User login
Don’t overlook these uses of point-of-care ultrasound
In the article, “Point-of-care ultrasound: Coming soon to primary care?” (J Fam Pract. 2018;67:70-79), Bornemann et al outline potential uses for point-of-care ultrasound (POCUS), describing in detail its role in cardiovascular and pulmonary exams, screening for abdominal aortic aneurysms, and diagnosing deep vein thrombosis. The American Academy of Family Physicians, in the Recommended Curriculum Guidelines for Family Medicine Residents (available at: https://www.aafp.org/medical-school-residency/program-directors/curriculum.html), also discusses obstetric and gynecologic uses for POCUS, such as determining fetal presentation and distinguishing viable pregnancy from miscarriage.
In my practice, I most often use POCUS for gynecologic and pregnancy-related issues, such as to ensure proper placement of an intrauterine device (IUD) when the strings are not visible, to determine gestational age in patients with uncertain last menstrual periods, and to confirm pregnancy location when patients have risk factors for, or symptoms suggestive of, ectopic pregnancy.
The breadth of care provided in family medicine is what makes it special. We must make sure that as we expand our care with new technologies, we do not trade tried and true uses of those technologies for newer ones.
Zoey Thill, MD, MPP
Bronx, NY
In the article, “Point-of-care ultrasound: Coming soon to primary care?” (J Fam Pract. 2018;67:70-79), Bornemann et al outline potential uses for point-of-care ultrasound (POCUS), describing in detail its role in cardiovascular and pulmonary exams, screening for abdominal aortic aneurysms, and diagnosing deep vein thrombosis. The American Academy of Family Physicians, in the Recommended Curriculum Guidelines for Family Medicine Residents (available at: https://www.aafp.org/medical-school-residency/program-directors/curriculum.html), also discusses obstetric and gynecologic uses for POCUS, such as determining fetal presentation and distinguishing viable pregnancy from miscarriage.
In my practice, I most often use POCUS for gynecologic and pregnancy-related issues, such as to ensure proper placement of an intrauterine device (IUD) when the strings are not visible, to determine gestational age in patients with uncertain last menstrual periods, and to confirm pregnancy location when patients have risk factors for, or symptoms suggestive of, ectopic pregnancy.
The breadth of care provided in family medicine is what makes it special. We must make sure that as we expand our care with new technologies, we do not trade tried and true uses of those technologies for newer ones.
Zoey Thill, MD, MPP
Bronx, NY
In the article, “Point-of-care ultrasound: Coming soon to primary care?” (J Fam Pract. 2018;67:70-79), Bornemann et al outline potential uses for point-of-care ultrasound (POCUS), describing in detail its role in cardiovascular and pulmonary exams, screening for abdominal aortic aneurysms, and diagnosing deep vein thrombosis. The American Academy of Family Physicians, in the Recommended Curriculum Guidelines for Family Medicine Residents (available at: https://www.aafp.org/medical-school-residency/program-directors/curriculum.html), also discusses obstetric and gynecologic uses for POCUS, such as determining fetal presentation and distinguishing viable pregnancy from miscarriage.
In my practice, I most often use POCUS for gynecologic and pregnancy-related issues, such as to ensure proper placement of an intrauterine device (IUD) when the strings are not visible, to determine gestational age in patients with uncertain last menstrual periods, and to confirm pregnancy location when patients have risk factors for, or symptoms suggestive of, ectopic pregnancy.
The breadth of care provided in family medicine is what makes it special. We must make sure that as we expand our care with new technologies, we do not trade tried and true uses of those technologies for newer ones.
Zoey Thill, MD, MPP
Bronx, NY
Restoring healing to the patient-provider conversation
This country continues to struggle with the issue of how to pay for health care. But regardless of the source of payment, primary care usually gets caught in the middle. Squeezed between volume and value, family physicians know all too well the gap that exists between what our patients need and what our training and health care system allow us to provide.
This knowledge prompted me to change how I conduct my day-to-day office visits. To routinely restore healing to the patient-provider conversation, I developed a tool called the HOPE (Healing Oriented Practices and Environments) Note. It consists of a set of questions to ask during a routine office visit that are specifically geared toward uncovering and addressing patients’ personal determinants of health and healing.
During a HOPE consultation, I seek to reframe the orientation from one that focuses only on
From there, I develop a personalized health promotion plan adjusted to the patient’s needs, personality, readiness, resources, and circumstances. Usually, patients benefit from additional assistance, such as health coaching and ways to measure and track progress. I have created a HOPE Note Checklist to teach students and residents about this approach, and a patient guide to help prepare patients for the visit ahead of time. (To access the guide and other free HOPE Note tools, see www.drwaynejonas.com/hope.)
Of course, these tools won’t single-handedly solve the issue of health care costs. But by practicing in a way that prioritizes what really matters to patients, we begin to take health care reform into our own hands.
Wayne B. Jonas, MD
Alexandria, Va
This country continues to struggle with the issue of how to pay for health care. But regardless of the source of payment, primary care usually gets caught in the middle. Squeezed between volume and value, family physicians know all too well the gap that exists between what our patients need and what our training and health care system allow us to provide.
This knowledge prompted me to change how I conduct my day-to-day office visits. To routinely restore healing to the patient-provider conversation, I developed a tool called the HOPE (Healing Oriented Practices and Environments) Note. It consists of a set of questions to ask during a routine office visit that are specifically geared toward uncovering and addressing patients’ personal determinants of health and healing.
During a HOPE consultation, I seek to reframe the orientation from one that focuses only on
From there, I develop a personalized health promotion plan adjusted to the patient’s needs, personality, readiness, resources, and circumstances. Usually, patients benefit from additional assistance, such as health coaching and ways to measure and track progress. I have created a HOPE Note Checklist to teach students and residents about this approach, and a patient guide to help prepare patients for the visit ahead of time. (To access the guide and other free HOPE Note tools, see www.drwaynejonas.com/hope.)
Of course, these tools won’t single-handedly solve the issue of health care costs. But by practicing in a way that prioritizes what really matters to patients, we begin to take health care reform into our own hands.
Wayne B. Jonas, MD
Alexandria, Va
This country continues to struggle with the issue of how to pay for health care. But regardless of the source of payment, primary care usually gets caught in the middle. Squeezed between volume and value, family physicians know all too well the gap that exists between what our patients need and what our training and health care system allow us to provide.
This knowledge prompted me to change how I conduct my day-to-day office visits. To routinely restore healing to the patient-provider conversation, I developed a tool called the HOPE (Healing Oriented Practices and Environments) Note. It consists of a set of questions to ask during a routine office visit that are specifically geared toward uncovering and addressing patients’ personal determinants of health and healing.
During a HOPE consultation, I seek to reframe the orientation from one that focuses only on
From there, I develop a personalized health promotion plan adjusted to the patient’s needs, personality, readiness, resources, and circumstances. Usually, patients benefit from additional assistance, such as health coaching and ways to measure and track progress. I have created a HOPE Note Checklist to teach students and residents about this approach, and a patient guide to help prepare patients for the visit ahead of time. (To access the guide and other free HOPE Note tools, see www.drwaynejonas.com/hope.)
Of course, these tools won’t single-handedly solve the issue of health care costs. But by practicing in a way that prioritizes what really matters to patients, we begin to take health care reform into our own hands.
Wayne B. Jonas, MD
Alexandria, Va
When our biases derail the diagnosis
This month's article by Dr. Yuen and colleagues on cognitive biases and the diagnostic errors that can result is a humbling reminder of the limitations of our brains and the need for us to be ever vigilant about the accuracy of our clinical diagnoses.
According to the article, at least 8 different kinds of bias can unintentionally derail our efforts to make the correct diagnosis. In my editorial last month (J Fam Pract. 2018;67:268), I presented data showing that up to 30% of patients with a physician’s diagnosis of asthma do not, in fact, have asthma. These mistaken diagnoses are most likely due to the bias known as “diagnostic momentum,” which is the tendency of physicians to accept a diagnosis without questioning its validity.
We are also prone to anchoring. Because family physicians (FPs) are very busy and use type 1 reasoning (pattern recognition or intuitive reasoning) more frequently than type 2 reasoning (analytical thinking, which requires more time), I suspect we are most susceptible to the bias of premature closure of the diagnostic process, also called anchoring. At times we attach too much weight to preliminary findings and don’t dig deep enough into the history or physical findings to confirm or support our diagnoses.
A memorable example of my own cognitive bias was my treatment of a middle-aged woman with hyperlipidemia. I thought I was being a good doctor, treating her appropriately with a statin. Luckily for her, she saw one of my partners when I was on vacation. My partner walked into the room and immediately recognized her myxedematous face as a sign of hypothyroidism. Her thyroid stimulating hormone level was 124 mIU/L! She was cured with thyroid hormone replacement and did not need a statin at all. I had not taken the time to think through the case carefully. And I had not noticed her gradual weight gain or the changes to her face.
Lulled by common diagnoses. Another difficulty for FPs and other primary care practitioners is that most of the patients we see have a common illness that is easy to diagnose. Recognizing shingles, eczema, acute appendicitis, and viral respiratory infections and managing chronic illnesses such as hypertension, diabetes, and chronic obstructive pulmonary disease (COPD) is second nature to us. But we must constantly be on the lookout for uncommon and potentially serious conditions. A classic example is not considering alpha-1 antitrypsin deficiency in a patient with COPD who does not smoke.
The bottom line: Take an extra minute or 2 to think through every diagnosis carefully—especially when one or more of the puzzle pieces do not fit together properly.
This month's article by Dr. Yuen and colleagues on cognitive biases and the diagnostic errors that can result is a humbling reminder of the limitations of our brains and the need for us to be ever vigilant about the accuracy of our clinical diagnoses.
According to the article, at least 8 different kinds of bias can unintentionally derail our efforts to make the correct diagnosis. In my editorial last month (J Fam Pract. 2018;67:268), I presented data showing that up to 30% of patients with a physician’s diagnosis of asthma do not, in fact, have asthma. These mistaken diagnoses are most likely due to the bias known as “diagnostic momentum,” which is the tendency of physicians to accept a diagnosis without questioning its validity.
We are also prone to anchoring. Because family physicians (FPs) are very busy and use type 1 reasoning (pattern recognition or intuitive reasoning) more frequently than type 2 reasoning (analytical thinking, which requires more time), I suspect we are most susceptible to the bias of premature closure of the diagnostic process, also called anchoring. At times we attach too much weight to preliminary findings and don’t dig deep enough into the history or physical findings to confirm or support our diagnoses.
A memorable example of my own cognitive bias was my treatment of a middle-aged woman with hyperlipidemia. I thought I was being a good doctor, treating her appropriately with a statin. Luckily for her, she saw one of my partners when I was on vacation. My partner walked into the room and immediately recognized her myxedematous face as a sign of hypothyroidism. Her thyroid stimulating hormone level was 124 mIU/L! She was cured with thyroid hormone replacement and did not need a statin at all. I had not taken the time to think through the case carefully. And I had not noticed her gradual weight gain or the changes to her face.
Lulled by common diagnoses. Another difficulty for FPs and other primary care practitioners is that most of the patients we see have a common illness that is easy to diagnose. Recognizing shingles, eczema, acute appendicitis, and viral respiratory infections and managing chronic illnesses such as hypertension, diabetes, and chronic obstructive pulmonary disease (COPD) is second nature to us. But we must constantly be on the lookout for uncommon and potentially serious conditions. A classic example is not considering alpha-1 antitrypsin deficiency in a patient with COPD who does not smoke.
The bottom line: Take an extra minute or 2 to think through every diagnosis carefully—especially when one or more of the puzzle pieces do not fit together properly.
This month's article by Dr. Yuen and colleagues on cognitive biases and the diagnostic errors that can result is a humbling reminder of the limitations of our brains and the need for us to be ever vigilant about the accuracy of our clinical diagnoses.
According to the article, at least 8 different kinds of bias can unintentionally derail our efforts to make the correct diagnosis. In my editorial last month (J Fam Pract. 2018;67:268), I presented data showing that up to 30% of patients with a physician’s diagnosis of asthma do not, in fact, have asthma. These mistaken diagnoses are most likely due to the bias known as “diagnostic momentum,” which is the tendency of physicians to accept a diagnosis without questioning its validity.
We are also prone to anchoring. Because family physicians (FPs) are very busy and use type 1 reasoning (pattern recognition or intuitive reasoning) more frequently than type 2 reasoning (analytical thinking, which requires more time), I suspect we are most susceptible to the bias of premature closure of the diagnostic process, also called anchoring. At times we attach too much weight to preliminary findings and don’t dig deep enough into the history or physical findings to confirm or support our diagnoses.
A memorable example of my own cognitive bias was my treatment of a middle-aged woman with hyperlipidemia. I thought I was being a good doctor, treating her appropriately with a statin. Luckily for her, she saw one of my partners when I was on vacation. My partner walked into the room and immediately recognized her myxedematous face as a sign of hypothyroidism. Her thyroid stimulating hormone level was 124 mIU/L! She was cured with thyroid hormone replacement and did not need a statin at all. I had not taken the time to think through the case carefully. And I had not noticed her gradual weight gain or the changes to her face.
Lulled by common diagnoses. Another difficulty for FPs and other primary care practitioners is that most of the patients we see have a common illness that is easy to diagnose. Recognizing shingles, eczema, acute appendicitis, and viral respiratory infections and managing chronic illnesses such as hypertension, diabetes, and chronic obstructive pulmonary disease (COPD) is second nature to us. But we must constantly be on the lookout for uncommon and potentially serious conditions. A classic example is not considering alpha-1 antitrypsin deficiency in a patient with COPD who does not smoke.
The bottom line: Take an extra minute or 2 to think through every diagnosis carefully—especially when one or more of the puzzle pieces do not fit together properly.
Sexual harassment and medicine
Sexual harassment hit a peak of cultural awareness over the past year. Will medicine be the next field to experience a reckoning?
In 2017, Time magazine’s Person of the Year Award went to the Silence Breakers who spoke out against sexual assault and harassment.1 The exposure of predatory behavior exhibited by once-celebrated movie producers, newscasters, and actors has given rise to a powerful change. The #MeToo movement has risen to support survivors and end sexual violence.
Just like show business, other industries have rich histories of discrimination and power. Think Wall Street, Silicon Valley, hospitality services, and the list goes on and on.2 But what about medicine? To answer this question, this article aims to:
- review the dilemma
- explore our duty to our patients and each other
- discuss solutions to address the problem.
Sexual harassment: A brief history
Decades ago, Anita Hill accused U.S. Supreme Court nominee Clarence Thomas, her boss at the U.S. Department of Education and the Equal Employment Opportunity Commission (EEOC), of sexual harassment.3
The year was 1991, and President George H. W. Bush had nominated Thomas, a federal Circuit Judge, to succeed retiring Associate Supreme Court Justice Thurgood Marshall. With Thomas’s good character presented as a primary qualification, he appeared to be a sure thing.
Continue to: That was until an FBI interview...
That was until an FBI interview of Hill was leaked to the press. Hill asserted that Thomas had sexually harassed her while he was her supervisor at the Department of Education and the EEOC.4 Heavily scrutinized for her choice to follow Thomas to a second job after he had already allegedly harassed her, Hill was in a conundrum shared by many women—putting up with abuse in exchange for a reputable position and the opportunity to fulfill a career ambition.
Hill is a trailblazer for women yearning to speak the truth, and she brought national attention to sexual harassment in the early 1990s. On December 16, 2017, the Commission on Sexual Harassment and Advancing Equality in the Workplace was formed. Hill was selected to lead the charge against sexual harassment in the entertainment industry.5
A forensic assessment of harassment
Hill’s courageous story is one of many touched upon in the 2016 book Because of Sex.6 Author Gillian Thomas, a senior staff attorney with the American Civil Liberties Union’s Women’s Rights Project, explores how Title VII of the Civil Rights Act of 1964 made it illegal to discriminate “because of sex.”
The field of forensic psychiatry has long been attentive to themes of sexual harassment and discrimination. The American Academy of Psychiatry and Law has a robust list of landmark cases thought to be especially important and significant for forensic psychiatry.7 This list includes cases brought forth by tenacious, yet ordinary women who used the law to advocate, and some have taken their fight all the way to the Supreme Court. Let’s consider 2 such cases:
Meritor Savings Bank, FSB v Vinson (1986).8 This was a U.S. labor law case. Michelle Vinson rose through the ranks at Meritor Savings Bank, only to be fired for excessive sick leave. She filed a Title VII suit against the bank. Vinson alleged that the bank was liable for sexual harassment perpetrated by its employee and vice president, Sidney Taylor. Vinson claimed that there had been 40 to 50 sexual encounters over 4 years, ranging from fondling to indecent exposure to rape. Vinson asserted that she never reported these events for fear of losing her job. The Supreme Court, in a 9-to-0 decision, recognized sexual harassment as a violation of Title VII of the Civil Rights Act of 1964.
Continue to: Harris v Forklift Systems, Inc. (1993)
Harris v Forklift Systems, Inc. (1993).9 Teresa Harris, a manager at Forklift Systems, Inc., claimed that the company’s president frequently directed offensive remarks at her that were sexual and discriminatory. The Supreme Court clarified the definition of a “hostile” or “abusive” work environment under Title VII of the Civil Rights Act of 1964. Associate Justice Sandra Day O’Connor was joined by a unanimous majority opinion in agreement with Harris.
Physicians are not immune
Clinicians are affected by sexual harassment, too. We have a duty to protect our patients, colleagues, and ourselves. Psychiatrists in particular often are on the frontlines of helping victims process their trauma.10
But will the field of medicine also face a reckoning when it comes to perpetrating harassment? It seems likely that the medical field would be ripe with harassment when you consider its history of male domination and a hierarchical structure with strong power differentials—not to mention the late nights, exhaustion, easy access to beds, and late-night encounters where inhibitions may be lowered.11
A shocking number of female doctors are sexually harassed. Thirty percent of the top female clinician-researchers have experienced blatant sexual harassment on the job, according to a survey of 573 men and 493 women who received career development awards from the National Institutes of Health in 2006 to 2009.12 In this survey, harassment covered the scope of sexist remarks or behavior, unwanted sexual advances, bribery, threats, and coercion. The majority of those affected said the experience undermined their confidence as professionals, and many said the harassment negatively affected their career advancement.12
Continue to: But what about the progress women have made...
But what about the progress women have made in medicine? Women are surpassing men in terms of admittance to medical school. Last year, for the first time, women accounted for more than half of the enrollees in U.S. medical schools, according to the Association of American Medical Colleges.13 Yet there has been a stalling in terms of change when it comes to harassment.12 Women may be more vulnerable to harassment, both when they’re perceived as weak and when they’re so strong that they challenge traditional hierarchies.
Perpetuating the problem is the trouble with reporting sexual harassment. Victims do not fare well in our society. Even in the #MeToo era, reporting such behavior is far from straightforward.11 Women fear that reporting any harassment will make them a target. Think of Anita Hill—her testimony against Clarence Thomas during his confirmation hearings for the Supreme Court showed that women who report sexual harassment experience marginalization, retaliation, stigmatization, and worse.
The result is that medical professionals tend to suppress the recognition of harassment. We make excuses for it, blame ourselves, or just take it on the chin and move on. There’s also confusion regarding what constitutes harassment. As doctors, especially psychiatrists, we hear harrowing stories. It’s reasonable to downplay our own experiences. Turning everyone into a victim of sexual harassment could detract from the stories of women who were raped, molested, and severely taken advantage of. There is a reasonable fear that diluting their message could be further damaging.14
Time for action
The field of medicine needs to do better in terms of education, support, anticipation, prevention, and reaction to harassment. We have the awareness. Now, we need action.
Continue to: One way to change any culture...
One way to change any culture of harassment or discrimination would be the advancement of more female physicians into leadership positions. The Association of American Medical Colleges has reported that fewer women than men hold faculty positions and full professorships.15,16 There’s also a striking imbalance among fields of medicine practiced by men and women, with more women seen in pediatrics, obstetrics, and gynecology as opposed to surgery. Advancement into policy-setting echelons of medicine is essential for change. Sexual harassment can be a silent problem that will be corrected only when institutions and leaders put it on the forefront of discussions.17
Another possible solution would be to shift problem-solving from punishment to prevention. Many institutions set expectations about intolerance of sexual harassment and conduct occasional lectures about it. However, enforcing protocols and safeguards that support and enforce policy are difficult on the ground level. In any event, punishment alone won’t change a culture.17
Working with students until they are comfortable disclosing details of incidents can be helpful. For example, the University of Wisconsin-Madison employs an ombuds to help with this process.18 All institutions should encourage reporting along confidential pathways and have multiple ways to report.17 Tracking complaints, even seemingly minor infractions, can help identify patterns of behavior and anticipate future incidents.
Some solutions seem obvious, such as informal and retaliation-free reporting that allows institutions to track perpetrators’ behavior; mandatory training that includes bystander training; and disciplining and monitoring transgressors and terminating their employment when appropriate—something along the lines of a zero-tolerance policy. There needs to be more research on the prevalence, severity, and outcomes of sexual harassment, and subsequent investigations, along with research into evidence-based prevention and intervention strategies.17
Continue to: Although this article focuses...
Although this article focuses on harassment of women, men are equally important to this conversation because they, too, can be victims. Men also can serve a pivotal role in mentoring and championing their female counterparts as they strive for advancement, equality, and respect.
The task ahead is large, and this discussion is not over.
1. Felsenthal E. TIME’s 2017 Person of the Year: the Silence Breakers. TIME. http://time.com/magazine/us/5055335/december-18th-2017-vol-190-no-25-u-s/. Published December 18, 2017. Accessed April 23, 2018.
2. Hiltzik M. Los Angeles Times. Will medicine be the next field to face a sexual harassment reckoning? http://www.latimes.com/business/hiltzik/la-fi-hiltzik-medicine-harassment-20180110-story.html. Published January 10, 2018. Accessed April 23, 2018.
3. Thompson K. For Anita Hill, the Clarence Thomas hearings haven’t really ended. The Washington Post. https://www.washingtonpost.com/politics/for-anita-hill-the-clarence-thomas-hearings-havent-really-ended/2011/10/05/gIQAy2b5QL_story.html. Published October 6, 2011. Accessed April 23, 2018.
4. Toobin J. Good versus evil. In: Toobin J. The nine: inside the secret world of the Supreme Court. New York, NY: Doubleday; 2007:30-32.
5. Barnes B. Motion picture academy finds no merit to accusations against its president. https://www.nytimes.com/2018/03/28/business/media/john-bailey-sexual-harassment-academy.html. The New York Times. Published March 28, 2018. Accessed April 23, 2018.
6. Thomas G. Because of sex: one law, ten cases, and fifty years that changed American women’s lives at work. New York, NY: Picador; 2016.
7. Landmark cases 2014. American Academy of Psychiatry and Law. http://www.aapl.org/landmark_list.htm. 2014. Accessed April 22, 2018.
8. Meritor Savings Bank v Vinson, 477 US 57 (1986).
9. Harris v Forklift Systems, Inc., 114 S Ct 367 (1993).
10. Okwerekwu JA. #MeToo: so many of my patients have a story. And absorbing them is taking its toll. STAT. https://www.scribd.com/article/367482959/Me-Too-So-Many-Of-My-Patients-Have-A-Story-And-Absorbing-Them-Is-Taking-Its-Toll. Published December 18, 2017. Accessed April 23, 2018.
11. Jagsi R. Sexual harassment in medicine—#MeToo. N Engl J Med. 2018;378:209-211.
12. Jagsi R, Griffith KA, Jones R. et al. Sexual harassment and discrimination experiences of academic medical faculty. JAMA. 2016;315(19):2120-2121.
13. AAMCNEWS. More women than men enrolled in U.S. medical schools in 2017. https://news.aamc.org/press-releases/article/applicant-enrollment-2017/. Published December 18, 2017. Accessed May 4, 2018.
14. Miller D. #MeToo: does it help? Clinical Psychiatry News. https://www.mdedge.com/psychiatry/article/150148/depression/metoo-does-it-help. Published October 24, 2017. Accessed April 23, 2018.
15. Chang S, Morahan PS, Magrane D, et al. Retaining faculty in academic medicine: the impact of career development programs for women. J Womens Health (Larchmt). 2016;25(7):687-696.
16. Lautenberger DM, Dandar, VM, Raezer CL, et al. The state of women in academic medicine: the pipeline and pathways to leadership, 2013-2014. AAMC. https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Published 2014. Accessed May 4, 2018.
17. Jablow M. Zero tolerance: combating sexual harassment in academic medicine. AAMCNews. https://news.aamc.org/diversity/article/combating-sexual-harassment-academic-medicine. Published April 4, 2017. Accessed April 23, 2018.
18. University of Wisconsin-Madison, the School of Medicine and Public Health. UW-Madison Policy on Sexual Harassment and Sexual Violence. https://compliance.wiscweb.wisc.edu/wp-content/uploads/sites/102/2018/01/UW-Madison-Policy-on-Sexual-Harassment-And-Sexual-Violence-January-2018.pdf. Published January 2018. Accessed April 22, 2018.
Sexual harassment hit a peak of cultural awareness over the past year. Will medicine be the next field to experience a reckoning?
In 2017, Time magazine’s Person of the Year Award went to the Silence Breakers who spoke out against sexual assault and harassment.1 The exposure of predatory behavior exhibited by once-celebrated movie producers, newscasters, and actors has given rise to a powerful change. The #MeToo movement has risen to support survivors and end sexual violence.
Just like show business, other industries have rich histories of discrimination and power. Think Wall Street, Silicon Valley, hospitality services, and the list goes on and on.2 But what about medicine? To answer this question, this article aims to:
- review the dilemma
- explore our duty to our patients and each other
- discuss solutions to address the problem.
Sexual harassment: A brief history
Decades ago, Anita Hill accused U.S. Supreme Court nominee Clarence Thomas, her boss at the U.S. Department of Education and the Equal Employment Opportunity Commission (EEOC), of sexual harassment.3
The year was 1991, and President George H. W. Bush had nominated Thomas, a federal Circuit Judge, to succeed retiring Associate Supreme Court Justice Thurgood Marshall. With Thomas’s good character presented as a primary qualification, he appeared to be a sure thing.
Continue to: That was until an FBI interview...
That was until an FBI interview of Hill was leaked to the press. Hill asserted that Thomas had sexually harassed her while he was her supervisor at the Department of Education and the EEOC.4 Heavily scrutinized for her choice to follow Thomas to a second job after he had already allegedly harassed her, Hill was in a conundrum shared by many women—putting up with abuse in exchange for a reputable position and the opportunity to fulfill a career ambition.
Hill is a trailblazer for women yearning to speak the truth, and she brought national attention to sexual harassment in the early 1990s. On December 16, 2017, the Commission on Sexual Harassment and Advancing Equality in the Workplace was formed. Hill was selected to lead the charge against sexual harassment in the entertainment industry.5
A forensic assessment of harassment
Hill’s courageous story is one of many touched upon in the 2016 book Because of Sex.6 Author Gillian Thomas, a senior staff attorney with the American Civil Liberties Union’s Women’s Rights Project, explores how Title VII of the Civil Rights Act of 1964 made it illegal to discriminate “because of sex.”
The field of forensic psychiatry has long been attentive to themes of sexual harassment and discrimination. The American Academy of Psychiatry and Law has a robust list of landmark cases thought to be especially important and significant for forensic psychiatry.7 This list includes cases brought forth by tenacious, yet ordinary women who used the law to advocate, and some have taken their fight all the way to the Supreme Court. Let’s consider 2 such cases:
Meritor Savings Bank, FSB v Vinson (1986).8 This was a U.S. labor law case. Michelle Vinson rose through the ranks at Meritor Savings Bank, only to be fired for excessive sick leave. She filed a Title VII suit against the bank. Vinson alleged that the bank was liable for sexual harassment perpetrated by its employee and vice president, Sidney Taylor. Vinson claimed that there had been 40 to 50 sexual encounters over 4 years, ranging from fondling to indecent exposure to rape. Vinson asserted that she never reported these events for fear of losing her job. The Supreme Court, in a 9-to-0 decision, recognized sexual harassment as a violation of Title VII of the Civil Rights Act of 1964.
Continue to: Harris v Forklift Systems, Inc. (1993)
Harris v Forklift Systems, Inc. (1993).9 Teresa Harris, a manager at Forklift Systems, Inc., claimed that the company’s president frequently directed offensive remarks at her that were sexual and discriminatory. The Supreme Court clarified the definition of a “hostile” or “abusive” work environment under Title VII of the Civil Rights Act of 1964. Associate Justice Sandra Day O’Connor was joined by a unanimous majority opinion in agreement with Harris.
Physicians are not immune
Clinicians are affected by sexual harassment, too. We have a duty to protect our patients, colleagues, and ourselves. Psychiatrists in particular often are on the frontlines of helping victims process their trauma.10
But will the field of medicine also face a reckoning when it comes to perpetrating harassment? It seems likely that the medical field would be ripe with harassment when you consider its history of male domination and a hierarchical structure with strong power differentials—not to mention the late nights, exhaustion, easy access to beds, and late-night encounters where inhibitions may be lowered.11
A shocking number of female doctors are sexually harassed. Thirty percent of the top female clinician-researchers have experienced blatant sexual harassment on the job, according to a survey of 573 men and 493 women who received career development awards from the National Institutes of Health in 2006 to 2009.12 In this survey, harassment covered the scope of sexist remarks or behavior, unwanted sexual advances, bribery, threats, and coercion. The majority of those affected said the experience undermined their confidence as professionals, and many said the harassment negatively affected their career advancement.12
Continue to: But what about the progress women have made...
But what about the progress women have made in medicine? Women are surpassing men in terms of admittance to medical school. Last year, for the first time, women accounted for more than half of the enrollees in U.S. medical schools, according to the Association of American Medical Colleges.13 Yet there has been a stalling in terms of change when it comes to harassment.12 Women may be more vulnerable to harassment, both when they’re perceived as weak and when they’re so strong that they challenge traditional hierarchies.
Perpetuating the problem is the trouble with reporting sexual harassment. Victims do not fare well in our society. Even in the #MeToo era, reporting such behavior is far from straightforward.11 Women fear that reporting any harassment will make them a target. Think of Anita Hill—her testimony against Clarence Thomas during his confirmation hearings for the Supreme Court showed that women who report sexual harassment experience marginalization, retaliation, stigmatization, and worse.
The result is that medical professionals tend to suppress the recognition of harassment. We make excuses for it, blame ourselves, or just take it on the chin and move on. There’s also confusion regarding what constitutes harassment. As doctors, especially psychiatrists, we hear harrowing stories. It’s reasonable to downplay our own experiences. Turning everyone into a victim of sexual harassment could detract from the stories of women who were raped, molested, and severely taken advantage of. There is a reasonable fear that diluting their message could be further damaging.14
Time for action
The field of medicine needs to do better in terms of education, support, anticipation, prevention, and reaction to harassment. We have the awareness. Now, we need action.
Continue to: One way to change any culture...
One way to change any culture of harassment or discrimination would be the advancement of more female physicians into leadership positions. The Association of American Medical Colleges has reported that fewer women than men hold faculty positions and full professorships.15,16 There’s also a striking imbalance among fields of medicine practiced by men and women, with more women seen in pediatrics, obstetrics, and gynecology as opposed to surgery. Advancement into policy-setting echelons of medicine is essential for change. Sexual harassment can be a silent problem that will be corrected only when institutions and leaders put it on the forefront of discussions.17
Another possible solution would be to shift problem-solving from punishment to prevention. Many institutions set expectations about intolerance of sexual harassment and conduct occasional lectures about it. However, enforcing protocols and safeguards that support and enforce policy are difficult on the ground level. In any event, punishment alone won’t change a culture.17
Working with students until they are comfortable disclosing details of incidents can be helpful. For example, the University of Wisconsin-Madison employs an ombuds to help with this process.18 All institutions should encourage reporting along confidential pathways and have multiple ways to report.17 Tracking complaints, even seemingly minor infractions, can help identify patterns of behavior and anticipate future incidents.
Some solutions seem obvious, such as informal and retaliation-free reporting that allows institutions to track perpetrators’ behavior; mandatory training that includes bystander training; and disciplining and monitoring transgressors and terminating their employment when appropriate—something along the lines of a zero-tolerance policy. There needs to be more research on the prevalence, severity, and outcomes of sexual harassment, and subsequent investigations, along with research into evidence-based prevention and intervention strategies.17
Continue to: Although this article focuses...
Although this article focuses on harassment of women, men are equally important to this conversation because they, too, can be victims. Men also can serve a pivotal role in mentoring and championing their female counterparts as they strive for advancement, equality, and respect.
The task ahead is large, and this discussion is not over.
Sexual harassment hit a peak of cultural awareness over the past year. Will medicine be the next field to experience a reckoning?
In 2017, Time magazine’s Person of the Year Award went to the Silence Breakers who spoke out against sexual assault and harassment.1 The exposure of predatory behavior exhibited by once-celebrated movie producers, newscasters, and actors has given rise to a powerful change. The #MeToo movement has risen to support survivors and end sexual violence.
Just like show business, other industries have rich histories of discrimination and power. Think Wall Street, Silicon Valley, hospitality services, and the list goes on and on.2 But what about medicine? To answer this question, this article aims to:
- review the dilemma
- explore our duty to our patients and each other
- discuss solutions to address the problem.
Sexual harassment: A brief history
Decades ago, Anita Hill accused U.S. Supreme Court nominee Clarence Thomas, her boss at the U.S. Department of Education and the Equal Employment Opportunity Commission (EEOC), of sexual harassment.3
The year was 1991, and President George H. W. Bush had nominated Thomas, a federal Circuit Judge, to succeed retiring Associate Supreme Court Justice Thurgood Marshall. With Thomas’s good character presented as a primary qualification, he appeared to be a sure thing.
Continue to: That was until an FBI interview...
That was until an FBI interview of Hill was leaked to the press. Hill asserted that Thomas had sexually harassed her while he was her supervisor at the Department of Education and the EEOC.4 Heavily scrutinized for her choice to follow Thomas to a second job after he had already allegedly harassed her, Hill was in a conundrum shared by many women—putting up with abuse in exchange for a reputable position and the opportunity to fulfill a career ambition.
Hill is a trailblazer for women yearning to speak the truth, and she brought national attention to sexual harassment in the early 1990s. On December 16, 2017, the Commission on Sexual Harassment and Advancing Equality in the Workplace was formed. Hill was selected to lead the charge against sexual harassment in the entertainment industry.5
A forensic assessment of harassment
Hill’s courageous story is one of many touched upon in the 2016 book Because of Sex.6 Author Gillian Thomas, a senior staff attorney with the American Civil Liberties Union’s Women’s Rights Project, explores how Title VII of the Civil Rights Act of 1964 made it illegal to discriminate “because of sex.”
The field of forensic psychiatry has long been attentive to themes of sexual harassment and discrimination. The American Academy of Psychiatry and Law has a robust list of landmark cases thought to be especially important and significant for forensic psychiatry.7 This list includes cases brought forth by tenacious, yet ordinary women who used the law to advocate, and some have taken their fight all the way to the Supreme Court. Let’s consider 2 such cases:
Meritor Savings Bank, FSB v Vinson (1986).8 This was a U.S. labor law case. Michelle Vinson rose through the ranks at Meritor Savings Bank, only to be fired for excessive sick leave. She filed a Title VII suit against the bank. Vinson alleged that the bank was liable for sexual harassment perpetrated by its employee and vice president, Sidney Taylor. Vinson claimed that there had been 40 to 50 sexual encounters over 4 years, ranging from fondling to indecent exposure to rape. Vinson asserted that she never reported these events for fear of losing her job. The Supreme Court, in a 9-to-0 decision, recognized sexual harassment as a violation of Title VII of the Civil Rights Act of 1964.
Continue to: Harris v Forklift Systems, Inc. (1993)
Harris v Forklift Systems, Inc. (1993).9 Teresa Harris, a manager at Forklift Systems, Inc., claimed that the company’s president frequently directed offensive remarks at her that were sexual and discriminatory. The Supreme Court clarified the definition of a “hostile” or “abusive” work environment under Title VII of the Civil Rights Act of 1964. Associate Justice Sandra Day O’Connor was joined by a unanimous majority opinion in agreement with Harris.
Physicians are not immune
Clinicians are affected by sexual harassment, too. We have a duty to protect our patients, colleagues, and ourselves. Psychiatrists in particular often are on the frontlines of helping victims process their trauma.10
But will the field of medicine also face a reckoning when it comes to perpetrating harassment? It seems likely that the medical field would be ripe with harassment when you consider its history of male domination and a hierarchical structure with strong power differentials—not to mention the late nights, exhaustion, easy access to beds, and late-night encounters where inhibitions may be lowered.11
A shocking number of female doctors are sexually harassed. Thirty percent of the top female clinician-researchers have experienced blatant sexual harassment on the job, according to a survey of 573 men and 493 women who received career development awards from the National Institutes of Health in 2006 to 2009.12 In this survey, harassment covered the scope of sexist remarks or behavior, unwanted sexual advances, bribery, threats, and coercion. The majority of those affected said the experience undermined their confidence as professionals, and many said the harassment negatively affected their career advancement.12
Continue to: But what about the progress women have made...
But what about the progress women have made in medicine? Women are surpassing men in terms of admittance to medical school. Last year, for the first time, women accounted for more than half of the enrollees in U.S. medical schools, according to the Association of American Medical Colleges.13 Yet there has been a stalling in terms of change when it comes to harassment.12 Women may be more vulnerable to harassment, both when they’re perceived as weak and when they’re so strong that they challenge traditional hierarchies.
Perpetuating the problem is the trouble with reporting sexual harassment. Victims do not fare well in our society. Even in the #MeToo era, reporting such behavior is far from straightforward.11 Women fear that reporting any harassment will make them a target. Think of Anita Hill—her testimony against Clarence Thomas during his confirmation hearings for the Supreme Court showed that women who report sexual harassment experience marginalization, retaliation, stigmatization, and worse.
The result is that medical professionals tend to suppress the recognition of harassment. We make excuses for it, blame ourselves, or just take it on the chin and move on. There’s also confusion regarding what constitutes harassment. As doctors, especially psychiatrists, we hear harrowing stories. It’s reasonable to downplay our own experiences. Turning everyone into a victim of sexual harassment could detract from the stories of women who were raped, molested, and severely taken advantage of. There is a reasonable fear that diluting their message could be further damaging.14
Time for action
The field of medicine needs to do better in terms of education, support, anticipation, prevention, and reaction to harassment. We have the awareness. Now, we need action.
Continue to: One way to change any culture...
One way to change any culture of harassment or discrimination would be the advancement of more female physicians into leadership positions. The Association of American Medical Colleges has reported that fewer women than men hold faculty positions and full professorships.15,16 There’s also a striking imbalance among fields of medicine practiced by men and women, with more women seen in pediatrics, obstetrics, and gynecology as opposed to surgery. Advancement into policy-setting echelons of medicine is essential for change. Sexual harassment can be a silent problem that will be corrected only when institutions and leaders put it on the forefront of discussions.17
Another possible solution would be to shift problem-solving from punishment to prevention. Many institutions set expectations about intolerance of sexual harassment and conduct occasional lectures about it. However, enforcing protocols and safeguards that support and enforce policy are difficult on the ground level. In any event, punishment alone won’t change a culture.17
Working with students until they are comfortable disclosing details of incidents can be helpful. For example, the University of Wisconsin-Madison employs an ombuds to help with this process.18 All institutions should encourage reporting along confidential pathways and have multiple ways to report.17 Tracking complaints, even seemingly minor infractions, can help identify patterns of behavior and anticipate future incidents.
Some solutions seem obvious, such as informal and retaliation-free reporting that allows institutions to track perpetrators’ behavior; mandatory training that includes bystander training; and disciplining and monitoring transgressors and terminating their employment when appropriate—something along the lines of a zero-tolerance policy. There needs to be more research on the prevalence, severity, and outcomes of sexual harassment, and subsequent investigations, along with research into evidence-based prevention and intervention strategies.17
Continue to: Although this article focuses...
Although this article focuses on harassment of women, men are equally important to this conversation because they, too, can be victims. Men also can serve a pivotal role in mentoring and championing their female counterparts as they strive for advancement, equality, and respect.
The task ahead is large, and this discussion is not over.
1. Felsenthal E. TIME’s 2017 Person of the Year: the Silence Breakers. TIME. http://time.com/magazine/us/5055335/december-18th-2017-vol-190-no-25-u-s/. Published December 18, 2017. Accessed April 23, 2018.
2. Hiltzik M. Los Angeles Times. Will medicine be the next field to face a sexual harassment reckoning? http://www.latimes.com/business/hiltzik/la-fi-hiltzik-medicine-harassment-20180110-story.html. Published January 10, 2018. Accessed April 23, 2018.
3. Thompson K. For Anita Hill, the Clarence Thomas hearings haven’t really ended. The Washington Post. https://www.washingtonpost.com/politics/for-anita-hill-the-clarence-thomas-hearings-havent-really-ended/2011/10/05/gIQAy2b5QL_story.html. Published October 6, 2011. Accessed April 23, 2018.
4. Toobin J. Good versus evil. In: Toobin J. The nine: inside the secret world of the Supreme Court. New York, NY: Doubleday; 2007:30-32.
5. Barnes B. Motion picture academy finds no merit to accusations against its president. https://www.nytimes.com/2018/03/28/business/media/john-bailey-sexual-harassment-academy.html. The New York Times. Published March 28, 2018. Accessed April 23, 2018.
6. Thomas G. Because of sex: one law, ten cases, and fifty years that changed American women’s lives at work. New York, NY: Picador; 2016.
7. Landmark cases 2014. American Academy of Psychiatry and Law. http://www.aapl.org/landmark_list.htm. 2014. Accessed April 22, 2018.
8. Meritor Savings Bank v Vinson, 477 US 57 (1986).
9. Harris v Forklift Systems, Inc., 114 S Ct 367 (1993).
10. Okwerekwu JA. #MeToo: so many of my patients have a story. And absorbing them is taking its toll. STAT. https://www.scribd.com/article/367482959/Me-Too-So-Many-Of-My-Patients-Have-A-Story-And-Absorbing-Them-Is-Taking-Its-Toll. Published December 18, 2017. Accessed April 23, 2018.
11. Jagsi R. Sexual harassment in medicine—#MeToo. N Engl J Med. 2018;378:209-211.
12. Jagsi R, Griffith KA, Jones R. et al. Sexual harassment and discrimination experiences of academic medical faculty. JAMA. 2016;315(19):2120-2121.
13. AAMCNEWS. More women than men enrolled in U.S. medical schools in 2017. https://news.aamc.org/press-releases/article/applicant-enrollment-2017/. Published December 18, 2017. Accessed May 4, 2018.
14. Miller D. #MeToo: does it help? Clinical Psychiatry News. https://www.mdedge.com/psychiatry/article/150148/depression/metoo-does-it-help. Published October 24, 2017. Accessed April 23, 2018.
15. Chang S, Morahan PS, Magrane D, et al. Retaining faculty in academic medicine: the impact of career development programs for women. J Womens Health (Larchmt). 2016;25(7):687-696.
16. Lautenberger DM, Dandar, VM, Raezer CL, et al. The state of women in academic medicine: the pipeline and pathways to leadership, 2013-2014. AAMC. https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Published 2014. Accessed May 4, 2018.
17. Jablow M. Zero tolerance: combating sexual harassment in academic medicine. AAMCNews. https://news.aamc.org/diversity/article/combating-sexual-harassment-academic-medicine. Published April 4, 2017. Accessed April 23, 2018.
18. University of Wisconsin-Madison, the School of Medicine and Public Health. UW-Madison Policy on Sexual Harassment and Sexual Violence. https://compliance.wiscweb.wisc.edu/wp-content/uploads/sites/102/2018/01/UW-Madison-Policy-on-Sexual-Harassment-And-Sexual-Violence-January-2018.pdf. Published January 2018. Accessed April 22, 2018.
1. Felsenthal E. TIME’s 2017 Person of the Year: the Silence Breakers. TIME. http://time.com/magazine/us/5055335/december-18th-2017-vol-190-no-25-u-s/. Published December 18, 2017. Accessed April 23, 2018.
2. Hiltzik M. Los Angeles Times. Will medicine be the next field to face a sexual harassment reckoning? http://www.latimes.com/business/hiltzik/la-fi-hiltzik-medicine-harassment-20180110-story.html. Published January 10, 2018. Accessed April 23, 2018.
3. Thompson K. For Anita Hill, the Clarence Thomas hearings haven’t really ended. The Washington Post. https://www.washingtonpost.com/politics/for-anita-hill-the-clarence-thomas-hearings-havent-really-ended/2011/10/05/gIQAy2b5QL_story.html. Published October 6, 2011. Accessed April 23, 2018.
4. Toobin J. Good versus evil. In: Toobin J. The nine: inside the secret world of the Supreme Court. New York, NY: Doubleday; 2007:30-32.
5. Barnes B. Motion picture academy finds no merit to accusations against its president. https://www.nytimes.com/2018/03/28/business/media/john-bailey-sexual-harassment-academy.html. The New York Times. Published March 28, 2018. Accessed April 23, 2018.
6. Thomas G. Because of sex: one law, ten cases, and fifty years that changed American women’s lives at work. New York, NY: Picador; 2016.
7. Landmark cases 2014. American Academy of Psychiatry and Law. http://www.aapl.org/landmark_list.htm. 2014. Accessed April 22, 2018.
8. Meritor Savings Bank v Vinson, 477 US 57 (1986).
9. Harris v Forklift Systems, Inc., 114 S Ct 367 (1993).
10. Okwerekwu JA. #MeToo: so many of my patients have a story. And absorbing them is taking its toll. STAT. https://www.scribd.com/article/367482959/Me-Too-So-Many-Of-My-Patients-Have-A-Story-And-Absorbing-Them-Is-Taking-Its-Toll. Published December 18, 2017. Accessed April 23, 2018.
11. Jagsi R. Sexual harassment in medicine—#MeToo. N Engl J Med. 2018;378:209-211.
12. Jagsi R, Griffith KA, Jones R. et al. Sexual harassment and discrimination experiences of academic medical faculty. JAMA. 2016;315(19):2120-2121.
13. AAMCNEWS. More women than men enrolled in U.S. medical schools in 2017. https://news.aamc.org/press-releases/article/applicant-enrollment-2017/. Published December 18, 2017. Accessed May 4, 2018.
14. Miller D. #MeToo: does it help? Clinical Psychiatry News. https://www.mdedge.com/psychiatry/article/150148/depression/metoo-does-it-help. Published October 24, 2017. Accessed April 23, 2018.
15. Chang S, Morahan PS, Magrane D, et al. Retaining faculty in academic medicine: the impact of career development programs for women. J Womens Health (Larchmt). 2016;25(7):687-696.
16. Lautenberger DM, Dandar, VM, Raezer CL, et al. The state of women in academic medicine: the pipeline and pathways to leadership, 2013-2014. AAMC. https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Published 2014. Accessed May 4, 2018.
17. Jablow M. Zero tolerance: combating sexual harassment in academic medicine. AAMCNews. https://news.aamc.org/diversity/article/combating-sexual-harassment-academic-medicine. Published April 4, 2017. Accessed April 23, 2018.
18. University of Wisconsin-Madison, the School of Medicine and Public Health. UW-Madison Policy on Sexual Harassment and Sexual Violence. https://compliance.wiscweb.wisc.edu/wp-content/uploads/sites/102/2018/01/UW-Madison-Policy-on-Sexual-Harassment-And-Sexual-Violence-January-2018.pdf. Published January 2018. Accessed April 22, 2018.
Letter from the Editor: A moment of grace
She was my 3:45 p.m. return visit. She had been a new patient with dyspepsia and I had found Helicobacter pylori–gastritis on endoscopy. She had marketplace-based coverage (silver, high-deductible plan), which was why she had to travel from her community to our university for care. That she did not look like me (older white male) was an understatement. She was so enthusiastic as she thanked me for helping her. Then she described how she, her husband (both hourly-wage, working adults) and their two young kids had gathered around the dinner table to discuss how they could reduce their food allowance for 2 months to have money for mom’s H. pylori medication. She said her entire family was grateful for the help to get her well. It was a moment of grace. She is why I keep fighting to make our health system great again.
Our cover articles this month discuss HCV treatment in patients with special risk factors or co-conditions. Fascinating information will emerge from studies like the article about artificial sweeteners. Scientists studied hunger-related enzyme levels and brain blood flow with functional MRI’s in obese and lean individuals after ingesting placebo and sucralose-containing solutions. Results might influence our weight loss advice to patients. Worried about malpractice? See our third front page article.
Additional articles discuss a reversal agent for one of the direct-acting oral anticoagulants and a hemospray for GI bleeding. Clinically impactful articles from the AGA journals are highlighted.
Finally, I would like to thank all of you who filled out the readership survey last fall. We are proud that you identified GI & Hepatology News as the best overall source for news information in gastroenterology.
John I. Allen, MD, MBA, AGAF
Editor in Chief
She was my 3:45 p.m. return visit. She had been a new patient with dyspepsia and I had found Helicobacter pylori–gastritis on endoscopy. She had marketplace-based coverage (silver, high-deductible plan), which was why she had to travel from her community to our university for care. That she did not look like me (older white male) was an understatement. She was so enthusiastic as she thanked me for helping her. Then she described how she, her husband (both hourly-wage, working adults) and their two young kids had gathered around the dinner table to discuss how they could reduce their food allowance for 2 months to have money for mom’s H. pylori medication. She said her entire family was grateful for the help to get her well. It was a moment of grace. She is why I keep fighting to make our health system great again.
Our cover articles this month discuss HCV treatment in patients with special risk factors or co-conditions. Fascinating information will emerge from studies like the article about artificial sweeteners. Scientists studied hunger-related enzyme levels and brain blood flow with functional MRI’s in obese and lean individuals after ingesting placebo and sucralose-containing solutions. Results might influence our weight loss advice to patients. Worried about malpractice? See our third front page article.
Additional articles discuss a reversal agent for one of the direct-acting oral anticoagulants and a hemospray for GI bleeding. Clinically impactful articles from the AGA journals are highlighted.
Finally, I would like to thank all of you who filled out the readership survey last fall. We are proud that you identified GI & Hepatology News as the best overall source for news information in gastroenterology.
John I. Allen, MD, MBA, AGAF
Editor in Chief
She was my 3:45 p.m. return visit. She had been a new patient with dyspepsia and I had found Helicobacter pylori–gastritis on endoscopy. She had marketplace-based coverage (silver, high-deductible plan), which was why she had to travel from her community to our university for care. That she did not look like me (older white male) was an understatement. She was so enthusiastic as she thanked me for helping her. Then she described how she, her husband (both hourly-wage, working adults) and their two young kids had gathered around the dinner table to discuss how they could reduce their food allowance for 2 months to have money for mom’s H. pylori medication. She said her entire family was grateful for the help to get her well. It was a moment of grace. She is why I keep fighting to make our health system great again.
Our cover articles this month discuss HCV treatment in patients with special risk factors or co-conditions. Fascinating information will emerge from studies like the article about artificial sweeteners. Scientists studied hunger-related enzyme levels and brain blood flow with functional MRI’s in obese and lean individuals after ingesting placebo and sucralose-containing solutions. Results might influence our weight loss advice to patients. Worried about malpractice? See our third front page article.
Additional articles discuss a reversal agent for one of the direct-acting oral anticoagulants and a hemospray for GI bleeding. Clinically impactful articles from the AGA journals are highlighted.
Finally, I would like to thank all of you who filled out the readership survey last fall. We are proud that you identified GI & Hepatology News as the best overall source for news information in gastroenterology.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Americans back from captivity need decompression period
The recent release of three Americans from North Korea has raised the question of how to bring back those who have been incarcerated abroad.
Jason Rezaian is the Iranian-American journalist who was detained in Iran for a year and a half. He recently discussed how beneficial it was for him to have time away from the spotlight after his release. He also expressed concern that the current administration’s tendency to parade former hostages before cameras right after their release could interfere with their ability to heal from their ordeal.
“I was so thankful that I had the opportunity to spend some time alone and with my family before that happened to me,” he said.
When I was in the Army, I was involved in planning for the release of an American pilot shot down over North Korea. Later, I talked on the Larry King Live about American soldiers taken prisoner in the beginning of the Iraq War who were being returned to Fort Bliss, Tex. And now, another American has been released from captivity, this time from Venezuela; by evening that same day, he was meeting with the president – and the press – at the White House.
In planning for repatriation, the military has built on the experience of former prisoners of war (POWs); in doing so, it has learned the best way to bring home those who have been captured. This experience builds on lessons learned from the return of POWs from the Korean war, the Vietnam war, the Gulf War, and other hostilities, according to the Borden Institute, an agency of the U.S. Army Medical Department Center and School now based in Fort Sam in Houston, Tex.
Optimal repatriation usually involves a decompression period, now often at the Army hospital in Landstuhl, Germany. About 3 days are allotted for medical and psychiatric exams, debriefing with intelligence agencies, and reunions with family members. Returning service members also catch up on sleep and nutrition; “three hots and a cot” is the Army mantra for dealing with combat stress, and it also applies here.
The returning service members also are prepared for the glare of media publicity which will follow. They learn how to avoid comments that might embarrass them later. If they have been held captive for a long period of time, they are brought up to date on recent events and news.
To quote the Borden Institute, “Most repatriated POWs, including those from the Persian Gulf War, have had little experience dealing with the media. The media are a substantial stressor that can have lifelong effects if a later, ‘Wish-I-had-never-said,’ statement is broadcast around the world. It is very important to both shield the POW and his family from early intrusive media coverage and to offer training in the management of media requests. This was done routinely for the POWs of the Persian Gulf War. Reminding POWs and their families that it is perfectly acceptable for them to say, ‘No,’ can be a most important intervention.”
So I would urge the current administration to take those lessons into account as it plans for the return of American hostages and returnees.
Dr. Ritchie, a forensic psychiatrist with expertise in military and veteran’s issues, is chief of psychiatry at MedStar Washington Hospital Center.
The recent release of three Americans from North Korea has raised the question of how to bring back those who have been incarcerated abroad.
Jason Rezaian is the Iranian-American journalist who was detained in Iran for a year and a half. He recently discussed how beneficial it was for him to have time away from the spotlight after his release. He also expressed concern that the current administration’s tendency to parade former hostages before cameras right after their release could interfere with their ability to heal from their ordeal.
“I was so thankful that I had the opportunity to spend some time alone and with my family before that happened to me,” he said.
When I was in the Army, I was involved in planning for the release of an American pilot shot down over North Korea. Later, I talked on the Larry King Live about American soldiers taken prisoner in the beginning of the Iraq War who were being returned to Fort Bliss, Tex. And now, another American has been released from captivity, this time from Venezuela; by evening that same day, he was meeting with the president – and the press – at the White House.
In planning for repatriation, the military has built on the experience of former prisoners of war (POWs); in doing so, it has learned the best way to bring home those who have been captured. This experience builds on lessons learned from the return of POWs from the Korean war, the Vietnam war, the Gulf War, and other hostilities, according to the Borden Institute, an agency of the U.S. Army Medical Department Center and School now based in Fort Sam in Houston, Tex.
Optimal repatriation usually involves a decompression period, now often at the Army hospital in Landstuhl, Germany. About 3 days are allotted for medical and psychiatric exams, debriefing with intelligence agencies, and reunions with family members. Returning service members also catch up on sleep and nutrition; “three hots and a cot” is the Army mantra for dealing with combat stress, and it also applies here.
The returning service members also are prepared for the glare of media publicity which will follow. They learn how to avoid comments that might embarrass them later. If they have been held captive for a long period of time, they are brought up to date on recent events and news.
To quote the Borden Institute, “Most repatriated POWs, including those from the Persian Gulf War, have had little experience dealing with the media. The media are a substantial stressor that can have lifelong effects if a later, ‘Wish-I-had-never-said,’ statement is broadcast around the world. It is very important to both shield the POW and his family from early intrusive media coverage and to offer training in the management of media requests. This was done routinely for the POWs of the Persian Gulf War. Reminding POWs and their families that it is perfectly acceptable for them to say, ‘No,’ can be a most important intervention.”
So I would urge the current administration to take those lessons into account as it plans for the return of American hostages and returnees.
Dr. Ritchie, a forensic psychiatrist with expertise in military and veteran’s issues, is chief of psychiatry at MedStar Washington Hospital Center.
The recent release of three Americans from North Korea has raised the question of how to bring back those who have been incarcerated abroad.
Jason Rezaian is the Iranian-American journalist who was detained in Iran for a year and a half. He recently discussed how beneficial it was for him to have time away from the spotlight after his release. He also expressed concern that the current administration’s tendency to parade former hostages before cameras right after their release could interfere with their ability to heal from their ordeal.
“I was so thankful that I had the opportunity to spend some time alone and with my family before that happened to me,” he said.
When I was in the Army, I was involved in planning for the release of an American pilot shot down over North Korea. Later, I talked on the Larry King Live about American soldiers taken prisoner in the beginning of the Iraq War who were being returned to Fort Bliss, Tex. And now, another American has been released from captivity, this time from Venezuela; by evening that same day, he was meeting with the president – and the press – at the White House.
In planning for repatriation, the military has built on the experience of former prisoners of war (POWs); in doing so, it has learned the best way to bring home those who have been captured. This experience builds on lessons learned from the return of POWs from the Korean war, the Vietnam war, the Gulf War, and other hostilities, according to the Borden Institute, an agency of the U.S. Army Medical Department Center and School now based in Fort Sam in Houston, Tex.
Optimal repatriation usually involves a decompression period, now often at the Army hospital in Landstuhl, Germany. About 3 days are allotted for medical and psychiatric exams, debriefing with intelligence agencies, and reunions with family members. Returning service members also catch up on sleep and nutrition; “three hots and a cot” is the Army mantra for dealing with combat stress, and it also applies here.
The returning service members also are prepared for the glare of media publicity which will follow. They learn how to avoid comments that might embarrass them later. If they have been held captive for a long period of time, they are brought up to date on recent events and news.
To quote the Borden Institute, “Most repatriated POWs, including those from the Persian Gulf War, have had little experience dealing with the media. The media are a substantial stressor that can have lifelong effects if a later, ‘Wish-I-had-never-said,’ statement is broadcast around the world. It is very important to both shield the POW and his family from early intrusive media coverage and to offer training in the management of media requests. This was done routinely for the POWs of the Persian Gulf War. Reminding POWs and their families that it is perfectly acceptable for them to say, ‘No,’ can be a most important intervention.”
So I would urge the current administration to take those lessons into account as it plans for the return of American hostages and returnees.
Dr. Ritchie, a forensic psychiatrist with expertise in military and veteran’s issues, is chief of psychiatry at MedStar Washington Hospital Center.
Detached parents: How to help
While most of the parents you will see in your office will be thoughtful, engaged, and even anxious, occasionally you will encounter parents who seem detached from their children. Spending just a few extra minutes to understand this detachment could mean an enormous difference in the psychological health and developmental well-being of your patient.
It is striking when you see it: Flat affect, little eye contact, no questions or comments. If the parents seem unconnected to their children, it is worth being curious about it. Whether they are constantly on their phones or just disengaged, you should start by directing a question straight to them. Perhaps a question about the child’s sleep, appetite, or school performance is a good place to start. You would like to assess their knowledge of the child’s development, performance at school, friendships, and interests, to ensure that they are up to date and paying attention.
Once alone, you might start by offering your impression of how the child is doing, then observe that you noticed that they (the parents) seem quiet or distant. The following questions should help you better understand the nature of their detachment.
Depression
Ask about how they are sleeping. If the child is very young or the parents have a difficult work schedule, they might simply be sleep deprived, which you might help them address. Difficulty sleeping also can be a symptom of depression. Have they noticed any changes in their appetite or energy? Is it harder to concentrate? Have they felt more tearful, sad, or irritable? Have they noticed that they don’t get as much pleasure from things that usually bring them joy? Do they worry about being a burden to others? Major depressive disorder is relatively common, affecting as many as one in five women in the postpartum period and one in ten women generally.
Men experience depression at about half that rate, according the Centers for Disease Control and Prevention. It is a condition that can cause feelings of guilt and shame, so many suffer silently, missing the chance for treatment and raising the risk for suicide. Infants of depressed mothers often appear listless and may be fussier about sleeping and eating, which can exacerbate poor attachment with their parents, and lead to problems in later years, including anxiety, mood, or behavioral problems. A parent’s depression, particularly in the postpartum period, represents a serious threat to the child’s healthy development and well-being.
Tell the parents that what they have described to you sounds like it could be a depressive episode and that depression has a serious impact on the whole family. Offer that their primary care physicians can evaluate and treat depression, or learn about other resources in your community that you can refer them to for accessible care.
Overwhelming stress
Is the newborn or special needs child feeling like more responsibility than the parents can handle? Where do the parents find support? Has there been a recent job loss or has there been a financial setback for the family? Is a spouse ill, or are they also caring for an aging parent? Has there been a separation from the spouse? Many adults face multiple significant stresses at the same time. It is not uncommon for working parents to be in “soldiering on” mode, just surviving. But this takes a toll on being present and engaged with the children, and puts them at risk for depression and substance abuse.
Traumatic stress
Have they recently experienced a crime or accident, the unexpected loss of a loved one, or threats or abuse at home? They may be grieving, or may be experiencing symptoms of posttraumatic stress disorder that lead them to appear distant and detached. Grief will improve with time, but they may benefit from extra support or from assistance with their responsibilities (a leave from work or more child care). If they have experienced a traumatic stress, they will need a clinical evaluation for potential treatment options. If they are being threatened or abused at home, you need to find out if their children have witnessed the abuse or may be victims as well. You can offer these parents resources for survivors of domestic abuse and speak with them about your obligation to file with your state’s agency responsible for children’s welfare. It is critical that you listen to any concerns they may have about this filing, from losing their children to enraging their abusers.
A detached parent may make a child feel worried, worthless, or guilty. There is no substitute for a loving, engaged parent, and your brief interventions to help a parent reconnect with the child will be invaluable.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected]
While most of the parents you will see in your office will be thoughtful, engaged, and even anxious, occasionally you will encounter parents who seem detached from their children. Spending just a few extra minutes to understand this detachment could mean an enormous difference in the psychological health and developmental well-being of your patient.
It is striking when you see it: Flat affect, little eye contact, no questions or comments. If the parents seem unconnected to their children, it is worth being curious about it. Whether they are constantly on their phones or just disengaged, you should start by directing a question straight to them. Perhaps a question about the child’s sleep, appetite, or school performance is a good place to start. You would like to assess their knowledge of the child’s development, performance at school, friendships, and interests, to ensure that they are up to date and paying attention.
Once alone, you might start by offering your impression of how the child is doing, then observe that you noticed that they (the parents) seem quiet or distant. The following questions should help you better understand the nature of their detachment.
Depression
Ask about how they are sleeping. If the child is very young or the parents have a difficult work schedule, they might simply be sleep deprived, which you might help them address. Difficulty sleeping also can be a symptom of depression. Have they noticed any changes in their appetite or energy? Is it harder to concentrate? Have they felt more tearful, sad, or irritable? Have they noticed that they don’t get as much pleasure from things that usually bring them joy? Do they worry about being a burden to others? Major depressive disorder is relatively common, affecting as many as one in five women in the postpartum period and one in ten women generally.
Men experience depression at about half that rate, according the Centers for Disease Control and Prevention. It is a condition that can cause feelings of guilt and shame, so many suffer silently, missing the chance for treatment and raising the risk for suicide. Infants of depressed mothers often appear listless and may be fussier about sleeping and eating, which can exacerbate poor attachment with their parents, and lead to problems in later years, including anxiety, mood, or behavioral problems. A parent’s depression, particularly in the postpartum period, represents a serious threat to the child’s healthy development and well-being.
Tell the parents that what they have described to you sounds like it could be a depressive episode and that depression has a serious impact on the whole family. Offer that their primary care physicians can evaluate and treat depression, or learn about other resources in your community that you can refer them to for accessible care.
Overwhelming stress
Is the newborn or special needs child feeling like more responsibility than the parents can handle? Where do the parents find support? Has there been a recent job loss or has there been a financial setback for the family? Is a spouse ill, or are they also caring for an aging parent? Has there been a separation from the spouse? Many adults face multiple significant stresses at the same time. It is not uncommon for working parents to be in “soldiering on” mode, just surviving. But this takes a toll on being present and engaged with the children, and puts them at risk for depression and substance abuse.
Traumatic stress
Have they recently experienced a crime or accident, the unexpected loss of a loved one, or threats or abuse at home? They may be grieving, or may be experiencing symptoms of posttraumatic stress disorder that lead them to appear distant and detached. Grief will improve with time, but they may benefit from extra support or from assistance with their responsibilities (a leave from work or more child care). If they have experienced a traumatic stress, they will need a clinical evaluation for potential treatment options. If they are being threatened or abused at home, you need to find out if their children have witnessed the abuse or may be victims as well. You can offer these parents resources for survivors of domestic abuse and speak with them about your obligation to file with your state’s agency responsible for children’s welfare. It is critical that you listen to any concerns they may have about this filing, from losing their children to enraging their abusers.
A detached parent may make a child feel worried, worthless, or guilty. There is no substitute for a loving, engaged parent, and your brief interventions to help a parent reconnect with the child will be invaluable.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected]
While most of the parents you will see in your office will be thoughtful, engaged, and even anxious, occasionally you will encounter parents who seem detached from their children. Spending just a few extra minutes to understand this detachment could mean an enormous difference in the psychological health and developmental well-being of your patient.
It is striking when you see it: Flat affect, little eye contact, no questions or comments. If the parents seem unconnected to their children, it is worth being curious about it. Whether they are constantly on their phones or just disengaged, you should start by directing a question straight to them. Perhaps a question about the child’s sleep, appetite, or school performance is a good place to start. You would like to assess their knowledge of the child’s development, performance at school, friendships, and interests, to ensure that they are up to date and paying attention.
Once alone, you might start by offering your impression of how the child is doing, then observe that you noticed that they (the parents) seem quiet or distant. The following questions should help you better understand the nature of their detachment.
Depression
Ask about how they are sleeping. If the child is very young or the parents have a difficult work schedule, they might simply be sleep deprived, which you might help them address. Difficulty sleeping also can be a symptom of depression. Have they noticed any changes in their appetite or energy? Is it harder to concentrate? Have they felt more tearful, sad, or irritable? Have they noticed that they don’t get as much pleasure from things that usually bring them joy? Do they worry about being a burden to others? Major depressive disorder is relatively common, affecting as many as one in five women in the postpartum period and one in ten women generally.
Men experience depression at about half that rate, according the Centers for Disease Control and Prevention. It is a condition that can cause feelings of guilt and shame, so many suffer silently, missing the chance for treatment and raising the risk for suicide. Infants of depressed mothers often appear listless and may be fussier about sleeping and eating, which can exacerbate poor attachment with their parents, and lead to problems in later years, including anxiety, mood, or behavioral problems. A parent’s depression, particularly in the postpartum period, represents a serious threat to the child’s healthy development and well-being.
Tell the parents that what they have described to you sounds like it could be a depressive episode and that depression has a serious impact on the whole family. Offer that their primary care physicians can evaluate and treat depression, or learn about other resources in your community that you can refer them to for accessible care.
Overwhelming stress
Is the newborn or special needs child feeling like more responsibility than the parents can handle? Where do the parents find support? Has there been a recent job loss or has there been a financial setback for the family? Is a spouse ill, or are they also caring for an aging parent? Has there been a separation from the spouse? Many adults face multiple significant stresses at the same time. It is not uncommon for working parents to be in “soldiering on” mode, just surviving. But this takes a toll on being present and engaged with the children, and puts them at risk for depression and substance abuse.
Traumatic stress
Have they recently experienced a crime or accident, the unexpected loss of a loved one, or threats or abuse at home? They may be grieving, or may be experiencing symptoms of posttraumatic stress disorder that lead them to appear distant and detached. Grief will improve with time, but they may benefit from extra support or from assistance with their responsibilities (a leave from work or more child care). If they have experienced a traumatic stress, they will need a clinical evaluation for potential treatment options. If they are being threatened or abused at home, you need to find out if their children have witnessed the abuse or may be victims as well. You can offer these parents resources for survivors of domestic abuse and speak with them about your obligation to file with your state’s agency responsible for children’s welfare. It is critical that you listen to any concerns they may have about this filing, from losing their children to enraging their abusers.
A detached parent may make a child feel worried, worthless, or guilty. There is no substitute for a loving, engaged parent, and your brief interventions to help a parent reconnect with the child will be invaluable.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected]
Under his IDH2: Epigenetic drivers of clonal hematopoiesis
The world has surely changed in recent years, leading television and Hollywood to recreate many former works of postapocalyptic fiction. Watching the recent Hulu drama “The Handmaid’s Tale” leads many to make modern-day comparisons, but to this hematologist the connection is bone deep.
Hematopoietic stem cells face a century of carefully regulated symmetric division. They are tasked with the mission to generate the heterogeneous and environmentally responsive progenitor populations that will undergo coordinated differentiation and maturation.1
Within this epic battle of Gilead, much like hematopoiesis, there is a hierarchy within the Sons of Jacob. At the top there are few who drive leukemogenicity and require no other co-conspirators. MLL fusions and core binding factor are the Commanders that can overthrow the regulated governance of normal marrow homeostasis. Other myeloid disease alleles are soldiers of Gilead (i.e. FLT3-ITD, IDH1, IDH2, NPM1c, Spliceosome/Cohesin). Their individual characteristics can influence the natural history of the disease and define its strengths and weaknesses, particularly as new targeted therapies are developed.
Recently, Jongen-Lavrencic et al. reported that all disease alleles that persist as minimal residual disease after induction have a negative influence on outcome, except for three – DNMT3A, TET2, and ASXL1.2 What do we make of the “DTA” mutations? Are they the “Eye” – spies embedded in the polyclonal background of the marrow – intrinsically wired with malevolent intent? Are they the innocent, abused Handmaids – reprogrammed by inflammatory “Aunts” at the marrow’s Red Center and forced to clonally procreate? Previous works have suggested the latter, that persistence of mutations in genes found in clonal hematopoiesis (CH) do not portend an equivalent risk of relapse.3,4
A more encompassing question remains as to the equivalency of CH in the absence of a hematopoietic tumor versus CH postleukemia therapy. Comparisons to small cell lymphomas after successful treatment of transformed disease are disingenuous; CH is not itself a malignant state.5 Forty months of median follow-up for post-AML CH is simply not enough time. Work presented at the 2017 annual meeting of the American Society of Hematology by Jaiswal et al. showed that the approximately 1% risk of transformation per year was consistent over a 20-year period of follow up in the Swedish Nurse’s Study.
The recent work in the New England Journal of Medicine adds to the growing understanding of CH, but requires the test of time to know if these cells are truly innocent Handmaids or the Eye in a red cloak. I’ll be exploring these issues and taking your questions during a live Twitter Q&A on June 14 at noon ET. Follow me at @TheDoctorIsVin and @HematologyNews1 for more details. Blessed be the fruit.
Dr. Viny is with the Memorial Sloan-Kettering Cancer Center, N.Y., where he is a clinical instructor, is on the staff of the leukemia service, and is a clinical researcher in the Ross Levine Lab.
References
1. Orkin SH and Zon L. Cell. 2008 Feb 22;132(4):631-44.
2. Jongen-Lavrencic M et al. N Engl J Med 2018; 378:1189-99.
3. Bhatnagar B et al. Br J Haematol. 2016 Oct;175(2):226-36.
4. Shlush LI et al. Nature. 2017;547:104-8.
5. Bowman RL et al. Cell Stem Cell. 2018 Feb 1;22(2):157-70.
The world has surely changed in recent years, leading television and Hollywood to recreate many former works of postapocalyptic fiction. Watching the recent Hulu drama “The Handmaid’s Tale” leads many to make modern-day comparisons, but to this hematologist the connection is bone deep.
Hematopoietic stem cells face a century of carefully regulated symmetric division. They are tasked with the mission to generate the heterogeneous and environmentally responsive progenitor populations that will undergo coordinated differentiation and maturation.1
Within this epic battle of Gilead, much like hematopoiesis, there is a hierarchy within the Sons of Jacob. At the top there are few who drive leukemogenicity and require no other co-conspirators. MLL fusions and core binding factor are the Commanders that can overthrow the regulated governance of normal marrow homeostasis. Other myeloid disease alleles are soldiers of Gilead (i.e. FLT3-ITD, IDH1, IDH2, NPM1c, Spliceosome/Cohesin). Their individual characteristics can influence the natural history of the disease and define its strengths and weaknesses, particularly as new targeted therapies are developed.
Recently, Jongen-Lavrencic et al. reported that all disease alleles that persist as minimal residual disease after induction have a negative influence on outcome, except for three – DNMT3A, TET2, and ASXL1.2 What do we make of the “DTA” mutations? Are they the “Eye” – spies embedded in the polyclonal background of the marrow – intrinsically wired with malevolent intent? Are they the innocent, abused Handmaids – reprogrammed by inflammatory “Aunts” at the marrow’s Red Center and forced to clonally procreate? Previous works have suggested the latter, that persistence of mutations in genes found in clonal hematopoiesis (CH) do not portend an equivalent risk of relapse.3,4
A more encompassing question remains as to the equivalency of CH in the absence of a hematopoietic tumor versus CH postleukemia therapy. Comparisons to small cell lymphomas after successful treatment of transformed disease are disingenuous; CH is not itself a malignant state.5 Forty months of median follow-up for post-AML CH is simply not enough time. Work presented at the 2017 annual meeting of the American Society of Hematology by Jaiswal et al. showed that the approximately 1% risk of transformation per year was consistent over a 20-year period of follow up in the Swedish Nurse’s Study.
The recent work in the New England Journal of Medicine adds to the growing understanding of CH, but requires the test of time to know if these cells are truly innocent Handmaids or the Eye in a red cloak. I’ll be exploring these issues and taking your questions during a live Twitter Q&A on June 14 at noon ET. Follow me at @TheDoctorIsVin and @HematologyNews1 for more details. Blessed be the fruit.
Dr. Viny is with the Memorial Sloan-Kettering Cancer Center, N.Y., where he is a clinical instructor, is on the staff of the leukemia service, and is a clinical researcher in the Ross Levine Lab.
References
1. Orkin SH and Zon L. Cell. 2008 Feb 22;132(4):631-44.
2. Jongen-Lavrencic M et al. N Engl J Med 2018; 378:1189-99.
3. Bhatnagar B et al. Br J Haematol. 2016 Oct;175(2):226-36.
4. Shlush LI et al. Nature. 2017;547:104-8.
5. Bowman RL et al. Cell Stem Cell. 2018 Feb 1;22(2):157-70.
The world has surely changed in recent years, leading television and Hollywood to recreate many former works of postapocalyptic fiction. Watching the recent Hulu drama “The Handmaid’s Tale” leads many to make modern-day comparisons, but to this hematologist the connection is bone deep.
Hematopoietic stem cells face a century of carefully regulated symmetric division. They are tasked with the mission to generate the heterogeneous and environmentally responsive progenitor populations that will undergo coordinated differentiation and maturation.1
Within this epic battle of Gilead, much like hematopoiesis, there is a hierarchy within the Sons of Jacob. At the top there are few who drive leukemogenicity and require no other co-conspirators. MLL fusions and core binding factor are the Commanders that can overthrow the regulated governance of normal marrow homeostasis. Other myeloid disease alleles are soldiers of Gilead (i.e. FLT3-ITD, IDH1, IDH2, NPM1c, Spliceosome/Cohesin). Their individual characteristics can influence the natural history of the disease and define its strengths and weaknesses, particularly as new targeted therapies are developed.
Recently, Jongen-Lavrencic et al. reported that all disease alleles that persist as minimal residual disease after induction have a negative influence on outcome, except for three – DNMT3A, TET2, and ASXL1.2 What do we make of the “DTA” mutations? Are they the “Eye” – spies embedded in the polyclonal background of the marrow – intrinsically wired with malevolent intent? Are they the innocent, abused Handmaids – reprogrammed by inflammatory “Aunts” at the marrow’s Red Center and forced to clonally procreate? Previous works have suggested the latter, that persistence of mutations in genes found in clonal hematopoiesis (CH) do not portend an equivalent risk of relapse.3,4
A more encompassing question remains as to the equivalency of CH in the absence of a hematopoietic tumor versus CH postleukemia therapy. Comparisons to small cell lymphomas after successful treatment of transformed disease are disingenuous; CH is not itself a malignant state.5 Forty months of median follow-up for post-AML CH is simply not enough time. Work presented at the 2017 annual meeting of the American Society of Hematology by Jaiswal et al. showed that the approximately 1% risk of transformation per year was consistent over a 20-year period of follow up in the Swedish Nurse’s Study.
The recent work in the New England Journal of Medicine adds to the growing understanding of CH, but requires the test of time to know if these cells are truly innocent Handmaids or the Eye in a red cloak. I’ll be exploring these issues and taking your questions during a live Twitter Q&A on June 14 at noon ET. Follow me at @TheDoctorIsVin and @HematologyNews1 for more details. Blessed be the fruit.
Dr. Viny is with the Memorial Sloan-Kettering Cancer Center, N.Y., where he is a clinical instructor, is on the staff of the leukemia service, and is a clinical researcher in the Ross Levine Lab.
References
1. Orkin SH and Zon L. Cell. 2008 Feb 22;132(4):631-44.
2. Jongen-Lavrencic M et al. N Engl J Med 2018; 378:1189-99.
3. Bhatnagar B et al. Br J Haematol. 2016 Oct;175(2):226-36.
4. Shlush LI et al. Nature. 2017;547:104-8.
5. Bowman RL et al. Cell Stem Cell. 2018 Feb 1;22(2):157-70.
Kawasaki disease: New info to enhance our index of suspicion
Most U.S. mainland pediatric practitioners will see only one or two cases of Kawasaki disease (KD) in their careers, but no one wants to miss even one case.
Making the diagnosis as early as possible is important to reduce the chance of sequelae, particularly the coronary artery aneurysms that will eventually lead to 5% of overall acute coronary syndromes in adults. And because there is no “KD test,” or sometimes incomplete KD. And there are some new data that complicate this. Despite the recently updated 2017 guideline,1 most cases end up being confirmed and managed by regional “experts.” But nearly all of the approximately 6,000 KD cases/year in U.S. children younger than 5 years old start out with one or more primary care, urgent care, or ED visits.
This means that every clinician in the trenches not only needs a high index of suspicion but also needs to be at least a partial expert, too. What raises our index of suspicion? Classic data tell us we need 5 consecutive days of fever plus four or five other principal clinical findings for a KD diagnosis. The principal findings are:
1. Eyes: Bilateral bulbar nonexudative conjunctival injection.
2. Mouth: Erythema of oral/pharyngeal mucosa or cracked lips or strawberry tongue or oral mucositis.
3. Rash.
4. Hands or feet findings: Swelling/erythema or later periungual desquamation.
5. Cervical adenopathy greater than 1.4 cm, usually unilateral.
Other factors that have classically increased suspicion are winter/early spring presentation in North America, male gender (1.5:1 ratio to females), and Asian (particularly Japanese) ancestry. The importance of genetics was initially based on epidemiology (Japan/Asian risk) but lately has been further associated with six gene polymorphisms. However, molecular genetic testing is not currently a practical tool.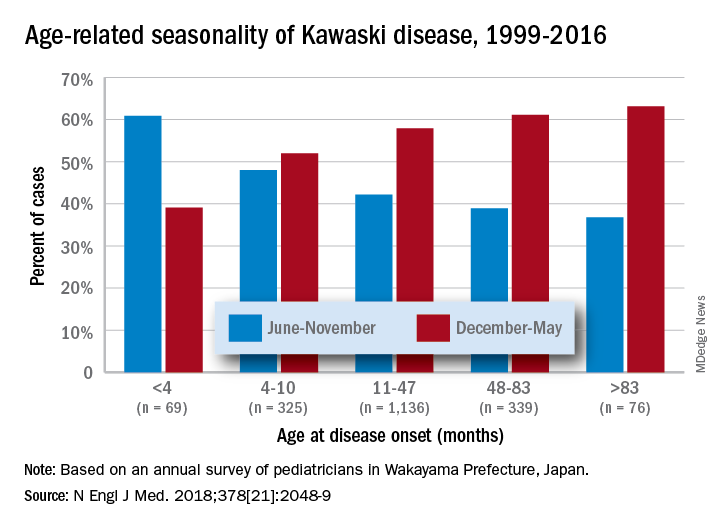
Clinical scenarios that also should raise suspicion include less-than-6-month-old infants with prolonged fever/irritability (may be the only clinical manifestations of KD) and children over 4 years old who more often may have incomplete KD. Both groups have higher prevalence of coronary artery abnormalities. Other high suspicion scenarios include prolonged fever with unexplained/culture-negative shock, or antibiotic treatment failure for cervical adenitis or retro/parapharyngeal phlegmon. Consultation with or referral to a regional KD expert may be needed.
Fuzzy KD math
Current guidelines list an exception to the 5-day fever requirement in that only 4 days of fever are needed with four or more principal clinical features, particularly when hand and feet findings exist. Some call this the “4X4 exception.” Then there is a sub-caveat: “Experienced clinicians who have treated many patients with KD may establish the diagnosis with 3 days of fever in rare cases.”1
Incomplete KD
This is another exception, which seems to be a more frequent diagnosis in the past decade. Incomplete KD requires the 5 days of fever duration plus an elevated C-reactive protein or erythrocyte sedimentation rate. But one needs only two or three of the five principal clinical KD criteria plus three or more of six other laboratory findings (anemia, low albumin, leukocytosis, thrombocytosis, pyuria, or elevated alanine aminotransferase). Incomplete KD can be confirmed by an abnormal echocardiogram – usually not until after 7 days of KD symptoms.1
New KD nuances
In a recent report on 20 years of data from Japan (n = 1,945 KD cases), more granularity on age, seasonal epidemiology, and outcome were seen.2 There was an inverse correlation of male predominance to age, i.e. as age groups got older, there was a gradual shift to female predominance by 7 years of age. The winter/spring predominance (60% of overall cases) did not hold true in younger age groups where summer/fall was the peak season (65% of cases).
With the goal of not missing any KD and diagnosing as early as possible to limit sequelae, we all need to be relative experts and keep alert for clinical scenarios that warrant our raising our index of suspicion. But now the seasonality trends appear blurred in the youngest cases and the male predominance is blurred in the oldest cases. And remember that fever and irritability for longer than 7 days in young infants may be the only clue to KD.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. Circulation. 2017 Mar 29. doi: 10.1161/CIR.0000000000000484
2. N Engl J Med. 2018 May 24. doi: 10.1056/NEJMc1804312.
Most U.S. mainland pediatric practitioners will see only one or two cases of Kawasaki disease (KD) in their careers, but no one wants to miss even one case.
Making the diagnosis as early as possible is important to reduce the chance of sequelae, particularly the coronary artery aneurysms that will eventually lead to 5% of overall acute coronary syndromes in adults. And because there is no “KD test,” or sometimes incomplete KD. And there are some new data that complicate this. Despite the recently updated 2017 guideline,1 most cases end up being confirmed and managed by regional “experts.” But nearly all of the approximately 6,000 KD cases/year in U.S. children younger than 5 years old start out with one or more primary care, urgent care, or ED visits.
This means that every clinician in the trenches not only needs a high index of suspicion but also needs to be at least a partial expert, too. What raises our index of suspicion? Classic data tell us we need 5 consecutive days of fever plus four or five other principal clinical findings for a KD diagnosis. The principal findings are:
1. Eyes: Bilateral bulbar nonexudative conjunctival injection.
2. Mouth: Erythema of oral/pharyngeal mucosa or cracked lips or strawberry tongue or oral mucositis.
3. Rash.
4. Hands or feet findings: Swelling/erythema or later periungual desquamation.
5. Cervical adenopathy greater than 1.4 cm, usually unilateral.
Other factors that have classically increased suspicion are winter/early spring presentation in North America, male gender (1.5:1 ratio to females), and Asian (particularly Japanese) ancestry. The importance of genetics was initially based on epidemiology (Japan/Asian risk) but lately has been further associated with six gene polymorphisms. However, molecular genetic testing is not currently a practical tool.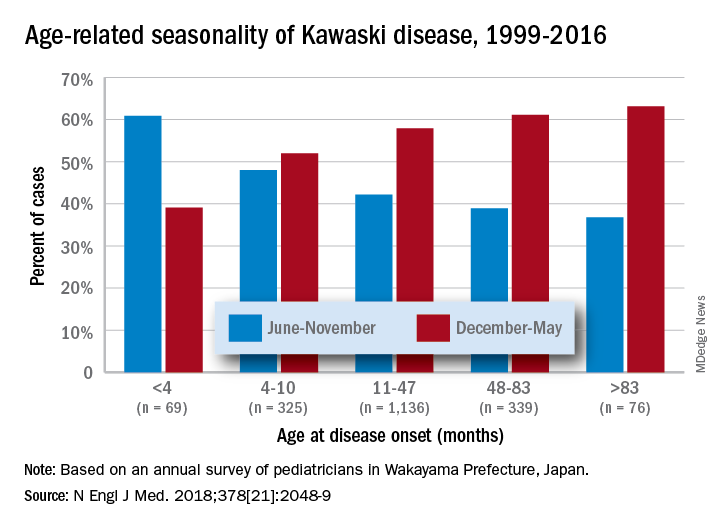
Clinical scenarios that also should raise suspicion include less-than-6-month-old infants with prolonged fever/irritability (may be the only clinical manifestations of KD) and children over 4 years old who more often may have incomplete KD. Both groups have higher prevalence of coronary artery abnormalities. Other high suspicion scenarios include prolonged fever with unexplained/culture-negative shock, or antibiotic treatment failure for cervical adenitis or retro/parapharyngeal phlegmon. Consultation with or referral to a regional KD expert may be needed.
Fuzzy KD math
Current guidelines list an exception to the 5-day fever requirement in that only 4 days of fever are needed with four or more principal clinical features, particularly when hand and feet findings exist. Some call this the “4X4 exception.” Then there is a sub-caveat: “Experienced clinicians who have treated many patients with KD may establish the diagnosis with 3 days of fever in rare cases.”1
Incomplete KD
This is another exception, which seems to be a more frequent diagnosis in the past decade. Incomplete KD requires the 5 days of fever duration plus an elevated C-reactive protein or erythrocyte sedimentation rate. But one needs only two or three of the five principal clinical KD criteria plus three or more of six other laboratory findings (anemia, low albumin, leukocytosis, thrombocytosis, pyuria, or elevated alanine aminotransferase). Incomplete KD can be confirmed by an abnormal echocardiogram – usually not until after 7 days of KD symptoms.1
New KD nuances
In a recent report on 20 years of data from Japan (n = 1,945 KD cases), more granularity on age, seasonal epidemiology, and outcome were seen.2 There was an inverse correlation of male predominance to age, i.e. as age groups got older, there was a gradual shift to female predominance by 7 years of age. The winter/spring predominance (60% of overall cases) did not hold true in younger age groups where summer/fall was the peak season (65% of cases).
With the goal of not missing any KD and diagnosing as early as possible to limit sequelae, we all need to be relative experts and keep alert for clinical scenarios that warrant our raising our index of suspicion. But now the seasonality trends appear blurred in the youngest cases and the male predominance is blurred in the oldest cases. And remember that fever and irritability for longer than 7 days in young infants may be the only clue to KD.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. Circulation. 2017 Mar 29. doi: 10.1161/CIR.0000000000000484
2. N Engl J Med. 2018 May 24. doi: 10.1056/NEJMc1804312.
Most U.S. mainland pediatric practitioners will see only one or two cases of Kawasaki disease (KD) in their careers, but no one wants to miss even one case.
Making the diagnosis as early as possible is important to reduce the chance of sequelae, particularly the coronary artery aneurysms that will eventually lead to 5% of overall acute coronary syndromes in adults. And because there is no “KD test,” or sometimes incomplete KD. And there are some new data that complicate this. Despite the recently updated 2017 guideline,1 most cases end up being confirmed and managed by regional “experts.” But nearly all of the approximately 6,000 KD cases/year in U.S. children younger than 5 years old start out with one or more primary care, urgent care, or ED visits.
This means that every clinician in the trenches not only needs a high index of suspicion but also needs to be at least a partial expert, too. What raises our index of suspicion? Classic data tell us we need 5 consecutive days of fever plus four or five other principal clinical findings for a KD diagnosis. The principal findings are:
1. Eyes: Bilateral bulbar nonexudative conjunctival injection.
2. Mouth: Erythema of oral/pharyngeal mucosa or cracked lips or strawberry tongue or oral mucositis.
3. Rash.
4. Hands or feet findings: Swelling/erythema or later periungual desquamation.
5. Cervical adenopathy greater than 1.4 cm, usually unilateral.
Other factors that have classically increased suspicion are winter/early spring presentation in North America, male gender (1.5:1 ratio to females), and Asian (particularly Japanese) ancestry. The importance of genetics was initially based on epidemiology (Japan/Asian risk) but lately has been further associated with six gene polymorphisms. However, molecular genetic testing is not currently a practical tool.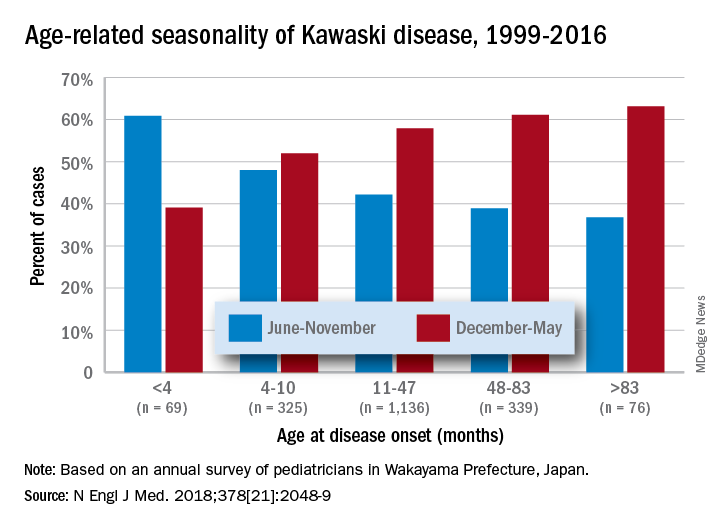
Clinical scenarios that also should raise suspicion include less-than-6-month-old infants with prolonged fever/irritability (may be the only clinical manifestations of KD) and children over 4 years old who more often may have incomplete KD. Both groups have higher prevalence of coronary artery abnormalities. Other high suspicion scenarios include prolonged fever with unexplained/culture-negative shock, or antibiotic treatment failure for cervical adenitis or retro/parapharyngeal phlegmon. Consultation with or referral to a regional KD expert may be needed.
Fuzzy KD math
Current guidelines list an exception to the 5-day fever requirement in that only 4 days of fever are needed with four or more principal clinical features, particularly when hand and feet findings exist. Some call this the “4X4 exception.” Then there is a sub-caveat: “Experienced clinicians who have treated many patients with KD may establish the diagnosis with 3 days of fever in rare cases.”1
Incomplete KD
This is another exception, which seems to be a more frequent diagnosis in the past decade. Incomplete KD requires the 5 days of fever duration plus an elevated C-reactive protein or erythrocyte sedimentation rate. But one needs only two or three of the five principal clinical KD criteria plus three or more of six other laboratory findings (anemia, low albumin, leukocytosis, thrombocytosis, pyuria, or elevated alanine aminotransferase). Incomplete KD can be confirmed by an abnormal echocardiogram – usually not until after 7 days of KD symptoms.1
New KD nuances
In a recent report on 20 years of data from Japan (n = 1,945 KD cases), more granularity on age, seasonal epidemiology, and outcome were seen.2 There was an inverse correlation of male predominance to age, i.e. as age groups got older, there was a gradual shift to female predominance by 7 years of age. The winter/spring predominance (60% of overall cases) did not hold true in younger age groups where summer/fall was the peak season (65% of cases).
With the goal of not missing any KD and diagnosing as early as possible to limit sequelae, we all need to be relative experts and keep alert for clinical scenarios that warrant our raising our index of suspicion. But now the seasonality trends appear blurred in the youngest cases and the male predominance is blurred in the oldest cases. And remember that fever and irritability for longer than 7 days in young infants may be the only clue to KD.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. Circulation. 2017 Mar 29. doi: 10.1161/CIR.0000000000000484
2. N Engl J Med. 2018 May 24. doi: 10.1056/NEJMc1804312.
Practice management pearls: Advice from seasoned doctors for residents looking to start a practice
The notion that residency training falls short when it comes to preparing residents and doctors for starting their own practice is a common thread across the board, whether you’re just getting started or have been managing your own practice for years. I did a survey on LinkedIn and over 50 dermatology and plastic surgery colleagues generously provided their own personal insights and words of wisdom to help young doctors avoid common practice management problems.
I could not quote everyone, but here are some of the best tips that I received:
Choose your staff carefully – and invest in the right candidates
One of the biggest pieces of practice management advice that doctors had to offer was to hire the right employees from the beginning, even if that means spending a little more time in the hiring process. This will eliminate headaches and frustration later.
In his own practice in Palm Beach Gardens, Fla., Dr. Lickstein has chosen a stable group of staff members who are, “first and foremost, nice, compassionate, and mature,” he said. “They need to be able to relate to cosmetic and medical patients of all ages. My office manager screens them, and then we have potential candidates shadow us for at least a half-day in the office. Afterward, we seek feedback from the current staff. I also try and talk with the candidate for a while, because I’ve found that once you get them to loosen up, you can get an actual sense of how they really are.”
Along the same lines, Cincinnati plastic surgeon Alex Donath, MD, suggests incentivizing employees and giving them an active role in the hiring process. “Give everyone in the office a chance to meet new employee candidates,” he said, “as that will both give the employees a sense of involvement in the process and allow more opportunities to catch glimpses of poor interpersonal skills that could hurt your reputation.”
Many doctors stressed the importance of the interview process, detailed job descriptions, a 60-day trial period, and background checks prior to hiring. This advice goes along with the famous quote “Be slow to hire and quick to fire (in the first 60 days)” that I have seen in many business books.
Foster teamwork
Another important aspect of managing your practice is building a sense of teamwork and camaraderie among employees and other doctors. Sean Weiss, MD, a facial plastic surgeon in New Orleans, has a great team-building tip that he uses daily.
“I plan a daily morning huddle with my staff. During the huddle, we review the prior day’s performance, those patients that need following up on, and whether or not the prior day’s goals were met. We then review the patient list for the current day to identify patient needs. We look specifically for ways to improve efficiency and avoid slowing down the work flow. We also try to identify opportunities to cross-promote our offerings to increase awareness of our services. In about 10 minutes, the entire team becomes focused and ready for a productive day.”
For Lacey Elwyn, DO, making staff feel appreciated can be as simple as telling them thank you on a regular basis. “The success of a dermatology practice encompasses every staff member of the team,” Dr. Elwyn, a medical and cosmetic dermatologist in South Florida, said. “The physician should respect and value all staff members. Tell them when they are doing a great job and tell them that you appreciate them every day, but also let them know right away when something is wrong.”
Don’t forget about patient education
Janet Trowbridge, MD, PhD, who practices in Edmond, Wash., expressed a great point that not only do patients need to be educated about their medical or cosmetic concerns, but they also need to be educated about the way that health care works in general. “I would say that 50% of my time as a physician is spent educating patients not about their disease, but about how medicine works – or doesn’t work,” she said. “I am constantly amazed by how little the average person understands about how health care is delivered. I talk about copays, coinsurance, annual deductibles, and why their prescriptions are not being covered. Patients feel that the system has let them down.”
Play the dual role of doctor and businessperson
At the end of the day, if you are managing your own practice, you must be able to split your time and skill set between being a physician and being a businessperson. Having realized the importance of the business aspect of running a practice, Justin Bryant, DO, a plastic and reconstructive surgeon in Walled Lake, Mich., enrolled in a dual-degree program during medical school in order to obtain his MBA.
“That investment already has proven priceless, as I’ve helped attendings and colleagues with their practice in marketing, finance, technology, and simply in translating business terms and contracts with physicians,” he said. “Although I don’t think it’s necessary for all physicians to pursue an MBA, and it’s not the answer to every business problem in the field of medicine, when applied, it can be very powerful!”
Build and protect your online reputation
Now more than ever, it is imperative to build and protect your online reputation, as online reviews can make or break your business. For plastic surgeon Nirmal Nathan, MD, in Plantation, Fla., managing your reputation is one of the most important considerations when starting a practice. “I would tell residents to start early on reputation management,” he said. “Reviews are so important, even with patients referred by word of mouth. Good reputation management also allows you to quickly ramp up if you decide to move your practice location.”
A large portion of building your online reputation now as to do with what you post (and don’t post) on social media. For Haena Kim, MD, a facial plastic and reconstructive surgeon practicing in Walnut Creek, Calif., figuring out how you would like others to perceive you is the first step.
“In this day and age of social media,” she said, “it’s so hard not to feel the pressure to follow the crowd and be the loudest person out there, and it’s incredibly hard to be patient with your practice growth. It’s important to figure out how you want to present yourself and what you want patients to come away with.”
Sweat the small stuff
Seemingly small administrative and business-related tasks can quickly add up and create much larger problems if not addressed early on. Tito Vasquez, MD, who practices in Southport, Conn., summed this up with an excellent piece of advice to remember: “Sweat the small stuff now, so you don’t have to sweat over the big stuff later.”
In terms of the “small stuff” you’ll need to manage, Dr. Vasquez points to items such as learning local economics and politics, daily finances, office regulations, and documentation, investment and planning, internal and external marketing, and human resources. “While most of us would view this as mundane or at least secondary to the craft we learn,” he said, “it will actually take far greater importance to taking care of patients if you really want your business to succeed and thrive.”
Another essential aspect of business planning that may seem daunting or mundane to many doctors when first starting out is putting together the necessary training manuals to effectively run your practice. Robert Bader, MD, stressed the importance of creating manuals for the front office, back office, Material Safety Data Sheets, and Occupational Safety and Health Administration.
“This is the time, while you have some extra time, to take an active role in forming the foundation of your practice,” Dr. Bader of Deerfield Beach, Fla., said. “Set aside time every year to go over and make necessary changes to these manuals.”
Make decisions now that reflect long-term goals
When you start your practice, deciding on a location might seem like a secondary detail, but the fact of the matter is that location will ultimately play a large role in the future of your business and your life. Beverly Hills, Calif., plastic surgeon John Layke, DO, suggested “choosing where you would like to live, and then building a practice around that location. Being happy in the area you live will make a big difference,” he says. “No one will ultimately be happy making $1 million-plus per year if they are miserable living in the area. In the beginning, share office space with reputable people where you become ‘visible,’ then build the office of your dreams when you are ready.”
Summary
I was amazed at the number of responses that I received in response to this survey. It is my goal to help doctors mentor each other on these important issues so that we do not all have to recreate the wheel. Connect with me on LinkedIn if you want to participate in these surveys or if you want to see the results of them. I want to wish the residents who are graduating and going into their own practice the best of luck. My final advice is to reach out for help – it’s obvious that many people are willing to provide advice.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients,” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems. She is the author of the monthly “Cosmeceutical Critique” column in Dermatology News.
The notion that residency training falls short when it comes to preparing residents and doctors for starting their own practice is a common thread across the board, whether you’re just getting started or have been managing your own practice for years. I did a survey on LinkedIn and over 50 dermatology and plastic surgery colleagues generously provided their own personal insights and words of wisdom to help young doctors avoid common practice management problems.
I could not quote everyone, but here are some of the best tips that I received:
Choose your staff carefully – and invest in the right candidates
One of the biggest pieces of practice management advice that doctors had to offer was to hire the right employees from the beginning, even if that means spending a little more time in the hiring process. This will eliminate headaches and frustration later.
In his own practice in Palm Beach Gardens, Fla., Dr. Lickstein has chosen a stable group of staff members who are, “first and foremost, nice, compassionate, and mature,” he said. “They need to be able to relate to cosmetic and medical patients of all ages. My office manager screens them, and then we have potential candidates shadow us for at least a half-day in the office. Afterward, we seek feedback from the current staff. I also try and talk with the candidate for a while, because I’ve found that once you get them to loosen up, you can get an actual sense of how they really are.”
Along the same lines, Cincinnati plastic surgeon Alex Donath, MD, suggests incentivizing employees and giving them an active role in the hiring process. “Give everyone in the office a chance to meet new employee candidates,” he said, “as that will both give the employees a sense of involvement in the process and allow more opportunities to catch glimpses of poor interpersonal skills that could hurt your reputation.”
Many doctors stressed the importance of the interview process, detailed job descriptions, a 60-day trial period, and background checks prior to hiring. This advice goes along with the famous quote “Be slow to hire and quick to fire (in the first 60 days)” that I have seen in many business books.
Foster teamwork
Another important aspect of managing your practice is building a sense of teamwork and camaraderie among employees and other doctors. Sean Weiss, MD, a facial plastic surgeon in New Orleans, has a great team-building tip that he uses daily.
“I plan a daily morning huddle with my staff. During the huddle, we review the prior day’s performance, those patients that need following up on, and whether or not the prior day’s goals were met. We then review the patient list for the current day to identify patient needs. We look specifically for ways to improve efficiency and avoid slowing down the work flow. We also try to identify opportunities to cross-promote our offerings to increase awareness of our services. In about 10 minutes, the entire team becomes focused and ready for a productive day.”
For Lacey Elwyn, DO, making staff feel appreciated can be as simple as telling them thank you on a regular basis. “The success of a dermatology practice encompasses every staff member of the team,” Dr. Elwyn, a medical and cosmetic dermatologist in South Florida, said. “The physician should respect and value all staff members. Tell them when they are doing a great job and tell them that you appreciate them every day, but also let them know right away when something is wrong.”
Don’t forget about patient education
Janet Trowbridge, MD, PhD, who practices in Edmond, Wash., expressed a great point that not only do patients need to be educated about their medical or cosmetic concerns, but they also need to be educated about the way that health care works in general. “I would say that 50% of my time as a physician is spent educating patients not about their disease, but about how medicine works – or doesn’t work,” she said. “I am constantly amazed by how little the average person understands about how health care is delivered. I talk about copays, coinsurance, annual deductibles, and why their prescriptions are not being covered. Patients feel that the system has let them down.”
Play the dual role of doctor and businessperson
At the end of the day, if you are managing your own practice, you must be able to split your time and skill set between being a physician and being a businessperson. Having realized the importance of the business aspect of running a practice, Justin Bryant, DO, a plastic and reconstructive surgeon in Walled Lake, Mich., enrolled in a dual-degree program during medical school in order to obtain his MBA.
“That investment already has proven priceless, as I’ve helped attendings and colleagues with their practice in marketing, finance, technology, and simply in translating business terms and contracts with physicians,” he said. “Although I don’t think it’s necessary for all physicians to pursue an MBA, and it’s not the answer to every business problem in the field of medicine, when applied, it can be very powerful!”
Build and protect your online reputation
Now more than ever, it is imperative to build and protect your online reputation, as online reviews can make or break your business. For plastic surgeon Nirmal Nathan, MD, in Plantation, Fla., managing your reputation is one of the most important considerations when starting a practice. “I would tell residents to start early on reputation management,” he said. “Reviews are so important, even with patients referred by word of mouth. Good reputation management also allows you to quickly ramp up if you decide to move your practice location.”
A large portion of building your online reputation now as to do with what you post (and don’t post) on social media. For Haena Kim, MD, a facial plastic and reconstructive surgeon practicing in Walnut Creek, Calif., figuring out how you would like others to perceive you is the first step.
“In this day and age of social media,” she said, “it’s so hard not to feel the pressure to follow the crowd and be the loudest person out there, and it’s incredibly hard to be patient with your practice growth. It’s important to figure out how you want to present yourself and what you want patients to come away with.”
Sweat the small stuff
Seemingly small administrative and business-related tasks can quickly add up and create much larger problems if not addressed early on. Tito Vasquez, MD, who practices in Southport, Conn., summed this up with an excellent piece of advice to remember: “Sweat the small stuff now, so you don’t have to sweat over the big stuff later.”
In terms of the “small stuff” you’ll need to manage, Dr. Vasquez points to items such as learning local economics and politics, daily finances, office regulations, and documentation, investment and planning, internal and external marketing, and human resources. “While most of us would view this as mundane or at least secondary to the craft we learn,” he said, “it will actually take far greater importance to taking care of patients if you really want your business to succeed and thrive.”
Another essential aspect of business planning that may seem daunting or mundane to many doctors when first starting out is putting together the necessary training manuals to effectively run your practice. Robert Bader, MD, stressed the importance of creating manuals for the front office, back office, Material Safety Data Sheets, and Occupational Safety and Health Administration.
“This is the time, while you have some extra time, to take an active role in forming the foundation of your practice,” Dr. Bader of Deerfield Beach, Fla., said. “Set aside time every year to go over and make necessary changes to these manuals.”
Make decisions now that reflect long-term goals
When you start your practice, deciding on a location might seem like a secondary detail, but the fact of the matter is that location will ultimately play a large role in the future of your business and your life. Beverly Hills, Calif., plastic surgeon John Layke, DO, suggested “choosing where you would like to live, and then building a practice around that location. Being happy in the area you live will make a big difference,” he says. “No one will ultimately be happy making $1 million-plus per year if they are miserable living in the area. In the beginning, share office space with reputable people where you become ‘visible,’ then build the office of your dreams when you are ready.”
Summary
I was amazed at the number of responses that I received in response to this survey. It is my goal to help doctors mentor each other on these important issues so that we do not all have to recreate the wheel. Connect with me on LinkedIn if you want to participate in these surveys or if you want to see the results of them. I want to wish the residents who are graduating and going into their own practice the best of luck. My final advice is to reach out for help – it’s obvious that many people are willing to provide advice.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients,” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems. She is the author of the monthly “Cosmeceutical Critique” column in Dermatology News.
The notion that residency training falls short when it comes to preparing residents and doctors for starting their own practice is a common thread across the board, whether you’re just getting started or have been managing your own practice for years. I did a survey on LinkedIn and over 50 dermatology and plastic surgery colleagues generously provided their own personal insights and words of wisdom to help young doctors avoid common practice management problems.
I could not quote everyone, but here are some of the best tips that I received:
Choose your staff carefully – and invest in the right candidates
One of the biggest pieces of practice management advice that doctors had to offer was to hire the right employees from the beginning, even if that means spending a little more time in the hiring process. This will eliminate headaches and frustration later.
In his own practice in Palm Beach Gardens, Fla., Dr. Lickstein has chosen a stable group of staff members who are, “first and foremost, nice, compassionate, and mature,” he said. “They need to be able to relate to cosmetic and medical patients of all ages. My office manager screens them, and then we have potential candidates shadow us for at least a half-day in the office. Afterward, we seek feedback from the current staff. I also try and talk with the candidate for a while, because I’ve found that once you get them to loosen up, you can get an actual sense of how they really are.”
Along the same lines, Cincinnati plastic surgeon Alex Donath, MD, suggests incentivizing employees and giving them an active role in the hiring process. “Give everyone in the office a chance to meet new employee candidates,” he said, “as that will both give the employees a sense of involvement in the process and allow more opportunities to catch glimpses of poor interpersonal skills that could hurt your reputation.”
Many doctors stressed the importance of the interview process, detailed job descriptions, a 60-day trial period, and background checks prior to hiring. This advice goes along with the famous quote “Be slow to hire and quick to fire (in the first 60 days)” that I have seen in many business books.
Foster teamwork
Another important aspect of managing your practice is building a sense of teamwork and camaraderie among employees and other doctors. Sean Weiss, MD, a facial plastic surgeon in New Orleans, has a great team-building tip that he uses daily.
“I plan a daily morning huddle with my staff. During the huddle, we review the prior day’s performance, those patients that need following up on, and whether or not the prior day’s goals were met. We then review the patient list for the current day to identify patient needs. We look specifically for ways to improve efficiency and avoid slowing down the work flow. We also try to identify opportunities to cross-promote our offerings to increase awareness of our services. In about 10 minutes, the entire team becomes focused and ready for a productive day.”
For Lacey Elwyn, DO, making staff feel appreciated can be as simple as telling them thank you on a regular basis. “The success of a dermatology practice encompasses every staff member of the team,” Dr. Elwyn, a medical and cosmetic dermatologist in South Florida, said. “The physician should respect and value all staff members. Tell them when they are doing a great job and tell them that you appreciate them every day, but also let them know right away when something is wrong.”
Don’t forget about patient education
Janet Trowbridge, MD, PhD, who practices in Edmond, Wash., expressed a great point that not only do patients need to be educated about their medical or cosmetic concerns, but they also need to be educated about the way that health care works in general. “I would say that 50% of my time as a physician is spent educating patients not about their disease, but about how medicine works – or doesn’t work,” she said. “I am constantly amazed by how little the average person understands about how health care is delivered. I talk about copays, coinsurance, annual deductibles, and why their prescriptions are not being covered. Patients feel that the system has let them down.”
Play the dual role of doctor and businessperson
At the end of the day, if you are managing your own practice, you must be able to split your time and skill set between being a physician and being a businessperson. Having realized the importance of the business aspect of running a practice, Justin Bryant, DO, a plastic and reconstructive surgeon in Walled Lake, Mich., enrolled in a dual-degree program during medical school in order to obtain his MBA.
“That investment already has proven priceless, as I’ve helped attendings and colleagues with their practice in marketing, finance, technology, and simply in translating business terms and contracts with physicians,” he said. “Although I don’t think it’s necessary for all physicians to pursue an MBA, and it’s not the answer to every business problem in the field of medicine, when applied, it can be very powerful!”
Build and protect your online reputation
Now more than ever, it is imperative to build and protect your online reputation, as online reviews can make or break your business. For plastic surgeon Nirmal Nathan, MD, in Plantation, Fla., managing your reputation is one of the most important considerations when starting a practice. “I would tell residents to start early on reputation management,” he said. “Reviews are so important, even with patients referred by word of mouth. Good reputation management also allows you to quickly ramp up if you decide to move your practice location.”
A large portion of building your online reputation now as to do with what you post (and don’t post) on social media. For Haena Kim, MD, a facial plastic and reconstructive surgeon practicing in Walnut Creek, Calif., figuring out how you would like others to perceive you is the first step.
“In this day and age of social media,” she said, “it’s so hard not to feel the pressure to follow the crowd and be the loudest person out there, and it’s incredibly hard to be patient with your practice growth. It’s important to figure out how you want to present yourself and what you want patients to come away with.”
Sweat the small stuff
Seemingly small administrative and business-related tasks can quickly add up and create much larger problems if not addressed early on. Tito Vasquez, MD, who practices in Southport, Conn., summed this up with an excellent piece of advice to remember: “Sweat the small stuff now, so you don’t have to sweat over the big stuff later.”
In terms of the “small stuff” you’ll need to manage, Dr. Vasquez points to items such as learning local economics and politics, daily finances, office regulations, and documentation, investment and planning, internal and external marketing, and human resources. “While most of us would view this as mundane or at least secondary to the craft we learn,” he said, “it will actually take far greater importance to taking care of patients if you really want your business to succeed and thrive.”
Another essential aspect of business planning that may seem daunting or mundane to many doctors when first starting out is putting together the necessary training manuals to effectively run your practice. Robert Bader, MD, stressed the importance of creating manuals for the front office, back office, Material Safety Data Sheets, and Occupational Safety and Health Administration.
“This is the time, while you have some extra time, to take an active role in forming the foundation of your practice,” Dr. Bader of Deerfield Beach, Fla., said. “Set aside time every year to go over and make necessary changes to these manuals.”
Make decisions now that reflect long-term goals
When you start your practice, deciding on a location might seem like a secondary detail, but the fact of the matter is that location will ultimately play a large role in the future of your business and your life. Beverly Hills, Calif., plastic surgeon John Layke, DO, suggested “choosing where you would like to live, and then building a practice around that location. Being happy in the area you live will make a big difference,” he says. “No one will ultimately be happy making $1 million-plus per year if they are miserable living in the area. In the beginning, share office space with reputable people where you become ‘visible,’ then build the office of your dreams when you are ready.”
Summary
I was amazed at the number of responses that I received in response to this survey. It is my goal to help doctors mentor each other on these important issues so that we do not all have to recreate the wheel. Connect with me on LinkedIn if you want to participate in these surveys or if you want to see the results of them. I want to wish the residents who are graduating and going into their own practice the best of luck. My final advice is to reach out for help – it’s obvious that many people are willing to provide advice.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients,” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems. She is the author of the monthly “Cosmeceutical Critique” column in Dermatology News.














