User login
Doctors treat osteoporosis with hormone therapy against guidelines
This type of hormone therapy (HT) can be given as estrogen or a combination of hormones including estrogen. The physicians interviewed for this piece who prescribe HT for osteoporosis suggest the benefits outweigh the downsides to its use for some of their patients. But such doctors may be a minority group, suggests Michael R. McClung, MD, founding director of the Oregon Osteoporosis Center, Portland.
According to Dr. McClung, HT is now rarely prescribed as treatment – as opposed to prevention – for osteoporosis in the absence of additional benefits such as reducing vasomotor symptoms.
Researchers’ findings on HT use in women with osteoporosis are complex. While HT is approved for menopausal prevention of osteoporosis, it is not indicated as a treatment for the disease by the Food and Drug Administration. See the prescribing information for Premarin tablets, which contain a mixture of estrogen hormones, for an example of the FDA’s indications and usage for the type of HT addressed in this article.
Women’s Health Initiative findings
The Women’s Health Initiative (WHI) hormone therapy trials showed that HT reduces the incidence of all osteoporosis-related fractures in postmenopausal women, even those at low risk of fracture, but osteoporosis-related fractures was not a study endpoint. These trials also revealed that HT was associated with increased risks of cardiovascular and cerebrovascular events, an increased risk of breast cancer, and other adverse health outcomes.
The release of the interim results of the WHI trials in 2002 led to a fair amount of fear and confusion about the use of HT after menopause. After the WHI findings were published, estrogen use dropped dramatically, but for everything, including for vasomotor symptoms and the prevention and treatment of osteoporosis.
Prior to the WHI study, it was very common for hormone therapy to be prescribed as women neared or entered menopause, said Risa Kagan MD, clinical professor of obstetrics, gynecology, and reproductive sciences, University of California, San Francisco.
“When a woman turned 50, that was one of the first things we did – was to put her on hormone therapy. All that changed with the WHI, but now we are coming full circle,” noted Dr. Kagan, who currently prescribes HT as first line treatment for osteoporosis to some women.
Hormone therapy’s complex history
HT’s ability to reduce bone loss in postmenopausal women is well-documented in many papers, including one published March 8, 2018, in Osteoporosis International, by Dr. Kagan and colleagues. This reduced bone loss has been shown to significantly reduce fractures in patients with low bone mass and osteoporosis.
While a growing number of therapies are now available to treat osteoporosis, HT was traditionally viewed as a standard method of preventing fractures in this population. It was also widely used to prevent other types of symptoms associated with the menopause, such as hot flashes, night sweats, and sleep disturbances, and multiple observational studies had demonstrated that its use appeared to reduce the incidence of cardiovascular disease (CVD) in symptomatic menopausal women who initiated HT in early menopause.
Even though the WHI studies were the largest randomized trials ever performed in postmenopausal women, they had notable limitations, according to Dr. Kagan.
“The women were older – the average age was 63 years,” she said. “And they only investigated one route and one dose of estrogen.”
Since then, many different formulations and routes of administration with more favorable safety profiles than what was used in the WHI have become available.
It’s both scientifically and clinically unsound to extrapolate the unfavorable risk-benefit profile of HT seen in the WHI trials to all women regardless of age, HT dosage or formulation, or the length of time they’re on it, she added.
Today’s use of HT in women with osteoporosis
Re-analyses and follow-up studies from the WHI trials, along with data from other studies, have suggested that the benefit-risk profiles of HT are affected by a variety of factors. These include the timing of use in relation to menopause and chronological age and the type of hormone regimen.
“Clinically, many advocate for [hormone therapy] use, especially in the newer younger postmenopausal women to prevent bone loss, but also in younger women who are diagnosed with osteoporosis and then as they get older transition to more bone specific agents,” noted Dr. Kagan.
“Some advocate preserving bone mass and preventing osteoporosis and even treating the younger newly postmenopausal women who have no contraindications with hormone therapy initially, and then gradually transitioning them to a bone specific agent as they get older and at risk for fracture.
“If a woman is already fractured and/or has very low bone density with no other obvious secondary metabolic reason, we also often advocate anabolic agents for 1-2 years then consider estrogen for maintenance – again, if [there is] no contraindication to using HT,” she added.
Thus, an individualized approach is recommended to determine a woman’s risk-benefit ratio of HT use based on the absolute risk of adverse effects, Dr. Kagan noted.
“Transdermal and low/ultra-low doses of HT, have a favorable risk profile, and are effective in preserving bone mineral density and bone quality in many women,” she said.
According to Dr. McClung, HT “is most often used for treatment in women in whom hormone therapy was begun for hot flashes and then, when osteoporosis was found later, was simply continued.
“Society guidelines are cautious about recommending hormone therapy for osteoporosis treatment since estrogen is not approved for treatment, despite the clear fracture protection benefit observed in the WHI study,” he said. “Since [women in the WHI trials] were not recruited as having osteoporosis, those results do not meet the FDA requirement for treatment approval, namely the reduction in fracture risk in patients with osteoporosis. However, knowing what we know about the salutary skeletal effects of estrogen, many of us do use them in our patients with osteoporosis – although not prescribed for that purpose.”
Additional scenarios when doctors may advise HT
“I often recommend – and I think colleagues do as well – that women with recent menopause and menopausal symptoms who also have low bone mineral density or even scores showing osteoporosis see their gynecologist to discuss HT for a few years, perhaps until age 60 if no contraindications, and if it is well tolerated,” said Ethel S. Siris, MD, professor of medicine at Columbia University Medical Center in New York.
“Once they stop it we can then give one of our other bone drugs, but it delays the need to start them since on adequate estrogen the bone density should remain stable while they take it,” added Dr. Siris, an endocrinologist and internist, and director of the Toni Stabile Osteoporosis Center in New York. “They may need a bisphosphonate or another bone drug to further protect them from bone loss and future fracture [after stopping HT].”
Victor L. Roberts, MD, founder of Endocrine Associates of Florida, Lake Mary, pointed out that women now have many options for treatment of osteoporosis.
“If a woman is in early menopause and is having other symptoms, then estrogen is warranted,” he said. “If she has osteoporosis, then it’s a bonus.”
“We have better agents that are bone specific,” for a patient who presents with osteoporosis and no other symptoms, he said.
“If a woman is intolerant of alendronate or other similar drugs, or chooses not to have an injectable, then estrogen or a SERM [selective estrogen receptor modulator] would be an option.”
Dr. Roberts added that HT would be more of a niche drug.
“It has a role and documented benefit and works,” he said. “There is good scientific data for the use of estrogen.”
Dr. Kagan is a consultant for Pfizer, Therapeutics MD, Amgen, on the Medical and Scientific Advisory Board of American Bone Health. The other experts interviewed for this piece reported no conflicts.
This type of hormone therapy (HT) can be given as estrogen or a combination of hormones including estrogen. The physicians interviewed for this piece who prescribe HT for osteoporosis suggest the benefits outweigh the downsides to its use for some of their patients. But such doctors may be a minority group, suggests Michael R. McClung, MD, founding director of the Oregon Osteoporosis Center, Portland.
According to Dr. McClung, HT is now rarely prescribed as treatment – as opposed to prevention – for osteoporosis in the absence of additional benefits such as reducing vasomotor symptoms.
Researchers’ findings on HT use in women with osteoporosis are complex. While HT is approved for menopausal prevention of osteoporosis, it is not indicated as a treatment for the disease by the Food and Drug Administration. See the prescribing information for Premarin tablets, which contain a mixture of estrogen hormones, for an example of the FDA’s indications and usage for the type of HT addressed in this article.
Women’s Health Initiative findings
The Women’s Health Initiative (WHI) hormone therapy trials showed that HT reduces the incidence of all osteoporosis-related fractures in postmenopausal women, even those at low risk of fracture, but osteoporosis-related fractures was not a study endpoint. These trials also revealed that HT was associated with increased risks of cardiovascular and cerebrovascular events, an increased risk of breast cancer, and other adverse health outcomes.
The release of the interim results of the WHI trials in 2002 led to a fair amount of fear and confusion about the use of HT after menopause. After the WHI findings were published, estrogen use dropped dramatically, but for everything, including for vasomotor symptoms and the prevention and treatment of osteoporosis.
Prior to the WHI study, it was very common for hormone therapy to be prescribed as women neared or entered menopause, said Risa Kagan MD, clinical professor of obstetrics, gynecology, and reproductive sciences, University of California, San Francisco.
“When a woman turned 50, that was one of the first things we did – was to put her on hormone therapy. All that changed with the WHI, but now we are coming full circle,” noted Dr. Kagan, who currently prescribes HT as first line treatment for osteoporosis to some women.
Hormone therapy’s complex history
HT’s ability to reduce bone loss in postmenopausal women is well-documented in many papers, including one published March 8, 2018, in Osteoporosis International, by Dr. Kagan and colleagues. This reduced bone loss has been shown to significantly reduce fractures in patients with low bone mass and osteoporosis.
While a growing number of therapies are now available to treat osteoporosis, HT was traditionally viewed as a standard method of preventing fractures in this population. It was also widely used to prevent other types of symptoms associated with the menopause, such as hot flashes, night sweats, and sleep disturbances, and multiple observational studies had demonstrated that its use appeared to reduce the incidence of cardiovascular disease (CVD) in symptomatic menopausal women who initiated HT in early menopause.
Even though the WHI studies were the largest randomized trials ever performed in postmenopausal women, they had notable limitations, according to Dr. Kagan.
“The women were older – the average age was 63 years,” she said. “And they only investigated one route and one dose of estrogen.”
Since then, many different formulations and routes of administration with more favorable safety profiles than what was used in the WHI have become available.
It’s both scientifically and clinically unsound to extrapolate the unfavorable risk-benefit profile of HT seen in the WHI trials to all women regardless of age, HT dosage or formulation, or the length of time they’re on it, she added.
Today’s use of HT in women with osteoporosis
Re-analyses and follow-up studies from the WHI trials, along with data from other studies, have suggested that the benefit-risk profiles of HT are affected by a variety of factors. These include the timing of use in relation to menopause and chronological age and the type of hormone regimen.
“Clinically, many advocate for [hormone therapy] use, especially in the newer younger postmenopausal women to prevent bone loss, but also in younger women who are diagnosed with osteoporosis and then as they get older transition to more bone specific agents,” noted Dr. Kagan.
“Some advocate preserving bone mass and preventing osteoporosis and even treating the younger newly postmenopausal women who have no contraindications with hormone therapy initially, and then gradually transitioning them to a bone specific agent as they get older and at risk for fracture.
“If a woman is already fractured and/or has very low bone density with no other obvious secondary metabolic reason, we also often advocate anabolic agents for 1-2 years then consider estrogen for maintenance – again, if [there is] no contraindication to using HT,” she added.
Thus, an individualized approach is recommended to determine a woman’s risk-benefit ratio of HT use based on the absolute risk of adverse effects, Dr. Kagan noted.
“Transdermal and low/ultra-low doses of HT, have a favorable risk profile, and are effective in preserving bone mineral density and bone quality in many women,” she said.
According to Dr. McClung, HT “is most often used for treatment in women in whom hormone therapy was begun for hot flashes and then, when osteoporosis was found later, was simply continued.
“Society guidelines are cautious about recommending hormone therapy for osteoporosis treatment since estrogen is not approved for treatment, despite the clear fracture protection benefit observed in the WHI study,” he said. “Since [women in the WHI trials] were not recruited as having osteoporosis, those results do not meet the FDA requirement for treatment approval, namely the reduction in fracture risk in patients with osteoporosis. However, knowing what we know about the salutary skeletal effects of estrogen, many of us do use them in our patients with osteoporosis – although not prescribed for that purpose.”
Additional scenarios when doctors may advise HT
“I often recommend – and I think colleagues do as well – that women with recent menopause and menopausal symptoms who also have low bone mineral density or even scores showing osteoporosis see their gynecologist to discuss HT for a few years, perhaps until age 60 if no contraindications, and if it is well tolerated,” said Ethel S. Siris, MD, professor of medicine at Columbia University Medical Center in New York.
“Once they stop it we can then give one of our other bone drugs, but it delays the need to start them since on adequate estrogen the bone density should remain stable while they take it,” added Dr. Siris, an endocrinologist and internist, and director of the Toni Stabile Osteoporosis Center in New York. “They may need a bisphosphonate or another bone drug to further protect them from bone loss and future fracture [after stopping HT].”
Victor L. Roberts, MD, founder of Endocrine Associates of Florida, Lake Mary, pointed out that women now have many options for treatment of osteoporosis.
“If a woman is in early menopause and is having other symptoms, then estrogen is warranted,” he said. “If she has osteoporosis, then it’s a bonus.”
“We have better agents that are bone specific,” for a patient who presents with osteoporosis and no other symptoms, he said.
“If a woman is intolerant of alendronate or other similar drugs, or chooses not to have an injectable, then estrogen or a SERM [selective estrogen receptor modulator] would be an option.”
Dr. Roberts added that HT would be more of a niche drug.
“It has a role and documented benefit and works,” he said. “There is good scientific data for the use of estrogen.”
Dr. Kagan is a consultant for Pfizer, Therapeutics MD, Amgen, on the Medical and Scientific Advisory Board of American Bone Health. The other experts interviewed for this piece reported no conflicts.
This type of hormone therapy (HT) can be given as estrogen or a combination of hormones including estrogen. The physicians interviewed for this piece who prescribe HT for osteoporosis suggest the benefits outweigh the downsides to its use for some of their patients. But such doctors may be a minority group, suggests Michael R. McClung, MD, founding director of the Oregon Osteoporosis Center, Portland.
According to Dr. McClung, HT is now rarely prescribed as treatment – as opposed to prevention – for osteoporosis in the absence of additional benefits such as reducing vasomotor symptoms.
Researchers’ findings on HT use in women with osteoporosis are complex. While HT is approved for menopausal prevention of osteoporosis, it is not indicated as a treatment for the disease by the Food and Drug Administration. See the prescribing information for Premarin tablets, which contain a mixture of estrogen hormones, for an example of the FDA’s indications and usage for the type of HT addressed in this article.
Women’s Health Initiative findings
The Women’s Health Initiative (WHI) hormone therapy trials showed that HT reduces the incidence of all osteoporosis-related fractures in postmenopausal women, even those at low risk of fracture, but osteoporosis-related fractures was not a study endpoint. These trials also revealed that HT was associated with increased risks of cardiovascular and cerebrovascular events, an increased risk of breast cancer, and other adverse health outcomes.
The release of the interim results of the WHI trials in 2002 led to a fair amount of fear and confusion about the use of HT after menopause. After the WHI findings were published, estrogen use dropped dramatically, but for everything, including for vasomotor symptoms and the prevention and treatment of osteoporosis.
Prior to the WHI study, it was very common for hormone therapy to be prescribed as women neared or entered menopause, said Risa Kagan MD, clinical professor of obstetrics, gynecology, and reproductive sciences, University of California, San Francisco.
“When a woman turned 50, that was one of the first things we did – was to put her on hormone therapy. All that changed with the WHI, but now we are coming full circle,” noted Dr. Kagan, who currently prescribes HT as first line treatment for osteoporosis to some women.
Hormone therapy’s complex history
HT’s ability to reduce bone loss in postmenopausal women is well-documented in many papers, including one published March 8, 2018, in Osteoporosis International, by Dr. Kagan and colleagues. This reduced bone loss has been shown to significantly reduce fractures in patients with low bone mass and osteoporosis.
While a growing number of therapies are now available to treat osteoporosis, HT was traditionally viewed as a standard method of preventing fractures in this population. It was also widely used to prevent other types of symptoms associated with the menopause, such as hot flashes, night sweats, and sleep disturbances, and multiple observational studies had demonstrated that its use appeared to reduce the incidence of cardiovascular disease (CVD) in symptomatic menopausal women who initiated HT in early menopause.
Even though the WHI studies were the largest randomized trials ever performed in postmenopausal women, they had notable limitations, according to Dr. Kagan.
“The women were older – the average age was 63 years,” she said. “And they only investigated one route and one dose of estrogen.”
Since then, many different formulations and routes of administration with more favorable safety profiles than what was used in the WHI have become available.
It’s both scientifically and clinically unsound to extrapolate the unfavorable risk-benefit profile of HT seen in the WHI trials to all women regardless of age, HT dosage or formulation, or the length of time they’re on it, she added.
Today’s use of HT in women with osteoporosis
Re-analyses and follow-up studies from the WHI trials, along with data from other studies, have suggested that the benefit-risk profiles of HT are affected by a variety of factors. These include the timing of use in relation to menopause and chronological age and the type of hormone regimen.
“Clinically, many advocate for [hormone therapy] use, especially in the newer younger postmenopausal women to prevent bone loss, but also in younger women who are diagnosed with osteoporosis and then as they get older transition to more bone specific agents,” noted Dr. Kagan.
“Some advocate preserving bone mass and preventing osteoporosis and even treating the younger newly postmenopausal women who have no contraindications with hormone therapy initially, and then gradually transitioning them to a bone specific agent as they get older and at risk for fracture.
“If a woman is already fractured and/or has very low bone density with no other obvious secondary metabolic reason, we also often advocate anabolic agents for 1-2 years then consider estrogen for maintenance – again, if [there is] no contraindication to using HT,” she added.
Thus, an individualized approach is recommended to determine a woman’s risk-benefit ratio of HT use based on the absolute risk of adverse effects, Dr. Kagan noted.
“Transdermal and low/ultra-low doses of HT, have a favorable risk profile, and are effective in preserving bone mineral density and bone quality in many women,” she said.
According to Dr. McClung, HT “is most often used for treatment in women in whom hormone therapy was begun for hot flashes and then, when osteoporosis was found later, was simply continued.
“Society guidelines are cautious about recommending hormone therapy for osteoporosis treatment since estrogen is not approved for treatment, despite the clear fracture protection benefit observed in the WHI study,” he said. “Since [women in the WHI trials] were not recruited as having osteoporosis, those results do not meet the FDA requirement for treatment approval, namely the reduction in fracture risk in patients with osteoporosis. However, knowing what we know about the salutary skeletal effects of estrogen, many of us do use them in our patients with osteoporosis – although not prescribed for that purpose.”
Additional scenarios when doctors may advise HT
“I often recommend – and I think colleagues do as well – that women with recent menopause and menopausal symptoms who also have low bone mineral density or even scores showing osteoporosis see their gynecologist to discuss HT for a few years, perhaps until age 60 if no contraindications, and if it is well tolerated,” said Ethel S. Siris, MD, professor of medicine at Columbia University Medical Center in New York.
“Once they stop it we can then give one of our other bone drugs, but it delays the need to start them since on adequate estrogen the bone density should remain stable while they take it,” added Dr. Siris, an endocrinologist and internist, and director of the Toni Stabile Osteoporosis Center in New York. “They may need a bisphosphonate or another bone drug to further protect them from bone loss and future fracture [after stopping HT].”
Victor L. Roberts, MD, founder of Endocrine Associates of Florida, Lake Mary, pointed out that women now have many options for treatment of osteoporosis.
“If a woman is in early menopause and is having other symptoms, then estrogen is warranted,” he said. “If she has osteoporosis, then it’s a bonus.”
“We have better agents that are bone specific,” for a patient who presents with osteoporosis and no other symptoms, he said.
“If a woman is intolerant of alendronate or other similar drugs, or chooses not to have an injectable, then estrogen or a SERM [selective estrogen receptor modulator] would be an option.”
Dr. Roberts added that HT would be more of a niche drug.
“It has a role and documented benefit and works,” he said. “There is good scientific data for the use of estrogen.”
Dr. Kagan is a consultant for Pfizer, Therapeutics MD, Amgen, on the Medical and Scientific Advisory Board of American Bone Health. The other experts interviewed for this piece reported no conflicts.
Ways to lessen toxic effects of chemo in older adults
Age-related changes that potentiate adverse drug reactions include alterations in absorption, distribution, metabolism, and excretion. As such, older patients often require adjustments in medications to optimize safety and use. Medication adjustment is especially important for older patients on complex medication regimens for multiple conditions, such as those undergoing cancer treatment. Three recent high-quality randomized trials evaluated the use of geriatric assessment (GA) in older adults with cancer.1-3
Interdisciplinary GA can identify aging-related conditions associated with poor outcomes in older patients with cancer (e.g., toxic effects of chemotherapy) and provide recommendations aimed at improving health outcomes. The results of these trials suggest that interdisciplinary GA can improve care outcomes and oncologists’ communication for older adults with cancer, and should be considered an emerging standard of care.
Geriatric assessment and chemotherapy-related toxic effects
A cluster randomized trial1 at City of Hope National Medical Center conducted between August 2015 and February 2019 enrolled 613 participants and randomly assigned them to receive a GA-guided intervention or usual standard of care in a 2-to-1 ratio. Participants were eligible for the study if they were aged ≥65 years; had a diagnosis of solid malignant neoplasm of any stage; were starting a new chemotherapy regimen; and were fluent in English, Spanish, or Chinese.
The intervention included a GA at baseline followed by assessments focused on six common areas: sleep problems, problems with eating and feeding, incontinence, confusion, evidence of falls, and skin breakdown. An interdisciplinary team (oncologist, nurse practitioner, pharmacist, physical therapist, occupational therapist, social worker, and nutritionist) performed the assessment and developed a plan of care. Interventions were multifactorial and could include referral to specialists; recommendations for medication changes; symptom management; nutritional intervention with diet recommendations and supplementation; and interventions targeting social, spiritual, and functional well-being. Follow-up by a nurse practitioner continued until completion of chemotherapy or 6 months after starting chemotherapy, whichever was earlier.
The primary outcome was grade 3 or higher chemotherapy-related toxic effects using National Cancer Institute criteria, and secondary outcomes were advance directive completion, emergency room visits and unplanned hospitalizations, and survival up to 12 months. Results showed a 10% absolute reduction in the incidence of grade 3 or higher toxic effects (P = .02), with a number needed to treat of 10. Advance directive completion also increased by 15%, but no differences were observed for other outcomes. This study offers high-quality evidence that a GA-based intervention can reduce toxic effects of chemotherapy regimens for older adults with cancer.
Geriatric assessment in community oncology practices
A recent study by Supriya G. Mohile, MD, and colleagues2 is the first nationwide multicenter clinical trial to demonstrate the effects of GA and GA-guided management. This study was conducted in 40 oncology practices from the University of Rochester National Cancer Institute Community Oncology Research Program network. Centers were randomly assigned to intervention or usual care (362 patients treated by 68 oncologists in the intervention group and 371 patients treated by 91 oncologists in the usual-care group). Eligibility criteria were age ≥70 years; impairment in at least one GA domain other than polypharmacy; incurable advanced solid tumor or lymphoma with a plan to start new cancer treatment with a high risk for toxic effects within 4 weeks; and English language fluency. Both study groups underwent a baseline GA that assessed patients’ physical performance, functional status, comorbidity, cognition, nutrition, social support, polypharmacy, and psychological status. For the intervention group, a summary and management recommendations were provided to the treating oncologists.
The primary outcome was grade 3 or higher toxic effects within 3 months of starting a new regimen; secondary outcomes included treatment intensity and survival and GA outcomes within 3 months. A smaller proportion of patients in the intervention group experienced toxicity (51% vs. 71%), with an absolute risk reduction of 20%. Patients in the intervention group also had fewer falls and a greater reduction in medications used; there were no other differences in secondary outcomes. This study offers very strong and generalizable evidence that incorporating GA in the care of older adults with cancer at risk for toxicity can reduce toxicity as well as improve other outcomes, such as falls and polypharmacy.
Geriatric assessment and oncologist-patient communication
A secondary analysis3 of data from Dr. Mohile and colleagues2 evaluated the effect of GA-guided recommendations on oncologist-patient communication regarding comorbidities. Patients (n = 541) included in this analysis were 76.6 years of age on average and had 3.2 (standard deviation, 1.9) comorbid conditions. All patients underwent GA, but only oncologists in the intervention arm received GA-based recommendations. Clinical encounters between oncologist and patient immediately following the GA were audio recorded and analyzed to examine communication between oncologists and participants as it relates to chronic comorbid conditions.
In the intervention arm, more discussions regarding comorbidities took place, and more participants’ concerns about comorbidities were acknowledged. More importantly, participants in the intervention group were 2.4 times more likely to have their concerns about comorbidities addressed through referral or education, compared with the usual-care group (P = .004). Moreover, 41% of oncologists in the intervention arm modified dosage or cancer treatment schedule because of concern about tolerability or comorbidities. This study demonstrates beneficial effects of GA in increasing communication and perhaps consideration of comorbidities of older adults when planning cancer treatment.
Dr. Hung is professor of geriatrics and palliative care at Mount Sinai Hospital, New York. He disclosed no relevant conflicts of interest.
References
1. Li D et al. JAMA Oncol. 2021;7:e214158.
2. Mohile SG et al. Lancet. 2021;398:1894-1904.
3. Kleckner AS et al. JCO Oncol Pract. 2022;18:e9-19.
A version of this article first appeared on Medscape.com.
Age-related changes that potentiate adverse drug reactions include alterations in absorption, distribution, metabolism, and excretion. As such, older patients often require adjustments in medications to optimize safety and use. Medication adjustment is especially important for older patients on complex medication regimens for multiple conditions, such as those undergoing cancer treatment. Three recent high-quality randomized trials evaluated the use of geriatric assessment (GA) in older adults with cancer.1-3
Interdisciplinary GA can identify aging-related conditions associated with poor outcomes in older patients with cancer (e.g., toxic effects of chemotherapy) and provide recommendations aimed at improving health outcomes. The results of these trials suggest that interdisciplinary GA can improve care outcomes and oncologists’ communication for older adults with cancer, and should be considered an emerging standard of care.
Geriatric assessment and chemotherapy-related toxic effects
A cluster randomized trial1 at City of Hope National Medical Center conducted between August 2015 and February 2019 enrolled 613 participants and randomly assigned them to receive a GA-guided intervention or usual standard of care in a 2-to-1 ratio. Participants were eligible for the study if they were aged ≥65 years; had a diagnosis of solid malignant neoplasm of any stage; were starting a new chemotherapy regimen; and were fluent in English, Spanish, or Chinese.
The intervention included a GA at baseline followed by assessments focused on six common areas: sleep problems, problems with eating and feeding, incontinence, confusion, evidence of falls, and skin breakdown. An interdisciplinary team (oncologist, nurse practitioner, pharmacist, physical therapist, occupational therapist, social worker, and nutritionist) performed the assessment and developed a plan of care. Interventions were multifactorial and could include referral to specialists; recommendations for medication changes; symptom management; nutritional intervention with diet recommendations and supplementation; and interventions targeting social, spiritual, and functional well-being. Follow-up by a nurse practitioner continued until completion of chemotherapy or 6 months after starting chemotherapy, whichever was earlier.
The primary outcome was grade 3 or higher chemotherapy-related toxic effects using National Cancer Institute criteria, and secondary outcomes were advance directive completion, emergency room visits and unplanned hospitalizations, and survival up to 12 months. Results showed a 10% absolute reduction in the incidence of grade 3 or higher toxic effects (P = .02), with a number needed to treat of 10. Advance directive completion also increased by 15%, but no differences were observed for other outcomes. This study offers high-quality evidence that a GA-based intervention can reduce toxic effects of chemotherapy regimens for older adults with cancer.
Geriatric assessment in community oncology practices
A recent study by Supriya G. Mohile, MD, and colleagues2 is the first nationwide multicenter clinical trial to demonstrate the effects of GA and GA-guided management. This study was conducted in 40 oncology practices from the University of Rochester National Cancer Institute Community Oncology Research Program network. Centers were randomly assigned to intervention or usual care (362 patients treated by 68 oncologists in the intervention group and 371 patients treated by 91 oncologists in the usual-care group). Eligibility criteria were age ≥70 years; impairment in at least one GA domain other than polypharmacy; incurable advanced solid tumor or lymphoma with a plan to start new cancer treatment with a high risk for toxic effects within 4 weeks; and English language fluency. Both study groups underwent a baseline GA that assessed patients’ physical performance, functional status, comorbidity, cognition, nutrition, social support, polypharmacy, and psychological status. For the intervention group, a summary and management recommendations were provided to the treating oncologists.
The primary outcome was grade 3 or higher toxic effects within 3 months of starting a new regimen; secondary outcomes included treatment intensity and survival and GA outcomes within 3 months. A smaller proportion of patients in the intervention group experienced toxicity (51% vs. 71%), with an absolute risk reduction of 20%. Patients in the intervention group also had fewer falls and a greater reduction in medications used; there were no other differences in secondary outcomes. This study offers very strong and generalizable evidence that incorporating GA in the care of older adults with cancer at risk for toxicity can reduce toxicity as well as improve other outcomes, such as falls and polypharmacy.
Geriatric assessment and oncologist-patient communication
A secondary analysis3 of data from Dr. Mohile and colleagues2 evaluated the effect of GA-guided recommendations on oncologist-patient communication regarding comorbidities. Patients (n = 541) included in this analysis were 76.6 years of age on average and had 3.2 (standard deviation, 1.9) comorbid conditions. All patients underwent GA, but only oncologists in the intervention arm received GA-based recommendations. Clinical encounters between oncologist and patient immediately following the GA were audio recorded and analyzed to examine communication between oncologists and participants as it relates to chronic comorbid conditions.
In the intervention arm, more discussions regarding comorbidities took place, and more participants’ concerns about comorbidities were acknowledged. More importantly, participants in the intervention group were 2.4 times more likely to have their concerns about comorbidities addressed through referral or education, compared with the usual-care group (P = .004). Moreover, 41% of oncologists in the intervention arm modified dosage or cancer treatment schedule because of concern about tolerability or comorbidities. This study demonstrates beneficial effects of GA in increasing communication and perhaps consideration of comorbidities of older adults when planning cancer treatment.
Dr. Hung is professor of geriatrics and palliative care at Mount Sinai Hospital, New York. He disclosed no relevant conflicts of interest.
References
1. Li D et al. JAMA Oncol. 2021;7:e214158.
2. Mohile SG et al. Lancet. 2021;398:1894-1904.
3. Kleckner AS et al. JCO Oncol Pract. 2022;18:e9-19.
A version of this article first appeared on Medscape.com.
Age-related changes that potentiate adverse drug reactions include alterations in absorption, distribution, metabolism, and excretion. As such, older patients often require adjustments in medications to optimize safety and use. Medication adjustment is especially important for older patients on complex medication regimens for multiple conditions, such as those undergoing cancer treatment. Three recent high-quality randomized trials evaluated the use of geriatric assessment (GA) in older adults with cancer.1-3
Interdisciplinary GA can identify aging-related conditions associated with poor outcomes in older patients with cancer (e.g., toxic effects of chemotherapy) and provide recommendations aimed at improving health outcomes. The results of these trials suggest that interdisciplinary GA can improve care outcomes and oncologists’ communication for older adults with cancer, and should be considered an emerging standard of care.
Geriatric assessment and chemotherapy-related toxic effects
A cluster randomized trial1 at City of Hope National Medical Center conducted between August 2015 and February 2019 enrolled 613 participants and randomly assigned them to receive a GA-guided intervention or usual standard of care in a 2-to-1 ratio. Participants were eligible for the study if they were aged ≥65 years; had a diagnosis of solid malignant neoplasm of any stage; were starting a new chemotherapy regimen; and were fluent in English, Spanish, or Chinese.
The intervention included a GA at baseline followed by assessments focused on six common areas: sleep problems, problems with eating and feeding, incontinence, confusion, evidence of falls, and skin breakdown. An interdisciplinary team (oncologist, nurse practitioner, pharmacist, physical therapist, occupational therapist, social worker, and nutritionist) performed the assessment and developed a plan of care. Interventions were multifactorial and could include referral to specialists; recommendations for medication changes; symptom management; nutritional intervention with diet recommendations and supplementation; and interventions targeting social, spiritual, and functional well-being. Follow-up by a nurse practitioner continued until completion of chemotherapy or 6 months after starting chemotherapy, whichever was earlier.
The primary outcome was grade 3 or higher chemotherapy-related toxic effects using National Cancer Institute criteria, and secondary outcomes were advance directive completion, emergency room visits and unplanned hospitalizations, and survival up to 12 months. Results showed a 10% absolute reduction in the incidence of grade 3 or higher toxic effects (P = .02), with a number needed to treat of 10. Advance directive completion also increased by 15%, but no differences were observed for other outcomes. This study offers high-quality evidence that a GA-based intervention can reduce toxic effects of chemotherapy regimens for older adults with cancer.
Geriatric assessment in community oncology practices
A recent study by Supriya G. Mohile, MD, and colleagues2 is the first nationwide multicenter clinical trial to demonstrate the effects of GA and GA-guided management. This study was conducted in 40 oncology practices from the University of Rochester National Cancer Institute Community Oncology Research Program network. Centers were randomly assigned to intervention or usual care (362 patients treated by 68 oncologists in the intervention group and 371 patients treated by 91 oncologists in the usual-care group). Eligibility criteria were age ≥70 years; impairment in at least one GA domain other than polypharmacy; incurable advanced solid tumor or lymphoma with a plan to start new cancer treatment with a high risk for toxic effects within 4 weeks; and English language fluency. Both study groups underwent a baseline GA that assessed patients’ physical performance, functional status, comorbidity, cognition, nutrition, social support, polypharmacy, and psychological status. For the intervention group, a summary and management recommendations were provided to the treating oncologists.
The primary outcome was grade 3 or higher toxic effects within 3 months of starting a new regimen; secondary outcomes included treatment intensity and survival and GA outcomes within 3 months. A smaller proportion of patients in the intervention group experienced toxicity (51% vs. 71%), with an absolute risk reduction of 20%. Patients in the intervention group also had fewer falls and a greater reduction in medications used; there were no other differences in secondary outcomes. This study offers very strong and generalizable evidence that incorporating GA in the care of older adults with cancer at risk for toxicity can reduce toxicity as well as improve other outcomes, such as falls and polypharmacy.
Geriatric assessment and oncologist-patient communication
A secondary analysis3 of data from Dr. Mohile and colleagues2 evaluated the effect of GA-guided recommendations on oncologist-patient communication regarding comorbidities. Patients (n = 541) included in this analysis were 76.6 years of age on average and had 3.2 (standard deviation, 1.9) comorbid conditions. All patients underwent GA, but only oncologists in the intervention arm received GA-based recommendations. Clinical encounters between oncologist and patient immediately following the GA were audio recorded and analyzed to examine communication between oncologists and participants as it relates to chronic comorbid conditions.
In the intervention arm, more discussions regarding comorbidities took place, and more participants’ concerns about comorbidities were acknowledged. More importantly, participants in the intervention group were 2.4 times more likely to have their concerns about comorbidities addressed through referral or education, compared with the usual-care group (P = .004). Moreover, 41% of oncologists in the intervention arm modified dosage or cancer treatment schedule because of concern about tolerability or comorbidities. This study demonstrates beneficial effects of GA in increasing communication and perhaps consideration of comorbidities of older adults when planning cancer treatment.
Dr. Hung is professor of geriatrics and palliative care at Mount Sinai Hospital, New York. He disclosed no relevant conflicts of interest.
References
1. Li D et al. JAMA Oncol. 2021;7:e214158.
2. Mohile SG et al. Lancet. 2021;398:1894-1904.
3. Kleckner AS et al. JCO Oncol Pract. 2022;18:e9-19.
A version of this article first appeared on Medscape.com.
Restoring ‘sixth sense’ may reduce falls in Alzheimer’s
(AD), new research confirms.
Falls are twice as common in patients with AD versu older individuals without the disorder and significantly increase the likelihood of institutionalization.
However, researchers recorded fewer falls in patients with a better functioning vestibular system, which detects head movements and plays a critical role in spatial orientation, posture, gait, and balance.
The results suggest that improving vestibular function with currently available therapies may prevent falls, something the researchers will investigate in a new clinical trial launching next month.
“One of the most dangerous and impactful symptoms in terms of function in patients with Alzheimer’s disease is their increased predisposition to falls,” study investigator Yuri Agrawal, MD, department of otolaryngology–head and neck surgery, Johns Hopkins University School of Medicine, Baltimore, said in an interview. “Alzheimer’s is the sixth leading cause of death in the U.S., and some people actually say that that high mortality rate is because of their predisposition to falls and the injuries that occur.”
The study was published online Feb. 14 in the Journal of Alzheimer’s Disease.
The ‘sixth hidden sense’
The vestibular system consists of three semicircular canals, which detect rotational head movement, and two otolith organs called the utricle and the saccule, which sense linear head movements and the orientation of the head with respect to gravity.
“We call the vestibular system the sixth hidden sense because it’s not a conscious perception like taste or smell,” Dr. Agrawal said. “It’s constantly providing input to our brain about where we are in space.”
Dr. Agrawal and colleagues previously reported that vestibular loss is twice as common in Alzheimer’s patients as in cognitively unimpaired age-matched controls. Now, they wanted to know if this sensory loss was associated with an increased risk for falls in this population.
The study included 48 patients age greater than or equal to 60 years with mild-to-moderate AD between 2018 and 2020. They also included an age-matched control group of healthy controls with no cognitive impairment.
Researchers assessed vestibular function at baseline by measuring semicircular canal and saccular function. One test required participants to wear goggles and complete a series of tests with their eyes open and closed while researchers recorded their eye movement with video-oculography. They also measured participants’ balance using the Berg Balance Scale.
Relative to matched controls, AD patients exhibited increased lateral instability when their eyes were open (P = .033) and closed (P = .042). Studies suggest that lateral stability declines more quickly with age and that instability with eyes closed is the single biggest predictor of incident falls in community-dwelling adults.
To determine if poor vestibular function increased fall risk in patients with AD, researchers followed the cohort for up to 2 years.
“We found that patients with vestibular loss at baseline were 50% more likely to fall, adjusting for other factors that could contribute to that,” Dr. Agrawal said.
Specifically, better semicircular canal function was significantly associated with lower likelihood of falls, even after adjusting for confounders (adjusted hazard ratio, 0.65; P = .009).
Can therapy help?
Commenting on the findings, James Burke, MD, PhD, professor of neurology at Duke University Medical Center, Durham, N.C., said that the finding that impaired vestibular function is associated with increased falls “significantly advances our understanding of the topic” and suggests that treating vestibular dysfunction could reduce falls in Alzheimer’s patients.
“Screening patients with Alzheimer’s disease for impaired vestibular function could lead to identification of individuals at high risk of falls and target those who would benefit from vestibular therapy,” he said.
Vestibular rehabilitation therapy is often used to treat a number of disorders related to vestibular function loss. There are also studies underway to measure the efficacy of a vestibular implant that works much like a cochlear implant.
While evaluation of vestibular function is currently not routinely included in AD care, studies such as these suggest it may be time to consider adding it to the standard of care, Jennifer Coto, PhD, assistant professor of otolaryngology at the University of Miami Miller School of Medicine, said in an interview.
“Best practice guidelines for management of Alzheimer’s patients should be revised to include routine vestibular evaluation and support from a multidisciplinary team that may address other crucial areas of functioning, particularly psychological functioning, sleep, and independence,” she said.
“Future research also needs to evaluate the effectiveness of vestibular therapy in patients with Alzheimer’s and the benefits of early identification and intervention for preventing recurrent falls.”
Dr. Agrawal is leading a 5-year, $3.5 million National Institute on Aging study that seeks to do just that. Enrollment in the study begins next month. Patients will complete an initial in-person screening, but the remainder of the study will be conducted virtually.
Therapies will be noninvasive, nonpharmaceutical, and performed in participants’ homes. If the therapy is successful at reducing falls, Dr. Agrawal said the virtual design would significantly broaden its potential patient reach.
The study was funded by the National Institute on Aging. Study authors’ disclosures are reported in the original article. Dr. Coto and Dr. Burke report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(AD), new research confirms.
Falls are twice as common in patients with AD versu older individuals without the disorder and significantly increase the likelihood of institutionalization.
However, researchers recorded fewer falls in patients with a better functioning vestibular system, which detects head movements and plays a critical role in spatial orientation, posture, gait, and balance.
The results suggest that improving vestibular function with currently available therapies may prevent falls, something the researchers will investigate in a new clinical trial launching next month.
“One of the most dangerous and impactful symptoms in terms of function in patients with Alzheimer’s disease is their increased predisposition to falls,” study investigator Yuri Agrawal, MD, department of otolaryngology–head and neck surgery, Johns Hopkins University School of Medicine, Baltimore, said in an interview. “Alzheimer’s is the sixth leading cause of death in the U.S., and some people actually say that that high mortality rate is because of their predisposition to falls and the injuries that occur.”
The study was published online Feb. 14 in the Journal of Alzheimer’s Disease.
The ‘sixth hidden sense’
The vestibular system consists of three semicircular canals, which detect rotational head movement, and two otolith organs called the utricle and the saccule, which sense linear head movements and the orientation of the head with respect to gravity.
“We call the vestibular system the sixth hidden sense because it’s not a conscious perception like taste or smell,” Dr. Agrawal said. “It’s constantly providing input to our brain about where we are in space.”
Dr. Agrawal and colleagues previously reported that vestibular loss is twice as common in Alzheimer’s patients as in cognitively unimpaired age-matched controls. Now, they wanted to know if this sensory loss was associated with an increased risk for falls in this population.
The study included 48 patients age greater than or equal to 60 years with mild-to-moderate AD between 2018 and 2020. They also included an age-matched control group of healthy controls with no cognitive impairment.
Researchers assessed vestibular function at baseline by measuring semicircular canal and saccular function. One test required participants to wear goggles and complete a series of tests with their eyes open and closed while researchers recorded their eye movement with video-oculography. They also measured participants’ balance using the Berg Balance Scale.
Relative to matched controls, AD patients exhibited increased lateral instability when their eyes were open (P = .033) and closed (P = .042). Studies suggest that lateral stability declines more quickly with age and that instability with eyes closed is the single biggest predictor of incident falls in community-dwelling adults.
To determine if poor vestibular function increased fall risk in patients with AD, researchers followed the cohort for up to 2 years.
“We found that patients with vestibular loss at baseline were 50% more likely to fall, adjusting for other factors that could contribute to that,” Dr. Agrawal said.
Specifically, better semicircular canal function was significantly associated with lower likelihood of falls, even after adjusting for confounders (adjusted hazard ratio, 0.65; P = .009).
Can therapy help?
Commenting on the findings, James Burke, MD, PhD, professor of neurology at Duke University Medical Center, Durham, N.C., said that the finding that impaired vestibular function is associated with increased falls “significantly advances our understanding of the topic” and suggests that treating vestibular dysfunction could reduce falls in Alzheimer’s patients.
“Screening patients with Alzheimer’s disease for impaired vestibular function could lead to identification of individuals at high risk of falls and target those who would benefit from vestibular therapy,” he said.
Vestibular rehabilitation therapy is often used to treat a number of disorders related to vestibular function loss. There are also studies underway to measure the efficacy of a vestibular implant that works much like a cochlear implant.
While evaluation of vestibular function is currently not routinely included in AD care, studies such as these suggest it may be time to consider adding it to the standard of care, Jennifer Coto, PhD, assistant professor of otolaryngology at the University of Miami Miller School of Medicine, said in an interview.
“Best practice guidelines for management of Alzheimer’s patients should be revised to include routine vestibular evaluation and support from a multidisciplinary team that may address other crucial areas of functioning, particularly psychological functioning, sleep, and independence,” she said.
“Future research also needs to evaluate the effectiveness of vestibular therapy in patients with Alzheimer’s and the benefits of early identification and intervention for preventing recurrent falls.”
Dr. Agrawal is leading a 5-year, $3.5 million National Institute on Aging study that seeks to do just that. Enrollment in the study begins next month. Patients will complete an initial in-person screening, but the remainder of the study will be conducted virtually.
Therapies will be noninvasive, nonpharmaceutical, and performed in participants’ homes. If the therapy is successful at reducing falls, Dr. Agrawal said the virtual design would significantly broaden its potential patient reach.
The study was funded by the National Institute on Aging. Study authors’ disclosures are reported in the original article. Dr. Coto and Dr. Burke report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(AD), new research confirms.
Falls are twice as common in patients with AD versu older individuals without the disorder and significantly increase the likelihood of institutionalization.
However, researchers recorded fewer falls in patients with a better functioning vestibular system, which detects head movements and plays a critical role in spatial orientation, posture, gait, and balance.
The results suggest that improving vestibular function with currently available therapies may prevent falls, something the researchers will investigate in a new clinical trial launching next month.
“One of the most dangerous and impactful symptoms in terms of function in patients with Alzheimer’s disease is their increased predisposition to falls,” study investigator Yuri Agrawal, MD, department of otolaryngology–head and neck surgery, Johns Hopkins University School of Medicine, Baltimore, said in an interview. “Alzheimer’s is the sixth leading cause of death in the U.S., and some people actually say that that high mortality rate is because of their predisposition to falls and the injuries that occur.”
The study was published online Feb. 14 in the Journal of Alzheimer’s Disease.
The ‘sixth hidden sense’
The vestibular system consists of three semicircular canals, which detect rotational head movement, and two otolith organs called the utricle and the saccule, which sense linear head movements and the orientation of the head with respect to gravity.
“We call the vestibular system the sixth hidden sense because it’s not a conscious perception like taste or smell,” Dr. Agrawal said. “It’s constantly providing input to our brain about where we are in space.”
Dr. Agrawal and colleagues previously reported that vestibular loss is twice as common in Alzheimer’s patients as in cognitively unimpaired age-matched controls. Now, they wanted to know if this sensory loss was associated with an increased risk for falls in this population.
The study included 48 patients age greater than or equal to 60 years with mild-to-moderate AD between 2018 and 2020. They also included an age-matched control group of healthy controls with no cognitive impairment.
Researchers assessed vestibular function at baseline by measuring semicircular canal and saccular function. One test required participants to wear goggles and complete a series of tests with their eyes open and closed while researchers recorded their eye movement with video-oculography. They also measured participants’ balance using the Berg Balance Scale.
Relative to matched controls, AD patients exhibited increased lateral instability when their eyes were open (P = .033) and closed (P = .042). Studies suggest that lateral stability declines more quickly with age and that instability with eyes closed is the single biggest predictor of incident falls in community-dwelling adults.
To determine if poor vestibular function increased fall risk in patients with AD, researchers followed the cohort for up to 2 years.
“We found that patients with vestibular loss at baseline were 50% more likely to fall, adjusting for other factors that could contribute to that,” Dr. Agrawal said.
Specifically, better semicircular canal function was significantly associated with lower likelihood of falls, even after adjusting for confounders (adjusted hazard ratio, 0.65; P = .009).
Can therapy help?
Commenting on the findings, James Burke, MD, PhD, professor of neurology at Duke University Medical Center, Durham, N.C., said that the finding that impaired vestibular function is associated with increased falls “significantly advances our understanding of the topic” and suggests that treating vestibular dysfunction could reduce falls in Alzheimer’s patients.
“Screening patients with Alzheimer’s disease for impaired vestibular function could lead to identification of individuals at high risk of falls and target those who would benefit from vestibular therapy,” he said.
Vestibular rehabilitation therapy is often used to treat a number of disorders related to vestibular function loss. There are also studies underway to measure the efficacy of a vestibular implant that works much like a cochlear implant.
While evaluation of vestibular function is currently not routinely included in AD care, studies such as these suggest it may be time to consider adding it to the standard of care, Jennifer Coto, PhD, assistant professor of otolaryngology at the University of Miami Miller School of Medicine, said in an interview.
“Best practice guidelines for management of Alzheimer’s patients should be revised to include routine vestibular evaluation and support from a multidisciplinary team that may address other crucial areas of functioning, particularly psychological functioning, sleep, and independence,” she said.
“Future research also needs to evaluate the effectiveness of vestibular therapy in patients with Alzheimer’s and the benefits of early identification and intervention for preventing recurrent falls.”
Dr. Agrawal is leading a 5-year, $3.5 million National Institute on Aging study that seeks to do just that. Enrollment in the study begins next month. Patients will complete an initial in-person screening, but the remainder of the study will be conducted virtually.
Therapies will be noninvasive, nonpharmaceutical, and performed in participants’ homes. If the therapy is successful at reducing falls, Dr. Agrawal said the virtual design would significantly broaden its potential patient reach.
The study was funded by the National Institute on Aging. Study authors’ disclosures are reported in the original article. Dr. Coto and Dr. Burke report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF ALZHEIMER’S DISEASE
FDA clears once-weekly transdermal patch for Alzheimer’s
Adlarity is the first and only once-weekly patch to continuously deliver consistent doses of the acetylcholinesterase inhibitor through the skin, bypassing the digestive system and resulting in low likelihood of gastrointestinal side effects associated with oral donepezil, the company said in a press release.
Each patch delivers either 5 mg or 10 mg of donepezil daily for 7 days. After that, it is removed and a new patch is applied.
“The availability of a once-weekly patch formulation of donepezil has the potential to substantially benefit patients, caregivers, and health care providers,” Pierre Tariot, MD, director of the Banner Alzheimer’s Institute, Phoenix, said in the release.
“It offers effective, well-tolerated, and stable dosing for 7 days for patients who cannot take daily oral donepezil reliably because of impaired memory. It can also offer benefits for those patients who have diminished ability to swallow or have GI side effects associated with ingestion of oral donepezil,” Dr. Tariot added.
The FDA approved Adlarity through the 505(b)(2) regulatory pathway, which allows the agency to refer to previous findings of safety and efficacy for an already-approved product, as well as to review findings from further studies of the product.
The company expects the donepezil transdermal patch to be available in early Fall 2022.
A version of this article first appeared on Medscape.com.
Adlarity is the first and only once-weekly patch to continuously deliver consistent doses of the acetylcholinesterase inhibitor through the skin, bypassing the digestive system and resulting in low likelihood of gastrointestinal side effects associated with oral donepezil, the company said in a press release.
Each patch delivers either 5 mg or 10 mg of donepezil daily for 7 days. After that, it is removed and a new patch is applied.
“The availability of a once-weekly patch formulation of donepezil has the potential to substantially benefit patients, caregivers, and health care providers,” Pierre Tariot, MD, director of the Banner Alzheimer’s Institute, Phoenix, said in the release.
“It offers effective, well-tolerated, and stable dosing for 7 days for patients who cannot take daily oral donepezil reliably because of impaired memory. It can also offer benefits for those patients who have diminished ability to swallow or have GI side effects associated with ingestion of oral donepezil,” Dr. Tariot added.
The FDA approved Adlarity through the 505(b)(2) regulatory pathway, which allows the agency to refer to previous findings of safety and efficacy for an already-approved product, as well as to review findings from further studies of the product.
The company expects the donepezil transdermal patch to be available in early Fall 2022.
A version of this article first appeared on Medscape.com.
Adlarity is the first and only once-weekly patch to continuously deliver consistent doses of the acetylcholinesterase inhibitor through the skin, bypassing the digestive system and resulting in low likelihood of gastrointestinal side effects associated with oral donepezil, the company said in a press release.
Each patch delivers either 5 mg or 10 mg of donepezil daily for 7 days. After that, it is removed and a new patch is applied.
“The availability of a once-weekly patch formulation of donepezil has the potential to substantially benefit patients, caregivers, and health care providers,” Pierre Tariot, MD, director of the Banner Alzheimer’s Institute, Phoenix, said in the release.
“It offers effective, well-tolerated, and stable dosing for 7 days for patients who cannot take daily oral donepezil reliably because of impaired memory. It can also offer benefits for those patients who have diminished ability to swallow or have GI side effects associated with ingestion of oral donepezil,” Dr. Tariot added.
The FDA approved Adlarity through the 505(b)(2) regulatory pathway, which allows the agency to refer to previous findings of safety and efficacy for an already-approved product, as well as to review findings from further studies of the product.
The company expects the donepezil transdermal patch to be available in early Fall 2022.
A version of this article first appeared on Medscape.com.
Handheld ECGs ease AFib screening in the very elderly
The use of handheld, single-lead electrocardiograms (ECGs) did not increase diagnoses of AFib overall in patients aged 65 and older, but it did in patients 85 and up, researchers reported in Circulation.
“Incorporating single-lead ECGs into routine medical assessments as a new vital sign was widely feasible. Over 90% of people who were offered screening agreed to it and underwent screening,” said Steven Lubitz, MD, of the Cardiac Arrhythmia Service and Cardiovascular Research Center at Massachusetts General Hospital, Boston, who led the study.
Because advanced age is associated with a substantially increased risk of both AFib and stroke, point-of-care screening might be an efficient use of handheld ECGs, Dr. Lubitz said.
“The technology simply requires patients to place their fingers on the device to record an electrocardiogram and can be easily embedded in the routine clinical practice of primary care physicians,” he said in an interview.
The typical person has a 30% lifetime risk of developing AFib, and the chances of experiencing a stroke associated with the arrhythmia can be reduced significantly with anticoagulants, Dr. Lubitz said.
Professional organizations are split about the utility of screening for AFib. The European Society of Cardiology recommends opportunistic screening with either pulse palpation or ECG rhythm strip at clinic visits for patients 65 and older. The National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand have issued similar guidelines.
However, screening for AFib is not considered standard of care in the United States – although Dr. Lubitz predicted that that would change.
“I think the guidelines in the United States will evolve in the next few years, because I think we’re getting closer to understanding who we should be screening for atrial fibrillation and how we should be screening,” Dr. Lubitz told this news organization.
‘Very reassuring’ results
The randomized controlled trial found that for patients 85 and older, use of handheld ECGs led to a nearly 2% increase in new diagnoses of AFib in the screening group compared to conventional care.
The researchers also demonstrated an increased likelihood of diagnosing AFib during the patient’s primary-care encounter than at other sites, such as the emergency department or inpatient settings that might be more costly and resource-intensive. Moreover, the study reported that point-of-care screening was associated with high rates of oral anticoagulation prescriptions written for patients with newly diagnosed AFib, a finding Dr. Lubitz called “very reassuring.”
The Mass General researchers used single-lead devices attached to a tablet computer to screen more than 35,000 men and women from 16 primary care sites affiliated with the hospital’s practice-based research network.
Half the sites were randomly selected to include the screening intervention, where medical assistants used handheld ECGs at the start of the visit while checking routine vital signs.
The 1-year study screened 91% of eligible patients, demonstrating that single-lead rhythm assessment is feasible as part of routine primary care practice, Dr. Lubitz said. This finding supports other studies suggesting that handheld devices can enable rapid and scalable mass screening.
“We demonstrated that integration into routine practice by clinical personnel – in this case, medical assistants – is feasible. No study has measured and demonstrated such a high integration with routine care, reflecting both patient interest in screening and feasibility of incorporating screening into busy clinical practices,” Dr. Lubitz said.
Mobile ECGs with the handheld device take about 30 seconds to perform. In contrast, standard ECGs used in outpatient practices are bulky, and recording the ECG can take roughly 10 minutes.
Anthony Leazzo, DO, chairman of family practice at Northwestern Medicine Delnor Hospital, in Geneva, Ill., noted that smartwatches provide an alternative technology for detecting AFib.
But “a handheld, one-lead device would be more beneficial and should be more sensitive by measuring electrical activity similar to a normal ECG,” he said.
However, Dr. Leazzo said using such technology would need to be cost-effective because the patients at highest risk for AFib usually are on fixed incomes. Consumer versions of the devices can cost under $100. Dr. Lubitz said the actual cost for devices and a software platform used for a medical enterprise may differ.
Handheld ECGs are gradually being integrated into clinical practices, a trend driven by the rapid growth of telemedicine to remotely assess patients, Dr. Lubitz said.
“Our work affirmed that single-lead devices generate information for the physician that is actionable, though the proportion of newly detected AFib cases using a point-of-care ECG screening approach is likely to be very small,” Dr. Lubitz said in an interview. “For that reason, we think handheld devices are best deployed for people at the highest risk of AFib and stroke, and age is an excellent surrogate for that determination.”
The study was funded by Bristol-Myers Squibb–Pfizer Alliance.
A version of this article first appeared on Medscape.com.
The use of handheld, single-lead electrocardiograms (ECGs) did not increase diagnoses of AFib overall in patients aged 65 and older, but it did in patients 85 and up, researchers reported in Circulation.
“Incorporating single-lead ECGs into routine medical assessments as a new vital sign was widely feasible. Over 90% of people who were offered screening agreed to it and underwent screening,” said Steven Lubitz, MD, of the Cardiac Arrhythmia Service and Cardiovascular Research Center at Massachusetts General Hospital, Boston, who led the study.
Because advanced age is associated with a substantially increased risk of both AFib and stroke, point-of-care screening might be an efficient use of handheld ECGs, Dr. Lubitz said.
“The technology simply requires patients to place their fingers on the device to record an electrocardiogram and can be easily embedded in the routine clinical practice of primary care physicians,” he said in an interview.
The typical person has a 30% lifetime risk of developing AFib, and the chances of experiencing a stroke associated with the arrhythmia can be reduced significantly with anticoagulants, Dr. Lubitz said.
Professional organizations are split about the utility of screening for AFib. The European Society of Cardiology recommends opportunistic screening with either pulse palpation or ECG rhythm strip at clinic visits for patients 65 and older. The National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand have issued similar guidelines.
However, screening for AFib is not considered standard of care in the United States – although Dr. Lubitz predicted that that would change.
“I think the guidelines in the United States will evolve in the next few years, because I think we’re getting closer to understanding who we should be screening for atrial fibrillation and how we should be screening,” Dr. Lubitz told this news organization.
‘Very reassuring’ results
The randomized controlled trial found that for patients 85 and older, use of handheld ECGs led to a nearly 2% increase in new diagnoses of AFib in the screening group compared to conventional care.
The researchers also demonstrated an increased likelihood of diagnosing AFib during the patient’s primary-care encounter than at other sites, such as the emergency department or inpatient settings that might be more costly and resource-intensive. Moreover, the study reported that point-of-care screening was associated with high rates of oral anticoagulation prescriptions written for patients with newly diagnosed AFib, a finding Dr. Lubitz called “very reassuring.”
The Mass General researchers used single-lead devices attached to a tablet computer to screen more than 35,000 men and women from 16 primary care sites affiliated with the hospital’s practice-based research network.
Half the sites were randomly selected to include the screening intervention, where medical assistants used handheld ECGs at the start of the visit while checking routine vital signs.
The 1-year study screened 91% of eligible patients, demonstrating that single-lead rhythm assessment is feasible as part of routine primary care practice, Dr. Lubitz said. This finding supports other studies suggesting that handheld devices can enable rapid and scalable mass screening.
“We demonstrated that integration into routine practice by clinical personnel – in this case, medical assistants – is feasible. No study has measured and demonstrated such a high integration with routine care, reflecting both patient interest in screening and feasibility of incorporating screening into busy clinical practices,” Dr. Lubitz said.
Mobile ECGs with the handheld device take about 30 seconds to perform. In contrast, standard ECGs used in outpatient practices are bulky, and recording the ECG can take roughly 10 minutes.
Anthony Leazzo, DO, chairman of family practice at Northwestern Medicine Delnor Hospital, in Geneva, Ill., noted that smartwatches provide an alternative technology for detecting AFib.
But “a handheld, one-lead device would be more beneficial and should be more sensitive by measuring electrical activity similar to a normal ECG,” he said.
However, Dr. Leazzo said using such technology would need to be cost-effective because the patients at highest risk for AFib usually are on fixed incomes. Consumer versions of the devices can cost under $100. Dr. Lubitz said the actual cost for devices and a software platform used for a medical enterprise may differ.
Handheld ECGs are gradually being integrated into clinical practices, a trend driven by the rapid growth of telemedicine to remotely assess patients, Dr. Lubitz said.
“Our work affirmed that single-lead devices generate information for the physician that is actionable, though the proportion of newly detected AFib cases using a point-of-care ECG screening approach is likely to be very small,” Dr. Lubitz said in an interview. “For that reason, we think handheld devices are best deployed for people at the highest risk of AFib and stroke, and age is an excellent surrogate for that determination.”
The study was funded by Bristol-Myers Squibb–Pfizer Alliance.
A version of this article first appeared on Medscape.com.
The use of handheld, single-lead electrocardiograms (ECGs) did not increase diagnoses of AFib overall in patients aged 65 and older, but it did in patients 85 and up, researchers reported in Circulation.
“Incorporating single-lead ECGs into routine medical assessments as a new vital sign was widely feasible. Over 90% of people who were offered screening agreed to it and underwent screening,” said Steven Lubitz, MD, of the Cardiac Arrhythmia Service and Cardiovascular Research Center at Massachusetts General Hospital, Boston, who led the study.
Because advanced age is associated with a substantially increased risk of both AFib and stroke, point-of-care screening might be an efficient use of handheld ECGs, Dr. Lubitz said.
“The technology simply requires patients to place their fingers on the device to record an electrocardiogram and can be easily embedded in the routine clinical practice of primary care physicians,” he said in an interview.
The typical person has a 30% lifetime risk of developing AFib, and the chances of experiencing a stroke associated with the arrhythmia can be reduced significantly with anticoagulants, Dr. Lubitz said.
Professional organizations are split about the utility of screening for AFib. The European Society of Cardiology recommends opportunistic screening with either pulse palpation or ECG rhythm strip at clinic visits for patients 65 and older. The National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand have issued similar guidelines.
However, screening for AFib is not considered standard of care in the United States – although Dr. Lubitz predicted that that would change.
“I think the guidelines in the United States will evolve in the next few years, because I think we’re getting closer to understanding who we should be screening for atrial fibrillation and how we should be screening,” Dr. Lubitz told this news organization.
‘Very reassuring’ results
The randomized controlled trial found that for patients 85 and older, use of handheld ECGs led to a nearly 2% increase in new diagnoses of AFib in the screening group compared to conventional care.
The researchers also demonstrated an increased likelihood of diagnosing AFib during the patient’s primary-care encounter than at other sites, such as the emergency department or inpatient settings that might be more costly and resource-intensive. Moreover, the study reported that point-of-care screening was associated with high rates of oral anticoagulation prescriptions written for patients with newly diagnosed AFib, a finding Dr. Lubitz called “very reassuring.”
The Mass General researchers used single-lead devices attached to a tablet computer to screen more than 35,000 men and women from 16 primary care sites affiliated with the hospital’s practice-based research network.
Half the sites were randomly selected to include the screening intervention, where medical assistants used handheld ECGs at the start of the visit while checking routine vital signs.
The 1-year study screened 91% of eligible patients, demonstrating that single-lead rhythm assessment is feasible as part of routine primary care practice, Dr. Lubitz said. This finding supports other studies suggesting that handheld devices can enable rapid and scalable mass screening.
“We demonstrated that integration into routine practice by clinical personnel – in this case, medical assistants – is feasible. No study has measured and demonstrated such a high integration with routine care, reflecting both patient interest in screening and feasibility of incorporating screening into busy clinical practices,” Dr. Lubitz said.
Mobile ECGs with the handheld device take about 30 seconds to perform. In contrast, standard ECGs used in outpatient practices are bulky, and recording the ECG can take roughly 10 minutes.
Anthony Leazzo, DO, chairman of family practice at Northwestern Medicine Delnor Hospital, in Geneva, Ill., noted that smartwatches provide an alternative technology for detecting AFib.
But “a handheld, one-lead device would be more beneficial and should be more sensitive by measuring electrical activity similar to a normal ECG,” he said.
However, Dr. Leazzo said using such technology would need to be cost-effective because the patients at highest risk for AFib usually are on fixed incomes. Consumer versions of the devices can cost under $100. Dr. Lubitz said the actual cost for devices and a software platform used for a medical enterprise may differ.
Handheld ECGs are gradually being integrated into clinical practices, a trend driven by the rapid growth of telemedicine to remotely assess patients, Dr. Lubitz said.
“Our work affirmed that single-lead devices generate information for the physician that is actionable, though the proportion of newly detected AFib cases using a point-of-care ECG screening approach is likely to be very small,” Dr. Lubitz said in an interview. “For that reason, we think handheld devices are best deployed for people at the highest risk of AFib and stroke, and age is an excellent surrogate for that determination.”
The study was funded by Bristol-Myers Squibb–Pfizer Alliance.
A version of this article first appeared on Medscape.com.
FROM CIRCULATION
Tremors and memory loss precede Parkinson’s in diverse population
Tremors and memory symptoms were identified among individuals in a primary care setting as early as 10 years before a Parkinson’s disease diagnosis in a new study.
Most research on the causes and early signs of Parkinson’s disease (PD) have involved patients of Northern European ancestry, Cristina Simonet, MD, of Queen Mary University of London, and colleagues wrote in their paper, published in JAMA Neurology.
Additionally, data on how PD might manifest in different ethnic groups are limited, they said.
In their nested case-control, the researchers examined data from electronic health records of an ethnically diverse population of 1,016,277 adults seen in primary care practices between 1990 and Feb. 6, 2018. They compared individuals with PD with those without PD or other neurologic conditions.
The researchers identified 10 age and sex-matched controls for each PD case, and also conducted an unmatched analysis after adjusting for age and sex. The final study population included 1,055 patients with PD and 1,009,523 controls. The population of PD cases was 15.7% Black, 19.7% South Asian, 50.9% White, and 8.3% other; the population of controls was 13.3% Black, 21.5% South Asian, 43.7% White, and 11.3% other.
“We observed a constellation of symptoms noted by general practitioners up to a decade before diagnosis of PD,” the researchers said. Symptoms were identified across three time intervals (less than 2 years, 2-5 years, and 5-10 years before diagnosis) to better evaluate exposure outcome associations.
In the matched analysis of midlife risk factors, epilepsy showed the strongest association with PD diagnosis across all time periods, and type 2 diabetes or hypertension 5-10 years before diagnosis was associated with later PD.
Prediagnostic signs of PD included both motor and nonmotor manifestations.
The matched analysis revealed a significant increased association between tremor and memory symptoms less than 2 years before diagnosis (adjusted odds ratios of 151.24 and 8.73, respectively) as well as up to 10 years before diagnosis for tremors and up to 5 years for memory symptoms (aOR, 11.4 and 3.09, respectively) in PD patients, compared with controls.
Other strong associations between PD and early nonmotor features in cases, compared with controls, included hypotension (aOR, 6.81), constipation (aOR, 3.29), and depression (aOR, 4.61).
In addition, the researchers found associations for epilepsy that had not been identified in previous studies, and these associations persisted in a replication analysis.
The study findings were limited by several factors, mainly the use of routine primary care data with underascertained factors of interest, and potential mislabeling of PD, the researchers noted. Other limitations included the lack of data on prescription medication for PD, and the recording of memory problems in primary care without supportive testing to confirm cognitive impairment.
The results support a range of comorbidities and symptoms that may present in primary care, and clinicians should consider PD as a possible cause, the researchers wrote.
Make early referral a priority
The study is important because of the lack of diversity in Parkinson’s disease research, lead author Dr. Simonet said in an interview.
“Over the last decade, the global population suffering from Parkinson’s disease has more than doubled,” she said. Causes may include the increasing numbers of older people with longer life expectancy. “However, it seems there are other factors, including environmental, genetic, and lifestyle, that might play a role in increasing the prevalence of Parkinson’s disease.”
“More representative studies, including minority ethnic groups and those living in areas of high social and economic deprivation, are needed,” Dr. Simonet emphasized.
She said that there is little research on the association with epilepsy and hearing loss in early PD, and “for that reason, our results should encourage further studies to confirm a possible link between these manifestations and Parkinson’s disease.”
Early detection may drive better diagnoses
The current study is important for understanding the prediagnostic features and risk factors that may allow for earlier detection of Parkinson’s disease, William Hung, MD, a geriatrics and palliative care specialist of the Icahn School of Medicine at Mount Sinai, New York, said in an interview. “Prior to this study, there was limited understanding of these features.
“One surprise [in the findings] was that ethnicity and socioeconomic deprivation do not appear to be associated with the risk of PD, in contrast to other illnesses such as dementia,” said Dr. Hung. “The array of prediagnostic features associated with PD is not surprising, but nonetheless important for clinicians to know to consider whether PD could be the underlying cause.”
The take-home message for primary care is that “there are features, such as hearing loss, history of epilepsy, autonomic symptoms, motor symptoms, among others, for which clinicians should consider PD as part of the differential diagnosis as underlying cause and consider referral to specialists for diagnostic clarification,” said Dr. Hung.
“Additional research is needed to translate these findings to care, perhaps developing decision aids, interventions that may help with diagnosis and evaluation,” as is work on understanding the link between PD and symptoms such as hearing loss and epilepsy, he said.
Primary care offers opportunity to identify risk factors
The current study represents an important step in early recognition of PD, with implications for helping patients access treatments promptly and improve their quality of life, Bhavana Patel, DO, Shannon Chiu, MD, and Melissa J. Armstrong, MD, of the University of Florida, Gainesville, wrote in an accompanying editorial.
“The primary care setting is commonly where symptoms heralding the onset of PD are first discussed. However, little is known regarding the prediagnostic manifestations of PD that are seen in primary care clinics, particularly in underserved populations,” they wrote.
The study included many risk factors and prodromal markers associated with research criteria for prodromal PD, but did not include several risk and prodromal markers in the Movement Disorders Society research criteria, “such as symptoms suggestive of REM sleep behavior disorder, excessive daytime sleepiness (which overlaps with, but is distinct from, fatigue), urinary dysfunction, pesticide and solvent exposure, caffeine use, level of physical activity, and family history,” they said.
Even in individuals with diagnosed PD, certain symptoms, particularly nonmotor symptoms, are commonly underreported,” and primary care clinicians may not recognize these symptoms as PD risk factors, the authors noted.
However, “in addition to contributing to possible models of modifiable risk factors for PD, study results may also further inform algorithms designed to predict PD diagnoses in primary care,” they said. The study also highlights the need for more multivariable models to better identify PD risk factors and strategies for early identification of PD in primary care.
Several study coauthors received funding related to the study from Barts Charity, Health Data Research UK, the Department of Health and Social Care (England) and the devolved administrations, and leading medical research charities, as well as the National Institute for Health Research UCLH Biomedical Research Centre. Lead author Dr. Simonet and Dr. Hung had no financial conflicts to disclose. Dr. Patel disclosed support from the National Institute on Aging, the Mangurian-Fixel-McKnight Collaboration for Pilot Studies in Lewy Body Dementia, and the American Brain Foundation and the Mary E. Groff Charitable Trust. Dr. Chiu reported receiving grants from Mangurian-Fixel-McKnight Collaboration for Pilot Studies in Lewy Body Dementia and the Smallwood Foundation. Dr. Armstrong disclosed funding from the National Institute on Aging, the Florida Department of Health, the Lewy Body Dementia Association, the Alzheimer’s Therapeutic Research Institute/Alzheimer’s Clinical Trial Consortium, the Alzheimer’s Disease Cooperative Study as Data Safety Monitoring Board the Parkinson’s Foundation, and the American Academy of Neurology.
Tremors and memory symptoms were identified among individuals in a primary care setting as early as 10 years before a Parkinson’s disease diagnosis in a new study.
Most research on the causes and early signs of Parkinson’s disease (PD) have involved patients of Northern European ancestry, Cristina Simonet, MD, of Queen Mary University of London, and colleagues wrote in their paper, published in JAMA Neurology.
Additionally, data on how PD might manifest in different ethnic groups are limited, they said.
In their nested case-control, the researchers examined data from electronic health records of an ethnically diverse population of 1,016,277 adults seen in primary care practices between 1990 and Feb. 6, 2018. They compared individuals with PD with those without PD or other neurologic conditions.
The researchers identified 10 age and sex-matched controls for each PD case, and also conducted an unmatched analysis after adjusting for age and sex. The final study population included 1,055 patients with PD and 1,009,523 controls. The population of PD cases was 15.7% Black, 19.7% South Asian, 50.9% White, and 8.3% other; the population of controls was 13.3% Black, 21.5% South Asian, 43.7% White, and 11.3% other.
“We observed a constellation of symptoms noted by general practitioners up to a decade before diagnosis of PD,” the researchers said. Symptoms were identified across three time intervals (less than 2 years, 2-5 years, and 5-10 years before diagnosis) to better evaluate exposure outcome associations.
In the matched analysis of midlife risk factors, epilepsy showed the strongest association with PD diagnosis across all time periods, and type 2 diabetes or hypertension 5-10 years before diagnosis was associated with later PD.
Prediagnostic signs of PD included both motor and nonmotor manifestations.
The matched analysis revealed a significant increased association between tremor and memory symptoms less than 2 years before diagnosis (adjusted odds ratios of 151.24 and 8.73, respectively) as well as up to 10 years before diagnosis for tremors and up to 5 years for memory symptoms (aOR, 11.4 and 3.09, respectively) in PD patients, compared with controls.
Other strong associations between PD and early nonmotor features in cases, compared with controls, included hypotension (aOR, 6.81), constipation (aOR, 3.29), and depression (aOR, 4.61).
In addition, the researchers found associations for epilepsy that had not been identified in previous studies, and these associations persisted in a replication analysis.
The study findings were limited by several factors, mainly the use of routine primary care data with underascertained factors of interest, and potential mislabeling of PD, the researchers noted. Other limitations included the lack of data on prescription medication for PD, and the recording of memory problems in primary care without supportive testing to confirm cognitive impairment.
The results support a range of comorbidities and symptoms that may present in primary care, and clinicians should consider PD as a possible cause, the researchers wrote.
Make early referral a priority
The study is important because of the lack of diversity in Parkinson’s disease research, lead author Dr. Simonet said in an interview.
“Over the last decade, the global population suffering from Parkinson’s disease has more than doubled,” she said. Causes may include the increasing numbers of older people with longer life expectancy. “However, it seems there are other factors, including environmental, genetic, and lifestyle, that might play a role in increasing the prevalence of Parkinson’s disease.”
“More representative studies, including minority ethnic groups and those living in areas of high social and economic deprivation, are needed,” Dr. Simonet emphasized.
She said that there is little research on the association with epilepsy and hearing loss in early PD, and “for that reason, our results should encourage further studies to confirm a possible link between these manifestations and Parkinson’s disease.”
Early detection may drive better diagnoses
The current study is important for understanding the prediagnostic features and risk factors that may allow for earlier detection of Parkinson’s disease, William Hung, MD, a geriatrics and palliative care specialist of the Icahn School of Medicine at Mount Sinai, New York, said in an interview. “Prior to this study, there was limited understanding of these features.
“One surprise [in the findings] was that ethnicity and socioeconomic deprivation do not appear to be associated with the risk of PD, in contrast to other illnesses such as dementia,” said Dr. Hung. “The array of prediagnostic features associated with PD is not surprising, but nonetheless important for clinicians to know to consider whether PD could be the underlying cause.”
The take-home message for primary care is that “there are features, such as hearing loss, history of epilepsy, autonomic symptoms, motor symptoms, among others, for which clinicians should consider PD as part of the differential diagnosis as underlying cause and consider referral to specialists for diagnostic clarification,” said Dr. Hung.
“Additional research is needed to translate these findings to care, perhaps developing decision aids, interventions that may help with diagnosis and evaluation,” as is work on understanding the link between PD and symptoms such as hearing loss and epilepsy, he said.
Primary care offers opportunity to identify risk factors
The current study represents an important step in early recognition of PD, with implications for helping patients access treatments promptly and improve their quality of life, Bhavana Patel, DO, Shannon Chiu, MD, and Melissa J. Armstrong, MD, of the University of Florida, Gainesville, wrote in an accompanying editorial.
“The primary care setting is commonly where symptoms heralding the onset of PD are first discussed. However, little is known regarding the prediagnostic manifestations of PD that are seen in primary care clinics, particularly in underserved populations,” they wrote.
The study included many risk factors and prodromal markers associated with research criteria for prodromal PD, but did not include several risk and prodromal markers in the Movement Disorders Society research criteria, “such as symptoms suggestive of REM sleep behavior disorder, excessive daytime sleepiness (which overlaps with, but is distinct from, fatigue), urinary dysfunction, pesticide and solvent exposure, caffeine use, level of physical activity, and family history,” they said.
Even in individuals with diagnosed PD, certain symptoms, particularly nonmotor symptoms, are commonly underreported,” and primary care clinicians may not recognize these symptoms as PD risk factors, the authors noted.
However, “in addition to contributing to possible models of modifiable risk factors for PD, study results may also further inform algorithms designed to predict PD diagnoses in primary care,” they said. The study also highlights the need for more multivariable models to better identify PD risk factors and strategies for early identification of PD in primary care.
Several study coauthors received funding related to the study from Barts Charity, Health Data Research UK, the Department of Health and Social Care (England) and the devolved administrations, and leading medical research charities, as well as the National Institute for Health Research UCLH Biomedical Research Centre. Lead author Dr. Simonet and Dr. Hung had no financial conflicts to disclose. Dr. Patel disclosed support from the National Institute on Aging, the Mangurian-Fixel-McKnight Collaboration for Pilot Studies in Lewy Body Dementia, and the American Brain Foundation and the Mary E. Groff Charitable Trust. Dr. Chiu reported receiving grants from Mangurian-Fixel-McKnight Collaboration for Pilot Studies in Lewy Body Dementia and the Smallwood Foundation. Dr. Armstrong disclosed funding from the National Institute on Aging, the Florida Department of Health, the Lewy Body Dementia Association, the Alzheimer’s Therapeutic Research Institute/Alzheimer’s Clinical Trial Consortium, the Alzheimer’s Disease Cooperative Study as Data Safety Monitoring Board the Parkinson’s Foundation, and the American Academy of Neurology.
Tremors and memory symptoms were identified among individuals in a primary care setting as early as 10 years before a Parkinson’s disease diagnosis in a new study.
Most research on the causes and early signs of Parkinson’s disease (PD) have involved patients of Northern European ancestry, Cristina Simonet, MD, of Queen Mary University of London, and colleagues wrote in their paper, published in JAMA Neurology.
Additionally, data on how PD might manifest in different ethnic groups are limited, they said.
In their nested case-control, the researchers examined data from electronic health records of an ethnically diverse population of 1,016,277 adults seen in primary care practices between 1990 and Feb. 6, 2018. They compared individuals with PD with those without PD or other neurologic conditions.
The researchers identified 10 age and sex-matched controls for each PD case, and also conducted an unmatched analysis after adjusting for age and sex. The final study population included 1,055 patients with PD and 1,009,523 controls. The population of PD cases was 15.7% Black, 19.7% South Asian, 50.9% White, and 8.3% other; the population of controls was 13.3% Black, 21.5% South Asian, 43.7% White, and 11.3% other.
“We observed a constellation of symptoms noted by general practitioners up to a decade before diagnosis of PD,” the researchers said. Symptoms were identified across three time intervals (less than 2 years, 2-5 years, and 5-10 years before diagnosis) to better evaluate exposure outcome associations.
In the matched analysis of midlife risk factors, epilepsy showed the strongest association with PD diagnosis across all time periods, and type 2 diabetes or hypertension 5-10 years before diagnosis was associated with later PD.
Prediagnostic signs of PD included both motor and nonmotor manifestations.
The matched analysis revealed a significant increased association between tremor and memory symptoms less than 2 years before diagnosis (adjusted odds ratios of 151.24 and 8.73, respectively) as well as up to 10 years before diagnosis for tremors and up to 5 years for memory symptoms (aOR, 11.4 and 3.09, respectively) in PD patients, compared with controls.
Other strong associations between PD and early nonmotor features in cases, compared with controls, included hypotension (aOR, 6.81), constipation (aOR, 3.29), and depression (aOR, 4.61).
In addition, the researchers found associations for epilepsy that had not been identified in previous studies, and these associations persisted in a replication analysis.
The study findings were limited by several factors, mainly the use of routine primary care data with underascertained factors of interest, and potential mislabeling of PD, the researchers noted. Other limitations included the lack of data on prescription medication for PD, and the recording of memory problems in primary care without supportive testing to confirm cognitive impairment.
The results support a range of comorbidities and symptoms that may present in primary care, and clinicians should consider PD as a possible cause, the researchers wrote.
Make early referral a priority
The study is important because of the lack of diversity in Parkinson’s disease research, lead author Dr. Simonet said in an interview.
“Over the last decade, the global population suffering from Parkinson’s disease has more than doubled,” she said. Causes may include the increasing numbers of older people with longer life expectancy. “However, it seems there are other factors, including environmental, genetic, and lifestyle, that might play a role in increasing the prevalence of Parkinson’s disease.”
“More representative studies, including minority ethnic groups and those living in areas of high social and economic deprivation, are needed,” Dr. Simonet emphasized.
She said that there is little research on the association with epilepsy and hearing loss in early PD, and “for that reason, our results should encourage further studies to confirm a possible link between these manifestations and Parkinson’s disease.”
Early detection may drive better diagnoses
The current study is important for understanding the prediagnostic features and risk factors that may allow for earlier detection of Parkinson’s disease, William Hung, MD, a geriatrics and palliative care specialist of the Icahn School of Medicine at Mount Sinai, New York, said in an interview. “Prior to this study, there was limited understanding of these features.
“One surprise [in the findings] was that ethnicity and socioeconomic deprivation do not appear to be associated with the risk of PD, in contrast to other illnesses such as dementia,” said Dr. Hung. “The array of prediagnostic features associated with PD is not surprising, but nonetheless important for clinicians to know to consider whether PD could be the underlying cause.”
The take-home message for primary care is that “there are features, such as hearing loss, history of epilepsy, autonomic symptoms, motor symptoms, among others, for which clinicians should consider PD as part of the differential diagnosis as underlying cause and consider referral to specialists for diagnostic clarification,” said Dr. Hung.
“Additional research is needed to translate these findings to care, perhaps developing decision aids, interventions that may help with diagnosis and evaluation,” as is work on understanding the link between PD and symptoms such as hearing loss and epilepsy, he said.
Primary care offers opportunity to identify risk factors
The current study represents an important step in early recognition of PD, with implications for helping patients access treatments promptly and improve their quality of life, Bhavana Patel, DO, Shannon Chiu, MD, and Melissa J. Armstrong, MD, of the University of Florida, Gainesville, wrote in an accompanying editorial.
“The primary care setting is commonly where symptoms heralding the onset of PD are first discussed. However, little is known regarding the prediagnostic manifestations of PD that are seen in primary care clinics, particularly in underserved populations,” they wrote.
The study included many risk factors and prodromal markers associated with research criteria for prodromal PD, but did not include several risk and prodromal markers in the Movement Disorders Society research criteria, “such as symptoms suggestive of REM sleep behavior disorder, excessive daytime sleepiness (which overlaps with, but is distinct from, fatigue), urinary dysfunction, pesticide and solvent exposure, caffeine use, level of physical activity, and family history,” they said.
Even in individuals with diagnosed PD, certain symptoms, particularly nonmotor symptoms, are commonly underreported,” and primary care clinicians may not recognize these symptoms as PD risk factors, the authors noted.
However, “in addition to contributing to possible models of modifiable risk factors for PD, study results may also further inform algorithms designed to predict PD diagnoses in primary care,” they said. The study also highlights the need for more multivariable models to better identify PD risk factors and strategies for early identification of PD in primary care.
Several study coauthors received funding related to the study from Barts Charity, Health Data Research UK, the Department of Health and Social Care (England) and the devolved administrations, and leading medical research charities, as well as the National Institute for Health Research UCLH Biomedical Research Centre. Lead author Dr. Simonet and Dr. Hung had no financial conflicts to disclose. Dr. Patel disclosed support from the National Institute on Aging, the Mangurian-Fixel-McKnight Collaboration for Pilot Studies in Lewy Body Dementia, and the American Brain Foundation and the Mary E. Groff Charitable Trust. Dr. Chiu reported receiving grants from Mangurian-Fixel-McKnight Collaboration for Pilot Studies in Lewy Body Dementia and the Smallwood Foundation. Dr. Armstrong disclosed funding from the National Institute on Aging, the Florida Department of Health, the Lewy Body Dementia Association, the Alzheimer’s Therapeutic Research Institute/Alzheimer’s Clinical Trial Consortium, the Alzheimer’s Disease Cooperative Study as Data Safety Monitoring Board the Parkinson’s Foundation, and the American Academy of Neurology.
FROM JAMA NEUROLOGY
Boosting daily exercise after age 70 tied to lower CVD risk
Increasingly active patterns of physical activity were linked with reduced rates of overall mortality and cardiovascular disease (CVD), but early rather than later in late life, in a 20-year follow-up cohort study.
In this population of people older than 65 years, researchers found that physical activity overall was associated with lower rates of incident CVD, particularly among men, and the association was strongest in people 70 to 75 years of age, rather than in older age groups.
They also looked at “trajectories,” or changes in activity over time, and found that a stable-high trajectory of activity was associated with a significantly lower risk for cardiovascular outcomes in men than in those with a stable-low trajectory. For women, more physical activity was consistently associated with lower CVD outcomes, although not statistically significantly so, except for overall mortality, which did reach significance.
Notably, the greatest reduction in cardiovascular risk was reported in people who did more than 20 minutes of physical exercise each day, and it was more pronounced in those 70 years of age.
Physical activity was also associated with a lower incidence of heart failure and coronary heart disease in older people, again especially early on in late life, reported Claudio Barbiellini Amidei, MD, University of Padua, Italy, and colleagues.
The data suggest that physical activity is more effective in preventing CVD onset when implemented early rather than later in life, noted Dr. Amidei in an email.
“The findings of our study are suggestive of a protective effect of physical activity in late-life on cardiovascular health. WHO recommendations for adults and older adults are to practice at least 20 minutes of moderate to vigorous physical activity per day. I believe this is a realistic target, and policy makers should raise awareness on the importance of achieving this goal at all ages, including in late-life,” Dr. Amidei said.
The study was published online Feb. 14 in Heart.
Previous research has demonstrated that the most benefit of high physical activity, compared with low, begins at about 60 years of age, and that is because younger people are at much lower risk, noted Carl “Chip” Lavie MD, FACC, medical director of cardiac rehabilitation and prevention, Ochsner Clinical School–The University of Queensland School of Medicine, New Orleans, who was not involved in the study.
“At quite old ages, for example over age 80, resistance exercise or weight training and balance training may be even more important than aerobic training,” he added.
Activity ‘trajectories’
The benefits of physical activity on cardiovascular risk are well established, the researchers note. Less clear is the role that trajectories of activity over time play, although research to date suggests a reduction in risk with increasing activity from mid-life to early old age, they write.
For the current analysis, the researchers assessed 3,099 Italian participants. Mean age was about 75 years, and baseline data were collected from 1995 to 1997.
Follow-up visits were conducted after 4 years and again after 7 years. Using hospital medical records and mortality data, the researchers were able to collect surveillance data through 2018. Hospital records, surveys, and clinical assessments helped them identify incident and prevalent cardiovascular diseases, such as stroke, coronary heart disease, and heart failure.
Participants’ physical activity patterns were classified as stable-high, low-increasing, high-decreasing, and stable-low. Exposure was evaluated at 70, 75, 80, and 85 years of age.
“In our analyses, we focused on moderate to vigorous physical activity, and these include a broad range of exercises, such as walking very briskly, playing tennis, [and] jogging, but comprise also other activities, such as gardening or doing household chores,” said Dr. Amidei.
Patterns of stable-low physical activity were linked to a significantly greater risk for cardiovascular outcomes in men than patterns of stable-high physical activity (hazard ratio, 0.48; 95% confidence interval, 0.27-0.86; P for trend = .002).
No significant relation was found between physical activity and stroke, the researchers note.
“The benefits of physical activity seem to lessen above the age of 75 years and seem more important in men,” noted Dr. Lavie. “This may be partly due to the higher risk of CVD in men. Women typically lag 13 to 15 years behind men for CVD but start catching up in older years.”
Limitations of the study include lack of information regarding physical activity during mid-life, the limited number of stroke events, the relatively few participants older than 85 years, and potential recall bias, the researchers note.
Another limitation was that the physical activity data were based on patient surveys collected 3 years apart and did not involve the use of an accelerometer, the researchers add.
“Future observational studies are required to confirm our findings and pathophysiological studies are warranted to examine the underlying biological mechanisms. Physical activity is likely to be beneficial at any age, but to summarize our findings, we could say that when it comes to being physically active, the sooner the better,” concluded Dr. Amidei.
Dr. Amidei reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Increasingly active patterns of physical activity were linked with reduced rates of overall mortality and cardiovascular disease (CVD), but early rather than later in late life, in a 20-year follow-up cohort study.
In this population of people older than 65 years, researchers found that physical activity overall was associated with lower rates of incident CVD, particularly among men, and the association was strongest in people 70 to 75 years of age, rather than in older age groups.
They also looked at “trajectories,” or changes in activity over time, and found that a stable-high trajectory of activity was associated with a significantly lower risk for cardiovascular outcomes in men than in those with a stable-low trajectory. For women, more physical activity was consistently associated with lower CVD outcomes, although not statistically significantly so, except for overall mortality, which did reach significance.
Notably, the greatest reduction in cardiovascular risk was reported in people who did more than 20 minutes of physical exercise each day, and it was more pronounced in those 70 years of age.
Physical activity was also associated with a lower incidence of heart failure and coronary heart disease in older people, again especially early on in late life, reported Claudio Barbiellini Amidei, MD, University of Padua, Italy, and colleagues.
The data suggest that physical activity is more effective in preventing CVD onset when implemented early rather than later in life, noted Dr. Amidei in an email.
“The findings of our study are suggestive of a protective effect of physical activity in late-life on cardiovascular health. WHO recommendations for adults and older adults are to practice at least 20 minutes of moderate to vigorous physical activity per day. I believe this is a realistic target, and policy makers should raise awareness on the importance of achieving this goal at all ages, including in late-life,” Dr. Amidei said.
The study was published online Feb. 14 in Heart.
Previous research has demonstrated that the most benefit of high physical activity, compared with low, begins at about 60 years of age, and that is because younger people are at much lower risk, noted Carl “Chip” Lavie MD, FACC, medical director of cardiac rehabilitation and prevention, Ochsner Clinical School–The University of Queensland School of Medicine, New Orleans, who was not involved in the study.
“At quite old ages, for example over age 80, resistance exercise or weight training and balance training may be even more important than aerobic training,” he added.
Activity ‘trajectories’
The benefits of physical activity on cardiovascular risk are well established, the researchers note. Less clear is the role that trajectories of activity over time play, although research to date suggests a reduction in risk with increasing activity from mid-life to early old age, they write.
For the current analysis, the researchers assessed 3,099 Italian participants. Mean age was about 75 years, and baseline data were collected from 1995 to 1997.
Follow-up visits were conducted after 4 years and again after 7 years. Using hospital medical records and mortality data, the researchers were able to collect surveillance data through 2018. Hospital records, surveys, and clinical assessments helped them identify incident and prevalent cardiovascular diseases, such as stroke, coronary heart disease, and heart failure.
Participants’ physical activity patterns were classified as stable-high, low-increasing, high-decreasing, and stable-low. Exposure was evaluated at 70, 75, 80, and 85 years of age.
“In our analyses, we focused on moderate to vigorous physical activity, and these include a broad range of exercises, such as walking very briskly, playing tennis, [and] jogging, but comprise also other activities, such as gardening or doing household chores,” said Dr. Amidei.
Patterns of stable-low physical activity were linked to a significantly greater risk for cardiovascular outcomes in men than patterns of stable-high physical activity (hazard ratio, 0.48; 95% confidence interval, 0.27-0.86; P for trend = .002).
No significant relation was found between physical activity and stroke, the researchers note.
“The benefits of physical activity seem to lessen above the age of 75 years and seem more important in men,” noted Dr. Lavie. “This may be partly due to the higher risk of CVD in men. Women typically lag 13 to 15 years behind men for CVD but start catching up in older years.”
Limitations of the study include lack of information regarding physical activity during mid-life, the limited number of stroke events, the relatively few participants older than 85 years, and potential recall bias, the researchers note.
Another limitation was that the physical activity data were based on patient surveys collected 3 years apart and did not involve the use of an accelerometer, the researchers add.
“Future observational studies are required to confirm our findings and pathophysiological studies are warranted to examine the underlying biological mechanisms. Physical activity is likely to be beneficial at any age, but to summarize our findings, we could say that when it comes to being physically active, the sooner the better,” concluded Dr. Amidei.
Dr. Amidei reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Increasingly active patterns of physical activity were linked with reduced rates of overall mortality and cardiovascular disease (CVD), but early rather than later in late life, in a 20-year follow-up cohort study.
In this population of people older than 65 years, researchers found that physical activity overall was associated with lower rates of incident CVD, particularly among men, and the association was strongest in people 70 to 75 years of age, rather than in older age groups.
They also looked at “trajectories,” or changes in activity over time, and found that a stable-high trajectory of activity was associated with a significantly lower risk for cardiovascular outcomes in men than in those with a stable-low trajectory. For women, more physical activity was consistently associated with lower CVD outcomes, although not statistically significantly so, except for overall mortality, which did reach significance.
Notably, the greatest reduction in cardiovascular risk was reported in people who did more than 20 minutes of physical exercise each day, and it was more pronounced in those 70 years of age.
Physical activity was also associated with a lower incidence of heart failure and coronary heart disease in older people, again especially early on in late life, reported Claudio Barbiellini Amidei, MD, University of Padua, Italy, and colleagues.
The data suggest that physical activity is more effective in preventing CVD onset when implemented early rather than later in life, noted Dr. Amidei in an email.
“The findings of our study are suggestive of a protective effect of physical activity in late-life on cardiovascular health. WHO recommendations for adults and older adults are to practice at least 20 minutes of moderate to vigorous physical activity per day. I believe this is a realistic target, and policy makers should raise awareness on the importance of achieving this goal at all ages, including in late-life,” Dr. Amidei said.
The study was published online Feb. 14 in Heart.
Previous research has demonstrated that the most benefit of high physical activity, compared with low, begins at about 60 years of age, and that is because younger people are at much lower risk, noted Carl “Chip” Lavie MD, FACC, medical director of cardiac rehabilitation and prevention, Ochsner Clinical School–The University of Queensland School of Medicine, New Orleans, who was not involved in the study.
“At quite old ages, for example over age 80, resistance exercise or weight training and balance training may be even more important than aerobic training,” he added.
Activity ‘trajectories’
The benefits of physical activity on cardiovascular risk are well established, the researchers note. Less clear is the role that trajectories of activity over time play, although research to date suggests a reduction in risk with increasing activity from mid-life to early old age, they write.
For the current analysis, the researchers assessed 3,099 Italian participants. Mean age was about 75 years, and baseline data were collected from 1995 to 1997.
Follow-up visits were conducted after 4 years and again after 7 years. Using hospital medical records and mortality data, the researchers were able to collect surveillance data through 2018. Hospital records, surveys, and clinical assessments helped them identify incident and prevalent cardiovascular diseases, such as stroke, coronary heart disease, and heart failure.
Participants’ physical activity patterns were classified as stable-high, low-increasing, high-decreasing, and stable-low. Exposure was evaluated at 70, 75, 80, and 85 years of age.
“In our analyses, we focused on moderate to vigorous physical activity, and these include a broad range of exercises, such as walking very briskly, playing tennis, [and] jogging, but comprise also other activities, such as gardening or doing household chores,” said Dr. Amidei.
Patterns of stable-low physical activity were linked to a significantly greater risk for cardiovascular outcomes in men than patterns of stable-high physical activity (hazard ratio, 0.48; 95% confidence interval, 0.27-0.86; P for trend = .002).
No significant relation was found between physical activity and stroke, the researchers note.
“The benefits of physical activity seem to lessen above the age of 75 years and seem more important in men,” noted Dr. Lavie. “This may be partly due to the higher risk of CVD in men. Women typically lag 13 to 15 years behind men for CVD but start catching up in older years.”
Limitations of the study include lack of information regarding physical activity during mid-life, the limited number of stroke events, the relatively few participants older than 85 years, and potential recall bias, the researchers note.
Another limitation was that the physical activity data were based on patient surveys collected 3 years apart and did not involve the use of an accelerometer, the researchers add.
“Future observational studies are required to confirm our findings and pathophysiological studies are warranted to examine the underlying biological mechanisms. Physical activity is likely to be beneficial at any age, but to summarize our findings, we could say that when it comes to being physically active, the sooner the better,” concluded Dr. Amidei.
Dr. Amidei reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Right place, right time: Facilitating end-of-life conversations
As the geriatric population continues to grow and treatment advances blur the lines between improving the length of life vs improving its quality, end-of-life (EOL) conversations are becoming increasingly important. These discussions are a crucial part of the advance care planning (ACP) process, in which patients discuss their treatment preferences and values with their caregiver/surrogate decision maker and health care provider to ultimately improve EOL decision-making and care. 1,2
EOL conversations are most helpful when incorporated in the outpatient setting as part of the patient’s ongoing health care plan or when initiating treatment for a chronic or life-threatening disease. Because family physicians promote general wellness, understand the patient’s health status and medical history, and have an ongoing—and often longstanding—relationship with patients and their families, we are ideally positioned to engage patients in EOL discussions. However, these conversations can be challenging in the outpatient setting, and often clinicians struggle not only to find ways to raise the subject, but also to find the time to have these supportive, meaningful conversations.3
In this article, we will address the importance of having EOL discussions in the outpatient setting, specifically about advance directives (ADs), and the reasons why patients and physicians might avoid these discussions. The role of palliative care in EOL care, along with its benefits and methods for overcoming patient and physician barriers to its successful use, are reviewed. Finally, we examine specific challenges associated with discussing EOL care with patients with decreased mental capacity, such as those with dementia, and provide strategies to successfully facilitate EOL discussions in these populations.
Moving patients toward completion of advance directives
Although many older patients express a desire to document their wishes before EOL situations arise, they may not fully understand the benefits of an AD or how to complete one. 4 Often the family physician is best equipped to address the patient’s concerns and discuss their goals for EOL care, as well as the potential situations that might arise.
Managing an aging population. Projections suggest that primary care physicians will encounter increasing numbers of geriatric patients in the next 2 decades. Thus it is essential for those in primary care to receive proper training during their residency for the care of this group of patients. According to a group of academic educators and geriatricians from internal medicine and family medicine whose goal was to define a set of minimal and essential competencies in the care of older adults, this includes training on how to discuss and document “advance care planning and goals of care with all patients with chronic or complex illness,” as well as how to differentiate among “types of code status, health care proxies, and advanced directives” within the state in which training occurs. 5
Educate patients and ease fears. Patients often avoid EOL conversations or wait for their family physician to start the conversation. They may not understand how ADs can help guide care or they may believe they are “too healthy” to have these conversations at this time. 4 Simply asking about existing ADs or providing forms to patients during an outpatient visit can open the door to more in-depth discussions. Some examples of opening phrases include:
- Do you have a living will or durable power of attorney for health care?
- Have you ever discussed your health care wishes with your loved ones?
- Who would you want to speak for you regarding your health care if you could not speak for yourself? Have you discussed your health care wishes with that person?
By normalizing the conversation as a routine part of comprehensive, patient-centered care, the family physician can allay patient fears, foster open and honest conversations, and encourage ongoing discussions with loved ones as situations arise.6
Continue to: When ADs are executed...
When ADs are executed, patients often fail to have meaningful conversations with their surrogates about specific treatment wishes or EOL scenarios. As a result, the surrogate may not feel prepared to serve as a proxy decision maker or may find the role extremely stressful.7 Physicians should encourage open conversations between patients and their surrogates about potential EOL scenarios when possible. When possible and appropriate, it is also important to encourage the patient to include the surrogate in future outpatient visits so that the surrogate can understand the patient’s health status and potential decisions they may need to make.
Don’t overlook clinician barriers. Family physicians also might avoid AD discussions because they do not understand laws that govern ADs, which vary from state to state. Various online resources for patients and physicians exist that clarify state-specific regulations and provide state-specific forms (TABLE).
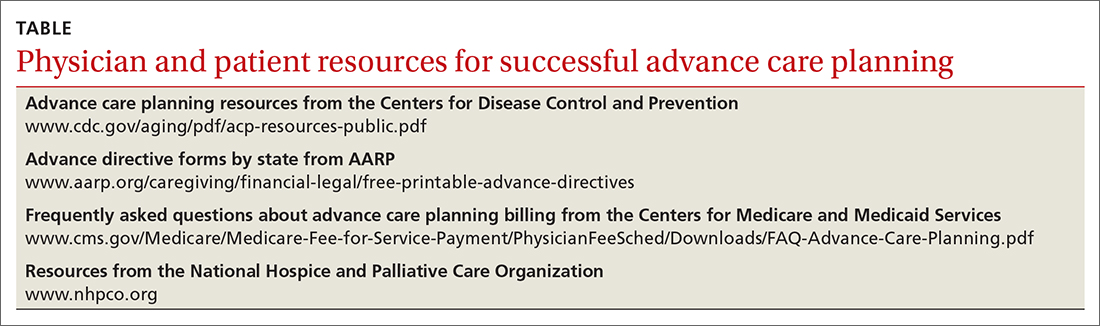
Time constraints present another challenge for family physicians. This can be addressed by establishing workflows that include EOL elements. Also, the Centers for Medicare and Medicaid Services (CMS) has provided separate billing codes for AD discussion based on time spent explaining and discussing how to complete forms.8 CPT codes 99497 and 99498 are time-based codes that cover the first 30 minutes and each additional 30 minutes, respectively, of time spent explaining and discussing how to complete standard forms in a face-to-face setting (TABLE).9 CMS also includes discussion of AD documents as an optional element of the annual Medicare wellness visit.8
Improve quality of life for patients with any serious illness
Unlike hospice, which focuses on providing comfort rather than cure in the final months of a patient’s life, palliative care strives to prevent and relieve the patient’s suffering from a serious illness that is not immediately life-threatening. Palliative care focuses on the early identification, careful assessment, and treatment of the physical, psychosocial, and spiritual symptoms associated with a patient’s condition(s).10,11 It has been well established that palliative care has a positive effect on many clinical outcomes including symptom burden, quality of life, satisfaction with care, and survival.12-14 Patients who receive palliative care consultation also tend to perceive a higher quality of care.15
Conversations lead to better outcomes. Palliative care consultation is being increasingly used in the outpatient setting and can be introduced early in a disease process. Doing so provides an additional opportunity for the family physician to introduce an EOL discussion. A comparison of outcomes between patients who had initial inpatient palliative care consultation vs outpatient palliative care referral found that outpatient referral improved quality EOL care and was associated with significantly fewer emergency department visits (68% vs 48%; P < .001) and hospital admissions (86% vs 52%; P < .001), as well as shorter hospital stays in the last 30 days of life (3-11 vs 5-14 days; P = .01).14 Despite these benefits, 60% to 90% of patients with a serious illness report never having discussed EOL care issues with their clinician.16,17
Continue to: Early EOL discussions...
Early EOL discussions have also been shown to have a positive impact on families. In a US study, family members stated that timely EOL care discussions allowed them to make use of hospice and palliative care services sooner and to make the most of their time with the patient.18
Timing and communication are key
Logistically it can be difficult to gather the right people (patient, family, etc) in the right place and at the right time. For physicians, the most often cited barriers include inadequate time to conduct an EOL discussion, 19 a perceived lack of competence in EOL conversations, 1,20 difficulty navigating patient readiness, 21 and a fear of destroying hope due to prognostic uncertainty. 19,20
A prospective, observational study used the Quality of Communication (QOC) questionnaire to assess life-sustaining treatment preferences, ACP, and the quality of EOL care communication in Dutch outpatients with clinically stable but severe chronic obstructive pulmonary disease (n = 105) or congestive heart failure (n = 80). The QOC questionnaire is a validated instrument that asks patients to rate their physician on several communication skills from 0 (“the very worst” or “My doctor didn’t do this”) to 10 (“the very best”). In this study, quality communication was identified by patients as one of the most important skills for physicians to provide adequate EOL care. 22 While QOC ratings were high for general communication skills (median, 8.0 points), quality EOL care communication was rated very low (median, 0.0 points). Researchers say that this was primarily because most EOL topics were not discussed—especially spirituality, prognosis, and what dying might be like. 22 In a secondary analysis that evaluated quality of EOL care communication during 1-year follow-up of patients with advanced chronic organ failure (n = 265) with the QOC questionnaire, patient ratings improved to moderate to good (medians, 6-8 points) when these topics were addressed. 23
Pick a strategy and prepare. As the older population continues to grow, the demands of palliative care management cannot be met by specialists alone and the responsibility of discussing EOL care with patients and their families will increasingly fall to family physicians as well. 24 Several strategies and approaches have evolved to assist family physicians with acquiring the skills to conduct productive EOL discussions. These include widely referenced resources, such as VitalTalk 25 and the ABCDE Plan. 26 VitalTalk teaches skills to help clinicians navigate difficult conversations, 25 and the “ABCDE” method provides a pneumonic for recommendations for how to deliver bad news ( A dvance preparation; B uild a therapeutic environment/relationship; C ommunicate well; D eal with patient and family reactions; E ncourage and validate emotions). 26
Other strategies include familiarizing oneself with the patient’s medical history and present situation (eg, What are the patient’s symptoms? What do other involved clinicians think and recommend? What therapies have been attempted? What are the relevant social and emotional dynamics?); asking the patient who they want present for the EOL conversation; scheduling the conversation for when you can set aside an appropriate amount of time and in a private place where there will be no interruptions; and going into the meeting with your goal in mind, whether it is to deliver bad news, clarify the prognosis, establish goals of care, or communicate the patient’s goals and wishes for the EOL to those in attendance. 27 It can be very helpful to begin the conversation by clarifying what the patient and their family/surrogate understand about the current diagnosis and prognosis. From there, the family physician can present a “headline” that prepares them for the current conversation (eg, “I have your latest test results, and I need to share some serious news”). This can facilitate a more detailed discussion of the patient’s and surrogate’s goals of care. Using these strategies, family physicians can lead a productive EOL discussion that benefits everyone.
Continue to: How to navigate EOL discussions with patients with dementia
How to navigate EOL discussions with patients with dementia
EOL discussions with patients with dementia become even more complex and warrant specific discussion because one must consider the timing of such discussions, 2,28,29 the trajectory of the disease and how that affects the patient’s capacity for EOL conversations, and the critical importance of engaging caregivers/surrogate decision makers in these discussions. 2 ACP provides an opportunity for the physician, patient, and caregiver/surrogate to jointly explore the patient’s values, beliefs, and preferences for care through the EOL as the disease progresses and the patient’s decisional capacity declines.
Ensure meaningful participation with timing. EOL discussions should occur while the patient has the cognitive capacity to actively participate in the planning process. A National Institutes of Health stage I behavioral intervention development trial evaluated a structured psychoeducational intervention, known as SPIRIT (Sharing Patient’s Illness Representation to Increase Trust), that aimed to promote cognitive and emotional preparation for EOL decisions for patients and their surrogates.28 It was found to be effective in patients, including those with end-stage renal disease and advanced heart failure, and their surrogates.28 Preliminary results from the trial confirmed that people with mild-to-moderate dementia (recent Montreal Cognitive Assessment score ≥ 13) are able to participate meaningfully in EOL discussions and ACP.28
Song et al29 adapted SPIRIT for use with patients with dementia and conducted a feasibility study with 23 patient-surrogate dyads.The mixed-methods study involved an expert panel review of the adapted SPIRIT, followed by a randomized trial with qualitative interviews. All 23 patients with dementia, including 14 with moderate dementia, were able to articulate their values and EOL preferences somewhat or very coherently (91.3% inter-rater reliability).29 In addition, dyad care goal congruence (agreement between patient’s EOL preferences and surrogate’s understanding of those preferences) and surrogate decision-making confidence (comfort in performing as a surrogate) were high and patient decisional conflict (patient difficulty in weighing the benefits and burdens of life-sustaining treatments and decision-making) was low, both at baseline as well as post intervention.29 Although preparedness for EOL decision-making outcome measures did not change, people with dementia and their surrogates perceived SPIRIT to be beneficial, particularly in helping them be on the same page.29
The randomized trial portion of the study (phase 2) continues to recruit 120 patient-surrogate dyads. Patient and surrogate self-reported preparedness for EOL decision-making are the primary outcomes, measured at baseline and 2 to 3 days post intervention. The estimated study completion date is May 31, 2022.30
Evidence-based clinical guidance can improve the process. Following the Belgian Centre for Evidence-Based Medicine’s procedures as a sample methodology, Piers et al2 developed evidence-based clinical recommendations for providers to use in the practical application of ACP in their care of patients with dementia.The researchers searched the literature; developed recommendations based on the evidence obtained, as well as their collective expert opinion; and performed validation using expert and end-user feedback and peer review. The study resulted in 32 recommendations focused on 8 domains that ranged from the beginning of the process (preconditions for optimal implementation of ACP) to later stages (ACP when it is difficult/no longer possible to communicate).2Specific guidance for ACP in dementia care include the following:
- ACP initiation. Begin conversations around the time of diagnosis, continue them throughout ongoing care, and revisit them when changes occur in the patient’s health, financial, or residential status.
- ACP conversations. Use conversations to identify significant others in the patient’s life (potential caregivers and/or surrogate decision makers) and explore the patient’s awareness of the disease and its trajectory. Discuss the patient’s values and beliefs, as well as their fears about, and preferences for, future care and the EOL.
- Role of significant others in the ACP process. Involve a patient’s significant others early in the ACP process, educate them about the surrogate decision-maker role, assess their disease awareness, and inform them about the disease trajectory and anticipated EOL decisions. 2
Continue to: Incorporate and document patients' values and preferences with LEAD
Incorporate and document patients’ values and preferences with LEAD. Dassel et al31 developed the Life-planning in Early Alzheimer’s and Dementia (LEAD) tool, which is a validated dementia-focused EOL planning tool that can be used to promote discussion and document a patient’s care preferences and values within the context of their changing cognitive ability.Dassel et al31 used a 4-phase mixed-method design that included (1) focus groups of patients with early-stage dementia and family caregivers, (2) clinical utility evaluation by content experts, (3) instrument completion sampling to evaluate its psychometric properties, and (4) additional focus groups to inform how the instrument should be used by families and in clinical practice.Six scales with high internal consistency and high test-retest reliability were identified: 3 scales represented patient values (concern about being a burden, the importance of quality [vs length] of life, and the preference for autonomy in decision-making) and 3 scales represented patient preferences (use of life-prolonging measures, controlling the timing of death, and the location of EOL care).31
The LEAD Guide can be used as a self-assessment tool that is completed individually and then shared with the surrogate decision maker and health care provider.32 It also can be used to guide conversations with the surrogate and physician, as well as with trusted family and friends. Using this framework, family physicians can facilitate EOL planning with the patient and their surrogate that is based on the patient’s values and preferences for EOL care prior to, and in anticipation of, the patient’s loss of decisional capacity.31
Facilitate discussions that improve outcomes
Conversations about EOL care are taking on increased importance as the population ages and treatments advance. Understanding the concerns of patients and their surrogate decision makers, as well as the resources available to guide these difficult discussions ( TABLE ), will help family physicians conduct effective conversations that enhance care, reduce the burden on surrogate decision makers, and have a positive impact on many clinical outcomes.
CORRESPONDENCE
Shirley Bodi, MD, 3000 Arlington Avenue, Department of Family Medicine, Dowling Hall, Suite 2200, University of Toledo College of Medicine and Life Sciences, Toledo, OH 43614; [email protected]
1. Bergenholtz Heidi, Timm HU, Missel M. Talking about end of life in general palliative care – what’s going on? A qualitative study on end-of-life conversations in an acute care hospital in Denmark. BMC Palliat Care. 2019;18:62. doi: 10.1186/s12904-019-0448-z
2. Piers R, Albers G, Gilissen J, et al. Advance care planning in dementia: recommendations for healthcare professionals. BMC Palliat Care. 2018;17:88. doi: 10.1186/s12904-018-0332-2
3. Tunzi M, Ventres W. A reflective case study in family medicine advance care planning conversations. J Am Board Fam Med. 2019;32:108-114. doi: 10.3122/jabfm.2019.01.180198
4. Schickedanz AD, Schillinger D, Landefeld CS, et al. A clinical framework for improving the advance care planning process: start with patients’ self-identified barriers. J Am Geriatr Soc. 2009;57:31-39. doi: 10.1111/j.1532-5415.2008.02093.x
5. Williams BC, Warshaw G, Fabiny AR, et al. Medicine in the 21st century: recommended essential geriatrics competencies for internal medicine and family medicine residents. J Grad Med Ed. 2010;2:373-383. doi: 10.4300/JGME-D-10-00065.1
6. Alano G, Pekmezaris R, Tai J, et al. Factors influencing older adults to complete advance directives. Palliat Support Care. 2010;8:267-275. doi: 10.1017/S1478951510000064
7. Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med. 2011;154:336-346. doi: 10.7326/0003-4819-154-5-201103010-00008
8. Edelberg C. Advance care planning with and without an annual wellness visit. Ed Management website. June 1, 2016. Accessed November 16, 2021. ww.reliasmedia.com/articles/137829-advanced-care-planning-with-and-without-an-annual-wellness-visit
9. Centers for Medicare and Medicaid Services. Frequently asked questions about billing the physician fee schedule for advance care planning services. July 14, 2016. Accessed December 20, 2021. www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Downloads/FAQ-Advance-Care-Planning.pdf
10. World Health Organization. Palliative care fact sheet. August 5, 2020. Accessed November 16, 2021. www.who.int/news-room/fact-sheets/detail/palliative-care
11. National Institute on Aging. What are palliative care and hospice care? Reviewed May 14, 2021. Accessed December 20, 2021. www.nia.nih.gov/health/what-are-palliative-care-and-hospice-care#palliative-vs-hospice
12. Rabow MW, Dibble SL, Pantilat, SZ, et al. The comprehensive care team: a controlled trial of outpatient palliative medicine consultation. Arch Intern Med. 2004;164:83-91. doi: 10.1001/archinte.164.1.83
13. Muir JC, Daley F, Davis MS, et al. Integrating palliative care into the outpatient, private practice oncology setting. J Pain Symptom Manage. 2010;40:126-135. doi: 10.1016/j.jpainsymman.2009.12.017
14. Hui D, Kim SH, Roquemore J, et al. Impact of timing and setting of palliative care referral on quality of end-of-life care in cancer patients. Cancer. 2014;120:1743-1749. doi: 10.1002/cncr.28628
15. Leung JM, Udris EM, Uman J, e al. The effect of end-of-life discussions on perceived quality of care and health status among patients with COPD. Chest. 2012;142:128-133. doi: 10.1378/chest.11-2222
16. Davison SN. End-of-life care preferences and needs: perceptions of patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010;5:195-204. doi: 10.2215/CJN.05960809
17. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patients mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300:1665-1673. doi: 10.1001/jama.300.14.1665
18. Park E, Check DK, Yopp JM, et al. An exploratory study of end-of-life prognostic communication needs as reported by widowed fathers due to cancer. Psychooncology. 2015;24:1471-1476. doi: 10.1002/pon.3757
19. Tavares N, Jarrett N, Hunt K, et al. Palliative and end-of-life care conversations in COPD: a systematic literature review. ERJ Open Res. 2017;3:00068-2016. doi: 10.1183/23120541.00068-2016
20. Hancock K, Clayton JM, Parker SM, et al. Truth-telling in discussing prognosis in advanced life-limiting illnesses: a systematic review. Palliat Med. 2007;21:507-517. doi: 10.1177/0269216307080823
21. Parker SM, Clayton JM, Hancock K, et al. A systematic review of prognostic/end-of-life communication with adults in the advanced stages of a life-limiting illness: patient/caregiver preferences for the content, style, and timing of information. J Pain Symptom Manage. 2007;34:81-93. doi: 10.1016/j.jpainsymman.2006.09.035
22. Janssen DJA, Spruit MA, Schols JMGA, et al. A call for high-quality advance care planning in outpatients with severe COPD or chronic heart failure. Chest. 2011;139:1081-1088. doi: 10.1378/chest.10-1753
23. Houben CHM, Spruit MA, Schols JM, et al. Patient-clinician communication about end-of-life care on patients with advanced chronic organ failure during one year. J Pain Symptom Manage. 2015;49:1109-1115. doi: 10.1016/j.jpainsymman.2014.12.008
24. Brighton LJ, Bristowe K. Communication in palliative care: talking about the end of life, before the end of life. Postgrad Med J. 2016;92:466-470. doi: 10.1136/postgradmedj-2015-133368
25. VitalTalk website. Accessed December 20, 2021. vitaltalk.org
26. Rabow MQ, McPhee SJ. Beyond breaking bad news: how to help patients who suffer. Wes J Med. 1999;171:260-263. www.ncbi.nlm.nih.gov/pmc/articles/PMC1305864
27. Pfeifer M, Head B. Which critical communication skills are essential for interdisciplinary end-of-life discussions? AMA J Ethics. 2018;8:E724-E731. doi: 10.1001/amajethics.2018.724
28. Song M-K, Ward SE, Hepburn K, et al. SPIRIT advance care planning intervention in early stage dementias: an NIH stage I behavioral intervention development trial. Contemp Clin Trials. 2018;71:55-62. doi: 10.1016/j.cct.2018.06.005
29. Song M-K, Ward SE, Hepburn K, et al. Can persons with dementia meaningfully participate in advance care planning discussions? A mixed-methods study of SPIRIT. J Palliat Med. 2019;22:1410-1416. doi: 10.1089/jpm.2019.0088
30. Two-phased study of SPIRIT in mild dementia. ClinicalTrials.gov Identifier: NCT03311711. Updated August 23, 2021. Accessed December 20, 2021. clinicaltrials.gov/ct2/show/NCT03311711
31. Dassel K, Utz R, Supiano K, et al. Development of a dementia-focused end-of-life planning tool: the LEAD Guide (Life-planning in Early Alzheimer’s and Dementia). Innov Aging. 2019;3:igz024. doi: 10.1093/geroni/igz024
32. Dassel K, Supiano K, Utz R, et al. The LEAD Guide. Life-planning in Early Alzheimer’s and Dementia. 2019. Accessed December 20, 2021. utahgwep.org/resources/search-all-resources/send/10-dementia/27-the-lead-guide#:~:text=The%20LEAD%20Guide%20(Life%2DPlanning,your%20decisions%20about%20your%20care
As the geriatric population continues to grow and treatment advances blur the lines between improving the length of life vs improving its quality, end-of-life (EOL) conversations are becoming increasingly important. These discussions are a crucial part of the advance care planning (ACP) process, in which patients discuss their treatment preferences and values with their caregiver/surrogate decision maker and health care provider to ultimately improve EOL decision-making and care. 1,2
EOL conversations are most helpful when incorporated in the outpatient setting as part of the patient’s ongoing health care plan or when initiating treatment for a chronic or life-threatening disease. Because family physicians promote general wellness, understand the patient’s health status and medical history, and have an ongoing—and often longstanding—relationship with patients and their families, we are ideally positioned to engage patients in EOL discussions. However, these conversations can be challenging in the outpatient setting, and often clinicians struggle not only to find ways to raise the subject, but also to find the time to have these supportive, meaningful conversations.3
In this article, we will address the importance of having EOL discussions in the outpatient setting, specifically about advance directives (ADs), and the reasons why patients and physicians might avoid these discussions. The role of palliative care in EOL care, along with its benefits and methods for overcoming patient and physician barriers to its successful use, are reviewed. Finally, we examine specific challenges associated with discussing EOL care with patients with decreased mental capacity, such as those with dementia, and provide strategies to successfully facilitate EOL discussions in these populations.
Moving patients toward completion of advance directives
Although many older patients express a desire to document their wishes before EOL situations arise, they may not fully understand the benefits of an AD or how to complete one. 4 Often the family physician is best equipped to address the patient’s concerns and discuss their goals for EOL care, as well as the potential situations that might arise.
Managing an aging population. Projections suggest that primary care physicians will encounter increasing numbers of geriatric patients in the next 2 decades. Thus it is essential for those in primary care to receive proper training during their residency for the care of this group of patients. According to a group of academic educators and geriatricians from internal medicine and family medicine whose goal was to define a set of minimal and essential competencies in the care of older adults, this includes training on how to discuss and document “advance care planning and goals of care with all patients with chronic or complex illness,” as well as how to differentiate among “types of code status, health care proxies, and advanced directives” within the state in which training occurs. 5
Educate patients and ease fears. Patients often avoid EOL conversations or wait for their family physician to start the conversation. They may not understand how ADs can help guide care or they may believe they are “too healthy” to have these conversations at this time. 4 Simply asking about existing ADs or providing forms to patients during an outpatient visit can open the door to more in-depth discussions. Some examples of opening phrases include:
- Do you have a living will or durable power of attorney for health care?
- Have you ever discussed your health care wishes with your loved ones?
- Who would you want to speak for you regarding your health care if you could not speak for yourself? Have you discussed your health care wishes with that person?
By normalizing the conversation as a routine part of comprehensive, patient-centered care, the family physician can allay patient fears, foster open and honest conversations, and encourage ongoing discussions with loved ones as situations arise.6
Continue to: When ADs are executed...
When ADs are executed, patients often fail to have meaningful conversations with their surrogates about specific treatment wishes or EOL scenarios. As a result, the surrogate may not feel prepared to serve as a proxy decision maker or may find the role extremely stressful.7 Physicians should encourage open conversations between patients and their surrogates about potential EOL scenarios when possible. When possible and appropriate, it is also important to encourage the patient to include the surrogate in future outpatient visits so that the surrogate can understand the patient’s health status and potential decisions they may need to make.
Don’t overlook clinician barriers. Family physicians also might avoid AD discussions because they do not understand laws that govern ADs, which vary from state to state. Various online resources for patients and physicians exist that clarify state-specific regulations and provide state-specific forms (TABLE).
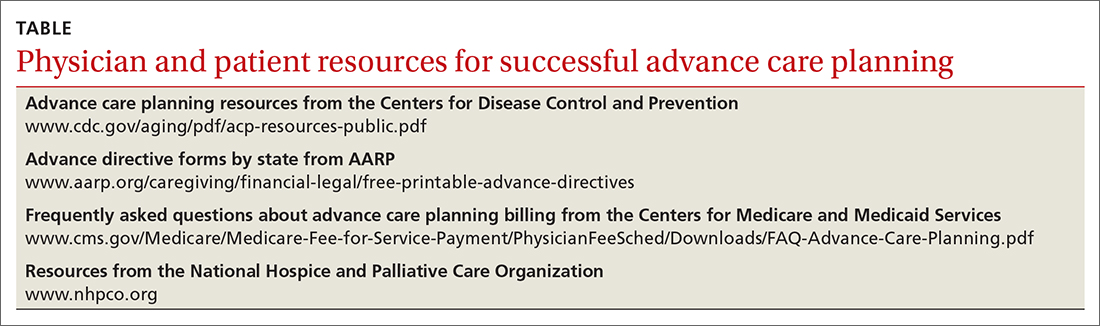
Time constraints present another challenge for family physicians. This can be addressed by establishing workflows that include EOL elements. Also, the Centers for Medicare and Medicaid Services (CMS) has provided separate billing codes for AD discussion based on time spent explaining and discussing how to complete forms.8 CPT codes 99497 and 99498 are time-based codes that cover the first 30 minutes and each additional 30 minutes, respectively, of time spent explaining and discussing how to complete standard forms in a face-to-face setting (TABLE).9 CMS also includes discussion of AD documents as an optional element of the annual Medicare wellness visit.8
Improve quality of life for patients with any serious illness
Unlike hospice, which focuses on providing comfort rather than cure in the final months of a patient’s life, palliative care strives to prevent and relieve the patient’s suffering from a serious illness that is not immediately life-threatening. Palliative care focuses on the early identification, careful assessment, and treatment of the physical, psychosocial, and spiritual symptoms associated with a patient’s condition(s).10,11 It has been well established that palliative care has a positive effect on many clinical outcomes including symptom burden, quality of life, satisfaction with care, and survival.12-14 Patients who receive palliative care consultation also tend to perceive a higher quality of care.15
Conversations lead to better outcomes. Palliative care consultation is being increasingly used in the outpatient setting and can be introduced early in a disease process. Doing so provides an additional opportunity for the family physician to introduce an EOL discussion. A comparison of outcomes between patients who had initial inpatient palliative care consultation vs outpatient palliative care referral found that outpatient referral improved quality EOL care and was associated with significantly fewer emergency department visits (68% vs 48%; P < .001) and hospital admissions (86% vs 52%; P < .001), as well as shorter hospital stays in the last 30 days of life (3-11 vs 5-14 days; P = .01).14 Despite these benefits, 60% to 90% of patients with a serious illness report never having discussed EOL care issues with their clinician.16,17
Continue to: Early EOL discussions...
Early EOL discussions have also been shown to have a positive impact on families. In a US study, family members stated that timely EOL care discussions allowed them to make use of hospice and palliative care services sooner and to make the most of their time with the patient.18
Timing and communication are key
Logistically it can be difficult to gather the right people (patient, family, etc) in the right place and at the right time. For physicians, the most often cited barriers include inadequate time to conduct an EOL discussion, 19 a perceived lack of competence in EOL conversations, 1,20 difficulty navigating patient readiness, 21 and a fear of destroying hope due to prognostic uncertainty. 19,20
A prospective, observational study used the Quality of Communication (QOC) questionnaire to assess life-sustaining treatment preferences, ACP, and the quality of EOL care communication in Dutch outpatients with clinically stable but severe chronic obstructive pulmonary disease (n = 105) or congestive heart failure (n = 80). The QOC questionnaire is a validated instrument that asks patients to rate their physician on several communication skills from 0 (“the very worst” or “My doctor didn’t do this”) to 10 (“the very best”). In this study, quality communication was identified by patients as one of the most important skills for physicians to provide adequate EOL care. 22 While QOC ratings were high for general communication skills (median, 8.0 points), quality EOL care communication was rated very low (median, 0.0 points). Researchers say that this was primarily because most EOL topics were not discussed—especially spirituality, prognosis, and what dying might be like. 22 In a secondary analysis that evaluated quality of EOL care communication during 1-year follow-up of patients with advanced chronic organ failure (n = 265) with the QOC questionnaire, patient ratings improved to moderate to good (medians, 6-8 points) when these topics were addressed. 23
Pick a strategy and prepare. As the older population continues to grow, the demands of palliative care management cannot be met by specialists alone and the responsibility of discussing EOL care with patients and their families will increasingly fall to family physicians as well. 24 Several strategies and approaches have evolved to assist family physicians with acquiring the skills to conduct productive EOL discussions. These include widely referenced resources, such as VitalTalk 25 and the ABCDE Plan. 26 VitalTalk teaches skills to help clinicians navigate difficult conversations, 25 and the “ABCDE” method provides a pneumonic for recommendations for how to deliver bad news ( A dvance preparation; B uild a therapeutic environment/relationship; C ommunicate well; D eal with patient and family reactions; E ncourage and validate emotions). 26
Other strategies include familiarizing oneself with the patient’s medical history and present situation (eg, What are the patient’s symptoms? What do other involved clinicians think and recommend? What therapies have been attempted? What are the relevant social and emotional dynamics?); asking the patient who they want present for the EOL conversation; scheduling the conversation for when you can set aside an appropriate amount of time and in a private place where there will be no interruptions; and going into the meeting with your goal in mind, whether it is to deliver bad news, clarify the prognosis, establish goals of care, or communicate the patient’s goals and wishes for the EOL to those in attendance. 27 It can be very helpful to begin the conversation by clarifying what the patient and their family/surrogate understand about the current diagnosis and prognosis. From there, the family physician can present a “headline” that prepares them for the current conversation (eg, “I have your latest test results, and I need to share some serious news”). This can facilitate a more detailed discussion of the patient’s and surrogate’s goals of care. Using these strategies, family physicians can lead a productive EOL discussion that benefits everyone.
Continue to: How to navigate EOL discussions with patients with dementia
How to navigate EOL discussions with patients with dementia
EOL discussions with patients with dementia become even more complex and warrant specific discussion because one must consider the timing of such discussions, 2,28,29 the trajectory of the disease and how that affects the patient’s capacity for EOL conversations, and the critical importance of engaging caregivers/surrogate decision makers in these discussions. 2 ACP provides an opportunity for the physician, patient, and caregiver/surrogate to jointly explore the patient’s values, beliefs, and preferences for care through the EOL as the disease progresses and the patient’s decisional capacity declines.
Ensure meaningful participation with timing. EOL discussions should occur while the patient has the cognitive capacity to actively participate in the planning process. A National Institutes of Health stage I behavioral intervention development trial evaluated a structured psychoeducational intervention, known as SPIRIT (Sharing Patient’s Illness Representation to Increase Trust), that aimed to promote cognitive and emotional preparation for EOL decisions for patients and their surrogates.28 It was found to be effective in patients, including those with end-stage renal disease and advanced heart failure, and their surrogates.28 Preliminary results from the trial confirmed that people with mild-to-moderate dementia (recent Montreal Cognitive Assessment score ≥ 13) are able to participate meaningfully in EOL discussions and ACP.28
Song et al29 adapted SPIRIT for use with patients with dementia and conducted a feasibility study with 23 patient-surrogate dyads.The mixed-methods study involved an expert panel review of the adapted SPIRIT, followed by a randomized trial with qualitative interviews. All 23 patients with dementia, including 14 with moderate dementia, were able to articulate their values and EOL preferences somewhat or very coherently (91.3% inter-rater reliability).29 In addition, dyad care goal congruence (agreement between patient’s EOL preferences and surrogate’s understanding of those preferences) and surrogate decision-making confidence (comfort in performing as a surrogate) were high and patient decisional conflict (patient difficulty in weighing the benefits and burdens of life-sustaining treatments and decision-making) was low, both at baseline as well as post intervention.29 Although preparedness for EOL decision-making outcome measures did not change, people with dementia and their surrogates perceived SPIRIT to be beneficial, particularly in helping them be on the same page.29
The randomized trial portion of the study (phase 2) continues to recruit 120 patient-surrogate dyads. Patient and surrogate self-reported preparedness for EOL decision-making are the primary outcomes, measured at baseline and 2 to 3 days post intervention. The estimated study completion date is May 31, 2022.30
Evidence-based clinical guidance can improve the process. Following the Belgian Centre for Evidence-Based Medicine’s procedures as a sample methodology, Piers et al2 developed evidence-based clinical recommendations for providers to use in the practical application of ACP in their care of patients with dementia.The researchers searched the literature; developed recommendations based on the evidence obtained, as well as their collective expert opinion; and performed validation using expert and end-user feedback and peer review. The study resulted in 32 recommendations focused on 8 domains that ranged from the beginning of the process (preconditions for optimal implementation of ACP) to later stages (ACP when it is difficult/no longer possible to communicate).2Specific guidance for ACP in dementia care include the following:
- ACP initiation. Begin conversations around the time of diagnosis, continue them throughout ongoing care, and revisit them when changes occur in the patient’s health, financial, or residential status.
- ACP conversations. Use conversations to identify significant others in the patient’s life (potential caregivers and/or surrogate decision makers) and explore the patient’s awareness of the disease and its trajectory. Discuss the patient’s values and beliefs, as well as their fears about, and preferences for, future care and the EOL.
- Role of significant others in the ACP process. Involve a patient’s significant others early in the ACP process, educate them about the surrogate decision-maker role, assess their disease awareness, and inform them about the disease trajectory and anticipated EOL decisions. 2
Continue to: Incorporate and document patients' values and preferences with LEAD
Incorporate and document patients’ values and preferences with LEAD. Dassel et al31 developed the Life-planning in Early Alzheimer’s and Dementia (LEAD) tool, which is a validated dementia-focused EOL planning tool that can be used to promote discussion and document a patient’s care preferences and values within the context of their changing cognitive ability.Dassel et al31 used a 4-phase mixed-method design that included (1) focus groups of patients with early-stage dementia and family caregivers, (2) clinical utility evaluation by content experts, (3) instrument completion sampling to evaluate its psychometric properties, and (4) additional focus groups to inform how the instrument should be used by families and in clinical practice.Six scales with high internal consistency and high test-retest reliability were identified: 3 scales represented patient values (concern about being a burden, the importance of quality [vs length] of life, and the preference for autonomy in decision-making) and 3 scales represented patient preferences (use of life-prolonging measures, controlling the timing of death, and the location of EOL care).31
The LEAD Guide can be used as a self-assessment tool that is completed individually and then shared with the surrogate decision maker and health care provider.32 It also can be used to guide conversations with the surrogate and physician, as well as with trusted family and friends. Using this framework, family physicians can facilitate EOL planning with the patient and their surrogate that is based on the patient’s values and preferences for EOL care prior to, and in anticipation of, the patient’s loss of decisional capacity.31
Facilitate discussions that improve outcomes
Conversations about EOL care are taking on increased importance as the population ages and treatments advance. Understanding the concerns of patients and their surrogate decision makers, as well as the resources available to guide these difficult discussions ( TABLE ), will help family physicians conduct effective conversations that enhance care, reduce the burden on surrogate decision makers, and have a positive impact on many clinical outcomes.
CORRESPONDENCE
Shirley Bodi, MD, 3000 Arlington Avenue, Department of Family Medicine, Dowling Hall, Suite 2200, University of Toledo College of Medicine and Life Sciences, Toledo, OH 43614; [email protected]
As the geriatric population continues to grow and treatment advances blur the lines between improving the length of life vs improving its quality, end-of-life (EOL) conversations are becoming increasingly important. These discussions are a crucial part of the advance care planning (ACP) process, in which patients discuss their treatment preferences and values with their caregiver/surrogate decision maker and health care provider to ultimately improve EOL decision-making and care. 1,2
EOL conversations are most helpful when incorporated in the outpatient setting as part of the patient’s ongoing health care plan or when initiating treatment for a chronic or life-threatening disease. Because family physicians promote general wellness, understand the patient’s health status and medical history, and have an ongoing—and often longstanding—relationship with patients and their families, we are ideally positioned to engage patients in EOL discussions. However, these conversations can be challenging in the outpatient setting, and often clinicians struggle not only to find ways to raise the subject, but also to find the time to have these supportive, meaningful conversations.3
In this article, we will address the importance of having EOL discussions in the outpatient setting, specifically about advance directives (ADs), and the reasons why patients and physicians might avoid these discussions. The role of palliative care in EOL care, along with its benefits and methods for overcoming patient and physician barriers to its successful use, are reviewed. Finally, we examine specific challenges associated with discussing EOL care with patients with decreased mental capacity, such as those with dementia, and provide strategies to successfully facilitate EOL discussions in these populations.
Moving patients toward completion of advance directives
Although many older patients express a desire to document their wishes before EOL situations arise, they may not fully understand the benefits of an AD or how to complete one. 4 Often the family physician is best equipped to address the patient’s concerns and discuss their goals for EOL care, as well as the potential situations that might arise.
Managing an aging population. Projections suggest that primary care physicians will encounter increasing numbers of geriatric patients in the next 2 decades. Thus it is essential for those in primary care to receive proper training during their residency for the care of this group of patients. According to a group of academic educators and geriatricians from internal medicine and family medicine whose goal was to define a set of minimal and essential competencies in the care of older adults, this includes training on how to discuss and document “advance care planning and goals of care with all patients with chronic or complex illness,” as well as how to differentiate among “types of code status, health care proxies, and advanced directives” within the state in which training occurs. 5
Educate patients and ease fears. Patients often avoid EOL conversations or wait for their family physician to start the conversation. They may not understand how ADs can help guide care or they may believe they are “too healthy” to have these conversations at this time. 4 Simply asking about existing ADs or providing forms to patients during an outpatient visit can open the door to more in-depth discussions. Some examples of opening phrases include:
- Do you have a living will or durable power of attorney for health care?
- Have you ever discussed your health care wishes with your loved ones?
- Who would you want to speak for you regarding your health care if you could not speak for yourself? Have you discussed your health care wishes with that person?
By normalizing the conversation as a routine part of comprehensive, patient-centered care, the family physician can allay patient fears, foster open and honest conversations, and encourage ongoing discussions with loved ones as situations arise.6
Continue to: When ADs are executed...
When ADs are executed, patients often fail to have meaningful conversations with their surrogates about specific treatment wishes or EOL scenarios. As a result, the surrogate may not feel prepared to serve as a proxy decision maker or may find the role extremely stressful.7 Physicians should encourage open conversations between patients and their surrogates about potential EOL scenarios when possible. When possible and appropriate, it is also important to encourage the patient to include the surrogate in future outpatient visits so that the surrogate can understand the patient’s health status and potential decisions they may need to make.
Don’t overlook clinician barriers. Family physicians also might avoid AD discussions because they do not understand laws that govern ADs, which vary from state to state. Various online resources for patients and physicians exist that clarify state-specific regulations and provide state-specific forms (TABLE).
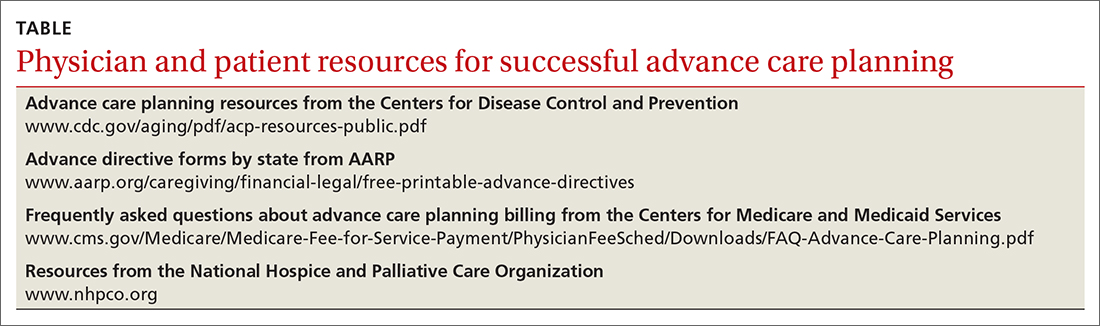
Time constraints present another challenge for family physicians. This can be addressed by establishing workflows that include EOL elements. Also, the Centers for Medicare and Medicaid Services (CMS) has provided separate billing codes for AD discussion based on time spent explaining and discussing how to complete forms.8 CPT codes 99497 and 99498 are time-based codes that cover the first 30 minutes and each additional 30 minutes, respectively, of time spent explaining and discussing how to complete standard forms in a face-to-face setting (TABLE).9 CMS also includes discussion of AD documents as an optional element of the annual Medicare wellness visit.8
Improve quality of life for patients with any serious illness
Unlike hospice, which focuses on providing comfort rather than cure in the final months of a patient’s life, palliative care strives to prevent and relieve the patient’s suffering from a serious illness that is not immediately life-threatening. Palliative care focuses on the early identification, careful assessment, and treatment of the physical, psychosocial, and spiritual symptoms associated with a patient’s condition(s).10,11 It has been well established that palliative care has a positive effect on many clinical outcomes including symptom burden, quality of life, satisfaction with care, and survival.12-14 Patients who receive palliative care consultation also tend to perceive a higher quality of care.15
Conversations lead to better outcomes. Palliative care consultation is being increasingly used in the outpatient setting and can be introduced early in a disease process. Doing so provides an additional opportunity for the family physician to introduce an EOL discussion. A comparison of outcomes between patients who had initial inpatient palliative care consultation vs outpatient palliative care referral found that outpatient referral improved quality EOL care and was associated with significantly fewer emergency department visits (68% vs 48%; P < .001) and hospital admissions (86% vs 52%; P < .001), as well as shorter hospital stays in the last 30 days of life (3-11 vs 5-14 days; P = .01).14 Despite these benefits, 60% to 90% of patients with a serious illness report never having discussed EOL care issues with their clinician.16,17
Continue to: Early EOL discussions...
Early EOL discussions have also been shown to have a positive impact on families. In a US study, family members stated that timely EOL care discussions allowed them to make use of hospice and palliative care services sooner and to make the most of their time with the patient.18
Timing and communication are key
Logistically it can be difficult to gather the right people (patient, family, etc) in the right place and at the right time. For physicians, the most often cited barriers include inadequate time to conduct an EOL discussion, 19 a perceived lack of competence in EOL conversations, 1,20 difficulty navigating patient readiness, 21 and a fear of destroying hope due to prognostic uncertainty. 19,20
A prospective, observational study used the Quality of Communication (QOC) questionnaire to assess life-sustaining treatment preferences, ACP, and the quality of EOL care communication in Dutch outpatients with clinically stable but severe chronic obstructive pulmonary disease (n = 105) or congestive heart failure (n = 80). The QOC questionnaire is a validated instrument that asks patients to rate their physician on several communication skills from 0 (“the very worst” or “My doctor didn’t do this”) to 10 (“the very best”). In this study, quality communication was identified by patients as one of the most important skills for physicians to provide adequate EOL care. 22 While QOC ratings were high for general communication skills (median, 8.0 points), quality EOL care communication was rated very low (median, 0.0 points). Researchers say that this was primarily because most EOL topics were not discussed—especially spirituality, prognosis, and what dying might be like. 22 In a secondary analysis that evaluated quality of EOL care communication during 1-year follow-up of patients with advanced chronic organ failure (n = 265) with the QOC questionnaire, patient ratings improved to moderate to good (medians, 6-8 points) when these topics were addressed. 23
Pick a strategy and prepare. As the older population continues to grow, the demands of palliative care management cannot be met by specialists alone and the responsibility of discussing EOL care with patients and their families will increasingly fall to family physicians as well. 24 Several strategies and approaches have evolved to assist family physicians with acquiring the skills to conduct productive EOL discussions. These include widely referenced resources, such as VitalTalk 25 and the ABCDE Plan. 26 VitalTalk teaches skills to help clinicians navigate difficult conversations, 25 and the “ABCDE” method provides a pneumonic for recommendations for how to deliver bad news ( A dvance preparation; B uild a therapeutic environment/relationship; C ommunicate well; D eal with patient and family reactions; E ncourage and validate emotions). 26
Other strategies include familiarizing oneself with the patient’s medical history and present situation (eg, What are the patient’s symptoms? What do other involved clinicians think and recommend? What therapies have been attempted? What are the relevant social and emotional dynamics?); asking the patient who they want present for the EOL conversation; scheduling the conversation for when you can set aside an appropriate amount of time and in a private place where there will be no interruptions; and going into the meeting with your goal in mind, whether it is to deliver bad news, clarify the prognosis, establish goals of care, or communicate the patient’s goals and wishes for the EOL to those in attendance. 27 It can be very helpful to begin the conversation by clarifying what the patient and their family/surrogate understand about the current diagnosis and prognosis. From there, the family physician can present a “headline” that prepares them for the current conversation (eg, “I have your latest test results, and I need to share some serious news”). This can facilitate a more detailed discussion of the patient’s and surrogate’s goals of care. Using these strategies, family physicians can lead a productive EOL discussion that benefits everyone.
Continue to: How to navigate EOL discussions with patients with dementia
How to navigate EOL discussions with patients with dementia
EOL discussions with patients with dementia become even more complex and warrant specific discussion because one must consider the timing of such discussions, 2,28,29 the trajectory of the disease and how that affects the patient’s capacity for EOL conversations, and the critical importance of engaging caregivers/surrogate decision makers in these discussions. 2 ACP provides an opportunity for the physician, patient, and caregiver/surrogate to jointly explore the patient’s values, beliefs, and preferences for care through the EOL as the disease progresses and the patient’s decisional capacity declines.
Ensure meaningful participation with timing. EOL discussions should occur while the patient has the cognitive capacity to actively participate in the planning process. A National Institutes of Health stage I behavioral intervention development trial evaluated a structured psychoeducational intervention, known as SPIRIT (Sharing Patient’s Illness Representation to Increase Trust), that aimed to promote cognitive and emotional preparation for EOL decisions for patients and their surrogates.28 It was found to be effective in patients, including those with end-stage renal disease and advanced heart failure, and their surrogates.28 Preliminary results from the trial confirmed that people with mild-to-moderate dementia (recent Montreal Cognitive Assessment score ≥ 13) are able to participate meaningfully in EOL discussions and ACP.28
Song et al29 adapted SPIRIT for use with patients with dementia and conducted a feasibility study with 23 patient-surrogate dyads.The mixed-methods study involved an expert panel review of the adapted SPIRIT, followed by a randomized trial with qualitative interviews. All 23 patients with dementia, including 14 with moderate dementia, were able to articulate their values and EOL preferences somewhat or very coherently (91.3% inter-rater reliability).29 In addition, dyad care goal congruence (agreement between patient’s EOL preferences and surrogate’s understanding of those preferences) and surrogate decision-making confidence (comfort in performing as a surrogate) were high and patient decisional conflict (patient difficulty in weighing the benefits and burdens of life-sustaining treatments and decision-making) was low, both at baseline as well as post intervention.29 Although preparedness for EOL decision-making outcome measures did not change, people with dementia and their surrogates perceived SPIRIT to be beneficial, particularly in helping them be on the same page.29
The randomized trial portion of the study (phase 2) continues to recruit 120 patient-surrogate dyads. Patient and surrogate self-reported preparedness for EOL decision-making are the primary outcomes, measured at baseline and 2 to 3 days post intervention. The estimated study completion date is May 31, 2022.30
Evidence-based clinical guidance can improve the process. Following the Belgian Centre for Evidence-Based Medicine’s procedures as a sample methodology, Piers et al2 developed evidence-based clinical recommendations for providers to use in the practical application of ACP in their care of patients with dementia.The researchers searched the literature; developed recommendations based on the evidence obtained, as well as their collective expert opinion; and performed validation using expert and end-user feedback and peer review. The study resulted in 32 recommendations focused on 8 domains that ranged from the beginning of the process (preconditions for optimal implementation of ACP) to later stages (ACP when it is difficult/no longer possible to communicate).2Specific guidance for ACP in dementia care include the following:
- ACP initiation. Begin conversations around the time of diagnosis, continue them throughout ongoing care, and revisit them when changes occur in the patient’s health, financial, or residential status.
- ACP conversations. Use conversations to identify significant others in the patient’s life (potential caregivers and/or surrogate decision makers) and explore the patient’s awareness of the disease and its trajectory. Discuss the patient’s values and beliefs, as well as their fears about, and preferences for, future care and the EOL.
- Role of significant others in the ACP process. Involve a patient’s significant others early in the ACP process, educate them about the surrogate decision-maker role, assess their disease awareness, and inform them about the disease trajectory and anticipated EOL decisions. 2
Continue to: Incorporate and document patients' values and preferences with LEAD
Incorporate and document patients’ values and preferences with LEAD. Dassel et al31 developed the Life-planning in Early Alzheimer’s and Dementia (LEAD) tool, which is a validated dementia-focused EOL planning tool that can be used to promote discussion and document a patient’s care preferences and values within the context of their changing cognitive ability.Dassel et al31 used a 4-phase mixed-method design that included (1) focus groups of patients with early-stage dementia and family caregivers, (2) clinical utility evaluation by content experts, (3) instrument completion sampling to evaluate its psychometric properties, and (4) additional focus groups to inform how the instrument should be used by families and in clinical practice.Six scales with high internal consistency and high test-retest reliability were identified: 3 scales represented patient values (concern about being a burden, the importance of quality [vs length] of life, and the preference for autonomy in decision-making) and 3 scales represented patient preferences (use of life-prolonging measures, controlling the timing of death, and the location of EOL care).31
The LEAD Guide can be used as a self-assessment tool that is completed individually and then shared with the surrogate decision maker and health care provider.32 It also can be used to guide conversations with the surrogate and physician, as well as with trusted family and friends. Using this framework, family physicians can facilitate EOL planning with the patient and their surrogate that is based on the patient’s values and preferences for EOL care prior to, and in anticipation of, the patient’s loss of decisional capacity.31
Facilitate discussions that improve outcomes
Conversations about EOL care are taking on increased importance as the population ages and treatments advance. Understanding the concerns of patients and their surrogate decision makers, as well as the resources available to guide these difficult discussions ( TABLE ), will help family physicians conduct effective conversations that enhance care, reduce the burden on surrogate decision makers, and have a positive impact on many clinical outcomes.
CORRESPONDENCE
Shirley Bodi, MD, 3000 Arlington Avenue, Department of Family Medicine, Dowling Hall, Suite 2200, University of Toledo College of Medicine and Life Sciences, Toledo, OH 43614; [email protected]
1. Bergenholtz Heidi, Timm HU, Missel M. Talking about end of life in general palliative care – what’s going on? A qualitative study on end-of-life conversations in an acute care hospital in Denmark. BMC Palliat Care. 2019;18:62. doi: 10.1186/s12904-019-0448-z
2. Piers R, Albers G, Gilissen J, et al. Advance care planning in dementia: recommendations for healthcare professionals. BMC Palliat Care. 2018;17:88. doi: 10.1186/s12904-018-0332-2
3. Tunzi M, Ventres W. A reflective case study in family medicine advance care planning conversations. J Am Board Fam Med. 2019;32:108-114. doi: 10.3122/jabfm.2019.01.180198
4. Schickedanz AD, Schillinger D, Landefeld CS, et al. A clinical framework for improving the advance care planning process: start with patients’ self-identified barriers. J Am Geriatr Soc. 2009;57:31-39. doi: 10.1111/j.1532-5415.2008.02093.x
5. Williams BC, Warshaw G, Fabiny AR, et al. Medicine in the 21st century: recommended essential geriatrics competencies for internal medicine and family medicine residents. J Grad Med Ed. 2010;2:373-383. doi: 10.4300/JGME-D-10-00065.1
6. Alano G, Pekmezaris R, Tai J, et al. Factors influencing older adults to complete advance directives. Palliat Support Care. 2010;8:267-275. doi: 10.1017/S1478951510000064
7. Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med. 2011;154:336-346. doi: 10.7326/0003-4819-154-5-201103010-00008
8. Edelberg C. Advance care planning with and without an annual wellness visit. Ed Management website. June 1, 2016. Accessed November 16, 2021. ww.reliasmedia.com/articles/137829-advanced-care-planning-with-and-without-an-annual-wellness-visit
9. Centers for Medicare and Medicaid Services. Frequently asked questions about billing the physician fee schedule for advance care planning services. July 14, 2016. Accessed December 20, 2021. www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Downloads/FAQ-Advance-Care-Planning.pdf
10. World Health Organization. Palliative care fact sheet. August 5, 2020. Accessed November 16, 2021. www.who.int/news-room/fact-sheets/detail/palliative-care
11. National Institute on Aging. What are palliative care and hospice care? Reviewed May 14, 2021. Accessed December 20, 2021. www.nia.nih.gov/health/what-are-palliative-care-and-hospice-care#palliative-vs-hospice
12. Rabow MW, Dibble SL, Pantilat, SZ, et al. The comprehensive care team: a controlled trial of outpatient palliative medicine consultation. Arch Intern Med. 2004;164:83-91. doi: 10.1001/archinte.164.1.83
13. Muir JC, Daley F, Davis MS, et al. Integrating palliative care into the outpatient, private practice oncology setting. J Pain Symptom Manage. 2010;40:126-135. doi: 10.1016/j.jpainsymman.2009.12.017
14. Hui D, Kim SH, Roquemore J, et al. Impact of timing and setting of palliative care referral on quality of end-of-life care in cancer patients. Cancer. 2014;120:1743-1749. doi: 10.1002/cncr.28628
15. Leung JM, Udris EM, Uman J, e al. The effect of end-of-life discussions on perceived quality of care and health status among patients with COPD. Chest. 2012;142:128-133. doi: 10.1378/chest.11-2222
16. Davison SN. End-of-life care preferences and needs: perceptions of patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010;5:195-204. doi: 10.2215/CJN.05960809
17. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patients mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300:1665-1673. doi: 10.1001/jama.300.14.1665
18. Park E, Check DK, Yopp JM, et al. An exploratory study of end-of-life prognostic communication needs as reported by widowed fathers due to cancer. Psychooncology. 2015;24:1471-1476. doi: 10.1002/pon.3757
19. Tavares N, Jarrett N, Hunt K, et al. Palliative and end-of-life care conversations in COPD: a systematic literature review. ERJ Open Res. 2017;3:00068-2016. doi: 10.1183/23120541.00068-2016
20. Hancock K, Clayton JM, Parker SM, et al. Truth-telling in discussing prognosis in advanced life-limiting illnesses: a systematic review. Palliat Med. 2007;21:507-517. doi: 10.1177/0269216307080823
21. Parker SM, Clayton JM, Hancock K, et al. A systematic review of prognostic/end-of-life communication with adults in the advanced stages of a life-limiting illness: patient/caregiver preferences for the content, style, and timing of information. J Pain Symptom Manage. 2007;34:81-93. doi: 10.1016/j.jpainsymman.2006.09.035
22. Janssen DJA, Spruit MA, Schols JMGA, et al. A call for high-quality advance care planning in outpatients with severe COPD or chronic heart failure. Chest. 2011;139:1081-1088. doi: 10.1378/chest.10-1753
23. Houben CHM, Spruit MA, Schols JM, et al. Patient-clinician communication about end-of-life care on patients with advanced chronic organ failure during one year. J Pain Symptom Manage. 2015;49:1109-1115. doi: 10.1016/j.jpainsymman.2014.12.008
24. Brighton LJ, Bristowe K. Communication in palliative care: talking about the end of life, before the end of life. Postgrad Med J. 2016;92:466-470. doi: 10.1136/postgradmedj-2015-133368
25. VitalTalk website. Accessed December 20, 2021. vitaltalk.org
26. Rabow MQ, McPhee SJ. Beyond breaking bad news: how to help patients who suffer. Wes J Med. 1999;171:260-263. www.ncbi.nlm.nih.gov/pmc/articles/PMC1305864
27. Pfeifer M, Head B. Which critical communication skills are essential for interdisciplinary end-of-life discussions? AMA J Ethics. 2018;8:E724-E731. doi: 10.1001/amajethics.2018.724
28. Song M-K, Ward SE, Hepburn K, et al. SPIRIT advance care planning intervention in early stage dementias: an NIH stage I behavioral intervention development trial. Contemp Clin Trials. 2018;71:55-62. doi: 10.1016/j.cct.2018.06.005
29. Song M-K, Ward SE, Hepburn K, et al. Can persons with dementia meaningfully participate in advance care planning discussions? A mixed-methods study of SPIRIT. J Palliat Med. 2019;22:1410-1416. doi: 10.1089/jpm.2019.0088
30. Two-phased study of SPIRIT in mild dementia. ClinicalTrials.gov Identifier: NCT03311711. Updated August 23, 2021. Accessed December 20, 2021. clinicaltrials.gov/ct2/show/NCT03311711
31. Dassel K, Utz R, Supiano K, et al. Development of a dementia-focused end-of-life planning tool: the LEAD Guide (Life-planning in Early Alzheimer’s and Dementia). Innov Aging. 2019;3:igz024. doi: 10.1093/geroni/igz024
32. Dassel K, Supiano K, Utz R, et al. The LEAD Guide. Life-planning in Early Alzheimer’s and Dementia. 2019. Accessed December 20, 2021. utahgwep.org/resources/search-all-resources/send/10-dementia/27-the-lead-guide#:~:text=The%20LEAD%20Guide%20(Life%2DPlanning,your%20decisions%20about%20your%20care
1. Bergenholtz Heidi, Timm HU, Missel M. Talking about end of life in general palliative care – what’s going on? A qualitative study on end-of-life conversations in an acute care hospital in Denmark. BMC Palliat Care. 2019;18:62. doi: 10.1186/s12904-019-0448-z
2. Piers R, Albers G, Gilissen J, et al. Advance care planning in dementia: recommendations for healthcare professionals. BMC Palliat Care. 2018;17:88. doi: 10.1186/s12904-018-0332-2
3. Tunzi M, Ventres W. A reflective case study in family medicine advance care planning conversations. J Am Board Fam Med. 2019;32:108-114. doi: 10.3122/jabfm.2019.01.180198
4. Schickedanz AD, Schillinger D, Landefeld CS, et al. A clinical framework for improving the advance care planning process: start with patients’ self-identified barriers. J Am Geriatr Soc. 2009;57:31-39. doi: 10.1111/j.1532-5415.2008.02093.x
5. Williams BC, Warshaw G, Fabiny AR, et al. Medicine in the 21st century: recommended essential geriatrics competencies for internal medicine and family medicine residents. J Grad Med Ed. 2010;2:373-383. doi: 10.4300/JGME-D-10-00065.1
6. Alano G, Pekmezaris R, Tai J, et al. Factors influencing older adults to complete advance directives. Palliat Support Care. 2010;8:267-275. doi: 10.1017/S1478951510000064
7. Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med. 2011;154:336-346. doi: 10.7326/0003-4819-154-5-201103010-00008
8. Edelberg C. Advance care planning with and without an annual wellness visit. Ed Management website. June 1, 2016. Accessed November 16, 2021. ww.reliasmedia.com/articles/137829-advanced-care-planning-with-and-without-an-annual-wellness-visit
9. Centers for Medicare and Medicaid Services. Frequently asked questions about billing the physician fee schedule for advance care planning services. July 14, 2016. Accessed December 20, 2021. www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Downloads/FAQ-Advance-Care-Planning.pdf
10. World Health Organization. Palliative care fact sheet. August 5, 2020. Accessed November 16, 2021. www.who.int/news-room/fact-sheets/detail/palliative-care
11. National Institute on Aging. What are palliative care and hospice care? Reviewed May 14, 2021. Accessed December 20, 2021. www.nia.nih.gov/health/what-are-palliative-care-and-hospice-care#palliative-vs-hospice
12. Rabow MW, Dibble SL, Pantilat, SZ, et al. The comprehensive care team: a controlled trial of outpatient palliative medicine consultation. Arch Intern Med. 2004;164:83-91. doi: 10.1001/archinte.164.1.83
13. Muir JC, Daley F, Davis MS, et al. Integrating palliative care into the outpatient, private practice oncology setting. J Pain Symptom Manage. 2010;40:126-135. doi: 10.1016/j.jpainsymman.2009.12.017
14. Hui D, Kim SH, Roquemore J, et al. Impact of timing and setting of palliative care referral on quality of end-of-life care in cancer patients. Cancer. 2014;120:1743-1749. doi: 10.1002/cncr.28628
15. Leung JM, Udris EM, Uman J, e al. The effect of end-of-life discussions on perceived quality of care and health status among patients with COPD. Chest. 2012;142:128-133. doi: 10.1378/chest.11-2222
16. Davison SN. End-of-life care preferences and needs: perceptions of patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010;5:195-204. doi: 10.2215/CJN.05960809
17. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patients mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300:1665-1673. doi: 10.1001/jama.300.14.1665
18. Park E, Check DK, Yopp JM, et al. An exploratory study of end-of-life prognostic communication needs as reported by widowed fathers due to cancer. Psychooncology. 2015;24:1471-1476. doi: 10.1002/pon.3757
19. Tavares N, Jarrett N, Hunt K, et al. Palliative and end-of-life care conversations in COPD: a systematic literature review. ERJ Open Res. 2017;3:00068-2016. doi: 10.1183/23120541.00068-2016
20. Hancock K, Clayton JM, Parker SM, et al. Truth-telling in discussing prognosis in advanced life-limiting illnesses: a systematic review. Palliat Med. 2007;21:507-517. doi: 10.1177/0269216307080823
21. Parker SM, Clayton JM, Hancock K, et al. A systematic review of prognostic/end-of-life communication with adults in the advanced stages of a life-limiting illness: patient/caregiver preferences for the content, style, and timing of information. J Pain Symptom Manage. 2007;34:81-93. doi: 10.1016/j.jpainsymman.2006.09.035
22. Janssen DJA, Spruit MA, Schols JMGA, et al. A call for high-quality advance care planning in outpatients with severe COPD or chronic heart failure. Chest. 2011;139:1081-1088. doi: 10.1378/chest.10-1753
23. Houben CHM, Spruit MA, Schols JM, et al. Patient-clinician communication about end-of-life care on patients with advanced chronic organ failure during one year. J Pain Symptom Manage. 2015;49:1109-1115. doi: 10.1016/j.jpainsymman.2014.12.008
24. Brighton LJ, Bristowe K. Communication in palliative care: talking about the end of life, before the end of life. Postgrad Med J. 2016;92:466-470. doi: 10.1136/postgradmedj-2015-133368
25. VitalTalk website. Accessed December 20, 2021. vitaltalk.org
26. Rabow MQ, McPhee SJ. Beyond breaking bad news: how to help patients who suffer. Wes J Med. 1999;171:260-263. www.ncbi.nlm.nih.gov/pmc/articles/PMC1305864
27. Pfeifer M, Head B. Which critical communication skills are essential for interdisciplinary end-of-life discussions? AMA J Ethics. 2018;8:E724-E731. doi: 10.1001/amajethics.2018.724
28. Song M-K, Ward SE, Hepburn K, et al. SPIRIT advance care planning intervention in early stage dementias: an NIH stage I behavioral intervention development trial. Contemp Clin Trials. 2018;71:55-62. doi: 10.1016/j.cct.2018.06.005
29. Song M-K, Ward SE, Hepburn K, et al. Can persons with dementia meaningfully participate in advance care planning discussions? A mixed-methods study of SPIRIT. J Palliat Med. 2019;22:1410-1416. doi: 10.1089/jpm.2019.0088
30. Two-phased study of SPIRIT in mild dementia. ClinicalTrials.gov Identifier: NCT03311711. Updated August 23, 2021. Accessed December 20, 2021. clinicaltrials.gov/ct2/show/NCT03311711
31. Dassel K, Utz R, Supiano K, et al. Development of a dementia-focused end-of-life planning tool: the LEAD Guide (Life-planning in Early Alzheimer’s and Dementia). Innov Aging. 2019;3:igz024. doi: 10.1093/geroni/igz024
32. Dassel K, Supiano K, Utz R, et al. The LEAD Guide. Life-planning in Early Alzheimer’s and Dementia. 2019. Accessed December 20, 2021. utahgwep.org/resources/search-all-resources/send/10-dementia/27-the-lead-guide#:~:text=The%20LEAD%20Guide%20(Life%2DPlanning,your%20decisions%20about%20your%20care
PRACTICE RECOMMENDATIONS
› Improve patients’ quality of life and satisfaction with care through the successful implementation of palliative care. C
› Initiate end-of-life (EOL) discussions with patients with dementia at diagnosis, while the patient is cognizant and able to actively express their values and preferences for EOL care. C
› Engage surrogate decision makers in conversations about dementia, its trajectory, and their role in EOL care early in the process. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Geriatric guideline implementation remains unrealistic in most EDs
Many emergency departments are currently unable to provide care for geriatric patients that meets best practices and guidelines recommended by several major medical organizations, but a panel discussion in 2021 at the American Academy of Emergency Medicine’s Scientific Assembly identified three areas in which realistic improvements might be achieved.
In an article published online in the Journal of Emergency Medicine, Richard D. Shih, MD, of Florida Atlantic University, Boca Raton, and colleagues synthesized the presentation and discussion of an expert panel on the topic of the GED guidelines and the current realities of patient care.
The Geriatric Emergency Department (GED) Guidelines, published in 2014 in Annals of Emergency Medicine, were endorsed by the American College of Emergency Physicians, American Geriatrics Society, Emergency Nurses Association, and Society for Academic Emergency Medicine.
“With the substantial challenges in providing guideline-recommended care in EDs, this article will explore three high-impact GED clinical conditions to highlight guideline recommendations, challenges, and opportunities, and discuss realistically achievable expectations for non–GED-accredited institutions,” the authors wrote.
Geriatric patients and delirium
When delirium in older adults is not identified in the ED, the patient’s 6-month mortality rate significantly increases, but few EDs have delirium screening protocols, the authors said. Challenges included the time and money needed to educate staff, on top of multiple mandatory training requirements on other topics. Delirium screening in the clinical setting also requires personnel to conduct assessments, and time to document symptoms and screening results in medical records.
“Perhaps the highest priority challenge for delirium experts is to evaluate and publish effective delirium intervention strategies because current evidence is completely lacking for ED-based delirium prevention or treatment,” they said. In the meantime, developing outcome measures for quality improvement of delirium care will require institutional support as well as education.
Geriatric patients and falls
Approximately one third of community-dwelling adults older than 65 years suffer falls, but data suggest that fewer than half of these individuals report falls to their doctors. “Older adults who present to an ED after a fall have an approximately 30% greater risk of functional decline and depression at 6 months after the event,” the authors noted.
The GED guidelines call for a comprehensive approach to evaluating and managing falls in older adults, but many of these “are untested in the ED,” the authors said. The recommended protocol includes an initial assessment of fall risk, followed by, for those at low risk, tailored recommendations for education and the use of community resources. Additional recommendations for those at high risk of falls include multifactorial assessment of modifiable risk factors, including peripheral neuropathy, balance/gait assessment, and medication review.
However, this best practice workflow is beyond the resource capacity of most EDs, the authors noted. “When ED resources are insufficient to support best practices, the care should focus on educating patients and caregivers about the significance of a fall event, providing educational materials (e.g., [the Centers for Disease Control and Prevention’s] STEADI materials), and assessing safety with respect to mobility for immediate return to the home environment and follow-up with a PCP.”
Geriatric patients and polypharmacy
Polypharmacy is common among older adults by virtue of their greater number of illnesses and comorbid conditions, and polypharmacy also has been associated with more adverse drug reactions, the authors said. The AGS Beers Criteria identifies medications associated with adverse drug reactions, but it is not practical for use in a busy ED setting. Instead, the authors suggested a more practical approach of focusing on a smaller list of common medications that tend to cause the adverse events that may result in ED visits.
“Perhaps targeting patients on multiple (three or more) psychoactive medications, drugs that can cause hypotension, or hypoglycemics could not only be done quickly, but identify patients in whom deprescribing should be considered in the ED,” the authors wrote. Deprescribing is a complicated process, however, and may be more effective when done via the patient’s primary care provider or in a geriatric consultation.
The GED Guidelines highlighted the specific needs of the geriatric population in the ED, the authors said. Widespread implementation remains a challenge, but many organizations provide resources to help improve care of geriatric patients in the ED and beyond.
In particular, the Geriatric Emergency Care Applied Research Network and Geriatric Emergency Department Collaborative provide funding opportunities, updated and focused published reviews, and webinars (some including free continuing medical education) for the entire health care team, including hospital administrators, the authors said.
Article brings attention to clinical realities
“The reality is that the overwhelming majority of emergency departments in the United States, if not globally, are simply not equipped – operationally or financially – to meet the rigorous standards that are required to fulfill the goals of operating an accredited geriatric ED,” Robert D. Glatter, MD, an emergency medicine physician at Lenox Hill Hospital, New York, said in an interview.
“Drawing attention to this important gap in accreditation is critical to not only inform hospitals, health care providers and stakeholders, but the public, patients, and their families about the important work that needs to be done to better equip all EDs with the proper tools and educational approaches to more effectively care for the geriatric community,” Dr. Glatter emphasized.
“There are currently three tiers of accreditation, with level 1 being the highest,” he explained, but there are only 100 geriatric ED accreditation-certified hospitals across the United States.
“I am not surprised at all by the challenges of implementing current GED guidelines,” said Dr. Glatter. “It comes down to operational and budget considerations, which ultimately compete with many other departments and regulatory constraints in any given hospital.”
However, “the bottom line is that such guidelines are designed with patient safety in mind, making them important issues in the eyes of any hospital administrator looking to improve outcomes and reduce medicolegal risk or exposure impacting geriatric patients in the emergency department,” he noted.
Ultimately, guideline adherence “comes down to budget decisions, and where hospitals must invest their money to meet the bottom line,” said Dr. Glatter. “Making modifications to hospital infrastructure and architecture to accommodate geriatric patients may not be the top priority of hospital administrators when confronted with multiple competing interests. But, if it impacts patient safety, the decision to invest in structural and operational improvements may certainly have additional and important considerations.
“Until Medicare, or even the Joint Commission on Accreditation of Hospitals, adopts geriatric guidelines in emergency departments as a requirement for accreditation, there may not be adequate incentives in place currently to satisfy the intent of having a rigorous set of guidelines in the first place,” Dr. Glatter added.
Despite the limitations of applying the current guidelines, there are some steps hospitals can take, said Dr. Glatter. “They can institute new measures in a graded fashion, with the goal of taking the important steps to satisfy at least some components of the guidelines. Attention to details can go a long way, such as rails in bathrooms, better lighting, and treads on floors that may reduce the risk of falls in the ED itself.
“Attention to fall prevention by assessing contributors including polypharmacy, gait instability, and quality of footwear can impact risk of future ED visits. Having incentives in place by Medicare or JACO may force the hand of hospital administrators to comply with geriatric guidelines and place emphasis on compliance,” noted Dr. Glatter.
More research is needed that “looks at costs of implementing geriatric guidelines in typical community and academic EDs and how this impacts key metrics such as length of stay, effect on reimbursement per ICD-10 code, and savings, if any, realized in reduced malpractice claims related to missed diagnoses (such as delirium), injuries, (patient falls), or medical misadventures due to polypharmacy,” he said.
The article received no outside funding. The authors disclosed no relevant financial relationships. Dr. Glatter disclosed no relevant financial relationships, and serves on the advisory board of Medscape Emergency Medicine.
A version of this article first appeared on Medscape.com.
Many emergency departments are currently unable to provide care for geriatric patients that meets best practices and guidelines recommended by several major medical organizations, but a panel discussion in 2021 at the American Academy of Emergency Medicine’s Scientific Assembly identified three areas in which realistic improvements might be achieved.
In an article published online in the Journal of Emergency Medicine, Richard D. Shih, MD, of Florida Atlantic University, Boca Raton, and colleagues synthesized the presentation and discussion of an expert panel on the topic of the GED guidelines and the current realities of patient care.
The Geriatric Emergency Department (GED) Guidelines, published in 2014 in Annals of Emergency Medicine, were endorsed by the American College of Emergency Physicians, American Geriatrics Society, Emergency Nurses Association, and Society for Academic Emergency Medicine.
“With the substantial challenges in providing guideline-recommended care in EDs, this article will explore three high-impact GED clinical conditions to highlight guideline recommendations, challenges, and opportunities, and discuss realistically achievable expectations for non–GED-accredited institutions,” the authors wrote.
Geriatric patients and delirium
When delirium in older adults is not identified in the ED, the patient’s 6-month mortality rate significantly increases, but few EDs have delirium screening protocols, the authors said. Challenges included the time and money needed to educate staff, on top of multiple mandatory training requirements on other topics. Delirium screening in the clinical setting also requires personnel to conduct assessments, and time to document symptoms and screening results in medical records.
“Perhaps the highest priority challenge for delirium experts is to evaluate and publish effective delirium intervention strategies because current evidence is completely lacking for ED-based delirium prevention or treatment,” they said. In the meantime, developing outcome measures for quality improvement of delirium care will require institutional support as well as education.
Geriatric patients and falls
Approximately one third of community-dwelling adults older than 65 years suffer falls, but data suggest that fewer than half of these individuals report falls to their doctors. “Older adults who present to an ED after a fall have an approximately 30% greater risk of functional decline and depression at 6 months after the event,” the authors noted.
The GED guidelines call for a comprehensive approach to evaluating and managing falls in older adults, but many of these “are untested in the ED,” the authors said. The recommended protocol includes an initial assessment of fall risk, followed by, for those at low risk, tailored recommendations for education and the use of community resources. Additional recommendations for those at high risk of falls include multifactorial assessment of modifiable risk factors, including peripheral neuropathy, balance/gait assessment, and medication review.
However, this best practice workflow is beyond the resource capacity of most EDs, the authors noted. “When ED resources are insufficient to support best practices, the care should focus on educating patients and caregivers about the significance of a fall event, providing educational materials (e.g., [the Centers for Disease Control and Prevention’s] STEADI materials), and assessing safety with respect to mobility for immediate return to the home environment and follow-up with a PCP.”
Geriatric patients and polypharmacy
Polypharmacy is common among older adults by virtue of their greater number of illnesses and comorbid conditions, and polypharmacy also has been associated with more adverse drug reactions, the authors said. The AGS Beers Criteria identifies medications associated with adverse drug reactions, but it is not practical for use in a busy ED setting. Instead, the authors suggested a more practical approach of focusing on a smaller list of common medications that tend to cause the adverse events that may result in ED visits.
“Perhaps targeting patients on multiple (three or more) psychoactive medications, drugs that can cause hypotension, or hypoglycemics could not only be done quickly, but identify patients in whom deprescribing should be considered in the ED,” the authors wrote. Deprescribing is a complicated process, however, and may be more effective when done via the patient’s primary care provider or in a geriatric consultation.
The GED Guidelines highlighted the specific needs of the geriatric population in the ED, the authors said. Widespread implementation remains a challenge, but many organizations provide resources to help improve care of geriatric patients in the ED and beyond.
In particular, the Geriatric Emergency Care Applied Research Network and Geriatric Emergency Department Collaborative provide funding opportunities, updated and focused published reviews, and webinars (some including free continuing medical education) for the entire health care team, including hospital administrators, the authors said.
Article brings attention to clinical realities
“The reality is that the overwhelming majority of emergency departments in the United States, if not globally, are simply not equipped – operationally or financially – to meet the rigorous standards that are required to fulfill the goals of operating an accredited geriatric ED,” Robert D. Glatter, MD, an emergency medicine physician at Lenox Hill Hospital, New York, said in an interview.
“Drawing attention to this important gap in accreditation is critical to not only inform hospitals, health care providers and stakeholders, but the public, patients, and their families about the important work that needs to be done to better equip all EDs with the proper tools and educational approaches to more effectively care for the geriatric community,” Dr. Glatter emphasized.
“There are currently three tiers of accreditation, with level 1 being the highest,” he explained, but there are only 100 geriatric ED accreditation-certified hospitals across the United States.
“I am not surprised at all by the challenges of implementing current GED guidelines,” said Dr. Glatter. “It comes down to operational and budget considerations, which ultimately compete with many other departments and regulatory constraints in any given hospital.”
However, “the bottom line is that such guidelines are designed with patient safety in mind, making them important issues in the eyes of any hospital administrator looking to improve outcomes and reduce medicolegal risk or exposure impacting geriatric patients in the emergency department,” he noted.
Ultimately, guideline adherence “comes down to budget decisions, and where hospitals must invest their money to meet the bottom line,” said Dr. Glatter. “Making modifications to hospital infrastructure and architecture to accommodate geriatric patients may not be the top priority of hospital administrators when confronted with multiple competing interests. But, if it impacts patient safety, the decision to invest in structural and operational improvements may certainly have additional and important considerations.
“Until Medicare, or even the Joint Commission on Accreditation of Hospitals, adopts geriatric guidelines in emergency departments as a requirement for accreditation, there may not be adequate incentives in place currently to satisfy the intent of having a rigorous set of guidelines in the first place,” Dr. Glatter added.
Despite the limitations of applying the current guidelines, there are some steps hospitals can take, said Dr. Glatter. “They can institute new measures in a graded fashion, with the goal of taking the important steps to satisfy at least some components of the guidelines. Attention to details can go a long way, such as rails in bathrooms, better lighting, and treads on floors that may reduce the risk of falls in the ED itself.
“Attention to fall prevention by assessing contributors including polypharmacy, gait instability, and quality of footwear can impact risk of future ED visits. Having incentives in place by Medicare or JACO may force the hand of hospital administrators to comply with geriatric guidelines and place emphasis on compliance,” noted Dr. Glatter.
More research is needed that “looks at costs of implementing geriatric guidelines in typical community and academic EDs and how this impacts key metrics such as length of stay, effect on reimbursement per ICD-10 code, and savings, if any, realized in reduced malpractice claims related to missed diagnoses (such as delirium), injuries, (patient falls), or medical misadventures due to polypharmacy,” he said.
The article received no outside funding. The authors disclosed no relevant financial relationships. Dr. Glatter disclosed no relevant financial relationships, and serves on the advisory board of Medscape Emergency Medicine.
A version of this article first appeared on Medscape.com.
Many emergency departments are currently unable to provide care for geriatric patients that meets best practices and guidelines recommended by several major medical organizations, but a panel discussion in 2021 at the American Academy of Emergency Medicine’s Scientific Assembly identified three areas in which realistic improvements might be achieved.
In an article published online in the Journal of Emergency Medicine, Richard D. Shih, MD, of Florida Atlantic University, Boca Raton, and colleagues synthesized the presentation and discussion of an expert panel on the topic of the GED guidelines and the current realities of patient care.
The Geriatric Emergency Department (GED) Guidelines, published in 2014 in Annals of Emergency Medicine, were endorsed by the American College of Emergency Physicians, American Geriatrics Society, Emergency Nurses Association, and Society for Academic Emergency Medicine.
“With the substantial challenges in providing guideline-recommended care in EDs, this article will explore three high-impact GED clinical conditions to highlight guideline recommendations, challenges, and opportunities, and discuss realistically achievable expectations for non–GED-accredited institutions,” the authors wrote.
Geriatric patients and delirium
When delirium in older adults is not identified in the ED, the patient’s 6-month mortality rate significantly increases, but few EDs have delirium screening protocols, the authors said. Challenges included the time and money needed to educate staff, on top of multiple mandatory training requirements on other topics. Delirium screening in the clinical setting also requires personnel to conduct assessments, and time to document symptoms and screening results in medical records.
“Perhaps the highest priority challenge for delirium experts is to evaluate and publish effective delirium intervention strategies because current evidence is completely lacking for ED-based delirium prevention or treatment,” they said. In the meantime, developing outcome measures for quality improvement of delirium care will require institutional support as well as education.
Geriatric patients and falls
Approximately one third of community-dwelling adults older than 65 years suffer falls, but data suggest that fewer than half of these individuals report falls to their doctors. “Older adults who present to an ED after a fall have an approximately 30% greater risk of functional decline and depression at 6 months after the event,” the authors noted.
The GED guidelines call for a comprehensive approach to evaluating and managing falls in older adults, but many of these “are untested in the ED,” the authors said. The recommended protocol includes an initial assessment of fall risk, followed by, for those at low risk, tailored recommendations for education and the use of community resources. Additional recommendations for those at high risk of falls include multifactorial assessment of modifiable risk factors, including peripheral neuropathy, balance/gait assessment, and medication review.
However, this best practice workflow is beyond the resource capacity of most EDs, the authors noted. “When ED resources are insufficient to support best practices, the care should focus on educating patients and caregivers about the significance of a fall event, providing educational materials (e.g., [the Centers for Disease Control and Prevention’s] STEADI materials), and assessing safety with respect to mobility for immediate return to the home environment and follow-up with a PCP.”
Geriatric patients and polypharmacy
Polypharmacy is common among older adults by virtue of their greater number of illnesses and comorbid conditions, and polypharmacy also has been associated with more adverse drug reactions, the authors said. The AGS Beers Criteria identifies medications associated with adverse drug reactions, but it is not practical for use in a busy ED setting. Instead, the authors suggested a more practical approach of focusing on a smaller list of common medications that tend to cause the adverse events that may result in ED visits.
“Perhaps targeting patients on multiple (three or more) psychoactive medications, drugs that can cause hypotension, or hypoglycemics could not only be done quickly, but identify patients in whom deprescribing should be considered in the ED,” the authors wrote. Deprescribing is a complicated process, however, and may be more effective when done via the patient’s primary care provider or in a geriatric consultation.
The GED Guidelines highlighted the specific needs of the geriatric population in the ED, the authors said. Widespread implementation remains a challenge, but many organizations provide resources to help improve care of geriatric patients in the ED and beyond.
In particular, the Geriatric Emergency Care Applied Research Network and Geriatric Emergency Department Collaborative provide funding opportunities, updated and focused published reviews, and webinars (some including free continuing medical education) for the entire health care team, including hospital administrators, the authors said.
Article brings attention to clinical realities
“The reality is that the overwhelming majority of emergency departments in the United States, if not globally, are simply not equipped – operationally or financially – to meet the rigorous standards that are required to fulfill the goals of operating an accredited geriatric ED,” Robert D. Glatter, MD, an emergency medicine physician at Lenox Hill Hospital, New York, said in an interview.
“Drawing attention to this important gap in accreditation is critical to not only inform hospitals, health care providers and stakeholders, but the public, patients, and their families about the important work that needs to be done to better equip all EDs with the proper tools and educational approaches to more effectively care for the geriatric community,” Dr. Glatter emphasized.
“There are currently three tiers of accreditation, with level 1 being the highest,” he explained, but there are only 100 geriatric ED accreditation-certified hospitals across the United States.
“I am not surprised at all by the challenges of implementing current GED guidelines,” said Dr. Glatter. “It comes down to operational and budget considerations, which ultimately compete with many other departments and regulatory constraints in any given hospital.”
However, “the bottom line is that such guidelines are designed with patient safety in mind, making them important issues in the eyes of any hospital administrator looking to improve outcomes and reduce medicolegal risk or exposure impacting geriatric patients in the emergency department,” he noted.
Ultimately, guideline adherence “comes down to budget decisions, and where hospitals must invest their money to meet the bottom line,” said Dr. Glatter. “Making modifications to hospital infrastructure and architecture to accommodate geriatric patients may not be the top priority of hospital administrators when confronted with multiple competing interests. But, if it impacts patient safety, the decision to invest in structural and operational improvements may certainly have additional and important considerations.
“Until Medicare, or even the Joint Commission on Accreditation of Hospitals, adopts geriatric guidelines in emergency departments as a requirement for accreditation, there may not be adequate incentives in place currently to satisfy the intent of having a rigorous set of guidelines in the first place,” Dr. Glatter added.
Despite the limitations of applying the current guidelines, there are some steps hospitals can take, said Dr. Glatter. “They can institute new measures in a graded fashion, with the goal of taking the important steps to satisfy at least some components of the guidelines. Attention to details can go a long way, such as rails in bathrooms, better lighting, and treads on floors that may reduce the risk of falls in the ED itself.
“Attention to fall prevention by assessing contributors including polypharmacy, gait instability, and quality of footwear can impact risk of future ED visits. Having incentives in place by Medicare or JACO may force the hand of hospital administrators to comply with geriatric guidelines and place emphasis on compliance,” noted Dr. Glatter.
More research is needed that “looks at costs of implementing geriatric guidelines in typical community and academic EDs and how this impacts key metrics such as length of stay, effect on reimbursement per ICD-10 code, and savings, if any, realized in reduced malpractice claims related to missed diagnoses (such as delirium), injuries, (patient falls), or medical misadventures due to polypharmacy,” he said.
The article received no outside funding. The authors disclosed no relevant financial relationships. Dr. Glatter disclosed no relevant financial relationships, and serves on the advisory board of Medscape Emergency Medicine.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF EMERGENCY MEDICINE
Handle with care: Managing IBD in older patients
As the saying goes: "Age is a case of mind over matter: If you don't mind, it don't matter."
But for older patients with inflammatory bowel disease (IBD) and the clinicians who treat them, it’s hard to ignore the complications that aging can bring, such as comorbidities, functional limitations, and polypharmacy, said Nana Bernasko, CRNP, DNP, WHNP-BC, a nurse practitioner in the department of gastroenterology at Penn State Milton S. Hershey Medical Center in Hershey, Pa.
“We are seeing a large number of patients in our clinics that are being diagnosed later on in life,” she said in an oral presentation at the annual Crohn’s & Colitis Congress®, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Between 10% and 30% of all patients with IBD are older than 60, and roughly 10%-15% of patients with IBD are diagnosed after age 60, she said.
The diagnosis of IBD is often delayed in older patients as well, with an estimated 60% of patients initially given an incorrect or incomplete diagnosis that may lead to significant delays in the initiation of appropriate therapy, she said.
Differential diagnoses for IBD in older patients include diverticulitis, ischemic colitis, infectious colitis, and radiation colitis.
Bharati Kochar, MD, MS, from the Crohn’s and Colitis Center at Massachusetts General Hospital in Boston, who was not involved in the presentation, agreed that older adults need special handling.
“The management of IBD in older adults is challenging for a number of reasons, but primarily because until very recently, we have not invested in understanding how IBD should be optimally managed at older ages,” she said in an interview.
“Additionally, like in all fields, older adults with IBD are disproportionately under-represented in clinical trials, meaning that we have less rigorous data guiding the management of older adults,” she added.
Clinical presentations
Older adults tend to differ in clinical presentation, compared with younger adults, Dr. Bernasko said.
For example, among patients with Crohn’s disease, rectal bleeding is a more common symptom among older adults, whereas diarrhea and weight loss are more common among younger adults.
Disease location may also differ, with more senior adults having predominantly colonic disease (L2 according to the Montreal Classification of IBD), compared with more prevalent ileocolonic disease (L3) among their more junior counterparts. And although both generations of patients have inflammatory behavior (B1) at diagnosis, younger patients have more prevalent structuring (B2) and penetrating disease (B3), Dr. Bernasko noted.
Among patients with ulcerative colitis, rectal bleeding, abdominal pain, and extraintestinal manifestations are more common among the younger set, whereas left-sided colitis is more common among older patients. In addition, extensive ulcerative colitis (E3) is more common in younger patients, compared with older patients.
Management considerations
Dr. Kochar noted that “older adults have higher baseline risks for all adverse events – like infections, malignancies, polypharmacy, procedural complications – than younger adults, so any additional risk conferred by treatments seem amplified, but that should not mean that we should avoid effectively treating older adults. It should mean we need to invest in understanding how to best mitigate those risks.”
While younger patients are sometimes on multiple medications prior to starting on IBD therapy, polypharmacy is common among the older set, who may be taking drugs for diabetes, hypertension, prostate disease, and so on.
“There’s just so much going on in terms of their medical background to start off with, so many medications, and then we’re adding more things to it,” Dr. Bernasko said.
She echoed Dr. Kochar in noting that older patients as a subgroup are under-represented in clinical trials, making it difficult to know what treatment approaches may work best for them.
In addition, older patients are at higher risk for malignancies, and for complications from surgery.
Medication adherence in older patients is frequently compromised by memory issues, she added, noting that “I can’t tell you enough how sometimes our older patients forget to take their medications.”
Other challenges for the management of older patients with IBD included psychosocial issues, cognitive decline, and malnutrition.
Medications and adverse events
Dr. Bernasko also discussed specific medications and potential adverse events and drug interactions in older patients.
For example, aminosalicylic acids (5-ASA) are associated with higher risk for nephrotoxicity and pancreatitis in older patients and can interact with thiopurines to cause leukopenia.
Steroids are associated with elevated risk for osteopenia, myopathy, cataracts, glaucoma, diabetes, and hypertension, and can interact with thiazide and loop diuretics to cause hypokalemia.
Methotrexate use in this population is linked to pancytopenia and hepatotoxicity, and it can interact with NSAIDs and multiple antibiotics to cause decreased renal secretion.
Thiopurines in older patients are associated with increased risk for leukopenia, myelosuppression, non-Hodgkin lymphoma, skin cancer, pancreatitis, and hepatotoxicity, and drugs in this class interact with allopurinol and angiotensin-converting enzyme inhibitors to increase risk for myelosuppression. Additionally, warfarin can inhibit the efficacy of thiopurines, and when these drugs are used in combination with tumor necrosis factor (TNF)–alpha inhibitors they can further increase risk of malignancy through immunosuppression.
Cyclosporine is associated with worsening hypertension and renal insufficiency among older patients.
TNF-alpha inhibitors are associated with increased risk for tuberculosis; hepatitis B; and fungal infections, malignant lymphoma, and New York Heart Association class 3 or 4 heart failure.
Ciprofloxacin in older patients with IBD has been linked to tendinopathy and increased risk for Clostridioides difficile infections. Metronidazole increases the likelihood of peripheral neuropathy in these patients.
Colon cancer screening
“When it comes to colon cancer screening, definitely assess the risk prior to doing this,” Dr. Bernasko recommended. “Weigh all the risks and benefits. Why are we doing this for these elderly patients, because there are definitely risks associated with this.”
Older patients with IBD may have difficulty with bowel prep and are at elevated risk, compared with younger patients, for cardiopulmonary complications, perforation, adverse events from sedation, and procedural complications, she cautioned.
“When it comes to our elderly patients, you want to focus on a more personalized approach – not all older people present the same way in terms of comorbidities or medications,” Dr. Bernasko advised in her summary.
Dr. Bernasko and Dr. Kochar reported having no relevant conflicts of interest to disclose. Dr. Kochar is a member of the board of editors for GI & Hepatology News.
This article was updated 2/18/22.
As the saying goes: "Age is a case of mind over matter: If you don't mind, it don't matter."
But for older patients with inflammatory bowel disease (IBD) and the clinicians who treat them, it’s hard to ignore the complications that aging can bring, such as comorbidities, functional limitations, and polypharmacy, said Nana Bernasko, CRNP, DNP, WHNP-BC, a nurse practitioner in the department of gastroenterology at Penn State Milton S. Hershey Medical Center in Hershey, Pa.
“We are seeing a large number of patients in our clinics that are being diagnosed later on in life,” she said in an oral presentation at the annual Crohn’s & Colitis Congress®, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Between 10% and 30% of all patients with IBD are older than 60, and roughly 10%-15% of patients with IBD are diagnosed after age 60, she said.
The diagnosis of IBD is often delayed in older patients as well, with an estimated 60% of patients initially given an incorrect or incomplete diagnosis that may lead to significant delays in the initiation of appropriate therapy, she said.
Differential diagnoses for IBD in older patients include diverticulitis, ischemic colitis, infectious colitis, and radiation colitis.
Bharati Kochar, MD, MS, from the Crohn’s and Colitis Center at Massachusetts General Hospital in Boston, who was not involved in the presentation, agreed that older adults need special handling.
“The management of IBD in older adults is challenging for a number of reasons, but primarily because until very recently, we have not invested in understanding how IBD should be optimally managed at older ages,” she said in an interview.
“Additionally, like in all fields, older adults with IBD are disproportionately under-represented in clinical trials, meaning that we have less rigorous data guiding the management of older adults,” she added.
Clinical presentations
Older adults tend to differ in clinical presentation, compared with younger adults, Dr. Bernasko said.
For example, among patients with Crohn’s disease, rectal bleeding is a more common symptom among older adults, whereas diarrhea and weight loss are more common among younger adults.
Disease location may also differ, with more senior adults having predominantly colonic disease (L2 according to the Montreal Classification of IBD), compared with more prevalent ileocolonic disease (L3) among their more junior counterparts. And although both generations of patients have inflammatory behavior (B1) at diagnosis, younger patients have more prevalent structuring (B2) and penetrating disease (B3), Dr. Bernasko noted.
Among patients with ulcerative colitis, rectal bleeding, abdominal pain, and extraintestinal manifestations are more common among the younger set, whereas left-sided colitis is more common among older patients. In addition, extensive ulcerative colitis (E3) is more common in younger patients, compared with older patients.
Management considerations
Dr. Kochar noted that “older adults have higher baseline risks for all adverse events – like infections, malignancies, polypharmacy, procedural complications – than younger adults, so any additional risk conferred by treatments seem amplified, but that should not mean that we should avoid effectively treating older adults. It should mean we need to invest in understanding how to best mitigate those risks.”
While younger patients are sometimes on multiple medications prior to starting on IBD therapy, polypharmacy is common among the older set, who may be taking drugs for diabetes, hypertension, prostate disease, and so on.
“There’s just so much going on in terms of their medical background to start off with, so many medications, and then we’re adding more things to it,” Dr. Bernasko said.
She echoed Dr. Kochar in noting that older patients as a subgroup are under-represented in clinical trials, making it difficult to know what treatment approaches may work best for them.
In addition, older patients are at higher risk for malignancies, and for complications from surgery.
Medication adherence in older patients is frequently compromised by memory issues, she added, noting that “I can’t tell you enough how sometimes our older patients forget to take their medications.”
Other challenges for the management of older patients with IBD included psychosocial issues, cognitive decline, and malnutrition.
Medications and adverse events
Dr. Bernasko also discussed specific medications and potential adverse events and drug interactions in older patients.
For example, aminosalicylic acids (5-ASA) are associated with higher risk for nephrotoxicity and pancreatitis in older patients and can interact with thiopurines to cause leukopenia.
Steroids are associated with elevated risk for osteopenia, myopathy, cataracts, glaucoma, diabetes, and hypertension, and can interact with thiazide and loop diuretics to cause hypokalemia.
Methotrexate use in this population is linked to pancytopenia and hepatotoxicity, and it can interact with NSAIDs and multiple antibiotics to cause decreased renal secretion.
Thiopurines in older patients are associated with increased risk for leukopenia, myelosuppression, non-Hodgkin lymphoma, skin cancer, pancreatitis, and hepatotoxicity, and drugs in this class interact with allopurinol and angiotensin-converting enzyme inhibitors to increase risk for myelosuppression. Additionally, warfarin can inhibit the efficacy of thiopurines, and when these drugs are used in combination with tumor necrosis factor (TNF)–alpha inhibitors they can further increase risk of malignancy through immunosuppression.
Cyclosporine is associated with worsening hypertension and renal insufficiency among older patients.
TNF-alpha inhibitors are associated with increased risk for tuberculosis; hepatitis B; and fungal infections, malignant lymphoma, and New York Heart Association class 3 or 4 heart failure.
Ciprofloxacin in older patients with IBD has been linked to tendinopathy and increased risk for Clostridioides difficile infections. Metronidazole increases the likelihood of peripheral neuropathy in these patients.
Colon cancer screening
“When it comes to colon cancer screening, definitely assess the risk prior to doing this,” Dr. Bernasko recommended. “Weigh all the risks and benefits. Why are we doing this for these elderly patients, because there are definitely risks associated with this.”
Older patients with IBD may have difficulty with bowel prep and are at elevated risk, compared with younger patients, for cardiopulmonary complications, perforation, adverse events from sedation, and procedural complications, she cautioned.
“When it comes to our elderly patients, you want to focus on a more personalized approach – not all older people present the same way in terms of comorbidities or medications,” Dr. Bernasko advised in her summary.
Dr. Bernasko and Dr. Kochar reported having no relevant conflicts of interest to disclose. Dr. Kochar is a member of the board of editors for GI & Hepatology News.
This article was updated 2/18/22.
As the saying goes: "Age is a case of mind over matter: If you don't mind, it don't matter."
But for older patients with inflammatory bowel disease (IBD) and the clinicians who treat them, it’s hard to ignore the complications that aging can bring, such as comorbidities, functional limitations, and polypharmacy, said Nana Bernasko, CRNP, DNP, WHNP-BC, a nurse practitioner in the department of gastroenterology at Penn State Milton S. Hershey Medical Center in Hershey, Pa.
“We are seeing a large number of patients in our clinics that are being diagnosed later on in life,” she said in an oral presentation at the annual Crohn’s & Colitis Congress®, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Between 10% and 30% of all patients with IBD are older than 60, and roughly 10%-15% of patients with IBD are diagnosed after age 60, she said.
The diagnosis of IBD is often delayed in older patients as well, with an estimated 60% of patients initially given an incorrect or incomplete diagnosis that may lead to significant delays in the initiation of appropriate therapy, she said.
Differential diagnoses for IBD in older patients include diverticulitis, ischemic colitis, infectious colitis, and radiation colitis.
Bharati Kochar, MD, MS, from the Crohn’s and Colitis Center at Massachusetts General Hospital in Boston, who was not involved in the presentation, agreed that older adults need special handling.
“The management of IBD in older adults is challenging for a number of reasons, but primarily because until very recently, we have not invested in understanding how IBD should be optimally managed at older ages,” she said in an interview.
“Additionally, like in all fields, older adults with IBD are disproportionately under-represented in clinical trials, meaning that we have less rigorous data guiding the management of older adults,” she added.
Clinical presentations
Older adults tend to differ in clinical presentation, compared with younger adults, Dr. Bernasko said.
For example, among patients with Crohn’s disease, rectal bleeding is a more common symptom among older adults, whereas diarrhea and weight loss are more common among younger adults.
Disease location may also differ, with more senior adults having predominantly colonic disease (L2 according to the Montreal Classification of IBD), compared with more prevalent ileocolonic disease (L3) among their more junior counterparts. And although both generations of patients have inflammatory behavior (B1) at diagnosis, younger patients have more prevalent structuring (B2) and penetrating disease (B3), Dr. Bernasko noted.
Among patients with ulcerative colitis, rectal bleeding, abdominal pain, and extraintestinal manifestations are more common among the younger set, whereas left-sided colitis is more common among older patients. In addition, extensive ulcerative colitis (E3) is more common in younger patients, compared with older patients.
Management considerations
Dr. Kochar noted that “older adults have higher baseline risks for all adverse events – like infections, malignancies, polypharmacy, procedural complications – than younger adults, so any additional risk conferred by treatments seem amplified, but that should not mean that we should avoid effectively treating older adults. It should mean we need to invest in understanding how to best mitigate those risks.”
While younger patients are sometimes on multiple medications prior to starting on IBD therapy, polypharmacy is common among the older set, who may be taking drugs for diabetes, hypertension, prostate disease, and so on.
“There’s just so much going on in terms of their medical background to start off with, so many medications, and then we’re adding more things to it,” Dr. Bernasko said.
She echoed Dr. Kochar in noting that older patients as a subgroup are under-represented in clinical trials, making it difficult to know what treatment approaches may work best for them.
In addition, older patients are at higher risk for malignancies, and for complications from surgery.
Medication adherence in older patients is frequently compromised by memory issues, she added, noting that “I can’t tell you enough how sometimes our older patients forget to take their medications.”
Other challenges for the management of older patients with IBD included psychosocial issues, cognitive decline, and malnutrition.
Medications and adverse events
Dr. Bernasko also discussed specific medications and potential adverse events and drug interactions in older patients.
For example, aminosalicylic acids (5-ASA) are associated with higher risk for nephrotoxicity and pancreatitis in older patients and can interact with thiopurines to cause leukopenia.
Steroids are associated with elevated risk for osteopenia, myopathy, cataracts, glaucoma, diabetes, and hypertension, and can interact with thiazide and loop diuretics to cause hypokalemia.
Methotrexate use in this population is linked to pancytopenia and hepatotoxicity, and it can interact with NSAIDs and multiple antibiotics to cause decreased renal secretion.
Thiopurines in older patients are associated with increased risk for leukopenia, myelosuppression, non-Hodgkin lymphoma, skin cancer, pancreatitis, and hepatotoxicity, and drugs in this class interact with allopurinol and angiotensin-converting enzyme inhibitors to increase risk for myelosuppression. Additionally, warfarin can inhibit the efficacy of thiopurines, and when these drugs are used in combination with tumor necrosis factor (TNF)–alpha inhibitors they can further increase risk of malignancy through immunosuppression.
Cyclosporine is associated with worsening hypertension and renal insufficiency among older patients.
TNF-alpha inhibitors are associated with increased risk for tuberculosis; hepatitis B; and fungal infections, malignant lymphoma, and New York Heart Association class 3 or 4 heart failure.
Ciprofloxacin in older patients with IBD has been linked to tendinopathy and increased risk for Clostridioides difficile infections. Metronidazole increases the likelihood of peripheral neuropathy in these patients.
Colon cancer screening
“When it comes to colon cancer screening, definitely assess the risk prior to doing this,” Dr. Bernasko recommended. “Weigh all the risks and benefits. Why are we doing this for these elderly patients, because there are definitely risks associated with this.”
Older patients with IBD may have difficulty with bowel prep and are at elevated risk, compared with younger patients, for cardiopulmonary complications, perforation, adverse events from sedation, and procedural complications, she cautioned.
“When it comes to our elderly patients, you want to focus on a more personalized approach – not all older people present the same way in terms of comorbidities or medications,” Dr. Bernasko advised in her summary.
Dr. Bernasko and Dr. Kochar reported having no relevant conflicts of interest to disclose. Dr. Kochar is a member of the board of editors for GI & Hepatology News.
This article was updated 2/18/22.
FROM CROHN’S & COLITIS CONGRESS






