User login
Sharpen your ax
Recently, I had a trauma call at my scenic little hospital in Maine. “Bleeding leg wound, Dr, Crosslin. We’ve got pressure on it. Come soon.” During my jog across the parking lot to the ER, I drifted into my residency mantra and started reciting the ABCs of trauma care:
Airway, Breathing, CT scan.
Airway, Breathing, C-spine collar.
Airway, Breathing, Consult with ortho.
Okay, so it’s been a while. Four years doesn’t seem like a long time, but that little span serves up a lot of change. You settle into a routine in your isolated, bucolic New England coastal town, where most trauma is related to hauling up lobster crates and having Massachusetts drivers scare the moxie out of locals in the crosswalks, and you forget about the hundreds of Level 1 traumas you managed over 5 years in Boston. The drilled-down, rapid sequence of the primary and secondary surveys gets lost, if just for a moment. Your confident swagger is replaced with a measured, humble shuffle into Trauma Bay 1. Do I scan the leg now? Did I feel for pulses in the foot? Wait, where do the major vessels branch again?
After addressing the issue at hand (or in this case, at foot), I kept thinking about the woodsman’s statement. I reflected on how I felt when I entered the trauma bay. Had I been doing enough to keep my own mental tools sharp? Well, actually, no. When did things slip just enough to allow hesitation and a bit of doubt to creep in? Probably sooner than I would care to admit. I certainly don’t think it took all of these 4 years for it to happen.
There has been some discussion of late surrounding the changes to maintenance of certification requirements from the American Board of Surgery. As with anything in surgery, we all need a chance to grumble about how things were better in the good old days. But then we grudgingly have to acknowledge that maybe – just maybe – the new approach makes some sense.
Did anyone really enjoy reporting on a 3-year cycle and taking a high-stakes, nausea-inducing exam every 10 years? I certainly wasn’t looking forward to reporting in this year about my “progress,” especially given how dull I seem to have become in so many subcategories just 4 years after graduation. But reporting every 5 years? That appeals to my inner slacker. Having a more-frequent-but-way-less-stressful examination that can be tailored to my practice? Yes, I’ll give that a shot.
It’s no secret we all are driven to care more about the things we enjoy doing, and educational science has established, quite firmly, the increased likelihood of concrete learning in higher numbers of loosely related fields when the primary subject is of particular interest to the learner. Elementary school teachers implemented that particular tidbit a long time ago. For me, the drive to excel leads me to the oncology, endocrine, and complex hernia reconstruction arenas. I do not pretend to be the world’s authority on trauma surgery, or anorectal surgery, or vascular surgery. I leave that expertise to others I secretly have judged to be far more pathological than myself. But I would be willing to glean more from reviewing those particular subjects if the overall focus is geared toward improving my knowledge and skill in cancer surgery.
In this ultramodern era, when the compendium of medical and surgical knowledge infinitely outpaces our ability to provide “one-stop shopping” services, perhaps it is time we accept the limitations of our interests and our abilities as part of the natural, beneficial evolution of good medical practice. The College’s willingness to work with the ABS to address the hot-button issue of continuing education in an interactive, relevant, timely manner should be a major point of pride. Rather than clinging to the dull ways of the past, I think we all are going to benefit from carrying a collectively sharper ax.
Dr. Crosslin is a general surgeon practicing in Rockport, Maine.
Recently, I had a trauma call at my scenic little hospital in Maine. “Bleeding leg wound, Dr, Crosslin. We’ve got pressure on it. Come soon.” During my jog across the parking lot to the ER, I drifted into my residency mantra and started reciting the ABCs of trauma care:
Airway, Breathing, CT scan.
Airway, Breathing, C-spine collar.
Airway, Breathing, Consult with ortho.
Okay, so it’s been a while. Four years doesn’t seem like a long time, but that little span serves up a lot of change. You settle into a routine in your isolated, bucolic New England coastal town, where most trauma is related to hauling up lobster crates and having Massachusetts drivers scare the moxie out of locals in the crosswalks, and you forget about the hundreds of Level 1 traumas you managed over 5 years in Boston. The drilled-down, rapid sequence of the primary and secondary surveys gets lost, if just for a moment. Your confident swagger is replaced with a measured, humble shuffle into Trauma Bay 1. Do I scan the leg now? Did I feel for pulses in the foot? Wait, where do the major vessels branch again?
After addressing the issue at hand (or in this case, at foot), I kept thinking about the woodsman’s statement. I reflected on how I felt when I entered the trauma bay. Had I been doing enough to keep my own mental tools sharp? Well, actually, no. When did things slip just enough to allow hesitation and a bit of doubt to creep in? Probably sooner than I would care to admit. I certainly don’t think it took all of these 4 years for it to happen.
There has been some discussion of late surrounding the changes to maintenance of certification requirements from the American Board of Surgery. As with anything in surgery, we all need a chance to grumble about how things were better in the good old days. But then we grudgingly have to acknowledge that maybe – just maybe – the new approach makes some sense.
Did anyone really enjoy reporting on a 3-year cycle and taking a high-stakes, nausea-inducing exam every 10 years? I certainly wasn’t looking forward to reporting in this year about my “progress,” especially given how dull I seem to have become in so many subcategories just 4 years after graduation. But reporting every 5 years? That appeals to my inner slacker. Having a more-frequent-but-way-less-stressful examination that can be tailored to my practice? Yes, I’ll give that a shot.
It’s no secret we all are driven to care more about the things we enjoy doing, and educational science has established, quite firmly, the increased likelihood of concrete learning in higher numbers of loosely related fields when the primary subject is of particular interest to the learner. Elementary school teachers implemented that particular tidbit a long time ago. For me, the drive to excel leads me to the oncology, endocrine, and complex hernia reconstruction arenas. I do not pretend to be the world’s authority on trauma surgery, or anorectal surgery, or vascular surgery. I leave that expertise to others I secretly have judged to be far more pathological than myself. But I would be willing to glean more from reviewing those particular subjects if the overall focus is geared toward improving my knowledge and skill in cancer surgery.
In this ultramodern era, when the compendium of medical and surgical knowledge infinitely outpaces our ability to provide “one-stop shopping” services, perhaps it is time we accept the limitations of our interests and our abilities as part of the natural, beneficial evolution of good medical practice. The College’s willingness to work with the ABS to address the hot-button issue of continuing education in an interactive, relevant, timely manner should be a major point of pride. Rather than clinging to the dull ways of the past, I think we all are going to benefit from carrying a collectively sharper ax.
Dr. Crosslin is a general surgeon practicing in Rockport, Maine.
Recently, I had a trauma call at my scenic little hospital in Maine. “Bleeding leg wound, Dr, Crosslin. We’ve got pressure on it. Come soon.” During my jog across the parking lot to the ER, I drifted into my residency mantra and started reciting the ABCs of trauma care:
Airway, Breathing, CT scan.
Airway, Breathing, C-spine collar.
Airway, Breathing, Consult with ortho.
Okay, so it’s been a while. Four years doesn’t seem like a long time, but that little span serves up a lot of change. You settle into a routine in your isolated, bucolic New England coastal town, where most trauma is related to hauling up lobster crates and having Massachusetts drivers scare the moxie out of locals in the crosswalks, and you forget about the hundreds of Level 1 traumas you managed over 5 years in Boston. The drilled-down, rapid sequence of the primary and secondary surveys gets lost, if just for a moment. Your confident swagger is replaced with a measured, humble shuffle into Trauma Bay 1. Do I scan the leg now? Did I feel for pulses in the foot? Wait, where do the major vessels branch again?
After addressing the issue at hand (or in this case, at foot), I kept thinking about the woodsman’s statement. I reflected on how I felt when I entered the trauma bay. Had I been doing enough to keep my own mental tools sharp? Well, actually, no. When did things slip just enough to allow hesitation and a bit of doubt to creep in? Probably sooner than I would care to admit. I certainly don’t think it took all of these 4 years for it to happen.
There has been some discussion of late surrounding the changes to maintenance of certification requirements from the American Board of Surgery. As with anything in surgery, we all need a chance to grumble about how things were better in the good old days. But then we grudgingly have to acknowledge that maybe – just maybe – the new approach makes some sense.
Did anyone really enjoy reporting on a 3-year cycle and taking a high-stakes, nausea-inducing exam every 10 years? I certainly wasn’t looking forward to reporting in this year about my “progress,” especially given how dull I seem to have become in so many subcategories just 4 years after graduation. But reporting every 5 years? That appeals to my inner slacker. Having a more-frequent-but-way-less-stressful examination that can be tailored to my practice? Yes, I’ll give that a shot.
It’s no secret we all are driven to care more about the things we enjoy doing, and educational science has established, quite firmly, the increased likelihood of concrete learning in higher numbers of loosely related fields when the primary subject is of particular interest to the learner. Elementary school teachers implemented that particular tidbit a long time ago. For me, the drive to excel leads me to the oncology, endocrine, and complex hernia reconstruction arenas. I do not pretend to be the world’s authority on trauma surgery, or anorectal surgery, or vascular surgery. I leave that expertise to others I secretly have judged to be far more pathological than myself. But I would be willing to glean more from reviewing those particular subjects if the overall focus is geared toward improving my knowledge and skill in cancer surgery.
In this ultramodern era, when the compendium of medical and surgical knowledge infinitely outpaces our ability to provide “one-stop shopping” services, perhaps it is time we accept the limitations of our interests and our abilities as part of the natural, beneficial evolution of good medical practice. The College’s willingness to work with the ABS to address the hot-button issue of continuing education in an interactive, relevant, timely manner should be a major point of pride. Rather than clinging to the dull ways of the past, I think we all are going to benefit from carrying a collectively sharper ax.
Dr. Crosslin is a general surgeon practicing in Rockport, Maine.
Summer colds
Enteroviruses cause most summer colds. The enteroviruses include echoviruses, coxsackieviruses, numbered enteroviruses, and the polioviruses. Most summer colds seen in private practice are self limited, presenting with fever alone or clinically distinctive pictures such as hand-foot-and-mouth disease (HFMD), herpangina, or pleurodynia. However, enteroviruses also cause serious illnesses such as meningitis, myocarditis, encephalitis, and neonatal sepsis. Enterovirus infections often are confused with bacterial infections and treated unnecessarily with antibiotics.
Enteroviral infections spread predominantly by the fecal-oral route. Contaminated swimming pools also may serve as a source of transmission. Enteroviruses colonize the respiratory and the gastrointestinal tract. The infection spreads to the lymph nodes, where the virus replicates and an initial viremia occurs on approximately the third postexposure day. The viremia results in subsequent spread to the throat (herpangina), and/or hands and feet (HFMD), lungs (pleurodynia), heart (myocarditis) or meninges (viral meningitis). Infection at the secondary sites corresponds to the onset of clinical symptoms 4-6 days after exposure. The clinical manifestations of enteroviral infections result from the damage caused by the virus at the secondary sites of infection.
Enterovirus pharyngitis starts abruptly and often is accompanied by fever. Younger children may present with increased drooling, hands in the mouth, and refusal to eat. Older children complain of sore throat as well as headache, myalgias, and malaise. Mild vomiting and diarrhea commonly accompany the respiratory symptoms. Herpangina is a specific syndrome of enterovirus pharyngitis; children with this syndrome have fever and characteristic papulovesicular lesions on the anterior tonsillar pillars, soft palate, uvula, tonsils, and pharyngeal wall. The lesions are discrete and average five per patient. They do not appear in the anterior part of the mouth.
Hand-foot-and-mouth disease is well recognized by clinicians who care for young children. The child presents with fever and papulovesicular lesions within the mouth that quickly become ulcerated and papulovesicular lesions on the palms and soles. The palms and soles often are puffy and red, and the child may act as though her hands and feet hurt, refusing to use her hands or walk. The fever accompanying herpangina and HFMD usually lasts 3 or 4 days, but fever that persists for a week is not uncommon. The pharyngitis follows a pattern similar to the fever.
Pleurodynia has a sudden onset of pain in the chest or upper abdomen. The pain appears to be muscular in origin; its intensity varies. It can be excruciatingly severe and accompanied by sweating and pallor. Older children describe the pain as sharp and stabbing. It occurs in spasms that can last for a few minutes to a few hours. During spasms, the patient has rapid, shallow respirations that suggest pneumonia. The symptoms usually last 1 or 2 days, but the illness can be biphasic, with symptoms resolving only to reappear a few days later.
Gastrointestinal manifestations are almost universal in enterovirus infections. The most common symptoms are anorexia, nausea, vomiting, and diarrhea. They usually are not severe and often occur in combination with other symptoms, such as fever and sore throat. Abdominal pain may be the only manifestation of infection; when severe, it can mimic appendicitis.
Enterovirus infections once were thought to be mild diseases that lasted 2-3 days. But a study of 380 children aged 4-18 years during July to October from private pediatric practices found that illness is prolonged in many patients (Pediatrics. 1998 Nov;102[5]:1126-34). The mean duration of illness was found to be 10 days for myalgia-malaise syndrome, 7 days for herpangina, and 7 days for HFMD.
Spread of enteroviral infections within a household was common. More than 50% of children studied had a family member with enterovirus illness. Half of siblings and 25% of adults within the household of the index case contracted an enteroviral infection. Some had the same presentation as the index patient, but it was not uncommon for other household members to have quite different presentations. For example, the first child seen might present with hand-foot-and-mouth disease, and a few days later a sibling might be brought for care with myalgia-malaise, and the parent might appear ill and complain of pleurodynia.
Summer colds can be costly to families. The duration of the illness and the multitude of nonspecific symptoms sometimes leads to concern about a possible bacterial cause, which prompts a diagnostic workup, including laboratory tests and empiric treatment with antibiotics. The direct costs vary with the syndrome; stomatitis and HFMD are the least expensive to treat because the clinical picture is diagnostic with a single office visit, but a severe manifestation such as aseptic meningitis are expensive to treat with associated emergency department visits, spinal tap, and sometimes hospitalization.
Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. He reported having no conflicts of interest. Email him at [email protected].
Enteroviruses cause most summer colds. The enteroviruses include echoviruses, coxsackieviruses, numbered enteroviruses, and the polioviruses. Most summer colds seen in private practice are self limited, presenting with fever alone or clinically distinctive pictures such as hand-foot-and-mouth disease (HFMD), herpangina, or pleurodynia. However, enteroviruses also cause serious illnesses such as meningitis, myocarditis, encephalitis, and neonatal sepsis. Enterovirus infections often are confused with bacterial infections and treated unnecessarily with antibiotics.
Enteroviral infections spread predominantly by the fecal-oral route. Contaminated swimming pools also may serve as a source of transmission. Enteroviruses colonize the respiratory and the gastrointestinal tract. The infection spreads to the lymph nodes, where the virus replicates and an initial viremia occurs on approximately the third postexposure day. The viremia results in subsequent spread to the throat (herpangina), and/or hands and feet (HFMD), lungs (pleurodynia), heart (myocarditis) or meninges (viral meningitis). Infection at the secondary sites corresponds to the onset of clinical symptoms 4-6 days after exposure. The clinical manifestations of enteroviral infections result from the damage caused by the virus at the secondary sites of infection.
Enterovirus pharyngitis starts abruptly and often is accompanied by fever. Younger children may present with increased drooling, hands in the mouth, and refusal to eat. Older children complain of sore throat as well as headache, myalgias, and malaise. Mild vomiting and diarrhea commonly accompany the respiratory symptoms. Herpangina is a specific syndrome of enterovirus pharyngitis; children with this syndrome have fever and characteristic papulovesicular lesions on the anterior tonsillar pillars, soft palate, uvula, tonsils, and pharyngeal wall. The lesions are discrete and average five per patient. They do not appear in the anterior part of the mouth.
Hand-foot-and-mouth disease is well recognized by clinicians who care for young children. The child presents with fever and papulovesicular lesions within the mouth that quickly become ulcerated and papulovesicular lesions on the palms and soles. The palms and soles often are puffy and red, and the child may act as though her hands and feet hurt, refusing to use her hands or walk. The fever accompanying herpangina and HFMD usually lasts 3 or 4 days, but fever that persists for a week is not uncommon. The pharyngitis follows a pattern similar to the fever.
Pleurodynia has a sudden onset of pain in the chest or upper abdomen. The pain appears to be muscular in origin; its intensity varies. It can be excruciatingly severe and accompanied by sweating and pallor. Older children describe the pain as sharp and stabbing. It occurs in spasms that can last for a few minutes to a few hours. During spasms, the patient has rapid, shallow respirations that suggest pneumonia. The symptoms usually last 1 or 2 days, but the illness can be biphasic, with symptoms resolving only to reappear a few days later.
Gastrointestinal manifestations are almost universal in enterovirus infections. The most common symptoms are anorexia, nausea, vomiting, and diarrhea. They usually are not severe and often occur in combination with other symptoms, such as fever and sore throat. Abdominal pain may be the only manifestation of infection; when severe, it can mimic appendicitis.
Enterovirus infections once were thought to be mild diseases that lasted 2-3 days. But a study of 380 children aged 4-18 years during July to October from private pediatric practices found that illness is prolonged in many patients (Pediatrics. 1998 Nov;102[5]:1126-34). The mean duration of illness was found to be 10 days for myalgia-malaise syndrome, 7 days for herpangina, and 7 days for HFMD.
Spread of enteroviral infections within a household was common. More than 50% of children studied had a family member with enterovirus illness. Half of siblings and 25% of adults within the household of the index case contracted an enteroviral infection. Some had the same presentation as the index patient, but it was not uncommon for other household members to have quite different presentations. For example, the first child seen might present with hand-foot-and-mouth disease, and a few days later a sibling might be brought for care with myalgia-malaise, and the parent might appear ill and complain of pleurodynia.
Summer colds can be costly to families. The duration of the illness and the multitude of nonspecific symptoms sometimes leads to concern about a possible bacterial cause, which prompts a diagnostic workup, including laboratory tests and empiric treatment with antibiotics. The direct costs vary with the syndrome; stomatitis and HFMD are the least expensive to treat because the clinical picture is diagnostic with a single office visit, but a severe manifestation such as aseptic meningitis are expensive to treat with associated emergency department visits, spinal tap, and sometimes hospitalization.
Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. He reported having no conflicts of interest. Email him at [email protected].
Enteroviruses cause most summer colds. The enteroviruses include echoviruses, coxsackieviruses, numbered enteroviruses, and the polioviruses. Most summer colds seen in private practice are self limited, presenting with fever alone or clinically distinctive pictures such as hand-foot-and-mouth disease (HFMD), herpangina, or pleurodynia. However, enteroviruses also cause serious illnesses such as meningitis, myocarditis, encephalitis, and neonatal sepsis. Enterovirus infections often are confused with bacterial infections and treated unnecessarily with antibiotics.
Enteroviral infections spread predominantly by the fecal-oral route. Contaminated swimming pools also may serve as a source of transmission. Enteroviruses colonize the respiratory and the gastrointestinal tract. The infection spreads to the lymph nodes, where the virus replicates and an initial viremia occurs on approximately the third postexposure day. The viremia results in subsequent spread to the throat (herpangina), and/or hands and feet (HFMD), lungs (pleurodynia), heart (myocarditis) or meninges (viral meningitis). Infection at the secondary sites corresponds to the onset of clinical symptoms 4-6 days after exposure. The clinical manifestations of enteroviral infections result from the damage caused by the virus at the secondary sites of infection.
Enterovirus pharyngitis starts abruptly and often is accompanied by fever. Younger children may present with increased drooling, hands in the mouth, and refusal to eat. Older children complain of sore throat as well as headache, myalgias, and malaise. Mild vomiting and diarrhea commonly accompany the respiratory symptoms. Herpangina is a specific syndrome of enterovirus pharyngitis; children with this syndrome have fever and characteristic papulovesicular lesions on the anterior tonsillar pillars, soft palate, uvula, tonsils, and pharyngeal wall. The lesions are discrete and average five per patient. They do not appear in the anterior part of the mouth.
Hand-foot-and-mouth disease is well recognized by clinicians who care for young children. The child presents with fever and papulovesicular lesions within the mouth that quickly become ulcerated and papulovesicular lesions on the palms and soles. The palms and soles often are puffy and red, and the child may act as though her hands and feet hurt, refusing to use her hands or walk. The fever accompanying herpangina and HFMD usually lasts 3 or 4 days, but fever that persists for a week is not uncommon. The pharyngitis follows a pattern similar to the fever.
Pleurodynia has a sudden onset of pain in the chest or upper abdomen. The pain appears to be muscular in origin; its intensity varies. It can be excruciatingly severe and accompanied by sweating and pallor. Older children describe the pain as sharp and stabbing. It occurs in spasms that can last for a few minutes to a few hours. During spasms, the patient has rapid, shallow respirations that suggest pneumonia. The symptoms usually last 1 or 2 days, but the illness can be biphasic, with symptoms resolving only to reappear a few days later.
Gastrointestinal manifestations are almost universal in enterovirus infections. The most common symptoms are anorexia, nausea, vomiting, and diarrhea. They usually are not severe and often occur in combination with other symptoms, such as fever and sore throat. Abdominal pain may be the only manifestation of infection; when severe, it can mimic appendicitis.
Enterovirus infections once were thought to be mild diseases that lasted 2-3 days. But a study of 380 children aged 4-18 years during July to October from private pediatric practices found that illness is prolonged in many patients (Pediatrics. 1998 Nov;102[5]:1126-34). The mean duration of illness was found to be 10 days for myalgia-malaise syndrome, 7 days for herpangina, and 7 days for HFMD.
Spread of enteroviral infections within a household was common. More than 50% of children studied had a family member with enterovirus illness. Half of siblings and 25% of adults within the household of the index case contracted an enteroviral infection. Some had the same presentation as the index patient, but it was not uncommon for other household members to have quite different presentations. For example, the first child seen might present with hand-foot-and-mouth disease, and a few days later a sibling might be brought for care with myalgia-malaise, and the parent might appear ill and complain of pleurodynia.
Summer colds can be costly to families. The duration of the illness and the multitude of nonspecific symptoms sometimes leads to concern about a possible bacterial cause, which prompts a diagnostic workup, including laboratory tests and empiric treatment with antibiotics. The direct costs vary with the syndrome; stomatitis and HFMD are the least expensive to treat because the clinical picture is diagnostic with a single office visit, but a severe manifestation such as aseptic meningitis are expensive to treat with associated emergency department visits, spinal tap, and sometimes hospitalization.
Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. He reported having no conflicts of interest. Email him at [email protected].
‘Captain of the ship’ doctrine
Question: The “Captain of the Ship” doctrine:
A. Is a legal principle used mostly in maritime law.
B. Is applicable only to surgeons in the operating room.
C. Is good law in all jurisdictions.
D. May be used by plaintiffs in emergency department triage litigation.
E. Originated when hospitals lost their charitable immunity.
Answer: D. Historically, the Captain of the Ship doctrine imputes liability to the surgeon who has the authority and right to control the actions of his assistants in the operating room.
Pennsylvania famously saw the use of the phrase in a 1949 case: “In the course of an operation in the operating room of a hospital, and until the surgeon leaves that room at the conclusion of the operation … he is in the same complete charge of those who are present and assisting him as is the captain of a ship over all on board.”1
Public hospitals in the 1940s were immune from liability because they were charitable organizations, so the Captain of the Ship doctrine emerged as a means for injured patients to recover damages against the surgeon instead. Courts have used various legal theories to justify this doctrine, which is basically grounded in vicarious liability, e.g., master-servant relationship (respondeat superior), borrowed servant, a nondelegable duty, or more broadly, principles of agency.
Use of the doctrine to shift liability to the surgeon in the operating room is well exemplified in litigation over retained sponges, left-behind instruments, burns in the operating room, administration of the wrong blood type, and allergic reaction to penicillin. Actual control of the surgeon’s assistants is not essential, but the right to merely supervise is insufficient. What is dispositive is the right and authority to determine an assistant’s actions.
However, what constitutes an “operating room” has been in dispute. It may simply mean a circumscribed and controlled area for medical procedures and/or treatment. Thus, the term has been extended to a room where only local anesthesia was used for esophageal dilation. Reasoning by analogy, the modern-day heart catheterization lab or interventional radiology suite would arguably count as “operating rooms” where the procedurist-doctor, usually a nonsurgeon, may be deemed to function as the captain of the ship.
Another place where a nonsurgeon may be involved is the hospital ED. It has been stated that emergency physicians have been held liable for adverse outcomes resulting from the patients under triage, based on the Captain of the Ship doctrine.2 Once a patient arrives in the ED, a legal duty to provide care arises, even if the physician has yet to see the patient. The federal Emergency Medical Treatment and Labor Act, which regulates much of what happens in the nation’s emergency departments, covers “any individual ... [who] comes to the emergency department and a request is made on the individual’s behalf for examination or treatment for a medical condition.”
Still, the doctrine is less likely to be invoked in a more spread-out area such as a general medical ward, where a physician’s control cannot be reasonably expected.
For example, courts have held that ward nurses giving injections into the buttock causing permanent neuropathy to a patient’s leg were not the agents of the prescribing physician, but just of the hospital employing them. The doctrine also was rejected in Collins v. Hand by the Pennsylvania Supreme Court, which reversed a judgment against a psychiatrist defendant.3 In the Collins case, notwithstanding the fact that the psychiatrist, Dr. Hand, had personally arranged for the patient’s transfer to another hospital and wrote orders for electroconvulsive therapy (which was complicated by fractures), Dr. Hand did not choose the doctor who was to administer the therapy, nor did he hire, compensate, or control any of the team members.
In the 1960s, hospitals began losing their charitable immunity status and assumed direct as well as vicarious liability for injuries to patients from the negligent acts of their employees, such as nurses. The key policy reason for having the Captain of the Ship doctrine then no longer existed. Besides, operating rooms became increasingly complex, and the senior surgeon was thought to be incapable of being in charge of all activities there.
Wisconsin is typical: A retained sponge following a laparoscopic cholecystectomy led to complications, and the patient sued the hospital and surgeon, claiming each was responsible for the nurses’ sponge-count error. The lower court had found that “as a matter of law [the surgeon] is in fact responsible and liable for the actions of the parties that were in the operating room with him and working under his supervision ... [the] doctor is the captain of the ship. That doctor is responsible for everything.”
Upon appeal, the Wisconsin Supreme Court reversed the decision of the lower court by rejecting the doctrine altogether, finding that it failed to reflect the emergence of hospitals as modern health care facilities.5
Still, the doctrine is by no means obsolete. In a Colorado case, the court wrote that, even if the nurse were an employee of the hospital and her negligence caused the death of plaintiff’s husband, the Captain of the Ship doctrine would preclude recovery against the hospital.6 It relied on a precedent-setting case that held that once the operating surgeon assumed control in the operating room, the surgeon is liable for the negligence of all persons working there.
Likewise, California has recently breathed new life into the doctrine.7 A case in 2006 involved a patient who underwent arterial bypass surgery in his right leg. A case in which a nurse’s counting error led to a retained sponge ended up with the patient losing his leg. The surgeon initially escaped liability by virtue of the court’s refusal to include Captain of the Ship instructions to the jury, which found the doctor not negligent. The state court of appeals reversed, however, concluding that it was reasonably probable that the jury might have reached a different result had it been so instructed.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. McConnell v. Williams, 361 Pa. 355, 65 A.2d 243 (1949).
2. ED Legal Letter, Feb 1, 2018.
3. Collins v. Hand, 246 A.2d 398 (Pa 1968).
4. AORN J. 2001 Oct;74(4):525-8.
5. Lewis v. Physicians Insurance Company et al., 627 NW2d 484 (Wis 2001).
6. Krane v. St. Anthony Hospital Systems, 738 P.2d 75 (Co 1987).
7. Fields v. Yusuf, 144 Cal.App.4th 1381 (2006).
Question: The “Captain of the Ship” doctrine:
A. Is a legal principle used mostly in maritime law.
B. Is applicable only to surgeons in the operating room.
C. Is good law in all jurisdictions.
D. May be used by plaintiffs in emergency department triage litigation.
E. Originated when hospitals lost their charitable immunity.
Answer: D. Historically, the Captain of the Ship doctrine imputes liability to the surgeon who has the authority and right to control the actions of his assistants in the operating room.
Pennsylvania famously saw the use of the phrase in a 1949 case: “In the course of an operation in the operating room of a hospital, and until the surgeon leaves that room at the conclusion of the operation … he is in the same complete charge of those who are present and assisting him as is the captain of a ship over all on board.”1
Public hospitals in the 1940s were immune from liability because they were charitable organizations, so the Captain of the Ship doctrine emerged as a means for injured patients to recover damages against the surgeon instead. Courts have used various legal theories to justify this doctrine, which is basically grounded in vicarious liability, e.g., master-servant relationship (respondeat superior), borrowed servant, a nondelegable duty, or more broadly, principles of agency.
Use of the doctrine to shift liability to the surgeon in the operating room is well exemplified in litigation over retained sponges, left-behind instruments, burns in the operating room, administration of the wrong blood type, and allergic reaction to penicillin. Actual control of the surgeon’s assistants is not essential, but the right to merely supervise is insufficient. What is dispositive is the right and authority to determine an assistant’s actions.
However, what constitutes an “operating room” has been in dispute. It may simply mean a circumscribed and controlled area for medical procedures and/or treatment. Thus, the term has been extended to a room where only local anesthesia was used for esophageal dilation. Reasoning by analogy, the modern-day heart catheterization lab or interventional radiology suite would arguably count as “operating rooms” where the procedurist-doctor, usually a nonsurgeon, may be deemed to function as the captain of the ship.
Another place where a nonsurgeon may be involved is the hospital ED. It has been stated that emergency physicians have been held liable for adverse outcomes resulting from the patients under triage, based on the Captain of the Ship doctrine.2 Once a patient arrives in the ED, a legal duty to provide care arises, even if the physician has yet to see the patient. The federal Emergency Medical Treatment and Labor Act, which regulates much of what happens in the nation’s emergency departments, covers “any individual ... [who] comes to the emergency department and a request is made on the individual’s behalf for examination or treatment for a medical condition.”
Still, the doctrine is less likely to be invoked in a more spread-out area such as a general medical ward, where a physician’s control cannot be reasonably expected.
For example, courts have held that ward nurses giving injections into the buttock causing permanent neuropathy to a patient’s leg were not the agents of the prescribing physician, but just of the hospital employing them. The doctrine also was rejected in Collins v. Hand by the Pennsylvania Supreme Court, which reversed a judgment against a psychiatrist defendant.3 In the Collins case, notwithstanding the fact that the psychiatrist, Dr. Hand, had personally arranged for the patient’s transfer to another hospital and wrote orders for electroconvulsive therapy (which was complicated by fractures), Dr. Hand did not choose the doctor who was to administer the therapy, nor did he hire, compensate, or control any of the team members.
In the 1960s, hospitals began losing their charitable immunity status and assumed direct as well as vicarious liability for injuries to patients from the negligent acts of their employees, such as nurses. The key policy reason for having the Captain of the Ship doctrine then no longer existed. Besides, operating rooms became increasingly complex, and the senior surgeon was thought to be incapable of being in charge of all activities there.
Wisconsin is typical: A retained sponge following a laparoscopic cholecystectomy led to complications, and the patient sued the hospital and surgeon, claiming each was responsible for the nurses’ sponge-count error. The lower court had found that “as a matter of law [the surgeon] is in fact responsible and liable for the actions of the parties that were in the operating room with him and working under his supervision ... [the] doctor is the captain of the ship. That doctor is responsible for everything.”
Upon appeal, the Wisconsin Supreme Court reversed the decision of the lower court by rejecting the doctrine altogether, finding that it failed to reflect the emergence of hospitals as modern health care facilities.5
Still, the doctrine is by no means obsolete. In a Colorado case, the court wrote that, even if the nurse were an employee of the hospital and her negligence caused the death of plaintiff’s husband, the Captain of the Ship doctrine would preclude recovery against the hospital.6 It relied on a precedent-setting case that held that once the operating surgeon assumed control in the operating room, the surgeon is liable for the negligence of all persons working there.
Likewise, California has recently breathed new life into the doctrine.7 A case in 2006 involved a patient who underwent arterial bypass surgery in his right leg. A case in which a nurse’s counting error led to a retained sponge ended up with the patient losing his leg. The surgeon initially escaped liability by virtue of the court’s refusal to include Captain of the Ship instructions to the jury, which found the doctor not negligent. The state court of appeals reversed, however, concluding that it was reasonably probable that the jury might have reached a different result had it been so instructed.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. McConnell v. Williams, 361 Pa. 355, 65 A.2d 243 (1949).
2. ED Legal Letter, Feb 1, 2018.
3. Collins v. Hand, 246 A.2d 398 (Pa 1968).
4. AORN J. 2001 Oct;74(4):525-8.
5. Lewis v. Physicians Insurance Company et al., 627 NW2d 484 (Wis 2001).
6. Krane v. St. Anthony Hospital Systems, 738 P.2d 75 (Co 1987).
7. Fields v. Yusuf, 144 Cal.App.4th 1381 (2006).
Question: The “Captain of the Ship” doctrine:
A. Is a legal principle used mostly in maritime law.
B. Is applicable only to surgeons in the operating room.
C. Is good law in all jurisdictions.
D. May be used by plaintiffs in emergency department triage litigation.
E. Originated when hospitals lost their charitable immunity.
Answer: D. Historically, the Captain of the Ship doctrine imputes liability to the surgeon who has the authority and right to control the actions of his assistants in the operating room.
Pennsylvania famously saw the use of the phrase in a 1949 case: “In the course of an operation in the operating room of a hospital, and until the surgeon leaves that room at the conclusion of the operation … he is in the same complete charge of those who are present and assisting him as is the captain of a ship over all on board.”1
Public hospitals in the 1940s were immune from liability because they were charitable organizations, so the Captain of the Ship doctrine emerged as a means for injured patients to recover damages against the surgeon instead. Courts have used various legal theories to justify this doctrine, which is basically grounded in vicarious liability, e.g., master-servant relationship (respondeat superior), borrowed servant, a nondelegable duty, or more broadly, principles of agency.
Use of the doctrine to shift liability to the surgeon in the operating room is well exemplified in litigation over retained sponges, left-behind instruments, burns in the operating room, administration of the wrong blood type, and allergic reaction to penicillin. Actual control of the surgeon’s assistants is not essential, but the right to merely supervise is insufficient. What is dispositive is the right and authority to determine an assistant’s actions.
However, what constitutes an “operating room” has been in dispute. It may simply mean a circumscribed and controlled area for medical procedures and/or treatment. Thus, the term has been extended to a room where only local anesthesia was used for esophageal dilation. Reasoning by analogy, the modern-day heart catheterization lab or interventional radiology suite would arguably count as “operating rooms” where the procedurist-doctor, usually a nonsurgeon, may be deemed to function as the captain of the ship.
Another place where a nonsurgeon may be involved is the hospital ED. It has been stated that emergency physicians have been held liable for adverse outcomes resulting from the patients under triage, based on the Captain of the Ship doctrine.2 Once a patient arrives in the ED, a legal duty to provide care arises, even if the physician has yet to see the patient. The federal Emergency Medical Treatment and Labor Act, which regulates much of what happens in the nation’s emergency departments, covers “any individual ... [who] comes to the emergency department and a request is made on the individual’s behalf for examination or treatment for a medical condition.”
Still, the doctrine is less likely to be invoked in a more spread-out area such as a general medical ward, where a physician’s control cannot be reasonably expected.
For example, courts have held that ward nurses giving injections into the buttock causing permanent neuropathy to a patient’s leg were not the agents of the prescribing physician, but just of the hospital employing them. The doctrine also was rejected in Collins v. Hand by the Pennsylvania Supreme Court, which reversed a judgment against a psychiatrist defendant.3 In the Collins case, notwithstanding the fact that the psychiatrist, Dr. Hand, had personally arranged for the patient’s transfer to another hospital and wrote orders for electroconvulsive therapy (which was complicated by fractures), Dr. Hand did not choose the doctor who was to administer the therapy, nor did he hire, compensate, or control any of the team members.
In the 1960s, hospitals began losing their charitable immunity status and assumed direct as well as vicarious liability for injuries to patients from the negligent acts of their employees, such as nurses. The key policy reason for having the Captain of the Ship doctrine then no longer existed. Besides, operating rooms became increasingly complex, and the senior surgeon was thought to be incapable of being in charge of all activities there.
Wisconsin is typical: A retained sponge following a laparoscopic cholecystectomy led to complications, and the patient sued the hospital and surgeon, claiming each was responsible for the nurses’ sponge-count error. The lower court had found that “as a matter of law [the surgeon] is in fact responsible and liable for the actions of the parties that were in the operating room with him and working under his supervision ... [the] doctor is the captain of the ship. That doctor is responsible for everything.”
Upon appeal, the Wisconsin Supreme Court reversed the decision of the lower court by rejecting the doctrine altogether, finding that it failed to reflect the emergence of hospitals as modern health care facilities.5
Still, the doctrine is by no means obsolete. In a Colorado case, the court wrote that, even if the nurse were an employee of the hospital and her negligence caused the death of plaintiff’s husband, the Captain of the Ship doctrine would preclude recovery against the hospital.6 It relied on a precedent-setting case that held that once the operating surgeon assumed control in the operating room, the surgeon is liable for the negligence of all persons working there.
Likewise, California has recently breathed new life into the doctrine.7 A case in 2006 involved a patient who underwent arterial bypass surgery in his right leg. A case in which a nurse’s counting error led to a retained sponge ended up with the patient losing his leg. The surgeon initially escaped liability by virtue of the court’s refusal to include Captain of the Ship instructions to the jury, which found the doctor not negligent. The state court of appeals reversed, however, concluding that it was reasonably probable that the jury might have reached a different result had it been so instructed.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. McConnell v. Williams, 361 Pa. 355, 65 A.2d 243 (1949).
2. ED Legal Letter, Feb 1, 2018.
3. Collins v. Hand, 246 A.2d 398 (Pa 1968).
4. AORN J. 2001 Oct;74(4):525-8.
5. Lewis v. Physicians Insurance Company et al., 627 NW2d 484 (Wis 2001).
6. Krane v. St. Anthony Hospital Systems, 738 P.2d 75 (Co 1987).
7. Fields v. Yusuf, 144 Cal.App.4th 1381 (2006).
How congenital heart disease affects brain development
Congenital heart disease (CHD) is the most common congenital anomaly, with an estimated incidence of 6-12 per 1,000 live births. It is also the congenital anomaly that most often leads to death or significant morbidity. Advances in surgical procedures and operating room care as well as specialized care in the ICU have led to significant improvements in survival over the past 10-20 years – even for the most complex cases of CHD. We now expect the majority of newborns with CHD not only to survive, but to grow up into adulthood.
The focus of clinical research has thus transitioned from survival to issues of long-term morbidity and outcomes, and the more recent literature has clearly shown us that children with CHD are at high risk of learning disabilities and other neurodevelopmental abnormalities. The prevalence of impairment rises with the complexity of CHD, from a prevalence of approximately 20% in mild CHD to as much as 75% in severe CHD. Almost all neonates and infants who undergo palliative surgical procedures have neurodevelopmental impairments.
The neurobehavioral “signature” of CHD includes cognitive defects (usually mild), short attention span, fine and gross motor delays, speech and language delays, visual motor integration, and executive function deficits. Executive function deficits and attention deficits are among the problems that often do not present in children until they reach middle school and beyond, when they are expected to learn more complicated material and handle more complex tasks. Long-term surveillance and care have thus become a major focus at our institution and others throughout the country.
At the same time, evidence has increased in the past 5-10 years that adverse neurodevelopmental outcomes in children with complex CHD may stem from genetic factors as well as compromise to the brain in utero because of altered blood flow, compromise at the time of delivery, and insults during and after corrective or palliative surgery. Surgical strategies and operating room teams have become significantly better at protecting the brain, and new research now is directed toward understanding the neurologic abnormalities that are present in newborns prior to surgical intervention.
Increasingly, researchers are now focused on looking at the in utero origins of brain impairments in children with CHD and trying to understand specific prenatal causes, mechanisms, and potentially modifiable factors. We’re asking what we can do during pregnancy to improve neurodevelopmental outcomes.
Impaired brain growth
The question of how CHD affects blood flow to the fetal brain is an important one. We found some time ago in a study using Doppler ultrasound that 44% of fetuses with CHD had blood flow abnormalities in the middle cerebral artery at some point in the late second or third trimester, suggesting that the blood vessels had dilated to allow more cerebral perfusion. This phenomenon, termed “brain sparing,” is believed to be an autoregulatory mechanism that occurs as a result of diminished oxygen delivery or inadequate blood flow to the brain (Pediatr Cardiol. 2003 Jan;24[5]:436-43).
Subsequent studies have similarly documented abnormal cerebral blood flow in fetuses with various types of congenital heart lesions. What is left to be determined is whether this autoregulatory mechanism is adequate to maintain perfusion in the presence of specific, high-risk CHD.
Abnormalities were more often seen in CHD with obstructed aortic flow, such as hypoplastic left heart syndrome (HLHS) in which the aorta is perfused retrograde through the fetal ductus arteriosus (Circulation. 2010 Jan 4;121:26-33).
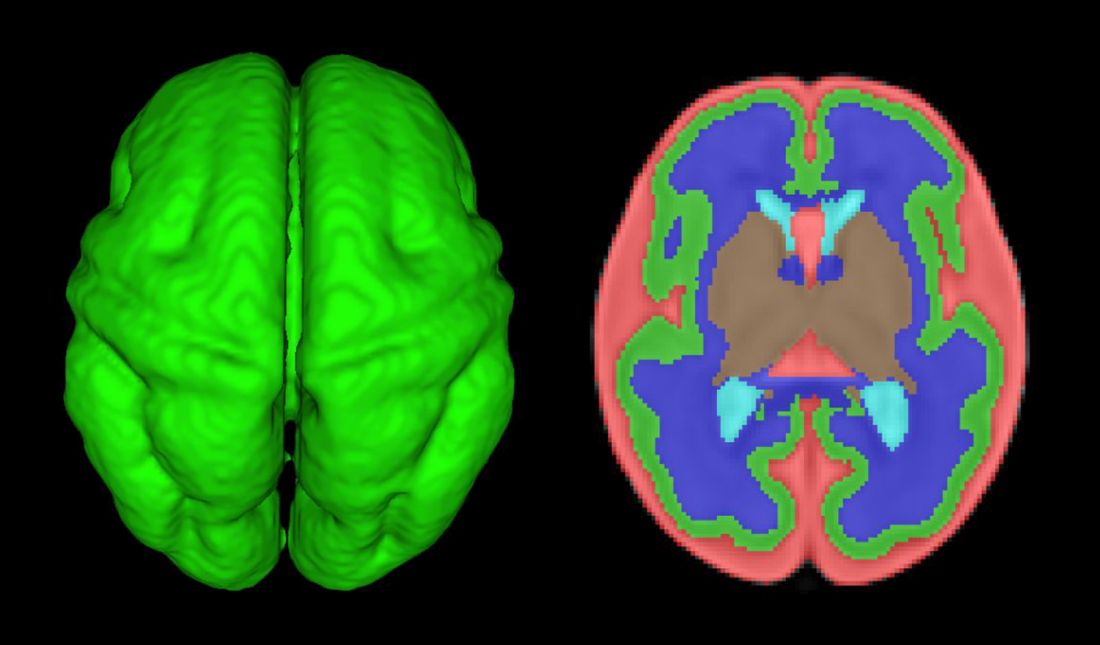
Other fetal imaging studies have similarly demonstrated a progressive third-trimester decrease in both cortical gray and white matter and in gyrification (cortical folding) (Cereb Cortex. 2013;23:2932-43), as well as decreased cerebral oxygen delivery and consumption (Circulation. 2015;131:1313-23) in fetuses with severe CHD. It appears that the brain may start out normal in size, but in the third trimester, the accelerated metabolic demands that come with rapid growth and development are not sufficiently met by the fetal cardiovascular circulation in CHD.
In the newborn with CHD, preoperative brain imaging studies have demonstrated structural abnormalities suggesting delayed development (for example, microcephaly and a widened operculum), microstructural abnormalities suggesting abnormal myelination and neuroaxonal development, and lower brain maturity scores (a composite score that combines multiple factors, such as myelination and cortical in-folding, to represent “brain age”).
Moreover, some of the newborn brain imaging studies have correlated brain MRI findings with neonatal neurodevelopmental assessments. For instance, investigators found that full-term newborns with CHD had decreased gray matter brain volume and increased cerebrospinal fluid volume and that these impairments were associated with poor behavioral state regulation and poor visual orienting (J Pediatr. 2014;164:1121-7).
Interestingly, it has been found that the full-term baby with specific complex CHD, including newborns with single ventricle CHD or transposition of the great arteries, is more likely to have a brain maturity score that is equivalent to that of a baby born at 35 weeks’ gestation. This means that, in some infants with CHD, the brain has lagged in growth by about a month, resulting in a pattern of disturbed development and subsequent injury that is similar to that of premature infants.
It also means that infants with CHD and an immature brain are especially vulnerable to brain injury when open-heart surgery is needed. In short, we now appreciate that the brain in patients with CHD is likely more fragile than we previously thought – and that this fragility is prenatal in its origins.
Delivery room planning
Ideally, our goal is to find ways of changing the circulation in utero to improve cerebral oxygenation and blood flow, and, consequently, improve brain development and long-term neurocognitive function. Despite significant efforts in this area, we’re not there yet.
Examples of strategies that are being tested include catheter intervention to open the aortic valve in utero for fetuses with critical aortic stenosis. This procedure currently is being performed to try to prevent progression of the valve abnormality to HLHS, but it has not been determined whether the intervention affects cerebral blood flow. Maternal oxygen therapy has been shown to change cerebral blood flow in the short term for fetuses with HLHS, but its long-term use has not been studied. At the time of birth, to prevent injury in the potentially more fragile brain of the newborn with CHD, what we can do is to identify those fetuses who are more likely to be at risk for hypoxia low cardiac output and hemodynamic compromise in the delivery room, and plan for specialized delivery room and perinatal management beyond standard neonatal care.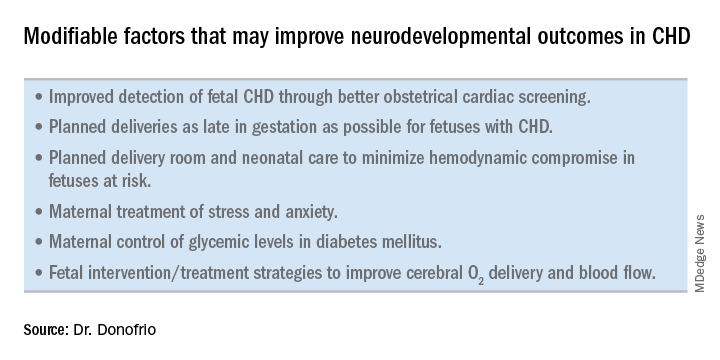
Most newborns with CHD are assigned to Level 1; they have no predicted risk of compromise in the delivery room – or even in the first couple weeks of life – and can deliver at a local hospital with neonatal evaluation and then consult with the pediatric cardiologist. Defects include shunt lesions such as septal defects or mild valve abnormalities.
Patients assigned to Level 2 have minimal risk of compromise in the delivery room but are expected to require postnatal surgery, cardiac catheterization, or another procedure before going home. They can be stabilized by the neonatologist, usually with initiation of a prostaglandin infusion, before transfer to the cardiac center for the planned intervention. Defects include single ventricle CHD and severe Tetralogy of Fallot.
Fetuses assigned to Level 3 and Level 4 are expected to have hemodynamic instability at cord clamping, requiring immediate specialty care in the delivery room that is likely to include urgent cardiac catheterization or surgical intervention. These defects are rare and include diagnoses such as transposition of the great arteries, HLHS with a restrictive or closed foramen ovale, and CHD with associated heart failure and hydrops.
We have found that fetal echocardiography accurately predicts postnatal risk and the need for specialized delivery room care in newborns diagnosed in utero with CHD and that level-of-care protocols ensure safe delivery and optimize fetal outcomes (J Am Soc Echocardiogr. 2015;28:1339-49; Am J Cardiol. 2013;111:737-47).
Such delivery planning, which is coordinated between obstetric, neonatal, cardiology, and surgical services with specialty teams as needed (for example, cardiac intensive care, interventional cardiology, and cardiac surgery), is recommended in a 2014 AHA statement on the diagnosis and treatment of fetal cardiac disease. In recent years it has become the standard of care in many health systems (Circulation. 2014;129[21]:2183-242).
The effect of maternal stress on the in utero environment is also getting increased attention in pediatric cardiology. Alterations in neurocognitive development and fetal and child cardiovascular health are likely to be associated with maternal stress during pregnancy, and studies have shown that maternal stress is high with prenatal diagnoses of CHD. We have to ask: Is stress a modifiable risk factor? There must be ways in which we can do better with prenatal counseling and support after a fetal diagnosis of CHD.
Screening for CHD
Initiating strategies to improve neurodevelopmental outcomes in infants with CHD rests partly on identifying babies with CHD before birth through improved fetal cardiac screening. Research cited in the 2014 AHA statement indicates that nearly all women giving birth to babies with CHD in the United States have obstetric ultrasound examinations in the second or third trimesters, but that only about 30% of the fetuses are diagnosed prenatally.
Current indications for referral for a fetal echocardiogram – in addition to suspicion of a structural heart abnormality on obstetric ultrasound – include maternal factors, such as diabetes mellitus, that raise the risk of CHD above the baseline population risk for low-risk pregnancies.
Women with pregestational diabetes mellitus have a nearly fivefold increase in CHD, compared with the general population (3%-5%), and should be referred for fetal echocardiography. Women with gestational diabetes mellitus have no or minimally increased risk for fetal CHD, but it has been shown that there is an increased risk for cardiac hypertrophy – particularly late in gestation – if glycemic levels are poorly controlled. The 2014 AHA guidelines recommend that fetal echocardiographic evaluation be considered in those who have HbA1c levels greater than 6% in the second half of pregnancy.
Dr. Mary T. Donofrio is a pediatric cardiologist and director of the fetal heart program and critical care delivery program at Children’s National Medical Center, Washington. She reported that she has no disclosures relevant to this article.
Congenital heart disease (CHD) is the most common congenital anomaly, with an estimated incidence of 6-12 per 1,000 live births. It is also the congenital anomaly that most often leads to death or significant morbidity. Advances in surgical procedures and operating room care as well as specialized care in the ICU have led to significant improvements in survival over the past 10-20 years – even for the most complex cases of CHD. We now expect the majority of newborns with CHD not only to survive, but to grow up into adulthood.
The focus of clinical research has thus transitioned from survival to issues of long-term morbidity and outcomes, and the more recent literature has clearly shown us that children with CHD are at high risk of learning disabilities and other neurodevelopmental abnormalities. The prevalence of impairment rises with the complexity of CHD, from a prevalence of approximately 20% in mild CHD to as much as 75% in severe CHD. Almost all neonates and infants who undergo palliative surgical procedures have neurodevelopmental impairments.
The neurobehavioral “signature” of CHD includes cognitive defects (usually mild), short attention span, fine and gross motor delays, speech and language delays, visual motor integration, and executive function deficits. Executive function deficits and attention deficits are among the problems that often do not present in children until they reach middle school and beyond, when they are expected to learn more complicated material and handle more complex tasks. Long-term surveillance and care have thus become a major focus at our institution and others throughout the country.
At the same time, evidence has increased in the past 5-10 years that adverse neurodevelopmental outcomes in children with complex CHD may stem from genetic factors as well as compromise to the brain in utero because of altered blood flow, compromise at the time of delivery, and insults during and after corrective or palliative surgery. Surgical strategies and operating room teams have become significantly better at protecting the brain, and new research now is directed toward understanding the neurologic abnormalities that are present in newborns prior to surgical intervention.
Increasingly, researchers are now focused on looking at the in utero origins of brain impairments in children with CHD and trying to understand specific prenatal causes, mechanisms, and potentially modifiable factors. We’re asking what we can do during pregnancy to improve neurodevelopmental outcomes.
Impaired brain growth
The question of how CHD affects blood flow to the fetal brain is an important one. We found some time ago in a study using Doppler ultrasound that 44% of fetuses with CHD had blood flow abnormalities in the middle cerebral artery at some point in the late second or third trimester, suggesting that the blood vessels had dilated to allow more cerebral perfusion. This phenomenon, termed “brain sparing,” is believed to be an autoregulatory mechanism that occurs as a result of diminished oxygen delivery or inadequate blood flow to the brain (Pediatr Cardiol. 2003 Jan;24[5]:436-43).
Subsequent studies have similarly documented abnormal cerebral blood flow in fetuses with various types of congenital heart lesions. What is left to be determined is whether this autoregulatory mechanism is adequate to maintain perfusion in the presence of specific, high-risk CHD.
Abnormalities were more often seen in CHD with obstructed aortic flow, such as hypoplastic left heart syndrome (HLHS) in which the aorta is perfused retrograde through the fetal ductus arteriosus (Circulation. 2010 Jan 4;121:26-33).
Other fetal imaging studies have similarly demonstrated a progressive third-trimester decrease in both cortical gray and white matter and in gyrification (cortical folding) (Cereb Cortex. 2013;23:2932-43), as well as decreased cerebral oxygen delivery and consumption (Circulation. 2015;131:1313-23) in fetuses with severe CHD. It appears that the brain may start out normal in size, but in the third trimester, the accelerated metabolic demands that come with rapid growth and development are not sufficiently met by the fetal cardiovascular circulation in CHD.
In the newborn with CHD, preoperative brain imaging studies have demonstrated structural abnormalities suggesting delayed development (for example, microcephaly and a widened operculum), microstructural abnormalities suggesting abnormal myelination and neuroaxonal development, and lower brain maturity scores (a composite score that combines multiple factors, such as myelination and cortical in-folding, to represent “brain age”).
Moreover, some of the newborn brain imaging studies have correlated brain MRI findings with neonatal neurodevelopmental assessments. For instance, investigators found that full-term newborns with CHD had decreased gray matter brain volume and increased cerebrospinal fluid volume and that these impairments were associated with poor behavioral state regulation and poor visual orienting (J Pediatr. 2014;164:1121-7).
Interestingly, it has been found that the full-term baby with specific complex CHD, including newborns with single ventricle CHD or transposition of the great arteries, is more likely to have a brain maturity score that is equivalent to that of a baby born at 35 weeks’ gestation. This means that, in some infants with CHD, the brain has lagged in growth by about a month, resulting in a pattern of disturbed development and subsequent injury that is similar to that of premature infants.
It also means that infants with CHD and an immature brain are especially vulnerable to brain injury when open-heart surgery is needed. In short, we now appreciate that the brain in patients with CHD is likely more fragile than we previously thought – and that this fragility is prenatal in its origins.
Delivery room planning
Ideally, our goal is to find ways of changing the circulation in utero to improve cerebral oxygenation and blood flow, and, consequently, improve brain development and long-term neurocognitive function. Despite significant efforts in this area, we’re not there yet.
Examples of strategies that are being tested include catheter intervention to open the aortic valve in utero for fetuses with critical aortic stenosis. This procedure currently is being performed to try to prevent progression of the valve abnormality to HLHS, but it has not been determined whether the intervention affects cerebral blood flow. Maternal oxygen therapy has been shown to change cerebral blood flow in the short term for fetuses with HLHS, but its long-term use has not been studied. At the time of birth, to prevent injury in the potentially more fragile brain of the newborn with CHD, what we can do is to identify those fetuses who are more likely to be at risk for hypoxia low cardiac output and hemodynamic compromise in the delivery room, and plan for specialized delivery room and perinatal management beyond standard neonatal care.
Most newborns with CHD are assigned to Level 1; they have no predicted risk of compromise in the delivery room – or even in the first couple weeks of life – and can deliver at a local hospital with neonatal evaluation and then consult with the pediatric cardiologist. Defects include shunt lesions such as septal defects or mild valve abnormalities.
Patients assigned to Level 2 have minimal risk of compromise in the delivery room but are expected to require postnatal surgery, cardiac catheterization, or another procedure before going home. They can be stabilized by the neonatologist, usually with initiation of a prostaglandin infusion, before transfer to the cardiac center for the planned intervention. Defects include single ventricle CHD and severe Tetralogy of Fallot.
Fetuses assigned to Level 3 and Level 4 are expected to have hemodynamic instability at cord clamping, requiring immediate specialty care in the delivery room that is likely to include urgent cardiac catheterization or surgical intervention. These defects are rare and include diagnoses such as transposition of the great arteries, HLHS with a restrictive or closed foramen ovale, and CHD with associated heart failure and hydrops.
We have found that fetal echocardiography accurately predicts postnatal risk and the need for specialized delivery room care in newborns diagnosed in utero with CHD and that level-of-care protocols ensure safe delivery and optimize fetal outcomes (J Am Soc Echocardiogr. 2015;28:1339-49; Am J Cardiol. 2013;111:737-47).
Such delivery planning, which is coordinated between obstetric, neonatal, cardiology, and surgical services with specialty teams as needed (for example, cardiac intensive care, interventional cardiology, and cardiac surgery), is recommended in a 2014 AHA statement on the diagnosis and treatment of fetal cardiac disease. In recent years it has become the standard of care in many health systems (Circulation. 2014;129[21]:2183-242).
The effect of maternal stress on the in utero environment is also getting increased attention in pediatric cardiology. Alterations in neurocognitive development and fetal and child cardiovascular health are likely to be associated with maternal stress during pregnancy, and studies have shown that maternal stress is high with prenatal diagnoses of CHD. We have to ask: Is stress a modifiable risk factor? There must be ways in which we can do better with prenatal counseling and support after a fetal diagnosis of CHD.
Screening for CHD
Initiating strategies to improve neurodevelopmental outcomes in infants with CHD rests partly on identifying babies with CHD before birth through improved fetal cardiac screening. Research cited in the 2014 AHA statement indicates that nearly all women giving birth to babies with CHD in the United States have obstetric ultrasound examinations in the second or third trimesters, but that only about 30% of the fetuses are diagnosed prenatally.
Current indications for referral for a fetal echocardiogram – in addition to suspicion of a structural heart abnormality on obstetric ultrasound – include maternal factors, such as diabetes mellitus, that raise the risk of CHD above the baseline population risk for low-risk pregnancies.
Women with pregestational diabetes mellitus have a nearly fivefold increase in CHD, compared with the general population (3%-5%), and should be referred for fetal echocardiography. Women with gestational diabetes mellitus have no or minimally increased risk for fetal CHD, but it has been shown that there is an increased risk for cardiac hypertrophy – particularly late in gestation – if glycemic levels are poorly controlled. The 2014 AHA guidelines recommend that fetal echocardiographic evaluation be considered in those who have HbA1c levels greater than 6% in the second half of pregnancy.
Dr. Mary T. Donofrio is a pediatric cardiologist and director of the fetal heart program and critical care delivery program at Children’s National Medical Center, Washington. She reported that she has no disclosures relevant to this article.
Congenital heart disease (CHD) is the most common congenital anomaly, with an estimated incidence of 6-12 per 1,000 live births. It is also the congenital anomaly that most often leads to death or significant morbidity. Advances in surgical procedures and operating room care as well as specialized care in the ICU have led to significant improvements in survival over the past 10-20 years – even for the most complex cases of CHD. We now expect the majority of newborns with CHD not only to survive, but to grow up into adulthood.
The focus of clinical research has thus transitioned from survival to issues of long-term morbidity and outcomes, and the more recent literature has clearly shown us that children with CHD are at high risk of learning disabilities and other neurodevelopmental abnormalities. The prevalence of impairment rises with the complexity of CHD, from a prevalence of approximately 20% in mild CHD to as much as 75% in severe CHD. Almost all neonates and infants who undergo palliative surgical procedures have neurodevelopmental impairments.
The neurobehavioral “signature” of CHD includes cognitive defects (usually mild), short attention span, fine and gross motor delays, speech and language delays, visual motor integration, and executive function deficits. Executive function deficits and attention deficits are among the problems that often do not present in children until they reach middle school and beyond, when they are expected to learn more complicated material and handle more complex tasks. Long-term surveillance and care have thus become a major focus at our institution and others throughout the country.
At the same time, evidence has increased in the past 5-10 years that adverse neurodevelopmental outcomes in children with complex CHD may stem from genetic factors as well as compromise to the brain in utero because of altered blood flow, compromise at the time of delivery, and insults during and after corrective or palliative surgery. Surgical strategies and operating room teams have become significantly better at protecting the brain, and new research now is directed toward understanding the neurologic abnormalities that are present in newborns prior to surgical intervention.
Increasingly, researchers are now focused on looking at the in utero origins of brain impairments in children with CHD and trying to understand specific prenatal causes, mechanisms, and potentially modifiable factors. We’re asking what we can do during pregnancy to improve neurodevelopmental outcomes.
Impaired brain growth
The question of how CHD affects blood flow to the fetal brain is an important one. We found some time ago in a study using Doppler ultrasound that 44% of fetuses with CHD had blood flow abnormalities in the middle cerebral artery at some point in the late second or third trimester, suggesting that the blood vessels had dilated to allow more cerebral perfusion. This phenomenon, termed “brain sparing,” is believed to be an autoregulatory mechanism that occurs as a result of diminished oxygen delivery or inadequate blood flow to the brain (Pediatr Cardiol. 2003 Jan;24[5]:436-43).
Subsequent studies have similarly documented abnormal cerebral blood flow in fetuses with various types of congenital heart lesions. What is left to be determined is whether this autoregulatory mechanism is adequate to maintain perfusion in the presence of specific, high-risk CHD.
Abnormalities were more often seen in CHD with obstructed aortic flow, such as hypoplastic left heart syndrome (HLHS) in which the aorta is perfused retrograde through the fetal ductus arteriosus (Circulation. 2010 Jan 4;121:26-33).
Other fetal imaging studies have similarly demonstrated a progressive third-trimester decrease in both cortical gray and white matter and in gyrification (cortical folding) (Cereb Cortex. 2013;23:2932-43), as well as decreased cerebral oxygen delivery and consumption (Circulation. 2015;131:1313-23) in fetuses with severe CHD. It appears that the brain may start out normal in size, but in the third trimester, the accelerated metabolic demands that come with rapid growth and development are not sufficiently met by the fetal cardiovascular circulation in CHD.
In the newborn with CHD, preoperative brain imaging studies have demonstrated structural abnormalities suggesting delayed development (for example, microcephaly and a widened operculum), microstructural abnormalities suggesting abnormal myelination and neuroaxonal development, and lower brain maturity scores (a composite score that combines multiple factors, such as myelination and cortical in-folding, to represent “brain age”).
Moreover, some of the newborn brain imaging studies have correlated brain MRI findings with neonatal neurodevelopmental assessments. For instance, investigators found that full-term newborns with CHD had decreased gray matter brain volume and increased cerebrospinal fluid volume and that these impairments were associated with poor behavioral state regulation and poor visual orienting (J Pediatr. 2014;164:1121-7).
Interestingly, it has been found that the full-term baby with specific complex CHD, including newborns with single ventricle CHD or transposition of the great arteries, is more likely to have a brain maturity score that is equivalent to that of a baby born at 35 weeks’ gestation. This means that, in some infants with CHD, the brain has lagged in growth by about a month, resulting in a pattern of disturbed development and subsequent injury that is similar to that of premature infants.
It also means that infants with CHD and an immature brain are especially vulnerable to brain injury when open-heart surgery is needed. In short, we now appreciate that the brain in patients with CHD is likely more fragile than we previously thought – and that this fragility is prenatal in its origins.
Delivery room planning
Ideally, our goal is to find ways of changing the circulation in utero to improve cerebral oxygenation and blood flow, and, consequently, improve brain development and long-term neurocognitive function. Despite significant efforts in this area, we’re not there yet.
Examples of strategies that are being tested include catheter intervention to open the aortic valve in utero for fetuses with critical aortic stenosis. This procedure currently is being performed to try to prevent progression of the valve abnormality to HLHS, but it has not been determined whether the intervention affects cerebral blood flow. Maternal oxygen therapy has been shown to change cerebral blood flow in the short term for fetuses with HLHS, but its long-term use has not been studied. At the time of birth, to prevent injury in the potentially more fragile brain of the newborn with CHD, what we can do is to identify those fetuses who are more likely to be at risk for hypoxia low cardiac output and hemodynamic compromise in the delivery room, and plan for specialized delivery room and perinatal management beyond standard neonatal care.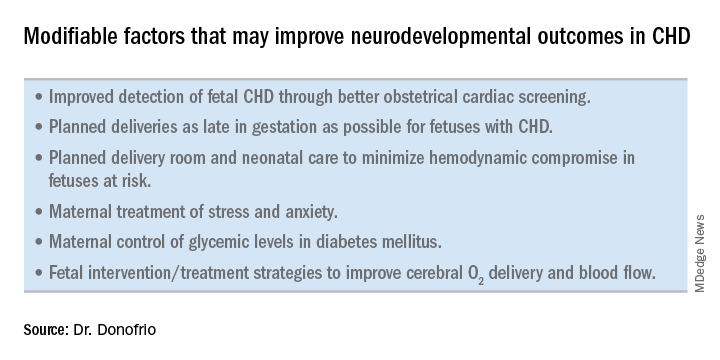
Most newborns with CHD are assigned to Level 1; they have no predicted risk of compromise in the delivery room – or even in the first couple weeks of life – and can deliver at a local hospital with neonatal evaluation and then consult with the pediatric cardiologist. Defects include shunt lesions such as septal defects or mild valve abnormalities.
Patients assigned to Level 2 have minimal risk of compromise in the delivery room but are expected to require postnatal surgery, cardiac catheterization, or another procedure before going home. They can be stabilized by the neonatologist, usually with initiation of a prostaglandin infusion, before transfer to the cardiac center for the planned intervention. Defects include single ventricle CHD and severe Tetralogy of Fallot.
Fetuses assigned to Level 3 and Level 4 are expected to have hemodynamic instability at cord clamping, requiring immediate specialty care in the delivery room that is likely to include urgent cardiac catheterization or surgical intervention. These defects are rare and include diagnoses such as transposition of the great arteries, HLHS with a restrictive or closed foramen ovale, and CHD with associated heart failure and hydrops.
We have found that fetal echocardiography accurately predicts postnatal risk and the need for specialized delivery room care in newborns diagnosed in utero with CHD and that level-of-care protocols ensure safe delivery and optimize fetal outcomes (J Am Soc Echocardiogr. 2015;28:1339-49; Am J Cardiol. 2013;111:737-47).
Such delivery planning, which is coordinated between obstetric, neonatal, cardiology, and surgical services with specialty teams as needed (for example, cardiac intensive care, interventional cardiology, and cardiac surgery), is recommended in a 2014 AHA statement on the diagnosis and treatment of fetal cardiac disease. In recent years it has become the standard of care in many health systems (Circulation. 2014;129[21]:2183-242).
The effect of maternal stress on the in utero environment is also getting increased attention in pediatric cardiology. Alterations in neurocognitive development and fetal and child cardiovascular health are likely to be associated with maternal stress during pregnancy, and studies have shown that maternal stress is high with prenatal diagnoses of CHD. We have to ask: Is stress a modifiable risk factor? There must be ways in which we can do better with prenatal counseling and support after a fetal diagnosis of CHD.
Screening for CHD
Initiating strategies to improve neurodevelopmental outcomes in infants with CHD rests partly on identifying babies with CHD before birth through improved fetal cardiac screening. Research cited in the 2014 AHA statement indicates that nearly all women giving birth to babies with CHD in the United States have obstetric ultrasound examinations in the second or third trimesters, but that only about 30% of the fetuses are diagnosed prenatally.
Current indications for referral for a fetal echocardiogram – in addition to suspicion of a structural heart abnormality on obstetric ultrasound – include maternal factors, such as diabetes mellitus, that raise the risk of CHD above the baseline population risk for low-risk pregnancies.
Women with pregestational diabetes mellitus have a nearly fivefold increase in CHD, compared with the general population (3%-5%), and should be referred for fetal echocardiography. Women with gestational diabetes mellitus have no or minimally increased risk for fetal CHD, but it has been shown that there is an increased risk for cardiac hypertrophy – particularly late in gestation – if glycemic levels are poorly controlled. The 2014 AHA guidelines recommend that fetal echocardiographic evaluation be considered in those who have HbA1c levels greater than 6% in the second half of pregnancy.
Dr. Mary T. Donofrio is a pediatric cardiologist and director of the fetal heart program and critical care delivery program at Children’s National Medical Center, Washington. She reported that she has no disclosures relevant to this article.
Is the suicide story fake – or just misleading?
Recently, a lot has been in the news about the increasing rates of suicide in all communities, including among African American youth, and two high-profile celebrities. Now that we have a CEO in the White House who has made the phrase “fake news” part of the national lexicon (and as a former CEO myself), I feel compelled to take a critical, clinical look at the way the suicide story has been reported.
CEOs tend to be unique people, and many of them are fond of hyperbole – as it promotes “followship” in employees and fosters business deals. I interpret fake news as the kind of information, or maybe spin is a better word, promulgated by CEOs.
While following a research letter published recently in JAMA Pediatrics – “Age-Related Racial Disparity in Suicide Rates Among U.S. Youths From 2001 Through 2015” (2018 May 21. doi: 10.001/jamapediatrics.2018.0399) – it occurred to me that this struck me as fake news. But as I thought about it, I realized that the conclusions in the research letter would be better characterized as perhaps misleading news. My basis for reaching those conclusions is rooted in the lessons I learned as a 2-year member of the Institute of Medicine’s Board on Neuroscience and Behavioral Health, Committee on Pathophysiology & Prevention of Adolescent & Adult Suicide. In fact, the report we produced was the first one referenced in the research letter. Unfortunately, however, the research letter’s authors seemed to miss the IOM report’s major take-away messages.
For example, the research letter authors compared the suicide rates among black children and white children in this way: “However, suicide rates increased from 1993 to 1997 and 2008 to 2012 among black children aged 5 to 11 years (from 1.36 to 2.54 per million) and decreased among white children of the same age (from 1.14 to 0.77 per million).” That sentence supports the conclusions of the IOM’s “Reducing Suicide” report, as it confirms that those are very low base rates. However, because the base rates are so low in most populations, it is difficult to determine scientifically whether a significant rise or decrease in rates occurred.
To quote page 377 of IOM report: “The base rate of completed suicide is sufficiently low to preclude all but the largest of studies. When such studies are performed, resultant comparisons are between extremely small and large groups of individuals (suicide completers versus non–suicide completers, or suicide attempters versus non–suicide attempters). Use of suicidal ideation as an outcome can increase incidence and alleviate the problem to some extent; however, it is unclear whether suicidal ideation is a strong predictor of suicide completion. Using both attempts and completions can confound the analysis since attempters may account for some of the suicides completed within the study period. Because the duration of the prevention studies is frequently too brief to collect sufficient data on the low frequency endpoints of suicide or suicide attempt, proximal measures such as changes in knowledge or attitude are used. Yet the predictive value of these variables is unconfirmed.”
Further, according to page 410 of the report: “As the statistical analysis above points out, at a suicide rate of 10 per 100,000 population, approximately 100,000 participants are needed to achieve statistical significance in an experimental context. In studying suicide among low-risk groups, the numbers needed are even greater.”
Let me break this down a bit. , because the numerator is so small and the dominator is so large. Let me put it this way – if the black female suicide rates are 2/100,000, and those rates quadrupled (sounds impressive, doesn’t it?) then there would be 8/100,000 black female suicides; the difference between 2 and 8 per 100,000 is not really a significant difference because the base-rates are so small. But to say the rates quadrupled sounds scary and impressive. “Figures don’t lie, but liars can figure.”
So, the premise of the research letter is whack.
I am not impressed that the rates of black children aged 5-7 increased from 1.36/1,000,000 to 2.54/1,000,000. I am not even sure those two numbers are significantly different, much less have clinical relevance. I have tried to make this point before, but it always gets lost by the hyperbolic press – which continues to yell about suicides in the United States rising by 30% or doubling, even quadrupling. The low base rates make drawing firm conclusions from this data like spitting into the ocean. I understand that one suicide is one suicide too many. But this is not science.
The characterizations about soaring U.S. suicide rates are not exactly fake news. Instead, I would call these interpretations misleading science and news.
Dr. Bell is staff psychiatrist at Jackson Park Hospital’s surgical-medical/psychiatric inpatient unit; clinical professor emeritus, department of psychiatry, University of Illinois at Chicago; former director of the Institute for Juvenile Research (the birthplace of child psychiatry), and former president/CEO of the Community Mental Health Council, all in Chicago. He also serves as chair of psychiatry at Windsor University, St. Kitts.
Recently, a lot has been in the news about the increasing rates of suicide in all communities, including among African American youth, and two high-profile celebrities. Now that we have a CEO in the White House who has made the phrase “fake news” part of the national lexicon (and as a former CEO myself), I feel compelled to take a critical, clinical look at the way the suicide story has been reported.
CEOs tend to be unique people, and many of them are fond of hyperbole – as it promotes “followship” in employees and fosters business deals. I interpret fake news as the kind of information, or maybe spin is a better word, promulgated by CEOs.
While following a research letter published recently in JAMA Pediatrics – “Age-Related Racial Disparity in Suicide Rates Among U.S. Youths From 2001 Through 2015” (2018 May 21. doi: 10.001/jamapediatrics.2018.0399) – it occurred to me that this struck me as fake news. But as I thought about it, I realized that the conclusions in the research letter would be better characterized as perhaps misleading news. My basis for reaching those conclusions is rooted in the lessons I learned as a 2-year member of the Institute of Medicine’s Board on Neuroscience and Behavioral Health, Committee on Pathophysiology & Prevention of Adolescent & Adult Suicide. In fact, the report we produced was the first one referenced in the research letter. Unfortunately, however, the research letter’s authors seemed to miss the IOM report’s major take-away messages.
For example, the research letter authors compared the suicide rates among black children and white children in this way: “However, suicide rates increased from 1993 to 1997 and 2008 to 2012 among black children aged 5 to 11 years (from 1.36 to 2.54 per million) and decreased among white children of the same age (from 1.14 to 0.77 per million).” That sentence supports the conclusions of the IOM’s “Reducing Suicide” report, as it confirms that those are very low base rates. However, because the base rates are so low in most populations, it is difficult to determine scientifically whether a significant rise or decrease in rates occurred.
To quote page 377 of IOM report: “The base rate of completed suicide is sufficiently low to preclude all but the largest of studies. When such studies are performed, resultant comparisons are between extremely small and large groups of individuals (suicide completers versus non–suicide completers, or suicide attempters versus non–suicide attempters). Use of suicidal ideation as an outcome can increase incidence and alleviate the problem to some extent; however, it is unclear whether suicidal ideation is a strong predictor of suicide completion. Using both attempts and completions can confound the analysis since attempters may account for some of the suicides completed within the study period. Because the duration of the prevention studies is frequently too brief to collect sufficient data on the low frequency endpoints of suicide or suicide attempt, proximal measures such as changes in knowledge or attitude are used. Yet the predictive value of these variables is unconfirmed.”
Further, according to page 410 of the report: “As the statistical analysis above points out, at a suicide rate of 10 per 100,000 population, approximately 100,000 participants are needed to achieve statistical significance in an experimental context. In studying suicide among low-risk groups, the numbers needed are even greater.”
Let me break this down a bit. , because the numerator is so small and the dominator is so large. Let me put it this way – if the black female suicide rates are 2/100,000, and those rates quadrupled (sounds impressive, doesn’t it?) then there would be 8/100,000 black female suicides; the difference between 2 and 8 per 100,000 is not really a significant difference because the base-rates are so small. But to say the rates quadrupled sounds scary and impressive. “Figures don’t lie, but liars can figure.”
So, the premise of the research letter is whack.
I am not impressed that the rates of black children aged 5-7 increased from 1.36/1,000,000 to 2.54/1,000,000. I am not even sure those two numbers are significantly different, much less have clinical relevance. I have tried to make this point before, but it always gets lost by the hyperbolic press – which continues to yell about suicides in the United States rising by 30% or doubling, even quadrupling. The low base rates make drawing firm conclusions from this data like spitting into the ocean. I understand that one suicide is one suicide too many. But this is not science.
The characterizations about soaring U.S. suicide rates are not exactly fake news. Instead, I would call these interpretations misleading science and news.
Dr. Bell is staff psychiatrist at Jackson Park Hospital’s surgical-medical/psychiatric inpatient unit; clinical professor emeritus, department of psychiatry, University of Illinois at Chicago; former director of the Institute for Juvenile Research (the birthplace of child psychiatry), and former president/CEO of the Community Mental Health Council, all in Chicago. He also serves as chair of psychiatry at Windsor University, St. Kitts.
Recently, a lot has been in the news about the increasing rates of suicide in all communities, including among African American youth, and two high-profile celebrities. Now that we have a CEO in the White House who has made the phrase “fake news” part of the national lexicon (and as a former CEO myself), I feel compelled to take a critical, clinical look at the way the suicide story has been reported.
CEOs tend to be unique people, and many of them are fond of hyperbole – as it promotes “followship” in employees and fosters business deals. I interpret fake news as the kind of information, or maybe spin is a better word, promulgated by CEOs.
While following a research letter published recently in JAMA Pediatrics – “Age-Related Racial Disparity in Suicide Rates Among U.S. Youths From 2001 Through 2015” (2018 May 21. doi: 10.001/jamapediatrics.2018.0399) – it occurred to me that this struck me as fake news. But as I thought about it, I realized that the conclusions in the research letter would be better characterized as perhaps misleading news. My basis for reaching those conclusions is rooted in the lessons I learned as a 2-year member of the Institute of Medicine’s Board on Neuroscience and Behavioral Health, Committee on Pathophysiology & Prevention of Adolescent & Adult Suicide. In fact, the report we produced was the first one referenced in the research letter. Unfortunately, however, the research letter’s authors seemed to miss the IOM report’s major take-away messages.
For example, the research letter authors compared the suicide rates among black children and white children in this way: “However, suicide rates increased from 1993 to 1997 and 2008 to 2012 among black children aged 5 to 11 years (from 1.36 to 2.54 per million) and decreased among white children of the same age (from 1.14 to 0.77 per million).” That sentence supports the conclusions of the IOM’s “Reducing Suicide” report, as it confirms that those are very low base rates. However, because the base rates are so low in most populations, it is difficult to determine scientifically whether a significant rise or decrease in rates occurred.
To quote page 377 of IOM report: “The base rate of completed suicide is sufficiently low to preclude all but the largest of studies. When such studies are performed, resultant comparisons are between extremely small and large groups of individuals (suicide completers versus non–suicide completers, or suicide attempters versus non–suicide attempters). Use of suicidal ideation as an outcome can increase incidence and alleviate the problem to some extent; however, it is unclear whether suicidal ideation is a strong predictor of suicide completion. Using both attempts and completions can confound the analysis since attempters may account for some of the suicides completed within the study period. Because the duration of the prevention studies is frequently too brief to collect sufficient data on the low frequency endpoints of suicide or suicide attempt, proximal measures such as changes in knowledge or attitude are used. Yet the predictive value of these variables is unconfirmed.”
Further, according to page 410 of the report: “As the statistical analysis above points out, at a suicide rate of 10 per 100,000 population, approximately 100,000 participants are needed to achieve statistical significance in an experimental context. In studying suicide among low-risk groups, the numbers needed are even greater.”
Let me break this down a bit. , because the numerator is so small and the dominator is so large. Let me put it this way – if the black female suicide rates are 2/100,000, and those rates quadrupled (sounds impressive, doesn’t it?) then there would be 8/100,000 black female suicides; the difference between 2 and 8 per 100,000 is not really a significant difference because the base-rates are so small. But to say the rates quadrupled sounds scary and impressive. “Figures don’t lie, but liars can figure.”
So, the premise of the research letter is whack.
I am not impressed that the rates of black children aged 5-7 increased from 1.36/1,000,000 to 2.54/1,000,000. I am not even sure those two numbers are significantly different, much less have clinical relevance. I have tried to make this point before, but it always gets lost by the hyperbolic press – which continues to yell about suicides in the United States rising by 30% or doubling, even quadrupling. The low base rates make drawing firm conclusions from this data like spitting into the ocean. I understand that one suicide is one suicide too many. But this is not science.
The characterizations about soaring U.S. suicide rates are not exactly fake news. Instead, I would call these interpretations misleading science and news.
Dr. Bell is staff psychiatrist at Jackson Park Hospital’s surgical-medical/psychiatric inpatient unit; clinical professor emeritus, department of psychiatry, University of Illinois at Chicago; former director of the Institute for Juvenile Research (the birthplace of child psychiatry), and former president/CEO of the Community Mental Health Council, all in Chicago. He also serves as chair of psychiatry at Windsor University, St. Kitts.
Stop extending credit
For as long as I have been writing this column, I have stressed that ; and yet, all these years later, AR is still the subject that generates the most questions.
Okay; let’s go over it one more time: Basically, physicians extend more credit than any business except banks. Despite what you may have read recently, banks are good at it, and they charge interest (and a myriad of fees) to do it. Doctors do it for free. Are we crazy? No business owner in his or her right mind allows customers to take away goods or services without paying for them; but doctors do it every day.
What to do? Common sense tells you to collect everything you can at the time of service; but some patients inevitably brandish the old “I forgot my checkbook” excuse and escape without paying. And the patient-owed portion of most insurance charges is often unknown, and unknowable, at the time of service.
That means you’ll need to send a bill; and every bill you send (or hire somebody to send) costs you a bundle. And when it arrives, it goes right to the bottom of your patient’s payment priority list. That is, each month your patients will pay their electric, water, gas, and telephone bills … and just about any other bill ... before getting around to yours. If there is no more money when your bill finally surfaces, that’s just too bad. The electric company can shut off their power; what can you do?
What we do is what every hotel, rental car agency, and many other businesses have done for years: We ask for a credit card number, keep it on file, and bill balances to it as they come in. Plastic runs the show everywhere you go – except in most medical offices.
New patients in my office receive a letter at their first visit explaining our policy. At the bottom is a brief consent for the patient to sign, and a place to write the credit card number and expiration date. (See below for a copy of our letter; feel free to use it as a template for creating your own.)
Do patients object? Some do – mostly older people, and fewer each year. But when we explain that we’re doing nothing different than a hotel does at each check-in, and that it will work to their advantage as well by decreasing the bills they will receive and the checks they must write, most come around. Make it an option at first if you wish; then, when everyone is accustomed to it, you can make it mandatory.
Do patients worry about confidentiality, or unauthorized use? They don’t anywhere else. They think nothing of handing a card to a waiter or waitress in a restaurant with no thought of what he or she might do with it in the kitchen. They hand cards over to hotel clerks, and never think to ask how long they keep the information or who has access to it. They blithely shoot their numbers into black holes on the Internet. We explain that we guard our patients’ financial information as carefully as we do their medical information. (If you have EHR, it can go in the chart with everything else; if not, I suggest a separate portable Rolodex-type file that can be locked up each night.)
Does it work? In only a year, our accounts receivable totals dropped by nearly 50%; after another year, they stabilized at 30%-35% of previous levels and have remained there ever since. When my accountant retired a few years ago, I hired a new one. Something must be wrong, he said nervously, after his first look at our books; AR totals are “never” that low in a practice with our level of volume. His eyes widened as I explained our system. “Why doesn’t every medical office do that?” he asked.
Why indeed? The business of health care delivery is being rocked to its very foundations as we speak. In my humble opinion, private practice will only survive those changes if physicians learn to do more of what we do best – treating patients – and leave the business of extending credit to the banks.
Patient consent form
This generic letter is intended to be used as an example for a letter you might draft for a similar purpose. We take no responsibility for your use of its content, either verbatim or altered, or for any inappropriate usage. Click on the attachment below for a printable copy of the letter.
To Our Patients:
As you know if you have ever checked into a hotel or rented a car, the first thing you are asked for is a credit card, which is imprinted and later used to pay your bill. This is an advantage for both you and the hotel or rental company, since it makes checkout easier, faster, and more efficient.
We have implemented a similar policy. You will be asked for a credit card number at the time you check in and the information will be held securely until your insurances have paid their portion and notified us of the amount of your share. At that time, any remaining balance owed by you will be charged to your credit card, and a copy of the charge will be mailed to you.
This will be an advantage to you, since you will no longer have to write out and mail us checks. It will be an advantage to us as well, since it will greatly decrease the number of statements that we have to generate and send out. The combination will benefit everybody in helping to keep the cost of health care down.
This in no way will compromise your ability to dispute a charge or question your insurance company’s determination of payment.
Copays due at the time of the visit will, of course, still be due at the time of the visit.
If you have any questions about this payment method, do not hesitate to ask.
Sincerely yours,
I authorize ********************, PA to charge outstanding balances on my account to the following credit card:
Visa Mastercard American Express Other: ____________________________
Account number _______________________Expiration Date ____________CVV_____
Name on card (please print) _________________________________________________
Signature _____________________________________ Date ______________________
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]
For as long as I have been writing this column, I have stressed that ; and yet, all these years later, AR is still the subject that generates the most questions.
Okay; let’s go over it one more time: Basically, physicians extend more credit than any business except banks. Despite what you may have read recently, banks are good at it, and they charge interest (and a myriad of fees) to do it. Doctors do it for free. Are we crazy? No business owner in his or her right mind allows customers to take away goods or services without paying for them; but doctors do it every day.
What to do? Common sense tells you to collect everything you can at the time of service; but some patients inevitably brandish the old “I forgot my checkbook” excuse and escape without paying. And the patient-owed portion of most insurance charges is often unknown, and unknowable, at the time of service.
That means you’ll need to send a bill; and every bill you send (or hire somebody to send) costs you a bundle. And when it arrives, it goes right to the bottom of your patient’s payment priority list. That is, each month your patients will pay their electric, water, gas, and telephone bills … and just about any other bill ... before getting around to yours. If there is no more money when your bill finally surfaces, that’s just too bad. The electric company can shut off their power; what can you do?
What we do is what every hotel, rental car agency, and many other businesses have done for years: We ask for a credit card number, keep it on file, and bill balances to it as they come in. Plastic runs the show everywhere you go – except in most medical offices.
New patients in my office receive a letter at their first visit explaining our policy. At the bottom is a brief consent for the patient to sign, and a place to write the credit card number and expiration date. (See below for a copy of our letter; feel free to use it as a template for creating your own.)
Do patients object? Some do – mostly older people, and fewer each year. But when we explain that we’re doing nothing different than a hotel does at each check-in, and that it will work to their advantage as well by decreasing the bills they will receive and the checks they must write, most come around. Make it an option at first if you wish; then, when everyone is accustomed to it, you can make it mandatory.
Do patients worry about confidentiality, or unauthorized use? They don’t anywhere else. They think nothing of handing a card to a waiter or waitress in a restaurant with no thought of what he or she might do with it in the kitchen. They hand cards over to hotel clerks, and never think to ask how long they keep the information or who has access to it. They blithely shoot their numbers into black holes on the Internet. We explain that we guard our patients’ financial information as carefully as we do their medical information. (If you have EHR, it can go in the chart with everything else; if not, I suggest a separate portable Rolodex-type file that can be locked up each night.)
Does it work? In only a year, our accounts receivable totals dropped by nearly 50%; after another year, they stabilized at 30%-35% of previous levels and have remained there ever since. When my accountant retired a few years ago, I hired a new one. Something must be wrong, he said nervously, after his first look at our books; AR totals are “never” that low in a practice with our level of volume. His eyes widened as I explained our system. “Why doesn’t every medical office do that?” he asked.
Why indeed? The business of health care delivery is being rocked to its very foundations as we speak. In my humble opinion, private practice will only survive those changes if physicians learn to do more of what we do best – treating patients – and leave the business of extending credit to the banks.
Patient consent form
This generic letter is intended to be used as an example for a letter you might draft for a similar purpose. We take no responsibility for your use of its content, either verbatim or altered, or for any inappropriate usage. Click on the attachment below for a printable copy of the letter.
To Our Patients:
As you know if you have ever checked into a hotel or rented a car, the first thing you are asked for is a credit card, which is imprinted and later used to pay your bill. This is an advantage for both you and the hotel or rental company, since it makes checkout easier, faster, and more efficient.
We have implemented a similar policy. You will be asked for a credit card number at the time you check in and the information will be held securely until your insurances have paid their portion and notified us of the amount of your share. At that time, any remaining balance owed by you will be charged to your credit card, and a copy of the charge will be mailed to you.
This will be an advantage to you, since you will no longer have to write out and mail us checks. It will be an advantage to us as well, since it will greatly decrease the number of statements that we have to generate and send out. The combination will benefit everybody in helping to keep the cost of health care down.
This in no way will compromise your ability to dispute a charge or question your insurance company’s determination of payment.
Copays due at the time of the visit will, of course, still be due at the time of the visit.
If you have any questions about this payment method, do not hesitate to ask.
Sincerely yours,
I authorize ********************, PA to charge outstanding balances on my account to the following credit card:
Visa Mastercard American Express Other: ____________________________
Account number _______________________Expiration Date ____________CVV_____
Name on card (please print) _________________________________________________
Signature _____________________________________ Date ______________________
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]
For as long as I have been writing this column, I have stressed that ; and yet, all these years later, AR is still the subject that generates the most questions.
Okay; let’s go over it one more time: Basically, physicians extend more credit than any business except banks. Despite what you may have read recently, banks are good at it, and they charge interest (and a myriad of fees) to do it. Doctors do it for free. Are we crazy? No business owner in his or her right mind allows customers to take away goods or services without paying for them; but doctors do it every day.
What to do? Common sense tells you to collect everything you can at the time of service; but some patients inevitably brandish the old “I forgot my checkbook” excuse and escape without paying. And the patient-owed portion of most insurance charges is often unknown, and unknowable, at the time of service.
That means you’ll need to send a bill; and every bill you send (or hire somebody to send) costs you a bundle. And when it arrives, it goes right to the bottom of your patient’s payment priority list. That is, each month your patients will pay their electric, water, gas, and telephone bills … and just about any other bill ... before getting around to yours. If there is no more money when your bill finally surfaces, that’s just too bad. The electric company can shut off their power; what can you do?
What we do is what every hotel, rental car agency, and many other businesses have done for years: We ask for a credit card number, keep it on file, and bill balances to it as they come in. Plastic runs the show everywhere you go – except in most medical offices.
New patients in my office receive a letter at their first visit explaining our policy. At the bottom is a brief consent for the patient to sign, and a place to write the credit card number and expiration date. (See below for a copy of our letter; feel free to use it as a template for creating your own.)
Do patients object? Some do – mostly older people, and fewer each year. But when we explain that we’re doing nothing different than a hotel does at each check-in, and that it will work to their advantage as well by decreasing the bills they will receive and the checks they must write, most come around. Make it an option at first if you wish; then, when everyone is accustomed to it, you can make it mandatory.
Do patients worry about confidentiality, or unauthorized use? They don’t anywhere else. They think nothing of handing a card to a waiter or waitress in a restaurant with no thought of what he or she might do with it in the kitchen. They hand cards over to hotel clerks, and never think to ask how long they keep the information or who has access to it. They blithely shoot their numbers into black holes on the Internet. We explain that we guard our patients’ financial information as carefully as we do their medical information. (If you have EHR, it can go in the chart with everything else; if not, I suggest a separate portable Rolodex-type file that can be locked up each night.)
Does it work? In only a year, our accounts receivable totals dropped by nearly 50%; after another year, they stabilized at 30%-35% of previous levels and have remained there ever since. When my accountant retired a few years ago, I hired a new one. Something must be wrong, he said nervously, after his first look at our books; AR totals are “never” that low in a practice with our level of volume. His eyes widened as I explained our system. “Why doesn’t every medical office do that?” he asked.
Why indeed? The business of health care delivery is being rocked to its very foundations as we speak. In my humble opinion, private practice will only survive those changes if physicians learn to do more of what we do best – treating patients – and leave the business of extending credit to the banks.
Patient consent form
This generic letter is intended to be used as an example for a letter you might draft for a similar purpose. We take no responsibility for your use of its content, either verbatim or altered, or for any inappropriate usage. Click on the attachment below for a printable copy of the letter.
To Our Patients:
As you know if you have ever checked into a hotel or rented a car, the first thing you are asked for is a credit card, which is imprinted and later used to pay your bill. This is an advantage for both you and the hotel or rental company, since it makes checkout easier, faster, and more efficient.
We have implemented a similar policy. You will be asked for a credit card number at the time you check in and the information will be held securely until your insurances have paid their portion and notified us of the amount of your share. At that time, any remaining balance owed by you will be charged to your credit card, and a copy of the charge will be mailed to you.
This will be an advantage to you, since you will no longer have to write out and mail us checks. It will be an advantage to us as well, since it will greatly decrease the number of statements that we have to generate and send out. The combination will benefit everybody in helping to keep the cost of health care down.
This in no way will compromise your ability to dispute a charge or question your insurance company’s determination of payment.
Copays due at the time of the visit will, of course, still be due at the time of the visit.
If you have any questions about this payment method, do not hesitate to ask.
Sincerely yours,
I authorize ********************, PA to charge outstanding balances on my account to the following credit card:
Visa Mastercard American Express Other: ____________________________
Account number _______________________Expiration Date ____________CVV_____
Name on card (please print) _________________________________________________
Signature _____________________________________ Date ______________________
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]
A new way to classify endometrial cancer
We classify endometrial cancer so that we can communicate and define each patient’s disease status, the potential for harm, and the likelihood that adjuvant therapies might provide help. Traditional forms of classification have clearly fallen short in achieving this aim, as we all know of patients with apparent low-risk disease (such as stage IA grade 1 endometrioid carcinoma) who have had recurrences and died from their disease, and we know that many patients have been subjected to overtreatment for their cancer and have acquired lifelong toxicities of therapy. This column will explore the newer, more sophisticated molecular-based classifications that are being validated for endometrial cancer, and the ways in which this promises to personalize the treatment of endometrial cancer.
Breast cancer and melanoma are examples of the inclusion of molecular data such as hormone receptor status, HER2/neu status, or BRAF positivity resulting in advancements in personalizing therapeutics. We are now moving toward this for endometrial cancer.
What is the Cancer Genome Atlas?
In 2006 the National Institutes of Health announced an initiative to coordinate work between the National Cancer Institute and the National Human Genome Research Institute taking information about the human genome and analyzing it for key genomic alterations found in 33 common cancers. These data were combined with clinical information (such as survival) to classify the behaviors of those cancers with respect to their individual genomic alternations, in order to look for patterns in mutations and behaviors. The goal of this analysis was to shift the paradigm of cancer classification from being centered around primary organ site toward tumors’ shared genomic patterns.
In 2013 the Cancer Genome Atlas published their results of complete gene sequencing in endometrial cancer.3 The authors identified four discrete subgroups of endometrial cancer with distinct molecular mutational profiles and distinct clinical outcomes: polymerase epsilon (POLE, pronounced “pole-ee”) ultramutated, microsatellite instability (MSI) high, copy number high, and copy number low.
POLE ultramutated
An important subgroup identified in the Cancer Genome Atlas was a group of patients with a POLE ultramutated state. POLE encodes for a subunit of DNA polymerase, the enzyme responsible for replicating the leading DNA strand. Nonfunctioning POLE results in proofreading errors and a subsequent ultramutated cellular state with a predominance of single nucleotide variants. POLE proofreading domain mutations in endometrial cancer and colon cancer are associated with excellent prognosis, likely secondary to the immune response that is elicited by this ultramutated state from creation of “antigenic neoepitopes” that stimulate T-cell response. Effectively, the very mutated cell is seen as “more foreign” to the body’s immune system.
Approximately 10% of patients with endometrial cancer have a POLE ultramutated state, and, as stated above, prognosis is excellent, even if coexisting with a histologic cell type (such as serous) that is normally associated with adverse outcomes. These women tend to be younger, with a lower body mass index, higher-grade endometrioid cell type, the presence of lymphovascular space invasion, and low stage.
MSI high
MSI (microsatellite instability) is a result of epigenetic/hypermethylations or loss of expression in mismatch repair genes (such as MLH1, MSH2, MSH6, PMS2). These genes code for proteins critical in the repair of mismatches in short repeated sequences of DNA. Loss of their function results in an accumulation of errors in these sequences: MSI. It is a feature of the Lynch syndrome inherited state, but is also found sporadically in endometrial tumors. These tumors accumulate a number of mutations during cell replication that, as in POLE hypermutated tumors, are associated with eliciting an immune response.
These tumors tend to be associated with a higher-grade endometrioid cell type, the presence of lymphovascular space invasion, and an advanced stage. Patients with tumors that have been described as MSI high are candidates for “immune therapy” with the PDL1 inhibitor pembrolizumab because of their proinflammatory state and observed favorable responses in clinical trials.4
Copy number high/low
Copy number (CN) high and low refers to the results of microarrays in which hierarchical clustering was applied to identify reoccurring amplification or deletion regions. The CN-high group was associated with the poorest outcomes (recurrence and survival). There is significant overlap with mutations in TP53. Most serous carcinomas were CN high; however, 25% of patients with high-grade endometrioid cell type shared the CN-high classification. These tumors shared great molecular similarity to high-grade serous ovarian cancers and basal-like breast cancer.
Those patients who did not possess mutations that classified them as POLE hypermutated, MSI high, or CN high were classified as CN low. This group included predominantly grades 1 and 2 endometrioid adenocarcinomas of an early stage and had a favorable prognostic profile, though less favorable than those with a POLE ultramutated state, which appears to be somewhat protective.
Molecular/metabolic interactions
While molecular data are clearly important in driving a cancer cell’s behavior, other clinical and metabolic factors influence cancer behavior. For example, body mass index, adiposity, glucose, and lipid metabolism have been shown to be important drivers of cellular behavior and responsiveness to targeted therapies.5,6 Additionally age, race, and other metabolic states contribute to oncologic behavior. Future classifications of endometrial cancer are unlikely to use molecular profiles in isolation but will need to incorporate these additional patient-specific data to better predict and prognosticate outcomes.
Clinical applications
If researchers can better define and describe a patient’s endometrial cancer from the time of their biopsy, important clinical decisions might be able to be tackled. For example, in a premenopausal patient with an endometrial cancer who is considering fertility-sparing treatments, preoperative knowledge of a POLE ultramutated state (and therefore an anticipated good prognosis) might favor fertility preservation or avoid comprehensive staging which may be of limited value. Similarly, if an MSI-high profile is identified leading to a Lynch syndrome diagnosis, she may be more inclined to undergo a hysterectomy with bilateral salpingo-oophorectomy and staging as she is at known increased risk for a more advanced endometrial cancer, as well as the potential for ovarian cancer.
Postoperative incorporation of molecular data promises to be particularly helpful in guiding adjuvant therapies and sparing some women from unnecessary treatments. For example, women with high-grade endometrioid tumors who are CN high were historically treated with radiotherapy but might do better treated with systemic adjuvant therapies traditionally reserved for nonendometrioid carcinomas. Costly therapies such as immunotherapy can be directed toward those with MSI-high tumors, and the rare patient with a POLE ultramutated state who has a recurrence or advanced disease. Clinical trials will be able to cluster enrollment of patients with CN-high, serouslike cancers with those with serous cancers, rather than combining them with patients whose cancers predictably behave much differently.
Much work is still needed to validate this molecular profiling in endometrial cancer and define the algorithms associated with treatment decisions; however, it is likely that the way we describe endometrial cancer in the near future will be quite different.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no disclosures.
References
1. Bokhman JV. Two pathogenetic types of endometrial carcinoma. Gynecol Oncol. 1983;15(1):10-7.
2. Clarke BA et al. Endometrial carcinoma: controversies in histopathological assessment of grade and tumour cell type. J Clin Pathol. 2010;63(5):410-5.
3. Cancer Genome Atlas Research Network. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497(7447):67-73.
4. Ott PA et al. Pembrolizumab in advanced endometrial cancer: Preliminary results from the phase Ib KEYNOTE-028 study. J Clin Oncol. 2016;34(suppl):Abstract 5581.
5. Roque DR et al. Association between differential gene expression and body mass index among endometrial cancers from the Cancer Genome Atlas Project. Gynecol Oncol. 2016;142(2):317-22.
6. Talhouk A et al. New classification of endometrial cancers: The development and potential applications of genomic-based classification in research and clinical care. Gynecol Oncol Res Pract. 2016 Dec;3:14.
We classify endometrial cancer so that we can communicate and define each patient’s disease status, the potential for harm, and the likelihood that adjuvant therapies might provide help. Traditional forms of classification have clearly fallen short in achieving this aim, as we all know of patients with apparent low-risk disease (such as stage IA grade 1 endometrioid carcinoma) who have had recurrences and died from their disease, and we know that many patients have been subjected to overtreatment for their cancer and have acquired lifelong toxicities of therapy. This column will explore the newer, more sophisticated molecular-based classifications that are being validated for endometrial cancer, and the ways in which this promises to personalize the treatment of endometrial cancer.
Breast cancer and melanoma are examples of the inclusion of molecular data such as hormone receptor status, HER2/neu status, or BRAF positivity resulting in advancements in personalizing therapeutics. We are now moving toward this for endometrial cancer.
What is the Cancer Genome Atlas?
In 2006 the National Institutes of Health announced an initiative to coordinate work between the National Cancer Institute and the National Human Genome Research Institute taking information about the human genome and analyzing it for key genomic alterations found in 33 common cancers. These data were combined with clinical information (such as survival) to classify the behaviors of those cancers with respect to their individual genomic alternations, in order to look for patterns in mutations and behaviors. The goal of this analysis was to shift the paradigm of cancer classification from being centered around primary organ site toward tumors’ shared genomic patterns.
In 2013 the Cancer Genome Atlas published their results of complete gene sequencing in endometrial cancer.3 The authors identified four discrete subgroups of endometrial cancer with distinct molecular mutational profiles and distinct clinical outcomes: polymerase epsilon (POLE, pronounced “pole-ee”) ultramutated, microsatellite instability (MSI) high, copy number high, and copy number low.
POLE ultramutated
An important subgroup identified in the Cancer Genome Atlas was a group of patients with a POLE ultramutated state. POLE encodes for a subunit of DNA polymerase, the enzyme responsible for replicating the leading DNA strand. Nonfunctioning POLE results in proofreading errors and a subsequent ultramutated cellular state with a predominance of single nucleotide variants. POLE proofreading domain mutations in endometrial cancer and colon cancer are associated with excellent prognosis, likely secondary to the immune response that is elicited by this ultramutated state from creation of “antigenic neoepitopes” that stimulate T-cell response. Effectively, the very mutated cell is seen as “more foreign” to the body’s immune system.
Approximately 10% of patients with endometrial cancer have a POLE ultramutated state, and, as stated above, prognosis is excellent, even if coexisting with a histologic cell type (such as serous) that is normally associated with adverse outcomes. These women tend to be younger, with a lower body mass index, higher-grade endometrioid cell type, the presence of lymphovascular space invasion, and low stage.
MSI high
MSI (microsatellite instability) is a result of epigenetic/hypermethylations or loss of expression in mismatch repair genes (such as MLH1, MSH2, MSH6, PMS2). These genes code for proteins critical in the repair of mismatches in short repeated sequences of DNA. Loss of their function results in an accumulation of errors in these sequences: MSI. It is a feature of the Lynch syndrome inherited state, but is also found sporadically in endometrial tumors. These tumors accumulate a number of mutations during cell replication that, as in POLE hypermutated tumors, are associated with eliciting an immune response.
These tumors tend to be associated with a higher-grade endometrioid cell type, the presence of lymphovascular space invasion, and an advanced stage. Patients with tumors that have been described as MSI high are candidates for “immune therapy” with the PDL1 inhibitor pembrolizumab because of their proinflammatory state and observed favorable responses in clinical trials.4
Copy number high/low
Copy number (CN) high and low refers to the results of microarrays in which hierarchical clustering was applied to identify reoccurring amplification or deletion regions. The CN-high group was associated with the poorest outcomes (recurrence and survival). There is significant overlap with mutations in TP53. Most serous carcinomas were CN high; however, 25% of patients with high-grade endometrioid cell type shared the CN-high classification. These tumors shared great molecular similarity to high-grade serous ovarian cancers and basal-like breast cancer.
Those patients who did not possess mutations that classified them as POLE hypermutated, MSI high, or CN high were classified as CN low. This group included predominantly grades 1 and 2 endometrioid adenocarcinomas of an early stage and had a favorable prognostic profile, though less favorable than those with a POLE ultramutated state, which appears to be somewhat protective.
Molecular/metabolic interactions
While molecular data are clearly important in driving a cancer cell’s behavior, other clinical and metabolic factors influence cancer behavior. For example, body mass index, adiposity, glucose, and lipid metabolism have been shown to be important drivers of cellular behavior and responsiveness to targeted therapies.5,6 Additionally age, race, and other metabolic states contribute to oncologic behavior. Future classifications of endometrial cancer are unlikely to use molecular profiles in isolation but will need to incorporate these additional patient-specific data to better predict and prognosticate outcomes.
Clinical applications
If researchers can better define and describe a patient’s endometrial cancer from the time of their biopsy, important clinical decisions might be able to be tackled. For example, in a premenopausal patient with an endometrial cancer who is considering fertility-sparing treatments, preoperative knowledge of a POLE ultramutated state (and therefore an anticipated good prognosis) might favor fertility preservation or avoid comprehensive staging which may be of limited value. Similarly, if an MSI-high profile is identified leading to a Lynch syndrome diagnosis, she may be more inclined to undergo a hysterectomy with bilateral salpingo-oophorectomy and staging as she is at known increased risk for a more advanced endometrial cancer, as well as the potential for ovarian cancer.
Postoperative incorporation of molecular data promises to be particularly helpful in guiding adjuvant therapies and sparing some women from unnecessary treatments. For example, women with high-grade endometrioid tumors who are CN high were historically treated with radiotherapy but might do better treated with systemic adjuvant therapies traditionally reserved for nonendometrioid carcinomas. Costly therapies such as immunotherapy can be directed toward those with MSI-high tumors, and the rare patient with a POLE ultramutated state who has a recurrence or advanced disease. Clinical trials will be able to cluster enrollment of patients with CN-high, serouslike cancers with those with serous cancers, rather than combining them with patients whose cancers predictably behave much differently.
Much work is still needed to validate this molecular profiling in endometrial cancer and define the algorithms associated with treatment decisions; however, it is likely that the way we describe endometrial cancer in the near future will be quite different.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no disclosures.
References
1. Bokhman JV. Two pathogenetic types of endometrial carcinoma. Gynecol Oncol. 1983;15(1):10-7.
2. Clarke BA et al. Endometrial carcinoma: controversies in histopathological assessment of grade and tumour cell type. J Clin Pathol. 2010;63(5):410-5.
3. Cancer Genome Atlas Research Network. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497(7447):67-73.
4. Ott PA et al. Pembrolizumab in advanced endometrial cancer: Preliminary results from the phase Ib KEYNOTE-028 study. J Clin Oncol. 2016;34(suppl):Abstract 5581.
5. Roque DR et al. Association between differential gene expression and body mass index among endometrial cancers from the Cancer Genome Atlas Project. Gynecol Oncol. 2016;142(2):317-22.
6. Talhouk A et al. New classification of endometrial cancers: The development and potential applications of genomic-based classification in research and clinical care. Gynecol Oncol Res Pract. 2016 Dec;3:14.
We classify endometrial cancer so that we can communicate and define each patient’s disease status, the potential for harm, and the likelihood that adjuvant therapies might provide help. Traditional forms of classification have clearly fallen short in achieving this aim, as we all know of patients with apparent low-risk disease (such as stage IA grade 1 endometrioid carcinoma) who have had recurrences and died from their disease, and we know that many patients have been subjected to overtreatment for their cancer and have acquired lifelong toxicities of therapy. This column will explore the newer, more sophisticated molecular-based classifications that are being validated for endometrial cancer, and the ways in which this promises to personalize the treatment of endometrial cancer.
Breast cancer and melanoma are examples of the inclusion of molecular data such as hormone receptor status, HER2/neu status, or BRAF positivity resulting in advancements in personalizing therapeutics. We are now moving toward this for endometrial cancer.
What is the Cancer Genome Atlas?
In 2006 the National Institutes of Health announced an initiative to coordinate work between the National Cancer Institute and the National Human Genome Research Institute taking information about the human genome and analyzing it for key genomic alterations found in 33 common cancers. These data were combined with clinical information (such as survival) to classify the behaviors of those cancers with respect to their individual genomic alternations, in order to look for patterns in mutations and behaviors. The goal of this analysis was to shift the paradigm of cancer classification from being centered around primary organ site toward tumors’ shared genomic patterns.
In 2013 the Cancer Genome Atlas published their results of complete gene sequencing in endometrial cancer.3 The authors identified four discrete subgroups of endometrial cancer with distinct molecular mutational profiles and distinct clinical outcomes: polymerase epsilon (POLE, pronounced “pole-ee”) ultramutated, microsatellite instability (MSI) high, copy number high, and copy number low.
POLE ultramutated
An important subgroup identified in the Cancer Genome Atlas was a group of patients with a POLE ultramutated state. POLE encodes for a subunit of DNA polymerase, the enzyme responsible for replicating the leading DNA strand. Nonfunctioning POLE results in proofreading errors and a subsequent ultramutated cellular state with a predominance of single nucleotide variants. POLE proofreading domain mutations in endometrial cancer and colon cancer are associated with excellent prognosis, likely secondary to the immune response that is elicited by this ultramutated state from creation of “antigenic neoepitopes” that stimulate T-cell response. Effectively, the very mutated cell is seen as “more foreign” to the body’s immune system.
Approximately 10% of patients with endometrial cancer have a POLE ultramutated state, and, as stated above, prognosis is excellent, even if coexisting with a histologic cell type (such as serous) that is normally associated with adverse outcomes. These women tend to be younger, with a lower body mass index, higher-grade endometrioid cell type, the presence of lymphovascular space invasion, and low stage.
MSI high
MSI (microsatellite instability) is a result of epigenetic/hypermethylations or loss of expression in mismatch repair genes (such as MLH1, MSH2, MSH6, PMS2). These genes code for proteins critical in the repair of mismatches in short repeated sequences of DNA. Loss of their function results in an accumulation of errors in these sequences: MSI. It is a feature of the Lynch syndrome inherited state, but is also found sporadically in endometrial tumors. These tumors accumulate a number of mutations during cell replication that, as in POLE hypermutated tumors, are associated with eliciting an immune response.
These tumors tend to be associated with a higher-grade endometrioid cell type, the presence of lymphovascular space invasion, and an advanced stage. Patients with tumors that have been described as MSI high are candidates for “immune therapy” with the PDL1 inhibitor pembrolizumab because of their proinflammatory state and observed favorable responses in clinical trials.4
Copy number high/low
Copy number (CN) high and low refers to the results of microarrays in which hierarchical clustering was applied to identify reoccurring amplification or deletion regions. The CN-high group was associated with the poorest outcomes (recurrence and survival). There is significant overlap with mutations in TP53. Most serous carcinomas were CN high; however, 25% of patients with high-grade endometrioid cell type shared the CN-high classification. These tumors shared great molecular similarity to high-grade serous ovarian cancers and basal-like breast cancer.
Those patients who did not possess mutations that classified them as POLE hypermutated, MSI high, or CN high were classified as CN low. This group included predominantly grades 1 and 2 endometrioid adenocarcinomas of an early stage and had a favorable prognostic profile, though less favorable than those with a POLE ultramutated state, which appears to be somewhat protective.
Molecular/metabolic interactions
While molecular data are clearly important in driving a cancer cell’s behavior, other clinical and metabolic factors influence cancer behavior. For example, body mass index, adiposity, glucose, and lipid metabolism have been shown to be important drivers of cellular behavior and responsiveness to targeted therapies.5,6 Additionally age, race, and other metabolic states contribute to oncologic behavior. Future classifications of endometrial cancer are unlikely to use molecular profiles in isolation but will need to incorporate these additional patient-specific data to better predict and prognosticate outcomes.
Clinical applications
If researchers can better define and describe a patient’s endometrial cancer from the time of their biopsy, important clinical decisions might be able to be tackled. For example, in a premenopausal patient with an endometrial cancer who is considering fertility-sparing treatments, preoperative knowledge of a POLE ultramutated state (and therefore an anticipated good prognosis) might favor fertility preservation or avoid comprehensive staging which may be of limited value. Similarly, if an MSI-high profile is identified leading to a Lynch syndrome diagnosis, she may be more inclined to undergo a hysterectomy with bilateral salpingo-oophorectomy and staging as she is at known increased risk for a more advanced endometrial cancer, as well as the potential for ovarian cancer.
Postoperative incorporation of molecular data promises to be particularly helpful in guiding adjuvant therapies and sparing some women from unnecessary treatments. For example, women with high-grade endometrioid tumors who are CN high were historically treated with radiotherapy but might do better treated with systemic adjuvant therapies traditionally reserved for nonendometrioid carcinomas. Costly therapies such as immunotherapy can be directed toward those with MSI-high tumors, and the rare patient with a POLE ultramutated state who has a recurrence or advanced disease. Clinical trials will be able to cluster enrollment of patients with CN-high, serouslike cancers with those with serous cancers, rather than combining them with patients whose cancers predictably behave much differently.
Much work is still needed to validate this molecular profiling in endometrial cancer and define the algorithms associated with treatment decisions; however, it is likely that the way we describe endometrial cancer in the near future will be quite different.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no disclosures.
References
1. Bokhman JV. Two pathogenetic types of endometrial carcinoma. Gynecol Oncol. 1983;15(1):10-7.
2. Clarke BA et al. Endometrial carcinoma: controversies in histopathological assessment of grade and tumour cell type. J Clin Pathol. 2010;63(5):410-5.
3. Cancer Genome Atlas Research Network. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497(7447):67-73.
4. Ott PA et al. Pembrolizumab in advanced endometrial cancer: Preliminary results from the phase Ib KEYNOTE-028 study. J Clin Oncol. 2016;34(suppl):Abstract 5581.
5. Roque DR et al. Association between differential gene expression and body mass index among endometrial cancers from the Cancer Genome Atlas Project. Gynecol Oncol. 2016;142(2):317-22.
6. Talhouk A et al. New classification of endometrial cancers: The development and potential applications of genomic-based classification in research and clinical care. Gynecol Oncol Res Pract. 2016 Dec;3:14.
Marijuana use is affecting the job market
I have a friend who owns a large paving and excavating company. He currently is turning away large contracts because he can’t find employees to drive his dump trucks and operate his heavy machinery. The situation is so dire that he has begun to explore the possibility of recruiting employees out of the corrections system.
Like much of the country, Maine is experiencing a low level of unemployment that few of us over the age of 50 years can recall. Coupled with a confused and unwelcoming immigration policy at the federal level many small and large companies are struggling to find employees. The employment opportunities my friend’s company is offering are well above minimum wage, paying in the $30,000-$70,000 range with benefits. While the jobs require some special skills, his company is large enough that it can provide in-house training.
Maine residents recently have voted to decriminalize the possession of small amounts of marijuana. It is unclear exactly how this change in the official position of the state government will translate into a distribution network and a system of local codes. However, it does reflect a more tolerant attitude toward marijuana use. It also suggests that job seekers who are avoiding positions that require drug testing are not worried about the stigma of being identified as a user. They understand enough pharmacology to know that marijuana is detectable days and even weeks after it was last ingested or inhaled. Even the recreational users realize that the chances of being able to pass a drug test before employment and at any subsequent random testing are slim.
The problem is that these good-paying jobs are going unfilled because of the pharmacologic properties of a drug, and our current inability to devise a test that can accurately and consistently correlate a person’s blood level and his or her ability to safely operate a motor vehicle or piece of heavy equipment (“Establishing legal limit for driving under the influence of marijuana,” Inj Epidemiol. 2014 Dec.;1[1]: 26). There is some correlation between blood levels and whether a person is a heavy or infrequent user. Laws that rely on a zero tolerance philosophy are not bringing us any closer to a solution. And it is probably unrealistic to hope that in the near future scientists will develop a single, simply administered test that can provide a clear yes or no to the issue of impairment in the workplace.
I can envision a two-tier system in which all employees are blood or urine tested on a 3-month schedule. Those with a positive test must then take a 10-minute test on a laptop computer simulator with a joy stick each morning that they arrive on the job to demonstrate that, despite a history of marijuana use, they are not impaired.
Even if such a test is developed, we still owe our patients the reminder that, despite its decriminalization, marijuana is a drug and like any drug has side effects. One of them is that it can put limits on your employment opportunities.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
I have a friend who owns a large paving and excavating company. He currently is turning away large contracts because he can’t find employees to drive his dump trucks and operate his heavy machinery. The situation is so dire that he has begun to explore the possibility of recruiting employees out of the corrections system.
Like much of the country, Maine is experiencing a low level of unemployment that few of us over the age of 50 years can recall. Coupled with a confused and unwelcoming immigration policy at the federal level many small and large companies are struggling to find employees. The employment opportunities my friend’s company is offering are well above minimum wage, paying in the $30,000-$70,000 range with benefits. While the jobs require some special skills, his company is large enough that it can provide in-house training.
Maine residents recently have voted to decriminalize the possession of small amounts of marijuana. It is unclear exactly how this change in the official position of the state government will translate into a distribution network and a system of local codes. However, it does reflect a more tolerant attitude toward marijuana use. It also suggests that job seekers who are avoiding positions that require drug testing are not worried about the stigma of being identified as a user. They understand enough pharmacology to know that marijuana is detectable days and even weeks after it was last ingested or inhaled. Even the recreational users realize that the chances of being able to pass a drug test before employment and at any subsequent random testing are slim.
The problem is that these good-paying jobs are going unfilled because of the pharmacologic properties of a drug, and our current inability to devise a test that can accurately and consistently correlate a person’s blood level and his or her ability to safely operate a motor vehicle or piece of heavy equipment (“Establishing legal limit for driving under the influence of marijuana,” Inj Epidemiol. 2014 Dec.;1[1]: 26). There is some correlation between blood levels and whether a person is a heavy or infrequent user. Laws that rely on a zero tolerance philosophy are not bringing us any closer to a solution. And it is probably unrealistic to hope that in the near future scientists will develop a single, simply administered test that can provide a clear yes or no to the issue of impairment in the workplace.
I can envision a two-tier system in which all employees are blood or urine tested on a 3-month schedule. Those with a positive test must then take a 10-minute test on a laptop computer simulator with a joy stick each morning that they arrive on the job to demonstrate that, despite a history of marijuana use, they are not impaired.
Even if such a test is developed, we still owe our patients the reminder that, despite its decriminalization, marijuana is a drug and like any drug has side effects. One of them is that it can put limits on your employment opportunities.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
I have a friend who owns a large paving and excavating company. He currently is turning away large contracts because he can’t find employees to drive his dump trucks and operate his heavy machinery. The situation is so dire that he has begun to explore the possibility of recruiting employees out of the corrections system.
Like much of the country, Maine is experiencing a low level of unemployment that few of us over the age of 50 years can recall. Coupled with a confused and unwelcoming immigration policy at the federal level many small and large companies are struggling to find employees. The employment opportunities my friend’s company is offering are well above minimum wage, paying in the $30,000-$70,000 range with benefits. While the jobs require some special skills, his company is large enough that it can provide in-house training.
Maine residents recently have voted to decriminalize the possession of small amounts of marijuana. It is unclear exactly how this change in the official position of the state government will translate into a distribution network and a system of local codes. However, it does reflect a more tolerant attitude toward marijuana use. It also suggests that job seekers who are avoiding positions that require drug testing are not worried about the stigma of being identified as a user. They understand enough pharmacology to know that marijuana is detectable days and even weeks after it was last ingested or inhaled. Even the recreational users realize that the chances of being able to pass a drug test before employment and at any subsequent random testing are slim.
The problem is that these good-paying jobs are going unfilled because of the pharmacologic properties of a drug, and our current inability to devise a test that can accurately and consistently correlate a person’s blood level and his or her ability to safely operate a motor vehicle or piece of heavy equipment (“Establishing legal limit for driving under the influence of marijuana,” Inj Epidemiol. 2014 Dec.;1[1]: 26). There is some correlation between blood levels and whether a person is a heavy or infrequent user. Laws that rely on a zero tolerance philosophy are not bringing us any closer to a solution. And it is probably unrealistic to hope that in the near future scientists will develop a single, simply administered test that can provide a clear yes or no to the issue of impairment in the workplace.
I can envision a two-tier system in which all employees are blood or urine tested on a 3-month schedule. Those with a positive test must then take a 10-minute test on a laptop computer simulator with a joy stick each morning that they arrive on the job to demonstrate that, despite a history of marijuana use, they are not impaired.
Even if such a test is developed, we still owe our patients the reminder that, despite its decriminalization, marijuana is a drug and like any drug has side effects. One of them is that it can put limits on your employment opportunities.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Dismantling the sports-betting ban: A mental health gamble
The Supreme Court decision to overturn the federal law that prohibited state-sanctioned college and professional sports betting is bad news for clinicians who treat patients with addictions.
On May 14, the high court ruled 7-2 that the 1992 law, called the Professional and Amateur Sports Protection Act (PASPA), was unconstitutional. Now every state is free to operate, sponsor, promote, license, advertise, or authorize gambling for any college or professional sport–based event.
Optimistic outlooks on the death of PASPA include the foreseen opportunity by the states to tax and generate revenue on such gambling. Proponents of the ruling also argue that illegal activity that thrived on sports betting will now end.
But to what extent will either of those scenarios benefit the public?
If passage of various state marijuana laws is any example, assumptions that legal avenues will usurp illegal enterprises are flawed. Also, taxation likely will generate a large sum of revenue for each state. But those revenues might be offset by subsequent changes that will be needed in mental health, addiction, and wellness programs – a difficult proposition given the opioid epidemic already overburdening the country. Remember the tobacco cases and promise of state support for education, treatment, and other noble activities? Addiction medicine specialists worry that taxes collected by the states, and promises to prevent and treat gambling problems – and prevent addiction – will not end up in those coffers.
As clinicians, perhaps our most important contribution to the debates on this ruling lies in raising awareness of pathological gambling as an addiction disorder.
Redefining the act of gambling
Breaking down previous barriers to access and increasing convenience to gambling undoubtedly will be associated with increased pathological engagement in gambling. This conclusion is clear, based on past national experiments with substances of addiction (such as alcohol prohibition).
Since the cocaine epidemic of the 1980s, and our increased understanding that addictions need not have prominent withdrawal syndromes, we have focused on addiction as a fatal attraction. Psychiatrists and other clinicians made the case – in some quarters, at least – for sugar, sex, and Internet compulsivity as addictions. Compared with those addictions, the evidence was clearest and most compelling for pathological gambling as an addiction disorder. Indeed, gambling disorder was introduced in 2013 to the DSM-5 as the very first non–substance-based addictive disorder. This was a decisive change, as it recognizes that gambling is more than an environmental hazard for those suffering from dopamine-driven obsessive-compulsive-like dysfunction (the DSM section where it had lived previously). Instead, gambling acts as an agent that can initiate a usurpation of the brain’s reward circuitry. (In addition, this change has reopened the door for other increasingly recognized non–substance-based disorder categories such as video game and pornography addiction, and others.)
Gambling disorder certainly fits well into what many experts view as the essential phenotype of any addiction: Continued use despite harm, waning self-control over engagement, a craving state, and compulsive use. Current research is expanding rapidly and filling in the theoretical framework, strongly supporting gambling disorder based on biological evidence. Much of what we now know about the biology of addiction has been through the efforts of the Yale University–based research group, led by psychiatrist Marc N. Potenza. Dr. Potenza and his colleagues have been investigating gambling disorder in a thorough manner (Harv Rev Psychiatry. 2015 Mar-Apr;23[2]:134-46) and (Curr Treat Options Psychiatry. 2014 Jun 1;1[2]:189-203). Indeed, gambling disorder is much like the other substance-use disorders in which it is grouped, in that it has been found to share some similarities/pathways common to all addictions while also carrying its own specific nuances.
Twin studies have unearthed a wealth of information, such as knowledge that environmental factors seem to be the predominant source of the comorbid development of gambling disorder with the more socially acceptable substances as associated use disorders (alcohol, tobacco, and marijuana) through mechanisms such as peer association and place preference conditioning. Similarly, genetic influences also might be meaningful to treatment. For example, one finding showed that patients with gambling disorder and a family history of alcoholism were found to more preferentially respond to opioid-receptor antagonists as treatment for gambling disorder, compared with individuals without such family history (Psychopharmacology [Berl]. 2008;200[4]:521-7).
Explorations of neurotransmitter involvement and brain connectivity also have been conducted for gambling behaviors. Dopaminergic underpinnings of addiction have been particularly indicated in imaging studies focused on the ventral striatum and other components of reward circuitry. In addition, functional MRI studies have identified both overlapping and discordant brain imaging findings between gambling and many other substance use disorders such as cocaine. All these indicate that gambling seems, like its use-disorder counterparts, to follow a similar but distinct course of hijacking reward systems and priming the brain to seek out further gambling in a pathological manner.
Vulnerable populations
Another key finding of recent research exploring the biological foundations of gambling disorder is gender dimorphism. In numerous studies, women have been found to experience a “telescoping effect” from gambling, compared with their male counterparts, where they seem to more quickly advance from first exposure to problematic use. This phenomenon also is seen in women who use cocaine. Also, functional MRI studies also have found that women appear to have alternative signal changes in regions germane to addiction, compared with their male counterparts. One such example was greater activity in the hippocampus and middle temporal gyrus in women, suggestive of stronger activation of regions key for memory retrieval used in craving/urge-related emotions. These data highlight the need for not only understanding how gambling and other addictions diverge between men and women, but also for how prevention and treatment of these disorders might differ based on sex.
Adolescents also get special consideration: How will they be affected by this expected growth in gambling avenues? Adolescence and young adulthood are periods of development defined by increased impulsivity and risk taking, making this population particularly vulnerable to addiction that can then persist into adulthood. It is expected that age laws will persist and prevent the legal access adults might enjoy, but shifts in opinions of harm and ease of access are likely to contribute to increased gambling exposure. To use another addictive phenomena as an example, data from the Substance Abuse and Mental Health Services Administration show a clear correlation between marijuana use, marijuana legal status, and perceptions of risk. Specifically, areas with unfettered/loosened marijuana regulation have much lower levels of perceived risk among youth and much higher levels of use. Gambling could follow a similar course.
Perhaps the most crucial observation is that the most severe pathological gamblers began gambling before adulthood. Many factors have been identified that seem to increase rates of gambling in youth: Receiving scratch-off lotto cards as gifts, gambling on school grounds, and even smoking status (quite significant given the advent of e-cigarettes now common to many high school students). All of these essentially boil down to the common pathway of proximity and social referencing. As such, the notion that an increased social presence of (what will likely be) large scale, polished, mass televised sports gambling events will be associated with increased gambling behavior (and other mental health comorbidities) among youth is not far-fetched. What also is known for gambling, as well as for other addictive disorders, is that earlier age of onset is correlated to a worse prognosis of gambling disorder in adulthood. In other words, the earlier an addiction strikes, the deeper and more severe it is in the individual – further highlighting the impetus to focus concerns about the PASPA ruling toward the impact on youth.
Prevention and treatment
Lastly, it is important to consider the ground gained in preventing and treating gambling addiction. Many groups focused on treating and preventing gambling already are well established, such as Gamblers Anonymous, and these groups have produced favorable results. More targeted interventions such as cognitive-behavioral therapy adjusted for addiction disorders also have proved effective, as they often not only tackle the gambling disorder but also the collection of conditions it is so often comorbid with (affective illnesses, anxiety disorders).
Pharmacotherapy also has a role, further justifying the view of gambling disorder, and indeed all addiction disorders, as biological processes with biological solutions. Examinations into opiate antagonism and glutamatergic modulation (N-acetylcysteine) also have shown some promise. Prevention programs offer perhaps the best cost-effective ratio in reducing the societal burden of gambling, which is about $7 billion annually, according to 2013 estimates by the National Council on Problem Gambling). These programs have been conducted in schools through parent-teacher groups as well as publicly through distribution of informative psychoeducation via TV and advertising channels.
All available research conducted on treatment shows that further research and validation are needed. We should not pretend that increasing access to sports betting and normalizing the activity will not have an effect on gambling prevalence and problems. Prevention, even simple cautionary public warnings, requires time, money, and planning for effective execution.
Dr. Wenzinger is a clinical fellow, PGY-4, in the department of child and adolescent psychiatry at St. Louis Children’s Hospital. Dr. Gold is the 17th Distinguished Alumni Professor at the University of Florida, Gainesville, and professor of psychiatry (adjunct) at Washington University in St. Louis. He also serves as chairman of the scientific advisory boards for RiverMend Health.
The Supreme Court decision to overturn the federal law that prohibited state-sanctioned college and professional sports betting is bad news for clinicians who treat patients with addictions.
On May 14, the high court ruled 7-2 that the 1992 law, called the Professional and Amateur Sports Protection Act (PASPA), was unconstitutional. Now every state is free to operate, sponsor, promote, license, advertise, or authorize gambling for any college or professional sport–based event.
Optimistic outlooks on the death of PASPA include the foreseen opportunity by the states to tax and generate revenue on such gambling. Proponents of the ruling also argue that illegal activity that thrived on sports betting will now end.
But to what extent will either of those scenarios benefit the public?
If passage of various state marijuana laws is any example, assumptions that legal avenues will usurp illegal enterprises are flawed. Also, taxation likely will generate a large sum of revenue for each state. But those revenues might be offset by subsequent changes that will be needed in mental health, addiction, and wellness programs – a difficult proposition given the opioid epidemic already overburdening the country. Remember the tobacco cases and promise of state support for education, treatment, and other noble activities? Addiction medicine specialists worry that taxes collected by the states, and promises to prevent and treat gambling problems – and prevent addiction – will not end up in those coffers.
As clinicians, perhaps our most important contribution to the debates on this ruling lies in raising awareness of pathological gambling as an addiction disorder.
Redefining the act of gambling
Breaking down previous barriers to access and increasing convenience to gambling undoubtedly will be associated with increased pathological engagement in gambling. This conclusion is clear, based on past national experiments with substances of addiction (such as alcohol prohibition).
Since the cocaine epidemic of the 1980s, and our increased understanding that addictions need not have prominent withdrawal syndromes, we have focused on addiction as a fatal attraction. Psychiatrists and other clinicians made the case – in some quarters, at least – for sugar, sex, and Internet compulsivity as addictions. Compared with those addictions, the evidence was clearest and most compelling for pathological gambling as an addiction disorder. Indeed, gambling disorder was introduced in 2013 to the DSM-5 as the very first non–substance-based addictive disorder. This was a decisive change, as it recognizes that gambling is more than an environmental hazard for those suffering from dopamine-driven obsessive-compulsive-like dysfunction (the DSM section where it had lived previously). Instead, gambling acts as an agent that can initiate a usurpation of the brain’s reward circuitry. (In addition, this change has reopened the door for other increasingly recognized non–substance-based disorder categories such as video game and pornography addiction, and others.)
Gambling disorder certainly fits well into what many experts view as the essential phenotype of any addiction: Continued use despite harm, waning self-control over engagement, a craving state, and compulsive use. Current research is expanding rapidly and filling in the theoretical framework, strongly supporting gambling disorder based on biological evidence. Much of what we now know about the biology of addiction has been through the efforts of the Yale University–based research group, led by psychiatrist Marc N. Potenza. Dr. Potenza and his colleagues have been investigating gambling disorder in a thorough manner (Harv Rev Psychiatry. 2015 Mar-Apr;23[2]:134-46) and (Curr Treat Options Psychiatry. 2014 Jun 1;1[2]:189-203). Indeed, gambling disorder is much like the other substance-use disorders in which it is grouped, in that it has been found to share some similarities/pathways common to all addictions while also carrying its own specific nuances.
Twin studies have unearthed a wealth of information, such as knowledge that environmental factors seem to be the predominant source of the comorbid development of gambling disorder with the more socially acceptable substances as associated use disorders (alcohol, tobacco, and marijuana) through mechanisms such as peer association and place preference conditioning. Similarly, genetic influences also might be meaningful to treatment. For example, one finding showed that patients with gambling disorder and a family history of alcoholism were found to more preferentially respond to opioid-receptor antagonists as treatment for gambling disorder, compared with individuals without such family history (Psychopharmacology [Berl]. 2008;200[4]:521-7).
Explorations of neurotransmitter involvement and brain connectivity also have been conducted for gambling behaviors. Dopaminergic underpinnings of addiction have been particularly indicated in imaging studies focused on the ventral striatum and other components of reward circuitry. In addition, functional MRI studies have identified both overlapping and discordant brain imaging findings between gambling and many other substance use disorders such as cocaine. All these indicate that gambling seems, like its use-disorder counterparts, to follow a similar but distinct course of hijacking reward systems and priming the brain to seek out further gambling in a pathological manner.
Vulnerable populations
Another key finding of recent research exploring the biological foundations of gambling disorder is gender dimorphism. In numerous studies, women have been found to experience a “telescoping effect” from gambling, compared with their male counterparts, where they seem to more quickly advance from first exposure to problematic use. This phenomenon also is seen in women who use cocaine. Also, functional MRI studies also have found that women appear to have alternative signal changes in regions germane to addiction, compared with their male counterparts. One such example was greater activity in the hippocampus and middle temporal gyrus in women, suggestive of stronger activation of regions key for memory retrieval used in craving/urge-related emotions. These data highlight the need for not only understanding how gambling and other addictions diverge between men and women, but also for how prevention and treatment of these disorders might differ based on sex.
Adolescents also get special consideration: How will they be affected by this expected growth in gambling avenues? Adolescence and young adulthood are periods of development defined by increased impulsivity and risk taking, making this population particularly vulnerable to addiction that can then persist into adulthood. It is expected that age laws will persist and prevent the legal access adults might enjoy, but shifts in opinions of harm and ease of access are likely to contribute to increased gambling exposure. To use another addictive phenomena as an example, data from the Substance Abuse and Mental Health Services Administration show a clear correlation between marijuana use, marijuana legal status, and perceptions of risk. Specifically, areas with unfettered/loosened marijuana regulation have much lower levels of perceived risk among youth and much higher levels of use. Gambling could follow a similar course.
Perhaps the most crucial observation is that the most severe pathological gamblers began gambling before adulthood. Many factors have been identified that seem to increase rates of gambling in youth: Receiving scratch-off lotto cards as gifts, gambling on school grounds, and even smoking status (quite significant given the advent of e-cigarettes now common to many high school students). All of these essentially boil down to the common pathway of proximity and social referencing. As such, the notion that an increased social presence of (what will likely be) large scale, polished, mass televised sports gambling events will be associated with increased gambling behavior (and other mental health comorbidities) among youth is not far-fetched. What also is known for gambling, as well as for other addictive disorders, is that earlier age of onset is correlated to a worse prognosis of gambling disorder in adulthood. In other words, the earlier an addiction strikes, the deeper and more severe it is in the individual – further highlighting the impetus to focus concerns about the PASPA ruling toward the impact on youth.
Prevention and treatment
Lastly, it is important to consider the ground gained in preventing and treating gambling addiction. Many groups focused on treating and preventing gambling already are well established, such as Gamblers Anonymous, and these groups have produced favorable results. More targeted interventions such as cognitive-behavioral therapy adjusted for addiction disorders also have proved effective, as they often not only tackle the gambling disorder but also the collection of conditions it is so often comorbid with (affective illnesses, anxiety disorders).
Pharmacotherapy also has a role, further justifying the view of gambling disorder, and indeed all addiction disorders, as biological processes with biological solutions. Examinations into opiate antagonism and glutamatergic modulation (N-acetylcysteine) also have shown some promise. Prevention programs offer perhaps the best cost-effective ratio in reducing the societal burden of gambling, which is about $7 billion annually, according to 2013 estimates by the National Council on Problem Gambling). These programs have been conducted in schools through parent-teacher groups as well as publicly through distribution of informative psychoeducation via TV and advertising channels.
All available research conducted on treatment shows that further research and validation are needed. We should not pretend that increasing access to sports betting and normalizing the activity will not have an effect on gambling prevalence and problems. Prevention, even simple cautionary public warnings, requires time, money, and planning for effective execution.
Dr. Wenzinger is a clinical fellow, PGY-4, in the department of child and adolescent psychiatry at St. Louis Children’s Hospital. Dr. Gold is the 17th Distinguished Alumni Professor at the University of Florida, Gainesville, and professor of psychiatry (adjunct) at Washington University in St. Louis. He also serves as chairman of the scientific advisory boards for RiverMend Health.
The Supreme Court decision to overturn the federal law that prohibited state-sanctioned college and professional sports betting is bad news for clinicians who treat patients with addictions.
On May 14, the high court ruled 7-2 that the 1992 law, called the Professional and Amateur Sports Protection Act (PASPA), was unconstitutional. Now every state is free to operate, sponsor, promote, license, advertise, or authorize gambling for any college or professional sport–based event.
Optimistic outlooks on the death of PASPA include the foreseen opportunity by the states to tax and generate revenue on such gambling. Proponents of the ruling also argue that illegal activity that thrived on sports betting will now end.
But to what extent will either of those scenarios benefit the public?
If passage of various state marijuana laws is any example, assumptions that legal avenues will usurp illegal enterprises are flawed. Also, taxation likely will generate a large sum of revenue for each state. But those revenues might be offset by subsequent changes that will be needed in mental health, addiction, and wellness programs – a difficult proposition given the opioid epidemic already overburdening the country. Remember the tobacco cases and promise of state support for education, treatment, and other noble activities? Addiction medicine specialists worry that taxes collected by the states, and promises to prevent and treat gambling problems – and prevent addiction – will not end up in those coffers.
As clinicians, perhaps our most important contribution to the debates on this ruling lies in raising awareness of pathological gambling as an addiction disorder.
Redefining the act of gambling
Breaking down previous barriers to access and increasing convenience to gambling undoubtedly will be associated with increased pathological engagement in gambling. This conclusion is clear, based on past national experiments with substances of addiction (such as alcohol prohibition).
Since the cocaine epidemic of the 1980s, and our increased understanding that addictions need not have prominent withdrawal syndromes, we have focused on addiction as a fatal attraction. Psychiatrists and other clinicians made the case – in some quarters, at least – for sugar, sex, and Internet compulsivity as addictions. Compared with those addictions, the evidence was clearest and most compelling for pathological gambling as an addiction disorder. Indeed, gambling disorder was introduced in 2013 to the DSM-5 as the very first non–substance-based addictive disorder. This was a decisive change, as it recognizes that gambling is more than an environmental hazard for those suffering from dopamine-driven obsessive-compulsive-like dysfunction (the DSM section where it had lived previously). Instead, gambling acts as an agent that can initiate a usurpation of the brain’s reward circuitry. (In addition, this change has reopened the door for other increasingly recognized non–substance-based disorder categories such as video game and pornography addiction, and others.)
Gambling disorder certainly fits well into what many experts view as the essential phenotype of any addiction: Continued use despite harm, waning self-control over engagement, a craving state, and compulsive use. Current research is expanding rapidly and filling in the theoretical framework, strongly supporting gambling disorder based on biological evidence. Much of what we now know about the biology of addiction has been through the efforts of the Yale University–based research group, led by psychiatrist Marc N. Potenza. Dr. Potenza and his colleagues have been investigating gambling disorder in a thorough manner (Harv Rev Psychiatry. 2015 Mar-Apr;23[2]:134-46) and (Curr Treat Options Psychiatry. 2014 Jun 1;1[2]:189-203). Indeed, gambling disorder is much like the other substance-use disorders in which it is grouped, in that it has been found to share some similarities/pathways common to all addictions while also carrying its own specific nuances.
Twin studies have unearthed a wealth of information, such as knowledge that environmental factors seem to be the predominant source of the comorbid development of gambling disorder with the more socially acceptable substances as associated use disorders (alcohol, tobacco, and marijuana) through mechanisms such as peer association and place preference conditioning. Similarly, genetic influences also might be meaningful to treatment. For example, one finding showed that patients with gambling disorder and a family history of alcoholism were found to more preferentially respond to opioid-receptor antagonists as treatment for gambling disorder, compared with individuals without such family history (Psychopharmacology [Berl]. 2008;200[4]:521-7).
Explorations of neurotransmitter involvement and brain connectivity also have been conducted for gambling behaviors. Dopaminergic underpinnings of addiction have been particularly indicated in imaging studies focused on the ventral striatum and other components of reward circuitry. In addition, functional MRI studies have identified both overlapping and discordant brain imaging findings between gambling and many other substance use disorders such as cocaine. All these indicate that gambling seems, like its use-disorder counterparts, to follow a similar but distinct course of hijacking reward systems and priming the brain to seek out further gambling in a pathological manner.
Vulnerable populations
Another key finding of recent research exploring the biological foundations of gambling disorder is gender dimorphism. In numerous studies, women have been found to experience a “telescoping effect” from gambling, compared with their male counterparts, where they seem to more quickly advance from first exposure to problematic use. This phenomenon also is seen in women who use cocaine. Also, functional MRI studies also have found that women appear to have alternative signal changes in regions germane to addiction, compared with their male counterparts. One such example was greater activity in the hippocampus and middle temporal gyrus in women, suggestive of stronger activation of regions key for memory retrieval used in craving/urge-related emotions. These data highlight the need for not only understanding how gambling and other addictions diverge between men and women, but also for how prevention and treatment of these disorders might differ based on sex.
Adolescents also get special consideration: How will they be affected by this expected growth in gambling avenues? Adolescence and young adulthood are periods of development defined by increased impulsivity and risk taking, making this population particularly vulnerable to addiction that can then persist into adulthood. It is expected that age laws will persist and prevent the legal access adults might enjoy, but shifts in opinions of harm and ease of access are likely to contribute to increased gambling exposure. To use another addictive phenomena as an example, data from the Substance Abuse and Mental Health Services Administration show a clear correlation between marijuana use, marijuana legal status, and perceptions of risk. Specifically, areas with unfettered/loosened marijuana regulation have much lower levels of perceived risk among youth and much higher levels of use. Gambling could follow a similar course.
Perhaps the most crucial observation is that the most severe pathological gamblers began gambling before adulthood. Many factors have been identified that seem to increase rates of gambling in youth: Receiving scratch-off lotto cards as gifts, gambling on school grounds, and even smoking status (quite significant given the advent of e-cigarettes now common to many high school students). All of these essentially boil down to the common pathway of proximity and social referencing. As such, the notion that an increased social presence of (what will likely be) large scale, polished, mass televised sports gambling events will be associated with increased gambling behavior (and other mental health comorbidities) among youth is not far-fetched. What also is known for gambling, as well as for other addictive disorders, is that earlier age of onset is correlated to a worse prognosis of gambling disorder in adulthood. In other words, the earlier an addiction strikes, the deeper and more severe it is in the individual – further highlighting the impetus to focus concerns about the PASPA ruling toward the impact on youth.
Prevention and treatment
Lastly, it is important to consider the ground gained in preventing and treating gambling addiction. Many groups focused on treating and preventing gambling already are well established, such as Gamblers Anonymous, and these groups have produced favorable results. More targeted interventions such as cognitive-behavioral therapy adjusted for addiction disorders also have proved effective, as they often not only tackle the gambling disorder but also the collection of conditions it is so often comorbid with (affective illnesses, anxiety disorders).
Pharmacotherapy also has a role, further justifying the view of gambling disorder, and indeed all addiction disorders, as biological processes with biological solutions. Examinations into opiate antagonism and glutamatergic modulation (N-acetylcysteine) also have shown some promise. Prevention programs offer perhaps the best cost-effective ratio in reducing the societal burden of gambling, which is about $7 billion annually, according to 2013 estimates by the National Council on Problem Gambling). These programs have been conducted in schools through parent-teacher groups as well as publicly through distribution of informative psychoeducation via TV and advertising channels.
All available research conducted on treatment shows that further research and validation are needed. We should not pretend that increasing access to sports betting and normalizing the activity will not have an effect on gambling prevalence and problems. Prevention, even simple cautionary public warnings, requires time, money, and planning for effective execution.
Dr. Wenzinger is a clinical fellow, PGY-4, in the department of child and adolescent psychiatry at St. Louis Children’s Hospital. Dr. Gold is the 17th Distinguished Alumni Professor at the University of Florida, Gainesville, and professor of psychiatry (adjunct) at Washington University in St. Louis. He also serves as chairman of the scientific advisory boards for RiverMend Health.
The demise of family dinners may play role in picky eating
My wife and I have dinner together almost every evening. There is a candle on the table regardless of the menu. And the meal begins with a toast, usually “To this chance to be together.” I can hear you muttering to yourself, “They must be one of those sappy, sweet hand-holding couples that appear to be joined at the hip.” Far from it, we lead very busy, active, but separate lives that only rarely intersect. But we make it a priority that one of those intersections occurs at a meal. For us, an evening dinner works best.
Listening to our friends, we have learned that an increasing number of them have drifted away from sharing a meal together. This phenomenon is surprising because most of them are retired, and time is not an issue. Of course, it is no secret that, for young overscheduled families, sitting down for a shared dining experience is becoming increasingly less frequent. Like some of you, I would like to claim that a return to family meal times would solve all of society’s ills. But some of the literature supporting this claim suggests shared family experiences in general, not particularly those associated with eating, may be just as important in supporting emotional health. But because everyone needs to eat, meals seem to me to be the easy target, low-hanging fruit if you will.
It is interesting that parents’ reports of their children’s eating patterns were validated by the behaviors videotaped by the researchers. But what is really interesting is that children who grew up in households where mealtimes followed a routine were more likely to be in the low–picky eating group. Routines included things like having a specific place times for eating, a habitual way of serving food, and other rituals such as saying grace.
Unfortunately, because this Michigan study began at age 4 years it doesn’t tell us if the worst picky eaters were that way from the beginning. I suspect that some were. But my hunch is that picky eaters who are managed in a home environment that includes mealtime rituals and puts dining together as a high priority are more likely to outgrow their pickiness.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater: A Guide for the Perplexed Parent.” Email him at [email protected].
My wife and I have dinner together almost every evening. There is a candle on the table regardless of the menu. And the meal begins with a toast, usually “To this chance to be together.” I can hear you muttering to yourself, “They must be one of those sappy, sweet hand-holding couples that appear to be joined at the hip.” Far from it, we lead very busy, active, but separate lives that only rarely intersect. But we make it a priority that one of those intersections occurs at a meal. For us, an evening dinner works best.
Listening to our friends, we have learned that an increasing number of them have drifted away from sharing a meal together. This phenomenon is surprising because most of them are retired, and time is not an issue. Of course, it is no secret that, for young overscheduled families, sitting down for a shared dining experience is becoming increasingly less frequent. Like some of you, I would like to claim that a return to family meal times would solve all of society’s ills. But some of the literature supporting this claim suggests shared family experiences in general, not particularly those associated with eating, may be just as important in supporting emotional health. But because everyone needs to eat, meals seem to me to be the easy target, low-hanging fruit if you will.
It is interesting that parents’ reports of their children’s eating patterns were validated by the behaviors videotaped by the researchers. But what is really interesting is that children who grew up in households where mealtimes followed a routine were more likely to be in the low–picky eating group. Routines included things like having a specific place times for eating, a habitual way of serving food, and other rituals such as saying grace.
Unfortunately, because this Michigan study began at age 4 years it doesn’t tell us if the worst picky eaters were that way from the beginning. I suspect that some were. But my hunch is that picky eaters who are managed in a home environment that includes mealtime rituals and puts dining together as a high priority are more likely to outgrow their pickiness.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater: A Guide for the Perplexed Parent.” Email him at [email protected].
My wife and I have dinner together almost every evening. There is a candle on the table regardless of the menu. And the meal begins with a toast, usually “To this chance to be together.” I can hear you muttering to yourself, “They must be one of those sappy, sweet hand-holding couples that appear to be joined at the hip.” Far from it, we lead very busy, active, but separate lives that only rarely intersect. But we make it a priority that one of those intersections occurs at a meal. For us, an evening dinner works best.
Listening to our friends, we have learned that an increasing number of them have drifted away from sharing a meal together. This phenomenon is surprising because most of them are retired, and time is not an issue. Of course, it is no secret that, for young overscheduled families, sitting down for a shared dining experience is becoming increasingly less frequent. Like some of you, I would like to claim that a return to family meal times would solve all of society’s ills. But some of the literature supporting this claim suggests shared family experiences in general, not particularly those associated with eating, may be just as important in supporting emotional health. But because everyone needs to eat, meals seem to me to be the easy target, low-hanging fruit if you will.
It is interesting that parents’ reports of their children’s eating patterns were validated by the behaviors videotaped by the researchers. But what is really interesting is that children who grew up in households where mealtimes followed a routine were more likely to be in the low–picky eating group. Routines included things like having a specific place times for eating, a habitual way of serving food, and other rituals such as saying grace.
Unfortunately, because this Michigan study began at age 4 years it doesn’t tell us if the worst picky eaters were that way from the beginning. I suspect that some were. But my hunch is that picky eaters who are managed in a home environment that includes mealtime rituals and puts dining together as a high priority are more likely to outgrow their pickiness.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater: A Guide for the Perplexed Parent.” Email him at [email protected].