User login
Childhood cancer survivors face several long-term risks
Chicago – Survivors of childhood cancers face several later risks from treatment, and investigators presented studies evaluating risks in three specific areas – secondary neoplasms, premature menopause, and neurocognitive function – at the annual meeting of the American Society of Clinical Oncology.
Discussant Paul Nathan, M.D., of The Hospital for Sick Children in Toronto, said “the whole purpose” of research in this area “is to start to understand the predictors and modifiers of late effects” and then to design risk assessment tools and interventions to reduce long-term toxicity. These interventions include modification of chemotherapy and radiation doses, protective strategies, and disease risk stratification to adjust intensity of therapies.
Other strategies are to use behavioral interventions directed at improving compliance with follow-up to detect problems earlier and the use of real-time monitoring, such as with smart phones or fitness trackers. He said one limitation of this sort of research and implementing interventions to reduce late toxicities is that “you need time to document long-term outcomes.” So tracking newer therapies, such as proton beam radiation, small molecule drugs, and immunotherapy, is “going to take time, perhaps decades, before you understand their impact on patients.”
Risk of secondary neoplasms reduced
Risk-stratifying of disease “has allowed us to make attempts to minimize late effects by modifying therapy over time in certain subgroups of lower-risk patients,” said Dr. Lucie Turcotte of the University of Minnesota in Minneapolis.
To study the effects of these changes, she determined the risk of certain subsequent malignant or benign neoplasms over three periods of therapeutic exposure among 23,603 5-year survivors of childhood cancers diagnosed at less than 21 years of age from 1970 to 1999, drawing from the cohort of the Childhood Cancer Survivor Study (CCSS). The CCSS represents about 20% of childhood cancer survivors in the United States for the study period.
Over the decades of 1970-1979, 1980-1989, and 1990-1999, the use of any radiation went from 77% to 58% to 41%, respectively. Cranial radiation for acute lymphoblastic leukemia (ALL) decreased from 85% to 19%, abdominal radiation for Wilms tumor from 78% to 43%, and chest radiotherapy for Hodgkin lymphoma from 87% to 61%. The proportion of children receiving alkylating agents, anthracyclines, and epipodophyllotoxins went up, but the cumulative doses went down (N Engl J Med. 2016 Mar 3;374(9):833-42).
Dr. Nathan said today, almost no child gets cranial radiation for ALL. “So we’ve slowly learned that our treatments are toxic, and we’ve certainly done what we can to change them.”
But have these changes made a difference? Dr. Turcotte found that survivors remain at increased risk of a secondary neoplasm, but the risk was lower for children treated in later time periods.
Dr. Nathan pointed to Dr. Turcotte’s data showing that the incidence of subsequent malignant neoplasms decreased from 1970 to 1999 by 7% for each 5-year era (15-year risk: 2.3% to 1.6%; P = .001; number needed to treat, NNT = 143). Similarly, non-melanoma skin cancer 15-year risk decreased from 0.7% to 0.1% (P less than .001; NNT = 167). The NNT’s are “certainly important, but these are not major differences over time,” Dr. Nathan said. Knowing the impact of newer, targeted therapeutic approaches will take some time.
Predicting risk of premature menopause
Also using the CCSS data, Dr. Jennifer Levine of Columbia University Medical Center, New York, N.Y., studied the prevalence of and risk factors for nonsurgical premature menopause (NSPM), defined as cessation of menses prior to age 40 years, as well as the effect on reproductive outcomes for survivors of childhood cancers.
Dr. Nathan said when a child is first diagnosed with cancer, seldom does the issue of fertility come up early in the discussion, “but when you treat young adults who are survivors, the number one thing they talk about often is fertility. And so doing a better job in predicting who is at risk for infertility is clearly a priority for survivorship research.”
He said the development of the cyclophosphamide equivalent dose (CED) by D.M Green et al. (Pediatr Blood Cancer. 2014 Jan;61(1):53-67) has been very helpful for quantifying alkylating agent exposure to make comparisons between studies. The goal is to develop a risk assessment tool to be able to tell patients and families their fertility risk based on demographics, therapy, and biomarkers.
Being able to evaluate risk is critically important because for girls, oocyte or ovarian harvesting or even transvaginal ultrasound is highly invasive, and these procedures should be recommended only if their risk for infertility is very high.
Dr. Levine studied 2,930 female cancer survivors diagnosed at a median age of 6 years between 1979 and 1986 and a median age at follow-up of 34 years, who were compared with 1,399 healthy siblings. Of the survivor cohort, 110 developed NSPM at a median age of 32 years, and the prevalence of NSPM at age 40 years for the entire cohort was 9.1%, giving a relative risk of NSPM of 10.5 compared with siblings, who had a 0.9% NSPM prevalence at age 40.
She found that exposure to alkylating agents and older age at diagnosis put childhood cancer survivors at increased risk of NSPM, which was associated with lower rates of pregnancy and live births after age 31 years. The greatest risk of NSPM occurred if the cyclophosphamide equivalent dose was greater than 6000 mg/m2 (odds ratio = 3.6 compared with no CED); if there had been any radiation to the ovaries (less than 5 Gy: OR = 4.0; 5 Gy or more: OR = 20.4); or if the age at diagnosis was greater than 14 years (OR = 2.3).
Women with NSPM, compared with survivors without NSPM, were less likely ever to be pregnant (OR = 0.41) or to have a live birth after age 30 (OR = 0.35). However, these outcomes were no different between the ages of 21 and 30. Dr. Levine said this information can assist clinicians in counseling their patients about the risk for early menopause and planning for alternative reproductive means, such as oocyte or embryo harvesting and preservation.
Neurocognitive functioning after treatment
Dr. Wei Liu of St. Jude Children’s Research Hospital, Memphis, Tenn., studied the neurocognitive function of long-term survivors of ALL.
Dr. Nathan called ALL “the paradigm for how we’ve sort of learned and adjusted how we treat patients based on late effects.” Early on, the disease was treated with craniospinal radiation and intrathecal chemotherapy, and while patients survived, it became obvious that they suffered neurocognitive and endocrine problems, growth abnormalities, and secondary malignancies. These findings forced a reevaluatuon of treatments, leading to elimination of spinal radiation, reduction of cranial radiation dose, intensification of systemic therapy, including methotrexate, and risk stratification allowing modification of therapies.
Survival was sustained, but long-term outcomes were still based on children treated with radiation. So long-term cognitive consequences in the more modern era of therapy were unknown. Only recently have adult cohorts become available who were treated in the chemotherapy-only era.
Dr. Liu studied 159 ALL survivors who had been treated with chemotherapy alone at a mean age of 9.2 years. The follow-up was at a median of 7.6 years off therapy at a mean age of 13.7 years. At the end of the chemotherapy protocol, patients completed tests of sustained attention, and parents rated survivors’ behavior on standard scales.
She found that for these childhood cancer survivors, sustained attention and behavior functioning at the end of chemotherapy predicted long-term attention and processing speed outcomes. Only exposure to chemotherapy, and not end-of-therapy function, predicted that survivors would have poor executive function of fluency and flexibility at long-term follow up.
Dr. Nathan praised the investigators for their foresight to collect data on the methotrexate area under the curve, number of triple intrathecal therapies (cytarabine, methotrexate, and hydrocortisone), and neurocognitive functioning at the end of chemotherapy. “What’s clear is that chemotherapy alone can lead to neurocognitive late effects,” he said. “But what’s also important is that not all late effects can be predicted by end of therapy assessments.” These late effects appear to evolve over time, so ongoing assessments are needed.
Dr. Turcotte, Dr. Liu, Dr. Levine, and Dr. Nathan each reported no financial disclosures.
Chicago – Survivors of childhood cancers face several later risks from treatment, and investigators presented studies evaluating risks in three specific areas – secondary neoplasms, premature menopause, and neurocognitive function – at the annual meeting of the American Society of Clinical Oncology.
Discussant Paul Nathan, M.D., of The Hospital for Sick Children in Toronto, said “the whole purpose” of research in this area “is to start to understand the predictors and modifiers of late effects” and then to design risk assessment tools and interventions to reduce long-term toxicity. These interventions include modification of chemotherapy and radiation doses, protective strategies, and disease risk stratification to adjust intensity of therapies.
Other strategies are to use behavioral interventions directed at improving compliance with follow-up to detect problems earlier and the use of real-time monitoring, such as with smart phones or fitness trackers. He said one limitation of this sort of research and implementing interventions to reduce late toxicities is that “you need time to document long-term outcomes.” So tracking newer therapies, such as proton beam radiation, small molecule drugs, and immunotherapy, is “going to take time, perhaps decades, before you understand their impact on patients.”
Risk of secondary neoplasms reduced
Risk-stratifying of disease “has allowed us to make attempts to minimize late effects by modifying therapy over time in certain subgroups of lower-risk patients,” said Dr. Lucie Turcotte of the University of Minnesota in Minneapolis.
To study the effects of these changes, she determined the risk of certain subsequent malignant or benign neoplasms over three periods of therapeutic exposure among 23,603 5-year survivors of childhood cancers diagnosed at less than 21 years of age from 1970 to 1999, drawing from the cohort of the Childhood Cancer Survivor Study (CCSS). The CCSS represents about 20% of childhood cancer survivors in the United States for the study period.
Over the decades of 1970-1979, 1980-1989, and 1990-1999, the use of any radiation went from 77% to 58% to 41%, respectively. Cranial radiation for acute lymphoblastic leukemia (ALL) decreased from 85% to 19%, abdominal radiation for Wilms tumor from 78% to 43%, and chest radiotherapy for Hodgkin lymphoma from 87% to 61%. The proportion of children receiving alkylating agents, anthracyclines, and epipodophyllotoxins went up, but the cumulative doses went down (N Engl J Med. 2016 Mar 3;374(9):833-42).
Dr. Nathan said today, almost no child gets cranial radiation for ALL. “So we’ve slowly learned that our treatments are toxic, and we’ve certainly done what we can to change them.”
But have these changes made a difference? Dr. Turcotte found that survivors remain at increased risk of a secondary neoplasm, but the risk was lower for children treated in later time periods.
Dr. Nathan pointed to Dr. Turcotte’s data showing that the incidence of subsequent malignant neoplasms decreased from 1970 to 1999 by 7% for each 5-year era (15-year risk: 2.3% to 1.6%; P = .001; number needed to treat, NNT = 143). Similarly, non-melanoma skin cancer 15-year risk decreased from 0.7% to 0.1% (P less than .001; NNT = 167). The NNT’s are “certainly important, but these are not major differences over time,” Dr. Nathan said. Knowing the impact of newer, targeted therapeutic approaches will take some time.
Predicting risk of premature menopause
Also using the CCSS data, Dr. Jennifer Levine of Columbia University Medical Center, New York, N.Y., studied the prevalence of and risk factors for nonsurgical premature menopause (NSPM), defined as cessation of menses prior to age 40 years, as well as the effect on reproductive outcomes for survivors of childhood cancers.
Dr. Nathan said when a child is first diagnosed with cancer, seldom does the issue of fertility come up early in the discussion, “but when you treat young adults who are survivors, the number one thing they talk about often is fertility. And so doing a better job in predicting who is at risk for infertility is clearly a priority for survivorship research.”
He said the development of the cyclophosphamide equivalent dose (CED) by D.M Green et al. (Pediatr Blood Cancer. 2014 Jan;61(1):53-67) has been very helpful for quantifying alkylating agent exposure to make comparisons between studies. The goal is to develop a risk assessment tool to be able to tell patients and families their fertility risk based on demographics, therapy, and biomarkers.
Being able to evaluate risk is critically important because for girls, oocyte or ovarian harvesting or even transvaginal ultrasound is highly invasive, and these procedures should be recommended only if their risk for infertility is very high.
Dr. Levine studied 2,930 female cancer survivors diagnosed at a median age of 6 years between 1979 and 1986 and a median age at follow-up of 34 years, who were compared with 1,399 healthy siblings. Of the survivor cohort, 110 developed NSPM at a median age of 32 years, and the prevalence of NSPM at age 40 years for the entire cohort was 9.1%, giving a relative risk of NSPM of 10.5 compared with siblings, who had a 0.9% NSPM prevalence at age 40.
She found that exposure to alkylating agents and older age at diagnosis put childhood cancer survivors at increased risk of NSPM, which was associated with lower rates of pregnancy and live births after age 31 years. The greatest risk of NSPM occurred if the cyclophosphamide equivalent dose was greater than 6000 mg/m2 (odds ratio = 3.6 compared with no CED); if there had been any radiation to the ovaries (less than 5 Gy: OR = 4.0; 5 Gy or more: OR = 20.4); or if the age at diagnosis was greater than 14 years (OR = 2.3).
Women with NSPM, compared with survivors without NSPM, were less likely ever to be pregnant (OR = 0.41) or to have a live birth after age 30 (OR = 0.35). However, these outcomes were no different between the ages of 21 and 30. Dr. Levine said this information can assist clinicians in counseling their patients about the risk for early menopause and planning for alternative reproductive means, such as oocyte or embryo harvesting and preservation.
Neurocognitive functioning after treatment
Dr. Wei Liu of St. Jude Children’s Research Hospital, Memphis, Tenn., studied the neurocognitive function of long-term survivors of ALL.
Dr. Nathan called ALL “the paradigm for how we’ve sort of learned and adjusted how we treat patients based on late effects.” Early on, the disease was treated with craniospinal radiation and intrathecal chemotherapy, and while patients survived, it became obvious that they suffered neurocognitive and endocrine problems, growth abnormalities, and secondary malignancies. These findings forced a reevaluatuon of treatments, leading to elimination of spinal radiation, reduction of cranial radiation dose, intensification of systemic therapy, including methotrexate, and risk stratification allowing modification of therapies.
Survival was sustained, but long-term outcomes were still based on children treated with radiation. So long-term cognitive consequences in the more modern era of therapy were unknown. Only recently have adult cohorts become available who were treated in the chemotherapy-only era.
Dr. Liu studied 159 ALL survivors who had been treated with chemotherapy alone at a mean age of 9.2 years. The follow-up was at a median of 7.6 years off therapy at a mean age of 13.7 years. At the end of the chemotherapy protocol, patients completed tests of sustained attention, and parents rated survivors’ behavior on standard scales.
She found that for these childhood cancer survivors, sustained attention and behavior functioning at the end of chemotherapy predicted long-term attention and processing speed outcomes. Only exposure to chemotherapy, and not end-of-therapy function, predicted that survivors would have poor executive function of fluency and flexibility at long-term follow up.
Dr. Nathan praised the investigators for their foresight to collect data on the methotrexate area under the curve, number of triple intrathecal therapies (cytarabine, methotrexate, and hydrocortisone), and neurocognitive functioning at the end of chemotherapy. “What’s clear is that chemotherapy alone can lead to neurocognitive late effects,” he said. “But what’s also important is that not all late effects can be predicted by end of therapy assessments.” These late effects appear to evolve over time, so ongoing assessments are needed.
Dr. Turcotte, Dr. Liu, Dr. Levine, and Dr. Nathan each reported no financial disclosures.
Chicago – Survivors of childhood cancers face several later risks from treatment, and investigators presented studies evaluating risks in three specific areas – secondary neoplasms, premature menopause, and neurocognitive function – at the annual meeting of the American Society of Clinical Oncology.
Discussant Paul Nathan, M.D., of The Hospital for Sick Children in Toronto, said “the whole purpose” of research in this area “is to start to understand the predictors and modifiers of late effects” and then to design risk assessment tools and interventions to reduce long-term toxicity. These interventions include modification of chemotherapy and radiation doses, protective strategies, and disease risk stratification to adjust intensity of therapies.
Other strategies are to use behavioral interventions directed at improving compliance with follow-up to detect problems earlier and the use of real-time monitoring, such as with smart phones or fitness trackers. He said one limitation of this sort of research and implementing interventions to reduce late toxicities is that “you need time to document long-term outcomes.” So tracking newer therapies, such as proton beam radiation, small molecule drugs, and immunotherapy, is “going to take time, perhaps decades, before you understand their impact on patients.”
Risk of secondary neoplasms reduced
Risk-stratifying of disease “has allowed us to make attempts to minimize late effects by modifying therapy over time in certain subgroups of lower-risk patients,” said Dr. Lucie Turcotte of the University of Minnesota in Minneapolis.
To study the effects of these changes, she determined the risk of certain subsequent malignant or benign neoplasms over three periods of therapeutic exposure among 23,603 5-year survivors of childhood cancers diagnosed at less than 21 years of age from 1970 to 1999, drawing from the cohort of the Childhood Cancer Survivor Study (CCSS). The CCSS represents about 20% of childhood cancer survivors in the United States for the study period.
Over the decades of 1970-1979, 1980-1989, and 1990-1999, the use of any radiation went from 77% to 58% to 41%, respectively. Cranial radiation for acute lymphoblastic leukemia (ALL) decreased from 85% to 19%, abdominal radiation for Wilms tumor from 78% to 43%, and chest radiotherapy for Hodgkin lymphoma from 87% to 61%. The proportion of children receiving alkylating agents, anthracyclines, and epipodophyllotoxins went up, but the cumulative doses went down (N Engl J Med. 2016 Mar 3;374(9):833-42).
Dr. Nathan said today, almost no child gets cranial radiation for ALL. “So we’ve slowly learned that our treatments are toxic, and we’ve certainly done what we can to change them.”
But have these changes made a difference? Dr. Turcotte found that survivors remain at increased risk of a secondary neoplasm, but the risk was lower for children treated in later time periods.
Dr. Nathan pointed to Dr. Turcotte’s data showing that the incidence of subsequent malignant neoplasms decreased from 1970 to 1999 by 7% for each 5-year era (15-year risk: 2.3% to 1.6%; P = .001; number needed to treat, NNT = 143). Similarly, non-melanoma skin cancer 15-year risk decreased from 0.7% to 0.1% (P less than .001; NNT = 167). The NNT’s are “certainly important, but these are not major differences over time,” Dr. Nathan said. Knowing the impact of newer, targeted therapeutic approaches will take some time.
Predicting risk of premature menopause
Also using the CCSS data, Dr. Jennifer Levine of Columbia University Medical Center, New York, N.Y., studied the prevalence of and risk factors for nonsurgical premature menopause (NSPM), defined as cessation of menses prior to age 40 years, as well as the effect on reproductive outcomes for survivors of childhood cancers.
Dr. Nathan said when a child is first diagnosed with cancer, seldom does the issue of fertility come up early in the discussion, “but when you treat young adults who are survivors, the number one thing they talk about often is fertility. And so doing a better job in predicting who is at risk for infertility is clearly a priority for survivorship research.”
He said the development of the cyclophosphamide equivalent dose (CED) by D.M Green et al. (Pediatr Blood Cancer. 2014 Jan;61(1):53-67) has been very helpful for quantifying alkylating agent exposure to make comparisons between studies. The goal is to develop a risk assessment tool to be able to tell patients and families their fertility risk based on demographics, therapy, and biomarkers.
Being able to evaluate risk is critically important because for girls, oocyte or ovarian harvesting or even transvaginal ultrasound is highly invasive, and these procedures should be recommended only if their risk for infertility is very high.
Dr. Levine studied 2,930 female cancer survivors diagnosed at a median age of 6 years between 1979 and 1986 and a median age at follow-up of 34 years, who were compared with 1,399 healthy siblings. Of the survivor cohort, 110 developed NSPM at a median age of 32 years, and the prevalence of NSPM at age 40 years for the entire cohort was 9.1%, giving a relative risk of NSPM of 10.5 compared with siblings, who had a 0.9% NSPM prevalence at age 40.
She found that exposure to alkylating agents and older age at diagnosis put childhood cancer survivors at increased risk of NSPM, which was associated with lower rates of pregnancy and live births after age 31 years. The greatest risk of NSPM occurred if the cyclophosphamide equivalent dose was greater than 6000 mg/m2 (odds ratio = 3.6 compared with no CED); if there had been any radiation to the ovaries (less than 5 Gy: OR = 4.0; 5 Gy or more: OR = 20.4); or if the age at diagnosis was greater than 14 years (OR = 2.3).
Women with NSPM, compared with survivors without NSPM, were less likely ever to be pregnant (OR = 0.41) or to have a live birth after age 30 (OR = 0.35). However, these outcomes were no different between the ages of 21 and 30. Dr. Levine said this information can assist clinicians in counseling their patients about the risk for early menopause and planning for alternative reproductive means, such as oocyte or embryo harvesting and preservation.
Neurocognitive functioning after treatment
Dr. Wei Liu of St. Jude Children’s Research Hospital, Memphis, Tenn., studied the neurocognitive function of long-term survivors of ALL.
Dr. Nathan called ALL “the paradigm for how we’ve sort of learned and adjusted how we treat patients based on late effects.” Early on, the disease was treated with craniospinal radiation and intrathecal chemotherapy, and while patients survived, it became obvious that they suffered neurocognitive and endocrine problems, growth abnormalities, and secondary malignancies. These findings forced a reevaluatuon of treatments, leading to elimination of spinal radiation, reduction of cranial radiation dose, intensification of systemic therapy, including methotrexate, and risk stratification allowing modification of therapies.
Survival was sustained, but long-term outcomes were still based on children treated with radiation. So long-term cognitive consequences in the more modern era of therapy were unknown. Only recently have adult cohorts become available who were treated in the chemotherapy-only era.
Dr. Liu studied 159 ALL survivors who had been treated with chemotherapy alone at a mean age of 9.2 years. The follow-up was at a median of 7.6 years off therapy at a mean age of 13.7 years. At the end of the chemotherapy protocol, patients completed tests of sustained attention, and parents rated survivors’ behavior on standard scales.
She found that for these childhood cancer survivors, sustained attention and behavior functioning at the end of chemotherapy predicted long-term attention and processing speed outcomes. Only exposure to chemotherapy, and not end-of-therapy function, predicted that survivors would have poor executive function of fluency and flexibility at long-term follow up.
Dr. Nathan praised the investigators for their foresight to collect data on the methotrexate area under the curve, number of triple intrathecal therapies (cytarabine, methotrexate, and hydrocortisone), and neurocognitive functioning at the end of chemotherapy. “What’s clear is that chemotherapy alone can lead to neurocognitive late effects,” he said. “But what’s also important is that not all late effects can be predicted by end of therapy assessments.” These late effects appear to evolve over time, so ongoing assessments are needed.
Dr. Turcotte, Dr. Liu, Dr. Levine, and Dr. Nathan each reported no financial disclosures.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF CLINICAL ONCOLOGY
Key clinical point: Despite improvements, survivors of childhood cancers still face long-term risks in terms of secondary neoplasms, nonsurgical premature menopause (NSPM), and neurocognitive function.
Major finding: Of the survivor cohort, 110 developed NSPM at a median age of 32 years, so the prevalence of NSPM at age 40 years for the entire cohort was 9.1%, while siblings had a 0.9% NSPM prevalence at age 40.
Data source: Retrospective study of 2,930 childhood cancer survivors diagnosed at age 6 years and follow-up at median age 34 years and 1,390 healthy siblings. Also cross-sectional prospective study for neurocognitive assessment of 159 ALL survivors, and risks of secondary neoplasms in 23,603 5-year survivors of childhood cancers .
Disclosures: Dr. Turcotte, Dr. Liu, Dr. Levine, and Dr. Nathan each reported no financial disclosures.
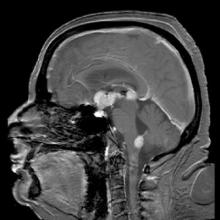
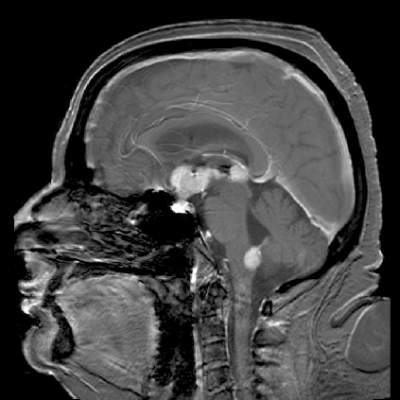
Temozolomide + RT boosts survival in elderly with glioblastoma
CHICAGO – Adding concomitant and adjuvant temozolomide to a shorter course of radiotherapy (RT) for elderly patients with glioblastoma improves progression-free survival, according to a phase III study presented at the annual meeting of the American Society of Clinical Oncology.
Both patients with and without MGMT methylated promoters in their tumors benefited, with the greatest benefit accruing to patients with promoter methylation, reported Dr. James Perry, head of the division of neurology at Sunnybrook Health Sciences Centre, Toronto.
The age of peak incidence of glioblastoma is 64 years, and the incidence is increasing. Best practice has been surgical resection and 6 weeks of radiation combined with oral temozolomide. A pivotal trial just over 10 years ago was restricted to patients younger than age 70 years and included few patients older than 65 years. It showed decreasing benefit of temozolomide with increasing age. Furthermore, trials in the elderly have compared only head-to-head radiation schedules or radiation alone with temozolomide alone. There has been no evidence on which to base practice for combining radiotherapy with temozolomide, Dr. Perry said.
To address this deficiency, Dr. Perry and his colleagues randomly assigned patients 65 years or older with newly diagnosed glioblastoma either to a short course of RT, consisting of 40 Gy in 15 fractions over 3 weeks or to the same radiotherapy plus 3 weeks of concomitant temozolomide and then adjuvant temozolomide for 12 months or until progression.
Patients (n = 562; 281 in each arm) averaged 73 years (range, 65-90 years), 77% had Eastern Cooperative Oncology Group performance score (PS) 0/1 and the rest PS 2, and 58% had had tumor resection.
Median overall survival was 9.3 months with the combined therapy and 7.6 months with radiation alone. Median progression-free survival was 5.3 vs. 3.9 months, respectively, with a hazard ratio of 0.50 (P less than .0001).
MGMT promoter methylation is a predictive marker for benefit from chemotherapy and a prognostic factor for survival. Forty-six percent of the tumors had this promoter methylation.
Temozolomide use added relatively more benefit if promoters were methylated. Patients with methylated promoters had an overall survival of 7.7 months with radiation alone and 13.5 months with combined radiation and temozolomide (HR, 0.53; P = .0001). For unmethylated promoters, overall survival with radiation alone was 7.9 months and was 10.0 months when temozolomide was added (HR, 0.75; P = .055), suggesting some benefit from temozolomide, although not as great as with tumors with methylated promoters.
“The advantage of this combined treatment with chemoradiation was achieved with minimal side effects,” Dr. Perry reported. Mild nausea and vomiting occurred mostly in the first weeks of therapy, and a slight increase in grade 3/4 hematologic toxicity was seen but occurred in less than 5% of patients. No differences in quality of life were reported between the treatment arms.
Most patients could easily complete the treatment plan, with 97% adherence to the 3 weeks of chemoradiation. “This is quite important because the elderly often have difficulties with mobility, distance from treatment centers, and sometimes don’t have caregivers [who] are able to bring them back and forth for treatment,” Dr. Perry said. He suggested that the shorter course of radiotherapy may have been one factor in the high adherence rate.
Based on these results of higher efficacy using concomitant and adjuvant temozolomide with manageable toxicities and no sacrifice in quality of life, “oncologists now have evidence to consider radiation with chemotherapy in all newly diagnosed elderly patients with glioblastoma,” he said.
Dr. Julie Vose, president of the American Society of Clinical Oncology, said the study was important because it compared the treatments in the appropriate patient population, that is, in the elderly who have the highest incidence of glioblastoma.
CHICAGO – Adding concomitant and adjuvant temozolomide to a shorter course of radiotherapy (RT) for elderly patients with glioblastoma improves progression-free survival, according to a phase III study presented at the annual meeting of the American Society of Clinical Oncology.
Both patients with and without MGMT methylated promoters in their tumors benefited, with the greatest benefit accruing to patients with promoter methylation, reported Dr. James Perry, head of the division of neurology at Sunnybrook Health Sciences Centre, Toronto.
The age of peak incidence of glioblastoma is 64 years, and the incidence is increasing. Best practice has been surgical resection and 6 weeks of radiation combined with oral temozolomide. A pivotal trial just over 10 years ago was restricted to patients younger than age 70 years and included few patients older than 65 years. It showed decreasing benefit of temozolomide with increasing age. Furthermore, trials in the elderly have compared only head-to-head radiation schedules or radiation alone with temozolomide alone. There has been no evidence on which to base practice for combining radiotherapy with temozolomide, Dr. Perry said.
To address this deficiency, Dr. Perry and his colleagues randomly assigned patients 65 years or older with newly diagnosed glioblastoma either to a short course of RT, consisting of 40 Gy in 15 fractions over 3 weeks or to the same radiotherapy plus 3 weeks of concomitant temozolomide and then adjuvant temozolomide for 12 months or until progression.
Patients (n = 562; 281 in each arm) averaged 73 years (range, 65-90 years), 77% had Eastern Cooperative Oncology Group performance score (PS) 0/1 and the rest PS 2, and 58% had had tumor resection.
Median overall survival was 9.3 months with the combined therapy and 7.6 months with radiation alone. Median progression-free survival was 5.3 vs. 3.9 months, respectively, with a hazard ratio of 0.50 (P less than .0001).
MGMT promoter methylation is a predictive marker for benefit from chemotherapy and a prognostic factor for survival. Forty-six percent of the tumors had this promoter methylation.
Temozolomide use added relatively more benefit if promoters were methylated. Patients with methylated promoters had an overall survival of 7.7 months with radiation alone and 13.5 months with combined radiation and temozolomide (HR, 0.53; P = .0001). For unmethylated promoters, overall survival with radiation alone was 7.9 months and was 10.0 months when temozolomide was added (HR, 0.75; P = .055), suggesting some benefit from temozolomide, although not as great as with tumors with methylated promoters.
“The advantage of this combined treatment with chemoradiation was achieved with minimal side effects,” Dr. Perry reported. Mild nausea and vomiting occurred mostly in the first weeks of therapy, and a slight increase in grade 3/4 hematologic toxicity was seen but occurred in less than 5% of patients. No differences in quality of life were reported between the treatment arms.
Most patients could easily complete the treatment plan, with 97% adherence to the 3 weeks of chemoradiation. “This is quite important because the elderly often have difficulties with mobility, distance from treatment centers, and sometimes don’t have caregivers [who] are able to bring them back and forth for treatment,” Dr. Perry said. He suggested that the shorter course of radiotherapy may have been one factor in the high adherence rate.
Based on these results of higher efficacy using concomitant and adjuvant temozolomide with manageable toxicities and no sacrifice in quality of life, “oncologists now have evidence to consider radiation with chemotherapy in all newly diagnosed elderly patients with glioblastoma,” he said.
Dr. Julie Vose, president of the American Society of Clinical Oncology, said the study was important because it compared the treatments in the appropriate patient population, that is, in the elderly who have the highest incidence of glioblastoma.
CHICAGO – Adding concomitant and adjuvant temozolomide to a shorter course of radiotherapy (RT) for elderly patients with glioblastoma improves progression-free survival, according to a phase III study presented at the annual meeting of the American Society of Clinical Oncology.
Both patients with and without MGMT methylated promoters in their tumors benefited, with the greatest benefit accruing to patients with promoter methylation, reported Dr. James Perry, head of the division of neurology at Sunnybrook Health Sciences Centre, Toronto.
The age of peak incidence of glioblastoma is 64 years, and the incidence is increasing. Best practice has been surgical resection and 6 weeks of radiation combined with oral temozolomide. A pivotal trial just over 10 years ago was restricted to patients younger than age 70 years and included few patients older than 65 years. It showed decreasing benefit of temozolomide with increasing age. Furthermore, trials in the elderly have compared only head-to-head radiation schedules or radiation alone with temozolomide alone. There has been no evidence on which to base practice for combining radiotherapy with temozolomide, Dr. Perry said.
To address this deficiency, Dr. Perry and his colleagues randomly assigned patients 65 years or older with newly diagnosed glioblastoma either to a short course of RT, consisting of 40 Gy in 15 fractions over 3 weeks or to the same radiotherapy plus 3 weeks of concomitant temozolomide and then adjuvant temozolomide for 12 months or until progression.
Patients (n = 562; 281 in each arm) averaged 73 years (range, 65-90 years), 77% had Eastern Cooperative Oncology Group performance score (PS) 0/1 and the rest PS 2, and 58% had had tumor resection.
Median overall survival was 9.3 months with the combined therapy and 7.6 months with radiation alone. Median progression-free survival was 5.3 vs. 3.9 months, respectively, with a hazard ratio of 0.50 (P less than .0001).
MGMT promoter methylation is a predictive marker for benefit from chemotherapy and a prognostic factor for survival. Forty-six percent of the tumors had this promoter methylation.
Temozolomide use added relatively more benefit if promoters were methylated. Patients with methylated promoters had an overall survival of 7.7 months with radiation alone and 13.5 months with combined radiation and temozolomide (HR, 0.53; P = .0001). For unmethylated promoters, overall survival with radiation alone was 7.9 months and was 10.0 months when temozolomide was added (HR, 0.75; P = .055), suggesting some benefit from temozolomide, although not as great as with tumors with methylated promoters.
“The advantage of this combined treatment with chemoradiation was achieved with minimal side effects,” Dr. Perry reported. Mild nausea and vomiting occurred mostly in the first weeks of therapy, and a slight increase in grade 3/4 hematologic toxicity was seen but occurred in less than 5% of patients. No differences in quality of life were reported between the treatment arms.
Most patients could easily complete the treatment plan, with 97% adherence to the 3 weeks of chemoradiation. “This is quite important because the elderly often have difficulties with mobility, distance from treatment centers, and sometimes don’t have caregivers [who] are able to bring them back and forth for treatment,” Dr. Perry said. He suggested that the shorter course of radiotherapy may have been one factor in the high adherence rate.
Based on these results of higher efficacy using concomitant and adjuvant temozolomide with manageable toxicities and no sacrifice in quality of life, “oncologists now have evidence to consider radiation with chemotherapy in all newly diagnosed elderly patients with glioblastoma,” he said.
Dr. Julie Vose, president of the American Society of Clinical Oncology, said the study was important because it compared the treatments in the appropriate patient population, that is, in the elderly who have the highest incidence of glioblastoma.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Combining temozolomide with radiotherapy prolongs survival for elderly with glioblastoma.
Major finding: Combining temozolomide with radiotherapy increased survival by 33% vs. radiation alone.
Data source: Global phase III study of 562 elderly patients with newly diagnosed glioblastoma randomized to temozolomide plus radiation vs radiation alone.
Disclosures: Dr. Perry reported stock or other ownership interests in DelMar Pharmaceuticals and VBL Therapeutics. Dr. Vose reported receiving honoraria from Sanofi-Aventis and Seattle Genetics; consulting for Bio Connections; and receiving research funding to her institution from Acerta, Bristol-Myers Squibb, Celgene, Genentech, GlaxoSmithKline, Incyte, Janssen Biotech, Kite Pharma, Pharmacyclics, and Spectrum Pharmaceuticals.
Tandem beats single ASCT for childhood neuroblastoma
CHICAGO – More children treated for high-risk neuroblastoma who received a second autologous stem cell transplant in consolidation after induction chemotherapy were alive after 3 years compared with children getting a single transplant, Dr. Julie R. Park reported at the annual meeting of the American Society of Clinical Oncology.
Neuroblastoma (NB) is the most common extracranial tumor of childhood and arises in the sympathetic nervous system of very young children. Fewer than 50% of children with high-risk NB survive 5 years following today’s multiagent, aggressive therapy. Single autologous hematopoietic stem cell transplant (ASCT) has improved outcomes, and in pilot studies, tandem ASCT appeared tolerable with better efficacy as consolidation therapy for high-risk NB.
The present trial enrolled 665 patients (mean age 3.1 years), who received an induction regimen of six cycles of chemotherapy, with harvest of peripheral blood stem cells after the first two cycles and surgery after five cycles. Patients with adequate stem cell collection, adequate organ function, and no evidence of disease progression were randomized to either standard therapy with a single ASCT with carboplatin, etoposide, melphalan and local radiotherapy (n = 179); or to a double (tandem) ASCT with cyclophosphamide and thiotepa prior to the first ASCT followed 6 weeks later by a dose-modified regimen of carboplatin, etoposide, melphalan and radiotherapy prior to a second ASCT (n = 176). The two transplants were separated by 6-8 weeks.
About 70% of patients in each arm received dinutuximab plus cytokine immunotherapy after their transplants. Dinutuximab is an antibody directed against GD2, an antigen present on neuroblastoma cells. About 38% of patients had high-risk tumors based on the presence of MYCN gene amplification.
The children who were randomized to receive a tandem transplant had a statistically significant, improved event-free survival, with a 3-year event-free survival of 61%, compared to those children receiving a single transplant, with a 3-year event-free survival of 48% (P = .0081), reported Dr. Park, professor of pediatrics at the University of Washington, Seattle.
Three-year overall survival did not differ between the two groups, at 74% for the tandem transplant group and 69% for the single transplant group (P = .185). The study was powered to see a difference in event-free survival, and the study was probably not long enough to detect a difference in overall survival, Dr. Park said.
Anti-GD2 immunotherapy improved both event-free and overall survival for both the tandem and single ASCT groups. At 3 years from the time of the patients’ receiving immunotherapy, event-free survival was 73.7% and 56%, respectively (P = .0033), and overall survival was 83.7% and 74.4% (P = .0322), respectively.
The benefit of tandem transplant occurred without an increase in toxicity or regimen-related mortality. The rates of severe toxicities were similar in the two arms. Two patients receiving a tandem ASCT died, compared with eight receiving a single ASCT.
“This finding will change the way we treat children with high-risk neuroblastoma in North America, which still claims many young lives and is in urgent need of better treatments,” Dr. Park said in a press release.
Dr. Park noted that most NB recurrences happen within 2-3 years from diagnosis and that patients who have not had a recurrence by 3 years have a better chance of long-term survival. Patients in this study will continue to be followed for 10 years.
Dr. Park disclosed ties with Roche. Dr. Hunger reported ties with Merck, Sigma Tau, Jazz Pharmaceuticals, and Spectrum Pharmaceuticals.
CHICAGO – More children treated for high-risk neuroblastoma who received a second autologous stem cell transplant in consolidation after induction chemotherapy were alive after 3 years compared with children getting a single transplant, Dr. Julie R. Park reported at the annual meeting of the American Society of Clinical Oncology.
Neuroblastoma (NB) is the most common extracranial tumor of childhood and arises in the sympathetic nervous system of very young children. Fewer than 50% of children with high-risk NB survive 5 years following today’s multiagent, aggressive therapy. Single autologous hematopoietic stem cell transplant (ASCT) has improved outcomes, and in pilot studies, tandem ASCT appeared tolerable with better efficacy as consolidation therapy for high-risk NB.
The present trial enrolled 665 patients (mean age 3.1 years), who received an induction regimen of six cycles of chemotherapy, with harvest of peripheral blood stem cells after the first two cycles and surgery after five cycles. Patients with adequate stem cell collection, adequate organ function, and no evidence of disease progression were randomized to either standard therapy with a single ASCT with carboplatin, etoposide, melphalan and local radiotherapy (n = 179); or to a double (tandem) ASCT with cyclophosphamide and thiotepa prior to the first ASCT followed 6 weeks later by a dose-modified regimen of carboplatin, etoposide, melphalan and radiotherapy prior to a second ASCT (n = 176). The two transplants were separated by 6-8 weeks.
About 70% of patients in each arm received dinutuximab plus cytokine immunotherapy after their transplants. Dinutuximab is an antibody directed against GD2, an antigen present on neuroblastoma cells. About 38% of patients had high-risk tumors based on the presence of MYCN gene amplification.
The children who were randomized to receive a tandem transplant had a statistically significant, improved event-free survival, with a 3-year event-free survival of 61%, compared to those children receiving a single transplant, with a 3-year event-free survival of 48% (P = .0081), reported Dr. Park, professor of pediatrics at the University of Washington, Seattle.
Three-year overall survival did not differ between the two groups, at 74% for the tandem transplant group and 69% for the single transplant group (P = .185). The study was powered to see a difference in event-free survival, and the study was probably not long enough to detect a difference in overall survival, Dr. Park said.
Anti-GD2 immunotherapy improved both event-free and overall survival for both the tandem and single ASCT groups. At 3 years from the time of the patients’ receiving immunotherapy, event-free survival was 73.7% and 56%, respectively (P = .0033), and overall survival was 83.7% and 74.4% (P = .0322), respectively.
The benefit of tandem transplant occurred without an increase in toxicity or regimen-related mortality. The rates of severe toxicities were similar in the two arms. Two patients receiving a tandem ASCT died, compared with eight receiving a single ASCT.
“This finding will change the way we treat children with high-risk neuroblastoma in North America, which still claims many young lives and is in urgent need of better treatments,” Dr. Park said in a press release.
Dr. Park noted that most NB recurrences happen within 2-3 years from diagnosis and that patients who have not had a recurrence by 3 years have a better chance of long-term survival. Patients in this study will continue to be followed for 10 years.
Dr. Park disclosed ties with Roche. Dr. Hunger reported ties with Merck, Sigma Tau, Jazz Pharmaceuticals, and Spectrum Pharmaceuticals.
CHICAGO – More children treated for high-risk neuroblastoma who received a second autologous stem cell transplant in consolidation after induction chemotherapy were alive after 3 years compared with children getting a single transplant, Dr. Julie R. Park reported at the annual meeting of the American Society of Clinical Oncology.
Neuroblastoma (NB) is the most common extracranial tumor of childhood and arises in the sympathetic nervous system of very young children. Fewer than 50% of children with high-risk NB survive 5 years following today’s multiagent, aggressive therapy. Single autologous hematopoietic stem cell transplant (ASCT) has improved outcomes, and in pilot studies, tandem ASCT appeared tolerable with better efficacy as consolidation therapy for high-risk NB.
The present trial enrolled 665 patients (mean age 3.1 years), who received an induction regimen of six cycles of chemotherapy, with harvest of peripheral blood stem cells after the first two cycles and surgery after five cycles. Patients with adequate stem cell collection, adequate organ function, and no evidence of disease progression were randomized to either standard therapy with a single ASCT with carboplatin, etoposide, melphalan and local radiotherapy (n = 179); or to a double (tandem) ASCT with cyclophosphamide and thiotepa prior to the first ASCT followed 6 weeks later by a dose-modified regimen of carboplatin, etoposide, melphalan and radiotherapy prior to a second ASCT (n = 176). The two transplants were separated by 6-8 weeks.
About 70% of patients in each arm received dinutuximab plus cytokine immunotherapy after their transplants. Dinutuximab is an antibody directed against GD2, an antigen present on neuroblastoma cells. About 38% of patients had high-risk tumors based on the presence of MYCN gene amplification.
The children who were randomized to receive a tandem transplant had a statistically significant, improved event-free survival, with a 3-year event-free survival of 61%, compared to those children receiving a single transplant, with a 3-year event-free survival of 48% (P = .0081), reported Dr. Park, professor of pediatrics at the University of Washington, Seattle.
Three-year overall survival did not differ between the two groups, at 74% for the tandem transplant group and 69% for the single transplant group (P = .185). The study was powered to see a difference in event-free survival, and the study was probably not long enough to detect a difference in overall survival, Dr. Park said.
Anti-GD2 immunotherapy improved both event-free and overall survival for both the tandem and single ASCT groups. At 3 years from the time of the patients’ receiving immunotherapy, event-free survival was 73.7% and 56%, respectively (P = .0033), and overall survival was 83.7% and 74.4% (P = .0322), respectively.
The benefit of tandem transplant occurred without an increase in toxicity or regimen-related mortality. The rates of severe toxicities were similar in the two arms. Two patients receiving a tandem ASCT died, compared with eight receiving a single ASCT.
“This finding will change the way we treat children with high-risk neuroblastoma in North America, which still claims many young lives and is in urgent need of better treatments,” Dr. Park said in a press release.
Dr. Park noted that most NB recurrences happen within 2-3 years from diagnosis and that patients who have not had a recurrence by 3 years have a better chance of long-term survival. Patients in this study will continue to be followed for 10 years.
Dr. Park disclosed ties with Roche. Dr. Hunger reported ties with Merck, Sigma Tau, Jazz Pharmaceuticals, and Spectrum Pharmaceuticals.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Neuroblastoma event-free survival was better with tandem than with single ASCT.
Major finding: Event-free survival was 61% with tandem vs. 48% with single ASCT.
Data source: Randomized phase III trial of 355 patients assigned equally to single vs. tandem autologous stem cell transplant.
Disclosures: Dr. Park disclosed ties with Roche. Dr. Hunger reported ties with Merck, Sigma Tau, Jazz Pharmaceuticals, and Spectrum Pharmaceuticals.
IL-2 adds only toxicity to neuroblastoma antibody tx
CHICAGO – Adding the cytokine IL-2 to front-line therapy with the anti-GD2 antibody ch14.18/CHO provided no additional survival benefit and only added to toxicity in the treatment of pediatric patients with high-risk neuroblastoma (NB), Dr. Ruth Ladenstein reported at the annual meeting of the American Society of Clinical Oncology.
A form of the antibody (dinutuximab) is approved for use in combination with granulocyte-macrophage colony stimulating factor, IL-2, and 13-cis-retinoic acid (RA) to treat high risk NB. A previous study (N Engl J Med. 2010;363:1324-34) showed that a combination of ch14.18 and the cytokines improved event free survival to 66% at 2 years, but the role of cytokines in this context remained unclear. Dr. Ladenstein and associates therefore performed a phase III trial that randomized patients to the antibody with or without subcutaneous (sc) IL-2.
High-risk NB was defined as patients with International Neuroblastoma Staging System stage 4 disease 1 year old or older, stage 4 less than 1 year old with MYCN amplification, or stage 2,3 patients up to age 21 years with MYCN amplification. Patients underwent a rapid induction therapy, followed by peripheral stem cell harvest, local control with complete tumor resection, myeloablative therapy with peripheral stem cell transplant, local control with radiotherapy, and then ch14.18 anti-GD2 monoclonal immunotherapy with RA, with or without sc IL-2.
Inclusion criteria were a complete response or partial response with three or fewer skeletal metastatic spots and no positive bone marrow biopsies on two aspirates. Randomization occurred between day 60 and 90 post stem cell infusion. RA was given on days 1-14 post randomization. For the arm receiving IL-2, it was given as 5 daily injections of 6 x 106 IU/m2 per day over 8 hours on days 15-19. IL-2 was repeated on days 22-26. Both groups also received the ch14.18 antibody on days 22-26. All patients received high-dose morphine for pain management.
For event free survival (EFS), the primary endpoint of the trial, “if we look at 3 years, we see with antibody alone it’s 57%. With IL-2, it’s 60%. It’s completely clear that there’s no superiority for the IL-2 arm,” said Dr. Ladenstein, professor of pediatrics at the Children’s Cancer Research Institute, Austria.
At 5 years, the EFS was no different for the two treatment arms, at 51% for antibody alone and 56% for antibody plus IL-2 (P = .561). There were 199/200 patients in the antibody-alone arm with follow-up after randomization and 203/206 in the antibody plus IL-2 arm. The same was true for the secondary endpoint of overall survival, with 66% survival with antibody-alone and 58% in the antibody plus IL-2 at 5 years.
The EFS for patients with a complete response prior to immunotherapy was 66% at 3 years and was 50% for patients with less than a complete response, a significant difference (P = .003) in favor of those with a complete response. IL-2 administration had no effect on the EFS of the patients with a complete response if it was given with the immunotherapy. Similarly, IL-2 made no difference for patients who had had a very good partial response or a partial response prior to immunotherapy. For complete, very good partial, or partial responses prior to immunotherapy, the overall response to immunotherapy was 51%.
“However, feasibility is a concern, particularly in the IL-2 arm. Only 61% of the cycles were completed whereas it was 85% in the antibody-only arm, and the interruptions are definitely related mainly to the IL-2 component,” Dr. Ladenstein said.
Toxicity was higher for those patients receiving IL-2 compared to those getting antibody alone: Lansky performance status of 30% or less was 41% vs. 17%, early termination of therapy was 39% vs. 15%, and Common Terminology Criteria grade 3/4 fever was 41% vs. 14%, respectively (all P less than .001). There were also significantly more grade 3/4 allergic reactions and incidences of capillary leak, as well as diarrhea, hypotension, central nervous toxicity, and pain with IL-2.
The outcomes were favorable with antibody immunotherapy alone, but the higher toxicity with IL-2 shows that “a less toxic treatment schedule therefore is needed for this late treatment phase,” Dr. Ladenstein said.
Commenting on the trial, Dr. Barbara Hero of University Children’s Hospital in Cologne, Germany, asked whether cytokines are a useful part of the regimen “because we know the cytokines add quite a lot of toxicity to the regimens.” Even if they are potentially useful, researchers still do not know which cytokines, route of administration, and at what doses and timing would be best. Also, it is not known if a different induction regimen or antibody treatment could make a difference in using cytokines.
Another question is whether cytokines may be of benefit in patients with a higher tumor burden, e.g., more than three skeletal spots, used as the eligibility cut-off in this trial, Dr. Hero said.
CHICAGO – Adding the cytokine IL-2 to front-line therapy with the anti-GD2 antibody ch14.18/CHO provided no additional survival benefit and only added to toxicity in the treatment of pediatric patients with high-risk neuroblastoma (NB), Dr. Ruth Ladenstein reported at the annual meeting of the American Society of Clinical Oncology.
A form of the antibody (dinutuximab) is approved for use in combination with granulocyte-macrophage colony stimulating factor, IL-2, and 13-cis-retinoic acid (RA) to treat high risk NB. A previous study (N Engl J Med. 2010;363:1324-34) showed that a combination of ch14.18 and the cytokines improved event free survival to 66% at 2 years, but the role of cytokines in this context remained unclear. Dr. Ladenstein and associates therefore performed a phase III trial that randomized patients to the antibody with or without subcutaneous (sc) IL-2.
High-risk NB was defined as patients with International Neuroblastoma Staging System stage 4 disease 1 year old or older, stage 4 less than 1 year old with MYCN amplification, or stage 2,3 patients up to age 21 years with MYCN amplification. Patients underwent a rapid induction therapy, followed by peripheral stem cell harvest, local control with complete tumor resection, myeloablative therapy with peripheral stem cell transplant, local control with radiotherapy, and then ch14.18 anti-GD2 monoclonal immunotherapy with RA, with or without sc IL-2.
Inclusion criteria were a complete response or partial response with three or fewer skeletal metastatic spots and no positive bone marrow biopsies on two aspirates. Randomization occurred between day 60 and 90 post stem cell infusion. RA was given on days 1-14 post randomization. For the arm receiving IL-2, it was given as 5 daily injections of 6 x 106 IU/m2 per day over 8 hours on days 15-19. IL-2 was repeated on days 22-26. Both groups also received the ch14.18 antibody on days 22-26. All patients received high-dose morphine for pain management.
For event free survival (EFS), the primary endpoint of the trial, “if we look at 3 years, we see with antibody alone it’s 57%. With IL-2, it’s 60%. It’s completely clear that there’s no superiority for the IL-2 arm,” said Dr. Ladenstein, professor of pediatrics at the Children’s Cancer Research Institute, Austria.
At 5 years, the EFS was no different for the two treatment arms, at 51% for antibody alone and 56% for antibody plus IL-2 (P = .561). There were 199/200 patients in the antibody-alone arm with follow-up after randomization and 203/206 in the antibody plus IL-2 arm. The same was true for the secondary endpoint of overall survival, with 66% survival with antibody-alone and 58% in the antibody plus IL-2 at 5 years.
The EFS for patients with a complete response prior to immunotherapy was 66% at 3 years and was 50% for patients with less than a complete response, a significant difference (P = .003) in favor of those with a complete response. IL-2 administration had no effect on the EFS of the patients with a complete response if it was given with the immunotherapy. Similarly, IL-2 made no difference for patients who had had a very good partial response or a partial response prior to immunotherapy. For complete, very good partial, or partial responses prior to immunotherapy, the overall response to immunotherapy was 51%.
“However, feasibility is a concern, particularly in the IL-2 arm. Only 61% of the cycles were completed whereas it was 85% in the antibody-only arm, and the interruptions are definitely related mainly to the IL-2 component,” Dr. Ladenstein said.
Toxicity was higher for those patients receiving IL-2 compared to those getting antibody alone: Lansky performance status of 30% or less was 41% vs. 17%, early termination of therapy was 39% vs. 15%, and Common Terminology Criteria grade 3/4 fever was 41% vs. 14%, respectively (all P less than .001). There were also significantly more grade 3/4 allergic reactions and incidences of capillary leak, as well as diarrhea, hypotension, central nervous toxicity, and pain with IL-2.
The outcomes were favorable with antibody immunotherapy alone, but the higher toxicity with IL-2 shows that “a less toxic treatment schedule therefore is needed for this late treatment phase,” Dr. Ladenstein said.
Commenting on the trial, Dr. Barbara Hero of University Children’s Hospital in Cologne, Germany, asked whether cytokines are a useful part of the regimen “because we know the cytokines add quite a lot of toxicity to the regimens.” Even if they are potentially useful, researchers still do not know which cytokines, route of administration, and at what doses and timing would be best. Also, it is not known if a different induction regimen or antibody treatment could make a difference in using cytokines.
Another question is whether cytokines may be of benefit in patients with a higher tumor burden, e.g., more than three skeletal spots, used as the eligibility cut-off in this trial, Dr. Hero said.
CHICAGO – Adding the cytokine IL-2 to front-line therapy with the anti-GD2 antibody ch14.18/CHO provided no additional survival benefit and only added to toxicity in the treatment of pediatric patients with high-risk neuroblastoma (NB), Dr. Ruth Ladenstein reported at the annual meeting of the American Society of Clinical Oncology.
A form of the antibody (dinutuximab) is approved for use in combination with granulocyte-macrophage colony stimulating factor, IL-2, and 13-cis-retinoic acid (RA) to treat high risk NB. A previous study (N Engl J Med. 2010;363:1324-34) showed that a combination of ch14.18 and the cytokines improved event free survival to 66% at 2 years, but the role of cytokines in this context remained unclear. Dr. Ladenstein and associates therefore performed a phase III trial that randomized patients to the antibody with or without subcutaneous (sc) IL-2.
High-risk NB was defined as patients with International Neuroblastoma Staging System stage 4 disease 1 year old or older, stage 4 less than 1 year old with MYCN amplification, or stage 2,3 patients up to age 21 years with MYCN amplification. Patients underwent a rapid induction therapy, followed by peripheral stem cell harvest, local control with complete tumor resection, myeloablative therapy with peripheral stem cell transplant, local control with radiotherapy, and then ch14.18 anti-GD2 monoclonal immunotherapy with RA, with or without sc IL-2.
Inclusion criteria were a complete response or partial response with three or fewer skeletal metastatic spots and no positive bone marrow biopsies on two aspirates. Randomization occurred between day 60 and 90 post stem cell infusion. RA was given on days 1-14 post randomization. For the arm receiving IL-2, it was given as 5 daily injections of 6 x 106 IU/m2 per day over 8 hours on days 15-19. IL-2 was repeated on days 22-26. Both groups also received the ch14.18 antibody on days 22-26. All patients received high-dose morphine for pain management.
For event free survival (EFS), the primary endpoint of the trial, “if we look at 3 years, we see with antibody alone it’s 57%. With IL-2, it’s 60%. It’s completely clear that there’s no superiority for the IL-2 arm,” said Dr. Ladenstein, professor of pediatrics at the Children’s Cancer Research Institute, Austria.
At 5 years, the EFS was no different for the two treatment arms, at 51% for antibody alone and 56% for antibody plus IL-2 (P = .561). There were 199/200 patients in the antibody-alone arm with follow-up after randomization and 203/206 in the antibody plus IL-2 arm. The same was true for the secondary endpoint of overall survival, with 66% survival with antibody-alone and 58% in the antibody plus IL-2 at 5 years.
The EFS for patients with a complete response prior to immunotherapy was 66% at 3 years and was 50% for patients with less than a complete response, a significant difference (P = .003) in favor of those with a complete response. IL-2 administration had no effect on the EFS of the patients with a complete response if it was given with the immunotherapy. Similarly, IL-2 made no difference for patients who had had a very good partial response or a partial response prior to immunotherapy. For complete, very good partial, or partial responses prior to immunotherapy, the overall response to immunotherapy was 51%.
“However, feasibility is a concern, particularly in the IL-2 arm. Only 61% of the cycles were completed whereas it was 85% in the antibody-only arm, and the interruptions are definitely related mainly to the IL-2 component,” Dr. Ladenstein said.
Toxicity was higher for those patients receiving IL-2 compared to those getting antibody alone: Lansky performance status of 30% or less was 41% vs. 17%, early termination of therapy was 39% vs. 15%, and Common Terminology Criteria grade 3/4 fever was 41% vs. 14%, respectively (all P less than .001). There were also significantly more grade 3/4 allergic reactions and incidences of capillary leak, as well as diarrhea, hypotension, central nervous toxicity, and pain with IL-2.
The outcomes were favorable with antibody immunotherapy alone, but the higher toxicity with IL-2 shows that “a less toxic treatment schedule therefore is needed for this late treatment phase,” Dr. Ladenstein said.
Commenting on the trial, Dr. Barbara Hero of University Children’s Hospital in Cologne, Germany, asked whether cytokines are a useful part of the regimen “because we know the cytokines add quite a lot of toxicity to the regimens.” Even if they are potentially useful, researchers still do not know which cytokines, route of administration, and at what doses and timing would be best. Also, it is not known if a different induction regimen or antibody treatment could make a difference in using cytokines.
Another question is whether cytokines may be of benefit in patients with a higher tumor burden, e.g., more than three skeletal spots, used as the eligibility cut-off in this trial, Dr. Hero said.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: IL-2 adds no benefit, only toxicity, to neuroblastoma antibody therapy.
Major finding: Only 61% of treatment cycles were completed with IL-2.
Data source: Phase III, randomized, two-arm study of 402 pediatric/adolescent neuroblastoma patients.
Disclosures: Dr. Ladenstein has received honoraria and has had a consulting or advisory role with Apeiron Biologics and Boehringer Ingelheim, and has research funding from, patents with, has provided expert testimony for, and has received travel expenses from Apeiron. Dr. Hero had no disclosures.
Adjuvant temozolomide increases survival in rare anaplastic glioma
CHICAGO – Adjuvant temozolomide given after radiation therapy improves survival of patients with a form of anaplastic glioma, a rare brain tumor. The patients had anaplastic glioma without 1p/19q co-deletion.
This co-deletion – the short arm of chromosome 1 and the long arm of chromosome 19 – is a favorable marker in the tumor, and patients without the deletion have traditionally done worse than those with the deletion. Until this study, no one knew if temozolomide would improve outcomes of patients without the co-deletion.
The four-arm, Phase III Trial on Concurrent and Adjuvant Temozolomide [TMZ] Chemotherapy in NON-1p/19q Deleted Anaplastic Glioma: The CATNON Intergroup Trial (EORTC 26053-22054), still ongoing, is testing radiotherapy, radiotherapy plus concurrent TMZ, radiotherapy plus 12 months of adjuvant TMZ, or radiotherapy plus concurrent TMZ plus 12 months of adjuvant TMZ. Adjuvant TMZ was given in 12 cycles.
Given the rarity of the tumor, the trial involved 118 institutions on three continents and ran for eight years between 2007 and 2015. From 1407 patients 18 years or older with World Health Organization performance status 0-2 screened, 751 were confirmed to have grade III anaplastic gliomas that were intact for 1p/19q (ie, no deletions). After radiation therapy with 59.4 Gy in 33 fractions, these patients were randomly assigned to one of the four treatment arms.
The trial asked two questions: Does adjuvant chemotherapy after radiotherapy improve outcome, and does chemotherapy concurrent with radiotherapy improve outcomes?
Just after enrollment was completed, a data monitoring committee recommended, based on an interim analysis in October 2015, that the data for the adjuvant arm be released, reported Dr. Martin van den Bent, professor of neuro-oncology at Erasmus MC Cancer Center in Rotterdam, The Netherlands. “It completely came as a surprise,” he said at a press conference at the annual meeting of the American Society of Clinical Oncology.
Comparing radiation with or without concurrent TMZ followed by adjuvant TMZ to treatment without adjuvant therapy, the overall survival at five years increased from 44% without any TMZ or with TMZ concurrent with radiation (n = 372) to 56% with adjuvant temozolomide (n = 373). “This corresponds to a hazard ratio of 0.67, a highly statistically significant increment,” Dr. van den Bent said.
Adjuvant TMZ was also associated with a statistically significant increase in median progression free survival from 19 months without adjuvant therapy to almost 43 months with it.
When patients were stratified by O6-methyl-guanine DNA methyltransferase (MGMT) promoter methylation status, the researchers found that MGMT methylation was prognostic for overall survival but not predictive of improved outcome to adjuvant TMZ.
For the nonadjuvant group, the median overall survival was 41 months (95% CI, 37-61 months), but the groups receiving adjuvant TMZ had not yet reached a median overall survival. “We know now that temozolomide given after radiation therapy improves survival in this disease,” Dr. van den Bent said.
A trial of such a rare disease requires many collaborating centers and oncology groups and a long duration to show improvements in outcome. Collaborating oncology groups across many countries “have shown the capacity to answer important clinical questions in orphan diseases,” he said.
Press conference moderator Dr. Don Dizon of Massachusetts General Hospital, Boston, said, “I think this illustrates… the theme of this year’s meeting, which is Collective Wisdom, and even more than that it illustrates that even with a rare tumor type and using standard chemotherapy it’s very important, and we can select patients who are most likely to benefit from treatment and at the same time potentially spare patients from the toxicities of therapy that they’re unlikely to benefit from.”
Results from the arm of the trial testing temozolomide given only at the time of radiation therapy are not yet available and are expected in 2020. In addition, investigators plan to assess genetic abnormalities that are known to affect prognosis in the disease, specifically MGMT promoter methylation and IDH (isocitrate dehydrogenase) mutation.
Common toxicities with temozolomide were mainly low platelet and white cell counts with severe toxicity in 5-10% of patients.
CHICAGO – Adjuvant temozolomide given after radiation therapy improves survival of patients with a form of anaplastic glioma, a rare brain tumor. The patients had anaplastic glioma without 1p/19q co-deletion.
This co-deletion – the short arm of chromosome 1 and the long arm of chromosome 19 – is a favorable marker in the tumor, and patients without the deletion have traditionally done worse than those with the deletion. Until this study, no one knew if temozolomide would improve outcomes of patients without the co-deletion.
The four-arm, Phase III Trial on Concurrent and Adjuvant Temozolomide [TMZ] Chemotherapy in NON-1p/19q Deleted Anaplastic Glioma: The CATNON Intergroup Trial (EORTC 26053-22054), still ongoing, is testing radiotherapy, radiotherapy plus concurrent TMZ, radiotherapy plus 12 months of adjuvant TMZ, or radiotherapy plus concurrent TMZ plus 12 months of adjuvant TMZ. Adjuvant TMZ was given in 12 cycles.
Given the rarity of the tumor, the trial involved 118 institutions on three continents and ran for eight years between 2007 and 2015. From 1407 patients 18 years or older with World Health Organization performance status 0-2 screened, 751 were confirmed to have grade III anaplastic gliomas that were intact for 1p/19q (ie, no deletions). After radiation therapy with 59.4 Gy in 33 fractions, these patients were randomly assigned to one of the four treatment arms.
The trial asked two questions: Does adjuvant chemotherapy after radiotherapy improve outcome, and does chemotherapy concurrent with radiotherapy improve outcomes?
Just after enrollment was completed, a data monitoring committee recommended, based on an interim analysis in October 2015, that the data for the adjuvant arm be released, reported Dr. Martin van den Bent, professor of neuro-oncology at Erasmus MC Cancer Center in Rotterdam, The Netherlands. “It completely came as a surprise,” he said at a press conference at the annual meeting of the American Society of Clinical Oncology.
Comparing radiation with or without concurrent TMZ followed by adjuvant TMZ to treatment without adjuvant therapy, the overall survival at five years increased from 44% without any TMZ or with TMZ concurrent with radiation (n = 372) to 56% with adjuvant temozolomide (n = 373). “This corresponds to a hazard ratio of 0.67, a highly statistically significant increment,” Dr. van den Bent said.
Adjuvant TMZ was also associated with a statistically significant increase in median progression free survival from 19 months without adjuvant therapy to almost 43 months with it.
When patients were stratified by O6-methyl-guanine DNA methyltransferase (MGMT) promoter methylation status, the researchers found that MGMT methylation was prognostic for overall survival but not predictive of improved outcome to adjuvant TMZ.
For the nonadjuvant group, the median overall survival was 41 months (95% CI, 37-61 months), but the groups receiving adjuvant TMZ had not yet reached a median overall survival. “We know now that temozolomide given after radiation therapy improves survival in this disease,” Dr. van den Bent said.
A trial of such a rare disease requires many collaborating centers and oncology groups and a long duration to show improvements in outcome. Collaborating oncology groups across many countries “have shown the capacity to answer important clinical questions in orphan diseases,” he said.
Press conference moderator Dr. Don Dizon of Massachusetts General Hospital, Boston, said, “I think this illustrates… the theme of this year’s meeting, which is Collective Wisdom, and even more than that it illustrates that even with a rare tumor type and using standard chemotherapy it’s very important, and we can select patients who are most likely to benefit from treatment and at the same time potentially spare patients from the toxicities of therapy that they’re unlikely to benefit from.”
Results from the arm of the trial testing temozolomide given only at the time of radiation therapy are not yet available and are expected in 2020. In addition, investigators plan to assess genetic abnormalities that are known to affect prognosis in the disease, specifically MGMT promoter methylation and IDH (isocitrate dehydrogenase) mutation.
Common toxicities with temozolomide were mainly low platelet and white cell counts with severe toxicity in 5-10% of patients.
CHICAGO – Adjuvant temozolomide given after radiation therapy improves survival of patients with a form of anaplastic glioma, a rare brain tumor. The patients had anaplastic glioma without 1p/19q co-deletion.
This co-deletion – the short arm of chromosome 1 and the long arm of chromosome 19 – is a favorable marker in the tumor, and patients without the deletion have traditionally done worse than those with the deletion. Until this study, no one knew if temozolomide would improve outcomes of patients without the co-deletion.
The four-arm, Phase III Trial on Concurrent and Adjuvant Temozolomide [TMZ] Chemotherapy in NON-1p/19q Deleted Anaplastic Glioma: The CATNON Intergroup Trial (EORTC 26053-22054), still ongoing, is testing radiotherapy, radiotherapy plus concurrent TMZ, radiotherapy plus 12 months of adjuvant TMZ, or radiotherapy plus concurrent TMZ plus 12 months of adjuvant TMZ. Adjuvant TMZ was given in 12 cycles.
Given the rarity of the tumor, the trial involved 118 institutions on three continents and ran for eight years between 2007 and 2015. From 1407 patients 18 years or older with World Health Organization performance status 0-2 screened, 751 were confirmed to have grade III anaplastic gliomas that were intact for 1p/19q (ie, no deletions). After radiation therapy with 59.4 Gy in 33 fractions, these patients were randomly assigned to one of the four treatment arms.
The trial asked two questions: Does adjuvant chemotherapy after radiotherapy improve outcome, and does chemotherapy concurrent with radiotherapy improve outcomes?
Just after enrollment was completed, a data monitoring committee recommended, based on an interim analysis in October 2015, that the data for the adjuvant arm be released, reported Dr. Martin van den Bent, professor of neuro-oncology at Erasmus MC Cancer Center in Rotterdam, The Netherlands. “It completely came as a surprise,” he said at a press conference at the annual meeting of the American Society of Clinical Oncology.
Comparing radiation with or without concurrent TMZ followed by adjuvant TMZ to treatment without adjuvant therapy, the overall survival at five years increased from 44% without any TMZ or with TMZ concurrent with radiation (n = 372) to 56% with adjuvant temozolomide (n = 373). “This corresponds to a hazard ratio of 0.67, a highly statistically significant increment,” Dr. van den Bent said.
Adjuvant TMZ was also associated with a statistically significant increase in median progression free survival from 19 months without adjuvant therapy to almost 43 months with it.
When patients were stratified by O6-methyl-guanine DNA methyltransferase (MGMT) promoter methylation status, the researchers found that MGMT methylation was prognostic for overall survival but not predictive of improved outcome to adjuvant TMZ.
For the nonadjuvant group, the median overall survival was 41 months (95% CI, 37-61 months), but the groups receiving adjuvant TMZ had not yet reached a median overall survival. “We know now that temozolomide given after radiation therapy improves survival in this disease,” Dr. van den Bent said.
A trial of such a rare disease requires many collaborating centers and oncology groups and a long duration to show improvements in outcome. Collaborating oncology groups across many countries “have shown the capacity to answer important clinical questions in orphan diseases,” he said.
Press conference moderator Dr. Don Dizon of Massachusetts General Hospital, Boston, said, “I think this illustrates… the theme of this year’s meeting, which is Collective Wisdom, and even more than that it illustrates that even with a rare tumor type and using standard chemotherapy it’s very important, and we can select patients who are most likely to benefit from treatment and at the same time potentially spare patients from the toxicities of therapy that they’re unlikely to benefit from.”
Results from the arm of the trial testing temozolomide given only at the time of radiation therapy are not yet available and are expected in 2020. In addition, investigators plan to assess genetic abnormalities that are known to affect prognosis in the disease, specifically MGMT promoter methylation and IDH (isocitrate dehydrogenase) mutation.
Common toxicities with temozolomide were mainly low platelet and white cell counts with severe toxicity in 5-10% of patients.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Adjuvant temozolomide post-radiation improves survival in non-1p/19q-deleted anaplastic glioma.
Major finding: Adjuvant temozolomide improved overall survival to 56% from 44%.
Data source: Randomized, 4-arm trial of adjuvant temozolomide or not among 751 patients with non-1p/19q-deleted anaplastic glioma.
Disclosures: Schering Plough/MSD provided an unrestricted grant for the research and supplied temozolomide. Dr. van den Bent has consulting or advisory roles with Merck, Roche, Celldex, Novocure, Abbvie, and Amgen; has received honoraria from Roche, Actelion, Celldex, Bristol-Myers Squibb, Merck, Abbvie, and Novocure; and has research funding from Abbvie and Roche.
Early results positive for treating high-grade gliomas with virus-based therapy
An investigational virus-based therapy was safely given to patients with high-grade or recurrent gliomas in a phase I study, improving survival for some, investigators report.
In the phase I trial of Toca 511 (vocimagene amiretrorepvec) in combination with surgical resection, median overall survival was 13.6 months (95% confidence interval, 10.8-20.0) among all evaluable patients with high-grade glioblastoma (n = 43) and 14.4 months (95% CI, 11.3-32.3) for patients with first or second recurrence (n = 32), Dr. Timothy Cloughesy of the University of California, Los Angeles, and his associates reported (Sci Transl Med. 2016;8:1-11).
Investigators compared their data to those of external controls with glioblastoma at first and second recurrence treated with lomustine and saw an almost twofold improvement in overall survival (13.6 months vs. 7.1 months (hazard ratio, 0.45; P = .003).
Toca 511 dispatches a virus to rapidly dividing cancer cells, then delivers a gene encoding an enzyme that converts a nontoxic prodrug, Toca FC (extended-release 5-fluorocytosine), into its active form, 5-fluorouracil.
There were no treatment-related deaths, and there were fewer grade 3 adverse events, compared with the external lomustine control group.
“Recurrent HGG [high-grade glioblastoma] is associated with dismal clinical outcomes, and patients are in need of safe and more efficacious therapy. The nonlytic RRV [retroviral replicating vector] Toca 511 and an extended-release 5-FC [5-fluorocytosine] have the potential to fill this medical need,” the researchers said.
A randomized phase II/III trial in patients with recurrent glioblastoma and anaplastic astrocytoma is underway, they said.
This study was supported by the Accelerate Brain Cancer Cure Foundation, the National Brain Tumor Society, the American Brain Tumor Association, the Musela Foundation, Voices Against Brain Cancer, and the National Institute of Neurological Disorders and Stroke. Thirteen investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies.
On Twitter @JessCraig_OP
An investigational virus-based therapy was safely given to patients with high-grade or recurrent gliomas in a phase I study, improving survival for some, investigators report.
In the phase I trial of Toca 511 (vocimagene amiretrorepvec) in combination with surgical resection, median overall survival was 13.6 months (95% confidence interval, 10.8-20.0) among all evaluable patients with high-grade glioblastoma (n = 43) and 14.4 months (95% CI, 11.3-32.3) for patients with first or second recurrence (n = 32), Dr. Timothy Cloughesy of the University of California, Los Angeles, and his associates reported (Sci Transl Med. 2016;8:1-11).
Investigators compared their data to those of external controls with glioblastoma at first and second recurrence treated with lomustine and saw an almost twofold improvement in overall survival (13.6 months vs. 7.1 months (hazard ratio, 0.45; P = .003).
Toca 511 dispatches a virus to rapidly dividing cancer cells, then delivers a gene encoding an enzyme that converts a nontoxic prodrug, Toca FC (extended-release 5-fluorocytosine), into its active form, 5-fluorouracil.
There were no treatment-related deaths, and there were fewer grade 3 adverse events, compared with the external lomustine control group.
“Recurrent HGG [high-grade glioblastoma] is associated with dismal clinical outcomes, and patients are in need of safe and more efficacious therapy. The nonlytic RRV [retroviral replicating vector] Toca 511 and an extended-release 5-FC [5-fluorocytosine] have the potential to fill this medical need,” the researchers said.
A randomized phase II/III trial in patients with recurrent glioblastoma and anaplastic astrocytoma is underway, they said.
This study was supported by the Accelerate Brain Cancer Cure Foundation, the National Brain Tumor Society, the American Brain Tumor Association, the Musela Foundation, Voices Against Brain Cancer, and the National Institute of Neurological Disorders and Stroke. Thirteen investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies.
On Twitter @JessCraig_OP
An investigational virus-based therapy was safely given to patients with high-grade or recurrent gliomas in a phase I study, improving survival for some, investigators report.
In the phase I trial of Toca 511 (vocimagene amiretrorepvec) in combination with surgical resection, median overall survival was 13.6 months (95% confidence interval, 10.8-20.0) among all evaluable patients with high-grade glioblastoma (n = 43) and 14.4 months (95% CI, 11.3-32.3) for patients with first or second recurrence (n = 32), Dr. Timothy Cloughesy of the University of California, Los Angeles, and his associates reported (Sci Transl Med. 2016;8:1-11).
Investigators compared their data to those of external controls with glioblastoma at first and second recurrence treated with lomustine and saw an almost twofold improvement in overall survival (13.6 months vs. 7.1 months (hazard ratio, 0.45; P = .003).
Toca 511 dispatches a virus to rapidly dividing cancer cells, then delivers a gene encoding an enzyme that converts a nontoxic prodrug, Toca FC (extended-release 5-fluorocytosine), into its active form, 5-fluorouracil.
There were no treatment-related deaths, and there were fewer grade 3 adverse events, compared with the external lomustine control group.
“Recurrent HGG [high-grade glioblastoma] is associated with dismal clinical outcomes, and patients are in need of safe and more efficacious therapy. The nonlytic RRV [retroviral replicating vector] Toca 511 and an extended-release 5-FC [5-fluorocytosine] have the potential to fill this medical need,” the researchers said.
A randomized phase II/III trial in patients with recurrent glioblastoma and anaplastic astrocytoma is underway, they said.
This study was supported by the Accelerate Brain Cancer Cure Foundation, the National Brain Tumor Society, the American Brain Tumor Association, the Musela Foundation, Voices Against Brain Cancer, and the National Institute of Neurological Disorders and Stroke. Thirteen investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies.
On Twitter @JessCraig_OP
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point: A phase I trial indicates that Toca 511 is safe and shows activity in treating patients with high-grade or recurrent glioblastoma.
Major finding: Median overall survival was 13.6 months (95% CI, 10.8-20.0) for patients with high-grade glioblastoma (n = 43), almost twice as long as that of similar patients from a separate trial treated with standard therapy (hazard ratio, 0.45; P = .003).
Data source: A phase I trial of 45 patients with glioblastoma, compared with an external control group.
Disclosures: This study was supported by the Accelerate Brain Cancer Cure Foundation, the National Brain Tumor Society, the American Brain Tumor Association, the Musela Foundation, Voices Against Brain Cancer, and the National Institute of Neurological Disorders and Stroke. Thirteen investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies.
Investigational CDK4/6 inhibitor shows activity, less toxicity
Abemaciclib, a CDK4/6 inhibitor, showed durable clinical activity when given as continuous single-agent therapy to patients with advanced cancer, including breast cancer and non–small-cell lung cancer, according to investigators.
Neutropenia was rarely observed in patients treated with abemaciclib, the toxicity observed in some patients who receive the only Food and Drug Administration–approved CDK4/6 inhibitor, palbociclib.
“Abemaciclib is a small-molecule inhibitor of CDK4 and CDK6 that is structurally distinct from other dual inhibitors (such as palbociclib and ribociclib) and notably exhibits greater selectivity for CDK4 compared with CDK6,” wrote Dr. Amita Patnaik of South Texas Accelerated Research Therapeutics and her associates (Cancer Discov. 2016 May 23. doi: 10.1158/2159-8290.CD-16-0095).
Furthermore, preclinical models indicate that the drug can cross the blood-brain barrier, suggesting potential efficacy against primary and metastatic tumors involving the central nervous system, they said.
A total of 225 patients with various types of advanced cancers were enrolled in this multicohort phase I study (dose escalation, n = 33; single-agent abemaciclib therapy for breast cancer, n = 47; non–small-cell lung cancer, n = 68; glioblastoma, n = 17; melanoma, n = 26; colorectal cancer, n = 15; abemaciclib plus fulvestrant combination therapy for hormone receptor–positive breast cancer, n = 19). Abemaciclib was given orally to all patients.
Neither dose-limiting toxicity nor maximum tolerated dose was reached in patients treated at levels of 50 mg, 100 mg, 150 mg, or 225 mg once daily. The maximum tolerated dose was 200 mg for patients treated with abemaciclib twice daily.
In the single-agent breast cancer cohort, the disease control rate was 81% for hormone receptor–positive (HR-positive) tumors, 33% for HR-negative tumors, 100% for HR-positive HER2-positive tumors, 72% for HR-positive HER2-negative tumors, and 70% overall. The response rate was 31% for HR-positive tumors, 0% for HR-negative tumors, 36% for HR-positive HER2-positive tumors, 28% for HR-positive HER2-negative tumors, and 23% overall.
The overall response rate was 21% for breast cancer patients receiving abemaciclib plus fulvestrant.
Among the 68 patients with non–small-cell lung cancer, 2 had a partial response and 31 had stable disease. Of the 26 patients with melanoma, 1 had a partial response and 6 had stable disease. Of the 17 patients with glioblastoma, 3 had stable disease.
Overall, there were no study-related deaths. Diarrhea, nausea, and fatigue were the most common adverse events; all were reversible.
Neutropenia was observed in 39 patients (23% of 173 patients in the single-agent tumor-specific cohort) – 2 were grade 4 events. Grade 3 neutropenia occurred in 6 patients (32% of 19 patients with HR-positive breast cancer receiving combination therapy with abemaciclib plus fulvestrant).
“Previous reports have identified neutropenia as an adverse event associated with dual inhibition of CDK4 and CDK6. However, abemaciclib given as a single agent on a continuous schedule in the tumor-specific cohorts was associated with an acceptable incidence of investigator-reported grade 3 (9%, 16 of 173 patients) or grade 4 (1%, 2 of 173 patients) neutropenia,” wrote the investigators.
“In summary, the results of this clinical trial demonstrate the safety and antitumor activity of abemaciclib as a single agent and support its further development both as monotherapy and in rational combinations. Furthermore, these findings validate CDK4 and CDK6 as anticancer drug targets and translate preclinical predictions regarding therapeutic targeting of cell-cycle derangements in cancer into clinical efficacy,”they wrote.
Eli Lilly funded the study. Eight investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies including Eli Lilly.
On Twitter @JessCraig_OP
Abemaciclib, a CDK4/6 inhibitor, showed durable clinical activity when given as continuous single-agent therapy to patients with advanced cancer, including breast cancer and non–small-cell lung cancer, according to investigators.
Neutropenia was rarely observed in patients treated with abemaciclib, the toxicity observed in some patients who receive the only Food and Drug Administration–approved CDK4/6 inhibitor, palbociclib.
“Abemaciclib is a small-molecule inhibitor of CDK4 and CDK6 that is structurally distinct from other dual inhibitors (such as palbociclib and ribociclib) and notably exhibits greater selectivity for CDK4 compared with CDK6,” wrote Dr. Amita Patnaik of South Texas Accelerated Research Therapeutics and her associates (Cancer Discov. 2016 May 23. doi: 10.1158/2159-8290.CD-16-0095).
Furthermore, preclinical models indicate that the drug can cross the blood-brain barrier, suggesting potential efficacy against primary and metastatic tumors involving the central nervous system, they said.
A total of 225 patients with various types of advanced cancers were enrolled in this multicohort phase I study (dose escalation, n = 33; single-agent abemaciclib therapy for breast cancer, n = 47; non–small-cell lung cancer, n = 68; glioblastoma, n = 17; melanoma, n = 26; colorectal cancer, n = 15; abemaciclib plus fulvestrant combination therapy for hormone receptor–positive breast cancer, n = 19). Abemaciclib was given orally to all patients.
Neither dose-limiting toxicity nor maximum tolerated dose was reached in patients treated at levels of 50 mg, 100 mg, 150 mg, or 225 mg once daily. The maximum tolerated dose was 200 mg for patients treated with abemaciclib twice daily.
In the single-agent breast cancer cohort, the disease control rate was 81% for hormone receptor–positive (HR-positive) tumors, 33% for HR-negative tumors, 100% for HR-positive HER2-positive tumors, 72% for HR-positive HER2-negative tumors, and 70% overall. The response rate was 31% for HR-positive tumors, 0% for HR-negative tumors, 36% for HR-positive HER2-positive tumors, 28% for HR-positive HER2-negative tumors, and 23% overall.
The overall response rate was 21% for breast cancer patients receiving abemaciclib plus fulvestrant.
Among the 68 patients with non–small-cell lung cancer, 2 had a partial response and 31 had stable disease. Of the 26 patients with melanoma, 1 had a partial response and 6 had stable disease. Of the 17 patients with glioblastoma, 3 had stable disease.
Overall, there were no study-related deaths. Diarrhea, nausea, and fatigue were the most common adverse events; all were reversible.
Neutropenia was observed in 39 patients (23% of 173 patients in the single-agent tumor-specific cohort) – 2 were grade 4 events. Grade 3 neutropenia occurred in 6 patients (32% of 19 patients with HR-positive breast cancer receiving combination therapy with abemaciclib plus fulvestrant).
“Previous reports have identified neutropenia as an adverse event associated with dual inhibition of CDK4 and CDK6. However, abemaciclib given as a single agent on a continuous schedule in the tumor-specific cohorts was associated with an acceptable incidence of investigator-reported grade 3 (9%, 16 of 173 patients) or grade 4 (1%, 2 of 173 patients) neutropenia,” wrote the investigators.
“In summary, the results of this clinical trial demonstrate the safety and antitumor activity of abemaciclib as a single agent and support its further development both as monotherapy and in rational combinations. Furthermore, these findings validate CDK4 and CDK6 as anticancer drug targets and translate preclinical predictions regarding therapeutic targeting of cell-cycle derangements in cancer into clinical efficacy,”they wrote.
Eli Lilly funded the study. Eight investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies including Eli Lilly.
On Twitter @JessCraig_OP
Abemaciclib, a CDK4/6 inhibitor, showed durable clinical activity when given as continuous single-agent therapy to patients with advanced cancer, including breast cancer and non–small-cell lung cancer, according to investigators.
Neutropenia was rarely observed in patients treated with abemaciclib, the toxicity observed in some patients who receive the only Food and Drug Administration–approved CDK4/6 inhibitor, palbociclib.
“Abemaciclib is a small-molecule inhibitor of CDK4 and CDK6 that is structurally distinct from other dual inhibitors (such as palbociclib and ribociclib) and notably exhibits greater selectivity for CDK4 compared with CDK6,” wrote Dr. Amita Patnaik of South Texas Accelerated Research Therapeutics and her associates (Cancer Discov. 2016 May 23. doi: 10.1158/2159-8290.CD-16-0095).
Furthermore, preclinical models indicate that the drug can cross the blood-brain barrier, suggesting potential efficacy against primary and metastatic tumors involving the central nervous system, they said.
A total of 225 patients with various types of advanced cancers were enrolled in this multicohort phase I study (dose escalation, n = 33; single-agent abemaciclib therapy for breast cancer, n = 47; non–small-cell lung cancer, n = 68; glioblastoma, n = 17; melanoma, n = 26; colorectal cancer, n = 15; abemaciclib plus fulvestrant combination therapy for hormone receptor–positive breast cancer, n = 19). Abemaciclib was given orally to all patients.
Neither dose-limiting toxicity nor maximum tolerated dose was reached in patients treated at levels of 50 mg, 100 mg, 150 mg, or 225 mg once daily. The maximum tolerated dose was 200 mg for patients treated with abemaciclib twice daily.
In the single-agent breast cancer cohort, the disease control rate was 81% for hormone receptor–positive (HR-positive) tumors, 33% for HR-negative tumors, 100% for HR-positive HER2-positive tumors, 72% for HR-positive HER2-negative tumors, and 70% overall. The response rate was 31% for HR-positive tumors, 0% for HR-negative tumors, 36% for HR-positive HER2-positive tumors, 28% for HR-positive HER2-negative tumors, and 23% overall.
The overall response rate was 21% for breast cancer patients receiving abemaciclib plus fulvestrant.
Among the 68 patients with non–small-cell lung cancer, 2 had a partial response and 31 had stable disease. Of the 26 patients with melanoma, 1 had a partial response and 6 had stable disease. Of the 17 patients with glioblastoma, 3 had stable disease.
Overall, there were no study-related deaths. Diarrhea, nausea, and fatigue were the most common adverse events; all were reversible.
Neutropenia was observed in 39 patients (23% of 173 patients in the single-agent tumor-specific cohort) – 2 were grade 4 events. Grade 3 neutropenia occurred in 6 patients (32% of 19 patients with HR-positive breast cancer receiving combination therapy with abemaciclib plus fulvestrant).
“Previous reports have identified neutropenia as an adverse event associated with dual inhibition of CDK4 and CDK6. However, abemaciclib given as a single agent on a continuous schedule in the tumor-specific cohorts was associated with an acceptable incidence of investigator-reported grade 3 (9%, 16 of 173 patients) or grade 4 (1%, 2 of 173 patients) neutropenia,” wrote the investigators.
“In summary, the results of this clinical trial demonstrate the safety and antitumor activity of abemaciclib as a single agent and support its further development both as monotherapy and in rational combinations. Furthermore, these findings validate CDK4 and CDK6 as anticancer drug targets and translate preclinical predictions regarding therapeutic targeting of cell-cycle derangements in cancer into clinical efficacy,”they wrote.
Eli Lilly funded the study. Eight investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies including Eli Lilly.
On Twitter @JessCraig_OP
FROM CANCER DISCOVERY
Key clinical point: A phase I trial indicates that abemaciclib is safe and shows activity in treating patients with advanced breast and other cancers.
Major finding: In the single-agent breast cancer cohort, the overall disease control rate was 70%. Incidence of neutropenia was 9% for grade 3 and 1% for grade 4.
Data source: A multicenter phase I dose-escalation and tumor-specific cohort study of 225 patients with advanced cancers.
Disclosures: Eli Lilly funded the study. Eight investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies including Eli Lilly.
Targeting gene rearrangements shows promise in early study
Entrectinib, an investigational drug that targets several abnormal fusion proteins, showed antitumor activity and was safe in patients with several different types of advanced solid tumors. The patients had never before been exposed to drugs targeting these same genetic alterations.
“Responses can be very rapid and durable … which include colorectal, primary brain tumor, astrocytoma, fibrosarcoma, lung, and mammary analog secretory carcinoma,” Dr. Alexander Drilon of Memorial Sloan Kettering Cancer Center in New York said in a news conference at the annual meeting of the American Association for Cancer Research. “Dramatic intracranial activity … has been demonstrated both in primary brain tumor and also in metastatic.”
NTRK1/2/3, ROS1, and ALK gene–rearranged cancers produce fusion proteins that are ligand independent for their activity and thus constitutively active, driving tumor growth. Entrectinib is a pan-TRK, ROS1, ALK tyrosine kinase inhibitor that targets the abnormal fusion protein products of the genes, is highly potent at low concentrations, and has been designed to cross the blood-brain barrier (BBB). The targeted proteins are present across multiple cancers and are especially prevalent (greater than 80%) among some rare adult and pediatric cancers.
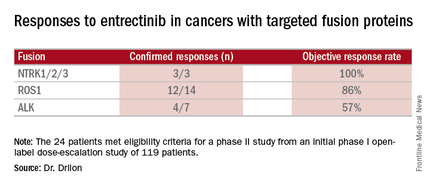
Combined data on 119 patients in two phase I trials established 600 mg orally once daily as the recommended dose to go into phase II trials. Among the 24 patients meeting eligibility criteria for a phase II trial (presence of the targeted gene fusions in their tumors, no prior treatment against these targets, and treatment at or above 600 mg daily), the confirmed response rate was 79% (19/24). Most were partial responses in terms of tumor shrinkage, but two patients had complete responses. Response rates appeared to vary according to the specific fusion protein defect.
All three cases of CNS disease with NTRK-rearranged cancers had intracranial responses, demonstrating that the drug crosses the BBB and is active. In one case, a 46-year-old man with brain metastases heavily pretreated for non–small cell lung cancer with an NTRK1 rearrangement experienced a dramatic response.
“The patient at that point was actually on hospice and was doing extremely poorly on supplemental oxygen,” Dr. Drilon said. “Within a few weeks, the patient had a dramatic clinical response to therapy … At day 26 there was almost a 50% reduction in tumor burden.” At day 317 scans showed he had a complete intracranial response to entrectinib, but he still has visceral disease on therapy past 1 year.
Responses often occurred within the first month of therapy, and many persisted for several months without disease progression, with one patient being followed for more than 2 years with clinical benefit. Nineteen of 24 patients have been on the therapy for more than 6 months, and the therapy appears to be safe and well tolerated.
Commenting on this study and others targeting specific genetic alterations leading to cancer, Dr. Louis Weiner, director of the Georgetown Lombardi Comprehensive Cancer Center in Washington, said, “You’re seeing a series of clinical trials described that aren’t necessarily targeting people with a particular cancer but rather people who have cancers characterized by particular molecular abnormalities.” Not all cancers will have identified molecular abnormalities driving them. “However, I think where you have these drivers, the proper thing to do is not to worry about whether [a drug] works in a given disease but rather whether it works for people with that particular abnormality,” he said.
For the future, the investigators plan a phase II trial called STARTRK-2. It is a multicenter, open-label, global basket study to include any solid tumors with the targeted rearrangements.
Dr. Drilon disclosed ties with Ignyta, which funded the study, and has received research funding from Foundation Medicine. Dr. Weiner disclosed ties with several pharmaceutical companies.
Entrectinib, an investigational drug that targets several abnormal fusion proteins, showed antitumor activity and was safe in patients with several different types of advanced solid tumors. The patients had never before been exposed to drugs targeting these same genetic alterations.
“Responses can be very rapid and durable … which include colorectal, primary brain tumor, astrocytoma, fibrosarcoma, lung, and mammary analog secretory carcinoma,” Dr. Alexander Drilon of Memorial Sloan Kettering Cancer Center in New York said in a news conference at the annual meeting of the American Association for Cancer Research. “Dramatic intracranial activity … has been demonstrated both in primary brain tumor and also in metastatic.”
NTRK1/2/3, ROS1, and ALK gene–rearranged cancers produce fusion proteins that are ligand independent for their activity and thus constitutively active, driving tumor growth. Entrectinib is a pan-TRK, ROS1, ALK tyrosine kinase inhibitor that targets the abnormal fusion protein products of the genes, is highly potent at low concentrations, and has been designed to cross the blood-brain barrier (BBB). The targeted proteins are present across multiple cancers and are especially prevalent (greater than 80%) among some rare adult and pediatric cancers.
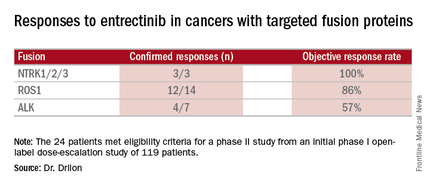
Combined data on 119 patients in two phase I trials established 600 mg orally once daily as the recommended dose to go into phase II trials. Among the 24 patients meeting eligibility criteria for a phase II trial (presence of the targeted gene fusions in their tumors, no prior treatment against these targets, and treatment at or above 600 mg daily), the confirmed response rate was 79% (19/24). Most were partial responses in terms of tumor shrinkage, but two patients had complete responses. Response rates appeared to vary according to the specific fusion protein defect.
All three cases of CNS disease with NTRK-rearranged cancers had intracranial responses, demonstrating that the drug crosses the BBB and is active. In one case, a 46-year-old man with brain metastases heavily pretreated for non–small cell lung cancer with an NTRK1 rearrangement experienced a dramatic response.
“The patient at that point was actually on hospice and was doing extremely poorly on supplemental oxygen,” Dr. Drilon said. “Within a few weeks, the patient had a dramatic clinical response to therapy … At day 26 there was almost a 50% reduction in tumor burden.” At day 317 scans showed he had a complete intracranial response to entrectinib, but he still has visceral disease on therapy past 1 year.
Responses often occurred within the first month of therapy, and many persisted for several months without disease progression, with one patient being followed for more than 2 years with clinical benefit. Nineteen of 24 patients have been on the therapy for more than 6 months, and the therapy appears to be safe and well tolerated.
Commenting on this study and others targeting specific genetic alterations leading to cancer, Dr. Louis Weiner, director of the Georgetown Lombardi Comprehensive Cancer Center in Washington, said, “You’re seeing a series of clinical trials described that aren’t necessarily targeting people with a particular cancer but rather people who have cancers characterized by particular molecular abnormalities.” Not all cancers will have identified molecular abnormalities driving them. “However, I think where you have these drivers, the proper thing to do is not to worry about whether [a drug] works in a given disease but rather whether it works for people with that particular abnormality,” he said.
For the future, the investigators plan a phase II trial called STARTRK-2. It is a multicenter, open-label, global basket study to include any solid tumors with the targeted rearrangements.
Dr. Drilon disclosed ties with Ignyta, which funded the study, and has received research funding from Foundation Medicine. Dr. Weiner disclosed ties with several pharmaceutical companies.
Entrectinib, an investigational drug that targets several abnormal fusion proteins, showed antitumor activity and was safe in patients with several different types of advanced solid tumors. The patients had never before been exposed to drugs targeting these same genetic alterations.
“Responses can be very rapid and durable … which include colorectal, primary brain tumor, astrocytoma, fibrosarcoma, lung, and mammary analog secretory carcinoma,” Dr. Alexander Drilon of Memorial Sloan Kettering Cancer Center in New York said in a news conference at the annual meeting of the American Association for Cancer Research. “Dramatic intracranial activity … has been demonstrated both in primary brain tumor and also in metastatic.”
NTRK1/2/3, ROS1, and ALK gene–rearranged cancers produce fusion proteins that are ligand independent for their activity and thus constitutively active, driving tumor growth. Entrectinib is a pan-TRK, ROS1, ALK tyrosine kinase inhibitor that targets the abnormal fusion protein products of the genes, is highly potent at low concentrations, and has been designed to cross the blood-brain barrier (BBB). The targeted proteins are present across multiple cancers and are especially prevalent (greater than 80%) among some rare adult and pediatric cancers.
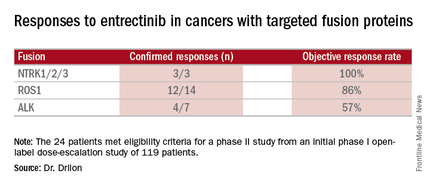
Combined data on 119 patients in two phase I trials established 600 mg orally once daily as the recommended dose to go into phase II trials. Among the 24 patients meeting eligibility criteria for a phase II trial (presence of the targeted gene fusions in their tumors, no prior treatment against these targets, and treatment at or above 600 mg daily), the confirmed response rate was 79% (19/24). Most were partial responses in terms of tumor shrinkage, but two patients had complete responses. Response rates appeared to vary according to the specific fusion protein defect.
All three cases of CNS disease with NTRK-rearranged cancers had intracranial responses, demonstrating that the drug crosses the BBB and is active. In one case, a 46-year-old man with brain metastases heavily pretreated for non–small cell lung cancer with an NTRK1 rearrangement experienced a dramatic response.
“The patient at that point was actually on hospice and was doing extremely poorly on supplemental oxygen,” Dr. Drilon said. “Within a few weeks, the patient had a dramatic clinical response to therapy … At day 26 there was almost a 50% reduction in tumor burden.” At day 317 scans showed he had a complete intracranial response to entrectinib, but he still has visceral disease on therapy past 1 year.
Responses often occurred within the first month of therapy, and many persisted for several months without disease progression, with one patient being followed for more than 2 years with clinical benefit. Nineteen of 24 patients have been on the therapy for more than 6 months, and the therapy appears to be safe and well tolerated.
Commenting on this study and others targeting specific genetic alterations leading to cancer, Dr. Louis Weiner, director of the Georgetown Lombardi Comprehensive Cancer Center in Washington, said, “You’re seeing a series of clinical trials described that aren’t necessarily targeting people with a particular cancer but rather people who have cancers characterized by particular molecular abnormalities.” Not all cancers will have identified molecular abnormalities driving them. “However, I think where you have these drivers, the proper thing to do is not to worry about whether [a drug] works in a given disease but rather whether it works for people with that particular abnormality,” he said.
For the future, the investigators plan a phase II trial called STARTRK-2. It is a multicenter, open-label, global basket study to include any solid tumors with the targeted rearrangements.
Dr. Drilon disclosed ties with Ignyta, which funded the study, and has received research funding from Foundation Medicine. Dr. Weiner disclosed ties with several pharmaceutical companies.
FROM THE AACR ANNUAL MEETING
Key clinical point: Entrectinib showed antitumor activity including intracranial responses.
Major finding: Patients with the targeted abnormalities had a 79% response rate.
Data source: Twenty-four patients meeting eligibility criteria for a phase II study from an initial phase I open-label dose-escalation study of 119 patients.
Disclosures: Dr. Drilon disclosed ties with Ignyta, which funded the study, and has received research funding from Foundation Medicine. Dr. Weiner disclosed ties with several pharmaceutical companies.
Adding chemo to radiation boosts survival from low-grade gliomas
Adding a chemotherapy combination to radiation therapy for initial treatment of low-grade gliomas significantly improved overall survival and progression-free survival, regardless of the tumor type, investigators report in the New England Journal of Medicine.
Grade 2 glioma patients who received radiation plus the combination of procarbazine, lomustine (also called CCNU), and vincristine (PCV) had a longer median overall survival than those who received radiation alone (13.3 vs. 7.8 years; hazard ratio for death, 0.59; P = .003). Of those who received radiation plus chemotherapy, the progression-free survival rate at 10 years was 51%, compared with 21% for the group who received radiation alone, Dr. Jan Buckner and his colleagues report (N Engl J Med. 2016;374:1344-55. doi: 10.1056/NEJMoa1500925).
“The magnitude of treatment benefit from combined chemotherapy plus radiation therapy is substantial, but the toxic effects are greater than those observed with radiation therapy alone,” wrote Dr. Buckner, professor of oncology at the Mayo Clinic, Rochester, Minn., and associates. Patients who received radiation plus PCV had more toxic side effects from their therapy, though most effects were grade 1 and 2.
For this study, 254 patients were randomized, with 128 assigned to radiotherapy alone, and 126 assigned to radiotherapy plus PCV. A total of 126 patients in the radiotherapy arm were included in the analysis, with one patient not receiving the intervention and 14 patients lost to follow-up at some point during the 10 years of the study. In the radiotherapy plus PCV arm, 125 patients were eligible for evaluation, and all of those patients were included in the analysis. Twenty-six patients in this arm were lost to follow-up, and 72 patients discontinued the intervention in this arm (this figure included four patients who died).
Tumor types included in the study were grade 2 astrocytoma, oligoastrocytoma, or oligodendroglioma.
Patients were included if they were between 18 and 39 years of age and had received a subtotal resection or biopsy of their tumor, or if they were 40 years of age or older and had any resection or biopsy of their tumor. Exclusion criteria included previous radiation to the head or neck, any previous chemotherapy, significant pulmonary disease, and a 5-year history of other cancers except cervical cancer in situ and non-melanoma skin cancer. Tumors could not have spread to noncontiguous leptomeninges, and patients could not have gliomatosis cerebri. Patients had to have a Karnofsky performance score of 60 or higher, and a neurological function score of 3 or less.
Dr. Buckner and his collaborators also assessed tumors for IDH1 mutational status by performing immunostaining with the mutation-specific monoclonal antibody IDH1 R132H; appropriate tissue was available for testing in slightly less than half of the patients in each study arm. The mutation was present in 35/57 patients (61%) in the radiotherapy-only arm, and 36/56 patients (64%) in the radiotherapy plus PCV arm. Patients with oligodendroglioma were most likely to have IDH1 R132H mutations. Sample sizes were too small to determine the effect of other IDH mutations or co-deletion of chromosome arms 1p and 19q.
In multivariable analysis, the presence of the IDH1 R132H mutation was identified as an independent prognostic factor for better overall survival (OS) and progression-free survival (PFS), regardless of the treatment administered. Those with the mutation still benefited significantly from receiving radiotherapy plus PCV rather than radiotherapy alone (P = .02 for OS, P less than .001 for PFS).
Exploratory analysis that broke down OS and PFS by cancer type showed that “the superiority of radiation therapy plus chemotherapy over radiation therapy alone was seen with all histologic diagnoses, although the difference did not reach significance among patients with astrocytoma,” wrote Dr. Buckner and his collaborators.
When all patients lost to follow-up in both groups were assessed as having died, the sensitivity analysis still showed benefit for radiotherapy plus PCV (HR for death, compared with radiotherapy alone, 0.72; P = .03).
The value of the long-term follow-up, wrote Dr. Buckner and his colleagues, was that “The separation of the progression-free survival curves of the two treatment groups did not begin until 2 to 3 years after randomization, although approximately 25% of the patients in each group had disease progression by then.”
Dr. Buckner and his collaborators emphasized that the patient-physician team should consider all factors in making treatment decisions, saying, “Patients and their physicians will have to weigh whether the longer survival justified the more toxic therapeutic approach.“
On Twitter @karioakes
Adding a chemotherapy combination to radiation therapy for initial treatment of low-grade gliomas significantly improved overall survival and progression-free survival, regardless of the tumor type, investigators report in the New England Journal of Medicine.
Grade 2 glioma patients who received radiation plus the combination of procarbazine, lomustine (also called CCNU), and vincristine (PCV) had a longer median overall survival than those who received radiation alone (13.3 vs. 7.8 years; hazard ratio for death, 0.59; P = .003). Of those who received radiation plus chemotherapy, the progression-free survival rate at 10 years was 51%, compared with 21% for the group who received radiation alone, Dr. Jan Buckner and his colleagues report (N Engl J Med. 2016;374:1344-55. doi: 10.1056/NEJMoa1500925).
“The magnitude of treatment benefit from combined chemotherapy plus radiation therapy is substantial, but the toxic effects are greater than those observed with radiation therapy alone,” wrote Dr. Buckner, professor of oncology at the Mayo Clinic, Rochester, Minn., and associates. Patients who received radiation plus PCV had more toxic side effects from their therapy, though most effects were grade 1 and 2.
For this study, 254 patients were randomized, with 128 assigned to radiotherapy alone, and 126 assigned to radiotherapy plus PCV. A total of 126 patients in the radiotherapy arm were included in the analysis, with one patient not receiving the intervention and 14 patients lost to follow-up at some point during the 10 years of the study. In the radiotherapy plus PCV arm, 125 patients were eligible for evaluation, and all of those patients were included in the analysis. Twenty-six patients in this arm were lost to follow-up, and 72 patients discontinued the intervention in this arm (this figure included four patients who died).
Tumor types included in the study were grade 2 astrocytoma, oligoastrocytoma, or oligodendroglioma.
Patients were included if they were between 18 and 39 years of age and had received a subtotal resection or biopsy of their tumor, or if they were 40 years of age or older and had any resection or biopsy of their tumor. Exclusion criteria included previous radiation to the head or neck, any previous chemotherapy, significant pulmonary disease, and a 5-year history of other cancers except cervical cancer in situ and non-melanoma skin cancer. Tumors could not have spread to noncontiguous leptomeninges, and patients could not have gliomatosis cerebri. Patients had to have a Karnofsky performance score of 60 or higher, and a neurological function score of 3 or less.
Dr. Buckner and his collaborators also assessed tumors for IDH1 mutational status by performing immunostaining with the mutation-specific monoclonal antibody IDH1 R132H; appropriate tissue was available for testing in slightly less than half of the patients in each study arm. The mutation was present in 35/57 patients (61%) in the radiotherapy-only arm, and 36/56 patients (64%) in the radiotherapy plus PCV arm. Patients with oligodendroglioma were most likely to have IDH1 R132H mutations. Sample sizes were too small to determine the effect of other IDH mutations or co-deletion of chromosome arms 1p and 19q.
In multivariable analysis, the presence of the IDH1 R132H mutation was identified as an independent prognostic factor for better overall survival (OS) and progression-free survival (PFS), regardless of the treatment administered. Those with the mutation still benefited significantly from receiving radiotherapy plus PCV rather than radiotherapy alone (P = .02 for OS, P less than .001 for PFS).
Exploratory analysis that broke down OS and PFS by cancer type showed that “the superiority of radiation therapy plus chemotherapy over radiation therapy alone was seen with all histologic diagnoses, although the difference did not reach significance among patients with astrocytoma,” wrote Dr. Buckner and his collaborators.
When all patients lost to follow-up in both groups were assessed as having died, the sensitivity analysis still showed benefit for radiotherapy plus PCV (HR for death, compared with radiotherapy alone, 0.72; P = .03).
The value of the long-term follow-up, wrote Dr. Buckner and his colleagues, was that “The separation of the progression-free survival curves of the two treatment groups did not begin until 2 to 3 years after randomization, although approximately 25% of the patients in each group had disease progression by then.”
Dr. Buckner and his collaborators emphasized that the patient-physician team should consider all factors in making treatment decisions, saying, “Patients and their physicians will have to weigh whether the longer survival justified the more toxic therapeutic approach.“
On Twitter @karioakes
Adding a chemotherapy combination to radiation therapy for initial treatment of low-grade gliomas significantly improved overall survival and progression-free survival, regardless of the tumor type, investigators report in the New England Journal of Medicine.
Grade 2 glioma patients who received radiation plus the combination of procarbazine, lomustine (also called CCNU), and vincristine (PCV) had a longer median overall survival than those who received radiation alone (13.3 vs. 7.8 years; hazard ratio for death, 0.59; P = .003). Of those who received radiation plus chemotherapy, the progression-free survival rate at 10 years was 51%, compared with 21% for the group who received radiation alone, Dr. Jan Buckner and his colleagues report (N Engl J Med. 2016;374:1344-55. doi: 10.1056/NEJMoa1500925).
“The magnitude of treatment benefit from combined chemotherapy plus radiation therapy is substantial, but the toxic effects are greater than those observed with radiation therapy alone,” wrote Dr. Buckner, professor of oncology at the Mayo Clinic, Rochester, Minn., and associates. Patients who received radiation plus PCV had more toxic side effects from their therapy, though most effects were grade 1 and 2.
For this study, 254 patients were randomized, with 128 assigned to radiotherapy alone, and 126 assigned to radiotherapy plus PCV. A total of 126 patients in the radiotherapy arm were included in the analysis, with one patient not receiving the intervention and 14 patients lost to follow-up at some point during the 10 years of the study. In the radiotherapy plus PCV arm, 125 patients were eligible for evaluation, and all of those patients were included in the analysis. Twenty-six patients in this arm were lost to follow-up, and 72 patients discontinued the intervention in this arm (this figure included four patients who died).
Tumor types included in the study were grade 2 astrocytoma, oligoastrocytoma, or oligodendroglioma.
Patients were included if they were between 18 and 39 years of age and had received a subtotal resection or biopsy of their tumor, or if they were 40 years of age or older and had any resection or biopsy of their tumor. Exclusion criteria included previous radiation to the head or neck, any previous chemotherapy, significant pulmonary disease, and a 5-year history of other cancers except cervical cancer in situ and non-melanoma skin cancer. Tumors could not have spread to noncontiguous leptomeninges, and patients could not have gliomatosis cerebri. Patients had to have a Karnofsky performance score of 60 or higher, and a neurological function score of 3 or less.
Dr. Buckner and his collaborators also assessed tumors for IDH1 mutational status by performing immunostaining with the mutation-specific monoclonal antibody IDH1 R132H; appropriate tissue was available for testing in slightly less than half of the patients in each study arm. The mutation was present in 35/57 patients (61%) in the radiotherapy-only arm, and 36/56 patients (64%) in the radiotherapy plus PCV arm. Patients with oligodendroglioma were most likely to have IDH1 R132H mutations. Sample sizes were too small to determine the effect of other IDH mutations or co-deletion of chromosome arms 1p and 19q.
In multivariable analysis, the presence of the IDH1 R132H mutation was identified as an independent prognostic factor for better overall survival (OS) and progression-free survival (PFS), regardless of the treatment administered. Those with the mutation still benefited significantly from receiving radiotherapy plus PCV rather than radiotherapy alone (P = .02 for OS, P less than .001 for PFS).
Exploratory analysis that broke down OS and PFS by cancer type showed that “the superiority of radiation therapy plus chemotherapy over radiation therapy alone was seen with all histologic diagnoses, although the difference did not reach significance among patients with astrocytoma,” wrote Dr. Buckner and his collaborators.
When all patients lost to follow-up in both groups were assessed as having died, the sensitivity analysis still showed benefit for radiotherapy plus PCV (HR for death, compared with radiotherapy alone, 0.72; P = .03).
The value of the long-term follow-up, wrote Dr. Buckner and his colleagues, was that “The separation of the progression-free survival curves of the two treatment groups did not begin until 2 to 3 years after randomization, although approximately 25% of the patients in each group had disease progression by then.”
Dr. Buckner and his collaborators emphasized that the patient-physician team should consider all factors in making treatment decisions, saying, “Patients and their physicians will have to weigh whether the longer survival justified the more toxic therapeutic approach.“
On Twitter @karioakes
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Adding chemotherapy to radiotherapy improved progression-free survival and overall survival in patients with low-grade glioma.
Major finding: Median overall survival was 13.3 years for those receiving radiotherapy plus chemotherapy, compared with 7.8 years for radiotherapy alone (hazard ratio for death, 0.59; P = .003).
Data source: Longitudinal study of 254 patients with grade 2 gliomas receiving radiation therapy alone or radiation therapy plus procarbazine, lomustine, and vincristine.
Disclosures: The study was supported by the National Cancer Institute and did not receive funding from commercial sources. Dr. Bell and Dr. Chakravarti reported a planned patent application related to this work. Dr. Buckner, Dr. Gilbert, Dr. Mehta, and Dr. Suh reported support from pharmaceutical companies outside the scope of this study.
Temsirolimus results in good but short-duration responses in primary CNS lymphoma
Single-agent therapy with temsirolimus was active in patients with relapsed/refractory primary central nervous system lymphoma, but most of the responses were short lived, results of a phase II trial show.
Among 37 patients with primary CNS lymphoma (PCNSL) for whom firstline therapy had failed, there were five complete responses (CR), three CR unconfirmed, and 12 partial responses (PR), for an overall response rate (ORR) of 54%, reported Dr. Agnieszka Korfel from Charité University Medicine Berlin (Germany) and colleagues.
The median progression-free survival (PFS), however, was just 2.1 months, although 1 patient had PFS of 15.8 months duration, and another had a response lasting for more than 44 months, the investigators noted in a study published online in the Journal of Clinical Oncology (doi: 10.1200/JCO.2015.64.9897).
The rationale for trying temsirolimus (Torisel), an inhibitor of the mammalian target of rapamycin (mTOR), came from studies showing the drug’s efficacy against relapsed/refractory mantle-cell lymphoma and against other, more aggressive forms of non-Hodgkin lymphoma. Patients with relapsed/refractory aggressive lymphomas tolerate temsirolimus relatively well, and the drug has the ability to penetrate brain tumor tissue, the authors noted.
They enrolled 37 patients with a median age of 70 years and a median time since their last treatment of 3.9 months into an open-label trial. The patients were all immuncompetent with histologically confirmed primary central nervous system lymphoma for whom high-dose methotrexate-based chemotherapy had failed and for whom high-dose chemotherapy with autologous stem cell transplant had either failed or was not an option.
The first six patients were treated with temsirolimus 25 mg intravenously once weekly, and the remaining 31 were treated with 75 mg IV once weekly until disease progression, intolerable toxicity, patient or physician decision to terminate, or death.
As noted before, ORR, the primary endpoint, was 54%. Median overall survival (OS), a secondary endpoint, was 3.7 months, and 1-year and 2-year OS were 19% and 16.2%, respectively.
The most frequently occurring toxicities include hyperglycemia, myelosuppression, pneumonias and other infections, and fatigue. A total of 28 severe adverse events occurred in 21 patients, including infectious episodes, hospitalizations because of disease progression, deep-vein thromboses, hyperglycemia, and one case each of seizures, grade 4 thrombocytopenia, drug fever, hyponatremia, renal insufficiency, and atrial fibrillation.
“Although most responses were short lived, some patients achieved long-term control. Thus, further evaluation in combination with other drugs seems reasonable. However, one has to be aware of the risk of hematotoxicity and infections necessitating primary antibiotic prophylaxis. Definition of biomarkers allowing identification of potential responders and those who are at particular risk for toxicity would be highly desirable,” the investigators concluded.
Single-agent therapy with temsirolimus was active in patients with relapsed/refractory primary central nervous system lymphoma, but most of the responses were short lived, results of a phase II trial show.
Among 37 patients with primary CNS lymphoma (PCNSL) for whom firstline therapy had failed, there were five complete responses (CR), three CR unconfirmed, and 12 partial responses (PR), for an overall response rate (ORR) of 54%, reported Dr. Agnieszka Korfel from Charité University Medicine Berlin (Germany) and colleagues.
The median progression-free survival (PFS), however, was just 2.1 months, although 1 patient had PFS of 15.8 months duration, and another had a response lasting for more than 44 months, the investigators noted in a study published online in the Journal of Clinical Oncology (doi: 10.1200/JCO.2015.64.9897).
The rationale for trying temsirolimus (Torisel), an inhibitor of the mammalian target of rapamycin (mTOR), came from studies showing the drug’s efficacy against relapsed/refractory mantle-cell lymphoma and against other, more aggressive forms of non-Hodgkin lymphoma. Patients with relapsed/refractory aggressive lymphomas tolerate temsirolimus relatively well, and the drug has the ability to penetrate brain tumor tissue, the authors noted.
They enrolled 37 patients with a median age of 70 years and a median time since their last treatment of 3.9 months into an open-label trial. The patients were all immuncompetent with histologically confirmed primary central nervous system lymphoma for whom high-dose methotrexate-based chemotherapy had failed and for whom high-dose chemotherapy with autologous stem cell transplant had either failed or was not an option.
The first six patients were treated with temsirolimus 25 mg intravenously once weekly, and the remaining 31 were treated with 75 mg IV once weekly until disease progression, intolerable toxicity, patient or physician decision to terminate, or death.
As noted before, ORR, the primary endpoint, was 54%. Median overall survival (OS), a secondary endpoint, was 3.7 months, and 1-year and 2-year OS were 19% and 16.2%, respectively.
The most frequently occurring toxicities include hyperglycemia, myelosuppression, pneumonias and other infections, and fatigue. A total of 28 severe adverse events occurred in 21 patients, including infectious episodes, hospitalizations because of disease progression, deep-vein thromboses, hyperglycemia, and one case each of seizures, grade 4 thrombocytopenia, drug fever, hyponatremia, renal insufficiency, and atrial fibrillation.
“Although most responses were short lived, some patients achieved long-term control. Thus, further evaluation in combination with other drugs seems reasonable. However, one has to be aware of the risk of hematotoxicity and infections necessitating primary antibiotic prophylaxis. Definition of biomarkers allowing identification of potential responders and those who are at particular risk for toxicity would be highly desirable,” the investigators concluded.
Single-agent therapy with temsirolimus was active in patients with relapsed/refractory primary central nervous system lymphoma, but most of the responses were short lived, results of a phase II trial show.
Among 37 patients with primary CNS lymphoma (PCNSL) for whom firstline therapy had failed, there were five complete responses (CR), three CR unconfirmed, and 12 partial responses (PR), for an overall response rate (ORR) of 54%, reported Dr. Agnieszka Korfel from Charité University Medicine Berlin (Germany) and colleagues.
The median progression-free survival (PFS), however, was just 2.1 months, although 1 patient had PFS of 15.8 months duration, and another had a response lasting for more than 44 months, the investigators noted in a study published online in the Journal of Clinical Oncology (doi: 10.1200/JCO.2015.64.9897).
The rationale for trying temsirolimus (Torisel), an inhibitor of the mammalian target of rapamycin (mTOR), came from studies showing the drug’s efficacy against relapsed/refractory mantle-cell lymphoma and against other, more aggressive forms of non-Hodgkin lymphoma. Patients with relapsed/refractory aggressive lymphomas tolerate temsirolimus relatively well, and the drug has the ability to penetrate brain tumor tissue, the authors noted.
They enrolled 37 patients with a median age of 70 years and a median time since their last treatment of 3.9 months into an open-label trial. The patients were all immuncompetent with histologically confirmed primary central nervous system lymphoma for whom high-dose methotrexate-based chemotherapy had failed and for whom high-dose chemotherapy with autologous stem cell transplant had either failed or was not an option.
The first six patients were treated with temsirolimus 25 mg intravenously once weekly, and the remaining 31 were treated with 75 mg IV once weekly until disease progression, intolerable toxicity, patient or physician decision to terminate, or death.
As noted before, ORR, the primary endpoint, was 54%. Median overall survival (OS), a secondary endpoint, was 3.7 months, and 1-year and 2-year OS were 19% and 16.2%, respectively.
The most frequently occurring toxicities include hyperglycemia, myelosuppression, pneumonias and other infections, and fatigue. A total of 28 severe adverse events occurred in 21 patients, including infectious episodes, hospitalizations because of disease progression, deep-vein thromboses, hyperglycemia, and one case each of seizures, grade 4 thrombocytopenia, drug fever, hyponatremia, renal insufficiency, and atrial fibrillation.
“Although most responses were short lived, some patients achieved long-term control. Thus, further evaluation in combination with other drugs seems reasonable. However, one has to be aware of the risk of hematotoxicity and infections necessitating primary antibiotic prophylaxis. Definition of biomarkers allowing identification of potential responders and those who are at particular risk for toxicity would be highly desirable,” the investigators concluded.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Relapsed/refractory primary CNS lymphoma has a poor prognosis and no standard treatment option.
Major finding: The overall response rate to once-weekly temsirolimus was 54%; most responses were short lived.
Data source: Open-label phase 2 study in 37 adults with relapsed/refractory primary CNS lymphoma.
Disclosures: The study was supported by Pfizer Germany. Dr. Korfel and several colleagues disclosed research support from or consulting/advising for the company.