User login
Lonely in the middle
Those of us who consider ourselves centrists are feeling pretty lonely right now. It seems everyone else, or at least all of the folks in Washington, have fled to the extreme political poles and left us to search for a patch of middle ground to stand on. It appears that without courageous leadership the silent majority has splintered and gravitated to the tails of what was once a bell-shaped curve.
One issue that might attract support from both sides of the political spectrum emerged from the Nov. 18, 2016, report from the United States Department of Agriculture that listed sweetened drinks as the No. 1 purchase by households participating in SNAP (“Foods Typically Purchased by Supplemental Nutrition Assistance Program (SNAP) Households”). The data reveal that households in this $74 billion program are spending 5% of their food dollars on soft drinks and almost 10% on sweetened beverages – soft drinks, fruit juices, energy drinks, and sweetened teas.
Several states (including Maine), dozens of other municipalities (most notably New York City under Mayor Michael Bloomberg), and a variety of medical groups have asked the USDA to reconsider its guidelines. Arguing that selectively banning certain items would generate too much red tape and be unfair to food stamp recipients, the department has been resistant to change (“In the Shopping Cart of a Food Stamp Household: Lots of Soda,” by Anahad O’Connor, New York Times, Jan. 13, 2017). One has to wonder how much of the department’s hesitancy is a reflection of the millions of dollars the food and beverage industries have invested in lobbying against change.
There are some ultra liberals (or progressives if you prefer) who feel that no one should be deprived of the privilege of buying unhealthy food simply because he or she is poor. At the other end of the spectrum there are conservatives who would prefer to scrap the whole SNAP program because it is a wasteful frill of the welfare state. However, I have to believe that the vast majority of folks on both sides of the political divide believe that feeding the less fortunate is important, but that spending their tax money on junk food and soft drinks is a bad idea.
While we still are learning that the causes of our obesity epidemic are far more complex than we once imagined, I think most people believe that soft drinks and junk food are playing a significant role – even though these same folks may have found it difficult to change their own behavior. According to the New York Times article mentioned above, Kevin Concannon, the USDA undersecretary for food, nutrition, and consumer services, said that instead of restricting food, the USDA has prioritized incentive programs to encourage participants to purchase more nutritious foods. However, a 2014 study of more than 19,000 SNAP recipients by Stanford researchers determined that an incentive program would not affect obesity rates, while banning sugary drinks would “significantly reduce obesity prevalence and type 2 diabetes incidence” (Health Aff. Jun 2014;33[6]:1032-9).
All we need now are a few courageous senators and congressmen to buck the soft drink lobby and bring this issue to the front burner. I have to believe that there are more than enough people, both liberals and conservatives, who would venture together on the middle ground and support removing sweetened drinks from the SNAP program. If I’m correct, it would be a refreshing example of some much needed legislative cooperation. Or, am I just a lonely dreamer longing for some company here in the center?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Those of us who consider ourselves centrists are feeling pretty lonely right now. It seems everyone else, or at least all of the folks in Washington, have fled to the extreme political poles and left us to search for a patch of middle ground to stand on. It appears that without courageous leadership the silent majority has splintered and gravitated to the tails of what was once a bell-shaped curve.
One issue that might attract support from both sides of the political spectrum emerged from the Nov. 18, 2016, report from the United States Department of Agriculture that listed sweetened drinks as the No. 1 purchase by households participating in SNAP (“Foods Typically Purchased by Supplemental Nutrition Assistance Program (SNAP) Households”). The data reveal that households in this $74 billion program are spending 5% of their food dollars on soft drinks and almost 10% on sweetened beverages – soft drinks, fruit juices, energy drinks, and sweetened teas.
Several states (including Maine), dozens of other municipalities (most notably New York City under Mayor Michael Bloomberg), and a variety of medical groups have asked the USDA to reconsider its guidelines. Arguing that selectively banning certain items would generate too much red tape and be unfair to food stamp recipients, the department has been resistant to change (“In the Shopping Cart of a Food Stamp Household: Lots of Soda,” by Anahad O’Connor, New York Times, Jan. 13, 2017). One has to wonder how much of the department’s hesitancy is a reflection of the millions of dollars the food and beverage industries have invested in lobbying against change.
There are some ultra liberals (or progressives if you prefer) who feel that no one should be deprived of the privilege of buying unhealthy food simply because he or she is poor. At the other end of the spectrum there are conservatives who would prefer to scrap the whole SNAP program because it is a wasteful frill of the welfare state. However, I have to believe that the vast majority of folks on both sides of the political divide believe that feeding the less fortunate is important, but that spending their tax money on junk food and soft drinks is a bad idea.
While we still are learning that the causes of our obesity epidemic are far more complex than we once imagined, I think most people believe that soft drinks and junk food are playing a significant role – even though these same folks may have found it difficult to change their own behavior. According to the New York Times article mentioned above, Kevin Concannon, the USDA undersecretary for food, nutrition, and consumer services, said that instead of restricting food, the USDA has prioritized incentive programs to encourage participants to purchase more nutritious foods. However, a 2014 study of more than 19,000 SNAP recipients by Stanford researchers determined that an incentive program would not affect obesity rates, while banning sugary drinks would “significantly reduce obesity prevalence and type 2 diabetes incidence” (Health Aff. Jun 2014;33[6]:1032-9).
All we need now are a few courageous senators and congressmen to buck the soft drink lobby and bring this issue to the front burner. I have to believe that there are more than enough people, both liberals and conservatives, who would venture together on the middle ground and support removing sweetened drinks from the SNAP program. If I’m correct, it would be a refreshing example of some much needed legislative cooperation. Or, am I just a lonely dreamer longing for some company here in the center?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Those of us who consider ourselves centrists are feeling pretty lonely right now. It seems everyone else, or at least all of the folks in Washington, have fled to the extreme political poles and left us to search for a patch of middle ground to stand on. It appears that without courageous leadership the silent majority has splintered and gravitated to the tails of what was once a bell-shaped curve.
One issue that might attract support from both sides of the political spectrum emerged from the Nov. 18, 2016, report from the United States Department of Agriculture that listed sweetened drinks as the No. 1 purchase by households participating in SNAP (“Foods Typically Purchased by Supplemental Nutrition Assistance Program (SNAP) Households”). The data reveal that households in this $74 billion program are spending 5% of their food dollars on soft drinks and almost 10% on sweetened beverages – soft drinks, fruit juices, energy drinks, and sweetened teas.
Several states (including Maine), dozens of other municipalities (most notably New York City under Mayor Michael Bloomberg), and a variety of medical groups have asked the USDA to reconsider its guidelines. Arguing that selectively banning certain items would generate too much red tape and be unfair to food stamp recipients, the department has been resistant to change (“In the Shopping Cart of a Food Stamp Household: Lots of Soda,” by Anahad O’Connor, New York Times, Jan. 13, 2017). One has to wonder how much of the department’s hesitancy is a reflection of the millions of dollars the food and beverage industries have invested in lobbying against change.
There are some ultra liberals (or progressives if you prefer) who feel that no one should be deprived of the privilege of buying unhealthy food simply because he or she is poor. At the other end of the spectrum there are conservatives who would prefer to scrap the whole SNAP program because it is a wasteful frill of the welfare state. However, I have to believe that the vast majority of folks on both sides of the political divide believe that feeding the less fortunate is important, but that spending their tax money on junk food and soft drinks is a bad idea.
While we still are learning that the causes of our obesity epidemic are far more complex than we once imagined, I think most people believe that soft drinks and junk food are playing a significant role – even though these same folks may have found it difficult to change their own behavior. According to the New York Times article mentioned above, Kevin Concannon, the USDA undersecretary for food, nutrition, and consumer services, said that instead of restricting food, the USDA has prioritized incentive programs to encourage participants to purchase more nutritious foods. However, a 2014 study of more than 19,000 SNAP recipients by Stanford researchers determined that an incentive program would not affect obesity rates, while banning sugary drinks would “significantly reduce obesity prevalence and type 2 diabetes incidence” (Health Aff. Jun 2014;33[6]:1032-9).
All we need now are a few courageous senators and congressmen to buck the soft drink lobby and bring this issue to the front burner. I have to believe that there are more than enough people, both liberals and conservatives, who would venture together on the middle ground and support removing sweetened drinks from the SNAP program. If I’m correct, it would be a refreshing example of some much needed legislative cooperation. Or, am I just a lonely dreamer longing for some company here in the center?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
The power of interaction – Supporting language and play development
Engaging caregivers in the management and treatment of early childhood developmental challenges is a critical component of effective intervention.1 Family-centered care helps to promote positive outcomes with early intervention (across developmental domains), and there’s increasing evidence that parent-training programs can be effective in promoting skill generalization and targeting core impairments in toddlers with autism.2
Furthermore, a 2014 randomized controlled trial revealed that individual Early Social Interaction (ESI) with home coaching using the SCERTS (Social Communication, Emotional Regulation, and Transactional Support) curriculum was associated with improvement of a range of child outcomes, compared with group ESI. The authors commented on the importance of individualized parent coaching in natural environments as a way to improve social components of communication and receptive language for toddlers with autism.3
For many parents and at-home caregivers, however, engaging in home-based and parent-delivered interventions can be overwhelming and anxiety-provoking, as well as complicated by other barriers (competing responsibilities, cultural beliefs, and so on). Additionally, these interventions can themselves be a source of stress for some families.
Case
Jake is a 3-year-old boy with a history of global developmental delays, who presents with particular struggles: relating his expressive communication, ability to engage peers in an age-appropriate manner, and capacity to self-regulate when frustrated. He and his family participated in an comprehensive autism diagnostic assessment. In reviewing the history and presentation, considerable challenges in the two core symptom domains that characterize an autism spectrum disorder were noted. A diagnosis of autism was provided, and treatment recommendations were discussed. “What can I do at home to help Jake learn?” his mother asked, noting that, with one-on-one attention, he does seem to demonstrate increased responsiveness, less use of echolalic language, and improved eye contact.
Discussion
To complement the autism services that Jake would likely qualify for through an Early Education program, in-home interaction and play to ensure skill development was discussed at length with his mother, who readily acknowledged her own care-giving struggles that, in part, are informed by her own mental health troubles.
We openly explored Jake’s mother’s perceived challenges in engaging with her son at home and developed initial recommendations for interaction that didn’t risk overwhelming her. We impressed upon Jake’s mother that, regardless of a child’s developmental profile, toddlers use play to learn and she can be Jake’s “favorite toy.” After all, “play is really the work of childhood,” as Fred Rogers said.
With all children, back-and-forth interactions serve as the foundation for future development. Using scaffolding techniques, parent support is a primary driver of “how children develop cognitive, language, social-emotional, and higher-level thinking skills.”4 In particular, the quality of parental interaction can influence language development, and, when considering children with autism, there are several recommendations for what parents can do to help build social, play, and communication skills.5 The Hanen Program is a great resource for providers and parents to learn more about parent engagement in early learning, the power of building communication through everyday experiences and attention to responsiveness, and the use of a child’s strengths to help make family interactions more meaningful and enjoyable. Additionally, the 2012 book “An Early Start for Your Child with Autism: Using Everyday Activities to Help Kids Connect, Communicate, and Learn” by Sally Rogers, PhD, et al. is an easy-to-read text for parents and caregivers for learning effective and practical strategies for engaging their child with autism.
With Jake and his mother, our team offered the following in-home recommendations:
- Try to keep interaction fun. Be enthusiastic when encouraging Jake’s attempts to communicate.
- Teach Jake song-gesture games. Encourage him to produce routine, predictable gestures to keep the song going (in imitation of mom). Using songs with vowel emphasis is encouraged (for example: Farmer in the Dell with “E I E I OOOOO”).
- Encourage Jake to produce responsive gestures in play and daily routines not involving songs, such as open arms to receive a ball, reaching to mom when about to be tickled, or having his arms up to have his shirt taken off.
- Capitalize on Jake’s natural desires and personal preferences. Activate a wind-up toy, let it deactivate, and then hand it to Jake.
- Initiate a familiar social game with Jake until he expresses pleasure. Then stop the game and wait for him to initiate continuance.
- Adapt the environment so that Jake will need to frequently request objects of assistance to make choices (place favorite toys in clear containers which may be difficult to open so that he must request help).
Clinical pearl
The United States Department of Education recognizes the importance of family engagement in a child’s early years. Their 2015 policy statement notes that “families are their children’s first and most important teachers, advocates, and nurturers. As such, strong family engagement is central – not supplemental – to the success of early childhood systems and programs that promote children’s healthy development, learning, and wellness.”
By recognizing this principle, primary care providers are in a position to talk with parents about how much youth learn through play and regular interaction. This especially holds true for children with autism. Developing in-home strategies to facilitate active engagement, even strategies that may not be a formal component of a home-based intervention program, are instrumental in fostering positive family- and child-based outcomes and wellness.
Dr. Dickerson, a child and adolescent psychiatrist, is assistant professor of psychiatry at the University of Vermont, Burlington, where he is director of the autism diagnostic clinic. Email him at [email protected].
References
1. Annu Rev Clin Psychol. 2010;6:447-68.
2. J Autism Dev Disord. 2010 Sep;40(9):1045-56.
3. Pediatrics. 2014 Dec;134(6):1084-93.
4. JAMA Pediatr. 2016 Feb;170(2):112-3.
5. Child Dev. 2012 Sep-Oct;83(5):1762-74.
Engaging caregivers in the management and treatment of early childhood developmental challenges is a critical component of effective intervention.1 Family-centered care helps to promote positive outcomes with early intervention (across developmental domains), and there’s increasing evidence that parent-training programs can be effective in promoting skill generalization and targeting core impairments in toddlers with autism.2
Furthermore, a 2014 randomized controlled trial revealed that individual Early Social Interaction (ESI) with home coaching using the SCERTS (Social Communication, Emotional Regulation, and Transactional Support) curriculum was associated with improvement of a range of child outcomes, compared with group ESI. The authors commented on the importance of individualized parent coaching in natural environments as a way to improve social components of communication and receptive language for toddlers with autism.3
For many parents and at-home caregivers, however, engaging in home-based and parent-delivered interventions can be overwhelming and anxiety-provoking, as well as complicated by other barriers (competing responsibilities, cultural beliefs, and so on). Additionally, these interventions can themselves be a source of stress for some families.
Case
Jake is a 3-year-old boy with a history of global developmental delays, who presents with particular struggles: relating his expressive communication, ability to engage peers in an age-appropriate manner, and capacity to self-regulate when frustrated. He and his family participated in an comprehensive autism diagnostic assessment. In reviewing the history and presentation, considerable challenges in the two core symptom domains that characterize an autism spectrum disorder were noted. A diagnosis of autism was provided, and treatment recommendations were discussed. “What can I do at home to help Jake learn?” his mother asked, noting that, with one-on-one attention, he does seem to demonstrate increased responsiveness, less use of echolalic language, and improved eye contact.
Discussion
To complement the autism services that Jake would likely qualify for through an Early Education program, in-home interaction and play to ensure skill development was discussed at length with his mother, who readily acknowledged her own care-giving struggles that, in part, are informed by her own mental health troubles.
We openly explored Jake’s mother’s perceived challenges in engaging with her son at home and developed initial recommendations for interaction that didn’t risk overwhelming her. We impressed upon Jake’s mother that, regardless of a child’s developmental profile, toddlers use play to learn and she can be Jake’s “favorite toy.” After all, “play is really the work of childhood,” as Fred Rogers said.
With all children, back-and-forth interactions serve as the foundation for future development. Using scaffolding techniques, parent support is a primary driver of “how children develop cognitive, language, social-emotional, and higher-level thinking skills.”4 In particular, the quality of parental interaction can influence language development, and, when considering children with autism, there are several recommendations for what parents can do to help build social, play, and communication skills.5 The Hanen Program is a great resource for providers and parents to learn more about parent engagement in early learning, the power of building communication through everyday experiences and attention to responsiveness, and the use of a child’s strengths to help make family interactions more meaningful and enjoyable. Additionally, the 2012 book “An Early Start for Your Child with Autism: Using Everyday Activities to Help Kids Connect, Communicate, and Learn” by Sally Rogers, PhD, et al. is an easy-to-read text for parents and caregivers for learning effective and practical strategies for engaging their child with autism.
With Jake and his mother, our team offered the following in-home recommendations:
- Try to keep interaction fun. Be enthusiastic when encouraging Jake’s attempts to communicate.
- Teach Jake song-gesture games. Encourage him to produce routine, predictable gestures to keep the song going (in imitation of mom). Using songs with vowel emphasis is encouraged (for example: Farmer in the Dell with “E I E I OOOOO”).
- Encourage Jake to produce responsive gestures in play and daily routines not involving songs, such as open arms to receive a ball, reaching to mom when about to be tickled, or having his arms up to have his shirt taken off.
- Capitalize on Jake’s natural desires and personal preferences. Activate a wind-up toy, let it deactivate, and then hand it to Jake.
- Initiate a familiar social game with Jake until he expresses pleasure. Then stop the game and wait for him to initiate continuance.
- Adapt the environment so that Jake will need to frequently request objects of assistance to make choices (place favorite toys in clear containers which may be difficult to open so that he must request help).
Clinical pearl
The United States Department of Education recognizes the importance of family engagement in a child’s early years. Their 2015 policy statement notes that “families are their children’s first and most important teachers, advocates, and nurturers. As such, strong family engagement is central – not supplemental – to the success of early childhood systems and programs that promote children’s healthy development, learning, and wellness.”
By recognizing this principle, primary care providers are in a position to talk with parents about how much youth learn through play and regular interaction. This especially holds true for children with autism. Developing in-home strategies to facilitate active engagement, even strategies that may not be a formal component of a home-based intervention program, are instrumental in fostering positive family- and child-based outcomes and wellness.
Dr. Dickerson, a child and adolescent psychiatrist, is assistant professor of psychiatry at the University of Vermont, Burlington, where he is director of the autism diagnostic clinic. Email him at [email protected].
References
1. Annu Rev Clin Psychol. 2010;6:447-68.
2. J Autism Dev Disord. 2010 Sep;40(9):1045-56.
3. Pediatrics. 2014 Dec;134(6):1084-93.
4. JAMA Pediatr. 2016 Feb;170(2):112-3.
5. Child Dev. 2012 Sep-Oct;83(5):1762-74.
Engaging caregivers in the management and treatment of early childhood developmental challenges is a critical component of effective intervention.1 Family-centered care helps to promote positive outcomes with early intervention (across developmental domains), and there’s increasing evidence that parent-training programs can be effective in promoting skill generalization and targeting core impairments in toddlers with autism.2
Furthermore, a 2014 randomized controlled trial revealed that individual Early Social Interaction (ESI) with home coaching using the SCERTS (Social Communication, Emotional Regulation, and Transactional Support) curriculum was associated with improvement of a range of child outcomes, compared with group ESI. The authors commented on the importance of individualized parent coaching in natural environments as a way to improve social components of communication and receptive language for toddlers with autism.3
For many parents and at-home caregivers, however, engaging in home-based and parent-delivered interventions can be overwhelming and anxiety-provoking, as well as complicated by other barriers (competing responsibilities, cultural beliefs, and so on). Additionally, these interventions can themselves be a source of stress for some families.
Case
Jake is a 3-year-old boy with a history of global developmental delays, who presents with particular struggles: relating his expressive communication, ability to engage peers in an age-appropriate manner, and capacity to self-regulate when frustrated. He and his family participated in an comprehensive autism diagnostic assessment. In reviewing the history and presentation, considerable challenges in the two core symptom domains that characterize an autism spectrum disorder were noted. A diagnosis of autism was provided, and treatment recommendations were discussed. “What can I do at home to help Jake learn?” his mother asked, noting that, with one-on-one attention, he does seem to demonstrate increased responsiveness, less use of echolalic language, and improved eye contact.
Discussion
To complement the autism services that Jake would likely qualify for through an Early Education program, in-home interaction and play to ensure skill development was discussed at length with his mother, who readily acknowledged her own care-giving struggles that, in part, are informed by her own mental health troubles.
We openly explored Jake’s mother’s perceived challenges in engaging with her son at home and developed initial recommendations for interaction that didn’t risk overwhelming her. We impressed upon Jake’s mother that, regardless of a child’s developmental profile, toddlers use play to learn and she can be Jake’s “favorite toy.” After all, “play is really the work of childhood,” as Fred Rogers said.
With all children, back-and-forth interactions serve as the foundation for future development. Using scaffolding techniques, parent support is a primary driver of “how children develop cognitive, language, social-emotional, and higher-level thinking skills.”4 In particular, the quality of parental interaction can influence language development, and, when considering children with autism, there are several recommendations for what parents can do to help build social, play, and communication skills.5 The Hanen Program is a great resource for providers and parents to learn more about parent engagement in early learning, the power of building communication through everyday experiences and attention to responsiveness, and the use of a child’s strengths to help make family interactions more meaningful and enjoyable. Additionally, the 2012 book “An Early Start for Your Child with Autism: Using Everyday Activities to Help Kids Connect, Communicate, and Learn” by Sally Rogers, PhD, et al. is an easy-to-read text for parents and caregivers for learning effective and practical strategies for engaging their child with autism.
With Jake and his mother, our team offered the following in-home recommendations:
- Try to keep interaction fun. Be enthusiastic when encouraging Jake’s attempts to communicate.
- Teach Jake song-gesture games. Encourage him to produce routine, predictable gestures to keep the song going (in imitation of mom). Using songs with vowel emphasis is encouraged (for example: Farmer in the Dell with “E I E I OOOOO”).
- Encourage Jake to produce responsive gestures in play and daily routines not involving songs, such as open arms to receive a ball, reaching to mom when about to be tickled, or having his arms up to have his shirt taken off.
- Capitalize on Jake’s natural desires and personal preferences. Activate a wind-up toy, let it deactivate, and then hand it to Jake.
- Initiate a familiar social game with Jake until he expresses pleasure. Then stop the game and wait for him to initiate continuance.
- Adapt the environment so that Jake will need to frequently request objects of assistance to make choices (place favorite toys in clear containers which may be difficult to open so that he must request help).
Clinical pearl
The United States Department of Education recognizes the importance of family engagement in a child’s early years. Their 2015 policy statement notes that “families are their children’s first and most important teachers, advocates, and nurturers. As such, strong family engagement is central – not supplemental – to the success of early childhood systems and programs that promote children’s healthy development, learning, and wellness.”
By recognizing this principle, primary care providers are in a position to talk with parents about how much youth learn through play and regular interaction. This especially holds true for children with autism. Developing in-home strategies to facilitate active engagement, even strategies that may not be a formal component of a home-based intervention program, are instrumental in fostering positive family- and child-based outcomes and wellness.
Dr. Dickerson, a child and adolescent psychiatrist, is assistant professor of psychiatry at the University of Vermont, Burlington, where he is director of the autism diagnostic clinic. Email him at [email protected].
References
1. Annu Rev Clin Psychol. 2010;6:447-68.
2. J Autism Dev Disord. 2010 Sep;40(9):1045-56.
3. Pediatrics. 2014 Dec;134(6):1084-93.
4. JAMA Pediatr. 2016 Feb;170(2):112-3.
5. Child Dev. 2012 Sep-Oct;83(5):1762-74.
Update on malpractice trends
Question: Recent developments in malpractice include the following:
A. Severity and frequency rates continue to rise.
B. Apology laws appear to be very effective in reducing claims.
C. Litigation surrounds whether an assistant may obtain a patient’s informed consent on behalf of the doctor.
D. A and B.
E. A, B, and C.
Answer: C. Over the past decade, malpractice claims have in fact diminished, accompanied by a leveling or reduction in premiums.1 Rates have plummeted to roughly half of previous levels, averaging six claims per 100 doctors in 2016.
According to The Doctors Company, internists paid an average premium of $15,853, compared with an average of $19,900 in 2006, general surgeons $52,905 instead of $68,186, and obstetricians $72,999, a drop from $93,230. Even claims-plagued Florida’s Dade County has seen a dramatic drop in internist premiums by some $27,000, down to $47,707.2
The latest attack on MICRA, in 2015, concerned a wrongful death suit brought by a woman whose mother died from hemorrhagic complications related to Coumadin use following heart surgery.4 Her constitutional challenges included violation of equal protection, due process, and the right to a jury trial. But these were essentially all grounded on an entitlement to recover additional noneconomic damages sufficient to cover attorney fees. The trial court had reduced her $1 million noneconomic damages to $250,000 as required by MICRA. A California appeals court rejected her claim as being “contrary to many well-established legal principles.”
Disclosure of medical errors is a relative newcomer as an ethical and effective way of thwarting potential malpractice claims. Many states have enacted so-called “apology laws,” an outgrowth of the communication and resolution programs popularized by the Lexington (Ky.) VA Medical Center, University of Michigan Health System, Harvard’s affiliated institutions, and Colorado’s COPIC Insurance.
Apology laws disallow statements of sympathy from being admitted into evidence. In some cases, these laws may assist the physician. For example, the Ohio Supreme Court has ruled that a surgeon’s comments and alleged admission of guilt (“I take full responsibility for this” regarding accidentally sectioning the common bile duct) were properly shielded from discovery by the state’s apology statute, even though the incident took place before the law went into effect.5
However, apology laws do vary from state to state, and some do not shield admissions regarding causation of error or fault.
A recent study suggests that apology laws don’t work. A Vanderbilt University study published online used a unique dataset covering all malpractice claims for 90% of physicians practicing in a single specialty across the country.6 The findings revealed that, for physicians who do not regularly perform surgery, apology laws actually increased the probability of facing a lawsuit. For surgeons, apology laws do not have a substantial effect on the probability of facing a claim or the average payment made to resolve a claim.
The study’s authors concluded that “apology laws are not substitutes for specific physician disclosure programs, and that the experiences of these types of programs are not generalizable to the physician population at large. In other words, simply being allowed to apologize is not enough to reduce malpractice risk.”
In the informed consent arena, the latest development in the law revolves around whether a physician assistant, in lieu of the surgeon himself, can obtain informed consent from a patient.
In Shinal v. Toms,7 Megan Shinal underwent surgery to remove a craniopharyngioma, but it regrew and required re-exploration by Dr. Steven Toms. Dr. Toms testified that Ms. Shinal had agreed that he would determine during the surgery whether he should remove the entire tumor or perform a partial resection. The operation was complicated by a carotid artery perforation, which left the patient with impaired vision and ambulation.
The complaint asserted that Dr. Toms’s physician assistant, not Dr. Toms himself, had provided the actual discussion during the informed consent process, and thus the patient’s consent was invalid.
The jury was allowed to consider the information provided by the doctor’s support staff, and the Superior Court of Pennsylvania affirmed the validity of the patient’s consent, holding that consent is based on the scope of information relayed rather than the identity of the individual communicating the information. This carefully watched case is now on final appeal before the Supreme Court of Pennsylvania.
At a personal level, physicians dread the stress surrounding medical malpractice litigation. The process frontally attacks their competence and consumes much time and energy, notwithstanding there being little or no exposure of personal assets because of insurance protection. Virtually all doctors practice defensive medicine, which has been defined as “deviation from sound medical practice that is induced primarily by a threat of liability.”
At a societal level, defensive medicine is reported to add substantially to the nation’s medical bill. The figure tossed around is $12 billion to $50 billion a year, based mostly on estimates by the American Medical Association and an older study extrapolating potential Medicare savings from litigation over heart disease.8
A more recent report continues to emphasize the high cost of defensive medicine.9 Jackson Healthcare invited 138,686 physicians to participate in a confidential online survey to quantify the costs and impact of defensive medicine. More than 3,000 physicians spanning all states and medical specialties completed the survey; however, this represented only a 2.21% response rate.
The authors concluded that defensive medicine is a significant force driving the high cost of health care in the United States, and that physicians estimate the cost of defensive medicine to be in the $650 billion to $850 billion range, or between 26% and 34% of annual health care costs.
Skeptics question the way the profession defines defensive medicine, pointing out that malpractice concerns may not be the primary reason, as most interventions add some marginal value to patient care. There may also be conflicting motivations of physicians, such as financial or other personal rewards.
Above all, there is no acceptable method for measuring the extent and use of defensive medicine, and survey reports are apt to be misleading because of bias and the lack of controls and baseline data.
Looking ahead, what can we expect for malpractice law under the Trump administration? Tom Price, MD, a former Republican congressman from Georgia, is an orthopedic surgeon and the new secretary of the Department of Health & Human Services. He has previously spoken passionately about tort reforms such as defensive medicine, damage caps, health tribunals, and practice guidelines. Many states have already incorporated some of these measures into their own tort reforms – with salutary results. It remains to be seen whether HHS will deem any omnibus federal legislation necessary at this point.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the materials have been taken from my earlier columns in Internal Medicine News. For additional information, readers may contact the author at [email protected].
References
1. JAMA. 2014 Nov 26;312(20):2146-55.
2. “Malpractice 2017: Do We Need Reform?” Internal Medicine News, March 1, 2017, page 1.
3. Fein v. Permanente, 38 Cal.3d 137 (1985).
4. Chan v. Curran, 237 CA 4th 601 (2015).
5. Estate of Johnson v. Randall Smith, Inc., 135 Ohio St.3d 440 (2013).
6. Available at https://papers.ssrn.com/sol3/papers2.cfm?abstract_id=2883693.
7. Shinal v. Toms, 122 A. 3d 1066 (Pa. Super. Ct. 2015).
8. Q J Econ. (1996) 111 (2): 353-390.
9. Available at www.jacksonhealthcare.com/media/8968/defensivemedicine_ebook_final.pdf.
Question: Recent developments in malpractice include the following:
A. Severity and frequency rates continue to rise.
B. Apology laws appear to be very effective in reducing claims.
C. Litigation surrounds whether an assistant may obtain a patient’s informed consent on behalf of the doctor.
D. A and B.
E. A, B, and C.
Answer: C. Over the past decade, malpractice claims have in fact diminished, accompanied by a leveling or reduction in premiums.1 Rates have plummeted to roughly half of previous levels, averaging six claims per 100 doctors in 2016.
According to The Doctors Company, internists paid an average premium of $15,853, compared with an average of $19,900 in 2006, general surgeons $52,905 instead of $68,186, and obstetricians $72,999, a drop from $93,230. Even claims-plagued Florida’s Dade County has seen a dramatic drop in internist premiums by some $27,000, down to $47,707.2
The latest attack on MICRA, in 2015, concerned a wrongful death suit brought by a woman whose mother died from hemorrhagic complications related to Coumadin use following heart surgery.4 Her constitutional challenges included violation of equal protection, due process, and the right to a jury trial. But these were essentially all grounded on an entitlement to recover additional noneconomic damages sufficient to cover attorney fees. The trial court had reduced her $1 million noneconomic damages to $250,000 as required by MICRA. A California appeals court rejected her claim as being “contrary to many well-established legal principles.”
Disclosure of medical errors is a relative newcomer as an ethical and effective way of thwarting potential malpractice claims. Many states have enacted so-called “apology laws,” an outgrowth of the communication and resolution programs popularized by the Lexington (Ky.) VA Medical Center, University of Michigan Health System, Harvard’s affiliated institutions, and Colorado’s COPIC Insurance.
Apology laws disallow statements of sympathy from being admitted into evidence. In some cases, these laws may assist the physician. For example, the Ohio Supreme Court has ruled that a surgeon’s comments and alleged admission of guilt (“I take full responsibility for this” regarding accidentally sectioning the common bile duct) were properly shielded from discovery by the state’s apology statute, even though the incident took place before the law went into effect.5
However, apology laws do vary from state to state, and some do not shield admissions regarding causation of error or fault.
A recent study suggests that apology laws don’t work. A Vanderbilt University study published online used a unique dataset covering all malpractice claims for 90% of physicians practicing in a single specialty across the country.6 The findings revealed that, for physicians who do not regularly perform surgery, apology laws actually increased the probability of facing a lawsuit. For surgeons, apology laws do not have a substantial effect on the probability of facing a claim or the average payment made to resolve a claim.
The study’s authors concluded that “apology laws are not substitutes for specific physician disclosure programs, and that the experiences of these types of programs are not generalizable to the physician population at large. In other words, simply being allowed to apologize is not enough to reduce malpractice risk.”
In the informed consent arena, the latest development in the law revolves around whether a physician assistant, in lieu of the surgeon himself, can obtain informed consent from a patient.
In Shinal v. Toms,7 Megan Shinal underwent surgery to remove a craniopharyngioma, but it regrew and required re-exploration by Dr. Steven Toms. Dr. Toms testified that Ms. Shinal had agreed that he would determine during the surgery whether he should remove the entire tumor or perform a partial resection. The operation was complicated by a carotid artery perforation, which left the patient with impaired vision and ambulation.
The complaint asserted that Dr. Toms’s physician assistant, not Dr. Toms himself, had provided the actual discussion during the informed consent process, and thus the patient’s consent was invalid.
The jury was allowed to consider the information provided by the doctor’s support staff, and the Superior Court of Pennsylvania affirmed the validity of the patient’s consent, holding that consent is based on the scope of information relayed rather than the identity of the individual communicating the information. This carefully watched case is now on final appeal before the Supreme Court of Pennsylvania.
At a personal level, physicians dread the stress surrounding medical malpractice litigation. The process frontally attacks their competence and consumes much time and energy, notwithstanding there being little or no exposure of personal assets because of insurance protection. Virtually all doctors practice defensive medicine, which has been defined as “deviation from sound medical practice that is induced primarily by a threat of liability.”
At a societal level, defensive medicine is reported to add substantially to the nation’s medical bill. The figure tossed around is $12 billion to $50 billion a year, based mostly on estimates by the American Medical Association and an older study extrapolating potential Medicare savings from litigation over heart disease.8
A more recent report continues to emphasize the high cost of defensive medicine.9 Jackson Healthcare invited 138,686 physicians to participate in a confidential online survey to quantify the costs and impact of defensive medicine. More than 3,000 physicians spanning all states and medical specialties completed the survey; however, this represented only a 2.21% response rate.
The authors concluded that defensive medicine is a significant force driving the high cost of health care in the United States, and that physicians estimate the cost of defensive medicine to be in the $650 billion to $850 billion range, or between 26% and 34% of annual health care costs.
Skeptics question the way the profession defines defensive medicine, pointing out that malpractice concerns may not be the primary reason, as most interventions add some marginal value to patient care. There may also be conflicting motivations of physicians, such as financial or other personal rewards.
Above all, there is no acceptable method for measuring the extent and use of defensive medicine, and survey reports are apt to be misleading because of bias and the lack of controls and baseline data.
Looking ahead, what can we expect for malpractice law under the Trump administration? Tom Price, MD, a former Republican congressman from Georgia, is an orthopedic surgeon and the new secretary of the Department of Health & Human Services. He has previously spoken passionately about tort reforms such as defensive medicine, damage caps, health tribunals, and practice guidelines. Many states have already incorporated some of these measures into their own tort reforms – with salutary results. It remains to be seen whether HHS will deem any omnibus federal legislation necessary at this point.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the materials have been taken from my earlier columns in Internal Medicine News. For additional information, readers may contact the author at [email protected].
References
1. JAMA. 2014 Nov 26;312(20):2146-55.
2. “Malpractice 2017: Do We Need Reform?” Internal Medicine News, March 1, 2017, page 1.
3. Fein v. Permanente, 38 Cal.3d 137 (1985).
4. Chan v. Curran, 237 CA 4th 601 (2015).
5. Estate of Johnson v. Randall Smith, Inc., 135 Ohio St.3d 440 (2013).
6. Available at https://papers.ssrn.com/sol3/papers2.cfm?abstract_id=2883693.
7. Shinal v. Toms, 122 A. 3d 1066 (Pa. Super. Ct. 2015).
8. Q J Econ. (1996) 111 (2): 353-390.
9. Available at www.jacksonhealthcare.com/media/8968/defensivemedicine_ebook_final.pdf.
Question: Recent developments in malpractice include the following:
A. Severity and frequency rates continue to rise.
B. Apology laws appear to be very effective in reducing claims.
C. Litigation surrounds whether an assistant may obtain a patient’s informed consent on behalf of the doctor.
D. A and B.
E. A, B, and C.
Answer: C. Over the past decade, malpractice claims have in fact diminished, accompanied by a leveling or reduction in premiums.1 Rates have plummeted to roughly half of previous levels, averaging six claims per 100 doctors in 2016.
According to The Doctors Company, internists paid an average premium of $15,853, compared with an average of $19,900 in 2006, general surgeons $52,905 instead of $68,186, and obstetricians $72,999, a drop from $93,230. Even claims-plagued Florida’s Dade County has seen a dramatic drop in internist premiums by some $27,000, down to $47,707.2
The latest attack on MICRA, in 2015, concerned a wrongful death suit brought by a woman whose mother died from hemorrhagic complications related to Coumadin use following heart surgery.4 Her constitutional challenges included violation of equal protection, due process, and the right to a jury trial. But these were essentially all grounded on an entitlement to recover additional noneconomic damages sufficient to cover attorney fees. The trial court had reduced her $1 million noneconomic damages to $250,000 as required by MICRA. A California appeals court rejected her claim as being “contrary to many well-established legal principles.”
Disclosure of medical errors is a relative newcomer as an ethical and effective way of thwarting potential malpractice claims. Many states have enacted so-called “apology laws,” an outgrowth of the communication and resolution programs popularized by the Lexington (Ky.) VA Medical Center, University of Michigan Health System, Harvard’s affiliated institutions, and Colorado’s COPIC Insurance.
Apology laws disallow statements of sympathy from being admitted into evidence. In some cases, these laws may assist the physician. For example, the Ohio Supreme Court has ruled that a surgeon’s comments and alleged admission of guilt (“I take full responsibility for this” regarding accidentally sectioning the common bile duct) were properly shielded from discovery by the state’s apology statute, even though the incident took place before the law went into effect.5
However, apology laws do vary from state to state, and some do not shield admissions regarding causation of error or fault.
A recent study suggests that apology laws don’t work. A Vanderbilt University study published online used a unique dataset covering all malpractice claims for 90% of physicians practicing in a single specialty across the country.6 The findings revealed that, for physicians who do not regularly perform surgery, apology laws actually increased the probability of facing a lawsuit. For surgeons, apology laws do not have a substantial effect on the probability of facing a claim or the average payment made to resolve a claim.
The study’s authors concluded that “apology laws are not substitutes for specific physician disclosure programs, and that the experiences of these types of programs are not generalizable to the physician population at large. In other words, simply being allowed to apologize is not enough to reduce malpractice risk.”
In the informed consent arena, the latest development in the law revolves around whether a physician assistant, in lieu of the surgeon himself, can obtain informed consent from a patient.
In Shinal v. Toms,7 Megan Shinal underwent surgery to remove a craniopharyngioma, but it regrew and required re-exploration by Dr. Steven Toms. Dr. Toms testified that Ms. Shinal had agreed that he would determine during the surgery whether he should remove the entire tumor or perform a partial resection. The operation was complicated by a carotid artery perforation, which left the patient with impaired vision and ambulation.
The complaint asserted that Dr. Toms’s physician assistant, not Dr. Toms himself, had provided the actual discussion during the informed consent process, and thus the patient’s consent was invalid.
The jury was allowed to consider the information provided by the doctor’s support staff, and the Superior Court of Pennsylvania affirmed the validity of the patient’s consent, holding that consent is based on the scope of information relayed rather than the identity of the individual communicating the information. This carefully watched case is now on final appeal before the Supreme Court of Pennsylvania.
At a personal level, physicians dread the stress surrounding medical malpractice litigation. The process frontally attacks their competence and consumes much time and energy, notwithstanding there being little or no exposure of personal assets because of insurance protection. Virtually all doctors practice defensive medicine, which has been defined as “deviation from sound medical practice that is induced primarily by a threat of liability.”
At a societal level, defensive medicine is reported to add substantially to the nation’s medical bill. The figure tossed around is $12 billion to $50 billion a year, based mostly on estimates by the American Medical Association and an older study extrapolating potential Medicare savings from litigation over heart disease.8
A more recent report continues to emphasize the high cost of defensive medicine.9 Jackson Healthcare invited 138,686 physicians to participate in a confidential online survey to quantify the costs and impact of defensive medicine. More than 3,000 physicians spanning all states and medical specialties completed the survey; however, this represented only a 2.21% response rate.
The authors concluded that defensive medicine is a significant force driving the high cost of health care in the United States, and that physicians estimate the cost of defensive medicine to be in the $650 billion to $850 billion range, or between 26% and 34% of annual health care costs.
Skeptics question the way the profession defines defensive medicine, pointing out that malpractice concerns may not be the primary reason, as most interventions add some marginal value to patient care. There may also be conflicting motivations of physicians, such as financial or other personal rewards.
Above all, there is no acceptable method for measuring the extent and use of defensive medicine, and survey reports are apt to be misleading because of bias and the lack of controls and baseline data.
Looking ahead, what can we expect for malpractice law under the Trump administration? Tom Price, MD, a former Republican congressman from Georgia, is an orthopedic surgeon and the new secretary of the Department of Health & Human Services. He has previously spoken passionately about tort reforms such as defensive medicine, damage caps, health tribunals, and practice guidelines. Many states have already incorporated some of these measures into their own tort reforms – with salutary results. It remains to be seen whether HHS will deem any omnibus federal legislation necessary at this point.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the materials have been taken from my earlier columns in Internal Medicine News. For additional information, readers may contact the author at [email protected].
References
1. JAMA. 2014 Nov 26;312(20):2146-55.
2. “Malpractice 2017: Do We Need Reform?” Internal Medicine News, March 1, 2017, page 1.
3. Fein v. Permanente, 38 Cal.3d 137 (1985).
4. Chan v. Curran, 237 CA 4th 601 (2015).
5. Estate of Johnson v. Randall Smith, Inc., 135 Ohio St.3d 440 (2013).
6. Available at https://papers.ssrn.com/sol3/papers2.cfm?abstract_id=2883693.
7. Shinal v. Toms, 122 A. 3d 1066 (Pa. Super. Ct. 2015).
8. Q J Econ. (1996) 111 (2): 353-390.
9. Available at www.jacksonhealthcare.com/media/8968/defensivemedicine_ebook_final.pdf.
Hold your breath
“Exercising my ‘reasoned judgment,’ I have no doubt that the right to a climate system capable of sustaining human life is fundamental to a free and ordered society.”
– U.S. District Judge Ann Aiken in Kelsey Cascadia Rose Juliana vs. United States of America, et al.
In many areas of the world, the simple act of breathing has become hazardous to people’s health.
According to the World Health Organization, more people die every day from air pollution than from HIV/AIDS, tuberculosis, and road injuries combined. In China, more than 1 million deaths annually are linked to polluted air (76/100,000); in India the number of deaths is more than 600,000 annually (49/100,000); and in the United States, that figure comes to more than 38,000 (12/100,000).
And yet, nonpolluting, alternative options – such as sun and wind power – are readily available.
Dirty air is visible on a hot summer day – when, mixed with other substances, it forms smog. Higher temperatures can then speed up the chemical reactions that form smog. We breathe in that polluted air, especially on days when the air is stagnant or there is temperature inversion.
The health effects of climate change
Black carbon found in air pollution leads to drug-resistant bacteria and alters antibiotic tolerance.1 The pollution also is associated with multiple cancers: lung, liver, ovarian, and, possibly, breast.2,3,4,5 It causes inflammation linked to the development of coronary artery disease (seen even in children!) and plaque formation leading to heart attacks and cardiac arrhythmias – including atrial fibrillation. Air pollution causes, triggers, or worsens respiratory illnesses – chronic obstructive pulmonary disease, emphysema, asthma, infections – and is responsible for lifelong diminished lung volume in children (a reason families are leaving Beijing.) Exponentially increased rates of autism are linked to bad air quality, as are autoimmune diseases, which also are on the rise.6,7 Polluted air causes brain inflammation – living near sources of air pollution increases the risk of dementia – and other neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s, and amyotrophic lateral sclerosis.8 The blood brain barrier protects the brain from most foreign matter, but particulate matter, especially ultrafine particulate matter of less than 1 mcm such as magnetite, can cross directly into the brain via the olfactory nerve. (Magnetite has been identified in the brain tissue of residents living in areas where the substance is produced as a result of industrial waste.) While particulate matter of 2.5 mcmis measured in the United States, ultrafine particulate matter is not.
Psychiatric symptoms and chronic psychiatric disorders also are associated with polluted air: On days with poor air quality, a statistically significant increase is seen in suicide threats and visits to emergency departments for panic attacks.9,10
A rise in aggression occurs when there are abnormally high temperatures and significant changes in rainfall. More assaults, murders, suicides, domestic violence, and child abuse can be expected, and a rise in unrest around the world should come as no surprise.
As a consequence of increased CO2 in the atmosphere, temperatures have already risen by 2° F: Sixteen of the hottest years on record have occurred in the last 17 years, with 2016 as the hottest year ever recorded. In Iraq and Kuwait, the temperature last summer reached 129.2° F.
We are experiencing more frequent and extreme weather events, chronic climate conditions, and the cascading disruption of ecosystems. Drought and sea level rise are leading to physical and psychological impacts – both direct and indirect. Some regions of the world have become destabilized, triggering migrations and the refugee crisis.
Along with these psychological impacts, CO2 affects cognition: A recent study by the Harvard School of Public Health, Boston, shows that the indoor levels of CO2 to which American workers typically are exposed impair cognitive functioning, particularly in the areas of strategic thinking, information processing, and crisis management.11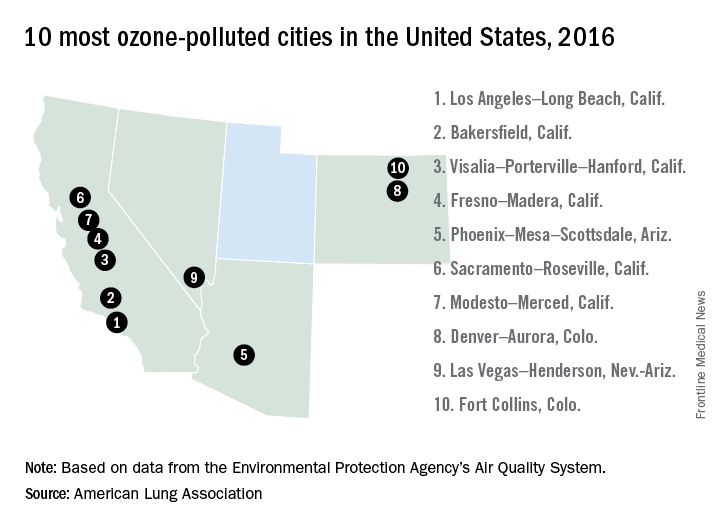
What do we do about it?
As mental health professionals, we know that aggression can be overt or passive (from inaction). Overwhelming evidence shows harm to public health from burning fossil fuels, and yet, though we are making progress, resistance still exists in the transition to clean, renewable energy critical for the health of our families and communities. When political will is what stands between us and getting back on a path to breathing clean air, how can inaction be understood as anything but an act of aggression?
This issue has reached U.S. courts: In a landmark case, 21 youths aged 9-20 years represented by “Our Children’s Trust” are suing the U.S. government in the Oregon U.S. District Court for failure to act on climate. The case, heard by Judge Ann Aiken, is now headed to trial.
All of us have a duty to collectively, repeatedly, and forcefully call on policy makers to take action.
That leads me to what we can do as doctors. In this effort to quickly transition to safe, clean renewable energy, we all have a role to play. The notion that we can’t do anything as individuals is no more credible than saying “my vote doesn’t matter.” Just as our actions as voters in a democracy demonstrate the collective civic responsibility we owe one another, so too do our actions on climate. As global citizens, all actions that we take to help us live within the planet’s means are opportunities to restore balance.
What we do collectively drives markets and determines the social norms that powerfully influence the decisions of others – sometimes even unconsciously.
As doctors, we have a unique role to play in the places we work – urging hospitals, clinics, academic centers, and other organizations and facilities to lead by example, become role models for energy efficiency, and choose clean renewable energy sources over the ones harming our health. We can start by choosing wind and solar to power our homes and influencing others to do the same.
We are the voices because this is a health message.
Dr. Van Susteren is a practicing general and forensic psychiatrist in Washington. She serves on the advisory board of the Center for Health and the Global Environment at Harvard T.H. Chan School of Public Health, Boston. Dr. Van Susteren is a former member of the board of directors of the National Wildlife Federation and coauthor of group’s report, “The Psychological Effects of Global Warming on the United States – Why the U.S. Mental Health System is Not Prepared.” In 2006, Dr. Van Susteren sought the Democratic nomination for a U.S. Senate seat in Maryland. She also founded Lucky Planet Foods, a company that provides plant-based, low carbon foods.
References
1. Environ Microbiol. 2017 Feb 14. doi: 10.1111/1462-2920.13686.
2. Environ Health Perspect. 2017 Mar;125[3]:378-84.
3. J Hepatol. 2015;63[6]:1397-1404.
4. J Toxicol Environ Health A. 2012;75[3]:174-82.
5. Environ Health Perspect. 2012 Nov; 118[11]:1578-83.
6. J Child Psychol Psychiatry. 2016; 57[3]:271-92.
7. Curr Opin Pediatr. 2010;22[2]219-25.
8. Inhal Toxicol. 2008;20[5]:499-506.
9. J Psychiatr Res. 2015 Mar;62:130-5.
10. Schizophr Res. 2016 Oct 5. doi: 10.1016/j.schres.2016.10.003.
11. Environ Health Perspect. 2016 Jun;124[6]:805-12.
“Exercising my ‘reasoned judgment,’ I have no doubt that the right to a climate system capable of sustaining human life is fundamental to a free and ordered society.”
– U.S. District Judge Ann Aiken in Kelsey Cascadia Rose Juliana vs. United States of America, et al.
In many areas of the world, the simple act of breathing has become hazardous to people’s health.
According to the World Health Organization, more people die every day from air pollution than from HIV/AIDS, tuberculosis, and road injuries combined. In China, more than 1 million deaths annually are linked to polluted air (76/100,000); in India the number of deaths is more than 600,000 annually (49/100,000); and in the United States, that figure comes to more than 38,000 (12/100,000).
And yet, nonpolluting, alternative options – such as sun and wind power – are readily available.
Dirty air is visible on a hot summer day – when, mixed with other substances, it forms smog. Higher temperatures can then speed up the chemical reactions that form smog. We breathe in that polluted air, especially on days when the air is stagnant or there is temperature inversion.
The health effects of climate change
Black carbon found in air pollution leads to drug-resistant bacteria and alters antibiotic tolerance.1 The pollution also is associated with multiple cancers: lung, liver, ovarian, and, possibly, breast.2,3,4,5 It causes inflammation linked to the development of coronary artery disease (seen even in children!) and plaque formation leading to heart attacks and cardiac arrhythmias – including atrial fibrillation. Air pollution causes, triggers, or worsens respiratory illnesses – chronic obstructive pulmonary disease, emphysema, asthma, infections – and is responsible for lifelong diminished lung volume in children (a reason families are leaving Beijing.) Exponentially increased rates of autism are linked to bad air quality, as are autoimmune diseases, which also are on the rise.6,7 Polluted air causes brain inflammation – living near sources of air pollution increases the risk of dementia – and other neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s, and amyotrophic lateral sclerosis.8 The blood brain barrier protects the brain from most foreign matter, but particulate matter, especially ultrafine particulate matter of less than 1 mcm such as magnetite, can cross directly into the brain via the olfactory nerve. (Magnetite has been identified in the brain tissue of residents living in areas where the substance is produced as a result of industrial waste.) While particulate matter of 2.5 mcmis measured in the United States, ultrafine particulate matter is not.
Psychiatric symptoms and chronic psychiatric disorders also are associated with polluted air: On days with poor air quality, a statistically significant increase is seen in suicide threats and visits to emergency departments for panic attacks.9,10
A rise in aggression occurs when there are abnormally high temperatures and significant changes in rainfall. More assaults, murders, suicides, domestic violence, and child abuse can be expected, and a rise in unrest around the world should come as no surprise.
As a consequence of increased CO2 in the atmosphere, temperatures have already risen by 2° F: Sixteen of the hottest years on record have occurred in the last 17 years, with 2016 as the hottest year ever recorded. In Iraq and Kuwait, the temperature last summer reached 129.2° F.
We are experiencing more frequent and extreme weather events, chronic climate conditions, and the cascading disruption of ecosystems. Drought and sea level rise are leading to physical and psychological impacts – both direct and indirect. Some regions of the world have become destabilized, triggering migrations and the refugee crisis.
Along with these psychological impacts, CO2 affects cognition: A recent study by the Harvard School of Public Health, Boston, shows that the indoor levels of CO2 to which American workers typically are exposed impair cognitive functioning, particularly in the areas of strategic thinking, information processing, and crisis management.11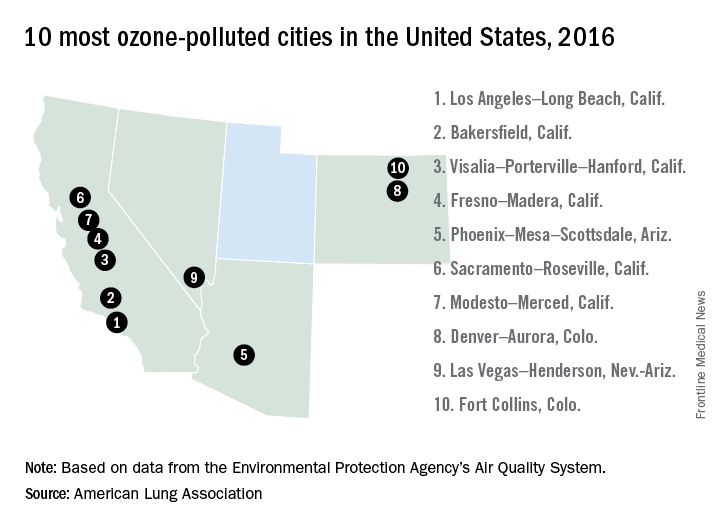
What do we do about it?
As mental health professionals, we know that aggression can be overt or passive (from inaction). Overwhelming evidence shows harm to public health from burning fossil fuels, and yet, though we are making progress, resistance still exists in the transition to clean, renewable energy critical for the health of our families and communities. When political will is what stands between us and getting back on a path to breathing clean air, how can inaction be understood as anything but an act of aggression?
This issue has reached U.S. courts: In a landmark case, 21 youths aged 9-20 years represented by “Our Children’s Trust” are suing the U.S. government in the Oregon U.S. District Court for failure to act on climate. The case, heard by Judge Ann Aiken, is now headed to trial.
All of us have a duty to collectively, repeatedly, and forcefully call on policy makers to take action.
That leads me to what we can do as doctors. In this effort to quickly transition to safe, clean renewable energy, we all have a role to play. The notion that we can’t do anything as individuals is no more credible than saying “my vote doesn’t matter.” Just as our actions as voters in a democracy demonstrate the collective civic responsibility we owe one another, so too do our actions on climate. As global citizens, all actions that we take to help us live within the planet’s means are opportunities to restore balance.
What we do collectively drives markets and determines the social norms that powerfully influence the decisions of others – sometimes even unconsciously.
As doctors, we have a unique role to play in the places we work – urging hospitals, clinics, academic centers, and other organizations and facilities to lead by example, become role models for energy efficiency, and choose clean renewable energy sources over the ones harming our health. We can start by choosing wind and solar to power our homes and influencing others to do the same.
We are the voices because this is a health message.
Dr. Van Susteren is a practicing general and forensic psychiatrist in Washington. She serves on the advisory board of the Center for Health and the Global Environment at Harvard T.H. Chan School of Public Health, Boston. Dr. Van Susteren is a former member of the board of directors of the National Wildlife Federation and coauthor of group’s report, “The Psychological Effects of Global Warming on the United States – Why the U.S. Mental Health System is Not Prepared.” In 2006, Dr. Van Susteren sought the Democratic nomination for a U.S. Senate seat in Maryland. She also founded Lucky Planet Foods, a company that provides plant-based, low carbon foods.
References
1. Environ Microbiol. 2017 Feb 14. doi: 10.1111/1462-2920.13686.
2. Environ Health Perspect. 2017 Mar;125[3]:378-84.
3. J Hepatol. 2015;63[6]:1397-1404.
4. J Toxicol Environ Health A. 2012;75[3]:174-82.
5. Environ Health Perspect. 2012 Nov; 118[11]:1578-83.
6. J Child Psychol Psychiatry. 2016; 57[3]:271-92.
7. Curr Opin Pediatr. 2010;22[2]219-25.
8. Inhal Toxicol. 2008;20[5]:499-506.
9. J Psychiatr Res. 2015 Mar;62:130-5.
10. Schizophr Res. 2016 Oct 5. doi: 10.1016/j.schres.2016.10.003.
11. Environ Health Perspect. 2016 Jun;124[6]:805-12.
“Exercising my ‘reasoned judgment,’ I have no doubt that the right to a climate system capable of sustaining human life is fundamental to a free and ordered society.”
– U.S. District Judge Ann Aiken in Kelsey Cascadia Rose Juliana vs. United States of America, et al.
In many areas of the world, the simple act of breathing has become hazardous to people’s health.
According to the World Health Organization, more people die every day from air pollution than from HIV/AIDS, tuberculosis, and road injuries combined. In China, more than 1 million deaths annually are linked to polluted air (76/100,000); in India the number of deaths is more than 600,000 annually (49/100,000); and in the United States, that figure comes to more than 38,000 (12/100,000).
And yet, nonpolluting, alternative options – such as sun and wind power – are readily available.
Dirty air is visible on a hot summer day – when, mixed with other substances, it forms smog. Higher temperatures can then speed up the chemical reactions that form smog. We breathe in that polluted air, especially on days when the air is stagnant or there is temperature inversion.
The health effects of climate change
Black carbon found in air pollution leads to drug-resistant bacteria and alters antibiotic tolerance.1 The pollution also is associated with multiple cancers: lung, liver, ovarian, and, possibly, breast.2,3,4,5 It causes inflammation linked to the development of coronary artery disease (seen even in children!) and plaque formation leading to heart attacks and cardiac arrhythmias – including atrial fibrillation. Air pollution causes, triggers, or worsens respiratory illnesses – chronic obstructive pulmonary disease, emphysema, asthma, infections – and is responsible for lifelong diminished lung volume in children (a reason families are leaving Beijing.) Exponentially increased rates of autism are linked to bad air quality, as are autoimmune diseases, which also are on the rise.6,7 Polluted air causes brain inflammation – living near sources of air pollution increases the risk of dementia – and other neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s, and amyotrophic lateral sclerosis.8 The blood brain barrier protects the brain from most foreign matter, but particulate matter, especially ultrafine particulate matter of less than 1 mcm such as magnetite, can cross directly into the brain via the olfactory nerve. (Magnetite has been identified in the brain tissue of residents living in areas where the substance is produced as a result of industrial waste.) While particulate matter of 2.5 mcmis measured in the United States, ultrafine particulate matter is not.
Psychiatric symptoms and chronic psychiatric disorders also are associated with polluted air: On days with poor air quality, a statistically significant increase is seen in suicide threats and visits to emergency departments for panic attacks.9,10
A rise in aggression occurs when there are abnormally high temperatures and significant changes in rainfall. More assaults, murders, suicides, domestic violence, and child abuse can be expected, and a rise in unrest around the world should come as no surprise.
As a consequence of increased CO2 in the atmosphere, temperatures have already risen by 2° F: Sixteen of the hottest years on record have occurred in the last 17 years, with 2016 as the hottest year ever recorded. In Iraq and Kuwait, the temperature last summer reached 129.2° F.
We are experiencing more frequent and extreme weather events, chronic climate conditions, and the cascading disruption of ecosystems. Drought and sea level rise are leading to physical and psychological impacts – both direct and indirect. Some regions of the world have become destabilized, triggering migrations and the refugee crisis.
Along with these psychological impacts, CO2 affects cognition: A recent study by the Harvard School of Public Health, Boston, shows that the indoor levels of CO2 to which American workers typically are exposed impair cognitive functioning, particularly in the areas of strategic thinking, information processing, and crisis management.11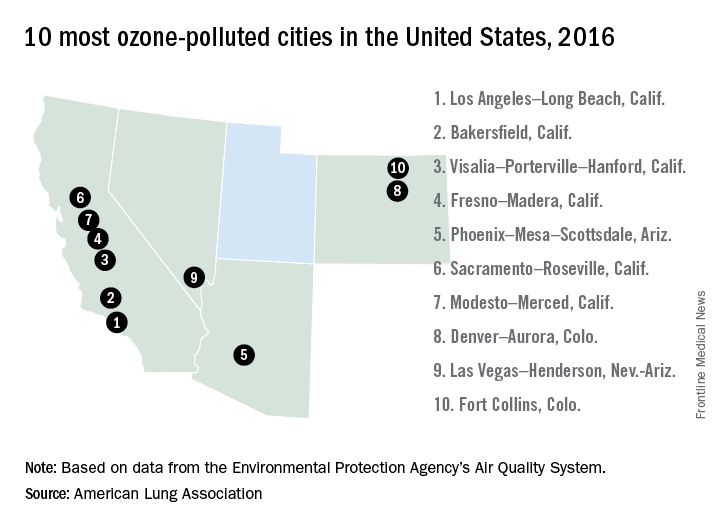
What do we do about it?
As mental health professionals, we know that aggression can be overt or passive (from inaction). Overwhelming evidence shows harm to public health from burning fossil fuels, and yet, though we are making progress, resistance still exists in the transition to clean, renewable energy critical for the health of our families and communities. When political will is what stands between us and getting back on a path to breathing clean air, how can inaction be understood as anything but an act of aggression?
This issue has reached U.S. courts: In a landmark case, 21 youths aged 9-20 years represented by “Our Children’s Trust” are suing the U.S. government in the Oregon U.S. District Court for failure to act on climate. The case, heard by Judge Ann Aiken, is now headed to trial.
All of us have a duty to collectively, repeatedly, and forcefully call on policy makers to take action.
That leads me to what we can do as doctors. In this effort to quickly transition to safe, clean renewable energy, we all have a role to play. The notion that we can’t do anything as individuals is no more credible than saying “my vote doesn’t matter.” Just as our actions as voters in a democracy demonstrate the collective civic responsibility we owe one another, so too do our actions on climate. As global citizens, all actions that we take to help us live within the planet’s means are opportunities to restore balance.
What we do collectively drives markets and determines the social norms that powerfully influence the decisions of others – sometimes even unconsciously.
As doctors, we have a unique role to play in the places we work – urging hospitals, clinics, academic centers, and other organizations and facilities to lead by example, become role models for energy efficiency, and choose clean renewable energy sources over the ones harming our health. We can start by choosing wind and solar to power our homes and influencing others to do the same.
We are the voices because this is a health message.
Dr. Van Susteren is a practicing general and forensic psychiatrist in Washington. She serves on the advisory board of the Center for Health and the Global Environment at Harvard T.H. Chan School of Public Health, Boston. Dr. Van Susteren is a former member of the board of directors of the National Wildlife Federation and coauthor of group’s report, “The Psychological Effects of Global Warming on the United States – Why the U.S. Mental Health System is Not Prepared.” In 2006, Dr. Van Susteren sought the Democratic nomination for a U.S. Senate seat in Maryland. She also founded Lucky Planet Foods, a company that provides plant-based, low carbon foods.
References
1. Environ Microbiol. 2017 Feb 14. doi: 10.1111/1462-2920.13686.
2. Environ Health Perspect. 2017 Mar;125[3]:378-84.
3. J Hepatol. 2015;63[6]:1397-1404.
4. J Toxicol Environ Health A. 2012;75[3]:174-82.
5. Environ Health Perspect. 2012 Nov; 118[11]:1578-83.
6. J Child Psychol Psychiatry. 2016; 57[3]:271-92.
7. Curr Opin Pediatr. 2010;22[2]219-25.
8. Inhal Toxicol. 2008;20[5]:499-506.
9. J Psychiatr Res. 2015 Mar;62:130-5.
10. Schizophr Res. 2016 Oct 5. doi: 10.1016/j.schres.2016.10.003.
11. Environ Health Perspect. 2016 Jun;124[6]:805-12.
MACRA: Not going away any time soon
MACRA is now a fact of life.
Implementation of the Medicare Access and CHIP Reauthorization Act (MACRA), the historic Medicare reform law that replaced the Sustainable Growth Rate (SGR) formula in 2015, began in January 2017. Patrick V. Bailey, MD, FACS, Medical Director, Advocacy, in the American College of Surgeons (ACS) Division of Advocacy and Health Policy (DAHP) office in Washington DC has, for the past several years, been involved with ensuring that the policy implemented takes into account the interests of surgeons and their patients. He has seen MACRA develop from its beginnings. Dr. Bailey, a pediatric surgeon, has deep knowledge about the program, both from the policy perspective and as a surgeon. We asked Dr. Bailey to share with us his insights on what surgeons can expect and what surgeons can do to avoid penalties.
1) Many surgeons are overwhelmed by the perceived complexity of the new MACRA law. What do you say to those who have so far tuned out much of the information they have been given?
A few thoughts. First, we really do understand that the concerns about the complexity are real. Some of those very real feelings come out of a basic aversion to change. Some come from the overall stress and uncertainty surrounding the constant changes in our health care system that have been ongoing for years. And some are the result of the continuously expanding administrative burden. We get it.
Is MACRA exactly what we surgeons would wish for? No, but those of us who have worked in the policy process feel our efforts had a positive impact on how this legislation played out. More importantly, we are absolutely confident that, for 2017, ALL surgeons can avoid a penalty.
From a pragmatic perspective, the implementation of MACRA is going forward, and burying one’s head in the sand will not make it go away. Therefore, it is imperative that surgeons devote some time to understanding the new Quality Payment Program, or QPP, which is the operationalization of the MACRA law. Even a very limited time investment will pay dividends in the Medicare payment they receive in 2019, based on their performance in 2017.
So, if you have avoided dealing with this up until now, I urge you to set aside an hour or so to look at the materials that the ACS has prepared. The reporting requirements may look much less daunting once you become familiar with them.
Again, I am confident that surgeons can and will be successful (as defined by either avoiding a penalty or receiving a small positive rate update), if they take some time to acquire some basic knowledge about the program, make an assessment of their individual practice situation, determine the best course for their individual situation, and take the necessary actions to meet the requirements for the choices they have made.
Fortunately, there is still more than ample time to get started and ACS has developed resources for Fellows to assist them in educating themselves about the program and making their individual choices about their level of participation.
2) With all the talk of change to the Affordable Care Act (ACA), how likely is it that all of this will simply “go away”?
The ACA and MACRA are separate and different pieces of legislation from a temporal, process, policy, and political perspective. In fact, despite the fact that the ACS and other medical specialty groups specifically advocated for language repealing the SGR be included in the ACA in 2010, that did not occur. Therefore, the efforts directed at repealing the SGR took another 5 years and ultimately culminated in the passage of MACRA in 2015.
Many will recall the contentious process and political repercussions that resulted in the passage of the ACA. In contrast, leaders from both political parties worked cooperatively on the SGR repeal legislation we now know as MACRA. This resulted in the MACRA legislation being passed in a very bipartisan manner with only 37 of the 435 members of the House and 8 of the 100 members of the Senate voting against the law.
Accordingly, while we believe there will be a need for some specific, targeted legislative “fixes” and regulatory relief actions from CMS (Centers for Medicare and Medicaid Services) to address faults in the QPP (and the ACS will continue our efforts in this direction), it is highly unlikely that MACRA will be repealed or that it will change significantly in the near-term future.
3) What is the starting point for surgeons who want to learn more and begin the process of determining how best to participate?
There is a relatively straightforward process, which revolves around a series of questions and individual decisions.
First, surgeons should determine if all their Merit-based Incentive Payment System (MIPS) data will be reported by their institution or group via a group reporting option (GPRO). For those surgeons, whose data are so reported, they are done and there is nothing further for them to do.
If their data are not reported for them via a GPRO, then they should determine if CMS has notified them that they are exempt from participating in MIPS due to the low volume threshold. If you see 100 or fewer Medicare patients annually or one submits $30,000 or less in Medicare claims, you are not eligible for MIPS incentives or subject to its penalties.
However, this is not a determination that individual Fellows can make on their own based on data they may have on hand based on prior calendar or fiscal years. Instead, CMS makes the determination based on a specific period and notifies individual providers who are so exempted. It is also our understanding that a website, where one can check whether they have been excluded based on the low volume threshold, is forthcoming from CMS. When this website becomes available, ACS will make sure Fellows are informed.
If your data are not reported via a GPRO and you do not receive notification from CMS that you are exempt based on the low-volume threshold, then you have choices to make – having choices is a good thing.
For those who want to compete for positive updates in their Medicare payment rates in 2019 based on their reporting in 2017, I recommend they first visit facs.org/qpp where we have made available a variety of resources in print, video, and PowerPoint formats to assist Fellows in making their plans for participating for either a full or partial year. The update received will depend on performance and not on the amount of data submitted or the time of participation. That said, for those who plan to fully engage, participation over a longer period of time provides more opportunity for improvement and, thus, increases the potential for better performance.
4) What about surgeons who simply want to avoid a penalty and forgo any chance for a positive update?
If your goal for 2017 is to simply avoid a penalty, CMS only requires data be submitted for only one of the three components of MIPS that will be reported this year. Here again for 2017, you have a choice to submit:
A) The required base score measures for your EHR (now known as Advancing Care Information) OR
B) Participation in one Improvement Activity for 90 days, which is reported by simple attestation OR
C) Submit one Quality measure on one patient, which may be reported by a registry, a qualified clinical data registry (QCDR), an EHR or, traditional claims
One very important point to note is that one is NOT required to have a certified EHR to avoid a penalty for 2017. I believe this point alone has been the source of a lot of misunderstanding and anxiety about the QPP and MIPS.
Another key point is that, by simply engaging in one Improvement Activity (such as Maintenance of Certification Part IV, registering with your state’s prescription drug monitoring program, or use of the ACS’ Surgical Risk Calculator) and attesting to having done so with the ACS Surgeon Specific Registry (SSR) or the CMS web portal, one can avoid a penalty.
Alternatively, using the SSR to submit one Quality measure on one patient will also suffice to prevent one from receiving a penalty in 2019 based on their 2017 performance.
It is relatively easy to avoid any negative financial implications of MIPS in 2017, but it does require some effort, albeit minimal. It is also important for Fellows to remember that, since MIPS is essentially a tournament model, those who choose not to participate will take the penalty that provides the funds used to reward those who do participate. I think most surgeons will want to participate, even if only at the minimal levels outlined above, in order to avoid “paying for” another provider’s positive update.
5) What are the consequences of not participating at the minimal levels you just described and choosing to submit no data?
That question is perhaps best addressed in the form of a comparison between 2016 and 2017.
In 2016, if one did not report any PQRS (Physician Quality Reporting System) data and did not participate in the electronic health record meaningful use program, their lack of participation would result in a 10% negative payment adjustment in 2018. In 2017, if one chooses not to submit the minimal amount of data for either the ACI, Improvement Activity, or Quality components as discussed previously, that lack of participation will lead to a 4% negative payment adjustment in 2019.
In effect, those who have never participated and continue to not do so will see a 6% increase in their Medicare reimbursement in 2019 compared to what they receive in 2018.
However, we DO NOT recommend this option because, in future years, the negative payment adjustments will gradually increase to 9%. Accordingly, we encourage Fellows to use 2017 as a period to learn and get familiar and more comfortable with the reporting of data so that they will be better prepared to be successful in those future years when the stakes are higher.
6) You have mentioned the resources ACS has prepared to assist Fellows with this transition. Can you be more specific about what is available?
The ACS one-stop shop is the Quality Payment Program Resource Center found at www.facs.org/qpp.
Fellows who attended the Clinical Congress in Washington last October likely received a copy of the MACRA Quality Payment Manual which was developed to help educate Fellows about the QPP. That manual has subsequently been totally revamped and updated to reflect the changes to the QPP as reflected in the final rule. We highly encourage Fellows to obtain and read the latest version – it is available as individual sections or as the complete publication on the facs.org/qpp webpage.
Also available on the QPP webpage is the second generation of the video series we first created last fall. There are now a total of 6 videos with a run time for the entire series of approximately 30 minutes. The videos cover a wide spectrum of topics including the historical background and context of MACRA, an introduction to MIPS, and three individual videos dedicated to MIPS components: Quality, Advancing Care Information and Improvement Activity, and a video outlining the options for participation in 2017.
The PowerPoint presentations seen in the videos are also available, as are links to specific CMS web pages and more information on ACS’ efforts to develop advanced alternative payment models (APMs) for surgeons.
We will continue to update the website throughout the year in our ongoing efforts to refine the resources to be the most useful to Fellows.
I would encourage all Fellows to visit the website, watch the videos, and read the manual. I realize time is a precious commodity, but with a total time investment of 60-90 minutes, one can acquire an operational knowledge of the QPP and make a determination as to how they wish to participate.
Again, no Fellow should settle for accepting a penalty in 2019 based on what they do this year. With the multiple options available, it is simply too easy to avoid and to do so would effectively serve to put their money in someone else’s pocket. For those who feel more prepared (that is, they have previously reported PQRS data and have a 2014 or 2015 edition EHR) and wish to seek a positive rate update, investment of more time will obviously be required. However, in addition to the small positive payment update they will likely receive, probably the most substantial benefit to be derived is their preparation for future years when the incentives and penalties increase to +/- 9%.
Finally, ACS “has your back” on coping with MACRA and as always, ACS staff in Chicago and Washington are available to assist Fellows with their preparation, to answer questions about the program and the reporting requirements, or to provide general or specific direction in their efforts to navigate the QPP.
MACRA is now a fact of life.
Implementation of the Medicare Access and CHIP Reauthorization Act (MACRA), the historic Medicare reform law that replaced the Sustainable Growth Rate (SGR) formula in 2015, began in January 2017. Patrick V. Bailey, MD, FACS, Medical Director, Advocacy, in the American College of Surgeons (ACS) Division of Advocacy and Health Policy (DAHP) office in Washington DC has, for the past several years, been involved with ensuring that the policy implemented takes into account the interests of surgeons and their patients. He has seen MACRA develop from its beginnings. Dr. Bailey, a pediatric surgeon, has deep knowledge about the program, both from the policy perspective and as a surgeon. We asked Dr. Bailey to share with us his insights on what surgeons can expect and what surgeons can do to avoid penalties.
1) Many surgeons are overwhelmed by the perceived complexity of the new MACRA law. What do you say to those who have so far tuned out much of the information they have been given?
A few thoughts. First, we really do understand that the concerns about the complexity are real. Some of those very real feelings come out of a basic aversion to change. Some come from the overall stress and uncertainty surrounding the constant changes in our health care system that have been ongoing for years. And some are the result of the continuously expanding administrative burden. We get it.
Is MACRA exactly what we surgeons would wish for? No, but those of us who have worked in the policy process feel our efforts had a positive impact on how this legislation played out. More importantly, we are absolutely confident that, for 2017, ALL surgeons can avoid a penalty.
From a pragmatic perspective, the implementation of MACRA is going forward, and burying one’s head in the sand will not make it go away. Therefore, it is imperative that surgeons devote some time to understanding the new Quality Payment Program, or QPP, which is the operationalization of the MACRA law. Even a very limited time investment will pay dividends in the Medicare payment they receive in 2019, based on their performance in 2017.
So, if you have avoided dealing with this up until now, I urge you to set aside an hour or so to look at the materials that the ACS has prepared. The reporting requirements may look much less daunting once you become familiar with them.
Again, I am confident that surgeons can and will be successful (as defined by either avoiding a penalty or receiving a small positive rate update), if they take some time to acquire some basic knowledge about the program, make an assessment of their individual practice situation, determine the best course for their individual situation, and take the necessary actions to meet the requirements for the choices they have made.
Fortunately, there is still more than ample time to get started and ACS has developed resources for Fellows to assist them in educating themselves about the program and making their individual choices about their level of participation.
2) With all the talk of change to the Affordable Care Act (ACA), how likely is it that all of this will simply “go away”?
The ACA and MACRA are separate and different pieces of legislation from a temporal, process, policy, and political perspective. In fact, despite the fact that the ACS and other medical specialty groups specifically advocated for language repealing the SGR be included in the ACA in 2010, that did not occur. Therefore, the efforts directed at repealing the SGR took another 5 years and ultimately culminated in the passage of MACRA in 2015.
Many will recall the contentious process and political repercussions that resulted in the passage of the ACA. In contrast, leaders from both political parties worked cooperatively on the SGR repeal legislation we now know as MACRA. This resulted in the MACRA legislation being passed in a very bipartisan manner with only 37 of the 435 members of the House and 8 of the 100 members of the Senate voting against the law.
Accordingly, while we believe there will be a need for some specific, targeted legislative “fixes” and regulatory relief actions from CMS (Centers for Medicare and Medicaid Services) to address faults in the QPP (and the ACS will continue our efforts in this direction), it is highly unlikely that MACRA will be repealed or that it will change significantly in the near-term future.
3) What is the starting point for surgeons who want to learn more and begin the process of determining how best to participate?
There is a relatively straightforward process, which revolves around a series of questions and individual decisions.
First, surgeons should determine if all their Merit-based Incentive Payment System (MIPS) data will be reported by their institution or group via a group reporting option (GPRO). For those surgeons, whose data are so reported, they are done and there is nothing further for them to do.
If their data are not reported for them via a GPRO, then they should determine if CMS has notified them that they are exempt from participating in MIPS due to the low volume threshold. If you see 100 or fewer Medicare patients annually or one submits $30,000 or less in Medicare claims, you are not eligible for MIPS incentives or subject to its penalties.
However, this is not a determination that individual Fellows can make on their own based on data they may have on hand based on prior calendar or fiscal years. Instead, CMS makes the determination based on a specific period and notifies individual providers who are so exempted. It is also our understanding that a website, where one can check whether they have been excluded based on the low volume threshold, is forthcoming from CMS. When this website becomes available, ACS will make sure Fellows are informed.
If your data are not reported via a GPRO and you do not receive notification from CMS that you are exempt based on the low-volume threshold, then you have choices to make – having choices is a good thing.
For those who want to compete for positive updates in their Medicare payment rates in 2019 based on their reporting in 2017, I recommend they first visit facs.org/qpp where we have made available a variety of resources in print, video, and PowerPoint formats to assist Fellows in making their plans for participating for either a full or partial year. The update received will depend on performance and not on the amount of data submitted or the time of participation. That said, for those who plan to fully engage, participation over a longer period of time provides more opportunity for improvement and, thus, increases the potential for better performance.
4) What about surgeons who simply want to avoid a penalty and forgo any chance for a positive update?
If your goal for 2017 is to simply avoid a penalty, CMS only requires data be submitted for only one of the three components of MIPS that will be reported this year. Here again for 2017, you have a choice to submit:
A) The required base score measures for your EHR (now known as Advancing Care Information) OR
B) Participation in one Improvement Activity for 90 days, which is reported by simple attestation OR
C) Submit one Quality measure on one patient, which may be reported by a registry, a qualified clinical data registry (QCDR), an EHR or, traditional claims
One very important point to note is that one is NOT required to have a certified EHR to avoid a penalty for 2017. I believe this point alone has been the source of a lot of misunderstanding and anxiety about the QPP and MIPS.
Another key point is that, by simply engaging in one Improvement Activity (such as Maintenance of Certification Part IV, registering with your state’s prescription drug monitoring program, or use of the ACS’ Surgical Risk Calculator) and attesting to having done so with the ACS Surgeon Specific Registry (SSR) or the CMS web portal, one can avoid a penalty.
Alternatively, using the SSR to submit one Quality measure on one patient will also suffice to prevent one from receiving a penalty in 2019 based on their 2017 performance.
It is relatively easy to avoid any negative financial implications of MIPS in 2017, but it does require some effort, albeit minimal. It is also important for Fellows to remember that, since MIPS is essentially a tournament model, those who choose not to participate will take the penalty that provides the funds used to reward those who do participate. I think most surgeons will want to participate, even if only at the minimal levels outlined above, in order to avoid “paying for” another provider’s positive update.
5) What are the consequences of not participating at the minimal levels you just described and choosing to submit no data?
That question is perhaps best addressed in the form of a comparison between 2016 and 2017.
In 2016, if one did not report any PQRS (Physician Quality Reporting System) data and did not participate in the electronic health record meaningful use program, their lack of participation would result in a 10% negative payment adjustment in 2018. In 2017, if one chooses not to submit the minimal amount of data for either the ACI, Improvement Activity, or Quality components as discussed previously, that lack of participation will lead to a 4% negative payment adjustment in 2019.
In effect, those who have never participated and continue to not do so will see a 6% increase in their Medicare reimbursement in 2019 compared to what they receive in 2018.
However, we DO NOT recommend this option because, in future years, the negative payment adjustments will gradually increase to 9%. Accordingly, we encourage Fellows to use 2017 as a period to learn and get familiar and more comfortable with the reporting of data so that they will be better prepared to be successful in those future years when the stakes are higher.
6) You have mentioned the resources ACS has prepared to assist Fellows with this transition. Can you be more specific about what is available?
The ACS one-stop shop is the Quality Payment Program Resource Center found at www.facs.org/qpp.
Fellows who attended the Clinical Congress in Washington last October likely received a copy of the MACRA Quality Payment Manual which was developed to help educate Fellows about the QPP. That manual has subsequently been totally revamped and updated to reflect the changes to the QPP as reflected in the final rule. We highly encourage Fellows to obtain and read the latest version – it is available as individual sections or as the complete publication on the facs.org/qpp webpage.
Also available on the QPP webpage is the second generation of the video series we first created last fall. There are now a total of 6 videos with a run time for the entire series of approximately 30 minutes. The videos cover a wide spectrum of topics including the historical background and context of MACRA, an introduction to MIPS, and three individual videos dedicated to MIPS components: Quality, Advancing Care Information and Improvement Activity, and a video outlining the options for participation in 2017.
The PowerPoint presentations seen in the videos are also available, as are links to specific CMS web pages and more information on ACS’ efforts to develop advanced alternative payment models (APMs) for surgeons.
We will continue to update the website throughout the year in our ongoing efforts to refine the resources to be the most useful to Fellows.
I would encourage all Fellows to visit the website, watch the videos, and read the manual. I realize time is a precious commodity, but with a total time investment of 60-90 minutes, one can acquire an operational knowledge of the QPP and make a determination as to how they wish to participate.
Again, no Fellow should settle for accepting a penalty in 2019 based on what they do this year. With the multiple options available, it is simply too easy to avoid and to do so would effectively serve to put their money in someone else’s pocket. For those who feel more prepared (that is, they have previously reported PQRS data and have a 2014 or 2015 edition EHR) and wish to seek a positive rate update, investment of more time will obviously be required. However, in addition to the small positive payment update they will likely receive, probably the most substantial benefit to be derived is their preparation for future years when the incentives and penalties increase to +/- 9%.
Finally, ACS “has your back” on coping with MACRA and as always, ACS staff in Chicago and Washington are available to assist Fellows with their preparation, to answer questions about the program and the reporting requirements, or to provide general or specific direction in their efforts to navigate the QPP.
MACRA is now a fact of life.
Implementation of the Medicare Access and CHIP Reauthorization Act (MACRA), the historic Medicare reform law that replaced the Sustainable Growth Rate (SGR) formula in 2015, began in January 2017. Patrick V. Bailey, MD, FACS, Medical Director, Advocacy, in the American College of Surgeons (ACS) Division of Advocacy and Health Policy (DAHP) office in Washington DC has, for the past several years, been involved with ensuring that the policy implemented takes into account the interests of surgeons and their patients. He has seen MACRA develop from its beginnings. Dr. Bailey, a pediatric surgeon, has deep knowledge about the program, both from the policy perspective and as a surgeon. We asked Dr. Bailey to share with us his insights on what surgeons can expect and what surgeons can do to avoid penalties.
1) Many surgeons are overwhelmed by the perceived complexity of the new MACRA law. What do you say to those who have so far tuned out much of the information they have been given?
A few thoughts. First, we really do understand that the concerns about the complexity are real. Some of those very real feelings come out of a basic aversion to change. Some come from the overall stress and uncertainty surrounding the constant changes in our health care system that have been ongoing for years. And some are the result of the continuously expanding administrative burden. We get it.
Is MACRA exactly what we surgeons would wish for? No, but those of us who have worked in the policy process feel our efforts had a positive impact on how this legislation played out. More importantly, we are absolutely confident that, for 2017, ALL surgeons can avoid a penalty.
From a pragmatic perspective, the implementation of MACRA is going forward, and burying one’s head in the sand will not make it go away. Therefore, it is imperative that surgeons devote some time to understanding the new Quality Payment Program, or QPP, which is the operationalization of the MACRA law. Even a very limited time investment will pay dividends in the Medicare payment they receive in 2019, based on their performance in 2017.
So, if you have avoided dealing with this up until now, I urge you to set aside an hour or so to look at the materials that the ACS has prepared. The reporting requirements may look much less daunting once you become familiar with them.
Again, I am confident that surgeons can and will be successful (as defined by either avoiding a penalty or receiving a small positive rate update), if they take some time to acquire some basic knowledge about the program, make an assessment of their individual practice situation, determine the best course for their individual situation, and take the necessary actions to meet the requirements for the choices they have made.
Fortunately, there is still more than ample time to get started and ACS has developed resources for Fellows to assist them in educating themselves about the program and making their individual choices about their level of participation.
2) With all the talk of change to the Affordable Care Act (ACA), how likely is it that all of this will simply “go away”?
The ACA and MACRA are separate and different pieces of legislation from a temporal, process, policy, and political perspective. In fact, despite the fact that the ACS and other medical specialty groups specifically advocated for language repealing the SGR be included in the ACA in 2010, that did not occur. Therefore, the efforts directed at repealing the SGR took another 5 years and ultimately culminated in the passage of MACRA in 2015.
Many will recall the contentious process and political repercussions that resulted in the passage of the ACA. In contrast, leaders from both political parties worked cooperatively on the SGR repeal legislation we now know as MACRA. This resulted in the MACRA legislation being passed in a very bipartisan manner with only 37 of the 435 members of the House and 8 of the 100 members of the Senate voting against the law.
Accordingly, while we believe there will be a need for some specific, targeted legislative “fixes” and regulatory relief actions from CMS (Centers for Medicare and Medicaid Services) to address faults in the QPP (and the ACS will continue our efforts in this direction), it is highly unlikely that MACRA will be repealed or that it will change significantly in the near-term future.
3) What is the starting point for surgeons who want to learn more and begin the process of determining how best to participate?
There is a relatively straightforward process, which revolves around a series of questions and individual decisions.
First, surgeons should determine if all their Merit-based Incentive Payment System (MIPS) data will be reported by their institution or group via a group reporting option (GPRO). For those surgeons, whose data are so reported, they are done and there is nothing further for them to do.
If their data are not reported for them via a GPRO, then they should determine if CMS has notified them that they are exempt from participating in MIPS due to the low volume threshold. If you see 100 or fewer Medicare patients annually or one submits $30,000 or less in Medicare claims, you are not eligible for MIPS incentives or subject to its penalties.
However, this is not a determination that individual Fellows can make on their own based on data they may have on hand based on prior calendar or fiscal years. Instead, CMS makes the determination based on a specific period and notifies individual providers who are so exempted. It is also our understanding that a website, where one can check whether they have been excluded based on the low volume threshold, is forthcoming from CMS. When this website becomes available, ACS will make sure Fellows are informed.
If your data are not reported via a GPRO and you do not receive notification from CMS that you are exempt based on the low-volume threshold, then you have choices to make – having choices is a good thing.
For those who want to compete for positive updates in their Medicare payment rates in 2019 based on their reporting in 2017, I recommend they first visit facs.org/qpp where we have made available a variety of resources in print, video, and PowerPoint formats to assist Fellows in making their plans for participating for either a full or partial year. The update received will depend on performance and not on the amount of data submitted or the time of participation. That said, for those who plan to fully engage, participation over a longer period of time provides more opportunity for improvement and, thus, increases the potential for better performance.
4) What about surgeons who simply want to avoid a penalty and forgo any chance for a positive update?
If your goal for 2017 is to simply avoid a penalty, CMS only requires data be submitted for only one of the three components of MIPS that will be reported this year. Here again for 2017, you have a choice to submit:
A) The required base score measures for your EHR (now known as Advancing Care Information) OR
B) Participation in one Improvement Activity for 90 days, which is reported by simple attestation OR
C) Submit one Quality measure on one patient, which may be reported by a registry, a qualified clinical data registry (QCDR), an EHR or, traditional claims
One very important point to note is that one is NOT required to have a certified EHR to avoid a penalty for 2017. I believe this point alone has been the source of a lot of misunderstanding and anxiety about the QPP and MIPS.
Another key point is that, by simply engaging in one Improvement Activity (such as Maintenance of Certification Part IV, registering with your state’s prescription drug monitoring program, or use of the ACS’ Surgical Risk Calculator) and attesting to having done so with the ACS Surgeon Specific Registry (SSR) or the CMS web portal, one can avoid a penalty.
Alternatively, using the SSR to submit one Quality measure on one patient will also suffice to prevent one from receiving a penalty in 2019 based on their 2017 performance.
It is relatively easy to avoid any negative financial implications of MIPS in 2017, but it does require some effort, albeit minimal. It is also important for Fellows to remember that, since MIPS is essentially a tournament model, those who choose not to participate will take the penalty that provides the funds used to reward those who do participate. I think most surgeons will want to participate, even if only at the minimal levels outlined above, in order to avoid “paying for” another provider’s positive update.
5) What are the consequences of not participating at the minimal levels you just described and choosing to submit no data?
That question is perhaps best addressed in the form of a comparison between 2016 and 2017.
In 2016, if one did not report any PQRS (Physician Quality Reporting System) data and did not participate in the electronic health record meaningful use program, their lack of participation would result in a 10% negative payment adjustment in 2018. In 2017, if one chooses not to submit the minimal amount of data for either the ACI, Improvement Activity, or Quality components as discussed previously, that lack of participation will lead to a 4% negative payment adjustment in 2019.
In effect, those who have never participated and continue to not do so will see a 6% increase in their Medicare reimbursement in 2019 compared to what they receive in 2018.
However, we DO NOT recommend this option because, in future years, the negative payment adjustments will gradually increase to 9%. Accordingly, we encourage Fellows to use 2017 as a period to learn and get familiar and more comfortable with the reporting of data so that they will be better prepared to be successful in those future years when the stakes are higher.
6) You have mentioned the resources ACS has prepared to assist Fellows with this transition. Can you be more specific about what is available?
The ACS one-stop shop is the Quality Payment Program Resource Center found at www.facs.org/qpp.
Fellows who attended the Clinical Congress in Washington last October likely received a copy of the MACRA Quality Payment Manual which was developed to help educate Fellows about the QPP. That manual has subsequently been totally revamped and updated to reflect the changes to the QPP as reflected in the final rule. We highly encourage Fellows to obtain and read the latest version – it is available as individual sections or as the complete publication on the facs.org/qpp webpage.
Also available on the QPP webpage is the second generation of the video series we first created last fall. There are now a total of 6 videos with a run time for the entire series of approximately 30 minutes. The videos cover a wide spectrum of topics including the historical background and context of MACRA, an introduction to MIPS, and three individual videos dedicated to MIPS components: Quality, Advancing Care Information and Improvement Activity, and a video outlining the options for participation in 2017.
The PowerPoint presentations seen in the videos are also available, as are links to specific CMS web pages and more information on ACS’ efforts to develop advanced alternative payment models (APMs) for surgeons.
We will continue to update the website throughout the year in our ongoing efforts to refine the resources to be the most useful to Fellows.
I would encourage all Fellows to visit the website, watch the videos, and read the manual. I realize time is a precious commodity, but with a total time investment of 60-90 minutes, one can acquire an operational knowledge of the QPP and make a determination as to how they wish to participate.
Again, no Fellow should settle for accepting a penalty in 2019 based on what they do this year. With the multiple options available, it is simply too easy to avoid and to do so would effectively serve to put their money in someone else’s pocket. For those who feel more prepared (that is, they have previously reported PQRS data and have a 2014 or 2015 edition EHR) and wish to seek a positive rate update, investment of more time will obviously be required. However, in addition to the small positive payment update they will likely receive, probably the most substantial benefit to be derived is their preparation for future years when the incentives and penalties increase to +/- 9%.
Finally, ACS “has your back” on coping with MACRA and as always, ACS staff in Chicago and Washington are available to assist Fellows with their preparation, to answer questions about the program and the reporting requirements, or to provide general or specific direction in their efforts to navigate the QPP.
The dermatologic tourist
I’m not much of a traveler. I like to see the world through the adventures of my patients.
This is especially nice in the winter, such as during school vacation week. Within the past 24 hours, I’ve gotten messages from patients in Hawaii, Arizona, and Orlando.
Writing from Hawaii, Melvin showed me a photo of a small white spot that appeared on the outer aspect of his arm. I couldn’t make much of it except to tell him that it doesn’t look like anything that warrants a 9-hour flight to show it to me, at least not until he gets back to town.
Finally, Svetlana forwarded a photograph of a rash on her foot that she said had “just come yesterday.” This was the nicest case of cutaneous larva migrans that I’ve seen in quite some time, although I am fairly sure it has been there for more than a day. I tried not to sound too excited about her diagnosis, of course (“You’ve got the coolest parasite!”), and just suggested that she come in to see me on her return next week.
North, South, West. I’ve been all over, without leaving the chair facing my computer screen. (Nobody seems to have gotten a volcanic eruption in Iceland this year.) All this with no packing, no waiting in airports, no TSA lines. Who says traveling can’t be a pleasure?
Practice dermatology – see the world!
* * * * * * * * * * * * * * * * * * * * * * *
Brian was delighted. The fungal infection on his calf, treated for weeks with a topical steroid that had produced only intolerable itch, was subsiding nicely with oral terbinafine and topical ketoconazole.
“Can I drink when I take this medicine?” he asked. “The Internet says I shouldn’t.”
“It’s only another week, Brian,” I said. “Best to hold off ‘till then.”
“Because I really needed a drink last week,” he said.
“Why was that?”
“I was on a vacation with my father.”
“I see.”
“It was my father and his 70-year-old girlfriend.”
“Oh.”
“We were at a nudist colony.”
“You know, Brian,” I said. “Just hearing about that makes me want a drink myself.”
Practice can take you places you never went, places you’ll never get to, places you never want to get to.
* * * * * * * * * * * * * * * * * * * * * * *
Although I have patients fill out the usual consent form on oral isotretinoin, on which they promise to contact me if they become depressed, I rarely find anyone who does. Instead, people tend to become rather happy once their acne improves.
Since I’m not a psychiatrist, I try to do an amateur job of assessing mood when patients come in for their monthly follow-up. I pass on my technique for any of you might find it useful.
“Hello, Peter, are you having any problems?”
“No.”
“Do you get headaches?”
“No.”
“Nosebleeds?”
“No.”
“Any aches and pains in your muscles?”
“No.”
“Are you depressed?”
“No.”
“Are you always this negative?”
If the patient smiles while saying, “No,” you’re in good shape. If not, consider suggesting a therapist.
Better still, send the patient to the Caribbean. Then propose that you go come along yourself as a consultant, just to keep an eye on things.
And bring sunscreen. For the two of you.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His new book “Act Like a Doctor, Think Like a Patient” is now available at amazon.com and barnesandnoble.com. This is his second book. Write to him at [email protected].
I’m not much of a traveler. I like to see the world through the adventures of my patients.
This is especially nice in the winter, such as during school vacation week. Within the past 24 hours, I’ve gotten messages from patients in Hawaii, Arizona, and Orlando.
Writing from Hawaii, Melvin showed me a photo of a small white spot that appeared on the outer aspect of his arm. I couldn’t make much of it except to tell him that it doesn’t look like anything that warrants a 9-hour flight to show it to me, at least not until he gets back to town.
Finally, Svetlana forwarded a photograph of a rash on her foot that she said had “just come yesterday.” This was the nicest case of cutaneous larva migrans that I’ve seen in quite some time, although I am fairly sure it has been there for more than a day. I tried not to sound too excited about her diagnosis, of course (“You’ve got the coolest parasite!”), and just suggested that she come in to see me on her return next week.
North, South, West. I’ve been all over, without leaving the chair facing my computer screen. (Nobody seems to have gotten a volcanic eruption in Iceland this year.) All this with no packing, no waiting in airports, no TSA lines. Who says traveling can’t be a pleasure?
Practice dermatology – see the world!
* * * * * * * * * * * * * * * * * * * * * * *
Brian was delighted. The fungal infection on his calf, treated for weeks with a topical steroid that had produced only intolerable itch, was subsiding nicely with oral terbinafine and topical ketoconazole.
“Can I drink when I take this medicine?” he asked. “The Internet says I shouldn’t.”
“It’s only another week, Brian,” I said. “Best to hold off ‘till then.”
“Because I really needed a drink last week,” he said.
“Why was that?”
“I was on a vacation with my father.”
“I see.”
“It was my father and his 70-year-old girlfriend.”
“Oh.”
“We were at a nudist colony.”
“You know, Brian,” I said. “Just hearing about that makes me want a drink myself.”
Practice can take you places you never went, places you’ll never get to, places you never want to get to.
* * * * * * * * * * * * * * * * * * * * * * *
Although I have patients fill out the usual consent form on oral isotretinoin, on which they promise to contact me if they become depressed, I rarely find anyone who does. Instead, people tend to become rather happy once their acne improves.
Since I’m not a psychiatrist, I try to do an amateur job of assessing mood when patients come in for their monthly follow-up. I pass on my technique for any of you might find it useful.
“Hello, Peter, are you having any problems?”
“No.”
“Do you get headaches?”
“No.”
“Nosebleeds?”
“No.”
“Any aches and pains in your muscles?”
“No.”
“Are you depressed?”
“No.”
“Are you always this negative?”
If the patient smiles while saying, “No,” you’re in good shape. If not, consider suggesting a therapist.
Better still, send the patient to the Caribbean. Then propose that you go come along yourself as a consultant, just to keep an eye on things.
And bring sunscreen. For the two of you.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His new book “Act Like a Doctor, Think Like a Patient” is now available at amazon.com and barnesandnoble.com. This is his second book. Write to him at [email protected].
I’m not much of a traveler. I like to see the world through the adventures of my patients.
This is especially nice in the winter, such as during school vacation week. Within the past 24 hours, I’ve gotten messages from patients in Hawaii, Arizona, and Orlando.
Writing from Hawaii, Melvin showed me a photo of a small white spot that appeared on the outer aspect of his arm. I couldn’t make much of it except to tell him that it doesn’t look like anything that warrants a 9-hour flight to show it to me, at least not until he gets back to town.
Finally, Svetlana forwarded a photograph of a rash on her foot that she said had “just come yesterday.” This was the nicest case of cutaneous larva migrans that I’ve seen in quite some time, although I am fairly sure it has been there for more than a day. I tried not to sound too excited about her diagnosis, of course (“You’ve got the coolest parasite!”), and just suggested that she come in to see me on her return next week.
North, South, West. I’ve been all over, without leaving the chair facing my computer screen. (Nobody seems to have gotten a volcanic eruption in Iceland this year.) All this with no packing, no waiting in airports, no TSA lines. Who says traveling can’t be a pleasure?
Practice dermatology – see the world!
* * * * * * * * * * * * * * * * * * * * * * *
Brian was delighted. The fungal infection on his calf, treated for weeks with a topical steroid that had produced only intolerable itch, was subsiding nicely with oral terbinafine and topical ketoconazole.
“Can I drink when I take this medicine?” he asked. “The Internet says I shouldn’t.”
“It’s only another week, Brian,” I said. “Best to hold off ‘till then.”
“Because I really needed a drink last week,” he said.
“Why was that?”
“I was on a vacation with my father.”
“I see.”
“It was my father and his 70-year-old girlfriend.”
“Oh.”
“We were at a nudist colony.”
“You know, Brian,” I said. “Just hearing about that makes me want a drink myself.”
Practice can take you places you never went, places you’ll never get to, places you never want to get to.
* * * * * * * * * * * * * * * * * * * * * * *
Although I have patients fill out the usual consent form on oral isotretinoin, on which they promise to contact me if they become depressed, I rarely find anyone who does. Instead, people tend to become rather happy once their acne improves.
Since I’m not a psychiatrist, I try to do an amateur job of assessing mood when patients come in for their monthly follow-up. I pass on my technique for any of you might find it useful.
“Hello, Peter, are you having any problems?”
“No.”
“Do you get headaches?”
“No.”
“Nosebleeds?”
“No.”
“Any aches and pains in your muscles?”
“No.”
“Are you depressed?”
“No.”
“Are you always this negative?”
If the patient smiles while saying, “No,” you’re in good shape. If not, consider suggesting a therapist.
Better still, send the patient to the Caribbean. Then propose that you go come along yourself as a consultant, just to keep an eye on things.
And bring sunscreen. For the two of you.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His new book “Act Like a Doctor, Think Like a Patient” is now available at amazon.com and barnesandnoble.com. This is his second book. Write to him at [email protected].
Surveillance
A few weeks ago I received an email from a pediatrician thanking me for supporting her decision to quit work so that she could be home when her teenage son came home from school. She felt that by being home during her son’s adolescence, not only had she provided him a secure base but she also had helped protect him from a drug-dominated culture that permeated the community where they lived. While I hadn’t touched on it in my column, “Perfect Attendance” (Pediatric News, March 2017), this pediatrician’s experience highlights another benefit of a parental presence during those potentially stormy adolescent years.
In a recent article in the New York Times (“Teenagers Do Dumb Things, but There Are Ways to Limit Recklessness,” by Lisa Damour, March 8, 2017), Dr. Laurence Steinberg, a psychology professor at Temple University, is quoted as saying that “the context in which kids grow up must matter a great deal, and that recklessness isn’t the inevitable byproduct of the period’s biology.”
As writer Lisa Damour cogently states in her article, “For teenagers to find trouble, temptation must meet opportunity.”
Here in Brunswick, high school students finish their school day at 2:10 pm. If the student doesn’t play on a sports team and even if his or her home is at the end of the longest bus route, he or she is going to be home before 3 p.m. ... probably unsupervised. And stuff happens.
Although I may have been unsupervised, I was – or at least I believed that I was – always under constant surveillance. In the 1950s and 1960s, the population of Pleasantville, N.Y. was 5,000 and my mother had me convinced that she knew 4,000 of them. She recounted enough little things she had heard to make me believe that I was being watched by 8,000 eyes. She and the other mothers in town were masters of information sharing long before anyone had heard of networking.
These were not helicopter mothers hovering over every shady corner of our lives. They were simply concerned parents and fellow citizens going about their daily business who were not afraid to say something if they saw something. My mother’s apparent omniscience was a powerful deterrent to my adolescent recklessness. Only after I could afford to buy a car did I feel I could escape her surveillance network. And even then I wasn’t always sure.
The Internet has opened opportunities for mischief that are several orders of magnitude greater than the ones my friends and I sought to exploit in the 1950s and 1960s. However, parents today do have tools with which they can create a surveillance network to protect adolescents from their biologically predetermined urges. They simply need to have to courage to use them and not be afraid to say something if they see something.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
A few weeks ago I received an email from a pediatrician thanking me for supporting her decision to quit work so that she could be home when her teenage son came home from school. She felt that by being home during her son’s adolescence, not only had she provided him a secure base but she also had helped protect him from a drug-dominated culture that permeated the community where they lived. While I hadn’t touched on it in my column, “Perfect Attendance” (Pediatric News, March 2017), this pediatrician’s experience highlights another benefit of a parental presence during those potentially stormy adolescent years.
In a recent article in the New York Times (“Teenagers Do Dumb Things, but There Are Ways to Limit Recklessness,” by Lisa Damour, March 8, 2017), Dr. Laurence Steinberg, a psychology professor at Temple University, is quoted as saying that “the context in which kids grow up must matter a great deal, and that recklessness isn’t the inevitable byproduct of the period’s biology.”
As writer Lisa Damour cogently states in her article, “For teenagers to find trouble, temptation must meet opportunity.”
Here in Brunswick, high school students finish their school day at 2:10 pm. If the student doesn’t play on a sports team and even if his or her home is at the end of the longest bus route, he or she is going to be home before 3 p.m. ... probably unsupervised. And stuff happens.
Although I may have been unsupervised, I was – or at least I believed that I was – always under constant surveillance. In the 1950s and 1960s, the population of Pleasantville, N.Y. was 5,000 and my mother had me convinced that she knew 4,000 of them. She recounted enough little things she had heard to make me believe that I was being watched by 8,000 eyes. She and the other mothers in town were masters of information sharing long before anyone had heard of networking.
These were not helicopter mothers hovering over every shady corner of our lives. They were simply concerned parents and fellow citizens going about their daily business who were not afraid to say something if they saw something. My mother’s apparent omniscience was a powerful deterrent to my adolescent recklessness. Only after I could afford to buy a car did I feel I could escape her surveillance network. And even then I wasn’t always sure.
The Internet has opened opportunities for mischief that are several orders of magnitude greater than the ones my friends and I sought to exploit in the 1950s and 1960s. However, parents today do have tools with which they can create a surveillance network to protect adolescents from their biologically predetermined urges. They simply need to have to courage to use them and not be afraid to say something if they see something.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
A few weeks ago I received an email from a pediatrician thanking me for supporting her decision to quit work so that she could be home when her teenage son came home from school. She felt that by being home during her son’s adolescence, not only had she provided him a secure base but she also had helped protect him from a drug-dominated culture that permeated the community where they lived. While I hadn’t touched on it in my column, “Perfect Attendance” (Pediatric News, March 2017), this pediatrician’s experience highlights another benefit of a parental presence during those potentially stormy adolescent years.
In a recent article in the New York Times (“Teenagers Do Dumb Things, but There Are Ways to Limit Recklessness,” by Lisa Damour, March 8, 2017), Dr. Laurence Steinberg, a psychology professor at Temple University, is quoted as saying that “the context in which kids grow up must matter a great deal, and that recklessness isn’t the inevitable byproduct of the period’s biology.”
As writer Lisa Damour cogently states in her article, “For teenagers to find trouble, temptation must meet opportunity.”
Here in Brunswick, high school students finish their school day at 2:10 pm. If the student doesn’t play on a sports team and even if his or her home is at the end of the longest bus route, he or she is going to be home before 3 p.m. ... probably unsupervised. And stuff happens.
Although I may have been unsupervised, I was – or at least I believed that I was – always under constant surveillance. In the 1950s and 1960s, the population of Pleasantville, N.Y. was 5,000 and my mother had me convinced that she knew 4,000 of them. She recounted enough little things she had heard to make me believe that I was being watched by 8,000 eyes. She and the other mothers in town were masters of information sharing long before anyone had heard of networking.
These were not helicopter mothers hovering over every shady corner of our lives. They were simply concerned parents and fellow citizens going about their daily business who were not afraid to say something if they saw something. My mother’s apparent omniscience was a powerful deterrent to my adolescent recklessness. Only after I could afford to buy a car did I feel I could escape her surveillance network. And even then I wasn’t always sure.
The Internet has opened opportunities for mischief that are several orders of magnitude greater than the ones my friends and I sought to exploit in the 1950s and 1960s. However, parents today do have tools with which they can create a surveillance network to protect adolescents from their biologically predetermined urges. They simply need to have to courage to use them and not be afraid to say something if they see something.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
On vacation, my patients go with me
I’m in the process of planning our family vacations for the summer. I do something different from most when on the road: I take my patients with me.
Well, obviously not physically, but I do cover everything, no matter where I am.
Yes, it takes time. In a ritual my family is used to, two to three times a day I’ll call my staff and go over a list of calls that came in, refills needed, and test results. We go back and forth for a bit. For more complicated questions, I may have to wait until I have my laptop, with the charts on it. If there’s an emergency they’ll call me, and if I can’t be reached, they’ll dial up my call partners.
• I know my patients. I think we all feel that way. I’m more comfortable, and I hope they are too, with the doc who knows them making the decisions.
• My call partners don’t know them. We’re all in solo practice. They don’t have access to my charts any more than I do to theirs. That’s an okay arrangement for a weekend call, but not 2 weeks.
• No surprises. I know that I’m not going to be coming home to a pile of MRI and lab reports that I need to review and act on. If my patient was in the ER or admitted, I spoke to the physician handling it.
A long time ago, when I first started out, I asked another neurologist in my building to cover for me when I was leaving town. I didn’t know him very well, but I was still learning the ropes. He said fine.
When I came home, I found he’d actually “poached” several who’d called, having them come in and convincing them to switch doctors. He’d also changed medications on well-controlled epilepsy and migraine patients who’d needed refills, leaving me to deal with the complications of it when I returned.
Granted, I’ve since learned that he was unusual in that degree, but it really rattled me. I decided I’d rather handle things on my own from then on.
This isn’t an easy decision, but I’m glad I do it. I come home to an office with no surprises, no test results piled up to review, no medication changes that I look at and wonder about.
Does it ruin my vacation? Not at all. Yes, it’s 30-60 minutes out of each day that I have to spend with my office, but I think it’s worth it. It’s peace of mind for me, my staff, and my patients, at least as much as you can ever have in this field.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
[polldaddy:9696724]
I’m in the process of planning our family vacations for the summer. I do something different from most when on the road: I take my patients with me.
Well, obviously not physically, but I do cover everything, no matter where I am.
Yes, it takes time. In a ritual my family is used to, two to three times a day I’ll call my staff and go over a list of calls that came in, refills needed, and test results. We go back and forth for a bit. For more complicated questions, I may have to wait until I have my laptop, with the charts on it. If there’s an emergency they’ll call me, and if I can’t be reached, they’ll dial up my call partners.
• I know my patients. I think we all feel that way. I’m more comfortable, and I hope they are too, with the doc who knows them making the decisions.
• My call partners don’t know them. We’re all in solo practice. They don’t have access to my charts any more than I do to theirs. That’s an okay arrangement for a weekend call, but not 2 weeks.
• No surprises. I know that I’m not going to be coming home to a pile of MRI and lab reports that I need to review and act on. If my patient was in the ER or admitted, I spoke to the physician handling it.
A long time ago, when I first started out, I asked another neurologist in my building to cover for me when I was leaving town. I didn’t know him very well, but I was still learning the ropes. He said fine.
When I came home, I found he’d actually “poached” several who’d called, having them come in and convincing them to switch doctors. He’d also changed medications on well-controlled epilepsy and migraine patients who’d needed refills, leaving me to deal with the complications of it when I returned.
Granted, I’ve since learned that he was unusual in that degree, but it really rattled me. I decided I’d rather handle things on my own from then on.
This isn’t an easy decision, but I’m glad I do it. I come home to an office with no surprises, no test results piled up to review, no medication changes that I look at and wonder about.
Does it ruin my vacation? Not at all. Yes, it’s 30-60 minutes out of each day that I have to spend with my office, but I think it’s worth it. It’s peace of mind for me, my staff, and my patients, at least as much as you can ever have in this field.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
[polldaddy:9696724]
I’m in the process of planning our family vacations for the summer. I do something different from most when on the road: I take my patients with me.
Well, obviously not physically, but I do cover everything, no matter where I am.
Yes, it takes time. In a ritual my family is used to, two to three times a day I’ll call my staff and go over a list of calls that came in, refills needed, and test results. We go back and forth for a bit. For more complicated questions, I may have to wait until I have my laptop, with the charts on it. If there’s an emergency they’ll call me, and if I can’t be reached, they’ll dial up my call partners.
• I know my patients. I think we all feel that way. I’m more comfortable, and I hope they are too, with the doc who knows them making the decisions.
• My call partners don’t know them. We’re all in solo practice. They don’t have access to my charts any more than I do to theirs. That’s an okay arrangement for a weekend call, but not 2 weeks.
• No surprises. I know that I’m not going to be coming home to a pile of MRI and lab reports that I need to review and act on. If my patient was in the ER or admitted, I spoke to the physician handling it.
A long time ago, when I first started out, I asked another neurologist in my building to cover for me when I was leaving town. I didn’t know him very well, but I was still learning the ropes. He said fine.
When I came home, I found he’d actually “poached” several who’d called, having them come in and convincing them to switch doctors. He’d also changed medications on well-controlled epilepsy and migraine patients who’d needed refills, leaving me to deal with the complications of it when I returned.
Granted, I’ve since learned that he was unusual in that degree, but it really rattled me. I decided I’d rather handle things on my own from then on.
This isn’t an easy decision, but I’m glad I do it. I come home to an office with no surprises, no test results piled up to review, no medication changes that I look at and wonder about.
Does it ruin my vacation? Not at all. Yes, it’s 30-60 minutes out of each day that I have to spend with my office, but I think it’s worth it. It’s peace of mind for me, my staff, and my patients, at least as much as you can ever have in this field.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
[polldaddy:9696724]
Ursolic acid
Ursolic acid (3beta-hydroxy-urs-12-en-28-oic acid) is a pentacyclic triterpenoid found naturally in apples, waxy berries, rosemary, oregano, and several other plants and herbs used in medicine and the diet.1,2 It is known to have significant antioxidant, anti-inflammatory, and antiproliferative properties, and has also been associated with a wider range of biologic activities, including anticancer, antimicrobial, antitumor, antiwrinkle, anti-HIV, cytotoxic, and hepatoprotective.3,4 In addition, ursolic acid is the focus of human clinical trials for potential uses in cancer and skin wrinkles.4 While this triterpenoid is known to suppress tumor formation and viability in various kinds of cancer, including skin cancer, several forms of cancer are resistant to ursolic acid.
Anti-inflammatory activity
In a 2013 study of the antibacterial and anti-inflammatory effects of Syzygium jambos on acne, Sharma et al. found that ursolic acid was one of the constituents of the leaf extracts that contributed to a significant suppression of the release of inflammatory cytokines interleukin (IL)-8 and tumor necrosis factor-alpha.5
In 2010, Yang et al. identified ursolic acid as a key constituent of Acanthopanax koreanum fruit, a popular fruit in Jeju Island, South Korea, extracts of which they found to exhibit significant anti-inflammatory activity and suitability as a topical agent.6
Yasukawa et al. conducted an in vivo two-stage carcinogenesis test in mice in 2009 in which extracts of the branches of Hippophae rhamnoides displayed significant antitumor activity after initiation with 7,12-dimethylbenz[a]anthracene (DMBA) and promotion with 12-O-tetradecanoylphorbol-13-acetate (TPA). Ursolic acid and (-)-epigallocatechin were the constituents found to have the greatest inhibitory effects on TPA-induced inflammation.7
A 2002 study by Chattopadhyay et al. revealed that the ursolic acid present in Mallotus peltatus extract (long used in traditional folk medicine to treat skin infections and intestinal disorders) may partially account for the broad anti-inflammatory and antimicrobial activity of the plant.9
In 1997, Máñez et al. noted that ursolic acid was among two of the four selected natural triterpenoids tested and found to be significantly effective against inflammation in a TPA multiple-dose model of chronic skin inflammation.10
Anticancer activity
In 2015, Cho et al. reported on the inhibitory effects on skin tumor promotion from the topical application of ursolic acid, resveratrol, or the combination of the two prior to TPA treatment on mouse skin. The combination of the two botanical agents yielded the strongest suppression of TPA-induced epidermal hyperproliferation, skin inflammation, inflammatory gene expression, and skin tumor promotion.11
In another study that year buttressing the combination of the two botanical agents, Junco et al. demonstrated that chloroquine could be used to sensitize B16F10 metastatic mouse melanoma to the anticancer activities of ursolic acid and resveratrol. The investigators concluded that the combination of ursolic acid or resveratrol with chloroquine has potential for inclusion in melanoma treatment in humans.12 Previously, Junco et al. observed that the anti–skin cancer effects of ursolic acid are augmented by P-glycoprotein inhibitors, and that ursolic acid and the stilbene resveratrol, a potent antioxidant, work synergistically, although not by blocking P-glycoprotein. The investigators suggested that ursolic acid along with resveratrol and/or P-glycoprotein inhibitors have potential as effective anti–skin cancer regimens.
In 2014, Lee et al. showed that ursolic acid can differentially modulate apoptosis in cutaneous melanoma and retinal pigment epithelial cells exposed to ultraviolet to visible broadband radiation, exhibiting the potential to protect normal cells while sensitizing melanoma cells to the effects of UV radiation.13 These findings supported earlier work by the team showing that pretreatment of human cells derived from a malignant skin melanoma markedly enhanced the sensitivity of melanoma cells to UV radiation, while providing some photoprotection to retinal pigment epithelium.
Also that year, Soica et al. demonstrated, using in vitro tests and in vivo skin cancer models, that the mixture of oleanolic and ursolic acids and in complex with cyclodextrin rendered a synergistic antitumor activity.14
A year earlier, Kowalczyk et al. showed that the combined action of phytochemicals – dietary calcium D-glucarate and topical ursolic acid and resveratrol – was effective in suppressing the initiation (with 7,12-dimethylbenz[a]anthracene [DMBA]) and promotion (with TPA) of skin tumorigenesis in SENCAR mice. Ursolic acid alone or in combination with calcium D-glucarate significantly diminished epidermal hyperplasia when applied during promotion. All of the antipromotion protocols led to significant decreases in cyclooxygenase-2 and interleukin (IL)-6 expression. The researchers concluded that ursolic acid strongly inhibits skin tumor promotion and inflammatory signaling, and warrants attention as a potential preventive agent against skin and other epithelial cancers.15 Kowalczyk et al. had previously found that ursolic acid and other phytochemicals displayed significant in vitro and in vivo antioxidant and antitumorigenic activity, inhibiting murine skin carcinogenesis by blunting tumor initiation and tumor promotion/progression.16
In 2006, beta-ursolic acid isolated from Salvia officinalis was found by Jedinák et al. to be effective in suppressing lung colonization of beta16 mouse melanoma cells in vivo.17
Huang et al. showed in 1994 that extracts of the leaves of Rosmarinus officinalis (rosemary) were effective in suppressing tumor initiation and promotion in a two-stage skin tumorigenesis mouse model. Topically applied ursolic acid isolated from the leaves was found to hinder TPA-induced ear inflammation, ornithine decarboxylase activity, and tumor promotion. The number of tumors per mouse also declined significantly due to the topical application of ursolic acid concurrent with twice weekly application of the tumor-promoter TPA in DMBA-initiated mice.18
Antiaging and other activities
In 2015, Herndon et al. conducted an open-label clinical trial in 37 females (aged 35-60 years) to ascertain the effectiveness of an anti-aging moisturizer containing Astragalus membranaceus root extract, a peptide blend including palmitoyl tripeptide-38, standardized rosemary leaf extract (ursolic acid), tetrahexyldecyl ascorbate (THD ascorbate), and ubiquinone (coenzyme Q10). Subjects were instructed to apply the moisturizer once in the morning and once in the evening, and were assessed at baseline, and after 4, 8, and 12 weeks of twice daily application. Clinical evaluations after 8 weeks revealed a statistically significant improvement in all grading parameters (fine lines and wrinkles, clarity/brightness, visual roughness, tactile roughness, redness, hyperpigmentation, and overall appearance), with even more pronounced improvement at 12 weeks. The product was found to be mild and well tolerated, and digital photography reinforced clinical assessments and self-evaluations.19
Lee et al. reported in 2012 on in vitro results suggesting that ursolic acid was effective as an inhibitor of matrix metalloproteinase (MMP)-1 after UVB exposure and was more effective than retinoic acid.20
Based on studies with hairless mice, Lim et al. found in 2007 that ursolic and oleanolic acids can enhance the recovery of skin barrier function and, via peroxisome proliferator-activated receptor-alpha, spur epidermal keratinocyte differentiation. They concluded that both acids have potential for use as agents to promote epidermal permeability barrier function.21
In 2003, Soo et al. observed that pretreatment with ursolic acid inhibited UVA-induced oxidative stress and activation and expression of MMP-2 in HaCaT human keratinocytes. They concluded that ursolic acid may merit attention for the prevention of UVA-induced photoaging.22
Three years earlier, Yarosh et al. showed that liposomes containing ursolic acid augmented ceramide content in cultured normal human epidermal keratinocytes and collagen content in cultured normal human dermal fibroblasts. Over an 11-day period, clinical tests with the ursolic acid–containing liposome (Merotaine) revealed increases in the ceramide content in human skin.23 Two years later, many of the same researchers duplicated their results. This new study also demonstrated that ursolic acid liposomes raise ceramide levels in normal human epidermal keratinocytes, in contrast to the effects of retinoic acid, earlier shown to reduce such levels. They concluded that ursolic acid liposomes show promise for use alone or in combination to replenish or maintain cutaneous ceramide and collagen levels.24 Notably, ursolic acid is incorporated into topical oils and creams intended to confer rejuvenating effects to the skin.
Conclusion
Ursolic acid is a compelling ingredient. I especially will be interested in the results of ongoing human clinical trials of this triterpenoid for treating cancer and skin wrinkles. As it is, ursolic acid is known to exert significant inhibitory activity against tumor formation and tumor cell viability in the laboratory. Given its wide range of biologic activity, and some promising cutaneous results, there is reason to believe that ursolic acid has the potential to play an increasingly useful role in topical skin care agents and dermatologic practice.
References
1. J Dermatol. 2007 Sep;34(9):625-34.
2. Folia Histochem Cytobiol. 2011;49(4):664-9.
3. J Cosmet Dermatol. 2004 Jan;3(1):26-34.
4. J Enzyme Inhib Med Chem. 2011 Oct;26(5):616-42.
5. BMC Complement Altern Med. 2013 Oct 29;13:292.
6. J Biomed Biotechnol. 2010;2010:715739.
7. Fitoterapia. 2009 Apr;80(3):164-7.
8. Biosci Biotechnol Biochem. 2004 Jan;68(1):85-90.
9. J Ethnopharmacol. 2002 Oct;82(2-3):229-37.
10. Eur J Pharmacol. 1997 Sep 3;334(1):103-5.
11. Cancer Prev Res (Phila). 2015 Sep;8(9):817-25.
12. Melanoma Res. 2015 Apr;25(2):103-12.
13. Apoptosis. 2014 May;19(5):816-28.
14. Molecules. 2014 Apr 17;19(4):4924-40.
15. Int J Oncol. 2013 Sep;43(3):911-8.
16. Carcinogenesis. 2009 Jun;30(6):1008-15.
17. Z Naturforsch C. 2006 Nov-Dec;61(11-12):777-82.
18. Cancer Res. 1994 Feb 1;54(3):701-8.
19. J Drugs Dermatol. 2015 Jul;14(7):699-704.
20. Bioorg Khim. 2012 May-Jun;38(3):374-81.
21. J Dermatol. 2007;34(9):625-34.
22. Eur J Pharmacol. 2003 Aug 29;476(3):173-8.
23. Horm Res. 2000;54(5-6):318-21.
24. Arch Dermatol Res. 2002 Jan;293(11):569-75.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever. Dr. Baumann also developed and owns the Baumann Skin Type Solution skin typing systems and related products.
Ursolic acid (3beta-hydroxy-urs-12-en-28-oic acid) is a pentacyclic triterpenoid found naturally in apples, waxy berries, rosemary, oregano, and several other plants and herbs used in medicine and the diet.1,2 It is known to have significant antioxidant, anti-inflammatory, and antiproliferative properties, and has also been associated with a wider range of biologic activities, including anticancer, antimicrobial, antitumor, antiwrinkle, anti-HIV, cytotoxic, and hepatoprotective.3,4 In addition, ursolic acid is the focus of human clinical trials for potential uses in cancer and skin wrinkles.4 While this triterpenoid is known to suppress tumor formation and viability in various kinds of cancer, including skin cancer, several forms of cancer are resistant to ursolic acid.
Anti-inflammatory activity
In a 2013 study of the antibacterial and anti-inflammatory effects of Syzygium jambos on acne, Sharma et al. found that ursolic acid was one of the constituents of the leaf extracts that contributed to a significant suppression of the release of inflammatory cytokines interleukin (IL)-8 and tumor necrosis factor-alpha.5
In 2010, Yang et al. identified ursolic acid as a key constituent of Acanthopanax koreanum fruit, a popular fruit in Jeju Island, South Korea, extracts of which they found to exhibit significant anti-inflammatory activity and suitability as a topical agent.6
Yasukawa et al. conducted an in vivo two-stage carcinogenesis test in mice in 2009 in which extracts of the branches of Hippophae rhamnoides displayed significant antitumor activity after initiation with 7,12-dimethylbenz[a]anthracene (DMBA) and promotion with 12-O-tetradecanoylphorbol-13-acetate (TPA). Ursolic acid and (-)-epigallocatechin were the constituents found to have the greatest inhibitory effects on TPA-induced inflammation.7
A 2002 study by Chattopadhyay et al. revealed that the ursolic acid present in Mallotus peltatus extract (long used in traditional folk medicine to treat skin infections and intestinal disorders) may partially account for the broad anti-inflammatory and antimicrobial activity of the plant.9
In 1997, Máñez et al. noted that ursolic acid was among two of the four selected natural triterpenoids tested and found to be significantly effective against inflammation in a TPA multiple-dose model of chronic skin inflammation.10
Anticancer activity
In 2015, Cho et al. reported on the inhibitory effects on skin tumor promotion from the topical application of ursolic acid, resveratrol, or the combination of the two prior to TPA treatment on mouse skin. The combination of the two botanical agents yielded the strongest suppression of TPA-induced epidermal hyperproliferation, skin inflammation, inflammatory gene expression, and skin tumor promotion.11
In another study that year buttressing the combination of the two botanical agents, Junco et al. demonstrated that chloroquine could be used to sensitize B16F10 metastatic mouse melanoma to the anticancer activities of ursolic acid and resveratrol. The investigators concluded that the combination of ursolic acid or resveratrol with chloroquine has potential for inclusion in melanoma treatment in humans.12 Previously, Junco et al. observed that the anti–skin cancer effects of ursolic acid are augmented by P-glycoprotein inhibitors, and that ursolic acid and the stilbene resveratrol, a potent antioxidant, work synergistically, although not by blocking P-glycoprotein. The investigators suggested that ursolic acid along with resveratrol and/or P-glycoprotein inhibitors have potential as effective anti–skin cancer regimens.
In 2014, Lee et al. showed that ursolic acid can differentially modulate apoptosis in cutaneous melanoma and retinal pigment epithelial cells exposed to ultraviolet to visible broadband radiation, exhibiting the potential to protect normal cells while sensitizing melanoma cells to the effects of UV radiation.13 These findings supported earlier work by the team showing that pretreatment of human cells derived from a malignant skin melanoma markedly enhanced the sensitivity of melanoma cells to UV radiation, while providing some photoprotection to retinal pigment epithelium.
Also that year, Soica et al. demonstrated, using in vitro tests and in vivo skin cancer models, that the mixture of oleanolic and ursolic acids and in complex with cyclodextrin rendered a synergistic antitumor activity.14
A year earlier, Kowalczyk et al. showed that the combined action of phytochemicals – dietary calcium D-glucarate and topical ursolic acid and resveratrol – was effective in suppressing the initiation (with 7,12-dimethylbenz[a]anthracene [DMBA]) and promotion (with TPA) of skin tumorigenesis in SENCAR mice. Ursolic acid alone or in combination with calcium D-glucarate significantly diminished epidermal hyperplasia when applied during promotion. All of the antipromotion protocols led to significant decreases in cyclooxygenase-2 and interleukin (IL)-6 expression. The researchers concluded that ursolic acid strongly inhibits skin tumor promotion and inflammatory signaling, and warrants attention as a potential preventive agent against skin and other epithelial cancers.15 Kowalczyk et al. had previously found that ursolic acid and other phytochemicals displayed significant in vitro and in vivo antioxidant and antitumorigenic activity, inhibiting murine skin carcinogenesis by blunting tumor initiation and tumor promotion/progression.16
In 2006, beta-ursolic acid isolated from Salvia officinalis was found by Jedinák et al. to be effective in suppressing lung colonization of beta16 mouse melanoma cells in vivo.17
Huang et al. showed in 1994 that extracts of the leaves of Rosmarinus officinalis (rosemary) were effective in suppressing tumor initiation and promotion in a two-stage skin tumorigenesis mouse model. Topically applied ursolic acid isolated from the leaves was found to hinder TPA-induced ear inflammation, ornithine decarboxylase activity, and tumor promotion. The number of tumors per mouse also declined significantly due to the topical application of ursolic acid concurrent with twice weekly application of the tumor-promoter TPA in DMBA-initiated mice.18
Antiaging and other activities
In 2015, Herndon et al. conducted an open-label clinical trial in 37 females (aged 35-60 years) to ascertain the effectiveness of an anti-aging moisturizer containing Astragalus membranaceus root extract, a peptide blend including palmitoyl tripeptide-38, standardized rosemary leaf extract (ursolic acid), tetrahexyldecyl ascorbate (THD ascorbate), and ubiquinone (coenzyme Q10). Subjects were instructed to apply the moisturizer once in the morning and once in the evening, and were assessed at baseline, and after 4, 8, and 12 weeks of twice daily application. Clinical evaluations after 8 weeks revealed a statistically significant improvement in all grading parameters (fine lines and wrinkles, clarity/brightness, visual roughness, tactile roughness, redness, hyperpigmentation, and overall appearance), with even more pronounced improvement at 12 weeks. The product was found to be mild and well tolerated, and digital photography reinforced clinical assessments and self-evaluations.19
Lee et al. reported in 2012 on in vitro results suggesting that ursolic acid was effective as an inhibitor of matrix metalloproteinase (MMP)-1 after UVB exposure and was more effective than retinoic acid.20
Based on studies with hairless mice, Lim et al. found in 2007 that ursolic and oleanolic acids can enhance the recovery of skin barrier function and, via peroxisome proliferator-activated receptor-alpha, spur epidermal keratinocyte differentiation. They concluded that both acids have potential for use as agents to promote epidermal permeability barrier function.21
In 2003, Soo et al. observed that pretreatment with ursolic acid inhibited UVA-induced oxidative stress and activation and expression of MMP-2 in HaCaT human keratinocytes. They concluded that ursolic acid may merit attention for the prevention of UVA-induced photoaging.22
Three years earlier, Yarosh et al. showed that liposomes containing ursolic acid augmented ceramide content in cultured normal human epidermal keratinocytes and collagen content in cultured normal human dermal fibroblasts. Over an 11-day period, clinical tests with the ursolic acid–containing liposome (Merotaine) revealed increases in the ceramide content in human skin.23 Two years later, many of the same researchers duplicated their results. This new study also demonstrated that ursolic acid liposomes raise ceramide levels in normal human epidermal keratinocytes, in contrast to the effects of retinoic acid, earlier shown to reduce such levels. They concluded that ursolic acid liposomes show promise for use alone or in combination to replenish or maintain cutaneous ceramide and collagen levels.24 Notably, ursolic acid is incorporated into topical oils and creams intended to confer rejuvenating effects to the skin.
Conclusion
Ursolic acid is a compelling ingredient. I especially will be interested in the results of ongoing human clinical trials of this triterpenoid for treating cancer and skin wrinkles. As it is, ursolic acid is known to exert significant inhibitory activity against tumor formation and tumor cell viability in the laboratory. Given its wide range of biologic activity, and some promising cutaneous results, there is reason to believe that ursolic acid has the potential to play an increasingly useful role in topical skin care agents and dermatologic practice.
References
1. J Dermatol. 2007 Sep;34(9):625-34.
2. Folia Histochem Cytobiol. 2011;49(4):664-9.
3. J Cosmet Dermatol. 2004 Jan;3(1):26-34.
4. J Enzyme Inhib Med Chem. 2011 Oct;26(5):616-42.
5. BMC Complement Altern Med. 2013 Oct 29;13:292.
6. J Biomed Biotechnol. 2010;2010:715739.
7. Fitoterapia. 2009 Apr;80(3):164-7.
8. Biosci Biotechnol Biochem. 2004 Jan;68(1):85-90.
9. J Ethnopharmacol. 2002 Oct;82(2-3):229-37.
10. Eur J Pharmacol. 1997 Sep 3;334(1):103-5.
11. Cancer Prev Res (Phila). 2015 Sep;8(9):817-25.
12. Melanoma Res. 2015 Apr;25(2):103-12.
13. Apoptosis. 2014 May;19(5):816-28.
14. Molecules. 2014 Apr 17;19(4):4924-40.
15. Int J Oncol. 2013 Sep;43(3):911-8.
16. Carcinogenesis. 2009 Jun;30(6):1008-15.
17. Z Naturforsch C. 2006 Nov-Dec;61(11-12):777-82.
18. Cancer Res. 1994 Feb 1;54(3):701-8.
19. J Drugs Dermatol. 2015 Jul;14(7):699-704.
20. Bioorg Khim. 2012 May-Jun;38(3):374-81.
21. J Dermatol. 2007;34(9):625-34.
22. Eur J Pharmacol. 2003 Aug 29;476(3):173-8.
23. Horm Res. 2000;54(5-6):318-21.
24. Arch Dermatol Res. 2002 Jan;293(11):569-75.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever. Dr. Baumann also developed and owns the Baumann Skin Type Solution skin typing systems and related products.
Ursolic acid (3beta-hydroxy-urs-12-en-28-oic acid) is a pentacyclic triterpenoid found naturally in apples, waxy berries, rosemary, oregano, and several other plants and herbs used in medicine and the diet.1,2 It is known to have significant antioxidant, anti-inflammatory, and antiproliferative properties, and has also been associated with a wider range of biologic activities, including anticancer, antimicrobial, antitumor, antiwrinkle, anti-HIV, cytotoxic, and hepatoprotective.3,4 In addition, ursolic acid is the focus of human clinical trials for potential uses in cancer and skin wrinkles.4 While this triterpenoid is known to suppress tumor formation and viability in various kinds of cancer, including skin cancer, several forms of cancer are resistant to ursolic acid.
Anti-inflammatory activity
In a 2013 study of the antibacterial and anti-inflammatory effects of Syzygium jambos on acne, Sharma et al. found that ursolic acid was one of the constituents of the leaf extracts that contributed to a significant suppression of the release of inflammatory cytokines interleukin (IL)-8 and tumor necrosis factor-alpha.5
In 2010, Yang et al. identified ursolic acid as a key constituent of Acanthopanax koreanum fruit, a popular fruit in Jeju Island, South Korea, extracts of which they found to exhibit significant anti-inflammatory activity and suitability as a topical agent.6
Yasukawa et al. conducted an in vivo two-stage carcinogenesis test in mice in 2009 in which extracts of the branches of Hippophae rhamnoides displayed significant antitumor activity after initiation with 7,12-dimethylbenz[a]anthracene (DMBA) and promotion with 12-O-tetradecanoylphorbol-13-acetate (TPA). Ursolic acid and (-)-epigallocatechin were the constituents found to have the greatest inhibitory effects on TPA-induced inflammation.7
A 2002 study by Chattopadhyay et al. revealed that the ursolic acid present in Mallotus peltatus extract (long used in traditional folk medicine to treat skin infections and intestinal disorders) may partially account for the broad anti-inflammatory and antimicrobial activity of the plant.9
In 1997, Máñez et al. noted that ursolic acid was among two of the four selected natural triterpenoids tested and found to be significantly effective against inflammation in a TPA multiple-dose model of chronic skin inflammation.10
Anticancer activity
In 2015, Cho et al. reported on the inhibitory effects on skin tumor promotion from the topical application of ursolic acid, resveratrol, or the combination of the two prior to TPA treatment on mouse skin. The combination of the two botanical agents yielded the strongest suppression of TPA-induced epidermal hyperproliferation, skin inflammation, inflammatory gene expression, and skin tumor promotion.11
In another study that year buttressing the combination of the two botanical agents, Junco et al. demonstrated that chloroquine could be used to sensitize B16F10 metastatic mouse melanoma to the anticancer activities of ursolic acid and resveratrol. The investigators concluded that the combination of ursolic acid or resveratrol with chloroquine has potential for inclusion in melanoma treatment in humans.12 Previously, Junco et al. observed that the anti–skin cancer effects of ursolic acid are augmented by P-glycoprotein inhibitors, and that ursolic acid and the stilbene resveratrol, a potent antioxidant, work synergistically, although not by blocking P-glycoprotein. The investigators suggested that ursolic acid along with resveratrol and/or P-glycoprotein inhibitors have potential as effective anti–skin cancer regimens.
In 2014, Lee et al. showed that ursolic acid can differentially modulate apoptosis in cutaneous melanoma and retinal pigment epithelial cells exposed to ultraviolet to visible broadband radiation, exhibiting the potential to protect normal cells while sensitizing melanoma cells to the effects of UV radiation.13 These findings supported earlier work by the team showing that pretreatment of human cells derived from a malignant skin melanoma markedly enhanced the sensitivity of melanoma cells to UV radiation, while providing some photoprotection to retinal pigment epithelium.
Also that year, Soica et al. demonstrated, using in vitro tests and in vivo skin cancer models, that the mixture of oleanolic and ursolic acids and in complex with cyclodextrin rendered a synergistic antitumor activity.14
A year earlier, Kowalczyk et al. showed that the combined action of phytochemicals – dietary calcium D-glucarate and topical ursolic acid and resveratrol – was effective in suppressing the initiation (with 7,12-dimethylbenz[a]anthracene [DMBA]) and promotion (with TPA) of skin tumorigenesis in SENCAR mice. Ursolic acid alone or in combination with calcium D-glucarate significantly diminished epidermal hyperplasia when applied during promotion. All of the antipromotion protocols led to significant decreases in cyclooxygenase-2 and interleukin (IL)-6 expression. The researchers concluded that ursolic acid strongly inhibits skin tumor promotion and inflammatory signaling, and warrants attention as a potential preventive agent against skin and other epithelial cancers.15 Kowalczyk et al. had previously found that ursolic acid and other phytochemicals displayed significant in vitro and in vivo antioxidant and antitumorigenic activity, inhibiting murine skin carcinogenesis by blunting tumor initiation and tumor promotion/progression.16
In 2006, beta-ursolic acid isolated from Salvia officinalis was found by Jedinák et al. to be effective in suppressing lung colonization of beta16 mouse melanoma cells in vivo.17
Huang et al. showed in 1994 that extracts of the leaves of Rosmarinus officinalis (rosemary) were effective in suppressing tumor initiation and promotion in a two-stage skin tumorigenesis mouse model. Topically applied ursolic acid isolated from the leaves was found to hinder TPA-induced ear inflammation, ornithine decarboxylase activity, and tumor promotion. The number of tumors per mouse also declined significantly due to the topical application of ursolic acid concurrent with twice weekly application of the tumor-promoter TPA in DMBA-initiated mice.18
Antiaging and other activities
In 2015, Herndon et al. conducted an open-label clinical trial in 37 females (aged 35-60 years) to ascertain the effectiveness of an anti-aging moisturizer containing Astragalus membranaceus root extract, a peptide blend including palmitoyl tripeptide-38, standardized rosemary leaf extract (ursolic acid), tetrahexyldecyl ascorbate (THD ascorbate), and ubiquinone (coenzyme Q10). Subjects were instructed to apply the moisturizer once in the morning and once in the evening, and were assessed at baseline, and after 4, 8, and 12 weeks of twice daily application. Clinical evaluations after 8 weeks revealed a statistically significant improvement in all grading parameters (fine lines and wrinkles, clarity/brightness, visual roughness, tactile roughness, redness, hyperpigmentation, and overall appearance), with even more pronounced improvement at 12 weeks. The product was found to be mild and well tolerated, and digital photography reinforced clinical assessments and self-evaluations.19
Lee et al. reported in 2012 on in vitro results suggesting that ursolic acid was effective as an inhibitor of matrix metalloproteinase (MMP)-1 after UVB exposure and was more effective than retinoic acid.20
Based on studies with hairless mice, Lim et al. found in 2007 that ursolic and oleanolic acids can enhance the recovery of skin barrier function and, via peroxisome proliferator-activated receptor-alpha, spur epidermal keratinocyte differentiation. They concluded that both acids have potential for use as agents to promote epidermal permeability barrier function.21
In 2003, Soo et al. observed that pretreatment with ursolic acid inhibited UVA-induced oxidative stress and activation and expression of MMP-2 in HaCaT human keratinocytes. They concluded that ursolic acid may merit attention for the prevention of UVA-induced photoaging.22
Three years earlier, Yarosh et al. showed that liposomes containing ursolic acid augmented ceramide content in cultured normal human epidermal keratinocytes and collagen content in cultured normal human dermal fibroblasts. Over an 11-day period, clinical tests with the ursolic acid–containing liposome (Merotaine) revealed increases in the ceramide content in human skin.23 Two years later, many of the same researchers duplicated their results. This new study also demonstrated that ursolic acid liposomes raise ceramide levels in normal human epidermal keratinocytes, in contrast to the effects of retinoic acid, earlier shown to reduce such levels. They concluded that ursolic acid liposomes show promise for use alone or in combination to replenish or maintain cutaneous ceramide and collagen levels.24 Notably, ursolic acid is incorporated into topical oils and creams intended to confer rejuvenating effects to the skin.
Conclusion
Ursolic acid is a compelling ingredient. I especially will be interested in the results of ongoing human clinical trials of this triterpenoid for treating cancer and skin wrinkles. As it is, ursolic acid is known to exert significant inhibitory activity against tumor formation and tumor cell viability in the laboratory. Given its wide range of biologic activity, and some promising cutaneous results, there is reason to believe that ursolic acid has the potential to play an increasingly useful role in topical skin care agents and dermatologic practice.
References
1. J Dermatol. 2007 Sep;34(9):625-34.
2. Folia Histochem Cytobiol. 2011;49(4):664-9.
3. J Cosmet Dermatol. 2004 Jan;3(1):26-34.
4. J Enzyme Inhib Med Chem. 2011 Oct;26(5):616-42.
5. BMC Complement Altern Med. 2013 Oct 29;13:292.
6. J Biomed Biotechnol. 2010;2010:715739.
7. Fitoterapia. 2009 Apr;80(3):164-7.
8. Biosci Biotechnol Biochem. 2004 Jan;68(1):85-90.
9. J Ethnopharmacol. 2002 Oct;82(2-3):229-37.
10. Eur J Pharmacol. 1997 Sep 3;334(1):103-5.
11. Cancer Prev Res (Phila). 2015 Sep;8(9):817-25.
12. Melanoma Res. 2015 Apr;25(2):103-12.
13. Apoptosis. 2014 May;19(5):816-28.
14. Molecules. 2014 Apr 17;19(4):4924-40.
15. Int J Oncol. 2013 Sep;43(3):911-8.
16. Carcinogenesis. 2009 Jun;30(6):1008-15.
17. Z Naturforsch C. 2006 Nov-Dec;61(11-12):777-82.
18. Cancer Res. 1994 Feb 1;54(3):701-8.
19. J Drugs Dermatol. 2015 Jul;14(7):699-704.
20. Bioorg Khim. 2012 May-Jun;38(3):374-81.
21. J Dermatol. 2007;34(9):625-34.
22. Eur J Pharmacol. 2003 Aug 29;476(3):173-8.
23. Horm Res. 2000;54(5-6):318-21.
24. Arch Dermatol Res. 2002 Jan;293(11):569-75.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever. Dr. Baumann also developed and owns the Baumann Skin Type Solution skin typing systems and related products.