User login
Mounjaro Beats Ozempic, So Why Isn’t It More Popular?
This transcript has been edited for clarity.
It’s July, which means our hospital is filled with new interns, residents, and fellows all eager to embark on a new stage of their career. It’s an exciting time — a bit of a scary time — but it’s also the time when the medical strategies I’ve been taking for granted get called into question. At this point in the year, I tend to get a lot of “why” questions. Why did you order that test? Why did you suspect that diagnosis? Why did you choose that medication?
Meds are the hardest, I find. Sure, I can explain that I prescribed a glucagon-like peptide 1 (GLP-1) receptor agonist because the patient had diabetes and was overweight, and multiple studies show that this class of drug leads to weight loss and reduced mortality risk. But then I get the follow-up: Sure, but why THAT GLP-1 drug? Why did you pick semaglutide (Ozempic) over tirzepatide (Mounjaro)?
Here’s where I run out of good answers. Sometimes I choose a drug because that’s what the patient’s insurance has on their formulary. Sometimes it’s because it’s cheaper in general. Sometimes, it’s just force of habit. I know the correct dose, I have experience with the side effects — it’s comfortable.
What I can’t say is that I have solid evidence that one drug is superior to another, say from a randomized trial of semaglutide vs tirzepatide. I don’t have that evidence because that trial has never happened and, as I’ll explain in a minute, may never happen at all.
But we might have the next best thing. And the results may surprise you.
Why don’t we see more head-to-head trials of competitor drugs? The answer is pretty simple, honestly: risk management. For drugs that are on patent, like the GLP-1s, conducting a trial without the buy-in of the pharmaceutical company is simply too expensive — we can’t run a trial unless someone provides the drug for free. That gives the companies a lot of say in what trials get done, and it seems that most pharma companies have reached the same conclusion: A head-to-head trial is too risky. Be happy with the market share you have, and try to nibble away at the edges through good old-fashioned marketing.
But if you look at the data that are out there, you might wonder why Ozempic is the market leader. I mean, sure, it’s a heck of a weight loss drug. But the weight loss in the trials of Mounjaro was actually a bit higher. It’s worth noting here that tirzepatide (Mounjaro) is not just a GLP-1 receptor agonist; it is also a gastric inhibitory polypeptide agonist. 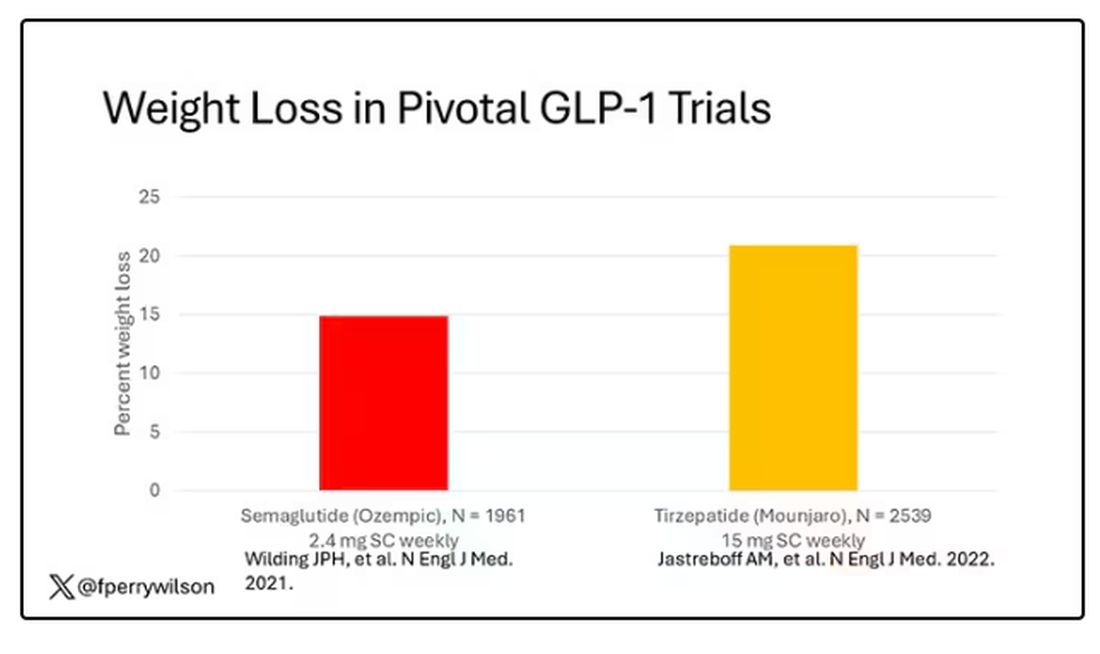
But it’s very hard to compare the results of a trial pitting Ozempic against placebo with a totally different trial pitting Mounjaro against placebo. You can always argue that the patients studied were just too different at baseline — an apples and oranges situation.
Newly published, a study appearing in JAMA Internal Medicine uses real-world data and propensity-score matching to turn oranges back into apples. I’ll walk you through it.
The data and analysis here come from Truveta, a collective of various US healthcare systems that share a broad swath of electronic health record data. Researchers identified 41,222 adults with overweight or obesity who were prescribed semaglutide or tirzepatide between May 2022 and September 2023.
You’d be tempted to just see which group lost more weight over time, but that is the apples and oranges problem. People prescribed Mounjaro were different from people who were prescribed Ozempic. There are a variety of factors to look at here, but the vibe is that the Mounjaro group seems healthier at baseline. They were younger and had less kidney disease, less hypertension, and less hyperlipidemia. They had higher incomes and were more likely to be White. They were also dramatically less likely to have diabetes. 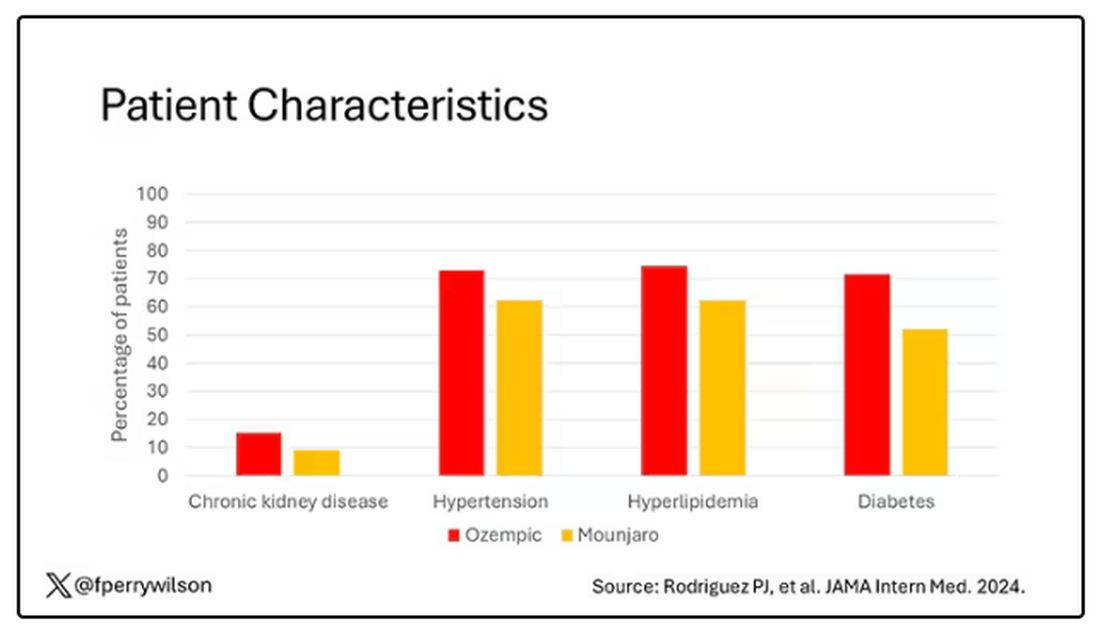
To account for this, the researchers used a statistical technique called propensity-score matching. Briefly, you create a model based on a variety of patient factors to predict who would be prescribed Ozempic and who would be prescribed Mounjaro. You then identify pairs of patients with similar probability (or propensity) of receiving, say, Ozempic, where one member of the pair got Ozempic and one got Mounjaro. Any unmatched individuals simply get dropped from the analysis.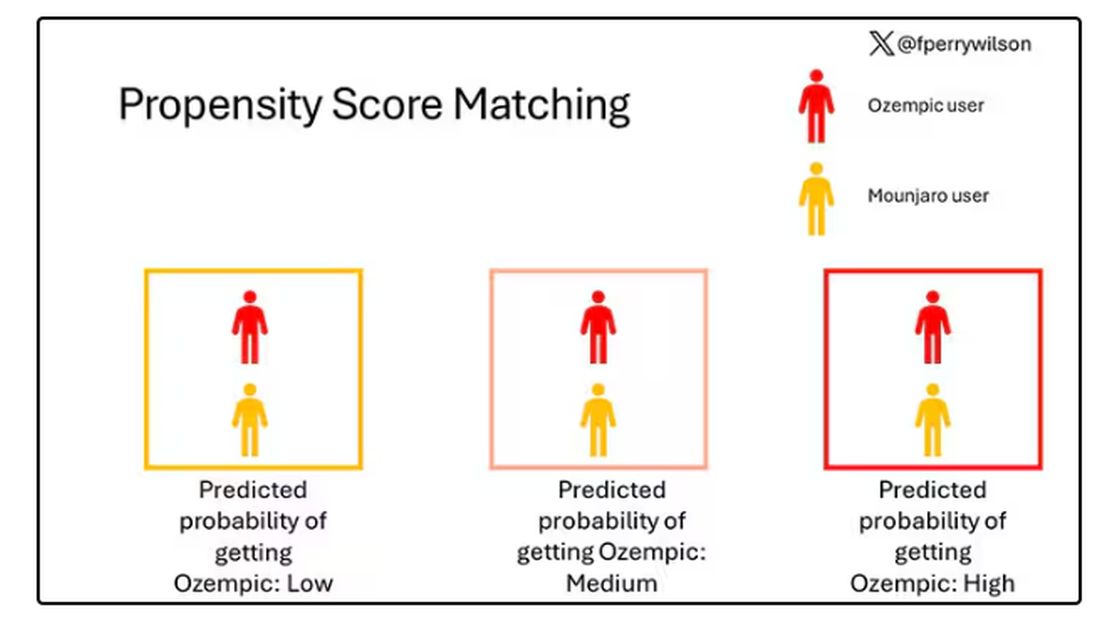
Thus, the researchers took the 41,222 individuals who started the analysis, of whom 9193 received Mounjaro, and identified the 9193 patients who got Ozempic that most closely matched the Mounjaro crowd. I know, it sounds confusing. But as an example, in the original dataset, 51.9% of those who got Mounjaro had diabetes compared with 71.5% of those who got Ozempic. Among the 9193 individuals who remained in the Ozempic group after matching, 52.1% had diabetes. By matching in this way, you balance your baseline characteristics. Turning apples into oranges. Or, maybe the better metaphor would be plucking the oranges out of a big pile of mostly apples.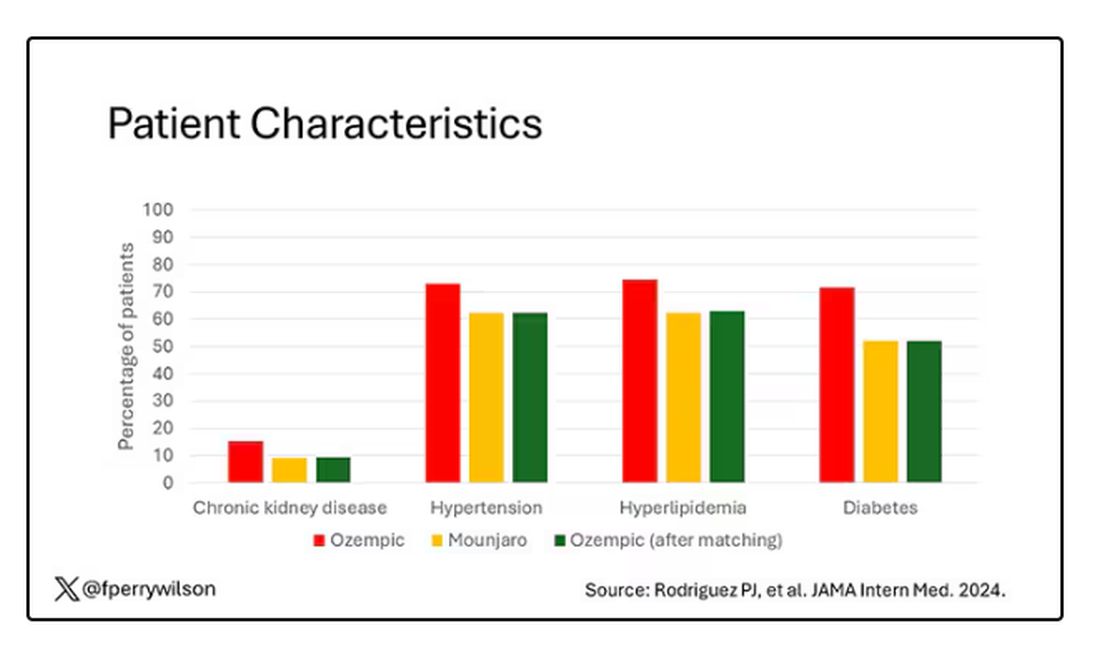
Once that’s done, we can go back to do what we wanted to do in the beginning, which is to look at the weight loss between the groups.
What I’m showing you here is the average percent change in body weight at 3, 6, and 12 months across the two drugs in the matched cohort. By a year out, you have basically 15% weight loss in the Mounjaro group compared with 8% or so in the Ozempic group. 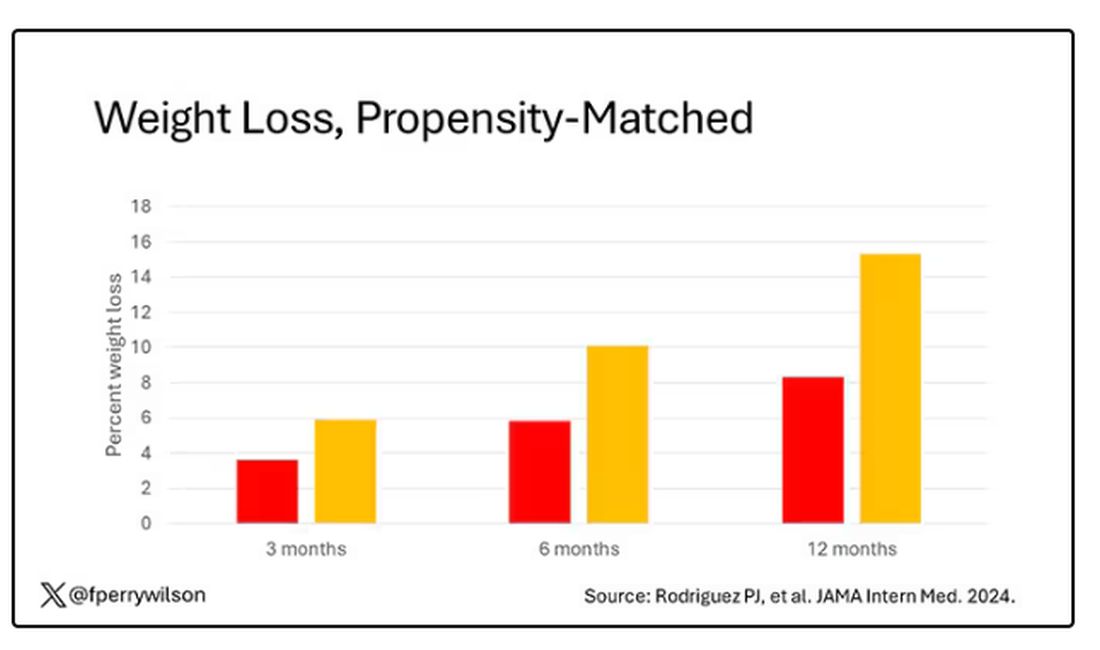
We can slice this a different way as well — asking what percent of people in each group achieve, say, 10% weight loss? This graph examines the percentage of each treatment group who hit that weight loss target over time. Mounjaro gets there faster.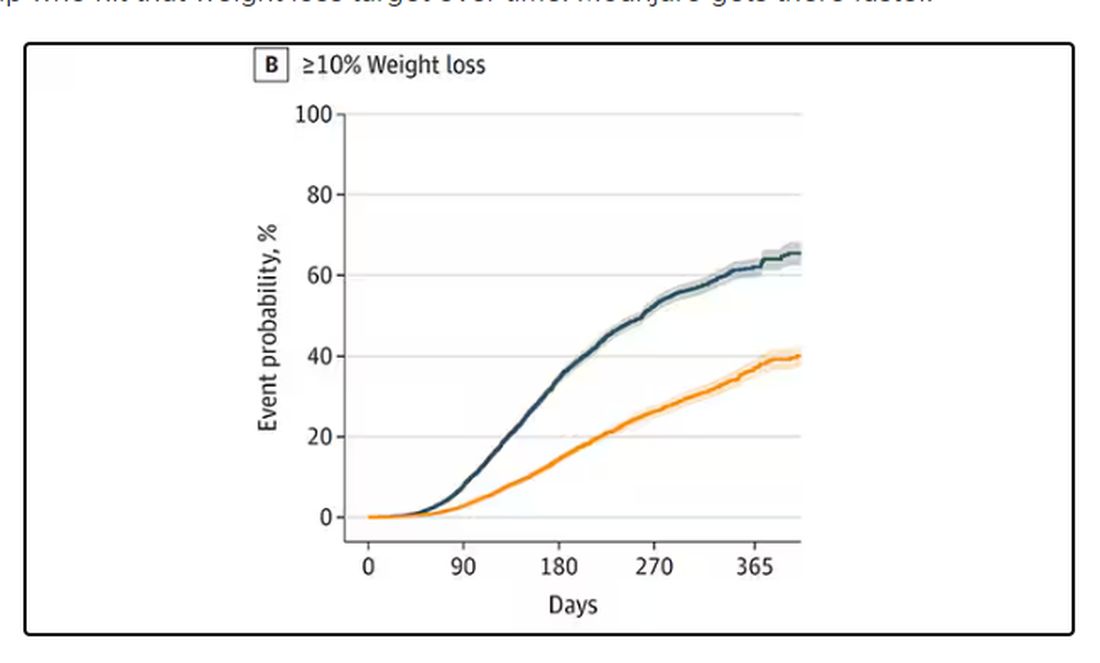
I should point out that this was a so-called “on treatment” analysis: If people stopped taking either of the drugs, they were no longer included in the study. That tends to make drugs like this appear better than they are because as time goes on, you may weed out the people who stop the drug owing to lack of efficacy or to side effects. But in a sensitivity analysis, the authors see what happens if they just treat people as if they were taking the drug for the entire year once they had it prescribed, and the results, while not as dramatic, were broadly similar. Mounjaro still came out on top.
Adverse events— stuff like gastroparesis and pancreatitis — were rare, but rates were similar between the two groups.
It’s great to see studies like this that leverage real world data and a solid statistical underpinning to give us providers actionable information. Is it 100% definitive? No. But, especially considering the clinical trial data, I don’t think I’m going out on a limb to say that Mounjaro seems to be the more effective weight loss agent. That said, we don’t actually live in a world where we can prescribe medications based on a silly little thing like which is the most effective. Especially given the cost of these agents — the patient’s insurance status is going to guide our prescription pen more than this study ever could. And of course, given the demand for this class of agents and the fact that both are actually quite effective, you may be best off prescribing whatever you can get your hands on.
But I’d like to see more of this. When I do have a choice of a medication, when costs and availability are similar, I’d like to be able to answer that question of “why did you choose that one?” with an evidence-based answer: “It’s better.”
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It’s July, which means our hospital is filled with new interns, residents, and fellows all eager to embark on a new stage of their career. It’s an exciting time — a bit of a scary time — but it’s also the time when the medical strategies I’ve been taking for granted get called into question. At this point in the year, I tend to get a lot of “why” questions. Why did you order that test? Why did you suspect that diagnosis? Why did you choose that medication?
Meds are the hardest, I find. Sure, I can explain that I prescribed a glucagon-like peptide 1 (GLP-1) receptor agonist because the patient had diabetes and was overweight, and multiple studies show that this class of drug leads to weight loss and reduced mortality risk. But then I get the follow-up: Sure, but why THAT GLP-1 drug? Why did you pick semaglutide (Ozempic) over tirzepatide (Mounjaro)?
Here’s where I run out of good answers. Sometimes I choose a drug because that’s what the patient’s insurance has on their formulary. Sometimes it’s because it’s cheaper in general. Sometimes, it’s just force of habit. I know the correct dose, I have experience with the side effects — it’s comfortable.
What I can’t say is that I have solid evidence that one drug is superior to another, say from a randomized trial of semaglutide vs tirzepatide. I don’t have that evidence because that trial has never happened and, as I’ll explain in a minute, may never happen at all.
But we might have the next best thing. And the results may surprise you.
Why don’t we see more head-to-head trials of competitor drugs? The answer is pretty simple, honestly: risk management. For drugs that are on patent, like the GLP-1s, conducting a trial without the buy-in of the pharmaceutical company is simply too expensive — we can’t run a trial unless someone provides the drug for free. That gives the companies a lot of say in what trials get done, and it seems that most pharma companies have reached the same conclusion: A head-to-head trial is too risky. Be happy with the market share you have, and try to nibble away at the edges through good old-fashioned marketing.
But if you look at the data that are out there, you might wonder why Ozempic is the market leader. I mean, sure, it’s a heck of a weight loss drug. But the weight loss in the trials of Mounjaro was actually a bit higher. It’s worth noting here that tirzepatide (Mounjaro) is not just a GLP-1 receptor agonist; it is also a gastric inhibitory polypeptide agonist. 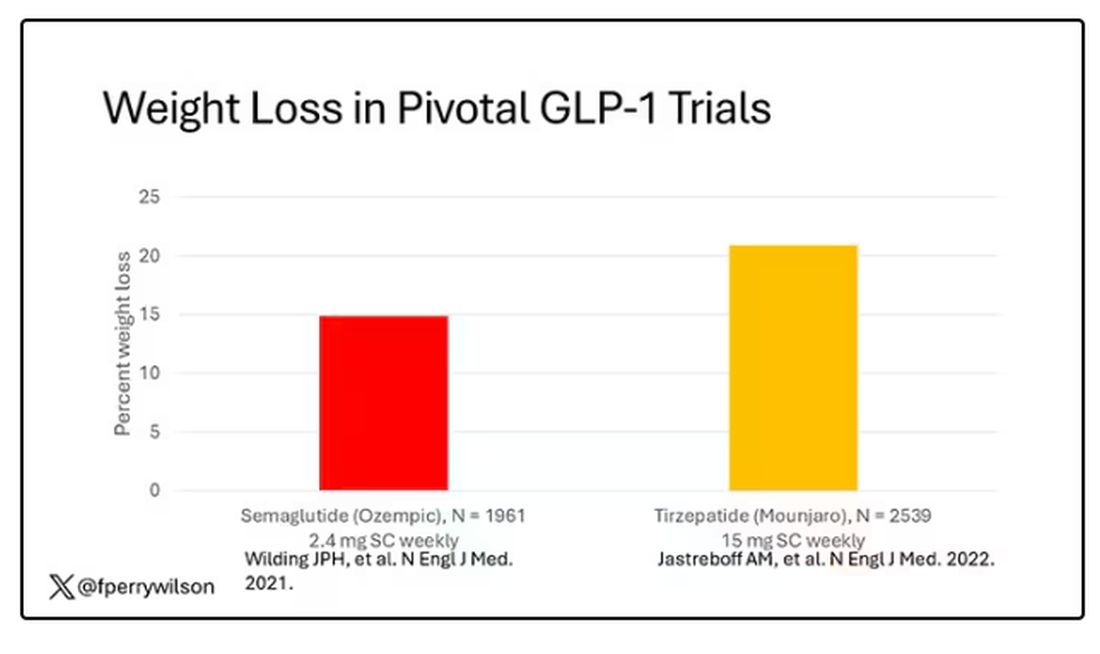
But it’s very hard to compare the results of a trial pitting Ozempic against placebo with a totally different trial pitting Mounjaro against placebo. You can always argue that the patients studied were just too different at baseline — an apples and oranges situation.
Newly published, a study appearing in JAMA Internal Medicine uses real-world data and propensity-score matching to turn oranges back into apples. I’ll walk you through it.
The data and analysis here come from Truveta, a collective of various US healthcare systems that share a broad swath of electronic health record data. Researchers identified 41,222 adults with overweight or obesity who were prescribed semaglutide or tirzepatide between May 2022 and September 2023.
You’d be tempted to just see which group lost more weight over time, but that is the apples and oranges problem. People prescribed Mounjaro were different from people who were prescribed Ozempic. There are a variety of factors to look at here, but the vibe is that the Mounjaro group seems healthier at baseline. They were younger and had less kidney disease, less hypertension, and less hyperlipidemia. They had higher incomes and were more likely to be White. They were also dramatically less likely to have diabetes. 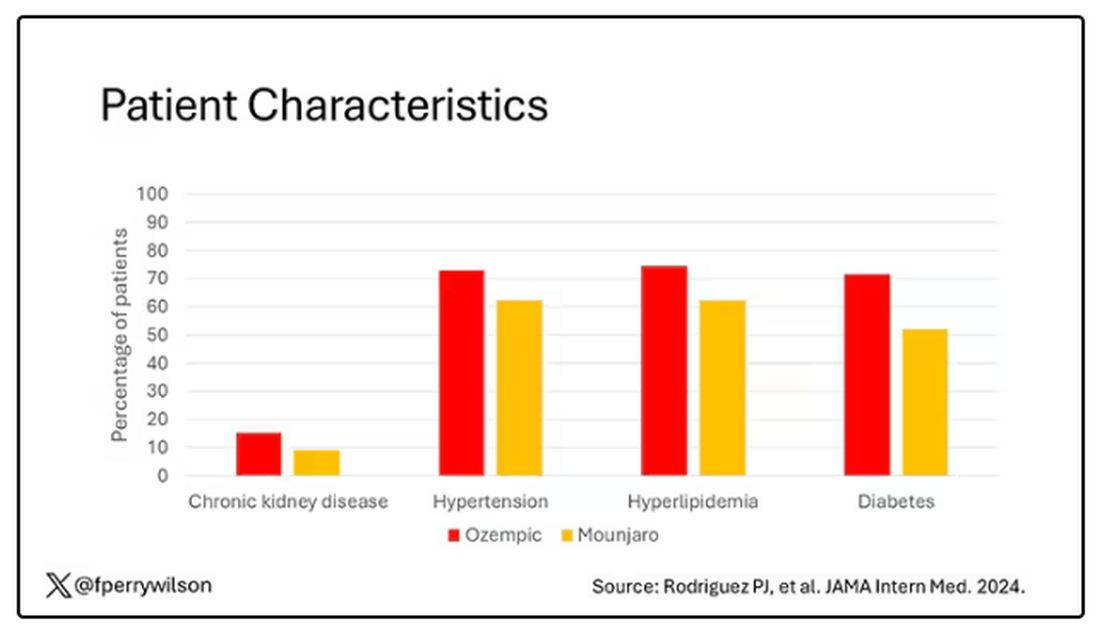
To account for this, the researchers used a statistical technique called propensity-score matching. Briefly, you create a model based on a variety of patient factors to predict who would be prescribed Ozempic and who would be prescribed Mounjaro. You then identify pairs of patients with similar probability (or propensity) of receiving, say, Ozempic, where one member of the pair got Ozempic and one got Mounjaro. Any unmatched individuals simply get dropped from the analysis.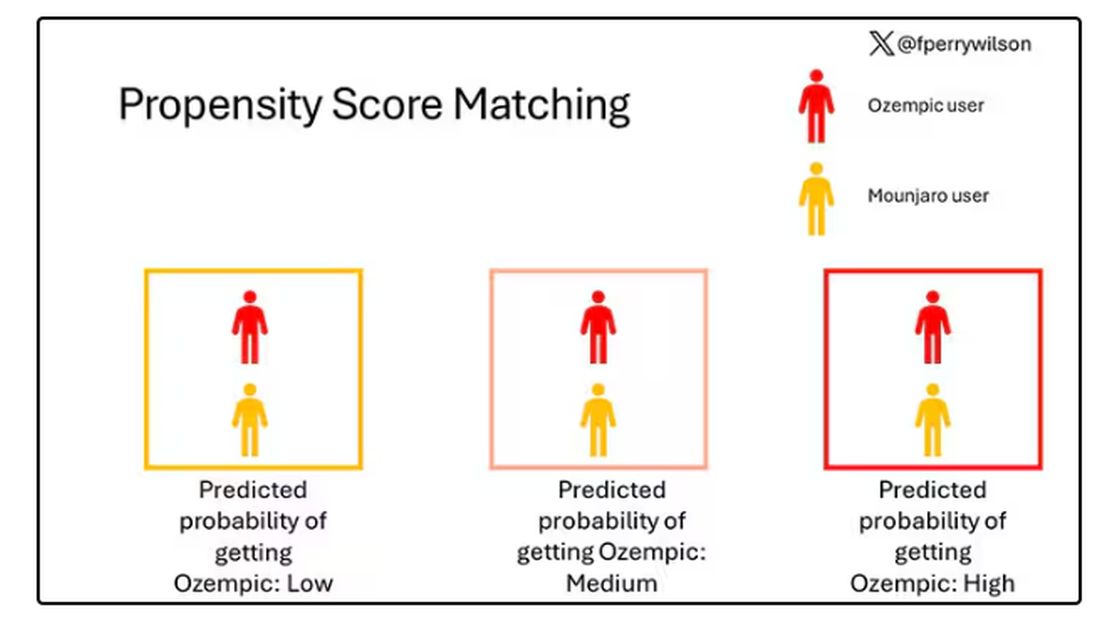
Thus, the researchers took the 41,222 individuals who started the analysis, of whom 9193 received Mounjaro, and identified the 9193 patients who got Ozempic that most closely matched the Mounjaro crowd. I know, it sounds confusing. But as an example, in the original dataset, 51.9% of those who got Mounjaro had diabetes compared with 71.5% of those who got Ozempic. Among the 9193 individuals who remained in the Ozempic group after matching, 52.1% had diabetes. By matching in this way, you balance your baseline characteristics. Turning apples into oranges. Or, maybe the better metaphor would be plucking the oranges out of a big pile of mostly apples.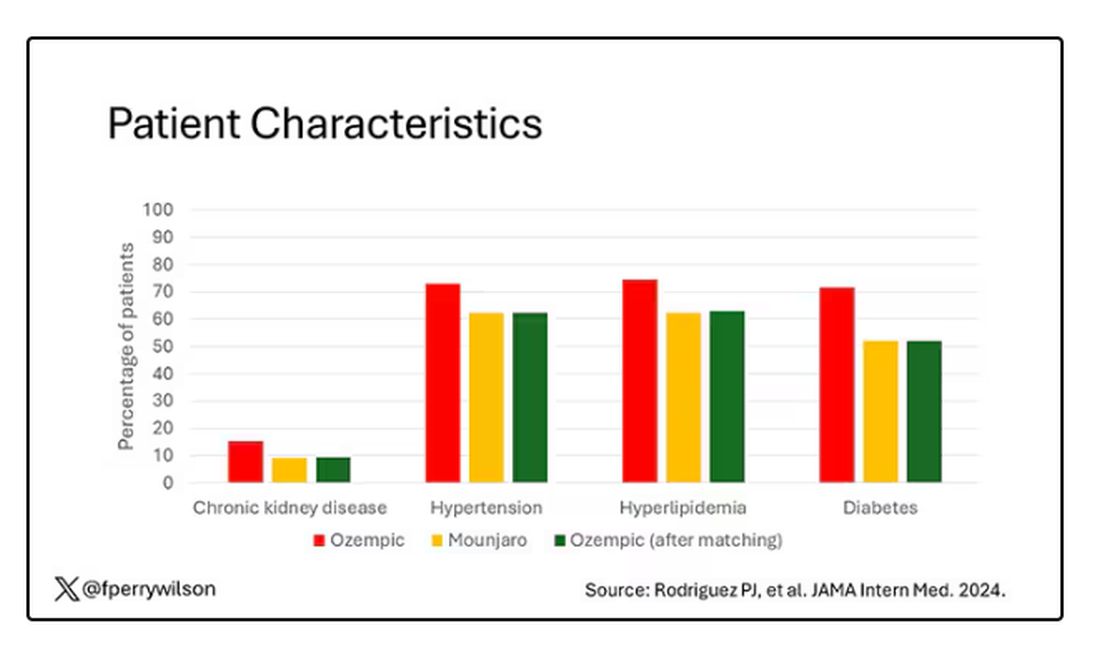
Once that’s done, we can go back to do what we wanted to do in the beginning, which is to look at the weight loss between the groups.
What I’m showing you here is the average percent change in body weight at 3, 6, and 12 months across the two drugs in the matched cohort. By a year out, you have basically 15% weight loss in the Mounjaro group compared with 8% or so in the Ozempic group. 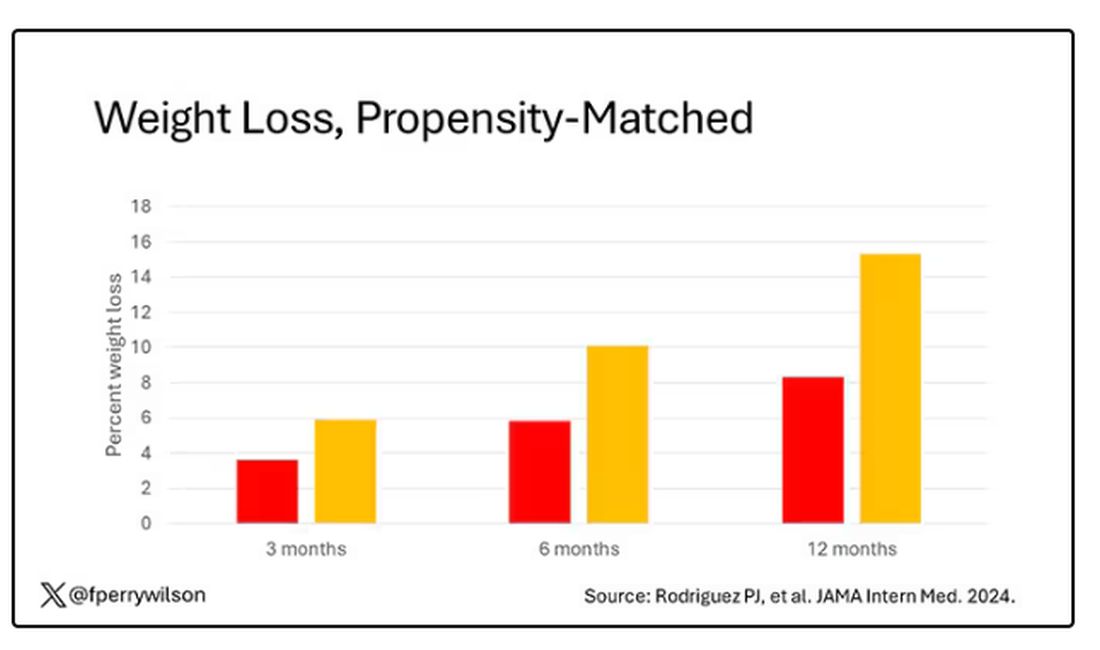
We can slice this a different way as well — asking what percent of people in each group achieve, say, 10% weight loss? This graph examines the percentage of each treatment group who hit that weight loss target over time. Mounjaro gets there faster.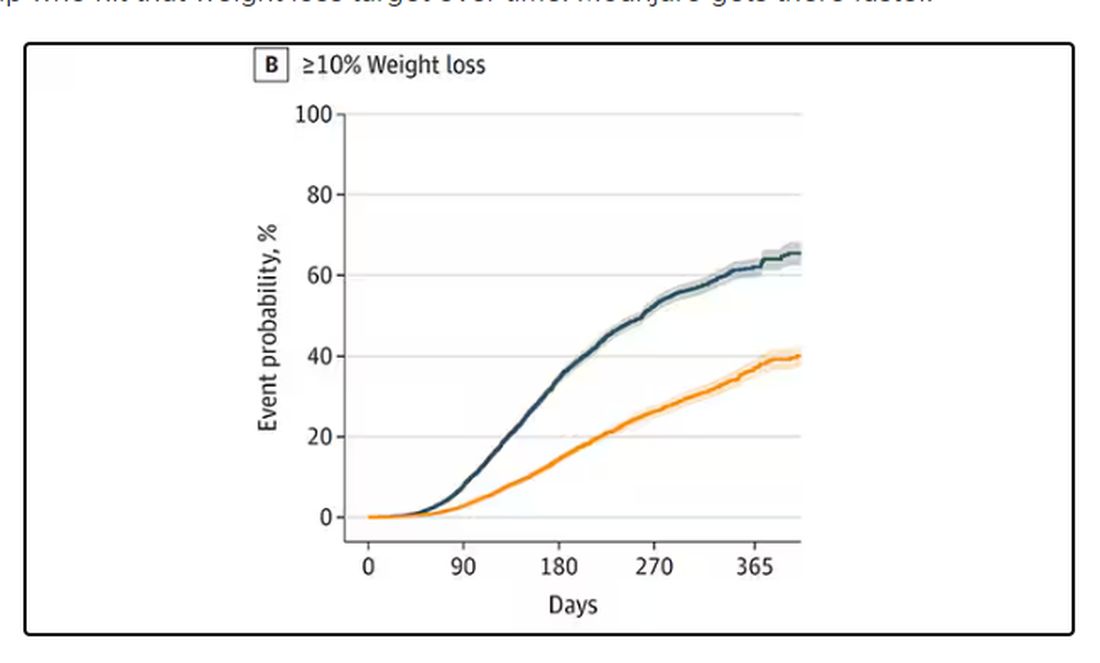
I should point out that this was a so-called “on treatment” analysis: If people stopped taking either of the drugs, they were no longer included in the study. That tends to make drugs like this appear better than they are because as time goes on, you may weed out the people who stop the drug owing to lack of efficacy or to side effects. But in a sensitivity analysis, the authors see what happens if they just treat people as if they were taking the drug for the entire year once they had it prescribed, and the results, while not as dramatic, were broadly similar. Mounjaro still came out on top.
Adverse events— stuff like gastroparesis and pancreatitis — were rare, but rates were similar between the two groups.
It’s great to see studies like this that leverage real world data and a solid statistical underpinning to give us providers actionable information. Is it 100% definitive? No. But, especially considering the clinical trial data, I don’t think I’m going out on a limb to say that Mounjaro seems to be the more effective weight loss agent. That said, we don’t actually live in a world where we can prescribe medications based on a silly little thing like which is the most effective. Especially given the cost of these agents — the patient’s insurance status is going to guide our prescription pen more than this study ever could. And of course, given the demand for this class of agents and the fact that both are actually quite effective, you may be best off prescribing whatever you can get your hands on.
But I’d like to see more of this. When I do have a choice of a medication, when costs and availability are similar, I’d like to be able to answer that question of “why did you choose that one?” with an evidence-based answer: “It’s better.”
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It’s July, which means our hospital is filled with new interns, residents, and fellows all eager to embark on a new stage of their career. It’s an exciting time — a bit of a scary time — but it’s also the time when the medical strategies I’ve been taking for granted get called into question. At this point in the year, I tend to get a lot of “why” questions. Why did you order that test? Why did you suspect that diagnosis? Why did you choose that medication?
Meds are the hardest, I find. Sure, I can explain that I prescribed a glucagon-like peptide 1 (GLP-1) receptor agonist because the patient had diabetes and was overweight, and multiple studies show that this class of drug leads to weight loss and reduced mortality risk. But then I get the follow-up: Sure, but why THAT GLP-1 drug? Why did you pick semaglutide (Ozempic) over tirzepatide (Mounjaro)?
Here’s where I run out of good answers. Sometimes I choose a drug because that’s what the patient’s insurance has on their formulary. Sometimes it’s because it’s cheaper in general. Sometimes, it’s just force of habit. I know the correct dose, I have experience with the side effects — it’s comfortable.
What I can’t say is that I have solid evidence that one drug is superior to another, say from a randomized trial of semaglutide vs tirzepatide. I don’t have that evidence because that trial has never happened and, as I’ll explain in a minute, may never happen at all.
But we might have the next best thing. And the results may surprise you.
Why don’t we see more head-to-head trials of competitor drugs? The answer is pretty simple, honestly: risk management. For drugs that are on patent, like the GLP-1s, conducting a trial without the buy-in of the pharmaceutical company is simply too expensive — we can’t run a trial unless someone provides the drug for free. That gives the companies a lot of say in what trials get done, and it seems that most pharma companies have reached the same conclusion: A head-to-head trial is too risky. Be happy with the market share you have, and try to nibble away at the edges through good old-fashioned marketing.
But if you look at the data that are out there, you might wonder why Ozempic is the market leader. I mean, sure, it’s a heck of a weight loss drug. But the weight loss in the trials of Mounjaro was actually a bit higher. It’s worth noting here that tirzepatide (Mounjaro) is not just a GLP-1 receptor agonist; it is also a gastric inhibitory polypeptide agonist. 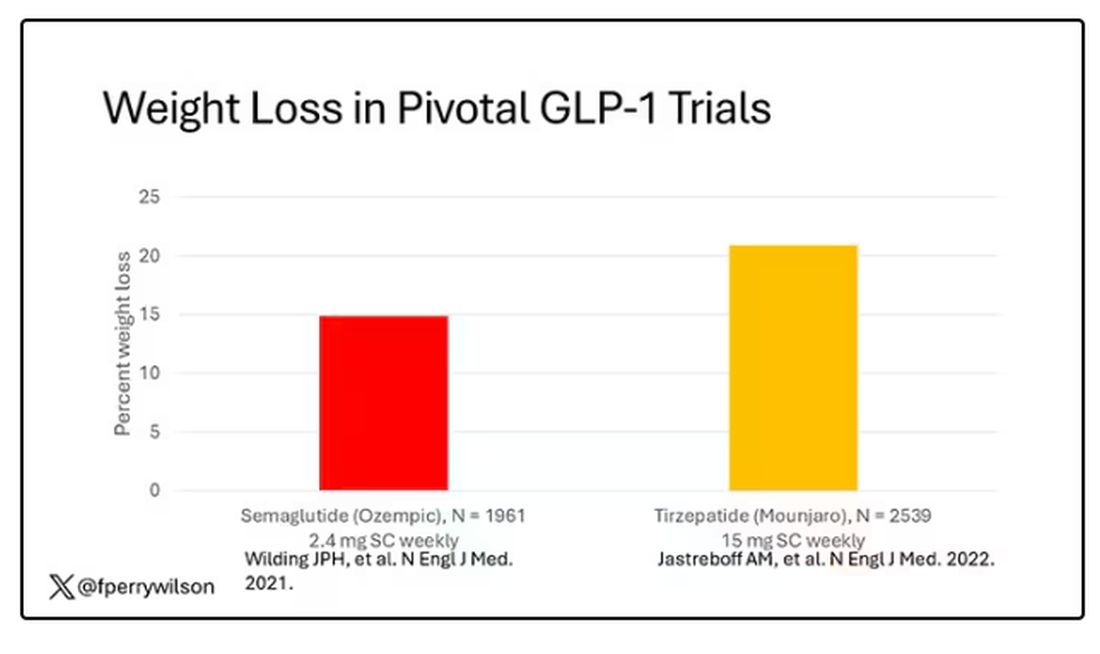
But it’s very hard to compare the results of a trial pitting Ozempic against placebo with a totally different trial pitting Mounjaro against placebo. You can always argue that the patients studied were just too different at baseline — an apples and oranges situation.
Newly published, a study appearing in JAMA Internal Medicine uses real-world data and propensity-score matching to turn oranges back into apples. I’ll walk you through it.
The data and analysis here come from Truveta, a collective of various US healthcare systems that share a broad swath of electronic health record data. Researchers identified 41,222 adults with overweight or obesity who were prescribed semaglutide or tirzepatide between May 2022 and September 2023.
You’d be tempted to just see which group lost more weight over time, but that is the apples and oranges problem. People prescribed Mounjaro were different from people who were prescribed Ozempic. There are a variety of factors to look at here, but the vibe is that the Mounjaro group seems healthier at baseline. They were younger and had less kidney disease, less hypertension, and less hyperlipidemia. They had higher incomes and were more likely to be White. They were also dramatically less likely to have diabetes. 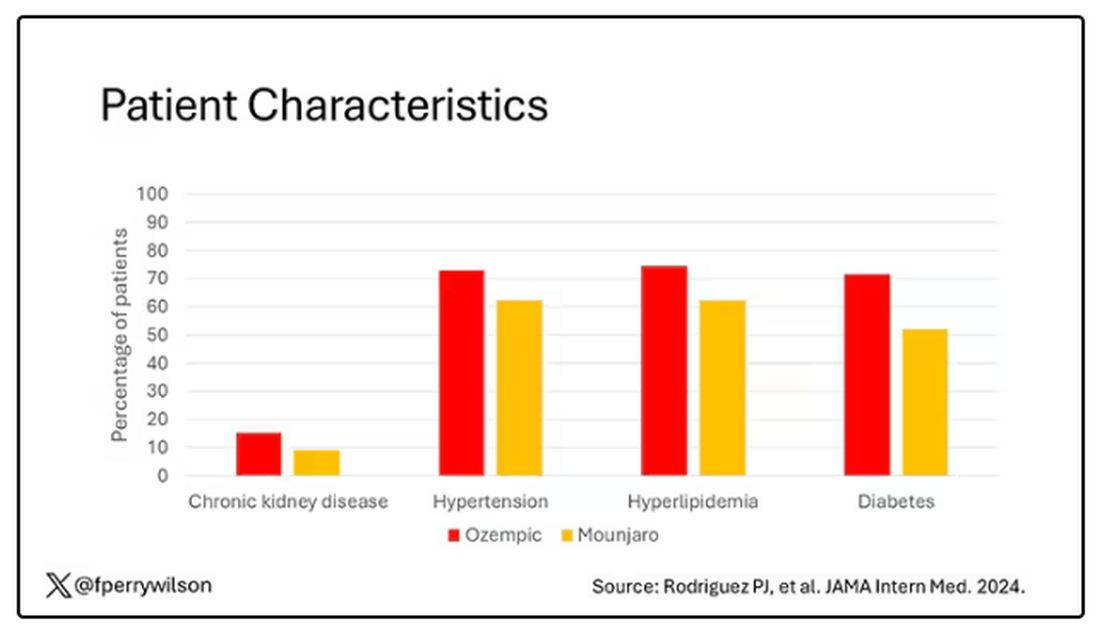
To account for this, the researchers used a statistical technique called propensity-score matching. Briefly, you create a model based on a variety of patient factors to predict who would be prescribed Ozempic and who would be prescribed Mounjaro. You then identify pairs of patients with similar probability (or propensity) of receiving, say, Ozempic, where one member of the pair got Ozempic and one got Mounjaro. Any unmatched individuals simply get dropped from the analysis.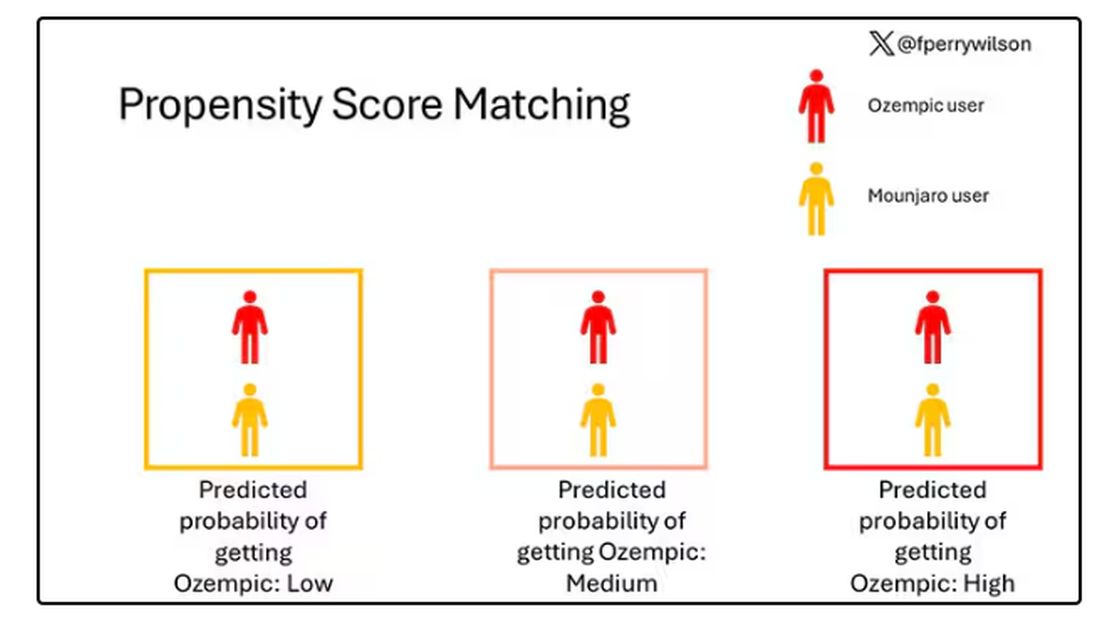
Thus, the researchers took the 41,222 individuals who started the analysis, of whom 9193 received Mounjaro, and identified the 9193 patients who got Ozempic that most closely matched the Mounjaro crowd. I know, it sounds confusing. But as an example, in the original dataset, 51.9% of those who got Mounjaro had diabetes compared with 71.5% of those who got Ozempic. Among the 9193 individuals who remained in the Ozempic group after matching, 52.1% had diabetes. By matching in this way, you balance your baseline characteristics. Turning apples into oranges. Or, maybe the better metaphor would be plucking the oranges out of a big pile of mostly apples.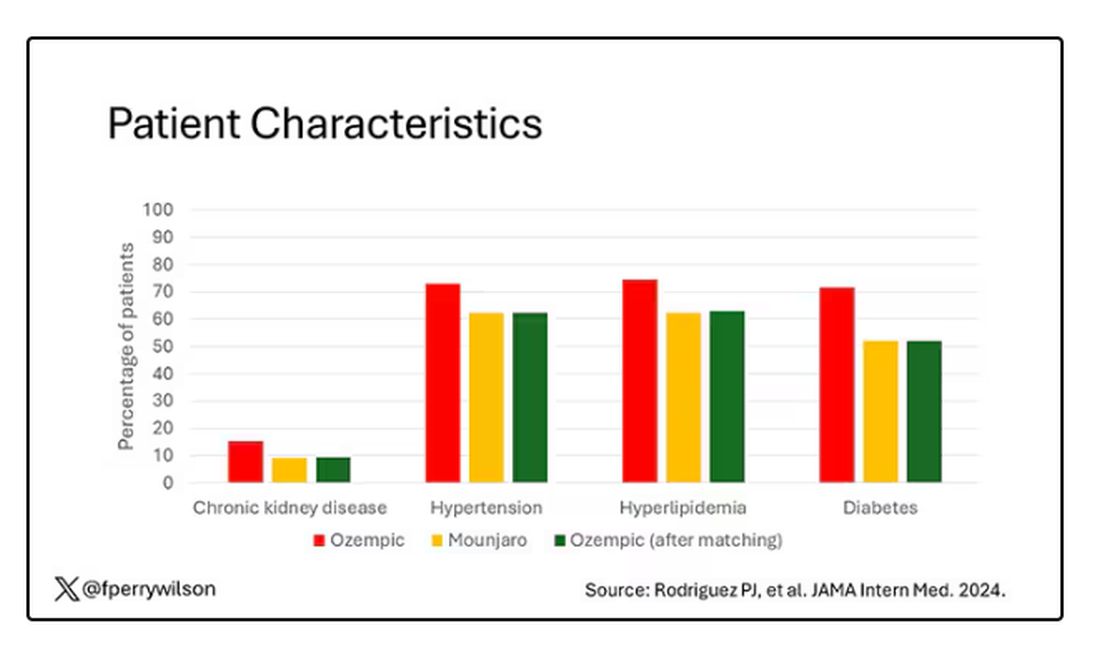
Once that’s done, we can go back to do what we wanted to do in the beginning, which is to look at the weight loss between the groups.
What I’m showing you here is the average percent change in body weight at 3, 6, and 12 months across the two drugs in the matched cohort. By a year out, you have basically 15% weight loss in the Mounjaro group compared with 8% or so in the Ozempic group. 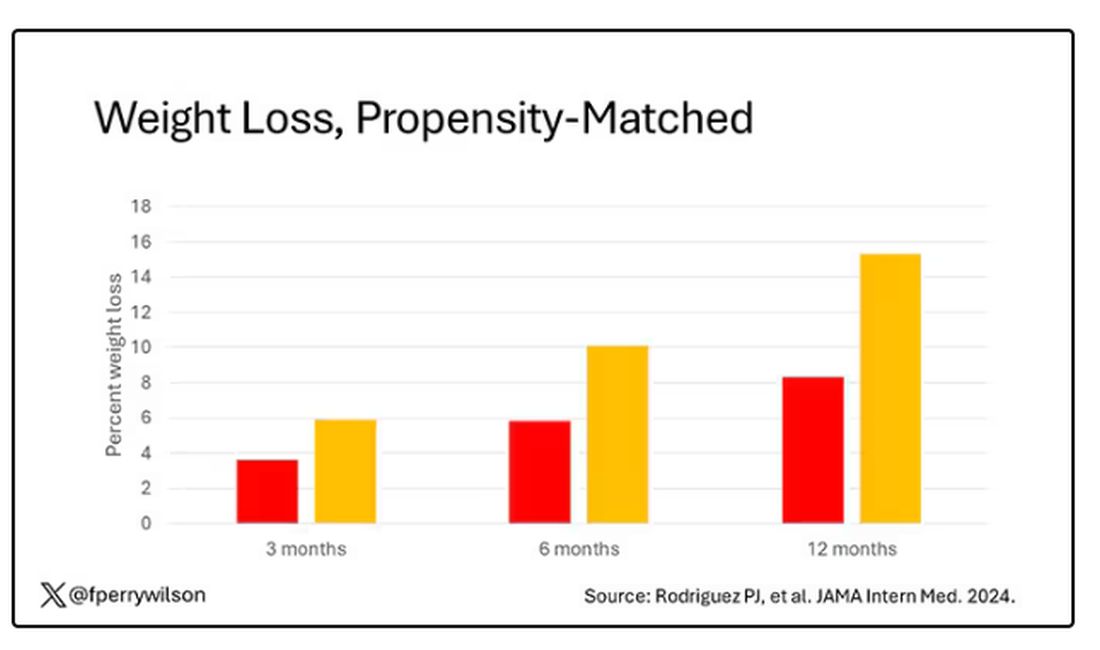
We can slice this a different way as well — asking what percent of people in each group achieve, say, 10% weight loss? This graph examines the percentage of each treatment group who hit that weight loss target over time. Mounjaro gets there faster.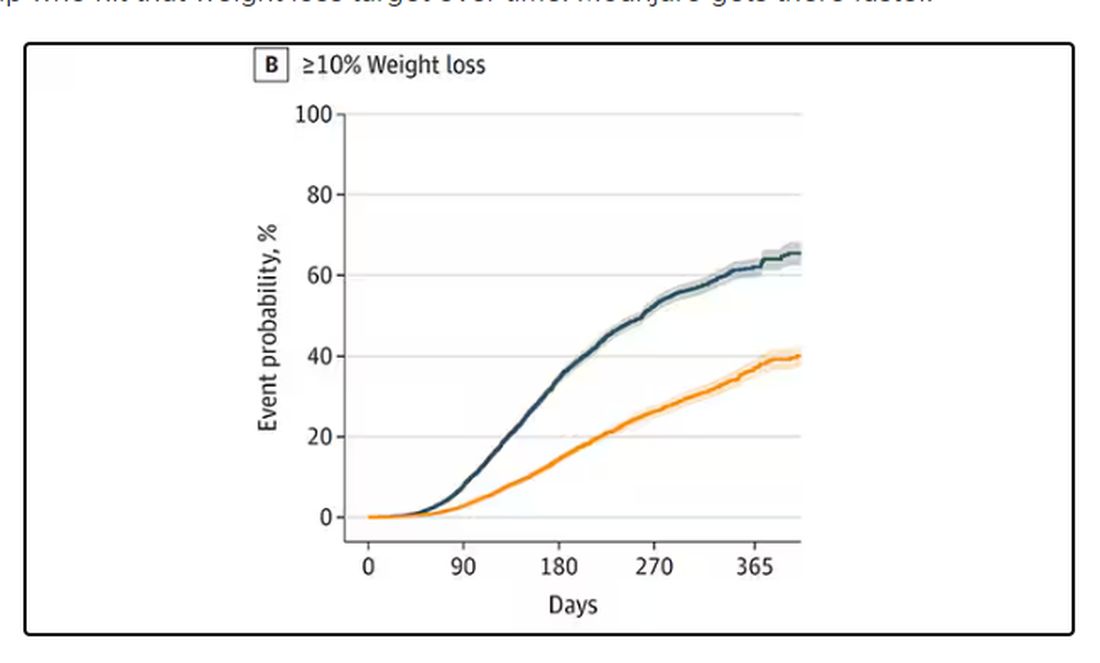
I should point out that this was a so-called “on treatment” analysis: If people stopped taking either of the drugs, they were no longer included in the study. That tends to make drugs like this appear better than they are because as time goes on, you may weed out the people who stop the drug owing to lack of efficacy or to side effects. But in a sensitivity analysis, the authors see what happens if they just treat people as if they were taking the drug for the entire year once they had it prescribed, and the results, while not as dramatic, were broadly similar. Mounjaro still came out on top.
Adverse events— stuff like gastroparesis and pancreatitis — were rare, but rates were similar between the two groups.
It’s great to see studies like this that leverage real world data and a solid statistical underpinning to give us providers actionable information. Is it 100% definitive? No. But, especially considering the clinical trial data, I don’t think I’m going out on a limb to say that Mounjaro seems to be the more effective weight loss agent. That said, we don’t actually live in a world where we can prescribe medications based on a silly little thing like which is the most effective. Especially given the cost of these agents — the patient’s insurance status is going to guide our prescription pen more than this study ever could. And of course, given the demand for this class of agents and the fact that both are actually quite effective, you may be best off prescribing whatever you can get your hands on.
But I’d like to see more of this. When I do have a choice of a medication, when costs and availability are similar, I’d like to be able to answer that question of “why did you choose that one?” with an evidence-based answer: “It’s better.”
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Chronic Neck Pain: A Primary Care Approach
This transcript has been edited for clarity.
Matthew F. Watto, MD: Welcome to The Curbsiders. I’m here with my great friend and America’s primary care physician, Dr. Paul Nelson Williams. We’re going to be talking about the evaluation of chronic neck pain, which is a really common complaint in primary care. So, Paul, what are the three buckets of neck pain?
Paul N. Williams, MD: Well, as our listeners probably know, neck pain is extraordinarily common. There are three big buckets. There is mechanical neck pain, which is sort of the bread-and-butter “my neck just hurts” — probably the one you’re going to see most commonly in the office. We’ll get into that in just a second.
The second bucket is cervical radiculopathy. We see a little bit more neurologic symptoms as part of the presentation. They may have weakness. They may have pain.
The third type of neck pain is cervical myelopathy, which is the one that probably warrants more aggressive follow-up and evaluation, and potentially even management. And that is typically your older patients in nontraumatic cases, who have bony impingement on the central spinal cord, often with upper motor neuron signs, and it can ultimately be very devastating. It’s almost a spectrum of presentations to worry about in terms of severity and outcomes.
We’ll start with the mechanical neck pain. It’s the one that we see the most commonly in the primary care office. We’ve all dealt with this. This is the patient who’s got localized neck pain that doesn’t really radiate anywhere; it kind of sits in the middle of the neck. In fact, if you actually poke back there where the patient says “ouch,” you’re probably in the right ballpark. The etiology and pathophysiology, weirdly, are still not super well-defined, but it’s probably mostly myofascial in etiology. And as such, it often gets better no matter what you do. It will probably get better with time.
You are not going to have neurologic deficits with this type of neck pain. There’s not going to be weakness, or radiation down the arm, or upper motor neuron signs. No one is mentioning the urinary symptoms with this. You can treat it with NSAIDs and physical therapy, which may be necessary if it persists. Massage can sometimes be helpful, but basically you’re just kind of supporting the patients through their own natural healing process. Physical therapy might help with the ergonomics and help make sure that they position themselves and move in a way that does not exacerbate the underlying structures. That is probably the one that we see the most and in some ways is probably the easiest to manage.
Dr. Watto: This is the one that we generally should be least worried about. But cervical radiculopathy, which is the second bucket, is not as severe as cervical myelopathy, so it’s kind of in between the two. Cervical radiculopathy is basically the patient who has neck pain that’s going down one arm or the other, usually not both arms because that would be weird for them to have symmetric radiculopathy. It’s a nerve being pinched somewhere, usually more on one side than the other.
The good news for patients is that the natural history is that it’s going to get better over time, almost no matter what we do. I almost think of this akin to sciatica. Usually sciatica and cervical radiculopathy do not have any motor weakness along with them. It’s really just the pain and maybe a little bit of mild sensory symptoms. So, you can reassure the patient that this usually goes away. Our guest said he sometimes gives gabapentin for this. That’s not my practice. I would be more likely to refer to physical therapy or try some NSAIDs if they’re really having trouble functioning or maybe some muscle relaxants. But they aren’t going to need to go to surgery.
What about cervical myelopathy, Paul? Do those patients need surgery?
Dr. Williams: Yes. The idea with cervical myelopathy is to keep it from progressing. It typically occurs in older patients. It’s like arthritis — a sort of bony buildup that compresses on the spinal cord itself. These patients will often have neck pain but not always. It’s also associated with impairments in motor function and other neurologic deficits. So, the patients may report that they have difficulty buttoning their buttons or managing fine-motor skills. They may have radicular symptoms down their arms. They may have an abnormal physical examination. They may have weakness on exam, but they’ll have a positive Hoffmann’s test where you flick the middle finger and look for flexion of the first finger and the thumb. They may have abnormal tandem gait, or patellar or Achilles hyperreflexia. Their neuro exam will not be normal much of the time, and in later cases because it’s upper motor neuron disease, they may even report urinary symptoms like urinary hesitancy or just a feeling of general unsteadiness of the gait, even though we’re at the cervical level. If you suspect myelopathy — and the trick is to think about it and recognize it when you see it — then you should send them for an MRI. If it persists or they have rapid regression, you get the MRI and refer them to neurosurgery. It’s not necessarily a neurosurgical emergency, but things should move along fairly briskly once you’ve actually identified it.
Dr. Watto: Dr. Mikula made the point that if someone comes to you in a wheelchair, they are probably not going to regain the ability to walk. You’re really trying to prevent progression. If they are already severely disabled, they’re probably not going to get totally back to full functioning, even with surgery. You’re just trying to prevent things from getting worse. That’s the main reason to identify this and get the patient to surgery.
We covered a lot more about neck pain. This was a very superficial review of what we talked about with Dr. Anthony Mikula. Click here to listen to the full podcast.
Matthew F. Watto is clinical assistant professor, Department of Medicine, Perelman School of Medicine at University of Pennsylvania, and internist, Department of Medicine, Hospital Medicine Section, Pennsylvania Hospital, Philadelphia, Pennsylvania. He has disclosed no relevant financial relationships. Paul N. Williams is associate professor of clinical medicine, Department of General Internal Medicine, Lewis Katz School of Medicine, and staff physician, Department of General Internal Medicine, Temple Internal Medicine Associates, Philadelphia, Pennsylvania. He has disclosed the following relevant financial relationships: serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for The Curbsiders; received income in an amount equal to or greater than $250 from The Curbsiders.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Matthew F. Watto, MD: Welcome to The Curbsiders. I’m here with my great friend and America’s primary care physician, Dr. Paul Nelson Williams. We’re going to be talking about the evaluation of chronic neck pain, which is a really common complaint in primary care. So, Paul, what are the three buckets of neck pain?
Paul N. Williams, MD: Well, as our listeners probably know, neck pain is extraordinarily common. There are three big buckets. There is mechanical neck pain, which is sort of the bread-and-butter “my neck just hurts” — probably the one you’re going to see most commonly in the office. We’ll get into that in just a second.
The second bucket is cervical radiculopathy. We see a little bit more neurologic symptoms as part of the presentation. They may have weakness. They may have pain.
The third type of neck pain is cervical myelopathy, which is the one that probably warrants more aggressive follow-up and evaluation, and potentially even management. And that is typically your older patients in nontraumatic cases, who have bony impingement on the central spinal cord, often with upper motor neuron signs, and it can ultimately be very devastating. It’s almost a spectrum of presentations to worry about in terms of severity and outcomes.
We’ll start with the mechanical neck pain. It’s the one that we see the most commonly in the primary care office. We’ve all dealt with this. This is the patient who’s got localized neck pain that doesn’t really radiate anywhere; it kind of sits in the middle of the neck. In fact, if you actually poke back there where the patient says “ouch,” you’re probably in the right ballpark. The etiology and pathophysiology, weirdly, are still not super well-defined, but it’s probably mostly myofascial in etiology. And as such, it often gets better no matter what you do. It will probably get better with time.
You are not going to have neurologic deficits with this type of neck pain. There’s not going to be weakness, or radiation down the arm, or upper motor neuron signs. No one is mentioning the urinary symptoms with this. You can treat it with NSAIDs and physical therapy, which may be necessary if it persists. Massage can sometimes be helpful, but basically you’re just kind of supporting the patients through their own natural healing process. Physical therapy might help with the ergonomics and help make sure that they position themselves and move in a way that does not exacerbate the underlying structures. That is probably the one that we see the most and in some ways is probably the easiest to manage.
Dr. Watto: This is the one that we generally should be least worried about. But cervical radiculopathy, which is the second bucket, is not as severe as cervical myelopathy, so it’s kind of in between the two. Cervical radiculopathy is basically the patient who has neck pain that’s going down one arm or the other, usually not both arms because that would be weird for them to have symmetric radiculopathy. It’s a nerve being pinched somewhere, usually more on one side than the other.
The good news for patients is that the natural history is that it’s going to get better over time, almost no matter what we do. I almost think of this akin to sciatica. Usually sciatica and cervical radiculopathy do not have any motor weakness along with them. It’s really just the pain and maybe a little bit of mild sensory symptoms. So, you can reassure the patient that this usually goes away. Our guest said he sometimes gives gabapentin for this. That’s not my practice. I would be more likely to refer to physical therapy or try some NSAIDs if they’re really having trouble functioning or maybe some muscle relaxants. But they aren’t going to need to go to surgery.
What about cervical myelopathy, Paul? Do those patients need surgery?
Dr. Williams: Yes. The idea with cervical myelopathy is to keep it from progressing. It typically occurs in older patients. It’s like arthritis — a sort of bony buildup that compresses on the spinal cord itself. These patients will often have neck pain but not always. It’s also associated with impairments in motor function and other neurologic deficits. So, the patients may report that they have difficulty buttoning their buttons or managing fine-motor skills. They may have radicular symptoms down their arms. They may have an abnormal physical examination. They may have weakness on exam, but they’ll have a positive Hoffmann’s test where you flick the middle finger and look for flexion of the first finger and the thumb. They may have abnormal tandem gait, or patellar or Achilles hyperreflexia. Their neuro exam will not be normal much of the time, and in later cases because it’s upper motor neuron disease, they may even report urinary symptoms like urinary hesitancy or just a feeling of general unsteadiness of the gait, even though we’re at the cervical level. If you suspect myelopathy — and the trick is to think about it and recognize it when you see it — then you should send them for an MRI. If it persists or they have rapid regression, you get the MRI and refer them to neurosurgery. It’s not necessarily a neurosurgical emergency, but things should move along fairly briskly once you’ve actually identified it.
Dr. Watto: Dr. Mikula made the point that if someone comes to you in a wheelchair, they are probably not going to regain the ability to walk. You’re really trying to prevent progression. If they are already severely disabled, they’re probably not going to get totally back to full functioning, even with surgery. You’re just trying to prevent things from getting worse. That’s the main reason to identify this and get the patient to surgery.
We covered a lot more about neck pain. This was a very superficial review of what we talked about with Dr. Anthony Mikula. Click here to listen to the full podcast.
Matthew F. Watto is clinical assistant professor, Department of Medicine, Perelman School of Medicine at University of Pennsylvania, and internist, Department of Medicine, Hospital Medicine Section, Pennsylvania Hospital, Philadelphia, Pennsylvania. He has disclosed no relevant financial relationships. Paul N. Williams is associate professor of clinical medicine, Department of General Internal Medicine, Lewis Katz School of Medicine, and staff physician, Department of General Internal Medicine, Temple Internal Medicine Associates, Philadelphia, Pennsylvania. He has disclosed the following relevant financial relationships: serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for The Curbsiders; received income in an amount equal to or greater than $250 from The Curbsiders.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Matthew F. Watto, MD: Welcome to The Curbsiders. I’m here with my great friend and America’s primary care physician, Dr. Paul Nelson Williams. We’re going to be talking about the evaluation of chronic neck pain, which is a really common complaint in primary care. So, Paul, what are the three buckets of neck pain?
Paul N. Williams, MD: Well, as our listeners probably know, neck pain is extraordinarily common. There are three big buckets. There is mechanical neck pain, which is sort of the bread-and-butter “my neck just hurts” — probably the one you’re going to see most commonly in the office. We’ll get into that in just a second.
The second bucket is cervical radiculopathy. We see a little bit more neurologic symptoms as part of the presentation. They may have weakness. They may have pain.
The third type of neck pain is cervical myelopathy, which is the one that probably warrants more aggressive follow-up and evaluation, and potentially even management. And that is typically your older patients in nontraumatic cases, who have bony impingement on the central spinal cord, often with upper motor neuron signs, and it can ultimately be very devastating. It’s almost a spectrum of presentations to worry about in terms of severity and outcomes.
We’ll start with the mechanical neck pain. It’s the one that we see the most commonly in the primary care office. We’ve all dealt with this. This is the patient who’s got localized neck pain that doesn’t really radiate anywhere; it kind of sits in the middle of the neck. In fact, if you actually poke back there where the patient says “ouch,” you’re probably in the right ballpark. The etiology and pathophysiology, weirdly, are still not super well-defined, but it’s probably mostly myofascial in etiology. And as such, it often gets better no matter what you do. It will probably get better with time.
You are not going to have neurologic deficits with this type of neck pain. There’s not going to be weakness, or radiation down the arm, or upper motor neuron signs. No one is mentioning the urinary symptoms with this. You can treat it with NSAIDs and physical therapy, which may be necessary if it persists. Massage can sometimes be helpful, but basically you’re just kind of supporting the patients through their own natural healing process. Physical therapy might help with the ergonomics and help make sure that they position themselves and move in a way that does not exacerbate the underlying structures. That is probably the one that we see the most and in some ways is probably the easiest to manage.
Dr. Watto: This is the one that we generally should be least worried about. But cervical radiculopathy, which is the second bucket, is not as severe as cervical myelopathy, so it’s kind of in between the two. Cervical radiculopathy is basically the patient who has neck pain that’s going down one arm or the other, usually not both arms because that would be weird for them to have symmetric radiculopathy. It’s a nerve being pinched somewhere, usually more on one side than the other.
The good news for patients is that the natural history is that it’s going to get better over time, almost no matter what we do. I almost think of this akin to sciatica. Usually sciatica and cervical radiculopathy do not have any motor weakness along with them. It’s really just the pain and maybe a little bit of mild sensory symptoms. So, you can reassure the patient that this usually goes away. Our guest said he sometimes gives gabapentin for this. That’s not my practice. I would be more likely to refer to physical therapy or try some NSAIDs if they’re really having trouble functioning or maybe some muscle relaxants. But they aren’t going to need to go to surgery.
What about cervical myelopathy, Paul? Do those patients need surgery?
Dr. Williams: Yes. The idea with cervical myelopathy is to keep it from progressing. It typically occurs in older patients. It’s like arthritis — a sort of bony buildup that compresses on the spinal cord itself. These patients will often have neck pain but not always. It’s also associated with impairments in motor function and other neurologic deficits. So, the patients may report that they have difficulty buttoning their buttons or managing fine-motor skills. They may have radicular symptoms down their arms. They may have an abnormal physical examination. They may have weakness on exam, but they’ll have a positive Hoffmann’s test where you flick the middle finger and look for flexion of the first finger and the thumb. They may have abnormal tandem gait, or patellar or Achilles hyperreflexia. Their neuro exam will not be normal much of the time, and in later cases because it’s upper motor neuron disease, they may even report urinary symptoms like urinary hesitancy or just a feeling of general unsteadiness of the gait, even though we’re at the cervical level. If you suspect myelopathy — and the trick is to think about it and recognize it when you see it — then you should send them for an MRI. If it persists or they have rapid regression, you get the MRI and refer them to neurosurgery. It’s not necessarily a neurosurgical emergency, but things should move along fairly briskly once you’ve actually identified it.
Dr. Watto: Dr. Mikula made the point that if someone comes to you in a wheelchair, they are probably not going to regain the ability to walk. You’re really trying to prevent progression. If they are already severely disabled, they’re probably not going to get totally back to full functioning, even with surgery. You’re just trying to prevent things from getting worse. That’s the main reason to identify this and get the patient to surgery.
We covered a lot more about neck pain. This was a very superficial review of what we talked about with Dr. Anthony Mikula. Click here to listen to the full podcast.
Matthew F. Watto is clinical assistant professor, Department of Medicine, Perelman School of Medicine at University of Pennsylvania, and internist, Department of Medicine, Hospital Medicine Section, Pennsylvania Hospital, Philadelphia, Pennsylvania. He has disclosed no relevant financial relationships. Paul N. Williams is associate professor of clinical medicine, Department of General Internal Medicine, Lewis Katz School of Medicine, and staff physician, Department of General Internal Medicine, Temple Internal Medicine Associates, Philadelphia, Pennsylvania. He has disclosed the following relevant financial relationships: serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for The Curbsiders; received income in an amount equal to or greater than $250 from The Curbsiders.
A version of this article first appeared on Medscape.com.
‘The Oncologist Without the Pathologist Is Blind’: GI Cancer Updates at ASCO 2024
This transcript has been edited for clarity.
Hello. I’m Mark Lewis, director of gastrointestinal (GI) oncology at Intermountain Health in Utah.
If you allow me, I’d like to go in a craniocaudal fashion. It’s my anatomic mnemonic. I think that’s appropriate because our plenary session yesterday kicked off with some exciting data in esophageal cancer, specifically esophageal adenocarcinoma.
This was the long-awaited ESOPEC trial. It’s a phase 3 study looking at perioperative FLOT (5-FU/leucovorin/oxaliplatin/docetaxel), a chemo triplet, vs the CROSS protocol, which is neoadjuvant chemoradiation with carboplatin and paclitaxel. The primary endpoint was overall survival, and at first blush, FLOT looked to be the true winner. There were some really remarkable milestones in this study, and I have some reservations about the FLOT arm that I’ll raise in just a second.
The investigators are to be commended because in a truly deadly disease, they reported a 5-year overall survival in half of the patients who were receiving FLOT. That is truly commendable and really a milestone in our field. The reason I take a little bit of issue with the trial is that I still have some questions about methodology.
It wasn’t that long ago at ASCO GI that there was a really heated debate called “FLOT or Not” — not in this precise setting, but asking the question, do we think that patients with upper GI malignancy are even fit enough to handle a chemo triplet like FLOT?
The reason I bring that up now in 2024 is that, to my surprise, and I think to many others’, there was a lower-than-expected completion rate of the patients in this trial who were receiving the CROSS regimen. The number of people who were able to complete that in full was about two-thirds, which compared with a historical control from a trial scheme that first emerged over a decade ago that used to be over 90% completion. I found that quite strange.
I also think this trial suffers a little bit, and unavoidably, from the evolution of care that’s happened since it was first enrolling. Of course, I refer to adjuvant immunotherapy. Now, the real question is whether there is synergy between patients who receive radiation upfront and then adjuvant nivolumab, as per CheckMate 577.
In her plenary discussion, I thought Dr. Karyn Goodman did a masterful job — I would encourage you to watch it on ASCO’s website —discussing how we can take all these data and reconcile them for optimal patient outcome. She ultimately suggested that we might deploy all four modalities in the management of these people.
She proposed a paradigm with a PET-adapted, upfront induction chemotherapy, then moving to chemoradiation, then moving to surgery, and finally moving to immunotherapy. That is all four of the traditional arms of oncology. I find that really rather remarkable. Watch that space. This is a great trial with really remarkable survival data, but I’m not entirely convinced that the CROSS arm was given its due.
Next up, I want to talk about pancreas cancer, which is something near and dear to my heart. It affects about one in four of my patients and it remains, unfortunately, a highly lethal disease. I think the top-line news from this meeting is that the KRAS mutation is druggable. I’m probably showing my age, but when I did my fellowship in 2009 through 2012, I was taught that KRAS was sort of the undruggable mutation par excellence. At this meeting, we’ve seen maturing data in regard to targeting KRAS G12C with both sotorasib and adagrasib. The disease control rates are astounding, at 80% and more, which is really remarkable. I wouldn’t have believed that even a few years ago.
I’m even more excited about how we bring a rising tide that can lift all boats and apply this to other KRAS mutations, and not just KRAS G12C but all KRAS mutations. I think that’s coming, hopefully, with the pan-RAS inhibitors, because once that happens — if that happens; I’ll try not to be irrationally exuberant — that would take the traditional mutation found in almost all pancreas cancers and really make it its own Achilles heel. I think that could be such a huge leap forward.
Another matter, however, that remains unresolved at this meeting is in the neoadjuvant setting with pancreatic ductal adenocarcinoma. There’s still equipoise, actually, between neoadjuvant gemcitabine, paclitaxel, and FOLFIRINOX. I thought that that was very well spelled out by some of our Dutch colleagues, who continue to do great work in a variety of cancers, including colorectal.
Where I’d like to move next is colorectal cancer. Of course, immunotherapy remains a hot topic at all of these conferences. There were three different aspects of immunotherapy I’d like to highlight at this conference in regard to colon and rectal cancer.
First, Dr. Heinz-Josef Lenz presented updated data from CheckMate 8HW, which looked at nivolumab and ipilimumab (nivo/ipi) vs chemotherapy in the first line for MSI-high or mismatch repair–deficient colon cancer. Once again, the data we’ve had now for several years at the 2-year mark are incredibly impressive. The 2-year progression-free survival (PFS) rates for nivo/ipi are above 70% and down at around 14% for chemo.
What was impressive about this meeting is that Dr. Lenz presented PFS2, trying to determine the impact, if any, of subsequent therapy. What was going on here, which I think was ethically responsible by the investigators, was crossover. About two-thirds of the chemo arm crossed over to any form of immuno-oncology (IO), and just under a half crossed over to nivo and ipi. The PFS benefits continued with up-front IO. The way that Dr. Lenz phrased it is that you really never get the chance to win back the benefit that you would derive by giving immunotherapy first line to someone who has MSI-high or mismatch repair–deficient metastatic colon cancer.
One thing that’s still not settled in my mind, though, is, does this really dethrone single-agent immunotherapy, such as pembrolizumab in KEYNOTE-177? What I’m really driving at is the ipilimumab. Is the juice worth the squeeze? Is the addition of an anti-CTLA4 agent worth the toxicity that we know comes along with that mechanism of action? Watch this space.
I was also really interested in NEOPRISM-CRC, which looked at the role of immunotherapy in neoadjuvant down-staging of radiographically high-risk stage II or stage III colon cancer. Here, the investigators really make a strong case that, up front in these potentially respectable cases, not only should we know about mismatch repair deficiency but we should actually be interrogating further for tumor mutational burden (TMB).
They had TMB-high patients. In fact, the median TMB was 42 mutations per megabase, with really impressive down-staging using three cycles of every-3-week pembrolizumab before surgery. Again, I really think we’re at an exciting time where, even for colon cancer that looks operable up front, we might actually have the opportunity to improve pathologic and clinical complete responses before and after surgery.
Finally, I want to bring up what continues to amaze me. Two years ago, at ASCO 2022, we heard from Dr. Andrea Cercek and the Memorial Sloan Kettering group about the incredible experience they were having with neoadjuvant, or frankly, definitive dostarlimab in mismatch repair–deficient locally advanced rectal cancer.
I remember being at the conference and there was simultaneous publication of that abstract in The New York Times because it was so remarkable. There was a 100% clinical complete response. The patients didn’t require radiation, they didn’t require chemotherapy, and they didn’t require surgery for locally advanced rectal cancer, provided there was this vulnerability of mismatch-repair deficiency.
Now, 2 years later, Dr. Cercek and her group have updated those data with more than 40 patients, and again, a 100% clinical complete response, including mature, complete responses at over a year in about 20 patients. Again, we are really doing our rectal cancer patients a disservice if we’re not checking for mismatch-repair deficiency upfront, and especially if we’re not talking about them in multidisciplinary conferences.
One of the things that absolutely blows my mind about rectal cancer is just how complicated it’s becoming. I think it is the standard of care to discuss these cases upfront with radiation oncology, surgical oncology, medical oncology, and pathology.
Maybe the overarching message I would take from everything I’ve said today is that the oncologist without the pathologist is blind. It’s really a dyad, a partnership that guides optimal medical oncology care. As much as I love ASCO, I often wish we had more of our pathology colleagues here. I look forward to taking all the findings from this meeting back to the tumor board and really having a dynamic dialogue.
Dr. Lewis is director, Department of Gastrointestinal Oncology, Intermountain Health, Salt Lake City, Utah. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. I’m Mark Lewis, director of gastrointestinal (GI) oncology at Intermountain Health in Utah.
If you allow me, I’d like to go in a craniocaudal fashion. It’s my anatomic mnemonic. I think that’s appropriate because our plenary session yesterday kicked off with some exciting data in esophageal cancer, specifically esophageal adenocarcinoma.
This was the long-awaited ESOPEC trial. It’s a phase 3 study looking at perioperative FLOT (5-FU/leucovorin/oxaliplatin/docetaxel), a chemo triplet, vs the CROSS protocol, which is neoadjuvant chemoradiation with carboplatin and paclitaxel. The primary endpoint was overall survival, and at first blush, FLOT looked to be the true winner. There were some really remarkable milestones in this study, and I have some reservations about the FLOT arm that I’ll raise in just a second.
The investigators are to be commended because in a truly deadly disease, they reported a 5-year overall survival in half of the patients who were receiving FLOT. That is truly commendable and really a milestone in our field. The reason I take a little bit of issue with the trial is that I still have some questions about methodology.
It wasn’t that long ago at ASCO GI that there was a really heated debate called “FLOT or Not” — not in this precise setting, but asking the question, do we think that patients with upper GI malignancy are even fit enough to handle a chemo triplet like FLOT?
The reason I bring that up now in 2024 is that, to my surprise, and I think to many others’, there was a lower-than-expected completion rate of the patients in this trial who were receiving the CROSS regimen. The number of people who were able to complete that in full was about two-thirds, which compared with a historical control from a trial scheme that first emerged over a decade ago that used to be over 90% completion. I found that quite strange.
I also think this trial suffers a little bit, and unavoidably, from the evolution of care that’s happened since it was first enrolling. Of course, I refer to adjuvant immunotherapy. Now, the real question is whether there is synergy between patients who receive radiation upfront and then adjuvant nivolumab, as per CheckMate 577.
In her plenary discussion, I thought Dr. Karyn Goodman did a masterful job — I would encourage you to watch it on ASCO’s website —discussing how we can take all these data and reconcile them for optimal patient outcome. She ultimately suggested that we might deploy all four modalities in the management of these people.
She proposed a paradigm with a PET-adapted, upfront induction chemotherapy, then moving to chemoradiation, then moving to surgery, and finally moving to immunotherapy. That is all four of the traditional arms of oncology. I find that really rather remarkable. Watch that space. This is a great trial with really remarkable survival data, but I’m not entirely convinced that the CROSS arm was given its due.
Next up, I want to talk about pancreas cancer, which is something near and dear to my heart. It affects about one in four of my patients and it remains, unfortunately, a highly lethal disease. I think the top-line news from this meeting is that the KRAS mutation is druggable. I’m probably showing my age, but when I did my fellowship in 2009 through 2012, I was taught that KRAS was sort of the undruggable mutation par excellence. At this meeting, we’ve seen maturing data in regard to targeting KRAS G12C with both sotorasib and adagrasib. The disease control rates are astounding, at 80% and more, which is really remarkable. I wouldn’t have believed that even a few years ago.
I’m even more excited about how we bring a rising tide that can lift all boats and apply this to other KRAS mutations, and not just KRAS G12C but all KRAS mutations. I think that’s coming, hopefully, with the pan-RAS inhibitors, because once that happens — if that happens; I’ll try not to be irrationally exuberant — that would take the traditional mutation found in almost all pancreas cancers and really make it its own Achilles heel. I think that could be such a huge leap forward.
Another matter, however, that remains unresolved at this meeting is in the neoadjuvant setting with pancreatic ductal adenocarcinoma. There’s still equipoise, actually, between neoadjuvant gemcitabine, paclitaxel, and FOLFIRINOX. I thought that that was very well spelled out by some of our Dutch colleagues, who continue to do great work in a variety of cancers, including colorectal.
Where I’d like to move next is colorectal cancer. Of course, immunotherapy remains a hot topic at all of these conferences. There were three different aspects of immunotherapy I’d like to highlight at this conference in regard to colon and rectal cancer.
First, Dr. Heinz-Josef Lenz presented updated data from CheckMate 8HW, which looked at nivolumab and ipilimumab (nivo/ipi) vs chemotherapy in the first line for MSI-high or mismatch repair–deficient colon cancer. Once again, the data we’ve had now for several years at the 2-year mark are incredibly impressive. The 2-year progression-free survival (PFS) rates for nivo/ipi are above 70% and down at around 14% for chemo.
What was impressive about this meeting is that Dr. Lenz presented PFS2, trying to determine the impact, if any, of subsequent therapy. What was going on here, which I think was ethically responsible by the investigators, was crossover. About two-thirds of the chemo arm crossed over to any form of immuno-oncology (IO), and just under a half crossed over to nivo and ipi. The PFS benefits continued with up-front IO. The way that Dr. Lenz phrased it is that you really never get the chance to win back the benefit that you would derive by giving immunotherapy first line to someone who has MSI-high or mismatch repair–deficient metastatic colon cancer.
One thing that’s still not settled in my mind, though, is, does this really dethrone single-agent immunotherapy, such as pembrolizumab in KEYNOTE-177? What I’m really driving at is the ipilimumab. Is the juice worth the squeeze? Is the addition of an anti-CTLA4 agent worth the toxicity that we know comes along with that mechanism of action? Watch this space.
I was also really interested in NEOPRISM-CRC, which looked at the role of immunotherapy in neoadjuvant down-staging of radiographically high-risk stage II or stage III colon cancer. Here, the investigators really make a strong case that, up front in these potentially respectable cases, not only should we know about mismatch repair deficiency but we should actually be interrogating further for tumor mutational burden (TMB).
They had TMB-high patients. In fact, the median TMB was 42 mutations per megabase, with really impressive down-staging using three cycles of every-3-week pembrolizumab before surgery. Again, I really think we’re at an exciting time where, even for colon cancer that looks operable up front, we might actually have the opportunity to improve pathologic and clinical complete responses before and after surgery.
Finally, I want to bring up what continues to amaze me. Two years ago, at ASCO 2022, we heard from Dr. Andrea Cercek and the Memorial Sloan Kettering group about the incredible experience they were having with neoadjuvant, or frankly, definitive dostarlimab in mismatch repair–deficient locally advanced rectal cancer.
I remember being at the conference and there was simultaneous publication of that abstract in The New York Times because it was so remarkable. There was a 100% clinical complete response. The patients didn’t require radiation, they didn’t require chemotherapy, and they didn’t require surgery for locally advanced rectal cancer, provided there was this vulnerability of mismatch-repair deficiency.
Now, 2 years later, Dr. Cercek and her group have updated those data with more than 40 patients, and again, a 100% clinical complete response, including mature, complete responses at over a year in about 20 patients. Again, we are really doing our rectal cancer patients a disservice if we’re not checking for mismatch-repair deficiency upfront, and especially if we’re not talking about them in multidisciplinary conferences.
One of the things that absolutely blows my mind about rectal cancer is just how complicated it’s becoming. I think it is the standard of care to discuss these cases upfront with radiation oncology, surgical oncology, medical oncology, and pathology.
Maybe the overarching message I would take from everything I’ve said today is that the oncologist without the pathologist is blind. It’s really a dyad, a partnership that guides optimal medical oncology care. As much as I love ASCO, I often wish we had more of our pathology colleagues here. I look forward to taking all the findings from this meeting back to the tumor board and really having a dynamic dialogue.
Dr. Lewis is director, Department of Gastrointestinal Oncology, Intermountain Health, Salt Lake City, Utah. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. I’m Mark Lewis, director of gastrointestinal (GI) oncology at Intermountain Health in Utah.
If you allow me, I’d like to go in a craniocaudal fashion. It’s my anatomic mnemonic. I think that’s appropriate because our plenary session yesterday kicked off with some exciting data in esophageal cancer, specifically esophageal adenocarcinoma.
This was the long-awaited ESOPEC trial. It’s a phase 3 study looking at perioperative FLOT (5-FU/leucovorin/oxaliplatin/docetaxel), a chemo triplet, vs the CROSS protocol, which is neoadjuvant chemoradiation with carboplatin and paclitaxel. The primary endpoint was overall survival, and at first blush, FLOT looked to be the true winner. There were some really remarkable milestones in this study, and I have some reservations about the FLOT arm that I’ll raise in just a second.
The investigators are to be commended because in a truly deadly disease, they reported a 5-year overall survival in half of the patients who were receiving FLOT. That is truly commendable and really a milestone in our field. The reason I take a little bit of issue with the trial is that I still have some questions about methodology.
It wasn’t that long ago at ASCO GI that there was a really heated debate called “FLOT or Not” — not in this precise setting, but asking the question, do we think that patients with upper GI malignancy are even fit enough to handle a chemo triplet like FLOT?
The reason I bring that up now in 2024 is that, to my surprise, and I think to many others’, there was a lower-than-expected completion rate of the patients in this trial who were receiving the CROSS regimen. The number of people who were able to complete that in full was about two-thirds, which compared with a historical control from a trial scheme that first emerged over a decade ago that used to be over 90% completion. I found that quite strange.
I also think this trial suffers a little bit, and unavoidably, from the evolution of care that’s happened since it was first enrolling. Of course, I refer to adjuvant immunotherapy. Now, the real question is whether there is synergy between patients who receive radiation upfront and then adjuvant nivolumab, as per CheckMate 577.
In her plenary discussion, I thought Dr. Karyn Goodman did a masterful job — I would encourage you to watch it on ASCO’s website —discussing how we can take all these data and reconcile them for optimal patient outcome. She ultimately suggested that we might deploy all four modalities in the management of these people.
She proposed a paradigm with a PET-adapted, upfront induction chemotherapy, then moving to chemoradiation, then moving to surgery, and finally moving to immunotherapy. That is all four of the traditional arms of oncology. I find that really rather remarkable. Watch that space. This is a great trial with really remarkable survival data, but I’m not entirely convinced that the CROSS arm was given its due.
Next up, I want to talk about pancreas cancer, which is something near and dear to my heart. It affects about one in four of my patients and it remains, unfortunately, a highly lethal disease. I think the top-line news from this meeting is that the KRAS mutation is druggable. I’m probably showing my age, but when I did my fellowship in 2009 through 2012, I was taught that KRAS was sort of the undruggable mutation par excellence. At this meeting, we’ve seen maturing data in regard to targeting KRAS G12C with both sotorasib and adagrasib. The disease control rates are astounding, at 80% and more, which is really remarkable. I wouldn’t have believed that even a few years ago.
I’m even more excited about how we bring a rising tide that can lift all boats and apply this to other KRAS mutations, and not just KRAS G12C but all KRAS mutations. I think that’s coming, hopefully, with the pan-RAS inhibitors, because once that happens — if that happens; I’ll try not to be irrationally exuberant — that would take the traditional mutation found in almost all pancreas cancers and really make it its own Achilles heel. I think that could be such a huge leap forward.
Another matter, however, that remains unresolved at this meeting is in the neoadjuvant setting with pancreatic ductal adenocarcinoma. There’s still equipoise, actually, between neoadjuvant gemcitabine, paclitaxel, and FOLFIRINOX. I thought that that was very well spelled out by some of our Dutch colleagues, who continue to do great work in a variety of cancers, including colorectal.
Where I’d like to move next is colorectal cancer. Of course, immunotherapy remains a hot topic at all of these conferences. There were three different aspects of immunotherapy I’d like to highlight at this conference in regard to colon and rectal cancer.
First, Dr. Heinz-Josef Lenz presented updated data from CheckMate 8HW, which looked at nivolumab and ipilimumab (nivo/ipi) vs chemotherapy in the first line for MSI-high or mismatch repair–deficient colon cancer. Once again, the data we’ve had now for several years at the 2-year mark are incredibly impressive. The 2-year progression-free survival (PFS) rates for nivo/ipi are above 70% and down at around 14% for chemo.
What was impressive about this meeting is that Dr. Lenz presented PFS2, trying to determine the impact, if any, of subsequent therapy. What was going on here, which I think was ethically responsible by the investigators, was crossover. About two-thirds of the chemo arm crossed over to any form of immuno-oncology (IO), and just under a half crossed over to nivo and ipi. The PFS benefits continued with up-front IO. The way that Dr. Lenz phrased it is that you really never get the chance to win back the benefit that you would derive by giving immunotherapy first line to someone who has MSI-high or mismatch repair–deficient metastatic colon cancer.
One thing that’s still not settled in my mind, though, is, does this really dethrone single-agent immunotherapy, such as pembrolizumab in KEYNOTE-177? What I’m really driving at is the ipilimumab. Is the juice worth the squeeze? Is the addition of an anti-CTLA4 agent worth the toxicity that we know comes along with that mechanism of action? Watch this space.
I was also really interested in NEOPRISM-CRC, which looked at the role of immunotherapy in neoadjuvant down-staging of radiographically high-risk stage II or stage III colon cancer. Here, the investigators really make a strong case that, up front in these potentially respectable cases, not only should we know about mismatch repair deficiency but we should actually be interrogating further for tumor mutational burden (TMB).
They had TMB-high patients. In fact, the median TMB was 42 mutations per megabase, with really impressive down-staging using three cycles of every-3-week pembrolizumab before surgery. Again, I really think we’re at an exciting time where, even for colon cancer that looks operable up front, we might actually have the opportunity to improve pathologic and clinical complete responses before and after surgery.
Finally, I want to bring up what continues to amaze me. Two years ago, at ASCO 2022, we heard from Dr. Andrea Cercek and the Memorial Sloan Kettering group about the incredible experience they were having with neoadjuvant, or frankly, definitive dostarlimab in mismatch repair–deficient locally advanced rectal cancer.
I remember being at the conference and there was simultaneous publication of that abstract in The New York Times because it was so remarkable. There was a 100% clinical complete response. The patients didn’t require radiation, they didn’t require chemotherapy, and they didn’t require surgery for locally advanced rectal cancer, provided there was this vulnerability of mismatch-repair deficiency.
Now, 2 years later, Dr. Cercek and her group have updated those data with more than 40 patients, and again, a 100% clinical complete response, including mature, complete responses at over a year in about 20 patients. Again, we are really doing our rectal cancer patients a disservice if we’re not checking for mismatch-repair deficiency upfront, and especially if we’re not talking about them in multidisciplinary conferences.
One of the things that absolutely blows my mind about rectal cancer is just how complicated it’s becoming. I think it is the standard of care to discuss these cases upfront with radiation oncology, surgical oncology, medical oncology, and pathology.
Maybe the overarching message I would take from everything I’ve said today is that the oncologist without the pathologist is blind. It’s really a dyad, a partnership that guides optimal medical oncology care. As much as I love ASCO, I often wish we had more of our pathology colleagues here. I look forward to taking all the findings from this meeting back to the tumor board and really having a dynamic dialogue.
Dr. Lewis is director, Department of Gastrointestinal Oncology, Intermountain Health, Salt Lake City, Utah. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
An Overview of Gender-Affirming Care for Children and Adolescents
As Pride Month drew to a close, the Supreme Court made a shocking announcement. For the first time in the history of the court, it is willing to hear a legal challenge regarding gender-affirming care for minors. The justices will review whether a 2023 Tennessee law, SB1, which bans hormone therapy, puberty blockers, and surgery for transgender minors, is unconstitutional. This is the first time the Supreme Court will directly weigh in on gender-affirming care.
There are few topics as politically and medically divisive as gender-affirming care for minors. When the World Professional Association for Transgender Health (WPATH) released its updated Standards of Care, SOC8, one of the noticeable changes to the document was its approach to caring for transgender children and adolescents.
Before I highlight these recommendations and the ensuing controversy, it is imperative to establish proper terminology. Unfortunately, medical and legal terms often differ. Both activists and opponents use these terms interchangeably, which makes discourse about an already emotionally charged topic extremely difficult. From a legal perspective, the terms “minor” and “child” often refer to individuals under the age of majority. In the United States, the age of majority is 18. However, the term child also has a well-established medical definition. A child is an individual between the stages of infancy and puberty. Adolescence is a transitional period marked by the onset of puberty until adulthood (typically the age of majority). As medical providers, understanding these definitions is essential to identifying misinformation pertaining to this type of healthcare.
For the purposes of this article, I will be adhering to the medical terminology. Now, I want to be very clear. WPATH does not endorse surgical procedures on children. Furthermore, surgeons are not performing gender-affirming surgeries on children. On adolescents, rarely. But children, never.
According to the updated SOC8, the only acceptable gender-affirming intervention for children is psychosocial support.1 This does not include puberty blockers, hormones, or surgery, but rather allowing a child to explore their gender identity by experimenting with different clothing, toys, hairstyles, and even an alternative name that aligns more closely with their gender identity.1
It is only after children reach adolescence that medical, and in rare cases, surgical interventions, can be considered. Puberty blockers are appropriate for patients who have started puberty and experience gender dysphoria. These medications are reversible, and their purpose is to temporarily pause puberty to allow the adolescent to further explore their gender identity.
The most significant side effect of puberty blockers is decreased bone density.1 As a result, providers typically do not prescribe these medications for more than 2-3 years. After discontinuation of the medication, bone density returns to baseline.1 If the adolescent’s gender identity is marked and sustained over time, hormone therapy, such as testosterone or estrogen is then considered. Unlike puberty blockers, these medications can have permanent side effects. Testosterone use can lead to irreversible hair growth, alopecia, clitoromegaly, and voice deepening, while estrogen can cause permanent breast growth and halt sperm production.1 Future fertility and these side effects are discussed with the patient in detail prior to the initiation of these medications.
Contrary to the current political narrative, gender-affirming care for children and adolescents is not taken lightly. These individuals often receive years of multidisciplinary assessments, with a focus on gender identity development, social development and support, and diagnostic assessment of possible co-occurring mental health or developmental concerns and capacity for decision making.1 The clinical visits also occur with parental support and consent.
WPATH SOC8 also delineates the provider qualifications for health care professionals assessing these patients. Providers must be licensed by their statutory bodies and hold a postgraduate degree by a nationally accredited statutory institution; receive theoretical and evidence-based training and develop expertise in child, adolescent, and family mental health across the developmental spectrum; receive training and have expertise in gender identity development and gender diversity in children and adolescence; have the ability to assess capacity to assent/consent; receive training and develop expertise in autism spectrum disorders and other neurodevelopmental presentations; and to continue engaging in professional development in all areas relevant to gender-diverse children, adolescents, and families.1
The most controversial aspect of gender-affirming care for children and adolescents relates to surgical treatment. While the rates of gender-affirming surgeries have increased for this age group over the years, the overall rate of gender-affirming surgery for adolescents is markedly lower compared with other adolescents seeking cosmetic surgeries and compared with transgender adults undergoing gender-affirming surgery.
In a cohort study conducted between 2016 to 2020, 48,019 patients were identified who had undergone gender-affirming surgery.2 Only 3678 or 7.7% of patients were aged between 12 and 18, with the most common procedure being chest/breast surgery.2 So, under about 1000 cases per year were gender-affirming surgeries on patients under 18.
During 2020 alone, the number of cisgender adolescents between the ages of 13 and 19 who underwent breast augmentation and breast reduction was 3233 and 4666, respectively.3 The outrage about gender-affirming surgeries on transgender youth, yet the silence on cosmetic procedures in this same age group, speaks volumes.
All surgeries on adolescents should be taken seriously and with caution, regardless of gender identity. However, current legislation disproportionately targets only transgender youth. For whatever reason, surgeries on transgender individuals are labeled as “body mutilation,” whereas surgeries on cisgender youth are not even discussed. Such inflammatory rhetoric and complete lack of empathy impedes the common goal of all parties: what is in the best interest of the minor? Unfortunately, in a few short months, the answer to this question will be determined by a group of nine justices who have no experience in medicine or transgender health care, instead of by medical experts and the parents who care for these individuals.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pennsylvania. She has no conflicts of interest.
References
1. Coleman E et al. Standards of care for the health of transgender and gender diverse people, version 8. Int J Transgender Health. 2022;23(sup):S1-S259.
2. Wright JD et al. National estimates of gender affirming surgery in the US. JAMA Netw Open. 2023 Aug 1;6(8):e2330348.
3. American Society of Plastic Surgeons. Plastic Surgery Statistics Report. ASPS National Clearinghouse of Plastic Surgery Procedural Statistics. 2020.
As Pride Month drew to a close, the Supreme Court made a shocking announcement. For the first time in the history of the court, it is willing to hear a legal challenge regarding gender-affirming care for minors. The justices will review whether a 2023 Tennessee law, SB1, which bans hormone therapy, puberty blockers, and surgery for transgender minors, is unconstitutional. This is the first time the Supreme Court will directly weigh in on gender-affirming care.
There are few topics as politically and medically divisive as gender-affirming care for minors. When the World Professional Association for Transgender Health (WPATH) released its updated Standards of Care, SOC8, one of the noticeable changes to the document was its approach to caring for transgender children and adolescents.
Before I highlight these recommendations and the ensuing controversy, it is imperative to establish proper terminology. Unfortunately, medical and legal terms often differ. Both activists and opponents use these terms interchangeably, which makes discourse about an already emotionally charged topic extremely difficult. From a legal perspective, the terms “minor” and “child” often refer to individuals under the age of majority. In the United States, the age of majority is 18. However, the term child also has a well-established medical definition. A child is an individual between the stages of infancy and puberty. Adolescence is a transitional period marked by the onset of puberty until adulthood (typically the age of majority). As medical providers, understanding these definitions is essential to identifying misinformation pertaining to this type of healthcare.
For the purposes of this article, I will be adhering to the medical terminology. Now, I want to be very clear. WPATH does not endorse surgical procedures on children. Furthermore, surgeons are not performing gender-affirming surgeries on children. On adolescents, rarely. But children, never.
According to the updated SOC8, the only acceptable gender-affirming intervention for children is psychosocial support.1 This does not include puberty blockers, hormones, or surgery, but rather allowing a child to explore their gender identity by experimenting with different clothing, toys, hairstyles, and even an alternative name that aligns more closely with their gender identity.1
It is only after children reach adolescence that medical, and in rare cases, surgical interventions, can be considered. Puberty blockers are appropriate for patients who have started puberty and experience gender dysphoria. These medications are reversible, and their purpose is to temporarily pause puberty to allow the adolescent to further explore their gender identity.
The most significant side effect of puberty blockers is decreased bone density.1 As a result, providers typically do not prescribe these medications for more than 2-3 years. After discontinuation of the medication, bone density returns to baseline.1 If the adolescent’s gender identity is marked and sustained over time, hormone therapy, such as testosterone or estrogen is then considered. Unlike puberty blockers, these medications can have permanent side effects. Testosterone use can lead to irreversible hair growth, alopecia, clitoromegaly, and voice deepening, while estrogen can cause permanent breast growth and halt sperm production.1 Future fertility and these side effects are discussed with the patient in detail prior to the initiation of these medications.
Contrary to the current political narrative, gender-affirming care for children and adolescents is not taken lightly. These individuals often receive years of multidisciplinary assessments, with a focus on gender identity development, social development and support, and diagnostic assessment of possible co-occurring mental health or developmental concerns and capacity for decision making.1 The clinical visits also occur with parental support and consent.
WPATH SOC8 also delineates the provider qualifications for health care professionals assessing these patients. Providers must be licensed by their statutory bodies and hold a postgraduate degree by a nationally accredited statutory institution; receive theoretical and evidence-based training and develop expertise in child, adolescent, and family mental health across the developmental spectrum; receive training and have expertise in gender identity development and gender diversity in children and adolescence; have the ability to assess capacity to assent/consent; receive training and develop expertise in autism spectrum disorders and other neurodevelopmental presentations; and to continue engaging in professional development in all areas relevant to gender-diverse children, adolescents, and families.1
The most controversial aspect of gender-affirming care for children and adolescents relates to surgical treatment. While the rates of gender-affirming surgeries have increased for this age group over the years, the overall rate of gender-affirming surgery for adolescents is markedly lower compared with other adolescents seeking cosmetic surgeries and compared with transgender adults undergoing gender-affirming surgery.
In a cohort study conducted between 2016 to 2020, 48,019 patients were identified who had undergone gender-affirming surgery.2 Only 3678 or 7.7% of patients were aged between 12 and 18, with the most common procedure being chest/breast surgery.2 So, under about 1000 cases per year were gender-affirming surgeries on patients under 18.
During 2020 alone, the number of cisgender adolescents between the ages of 13 and 19 who underwent breast augmentation and breast reduction was 3233 and 4666, respectively.3 The outrage about gender-affirming surgeries on transgender youth, yet the silence on cosmetic procedures in this same age group, speaks volumes.
All surgeries on adolescents should be taken seriously and with caution, regardless of gender identity. However, current legislation disproportionately targets only transgender youth. For whatever reason, surgeries on transgender individuals are labeled as “body mutilation,” whereas surgeries on cisgender youth are not even discussed. Such inflammatory rhetoric and complete lack of empathy impedes the common goal of all parties: what is in the best interest of the minor? Unfortunately, in a few short months, the answer to this question will be determined by a group of nine justices who have no experience in medicine or transgender health care, instead of by medical experts and the parents who care for these individuals.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pennsylvania. She has no conflicts of interest.
References
1. Coleman E et al. Standards of care for the health of transgender and gender diverse people, version 8. Int J Transgender Health. 2022;23(sup):S1-S259.
2. Wright JD et al. National estimates of gender affirming surgery in the US. JAMA Netw Open. 2023 Aug 1;6(8):e2330348.
3. American Society of Plastic Surgeons. Plastic Surgery Statistics Report. ASPS National Clearinghouse of Plastic Surgery Procedural Statistics. 2020.
As Pride Month drew to a close, the Supreme Court made a shocking announcement. For the first time in the history of the court, it is willing to hear a legal challenge regarding gender-affirming care for minors. The justices will review whether a 2023 Tennessee law, SB1, which bans hormone therapy, puberty blockers, and surgery for transgender minors, is unconstitutional. This is the first time the Supreme Court will directly weigh in on gender-affirming care.
There are few topics as politically and medically divisive as gender-affirming care for minors. When the World Professional Association for Transgender Health (WPATH) released its updated Standards of Care, SOC8, one of the noticeable changes to the document was its approach to caring for transgender children and adolescents.
Before I highlight these recommendations and the ensuing controversy, it is imperative to establish proper terminology. Unfortunately, medical and legal terms often differ. Both activists and opponents use these terms interchangeably, which makes discourse about an already emotionally charged topic extremely difficult. From a legal perspective, the terms “minor” and “child” often refer to individuals under the age of majority. In the United States, the age of majority is 18. However, the term child also has a well-established medical definition. A child is an individual between the stages of infancy and puberty. Adolescence is a transitional period marked by the onset of puberty until adulthood (typically the age of majority). As medical providers, understanding these definitions is essential to identifying misinformation pertaining to this type of healthcare.
For the purposes of this article, I will be adhering to the medical terminology. Now, I want to be very clear. WPATH does not endorse surgical procedures on children. Furthermore, surgeons are not performing gender-affirming surgeries on children. On adolescents, rarely. But children, never.
According to the updated SOC8, the only acceptable gender-affirming intervention for children is psychosocial support.1 This does not include puberty blockers, hormones, or surgery, but rather allowing a child to explore their gender identity by experimenting with different clothing, toys, hairstyles, and even an alternative name that aligns more closely with their gender identity.1
It is only after children reach adolescence that medical, and in rare cases, surgical interventions, can be considered. Puberty blockers are appropriate for patients who have started puberty and experience gender dysphoria. These medications are reversible, and their purpose is to temporarily pause puberty to allow the adolescent to further explore their gender identity.
The most significant side effect of puberty blockers is decreased bone density.1 As a result, providers typically do not prescribe these medications for more than 2-3 years. After discontinuation of the medication, bone density returns to baseline.1 If the adolescent’s gender identity is marked and sustained over time, hormone therapy, such as testosterone or estrogen is then considered. Unlike puberty blockers, these medications can have permanent side effects. Testosterone use can lead to irreversible hair growth, alopecia, clitoromegaly, and voice deepening, while estrogen can cause permanent breast growth and halt sperm production.1 Future fertility and these side effects are discussed with the patient in detail prior to the initiation of these medications.
Contrary to the current political narrative, gender-affirming care for children and adolescents is not taken lightly. These individuals often receive years of multidisciplinary assessments, with a focus on gender identity development, social development and support, and diagnostic assessment of possible co-occurring mental health or developmental concerns and capacity for decision making.1 The clinical visits also occur with parental support and consent.
WPATH SOC8 also delineates the provider qualifications for health care professionals assessing these patients. Providers must be licensed by their statutory bodies and hold a postgraduate degree by a nationally accredited statutory institution; receive theoretical and evidence-based training and develop expertise in child, adolescent, and family mental health across the developmental spectrum; receive training and have expertise in gender identity development and gender diversity in children and adolescence; have the ability to assess capacity to assent/consent; receive training and develop expertise in autism spectrum disorders and other neurodevelopmental presentations; and to continue engaging in professional development in all areas relevant to gender-diverse children, adolescents, and families.1
The most controversial aspect of gender-affirming care for children and adolescents relates to surgical treatment. While the rates of gender-affirming surgeries have increased for this age group over the years, the overall rate of gender-affirming surgery for adolescents is markedly lower compared with other adolescents seeking cosmetic surgeries and compared with transgender adults undergoing gender-affirming surgery.
In a cohort study conducted between 2016 to 2020, 48,019 patients were identified who had undergone gender-affirming surgery.2 Only 3678 or 7.7% of patients were aged between 12 and 18, with the most common procedure being chest/breast surgery.2 So, under about 1000 cases per year were gender-affirming surgeries on patients under 18.
During 2020 alone, the number of cisgender adolescents between the ages of 13 and 19 who underwent breast augmentation and breast reduction was 3233 and 4666, respectively.3 The outrage about gender-affirming surgeries on transgender youth, yet the silence on cosmetic procedures in this same age group, speaks volumes.
All surgeries on adolescents should be taken seriously and with caution, regardless of gender identity. However, current legislation disproportionately targets only transgender youth. For whatever reason, surgeries on transgender individuals are labeled as “body mutilation,” whereas surgeries on cisgender youth are not even discussed. Such inflammatory rhetoric and complete lack of empathy impedes the common goal of all parties: what is in the best interest of the minor? Unfortunately, in a few short months, the answer to this question will be determined by a group of nine justices who have no experience in medicine or transgender health care, instead of by medical experts and the parents who care for these individuals.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pennsylvania. She has no conflicts of interest.
References
1. Coleman E et al. Standards of care for the health of transgender and gender diverse people, version 8. Int J Transgender Health. 2022;23(sup):S1-S259.
2. Wright JD et al. National estimates of gender affirming surgery in the US. JAMA Netw Open. 2023 Aug 1;6(8):e2330348.
3. American Society of Plastic Surgeons. Plastic Surgery Statistics Report. ASPS National Clearinghouse of Plastic Surgery Procedural Statistics. 2020.
Should South Park: The End of Obesity Be Required Viewing in Medical School?
Yes, there’s still much to find offensive, but South Park: The End of Obesity, in just 51 minutes, does more to explain some of obesity’s realities, its pharmacotherapy, and weight bias than the mainstream media has done perhaps ever.
The mini-movie follows the plight of Eric Cartman, the fictional South Parkian child with severe obesity.
South Park got everything right. The movie starts in a medical center where discussions with Cartman, his mother, and his doctor make it clear that obesity isn’t something that Cartman chose and is perhaps the most distressing aspect of his life. This certainly echoes study findings which report that quality-of-life scores in children with severe obesity are lower than those of children with newly diagnosed on-treatment cancers. As to how obesity erodes a child’s quality of life, no doubt part of its impact stems from obesity being a top source of schoolyard bullying, which is reflected by Cartman as he imagines his life without it.
Cartman’s mother explains that of course they’ve tried diet and exercise, but that intentional behavior change alone hasn’t been sufficient to sustainably move the scale’s needle — a truth for the vast majority of people with obesity. But here, unlike in many actual doctors’ offices, Cartman’s doctor doesn’t spend time doubting or cajoling; instead, he does his job — which is to inform his patient, without judgment, about a pharmaceutical option that has proved to be beneficial. He accurately describes these medications as ushering in “a whole new era of medicine, a miracle really” that can “help people lose vast amounts of weight.”
The kicker, though, comes next. The doctor explains that insurance companies cover the medications only for patients with diabetes, “so if you can’t afford them, you’re just kind of out of luck.” This is changing somewhat now, at least here in Canada, where two of our main private insurers have changed their base coverages to make antiobesity medications something employers need to opt out of rather than opt into, but certainly they’re not covered by US Medicare for weight management, nor by our version of the same here in Canada.
But even for those who have coverage, there are hoops to jump through, which is highlighted by the incredible efforts made by Cartman and his friends to get his insurance plan to cover the medications. Thwarted at every turn, despite the undeniable benefits of these medications to health and quality of life, they are forced to turn to compounding — a phenomenon certainly pervasive here in North America whereby compounding pharmacies claim to be able to provide glucagon-like peptide-1 (GLP-1) analogs with comparable efficacy at a fraction of the price, but without the same rigor of proof of purity or efficacy.
Also covered by South Park is that the GLP-1 analog supply is impacted by use by people who don’t meet approved medical criteria and are using the medications for aesthetic purposes. This speaks to the incredible societal pressure to be thin and to the comfort of some physicians to inappropriately prescribe these medications. This is covered by the subplot of South Park’s weed farmer, Randy, who in turn delivers an important insight into how it feels to use a GLP-1 analog: “I think there’s something wrong with these drugs ... I feel satisfied. With any drugs I want to do more and more, but with these drugs I feel like I want things less. With these drugs you don’t really crave anything.” The sentiment is echoed by Cartman, who exclaims, “I think I’m full. I’ve never known that feeling before in my life, but I’m full.”
It’s remarkable that South Park, a show built on serving up politically incorrect offense, covers obesity and its treatment with more accuracy, nuance, and compassion than does society as a whole. The show notes that obesity is a biological condition (it is), that when it comes to health (in America) “you have to have some f-ing willpower.” But where they explicitly mean having willpower in terms of filing and pursing insurance claims (you do), explains that drug companies are making antiobesity medications more expensive in America than anywhere else in the world (they are), and finally delivers this quote, which, while missing the biological basis of behavior and hunger with respect to obesity, certainly sums up why blame has no place in the discourse:
“We have sugar companies, pharmaceutical companies, and insurance companies all just trying to figure out how to make money off our health. It isn’t fair to put the blame on anyone for their weight.”
No, it’s not.
This movie should be required viewing in medical schools.
Dr. Freedhoff is associate professor, department of family medicine, University of Ottawa, and medical director, Bariatric Medical Institute, Ottawa, Ontario, Canada. He disclosed ties with Bariatric Medical Institute, Constant Health, Novo Nordisk, and Weighty Matters.
A version of this article appeared on Medscape.com.
Yes, there’s still much to find offensive, but South Park: The End of Obesity, in just 51 minutes, does more to explain some of obesity’s realities, its pharmacotherapy, and weight bias than the mainstream media has done perhaps ever.
The mini-movie follows the plight of Eric Cartman, the fictional South Parkian child with severe obesity.
South Park got everything right. The movie starts in a medical center where discussions with Cartman, his mother, and his doctor make it clear that obesity isn’t something that Cartman chose and is perhaps the most distressing aspect of his life. This certainly echoes study findings which report that quality-of-life scores in children with severe obesity are lower than those of children with newly diagnosed on-treatment cancers. As to how obesity erodes a child’s quality of life, no doubt part of its impact stems from obesity being a top source of schoolyard bullying, which is reflected by Cartman as he imagines his life without it.
Cartman’s mother explains that of course they’ve tried diet and exercise, but that intentional behavior change alone hasn’t been sufficient to sustainably move the scale’s needle — a truth for the vast majority of people with obesity. But here, unlike in many actual doctors’ offices, Cartman’s doctor doesn’t spend time doubting or cajoling; instead, he does his job — which is to inform his patient, without judgment, about a pharmaceutical option that has proved to be beneficial. He accurately describes these medications as ushering in “a whole new era of medicine, a miracle really” that can “help people lose vast amounts of weight.”
The kicker, though, comes next. The doctor explains that insurance companies cover the medications only for patients with diabetes, “so if you can’t afford them, you’re just kind of out of luck.” This is changing somewhat now, at least here in Canada, where two of our main private insurers have changed their base coverages to make antiobesity medications something employers need to opt out of rather than opt into, but certainly they’re not covered by US Medicare for weight management, nor by our version of the same here in Canada.
But even for those who have coverage, there are hoops to jump through, which is highlighted by the incredible efforts made by Cartman and his friends to get his insurance plan to cover the medications. Thwarted at every turn, despite the undeniable benefits of these medications to health and quality of life, they are forced to turn to compounding — a phenomenon certainly pervasive here in North America whereby compounding pharmacies claim to be able to provide glucagon-like peptide-1 (GLP-1) analogs with comparable efficacy at a fraction of the price, but without the same rigor of proof of purity or efficacy.
Also covered by South Park is that the GLP-1 analog supply is impacted by use by people who don’t meet approved medical criteria and are using the medications for aesthetic purposes. This speaks to the incredible societal pressure to be thin and to the comfort of some physicians to inappropriately prescribe these medications. This is covered by the subplot of South Park’s weed farmer, Randy, who in turn delivers an important insight into how it feels to use a GLP-1 analog: “I think there’s something wrong with these drugs ... I feel satisfied. With any drugs I want to do more and more, but with these drugs I feel like I want things less. With these drugs you don’t really crave anything.” The sentiment is echoed by Cartman, who exclaims, “I think I’m full. I’ve never known that feeling before in my life, but I’m full.”
It’s remarkable that South Park, a show built on serving up politically incorrect offense, covers obesity and its treatment with more accuracy, nuance, and compassion than does society as a whole. The show notes that obesity is a biological condition (it is), that when it comes to health (in America) “you have to have some f-ing willpower.” But where they explicitly mean having willpower in terms of filing and pursing insurance claims (you do), explains that drug companies are making antiobesity medications more expensive in America than anywhere else in the world (they are), and finally delivers this quote, which, while missing the biological basis of behavior and hunger with respect to obesity, certainly sums up why blame has no place in the discourse:
“We have sugar companies, pharmaceutical companies, and insurance companies all just trying to figure out how to make money off our health. It isn’t fair to put the blame on anyone for their weight.”
No, it’s not.
This movie should be required viewing in medical schools.
Dr. Freedhoff is associate professor, department of family medicine, University of Ottawa, and medical director, Bariatric Medical Institute, Ottawa, Ontario, Canada. He disclosed ties with Bariatric Medical Institute, Constant Health, Novo Nordisk, and Weighty Matters.
A version of this article appeared on Medscape.com.
Yes, there’s still much to find offensive, but South Park: The End of Obesity, in just 51 minutes, does more to explain some of obesity’s realities, its pharmacotherapy, and weight bias than the mainstream media has done perhaps ever.
The mini-movie follows the plight of Eric Cartman, the fictional South Parkian child with severe obesity.
South Park got everything right. The movie starts in a medical center where discussions with Cartman, his mother, and his doctor make it clear that obesity isn’t something that Cartman chose and is perhaps the most distressing aspect of his life. This certainly echoes study findings which report that quality-of-life scores in children with severe obesity are lower than those of children with newly diagnosed on-treatment cancers. As to how obesity erodes a child’s quality of life, no doubt part of its impact stems from obesity being a top source of schoolyard bullying, which is reflected by Cartman as he imagines his life without it.
Cartman’s mother explains that of course they’ve tried diet and exercise, but that intentional behavior change alone hasn’t been sufficient to sustainably move the scale’s needle — a truth for the vast majority of people with obesity. But here, unlike in many actual doctors’ offices, Cartman’s doctor doesn’t spend time doubting or cajoling; instead, he does his job — which is to inform his patient, without judgment, about a pharmaceutical option that has proved to be beneficial. He accurately describes these medications as ushering in “a whole new era of medicine, a miracle really” that can “help people lose vast amounts of weight.”
The kicker, though, comes next. The doctor explains that insurance companies cover the medications only for patients with diabetes, “so if you can’t afford them, you’re just kind of out of luck.” This is changing somewhat now, at least here in Canada, where two of our main private insurers have changed their base coverages to make antiobesity medications something employers need to opt out of rather than opt into, but certainly they’re not covered by US Medicare for weight management, nor by our version of the same here in Canada.
But even for those who have coverage, there are hoops to jump through, which is highlighted by the incredible efforts made by Cartman and his friends to get his insurance plan to cover the medications. Thwarted at every turn, despite the undeniable benefits of these medications to health and quality of life, they are forced to turn to compounding — a phenomenon certainly pervasive here in North America whereby compounding pharmacies claim to be able to provide glucagon-like peptide-1 (GLP-1) analogs with comparable efficacy at a fraction of the price, but without the same rigor of proof of purity or efficacy.
Also covered by South Park is that the GLP-1 analog supply is impacted by use by people who don’t meet approved medical criteria and are using the medications for aesthetic purposes. This speaks to the incredible societal pressure to be thin and to the comfort of some physicians to inappropriately prescribe these medications. This is covered by the subplot of South Park’s weed farmer, Randy, who in turn delivers an important insight into how it feels to use a GLP-1 analog: “I think there’s something wrong with these drugs ... I feel satisfied. With any drugs I want to do more and more, but with these drugs I feel like I want things less. With these drugs you don’t really crave anything.” The sentiment is echoed by Cartman, who exclaims, “I think I’m full. I’ve never known that feeling before in my life, but I’m full.”
It’s remarkable that South Park, a show built on serving up politically incorrect offense, covers obesity and its treatment with more accuracy, nuance, and compassion than does society as a whole. The show notes that obesity is a biological condition (it is), that when it comes to health (in America) “you have to have some f-ing willpower.” But where they explicitly mean having willpower in terms of filing and pursing insurance claims (you do), explains that drug companies are making antiobesity medications more expensive in America than anywhere else in the world (they are), and finally delivers this quote, which, while missing the biological basis of behavior and hunger with respect to obesity, certainly sums up why blame has no place in the discourse:
“We have sugar companies, pharmaceutical companies, and insurance companies all just trying to figure out how to make money off our health. It isn’t fair to put the blame on anyone for their weight.”
No, it’s not.
This movie should be required viewing in medical schools.
Dr. Freedhoff is associate professor, department of family medicine, University of Ottawa, and medical director, Bariatric Medical Institute, Ottawa, Ontario, Canada. He disclosed ties with Bariatric Medical Institute, Constant Health, Novo Nordisk, and Weighty Matters.
A version of this article appeared on Medscape.com.
Facial Temperature Can Reveal Age and Disease
This transcript has been edited for clarity.
My oldest daughter is at sleepaway camp for a couple of weeks, and the camp has a photographer who goes around all day taking pictures of the kids, which get uploaded to a private Facebook group. In the past, I would go online every day (or, okay, several times a day) and scroll through all those pictures looking for one that features my kid.
I don’t have to do that anymore. This year, I simply uploaded a picture of my daughter to an app and artificial intelligence (AI) takes care of the rest, recognizing her face amidst the sea of smiling children, and flagging just those photos for me to peruse. It’s amazing, really. And a bit scary.
The fact that facial recognition has penetrated the summer camp market should tell you that the tech is truly ubiquitous. But today we’re going to think a bit more about what AI can do with a picture of your face, because the power of facial recognition is not just skin deep.
What’s got me hot and bothered about facial images is this paper, appearing in Cell Metabolism, which adds a new layer to the standard facial-analysis playbook: facial temperature.
To understand this paper, you need to understand a whole field of research that is developing various different “clocks” for age.
It turns out that age really is just a number. Our cells, our proteins, our biochemistry can be analyzed to give different numbers. These “clocks,” as distinct from the calendar we usually use to measure our age, might have more predictive power than the number itself.
There are numerous molecular clocks, such as telomere length, that not only correlate with calendar age but are superior to calendar age in predicting age-related complications. Testing telomere length typically requires a blood sample — and remains costly. But we can use other sources to estimate age; how about a photo?
I mean, we do this all the time when we meet someone new or, as a physician, when we meet a new patient. I have often written that a patient “appears younger than their stated age,” and we’ve all had the experience of hearing how old someone is and being shocked. I mean, have you seen Sharon Stone recently? She’s 66 years old. Okay — to be fair, there might be some outside help there. But you get the point.
Back to the Cell Metabolism paper. Researchers report on multiple algorithms to obtain an “age” from a picture of an individual’s face.
The first algorithm is pretty straightforward. Researchers collected 2811 images, all of Han Chinese individuals ranging in age from 20 to 90 years, and reconstructed a 3D facial map from those. 
They then trained a convolutional neural network to predict the individuals’ ages from the pictures. It was quite accurate, as you can see here.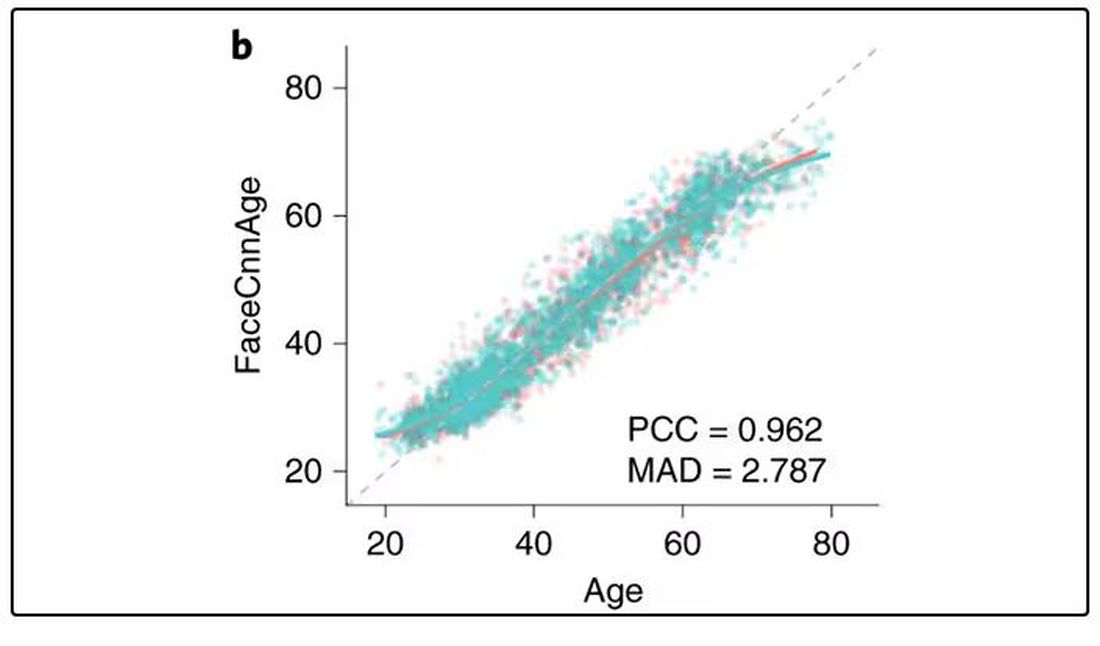
In the AI age, this may not seem that impressive. A brief search online turned up dozens of apps that promised to guess my age from a photo.
I sent this rather unflattering picture of myself to ChatGPT which, after initially demurring and saying it was not designed to guess ages, pegged me at somewhere between 35 and 45, which I am taking as a major victory.
But the Cell Metabolism paper goes deeper. Literally. 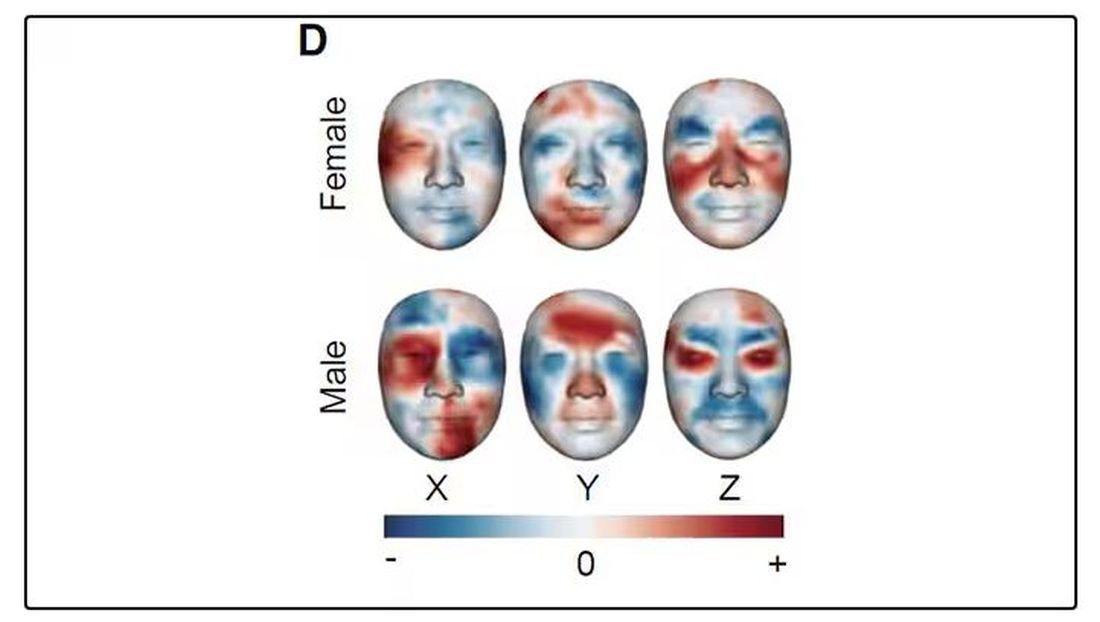
And this is where things start to get interesting. Because sure, the visible part of your face can change depending on makeup, expression, plastic surgery, and the like. But the temperature? That’s harder to fake.
It turns out that the temperature distribution in your face changes as you get older. There is a cooling of the nose and the cheeks, for example.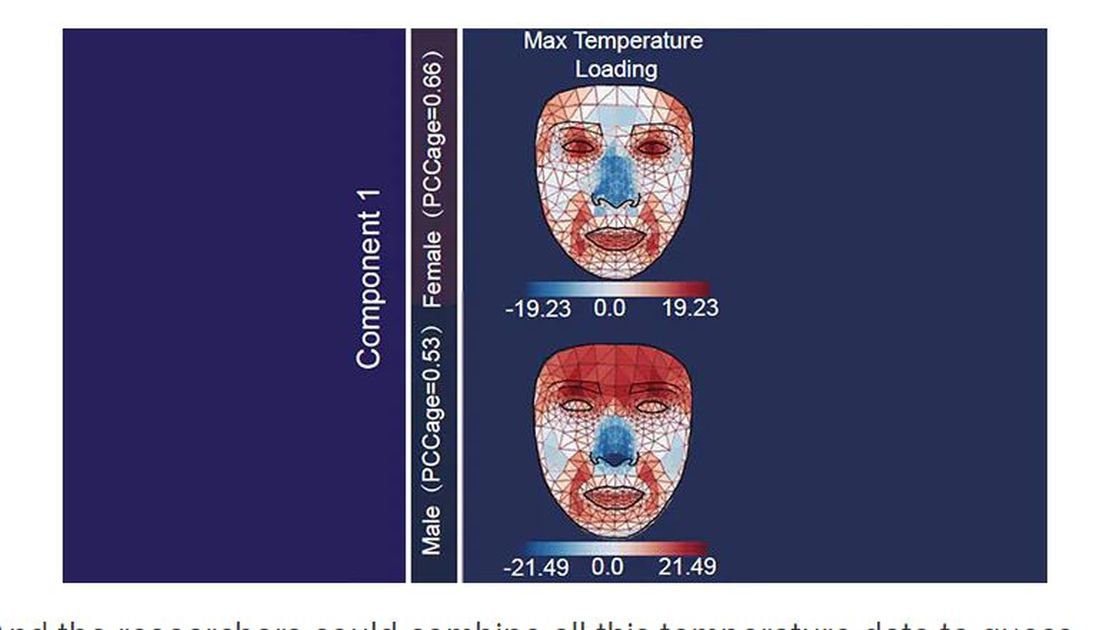
And the researchers could combine all this temperature data to guess someone’s calendar age fairly accurately, though notably not as accurately as the model that just looks at the pictures.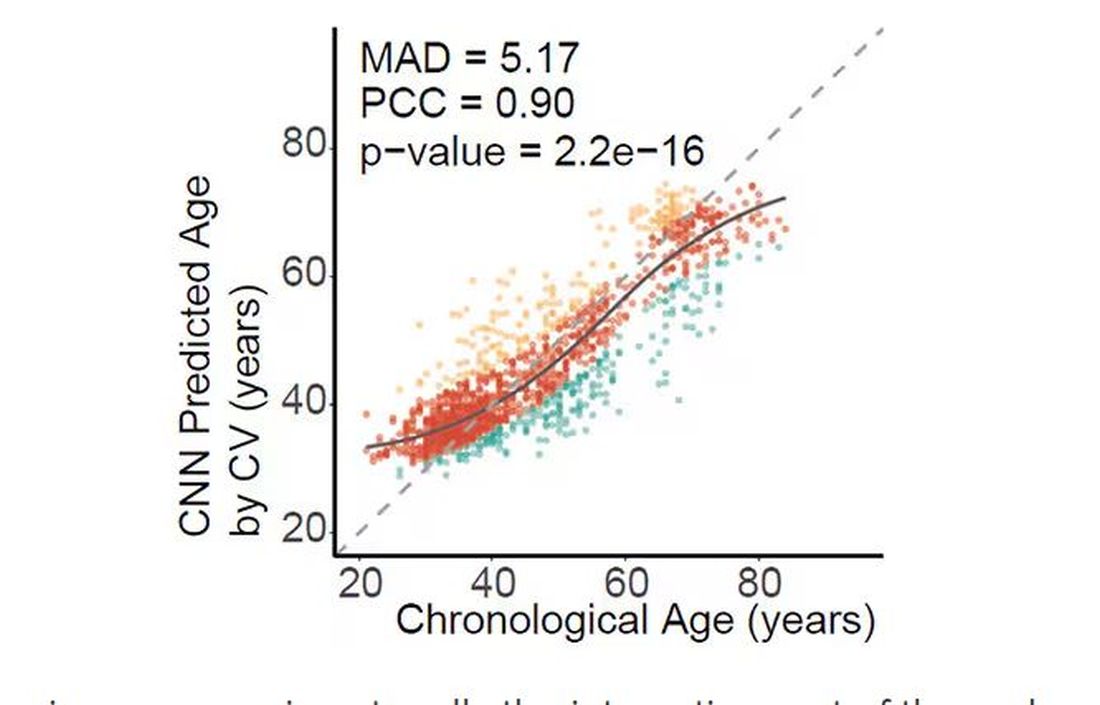
But guessing your age is not really the interesting part of thermal imaging of the face. It’s guessing — or, rather, predicting — the state of your metabolism. All these study participants had extensive metabolic testing performed, as well as detailed analysis of their lifestyle behaviors. And facial images could be used to predict those factors.
For example, the 3D reconstruction of the faces could predict who ate seafood (they tend to look younger than their actual age) compared with who ate poultry and meat (they tend to look older). The thermal imaging could predict who got more sleep (they look younger from a temperature perspective) and who ate more yogurt (also younger-appearing, temperature-wise). Facial temperature patterns could identify those with higher BMI, higher blood pressure, higher fasting glucose.
The researchers used the difference between actual and predicted age as a metric to measure illness as well. You can see here how, on average, individuals with hypertension, diabetes, and even liver cysts are “older,” at least by face temperature.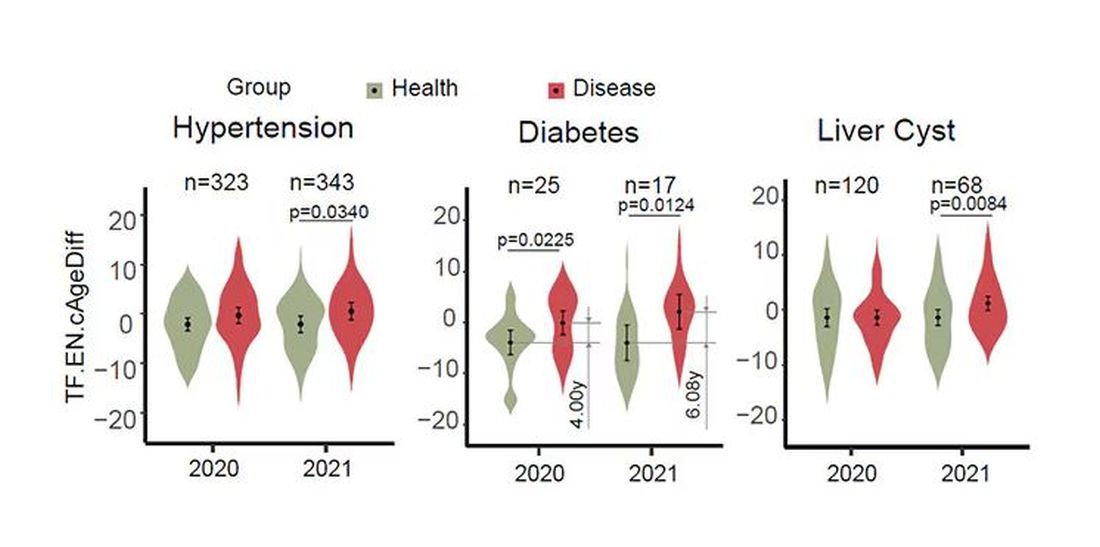
It may even be possible to use facial temperature as biofeedback. In a small study, the researchers measured the difference between facial temperature age and real age before and after 2 weeks of jump-roping. It turns out that 2 weeks of jump-roping can make you look about 5 years younger, at least as judged by a thermal camera. Or like the Predator.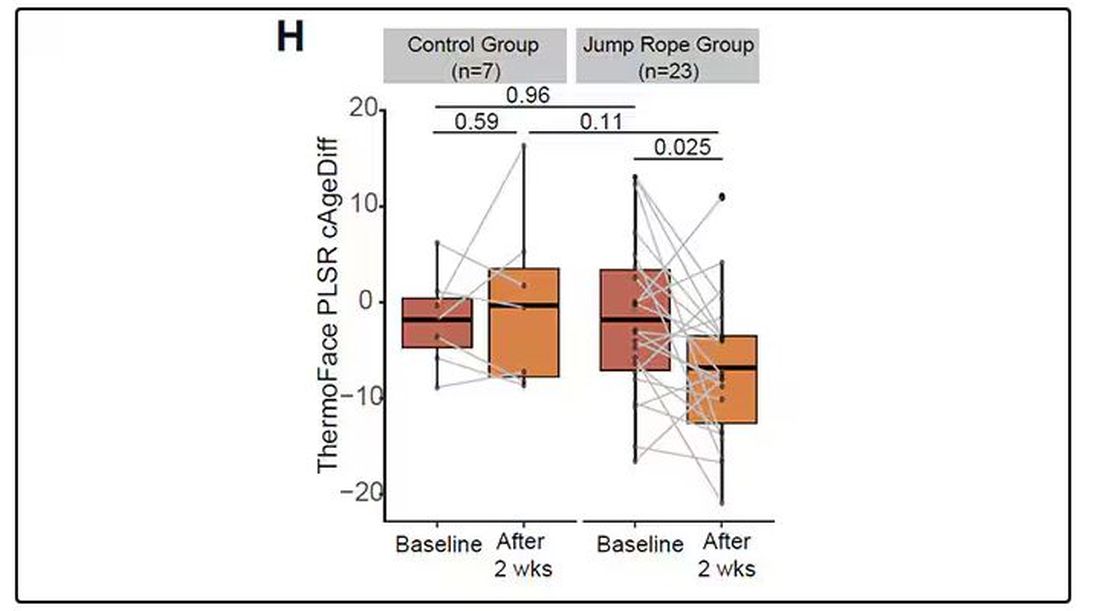
Okay, this is all very cool, but I’m not saying we’ll all be doing facial temperature tests in the near future. No; what this study highlights for me is how much information about ourselves is available to those who know how to decode it. Maybe those data come from the wrinkles in our faces, or the angles of our smiles, or the speed with which we type, or the temperature of our elbows. The data have always been there, actually, but we’ve never had the tools powerful enough to analyze them until now.
When I was a kid, I was obsessed with Star Trek — I know, you’re shocked — and, of course, the famous tricorder, a scanner that could tell everything about someone’s state of health in 5 seconds from 3 feet away. That’s how I thought medicine really would be in the future. Once I got to medical school, I was disabused of that notion. But the age of data, the age of AI, may mean the tricorder age is not actually that far away.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
My oldest daughter is at sleepaway camp for a couple of weeks, and the camp has a photographer who goes around all day taking pictures of the kids, which get uploaded to a private Facebook group. In the past, I would go online every day (or, okay, several times a day) and scroll through all those pictures looking for one that features my kid.
I don’t have to do that anymore. This year, I simply uploaded a picture of my daughter to an app and artificial intelligence (AI) takes care of the rest, recognizing her face amidst the sea of smiling children, and flagging just those photos for me to peruse. It’s amazing, really. And a bit scary.
The fact that facial recognition has penetrated the summer camp market should tell you that the tech is truly ubiquitous. But today we’re going to think a bit more about what AI can do with a picture of your face, because the power of facial recognition is not just skin deep.
What’s got me hot and bothered about facial images is this paper, appearing in Cell Metabolism, which adds a new layer to the standard facial-analysis playbook: facial temperature.
To understand this paper, you need to understand a whole field of research that is developing various different “clocks” for age.
It turns out that age really is just a number. Our cells, our proteins, our biochemistry can be analyzed to give different numbers. These “clocks,” as distinct from the calendar we usually use to measure our age, might have more predictive power than the number itself.
There are numerous molecular clocks, such as telomere length, that not only correlate with calendar age but are superior to calendar age in predicting age-related complications. Testing telomere length typically requires a blood sample — and remains costly. But we can use other sources to estimate age; how about a photo?
I mean, we do this all the time when we meet someone new or, as a physician, when we meet a new patient. I have often written that a patient “appears younger than their stated age,” and we’ve all had the experience of hearing how old someone is and being shocked. I mean, have you seen Sharon Stone recently? She’s 66 years old. Okay — to be fair, there might be some outside help there. But you get the point.
Back to the Cell Metabolism paper. Researchers report on multiple algorithms to obtain an “age” from a picture of an individual’s face.
The first algorithm is pretty straightforward. Researchers collected 2811 images, all of Han Chinese individuals ranging in age from 20 to 90 years, and reconstructed a 3D facial map from those. 
They then trained a convolutional neural network to predict the individuals’ ages from the pictures. It was quite accurate, as you can see here.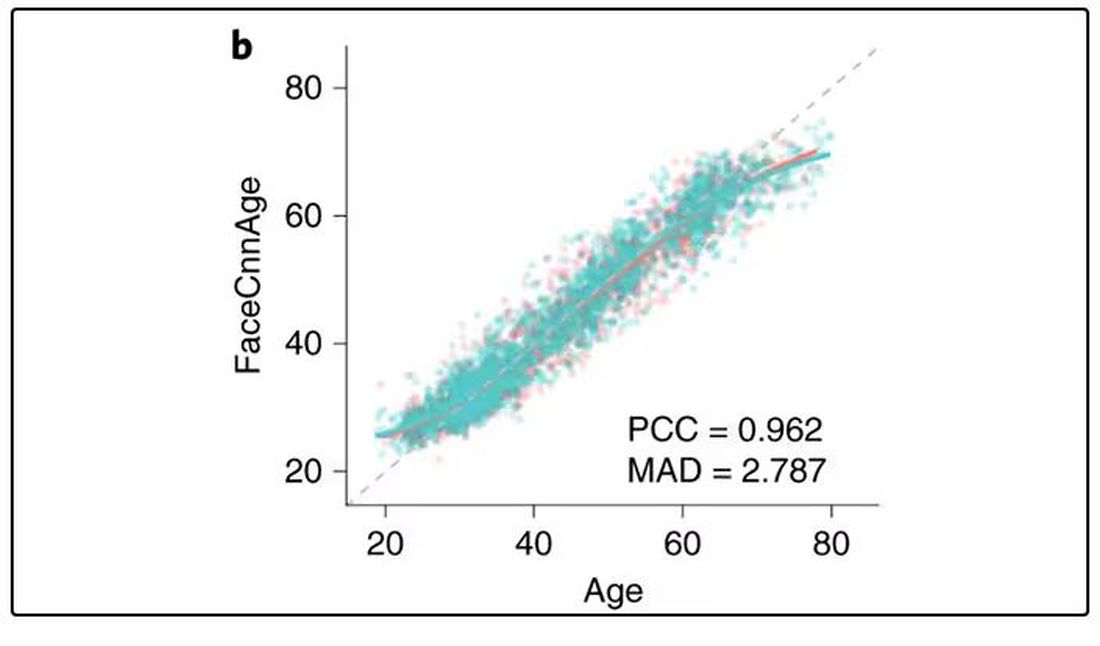
In the AI age, this may not seem that impressive. A brief search online turned up dozens of apps that promised to guess my age from a photo.
I sent this rather unflattering picture of myself to ChatGPT which, after initially demurring and saying it was not designed to guess ages, pegged me at somewhere between 35 and 45, which I am taking as a major victory.
But the Cell Metabolism paper goes deeper. Literally. 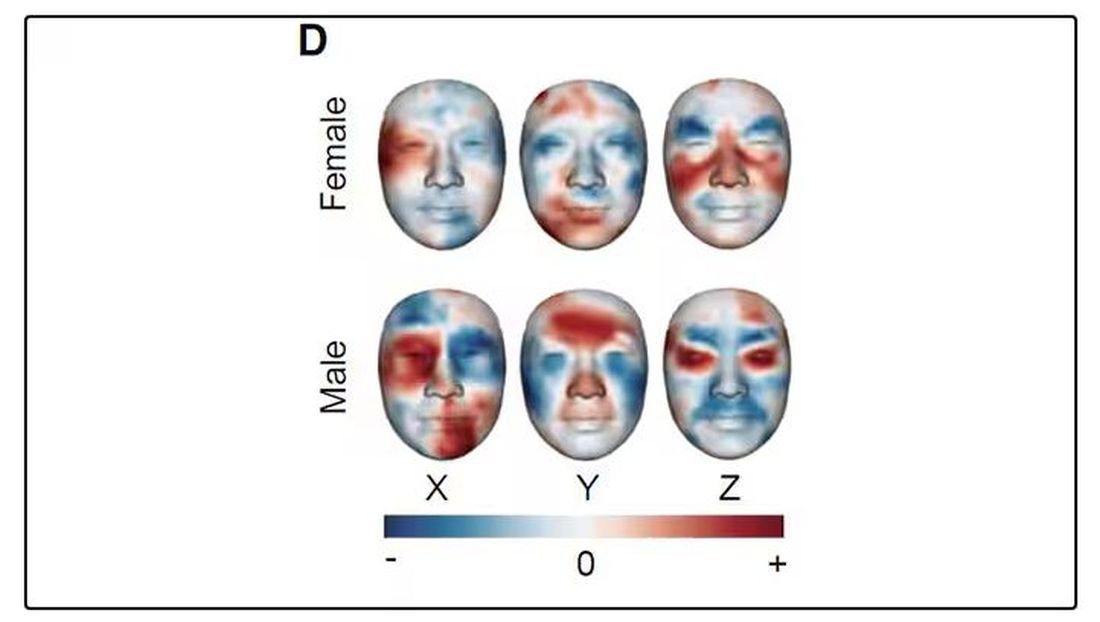
And this is where things start to get interesting. Because sure, the visible part of your face can change depending on makeup, expression, plastic surgery, and the like. But the temperature? That’s harder to fake.
It turns out that the temperature distribution in your face changes as you get older. There is a cooling of the nose and the cheeks, for example.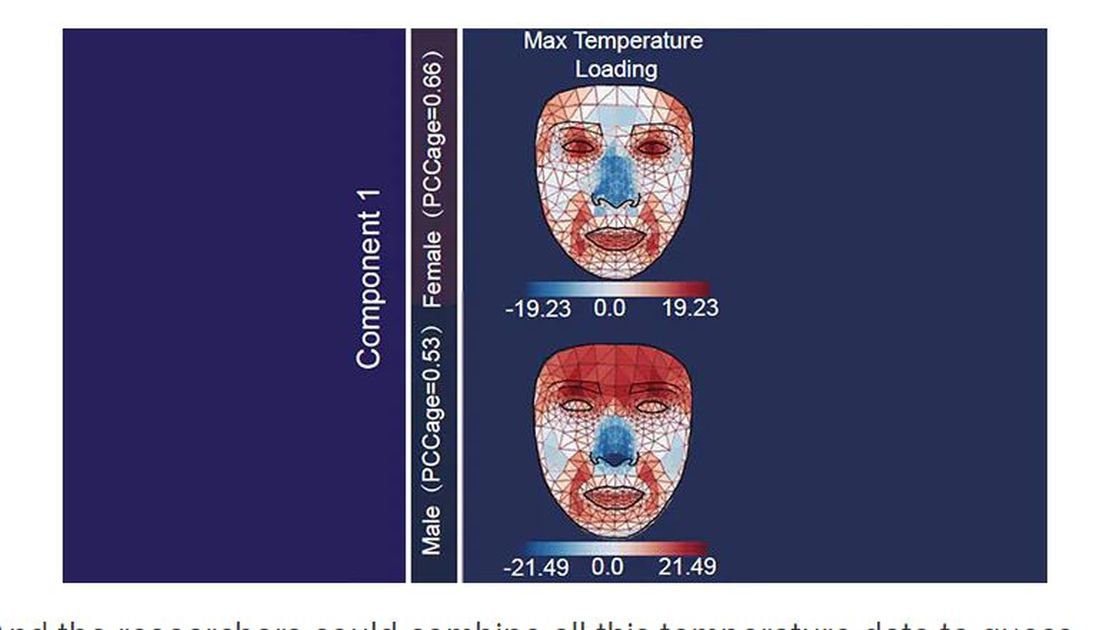
And the researchers could combine all this temperature data to guess someone’s calendar age fairly accurately, though notably not as accurately as the model that just looks at the pictures.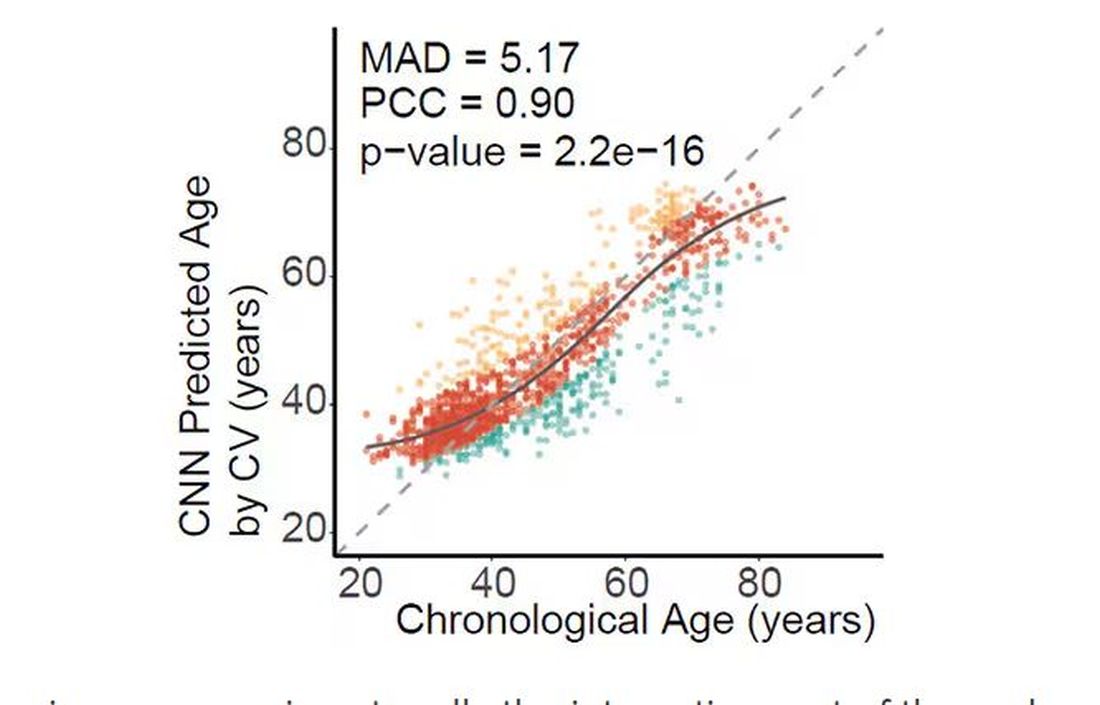
But guessing your age is not really the interesting part of thermal imaging of the face. It’s guessing — or, rather, predicting — the state of your metabolism. All these study participants had extensive metabolic testing performed, as well as detailed analysis of their lifestyle behaviors. And facial images could be used to predict those factors.
For example, the 3D reconstruction of the faces could predict who ate seafood (they tend to look younger than their actual age) compared with who ate poultry and meat (they tend to look older). The thermal imaging could predict who got more sleep (they look younger from a temperature perspective) and who ate more yogurt (also younger-appearing, temperature-wise). Facial temperature patterns could identify those with higher BMI, higher blood pressure, higher fasting glucose.
The researchers used the difference between actual and predicted age as a metric to measure illness as well. You can see here how, on average, individuals with hypertension, diabetes, and even liver cysts are “older,” at least by face temperature.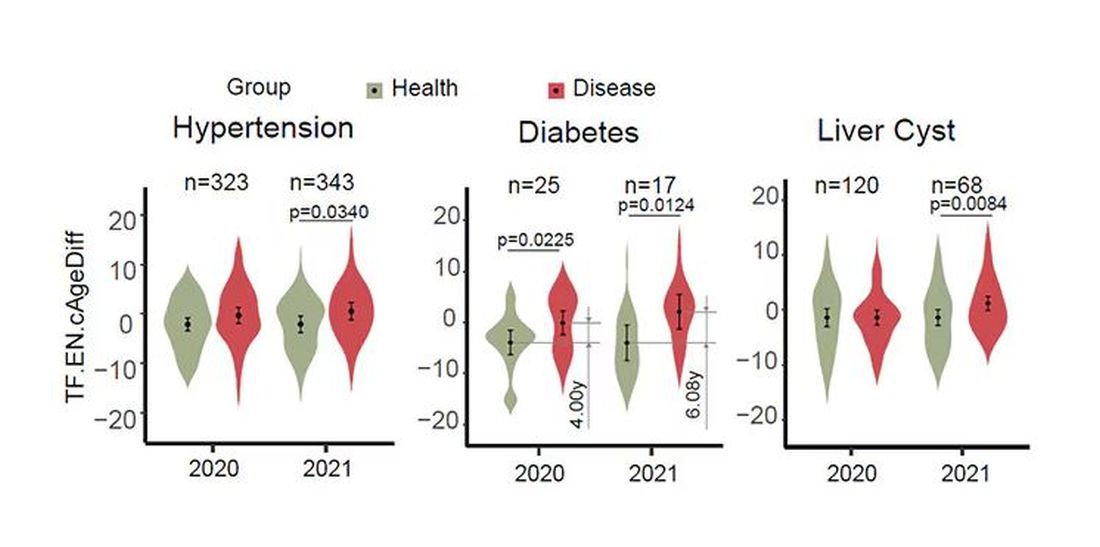
It may even be possible to use facial temperature as biofeedback. In a small study, the researchers measured the difference between facial temperature age and real age before and after 2 weeks of jump-roping. It turns out that 2 weeks of jump-roping can make you look about 5 years younger, at least as judged by a thermal camera. Or like the Predator.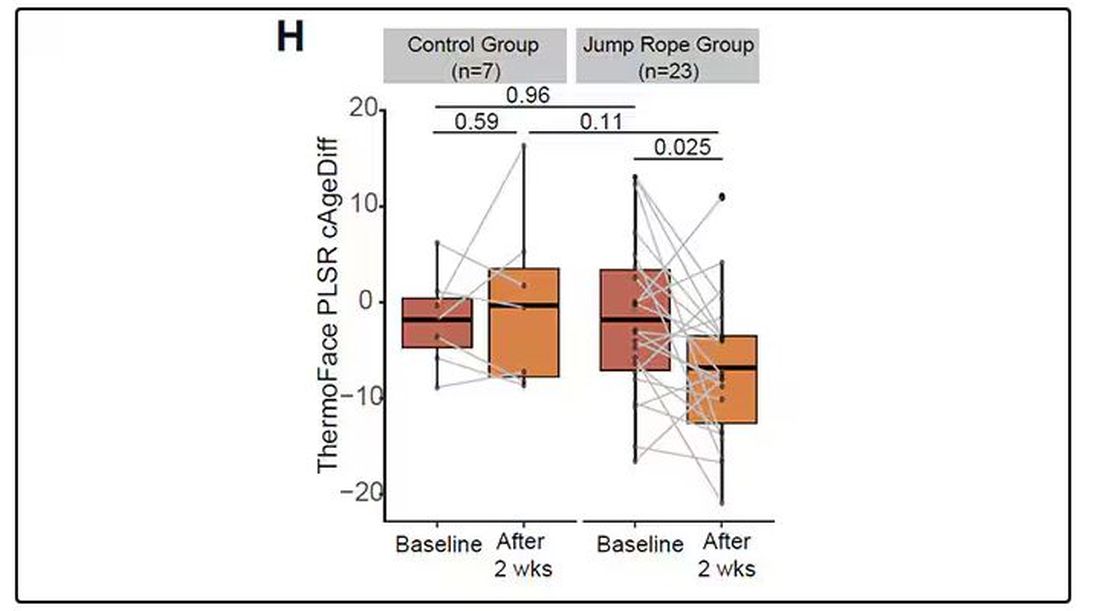
Okay, this is all very cool, but I’m not saying we’ll all be doing facial temperature tests in the near future. No; what this study highlights for me is how much information about ourselves is available to those who know how to decode it. Maybe those data come from the wrinkles in our faces, or the angles of our smiles, or the speed with which we type, or the temperature of our elbows. The data have always been there, actually, but we’ve never had the tools powerful enough to analyze them until now.
When I was a kid, I was obsessed with Star Trek — I know, you’re shocked — and, of course, the famous tricorder, a scanner that could tell everything about someone’s state of health in 5 seconds from 3 feet away. That’s how I thought medicine really would be in the future. Once I got to medical school, I was disabused of that notion. But the age of data, the age of AI, may mean the tricorder age is not actually that far away.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
My oldest daughter is at sleepaway camp for a couple of weeks, and the camp has a photographer who goes around all day taking pictures of the kids, which get uploaded to a private Facebook group. In the past, I would go online every day (or, okay, several times a day) and scroll through all those pictures looking for one that features my kid.
I don’t have to do that anymore. This year, I simply uploaded a picture of my daughter to an app and artificial intelligence (AI) takes care of the rest, recognizing her face amidst the sea of smiling children, and flagging just those photos for me to peruse. It’s amazing, really. And a bit scary.
The fact that facial recognition has penetrated the summer camp market should tell you that the tech is truly ubiquitous. But today we’re going to think a bit more about what AI can do with a picture of your face, because the power of facial recognition is not just skin deep.
What’s got me hot and bothered about facial images is this paper, appearing in Cell Metabolism, which adds a new layer to the standard facial-analysis playbook: facial temperature.
To understand this paper, you need to understand a whole field of research that is developing various different “clocks” for age.
It turns out that age really is just a number. Our cells, our proteins, our biochemistry can be analyzed to give different numbers. These “clocks,” as distinct from the calendar we usually use to measure our age, might have more predictive power than the number itself.
There are numerous molecular clocks, such as telomere length, that not only correlate with calendar age but are superior to calendar age in predicting age-related complications. Testing telomere length typically requires a blood sample — and remains costly. But we can use other sources to estimate age; how about a photo?
I mean, we do this all the time when we meet someone new or, as a physician, when we meet a new patient. I have often written that a patient “appears younger than their stated age,” and we’ve all had the experience of hearing how old someone is and being shocked. I mean, have you seen Sharon Stone recently? She’s 66 years old. Okay — to be fair, there might be some outside help there. But you get the point.
Back to the Cell Metabolism paper. Researchers report on multiple algorithms to obtain an “age” from a picture of an individual’s face.
The first algorithm is pretty straightforward. Researchers collected 2811 images, all of Han Chinese individuals ranging in age from 20 to 90 years, and reconstructed a 3D facial map from those. 
They then trained a convolutional neural network to predict the individuals’ ages from the pictures. It was quite accurate, as you can see here.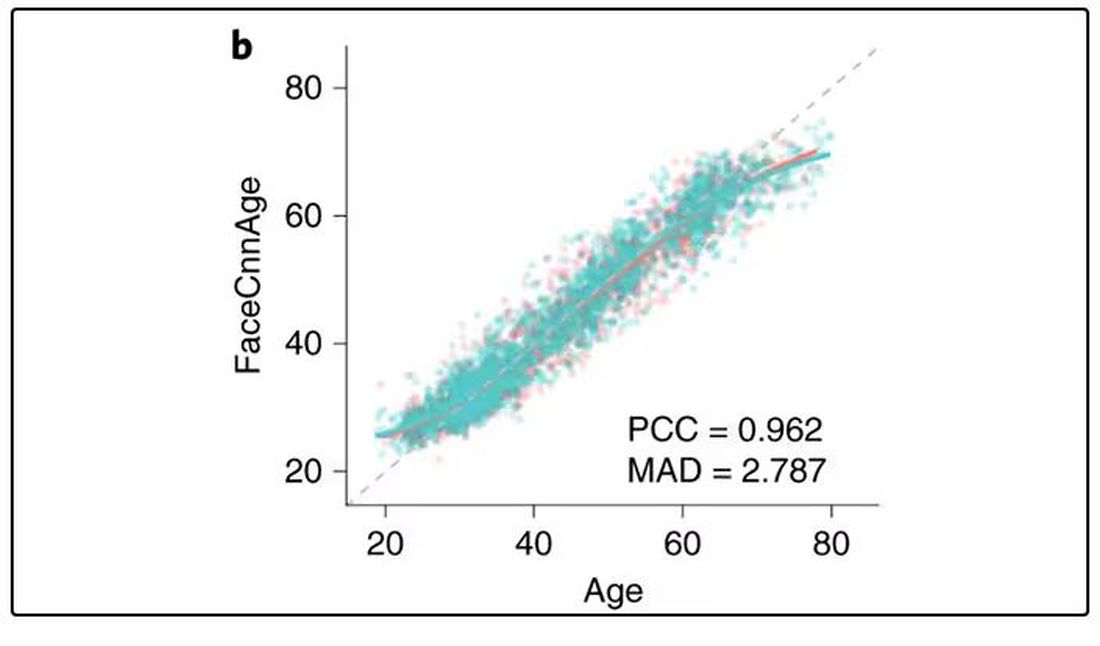
In the AI age, this may not seem that impressive. A brief search online turned up dozens of apps that promised to guess my age from a photo.
I sent this rather unflattering picture of myself to ChatGPT which, after initially demurring and saying it was not designed to guess ages, pegged me at somewhere between 35 and 45, which I am taking as a major victory.
But the Cell Metabolism paper goes deeper. Literally. 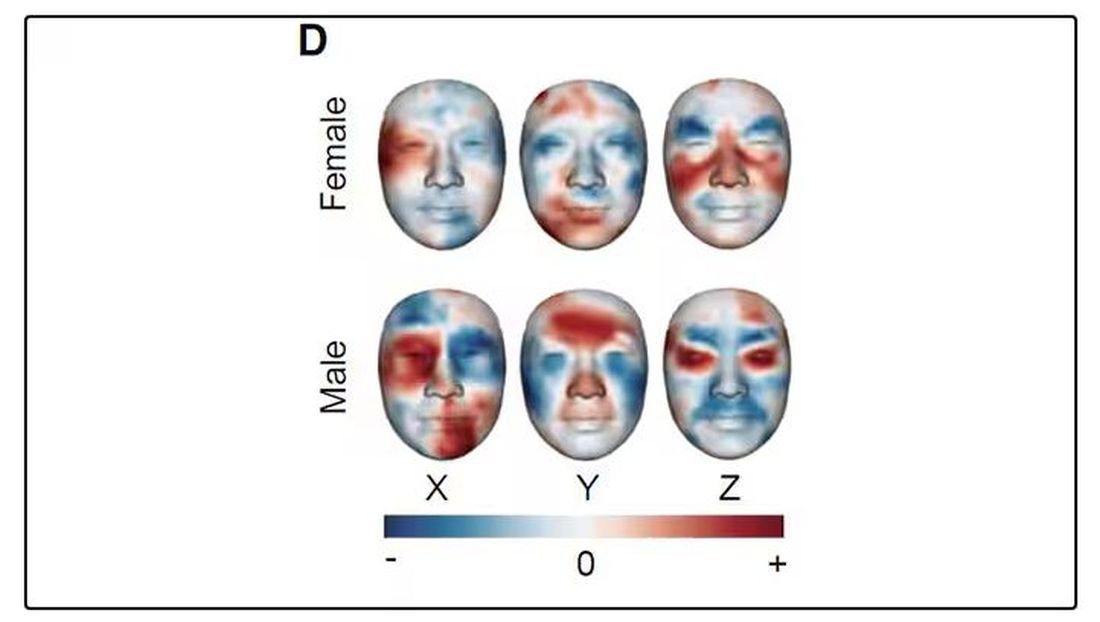
And this is where things start to get interesting. Because sure, the visible part of your face can change depending on makeup, expression, plastic surgery, and the like. But the temperature? That’s harder to fake.
It turns out that the temperature distribution in your face changes as you get older. There is a cooling of the nose and the cheeks, for example.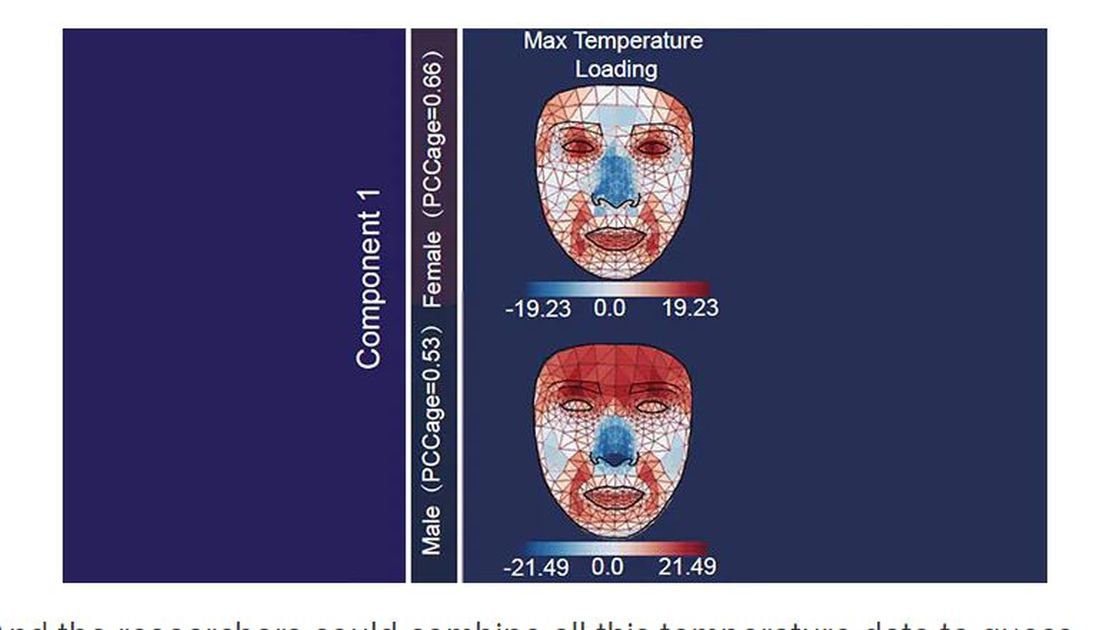
And the researchers could combine all this temperature data to guess someone’s calendar age fairly accurately, though notably not as accurately as the model that just looks at the pictures.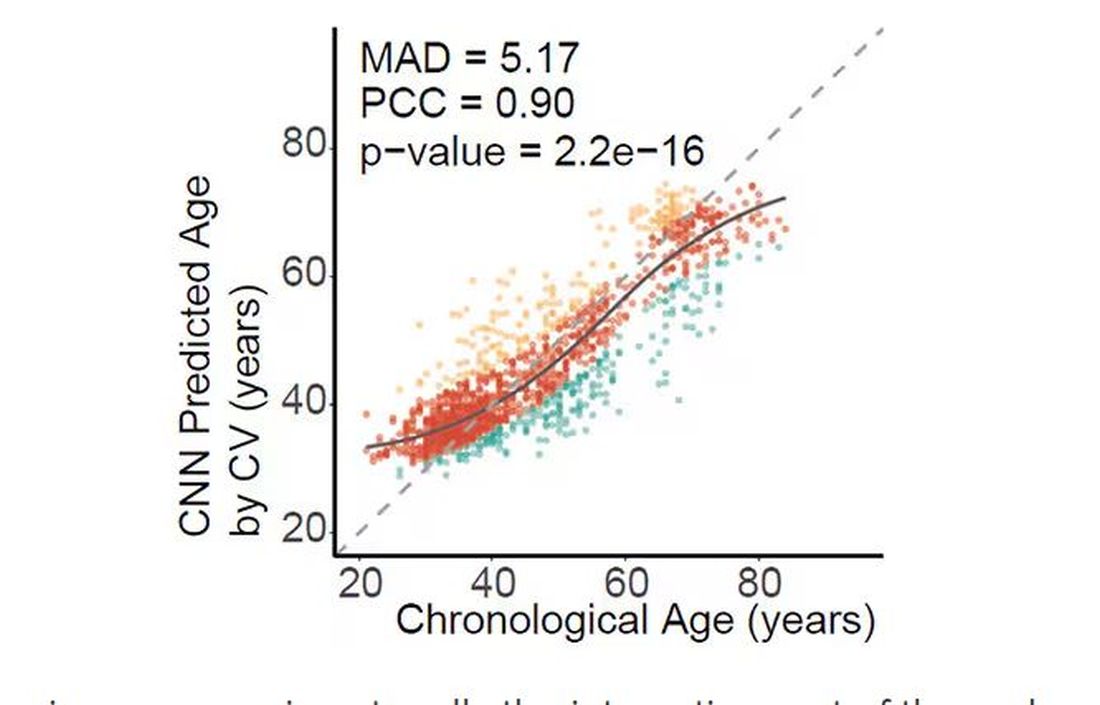
But guessing your age is not really the interesting part of thermal imaging of the face. It’s guessing — or, rather, predicting — the state of your metabolism. All these study participants had extensive metabolic testing performed, as well as detailed analysis of their lifestyle behaviors. And facial images could be used to predict those factors.
For example, the 3D reconstruction of the faces could predict who ate seafood (they tend to look younger than their actual age) compared with who ate poultry and meat (they tend to look older). The thermal imaging could predict who got more sleep (they look younger from a temperature perspective) and who ate more yogurt (also younger-appearing, temperature-wise). Facial temperature patterns could identify those with higher BMI, higher blood pressure, higher fasting glucose.
The researchers used the difference between actual and predicted age as a metric to measure illness as well. You can see here how, on average, individuals with hypertension, diabetes, and even liver cysts are “older,” at least by face temperature.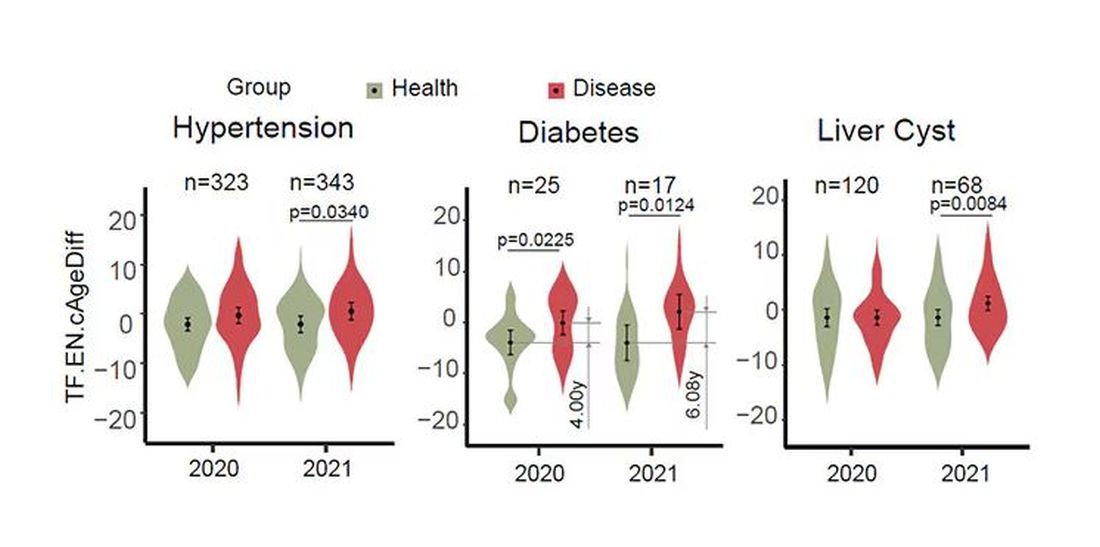
It may even be possible to use facial temperature as biofeedback. In a small study, the researchers measured the difference between facial temperature age and real age before and after 2 weeks of jump-roping. It turns out that 2 weeks of jump-roping can make you look about 5 years younger, at least as judged by a thermal camera. Or like the Predator.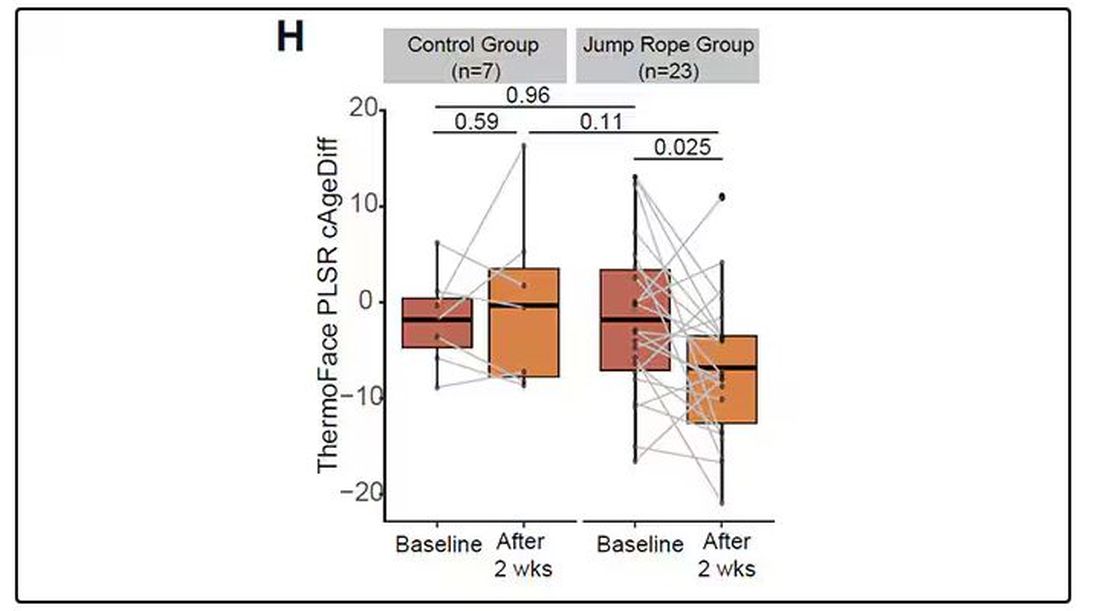
Okay, this is all very cool, but I’m not saying we’ll all be doing facial temperature tests in the near future. No; what this study highlights for me is how much information about ourselves is available to those who know how to decode it. Maybe those data come from the wrinkles in our faces, or the angles of our smiles, or the speed with which we type, or the temperature of our elbows. The data have always been there, actually, but we’ve never had the tools powerful enough to analyze them until now.
When I was a kid, I was obsessed with Star Trek — I know, you’re shocked — and, of course, the famous tricorder, a scanner that could tell everything about someone’s state of health in 5 seconds from 3 feet away. That’s how I thought medicine really would be in the future. Once I got to medical school, I was disabused of that notion. But the age of data, the age of AI, may mean the tricorder age is not actually that far away.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Benzoyl Peroxide, Benzene, and Lots of Unanswered Questions: Where Are We Now?
March 2024 proved to be a busy month for benzoyl peroxide in the media! We are now at almost 4 months since Valisure, an independent analytical laboratory located in Connecticut, filed a Citizen Petition on benzene in benzoyl peroxide drug products with the US Food and Drug Administration (FDA) on March 5, 2024.1 This petition was filed shortly before the annual meeting of the American Academy of Dermatology was held in San Diego, California, creating quite a stir of concern in the dermatology world. Further information on the degradation of benzoyl peroxide with production of benzene was published in the medical literature in March 2024.2 As benzene is recognized as a human carcinogen, manufacturing regulations exist to assure that it does not appear in topical products either through contamination or degradation over the course of a product’s shelf-life.3
As anticipated, several opinions and commentaries appeared quickly, both on video and in various articles. The American Acne & Rosacea Society (AARS) released a statement on this issue on March 20, 2024.4 The safety of the public is the overarching primary concern. This AARS statement does include some general suggestions related to benzoyl peroxide use based on the best assessment to date while awaiting further guidance from the FDA on this issue. Benzoyl peroxide is approved for use by the FDA as an over-the-counter (OTC) topical product for acne and also is in several FDA-approved prescription topical products.5,6
The following reflects my personal viewpoint as both a dermatologist and a grandfather who has grandchildren who use acne products. My views are not necessarily those of AARS. Since early March 2024, I have read several documents and spoken to several dermatologists, scientists, and formulators with knowledge in this area, including contacts at Valisure. I was hoping to get to some reasonable definitive answer but have not been able to achieve this to my full satisfaction. There are many opinions and concerns, and each one makes sense based on the vantage point of the presenter. However, several unanswered questions remain related to what testing and data are currently required of companies to gain FDA approval of a benzoyl peroxide product, including:
- assessment of stability and degradation products (including benzene),
- validation of testing methods,
- the issue of benzoyl peroxide stability in commercial products, and
- the relevant magnitude of resultant benzene exposures, especially as we are all exposed to benzene from several sources each day.
I am certain that companies with benzoyl peroxide products will evaluate their already-approved products and also do further testing. However, in this situation, which impacts millions of people on so many levels, I feel there needs to be an organized approach to evaluate and resolve the issue, otherwise the likelihood of continued confusion and uncertainty is high. As the FDA is the approval body, I am hoping it will provide definitive guidance within a reasonable timeline so that clinicians, patients, and manufacturers of benzoyl peroxide can proceed with full confidence. Right now, we all remain in a state of limbo. It is time for less talk and more definitive action to sort out this issue.
- Valisure Citizen Petition on Benzene in Benzoyl Peroxide Products. March 5, 2024. Accessed June 5, 2024. https://assets-global.website-files.com/6215052733f8bb8fea016220/65e8560962ed23f744902a7b_Valisure%20Citizen%20Petition%20on%20Benzene%20in%20Benzoyl%20Peroxide%20Drug%20Products.pdf
- Kucera K, Zenzola N, Hudspeth A, et al. Benzoyl peroxide drug products form benzene. Environ Health Perspect. 2024;132:37702. doi:10.1289/EHP13984
- US Food and Drug Administration. Reformulating drug products that contain carbomers manufactured with benzene. December 2023. Accessed June 12, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/reformulating-drug-products-contain-carbomers-manufactured-benzene
- American Acne & Rosacea Society. Response Statement from the AARS to the Valisure Citizen Petition on Benzene in Benzoyl Peroxide Drug Products. March 20, 2024. Accessed June 12, 2024. https://www.einpresswire.com/article/697481595/response-statement-from-the-aars-to-the-valisure-citizen-petition-on-benzene-in-benzoyl-peroxide-drug-products
- Department of Health and Human Services. Classification of benzoyl peroxide as safe and effective and revision of labeling to drug facts format; topical acne drug products for over-the-counter human use; Final Rule. Fed Registr. 2010;75:9767-9777.
- US Food and Drug Administration. Topical acne drug products for over-the-counter human use—revision of labeling and classification of benzoyl peroxide as safe and effective. June 2011. Accessed June 12, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/topical-acne-drug-products-over-counter-human-use-revision-labeling-and-classification-benzoyl
March 2024 proved to be a busy month for benzoyl peroxide in the media! We are now at almost 4 months since Valisure, an independent analytical laboratory located in Connecticut, filed a Citizen Petition on benzene in benzoyl peroxide drug products with the US Food and Drug Administration (FDA) on March 5, 2024.1 This petition was filed shortly before the annual meeting of the American Academy of Dermatology was held in San Diego, California, creating quite a stir of concern in the dermatology world. Further information on the degradation of benzoyl peroxide with production of benzene was published in the medical literature in March 2024.2 As benzene is recognized as a human carcinogen, manufacturing regulations exist to assure that it does not appear in topical products either through contamination or degradation over the course of a product’s shelf-life.3
As anticipated, several opinions and commentaries appeared quickly, both on video and in various articles. The American Acne & Rosacea Society (AARS) released a statement on this issue on March 20, 2024.4 The safety of the public is the overarching primary concern. This AARS statement does include some general suggestions related to benzoyl peroxide use based on the best assessment to date while awaiting further guidance from the FDA on this issue. Benzoyl peroxide is approved for use by the FDA as an over-the-counter (OTC) topical product for acne and also is in several FDA-approved prescription topical products.5,6
The following reflects my personal viewpoint as both a dermatologist and a grandfather who has grandchildren who use acne products. My views are not necessarily those of AARS. Since early March 2024, I have read several documents and spoken to several dermatologists, scientists, and formulators with knowledge in this area, including contacts at Valisure. I was hoping to get to some reasonable definitive answer but have not been able to achieve this to my full satisfaction. There are many opinions and concerns, and each one makes sense based on the vantage point of the presenter. However, several unanswered questions remain related to what testing and data are currently required of companies to gain FDA approval of a benzoyl peroxide product, including:
- assessment of stability and degradation products (including benzene),
- validation of testing methods,
- the issue of benzoyl peroxide stability in commercial products, and
- the relevant magnitude of resultant benzene exposures, especially as we are all exposed to benzene from several sources each day.
I am certain that companies with benzoyl peroxide products will evaluate their already-approved products and also do further testing. However, in this situation, which impacts millions of people on so many levels, I feel there needs to be an organized approach to evaluate and resolve the issue, otherwise the likelihood of continued confusion and uncertainty is high. As the FDA is the approval body, I am hoping it will provide definitive guidance within a reasonable timeline so that clinicians, patients, and manufacturers of benzoyl peroxide can proceed with full confidence. Right now, we all remain in a state of limbo. It is time for less talk and more definitive action to sort out this issue.
March 2024 proved to be a busy month for benzoyl peroxide in the media! We are now at almost 4 months since Valisure, an independent analytical laboratory located in Connecticut, filed a Citizen Petition on benzene in benzoyl peroxide drug products with the US Food and Drug Administration (FDA) on March 5, 2024.1 This petition was filed shortly before the annual meeting of the American Academy of Dermatology was held in San Diego, California, creating quite a stir of concern in the dermatology world. Further information on the degradation of benzoyl peroxide with production of benzene was published in the medical literature in March 2024.2 As benzene is recognized as a human carcinogen, manufacturing regulations exist to assure that it does not appear in topical products either through contamination or degradation over the course of a product’s shelf-life.3
As anticipated, several opinions and commentaries appeared quickly, both on video and in various articles. The American Acne & Rosacea Society (AARS) released a statement on this issue on March 20, 2024.4 The safety of the public is the overarching primary concern. This AARS statement does include some general suggestions related to benzoyl peroxide use based on the best assessment to date while awaiting further guidance from the FDA on this issue. Benzoyl peroxide is approved for use by the FDA as an over-the-counter (OTC) topical product for acne and also is in several FDA-approved prescription topical products.5,6
The following reflects my personal viewpoint as both a dermatologist and a grandfather who has grandchildren who use acne products. My views are not necessarily those of AARS. Since early March 2024, I have read several documents and spoken to several dermatologists, scientists, and formulators with knowledge in this area, including contacts at Valisure. I was hoping to get to some reasonable definitive answer but have not been able to achieve this to my full satisfaction. There are many opinions and concerns, and each one makes sense based on the vantage point of the presenter. However, several unanswered questions remain related to what testing and data are currently required of companies to gain FDA approval of a benzoyl peroxide product, including:
- assessment of stability and degradation products (including benzene),
- validation of testing methods,
- the issue of benzoyl peroxide stability in commercial products, and
- the relevant magnitude of resultant benzene exposures, especially as we are all exposed to benzene from several sources each day.
I am certain that companies with benzoyl peroxide products will evaluate their already-approved products and also do further testing. However, in this situation, which impacts millions of people on so many levels, I feel there needs to be an organized approach to evaluate and resolve the issue, otherwise the likelihood of continued confusion and uncertainty is high. As the FDA is the approval body, I am hoping it will provide definitive guidance within a reasonable timeline so that clinicians, patients, and manufacturers of benzoyl peroxide can proceed with full confidence. Right now, we all remain in a state of limbo. It is time for less talk and more definitive action to sort out this issue.
- Valisure Citizen Petition on Benzene in Benzoyl Peroxide Products. March 5, 2024. Accessed June 5, 2024. https://assets-global.website-files.com/6215052733f8bb8fea016220/65e8560962ed23f744902a7b_Valisure%20Citizen%20Petition%20on%20Benzene%20in%20Benzoyl%20Peroxide%20Drug%20Products.pdf
- Kucera K, Zenzola N, Hudspeth A, et al. Benzoyl peroxide drug products form benzene. Environ Health Perspect. 2024;132:37702. doi:10.1289/EHP13984
- US Food and Drug Administration. Reformulating drug products that contain carbomers manufactured with benzene. December 2023. Accessed June 12, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/reformulating-drug-products-contain-carbomers-manufactured-benzene
- American Acne & Rosacea Society. Response Statement from the AARS to the Valisure Citizen Petition on Benzene in Benzoyl Peroxide Drug Products. March 20, 2024. Accessed June 12, 2024. https://www.einpresswire.com/article/697481595/response-statement-from-the-aars-to-the-valisure-citizen-petition-on-benzene-in-benzoyl-peroxide-drug-products
- Department of Health and Human Services. Classification of benzoyl peroxide as safe and effective and revision of labeling to drug facts format; topical acne drug products for over-the-counter human use; Final Rule. Fed Registr. 2010;75:9767-9777.
- US Food and Drug Administration. Topical acne drug products for over-the-counter human use—revision of labeling and classification of benzoyl peroxide as safe and effective. June 2011. Accessed June 12, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/topical-acne-drug-products-over-counter-human-use-revision-labeling-and-classification-benzoyl
- Valisure Citizen Petition on Benzene in Benzoyl Peroxide Products. March 5, 2024. Accessed June 5, 2024. https://assets-global.website-files.com/6215052733f8bb8fea016220/65e8560962ed23f744902a7b_Valisure%20Citizen%20Petition%20on%20Benzene%20in%20Benzoyl%20Peroxide%20Drug%20Products.pdf
- Kucera K, Zenzola N, Hudspeth A, et al. Benzoyl peroxide drug products form benzene. Environ Health Perspect. 2024;132:37702. doi:10.1289/EHP13984
- US Food and Drug Administration. Reformulating drug products that contain carbomers manufactured with benzene. December 2023. Accessed June 12, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/reformulating-drug-products-contain-carbomers-manufactured-benzene
- American Acne & Rosacea Society. Response Statement from the AARS to the Valisure Citizen Petition on Benzene in Benzoyl Peroxide Drug Products. March 20, 2024. Accessed June 12, 2024. https://www.einpresswire.com/article/697481595/response-statement-from-the-aars-to-the-valisure-citizen-petition-on-benzene-in-benzoyl-peroxide-drug-products
- Department of Health and Human Services. Classification of benzoyl peroxide as safe and effective and revision of labeling to drug facts format; topical acne drug products for over-the-counter human use; Final Rule. Fed Registr. 2010;75:9767-9777.
- US Food and Drug Administration. Topical acne drug products for over-the-counter human use—revision of labeling and classification of benzoyl peroxide as safe and effective. June 2011. Accessed June 12, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/topical-acne-drug-products-over-counter-human-use-revision-labeling-and-classification-benzoyl
Medication Overuse in Mental Health Facilities: Not the Answer, Regardless of Consent, Says Ethicist
This transcript has been edited for clarity.
There’s a growing scandal in mental health care. Recent studies are showing that certain medications that basically are used to, if you will, quiet patients — antipsychotic drugs — are being overused, particularly in facilities that serve poorer people and people who are minorities. This situation is utterly, ethically unacceptable and it’s something that we are starting to get really pressed to solve.
Part of this is due to the fact that numbers of caregivers are in short supply. We need to get more people trained. We need to get more mental health providers at all levels into facilities in order to provide care, and not substitute that inability to have a provider present and minimize risk to patients by having drug-induced sleepiness, soporific behavior, or, if you will, snowing them just because we don’t have enough people to keep an eye on them. Furthermore, we can’t let them engage in some activities, even things like walking around, because we’re worried about falls. The nursing homes or mental health facilities don’t want anybody to get injured, much less killed, because that’s going to really bring government agencies down on them.
What do we do, aside from trying to get more numbers in there? California came up with a law not too long ago that basically put the burden of using these drugs on consent. They passed a law that said the patient, before going under and being administered any type of psychoactive drug, has to consent; or if they’re really unable to do that, their relative or next of kin should have to consent.
California law now puts the burden on getting consent from the patient in order to use these drugs. It’s not a good solution. It still permits the use of the drugs to substitute for the inability to provide adequate numbers of people to provide care in safe environments. It’s almost like saying, “We know you’re going into a dangerous place. We can’t really reduce the danger, so we’re going to make sure that you stay in your seat. You better consent to that because otherwise things could not go well for you in this mental institution.”
That’s not a sound argument for the use of informed consent. Moreover, I’m very skeptical that many of these people in mental institutions do have the capacity to either say, “Fine, give me psychoactive drugs if I have to stay here,” or “No, I don’t want that. I’ll take my chances.”
They’re vulnerable people. Many of them may not be fully incompetent, but they often have compromised competency. Relatives may be thinking, Well, the right thing to do is just to make sure they don’t get hurt or injure themselves. Yes, give them the drugs.
Consent, while I support it, is not the solution to what is fundamentally an infrastructure problem, a personnel problem, and one of the shames of American healthcare, which is lousy long-term mental health care. For too many people, their care is in the street. For too many people, their care is taking place in institutions that have dangerous designs where people either get injured, can’t provide enough spacing, or just don’t have the people to do it.
Let’s move to fix the mental health care system and not be in a situation where we say to people, “The system stinks and you’re at risk. Is it okay with you if we drug you because we can’t think of any other way to keep you safe, given the rotten nature of the institutions that we’ve got?”
Dr. Caplan is director, Division of Medical Ethics, New York University Langone Medical Center, New York. He disclosed ties with Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position) and serves as a contributing author and adviser for Medscape.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
There’s a growing scandal in mental health care. Recent studies are showing that certain medications that basically are used to, if you will, quiet patients — antipsychotic drugs — are being overused, particularly in facilities that serve poorer people and people who are minorities. This situation is utterly, ethically unacceptable and it’s something that we are starting to get really pressed to solve.
Part of this is due to the fact that numbers of caregivers are in short supply. We need to get more people trained. We need to get more mental health providers at all levels into facilities in order to provide care, and not substitute that inability to have a provider present and minimize risk to patients by having drug-induced sleepiness, soporific behavior, or, if you will, snowing them just because we don’t have enough people to keep an eye on them. Furthermore, we can’t let them engage in some activities, even things like walking around, because we’re worried about falls. The nursing homes or mental health facilities don’t want anybody to get injured, much less killed, because that’s going to really bring government agencies down on them.
What do we do, aside from trying to get more numbers in there? California came up with a law not too long ago that basically put the burden of using these drugs on consent. They passed a law that said the patient, before going under and being administered any type of psychoactive drug, has to consent; or if they’re really unable to do that, their relative or next of kin should have to consent.
California law now puts the burden on getting consent from the patient in order to use these drugs. It’s not a good solution. It still permits the use of the drugs to substitute for the inability to provide adequate numbers of people to provide care in safe environments. It’s almost like saying, “We know you’re going into a dangerous place. We can’t really reduce the danger, so we’re going to make sure that you stay in your seat. You better consent to that because otherwise things could not go well for you in this mental institution.”
That’s not a sound argument for the use of informed consent. Moreover, I’m very skeptical that many of these people in mental institutions do have the capacity to either say, “Fine, give me psychoactive drugs if I have to stay here,” or “No, I don’t want that. I’ll take my chances.”
They’re vulnerable people. Many of them may not be fully incompetent, but they often have compromised competency. Relatives may be thinking, Well, the right thing to do is just to make sure they don’t get hurt or injure themselves. Yes, give them the drugs.
Consent, while I support it, is not the solution to what is fundamentally an infrastructure problem, a personnel problem, and one of the shames of American healthcare, which is lousy long-term mental health care. For too many people, their care is in the street. For too many people, their care is taking place in institutions that have dangerous designs where people either get injured, can’t provide enough spacing, or just don’t have the people to do it.
Let’s move to fix the mental health care system and not be in a situation where we say to people, “The system stinks and you’re at risk. Is it okay with you if we drug you because we can’t think of any other way to keep you safe, given the rotten nature of the institutions that we’ve got?”
Dr. Caplan is director, Division of Medical Ethics, New York University Langone Medical Center, New York. He disclosed ties with Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position) and serves as a contributing author and adviser for Medscape.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
There’s a growing scandal in mental health care. Recent studies are showing that certain medications that basically are used to, if you will, quiet patients — antipsychotic drugs — are being overused, particularly in facilities that serve poorer people and people who are minorities. This situation is utterly, ethically unacceptable and it’s something that we are starting to get really pressed to solve.
Part of this is due to the fact that numbers of caregivers are in short supply. We need to get more people trained. We need to get more mental health providers at all levels into facilities in order to provide care, and not substitute that inability to have a provider present and minimize risk to patients by having drug-induced sleepiness, soporific behavior, or, if you will, snowing them just because we don’t have enough people to keep an eye on them. Furthermore, we can’t let them engage in some activities, even things like walking around, because we’re worried about falls. The nursing homes or mental health facilities don’t want anybody to get injured, much less killed, because that’s going to really bring government agencies down on them.
What do we do, aside from trying to get more numbers in there? California came up with a law not too long ago that basically put the burden of using these drugs on consent. They passed a law that said the patient, before going under and being administered any type of psychoactive drug, has to consent; or if they’re really unable to do that, their relative or next of kin should have to consent.
California law now puts the burden on getting consent from the patient in order to use these drugs. It’s not a good solution. It still permits the use of the drugs to substitute for the inability to provide adequate numbers of people to provide care in safe environments. It’s almost like saying, “We know you’re going into a dangerous place. We can’t really reduce the danger, so we’re going to make sure that you stay in your seat. You better consent to that because otherwise things could not go well for you in this mental institution.”
That’s not a sound argument for the use of informed consent. Moreover, I’m very skeptical that many of these people in mental institutions do have the capacity to either say, “Fine, give me psychoactive drugs if I have to stay here,” or “No, I don’t want that. I’ll take my chances.”
They’re vulnerable people. Many of them may not be fully incompetent, but they often have compromised competency. Relatives may be thinking, Well, the right thing to do is just to make sure they don’t get hurt or injure themselves. Yes, give them the drugs.
Consent, while I support it, is not the solution to what is fundamentally an infrastructure problem, a personnel problem, and one of the shames of American healthcare, which is lousy long-term mental health care. For too many people, their care is in the street. For too many people, their care is taking place in institutions that have dangerous designs where people either get injured, can’t provide enough spacing, or just don’t have the people to do it.
Let’s move to fix the mental health care system and not be in a situation where we say to people, “The system stinks and you’re at risk. Is it okay with you if we drug you because we can’t think of any other way to keep you safe, given the rotten nature of the institutions that we’ve got?”
Dr. Caplan is director, Division of Medical Ethics, New York University Langone Medical Center, New York. He disclosed ties with Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position) and serves as a contributing author and adviser for Medscape.
A version of this article first appeared on Medscape.com.
ASCO 2024: Treating Myeloma Just Got More Complicated
For brevity’s sake, I’ll focus on trials about newly diagnosed MM and myeloma at first relapse. Here’s my take on how to interpret those studies in light of broader evidence, what I view as their key limitations, and how what came out of ASCO 2024 changes my approach.
The Return of Belantamab
Belantamab, a BCMA targeting antibody-drug conjugate, previously had shown a response rate of 34% in a single-arm, heavily pretreated population, albeit with modest progression free survival (PFS), only to fail its confirmatory randomized study against pomalidomide/dexamethasone. Given the ocular toxicity associated with belantamab, many — including myself — had written off this drug (save in exceptional/unique circumstances), especially with the rise of novel immunotherapies targeting BCMA, such as chimeric antigen receptor (CAR T-cell) therapy and bispecific antibodies.
However, this year at ASCO, two key randomized trials were presented with concurrent publications, a trial of belantamab/bortezomib/dexamethasone versus daratumumab/bortezomib/dexamethasone (DVd) (DREAMM-7), and a trial of belantamab/pomalidomide/dexamethasone versus bortezomib/pomalidomide/dexamethasone (DREAMM-8). Both trials evaluated patients with myeloma who had relapsed disease and had received at least one prior line of therapy.
In both trials, the belantamab triplet beat the other triplets for the endpoint of PFS (median PFS 36.6 vs 13 months for DREAMM-7, and 12 months PFS 71% vs 51% for DREAMM-8). We must commend the bold three-versus-three design and a convincing result.
What are the caveats? Some censoring of information happened in DREAMM-7, which helped make the intervention arm look better than reality and the control arm look even worse than reality. To illustrate this point: the control arm of DVd (PFS 13 months) underperformed, compared to the CASTOR trial, where DVd led to a PFS of 16.7 months. The drug remains toxic, with high rates of keratopathy and vision problems in its current dosing schema. (Perhaps the future lies in less frequent dosing.) This toxicity is almost always reversible, but it is a huge problem to deal with, and our current quality-of-life instruments fail miserably at capturing this.
Furthermore, DVd is now emerging as perhaps the weakest daratumumab triplet that exists. Almost all patients in this trial had disease sensitivity to lenalidomide, and daratumumab/lenalidomide/dexamethasone (PFS of 45 months in the POLLUX trial) is unequivocally easier to use and handle (in my opinion) than this belantamab triplet--which is quite literally “an eyesore.” Would belantamab-based triplets beat dara/len/dex for patients with lenalidomide sensitive disease? Or, for that matter, would belantamab combos beat anti-CD38+carfilzomib+dex combinations, or cilta-cel (which is also now approved for first relapse)?
How do I foresee the future of belantamab? Despite these unequivocally positive results, I am not enthused about using it for most patients at first relapse. When trials for bispecifics at first relapse read out, my enthusiasm will likely wane even more. Still, it is useful to have belantamab in the armamentarium. For some patients perceived to be at very high risk of infection, belantamab-based triplets may indeed prove to be a better option than bispecifics. However, I suspect that with better dosing strategies for bispecifics, perhaps even that trend may be mitigated. Since we do not yet have bispecifics available in this line, my suggested algorithm for first relapse is as follows:
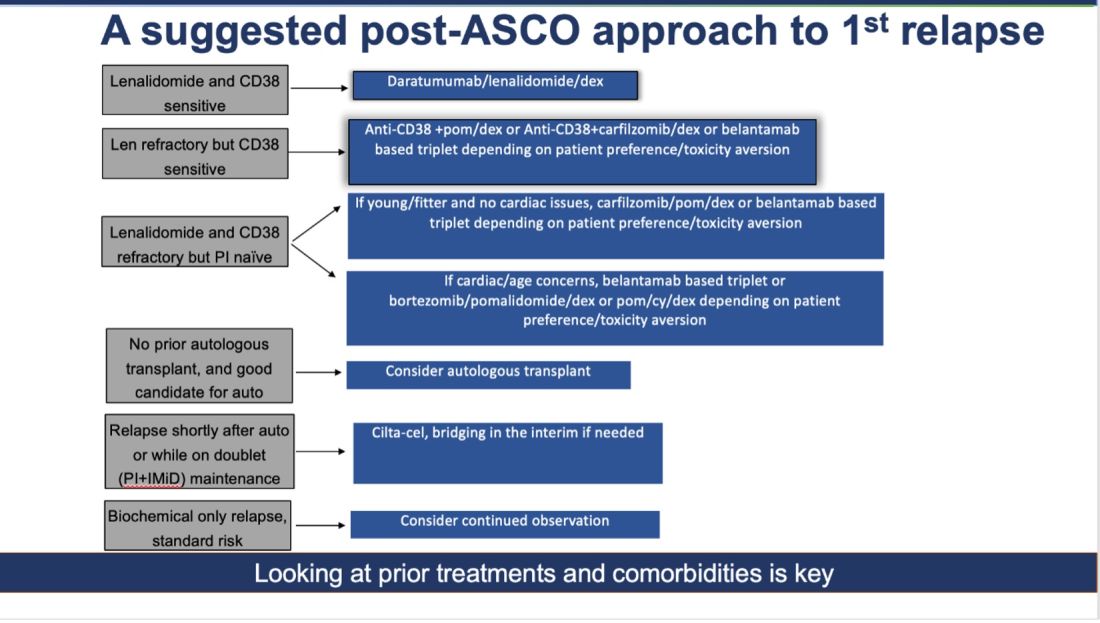
Newly Diagnosed MM: The Era of Quads Solidifies
At ASCO 2024, two key trials with concurrent publications assessed the role of quadruplets (without the use of transplant): the IMROZ trial of a quadruplet of isatuximab/bortezomib/lenalidomide/dexamethasone versus bortezomib/lenalidomide/dexamethasone (VRd), and the BENEFIT trial (isatuximab/lenalidomide/bortezomib/dexamethasone versus isatuximab/lenalidomide/dexamethasone).
The IMROZ trial tested the addition of an anti-CD38 antibody to a triplet backbone, and the results are compelling. The PFS was not reached for the quad vs 54 months for VRd. Unlike in the belantamab trial (where the control arm underperformed), here the control arm really overperformed. In this case, we have never seen such a compelling PFS of 54 months for VRd before. (Based on other trials, VRd PFS has been more in the ballpark of 35-43 months.) This speaks to the fitness and biology of the patients enrolled in this trial, and perhaps to how we will not see such stellar results with this quad recreated in real life.
The addition of isatuximab did not seem to impair quality of life, and although there were more treatment-related deaths with isatuximab, those higher numbers seem to have been driven by longer treatment durations. For this study, the upper age limit was 80 years, and most patients enrolled had an excellent functional status--making it clear that frail patients were greatly underrepresented.
What can we conclude from this study? For fit, older patients (who would have been transplant-eligible in the United States), this study provides excellent proof of concept that very good outcomes can be obtained without the use of transplantation. In treating frail patients, we do not know if quads are safe (or even necessary, compared to gentler sequencing), so these data are not applicable.
High-risk cytogenetics were underrepresented, and although the subgroup analysis for such patients did not show a benefit, it is hard to draw conclusions either way. For me, this trial is further evidence that for many older patients with MM, even if you “can” do a transplant, you probably “shouldn’t, they will experience increasingly better outcomes.
The standard for newly diagnosed MM in older patients for whom transplant is not intended is currently dara/len/dex. Is isa/bort/len/dex better? I do not know. It may give a better PFS, but the addition of bortezomib will lead to more neuropathy: 60% of patients developed neuropathy here, with 7% developing Grade III/IV peripheral neuropathy.
To resolve this issue, highly individualized discussions with patients will be needed. The BENEFIT trial evaluated this question more directly, with a randomized comparison of Isa-VRd versus Isa-Rd (the role of bortezomib being the main variable assessed here) with a primary endpoint of MRD negativity at 10-5 at 18 months. Although MRD negativity allows for a quick read-out, having MRD as an endpoint is a foregone conclusion. Adding another drug will almost certainly lead to deeper responses. But is it worth it?
In the BENEFIT trial, the MRD negativity at 10-5 was 26% versus 53% with the quad. However, peripheral neuropathy rates were much higher with the quad (28% vs 52%). Without longer-term data such as PFS and OS, I do not know whether it is worth the extra risks of neuropathy for older patients. Their priority may not be eradication of cancer cells at all costs. Instead, it may be better quality of life and functioning while preserving survival.
To sum up: Post-ASCO 2024, the approach to newly diagnosed MM just got a lot more complicated. For fit, older patients willing to endure extra toxicities of neuropathy (and acknowledging that we do not know whether survival will be any better with this approach), a quad is a very reasonable option to offer while forgoing transplant, in resource-rich areas of the world, such as the United States. Omitting a transplant now seems very reasonable for most older adults. However, a nuanced and individualized approach remains paramount. And given the speed of new developments, even this suggested approach will be outdated soon!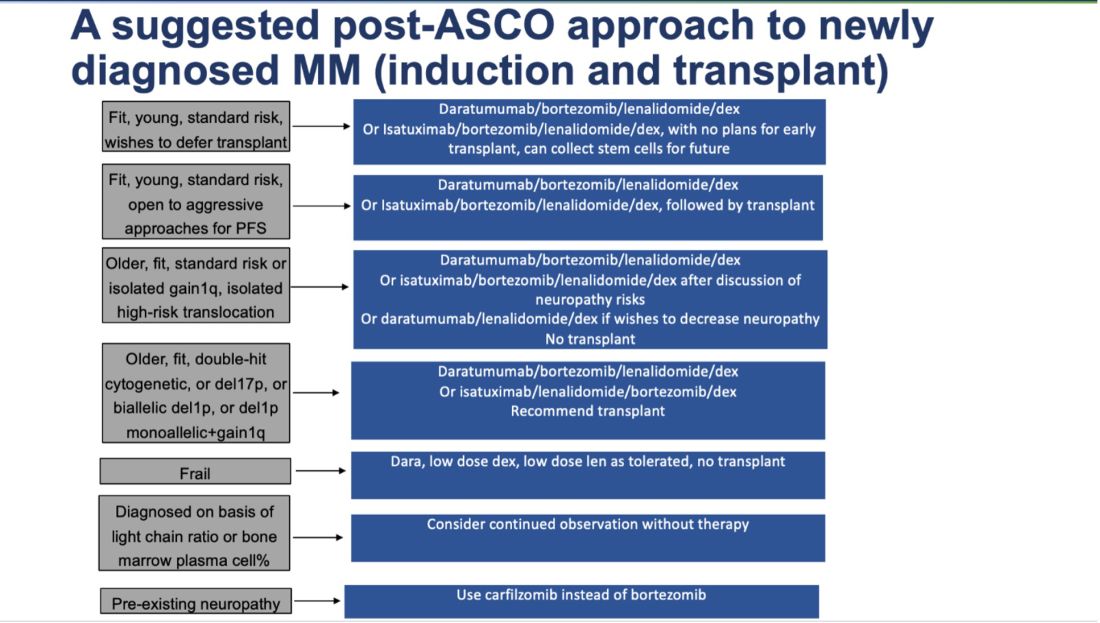
Dr. Mohyuddin is assistant professor in the multiple myeloma program at the Huntsman Cancer Institute at the University of Utah in Salt Lake City.
For brevity’s sake, I’ll focus on trials about newly diagnosed MM and myeloma at first relapse. Here’s my take on how to interpret those studies in light of broader evidence, what I view as their key limitations, and how what came out of ASCO 2024 changes my approach.
The Return of Belantamab
Belantamab, a BCMA targeting antibody-drug conjugate, previously had shown a response rate of 34% in a single-arm, heavily pretreated population, albeit with modest progression free survival (PFS), only to fail its confirmatory randomized study against pomalidomide/dexamethasone. Given the ocular toxicity associated with belantamab, many — including myself — had written off this drug (save in exceptional/unique circumstances), especially with the rise of novel immunotherapies targeting BCMA, such as chimeric antigen receptor (CAR T-cell) therapy and bispecific antibodies.
However, this year at ASCO, two key randomized trials were presented with concurrent publications, a trial of belantamab/bortezomib/dexamethasone versus daratumumab/bortezomib/dexamethasone (DVd) (DREAMM-7), and a trial of belantamab/pomalidomide/dexamethasone versus bortezomib/pomalidomide/dexamethasone (DREAMM-8). Both trials evaluated patients with myeloma who had relapsed disease and had received at least one prior line of therapy.
In both trials, the belantamab triplet beat the other triplets for the endpoint of PFS (median PFS 36.6 vs 13 months for DREAMM-7, and 12 months PFS 71% vs 51% for DREAMM-8). We must commend the bold three-versus-three design and a convincing result.
What are the caveats? Some censoring of information happened in DREAMM-7, which helped make the intervention arm look better than reality and the control arm look even worse than reality. To illustrate this point: the control arm of DVd (PFS 13 months) underperformed, compared to the CASTOR trial, where DVd led to a PFS of 16.7 months. The drug remains toxic, with high rates of keratopathy and vision problems in its current dosing schema. (Perhaps the future lies in less frequent dosing.) This toxicity is almost always reversible, but it is a huge problem to deal with, and our current quality-of-life instruments fail miserably at capturing this.
Furthermore, DVd is now emerging as perhaps the weakest daratumumab triplet that exists. Almost all patients in this trial had disease sensitivity to lenalidomide, and daratumumab/lenalidomide/dexamethasone (PFS of 45 months in the POLLUX trial) is unequivocally easier to use and handle (in my opinion) than this belantamab triplet--which is quite literally “an eyesore.” Would belantamab-based triplets beat dara/len/dex for patients with lenalidomide sensitive disease? Or, for that matter, would belantamab combos beat anti-CD38+carfilzomib+dex combinations, or cilta-cel (which is also now approved for first relapse)?
How do I foresee the future of belantamab? Despite these unequivocally positive results, I am not enthused about using it for most patients at first relapse. When trials for bispecifics at first relapse read out, my enthusiasm will likely wane even more. Still, it is useful to have belantamab in the armamentarium. For some patients perceived to be at very high risk of infection, belantamab-based triplets may indeed prove to be a better option than bispecifics. However, I suspect that with better dosing strategies for bispecifics, perhaps even that trend may be mitigated. Since we do not yet have bispecifics available in this line, my suggested algorithm for first relapse is as follows:
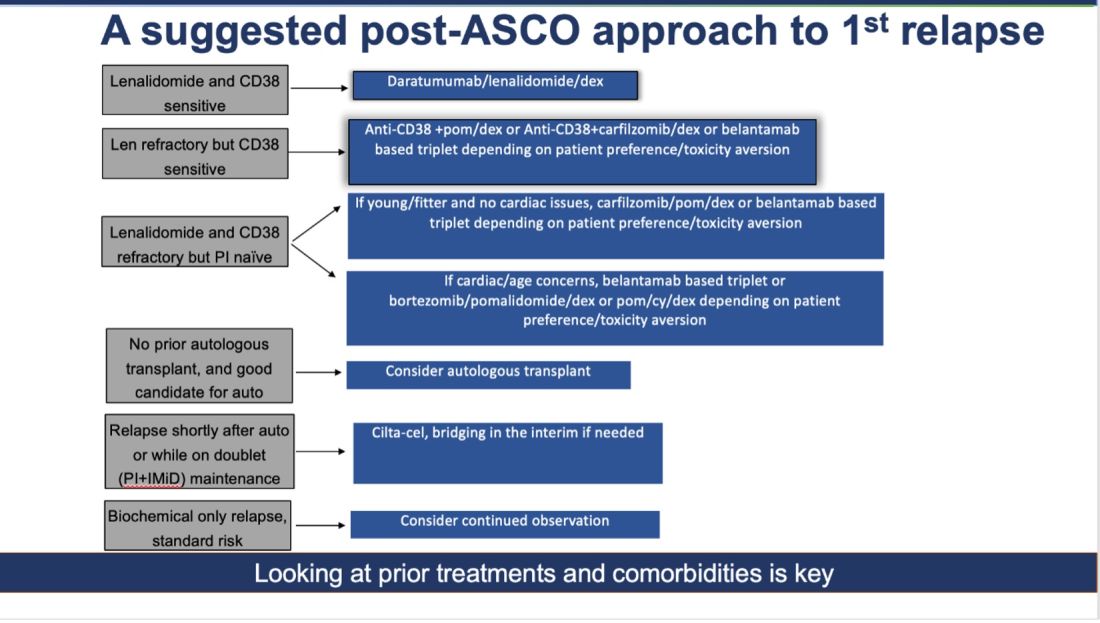
Newly Diagnosed MM: The Era of Quads Solidifies
At ASCO 2024, two key trials with concurrent publications assessed the role of quadruplets (without the use of transplant): the IMROZ trial of a quadruplet of isatuximab/bortezomib/lenalidomide/dexamethasone versus bortezomib/lenalidomide/dexamethasone (VRd), and the BENEFIT trial (isatuximab/lenalidomide/bortezomib/dexamethasone versus isatuximab/lenalidomide/dexamethasone).
The IMROZ trial tested the addition of an anti-CD38 antibody to a triplet backbone, and the results are compelling. The PFS was not reached for the quad vs 54 months for VRd. Unlike in the belantamab trial (where the control arm underperformed), here the control arm really overperformed. In this case, we have never seen such a compelling PFS of 54 months for VRd before. (Based on other trials, VRd PFS has been more in the ballpark of 35-43 months.) This speaks to the fitness and biology of the patients enrolled in this trial, and perhaps to how we will not see such stellar results with this quad recreated in real life.
The addition of isatuximab did not seem to impair quality of life, and although there were more treatment-related deaths with isatuximab, those higher numbers seem to have been driven by longer treatment durations. For this study, the upper age limit was 80 years, and most patients enrolled had an excellent functional status--making it clear that frail patients were greatly underrepresented.
What can we conclude from this study? For fit, older patients (who would have been transplant-eligible in the United States), this study provides excellent proof of concept that very good outcomes can be obtained without the use of transplantation. In treating frail patients, we do not know if quads are safe (or even necessary, compared to gentler sequencing), so these data are not applicable.
High-risk cytogenetics were underrepresented, and although the subgroup analysis for such patients did not show a benefit, it is hard to draw conclusions either way. For me, this trial is further evidence that for many older patients with MM, even if you “can” do a transplant, you probably “shouldn’t, they will experience increasingly better outcomes.
The standard for newly diagnosed MM in older patients for whom transplant is not intended is currently dara/len/dex. Is isa/bort/len/dex better? I do not know. It may give a better PFS, but the addition of bortezomib will lead to more neuropathy: 60% of patients developed neuropathy here, with 7% developing Grade III/IV peripheral neuropathy.
To resolve this issue, highly individualized discussions with patients will be needed. The BENEFIT trial evaluated this question more directly, with a randomized comparison of Isa-VRd versus Isa-Rd (the role of bortezomib being the main variable assessed here) with a primary endpoint of MRD negativity at 10-5 at 18 months. Although MRD negativity allows for a quick read-out, having MRD as an endpoint is a foregone conclusion. Adding another drug will almost certainly lead to deeper responses. But is it worth it?
In the BENEFIT trial, the MRD negativity at 10-5 was 26% versus 53% with the quad. However, peripheral neuropathy rates were much higher with the quad (28% vs 52%). Without longer-term data such as PFS and OS, I do not know whether it is worth the extra risks of neuropathy for older patients. Their priority may not be eradication of cancer cells at all costs. Instead, it may be better quality of life and functioning while preserving survival.
To sum up: Post-ASCO 2024, the approach to newly diagnosed MM just got a lot more complicated. For fit, older patients willing to endure extra toxicities of neuropathy (and acknowledging that we do not know whether survival will be any better with this approach), a quad is a very reasonable option to offer while forgoing transplant, in resource-rich areas of the world, such as the United States. Omitting a transplant now seems very reasonable for most older adults. However, a nuanced and individualized approach remains paramount. And given the speed of new developments, even this suggested approach will be outdated soon!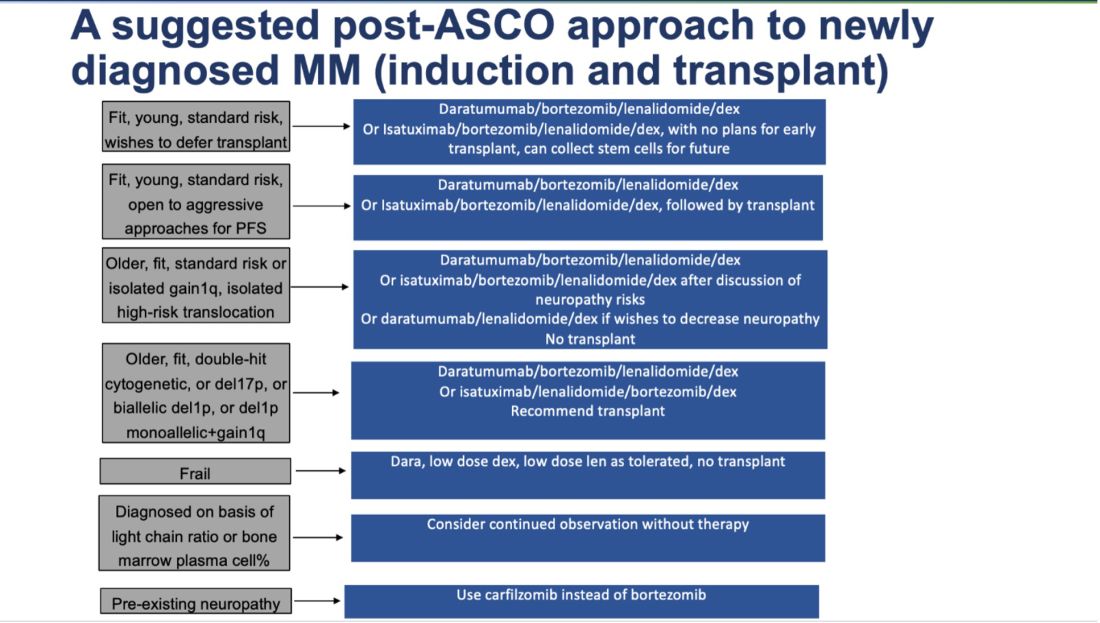
Dr. Mohyuddin is assistant professor in the multiple myeloma program at the Huntsman Cancer Institute at the University of Utah in Salt Lake City.
For brevity’s sake, I’ll focus on trials about newly diagnosed MM and myeloma at first relapse. Here’s my take on how to interpret those studies in light of broader evidence, what I view as their key limitations, and how what came out of ASCO 2024 changes my approach.
The Return of Belantamab
Belantamab, a BCMA targeting antibody-drug conjugate, previously had shown a response rate of 34% in a single-arm, heavily pretreated population, albeit with modest progression free survival (PFS), only to fail its confirmatory randomized study against pomalidomide/dexamethasone. Given the ocular toxicity associated with belantamab, many — including myself — had written off this drug (save in exceptional/unique circumstances), especially with the rise of novel immunotherapies targeting BCMA, such as chimeric antigen receptor (CAR T-cell) therapy and bispecific antibodies.
However, this year at ASCO, two key randomized trials were presented with concurrent publications, a trial of belantamab/bortezomib/dexamethasone versus daratumumab/bortezomib/dexamethasone (DVd) (DREAMM-7), and a trial of belantamab/pomalidomide/dexamethasone versus bortezomib/pomalidomide/dexamethasone (DREAMM-8). Both trials evaluated patients with myeloma who had relapsed disease and had received at least one prior line of therapy.
In both trials, the belantamab triplet beat the other triplets for the endpoint of PFS (median PFS 36.6 vs 13 months for DREAMM-7, and 12 months PFS 71% vs 51% for DREAMM-8). We must commend the bold three-versus-three design and a convincing result.
What are the caveats? Some censoring of information happened in DREAMM-7, which helped make the intervention arm look better than reality and the control arm look even worse than reality. To illustrate this point: the control arm of DVd (PFS 13 months) underperformed, compared to the CASTOR trial, where DVd led to a PFS of 16.7 months. The drug remains toxic, with high rates of keratopathy and vision problems in its current dosing schema. (Perhaps the future lies in less frequent dosing.) This toxicity is almost always reversible, but it is a huge problem to deal with, and our current quality-of-life instruments fail miserably at capturing this.
Furthermore, DVd is now emerging as perhaps the weakest daratumumab triplet that exists. Almost all patients in this trial had disease sensitivity to lenalidomide, and daratumumab/lenalidomide/dexamethasone (PFS of 45 months in the POLLUX trial) is unequivocally easier to use and handle (in my opinion) than this belantamab triplet--which is quite literally “an eyesore.” Would belantamab-based triplets beat dara/len/dex for patients with lenalidomide sensitive disease? Or, for that matter, would belantamab combos beat anti-CD38+carfilzomib+dex combinations, or cilta-cel (which is also now approved for first relapse)?
How do I foresee the future of belantamab? Despite these unequivocally positive results, I am not enthused about using it for most patients at first relapse. When trials for bispecifics at first relapse read out, my enthusiasm will likely wane even more. Still, it is useful to have belantamab in the armamentarium. For some patients perceived to be at very high risk of infection, belantamab-based triplets may indeed prove to be a better option than bispecifics. However, I suspect that with better dosing strategies for bispecifics, perhaps even that trend may be mitigated. Since we do not yet have bispecifics available in this line, my suggested algorithm for first relapse is as follows:
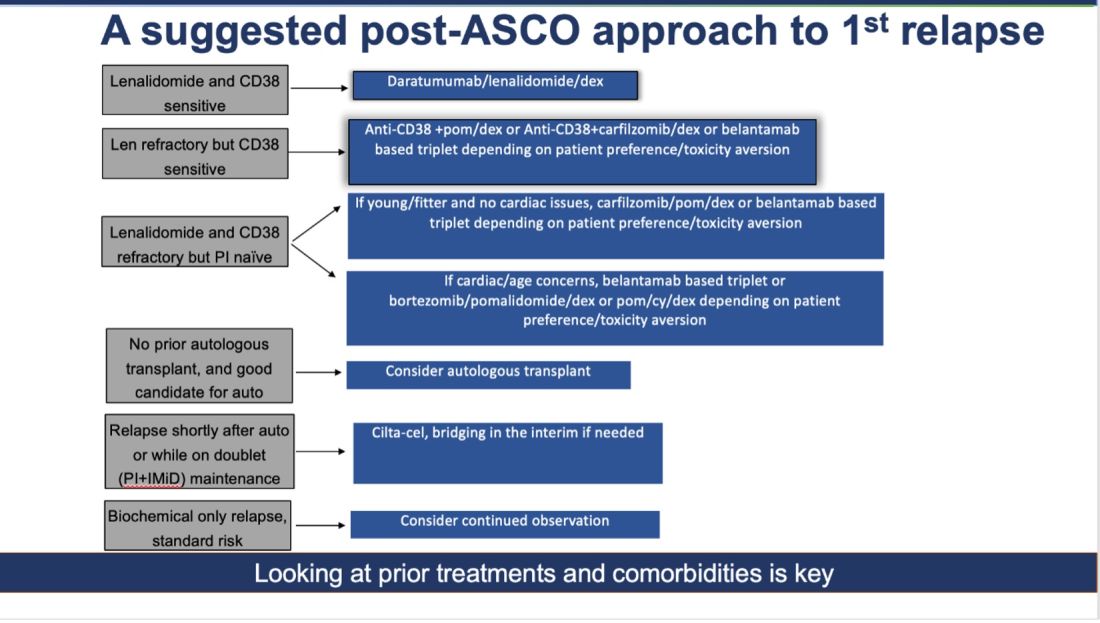
Newly Diagnosed MM: The Era of Quads Solidifies
At ASCO 2024, two key trials with concurrent publications assessed the role of quadruplets (without the use of transplant): the IMROZ trial of a quadruplet of isatuximab/bortezomib/lenalidomide/dexamethasone versus bortezomib/lenalidomide/dexamethasone (VRd), and the BENEFIT trial (isatuximab/lenalidomide/bortezomib/dexamethasone versus isatuximab/lenalidomide/dexamethasone).
The IMROZ trial tested the addition of an anti-CD38 antibody to a triplet backbone, and the results are compelling. The PFS was not reached for the quad vs 54 months for VRd. Unlike in the belantamab trial (where the control arm underperformed), here the control arm really overperformed. In this case, we have never seen such a compelling PFS of 54 months for VRd before. (Based on other trials, VRd PFS has been more in the ballpark of 35-43 months.) This speaks to the fitness and biology of the patients enrolled in this trial, and perhaps to how we will not see such stellar results with this quad recreated in real life.
The addition of isatuximab did not seem to impair quality of life, and although there were more treatment-related deaths with isatuximab, those higher numbers seem to have been driven by longer treatment durations. For this study, the upper age limit was 80 years, and most patients enrolled had an excellent functional status--making it clear that frail patients were greatly underrepresented.
What can we conclude from this study? For fit, older patients (who would have been transplant-eligible in the United States), this study provides excellent proof of concept that very good outcomes can be obtained without the use of transplantation. In treating frail patients, we do not know if quads are safe (or even necessary, compared to gentler sequencing), so these data are not applicable.
High-risk cytogenetics were underrepresented, and although the subgroup analysis for such patients did not show a benefit, it is hard to draw conclusions either way. For me, this trial is further evidence that for many older patients with MM, even if you “can” do a transplant, you probably “shouldn’t, they will experience increasingly better outcomes.
The standard for newly diagnosed MM in older patients for whom transplant is not intended is currently dara/len/dex. Is isa/bort/len/dex better? I do not know. It may give a better PFS, but the addition of bortezomib will lead to more neuropathy: 60% of patients developed neuropathy here, with 7% developing Grade III/IV peripheral neuropathy.
To resolve this issue, highly individualized discussions with patients will be needed. The BENEFIT trial evaluated this question more directly, with a randomized comparison of Isa-VRd versus Isa-Rd (the role of bortezomib being the main variable assessed here) with a primary endpoint of MRD negativity at 10-5 at 18 months. Although MRD negativity allows for a quick read-out, having MRD as an endpoint is a foregone conclusion. Adding another drug will almost certainly lead to deeper responses. But is it worth it?
In the BENEFIT trial, the MRD negativity at 10-5 was 26% versus 53% with the quad. However, peripheral neuropathy rates were much higher with the quad (28% vs 52%). Without longer-term data such as PFS and OS, I do not know whether it is worth the extra risks of neuropathy for older patients. Their priority may not be eradication of cancer cells at all costs. Instead, it may be better quality of life and functioning while preserving survival.
To sum up: Post-ASCO 2024, the approach to newly diagnosed MM just got a lot more complicated. For fit, older patients willing to endure extra toxicities of neuropathy (and acknowledging that we do not know whether survival will be any better with this approach), a quad is a very reasonable option to offer while forgoing transplant, in resource-rich areas of the world, such as the United States. Omitting a transplant now seems very reasonable for most older adults. However, a nuanced and individualized approach remains paramount. And given the speed of new developments, even this suggested approach will be outdated soon!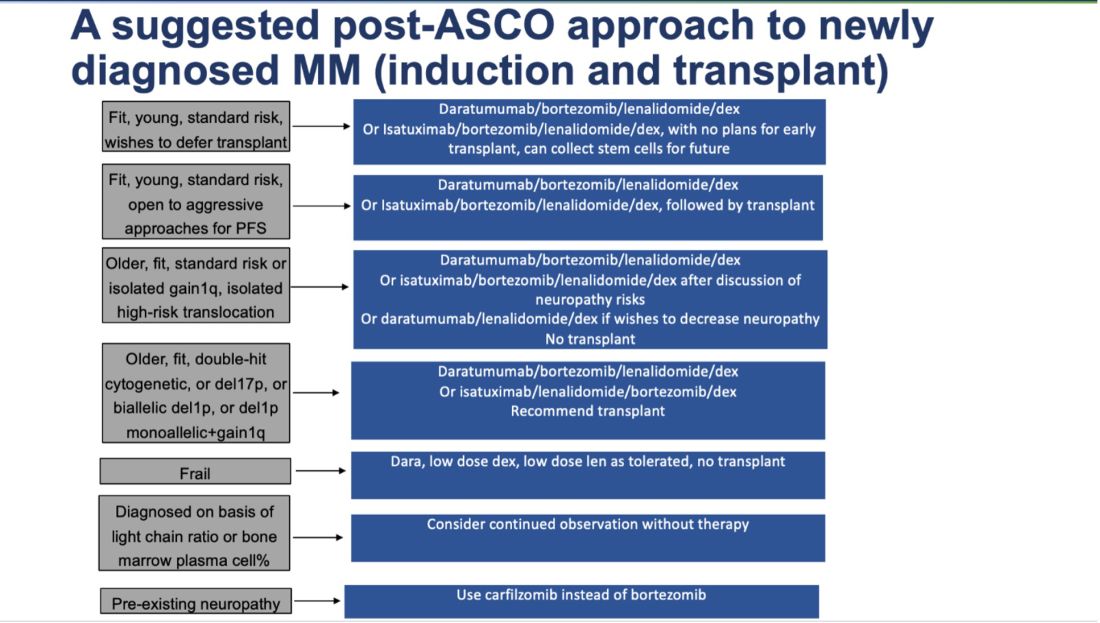
Dr. Mohyuddin is assistant professor in the multiple myeloma program at the Huntsman Cancer Institute at the University of Utah in Salt Lake City.
GLP-1 Receptor Agonists in Endoscopy
Dear colleagues,
Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are revolutionizing the field of obesity management and are now common medication in patients presenting for endoscopy. With their effect on gastric emptying, the American Society of Anesthesiologists has recommended cessation of such agents prior to endoscopy. However, is this necessary in patients who have been on a clear liquid diet in preparation for a colonoscopy or who are undergoing moderate sedation? Additionally, there are risks to holding GLP-1 RAs, especially for those taking them for glycemic control.
In this issue of Perspectives, Dr. Thomas Hickey and Dr. Ryan Pouliot discuss the nuances of pre-procedure cessation from an anesthesiologist’s perspective. Dr. Jana Al Hashash provides a gastroenterologist’s view, also highlighting the current paucity of evidence guiding management strategies. We hope these pieces will help your discussions in managing GLP-1 RAs prior to endoscopy in your own practice. We welcome your thoughts on this issue on X @AGA_GIHN.
Gyanprakash A. Ketwaroo, MD, MSc, is associate professor of medicine, Yale University, New Haven, Connecticut, and chief of endoscopy at West Haven (Connecticut) VA Medical Center. He is an associate editor for GI & Hepatology News.
GLP-1 Receptor Agonists in Endoscopy
BY THOMAS R. HICKEY, MD; RYAN C. POULIOT, MD
In response to the recent dramatic increase in GLP-1 receptor agonist (GLP-1RA) prescribing and at the urging of its membership, the American Society of Anesthesiologists issued guidance on the preoperative management of these medications. The big takeaways were recommendations that patients on daily dosing should hold their dose on the day of a procedure, and that patients on weekly dosing should hold their dose a week prior.
The ASA guidance recognizes the sparse available evidence base and makes its recommendations in the spirit of patient safety, presuming that a more conservative approach will mitigate risk of rare but potentially devastating pulmonary aspiration, until prospective evidence informs the ideal approach. Until that approach is defined, whether more or less conservative, it is expected that anesthesiologists will adhere to their professional society’s recommendations.
Meanwhile, the American Gastroenterological Association Institute Rapid Clinical Practice Update (CPU) makes little distinction in the management of the endoscopy patient on GLP-1RA. A key refrain throughout the CPU is that there is no actionable data to justify the harms that may come to patients from stopping these medications (e.g., withdrawal of benefit to glycemic control and cardiovascular health) and in delaying or canceling procedures, which could lead to further stress on an overburdened workforce and add complexity to periprocedural processes.
Anesthesiologists should rightly consider themselves leaders in patient safety. As such, when a serious safety concern emerges they should be compelled to caution despite the possibility of other harms, until their concerns are mitigated by robust clinical evidence. Thankfully these questions are quite amenable to research, and prospective trials are already reporting compelling data that residual gastric contents, clearly a risk factor for aspiration, are increased in GLP-1RA groups compared to controls. This is evident even while following recommended fasting times and abstinences from these medications, and adjusting for confounders (e.g., age, diabetes, body mass index).1,2 It logically follows that large studies are likely to find an increased aspiration risk in GLP-1RA populations. Indeed, this increased risk has already been identified in a large retrospective study of endoscopy patients.3 These findings support the ASA’s caution. Additional data indicate that standard fasting guidelines in this patient population may be inadequate.4
The ASA guidance does not differentiate between patients undergoing surgery in the operating room and procedures in the endoscopy suite. Part of our task is to provide perspective on whether GLP-1RA management deserves different treatment for endoscopy patients. We can only speculate pending further data. For example, a prolonged fasting period including a full day of clears, with or without a bowel prep, intuitively protects against pulmonary aspiration. However, this is unlikely to mitigate an anesthesiologist’s concern that administration of propofol, frequently to a state of general anesthesia with an unsecured airway and resulting in a patient devoid of airway protection reflexes, is an inherently higher risk scenario for aspiration compared to surgery in the operating room with a secured airway. We also expect prospective trials will confirm retrospective findings that both propofol and procedures including upper endoscopy confer a higher risk for aspiration compared with conscious sedation and colonoscopy.3
We suggest a reasonable approach based on society guidance and existing evidence, pending additional data. Endoscopists and anesthesiologists should continue this important conversation with a specific focus on risks and benefits in order to decrease conflict and achieve consensus. If anesthesia care is desired, the patient instructions should be updated to reflect ASA guidance. Special attention should be paid to the “gray area,” for example those who did not hold the GLP-1 agonist as recommended.
This category of patients can be considered on a case-by-case basis by the anesthesiologist, proceduralist, and patient, with a range of options including: proceeding with endoscopist-directed sedation, proceeding with anesthesiology-administered conscious sedation, rescheduling the procedure, and proceeding with general anesthesia with rapid-sequence intubation. In addition to patient factors (e.g., GI symptoms, urgency of procedure), this consideration would vary based on local resources (e.g., presence or absence of anesthesia support staff, emergency airway equipment, nursing staff to comfort recovering patients after general endotracheal anesthesia), and aspiration risk inherent to the procedure (e.g., upper and or combination upper and lower endoscopy vs colonoscopy alone). Proficiency and availability of point-of-care ultrasound are rapidly increasing; adoption of a pre-procedure gastric ultrasound to assess for solids, thick liquids, or large volume of clear liquids may provide a less nuanced, more objective means to address this question.
While the question of periprocedural management of these medications has generated intense interest among anesthesiologists and endoscopists alike, it is worth noting the net positive health effects these drugs are likely to have on our patients, including improved glycemic control, significant weight loss, and decreased cardiovascular risk. We are eager to see whether these benefits translate into an overall improvement in periprocedural outcomes, including in our endoscopy patients.
Dr. Hickey is assistant professor of anesthesiology at the Yale University School of Medicine, New Haven, Connecticut, and the VA Connecticut Healthcare System. Dr. Pouliot is assistant professor of anesthesiology at the Geisel School of Medicine at Dartmouth, Hanover, New Hampshire, and Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire.
References
1. Sherwin M et al. Influence of semaglutide use on the presence of residual gastric solids on gastric ultrasound: A prospective observational study in volunteers without obesity recently started on semaglutide. Can J Anaesth. 2023 Aug. doi:10.1007/s12630-023-02549-5.
2. Wu F et al. Association of glucagon-like peptide receptor 1 agonist therapy with the presence of gastric contents in fasting patients undergoing endoscopy under anesthesia care: A historical cohort study. Can J Anaesth. 2024 Mar 14. doi:10.1007/s12630-024-02719-z.
3. Yeo YH et al. Increased risk of aspiration pneumonia associated with endoscopic procedures among patients with glucagon-like peptide 1 receptor agonist use. Gastroenterology. 2024 Mar 27. doi:10.1053/j.gastro.2024.03.015.
4. Sen S et al. Glucagon-like peptide-1 receptor agonist use and residual gastric content before anesthesia. JAMA Surg. 2024 Mar 6. doi:10.1001/jamasurg.2024.0111.
The Impact of GLP-1 Receptor Agonists On Endoscopy
BY JANA G. AL HASHASH, MD, MSc, AGAF
Glucagon-like peptide 1 receptor agonists (GLP-1 RAs) have been approved for the treatment of type 2 diabetes mellitus since 2005. They have become more widely used over the last couple of years for weight loss in individuals who suffer from adiposity-based chronic disease.
The remarkable positive effects that GLP-1 RAs have had on weight loss as well as other medical conditions such as heart disease, hypertension, metabolic dysfunction–associated steatotic liver disease, among many others, have gained these drugs more traction. Even in situations when insurance companies deny coverage of GLP-1 RAs, many patients have been resorting to other routes to obtain these medications, commonly by purchasing them from online compounding pharmacies.
As such, more and more of our patients who present to endoscopy suites across the country are on one of the available GLP-1 RAs. This has necessitated endoscopists and anesthesiologists to become more familiar with the impact of GLP-1 RAs on patients undergoing endoscopic procedures.
Similar to narcotics, GLP-1 RAs affect gastrointestinal motility and delay gastric emptying. Common side effects of patients receiving GLP-1 RAs include nausea, vomiting, and increased satiety. Patients on GLP-1 RAs for weight loss may also have other contributing risk factors for gastroparesis such as diabetes mellitus which may further delay gastric emptying.
For endoscopists, our goals are to achieve the highest quality examination in the safest way possible. As such, being on a GLP-1 RAs could compromise both goals; but to date, the exact impact of these drugs on exam quality and patient safety is yet to be determined.
Studies have shown that patients on GLP-1 RAs have increased gastric residue on upper endoscopy compared with patients not on GLP-1 RAs. The effect of this increased residue on aspiration risk and clinically meaningful patient outcomes is being investigated, and the available published data are conflicting. Additionally, other published cases have shown that GLP-1 RAs are associated with increased solid gastric residue but not liquids, and that symptoms of dyspepsia and abdominal bloating are associated with an increased probability of residual gastric content.
Given the valid concern for increased gastric content residue, anesthesia specialists became more strict about which GLP-1 RA users they would agree to sedate, which ones they would intubate, and which procedures they would cancel. As one would imagine, cancellation and intubation rates have been increasing, and these have affected the schedules of patients, their families, and physicians.
The concern with GLP-1 RAs does not only apply to upper endoscopies, but also impacts colonoscopies. In addition to the concerns of aspiration and pneumonia, studies have shown that the use of GLP-1 RAs may be associated with a lower quality of bowel preparation and higher need for repeat colonoscopy. A study, which I believe is critical, showed that patients on GLP-1 RAs who were scheduled for upper endoscopy and colonoscopy were found to have less gastric residue and less risk of complications when compared with patients who were only having an upper endoscopy. This study sets the stage for a modified prep for patients on GLP-1 RAs prior to their procedures, since patients who received a modified/extended liquid diet on the day prior to their procedure (those preparing for a colonoscopy), had a protective effect against retained gastric content.
Clearly, there is a knowledge gap and a need for guidance. In our recently published AGA Rapid CPU, we advised an individualized approach to managing patients on GLP-1 RAs in the pre-endoscopic setting. Factors to consider are the indication for the GLP-1 RAs, the dose being used, duration of use, and indication and urgency of the procedure, as well as the presence of symptoms in the preoperative area (i.e., do patients have any nausea, vomiting, dyspepsia, etc.). Also an important factor is the facility in which the endoscopy will be taking place, as certain centers have the capacity to act fast and prevent complications or address them in a timely manner while other centers may not be prepared.
We proposed that a modified liquid diet be considered in patients prior to their endoscopies by advising patients to adhere to a clear liquid diet the day before the procedure, as this may help decrease gastric residue and be the safest and best approach for patients on GLP-1 RAs. Of course, it is important to note that more prospective studies are needed to inform clinical practice, and until then, we will have to individualize our approach and continue to put patient safety first.
Dr. Al Hashash is a gastroenterologist and associate professor of medicine at Mayo Clinic, Jacksonville, Florida.
Dear colleagues,
Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are revolutionizing the field of obesity management and are now common medication in patients presenting for endoscopy. With their effect on gastric emptying, the American Society of Anesthesiologists has recommended cessation of such agents prior to endoscopy. However, is this necessary in patients who have been on a clear liquid diet in preparation for a colonoscopy or who are undergoing moderate sedation? Additionally, there are risks to holding GLP-1 RAs, especially for those taking them for glycemic control.
In this issue of Perspectives, Dr. Thomas Hickey and Dr. Ryan Pouliot discuss the nuances of pre-procedure cessation from an anesthesiologist’s perspective. Dr. Jana Al Hashash provides a gastroenterologist’s view, also highlighting the current paucity of evidence guiding management strategies. We hope these pieces will help your discussions in managing GLP-1 RAs prior to endoscopy in your own practice. We welcome your thoughts on this issue on X @AGA_GIHN.
Gyanprakash A. Ketwaroo, MD, MSc, is associate professor of medicine, Yale University, New Haven, Connecticut, and chief of endoscopy at West Haven (Connecticut) VA Medical Center. He is an associate editor for GI & Hepatology News.
GLP-1 Receptor Agonists in Endoscopy
BY THOMAS R. HICKEY, MD; RYAN C. POULIOT, MD
In response to the recent dramatic increase in GLP-1 receptor agonist (GLP-1RA) prescribing and at the urging of its membership, the American Society of Anesthesiologists issued guidance on the preoperative management of these medications. The big takeaways were recommendations that patients on daily dosing should hold their dose on the day of a procedure, and that patients on weekly dosing should hold their dose a week prior.
The ASA guidance recognizes the sparse available evidence base and makes its recommendations in the spirit of patient safety, presuming that a more conservative approach will mitigate risk of rare but potentially devastating pulmonary aspiration, until prospective evidence informs the ideal approach. Until that approach is defined, whether more or less conservative, it is expected that anesthesiologists will adhere to their professional society’s recommendations.
Meanwhile, the American Gastroenterological Association Institute Rapid Clinical Practice Update (CPU) makes little distinction in the management of the endoscopy patient on GLP-1RA. A key refrain throughout the CPU is that there is no actionable data to justify the harms that may come to patients from stopping these medications (e.g., withdrawal of benefit to glycemic control and cardiovascular health) and in delaying or canceling procedures, which could lead to further stress on an overburdened workforce and add complexity to periprocedural processes.
Anesthesiologists should rightly consider themselves leaders in patient safety. As such, when a serious safety concern emerges they should be compelled to caution despite the possibility of other harms, until their concerns are mitigated by robust clinical evidence. Thankfully these questions are quite amenable to research, and prospective trials are already reporting compelling data that residual gastric contents, clearly a risk factor for aspiration, are increased in GLP-1RA groups compared to controls. This is evident even while following recommended fasting times and abstinences from these medications, and adjusting for confounders (e.g., age, diabetes, body mass index).1,2 It logically follows that large studies are likely to find an increased aspiration risk in GLP-1RA populations. Indeed, this increased risk has already been identified in a large retrospective study of endoscopy patients.3 These findings support the ASA’s caution. Additional data indicate that standard fasting guidelines in this patient population may be inadequate.4
The ASA guidance does not differentiate between patients undergoing surgery in the operating room and procedures in the endoscopy suite. Part of our task is to provide perspective on whether GLP-1RA management deserves different treatment for endoscopy patients. We can only speculate pending further data. For example, a prolonged fasting period including a full day of clears, with or without a bowel prep, intuitively protects against pulmonary aspiration. However, this is unlikely to mitigate an anesthesiologist’s concern that administration of propofol, frequently to a state of general anesthesia with an unsecured airway and resulting in a patient devoid of airway protection reflexes, is an inherently higher risk scenario for aspiration compared to surgery in the operating room with a secured airway. We also expect prospective trials will confirm retrospective findings that both propofol and procedures including upper endoscopy confer a higher risk for aspiration compared with conscious sedation and colonoscopy.3
We suggest a reasonable approach based on society guidance and existing evidence, pending additional data. Endoscopists and anesthesiologists should continue this important conversation with a specific focus on risks and benefits in order to decrease conflict and achieve consensus. If anesthesia care is desired, the patient instructions should be updated to reflect ASA guidance. Special attention should be paid to the “gray area,” for example those who did not hold the GLP-1 agonist as recommended.
This category of patients can be considered on a case-by-case basis by the anesthesiologist, proceduralist, and patient, with a range of options including: proceeding with endoscopist-directed sedation, proceeding with anesthesiology-administered conscious sedation, rescheduling the procedure, and proceeding with general anesthesia with rapid-sequence intubation. In addition to patient factors (e.g., GI symptoms, urgency of procedure), this consideration would vary based on local resources (e.g., presence or absence of anesthesia support staff, emergency airway equipment, nursing staff to comfort recovering patients after general endotracheal anesthesia), and aspiration risk inherent to the procedure (e.g., upper and or combination upper and lower endoscopy vs colonoscopy alone). Proficiency and availability of point-of-care ultrasound are rapidly increasing; adoption of a pre-procedure gastric ultrasound to assess for solids, thick liquids, or large volume of clear liquids may provide a less nuanced, more objective means to address this question.
While the question of periprocedural management of these medications has generated intense interest among anesthesiologists and endoscopists alike, it is worth noting the net positive health effects these drugs are likely to have on our patients, including improved glycemic control, significant weight loss, and decreased cardiovascular risk. We are eager to see whether these benefits translate into an overall improvement in periprocedural outcomes, including in our endoscopy patients.
Dr. Hickey is assistant professor of anesthesiology at the Yale University School of Medicine, New Haven, Connecticut, and the VA Connecticut Healthcare System. Dr. Pouliot is assistant professor of anesthesiology at the Geisel School of Medicine at Dartmouth, Hanover, New Hampshire, and Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire.
References
1. Sherwin M et al. Influence of semaglutide use on the presence of residual gastric solids on gastric ultrasound: A prospective observational study in volunteers without obesity recently started on semaglutide. Can J Anaesth. 2023 Aug. doi:10.1007/s12630-023-02549-5.
2. Wu F et al. Association of glucagon-like peptide receptor 1 agonist therapy with the presence of gastric contents in fasting patients undergoing endoscopy under anesthesia care: A historical cohort study. Can J Anaesth. 2024 Mar 14. doi:10.1007/s12630-024-02719-z.
3. Yeo YH et al. Increased risk of aspiration pneumonia associated with endoscopic procedures among patients with glucagon-like peptide 1 receptor agonist use. Gastroenterology. 2024 Mar 27. doi:10.1053/j.gastro.2024.03.015.
4. Sen S et al. Glucagon-like peptide-1 receptor agonist use and residual gastric content before anesthesia. JAMA Surg. 2024 Mar 6. doi:10.1001/jamasurg.2024.0111.
The Impact of GLP-1 Receptor Agonists On Endoscopy
BY JANA G. AL HASHASH, MD, MSc, AGAF
Glucagon-like peptide 1 receptor agonists (GLP-1 RAs) have been approved for the treatment of type 2 diabetes mellitus since 2005. They have become more widely used over the last couple of years for weight loss in individuals who suffer from adiposity-based chronic disease.
The remarkable positive effects that GLP-1 RAs have had on weight loss as well as other medical conditions such as heart disease, hypertension, metabolic dysfunction–associated steatotic liver disease, among many others, have gained these drugs more traction. Even in situations when insurance companies deny coverage of GLP-1 RAs, many patients have been resorting to other routes to obtain these medications, commonly by purchasing them from online compounding pharmacies.
As such, more and more of our patients who present to endoscopy suites across the country are on one of the available GLP-1 RAs. This has necessitated endoscopists and anesthesiologists to become more familiar with the impact of GLP-1 RAs on patients undergoing endoscopic procedures.
Similar to narcotics, GLP-1 RAs affect gastrointestinal motility and delay gastric emptying. Common side effects of patients receiving GLP-1 RAs include nausea, vomiting, and increased satiety. Patients on GLP-1 RAs for weight loss may also have other contributing risk factors for gastroparesis such as diabetes mellitus which may further delay gastric emptying.
For endoscopists, our goals are to achieve the highest quality examination in the safest way possible. As such, being on a GLP-1 RAs could compromise both goals; but to date, the exact impact of these drugs on exam quality and patient safety is yet to be determined.
Studies have shown that patients on GLP-1 RAs have increased gastric residue on upper endoscopy compared with patients not on GLP-1 RAs. The effect of this increased residue on aspiration risk and clinically meaningful patient outcomes is being investigated, and the available published data are conflicting. Additionally, other published cases have shown that GLP-1 RAs are associated with increased solid gastric residue but not liquids, and that symptoms of dyspepsia and abdominal bloating are associated with an increased probability of residual gastric content.
Given the valid concern for increased gastric content residue, anesthesia specialists became more strict about which GLP-1 RA users they would agree to sedate, which ones they would intubate, and which procedures they would cancel. As one would imagine, cancellation and intubation rates have been increasing, and these have affected the schedules of patients, their families, and physicians.
The concern with GLP-1 RAs does not only apply to upper endoscopies, but also impacts colonoscopies. In addition to the concerns of aspiration and pneumonia, studies have shown that the use of GLP-1 RAs may be associated with a lower quality of bowel preparation and higher need for repeat colonoscopy. A study, which I believe is critical, showed that patients on GLP-1 RAs who were scheduled for upper endoscopy and colonoscopy were found to have less gastric residue and less risk of complications when compared with patients who were only having an upper endoscopy. This study sets the stage for a modified prep for patients on GLP-1 RAs prior to their procedures, since patients who received a modified/extended liquid diet on the day prior to their procedure (those preparing for a colonoscopy), had a protective effect against retained gastric content.
Clearly, there is a knowledge gap and a need for guidance. In our recently published AGA Rapid CPU, we advised an individualized approach to managing patients on GLP-1 RAs in the pre-endoscopic setting. Factors to consider are the indication for the GLP-1 RAs, the dose being used, duration of use, and indication and urgency of the procedure, as well as the presence of symptoms in the preoperative area (i.e., do patients have any nausea, vomiting, dyspepsia, etc.). Also an important factor is the facility in which the endoscopy will be taking place, as certain centers have the capacity to act fast and prevent complications or address them in a timely manner while other centers may not be prepared.
We proposed that a modified liquid diet be considered in patients prior to their endoscopies by advising patients to adhere to a clear liquid diet the day before the procedure, as this may help decrease gastric residue and be the safest and best approach for patients on GLP-1 RAs. Of course, it is important to note that more prospective studies are needed to inform clinical practice, and until then, we will have to individualize our approach and continue to put patient safety first.
Dr. Al Hashash is a gastroenterologist and associate professor of medicine at Mayo Clinic, Jacksonville, Florida.
Dear colleagues,
Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are revolutionizing the field of obesity management and are now common medication in patients presenting for endoscopy. With their effect on gastric emptying, the American Society of Anesthesiologists has recommended cessation of such agents prior to endoscopy. However, is this necessary in patients who have been on a clear liquid diet in preparation for a colonoscopy or who are undergoing moderate sedation? Additionally, there are risks to holding GLP-1 RAs, especially for those taking them for glycemic control.
In this issue of Perspectives, Dr. Thomas Hickey and Dr. Ryan Pouliot discuss the nuances of pre-procedure cessation from an anesthesiologist’s perspective. Dr. Jana Al Hashash provides a gastroenterologist’s view, also highlighting the current paucity of evidence guiding management strategies. We hope these pieces will help your discussions in managing GLP-1 RAs prior to endoscopy in your own practice. We welcome your thoughts on this issue on X @AGA_GIHN.
Gyanprakash A. Ketwaroo, MD, MSc, is associate professor of medicine, Yale University, New Haven, Connecticut, and chief of endoscopy at West Haven (Connecticut) VA Medical Center. He is an associate editor for GI & Hepatology News.
GLP-1 Receptor Agonists in Endoscopy
BY THOMAS R. HICKEY, MD; RYAN C. POULIOT, MD
In response to the recent dramatic increase in GLP-1 receptor agonist (GLP-1RA) prescribing and at the urging of its membership, the American Society of Anesthesiologists issued guidance on the preoperative management of these medications. The big takeaways were recommendations that patients on daily dosing should hold their dose on the day of a procedure, and that patients on weekly dosing should hold their dose a week prior.
The ASA guidance recognizes the sparse available evidence base and makes its recommendations in the spirit of patient safety, presuming that a more conservative approach will mitigate risk of rare but potentially devastating pulmonary aspiration, until prospective evidence informs the ideal approach. Until that approach is defined, whether more or less conservative, it is expected that anesthesiologists will adhere to their professional society’s recommendations.
Meanwhile, the American Gastroenterological Association Institute Rapid Clinical Practice Update (CPU) makes little distinction in the management of the endoscopy patient on GLP-1RA. A key refrain throughout the CPU is that there is no actionable data to justify the harms that may come to patients from stopping these medications (e.g., withdrawal of benefit to glycemic control and cardiovascular health) and in delaying or canceling procedures, which could lead to further stress on an overburdened workforce and add complexity to periprocedural processes.
Anesthesiologists should rightly consider themselves leaders in patient safety. As such, when a serious safety concern emerges they should be compelled to caution despite the possibility of other harms, until their concerns are mitigated by robust clinical evidence. Thankfully these questions are quite amenable to research, and prospective trials are already reporting compelling data that residual gastric contents, clearly a risk factor for aspiration, are increased in GLP-1RA groups compared to controls. This is evident even while following recommended fasting times and abstinences from these medications, and adjusting for confounders (e.g., age, diabetes, body mass index).1,2 It logically follows that large studies are likely to find an increased aspiration risk in GLP-1RA populations. Indeed, this increased risk has already been identified in a large retrospective study of endoscopy patients.3 These findings support the ASA’s caution. Additional data indicate that standard fasting guidelines in this patient population may be inadequate.4
The ASA guidance does not differentiate between patients undergoing surgery in the operating room and procedures in the endoscopy suite. Part of our task is to provide perspective on whether GLP-1RA management deserves different treatment for endoscopy patients. We can only speculate pending further data. For example, a prolonged fasting period including a full day of clears, with or without a bowel prep, intuitively protects against pulmonary aspiration. However, this is unlikely to mitigate an anesthesiologist’s concern that administration of propofol, frequently to a state of general anesthesia with an unsecured airway and resulting in a patient devoid of airway protection reflexes, is an inherently higher risk scenario for aspiration compared to surgery in the operating room with a secured airway. We also expect prospective trials will confirm retrospective findings that both propofol and procedures including upper endoscopy confer a higher risk for aspiration compared with conscious sedation and colonoscopy.3
We suggest a reasonable approach based on society guidance and existing evidence, pending additional data. Endoscopists and anesthesiologists should continue this important conversation with a specific focus on risks and benefits in order to decrease conflict and achieve consensus. If anesthesia care is desired, the patient instructions should be updated to reflect ASA guidance. Special attention should be paid to the “gray area,” for example those who did not hold the GLP-1 agonist as recommended.
This category of patients can be considered on a case-by-case basis by the anesthesiologist, proceduralist, and patient, with a range of options including: proceeding with endoscopist-directed sedation, proceeding with anesthesiology-administered conscious sedation, rescheduling the procedure, and proceeding with general anesthesia with rapid-sequence intubation. In addition to patient factors (e.g., GI symptoms, urgency of procedure), this consideration would vary based on local resources (e.g., presence or absence of anesthesia support staff, emergency airway equipment, nursing staff to comfort recovering patients after general endotracheal anesthesia), and aspiration risk inherent to the procedure (e.g., upper and or combination upper and lower endoscopy vs colonoscopy alone). Proficiency and availability of point-of-care ultrasound are rapidly increasing; adoption of a pre-procedure gastric ultrasound to assess for solids, thick liquids, or large volume of clear liquids may provide a less nuanced, more objective means to address this question.
While the question of periprocedural management of these medications has generated intense interest among anesthesiologists and endoscopists alike, it is worth noting the net positive health effects these drugs are likely to have on our patients, including improved glycemic control, significant weight loss, and decreased cardiovascular risk. We are eager to see whether these benefits translate into an overall improvement in periprocedural outcomes, including in our endoscopy patients.
Dr. Hickey is assistant professor of anesthesiology at the Yale University School of Medicine, New Haven, Connecticut, and the VA Connecticut Healthcare System. Dr. Pouliot is assistant professor of anesthesiology at the Geisel School of Medicine at Dartmouth, Hanover, New Hampshire, and Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire.
References
1. Sherwin M et al. Influence of semaglutide use on the presence of residual gastric solids on gastric ultrasound: A prospective observational study in volunteers without obesity recently started on semaglutide. Can J Anaesth. 2023 Aug. doi:10.1007/s12630-023-02549-5.
2. Wu F et al. Association of glucagon-like peptide receptor 1 agonist therapy with the presence of gastric contents in fasting patients undergoing endoscopy under anesthesia care: A historical cohort study. Can J Anaesth. 2024 Mar 14. doi:10.1007/s12630-024-02719-z.
3. Yeo YH et al. Increased risk of aspiration pneumonia associated with endoscopic procedures among patients with glucagon-like peptide 1 receptor agonist use. Gastroenterology. 2024 Mar 27. doi:10.1053/j.gastro.2024.03.015.
4. Sen S et al. Glucagon-like peptide-1 receptor agonist use and residual gastric content before anesthesia. JAMA Surg. 2024 Mar 6. doi:10.1001/jamasurg.2024.0111.
The Impact of GLP-1 Receptor Agonists On Endoscopy
BY JANA G. AL HASHASH, MD, MSc, AGAF
Glucagon-like peptide 1 receptor agonists (GLP-1 RAs) have been approved for the treatment of type 2 diabetes mellitus since 2005. They have become more widely used over the last couple of years for weight loss in individuals who suffer from adiposity-based chronic disease.
The remarkable positive effects that GLP-1 RAs have had on weight loss as well as other medical conditions such as heart disease, hypertension, metabolic dysfunction–associated steatotic liver disease, among many others, have gained these drugs more traction. Even in situations when insurance companies deny coverage of GLP-1 RAs, many patients have been resorting to other routes to obtain these medications, commonly by purchasing them from online compounding pharmacies.
As such, more and more of our patients who present to endoscopy suites across the country are on one of the available GLP-1 RAs. This has necessitated endoscopists and anesthesiologists to become more familiar with the impact of GLP-1 RAs on patients undergoing endoscopic procedures.
Similar to narcotics, GLP-1 RAs affect gastrointestinal motility and delay gastric emptying. Common side effects of patients receiving GLP-1 RAs include nausea, vomiting, and increased satiety. Patients on GLP-1 RAs for weight loss may also have other contributing risk factors for gastroparesis such as diabetes mellitus which may further delay gastric emptying.
For endoscopists, our goals are to achieve the highest quality examination in the safest way possible. As such, being on a GLP-1 RAs could compromise both goals; but to date, the exact impact of these drugs on exam quality and patient safety is yet to be determined.
Studies have shown that patients on GLP-1 RAs have increased gastric residue on upper endoscopy compared with patients not on GLP-1 RAs. The effect of this increased residue on aspiration risk and clinically meaningful patient outcomes is being investigated, and the available published data are conflicting. Additionally, other published cases have shown that GLP-1 RAs are associated with increased solid gastric residue but not liquids, and that symptoms of dyspepsia and abdominal bloating are associated with an increased probability of residual gastric content.
Given the valid concern for increased gastric content residue, anesthesia specialists became more strict about which GLP-1 RA users they would agree to sedate, which ones they would intubate, and which procedures they would cancel. As one would imagine, cancellation and intubation rates have been increasing, and these have affected the schedules of patients, their families, and physicians.
The concern with GLP-1 RAs does not only apply to upper endoscopies, but also impacts colonoscopies. In addition to the concerns of aspiration and pneumonia, studies have shown that the use of GLP-1 RAs may be associated with a lower quality of bowel preparation and higher need for repeat colonoscopy. A study, which I believe is critical, showed that patients on GLP-1 RAs who were scheduled for upper endoscopy and colonoscopy were found to have less gastric residue and less risk of complications when compared with patients who were only having an upper endoscopy. This study sets the stage for a modified prep for patients on GLP-1 RAs prior to their procedures, since patients who received a modified/extended liquid diet on the day prior to their procedure (those preparing for a colonoscopy), had a protective effect against retained gastric content.
Clearly, there is a knowledge gap and a need for guidance. In our recently published AGA Rapid CPU, we advised an individualized approach to managing patients on GLP-1 RAs in the pre-endoscopic setting. Factors to consider are the indication for the GLP-1 RAs, the dose being used, duration of use, and indication and urgency of the procedure, as well as the presence of symptoms in the preoperative area (i.e., do patients have any nausea, vomiting, dyspepsia, etc.). Also an important factor is the facility in which the endoscopy will be taking place, as certain centers have the capacity to act fast and prevent complications or address them in a timely manner while other centers may not be prepared.
We proposed that a modified liquid diet be considered in patients prior to their endoscopies by advising patients to adhere to a clear liquid diet the day before the procedure, as this may help decrease gastric residue and be the safest and best approach for patients on GLP-1 RAs. Of course, it is important to note that more prospective studies are needed to inform clinical practice, and until then, we will have to individualize our approach and continue to put patient safety first.
Dr. Al Hashash is a gastroenterologist and associate professor of medicine at Mayo Clinic, Jacksonville, Florida.









