User login
Genetic signature helps identify those at risk of MS
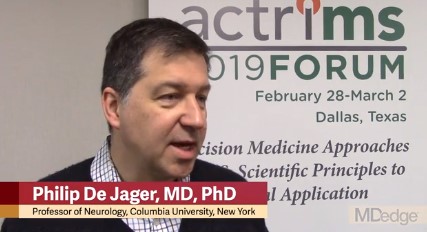
DALLAS – in a precision medicine–focused session at the meeting of the Americas Committee on Treatment and Research in Multiple Sclerosis.
“MS remains a diagnosis of exclusion ... But we’re now beginning to understand a lot more about the earliest stages of the disease, and we’re constantly redefining the disease in terms of when it starts, and what it consists of,” said Dr. De Jager, professor of neurology and chief of neuroimmunology at Columbia University, New York, in an interview.
For example, physicians are now starting to treat asymptomatic individuals with radiologically isolated syndrome, he said. “Is that part of the disease? Well, a lot of us think so, and we’re currently doing the studies to see whether treating them has an impact on long-term disability.”
“In this effort to redefine this disease and when it starts, these molecular and cellular studies are becoming very important,” Dr. De Jager said. Both individuals in the general population and high-risk individuals, such as family members of people with MS, will benefit from these research approaches, he said.
Right now, it’s hard to know who could benefit most from future preventive therapies, or who should have the most rigorous surveillance.
Dr. De Jager pointed to a presentation by his collaborator, Nikolaos Patsopoulos, MD, PhD, of Brigham and Women’s Hospital, Boston, who reported on the activities of the International MS Genetics Consortium. The consortium has collected and is nearing publication of data from more than 45,000 people with MS and 65,000 control participants to identify the genetic architecture of MS onset.
“We’re going to be reporting that there are over 234 genetic variations” that contribute to the onset of MS, Dr. De Jager said. “There are more to be found, but that’s a large number,” he said. The data point toward a genetic fingerprint that’s close to lupus, type 1 diabetes, and other inflammatory diseases. This shared genetic architecture means that there’s overlapping susceptibility for many diseases in this spectrum.
DALLAS – in a precision medicine–focused session at the meeting of the Americas Committee on Treatment and Research in Multiple Sclerosis.
“MS remains a diagnosis of exclusion ... But we’re now beginning to understand a lot more about the earliest stages of the disease, and we’re constantly redefining the disease in terms of when it starts, and what it consists of,” said Dr. De Jager, professor of neurology and chief of neuroimmunology at Columbia University, New York, in an interview.
For example, physicians are now starting to treat asymptomatic individuals with radiologically isolated syndrome, he said. “Is that part of the disease? Well, a lot of us think so, and we’re currently doing the studies to see whether treating them has an impact on long-term disability.”
“In this effort to redefine this disease and when it starts, these molecular and cellular studies are becoming very important,” Dr. De Jager said. Both individuals in the general population and high-risk individuals, such as family members of people with MS, will benefit from these research approaches, he said.
Right now, it’s hard to know who could benefit most from future preventive therapies, or who should have the most rigorous surveillance.
Dr. De Jager pointed to a presentation by his collaborator, Nikolaos Patsopoulos, MD, PhD, of Brigham and Women’s Hospital, Boston, who reported on the activities of the International MS Genetics Consortium. The consortium has collected and is nearing publication of data from more than 45,000 people with MS and 65,000 control participants to identify the genetic architecture of MS onset.
“We’re going to be reporting that there are over 234 genetic variations” that contribute to the onset of MS, Dr. De Jager said. “There are more to be found, but that’s a large number,” he said. The data point toward a genetic fingerprint that’s close to lupus, type 1 diabetes, and other inflammatory diseases. This shared genetic architecture means that there’s overlapping susceptibility for many diseases in this spectrum.
DALLAS – in a precision medicine–focused session at the meeting of the Americas Committee on Treatment and Research in Multiple Sclerosis.
“MS remains a diagnosis of exclusion ... But we’re now beginning to understand a lot more about the earliest stages of the disease, and we’re constantly redefining the disease in terms of when it starts, and what it consists of,” said Dr. De Jager, professor of neurology and chief of neuroimmunology at Columbia University, New York, in an interview.
For example, physicians are now starting to treat asymptomatic individuals with radiologically isolated syndrome, he said. “Is that part of the disease? Well, a lot of us think so, and we’re currently doing the studies to see whether treating them has an impact on long-term disability.”
“In this effort to redefine this disease and when it starts, these molecular and cellular studies are becoming very important,” Dr. De Jager said. Both individuals in the general population and high-risk individuals, such as family members of people with MS, will benefit from these research approaches, he said.
Right now, it’s hard to know who could benefit most from future preventive therapies, or who should have the most rigorous surveillance.
Dr. De Jager pointed to a presentation by his collaborator, Nikolaos Patsopoulos, MD, PhD, of Brigham and Women’s Hospital, Boston, who reported on the activities of the International MS Genetics Consortium. The consortium has collected and is nearing publication of data from more than 45,000 people with MS and 65,000 control participants to identify the genetic architecture of MS onset.
“We’re going to be reporting that there are over 234 genetic variations” that contribute to the onset of MS, Dr. De Jager said. “There are more to be found, but that’s a large number,” he said. The data point toward a genetic fingerprint that’s close to lupus, type 1 diabetes, and other inflammatory diseases. This shared genetic architecture means that there’s overlapping susceptibility for many diseases in this spectrum.
REPORTING FROM ACTRIMS FORUM 2019
Andexanet alfa effectively reverses factor Xa inhibition
HONOLULU – according to a study presented at the International Stroke Conference sponsored by the American Heart Association. The medication is associated with a low rate of mortality resulting from intracerebral hemorrhage (ICH), compared with the general population of patients with ICH receiving anticoagulation.
Factor Xa inhibitors such as apixaban and rivaroxaban effectively prevent thromboembolic events but may cause or exacerbate acute major bleeding. Andexanet alfa, a modified, recombinant, inactive form of human factor Xa, was developed and approved as a reversal agent for factor Xa inhibitors. In a 2015 study, andexanet rapidly and safely reversed anti–factor Xa activity in large cohorts of patients without bleeding.
A single-cohort study
Truman John Milling Jr., MD, an emergency medicine physician at Dell Seton Medical Center at the University of Texas in Austin, and his colleagues conducted the Andexanet Alfa, a Novel Antidote to the Anticoagulation Effects of Factor Xa Inhibitors (ANNEXA-4) study to evaluate the drug’s safety and efficacy in patients with acute major bleeding associated with treatment with a factor Xa inhibitor. For participants to be eligible, their bleeding had to be life threatening with signs of hemodynamic compromise, be associated with a decrease in hemoglobin level of at least 2 g/dL, or occur in a critical organ such as the brain. An independent academic committee determined whether patients met these criteria.
The trial’s primary efficacy outcomes were change from baseline in anti–factor Xa activity and the percentage of patients with excellent or good hemostatic efficacy at 12 hours. The primary safety endpoints were death, thrombotic events, and the development of neutralizing antibodies to andexanet or to native factor X and factor Xa. The efficacy population included patients with major bleeding and baseline anti–factor Xa activity of at least 75 ng/mL. The safety population included all patients who received a dose of andexanet. The independent committee adjudicated the efficacy and safety outcomes.
Hemostasis was sustained for 12 hours
The investigators enrolled 352 participants into the study, all of whom received andexanet and were followed for at least 30 days or until death. The population’s mean age was 77 years. “These were older and sicker patients with a significant amount of comorbid disease,” said Dr. Milling. The primary indication for anticoagulation was atrial fibrillation in 80% of patients. The primary site of bleeding was intracranial in 64% of patients and gastrointestinal in 26% of patients. The remaining 10% of patients had bleeding affecting other areas (such as pericardial or intramuscular bleeding).
The investigators included 254 patients in the efficacy population. At the end of the administration of the andexanet bolus, the median value for anti–factor Xa activity decreased by 92% among participants receiving apixaban, 92% among participants receiving rivaroxaban, and 75% among patients receiving enoxaparin. Among patients receiving apixaban, the median value for anti–factor Xa activity was decreased by 32% at 4 hours, 34% at 8 hours, and 38% at 12 hours. Among patients receiving rivaroxaban, the median value for anti–factor Xa activity was decreased by 42% at 4 hours, 48% at 8 hours, and 62% at 12 hours.
Dr. Milling and his colleagues assessed hemostatic efficacy in 249 patients. Of this group, 82% achieved good or excellent hemostasis. Among participants with good or excellent hemostasis, 84% had excellent results, and 16% had good results. Subanalysis by factor Xa inhibitor, type of bleed, age, and dose of andexanet did not alter the findings significantly.
To determine whether hemostasis had been sustained sufficiently to prevent clinical deterioration, the investigators examined 71 patients with ICH and a single-compartment bleed. From 1 hour to 12 hours, one patient’s outcome changed from excellent/good to poor/none, and one patient’s outcome changed from excellent to good. For the majority of these patients, however, good hemostasis was sustained from 1 to 12 hours.
The rate of thromboembolic events was 9.7%, which is in the expected range for this population, said Dr. Milling. These events were distributed evenly among the 4 weeks of the study. Stroke and deep vein thrombosis accounted for most of these events, and pulmonary emboli and heart attacks occurred as well. “Once we restarted oral anticoagulation ... there were no more thrombotic events,” said Dr. Milling. No patient developed neutralizing antibodies to factor X or factor Xa, nor did any patient develop neutralizing antibodies to andexanet.
The overall mortality rate was 13.9%. The rate of mortality resulting from ICH was 15%, and the rate of mortality resulting from gastrointestinal bleeding was 11%. These results are impressive, considering that patients had received anticoagulants, said Dr. Milling.
Portola Pharmaceuticals, the maker of andexanet alfa, funded the study. Dr. Milling reported receiving funding and honoraria from the Population Health Research Institute at McMasters University, Janssen, CSL Behring, and Octapharma. He also received a small research payment from Portola Pharmaceuticals. Several of the investigators reported receiving funding from Portola Pharmaceuticals.
SOURCE: Milling TJ et al. ISC 2019, Abstract LB7.
HONOLULU – according to a study presented at the International Stroke Conference sponsored by the American Heart Association. The medication is associated with a low rate of mortality resulting from intracerebral hemorrhage (ICH), compared with the general population of patients with ICH receiving anticoagulation.
Factor Xa inhibitors such as apixaban and rivaroxaban effectively prevent thromboembolic events but may cause or exacerbate acute major bleeding. Andexanet alfa, a modified, recombinant, inactive form of human factor Xa, was developed and approved as a reversal agent for factor Xa inhibitors. In a 2015 study, andexanet rapidly and safely reversed anti–factor Xa activity in large cohorts of patients without bleeding.
A single-cohort study
Truman John Milling Jr., MD, an emergency medicine physician at Dell Seton Medical Center at the University of Texas in Austin, and his colleagues conducted the Andexanet Alfa, a Novel Antidote to the Anticoagulation Effects of Factor Xa Inhibitors (ANNEXA-4) study to evaluate the drug’s safety and efficacy in patients with acute major bleeding associated with treatment with a factor Xa inhibitor. For participants to be eligible, their bleeding had to be life threatening with signs of hemodynamic compromise, be associated with a decrease in hemoglobin level of at least 2 g/dL, or occur in a critical organ such as the brain. An independent academic committee determined whether patients met these criteria.
The trial’s primary efficacy outcomes were change from baseline in anti–factor Xa activity and the percentage of patients with excellent or good hemostatic efficacy at 12 hours. The primary safety endpoints were death, thrombotic events, and the development of neutralizing antibodies to andexanet or to native factor X and factor Xa. The efficacy population included patients with major bleeding and baseline anti–factor Xa activity of at least 75 ng/mL. The safety population included all patients who received a dose of andexanet. The independent committee adjudicated the efficacy and safety outcomes.
Hemostasis was sustained for 12 hours
The investigators enrolled 352 participants into the study, all of whom received andexanet and were followed for at least 30 days or until death. The population’s mean age was 77 years. “These were older and sicker patients with a significant amount of comorbid disease,” said Dr. Milling. The primary indication for anticoagulation was atrial fibrillation in 80% of patients. The primary site of bleeding was intracranial in 64% of patients and gastrointestinal in 26% of patients. The remaining 10% of patients had bleeding affecting other areas (such as pericardial or intramuscular bleeding).
The investigators included 254 patients in the efficacy population. At the end of the administration of the andexanet bolus, the median value for anti–factor Xa activity decreased by 92% among participants receiving apixaban, 92% among participants receiving rivaroxaban, and 75% among patients receiving enoxaparin. Among patients receiving apixaban, the median value for anti–factor Xa activity was decreased by 32% at 4 hours, 34% at 8 hours, and 38% at 12 hours. Among patients receiving rivaroxaban, the median value for anti–factor Xa activity was decreased by 42% at 4 hours, 48% at 8 hours, and 62% at 12 hours.
Dr. Milling and his colleagues assessed hemostatic efficacy in 249 patients. Of this group, 82% achieved good or excellent hemostasis. Among participants with good or excellent hemostasis, 84% had excellent results, and 16% had good results. Subanalysis by factor Xa inhibitor, type of bleed, age, and dose of andexanet did not alter the findings significantly.
To determine whether hemostasis had been sustained sufficiently to prevent clinical deterioration, the investigators examined 71 patients with ICH and a single-compartment bleed. From 1 hour to 12 hours, one patient’s outcome changed from excellent/good to poor/none, and one patient’s outcome changed from excellent to good. For the majority of these patients, however, good hemostasis was sustained from 1 to 12 hours.
The rate of thromboembolic events was 9.7%, which is in the expected range for this population, said Dr. Milling. These events were distributed evenly among the 4 weeks of the study. Stroke and deep vein thrombosis accounted for most of these events, and pulmonary emboli and heart attacks occurred as well. “Once we restarted oral anticoagulation ... there were no more thrombotic events,” said Dr. Milling. No patient developed neutralizing antibodies to factor X or factor Xa, nor did any patient develop neutralizing antibodies to andexanet.
The overall mortality rate was 13.9%. The rate of mortality resulting from ICH was 15%, and the rate of mortality resulting from gastrointestinal bleeding was 11%. These results are impressive, considering that patients had received anticoagulants, said Dr. Milling.
Portola Pharmaceuticals, the maker of andexanet alfa, funded the study. Dr. Milling reported receiving funding and honoraria from the Population Health Research Institute at McMasters University, Janssen, CSL Behring, and Octapharma. He also received a small research payment from Portola Pharmaceuticals. Several of the investigators reported receiving funding from Portola Pharmaceuticals.
SOURCE: Milling TJ et al. ISC 2019, Abstract LB7.
HONOLULU – according to a study presented at the International Stroke Conference sponsored by the American Heart Association. The medication is associated with a low rate of mortality resulting from intracerebral hemorrhage (ICH), compared with the general population of patients with ICH receiving anticoagulation.
Factor Xa inhibitors such as apixaban and rivaroxaban effectively prevent thromboembolic events but may cause or exacerbate acute major bleeding. Andexanet alfa, a modified, recombinant, inactive form of human factor Xa, was developed and approved as a reversal agent for factor Xa inhibitors. In a 2015 study, andexanet rapidly and safely reversed anti–factor Xa activity in large cohorts of patients without bleeding.
A single-cohort study
Truman John Milling Jr., MD, an emergency medicine physician at Dell Seton Medical Center at the University of Texas in Austin, and his colleagues conducted the Andexanet Alfa, a Novel Antidote to the Anticoagulation Effects of Factor Xa Inhibitors (ANNEXA-4) study to evaluate the drug’s safety and efficacy in patients with acute major bleeding associated with treatment with a factor Xa inhibitor. For participants to be eligible, their bleeding had to be life threatening with signs of hemodynamic compromise, be associated with a decrease in hemoglobin level of at least 2 g/dL, or occur in a critical organ such as the brain. An independent academic committee determined whether patients met these criteria.
The trial’s primary efficacy outcomes were change from baseline in anti–factor Xa activity and the percentage of patients with excellent or good hemostatic efficacy at 12 hours. The primary safety endpoints were death, thrombotic events, and the development of neutralizing antibodies to andexanet or to native factor X and factor Xa. The efficacy population included patients with major bleeding and baseline anti–factor Xa activity of at least 75 ng/mL. The safety population included all patients who received a dose of andexanet. The independent committee adjudicated the efficacy and safety outcomes.
Hemostasis was sustained for 12 hours
The investigators enrolled 352 participants into the study, all of whom received andexanet and were followed for at least 30 days or until death. The population’s mean age was 77 years. “These were older and sicker patients with a significant amount of comorbid disease,” said Dr. Milling. The primary indication for anticoagulation was atrial fibrillation in 80% of patients. The primary site of bleeding was intracranial in 64% of patients and gastrointestinal in 26% of patients. The remaining 10% of patients had bleeding affecting other areas (such as pericardial or intramuscular bleeding).
The investigators included 254 patients in the efficacy population. At the end of the administration of the andexanet bolus, the median value for anti–factor Xa activity decreased by 92% among participants receiving apixaban, 92% among participants receiving rivaroxaban, and 75% among patients receiving enoxaparin. Among patients receiving apixaban, the median value for anti–factor Xa activity was decreased by 32% at 4 hours, 34% at 8 hours, and 38% at 12 hours. Among patients receiving rivaroxaban, the median value for anti–factor Xa activity was decreased by 42% at 4 hours, 48% at 8 hours, and 62% at 12 hours.
Dr. Milling and his colleagues assessed hemostatic efficacy in 249 patients. Of this group, 82% achieved good or excellent hemostasis. Among participants with good or excellent hemostasis, 84% had excellent results, and 16% had good results. Subanalysis by factor Xa inhibitor, type of bleed, age, and dose of andexanet did not alter the findings significantly.
To determine whether hemostasis had been sustained sufficiently to prevent clinical deterioration, the investigators examined 71 patients with ICH and a single-compartment bleed. From 1 hour to 12 hours, one patient’s outcome changed from excellent/good to poor/none, and one patient’s outcome changed from excellent to good. For the majority of these patients, however, good hemostasis was sustained from 1 to 12 hours.
The rate of thromboembolic events was 9.7%, which is in the expected range for this population, said Dr. Milling. These events were distributed evenly among the 4 weeks of the study. Stroke and deep vein thrombosis accounted for most of these events, and pulmonary emboli and heart attacks occurred as well. “Once we restarted oral anticoagulation ... there were no more thrombotic events,” said Dr. Milling. No patient developed neutralizing antibodies to factor X or factor Xa, nor did any patient develop neutralizing antibodies to andexanet.
The overall mortality rate was 13.9%. The rate of mortality resulting from ICH was 15%, and the rate of mortality resulting from gastrointestinal bleeding was 11%. These results are impressive, considering that patients had received anticoagulants, said Dr. Milling.
Portola Pharmaceuticals, the maker of andexanet alfa, funded the study. Dr. Milling reported receiving funding and honoraria from the Population Health Research Institute at McMasters University, Janssen, CSL Behring, and Octapharma. He also received a small research payment from Portola Pharmaceuticals. Several of the investigators reported receiving funding from Portola Pharmaceuticals.
SOURCE: Milling TJ et al. ISC 2019, Abstract LB7.
REPORTING FROM ISC 2019
Through the eyes of migraine: Ocular considerations
STOWE, VT. – said Kathleen Digre, MD, at the annual meeting of the Headache Cooperative of New England. Specifically, she said, dry eye and photophobia are two symptoms that have biologic underpinnings, can be diagnosed, and can be treated. Dr. Digre is a professor of neurology and ophthalmology at the University of Utah, Salt Lake City, and is the current president of the American Headache Society.

Dr. Digre explained that dry eyes and migraine could have a cyclical relationship where dry eyes provoke the migraine, and the migraine may provoke the feeling of dry eye, regardless of whether it can be objectively measured.
Regarding photophobia, Dr. Digre stressed the importance of an accurate diagnosis that rules out eye disorders and other causes of photophobia. She discussed the problem of patient overreliance on dark glasses and encourages a return to light to break the cycle of dark adapting the retina.
Finally, Dr. Digre discussed how proper treatment of migraine and any associated anxiety or depression can help resolve eye issues that may be contributing to migraine.
STOWE, VT. – said Kathleen Digre, MD, at the annual meeting of the Headache Cooperative of New England. Specifically, she said, dry eye and photophobia are two symptoms that have biologic underpinnings, can be diagnosed, and can be treated. Dr. Digre is a professor of neurology and ophthalmology at the University of Utah, Salt Lake City, and is the current president of the American Headache Society.

Dr. Digre explained that dry eyes and migraine could have a cyclical relationship where dry eyes provoke the migraine, and the migraine may provoke the feeling of dry eye, regardless of whether it can be objectively measured.
Regarding photophobia, Dr. Digre stressed the importance of an accurate diagnosis that rules out eye disorders and other causes of photophobia. She discussed the problem of patient overreliance on dark glasses and encourages a return to light to break the cycle of dark adapting the retina.
Finally, Dr. Digre discussed how proper treatment of migraine and any associated anxiety or depression can help resolve eye issues that may be contributing to migraine.
STOWE, VT. – said Kathleen Digre, MD, at the annual meeting of the Headache Cooperative of New England. Specifically, she said, dry eye and photophobia are two symptoms that have biologic underpinnings, can be diagnosed, and can be treated. Dr. Digre is a professor of neurology and ophthalmology at the University of Utah, Salt Lake City, and is the current president of the American Headache Society.

Dr. Digre explained that dry eyes and migraine could have a cyclical relationship where dry eyes provoke the migraine, and the migraine may provoke the feeling of dry eye, regardless of whether it can be objectively measured.
Regarding photophobia, Dr. Digre stressed the importance of an accurate diagnosis that rules out eye disorders and other causes of photophobia. She discussed the problem of patient overreliance on dark glasses and encourages a return to light to break the cycle of dark adapting the retina.
Finally, Dr. Digre discussed how proper treatment of migraine and any associated anxiety or depression can help resolve eye issues that may be contributing to migraine.
REPORTING FROM HCNE STOWE 2019
CGRP drugs: How is it going?
STOWE, VT. – These are the early days of the “CGRP monoclonal antibody era,”

In an interview at the annual meeting of the Headache Cooperative of New England, Dr. McAllister said, “We are comforted that we have now 1-year, 3-year, and 5-year data” from clinical trials, but the sample size is small.
In the time since the first three drugs were approved, “we have probably in the ballpark of over 200,000 patients who have received a monoclonal antibody, and so far there has been nothing that makes us stop cold in our tracks and say there’s something wrong here. That is very comforting,” he said. Dr. McAllister is the medical director of the New England Institute for Neurology and Headache in Stamford, Conn.
What is still unknown, however, is the long-term safety and efficacy; what happens in a larger pool of patients taking these drugs; what happens in pregnancy and effects on the fetus; how and when to safely switch from one monoclonal antibody to another; the systemic effects of these drugs; and other concerns that may arise in postmarketing studies.
STOWE, VT. – These are the early days of the “CGRP monoclonal antibody era,”

In an interview at the annual meeting of the Headache Cooperative of New England, Dr. McAllister said, “We are comforted that we have now 1-year, 3-year, and 5-year data” from clinical trials, but the sample size is small.
In the time since the first three drugs were approved, “we have probably in the ballpark of over 200,000 patients who have received a monoclonal antibody, and so far there has been nothing that makes us stop cold in our tracks and say there’s something wrong here. That is very comforting,” he said. Dr. McAllister is the medical director of the New England Institute for Neurology and Headache in Stamford, Conn.
What is still unknown, however, is the long-term safety and efficacy; what happens in a larger pool of patients taking these drugs; what happens in pregnancy and effects on the fetus; how and when to safely switch from one monoclonal antibody to another; the systemic effects of these drugs; and other concerns that may arise in postmarketing studies.
STOWE, VT. – These are the early days of the “CGRP monoclonal antibody era,”

In an interview at the annual meeting of the Headache Cooperative of New England, Dr. McAllister said, “We are comforted that we have now 1-year, 3-year, and 5-year data” from clinical trials, but the sample size is small.
In the time since the first three drugs were approved, “we have probably in the ballpark of over 200,000 patients who have received a monoclonal antibody, and so far there has been nothing that makes us stop cold in our tracks and say there’s something wrong here. That is very comforting,” he said. Dr. McAllister is the medical director of the New England Institute for Neurology and Headache in Stamford, Conn.
What is still unknown, however, is the long-term safety and efficacy; what happens in a larger pool of patients taking these drugs; what happens in pregnancy and effects on the fetus; how and when to safely switch from one monoclonal antibody to another; the systemic effects of these drugs; and other concerns that may arise in postmarketing studies.
REPORTING FROM HCNE STOWE 2019
Which comorbidities most diminish quality of life in patients with MS?
DALLAS – (MS), according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. In addition, comorbidities account for about 18% of the variance in health-related quality of life, and a higher number of comorbidities correlates with lower health-related quality of life in a “clear dose–response” manner, the researchers said.
The “magnitude of effect emphasizes the need for recognition and appropriate management of comorbidities,” said presenting author Lara Marie Pangan Lo, a researcher at Menzies Institute for Medical Research at the University of Tasmania, Australia, and her research colleagues. “The individual effect sizes may assist with the prioritizing of comorbidities that require more or less aggressive treatment in order to minimize” their impact.
Prior studies have found that patients with MS have lower health-related quality of life, compared with the general population, and that comorbidities affect patients’ quality of life, but few studies have looked at the effects of individual comorbidities on quality of life, Ms. Lo and her colleagues said. To examine the total impact and relative importance of comorbidities on psychosocial, physical, and overall health-related quality of life in people with MS, the investigators analyzed survey data from 902 participants in the survey-based Australian MS Longitudinal Study. They used linear regression and dominance analysis to assess relationships between comorbidities and participants’ Assessment of Quality of Life-8 Dimensions scores, which can range from 0 (death) to 1 (perfect health).
The predicted health-related quality of life for patients without comorbidities was 0.74. After the researchers adjusted for age, sex, and education, they found that systemic lupus erythematosus (reported by 1.56% of patients), depression (41.25%), hyperthyroidism (3.01%), and anxiety (38.35%) were associated with the greatest estimated decreases in health-related quality of life (–0.16, –0.15, –0.12, and –0.11, respectively). Depression and anxiety had the largest effect on psychosocial health–related quality of life, whereas systemic lupus erythematosus, rheumatoid arthritis, and hyperthyroidism had the largest impact on physical health–related quality of life. Other comorbidities that significantly correlated with quality of life included osteoporosis, type 2 diabetes, migraine, and inflammatory bowel disease.
The study was supported by Multiple Sclerosis Research Australia. The authors had no relevant disclosures.
SOURCE: Lo LMP et al. ACTRIMS Forum 2019, Abstract 80.
DALLAS – (MS), according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. In addition, comorbidities account for about 18% of the variance in health-related quality of life, and a higher number of comorbidities correlates with lower health-related quality of life in a “clear dose–response” manner, the researchers said.
The “magnitude of effect emphasizes the need for recognition and appropriate management of comorbidities,” said presenting author Lara Marie Pangan Lo, a researcher at Menzies Institute for Medical Research at the University of Tasmania, Australia, and her research colleagues. “The individual effect sizes may assist with the prioritizing of comorbidities that require more or less aggressive treatment in order to minimize” their impact.
Prior studies have found that patients with MS have lower health-related quality of life, compared with the general population, and that comorbidities affect patients’ quality of life, but few studies have looked at the effects of individual comorbidities on quality of life, Ms. Lo and her colleagues said. To examine the total impact and relative importance of comorbidities on psychosocial, physical, and overall health-related quality of life in people with MS, the investigators analyzed survey data from 902 participants in the survey-based Australian MS Longitudinal Study. They used linear regression and dominance analysis to assess relationships between comorbidities and participants’ Assessment of Quality of Life-8 Dimensions scores, which can range from 0 (death) to 1 (perfect health).
The predicted health-related quality of life for patients without comorbidities was 0.74. After the researchers adjusted for age, sex, and education, they found that systemic lupus erythematosus (reported by 1.56% of patients), depression (41.25%), hyperthyroidism (3.01%), and anxiety (38.35%) were associated with the greatest estimated decreases in health-related quality of life (–0.16, –0.15, –0.12, and –0.11, respectively). Depression and anxiety had the largest effect on psychosocial health–related quality of life, whereas systemic lupus erythematosus, rheumatoid arthritis, and hyperthyroidism had the largest impact on physical health–related quality of life. Other comorbidities that significantly correlated with quality of life included osteoporosis, type 2 diabetes, migraine, and inflammatory bowel disease.
The study was supported by Multiple Sclerosis Research Australia. The authors had no relevant disclosures.
SOURCE: Lo LMP et al. ACTRIMS Forum 2019, Abstract 80.
DALLAS – (MS), according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. In addition, comorbidities account for about 18% of the variance in health-related quality of life, and a higher number of comorbidities correlates with lower health-related quality of life in a “clear dose–response” manner, the researchers said.
The “magnitude of effect emphasizes the need for recognition and appropriate management of comorbidities,” said presenting author Lara Marie Pangan Lo, a researcher at Menzies Institute for Medical Research at the University of Tasmania, Australia, and her research colleagues. “The individual effect sizes may assist with the prioritizing of comorbidities that require more or less aggressive treatment in order to minimize” their impact.
Prior studies have found that patients with MS have lower health-related quality of life, compared with the general population, and that comorbidities affect patients’ quality of life, but few studies have looked at the effects of individual comorbidities on quality of life, Ms. Lo and her colleagues said. To examine the total impact and relative importance of comorbidities on psychosocial, physical, and overall health-related quality of life in people with MS, the investigators analyzed survey data from 902 participants in the survey-based Australian MS Longitudinal Study. They used linear regression and dominance analysis to assess relationships between comorbidities and participants’ Assessment of Quality of Life-8 Dimensions scores, which can range from 0 (death) to 1 (perfect health).
The predicted health-related quality of life for patients without comorbidities was 0.74. After the researchers adjusted for age, sex, and education, they found that systemic lupus erythematosus (reported by 1.56% of patients), depression (41.25%), hyperthyroidism (3.01%), and anxiety (38.35%) were associated with the greatest estimated decreases in health-related quality of life (–0.16, –0.15, –0.12, and –0.11, respectively). Depression and anxiety had the largest effect on psychosocial health–related quality of life, whereas systemic lupus erythematosus, rheumatoid arthritis, and hyperthyroidism had the largest impact on physical health–related quality of life. Other comorbidities that significantly correlated with quality of life included osteoporosis, type 2 diabetes, migraine, and inflammatory bowel disease.
The study was supported by Multiple Sclerosis Research Australia. The authors had no relevant disclosures.
SOURCE: Lo LMP et al. ACTRIMS Forum 2019, Abstract 80.
REPORTING FROM ACTRIMS FORUM 2019
MI, strokes spike during 30 days after cancer diagnosis
HONOLULU – During the first month after a new cancer diagnosis, patients face a substantially elevated risk for an arterial thromboembolic event – an MI or stroke – consistent with the well-described increased risk newly diagnosed cancer patients face from venous thromboembolism, based on findings from a prospective study of more than 4,000 people.
In the new study, 836 patients newly diagnosed with cancer had a 480% increased rate of a fatal or nonfatal MI or stroke during the 30 days following their diagnosis, compared with 3,339 matched people without cancer and after adjustment for baseline differences in demographics and cardiovascular risk factors, Babak B. Navi, MD, said while presenting a poster at the International Stroke Conference sponsored by the American Heart Association.
An additional analysis that focused on 210 of the 836 patients with incident cancer who had any of seven of the cancers known to pose the highest venous thromboembolism risk (lymphoma; gynecologic cancer; or cancer of the pancreas, stomach, lung, bladder, or testes) showed an 1,750% greater rate of incident MI or stroke during the first 30 days after diagnosis, compared with matched people without cancer, reported Dr. Navi, chief of the stroke and hospital neurology at Weill Cornell Medicine, New York.
In contrast, during both the period 1-3 months after the cancer diagnosis and more than 3 months after, the rate of MI or stroke among recently diagnosed cancer patients was not significantly different from the rate in comparator individuals, although the data showed modest trends toward more arterial thromboembolic events after a month, and the lack of statistically significant differences may have been a power issue, Dr. Navi suggested.
The reasons for this acutely increased risk for arterial thromboembolic events, as well as the early spike in venous thromboembolic events, are not completely clear, but they likely result from factors released by tumors, effects from the drugs that patients receive for cancer treatment, stress, and interruption of antithrombotic treatment. Dr. Navi fingered cancer-induced hypercoagulability as likely the biggest culprit. It may now be reasonable to test the idea of treating newly diagnosed cancer patients with agents that could reduce their risk for MI or stroke, such as aspirin or a statin, he said in an interview.
The new analysis used data collected in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study, which during 2003-2007 enrolled more than 30,000 U.S. residents who were at least 45 years old. Dr. Navi and his associates used data collected from all REGARDS participants who developed incident cancer and had continuous Medicare coverage for at least 1 year before entering REGARDS, excluding those with cancer before enrollment. They used the Medicare records to identify the cancer diagnoses, and matched each of these people with four similar but cancer-free people enrolled in the study. Follow-up continued through September 2015. The average age of this REGARDS subgroup at enrollment was 72 years old, and nearly half were women. The incident cancers included 640 patients with a solid tumor, 71 with hematologic cancers, 13 with brain tumors, and 112 with an unknown primary cancer site.
Dr. Navi and his associates designed this study to validate previously reported findings of increased arterial thromboembolic events in newly diagnosed cancer patients from studies of insurance claims databases. Although the increased risk for venous thromboembolism in cancer patients is already well established, documenting a similar risk for arterial events is important because they are “generally more impactful for patients than venous thromboembolism,” Dr. Navi said.
REGARDS has received no commercial funding. Dr. Navi reported no disclosures.
SOURCE: Navi BB et al. Stroke. 2019 Feb;50(Suppl_1): Abstract WMP53.
HONOLULU – During the first month after a new cancer diagnosis, patients face a substantially elevated risk for an arterial thromboembolic event – an MI or stroke – consistent with the well-described increased risk newly diagnosed cancer patients face from venous thromboembolism, based on findings from a prospective study of more than 4,000 people.
In the new study, 836 patients newly diagnosed with cancer had a 480% increased rate of a fatal or nonfatal MI or stroke during the 30 days following their diagnosis, compared with 3,339 matched people without cancer and after adjustment for baseline differences in demographics and cardiovascular risk factors, Babak B. Navi, MD, said while presenting a poster at the International Stroke Conference sponsored by the American Heart Association.
An additional analysis that focused on 210 of the 836 patients with incident cancer who had any of seven of the cancers known to pose the highest venous thromboembolism risk (lymphoma; gynecologic cancer; or cancer of the pancreas, stomach, lung, bladder, or testes) showed an 1,750% greater rate of incident MI or stroke during the first 30 days after diagnosis, compared with matched people without cancer, reported Dr. Navi, chief of the stroke and hospital neurology at Weill Cornell Medicine, New York.
In contrast, during both the period 1-3 months after the cancer diagnosis and more than 3 months after, the rate of MI or stroke among recently diagnosed cancer patients was not significantly different from the rate in comparator individuals, although the data showed modest trends toward more arterial thromboembolic events after a month, and the lack of statistically significant differences may have been a power issue, Dr. Navi suggested.
The reasons for this acutely increased risk for arterial thromboembolic events, as well as the early spike in venous thromboembolic events, are not completely clear, but they likely result from factors released by tumors, effects from the drugs that patients receive for cancer treatment, stress, and interruption of antithrombotic treatment. Dr. Navi fingered cancer-induced hypercoagulability as likely the biggest culprit. It may now be reasonable to test the idea of treating newly diagnosed cancer patients with agents that could reduce their risk for MI or stroke, such as aspirin or a statin, he said in an interview.
The new analysis used data collected in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study, which during 2003-2007 enrolled more than 30,000 U.S. residents who were at least 45 years old. Dr. Navi and his associates used data collected from all REGARDS participants who developed incident cancer and had continuous Medicare coverage for at least 1 year before entering REGARDS, excluding those with cancer before enrollment. They used the Medicare records to identify the cancer diagnoses, and matched each of these people with four similar but cancer-free people enrolled in the study. Follow-up continued through September 2015. The average age of this REGARDS subgroup at enrollment was 72 years old, and nearly half were women. The incident cancers included 640 patients with a solid tumor, 71 with hematologic cancers, 13 with brain tumors, and 112 with an unknown primary cancer site.
Dr. Navi and his associates designed this study to validate previously reported findings of increased arterial thromboembolic events in newly diagnosed cancer patients from studies of insurance claims databases. Although the increased risk for venous thromboembolism in cancer patients is already well established, documenting a similar risk for arterial events is important because they are “generally more impactful for patients than venous thromboembolism,” Dr. Navi said.
REGARDS has received no commercial funding. Dr. Navi reported no disclosures.
SOURCE: Navi BB et al. Stroke. 2019 Feb;50(Suppl_1): Abstract WMP53.
HONOLULU – During the first month after a new cancer diagnosis, patients face a substantially elevated risk for an arterial thromboembolic event – an MI or stroke – consistent with the well-described increased risk newly diagnosed cancer patients face from venous thromboembolism, based on findings from a prospective study of more than 4,000 people.
In the new study, 836 patients newly diagnosed with cancer had a 480% increased rate of a fatal or nonfatal MI or stroke during the 30 days following their diagnosis, compared with 3,339 matched people without cancer and after adjustment for baseline differences in demographics and cardiovascular risk factors, Babak B. Navi, MD, said while presenting a poster at the International Stroke Conference sponsored by the American Heart Association.
An additional analysis that focused on 210 of the 836 patients with incident cancer who had any of seven of the cancers known to pose the highest venous thromboembolism risk (lymphoma; gynecologic cancer; or cancer of the pancreas, stomach, lung, bladder, or testes) showed an 1,750% greater rate of incident MI or stroke during the first 30 days after diagnosis, compared with matched people without cancer, reported Dr. Navi, chief of the stroke and hospital neurology at Weill Cornell Medicine, New York.
In contrast, during both the period 1-3 months after the cancer diagnosis and more than 3 months after, the rate of MI or stroke among recently diagnosed cancer patients was not significantly different from the rate in comparator individuals, although the data showed modest trends toward more arterial thromboembolic events after a month, and the lack of statistically significant differences may have been a power issue, Dr. Navi suggested.
The reasons for this acutely increased risk for arterial thromboembolic events, as well as the early spike in venous thromboembolic events, are not completely clear, but they likely result from factors released by tumors, effects from the drugs that patients receive for cancer treatment, stress, and interruption of antithrombotic treatment. Dr. Navi fingered cancer-induced hypercoagulability as likely the biggest culprit. It may now be reasonable to test the idea of treating newly diagnosed cancer patients with agents that could reduce their risk for MI or stroke, such as aspirin or a statin, he said in an interview.
The new analysis used data collected in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study, which during 2003-2007 enrolled more than 30,000 U.S. residents who were at least 45 years old. Dr. Navi and his associates used data collected from all REGARDS participants who developed incident cancer and had continuous Medicare coverage for at least 1 year before entering REGARDS, excluding those with cancer before enrollment. They used the Medicare records to identify the cancer diagnoses, and matched each of these people with four similar but cancer-free people enrolled in the study. Follow-up continued through September 2015. The average age of this REGARDS subgroup at enrollment was 72 years old, and nearly half were women. The incident cancers included 640 patients with a solid tumor, 71 with hematologic cancers, 13 with brain tumors, and 112 with an unknown primary cancer site.
Dr. Navi and his associates designed this study to validate previously reported findings of increased arterial thromboembolic events in newly diagnosed cancer patients from studies of insurance claims databases. Although the increased risk for venous thromboembolism in cancer patients is already well established, documenting a similar risk for arterial events is important because they are “generally more impactful for patients than venous thromboembolism,” Dr. Navi said.
REGARDS has received no commercial funding. Dr. Navi reported no disclosures.
SOURCE: Navi BB et al. Stroke. 2019 Feb;50(Suppl_1): Abstract WMP53.
REPORTING FROM ISC 2019
Higher blood pressure after thrombectomy links with bad stroke outcomes
HONOLULU – Acute ischemic stroke patients who underwent endovascular thrombectomy and then had a peak systolic blood pressure of greater than 158 mm Hg during the next 24 hours had worse 90-day outcomes than did patients whose peak systolic pressure remained at or below 158 mm Hg in a prospective, multicenter, observational study with 485 patients.
The results hint that maintaining a lower systolic blood pressure after thrombectomy in acute ischemic stroke patients may improve outcomes, but because the current study was observational, the hypothesis that patients benefit when treatment keeps their systolic pressure at or below 158 mm Hg must undergo testing in a prospective, randomized trial, Eva A. Mistry, MBBS, said at the International Stroke Conference, sponsored by the American Heart Association.
The finding from this study that 158 mm Hg provided the best dichotomous division between systolic blood pressures linked with good or bad outcomes is a first step toward trying to devise a more systematic and evidence-based approach to blood pressure management in acute ischemic stroke patients following endovascular thrombectomy, said Dr. Mistry, a neurologist at Vanderbilt University in Nashville, Tenn.
Neither Vanderbilt nor any of the other 11 major U.S. stroke centers that participated in the current study currently have an established protocol for blood pressure management after thrombectomy, Dr. Mistry said in an interview.
“We usually treat to reduce blood pressure, but we don’t have a [broadly agreed on] threshold” to trigger treatment. “It depends on a collective decision” by the various medical specialists who care for an individual acute stroke patient. In addition, no consensus yet exists for the best treatment strategy for blood pressure lowering in acute ischemic stroke patients. Intravenous nicardipine is often the top choice because it is fast-acting and easy to administer and control as an intravenous agent. Those same properties make the beta blocker labetalol a frequently used second drug, she said.
The BEST (Blood Pressure After Endovascular Stroke Therapy) study ran at 12 U.S. centers and enrolled 485 patients who underwent endovascular thrombectomy to treat an acute ischemic stroke. The patients averaged 69 years old, and 48% also underwent thrombolytic treatment. The study’s primary outcome was the percentage of patients with a modified Rankin Scale score of 0-2 at 90 days after their stroke, an outcome reached by 39% of all patients in the study.
Statistical analysis of the collected data showed that a peak systolic blood pressure of 158 mm Hg reached during the 24 hours following thrombectomy best divided patients with good 90-day outcomes from those with worse outcomes. Patients with a postthrombectomy peak systolic pressure above 158 mm Hg had a 2.2-fold increased rate of having a modified Rankin Scale score of 3 or higher after 90 days, a statistically significant relationship, Dr. Mistry reported. However, in an analysis that also adjusted for age, baseline stroke severity, glucose level, time to reperfusion, ASPECTS score, history of hypertension, and recanalization status, the elevated risk for a bad outcome linked with higher systolic pressure dropped to 39% greater than that for patients with systolic pressures that did not rise above 158 mm Hg, a difference that was not statistically significant. This suggests that these adjustments were unable to account for all confounders and further highlighted the need for a prospective, randomized trial to test the value of controlling blood pressure following thrombectomy, Dr. Mistry said. The unadjusted results confirmed a prior report from Dr. Mistry and her associates that found a link between higher blood pressure after stroke thrombectomy and worse outcomes (J Am Heart Assoc. 2017 May 18. doi: 10.1161/JAHA.117.006167).
The analysis also showed that patients who were successfully recanalized by thrombectomy, achieving a thrombolysis in cerebral infarction (TICI) score of 2b or 3, had lower peak systolic blood pressures than did patients who failed to get this level of restored cerebral blood flow from thrombectomy.
BEST received no commercial funding. Dr. Mistry had no disclosures.
SOURCE: Mistry EA et al. Stroke. 2019 Feb;50(Suppl_1): Abstract 94.
HONOLULU – Acute ischemic stroke patients who underwent endovascular thrombectomy and then had a peak systolic blood pressure of greater than 158 mm Hg during the next 24 hours had worse 90-day outcomes than did patients whose peak systolic pressure remained at or below 158 mm Hg in a prospective, multicenter, observational study with 485 patients.
The results hint that maintaining a lower systolic blood pressure after thrombectomy in acute ischemic stroke patients may improve outcomes, but because the current study was observational, the hypothesis that patients benefit when treatment keeps their systolic pressure at or below 158 mm Hg must undergo testing in a prospective, randomized trial, Eva A. Mistry, MBBS, said at the International Stroke Conference, sponsored by the American Heart Association.
The finding from this study that 158 mm Hg provided the best dichotomous division between systolic blood pressures linked with good or bad outcomes is a first step toward trying to devise a more systematic and evidence-based approach to blood pressure management in acute ischemic stroke patients following endovascular thrombectomy, said Dr. Mistry, a neurologist at Vanderbilt University in Nashville, Tenn.
Neither Vanderbilt nor any of the other 11 major U.S. stroke centers that participated in the current study currently have an established protocol for blood pressure management after thrombectomy, Dr. Mistry said in an interview.
“We usually treat to reduce blood pressure, but we don’t have a [broadly agreed on] threshold” to trigger treatment. “It depends on a collective decision” by the various medical specialists who care for an individual acute stroke patient. In addition, no consensus yet exists for the best treatment strategy for blood pressure lowering in acute ischemic stroke patients. Intravenous nicardipine is often the top choice because it is fast-acting and easy to administer and control as an intravenous agent. Those same properties make the beta blocker labetalol a frequently used second drug, she said.
The BEST (Blood Pressure After Endovascular Stroke Therapy) study ran at 12 U.S. centers and enrolled 485 patients who underwent endovascular thrombectomy to treat an acute ischemic stroke. The patients averaged 69 years old, and 48% also underwent thrombolytic treatment. The study’s primary outcome was the percentage of patients with a modified Rankin Scale score of 0-2 at 90 days after their stroke, an outcome reached by 39% of all patients in the study.
Statistical analysis of the collected data showed that a peak systolic blood pressure of 158 mm Hg reached during the 24 hours following thrombectomy best divided patients with good 90-day outcomes from those with worse outcomes. Patients with a postthrombectomy peak systolic pressure above 158 mm Hg had a 2.2-fold increased rate of having a modified Rankin Scale score of 3 or higher after 90 days, a statistically significant relationship, Dr. Mistry reported. However, in an analysis that also adjusted for age, baseline stroke severity, glucose level, time to reperfusion, ASPECTS score, history of hypertension, and recanalization status, the elevated risk for a bad outcome linked with higher systolic pressure dropped to 39% greater than that for patients with systolic pressures that did not rise above 158 mm Hg, a difference that was not statistically significant. This suggests that these adjustments were unable to account for all confounders and further highlighted the need for a prospective, randomized trial to test the value of controlling blood pressure following thrombectomy, Dr. Mistry said. The unadjusted results confirmed a prior report from Dr. Mistry and her associates that found a link between higher blood pressure after stroke thrombectomy and worse outcomes (J Am Heart Assoc. 2017 May 18. doi: 10.1161/JAHA.117.006167).
The analysis also showed that patients who were successfully recanalized by thrombectomy, achieving a thrombolysis in cerebral infarction (TICI) score of 2b or 3, had lower peak systolic blood pressures than did patients who failed to get this level of restored cerebral blood flow from thrombectomy.
BEST received no commercial funding. Dr. Mistry had no disclosures.
SOURCE: Mistry EA et al. Stroke. 2019 Feb;50(Suppl_1): Abstract 94.
HONOLULU – Acute ischemic stroke patients who underwent endovascular thrombectomy and then had a peak systolic blood pressure of greater than 158 mm Hg during the next 24 hours had worse 90-day outcomes than did patients whose peak systolic pressure remained at or below 158 mm Hg in a prospective, multicenter, observational study with 485 patients.
The results hint that maintaining a lower systolic blood pressure after thrombectomy in acute ischemic stroke patients may improve outcomes, but because the current study was observational, the hypothesis that patients benefit when treatment keeps their systolic pressure at or below 158 mm Hg must undergo testing in a prospective, randomized trial, Eva A. Mistry, MBBS, said at the International Stroke Conference, sponsored by the American Heart Association.
The finding from this study that 158 mm Hg provided the best dichotomous division between systolic blood pressures linked with good or bad outcomes is a first step toward trying to devise a more systematic and evidence-based approach to blood pressure management in acute ischemic stroke patients following endovascular thrombectomy, said Dr. Mistry, a neurologist at Vanderbilt University in Nashville, Tenn.
Neither Vanderbilt nor any of the other 11 major U.S. stroke centers that participated in the current study currently have an established protocol for blood pressure management after thrombectomy, Dr. Mistry said in an interview.
“We usually treat to reduce blood pressure, but we don’t have a [broadly agreed on] threshold” to trigger treatment. “It depends on a collective decision” by the various medical specialists who care for an individual acute stroke patient. In addition, no consensus yet exists for the best treatment strategy for blood pressure lowering in acute ischemic stroke patients. Intravenous nicardipine is often the top choice because it is fast-acting and easy to administer and control as an intravenous agent. Those same properties make the beta blocker labetalol a frequently used second drug, she said.
The BEST (Blood Pressure After Endovascular Stroke Therapy) study ran at 12 U.S. centers and enrolled 485 patients who underwent endovascular thrombectomy to treat an acute ischemic stroke. The patients averaged 69 years old, and 48% also underwent thrombolytic treatment. The study’s primary outcome was the percentage of patients with a modified Rankin Scale score of 0-2 at 90 days after their stroke, an outcome reached by 39% of all patients in the study.
Statistical analysis of the collected data showed that a peak systolic blood pressure of 158 mm Hg reached during the 24 hours following thrombectomy best divided patients with good 90-day outcomes from those with worse outcomes. Patients with a postthrombectomy peak systolic pressure above 158 mm Hg had a 2.2-fold increased rate of having a modified Rankin Scale score of 3 or higher after 90 days, a statistically significant relationship, Dr. Mistry reported. However, in an analysis that also adjusted for age, baseline stroke severity, glucose level, time to reperfusion, ASPECTS score, history of hypertension, and recanalization status, the elevated risk for a bad outcome linked with higher systolic pressure dropped to 39% greater than that for patients with systolic pressures that did not rise above 158 mm Hg, a difference that was not statistically significant. This suggests that these adjustments were unable to account for all confounders and further highlighted the need for a prospective, randomized trial to test the value of controlling blood pressure following thrombectomy, Dr. Mistry said. The unadjusted results confirmed a prior report from Dr. Mistry and her associates that found a link between higher blood pressure after stroke thrombectomy and worse outcomes (J Am Heart Assoc. 2017 May 18. doi: 10.1161/JAHA.117.006167).
The analysis also showed that patients who were successfully recanalized by thrombectomy, achieving a thrombolysis in cerebral infarction (TICI) score of 2b or 3, had lower peak systolic blood pressures than did patients who failed to get this level of restored cerebral blood flow from thrombectomy.
BEST received no commercial funding. Dr. Mistry had no disclosures.
SOURCE: Mistry EA et al. Stroke. 2019 Feb;50(Suppl_1): Abstract 94.
REPORTING FROM ISC 2019
Survey of MS patients reveals numerous pregnancy-related concerns
DALLAS – When it comes to family planning and pregnancy-related decisions such as breastfeeding and medication management, patients with multiple sclerosis (MS) receive a wide variety of advice, guidance, and engagement from their health care providers, results from a single-center survey demonstrated.
“We want our patients to feel comfortable when they come to us in their 20s or 30s and they get diagnosed, they’re scared, and it’s all new to them,” one of the study authors, Casey E. Engel said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “We want them to know that family planning is something to consider and that they can proceed with having a family with our help and guidance.”
In an effort to collect patient-experience data around family planning, pregnancy, and breastfeeding post-MS diagnosis, Ms. Engel and senior author Myla D. Goldman, MD, mailed a survey to 1,000 women with confirmed MS diagnosis who had received care at the University of Virginia Medical Center in Charlottesville. The researchers reported findings from 173 respondents, of whom 70% were receiving specialty care for MS. Most of the survey participants (137) did not become pregnant following their diagnosis, while 36 did.
Of the 137 respondents who did not become pregnant following diagnosis, 22 (16%) indicated that their decision was driven by MS-related concerns, including MS worsening with pregnancy (64%), ability to care for child secondary to MS (46%), lack of knowledge about options for pregnancy and MS (18%), passing MS onto child (18%), and stopping disease-modifying therapy (DMT) to attempt pregnancy (9%).
Of the 36 women who had a pregnancy following diagnosis, 20% reported postpartum depression or anxiety, higher than the national average of 10%-15%. In addition, 79% reported not being on DMT at the time of conception, 9% were on either glatiramer acetate injection or interferon beta-1a at time of conception, and 3% were on fingolimod (Gilenya) at time of conception. The majority reported receiving inconsistent advice about when to discontinue DMT before attempting pregnancy (a range from 0 to 6 months).
“It’s also noteworthy that 20% took a year to achieve pregnancy,” said Dr. Goldman, a neurologist who directs the university’s MS clinic. “If these women stop [their DMT] 6 months in advance and they take a year to achieve pregnancy, that’s 18 months without therapeutic coverage. That’s a concern to bring to light.”
Breastfeeding was reported in 71% of mothers in postdiagnosis pregnancy with a range between 1 week and 10 months, driven in part by variable guidelines regarding DMT reinitiation. In the meantime, respondents who did not breastfeed made this decision due to fear of relapse, glucocorticoids, or desire to reinitiate medication.
“Though our study was limited by low survey response, we hope that our work may highlight the difficulty our patients face and foster discussions within the MS community around these issues to improve the individual patient experience,” the researchers wrote in their poster.
Ms. Engel worked on the study while an undergraduate at the University of Virginia. The study was supported by the ziMS Foundation.
SOURCE: Engel CE et al. ACTRIMS Forum 2019, Poster 307.
DALLAS – When it comes to family planning and pregnancy-related decisions such as breastfeeding and medication management, patients with multiple sclerosis (MS) receive a wide variety of advice, guidance, and engagement from their health care providers, results from a single-center survey demonstrated.
“We want our patients to feel comfortable when they come to us in their 20s or 30s and they get diagnosed, they’re scared, and it’s all new to them,” one of the study authors, Casey E. Engel said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “We want them to know that family planning is something to consider and that they can proceed with having a family with our help and guidance.”
In an effort to collect patient-experience data around family planning, pregnancy, and breastfeeding post-MS diagnosis, Ms. Engel and senior author Myla D. Goldman, MD, mailed a survey to 1,000 women with confirmed MS diagnosis who had received care at the University of Virginia Medical Center in Charlottesville. The researchers reported findings from 173 respondents, of whom 70% were receiving specialty care for MS. Most of the survey participants (137) did not become pregnant following their diagnosis, while 36 did.
Of the 137 respondents who did not become pregnant following diagnosis, 22 (16%) indicated that their decision was driven by MS-related concerns, including MS worsening with pregnancy (64%), ability to care for child secondary to MS (46%), lack of knowledge about options for pregnancy and MS (18%), passing MS onto child (18%), and stopping disease-modifying therapy (DMT) to attempt pregnancy (9%).
Of the 36 women who had a pregnancy following diagnosis, 20% reported postpartum depression or anxiety, higher than the national average of 10%-15%. In addition, 79% reported not being on DMT at the time of conception, 9% were on either glatiramer acetate injection or interferon beta-1a at time of conception, and 3% were on fingolimod (Gilenya) at time of conception. The majority reported receiving inconsistent advice about when to discontinue DMT before attempting pregnancy (a range from 0 to 6 months).
“It’s also noteworthy that 20% took a year to achieve pregnancy,” said Dr. Goldman, a neurologist who directs the university’s MS clinic. “If these women stop [their DMT] 6 months in advance and they take a year to achieve pregnancy, that’s 18 months without therapeutic coverage. That’s a concern to bring to light.”
Breastfeeding was reported in 71% of mothers in postdiagnosis pregnancy with a range between 1 week and 10 months, driven in part by variable guidelines regarding DMT reinitiation. In the meantime, respondents who did not breastfeed made this decision due to fear of relapse, glucocorticoids, or desire to reinitiate medication.
“Though our study was limited by low survey response, we hope that our work may highlight the difficulty our patients face and foster discussions within the MS community around these issues to improve the individual patient experience,” the researchers wrote in their poster.
Ms. Engel worked on the study while an undergraduate at the University of Virginia. The study was supported by the ziMS Foundation.
SOURCE: Engel CE et al. ACTRIMS Forum 2019, Poster 307.
DALLAS – When it comes to family planning and pregnancy-related decisions such as breastfeeding and medication management, patients with multiple sclerosis (MS) receive a wide variety of advice, guidance, and engagement from their health care providers, results from a single-center survey demonstrated.
“We want our patients to feel comfortable when they come to us in their 20s or 30s and they get diagnosed, they’re scared, and it’s all new to them,” one of the study authors, Casey E. Engel said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “We want them to know that family planning is something to consider and that they can proceed with having a family with our help and guidance.”
In an effort to collect patient-experience data around family planning, pregnancy, and breastfeeding post-MS diagnosis, Ms. Engel and senior author Myla D. Goldman, MD, mailed a survey to 1,000 women with confirmed MS diagnosis who had received care at the University of Virginia Medical Center in Charlottesville. The researchers reported findings from 173 respondents, of whom 70% were receiving specialty care for MS. Most of the survey participants (137) did not become pregnant following their diagnosis, while 36 did.
Of the 137 respondents who did not become pregnant following diagnosis, 22 (16%) indicated that their decision was driven by MS-related concerns, including MS worsening with pregnancy (64%), ability to care for child secondary to MS (46%), lack of knowledge about options for pregnancy and MS (18%), passing MS onto child (18%), and stopping disease-modifying therapy (DMT) to attempt pregnancy (9%).
Of the 36 women who had a pregnancy following diagnosis, 20% reported postpartum depression or anxiety, higher than the national average of 10%-15%. In addition, 79% reported not being on DMT at the time of conception, 9% were on either glatiramer acetate injection or interferon beta-1a at time of conception, and 3% were on fingolimod (Gilenya) at time of conception. The majority reported receiving inconsistent advice about when to discontinue DMT before attempting pregnancy (a range from 0 to 6 months).
“It’s also noteworthy that 20% took a year to achieve pregnancy,” said Dr. Goldman, a neurologist who directs the university’s MS clinic. “If these women stop [their DMT] 6 months in advance and they take a year to achieve pregnancy, that’s 18 months without therapeutic coverage. That’s a concern to bring to light.”
Breastfeeding was reported in 71% of mothers in postdiagnosis pregnancy with a range between 1 week and 10 months, driven in part by variable guidelines regarding DMT reinitiation. In the meantime, respondents who did not breastfeed made this decision due to fear of relapse, glucocorticoids, or desire to reinitiate medication.
“Though our study was limited by low survey response, we hope that our work may highlight the difficulty our patients face and foster discussions within the MS community around these issues to improve the individual patient experience,” the researchers wrote in their poster.
Ms. Engel worked on the study while an undergraduate at the University of Virginia. The study was supported by the ziMS Foundation.
SOURCE: Engel CE et al. ACTRIMS Forum 2019, Poster 307.
REPORTING FROM ACTRIMS FORUM 2019
Teriflunomide transmission can occur in female partners of men taking the drug
DALLAS – Low or undetectable levels of teriflunomide (Aubagio) occur in women who are sexually active with men taking the drug for relapsing multiple sclerosis, results from a small study demonstrated.
“One of the issues with this particular drug is that it carries a strong pregnancy warning because in animal studies the drug has been teratogenic,” Joseph B. Guarnaccia, MD, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “The other issue is that it remains detectable in the body for some time. The issue of females taking this drug and conception are well known. There are strong warnings that, if a woman wants to become pregnant, the drug should be removed quickly from the system. But if their male partner is on the drug, does that pose a risk to their female partner? That question has never been addressed in a human study.”
The Food and Drug Administration prescribing information recommends that men wishing to father a child should discontinue use of teriflunomide and undergo the accelerated elimination procedure. It also recommends that female partners wishing to become pregnant should discontinue the drug and undergo an accelerated elimination procedure to verify that the plasma teriflunomide concentration is less than 0.020 mcg/mL.
In an effort to test the risk of female exposure to potentially teratogenic levels of teriflunomide through sexual intercourse, Dr. Guarnaccia, a neurologist with the Multiple Sclerosis Treatment Center at Griffin Hospital in Derby, Conn., and his colleagues recruited 10 couples and compared serum levels of teriflunomide in men with relapsing multiple sclerosis with those of their female partners. Enrollment criteria for men included a diagnosis of relapsing multiple sclerosis, age between 18 and 55 years, treatment with teriflunomide for at least 2 months prior to study entry, and frequency of sexual intercourse with their female partners at least twice a month. Pregnancy was excluded in females, and couples could not use barrier or withdrawal methods of contraception. The couples completed a brief questionnaire and underwent a one-time blood draw for teriflunomide levels either at the investigator’s office or at a LabCorp facility.
The mean age of study participants was 47 years and the mean frequency of intercourse was seven episodes per month. The mean teriflunomide concentration in men was 42.30 mcg/mL (ranged from 10.07 to 142.84 mcg/mL). Six women had teriflunomide below detection levels (0.020 mcg/mL). However, four women had detectable levels that averaged 0.045 mcg/mL (ranging from 0.022 to 0.077 mcg/mL).
“This small study demonstrates that low or undetectable levels of teriflunomide occur in females who are sexually active with males taking teriflunomide for relapsing multiple sclerosis,” the researchers wrote in their poster. They found that women who had low detectable levels of teriflunomide, compared with women with undetectable levels, did not engage in more frequent sexual intercourse nor were their levels associated with higher levels of teriflunomide in their male partners.
“Indeed, one might have expected a positive correlation between serum levels of teriflunomide in females and the frequency or concentration of inoculation in semen from their partners,” the researchers wrote. “While semen levels of teriflunomide were not measured in this study, it might be assumed that serum and semen concentrations of small molecules like teriflunomide are similar.”
The study was supported by a investigator-sponsored research grant from Sanofi-Genzyme. Dr. Guarnaccia reported that he has received speaking honoraria and educational grants from Sanofi-Genzyme, Biogen, Teva, Acorda Therapeutics, Bayer, EMD Serono, and Genentech.
SOURCE: Guarnaccia JB et al. ACTRIMS Forum 2019, Poster 115.
DALLAS – Low or undetectable levels of teriflunomide (Aubagio) occur in women who are sexually active with men taking the drug for relapsing multiple sclerosis, results from a small study demonstrated.
“One of the issues with this particular drug is that it carries a strong pregnancy warning because in animal studies the drug has been teratogenic,” Joseph B. Guarnaccia, MD, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “The other issue is that it remains detectable in the body for some time. The issue of females taking this drug and conception are well known. There are strong warnings that, if a woman wants to become pregnant, the drug should be removed quickly from the system. But if their male partner is on the drug, does that pose a risk to their female partner? That question has never been addressed in a human study.”
The Food and Drug Administration prescribing information recommends that men wishing to father a child should discontinue use of teriflunomide and undergo the accelerated elimination procedure. It also recommends that female partners wishing to become pregnant should discontinue the drug and undergo an accelerated elimination procedure to verify that the plasma teriflunomide concentration is less than 0.020 mcg/mL.
In an effort to test the risk of female exposure to potentially teratogenic levels of teriflunomide through sexual intercourse, Dr. Guarnaccia, a neurologist with the Multiple Sclerosis Treatment Center at Griffin Hospital in Derby, Conn., and his colleagues recruited 10 couples and compared serum levels of teriflunomide in men with relapsing multiple sclerosis with those of their female partners. Enrollment criteria for men included a diagnosis of relapsing multiple sclerosis, age between 18 and 55 years, treatment with teriflunomide for at least 2 months prior to study entry, and frequency of sexual intercourse with their female partners at least twice a month. Pregnancy was excluded in females, and couples could not use barrier or withdrawal methods of contraception. The couples completed a brief questionnaire and underwent a one-time blood draw for teriflunomide levels either at the investigator’s office or at a LabCorp facility.
The mean age of study participants was 47 years and the mean frequency of intercourse was seven episodes per month. The mean teriflunomide concentration in men was 42.30 mcg/mL (ranged from 10.07 to 142.84 mcg/mL). Six women had teriflunomide below detection levels (0.020 mcg/mL). However, four women had detectable levels that averaged 0.045 mcg/mL (ranging from 0.022 to 0.077 mcg/mL).
“This small study demonstrates that low or undetectable levels of teriflunomide occur in females who are sexually active with males taking teriflunomide for relapsing multiple sclerosis,” the researchers wrote in their poster. They found that women who had low detectable levels of teriflunomide, compared with women with undetectable levels, did not engage in more frequent sexual intercourse nor were their levels associated with higher levels of teriflunomide in their male partners.
“Indeed, one might have expected a positive correlation between serum levels of teriflunomide in females and the frequency or concentration of inoculation in semen from their partners,” the researchers wrote. “While semen levels of teriflunomide were not measured in this study, it might be assumed that serum and semen concentrations of small molecules like teriflunomide are similar.”
The study was supported by a investigator-sponsored research grant from Sanofi-Genzyme. Dr. Guarnaccia reported that he has received speaking honoraria and educational grants from Sanofi-Genzyme, Biogen, Teva, Acorda Therapeutics, Bayer, EMD Serono, and Genentech.
SOURCE: Guarnaccia JB et al. ACTRIMS Forum 2019, Poster 115.
DALLAS – Low or undetectable levels of teriflunomide (Aubagio) occur in women who are sexually active with men taking the drug for relapsing multiple sclerosis, results from a small study demonstrated.
“One of the issues with this particular drug is that it carries a strong pregnancy warning because in animal studies the drug has been teratogenic,” Joseph B. Guarnaccia, MD, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “The other issue is that it remains detectable in the body for some time. The issue of females taking this drug and conception are well known. There are strong warnings that, if a woman wants to become pregnant, the drug should be removed quickly from the system. But if their male partner is on the drug, does that pose a risk to their female partner? That question has never been addressed in a human study.”
The Food and Drug Administration prescribing information recommends that men wishing to father a child should discontinue use of teriflunomide and undergo the accelerated elimination procedure. It also recommends that female partners wishing to become pregnant should discontinue the drug and undergo an accelerated elimination procedure to verify that the plasma teriflunomide concentration is less than 0.020 mcg/mL.
In an effort to test the risk of female exposure to potentially teratogenic levels of teriflunomide through sexual intercourse, Dr. Guarnaccia, a neurologist with the Multiple Sclerosis Treatment Center at Griffin Hospital in Derby, Conn., and his colleagues recruited 10 couples and compared serum levels of teriflunomide in men with relapsing multiple sclerosis with those of their female partners. Enrollment criteria for men included a diagnosis of relapsing multiple sclerosis, age between 18 and 55 years, treatment with teriflunomide for at least 2 months prior to study entry, and frequency of sexual intercourse with their female partners at least twice a month. Pregnancy was excluded in females, and couples could not use barrier or withdrawal methods of contraception. The couples completed a brief questionnaire and underwent a one-time blood draw for teriflunomide levels either at the investigator’s office or at a LabCorp facility.
The mean age of study participants was 47 years and the mean frequency of intercourse was seven episodes per month. The mean teriflunomide concentration in men was 42.30 mcg/mL (ranged from 10.07 to 142.84 mcg/mL). Six women had teriflunomide below detection levels (0.020 mcg/mL). However, four women had detectable levels that averaged 0.045 mcg/mL (ranging from 0.022 to 0.077 mcg/mL).
“This small study demonstrates that low or undetectable levels of teriflunomide occur in females who are sexually active with males taking teriflunomide for relapsing multiple sclerosis,” the researchers wrote in their poster. They found that women who had low detectable levels of teriflunomide, compared with women with undetectable levels, did not engage in more frequent sexual intercourse nor were their levels associated with higher levels of teriflunomide in their male partners.
“Indeed, one might have expected a positive correlation between serum levels of teriflunomide in females and the frequency or concentration of inoculation in semen from their partners,” the researchers wrote. “While semen levels of teriflunomide were not measured in this study, it might be assumed that serum and semen concentrations of small molecules like teriflunomide are similar.”
The study was supported by a investigator-sponsored research grant from Sanofi-Genzyme. Dr. Guarnaccia reported that he has received speaking honoraria and educational grants from Sanofi-Genzyme, Biogen, Teva, Acorda Therapeutics, Bayer, EMD Serono, and Genentech.
SOURCE: Guarnaccia JB et al. ACTRIMS Forum 2019, Poster 115.
REPORTING FROM ACTRIMS FORUM 2019
Boosting Alzheimer’s trial participation via Medicare Advantage ‘memory fitness programs’
Clinical trials represent future hope for patients seeking better care, and there is no disease more in need of better care than Alzheimer’s disease. While death rates among most cancers, as well as heart disease, HIV-related illness, and other categories, have declined in the past decade, there has been no progress for Alzheimer’s disease. Better health and wellness overall may be having a beneficial effect that has produced a reduction in age-adjusted dementia rates, but with the aging of the population there are a greater absolute number of dementia cases than ever before, and that number is expected to continue rising. Finding a disease-modifying therapy seems to be the best hope for changing this dim outlook. Clinical trials intend to do just that but are hampered by patient enrollment rates that remain low. Far fewer eligible patients enroll than are needed, causing studies to take longer to complete, driving up their costs and essentially slowing progress. There is a need to increase patient enrollment, and there has been a variety of efforts intended to address this, not the least of which has been an explosion of media coverage of Alzheimer’s disease.
The Global Alzheimer’s Platform (GAP) Foundation, a nonprofit, self-described patient-centric entity dedicated to reducing the time and cost of Alzheimer’s disease clinical trials, recently announced an initiative to increase participation in Alzheimer’s clinical trials by supporting and collaborating with “memory fitness programs” through select Medicare Advantage plans. At worst, this seems a harmless way to increase attention and hopefully interest in clinical trial participation. At best, this may be a cost-effective way to increase enrollment and even improve dementia care. Dementia is notoriously underdiagnosed, especially by overworked, busy primary care providers who simply lack the time to perform the time-consuming testing that is typically required to diagnose and follow such patients.
There are some caveats to consider. First, memory fitness programs are of dubious benefit. They generally fit the description of being harmless, but there is little compelling evidence that they preserve or improve memory.
Second, enrollment in a clinical trial, for a patient, is not always a winning proposition. To date, there has been little success and in the absence of benefit, any downside – even if simply an inconvenience – is a net negative. Recently at the 2018 Clinical Trials on Alzheimer’s Disease meeting, Merck reported that patients with mild cognitive impairment receiving active treatment in the BACE1 inhibitor verubecestat trial actually declined at a more rapid rate than did those on placebo. While the absolute difference was small, and one could argue whether it was clinically significant or simply a random occurrence, it was a reminder that intervention with an experimental agent is not necessarily benign.
Third, Medicare Advantage plans, while popular in some circles, are not considered advantageous to providers so that the proliferation of inadequate reimbursement will potentially fuel the accelerating number of providers who opt out of insurance plans altogether. This is not necessarily an issue for the GAP Foundation specifically but is nonetheless an issue for anything that promotes MA plans).
Finally, it remains important to help patients and families maintain a positive outlook, especially when we have nothing better to offer. Alzheimer’s disease is not a death sentence for every patient affected. While many have difficult and heartbreaking courses, some have slowly progressive courses with relatively little impairment for an extended period of time. There are also the dementia-phobic, cognitively unimpaired individuals (or who simply have normal age-associated cognitive changes) in whom the continued drumbeat of dementia awareness and memory testing raises their paranoia ever higher. We treat deficits (or try to), but we have to live based on our preserved skills. The challenge clinicians must face with patients and families is how to maximize function while compensating for deficits and making sure that patients and families maintain their hope.
Dr. Caselli is professor of neurology at the Mayo Clinic Arizona in Scottsdale and associate director and clinical core director of the Arizona Alzheimer’s Disease Center.
Clinical trials represent future hope for patients seeking better care, and there is no disease more in need of better care than Alzheimer’s disease. While death rates among most cancers, as well as heart disease, HIV-related illness, and other categories, have declined in the past decade, there has been no progress for Alzheimer’s disease. Better health and wellness overall may be having a beneficial effect that has produced a reduction in age-adjusted dementia rates, but with the aging of the population there are a greater absolute number of dementia cases than ever before, and that number is expected to continue rising. Finding a disease-modifying therapy seems to be the best hope for changing this dim outlook. Clinical trials intend to do just that but are hampered by patient enrollment rates that remain low. Far fewer eligible patients enroll than are needed, causing studies to take longer to complete, driving up their costs and essentially slowing progress. There is a need to increase patient enrollment, and there has been a variety of efforts intended to address this, not the least of which has been an explosion of media coverage of Alzheimer’s disease.
The Global Alzheimer’s Platform (GAP) Foundation, a nonprofit, self-described patient-centric entity dedicated to reducing the time and cost of Alzheimer’s disease clinical trials, recently announced an initiative to increase participation in Alzheimer’s clinical trials by supporting and collaborating with “memory fitness programs” through select Medicare Advantage plans. At worst, this seems a harmless way to increase attention and hopefully interest in clinical trial participation. At best, this may be a cost-effective way to increase enrollment and even improve dementia care. Dementia is notoriously underdiagnosed, especially by overworked, busy primary care providers who simply lack the time to perform the time-consuming testing that is typically required to diagnose and follow such patients.
There are some caveats to consider. First, memory fitness programs are of dubious benefit. They generally fit the description of being harmless, but there is little compelling evidence that they preserve or improve memory.
Second, enrollment in a clinical trial, for a patient, is not always a winning proposition. To date, there has been little success and in the absence of benefit, any downside – even if simply an inconvenience – is a net negative. Recently at the 2018 Clinical Trials on Alzheimer’s Disease meeting, Merck reported that patients with mild cognitive impairment receiving active treatment in the BACE1 inhibitor verubecestat trial actually declined at a more rapid rate than did those on placebo. While the absolute difference was small, and one could argue whether it was clinically significant or simply a random occurrence, it was a reminder that intervention with an experimental agent is not necessarily benign.
Third, Medicare Advantage plans, while popular in some circles, are not considered advantageous to providers so that the proliferation of inadequate reimbursement will potentially fuel the accelerating number of providers who opt out of insurance plans altogether. This is not necessarily an issue for the GAP Foundation specifically but is nonetheless an issue for anything that promotes MA plans).
Finally, it remains important to help patients and families maintain a positive outlook, especially when we have nothing better to offer. Alzheimer’s disease is not a death sentence for every patient affected. While many have difficult and heartbreaking courses, some have slowly progressive courses with relatively little impairment for an extended period of time. There are also the dementia-phobic, cognitively unimpaired individuals (or who simply have normal age-associated cognitive changes) in whom the continued drumbeat of dementia awareness and memory testing raises their paranoia ever higher. We treat deficits (or try to), but we have to live based on our preserved skills. The challenge clinicians must face with patients and families is how to maximize function while compensating for deficits and making sure that patients and families maintain their hope.
Dr. Caselli is professor of neurology at the Mayo Clinic Arizona in Scottsdale and associate director and clinical core director of the Arizona Alzheimer’s Disease Center.
Clinical trials represent future hope for patients seeking better care, and there is no disease more in need of better care than Alzheimer’s disease. While death rates among most cancers, as well as heart disease, HIV-related illness, and other categories, have declined in the past decade, there has been no progress for Alzheimer’s disease. Better health and wellness overall may be having a beneficial effect that has produced a reduction in age-adjusted dementia rates, but with the aging of the population there are a greater absolute number of dementia cases than ever before, and that number is expected to continue rising. Finding a disease-modifying therapy seems to be the best hope for changing this dim outlook. Clinical trials intend to do just that but are hampered by patient enrollment rates that remain low. Far fewer eligible patients enroll than are needed, causing studies to take longer to complete, driving up their costs and essentially slowing progress. There is a need to increase patient enrollment, and there has been a variety of efforts intended to address this, not the least of which has been an explosion of media coverage of Alzheimer’s disease.
The Global Alzheimer’s Platform (GAP) Foundation, a nonprofit, self-described patient-centric entity dedicated to reducing the time and cost of Alzheimer’s disease clinical trials, recently announced an initiative to increase participation in Alzheimer’s clinical trials by supporting and collaborating with “memory fitness programs” through select Medicare Advantage plans. At worst, this seems a harmless way to increase attention and hopefully interest in clinical trial participation. At best, this may be a cost-effective way to increase enrollment and even improve dementia care. Dementia is notoriously underdiagnosed, especially by overworked, busy primary care providers who simply lack the time to perform the time-consuming testing that is typically required to diagnose and follow such patients.
There are some caveats to consider. First, memory fitness programs are of dubious benefit. They generally fit the description of being harmless, but there is little compelling evidence that they preserve or improve memory.
Second, enrollment in a clinical trial, for a patient, is not always a winning proposition. To date, there has been little success and in the absence of benefit, any downside – even if simply an inconvenience – is a net negative. Recently at the 2018 Clinical Trials on Alzheimer’s Disease meeting, Merck reported that patients with mild cognitive impairment receiving active treatment in the BACE1 inhibitor verubecestat trial actually declined at a more rapid rate than did those on placebo. While the absolute difference was small, and one could argue whether it was clinically significant or simply a random occurrence, it was a reminder that intervention with an experimental agent is not necessarily benign.
Third, Medicare Advantage plans, while popular in some circles, are not considered advantageous to providers so that the proliferation of inadequate reimbursement will potentially fuel the accelerating number of providers who opt out of insurance plans altogether. This is not necessarily an issue for the GAP Foundation specifically but is nonetheless an issue for anything that promotes MA plans).
Finally, it remains important to help patients and families maintain a positive outlook, especially when we have nothing better to offer. Alzheimer’s disease is not a death sentence for every patient affected. While many have difficult and heartbreaking courses, some have slowly progressive courses with relatively little impairment for an extended period of time. There are also the dementia-phobic, cognitively unimpaired individuals (or who simply have normal age-associated cognitive changes) in whom the continued drumbeat of dementia awareness and memory testing raises their paranoia ever higher. We treat deficits (or try to), but we have to live based on our preserved skills. The challenge clinicians must face with patients and families is how to maximize function while compensating for deficits and making sure that patients and families maintain their hope.
Dr. Caselli is professor of neurology at the Mayo Clinic Arizona in Scottsdale and associate director and clinical core director of the Arizona Alzheimer’s Disease Center.