User login
Guidance on infection prevention for health care personnel
As we reopen our offices we are faced with the challenge of determining the best way to do it safely – protecting ourselves, our staff, and our patients.
In this column we will focus on selected details of the recommendations from IDSA and the CDC that may be helpful in primary care offices.
Face masks
Many clinicians have asked whether a physician should use a mask while seeing patients without COVID-19 in the office, and if yes, which type. The IDSA guideline states that mask usage is imperative for reducing the risk of health care workers contracting COVID-19.1 The evidence is derived from a number of sources, including a retrospective study from Wuhan (China) University that examined two groups of health care workers during the outbreak. The first group wore N95 masks and washed their hands frequently, while the second group did not wear masks and washed their hands less frequently. In the group that took greater actions to protect themselves, none of the 493 staff members contracted COVID-19, compared with 10 of 213 staff members in the other group. The decrease in infection rate occurred in the group that wore masks despite the fact that this group had 733% more exposure to COVID-19 patients.2 Further evidence came from a case-control study done in hospitals in Hong Kong during the 2003 SARS-CoV outbreak.3 This study showed that mask wearing was the most significant intervention for reducing infection, followed by gowning, and then handwashing. These findings make it clear that mask usage is a must for all health care providers who may be caring for patients who could have COVID-19.
The guideline also reviews evidence about the use of surgical masks versus N95 masks. On reviewing indirect evidence from the SARS-CoV epidemic, IDSA found that wearing any mask – surgical or N95 – led to a large reduction in the risk of developing an infection. In this systematic review of five observational studies in health care personnel, for those wearing surgical masks, the odds ratio for developing an infection was 0.13 (95% CI, 0.03-0.62), and for those wearing N95 masks, the odds ratio was 0.12 (95% CI, 0.06-0.26). There was not a significant difference between risk reductions for those who wore surgical masks and N95 masks, respectively.1,4 The IDSA guideline panel recommended “that health care personnel caring for patients with suspected or known COVID-19 use either a surgical mask or N95 respirator ... as part of appropriate PPE.” Since there is not a significant difference in outcomes between those who use surgical masks and those who use N95 respirators, and the IDSA guideline states either type of mask is considered appropriate when taking care of patients with suspected or known COVID-19, in our opinion, use of surgical masks rather than N95s is sufficient when performing low-risk activities. Such activities include seeing patients who do not have a high likelihood of COVID-19 in the office setting.
The IDSA recommendation also discusses universal masking, defined as both patients and clinicians wearing masks. The recommendation is supported by the findings of a study in which universal mask usage was used to prevent the spread of H1N 1 during the 2009 outbreak. In this study of staff members and patients exposed to H1N1 who all wore masks, only 0.48% of 836 acquired infection. In the same study, not wearing a mask by either the provider or patient increased the risk of infection.5 Also, in a prospective study of hematopoietic stem cell transplant patients, universal masking caused infection rates to drop from 10.3% to 4.4%.6
The IDSA guideline states the following: “There may be some, albeit uncertain, benefit to universal masking in the absence of resource constraints. However, the benefits of universal masking with surgical masks should be weighed against the risk of increasing the PPE burn rate and contextualized to the background COVID-19 prevalence rate for asymptomatic or minimally symptomatic HCPs [health care providers] and visitors.”1
The CDC’s guidance statement says the following: “Continued community transmission has increased the number of individuals potentially exposed to and infectious with SARS-CoV-2. Fever and symptom screening have proven to be relatively ineffective in identifying all infected individuals, including HCPs. Symptom screening also will not identify individuals who are infected but otherwise asymptomatic or pre-symptomatic; additional interventions are needed to limit the unrecognized introduction of SARS-CoV-2 into healthcare settings by these individuals. As part of aggressive source control measures, healthcare facilities should consider implementing policies requiring everyone entering the facility to wear a cloth face covering (if tolerated) while in the building, regardless of symptoms.”7
It is our opinion, based on the CDC and IDSA recommendations, that both clinicians and patients should be required to wear masks when patients are seen in the office if possible. Many offices have instituted a policy that says, if a patient refuses to wear a mask during an office visit, then the patient will not be seen.
Eye protection
Many clinicians are uncertain about whether eye protection needs to be used when seeing asymptomatic patients. The IDSA acknowledges that there are not studies that have looked critically at eye protection, but the society also acknowledges “appropriate personal protective equipment includes, in addition to a mask or respirator, eye protection, gown and gloves.”1 In addition, the CDC recommends that, for healthcare workers located in areas with moderate or higher prevalence of COVID-19, HCPs should wear eye protection in addition to facemasks since they may encounter asymptomatic individuals with COVID-19.
Gowns and gloves
Gowns and gloves are recommended as a part of personal protective gear when caring for patients who have COVID-19. The IDSA guideline is clear in its recommendations, but does not cite evidence for having no gloves versus having gloves. Furthermore, they state that the evidence is insufficient to recommend double gloves, with the top glove used to take off a personal protective gown, and the inner glove discarded after the gown is removed. The CDC do not make recommendations for routine use of gloves in the care of patients who do not have COVID-19, even in areas where there may be asymptomatic COVID-19, and recommends standard precautions, specifically practicing hand hygiene before and after patient contact.8
The Bottom Line
When seeing patients with COVID-19, N-95 masks, goggles or face shields, gowns, and gloves should be used, with hand hygiene routinely practiced before and after seeing patients. For offices seeing patients not suspected of having COVID-19, the IDSA guideline clarifies that there is not a statistical difference in acquisition of infection with the use of surgical face masks vs N95 respirators. According to the CDC recommendations, eye protection in addition to facemasks should be used by the health care provider, and masks should be worn by patients. Hand hygiene should be used routinely before and after all patient contact. With use of these approaches, it should be safe for offices to reopen and see patients.
Neil Skolnik, MD, is professor of family and community medicine at the Thomas Jefferson University, Philadelphia, and associate director of the Family Medicine Residency Program at Abington (Pa.) Jefferson Health. Jeffrey Matthews, DO, is a second-year resident in the Family Medicine Residency at Abington Jefferson Health. For questions or comments, feel free to contact Dr. Skolnik on Twitter @NeilSkolnik.
References
1. Lynch JB, Davitkov P, Anderson DJ, et al. COVID-19 Guideline, Part 2: Infection Prevention. IDSA Home. https://www.idsociety.org/practice-guideline/covid-19-guideline-infection-prevention/. April 27, 2020. Accessed June 10, 2020.
2. J Hosp Infect. 2020 May;105(1):104-5.
3. Lancet. 2003;361(9368):1519-20.
4. Influenza Other Respir Viruses. 2020 Apr 4. doi: 2020;10.1111/irv.12745.
5. J Hosp Infect. 2010;74(3):271-7.
6. Clin Infect Dis. 2016;63(8):999-1006.
7. Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Accessed Jun 16, 2020.
8. Centers for Disease Control and Prevention. Healthcare Infection Prevention and Control FAQs for COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-faq.html. Accessed June 15, 2020.
As we reopen our offices we are faced with the challenge of determining the best way to do it safely – protecting ourselves, our staff, and our patients.
In this column we will focus on selected details of the recommendations from IDSA and the CDC that may be helpful in primary care offices.
Face masks
Many clinicians have asked whether a physician should use a mask while seeing patients without COVID-19 in the office, and if yes, which type. The IDSA guideline states that mask usage is imperative for reducing the risk of health care workers contracting COVID-19.1 The evidence is derived from a number of sources, including a retrospective study from Wuhan (China) University that examined two groups of health care workers during the outbreak. The first group wore N95 masks and washed their hands frequently, while the second group did not wear masks and washed their hands less frequently. In the group that took greater actions to protect themselves, none of the 493 staff members contracted COVID-19, compared with 10 of 213 staff members in the other group. The decrease in infection rate occurred in the group that wore masks despite the fact that this group had 733% more exposure to COVID-19 patients.2 Further evidence came from a case-control study done in hospitals in Hong Kong during the 2003 SARS-CoV outbreak.3 This study showed that mask wearing was the most significant intervention for reducing infection, followed by gowning, and then handwashing. These findings make it clear that mask usage is a must for all health care providers who may be caring for patients who could have COVID-19.
The guideline also reviews evidence about the use of surgical masks versus N95 masks. On reviewing indirect evidence from the SARS-CoV epidemic, IDSA found that wearing any mask – surgical or N95 – led to a large reduction in the risk of developing an infection. In this systematic review of five observational studies in health care personnel, for those wearing surgical masks, the odds ratio for developing an infection was 0.13 (95% CI, 0.03-0.62), and for those wearing N95 masks, the odds ratio was 0.12 (95% CI, 0.06-0.26). There was not a significant difference between risk reductions for those who wore surgical masks and N95 masks, respectively.1,4 The IDSA guideline panel recommended “that health care personnel caring for patients with suspected or known COVID-19 use either a surgical mask or N95 respirator ... as part of appropriate PPE.” Since there is not a significant difference in outcomes between those who use surgical masks and those who use N95 respirators, and the IDSA guideline states either type of mask is considered appropriate when taking care of patients with suspected or known COVID-19, in our opinion, use of surgical masks rather than N95s is sufficient when performing low-risk activities. Such activities include seeing patients who do not have a high likelihood of COVID-19 in the office setting.
The IDSA recommendation also discusses universal masking, defined as both patients and clinicians wearing masks. The recommendation is supported by the findings of a study in which universal mask usage was used to prevent the spread of H1N 1 during the 2009 outbreak. In this study of staff members and patients exposed to H1N1 who all wore masks, only 0.48% of 836 acquired infection. In the same study, not wearing a mask by either the provider or patient increased the risk of infection.5 Also, in a prospective study of hematopoietic stem cell transplant patients, universal masking caused infection rates to drop from 10.3% to 4.4%.6
The IDSA guideline states the following: “There may be some, albeit uncertain, benefit to universal masking in the absence of resource constraints. However, the benefits of universal masking with surgical masks should be weighed against the risk of increasing the PPE burn rate and contextualized to the background COVID-19 prevalence rate for asymptomatic or minimally symptomatic HCPs [health care providers] and visitors.”1
The CDC’s guidance statement says the following: “Continued community transmission has increased the number of individuals potentially exposed to and infectious with SARS-CoV-2. Fever and symptom screening have proven to be relatively ineffective in identifying all infected individuals, including HCPs. Symptom screening also will not identify individuals who are infected but otherwise asymptomatic or pre-symptomatic; additional interventions are needed to limit the unrecognized introduction of SARS-CoV-2 into healthcare settings by these individuals. As part of aggressive source control measures, healthcare facilities should consider implementing policies requiring everyone entering the facility to wear a cloth face covering (if tolerated) while in the building, regardless of symptoms.”7
It is our opinion, based on the CDC and IDSA recommendations, that both clinicians and patients should be required to wear masks when patients are seen in the office if possible. Many offices have instituted a policy that says, if a patient refuses to wear a mask during an office visit, then the patient will not be seen.
Eye protection
Many clinicians are uncertain about whether eye protection needs to be used when seeing asymptomatic patients. The IDSA acknowledges that there are not studies that have looked critically at eye protection, but the society also acknowledges “appropriate personal protective equipment includes, in addition to a mask or respirator, eye protection, gown and gloves.”1 In addition, the CDC recommends that, for healthcare workers located in areas with moderate or higher prevalence of COVID-19, HCPs should wear eye protection in addition to facemasks since they may encounter asymptomatic individuals with COVID-19.
Gowns and gloves
Gowns and gloves are recommended as a part of personal protective gear when caring for patients who have COVID-19. The IDSA guideline is clear in its recommendations, but does not cite evidence for having no gloves versus having gloves. Furthermore, they state that the evidence is insufficient to recommend double gloves, with the top glove used to take off a personal protective gown, and the inner glove discarded after the gown is removed. The CDC do not make recommendations for routine use of gloves in the care of patients who do not have COVID-19, even in areas where there may be asymptomatic COVID-19, and recommends standard precautions, specifically practicing hand hygiene before and after patient contact.8
The Bottom Line
When seeing patients with COVID-19, N-95 masks, goggles or face shields, gowns, and gloves should be used, with hand hygiene routinely practiced before and after seeing patients. For offices seeing patients not suspected of having COVID-19, the IDSA guideline clarifies that there is not a statistical difference in acquisition of infection with the use of surgical face masks vs N95 respirators. According to the CDC recommendations, eye protection in addition to facemasks should be used by the health care provider, and masks should be worn by patients. Hand hygiene should be used routinely before and after all patient contact. With use of these approaches, it should be safe for offices to reopen and see patients.
Neil Skolnik, MD, is professor of family and community medicine at the Thomas Jefferson University, Philadelphia, and associate director of the Family Medicine Residency Program at Abington (Pa.) Jefferson Health. Jeffrey Matthews, DO, is a second-year resident in the Family Medicine Residency at Abington Jefferson Health. For questions or comments, feel free to contact Dr. Skolnik on Twitter @NeilSkolnik.
References
1. Lynch JB, Davitkov P, Anderson DJ, et al. COVID-19 Guideline, Part 2: Infection Prevention. IDSA Home. https://www.idsociety.org/practice-guideline/covid-19-guideline-infection-prevention/. April 27, 2020. Accessed June 10, 2020.
2. J Hosp Infect. 2020 May;105(1):104-5.
3. Lancet. 2003;361(9368):1519-20.
4. Influenza Other Respir Viruses. 2020 Apr 4. doi: 2020;10.1111/irv.12745.
5. J Hosp Infect. 2010;74(3):271-7.
6. Clin Infect Dis. 2016;63(8):999-1006.
7. Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Accessed Jun 16, 2020.
8. Centers for Disease Control and Prevention. Healthcare Infection Prevention and Control FAQs for COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-faq.html. Accessed June 15, 2020.
As we reopen our offices we are faced with the challenge of determining the best way to do it safely – protecting ourselves, our staff, and our patients.
In this column we will focus on selected details of the recommendations from IDSA and the CDC that may be helpful in primary care offices.
Face masks
Many clinicians have asked whether a physician should use a mask while seeing patients without COVID-19 in the office, and if yes, which type. The IDSA guideline states that mask usage is imperative for reducing the risk of health care workers contracting COVID-19.1 The evidence is derived from a number of sources, including a retrospective study from Wuhan (China) University that examined two groups of health care workers during the outbreak. The first group wore N95 masks and washed their hands frequently, while the second group did not wear masks and washed their hands less frequently. In the group that took greater actions to protect themselves, none of the 493 staff members contracted COVID-19, compared with 10 of 213 staff members in the other group. The decrease in infection rate occurred in the group that wore masks despite the fact that this group had 733% more exposure to COVID-19 patients.2 Further evidence came from a case-control study done in hospitals in Hong Kong during the 2003 SARS-CoV outbreak.3 This study showed that mask wearing was the most significant intervention for reducing infection, followed by gowning, and then handwashing. These findings make it clear that mask usage is a must for all health care providers who may be caring for patients who could have COVID-19.
The guideline also reviews evidence about the use of surgical masks versus N95 masks. On reviewing indirect evidence from the SARS-CoV epidemic, IDSA found that wearing any mask – surgical or N95 – led to a large reduction in the risk of developing an infection. In this systematic review of five observational studies in health care personnel, for those wearing surgical masks, the odds ratio for developing an infection was 0.13 (95% CI, 0.03-0.62), and for those wearing N95 masks, the odds ratio was 0.12 (95% CI, 0.06-0.26). There was not a significant difference between risk reductions for those who wore surgical masks and N95 masks, respectively.1,4 The IDSA guideline panel recommended “that health care personnel caring for patients with suspected or known COVID-19 use either a surgical mask or N95 respirator ... as part of appropriate PPE.” Since there is not a significant difference in outcomes between those who use surgical masks and those who use N95 respirators, and the IDSA guideline states either type of mask is considered appropriate when taking care of patients with suspected or known COVID-19, in our opinion, use of surgical masks rather than N95s is sufficient when performing low-risk activities. Such activities include seeing patients who do not have a high likelihood of COVID-19 in the office setting.
The IDSA recommendation also discusses universal masking, defined as both patients and clinicians wearing masks. The recommendation is supported by the findings of a study in which universal mask usage was used to prevent the spread of H1N 1 during the 2009 outbreak. In this study of staff members and patients exposed to H1N1 who all wore masks, only 0.48% of 836 acquired infection. In the same study, not wearing a mask by either the provider or patient increased the risk of infection.5 Also, in a prospective study of hematopoietic stem cell transplant patients, universal masking caused infection rates to drop from 10.3% to 4.4%.6
The IDSA guideline states the following: “There may be some, albeit uncertain, benefit to universal masking in the absence of resource constraints. However, the benefits of universal masking with surgical masks should be weighed against the risk of increasing the PPE burn rate and contextualized to the background COVID-19 prevalence rate for asymptomatic or minimally symptomatic HCPs [health care providers] and visitors.”1
The CDC’s guidance statement says the following: “Continued community transmission has increased the number of individuals potentially exposed to and infectious with SARS-CoV-2. Fever and symptom screening have proven to be relatively ineffective in identifying all infected individuals, including HCPs. Symptom screening also will not identify individuals who are infected but otherwise asymptomatic or pre-symptomatic; additional interventions are needed to limit the unrecognized introduction of SARS-CoV-2 into healthcare settings by these individuals. As part of aggressive source control measures, healthcare facilities should consider implementing policies requiring everyone entering the facility to wear a cloth face covering (if tolerated) while in the building, regardless of symptoms.”7
It is our opinion, based on the CDC and IDSA recommendations, that both clinicians and patients should be required to wear masks when patients are seen in the office if possible. Many offices have instituted a policy that says, if a patient refuses to wear a mask during an office visit, then the patient will not be seen.
Eye protection
Many clinicians are uncertain about whether eye protection needs to be used when seeing asymptomatic patients. The IDSA acknowledges that there are not studies that have looked critically at eye protection, but the society also acknowledges “appropriate personal protective equipment includes, in addition to a mask or respirator, eye protection, gown and gloves.”1 In addition, the CDC recommends that, for healthcare workers located in areas with moderate or higher prevalence of COVID-19, HCPs should wear eye protection in addition to facemasks since they may encounter asymptomatic individuals with COVID-19.
Gowns and gloves
Gowns and gloves are recommended as a part of personal protective gear when caring for patients who have COVID-19. The IDSA guideline is clear in its recommendations, but does not cite evidence for having no gloves versus having gloves. Furthermore, they state that the evidence is insufficient to recommend double gloves, with the top glove used to take off a personal protective gown, and the inner glove discarded after the gown is removed. The CDC do not make recommendations for routine use of gloves in the care of patients who do not have COVID-19, even in areas where there may be asymptomatic COVID-19, and recommends standard precautions, specifically practicing hand hygiene before and after patient contact.8
The Bottom Line
When seeing patients with COVID-19, N-95 masks, goggles or face shields, gowns, and gloves should be used, with hand hygiene routinely practiced before and after seeing patients. For offices seeing patients not suspected of having COVID-19, the IDSA guideline clarifies that there is not a statistical difference in acquisition of infection with the use of surgical face masks vs N95 respirators. According to the CDC recommendations, eye protection in addition to facemasks should be used by the health care provider, and masks should be worn by patients. Hand hygiene should be used routinely before and after all patient contact. With use of these approaches, it should be safe for offices to reopen and see patients.
Neil Skolnik, MD, is professor of family and community medicine at the Thomas Jefferson University, Philadelphia, and associate director of the Family Medicine Residency Program at Abington (Pa.) Jefferson Health. Jeffrey Matthews, DO, is a second-year resident in the Family Medicine Residency at Abington Jefferson Health. For questions or comments, feel free to contact Dr. Skolnik on Twitter @NeilSkolnik.
References
1. Lynch JB, Davitkov P, Anderson DJ, et al. COVID-19 Guideline, Part 2: Infection Prevention. IDSA Home. https://www.idsociety.org/practice-guideline/covid-19-guideline-infection-prevention/. April 27, 2020. Accessed June 10, 2020.
2. J Hosp Infect. 2020 May;105(1):104-5.
3. Lancet. 2003;361(9368):1519-20.
4. Influenza Other Respir Viruses. 2020 Apr 4. doi: 2020;10.1111/irv.12745.
5. J Hosp Infect. 2010;74(3):271-7.
6. Clin Infect Dis. 2016;63(8):999-1006.
7. Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Accessed Jun 16, 2020.
8. Centers for Disease Control and Prevention. Healthcare Infection Prevention and Control FAQs for COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-faq.html. Accessed June 15, 2020.
Summary of the IDSA guidelines on the diagnosis of COVID-19
These guidelines were developed using a rigorous evidence-based approach, the GRADE framework, which involved identifying the important questions that need to be addressed ahead of time and, later, integrating the best available evidence into the recommendations.
The Food and Drug Administration’s Emergency Use Authorization is useful for understanding any recommendations related to COVID-19 testing. Under usual FDA approval, a manufacturer has to submit data on the performance of a test in human subjects. Under the Emergency Use Authorization for development and approval of SARS-CoV-2 testing, approval is based on “acceptable analytical accuracy,” meaning that a test is assessed using manufactured reagents. The approved test is not tested in real-world clinical situations prior to FDA approval, and the test’s sensitivity and specificity are not well described.
IDSA formulated 15 recommendations, of which the most relevant to primary care clinicians are described and discussed below. The complete set of recommendations can be viewed on the IDSA website:
Recommendation 1
The IDSA panel recommends a SARS-CoV-2 nucleic acid amplification test in symptomatic individuals in the community suspected of having COVID-19, even when the clinical suspicion is low (strong recommendation, very low certainty of evidence). The panel placed a high value on accurate assessment of COVID-19 with the intent of minimizing overdiagnosis of COVID-19 using clinical diagnosis alone. Without testing, the rate of overdiagnosis ranges from 62% to 98%.
If patients are misdiagnosed as having COVID-19, they may spend unnecessary time in quarantine and then may stop taking appropriate safety precautions to protect themselves from infection.
Recommendation 2
The IDSA panel suggests collecting nasopharyngeal, or mid-turbinate or nasal swabs, rather than oropharyngeal swabs or saliva alone for SARS-CoV-2 RNA testing in symptomatic individuals with upper respiratory tract infection or influenza-like illness suspected of having COVID-19 (conditional recommendation, very low certainty of evidence).
The rationale for this recommendation is that comparative data showed a much lower sensitivity for oral sampling, compared with nasopharyngeal, mid-turbinate, or nasal sampling.
The average sensitivity of oral swabs is 56%, compared with nasopharyngeal at 97%, mid-turbinate at 100%, and nasal sampling at 95%. Given these test characteristics, there are far less false-negative tests with nasopharyngeal, mid-turbinate, and nasal swabs. Fewer false negatives means fewer instances of incorrectly telling COVID-19–positive patients that they do not have the illness. An exciting new area of testing that is being evaluated is saliva, which appears to have a sensitivity of 85%.
Recommendation 3
The IDSA panel suggests that nasal and mid-turbinate swab specimens may be collected for SARS-CoV-2 RNA testing by either patients or health care providers in symptomatic individuals with upper respiratory tract infection or influenza-like illness suspected of having COVID-19 (conditional recommendation, low certainty of evidence).
This recommendation is particularly exciting because patient self-collection provides the potential for health care personnel to avoid exposure to infection, as can occur when health care personnel are swabbing a patient; this is ow testing has been done at most testing centers.
While the data are limited, it appears that patient self-collection of nasal or mid-turbinate swabs results in similar detection rates as occurs with health care personnel–collected nasopharyngeal swabs.
Recommendation 6
The IDSA panel suggests repeating viral RNA testing when the initial test is negative (versus performing a single test) in symptomatic individuals with an intermediate or high clinical suspicion of COVID-19 (conditional recommendation, low certainty of evidence).
Since none of the tests are perfect and any can have false negatives, the panel places a high value on detecting infection when present. If there is a low clinical likelihood of disease, the panel recommends not retesting. When the clinical likelihood of COVID-19 is moderate to high, in the event that the initial test is negative, the panel recommends retesting for COVID-19 1-2 days after the initial test.
Recommendation 8
The IDSA panel suggests SARS-CoV-2 RNA testing in asymptomatic individuals who are either known or suspected to have been exposed to COVID-19 (conditional recommendation, very low certainty of evidence).
For this recommendation, a known contact is defined as someone who has had direct contact with a confirmed case.
A suspected exposure occurs when someone is working or living in a congregate setting such as long-term care, a correctional facility, or a cruise ship in which there is an outbreak. The time frame during which to do post-exposure testing is five to seven days after the exposure.
Recommendation 10
The IDSA panel recommends direct SARS-CoV-2 RNA testing in asymptomatic individuals with no known contact with COVID-19 who are being hospitalized in areas with a high prevalence of COVID-19 in the community (conditional recommendation, very low certainty of evidence).
The idea is to do rapid testing to identify individuals entering the hospital either for other illnesses or for procedures, in order to be able to institute appropriate precautions and decrease the likelihood of nosocomial transmission and/or transmission to health care personnel. It is worth noting that the recommendations do not address testing in areas with a low or intermediate prevalence of COVID-19. In the absence of an official guideline-based-recommendation, the decision about testing needs to made by the local hospital system.
Recommendations 11, 12, and 13
The IDSA panel recommends SARS-CoV-2 RNA testing in immunocompromised asymptomatic individuals who are being admitted to the hospital and in asymptomatic individuals prior to receiving immunosuppressive therapy regardless of exposure to COVID-19. It is also recommended to test asymptomatic individuals planning to undergo major surgery.
The rationale for this recommendation is that patients who are to receive chemotherapy, other immunosuppressive procedures, or surgery are at high risk if they have COVID-19 and may be better off delaying the procedure.
Some additional issues were addressed, though not in the form of additional recommendations. It was clarified that some individuals remain nucleic acid positive after their symptoms resolve, and sometimes even after seroconversion. It is not clear if those individuals remain infectious to others. The recommendations did not address serologic testing for public health surveillance.
Dr. Skolnik is professor of family and community medicine at the Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
SOURCE: Hanson KE et al. Infectious Diseases Society of America guidelines on the diagnosis of COVID-19.
These guidelines were developed using a rigorous evidence-based approach, the GRADE framework, which involved identifying the important questions that need to be addressed ahead of time and, later, integrating the best available evidence into the recommendations.
The Food and Drug Administration’s Emergency Use Authorization is useful for understanding any recommendations related to COVID-19 testing. Under usual FDA approval, a manufacturer has to submit data on the performance of a test in human subjects. Under the Emergency Use Authorization for development and approval of SARS-CoV-2 testing, approval is based on “acceptable analytical accuracy,” meaning that a test is assessed using manufactured reagents. The approved test is not tested in real-world clinical situations prior to FDA approval, and the test’s sensitivity and specificity are not well described.
IDSA formulated 15 recommendations, of which the most relevant to primary care clinicians are described and discussed below. The complete set of recommendations can be viewed on the IDSA website:
Recommendation 1
The IDSA panel recommends a SARS-CoV-2 nucleic acid amplification test in symptomatic individuals in the community suspected of having COVID-19, even when the clinical suspicion is low (strong recommendation, very low certainty of evidence). The panel placed a high value on accurate assessment of COVID-19 with the intent of minimizing overdiagnosis of COVID-19 using clinical diagnosis alone. Without testing, the rate of overdiagnosis ranges from 62% to 98%.
If patients are misdiagnosed as having COVID-19, they may spend unnecessary time in quarantine and then may stop taking appropriate safety precautions to protect themselves from infection.
Recommendation 2
The IDSA panel suggests collecting nasopharyngeal, or mid-turbinate or nasal swabs, rather than oropharyngeal swabs or saliva alone for SARS-CoV-2 RNA testing in symptomatic individuals with upper respiratory tract infection or influenza-like illness suspected of having COVID-19 (conditional recommendation, very low certainty of evidence).
The rationale for this recommendation is that comparative data showed a much lower sensitivity for oral sampling, compared with nasopharyngeal, mid-turbinate, or nasal sampling.
The average sensitivity of oral swabs is 56%, compared with nasopharyngeal at 97%, mid-turbinate at 100%, and nasal sampling at 95%. Given these test characteristics, there are far less false-negative tests with nasopharyngeal, mid-turbinate, and nasal swabs. Fewer false negatives means fewer instances of incorrectly telling COVID-19–positive patients that they do not have the illness. An exciting new area of testing that is being evaluated is saliva, which appears to have a sensitivity of 85%.
Recommendation 3
The IDSA panel suggests that nasal and mid-turbinate swab specimens may be collected for SARS-CoV-2 RNA testing by either patients or health care providers in symptomatic individuals with upper respiratory tract infection or influenza-like illness suspected of having COVID-19 (conditional recommendation, low certainty of evidence).
This recommendation is particularly exciting because patient self-collection provides the potential for health care personnel to avoid exposure to infection, as can occur when health care personnel are swabbing a patient; this is ow testing has been done at most testing centers.
While the data are limited, it appears that patient self-collection of nasal or mid-turbinate swabs results in similar detection rates as occurs with health care personnel–collected nasopharyngeal swabs.
Recommendation 6
The IDSA panel suggests repeating viral RNA testing when the initial test is negative (versus performing a single test) in symptomatic individuals with an intermediate or high clinical suspicion of COVID-19 (conditional recommendation, low certainty of evidence).
Since none of the tests are perfect and any can have false negatives, the panel places a high value on detecting infection when present. If there is a low clinical likelihood of disease, the panel recommends not retesting. When the clinical likelihood of COVID-19 is moderate to high, in the event that the initial test is negative, the panel recommends retesting for COVID-19 1-2 days after the initial test.
Recommendation 8
The IDSA panel suggests SARS-CoV-2 RNA testing in asymptomatic individuals who are either known or suspected to have been exposed to COVID-19 (conditional recommendation, very low certainty of evidence).
For this recommendation, a known contact is defined as someone who has had direct contact with a confirmed case.
A suspected exposure occurs when someone is working or living in a congregate setting such as long-term care, a correctional facility, or a cruise ship in which there is an outbreak. The time frame during which to do post-exposure testing is five to seven days after the exposure.
Recommendation 10
The IDSA panel recommends direct SARS-CoV-2 RNA testing in asymptomatic individuals with no known contact with COVID-19 who are being hospitalized in areas with a high prevalence of COVID-19 in the community (conditional recommendation, very low certainty of evidence).
The idea is to do rapid testing to identify individuals entering the hospital either for other illnesses or for procedures, in order to be able to institute appropriate precautions and decrease the likelihood of nosocomial transmission and/or transmission to health care personnel. It is worth noting that the recommendations do not address testing in areas with a low or intermediate prevalence of COVID-19. In the absence of an official guideline-based-recommendation, the decision about testing needs to made by the local hospital system.
Recommendations 11, 12, and 13
The IDSA panel recommends SARS-CoV-2 RNA testing in immunocompromised asymptomatic individuals who are being admitted to the hospital and in asymptomatic individuals prior to receiving immunosuppressive therapy regardless of exposure to COVID-19. It is also recommended to test asymptomatic individuals planning to undergo major surgery.
The rationale for this recommendation is that patients who are to receive chemotherapy, other immunosuppressive procedures, or surgery are at high risk if they have COVID-19 and may be better off delaying the procedure.
Some additional issues were addressed, though not in the form of additional recommendations. It was clarified that some individuals remain nucleic acid positive after their symptoms resolve, and sometimes even after seroconversion. It is not clear if those individuals remain infectious to others. The recommendations did not address serologic testing for public health surveillance.
Dr. Skolnik is professor of family and community medicine at the Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
SOURCE: Hanson KE et al. Infectious Diseases Society of America guidelines on the diagnosis of COVID-19.
These guidelines were developed using a rigorous evidence-based approach, the GRADE framework, which involved identifying the important questions that need to be addressed ahead of time and, later, integrating the best available evidence into the recommendations.
The Food and Drug Administration’s Emergency Use Authorization is useful for understanding any recommendations related to COVID-19 testing. Under usual FDA approval, a manufacturer has to submit data on the performance of a test in human subjects. Under the Emergency Use Authorization for development and approval of SARS-CoV-2 testing, approval is based on “acceptable analytical accuracy,” meaning that a test is assessed using manufactured reagents. The approved test is not tested in real-world clinical situations prior to FDA approval, and the test’s sensitivity and specificity are not well described.
IDSA formulated 15 recommendations, of which the most relevant to primary care clinicians are described and discussed below. The complete set of recommendations can be viewed on the IDSA website:
Recommendation 1
The IDSA panel recommends a SARS-CoV-2 nucleic acid amplification test in symptomatic individuals in the community suspected of having COVID-19, even when the clinical suspicion is low (strong recommendation, very low certainty of evidence). The panel placed a high value on accurate assessment of COVID-19 with the intent of minimizing overdiagnosis of COVID-19 using clinical diagnosis alone. Without testing, the rate of overdiagnosis ranges from 62% to 98%.
If patients are misdiagnosed as having COVID-19, they may spend unnecessary time in quarantine and then may stop taking appropriate safety precautions to protect themselves from infection.
Recommendation 2
The IDSA panel suggests collecting nasopharyngeal, or mid-turbinate or nasal swabs, rather than oropharyngeal swabs or saliva alone for SARS-CoV-2 RNA testing in symptomatic individuals with upper respiratory tract infection or influenza-like illness suspected of having COVID-19 (conditional recommendation, very low certainty of evidence).
The rationale for this recommendation is that comparative data showed a much lower sensitivity for oral sampling, compared with nasopharyngeal, mid-turbinate, or nasal sampling.
The average sensitivity of oral swabs is 56%, compared with nasopharyngeal at 97%, mid-turbinate at 100%, and nasal sampling at 95%. Given these test characteristics, there are far less false-negative tests with nasopharyngeal, mid-turbinate, and nasal swabs. Fewer false negatives means fewer instances of incorrectly telling COVID-19–positive patients that they do not have the illness. An exciting new area of testing that is being evaluated is saliva, which appears to have a sensitivity of 85%.
Recommendation 3
The IDSA panel suggests that nasal and mid-turbinate swab specimens may be collected for SARS-CoV-2 RNA testing by either patients or health care providers in symptomatic individuals with upper respiratory tract infection or influenza-like illness suspected of having COVID-19 (conditional recommendation, low certainty of evidence).
This recommendation is particularly exciting because patient self-collection provides the potential for health care personnel to avoid exposure to infection, as can occur when health care personnel are swabbing a patient; this is ow testing has been done at most testing centers.
While the data are limited, it appears that patient self-collection of nasal or mid-turbinate swabs results in similar detection rates as occurs with health care personnel–collected nasopharyngeal swabs.
Recommendation 6
The IDSA panel suggests repeating viral RNA testing when the initial test is negative (versus performing a single test) in symptomatic individuals with an intermediate or high clinical suspicion of COVID-19 (conditional recommendation, low certainty of evidence).
Since none of the tests are perfect and any can have false negatives, the panel places a high value on detecting infection when present. If there is a low clinical likelihood of disease, the panel recommends not retesting. When the clinical likelihood of COVID-19 is moderate to high, in the event that the initial test is negative, the panel recommends retesting for COVID-19 1-2 days after the initial test.
Recommendation 8
The IDSA panel suggests SARS-CoV-2 RNA testing in asymptomatic individuals who are either known or suspected to have been exposed to COVID-19 (conditional recommendation, very low certainty of evidence).
For this recommendation, a known contact is defined as someone who has had direct contact with a confirmed case.
A suspected exposure occurs when someone is working or living in a congregate setting such as long-term care, a correctional facility, or a cruise ship in which there is an outbreak. The time frame during which to do post-exposure testing is five to seven days after the exposure.
Recommendation 10
The IDSA panel recommends direct SARS-CoV-2 RNA testing in asymptomatic individuals with no known contact with COVID-19 who are being hospitalized in areas with a high prevalence of COVID-19 in the community (conditional recommendation, very low certainty of evidence).
The idea is to do rapid testing to identify individuals entering the hospital either for other illnesses or for procedures, in order to be able to institute appropriate precautions and decrease the likelihood of nosocomial transmission and/or transmission to health care personnel. It is worth noting that the recommendations do not address testing in areas with a low or intermediate prevalence of COVID-19. In the absence of an official guideline-based-recommendation, the decision about testing needs to made by the local hospital system.
Recommendations 11, 12, and 13
The IDSA panel recommends SARS-CoV-2 RNA testing in immunocompromised asymptomatic individuals who are being admitted to the hospital and in asymptomatic individuals prior to receiving immunosuppressive therapy regardless of exposure to COVID-19. It is also recommended to test asymptomatic individuals planning to undergo major surgery.
The rationale for this recommendation is that patients who are to receive chemotherapy, other immunosuppressive procedures, or surgery are at high risk if they have COVID-19 and may be better off delaying the procedure.
Some additional issues were addressed, though not in the form of additional recommendations. It was clarified that some individuals remain nucleic acid positive after their symptoms resolve, and sometimes even after seroconversion. It is not clear if those individuals remain infectious to others. The recommendations did not address serologic testing for public health surveillance.
Dr. Skolnik is professor of family and community medicine at the Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
SOURCE: Hanson KE et al. Infectious Diseases Society of America guidelines on the diagnosis of COVID-19.
COVID-19: Frequently asked clinical questions
Question
How should patients on immunosuppressive therapy be advised during the COVID-19 pandemic?
Answer
In general, those patients who have not tested positive, have not been exposed, and are asymptomatic should continue their medications as prescribed.
The American College of Rheumatology issued a statement on April 14, recommending that stable patients continue their medications. Those with known exposure but without confirmed infection may continue hydroxychloroquine, sulfasalazine, and NSAIDs.
Immunosuppressants, non–IL-6 biologics, and JAK inhibitors should be stopped temporarily, pending a negative test or after two weeks without symptoms. In patients with confirmed positive COVID-19 infection, sulfasalazine, methotrexate, leflunomide, immunosuppressants, non-IL-6 biologics, and JAK inhibitors should be stopped temporarily, pending a negative test or after two weeks without symptoms. In patients with confirmed positive COVID-19 infection, sulfasalazine, methotrexate, leflunomide, immunosuppressants, non-IL-6 biologics, and JAK inhibitors should be stopped temporarily. Anti-malarial therapies (hydroxycholoroquine and chloroquine) may be continued and IL-6 inhibitors may be continued in select circumstances.1
The American Academy of Dermatology recommends that the discussion of continuation of biologics be based on a case-by-case basis, citing insufficient evidence to recommend against discontinuation at this time in those patients who have not tested positive. In patients who have tested positive for COVID-19 it is recommended that biologic therapy be suspended until symptoms have resolved.2
Question
Should I continue preventive services during peak COVID-19?
Answer
The Centers for Disease Control and Prevention recommends delaying all elective ambulatory provider visits. In general, preventative services, such as adult immunizations, lipid screening, and cancer screenings, should be delayed. Additionally, the CDC recommends reaching out to patients who are at high risk for complications from respiratory diseases to ensure medication adherence and provide resources if these patients become ill. Facilities can reduce transmission of COVID-19 by triaging and assessing patients through virtual visits through phone calls, video conferences, text-monitoring systems, and other telemedicine tools. Physicians should try to provide routine and chronic care through virtual visits when possible over in-person visits.3
Question
Should I continue to vaccinate my pediatric population during peak COVID-19?
Answer
Practices that schedule separate well visits and sick visits in different sessions or locations can continue to provide well child visits. A practice could, for example, schedule well visits in the morning and sick visits in the afternoon if a single facility is used. These practices should prioritize newborn care and vaccinations of children, especially for those under the age of 24 months.4
Question
Can physicians use telehealth (phone only or audiovisual) to conduct visits with Medicare patients even if they are new patients?
Answer
Effective March 1 through the duration of the pandemic, Medicare will pay physicians for telehealth services at the same rate as an in-office visit. On March 30th, the Centers for Medicare & Medcaid Services announced new policies for physicians and hospitals during the COVID-19 pandemic. These guidelines were updated on April 9.
Audio-only visits are now permitted and the limit on the number of these kinds of visits allowed per month has been waived. Controlled substances can be prescribed via telehealth; however, complying with each state’s individual laws is still required.
Use of any two-way, audiovisual device is permitted. The level of service billed for visits with both audio and visual components is the same as an in-office visit. Telemedicine can be used for both new and existing patients.5
A list of services that may be rendered via telehealth are available on the CMS website.6
It will be important to regularly check the references given, as information on some of these topics is updated frequently.
Dr. Chuong is a second-year resident in the family medicine residency, Dr. Flanagan is a third-year resident, and Dr. Matthews is an intern, all at Abington (Pa.) Jefferson Health. Dr. Skolnik is professor of family and community medicine at the Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
References
1. ACR issues COVID-19 treatment guidance for rheumatic disease patients.
2. American Academy of Dermatology: Guidance on the use of biologic agents during COVID-19 outbreak.
3. Centers for Disease Control and Prevention. Actions to take in response to community transmission of COVID-19.
4. Centers for Disease Control and Prevention. Maintaining childhood immunizations during COVID19 pandemic.
5. Centers for Medicare & Medcaid Services. COVID-19 frequently asked questions (FAQs) on Medicare Fee-for-Service (FFS) billing.
6. Centers for Medicare & Medcaid Services. List of telehealth services.
Question
How should patients on immunosuppressive therapy be advised during the COVID-19 pandemic?
Answer
In general, those patients who have not tested positive, have not been exposed, and are asymptomatic should continue their medications as prescribed.
The American College of Rheumatology issued a statement on April 14, recommending that stable patients continue their medications. Those with known exposure but without confirmed infection may continue hydroxychloroquine, sulfasalazine, and NSAIDs.
Immunosuppressants, non–IL-6 biologics, and JAK inhibitors should be stopped temporarily, pending a negative test or after two weeks without symptoms. In patients with confirmed positive COVID-19 infection, sulfasalazine, methotrexate, leflunomide, immunosuppressants, non-IL-6 biologics, and JAK inhibitors should be stopped temporarily, pending a negative test or after two weeks without symptoms. In patients with confirmed positive COVID-19 infection, sulfasalazine, methotrexate, leflunomide, immunosuppressants, non-IL-6 biologics, and JAK inhibitors should be stopped temporarily. Anti-malarial therapies (hydroxycholoroquine and chloroquine) may be continued and IL-6 inhibitors may be continued in select circumstances.1
The American Academy of Dermatology recommends that the discussion of continuation of biologics be based on a case-by-case basis, citing insufficient evidence to recommend against discontinuation at this time in those patients who have not tested positive. In patients who have tested positive for COVID-19 it is recommended that biologic therapy be suspended until symptoms have resolved.2
Question
Should I continue preventive services during peak COVID-19?
Answer
The Centers for Disease Control and Prevention recommends delaying all elective ambulatory provider visits. In general, preventative services, such as adult immunizations, lipid screening, and cancer screenings, should be delayed. Additionally, the CDC recommends reaching out to patients who are at high risk for complications from respiratory diseases to ensure medication adherence and provide resources if these patients become ill. Facilities can reduce transmission of COVID-19 by triaging and assessing patients through virtual visits through phone calls, video conferences, text-monitoring systems, and other telemedicine tools. Physicians should try to provide routine and chronic care through virtual visits when possible over in-person visits.3
Question
Should I continue to vaccinate my pediatric population during peak COVID-19?
Answer
Practices that schedule separate well visits and sick visits in different sessions or locations can continue to provide well child visits. A practice could, for example, schedule well visits in the morning and sick visits in the afternoon if a single facility is used. These practices should prioritize newborn care and vaccinations of children, especially for those under the age of 24 months.4
Question
Can physicians use telehealth (phone only or audiovisual) to conduct visits with Medicare patients even if they are new patients?
Answer
Effective March 1 through the duration of the pandemic, Medicare will pay physicians for telehealth services at the same rate as an in-office visit. On March 30th, the Centers for Medicare & Medcaid Services announced new policies for physicians and hospitals during the COVID-19 pandemic. These guidelines were updated on April 9.
Audio-only visits are now permitted and the limit on the number of these kinds of visits allowed per month has been waived. Controlled substances can be prescribed via telehealth; however, complying with each state’s individual laws is still required.
Use of any two-way, audiovisual device is permitted. The level of service billed for visits with both audio and visual components is the same as an in-office visit. Telemedicine can be used for both new and existing patients.5
A list of services that may be rendered via telehealth are available on the CMS website.6
It will be important to regularly check the references given, as information on some of these topics is updated frequently.
Dr. Chuong is a second-year resident in the family medicine residency, Dr. Flanagan is a third-year resident, and Dr. Matthews is an intern, all at Abington (Pa.) Jefferson Health. Dr. Skolnik is professor of family and community medicine at the Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
References
1. ACR issues COVID-19 treatment guidance for rheumatic disease patients.
2. American Academy of Dermatology: Guidance on the use of biologic agents during COVID-19 outbreak.
3. Centers for Disease Control and Prevention. Actions to take in response to community transmission of COVID-19.
4. Centers for Disease Control and Prevention. Maintaining childhood immunizations during COVID19 pandemic.
5. Centers for Medicare & Medcaid Services. COVID-19 frequently asked questions (FAQs) on Medicare Fee-for-Service (FFS) billing.
6. Centers for Medicare & Medcaid Services. List of telehealth services.
Question
How should patients on immunosuppressive therapy be advised during the COVID-19 pandemic?
Answer
In general, those patients who have not tested positive, have not been exposed, and are asymptomatic should continue their medications as prescribed.
The American College of Rheumatology issued a statement on April 14, recommending that stable patients continue their medications. Those with known exposure but without confirmed infection may continue hydroxychloroquine, sulfasalazine, and NSAIDs.
Immunosuppressants, non–IL-6 biologics, and JAK inhibitors should be stopped temporarily, pending a negative test or after two weeks without symptoms. In patients with confirmed positive COVID-19 infection, sulfasalazine, methotrexate, leflunomide, immunosuppressants, non-IL-6 biologics, and JAK inhibitors should be stopped temporarily, pending a negative test or after two weeks without symptoms. In patients with confirmed positive COVID-19 infection, sulfasalazine, methotrexate, leflunomide, immunosuppressants, non-IL-6 biologics, and JAK inhibitors should be stopped temporarily. Anti-malarial therapies (hydroxycholoroquine and chloroquine) may be continued and IL-6 inhibitors may be continued in select circumstances.1
The American Academy of Dermatology recommends that the discussion of continuation of biologics be based on a case-by-case basis, citing insufficient evidence to recommend against discontinuation at this time in those patients who have not tested positive. In patients who have tested positive for COVID-19 it is recommended that biologic therapy be suspended until symptoms have resolved.2
Question
Should I continue preventive services during peak COVID-19?
Answer
The Centers for Disease Control and Prevention recommends delaying all elective ambulatory provider visits. In general, preventative services, such as adult immunizations, lipid screening, and cancer screenings, should be delayed. Additionally, the CDC recommends reaching out to patients who are at high risk for complications from respiratory diseases to ensure medication adherence and provide resources if these patients become ill. Facilities can reduce transmission of COVID-19 by triaging and assessing patients through virtual visits through phone calls, video conferences, text-monitoring systems, and other telemedicine tools. Physicians should try to provide routine and chronic care through virtual visits when possible over in-person visits.3
Question
Should I continue to vaccinate my pediatric population during peak COVID-19?
Answer
Practices that schedule separate well visits and sick visits in different sessions or locations can continue to provide well child visits. A practice could, for example, schedule well visits in the morning and sick visits in the afternoon if a single facility is used. These practices should prioritize newborn care and vaccinations of children, especially for those under the age of 24 months.4
Question
Can physicians use telehealth (phone only or audiovisual) to conduct visits with Medicare patients even if they are new patients?
Answer
Effective March 1 through the duration of the pandemic, Medicare will pay physicians for telehealth services at the same rate as an in-office visit. On March 30th, the Centers for Medicare & Medcaid Services announced new policies for physicians and hospitals during the COVID-19 pandemic. These guidelines were updated on April 9.
Audio-only visits are now permitted and the limit on the number of these kinds of visits allowed per month has been waived. Controlled substances can be prescribed via telehealth; however, complying with each state’s individual laws is still required.
Use of any two-way, audiovisual device is permitted. The level of service billed for visits with both audio and visual components is the same as an in-office visit. Telemedicine can be used for both new and existing patients.5
A list of services that may be rendered via telehealth are available on the CMS website.6
It will be important to regularly check the references given, as information on some of these topics is updated frequently.
Dr. Chuong is a second-year resident in the family medicine residency, Dr. Flanagan is a third-year resident, and Dr. Matthews is an intern, all at Abington (Pa.) Jefferson Health. Dr. Skolnik is professor of family and community medicine at the Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
References
1. ACR issues COVID-19 treatment guidance for rheumatic disease patients.
2. American Academy of Dermatology: Guidance on the use of biologic agents during COVID-19 outbreak.
3. Centers for Disease Control and Prevention. Actions to take in response to community transmission of COVID-19.
4. Centers for Disease Control and Prevention. Maintaining childhood immunizations during COVID19 pandemic.
5. Centers for Medicare & Medcaid Services. COVID-19 frequently asked questions (FAQs) on Medicare Fee-for-Service (FFS) billing.
6. Centers for Medicare & Medcaid Services. List of telehealth services.
New guidelines for testosterone treatment in adult men with age-related low testosterone
Testosterone normally decreases with age in men beginning in their mid-30s, with a rate of decline averaging approximately 1.6% per year. Using a cutoff of a total testosterone less than 325 ng/dL, the incidence of low testosterone is approximately 20% after age 60 years, and 30% after age 70. While the change in labs values has been reasonably validated,
Additional potential symptoms of testosterone deficiency include changes in bone mineral density, decreased libido, depression, erectile dysfunction, loss of hair, and general weakness. Since the symptoms are nonspecific, it is often unclear if someone should be tested or treated for testosterone deficiency. To address this issue, the American College of Physicians commissioned a systematic review of the evidence on testosterone-replacement therapy for age-related testosterone deficiency.1
The evidence review of testosterone replacement in men with age-related low testosterone found the following.
- Low-certainty evidence of improvement in quality of life
- Moderate-certainty evidence of a small improvement in sexual function
- Low-certainty evidence of a small improvement in erectile function
- Low-certainty evidence showing little to no improvement in physical function
- Low-certainty evidence of a small increase to no difference in adverse cardiovascular events
- Moderate-certainty evidence of no increase in the risk for serious adverse events
The trials were not powered to assess mortality, but pool analysis showed fewer deaths among patients treated with testosterone than those who received placebo (odds ratio, 0.47; 95% confidence interval, 0.25-0.89). There were no differences in cognitive function, and the improvement in vitality and fatigue was “less than a small amount.” Evidence from an observational trial showed no increased risk for mortality, cardiovascular events, prostate cancer, or pulmonary embolus or deep vein thrombosis. Of note, most studies excluded men with recent cardiovascular disease.
This evidence review led to the following recommendations.2
Recommendation 1a
Clinicians should have a discussion regarding the potential risk and benefits of treatment with the patients who have documented age-related low testosterone (testosterone levels less than 10.4 nmol/L or 300 ng/dL) and are suffering from sexual dysfunction or have a desire to enhance their sexual function.
This recommendation was based on evidence showing small improvement in sexual function and erectile dysfunction.
Recommendation 1b
For patients who opt for treatment based on recommendation 1a, clinicians should reevaluate the benefit of treatment within 12 months. If a patient is not receiving any benefit in sexual function by 12 months, it is recommended that treatment be stopped at that time.
The ACP recommendation to stop treatment if a patient lacks improvement of sexual function within 12 months stems from low or insufficient evidence regarding potential harm of treatment. If the treatment is not helping the target symptom then the benefit no longer outweighs the potential harm.
Recommendation 1c
For patients who opt for treatment based on recommendation 1a, intramuscular replacement therapy rather than transdermal replacement therapy is recommended because of substantial differences in the cost.
It is important to note that both intramuscular and transdermal testosterone applications have been associated with improvements in sexual function, without any significant differences noted in benefit or harm for the patients. This recommendation is based on a per-person per-year average cost of the intramuscular formulation – $156.32, compared with the transdermal formulation – $2,135.32.
Recommendation 2
The ACP does not endorse the use of testosterone treatment for age-related low testosterone in patients desiring improvement in physical function, mood, energy, or cognitive function.
This clear recommendation is critical, as this might be the most common reason for prescriptions of testosterone – a misplaced belief that testosterone will help general quality of life. The evidence simply does not support this effect of testosterone replacement for age-related testosterone deficiency.
The bottom line
Testosterone levels in men decrease steadily with age, with a great deal of variability. Testosterone replacement therapy may be considered for men with age-related testosterone deficiency and sexual dysfunction. Testosterone replacement therapy is not recommended as a treatment for general fatigue, weakness or with an expectation that it will improve physical function, mood, energy, or cognitive function.
Dr. Hansen is a third-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Hospital–Jefferson Health.
References
1. Diem SJ et al. Efficacy and safety of testosterone treatment in men: An evidence report for a clinical practice guideline by the American College of Physicians. Ann Intern Med. 2020 Jan 21. doi: 10.7326/M19-0830.
2. Qaseem A et al. Testosterone treatment in adult men with age-related low testosterone: A clinical guideline from the American College of Physicians. Ann Intern Med. 2020 Jan 21. doi: 10.7326/M19-0882.
Testosterone normally decreases with age in men beginning in their mid-30s, with a rate of decline averaging approximately 1.6% per year. Using a cutoff of a total testosterone less than 325 ng/dL, the incidence of low testosterone is approximately 20% after age 60 years, and 30% after age 70. While the change in labs values has been reasonably validated,
Additional potential symptoms of testosterone deficiency include changes in bone mineral density, decreased libido, depression, erectile dysfunction, loss of hair, and general weakness. Since the symptoms are nonspecific, it is often unclear if someone should be tested or treated for testosterone deficiency. To address this issue, the American College of Physicians commissioned a systematic review of the evidence on testosterone-replacement therapy for age-related testosterone deficiency.1
The evidence review of testosterone replacement in men with age-related low testosterone found the following.
- Low-certainty evidence of improvement in quality of life
- Moderate-certainty evidence of a small improvement in sexual function
- Low-certainty evidence of a small improvement in erectile function
- Low-certainty evidence showing little to no improvement in physical function
- Low-certainty evidence of a small increase to no difference in adverse cardiovascular events
- Moderate-certainty evidence of no increase in the risk for serious adverse events
The trials were not powered to assess mortality, but pool analysis showed fewer deaths among patients treated with testosterone than those who received placebo (odds ratio, 0.47; 95% confidence interval, 0.25-0.89). There were no differences in cognitive function, and the improvement in vitality and fatigue was “less than a small amount.” Evidence from an observational trial showed no increased risk for mortality, cardiovascular events, prostate cancer, or pulmonary embolus or deep vein thrombosis. Of note, most studies excluded men with recent cardiovascular disease.
This evidence review led to the following recommendations.2
Recommendation 1a
Clinicians should have a discussion regarding the potential risk and benefits of treatment with the patients who have documented age-related low testosterone (testosterone levels less than 10.4 nmol/L or 300 ng/dL) and are suffering from sexual dysfunction or have a desire to enhance their sexual function.
This recommendation was based on evidence showing small improvement in sexual function and erectile dysfunction.
Recommendation 1b
For patients who opt for treatment based on recommendation 1a, clinicians should reevaluate the benefit of treatment within 12 months. If a patient is not receiving any benefit in sexual function by 12 months, it is recommended that treatment be stopped at that time.
The ACP recommendation to stop treatment if a patient lacks improvement of sexual function within 12 months stems from low or insufficient evidence regarding potential harm of treatment. If the treatment is not helping the target symptom then the benefit no longer outweighs the potential harm.
Recommendation 1c
For patients who opt for treatment based on recommendation 1a, intramuscular replacement therapy rather than transdermal replacement therapy is recommended because of substantial differences in the cost.
It is important to note that both intramuscular and transdermal testosterone applications have been associated with improvements in sexual function, without any significant differences noted in benefit or harm for the patients. This recommendation is based on a per-person per-year average cost of the intramuscular formulation – $156.32, compared with the transdermal formulation – $2,135.32.
Recommendation 2
The ACP does not endorse the use of testosterone treatment for age-related low testosterone in patients desiring improvement in physical function, mood, energy, or cognitive function.
This clear recommendation is critical, as this might be the most common reason for prescriptions of testosterone – a misplaced belief that testosterone will help general quality of life. The evidence simply does not support this effect of testosterone replacement for age-related testosterone deficiency.
The bottom line
Testosterone levels in men decrease steadily with age, with a great deal of variability. Testosterone replacement therapy may be considered for men with age-related testosterone deficiency and sexual dysfunction. Testosterone replacement therapy is not recommended as a treatment for general fatigue, weakness or with an expectation that it will improve physical function, mood, energy, or cognitive function.
Dr. Hansen is a third-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Hospital–Jefferson Health.
References
1. Diem SJ et al. Efficacy and safety of testosterone treatment in men: An evidence report for a clinical practice guideline by the American College of Physicians. Ann Intern Med. 2020 Jan 21. doi: 10.7326/M19-0830.
2. Qaseem A et al. Testosterone treatment in adult men with age-related low testosterone: A clinical guideline from the American College of Physicians. Ann Intern Med. 2020 Jan 21. doi: 10.7326/M19-0882.
Testosterone normally decreases with age in men beginning in their mid-30s, with a rate of decline averaging approximately 1.6% per year. Using a cutoff of a total testosterone less than 325 ng/dL, the incidence of low testosterone is approximately 20% after age 60 years, and 30% after age 70. While the change in labs values has been reasonably validated,
Additional potential symptoms of testosterone deficiency include changes in bone mineral density, decreased libido, depression, erectile dysfunction, loss of hair, and general weakness. Since the symptoms are nonspecific, it is often unclear if someone should be tested or treated for testosterone deficiency. To address this issue, the American College of Physicians commissioned a systematic review of the evidence on testosterone-replacement therapy for age-related testosterone deficiency.1
The evidence review of testosterone replacement in men with age-related low testosterone found the following.
- Low-certainty evidence of improvement in quality of life
- Moderate-certainty evidence of a small improvement in sexual function
- Low-certainty evidence of a small improvement in erectile function
- Low-certainty evidence showing little to no improvement in physical function
- Low-certainty evidence of a small increase to no difference in adverse cardiovascular events
- Moderate-certainty evidence of no increase in the risk for serious adverse events
The trials were not powered to assess mortality, but pool analysis showed fewer deaths among patients treated with testosterone than those who received placebo (odds ratio, 0.47; 95% confidence interval, 0.25-0.89). There were no differences in cognitive function, and the improvement in vitality and fatigue was “less than a small amount.” Evidence from an observational trial showed no increased risk for mortality, cardiovascular events, prostate cancer, or pulmonary embolus or deep vein thrombosis. Of note, most studies excluded men with recent cardiovascular disease.
This evidence review led to the following recommendations.2
Recommendation 1a
Clinicians should have a discussion regarding the potential risk and benefits of treatment with the patients who have documented age-related low testosterone (testosterone levels less than 10.4 nmol/L or 300 ng/dL) and are suffering from sexual dysfunction or have a desire to enhance their sexual function.
This recommendation was based on evidence showing small improvement in sexual function and erectile dysfunction.
Recommendation 1b
For patients who opt for treatment based on recommendation 1a, clinicians should reevaluate the benefit of treatment within 12 months. If a patient is not receiving any benefit in sexual function by 12 months, it is recommended that treatment be stopped at that time.
The ACP recommendation to stop treatment if a patient lacks improvement of sexual function within 12 months stems from low or insufficient evidence regarding potential harm of treatment. If the treatment is not helping the target symptom then the benefit no longer outweighs the potential harm.
Recommendation 1c
For patients who opt for treatment based on recommendation 1a, intramuscular replacement therapy rather than transdermal replacement therapy is recommended because of substantial differences in the cost.
It is important to note that both intramuscular and transdermal testosterone applications have been associated with improvements in sexual function, without any significant differences noted in benefit or harm for the patients. This recommendation is based on a per-person per-year average cost of the intramuscular formulation – $156.32, compared with the transdermal formulation – $2,135.32.
Recommendation 2
The ACP does not endorse the use of testosterone treatment for age-related low testosterone in patients desiring improvement in physical function, mood, energy, or cognitive function.
This clear recommendation is critical, as this might be the most common reason for prescriptions of testosterone – a misplaced belief that testosterone will help general quality of life. The evidence simply does not support this effect of testosterone replacement for age-related testosterone deficiency.
The bottom line
Testosterone levels in men decrease steadily with age, with a great deal of variability. Testosterone replacement therapy may be considered for men with age-related testosterone deficiency and sexual dysfunction. Testosterone replacement therapy is not recommended as a treatment for general fatigue, weakness or with an expectation that it will improve physical function, mood, energy, or cognitive function.
Dr. Hansen is a third-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Hospital–Jefferson Health.
References
1. Diem SJ et al. Efficacy and safety of testosterone treatment in men: An evidence report for a clinical practice guideline by the American College of Physicians. Ann Intern Med. 2020 Jan 21. doi: 10.7326/M19-0830.
2. Qaseem A et al. Testosterone treatment in adult men with age-related low testosterone: A clinical guideline from the American College of Physicians. Ann Intern Med. 2020 Jan 21. doi: 10.7326/M19-0882.
Clinical management guidelines for hidradenitis suppurativa
Hidradenitis suppurativa (HS) is a chronic inflammatory skin disease that affects hair follicles, with predilection for intertriginous sites. The prevalence of HS ranges from 0.1% to 2%, with HS significantly affecting the quality of life for patients, with both physical and emotional consequences.
Guidelines from the U.S. and Canadian Hidradenitis Suppurativa Foundations provide a summary of management and treatment for patients.
Grading
Hurley staging is recommended to determine therapies. Stage I is classified by recurrent nodules and abscesses with minimal scars. Stage II is classified by one or a limited number of sinuses and/or scarring within a body region. Stage III is classified by multiple or extensive sinuses and/or scarring. The Dermatology Life Quality Index and pain visual analog scale scores can be used in addition to the Hurley staging for management.
Diagnostic testing/comorbidities screening
There is limited evidence for microbiological testing for HS because skin flora is the main bacteria cultured. Patients should be screened for smoking use, diabetes, metabolic syndrome, depression/anxiety, follicular occlusion tetrad, and squamous cell carcinoma. Some studies have suggested an association between the severity of HS and smoking; therefore, smoking cessation is recommended. Patients should also be counseled on weight loss.
Zinc supplementation (90 mg daily) may be helpful. However, there is insufficient evidence for recommendations to avoid diary, brewer’s yeast, friction, deodorant, depilation, or shaving. There is also insufficient data to support vitamin D supplementation.
Topical/intralesional therapies
Expert opinion supports the use of chlorhexidine, benzoyl peroxide, or zinc pyrithione. A keratolytic and antiseptic cream such as resorcinol 15% cream may be used but can cause contact dermatitis. Topical clindamycin may decrease pustules formation, but it can increase resistance to Staphylococcus aureus. Triamcinolone intravlesional injections may decrease inflamed HS lesions in the short term.
Systemic antibiotics
Systemic antibiotics have been used for decades to treat HS. Tetracyclines for a 12-week course or long-term maintenance can be used in mild to moderate HS. Clindamycin and rifampin combination can be used as second-line therapy for mild to moderate HS. Moxifloxacin, metronidazole, and rifampin combination can also be considered second-line treatment for moderate to severe disease. Dapsone can be used in patients with Hurley stage I or II for maintenance therapy. Ertapenem IV can be used as a rescue or as bridge therapy for severe disease.
The duration of antibiotics and frequency of use depends on each patient and resistance.
Hormonal agents and retinoids
Although androgens may influence HS, evidence for hormonal agents is limited. Hormonal agents, such as ethinyl estradiol and spironolactone, can be considered for females with mild to moderate HS. Retinoids may be considered as a second- or third-line agent, especially in patients with severe acne and HS.
Immunosuppressants and biologics
Immunosuppressants such as methotrexate and azathioprine provide limited benefit; therefore, they are not recommended. Colchicine with minocycline may provide slight benefit in refractory mild to moderate HS. Cyclosporine may be considered in recalcitrant, severe HS. Systemic corticosteroids can be used short term for acute flares or long term for severe HS.
Biologic therapy is becoming more common and the choice of therapy for moderate to severe HS. Adalimumab is currently the only Food and Drug Administration–approved tumor necrosis factor–inhibitor treatment for HS. Other biologics – including infliximab, anakinra, and ustekinumab – may be effective for HS, but optimal dosing needs to be determined.
Pain management
While there are no studies about pain in HS, acute pain management should include topical analgesics and oral nonsteroidal anti-inflammatory drugs. Anticonvulsants such as pregabalin or gabapentin may help with neuropathic pain, and opioids can be considered if there is no improvement with first-line agents.
Surgical management
Recurrent nodules and tunnels can be deroofed or excised. Acute abscesses may be relieved by incision and drainage. Extensive lesions may require wide local scalpel excision, carbon dioxide laser excision, or electrosurgical excision. Surgery alone does not affect the biology of HS; therefore, surgical interventions should be reserved for disease that is not managed by medical therapy.
The bottom line
HS is a chronic inflammatory condition with complex medical management and surgical treatment options. Hurley staging I-III can be used to grade severity and determine therapy. Management of pain, tobacco cessation, weight loss, and mental health are important aspects of HS. Zinc supplementation (90 mg daily) may be helpful. Experts opinion supports the use of chlorhexidine, benzoyl peroxide or zinc pyrithione.
Acute lesions may be managed with short-term oral or intralesional corticosteroids, as well as deroofing or incision and drainage. Moderate-to-severe HS may be managed with systemic antibiotics or biologics and surgical therapy. Adalimumab is the only FDA-approved biologic for treatment of HS.
Dr. Chuong is a second-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
References
Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: A publication from the United States and Canadian Hidradenitis Suppurativa Foundations. Part I: Diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol. 2019 Jul;81(1):76-90.
Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: A publication form the United States and Canadian Hidradenitis Suppurativa Foundations. Part II: Topical, intralesional, and systemic medical management. J Am Acad Dermatol. 2019 Jul;81(1):91-101.
Hidradenitis suppurativa (HS) is a chronic inflammatory skin disease that affects hair follicles, with predilection for intertriginous sites. The prevalence of HS ranges from 0.1% to 2%, with HS significantly affecting the quality of life for patients, with both physical and emotional consequences.
Guidelines from the U.S. and Canadian Hidradenitis Suppurativa Foundations provide a summary of management and treatment for patients.
Grading
Hurley staging is recommended to determine therapies. Stage I is classified by recurrent nodules and abscesses with minimal scars. Stage II is classified by one or a limited number of sinuses and/or scarring within a body region. Stage III is classified by multiple or extensive sinuses and/or scarring. The Dermatology Life Quality Index and pain visual analog scale scores can be used in addition to the Hurley staging for management.
Diagnostic testing/comorbidities screening
There is limited evidence for microbiological testing for HS because skin flora is the main bacteria cultured. Patients should be screened for smoking use, diabetes, metabolic syndrome, depression/anxiety, follicular occlusion tetrad, and squamous cell carcinoma. Some studies have suggested an association between the severity of HS and smoking; therefore, smoking cessation is recommended. Patients should also be counseled on weight loss.
Zinc supplementation (90 mg daily) may be helpful. However, there is insufficient evidence for recommendations to avoid diary, brewer’s yeast, friction, deodorant, depilation, or shaving. There is also insufficient data to support vitamin D supplementation.
Topical/intralesional therapies
Expert opinion supports the use of chlorhexidine, benzoyl peroxide, or zinc pyrithione. A keratolytic and antiseptic cream such as resorcinol 15% cream may be used but can cause contact dermatitis. Topical clindamycin may decrease pustules formation, but it can increase resistance to Staphylococcus aureus. Triamcinolone intravlesional injections may decrease inflamed HS lesions in the short term.
Systemic antibiotics
Systemic antibiotics have been used for decades to treat HS. Tetracyclines for a 12-week course or long-term maintenance can be used in mild to moderate HS. Clindamycin and rifampin combination can be used as second-line therapy for mild to moderate HS. Moxifloxacin, metronidazole, and rifampin combination can also be considered second-line treatment for moderate to severe disease. Dapsone can be used in patients with Hurley stage I or II for maintenance therapy. Ertapenem IV can be used as a rescue or as bridge therapy for severe disease.
The duration of antibiotics and frequency of use depends on each patient and resistance.
Hormonal agents and retinoids
Although androgens may influence HS, evidence for hormonal agents is limited. Hormonal agents, such as ethinyl estradiol and spironolactone, can be considered for females with mild to moderate HS. Retinoids may be considered as a second- or third-line agent, especially in patients with severe acne and HS.
Immunosuppressants and biologics
Immunosuppressants such as methotrexate and azathioprine provide limited benefit; therefore, they are not recommended. Colchicine with minocycline may provide slight benefit in refractory mild to moderate HS. Cyclosporine may be considered in recalcitrant, severe HS. Systemic corticosteroids can be used short term for acute flares or long term for severe HS.
Biologic therapy is becoming more common and the choice of therapy for moderate to severe HS. Adalimumab is currently the only Food and Drug Administration–approved tumor necrosis factor–inhibitor treatment for HS. Other biologics – including infliximab, anakinra, and ustekinumab – may be effective for HS, but optimal dosing needs to be determined.
Pain management
While there are no studies about pain in HS, acute pain management should include topical analgesics and oral nonsteroidal anti-inflammatory drugs. Anticonvulsants such as pregabalin or gabapentin may help with neuropathic pain, and opioids can be considered if there is no improvement with first-line agents.
Surgical management
Recurrent nodules and tunnels can be deroofed or excised. Acute abscesses may be relieved by incision and drainage. Extensive lesions may require wide local scalpel excision, carbon dioxide laser excision, or electrosurgical excision. Surgery alone does not affect the biology of HS; therefore, surgical interventions should be reserved for disease that is not managed by medical therapy.
The bottom line
HS is a chronic inflammatory condition with complex medical management and surgical treatment options. Hurley staging I-III can be used to grade severity and determine therapy. Management of pain, tobacco cessation, weight loss, and mental health are important aspects of HS. Zinc supplementation (90 mg daily) may be helpful. Experts opinion supports the use of chlorhexidine, benzoyl peroxide or zinc pyrithione.
Acute lesions may be managed with short-term oral or intralesional corticosteroids, as well as deroofing or incision and drainage. Moderate-to-severe HS may be managed with systemic antibiotics or biologics and surgical therapy. Adalimumab is the only FDA-approved biologic for treatment of HS.
Dr. Chuong is a second-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
References
Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: A publication from the United States and Canadian Hidradenitis Suppurativa Foundations. Part I: Diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol. 2019 Jul;81(1):76-90.
Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: A publication form the United States and Canadian Hidradenitis Suppurativa Foundations. Part II: Topical, intralesional, and systemic medical management. J Am Acad Dermatol. 2019 Jul;81(1):91-101.
Hidradenitis suppurativa (HS) is a chronic inflammatory skin disease that affects hair follicles, with predilection for intertriginous sites. The prevalence of HS ranges from 0.1% to 2%, with HS significantly affecting the quality of life for patients, with both physical and emotional consequences.
Guidelines from the U.S. and Canadian Hidradenitis Suppurativa Foundations provide a summary of management and treatment for patients.
Grading
Hurley staging is recommended to determine therapies. Stage I is classified by recurrent nodules and abscesses with minimal scars. Stage II is classified by one or a limited number of sinuses and/or scarring within a body region. Stage III is classified by multiple or extensive sinuses and/or scarring. The Dermatology Life Quality Index and pain visual analog scale scores can be used in addition to the Hurley staging for management.
Diagnostic testing/comorbidities screening
There is limited evidence for microbiological testing for HS because skin flora is the main bacteria cultured. Patients should be screened for smoking use, diabetes, metabolic syndrome, depression/anxiety, follicular occlusion tetrad, and squamous cell carcinoma. Some studies have suggested an association between the severity of HS and smoking; therefore, smoking cessation is recommended. Patients should also be counseled on weight loss.
Zinc supplementation (90 mg daily) may be helpful. However, there is insufficient evidence for recommendations to avoid diary, brewer’s yeast, friction, deodorant, depilation, or shaving. There is also insufficient data to support vitamin D supplementation.
Topical/intralesional therapies
Expert opinion supports the use of chlorhexidine, benzoyl peroxide, or zinc pyrithione. A keratolytic and antiseptic cream such as resorcinol 15% cream may be used but can cause contact dermatitis. Topical clindamycin may decrease pustules formation, but it can increase resistance to Staphylococcus aureus. Triamcinolone intravlesional injections may decrease inflamed HS lesions in the short term.
Systemic antibiotics
Systemic antibiotics have been used for decades to treat HS. Tetracyclines for a 12-week course or long-term maintenance can be used in mild to moderate HS. Clindamycin and rifampin combination can be used as second-line therapy for mild to moderate HS. Moxifloxacin, metronidazole, and rifampin combination can also be considered second-line treatment for moderate to severe disease. Dapsone can be used in patients with Hurley stage I or II for maintenance therapy. Ertapenem IV can be used as a rescue or as bridge therapy for severe disease.
The duration of antibiotics and frequency of use depends on each patient and resistance.
Hormonal agents and retinoids
Although androgens may influence HS, evidence for hormonal agents is limited. Hormonal agents, such as ethinyl estradiol and spironolactone, can be considered for females with mild to moderate HS. Retinoids may be considered as a second- or third-line agent, especially in patients with severe acne and HS.
Immunosuppressants and biologics
Immunosuppressants such as methotrexate and azathioprine provide limited benefit; therefore, they are not recommended. Colchicine with minocycline may provide slight benefit in refractory mild to moderate HS. Cyclosporine may be considered in recalcitrant, severe HS. Systemic corticosteroids can be used short term for acute flares or long term for severe HS.
Biologic therapy is becoming more common and the choice of therapy for moderate to severe HS. Adalimumab is currently the only Food and Drug Administration–approved tumor necrosis factor–inhibitor treatment for HS. Other biologics – including infliximab, anakinra, and ustekinumab – may be effective for HS, but optimal dosing needs to be determined.
Pain management
While there are no studies about pain in HS, acute pain management should include topical analgesics and oral nonsteroidal anti-inflammatory drugs. Anticonvulsants such as pregabalin or gabapentin may help with neuropathic pain, and opioids can be considered if there is no improvement with first-line agents.
Surgical management
Recurrent nodules and tunnels can be deroofed or excised. Acute abscesses may be relieved by incision and drainage. Extensive lesions may require wide local scalpel excision, carbon dioxide laser excision, or electrosurgical excision. Surgery alone does not affect the biology of HS; therefore, surgical interventions should be reserved for disease that is not managed by medical therapy.
The bottom line
HS is a chronic inflammatory condition with complex medical management and surgical treatment options. Hurley staging I-III can be used to grade severity and determine therapy. Management of pain, tobacco cessation, weight loss, and mental health are important aspects of HS. Zinc supplementation (90 mg daily) may be helpful. Experts opinion supports the use of chlorhexidine, benzoyl peroxide or zinc pyrithione.
Acute lesions may be managed with short-term oral or intralesional corticosteroids, as well as deroofing or incision and drainage. Moderate-to-severe HS may be managed with systemic antibiotics or biologics and surgical therapy. Adalimumab is the only FDA-approved biologic for treatment of HS.
Dr. Chuong is a second-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
References
Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: A publication from the United States and Canadian Hidradenitis Suppurativa Foundations. Part I: Diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol. 2019 Jul;81(1):76-90.
Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: A publication form the United States and Canadian Hidradenitis Suppurativa Foundations. Part II: Topical, intralesional, and systemic medical management. J Am Acad Dermatol. 2019 Jul;81(1):91-101.
USPSTF recommendations on screening for abdominal aortic aneurysm
The prevalence of abdominal aortic aneurysms (AAAs) is decreasing, thought to be caused by a decrease in smoking. But the risk of death if one ruptures is as high as 81%. So, screening is still an important part of preventive medicine.
When the abdominal aorta enlarges to greater than 3.0 cm, it is considered an aneurysm. Risk factors that can lead to an enlarged aorta include older age, male sex, smoking, history of AAA in a first-degree relative, hypertension, history of other aneurysms, coronary artery disease, cerebrovascular disease, atherosclerosis, and hypercholesterolemia.
History of AAA in a first-degree relative puts patients at double the risk of developing an abdominal aortic aneurysm. Interestingly, diabetes has been associated with a reduced risk of AAA. People of African American, Asian, and Hispanic descent have a reduced risk of AAA.
Screening
Screening is performed using abdominal duplex ultrasound. It has high sensitivity (94%-100%) and specificity (98%-100%), is low cost, and has low risk to the patient. The U.S. Preventive Services Task Force breaks its screening recommendations into four categories:
1. Men aged 65-75 years who have ever smoked (at least 100 cigarettes in their lifetime): One-time screening (grade B, moderate net benefit).
2. Men aged 65-75 years who have never smoked: Selectively offer screening (grade C, small net benefit). “To determine whether this service is appropriate, patients and clinicians should consider the patient’s medical history, family history, other risk factors, and personal values.”
3. Women without a smoking history or family history of AAA: Do not perform screening (grade D, recommendation against the service).
4. Women aged 65-75 years who have a smoking history or family history of AAA: There is insufficient evidence on whether or not to screen for AAA (grade I, insufficient evidence).
To assess screening and treatment of AAAs, the USPSTF looked at four randomized, controlled trials largely focused on men older than 65 years. With the combined data, they found 246 men would need to be screened to prevent 1 AAA rupture, and 305 men would need to be screened to prevent 1 death from AAA.
The USPSTF does note that, while the risk of death is lower for elective AAA repair than ruptured AAA, there is still increased risk with elective surgery. In addition, increased screening and detection increases the rate of elective surgery. Overdiagnosis and overtreatment could represent a harm.
Treatment
Surgical repair of AAA in men depends on the size of the aneurysm and rate of growth.
For men, surgical repair is standard when the AAA reaches 5.5 cm or if the AAA is growing faster than 1.0 cm per year and is larger than 4.0 cm. For women, surgical repair is often recommended between 5.0 cm and 5.4 cm in size.
Surgical repair is not recommended for AAAs that are less than 5.0 cm because the annual risk of rupture is 0%-1% below 5.0 cm. The risk increases to 11% for aneurysms that are 5.0-5.9 cm in size.
There are two methods of surgical repair: endovascular aneurysm repair and open repair. Recommendations for the surveillance of AAA between 3.0 cm and 5.5 cm is regular ultrasound surveillance, with the interval becoming shorter as the aneurysm size becomes larger. Exact intervals differ from one guideline group to another.
Screening and treatment in women
While it is true that AAAs in women are more likely to rupture at smaller sizes than AAAs in men, the AAAs that rupture in women are more likely to rupture at an older age than AAAs rupture in men.
The prevalence of AAAs in women is thought to be one-sixth of the prevalence of men. In addition, women had a higher 30-day mortality after surgical repair. They also had higher rates of complications for elective surgical repair of AAAs.
For these reasons, it is unclear that the benefits of AAA screening and treatment in women outweigh the risks, and the USPSTF cannot come to a conclusive recommendation for women who have ever smoked or women who have a family history of AAA.
The USPSTF is able to state definitively that they do not recommend screening in women with no smoking history or family history of AAA.
Bottom line
The USPSTF recommends screening men aged 65-75 years who have ever smoked and selectively screening men aged 65-75 years with no smoking history. The USPSTF recommends against screening women aged 65-75 years who have never smoked and have no family history of AAA. There is insufficient evidence to either recommend for or against screening women aged 65-75 years who have smoked or have a family history of AAA.
Reference
Owens DK et al. Screening for abdominal aortic aneurysm: U.S. Preventive Services Task Force Recommendation Statement. JAMA. 2019 Dec 10;322(22):2211-18.
Dr. Sprogell is a second-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health.
The prevalence of abdominal aortic aneurysms (AAAs) is decreasing, thought to be caused by a decrease in smoking. But the risk of death if one ruptures is as high as 81%. So, screening is still an important part of preventive medicine.
When the abdominal aorta enlarges to greater than 3.0 cm, it is considered an aneurysm. Risk factors that can lead to an enlarged aorta include older age, male sex, smoking, history of AAA in a first-degree relative, hypertension, history of other aneurysms, coronary artery disease, cerebrovascular disease, atherosclerosis, and hypercholesterolemia.
History of AAA in a first-degree relative puts patients at double the risk of developing an abdominal aortic aneurysm. Interestingly, diabetes has been associated with a reduced risk of AAA. People of African American, Asian, and Hispanic descent have a reduced risk of AAA.
Screening
Screening is performed using abdominal duplex ultrasound. It has high sensitivity (94%-100%) and specificity (98%-100%), is low cost, and has low risk to the patient. The U.S. Preventive Services Task Force breaks its screening recommendations into four categories:
1. Men aged 65-75 years who have ever smoked (at least 100 cigarettes in their lifetime): One-time screening (grade B, moderate net benefit).
2. Men aged 65-75 years who have never smoked: Selectively offer screening (grade C, small net benefit). “To determine whether this service is appropriate, patients and clinicians should consider the patient’s medical history, family history, other risk factors, and personal values.”
3. Women without a smoking history or family history of AAA: Do not perform screening (grade D, recommendation against the service).
4. Women aged 65-75 years who have a smoking history or family history of AAA: There is insufficient evidence on whether or not to screen for AAA (grade I, insufficient evidence).
To assess screening and treatment of AAAs, the USPSTF looked at four randomized, controlled trials largely focused on men older than 65 years. With the combined data, they found 246 men would need to be screened to prevent 1 AAA rupture, and 305 men would need to be screened to prevent 1 death from AAA.
The USPSTF does note that, while the risk of death is lower for elective AAA repair than ruptured AAA, there is still increased risk with elective surgery. In addition, increased screening and detection increases the rate of elective surgery. Overdiagnosis and overtreatment could represent a harm.
Treatment
Surgical repair of AAA in men depends on the size of the aneurysm and rate of growth.
For men, surgical repair is standard when the AAA reaches 5.5 cm or if the AAA is growing faster than 1.0 cm per year and is larger than 4.0 cm. For women, surgical repair is often recommended between 5.0 cm and 5.4 cm in size.
Surgical repair is not recommended for AAAs that are less than 5.0 cm because the annual risk of rupture is 0%-1% below 5.0 cm. The risk increases to 11% for aneurysms that are 5.0-5.9 cm in size.
There are two methods of surgical repair: endovascular aneurysm repair and open repair. Recommendations for the surveillance of AAA between 3.0 cm and 5.5 cm is regular ultrasound surveillance, with the interval becoming shorter as the aneurysm size becomes larger. Exact intervals differ from one guideline group to another.
Screening and treatment in women
While it is true that AAAs in women are more likely to rupture at smaller sizes than AAAs in men, the AAAs that rupture in women are more likely to rupture at an older age than AAAs rupture in men.
The prevalence of AAAs in women is thought to be one-sixth of the prevalence of men. In addition, women had a higher 30-day mortality after surgical repair. They also had higher rates of complications for elective surgical repair of AAAs.
For these reasons, it is unclear that the benefits of AAA screening and treatment in women outweigh the risks, and the USPSTF cannot come to a conclusive recommendation for women who have ever smoked or women who have a family history of AAA.
The USPSTF is able to state definitively that they do not recommend screening in women with no smoking history or family history of AAA.
Bottom line
The USPSTF recommends screening men aged 65-75 years who have ever smoked and selectively screening men aged 65-75 years with no smoking history. The USPSTF recommends against screening women aged 65-75 years who have never smoked and have no family history of AAA. There is insufficient evidence to either recommend for or against screening women aged 65-75 years who have smoked or have a family history of AAA.
Reference
Owens DK et al. Screening for abdominal aortic aneurysm: U.S. Preventive Services Task Force Recommendation Statement. JAMA. 2019 Dec 10;322(22):2211-18.
Dr. Sprogell is a second-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health.
The prevalence of abdominal aortic aneurysms (AAAs) is decreasing, thought to be caused by a decrease in smoking. But the risk of death if one ruptures is as high as 81%. So, screening is still an important part of preventive medicine.
When the abdominal aorta enlarges to greater than 3.0 cm, it is considered an aneurysm. Risk factors that can lead to an enlarged aorta include older age, male sex, smoking, history of AAA in a first-degree relative, hypertension, history of other aneurysms, coronary artery disease, cerebrovascular disease, atherosclerosis, and hypercholesterolemia.
History of AAA in a first-degree relative puts patients at double the risk of developing an abdominal aortic aneurysm. Interestingly, diabetes has been associated with a reduced risk of AAA. People of African American, Asian, and Hispanic descent have a reduced risk of AAA.
Screening
Screening is performed using abdominal duplex ultrasound. It has high sensitivity (94%-100%) and specificity (98%-100%), is low cost, and has low risk to the patient. The U.S. Preventive Services Task Force breaks its screening recommendations into four categories:
1. Men aged 65-75 years who have ever smoked (at least 100 cigarettes in their lifetime): One-time screening (grade B, moderate net benefit).
2. Men aged 65-75 years who have never smoked: Selectively offer screening (grade C, small net benefit). “To determine whether this service is appropriate, patients and clinicians should consider the patient’s medical history, family history, other risk factors, and personal values.”
3. Women without a smoking history or family history of AAA: Do not perform screening (grade D, recommendation against the service).
4. Women aged 65-75 years who have a smoking history or family history of AAA: There is insufficient evidence on whether or not to screen for AAA (grade I, insufficient evidence).
To assess screening and treatment of AAAs, the USPSTF looked at four randomized, controlled trials largely focused on men older than 65 years. With the combined data, they found 246 men would need to be screened to prevent 1 AAA rupture, and 305 men would need to be screened to prevent 1 death from AAA.
The USPSTF does note that, while the risk of death is lower for elective AAA repair than ruptured AAA, there is still increased risk with elective surgery. In addition, increased screening and detection increases the rate of elective surgery. Overdiagnosis and overtreatment could represent a harm.
Treatment
Surgical repair of AAA in men depends on the size of the aneurysm and rate of growth.
For men, surgical repair is standard when the AAA reaches 5.5 cm or if the AAA is growing faster than 1.0 cm per year and is larger than 4.0 cm. For women, surgical repair is often recommended between 5.0 cm and 5.4 cm in size.
Surgical repair is not recommended for AAAs that are less than 5.0 cm because the annual risk of rupture is 0%-1% below 5.0 cm. The risk increases to 11% for aneurysms that are 5.0-5.9 cm in size.
There are two methods of surgical repair: endovascular aneurysm repair and open repair. Recommendations for the surveillance of AAA between 3.0 cm and 5.5 cm is regular ultrasound surveillance, with the interval becoming shorter as the aneurysm size becomes larger. Exact intervals differ from one guideline group to another.
Screening and treatment in women
While it is true that AAAs in women are more likely to rupture at smaller sizes than AAAs in men, the AAAs that rupture in women are more likely to rupture at an older age than AAAs rupture in men.
The prevalence of AAAs in women is thought to be one-sixth of the prevalence of men. In addition, women had a higher 30-day mortality after surgical repair. They also had higher rates of complications for elective surgical repair of AAAs.
For these reasons, it is unclear that the benefits of AAA screening and treatment in women outweigh the risks, and the USPSTF cannot come to a conclusive recommendation for women who have ever smoked or women who have a family history of AAA.
The USPSTF is able to state definitively that they do not recommend screening in women with no smoking history or family history of AAA.
Bottom line
The USPSTF recommends screening men aged 65-75 years who have ever smoked and selectively screening men aged 65-75 years with no smoking history. The USPSTF recommends against screening women aged 65-75 years who have never smoked and have no family history of AAA. There is insufficient evidence to either recommend for or against screening women aged 65-75 years who have smoked or have a family history of AAA.
Reference
Owens DK et al. Screening for abdominal aortic aneurysm: U.S. Preventive Services Task Force Recommendation Statement. JAMA. 2019 Dec 10;322(22):2211-18.
Dr. Sprogell is a second-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health.
Guideline: Diagnosis and treatment of adults with community-acquired pneumonia
A new guideline has been published to update the 2007 guidelines for the management of adults with community-acquired pneumonia (CAP).
The practice guideline was jointly written by an ad hoc committee of the American Thoracic Society and Infectious Diseases Society of America. CAP refers to a pneumonia infection that was acquired by a patient in his or her community. Decisions about which antibiotics to use to treat this kind of infection are based on risk factors for resistant organisms and the severity of illness.
Pathogens
Traditionally, CAP is caused by common bacterial pathogens that include Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae, Staphylococcus aureus, Legionella species, Chlamydia pneumonia, and Moraxella catarrhalis. Risk factors for multidrug resistant pathogens such as methicillin-resistant S. aureus (MRSA) and Pseudomonas aeruginosa include previous infection with MRSA or P. aeruginosa, recent hospitalization, and requiring parenteral antibiotics in the last 90 days.
Defining severe community-acquired pneumonia
The health care–associated pneumonia, or HCAP, classification should no longer be used to determine empiric treatment. The recommendations for which antibiotics to use are linked to the severity of illness. Previously the site of treatment drove antibiotic selection, but since decision about the site of care can be affected by many considerations, the guidelines recommend using the CAP severity criteria. Severe CAP includes either one major or at least three minor criteria.
Major criteria are:
- Septic shock requiring vasopressors.
- Respiratory failure requiring mechanical ventilation.
Minor criteria are:
- Respiratory rate greater than or equal to 30 breaths/min.
- Ratio of arterial O2 partial pressure to fractional inspired O2 less than or equal to 250.
- Multilobar infiltrates.
- Confusion/disorientation.
- Uremia (blood urea nitrogen level greater than or equal to 20 mg/dL).
- Leukopenia (white blood cell count less than 4,000 cells/mcL).
- Thrombocytopenia (platelet count less than 100,000 mcL)
- Hypothermia (core temperature less than 36º C).
- Hypotension requiring aggressive fluid resuscitation.
Management and diagnostic testing
Clinicians should use the Pneumonia Severity Index (PSI) and clinical judgment to guide the site of treatment for patients. Gram stain, sputum, and blood culture should not be routinely obtained in an outpatient setting. Legionella antigen should not be routinely obtained unless indicated by epidemiological factors. During influenza season, a rapid influenza assay, preferably a nucleic acid amplification test, should be obtained to help guide treatment.
For patients with severe CAP or risk factors for MRSA or P. aeruginosa, gram stain and culture and Legionella antigen should be obtained to manage antibiotic choices. Also, blood cultures should be obtained for these patients.
Empiric antibiotic therapy should be initiated based on clinical judgment and radiographic confirmation of CAP. Serum procalcitonin should not be used to assess initiation of antibiotic therapy.
Empiric antibiotic therapy
Healthy adults without comorbidities should be treated with monotherapy of either:
- Amoxicillin 1 g three times daily.
- OR doxycycline 100 mg twice daily.
- OR a macrolide (azithromycin 500 mg on first day then 250 mg daily or clarithromycin 500 mg twice daily or clarithromycin extended release 1,000 mg daily) only in areas with pneumococcal resistance to macrolides less than 25%.
Adults with comorbidities such as chronic heart, lung, liver, or renal disease; diabetes mellitus; alcoholism; malignancy; or asplenia should be treated with:
- Amoxicillin/clavulanate 500 mg/125 mg three times daily, or amoxicillin/ clavulanate 875 mg/125 mg twice daily, or 2,000 mg/125 mg twice daily, or a cephalosporin (cefpodoxime 200 mg twice daily or cefuroxime 500 mg twice daily); and a macrolide (azithromycin 500 mg on first day then 250 mg daily, clarithromycin [500 mg twice daily or extended release 1,000 mg once daily]), or doxycycline 100 mg twice daily. (Some experts recommend that the first dose of doxycycline should be 200 mg.)
- OR monotherapy with respiratory fluoroquinolone (levofloxacin 750 mg daily, moxifloxacin 400 mg daily, or gemifloxacin 320 mg daily).
Inpatient pneumonia that is not severe, without risk factors for resistant organisms should be treated with:
- Beta-lactam (ampicillin 1 sulbactam 1.5-3 g every 6 h, cefotaxime 1-2 g every 8 h, ceftriaxone 1-2 g daily, or ceftaroline 600 mg every 12 h) and a macrolide (azithromycin 500 mg daily or clarithromycin 500 mg twice daily).
- OR monotherapy with a respiratory fluoroquinolone (levofloxacin 750 mg daily, moxifloxacin 400 mg daily).
If there is a contraindication for the use of both a macrolide and a fluoroquinolone, then doxycycline can be used instead.
Severe inpatient pneumonia without risk factors for resistant organisms should be treated with combination therapy of either (agents and doses the same as above):
- Beta-lactam and macrolide.
- OR fluoroquinolone and beta-lactam.
It is recommended to not routinely add anaerobic coverage for suspected aspiration pneumonia unless lung abscess or empyema is suspected. Clinicians should identify risk factors for MRSA or P. aeruginosa before adding additional agents.
Duration of antibiotic therapy is determined by the patient achieving clinical stability with no less than 5 days of antibiotics. In adults with symptom resolution within 5-7 days, no additional follow-up chest imaging is recommended. If patients test positive for influenza, then anti-influenza treatment such as oseltamivir should be used in addition to antibiotics regardless of length of influenza symptoms before presentation.
The bottom line
CAP treatment should be based on severity of illness and risk factors for resistant organisms. Blood and sputum cultures are recommended only for patients with severe pneumonia. There have been important changes in the recommendations for antibiotic treatment of CAP, with high-dose amoxicillin recommended for most patients with CAP who are treated as outpatients. Patients who exhibit clinical stability should be treated for at least 5 days and do not require follow up imaging studies.
For a podcast of this guideline, go to iTunes and download the Infectious Diseases Society of America guideline podcast.
Reference
Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019 Oct 1;200(7):e45-e67.
Tina Chuong, DO, is a second-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
A new guideline has been published to update the 2007 guidelines for the management of adults with community-acquired pneumonia (CAP).
The practice guideline was jointly written by an ad hoc committee of the American Thoracic Society and Infectious Diseases Society of America. CAP refers to a pneumonia infection that was acquired by a patient in his or her community. Decisions about which antibiotics to use to treat this kind of infection are based on risk factors for resistant organisms and the severity of illness.
Pathogens
Traditionally, CAP is caused by common bacterial pathogens that include Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae, Staphylococcus aureus, Legionella species, Chlamydia pneumonia, and Moraxella catarrhalis. Risk factors for multidrug resistant pathogens such as methicillin-resistant S. aureus (MRSA) and Pseudomonas aeruginosa include previous infection with MRSA or P. aeruginosa, recent hospitalization, and requiring parenteral antibiotics in the last 90 days.
Defining severe community-acquired pneumonia
The health care–associated pneumonia, or HCAP, classification should no longer be used to determine empiric treatment. The recommendations for which antibiotics to use are linked to the severity of illness. Previously the site of treatment drove antibiotic selection, but since decision about the site of care can be affected by many considerations, the guidelines recommend using the CAP severity criteria. Severe CAP includes either one major or at least three minor criteria.
Major criteria are:
- Septic shock requiring vasopressors.
- Respiratory failure requiring mechanical ventilation.
Minor criteria are:
- Respiratory rate greater than or equal to 30 breaths/min.
- Ratio of arterial O2 partial pressure to fractional inspired O2 less than or equal to 250.
- Multilobar infiltrates.
- Confusion/disorientation.
- Uremia (blood urea nitrogen level greater than or equal to 20 mg/dL).
- Leukopenia (white blood cell count less than 4,000 cells/mcL).
- Thrombocytopenia (platelet count less than 100,000 mcL)
- Hypothermia (core temperature less than 36º C).
- Hypotension requiring aggressive fluid resuscitation.
Management and diagnostic testing
Clinicians should use the Pneumonia Severity Index (PSI) and clinical judgment to guide the site of treatment for patients. Gram stain, sputum, and blood culture should not be routinely obtained in an outpatient setting. Legionella antigen should not be routinely obtained unless indicated by epidemiological factors. During influenza season, a rapid influenza assay, preferably a nucleic acid amplification test, should be obtained to help guide treatment.
For patients with severe CAP or risk factors for MRSA or P. aeruginosa, gram stain and culture and Legionella antigen should be obtained to manage antibiotic choices. Also, blood cultures should be obtained for these patients.
Empiric antibiotic therapy should be initiated based on clinical judgment and radiographic confirmation of CAP. Serum procalcitonin should not be used to assess initiation of antibiotic therapy.
Empiric antibiotic therapy
Healthy adults without comorbidities should be treated with monotherapy of either:
- Amoxicillin 1 g three times daily.
- OR doxycycline 100 mg twice daily.
- OR a macrolide (azithromycin 500 mg on first day then 250 mg daily or clarithromycin 500 mg twice daily or clarithromycin extended release 1,000 mg daily) only in areas with pneumococcal resistance to macrolides less than 25%.
Adults with comorbidities such as chronic heart, lung, liver, or renal disease; diabetes mellitus; alcoholism; malignancy; or asplenia should be treated with:
- Amoxicillin/clavulanate 500 mg/125 mg three times daily, or amoxicillin/ clavulanate 875 mg/125 mg twice daily, or 2,000 mg/125 mg twice daily, or a cephalosporin (cefpodoxime 200 mg twice daily or cefuroxime 500 mg twice daily); and a macrolide (azithromycin 500 mg on first day then 250 mg daily, clarithromycin [500 mg twice daily or extended release 1,000 mg once daily]), or doxycycline 100 mg twice daily. (Some experts recommend that the first dose of doxycycline should be 200 mg.)
- OR monotherapy with respiratory fluoroquinolone (levofloxacin 750 mg daily, moxifloxacin 400 mg daily, or gemifloxacin 320 mg daily).
Inpatient pneumonia that is not severe, without risk factors for resistant organisms should be treated with:
- Beta-lactam (ampicillin 1 sulbactam 1.5-3 g every 6 h, cefotaxime 1-2 g every 8 h, ceftriaxone 1-2 g daily, or ceftaroline 600 mg every 12 h) and a macrolide (azithromycin 500 mg daily or clarithromycin 500 mg twice daily).
- OR monotherapy with a respiratory fluoroquinolone (levofloxacin 750 mg daily, moxifloxacin 400 mg daily).
If there is a contraindication for the use of both a macrolide and a fluoroquinolone, then doxycycline can be used instead.
Severe inpatient pneumonia without risk factors for resistant organisms should be treated with combination therapy of either (agents and doses the same as above):
- Beta-lactam and macrolide.
- OR fluoroquinolone and beta-lactam.
It is recommended to not routinely add anaerobic coverage for suspected aspiration pneumonia unless lung abscess or empyema is suspected. Clinicians should identify risk factors for MRSA or P. aeruginosa before adding additional agents.
Duration of antibiotic therapy is determined by the patient achieving clinical stability with no less than 5 days of antibiotics. In adults with symptom resolution within 5-7 days, no additional follow-up chest imaging is recommended. If patients test positive for influenza, then anti-influenza treatment such as oseltamivir should be used in addition to antibiotics regardless of length of influenza symptoms before presentation.
The bottom line
CAP treatment should be based on severity of illness and risk factors for resistant organisms. Blood and sputum cultures are recommended only for patients with severe pneumonia. There have been important changes in the recommendations for antibiotic treatment of CAP, with high-dose amoxicillin recommended for most patients with CAP who are treated as outpatients. Patients who exhibit clinical stability should be treated for at least 5 days and do not require follow up imaging studies.
For a podcast of this guideline, go to iTunes and download the Infectious Diseases Society of America guideline podcast.
Reference
Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019 Oct 1;200(7):e45-e67.
Tina Chuong, DO, is a second-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
A new guideline has been published to update the 2007 guidelines for the management of adults with community-acquired pneumonia (CAP).
The practice guideline was jointly written by an ad hoc committee of the American Thoracic Society and Infectious Diseases Society of America. CAP refers to a pneumonia infection that was acquired by a patient in his or her community. Decisions about which antibiotics to use to treat this kind of infection are based on risk factors for resistant organisms and the severity of illness.
Pathogens
Traditionally, CAP is caused by common bacterial pathogens that include Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae, Staphylococcus aureus, Legionella species, Chlamydia pneumonia, and Moraxella catarrhalis. Risk factors for multidrug resistant pathogens such as methicillin-resistant S. aureus (MRSA) and Pseudomonas aeruginosa include previous infection with MRSA or P. aeruginosa, recent hospitalization, and requiring parenteral antibiotics in the last 90 days.
Defining severe community-acquired pneumonia
The health care–associated pneumonia, or HCAP, classification should no longer be used to determine empiric treatment. The recommendations for which antibiotics to use are linked to the severity of illness. Previously the site of treatment drove antibiotic selection, but since decision about the site of care can be affected by many considerations, the guidelines recommend using the CAP severity criteria. Severe CAP includes either one major or at least three minor criteria.
Major criteria are:
- Septic shock requiring vasopressors.
- Respiratory failure requiring mechanical ventilation.
Minor criteria are:
- Respiratory rate greater than or equal to 30 breaths/min.
- Ratio of arterial O2 partial pressure to fractional inspired O2 less than or equal to 250.
- Multilobar infiltrates.
- Confusion/disorientation.
- Uremia (blood urea nitrogen level greater than or equal to 20 mg/dL).
- Leukopenia (white blood cell count less than 4,000 cells/mcL).
- Thrombocytopenia (platelet count less than 100,000 mcL)
- Hypothermia (core temperature less than 36º C).
- Hypotension requiring aggressive fluid resuscitation.
Management and diagnostic testing
Clinicians should use the Pneumonia Severity Index (PSI) and clinical judgment to guide the site of treatment for patients. Gram stain, sputum, and blood culture should not be routinely obtained in an outpatient setting. Legionella antigen should not be routinely obtained unless indicated by epidemiological factors. During influenza season, a rapid influenza assay, preferably a nucleic acid amplification test, should be obtained to help guide treatment.
For patients with severe CAP or risk factors for MRSA or P. aeruginosa, gram stain and culture and Legionella antigen should be obtained to manage antibiotic choices. Also, blood cultures should be obtained for these patients.
Empiric antibiotic therapy should be initiated based on clinical judgment and radiographic confirmation of CAP. Serum procalcitonin should not be used to assess initiation of antibiotic therapy.
Empiric antibiotic therapy
Healthy adults without comorbidities should be treated with monotherapy of either:
- Amoxicillin 1 g three times daily.
- OR doxycycline 100 mg twice daily.
- OR a macrolide (azithromycin 500 mg on first day then 250 mg daily or clarithromycin 500 mg twice daily or clarithromycin extended release 1,000 mg daily) only in areas with pneumococcal resistance to macrolides less than 25%.
Adults with comorbidities such as chronic heart, lung, liver, or renal disease; diabetes mellitus; alcoholism; malignancy; or asplenia should be treated with:
- Amoxicillin/clavulanate 500 mg/125 mg three times daily, or amoxicillin/ clavulanate 875 mg/125 mg twice daily, or 2,000 mg/125 mg twice daily, or a cephalosporin (cefpodoxime 200 mg twice daily or cefuroxime 500 mg twice daily); and a macrolide (azithromycin 500 mg on first day then 250 mg daily, clarithromycin [500 mg twice daily or extended release 1,000 mg once daily]), or doxycycline 100 mg twice daily. (Some experts recommend that the first dose of doxycycline should be 200 mg.)
- OR monotherapy with respiratory fluoroquinolone (levofloxacin 750 mg daily, moxifloxacin 400 mg daily, or gemifloxacin 320 mg daily).
Inpatient pneumonia that is not severe, without risk factors for resistant organisms should be treated with:
- Beta-lactam (ampicillin 1 sulbactam 1.5-3 g every 6 h, cefotaxime 1-2 g every 8 h, ceftriaxone 1-2 g daily, or ceftaroline 600 mg every 12 h) and a macrolide (azithromycin 500 mg daily or clarithromycin 500 mg twice daily).
- OR monotherapy with a respiratory fluoroquinolone (levofloxacin 750 mg daily, moxifloxacin 400 mg daily).
If there is a contraindication for the use of both a macrolide and a fluoroquinolone, then doxycycline can be used instead.
Severe inpatient pneumonia without risk factors for resistant organisms should be treated with combination therapy of either (agents and doses the same as above):
- Beta-lactam and macrolide.
- OR fluoroquinolone and beta-lactam.
It is recommended to not routinely add anaerobic coverage for suspected aspiration pneumonia unless lung abscess or empyema is suspected. Clinicians should identify risk factors for MRSA or P. aeruginosa before adding additional agents.
Duration of antibiotic therapy is determined by the patient achieving clinical stability with no less than 5 days of antibiotics. In adults with symptom resolution within 5-7 days, no additional follow-up chest imaging is recommended. If patients test positive for influenza, then anti-influenza treatment such as oseltamivir should be used in addition to antibiotics regardless of length of influenza symptoms before presentation.
The bottom line
CAP treatment should be based on severity of illness and risk factors for resistant organisms. Blood and sputum cultures are recommended only for patients with severe pneumonia. There have been important changes in the recommendations for antibiotic treatment of CAP, with high-dose amoxicillin recommended for most patients with CAP who are treated as outpatients. Patients who exhibit clinical stability should be treated for at least 5 days and do not require follow up imaging studies.
For a podcast of this guideline, go to iTunes and download the Infectious Diseases Society of America guideline podcast.
Reference
Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019 Oct 1;200(7):e45-e67.
Tina Chuong, DO, is a second-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
USPSTF recommendations on risk assessment, genetic counseling, and genetic testing for BRCA-related cancer
Breast cancer screening recommendations have evolved over the past decade. BRCA1/2 genes are tumor-suppressor genes. Mutations in these genes place women at an increased risk for developing breast, ovarian, fallopian tube, and peritoneal cancer. Detection of BRCA1/2 mutations through genetic screening can provide patients with more information about their cancer risk and can lead to discussion of prophylactic therapies. This includes increased screening frequency, medical therapy, and surgical interventions.
New USPSTF recommendations address who is at an increased risk for BRCA1/2 mutations. They recommend using screening tools focusing on family history that primary care physicians can utilize to determine who should be referred for genetic counseling to discuss the risks and benefits of genetic screening. The following are the task force’s two primary recommendations:
The USPSTF recommends that primary care clinicians assess women with a personal or family history of breast, ovarian, tubal, or peritoneal cancer or who have an ancestry associated with BRCA1/2 gene mutations with an appropriate brief familial risk assessment tool. Women with a positive result on the risk assessment tool should receive genetic counseling and, if indicated after counseling, genetic testing. (B recommendation)
The USPSTF recommends against routine risk assessment, genetic counseling, or genetic testing for women whose personal or family history or ancestry is not associated with potentially harmful BRCA1/2 gene mutations. (D recommendation)
Breast cancer is the second leading cause of cancer and cancer death for women in the United States. Ovarian cancer ranks fifth in cancer deaths for women in the U.S. By age 70, women with BRCA1/2 mutations have a 45%-65% cumulative lifetime risk of developing breast cancer.
Mutations in BRCA1, specifically, are associated with a 39% lifetime risk for ovarian, fallopian tube, and peritoneal cancer. In contrast, mutations in BRCA2 are associated with a 10%-17% lifetime risk.
The USPSTF also underscores the increased prevalence of BRCA1/2 mutations in the Ashkenazi Jewish population. Three out of seven familial risk assessment tools inquire about Jewish ancestry. This is because the Ashkenazi Jewish population have a higher prevalence of three founder mutations in the BRCA1/2 gene. A member of this population has a 1 in 40 chance of carrying one of these three mutations, whereas the general population has a 1 in 300 chance.
The USPSTF recommends a multistep process of screening. The first step is taking a family history of cancer. For women who have a family history of breast, ovarian, tubal, or peritoneal cancer or a personal history of these cancers, a brief familial risk assessment tool should be used to determine the need for referral for in-depth genetic counseling to determine the need for genetic testing.
It is important to recognize that the validated tools recommended by the USPSTF are specific for genetic risk assessment. General breast cancer risk assessment tools, including the National Cancer Institute Breast Cancer Risk Assessment Tool, which is based on the Gail model, are not recommended.
The sensitivity of the tools recommended by the USPSTF range between 77% and 100%. A number of tools are given as an option with no one tool being better than the other. Perhaps the easiest to implement of the validated tools recommended is the Pedigree Assessment Tool. For this tool, points are assigned for every family member with breast or ovarian cancer as indicated in the table below.
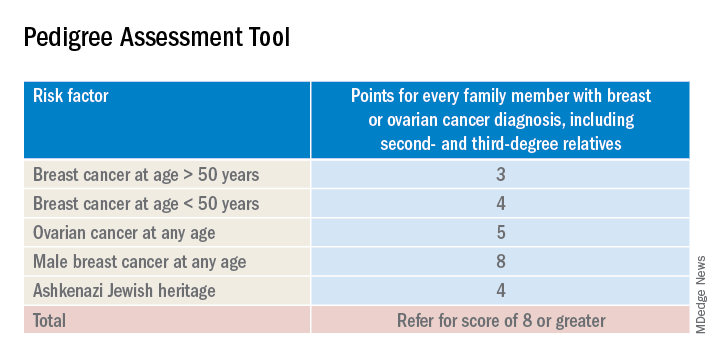
A positive result on a screening tool will lead primary care physicians to appropriately refer patients for genetic counseling. Genetic testing for BRCA1/2 mutations should be limited to those individuals whose personal and/or family history reflects an increased risk for gene mutations after detailed genetic assessment and counseling. The results of the genetic screening should assist a patient in their decision making.
Prophylactic treatment for BRCA1/2 mutation carriers are outside the scope of this recommendation. However the guidelines briefly review risk-reducing therapies including screening, medical, and surgical options. Medical therapy for patients who have BRCA1/2 mutations include the use of tamoxifen, raloxifene, and aromatase inhibitors. Surgical interventions include bilateral mastectomy and salpingo-oopherectomy.
Screening options include earlier and more frequent mammograms and breast MRIs. Screening is largely based on family history and the USPSTF acknowledges their uncertainty when screening women with an unknown family history. Male breast cancer, pancreatic cancer, prostate cancer, and melanoma are also associated with BRCA1/2 mutations. They are not included in this recommendation.
The bottom line
USPSTF recommended that primary care physicians should use familial risk assessment tools to screen women for BRCA1/2 mutations. This includes women with a personal and/or family history of breast, ovarian, tubal, or peritoneal cancer or women with a family history of BRCA1/2 gene mutations. Patients who test positive through one of the suggested screening tools should be referred for genetic counseling. This could lead to genetic testing and subsequent prophylactic therapies and/or increased screenings if the patient so desires. It is of importance to note the USPSTF recommends against routine screening of BRCA1/2 gene mutations for women who do not meet the above requirements.
Reference
USPSTF Recommendation: Assessment, counseling, and testing for BRCA-related cancer. JAMA. 2019;322(7):652-65. doi: 10.1001/jama.2019.10987.
Dr. Style is a second-year resident in the Family Medicine Residency Program at Abington (Pa.) Jefferson Health. Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
Breast cancer screening recommendations have evolved over the past decade. BRCA1/2 genes are tumor-suppressor genes. Mutations in these genes place women at an increased risk for developing breast, ovarian, fallopian tube, and peritoneal cancer. Detection of BRCA1/2 mutations through genetic screening can provide patients with more information about their cancer risk and can lead to discussion of prophylactic therapies. This includes increased screening frequency, medical therapy, and surgical interventions.
New USPSTF recommendations address who is at an increased risk for BRCA1/2 mutations. They recommend using screening tools focusing on family history that primary care physicians can utilize to determine who should be referred for genetic counseling to discuss the risks and benefits of genetic screening. The following are the task force’s two primary recommendations:
The USPSTF recommends that primary care clinicians assess women with a personal or family history of breast, ovarian, tubal, or peritoneal cancer or who have an ancestry associated with BRCA1/2 gene mutations with an appropriate brief familial risk assessment tool. Women with a positive result on the risk assessment tool should receive genetic counseling and, if indicated after counseling, genetic testing. (B recommendation)
The USPSTF recommends against routine risk assessment, genetic counseling, or genetic testing for women whose personal or family history or ancestry is not associated with potentially harmful BRCA1/2 gene mutations. (D recommendation)
Breast cancer is the second leading cause of cancer and cancer death for women in the United States. Ovarian cancer ranks fifth in cancer deaths for women in the U.S. By age 70, women with BRCA1/2 mutations have a 45%-65% cumulative lifetime risk of developing breast cancer.
Mutations in BRCA1, specifically, are associated with a 39% lifetime risk for ovarian, fallopian tube, and peritoneal cancer. In contrast, mutations in BRCA2 are associated with a 10%-17% lifetime risk.
The USPSTF also underscores the increased prevalence of BRCA1/2 mutations in the Ashkenazi Jewish population. Three out of seven familial risk assessment tools inquire about Jewish ancestry. This is because the Ashkenazi Jewish population have a higher prevalence of three founder mutations in the BRCA1/2 gene. A member of this population has a 1 in 40 chance of carrying one of these three mutations, whereas the general population has a 1 in 300 chance.
The USPSTF recommends a multistep process of screening. The first step is taking a family history of cancer. For women who have a family history of breast, ovarian, tubal, or peritoneal cancer or a personal history of these cancers, a brief familial risk assessment tool should be used to determine the need for referral for in-depth genetic counseling to determine the need for genetic testing.
It is important to recognize that the validated tools recommended by the USPSTF are specific for genetic risk assessment. General breast cancer risk assessment tools, including the National Cancer Institute Breast Cancer Risk Assessment Tool, which is based on the Gail model, are not recommended.
The sensitivity of the tools recommended by the USPSTF range between 77% and 100%. A number of tools are given as an option with no one tool being better than the other. Perhaps the easiest to implement of the validated tools recommended is the Pedigree Assessment Tool. For this tool, points are assigned for every family member with breast or ovarian cancer as indicated in the table below.
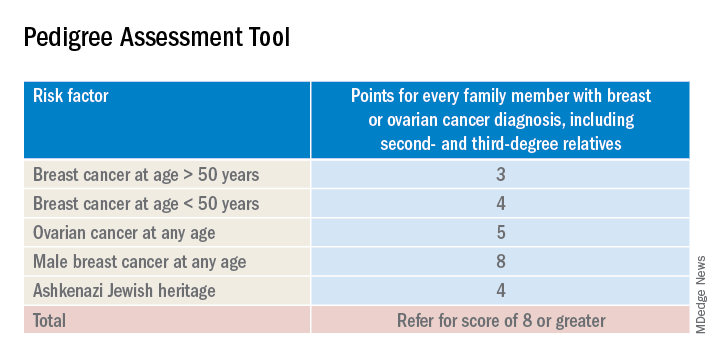
A positive result on a screening tool will lead primary care physicians to appropriately refer patients for genetic counseling. Genetic testing for BRCA1/2 mutations should be limited to those individuals whose personal and/or family history reflects an increased risk for gene mutations after detailed genetic assessment and counseling. The results of the genetic screening should assist a patient in their decision making.
Prophylactic treatment for BRCA1/2 mutation carriers are outside the scope of this recommendation. However the guidelines briefly review risk-reducing therapies including screening, medical, and surgical options. Medical therapy for patients who have BRCA1/2 mutations include the use of tamoxifen, raloxifene, and aromatase inhibitors. Surgical interventions include bilateral mastectomy and salpingo-oopherectomy.
Screening options include earlier and more frequent mammograms and breast MRIs. Screening is largely based on family history and the USPSTF acknowledges their uncertainty when screening women with an unknown family history. Male breast cancer, pancreatic cancer, prostate cancer, and melanoma are also associated with BRCA1/2 mutations. They are not included in this recommendation.
The bottom line
USPSTF recommended that primary care physicians should use familial risk assessment tools to screen women for BRCA1/2 mutations. This includes women with a personal and/or family history of breast, ovarian, tubal, or peritoneal cancer or women with a family history of BRCA1/2 gene mutations. Patients who test positive through one of the suggested screening tools should be referred for genetic counseling. This could lead to genetic testing and subsequent prophylactic therapies and/or increased screenings if the patient so desires. It is of importance to note the USPSTF recommends against routine screening of BRCA1/2 gene mutations for women who do not meet the above requirements.
Reference
USPSTF Recommendation: Assessment, counseling, and testing for BRCA-related cancer. JAMA. 2019;322(7):652-65. doi: 10.1001/jama.2019.10987.
Dr. Style is a second-year resident in the Family Medicine Residency Program at Abington (Pa.) Jefferson Health. Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
Breast cancer screening recommendations have evolved over the past decade. BRCA1/2 genes are tumor-suppressor genes. Mutations in these genes place women at an increased risk for developing breast, ovarian, fallopian tube, and peritoneal cancer. Detection of BRCA1/2 mutations through genetic screening can provide patients with more information about their cancer risk and can lead to discussion of prophylactic therapies. This includes increased screening frequency, medical therapy, and surgical interventions.
New USPSTF recommendations address who is at an increased risk for BRCA1/2 mutations. They recommend using screening tools focusing on family history that primary care physicians can utilize to determine who should be referred for genetic counseling to discuss the risks and benefits of genetic screening. The following are the task force’s two primary recommendations:
The USPSTF recommends that primary care clinicians assess women with a personal or family history of breast, ovarian, tubal, or peritoneal cancer or who have an ancestry associated with BRCA1/2 gene mutations with an appropriate brief familial risk assessment tool. Women with a positive result on the risk assessment tool should receive genetic counseling and, if indicated after counseling, genetic testing. (B recommendation)
The USPSTF recommends against routine risk assessment, genetic counseling, or genetic testing for women whose personal or family history or ancestry is not associated with potentially harmful BRCA1/2 gene mutations. (D recommendation)
Breast cancer is the second leading cause of cancer and cancer death for women in the United States. Ovarian cancer ranks fifth in cancer deaths for women in the U.S. By age 70, women with BRCA1/2 mutations have a 45%-65% cumulative lifetime risk of developing breast cancer.
Mutations in BRCA1, specifically, are associated with a 39% lifetime risk for ovarian, fallopian tube, and peritoneal cancer. In contrast, mutations in BRCA2 are associated with a 10%-17% lifetime risk.
The USPSTF also underscores the increased prevalence of BRCA1/2 mutations in the Ashkenazi Jewish population. Three out of seven familial risk assessment tools inquire about Jewish ancestry. This is because the Ashkenazi Jewish population have a higher prevalence of three founder mutations in the BRCA1/2 gene. A member of this population has a 1 in 40 chance of carrying one of these three mutations, whereas the general population has a 1 in 300 chance.
The USPSTF recommends a multistep process of screening. The first step is taking a family history of cancer. For women who have a family history of breast, ovarian, tubal, or peritoneal cancer or a personal history of these cancers, a brief familial risk assessment tool should be used to determine the need for referral for in-depth genetic counseling to determine the need for genetic testing.
It is important to recognize that the validated tools recommended by the USPSTF are specific for genetic risk assessment. General breast cancer risk assessment tools, including the National Cancer Institute Breast Cancer Risk Assessment Tool, which is based on the Gail model, are not recommended.
The sensitivity of the tools recommended by the USPSTF range between 77% and 100%. A number of tools are given as an option with no one tool being better than the other. Perhaps the easiest to implement of the validated tools recommended is the Pedigree Assessment Tool. For this tool, points are assigned for every family member with breast or ovarian cancer as indicated in the table below.
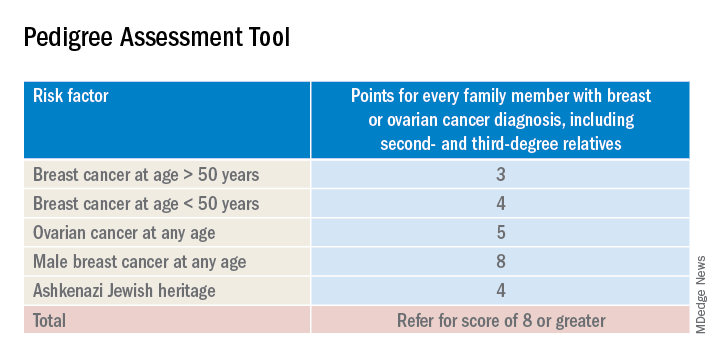
A positive result on a screening tool will lead primary care physicians to appropriately refer patients for genetic counseling. Genetic testing for BRCA1/2 mutations should be limited to those individuals whose personal and/or family history reflects an increased risk for gene mutations after detailed genetic assessment and counseling. The results of the genetic screening should assist a patient in their decision making.
Prophylactic treatment for BRCA1/2 mutation carriers are outside the scope of this recommendation. However the guidelines briefly review risk-reducing therapies including screening, medical, and surgical options. Medical therapy for patients who have BRCA1/2 mutations include the use of tamoxifen, raloxifene, and aromatase inhibitors. Surgical interventions include bilateral mastectomy and salpingo-oopherectomy.
Screening options include earlier and more frequent mammograms and breast MRIs. Screening is largely based on family history and the USPSTF acknowledges their uncertainty when screening women with an unknown family history. Male breast cancer, pancreatic cancer, prostate cancer, and melanoma are also associated with BRCA1/2 mutations. They are not included in this recommendation.
The bottom line
USPSTF recommended that primary care physicians should use familial risk assessment tools to screen women for BRCA1/2 mutations. This includes women with a personal and/or family history of breast, ovarian, tubal, or peritoneal cancer or women with a family history of BRCA1/2 gene mutations. Patients who test positive through one of the suggested screening tools should be referred for genetic counseling. This could lead to genetic testing and subsequent prophylactic therapies and/or increased screenings if the patient so desires. It is of importance to note the USPSTF recommends against routine screening of BRCA1/2 gene mutations for women who do not meet the above requirements.
Reference
USPSTF Recommendation: Assessment, counseling, and testing for BRCA-related cancer. JAMA. 2019;322(7):652-65. doi: 10.1001/jama.2019.10987.
Dr. Style is a second-year resident in the Family Medicine Residency Program at Abington (Pa.) Jefferson Health. Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
Summary: Preexposure prophylaxis for the prevention of HIV infection USPSTF recommendation statement
It is estimated that there are 1.1 million people in the United States living with HIV and that 15% of those people do not know they have HIV. Although the number of new cases reported each year is decreasing, there were still 38,281 new diagnoses in 2017. New cases might be decreasing overall, but the incidence of HIV is rising in some groups including people aged 25-29 years old and American Indian/Alaska Native and Asian populations. In addition, HIV disproportionately affects men who have sex with men, black/African American populations, and Hispanic/Latino populations, according to the USPSTF statement.
Given the prevalence of HIV and rising new cases in certain groups, it is thought that preexposure prophylaxis (PrEP) is being underutilized. The CDC reported that, in 2015, 1.2 million people were candidates for PrEP, but in 2017, only 100,282 people were using PrEP. The USPSTF performed a meta-analysis of 12 RCTs comparing rates of HIV infection in groups treated with PrEP versus those treated with placebo or no treatment and found a risk ratio of 0.46 (95% confidence interval, 0.33-0.66) and absolute risk reduction of –2% (95% CI, –2.8% to –1.2%) after 4 months and 4 years.
With this epidemiologic data and the meta-analysis, the USPSTF offered the following recommendations.
Screening
In order to decrease the rates of transmission and incidence of HIV infection, we must appropriately identify those who would be good candidates for PrEP. That begins with taking a complete and thorough sexual and injection drug use history in a manner that does not make patients feel stigmatized or discriminated against. The USPSTF recommends screening for HIV infection in patients aged 15-65 years old, in younger and older patients who have increased risk factors, and all pregnant patients. PrEP is not an appropriate choice in those who have HIV because it can lead to drug resistance.
When screening for HIV and considering starting PrEP, it is recommended that clinicians also test for kidney function, hepatitis B and C, other STIs, and pregnancy. The USPSTF suggests that the following groups be considered for PrEP given the increased risk of HIV infection:
- Men who have sex with men, are sexually active, and have one of these additional characteristics: a serodiscordant sex partner, inconsistent use of condoms during receptive or insertive anal sex, or infection with syphilis, gonorrhea, or chlamydia in the past 6 months.
- Heterosexual men or women who are sexually active with one or more of these additional characteristics: a serodiscordant sex partner, inconsistent use of condoms during sex with a partner whose HIV status is unknown and who is at high risk, and infection with syphilis or gonorrhea in the past 6 months.
- Patients who inject drugs with one or more of the following characteristics: shared use of drug injection equipment and risk of sexual acquisition (as in the categories above).
The USPSTF also notes that those who engage in transactional sex (for money, drugs, or housing) and transgender patients are at an increased risk of HIV infection.
Treatment
The only FDA approved treatment for the prevention HIV infection is once daily oral combined tenofovir disoproxil fumarate and emtricitabine; however, some studies have found that tenofovir disproxil fumarate monotherapy is also effective. Considering these trials, the CDC has suggested that tenofovir disoproxil fumarate monotherapy can be used as an alternative for men and women at high risk and those who inject drugs.
Tenofovir disoproxil fumarate/emtricitabine can also be used in pregnant patients, however the USPSTF notes that no PrEP trials included pregnant women. Additionally, tenofovir disoproxil fumarate/emtricitabine can be used in adolescents who weigh more than 35 kg. It is unknown how much time it takes to achieve protection against HIV infection after starting PrEP, and there is no clear timeline for how long patients should be on PrEP. Patients may discontinue medication because of preference, decreased risk of HIV exposure, or side effects.
Side effects include renal adverse events (serum creatinine rise), gastrointestinal adverse events (mostly nausea), and bone loss and increased fracture risk, although none were statistically significant when PrEP and placebo groups were compared. The USPSTF’s recommendations note that the effectiveness of PrEP is dependent on medication adherence.
While PrEP is an important part of preventing HIV, it is always important to counsel patients on other ways to reduce risk. The USPSTF notes that consistent condom use reduces the risk of HIV infection by around 80% in addition to reducing the risk of other STIs. All trials studied by the USPSTF for these recommendations included counseling on behavior, adherence, and condom use.
Bottom Line
It is estimated that 1.1 million Americans are living with HIV and 15% are unaware that they are positive for HIV. Overall cases of new HIV diagnoses are down, but they are rising in some groups. Every patient should be screened for high-risk sexual behavior and drug use with a thorough history. Patients aged 15-65 years should be screened for HIV. If patients are negative for HIV, but participate in high-risk sexual behaviors and drug injection, they should be offered PrEP along with counseling on, medication adherence, condom use, and reduction of high-risk behaviors.
Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Sprogell is a second-year resident in the Family Medicine Residency Program at Abington Jefferson Health
Reference
Owens DK et al. “Preexposure prophylaxis for the prevention of HIV infection: US Preventive Services Task Force recommendation statement.” JAMA. 2019 Jun 11;321(22):2203-13.
It is estimated that there are 1.1 million people in the United States living with HIV and that 15% of those people do not know they have HIV. Although the number of new cases reported each year is decreasing, there were still 38,281 new diagnoses in 2017. New cases might be decreasing overall, but the incidence of HIV is rising in some groups including people aged 25-29 years old and American Indian/Alaska Native and Asian populations. In addition, HIV disproportionately affects men who have sex with men, black/African American populations, and Hispanic/Latino populations, according to the USPSTF statement.
Given the prevalence of HIV and rising new cases in certain groups, it is thought that preexposure prophylaxis (PrEP) is being underutilized. The CDC reported that, in 2015, 1.2 million people were candidates for PrEP, but in 2017, only 100,282 people were using PrEP. The USPSTF performed a meta-analysis of 12 RCTs comparing rates of HIV infection in groups treated with PrEP versus those treated with placebo or no treatment and found a risk ratio of 0.46 (95% confidence interval, 0.33-0.66) and absolute risk reduction of –2% (95% CI, –2.8% to –1.2%) after 4 months and 4 years.
With this epidemiologic data and the meta-analysis, the USPSTF offered the following recommendations.
Screening
In order to decrease the rates of transmission and incidence of HIV infection, we must appropriately identify those who would be good candidates for PrEP. That begins with taking a complete and thorough sexual and injection drug use history in a manner that does not make patients feel stigmatized or discriminated against. The USPSTF recommends screening for HIV infection in patients aged 15-65 years old, in younger and older patients who have increased risk factors, and all pregnant patients. PrEP is not an appropriate choice in those who have HIV because it can lead to drug resistance.
When screening for HIV and considering starting PrEP, it is recommended that clinicians also test for kidney function, hepatitis B and C, other STIs, and pregnancy. The USPSTF suggests that the following groups be considered for PrEP given the increased risk of HIV infection:
- Men who have sex with men, are sexually active, and have one of these additional characteristics: a serodiscordant sex partner, inconsistent use of condoms during receptive or insertive anal sex, or infection with syphilis, gonorrhea, or chlamydia in the past 6 months.
- Heterosexual men or women who are sexually active with one or more of these additional characteristics: a serodiscordant sex partner, inconsistent use of condoms during sex with a partner whose HIV status is unknown and who is at high risk, and infection with syphilis or gonorrhea in the past 6 months.
- Patients who inject drugs with one or more of the following characteristics: shared use of drug injection equipment and risk of sexual acquisition (as in the categories above).
The USPSTF also notes that those who engage in transactional sex (for money, drugs, or housing) and transgender patients are at an increased risk of HIV infection.
Treatment
The only FDA approved treatment for the prevention HIV infection is once daily oral combined tenofovir disoproxil fumarate and emtricitabine; however, some studies have found that tenofovir disproxil fumarate monotherapy is also effective. Considering these trials, the CDC has suggested that tenofovir disoproxil fumarate monotherapy can be used as an alternative for men and women at high risk and those who inject drugs.
Tenofovir disoproxil fumarate/emtricitabine can also be used in pregnant patients, however the USPSTF notes that no PrEP trials included pregnant women. Additionally, tenofovir disoproxil fumarate/emtricitabine can be used in adolescents who weigh more than 35 kg. It is unknown how much time it takes to achieve protection against HIV infection after starting PrEP, and there is no clear timeline for how long patients should be on PrEP. Patients may discontinue medication because of preference, decreased risk of HIV exposure, or side effects.
Side effects include renal adverse events (serum creatinine rise), gastrointestinal adverse events (mostly nausea), and bone loss and increased fracture risk, although none were statistically significant when PrEP and placebo groups were compared. The USPSTF’s recommendations note that the effectiveness of PrEP is dependent on medication adherence.
While PrEP is an important part of preventing HIV, it is always important to counsel patients on other ways to reduce risk. The USPSTF notes that consistent condom use reduces the risk of HIV infection by around 80% in addition to reducing the risk of other STIs. All trials studied by the USPSTF for these recommendations included counseling on behavior, adherence, and condom use.
Bottom Line
It is estimated that 1.1 million Americans are living with HIV and 15% are unaware that they are positive for HIV. Overall cases of new HIV diagnoses are down, but they are rising in some groups. Every patient should be screened for high-risk sexual behavior and drug use with a thorough history. Patients aged 15-65 years should be screened for HIV. If patients are negative for HIV, but participate in high-risk sexual behaviors and drug injection, they should be offered PrEP along with counseling on, medication adherence, condom use, and reduction of high-risk behaviors.
Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Sprogell is a second-year resident in the Family Medicine Residency Program at Abington Jefferson Health
Reference
Owens DK et al. “Preexposure prophylaxis for the prevention of HIV infection: US Preventive Services Task Force recommendation statement.” JAMA. 2019 Jun 11;321(22):2203-13.
It is estimated that there are 1.1 million people in the United States living with HIV and that 15% of those people do not know they have HIV. Although the number of new cases reported each year is decreasing, there were still 38,281 new diagnoses in 2017. New cases might be decreasing overall, but the incidence of HIV is rising in some groups including people aged 25-29 years old and American Indian/Alaska Native and Asian populations. In addition, HIV disproportionately affects men who have sex with men, black/African American populations, and Hispanic/Latino populations, according to the USPSTF statement.
Given the prevalence of HIV and rising new cases in certain groups, it is thought that preexposure prophylaxis (PrEP) is being underutilized. The CDC reported that, in 2015, 1.2 million people were candidates for PrEP, but in 2017, only 100,282 people were using PrEP. The USPSTF performed a meta-analysis of 12 RCTs comparing rates of HIV infection in groups treated with PrEP versus those treated with placebo or no treatment and found a risk ratio of 0.46 (95% confidence interval, 0.33-0.66) and absolute risk reduction of –2% (95% CI, –2.8% to –1.2%) after 4 months and 4 years.
With this epidemiologic data and the meta-analysis, the USPSTF offered the following recommendations.
Screening
In order to decrease the rates of transmission and incidence of HIV infection, we must appropriately identify those who would be good candidates for PrEP. That begins with taking a complete and thorough sexual and injection drug use history in a manner that does not make patients feel stigmatized or discriminated against. The USPSTF recommends screening for HIV infection in patients aged 15-65 years old, in younger and older patients who have increased risk factors, and all pregnant patients. PrEP is not an appropriate choice in those who have HIV because it can lead to drug resistance.
When screening for HIV and considering starting PrEP, it is recommended that clinicians also test for kidney function, hepatitis B and C, other STIs, and pregnancy. The USPSTF suggests that the following groups be considered for PrEP given the increased risk of HIV infection:
- Men who have sex with men, are sexually active, and have one of these additional characteristics: a serodiscordant sex partner, inconsistent use of condoms during receptive or insertive anal sex, or infection with syphilis, gonorrhea, or chlamydia in the past 6 months.
- Heterosexual men or women who are sexually active with one or more of these additional characteristics: a serodiscordant sex partner, inconsistent use of condoms during sex with a partner whose HIV status is unknown and who is at high risk, and infection with syphilis or gonorrhea in the past 6 months.
- Patients who inject drugs with one or more of the following characteristics: shared use of drug injection equipment and risk of sexual acquisition (as in the categories above).
The USPSTF also notes that those who engage in transactional sex (for money, drugs, or housing) and transgender patients are at an increased risk of HIV infection.
Treatment
The only FDA approved treatment for the prevention HIV infection is once daily oral combined tenofovir disoproxil fumarate and emtricitabine; however, some studies have found that tenofovir disproxil fumarate monotherapy is also effective. Considering these trials, the CDC has suggested that tenofovir disoproxil fumarate monotherapy can be used as an alternative for men and women at high risk and those who inject drugs.
Tenofovir disoproxil fumarate/emtricitabine can also be used in pregnant patients, however the USPSTF notes that no PrEP trials included pregnant women. Additionally, tenofovir disoproxil fumarate/emtricitabine can be used in adolescents who weigh more than 35 kg. It is unknown how much time it takes to achieve protection against HIV infection after starting PrEP, and there is no clear timeline for how long patients should be on PrEP. Patients may discontinue medication because of preference, decreased risk of HIV exposure, or side effects.
Side effects include renal adverse events (serum creatinine rise), gastrointestinal adverse events (mostly nausea), and bone loss and increased fracture risk, although none were statistically significant when PrEP and placebo groups were compared. The USPSTF’s recommendations note that the effectiveness of PrEP is dependent on medication adherence.
While PrEP is an important part of preventing HIV, it is always important to counsel patients on other ways to reduce risk. The USPSTF notes that consistent condom use reduces the risk of HIV infection by around 80% in addition to reducing the risk of other STIs. All trials studied by the USPSTF for these recommendations included counseling on behavior, adherence, and condom use.
Bottom Line
It is estimated that 1.1 million Americans are living with HIV and 15% are unaware that they are positive for HIV. Overall cases of new HIV diagnoses are down, but they are rising in some groups. Every patient should be screened for high-risk sexual behavior and drug use with a thorough history. Patients aged 15-65 years should be screened for HIV. If patients are negative for HIV, but participate in high-risk sexual behaviors and drug injection, they should be offered PrEP along with counseling on, medication adherence, condom use, and reduction of high-risk behaviors.
Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Sprogell is a second-year resident in the Family Medicine Residency Program at Abington Jefferson Health
Reference
Owens DK et al. “Preexposure prophylaxis for the prevention of HIV infection: US Preventive Services Task Force recommendation statement.” JAMA. 2019 Jun 11;321(22):2203-13.
Summary: American Medical Society for Sports Medicine position statement on concussion in sport
An estimated 1-1.8 million sport-related concussions (SRC) occur per year in patients younger than 18 years of age. Concussion is defined as “a traumatically induced transient disturbance of brain function.” More than 50% of concussions among high school youth are not related to organized sports and between 2% and 15% of athletes in organized sports will sustain a concussion during a season of play.
which will be described in this article. The guidelines include recommendations for imaging, treatment, and decision making regarding when as well as whether to return to play. Here is a brief summary of those recommendations.
Preseason: Preseason evaluation includes a preparticipation physical evaluation and discussion of concussion history as well as risk factors associated with prolonged concussion recovery. Neurocognitive tests are available for baseline evaluation. While these may assist with diagnosis and return-to-play decisions, there can be considerable variation in an individual’s baseline score as well as the possibility of changes in that baseline over time. Because of this potential for variability, these tests are not required or accepted as the standard of care.
Sideline assessment: Familiarity with the athlete is the best way to detect subtle changes in personality or performance. Looking at symptoms is still the most sensitive way to diagnose a concussion. Loss of consciousness, seizure, tonic posturing, lack of motor coordination, confusion, amnesia, difficulty with balance, or any cognitive difficulty should prompt removal from play for possible concussion. Once a potential injury is identified, how the athlete responds to the elements of orientation, memory, concentration, speech pattern, and balance should be evaluated. If an athlete has a probable or definite concussion, the athlete needs to be removed from play and cannot return to same-day play, and a more detailed evaluation needs to be done.
Office assessment: It is not unusual for symptoms and testing to normalize by the time an office visit occurs. If this is the case, the visit should focus on recommendations for safe return to school and sport. A standard office evaluation should include taking a history with details of the mechanism of injury and preexisting conditions – such as depression and prior concussion – that can affect concussion recovery. The history should focus on detecting symptoms that typically cause impairment from concussion: headache, ocular-vestibular issues leading to problems with balance, and cognitive issues with difficulty concentrating and remembering, as well as fatigue and mood issues such as anxiety, irritability, and depression. The physical exam should include assessment of ocular and vestibular function, gait, and balance in addition to a neurological exam.
Imaging: Head CT or MRI are rarely indicated. Intracranial bleeds are rare in the context of SRC but can occur. If there is concern for a bleed, then CT scan is the imaging test of choice. MRI may have value for evaluation for atypical or prolonged recovery.
Recovery time: The large majority (80%-90%) of concussed older adolescents and adults return to preinjury levels of function within 2 weeks; in younger athletes, clinical recovery may take up to 4 weeks. The best predictor of recovery from SRC is the number and severity of symptoms.
Treatment: For decades, cognitive and physical rest has been the standard of treatment. However, this is no longer the “gold standard” as it has been shown that strict rest (“cocoon therapy”) after SRC slows recovery and leads to an increased chance of prolonged symptoms. Current consensus guidelines support 24-48 hours of symptom-limited rest, both cognitive and physical, followed by a gradual increase in activity, staying below symptom-exacerbation thresholds. Activity, along with good sleep hygiene, appears to be helpful in facilitating recovery from SRC. In athletes with persistent post concussive symptoms that continue beyond the expected recovery time frame, activities of daily living, school, and exercise that do not significantly exacerbate symptoms are recommended.
Return to learning/play: A concussion can cause temporary deficits in attention, cognitive processing, short-term memory, and executive functioning. School personnel should be informed of the injury and assist in employing an individualized return to learn plan, including academic accommodations. Ultimately, return to sports activities should follow a successful return to the classroom. Return to play involves a stepwise increase in physical demands/activity without symptoms before a student is allowed to participate in full contact play.
Concussion-related risks: Continuing to participate in sports before resolution of concussion can worsen and prolong symptoms of SRC. Returning too early after concussion, before full recovery, increases the risk of recurrent SRC. During the initial post-injury period, returning to sports too early increases the risk for a rare but devastating possibility of second impact syndrome that can be a life-threatening repeat head injury. Studies of long-term mental health diagnoses are conflicting and inconsistent. Chronic traumatic encephalopathy has been described in athletes with a long history of concussions and repetitive sub-symptom head impacts. The degree of exposure needed appears to be variable and dependent on the individual.
Disqualification from play: Because each athlete is individually assessed after SRC, there are no evidence-based studies indicating how many concussions are “safe” for an athlete to have in a lifetime. The decision to stop playing sports is both serious and difficult for most athletes and requires shared decision making between clinician, the athlete, and the athlete’s parents. Factors to consider when determining if disqualification from play is warranted include:
- The total number of concussions experienced by a patient.
- Whether a patient has sustained subsequent concussions with progressively less forceful blows to the head.
- If a patient has sustained multiple concussions,whether the time to complete a full recovery after each concussion event increased.
The bottom line: “Cocoon therapy” is no longer recommended. Consensus guidelines endorse 24-48 hours of symptom-limited cognitive and physical rest followed by a gradual increase in activity, including noncontact physical activity that does not provoke symptoms.
Dr. Belogorodsky is a second-year resident and Dr. Fidler is an associate director in the Family Medicine Residency Program at Abington (Pa.) Jefferson Health. Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
Reference
Harmon KG et al. American Medical Society for Sports Medicine position statement on concussion in sport. Br J Sports Med. 2019;53:213-25.
An estimated 1-1.8 million sport-related concussions (SRC) occur per year in patients younger than 18 years of age. Concussion is defined as “a traumatically induced transient disturbance of brain function.” More than 50% of concussions among high school youth are not related to organized sports and between 2% and 15% of athletes in organized sports will sustain a concussion during a season of play.
which will be described in this article. The guidelines include recommendations for imaging, treatment, and decision making regarding when as well as whether to return to play. Here is a brief summary of those recommendations.
Preseason: Preseason evaluation includes a preparticipation physical evaluation and discussion of concussion history as well as risk factors associated with prolonged concussion recovery. Neurocognitive tests are available for baseline evaluation. While these may assist with diagnosis and return-to-play decisions, there can be considerable variation in an individual’s baseline score as well as the possibility of changes in that baseline over time. Because of this potential for variability, these tests are not required or accepted as the standard of care.
Sideline assessment: Familiarity with the athlete is the best way to detect subtle changes in personality or performance. Looking at symptoms is still the most sensitive way to diagnose a concussion. Loss of consciousness, seizure, tonic posturing, lack of motor coordination, confusion, amnesia, difficulty with balance, or any cognitive difficulty should prompt removal from play for possible concussion. Once a potential injury is identified, how the athlete responds to the elements of orientation, memory, concentration, speech pattern, and balance should be evaluated. If an athlete has a probable or definite concussion, the athlete needs to be removed from play and cannot return to same-day play, and a more detailed evaluation needs to be done.
Office assessment: It is not unusual for symptoms and testing to normalize by the time an office visit occurs. If this is the case, the visit should focus on recommendations for safe return to school and sport. A standard office evaluation should include taking a history with details of the mechanism of injury and preexisting conditions – such as depression and prior concussion – that can affect concussion recovery. The history should focus on detecting symptoms that typically cause impairment from concussion: headache, ocular-vestibular issues leading to problems with balance, and cognitive issues with difficulty concentrating and remembering, as well as fatigue and mood issues such as anxiety, irritability, and depression. The physical exam should include assessment of ocular and vestibular function, gait, and balance in addition to a neurological exam.
Imaging: Head CT or MRI are rarely indicated. Intracranial bleeds are rare in the context of SRC but can occur. If there is concern for a bleed, then CT scan is the imaging test of choice. MRI may have value for evaluation for atypical or prolonged recovery.
Recovery time: The large majority (80%-90%) of concussed older adolescents and adults return to preinjury levels of function within 2 weeks; in younger athletes, clinical recovery may take up to 4 weeks. The best predictor of recovery from SRC is the number and severity of symptoms.
Treatment: For decades, cognitive and physical rest has been the standard of treatment. However, this is no longer the “gold standard” as it has been shown that strict rest (“cocoon therapy”) after SRC slows recovery and leads to an increased chance of prolonged symptoms. Current consensus guidelines support 24-48 hours of symptom-limited rest, both cognitive and physical, followed by a gradual increase in activity, staying below symptom-exacerbation thresholds. Activity, along with good sleep hygiene, appears to be helpful in facilitating recovery from SRC. In athletes with persistent post concussive symptoms that continue beyond the expected recovery time frame, activities of daily living, school, and exercise that do not significantly exacerbate symptoms are recommended.
Return to learning/play: A concussion can cause temporary deficits in attention, cognitive processing, short-term memory, and executive functioning. School personnel should be informed of the injury and assist in employing an individualized return to learn plan, including academic accommodations. Ultimately, return to sports activities should follow a successful return to the classroom. Return to play involves a stepwise increase in physical demands/activity without symptoms before a student is allowed to participate in full contact play.
Concussion-related risks: Continuing to participate in sports before resolution of concussion can worsen and prolong symptoms of SRC. Returning too early after concussion, before full recovery, increases the risk of recurrent SRC. During the initial post-injury period, returning to sports too early increases the risk for a rare but devastating possibility of second impact syndrome that can be a life-threatening repeat head injury. Studies of long-term mental health diagnoses are conflicting and inconsistent. Chronic traumatic encephalopathy has been described in athletes with a long history of concussions and repetitive sub-symptom head impacts. The degree of exposure needed appears to be variable and dependent on the individual.
Disqualification from play: Because each athlete is individually assessed after SRC, there are no evidence-based studies indicating how many concussions are “safe” for an athlete to have in a lifetime. The decision to stop playing sports is both serious and difficult for most athletes and requires shared decision making between clinician, the athlete, and the athlete’s parents. Factors to consider when determining if disqualification from play is warranted include:
- The total number of concussions experienced by a patient.
- Whether a patient has sustained subsequent concussions with progressively less forceful blows to the head.
- If a patient has sustained multiple concussions,whether the time to complete a full recovery after each concussion event increased.
The bottom line: “Cocoon therapy” is no longer recommended. Consensus guidelines endorse 24-48 hours of symptom-limited cognitive and physical rest followed by a gradual increase in activity, including noncontact physical activity that does not provoke symptoms.
Dr. Belogorodsky is a second-year resident and Dr. Fidler is an associate director in the Family Medicine Residency Program at Abington (Pa.) Jefferson Health. Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
Reference
Harmon KG et al. American Medical Society for Sports Medicine position statement on concussion in sport. Br J Sports Med. 2019;53:213-25.
An estimated 1-1.8 million sport-related concussions (SRC) occur per year in patients younger than 18 years of age. Concussion is defined as “a traumatically induced transient disturbance of brain function.” More than 50% of concussions among high school youth are not related to organized sports and between 2% and 15% of athletes in organized sports will sustain a concussion during a season of play.
which will be described in this article. The guidelines include recommendations for imaging, treatment, and decision making regarding when as well as whether to return to play. Here is a brief summary of those recommendations.
Preseason: Preseason evaluation includes a preparticipation physical evaluation and discussion of concussion history as well as risk factors associated with prolonged concussion recovery. Neurocognitive tests are available for baseline evaluation. While these may assist with diagnosis and return-to-play decisions, there can be considerable variation in an individual’s baseline score as well as the possibility of changes in that baseline over time. Because of this potential for variability, these tests are not required or accepted as the standard of care.
Sideline assessment: Familiarity with the athlete is the best way to detect subtle changes in personality or performance. Looking at symptoms is still the most sensitive way to diagnose a concussion. Loss of consciousness, seizure, tonic posturing, lack of motor coordination, confusion, amnesia, difficulty with balance, or any cognitive difficulty should prompt removal from play for possible concussion. Once a potential injury is identified, how the athlete responds to the elements of orientation, memory, concentration, speech pattern, and balance should be evaluated. If an athlete has a probable or definite concussion, the athlete needs to be removed from play and cannot return to same-day play, and a more detailed evaluation needs to be done.
Office assessment: It is not unusual for symptoms and testing to normalize by the time an office visit occurs. If this is the case, the visit should focus on recommendations for safe return to school and sport. A standard office evaluation should include taking a history with details of the mechanism of injury and preexisting conditions – such as depression and prior concussion – that can affect concussion recovery. The history should focus on detecting symptoms that typically cause impairment from concussion: headache, ocular-vestibular issues leading to problems with balance, and cognitive issues with difficulty concentrating and remembering, as well as fatigue and mood issues such as anxiety, irritability, and depression. The physical exam should include assessment of ocular and vestibular function, gait, and balance in addition to a neurological exam.
Imaging: Head CT or MRI are rarely indicated. Intracranial bleeds are rare in the context of SRC but can occur. If there is concern for a bleed, then CT scan is the imaging test of choice. MRI may have value for evaluation for atypical or prolonged recovery.
Recovery time: The large majority (80%-90%) of concussed older adolescents and adults return to preinjury levels of function within 2 weeks; in younger athletes, clinical recovery may take up to 4 weeks. The best predictor of recovery from SRC is the number and severity of symptoms.
Treatment: For decades, cognitive and physical rest has been the standard of treatment. However, this is no longer the “gold standard” as it has been shown that strict rest (“cocoon therapy”) after SRC slows recovery and leads to an increased chance of prolonged symptoms. Current consensus guidelines support 24-48 hours of symptom-limited rest, both cognitive and physical, followed by a gradual increase in activity, staying below symptom-exacerbation thresholds. Activity, along with good sleep hygiene, appears to be helpful in facilitating recovery from SRC. In athletes with persistent post concussive symptoms that continue beyond the expected recovery time frame, activities of daily living, school, and exercise that do not significantly exacerbate symptoms are recommended.
Return to learning/play: A concussion can cause temporary deficits in attention, cognitive processing, short-term memory, and executive functioning. School personnel should be informed of the injury and assist in employing an individualized return to learn plan, including academic accommodations. Ultimately, return to sports activities should follow a successful return to the classroom. Return to play involves a stepwise increase in physical demands/activity without symptoms before a student is allowed to participate in full contact play.
Concussion-related risks: Continuing to participate in sports before resolution of concussion can worsen and prolong symptoms of SRC. Returning too early after concussion, before full recovery, increases the risk of recurrent SRC. During the initial post-injury period, returning to sports too early increases the risk for a rare but devastating possibility of second impact syndrome that can be a life-threatening repeat head injury. Studies of long-term mental health diagnoses are conflicting and inconsistent. Chronic traumatic encephalopathy has been described in athletes with a long history of concussions and repetitive sub-symptom head impacts. The degree of exposure needed appears to be variable and dependent on the individual.
Disqualification from play: Because each athlete is individually assessed after SRC, there are no evidence-based studies indicating how many concussions are “safe” for an athlete to have in a lifetime. The decision to stop playing sports is both serious and difficult for most athletes and requires shared decision making between clinician, the athlete, and the athlete’s parents. Factors to consider when determining if disqualification from play is warranted include:
- The total number of concussions experienced by a patient.
- Whether a patient has sustained subsequent concussions with progressively less forceful blows to the head.
- If a patient has sustained multiple concussions,whether the time to complete a full recovery after each concussion event increased.
The bottom line: “Cocoon therapy” is no longer recommended. Consensus guidelines endorse 24-48 hours of symptom-limited cognitive and physical rest followed by a gradual increase in activity, including noncontact physical activity that does not provoke symptoms.
Dr. Belogorodsky is a second-year resident and Dr. Fidler is an associate director in the Family Medicine Residency Program at Abington (Pa.) Jefferson Health. Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
Reference
Harmon KG et al. American Medical Society for Sports Medicine position statement on concussion in sport. Br J Sports Med. 2019;53:213-25.