures serve to convert the round punch defect into a linear wound, preferably matching skin tension lines. The tissue thus removed is always sent for pathologic examination to rule out basal cell carcinoma.
But for the vast majority of patients affected by dilated pore of Winer, the best treatment is to leave the lesions alone.
ANSWER
The correct answer is dilated pore of Winer (choice “b”), a hair structure anomaly discussed below. Sebaceous cysts (choice “a”) often present with a surface punctum, but the depth and appearance of this pore are not consistent with a simple punctum. The same could be said of the other two choices: ice-pick scar secondary to acne (choice “c”) and ingrown hair (choice “d”).
DISCUSSION
Dilated pore of Winer is actually a tumor of the intraepidermal follicle and related infundibulum of the pilosebaceous apparatus, a fact confirmed by immunohistochemical studies. It has no implication for health, but its appearance is occasionally distressing. Unfortunately, this patient has matching dilated pores on either side of his nose.
These scar-like pits are most commonly seen on the face, especially the maxillae. Even though they resemble one another, dilated pore of Winer differs significantly from a simple comedone: The former is considerably deeper, as well as markedly different in structure.
TREATMENT
The only effective treatment for dilated pore of Winer is surgical excision, which is easily accomplished under local anesthesia. A 4- to 5-mm punch biopsy tool is introduced into the skin at the same angle as the course of the pore, then taken down to adipose tissue, which ensures complete removal. Two interrupted skin sutures serve to convert the round punch defect into a linear wound, preferably matching skin tension lines. The tissue thus removed is always sent for pathologic examination to rule out basal cell carcinoma.
But for the vast majority of patients affected by dilated pore of Winer, the best treatment is to leave the lesions alone.
ANSWER
The correct answer is dilated pore of Winer (choice “b”), a hair structure anomaly discussed below. Sebaceous cysts (choice “a”) often present with a surface punctum, but the depth and appearance of this pore are not consistent with a simple punctum. The same could be said of the other two choices: ice-pick scar secondary to acne (choice “c”) and ingrown hair (choice “d”).
DISCUSSION
Dilated pore of Winer is actually a tumor of the intraepidermal follicle and related infundibulum of the pilosebaceous apparatus, a fact confirmed by immunohistochemical studies. It has no implication for health, but its appearance is occasionally distressing. Unfortunately, this patient has matching dilated pores on either side of his nose.
These scar-like pits are most commonly seen on the face, especially the maxillae. Even though they resemble one another, dilated pore of Winer differs significantly from a simple comedone: The former is considerably deeper, as well as markedly different in structure.
TREATMENT
The only effective treatment for dilated pore of Winer is surgical excision, which is easily accomplished under local anesthesia. A 4- to 5-mm punch biopsy tool is introduced into the skin at the same angle as the course of the pore, then taken down to adipose tissue, which ensures complete removal. Two interrupted skin sutures serve to convert the round punch defect into a linear wound, preferably matching skin tension lines. The tissue thus removed is always sent for pathologic examination to rule out basal cell carcinoma.
But for the vast majority of patients affected by dilated pore of Winer, the best treatment is to leave the lesions alone.

A 52-year-old man self-refers to dermatology, at his wife’s insistence, for evaluation of “big black-heads” that have been present on his maxillae for as long as he can remember. Periodically, he ex-presses cheesy, odoriferous material from them. He denies ever experiencing trauma in the area, and there is no history of other skin problems (eg, acne). His wife wants him to get these “black-heads” removed, because there is “dirt” in them. Small “holes” are seen on each side of the nose, about 3 cm lateral to midline. Each lesion is 2 to 3 mm wide and obviously deep. There is no comedonal material or protruding hair seen in the lesions; the surrounding skin is unchanged. Induration is absent in or around the lesions. No signs of active acne are seen elsewhere.
Hospitalists' Challenge and Opportunity
Can you explain why Dr. Johnson thinks I should be taking antibiotics, while your note says I shouldn't?
Today you may be surprised by such an inquiry during morning rounds, but such questions are likely coming to your wards. At a time of societal fascination both with transparency and the explosion of health information technologies, a growing number of hospitals are offering, or will soon offer, patients and their family instantaneous access to their doctors' and nurses' notes. What will this new opportunity for patient engagement mean for the hospitalist?
BACKGROUND
Helping patients through highly complicated care processes is no easy feat, and enabling patients and their families to deal successfully with a constantly changing scenario is a particular challenge for hospitalists. Multiple studies show how poorly patients recall information offered them in office visits,[1, 2] and such settings are far less stressful than the rapid fire mixture of procedures, multiple medications, and morbid disease processes that take center stage in so many hospitalizations. And now something new: What is in store for patients and their doctors when patients in a hospital room gain access in real time not only to test results, but also to notes written by their hospitalists, nurses, and consultants?
ENGAGING PATIENTS
With the principal goal of promoting more active patient engagement in care, patient portals designed primarily for ambulatory practice are proliferating rapidly. Not only do they offer patients windows into their records and secure ways to communicate with their providers, their goal is also to automate chores such as reporting results or other administrative tasks that take away from valuable face‐to‐face time between providers and patients. First appearing shortly after the dawn of the Internet, secure electronic portals began to offer patients access to much of their chart.[3] Rapidly evolving beyond limited data feeds over very simple connections, portals today share far more data, are spreading rapidly, and in some cases offer patients access to their entire records. Whether or not 1 record can serve all the traditional users and also the patient and family is a fascinating question,[4] but the fact is that patients can now access their records from their computers, and via smartphones and tablets on the go. While lying in hospital beds, they can gain access to their laboratory and test data as the data evolve, and sometimes the patients see the findings well before their busy clinicians. Moreover, family members, other informal caregivers, or a formally designated health care proxy, will access the patient's record as well, whether through documented proxy functions or by informally peering at the patient's tablet.
MEANINGFUL USE INCENTIVES
Today, state and federal government regulations either encourage or require healthcare providers to grant patients access to their clinical information. But despite the rules embedded in the federal Health Insurance Portability and Accountability Act, patients often face time‐consuming obstacles in their quest for access, and many providers view compliance as a burden. We suggest an alternative view. Over time, we anticipate that inviting patients to review their medical record will reduce risk, increase knowledge, foster active engagement, and help them take more control of their care.
With the goal also of reducing medical errors and improving outcomes, the expansion of portals is accompanied by a combination of incentives, and in the future, sanctions, as the Center for Medicare and Medicaid Services (CMS) refines efforts to promote certified electronic health record technologies that focus on meaningful use (MU), which often include patient engagement tools such as portals. In the fall of 2012, CMS announced stage 2 MU objectives, with several having substantial implications for hospitalists and their patients. One calls for providing patients the ability to view online, download and transmit their health information within 4 business days of the information being available to the provider. Rather than an outpatient‐only requirement, it is a practice‐based requirement, and we can soon expect hospitalist data to appear on portals.
INSIGHTS FROM TRANSPARENCY IN PRIMARY CARE
The OpenNotes trial provides clues as to how such practice will affect both patients and providers.[5, 6] The trial included patients and primary care physicians (PCPs) from 3 diverse settings: Beth Israel Deaconess Medical Center (BIDMC), an urban academic health center in Boston, Massachusetts, and affiliated community practices near Boston; Geisinger Health System, a primarily rural integrated health system in Pennsylvania; and adult medicine and human immunodeficiency virus clinics at Harborview Medical Center, a safety net hospital in Seattle, Washington. More than 100 volunteering PCPs invited 20,000 of their patients enrolled in their institution's portals to read their office visit notes over a 1‐year period. Physicianpatient messaging was tracked to examine impact on physician workloads, and patients and physicians were surveyed before and after the intervention.
The experience generated considerable enthusiasm and potential clinical benefits among the patients, with little adverse impact on patients and providers. Of particular relevance for hospitalists, more than 4 in 5 patients read their notes, with more than 70% reporting they understood their medical conditions better and felt more in control of their care, and two‐thirds reported increased adherence to their medicines, a finding both unanticipated and striking. More than 1 in 5 shared their notes with others. And in spite of doctors' worries, few found their notes confusing (2%8% of patients at the 3 sites), worried more (5%8%), or felt offended by their notes (1%2%). At the end of the year‐long intervention, 99% of patients returning surveys recommended that the practice continue.
PCPs reported virtually no impact on their workflow, although about 1 in 3 reported changing their documentation, given the knowledge that their patients might read their notes. Fewer than 5% of physicians reported visits taking more time, whereas 15% to 20% of physicians reported taking longer to write their notes. Approximately 30% of physicians reported changing the content of their notes to address obesity, substance abuse, mental health, or issues concerning malignancies. Of note, physicians were given an opt out function for any note, but they called on this very rarely during the study. And at the end of the year, not 1 PCP chose to discontinue offering patients his or her notes.
The 3 participating institutions felt that the trial was so successful that they decided to expand this practice aggressively. At BIDMC, OpenNotes will soon extend to all clinical departments and include all notes signed in the online record by doctors (including housestaff and fellows), nurses, social workers, physician assistants, clinical pharmacists, nutritionists, and occupational and physical therapists. The only exceptions will be those notes authored primarily by students, and those the clinician chooses to monitor, thereby blinding access to patients.
With stage 2 MU incentives in place, and the patient engagement movement accelerating, such practice will likely spread rapidly nationwide. We expect that more and more patients will be soon able to read all signed notes by hospitalists in real time. But differences abound among outpatients and inpatients, and PCPs and hospitalists, and inpatient notes are vastly different from those describing office visits. How may this change in practice affect hospitalized patients and their clinicians?
IMPLICATIONS FOR HOSPITALISTS
Most inpatients meet their hospitalists for the first time at admission. During their stay, they may encounter many hospitalists, along with multiple specialty consultants, house officers, nurses, and ancillary providers. Moreover, inpatient notes vary widely in their content and context. They may describe the patient tersely, while spelling out both a broad (and frightening) differential diagnosis, along with options for addressing a range of contingencies. Such notes, written during the acute diagnostic and treatment phase of an admission, tend to focus primarily on acute and discrete issues at hand, in contrast to outpatient notes that may take a more comprehensive approach. Moreover, given the enormous burden and acuity of illness today among many hospitalized patients, a large volume of data is generated in a very short period of time. Due both to time constraints and complexity, decisions are made quickly, often without the patient's input. When did you last ask a hospitalized patient if you could order specific blood tests? Unless a major therapeutic change is anticipated, how often are your patients told their results as a matter of course?
As acutely ill patients suddenly experience a life out of their control, how will they and their families respond to new access to a large volume of information? Should hospitalists expect an avalanche of questions, or might the prime impact be a change in the nature of those questions, as patients and their families move from What was the result? to What is the meaning of this result, given my condition? When the patient sees test results and reads consultant notes before the hospitalist has had a chance to review them, how will this impact the process of care and shape the patient's view of the hospitalist? When questions arise, will they discuss them immediately with their hospitalists, might they try to contact the doctor with whom they have an ongoing relationship, or will they wait until discharge to contact their PCPs? One hopes that offering patients ready access to their hospital record will foster trust and facilitate a positive relationship with hospitalists. But notes could also foster confusion and distrust, particularly if patients feel out of the loop and perceive differing opinions among those caring for them.
We anticipate that transparent records will stimulate hospitalists, PCPs, and other caregivers to improve communication throughout the patient's hospital stay. We know that medical errors occur with alarming frequency in all care settings, and unfortunately electronic medical records make it easier to spread erroneous information widely. As providers we are both morally and legally responsible for eliminating such errors, inviting the patient (and family) to review the chart may help prevent mistakes well before an adverse outcome ensues.
OPPORTUNITIES FOR IMPROVED CARE
Open notes will be viewed by many as a disruptive change, and the best strategy for adapting will be to move proactively to create policies that establish clear guidelines. Consider the following strategies:
- Draw on complex provider notes that may include potentially alarming differential diagnoses as an opportunity for engaging and educating the patient and caregiver.
- Try to avoid jargon and wording that patients may find objectionable, such as patient denies, poor historian, or even obese. Instead, use more situational wording, such as the patient was unclear on his history.
- Avoid abbreviations when possible. They are a frequent source of confusion among clinicians, let alone patients.
- When it is likely that a treatment may not succeed or a diagnosis may prove wrong, address contingency plans in your notes. Where possible, express likelihoods in terms consistent with the patient's level of comfort with numbers.
- Teach trainees to review notes with supervisors before signing.
- Explain to patients and families when they may expect to see your notes.
- Try rephrasing some of the technical content of notes. Move from incr. Cr FeNa=Prerenal, 1L IVF, to Due to dehydration (creatinine rising to 1.8, and fena 0.8), will give 1L IV fluids. Although at first blush this seems like more work, short circuiting need for explanation may save the hospitalist or nurse time later on. And clarity may lead to important additional history from the patient, furnishing perhaps insight into how he or she became dehydrated.
- Expect patients to download, copy, paste, and forward your note. Document with this in mind.
- Discuss with providers concerns about potential medicallegal risks and how to address them.
OpenNotes offers a special opportunity for improving the patient experience after leaving the hospital. For example, providing patients and their families with a medication list may be helpful, but a note adding context to medications may drive the reasoning home and prove vitally important, especially for those faced with complex medical regimens who may have poor health literacy.[7] Moreover, though providers are learning to focus on patient and family education during the discharge transition period in the hope of minimizing rehospitalizations, time spent at the bedside may have little impact.[8] Methods to improve patient/family understanding are often time consuming,[9, 10] and time is a luxury hospitalists rarely have. Providing patients full access to their providers' notes may mitigate confusion about salient aspects of the hospitalization or prompt timely questions, thereby facilitating a safe transition home.
Open access to notes should also help hospitalized patients engage a range of individuals well beyond those directly involved in their care. Patients will be increasingly likely to grant access to surrogates, whether through formal or informal mechanisms. Patients and their families may also forward notes to providers in other institutions, an activity that all too often falls between cracks. But such capabilities create both new opportunities and new challenges for hospitalists. On the 1 hand, they may find themselves more often in the difficult position of trying to arbitrate differences of opinion within a family. Alternatively, family members or friends, including health professionals offering informal consultation, may prove invaluable in helping hospitalists and patients agree on a plan of care developed collaboratively by a wide range of individuals.
FUTURE WORK
Opening hospital notes to patients will affect both clinicians and patients, and the hospital medicine community should begin to consider its options:
- Should we establish a formal curriculum designed to help hospitalists compose notes that will intelligently and efficiently engage patients?
- Can we identify best practice techniques for preparing notes that engage patients and families without overwhelming them?
- How can we use such notes to assure respect for the individual needs of patients and their families? How can we best assure maintaining their dignity?
- How can we use open notes to support patient safety? Can they reduce malpractice claims?
- How should we handle unsolicited second opinions initiated by patients and families who shared open notes with providers and others outside the care team?
- Should we encourage hospitals to offer portal access to all patients, including those who may have only a brief, passing relationship with the institution?
- What patient portal functions could best assist patients and families in understanding the content of inpatient notes?
- In the rapidly changing inpatient environment, how should we deal with patient‐initiated requests for corrections and changes to notes?
- Should all hospital notes be opened? Should clinicians be able to hide specific notes? Clinicians worry about medical record access for patients with mental illness; should patients with these or other specified conditions be exempted, and if so, how can one structure such processes openly and honestly?
The inexorable spread of fully open medical records requires rapid and intense intellectual scrutiny. Benefits will accompany risks, and unforeseen consequences are virtually inevitable. But this expression of transparency may soon constitute the standard of care in hospital medicine. We need to shape it carefully so that in inures to the benefit of both our patients and ourselves. Over time, we expect that inviting patients and their families to read notes openly will improve the quality of care and promote patient safety. We should take full advantage of such opportunity.
- , . New prescriptions: how well do patients remember important information? Fam Med. 2011;43(4):254–259.
- . Do physicians tell patients enough about prescription drugs? Do patients think so? Postgrad Med. 1983;74:169–175.
- , , . Early experiences with personal health records. J Am Med Inform Assoc. 2008;15:1–7.
- , , , et al. Open notes: doctors and patients signing on. Ann Intern Med. 2010;153(2):121–125.
- , , , Vodicka E, Darer JD, Dhanireddy S, Elmore JG, Feldman HJ, Lichtenfeld MJ, Oster N, Ralston JD, Ross S, Delbanco T. Inviting patients to read their doctors' notes: patients and doctors look ahead: patient and physician surveys. Ann Intern Med. 2011;155:811–819.
- , , , Darer JD, Elmore JG, Farag N, Feldman HJ, Mejilla R, Ngo L, Ralston JD, Ross SE, Trivedi N, Vodicka E, Leveille SG. Inviting patients to read their doctors' notes: a quasi‐experimental study and a look ahead. Ann Intern Med. 2012;157(7):461–470.
- , , , , . Hospital quality and patient safety competencies: development, description, and recommendations for use. J Hosp Med. 2011;6(9):530–536.
- , , , , , . The relationship between time spent communicating and communication outcomes on a hospital medicine service. J Gen Intern Med. 2012;27(2):185–189.
- , , , , . Is “teach‐back” associated with knowledge retention and hospital readmission in hospitalized heart failure patients? J Cardiovasc Nurs. 2013;28(2):137–146.
- , , ., “They never told us anything”: postdischarge instruction for families of persons with brain injuries. Rehabil Nurs.2001;26(2):48–53.
Can you explain why Dr. Johnson thinks I should be taking antibiotics, while your note says I shouldn't?
Today you may be surprised by such an inquiry during morning rounds, but such questions are likely coming to your wards. At a time of societal fascination both with transparency and the explosion of health information technologies, a growing number of hospitals are offering, or will soon offer, patients and their family instantaneous access to their doctors' and nurses' notes. What will this new opportunity for patient engagement mean for the hospitalist?
BACKGROUND
Helping patients through highly complicated care processes is no easy feat, and enabling patients and their families to deal successfully with a constantly changing scenario is a particular challenge for hospitalists. Multiple studies show how poorly patients recall information offered them in office visits,[1, 2] and such settings are far less stressful than the rapid fire mixture of procedures, multiple medications, and morbid disease processes that take center stage in so many hospitalizations. And now something new: What is in store for patients and their doctors when patients in a hospital room gain access in real time not only to test results, but also to notes written by their hospitalists, nurses, and consultants?
ENGAGING PATIENTS
With the principal goal of promoting more active patient engagement in care, patient portals designed primarily for ambulatory practice are proliferating rapidly. Not only do they offer patients windows into their records and secure ways to communicate with their providers, their goal is also to automate chores such as reporting results or other administrative tasks that take away from valuable face‐to‐face time between providers and patients. First appearing shortly after the dawn of the Internet, secure electronic portals began to offer patients access to much of their chart.[3] Rapidly evolving beyond limited data feeds over very simple connections, portals today share far more data, are spreading rapidly, and in some cases offer patients access to their entire records. Whether or not 1 record can serve all the traditional users and also the patient and family is a fascinating question,[4] but the fact is that patients can now access their records from their computers, and via smartphones and tablets on the go. While lying in hospital beds, they can gain access to their laboratory and test data as the data evolve, and sometimes the patients see the findings well before their busy clinicians. Moreover, family members, other informal caregivers, or a formally designated health care proxy, will access the patient's record as well, whether through documented proxy functions or by informally peering at the patient's tablet.
MEANINGFUL USE INCENTIVES
Today, state and federal government regulations either encourage or require healthcare providers to grant patients access to their clinical information. But despite the rules embedded in the federal Health Insurance Portability and Accountability Act, patients often face time‐consuming obstacles in their quest for access, and many providers view compliance as a burden. We suggest an alternative view. Over time, we anticipate that inviting patients to review their medical record will reduce risk, increase knowledge, foster active engagement, and help them take more control of their care.
With the goal also of reducing medical errors and improving outcomes, the expansion of portals is accompanied by a combination of incentives, and in the future, sanctions, as the Center for Medicare and Medicaid Services (CMS) refines efforts to promote certified electronic health record technologies that focus on meaningful use (MU), which often include patient engagement tools such as portals. In the fall of 2012, CMS announced stage 2 MU objectives, with several having substantial implications for hospitalists and their patients. One calls for providing patients the ability to view online, download and transmit their health information within 4 business days of the information being available to the provider. Rather than an outpatient‐only requirement, it is a practice‐based requirement, and we can soon expect hospitalist data to appear on portals.
INSIGHTS FROM TRANSPARENCY IN PRIMARY CARE
The OpenNotes trial provides clues as to how such practice will affect both patients and providers.[5, 6] The trial included patients and primary care physicians (PCPs) from 3 diverse settings: Beth Israel Deaconess Medical Center (BIDMC), an urban academic health center in Boston, Massachusetts, and affiliated community practices near Boston; Geisinger Health System, a primarily rural integrated health system in Pennsylvania; and adult medicine and human immunodeficiency virus clinics at Harborview Medical Center, a safety net hospital in Seattle, Washington. More than 100 volunteering PCPs invited 20,000 of their patients enrolled in their institution's portals to read their office visit notes over a 1‐year period. Physicianpatient messaging was tracked to examine impact on physician workloads, and patients and physicians were surveyed before and after the intervention.
The experience generated considerable enthusiasm and potential clinical benefits among the patients, with little adverse impact on patients and providers. Of particular relevance for hospitalists, more than 4 in 5 patients read their notes, with more than 70% reporting they understood their medical conditions better and felt more in control of their care, and two‐thirds reported increased adherence to their medicines, a finding both unanticipated and striking. More than 1 in 5 shared their notes with others. And in spite of doctors' worries, few found their notes confusing (2%8% of patients at the 3 sites), worried more (5%8%), or felt offended by their notes (1%2%). At the end of the year‐long intervention, 99% of patients returning surveys recommended that the practice continue.
PCPs reported virtually no impact on their workflow, although about 1 in 3 reported changing their documentation, given the knowledge that their patients might read their notes. Fewer than 5% of physicians reported visits taking more time, whereas 15% to 20% of physicians reported taking longer to write their notes. Approximately 30% of physicians reported changing the content of their notes to address obesity, substance abuse, mental health, or issues concerning malignancies. Of note, physicians were given an opt out function for any note, but they called on this very rarely during the study. And at the end of the year, not 1 PCP chose to discontinue offering patients his or her notes.
The 3 participating institutions felt that the trial was so successful that they decided to expand this practice aggressively. At BIDMC, OpenNotes will soon extend to all clinical departments and include all notes signed in the online record by doctors (including housestaff and fellows), nurses, social workers, physician assistants, clinical pharmacists, nutritionists, and occupational and physical therapists. The only exceptions will be those notes authored primarily by students, and those the clinician chooses to monitor, thereby blinding access to patients.
With stage 2 MU incentives in place, and the patient engagement movement accelerating, such practice will likely spread rapidly nationwide. We expect that more and more patients will be soon able to read all signed notes by hospitalists in real time. But differences abound among outpatients and inpatients, and PCPs and hospitalists, and inpatient notes are vastly different from those describing office visits. How may this change in practice affect hospitalized patients and their clinicians?
IMPLICATIONS FOR HOSPITALISTS
Most inpatients meet their hospitalists for the first time at admission. During their stay, they may encounter many hospitalists, along with multiple specialty consultants, house officers, nurses, and ancillary providers. Moreover, inpatient notes vary widely in their content and context. They may describe the patient tersely, while spelling out both a broad (and frightening) differential diagnosis, along with options for addressing a range of contingencies. Such notes, written during the acute diagnostic and treatment phase of an admission, tend to focus primarily on acute and discrete issues at hand, in contrast to outpatient notes that may take a more comprehensive approach. Moreover, given the enormous burden and acuity of illness today among many hospitalized patients, a large volume of data is generated in a very short period of time. Due both to time constraints and complexity, decisions are made quickly, often without the patient's input. When did you last ask a hospitalized patient if you could order specific blood tests? Unless a major therapeutic change is anticipated, how often are your patients told their results as a matter of course?
As acutely ill patients suddenly experience a life out of their control, how will they and their families respond to new access to a large volume of information? Should hospitalists expect an avalanche of questions, or might the prime impact be a change in the nature of those questions, as patients and their families move from What was the result? to What is the meaning of this result, given my condition? When the patient sees test results and reads consultant notes before the hospitalist has had a chance to review them, how will this impact the process of care and shape the patient's view of the hospitalist? When questions arise, will they discuss them immediately with their hospitalists, might they try to contact the doctor with whom they have an ongoing relationship, or will they wait until discharge to contact their PCPs? One hopes that offering patients ready access to their hospital record will foster trust and facilitate a positive relationship with hospitalists. But notes could also foster confusion and distrust, particularly if patients feel out of the loop and perceive differing opinions among those caring for them.
We anticipate that transparent records will stimulate hospitalists, PCPs, and other caregivers to improve communication throughout the patient's hospital stay. We know that medical errors occur with alarming frequency in all care settings, and unfortunately electronic medical records make it easier to spread erroneous information widely. As providers we are both morally and legally responsible for eliminating such errors, inviting the patient (and family) to review the chart may help prevent mistakes well before an adverse outcome ensues.
OPPORTUNITIES FOR IMPROVED CARE
Open notes will be viewed by many as a disruptive change, and the best strategy for adapting will be to move proactively to create policies that establish clear guidelines. Consider the following strategies:
- Draw on complex provider notes that may include potentially alarming differential diagnoses as an opportunity for engaging and educating the patient and caregiver.
- Try to avoid jargon and wording that patients may find objectionable, such as patient denies, poor historian, or even obese. Instead, use more situational wording, such as the patient was unclear on his history.
- Avoid abbreviations when possible. They are a frequent source of confusion among clinicians, let alone patients.
- When it is likely that a treatment may not succeed or a diagnosis may prove wrong, address contingency plans in your notes. Where possible, express likelihoods in terms consistent with the patient's level of comfort with numbers.
- Teach trainees to review notes with supervisors before signing.
- Explain to patients and families when they may expect to see your notes.
- Try rephrasing some of the technical content of notes. Move from incr. Cr FeNa=Prerenal, 1L IVF, to Due to dehydration (creatinine rising to 1.8, and fena 0.8), will give 1L IV fluids. Although at first blush this seems like more work, short circuiting need for explanation may save the hospitalist or nurse time later on. And clarity may lead to important additional history from the patient, furnishing perhaps insight into how he or she became dehydrated.
- Expect patients to download, copy, paste, and forward your note. Document with this in mind.
- Discuss with providers concerns about potential medicallegal risks and how to address them.
OpenNotes offers a special opportunity for improving the patient experience after leaving the hospital. For example, providing patients and their families with a medication list may be helpful, but a note adding context to medications may drive the reasoning home and prove vitally important, especially for those faced with complex medical regimens who may have poor health literacy.[7] Moreover, though providers are learning to focus on patient and family education during the discharge transition period in the hope of minimizing rehospitalizations, time spent at the bedside may have little impact.[8] Methods to improve patient/family understanding are often time consuming,[9, 10] and time is a luxury hospitalists rarely have. Providing patients full access to their providers' notes may mitigate confusion about salient aspects of the hospitalization or prompt timely questions, thereby facilitating a safe transition home.
Open access to notes should also help hospitalized patients engage a range of individuals well beyond those directly involved in their care. Patients will be increasingly likely to grant access to surrogates, whether through formal or informal mechanisms. Patients and their families may also forward notes to providers in other institutions, an activity that all too often falls between cracks. But such capabilities create both new opportunities and new challenges for hospitalists. On the 1 hand, they may find themselves more often in the difficult position of trying to arbitrate differences of opinion within a family. Alternatively, family members or friends, including health professionals offering informal consultation, may prove invaluable in helping hospitalists and patients agree on a plan of care developed collaboratively by a wide range of individuals.
FUTURE WORK
Opening hospital notes to patients will affect both clinicians and patients, and the hospital medicine community should begin to consider its options:
- Should we establish a formal curriculum designed to help hospitalists compose notes that will intelligently and efficiently engage patients?
- Can we identify best practice techniques for preparing notes that engage patients and families without overwhelming them?
- How can we use such notes to assure respect for the individual needs of patients and their families? How can we best assure maintaining their dignity?
- How can we use open notes to support patient safety? Can they reduce malpractice claims?
- How should we handle unsolicited second opinions initiated by patients and families who shared open notes with providers and others outside the care team?
- Should we encourage hospitals to offer portal access to all patients, including those who may have only a brief, passing relationship with the institution?
- What patient portal functions could best assist patients and families in understanding the content of inpatient notes?
- In the rapidly changing inpatient environment, how should we deal with patient‐initiated requests for corrections and changes to notes?
- Should all hospital notes be opened? Should clinicians be able to hide specific notes? Clinicians worry about medical record access for patients with mental illness; should patients with these or other specified conditions be exempted, and if so, how can one structure such processes openly and honestly?
The inexorable spread of fully open medical records requires rapid and intense intellectual scrutiny. Benefits will accompany risks, and unforeseen consequences are virtually inevitable. But this expression of transparency may soon constitute the standard of care in hospital medicine. We need to shape it carefully so that in inures to the benefit of both our patients and ourselves. Over time, we expect that inviting patients and their families to read notes openly will improve the quality of care and promote patient safety. We should take full advantage of such opportunity.
Can you explain why Dr. Johnson thinks I should be taking antibiotics, while your note says I shouldn't?
Today you may be surprised by such an inquiry during morning rounds, but such questions are likely coming to your wards. At a time of societal fascination both with transparency and the explosion of health information technologies, a growing number of hospitals are offering, or will soon offer, patients and their family instantaneous access to their doctors' and nurses' notes. What will this new opportunity for patient engagement mean for the hospitalist?
BACKGROUND
Helping patients through highly complicated care processes is no easy feat, and enabling patients and their families to deal successfully with a constantly changing scenario is a particular challenge for hospitalists. Multiple studies show how poorly patients recall information offered them in office visits,[1, 2] and such settings are far less stressful than the rapid fire mixture of procedures, multiple medications, and morbid disease processes that take center stage in so many hospitalizations. And now something new: What is in store for patients and their doctors when patients in a hospital room gain access in real time not only to test results, but also to notes written by their hospitalists, nurses, and consultants?
ENGAGING PATIENTS
With the principal goal of promoting more active patient engagement in care, patient portals designed primarily for ambulatory practice are proliferating rapidly. Not only do they offer patients windows into their records and secure ways to communicate with their providers, their goal is also to automate chores such as reporting results or other administrative tasks that take away from valuable face‐to‐face time between providers and patients. First appearing shortly after the dawn of the Internet, secure electronic portals began to offer patients access to much of their chart.[3] Rapidly evolving beyond limited data feeds over very simple connections, portals today share far more data, are spreading rapidly, and in some cases offer patients access to their entire records. Whether or not 1 record can serve all the traditional users and also the patient and family is a fascinating question,[4] but the fact is that patients can now access their records from their computers, and via smartphones and tablets on the go. While lying in hospital beds, they can gain access to their laboratory and test data as the data evolve, and sometimes the patients see the findings well before their busy clinicians. Moreover, family members, other informal caregivers, or a formally designated health care proxy, will access the patient's record as well, whether through documented proxy functions or by informally peering at the patient's tablet.
MEANINGFUL USE INCENTIVES
Today, state and federal government regulations either encourage or require healthcare providers to grant patients access to their clinical information. But despite the rules embedded in the federal Health Insurance Portability and Accountability Act, patients often face time‐consuming obstacles in their quest for access, and many providers view compliance as a burden. We suggest an alternative view. Over time, we anticipate that inviting patients to review their medical record will reduce risk, increase knowledge, foster active engagement, and help them take more control of their care.
With the goal also of reducing medical errors and improving outcomes, the expansion of portals is accompanied by a combination of incentives, and in the future, sanctions, as the Center for Medicare and Medicaid Services (CMS) refines efforts to promote certified electronic health record technologies that focus on meaningful use (MU), which often include patient engagement tools such as portals. In the fall of 2012, CMS announced stage 2 MU objectives, with several having substantial implications for hospitalists and their patients. One calls for providing patients the ability to view online, download and transmit their health information within 4 business days of the information being available to the provider. Rather than an outpatient‐only requirement, it is a practice‐based requirement, and we can soon expect hospitalist data to appear on portals.
INSIGHTS FROM TRANSPARENCY IN PRIMARY CARE
The OpenNotes trial provides clues as to how such practice will affect both patients and providers.[5, 6] The trial included patients and primary care physicians (PCPs) from 3 diverse settings: Beth Israel Deaconess Medical Center (BIDMC), an urban academic health center in Boston, Massachusetts, and affiliated community practices near Boston; Geisinger Health System, a primarily rural integrated health system in Pennsylvania; and adult medicine and human immunodeficiency virus clinics at Harborview Medical Center, a safety net hospital in Seattle, Washington. More than 100 volunteering PCPs invited 20,000 of their patients enrolled in their institution's portals to read their office visit notes over a 1‐year period. Physicianpatient messaging was tracked to examine impact on physician workloads, and patients and physicians were surveyed before and after the intervention.
The experience generated considerable enthusiasm and potential clinical benefits among the patients, with little adverse impact on patients and providers. Of particular relevance for hospitalists, more than 4 in 5 patients read their notes, with more than 70% reporting they understood their medical conditions better and felt more in control of their care, and two‐thirds reported increased adherence to their medicines, a finding both unanticipated and striking. More than 1 in 5 shared their notes with others. And in spite of doctors' worries, few found their notes confusing (2%8% of patients at the 3 sites), worried more (5%8%), or felt offended by their notes (1%2%). At the end of the year‐long intervention, 99% of patients returning surveys recommended that the practice continue.
PCPs reported virtually no impact on their workflow, although about 1 in 3 reported changing their documentation, given the knowledge that their patients might read their notes. Fewer than 5% of physicians reported visits taking more time, whereas 15% to 20% of physicians reported taking longer to write their notes. Approximately 30% of physicians reported changing the content of their notes to address obesity, substance abuse, mental health, or issues concerning malignancies. Of note, physicians were given an opt out function for any note, but they called on this very rarely during the study. And at the end of the year, not 1 PCP chose to discontinue offering patients his or her notes.
The 3 participating institutions felt that the trial was so successful that they decided to expand this practice aggressively. At BIDMC, OpenNotes will soon extend to all clinical departments and include all notes signed in the online record by doctors (including housestaff and fellows), nurses, social workers, physician assistants, clinical pharmacists, nutritionists, and occupational and physical therapists. The only exceptions will be those notes authored primarily by students, and those the clinician chooses to monitor, thereby blinding access to patients.
With stage 2 MU incentives in place, and the patient engagement movement accelerating, such practice will likely spread rapidly nationwide. We expect that more and more patients will be soon able to read all signed notes by hospitalists in real time. But differences abound among outpatients and inpatients, and PCPs and hospitalists, and inpatient notes are vastly different from those describing office visits. How may this change in practice affect hospitalized patients and their clinicians?
IMPLICATIONS FOR HOSPITALISTS
Most inpatients meet their hospitalists for the first time at admission. During their stay, they may encounter many hospitalists, along with multiple specialty consultants, house officers, nurses, and ancillary providers. Moreover, inpatient notes vary widely in their content and context. They may describe the patient tersely, while spelling out both a broad (and frightening) differential diagnosis, along with options for addressing a range of contingencies. Such notes, written during the acute diagnostic and treatment phase of an admission, tend to focus primarily on acute and discrete issues at hand, in contrast to outpatient notes that may take a more comprehensive approach. Moreover, given the enormous burden and acuity of illness today among many hospitalized patients, a large volume of data is generated in a very short period of time. Due both to time constraints and complexity, decisions are made quickly, often without the patient's input. When did you last ask a hospitalized patient if you could order specific blood tests? Unless a major therapeutic change is anticipated, how often are your patients told their results as a matter of course?
As acutely ill patients suddenly experience a life out of their control, how will they and their families respond to new access to a large volume of information? Should hospitalists expect an avalanche of questions, or might the prime impact be a change in the nature of those questions, as patients and their families move from What was the result? to What is the meaning of this result, given my condition? When the patient sees test results and reads consultant notes before the hospitalist has had a chance to review them, how will this impact the process of care and shape the patient's view of the hospitalist? When questions arise, will they discuss them immediately with their hospitalists, might they try to contact the doctor with whom they have an ongoing relationship, or will they wait until discharge to contact their PCPs? One hopes that offering patients ready access to their hospital record will foster trust and facilitate a positive relationship with hospitalists. But notes could also foster confusion and distrust, particularly if patients feel out of the loop and perceive differing opinions among those caring for them.
We anticipate that transparent records will stimulate hospitalists, PCPs, and other caregivers to improve communication throughout the patient's hospital stay. We know that medical errors occur with alarming frequency in all care settings, and unfortunately electronic medical records make it easier to spread erroneous information widely. As providers we are both morally and legally responsible for eliminating such errors, inviting the patient (and family) to review the chart may help prevent mistakes well before an adverse outcome ensues.
OPPORTUNITIES FOR IMPROVED CARE
Open notes will be viewed by many as a disruptive change, and the best strategy for adapting will be to move proactively to create policies that establish clear guidelines. Consider the following strategies:
- Draw on complex provider notes that may include potentially alarming differential diagnoses as an opportunity for engaging and educating the patient and caregiver.
- Try to avoid jargon and wording that patients may find objectionable, such as patient denies, poor historian, or even obese. Instead, use more situational wording, such as the patient was unclear on his history.
- Avoid abbreviations when possible. They are a frequent source of confusion among clinicians, let alone patients.
- When it is likely that a treatment may not succeed or a diagnosis may prove wrong, address contingency plans in your notes. Where possible, express likelihoods in terms consistent with the patient's level of comfort with numbers.
- Teach trainees to review notes with supervisors before signing.
- Explain to patients and families when they may expect to see your notes.
- Try rephrasing some of the technical content of notes. Move from incr. Cr FeNa=Prerenal, 1L IVF, to Due to dehydration (creatinine rising to 1.8, and fena 0.8), will give 1L IV fluids. Although at first blush this seems like more work, short circuiting need for explanation may save the hospitalist or nurse time later on. And clarity may lead to important additional history from the patient, furnishing perhaps insight into how he or she became dehydrated.
- Expect patients to download, copy, paste, and forward your note. Document with this in mind.
- Discuss with providers concerns about potential medicallegal risks and how to address them.
OpenNotes offers a special opportunity for improving the patient experience after leaving the hospital. For example, providing patients and their families with a medication list may be helpful, but a note adding context to medications may drive the reasoning home and prove vitally important, especially for those faced with complex medical regimens who may have poor health literacy.[7] Moreover, though providers are learning to focus on patient and family education during the discharge transition period in the hope of minimizing rehospitalizations, time spent at the bedside may have little impact.[8] Methods to improve patient/family understanding are often time consuming,[9, 10] and time is a luxury hospitalists rarely have. Providing patients full access to their providers' notes may mitigate confusion about salient aspects of the hospitalization or prompt timely questions, thereby facilitating a safe transition home.
Open access to notes should also help hospitalized patients engage a range of individuals well beyond those directly involved in their care. Patients will be increasingly likely to grant access to surrogates, whether through formal or informal mechanisms. Patients and their families may also forward notes to providers in other institutions, an activity that all too often falls between cracks. But such capabilities create both new opportunities and new challenges for hospitalists. On the 1 hand, they may find themselves more often in the difficult position of trying to arbitrate differences of opinion within a family. Alternatively, family members or friends, including health professionals offering informal consultation, may prove invaluable in helping hospitalists and patients agree on a plan of care developed collaboratively by a wide range of individuals.
FUTURE WORK
Opening hospital notes to patients will affect both clinicians and patients, and the hospital medicine community should begin to consider its options:
- Should we establish a formal curriculum designed to help hospitalists compose notes that will intelligently and efficiently engage patients?
- Can we identify best practice techniques for preparing notes that engage patients and families without overwhelming them?
- How can we use such notes to assure respect for the individual needs of patients and their families? How can we best assure maintaining their dignity?
- How can we use open notes to support patient safety? Can they reduce malpractice claims?
- How should we handle unsolicited second opinions initiated by patients and families who shared open notes with providers and others outside the care team?
- Should we encourage hospitals to offer portal access to all patients, including those who may have only a brief, passing relationship with the institution?
- What patient portal functions could best assist patients and families in understanding the content of inpatient notes?
- In the rapidly changing inpatient environment, how should we deal with patient‐initiated requests for corrections and changes to notes?
- Should all hospital notes be opened? Should clinicians be able to hide specific notes? Clinicians worry about medical record access for patients with mental illness; should patients with these or other specified conditions be exempted, and if so, how can one structure such processes openly and honestly?
The inexorable spread of fully open medical records requires rapid and intense intellectual scrutiny. Benefits will accompany risks, and unforeseen consequences are virtually inevitable. But this expression of transparency may soon constitute the standard of care in hospital medicine. We need to shape it carefully so that in inures to the benefit of both our patients and ourselves. Over time, we expect that inviting patients and their families to read notes openly will improve the quality of care and promote patient safety. We should take full advantage of such opportunity.
- , . New prescriptions: how well do patients remember important information? Fam Med. 2011;43(4):254–259.
- . Do physicians tell patients enough about prescription drugs? Do patients think so? Postgrad Med. 1983;74:169–175.
- , , . Early experiences with personal health records. J Am Med Inform Assoc. 2008;15:1–7.
- , , , et al. Open notes: doctors and patients signing on. Ann Intern Med. 2010;153(2):121–125.
- , , , Vodicka E, Darer JD, Dhanireddy S, Elmore JG, Feldman HJ, Lichtenfeld MJ, Oster N, Ralston JD, Ross S, Delbanco T. Inviting patients to read their doctors' notes: patients and doctors look ahead: patient and physician surveys. Ann Intern Med. 2011;155:811–819.
- , , , Darer JD, Elmore JG, Farag N, Feldman HJ, Mejilla R, Ngo L, Ralston JD, Ross SE, Trivedi N, Vodicka E, Leveille SG. Inviting patients to read their doctors' notes: a quasi‐experimental study and a look ahead. Ann Intern Med. 2012;157(7):461–470.
- , , , , . Hospital quality and patient safety competencies: development, description, and recommendations for use. J Hosp Med. 2011;6(9):530–536.
- , , , , , . The relationship between time spent communicating and communication outcomes on a hospital medicine service. J Gen Intern Med. 2012;27(2):185–189.
- , , , , . Is “teach‐back” associated with knowledge retention and hospital readmission in hospitalized heart failure patients? J Cardiovasc Nurs. 2013;28(2):137–146.
- , , ., “They never told us anything”: postdischarge instruction for families of persons with brain injuries. Rehabil Nurs.2001;26(2):48–53.
- , . New prescriptions: how well do patients remember important information? Fam Med. 2011;43(4):254–259.
- . Do physicians tell patients enough about prescription drugs? Do patients think so? Postgrad Med. 1983;74:169–175.
- , , . Early experiences with personal health records. J Am Med Inform Assoc. 2008;15:1–7.
- , , , et al. Open notes: doctors and patients signing on. Ann Intern Med. 2010;153(2):121–125.
- , , , Vodicka E, Darer JD, Dhanireddy S, Elmore JG, Feldman HJ, Lichtenfeld MJ, Oster N, Ralston JD, Ross S, Delbanco T. Inviting patients to read their doctors' notes: patients and doctors look ahead: patient and physician surveys. Ann Intern Med. 2011;155:811–819.
- , , , Darer JD, Elmore JG, Farag N, Feldman HJ, Mejilla R, Ngo L, Ralston JD, Ross SE, Trivedi N, Vodicka E, Leveille SG. Inviting patients to read their doctors' notes: a quasi‐experimental study and a look ahead. Ann Intern Med. 2012;157(7):461–470.
- , , , , . Hospital quality and patient safety competencies: development, description, and recommendations for use. J Hosp Med. 2011;6(9):530–536.
- , , , , , . The relationship between time spent communicating and communication outcomes on a hospital medicine service. J Gen Intern Med. 2012;27(2):185–189.
- , , , , . Is “teach‐back” associated with knowledge retention and hospital readmission in hospitalized heart failure patients? J Cardiovasc Nurs. 2013;28(2):137–146.
- , , ., “They never told us anything”: postdischarge instruction for families of persons with brain injuries. Rehabil Nurs.2001;26(2):48–53.
Cardiotoxicity of chemotherapeutic agents
The successful treatment of cancer with chemotherapeutic agents has led to a new set of cardiac problems related to their acute and chronic cardiac toxicity. It should not be surprising that drugs that impact so potently on intrinsic cell function and energy production to cause tumor cell death also impact on other systems, including the heart. An unfortunate by-product of the success of adjuvant therapy has been development of cardiomyocyte dysfunction and death and the development of heart failure.
Current estimates indicate that cardiovascular disease has become a competing comortality risk in women undergoing cancer chemotherapy. Cohort studies indicate that breast cancer patients who have undergone chemotherapy are at an increased cardiovascular mortality risk, compared with age matched controls. The National Cancer Institute and the Centers for Disease Control and Prevention estimate that there are more than 10 million cancer survivors in the United States and that 60% of adults newly diagnosed with cancer will be alive 5 or more years later. Many of these survivors will have significant heart failure as a result of their "successful" chemotherapy (J. Clin. Oncol. 2007;25:3991-4008).
Most of these survivors will have been treated either acutely or chronically with anthracycline drugs (such as doxorubicin), drugs directed at HER2 monoclonal antibodies (trastuzumab), or endocrine-like drugs (tamoxifen). Treatment protocols vary widely and have focused primarily on the acute, chronic, and recurrent therapy for tumor eradication with limited regard – until recently – for the acute or chronic cardiotoxic effects of the drugs. The precise incidence of cardiac toxicity is poorly understood since there are very few long-term follow-up data regarding cardiac morbidity and mortality. In these long-term survivors, cardiovascular mortality will be the predominant cause of death in women over age 60 treated for breast cancer (Circulation 2012;126:2749-63). It is estimated that half of the patients treated with anthracyclines will exhibit some cardiac dysfunction within 10-20 years and 5% will develop overt heart failure.
The mechanism by which cardiac dysfunction occurs varies depending upon the drug used. Anthracycline drugs cause ultrastructural cell changes, vacuolar degeneration, myofibrillar loss, and apoptosis. This change can be observed during early administration but may manifest years later, seemingly without any early evidence of dysfunction. Trastuzumab causes cardiac function as a result of deletion of HER2, which is essential for cardiomyocyte survival and stress adaptation. Tamoxifen-like drugs can lead to the acceleration of typical cardiac risk factors. Interaction of any of these classes of drugs when used in combination for recurrent or resistant disease can accelerate the occurrence of cardiac pathology.
The degree of adverse acute and chronic cardiac effects is related to the dose and duration of therapy. Early recognition of cardiac toxicity appears to be critical in order to mitigate the toxic drug effects. Clinical data suggest that early administration of ACE inhibitors or beta-blockers may limit or reverse cardiac dysfunction (Circulation 2006;114:2474-81). The measurement of LVEF has been used to identify early cardiac dysfunction. A symptomatic decrease in LVEF from 5% to 55% or an asymptomatic decrease of 10% is considered to be diagnostic of cardiac toxicity. Serum troponin I of greater than 0.08% also has been reported to increase the occurrence of cardiac toxicity 24-fold. Recent studies suggest that measurement of myocardial contractile velocity and strain and rate of strain by tissue Doppler imaging may provide earlier identification of myocardial dysfunction than that achieved with LVEF alone (Circulation 2012;126:2749-63).
The increased development of heart failure as a result of cancer chemotherapy has largely slipped under the cardiologist’s radar. The recent awareness of the adverse cardiac effect of these agents has generated investigation into the development of early and more sensitive biological markers and methods of mitigating cell dysfunction with concomitant medical therapy.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
The successful treatment of cancer with chemotherapeutic agents has led to a new set of cardiac problems related to their acute and chronic cardiac toxicity. It should not be surprising that drugs that impact so potently on intrinsic cell function and energy production to cause tumor cell death also impact on other systems, including the heart. An unfortunate by-product of the success of adjuvant therapy has been development of cardiomyocyte dysfunction and death and the development of heart failure.
Current estimates indicate that cardiovascular disease has become a competing comortality risk in women undergoing cancer chemotherapy. Cohort studies indicate that breast cancer patients who have undergone chemotherapy are at an increased cardiovascular mortality risk, compared with age matched controls. The National Cancer Institute and the Centers for Disease Control and Prevention estimate that there are more than 10 million cancer survivors in the United States and that 60% of adults newly diagnosed with cancer will be alive 5 or more years later. Many of these survivors will have significant heart failure as a result of their "successful" chemotherapy (J. Clin. Oncol. 2007;25:3991-4008).
Most of these survivors will have been treated either acutely or chronically with anthracycline drugs (such as doxorubicin), drugs directed at HER2 monoclonal antibodies (trastuzumab), or endocrine-like drugs (tamoxifen). Treatment protocols vary widely and have focused primarily on the acute, chronic, and recurrent therapy for tumor eradication with limited regard – until recently – for the acute or chronic cardiotoxic effects of the drugs. The precise incidence of cardiac toxicity is poorly understood since there are very few long-term follow-up data regarding cardiac morbidity and mortality. In these long-term survivors, cardiovascular mortality will be the predominant cause of death in women over age 60 treated for breast cancer (Circulation 2012;126:2749-63). It is estimated that half of the patients treated with anthracyclines will exhibit some cardiac dysfunction within 10-20 years and 5% will develop overt heart failure.
The mechanism by which cardiac dysfunction occurs varies depending upon the drug used. Anthracycline drugs cause ultrastructural cell changes, vacuolar degeneration, myofibrillar loss, and apoptosis. This change can be observed during early administration but may manifest years later, seemingly without any early evidence of dysfunction. Trastuzumab causes cardiac function as a result of deletion of HER2, which is essential for cardiomyocyte survival and stress adaptation. Tamoxifen-like drugs can lead to the acceleration of typical cardiac risk factors. Interaction of any of these classes of drugs when used in combination for recurrent or resistant disease can accelerate the occurrence of cardiac pathology.
The degree of adverse acute and chronic cardiac effects is related to the dose and duration of therapy. Early recognition of cardiac toxicity appears to be critical in order to mitigate the toxic drug effects. Clinical data suggest that early administration of ACE inhibitors or beta-blockers may limit or reverse cardiac dysfunction (Circulation 2006;114:2474-81). The measurement of LVEF has been used to identify early cardiac dysfunction. A symptomatic decrease in LVEF from 5% to 55% or an asymptomatic decrease of 10% is considered to be diagnostic of cardiac toxicity. Serum troponin I of greater than 0.08% also has been reported to increase the occurrence of cardiac toxicity 24-fold. Recent studies suggest that measurement of myocardial contractile velocity and strain and rate of strain by tissue Doppler imaging may provide earlier identification of myocardial dysfunction than that achieved with LVEF alone (Circulation 2012;126:2749-63).
The increased development of heart failure as a result of cancer chemotherapy has largely slipped under the cardiologist’s radar. The recent awareness of the adverse cardiac effect of these agents has generated investigation into the development of early and more sensitive biological markers and methods of mitigating cell dysfunction with concomitant medical therapy.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
The successful treatment of cancer with chemotherapeutic agents has led to a new set of cardiac problems related to their acute and chronic cardiac toxicity. It should not be surprising that drugs that impact so potently on intrinsic cell function and energy production to cause tumor cell death also impact on other systems, including the heart. An unfortunate by-product of the success of adjuvant therapy has been development of cardiomyocyte dysfunction and death and the development of heart failure.
Current estimates indicate that cardiovascular disease has become a competing comortality risk in women undergoing cancer chemotherapy. Cohort studies indicate that breast cancer patients who have undergone chemotherapy are at an increased cardiovascular mortality risk, compared with age matched controls. The National Cancer Institute and the Centers for Disease Control and Prevention estimate that there are more than 10 million cancer survivors in the United States and that 60% of adults newly diagnosed with cancer will be alive 5 or more years later. Many of these survivors will have significant heart failure as a result of their "successful" chemotherapy (J. Clin. Oncol. 2007;25:3991-4008).
Most of these survivors will have been treated either acutely or chronically with anthracycline drugs (such as doxorubicin), drugs directed at HER2 monoclonal antibodies (trastuzumab), or endocrine-like drugs (tamoxifen). Treatment protocols vary widely and have focused primarily on the acute, chronic, and recurrent therapy for tumor eradication with limited regard – until recently – for the acute or chronic cardiotoxic effects of the drugs. The precise incidence of cardiac toxicity is poorly understood since there are very few long-term follow-up data regarding cardiac morbidity and mortality. In these long-term survivors, cardiovascular mortality will be the predominant cause of death in women over age 60 treated for breast cancer (Circulation 2012;126:2749-63). It is estimated that half of the patients treated with anthracyclines will exhibit some cardiac dysfunction within 10-20 years and 5% will develop overt heart failure.
The mechanism by which cardiac dysfunction occurs varies depending upon the drug used. Anthracycline drugs cause ultrastructural cell changes, vacuolar degeneration, myofibrillar loss, and apoptosis. This change can be observed during early administration but may manifest years later, seemingly without any early evidence of dysfunction. Trastuzumab causes cardiac function as a result of deletion of HER2, which is essential for cardiomyocyte survival and stress adaptation. Tamoxifen-like drugs can lead to the acceleration of typical cardiac risk factors. Interaction of any of these classes of drugs when used in combination for recurrent or resistant disease can accelerate the occurrence of cardiac pathology.
The degree of adverse acute and chronic cardiac effects is related to the dose and duration of therapy. Early recognition of cardiac toxicity appears to be critical in order to mitigate the toxic drug effects. Clinical data suggest that early administration of ACE inhibitors or beta-blockers may limit or reverse cardiac dysfunction (Circulation 2006;114:2474-81). The measurement of LVEF has been used to identify early cardiac dysfunction. A symptomatic decrease in LVEF from 5% to 55% or an asymptomatic decrease of 10% is considered to be diagnostic of cardiac toxicity. Serum troponin I of greater than 0.08% also has been reported to increase the occurrence of cardiac toxicity 24-fold. Recent studies suggest that measurement of myocardial contractile velocity and strain and rate of strain by tissue Doppler imaging may provide earlier identification of myocardial dysfunction than that achieved with LVEF alone (Circulation 2012;126:2749-63).
The increased development of heart failure as a result of cancer chemotherapy has largely slipped under the cardiologist’s radar. The recent awareness of the adverse cardiac effect of these agents has generated investigation into the development of early and more sensitive biological markers and methods of mitigating cell dysfunction with concomitant medical therapy.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
The Biologic Holy Grail: Will It Ever Be Found?
The problem is not new. A routine arthroscopic knee surgery is performed and an isolated Grade 4 cartilage is seen. So what is a surgeon to do? Certainly one could easily perform a microfracture but is the patient going to accept the often-prescribed 6 weeks of limited weight-bearing? Other options do exist, but once again, not all patients are accepting of a more invasive procedure with a prolonged rehabilitation period.
We thought we had an answer in the mid 1990s with the popularization of autologous chondrocyte transplantations (Carticel; Genzyme Corp, a Sanofi company, Cambridge, Massachusetts). There was a sense of excitement and theorthopedic community went biopsy crazy. Mandatory training was required, initially in Gothenburg, Sweden, and a new dawn of cartilage restoration was born. This excitement spilled over into other forms of cartilage treatments including Osteochondral Autograft Transfer Systems (OATS), with improved instrumentation and more options for the treatment of these cartilage lesions. This time period was the Renaissance Period of cartilage restoration: a period of excitement that led to the establishment of the International Cartilage Repair Society.
But as cartilage restoration became more popular, so did the amount of obstacles surgeons would encounter to be able to perform these procedures. Because of a paucity of literature describing the efficacy of these procedures, insurance companies were quick to describe the procedures as experimental, often refusing to approve the procedures or denying claims once performed.
While good results were eventually reported, some limitations remained. The procedure was expensive, two procedures, including an open arthrotomy was required, rehabilitation was slow and a high reoperation rate was reported. In addition, while this procedure is still being performed, it falls short of being the ultimate answer to isolated cartilage lesions of the knee.
What is the ideal method of cartilage repair? In a perfect world, all patients would be consented to routine arthroscopy and cartilage procedures as indicated (Figure 1). If an isolated lesion is seen, then the method of repair should be not only efficacious but should be performed arthroscopically, an off the shelf option, that can be performed at the same time as the diagnostic arthroscopy.
Over the last several years, we have seen a resurgence in cartilage restoration biologic options. DeNovo juvenile cartilage (Zimmer Inc, Warsaw, Indiana) has been introduced but does have its limitations. It is juvenile allograft cartilage that is prepared with a fibrin glue and placed currently as a second procedure. The lesion is seen at the time of diagnostic arthroscopy, lesion is sized, and how much of the cartilage to order is determined. Limits include not only the cost, but also the requirement of a second procedure, an arthrotomy, and lets not forget the need to bone graft the defect bed if significant subchondral bone loss has occurred.
Another recent advancement is the use of allograft cartilage plugs, Chondrofix, (Zimmer Inc) (Figures 2A, 2B). These are human allograft osteochondral plugs, irradiated for safety, have a long shelf life, and can be available as needed. Due to the radiation, the cartilage plugs may be disease-free, have been FDA approved, but there is a lack of long-term studies not only demonstrating efficacy but also long-term durability. Perhaps we are approaching the Holy Grail with biologic products such as this, but long-term acceptance will not occur until proper long-term studies are performed. Cost will remain an issue as well, since it is quite easy to place 3 to 4 plugs at one sitting and approach implant costs as high as a revision knee implant (Figure 3).
I am sad to say that the Holy Grail for biologic restoration of isolated cartilage lesions has yet to be found. We still do not have the perfect method for cartilage restoration at this time. While new attempts to restore cartilage remain in the pipeline, we must move away from pure animal studies, case reports, white papers, and small surgeon experience. Randomized controlled studies are needed to test these biologic advances, and finally find the ideal treatment for these isolated cartilage defects. We owe it to our patients to finally find the ideal treatment for these cartilage lesions.
Dr. Cushner is Editorial Review Board member of the journal; Chief of Orthopedics, Southside Hospital, Bay Shore, New York; and Director, Insall Scott Kelly, New York, New York.
Author’s Disclosure Statement: The author wishes to report that he will be a Speaker Bureau for Zimmer, Inc.
Am J Orthop. 2013;42(5):206-207. Copyright Frontline Medical Communications Inc. 2013. All rights reserved.
The problem is not new. A routine arthroscopic knee surgery is performed and an isolated Grade 4 cartilage is seen. So what is a surgeon to do? Certainly one could easily perform a microfracture but is the patient going to accept the often-prescribed 6 weeks of limited weight-bearing? Other options do exist, but once again, not all patients are accepting of a more invasive procedure with a prolonged rehabilitation period.
We thought we had an answer in the mid 1990s with the popularization of autologous chondrocyte transplantations (Carticel; Genzyme Corp, a Sanofi company, Cambridge, Massachusetts). There was a sense of excitement and theorthopedic community went biopsy crazy. Mandatory training was required, initially in Gothenburg, Sweden, and a new dawn of cartilage restoration was born. This excitement spilled over into other forms of cartilage treatments including Osteochondral Autograft Transfer Systems (OATS), with improved instrumentation and more options for the treatment of these cartilage lesions. This time period was the Renaissance Period of cartilage restoration: a period of excitement that led to the establishment of the International Cartilage Repair Society.
But as cartilage restoration became more popular, so did the amount of obstacles surgeons would encounter to be able to perform these procedures. Because of a paucity of literature describing the efficacy of these procedures, insurance companies were quick to describe the procedures as experimental, often refusing to approve the procedures or denying claims once performed.
While good results were eventually reported, some limitations remained. The procedure was expensive, two procedures, including an open arthrotomy was required, rehabilitation was slow and a high reoperation rate was reported. In addition, while this procedure is still being performed, it falls short of being the ultimate answer to isolated cartilage lesions of the knee.
What is the ideal method of cartilage repair? In a perfect world, all patients would be consented to routine arthroscopy and cartilage procedures as indicated (Figure 1). If an isolated lesion is seen, then the method of repair should be not only efficacious but should be performed arthroscopically, an off the shelf option, that can be performed at the same time as the diagnostic arthroscopy.
Over the last several years, we have seen a resurgence in cartilage restoration biologic options. DeNovo juvenile cartilage (Zimmer Inc, Warsaw, Indiana) has been introduced but does have its limitations. It is juvenile allograft cartilage that is prepared with a fibrin glue and placed currently as a second procedure. The lesion is seen at the time of diagnostic arthroscopy, lesion is sized, and how much of the cartilage to order is determined. Limits include not only the cost, but also the requirement of a second procedure, an arthrotomy, and lets not forget the need to bone graft the defect bed if significant subchondral bone loss has occurred.
Another recent advancement is the use of allograft cartilage plugs, Chondrofix, (Zimmer Inc) (Figures 2A, 2B). These are human allograft osteochondral plugs, irradiated for safety, have a long shelf life, and can be available as needed. Due to the radiation, the cartilage plugs may be disease-free, have been FDA approved, but there is a lack of long-term studies not only demonstrating efficacy but also long-term durability. Perhaps we are approaching the Holy Grail with biologic products such as this, but long-term acceptance will not occur until proper long-term studies are performed. Cost will remain an issue as well, since it is quite easy to place 3 to 4 plugs at one sitting and approach implant costs as high as a revision knee implant (Figure 3).
I am sad to say that the Holy Grail for biologic restoration of isolated cartilage lesions has yet to be found. We still do not have the perfect method for cartilage restoration at this time. While new attempts to restore cartilage remain in the pipeline, we must move away from pure animal studies, case reports, white papers, and small surgeon experience. Randomized controlled studies are needed to test these biologic advances, and finally find the ideal treatment for these isolated cartilage defects. We owe it to our patients to finally find the ideal treatment for these cartilage lesions.
Dr. Cushner is Editorial Review Board member of the journal; Chief of Orthopedics, Southside Hospital, Bay Shore, New York; and Director, Insall Scott Kelly, New York, New York.
Author’s Disclosure Statement: The author wishes to report that he will be a Speaker Bureau for Zimmer, Inc.
Am J Orthop. 2013;42(5):206-207. Copyright Frontline Medical Communications Inc. 2013. All rights reserved.
The problem is not new. A routine arthroscopic knee surgery is performed and an isolated Grade 4 cartilage is seen. So what is a surgeon to do? Certainly one could easily perform a microfracture but is the patient going to accept the often-prescribed 6 weeks of limited weight-bearing? Other options do exist, but once again, not all patients are accepting of a more invasive procedure with a prolonged rehabilitation period.
We thought we had an answer in the mid 1990s with the popularization of autologous chondrocyte transplantations (Carticel; Genzyme Corp, a Sanofi company, Cambridge, Massachusetts). There was a sense of excitement and theorthopedic community went biopsy crazy. Mandatory training was required, initially in Gothenburg, Sweden, and a new dawn of cartilage restoration was born. This excitement spilled over into other forms of cartilage treatments including Osteochondral Autograft Transfer Systems (OATS), with improved instrumentation and more options for the treatment of these cartilage lesions. This time period was the Renaissance Period of cartilage restoration: a period of excitement that led to the establishment of the International Cartilage Repair Society.
But as cartilage restoration became more popular, so did the amount of obstacles surgeons would encounter to be able to perform these procedures. Because of a paucity of literature describing the efficacy of these procedures, insurance companies were quick to describe the procedures as experimental, often refusing to approve the procedures or denying claims once performed.
While good results were eventually reported, some limitations remained. The procedure was expensive, two procedures, including an open arthrotomy was required, rehabilitation was slow and a high reoperation rate was reported. In addition, while this procedure is still being performed, it falls short of being the ultimate answer to isolated cartilage lesions of the knee.
What is the ideal method of cartilage repair? In a perfect world, all patients would be consented to routine arthroscopy and cartilage procedures as indicated (Figure 1). If an isolated lesion is seen, then the method of repair should be not only efficacious but should be performed arthroscopically, an off the shelf option, that can be performed at the same time as the diagnostic arthroscopy.
Over the last several years, we have seen a resurgence in cartilage restoration biologic options. DeNovo juvenile cartilage (Zimmer Inc, Warsaw, Indiana) has been introduced but does have its limitations. It is juvenile allograft cartilage that is prepared with a fibrin glue and placed currently as a second procedure. The lesion is seen at the time of diagnostic arthroscopy, lesion is sized, and how much of the cartilage to order is determined. Limits include not only the cost, but also the requirement of a second procedure, an arthrotomy, and lets not forget the need to bone graft the defect bed if significant subchondral bone loss has occurred.
Another recent advancement is the use of allograft cartilage plugs, Chondrofix, (Zimmer Inc) (Figures 2A, 2B). These are human allograft osteochondral plugs, irradiated for safety, have a long shelf life, and can be available as needed. Due to the radiation, the cartilage plugs may be disease-free, have been FDA approved, but there is a lack of long-term studies not only demonstrating efficacy but also long-term durability. Perhaps we are approaching the Holy Grail with biologic products such as this, but long-term acceptance will not occur until proper long-term studies are performed. Cost will remain an issue as well, since it is quite easy to place 3 to 4 plugs at one sitting and approach implant costs as high as a revision knee implant (Figure 3).
I am sad to say that the Holy Grail for biologic restoration of isolated cartilage lesions has yet to be found. We still do not have the perfect method for cartilage restoration at this time. While new attempts to restore cartilage remain in the pipeline, we must move away from pure animal studies, case reports, white papers, and small surgeon experience. Randomized controlled studies are needed to test these biologic advances, and finally find the ideal treatment for these isolated cartilage defects. We owe it to our patients to finally find the ideal treatment for these cartilage lesions.
Dr. Cushner is Editorial Review Board member of the journal; Chief of Orthopedics, Southside Hospital, Bay Shore, New York; and Director, Insall Scott Kelly, New York, New York.
Author’s Disclosure Statement: The author wishes to report that he will be a Speaker Bureau for Zimmer, Inc.
Am J Orthop. 2013;42(5):206-207. Copyright Frontline Medical Communications Inc. 2013. All rights reserved.
Four pillars of a successful practice: 3. Obtain and maintain physician referrals
READ THE REST OF THE SERIES
Pillar 1: Keep your current patients happy (March 2013)
Dr. Baum describes his number one strategy to retain patients (Audiocast, March 2013)
Pillar 2: Attract new patients (May 2013)
Pillar 4: Motivate your staff (August 2013)
Discussions of medical marketing often begin with the three As: availability, affability, and affordability. But most physicians already think of themselves as available, likeable, and offering appropriately priced services.
How do you differentiate yourself from the competition?
Fancy stationery; a slick, three-color brochure; a catchy logo; and a Web site will not do the trick. In fact, these are the last things you need.
One of the biggest misconceptions about marketing is that, to do it well, you must spend lots of money on peripherals. In truth, there are many other actions that are far more effective and essential to marketing than merely polishing your public relations image. The most essential element of your marketing plan is to make your practice user-friendly.
Nowhere is this need greater than when it comes to working with colleagues who are capable of referring patients to you—or are already doing so. In this article, I describe 10 strategies you can use to enhance your relationships with referring physicians.
1. WRITE AN EFFECTIVE REFERRAL LETTER
To obtain referrals from your colleagues, you need to ensure that your name crosses their mind and desk as frequently as possible—and in a positive fashion.
If you interview referring physicians, you will find that prompt communication is one of the most important reasons they refer a patient to a particular provider. According to the Annals of Family Medicine, more than 50% of physicians state that effective communication is the reason they select a doctor for referral (TABLE).1
| How primary care physicians select a doctor for referral | |
| Medical skill of the specialist | 87.5% |
| Access to the practice and acceptance of insurance | 59.0% |
| Previous experience with the specialist | 59.2% |
| Quality of communication | 52.5% |
| Board certification of the specialist | 33.9% |
| Medical school, residency | <1% |
Source: Kinchen et al1
Keep your referral letter short
The traditional referral letter is far too long, often 2 or 3 pages. It usually arrives 10 to 14 days after the patient was seen and is very expensive, costing a practice $12–$15 for each letter sent. The goal of an effective referral letter: Get it there before the patient returns to the primary care provider.
The key ingredients of an effective referral letter are:
diagnosis
medications you have prescribed for the patient
your treatment plan.
The referring doctor is not interested in the nuances of your history or physical exam. They just want the three ingredients listed above.
For example, let’s say that Dr. Bill Smith refers Jane Doe, who has an overactive bladder and cystocele. Her urinalysis is negative, so you prescribe an anticholinergic agent and schedule a follow-up visit in 1 month to check symptoms and to conduct a urodynamic study if she has not improved. Your letter to Dr. Smith would read as follows:
Now the letter can be faxed to the referring doctor, often before the patient leaves the office. That way you can be certain that the letter arrives before the patient calls the physician with questions or concerns.
This is the best way to keep the referring physician informed and to function as the captain of the patient’s health-care ship.
EHRs can smooth the referral process
Most electronic health records (EHRs) have the capability to fax the entire note to the referring physician. However, if you were to ask a referring physician if she would like to read your entire note, the answer would probably be “No.” Most EHRs will allow you to select fields that contain the diagnosis, medications prescribed, and the treatment plan. A sample of this kind of letter appears in the FIGURE.
2. MAKE AN EFFORT TO PERSONALLY MEET EVERY PHYSICIAN WHO REFERS A PATIENT
Not only that, but try to meet all new physicians in your area. It is important to coddle your existing sources of referrals, but don’t forget to reach out to new physicians to let them know about your areas of interest or expertise.
3. REFER YOUR NEW PATIENTS TO REFERRING PHYSICIANS
Don’t refer to the same colleagues time after time. If a doctor starts sending new patients your way, it’s in your best interest to “reverse-refer” when a patient needs a primary care doctor, endocrinologist, or cardiologist.
You can be sure these referring doctors will appreciate your recommendations.
Related Article Complex atypical endometrial hyperplasia: When to refer
4. CREATE A LUNCH-AND-LEARN PROGRAM
You want other offices and medical staffs to get to know your staff and to be familiar with what you do. There’s no better way than to create a lunch-and-learn program in your office and extend an invitation to other offices in the area. At the program, have all of the staff members introduce themselves. Provide a tour of your office and give a 3- to 5-minute lecture on areas of your gynecologic interest and expertise.
5. ACKNOWLEDGE THE ACCOMPLISHMENTS OF REFERRING PHYSICIANS AND THEIR FAMILIES
If you see that one of your referring physicians has received an honor or award, send him a congratulatory note. If her children have been recognized for academic or athletic achievement, acknowledge this accomplishment with a note. You can be sure it will be one of the only acknowledgments they receive and will be deeply appreciated.
6. SHARE INFORMATION WITH A NO-MEETING JOURNAL CLUB
It’s very difficult to keep up with the medical literature. It’s challenging enough to keep up with the literature in your own specialty, let alone articles appearing in other specialty publications. One of the nicest gestures you can make is to copy any article that may be of interest to your colleagues and send it to them. Include a sticky note indicating where you would like them to look so that they don’t have to read the entire article.
7. SHARE NONMEDICAL INFORMATION, TOO
Your colleagues will appreciate it when you share nonmedical information to let them know you are thinking of them even when you are not discussing patient care. For example, one of my colleagues collects fine pens. When I saw an article about a very expensive pen made with diamonds, I sent the story to my friend, suggesting that he tell his wife what was on his wish list.
8. KEEP THE REFERRING DOCTOR IN THE MEDICAL LOOP
If you are caring for a patient and plan to discharge her from the hospital, make sure that you or someone in your office contacts the referring doctor to inform him that the patient is being discharged so he doesn’t make unnecessary rounds. Other times to notify the referring doctor:
upon admission of her patient to the hospital
after surgery or a procedure
when you receive a significant laboratory or pathology report.
9. BE USER-FRIENDLY
If you perform gynecologic surgery on a referred patient, be sure to dictate a discharge summary. If the patient is to be discharged with gynecologic medications, give the patient their names in writing. Another convenience for the patient: Arrange your follow-up appointment on the same day she is to return to see the referring physician.
10. DON’T FORGET NONPHYSICIAN REFERRAL SOURCES
Nurses, pharmacists, pharmaceutical representatives, social workers, lawyers, beauticians, and manicurists—all of these professionals are likely to refer patients to you if you keep them in the loop.
11. BOTTOM LINE
You can build a practice by word of mouth by doing a great job of caring for patients, hoping that they will tell others about their positive experience. However, there are other opportunities to enhance your practice—notably, by nurturing your relationship with referring physicians. Try a few of these ideas and you will certainly see your referrals increase significantly.
READ THE REST OF THE SERIES
Pillar 1: Keep your current patients happy (March 2013)
Dr. Baum describes his number one strategy to retain patients (Audiocast, March 2013)
Pillar 2: Attract new patients (May 2013)
Pillar 4: Motivate your staff (August 2013)
Discussions of medical marketing often begin with the three As: availability, affability, and affordability. But most physicians already think of themselves as available, likeable, and offering appropriately priced services.
How do you differentiate yourself from the competition?
Fancy stationery; a slick, three-color brochure; a catchy logo; and a Web site will not do the trick. In fact, these are the last things you need.
One of the biggest misconceptions about marketing is that, to do it well, you must spend lots of money on peripherals. In truth, there are many other actions that are far more effective and essential to marketing than merely polishing your public relations image. The most essential element of your marketing plan is to make your practice user-friendly.
Nowhere is this need greater than when it comes to working with colleagues who are capable of referring patients to you—or are already doing so. In this article, I describe 10 strategies you can use to enhance your relationships with referring physicians.
1. WRITE AN EFFECTIVE REFERRAL LETTER
To obtain referrals from your colleagues, you need to ensure that your name crosses their mind and desk as frequently as possible—and in a positive fashion.
If you interview referring physicians, you will find that prompt communication is one of the most important reasons they refer a patient to a particular provider. According to the Annals of Family Medicine, more than 50% of physicians state that effective communication is the reason they select a doctor for referral (TABLE).1
| How primary care physicians select a doctor for referral | |
| Medical skill of the specialist | 87.5% |
| Access to the practice and acceptance of insurance | 59.0% |
| Previous experience with the specialist | 59.2% |
| Quality of communication | 52.5% |
| Board certification of the specialist | 33.9% |
| Medical school, residency | <1% |
Source: Kinchen et al1
Keep your referral letter short
The traditional referral letter is far too long, often 2 or 3 pages. It usually arrives 10 to 14 days after the patient was seen and is very expensive, costing a practice $12–$15 for each letter sent. The goal of an effective referral letter: Get it there before the patient returns to the primary care provider.
The key ingredients of an effective referral letter are:
diagnosis
medications you have prescribed for the patient
your treatment plan.
The referring doctor is not interested in the nuances of your history or physical exam. They just want the three ingredients listed above.
For example, let’s say that Dr. Bill Smith refers Jane Doe, who has an overactive bladder and cystocele. Her urinalysis is negative, so you prescribe an anticholinergic agent and schedule a follow-up visit in 1 month to check symptoms and to conduct a urodynamic study if she has not improved. Your letter to Dr. Smith would read as follows:
Now the letter can be faxed to the referring doctor, often before the patient leaves the office. That way you can be certain that the letter arrives before the patient calls the physician with questions or concerns.
This is the best way to keep the referring physician informed and to function as the captain of the patient’s health-care ship.
EHRs can smooth the referral process
Most electronic health records (EHRs) have the capability to fax the entire note to the referring physician. However, if you were to ask a referring physician if she would like to read your entire note, the answer would probably be “No.” Most EHRs will allow you to select fields that contain the diagnosis, medications prescribed, and the treatment plan. A sample of this kind of letter appears in the FIGURE.
2. MAKE AN EFFORT TO PERSONALLY MEET EVERY PHYSICIAN WHO REFERS A PATIENT
Not only that, but try to meet all new physicians in your area. It is important to coddle your existing sources of referrals, but don’t forget to reach out to new physicians to let them know about your areas of interest or expertise.
3. REFER YOUR NEW PATIENTS TO REFERRING PHYSICIANS
Don’t refer to the same colleagues time after time. If a doctor starts sending new patients your way, it’s in your best interest to “reverse-refer” when a patient needs a primary care doctor, endocrinologist, or cardiologist.
You can be sure these referring doctors will appreciate your recommendations.
Related Article Complex atypical endometrial hyperplasia: When to refer
4. CREATE A LUNCH-AND-LEARN PROGRAM
You want other offices and medical staffs to get to know your staff and to be familiar with what you do. There’s no better way than to create a lunch-and-learn program in your office and extend an invitation to other offices in the area. At the program, have all of the staff members introduce themselves. Provide a tour of your office and give a 3- to 5-minute lecture on areas of your gynecologic interest and expertise.
5. ACKNOWLEDGE THE ACCOMPLISHMENTS OF REFERRING PHYSICIANS AND THEIR FAMILIES
If you see that one of your referring physicians has received an honor or award, send him a congratulatory note. If her children have been recognized for academic or athletic achievement, acknowledge this accomplishment with a note. You can be sure it will be one of the only acknowledgments they receive and will be deeply appreciated.
6. SHARE INFORMATION WITH A NO-MEETING JOURNAL CLUB
It’s very difficult to keep up with the medical literature. It’s challenging enough to keep up with the literature in your own specialty, let alone articles appearing in other specialty publications. One of the nicest gestures you can make is to copy any article that may be of interest to your colleagues and send it to them. Include a sticky note indicating where you would like them to look so that they don’t have to read the entire article.
7. SHARE NONMEDICAL INFORMATION, TOO
Your colleagues will appreciate it when you share nonmedical information to let them know you are thinking of them even when you are not discussing patient care. For example, one of my colleagues collects fine pens. When I saw an article about a very expensive pen made with diamonds, I sent the story to my friend, suggesting that he tell his wife what was on his wish list.
8. KEEP THE REFERRING DOCTOR IN THE MEDICAL LOOP
If you are caring for a patient and plan to discharge her from the hospital, make sure that you or someone in your office contacts the referring doctor to inform him that the patient is being discharged so he doesn’t make unnecessary rounds. Other times to notify the referring doctor:
upon admission of her patient to the hospital
after surgery or a procedure
when you receive a significant laboratory or pathology report.
9. BE USER-FRIENDLY
If you perform gynecologic surgery on a referred patient, be sure to dictate a discharge summary. If the patient is to be discharged with gynecologic medications, give the patient their names in writing. Another convenience for the patient: Arrange your follow-up appointment on the same day she is to return to see the referring physician.
10. DON’T FORGET NONPHYSICIAN REFERRAL SOURCES
Nurses, pharmacists, pharmaceutical representatives, social workers, lawyers, beauticians, and manicurists—all of these professionals are likely to refer patients to you if you keep them in the loop.
11. BOTTOM LINE
You can build a practice by word of mouth by doing a great job of caring for patients, hoping that they will tell others about their positive experience. However, there are other opportunities to enhance your practice—notably, by nurturing your relationship with referring physicians. Try a few of these ideas and you will certainly see your referrals increase significantly.
READ THE REST OF THE SERIES
Pillar 1: Keep your current patients happy (March 2013)
Dr. Baum describes his number one strategy to retain patients (Audiocast, March 2013)
Pillar 2: Attract new patients (May 2013)
Pillar 4: Motivate your staff (August 2013)
Discussions of medical marketing often begin with the three As: availability, affability, and affordability. But most physicians already think of themselves as available, likeable, and offering appropriately priced services.
How do you differentiate yourself from the competition?
Fancy stationery; a slick, three-color brochure; a catchy logo; and a Web site will not do the trick. In fact, these are the last things you need.
One of the biggest misconceptions about marketing is that, to do it well, you must spend lots of money on peripherals. In truth, there are many other actions that are far more effective and essential to marketing than merely polishing your public relations image. The most essential element of your marketing plan is to make your practice user-friendly.
Nowhere is this need greater than when it comes to working with colleagues who are capable of referring patients to you—or are already doing so. In this article, I describe 10 strategies you can use to enhance your relationships with referring physicians.
1. WRITE AN EFFECTIVE REFERRAL LETTER
To obtain referrals from your colleagues, you need to ensure that your name crosses their mind and desk as frequently as possible—and in a positive fashion.
If you interview referring physicians, you will find that prompt communication is one of the most important reasons they refer a patient to a particular provider. According to the Annals of Family Medicine, more than 50% of physicians state that effective communication is the reason they select a doctor for referral (TABLE).1
| How primary care physicians select a doctor for referral | |
| Medical skill of the specialist | 87.5% |
| Access to the practice and acceptance of insurance | 59.0% |
| Previous experience with the specialist | 59.2% |
| Quality of communication | 52.5% |
| Board certification of the specialist | 33.9% |
| Medical school, residency | <1% |
Source: Kinchen et al1
Keep your referral letter short
The traditional referral letter is far too long, often 2 or 3 pages. It usually arrives 10 to 14 days after the patient was seen and is very expensive, costing a practice $12–$15 for each letter sent. The goal of an effective referral letter: Get it there before the patient returns to the primary care provider.
The key ingredients of an effective referral letter are:
diagnosis
medications you have prescribed for the patient
your treatment plan.
The referring doctor is not interested in the nuances of your history or physical exam. They just want the three ingredients listed above.
For example, let’s say that Dr. Bill Smith refers Jane Doe, who has an overactive bladder and cystocele. Her urinalysis is negative, so you prescribe an anticholinergic agent and schedule a follow-up visit in 1 month to check symptoms and to conduct a urodynamic study if she has not improved. Your letter to Dr. Smith would read as follows:
Now the letter can be faxed to the referring doctor, often before the patient leaves the office. That way you can be certain that the letter arrives before the patient calls the physician with questions or concerns.
This is the best way to keep the referring physician informed and to function as the captain of the patient’s health-care ship.
EHRs can smooth the referral process
Most electronic health records (EHRs) have the capability to fax the entire note to the referring physician. However, if you were to ask a referring physician if she would like to read your entire note, the answer would probably be “No.” Most EHRs will allow you to select fields that contain the diagnosis, medications prescribed, and the treatment plan. A sample of this kind of letter appears in the FIGURE.
2. MAKE AN EFFORT TO PERSONALLY MEET EVERY PHYSICIAN WHO REFERS A PATIENT
Not only that, but try to meet all new physicians in your area. It is important to coddle your existing sources of referrals, but don’t forget to reach out to new physicians to let them know about your areas of interest or expertise.
3. REFER YOUR NEW PATIENTS TO REFERRING PHYSICIANS
Don’t refer to the same colleagues time after time. If a doctor starts sending new patients your way, it’s in your best interest to “reverse-refer” when a patient needs a primary care doctor, endocrinologist, or cardiologist.
You can be sure these referring doctors will appreciate your recommendations.
Related Article Complex atypical endometrial hyperplasia: When to refer
4. CREATE A LUNCH-AND-LEARN PROGRAM
You want other offices and medical staffs to get to know your staff and to be familiar with what you do. There’s no better way than to create a lunch-and-learn program in your office and extend an invitation to other offices in the area. At the program, have all of the staff members introduce themselves. Provide a tour of your office and give a 3- to 5-minute lecture on areas of your gynecologic interest and expertise.
5. ACKNOWLEDGE THE ACCOMPLISHMENTS OF REFERRING PHYSICIANS AND THEIR FAMILIES
If you see that one of your referring physicians has received an honor or award, send him a congratulatory note. If her children have been recognized for academic or athletic achievement, acknowledge this accomplishment with a note. You can be sure it will be one of the only acknowledgments they receive and will be deeply appreciated.
6. SHARE INFORMATION WITH A NO-MEETING JOURNAL CLUB
It’s very difficult to keep up with the medical literature. It’s challenging enough to keep up with the literature in your own specialty, let alone articles appearing in other specialty publications. One of the nicest gestures you can make is to copy any article that may be of interest to your colleagues and send it to them. Include a sticky note indicating where you would like them to look so that they don’t have to read the entire article.
7. SHARE NONMEDICAL INFORMATION, TOO
Your colleagues will appreciate it when you share nonmedical information to let them know you are thinking of them even when you are not discussing patient care. For example, one of my colleagues collects fine pens. When I saw an article about a very expensive pen made with diamonds, I sent the story to my friend, suggesting that he tell his wife what was on his wish list.
8. KEEP THE REFERRING DOCTOR IN THE MEDICAL LOOP
If you are caring for a patient and plan to discharge her from the hospital, make sure that you or someone in your office contacts the referring doctor to inform him that the patient is being discharged so he doesn’t make unnecessary rounds. Other times to notify the referring doctor:
upon admission of her patient to the hospital
after surgery or a procedure
when you receive a significant laboratory or pathology report.
9. BE USER-FRIENDLY
If you perform gynecologic surgery on a referred patient, be sure to dictate a discharge summary. If the patient is to be discharged with gynecologic medications, give the patient their names in writing. Another convenience for the patient: Arrange your follow-up appointment on the same day she is to return to see the referring physician.
10. DON’T FORGET NONPHYSICIAN REFERRAL SOURCES
Nurses, pharmacists, pharmaceutical representatives, social workers, lawyers, beauticians, and manicurists—all of these professionals are likely to refer patients to you if you keep them in the loop.
11. BOTTOM LINE
You can build a practice by word of mouth by doing a great job of caring for patients, hoping that they will tell others about their positive experience. However, there are other opportunities to enhance your practice—notably, by nurturing your relationship with referring physicians. Try a few of these ideas and you will certainly see your referrals increase significantly.
Grassroots Efforts to Improve Patient Care
When it joined with 15 other medical specialty societies at a Feb. 21 press conference to announce updates to the ABIM Foundation’s Choosing Wisely campaign to combat cost and waste reduction in healthcare , SHM leaders said they hoped the hospitalist-focused quality guidelines would trickle down from the national level to clinicians in the field (see “Stop! Think Twice Before You Order"). The lists of treatments adult and pediatric hospitalists should consider questioning in the absence of evidence or protocols include the urinary catheters, blood transfusions, telemetry monitoring outside of the ICU, and certain lab tests and medications for preventing stress ulcers.
Ian Jenkins, MD, a hospitalist at the University of California, San Diego, who presented during both Choosing Wisely sessions, said hospitalists are at the intersection of healthcare cost and quality improvement. “People recognize the moral imperatives,” he said.
Pre-course participants split into four teams and drilled deeper into questionable treatments and practices outlined by the campaign. SHM plans to make results of those small-group discussions available to its members, along with enhanced reference lists and best practices from the field. “We can contribute a bunch of stuff,” Dr. Jenkins told pre-course participants. “Tell us what you can contribute, and what you’d like to see from us.”
Hospitalist George Dimitriou, MD, of Allegheny General Hospital in Pittsburgh, said his hospital has spent the past couple of years working on several of the same hospital-focused quality issues outlined in the Choosing Wisely campaign.
“Our transfusion initiative was driven by the local blood bank, knowing we were over-transfusing,” he said. “We had an order set, but we recently put in place a more restrictive transfusion policy, following national guidelines.
“Our Foley catheter protocol was in response to the national recommendations to reduce urinary tract infections, mostly driven by our infectious disease department,” Dr. Dimitriou added. The hospital has not yet tackled the problem of overuse of telemetry services, “although that’s something I have wanted to do for a long time.”
Another hot-button issue, the daily ordering of lab tests, should be rectified by simply “taking it out of the electronic medical record as a default option.”
According to SHM staff, a Choosing Wisely case study competition will be held next year, with $10,000 in cash prizes awarded for adult and pediatric quality initiatives showing improvement in utilization, innovation, sustainability, and institutional commitment. An independent review panel will develop evaluation criteria, with a projected application deadline of Fall 2014. The competition is supported by a $50,000 grant from the ABIM Foundation. TH
Larry Beresford is a freelance writer in Oakland, Calif.
When it joined with 15 other medical specialty societies at a Feb. 21 press conference to announce updates to the ABIM Foundation’s Choosing Wisely campaign to combat cost and waste reduction in healthcare , SHM leaders said they hoped the hospitalist-focused quality guidelines would trickle down from the national level to clinicians in the field (see “Stop! Think Twice Before You Order"). The lists of treatments adult and pediatric hospitalists should consider questioning in the absence of evidence or protocols include the urinary catheters, blood transfusions, telemetry monitoring outside of the ICU, and certain lab tests and medications for preventing stress ulcers.
Ian Jenkins, MD, a hospitalist at the University of California, San Diego, who presented during both Choosing Wisely sessions, said hospitalists are at the intersection of healthcare cost and quality improvement. “People recognize the moral imperatives,” he said.
Pre-course participants split into four teams and drilled deeper into questionable treatments and practices outlined by the campaign. SHM plans to make results of those small-group discussions available to its members, along with enhanced reference lists and best practices from the field. “We can contribute a bunch of stuff,” Dr. Jenkins told pre-course participants. “Tell us what you can contribute, and what you’d like to see from us.”
Hospitalist George Dimitriou, MD, of Allegheny General Hospital in Pittsburgh, said his hospital has spent the past couple of years working on several of the same hospital-focused quality issues outlined in the Choosing Wisely campaign.
“Our transfusion initiative was driven by the local blood bank, knowing we were over-transfusing,” he said. “We had an order set, but we recently put in place a more restrictive transfusion policy, following national guidelines.
“Our Foley catheter protocol was in response to the national recommendations to reduce urinary tract infections, mostly driven by our infectious disease department,” Dr. Dimitriou added. The hospital has not yet tackled the problem of overuse of telemetry services, “although that’s something I have wanted to do for a long time.”
Another hot-button issue, the daily ordering of lab tests, should be rectified by simply “taking it out of the electronic medical record as a default option.”
According to SHM staff, a Choosing Wisely case study competition will be held next year, with $10,000 in cash prizes awarded for adult and pediatric quality initiatives showing improvement in utilization, innovation, sustainability, and institutional commitment. An independent review panel will develop evaluation criteria, with a projected application deadline of Fall 2014. The competition is supported by a $50,000 grant from the ABIM Foundation. TH
Larry Beresford is a freelance writer in Oakland, Calif.
When it joined with 15 other medical specialty societies at a Feb. 21 press conference to announce updates to the ABIM Foundation’s Choosing Wisely campaign to combat cost and waste reduction in healthcare , SHM leaders said they hoped the hospitalist-focused quality guidelines would trickle down from the national level to clinicians in the field (see “Stop! Think Twice Before You Order"). The lists of treatments adult and pediatric hospitalists should consider questioning in the absence of evidence or protocols include the urinary catheters, blood transfusions, telemetry monitoring outside of the ICU, and certain lab tests and medications for preventing stress ulcers.
Ian Jenkins, MD, a hospitalist at the University of California, San Diego, who presented during both Choosing Wisely sessions, said hospitalists are at the intersection of healthcare cost and quality improvement. “People recognize the moral imperatives,” he said.
Pre-course participants split into four teams and drilled deeper into questionable treatments and practices outlined by the campaign. SHM plans to make results of those small-group discussions available to its members, along with enhanced reference lists and best practices from the field. “We can contribute a bunch of stuff,” Dr. Jenkins told pre-course participants. “Tell us what you can contribute, and what you’d like to see from us.”
Hospitalist George Dimitriou, MD, of Allegheny General Hospital in Pittsburgh, said his hospital has spent the past couple of years working on several of the same hospital-focused quality issues outlined in the Choosing Wisely campaign.
“Our transfusion initiative was driven by the local blood bank, knowing we were over-transfusing,” he said. “We had an order set, but we recently put in place a more restrictive transfusion policy, following national guidelines.
“Our Foley catheter protocol was in response to the national recommendations to reduce urinary tract infections, mostly driven by our infectious disease department,” Dr. Dimitriou added. The hospital has not yet tackled the problem of overuse of telemetry services, “although that’s something I have wanted to do for a long time.”
Another hot-button issue, the daily ordering of lab tests, should be rectified by simply “taking it out of the electronic medical record as a default option.”
According to SHM staff, a Choosing Wisely case study competition will be held next year, with $10,000 in cash prizes awarded for adult and pediatric quality initiatives showing improvement in utilization, innovation, sustainability, and institutional commitment. An independent review panel will develop evaluation criteria, with a projected application deadline of Fall 2014. The competition is supported by a $50,000 grant from the ABIM Foundation. TH
Larry Beresford is a freelance writer in Oakland, Calif.
School nurses
When my children were in school and got head lice, I learned the full metaphorical scope of words like "lousy" and "nit-picking." I also learned that school nurses didn’t give a hoot for my opinions.
Despite my boards in pediatrics and dermatology, my protests against schools’ policies of dragging parents out of work to pick up a kid on whom the nurse found a nit, or thought she did, even after multiple treatments and fine-tooth combing (another nice, real-life metaphor) went unheard.
In vain did I cite policy statements by august professional organizations that no-nit policies were unnecessary. No sir – they find one dead egg case, and Johnny goes home. His parents are obviously irresponsible anyway, not to mention unhygienic. So I gave up, and my children grew up.
What reawakened these memories was my annual visit to Marcie, my eye doctor. "I really like your PA," she said. "Jared saw her when the school nurse sent him home with a rash. Your PA asked him why he was there. ‘The nurse sent me home,’ he said. ‘OK,’ said your PA, ‘now you can go back.’
"They once sent Jared home because of a chalazion," Marcie continued. "I called them up. ‘He’s on tobramycin,’ I told them. ‘And a chalazion isn’t contagious anyway.’ But they didn’t believe me!
"My husband called them. ‘My wife is an eye doctor,’ he said. ‘Oh,’ they said, ‘We didn’t know what kind of doctor she was.’ "
Probably the most egregious example of high-handed school medical behavior I have ever seen played out in my office just last month. The Hightowers brought in 4-year-old Jeffrey with an impetiginized rash. We started cephalexin, pending culture results. When these showed MRSA on Friday afternoon, we called the family to switch Jeffrey to trimethoprim-sulfamethoxazole.
Janice Hightower became very upset. "Should I call the school?" We suggested she use her discretion, because by Monday Jeffrey would no longer be contagious. "But I’m a teacher," she said. "I feel responsible." So she did.
The next day, Jeffrey’s dad, Brian Hightower, came to school to coach baseball (his kids stayed home). During the game, all the parents got text messages informing them: "Someone in the school is infected with MRSA, and school is closed until further notice." He then sat in stunned silence as the other parents commiserated with each other about what happens when their children have to hang around with other kids whose parents are irresponsible, dirty, and a lot of other unpleasant things.
On Monday, Brian Hightower brought Jeffrey’s older brother, Jason, to the office. Jason had no skin lesions at all. "My wife won’t let me go home without antibiotics for him," insisted Brian. We told him there was nothing to treat, and he left. Later, Janice Hightower called. "This is like ‘The Scarlet Letter,’ " she said. "We’ll never be able to show our faces in the community again."
We tried to reassure her (the MRSA culprit’s identity had mercifully not been divulged), but she pressed on. "When he grows up and kisses his first girl," she asked, "will he have to tell her about this?"
Things went downhill from there. Several days and many phone calls later, the Hightowers began to calm down. Jeffrey and Jason returned to school, which had somehow managed to reopen. I have no idea which medical authority authorized the reopening, any more than I know who told them to close it in the first place. Jeffrey hasn’t been sighted kissing any girls yet, other than possibly Aunt Susie.
What this episode says about how people judge and treat others who are ill, not to mention how ancient ideas about disease persist long after they are supposed to have been discarded, doesn’t need to be spelled out. Better to take polite notice and move on.
But it also says quite a lot about the limitations of our professional authority outside the spheres where we’re in charge. In the office, people may or may not listen to us, but at least they act as though they might.
But outside the office, in schools for instance, what we have to say often doesn’t count for much. Or anything.
Dr. Rockoff practices dermatology in Brookline, Mass. To respond to this column, e-mail him at our editorial offices at [email protected].
When my children were in school and got head lice, I learned the full metaphorical scope of words like "lousy" and "nit-picking." I also learned that school nurses didn’t give a hoot for my opinions.
Despite my boards in pediatrics and dermatology, my protests against schools’ policies of dragging parents out of work to pick up a kid on whom the nurse found a nit, or thought she did, even after multiple treatments and fine-tooth combing (another nice, real-life metaphor) went unheard.
In vain did I cite policy statements by august professional organizations that no-nit policies were unnecessary. No sir – they find one dead egg case, and Johnny goes home. His parents are obviously irresponsible anyway, not to mention unhygienic. So I gave up, and my children grew up.
What reawakened these memories was my annual visit to Marcie, my eye doctor. "I really like your PA," she said. "Jared saw her when the school nurse sent him home with a rash. Your PA asked him why he was there. ‘The nurse sent me home,’ he said. ‘OK,’ said your PA, ‘now you can go back.’
"They once sent Jared home because of a chalazion," Marcie continued. "I called them up. ‘He’s on tobramycin,’ I told them. ‘And a chalazion isn’t contagious anyway.’ But they didn’t believe me!
"My husband called them. ‘My wife is an eye doctor,’ he said. ‘Oh,’ they said, ‘We didn’t know what kind of doctor she was.’ "
Probably the most egregious example of high-handed school medical behavior I have ever seen played out in my office just last month. The Hightowers brought in 4-year-old Jeffrey with an impetiginized rash. We started cephalexin, pending culture results. When these showed MRSA on Friday afternoon, we called the family to switch Jeffrey to trimethoprim-sulfamethoxazole.
Janice Hightower became very upset. "Should I call the school?" We suggested she use her discretion, because by Monday Jeffrey would no longer be contagious. "But I’m a teacher," she said. "I feel responsible." So she did.
The next day, Jeffrey’s dad, Brian Hightower, came to school to coach baseball (his kids stayed home). During the game, all the parents got text messages informing them: "Someone in the school is infected with MRSA, and school is closed until further notice." He then sat in stunned silence as the other parents commiserated with each other about what happens when their children have to hang around with other kids whose parents are irresponsible, dirty, and a lot of other unpleasant things.
On Monday, Brian Hightower brought Jeffrey’s older brother, Jason, to the office. Jason had no skin lesions at all. "My wife won’t let me go home without antibiotics for him," insisted Brian. We told him there was nothing to treat, and he left. Later, Janice Hightower called. "This is like ‘The Scarlet Letter,’ " she said. "We’ll never be able to show our faces in the community again."
We tried to reassure her (the MRSA culprit’s identity had mercifully not been divulged), but she pressed on. "When he grows up and kisses his first girl," she asked, "will he have to tell her about this?"
Things went downhill from there. Several days and many phone calls later, the Hightowers began to calm down. Jeffrey and Jason returned to school, which had somehow managed to reopen. I have no idea which medical authority authorized the reopening, any more than I know who told them to close it in the first place. Jeffrey hasn’t been sighted kissing any girls yet, other than possibly Aunt Susie.
What this episode says about how people judge and treat others who are ill, not to mention how ancient ideas about disease persist long after they are supposed to have been discarded, doesn’t need to be spelled out. Better to take polite notice and move on.
But it also says quite a lot about the limitations of our professional authority outside the spheres where we’re in charge. In the office, people may or may not listen to us, but at least they act as though they might.
But outside the office, in schools for instance, what we have to say often doesn’t count for much. Or anything.
Dr. Rockoff practices dermatology in Brookline, Mass. To respond to this column, e-mail him at our editorial offices at [email protected].
When my children were in school and got head lice, I learned the full metaphorical scope of words like "lousy" and "nit-picking." I also learned that school nurses didn’t give a hoot for my opinions.
Despite my boards in pediatrics and dermatology, my protests against schools’ policies of dragging parents out of work to pick up a kid on whom the nurse found a nit, or thought she did, even after multiple treatments and fine-tooth combing (another nice, real-life metaphor) went unheard.
In vain did I cite policy statements by august professional organizations that no-nit policies were unnecessary. No sir – they find one dead egg case, and Johnny goes home. His parents are obviously irresponsible anyway, not to mention unhygienic. So I gave up, and my children grew up.
What reawakened these memories was my annual visit to Marcie, my eye doctor. "I really like your PA," she said. "Jared saw her when the school nurse sent him home with a rash. Your PA asked him why he was there. ‘The nurse sent me home,’ he said. ‘OK,’ said your PA, ‘now you can go back.’
"They once sent Jared home because of a chalazion," Marcie continued. "I called them up. ‘He’s on tobramycin,’ I told them. ‘And a chalazion isn’t contagious anyway.’ But they didn’t believe me!
"My husband called them. ‘My wife is an eye doctor,’ he said. ‘Oh,’ they said, ‘We didn’t know what kind of doctor she was.’ "
Probably the most egregious example of high-handed school medical behavior I have ever seen played out in my office just last month. The Hightowers brought in 4-year-old Jeffrey with an impetiginized rash. We started cephalexin, pending culture results. When these showed MRSA on Friday afternoon, we called the family to switch Jeffrey to trimethoprim-sulfamethoxazole.
Janice Hightower became very upset. "Should I call the school?" We suggested she use her discretion, because by Monday Jeffrey would no longer be contagious. "But I’m a teacher," she said. "I feel responsible." So she did.
The next day, Jeffrey’s dad, Brian Hightower, came to school to coach baseball (his kids stayed home). During the game, all the parents got text messages informing them: "Someone in the school is infected with MRSA, and school is closed until further notice." He then sat in stunned silence as the other parents commiserated with each other about what happens when their children have to hang around with other kids whose parents are irresponsible, dirty, and a lot of other unpleasant things.
On Monday, Brian Hightower brought Jeffrey’s older brother, Jason, to the office. Jason had no skin lesions at all. "My wife won’t let me go home without antibiotics for him," insisted Brian. We told him there was nothing to treat, and he left. Later, Janice Hightower called. "This is like ‘The Scarlet Letter,’ " she said. "We’ll never be able to show our faces in the community again."
We tried to reassure her (the MRSA culprit’s identity had mercifully not been divulged), but she pressed on. "When he grows up and kisses his first girl," she asked, "will he have to tell her about this?"
Things went downhill from there. Several days and many phone calls later, the Hightowers began to calm down. Jeffrey and Jason returned to school, which had somehow managed to reopen. I have no idea which medical authority authorized the reopening, any more than I know who told them to close it in the first place. Jeffrey hasn’t been sighted kissing any girls yet, other than possibly Aunt Susie.
What this episode says about how people judge and treat others who are ill, not to mention how ancient ideas about disease persist long after they are supposed to have been discarded, doesn’t need to be spelled out. Better to take polite notice and move on.
But it also says quite a lot about the limitations of our professional authority outside the spheres where we’re in charge. In the office, people may or may not listen to us, but at least they act as though they might.
But outside the office, in schools for instance, what we have to say often doesn’t count for much. Or anything.
Dr. Rockoff practices dermatology in Brookline, Mass. To respond to this column, e-mail him at our editorial offices at [email protected].