User login
Managing menopause symptoms in gynecologic cancer survivors
Due to advancements in surgical treatment, chemotherapy, and radiation therapy, gynecologic cancer survival rates are continuing to improve and quality of life is evolving into an even more significant focus in cancer care.
Roughly 30%-40% of all women with a gynecologic malignancy will experience climacteric symptoms and menopause prior to the anticipated time of natural menopause (J Clin Oncol. 2009 Mar 10;27[8]:1214-9). Cessation of ovarian estrogen and progesterone production can result in short-term as well as long-term sequelae, including vasomotor symptoms, vaginal dryness, osteoporosis, and mood disturbances. Iatrogenic menopause after cancer treatment can be more sudden and severe when compared with the natural course of physiologic menopause. As a result, determination of safe, effective modalities for treating these symptoms is of particular importance for survivor quality of life.
Both combination and estrogen-only hormone replacement therapy (HT) provide greater improvement in these specific symptoms and overall quality of life than placebo as demonstrated in several observational and randomized control trials (Cochrane Database Syst Rev. 2009 Apr 15;[2]:CD004143).
Endometrial cancer
Endometrial cancer is the most common gynecologic malignancy, with approximately 54,000 new cases anticipated in the United States in 2015. Twenty-five percent of these new cases will be in premenopausal women, and with an ever-increasing obesity rate, this number may continue to climb.
Women with early-stage Type 1 endometrial cancer who have vasomotor symptoms after surgery may be offered a short course of estrogen-based HT at the lowest effective dose following hysterectomy/bilateral salpingo-oophorectomy and staging procedure (J Clin Oncol. 2006 Feb 1;24[4]:587-92). For women with genitourinary symptoms, vaginal moisturizers and/or low-dose vaginal estrogen are reasonable options. Unfortunately, there are no data to guide the use of estrogen replacement therapy in women with Type 2 endometrial cancers (Gynecol Oncol. 2011 Aug;122[2]:447-54).
Ovarian cancer
There is minimal data implicating a hormonal causation to ovarian carcinogenesis. Most women with epithelial ovarian cancer do not express tumor estrogen or progesterone receptors. Treatment will result in abrupt, iatrogenic menopause, raising the question of whether it is safe to use HT in patients with epithelial ovarian cancer.
Multiple studies have failed to demonstrate a difference in 5-year survival rates in women with epithelial cancer using HT for 2 years or less (JAMA. 2009 Jul 15;302[3]:298-305, Eur J Gynaecol Oncol. 2000;21[2]:192-6, Cancer. 1999 Sep 15;86[6]:1013-8). As such, symptomatic patients could be offered a course of HT; however, caution should be exercised in women with estrogen/progesterone–expressing tumors or nonepithelial tumors. As with endometrial cancer patients, the lowest effective doses should be prescribed.
Cervical cancer
Most cervical squamous and adenocarcinomas are not hormone dependent. For women with early-stage squamous cell carcinoma, ovarian conservation may be possible or oophoropexy may be offered. However, for many patients, bilateral salpingo-oophorectomy at the time of hysterectomy is more common, and the local effect of radiation therapy can result in vaginal atrophy with subsequent dyspareunia or ovarian failure from radiation scatter. Even for patients who undergo oophoropexy, radiation scatter may still result in ovarian failure. In a few observational studies, there are no data to infer that cervical cancer is hormonally related or that survival rates are decreased.
Currently, HT use in cervical cancer survivors is considered safe. Of note, for women with more advanced-stage cervical cancer and who received chemoradiation for primary treatment, combination therapy with estrogen and progesterone may be more appropriate if the uterus remains in situ. However, for women who have undergone hysterectomy, combination therapy with progesterone may not be warranted and estrogen alone (orally or vaginally) is acceptable (Gynecol Oncol. 2011 Aug;122[2]:447-54)
Nonhormonal therapies
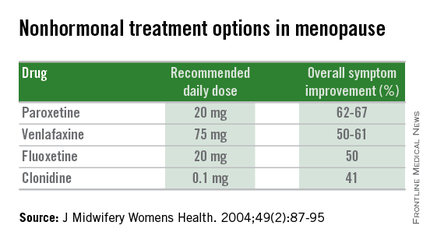
Women presenting with menopausal symptoms in whom estrogen therapy is contraindicated or not desired can also consider using nonhormonal therapies as an alternative. These include selective serotonin reuptake inhibitors (SSRIs) and alpha-2 adrenergic agonists, such as clonidine. Albeit not as effective as HT, these alternative therapies are reasonable options, particularly for management of vasomotor symptoms.
From a limited number of observational studies and a few randomized trials, short-term hormone replacement therapy does not present increased risk to survivors of gynecologic cancers. Additionally, patients have the added option of using nonhormonal therapies, which may provide some benefit. The decision to institute HT should occur after a thorough discussion of the potential to optimize symptom control and the theoretical risk of stimulating quiescent malignant disease.
Dr. Staley is a resident physician in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill. Dr. Gehrig is professor and director of gynecologic oncology at the university. They reported having no relevant financial disclosures.
Due to advancements in surgical treatment, chemotherapy, and radiation therapy, gynecologic cancer survival rates are continuing to improve and quality of life is evolving into an even more significant focus in cancer care.
Roughly 30%-40% of all women with a gynecologic malignancy will experience climacteric symptoms and menopause prior to the anticipated time of natural menopause (J Clin Oncol. 2009 Mar 10;27[8]:1214-9). Cessation of ovarian estrogen and progesterone production can result in short-term as well as long-term sequelae, including vasomotor symptoms, vaginal dryness, osteoporosis, and mood disturbances. Iatrogenic menopause after cancer treatment can be more sudden and severe when compared with the natural course of physiologic menopause. As a result, determination of safe, effective modalities for treating these symptoms is of particular importance for survivor quality of life.
Both combination and estrogen-only hormone replacement therapy (HT) provide greater improvement in these specific symptoms and overall quality of life than placebo as demonstrated in several observational and randomized control trials (Cochrane Database Syst Rev. 2009 Apr 15;[2]:CD004143).
Endometrial cancer
Endometrial cancer is the most common gynecologic malignancy, with approximately 54,000 new cases anticipated in the United States in 2015. Twenty-five percent of these new cases will be in premenopausal women, and with an ever-increasing obesity rate, this number may continue to climb.
Women with early-stage Type 1 endometrial cancer who have vasomotor symptoms after surgery may be offered a short course of estrogen-based HT at the lowest effective dose following hysterectomy/bilateral salpingo-oophorectomy and staging procedure (J Clin Oncol. 2006 Feb 1;24[4]:587-92). For women with genitourinary symptoms, vaginal moisturizers and/or low-dose vaginal estrogen are reasonable options. Unfortunately, there are no data to guide the use of estrogen replacement therapy in women with Type 2 endometrial cancers (Gynecol Oncol. 2011 Aug;122[2]:447-54).
Ovarian cancer
There is minimal data implicating a hormonal causation to ovarian carcinogenesis. Most women with epithelial ovarian cancer do not express tumor estrogen or progesterone receptors. Treatment will result in abrupt, iatrogenic menopause, raising the question of whether it is safe to use HT in patients with epithelial ovarian cancer.
Multiple studies have failed to demonstrate a difference in 5-year survival rates in women with epithelial cancer using HT for 2 years or less (JAMA. 2009 Jul 15;302[3]:298-305, Eur J Gynaecol Oncol. 2000;21[2]:192-6, Cancer. 1999 Sep 15;86[6]:1013-8). As such, symptomatic patients could be offered a course of HT; however, caution should be exercised in women with estrogen/progesterone–expressing tumors or nonepithelial tumors. As with endometrial cancer patients, the lowest effective doses should be prescribed.
Cervical cancer
Most cervical squamous and adenocarcinomas are not hormone dependent. For women with early-stage squamous cell carcinoma, ovarian conservation may be possible or oophoropexy may be offered. However, for many patients, bilateral salpingo-oophorectomy at the time of hysterectomy is more common, and the local effect of radiation therapy can result in vaginal atrophy with subsequent dyspareunia or ovarian failure from radiation scatter. Even for patients who undergo oophoropexy, radiation scatter may still result in ovarian failure. In a few observational studies, there are no data to infer that cervical cancer is hormonally related or that survival rates are decreased.
Currently, HT use in cervical cancer survivors is considered safe. Of note, for women with more advanced-stage cervical cancer and who received chemoradiation for primary treatment, combination therapy with estrogen and progesterone may be more appropriate if the uterus remains in situ. However, for women who have undergone hysterectomy, combination therapy with progesterone may not be warranted and estrogen alone (orally or vaginally) is acceptable (Gynecol Oncol. 2011 Aug;122[2]:447-54)
Nonhormonal therapies
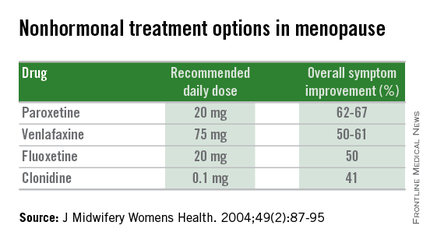
Women presenting with menopausal symptoms in whom estrogen therapy is contraindicated or not desired can also consider using nonhormonal therapies as an alternative. These include selective serotonin reuptake inhibitors (SSRIs) and alpha-2 adrenergic agonists, such as clonidine. Albeit not as effective as HT, these alternative therapies are reasonable options, particularly for management of vasomotor symptoms.
From a limited number of observational studies and a few randomized trials, short-term hormone replacement therapy does not present increased risk to survivors of gynecologic cancers. Additionally, patients have the added option of using nonhormonal therapies, which may provide some benefit. The decision to institute HT should occur after a thorough discussion of the potential to optimize symptom control and the theoretical risk of stimulating quiescent malignant disease.
Dr. Staley is a resident physician in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill. Dr. Gehrig is professor and director of gynecologic oncology at the university. They reported having no relevant financial disclosures.
Due to advancements in surgical treatment, chemotherapy, and radiation therapy, gynecologic cancer survival rates are continuing to improve and quality of life is evolving into an even more significant focus in cancer care.
Roughly 30%-40% of all women with a gynecologic malignancy will experience climacteric symptoms and menopause prior to the anticipated time of natural menopause (J Clin Oncol. 2009 Mar 10;27[8]:1214-9). Cessation of ovarian estrogen and progesterone production can result in short-term as well as long-term sequelae, including vasomotor symptoms, vaginal dryness, osteoporosis, and mood disturbances. Iatrogenic menopause after cancer treatment can be more sudden and severe when compared with the natural course of physiologic menopause. As a result, determination of safe, effective modalities for treating these symptoms is of particular importance for survivor quality of life.
Both combination and estrogen-only hormone replacement therapy (HT) provide greater improvement in these specific symptoms and overall quality of life than placebo as demonstrated in several observational and randomized control trials (Cochrane Database Syst Rev. 2009 Apr 15;[2]:CD004143).
Endometrial cancer
Endometrial cancer is the most common gynecologic malignancy, with approximately 54,000 new cases anticipated in the United States in 2015. Twenty-five percent of these new cases will be in premenopausal women, and with an ever-increasing obesity rate, this number may continue to climb.
Women with early-stage Type 1 endometrial cancer who have vasomotor symptoms after surgery may be offered a short course of estrogen-based HT at the lowest effective dose following hysterectomy/bilateral salpingo-oophorectomy and staging procedure (J Clin Oncol. 2006 Feb 1;24[4]:587-92). For women with genitourinary symptoms, vaginal moisturizers and/or low-dose vaginal estrogen are reasonable options. Unfortunately, there are no data to guide the use of estrogen replacement therapy in women with Type 2 endometrial cancers (Gynecol Oncol. 2011 Aug;122[2]:447-54).
Ovarian cancer
There is minimal data implicating a hormonal causation to ovarian carcinogenesis. Most women with epithelial ovarian cancer do not express tumor estrogen or progesterone receptors. Treatment will result in abrupt, iatrogenic menopause, raising the question of whether it is safe to use HT in patients with epithelial ovarian cancer.
Multiple studies have failed to demonstrate a difference in 5-year survival rates in women with epithelial cancer using HT for 2 years or less (JAMA. 2009 Jul 15;302[3]:298-305, Eur J Gynaecol Oncol. 2000;21[2]:192-6, Cancer. 1999 Sep 15;86[6]:1013-8). As such, symptomatic patients could be offered a course of HT; however, caution should be exercised in women with estrogen/progesterone–expressing tumors or nonepithelial tumors. As with endometrial cancer patients, the lowest effective doses should be prescribed.
Cervical cancer
Most cervical squamous and adenocarcinomas are not hormone dependent. For women with early-stage squamous cell carcinoma, ovarian conservation may be possible or oophoropexy may be offered. However, for many patients, bilateral salpingo-oophorectomy at the time of hysterectomy is more common, and the local effect of radiation therapy can result in vaginal atrophy with subsequent dyspareunia or ovarian failure from radiation scatter. Even for patients who undergo oophoropexy, radiation scatter may still result in ovarian failure. In a few observational studies, there are no data to infer that cervical cancer is hormonally related or that survival rates are decreased.
Currently, HT use in cervical cancer survivors is considered safe. Of note, for women with more advanced-stage cervical cancer and who received chemoradiation for primary treatment, combination therapy with estrogen and progesterone may be more appropriate if the uterus remains in situ. However, for women who have undergone hysterectomy, combination therapy with progesterone may not be warranted and estrogen alone (orally or vaginally) is acceptable (Gynecol Oncol. 2011 Aug;122[2]:447-54)
Nonhormonal therapies
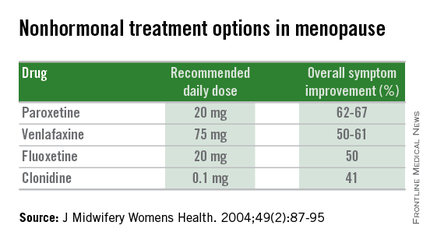
Women presenting with menopausal symptoms in whom estrogen therapy is contraindicated or not desired can also consider using nonhormonal therapies as an alternative. These include selective serotonin reuptake inhibitors (SSRIs) and alpha-2 adrenergic agonists, such as clonidine. Albeit not as effective as HT, these alternative therapies are reasonable options, particularly for management of vasomotor symptoms.
From a limited number of observational studies and a few randomized trials, short-term hormone replacement therapy does not present increased risk to survivors of gynecologic cancers. Additionally, patients have the added option of using nonhormonal therapies, which may provide some benefit. The decision to institute HT should occur after a thorough discussion of the potential to optimize symptom control and the theoretical risk of stimulating quiescent malignant disease.
Dr. Staley is a resident physician in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill. Dr. Gehrig is professor and director of gynecologic oncology at the university. They reported having no relevant financial disclosures.
Naloxone to revive an addict
We are in the midst of an epidemic of heroin and prescription opioid abuse. While the two do not completely explain each other, they are tragically and irrevocably linked.
From 2001 to 2013, we have observed a threefold increase in the total number of overdose deaths from opioid pain relievers (about 16,000 in 2013) and a fivefold increase in the total number of overdose deaths from heroin (about 8,000 in 2013).
Heroin initiation is almost 20 times higher among individuals reporting nonmedical prescription pain reliever use. Among opioid-treatment seekers, the majority of individuals who initiated opioid use in the 1960s were first exposed to heroin. This is in contrast to those who initiated in the 2000s, among whom the majority were exposed to prescription opioids. For young adults, the main sources of opioids are family, friends … and clinicians.
Opioids are powerfully addictive and can be snorted, swallowed, smoked, or shot. Data from the START (Starting Treatment with Agonist Replacement Therapies) trial suggest that individuals who inject opioids are less likely to remain in treatment than noninjectors. This necessarily increases the risk for injectors to inject again and be at risk for overdose.
Opioid overdose can be reversed with the use of naloxone. But naloxone has to be immediately or quickly available for it to be effective. Take-home naloxone programs are located in 30 U.S. states and the District of Columbia. Since 1996, home naloxone programs have reported more than 26,000 drug overdose reversals with naloxone.
On Nov. 18, the Food and Drug Administration announced the approval of a naloxone nasal spray. Prior to this approval, naloxone was only available in the injectable form (syringe or auto-injector), and needle management likely posed a barrier to first responders. The nasal spray can be administered easily without medical training. Naloxone nasal spray administered in one nostril delivered approximately the same levels or higher of naloxone as a single dose of an FDA-approved naloxone intramuscular injection in approximately the same time frame.
It is one thing to save a heroin addict who has just overdosed with nasal naloxone followed by appropriate medical attention. It is entirely another to engage them in an effective drug treatment program.
If naloxone revives them, it is treatment that can save them.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article.
We are in the midst of an epidemic of heroin and prescription opioid abuse. While the two do not completely explain each other, they are tragically and irrevocably linked.
From 2001 to 2013, we have observed a threefold increase in the total number of overdose deaths from opioid pain relievers (about 16,000 in 2013) and a fivefold increase in the total number of overdose deaths from heroin (about 8,000 in 2013).
Heroin initiation is almost 20 times higher among individuals reporting nonmedical prescription pain reliever use. Among opioid-treatment seekers, the majority of individuals who initiated opioid use in the 1960s were first exposed to heroin. This is in contrast to those who initiated in the 2000s, among whom the majority were exposed to prescription opioids. For young adults, the main sources of opioids are family, friends … and clinicians.
Opioids are powerfully addictive and can be snorted, swallowed, smoked, or shot. Data from the START (Starting Treatment with Agonist Replacement Therapies) trial suggest that individuals who inject opioids are less likely to remain in treatment than noninjectors. This necessarily increases the risk for injectors to inject again and be at risk for overdose.
Opioid overdose can be reversed with the use of naloxone. But naloxone has to be immediately or quickly available for it to be effective. Take-home naloxone programs are located in 30 U.S. states and the District of Columbia. Since 1996, home naloxone programs have reported more than 26,000 drug overdose reversals with naloxone.
On Nov. 18, the Food and Drug Administration announced the approval of a naloxone nasal spray. Prior to this approval, naloxone was only available in the injectable form (syringe or auto-injector), and needle management likely posed a barrier to first responders. The nasal spray can be administered easily without medical training. Naloxone nasal spray administered in one nostril delivered approximately the same levels or higher of naloxone as a single dose of an FDA-approved naloxone intramuscular injection in approximately the same time frame.
It is one thing to save a heroin addict who has just overdosed with nasal naloxone followed by appropriate medical attention. It is entirely another to engage them in an effective drug treatment program.
If naloxone revives them, it is treatment that can save them.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article.
We are in the midst of an epidemic of heroin and prescription opioid abuse. While the two do not completely explain each other, they are tragically and irrevocably linked.
From 2001 to 2013, we have observed a threefold increase in the total number of overdose deaths from opioid pain relievers (about 16,000 in 2013) and a fivefold increase in the total number of overdose deaths from heroin (about 8,000 in 2013).
Heroin initiation is almost 20 times higher among individuals reporting nonmedical prescription pain reliever use. Among opioid-treatment seekers, the majority of individuals who initiated opioid use in the 1960s were first exposed to heroin. This is in contrast to those who initiated in the 2000s, among whom the majority were exposed to prescription opioids. For young adults, the main sources of opioids are family, friends … and clinicians.
Opioids are powerfully addictive and can be snorted, swallowed, smoked, or shot. Data from the START (Starting Treatment with Agonist Replacement Therapies) trial suggest that individuals who inject opioids are less likely to remain in treatment than noninjectors. This necessarily increases the risk for injectors to inject again and be at risk for overdose.
Opioid overdose can be reversed with the use of naloxone. But naloxone has to be immediately or quickly available for it to be effective. Take-home naloxone programs are located in 30 U.S. states and the District of Columbia. Since 1996, home naloxone programs have reported more than 26,000 drug overdose reversals with naloxone.
On Nov. 18, the Food and Drug Administration announced the approval of a naloxone nasal spray. Prior to this approval, naloxone was only available in the injectable form (syringe or auto-injector), and needle management likely posed a barrier to first responders. The nasal spray can be administered easily without medical training. Naloxone nasal spray administered in one nostril delivered approximately the same levels or higher of naloxone as a single dose of an FDA-approved naloxone intramuscular injection in approximately the same time frame.
It is one thing to save a heroin addict who has just overdosed with nasal naloxone followed by appropriate medical attention. It is entirely another to engage them in an effective drug treatment program.
If naloxone revives them, it is treatment that can save them.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article.
Polymyxin resistance is bad news
The finding of British and Chinese colleagues of a new plasmid-borne resistance, MCR-1, encoding for resistance to colistin/polymyxin in Escherichia coli, Klebsiella, and Pseudomonas aeruginosa is, as many have pointed out, very bad news (Lancet Infec Dis. 2015 Nov 18. doi: 10.1016/S1473-3099[15]00424-7).
The fact that it may have infiltrated large areas of East and Southeast Asia forebodes an era where no antibiotic will be available to treat some of our patients. It is not the end of mankind, and it will not bring us back to the Middle Ages, after all we managed to rather successfully experience the end of the Second World War without having experienced extinction as a species.
BUT, here is the crunch of the matter – we have since then developed what is today ‘modern medicine’ and modern medicine as we know it with successful treatment of malignant blood disorders, cancer, transplantations, intensive care, neonatal care, and foreign body surgery is very much dependent on managing to prevent and treat complications in the form of infections. If panresistance becomes common we may have to reevaluate our strategies when dealing with these disorders and procedures.
What did we do to deserve this? We have behaved the way we behave with most natural resources available to us. We have abused antibiotics since we discovered them, and we continue to squander them for economical gain in areas where antibiotics have no place at all. We look for evidence that using 600 tons of antibiotics to successfully rear pigs is not harmful instead of saying ‘why take the risk?’
In the latest case, that of the new gene MCR-1 encoding resistance to colistin/polymyxin, it is now believed that the frequent use of colistin in animal husbandry in China and other East Asian countries may be behind the catastrophe.
Evolution is a harsh but fair task master. We deserve everything we get. But again we have squandered the resources of our children and grandchildren.
Dr. Gunnar Kahlmeter is communications officer at the European Society of Clinical Microbiology and Infectious Diseases and practices in the department of clinical microbiology at Central Hospital in Växjö, Sweden.
The finding of British and Chinese colleagues of a new plasmid-borne resistance, MCR-1, encoding for resistance to colistin/polymyxin in Escherichia coli, Klebsiella, and Pseudomonas aeruginosa is, as many have pointed out, very bad news (Lancet Infec Dis. 2015 Nov 18. doi: 10.1016/S1473-3099[15]00424-7).
The fact that it may have infiltrated large areas of East and Southeast Asia forebodes an era where no antibiotic will be available to treat some of our patients. It is not the end of mankind, and it will not bring us back to the Middle Ages, after all we managed to rather successfully experience the end of the Second World War without having experienced extinction as a species.
BUT, here is the crunch of the matter – we have since then developed what is today ‘modern medicine’ and modern medicine as we know it with successful treatment of malignant blood disorders, cancer, transplantations, intensive care, neonatal care, and foreign body surgery is very much dependent on managing to prevent and treat complications in the form of infections. If panresistance becomes common we may have to reevaluate our strategies when dealing with these disorders and procedures.
What did we do to deserve this? We have behaved the way we behave with most natural resources available to us. We have abused antibiotics since we discovered them, and we continue to squander them for economical gain in areas where antibiotics have no place at all. We look for evidence that using 600 tons of antibiotics to successfully rear pigs is not harmful instead of saying ‘why take the risk?’
In the latest case, that of the new gene MCR-1 encoding resistance to colistin/polymyxin, it is now believed that the frequent use of colistin in animal husbandry in China and other East Asian countries may be behind the catastrophe.
Evolution is a harsh but fair task master. We deserve everything we get. But again we have squandered the resources of our children and grandchildren.
Dr. Gunnar Kahlmeter is communications officer at the European Society of Clinical Microbiology and Infectious Diseases and practices in the department of clinical microbiology at Central Hospital in Växjö, Sweden.
The finding of British and Chinese colleagues of a new plasmid-borne resistance, MCR-1, encoding for resistance to colistin/polymyxin in Escherichia coli, Klebsiella, and Pseudomonas aeruginosa is, as many have pointed out, very bad news (Lancet Infec Dis. 2015 Nov 18. doi: 10.1016/S1473-3099[15]00424-7).
The fact that it may have infiltrated large areas of East and Southeast Asia forebodes an era where no antibiotic will be available to treat some of our patients. It is not the end of mankind, and it will not bring us back to the Middle Ages, after all we managed to rather successfully experience the end of the Second World War without having experienced extinction as a species.
BUT, here is the crunch of the matter – we have since then developed what is today ‘modern medicine’ and modern medicine as we know it with successful treatment of malignant blood disorders, cancer, transplantations, intensive care, neonatal care, and foreign body surgery is very much dependent on managing to prevent and treat complications in the form of infections. If panresistance becomes common we may have to reevaluate our strategies when dealing with these disorders and procedures.
What did we do to deserve this? We have behaved the way we behave with most natural resources available to us. We have abused antibiotics since we discovered them, and we continue to squander them for economical gain in areas where antibiotics have no place at all. We look for evidence that using 600 tons of antibiotics to successfully rear pigs is not harmful instead of saying ‘why take the risk?’
In the latest case, that of the new gene MCR-1 encoding resistance to colistin/polymyxin, it is now believed that the frequent use of colistin in animal husbandry in China and other East Asian countries may be behind the catastrophe.
Evolution is a harsh but fair task master. We deserve everything we get. But again we have squandered the resources of our children and grandchildren.
Dr. Gunnar Kahlmeter is communications officer at the European Society of Clinical Microbiology and Infectious Diseases and practices in the department of clinical microbiology at Central Hospital in Växjö, Sweden.
Relationship-Based Care: A novel approach for patients and providers
When I think of the word “relationship,” I imagine gazing into the loving eyes of my husband, playing hide and seek with my children, or texting my best friend for no good reason other than to just say hello.
There is a special comfort zone we expect from people who are close to us; a feeling of love and acceptance that we can’t find elsewhere.
But in a much broader sense, our important relationships extend far beyond our inner circle to include every single person who is involved with our health care team. Our team includes the hospital executives who create new safety initiatives, develop budgets, and oversee a host of other patient care and fiscal functions. The physical therapists who evaluate our patients and make recommendations on how to safely transition them out of the hospital are on our team. The housekeepers who scrub the toilets and wash the linens to prevent nosocomial infections are on our team. They, along with many others, play a pivotal role in our patients’ care, although many important players make their impact behind the scenes.
Yet, of course, our most important professional relationships are not with the CEO, the pharmacist, or even the nursing staff. Our most important relationships are with our patients and their families. I recently attended an all-day conference on a little-known gem called Relationship-Based Care (RBC), a culture transformation and operational model that is gaining steam globally. The RBC model focuses not only on well-known metrics, such as patient safety, quality care, and patient satisfaction; it also emphasizes staff satisfaction by improving each and every relationship. Specifically, it creates therapeutic relationships between caregivers and the patients and families they serve, strengthens relationships between members of the health care team, and last, but certainly not least, it nurtures each caregiver’s relationship with himself or herself. What a novel, and much needed concept!
Numerous hospitals that have implemented this training model have achieved impressive outcomes, including significant improvement in HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores, and staff satisfaction survey scores so high that one hospital gained national recognition as one of the best places to work in America.
I look forward to future training on RBC and am glad to see that addressing the needs of caregivers, not just care receivers, is starting to take center stage, as it rightfully should. After all, how can we give our all to our patients when we are not whole?
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
When I think of the word “relationship,” I imagine gazing into the loving eyes of my husband, playing hide and seek with my children, or texting my best friend for no good reason other than to just say hello.
There is a special comfort zone we expect from people who are close to us; a feeling of love and acceptance that we can’t find elsewhere.
But in a much broader sense, our important relationships extend far beyond our inner circle to include every single person who is involved with our health care team. Our team includes the hospital executives who create new safety initiatives, develop budgets, and oversee a host of other patient care and fiscal functions. The physical therapists who evaluate our patients and make recommendations on how to safely transition them out of the hospital are on our team. The housekeepers who scrub the toilets and wash the linens to prevent nosocomial infections are on our team. They, along with many others, play a pivotal role in our patients’ care, although many important players make their impact behind the scenes.
Yet, of course, our most important professional relationships are not with the CEO, the pharmacist, or even the nursing staff. Our most important relationships are with our patients and their families. I recently attended an all-day conference on a little-known gem called Relationship-Based Care (RBC), a culture transformation and operational model that is gaining steam globally. The RBC model focuses not only on well-known metrics, such as patient safety, quality care, and patient satisfaction; it also emphasizes staff satisfaction by improving each and every relationship. Specifically, it creates therapeutic relationships between caregivers and the patients and families they serve, strengthens relationships between members of the health care team, and last, but certainly not least, it nurtures each caregiver’s relationship with himself or herself. What a novel, and much needed concept!
Numerous hospitals that have implemented this training model have achieved impressive outcomes, including significant improvement in HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores, and staff satisfaction survey scores so high that one hospital gained national recognition as one of the best places to work in America.
I look forward to future training on RBC and am glad to see that addressing the needs of caregivers, not just care receivers, is starting to take center stage, as it rightfully should. After all, how can we give our all to our patients when we are not whole?
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
When I think of the word “relationship,” I imagine gazing into the loving eyes of my husband, playing hide and seek with my children, or texting my best friend for no good reason other than to just say hello.
There is a special comfort zone we expect from people who are close to us; a feeling of love and acceptance that we can’t find elsewhere.
But in a much broader sense, our important relationships extend far beyond our inner circle to include every single person who is involved with our health care team. Our team includes the hospital executives who create new safety initiatives, develop budgets, and oversee a host of other patient care and fiscal functions. The physical therapists who evaluate our patients and make recommendations on how to safely transition them out of the hospital are on our team. The housekeepers who scrub the toilets and wash the linens to prevent nosocomial infections are on our team. They, along with many others, play a pivotal role in our patients’ care, although many important players make their impact behind the scenes.
Yet, of course, our most important professional relationships are not with the CEO, the pharmacist, or even the nursing staff. Our most important relationships are with our patients and their families. I recently attended an all-day conference on a little-known gem called Relationship-Based Care (RBC), a culture transformation and operational model that is gaining steam globally. The RBC model focuses not only on well-known metrics, such as patient safety, quality care, and patient satisfaction; it also emphasizes staff satisfaction by improving each and every relationship. Specifically, it creates therapeutic relationships between caregivers and the patients and families they serve, strengthens relationships between members of the health care team, and last, but certainly not least, it nurtures each caregiver’s relationship with himself or herself. What a novel, and much needed concept!
Numerous hospitals that have implemented this training model have achieved impressive outcomes, including significant improvement in HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores, and staff satisfaction survey scores so high that one hospital gained national recognition as one of the best places to work in America.
I look forward to future training on RBC and am glad to see that addressing the needs of caregivers, not just care receivers, is starting to take center stage, as it rightfully should. After all, how can we give our all to our patients when we are not whole?
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
An open letter to the FDA regarding the use of morcellation procedures for women having surgery for presumed uterine fibroids
In November 2014, the FDA ruled that power morcellation was contraindicated in "the majority of women" having surgery for uterine fibroids due to the potential risk of spreading occult uterine sarcoma.1 Although problems with this ruling were immediately apparent, the passage of time has allowed for more clarity on the related medical issues.
Prevalence of leiomyosarcoma among women having surgery for presumed uterine fibroids
The prevalence of occult leiomyosarcoma among women with fibroids is critical for every patient. All medical procedures have potential risk and the patient's understanding of risk is the foundation of medical decision making.
The FDA estimated that for every 458 women having surgery for fibroids, one woman would be found to have an occult leiomyosarcoma (LMS). We challenge this calculation. To estimate this risk, the FDA searched medical databases using the terms “uterine cancer” AND “hysterectomy or myomectomy.” Because “uterine cancer” was required, studies where cancer was not found or discussed were not identified. Nine studies, all but one of which were retrospective, were analyzed including a non–peer-reviewed Letter to the Editor and an abstract from an unpublished study.2,3
Additionally, 3 leiomyosarcoma cases identified by the FDA do not meet current pathologic criteria for cancer and would now be classified as benign "atypical" leiomyomas. If atypical leiomyomas and non–peer-reviewed data are excluded, the FDA identified 8 cases of LMS among 12,402 women having surgery for presumed leiomyomas, a prevalence of 1 in 1,550 (0.064%).
Pritts and colleagues4 recently published a more rigorous meta-analysis of 133 studies and determined that the prevalence of LMS among women having surgery for presumed fibroids was 1 in 1,960, or 0.051%. All peer-reviewed reports in which surgery was performed for presumed fibroids were analyzed, including reports where cancer was not found. Inclusion criteria required that histopathology results be explicitly provided and available for interpretation. Among the 26 randomized controlled trials analyzed, 1,582 women had surgery for fibroids and none were found to have LMS.
Bojahr and colleagues5 recently published a large population-based prospective registry study and reported 2 occult LMS among 8,720 women having surgery for fibroids (0.023%).
In summary: The re-analyzed FDA dataset yields a prevalence of 1 in 1,550 (0.064%); the Pritts study reports a prevalence of 1 in 1,960 (0.051%), with the RCTs having a prevalence of 0; and the Bojahr study reports a prevalence of 2 of 8,720 (0.023%). We acknowledge that with rare events statistical analysis may be uncertain and confidence intervals may be wide. However, these numbers do not support the FDA's estimated prevalence of LMS among women having surgery for presumed fibroids and those at risk for morcellation of an LMS.
Prognosis for women with morcellated LMS
Women with LMS, removed intact without morcellation, have a poor prognosis. Based on SEER data, the 5-year survival of stage I and II LMS is only 61%.6 Whether morcellation influences the prognosis of women with LMS is not known, and the biology of this tumor has not been well studied. Distant metastases occur early in the disease process, primarily hematogenous dissemination. Four frequently quoted published studies examine survival following power morcellation. Surprisingly, virtually none of the women in these studies had power morcellation. Furthermore, the data presented in these reports are poorly analyzed and patient numbers are very small.
Park and colleagues7 reported only one of the 25 morcellated cases had laparoscopic surgery with power morcellation. Eighteen women had a laparoscopically-assisted vaginal hysterectomy with scalpel morcellation performed through the vagina, one had a vaginal hysterectomy with scalpel-morcellation, and 5 had mini-laparotomy with scalpel morcellation through small lower abdominal incisions. Seventeen of the 25 patients plotted in the published survival curve were referred to the hospital after initial diagnosis or the discovery of a recurrence at another institution. Since the number of nonreferred women with less aggressive disease or without recurrence is not known, it is not possible to determine differences in survival between patients with and without morcellation.
In a study by Perri and colleagues,8 none of the patients had power morcellation: 4 women had abdominal myomectomy; 4 had hysteroscopic myomectomy with tissue confined within the uterine cavity; 2 had laparoscopic hysterectomy with scalpel morcellation; 4 had supracervical abdominal hysterectomy with cut-through at the cervix; and 2 had abdominal hysterectomy with injury to the uterus with a sharp instrument.
When comparing the outcomes for women with morcellated and nonmorcellated LMS, Morice and colleagues9 found no difference in recurrence rates or overall and disease-free survival at 6 months.
In the only study to compare use of power with scalpel morcellation in women with LMS, Oduyebo and colleagues10 found no difference in outcomes for the 10 women with power morcellation and 5 with scalpel morcellation followed for a median of 27 months (range, 2–93 months). Notably, a life table analysis of the above studies showed no difference in survival between morcellation methods.11
Of note, laparoscopic-aided morcellation allows the surgeon to inspect the pelvic and abdominal cavities and irrigate and remove tissue fragments under visual control. In contrast, the surgeon cannot visually inspect the peritoneal cavity during vaginal or mini-laparotomy procedures. Morcellation within containment bags has recently been utilized in an attempt to avoid spread of tissue. This method has not yet been proven effective or safe, and there is concern that bags may make morcellation more cumbersome and less safe.
What the FDA restrictions mean for women
The FDA communication states, "the FDA is warning against the use of laparoscopic power morcellators in the majority of women undergoing hysterectomy or myomectomy for uterine fibroids."1 This statement is not consistent with current evidence.
Moreover, a severe restriction of morcellation, including vaginal and mini-laparotomy morcellation, would limit women with symptomatic leiomyomas to one option: total abdominal hysterectomy. For women with fibroids larger than a 10-week pregnancy size, which most often require either scalpel or power morcellation in order to remove tissue, a ban on morcellation would eliminate the following procedures:
- vaginal hysterectomy (scalpel morcellation)
- mini-laparotomy hysterectomy (scalpel morcellation)
- laparoscopic hysterectomy (scalpel morcellation)
- laparoscopic supracervical hysterectomy (cervix cut-through)
- open supracervical hysterectomy (cervix cut-through)
- laparoscopic myomectomy (power morcellation)
- mini-laparotomy myomectomy (scalpel morcellation)
- hysteroscopic myomectomy (intrauterine morcellation)
- uterine artery embolization (no specimen and will delay diagnosis)
- high-intensity focused ultrasound (no specimen and will delay diagnosis)
If abdominal hysterectomy is recommended to women with fibroids, will women be better off?
By focusing exclusively on the risk of LMS, the FDA failed to take into account other risks associated with surgery. Laparoscopic surgery uses small incisions, is performed as an outpatient procedure (or overnight stay), has a faster recovery (2 weeks vs 4–6 weeks for open surgery), and is associated with lower mortality and fewer complications. These benefits of minimally invasive surgery are now well established in gynecologic and general surgery.
Using published best-evidence data, a recent decision analysis12 showed that, comparing 100,000 women undergoing laparoscopic hysterectomy with 100,000 undergoing open hysterectomy, the group undergoing laparoscopic surgery would experience 20 fewer perioperative deaths, 150 fewer pulmonary or venous embolus, and 4,800 fewer wound infections. Importantly, women having open surgery would have 8,000 fewer quality-of-life years.
A recently published study13 found that, in the 8 months following the FDA safety communication, utilization of laparoscopic hysterectomies decreased by 4.1% (P = .005), and abdominal and vaginal hysterectomies increased by 1.7% (P = .112) and 2.4% (P = .012), respectively. Major surgical complications (not including blood transfusions) increased from 2.2% to 2.8% (P = .015), and the rate of hospital readmission within 30 days also increased from 3.4% to 4.2% (P = .025). These observations merit consideration as women weigh the pros and cons of minimally invasive surgery with morcellation versus open surgery. These observations merit consideration as women weigh the pros and cons of minimally invasive surgery with possible morcellation versus open surgery.
Clinical recommendations
Recent attention to surgical options for women with uterine leiomyomas and the risk of an occult leiomyosarcoma are positive developments in that the gynecologic community is re-examining relevant issues. We respectfully suggest that the following clinical recommendations be considered:
- The risk of LMS is higher in older postmenopausal women; greater caution should be exercised prior to recommending morcellation procedures for these women.
- Preoperative consideration of LMS is important. Women aged 35 years and older with irregular uterine bleeding and presumed fibroids should have an endometrial biopsy, which occasionally may detect LMS prior to surgery. Women should have normal results of cervical cancer screening.
- Ultrasound or MRI findings of a large irregular vascular mass, often with irregular anechoic (cystic) areas reflecting necrosis, may cause suspicion of LMS.
- Women wishing minimally invasive procedures with morcellation, including scalpel morcellation via the vagina or mini-laparotomy, or power morcellation using laparoscopic guidance, should understand the potential risk of decreased survival should LMS be present. Open procedures should be offered to all women who are considering minimally invasive procedures for "fibroids."
- Following morcellation, careful inspection for tissue fragments should be undertaken and copious irrigation of the pelvic and abdominal cavities should be performed to minimize the risk of retained tissue.
- Further investigations of a means to identify LMS preoperatively should be supported. Likewise, investigation into the biology of LMS should be funded to better understand the propensity of tissue fragments or cells to implant and grow. With that knowledge, minimally invasive procedures could be avoided for women with LMS and women choosing minimally invasive surgery could be reassured that they do not have LMS.
Respecting women who suffer from leiomyosarcoma, we conclude that the FDA directive was based on a misleading analysis. Consequently, more accurate estimates regarding the prevalence of LMS among women having surgery for fibroids should be issued. Women have a right to self determination. Modification of the FDA's current restrictive guidance regarding power morcellation would empower each woman to consider the pertinent issues and have the freedom to undertake shared decision making with her surgeon in order to select the procedure that is most appropriate for her.
William Parker, MD
Clinical Professor, University of California Los Angeles (UCLA) School of Medicine, Director, Minimally Invasive Gynecologic Surgery, Santa Monica-UCLA Medical Center, Santa Monica, California
Jonathan S. Berek, MD, MMS
Laurie Kraus Lacob Professor and Director, Stanford Women's Cancer Center, Director, Stanford Health Care Communication Program, Chair, Department of Obstetrics and Gynecology, Stanford University School of Medicine, Stanford, California
Elizabeth Pritts, MD
Wisconsin Fertility Institute, Middleton, Wisconsin
David Olive, MD
Wisconsin Fertility Institute, Middleton, Wisconsin
Andrew M. Kaunitz, MD
University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology, University of Florida College of Medicine–Jacksonville; Director, Menopause and Gynecologic Ultrasound Services, UF Women’s Health Specialists at Emerson, Jacksonville, Florida.
Eva Chalas, MD
Chief, Division of Gynecologic Oncology, Director, Clinical Cancer Services, Vice-Chair, Department of Obstetrics and Gynecology, Winthrop-University Hospital, Mineola, New York
Daniel Clarke-Pearson, MD
Professor and Chair, Clinical Research, Gynecologic Oncology Program, University of North Carolina at Chapel Hill
Barbara Goff, MD
Professor, Obstetrics and Gynecology, Director, Division of Gynecologic Oncology, University of Washington, Seattle, Washington
Robert E. Bristow, MD, MBA
Professor and Chair, Department of Obstetrics and Gynecology, University of California Irvine School of Medicine, Orange, California
Hugh S. Taylor, MD
Anita O'Keeffe Young Professor and Chair, Department of Obstetrics, Gynecology, and Reproductive Sciences, Yale School of Medicin; Chief of Obstetrics and Gynecology, Yale-New Haven Hospital, New Haven, Connecticut
Robin Farias-Eisner, MD
Chief, Gynecology and Gynecologic Oncology, Department of Obstetrics and Gynecology, David Geffen School of Medicine at University of California Los Angeles
Amanda Nickles Fader, MD
Director, Kelly Gynecologic Oncology Service, Associate Professor of Gynecology and Obstetrics, Director, FJ Montz Fellowship in Gynecologic Oncology, Johns Hopkins Medicine, Baltimore, Maryland
G. Larry Maxwell, MD, COL (ret) US Army
Chairman, Department of Obstetrics and Gynecology, Inova Fairfax Hospital, Falls Church, Virginia; Co-Investigator and Deputy Director of Science, Department of Defense Gynecologic Cancer Translational Research Center of Excellence, Bethesda, Maryland; Professor of Virginia Commonwealth School of Medicine, Richmond, Virginia; and Executive Director of Globeathon to End Women’s Cancer
Scott C. Goodwin, MD
Hasso Brothers Professor and Chairman, Radiological Sciences, University of California Irvine Medical Center, Orange, California
Susan Love, MD, MBA
Dr. Susan Love Research Foundation, Encino, California
William E. Gibbons, MD
Professor and Director, Division of Reproductive Medicine, Director of Fellowship Training, Department of Obstetrics and Gynecology, Baylor College of Medicine; Chief of Reproductive Medicine at the Pavilion For Women at Texas Children’s Hospital, Houston, Texas
Leland J. Foshag, MD
Surgical Oncology, Melanoma and Sarcoma, John Wayne Cancer Institute, Santa Monica, California
Phyllis C. Leppert, MD, PhD
Emerita Professor of Obstetrics and Gynecology, Duke University School of Medicine; President of The Campion Fund, Phyllis and Mark Leppert Foundation for Fertility Research, Durham, North Carolina
Judy Norsigian
Co-founder of Our Bodies, Ourselves, Boston, Massachusetts
Charles W. Nager, MD
Professor and Chairman, Department of Reproductive Medicine, University of California San Diego Health System
Timothy Robert B. Johnson, MD
Arthur F. Thurnau Professor and Chair, Department of Obstetrics and Gynecology, Professor of Women’s Studies, and Research Professor in the Center for Human Growth and Development, University of Michigan, Ann Arbor, Michigan
David S. Guzick, MD, PhD
Senior Vice President of Health Affairs, President of UF Health, University of Florida, Gainesville, Florida
Sawsan As-Sanie, MD, MPH
Assistant Professor and Director, Minimally Invasive Gynecologic Surgery, Fellowship Director of Endometriosis Center, University of Michigan, Ann Arbor, Michigan
Richard J. Paulson, MD
Alia Tutor Chair in Reproductive Medicine, Professor and Vice-Chair, Department of Obstetrics and Gynecology, Chief, Division of Reproductive Endocrinology and Infertility, Keck School of Medicine, University of Southern California, Los Angeles, California
Cindy Farquhar
Professor of Obstetrics and Gynaecology and National Women's Health, University of Auckland, New Zealand
Linda Bradley, MD
Vice Chair of Obstetrics, Gynecology, and Women’s Health Institute, Director of the Fibroid and Menstrual Disorders Center, Department of Obstetrics and Gynecology, Cleveland Clinic, Cleveland, Ohio.
Stacey A. Scheib, MD
Assistant Professor and Director, Hopkins Multidisciplinary Fibroid Center, Director of Minimally Invasive Gynecologic Surgery, Johns Hopkins Hospital, Baltimore, Maryland
Anton J. Bilchik, MD, PhD
Professor of Surgery, Chief of Medicine at John Wayne Cancer Institute, Santa Monica, California
Laurel W. Rice, MD
Chair, Department of Obstetrics and Gynecology, Professor, Division of Gynecology Oncology, University of Wisconsin-Madison School of Medicine and Public Health, Madison, Wisconsin
Carla Dionne
Founder of National Uterine Fibroid Foundation, Colorado Springs, Colorado
Alison Jacoby, MD
Director, University of California-San Francisco Comprehensive Fibroid Center, Interim Chief, Division of Gynecology, University of California San Francisco
Charles Ascher-Walsh, MD
Director of Gynecology, Urogynecology, and Minimally Invasive Surgery, Mt. Sinai School of Medicine, New York, New York
Sarah J. Kilpatrick, MD, PhD
Chair of Department of Obstetrics and Gynecology, Associate Dean of Faculty Development, Helping Hand of Los Angeles Chair in Obstetrics and Gynecology, Cedars-Sinai Medical Center, Los Angeles, California
G. David Adamson, MD
Clinical Professor, Stanford University School of Medicine, Stanford, California; Past President of the American Society for Reproductive Medicine
Matthew Siedhoff, MD, MSCR
Assistant Professor and Division Director, Minimally Invasive Gynecologic Surgery, Department of Obstetrics and Gynecology, University of North Carolina at Chapel Hill
Robert Israel, MD
Professor, Department of Obstetrics and Gynecology, Chair, Quality Improvement, Director, Women's Health Clinics and Referrals, LAC+USC Medical Center, Los Angeles, California
Marie Fidela Paraiso, MD
Head, Female Pelvic Medicine & Reconstructive Surgery, Department of Obstetrics and Gynecology, Cleveland Clinic, Cleveland, Ohio
Michael M. Frumovitz, MD, MPH
Fellowship Program Director, Department of Gynecologic Oncology and Reproductive Medicine, University of Texas MD Anderson Cancer Center, Houston, Texas
John R. Lurain, MD
Marcia Stenn Professor of Gynecologic Oncology, Program Director, Fellowship in Gynecologic Oncology, Northwestern University Feinberg School of Medicine, Chicago, Illinois
Ayman Al-Hendy, MD, PhD
Georgia Regents University Director of Interdisciplinary Translational Research; Medical College of Georgia Assistant Dean for Global Translational Research; Professor and Director, Division of Translational Research, Department of Obstetrics and Gynecology, Georgia Regents Health, Augusta, Georgia
Guy I. Benrubi, MD
Senior Associate Dean for Faculty Affairs, Robert J. Thompson Professor and Chair of Department of Obstetrics and Gynecology, University of Florida College of Medicine – Jacksonville
Steven S. Raman, MD
Professor, Radiology, Urology, and Surgery, Co-director, Fibroid Treatment Program, David Geffen School of Medicine at University of California Los Angeles
Rosanne M. Kho, MD
Associate Professor and Head, Section of Urogynecology and Female Pelvic Medicine & Reconstructive Surgery; Co-Director of Minimally Invasive Gynecologic Surgery Fellowship Program, Columbia University Medical Center, New York, New York
Ted L. Anderson, MD, PhD
Betty and Lonnie S. Burnett Professor and Chair, Obstetrics and Gynecology, Division Director of Gynecology, Vanderbilt University School of Medicine, Nashville, Tennessee
R. Kevin Reynolds, MD
The George W. Morley Professor and Chief, Division of Gynecologic Oncology, University of Michigan Health System, Ann Arbor, Michigan
John DeLancey, MD
Norman F. Miller Professor of Obstetrics & Gynecology, University of Michigan Health System, Ann Arbor, Michigan
- US Food and Drug Administration. Medical Devices Safety Communications. UPDATED Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy: FDA Safety Communication. http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm424443.htm. Published November 24, 2014. Accessed December 7, 2015.
- Leung F, Terzibachian JJ. Re: "The impact of tumor morcellation during surgery on the prognosis of patients with apparently early uterine leiomyosarcoma” [letter]. Gynecol Oncol. 2012;124(1):172–173.
- Rowland M, Lesnock J, Edwards R, et al. Occult uterine cancer in patients undergoing laparoscopic hysterectomy with morcellation [abstract]. Gynecol Oncol. 2012;127(1):S29.
- Pritts E, Vanness D, Berek J, et al. The prevalence of occult leiomyosarcoma at surgery for presumed uterine fibroids: a meta-analysis. Gynecol Surg. 2015;12(3):165–177.
- Bojahr B, De Wilde R, Tchartchian G. Malignancy rate of 10,731 uteri morcellated during laparoscopic supracervical hysterectomy (LASH). Arch Gynecol Obstet. 2015;292:665–672.
- Kosary CL. SEER survival monograph: Cancer survival among adults: U.S. SEER program, 1988-2001, patient and tumor characteristics. In: Ries LAG, Young JL, Keel GE, et al, eds. Cancer of the corpus uteri. Bethesda, Maryland: National Cancer Institute, SEER Program, NIH; 2007:123–132.
- Park JY, Park SK, Kim DY, et al. The impact of tumor morcellation during surgery on the prognosis of patients with apparently early uterine leiomyosarcoma. Gynecol Oncol. 2011;122(2):255–259.
- Perri T, Korach J, Sadetzki S, Oberman B, Fridman E, Ben-Baruch G. Uterine leiomyosarcoma: does the primary surgical procedure matter? Int J Gynecol Cancer. 2009;19(2):257–260.
- Morice P, Rodriguez A, Rey A, et al. Prognostic value of initial surgical procedure for patients with uterine sarcoma: analysis of 123 patients. Eur J Gynaecol Oncol. 2003;24(3–4):237–240.
- Oduyebo T, Rauh-Hain AJ, Meserve EE, et al. The value of re-exploration in patients with inadvertently morcellated uterine sarcoma. Gynecol Oncol. 2014;132(2):360–365.
- Pritts E, Parker W, Brown J, Olive D. Outcome of occult uterine leiomyosarcoma after surgery for presumed uterine fibroids: a systematic review. J Minim Invasive Gynecol. 2015;22(1):26–33.
- Siedhoff MT, Wheeler SB, Rutstein SE, et al. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis. Am J Obstet Gynecol. 2015;212(5):591.e1–e8.
- Harris JA, Swenson CW, Uppal S, et al. Practice patterns and postoperative complications before and after Food and Drug Administration Safety Communication on power morcellation [published online ahead of print August 24, 2015]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2015.08.047.
In November 2014, the FDA ruled that power morcellation was contraindicated in "the majority of women" having surgery for uterine fibroids due to the potential risk of spreading occult uterine sarcoma.1 Although problems with this ruling were immediately apparent, the passage of time has allowed for more clarity on the related medical issues.
Prevalence of leiomyosarcoma among women having surgery for presumed uterine fibroids
The prevalence of occult leiomyosarcoma among women with fibroids is critical for every patient. All medical procedures have potential risk and the patient's understanding of risk is the foundation of medical decision making.
The FDA estimated that for every 458 women having surgery for fibroids, one woman would be found to have an occult leiomyosarcoma (LMS). We challenge this calculation. To estimate this risk, the FDA searched medical databases using the terms “uterine cancer” AND “hysterectomy or myomectomy.” Because “uterine cancer” was required, studies where cancer was not found or discussed were not identified. Nine studies, all but one of which were retrospective, were analyzed including a non–peer-reviewed Letter to the Editor and an abstract from an unpublished study.2,3
Additionally, 3 leiomyosarcoma cases identified by the FDA do not meet current pathologic criteria for cancer and would now be classified as benign "atypical" leiomyomas. If atypical leiomyomas and non–peer-reviewed data are excluded, the FDA identified 8 cases of LMS among 12,402 women having surgery for presumed leiomyomas, a prevalence of 1 in 1,550 (0.064%).
Pritts and colleagues4 recently published a more rigorous meta-analysis of 133 studies and determined that the prevalence of LMS among women having surgery for presumed fibroids was 1 in 1,960, or 0.051%. All peer-reviewed reports in which surgery was performed for presumed fibroids were analyzed, including reports where cancer was not found. Inclusion criteria required that histopathology results be explicitly provided and available for interpretation. Among the 26 randomized controlled trials analyzed, 1,582 women had surgery for fibroids and none were found to have LMS.
Bojahr and colleagues5 recently published a large population-based prospective registry study and reported 2 occult LMS among 8,720 women having surgery for fibroids (0.023%).
In summary: The re-analyzed FDA dataset yields a prevalence of 1 in 1,550 (0.064%); the Pritts study reports a prevalence of 1 in 1,960 (0.051%), with the RCTs having a prevalence of 0; and the Bojahr study reports a prevalence of 2 of 8,720 (0.023%). We acknowledge that with rare events statistical analysis may be uncertain and confidence intervals may be wide. However, these numbers do not support the FDA's estimated prevalence of LMS among women having surgery for presumed fibroids and those at risk for morcellation of an LMS.
Prognosis for women with morcellated LMS
Women with LMS, removed intact without morcellation, have a poor prognosis. Based on SEER data, the 5-year survival of stage I and II LMS is only 61%.6 Whether morcellation influences the prognosis of women with LMS is not known, and the biology of this tumor has not been well studied. Distant metastases occur early in the disease process, primarily hematogenous dissemination. Four frequently quoted published studies examine survival following power morcellation. Surprisingly, virtually none of the women in these studies had power morcellation. Furthermore, the data presented in these reports are poorly analyzed and patient numbers are very small.
Park and colleagues7 reported only one of the 25 morcellated cases had laparoscopic surgery with power morcellation. Eighteen women had a laparoscopically-assisted vaginal hysterectomy with scalpel morcellation performed through the vagina, one had a vaginal hysterectomy with scalpel-morcellation, and 5 had mini-laparotomy with scalpel morcellation through small lower abdominal incisions. Seventeen of the 25 patients plotted in the published survival curve were referred to the hospital after initial diagnosis or the discovery of a recurrence at another institution. Since the number of nonreferred women with less aggressive disease or without recurrence is not known, it is not possible to determine differences in survival between patients with and without morcellation.
In a study by Perri and colleagues,8 none of the patients had power morcellation: 4 women had abdominal myomectomy; 4 had hysteroscopic myomectomy with tissue confined within the uterine cavity; 2 had laparoscopic hysterectomy with scalpel morcellation; 4 had supracervical abdominal hysterectomy with cut-through at the cervix; and 2 had abdominal hysterectomy with injury to the uterus with a sharp instrument.
When comparing the outcomes for women with morcellated and nonmorcellated LMS, Morice and colleagues9 found no difference in recurrence rates or overall and disease-free survival at 6 months.
In the only study to compare use of power with scalpel morcellation in women with LMS, Oduyebo and colleagues10 found no difference in outcomes for the 10 women with power morcellation and 5 with scalpel morcellation followed for a median of 27 months (range, 2–93 months). Notably, a life table analysis of the above studies showed no difference in survival between morcellation methods.11
Of note, laparoscopic-aided morcellation allows the surgeon to inspect the pelvic and abdominal cavities and irrigate and remove tissue fragments under visual control. In contrast, the surgeon cannot visually inspect the peritoneal cavity during vaginal or mini-laparotomy procedures. Morcellation within containment bags has recently been utilized in an attempt to avoid spread of tissue. This method has not yet been proven effective or safe, and there is concern that bags may make morcellation more cumbersome and less safe.
What the FDA restrictions mean for women
The FDA communication states, "the FDA is warning against the use of laparoscopic power morcellators in the majority of women undergoing hysterectomy or myomectomy for uterine fibroids."1 This statement is not consistent with current evidence.
Moreover, a severe restriction of morcellation, including vaginal and mini-laparotomy morcellation, would limit women with symptomatic leiomyomas to one option: total abdominal hysterectomy. For women with fibroids larger than a 10-week pregnancy size, which most often require either scalpel or power morcellation in order to remove tissue, a ban on morcellation would eliminate the following procedures:
- vaginal hysterectomy (scalpel morcellation)
- mini-laparotomy hysterectomy (scalpel morcellation)
- laparoscopic hysterectomy (scalpel morcellation)
- laparoscopic supracervical hysterectomy (cervix cut-through)
- open supracervical hysterectomy (cervix cut-through)
- laparoscopic myomectomy (power morcellation)
- mini-laparotomy myomectomy (scalpel morcellation)
- hysteroscopic myomectomy (intrauterine morcellation)
- uterine artery embolization (no specimen and will delay diagnosis)
- high-intensity focused ultrasound (no specimen and will delay diagnosis)
If abdominal hysterectomy is recommended to women with fibroids, will women be better off?
By focusing exclusively on the risk of LMS, the FDA failed to take into account other risks associated with surgery. Laparoscopic surgery uses small incisions, is performed as an outpatient procedure (or overnight stay), has a faster recovery (2 weeks vs 4–6 weeks for open surgery), and is associated with lower mortality and fewer complications. These benefits of minimally invasive surgery are now well established in gynecologic and general surgery.
Using published best-evidence data, a recent decision analysis12 showed that, comparing 100,000 women undergoing laparoscopic hysterectomy with 100,000 undergoing open hysterectomy, the group undergoing laparoscopic surgery would experience 20 fewer perioperative deaths, 150 fewer pulmonary or venous embolus, and 4,800 fewer wound infections. Importantly, women having open surgery would have 8,000 fewer quality-of-life years.
A recently published study13 found that, in the 8 months following the FDA safety communication, utilization of laparoscopic hysterectomies decreased by 4.1% (P = .005), and abdominal and vaginal hysterectomies increased by 1.7% (P = .112) and 2.4% (P = .012), respectively. Major surgical complications (not including blood transfusions) increased from 2.2% to 2.8% (P = .015), and the rate of hospital readmission within 30 days also increased from 3.4% to 4.2% (P = .025). These observations merit consideration as women weigh the pros and cons of minimally invasive surgery with morcellation versus open surgery. These observations merit consideration as women weigh the pros and cons of minimally invasive surgery with possible morcellation versus open surgery.
Clinical recommendations
Recent attention to surgical options for women with uterine leiomyomas and the risk of an occult leiomyosarcoma are positive developments in that the gynecologic community is re-examining relevant issues. We respectfully suggest that the following clinical recommendations be considered:
- The risk of LMS is higher in older postmenopausal women; greater caution should be exercised prior to recommending morcellation procedures for these women.
- Preoperative consideration of LMS is important. Women aged 35 years and older with irregular uterine bleeding and presumed fibroids should have an endometrial biopsy, which occasionally may detect LMS prior to surgery. Women should have normal results of cervical cancer screening.
- Ultrasound or MRI findings of a large irregular vascular mass, often with irregular anechoic (cystic) areas reflecting necrosis, may cause suspicion of LMS.
- Women wishing minimally invasive procedures with morcellation, including scalpel morcellation via the vagina or mini-laparotomy, or power morcellation using laparoscopic guidance, should understand the potential risk of decreased survival should LMS be present. Open procedures should be offered to all women who are considering minimally invasive procedures for "fibroids."
- Following morcellation, careful inspection for tissue fragments should be undertaken and copious irrigation of the pelvic and abdominal cavities should be performed to minimize the risk of retained tissue.
- Further investigations of a means to identify LMS preoperatively should be supported. Likewise, investigation into the biology of LMS should be funded to better understand the propensity of tissue fragments or cells to implant and grow. With that knowledge, minimally invasive procedures could be avoided for women with LMS and women choosing minimally invasive surgery could be reassured that they do not have LMS.
Respecting women who suffer from leiomyosarcoma, we conclude that the FDA directive was based on a misleading analysis. Consequently, more accurate estimates regarding the prevalence of LMS among women having surgery for fibroids should be issued. Women have a right to self determination. Modification of the FDA's current restrictive guidance regarding power morcellation would empower each woman to consider the pertinent issues and have the freedom to undertake shared decision making with her surgeon in order to select the procedure that is most appropriate for her.
William Parker, MD
Clinical Professor, University of California Los Angeles (UCLA) School of Medicine, Director, Minimally Invasive Gynecologic Surgery, Santa Monica-UCLA Medical Center, Santa Monica, California
Jonathan S. Berek, MD, MMS
Laurie Kraus Lacob Professor and Director, Stanford Women's Cancer Center, Director, Stanford Health Care Communication Program, Chair, Department of Obstetrics and Gynecology, Stanford University School of Medicine, Stanford, California
Elizabeth Pritts, MD
Wisconsin Fertility Institute, Middleton, Wisconsin
David Olive, MD
Wisconsin Fertility Institute, Middleton, Wisconsin
Andrew M. Kaunitz, MD
University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology, University of Florida College of Medicine–Jacksonville; Director, Menopause and Gynecologic Ultrasound Services, UF Women’s Health Specialists at Emerson, Jacksonville, Florida.
Eva Chalas, MD
Chief, Division of Gynecologic Oncology, Director, Clinical Cancer Services, Vice-Chair, Department of Obstetrics and Gynecology, Winthrop-University Hospital, Mineola, New York
Daniel Clarke-Pearson, MD
Professor and Chair, Clinical Research, Gynecologic Oncology Program, University of North Carolina at Chapel Hill
Barbara Goff, MD
Professor, Obstetrics and Gynecology, Director, Division of Gynecologic Oncology, University of Washington, Seattle, Washington
Robert E. Bristow, MD, MBA
Professor and Chair, Department of Obstetrics and Gynecology, University of California Irvine School of Medicine, Orange, California
Hugh S. Taylor, MD
Anita O'Keeffe Young Professor and Chair, Department of Obstetrics, Gynecology, and Reproductive Sciences, Yale School of Medicin; Chief of Obstetrics and Gynecology, Yale-New Haven Hospital, New Haven, Connecticut
Robin Farias-Eisner, MD
Chief, Gynecology and Gynecologic Oncology, Department of Obstetrics and Gynecology, David Geffen School of Medicine at University of California Los Angeles
Amanda Nickles Fader, MD
Director, Kelly Gynecologic Oncology Service, Associate Professor of Gynecology and Obstetrics, Director, FJ Montz Fellowship in Gynecologic Oncology, Johns Hopkins Medicine, Baltimore, Maryland
G. Larry Maxwell, MD, COL (ret) US Army
Chairman, Department of Obstetrics and Gynecology, Inova Fairfax Hospital, Falls Church, Virginia; Co-Investigator and Deputy Director of Science, Department of Defense Gynecologic Cancer Translational Research Center of Excellence, Bethesda, Maryland; Professor of Virginia Commonwealth School of Medicine, Richmond, Virginia; and Executive Director of Globeathon to End Women’s Cancer
Scott C. Goodwin, MD
Hasso Brothers Professor and Chairman, Radiological Sciences, University of California Irvine Medical Center, Orange, California
Susan Love, MD, MBA
Dr. Susan Love Research Foundation, Encino, California
William E. Gibbons, MD
Professor and Director, Division of Reproductive Medicine, Director of Fellowship Training, Department of Obstetrics and Gynecology, Baylor College of Medicine; Chief of Reproductive Medicine at the Pavilion For Women at Texas Children’s Hospital, Houston, Texas
Leland J. Foshag, MD
Surgical Oncology, Melanoma and Sarcoma, John Wayne Cancer Institute, Santa Monica, California
Phyllis C. Leppert, MD, PhD
Emerita Professor of Obstetrics and Gynecology, Duke University School of Medicine; President of The Campion Fund, Phyllis and Mark Leppert Foundation for Fertility Research, Durham, North Carolina
Judy Norsigian
Co-founder of Our Bodies, Ourselves, Boston, Massachusetts
Charles W. Nager, MD
Professor and Chairman, Department of Reproductive Medicine, University of California San Diego Health System
Timothy Robert B. Johnson, MD
Arthur F. Thurnau Professor and Chair, Department of Obstetrics and Gynecology, Professor of Women’s Studies, and Research Professor in the Center for Human Growth and Development, University of Michigan, Ann Arbor, Michigan
David S. Guzick, MD, PhD
Senior Vice President of Health Affairs, President of UF Health, University of Florida, Gainesville, Florida
Sawsan As-Sanie, MD, MPH
Assistant Professor and Director, Minimally Invasive Gynecologic Surgery, Fellowship Director of Endometriosis Center, University of Michigan, Ann Arbor, Michigan
Richard J. Paulson, MD
Alia Tutor Chair in Reproductive Medicine, Professor and Vice-Chair, Department of Obstetrics and Gynecology, Chief, Division of Reproductive Endocrinology and Infertility, Keck School of Medicine, University of Southern California, Los Angeles, California
Cindy Farquhar
Professor of Obstetrics and Gynaecology and National Women's Health, University of Auckland, New Zealand
Linda Bradley, MD
Vice Chair of Obstetrics, Gynecology, and Women’s Health Institute, Director of the Fibroid and Menstrual Disorders Center, Department of Obstetrics and Gynecology, Cleveland Clinic, Cleveland, Ohio.
Stacey A. Scheib, MD
Assistant Professor and Director, Hopkins Multidisciplinary Fibroid Center, Director of Minimally Invasive Gynecologic Surgery, Johns Hopkins Hospital, Baltimore, Maryland
Anton J. Bilchik, MD, PhD
Professor of Surgery, Chief of Medicine at John Wayne Cancer Institute, Santa Monica, California
Laurel W. Rice, MD
Chair, Department of Obstetrics and Gynecology, Professor, Division of Gynecology Oncology, University of Wisconsin-Madison School of Medicine and Public Health, Madison, Wisconsin
Carla Dionne
Founder of National Uterine Fibroid Foundation, Colorado Springs, Colorado
Alison Jacoby, MD
Director, University of California-San Francisco Comprehensive Fibroid Center, Interim Chief, Division of Gynecology, University of California San Francisco
Charles Ascher-Walsh, MD
Director of Gynecology, Urogynecology, and Minimally Invasive Surgery, Mt. Sinai School of Medicine, New York, New York
Sarah J. Kilpatrick, MD, PhD
Chair of Department of Obstetrics and Gynecology, Associate Dean of Faculty Development, Helping Hand of Los Angeles Chair in Obstetrics and Gynecology, Cedars-Sinai Medical Center, Los Angeles, California
G. David Adamson, MD
Clinical Professor, Stanford University School of Medicine, Stanford, California; Past President of the American Society for Reproductive Medicine
Matthew Siedhoff, MD, MSCR
Assistant Professor and Division Director, Minimally Invasive Gynecologic Surgery, Department of Obstetrics and Gynecology, University of North Carolina at Chapel Hill
Robert Israel, MD
Professor, Department of Obstetrics and Gynecology, Chair, Quality Improvement, Director, Women's Health Clinics and Referrals, LAC+USC Medical Center, Los Angeles, California
Marie Fidela Paraiso, MD
Head, Female Pelvic Medicine & Reconstructive Surgery, Department of Obstetrics and Gynecology, Cleveland Clinic, Cleveland, Ohio
Michael M. Frumovitz, MD, MPH
Fellowship Program Director, Department of Gynecologic Oncology and Reproductive Medicine, University of Texas MD Anderson Cancer Center, Houston, Texas
John R. Lurain, MD
Marcia Stenn Professor of Gynecologic Oncology, Program Director, Fellowship in Gynecologic Oncology, Northwestern University Feinberg School of Medicine, Chicago, Illinois
Ayman Al-Hendy, MD, PhD
Georgia Regents University Director of Interdisciplinary Translational Research; Medical College of Georgia Assistant Dean for Global Translational Research; Professor and Director, Division of Translational Research, Department of Obstetrics and Gynecology, Georgia Regents Health, Augusta, Georgia
Guy I. Benrubi, MD
Senior Associate Dean for Faculty Affairs, Robert J. Thompson Professor and Chair of Department of Obstetrics and Gynecology, University of Florida College of Medicine – Jacksonville
Steven S. Raman, MD
Professor, Radiology, Urology, and Surgery, Co-director, Fibroid Treatment Program, David Geffen School of Medicine at University of California Los Angeles
Rosanne M. Kho, MD
Associate Professor and Head, Section of Urogynecology and Female Pelvic Medicine & Reconstructive Surgery; Co-Director of Minimally Invasive Gynecologic Surgery Fellowship Program, Columbia University Medical Center, New York, New York
Ted L. Anderson, MD, PhD
Betty and Lonnie S. Burnett Professor and Chair, Obstetrics and Gynecology, Division Director of Gynecology, Vanderbilt University School of Medicine, Nashville, Tennessee
R. Kevin Reynolds, MD
The George W. Morley Professor and Chief, Division of Gynecologic Oncology, University of Michigan Health System, Ann Arbor, Michigan
John DeLancey, MD
Norman F. Miller Professor of Obstetrics & Gynecology, University of Michigan Health System, Ann Arbor, Michigan
In November 2014, the FDA ruled that power morcellation was contraindicated in "the majority of women" having surgery for uterine fibroids due to the potential risk of spreading occult uterine sarcoma.1 Although problems with this ruling were immediately apparent, the passage of time has allowed for more clarity on the related medical issues.
Prevalence of leiomyosarcoma among women having surgery for presumed uterine fibroids
The prevalence of occult leiomyosarcoma among women with fibroids is critical for every patient. All medical procedures have potential risk and the patient's understanding of risk is the foundation of medical decision making.
The FDA estimated that for every 458 women having surgery for fibroids, one woman would be found to have an occult leiomyosarcoma (LMS). We challenge this calculation. To estimate this risk, the FDA searched medical databases using the terms “uterine cancer” AND “hysterectomy or myomectomy.” Because “uterine cancer” was required, studies where cancer was not found or discussed were not identified. Nine studies, all but one of which were retrospective, were analyzed including a non–peer-reviewed Letter to the Editor and an abstract from an unpublished study.2,3
Additionally, 3 leiomyosarcoma cases identified by the FDA do not meet current pathologic criteria for cancer and would now be classified as benign "atypical" leiomyomas. If atypical leiomyomas and non–peer-reviewed data are excluded, the FDA identified 8 cases of LMS among 12,402 women having surgery for presumed leiomyomas, a prevalence of 1 in 1,550 (0.064%).
Pritts and colleagues4 recently published a more rigorous meta-analysis of 133 studies and determined that the prevalence of LMS among women having surgery for presumed fibroids was 1 in 1,960, or 0.051%. All peer-reviewed reports in which surgery was performed for presumed fibroids were analyzed, including reports where cancer was not found. Inclusion criteria required that histopathology results be explicitly provided and available for interpretation. Among the 26 randomized controlled trials analyzed, 1,582 women had surgery for fibroids and none were found to have LMS.
Bojahr and colleagues5 recently published a large population-based prospective registry study and reported 2 occult LMS among 8,720 women having surgery for fibroids (0.023%).
In summary: The re-analyzed FDA dataset yields a prevalence of 1 in 1,550 (0.064%); the Pritts study reports a prevalence of 1 in 1,960 (0.051%), with the RCTs having a prevalence of 0; and the Bojahr study reports a prevalence of 2 of 8,720 (0.023%). We acknowledge that with rare events statistical analysis may be uncertain and confidence intervals may be wide. However, these numbers do not support the FDA's estimated prevalence of LMS among women having surgery for presumed fibroids and those at risk for morcellation of an LMS.
Prognosis for women with morcellated LMS
Women with LMS, removed intact without morcellation, have a poor prognosis. Based on SEER data, the 5-year survival of stage I and II LMS is only 61%.6 Whether morcellation influences the prognosis of women with LMS is not known, and the biology of this tumor has not been well studied. Distant metastases occur early in the disease process, primarily hematogenous dissemination. Four frequently quoted published studies examine survival following power morcellation. Surprisingly, virtually none of the women in these studies had power morcellation. Furthermore, the data presented in these reports are poorly analyzed and patient numbers are very small.
Park and colleagues7 reported only one of the 25 morcellated cases had laparoscopic surgery with power morcellation. Eighteen women had a laparoscopically-assisted vaginal hysterectomy with scalpel morcellation performed through the vagina, one had a vaginal hysterectomy with scalpel-morcellation, and 5 had mini-laparotomy with scalpel morcellation through small lower abdominal incisions. Seventeen of the 25 patients plotted in the published survival curve were referred to the hospital after initial diagnosis or the discovery of a recurrence at another institution. Since the number of nonreferred women with less aggressive disease or without recurrence is not known, it is not possible to determine differences in survival between patients with and without morcellation.
In a study by Perri and colleagues,8 none of the patients had power morcellation: 4 women had abdominal myomectomy; 4 had hysteroscopic myomectomy with tissue confined within the uterine cavity; 2 had laparoscopic hysterectomy with scalpel morcellation; 4 had supracervical abdominal hysterectomy with cut-through at the cervix; and 2 had abdominal hysterectomy with injury to the uterus with a sharp instrument.
When comparing the outcomes for women with morcellated and nonmorcellated LMS, Morice and colleagues9 found no difference in recurrence rates or overall and disease-free survival at 6 months.
In the only study to compare use of power with scalpel morcellation in women with LMS, Oduyebo and colleagues10 found no difference in outcomes for the 10 women with power morcellation and 5 with scalpel morcellation followed for a median of 27 months (range, 2–93 months). Notably, a life table analysis of the above studies showed no difference in survival between morcellation methods.11
Of note, laparoscopic-aided morcellation allows the surgeon to inspect the pelvic and abdominal cavities and irrigate and remove tissue fragments under visual control. In contrast, the surgeon cannot visually inspect the peritoneal cavity during vaginal or mini-laparotomy procedures. Morcellation within containment bags has recently been utilized in an attempt to avoid spread of tissue. This method has not yet been proven effective or safe, and there is concern that bags may make morcellation more cumbersome and less safe.
What the FDA restrictions mean for women
The FDA communication states, "the FDA is warning against the use of laparoscopic power morcellators in the majority of women undergoing hysterectomy or myomectomy for uterine fibroids."1 This statement is not consistent with current evidence.
Moreover, a severe restriction of morcellation, including vaginal and mini-laparotomy morcellation, would limit women with symptomatic leiomyomas to one option: total abdominal hysterectomy. For women with fibroids larger than a 10-week pregnancy size, which most often require either scalpel or power morcellation in order to remove tissue, a ban on morcellation would eliminate the following procedures:
- vaginal hysterectomy (scalpel morcellation)
- mini-laparotomy hysterectomy (scalpel morcellation)
- laparoscopic hysterectomy (scalpel morcellation)
- laparoscopic supracervical hysterectomy (cervix cut-through)
- open supracervical hysterectomy (cervix cut-through)
- laparoscopic myomectomy (power morcellation)
- mini-laparotomy myomectomy (scalpel morcellation)
- hysteroscopic myomectomy (intrauterine morcellation)
- uterine artery embolization (no specimen and will delay diagnosis)
- high-intensity focused ultrasound (no specimen and will delay diagnosis)
If abdominal hysterectomy is recommended to women with fibroids, will women be better off?
By focusing exclusively on the risk of LMS, the FDA failed to take into account other risks associated with surgery. Laparoscopic surgery uses small incisions, is performed as an outpatient procedure (or overnight stay), has a faster recovery (2 weeks vs 4–6 weeks for open surgery), and is associated with lower mortality and fewer complications. These benefits of minimally invasive surgery are now well established in gynecologic and general surgery.
Using published best-evidence data, a recent decision analysis12 showed that, comparing 100,000 women undergoing laparoscopic hysterectomy with 100,000 undergoing open hysterectomy, the group undergoing laparoscopic surgery would experience 20 fewer perioperative deaths, 150 fewer pulmonary or venous embolus, and 4,800 fewer wound infections. Importantly, women having open surgery would have 8,000 fewer quality-of-life years.
A recently published study13 found that, in the 8 months following the FDA safety communication, utilization of laparoscopic hysterectomies decreased by 4.1% (P = .005), and abdominal and vaginal hysterectomies increased by 1.7% (P = .112) and 2.4% (P = .012), respectively. Major surgical complications (not including blood transfusions) increased from 2.2% to 2.8% (P = .015), and the rate of hospital readmission within 30 days also increased from 3.4% to 4.2% (P = .025). These observations merit consideration as women weigh the pros and cons of minimally invasive surgery with morcellation versus open surgery. These observations merit consideration as women weigh the pros and cons of minimally invasive surgery with possible morcellation versus open surgery.
Clinical recommendations
Recent attention to surgical options for women with uterine leiomyomas and the risk of an occult leiomyosarcoma are positive developments in that the gynecologic community is re-examining relevant issues. We respectfully suggest that the following clinical recommendations be considered:
- The risk of LMS is higher in older postmenopausal women; greater caution should be exercised prior to recommending morcellation procedures for these women.
- Preoperative consideration of LMS is important. Women aged 35 years and older with irregular uterine bleeding and presumed fibroids should have an endometrial biopsy, which occasionally may detect LMS prior to surgery. Women should have normal results of cervical cancer screening.
- Ultrasound or MRI findings of a large irregular vascular mass, often with irregular anechoic (cystic) areas reflecting necrosis, may cause suspicion of LMS.
- Women wishing minimally invasive procedures with morcellation, including scalpel morcellation via the vagina or mini-laparotomy, or power morcellation using laparoscopic guidance, should understand the potential risk of decreased survival should LMS be present. Open procedures should be offered to all women who are considering minimally invasive procedures for "fibroids."
- Following morcellation, careful inspection for tissue fragments should be undertaken and copious irrigation of the pelvic and abdominal cavities should be performed to minimize the risk of retained tissue.
- Further investigations of a means to identify LMS preoperatively should be supported. Likewise, investigation into the biology of LMS should be funded to better understand the propensity of tissue fragments or cells to implant and grow. With that knowledge, minimally invasive procedures could be avoided for women with LMS and women choosing minimally invasive surgery could be reassured that they do not have LMS.
Respecting women who suffer from leiomyosarcoma, we conclude that the FDA directive was based on a misleading analysis. Consequently, more accurate estimates regarding the prevalence of LMS among women having surgery for fibroids should be issued. Women have a right to self determination. Modification of the FDA's current restrictive guidance regarding power morcellation would empower each woman to consider the pertinent issues and have the freedom to undertake shared decision making with her surgeon in order to select the procedure that is most appropriate for her.
William Parker, MD
Clinical Professor, University of California Los Angeles (UCLA) School of Medicine, Director, Minimally Invasive Gynecologic Surgery, Santa Monica-UCLA Medical Center, Santa Monica, California
Jonathan S. Berek, MD, MMS
Laurie Kraus Lacob Professor and Director, Stanford Women's Cancer Center, Director, Stanford Health Care Communication Program, Chair, Department of Obstetrics and Gynecology, Stanford University School of Medicine, Stanford, California
Elizabeth Pritts, MD
Wisconsin Fertility Institute, Middleton, Wisconsin
David Olive, MD
Wisconsin Fertility Institute, Middleton, Wisconsin
Andrew M. Kaunitz, MD
University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology, University of Florida College of Medicine–Jacksonville; Director, Menopause and Gynecologic Ultrasound Services, UF Women’s Health Specialists at Emerson, Jacksonville, Florida.
Eva Chalas, MD
Chief, Division of Gynecologic Oncology, Director, Clinical Cancer Services, Vice-Chair, Department of Obstetrics and Gynecology, Winthrop-University Hospital, Mineola, New York
Daniel Clarke-Pearson, MD
Professor and Chair, Clinical Research, Gynecologic Oncology Program, University of North Carolina at Chapel Hill
Barbara Goff, MD
Professor, Obstetrics and Gynecology, Director, Division of Gynecologic Oncology, University of Washington, Seattle, Washington
Robert E. Bristow, MD, MBA
Professor and Chair, Department of Obstetrics and Gynecology, University of California Irvine School of Medicine, Orange, California
Hugh S. Taylor, MD
Anita O'Keeffe Young Professor and Chair, Department of Obstetrics, Gynecology, and Reproductive Sciences, Yale School of Medicin; Chief of Obstetrics and Gynecology, Yale-New Haven Hospital, New Haven, Connecticut
Robin Farias-Eisner, MD
Chief, Gynecology and Gynecologic Oncology, Department of Obstetrics and Gynecology, David Geffen School of Medicine at University of California Los Angeles
Amanda Nickles Fader, MD
Director, Kelly Gynecologic Oncology Service, Associate Professor of Gynecology and Obstetrics, Director, FJ Montz Fellowship in Gynecologic Oncology, Johns Hopkins Medicine, Baltimore, Maryland
G. Larry Maxwell, MD, COL (ret) US Army
Chairman, Department of Obstetrics and Gynecology, Inova Fairfax Hospital, Falls Church, Virginia; Co-Investigator and Deputy Director of Science, Department of Defense Gynecologic Cancer Translational Research Center of Excellence, Bethesda, Maryland; Professor of Virginia Commonwealth School of Medicine, Richmond, Virginia; and Executive Director of Globeathon to End Women’s Cancer
Scott C. Goodwin, MD
Hasso Brothers Professor and Chairman, Radiological Sciences, University of California Irvine Medical Center, Orange, California
Susan Love, MD, MBA
Dr. Susan Love Research Foundation, Encino, California
William E. Gibbons, MD
Professor and Director, Division of Reproductive Medicine, Director of Fellowship Training, Department of Obstetrics and Gynecology, Baylor College of Medicine; Chief of Reproductive Medicine at the Pavilion For Women at Texas Children’s Hospital, Houston, Texas
Leland J. Foshag, MD
Surgical Oncology, Melanoma and Sarcoma, John Wayne Cancer Institute, Santa Monica, California
Phyllis C. Leppert, MD, PhD
Emerita Professor of Obstetrics and Gynecology, Duke University School of Medicine; President of The Campion Fund, Phyllis and Mark Leppert Foundation for Fertility Research, Durham, North Carolina
Judy Norsigian
Co-founder of Our Bodies, Ourselves, Boston, Massachusetts
Charles W. Nager, MD
Professor and Chairman, Department of Reproductive Medicine, University of California San Diego Health System
Timothy Robert B. Johnson, MD
Arthur F. Thurnau Professor and Chair, Department of Obstetrics and Gynecology, Professor of Women’s Studies, and Research Professor in the Center for Human Growth and Development, University of Michigan, Ann Arbor, Michigan
David S. Guzick, MD, PhD
Senior Vice President of Health Affairs, President of UF Health, University of Florida, Gainesville, Florida
Sawsan As-Sanie, MD, MPH
Assistant Professor and Director, Minimally Invasive Gynecologic Surgery, Fellowship Director of Endometriosis Center, University of Michigan, Ann Arbor, Michigan
Richard J. Paulson, MD
Alia Tutor Chair in Reproductive Medicine, Professor and Vice-Chair, Department of Obstetrics and Gynecology, Chief, Division of Reproductive Endocrinology and Infertility, Keck School of Medicine, University of Southern California, Los Angeles, California
Cindy Farquhar
Professor of Obstetrics and Gynaecology and National Women's Health, University of Auckland, New Zealand
Linda Bradley, MD
Vice Chair of Obstetrics, Gynecology, and Women’s Health Institute, Director of the Fibroid and Menstrual Disorders Center, Department of Obstetrics and Gynecology, Cleveland Clinic, Cleveland, Ohio.
Stacey A. Scheib, MD
Assistant Professor and Director, Hopkins Multidisciplinary Fibroid Center, Director of Minimally Invasive Gynecologic Surgery, Johns Hopkins Hospital, Baltimore, Maryland
Anton J. Bilchik, MD, PhD
Professor of Surgery, Chief of Medicine at John Wayne Cancer Institute, Santa Monica, California
Laurel W. Rice, MD
Chair, Department of Obstetrics and Gynecology, Professor, Division of Gynecology Oncology, University of Wisconsin-Madison School of Medicine and Public Health, Madison, Wisconsin
Carla Dionne
Founder of National Uterine Fibroid Foundation, Colorado Springs, Colorado
Alison Jacoby, MD
Director, University of California-San Francisco Comprehensive Fibroid Center, Interim Chief, Division of Gynecology, University of California San Francisco
Charles Ascher-Walsh, MD
Director of Gynecology, Urogynecology, and Minimally Invasive Surgery, Mt. Sinai School of Medicine, New York, New York
Sarah J. Kilpatrick, MD, PhD
Chair of Department of Obstetrics and Gynecology, Associate Dean of Faculty Development, Helping Hand of Los Angeles Chair in Obstetrics and Gynecology, Cedars-Sinai Medical Center, Los Angeles, California
G. David Adamson, MD
Clinical Professor, Stanford University School of Medicine, Stanford, California; Past President of the American Society for Reproductive Medicine
Matthew Siedhoff, MD, MSCR
Assistant Professor and Division Director, Minimally Invasive Gynecologic Surgery, Department of Obstetrics and Gynecology, University of North Carolina at Chapel Hill
Robert Israel, MD
Professor, Department of Obstetrics and Gynecology, Chair, Quality Improvement, Director, Women's Health Clinics and Referrals, LAC+USC Medical Center, Los Angeles, California
Marie Fidela Paraiso, MD
Head, Female Pelvic Medicine & Reconstructive Surgery, Department of Obstetrics and Gynecology, Cleveland Clinic, Cleveland, Ohio
Michael M. Frumovitz, MD, MPH
Fellowship Program Director, Department of Gynecologic Oncology and Reproductive Medicine, University of Texas MD Anderson Cancer Center, Houston, Texas
John R. Lurain, MD
Marcia Stenn Professor of Gynecologic Oncology, Program Director, Fellowship in Gynecologic Oncology, Northwestern University Feinberg School of Medicine, Chicago, Illinois
Ayman Al-Hendy, MD, PhD
Georgia Regents University Director of Interdisciplinary Translational Research; Medical College of Georgia Assistant Dean for Global Translational Research; Professor and Director, Division of Translational Research, Department of Obstetrics and Gynecology, Georgia Regents Health, Augusta, Georgia
Guy I. Benrubi, MD
Senior Associate Dean for Faculty Affairs, Robert J. Thompson Professor and Chair of Department of Obstetrics and Gynecology, University of Florida College of Medicine – Jacksonville
Steven S. Raman, MD
Professor, Radiology, Urology, and Surgery, Co-director, Fibroid Treatment Program, David Geffen School of Medicine at University of California Los Angeles
Rosanne M. Kho, MD
Associate Professor and Head, Section of Urogynecology and Female Pelvic Medicine & Reconstructive Surgery; Co-Director of Minimally Invasive Gynecologic Surgery Fellowship Program, Columbia University Medical Center, New York, New York
Ted L. Anderson, MD, PhD
Betty and Lonnie S. Burnett Professor and Chair, Obstetrics and Gynecology, Division Director of Gynecology, Vanderbilt University School of Medicine, Nashville, Tennessee
R. Kevin Reynolds, MD
The George W. Morley Professor and Chief, Division of Gynecologic Oncology, University of Michigan Health System, Ann Arbor, Michigan
John DeLancey, MD
Norman F. Miller Professor of Obstetrics & Gynecology, University of Michigan Health System, Ann Arbor, Michigan
- US Food and Drug Administration. Medical Devices Safety Communications. UPDATED Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy: FDA Safety Communication. http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm424443.htm. Published November 24, 2014. Accessed December 7, 2015.
- Leung F, Terzibachian JJ. Re: "The impact of tumor morcellation during surgery on the prognosis of patients with apparently early uterine leiomyosarcoma” [letter]. Gynecol Oncol. 2012;124(1):172–173.
- Rowland M, Lesnock J, Edwards R, et al. Occult uterine cancer in patients undergoing laparoscopic hysterectomy with morcellation [abstract]. Gynecol Oncol. 2012;127(1):S29.
- Pritts E, Vanness D, Berek J, et al. The prevalence of occult leiomyosarcoma at surgery for presumed uterine fibroids: a meta-analysis. Gynecol Surg. 2015;12(3):165–177.
- Bojahr B, De Wilde R, Tchartchian G. Malignancy rate of 10,731 uteri morcellated during laparoscopic supracervical hysterectomy (LASH). Arch Gynecol Obstet. 2015;292:665–672.
- Kosary CL. SEER survival monograph: Cancer survival among adults: U.S. SEER program, 1988-2001, patient and tumor characteristics. In: Ries LAG, Young JL, Keel GE, et al, eds. Cancer of the corpus uteri. Bethesda, Maryland: National Cancer Institute, SEER Program, NIH; 2007:123–132.
- Park JY, Park SK, Kim DY, et al. The impact of tumor morcellation during surgery on the prognosis of patients with apparently early uterine leiomyosarcoma. Gynecol Oncol. 2011;122(2):255–259.
- Perri T, Korach J, Sadetzki S, Oberman B, Fridman E, Ben-Baruch G. Uterine leiomyosarcoma: does the primary surgical procedure matter? Int J Gynecol Cancer. 2009;19(2):257–260.
- Morice P, Rodriguez A, Rey A, et al. Prognostic value of initial surgical procedure for patients with uterine sarcoma: analysis of 123 patients. Eur J Gynaecol Oncol. 2003;24(3–4):237–240.
- Oduyebo T, Rauh-Hain AJ, Meserve EE, et al. The value of re-exploration in patients with inadvertently morcellated uterine sarcoma. Gynecol Oncol. 2014;132(2):360–365.
- Pritts E, Parker W, Brown J, Olive D. Outcome of occult uterine leiomyosarcoma after surgery for presumed uterine fibroids: a systematic review. J Minim Invasive Gynecol. 2015;22(1):26–33.
- Siedhoff MT, Wheeler SB, Rutstein SE, et al. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis. Am J Obstet Gynecol. 2015;212(5):591.e1–e8.
- Harris JA, Swenson CW, Uppal S, et al. Practice patterns and postoperative complications before and after Food and Drug Administration Safety Communication on power morcellation [published online ahead of print August 24, 2015]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2015.08.047.
- US Food and Drug Administration. Medical Devices Safety Communications. UPDATED Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy: FDA Safety Communication. http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm424443.htm. Published November 24, 2014. Accessed December 7, 2015.
- Leung F, Terzibachian JJ. Re: "The impact of tumor morcellation during surgery on the prognosis of patients with apparently early uterine leiomyosarcoma” [letter]. Gynecol Oncol. 2012;124(1):172–173.
- Rowland M, Lesnock J, Edwards R, et al. Occult uterine cancer in patients undergoing laparoscopic hysterectomy with morcellation [abstract]. Gynecol Oncol. 2012;127(1):S29.
- Pritts E, Vanness D, Berek J, et al. The prevalence of occult leiomyosarcoma at surgery for presumed uterine fibroids: a meta-analysis. Gynecol Surg. 2015;12(3):165–177.
- Bojahr B, De Wilde R, Tchartchian G. Malignancy rate of 10,731 uteri morcellated during laparoscopic supracervical hysterectomy (LASH). Arch Gynecol Obstet. 2015;292:665–672.
- Kosary CL. SEER survival monograph: Cancer survival among adults: U.S. SEER program, 1988-2001, patient and tumor characteristics. In: Ries LAG, Young JL, Keel GE, et al, eds. Cancer of the corpus uteri. Bethesda, Maryland: National Cancer Institute, SEER Program, NIH; 2007:123–132.
- Park JY, Park SK, Kim DY, et al. The impact of tumor morcellation during surgery on the prognosis of patients with apparently early uterine leiomyosarcoma. Gynecol Oncol. 2011;122(2):255–259.
- Perri T, Korach J, Sadetzki S, Oberman B, Fridman E, Ben-Baruch G. Uterine leiomyosarcoma: does the primary surgical procedure matter? Int J Gynecol Cancer. 2009;19(2):257–260.
- Morice P, Rodriguez A, Rey A, et al. Prognostic value of initial surgical procedure for patients with uterine sarcoma: analysis of 123 patients. Eur J Gynaecol Oncol. 2003;24(3–4):237–240.
- Oduyebo T, Rauh-Hain AJ, Meserve EE, et al. The value of re-exploration in patients with inadvertently morcellated uterine sarcoma. Gynecol Oncol. 2014;132(2):360–365.
- Pritts E, Parker W, Brown J, Olive D. Outcome of occult uterine leiomyosarcoma after surgery for presumed uterine fibroids: a systematic review. J Minim Invasive Gynecol. 2015;22(1):26–33.
- Siedhoff MT, Wheeler SB, Rutstein SE, et al. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis. Am J Obstet Gynecol. 2015;212(5):591.e1–e8.
- Harris JA, Swenson CW, Uppal S, et al. Practice patterns and postoperative complications before and after Food and Drug Administration Safety Communication on power morcellation [published online ahead of print August 24, 2015]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2015.08.047.
Click here to listen to an interview with letter signatory Eva Chalas, MD
The Changing Landscape of Orthopedic Practice: Challenges and Opportunities
Orthopedic surgery is going through a time of remarkable change. Health care reform, heightened public scrutiny, shifting population demographics, increased reliance on the Internet for information, ongoing metamorphosis of our profession into a business, and lack of consistent high-quality clinical evidence have created a new frontier of challenges and opportunities. At heart are the needs to deliver high-quality education that is in line with new technological media, to reclaim our ability to guide musculoskeletal care at the policymaking level, to fortify our long-held tradition of ethical responsibility, to invest in research and the training of physician-scientists, to maintain unity among the different subspecialties, and to increase female and minority representation. Never before has understanding and applying the key tenets of our philosophy as orthopedic surgeons been more crucial.
The changing landscape of orthopedic practice has been an unsettling topic in many of the American Academy of Orthopaedic Surgeons (AAOS) presidential addresses in recent years.1-11 What are the challenges and what can we learn moving forward? In this article, we seek to answer these questions by drawing insights from the combined experience and wisdom of past AAOS presidents since the turn of the 21st century.
Education
Education is the cornerstone of providing quality musculoskeletal care12 and staying up to date with technological advances.13 The modes of education delivery, however, have changed. No longer is orthopedic education confined to tangible textbooks and journal articles, nor is it limited to those of us in the profession. Instead, orthopedic education has shifted toward online learning14 and is available to patients and nonorthopedic providers.12 With more patients gaining access to rapidly growing online resources, a unique challenge has arisen: an abundance of data with variable quality of evidence influencing the decision-making process. This has created what Richard Kyle15 described as the “trap of the new technology war,” where patient misinformation and direct-to-consumer marketing can lead to dangerous musculoskeletal care delivery, including unrealistic patient expectations.3 To compound the problem, our ability to provide orthopedic education in formats compatible with the new learning mediums has not been up to the demand, with issues of cost, accessibility, and efficacy plaguing the current process.3,5 Also, we have yet to unlock the benefits of surgical simulation, which has the potential to provide more effective training at no risk to the patient.4,13 By adapting to the new learning formats, we can provide numerous new opportunities for keeping up to date on evolving practice management principles, which, with added accessibility, will be used more often by orthopedic surgeons and the public.13
Research
Research is vital for quality improvement and the continuation of excellence.5 It is only with research that we can provide groundbreaking advances and measure the outcomes of our interventions.2 Unfortunately, orthopedic research funding continues to be disproportionately low, especially given that musculoskeletal ailments are the leading cause of both physician visits and chronic impairment in the United States.2 For example, the National Institute of Arthritis and Musculoskeletal and Skin Diseases receives only 10% of what our country spends on cancer research and 15% of what is spent on heart- and lung-disease research.2 To compound the problem of limited funding, the number of physician-scientists has been dropping at an alarming rate.2 As a result, we must not only refocus our research efforts so that they are efficient and effective, but we must also invest in the training of orthopedic physician-scientists to ensure a continuous stream of groundbreaking discoveries. We owe it to our patients to provide them with proven, effective, and high-quality care.
Industry Relationships
Local and national attention will continue to focus on our relationships with industry. The challenge is twofold: mitigating the negative portrayal of industry relationships and navigating the changes applied to industry funding for research and education.9 Our collaboration with industry is important for the development and advancement of orthopedics,15 but it must be guided by the professional and ethical guidelines established by the AAOS, ensuring that the best interest of patients remains a top priority.8,15 We must maintain the public’s trust by using every opportunity to convey our lone goal in collaborating with industry, ie, improving patient care.9 According to James Beaty,7 any relationship with industry should be “so ethical that it could be printed on the front page of the newspaper and we could face our neighbors with our heads held high.”
Gender and Minority Representation
The racial and ethnic makeup of the United States is undergoing a rapid change. Over the next 4 decades, the white population is projected to become the minority, while women will continue to outnumber men.16 Despite the rapidly changing demographics of the United States, health care disparities persist. As of 2011, minorities and women made up only 22.55% and 14.52%, respectively, of all orthopedic surgery residents.17 This limited diversity in orthopedic training programs is alarming and may lead to suboptimal physician–patient relationships, because patients tend to be more comfortable with and respond better to the care provided by physicians of similar background.3 In addition, if we do not integrate women into orthopedics, the number of female medical students applying to orthopedic residency programs might decline.3
Equating excellent medical care with diversity and cultural competence requires that we bridge the gap that has prevented patients from obtaining high-quality care.8 To achieve this goal, we need to continue recruiting orthopedic surgeons from all segments of our population. Ultimately, health care disparities can be effectively reduced through the delivery of culturally competent care.8
Physician–Patient Relationship
Medical liability has resulted in the development of damaging attitudes among physicians, with many viewing patients as potential adversaries and even avoiding high-risk procedures altogether.6 This deterioration of the physician–patient relationship has been another troubling consequence of managed care that emphasizes quantity and speed.1 As a result, we are perceived by the public as impersonal, poor listeners, and difficult to see on short notice.1
The poor perception of orthopedic surgeons by the general public is not acceptable for a field that places such a high value on excellence. Patient-centered care is at the core of quality improvement, and improving patient relationships starts and ends with us and with each patient we treat.6 In a health care environment in which the average orthopedic surgeon cares for thousands of patients each year, we must make certain to use each opportunity to engage our patients and enhance our relationships with them.6 The basic necessities of patient-centered care include empowerment of the patient through education, better communication, and transparency; providing accurate and evidence-based information; and cooperation among physicians.3,6 The benefits of improving personal relationships with patients are multifold and could have lasting positive effects: increased physician and patient satisfaction, better patient compliance, greater practice efficiency, and fewer malpractice lawsuits.1 We can also benefit from mobilizing a greater constituency to advocate alongside us.6
Unity
Despite accounting for less than 3% of all physicians, orthopedic surgeons have assumed an influential voice in the field of medicine.13 This is attributed not only to the success of our interventions but, more importantly, to the fact that we have “stuck together.”13 The concept of “sticking together” may seem a cliché and facile but will certainly be a pressing need as we move ahead. We draw strength from the breadth and diversity of our subspecialties, but this strength may become a weakness if we do not join in promoting the betterment of our profession as a whole.14 To avoid duplications and bring synergy to all our efforts, we should continue to develop new partnerships in our specialty societies6 and speak with one voice to our patients and to the public.15 Joshua Jacobs11 reminds us of the warning Benjamin Franklin imparted to the signers of the Declaration of Independence, “We must hang together, or most assuredly, we will all hang separately.” To ensure the continued strength of the house of orthopedics, we must live by this tenet.
Advocacy
The federal government has become increasingly involved in regulating the practice of medicine.9 Orthopedic surgery has been hit especially hard, because the cost of implants and continued innovation has fueled the belief that our profession is a major contributor to unsustainable health care costs.11 We now face multiple legislative regulations related to physician reimbursement, ownership, self-referral, medical liability, and mandates of the Affordable Care Act.9 As a result, there has been a decreasing role for orthopedic surgeons as independent practitioners, with more orthopedists forgoing physician-owned practices for large hospital corporations. We are also in increasing competition for limited resources.10 This is compounded by the fact that those regulating health care, paying for health care, and allocating research funding fail to comprehend the high societal needs for treatment of musculoskeletal diseases and injuries,6 which will only increase in the coming decades.14
The aforementioned challenges make our involvement at all levels of the political process more necessary than ever before.5,9 E. Anthony Rankin8 reminds us, “As physicians, we cannot in good conscience allow our patients’ access to quality orthopedic care to be determined solely by the government, the insurance companies, the trial lawyers, or others…. Either we will have a voice in defining the future of health care, or it will be defined by others for us.” Our advocacy approach, however, should be very careful. Joshua Jacobs11 cautions that “we will be most effective if our advocacy message is presented as a potential solution to the current health care crisis, not just as a demand for fair reimbursement.” Instead, we can achieve this goal with what Richard Gelberman2 summarized as “doing what we do best: accumulating knowledge, positioning ourselves as the authorities that we are, and using what we learn to advocate for better patient care and research.”
Value Medicine
Orthopedic surgeons are now expected to provide not just high-quality care but low-cost care. In line with the emerging emphasis on value, sharp focus has been placed on the assessment of physician performance and treatment outcomes as quality-of-care measures.6 But how have we measured the quality of the care we provide? We have not, or, at least, we have not had valid or reliable means of doing so.6 Gone are the days of telling the world of the excellence of our profession in the treatment of musculoskeletal disease. We now must prove to our patients, the government, and payers that what we do works.12,13 If we fail to communicate the cost effectiveness of our interventions, our new knowledge and technologies will not be accepted or funded.10 We should, however, not be discouraged by the new “value equation,” but use it as an incentive to provide evidence-based care and to improve the efficiency of resource utilization.14 Today, we are urged to be leaders in quality improvement, both in our individual orthopedic practices and as a profession.10,12,13
Conclusion
Meeting increasingly higher demands for musculoskeletal care in an evolving medical landscape will bring a new set of challenges that will be more frequent and more intense than those in the past.14 Today, we are tasked with providing fiscally efficient, culturally competent, high-quality, evidence-based, and compassionate care. We are also tasked with reclaiming our ability to shape the future of our profession at the policymaking level. In doing so, the need for unity, advocacy, commitment to education and research, women and minority representation, and open communication with the public has never been more relevant. As we continue to advance as a profession, we must resist the temptation to look back in defiance of change but move forward, confident in our ability to evolve. ◾
1. Canale ST. The orthopaedic forum. Falling in love again. J Bone Joint Surg Am. 2000;82(5):739-742.
2. Gelberman RH. The Academy on the edge: taking charge of our future. J Bone Joint Surg Am. 2001;83(6):946-950.
3. Tolo VT. The challenges of change: is orthopaedics ready? J Bone Joint Surg Am. 2002;84(9):1707-1713.
4. Herndon JH. One more turn of the wrench. J Bone Joint Surg Am. 2003;85(10):2036-2048.
5. Bucholz RW. Knowledge is our business. J Bone Joint Surg Am. 2004;86(7):1575-1578.
6. Weinstein SL. Nothing about you...without you. J Bone Joint Surg Am. 2005;87(7):1648-1652.
7. Beaty JH. Presidential address: “Building the best . . . Lifelong learning”. J Am Acad Orthop Surg. 2007;15(9):515-518.
8. Rankin EA. Presidential Address: advocacy now... for our patients and our profession. J Am Acad Orthop Surg. 2008;16(6):303-305.
9. Zuckerman JD. Silk purses, sows’ ears, and heap ash—turning challenges into opportunities. J Am Acad Orthop Surg. 2009;17(5):271-275.
10. Tongue JR. Strong on vision, flexible on details. J Am Acad Orthop Surg. 2012;20(4):187-189.
11. Jacobs JJ. Moving forward: from curses to blessings. J Am Acad Orthop Surg. 2013;21(5):261-265.
12. Callaghan JJ. Quality of care: getting from good to great. J Am Acad Orthop Surg. 2010;8(9):516-519.
13. Berry DJ. Informed by our past, building our future. J Am Acad Orthop Surg. 2011;19(4):187-190.
14. Azar FM. Building a bigger box. J Am Acad Orthop Surg. 2014;22(6):341-345.
15. Kyle RF. Presidential Address: Together we are one. J Am Acad Orthop Surg. 2006;14(5):261-264.
16. Vincent GK, Velkoff VA. The Next Four Decades: The Older Population in the United States: 2010 to 2050. Washington, DC: Economics and Statistics Administration, US Census Bureau, US Dept of Commerce; 2010.
17. American Academy of Orthopaedic Surgeons Department of Research and Scientific Affairs. 1998-2011 Resident Diversity Survey Report. American Academy of Orthopaedic Surgeons website. http://www3.aaos.org/about/diversity/pdfs/resident_trend.pdf. Published March 9, 2012. Accessed October 26, 2015.
Orthopedic surgery is going through a time of remarkable change. Health care reform, heightened public scrutiny, shifting population demographics, increased reliance on the Internet for information, ongoing metamorphosis of our profession into a business, and lack of consistent high-quality clinical evidence have created a new frontier of challenges and opportunities. At heart are the needs to deliver high-quality education that is in line with new technological media, to reclaim our ability to guide musculoskeletal care at the policymaking level, to fortify our long-held tradition of ethical responsibility, to invest in research and the training of physician-scientists, to maintain unity among the different subspecialties, and to increase female and minority representation. Never before has understanding and applying the key tenets of our philosophy as orthopedic surgeons been more crucial.
The changing landscape of orthopedic practice has been an unsettling topic in many of the American Academy of Orthopaedic Surgeons (AAOS) presidential addresses in recent years.1-11 What are the challenges and what can we learn moving forward? In this article, we seek to answer these questions by drawing insights from the combined experience and wisdom of past AAOS presidents since the turn of the 21st century.
Education
Education is the cornerstone of providing quality musculoskeletal care12 and staying up to date with technological advances.13 The modes of education delivery, however, have changed. No longer is orthopedic education confined to tangible textbooks and journal articles, nor is it limited to those of us in the profession. Instead, orthopedic education has shifted toward online learning14 and is available to patients and nonorthopedic providers.12 With more patients gaining access to rapidly growing online resources, a unique challenge has arisen: an abundance of data with variable quality of evidence influencing the decision-making process. This has created what Richard Kyle15 described as the “trap of the new technology war,” where patient misinformation and direct-to-consumer marketing can lead to dangerous musculoskeletal care delivery, including unrealistic patient expectations.3 To compound the problem, our ability to provide orthopedic education in formats compatible with the new learning mediums has not been up to the demand, with issues of cost, accessibility, and efficacy plaguing the current process.3,5 Also, we have yet to unlock the benefits of surgical simulation, which has the potential to provide more effective training at no risk to the patient.4,13 By adapting to the new learning formats, we can provide numerous new opportunities for keeping up to date on evolving practice management principles, which, with added accessibility, will be used more often by orthopedic surgeons and the public.13
Research
Research is vital for quality improvement and the continuation of excellence.5 It is only with research that we can provide groundbreaking advances and measure the outcomes of our interventions.2 Unfortunately, orthopedic research funding continues to be disproportionately low, especially given that musculoskeletal ailments are the leading cause of both physician visits and chronic impairment in the United States.2 For example, the National Institute of Arthritis and Musculoskeletal and Skin Diseases receives only 10% of what our country spends on cancer research and 15% of what is spent on heart- and lung-disease research.2 To compound the problem of limited funding, the number of physician-scientists has been dropping at an alarming rate.2 As a result, we must not only refocus our research efforts so that they are efficient and effective, but we must also invest in the training of orthopedic physician-scientists to ensure a continuous stream of groundbreaking discoveries. We owe it to our patients to provide them with proven, effective, and high-quality care.
Industry Relationships
Local and national attention will continue to focus on our relationships with industry. The challenge is twofold: mitigating the negative portrayal of industry relationships and navigating the changes applied to industry funding for research and education.9 Our collaboration with industry is important for the development and advancement of orthopedics,15 but it must be guided by the professional and ethical guidelines established by the AAOS, ensuring that the best interest of patients remains a top priority.8,15 We must maintain the public’s trust by using every opportunity to convey our lone goal in collaborating with industry, ie, improving patient care.9 According to James Beaty,7 any relationship with industry should be “so ethical that it could be printed on the front page of the newspaper and we could face our neighbors with our heads held high.”
Gender and Minority Representation
The racial and ethnic makeup of the United States is undergoing a rapid change. Over the next 4 decades, the white population is projected to become the minority, while women will continue to outnumber men.16 Despite the rapidly changing demographics of the United States, health care disparities persist. As of 2011, minorities and women made up only 22.55% and 14.52%, respectively, of all orthopedic surgery residents.17 This limited diversity in orthopedic training programs is alarming and may lead to suboptimal physician–patient relationships, because patients tend to be more comfortable with and respond better to the care provided by physicians of similar background.3 In addition, if we do not integrate women into orthopedics, the number of female medical students applying to orthopedic residency programs might decline.3
Equating excellent medical care with diversity and cultural competence requires that we bridge the gap that has prevented patients from obtaining high-quality care.8 To achieve this goal, we need to continue recruiting orthopedic surgeons from all segments of our population. Ultimately, health care disparities can be effectively reduced through the delivery of culturally competent care.8
Physician–Patient Relationship
Medical liability has resulted in the development of damaging attitudes among physicians, with many viewing patients as potential adversaries and even avoiding high-risk procedures altogether.6 This deterioration of the physician–patient relationship has been another troubling consequence of managed care that emphasizes quantity and speed.1 As a result, we are perceived by the public as impersonal, poor listeners, and difficult to see on short notice.1
The poor perception of orthopedic surgeons by the general public is not acceptable for a field that places such a high value on excellence. Patient-centered care is at the core of quality improvement, and improving patient relationships starts and ends with us and with each patient we treat.6 In a health care environment in which the average orthopedic surgeon cares for thousands of patients each year, we must make certain to use each opportunity to engage our patients and enhance our relationships with them.6 The basic necessities of patient-centered care include empowerment of the patient through education, better communication, and transparency; providing accurate and evidence-based information; and cooperation among physicians.3,6 The benefits of improving personal relationships with patients are multifold and could have lasting positive effects: increased physician and patient satisfaction, better patient compliance, greater practice efficiency, and fewer malpractice lawsuits.1 We can also benefit from mobilizing a greater constituency to advocate alongside us.6
Unity
Despite accounting for less than 3% of all physicians, orthopedic surgeons have assumed an influential voice in the field of medicine.13 This is attributed not only to the success of our interventions but, more importantly, to the fact that we have “stuck together.”13 The concept of “sticking together” may seem a cliché and facile but will certainly be a pressing need as we move ahead. We draw strength from the breadth and diversity of our subspecialties, but this strength may become a weakness if we do not join in promoting the betterment of our profession as a whole.14 To avoid duplications and bring synergy to all our efforts, we should continue to develop new partnerships in our specialty societies6 and speak with one voice to our patients and to the public.15 Joshua Jacobs11 reminds us of the warning Benjamin Franklin imparted to the signers of the Declaration of Independence, “We must hang together, or most assuredly, we will all hang separately.” To ensure the continued strength of the house of orthopedics, we must live by this tenet.
Advocacy
The federal government has become increasingly involved in regulating the practice of medicine.9 Orthopedic surgery has been hit especially hard, because the cost of implants and continued innovation has fueled the belief that our profession is a major contributor to unsustainable health care costs.11 We now face multiple legislative regulations related to physician reimbursement, ownership, self-referral, medical liability, and mandates of the Affordable Care Act.9 As a result, there has been a decreasing role for orthopedic surgeons as independent practitioners, with more orthopedists forgoing physician-owned practices for large hospital corporations. We are also in increasing competition for limited resources.10 This is compounded by the fact that those regulating health care, paying for health care, and allocating research funding fail to comprehend the high societal needs for treatment of musculoskeletal diseases and injuries,6 which will only increase in the coming decades.14
The aforementioned challenges make our involvement at all levels of the political process more necessary than ever before.5,9 E. Anthony Rankin8 reminds us, “As physicians, we cannot in good conscience allow our patients’ access to quality orthopedic care to be determined solely by the government, the insurance companies, the trial lawyers, or others…. Either we will have a voice in defining the future of health care, or it will be defined by others for us.” Our advocacy approach, however, should be very careful. Joshua Jacobs11 cautions that “we will be most effective if our advocacy message is presented as a potential solution to the current health care crisis, not just as a demand for fair reimbursement.” Instead, we can achieve this goal with what Richard Gelberman2 summarized as “doing what we do best: accumulating knowledge, positioning ourselves as the authorities that we are, and using what we learn to advocate for better patient care and research.”
Value Medicine
Orthopedic surgeons are now expected to provide not just high-quality care but low-cost care. In line with the emerging emphasis on value, sharp focus has been placed on the assessment of physician performance and treatment outcomes as quality-of-care measures.6 But how have we measured the quality of the care we provide? We have not, or, at least, we have not had valid or reliable means of doing so.6 Gone are the days of telling the world of the excellence of our profession in the treatment of musculoskeletal disease. We now must prove to our patients, the government, and payers that what we do works.12,13 If we fail to communicate the cost effectiveness of our interventions, our new knowledge and technologies will not be accepted or funded.10 We should, however, not be discouraged by the new “value equation,” but use it as an incentive to provide evidence-based care and to improve the efficiency of resource utilization.14 Today, we are urged to be leaders in quality improvement, both in our individual orthopedic practices and as a profession.10,12,13
Conclusion
Meeting increasingly higher demands for musculoskeletal care in an evolving medical landscape will bring a new set of challenges that will be more frequent and more intense than those in the past.14 Today, we are tasked with providing fiscally efficient, culturally competent, high-quality, evidence-based, and compassionate care. We are also tasked with reclaiming our ability to shape the future of our profession at the policymaking level. In doing so, the need for unity, advocacy, commitment to education and research, women and minority representation, and open communication with the public has never been more relevant. As we continue to advance as a profession, we must resist the temptation to look back in defiance of change but move forward, confident in our ability to evolve. ◾
Orthopedic surgery is going through a time of remarkable change. Health care reform, heightened public scrutiny, shifting population demographics, increased reliance on the Internet for information, ongoing metamorphosis of our profession into a business, and lack of consistent high-quality clinical evidence have created a new frontier of challenges and opportunities. At heart are the needs to deliver high-quality education that is in line with new technological media, to reclaim our ability to guide musculoskeletal care at the policymaking level, to fortify our long-held tradition of ethical responsibility, to invest in research and the training of physician-scientists, to maintain unity among the different subspecialties, and to increase female and minority representation. Never before has understanding and applying the key tenets of our philosophy as orthopedic surgeons been more crucial.
The changing landscape of orthopedic practice has been an unsettling topic in many of the American Academy of Orthopaedic Surgeons (AAOS) presidential addresses in recent years.1-11 What are the challenges and what can we learn moving forward? In this article, we seek to answer these questions by drawing insights from the combined experience and wisdom of past AAOS presidents since the turn of the 21st century.
Education
Education is the cornerstone of providing quality musculoskeletal care12 and staying up to date with technological advances.13 The modes of education delivery, however, have changed. No longer is orthopedic education confined to tangible textbooks and journal articles, nor is it limited to those of us in the profession. Instead, orthopedic education has shifted toward online learning14 and is available to patients and nonorthopedic providers.12 With more patients gaining access to rapidly growing online resources, a unique challenge has arisen: an abundance of data with variable quality of evidence influencing the decision-making process. This has created what Richard Kyle15 described as the “trap of the new technology war,” where patient misinformation and direct-to-consumer marketing can lead to dangerous musculoskeletal care delivery, including unrealistic patient expectations.3 To compound the problem, our ability to provide orthopedic education in formats compatible with the new learning mediums has not been up to the demand, with issues of cost, accessibility, and efficacy plaguing the current process.3,5 Also, we have yet to unlock the benefits of surgical simulation, which has the potential to provide more effective training at no risk to the patient.4,13 By adapting to the new learning formats, we can provide numerous new opportunities for keeping up to date on evolving practice management principles, which, with added accessibility, will be used more often by orthopedic surgeons and the public.13
Research
Research is vital for quality improvement and the continuation of excellence.5 It is only with research that we can provide groundbreaking advances and measure the outcomes of our interventions.2 Unfortunately, orthopedic research funding continues to be disproportionately low, especially given that musculoskeletal ailments are the leading cause of both physician visits and chronic impairment in the United States.2 For example, the National Institute of Arthritis and Musculoskeletal and Skin Diseases receives only 10% of what our country spends on cancer research and 15% of what is spent on heart- and lung-disease research.2 To compound the problem of limited funding, the number of physician-scientists has been dropping at an alarming rate.2 As a result, we must not only refocus our research efforts so that they are efficient and effective, but we must also invest in the training of orthopedic physician-scientists to ensure a continuous stream of groundbreaking discoveries. We owe it to our patients to provide them with proven, effective, and high-quality care.
Industry Relationships
Local and national attention will continue to focus on our relationships with industry. The challenge is twofold: mitigating the negative portrayal of industry relationships and navigating the changes applied to industry funding for research and education.9 Our collaboration with industry is important for the development and advancement of orthopedics,15 but it must be guided by the professional and ethical guidelines established by the AAOS, ensuring that the best interest of patients remains a top priority.8,15 We must maintain the public’s trust by using every opportunity to convey our lone goal in collaborating with industry, ie, improving patient care.9 According to James Beaty,7 any relationship with industry should be “so ethical that it could be printed on the front page of the newspaper and we could face our neighbors with our heads held high.”
Gender and Minority Representation
The racial and ethnic makeup of the United States is undergoing a rapid change. Over the next 4 decades, the white population is projected to become the minority, while women will continue to outnumber men.16 Despite the rapidly changing demographics of the United States, health care disparities persist. As of 2011, minorities and women made up only 22.55% and 14.52%, respectively, of all orthopedic surgery residents.17 This limited diversity in orthopedic training programs is alarming and may lead to suboptimal physician–patient relationships, because patients tend to be more comfortable with and respond better to the care provided by physicians of similar background.3 In addition, if we do not integrate women into orthopedics, the number of female medical students applying to orthopedic residency programs might decline.3
Equating excellent medical care with diversity and cultural competence requires that we bridge the gap that has prevented patients from obtaining high-quality care.8 To achieve this goal, we need to continue recruiting orthopedic surgeons from all segments of our population. Ultimately, health care disparities can be effectively reduced through the delivery of culturally competent care.8
Physician–Patient Relationship
Medical liability has resulted in the development of damaging attitudes among physicians, with many viewing patients as potential adversaries and even avoiding high-risk procedures altogether.6 This deterioration of the physician–patient relationship has been another troubling consequence of managed care that emphasizes quantity and speed.1 As a result, we are perceived by the public as impersonal, poor listeners, and difficult to see on short notice.1
The poor perception of orthopedic surgeons by the general public is not acceptable for a field that places such a high value on excellence. Patient-centered care is at the core of quality improvement, and improving patient relationships starts and ends with us and with each patient we treat.6 In a health care environment in which the average orthopedic surgeon cares for thousands of patients each year, we must make certain to use each opportunity to engage our patients and enhance our relationships with them.6 The basic necessities of patient-centered care include empowerment of the patient through education, better communication, and transparency; providing accurate and evidence-based information; and cooperation among physicians.3,6 The benefits of improving personal relationships with patients are multifold and could have lasting positive effects: increased physician and patient satisfaction, better patient compliance, greater practice efficiency, and fewer malpractice lawsuits.1 We can also benefit from mobilizing a greater constituency to advocate alongside us.6
Unity
Despite accounting for less than 3% of all physicians, orthopedic surgeons have assumed an influential voice in the field of medicine.13 This is attributed not only to the success of our interventions but, more importantly, to the fact that we have “stuck together.”13 The concept of “sticking together” may seem a cliché and facile but will certainly be a pressing need as we move ahead. We draw strength from the breadth and diversity of our subspecialties, but this strength may become a weakness if we do not join in promoting the betterment of our profession as a whole.14 To avoid duplications and bring synergy to all our efforts, we should continue to develop new partnerships in our specialty societies6 and speak with one voice to our patients and to the public.15 Joshua Jacobs11 reminds us of the warning Benjamin Franklin imparted to the signers of the Declaration of Independence, “We must hang together, or most assuredly, we will all hang separately.” To ensure the continued strength of the house of orthopedics, we must live by this tenet.
Advocacy
The federal government has become increasingly involved in regulating the practice of medicine.9 Orthopedic surgery has been hit especially hard, because the cost of implants and continued innovation has fueled the belief that our profession is a major contributor to unsustainable health care costs.11 We now face multiple legislative regulations related to physician reimbursement, ownership, self-referral, medical liability, and mandates of the Affordable Care Act.9 As a result, there has been a decreasing role for orthopedic surgeons as independent practitioners, with more orthopedists forgoing physician-owned practices for large hospital corporations. We are also in increasing competition for limited resources.10 This is compounded by the fact that those regulating health care, paying for health care, and allocating research funding fail to comprehend the high societal needs for treatment of musculoskeletal diseases and injuries,6 which will only increase in the coming decades.14
The aforementioned challenges make our involvement at all levels of the political process more necessary than ever before.5,9 E. Anthony Rankin8 reminds us, “As physicians, we cannot in good conscience allow our patients’ access to quality orthopedic care to be determined solely by the government, the insurance companies, the trial lawyers, or others…. Either we will have a voice in defining the future of health care, or it will be defined by others for us.” Our advocacy approach, however, should be very careful. Joshua Jacobs11 cautions that “we will be most effective if our advocacy message is presented as a potential solution to the current health care crisis, not just as a demand for fair reimbursement.” Instead, we can achieve this goal with what Richard Gelberman2 summarized as “doing what we do best: accumulating knowledge, positioning ourselves as the authorities that we are, and using what we learn to advocate for better patient care and research.”
Value Medicine
Orthopedic surgeons are now expected to provide not just high-quality care but low-cost care. In line with the emerging emphasis on value, sharp focus has been placed on the assessment of physician performance and treatment outcomes as quality-of-care measures.6 But how have we measured the quality of the care we provide? We have not, or, at least, we have not had valid or reliable means of doing so.6 Gone are the days of telling the world of the excellence of our profession in the treatment of musculoskeletal disease. We now must prove to our patients, the government, and payers that what we do works.12,13 If we fail to communicate the cost effectiveness of our interventions, our new knowledge and technologies will not be accepted or funded.10 We should, however, not be discouraged by the new “value equation,” but use it as an incentive to provide evidence-based care and to improve the efficiency of resource utilization.14 Today, we are urged to be leaders in quality improvement, both in our individual orthopedic practices and as a profession.10,12,13
Conclusion
Meeting increasingly higher demands for musculoskeletal care in an evolving medical landscape will bring a new set of challenges that will be more frequent and more intense than those in the past.14 Today, we are tasked with providing fiscally efficient, culturally competent, high-quality, evidence-based, and compassionate care. We are also tasked with reclaiming our ability to shape the future of our profession at the policymaking level. In doing so, the need for unity, advocacy, commitment to education and research, women and minority representation, and open communication with the public has never been more relevant. As we continue to advance as a profession, we must resist the temptation to look back in defiance of change but move forward, confident in our ability to evolve. ◾
1. Canale ST. The orthopaedic forum. Falling in love again. J Bone Joint Surg Am. 2000;82(5):739-742.
2. Gelberman RH. The Academy on the edge: taking charge of our future. J Bone Joint Surg Am. 2001;83(6):946-950.
3. Tolo VT. The challenges of change: is orthopaedics ready? J Bone Joint Surg Am. 2002;84(9):1707-1713.
4. Herndon JH. One more turn of the wrench. J Bone Joint Surg Am. 2003;85(10):2036-2048.
5. Bucholz RW. Knowledge is our business. J Bone Joint Surg Am. 2004;86(7):1575-1578.
6. Weinstein SL. Nothing about you...without you. J Bone Joint Surg Am. 2005;87(7):1648-1652.
7. Beaty JH. Presidential address: “Building the best . . . Lifelong learning”. J Am Acad Orthop Surg. 2007;15(9):515-518.
8. Rankin EA. Presidential Address: advocacy now... for our patients and our profession. J Am Acad Orthop Surg. 2008;16(6):303-305.
9. Zuckerman JD. Silk purses, sows’ ears, and heap ash—turning challenges into opportunities. J Am Acad Orthop Surg. 2009;17(5):271-275.
10. Tongue JR. Strong on vision, flexible on details. J Am Acad Orthop Surg. 2012;20(4):187-189.
11. Jacobs JJ. Moving forward: from curses to blessings. J Am Acad Orthop Surg. 2013;21(5):261-265.
12. Callaghan JJ. Quality of care: getting from good to great. J Am Acad Orthop Surg. 2010;8(9):516-519.
13. Berry DJ. Informed by our past, building our future. J Am Acad Orthop Surg. 2011;19(4):187-190.
14. Azar FM. Building a bigger box. J Am Acad Orthop Surg. 2014;22(6):341-345.
15. Kyle RF. Presidential Address: Together we are one. J Am Acad Orthop Surg. 2006;14(5):261-264.
16. Vincent GK, Velkoff VA. The Next Four Decades: The Older Population in the United States: 2010 to 2050. Washington, DC: Economics and Statistics Administration, US Census Bureau, US Dept of Commerce; 2010.
17. American Academy of Orthopaedic Surgeons Department of Research and Scientific Affairs. 1998-2011 Resident Diversity Survey Report. American Academy of Orthopaedic Surgeons website. http://www3.aaos.org/about/diversity/pdfs/resident_trend.pdf. Published March 9, 2012. Accessed October 26, 2015.
1. Canale ST. The orthopaedic forum. Falling in love again. J Bone Joint Surg Am. 2000;82(5):739-742.
2. Gelberman RH. The Academy on the edge: taking charge of our future. J Bone Joint Surg Am. 2001;83(6):946-950.
3. Tolo VT. The challenges of change: is orthopaedics ready? J Bone Joint Surg Am. 2002;84(9):1707-1713.
4. Herndon JH. One more turn of the wrench. J Bone Joint Surg Am. 2003;85(10):2036-2048.
5. Bucholz RW. Knowledge is our business. J Bone Joint Surg Am. 2004;86(7):1575-1578.
6. Weinstein SL. Nothing about you...without you. J Bone Joint Surg Am. 2005;87(7):1648-1652.
7. Beaty JH. Presidential address: “Building the best . . . Lifelong learning”. J Am Acad Orthop Surg. 2007;15(9):515-518.
8. Rankin EA. Presidential Address: advocacy now... for our patients and our profession. J Am Acad Orthop Surg. 2008;16(6):303-305.
9. Zuckerman JD. Silk purses, sows’ ears, and heap ash—turning challenges into opportunities. J Am Acad Orthop Surg. 2009;17(5):271-275.
10. Tongue JR. Strong on vision, flexible on details. J Am Acad Orthop Surg. 2012;20(4):187-189.
11. Jacobs JJ. Moving forward: from curses to blessings. J Am Acad Orthop Surg. 2013;21(5):261-265.
12. Callaghan JJ. Quality of care: getting from good to great. J Am Acad Orthop Surg. 2010;8(9):516-519.
13. Berry DJ. Informed by our past, building our future. J Am Acad Orthop Surg. 2011;19(4):187-190.
14. Azar FM. Building a bigger box. J Am Acad Orthop Surg. 2014;22(6):341-345.
15. Kyle RF. Presidential Address: Together we are one. J Am Acad Orthop Surg. 2006;14(5):261-264.
16. Vincent GK, Velkoff VA. The Next Four Decades: The Older Population in the United States: 2010 to 2050. Washington, DC: Economics and Statistics Administration, US Census Bureau, US Dept of Commerce; 2010.
17. American Academy of Orthopaedic Surgeons Department of Research and Scientific Affairs. 1998-2011 Resident Diversity Survey Report. American Academy of Orthopaedic Surgeons website. http://www3.aaos.org/about/diversity/pdfs/resident_trend.pdf. Published March 9, 2012. Accessed October 26, 2015.
Pardon the interruption
It’s 7:30 Monday evening and the good news is that you were able to leave the office a little after 7:00 and are now at home. The bad news is that you are on call tonight and you are scheduled to work a usual 10-hour day tomorrow.
Should you:
A) Tuck the kids in, warm up a bowl of chili, and lie down on the couch in the den and hope to get a few hours of prophylactic sleep?
B) Go to bed at your usual bedtime of 10:30?
C) Stay up until midnight when experience tells you that the likelihood of getting a call drops significantly ... but unfortunately never approaches zero?
D) Say “To hell with it” and stay up all night binge-watching a whole season of “Justified?”
E) Or, stay up all night surfing the Internet looking for job opportunities that don’t include night call?
Of course, there is no correct answer because stuff happens whenever it chooses to and no strategy will ever guarantee you an uninterrupted 8 hours of sleep when you are on call. However, I learned from a recent article in the Wall Street Journal (A Good Night’s Sleep Is Tied to Interruptions, Not Just Hours – Sumathi Reddy – Nov. 30, 2015) that there is some evidence that “C” clearly is the best choice.
A study from John Hopkins University, Baltimore, published in the journal Sleep found that subjects who were awakened multiple times during the night exhibited a greater decline in positive mood than did those subjects who were sleep deprived by being made to stay up past their usual bedtime (2015 Nov 1;38[11]:1735-42).
Another study from the University of Pittsburgh discovered that elderly subjects’ cognitive performance was impaired when their sleep was interrupted but not when they were allowed to sleep uninterrupted for a shorter period of time (J Gerontol B Psychol Sci Soc Sci. 2009 Mar;64B[2]:180-7).
And, investigators at the University of Tel Aviv have found that subjects who endured 8 hours of fragmented sleep demonstrated declines in their positive mood and ability to attend that were similar to subjects who were allowed only 4 hours of uninterrupted sleep (Sleep Med. 2011 Mar;12[3]:257-61).
Where were these sleep researchers 45 years ago, when I was experimenting with my own strategies for navigating a night on call with a minimum of emotional and cognitive damage? It took me several years to discover that it was fruitless to try grabbing an hour or two of prophylactic sleep early in the evening when the risk of being awakened by a call was still relatively high. The rare occasion when I slept without interruption was of little comfort on the other nights when I could feel every wakening erode my feeble attempts at projecting a pleasant bedside (my bed that is) manner.
It took another few years of trial and error to improve my skill at determining the optimal time to turn in on a given night. It was never perfect, but eventually, I developed an instinct – based on the level of disease in the community, the pulse of the office during the day, and the weather – that kept the interruptions to a minimum. Despite what you may have heard, I never found the phase of moon to be terribly helpful in predicting when I could more safely go to bed.
There is no avoiding the unpleasant truth that being on call puts you at risk for sleep deprivation. One way or another, you are going to be sleep deprived when you show up at the office the next day. But, your best chance of continuing to appear to be a sensitive and intelligent physician is staying up late until the likelihood you will be awakened by a call has reached its traditional nadir.
It’s 7:30 Monday evening and the good news is that you were able to leave the office a little after 7:00 and are now at home. The bad news is that you are on call tonight and you are scheduled to work a usual 10-hour day tomorrow.
Should you:
A) Tuck the kids in, warm up a bowl of chili, and lie down on the couch in the den and hope to get a few hours of prophylactic sleep?
B) Go to bed at your usual bedtime of 10:30?
C) Stay up until midnight when experience tells you that the likelihood of getting a call drops significantly ... but unfortunately never approaches zero?
D) Say “To hell with it” and stay up all night binge-watching a whole season of “Justified?”
E) Or, stay up all night surfing the Internet looking for job opportunities that don’t include night call?
Of course, there is no correct answer because stuff happens whenever it chooses to and no strategy will ever guarantee you an uninterrupted 8 hours of sleep when you are on call. However, I learned from a recent article in the Wall Street Journal (A Good Night’s Sleep Is Tied to Interruptions, Not Just Hours – Sumathi Reddy – Nov. 30, 2015) that there is some evidence that “C” clearly is the best choice.
A study from John Hopkins University, Baltimore, published in the journal Sleep found that subjects who were awakened multiple times during the night exhibited a greater decline in positive mood than did those subjects who were sleep deprived by being made to stay up past their usual bedtime (2015 Nov 1;38[11]:1735-42).
Another study from the University of Pittsburgh discovered that elderly subjects’ cognitive performance was impaired when their sleep was interrupted but not when they were allowed to sleep uninterrupted for a shorter period of time (J Gerontol B Psychol Sci Soc Sci. 2009 Mar;64B[2]:180-7).
And, investigators at the University of Tel Aviv have found that subjects who endured 8 hours of fragmented sleep demonstrated declines in their positive mood and ability to attend that were similar to subjects who were allowed only 4 hours of uninterrupted sleep (Sleep Med. 2011 Mar;12[3]:257-61).
Where were these sleep researchers 45 years ago, when I was experimenting with my own strategies for navigating a night on call with a minimum of emotional and cognitive damage? It took me several years to discover that it was fruitless to try grabbing an hour or two of prophylactic sleep early in the evening when the risk of being awakened by a call was still relatively high. The rare occasion when I slept without interruption was of little comfort on the other nights when I could feel every wakening erode my feeble attempts at projecting a pleasant bedside (my bed that is) manner.
It took another few years of trial and error to improve my skill at determining the optimal time to turn in on a given night. It was never perfect, but eventually, I developed an instinct – based on the level of disease in the community, the pulse of the office during the day, and the weather – that kept the interruptions to a minimum. Despite what you may have heard, I never found the phase of moon to be terribly helpful in predicting when I could more safely go to bed.
There is no avoiding the unpleasant truth that being on call puts you at risk for sleep deprivation. One way or another, you are going to be sleep deprived when you show up at the office the next day. But, your best chance of continuing to appear to be a sensitive and intelligent physician is staying up late until the likelihood you will be awakened by a call has reached its traditional nadir.
It’s 7:30 Monday evening and the good news is that you were able to leave the office a little after 7:00 and are now at home. The bad news is that you are on call tonight and you are scheduled to work a usual 10-hour day tomorrow.
Should you:
A) Tuck the kids in, warm up a bowl of chili, and lie down on the couch in the den and hope to get a few hours of prophylactic sleep?
B) Go to bed at your usual bedtime of 10:30?
C) Stay up until midnight when experience tells you that the likelihood of getting a call drops significantly ... but unfortunately never approaches zero?
D) Say “To hell with it” and stay up all night binge-watching a whole season of “Justified?”
E) Or, stay up all night surfing the Internet looking for job opportunities that don’t include night call?
Of course, there is no correct answer because stuff happens whenever it chooses to and no strategy will ever guarantee you an uninterrupted 8 hours of sleep when you are on call. However, I learned from a recent article in the Wall Street Journal (A Good Night’s Sleep Is Tied to Interruptions, Not Just Hours – Sumathi Reddy – Nov. 30, 2015) that there is some evidence that “C” clearly is the best choice.
A study from John Hopkins University, Baltimore, published in the journal Sleep found that subjects who were awakened multiple times during the night exhibited a greater decline in positive mood than did those subjects who were sleep deprived by being made to stay up past their usual bedtime (2015 Nov 1;38[11]:1735-42).
Another study from the University of Pittsburgh discovered that elderly subjects’ cognitive performance was impaired when their sleep was interrupted but not when they were allowed to sleep uninterrupted for a shorter period of time (J Gerontol B Psychol Sci Soc Sci. 2009 Mar;64B[2]:180-7).
And, investigators at the University of Tel Aviv have found that subjects who endured 8 hours of fragmented sleep demonstrated declines in their positive mood and ability to attend that were similar to subjects who were allowed only 4 hours of uninterrupted sleep (Sleep Med. 2011 Mar;12[3]:257-61).
Where were these sleep researchers 45 years ago, when I was experimenting with my own strategies for navigating a night on call with a minimum of emotional and cognitive damage? It took me several years to discover that it was fruitless to try grabbing an hour or two of prophylactic sleep early in the evening when the risk of being awakened by a call was still relatively high. The rare occasion when I slept without interruption was of little comfort on the other nights when I could feel every wakening erode my feeble attempts at projecting a pleasant bedside (my bed that is) manner.
It took another few years of trial and error to improve my skill at determining the optimal time to turn in on a given night. It was never perfect, but eventually, I developed an instinct – based on the level of disease in the community, the pulse of the office during the day, and the weather – that kept the interruptions to a minimum. Despite what you may have heard, I never found the phase of moon to be terribly helpful in predicting when I could more safely go to bed.
There is no avoiding the unpleasant truth that being on call puts you at risk for sleep deprivation. One way or another, you are going to be sleep deprived when you show up at the office the next day. But, your best chance of continuing to appear to be a sensitive and intelligent physician is staying up late until the likelihood you will be awakened by a call has reached its traditional nadir.
Bearing the wait
If you have ever waited anxiously for the results of a blood test or biopsy, you may be surprised to learn that some psychologists at the University of California, Riverside, believe that there can be a bright side to those dark days you spent worrying (“Two Definitions of Waiting Well.” Emotion 2015 Oct 12 [epub ahead of print]).
Surveying more than 200 recent law school graduates every 2 weeks during their 4-month wait for the results of the California bar exam, the researchers discovered that those who rode it out anxiously and pessimistically handled the bad news of failure “more productively.” And they welcomed the good news “more joyously” than did their peers who had “suffered little during the wait.”
While these psychologists’ findings may be of some help to aspiring lawyers or freshly minted physicians waiting to hear if they have passed their boards, I don’t think we should take them to heart when ordering lab work or imaging studies on our patients. After all, flunking the bar exam may be a life-altering event, but it isn’t a life-ending one such as learning that the biopsy you waited a week for has detected a cancer that has metastasized beyond the reaches of radiation and chemotherapy.
The bottom line is that waiting for potentially bad news is anxiety provoking regardless of whether it is for the results of a qualifying exam or a simple CBC. And, as physicians, it is our responsibility to do whatever we can to minimize that anxiety by following some simple commonsense rules of courtesy and decency.
First, we must understand that even low-risk preop screening lab work that we may view as innocuous may trigger significant anxiety in many patients. For example, a patient who knew someone whose leukemia was discovered as the result of a preop screening CBC may worry that a similar fate will be revealed by his blood test.
Second, we should ask ourselves every time we order some lab work or imaging study if it is really necessary. Are we just trying to cover our behinds and protect ourselves from a malpractice suit? Do we know what we are going to do with an equivocal borderline result? An unnecessary blood test isn’t just a waste of someone’s money and a symptom of sloppy medicine. It can be the cause of an anxiety-provoking wait for the patient.
Finally, if we are going to order a lab test, even if it is just for preop screening, it is our obligation to inform the patient of the result in a timely fashion. In my universe, that means the same day that the physician receives the result. In today’s world with its panoply of communication platforms, informing the patient can be as simple as leaving a message on a system previously approved by the patient. Obviously, bad or complicated news should be delivered directly by the physician with a phone call. Of course, informing the patient of even normal lab work results takes time, but it is the courteous and decent thing to do and signals to the patient that she has a physician who cares. If it seems like too much work, it may be that the physician is ordering too much lab work.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
If you have ever waited anxiously for the results of a blood test or biopsy, you may be surprised to learn that some psychologists at the University of California, Riverside, believe that there can be a bright side to those dark days you spent worrying (“Two Definitions of Waiting Well.” Emotion 2015 Oct 12 [epub ahead of print]).
Surveying more than 200 recent law school graduates every 2 weeks during their 4-month wait for the results of the California bar exam, the researchers discovered that those who rode it out anxiously and pessimistically handled the bad news of failure “more productively.” And they welcomed the good news “more joyously” than did their peers who had “suffered little during the wait.”
While these psychologists’ findings may be of some help to aspiring lawyers or freshly minted physicians waiting to hear if they have passed their boards, I don’t think we should take them to heart when ordering lab work or imaging studies on our patients. After all, flunking the bar exam may be a life-altering event, but it isn’t a life-ending one such as learning that the biopsy you waited a week for has detected a cancer that has metastasized beyond the reaches of radiation and chemotherapy.
The bottom line is that waiting for potentially bad news is anxiety provoking regardless of whether it is for the results of a qualifying exam or a simple CBC. And, as physicians, it is our responsibility to do whatever we can to minimize that anxiety by following some simple commonsense rules of courtesy and decency.
First, we must understand that even low-risk preop screening lab work that we may view as innocuous may trigger significant anxiety in many patients. For example, a patient who knew someone whose leukemia was discovered as the result of a preop screening CBC may worry that a similar fate will be revealed by his blood test.
Second, we should ask ourselves every time we order some lab work or imaging study if it is really necessary. Are we just trying to cover our behinds and protect ourselves from a malpractice suit? Do we know what we are going to do with an equivocal borderline result? An unnecessary blood test isn’t just a waste of someone’s money and a symptom of sloppy medicine. It can be the cause of an anxiety-provoking wait for the patient.
Finally, if we are going to order a lab test, even if it is just for preop screening, it is our obligation to inform the patient of the result in a timely fashion. In my universe, that means the same day that the physician receives the result. In today’s world with its panoply of communication platforms, informing the patient can be as simple as leaving a message on a system previously approved by the patient. Obviously, bad or complicated news should be delivered directly by the physician with a phone call. Of course, informing the patient of even normal lab work results takes time, but it is the courteous and decent thing to do and signals to the patient that she has a physician who cares. If it seems like too much work, it may be that the physician is ordering too much lab work.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
If you have ever waited anxiously for the results of a blood test or biopsy, you may be surprised to learn that some psychologists at the University of California, Riverside, believe that there can be a bright side to those dark days you spent worrying (“Two Definitions of Waiting Well.” Emotion 2015 Oct 12 [epub ahead of print]).
Surveying more than 200 recent law school graduates every 2 weeks during their 4-month wait for the results of the California bar exam, the researchers discovered that those who rode it out anxiously and pessimistically handled the bad news of failure “more productively.” And they welcomed the good news “more joyously” than did their peers who had “suffered little during the wait.”
While these psychologists’ findings may be of some help to aspiring lawyers or freshly minted physicians waiting to hear if they have passed their boards, I don’t think we should take them to heart when ordering lab work or imaging studies on our patients. After all, flunking the bar exam may be a life-altering event, but it isn’t a life-ending one such as learning that the biopsy you waited a week for has detected a cancer that has metastasized beyond the reaches of radiation and chemotherapy.
The bottom line is that waiting for potentially bad news is anxiety provoking regardless of whether it is for the results of a qualifying exam or a simple CBC. And, as physicians, it is our responsibility to do whatever we can to minimize that anxiety by following some simple commonsense rules of courtesy and decency.
First, we must understand that even low-risk preop screening lab work that we may view as innocuous may trigger significant anxiety in many patients. For example, a patient who knew someone whose leukemia was discovered as the result of a preop screening CBC may worry that a similar fate will be revealed by his blood test.
Second, we should ask ourselves every time we order some lab work or imaging study if it is really necessary. Are we just trying to cover our behinds and protect ourselves from a malpractice suit? Do we know what we are going to do with an equivocal borderline result? An unnecessary blood test isn’t just a waste of someone’s money and a symptom of sloppy medicine. It can be the cause of an anxiety-provoking wait for the patient.
Finally, if we are going to order a lab test, even if it is just for preop screening, it is our obligation to inform the patient of the result in a timely fashion. In my universe, that means the same day that the physician receives the result. In today’s world with its panoply of communication platforms, informing the patient can be as simple as leaving a message on a system previously approved by the patient. Obviously, bad or complicated news should be delivered directly by the physician with a phone call. Of course, informing the patient of even normal lab work results takes time, but it is the courteous and decent thing to do and signals to the patient that she has a physician who cares. If it seems like too much work, it may be that the physician is ordering too much lab work.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
Melia azedarach
Native to China, India, and Iran, Melia azedarach – also known as Chinaberry (Ku-lian), Pride of China, Indian lilac, Persian lilac, and white cedar – is a large nondeciduous tree now cultivated throughout the world.1-3 The leaves and fruits of this member of the Meliaceae family have been found to exhibit anthelmintic and antifeedant activity toward insects.4 The root bark or dried stem bark of the plant is used in traditional Chinese medicine to treat dermatoses and to expel and repel worms.5,6M. azedarach has also been used in Ayurveda3; it is known as Bakayn in India and Pakistan, where it has been used in traditional medicine to treat leprosy, scrofula, nausea, vomiting, thirst, and eruptive skin conditions.3,7
Traditional indications
Cropley and Hasegawa noted in 2007 that M. azedarach was used in the 19th century in the United States primarily as an anthelmintic, but also to treat tinea capitis and to eliminate lice.Further, they noted that the plant, which was widely cultivated in the South, was used, according to the literature of the 1800s, as a diuretic, as well as to promote hair growth, and treat scalp eruptions, fever, and malaria.8
A 2006 ethnopharmacologic study by Saikia et al. of medicinal plants used in Assam (Northeast India) to treat skin disorders and for cosmetic purposes revealed that M. azedarach was one of the primary plants used for medicinal purposes, including 18 skin conditions such as acne, burns, carbuncles, abscesses, measles, pediculosis, cellulitis, and prickly heat.9
Four years later, in an ethnopharmacologic study of medicinal plants used to treat cutaneous disorders and in folk cosmetics, Abbasi et al. interviewed residents in 30 remote tribal communities in the Northwest Frontier Province of Pakistan, finding that M. azedarach was one of 15 plant species identified as curative for numerous skin diseases, including boils, acne, and scabies.10
Biologic activity
Various constituents of M. azedarach have been associated with a wide range of biologic activity. The antifungal activity of the plant has been attributed to its hydroxycoumarin content; anti-inflammatory activity to its monoterpenes; bacteriostatic properties to its beta-carboline alkaloids; antiviral effects to its meliacin and meliacarpin; and insecticidal and antifeedant activity to its limonoids, which belong to the tetranortriterpenoid class of compounds.7,11 Limonoids also are reputed to confer antibacterial, antiviral, and antifungal activities.12 Recent research suggests the potential of M. azedarach to offer a correspondingly broad impact on various conditions.
Anticancer potential
Zhou et al. isolated new ring C-seco limonoids from Brazilian M. azedarach in 2004 and evaluated their cytotoxic activity, finding that two limonoids significantly inhibited HeLa S3 cancer cells.4,11
In 2009, He et al. extracted water-soluble polysaccharides from the fruit of M. azedarach and assessed their cytotoxic activity against four human cell lines in vitro. They found that the major polysaccharide component exhibited potent cytotoxic activity in the BGC-823 cell line.3 Also that year, Wu et al. isolated three new and multiple known steroids from the leaves of Chinese M. azedarach, finding that two of the newly identified steroids – (20S)-5,24(28)-ergostadiene-3-beta,7-alpha,16-beta,20-tetrol and (20S)-5-ergostene-3-beta,7-alpha,16-beta,20-tetrol – and one of the known ones exerted significant cytotoxic impact in three human cancer cell lines (A-549, H460, U251).1
Two years later, Wu et al. isolated two new triterpenoids (21,24-cycloeupha-7-ene-3-beta,16beta,21-alpha,25-tetrol and 3-beta-acetoxy-12-beta-hydroxy-eupha-7,24-dien-21,16-beta-olide) and two new steroids (29-hydroperoxy-stigmasta-7,24(28) xi-dien-3-beta-ol and 24-xi-hydroperoxy-24-vinyl-lathosterol) along with several known related substances from M. azedarach bark. Five of the known compounds demonstrated cytotoxic activity against three human cancer cell lines (A-549, H460, HGC27).6
More recently, Yuan et al. isolated two limonoids, one triterpenoid, one steroid, and one sesquiterpenoid, as well as nine known limonoids from the bark of M. azedarach. In addition, the investigators observed that seven of the limonoids exhibited significant inhibitory properties against five human tumor cell lines (HL-60, SMM-C7721, A-549, MCF-7, and SW480).5
Efficacy against head lice
In 2007, Carpinella et al. investigated in vitro the pediculicidal and ovicidal activity of an M. azedarach extract against Pediculus humanus capitis, noting the increasing resistance of head lice to synthetic drugs. A combination of 20% ripe fruit extract with 10% ripe fruit oil was found to be the most effective in eradicating adult lice (96.5%). The investigators also prepared a formulation of extract and oil at 10% combined with an emulsifier and preservatives that yielded 92.3% mortality of adult lice and complete inhibition of nymph emergence. They concluded that the use of M. azedarach formulations may be a viable and natural way to control head lice.2M. azedarach also has been the key active ingredient in an antimicrobial cream and a preparation to treat tinea pedis.7
Topical cream
Saleem et al. reported in 2008 on an herbal cream preparation using a standardized extract of M. azedarach flowers that displayed strong antibacterial activity against cellulitis, pustules, and pyogenic infections, and other conditions in clinical trials in children under the age of 10 years in four different villages in Pakistan. Subjects with bacterial infections anywhere on the body were divided into three groups, one treated with M. azedarach cream, one with placebo (negative control), and one with neomycin (positive control). Each treatment was applied twice daily for 15 days. The investigators observed that the healing effects of M. azedarach were similar to those rendered by neomycin.7
Conclusion
Not only has M. azedarach been used in several traditional medical systems, but its uses have consistently included cutaneous indications. Its most convincing modern application may be for head lice, but recent evidence and traditional uses suggest that this versatile plant may indeed warrant a more prominent role in the current dermatologic armamentarium. Future research is needed, and should provide some interesting answers.
References
1. Steroids. 2009 Sep;74(9):761-5.
2. J Am Acad Dermatol. 2007 Feb;56(2):250-6.
3. Fitoterapia. 2009 Oct;80(7):399-403.
4. Chem Pharm Bull (Tokyo). 2005 Oct;53(10):1362-5.
5. Planta Med. 2013 Jan;79(2):163-8.
6. Planta Med. 2011 Jun;77(9):922-8.
7. Phytomedicine. 2008 Apr;15(4):231-6.
8. J Am Acad Dermatol. 2007 Aug;57(2):366-7.
9. J Ethnopharmacol. 2006 Jun 30;106(2):149-57.
10. J Ethnopharmacol. 2010 Mar 24;128(2):322-35.
11. J Nat Prod. 2004 Sep;67(9):1544-7.
12. Chem Biodivers. 2010 Apr;7(4):839-59.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Native to China, India, and Iran, Melia azedarach – also known as Chinaberry (Ku-lian), Pride of China, Indian lilac, Persian lilac, and white cedar – is a large nondeciduous tree now cultivated throughout the world.1-3 The leaves and fruits of this member of the Meliaceae family have been found to exhibit anthelmintic and antifeedant activity toward insects.4 The root bark or dried stem bark of the plant is used in traditional Chinese medicine to treat dermatoses and to expel and repel worms.5,6M. azedarach has also been used in Ayurveda3; it is known as Bakayn in India and Pakistan, where it has been used in traditional medicine to treat leprosy, scrofula, nausea, vomiting, thirst, and eruptive skin conditions.3,7
Traditional indications
Cropley and Hasegawa noted in 2007 that M. azedarach was used in the 19th century in the United States primarily as an anthelmintic, but also to treat tinea capitis and to eliminate lice.Further, they noted that the plant, which was widely cultivated in the South, was used, according to the literature of the 1800s, as a diuretic, as well as to promote hair growth, and treat scalp eruptions, fever, and malaria.8
A 2006 ethnopharmacologic study by Saikia et al. of medicinal plants used in Assam (Northeast India) to treat skin disorders and for cosmetic purposes revealed that M. azedarach was one of the primary plants used for medicinal purposes, including 18 skin conditions such as acne, burns, carbuncles, abscesses, measles, pediculosis, cellulitis, and prickly heat.9
Four years later, in an ethnopharmacologic study of medicinal plants used to treat cutaneous disorders and in folk cosmetics, Abbasi et al. interviewed residents in 30 remote tribal communities in the Northwest Frontier Province of Pakistan, finding that M. azedarach was one of 15 plant species identified as curative for numerous skin diseases, including boils, acne, and scabies.10
Biologic activity
Various constituents of M. azedarach have been associated with a wide range of biologic activity. The antifungal activity of the plant has been attributed to its hydroxycoumarin content; anti-inflammatory activity to its monoterpenes; bacteriostatic properties to its beta-carboline alkaloids; antiviral effects to its meliacin and meliacarpin; and insecticidal and antifeedant activity to its limonoids, which belong to the tetranortriterpenoid class of compounds.7,11 Limonoids also are reputed to confer antibacterial, antiviral, and antifungal activities.12 Recent research suggests the potential of M. azedarach to offer a correspondingly broad impact on various conditions.
Anticancer potential
Zhou et al. isolated new ring C-seco limonoids from Brazilian M. azedarach in 2004 and evaluated their cytotoxic activity, finding that two limonoids significantly inhibited HeLa S3 cancer cells.4,11
In 2009, He et al. extracted water-soluble polysaccharides from the fruit of M. azedarach and assessed their cytotoxic activity against four human cell lines in vitro. They found that the major polysaccharide component exhibited potent cytotoxic activity in the BGC-823 cell line.3 Also that year, Wu et al. isolated three new and multiple known steroids from the leaves of Chinese M. azedarach, finding that two of the newly identified steroids – (20S)-5,24(28)-ergostadiene-3-beta,7-alpha,16-beta,20-tetrol and (20S)-5-ergostene-3-beta,7-alpha,16-beta,20-tetrol – and one of the known ones exerted significant cytotoxic impact in three human cancer cell lines (A-549, H460, U251).1
Two years later, Wu et al. isolated two new triterpenoids (21,24-cycloeupha-7-ene-3-beta,16beta,21-alpha,25-tetrol and 3-beta-acetoxy-12-beta-hydroxy-eupha-7,24-dien-21,16-beta-olide) and two new steroids (29-hydroperoxy-stigmasta-7,24(28) xi-dien-3-beta-ol and 24-xi-hydroperoxy-24-vinyl-lathosterol) along with several known related substances from M. azedarach bark. Five of the known compounds demonstrated cytotoxic activity against three human cancer cell lines (A-549, H460, HGC27).6
More recently, Yuan et al. isolated two limonoids, one triterpenoid, one steroid, and one sesquiterpenoid, as well as nine known limonoids from the bark of M. azedarach. In addition, the investigators observed that seven of the limonoids exhibited significant inhibitory properties against five human tumor cell lines (HL-60, SMM-C7721, A-549, MCF-7, and SW480).5
Efficacy against head lice
In 2007, Carpinella et al. investigated in vitro the pediculicidal and ovicidal activity of an M. azedarach extract against Pediculus humanus capitis, noting the increasing resistance of head lice to synthetic drugs. A combination of 20% ripe fruit extract with 10% ripe fruit oil was found to be the most effective in eradicating adult lice (96.5%). The investigators also prepared a formulation of extract and oil at 10% combined with an emulsifier and preservatives that yielded 92.3% mortality of adult lice and complete inhibition of nymph emergence. They concluded that the use of M. azedarach formulations may be a viable and natural way to control head lice.2M. azedarach also has been the key active ingredient in an antimicrobial cream and a preparation to treat tinea pedis.7
Topical cream
Saleem et al. reported in 2008 on an herbal cream preparation using a standardized extract of M. azedarach flowers that displayed strong antibacterial activity against cellulitis, pustules, and pyogenic infections, and other conditions in clinical trials in children under the age of 10 years in four different villages in Pakistan. Subjects with bacterial infections anywhere on the body were divided into three groups, one treated with M. azedarach cream, one with placebo (negative control), and one with neomycin (positive control). Each treatment was applied twice daily for 15 days. The investigators observed that the healing effects of M. azedarach were similar to those rendered by neomycin.7
Conclusion
Not only has M. azedarach been used in several traditional medical systems, but its uses have consistently included cutaneous indications. Its most convincing modern application may be for head lice, but recent evidence and traditional uses suggest that this versatile plant may indeed warrant a more prominent role in the current dermatologic armamentarium. Future research is needed, and should provide some interesting answers.
References
1. Steroids. 2009 Sep;74(9):761-5.
2. J Am Acad Dermatol. 2007 Feb;56(2):250-6.
3. Fitoterapia. 2009 Oct;80(7):399-403.
4. Chem Pharm Bull (Tokyo). 2005 Oct;53(10):1362-5.
5. Planta Med. 2013 Jan;79(2):163-8.
6. Planta Med. 2011 Jun;77(9):922-8.
7. Phytomedicine. 2008 Apr;15(4):231-6.
8. J Am Acad Dermatol. 2007 Aug;57(2):366-7.
9. J Ethnopharmacol. 2006 Jun 30;106(2):149-57.
10. J Ethnopharmacol. 2010 Mar 24;128(2):322-35.
11. J Nat Prod. 2004 Sep;67(9):1544-7.
12. Chem Biodivers. 2010 Apr;7(4):839-59.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Native to China, India, and Iran, Melia azedarach – also known as Chinaberry (Ku-lian), Pride of China, Indian lilac, Persian lilac, and white cedar – is a large nondeciduous tree now cultivated throughout the world.1-3 The leaves and fruits of this member of the Meliaceae family have been found to exhibit anthelmintic and antifeedant activity toward insects.4 The root bark or dried stem bark of the plant is used in traditional Chinese medicine to treat dermatoses and to expel and repel worms.5,6M. azedarach has also been used in Ayurveda3; it is known as Bakayn in India and Pakistan, where it has been used in traditional medicine to treat leprosy, scrofula, nausea, vomiting, thirst, and eruptive skin conditions.3,7
Traditional indications
Cropley and Hasegawa noted in 2007 that M. azedarach was used in the 19th century in the United States primarily as an anthelmintic, but also to treat tinea capitis and to eliminate lice.Further, they noted that the plant, which was widely cultivated in the South, was used, according to the literature of the 1800s, as a diuretic, as well as to promote hair growth, and treat scalp eruptions, fever, and malaria.8
A 2006 ethnopharmacologic study by Saikia et al. of medicinal plants used in Assam (Northeast India) to treat skin disorders and for cosmetic purposes revealed that M. azedarach was one of the primary plants used for medicinal purposes, including 18 skin conditions such as acne, burns, carbuncles, abscesses, measles, pediculosis, cellulitis, and prickly heat.9
Four years later, in an ethnopharmacologic study of medicinal plants used to treat cutaneous disorders and in folk cosmetics, Abbasi et al. interviewed residents in 30 remote tribal communities in the Northwest Frontier Province of Pakistan, finding that M. azedarach was one of 15 plant species identified as curative for numerous skin diseases, including boils, acne, and scabies.10
Biologic activity
Various constituents of M. azedarach have been associated with a wide range of biologic activity. The antifungal activity of the plant has been attributed to its hydroxycoumarin content; anti-inflammatory activity to its monoterpenes; bacteriostatic properties to its beta-carboline alkaloids; antiviral effects to its meliacin and meliacarpin; and insecticidal and antifeedant activity to its limonoids, which belong to the tetranortriterpenoid class of compounds.7,11 Limonoids also are reputed to confer antibacterial, antiviral, and antifungal activities.12 Recent research suggests the potential of M. azedarach to offer a correspondingly broad impact on various conditions.
Anticancer potential
Zhou et al. isolated new ring C-seco limonoids from Brazilian M. azedarach in 2004 and evaluated their cytotoxic activity, finding that two limonoids significantly inhibited HeLa S3 cancer cells.4,11
In 2009, He et al. extracted water-soluble polysaccharides from the fruit of M. azedarach and assessed their cytotoxic activity against four human cell lines in vitro. They found that the major polysaccharide component exhibited potent cytotoxic activity in the BGC-823 cell line.3 Also that year, Wu et al. isolated three new and multiple known steroids from the leaves of Chinese M. azedarach, finding that two of the newly identified steroids – (20S)-5,24(28)-ergostadiene-3-beta,7-alpha,16-beta,20-tetrol and (20S)-5-ergostene-3-beta,7-alpha,16-beta,20-tetrol – and one of the known ones exerted significant cytotoxic impact in three human cancer cell lines (A-549, H460, U251).1
Two years later, Wu et al. isolated two new triterpenoids (21,24-cycloeupha-7-ene-3-beta,16beta,21-alpha,25-tetrol and 3-beta-acetoxy-12-beta-hydroxy-eupha-7,24-dien-21,16-beta-olide) and two new steroids (29-hydroperoxy-stigmasta-7,24(28) xi-dien-3-beta-ol and 24-xi-hydroperoxy-24-vinyl-lathosterol) along with several known related substances from M. azedarach bark. Five of the known compounds demonstrated cytotoxic activity against three human cancer cell lines (A-549, H460, HGC27).6
More recently, Yuan et al. isolated two limonoids, one triterpenoid, one steroid, and one sesquiterpenoid, as well as nine known limonoids from the bark of M. azedarach. In addition, the investigators observed that seven of the limonoids exhibited significant inhibitory properties against five human tumor cell lines (HL-60, SMM-C7721, A-549, MCF-7, and SW480).5
Efficacy against head lice
In 2007, Carpinella et al. investigated in vitro the pediculicidal and ovicidal activity of an M. azedarach extract against Pediculus humanus capitis, noting the increasing resistance of head lice to synthetic drugs. A combination of 20% ripe fruit extract with 10% ripe fruit oil was found to be the most effective in eradicating adult lice (96.5%). The investigators also prepared a formulation of extract and oil at 10% combined with an emulsifier and preservatives that yielded 92.3% mortality of adult lice and complete inhibition of nymph emergence. They concluded that the use of M. azedarach formulations may be a viable and natural way to control head lice.2M. azedarach also has been the key active ingredient in an antimicrobial cream and a preparation to treat tinea pedis.7
Topical cream
Saleem et al. reported in 2008 on an herbal cream preparation using a standardized extract of M. azedarach flowers that displayed strong antibacterial activity against cellulitis, pustules, and pyogenic infections, and other conditions in clinical trials in children under the age of 10 years in four different villages in Pakistan. Subjects with bacterial infections anywhere on the body were divided into three groups, one treated with M. azedarach cream, one with placebo (negative control), and one with neomycin (positive control). Each treatment was applied twice daily for 15 days. The investigators observed that the healing effects of M. azedarach were similar to those rendered by neomycin.7
Conclusion
Not only has M. azedarach been used in several traditional medical systems, but its uses have consistently included cutaneous indications. Its most convincing modern application may be for head lice, but recent evidence and traditional uses suggest that this versatile plant may indeed warrant a more prominent role in the current dermatologic armamentarium. Future research is needed, and should provide some interesting answers.
References
1. Steroids. 2009 Sep;74(9):761-5.
2. J Am Acad Dermatol. 2007 Feb;56(2):250-6.
3. Fitoterapia. 2009 Oct;80(7):399-403.
4. Chem Pharm Bull (Tokyo). 2005 Oct;53(10):1362-5.
5. Planta Med. 2013 Jan;79(2):163-8.
6. Planta Med. 2011 Jun;77(9):922-8.
7. Phytomedicine. 2008 Apr;15(4):231-6.
8. J Am Acad Dermatol. 2007 Aug;57(2):366-7.
9. J Ethnopharmacol. 2006 Jun 30;106(2):149-57.
10. J Ethnopharmacol. 2010 Mar 24;128(2):322-35.
11. J Nat Prod. 2004 Sep;67(9):1544-7.
12. Chem Biodivers. 2010 Apr;7(4):839-59.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Value and the Orthopedic Surgeon
Health care financing and the nature of orthopedic practice have changed dramatically in recent years and will continue to do so. Driving these changes is the emphasis on “value,” defined by Porter1 as the quality of care divided by the cost of care, as opposed to the traditional volume-based care, in which reimbursement is based on a fee for services rendered. Exploring this concept of value in orthopedic care is a favorite topic of mine, succinctly summarized by Black and Warner2 in their 2013 article in The American Journal of Orthopedics. Two papers in this current issue of The American Journal of Orthopedics make important points regarding value and the orthopedic surgeon.
In “Orthopedic Implant Waste: Analysis and Quantification” (pages 554-560), Payne and colleagues examine the costs of wasted implants across 8 orthopedic subspecialties at 1 academic institution over the course of 12 months. The take-home points were these: wasted implants accounted for nearly 2% of the implant cost of the institution; the incidence of waste was related to surgeons with less experience (in practice less than 10 years) but not case volumes (ie, busier surgeons); and nearly two-thirds of the cost of wasted implants occurred in total joint and spine fusion cases.
At my institution, orthopedic implants represent one of the 3 major costs of inpatient hospital care (the other 2 being operating room time and length of stay). Hence, a 2% savings of total implant costs by minimizing waste can make a significant difference in an institution’s profit margin. Since the attending surgeon makes the intraoperative decision on implant type, the burden of minimizing implant waste falls primarily on the orthopedic surgeon. This is just one example of how the individual orthopedic surgeon can improve “value” by decreasing the “cost” of care.
In “Orthopedics in US Health Care” (pages 538-541), Yu and Zuckerman review 5 points on the evolving role orthopedic surgery plays in the changing landscape of US health care. Among many important topics reviewed, the authors raise 2 important issues specifically related to value and the orthopedic surgeon that I believe warrant special attention.
In point 2, “The Cost Equation,” Yu and Zuckerman state that new technology (always more expensive than existing technology!) must “clearly improve outcomes” prior to its introduction to the market. The adage “newer is better” is sometimes true, but new and more expensive technology (which increases the denominator of the “value” quotient) must afford even greater improvement in quality outcomes to justify its widespread use. Hence, as practicing orthopedic surgeons, we should resist the temptation to embrace new technology without clear evidence that said new technology actually improves the quality of care.
The second topic of interest to me is how we measure “outcomes” in this new value-driven health care world. While many important outcome metrics can be measured by hospital data systems, such as length of stay, unscheduled returns to the operating room, transfusion and infection rates, and 30-day readmissions, equally important clinical outcomes (eg, pain and function scores, joint range of motion and strength, and radiographic findings) are obtained primarily from office-based outpatient medical records. These clinically based quality metrics are far more difficult to obtain for individual practicing orthopedic surgeons and require an investment of time and staff to gather meaningful data. How to record and incorporate these clinical outcomes remains a challenge for the practicing orthopedic surgeon, especially in the nonacademic setting, but these clinical metrics must be a component in the “value equation.”
The concept of value in orthopedic surgery will be the primary driver of future health care financing and policies. To succeed in this changing world, orthopedic surgeons will need to not only understand this new paradigm “value = quality/cost,” but be fundamentally involved in the process, institutionally and politically, that both defines and rewards value.
1. Porter ME. What is value in health care? N Engl J Med. 2010;363(26): 2477-2481.
2. Black EM, Warner JJP. 5 points on value in orthopedic surgery. Am J Orthop. 2013:42(1):22-25.
Health care financing and the nature of orthopedic practice have changed dramatically in recent years and will continue to do so. Driving these changes is the emphasis on “value,” defined by Porter1 as the quality of care divided by the cost of care, as opposed to the traditional volume-based care, in which reimbursement is based on a fee for services rendered. Exploring this concept of value in orthopedic care is a favorite topic of mine, succinctly summarized by Black and Warner2 in their 2013 article in The American Journal of Orthopedics. Two papers in this current issue of The American Journal of Orthopedics make important points regarding value and the orthopedic surgeon.
In “Orthopedic Implant Waste: Analysis and Quantification” (pages 554-560), Payne and colleagues examine the costs of wasted implants across 8 orthopedic subspecialties at 1 academic institution over the course of 12 months. The take-home points were these: wasted implants accounted for nearly 2% of the implant cost of the institution; the incidence of waste was related to surgeons with less experience (in practice less than 10 years) but not case volumes (ie, busier surgeons); and nearly two-thirds of the cost of wasted implants occurred in total joint and spine fusion cases.
At my institution, orthopedic implants represent one of the 3 major costs of inpatient hospital care (the other 2 being operating room time and length of stay). Hence, a 2% savings of total implant costs by minimizing waste can make a significant difference in an institution’s profit margin. Since the attending surgeon makes the intraoperative decision on implant type, the burden of minimizing implant waste falls primarily on the orthopedic surgeon. This is just one example of how the individual orthopedic surgeon can improve “value” by decreasing the “cost” of care.
In “Orthopedics in US Health Care” (pages 538-541), Yu and Zuckerman review 5 points on the evolving role orthopedic surgery plays in the changing landscape of US health care. Among many important topics reviewed, the authors raise 2 important issues specifically related to value and the orthopedic surgeon that I believe warrant special attention.
In point 2, “The Cost Equation,” Yu and Zuckerman state that new technology (always more expensive than existing technology!) must “clearly improve outcomes” prior to its introduction to the market. The adage “newer is better” is sometimes true, but new and more expensive technology (which increases the denominator of the “value” quotient) must afford even greater improvement in quality outcomes to justify its widespread use. Hence, as practicing orthopedic surgeons, we should resist the temptation to embrace new technology without clear evidence that said new technology actually improves the quality of care.
The second topic of interest to me is how we measure “outcomes” in this new value-driven health care world. While many important outcome metrics can be measured by hospital data systems, such as length of stay, unscheduled returns to the operating room, transfusion and infection rates, and 30-day readmissions, equally important clinical outcomes (eg, pain and function scores, joint range of motion and strength, and radiographic findings) are obtained primarily from office-based outpatient medical records. These clinically based quality metrics are far more difficult to obtain for individual practicing orthopedic surgeons and require an investment of time and staff to gather meaningful data. How to record and incorporate these clinical outcomes remains a challenge for the practicing orthopedic surgeon, especially in the nonacademic setting, but these clinical metrics must be a component in the “value equation.”
The concept of value in orthopedic surgery will be the primary driver of future health care financing and policies. To succeed in this changing world, orthopedic surgeons will need to not only understand this new paradigm “value = quality/cost,” but be fundamentally involved in the process, institutionally and politically, that both defines and rewards value.
Health care financing and the nature of orthopedic practice have changed dramatically in recent years and will continue to do so. Driving these changes is the emphasis on “value,” defined by Porter1 as the quality of care divided by the cost of care, as opposed to the traditional volume-based care, in which reimbursement is based on a fee for services rendered. Exploring this concept of value in orthopedic care is a favorite topic of mine, succinctly summarized by Black and Warner2 in their 2013 article in The American Journal of Orthopedics. Two papers in this current issue of The American Journal of Orthopedics make important points regarding value and the orthopedic surgeon.
In “Orthopedic Implant Waste: Analysis and Quantification” (pages 554-560), Payne and colleagues examine the costs of wasted implants across 8 orthopedic subspecialties at 1 academic institution over the course of 12 months. The take-home points were these: wasted implants accounted for nearly 2% of the implant cost of the institution; the incidence of waste was related to surgeons with less experience (in practice less than 10 years) but not case volumes (ie, busier surgeons); and nearly two-thirds of the cost of wasted implants occurred in total joint and spine fusion cases.
At my institution, orthopedic implants represent one of the 3 major costs of inpatient hospital care (the other 2 being operating room time and length of stay). Hence, a 2% savings of total implant costs by minimizing waste can make a significant difference in an institution’s profit margin. Since the attending surgeon makes the intraoperative decision on implant type, the burden of minimizing implant waste falls primarily on the orthopedic surgeon. This is just one example of how the individual orthopedic surgeon can improve “value” by decreasing the “cost” of care.
In “Orthopedics in US Health Care” (pages 538-541), Yu and Zuckerman review 5 points on the evolving role orthopedic surgery plays in the changing landscape of US health care. Among many important topics reviewed, the authors raise 2 important issues specifically related to value and the orthopedic surgeon that I believe warrant special attention.
In point 2, “The Cost Equation,” Yu and Zuckerman state that new technology (always more expensive than existing technology!) must “clearly improve outcomes” prior to its introduction to the market. The adage “newer is better” is sometimes true, but new and more expensive technology (which increases the denominator of the “value” quotient) must afford even greater improvement in quality outcomes to justify its widespread use. Hence, as practicing orthopedic surgeons, we should resist the temptation to embrace new technology without clear evidence that said new technology actually improves the quality of care.
The second topic of interest to me is how we measure “outcomes” in this new value-driven health care world. While many important outcome metrics can be measured by hospital data systems, such as length of stay, unscheduled returns to the operating room, transfusion and infection rates, and 30-day readmissions, equally important clinical outcomes (eg, pain and function scores, joint range of motion and strength, and radiographic findings) are obtained primarily from office-based outpatient medical records. These clinically based quality metrics are far more difficult to obtain for individual practicing orthopedic surgeons and require an investment of time and staff to gather meaningful data. How to record and incorporate these clinical outcomes remains a challenge for the practicing orthopedic surgeon, especially in the nonacademic setting, but these clinical metrics must be a component in the “value equation.”
The concept of value in orthopedic surgery will be the primary driver of future health care financing and policies. To succeed in this changing world, orthopedic surgeons will need to not only understand this new paradigm “value = quality/cost,” but be fundamentally involved in the process, institutionally and politically, that both defines and rewards value.
1. Porter ME. What is value in health care? N Engl J Med. 2010;363(26): 2477-2481.
2. Black EM, Warner JJP. 5 points on value in orthopedic surgery. Am J Orthop. 2013:42(1):22-25.
1. Porter ME. What is value in health care? N Engl J Med. 2010;363(26): 2477-2481.
2. Black EM, Warner JJP. 5 points on value in orthopedic surgery. Am J Orthop. 2013:42(1):22-25.