User login
ESMO gets creative with guidelines for breast cancer care in the COVID-19 era
Like other agencies, the European Society for Medical Oncology has developed guidelines for managing breast cancer patients during the COVID-19 pandemic, recommending when care should be prioritized, delayed, or modified.
ESMO’s breast cancer guidelines expand upon guidelines issued by other groups, addressing a broad spectrum of patient profiles and providing a creative array of treatment options in COVID-19–era clinical practice.
As with ESMO’s other disease-focused COVID-19 guidelines, the breast cancer guidelines are organized by priority levels – high, medium, and low – which are applied to several domains of diagnosis and treatment.
High-priority recommendations apply to patients whose condition is either clinically unstable or whose cancer burden is immediately life-threatening.
Medium-priority recommendations apply to patients for whom delaying care beyond 6 weeks would probably lower the likelihood of a significant benefit from the intervention.
Low-priority recommendations apply to patients for whom services can be delayed for the duration of the COVID-19 pandemic.
Personalized care and high-priority situations
ESMO’s guidelines suggest that multidisciplinary tumor boards should guide decisions about the urgency of care for individual patients, given the complexity of breast cancer biology, the multiplicity of evidence-based treatments, and the possibility of cure or durable high-quality remissions.
The guidelines deliver a clear message that prepandemic discussions about delivering personalized care are even more important now.
ESMO prioritizes investigating high-risk screening mammography results (i.e., BIRADS 5), lumps noted on breast self-examination, clinical evidence of local-regional recurrence, and breast cancer in pregnant women.
Making these scenarios “high priority” will facilitate the best long-term outcomes in time-sensitive scenarios and improve patient satisfaction with care.
Modifications to consider
ESMO provides explicit options for treatment of common breast cancer profiles in which short-term modifications of standard management strategies can safely be considered. Given the generally long natural history of most breast cancer subtypes, these temporary modifications are unlikely to compromise long-term outcomes.
For patients with a new diagnosis of localized breast cancer, the guidelines recommend neoadjuvant chemotherapy, targeted therapy, or hormonal therapy to achieve optimal breast cancer outcomes and safely delay surgery or radiotherapy.
In the metastatic setting, ESMO advises providers to consider:
- Symptom-oriented testing, recognizing the arguable benefit of frequent imaging or serum tumor marker measurement (J Clin Oncol. 2016 Aug 20;34[24]:2820-6).
- Drug holidays, de-escalated maintenance therapy, and protracted schedules of bone-modifying agents.
- Avoiding mTOR and PI3KCA inhibitors as an addition to standard hormonal therapy because of pneumonitis, hyperglycemia, and immunosuppression risks. The guidelines suggest careful thought about adding CDK4/6 inhibitors to standard hormonal therapy because of the added burden of remote safety monitoring with the biologic agents.
ESMO makes suggestions about trimming the duration of adjuvant trastuzumab to 6 months, as in the PERSEPHONE study (Lancet. 2019 Jun 29;393[10191]:2599-612), and modifying the schedule of luteinizing hormone–releasing hormone agonist administration, in an effort to reduce patient exposure to health care personnel (and vice versa).
The guidelines recommend continuing clinical trials if benefits to patients outweigh risks and trials can be modified to enhance patient safety while preserving study endpoint evaluations.
Lower-priority situations
ESMO pointedly assigns a low priority to follow-up of patients who are at high risk of relapse but lack signs or symptoms of relapse.
Like other groups, ESMO recommends that patients with equivocal (i.e., BIRADS 3) screening mammograms should have 6-month follow-up imaging in preference to immediate core needle biopsy of the area(s) of concern.
ESMO uses age to assign priority for postponing adjuvant breast radiation in patients with low- to moderate-risk lesions. However, the guidelines stop surprisingly short of recommending that adjuvant radiation be withheld for older patients with low-risk, stage I, hormonally sensitive, HER2-negative breast cancers who receive endocrine therapy.
Bottom line
The pragmatic adjustments ESMO suggests address the challenges of evaluating and treating breast cancer patients during the COVID-19 pandemic. The guidelines protect each patient’s right to care and safety as well as protecting the safety of caregivers.
The guidelines will likely heighten patients’ satisfaction with care and decrease concern about adequacy of timely evaluation and treatment.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Like other agencies, the European Society for Medical Oncology has developed guidelines for managing breast cancer patients during the COVID-19 pandemic, recommending when care should be prioritized, delayed, or modified.
ESMO’s breast cancer guidelines expand upon guidelines issued by other groups, addressing a broad spectrum of patient profiles and providing a creative array of treatment options in COVID-19–era clinical practice.
As with ESMO’s other disease-focused COVID-19 guidelines, the breast cancer guidelines are organized by priority levels – high, medium, and low – which are applied to several domains of diagnosis and treatment.
High-priority recommendations apply to patients whose condition is either clinically unstable or whose cancer burden is immediately life-threatening.
Medium-priority recommendations apply to patients for whom delaying care beyond 6 weeks would probably lower the likelihood of a significant benefit from the intervention.
Low-priority recommendations apply to patients for whom services can be delayed for the duration of the COVID-19 pandemic.
Personalized care and high-priority situations
ESMO’s guidelines suggest that multidisciplinary tumor boards should guide decisions about the urgency of care for individual patients, given the complexity of breast cancer biology, the multiplicity of evidence-based treatments, and the possibility of cure or durable high-quality remissions.
The guidelines deliver a clear message that prepandemic discussions about delivering personalized care are even more important now.
ESMO prioritizes investigating high-risk screening mammography results (i.e., BIRADS 5), lumps noted on breast self-examination, clinical evidence of local-regional recurrence, and breast cancer in pregnant women.
Making these scenarios “high priority” will facilitate the best long-term outcomes in time-sensitive scenarios and improve patient satisfaction with care.
Modifications to consider
ESMO provides explicit options for treatment of common breast cancer profiles in which short-term modifications of standard management strategies can safely be considered. Given the generally long natural history of most breast cancer subtypes, these temporary modifications are unlikely to compromise long-term outcomes.
For patients with a new diagnosis of localized breast cancer, the guidelines recommend neoadjuvant chemotherapy, targeted therapy, or hormonal therapy to achieve optimal breast cancer outcomes and safely delay surgery or radiotherapy.
In the metastatic setting, ESMO advises providers to consider:
- Symptom-oriented testing, recognizing the arguable benefit of frequent imaging or serum tumor marker measurement (J Clin Oncol. 2016 Aug 20;34[24]:2820-6).
- Drug holidays, de-escalated maintenance therapy, and protracted schedules of bone-modifying agents.
- Avoiding mTOR and PI3KCA inhibitors as an addition to standard hormonal therapy because of pneumonitis, hyperglycemia, and immunosuppression risks. The guidelines suggest careful thought about adding CDK4/6 inhibitors to standard hormonal therapy because of the added burden of remote safety monitoring with the biologic agents.
ESMO makes suggestions about trimming the duration of adjuvant trastuzumab to 6 months, as in the PERSEPHONE study (Lancet. 2019 Jun 29;393[10191]:2599-612), and modifying the schedule of luteinizing hormone–releasing hormone agonist administration, in an effort to reduce patient exposure to health care personnel (and vice versa).
The guidelines recommend continuing clinical trials if benefits to patients outweigh risks and trials can be modified to enhance patient safety while preserving study endpoint evaluations.
Lower-priority situations
ESMO pointedly assigns a low priority to follow-up of patients who are at high risk of relapse but lack signs or symptoms of relapse.
Like other groups, ESMO recommends that patients with equivocal (i.e., BIRADS 3) screening mammograms should have 6-month follow-up imaging in preference to immediate core needle biopsy of the area(s) of concern.
ESMO uses age to assign priority for postponing adjuvant breast radiation in patients with low- to moderate-risk lesions. However, the guidelines stop surprisingly short of recommending that adjuvant radiation be withheld for older patients with low-risk, stage I, hormonally sensitive, HER2-negative breast cancers who receive endocrine therapy.
Bottom line
The pragmatic adjustments ESMO suggests address the challenges of evaluating and treating breast cancer patients during the COVID-19 pandemic. The guidelines protect each patient’s right to care and safety as well as protecting the safety of caregivers.
The guidelines will likely heighten patients’ satisfaction with care and decrease concern about adequacy of timely evaluation and treatment.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Like other agencies, the European Society for Medical Oncology has developed guidelines for managing breast cancer patients during the COVID-19 pandemic, recommending when care should be prioritized, delayed, or modified.
ESMO’s breast cancer guidelines expand upon guidelines issued by other groups, addressing a broad spectrum of patient profiles and providing a creative array of treatment options in COVID-19–era clinical practice.
As with ESMO’s other disease-focused COVID-19 guidelines, the breast cancer guidelines are organized by priority levels – high, medium, and low – which are applied to several domains of diagnosis and treatment.
High-priority recommendations apply to patients whose condition is either clinically unstable or whose cancer burden is immediately life-threatening.
Medium-priority recommendations apply to patients for whom delaying care beyond 6 weeks would probably lower the likelihood of a significant benefit from the intervention.
Low-priority recommendations apply to patients for whom services can be delayed for the duration of the COVID-19 pandemic.
Personalized care and high-priority situations
ESMO’s guidelines suggest that multidisciplinary tumor boards should guide decisions about the urgency of care for individual patients, given the complexity of breast cancer biology, the multiplicity of evidence-based treatments, and the possibility of cure or durable high-quality remissions.
The guidelines deliver a clear message that prepandemic discussions about delivering personalized care are even more important now.
ESMO prioritizes investigating high-risk screening mammography results (i.e., BIRADS 5), lumps noted on breast self-examination, clinical evidence of local-regional recurrence, and breast cancer in pregnant women.
Making these scenarios “high priority” will facilitate the best long-term outcomes in time-sensitive scenarios and improve patient satisfaction with care.
Modifications to consider
ESMO provides explicit options for treatment of common breast cancer profiles in which short-term modifications of standard management strategies can safely be considered. Given the generally long natural history of most breast cancer subtypes, these temporary modifications are unlikely to compromise long-term outcomes.
For patients with a new diagnosis of localized breast cancer, the guidelines recommend neoadjuvant chemotherapy, targeted therapy, or hormonal therapy to achieve optimal breast cancer outcomes and safely delay surgery or radiotherapy.
In the metastatic setting, ESMO advises providers to consider:
- Symptom-oriented testing, recognizing the arguable benefit of frequent imaging or serum tumor marker measurement (J Clin Oncol. 2016 Aug 20;34[24]:2820-6).
- Drug holidays, de-escalated maintenance therapy, and protracted schedules of bone-modifying agents.
- Avoiding mTOR and PI3KCA inhibitors as an addition to standard hormonal therapy because of pneumonitis, hyperglycemia, and immunosuppression risks. The guidelines suggest careful thought about adding CDK4/6 inhibitors to standard hormonal therapy because of the added burden of remote safety monitoring with the biologic agents.
ESMO makes suggestions about trimming the duration of adjuvant trastuzumab to 6 months, as in the PERSEPHONE study (Lancet. 2019 Jun 29;393[10191]:2599-612), and modifying the schedule of luteinizing hormone–releasing hormone agonist administration, in an effort to reduce patient exposure to health care personnel (and vice versa).
The guidelines recommend continuing clinical trials if benefits to patients outweigh risks and trials can be modified to enhance patient safety while preserving study endpoint evaluations.
Lower-priority situations
ESMO pointedly assigns a low priority to follow-up of patients who are at high risk of relapse but lack signs or symptoms of relapse.
Like other groups, ESMO recommends that patients with equivocal (i.e., BIRADS 3) screening mammograms should have 6-month follow-up imaging in preference to immediate core needle biopsy of the area(s) of concern.
ESMO uses age to assign priority for postponing adjuvant breast radiation in patients with low- to moderate-risk lesions. However, the guidelines stop surprisingly short of recommending that adjuvant radiation be withheld for older patients with low-risk, stage I, hormonally sensitive, HER2-negative breast cancers who receive endocrine therapy.
Bottom line
The pragmatic adjustments ESMO suggests address the challenges of evaluating and treating breast cancer patients during the COVID-19 pandemic. The guidelines protect each patient’s right to care and safety as well as protecting the safety of caregivers.
The guidelines will likely heighten patients’ satisfaction with care and decrease concern about adequacy of timely evaluation and treatment.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
EHA webinar addresses treating AML patients with COVID-19
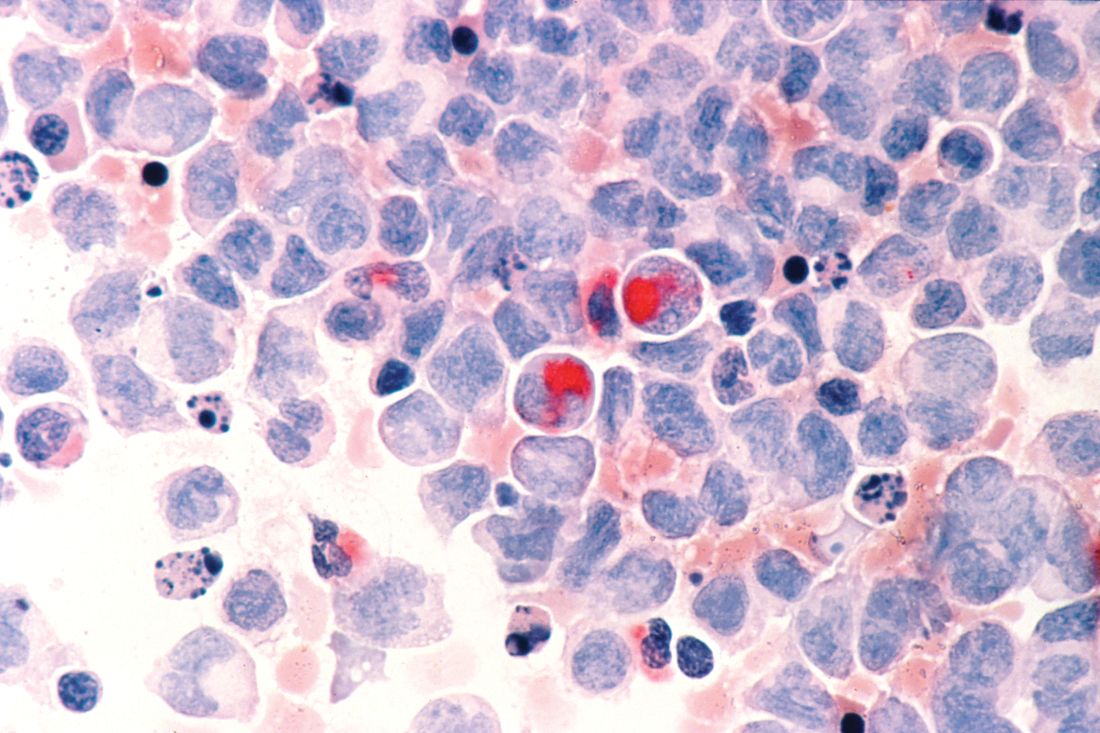
A hematologist in Italy shared his personal experience addressing the intersection of COVID-19 and the care of acute myeloid leukemia (AML) patients during a webinar hosted by the European Hematology Association (EHA).
Felicetto Ferrara, MD, of Cardarelli Hospital in Naples, Italy, discussed the main difficulties in administering optimal treatment for AML patients who become infected with SARS-CoV-2.
The major problems include the need to isolate patients while simultaneously allowing for collaboration with pulmonologists and intensivists, the delays in AML treatment caused by COVID-19, and the risk of drug-drug interactions while treating AML patients with COVID-19.
The need to isolate AML patients with COVID-19 is paramount, according to Dr. Ferrara. Isolation can be accomplished, ideally, by the creation of a dedicated COVID-19 unit or, alternatively, with the use of single-patient negative pressure rooms. Dr. Ferrara stressed that all patients with AML should be tested for COVID-19 before admission.
Delaying or reducing AML treatment
Treatment delays are of particular concern, according to Dr. Ferrara, and some patients may require dose reductions, especially for AML treatments that might have a detrimental effect on the immune system.
Decisions must be made as to whether planned approaches to induction or consolidation therapy should be changed, and special concern has to be paid to elderly AML patients, who have the highest risks of bad COVID-19 outcomes.
Specific attention should be paid to patients with acute promyelocytic leukemia as well, according to Dr. Ferrara. These patients are of concern in the COVID-19 era because of their risk of differentiation syndrome, which can induce respiratory distress.
In all cases, autologous or allogeneic stem cell transplant should be deferred until confirmed COVID-19–negative test results are obtained.
Continuing AML treatment
Of particular concern is the fact that, without a standard therapy for COVID-19, many different drugs might be used in treatment efforts. This raises the potential for serious drug-drug interactions with the patient’s AML medications, so close attention should be paid to an individual patient’s medications.
In terms of continuing AML treatment for younger adults (less than 65 years) who are positive for COVID-19, symptomatic and asymptomatic patients should be treated differently, Dr. Ferarra said.
Symptomatic patients should be given hydroxyurea until symptom resolution, and unless urgent, any further AML treatments should be delayed. However, if treatment is needed immediately, it should be given in a COVID-19–dedicated unit.
The restrictions are much looser for young adult asymptomatic COVID-19 patients with AML. Standard induction therapy should be given, with intermediate-dose cytarabine used as consolidation therapy.
Therapy in elderly patients with AML and COVID-19 should be based on symptom status as well, said Dr. Ferrara.
Asymptomatic but otherwise fit elderly patients should have standard induction therapy if they are in the European Leukemia Network favorable genetic subgroup. Asymptomatic elderly patients with high-risk molecular disease can receive venetoclax with a hypomethylating agent.
Symptomatic elderly patients should continue with hydroxyurea until symptom resolution, and any other treatments should be delayed in nonemergency cases.
Relapsed AML patients with COVID-19 should have their treatments postponed until they obtain negative COVID-19 test results whenever possible, Dr. Ferarra said. However, if treatment is necessary, molecularly targeted therapies (gilteritinib, ivosidenib, and enasidenib) are preferable to high-dose chemotherapy.
In all cases, treatment decisions should be made in conjunction with pulmonologists and intensivists, Dr. Ferrera noted.
Webinar moderator Francesco Cerisoli, MD, head of research and mentoring at EHA, highlighted the fact that EHA has published specific recommendations for treating AML patients during the COVID-19 pandemic. The majority of these were discussed by and are aligned with the recommendations presented by Dr. Ferrara.
The EHA webinar contains a disclaimer that the content discussed was based on the personal experiences and opinions of the speakers and that no general, evidence-based guidance could be derived from the discussion. There were no disclosures given.
A hematologist in Italy shared his personal experience addressing the intersection of COVID-19 and the care of acute myeloid leukemia (AML) patients during a webinar hosted by the European Hematology Association (EHA).
Felicetto Ferrara, MD, of Cardarelli Hospital in Naples, Italy, discussed the main difficulties in administering optimal treatment for AML patients who become infected with SARS-CoV-2.
The major problems include the need to isolate patients while simultaneously allowing for collaboration with pulmonologists and intensivists, the delays in AML treatment caused by COVID-19, and the risk of drug-drug interactions while treating AML patients with COVID-19.
The need to isolate AML patients with COVID-19 is paramount, according to Dr. Ferrara. Isolation can be accomplished, ideally, by the creation of a dedicated COVID-19 unit or, alternatively, with the use of single-patient negative pressure rooms. Dr. Ferrara stressed that all patients with AML should be tested for COVID-19 before admission.
Delaying or reducing AML treatment
Treatment delays are of particular concern, according to Dr. Ferrara, and some patients may require dose reductions, especially for AML treatments that might have a detrimental effect on the immune system.
Decisions must be made as to whether planned approaches to induction or consolidation therapy should be changed, and special concern has to be paid to elderly AML patients, who have the highest risks of bad COVID-19 outcomes.
Specific attention should be paid to patients with acute promyelocytic leukemia as well, according to Dr. Ferrara. These patients are of concern in the COVID-19 era because of their risk of differentiation syndrome, which can induce respiratory distress.
In all cases, autologous or allogeneic stem cell transplant should be deferred until confirmed COVID-19–negative test results are obtained.
Continuing AML treatment
Of particular concern is the fact that, without a standard therapy for COVID-19, many different drugs might be used in treatment efforts. This raises the potential for serious drug-drug interactions with the patient’s AML medications, so close attention should be paid to an individual patient’s medications.
In terms of continuing AML treatment for younger adults (less than 65 years) who are positive for COVID-19, symptomatic and asymptomatic patients should be treated differently, Dr. Ferarra said.
Symptomatic patients should be given hydroxyurea until symptom resolution, and unless urgent, any further AML treatments should be delayed. However, if treatment is needed immediately, it should be given in a COVID-19–dedicated unit.
The restrictions are much looser for young adult asymptomatic COVID-19 patients with AML. Standard induction therapy should be given, with intermediate-dose cytarabine used as consolidation therapy.
Therapy in elderly patients with AML and COVID-19 should be based on symptom status as well, said Dr. Ferrara.
Asymptomatic but otherwise fit elderly patients should have standard induction therapy if they are in the European Leukemia Network favorable genetic subgroup. Asymptomatic elderly patients with high-risk molecular disease can receive venetoclax with a hypomethylating agent.
Symptomatic elderly patients should continue with hydroxyurea until symptom resolution, and any other treatments should be delayed in nonemergency cases.
Relapsed AML patients with COVID-19 should have their treatments postponed until they obtain negative COVID-19 test results whenever possible, Dr. Ferarra said. However, if treatment is necessary, molecularly targeted therapies (gilteritinib, ivosidenib, and enasidenib) are preferable to high-dose chemotherapy.
In all cases, treatment decisions should be made in conjunction with pulmonologists and intensivists, Dr. Ferrera noted.
Webinar moderator Francesco Cerisoli, MD, head of research and mentoring at EHA, highlighted the fact that EHA has published specific recommendations for treating AML patients during the COVID-19 pandemic. The majority of these were discussed by and are aligned with the recommendations presented by Dr. Ferrara.
The EHA webinar contains a disclaimer that the content discussed was based on the personal experiences and opinions of the speakers and that no general, evidence-based guidance could be derived from the discussion. There were no disclosures given.
A hematologist in Italy shared his personal experience addressing the intersection of COVID-19 and the care of acute myeloid leukemia (AML) patients during a webinar hosted by the European Hematology Association (EHA).
Felicetto Ferrara, MD, of Cardarelli Hospital in Naples, Italy, discussed the main difficulties in administering optimal treatment for AML patients who become infected with SARS-CoV-2.
The major problems include the need to isolate patients while simultaneously allowing for collaboration with pulmonologists and intensivists, the delays in AML treatment caused by COVID-19, and the risk of drug-drug interactions while treating AML patients with COVID-19.
The need to isolate AML patients with COVID-19 is paramount, according to Dr. Ferrara. Isolation can be accomplished, ideally, by the creation of a dedicated COVID-19 unit or, alternatively, with the use of single-patient negative pressure rooms. Dr. Ferrara stressed that all patients with AML should be tested for COVID-19 before admission.
Delaying or reducing AML treatment
Treatment delays are of particular concern, according to Dr. Ferrara, and some patients may require dose reductions, especially for AML treatments that might have a detrimental effect on the immune system.
Decisions must be made as to whether planned approaches to induction or consolidation therapy should be changed, and special concern has to be paid to elderly AML patients, who have the highest risks of bad COVID-19 outcomes.
Specific attention should be paid to patients with acute promyelocytic leukemia as well, according to Dr. Ferrara. These patients are of concern in the COVID-19 era because of their risk of differentiation syndrome, which can induce respiratory distress.
In all cases, autologous or allogeneic stem cell transplant should be deferred until confirmed COVID-19–negative test results are obtained.
Continuing AML treatment
Of particular concern is the fact that, without a standard therapy for COVID-19, many different drugs might be used in treatment efforts. This raises the potential for serious drug-drug interactions with the patient’s AML medications, so close attention should be paid to an individual patient’s medications.
In terms of continuing AML treatment for younger adults (less than 65 years) who are positive for COVID-19, symptomatic and asymptomatic patients should be treated differently, Dr. Ferarra said.
Symptomatic patients should be given hydroxyurea until symptom resolution, and unless urgent, any further AML treatments should be delayed. However, if treatment is needed immediately, it should be given in a COVID-19–dedicated unit.
The restrictions are much looser for young adult asymptomatic COVID-19 patients with AML. Standard induction therapy should be given, with intermediate-dose cytarabine used as consolidation therapy.
Therapy in elderly patients with AML and COVID-19 should be based on symptom status as well, said Dr. Ferrara.
Asymptomatic but otherwise fit elderly patients should have standard induction therapy if they are in the European Leukemia Network favorable genetic subgroup. Asymptomatic elderly patients with high-risk molecular disease can receive venetoclax with a hypomethylating agent.
Symptomatic elderly patients should continue with hydroxyurea until symptom resolution, and any other treatments should be delayed in nonemergency cases.
Relapsed AML patients with COVID-19 should have their treatments postponed until they obtain negative COVID-19 test results whenever possible, Dr. Ferarra said. However, if treatment is necessary, molecularly targeted therapies (gilteritinib, ivosidenib, and enasidenib) are preferable to high-dose chemotherapy.
In all cases, treatment decisions should be made in conjunction with pulmonologists and intensivists, Dr. Ferrera noted.
Webinar moderator Francesco Cerisoli, MD, head of research and mentoring at EHA, highlighted the fact that EHA has published specific recommendations for treating AML patients during the COVID-19 pandemic. The majority of these were discussed by and are aligned with the recommendations presented by Dr. Ferrara.
The EHA webinar contains a disclaimer that the content discussed was based on the personal experiences and opinions of the speakers and that no general, evidence-based guidance could be derived from the discussion. There were no disclosures given.
COVID-19: Defer ‘bread and butter’ procedure for thyroid nodules
With a few notable exceptions, the majority of fine needle aspiration (FNA) biopsies of thyroid nodules should be delayed until the risk of COVID-19, and the burden on resources, has lessened, according to expert consensus.
“Our group recommends that FNA biopsy of most asymptomatic thyroid nodules – taking into account the sonographic characteristics and patients’ clinical picture – be deferred to a later time, when risk of exposure to COVID-19 is more manageable and resource restriction is no longer a concern,” said the endocrinologists, writing in a guest editorial in Clinical Thyroidology.
All elective procedures have been canceled under guidance of the Centers for Disease Control and Prevention, in conjunction with the U.S. surgeon general, in response to the COVID-19 pandemic. However, thyroid nodule FNAs, though elective, fall into the category of being considered medically necessary and potentially prolonging life expectancy
Yet, with approximately 90% of asymptomatic thyroid nodules turning out to be benign and little evidence that early detection and treatment affects disease outcomes, there is a strong argument for deferral in most cases, stressed Ming Lee, MD, and colleagues, of the endocrinology division at Phoenix (Ariz.) Veterans Affairs Health Care System (PVAHCS), who convened a multidisciplinary meeting to address the urgent issue.
Patients should instead be interviewed by an endocrinologist (preferably via telehealth) to collect their clinical history as well as assess their perception of the disease and risk of malignancy, senior author S. Mitchell Harman, MD, chief of PVAHCS, said in an interview.
“The principal guiding factor should be the objectively assessed likelihood of malignancy of the individual patient’s nodule(s),” he said.
“In my opinion, we should also factor in the patient’s level of anxiety, since some patients are more sanguine about risk than others and our goal is to provide relief of anxiety as well as to determine need for, and course of, subsequent treatment,” Dr. Harman added.
Vast majority of malignant thyroid nodules are DTC, which is ‘indolent’
Dr. Lee and colleagues noted that, even of the 10% of thyroid nodules that do prove to be malignant, the vast majority of these (90%) are differentiated thyroid cancers (DTC). In general, patients with DTC “follow an indolent course and have excellent outcomes.”
“There is little evidence that early detection and treatment of DTC significantly alters disease outcomes as the overall mortality rate for DTC has remained low, at around 0.5%,” they wrote.
They also noted that ultrasound features of thyroid nodules can help guide priority for the future timing of an FNA procedure, but should not be the sole basis for deciding on immediate thyroid FNA or surgery.
Exceptions to the rule
Exceptions for considering FNA include more urgent thyroid disease diagnoses, including those that are symptomatic:
Suspected medullary thyroid cancer
“Regarding medullary thyroid cancer (MTC), early diagnosis and surgery do significantly improve outcomes, therefore, delaying FNA of nodules harboring MTC could be potentially injurious,” the authors said.
They suggested, however, measuring calcitonin levels instead, which they noted “is still controversial” in the United States, but “we feel it would be justified in patients with thyroid nodules that would usually be indicated for FNA.”
Those with a family history of MTC, or nodules located in the posterior upper third of lateral lobes (the usual location of MTC), should have calcitonin levels measured.
If calcitonin levels are above 10 pg/mL, “FNA should be offered as early as possible.”
“Significantly elevated serum calcitonin levels (e.g., > 100 pg/mL) should be considered an indication for surgery without cytologic confirmation by FNA,” they added.
Anaplastic thyroid cancer
Anaplastic thyroid cancer, though rare, “is one of the few occasions when thyroid surgery should be performed on an urgent basis, as this condition can worsen very rapidly.
“Patients typically present with a rapidly enlarging thyroid mass that is associated with compressive symptoms, such as dysphagia and dyspnea,” they observed.
In this instance, although FNA is part of the preoperative work-up, it is often nondiagnostic and could require additional sampling.
“At the time of this pandemic, it is reasonable that after a multidisciplinary discussion, such patients with the appropriate clinical scenario be referred for thyroid surgery, with or without prior FNA, based on the team’s judgment,” the authors recommended.
Long-standing thyroid masses
These are usually large and/or closely associated with vital structures, such as the trachea and esophagus, and when such masses cause compressive symptoms, thyroid surgery typically is warranted.
And although prior FNA is helpful to obtain a cytologic diagnosis, as this may change the extent of surgery, it may not always be essential.
Broadly, symptomatic patients with compressive symptoms threatening vital structures can be directly referred to a surgeon, with the timing for surgery jointly decided based on the severity of symptoms, rapidity of disease progression, local COVID-19 status, and available resources.
“During the pandemic, we believe that the vast majority of thyroid FNAs should be considered optional, and extent of surgery can be determined by pathological analysis of frozen sections intraoperatively,” they wrote.
“The value of FNA in these situations is less compelling in the current COVID-19 setting, as the basis of decision for surgery has been already determined,” the authors explained.
If urgent FNA needed, screen patient for COVID-19 and use PPE
Should the need for an urgent thyroid FNA occur, patients should be screened and tested for COVID-19 by a clinician wearing personal protective equipment (PPE), said Dr. Lee and colleagues.
“It is crucial to carefully weigh the risks of COVID-19 exposure, availability of resources, and urgency of these procedures for each patient in our individual practice settings,” they noted.
As restrictions eventually loosen, precautions will still be necessary to some degree, Dr. Harman said.
“I do not consider FNA a ‘high-risk’ procedure in the era of COVID-19, since it does not routinely result in profuse aerosolization of respiratory fluids,” he said in an interview.
“However, patients do sometimes cough or choke due to pressure on the neck and the operator is, of necessity, very close to the patient’s face. Therefore, when we resume FNA, patients will be screened for symptoms of COVID-19 infection and both the operator and the patient will be masked,” Dr. Harman continued.
“We routinely wear gloves, [and] whether the operator will wear a surgical or an N95 mask, disposable gown, etc, will depend on CDC guidance and guidance received from our VA infectious disease experts as it is applied specifically to each patient evaluation.”
The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
With a few notable exceptions, the majority of fine needle aspiration (FNA) biopsies of thyroid nodules should be delayed until the risk of COVID-19, and the burden on resources, has lessened, according to expert consensus.
“Our group recommends that FNA biopsy of most asymptomatic thyroid nodules – taking into account the sonographic characteristics and patients’ clinical picture – be deferred to a later time, when risk of exposure to COVID-19 is more manageable and resource restriction is no longer a concern,” said the endocrinologists, writing in a guest editorial in Clinical Thyroidology.
All elective procedures have been canceled under guidance of the Centers for Disease Control and Prevention, in conjunction with the U.S. surgeon general, in response to the COVID-19 pandemic. However, thyroid nodule FNAs, though elective, fall into the category of being considered medically necessary and potentially prolonging life expectancy
Yet, with approximately 90% of asymptomatic thyroid nodules turning out to be benign and little evidence that early detection and treatment affects disease outcomes, there is a strong argument for deferral in most cases, stressed Ming Lee, MD, and colleagues, of the endocrinology division at Phoenix (Ariz.) Veterans Affairs Health Care System (PVAHCS), who convened a multidisciplinary meeting to address the urgent issue.
Patients should instead be interviewed by an endocrinologist (preferably via telehealth) to collect their clinical history as well as assess their perception of the disease and risk of malignancy, senior author S. Mitchell Harman, MD, chief of PVAHCS, said in an interview.
“The principal guiding factor should be the objectively assessed likelihood of malignancy of the individual patient’s nodule(s),” he said.
“In my opinion, we should also factor in the patient’s level of anxiety, since some patients are more sanguine about risk than others and our goal is to provide relief of anxiety as well as to determine need for, and course of, subsequent treatment,” Dr. Harman added.
Vast majority of malignant thyroid nodules are DTC, which is ‘indolent’
Dr. Lee and colleagues noted that, even of the 10% of thyroid nodules that do prove to be malignant, the vast majority of these (90%) are differentiated thyroid cancers (DTC). In general, patients with DTC “follow an indolent course and have excellent outcomes.”
“There is little evidence that early detection and treatment of DTC significantly alters disease outcomes as the overall mortality rate for DTC has remained low, at around 0.5%,” they wrote.
They also noted that ultrasound features of thyroid nodules can help guide priority for the future timing of an FNA procedure, but should not be the sole basis for deciding on immediate thyroid FNA or surgery.
Exceptions to the rule
Exceptions for considering FNA include more urgent thyroid disease diagnoses, including those that are symptomatic:
Suspected medullary thyroid cancer
“Regarding medullary thyroid cancer (MTC), early diagnosis and surgery do significantly improve outcomes, therefore, delaying FNA of nodules harboring MTC could be potentially injurious,” the authors said.
They suggested, however, measuring calcitonin levels instead, which they noted “is still controversial” in the United States, but “we feel it would be justified in patients with thyroid nodules that would usually be indicated for FNA.”
Those with a family history of MTC, or nodules located in the posterior upper third of lateral lobes (the usual location of MTC), should have calcitonin levels measured.
If calcitonin levels are above 10 pg/mL, “FNA should be offered as early as possible.”
“Significantly elevated serum calcitonin levels (e.g., > 100 pg/mL) should be considered an indication for surgery without cytologic confirmation by FNA,” they added.
Anaplastic thyroid cancer
Anaplastic thyroid cancer, though rare, “is one of the few occasions when thyroid surgery should be performed on an urgent basis, as this condition can worsen very rapidly.
“Patients typically present with a rapidly enlarging thyroid mass that is associated with compressive symptoms, such as dysphagia and dyspnea,” they observed.
In this instance, although FNA is part of the preoperative work-up, it is often nondiagnostic and could require additional sampling.
“At the time of this pandemic, it is reasonable that after a multidisciplinary discussion, such patients with the appropriate clinical scenario be referred for thyroid surgery, with or without prior FNA, based on the team’s judgment,” the authors recommended.
Long-standing thyroid masses
These are usually large and/or closely associated with vital structures, such as the trachea and esophagus, and when such masses cause compressive symptoms, thyroid surgery typically is warranted.
And although prior FNA is helpful to obtain a cytologic diagnosis, as this may change the extent of surgery, it may not always be essential.
Broadly, symptomatic patients with compressive symptoms threatening vital structures can be directly referred to a surgeon, with the timing for surgery jointly decided based on the severity of symptoms, rapidity of disease progression, local COVID-19 status, and available resources.
“During the pandemic, we believe that the vast majority of thyroid FNAs should be considered optional, and extent of surgery can be determined by pathological analysis of frozen sections intraoperatively,” they wrote.
“The value of FNA in these situations is less compelling in the current COVID-19 setting, as the basis of decision for surgery has been already determined,” the authors explained.
If urgent FNA needed, screen patient for COVID-19 and use PPE
Should the need for an urgent thyroid FNA occur, patients should be screened and tested for COVID-19 by a clinician wearing personal protective equipment (PPE), said Dr. Lee and colleagues.
“It is crucial to carefully weigh the risks of COVID-19 exposure, availability of resources, and urgency of these procedures for each patient in our individual practice settings,” they noted.
As restrictions eventually loosen, precautions will still be necessary to some degree, Dr. Harman said.
“I do not consider FNA a ‘high-risk’ procedure in the era of COVID-19, since it does not routinely result in profuse aerosolization of respiratory fluids,” he said in an interview.
“However, patients do sometimes cough or choke due to pressure on the neck and the operator is, of necessity, very close to the patient’s face. Therefore, when we resume FNA, patients will be screened for symptoms of COVID-19 infection and both the operator and the patient will be masked,” Dr. Harman continued.
“We routinely wear gloves, [and] whether the operator will wear a surgical or an N95 mask, disposable gown, etc, will depend on CDC guidance and guidance received from our VA infectious disease experts as it is applied specifically to each patient evaluation.”
The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
With a few notable exceptions, the majority of fine needle aspiration (FNA) biopsies of thyroid nodules should be delayed until the risk of COVID-19, and the burden on resources, has lessened, according to expert consensus.
“Our group recommends that FNA biopsy of most asymptomatic thyroid nodules – taking into account the sonographic characteristics and patients’ clinical picture – be deferred to a later time, when risk of exposure to COVID-19 is more manageable and resource restriction is no longer a concern,” said the endocrinologists, writing in a guest editorial in Clinical Thyroidology.
All elective procedures have been canceled under guidance of the Centers for Disease Control and Prevention, in conjunction with the U.S. surgeon general, in response to the COVID-19 pandemic. However, thyroid nodule FNAs, though elective, fall into the category of being considered medically necessary and potentially prolonging life expectancy
Yet, with approximately 90% of asymptomatic thyroid nodules turning out to be benign and little evidence that early detection and treatment affects disease outcomes, there is a strong argument for deferral in most cases, stressed Ming Lee, MD, and colleagues, of the endocrinology division at Phoenix (Ariz.) Veterans Affairs Health Care System (PVAHCS), who convened a multidisciplinary meeting to address the urgent issue.
Patients should instead be interviewed by an endocrinologist (preferably via telehealth) to collect their clinical history as well as assess their perception of the disease and risk of malignancy, senior author S. Mitchell Harman, MD, chief of PVAHCS, said in an interview.
“The principal guiding factor should be the objectively assessed likelihood of malignancy of the individual patient’s nodule(s),” he said.
“In my opinion, we should also factor in the patient’s level of anxiety, since some patients are more sanguine about risk than others and our goal is to provide relief of anxiety as well as to determine need for, and course of, subsequent treatment,” Dr. Harman added.
Vast majority of malignant thyroid nodules are DTC, which is ‘indolent’
Dr. Lee and colleagues noted that, even of the 10% of thyroid nodules that do prove to be malignant, the vast majority of these (90%) are differentiated thyroid cancers (DTC). In general, patients with DTC “follow an indolent course and have excellent outcomes.”
“There is little evidence that early detection and treatment of DTC significantly alters disease outcomes as the overall mortality rate for DTC has remained low, at around 0.5%,” they wrote.
They also noted that ultrasound features of thyroid nodules can help guide priority for the future timing of an FNA procedure, but should not be the sole basis for deciding on immediate thyroid FNA or surgery.
Exceptions to the rule
Exceptions for considering FNA include more urgent thyroid disease diagnoses, including those that are symptomatic:
Suspected medullary thyroid cancer
“Regarding medullary thyroid cancer (MTC), early diagnosis and surgery do significantly improve outcomes, therefore, delaying FNA of nodules harboring MTC could be potentially injurious,” the authors said.
They suggested, however, measuring calcitonin levels instead, which they noted “is still controversial” in the United States, but “we feel it would be justified in patients with thyroid nodules that would usually be indicated for FNA.”
Those with a family history of MTC, or nodules located in the posterior upper third of lateral lobes (the usual location of MTC), should have calcitonin levels measured.
If calcitonin levels are above 10 pg/mL, “FNA should be offered as early as possible.”
“Significantly elevated serum calcitonin levels (e.g., > 100 pg/mL) should be considered an indication for surgery without cytologic confirmation by FNA,” they added.
Anaplastic thyroid cancer
Anaplastic thyroid cancer, though rare, “is one of the few occasions when thyroid surgery should be performed on an urgent basis, as this condition can worsen very rapidly.
“Patients typically present with a rapidly enlarging thyroid mass that is associated with compressive symptoms, such as dysphagia and dyspnea,” they observed.
In this instance, although FNA is part of the preoperative work-up, it is often nondiagnostic and could require additional sampling.
“At the time of this pandemic, it is reasonable that after a multidisciplinary discussion, such patients with the appropriate clinical scenario be referred for thyroid surgery, with or without prior FNA, based on the team’s judgment,” the authors recommended.
Long-standing thyroid masses
These are usually large and/or closely associated with vital structures, such as the trachea and esophagus, and when such masses cause compressive symptoms, thyroid surgery typically is warranted.
And although prior FNA is helpful to obtain a cytologic diagnosis, as this may change the extent of surgery, it may not always be essential.
Broadly, symptomatic patients with compressive symptoms threatening vital structures can be directly referred to a surgeon, with the timing for surgery jointly decided based on the severity of symptoms, rapidity of disease progression, local COVID-19 status, and available resources.
“During the pandemic, we believe that the vast majority of thyroid FNAs should be considered optional, and extent of surgery can be determined by pathological analysis of frozen sections intraoperatively,” they wrote.
“The value of FNA in these situations is less compelling in the current COVID-19 setting, as the basis of decision for surgery has been already determined,” the authors explained.
If urgent FNA needed, screen patient for COVID-19 and use PPE
Should the need for an urgent thyroid FNA occur, patients should be screened and tested for COVID-19 by a clinician wearing personal protective equipment (PPE), said Dr. Lee and colleagues.
“It is crucial to carefully weigh the risks of COVID-19 exposure, availability of resources, and urgency of these procedures for each patient in our individual practice settings,” they noted.
As restrictions eventually loosen, precautions will still be necessary to some degree, Dr. Harman said.
“I do not consider FNA a ‘high-risk’ procedure in the era of COVID-19, since it does not routinely result in profuse aerosolization of respiratory fluids,” he said in an interview.
“However, patients do sometimes cough or choke due to pressure on the neck and the operator is, of necessity, very close to the patient’s face. Therefore, when we resume FNA, patients will be screened for symptoms of COVID-19 infection and both the operator and the patient will be masked,” Dr. Harman continued.
“We routinely wear gloves, [and] whether the operator will wear a surgical or an N95 mask, disposable gown, etc, will depend on CDC guidance and guidance received from our VA infectious disease experts as it is applied specifically to each patient evaluation.”
The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19 decimates outpatient visits
There has been a massive decline in outpatient office visits as patients have stayed home – likely deferring needed care – because of COVID-19, new research shows.
The number of visits to ambulatory practices dropped by a whopping 60% in mid-March, and continues to be down by at least 50% since early February, according to new data compiled and analyzed by Harvard University and Phreesia, a health care technology company.
Phreesia – which helps medical practices with patient registration, insurance verification, and payments – has data on 50,000 providers in all 50 states; in a typical year, Phreesia tracks 50 million outpatient visits.
The report was published online April 23 by the Commonwealth Fund.
The company captured data on visits from February 1 through April 16. The decline was greatest in New England and the Mid-Atlantic states, where, at the steepest end of the decline in late March, visits were down 66%.
They have rebounded slightly since then but are still down 64%. Practices in the mountain states had the smallest decline, but visits were down by 45% as of April 16.
Many practices have attempted to reach out to patients through telemedicine. As of April 16, about 30% of all visits tracked by Phreesia were provided via telemedicine – by phone or through video. That’s a monumental increase from mid-February, when zero visits were conducted virtually.
However, the Harvard researchers found that telemedicine visits barely made up for the huge decline in office visits.
Decline by specialty
Not surprisingly, declining visits have been steeper in procedure-oriented specialties.
Overall visits – including telemedicine – to ophthalmologists and otolaryngologists had declined by 79% and 75%, respectively, as of the week of April 5. Dermatology saw a 73% decline. Surgery, pulmonology, urology, orthopedics, cardiology, and gastroenterology all experienced declines ranging from 61% to 66%.
Primary care offices, oncology, endocrinology, and obstetrics/gynecology all fared slightly better, with visits down by half. Behavioral health experienced the lowest rate of decline (30%).
School-aged children were skipping care most often. The study showed a 71% drop in visits in 7- to 17-year-olds, and a 59% decline in visits by neonates, infants, and toddlers (up to age 6). Overall, pediatric practices experienced a 62% drop-off in visits.
Nearly two-thirds of Americans over age 65 also stayed away from their doctors. Only half of those aged 18 to 64 reduced their physician visits.
This article first appeared on Medscape.com.
There has been a massive decline in outpatient office visits as patients have stayed home – likely deferring needed care – because of COVID-19, new research shows.
The number of visits to ambulatory practices dropped by a whopping 60% in mid-March, and continues to be down by at least 50% since early February, according to new data compiled and analyzed by Harvard University and Phreesia, a health care technology company.
Phreesia – which helps medical practices with patient registration, insurance verification, and payments – has data on 50,000 providers in all 50 states; in a typical year, Phreesia tracks 50 million outpatient visits.
The report was published online April 23 by the Commonwealth Fund.
The company captured data on visits from February 1 through April 16. The decline was greatest in New England and the Mid-Atlantic states, where, at the steepest end of the decline in late March, visits were down 66%.
They have rebounded slightly since then but are still down 64%. Practices in the mountain states had the smallest decline, but visits were down by 45% as of April 16.
Many practices have attempted to reach out to patients through telemedicine. As of April 16, about 30% of all visits tracked by Phreesia were provided via telemedicine – by phone or through video. That’s a monumental increase from mid-February, when zero visits were conducted virtually.
However, the Harvard researchers found that telemedicine visits barely made up for the huge decline in office visits.
Decline by specialty
Not surprisingly, declining visits have been steeper in procedure-oriented specialties.
Overall visits – including telemedicine – to ophthalmologists and otolaryngologists had declined by 79% and 75%, respectively, as of the week of April 5. Dermatology saw a 73% decline. Surgery, pulmonology, urology, orthopedics, cardiology, and gastroenterology all experienced declines ranging from 61% to 66%.
Primary care offices, oncology, endocrinology, and obstetrics/gynecology all fared slightly better, with visits down by half. Behavioral health experienced the lowest rate of decline (30%).
School-aged children were skipping care most often. The study showed a 71% drop in visits in 7- to 17-year-olds, and a 59% decline in visits by neonates, infants, and toddlers (up to age 6). Overall, pediatric practices experienced a 62% drop-off in visits.
Nearly two-thirds of Americans over age 65 also stayed away from their doctors. Only half of those aged 18 to 64 reduced their physician visits.
This article first appeared on Medscape.com.
There has been a massive decline in outpatient office visits as patients have stayed home – likely deferring needed care – because of COVID-19, new research shows.
The number of visits to ambulatory practices dropped by a whopping 60% in mid-March, and continues to be down by at least 50% since early February, according to new data compiled and analyzed by Harvard University and Phreesia, a health care technology company.
Phreesia – which helps medical practices with patient registration, insurance verification, and payments – has data on 50,000 providers in all 50 states; in a typical year, Phreesia tracks 50 million outpatient visits.
The report was published online April 23 by the Commonwealth Fund.
The company captured data on visits from February 1 through April 16. The decline was greatest in New England and the Mid-Atlantic states, where, at the steepest end of the decline in late March, visits were down 66%.
They have rebounded slightly since then but are still down 64%. Practices in the mountain states had the smallest decline, but visits were down by 45% as of April 16.
Many practices have attempted to reach out to patients through telemedicine. As of April 16, about 30% of all visits tracked by Phreesia were provided via telemedicine – by phone or through video. That’s a monumental increase from mid-February, when zero visits were conducted virtually.
However, the Harvard researchers found that telemedicine visits barely made up for the huge decline in office visits.
Decline by specialty
Not surprisingly, declining visits have been steeper in procedure-oriented specialties.
Overall visits – including telemedicine – to ophthalmologists and otolaryngologists had declined by 79% and 75%, respectively, as of the week of April 5. Dermatology saw a 73% decline. Surgery, pulmonology, urology, orthopedics, cardiology, and gastroenterology all experienced declines ranging from 61% to 66%.
Primary care offices, oncology, endocrinology, and obstetrics/gynecology all fared slightly better, with visits down by half. Behavioral health experienced the lowest rate of decline (30%).
School-aged children were skipping care most often. The study showed a 71% drop in visits in 7- to 17-year-olds, and a 59% decline in visits by neonates, infants, and toddlers (up to age 6). Overall, pediatric practices experienced a 62% drop-off in visits.
Nearly two-thirds of Americans over age 65 also stayed away from their doctors. Only half of those aged 18 to 64 reduced their physician visits.
This article first appeared on Medscape.com.
ASCO panel outlines cancer care challenges during COVID-19 pandemic
The COVID-19 pandemic continues to exact a heavy price on cancer patients, cancer care, and clinical trials, an expert panel reported during a presscast.
“Limited data available thus far are sobering: In Italy, about 20% of COVID-related deaths occurred in people with cancer, and, in China, COVID-19 patients who had cancer were about five times more likely than others to die or be placed on a ventilator in an intensive care unit,” said Howard A “Skip” Burris, MD, president of the American Society of Clinical Oncology and president and CEO of the Sarah Cannon Cancer Institute in Nashville, Tenn.
“We also have little evidence on returning COVID-19 patients with cancer. Physicians have to rely on limited data, anecdotal reports, and their own professional expertise” regarding the extent of increased risk to cancer patients with COVID-19, whether to interrupt or modify treatment, and the effects of cancer on recovery from COVID-19 infection, Dr. Burris said during the ASCO-sponsored online presscast.
Care of COVID-free patients
For cancer patients without COVID-19, the picture is equally dim, with the prospect of delayed surgery, chemotherapy, or screening; shortages of medications and equipment needed for critical care; the shift to telemedicine that may increase patient anxiety; and the potential loss of access to innovative therapies through clinical trials, Dr. Burris said.
“We’re concerned that some hospitals have effectively deemed all cancer surgeries to be elective, requiring them to be postponed. For patients with fast-moving or hard-to-treat cancer, this delay may be devastating,” he said.
Dr. Burris also cited concerns about delayed cancer diagnosis. “In a typical month, roughly 150,000 Americans are diagnosed with cancer. But right now, routine screening visits are postponed, and patients with pain or other warning signs may put off a doctor’s visit because of social distancing,” he said.
The pandemic has also exacerbated shortages of sedatives and opioid analgesics required for intubation and mechanical ventilation of patients.
Trials halted or slowed
Dr. Burris also briefly discussed results of a new survey, which were posted online ahead of publication in JCO Oncology Practice. The survey showed that, of 14 academic and 18 community-based cancer programs, 59.4% reported halting screening and/or enrollment for at least some clinical trials and suspending research-based clinical visits except for those where cancer treatment was delivered.
“Half of respondents reported ceasing research-only blood and/or tissue collections,” the authors of the article reported.
“Trial interruptions are devastating news for thousands of patients; in many cases, clinical trials are the best or only appropriate option for care,” Dr. Burris said.
The article authors, led by David Waterhouse, MD, of Oncology Hematology Care in Cincinnati, pointed to a silver lining in the pandemic cloud in the form of opportunities to improve clinical trials going forward.
“Nearly all respondents (90.3%) identified telehealth visits for participants as a potential improvement to clinical trial conduct, and more than three-quarters (77.4%) indicated that remote patient review of symptoms held similar potential,” the authors wrote.
Other potential improvements included remote site visits from trial sponsors and/or contract research organizations, more efficient study enrollment through secure electronic platforms, direct shipment of oral drugs to patients, remote assessments of adverse events, and streamlined data collection.
Lessons from the front lines
Another member of the presscast panel, Melissa Dillmon, MD, of the Harbin Clinic Cancer Center in Rome, Georgia, described the experience of community oncologists during the pandemic.
Her community, located in northeastern Georgia, experienced a COVID-19 outbreak in early March linked to services at two large churches. Community public health authorities issued a shelter-in-place order before the state government issued stay-at-home guidelines and shuttered all but essential business, some of which were allowed by state order to reopen as of April 24.
Dr. Dillmon’s center began screening patients for COVID-19 symptoms at the door, limited visitors or companions, instituted virtual visits and tumor boards, and set up a cancer treatment triage system that would allow essential surgeries to proceed and most infusions to continue, while delaying the start of chemotherapy when possible.
“We have encouraged patients to continue on treatment, especially if treatment is being given with curative intent, or if the cancer is responding well already to treatment,” she said.
The center, located in a community with a high prevalence of comorbidities and high incidence of lung cancer, has seen a sharp decline in colonoscopies, mammograms, and lung scans as patient shelter in place.
“We have great concerns about patients missing their screening lung scans, as this program has already proven to be finding earlier lung cancers that are curable,” Dr. Dillmon said.
A view from Washington state
Another panel member, Gary Lyman, MD, of the Fred Hutchinson Cancer Research Center in Seattle, described the response by the state of Washington, the initial epicenter of the COVID-19 outbreak in the United States.
Following identification of infections in hospitalized patients and at a nursing home in Kirkland, Washington, “our response, which began in early March and progressed through the second and third week in March at the state level, was to restrict large gatherings; progressively, schools were closed; larger businesses closed; and, by March 23, a stay-at-home policy was implemented, and all nonessential businesses were closed,” Dr. Lyman said.
“We believe, based on what has happened since that time, that this has considerably flattened the curve,” he continued.
Lessons from the Washington experience include the need to plan for a long-term disruption or alteration of cancer care, expand COVID-19 testing to all patients coming into hospitals or major clinics, institute aggressive supportive care measures, prepare for subsequent waves of infection, collect and share data, and, for remote or rural areas, identify lifelines to needed resources, Dr. Lyman said.
ASCO resources
Also speaking at the presscast, Jonathan Marron, MD, of Boston Children’s Hospital and Harvard Medical School, Boston, outlined ASCO’s guidance on allocation of scarce resources during the COVID-19 pandemic.
Richard L. Schilsky, MD, ASCO chief medical officer and executive vice president, outlined community-wide collaborations, data initiatives, and online resources for both clinicians and patients.
The COVID-19 pandemic continues to exact a heavy price on cancer patients, cancer care, and clinical trials, an expert panel reported during a presscast.
“Limited data available thus far are sobering: In Italy, about 20% of COVID-related deaths occurred in people with cancer, and, in China, COVID-19 patients who had cancer were about five times more likely than others to die or be placed on a ventilator in an intensive care unit,” said Howard A “Skip” Burris, MD, president of the American Society of Clinical Oncology and president and CEO of the Sarah Cannon Cancer Institute in Nashville, Tenn.
“We also have little evidence on returning COVID-19 patients with cancer. Physicians have to rely on limited data, anecdotal reports, and their own professional expertise” regarding the extent of increased risk to cancer patients with COVID-19, whether to interrupt or modify treatment, and the effects of cancer on recovery from COVID-19 infection, Dr. Burris said during the ASCO-sponsored online presscast.
Care of COVID-free patients
For cancer patients without COVID-19, the picture is equally dim, with the prospect of delayed surgery, chemotherapy, or screening; shortages of medications and equipment needed for critical care; the shift to telemedicine that may increase patient anxiety; and the potential loss of access to innovative therapies through clinical trials, Dr. Burris said.
“We’re concerned that some hospitals have effectively deemed all cancer surgeries to be elective, requiring them to be postponed. For patients with fast-moving or hard-to-treat cancer, this delay may be devastating,” he said.
Dr. Burris also cited concerns about delayed cancer diagnosis. “In a typical month, roughly 150,000 Americans are diagnosed with cancer. But right now, routine screening visits are postponed, and patients with pain or other warning signs may put off a doctor’s visit because of social distancing,” he said.
The pandemic has also exacerbated shortages of sedatives and opioid analgesics required for intubation and mechanical ventilation of patients.
Trials halted or slowed
Dr. Burris also briefly discussed results of a new survey, which were posted online ahead of publication in JCO Oncology Practice. The survey showed that, of 14 academic and 18 community-based cancer programs, 59.4% reported halting screening and/or enrollment for at least some clinical trials and suspending research-based clinical visits except for those where cancer treatment was delivered.
“Half of respondents reported ceasing research-only blood and/or tissue collections,” the authors of the article reported.
“Trial interruptions are devastating news for thousands of patients; in many cases, clinical trials are the best or only appropriate option for care,” Dr. Burris said.
The article authors, led by David Waterhouse, MD, of Oncology Hematology Care in Cincinnati, pointed to a silver lining in the pandemic cloud in the form of opportunities to improve clinical trials going forward.
“Nearly all respondents (90.3%) identified telehealth visits for participants as a potential improvement to clinical trial conduct, and more than three-quarters (77.4%) indicated that remote patient review of symptoms held similar potential,” the authors wrote.
Other potential improvements included remote site visits from trial sponsors and/or contract research organizations, more efficient study enrollment through secure electronic platforms, direct shipment of oral drugs to patients, remote assessments of adverse events, and streamlined data collection.
Lessons from the front lines
Another member of the presscast panel, Melissa Dillmon, MD, of the Harbin Clinic Cancer Center in Rome, Georgia, described the experience of community oncologists during the pandemic.
Her community, located in northeastern Georgia, experienced a COVID-19 outbreak in early March linked to services at two large churches. Community public health authorities issued a shelter-in-place order before the state government issued stay-at-home guidelines and shuttered all but essential business, some of which were allowed by state order to reopen as of April 24.
Dr. Dillmon’s center began screening patients for COVID-19 symptoms at the door, limited visitors or companions, instituted virtual visits and tumor boards, and set up a cancer treatment triage system that would allow essential surgeries to proceed and most infusions to continue, while delaying the start of chemotherapy when possible.
“We have encouraged patients to continue on treatment, especially if treatment is being given with curative intent, or if the cancer is responding well already to treatment,” she said.
The center, located in a community with a high prevalence of comorbidities and high incidence of lung cancer, has seen a sharp decline in colonoscopies, mammograms, and lung scans as patient shelter in place.
“We have great concerns about patients missing their screening lung scans, as this program has already proven to be finding earlier lung cancers that are curable,” Dr. Dillmon said.
A view from Washington state
Another panel member, Gary Lyman, MD, of the Fred Hutchinson Cancer Research Center in Seattle, described the response by the state of Washington, the initial epicenter of the COVID-19 outbreak in the United States.
Following identification of infections in hospitalized patients and at a nursing home in Kirkland, Washington, “our response, which began in early March and progressed through the second and third week in March at the state level, was to restrict large gatherings; progressively, schools were closed; larger businesses closed; and, by March 23, a stay-at-home policy was implemented, and all nonessential businesses were closed,” Dr. Lyman said.
“We believe, based on what has happened since that time, that this has considerably flattened the curve,” he continued.
Lessons from the Washington experience include the need to plan for a long-term disruption or alteration of cancer care, expand COVID-19 testing to all patients coming into hospitals or major clinics, institute aggressive supportive care measures, prepare for subsequent waves of infection, collect and share data, and, for remote or rural areas, identify lifelines to needed resources, Dr. Lyman said.
ASCO resources
Also speaking at the presscast, Jonathan Marron, MD, of Boston Children’s Hospital and Harvard Medical School, Boston, outlined ASCO’s guidance on allocation of scarce resources during the COVID-19 pandemic.
Richard L. Schilsky, MD, ASCO chief medical officer and executive vice president, outlined community-wide collaborations, data initiatives, and online resources for both clinicians and patients.
The COVID-19 pandemic continues to exact a heavy price on cancer patients, cancer care, and clinical trials, an expert panel reported during a presscast.
“Limited data available thus far are sobering: In Italy, about 20% of COVID-related deaths occurred in people with cancer, and, in China, COVID-19 patients who had cancer were about five times more likely than others to die or be placed on a ventilator in an intensive care unit,” said Howard A “Skip” Burris, MD, president of the American Society of Clinical Oncology and president and CEO of the Sarah Cannon Cancer Institute in Nashville, Tenn.
“We also have little evidence on returning COVID-19 patients with cancer. Physicians have to rely on limited data, anecdotal reports, and their own professional expertise” regarding the extent of increased risk to cancer patients with COVID-19, whether to interrupt or modify treatment, and the effects of cancer on recovery from COVID-19 infection, Dr. Burris said during the ASCO-sponsored online presscast.
Care of COVID-free patients
For cancer patients without COVID-19, the picture is equally dim, with the prospect of delayed surgery, chemotherapy, or screening; shortages of medications and equipment needed for critical care; the shift to telemedicine that may increase patient anxiety; and the potential loss of access to innovative therapies through clinical trials, Dr. Burris said.
“We’re concerned that some hospitals have effectively deemed all cancer surgeries to be elective, requiring them to be postponed. For patients with fast-moving or hard-to-treat cancer, this delay may be devastating,” he said.
Dr. Burris also cited concerns about delayed cancer diagnosis. “In a typical month, roughly 150,000 Americans are diagnosed with cancer. But right now, routine screening visits are postponed, and patients with pain or other warning signs may put off a doctor’s visit because of social distancing,” he said.
The pandemic has also exacerbated shortages of sedatives and opioid analgesics required for intubation and mechanical ventilation of patients.
Trials halted or slowed
Dr. Burris also briefly discussed results of a new survey, which were posted online ahead of publication in JCO Oncology Practice. The survey showed that, of 14 academic and 18 community-based cancer programs, 59.4% reported halting screening and/or enrollment for at least some clinical trials and suspending research-based clinical visits except for those where cancer treatment was delivered.
“Half of respondents reported ceasing research-only blood and/or tissue collections,” the authors of the article reported.
“Trial interruptions are devastating news for thousands of patients; in many cases, clinical trials are the best or only appropriate option for care,” Dr. Burris said.
The article authors, led by David Waterhouse, MD, of Oncology Hematology Care in Cincinnati, pointed to a silver lining in the pandemic cloud in the form of opportunities to improve clinical trials going forward.
“Nearly all respondents (90.3%) identified telehealth visits for participants as a potential improvement to clinical trial conduct, and more than three-quarters (77.4%) indicated that remote patient review of symptoms held similar potential,” the authors wrote.
Other potential improvements included remote site visits from trial sponsors and/or contract research organizations, more efficient study enrollment through secure electronic platforms, direct shipment of oral drugs to patients, remote assessments of adverse events, and streamlined data collection.
Lessons from the front lines
Another member of the presscast panel, Melissa Dillmon, MD, of the Harbin Clinic Cancer Center in Rome, Georgia, described the experience of community oncologists during the pandemic.
Her community, located in northeastern Georgia, experienced a COVID-19 outbreak in early March linked to services at two large churches. Community public health authorities issued a shelter-in-place order before the state government issued stay-at-home guidelines and shuttered all but essential business, some of which were allowed by state order to reopen as of April 24.
Dr. Dillmon’s center began screening patients for COVID-19 symptoms at the door, limited visitors or companions, instituted virtual visits and tumor boards, and set up a cancer treatment triage system that would allow essential surgeries to proceed and most infusions to continue, while delaying the start of chemotherapy when possible.
“We have encouraged patients to continue on treatment, especially if treatment is being given with curative intent, or if the cancer is responding well already to treatment,” she said.
The center, located in a community with a high prevalence of comorbidities and high incidence of lung cancer, has seen a sharp decline in colonoscopies, mammograms, and lung scans as patient shelter in place.
“We have great concerns about patients missing their screening lung scans, as this program has already proven to be finding earlier lung cancers that are curable,” Dr. Dillmon said.
A view from Washington state
Another panel member, Gary Lyman, MD, of the Fred Hutchinson Cancer Research Center in Seattle, described the response by the state of Washington, the initial epicenter of the COVID-19 outbreak in the United States.
Following identification of infections in hospitalized patients and at a nursing home in Kirkland, Washington, “our response, which began in early March and progressed through the second and third week in March at the state level, was to restrict large gatherings; progressively, schools were closed; larger businesses closed; and, by March 23, a stay-at-home policy was implemented, and all nonessential businesses were closed,” Dr. Lyman said.
“We believe, based on what has happened since that time, that this has considerably flattened the curve,” he continued.
Lessons from the Washington experience include the need to plan for a long-term disruption or alteration of cancer care, expand COVID-19 testing to all patients coming into hospitals or major clinics, institute aggressive supportive care measures, prepare for subsequent waves of infection, collect and share data, and, for remote or rural areas, identify lifelines to needed resources, Dr. Lyman said.
ASCO resources
Also speaking at the presscast, Jonathan Marron, MD, of Boston Children’s Hospital and Harvard Medical School, Boston, outlined ASCO’s guidance on allocation of scarce resources during the COVID-19 pandemic.
Richard L. Schilsky, MD, ASCO chief medical officer and executive vice president, outlined community-wide collaborations, data initiatives, and online resources for both clinicians and patients.
Global registry collects data on pediatric cancer patients with COVID-19
A week after its launch, a new online registry has information on more than 2 dozen cases of pediatric cancer patients with COVID-19.
The registry, created by St. Jude Children’s Research Hospital in Memphis, Tenn., and the International Society of Paediatric Oncology, is the first global COVID-19 registry for children with cancer.
Clinicians enter cases through an online form, then complete 30- and 60-day follow-up reports via email. St. Jude compiles the data and releases regularly updated summaries, including the number of cases by country and by treatment. Eventually, researchers might be able to apply for access to the raw data for their own projects.
It’s all free of charge, said Carlos Rodriguez-Galindo, MD, chair of the department of global pediatric medicine at St. Jude.
The registry is hosted on a website called “The Global COVID-19 Observatory and Resource Center for Childhood Cancer.” In addition to the registry, the website has a resource library and a discussion forum where clinicians can exchange information.
Other COVID-19 cancer registries have launched recently as well, including registries created by the COVID-19 and Cancer Consortium and the American Society of Clinical Oncology. The idea is to compile and disseminate best practices and other information quickly amid concerns that immunosuppressed cancer patients might be especially vulnerable.
So far, that doesn’t seem to be the case for children. Their relative protection from the disease and serious complications seems to hold even when they have cancer, Dr. Rodriguez-Galindo said.
“When we talk with the people in China” the number of COVID-19 cases in children with cancer is “very small,” he said. There are a couple of reports from Europe finding the same thing, and the severity of COVID-19 also “seems to be lower than you would expect,” he added.
The new registry will help better define the situation, according to Dr. Rodriguez-Galindo.
St. Jude is working with European countries that have their own national pediatric cancer COVID-19 registries to share information. St. Jude’s ties with lower- and middle-income countries, established via the department of global pediatric medicine, should help populate the global registry as well.
Furthermore, international surveys are being planned to gauge the impact of COVID-19 on children with cancer and their access to care.
A week after its launch, a new online registry has information on more than 2 dozen cases of pediatric cancer patients with COVID-19.
The registry, created by St. Jude Children’s Research Hospital in Memphis, Tenn., and the International Society of Paediatric Oncology, is the first global COVID-19 registry for children with cancer.
Clinicians enter cases through an online form, then complete 30- and 60-day follow-up reports via email. St. Jude compiles the data and releases regularly updated summaries, including the number of cases by country and by treatment. Eventually, researchers might be able to apply for access to the raw data for their own projects.
It’s all free of charge, said Carlos Rodriguez-Galindo, MD, chair of the department of global pediatric medicine at St. Jude.
The registry is hosted on a website called “The Global COVID-19 Observatory and Resource Center for Childhood Cancer.” In addition to the registry, the website has a resource library and a discussion forum where clinicians can exchange information.
Other COVID-19 cancer registries have launched recently as well, including registries created by the COVID-19 and Cancer Consortium and the American Society of Clinical Oncology. The idea is to compile and disseminate best practices and other information quickly amid concerns that immunosuppressed cancer patients might be especially vulnerable.
So far, that doesn’t seem to be the case for children. Their relative protection from the disease and serious complications seems to hold even when they have cancer, Dr. Rodriguez-Galindo said.
“When we talk with the people in China” the number of COVID-19 cases in children with cancer is “very small,” he said. There are a couple of reports from Europe finding the same thing, and the severity of COVID-19 also “seems to be lower than you would expect,” he added.
The new registry will help better define the situation, according to Dr. Rodriguez-Galindo.
St. Jude is working with European countries that have their own national pediatric cancer COVID-19 registries to share information. St. Jude’s ties with lower- and middle-income countries, established via the department of global pediatric medicine, should help populate the global registry as well.
Furthermore, international surveys are being planned to gauge the impact of COVID-19 on children with cancer and their access to care.
A week after its launch, a new online registry has information on more than 2 dozen cases of pediatric cancer patients with COVID-19.
The registry, created by St. Jude Children’s Research Hospital in Memphis, Tenn., and the International Society of Paediatric Oncology, is the first global COVID-19 registry for children with cancer.
Clinicians enter cases through an online form, then complete 30- and 60-day follow-up reports via email. St. Jude compiles the data and releases regularly updated summaries, including the number of cases by country and by treatment. Eventually, researchers might be able to apply for access to the raw data for their own projects.
It’s all free of charge, said Carlos Rodriguez-Galindo, MD, chair of the department of global pediatric medicine at St. Jude.
The registry is hosted on a website called “The Global COVID-19 Observatory and Resource Center for Childhood Cancer.” In addition to the registry, the website has a resource library and a discussion forum where clinicians can exchange information.
Other COVID-19 cancer registries have launched recently as well, including registries created by the COVID-19 and Cancer Consortium and the American Society of Clinical Oncology. The idea is to compile and disseminate best practices and other information quickly amid concerns that immunosuppressed cancer patients might be especially vulnerable.
So far, that doesn’t seem to be the case for children. Their relative protection from the disease and serious complications seems to hold even when they have cancer, Dr. Rodriguez-Galindo said.
“When we talk with the people in China” the number of COVID-19 cases in children with cancer is “very small,” he said. There are a couple of reports from Europe finding the same thing, and the severity of COVID-19 also “seems to be lower than you would expect,” he added.
The new registry will help better define the situation, according to Dr. Rodriguez-Galindo.
St. Jude is working with European countries that have their own national pediatric cancer COVID-19 registries to share information. St. Jude’s ties with lower- and middle-income countries, established via the department of global pediatric medicine, should help populate the global registry as well.
Furthermore, international surveys are being planned to gauge the impact of COVID-19 on children with cancer and their access to care.
Will coronavirus restrictions lead to more advanced cancers?
My pathology lab once faced a daily flood of colon polyps, pap smears, and prostate biopsies. Suddenly, our work has dried up. The coronavirus pandemic has cleared out operating rooms and clinics across the country. Endoscopy and radiology suites have gone dark.
Pathology is largely driven by mass screening programs, and the machinery of screening has grinded to a halt during the COVID-19 pandemic. The American Cancer Society currently recommends that “no one should go to a health care facility for routine cancer screening at this time.”
But malignancies are still growing and spreading even though a great deal of medical care is on hold. The most urgent cancer care is still taking place; the risks of delaying treatment for patients with advanced or symptomatic cancer are obvious—these tumors can cause severe pain and life-threatening complications.
But that leaves us with a more complex and uncomfortable question: Will the pause in screening ultimately leave patients with tiny, asymptomatic cancers or precursor lesions worse off? What will a delay mean for those with ductal carcinoma in situ or small breast cancers? What’s the long-term effect of all those dysplastic nevi and early melanoma left unexcised by dermatologists? Perhaps more troubling, what about the spreading kidney cancer that may have turned up as an incidental finding on a CT scan?
COVID-19: A natural experiment
For many years, we’ve been dealing with the other side of the screening question: overdiagnosing and treating cancers that would probably never harm the patient. Overdiagnosis has been on a decades-long rise due to organized screening like PSA testing and mammography, as well as through ad hoc detection from heavier use of medical imaging. All of these have been disrupted by the pandemic.
Because the correlation between medical interventions and cancer overdiagnosis is clear, we can safely assume that overdiagnosis will decline during the pandemic. But what will be the net effect? Early detection of cancer undoubtedly saves some lives, but how many and at what cost has been a seemingly intractable debate.
Until now.
The coronavirus outbreak will be a natural experiment like no other. Economists and epidemiologists love to study “natural experiments” – systemic shocks that shed light on a complex phenomenon.
The unexpected nationwide delay in screening will undoubtedly inform the debate on overdiagnosis. For one, we can learn whether less intensive screening leads to more advanced cancers. Because screening will probably return to normal at different times across the country, we can almost simulate a randomized trial. Will this transformative data be a silver lining to this awful time?
The pressure to ‘fight’
The pandemic has also raised a question about cancer screening that goes beyond data: Why has the loud epidemic of coronavirus so thoroughly trumped cancer’s silent one? To me, the necessary urgency of our coronavirus response stands in stark contrast to the overly aggressive public health messaging used for cancer screening.
The tools used to fight the coronavirus epidemic have been forceful. We’re all diligently washing our hands and staying inside. We’re making sacrifices in our jobs and personal lives to stop the virus’ spread.
Cancer screening has similarly been touted as dogma – an urgent public health intervention that only a fool would turn down. The American Cancer Society once ran an infamous advertisement suggesting that if you decline mammography, you “need more than your breasts examined.” Even today, well-intentioned organizations run cancer screening drives pushing people to pledge to “get screened now.” It is no surprise, then, that I have had patients and family members confide in me that they feel guilty about not pursuing all of their recommended screening tests. The thought of anyone feeling like they caused their own cancer appalls me.
This pressure extends into the clinic. In many practices, primary care doctors are evaluated based on how many patients “comply” with screening recommendations. There seems to be a relentless drive to reach 100% screening penetration. These oversimplified tactics run counter to the shared decision making and informed consent we profess to value in medicine.
The tricky thing about cancer screening is that because most people will never develop the cancer being screened for, we know that most people can also never be helped by it. This doesn’t make screening useless, just as washing your hands can help even if it doesn’t guarantee that you won’t catch coronavirus. We know that some individuals benefit, which we detect at the population level. Overdiagnosis arises in the same way, as a phenomenon detected within populations and not individuals. These aspects of screening are what has led to cancer being viewed as a “societal disease” requiring a uniform response – 100% screening compliance.
Metaphors of war
These assumptions fall apart now that we are facing a real societal disease, an infectious disease outbreak. Coronavirus has made us reflect on what actions individuals should take in order to protect others. But cancer is not a contagion. When we decide whether and how to screen, we make intimate decisions affecting primarily ourselves and our family – not society at large.
Countless articles have been written about the use of metaphor in cancer, perhaps most famously by essayist and breast cancer patient Susan Sontag. Sontag and others have been critical of the rampant use of war metaphors in the cancer community. Wars invoke sacrifice, duty, and suffering. The “battle” against coronavirus really puts the “war on cancer” in perspective. These pandemic weeks have terrified me. I have been willing to do anything to protect myself and others. They’ve also exhausted me. We can’t be at war forever.
When this current war ends, will the “war on cancer” resume unchanged? Screening will no doubt begin again, hopefully improved by data from the coronavirus natural experiment. But I wonder whether we will tolerate the same kinds of public health messages – and whether we should – having now experienced an infectious disease outbreak where our actions as individuals really do have an impact on the health of others.
After feeling helpless, besieged, and even guilt-ridden during the pandemic, I think many people would appreciate regaining a sense of control over other aspects of their health. Cancer screening can save lives, but it’s a choice we should make for ourselves based on an understanding of the trade-offs and our own preferences. When screening restarts, I hope its paternalistic dogma can be replaced by nuanced, empowering tactics more appropriate for peacetime.
Benjamin Mazer, MD, MBA, is an anatomic and clinical pathology resident at Yale with interests in diagnostic surgical pathology, laboratory management, and evidence-based medicine.
This article first appeared on Medscape.com.
My pathology lab once faced a daily flood of colon polyps, pap smears, and prostate biopsies. Suddenly, our work has dried up. The coronavirus pandemic has cleared out operating rooms and clinics across the country. Endoscopy and radiology suites have gone dark.
Pathology is largely driven by mass screening programs, and the machinery of screening has grinded to a halt during the COVID-19 pandemic. The American Cancer Society currently recommends that “no one should go to a health care facility for routine cancer screening at this time.”
But malignancies are still growing and spreading even though a great deal of medical care is on hold. The most urgent cancer care is still taking place; the risks of delaying treatment for patients with advanced or symptomatic cancer are obvious—these tumors can cause severe pain and life-threatening complications.
But that leaves us with a more complex and uncomfortable question: Will the pause in screening ultimately leave patients with tiny, asymptomatic cancers or precursor lesions worse off? What will a delay mean for those with ductal carcinoma in situ or small breast cancers? What’s the long-term effect of all those dysplastic nevi and early melanoma left unexcised by dermatologists? Perhaps more troubling, what about the spreading kidney cancer that may have turned up as an incidental finding on a CT scan?
COVID-19: A natural experiment
For many years, we’ve been dealing with the other side of the screening question: overdiagnosing and treating cancers that would probably never harm the patient. Overdiagnosis has been on a decades-long rise due to organized screening like PSA testing and mammography, as well as through ad hoc detection from heavier use of medical imaging. All of these have been disrupted by the pandemic.
Because the correlation between medical interventions and cancer overdiagnosis is clear, we can safely assume that overdiagnosis will decline during the pandemic. But what will be the net effect? Early detection of cancer undoubtedly saves some lives, but how many and at what cost has been a seemingly intractable debate.
Until now.
The coronavirus outbreak will be a natural experiment like no other. Economists and epidemiologists love to study “natural experiments” – systemic shocks that shed light on a complex phenomenon.
The unexpected nationwide delay in screening will undoubtedly inform the debate on overdiagnosis. For one, we can learn whether less intensive screening leads to more advanced cancers. Because screening will probably return to normal at different times across the country, we can almost simulate a randomized trial. Will this transformative data be a silver lining to this awful time?
The pressure to ‘fight’
The pandemic has also raised a question about cancer screening that goes beyond data: Why has the loud epidemic of coronavirus so thoroughly trumped cancer’s silent one? To me, the necessary urgency of our coronavirus response stands in stark contrast to the overly aggressive public health messaging used for cancer screening.
The tools used to fight the coronavirus epidemic have been forceful. We’re all diligently washing our hands and staying inside. We’re making sacrifices in our jobs and personal lives to stop the virus’ spread.
Cancer screening has similarly been touted as dogma – an urgent public health intervention that only a fool would turn down. The American Cancer Society once ran an infamous advertisement suggesting that if you decline mammography, you “need more than your breasts examined.” Even today, well-intentioned organizations run cancer screening drives pushing people to pledge to “get screened now.” It is no surprise, then, that I have had patients and family members confide in me that they feel guilty about not pursuing all of their recommended screening tests. The thought of anyone feeling like they caused their own cancer appalls me.
This pressure extends into the clinic. In many practices, primary care doctors are evaluated based on how many patients “comply” with screening recommendations. There seems to be a relentless drive to reach 100% screening penetration. These oversimplified tactics run counter to the shared decision making and informed consent we profess to value in medicine.
The tricky thing about cancer screening is that because most people will never develop the cancer being screened for, we know that most people can also never be helped by it. This doesn’t make screening useless, just as washing your hands can help even if it doesn’t guarantee that you won’t catch coronavirus. We know that some individuals benefit, which we detect at the population level. Overdiagnosis arises in the same way, as a phenomenon detected within populations and not individuals. These aspects of screening are what has led to cancer being viewed as a “societal disease” requiring a uniform response – 100% screening compliance.
Metaphors of war
These assumptions fall apart now that we are facing a real societal disease, an infectious disease outbreak. Coronavirus has made us reflect on what actions individuals should take in order to protect others. But cancer is not a contagion. When we decide whether and how to screen, we make intimate decisions affecting primarily ourselves and our family – not society at large.
Countless articles have been written about the use of metaphor in cancer, perhaps most famously by essayist and breast cancer patient Susan Sontag. Sontag and others have been critical of the rampant use of war metaphors in the cancer community. Wars invoke sacrifice, duty, and suffering. The “battle” against coronavirus really puts the “war on cancer” in perspective. These pandemic weeks have terrified me. I have been willing to do anything to protect myself and others. They’ve also exhausted me. We can’t be at war forever.
When this current war ends, will the “war on cancer” resume unchanged? Screening will no doubt begin again, hopefully improved by data from the coronavirus natural experiment. But I wonder whether we will tolerate the same kinds of public health messages – and whether we should – having now experienced an infectious disease outbreak where our actions as individuals really do have an impact on the health of others.
After feeling helpless, besieged, and even guilt-ridden during the pandemic, I think many people would appreciate regaining a sense of control over other aspects of their health. Cancer screening can save lives, but it’s a choice we should make for ourselves based on an understanding of the trade-offs and our own preferences. When screening restarts, I hope its paternalistic dogma can be replaced by nuanced, empowering tactics more appropriate for peacetime.
Benjamin Mazer, MD, MBA, is an anatomic and clinical pathology resident at Yale with interests in diagnostic surgical pathology, laboratory management, and evidence-based medicine.
This article first appeared on Medscape.com.
My pathology lab once faced a daily flood of colon polyps, pap smears, and prostate biopsies. Suddenly, our work has dried up. The coronavirus pandemic has cleared out operating rooms and clinics across the country. Endoscopy and radiology suites have gone dark.
Pathology is largely driven by mass screening programs, and the machinery of screening has grinded to a halt during the COVID-19 pandemic. The American Cancer Society currently recommends that “no one should go to a health care facility for routine cancer screening at this time.”
But malignancies are still growing and spreading even though a great deal of medical care is on hold. The most urgent cancer care is still taking place; the risks of delaying treatment for patients with advanced or symptomatic cancer are obvious—these tumors can cause severe pain and life-threatening complications.
But that leaves us with a more complex and uncomfortable question: Will the pause in screening ultimately leave patients with tiny, asymptomatic cancers or precursor lesions worse off? What will a delay mean for those with ductal carcinoma in situ or small breast cancers? What’s the long-term effect of all those dysplastic nevi and early melanoma left unexcised by dermatologists? Perhaps more troubling, what about the spreading kidney cancer that may have turned up as an incidental finding on a CT scan?
COVID-19: A natural experiment
For many years, we’ve been dealing with the other side of the screening question: overdiagnosing and treating cancers that would probably never harm the patient. Overdiagnosis has been on a decades-long rise due to organized screening like PSA testing and mammography, as well as through ad hoc detection from heavier use of medical imaging. All of these have been disrupted by the pandemic.
Because the correlation between medical interventions and cancer overdiagnosis is clear, we can safely assume that overdiagnosis will decline during the pandemic. But what will be the net effect? Early detection of cancer undoubtedly saves some lives, but how many and at what cost has been a seemingly intractable debate.
Until now.
The coronavirus outbreak will be a natural experiment like no other. Economists and epidemiologists love to study “natural experiments” – systemic shocks that shed light on a complex phenomenon.
The unexpected nationwide delay in screening will undoubtedly inform the debate on overdiagnosis. For one, we can learn whether less intensive screening leads to more advanced cancers. Because screening will probably return to normal at different times across the country, we can almost simulate a randomized trial. Will this transformative data be a silver lining to this awful time?
The pressure to ‘fight’
The pandemic has also raised a question about cancer screening that goes beyond data: Why has the loud epidemic of coronavirus so thoroughly trumped cancer’s silent one? To me, the necessary urgency of our coronavirus response stands in stark contrast to the overly aggressive public health messaging used for cancer screening.
The tools used to fight the coronavirus epidemic have been forceful. We’re all diligently washing our hands and staying inside. We’re making sacrifices in our jobs and personal lives to stop the virus’ spread.
Cancer screening has similarly been touted as dogma – an urgent public health intervention that only a fool would turn down. The American Cancer Society once ran an infamous advertisement suggesting that if you decline mammography, you “need more than your breasts examined.” Even today, well-intentioned organizations run cancer screening drives pushing people to pledge to “get screened now.” It is no surprise, then, that I have had patients and family members confide in me that they feel guilty about not pursuing all of their recommended screening tests. The thought of anyone feeling like they caused their own cancer appalls me.
This pressure extends into the clinic. In many practices, primary care doctors are evaluated based on how many patients “comply” with screening recommendations. There seems to be a relentless drive to reach 100% screening penetration. These oversimplified tactics run counter to the shared decision making and informed consent we profess to value in medicine.
The tricky thing about cancer screening is that because most people will never develop the cancer being screened for, we know that most people can also never be helped by it. This doesn’t make screening useless, just as washing your hands can help even if it doesn’t guarantee that you won’t catch coronavirus. We know that some individuals benefit, which we detect at the population level. Overdiagnosis arises in the same way, as a phenomenon detected within populations and not individuals. These aspects of screening are what has led to cancer being viewed as a “societal disease” requiring a uniform response – 100% screening compliance.
Metaphors of war
These assumptions fall apart now that we are facing a real societal disease, an infectious disease outbreak. Coronavirus has made us reflect on what actions individuals should take in order to protect others. But cancer is not a contagion. When we decide whether and how to screen, we make intimate decisions affecting primarily ourselves and our family – not society at large.
Countless articles have been written about the use of metaphor in cancer, perhaps most famously by essayist and breast cancer patient Susan Sontag. Sontag and others have been critical of the rampant use of war metaphors in the cancer community. Wars invoke sacrifice, duty, and suffering. The “battle” against coronavirus really puts the “war on cancer” in perspective. These pandemic weeks have terrified me. I have been willing to do anything to protect myself and others. They’ve also exhausted me. We can’t be at war forever.
When this current war ends, will the “war on cancer” resume unchanged? Screening will no doubt begin again, hopefully improved by data from the coronavirus natural experiment. But I wonder whether we will tolerate the same kinds of public health messages – and whether we should – having now experienced an infectious disease outbreak where our actions as individuals really do have an impact on the health of others.
After feeling helpless, besieged, and even guilt-ridden during the pandemic, I think many people would appreciate regaining a sense of control over other aspects of their health. Cancer screening can save lives, but it’s a choice we should make for ourselves based on an understanding of the trade-offs and our own preferences. When screening restarts, I hope its paternalistic dogma can be replaced by nuanced, empowering tactics more appropriate for peacetime.
Benjamin Mazer, MD, MBA, is an anatomic and clinical pathology resident at Yale with interests in diagnostic surgical pathology, laboratory management, and evidence-based medicine.
This article first appeared on Medscape.com.
European cancer centers restructure care in the era of COVID-19
Delivering cancer care during the COVID-19 pandemic has proved particularly challenging, as minimizing the risk of infection must be balanced with maintaining optimal outcomes.
Healthcare systems and oncologists have had to reorganize standard oncologic care in order to protect vulnerable patients from exposure to COVID-19 as well as deal with pandemic-related issues of equipment and staffing shortages.
A new article now describes how seven cancer centers in Europe rapidly reorganized their oncologic services and are tackling this crisis, as well as offering guidance to other institutions.
This was a major undertaking, to work out a system where patients can still get care but in a safer manner, explained coauthor Emile Voest, MD, medical director of the Netherlands Cancer Institute in Amsterdam.
“Decisions needed to be taken based on availability of personnel, protective materials, and urgencies,” he told Medscape Medical News. “Because every country had its own speed of development of the COVID pandemic, there were different scenarios in all institutions, but all with a common factor of key expertise on how to de-escalate in a safe manner.”
The article was published April 16 in Nature Medicine.
The Netherlands Cancer Institute (the Netherlands), Karolinska Institute (Sweden), Institute Gustave Roussy (France), Cambridge Cancer Center (United Kingdom), Istituto Nazionale dei Tumori di Milano (Italy), German Cancer Research Center (Germany), and Vall d’Hebron Institute of Oncology (Spain) have been working closely together in a legal entity since 2014, and have created ‘Cancer Core Europe’ (CCE). The goal is to “maximize coherence and critical mass in cancer research,” the authors note.
The consortium represents roughly 60,000 patients with newly diagnosed cancer, delivers approximately 300,000 treatment courses, and conducts about 1.2 million consultations annually, with more than 1,500 ongoing clinical trials. In a joint effort, the centers collected, translated, and compared the guidelines that had been put in place to treat patients with cancer during the COVID-19 pandemic.
Cancer treatment is multidisciplinary and involves many specialties including surgery, radiology, pathology, radiation oncology, and medical oncology. Coordinating care among disciplines is a very complex process, Voest noted.
“Changing treatment also means that you need to reconsider capacities and requirements,” he said. “Hospitals have installed crisis teams that were very good at coordinating these efforts.”
Restructuring care
Cancer care had to be reorganized on multiple levels, and the CCE centers looked at several aspects that needed to be accounted for, to ensure continuity in cancer care.
“The biggest challenge for the NHS and other healthcare systems is the surge of patients requiring oxygen and/or intensive care, and the nature and infectiousness of the virus,” said coauthor Carlos Caldas, MD, FMedSci, professor of cancer medicine at the University of Cambridge, United Kingdom. “In hospitals that are mostly run close to capacity, and where all kinds of patients are treated, this has created major resource and logistical problems.”
For regular clinical activities, the institutions with dedicated cancer centers (German Cancer Research Center, Institute Gustave Roussy, Istituto Nazionale dei Tumori di Milano, and Netherlands Cancer Institute) have attempted to stay COVID-19 free. This policy would in turn help ensure that sufficient clinical and intensive-care capacity could be reserved for critical cancer surgeries or management of treatment-related side effects, and allow hospitals outside of the CCE to transfer patients with cancer to these centers. The general hospitals can then focus on caring for patients with COVID-19, as well as other illnesses/injuries that require inpatient care.
As the CCE centers located within general hospitals (Cambridge Cancer Center, Vall d’Hebron Institute of Oncology and Karolinska Institute) have to admit patients with suspected and positive cases of COVID-19, being “COVID-19 free” was never a realistic or pursued goal.
The authors note that it is the responsibility of all healthcare professionals to ensure patients are not exposed to COVID-19, and this has meant minimizing hospital visits and person-to-person contact. For example, whenever possible, consultations take place via telephone calls or over the Internet, and nonurgent appointments that would require a patient’s physical presence at the clinic have been postponed. Visitors are also not permitted to accompany patients when admitted to the hospital or during procedures.
Standard-of-care treatment regimens have been adapted across all centers to minimize the number of hospital visits and hospitalizations and prevent “anticancer treatment-induced” complications of COVID-19.
To minimize visits and hospitalizations, strategies include converting intravenous treatments to oral or subcutaneous regimens when possible; switching from cytotoxic chemotherapy to a less-toxic approach to minimize the risk of complications requiring hospitalization; or to pause therapies when possible (stable disease reached or better). In addition, nonemergency surgeries have been postponed or replaced by radiotherapy.
To prevent anticancer treatment-induced complications of COVID-19, most centers use the paradigm that the added benefit for tumor control should be weighed against the potential risk for COVID-19–related morbidity and mortality. To prevent or reduce the risk of neutropenia and lymphopenia, for example, all centers have suggested a de-escalation of cytotoxic chemotherapy or targeted treatment strategies, or to forgo second or subsequent lines of palliative treatments if response rates from up-front therapy are low.
Some of these changes may be here to stay, noted Caldas. “One of the positive messages that comes out of this is that, clearly, care can be delivered in a safe and compassionate manner without requiring as many hospital visits as in the pre-COVID-19 era,” he said. “In the future, we will take heed of the COVID-19 experience to improve delivery of cancer care.”
Capacity of facilities
Many healthcare systems have become overwhelmed as the pandemic has intensified, thus making it necessary to prioritize. To prepare for this possibility, CCE centers have established protocols to categorize and prioritize patients for systemic treatment or surgery. While the protocols vary by center, they are comparable with one another as they prioritize on the basis of anticipated treatment outcome, the authors note.
The guidelines in CCE centers unanimously recommend that neoadjuvant therapies and curative surgeries be the top priority, for the times when operating room and/or ICU capacity is limited. As an alternative, neoadjuvant systemic treatments may be initiated or extended to postpone surgery, and other nonsurgical interventions can be considered.
In addition, some centers agree that certain elective surgeries can be safely delayed if backed by scientific evidence. As an example, an 11-week deferment of surgery may be acceptable for patients with rectal cancer after downstaging.
Cancer centers may also need to upscale and downscale quickly, depending on how the pandemic evolves, and many have already outlined scenarios to prepare for increasing or decreasing their capacity using phased approaches.
The Netherlands Cancer Institute, for example, has defined four phases of increasing severity; in Germany, capacity planning has been coordinated among 18 hospitals and the federal ministry of health, in order to prevent shortages of cancer services.
“We note that the optimal downscaling strategies depend on country- and center-specific capacities and preferences,” they write. “Therefore, it is difficult to propose a common schedule, and it will be most effective if hospitals outline their own phase-specific downscaling strategies based on the prioritization schemes and practical handles discussed above.”
Future research
Better strategies will be needed to reduce the impact of COVID-19 in cancer care, and four research priorities were identified to allow for evidence-based adjustments of cancer care protocols while the pandemic continues:
- Collect real-world data about the effects of adjustment and de-escalation of treatment regimens on outcomes
- Determine the incidence of COVID-19 in both the general population and among patients with cancer who have received systemic therapies, with large-scale serological testing
- Develop an epidemiological model that will allow estimates of the cumulative incidence of COVID-19 for a patient with cancer, within a specific time frame
- Determine COVID-19 related morbidity and mortality in patients with cancer who have been treated with systemic therapies and/or granulocyte colony-stimulating factor (G-CSF). Several projects are currently underway, such as the UK Coronavirus Cancer Monitoring Project.
The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Delivering cancer care during the COVID-19 pandemic has proved particularly challenging, as minimizing the risk of infection must be balanced with maintaining optimal outcomes.
Healthcare systems and oncologists have had to reorganize standard oncologic care in order to protect vulnerable patients from exposure to COVID-19 as well as deal with pandemic-related issues of equipment and staffing shortages.
A new article now describes how seven cancer centers in Europe rapidly reorganized their oncologic services and are tackling this crisis, as well as offering guidance to other institutions.
This was a major undertaking, to work out a system where patients can still get care but in a safer manner, explained coauthor Emile Voest, MD, medical director of the Netherlands Cancer Institute in Amsterdam.
“Decisions needed to be taken based on availability of personnel, protective materials, and urgencies,” he told Medscape Medical News. “Because every country had its own speed of development of the COVID pandemic, there were different scenarios in all institutions, but all with a common factor of key expertise on how to de-escalate in a safe manner.”
The article was published April 16 in Nature Medicine.
The Netherlands Cancer Institute (the Netherlands), Karolinska Institute (Sweden), Institute Gustave Roussy (France), Cambridge Cancer Center (United Kingdom), Istituto Nazionale dei Tumori di Milano (Italy), German Cancer Research Center (Germany), and Vall d’Hebron Institute of Oncology (Spain) have been working closely together in a legal entity since 2014, and have created ‘Cancer Core Europe’ (CCE). The goal is to “maximize coherence and critical mass in cancer research,” the authors note.
The consortium represents roughly 60,000 patients with newly diagnosed cancer, delivers approximately 300,000 treatment courses, and conducts about 1.2 million consultations annually, with more than 1,500 ongoing clinical trials. In a joint effort, the centers collected, translated, and compared the guidelines that had been put in place to treat patients with cancer during the COVID-19 pandemic.
Cancer treatment is multidisciplinary and involves many specialties including surgery, radiology, pathology, radiation oncology, and medical oncology. Coordinating care among disciplines is a very complex process, Voest noted.
“Changing treatment also means that you need to reconsider capacities and requirements,” he said. “Hospitals have installed crisis teams that were very good at coordinating these efforts.”
Restructuring care
Cancer care had to be reorganized on multiple levels, and the CCE centers looked at several aspects that needed to be accounted for, to ensure continuity in cancer care.
“The biggest challenge for the NHS and other healthcare systems is the surge of patients requiring oxygen and/or intensive care, and the nature and infectiousness of the virus,” said coauthor Carlos Caldas, MD, FMedSci, professor of cancer medicine at the University of Cambridge, United Kingdom. “In hospitals that are mostly run close to capacity, and where all kinds of patients are treated, this has created major resource and logistical problems.”
For regular clinical activities, the institutions with dedicated cancer centers (German Cancer Research Center, Institute Gustave Roussy, Istituto Nazionale dei Tumori di Milano, and Netherlands Cancer Institute) have attempted to stay COVID-19 free. This policy would in turn help ensure that sufficient clinical and intensive-care capacity could be reserved for critical cancer surgeries or management of treatment-related side effects, and allow hospitals outside of the CCE to transfer patients with cancer to these centers. The general hospitals can then focus on caring for patients with COVID-19, as well as other illnesses/injuries that require inpatient care.
As the CCE centers located within general hospitals (Cambridge Cancer Center, Vall d’Hebron Institute of Oncology and Karolinska Institute) have to admit patients with suspected and positive cases of COVID-19, being “COVID-19 free” was never a realistic or pursued goal.
The authors note that it is the responsibility of all healthcare professionals to ensure patients are not exposed to COVID-19, and this has meant minimizing hospital visits and person-to-person contact. For example, whenever possible, consultations take place via telephone calls or over the Internet, and nonurgent appointments that would require a patient’s physical presence at the clinic have been postponed. Visitors are also not permitted to accompany patients when admitted to the hospital or during procedures.
Standard-of-care treatment regimens have been adapted across all centers to minimize the number of hospital visits and hospitalizations and prevent “anticancer treatment-induced” complications of COVID-19.
To minimize visits and hospitalizations, strategies include converting intravenous treatments to oral or subcutaneous regimens when possible; switching from cytotoxic chemotherapy to a less-toxic approach to minimize the risk of complications requiring hospitalization; or to pause therapies when possible (stable disease reached or better). In addition, nonemergency surgeries have been postponed or replaced by radiotherapy.
To prevent anticancer treatment-induced complications of COVID-19, most centers use the paradigm that the added benefit for tumor control should be weighed against the potential risk for COVID-19–related morbidity and mortality. To prevent or reduce the risk of neutropenia and lymphopenia, for example, all centers have suggested a de-escalation of cytotoxic chemotherapy or targeted treatment strategies, or to forgo second or subsequent lines of palliative treatments if response rates from up-front therapy are low.
Some of these changes may be here to stay, noted Caldas. “One of the positive messages that comes out of this is that, clearly, care can be delivered in a safe and compassionate manner without requiring as many hospital visits as in the pre-COVID-19 era,” he said. “In the future, we will take heed of the COVID-19 experience to improve delivery of cancer care.”
Capacity of facilities
Many healthcare systems have become overwhelmed as the pandemic has intensified, thus making it necessary to prioritize. To prepare for this possibility, CCE centers have established protocols to categorize and prioritize patients for systemic treatment or surgery. While the protocols vary by center, they are comparable with one another as they prioritize on the basis of anticipated treatment outcome, the authors note.
The guidelines in CCE centers unanimously recommend that neoadjuvant therapies and curative surgeries be the top priority, for the times when operating room and/or ICU capacity is limited. As an alternative, neoadjuvant systemic treatments may be initiated or extended to postpone surgery, and other nonsurgical interventions can be considered.
In addition, some centers agree that certain elective surgeries can be safely delayed if backed by scientific evidence. As an example, an 11-week deferment of surgery may be acceptable for patients with rectal cancer after downstaging.
Cancer centers may also need to upscale and downscale quickly, depending on how the pandemic evolves, and many have already outlined scenarios to prepare for increasing or decreasing their capacity using phased approaches.
The Netherlands Cancer Institute, for example, has defined four phases of increasing severity; in Germany, capacity planning has been coordinated among 18 hospitals and the federal ministry of health, in order to prevent shortages of cancer services.
“We note that the optimal downscaling strategies depend on country- and center-specific capacities and preferences,” they write. “Therefore, it is difficult to propose a common schedule, and it will be most effective if hospitals outline their own phase-specific downscaling strategies based on the prioritization schemes and practical handles discussed above.”
Future research
Better strategies will be needed to reduce the impact of COVID-19 in cancer care, and four research priorities were identified to allow for evidence-based adjustments of cancer care protocols while the pandemic continues:
- Collect real-world data about the effects of adjustment and de-escalation of treatment regimens on outcomes
- Determine the incidence of COVID-19 in both the general population and among patients with cancer who have received systemic therapies, with large-scale serological testing
- Develop an epidemiological model that will allow estimates of the cumulative incidence of COVID-19 for a patient with cancer, within a specific time frame
- Determine COVID-19 related morbidity and mortality in patients with cancer who have been treated with systemic therapies and/or granulocyte colony-stimulating factor (G-CSF). Several projects are currently underway, such as the UK Coronavirus Cancer Monitoring Project.
The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Delivering cancer care during the COVID-19 pandemic has proved particularly challenging, as minimizing the risk of infection must be balanced with maintaining optimal outcomes.
Healthcare systems and oncologists have had to reorganize standard oncologic care in order to protect vulnerable patients from exposure to COVID-19 as well as deal with pandemic-related issues of equipment and staffing shortages.
A new article now describes how seven cancer centers in Europe rapidly reorganized their oncologic services and are tackling this crisis, as well as offering guidance to other institutions.
This was a major undertaking, to work out a system where patients can still get care but in a safer manner, explained coauthor Emile Voest, MD, medical director of the Netherlands Cancer Institute in Amsterdam.
“Decisions needed to be taken based on availability of personnel, protective materials, and urgencies,” he told Medscape Medical News. “Because every country had its own speed of development of the COVID pandemic, there were different scenarios in all institutions, but all with a common factor of key expertise on how to de-escalate in a safe manner.”
The article was published April 16 in Nature Medicine.
The Netherlands Cancer Institute (the Netherlands), Karolinska Institute (Sweden), Institute Gustave Roussy (France), Cambridge Cancer Center (United Kingdom), Istituto Nazionale dei Tumori di Milano (Italy), German Cancer Research Center (Germany), and Vall d’Hebron Institute of Oncology (Spain) have been working closely together in a legal entity since 2014, and have created ‘Cancer Core Europe’ (CCE). The goal is to “maximize coherence and critical mass in cancer research,” the authors note.
The consortium represents roughly 60,000 patients with newly diagnosed cancer, delivers approximately 300,000 treatment courses, and conducts about 1.2 million consultations annually, with more than 1,500 ongoing clinical trials. In a joint effort, the centers collected, translated, and compared the guidelines that had been put in place to treat patients with cancer during the COVID-19 pandemic.
Cancer treatment is multidisciplinary and involves many specialties including surgery, radiology, pathology, radiation oncology, and medical oncology. Coordinating care among disciplines is a very complex process, Voest noted.
“Changing treatment also means that you need to reconsider capacities and requirements,” he said. “Hospitals have installed crisis teams that were very good at coordinating these efforts.”
Restructuring care
Cancer care had to be reorganized on multiple levels, and the CCE centers looked at several aspects that needed to be accounted for, to ensure continuity in cancer care.
“The biggest challenge for the NHS and other healthcare systems is the surge of patients requiring oxygen and/or intensive care, and the nature and infectiousness of the virus,” said coauthor Carlos Caldas, MD, FMedSci, professor of cancer medicine at the University of Cambridge, United Kingdom. “In hospitals that are mostly run close to capacity, and where all kinds of patients are treated, this has created major resource and logistical problems.”
For regular clinical activities, the institutions with dedicated cancer centers (German Cancer Research Center, Institute Gustave Roussy, Istituto Nazionale dei Tumori di Milano, and Netherlands Cancer Institute) have attempted to stay COVID-19 free. This policy would in turn help ensure that sufficient clinical and intensive-care capacity could be reserved for critical cancer surgeries or management of treatment-related side effects, and allow hospitals outside of the CCE to transfer patients with cancer to these centers. The general hospitals can then focus on caring for patients with COVID-19, as well as other illnesses/injuries that require inpatient care.
As the CCE centers located within general hospitals (Cambridge Cancer Center, Vall d’Hebron Institute of Oncology and Karolinska Institute) have to admit patients with suspected and positive cases of COVID-19, being “COVID-19 free” was never a realistic or pursued goal.
The authors note that it is the responsibility of all healthcare professionals to ensure patients are not exposed to COVID-19, and this has meant minimizing hospital visits and person-to-person contact. For example, whenever possible, consultations take place via telephone calls or over the Internet, and nonurgent appointments that would require a patient’s physical presence at the clinic have been postponed. Visitors are also not permitted to accompany patients when admitted to the hospital or during procedures.
Standard-of-care treatment regimens have been adapted across all centers to minimize the number of hospital visits and hospitalizations and prevent “anticancer treatment-induced” complications of COVID-19.
To minimize visits and hospitalizations, strategies include converting intravenous treatments to oral or subcutaneous regimens when possible; switching from cytotoxic chemotherapy to a less-toxic approach to minimize the risk of complications requiring hospitalization; or to pause therapies when possible (stable disease reached or better). In addition, nonemergency surgeries have been postponed or replaced by radiotherapy.
To prevent anticancer treatment-induced complications of COVID-19, most centers use the paradigm that the added benefit for tumor control should be weighed against the potential risk for COVID-19–related morbidity and mortality. To prevent or reduce the risk of neutropenia and lymphopenia, for example, all centers have suggested a de-escalation of cytotoxic chemotherapy or targeted treatment strategies, or to forgo second or subsequent lines of palliative treatments if response rates from up-front therapy are low.
Some of these changes may be here to stay, noted Caldas. “One of the positive messages that comes out of this is that, clearly, care can be delivered in a safe and compassionate manner without requiring as many hospital visits as in the pre-COVID-19 era,” he said. “In the future, we will take heed of the COVID-19 experience to improve delivery of cancer care.”
Capacity of facilities
Many healthcare systems have become overwhelmed as the pandemic has intensified, thus making it necessary to prioritize. To prepare for this possibility, CCE centers have established protocols to categorize and prioritize patients for systemic treatment or surgery. While the protocols vary by center, they are comparable with one another as they prioritize on the basis of anticipated treatment outcome, the authors note.
The guidelines in CCE centers unanimously recommend that neoadjuvant therapies and curative surgeries be the top priority, for the times when operating room and/or ICU capacity is limited. As an alternative, neoadjuvant systemic treatments may be initiated or extended to postpone surgery, and other nonsurgical interventions can be considered.
In addition, some centers agree that certain elective surgeries can be safely delayed if backed by scientific evidence. As an example, an 11-week deferment of surgery may be acceptable for patients with rectal cancer after downstaging.
Cancer centers may also need to upscale and downscale quickly, depending on how the pandemic evolves, and many have already outlined scenarios to prepare for increasing or decreasing their capacity using phased approaches.
The Netherlands Cancer Institute, for example, has defined four phases of increasing severity; in Germany, capacity planning has been coordinated among 18 hospitals and the federal ministry of health, in order to prevent shortages of cancer services.
“We note that the optimal downscaling strategies depend on country- and center-specific capacities and preferences,” they write. “Therefore, it is difficult to propose a common schedule, and it will be most effective if hospitals outline their own phase-specific downscaling strategies based on the prioritization schemes and practical handles discussed above.”
Future research
Better strategies will be needed to reduce the impact of COVID-19 in cancer care, and four research priorities were identified to allow for evidence-based adjustments of cancer care protocols while the pandemic continues:
- Collect real-world data about the effects of adjustment and de-escalation of treatment regimens on outcomes
- Determine the incidence of COVID-19 in both the general population and among patients with cancer who have received systemic therapies, with large-scale serological testing
- Develop an epidemiological model that will allow estimates of the cumulative incidence of COVID-19 for a patient with cancer, within a specific time frame
- Determine COVID-19 related morbidity and mortality in patients with cancer who have been treated with systemic therapies and/or granulocyte colony-stimulating factor (G-CSF). Several projects are currently underway, such as the UK Coronavirus Cancer Monitoring Project.
The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Prioritize lung cancer patients for COVID-19 testing, physicians recommend
Lung cancer patients should be prioritized for COVID-19 testing, according to an editorial published in Annals of Oncology.
In fact, treatment recommendations should call for baseline COVID-19 testing for all patients with lung cancer, Antonio Passaro, MD, PhD, of the European Institute of Oncology in Milan, Italy, and colleagues argued in the editorial.
“While all types of malignancies seem to be associated with high COVID-19 prevalence, morbidity, and mortality, lung cancer represents a specific scenario of cumulative risk factors for COVID-19 complications,” the authors wrote.
“[Lung cancer patients] are at a uniquely escalated risk of complications from COVID-19 due to the common features of smoking history, respiratory and cardiac disease, advanced age, and often predisposing risks from treatment, such as lung surgery and immunosuppressive chemotherapy,” said Howard (Jack) West, MD, of City of Hope Comprehensive Cancer Center in Duarte, Calif., who was not involved in the editorial.
“They also routinely experience a cough as well as chest imaging that may overlap between their underlying lung cancer, possible side effects of treatment, and potential COVID-19, leading to troubling ambiguity that can only be addressed by proactive and widespread testing of patients with lung cancer at the earliest opportunity and as a very high priority,” Dr. West added.
Dr. Passaro and colleagues’ editorial outlined these and other issues that suggest a need to prioritize testing in lung cancer patients.
Disease characteristics, treatment, and imaging
Lung cancer patients may have “defective pulmonary architecture,” such as mechanical obstruction from a tumor or previous lung surgery, that predisposes them to infection and can increase the risk of cytokine release. This is a concern because massive cytokine release during SARS-CoV-2 infection “has been postulated to be the major step in leading to the development of ARDS [acute respiratory distress syndrome],” Dr. Passaro and colleagues wrote.
The authors also argued that similar clinical symptoms among lung cancer patients and those with COVID-19 – such as cough, fever, and dyspnea – underscore the need for an accurate screening model to allow for early COVID-19 detection and potentially improve outcomes.
Similarly, lung cancer patients and COVID-19 patients may have overlapping findings on imaging. The radiologic effects of some common treatments for lung cancer can lead to the same kind of ground glass opacities and other findings seen in COVID-19 patients. Therefore, the authors predict an increase in “COVID-19-suspicious imaging, even in the absence of new symptoms” in the coming weeks.
Another issue to consider is the frequent use of corticosteroids in cancer patients. Corticosteroids may be harmful when used for COVID-19–related acute respiratory distress syndrome and could mask early symptoms of infection. Therefore, routine COVID-19 testing in patients receiving steroids may be warranted, according to Dr. Passaro and colleagues.
In addition, immunosuppression associated with cancer treatment “may impose specific consideration on the schedule and dose of cytotoxic chemotherapy for lung cancer patients in epidemic areas,” the authors wrote.
Increasing awareness: A registry and guidelines
“In the era of COVID-19, the optimal management of patients with lung cancer remains unknown, and the oncology community should have increased awareness to prevent the emergence of an increase in cancer-related and infectious mortality,” Dr. Passaro and colleagues wrote.
To that end, a novel global registry (TERAVOLT) has been launched and is collecting data worldwide with an aim of developing a tailored risk assessment strategy for lung cancer patients. The authors noted that developing international consensus with respect to COVID-19 testing in lung cancer is essential for achieving that goal.
The European Society for Medical Oncology recently released guidelines for treating lung cancer patients during the COVID-19 pandemic, but those guidelines do not include recommendations on COVID-19 testing.
“Baseline SARS-CoV-2 testing for all patients affected by lung cancer should be recommended,” Dr. Passaro and colleagues wrote. “In addition, for those patients with a negative swab test and new ground glass opacities detected on CT scan, with or without new respiratory symptoms, bronchoscopy should be considered to increase testing sensitivity.”
This work was partially supported by the Italian Ministry of Health. The authors reported having no relevant conflicts of interest. Dr. West is a regular correspondent for Medscape, which is owned by the same parent company as MDedge.
SOURCE: Passaro A et al. Annals of Oncology. doi: 10.1016/j.annonc.2020.04.002.
Lung cancer patients should be prioritized for COVID-19 testing, according to an editorial published in Annals of Oncology.
In fact, treatment recommendations should call for baseline COVID-19 testing for all patients with lung cancer, Antonio Passaro, MD, PhD, of the European Institute of Oncology in Milan, Italy, and colleagues argued in the editorial.
“While all types of malignancies seem to be associated with high COVID-19 prevalence, morbidity, and mortality, lung cancer represents a specific scenario of cumulative risk factors for COVID-19 complications,” the authors wrote.
“[Lung cancer patients] are at a uniquely escalated risk of complications from COVID-19 due to the common features of smoking history, respiratory and cardiac disease, advanced age, and often predisposing risks from treatment, such as lung surgery and immunosuppressive chemotherapy,” said Howard (Jack) West, MD, of City of Hope Comprehensive Cancer Center in Duarte, Calif., who was not involved in the editorial.
“They also routinely experience a cough as well as chest imaging that may overlap between their underlying lung cancer, possible side effects of treatment, and potential COVID-19, leading to troubling ambiguity that can only be addressed by proactive and widespread testing of patients with lung cancer at the earliest opportunity and as a very high priority,” Dr. West added.
Dr. Passaro and colleagues’ editorial outlined these and other issues that suggest a need to prioritize testing in lung cancer patients.
Disease characteristics, treatment, and imaging
Lung cancer patients may have “defective pulmonary architecture,” such as mechanical obstruction from a tumor or previous lung surgery, that predisposes them to infection and can increase the risk of cytokine release. This is a concern because massive cytokine release during SARS-CoV-2 infection “has been postulated to be the major step in leading to the development of ARDS [acute respiratory distress syndrome],” Dr. Passaro and colleagues wrote.
The authors also argued that similar clinical symptoms among lung cancer patients and those with COVID-19 – such as cough, fever, and dyspnea – underscore the need for an accurate screening model to allow for early COVID-19 detection and potentially improve outcomes.
Similarly, lung cancer patients and COVID-19 patients may have overlapping findings on imaging. The radiologic effects of some common treatments for lung cancer can lead to the same kind of ground glass opacities and other findings seen in COVID-19 patients. Therefore, the authors predict an increase in “COVID-19-suspicious imaging, even in the absence of new symptoms” in the coming weeks.
Another issue to consider is the frequent use of corticosteroids in cancer patients. Corticosteroids may be harmful when used for COVID-19–related acute respiratory distress syndrome and could mask early symptoms of infection. Therefore, routine COVID-19 testing in patients receiving steroids may be warranted, according to Dr. Passaro and colleagues.
In addition, immunosuppression associated with cancer treatment “may impose specific consideration on the schedule and dose of cytotoxic chemotherapy for lung cancer patients in epidemic areas,” the authors wrote.
Increasing awareness: A registry and guidelines
“In the era of COVID-19, the optimal management of patients with lung cancer remains unknown, and the oncology community should have increased awareness to prevent the emergence of an increase in cancer-related and infectious mortality,” Dr. Passaro and colleagues wrote.
To that end, a novel global registry (TERAVOLT) has been launched and is collecting data worldwide with an aim of developing a tailored risk assessment strategy for lung cancer patients. The authors noted that developing international consensus with respect to COVID-19 testing in lung cancer is essential for achieving that goal.
The European Society for Medical Oncology recently released guidelines for treating lung cancer patients during the COVID-19 pandemic, but those guidelines do not include recommendations on COVID-19 testing.
“Baseline SARS-CoV-2 testing for all patients affected by lung cancer should be recommended,” Dr. Passaro and colleagues wrote. “In addition, for those patients with a negative swab test and new ground glass opacities detected on CT scan, with or without new respiratory symptoms, bronchoscopy should be considered to increase testing sensitivity.”
This work was partially supported by the Italian Ministry of Health. The authors reported having no relevant conflicts of interest. Dr. West is a regular correspondent for Medscape, which is owned by the same parent company as MDedge.
SOURCE: Passaro A et al. Annals of Oncology. doi: 10.1016/j.annonc.2020.04.002.
Lung cancer patients should be prioritized for COVID-19 testing, according to an editorial published in Annals of Oncology.
In fact, treatment recommendations should call for baseline COVID-19 testing for all patients with lung cancer, Antonio Passaro, MD, PhD, of the European Institute of Oncology in Milan, Italy, and colleagues argued in the editorial.
“While all types of malignancies seem to be associated with high COVID-19 prevalence, morbidity, and mortality, lung cancer represents a specific scenario of cumulative risk factors for COVID-19 complications,” the authors wrote.
“[Lung cancer patients] are at a uniquely escalated risk of complications from COVID-19 due to the common features of smoking history, respiratory and cardiac disease, advanced age, and often predisposing risks from treatment, such as lung surgery and immunosuppressive chemotherapy,” said Howard (Jack) West, MD, of City of Hope Comprehensive Cancer Center in Duarte, Calif., who was not involved in the editorial.
“They also routinely experience a cough as well as chest imaging that may overlap between their underlying lung cancer, possible side effects of treatment, and potential COVID-19, leading to troubling ambiguity that can only be addressed by proactive and widespread testing of patients with lung cancer at the earliest opportunity and as a very high priority,” Dr. West added.
Dr. Passaro and colleagues’ editorial outlined these and other issues that suggest a need to prioritize testing in lung cancer patients.
Disease characteristics, treatment, and imaging
Lung cancer patients may have “defective pulmonary architecture,” such as mechanical obstruction from a tumor or previous lung surgery, that predisposes them to infection and can increase the risk of cytokine release. This is a concern because massive cytokine release during SARS-CoV-2 infection “has been postulated to be the major step in leading to the development of ARDS [acute respiratory distress syndrome],” Dr. Passaro and colleagues wrote.
The authors also argued that similar clinical symptoms among lung cancer patients and those with COVID-19 – such as cough, fever, and dyspnea – underscore the need for an accurate screening model to allow for early COVID-19 detection and potentially improve outcomes.
Similarly, lung cancer patients and COVID-19 patients may have overlapping findings on imaging. The radiologic effects of some common treatments for lung cancer can lead to the same kind of ground glass opacities and other findings seen in COVID-19 patients. Therefore, the authors predict an increase in “COVID-19-suspicious imaging, even in the absence of new symptoms” in the coming weeks.
Another issue to consider is the frequent use of corticosteroids in cancer patients. Corticosteroids may be harmful when used for COVID-19–related acute respiratory distress syndrome and could mask early symptoms of infection. Therefore, routine COVID-19 testing in patients receiving steroids may be warranted, according to Dr. Passaro and colleagues.
In addition, immunosuppression associated with cancer treatment “may impose specific consideration on the schedule and dose of cytotoxic chemotherapy for lung cancer patients in epidemic areas,” the authors wrote.
Increasing awareness: A registry and guidelines
“In the era of COVID-19, the optimal management of patients with lung cancer remains unknown, and the oncology community should have increased awareness to prevent the emergence of an increase in cancer-related and infectious mortality,” Dr. Passaro and colleagues wrote.
To that end, a novel global registry (TERAVOLT) has been launched and is collecting data worldwide with an aim of developing a tailored risk assessment strategy for lung cancer patients. The authors noted that developing international consensus with respect to COVID-19 testing in lung cancer is essential for achieving that goal.
The European Society for Medical Oncology recently released guidelines for treating lung cancer patients during the COVID-19 pandemic, but those guidelines do not include recommendations on COVID-19 testing.
“Baseline SARS-CoV-2 testing for all patients affected by lung cancer should be recommended,” Dr. Passaro and colleagues wrote. “In addition, for those patients with a negative swab test and new ground glass opacities detected on CT scan, with or without new respiratory symptoms, bronchoscopy should be considered to increase testing sensitivity.”
This work was partially supported by the Italian Ministry of Health. The authors reported having no relevant conflicts of interest. Dr. West is a regular correspondent for Medscape, which is owned by the same parent company as MDedge.
SOURCE: Passaro A et al. Annals of Oncology. doi: 10.1016/j.annonc.2020.04.002.
FROM ANNALS OF ONCOLOGY
COVID-19: New programs can provide money to keep your practice running
Family physician Frank Maselli, MD, saw approximately 30 patients a day in his office in the Bronx before COVID-19. But New York City has become a hot spot for the virus that has claimed the lives of the lives of more than 40,000 people nationwide.
Now Maselli and the other 10 physicians in the practice each treat only eight or nine patients a day via telemedicine. He spends most of his time on the phone answering patients’ questions about COVID-19 symptoms and potential exposure. Although he tries to bill for telemedicine and phone calls, he says many commercial payers reject the claims because their processing systems aren’t updated to reflect new coverage policies. He has enough cash in reserve to cover two payrolls, but he knows he needs a backup plan if patient volumes continue to decrease indefinitely.
“Our doctors will take a pay cut before we let people go,” says Maselli. “So far we’re OK because we’re getting paid for things we did two months ago before all of this happened.”
Ninety-seven percent of medical practices have experienced a negative financial impact directly or indirectly related to the COVID-19 pandemic, according to new data from the Medical Group Management Association (MGMA). On average, practices report a 60% decrease in patient volume and a 55% decrease in revenue since the beginning of the public health emergency.
Four options for financial assistance
However, there are ways to offset revenue loss and remain financially viable during the economic uncertainty of the COVID-19 pandemic. Options include the US Small Business Administration’s (SBA) Paycheck Protection Program; the SBA’s Emergency Economic Injury Disaster Loan (EIDL); Medicare’s advanced payment program; and an SBA Coronavirus Economic Stabilization Act (CESA) loan. These are in addition to several other strategies aimed at reducing costs and improving revenue.
1. Maselli, for example, applied for the Paycheck Protection Program, a short-term loan that helps small businesses (i.e., for physician offices, those with an annual revenue of under $12 million) keep staff employed during the COVID-19 crisis. The loan covers a variety of costs, including payroll, rent, utilities, mortgage interest, and interest on any other debt obligations incurred before February 15 of this year.
“We have no idea if this is coming and when, but it would be a big help,” he adds.
(As of press time, the Paycheck Protection Program had stopped accepting applications, having reached the limit of its $349 billion budget. Congress must now agree on legislation to add additional funding to assist small businesses.)
Practices can take out a loan of up to 2.5 times the average monthly payroll (excluding payroll for those making more than $100,000 annually) with a cap of $10 million. For example, if the average monthly payroll is $10,000 – and no employees earn more than $100,000 annually – the maximum loan amount is $25,000.
Practices approved for this loan can expect to receive the funds from their SBA-approved lender within 10 calendar days of the date of loan approval. Although it’s technically a loan, the good news is that it doesn’t need to be repaid if the practice complies with all of the loan requirements – particularly these two: The practice uses at least 75% of the loan specifically for payroll, and the practice keeps employees on the payroll (or rehire, when necessary) for 8 weeks after the loan origination date.
Forgiveness is reduced if full-time headcount declines, or if salaries and wages decrease. If a practice does need to repay all or a portion of the loan, it must do so within 2 years at an interest rate of 1%, and payments are deferred for 6 months.
Andrew D. McDonald, FACHE, practice leader of health care consulting at LBMC Healthcare, says it behooves practices to apply for this loan because it’s essentially free money during a time when revenue may be at an all-time low. “While the devil is in the details, on the surface, the paycheck protection funds appear to be a no-brainer. However, each practice will need to confirm with their lender that it’s a solid decision.”
One challenge with this loan is that some banks weren’t necessarily ready to accept applications on April 3, and many continue to lag behind in processing these applications.
2. A second option is the SBA’s EIDL, a low-interest, long-term loan (capped at 3.75% for small businesses) that practices with 500 or fewer employees can use to pay fixed debts, payrolls, accounts payable, and other bills that could have been paid had the disaster not occurred. Borrowers can ask for up to $2 million, and the maximum term of this loan is 30 years, though the overall process for obtaining these loans will depend on the lender.
Practices have until December 16 to apply for this loan. They can also apply for an expedited disbursement (i.e., an Economic Injury Disaster Advance) of up to $10,000 that’s paid within 3 days of the request.
3. A third option is Medicare’s COVID-19 advanced payment program. Under this program, eligible physicians are those who:
- Billed Medicare for claims within 180 days prior to the date of the request
- Are financially solvent (i.e., aren’t in bankruptcy)
- Are free from any active medical review or program integrity investigations
- Are in good standing with Medicare (i.e., don’t have an outstanding delinquent Medicare overpayment)
If physicians meet this criteria, they can ask their Medicare Administrative Contractor (MAC) to provide an advanced payment of up to 100% of the Medicare payment amount based on a 3-month lookback period.
Once requested, MACs will issue payment within 7 calendar days from the date of the request. Repayment will occur in the form of automatic recoupments beginning 120 days after the advanced payment is received. Medicare has already approved more than 21,000 requests totaling more than $51 billion. CMS has provided a fact sheet to learn more about how to request an accelerated payment.
“The key is that you need to repay this, so you want to set a reasonable goal,” says Sarah Hostetter, senior consultant at Advisory Board, a health care research & data consulting firm. She says practices should consider what they’ll realistically be able to repay within 120 days.
4. A fourth option – specifically for mid-size practices – is a CESA loan, the details of which have yet to be announced, that will enable practices to access funds with an annualized rate no greater than 2% and with no principal or interest due for at least 6 months. The CARES Act, signed into law 3 weeks ago, provides $454 billion for this program.
Selecting the right option for your practice
Which singular option – or combination of options – is best for your practice? McDonald says to ask these questions:
- How well are patient volumes holding up?
- How well are physicians pivoting to telehealth?
- What is the overall economic loss?
- What are the available liquid assets, and how long can the practice maintain its financial viability over the next couple of months and beyond?
Cheryl Mongillo, MBA, administrative director of two independent family practices in Delaware, applied for both the Paycheck Protection Program and Medicare advanced payments because she’s worried about being able to pay staff while also covering costs related to personal protective equipment, medical waste, and cleaning, all of which have tripled since the pandemic began. One of the practices includes one physician and four nurse practitioners. The other includes five physicians and three nurse practitioners. In total, both practices employ 35 additional staff.
“I want our staff to know how much we care about them. My hope is that after this is over, our business will pick back up pretty quickly,” she adds. “However, until I can get the business back, I needed something to keep us afloat.”
Others are being more cautious. Crystal Bruning, practice manager at an Ob/Gyn clinic in Orlando, Florida, says her practice applied for the Paycheck Protection Program but is waiting another month or so before deciding whether it will also take advantage of Medicare advanced payments.
The practice is still trying to assess the true financial impact of its 30% reduction in patient volume. Bruning says the advanced payments wouldn’t amount to much anyway because only 10% of the practice’s patients have Medicare.
Making tough financial decisions while awaiting assistance
Kansas-based family physician Jennifer Bacani McKenney, MD, says she hasn’t paid herself a salary in weeks because of the revenue loss her practice has incurred.
“I want to make sure we can pay [all 12] employees,” she says. “In my family, we have two incomes, and we’re pretty good at saving money. However, I know not every physician can afford to do this.”
Although McKenney’s practice has seen a 75% reduction in patient volume, staff continue to provide virtual visits – including Zoom-based nursing home visits – phone visits, and in-person visits for acute illnesses. They also provide curbside immunizations. Still, long-term revenue loss is a concern. “I have a threshold in mind based on what we have in reserves,” she says. “If we hit that point, we would need to talk about a loan or Medicare advanced payments.”
Arkansas-based family physician Lonnie S. Robinson, MD, says he immediately applied for the Paycheck Protection Program after it was announced. “We also made sure we had a line of credit with our local bank during the very first discussions about what the pandemic would mean for our revenue streams,” he says.
However, because he’s in a rural area of the state, he continues to struggle with telemedicine due to broadband and connectivity challenges. Cash flow is another challenge because a lot of insurance companies are waiving copayments.
“I didn’t realize the amount of money we collect immediately from the patient,” he says. “This was a substantial revenue stream, and it was immediate revenue – not revenue waiting on a claim to be paid.”
Illinois-based family physician Deborah L. Winiger, MD, says she also applied for the Paycheck Protection Program but in the meantime had to reduce staff hours by a third because her patient volume dropped by more than half. She will also encourage staff to pursue temporary positions at a local hospital if the federal funds don’t materialize.
Kelly Shackleton, practice manager at a New York-based internal medicine practice, says she laid off 7 of her 16 staff members (including lab technicians, licensed practical nurses, billers, a referral specialist, and a file clerk) due to a 70% decrease in patient volume.
“I didn’t lay them all off at once,” she says. “I kept them until things were all caught up in each department. I plan to get them all back when the time is right, but I want to be sure to keep the practice afloat so they have a place to return to.” If the Paycheck Protection Program for which she applied comes through, then she will rehire them. She also applied for Medicare advanced payments and increased the practice’s line of credit.
Bill properly – and for everything you are still doing
Accurate and complete coding is critical during this time of financial instability, says Maselli. “I keep telling doctors to bill for everything they do,” he says. This includes phone calls between patients and physicians or other qualified healthcare providers (CPT codes 99441-99443). Note that these are time-based codes, requiring a minimum of five minutes of medical discussion.
Remote physiologic monitoring (including monitoring a patient’s oxygen saturation levels using pulse oximetry), virtual check-ins, and online digital evaluation and management services are also covered by Medicare and some commercial payers.
Other good news is that the Centers for Medicare & Medicaid Services added more than 80 additional services that providers can furnish using telehealth, including new patient office visits, home visits, prolonged office visits, smoking and tobacco cessation counseling, annual depression and alcohol screenings, advanced care planning, and much more.
Mongillo, the family practice administrator in Delaware, agrees that physicians need to bill for as many services as possible. At one of the family medicine practices she manages, physicians perform wellness visits, when appropriate, if patients are already coming into the office for another ailment.
Also look for ways to cut costs. For example, Mongillo was able to renegotiate the practice’s telemedicine contract after she received several proposals from other vendors offering three months of complimentary service. Shackleton discontinued provider dictation services to save money.
Physicians need to take a hard look at what’s going on to help them sustain their business through times of uncertainty, says Advisory Board’s Hostetter. “Now is the time to evaluate options and figure out what’s right for your practice,” she adds.
This article first appeared on Medscape.com.
Family physician Frank Maselli, MD, saw approximately 30 patients a day in his office in the Bronx before COVID-19. But New York City has become a hot spot for the virus that has claimed the lives of the lives of more than 40,000 people nationwide.
Now Maselli and the other 10 physicians in the practice each treat only eight or nine patients a day via telemedicine. He spends most of his time on the phone answering patients’ questions about COVID-19 symptoms and potential exposure. Although he tries to bill for telemedicine and phone calls, he says many commercial payers reject the claims because their processing systems aren’t updated to reflect new coverage policies. He has enough cash in reserve to cover two payrolls, but he knows he needs a backup plan if patient volumes continue to decrease indefinitely.
“Our doctors will take a pay cut before we let people go,” says Maselli. “So far we’re OK because we’re getting paid for things we did two months ago before all of this happened.”
Ninety-seven percent of medical practices have experienced a negative financial impact directly or indirectly related to the COVID-19 pandemic, according to new data from the Medical Group Management Association (MGMA). On average, practices report a 60% decrease in patient volume and a 55% decrease in revenue since the beginning of the public health emergency.
Four options for financial assistance
However, there are ways to offset revenue loss and remain financially viable during the economic uncertainty of the COVID-19 pandemic. Options include the US Small Business Administration’s (SBA) Paycheck Protection Program; the SBA’s Emergency Economic Injury Disaster Loan (EIDL); Medicare’s advanced payment program; and an SBA Coronavirus Economic Stabilization Act (CESA) loan. These are in addition to several other strategies aimed at reducing costs and improving revenue.
1. Maselli, for example, applied for the Paycheck Protection Program, a short-term loan that helps small businesses (i.e., for physician offices, those with an annual revenue of under $12 million) keep staff employed during the COVID-19 crisis. The loan covers a variety of costs, including payroll, rent, utilities, mortgage interest, and interest on any other debt obligations incurred before February 15 of this year.
“We have no idea if this is coming and when, but it would be a big help,” he adds.
(As of press time, the Paycheck Protection Program had stopped accepting applications, having reached the limit of its $349 billion budget. Congress must now agree on legislation to add additional funding to assist small businesses.)
Practices can take out a loan of up to 2.5 times the average monthly payroll (excluding payroll for those making more than $100,000 annually) with a cap of $10 million. For example, if the average monthly payroll is $10,000 – and no employees earn more than $100,000 annually – the maximum loan amount is $25,000.
Practices approved for this loan can expect to receive the funds from their SBA-approved lender within 10 calendar days of the date of loan approval. Although it’s technically a loan, the good news is that it doesn’t need to be repaid if the practice complies with all of the loan requirements – particularly these two: The practice uses at least 75% of the loan specifically for payroll, and the practice keeps employees on the payroll (or rehire, when necessary) for 8 weeks after the loan origination date.
Forgiveness is reduced if full-time headcount declines, or if salaries and wages decrease. If a practice does need to repay all or a portion of the loan, it must do so within 2 years at an interest rate of 1%, and payments are deferred for 6 months.
Andrew D. McDonald, FACHE, practice leader of health care consulting at LBMC Healthcare, says it behooves practices to apply for this loan because it’s essentially free money during a time when revenue may be at an all-time low. “While the devil is in the details, on the surface, the paycheck protection funds appear to be a no-brainer. However, each practice will need to confirm with their lender that it’s a solid decision.”
One challenge with this loan is that some banks weren’t necessarily ready to accept applications on April 3, and many continue to lag behind in processing these applications.
2. A second option is the SBA’s EIDL, a low-interest, long-term loan (capped at 3.75% for small businesses) that practices with 500 or fewer employees can use to pay fixed debts, payrolls, accounts payable, and other bills that could have been paid had the disaster not occurred. Borrowers can ask for up to $2 million, and the maximum term of this loan is 30 years, though the overall process for obtaining these loans will depend on the lender.
Practices have until December 16 to apply for this loan. They can also apply for an expedited disbursement (i.e., an Economic Injury Disaster Advance) of up to $10,000 that’s paid within 3 days of the request.
3. A third option is Medicare’s COVID-19 advanced payment program. Under this program, eligible physicians are those who:
- Billed Medicare for claims within 180 days prior to the date of the request
- Are financially solvent (i.e., aren’t in bankruptcy)
- Are free from any active medical review or program integrity investigations
- Are in good standing with Medicare (i.e., don’t have an outstanding delinquent Medicare overpayment)
If physicians meet this criteria, they can ask their Medicare Administrative Contractor (MAC) to provide an advanced payment of up to 100% of the Medicare payment amount based on a 3-month lookback period.
Once requested, MACs will issue payment within 7 calendar days from the date of the request. Repayment will occur in the form of automatic recoupments beginning 120 days after the advanced payment is received. Medicare has already approved more than 21,000 requests totaling more than $51 billion. CMS has provided a fact sheet to learn more about how to request an accelerated payment.
“The key is that you need to repay this, so you want to set a reasonable goal,” says Sarah Hostetter, senior consultant at Advisory Board, a health care research & data consulting firm. She says practices should consider what they’ll realistically be able to repay within 120 days.
4. A fourth option – specifically for mid-size practices – is a CESA loan, the details of which have yet to be announced, that will enable practices to access funds with an annualized rate no greater than 2% and with no principal or interest due for at least 6 months. The CARES Act, signed into law 3 weeks ago, provides $454 billion for this program.
Selecting the right option for your practice
Which singular option – or combination of options – is best for your practice? McDonald says to ask these questions:
- How well are patient volumes holding up?
- How well are physicians pivoting to telehealth?
- What is the overall economic loss?
- What are the available liquid assets, and how long can the practice maintain its financial viability over the next couple of months and beyond?
Cheryl Mongillo, MBA, administrative director of two independent family practices in Delaware, applied for both the Paycheck Protection Program and Medicare advanced payments because she’s worried about being able to pay staff while also covering costs related to personal protective equipment, medical waste, and cleaning, all of which have tripled since the pandemic began. One of the practices includes one physician and four nurse practitioners. The other includes five physicians and three nurse practitioners. In total, both practices employ 35 additional staff.
“I want our staff to know how much we care about them. My hope is that after this is over, our business will pick back up pretty quickly,” she adds. “However, until I can get the business back, I needed something to keep us afloat.”
Others are being more cautious. Crystal Bruning, practice manager at an Ob/Gyn clinic in Orlando, Florida, says her practice applied for the Paycheck Protection Program but is waiting another month or so before deciding whether it will also take advantage of Medicare advanced payments.
The practice is still trying to assess the true financial impact of its 30% reduction in patient volume. Bruning says the advanced payments wouldn’t amount to much anyway because only 10% of the practice’s patients have Medicare.
Making tough financial decisions while awaiting assistance
Kansas-based family physician Jennifer Bacani McKenney, MD, says she hasn’t paid herself a salary in weeks because of the revenue loss her practice has incurred.
“I want to make sure we can pay [all 12] employees,” she says. “In my family, we have two incomes, and we’re pretty good at saving money. However, I know not every physician can afford to do this.”
Although McKenney’s practice has seen a 75% reduction in patient volume, staff continue to provide virtual visits – including Zoom-based nursing home visits – phone visits, and in-person visits for acute illnesses. They also provide curbside immunizations. Still, long-term revenue loss is a concern. “I have a threshold in mind based on what we have in reserves,” she says. “If we hit that point, we would need to talk about a loan or Medicare advanced payments.”
Arkansas-based family physician Lonnie S. Robinson, MD, says he immediately applied for the Paycheck Protection Program after it was announced. “We also made sure we had a line of credit with our local bank during the very first discussions about what the pandemic would mean for our revenue streams,” he says.
However, because he’s in a rural area of the state, he continues to struggle with telemedicine due to broadband and connectivity challenges. Cash flow is another challenge because a lot of insurance companies are waiving copayments.
“I didn’t realize the amount of money we collect immediately from the patient,” he says. “This was a substantial revenue stream, and it was immediate revenue – not revenue waiting on a claim to be paid.”
Illinois-based family physician Deborah L. Winiger, MD, says she also applied for the Paycheck Protection Program but in the meantime had to reduce staff hours by a third because her patient volume dropped by more than half. She will also encourage staff to pursue temporary positions at a local hospital if the federal funds don’t materialize.
Kelly Shackleton, practice manager at a New York-based internal medicine practice, says she laid off 7 of her 16 staff members (including lab technicians, licensed practical nurses, billers, a referral specialist, and a file clerk) due to a 70% decrease in patient volume.
“I didn’t lay them all off at once,” she says. “I kept them until things were all caught up in each department. I plan to get them all back when the time is right, but I want to be sure to keep the practice afloat so they have a place to return to.” If the Paycheck Protection Program for which she applied comes through, then she will rehire them. She also applied for Medicare advanced payments and increased the practice’s line of credit.
Bill properly – and for everything you are still doing
Accurate and complete coding is critical during this time of financial instability, says Maselli. “I keep telling doctors to bill for everything they do,” he says. This includes phone calls between patients and physicians or other qualified healthcare providers (CPT codes 99441-99443). Note that these are time-based codes, requiring a minimum of five minutes of medical discussion.
Remote physiologic monitoring (including monitoring a patient’s oxygen saturation levels using pulse oximetry), virtual check-ins, and online digital evaluation and management services are also covered by Medicare and some commercial payers.
Other good news is that the Centers for Medicare & Medicaid Services added more than 80 additional services that providers can furnish using telehealth, including new patient office visits, home visits, prolonged office visits, smoking and tobacco cessation counseling, annual depression and alcohol screenings, advanced care planning, and much more.
Mongillo, the family practice administrator in Delaware, agrees that physicians need to bill for as many services as possible. At one of the family medicine practices she manages, physicians perform wellness visits, when appropriate, if patients are already coming into the office for another ailment.
Also look for ways to cut costs. For example, Mongillo was able to renegotiate the practice’s telemedicine contract after she received several proposals from other vendors offering three months of complimentary service. Shackleton discontinued provider dictation services to save money.
Physicians need to take a hard look at what’s going on to help them sustain their business through times of uncertainty, says Advisory Board’s Hostetter. “Now is the time to evaluate options and figure out what’s right for your practice,” she adds.
This article first appeared on Medscape.com.
Family physician Frank Maselli, MD, saw approximately 30 patients a day in his office in the Bronx before COVID-19. But New York City has become a hot spot for the virus that has claimed the lives of the lives of more than 40,000 people nationwide.
Now Maselli and the other 10 physicians in the practice each treat only eight or nine patients a day via telemedicine. He spends most of his time on the phone answering patients’ questions about COVID-19 symptoms and potential exposure. Although he tries to bill for telemedicine and phone calls, he says many commercial payers reject the claims because their processing systems aren’t updated to reflect new coverage policies. He has enough cash in reserve to cover two payrolls, but he knows he needs a backup plan if patient volumes continue to decrease indefinitely.
“Our doctors will take a pay cut before we let people go,” says Maselli. “So far we’re OK because we’re getting paid for things we did two months ago before all of this happened.”
Ninety-seven percent of medical practices have experienced a negative financial impact directly or indirectly related to the COVID-19 pandemic, according to new data from the Medical Group Management Association (MGMA). On average, practices report a 60% decrease in patient volume and a 55% decrease in revenue since the beginning of the public health emergency.
Four options for financial assistance
However, there are ways to offset revenue loss and remain financially viable during the economic uncertainty of the COVID-19 pandemic. Options include the US Small Business Administration’s (SBA) Paycheck Protection Program; the SBA’s Emergency Economic Injury Disaster Loan (EIDL); Medicare’s advanced payment program; and an SBA Coronavirus Economic Stabilization Act (CESA) loan. These are in addition to several other strategies aimed at reducing costs and improving revenue.
1. Maselli, for example, applied for the Paycheck Protection Program, a short-term loan that helps small businesses (i.e., for physician offices, those with an annual revenue of under $12 million) keep staff employed during the COVID-19 crisis. The loan covers a variety of costs, including payroll, rent, utilities, mortgage interest, and interest on any other debt obligations incurred before February 15 of this year.
“We have no idea if this is coming and when, but it would be a big help,” he adds.
(As of press time, the Paycheck Protection Program had stopped accepting applications, having reached the limit of its $349 billion budget. Congress must now agree on legislation to add additional funding to assist small businesses.)
Practices can take out a loan of up to 2.5 times the average monthly payroll (excluding payroll for those making more than $100,000 annually) with a cap of $10 million. For example, if the average monthly payroll is $10,000 – and no employees earn more than $100,000 annually – the maximum loan amount is $25,000.
Practices approved for this loan can expect to receive the funds from their SBA-approved lender within 10 calendar days of the date of loan approval. Although it’s technically a loan, the good news is that it doesn’t need to be repaid if the practice complies with all of the loan requirements – particularly these two: The practice uses at least 75% of the loan specifically for payroll, and the practice keeps employees on the payroll (or rehire, when necessary) for 8 weeks after the loan origination date.
Forgiveness is reduced if full-time headcount declines, or if salaries and wages decrease. If a practice does need to repay all or a portion of the loan, it must do so within 2 years at an interest rate of 1%, and payments are deferred for 6 months.
Andrew D. McDonald, FACHE, practice leader of health care consulting at LBMC Healthcare, says it behooves practices to apply for this loan because it’s essentially free money during a time when revenue may be at an all-time low. “While the devil is in the details, on the surface, the paycheck protection funds appear to be a no-brainer. However, each practice will need to confirm with their lender that it’s a solid decision.”
One challenge with this loan is that some banks weren’t necessarily ready to accept applications on April 3, and many continue to lag behind in processing these applications.
2. A second option is the SBA’s EIDL, a low-interest, long-term loan (capped at 3.75% for small businesses) that practices with 500 or fewer employees can use to pay fixed debts, payrolls, accounts payable, and other bills that could have been paid had the disaster not occurred. Borrowers can ask for up to $2 million, and the maximum term of this loan is 30 years, though the overall process for obtaining these loans will depend on the lender.
Practices have until December 16 to apply for this loan. They can also apply for an expedited disbursement (i.e., an Economic Injury Disaster Advance) of up to $10,000 that’s paid within 3 days of the request.
3. A third option is Medicare’s COVID-19 advanced payment program. Under this program, eligible physicians are those who:
- Billed Medicare for claims within 180 days prior to the date of the request
- Are financially solvent (i.e., aren’t in bankruptcy)
- Are free from any active medical review or program integrity investigations
- Are in good standing with Medicare (i.e., don’t have an outstanding delinquent Medicare overpayment)
If physicians meet this criteria, they can ask their Medicare Administrative Contractor (MAC) to provide an advanced payment of up to 100% of the Medicare payment amount based on a 3-month lookback period.
Once requested, MACs will issue payment within 7 calendar days from the date of the request. Repayment will occur in the form of automatic recoupments beginning 120 days after the advanced payment is received. Medicare has already approved more than 21,000 requests totaling more than $51 billion. CMS has provided a fact sheet to learn more about how to request an accelerated payment.
“The key is that you need to repay this, so you want to set a reasonable goal,” says Sarah Hostetter, senior consultant at Advisory Board, a health care research & data consulting firm. She says practices should consider what they’ll realistically be able to repay within 120 days.
4. A fourth option – specifically for mid-size practices – is a CESA loan, the details of which have yet to be announced, that will enable practices to access funds with an annualized rate no greater than 2% and with no principal or interest due for at least 6 months. The CARES Act, signed into law 3 weeks ago, provides $454 billion for this program.
Selecting the right option for your practice
Which singular option – or combination of options – is best for your practice? McDonald says to ask these questions:
- How well are patient volumes holding up?
- How well are physicians pivoting to telehealth?
- What is the overall economic loss?
- What are the available liquid assets, and how long can the practice maintain its financial viability over the next couple of months and beyond?
Cheryl Mongillo, MBA, administrative director of two independent family practices in Delaware, applied for both the Paycheck Protection Program and Medicare advanced payments because she’s worried about being able to pay staff while also covering costs related to personal protective equipment, medical waste, and cleaning, all of which have tripled since the pandemic began. One of the practices includes one physician and four nurse practitioners. The other includes five physicians and three nurse practitioners. In total, both practices employ 35 additional staff.
“I want our staff to know how much we care about them. My hope is that after this is over, our business will pick back up pretty quickly,” she adds. “However, until I can get the business back, I needed something to keep us afloat.”
Others are being more cautious. Crystal Bruning, practice manager at an Ob/Gyn clinic in Orlando, Florida, says her practice applied for the Paycheck Protection Program but is waiting another month or so before deciding whether it will also take advantage of Medicare advanced payments.
The practice is still trying to assess the true financial impact of its 30% reduction in patient volume. Bruning says the advanced payments wouldn’t amount to much anyway because only 10% of the practice’s patients have Medicare.
Making tough financial decisions while awaiting assistance
Kansas-based family physician Jennifer Bacani McKenney, MD, says she hasn’t paid herself a salary in weeks because of the revenue loss her practice has incurred.
“I want to make sure we can pay [all 12] employees,” she says. “In my family, we have two incomes, and we’re pretty good at saving money. However, I know not every physician can afford to do this.”
Although McKenney’s practice has seen a 75% reduction in patient volume, staff continue to provide virtual visits – including Zoom-based nursing home visits – phone visits, and in-person visits for acute illnesses. They also provide curbside immunizations. Still, long-term revenue loss is a concern. “I have a threshold in mind based on what we have in reserves,” she says. “If we hit that point, we would need to talk about a loan or Medicare advanced payments.”
Arkansas-based family physician Lonnie S. Robinson, MD, says he immediately applied for the Paycheck Protection Program after it was announced. “We also made sure we had a line of credit with our local bank during the very first discussions about what the pandemic would mean for our revenue streams,” he says.
However, because he’s in a rural area of the state, he continues to struggle with telemedicine due to broadband and connectivity challenges. Cash flow is another challenge because a lot of insurance companies are waiving copayments.
“I didn’t realize the amount of money we collect immediately from the patient,” he says. “This was a substantial revenue stream, and it was immediate revenue – not revenue waiting on a claim to be paid.”
Illinois-based family physician Deborah L. Winiger, MD, says she also applied for the Paycheck Protection Program but in the meantime had to reduce staff hours by a third because her patient volume dropped by more than half. She will also encourage staff to pursue temporary positions at a local hospital if the federal funds don’t materialize.
Kelly Shackleton, practice manager at a New York-based internal medicine practice, says she laid off 7 of her 16 staff members (including lab technicians, licensed practical nurses, billers, a referral specialist, and a file clerk) due to a 70% decrease in patient volume.
“I didn’t lay them all off at once,” she says. “I kept them until things were all caught up in each department. I plan to get them all back when the time is right, but I want to be sure to keep the practice afloat so they have a place to return to.” If the Paycheck Protection Program for which she applied comes through, then she will rehire them. She also applied for Medicare advanced payments and increased the practice’s line of credit.
Bill properly – and for everything you are still doing
Accurate and complete coding is critical during this time of financial instability, says Maselli. “I keep telling doctors to bill for everything they do,” he says. This includes phone calls between patients and physicians or other qualified healthcare providers (CPT codes 99441-99443). Note that these are time-based codes, requiring a minimum of five minutes of medical discussion.
Remote physiologic monitoring (including monitoring a patient’s oxygen saturation levels using pulse oximetry), virtual check-ins, and online digital evaluation and management services are also covered by Medicare and some commercial payers.
Other good news is that the Centers for Medicare & Medicaid Services added more than 80 additional services that providers can furnish using telehealth, including new patient office visits, home visits, prolonged office visits, smoking and tobacco cessation counseling, annual depression and alcohol screenings, advanced care planning, and much more.
Mongillo, the family practice administrator in Delaware, agrees that physicians need to bill for as many services as possible. At one of the family medicine practices she manages, physicians perform wellness visits, when appropriate, if patients are already coming into the office for another ailment.
Also look for ways to cut costs. For example, Mongillo was able to renegotiate the practice’s telemedicine contract after she received several proposals from other vendors offering three months of complimentary service. Shackleton discontinued provider dictation services to save money.
Physicians need to take a hard look at what’s going on to help them sustain their business through times of uncertainty, says Advisory Board’s Hostetter. “Now is the time to evaluate options and figure out what’s right for your practice,” she adds.
This article first appeared on Medscape.com.