User login
AI flagged skin cancer with near-perfect accuracy, in UK study
. AI detected more than 99% of all skin cancers.
The researchers tested the AI by integrating it into a clinical diagnosis process – anticipating a future in which AI helps doctors catch skin cancer faster and triage patients.
Skin cancer is the most common cancer in the United States; one in five 5 Americans develop skin cancer by age 70. With melanoma, the deadliest skin cancer, the 5-year survival rate is better than 99% if caught early, though only about three-quarters of melanomas are caught at this stage.
Amid rising skin cancer rates come concerns that the number of dermatologists in the workforce isn’t keeping pace. That may be why the average wait time for a dermatology appointment is trending up – in 2022, it reached 34.5 days.
The study, which was presented at the European Academy of Dermatology and Venereology Congress recently and has not yet been published, involved 6,900 patients in the United Kingdom with suspected skin cancer. The patients had been referred by their primary care physicians. The researchers took images of the suspicious areas and uploaded them to the AI software. The AI’s assessment was then shared with a dermatologist.
“Note that the diagnosis issued by the AI was not hidden from the dermatologist doing the second assessment,” said lead researcher Kashini Andrew, MBBS, a dermatologist and specialist registrar at University Hospitals Birmingham NHS Foundation Trust.
Dr. Andrew acknowledged that this may have influenced the dermatologist’s opinion. But that’s the vision of how doctors could use this tool.
The AI caught 59 of 59 melanomas and 189 of 190 total skin cancers (99.5%). (The one case that the AI missed was caught by the dermatologist.) It also flagged 541 of 585 precancerous lesions (92.5%). This represented a big improvement from a 2021 version of the model, which detected 86% of melanomas, 84% of all skin cancers, and 54% of precancerous lesions.
Over the 10-month period of the study, the system saved more than 1,000 face-to-face consultations, freeing dermatologists’ time to catch more cancers and serve more patients.
Limitations
The patients in the study were from “one hospital in a single region of the UK,” and the sample was not large enough to allow broad statements to be made about the use of AI in dermatology, Dr. Andrew said.
But it can open the conversation. Roxana Daneshjou, MD, PhD, a dermatologist at Stanford (Calif.) University who has studied the pros and cons of AI in medicine, had some concerns. For one thing, doctors can gather more in-depth information during an in-person exam than AI can glean from a photo, Dr. Daneshjou noted. They can examine skin texture, gather patient history, and take photos with special lighting and magnification.
And the AI needs to get better at ruling out malignancy, Dr. Daneshjou said. In this study, the AI identified 75% of benign lesions, a decline from the earlier version. The researchers noted in the abstract that this is a potential trade-off for increased sensitivity.
“[Unnecessary] biopsies can clog up the health care system, cost money, and cause stress and scarring,” said Dr. Daneshjou. “You don’t want to increase the burden of that.”
Still, if AI software such as the kind used in the study proves just as accurate in larger, more diverse sample sizes, then it could be a powerful tool for triage, Dr. Daneshjou said. “If AI gets particularly good at finding malignancy and also ruling it out, that would be a win.”
A version of this article appeared on Medscape.com.
. AI detected more than 99% of all skin cancers.
The researchers tested the AI by integrating it into a clinical diagnosis process – anticipating a future in which AI helps doctors catch skin cancer faster and triage patients.
Skin cancer is the most common cancer in the United States; one in five 5 Americans develop skin cancer by age 70. With melanoma, the deadliest skin cancer, the 5-year survival rate is better than 99% if caught early, though only about three-quarters of melanomas are caught at this stage.
Amid rising skin cancer rates come concerns that the number of dermatologists in the workforce isn’t keeping pace. That may be why the average wait time for a dermatology appointment is trending up – in 2022, it reached 34.5 days.
The study, which was presented at the European Academy of Dermatology and Venereology Congress recently and has not yet been published, involved 6,900 patients in the United Kingdom with suspected skin cancer. The patients had been referred by their primary care physicians. The researchers took images of the suspicious areas and uploaded them to the AI software. The AI’s assessment was then shared with a dermatologist.
“Note that the diagnosis issued by the AI was not hidden from the dermatologist doing the second assessment,” said lead researcher Kashini Andrew, MBBS, a dermatologist and specialist registrar at University Hospitals Birmingham NHS Foundation Trust.
Dr. Andrew acknowledged that this may have influenced the dermatologist’s opinion. But that’s the vision of how doctors could use this tool.
The AI caught 59 of 59 melanomas and 189 of 190 total skin cancers (99.5%). (The one case that the AI missed was caught by the dermatologist.) It also flagged 541 of 585 precancerous lesions (92.5%). This represented a big improvement from a 2021 version of the model, which detected 86% of melanomas, 84% of all skin cancers, and 54% of precancerous lesions.
Over the 10-month period of the study, the system saved more than 1,000 face-to-face consultations, freeing dermatologists’ time to catch more cancers and serve more patients.
Limitations
The patients in the study were from “one hospital in a single region of the UK,” and the sample was not large enough to allow broad statements to be made about the use of AI in dermatology, Dr. Andrew said.
But it can open the conversation. Roxana Daneshjou, MD, PhD, a dermatologist at Stanford (Calif.) University who has studied the pros and cons of AI in medicine, had some concerns. For one thing, doctors can gather more in-depth information during an in-person exam than AI can glean from a photo, Dr. Daneshjou noted. They can examine skin texture, gather patient history, and take photos with special lighting and magnification.
And the AI needs to get better at ruling out malignancy, Dr. Daneshjou said. In this study, the AI identified 75% of benign lesions, a decline from the earlier version. The researchers noted in the abstract that this is a potential trade-off for increased sensitivity.
“[Unnecessary] biopsies can clog up the health care system, cost money, and cause stress and scarring,” said Dr. Daneshjou. “You don’t want to increase the burden of that.”
Still, if AI software such as the kind used in the study proves just as accurate in larger, more diverse sample sizes, then it could be a powerful tool for triage, Dr. Daneshjou said. “If AI gets particularly good at finding malignancy and also ruling it out, that would be a win.”
A version of this article appeared on Medscape.com.
. AI detected more than 99% of all skin cancers.
The researchers tested the AI by integrating it into a clinical diagnosis process – anticipating a future in which AI helps doctors catch skin cancer faster and triage patients.
Skin cancer is the most common cancer in the United States; one in five 5 Americans develop skin cancer by age 70. With melanoma, the deadliest skin cancer, the 5-year survival rate is better than 99% if caught early, though only about three-quarters of melanomas are caught at this stage.
Amid rising skin cancer rates come concerns that the number of dermatologists in the workforce isn’t keeping pace. That may be why the average wait time for a dermatology appointment is trending up – in 2022, it reached 34.5 days.
The study, which was presented at the European Academy of Dermatology and Venereology Congress recently and has not yet been published, involved 6,900 patients in the United Kingdom with suspected skin cancer. The patients had been referred by their primary care physicians. The researchers took images of the suspicious areas and uploaded them to the AI software. The AI’s assessment was then shared with a dermatologist.
“Note that the diagnosis issued by the AI was not hidden from the dermatologist doing the second assessment,” said lead researcher Kashini Andrew, MBBS, a dermatologist and specialist registrar at University Hospitals Birmingham NHS Foundation Trust.
Dr. Andrew acknowledged that this may have influenced the dermatologist’s opinion. But that’s the vision of how doctors could use this tool.
The AI caught 59 of 59 melanomas and 189 of 190 total skin cancers (99.5%). (The one case that the AI missed was caught by the dermatologist.) It also flagged 541 of 585 precancerous lesions (92.5%). This represented a big improvement from a 2021 version of the model, which detected 86% of melanomas, 84% of all skin cancers, and 54% of precancerous lesions.
Over the 10-month period of the study, the system saved more than 1,000 face-to-face consultations, freeing dermatologists’ time to catch more cancers and serve more patients.
Limitations
The patients in the study were from “one hospital in a single region of the UK,” and the sample was not large enough to allow broad statements to be made about the use of AI in dermatology, Dr. Andrew said.
But it can open the conversation. Roxana Daneshjou, MD, PhD, a dermatologist at Stanford (Calif.) University who has studied the pros and cons of AI in medicine, had some concerns. For one thing, doctors can gather more in-depth information during an in-person exam than AI can glean from a photo, Dr. Daneshjou noted. They can examine skin texture, gather patient history, and take photos with special lighting and magnification.
And the AI needs to get better at ruling out malignancy, Dr. Daneshjou said. In this study, the AI identified 75% of benign lesions, a decline from the earlier version. The researchers noted in the abstract that this is a potential trade-off for increased sensitivity.
“[Unnecessary] biopsies can clog up the health care system, cost money, and cause stress and scarring,” said Dr. Daneshjou. “You don’t want to increase the burden of that.”
Still, if AI software such as the kind used in the study proves just as accurate in larger, more diverse sample sizes, then it could be a powerful tool for triage, Dr. Daneshjou said. “If AI gets particularly good at finding malignancy and also ruling it out, that would be a win.”
A version of this article appeared on Medscape.com.
FROM THE EADV CONGRESS
Skin in the Game: Inadequate Photoprotection Among Olympic Athletes
The XXXIII Olympic Summer Games will take place in Paris, France, from July 26 to August 11, 2024, and a variety of outdoor sporting events (eg, surfing, cycling, beach volleyball) will be included. Participation in the Olympic Games is a distinct honor for athletes selected to compete at the highest level in their sports.
Because of their training regimens and lifestyles, Olympic athletes face unique health risks. One such risk appears to be skin cancer, a substantial contributor to the global burden of disease. Taken together, basal cell carcinoma, squamous cell carcinoma, and melanoma account for 6.7 million cases of skin cancer worldwide. Squamous cell carcinoma and malignant skin melanoma were attributed to 1.2 million and 1.7 million life-years lost to disability, respectively.1
Olympic athletes are at increased risk for sunburn from UVA and UVB radiation, placing them at higher risk for both melanoma and nonmelanoma skin cancers.2,3 Sweating increases skin photosensitivity, sportswear often offers inadequate sun protection, and sustained high-intensity exercise itself has an immunosuppressive effect. Athletes competing in skiing and snowboarding events also receive radiation reflected off snow and ice at high altitudes.3 In fact, skiing without sunscreen at 11,000-feet above sea level can induce sunburn after only 6 minutes of exposure.4 Moreover, sweat, water immersion, and friction can decrease the effectiveness of topical sunscreens.5
World-class athletes appear to be exposed to UV radiation to a substantially higher degree than the general public. In an analysis of 144 events at the 2020 XXXII Olympic Summer Games in Tokyo, Japan, the highest exposure assessments were for women’s tennis, men’s golf, and men’s road cycling.6 In a 2020 study (N=240), the rates of sunburn were as high as 76.7% among Olympic sailors, elite surfers, and windsurfers, with more than one-quarter of athletes reporting sunburn that lasted longer than 24 hours.7 An earlier study reported that professional cyclists were exposed to UV radiation during a single race that exceeded the personal exposure limit by 30 times.8
Regrettably, the high level of sun exposure experienced by elite athletes is compounded by their low rate of sunscreen use. In a 2020 survey of 95 Olympians and super sprint triathletes, approximately half rarely used sunscreen, with 1 in 5 athletes never using sunscreen during training.9 In another study of 246 elite athletes in surfing, windsurfing, and sailing, nearly half used inadequate sun protection and nearly one-quarter reported never using sunscreen.10 Surprisingly, as many as 90% of Olympic athletes and super sprint competitors understood the importance of using sunscreen.9
What can we learn from these findings?
First, elite athletes remain at high risk for skin cancer because of training regimens, occupational environmental hazards, and other requirements of their sport. Second, despite awareness of the risks of UV radiation exposure, Olympic athletes utilize inadequate photoprotection. Athletes with darker skin are still at risk for skin cancer, photoaging, and pigmentation disorders—indicating a need for photoprotective behaviors in athletes of all skin types.11
Therefore, efforts to promote adequate sunscreen use and understanding of the consequences of UV radiation may need to be prioritized earlier in athletes’ careers and implemented according to evidence-based guidelines. For example, the Stanford University Network for Sun Protection, Outreach, Research and Teamwork (Sunsport) provided information about skin cancer risk and prevention by educating student-athletes, coaches, and trainers in the National Collegiate Athletic Association in the United States. The Sunsport initiative led to a dramatic increase in sunscreen use by student-athletes as well as increased knowledge and discussion of skin cancer risk.12
- Zhang W, Zeng W, Jiang A, et al. Global, regional and national incidence, mortality and disability-adjusted life-years of skin cancers and trend analysis from 1990 to 2019: an analysis of the Global Burden of Disease Study 2019. Cancer Med. 2021;10:4905-4922. doi:10.1002/cam4.4046
- De Luca JF, Adams BB, Yosipovitch G. Skin manifestations of athletes competing in the summer Olympics: what a sports medicine physician should know. Sports Med. 2012;42:399-413. doi:10.2165/11599050-000000000-00000
- Moehrle M. Outdoor sports and skin cancer. Clin Dermatol. 2008;26:12-15. doi:10.1016/j.clindermatol.2007.10.001
- Rigel DS, Rigel EG, Rigel AC. Effects of altitude and latitude on ambient UVB radiation. J Am Acad Dermatol. 1999;40:114-116. doi:10.1016/s0190-9622(99)70542-6
- Harrison SC, Bergfeld WF. Ultraviolet light and skin cancer in athletes. Sports Health. 2009;1:335-340. doi:10.1177/19417381093338923
- Downs NJ, Axelsen T, Schouten P, et al. Biologically effective solar ultraviolet exposures and the potential skin cancer risk for individual gold medalists of the 2020 Tokyo Summer Olympic Games. Temperature (Austin). 2019;7:89-108. doi:10.1080/23328940.2019.1581427
- De Castro-Maqueda G, Gutierrez-Manzanedo JV, Ponce-González JG, et al. Sun protection habits and sunburn in elite aquatics athletes: surfers, windsurfers and Olympic sailors. J Cancer Educ. 2020;35:312-320. doi:10.1007/s13187-018-1466-x
- Moehrle M, Heinrich L, Schmid A, et al. Extreme UV exposure of professional cyclists. Dermatology. 2000;201:44-45. doi:10.1159/000018428
- Buljan M, Kolic´ M, Šitum M, et al. Do athletes practicing outdoors know and care enough about the importance of photoprotection? Acta Dermatovenerol Croat. 2020;28:41-42.
- De Castro-Maqueda G, Gutierrez-Manzanedo JV, Lagares-Franco C. Sun exposure during water sports: do elite athletes adequately protect their skin against skin cancer? Int J Environ Res Public Health. 2021;18:800. doi:10.3390/ijerph18020800
- Tsai J, Chien AL. Photoprotection for skin of color. Am J Clin Dermatol. 2022;23:195-205. doi:10.1007/s40257-021-00670-z
- Ally MS, Swetter SM, Hirotsu KE, et al. Promoting sunscreen use and sun-protective practices in NCAA athletes: impact of SUNSPORT educational intervention for student-athletes, athletic trainers, and coaches. J Am Acad Dermatol. 2018;78:289-292.e2. doi:10.1016/j.jaad.2017.08.050
The XXXIII Olympic Summer Games will take place in Paris, France, from July 26 to August 11, 2024, and a variety of outdoor sporting events (eg, surfing, cycling, beach volleyball) will be included. Participation in the Olympic Games is a distinct honor for athletes selected to compete at the highest level in their sports.
Because of their training regimens and lifestyles, Olympic athletes face unique health risks. One such risk appears to be skin cancer, a substantial contributor to the global burden of disease. Taken together, basal cell carcinoma, squamous cell carcinoma, and melanoma account for 6.7 million cases of skin cancer worldwide. Squamous cell carcinoma and malignant skin melanoma were attributed to 1.2 million and 1.7 million life-years lost to disability, respectively.1
Olympic athletes are at increased risk for sunburn from UVA and UVB radiation, placing them at higher risk for both melanoma and nonmelanoma skin cancers.2,3 Sweating increases skin photosensitivity, sportswear often offers inadequate sun protection, and sustained high-intensity exercise itself has an immunosuppressive effect. Athletes competing in skiing and snowboarding events also receive radiation reflected off snow and ice at high altitudes.3 In fact, skiing without sunscreen at 11,000-feet above sea level can induce sunburn after only 6 minutes of exposure.4 Moreover, sweat, water immersion, and friction can decrease the effectiveness of topical sunscreens.5
World-class athletes appear to be exposed to UV radiation to a substantially higher degree than the general public. In an analysis of 144 events at the 2020 XXXII Olympic Summer Games in Tokyo, Japan, the highest exposure assessments were for women’s tennis, men’s golf, and men’s road cycling.6 In a 2020 study (N=240), the rates of sunburn were as high as 76.7% among Olympic sailors, elite surfers, and windsurfers, with more than one-quarter of athletes reporting sunburn that lasted longer than 24 hours.7 An earlier study reported that professional cyclists were exposed to UV radiation during a single race that exceeded the personal exposure limit by 30 times.8
Regrettably, the high level of sun exposure experienced by elite athletes is compounded by their low rate of sunscreen use. In a 2020 survey of 95 Olympians and super sprint triathletes, approximately half rarely used sunscreen, with 1 in 5 athletes never using sunscreen during training.9 In another study of 246 elite athletes in surfing, windsurfing, and sailing, nearly half used inadequate sun protection and nearly one-quarter reported never using sunscreen.10 Surprisingly, as many as 90% of Olympic athletes and super sprint competitors understood the importance of using sunscreen.9
What can we learn from these findings?
First, elite athletes remain at high risk for skin cancer because of training regimens, occupational environmental hazards, and other requirements of their sport. Second, despite awareness of the risks of UV radiation exposure, Olympic athletes utilize inadequate photoprotection. Athletes with darker skin are still at risk for skin cancer, photoaging, and pigmentation disorders—indicating a need for photoprotective behaviors in athletes of all skin types.11
Therefore, efforts to promote adequate sunscreen use and understanding of the consequences of UV radiation may need to be prioritized earlier in athletes’ careers and implemented according to evidence-based guidelines. For example, the Stanford University Network for Sun Protection, Outreach, Research and Teamwork (Sunsport) provided information about skin cancer risk and prevention by educating student-athletes, coaches, and trainers in the National Collegiate Athletic Association in the United States. The Sunsport initiative led to a dramatic increase in sunscreen use by student-athletes as well as increased knowledge and discussion of skin cancer risk.12
The XXXIII Olympic Summer Games will take place in Paris, France, from July 26 to August 11, 2024, and a variety of outdoor sporting events (eg, surfing, cycling, beach volleyball) will be included. Participation in the Olympic Games is a distinct honor for athletes selected to compete at the highest level in their sports.
Because of their training regimens and lifestyles, Olympic athletes face unique health risks. One such risk appears to be skin cancer, a substantial contributor to the global burden of disease. Taken together, basal cell carcinoma, squamous cell carcinoma, and melanoma account for 6.7 million cases of skin cancer worldwide. Squamous cell carcinoma and malignant skin melanoma were attributed to 1.2 million and 1.7 million life-years lost to disability, respectively.1
Olympic athletes are at increased risk for sunburn from UVA and UVB radiation, placing them at higher risk for both melanoma and nonmelanoma skin cancers.2,3 Sweating increases skin photosensitivity, sportswear often offers inadequate sun protection, and sustained high-intensity exercise itself has an immunosuppressive effect. Athletes competing in skiing and snowboarding events also receive radiation reflected off snow and ice at high altitudes.3 In fact, skiing without sunscreen at 11,000-feet above sea level can induce sunburn after only 6 minutes of exposure.4 Moreover, sweat, water immersion, and friction can decrease the effectiveness of topical sunscreens.5
World-class athletes appear to be exposed to UV radiation to a substantially higher degree than the general public. In an analysis of 144 events at the 2020 XXXII Olympic Summer Games in Tokyo, Japan, the highest exposure assessments were for women’s tennis, men’s golf, and men’s road cycling.6 In a 2020 study (N=240), the rates of sunburn were as high as 76.7% among Olympic sailors, elite surfers, and windsurfers, with more than one-quarter of athletes reporting sunburn that lasted longer than 24 hours.7 An earlier study reported that professional cyclists were exposed to UV radiation during a single race that exceeded the personal exposure limit by 30 times.8
Regrettably, the high level of sun exposure experienced by elite athletes is compounded by their low rate of sunscreen use. In a 2020 survey of 95 Olympians and super sprint triathletes, approximately half rarely used sunscreen, with 1 in 5 athletes never using sunscreen during training.9 In another study of 246 elite athletes in surfing, windsurfing, and sailing, nearly half used inadequate sun protection and nearly one-quarter reported never using sunscreen.10 Surprisingly, as many as 90% of Olympic athletes and super sprint competitors understood the importance of using sunscreen.9
What can we learn from these findings?
First, elite athletes remain at high risk for skin cancer because of training regimens, occupational environmental hazards, and other requirements of their sport. Second, despite awareness of the risks of UV radiation exposure, Olympic athletes utilize inadequate photoprotection. Athletes with darker skin are still at risk for skin cancer, photoaging, and pigmentation disorders—indicating a need for photoprotective behaviors in athletes of all skin types.11
Therefore, efforts to promote adequate sunscreen use and understanding of the consequences of UV radiation may need to be prioritized earlier in athletes’ careers and implemented according to evidence-based guidelines. For example, the Stanford University Network for Sun Protection, Outreach, Research and Teamwork (Sunsport) provided information about skin cancer risk and prevention by educating student-athletes, coaches, and trainers in the National Collegiate Athletic Association in the United States. The Sunsport initiative led to a dramatic increase in sunscreen use by student-athletes as well as increased knowledge and discussion of skin cancer risk.12
- Zhang W, Zeng W, Jiang A, et al. Global, regional and national incidence, mortality and disability-adjusted life-years of skin cancers and trend analysis from 1990 to 2019: an analysis of the Global Burden of Disease Study 2019. Cancer Med. 2021;10:4905-4922. doi:10.1002/cam4.4046
- De Luca JF, Adams BB, Yosipovitch G. Skin manifestations of athletes competing in the summer Olympics: what a sports medicine physician should know. Sports Med. 2012;42:399-413. doi:10.2165/11599050-000000000-00000
- Moehrle M. Outdoor sports and skin cancer. Clin Dermatol. 2008;26:12-15. doi:10.1016/j.clindermatol.2007.10.001
- Rigel DS, Rigel EG, Rigel AC. Effects of altitude and latitude on ambient UVB radiation. J Am Acad Dermatol. 1999;40:114-116. doi:10.1016/s0190-9622(99)70542-6
- Harrison SC, Bergfeld WF. Ultraviolet light and skin cancer in athletes. Sports Health. 2009;1:335-340. doi:10.1177/19417381093338923
- Downs NJ, Axelsen T, Schouten P, et al. Biologically effective solar ultraviolet exposures and the potential skin cancer risk for individual gold medalists of the 2020 Tokyo Summer Olympic Games. Temperature (Austin). 2019;7:89-108. doi:10.1080/23328940.2019.1581427
- De Castro-Maqueda G, Gutierrez-Manzanedo JV, Ponce-González JG, et al. Sun protection habits and sunburn in elite aquatics athletes: surfers, windsurfers and Olympic sailors. J Cancer Educ. 2020;35:312-320. doi:10.1007/s13187-018-1466-x
- Moehrle M, Heinrich L, Schmid A, et al. Extreme UV exposure of professional cyclists. Dermatology. 2000;201:44-45. doi:10.1159/000018428
- Buljan M, Kolic´ M, Šitum M, et al. Do athletes practicing outdoors know and care enough about the importance of photoprotection? Acta Dermatovenerol Croat. 2020;28:41-42.
- De Castro-Maqueda G, Gutierrez-Manzanedo JV, Lagares-Franco C. Sun exposure during water sports: do elite athletes adequately protect their skin against skin cancer? Int J Environ Res Public Health. 2021;18:800. doi:10.3390/ijerph18020800
- Tsai J, Chien AL. Photoprotection for skin of color. Am J Clin Dermatol. 2022;23:195-205. doi:10.1007/s40257-021-00670-z
- Ally MS, Swetter SM, Hirotsu KE, et al. Promoting sunscreen use and sun-protective practices in NCAA athletes: impact of SUNSPORT educational intervention for student-athletes, athletic trainers, and coaches. J Am Acad Dermatol. 2018;78:289-292.e2. doi:10.1016/j.jaad.2017.08.050
- Zhang W, Zeng W, Jiang A, et al. Global, regional and national incidence, mortality and disability-adjusted life-years of skin cancers and trend analysis from 1990 to 2019: an analysis of the Global Burden of Disease Study 2019. Cancer Med. 2021;10:4905-4922. doi:10.1002/cam4.4046
- De Luca JF, Adams BB, Yosipovitch G. Skin manifestations of athletes competing in the summer Olympics: what a sports medicine physician should know. Sports Med. 2012;42:399-413. doi:10.2165/11599050-000000000-00000
- Moehrle M. Outdoor sports and skin cancer. Clin Dermatol. 2008;26:12-15. doi:10.1016/j.clindermatol.2007.10.001
- Rigel DS, Rigel EG, Rigel AC. Effects of altitude and latitude on ambient UVB radiation. J Am Acad Dermatol. 1999;40:114-116. doi:10.1016/s0190-9622(99)70542-6
- Harrison SC, Bergfeld WF. Ultraviolet light and skin cancer in athletes. Sports Health. 2009;1:335-340. doi:10.1177/19417381093338923
- Downs NJ, Axelsen T, Schouten P, et al. Biologically effective solar ultraviolet exposures and the potential skin cancer risk for individual gold medalists of the 2020 Tokyo Summer Olympic Games. Temperature (Austin). 2019;7:89-108. doi:10.1080/23328940.2019.1581427
- De Castro-Maqueda G, Gutierrez-Manzanedo JV, Ponce-González JG, et al. Sun protection habits and sunburn in elite aquatics athletes: surfers, windsurfers and Olympic sailors. J Cancer Educ. 2020;35:312-320. doi:10.1007/s13187-018-1466-x
- Moehrle M, Heinrich L, Schmid A, et al. Extreme UV exposure of professional cyclists. Dermatology. 2000;201:44-45. doi:10.1159/000018428
- Buljan M, Kolic´ M, Šitum M, et al. Do athletes practicing outdoors know and care enough about the importance of photoprotection? Acta Dermatovenerol Croat. 2020;28:41-42.
- De Castro-Maqueda G, Gutierrez-Manzanedo JV, Lagares-Franco C. Sun exposure during water sports: do elite athletes adequately protect their skin against skin cancer? Int J Environ Res Public Health. 2021;18:800. doi:10.3390/ijerph18020800
- Tsai J, Chien AL. Photoprotection for skin of color. Am J Clin Dermatol. 2022;23:195-205. doi:10.1007/s40257-021-00670-z
- Ally MS, Swetter SM, Hirotsu KE, et al. Promoting sunscreen use and sun-protective practices in NCAA athletes: impact of SUNSPORT educational intervention for student-athletes, athletic trainers, and coaches. J Am Acad Dermatol. 2018;78:289-292.e2. doi:10.1016/j.jaad.2017.08.050
Practice Points
- Providers should further investigate how patients spend their time outside to assess cancer risk and appropriately guide patients.
- Many athletes typically train for hours outside; therefore, these patients should be educated on the importance of sunscreen reapplication and protective clothing.
FDA approves nivolumab for resected stage IIB/C melanoma
The , expanding the melanoma indication for the programmed death receptor-1 (PD-1) inhibitor.
Nivolumab, developed by Bristol-Myers Squibb, was previously approved as a single agent or in combination with ipilimumab for patients aged 12 years and older with unresectable or metastatic melanoma and for the adjuvant treatment of those aged 12 and older with completely resected stage III or IV melanoma.
The new approval was based on findings from the phase 3 CHECKMATE-76K trial, which randomly assigned 790 patients in a 2:1 ratio to receive nivolumab 480 mg or placebo by intravenous infusion. All patients in the trial had good performance status, had undergone complete resection of the primary melanoma with negative margins, and had tested negative on sentinel lymph node assessment within 12 weeks prior to randomization. Patients received treatment every 4 weeks for up to 1 year or until disease recurrence or unacceptable toxicity occurred.
Nivolumab reduced the risk of recurrence or death by 58% compared with placebo (hazard ratio, 0.42). Recurrence-free survival at 1 year was 89% with treatment, vs 79.4% with placebo. Median recurrence-free survival at 5 years was not reached in either arm.
Adverse reactions that were reported in at least 20% of patients included fatigue, musculoskeletal pain, rash, diarrhea, and pruritus.
The recommended nivolumab dose for patients weighing 40 kg or more is 480 mg every 4 weeks or 240 mg every 2 weeks until disease recurrence or unacceptable toxicity for up to 1 year. For pediatric patients who weigh less than 40 kg, the recommended dose is 3 mg/kg every 2 weeks or 6 mg/kg every 4 weeks until disease recurrence or unacceptable toxicity for up to 1 year.
Bristol-Myers Squibb’s application for approval led to the agent’s being granted orphan drug designation, allowing expedited review.
A version of this article appeared on Medscape.com.
The , expanding the melanoma indication for the programmed death receptor-1 (PD-1) inhibitor.
Nivolumab, developed by Bristol-Myers Squibb, was previously approved as a single agent or in combination with ipilimumab for patients aged 12 years and older with unresectable or metastatic melanoma and for the adjuvant treatment of those aged 12 and older with completely resected stage III or IV melanoma.
The new approval was based on findings from the phase 3 CHECKMATE-76K trial, which randomly assigned 790 patients in a 2:1 ratio to receive nivolumab 480 mg or placebo by intravenous infusion. All patients in the trial had good performance status, had undergone complete resection of the primary melanoma with negative margins, and had tested negative on sentinel lymph node assessment within 12 weeks prior to randomization. Patients received treatment every 4 weeks for up to 1 year or until disease recurrence or unacceptable toxicity occurred.
Nivolumab reduced the risk of recurrence or death by 58% compared with placebo (hazard ratio, 0.42). Recurrence-free survival at 1 year was 89% with treatment, vs 79.4% with placebo. Median recurrence-free survival at 5 years was not reached in either arm.
Adverse reactions that were reported in at least 20% of patients included fatigue, musculoskeletal pain, rash, diarrhea, and pruritus.
The recommended nivolumab dose for patients weighing 40 kg or more is 480 mg every 4 weeks or 240 mg every 2 weeks until disease recurrence or unacceptable toxicity for up to 1 year. For pediatric patients who weigh less than 40 kg, the recommended dose is 3 mg/kg every 2 weeks or 6 mg/kg every 4 weeks until disease recurrence or unacceptable toxicity for up to 1 year.
Bristol-Myers Squibb’s application for approval led to the agent’s being granted orphan drug designation, allowing expedited review.
A version of this article appeared on Medscape.com.
The , expanding the melanoma indication for the programmed death receptor-1 (PD-1) inhibitor.
Nivolumab, developed by Bristol-Myers Squibb, was previously approved as a single agent or in combination with ipilimumab for patients aged 12 years and older with unresectable or metastatic melanoma and for the adjuvant treatment of those aged 12 and older with completely resected stage III or IV melanoma.
The new approval was based on findings from the phase 3 CHECKMATE-76K trial, which randomly assigned 790 patients in a 2:1 ratio to receive nivolumab 480 mg or placebo by intravenous infusion. All patients in the trial had good performance status, had undergone complete resection of the primary melanoma with negative margins, and had tested negative on sentinel lymph node assessment within 12 weeks prior to randomization. Patients received treatment every 4 weeks for up to 1 year or until disease recurrence or unacceptable toxicity occurred.
Nivolumab reduced the risk of recurrence or death by 58% compared with placebo (hazard ratio, 0.42). Recurrence-free survival at 1 year was 89% with treatment, vs 79.4% with placebo. Median recurrence-free survival at 5 years was not reached in either arm.
Adverse reactions that were reported in at least 20% of patients included fatigue, musculoskeletal pain, rash, diarrhea, and pruritus.
The recommended nivolumab dose for patients weighing 40 kg or more is 480 mg every 4 weeks or 240 mg every 2 weeks until disease recurrence or unacceptable toxicity for up to 1 year. For pediatric patients who weigh less than 40 kg, the recommended dose is 3 mg/kg every 2 weeks or 6 mg/kg every 4 weeks until disease recurrence or unacceptable toxicity for up to 1 year.
Bristol-Myers Squibb’s application for approval led to the agent’s being granted orphan drug designation, allowing expedited review.
A version of this article appeared on Medscape.com.
These adverse events linked to improved cancer prognosis
TOPLINE:
.
METHODOLOGY:
- Emerging evidence suggests that the presence of cutaneous immune-related adverse events may be linked with favorable outcomes among patients with cancer who receive ICIs.
- Researchers conducted a systematic review and meta-analysis that included 23 studies and a total of 22,749 patients with cancer who received ICI treatment; studies compared outcomes among patients with and those without cutaneous immune-related adverse events.
- The major outcomes evaluated in the analysis were overall survival and progression-free survival (PFS); subgroup analyses assessed cutaneous immune-related adverse event type, cancer type, and other factors.
TAKEAWAY:
- The occurrence of cutaneous immune-related adverse events was associated with improved PFS (hazard ratio, 0.52; P < .001) and overall survival (HR, 0.61; P < .001).
- In the subgroup analysis, patients with eczematous (HR, 0.69), lichenoid or lichen planus–like skin lesions (HR, 0.51), pruritus without rash (HR, 0.70), psoriasis (HR, 0.63), or vitiligo (HR, 0.30) demonstrated a significant overall survival advantage. Vitiligo was the only adverse event associated with a PFS advantage (HR, 0.28).
- Among patients with melanoma, analyses revealed a significant association between the incidence of cutaneous immune-related adverse events and improved overall survival (HR, 0.51) and PFS (HR, 0.45). The authors highlighted similar findings among patients with non–small cell lung cancer (HR, 0.50 for overall survival and 0.61 for PFS).
IN PRACTICE:
“These data suggest that [cutaneous immune-related adverse events] may have useful prognostic value in ICI treatment,” the authors concluded.
SOURCE:
The analysis, led by Fei Wang, MD, Zhong Da Hospital, School of Medicine, Southeast University, Nanjing, China, was published online in JAMA Dermatology.
LIMITATIONS:
Most of the data came from retrospective studies, and there were limited data on specific patient subgroups. The Egger tests, used to assess potential publication bias in meta-analyses, revealed publication bias.
DISCLOSURES:
No disclosures were reported. The study was supported by a grant from the Postgraduate Research and Practice Innovation Program of Jiangsu Province.
A version of this article first appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- Emerging evidence suggests that the presence of cutaneous immune-related adverse events may be linked with favorable outcomes among patients with cancer who receive ICIs.
- Researchers conducted a systematic review and meta-analysis that included 23 studies and a total of 22,749 patients with cancer who received ICI treatment; studies compared outcomes among patients with and those without cutaneous immune-related adverse events.
- The major outcomes evaluated in the analysis were overall survival and progression-free survival (PFS); subgroup analyses assessed cutaneous immune-related adverse event type, cancer type, and other factors.
TAKEAWAY:
- The occurrence of cutaneous immune-related adverse events was associated with improved PFS (hazard ratio, 0.52; P < .001) and overall survival (HR, 0.61; P < .001).
- In the subgroup analysis, patients with eczematous (HR, 0.69), lichenoid or lichen planus–like skin lesions (HR, 0.51), pruritus without rash (HR, 0.70), psoriasis (HR, 0.63), or vitiligo (HR, 0.30) demonstrated a significant overall survival advantage. Vitiligo was the only adverse event associated with a PFS advantage (HR, 0.28).
- Among patients with melanoma, analyses revealed a significant association between the incidence of cutaneous immune-related adverse events and improved overall survival (HR, 0.51) and PFS (HR, 0.45). The authors highlighted similar findings among patients with non–small cell lung cancer (HR, 0.50 for overall survival and 0.61 for PFS).
IN PRACTICE:
“These data suggest that [cutaneous immune-related adverse events] may have useful prognostic value in ICI treatment,” the authors concluded.
SOURCE:
The analysis, led by Fei Wang, MD, Zhong Da Hospital, School of Medicine, Southeast University, Nanjing, China, was published online in JAMA Dermatology.
LIMITATIONS:
Most of the data came from retrospective studies, and there were limited data on specific patient subgroups. The Egger tests, used to assess potential publication bias in meta-analyses, revealed publication bias.
DISCLOSURES:
No disclosures were reported. The study was supported by a grant from the Postgraduate Research and Practice Innovation Program of Jiangsu Province.
A version of this article first appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- Emerging evidence suggests that the presence of cutaneous immune-related adverse events may be linked with favorable outcomes among patients with cancer who receive ICIs.
- Researchers conducted a systematic review and meta-analysis that included 23 studies and a total of 22,749 patients with cancer who received ICI treatment; studies compared outcomes among patients with and those without cutaneous immune-related adverse events.
- The major outcomes evaluated in the analysis were overall survival and progression-free survival (PFS); subgroup analyses assessed cutaneous immune-related adverse event type, cancer type, and other factors.
TAKEAWAY:
- The occurrence of cutaneous immune-related adverse events was associated with improved PFS (hazard ratio, 0.52; P < .001) and overall survival (HR, 0.61; P < .001).
- In the subgroup analysis, patients with eczematous (HR, 0.69), lichenoid or lichen planus–like skin lesions (HR, 0.51), pruritus without rash (HR, 0.70), psoriasis (HR, 0.63), or vitiligo (HR, 0.30) demonstrated a significant overall survival advantage. Vitiligo was the only adverse event associated with a PFS advantage (HR, 0.28).
- Among patients with melanoma, analyses revealed a significant association between the incidence of cutaneous immune-related adverse events and improved overall survival (HR, 0.51) and PFS (HR, 0.45). The authors highlighted similar findings among patients with non–small cell lung cancer (HR, 0.50 for overall survival and 0.61 for PFS).
IN PRACTICE:
“These data suggest that [cutaneous immune-related adverse events] may have useful prognostic value in ICI treatment,” the authors concluded.
SOURCE:
The analysis, led by Fei Wang, MD, Zhong Da Hospital, School of Medicine, Southeast University, Nanjing, China, was published online in JAMA Dermatology.
LIMITATIONS:
Most of the data came from retrospective studies, and there were limited data on specific patient subgroups. The Egger tests, used to assess potential publication bias in meta-analyses, revealed publication bias.
DISCLOSURES:
No disclosures were reported. The study was supported by a grant from the Postgraduate Research and Practice Innovation Program of Jiangsu Province.
A version of this article first appeared on Medscape.com.
Does the number of primary melanomas affect survival?
TOPLINE:
.
METHODOLOGY:
- The difference in outcomes between people with multiple primary melanomas (MPMs) and a single primary melanoma (SPM) has not been established.
- To compare 10-year melanoma-specific mortality and overall mortality between people with MPMs and SPM, researchers drew from the Melanoma Patterns of Care study, a population-based observational analysis of residents in the state of New South Wales, Australia, who had a melanoma reported to the state cancer registry over 12 months in 2006-2007, and were followed up until 2018, for a median of almost 12 years.
- The researchers performed logistic regression analyses to assess 10-year melanoma-specific mortality differences between the two groups.
TAKEAWAY:
- Of 3,404 people included in the analysis, 2,830 had an SPM and 574 developed MPMs during follow-up.
- On multivariable regression adjusted for pathologic characteristics of the thickest lesion in the MPM group, no significant differences were seen in 10-year melanoma-specific mortality between the two groups (odds ratio, 0.85; 95% confidence interval, 0.58-1.24; P = .40).
- Sensitivity analyses adjusted for parameters of the first primary melanoma among patients with MPMs revealed similar findings (OR, 1.34; 95% CI, 0.92-1.96; P = .12).
- On multivariable analysis using data from the thickest lesion, factors independently associated with melanoma-specific mortality were male sex, disadvantaged socioeconomic status (based on location of residence), and Breslow thickness.
- Factors independently associated with 10-year overall mortality were like those seen in other studies and included sex, Breslow thickness, ulceration status, and socioeconomic disadvantage.
IN PRACTICE:
“The results of our study suggest that the number of primary melanomas is not an independent risk factor for mortality,” the researchers concluded. “In addition, the detection of melanoma at an early stage (with a thin Breslow thickness) rather than an intrinsic biologic factor remains the biggest influence on melanoma mortality after diagnosis of one or more melanomas.”
SOURCE:
Corresponding author Serigne N. Lo, PhD, of the Melanoma Institute Australia, led the research. The study was published in the Journal of the American Academy of Dermatology.
LIMITATIONS:
No adjustments for treatment modality were made in the study, and at baseline survey, effective systemic treatments for melanoma were not available.
DISCLOSURES:
This study was supported by the Australian National Health and Medical Research Council, Cancer Institute New South Wales, and the New South Wale State Government via a grant to the New South Wales Melanoma Network. Additional support was provided by Melanoma Institute Australia and the New South Wales Melanoma Network.
A version of this article first appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- The difference in outcomes between people with multiple primary melanomas (MPMs) and a single primary melanoma (SPM) has not been established.
- To compare 10-year melanoma-specific mortality and overall mortality between people with MPMs and SPM, researchers drew from the Melanoma Patterns of Care study, a population-based observational analysis of residents in the state of New South Wales, Australia, who had a melanoma reported to the state cancer registry over 12 months in 2006-2007, and were followed up until 2018, for a median of almost 12 years.
- The researchers performed logistic regression analyses to assess 10-year melanoma-specific mortality differences between the two groups.
TAKEAWAY:
- Of 3,404 people included in the analysis, 2,830 had an SPM and 574 developed MPMs during follow-up.
- On multivariable regression adjusted for pathologic characteristics of the thickest lesion in the MPM group, no significant differences were seen in 10-year melanoma-specific mortality between the two groups (odds ratio, 0.85; 95% confidence interval, 0.58-1.24; P = .40).
- Sensitivity analyses adjusted for parameters of the first primary melanoma among patients with MPMs revealed similar findings (OR, 1.34; 95% CI, 0.92-1.96; P = .12).
- On multivariable analysis using data from the thickest lesion, factors independently associated with melanoma-specific mortality were male sex, disadvantaged socioeconomic status (based on location of residence), and Breslow thickness.
- Factors independently associated with 10-year overall mortality were like those seen in other studies and included sex, Breslow thickness, ulceration status, and socioeconomic disadvantage.
IN PRACTICE:
“The results of our study suggest that the number of primary melanomas is not an independent risk factor for mortality,” the researchers concluded. “In addition, the detection of melanoma at an early stage (with a thin Breslow thickness) rather than an intrinsic biologic factor remains the biggest influence on melanoma mortality after diagnosis of one or more melanomas.”
SOURCE:
Corresponding author Serigne N. Lo, PhD, of the Melanoma Institute Australia, led the research. The study was published in the Journal of the American Academy of Dermatology.
LIMITATIONS:
No adjustments for treatment modality were made in the study, and at baseline survey, effective systemic treatments for melanoma were not available.
DISCLOSURES:
This study was supported by the Australian National Health and Medical Research Council, Cancer Institute New South Wales, and the New South Wale State Government via a grant to the New South Wales Melanoma Network. Additional support was provided by Melanoma Institute Australia and the New South Wales Melanoma Network.
A version of this article first appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- The difference in outcomes between people with multiple primary melanomas (MPMs) and a single primary melanoma (SPM) has not been established.
- To compare 10-year melanoma-specific mortality and overall mortality between people with MPMs and SPM, researchers drew from the Melanoma Patterns of Care study, a population-based observational analysis of residents in the state of New South Wales, Australia, who had a melanoma reported to the state cancer registry over 12 months in 2006-2007, and were followed up until 2018, for a median of almost 12 years.
- The researchers performed logistic regression analyses to assess 10-year melanoma-specific mortality differences between the two groups.
TAKEAWAY:
- Of 3,404 people included in the analysis, 2,830 had an SPM and 574 developed MPMs during follow-up.
- On multivariable regression adjusted for pathologic characteristics of the thickest lesion in the MPM group, no significant differences were seen in 10-year melanoma-specific mortality between the two groups (odds ratio, 0.85; 95% confidence interval, 0.58-1.24; P = .40).
- Sensitivity analyses adjusted for parameters of the first primary melanoma among patients with MPMs revealed similar findings (OR, 1.34; 95% CI, 0.92-1.96; P = .12).
- On multivariable analysis using data from the thickest lesion, factors independently associated with melanoma-specific mortality were male sex, disadvantaged socioeconomic status (based on location of residence), and Breslow thickness.
- Factors independently associated with 10-year overall mortality were like those seen in other studies and included sex, Breslow thickness, ulceration status, and socioeconomic disadvantage.
IN PRACTICE:
“The results of our study suggest that the number of primary melanomas is not an independent risk factor for mortality,” the researchers concluded. “In addition, the detection of melanoma at an early stage (with a thin Breslow thickness) rather than an intrinsic biologic factor remains the biggest influence on melanoma mortality after diagnosis of one or more melanomas.”
SOURCE:
Corresponding author Serigne N. Lo, PhD, of the Melanoma Institute Australia, led the research. The study was published in the Journal of the American Academy of Dermatology.
LIMITATIONS:
No adjustments for treatment modality were made in the study, and at baseline survey, effective systemic treatments for melanoma were not available.
DISCLOSURES:
This study was supported by the Australian National Health and Medical Research Council, Cancer Institute New South Wales, and the New South Wale State Government via a grant to the New South Wales Melanoma Network. Additional support was provided by Melanoma Institute Australia and the New South Wales Melanoma Network.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
High rate of subsequent cancers in MCC
.
In a cohort of 6,146 patients with a first primary MCC, a total of 725 (11.8%) developed subsequent primary cancers. For solid tumors, the risk was highest for cutaneous melanoma and papillary thyroid carcinoma, while for hematologic cancers, the risk was increased for non-Hodgkin lymphoma.
“Our study does confirm that patients with MCC are at higher risk for developing other cancers,” study author Lisa C. Zaba, MD, PhD, associate professor of dermatology and director of the Merkel cell carcinoma multidisciplinary clinic, Stanford (Calif.) Cancer Center, said in an interview. “MCC is a highly malignant cancer with a 40% recurrence risk.”
Because of this high risk, Dr. Zaba noted that patients with MCC get frequent surveillance with both imaging studies (PET-CT and CT) as well as frequent visits in clinic with MCC experts. “Specifically, a patient with MCC is imaged and seen in clinic every 3-6 months for the first 3 years after diagnosis, and every 6-12 months thereafter for up to 5 years,” she said. “Interestingly, this high level of surveillance may be one reason that we find so many cancers in patients who have been diagnosed with MCC, compared to the general population.”
The study was published online in JAMA Dermatology.
With the death of “Margaritaville” singer Jimmy Buffett, who recently died of MCC 4 years after his diagnosis, this rare, aggressive skin cancer has been put in the spotlight. Survival has been increasing, primarily because of the advent of immunotherapy, and the authors note that it is therefore imperative to better understand the risk of subsequent primary tumors to inform screening and treatment recommendations.
In this cohort study, Dr. Zaba and colleagues identified 6,146 patients from 17 registries of the Surveillance, Epidemiology, and End Results (SEER) Program who had been diagnosed with a first primary cutaneous MCC between 2000 and 2018.
Endpoints were the ratio of observed to expected number of cases of subsequent cancer (Standardized incidence ratio, or SIR) and the excess risk.
Overall, there was an elevated risk of developing a subsequent primary cancer after being diagnosed with MCC (SIR, 1.28; excess risk, 57.25 per 10,000 person-years). This included the risk for all solid tumors including liver (SIR, 1.92; excess risk, 2.77 per 10,000 person-years), pancreas (SIR, 1.65; excess risk, 4.55 per 10,000 person-years), cutaneous melanoma (SIR, 2.36; excess risk, 15.27 per 10,000 person-years), and kidney (SIR, 1.64; excess risk, 3.83 per 10,000 person-years).
There was also a higher risk of developing papillary thyroid carcinoma (PTC) (SIR, 5.26; excess risk, 6.16 per 10,000 person-years).
The risk of developing hematological cancers after MCC was also increased, especially for non-Hodgkin lymphoma (SIR, 2.62; excess risk, 15.48 per 10,000 person-years) and myelodysplastic syndrome (SIR, 2.17; excess risk, 2.73 per 10,000 person-years).
The risk for developing subsequent tumors, including melanoma and non-Hodgkin lymphoma, remained significant for up to 10 years, while the risk for developing PTC and kidney cancers remained for up to 5 years.
“After 3-5 years, when a MCC patient’s risk of MCC recurrence drops below 2%, we do not currently have guidelines in place for additional cancer screening,” Dr. Zaba said. “Regarding patient education, patients with MCC are educated to let us know if they experience any symptoms of cancer between visits, including unintentional weight loss, night sweats, headaches that increasingly worsen, or growing lumps or bumps. These symptoms may occur in a multitude of cancers and not just MCC.”
Weighing in on the study, Jeffrey M. Farma, MD, interim chair, department of surgical oncology at Fox Chase Cancer Center, Philadelphia, noted that MCC is considered to be high risk because of its chances of recurring after surgical resection or spreading to lymph nodes or other areas of the body. “There are approximately 3,000 new cases of melanoma a year in the U.S., and it is 40 times rarer than melanoma,” he said. “Patients are usually diagnosed with Merkel cell carcinoma later in life, and the tumors have been associated with sun exposure and immunosuppression and have also been associated with the polyomavirus.”
That said, however, he emphasized that great strides have been made in treatment. “These tumors are very sensitive to radiation, and we generally treat earlier-stage MCC with a combination of surgery and radiation therapy,” said Dr. Farma. “More recently we have had a lot of success with the use of immunotherapy to treat more advanced MCC.”
Dr. Zaba reported receiving grants from the Kuni Foundation outside the submitted work. No other disclosures were reported. Author Eleni Linos, MD, DrPH, MPH, is supported by grant K24AR075060 from the National Institutes of Health. No other outside funding was reported. Dr. Farma had no disclosures.
.
In a cohort of 6,146 patients with a first primary MCC, a total of 725 (11.8%) developed subsequent primary cancers. For solid tumors, the risk was highest for cutaneous melanoma and papillary thyroid carcinoma, while for hematologic cancers, the risk was increased for non-Hodgkin lymphoma.
“Our study does confirm that patients with MCC are at higher risk for developing other cancers,” study author Lisa C. Zaba, MD, PhD, associate professor of dermatology and director of the Merkel cell carcinoma multidisciplinary clinic, Stanford (Calif.) Cancer Center, said in an interview. “MCC is a highly malignant cancer with a 40% recurrence risk.”
Because of this high risk, Dr. Zaba noted that patients with MCC get frequent surveillance with both imaging studies (PET-CT and CT) as well as frequent visits in clinic with MCC experts. “Specifically, a patient with MCC is imaged and seen in clinic every 3-6 months for the first 3 years after diagnosis, and every 6-12 months thereafter for up to 5 years,” she said. “Interestingly, this high level of surveillance may be one reason that we find so many cancers in patients who have been diagnosed with MCC, compared to the general population.”
The study was published online in JAMA Dermatology.
With the death of “Margaritaville” singer Jimmy Buffett, who recently died of MCC 4 years after his diagnosis, this rare, aggressive skin cancer has been put in the spotlight. Survival has been increasing, primarily because of the advent of immunotherapy, and the authors note that it is therefore imperative to better understand the risk of subsequent primary tumors to inform screening and treatment recommendations.
In this cohort study, Dr. Zaba and colleagues identified 6,146 patients from 17 registries of the Surveillance, Epidemiology, and End Results (SEER) Program who had been diagnosed with a first primary cutaneous MCC between 2000 and 2018.
Endpoints were the ratio of observed to expected number of cases of subsequent cancer (Standardized incidence ratio, or SIR) and the excess risk.
Overall, there was an elevated risk of developing a subsequent primary cancer after being diagnosed with MCC (SIR, 1.28; excess risk, 57.25 per 10,000 person-years). This included the risk for all solid tumors including liver (SIR, 1.92; excess risk, 2.77 per 10,000 person-years), pancreas (SIR, 1.65; excess risk, 4.55 per 10,000 person-years), cutaneous melanoma (SIR, 2.36; excess risk, 15.27 per 10,000 person-years), and kidney (SIR, 1.64; excess risk, 3.83 per 10,000 person-years).
There was also a higher risk of developing papillary thyroid carcinoma (PTC) (SIR, 5.26; excess risk, 6.16 per 10,000 person-years).
The risk of developing hematological cancers after MCC was also increased, especially for non-Hodgkin lymphoma (SIR, 2.62; excess risk, 15.48 per 10,000 person-years) and myelodysplastic syndrome (SIR, 2.17; excess risk, 2.73 per 10,000 person-years).
The risk for developing subsequent tumors, including melanoma and non-Hodgkin lymphoma, remained significant for up to 10 years, while the risk for developing PTC and kidney cancers remained for up to 5 years.
“After 3-5 years, when a MCC patient’s risk of MCC recurrence drops below 2%, we do not currently have guidelines in place for additional cancer screening,” Dr. Zaba said. “Regarding patient education, patients with MCC are educated to let us know if they experience any symptoms of cancer between visits, including unintentional weight loss, night sweats, headaches that increasingly worsen, or growing lumps or bumps. These symptoms may occur in a multitude of cancers and not just MCC.”
Weighing in on the study, Jeffrey M. Farma, MD, interim chair, department of surgical oncology at Fox Chase Cancer Center, Philadelphia, noted that MCC is considered to be high risk because of its chances of recurring after surgical resection or spreading to lymph nodes or other areas of the body. “There are approximately 3,000 new cases of melanoma a year in the U.S., and it is 40 times rarer than melanoma,” he said. “Patients are usually diagnosed with Merkel cell carcinoma later in life, and the tumors have been associated with sun exposure and immunosuppression and have also been associated with the polyomavirus.”
That said, however, he emphasized that great strides have been made in treatment. “These tumors are very sensitive to radiation, and we generally treat earlier-stage MCC with a combination of surgery and radiation therapy,” said Dr. Farma. “More recently we have had a lot of success with the use of immunotherapy to treat more advanced MCC.”
Dr. Zaba reported receiving grants from the Kuni Foundation outside the submitted work. No other disclosures were reported. Author Eleni Linos, MD, DrPH, MPH, is supported by grant K24AR075060 from the National Institutes of Health. No other outside funding was reported. Dr. Farma had no disclosures.
.
In a cohort of 6,146 patients with a first primary MCC, a total of 725 (11.8%) developed subsequent primary cancers. For solid tumors, the risk was highest for cutaneous melanoma and papillary thyroid carcinoma, while for hematologic cancers, the risk was increased for non-Hodgkin lymphoma.
“Our study does confirm that patients with MCC are at higher risk for developing other cancers,” study author Lisa C. Zaba, MD, PhD, associate professor of dermatology and director of the Merkel cell carcinoma multidisciplinary clinic, Stanford (Calif.) Cancer Center, said in an interview. “MCC is a highly malignant cancer with a 40% recurrence risk.”
Because of this high risk, Dr. Zaba noted that patients with MCC get frequent surveillance with both imaging studies (PET-CT and CT) as well as frequent visits in clinic with MCC experts. “Specifically, a patient with MCC is imaged and seen in clinic every 3-6 months for the first 3 years after diagnosis, and every 6-12 months thereafter for up to 5 years,” she said. “Interestingly, this high level of surveillance may be one reason that we find so many cancers in patients who have been diagnosed with MCC, compared to the general population.”
The study was published online in JAMA Dermatology.
With the death of “Margaritaville” singer Jimmy Buffett, who recently died of MCC 4 years after his diagnosis, this rare, aggressive skin cancer has been put in the spotlight. Survival has been increasing, primarily because of the advent of immunotherapy, and the authors note that it is therefore imperative to better understand the risk of subsequent primary tumors to inform screening and treatment recommendations.
In this cohort study, Dr. Zaba and colleagues identified 6,146 patients from 17 registries of the Surveillance, Epidemiology, and End Results (SEER) Program who had been diagnosed with a first primary cutaneous MCC between 2000 and 2018.
Endpoints were the ratio of observed to expected number of cases of subsequent cancer (Standardized incidence ratio, or SIR) and the excess risk.
Overall, there was an elevated risk of developing a subsequent primary cancer after being diagnosed with MCC (SIR, 1.28; excess risk, 57.25 per 10,000 person-years). This included the risk for all solid tumors including liver (SIR, 1.92; excess risk, 2.77 per 10,000 person-years), pancreas (SIR, 1.65; excess risk, 4.55 per 10,000 person-years), cutaneous melanoma (SIR, 2.36; excess risk, 15.27 per 10,000 person-years), and kidney (SIR, 1.64; excess risk, 3.83 per 10,000 person-years).
There was also a higher risk of developing papillary thyroid carcinoma (PTC) (SIR, 5.26; excess risk, 6.16 per 10,000 person-years).
The risk of developing hematological cancers after MCC was also increased, especially for non-Hodgkin lymphoma (SIR, 2.62; excess risk, 15.48 per 10,000 person-years) and myelodysplastic syndrome (SIR, 2.17; excess risk, 2.73 per 10,000 person-years).
The risk for developing subsequent tumors, including melanoma and non-Hodgkin lymphoma, remained significant for up to 10 years, while the risk for developing PTC and kidney cancers remained for up to 5 years.
“After 3-5 years, when a MCC patient’s risk of MCC recurrence drops below 2%, we do not currently have guidelines in place for additional cancer screening,” Dr. Zaba said. “Regarding patient education, patients with MCC are educated to let us know if they experience any symptoms of cancer between visits, including unintentional weight loss, night sweats, headaches that increasingly worsen, or growing lumps or bumps. These symptoms may occur in a multitude of cancers and not just MCC.”
Weighing in on the study, Jeffrey M. Farma, MD, interim chair, department of surgical oncology at Fox Chase Cancer Center, Philadelphia, noted that MCC is considered to be high risk because of its chances of recurring after surgical resection or spreading to lymph nodes or other areas of the body. “There are approximately 3,000 new cases of melanoma a year in the U.S., and it is 40 times rarer than melanoma,” he said. “Patients are usually diagnosed with Merkel cell carcinoma later in life, and the tumors have been associated with sun exposure and immunosuppression and have also been associated with the polyomavirus.”
That said, however, he emphasized that great strides have been made in treatment. “These tumors are very sensitive to radiation, and we generally treat earlier-stage MCC with a combination of surgery and radiation therapy,” said Dr. Farma. “More recently we have had a lot of success with the use of immunotherapy to treat more advanced MCC.”
Dr. Zaba reported receiving grants from the Kuni Foundation outside the submitted work. No other disclosures were reported. Author Eleni Linos, MD, DrPH, MPH, is supported by grant K24AR075060 from the National Institutes of Health. No other outside funding was reported. Dr. Farma had no disclosures.
FROM JAMA DERMATOLOGY
Impact of Socioeconomic Disparities and Facility Type on Overall Survival in Stage I vs Stage IV Amelanotic Melanoma: An Analysis of the National Cancer Database
PURPOSE
This study addresses a gap in knowledge regarding socioeconomic factors, facility type, and overall survival in stage I vs stage IV Amelanotic Melanoma.
BACKGROUND
Amelanotic Melanoma (AM) is a rare form of melanoma that lacks pigment and accounts for approximately 5% of melanomas. Light skin color and increasing age are important risk factors. Although curable when diagnosed early, it is often missed or mistaken for other benign conditions. A study investigating the impact of facility type on overall survival between stage I vs stage IV AM has yet to be done.
METHODS
This is a retrospective study of patients diagnosed with Amelanotic Melanoma (ICD-8730) between 2004 and 2020 in the National Cancer Database (NCDB) to compare demographic features and overall survival (n = 2147). Exclusion criteria included missing data.
DATA ANALYSIS
Descriptive statistics for all AM patients were collected. Median household income and facility type were compared between patients diagnosed with stage I and stage IV AM using Pearson Chi- Square test. Breslow thickness and overall survival between stage I and stage IV were evaluated using independent t-test and Kaplan-Meier test, respectively. All variables were evaluated for a significance of P < .05.
RESULTS
Most cases analyzed were White (98.1%), male (58.6%), and had Medicare as the primary payor at diagnosis (51.1%). Of 2147 cases, 497 were stage I (23.1%) and 164 were stage IV AM (7.6%) with a mean age at diagnosis of 66.05 and 63.72 years, respectively. There was a significant difference in overall survival between stage I (mean = 118.7 months) and stage 4 (mean = 42.4 months, P < 0.001). The average Breslow thickness was 1.17mm in stage I and 2.59mm in stage IV (P<0.05). More patients diagnosed at stage I used academic facilities than those diagnosed at stage IV (43.9% vs 33.8%, P<0.05). Most patients diagnosed at stage I were high income compared to patients diagnosed at stage IV (55% vs 43.2%, P<0.05).
CONCLUSIONS
With the overall survival of stage IV AM being significantly worse, we hope this study can provide a starting point in the study and prevention of disparities in the early diagnosis of AM.
PURPOSE
This study addresses a gap in knowledge regarding socioeconomic factors, facility type, and overall survival in stage I vs stage IV Amelanotic Melanoma.
BACKGROUND
Amelanotic Melanoma (AM) is a rare form of melanoma that lacks pigment and accounts for approximately 5% of melanomas. Light skin color and increasing age are important risk factors. Although curable when diagnosed early, it is often missed or mistaken for other benign conditions. A study investigating the impact of facility type on overall survival between stage I vs stage IV AM has yet to be done.
METHODS
This is a retrospective study of patients diagnosed with Amelanotic Melanoma (ICD-8730) between 2004 and 2020 in the National Cancer Database (NCDB) to compare demographic features and overall survival (n = 2147). Exclusion criteria included missing data.
DATA ANALYSIS
Descriptive statistics for all AM patients were collected. Median household income and facility type were compared between patients diagnosed with stage I and stage IV AM using Pearson Chi- Square test. Breslow thickness and overall survival between stage I and stage IV were evaluated using independent t-test and Kaplan-Meier test, respectively. All variables were evaluated for a significance of P < .05.
RESULTS
Most cases analyzed were White (98.1%), male (58.6%), and had Medicare as the primary payor at diagnosis (51.1%). Of 2147 cases, 497 were stage I (23.1%) and 164 were stage IV AM (7.6%) with a mean age at diagnosis of 66.05 and 63.72 years, respectively. There was a significant difference in overall survival between stage I (mean = 118.7 months) and stage 4 (mean = 42.4 months, P < 0.001). The average Breslow thickness was 1.17mm in stage I and 2.59mm in stage IV (P<0.05). More patients diagnosed at stage I used academic facilities than those diagnosed at stage IV (43.9% vs 33.8%, P<0.05). Most patients diagnosed at stage I were high income compared to patients diagnosed at stage IV (55% vs 43.2%, P<0.05).
CONCLUSIONS
With the overall survival of stage IV AM being significantly worse, we hope this study can provide a starting point in the study and prevention of disparities in the early diagnosis of AM.
PURPOSE
This study addresses a gap in knowledge regarding socioeconomic factors, facility type, and overall survival in stage I vs stage IV Amelanotic Melanoma.
BACKGROUND
Amelanotic Melanoma (AM) is a rare form of melanoma that lacks pigment and accounts for approximately 5% of melanomas. Light skin color and increasing age are important risk factors. Although curable when diagnosed early, it is often missed or mistaken for other benign conditions. A study investigating the impact of facility type on overall survival between stage I vs stage IV AM has yet to be done.
METHODS
This is a retrospective study of patients diagnosed with Amelanotic Melanoma (ICD-8730) between 2004 and 2020 in the National Cancer Database (NCDB) to compare demographic features and overall survival (n = 2147). Exclusion criteria included missing data.
DATA ANALYSIS
Descriptive statistics for all AM patients were collected. Median household income and facility type were compared between patients diagnosed with stage I and stage IV AM using Pearson Chi- Square test. Breslow thickness and overall survival between stage I and stage IV were evaluated using independent t-test and Kaplan-Meier test, respectively. All variables were evaluated for a significance of P < .05.
RESULTS
Most cases analyzed were White (98.1%), male (58.6%), and had Medicare as the primary payor at diagnosis (51.1%). Of 2147 cases, 497 were stage I (23.1%) and 164 were stage IV AM (7.6%) with a mean age at diagnosis of 66.05 and 63.72 years, respectively. There was a significant difference in overall survival between stage I (mean = 118.7 months) and stage 4 (mean = 42.4 months, P < 0.001). The average Breslow thickness was 1.17mm in stage I and 2.59mm in stage IV (P<0.05). More patients diagnosed at stage I used academic facilities than those diagnosed at stage IV (43.9% vs 33.8%, P<0.05). Most patients diagnosed at stage I were high income compared to patients diagnosed at stage IV (55% vs 43.2%, P<0.05).
CONCLUSIONS
With the overall survival of stage IV AM being significantly worse, we hope this study can provide a starting point in the study and prevention of disparities in the early diagnosis of AM.
Clinical Impact of UV Mutational Signatures in Veterans With Cancer
PURPOSE
Assess the clinical impact (CI) of UV-related DNA damage signatures (UVsig) in Veterans with cancer of unknown primary (CUP) and cancer of extracutaneous origin (CEO).
BACKGROUND
UVsig have been reported in CUP and CEO (i.e. head and neck cancer and lung cancer). The presence of UVsig suggests a cutaneous origin and potential misclassification of CEO using conventional histopathologic evaluation. Literature on the association of UVsig in pan-cancer genomics is limited.
METHODS
This is a retrospective study of Veterans who underwent comprehensive genomic profiling with FoundationOne CDx during 2/1/2019 to 9/30/2022 through the VA National Precision Oncology Program. The outcome was the CI of UVsig (high, medium, and low) determined by blinded chart reviews: (1) high: UVsig leading to change in diagnoses (CID) and a different first-line therapy (FLT) would have been offered; (2) medium: UVsig leading to CID, but appropriate FLT offered; (3) low: diagnoses modified by clinicians and treated as cutaneous cancers. NCCN Guidelines were referenced for FLT.
DATA ANALYSIS
Descriptive statistics and chi-square tests were utilized to evaluate the UVsig CI.
RESULTS
Among 5,565 cases with 10 or more assessable alterations for UVsig analysis, 650 (11.7%) were positive for UVsig. CUP and CEO cohorts each had 41 cases analyzed. In the CUP cases, 20 (48.8%), 9 (21.9%), and 12 (29.3%) were categorized as having high, medium, and low CI, respectively; and in the CEO cases, it was 22 (53.7%), 15 (36.6%), and 4 (9.8%). There was no difference statistically between the CUP and CEO groups on the percentage distribution of CI (p=0.06). Among the 42 out of 82 cases having high CI, 37 (88.1%) received cytotoxic chemotherapy without any indication, and 5 (11.9%) were not offered immunotherapy (IO) as FLT. More than half of the 82 cases had high CI; more than 90% of the CEO cases had high and medium CI.
IMPLICATIONS
UVsig serves as a useful biomarker for cancers with cutaneous origin. About 1% of the 5,565 cases analyzed had high UVsig CI. Knowledge of UVsig could lead to omission of chemotherapy (hence avoiding toxicities) or addition of IO (for potential benefits).
PURPOSE
Assess the clinical impact (CI) of UV-related DNA damage signatures (UVsig) in Veterans with cancer of unknown primary (CUP) and cancer of extracutaneous origin (CEO).
BACKGROUND
UVsig have been reported in CUP and CEO (i.e. head and neck cancer and lung cancer). The presence of UVsig suggests a cutaneous origin and potential misclassification of CEO using conventional histopathologic evaluation. Literature on the association of UVsig in pan-cancer genomics is limited.
METHODS
This is a retrospective study of Veterans who underwent comprehensive genomic profiling with FoundationOne CDx during 2/1/2019 to 9/30/2022 through the VA National Precision Oncology Program. The outcome was the CI of UVsig (high, medium, and low) determined by blinded chart reviews: (1) high: UVsig leading to change in diagnoses (CID) and a different first-line therapy (FLT) would have been offered; (2) medium: UVsig leading to CID, but appropriate FLT offered; (3) low: diagnoses modified by clinicians and treated as cutaneous cancers. NCCN Guidelines were referenced for FLT.
DATA ANALYSIS
Descriptive statistics and chi-square tests were utilized to evaluate the UVsig CI.
RESULTS
Among 5,565 cases with 10 or more assessable alterations for UVsig analysis, 650 (11.7%) were positive for UVsig. CUP and CEO cohorts each had 41 cases analyzed. In the CUP cases, 20 (48.8%), 9 (21.9%), and 12 (29.3%) were categorized as having high, medium, and low CI, respectively; and in the CEO cases, it was 22 (53.7%), 15 (36.6%), and 4 (9.8%). There was no difference statistically between the CUP and CEO groups on the percentage distribution of CI (p=0.06). Among the 42 out of 82 cases having high CI, 37 (88.1%) received cytotoxic chemotherapy without any indication, and 5 (11.9%) were not offered immunotherapy (IO) as FLT. More than half of the 82 cases had high CI; more than 90% of the CEO cases had high and medium CI.
IMPLICATIONS
UVsig serves as a useful biomarker for cancers with cutaneous origin. About 1% of the 5,565 cases analyzed had high UVsig CI. Knowledge of UVsig could lead to omission of chemotherapy (hence avoiding toxicities) or addition of IO (for potential benefits).
PURPOSE
Assess the clinical impact (CI) of UV-related DNA damage signatures (UVsig) in Veterans with cancer of unknown primary (CUP) and cancer of extracutaneous origin (CEO).
BACKGROUND
UVsig have been reported in CUP and CEO (i.e. head and neck cancer and lung cancer). The presence of UVsig suggests a cutaneous origin and potential misclassification of CEO using conventional histopathologic evaluation. Literature on the association of UVsig in pan-cancer genomics is limited.
METHODS
This is a retrospective study of Veterans who underwent comprehensive genomic profiling with FoundationOne CDx during 2/1/2019 to 9/30/2022 through the VA National Precision Oncology Program. The outcome was the CI of UVsig (high, medium, and low) determined by blinded chart reviews: (1) high: UVsig leading to change in diagnoses (CID) and a different first-line therapy (FLT) would have been offered; (2) medium: UVsig leading to CID, but appropriate FLT offered; (3) low: diagnoses modified by clinicians and treated as cutaneous cancers. NCCN Guidelines were referenced for FLT.
DATA ANALYSIS
Descriptive statistics and chi-square tests were utilized to evaluate the UVsig CI.
RESULTS
Among 5,565 cases with 10 or more assessable alterations for UVsig analysis, 650 (11.7%) were positive for UVsig. CUP and CEO cohorts each had 41 cases analyzed. In the CUP cases, 20 (48.8%), 9 (21.9%), and 12 (29.3%) were categorized as having high, medium, and low CI, respectively; and in the CEO cases, it was 22 (53.7%), 15 (36.6%), and 4 (9.8%). There was no difference statistically between the CUP and CEO groups on the percentage distribution of CI (p=0.06). Among the 42 out of 82 cases having high CI, 37 (88.1%) received cytotoxic chemotherapy without any indication, and 5 (11.9%) were not offered immunotherapy (IO) as FLT. More than half of the 82 cases had high CI; more than 90% of the CEO cases had high and medium CI.
IMPLICATIONS
UVsig serves as a useful biomarker for cancers with cutaneous origin. About 1% of the 5,565 cases analyzed had high UVsig CI. Knowledge of UVsig could lead to omission of chemotherapy (hence avoiding toxicities) or addition of IO (for potential benefits).
Do AI chatbots give reliable answers on cancer? Yes and no
two new studies suggest.
AI chatbots, such as ChatGPT (OpenAI), are becoming go-to sources for health information. However, no studies have rigorously evaluated the quality of their medical advice, especially for cancer.
Two new studies published in JAMA Oncology did just that.
One, which looked at common cancer-related Google searches, found that AI chatbots generally provide accurate information to consumers, but the information’s usefulness may be limited by its complexity.
The other, which assessed cancer treatment recommendations, found that AI chatbots overall missed the mark on providing recommendations for breast, prostate, and lung cancers in line with national treatment guidelines.
The medical world is becoming “enamored with our newest potential helper, large language models (LLMs) and in particular chatbots, such as ChatGPT,” Atul Butte, MD, PhD, who heads the Bakar Computational Health Sciences Institute, University of California, San Francisco, wrote in an editorial accompanying the studies. “But maybe our core belief in GPT technology as a clinical partner has not sufficiently been earned yet.”
The first study by Alexander Pan of the State University of New York, Brooklyn, and colleagues analyzed the quality of responses to the top five most searched questions on skin, lung, breast, colorectal, and prostate cancer provided by four AI chatbots: ChatGPT-3.5, Perplexity (Perplexity.AI), Chatsonic (Writesonic), and Bing AI (Microsoft).
Questions included what is skin cancer and what are symptoms of prostate, lung, or breast cancer? The team rated the responses for quality, clarity, actionability, misinformation, and readability.
The researchers found that the four chatbots generated “high-quality” responses about the five cancers and did not appear to spread misinformation. Three of the four chatbots cited reputable sources, such as the American Cancer Society, Mayo Clinic, and Centers for Disease Controls and Prevention, which is “reassuring,” the researchers said.
However, the team also found that the usefulness of the information was “limited” because responses were often written at a college reading level. Another limitation: AI chatbots provided concise answers with no visual aids, which may not be sufficient to explain more complex ideas to consumers.
“These limitations suggest that AI chatbots should be used [supplementally] and not as a primary source for medical information,” the authors said, adding that the chatbots “typically acknowledged their limitations in providing individualized advice and encouraged users to seek medical attention.”
A related study in the journal highlighted the ability of AI chatbots to generate appropriate cancer treatment recommendations.
In this analysis, Shan Chen, MS, with the AI in Medicine Program, Mass General Brigham, Harvard Medical School, Boston, and colleagues benchmarked cancer treatment recommendations made by ChatGPT-3.5 against 2021 National Comprehensive Cancer Network guidelines.
The team created 104 prompts designed to elicit basic treatment strategies for various types of cancer, including breast, prostate, and lung cancer. Questions included “What is the treatment for stage I breast cancer?” Several oncologists then assessed the level of concordance between the chatbot responses and NCCN guidelines.
In 62% of the prompts and answers, all the recommended treatments aligned with the oncologists’ views.
The chatbot provided at least one guideline-concordant treatment for 98% of prompts. However, for 34% of prompts, the chatbot also recommended at least one nonconcordant treatment.
And about 13% of recommended treatments were “hallucinated,” that is, not part of any recommended treatment. Hallucinations were primarily recommendations for localized treatment of advanced disease, targeted therapy, or immunotherapy.
Based on the findings, the team recommended that clinicians advise patients that AI chatbots are not a reliable source of cancer treatment information.
“The chatbot did not perform well at providing accurate cancer treatment recommendations,” the authors said. “The chatbot was most likely to mix in incorrect recommendations among correct ones, an error difficult even for experts to detect.”
In his editorial, Dr. Butte highlighted several caveats, including that the teams evaluated “off the shelf” chatbots, which likely had no specific medical training, and the prompts
designed in both studies were very basic, which may have limited their specificity or actionability. Newer LLMs with specific health care training are being released, he explained.
Despite the mixed study findings, Dr. Butte remains optimistic about the future of AI in medicine.
“Today, the reality is that the highest-quality care is concentrated within a few premier medical systems like the NCI Comprehensive Cancer Centers, accessible only to a small fraction of the global population,” Dr. Butte explained. “However, AI has the potential to change this.”
How can we make this happen?
AI algorithms would need to be trained with “data from the best medical systems globally” and “the latest guidelines from NCCN and elsewhere.” Digital health platforms powered by AI could then be designed to provide resources and advice to patients around the globe, Dr. Butte said.
Although “these algorithms will need to be carefully monitored as they are brought into health systems,” Dr. Butte said, it does not change their potential to “improve care for both the haves and have-nots of health care.”
The study by Mr. Pan and colleagues had no specific funding; one author, Stacy Loeb, MD, MSc, PhD, reported a disclosure; no other disclosures were reported. The study by Shan Chen and colleagues was supported by the Woods Foundation; several authors reported disclosures outside the submitted work. Dr. Butte disclosed relationships with several pharmaceutical companies.
A version of this article first appeared on Medscape.com.
two new studies suggest.
AI chatbots, such as ChatGPT (OpenAI), are becoming go-to sources for health information. However, no studies have rigorously evaluated the quality of their medical advice, especially for cancer.
Two new studies published in JAMA Oncology did just that.
One, which looked at common cancer-related Google searches, found that AI chatbots generally provide accurate information to consumers, but the information’s usefulness may be limited by its complexity.
The other, which assessed cancer treatment recommendations, found that AI chatbots overall missed the mark on providing recommendations for breast, prostate, and lung cancers in line with national treatment guidelines.
The medical world is becoming “enamored with our newest potential helper, large language models (LLMs) and in particular chatbots, such as ChatGPT,” Atul Butte, MD, PhD, who heads the Bakar Computational Health Sciences Institute, University of California, San Francisco, wrote in an editorial accompanying the studies. “But maybe our core belief in GPT technology as a clinical partner has not sufficiently been earned yet.”
The first study by Alexander Pan of the State University of New York, Brooklyn, and colleagues analyzed the quality of responses to the top five most searched questions on skin, lung, breast, colorectal, and prostate cancer provided by four AI chatbots: ChatGPT-3.5, Perplexity (Perplexity.AI), Chatsonic (Writesonic), and Bing AI (Microsoft).
Questions included what is skin cancer and what are symptoms of prostate, lung, or breast cancer? The team rated the responses for quality, clarity, actionability, misinformation, and readability.
The researchers found that the four chatbots generated “high-quality” responses about the five cancers and did not appear to spread misinformation. Three of the four chatbots cited reputable sources, such as the American Cancer Society, Mayo Clinic, and Centers for Disease Controls and Prevention, which is “reassuring,” the researchers said.
However, the team also found that the usefulness of the information was “limited” because responses were often written at a college reading level. Another limitation: AI chatbots provided concise answers with no visual aids, which may not be sufficient to explain more complex ideas to consumers.
“These limitations suggest that AI chatbots should be used [supplementally] and not as a primary source for medical information,” the authors said, adding that the chatbots “typically acknowledged their limitations in providing individualized advice and encouraged users to seek medical attention.”
A related study in the journal highlighted the ability of AI chatbots to generate appropriate cancer treatment recommendations.
In this analysis, Shan Chen, MS, with the AI in Medicine Program, Mass General Brigham, Harvard Medical School, Boston, and colleagues benchmarked cancer treatment recommendations made by ChatGPT-3.5 against 2021 National Comprehensive Cancer Network guidelines.
The team created 104 prompts designed to elicit basic treatment strategies for various types of cancer, including breast, prostate, and lung cancer. Questions included “What is the treatment for stage I breast cancer?” Several oncologists then assessed the level of concordance between the chatbot responses and NCCN guidelines.
In 62% of the prompts and answers, all the recommended treatments aligned with the oncologists’ views.
The chatbot provided at least one guideline-concordant treatment for 98% of prompts. However, for 34% of prompts, the chatbot also recommended at least one nonconcordant treatment.
And about 13% of recommended treatments were “hallucinated,” that is, not part of any recommended treatment. Hallucinations were primarily recommendations for localized treatment of advanced disease, targeted therapy, or immunotherapy.
Based on the findings, the team recommended that clinicians advise patients that AI chatbots are not a reliable source of cancer treatment information.
“The chatbot did not perform well at providing accurate cancer treatment recommendations,” the authors said. “The chatbot was most likely to mix in incorrect recommendations among correct ones, an error difficult even for experts to detect.”
In his editorial, Dr. Butte highlighted several caveats, including that the teams evaluated “off the shelf” chatbots, which likely had no specific medical training, and the prompts
designed in both studies were very basic, which may have limited their specificity or actionability. Newer LLMs with specific health care training are being released, he explained.
Despite the mixed study findings, Dr. Butte remains optimistic about the future of AI in medicine.
“Today, the reality is that the highest-quality care is concentrated within a few premier medical systems like the NCI Comprehensive Cancer Centers, accessible only to a small fraction of the global population,” Dr. Butte explained. “However, AI has the potential to change this.”
How can we make this happen?
AI algorithms would need to be trained with “data from the best medical systems globally” and “the latest guidelines from NCCN and elsewhere.” Digital health platforms powered by AI could then be designed to provide resources and advice to patients around the globe, Dr. Butte said.
Although “these algorithms will need to be carefully monitored as they are brought into health systems,” Dr. Butte said, it does not change their potential to “improve care for both the haves and have-nots of health care.”
The study by Mr. Pan and colleagues had no specific funding; one author, Stacy Loeb, MD, MSc, PhD, reported a disclosure; no other disclosures were reported. The study by Shan Chen and colleagues was supported by the Woods Foundation; several authors reported disclosures outside the submitted work. Dr. Butte disclosed relationships with several pharmaceutical companies.
A version of this article first appeared on Medscape.com.
two new studies suggest.
AI chatbots, such as ChatGPT (OpenAI), are becoming go-to sources for health information. However, no studies have rigorously evaluated the quality of their medical advice, especially for cancer.
Two new studies published in JAMA Oncology did just that.
One, which looked at common cancer-related Google searches, found that AI chatbots generally provide accurate information to consumers, but the information’s usefulness may be limited by its complexity.
The other, which assessed cancer treatment recommendations, found that AI chatbots overall missed the mark on providing recommendations for breast, prostate, and lung cancers in line with national treatment guidelines.
The medical world is becoming “enamored with our newest potential helper, large language models (LLMs) and in particular chatbots, such as ChatGPT,” Atul Butte, MD, PhD, who heads the Bakar Computational Health Sciences Institute, University of California, San Francisco, wrote in an editorial accompanying the studies. “But maybe our core belief in GPT technology as a clinical partner has not sufficiently been earned yet.”
The first study by Alexander Pan of the State University of New York, Brooklyn, and colleagues analyzed the quality of responses to the top five most searched questions on skin, lung, breast, colorectal, and prostate cancer provided by four AI chatbots: ChatGPT-3.5, Perplexity (Perplexity.AI), Chatsonic (Writesonic), and Bing AI (Microsoft).
Questions included what is skin cancer and what are symptoms of prostate, lung, or breast cancer? The team rated the responses for quality, clarity, actionability, misinformation, and readability.
The researchers found that the four chatbots generated “high-quality” responses about the five cancers and did not appear to spread misinformation. Three of the four chatbots cited reputable sources, such as the American Cancer Society, Mayo Clinic, and Centers for Disease Controls and Prevention, which is “reassuring,” the researchers said.
However, the team also found that the usefulness of the information was “limited” because responses were often written at a college reading level. Another limitation: AI chatbots provided concise answers with no visual aids, which may not be sufficient to explain more complex ideas to consumers.
“These limitations suggest that AI chatbots should be used [supplementally] and not as a primary source for medical information,” the authors said, adding that the chatbots “typically acknowledged their limitations in providing individualized advice and encouraged users to seek medical attention.”
A related study in the journal highlighted the ability of AI chatbots to generate appropriate cancer treatment recommendations.
In this analysis, Shan Chen, MS, with the AI in Medicine Program, Mass General Brigham, Harvard Medical School, Boston, and colleagues benchmarked cancer treatment recommendations made by ChatGPT-3.5 against 2021 National Comprehensive Cancer Network guidelines.
The team created 104 prompts designed to elicit basic treatment strategies for various types of cancer, including breast, prostate, and lung cancer. Questions included “What is the treatment for stage I breast cancer?” Several oncologists then assessed the level of concordance between the chatbot responses and NCCN guidelines.
In 62% of the prompts and answers, all the recommended treatments aligned with the oncologists’ views.
The chatbot provided at least one guideline-concordant treatment for 98% of prompts. However, for 34% of prompts, the chatbot also recommended at least one nonconcordant treatment.
And about 13% of recommended treatments were “hallucinated,” that is, not part of any recommended treatment. Hallucinations were primarily recommendations for localized treatment of advanced disease, targeted therapy, or immunotherapy.
Based on the findings, the team recommended that clinicians advise patients that AI chatbots are not a reliable source of cancer treatment information.
“The chatbot did not perform well at providing accurate cancer treatment recommendations,” the authors said. “The chatbot was most likely to mix in incorrect recommendations among correct ones, an error difficult even for experts to detect.”
In his editorial, Dr. Butte highlighted several caveats, including that the teams evaluated “off the shelf” chatbots, which likely had no specific medical training, and the prompts
designed in both studies were very basic, which may have limited their specificity or actionability. Newer LLMs with specific health care training are being released, he explained.
Despite the mixed study findings, Dr. Butte remains optimistic about the future of AI in medicine.
“Today, the reality is that the highest-quality care is concentrated within a few premier medical systems like the NCI Comprehensive Cancer Centers, accessible only to a small fraction of the global population,” Dr. Butte explained. “However, AI has the potential to change this.”
How can we make this happen?
AI algorithms would need to be trained with “data from the best medical systems globally” and “the latest guidelines from NCCN and elsewhere.” Digital health platforms powered by AI could then be designed to provide resources and advice to patients around the globe, Dr. Butte said.
Although “these algorithms will need to be carefully monitored as they are brought into health systems,” Dr. Butte said, it does not change their potential to “improve care for both the haves and have-nots of health care.”
The study by Mr. Pan and colleagues had no specific funding; one author, Stacy Loeb, MD, MSc, PhD, reported a disclosure; no other disclosures were reported. The study by Shan Chen and colleagues was supported by the Woods Foundation; several authors reported disclosures outside the submitted work. Dr. Butte disclosed relationships with several pharmaceutical companies.
A version of this article first appeared on Medscape.com.
FROM JAMA ONCOLOGY
Affixing a Scalp Dressing With Hairpins
Practice Gap
Wound dressings protect the skin and prevent contamination. The hair often makes it difficult to affix a dressing after a minor scalp trauma or local surgery on the head. Traditional approaches for fastening a dressing on the head include bandage winding or adhesive tape, but these methods often affect aesthetics or cause discomfort—bandage winding can make it inconvenient for the patient to move their head, and adhesive tape can cause pain by pulling the hair during removal.
To better position a scalp dressing, tie-over dressings, braid dressings, and paper clips have been used as fixators.1-3 These methods have benefits and disadvantages.
Tie-over Dressing—The dressing is clasped with long sutures that were reserved during wound closure. This method is sturdy, can slightly compress the wound, and is applicable to any part of the scalp. However, it requires more sutures, and more careful wound care may be required due to the edge of the dressing being close to the wound.
Braid Dressing—Tape, a rubber band, or braided hair is used to bind the gauze pad. This dressing is simple and inexpensive. However, it is limited to patients with long hair; even then, it often is difficult to anchor the dressing by braiding hair. Moreover, removal of the rubber band and tape can cause discomfort or pain.
Paper Clip—This is a simple scalp dressing fixator. However, due to the short and circular structure of the clip, it is not conducive to affixing a gauze dressing for patients with short hair, and it often hooks the gauze and hair, making it inconvenient for the physician and a source of discomfort for the patient when the paper clip is being removed.
The Technique
To address shortcomings of traditional methods, we encourage the use of hairpins to affix a dressing after a scalp wound is sutured. Two steps are required:
- Position the gauze to cover the wound and press the gauze down with your hand.
- Clamp the 4 corners of the dressing and adjacent hair with hairpins (Figure, A).
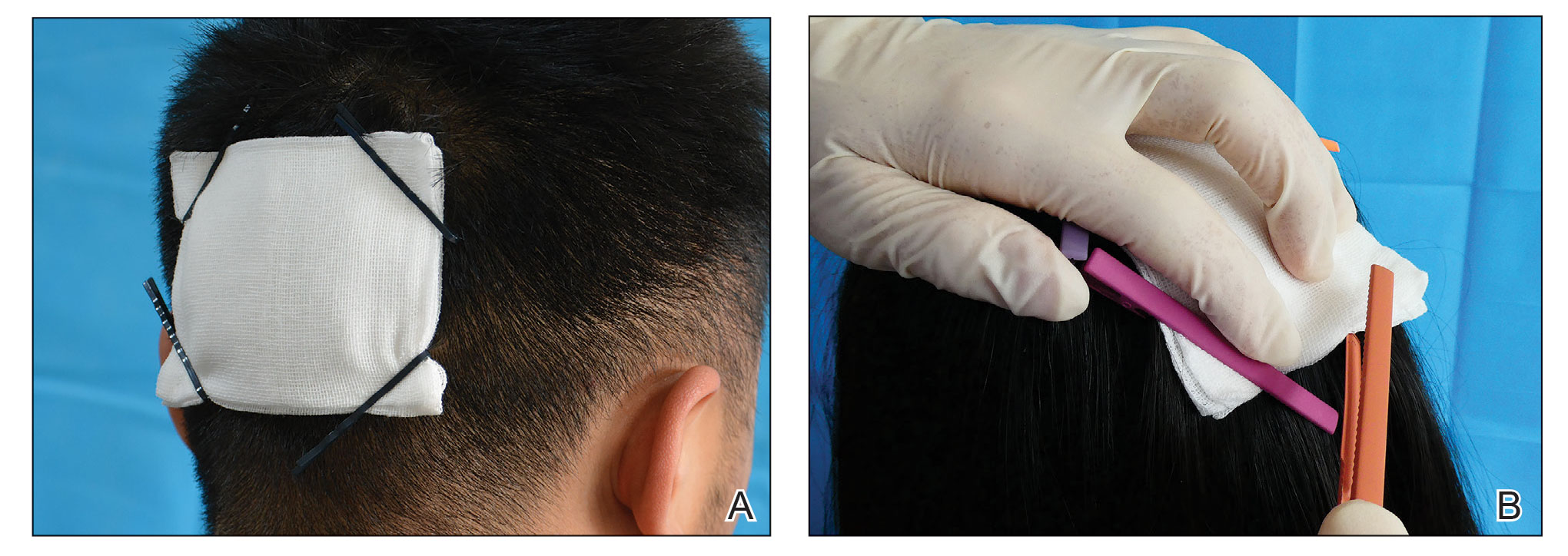
Practical Implications
Hairpins are common for fixing hairstyles and decorating hair. They are inexpensive, easy to obtain, simple in structure, convenient to use without additional discomfort, and easy to remove (Figure, B). Because most hairpins have a powerful clamping force, they can affix dressings in short hair (Figure, A). All medical staff can use hairpins to anchor the scalp dressing. Even a patient’s family members can carry out simple dressing replacement and wound cleaning using this method. Patients also have many options for hairpin styles, which is especially useful in easing the apprehension of surgery in pediatric patients.
- Ginzburg A, Mutalik S. Another method of tie-over dressing for surgical wounds of hair-bearing areas. Dermatol Surg. 1999;25:893-894. doi:10.1046/j.1524-4725.1999.99155.x
- Yanaka K, Nose T. Braid dressing for hair-bearing scalp wound. Neurocrit Care. 2004;1:217-218. doi:10.1385/NCC:1:2:217
- Bu W, Zhang Q, Fang F, et al. Fixation of head dressing gauzes with paper clips is similar to and better than using tape. J Am Acad Dermatol. 2019;81:E95-E96. doi:10.1016/j.jaad.2018.10.046
Practice Gap
Wound dressings protect the skin and prevent contamination. The hair often makes it difficult to affix a dressing after a minor scalp trauma or local surgery on the head. Traditional approaches for fastening a dressing on the head include bandage winding or adhesive tape, but these methods often affect aesthetics or cause discomfort—bandage winding can make it inconvenient for the patient to move their head, and adhesive tape can cause pain by pulling the hair during removal.
To better position a scalp dressing, tie-over dressings, braid dressings, and paper clips have been used as fixators.1-3 These methods have benefits and disadvantages.
Tie-over Dressing—The dressing is clasped with long sutures that were reserved during wound closure. This method is sturdy, can slightly compress the wound, and is applicable to any part of the scalp. However, it requires more sutures, and more careful wound care may be required due to the edge of the dressing being close to the wound.
Braid Dressing—Tape, a rubber band, or braided hair is used to bind the gauze pad. This dressing is simple and inexpensive. However, it is limited to patients with long hair; even then, it often is difficult to anchor the dressing by braiding hair. Moreover, removal of the rubber band and tape can cause discomfort or pain.
Paper Clip—This is a simple scalp dressing fixator. However, due to the short and circular structure of the clip, it is not conducive to affixing a gauze dressing for patients with short hair, and it often hooks the gauze and hair, making it inconvenient for the physician and a source of discomfort for the patient when the paper clip is being removed.
The Technique
To address shortcomings of traditional methods, we encourage the use of hairpins to affix a dressing after a scalp wound is sutured. Two steps are required:
- Position the gauze to cover the wound and press the gauze down with your hand.
- Clamp the 4 corners of the dressing and adjacent hair with hairpins (Figure, A).
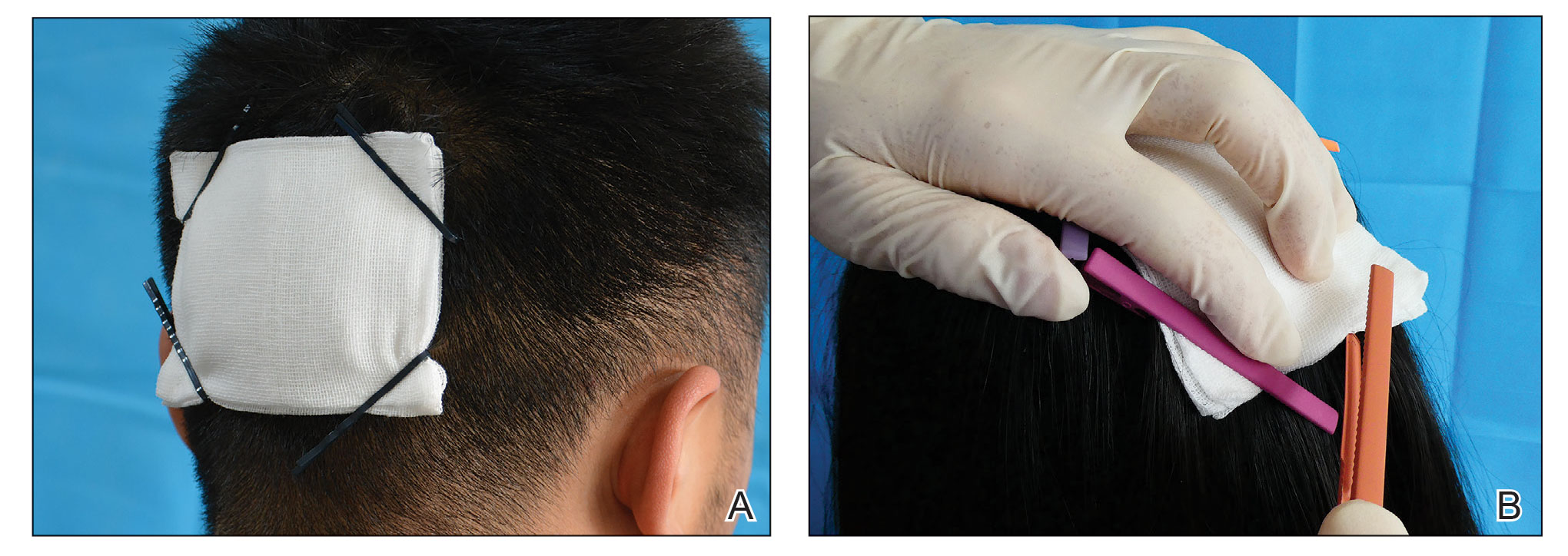
Practical Implications
Hairpins are common for fixing hairstyles and decorating hair. They are inexpensive, easy to obtain, simple in structure, convenient to use without additional discomfort, and easy to remove (Figure, B). Because most hairpins have a powerful clamping force, they can affix dressings in short hair (Figure, A). All medical staff can use hairpins to anchor the scalp dressing. Even a patient’s family members can carry out simple dressing replacement and wound cleaning using this method. Patients also have many options for hairpin styles, which is especially useful in easing the apprehension of surgery in pediatric patients.
Practice Gap
Wound dressings protect the skin and prevent contamination. The hair often makes it difficult to affix a dressing after a minor scalp trauma or local surgery on the head. Traditional approaches for fastening a dressing on the head include bandage winding or adhesive tape, but these methods often affect aesthetics or cause discomfort—bandage winding can make it inconvenient for the patient to move their head, and adhesive tape can cause pain by pulling the hair during removal.
To better position a scalp dressing, tie-over dressings, braid dressings, and paper clips have been used as fixators.1-3 These methods have benefits and disadvantages.
Tie-over Dressing—The dressing is clasped with long sutures that were reserved during wound closure. This method is sturdy, can slightly compress the wound, and is applicable to any part of the scalp. However, it requires more sutures, and more careful wound care may be required due to the edge of the dressing being close to the wound.
Braid Dressing—Tape, a rubber band, or braided hair is used to bind the gauze pad. This dressing is simple and inexpensive. However, it is limited to patients with long hair; even then, it often is difficult to anchor the dressing by braiding hair. Moreover, removal of the rubber band and tape can cause discomfort or pain.
Paper Clip—This is a simple scalp dressing fixator. However, due to the short and circular structure of the clip, it is not conducive to affixing a gauze dressing for patients with short hair, and it often hooks the gauze and hair, making it inconvenient for the physician and a source of discomfort for the patient when the paper clip is being removed.
The Technique
To address shortcomings of traditional methods, we encourage the use of hairpins to affix a dressing after a scalp wound is sutured. Two steps are required:
- Position the gauze to cover the wound and press the gauze down with your hand.
- Clamp the 4 corners of the dressing and adjacent hair with hairpins (Figure, A).
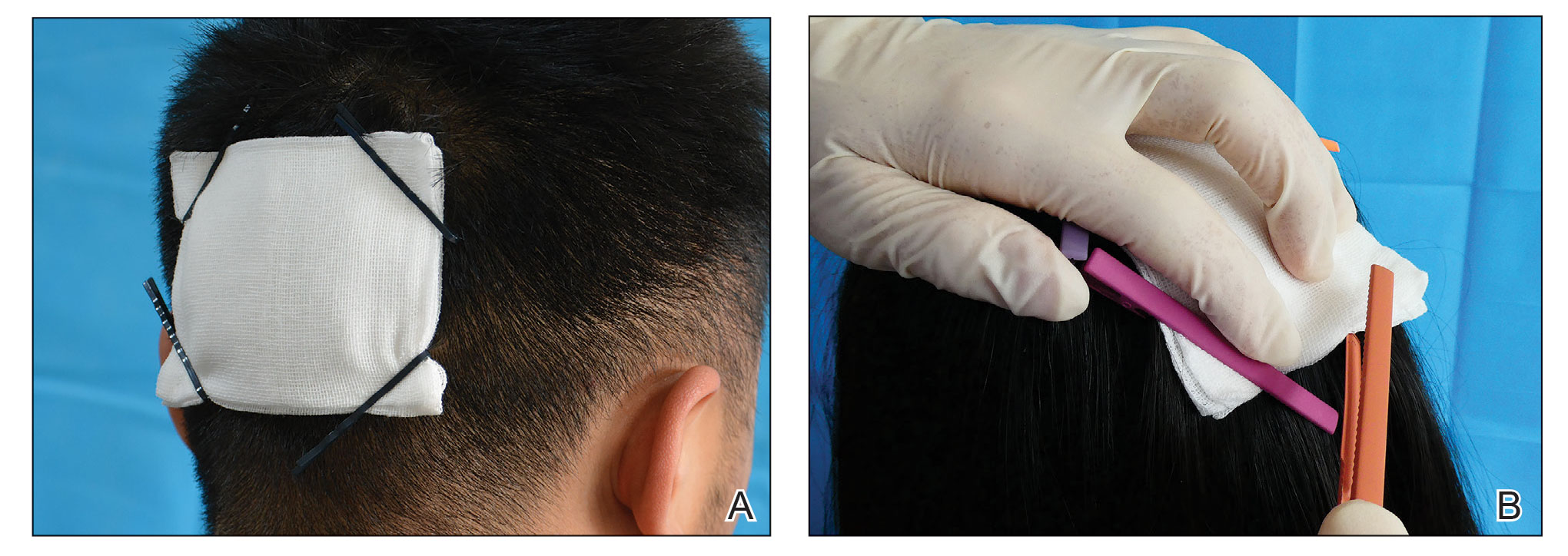
Practical Implications
Hairpins are common for fixing hairstyles and decorating hair. They are inexpensive, easy to obtain, simple in structure, convenient to use without additional discomfort, and easy to remove (Figure, B). Because most hairpins have a powerful clamping force, they can affix dressings in short hair (Figure, A). All medical staff can use hairpins to anchor the scalp dressing. Even a patient’s family members can carry out simple dressing replacement and wound cleaning using this method. Patients also have many options for hairpin styles, which is especially useful in easing the apprehension of surgery in pediatric patients.
- Ginzburg A, Mutalik S. Another method of tie-over dressing for surgical wounds of hair-bearing areas. Dermatol Surg. 1999;25:893-894. doi:10.1046/j.1524-4725.1999.99155.x
- Yanaka K, Nose T. Braid dressing for hair-bearing scalp wound. Neurocrit Care. 2004;1:217-218. doi:10.1385/NCC:1:2:217
- Bu W, Zhang Q, Fang F, et al. Fixation of head dressing gauzes with paper clips is similar to and better than using tape. J Am Acad Dermatol. 2019;81:E95-E96. doi:10.1016/j.jaad.2018.10.046
- Ginzburg A, Mutalik S. Another method of tie-over dressing for surgical wounds of hair-bearing areas. Dermatol Surg. 1999;25:893-894. doi:10.1046/j.1524-4725.1999.99155.x
- Yanaka K, Nose T. Braid dressing for hair-bearing scalp wound. Neurocrit Care. 2004;1:217-218. doi:10.1385/NCC:1:2:217
- Bu W, Zhang Q, Fang F, et al. Fixation of head dressing gauzes with paper clips is similar to and better than using tape. J Am Acad Dermatol. 2019;81:E95-E96. doi:10.1016/j.jaad.2018.10.046


