User login
The VA Cannot Be Privatized
As usual, it was a hectic Monday on the psychiatry consult service. All the trainees, from medical student to fellow, were seeing other patients when the call came from the surgery clinic. One of the pleasures of being a VA clinician is the ability to teach and supervise medical students and residents. The attending in that busy clinic said, “There is a patient down here who is refusing care for a gangrenous leg, but he is also talking about his life not being worth living. Could someone evaluate him?” That patient, Mr. S, declined to go to either the emergency department or the urgent care psychiatry clinic, so I went to see him. I realized that I had seen this patient in the hospital several times before.
One of the great clinical benefits of working in the VA, as opposed to in academic or community hospitals, is continuity. In my nearly 20 years at the same medical center, I have had the privilege of following many patients through multiple courses of treatment. This continuity is a huge advantage when there is what Hippocrates called a “critical day,” as on that Monday in the surgery clinic.2 Also, in many cases the continuity allows me to have a reservoir of trust that I can draw on for challenging consultations, like that of Mr. S.
The surgery resident and attending had spent more than an hour talking to Mr. S when I arrived but still they joined me for the conversation. Mr. S was a veteran in his sixties, and after a few minutes of listening to him, it was clear he was talking about ending his life because of its poor quality. He told us that he had acquired the infection in his leg secondary to unsanitary living conditions. The veteran was quite a storyteller, intelligent, and had a wry sense of humor, which only made his point that his living conditions were intolerable more poignant. He apparently had tried to talk to someone about his situation but felt frustrated that he had not obtained more help.
The surgery attending had already told Mr. S that he would respect his right to refuse the amputation but he feared that Mr. S’s refusal was an expression of his depression and hopelessness, hence, the psychiatry consult. Although Mr. S was not acutely suicidal, something about the combination of his despair and deliberation worried me.
The surgery attending offered to admit Mr. S to do a further workup of his leg. I encouraged him to accept this option and added that I would make sure a social worker saw him and the psychiatry service department also would follow him. Mr. S declined even a 24-hour admission, saying that he had just moved to a new apartment and “everything I have in the world is there and I don’t want to lose it.” This comment suggested to me that he was ambivalent about his wish to die and provided an opening to reduce his risk of harming himself either directly or indirectly.
After the discussion, Mr. S seemed to believe we cared about him and was more willing to participate in treatment planning. He agreed to let the surgeons draw blood and to pick up oral antibiotics from the pharmacy. I promised him that if he would come back to clinic that week, I would make sure a social worker met with him and that my team would talk with him more about his depression. Mr. S picked Friday for his return and assured me that now that he knew we were going to try and improve his situation, he would not hurt himself. Obviously, this was a risk on my part—but the show of compassion combined with flexibility had created a therapeutic alliance that I believed was sufficient to protect Mr. S until we met again.
I returned to my office and called the chief of social work: The dedication of career VA employees forges effective working relationships that can be leveraged for the benefit of the patients. At my facility and many others, many of the staff members who are now in positions of leadership rose through the ranks together, giving us a solidarity of purpose and mutual reliance that are rare in community health care settings. The chief of social work looked at the patient’s chart with me on the phone while I explained the circumstances and within a few minutes said, “We can help him. It looks like he is eligible for an increased pension, and I think we can find him better housing.”
I admit to some anxiety on Friday. One of the psychiatry residents on the service had volunteered to see Mr. S after studying his chart in the morning. Most of us are aware that the aging VA electronic health record system is due to be replaced. But having access to more than 20 years of medical history from episodes of inpatient, outpatient, and residential care all over the country is an unrivaled asset that brings a unique breadth that sharpens, deepens, and humanizes diagnosis and treatment planning.
Sure enough at 10
The social worker arranged new housing for Mr. S that day and help to move into his new place. The paperwork was submitted for the pension increase, and help for shopping and meals as well as transportation was either put in place or applied for. As he left to pack, Mr. S told the surgeon he might not want hospice just yet.
The coda to this narrative is equally uplifting. Several weeks after Mr. S was seen in the surgery clinic, I received a call from a midlevel psychiatric practitioner in the urgent care clinic who had been on leave for several weeks. He too had seen Mr. S before and shared my concern about his state of mind and well-being. He thanked me for having the consult service see him and remarked that it was a relief to know Mr. S had been taken care of and was in a better place in every sense of the word.
In response to a rising media tide of concern about the direction VA care is headed, Congress and the VA have issued a strong statements, “debunking” what they called the “myth” of privatization.3 Yet for the first time in my career, many thoughtful people discern a constellation of forces that could eventuate in this reality in our lifetimes. The title and message of this column is that the VA cannot be privatized, not that it will not be privatized. Also, I did not say that it should not be privatized. As I have written in other columns, that is because ethically I do not believe this is even a question.4 Privatization breaks President Abraham Lincoln’s promise to veterans, “to care for him who has borne the battle.” A promise that was kept for Mr. S and is fulfilled for thousands of other veterans every day all over this nation. A promise that far exceeds payments for medical services.
I also do not mean the title to be a rejection of the Veterans Choice Program. The VA has always provided—and should continue to offer—community-based care for veterans that complements VA care. For example, I live in one of the most rural states in the union and recognize that a patient should not have to drive 300 miles to get a routine colonoscopy.
The VA cannot be privatized because of the comprehensive care that it provides: the degree of integration; the wealth of resources; and the level of expertise in caring for the complex medical, psychiatric, and psychosocial problems of veterans cannot be replicated. Nor is this just my opinion—a recent RAND Corporation study documents the evidence.5 There are many medical services in the private sector that may be delivered more efficiently, and Congress has just passed the Mission Act to allocate the funds needed to ensure our veterans have wider and easier access to private care resources.6 Yet someone must coordinate, monitor, and center all these services on the veteran. It is not likely Mr. S’s story would have had this kind of ending in the community. The continuity of care, the access to staff with the knowledge of veterans benefits and health care needs, and the ability to listen and follow up without time or performance constraints is just not possible outside VA.
The other evening in the parking lot of the hospital, I encountered a physician who had left the VA to work in several other large health care organizations. He had some good things to say about their business processes and the volume of patients they saw. He came back to the VA, he said, because “No one else can provide this quality of care for the individual veteran.”
1. Conway E, Batalden P. Like magic? (“Every system is perfectly designed…”). http://www.ihi.org/communities/blogs/o rigin-of-every-system-is-perfectly-designed-quote. Published August 21, 2015. Accessed May 29, 2018.
2. Lloyd GER, ed. Hippocratic Writings . London: Penguin Books ; 1983.
3. US Department of Veterans Affairs, Office of Public and Intergovernmental Affairs. Debunking the VA privatization myth [press release]. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=4034. Published April 5, 2018. Accessed June 4, 2018.
4. Geppert CMA. Lessons from history: the ethical foundation of VA health care. Fed Pract. 2016;33(4):6-7.
5. Tanielian T, Farmer CM, Burns RM, Duffy EL, Messan Setodji C. Ready or Not? Assessing the Capacity of New York State Health Care Providers to Meet the Needs of Veterans. Santa Monica, CA: RAND Corporation, 2018.
6. VA MISSION Act of 2018, S 2372, 115th Congress, 2nd Sess (2018).
As usual, it was a hectic Monday on the psychiatry consult service. All the trainees, from medical student to fellow, were seeing other patients when the call came from the surgery clinic. One of the pleasures of being a VA clinician is the ability to teach and supervise medical students and residents. The attending in that busy clinic said, “There is a patient down here who is refusing care for a gangrenous leg, but he is also talking about his life not being worth living. Could someone evaluate him?” That patient, Mr. S, declined to go to either the emergency department or the urgent care psychiatry clinic, so I went to see him. I realized that I had seen this patient in the hospital several times before.
One of the great clinical benefits of working in the VA, as opposed to in academic or community hospitals, is continuity. In my nearly 20 years at the same medical center, I have had the privilege of following many patients through multiple courses of treatment. This continuity is a huge advantage when there is what Hippocrates called a “critical day,” as on that Monday in the surgery clinic.2 Also, in many cases the continuity allows me to have a reservoir of trust that I can draw on for challenging consultations, like that of Mr. S.
The surgery resident and attending had spent more than an hour talking to Mr. S when I arrived but still they joined me for the conversation. Mr. S was a veteran in his sixties, and after a few minutes of listening to him, it was clear he was talking about ending his life because of its poor quality. He told us that he had acquired the infection in his leg secondary to unsanitary living conditions. The veteran was quite a storyteller, intelligent, and had a wry sense of humor, which only made his point that his living conditions were intolerable more poignant. He apparently had tried to talk to someone about his situation but felt frustrated that he had not obtained more help.
The surgery attending had already told Mr. S that he would respect his right to refuse the amputation but he feared that Mr. S’s refusal was an expression of his depression and hopelessness, hence, the psychiatry consult. Although Mr. S was not acutely suicidal, something about the combination of his despair and deliberation worried me.
The surgery attending offered to admit Mr. S to do a further workup of his leg. I encouraged him to accept this option and added that I would make sure a social worker saw him and the psychiatry service department also would follow him. Mr. S declined even a 24-hour admission, saying that he had just moved to a new apartment and “everything I have in the world is there and I don’t want to lose it.” This comment suggested to me that he was ambivalent about his wish to die and provided an opening to reduce his risk of harming himself either directly or indirectly.
After the discussion, Mr. S seemed to believe we cared about him and was more willing to participate in treatment planning. He agreed to let the surgeons draw blood and to pick up oral antibiotics from the pharmacy. I promised him that if he would come back to clinic that week, I would make sure a social worker met with him and that my team would talk with him more about his depression. Mr. S picked Friday for his return and assured me that now that he knew we were going to try and improve his situation, he would not hurt himself. Obviously, this was a risk on my part—but the show of compassion combined with flexibility had created a therapeutic alliance that I believed was sufficient to protect Mr. S until we met again.
I returned to my office and called the chief of social work: The dedication of career VA employees forges effective working relationships that can be leveraged for the benefit of the patients. At my facility and many others, many of the staff members who are now in positions of leadership rose through the ranks together, giving us a solidarity of purpose and mutual reliance that are rare in community health care settings. The chief of social work looked at the patient’s chart with me on the phone while I explained the circumstances and within a few minutes said, “We can help him. It looks like he is eligible for an increased pension, and I think we can find him better housing.”
I admit to some anxiety on Friday. One of the psychiatry residents on the service had volunteered to see Mr. S after studying his chart in the morning. Most of us are aware that the aging VA electronic health record system is due to be replaced. But having access to more than 20 years of medical history from episodes of inpatient, outpatient, and residential care all over the country is an unrivaled asset that brings a unique breadth that sharpens, deepens, and humanizes diagnosis and treatment planning.
Sure enough at 10
The social worker arranged new housing for Mr. S that day and help to move into his new place. The paperwork was submitted for the pension increase, and help for shopping and meals as well as transportation was either put in place or applied for. As he left to pack, Mr. S told the surgeon he might not want hospice just yet.
The coda to this narrative is equally uplifting. Several weeks after Mr. S was seen in the surgery clinic, I received a call from a midlevel psychiatric practitioner in the urgent care clinic who had been on leave for several weeks. He too had seen Mr. S before and shared my concern about his state of mind and well-being. He thanked me for having the consult service see him and remarked that it was a relief to know Mr. S had been taken care of and was in a better place in every sense of the word.
In response to a rising media tide of concern about the direction VA care is headed, Congress and the VA have issued a strong statements, “debunking” what they called the “myth” of privatization.3 Yet for the first time in my career, many thoughtful people discern a constellation of forces that could eventuate in this reality in our lifetimes. The title and message of this column is that the VA cannot be privatized, not that it will not be privatized. Also, I did not say that it should not be privatized. As I have written in other columns, that is because ethically I do not believe this is even a question.4 Privatization breaks President Abraham Lincoln’s promise to veterans, “to care for him who has borne the battle.” A promise that was kept for Mr. S and is fulfilled for thousands of other veterans every day all over this nation. A promise that far exceeds payments for medical services.
I also do not mean the title to be a rejection of the Veterans Choice Program. The VA has always provided—and should continue to offer—community-based care for veterans that complements VA care. For example, I live in one of the most rural states in the union and recognize that a patient should not have to drive 300 miles to get a routine colonoscopy.
The VA cannot be privatized because of the comprehensive care that it provides: the degree of integration; the wealth of resources; and the level of expertise in caring for the complex medical, psychiatric, and psychosocial problems of veterans cannot be replicated. Nor is this just my opinion—a recent RAND Corporation study documents the evidence.5 There are many medical services in the private sector that may be delivered more efficiently, and Congress has just passed the Mission Act to allocate the funds needed to ensure our veterans have wider and easier access to private care resources.6 Yet someone must coordinate, monitor, and center all these services on the veteran. It is not likely Mr. S’s story would have had this kind of ending in the community. The continuity of care, the access to staff with the knowledge of veterans benefits and health care needs, and the ability to listen and follow up without time or performance constraints is just not possible outside VA.
The other evening in the parking lot of the hospital, I encountered a physician who had left the VA to work in several other large health care organizations. He had some good things to say about their business processes and the volume of patients they saw. He came back to the VA, he said, because “No one else can provide this quality of care for the individual veteran.”
As usual, it was a hectic Monday on the psychiatry consult service. All the trainees, from medical student to fellow, were seeing other patients when the call came from the surgery clinic. One of the pleasures of being a VA clinician is the ability to teach and supervise medical students and residents. The attending in that busy clinic said, “There is a patient down here who is refusing care for a gangrenous leg, but he is also talking about his life not being worth living. Could someone evaluate him?” That patient, Mr. S, declined to go to either the emergency department or the urgent care psychiatry clinic, so I went to see him. I realized that I had seen this patient in the hospital several times before.
One of the great clinical benefits of working in the VA, as opposed to in academic or community hospitals, is continuity. In my nearly 20 years at the same medical center, I have had the privilege of following many patients through multiple courses of treatment. This continuity is a huge advantage when there is what Hippocrates called a “critical day,” as on that Monday in the surgery clinic.2 Also, in many cases the continuity allows me to have a reservoir of trust that I can draw on for challenging consultations, like that of Mr. S.
The surgery resident and attending had spent more than an hour talking to Mr. S when I arrived but still they joined me for the conversation. Mr. S was a veteran in his sixties, and after a few minutes of listening to him, it was clear he was talking about ending his life because of its poor quality. He told us that he had acquired the infection in his leg secondary to unsanitary living conditions. The veteran was quite a storyteller, intelligent, and had a wry sense of humor, which only made his point that his living conditions were intolerable more poignant. He apparently had tried to talk to someone about his situation but felt frustrated that he had not obtained more help.
The surgery attending had already told Mr. S that he would respect his right to refuse the amputation but he feared that Mr. S’s refusal was an expression of his depression and hopelessness, hence, the psychiatry consult. Although Mr. S was not acutely suicidal, something about the combination of his despair and deliberation worried me.
The surgery attending offered to admit Mr. S to do a further workup of his leg. I encouraged him to accept this option and added that I would make sure a social worker saw him and the psychiatry service department also would follow him. Mr. S declined even a 24-hour admission, saying that he had just moved to a new apartment and “everything I have in the world is there and I don’t want to lose it.” This comment suggested to me that he was ambivalent about his wish to die and provided an opening to reduce his risk of harming himself either directly or indirectly.
After the discussion, Mr. S seemed to believe we cared about him and was more willing to participate in treatment planning. He agreed to let the surgeons draw blood and to pick up oral antibiotics from the pharmacy. I promised him that if he would come back to clinic that week, I would make sure a social worker met with him and that my team would talk with him more about his depression. Mr. S picked Friday for his return and assured me that now that he knew we were going to try and improve his situation, he would not hurt himself. Obviously, this was a risk on my part—but the show of compassion combined with flexibility had created a therapeutic alliance that I believed was sufficient to protect Mr. S until we met again.
I returned to my office and called the chief of social work: The dedication of career VA employees forges effective working relationships that can be leveraged for the benefit of the patients. At my facility and many others, many of the staff members who are now in positions of leadership rose through the ranks together, giving us a solidarity of purpose and mutual reliance that are rare in community health care settings. The chief of social work looked at the patient’s chart with me on the phone while I explained the circumstances and within a few minutes said, “We can help him. It looks like he is eligible for an increased pension, and I think we can find him better housing.”
I admit to some anxiety on Friday. One of the psychiatry residents on the service had volunteered to see Mr. S after studying his chart in the morning. Most of us are aware that the aging VA electronic health record system is due to be replaced. But having access to more than 20 years of medical history from episodes of inpatient, outpatient, and residential care all over the country is an unrivaled asset that brings a unique breadth that sharpens, deepens, and humanizes diagnosis and treatment planning.
Sure enough at 10
The social worker arranged new housing for Mr. S that day and help to move into his new place. The paperwork was submitted for the pension increase, and help for shopping and meals as well as transportation was either put in place or applied for. As he left to pack, Mr. S told the surgeon he might not want hospice just yet.
The coda to this narrative is equally uplifting. Several weeks after Mr. S was seen in the surgery clinic, I received a call from a midlevel psychiatric practitioner in the urgent care clinic who had been on leave for several weeks. He too had seen Mr. S before and shared my concern about his state of mind and well-being. He thanked me for having the consult service see him and remarked that it was a relief to know Mr. S had been taken care of and was in a better place in every sense of the word.
In response to a rising media tide of concern about the direction VA care is headed, Congress and the VA have issued a strong statements, “debunking” what they called the “myth” of privatization.3 Yet for the first time in my career, many thoughtful people discern a constellation of forces that could eventuate in this reality in our lifetimes. The title and message of this column is that the VA cannot be privatized, not that it will not be privatized. Also, I did not say that it should not be privatized. As I have written in other columns, that is because ethically I do not believe this is even a question.4 Privatization breaks President Abraham Lincoln’s promise to veterans, “to care for him who has borne the battle.” A promise that was kept for Mr. S and is fulfilled for thousands of other veterans every day all over this nation. A promise that far exceeds payments for medical services.
I also do not mean the title to be a rejection of the Veterans Choice Program. The VA has always provided—and should continue to offer—community-based care for veterans that complements VA care. For example, I live in one of the most rural states in the union and recognize that a patient should not have to drive 300 miles to get a routine colonoscopy.
The VA cannot be privatized because of the comprehensive care that it provides: the degree of integration; the wealth of resources; and the level of expertise in caring for the complex medical, psychiatric, and psychosocial problems of veterans cannot be replicated. Nor is this just my opinion—a recent RAND Corporation study documents the evidence.5 There are many medical services in the private sector that may be delivered more efficiently, and Congress has just passed the Mission Act to allocate the funds needed to ensure our veterans have wider and easier access to private care resources.6 Yet someone must coordinate, monitor, and center all these services on the veteran. It is not likely Mr. S’s story would have had this kind of ending in the community. The continuity of care, the access to staff with the knowledge of veterans benefits and health care needs, and the ability to listen and follow up without time or performance constraints is just not possible outside VA.
The other evening in the parking lot of the hospital, I encountered a physician who had left the VA to work in several other large health care organizations. He had some good things to say about their business processes and the volume of patients they saw. He came back to the VA, he said, because “No one else can provide this quality of care for the individual veteran.”
1. Conway E, Batalden P. Like magic? (“Every system is perfectly designed…”). http://www.ihi.org/communities/blogs/o rigin-of-every-system-is-perfectly-designed-quote. Published August 21, 2015. Accessed May 29, 2018.
2. Lloyd GER, ed. Hippocratic Writings . London: Penguin Books ; 1983.
3. US Department of Veterans Affairs, Office of Public and Intergovernmental Affairs. Debunking the VA privatization myth [press release]. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=4034. Published April 5, 2018. Accessed June 4, 2018.
4. Geppert CMA. Lessons from history: the ethical foundation of VA health care. Fed Pract. 2016;33(4):6-7.
5. Tanielian T, Farmer CM, Burns RM, Duffy EL, Messan Setodji C. Ready or Not? Assessing the Capacity of New York State Health Care Providers to Meet the Needs of Veterans. Santa Monica, CA: RAND Corporation, 2018.
6. VA MISSION Act of 2018, S 2372, 115th Congress, 2nd Sess (2018).
1. Conway E, Batalden P. Like magic? (“Every system is perfectly designed…”). http://www.ihi.org/communities/blogs/o rigin-of-every-system-is-perfectly-designed-quote. Published August 21, 2015. Accessed May 29, 2018.
2. Lloyd GER, ed. Hippocratic Writings . London: Penguin Books ; 1983.
3. US Department of Veterans Affairs, Office of Public and Intergovernmental Affairs. Debunking the VA privatization myth [press release]. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=4034. Published April 5, 2018. Accessed June 4, 2018.
4. Geppert CMA. Lessons from history: the ethical foundation of VA health care. Fed Pract. 2016;33(4):6-7.
5. Tanielian T, Farmer CM, Burns RM, Duffy EL, Messan Setodji C. Ready or Not? Assessing the Capacity of New York State Health Care Providers to Meet the Needs of Veterans. Santa Monica, CA: RAND Corporation, 2018.
6. VA MISSION Act of 2018, S 2372, 115th Congress, 2nd Sess (2018).
Medication management
This is the tenth in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
An important part of self-management (last month’s article) is medication management, often augmented by the use of a portal and always cognizant of the importance of medication reconciliation and drug interactions. These latter issues can be addressed with health information technology (health IT), which will be discussed the next two columns. This month, we examine some of AHRQ’s other tools and resources to assist with medication management.
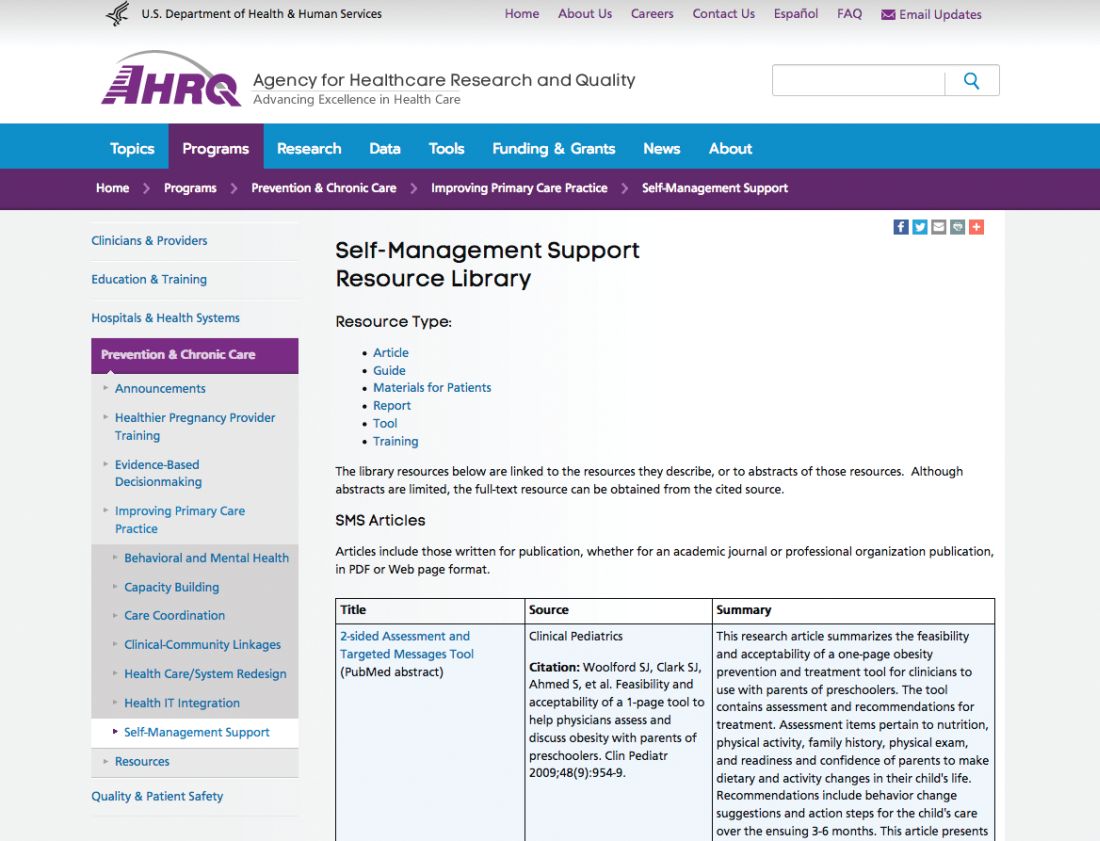
Patient understanding of the medications and medication schedule is important, and therefore health literacy key. The AHRQ Health Literacy Universal Precautions Toolkit – 2nd edition can help primary care practices reduce the complexity of health care, increase patient understanding of health information, and enhance support for patients of all health literacy levels. Also available are the companion guide, Implementing the AHRQ Health Literacy Universal Precautions Toolkit: Practical Ideas for Primary Care Practices, and a crosswalk showing how implementing health literacy tools can help meet standards for patient-centered medical home certification or recognition or meet Accreditation Canada standards.
Finally, How to Create a Pill Card helps users create an easy-to-use “pill card” for anyone who has a hard time keeping track of their medicines. Step-by-step instructions, sample clip art, and suggestions for design and use will help to customize a reminder card.
These and other tools can be found at the NCEPCR Web site: www.ahrq.gov/ncepcr.
Dr. Ganiats is director of the National Center for Excellence in Primary Care Research at AHRQ, Rockville, Md.
This is the tenth in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
An important part of self-management (last month’s article) is medication management, often augmented by the use of a portal and always cognizant of the importance of medication reconciliation and drug interactions. These latter issues can be addressed with health information technology (health IT), which will be discussed the next two columns. This month, we examine some of AHRQ’s other tools and resources to assist with medication management.
Patient understanding of the medications and medication schedule is important, and therefore health literacy key. The AHRQ Health Literacy Universal Precautions Toolkit – 2nd edition can help primary care practices reduce the complexity of health care, increase patient understanding of health information, and enhance support for patients of all health literacy levels. Also available are the companion guide, Implementing the AHRQ Health Literacy Universal Precautions Toolkit: Practical Ideas for Primary Care Practices, and a crosswalk showing how implementing health literacy tools can help meet standards for patient-centered medical home certification or recognition or meet Accreditation Canada standards.
Finally, How to Create a Pill Card helps users create an easy-to-use “pill card” for anyone who has a hard time keeping track of their medicines. Step-by-step instructions, sample clip art, and suggestions for design and use will help to customize a reminder card.
These and other tools can be found at the NCEPCR Web site: www.ahrq.gov/ncepcr.
Dr. Ganiats is director of the National Center for Excellence in Primary Care Research at AHRQ, Rockville, Md.
This is the tenth in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
An important part of self-management (last month’s article) is medication management, often augmented by the use of a portal and always cognizant of the importance of medication reconciliation and drug interactions. These latter issues can be addressed with health information technology (health IT), which will be discussed the next two columns. This month, we examine some of AHRQ’s other tools and resources to assist with medication management.
Patient understanding of the medications and medication schedule is important, and therefore health literacy key. The AHRQ Health Literacy Universal Precautions Toolkit – 2nd edition can help primary care practices reduce the complexity of health care, increase patient understanding of health information, and enhance support for patients of all health literacy levels. Also available are the companion guide, Implementing the AHRQ Health Literacy Universal Precautions Toolkit: Practical Ideas for Primary Care Practices, and a crosswalk showing how implementing health literacy tools can help meet standards for patient-centered medical home certification or recognition or meet Accreditation Canada standards.
Finally, How to Create a Pill Card helps users create an easy-to-use “pill card” for anyone who has a hard time keeping track of their medicines. Step-by-step instructions, sample clip art, and suggestions for design and use will help to customize a reminder card.
These and other tools can be found at the NCEPCR Web site: www.ahrq.gov/ncepcr.
Dr. Ganiats is director of the National Center for Excellence in Primary Care Research at AHRQ, Rockville, Md.
Updated Guidelines on Peanut Allergy Prevention in Infants With Atopic Dermatitis
It has been said that “extraordinary claims require extraordinary evidence.”1 In the pursuit of evidence-based medicine, we are encouraged to follow a similar standard, with an emphasis on waiting for multiple studies with good-quality data and high levels of agreement before changing any aspect of our clinical practice. The ostensible purpose is that studies can be flawed, conclusions can be incorrect, or biases can be overlooked. In such cases, acting on questionable results could imperil patients. It is for this reason that so many review articles sometimes frustratingly seem to conclude that further evidence is needed.2
Based on this standard, recently published addendum guidelines from the National Institute of Allergy and Infectious Diseases for prevention of peanut allergy in the United States3 are somewhat striking in that they make fairly bold recommendations based on results from the 2015 Learning Early about Peanut Allergy (LEAP) study,4 a randomized trial evaluating early peanut introduction as a preventive strategy for peanut allergy. Of note, this study was not placebo controlled, was conducted at only 1 site in the United Kingdom, and only included 640 children, though the number of participants was admittedly large for this type of study.4 Arguably, the LEAP study alone does not provide enough evidence upon which to base what essentially amounts to an about-face in the official recommendations for prevention of peanut and other food allergies, which emphasized delayed introduction of high-risk foods, especially in high-risk individuals.5-7 To better understand this shift, we need to briefly explore the context of the addendum guidelines.
As many as one-third of pediatric patients with atopic dermatitis (AD) have food allergies, thus diet often is invoked by patients and providers alike as an underlying cause of the disease.8 Many patients in my practice are so focused on potential food allergies that actual treatment of the affected skin is marginalized and often dismissed as a stopgap that does not address the root of the problem. A 2004 study of 100 children with AD found that diet was manipulated by the parents in 75% of patients in an attempt to manage the disease.9
Patients are not the only ones who consider food allergies to be a driving force in AD. The medical literature indicates that this theory has existed for centuries; for instance, with regard to the relationship between diet and AD, the author of an article from 1830 quipped, “There is probably no subject in which more deeply rooted convictions have been held . . . than the connection between diet and disease, both as regards the causation and treatment of the latter . . .”10 More apropos perhaps is a statement from the 2010 National Institute of Allergy and Infectious Diseases guidelines on food allergy management, which noted that while the expert group “does not mean to imply that AD results from [food allergies], the role of [food allergies] in the pathogenesis and severity of this condition remains controversial.”11
Prior to the LEAP study, food allergy recommendations for clinical practice in the United Kingdom in 199812 and the United States in 200013 recommended excluding allergenic foods (eg, peanuts, tree nuts, soy, milk, eggs) from the diet in infants with a family history of atopy until 3 years of age. However, those recommendations did not seem to be working, when in fact just the opposite was happening. From 1997 until the LEAP study was conducted in 2015, the prevalence of peanut allergy more than quadrupled and became the leading cause of anaphylaxis and death related to food allergy.14 Additionally, study after study concluded that elimination diets did not seem to help most patients with AD.15 As is required in good scientific thinking, when a hypothesis is proven false, other approaches must be considered.
The idea arose that perhaps delaying introduction of allergenic foods was the opposite of the answer.4 The LEAP study tested the notion that peanut allergies are rare in countries where peanuts are introduced early and if telling families to delay introduction of peanuts in infants might actually be causing development of a peanut allergy, and the tests bore fruit. It was found that giving infants peanut-containing foods resulted in a more than 80% reduction in peanut allergy at 5 years of age (P<.001).4 What was perhaps even more interesting was the connection between AD and peanut allergy. An important idea articulated in the LEAP study is in some ways revolutionary: Rather than foods causing AD, it could be that “early environmental exposure (through the skin) to peanut may account for early sensitization, whereas early oral exposure may lead to immune tolerance.”4 This concept—that impaired eczematous skin may actually lead to the development of food allergies—turns the whole thing upside down.
What do these updated guidelines actually suggest? The first guideline focuses on infants with severe AD, egg allergy, or both, who therefore are thought to be at the highest risk for developing peanut allergy.3 Because of the higher baseline risk in this subgroup, measurement of the peanut-specific IgE (peanut sIgE) level, skin prick testing (SPT), or both is strongly recommended before introducing peanut protein into the diet. This testing can be performed by qualified providers as a screening measure, but if positive (≥0.35 kUA/L for peanut sIgE or >2 mm on the peanut SPT), referral to an allergy specialist is warranted. If these studies are negative, it is thought the likelihood of peanut allergy is low, and it is recommended that caregivers introduce age-appropriate peanut-containing foods (eg, peanut butter snack puffs, diluted peanut butter) as early as 4 to 6 months of age. The second guideline recommends that peanut-containing foods should be introduced into the diets of infants with mild or moderate AD at approximately 6 months of age without the need for prior screening via peanut sIgE or SPT. Lastly, the third guideline recommends that caregivers freely introduce peanut-containing foods together with other solid foods in infants without AD or food allergies in accordance with family preference.3
The results of the LEAP study are certainly exciting, and although the theoretical basis makes good scientific sense and the updated guidelines truly address an important and growing problem, there are several issues with this update that are worth considering. Given the constraints of the LEAP study, it certainly seems possible that the results will not be applicable to all populations or foods. More research is needed to ensure that this robust finding applies to other children and to explore the introduction of other allergenic foods, which the LEAP study investigators also emphasized.4
In fairness, the updated guidelines clearly state the quality of evidence of their recommendations and make it clear that expert opinion is playing a large role.3 For the first guideline regarding recommendations for those with severe AD and/or egg allergy, the quality of evidence is deemed moderate, while the contribution of expert opinion is listed as significant. For the second and third guidelines regarding recommendations for mild to moderate AD and those without AD, respectively, the quality of evidence is low and expert opinion is again listed as significant.3
Importantly, delineating severe AD from moderate disease—which is necessary because only severe AD warrants evaluation with peanut sIgE and/or SPT—can be difficult, as the distinction relies on a degree of subjectivity that may vary between specialists. Indeed, 2 publications suggest extending the definition of severe AD to include infants with early-onset AD (<3 months of age) and those with moderate AD not responding to treatment.16,17
Despite these reservations, the updated guidelines represent a breakthrough in understanding in an area truly in need of advancement. Although the evidence may not be exactly extraordinary, the context for these developments and our deeper understanding suggest that we do indeed live in extraordinary times.
- Encyclopaedia Galactica [television transcript]. Cosmos: A Personal Voyage. Public Broadcasting Service. December 14, 1980.
- Ezzo J, Bausell B, Moerman DE, et al. Reviewing the reviews: how strong is the evidence? how clear are the conclusions? Int J Technol Assess Health Care. 2001;17:457-466.
- Togias A, Cooper SF, Acebal ML, et al. Addendum guidelines for the prevention of peanut allergy in the United States: report of the National Institute of Allergy and Infectious Diseases–sponsored expert panel.J Allergy Clin Immunol. 2017;139:29-44.
- Du Toit G, Roberts G, Sayre PH, et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372:803-813.
- Høst A, Koletzko B, Dreborg S, et al. Dietary products used in infants for treatment and prevention of food allergy. joint statement of the European Society for Paediatric Allergology and Clinical Immunology (ESPACI) Committee on Hypoallergenic Formulas and the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) Committee on Nutrition. Arch Dis Child. 1999;81:80-84.
- American Academy of Pediatrics. Committee on Nutrition. hypoallergenic infant formulas. Pediatrics. 2000;106(2, pt 1):346-349.
- Fiocchi A, Assa’ad A, Bahna S; Adverse Reactions to Foods Committee; American College of Allergy, Asthma and Immunology. Food allergy and the introduction of solid foods to infants: a consensus document. Ann Allergy Asthma Immunol. 2006;97:10-20.
- Thompson MM, Hanifin JM. Effective therapy of childhood atopic dermatitis allays food allergy concerns. J Am Acad Dermatol. 2005;53(2 suppl 2):S214-S219.
- Johnston GA, Bilbao RM, Graham-Brown RA. The use of dietary manipulation by parents of children with atopic dermatitis. Br J Dermatol. 2004;150:1186-1189.
- Mackenzie S. The inaugural address on the advantages to be derived from the study of dermatology. BMJ. 1830;1:193-197.
- Boyce JA, Assa’ad A, Burks AW, et al; NIAID-Sponsored Expert Panel. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126(6 suppl):S1-S58.
- Committee on Toxicity of Chemicals in Food, Consumer Products and the Environment. Peanut Allergy. London, England: Department of Health; 1998.
- American Academy of Pediatrics Committee on Nutrition. Hypoallergenic infant formulas. Pediatrics. 2000;106(2, pt 1):346-349.
- Gruchalla RS, Sampson HA. Preventing peanut allergy through early consumption—ready for prime time? N Engl J Med. 2015;372:875-877.
- Lim NR, Lohman ME, Lio PA. The role of elimination diets in atopic dermatitis: a comprehensive review. Pediatr Dermatol. 2017;34:516-527.
- Wong CC, Allen KJ, Orchard D. Changes to infant feeding guidelines: relevance to dermatologists. Australas J Dermatol. 2017;58:e171-e175.
- Martin PE, Eckert JK, Koplin JJ, et al. Which infants with eczema are at risk of food allergy? results from a population-based cohort. Clin Exp Allergy. 2015;45:255-264.
It has been said that “extraordinary claims require extraordinary evidence.”1 In the pursuit of evidence-based medicine, we are encouraged to follow a similar standard, with an emphasis on waiting for multiple studies with good-quality data and high levels of agreement before changing any aspect of our clinical practice. The ostensible purpose is that studies can be flawed, conclusions can be incorrect, or biases can be overlooked. In such cases, acting on questionable results could imperil patients. It is for this reason that so many review articles sometimes frustratingly seem to conclude that further evidence is needed.2
Based on this standard, recently published addendum guidelines from the National Institute of Allergy and Infectious Diseases for prevention of peanut allergy in the United States3 are somewhat striking in that they make fairly bold recommendations based on results from the 2015 Learning Early about Peanut Allergy (LEAP) study,4 a randomized trial evaluating early peanut introduction as a preventive strategy for peanut allergy. Of note, this study was not placebo controlled, was conducted at only 1 site in the United Kingdom, and only included 640 children, though the number of participants was admittedly large for this type of study.4 Arguably, the LEAP study alone does not provide enough evidence upon which to base what essentially amounts to an about-face in the official recommendations for prevention of peanut and other food allergies, which emphasized delayed introduction of high-risk foods, especially in high-risk individuals.5-7 To better understand this shift, we need to briefly explore the context of the addendum guidelines.
As many as one-third of pediatric patients with atopic dermatitis (AD) have food allergies, thus diet often is invoked by patients and providers alike as an underlying cause of the disease.8 Many patients in my practice are so focused on potential food allergies that actual treatment of the affected skin is marginalized and often dismissed as a stopgap that does not address the root of the problem. A 2004 study of 100 children with AD found that diet was manipulated by the parents in 75% of patients in an attempt to manage the disease.9
Patients are not the only ones who consider food allergies to be a driving force in AD. The medical literature indicates that this theory has existed for centuries; for instance, with regard to the relationship between diet and AD, the author of an article from 1830 quipped, “There is probably no subject in which more deeply rooted convictions have been held . . . than the connection between diet and disease, both as regards the causation and treatment of the latter . . .”10 More apropos perhaps is a statement from the 2010 National Institute of Allergy and Infectious Diseases guidelines on food allergy management, which noted that while the expert group “does not mean to imply that AD results from [food allergies], the role of [food allergies] in the pathogenesis and severity of this condition remains controversial.”11
Prior to the LEAP study, food allergy recommendations for clinical practice in the United Kingdom in 199812 and the United States in 200013 recommended excluding allergenic foods (eg, peanuts, tree nuts, soy, milk, eggs) from the diet in infants with a family history of atopy until 3 years of age. However, those recommendations did not seem to be working, when in fact just the opposite was happening. From 1997 until the LEAP study was conducted in 2015, the prevalence of peanut allergy more than quadrupled and became the leading cause of anaphylaxis and death related to food allergy.14 Additionally, study after study concluded that elimination diets did not seem to help most patients with AD.15 As is required in good scientific thinking, when a hypothesis is proven false, other approaches must be considered.
The idea arose that perhaps delaying introduction of allergenic foods was the opposite of the answer.4 The LEAP study tested the notion that peanut allergies are rare in countries where peanuts are introduced early and if telling families to delay introduction of peanuts in infants might actually be causing development of a peanut allergy, and the tests bore fruit. It was found that giving infants peanut-containing foods resulted in a more than 80% reduction in peanut allergy at 5 years of age (P<.001).4 What was perhaps even more interesting was the connection between AD and peanut allergy. An important idea articulated in the LEAP study is in some ways revolutionary: Rather than foods causing AD, it could be that “early environmental exposure (through the skin) to peanut may account for early sensitization, whereas early oral exposure may lead to immune tolerance.”4 This concept—that impaired eczematous skin may actually lead to the development of food allergies—turns the whole thing upside down.
What do these updated guidelines actually suggest? The first guideline focuses on infants with severe AD, egg allergy, or both, who therefore are thought to be at the highest risk for developing peanut allergy.3 Because of the higher baseline risk in this subgroup, measurement of the peanut-specific IgE (peanut sIgE) level, skin prick testing (SPT), or both is strongly recommended before introducing peanut protein into the diet. This testing can be performed by qualified providers as a screening measure, but if positive (≥0.35 kUA/L for peanut sIgE or >2 mm on the peanut SPT), referral to an allergy specialist is warranted. If these studies are negative, it is thought the likelihood of peanut allergy is low, and it is recommended that caregivers introduce age-appropriate peanut-containing foods (eg, peanut butter snack puffs, diluted peanut butter) as early as 4 to 6 months of age. The second guideline recommends that peanut-containing foods should be introduced into the diets of infants with mild or moderate AD at approximately 6 months of age without the need for prior screening via peanut sIgE or SPT. Lastly, the third guideline recommends that caregivers freely introduce peanut-containing foods together with other solid foods in infants without AD or food allergies in accordance with family preference.3
The results of the LEAP study are certainly exciting, and although the theoretical basis makes good scientific sense and the updated guidelines truly address an important and growing problem, there are several issues with this update that are worth considering. Given the constraints of the LEAP study, it certainly seems possible that the results will not be applicable to all populations or foods. More research is needed to ensure that this robust finding applies to other children and to explore the introduction of other allergenic foods, which the LEAP study investigators also emphasized.4
In fairness, the updated guidelines clearly state the quality of evidence of their recommendations and make it clear that expert opinion is playing a large role.3 For the first guideline regarding recommendations for those with severe AD and/or egg allergy, the quality of evidence is deemed moderate, while the contribution of expert opinion is listed as significant. For the second and third guidelines regarding recommendations for mild to moderate AD and those without AD, respectively, the quality of evidence is low and expert opinion is again listed as significant.3
Importantly, delineating severe AD from moderate disease—which is necessary because only severe AD warrants evaluation with peanut sIgE and/or SPT—can be difficult, as the distinction relies on a degree of subjectivity that may vary between specialists. Indeed, 2 publications suggest extending the definition of severe AD to include infants with early-onset AD (<3 months of age) and those with moderate AD not responding to treatment.16,17
Despite these reservations, the updated guidelines represent a breakthrough in understanding in an area truly in need of advancement. Although the evidence may not be exactly extraordinary, the context for these developments and our deeper understanding suggest that we do indeed live in extraordinary times.
It has been said that “extraordinary claims require extraordinary evidence.”1 In the pursuit of evidence-based medicine, we are encouraged to follow a similar standard, with an emphasis on waiting for multiple studies with good-quality data and high levels of agreement before changing any aspect of our clinical practice. The ostensible purpose is that studies can be flawed, conclusions can be incorrect, or biases can be overlooked. In such cases, acting on questionable results could imperil patients. It is for this reason that so many review articles sometimes frustratingly seem to conclude that further evidence is needed.2
Based on this standard, recently published addendum guidelines from the National Institute of Allergy and Infectious Diseases for prevention of peanut allergy in the United States3 are somewhat striking in that they make fairly bold recommendations based on results from the 2015 Learning Early about Peanut Allergy (LEAP) study,4 a randomized trial evaluating early peanut introduction as a preventive strategy for peanut allergy. Of note, this study was not placebo controlled, was conducted at only 1 site in the United Kingdom, and only included 640 children, though the number of participants was admittedly large for this type of study.4 Arguably, the LEAP study alone does not provide enough evidence upon which to base what essentially amounts to an about-face in the official recommendations for prevention of peanut and other food allergies, which emphasized delayed introduction of high-risk foods, especially in high-risk individuals.5-7 To better understand this shift, we need to briefly explore the context of the addendum guidelines.
As many as one-third of pediatric patients with atopic dermatitis (AD) have food allergies, thus diet often is invoked by patients and providers alike as an underlying cause of the disease.8 Many patients in my practice are so focused on potential food allergies that actual treatment of the affected skin is marginalized and often dismissed as a stopgap that does not address the root of the problem. A 2004 study of 100 children with AD found that diet was manipulated by the parents in 75% of patients in an attempt to manage the disease.9
Patients are not the only ones who consider food allergies to be a driving force in AD. The medical literature indicates that this theory has existed for centuries; for instance, with regard to the relationship between diet and AD, the author of an article from 1830 quipped, “There is probably no subject in which more deeply rooted convictions have been held . . . than the connection between diet and disease, both as regards the causation and treatment of the latter . . .”10 More apropos perhaps is a statement from the 2010 National Institute of Allergy and Infectious Diseases guidelines on food allergy management, which noted that while the expert group “does not mean to imply that AD results from [food allergies], the role of [food allergies] in the pathogenesis and severity of this condition remains controversial.”11
Prior to the LEAP study, food allergy recommendations for clinical practice in the United Kingdom in 199812 and the United States in 200013 recommended excluding allergenic foods (eg, peanuts, tree nuts, soy, milk, eggs) from the diet in infants with a family history of atopy until 3 years of age. However, those recommendations did not seem to be working, when in fact just the opposite was happening. From 1997 until the LEAP study was conducted in 2015, the prevalence of peanut allergy more than quadrupled and became the leading cause of anaphylaxis and death related to food allergy.14 Additionally, study after study concluded that elimination diets did not seem to help most patients with AD.15 As is required in good scientific thinking, when a hypothesis is proven false, other approaches must be considered.
The idea arose that perhaps delaying introduction of allergenic foods was the opposite of the answer.4 The LEAP study tested the notion that peanut allergies are rare in countries where peanuts are introduced early and if telling families to delay introduction of peanuts in infants might actually be causing development of a peanut allergy, and the tests bore fruit. It was found that giving infants peanut-containing foods resulted in a more than 80% reduction in peanut allergy at 5 years of age (P<.001).4 What was perhaps even more interesting was the connection between AD and peanut allergy. An important idea articulated in the LEAP study is in some ways revolutionary: Rather than foods causing AD, it could be that “early environmental exposure (through the skin) to peanut may account for early sensitization, whereas early oral exposure may lead to immune tolerance.”4 This concept—that impaired eczematous skin may actually lead to the development of food allergies—turns the whole thing upside down.
What do these updated guidelines actually suggest? The first guideline focuses on infants with severe AD, egg allergy, or both, who therefore are thought to be at the highest risk for developing peanut allergy.3 Because of the higher baseline risk in this subgroup, measurement of the peanut-specific IgE (peanut sIgE) level, skin prick testing (SPT), or both is strongly recommended before introducing peanut protein into the diet. This testing can be performed by qualified providers as a screening measure, but if positive (≥0.35 kUA/L for peanut sIgE or >2 mm on the peanut SPT), referral to an allergy specialist is warranted. If these studies are negative, it is thought the likelihood of peanut allergy is low, and it is recommended that caregivers introduce age-appropriate peanut-containing foods (eg, peanut butter snack puffs, diluted peanut butter) as early as 4 to 6 months of age. The second guideline recommends that peanut-containing foods should be introduced into the diets of infants with mild or moderate AD at approximately 6 months of age without the need for prior screening via peanut sIgE or SPT. Lastly, the third guideline recommends that caregivers freely introduce peanut-containing foods together with other solid foods in infants without AD or food allergies in accordance with family preference.3
The results of the LEAP study are certainly exciting, and although the theoretical basis makes good scientific sense and the updated guidelines truly address an important and growing problem, there are several issues with this update that are worth considering. Given the constraints of the LEAP study, it certainly seems possible that the results will not be applicable to all populations or foods. More research is needed to ensure that this robust finding applies to other children and to explore the introduction of other allergenic foods, which the LEAP study investigators also emphasized.4
In fairness, the updated guidelines clearly state the quality of evidence of their recommendations and make it clear that expert opinion is playing a large role.3 For the first guideline regarding recommendations for those with severe AD and/or egg allergy, the quality of evidence is deemed moderate, while the contribution of expert opinion is listed as significant. For the second and third guidelines regarding recommendations for mild to moderate AD and those without AD, respectively, the quality of evidence is low and expert opinion is again listed as significant.3
Importantly, delineating severe AD from moderate disease—which is necessary because only severe AD warrants evaluation with peanut sIgE and/or SPT—can be difficult, as the distinction relies on a degree of subjectivity that may vary between specialists. Indeed, 2 publications suggest extending the definition of severe AD to include infants with early-onset AD (<3 months of age) and those with moderate AD not responding to treatment.16,17
Despite these reservations, the updated guidelines represent a breakthrough in understanding in an area truly in need of advancement. Although the evidence may not be exactly extraordinary, the context for these developments and our deeper understanding suggest that we do indeed live in extraordinary times.
- Encyclopaedia Galactica [television transcript]. Cosmos: A Personal Voyage. Public Broadcasting Service. December 14, 1980.
- Ezzo J, Bausell B, Moerman DE, et al. Reviewing the reviews: how strong is the evidence? how clear are the conclusions? Int J Technol Assess Health Care. 2001;17:457-466.
- Togias A, Cooper SF, Acebal ML, et al. Addendum guidelines for the prevention of peanut allergy in the United States: report of the National Institute of Allergy and Infectious Diseases–sponsored expert panel.J Allergy Clin Immunol. 2017;139:29-44.
- Du Toit G, Roberts G, Sayre PH, et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372:803-813.
- Høst A, Koletzko B, Dreborg S, et al. Dietary products used in infants for treatment and prevention of food allergy. joint statement of the European Society for Paediatric Allergology and Clinical Immunology (ESPACI) Committee on Hypoallergenic Formulas and the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) Committee on Nutrition. Arch Dis Child. 1999;81:80-84.
- American Academy of Pediatrics. Committee on Nutrition. hypoallergenic infant formulas. Pediatrics. 2000;106(2, pt 1):346-349.
- Fiocchi A, Assa’ad A, Bahna S; Adverse Reactions to Foods Committee; American College of Allergy, Asthma and Immunology. Food allergy and the introduction of solid foods to infants: a consensus document. Ann Allergy Asthma Immunol. 2006;97:10-20.
- Thompson MM, Hanifin JM. Effective therapy of childhood atopic dermatitis allays food allergy concerns. J Am Acad Dermatol. 2005;53(2 suppl 2):S214-S219.
- Johnston GA, Bilbao RM, Graham-Brown RA. The use of dietary manipulation by parents of children with atopic dermatitis. Br J Dermatol. 2004;150:1186-1189.
- Mackenzie S. The inaugural address on the advantages to be derived from the study of dermatology. BMJ. 1830;1:193-197.
- Boyce JA, Assa’ad A, Burks AW, et al; NIAID-Sponsored Expert Panel. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126(6 suppl):S1-S58.
- Committee on Toxicity of Chemicals in Food, Consumer Products and the Environment. Peanut Allergy. London, England: Department of Health; 1998.
- American Academy of Pediatrics Committee on Nutrition. Hypoallergenic infant formulas. Pediatrics. 2000;106(2, pt 1):346-349.
- Gruchalla RS, Sampson HA. Preventing peanut allergy through early consumption—ready for prime time? N Engl J Med. 2015;372:875-877.
- Lim NR, Lohman ME, Lio PA. The role of elimination diets in atopic dermatitis: a comprehensive review. Pediatr Dermatol. 2017;34:516-527.
- Wong CC, Allen KJ, Orchard D. Changes to infant feeding guidelines: relevance to dermatologists. Australas J Dermatol. 2017;58:e171-e175.
- Martin PE, Eckert JK, Koplin JJ, et al. Which infants with eczema are at risk of food allergy? results from a population-based cohort. Clin Exp Allergy. 2015;45:255-264.
- Encyclopaedia Galactica [television transcript]. Cosmos: A Personal Voyage. Public Broadcasting Service. December 14, 1980.
- Ezzo J, Bausell B, Moerman DE, et al. Reviewing the reviews: how strong is the evidence? how clear are the conclusions? Int J Technol Assess Health Care. 2001;17:457-466.
- Togias A, Cooper SF, Acebal ML, et al. Addendum guidelines for the prevention of peanut allergy in the United States: report of the National Institute of Allergy and Infectious Diseases–sponsored expert panel.J Allergy Clin Immunol. 2017;139:29-44.
- Du Toit G, Roberts G, Sayre PH, et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372:803-813.
- Høst A, Koletzko B, Dreborg S, et al. Dietary products used in infants for treatment and prevention of food allergy. joint statement of the European Society for Paediatric Allergology and Clinical Immunology (ESPACI) Committee on Hypoallergenic Formulas and the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) Committee on Nutrition. Arch Dis Child. 1999;81:80-84.
- American Academy of Pediatrics. Committee on Nutrition. hypoallergenic infant formulas. Pediatrics. 2000;106(2, pt 1):346-349.
- Fiocchi A, Assa’ad A, Bahna S; Adverse Reactions to Foods Committee; American College of Allergy, Asthma and Immunology. Food allergy and the introduction of solid foods to infants: a consensus document. Ann Allergy Asthma Immunol. 2006;97:10-20.
- Thompson MM, Hanifin JM. Effective therapy of childhood atopic dermatitis allays food allergy concerns. J Am Acad Dermatol. 2005;53(2 suppl 2):S214-S219.
- Johnston GA, Bilbao RM, Graham-Brown RA. The use of dietary manipulation by parents of children with atopic dermatitis. Br J Dermatol. 2004;150:1186-1189.
- Mackenzie S. The inaugural address on the advantages to be derived from the study of dermatology. BMJ. 1830;1:193-197.
- Boyce JA, Assa’ad A, Burks AW, et al; NIAID-Sponsored Expert Panel. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126(6 suppl):S1-S58.
- Committee on Toxicity of Chemicals in Food, Consumer Products and the Environment. Peanut Allergy. London, England: Department of Health; 1998.
- American Academy of Pediatrics Committee on Nutrition. Hypoallergenic infant formulas. Pediatrics. 2000;106(2, pt 1):346-349.
- Gruchalla RS, Sampson HA. Preventing peanut allergy through early consumption—ready for prime time? N Engl J Med. 2015;372:875-877.
- Lim NR, Lohman ME, Lio PA. The role of elimination diets in atopic dermatitis: a comprehensive review. Pediatr Dermatol. 2017;34:516-527.
- Wong CC, Allen KJ, Orchard D. Changes to infant feeding guidelines: relevance to dermatologists. Australas J Dermatol. 2017;58:e171-e175.
- Martin PE, Eckert JK, Koplin JJ, et al. Which infants with eczema are at risk of food allergy? results from a population-based cohort. Clin Exp Allergy. 2015;45:255-264.
What is causing my patients’ macrocytosis?
A 56-year-old man presents for his annual physical. He brings in blood work done for all employees in his workplace (he is an aerospace engineer), and wants to talk about the lab that has an asterisk by it. All his labs are normal, except that his mean corpuscular volume (MCV) is 101. His hematocrit (HCT) is 42. He has no symptoms and a normal physical exam.
What test or tests would most likely be abnormal?
A. Thyroid-stimulating hormone.
B. Vitamin B12/folate.
C. Testosterone.
D. Gamma-glutamyl-transferase (GGT).
The finding of macrocytosis is fairly common in primary care, estimated to be found in 3% of complete blood count results.1 Most students in medical school quickly learn that vitamin B12 and folate deficiency can cause macrocytic anemias. The standard workups for patients with macrocytosis began and ended with checking vitamin B12 and folate levels, which are usually normal in the vast majority of patients with macrocytosis.
For this patient, the correct answer would be an abnormal GGT, because chronic moderate to heavy alcohol use can raise GGT levels, as well as MCVs.
Dr. David Savage and colleagues evaluated the etiology of macrocytosis in 300 consecutive hospitalized patients with macrocytosis.2 They found that the most common causes were medications, alcohol, liver disease, and reticulocytosis. The study was done in New York and was published in 2000, so zidovudine (AZT) was a common medication cause of the macrocytosis. This medication is much less commonly used today. Zidovudine causes macrocytosis in more than 80% of patients who take it. They also found in the study that very high MCVs (> 120) were most commonly associated with vitamin B12 deficiency.
Dr. Kaija Seppä and colleagues looked at all outpatients who had a blood count done over an 8-month period. A total of 9,527 blood counts were ordered, and 287 (3%) had macrocytosis.1 Further workup was done for 113 of the patients. The most common cause found for macrocytosis was alcohol abuse, in 74 (65%) of the patients (80% of the men and 36% of the women). No cause of the macrocytosis was found in 24 (21%) of the patients.
Dr. A. Wymer and colleagues looked at 2,800 adult outpatients who had complete blood counts. A total of 138 (3.7%) had macrocytosis, with 128 of these patients having charts that could be reviewed.3 A total of 73 patients had a workup for their macrocytosis. Alcohol was the diagnostic cause of the macrocytosis in 47 (64%). Only five of the patients had B12 deficiency (7%).
Dr. Seppä and colleagues also reported on hematologic morphologic features in nonanemic patients with macrocytosis due to alcohol abuse or vitamin B12 deficiency.4 They studied 136 patients with alcohol abuse and normal B12 levels, and 18 patients with pernicious anemia. The combination of a low red cell count or a high red cell distribution width with a normal platelet count was found in 94.4% of the vitamin-deficient patients but in only 14.6% of the abusers.
Pearl:
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the university. Contact Dr. Paauw at [email protected].
References
1. J Stud Alcohol. 1996 Jan;57(1):97-100.
2. Am J Med Sci. 2000 Jun;319(6):343-52.
3. J Gen Intern Med. 1990 May-Jun;5(3):192-7.
4. Alcohol. 1993 Sep-Oct;10(5):343-7.
5. South Med J. 2013 Feb;106(2):121-5.
A 56-year-old man presents for his annual physical. He brings in blood work done for all employees in his workplace (he is an aerospace engineer), and wants to talk about the lab that has an asterisk by it. All his labs are normal, except that his mean corpuscular volume (MCV) is 101. His hematocrit (HCT) is 42. He has no symptoms and a normal physical exam.
What test or tests would most likely be abnormal?
A. Thyroid-stimulating hormone.
B. Vitamin B12/folate.
C. Testosterone.
D. Gamma-glutamyl-transferase (GGT).
The finding of macrocytosis is fairly common in primary care, estimated to be found in 3% of complete blood count results.1 Most students in medical school quickly learn that vitamin B12 and folate deficiency can cause macrocytic anemias. The standard workups for patients with macrocytosis began and ended with checking vitamin B12 and folate levels, which are usually normal in the vast majority of patients with macrocytosis.
For this patient, the correct answer would be an abnormal GGT, because chronic moderate to heavy alcohol use can raise GGT levels, as well as MCVs.
Dr. David Savage and colleagues evaluated the etiology of macrocytosis in 300 consecutive hospitalized patients with macrocytosis.2 They found that the most common causes were medications, alcohol, liver disease, and reticulocytosis. The study was done in New York and was published in 2000, so zidovudine (AZT) was a common medication cause of the macrocytosis. This medication is much less commonly used today. Zidovudine causes macrocytosis in more than 80% of patients who take it. They also found in the study that very high MCVs (> 120) were most commonly associated with vitamin B12 deficiency.
Dr. Kaija Seppä and colleagues looked at all outpatients who had a blood count done over an 8-month period. A total of 9,527 blood counts were ordered, and 287 (3%) had macrocytosis.1 Further workup was done for 113 of the patients. The most common cause found for macrocytosis was alcohol abuse, in 74 (65%) of the patients (80% of the men and 36% of the women). No cause of the macrocytosis was found in 24 (21%) of the patients.
Dr. A. Wymer and colleagues looked at 2,800 adult outpatients who had complete blood counts. A total of 138 (3.7%) had macrocytosis, with 128 of these patients having charts that could be reviewed.3 A total of 73 patients had a workup for their macrocytosis. Alcohol was the diagnostic cause of the macrocytosis in 47 (64%). Only five of the patients had B12 deficiency (7%).
Dr. Seppä and colleagues also reported on hematologic morphologic features in nonanemic patients with macrocytosis due to alcohol abuse or vitamin B12 deficiency.4 They studied 136 patients with alcohol abuse and normal B12 levels, and 18 patients with pernicious anemia. The combination of a low red cell count or a high red cell distribution width with a normal platelet count was found in 94.4% of the vitamin-deficient patients but in only 14.6% of the abusers.
Pearl:
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the university. Contact Dr. Paauw at [email protected].
References
1. J Stud Alcohol. 1996 Jan;57(1):97-100.
2. Am J Med Sci. 2000 Jun;319(6):343-52.
3. J Gen Intern Med. 1990 May-Jun;5(3):192-7.
4. Alcohol. 1993 Sep-Oct;10(5):343-7.
5. South Med J. 2013 Feb;106(2):121-5.
A 56-year-old man presents for his annual physical. He brings in blood work done for all employees in his workplace (he is an aerospace engineer), and wants to talk about the lab that has an asterisk by it. All his labs are normal, except that his mean corpuscular volume (MCV) is 101. His hematocrit (HCT) is 42. He has no symptoms and a normal physical exam.
What test or tests would most likely be abnormal?
A. Thyroid-stimulating hormone.
B. Vitamin B12/folate.
C. Testosterone.
D. Gamma-glutamyl-transferase (GGT).
The finding of macrocytosis is fairly common in primary care, estimated to be found in 3% of complete blood count results.1 Most students in medical school quickly learn that vitamin B12 and folate deficiency can cause macrocytic anemias. The standard workups for patients with macrocytosis began and ended with checking vitamin B12 and folate levels, which are usually normal in the vast majority of patients with macrocytosis.
For this patient, the correct answer would be an abnormal GGT, because chronic moderate to heavy alcohol use can raise GGT levels, as well as MCVs.
Dr. David Savage and colleagues evaluated the etiology of macrocytosis in 300 consecutive hospitalized patients with macrocytosis.2 They found that the most common causes were medications, alcohol, liver disease, and reticulocytosis. The study was done in New York and was published in 2000, so zidovudine (AZT) was a common medication cause of the macrocytosis. This medication is much less commonly used today. Zidovudine causes macrocytosis in more than 80% of patients who take it. They also found in the study that very high MCVs (> 120) were most commonly associated with vitamin B12 deficiency.
Dr. Kaija Seppä and colleagues looked at all outpatients who had a blood count done over an 8-month period. A total of 9,527 blood counts were ordered, and 287 (3%) had macrocytosis.1 Further workup was done for 113 of the patients. The most common cause found for macrocytosis was alcohol abuse, in 74 (65%) of the patients (80% of the men and 36% of the women). No cause of the macrocytosis was found in 24 (21%) of the patients.
Dr. A. Wymer and colleagues looked at 2,800 adult outpatients who had complete blood counts. A total of 138 (3.7%) had macrocytosis, with 128 of these patients having charts that could be reviewed.3 A total of 73 patients had a workup for their macrocytosis. Alcohol was the diagnostic cause of the macrocytosis in 47 (64%). Only five of the patients had B12 deficiency (7%).
Dr. Seppä and colleagues also reported on hematologic morphologic features in nonanemic patients with macrocytosis due to alcohol abuse or vitamin B12 deficiency.4 They studied 136 patients with alcohol abuse and normal B12 levels, and 18 patients with pernicious anemia. The combination of a low red cell count or a high red cell distribution width with a normal platelet count was found in 94.4% of the vitamin-deficient patients but in only 14.6% of the abusers.
Pearl:
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the university. Contact Dr. Paauw at [email protected].
References
1. J Stud Alcohol. 1996 Jan;57(1):97-100.
2. Am J Med Sci. 2000 Jun;319(6):343-52.
3. J Gen Intern Med. 1990 May-Jun;5(3):192-7.
4. Alcohol. 1993 Sep-Oct;10(5):343-7.
5. South Med J. 2013 Feb;106(2):121-5.
Anorectal Evaluations: Are You Willing to Look?
Just over a year ago, I established a solo colorectal surgery clinic within a comprehensive academic medical center hospital system and have since seen a variety of cases: benign anorectal conditions, acute and chronic diseases, complex defecatory dysfunction, and colorectal surgery pre- and postop patients. I also manage a colorectal cancer survivorship clinic. As a PA in this field, I very much appreciated the November 2017 CE/CME, “Anorectal Evaluations: Diagnosing & Treating Benign Conditions” (Clinician Reviews. 2017;27[11]:28-37). The article offered useful highlights and clinical pearls for diagnosing common anorectal conditions. It supplied corresponding images for quick reference, discussed the need for a thorough history, and detailed the finesse of the often-dreaded-yet-so-important physical exam, reassuring providers that the majority of anorectal complaints are, indeed, benign and often treatable on first visit. However, the latter is contingent on one key factor: Are you willing to look?
Primary care is typically a patient’s first stop when experiencing anorectal symptoms. If you see a high volume of these cases and are comfortable and confident in your exam skills, the patient is likely well-served. But because it is not expected of general practitioners to have the experience or knowledge to recognize or discern the more minute features of anorectal atypia, I fully advocate the “when in doubt, refer it out” mentality without hesitation or judgement—and I quickly learned the importance of a quality referral network when I established my own clinic.
What concerns me, though, is how often a referral is made with no mention of an anorectal exam in the office note. I can certainly make a rare exception for the exam that mistakenly did not get recorded, but ultimately, if it wasn’t documented, it didn’t happen, right? And when questioned, most of these patients report that the referring provider didn’t look!
The greater issue therein occurs when a provider who doesn’t perform a physical exam recommends a course of treatment. For example—I see this on a weekly basis—a provider may prescribe a rectal preparation ointment for a patient complaining of “hemorrhoids.” Sometimes, that initial appointment is the only one before the patient is referred to my office; more often, the patient is subject to multiple office visits and excessive trials of prescription and/or homeopathic remedies before a referral is finally made. And all of this occurs without a proper exam!
The patient being treated for a presumed diagnosis of hemorrhoids may have a completely different problem altogether—if only the provider had looked. Optimistically, the patient may have an anal fissure, and the only downfall is a delay in appropriate treatment and symptom resolution. Unfortunately, grimmer outcomes can—and often do—result. I have diagnosed several cases of anal squamous cell cancer from referrals of this nature.
What’s more, recent studies have found that the incidence of anal cancer (all ages) and of colorectal cancer (adults ages 20-54) is on the rise.1,2 And because both may manifest with mild or seemingly benign symptoms, such as rectal bleeding, anorectal pain, or a change in bowel habits, making an early and accurate diagnosis can be challenging.
These data reinforce my belief that referral to a trusted colorectal specialist with whom you can easily communicate is the best option if any doubt exists. As a provider, I would rather see a patient who is urgently referred for what turns out to be a benign condition than diagnose a serious problem, such as cancer, in a patient who has been lost in the shuffle.
Continue to: Of course, the key in all this is...
Of course, the key in all this is the relationship you establish with your patients. In my case, building relationships with my patients encourages them to more freely discuss anorectal concerns and allows me to regularly perform necessary exams. Since I’ve created my own clinic
At the very least, I encourage you to read the CE/CME article that sparked this commentary. Incorporate the techniques into your patient care when someone presents with anorectal discomfort. In short, be willing to look. You never know when you might save a life!
1. American Cancer Society. Key Statistics for Anal Cancer. www.cancer.org/cancer/anal-cancer/about/what-is-key-statistics.html. Accessed May 10, 2018.
2. Siegel RL, Miller KD, Jemal A. Colorectal cancer mortality rates in adults aged 20 to 54 years in the United States, 1970-2014. JAMA.
Just over a year ago, I established a solo colorectal surgery clinic within a comprehensive academic medical center hospital system and have since seen a variety of cases: benign anorectal conditions, acute and chronic diseases, complex defecatory dysfunction, and colorectal surgery pre- and postop patients. I also manage a colorectal cancer survivorship clinic. As a PA in this field, I very much appreciated the November 2017 CE/CME, “Anorectal Evaluations: Diagnosing & Treating Benign Conditions” (Clinician Reviews. 2017;27[11]:28-37). The article offered useful highlights and clinical pearls for diagnosing common anorectal conditions. It supplied corresponding images for quick reference, discussed the need for a thorough history, and detailed the finesse of the often-dreaded-yet-so-important physical exam, reassuring providers that the majority of anorectal complaints are, indeed, benign and often treatable on first visit. However, the latter is contingent on one key factor: Are you willing to look?
Primary care is typically a patient’s first stop when experiencing anorectal symptoms. If you see a high volume of these cases and are comfortable and confident in your exam skills, the patient is likely well-served. But because it is not expected of general practitioners to have the experience or knowledge to recognize or discern the more minute features of anorectal atypia, I fully advocate the “when in doubt, refer it out” mentality without hesitation or judgement—and I quickly learned the importance of a quality referral network when I established my own clinic.
What concerns me, though, is how often a referral is made with no mention of an anorectal exam in the office note. I can certainly make a rare exception for the exam that mistakenly did not get recorded, but ultimately, if it wasn’t documented, it didn’t happen, right? And when questioned, most of these patients report that the referring provider didn’t look!
The greater issue therein occurs when a provider who doesn’t perform a physical exam recommends a course of treatment. For example—I see this on a weekly basis—a provider may prescribe a rectal preparation ointment for a patient complaining of “hemorrhoids.” Sometimes, that initial appointment is the only one before the patient is referred to my office; more often, the patient is subject to multiple office visits and excessive trials of prescription and/or homeopathic remedies before a referral is finally made. And all of this occurs without a proper exam!
The patient being treated for a presumed diagnosis of hemorrhoids may have a completely different problem altogether—if only the provider had looked. Optimistically, the patient may have an anal fissure, and the only downfall is a delay in appropriate treatment and symptom resolution. Unfortunately, grimmer outcomes can—and often do—result. I have diagnosed several cases of anal squamous cell cancer from referrals of this nature.
What’s more, recent studies have found that the incidence of anal cancer (all ages) and of colorectal cancer (adults ages 20-54) is on the rise.1,2 And because both may manifest with mild or seemingly benign symptoms, such as rectal bleeding, anorectal pain, or a change in bowel habits, making an early and accurate diagnosis can be challenging.
These data reinforce my belief that referral to a trusted colorectal specialist with whom you can easily communicate is the best option if any doubt exists. As a provider, I would rather see a patient who is urgently referred for what turns out to be a benign condition than diagnose a serious problem, such as cancer, in a patient who has been lost in the shuffle.
Continue to: Of course, the key in all this is...
Of course, the key in all this is the relationship you establish with your patients. In my case, building relationships with my patients encourages them to more freely discuss anorectal concerns and allows me to regularly perform necessary exams. Since I’ve created my own clinic
At the very least, I encourage you to read the CE/CME article that sparked this commentary. Incorporate the techniques into your patient care when someone presents with anorectal discomfort. In short, be willing to look. You never know when you might save a life!
Just over a year ago, I established a solo colorectal surgery clinic within a comprehensive academic medical center hospital system and have since seen a variety of cases: benign anorectal conditions, acute and chronic diseases, complex defecatory dysfunction, and colorectal surgery pre- and postop patients. I also manage a colorectal cancer survivorship clinic. As a PA in this field, I very much appreciated the November 2017 CE/CME, “Anorectal Evaluations: Diagnosing & Treating Benign Conditions” (Clinician Reviews. 2017;27[11]:28-37). The article offered useful highlights and clinical pearls for diagnosing common anorectal conditions. It supplied corresponding images for quick reference, discussed the need for a thorough history, and detailed the finesse of the often-dreaded-yet-so-important physical exam, reassuring providers that the majority of anorectal complaints are, indeed, benign and often treatable on first visit. However, the latter is contingent on one key factor: Are you willing to look?
Primary care is typically a patient’s first stop when experiencing anorectal symptoms. If you see a high volume of these cases and are comfortable and confident in your exam skills, the patient is likely well-served. But because it is not expected of general practitioners to have the experience or knowledge to recognize or discern the more minute features of anorectal atypia, I fully advocate the “when in doubt, refer it out” mentality without hesitation or judgement—and I quickly learned the importance of a quality referral network when I established my own clinic.
What concerns me, though, is how often a referral is made with no mention of an anorectal exam in the office note. I can certainly make a rare exception for the exam that mistakenly did not get recorded, but ultimately, if it wasn’t documented, it didn’t happen, right? And when questioned, most of these patients report that the referring provider didn’t look!
The greater issue therein occurs when a provider who doesn’t perform a physical exam recommends a course of treatment. For example—I see this on a weekly basis—a provider may prescribe a rectal preparation ointment for a patient complaining of “hemorrhoids.” Sometimes, that initial appointment is the only one before the patient is referred to my office; more often, the patient is subject to multiple office visits and excessive trials of prescription and/or homeopathic remedies before a referral is finally made. And all of this occurs without a proper exam!
The patient being treated for a presumed diagnosis of hemorrhoids may have a completely different problem altogether—if only the provider had looked. Optimistically, the patient may have an anal fissure, and the only downfall is a delay in appropriate treatment and symptom resolution. Unfortunately, grimmer outcomes can—and often do—result. I have diagnosed several cases of anal squamous cell cancer from referrals of this nature.
What’s more, recent studies have found that the incidence of anal cancer (all ages) and of colorectal cancer (adults ages 20-54) is on the rise.1,2 And because both may manifest with mild or seemingly benign symptoms, such as rectal bleeding, anorectal pain, or a change in bowel habits, making an early and accurate diagnosis can be challenging.
These data reinforce my belief that referral to a trusted colorectal specialist with whom you can easily communicate is the best option if any doubt exists. As a provider, I would rather see a patient who is urgently referred for what turns out to be a benign condition than diagnose a serious problem, such as cancer, in a patient who has been lost in the shuffle.
Continue to: Of course, the key in all this is...
Of course, the key in all this is the relationship you establish with your patients. In my case, building relationships with my patients encourages them to more freely discuss anorectal concerns and allows me to regularly perform necessary exams. Since I’ve created my own clinic
At the very least, I encourage you to read the CE/CME article that sparked this commentary. Incorporate the techniques into your patient care when someone presents with anorectal discomfort. In short, be willing to look. You never know when you might save a life!
1. American Cancer Society. Key Statistics for Anal Cancer. www.cancer.org/cancer/anal-cancer/about/what-is-key-statistics.html. Accessed May 10, 2018.
2. Siegel RL, Miller KD, Jemal A. Colorectal cancer mortality rates in adults aged 20 to 54 years in the United States, 1970-2014. JAMA.
1. American Cancer Society. Key Statistics for Anal Cancer. www.cancer.org/cancer/anal-cancer/about/what-is-key-statistics.html. Accessed May 10, 2018.
2. Siegel RL, Miller KD, Jemal A. Colorectal cancer mortality rates in adults aged 20 to 54 years in the United States, 1970-2014. JAMA.
What to eat
Where did you learn about nutrition? Was it primarily at home supplemented by a few teachers as you navigated K through 12? Studies have shown that it probably wasn’t during medical school (“How much does your doctor actually know about nutrition?” American Heart Association News, April 30, 2018). A survey of one-third of medicals schools done in 1985 found “inadequate exposure to nutrition,” which prompted the National Academy of Sciences to recommend a minimum of 25 classroom hours. A more recent survey in 2013 discovered that 71% percent of medical schools fail to meet that benchmark.
I certainly don’t recall receiving any teaching in medical school that was specifically targeted at nutrition. And to be perfectly honest I never felt that I had missed anything. It’s not that I don’t believe nutrition is important. What we eat joins exercise and sleep at the core of a healthy lifestyle. The problem is that I was never confident that I or anyone else knew what a healthy diet should be. I learned what happened if child didn’t eat enough fruits and vegetables or consume enough vitamin D. But the tide seemed to keep going in and out on how much of each category of food was optimal. What was the perfect nutritional pyramid? And then there was the whole apparent flip-flop on eggs. For myself, I tried to follow the old dictum “everything in moderation ... including moderation.”
Don’t misunderstand me. I think dietitians have a critical role in health maintenance and disease management and should be on the forefront of our efforts to seek the causes of those medical conditions that have yet to be fully explained. It would be a mistake to recommend a low-salt diet to a patient without encouraging him or her (and the family) to consult with a dietitian. However, is having a medical students spend an afternoon in a kitchen preparing a low-salt diet a worthwhile investment of 4 precious hours of their educational time? It sounds cool, and at the end of the day, the student will certainly have a better understanding of how difficult his dietary recommendations will be to follow. But if the student ends up being a pediatrician, how often will he look back on the kitchen experience as a positive?
Giving specific and detailed instruction on how to shop for and prepare a medically prescribed diet can be very time consuming, and it can’t be done well without close follow-up that might even include a home visit or two. In some practices, the best option is to have a dietitian on the team.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Where did you learn about nutrition? Was it primarily at home supplemented by a few teachers as you navigated K through 12? Studies have shown that it probably wasn’t during medical school (“How much does your doctor actually know about nutrition?” American Heart Association News, April 30, 2018). A survey of one-third of medicals schools done in 1985 found “inadequate exposure to nutrition,” which prompted the National Academy of Sciences to recommend a minimum of 25 classroom hours. A more recent survey in 2013 discovered that 71% percent of medical schools fail to meet that benchmark.
I certainly don’t recall receiving any teaching in medical school that was specifically targeted at nutrition. And to be perfectly honest I never felt that I had missed anything. It’s not that I don’t believe nutrition is important. What we eat joins exercise and sleep at the core of a healthy lifestyle. The problem is that I was never confident that I or anyone else knew what a healthy diet should be. I learned what happened if child didn’t eat enough fruits and vegetables or consume enough vitamin D. But the tide seemed to keep going in and out on how much of each category of food was optimal. What was the perfect nutritional pyramid? And then there was the whole apparent flip-flop on eggs. For myself, I tried to follow the old dictum “everything in moderation ... including moderation.”
Don’t misunderstand me. I think dietitians have a critical role in health maintenance and disease management and should be on the forefront of our efforts to seek the causes of those medical conditions that have yet to be fully explained. It would be a mistake to recommend a low-salt diet to a patient without encouraging him or her (and the family) to consult with a dietitian. However, is having a medical students spend an afternoon in a kitchen preparing a low-salt diet a worthwhile investment of 4 precious hours of their educational time? It sounds cool, and at the end of the day, the student will certainly have a better understanding of how difficult his dietary recommendations will be to follow. But if the student ends up being a pediatrician, how often will he look back on the kitchen experience as a positive?
Giving specific and detailed instruction on how to shop for and prepare a medically prescribed diet can be very time consuming, and it can’t be done well without close follow-up that might even include a home visit or two. In some practices, the best option is to have a dietitian on the team.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Where did you learn about nutrition? Was it primarily at home supplemented by a few teachers as you navigated K through 12? Studies have shown that it probably wasn’t during medical school (“How much does your doctor actually know about nutrition?” American Heart Association News, April 30, 2018). A survey of one-third of medicals schools done in 1985 found “inadequate exposure to nutrition,” which prompted the National Academy of Sciences to recommend a minimum of 25 classroom hours. A more recent survey in 2013 discovered that 71% percent of medical schools fail to meet that benchmark.
I certainly don’t recall receiving any teaching in medical school that was specifically targeted at nutrition. And to be perfectly honest I never felt that I had missed anything. It’s not that I don’t believe nutrition is important. What we eat joins exercise and sleep at the core of a healthy lifestyle. The problem is that I was never confident that I or anyone else knew what a healthy diet should be. I learned what happened if child didn’t eat enough fruits and vegetables or consume enough vitamin D. But the tide seemed to keep going in and out on how much of each category of food was optimal. What was the perfect nutritional pyramid? And then there was the whole apparent flip-flop on eggs. For myself, I tried to follow the old dictum “everything in moderation ... including moderation.”
Don’t misunderstand me. I think dietitians have a critical role in health maintenance and disease management and should be on the forefront of our efforts to seek the causes of those medical conditions that have yet to be fully explained. It would be a mistake to recommend a low-salt diet to a patient without encouraging him or her (and the family) to consult with a dietitian. However, is having a medical students spend an afternoon in a kitchen preparing a low-salt diet a worthwhile investment of 4 precious hours of their educational time? It sounds cool, and at the end of the day, the student will certainly have a better understanding of how difficult his dietary recommendations will be to follow. But if the student ends up being a pediatrician, how often will he look back on the kitchen experience as a positive?
Giving specific and detailed instruction on how to shop for and prepare a medically prescribed diet can be very time consuming, and it can’t be done well without close follow-up that might even include a home visit or two. In some practices, the best option is to have a dietitian on the team.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
It’s not about time
Like most couples of retirement age, rituals dominate our breakfasts. I eat eggs. Marilyn leans toward baked goods. We each have a bowl of fruit and finish by working the New York Times mini-crossword on our electronic devices. Solving it usually takes somewhere between 40 seconds and 4 minutes. The challenge lies in how fast one can complete the puzzle. And, being who we are, Marilyn and I have ritualized this into a serious competition. She usually takes the first turn and then tries to psyche me out by announcing, “I did it in 2:34, but you should be able to solve it in less than 2 minutes.” This bit of gamesmanship often means that I am going to start the day with thin layer of nervous perspiration.
The claimed disabilities range from an anxiety disorder and ADHD to a problem with reading comprehension. The number of students requesting a test environment modification at Pomona College, Claremont, Calif., is 22% up from 5% in 2014. At Marlboro College in Vermont, one in three students asks for more time or a less distracting setting.
This phenomenon raises two obvious questions. First, what has happened to the bell-shaped curve? Was it too boring hanging out with all those people under the bell? Do folks feel safer and more secure in the tails? I guess we have to be happy that young people are less afraid to admit they are different. But it does make one wonder how we should go about defining a disability.
The second question is whether timed tests deserve a place in our educational toolbox? How often is processing speed important? I would like the woman piloting my flight to San Francisco to be quick-witted. But what about the research chemist working on a more durable tire compound? Is it a problem that it took him 30% longer than his classmates to successfully finish his college statistics final exam?
What about the lawyer who bills you $500 per hour to review the contract with your employer? It might have been helpful to know before you hired him that he routinely requested an extra hour and a half to complete his exams in law school. But I suspect that for the most part timed tests probably don’t produce better graduates. In the past they may have been used to thin oversubscribed disciplines, and certainly time limits have been the norm at every level of education I encountered. However, the best taught courses had exams with an abundance of time. Either you knew the information or you didn’t. An extra 2 hours wasn’t going to make a difference.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Like most couples of retirement age, rituals dominate our breakfasts. I eat eggs. Marilyn leans toward baked goods. We each have a bowl of fruit and finish by working the New York Times mini-crossword on our electronic devices. Solving it usually takes somewhere between 40 seconds and 4 minutes. The challenge lies in how fast one can complete the puzzle. And, being who we are, Marilyn and I have ritualized this into a serious competition. She usually takes the first turn and then tries to psyche me out by announcing, “I did it in 2:34, but you should be able to solve it in less than 2 minutes.” This bit of gamesmanship often means that I am going to start the day with thin layer of nervous perspiration.
The claimed disabilities range from an anxiety disorder and ADHD to a problem with reading comprehension. The number of students requesting a test environment modification at Pomona College, Claremont, Calif., is 22% up from 5% in 2014. At Marlboro College in Vermont, one in three students asks for more time or a less distracting setting.
This phenomenon raises two obvious questions. First, what has happened to the bell-shaped curve? Was it too boring hanging out with all those people under the bell? Do folks feel safer and more secure in the tails? I guess we have to be happy that young people are less afraid to admit they are different. But it does make one wonder how we should go about defining a disability.
The second question is whether timed tests deserve a place in our educational toolbox? How often is processing speed important? I would like the woman piloting my flight to San Francisco to be quick-witted. But what about the research chemist working on a more durable tire compound? Is it a problem that it took him 30% longer than his classmates to successfully finish his college statistics final exam?
What about the lawyer who bills you $500 per hour to review the contract with your employer? It might have been helpful to know before you hired him that he routinely requested an extra hour and a half to complete his exams in law school. But I suspect that for the most part timed tests probably don’t produce better graduates. In the past they may have been used to thin oversubscribed disciplines, and certainly time limits have been the norm at every level of education I encountered. However, the best taught courses had exams with an abundance of time. Either you knew the information or you didn’t. An extra 2 hours wasn’t going to make a difference.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Like most couples of retirement age, rituals dominate our breakfasts. I eat eggs. Marilyn leans toward baked goods. We each have a bowl of fruit and finish by working the New York Times mini-crossword on our electronic devices. Solving it usually takes somewhere between 40 seconds and 4 minutes. The challenge lies in how fast one can complete the puzzle. And, being who we are, Marilyn and I have ritualized this into a serious competition. She usually takes the first turn and then tries to psyche me out by announcing, “I did it in 2:34, but you should be able to solve it in less than 2 minutes.” This bit of gamesmanship often means that I am going to start the day with thin layer of nervous perspiration.
The claimed disabilities range from an anxiety disorder and ADHD to a problem with reading comprehension. The number of students requesting a test environment modification at Pomona College, Claremont, Calif., is 22% up from 5% in 2014. At Marlboro College in Vermont, one in three students asks for more time or a less distracting setting.
This phenomenon raises two obvious questions. First, what has happened to the bell-shaped curve? Was it too boring hanging out with all those people under the bell? Do folks feel safer and more secure in the tails? I guess we have to be happy that young people are less afraid to admit they are different. But it does make one wonder how we should go about defining a disability.
The second question is whether timed tests deserve a place in our educational toolbox? How often is processing speed important? I would like the woman piloting my flight to San Francisco to be quick-witted. But what about the research chemist working on a more durable tire compound? Is it a problem that it took him 30% longer than his classmates to successfully finish his college statistics final exam?
What about the lawyer who bills you $500 per hour to review the contract with your employer? It might have been helpful to know before you hired him that he routinely requested an extra hour and a half to complete his exams in law school. But I suspect that for the most part timed tests probably don’t produce better graduates. In the past they may have been used to thin oversubscribed disciplines, and certainly time limits have been the norm at every level of education I encountered. However, the best taught courses had exams with an abundance of time. Either you knew the information or you didn’t. An extra 2 hours wasn’t going to make a difference.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Pediatric Dermatology Consult - June 2018
The patient was diagnosed with granuloma annulare on the basis of history and clinical exam. A potassium hydroxide prep of skin scrapings was performed to rule out tinea corporis, and did not show evidence of fungal elements. The patient was treated with topical betamethasone with partial improvement.
First described as a “ringed eruption of the fingers” by Thomas Colcott Fox in 1895, granuloma annulare (GA) is a relatively common, benign, and self-limited condition whose precise etiology remains unclear. It is characterized commonly by pink to violaceous aciform or annular plaques on clinical examination. In some cases of GA, annular lesions are not present, or may be formed of grouped papules.
GA is characterized histologically by patchy interstitial lymphocytes and histiocytes palisading around mucin. Deep GA, an unusual subtype observed only in children, features a fibrin rather than a mucin core. This granulomatous picture is consistent with a Th1-mediated inflammatory process, and indeed, macrophage tumor necrosis factor production, as well as interleukin-2 and interferon-gamma production have been observed in GA. The reason for this exaggerated Th1 response is unknown, although in susceptible individuals trauma3 (an example of the Koebner phenomenon), arthropod assault,4 and herpes simplex infection5 (an example of Wolf isotopic response) all have been observed to trigger localized and/or generalized GA. Generalized GA has been associated with hyperlipidemia and the human leukocyte antigen–BW35 allele. GA has been described as a paraneoplastic eruption; atypical features such as associated pain or appearance in an uncharacteristic location often are present in such cases.6,7
Diagnosis of typical GA is clinical. If unusual features make you suspect tinea, leprosy, mycosis fungoides, or other annular lesions, then biopsy showing features typical of GA can reveal the correct diagnosis. Biopsy also can help to distinguish papular GA from warts or molluscum contagiosum. If extensive GA are present, then serum lipid testing for hypercholesterolemia or hypertriglyceridemia should be considered.
Other annular and raised lesions are on the differential for GA, but careful attention to the patient’s history and examination can clarify the diagnosis. Urticaria multiforme, a variant of annular urticaria, presents with numerous annular and polycyclic wheals, sometimes with central darkening that may be mistaken for necrosis. This patient did not present with polycyclic wheals. Furthermore, the lesions in urticaria multiforme are typically transient, with individual lesions lasting less than 24 hours, which was not the case with this patient. Wells syndrome, also known as eosinophilic cellulitis, is a condition marked by recurrent episodes of pruritus followed by appearance of edematous, painful, indurated, or edematous papules or plaques, although bullae and vesicles also may be present. The face and extremities are frequently involved and spontaneous resolution typically occurs in 2 months. Annular lesions are possible but papules, plaques, and nodules are more common in Wells syndrome. Annular elastolytic giant cell granuloma (AEGCG), also known as actinic granuloma and Miescher granuloma of the face, is an entity characterized clinically by chronic, persistent, sun-distributed, annular plaques typically seen in older women with significant sun damage. AEGCG is considered by some to be a variant of GA, but if this is the case, it is a distinct subtype with different epidemiologic, clinical, and histopathologic characteristics from GA. Interstitial granulomatous dermatitis is histologically and clinically distinct from GA, presenting as subtly erythematous cords or extensive annular or serpiginous plaques in the axilla, groin, buttocks, or chest, typically in adult patients with rheumatoid arthritis, reactive arthritis, psoriatic arthritis, or ankylosing spondylitis. Tinea corporis, the clinical manifestation of cutaneous dermatophyte infection, may be mistaken for granuloma annulare. However, tinea corporis lesions are scaly, whereas GA does not scale. Histologic examination of tinea corporis reveals hyphae, which are not present in GA.
GA is a relatively common, idiopathic, benign skin disease with numerous annular and papular mimics. Absence of scale, pain, and significant pruritus are important clues to the diagnosis, and biopsy can be helpful when the diagnosis is unclear. Treatment, although not necessary, may be offered using any of a number of modalities. The most consistent and effective healer of GA, however, is time.
References
1. J Am Acad Dermatol. 1980 Sep;3(3):217-30.
2. J Am Acad Dermatol. 2016 Sep;75(3):457-65.
3. Dermatol Online J. 2013 Dec 16;19(12):20719.
4. Acta Derm Venereol. 2008;88(5):519-20.
5. J Cutan Med Surg. 2014 Nov;18(6):413-9.
6. South Med J. 1997 Oct;90(10):1056-9.
7. Am J Dermatopathol. 2003 Apr;25(2):113-6.
8. Am J Clin Dermatol. 2013 Aug;14(4):279-90.
9. Br J Dermatol. 1994 Apr;130(4):494-7.
The patient was diagnosed with granuloma annulare on the basis of history and clinical exam. A potassium hydroxide prep of skin scrapings was performed to rule out tinea corporis, and did not show evidence of fungal elements. The patient was treated with topical betamethasone with partial improvement.
First described as a “ringed eruption of the fingers” by Thomas Colcott Fox in 1895, granuloma annulare (GA) is a relatively common, benign, and self-limited condition whose precise etiology remains unclear. It is characterized commonly by pink to violaceous aciform or annular plaques on clinical examination. In some cases of GA, annular lesions are not present, or may be formed of grouped papules.
GA is characterized histologically by patchy interstitial lymphocytes and histiocytes palisading around mucin. Deep GA, an unusual subtype observed only in children, features a fibrin rather than a mucin core. This granulomatous picture is consistent with a Th1-mediated inflammatory process, and indeed, macrophage tumor necrosis factor production, as well as interleukin-2 and interferon-gamma production have been observed in GA. The reason for this exaggerated Th1 response is unknown, although in susceptible individuals trauma3 (an example of the Koebner phenomenon), arthropod assault,4 and herpes simplex infection5 (an example of Wolf isotopic response) all have been observed to trigger localized and/or generalized GA. Generalized GA has been associated with hyperlipidemia and the human leukocyte antigen–BW35 allele. GA has been described as a paraneoplastic eruption; atypical features such as associated pain or appearance in an uncharacteristic location often are present in such cases.6,7
Diagnosis of typical GA is clinical. If unusual features make you suspect tinea, leprosy, mycosis fungoides, or other annular lesions, then biopsy showing features typical of GA can reveal the correct diagnosis. Biopsy also can help to distinguish papular GA from warts or molluscum contagiosum. If extensive GA are present, then serum lipid testing for hypercholesterolemia or hypertriglyceridemia should be considered.
Other annular and raised lesions are on the differential for GA, but careful attention to the patient’s history and examination can clarify the diagnosis. Urticaria multiforme, a variant of annular urticaria, presents with numerous annular and polycyclic wheals, sometimes with central darkening that may be mistaken for necrosis. This patient did not present with polycyclic wheals. Furthermore, the lesions in urticaria multiforme are typically transient, with individual lesions lasting less than 24 hours, which was not the case with this patient. Wells syndrome, also known as eosinophilic cellulitis, is a condition marked by recurrent episodes of pruritus followed by appearance of edematous, painful, indurated, or edematous papules or plaques, although bullae and vesicles also may be present. The face and extremities are frequently involved and spontaneous resolution typically occurs in 2 months. Annular lesions are possible but papules, plaques, and nodules are more common in Wells syndrome. Annular elastolytic giant cell granuloma (AEGCG), also known as actinic granuloma and Miescher granuloma of the face, is an entity characterized clinically by chronic, persistent, sun-distributed, annular plaques typically seen in older women with significant sun damage. AEGCG is considered by some to be a variant of GA, but if this is the case, it is a distinct subtype with different epidemiologic, clinical, and histopathologic characteristics from GA. Interstitial granulomatous dermatitis is histologically and clinically distinct from GA, presenting as subtly erythematous cords or extensive annular or serpiginous plaques in the axilla, groin, buttocks, or chest, typically in adult patients with rheumatoid arthritis, reactive arthritis, psoriatic arthritis, or ankylosing spondylitis. Tinea corporis, the clinical manifestation of cutaneous dermatophyte infection, may be mistaken for granuloma annulare. However, tinea corporis lesions are scaly, whereas GA does not scale. Histologic examination of tinea corporis reveals hyphae, which are not present in GA.
GA is a relatively common, idiopathic, benign skin disease with numerous annular and papular mimics. Absence of scale, pain, and significant pruritus are important clues to the diagnosis, and biopsy can be helpful when the diagnosis is unclear. Treatment, although not necessary, may be offered using any of a number of modalities. The most consistent and effective healer of GA, however, is time.
References
1. J Am Acad Dermatol. 1980 Sep;3(3):217-30.
2. J Am Acad Dermatol. 2016 Sep;75(3):457-65.
3. Dermatol Online J. 2013 Dec 16;19(12):20719.
4. Acta Derm Venereol. 2008;88(5):519-20.
5. J Cutan Med Surg. 2014 Nov;18(6):413-9.
6. South Med J. 1997 Oct;90(10):1056-9.
7. Am J Dermatopathol. 2003 Apr;25(2):113-6.
8. Am J Clin Dermatol. 2013 Aug;14(4):279-90.
9. Br J Dermatol. 1994 Apr;130(4):494-7.
The patient was diagnosed with granuloma annulare on the basis of history and clinical exam. A potassium hydroxide prep of skin scrapings was performed to rule out tinea corporis, and did not show evidence of fungal elements. The patient was treated with topical betamethasone with partial improvement.
First described as a “ringed eruption of the fingers” by Thomas Colcott Fox in 1895, granuloma annulare (GA) is a relatively common, benign, and self-limited condition whose precise etiology remains unclear. It is characterized commonly by pink to violaceous aciform or annular plaques on clinical examination. In some cases of GA, annular lesions are not present, or may be formed of grouped papules.
GA is characterized histologically by patchy interstitial lymphocytes and histiocytes palisading around mucin. Deep GA, an unusual subtype observed only in children, features a fibrin rather than a mucin core. This granulomatous picture is consistent with a Th1-mediated inflammatory process, and indeed, macrophage tumor necrosis factor production, as well as interleukin-2 and interferon-gamma production have been observed in GA. The reason for this exaggerated Th1 response is unknown, although in susceptible individuals trauma3 (an example of the Koebner phenomenon), arthropod assault,4 and herpes simplex infection5 (an example of Wolf isotopic response) all have been observed to trigger localized and/or generalized GA. Generalized GA has been associated with hyperlipidemia and the human leukocyte antigen–BW35 allele. GA has been described as a paraneoplastic eruption; atypical features such as associated pain or appearance in an uncharacteristic location often are present in such cases.6,7
Diagnosis of typical GA is clinical. If unusual features make you suspect tinea, leprosy, mycosis fungoides, or other annular lesions, then biopsy showing features typical of GA can reveal the correct diagnosis. Biopsy also can help to distinguish papular GA from warts or molluscum contagiosum. If extensive GA are present, then serum lipid testing for hypercholesterolemia or hypertriglyceridemia should be considered.
Other annular and raised lesions are on the differential for GA, but careful attention to the patient’s history and examination can clarify the diagnosis. Urticaria multiforme, a variant of annular urticaria, presents with numerous annular and polycyclic wheals, sometimes with central darkening that may be mistaken for necrosis. This patient did not present with polycyclic wheals. Furthermore, the lesions in urticaria multiforme are typically transient, with individual lesions lasting less than 24 hours, which was not the case with this patient. Wells syndrome, also known as eosinophilic cellulitis, is a condition marked by recurrent episodes of pruritus followed by appearance of edematous, painful, indurated, or edematous papules or plaques, although bullae and vesicles also may be present. The face and extremities are frequently involved and spontaneous resolution typically occurs in 2 months. Annular lesions are possible but papules, plaques, and nodules are more common in Wells syndrome. Annular elastolytic giant cell granuloma (AEGCG), also known as actinic granuloma and Miescher granuloma of the face, is an entity characterized clinically by chronic, persistent, sun-distributed, annular plaques typically seen in older women with significant sun damage. AEGCG is considered by some to be a variant of GA, but if this is the case, it is a distinct subtype with different epidemiologic, clinical, and histopathologic characteristics from GA. Interstitial granulomatous dermatitis is histologically and clinically distinct from GA, presenting as subtly erythematous cords or extensive annular or serpiginous plaques in the axilla, groin, buttocks, or chest, typically in adult patients with rheumatoid arthritis, reactive arthritis, psoriatic arthritis, or ankylosing spondylitis. Tinea corporis, the clinical manifestation of cutaneous dermatophyte infection, may be mistaken for granuloma annulare. However, tinea corporis lesions are scaly, whereas GA does not scale. Histologic examination of tinea corporis reveals hyphae, which are not present in GA.
GA is a relatively common, idiopathic, benign skin disease with numerous annular and papular mimics. Absence of scale, pain, and significant pruritus are important clues to the diagnosis, and biopsy can be helpful when the diagnosis is unclear. Treatment, although not necessary, may be offered using any of a number of modalities. The most consistent and effective healer of GA, however, is time.
References
1. J Am Acad Dermatol. 1980 Sep;3(3):217-30.
2. J Am Acad Dermatol. 2016 Sep;75(3):457-65.
3. Dermatol Online J. 2013 Dec 16;19(12):20719.
4. Acta Derm Venereol. 2008;88(5):519-20.
5. J Cutan Med Surg. 2014 Nov;18(6):413-9.
6. South Med J. 1997 Oct;90(10):1056-9.
7. Am J Dermatopathol. 2003 Apr;25(2):113-6.
8. Am J Clin Dermatol. 2013 Aug;14(4):279-90.
9. Br J Dermatol. 1994 Apr;130(4):494-7.
A 9-year-old girl presented to the dermatology clinic, referred by her pediatrician, for evaluation of asymptomatic lesions on her shins and feet for 2 months. She started developing one lesion over her right shin with other lesions appearing on the opposite leg a few weeks after, and treated the areas initially with an over-the-counter antifungal cream without improvement. She has been healthy and denied any recent fevers or upper respiratory infections, and said she had not taken any medications or vitamin supplements. She reported camping with her father occasionally but denied any bug or tick bites. No other family members were affected. There was no personal or family history of diabetes mellitus or high cholesterol, and there are no pets at home.
Reverse T3 or perverse T3? Still puzzling after 40 years
Four decades after reverse T3 (3,3´5´-triiodothyronine) was discovered, its physiologic and clinical relevance remains unclear and is still being studied. But scientific uncertainty has not stopped writers in the consumer press and on the Internet from making unsubstantiated claims about this hormone. Many patients believe their hypothyroid symptoms are due to high levels of reverse T3 and want to be tested for it, and some even bring in test results from independent laboratories.
HOW THYROID HORMONES WERE DISCOVERED
In 1970, Braverman et al9 showed that T4 is converted to T3 in athyreotic humans, and Sterling et al10 demonstrated the same in healthy humans. During that decade, techniques for measuring T4 were refined,11 and a specific radioimmunoassay for reverse T3 allowed a glimpse of its physiologic role.12 In 1975, Chopra et al13 noted reciprocal changes in the levels of T3 and reverse T3 in systemic illnesses—ie, when people are sick, their T3 levels go down and their reverse T3 levels go up.
The end of the 70s was marked by a surge of interest in T4 metabolites, including the development of a radioimmunoassay for 3,3´-diiodothyronine (3-3´ T2).18
The observed reciprocal changes in serum levels of T3 and reverse T3 suggested that T4 degradation is regulated into activating (T3) or inactivating (reverse T3) pathways, and that these changes are a presumed homeostatic process of energy conservation.19
HOW THYROID HORMONES ARE METABOLIZED
In the thyroid gland, for thyroid hormones to be synthesized, iodide must be oxidized and incorporated into the precursors 3-monoiodotyrosine (MIT) and 3,5-diiodotyrosine (DIT). This process is mediated by the enzyme thyroid peroxidase in the presence of hydrogen peroxide.20
The thyroid can make T4 and some T3
T4 is the main iodothyronine produced by the thyroid gland, at a rate of 80 to 100 µg per day.21 It is synthesized from the fusion of 2 DIT molecules.
The thyroid can also make T3 by fusing 1 DIT and 1 MIT molecule, but this process accounts for no more than 20% of the circulating T3 in humans. The rest of T3, and 95% to 98% of all reverse T3, is derived from peripheral conversion of T4 through deiodination.
T4 is converted to T3 or reverse T3
The metabolic transformation of thyroid hormones in peripheral tissues determines their biologic potency and regulates their biologic effects.
The number 4 in T4 means it has 4 iodine atoms. It can lose 1 of them, yielding either T3 or reverse T3, depending on which iodine atom it loses (Figure 3). Loss of iodine from the five-prime (5´) position on its outer ring yields T3, the most potent thyroid hormone, produced at a rate of 30 to 40 µg per day.21 On the other hand, when T4 loses an iodine atom from the five (5) position on its inner ring it yields reverse T3, produced at a rate slightly less than that of T3, 28 to 40 µg per day.21 Reverse T3 is inactive.
Both T3 and reverse T3 can shed more iodine atoms, forming in turn various isomers of T2, T1, and ultimately T0. Other pathways for thyroid hormone metabolism include glucuronidation, sulfation, oxidative deamination, and ether bond cleavage.20–22
D1 and D2 catalyze T3, D3 catalyzes reverse T3
Three types of enzymes that mediate deiodination have been identified and designated D1, D2, and D3. In humans they are expressed in variable amounts throughout the body:
- D1 mainly in the liver, kidneys, thyroid, and pituitary, but notably absent in the central nervous system
- D2 in the central nervous system, pituitary, brown adipose tissue, thyroid, placenta, skeletal muscle, and heart
- D3 in the central nervous system, skin, hemangiomas, fetal liver, placenta, and fetal tissues.23
D1 and D2 are responsible for converting T4 to T3, and D3 is responsible for converting T4 to reverse T3.
Plasma concentrations of free T4 and free T3 are relatively constant; however, tissue concentrations of free T3 vary in different tissues according to the amount of hormone transported and the activity of local deiodinases.23 Most thyroid hormone actions are initiated after T3 binds to its nuclear receptor. In this setting, deiodinases play a critical role in maintaining tissue and cellular thyroid hormone levels, so that thyroid hormone signaling can change irrespective of serum hormonal concentrations.22–24 For example, in the central nervous system, production of T3 by local D2 is significantly relevant for T3 homeostasis.22,23
Deiodinases also modulate the tissue-specific concentrations of T3 in response to iodine deficiency and to changes in thyroid state.23 During iodine deficiency and hypothyroidism, tissues that express D2, especially brain tissues, increase the activity of this enzyme in order to increase local conversion of T4 to T3. In hyperthyroidism, D1 overexpression contributes to the relative excess of T3 production, while D3 up-regulation in the brain protects the central nervous system from excessive amounts of thyroid hormone.23
REVERSE T3 AND SYSTEMIC ILLNESS
D3 is the main physiologic inactivator of thyroid hormones. This enzyme plays a central role in protecting tissues from an excess of thyroid hormone.23,24 This mechanism is crucial for fetal development and explains the high expression of D3 in the human placenta and fetal tissues.
In adult tissues, the importance of D3 in the regulation of thyroid hormone homeostasis becomes apparent under certain pathophysiologic conditions, such as nonthyroidal illness and malnutrition.
Whenever a reduction in metabolism is homeostatically desirable, such as in critically ill patients or during starvation, conversion to T3 is reduced and, alternatively, conversion to reverse T3 is increased. This pathway represents a metabolic adaptation that may protect the tissues from the catabolic effects of thyroid hormone that could otherwise worsen the patient’s basic clinical condition.
Euthyroid sick syndrome or hypothyroid?
In a variety of systemic illnesses, some patients with low T3, low or normal T4, and normal thyroid-stimulating hormone (TSH) levels could in fact be “sick euthyroid” rather than hypothyroid. The first reports of the euthyroid sick syndrome or low T3 syndrome date back to about 1976, and even though assays for reverse T3 were not widely available, some authors linked the syndrome to high levels of reverse T3.15,16 The syndrome is also known as nonthyroidal illness syndrome.
Advances in techniques for measuring T3, reverse T3, and other iodothyronines filled a gap in the understanding of the alterations that occur in thyroid hormone economy during severe nonthyroidal diseases. In 1982, Wartofsky and Burman25 reviewed the alterations in thyroid function in patients with systemic illness and discussed other factors that may alter thyroid economy, such as age, stress, and diverse drugs.
More recently, the low-T3 syndrome was revisited with a generalized concept regarding the role of D3 in the syndrome.26 D3, normally undetectable in mature tissues, is reactivated in diverse cell types in response to injury and is responsible for a fall in serum T3 levels. Hypoxia induces D3 activity and mRNA in vitro and in vivo.27 Recent studies have focused on the role of cytokines in the low T3 syndrome. For instance, interleukin 6 reduces D1 and D2 activity and increases D3 activity in vitro.28
In the outpatient setting, diverse conditions may affect thyroid hormone homeostasis, compatible with mild or atypical forms of low-T3 syndrome, including caloric deprivation, heart failure, and human immunodeficiency virus infection.29
POSSIBLE CLINICAL UTILITY OF MEASURING REVERSE T3
In inpatients
Unfortunately, measuring serum reverse T3 levels has not, in general, proven clinically useful for the diagnosis of hypothyroidism in systemically ill patients. Burmeister30 demonstrated, in a retrospective study, that when illness complicates the interpretation of thyroid function tests, serum reverse T3 measurements do not reliably distinguish the hypothyroid sick patient from the euthyroid sick patient. The best way to make the diagnosis, Burmeister suggested, is by clinical assessment, combined use of free T4 and TSH measurements, and patient follow-up.
In the outpatient setting, the utility of reverse T3 measurements is controversial. In intensive care units, the differential diagnosis between hypothyroidism and nonthyroidal illness syndrome can sometimes be difficult. Reverse T3 levels can be low, normal, or high regardless of the thyroidal state of the patient.30 Moreover, endogenous changes in the hypothalamic-pituitary-thyroid axis may be further complicated by medications commonly used in intensive care units, such as dopamine and glucocorticoids. Changes in thyroid function should be evaluated in the context of the patient’s clinical condition (Table 1).20 But regardless of the T3 level, treatment with T3 or T4 should not be started without taking into consideration the patient’s general clinical context; controlled trials have not shown such therapy to be beneficial.20
In outpatients
In noncritical conditions that may be associated with mild forms of low T3 syndrome, patients generally present with low T3 concentrations concurrently with low or normal TSH. Not infrequently, however, patients present with a serum reverse T3 measurement and impute their symptoms of hypothyroidism to “abnormal” reverse T3 levels, in spite of normal TSH levels.
There is no rationale for measuring reverse T3 to initiate or to adjust levothyroxine therapy—the single test relevant for these purposes is the TSH measurement. The risks of basing treatment decisions on reverse T3 levels include the use of excessive doses of levothyroxine that may lead to a state of subclinical or even clinical hyperthyroidism.
TAKE-HOME MESSAGE
The existence of an inactivating pathway of thyroid hormones represents a homeostatic mechanism, and in selected circumstances measuring serum reverse T3 may be useful, such as in euthyroid sick patients. The discovery of the molecular mechanisms that lead to the reactivation of D3 in illness is an important field of research.
- Kendall EC. Landmark article, June 19, 1915. The isolation in crystalline form of the compound containing iodin, which occurs in the thyroid. Its chemical nature and physiologic activity. By E.C. Kendall. JAMA 1983; 250(15):2045–2046. doi:10.1001/jama.1983.03340150087037
- Harington CR. Chemistry of thyroxine: isolation of thyroxine from the thyroid gland. Biochem J 1926; 20(2):293–299. pmid: 16743658
- Harington CR, Barger G. Chemistry of thyroxine: constitution and synthesis of thyroxine. Biochem J 1927; 21(1):169–183. pmid:16743801
- Gross J, Pitt-Rivers R. The identification of 3,5,3’L-triiodothyronine in human plasma. Lancet 1952; 1(6705):439–441. doi:10.1016/S0140-6736(52)91952-1
- Gross J, Pitt-Rivers R. 3:5:3’-triiodothyronine. 1. Isolation from thyroid gland and synthesis. Biochem J 1953; 53(4):645–650. pmid:13032123
- Pitt-Rivers R, Stanbury JB, Rapp B. Conversion of thyroxine to 3-5-3´-triiodothyronine in vivo. J Clin Endocrinol Metab 1955; 15(5):616–620. doi:10.1210/jcem-15-5-616
- Maclagan NF, Bowden CH, Wilkinson JH. The metabolism of thyroid hormones. 2. Detection of thyroxine and tri-iodothyronine in human plasma. Biochem J. 1957; 67(1):5–11. pmid:13471502
- Galton VA, Pitt-Rivers R. The identification of the acetic acid analogues of thyroxine and tri-iodothyronine in mammalian tissues. Biochem J 1959; 72(2):319–321. pmid: 13662303
- Braverman LE, Ingbar SH, Sterling K. Conversion of thyroxine (T4) to triiodothyronine (T3) in athyreotic human subjects. J Clin Invest 1970; 49(5):855–864. doi:10.1172/JCI106304
- Sterling K, Brenner MA, Newman ES. Conversion of thyroxine to triiodothyronine in normal human subjects. Science 1970; 169(3950):1099–1100. doi:10.1126/science.169.3950.1099
- Chopra IJ. A radioimmunoassay for measurement of thyroxine in unextracted serum. J Clin Endocrinol Metab 1972; 34:938–947. doi:10.1210/jcem-34-6-938
- Chopra IJ. A radioimmunoassay for measurement of 3,3´,5´-triiodothyronine (reverse T3). J Clin Invest 1974; 54(3):583–592. doi:10.1172/JCI107795
- Chopra IJ, Chopra U, Smith SR, Reza M, Solomon DH. Reciprocal changes in serum concentrations of 3,3´,5-triiodothyronine (T3) in systemic illnesses. J Clin Endocrinol Metab 1975; 41(6):1043–1049. doi:10.1210/jcem-41-6-1043
- Burman KD, Read J, Dimond RC, Strum D, et al. Measurement of 3,3’,5’-triiodothyroinine (reverse T3), 3,3’-L-diiodothyronine, T3 and T4 in human amniotic fluid and in cord and maternal serum. J Clin Endocrinol Metab 1976; 43(6):1351–1359. doi:10.1210/jcem-43-6-1351
- Rubenfeld S. Euthyroid sick syndrome. N Engl J Med 1978; 299(25):1414. doi:10.1056/NEJM197812212992514
- Burger A, Nicod P, Suter P, Vallotton MB, Vagenakis P, Braverman L. Reduced active thyroid hormone levels in acute illness. Lancet 1976; 1(7961):653–655. doi:10.1016/S0140-6736(76)92774-4
- Burman KD, Dimond RC, Wright FD, Earll JM, Bruton J, Wartofsky L. A radioimmunoassay for 3,3´,5´-L-triiodothyronine (reverse T3): assessment of thyroid gland content and serum measurements in conditions of normal and altered thyroidal economy and following administration of thyrotropin releasing hormone (TRH) and thyrotropin (TSH). J Clin Endocrinol Metab 1977; 44(4):660–672. doi:10.1210/jcem-44-4-660
- Burman KD, Strum D, Dimond RC, et al. A radioimmunoassay for 3,3´-L-diiodothyronine (3,3´T2). J Clin Endocrinol Metab 1977; 45(2):339–352. doi:10.1210/jcem-45-2-339
- Burman KD. Recent developments in thyroid hormone metabolism: interpretation and significance of measurements of reverse T3, 3,3´T2, and thyroglobulin. Metabolism 1978; 27(5):615–630. doi:10.1016/0026-0495(78)90028-8.
- Salvatore D, Davies TF, Schlumberger M, Hay ID, Larsen PR. Thyroid physiology and diagnostic evaluation of patients with thyroid disorders. In: Melmed S, Polonsky KS, Larsen PR, Kronenberg HM, eds. Williams Textbook of Endocrinology. 13th ed. Philadelphia, PA; Elsevier; 2016:334–368.
- Engler D, Burger AG. The deiodination of the iodothyronines and of their derivatives in man. Endocr Rev 1984; 5(2):151–184. doi:10.1210/edrv-5-2-151
- Peeters RP, Visser TJ, Peeters RP. Metabolism of thyroid hormone. Thyroid Disease Manager. www.thyroidmanager.org/chapter/metabolism-of-thyroid-hormone. Accessed March 14, 2018.
- Bianco AC, Salvatore D, Gereben B, Berry MJ, Larsen PR. Biochemistry, cellular and molecular biology, and physiological roles of the iodothyronine selenodeiodinases. Endocr Rev 2002; 23(1):38–89. doi:10.1210/edrv.23.1.0455
- Dentice M, Salvatore D. Deiodinases: the balance of thyroid hormone: local impact of thyroid hormone inactivation. J Endocrinol 2011; 209(3):273–282. doi:10.1530/JOE-11-0002
- Wartofsky L, Burman KD. Alterations in thyroid function in patients with systemic illness: the “euthyroid sick syndrome.” Endocr Rev 1982; 3(2):164–217. doi:10.1210/edrv-3-2-164
- Huang SA, Bianco AC. Reawakened interest in type III iodothyronine deiodinase in critical illness and injury. Nat Clin Pract Endocrinol Metab 2008; 4(3):148–155. doi:10.1038/ncpendmet0727
- Simonides WS, Mulcahey MA, Redout EM, et al. Hypoxia-inducible factor induces local thyroid hormone inactivation during hypoxic-ischemic disease in rats. J Clin Invest 2008; 118(3):975–983. doi:10.1172/JCI32824
- Wajner SM, Goemann IM, Bueno AL, Larsen PR, Maia AL. IL-6 promotes nonthyroidal illness syndrome by blocking thyroxine activation while promoting thyroid hormone inactivation in human cells. J Clin Invest 2011; 121(5):1834–1845. doi:10.1172/JCI44678
- Moura Neto A, Zantut-Wittmann DE. Abnormalities of thyroid hormone metabolism during systemic illness: the low T3 syndrome in different clinical settings. Int J Endocrinol 2016; 2016:2157583. doi:10.1155/2016/2157583
- Burmeister LA. Reverse T3 does not reliably differentiate hypothyroid sick syndrome from euthyroid sick syndrome. Thyroid 1995; 5(6):435–441. doi:10.1089/thy.1995.5.435
- Huang SA, Tu HM, Harney JW, et al. Severe hypothyroidism caused by type 3 iodothyronine deiodinase in infantile hemangiomas. N Engl J Med 2000; 343(3):185–189. doi:10.1056/NEJM200007203430305
Four decades after reverse T3 (3,3´5´-triiodothyronine) was discovered, its physiologic and clinical relevance remains unclear and is still being studied. But scientific uncertainty has not stopped writers in the consumer press and on the Internet from making unsubstantiated claims about this hormone. Many patients believe their hypothyroid symptoms are due to high levels of reverse T3 and want to be tested for it, and some even bring in test results from independent laboratories.
HOW THYROID HORMONES WERE DISCOVERED
In 1970, Braverman et al9 showed that T4 is converted to T3 in athyreotic humans, and Sterling et al10 demonstrated the same in healthy humans. During that decade, techniques for measuring T4 were refined,11 and a specific radioimmunoassay for reverse T3 allowed a glimpse of its physiologic role.12 In 1975, Chopra et al13 noted reciprocal changes in the levels of T3 and reverse T3 in systemic illnesses—ie, when people are sick, their T3 levels go down and their reverse T3 levels go up.
The end of the 70s was marked by a surge of interest in T4 metabolites, including the development of a radioimmunoassay for 3,3´-diiodothyronine (3-3´ T2).18
The observed reciprocal changes in serum levels of T3 and reverse T3 suggested that T4 degradation is regulated into activating (T3) or inactivating (reverse T3) pathways, and that these changes are a presumed homeostatic process of energy conservation.19
HOW THYROID HORMONES ARE METABOLIZED
In the thyroid gland, for thyroid hormones to be synthesized, iodide must be oxidized and incorporated into the precursors 3-monoiodotyrosine (MIT) and 3,5-diiodotyrosine (DIT). This process is mediated by the enzyme thyroid peroxidase in the presence of hydrogen peroxide.20
The thyroid can make T4 and some T3
T4 is the main iodothyronine produced by the thyroid gland, at a rate of 80 to 100 µg per day.21 It is synthesized from the fusion of 2 DIT molecules.
The thyroid can also make T3 by fusing 1 DIT and 1 MIT molecule, but this process accounts for no more than 20% of the circulating T3 in humans. The rest of T3, and 95% to 98% of all reverse T3, is derived from peripheral conversion of T4 through deiodination.
T4 is converted to T3 or reverse T3
The metabolic transformation of thyroid hormones in peripheral tissues determines their biologic potency and regulates their biologic effects.
The number 4 in T4 means it has 4 iodine atoms. It can lose 1 of them, yielding either T3 or reverse T3, depending on which iodine atom it loses (Figure 3). Loss of iodine from the five-prime (5´) position on its outer ring yields T3, the most potent thyroid hormone, produced at a rate of 30 to 40 µg per day.21 On the other hand, when T4 loses an iodine atom from the five (5) position on its inner ring it yields reverse T3, produced at a rate slightly less than that of T3, 28 to 40 µg per day.21 Reverse T3 is inactive.
Both T3 and reverse T3 can shed more iodine atoms, forming in turn various isomers of T2, T1, and ultimately T0. Other pathways for thyroid hormone metabolism include glucuronidation, sulfation, oxidative deamination, and ether bond cleavage.20–22
D1 and D2 catalyze T3, D3 catalyzes reverse T3
Three types of enzymes that mediate deiodination have been identified and designated D1, D2, and D3. In humans they are expressed in variable amounts throughout the body:
- D1 mainly in the liver, kidneys, thyroid, and pituitary, but notably absent in the central nervous system
- D2 in the central nervous system, pituitary, brown adipose tissue, thyroid, placenta, skeletal muscle, and heart
- D3 in the central nervous system, skin, hemangiomas, fetal liver, placenta, and fetal tissues.23
D1 and D2 are responsible for converting T4 to T3, and D3 is responsible for converting T4 to reverse T3.
Plasma concentrations of free T4 and free T3 are relatively constant; however, tissue concentrations of free T3 vary in different tissues according to the amount of hormone transported and the activity of local deiodinases.23 Most thyroid hormone actions are initiated after T3 binds to its nuclear receptor. In this setting, deiodinases play a critical role in maintaining tissue and cellular thyroid hormone levels, so that thyroid hormone signaling can change irrespective of serum hormonal concentrations.22–24 For example, in the central nervous system, production of T3 by local D2 is significantly relevant for T3 homeostasis.22,23
Deiodinases also modulate the tissue-specific concentrations of T3 in response to iodine deficiency and to changes in thyroid state.23 During iodine deficiency and hypothyroidism, tissues that express D2, especially brain tissues, increase the activity of this enzyme in order to increase local conversion of T4 to T3. In hyperthyroidism, D1 overexpression contributes to the relative excess of T3 production, while D3 up-regulation in the brain protects the central nervous system from excessive amounts of thyroid hormone.23
REVERSE T3 AND SYSTEMIC ILLNESS
D3 is the main physiologic inactivator of thyroid hormones. This enzyme plays a central role in protecting tissues from an excess of thyroid hormone.23,24 This mechanism is crucial for fetal development and explains the high expression of D3 in the human placenta and fetal tissues.
In adult tissues, the importance of D3 in the regulation of thyroid hormone homeostasis becomes apparent under certain pathophysiologic conditions, such as nonthyroidal illness and malnutrition.
Whenever a reduction in metabolism is homeostatically desirable, such as in critically ill patients or during starvation, conversion to T3 is reduced and, alternatively, conversion to reverse T3 is increased. This pathway represents a metabolic adaptation that may protect the tissues from the catabolic effects of thyroid hormone that could otherwise worsen the patient’s basic clinical condition.
Euthyroid sick syndrome or hypothyroid?
In a variety of systemic illnesses, some patients with low T3, low or normal T4, and normal thyroid-stimulating hormone (TSH) levels could in fact be “sick euthyroid” rather than hypothyroid. The first reports of the euthyroid sick syndrome or low T3 syndrome date back to about 1976, and even though assays for reverse T3 were not widely available, some authors linked the syndrome to high levels of reverse T3.15,16 The syndrome is also known as nonthyroidal illness syndrome.
Advances in techniques for measuring T3, reverse T3, and other iodothyronines filled a gap in the understanding of the alterations that occur in thyroid hormone economy during severe nonthyroidal diseases. In 1982, Wartofsky and Burman25 reviewed the alterations in thyroid function in patients with systemic illness and discussed other factors that may alter thyroid economy, such as age, stress, and diverse drugs.
More recently, the low-T3 syndrome was revisited with a generalized concept regarding the role of D3 in the syndrome.26 D3, normally undetectable in mature tissues, is reactivated in diverse cell types in response to injury and is responsible for a fall in serum T3 levels. Hypoxia induces D3 activity and mRNA in vitro and in vivo.27 Recent studies have focused on the role of cytokines in the low T3 syndrome. For instance, interleukin 6 reduces D1 and D2 activity and increases D3 activity in vitro.28
In the outpatient setting, diverse conditions may affect thyroid hormone homeostasis, compatible with mild or atypical forms of low-T3 syndrome, including caloric deprivation, heart failure, and human immunodeficiency virus infection.29
POSSIBLE CLINICAL UTILITY OF MEASURING REVERSE T3
In inpatients
Unfortunately, measuring serum reverse T3 levels has not, in general, proven clinically useful for the diagnosis of hypothyroidism in systemically ill patients. Burmeister30 demonstrated, in a retrospective study, that when illness complicates the interpretation of thyroid function tests, serum reverse T3 measurements do not reliably distinguish the hypothyroid sick patient from the euthyroid sick patient. The best way to make the diagnosis, Burmeister suggested, is by clinical assessment, combined use of free T4 and TSH measurements, and patient follow-up.
In the outpatient setting, the utility of reverse T3 measurements is controversial. In intensive care units, the differential diagnosis between hypothyroidism and nonthyroidal illness syndrome can sometimes be difficult. Reverse T3 levels can be low, normal, or high regardless of the thyroidal state of the patient.30 Moreover, endogenous changes in the hypothalamic-pituitary-thyroid axis may be further complicated by medications commonly used in intensive care units, such as dopamine and glucocorticoids. Changes in thyroid function should be evaluated in the context of the patient’s clinical condition (Table 1).20 But regardless of the T3 level, treatment with T3 or T4 should not be started without taking into consideration the patient’s general clinical context; controlled trials have not shown such therapy to be beneficial.20
In outpatients
In noncritical conditions that may be associated with mild forms of low T3 syndrome, patients generally present with low T3 concentrations concurrently with low or normal TSH. Not infrequently, however, patients present with a serum reverse T3 measurement and impute their symptoms of hypothyroidism to “abnormal” reverse T3 levels, in spite of normal TSH levels.
There is no rationale for measuring reverse T3 to initiate or to adjust levothyroxine therapy—the single test relevant for these purposes is the TSH measurement. The risks of basing treatment decisions on reverse T3 levels include the use of excessive doses of levothyroxine that may lead to a state of subclinical or even clinical hyperthyroidism.
TAKE-HOME MESSAGE
The existence of an inactivating pathway of thyroid hormones represents a homeostatic mechanism, and in selected circumstances measuring serum reverse T3 may be useful, such as in euthyroid sick patients. The discovery of the molecular mechanisms that lead to the reactivation of D3 in illness is an important field of research.
Four decades after reverse T3 (3,3´5´-triiodothyronine) was discovered, its physiologic and clinical relevance remains unclear and is still being studied. But scientific uncertainty has not stopped writers in the consumer press and on the Internet from making unsubstantiated claims about this hormone. Many patients believe their hypothyroid symptoms are due to high levels of reverse T3 and want to be tested for it, and some even bring in test results from independent laboratories.
HOW THYROID HORMONES WERE DISCOVERED
In 1970, Braverman et al9 showed that T4 is converted to T3 in athyreotic humans, and Sterling et al10 demonstrated the same in healthy humans. During that decade, techniques for measuring T4 were refined,11 and a specific radioimmunoassay for reverse T3 allowed a glimpse of its physiologic role.12 In 1975, Chopra et al13 noted reciprocal changes in the levels of T3 and reverse T3 in systemic illnesses—ie, when people are sick, their T3 levels go down and their reverse T3 levels go up.
The end of the 70s was marked by a surge of interest in T4 metabolites, including the development of a radioimmunoassay for 3,3´-diiodothyronine (3-3´ T2).18
The observed reciprocal changes in serum levels of T3 and reverse T3 suggested that T4 degradation is regulated into activating (T3) or inactivating (reverse T3) pathways, and that these changes are a presumed homeostatic process of energy conservation.19
HOW THYROID HORMONES ARE METABOLIZED
In the thyroid gland, for thyroid hormones to be synthesized, iodide must be oxidized and incorporated into the precursors 3-monoiodotyrosine (MIT) and 3,5-diiodotyrosine (DIT). This process is mediated by the enzyme thyroid peroxidase in the presence of hydrogen peroxide.20
The thyroid can make T4 and some T3
T4 is the main iodothyronine produced by the thyroid gland, at a rate of 80 to 100 µg per day.21 It is synthesized from the fusion of 2 DIT molecules.
The thyroid can also make T3 by fusing 1 DIT and 1 MIT molecule, but this process accounts for no more than 20% of the circulating T3 in humans. The rest of T3, and 95% to 98% of all reverse T3, is derived from peripheral conversion of T4 through deiodination.
T4 is converted to T3 or reverse T3
The metabolic transformation of thyroid hormones in peripheral tissues determines their biologic potency and regulates their biologic effects.
The number 4 in T4 means it has 4 iodine atoms. It can lose 1 of them, yielding either T3 or reverse T3, depending on which iodine atom it loses (Figure 3). Loss of iodine from the five-prime (5´) position on its outer ring yields T3, the most potent thyroid hormone, produced at a rate of 30 to 40 µg per day.21 On the other hand, when T4 loses an iodine atom from the five (5) position on its inner ring it yields reverse T3, produced at a rate slightly less than that of T3, 28 to 40 µg per day.21 Reverse T3 is inactive.
Both T3 and reverse T3 can shed more iodine atoms, forming in turn various isomers of T2, T1, and ultimately T0. Other pathways for thyroid hormone metabolism include glucuronidation, sulfation, oxidative deamination, and ether bond cleavage.20–22
D1 and D2 catalyze T3, D3 catalyzes reverse T3
Three types of enzymes that mediate deiodination have been identified and designated D1, D2, and D3. In humans they are expressed in variable amounts throughout the body:
- D1 mainly in the liver, kidneys, thyroid, and pituitary, but notably absent in the central nervous system
- D2 in the central nervous system, pituitary, brown adipose tissue, thyroid, placenta, skeletal muscle, and heart
- D3 in the central nervous system, skin, hemangiomas, fetal liver, placenta, and fetal tissues.23
D1 and D2 are responsible for converting T4 to T3, and D3 is responsible for converting T4 to reverse T3.
Plasma concentrations of free T4 and free T3 are relatively constant; however, tissue concentrations of free T3 vary in different tissues according to the amount of hormone transported and the activity of local deiodinases.23 Most thyroid hormone actions are initiated after T3 binds to its nuclear receptor. In this setting, deiodinases play a critical role in maintaining tissue and cellular thyroid hormone levels, so that thyroid hormone signaling can change irrespective of serum hormonal concentrations.22–24 For example, in the central nervous system, production of T3 by local D2 is significantly relevant for T3 homeostasis.22,23
Deiodinases also modulate the tissue-specific concentrations of T3 in response to iodine deficiency and to changes in thyroid state.23 During iodine deficiency and hypothyroidism, tissues that express D2, especially brain tissues, increase the activity of this enzyme in order to increase local conversion of T4 to T3. In hyperthyroidism, D1 overexpression contributes to the relative excess of T3 production, while D3 up-regulation in the brain protects the central nervous system from excessive amounts of thyroid hormone.23
REVERSE T3 AND SYSTEMIC ILLNESS
D3 is the main physiologic inactivator of thyroid hormones. This enzyme plays a central role in protecting tissues from an excess of thyroid hormone.23,24 This mechanism is crucial for fetal development and explains the high expression of D3 in the human placenta and fetal tissues.
In adult tissues, the importance of D3 in the regulation of thyroid hormone homeostasis becomes apparent under certain pathophysiologic conditions, such as nonthyroidal illness and malnutrition.
Whenever a reduction in metabolism is homeostatically desirable, such as in critically ill patients or during starvation, conversion to T3 is reduced and, alternatively, conversion to reverse T3 is increased. This pathway represents a metabolic adaptation that may protect the tissues from the catabolic effects of thyroid hormone that could otherwise worsen the patient’s basic clinical condition.
Euthyroid sick syndrome or hypothyroid?
In a variety of systemic illnesses, some patients with low T3, low or normal T4, and normal thyroid-stimulating hormone (TSH) levels could in fact be “sick euthyroid” rather than hypothyroid. The first reports of the euthyroid sick syndrome or low T3 syndrome date back to about 1976, and even though assays for reverse T3 were not widely available, some authors linked the syndrome to high levels of reverse T3.15,16 The syndrome is also known as nonthyroidal illness syndrome.
Advances in techniques for measuring T3, reverse T3, and other iodothyronines filled a gap in the understanding of the alterations that occur in thyroid hormone economy during severe nonthyroidal diseases. In 1982, Wartofsky and Burman25 reviewed the alterations in thyroid function in patients with systemic illness and discussed other factors that may alter thyroid economy, such as age, stress, and diverse drugs.
More recently, the low-T3 syndrome was revisited with a generalized concept regarding the role of D3 in the syndrome.26 D3, normally undetectable in mature tissues, is reactivated in diverse cell types in response to injury and is responsible for a fall in serum T3 levels. Hypoxia induces D3 activity and mRNA in vitro and in vivo.27 Recent studies have focused on the role of cytokines in the low T3 syndrome. For instance, interleukin 6 reduces D1 and D2 activity and increases D3 activity in vitro.28
In the outpatient setting, diverse conditions may affect thyroid hormone homeostasis, compatible with mild or atypical forms of low-T3 syndrome, including caloric deprivation, heart failure, and human immunodeficiency virus infection.29
POSSIBLE CLINICAL UTILITY OF MEASURING REVERSE T3
In inpatients
Unfortunately, measuring serum reverse T3 levels has not, in general, proven clinically useful for the diagnosis of hypothyroidism in systemically ill patients. Burmeister30 demonstrated, in a retrospective study, that when illness complicates the interpretation of thyroid function tests, serum reverse T3 measurements do not reliably distinguish the hypothyroid sick patient from the euthyroid sick patient. The best way to make the diagnosis, Burmeister suggested, is by clinical assessment, combined use of free T4 and TSH measurements, and patient follow-up.
In the outpatient setting, the utility of reverse T3 measurements is controversial. In intensive care units, the differential diagnosis between hypothyroidism and nonthyroidal illness syndrome can sometimes be difficult. Reverse T3 levels can be low, normal, or high regardless of the thyroidal state of the patient.30 Moreover, endogenous changes in the hypothalamic-pituitary-thyroid axis may be further complicated by medications commonly used in intensive care units, such as dopamine and glucocorticoids. Changes in thyroid function should be evaluated in the context of the patient’s clinical condition (Table 1).20 But regardless of the T3 level, treatment with T3 or T4 should not be started without taking into consideration the patient’s general clinical context; controlled trials have not shown such therapy to be beneficial.20
In outpatients
In noncritical conditions that may be associated with mild forms of low T3 syndrome, patients generally present with low T3 concentrations concurrently with low or normal TSH. Not infrequently, however, patients present with a serum reverse T3 measurement and impute their symptoms of hypothyroidism to “abnormal” reverse T3 levels, in spite of normal TSH levels.
There is no rationale for measuring reverse T3 to initiate or to adjust levothyroxine therapy—the single test relevant for these purposes is the TSH measurement. The risks of basing treatment decisions on reverse T3 levels include the use of excessive doses of levothyroxine that may lead to a state of subclinical or even clinical hyperthyroidism.
TAKE-HOME MESSAGE
The existence of an inactivating pathway of thyroid hormones represents a homeostatic mechanism, and in selected circumstances measuring serum reverse T3 may be useful, such as in euthyroid sick patients. The discovery of the molecular mechanisms that lead to the reactivation of D3 in illness is an important field of research.
- Kendall EC. Landmark article, June 19, 1915. The isolation in crystalline form of the compound containing iodin, which occurs in the thyroid. Its chemical nature and physiologic activity. By E.C. Kendall. JAMA 1983; 250(15):2045–2046. doi:10.1001/jama.1983.03340150087037
- Harington CR. Chemistry of thyroxine: isolation of thyroxine from the thyroid gland. Biochem J 1926; 20(2):293–299. pmid: 16743658
- Harington CR, Barger G. Chemistry of thyroxine: constitution and synthesis of thyroxine. Biochem J 1927; 21(1):169–183. pmid:16743801
- Gross J, Pitt-Rivers R. The identification of 3,5,3’L-triiodothyronine in human plasma. Lancet 1952; 1(6705):439–441. doi:10.1016/S0140-6736(52)91952-1
- Gross J, Pitt-Rivers R. 3:5:3’-triiodothyronine. 1. Isolation from thyroid gland and synthesis. Biochem J 1953; 53(4):645–650. pmid:13032123
- Pitt-Rivers R, Stanbury JB, Rapp B. Conversion of thyroxine to 3-5-3´-triiodothyronine in vivo. J Clin Endocrinol Metab 1955; 15(5):616–620. doi:10.1210/jcem-15-5-616
- Maclagan NF, Bowden CH, Wilkinson JH. The metabolism of thyroid hormones. 2. Detection of thyroxine and tri-iodothyronine in human plasma. Biochem J. 1957; 67(1):5–11. pmid:13471502
- Galton VA, Pitt-Rivers R. The identification of the acetic acid analogues of thyroxine and tri-iodothyronine in mammalian tissues. Biochem J 1959; 72(2):319–321. pmid: 13662303
- Braverman LE, Ingbar SH, Sterling K. Conversion of thyroxine (T4) to triiodothyronine (T3) in athyreotic human subjects. J Clin Invest 1970; 49(5):855–864. doi:10.1172/JCI106304
- Sterling K, Brenner MA, Newman ES. Conversion of thyroxine to triiodothyronine in normal human subjects. Science 1970; 169(3950):1099–1100. doi:10.1126/science.169.3950.1099
- Chopra IJ. A radioimmunoassay for measurement of thyroxine in unextracted serum. J Clin Endocrinol Metab 1972; 34:938–947. doi:10.1210/jcem-34-6-938
- Chopra IJ. A radioimmunoassay for measurement of 3,3´,5´-triiodothyronine (reverse T3). J Clin Invest 1974; 54(3):583–592. doi:10.1172/JCI107795
- Chopra IJ, Chopra U, Smith SR, Reza M, Solomon DH. Reciprocal changes in serum concentrations of 3,3´,5-triiodothyronine (T3) in systemic illnesses. J Clin Endocrinol Metab 1975; 41(6):1043–1049. doi:10.1210/jcem-41-6-1043
- Burman KD, Read J, Dimond RC, Strum D, et al. Measurement of 3,3’,5’-triiodothyroinine (reverse T3), 3,3’-L-diiodothyronine, T3 and T4 in human amniotic fluid and in cord and maternal serum. J Clin Endocrinol Metab 1976; 43(6):1351–1359. doi:10.1210/jcem-43-6-1351
- Rubenfeld S. Euthyroid sick syndrome. N Engl J Med 1978; 299(25):1414. doi:10.1056/NEJM197812212992514
- Burger A, Nicod P, Suter P, Vallotton MB, Vagenakis P, Braverman L. Reduced active thyroid hormone levels in acute illness. Lancet 1976; 1(7961):653–655. doi:10.1016/S0140-6736(76)92774-4
- Burman KD, Dimond RC, Wright FD, Earll JM, Bruton J, Wartofsky L. A radioimmunoassay for 3,3´,5´-L-triiodothyronine (reverse T3): assessment of thyroid gland content and serum measurements in conditions of normal and altered thyroidal economy and following administration of thyrotropin releasing hormone (TRH) and thyrotropin (TSH). J Clin Endocrinol Metab 1977; 44(4):660–672. doi:10.1210/jcem-44-4-660
- Burman KD, Strum D, Dimond RC, et al. A radioimmunoassay for 3,3´-L-diiodothyronine (3,3´T2). J Clin Endocrinol Metab 1977; 45(2):339–352. doi:10.1210/jcem-45-2-339
- Burman KD. Recent developments in thyroid hormone metabolism: interpretation and significance of measurements of reverse T3, 3,3´T2, and thyroglobulin. Metabolism 1978; 27(5):615–630. doi:10.1016/0026-0495(78)90028-8.
- Salvatore D, Davies TF, Schlumberger M, Hay ID, Larsen PR. Thyroid physiology and diagnostic evaluation of patients with thyroid disorders. In: Melmed S, Polonsky KS, Larsen PR, Kronenberg HM, eds. Williams Textbook of Endocrinology. 13th ed. Philadelphia, PA; Elsevier; 2016:334–368.
- Engler D, Burger AG. The deiodination of the iodothyronines and of their derivatives in man. Endocr Rev 1984; 5(2):151–184. doi:10.1210/edrv-5-2-151
- Peeters RP, Visser TJ, Peeters RP. Metabolism of thyroid hormone. Thyroid Disease Manager. www.thyroidmanager.org/chapter/metabolism-of-thyroid-hormone. Accessed March 14, 2018.
- Bianco AC, Salvatore D, Gereben B, Berry MJ, Larsen PR. Biochemistry, cellular and molecular biology, and physiological roles of the iodothyronine selenodeiodinases. Endocr Rev 2002; 23(1):38–89. doi:10.1210/edrv.23.1.0455
- Dentice M, Salvatore D. Deiodinases: the balance of thyroid hormone: local impact of thyroid hormone inactivation. J Endocrinol 2011; 209(3):273–282. doi:10.1530/JOE-11-0002
- Wartofsky L, Burman KD. Alterations in thyroid function in patients with systemic illness: the “euthyroid sick syndrome.” Endocr Rev 1982; 3(2):164–217. doi:10.1210/edrv-3-2-164
- Huang SA, Bianco AC. Reawakened interest in type III iodothyronine deiodinase in critical illness and injury. Nat Clin Pract Endocrinol Metab 2008; 4(3):148–155. doi:10.1038/ncpendmet0727
- Simonides WS, Mulcahey MA, Redout EM, et al. Hypoxia-inducible factor induces local thyroid hormone inactivation during hypoxic-ischemic disease in rats. J Clin Invest 2008; 118(3):975–983. doi:10.1172/JCI32824
- Wajner SM, Goemann IM, Bueno AL, Larsen PR, Maia AL. IL-6 promotes nonthyroidal illness syndrome by blocking thyroxine activation while promoting thyroid hormone inactivation in human cells. J Clin Invest 2011; 121(5):1834–1845. doi:10.1172/JCI44678
- Moura Neto A, Zantut-Wittmann DE. Abnormalities of thyroid hormone metabolism during systemic illness: the low T3 syndrome in different clinical settings. Int J Endocrinol 2016; 2016:2157583. doi:10.1155/2016/2157583
- Burmeister LA. Reverse T3 does not reliably differentiate hypothyroid sick syndrome from euthyroid sick syndrome. Thyroid 1995; 5(6):435–441. doi:10.1089/thy.1995.5.435
- Huang SA, Tu HM, Harney JW, et al. Severe hypothyroidism caused by type 3 iodothyronine deiodinase in infantile hemangiomas. N Engl J Med 2000; 343(3):185–189. doi:10.1056/NEJM200007203430305
- Kendall EC. Landmark article, June 19, 1915. The isolation in crystalline form of the compound containing iodin, which occurs in the thyroid. Its chemical nature and physiologic activity. By E.C. Kendall. JAMA 1983; 250(15):2045–2046. doi:10.1001/jama.1983.03340150087037
- Harington CR. Chemistry of thyroxine: isolation of thyroxine from the thyroid gland. Biochem J 1926; 20(2):293–299. pmid: 16743658
- Harington CR, Barger G. Chemistry of thyroxine: constitution and synthesis of thyroxine. Biochem J 1927; 21(1):169–183. pmid:16743801
- Gross J, Pitt-Rivers R. The identification of 3,5,3’L-triiodothyronine in human plasma. Lancet 1952; 1(6705):439–441. doi:10.1016/S0140-6736(52)91952-1
- Gross J, Pitt-Rivers R. 3:5:3’-triiodothyronine. 1. Isolation from thyroid gland and synthesis. Biochem J 1953; 53(4):645–650. pmid:13032123
- Pitt-Rivers R, Stanbury JB, Rapp B. Conversion of thyroxine to 3-5-3´-triiodothyronine in vivo. J Clin Endocrinol Metab 1955; 15(5):616–620. doi:10.1210/jcem-15-5-616
- Maclagan NF, Bowden CH, Wilkinson JH. The metabolism of thyroid hormones. 2. Detection of thyroxine and tri-iodothyronine in human plasma. Biochem J. 1957; 67(1):5–11. pmid:13471502
- Galton VA, Pitt-Rivers R. The identification of the acetic acid analogues of thyroxine and tri-iodothyronine in mammalian tissues. Biochem J 1959; 72(2):319–321. pmid: 13662303
- Braverman LE, Ingbar SH, Sterling K. Conversion of thyroxine (T4) to triiodothyronine (T3) in athyreotic human subjects. J Clin Invest 1970; 49(5):855–864. doi:10.1172/JCI106304
- Sterling K, Brenner MA, Newman ES. Conversion of thyroxine to triiodothyronine in normal human subjects. Science 1970; 169(3950):1099–1100. doi:10.1126/science.169.3950.1099
- Chopra IJ. A radioimmunoassay for measurement of thyroxine in unextracted serum. J Clin Endocrinol Metab 1972; 34:938–947. doi:10.1210/jcem-34-6-938
- Chopra IJ. A radioimmunoassay for measurement of 3,3´,5´-triiodothyronine (reverse T3). J Clin Invest 1974; 54(3):583–592. doi:10.1172/JCI107795
- Chopra IJ, Chopra U, Smith SR, Reza M, Solomon DH. Reciprocal changes in serum concentrations of 3,3´,5-triiodothyronine (T3) in systemic illnesses. J Clin Endocrinol Metab 1975; 41(6):1043–1049. doi:10.1210/jcem-41-6-1043
- Burman KD, Read J, Dimond RC, Strum D, et al. Measurement of 3,3’,5’-triiodothyroinine (reverse T3), 3,3’-L-diiodothyronine, T3 and T4 in human amniotic fluid and in cord and maternal serum. J Clin Endocrinol Metab 1976; 43(6):1351–1359. doi:10.1210/jcem-43-6-1351
- Rubenfeld S. Euthyroid sick syndrome. N Engl J Med 1978; 299(25):1414. doi:10.1056/NEJM197812212992514
- Burger A, Nicod P, Suter P, Vallotton MB, Vagenakis P, Braverman L. Reduced active thyroid hormone levels in acute illness. Lancet 1976; 1(7961):653–655. doi:10.1016/S0140-6736(76)92774-4
- Burman KD, Dimond RC, Wright FD, Earll JM, Bruton J, Wartofsky L. A radioimmunoassay for 3,3´,5´-L-triiodothyronine (reverse T3): assessment of thyroid gland content and serum measurements in conditions of normal and altered thyroidal economy and following administration of thyrotropin releasing hormone (TRH) and thyrotropin (TSH). J Clin Endocrinol Metab 1977; 44(4):660–672. doi:10.1210/jcem-44-4-660
- Burman KD, Strum D, Dimond RC, et al. A radioimmunoassay for 3,3´-L-diiodothyronine (3,3´T2). J Clin Endocrinol Metab 1977; 45(2):339–352. doi:10.1210/jcem-45-2-339
- Burman KD. Recent developments in thyroid hormone metabolism: interpretation and significance of measurements of reverse T3, 3,3´T2, and thyroglobulin. Metabolism 1978; 27(5):615–630. doi:10.1016/0026-0495(78)90028-8.
- Salvatore D, Davies TF, Schlumberger M, Hay ID, Larsen PR. Thyroid physiology and diagnostic evaluation of patients with thyroid disorders. In: Melmed S, Polonsky KS, Larsen PR, Kronenberg HM, eds. Williams Textbook of Endocrinology. 13th ed. Philadelphia, PA; Elsevier; 2016:334–368.
- Engler D, Burger AG. The deiodination of the iodothyronines and of their derivatives in man. Endocr Rev 1984; 5(2):151–184. doi:10.1210/edrv-5-2-151
- Peeters RP, Visser TJ, Peeters RP. Metabolism of thyroid hormone. Thyroid Disease Manager. www.thyroidmanager.org/chapter/metabolism-of-thyroid-hormone. Accessed March 14, 2018.
- Bianco AC, Salvatore D, Gereben B, Berry MJ, Larsen PR. Biochemistry, cellular and molecular biology, and physiological roles of the iodothyronine selenodeiodinases. Endocr Rev 2002; 23(1):38–89. doi:10.1210/edrv.23.1.0455
- Dentice M, Salvatore D. Deiodinases: the balance of thyroid hormone: local impact of thyroid hormone inactivation. J Endocrinol 2011; 209(3):273–282. doi:10.1530/JOE-11-0002
- Wartofsky L, Burman KD. Alterations in thyroid function in patients with systemic illness: the “euthyroid sick syndrome.” Endocr Rev 1982; 3(2):164–217. doi:10.1210/edrv-3-2-164
- Huang SA, Bianco AC. Reawakened interest in type III iodothyronine deiodinase in critical illness and injury. Nat Clin Pract Endocrinol Metab 2008; 4(3):148–155. doi:10.1038/ncpendmet0727
- Simonides WS, Mulcahey MA, Redout EM, et al. Hypoxia-inducible factor induces local thyroid hormone inactivation during hypoxic-ischemic disease in rats. J Clin Invest 2008; 118(3):975–983. doi:10.1172/JCI32824
- Wajner SM, Goemann IM, Bueno AL, Larsen PR, Maia AL. IL-6 promotes nonthyroidal illness syndrome by blocking thyroxine activation while promoting thyroid hormone inactivation in human cells. J Clin Invest 2011; 121(5):1834–1845. doi:10.1172/JCI44678
- Moura Neto A, Zantut-Wittmann DE. Abnormalities of thyroid hormone metabolism during systemic illness: the low T3 syndrome in different clinical settings. Int J Endocrinol 2016; 2016:2157583. doi:10.1155/2016/2157583
- Burmeister LA. Reverse T3 does not reliably differentiate hypothyroid sick syndrome from euthyroid sick syndrome. Thyroid 1995; 5(6):435–441. doi:10.1089/thy.1995.5.435
- Huang SA, Tu HM, Harney JW, et al. Severe hypothyroidism caused by type 3 iodothyronine deiodinase in infantile hemangiomas. N Engl J Med 2000; 343(3):185–189. doi:10.1056/NEJM200007203430305