User login
Data supporting cannabis for childhood epilepsy remain scarce
, according to two leading experts.
In a recent invited review article, Martin Kirkpatrick, MD, of the University of Dundee (Scotland), and Finbar O’Callaghan, MD, PhD, of University College London suggested that childhood epilepsy may be easy terrain for commercial interests to break ground, and from there, build their presence.
“Children with epilepsy are at risk of being used as the ‘Trojan horse’ for the cannabis industry,” Dr. Kirkpatrick and Dr. O’Callaghan wrote in Developmental Medicine & Child Neurology.
They noted that some of the first publicized success stories involving cannabis oil for epilepsy coincided with the rise of the medicinal and recreational cannabis markets, which will constitute an estimated 55-billion-dollar industry by 2027.
“Pediatric neurologists, imbued with the need to practice evidence-based medicine and wary of prescribing unlicensed medicines that had inadequate safety data, suddenly found themselves at odds with an array of vested interests and, most unfortunately, with the families of patients who were keen to try anything that would alleviate the effects of their child’s seizures,” the investigators wrote.
According to the review, fundamental questions about cannabis remain unanswered, including concerns about safety with long-term use, and the medicinal value of various plant components, such as myrcene, a terpene that gives cannabis its characteristic smell.
“A widely discussed issue is whether the terpenes add any therapeutic benefit, contributing to the so-called entourage effect of ‘whole-plant’ medicines,” the investigators wrote. “The concept is that all the constituents of the plant together create ‘the sum of all the parts that leads to the magic or power of cannabis.’ Although commonly referred to, there is little or no robust evidence to support the entourage effect as a credible clinical concept.”
Clinical evidence for treatment of pediatric epilepsy is also lacking, according to Dr. Kirkpatrick and Dr. O’Callaghan.
“Unfortunately, apart from the studies of pure cannabidiol (CBD) in Lennox–Gastaut and Dravet syndromes and tuberous sclerosis complex, level I evidence in the field of CBMPs and refractory epilepsy is lacking,” they wrote.
While other experts have pointed out that lower-level evidence – such as patient-reported outcomes and observational data – have previously been sufficient for drug licensing, Dr. Kirkpatrick and Dr. O’Callaghan noted that such exceptions “almost always” involve conditions without any effective treatments, or drugs that are undeniably effective.
“This is not the scenario with CBMPs,” they wrote, referring to current clinical data as “low-level” evidence “suggesting … possible efficacy.”
They highlighted concerns about placebo effect with open-label epilepsy studies, citing a randomized controlled trial for Dravet syndrome, in which 27% of patients given placebo had a 50% reduction in seizure frequency.
“We need carefully designed, good-quality CBMP studies that produce results on which we can rely,” Dr. Kirkpatrick and Dr. O’Callaghan concluded. “We can then work with families to choose the best treatments for children and young people with epilepsy. We owe this to them.”
A therapy of last resort
Jerzy P. Szaflarski, MD, PhD, of the University of Alabama at Birmingham, agreed that data are lacking for the use of CBMPs with patients who have epilepsy and other neurologic conditions; however, he also suggested that Dr. Kirkpatrick and Dr. O’Callaghan did not provide adequate real-world clinical context.
“Medical cannabis is not used as a first-, second-, or third-line therapy,” Dr. Szaflarski said. “It’s mostly used as a last resort in the sense that patients have already failed multiple other therapies.” In that respect, patients and parents are desperate to try anything that might work. “We have medical cannabis, and our patients want to try it, and at the point when multiple therapies have failed, it’s a reasonable option.”
While Dr. Szaflarski agreed that more high-quality clinical trials are needed, he also noted the practical challenges involved in such trials, largely because of variations in cannabis plants.
“The content of the cannabis plant changes depending on the day that it’s collected and the exposure to sun and how much water it has and what’s in the soil and many other things,” Dr. Szaflarski said. “It’s hard to get a very good, standardized product, and that’s why there needs to be a good-quality product delivered by the industry, which I have not seen thus far.”
For this reason, Dr. Szaflarski steers parents and patients away from over-the-counter CBMPs and toward Epidiolex, the only FDA-approved form of CBD.
“There is evidence that Epidiolex works,” he said. “I don’t know whether the products that are sold in a local cannabis store have the same high purity as Epidiolex. I tell [parents] that we should try Epidiolex first because it’s the one that is approved. But if it doesn’t work, we can go in that [other] direction.”
For those going the commercial route, Dr. Szaflarski advised close attention to product ingredients, to ensure that CBMPs are “devoid of any impurities, pesticides, fungicides, and other products that could be potentially dangerous.”
Parents considering CBMPs for their children also need to weigh concerns about long-term neurological safety, he added, noting that, on one hand, commercial products lack data, while on the other, epilepsy itself may cause harm.
“They need to consider the potential effects [of CBMPs] on their child’s brain and development versus … the effects of seizures on the brain,” Dr. Szaflarski said.
Dr. Kirkpatrick and Dr. O’Callaghan disclosed an application for a National Institute for Health Research–funded randomized controlled trial on CBMPs and joint authorship of British Paediatric Neurology Association Guidance on the use of CBMPs in children and young people with epilepsy. Dr. Szaflarski disclosed a relationship with Greenwich Biosciences and several other cannabis companies.
, according to two leading experts.
In a recent invited review article, Martin Kirkpatrick, MD, of the University of Dundee (Scotland), and Finbar O’Callaghan, MD, PhD, of University College London suggested that childhood epilepsy may be easy terrain for commercial interests to break ground, and from there, build their presence.
“Children with epilepsy are at risk of being used as the ‘Trojan horse’ for the cannabis industry,” Dr. Kirkpatrick and Dr. O’Callaghan wrote in Developmental Medicine & Child Neurology.
They noted that some of the first publicized success stories involving cannabis oil for epilepsy coincided with the rise of the medicinal and recreational cannabis markets, which will constitute an estimated 55-billion-dollar industry by 2027.
“Pediatric neurologists, imbued with the need to practice evidence-based medicine and wary of prescribing unlicensed medicines that had inadequate safety data, suddenly found themselves at odds with an array of vested interests and, most unfortunately, with the families of patients who were keen to try anything that would alleviate the effects of their child’s seizures,” the investigators wrote.
According to the review, fundamental questions about cannabis remain unanswered, including concerns about safety with long-term use, and the medicinal value of various plant components, such as myrcene, a terpene that gives cannabis its characteristic smell.
“A widely discussed issue is whether the terpenes add any therapeutic benefit, contributing to the so-called entourage effect of ‘whole-plant’ medicines,” the investigators wrote. “The concept is that all the constituents of the plant together create ‘the sum of all the parts that leads to the magic or power of cannabis.’ Although commonly referred to, there is little or no robust evidence to support the entourage effect as a credible clinical concept.”
Clinical evidence for treatment of pediatric epilepsy is also lacking, according to Dr. Kirkpatrick and Dr. O’Callaghan.
“Unfortunately, apart from the studies of pure cannabidiol (CBD) in Lennox–Gastaut and Dravet syndromes and tuberous sclerosis complex, level I evidence in the field of CBMPs and refractory epilepsy is lacking,” they wrote.
While other experts have pointed out that lower-level evidence – such as patient-reported outcomes and observational data – have previously been sufficient for drug licensing, Dr. Kirkpatrick and Dr. O’Callaghan noted that such exceptions “almost always” involve conditions without any effective treatments, or drugs that are undeniably effective.
“This is not the scenario with CBMPs,” they wrote, referring to current clinical data as “low-level” evidence “suggesting … possible efficacy.”
They highlighted concerns about placebo effect with open-label epilepsy studies, citing a randomized controlled trial for Dravet syndrome, in which 27% of patients given placebo had a 50% reduction in seizure frequency.
“We need carefully designed, good-quality CBMP studies that produce results on which we can rely,” Dr. Kirkpatrick and Dr. O’Callaghan concluded. “We can then work with families to choose the best treatments for children and young people with epilepsy. We owe this to them.”
A therapy of last resort
Jerzy P. Szaflarski, MD, PhD, of the University of Alabama at Birmingham, agreed that data are lacking for the use of CBMPs with patients who have epilepsy and other neurologic conditions; however, he also suggested that Dr. Kirkpatrick and Dr. O’Callaghan did not provide adequate real-world clinical context.
“Medical cannabis is not used as a first-, second-, or third-line therapy,” Dr. Szaflarski said. “It’s mostly used as a last resort in the sense that patients have already failed multiple other therapies.” In that respect, patients and parents are desperate to try anything that might work. “We have medical cannabis, and our patients want to try it, and at the point when multiple therapies have failed, it’s a reasonable option.”
While Dr. Szaflarski agreed that more high-quality clinical trials are needed, he also noted the practical challenges involved in such trials, largely because of variations in cannabis plants.
“The content of the cannabis plant changes depending on the day that it’s collected and the exposure to sun and how much water it has and what’s in the soil and many other things,” Dr. Szaflarski said. “It’s hard to get a very good, standardized product, and that’s why there needs to be a good-quality product delivered by the industry, which I have not seen thus far.”
For this reason, Dr. Szaflarski steers parents and patients away from over-the-counter CBMPs and toward Epidiolex, the only FDA-approved form of CBD.
“There is evidence that Epidiolex works,” he said. “I don’t know whether the products that are sold in a local cannabis store have the same high purity as Epidiolex. I tell [parents] that we should try Epidiolex first because it’s the one that is approved. But if it doesn’t work, we can go in that [other] direction.”
For those going the commercial route, Dr. Szaflarski advised close attention to product ingredients, to ensure that CBMPs are “devoid of any impurities, pesticides, fungicides, and other products that could be potentially dangerous.”
Parents considering CBMPs for their children also need to weigh concerns about long-term neurological safety, he added, noting that, on one hand, commercial products lack data, while on the other, epilepsy itself may cause harm.
“They need to consider the potential effects [of CBMPs] on their child’s brain and development versus … the effects of seizures on the brain,” Dr. Szaflarski said.
Dr. Kirkpatrick and Dr. O’Callaghan disclosed an application for a National Institute for Health Research–funded randomized controlled trial on CBMPs and joint authorship of British Paediatric Neurology Association Guidance on the use of CBMPs in children and young people with epilepsy. Dr. Szaflarski disclosed a relationship with Greenwich Biosciences and several other cannabis companies.
, according to two leading experts.
In a recent invited review article, Martin Kirkpatrick, MD, of the University of Dundee (Scotland), and Finbar O’Callaghan, MD, PhD, of University College London suggested that childhood epilepsy may be easy terrain for commercial interests to break ground, and from there, build their presence.
“Children with epilepsy are at risk of being used as the ‘Trojan horse’ for the cannabis industry,” Dr. Kirkpatrick and Dr. O’Callaghan wrote in Developmental Medicine & Child Neurology.
They noted that some of the first publicized success stories involving cannabis oil for epilepsy coincided with the rise of the medicinal and recreational cannabis markets, which will constitute an estimated 55-billion-dollar industry by 2027.
“Pediatric neurologists, imbued with the need to practice evidence-based medicine and wary of prescribing unlicensed medicines that had inadequate safety data, suddenly found themselves at odds with an array of vested interests and, most unfortunately, with the families of patients who were keen to try anything that would alleviate the effects of their child’s seizures,” the investigators wrote.
According to the review, fundamental questions about cannabis remain unanswered, including concerns about safety with long-term use, and the medicinal value of various plant components, such as myrcene, a terpene that gives cannabis its characteristic smell.
“A widely discussed issue is whether the terpenes add any therapeutic benefit, contributing to the so-called entourage effect of ‘whole-plant’ medicines,” the investigators wrote. “The concept is that all the constituents of the plant together create ‘the sum of all the parts that leads to the magic or power of cannabis.’ Although commonly referred to, there is little or no robust evidence to support the entourage effect as a credible clinical concept.”
Clinical evidence for treatment of pediatric epilepsy is also lacking, according to Dr. Kirkpatrick and Dr. O’Callaghan.
“Unfortunately, apart from the studies of pure cannabidiol (CBD) in Lennox–Gastaut and Dravet syndromes and tuberous sclerosis complex, level I evidence in the field of CBMPs and refractory epilepsy is lacking,” they wrote.
While other experts have pointed out that lower-level evidence – such as patient-reported outcomes and observational data – have previously been sufficient for drug licensing, Dr. Kirkpatrick and Dr. O’Callaghan noted that such exceptions “almost always” involve conditions without any effective treatments, or drugs that are undeniably effective.
“This is not the scenario with CBMPs,” they wrote, referring to current clinical data as “low-level” evidence “suggesting … possible efficacy.”
They highlighted concerns about placebo effect with open-label epilepsy studies, citing a randomized controlled trial for Dravet syndrome, in which 27% of patients given placebo had a 50% reduction in seizure frequency.
“We need carefully designed, good-quality CBMP studies that produce results on which we can rely,” Dr. Kirkpatrick and Dr. O’Callaghan concluded. “We can then work with families to choose the best treatments for children and young people with epilepsy. We owe this to them.”
A therapy of last resort
Jerzy P. Szaflarski, MD, PhD, of the University of Alabama at Birmingham, agreed that data are lacking for the use of CBMPs with patients who have epilepsy and other neurologic conditions; however, he also suggested that Dr. Kirkpatrick and Dr. O’Callaghan did not provide adequate real-world clinical context.
“Medical cannabis is not used as a first-, second-, or third-line therapy,” Dr. Szaflarski said. “It’s mostly used as a last resort in the sense that patients have already failed multiple other therapies.” In that respect, patients and parents are desperate to try anything that might work. “We have medical cannabis, and our patients want to try it, and at the point when multiple therapies have failed, it’s a reasonable option.”
While Dr. Szaflarski agreed that more high-quality clinical trials are needed, he also noted the practical challenges involved in such trials, largely because of variations in cannabis plants.
“The content of the cannabis plant changes depending on the day that it’s collected and the exposure to sun and how much water it has and what’s in the soil and many other things,” Dr. Szaflarski said. “It’s hard to get a very good, standardized product, and that’s why there needs to be a good-quality product delivered by the industry, which I have not seen thus far.”
For this reason, Dr. Szaflarski steers parents and patients away from over-the-counter CBMPs and toward Epidiolex, the only FDA-approved form of CBD.
“There is evidence that Epidiolex works,” he said. “I don’t know whether the products that are sold in a local cannabis store have the same high purity as Epidiolex. I tell [parents] that we should try Epidiolex first because it’s the one that is approved. But if it doesn’t work, we can go in that [other] direction.”
For those going the commercial route, Dr. Szaflarski advised close attention to product ingredients, to ensure that CBMPs are “devoid of any impurities, pesticides, fungicides, and other products that could be potentially dangerous.”
Parents considering CBMPs for their children also need to weigh concerns about long-term neurological safety, he added, noting that, on one hand, commercial products lack data, while on the other, epilepsy itself may cause harm.
“They need to consider the potential effects [of CBMPs] on their child’s brain and development versus … the effects of seizures on the brain,” Dr. Szaflarski said.
Dr. Kirkpatrick and Dr. O’Callaghan disclosed an application for a National Institute for Health Research–funded randomized controlled trial on CBMPs and joint authorship of British Paediatric Neurology Association Guidance on the use of CBMPs in children and young people with epilepsy. Dr. Szaflarski disclosed a relationship with Greenwich Biosciences and several other cannabis companies.
FROM DEVELOPMENTAL MEDICINE & CHILD NEUROLOGY
Atopic dermatitis subtype worsens into midlife, predicting poor health
giving reason to observe patients beyond the pediatric stage, according to a cohort study of more than 30,000 patients.
Early-life environmental factors, such as tobacco smoke exposure, were not reliable predictors of increasing AD into mid-adulthood, suggesting that a patient’s contemporaneous environment may impact disease course throughout life, reported lead author Katrina Abuabara, MD, associate professor of dermatology at the University of California, San Francisco, and colleagues.
“There is a lack of studies that prospectively examine the course of atopic eczema beyond adolescence/early adulthood, and a more comprehensive understanding of disease activity across the life span is needed,” the investigators wrote in JAMA Dermatology. “Data on long-term disease course may offer insight into mechanisms for disease onset and persistence, are important when counseling patients, and would establish baseline trajectories for future studies of whether new treatments can modify disease course and development of comorbidities.”
The present study included 30,905 patients from two population-based birth cohorts: the 1958 National Childhood Development Study (NCDS) and the 1970 British Cohort Study (BCS70). Follow-up data were collected between 1958 and 2016 via nine waves of standardized questionnaires, and subtypes of atopic eczema patterns were identified “based on parent-reported or self-reported atopic eczema period prevalence.”
This measure “was previously shown to coincide with standardized clinical examinations among children in the NCDS, and a similar questionnaire demonstrated high sensitivity and specificity for physician-diagnosed atopic eczema in U.S. populations,” the investigators noted.
Latent class analysis identified four disease subtypes based on probability of reporting prevalent AD into midlife: low (88%-91%), decreasing (4%), increasing (2%-6%), and persistently high (2%-3%) probability.
Next, the investigators looked for associations between these subtypes and established early-life risk factors, such as history of breastfeeding and childhood smoke exposure. None of the childhood environmental factors differentiated between high versus decreasing disease in adulthood, or increasing versus decreasing disease in adulthood. In contrast, female sex predicted the high versus decreasing adult subtype (odds ratio, 1.99; 95% confidence interval, 1.66-2.38), and the increasing versus decreasing adult subtype (OR, 1.99; 95% CI, 1.69-2.35).
These findings suggest that “disease trajectory is modifiable and may be influenced by environmental factors throughout life,” the investigators wrote.
Further analysis uncovered associations between adult AD subtypes and other health outcomes. For example, compared with adults in the low probability group, those in the high probability group were significantly more likely to report rhinitis (OR, 2.70; 95% CI, 2.24-3.26) and asthma (OR, 3.45; 95% CI, 2.82-4.21). Adults with the increasing subtype also had elevated rates of asthma and rhinitis, along with worse self-reported mental health at age 42 (OR, 1.45; 95% CI, 1.23-1.72) and poor general health at age 46/50 (OR, 1.29; 95% CI, 1.09-1.53).
“When extending the window of observation beyond childhood, clear subtypes of atopic eczema based on patterns of disease activity emerged,” the investigators concluded. “In particular, a newly identified subtype with increasing probability of activity in adulthood warrants additional attention given associations with poor self-reported physical and mental health in midlife.”
Commenting on these results, Robert Sidbury, MD, professor of dermatology at the University of Washington, Seattle, said that this is an “important study” because it adds to our understanding of natural disease course over time.
This knowledge, as a pediatric dermatologist, will help Dr. Sidbury answer one of the most common questions he hears from parents: When is it going to stop?
“Trying to put a little bit more evidence-based heft behind the answer ... is really important,” he said in an interview.
Based on available data, up to 10% of children with AD may have disease activity into adulthood, according to Dr. Sidbury, who is also chief of dermatology at Seattle Children’s Hospital.
“I would hazard to guess that most of those adults who have atopic dermatitis – at least the ones who had it in childhood – were told that they would grow out of it,” he said. “And so I think awareness is important – that [resolution with age] does not always happen.”
The findings also support the possibility that AD is a systemic disease, and that underlying immune dysregulation may be linked with serious health consequences later in life, Dr. Sidbury said, noting that “the stakes get higher and higher when you start speculating in that way.”
According to Dr. Sidbury, the reported link between childhood AD and poor midlife health raises questions about how modifiable the disease course may be, particularly in response to earlier intervention with emerging AD medications, which “seem to be much more effective and potent.”
“Will the advent of these medications and their adoption and use in treatment perhaps have a significant impact, not just on the prevention of atopic dermatitis itself, but maybe other comorbidities?” he asked.
For the time being, this question remains unanswered.
The study was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the Wellcome Trust. Dr. Abuabara received grants from the National Institutes of Health during the study, as well as personal fees from Target RWE and Pfizer outside of this study. One author reported receiving NIH grants during the study, another reported receiving grants from the Wellcome Trust and the Innovative Medicine Initiative Horizon 2020 (BIOMAP project) during the study; there were no other disclosures. Dr. Sidbury disclosed relationships with Galderma, Regeneron, and Pfizer.
giving reason to observe patients beyond the pediatric stage, according to a cohort study of more than 30,000 patients.
Early-life environmental factors, such as tobacco smoke exposure, were not reliable predictors of increasing AD into mid-adulthood, suggesting that a patient’s contemporaneous environment may impact disease course throughout life, reported lead author Katrina Abuabara, MD, associate professor of dermatology at the University of California, San Francisco, and colleagues.
“There is a lack of studies that prospectively examine the course of atopic eczema beyond adolescence/early adulthood, and a more comprehensive understanding of disease activity across the life span is needed,” the investigators wrote in JAMA Dermatology. “Data on long-term disease course may offer insight into mechanisms for disease onset and persistence, are important when counseling patients, and would establish baseline trajectories for future studies of whether new treatments can modify disease course and development of comorbidities.”
The present study included 30,905 patients from two population-based birth cohorts: the 1958 National Childhood Development Study (NCDS) and the 1970 British Cohort Study (BCS70). Follow-up data were collected between 1958 and 2016 via nine waves of standardized questionnaires, and subtypes of atopic eczema patterns were identified “based on parent-reported or self-reported atopic eczema period prevalence.”
This measure “was previously shown to coincide with standardized clinical examinations among children in the NCDS, and a similar questionnaire demonstrated high sensitivity and specificity for physician-diagnosed atopic eczema in U.S. populations,” the investigators noted.
Latent class analysis identified four disease subtypes based on probability of reporting prevalent AD into midlife: low (88%-91%), decreasing (4%), increasing (2%-6%), and persistently high (2%-3%) probability.
Next, the investigators looked for associations between these subtypes and established early-life risk factors, such as history of breastfeeding and childhood smoke exposure. None of the childhood environmental factors differentiated between high versus decreasing disease in adulthood, or increasing versus decreasing disease in adulthood. In contrast, female sex predicted the high versus decreasing adult subtype (odds ratio, 1.99; 95% confidence interval, 1.66-2.38), and the increasing versus decreasing adult subtype (OR, 1.99; 95% CI, 1.69-2.35).
These findings suggest that “disease trajectory is modifiable and may be influenced by environmental factors throughout life,” the investigators wrote.
Further analysis uncovered associations between adult AD subtypes and other health outcomes. For example, compared with adults in the low probability group, those in the high probability group were significantly more likely to report rhinitis (OR, 2.70; 95% CI, 2.24-3.26) and asthma (OR, 3.45; 95% CI, 2.82-4.21). Adults with the increasing subtype also had elevated rates of asthma and rhinitis, along with worse self-reported mental health at age 42 (OR, 1.45; 95% CI, 1.23-1.72) and poor general health at age 46/50 (OR, 1.29; 95% CI, 1.09-1.53).
“When extending the window of observation beyond childhood, clear subtypes of atopic eczema based on patterns of disease activity emerged,” the investigators concluded. “In particular, a newly identified subtype with increasing probability of activity in adulthood warrants additional attention given associations with poor self-reported physical and mental health in midlife.”
Commenting on these results, Robert Sidbury, MD, professor of dermatology at the University of Washington, Seattle, said that this is an “important study” because it adds to our understanding of natural disease course over time.
This knowledge, as a pediatric dermatologist, will help Dr. Sidbury answer one of the most common questions he hears from parents: When is it going to stop?
“Trying to put a little bit more evidence-based heft behind the answer ... is really important,” he said in an interview.
Based on available data, up to 10% of children with AD may have disease activity into adulthood, according to Dr. Sidbury, who is also chief of dermatology at Seattle Children’s Hospital.
“I would hazard to guess that most of those adults who have atopic dermatitis – at least the ones who had it in childhood – were told that they would grow out of it,” he said. “And so I think awareness is important – that [resolution with age] does not always happen.”
The findings also support the possibility that AD is a systemic disease, and that underlying immune dysregulation may be linked with serious health consequences later in life, Dr. Sidbury said, noting that “the stakes get higher and higher when you start speculating in that way.”
According to Dr. Sidbury, the reported link between childhood AD and poor midlife health raises questions about how modifiable the disease course may be, particularly in response to earlier intervention with emerging AD medications, which “seem to be much more effective and potent.”
“Will the advent of these medications and their adoption and use in treatment perhaps have a significant impact, not just on the prevention of atopic dermatitis itself, but maybe other comorbidities?” he asked.
For the time being, this question remains unanswered.
The study was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the Wellcome Trust. Dr. Abuabara received grants from the National Institutes of Health during the study, as well as personal fees from Target RWE and Pfizer outside of this study. One author reported receiving NIH grants during the study, another reported receiving grants from the Wellcome Trust and the Innovative Medicine Initiative Horizon 2020 (BIOMAP project) during the study; there were no other disclosures. Dr. Sidbury disclosed relationships with Galderma, Regeneron, and Pfizer.
giving reason to observe patients beyond the pediatric stage, according to a cohort study of more than 30,000 patients.
Early-life environmental factors, such as tobacco smoke exposure, were not reliable predictors of increasing AD into mid-adulthood, suggesting that a patient’s contemporaneous environment may impact disease course throughout life, reported lead author Katrina Abuabara, MD, associate professor of dermatology at the University of California, San Francisco, and colleagues.
“There is a lack of studies that prospectively examine the course of atopic eczema beyond adolescence/early adulthood, and a more comprehensive understanding of disease activity across the life span is needed,” the investigators wrote in JAMA Dermatology. “Data on long-term disease course may offer insight into mechanisms for disease onset and persistence, are important when counseling patients, and would establish baseline trajectories for future studies of whether new treatments can modify disease course and development of comorbidities.”
The present study included 30,905 patients from two population-based birth cohorts: the 1958 National Childhood Development Study (NCDS) and the 1970 British Cohort Study (BCS70). Follow-up data were collected between 1958 and 2016 via nine waves of standardized questionnaires, and subtypes of atopic eczema patterns were identified “based on parent-reported or self-reported atopic eczema period prevalence.”
This measure “was previously shown to coincide with standardized clinical examinations among children in the NCDS, and a similar questionnaire demonstrated high sensitivity and specificity for physician-diagnosed atopic eczema in U.S. populations,” the investigators noted.
Latent class analysis identified four disease subtypes based on probability of reporting prevalent AD into midlife: low (88%-91%), decreasing (4%), increasing (2%-6%), and persistently high (2%-3%) probability.
Next, the investigators looked for associations between these subtypes and established early-life risk factors, such as history of breastfeeding and childhood smoke exposure. None of the childhood environmental factors differentiated between high versus decreasing disease in adulthood, or increasing versus decreasing disease in adulthood. In contrast, female sex predicted the high versus decreasing adult subtype (odds ratio, 1.99; 95% confidence interval, 1.66-2.38), and the increasing versus decreasing adult subtype (OR, 1.99; 95% CI, 1.69-2.35).
These findings suggest that “disease trajectory is modifiable and may be influenced by environmental factors throughout life,” the investigators wrote.
Further analysis uncovered associations between adult AD subtypes and other health outcomes. For example, compared with adults in the low probability group, those in the high probability group were significantly more likely to report rhinitis (OR, 2.70; 95% CI, 2.24-3.26) and asthma (OR, 3.45; 95% CI, 2.82-4.21). Adults with the increasing subtype also had elevated rates of asthma and rhinitis, along with worse self-reported mental health at age 42 (OR, 1.45; 95% CI, 1.23-1.72) and poor general health at age 46/50 (OR, 1.29; 95% CI, 1.09-1.53).
“When extending the window of observation beyond childhood, clear subtypes of atopic eczema based on patterns of disease activity emerged,” the investigators concluded. “In particular, a newly identified subtype with increasing probability of activity in adulthood warrants additional attention given associations with poor self-reported physical and mental health in midlife.”
Commenting on these results, Robert Sidbury, MD, professor of dermatology at the University of Washington, Seattle, said that this is an “important study” because it adds to our understanding of natural disease course over time.
This knowledge, as a pediatric dermatologist, will help Dr. Sidbury answer one of the most common questions he hears from parents: When is it going to stop?
“Trying to put a little bit more evidence-based heft behind the answer ... is really important,” he said in an interview.
Based on available data, up to 10% of children with AD may have disease activity into adulthood, according to Dr. Sidbury, who is also chief of dermatology at Seattle Children’s Hospital.
“I would hazard to guess that most of those adults who have atopic dermatitis – at least the ones who had it in childhood – were told that they would grow out of it,” he said. “And so I think awareness is important – that [resolution with age] does not always happen.”
The findings also support the possibility that AD is a systemic disease, and that underlying immune dysregulation may be linked with serious health consequences later in life, Dr. Sidbury said, noting that “the stakes get higher and higher when you start speculating in that way.”
According to Dr. Sidbury, the reported link between childhood AD and poor midlife health raises questions about how modifiable the disease course may be, particularly in response to earlier intervention with emerging AD medications, which “seem to be much more effective and potent.”
“Will the advent of these medications and their adoption and use in treatment perhaps have a significant impact, not just on the prevention of atopic dermatitis itself, but maybe other comorbidities?” he asked.
For the time being, this question remains unanswered.
The study was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the Wellcome Trust. Dr. Abuabara received grants from the National Institutes of Health during the study, as well as personal fees from Target RWE and Pfizer outside of this study. One author reported receiving NIH grants during the study, another reported receiving grants from the Wellcome Trust and the Innovative Medicine Initiative Horizon 2020 (BIOMAP project) during the study; there were no other disclosures. Dr. Sidbury disclosed relationships with Galderma, Regeneron, and Pfizer.
FROM JAMA DERMATOLOGY
Pandemic-related school closures tied to mental health inequities
Back-to-school jitters are heightened this year, as children head back to the risk of COVID transmission in class, but one upside to the return of in-person school may be better mental health for students.
New research shows that virtual schooling, which dominated in many districts last year, was associated with worse mental health outcomes for students – especially older ones – and youth from Black, Hispanic, or lower-income families were hit hardest because they experienced the most closures.
“Schools with lower funding may have had more difficulty meeting guidelines for safe reopening, including updates to ventilation systems and finding the physical space to create safe distancing between children,” explained lead author Matt Hawrilenko, PhD, of the department of psychiatry and behavioral sciences at the University of Washington, Seattle, in an interview.
“In the context of complex school reopening decisions that balance competing risks and benefits, these findings suggest that allocating funding to support safe in-person instruction may reduce mental health inequities associated with race/ethnicity and income,” he and his coauthors noted in the study, published in JAMA Network Open. “Ensuring that all students have access to additional educational and mental health resources must be an important public health priority, met with appropriate funding and work force augmentation, during and beyond the COVID-19 pandemic.”
The study used a cross-sectional population-based survey of 2,324 parents of school-age children in the United States. It was administered in English and Spanish via web and telephone between Dec. 2 and Dec. 21, 2020, and used the parent-report version of the Strengths and Difficulties Questionnaire (SDQ) to assess mental health difficulties of one child per family in four domains: emotional problems, peer problems, conduct, and hyperactivity. Parents were also asked about what kind of schooling their child had received in the last year (remote, in-person, or hybrid) and about demographic information such as child age, gender, household income, parent race and ethnicity, and parent education.
The results showed that, during the 2020 school year, 58.0% of children attended school remotely, 24% attended fully in person, and 18.0% attended in a hybrid format. “Fully remote schooling was strongly patterned along lines of parent race and ethnicity as well as income,” the authors noted. “Parents of 336 children attending school in person (65.8%) but of 597 children attending school fully remotely (44.5%) were White, whereas all other racial/ethnic groups had larger proportions of children attending school fully remotely (P < .001).”
In terms of mental health, the findings showed that older children who attended school remotely had more difficulties, compared with those who attended in-person – but among younger children, remote learning was comparable or slightly better for mental health.
Specifically, “a child aged 17 years attending school remotely would be expected to have a total difficulty score 2.4 points higher than a child of the same age attending school in person, corresponding to a small effect size in favor of in-person schooling,” the authors wrote. “Conversely, a child aged 4 years attending school remotely would be expected to have a total difficulty score 0.5 points lower than a child of the same age attending school in person, corresponding to a very small effect size in favor of remote schooling.”
Age of child proves critical
“Our best estimate is that remote schooling was associated with no difference in mental health difficulties at age 6, and with slightly more difficulties with each year of age after that, with differences most clearly apparent for high school–aged kids,” explained Dr. Hawrilenko, adding the finding suggests that school reopenings should prioritize older children.
However, “what kids are doing at home matters,” he added. “In the youngest age group, the biggest work kids are doing in school and childcare settings is social and emotional development. … Finding opportunities for regular, safe social interactions with peers – perhaps during outdoor playdates – can help them build those skills.”
He emphasized with the anticipated starts and stutters of the new school year there is an important role that doctors can play.
“First, they can help families assess their own risk profile, and whether it makes sense for their children to attend school in person or remotely [to the extent that is an option]. Second, they can help families think through how school closures might impact their child specifically. For those kids who wind up with long chunks of remote schooling, scheduling in regular interactions with other kids in safe ways could make a big difference. Another driver of child anxiety might be learning loss, and this is a good place to reinforce that not every mental health problem needs a mental health solution.
“A lot of kids might be rightfully anxious about having fallen behind over the pandemic. These kids are preparing to transition to college or to the workforce and may be feeling increasingly behind while approaching these moments of transition. Pointing families toward the resources to help them navigate these issues could go a long way to helping quell child anxiety.”
Research helps fill vacuum
Elizabeth A. Stuart, PhD, who was not involved in the study, said in an interview that this research is particularly valuable because there have been very few data on this topic, especially on a large-scale national sample.
“Sadly, many of the results are not surprising,” said Dr. Stuart, a statistician and professor of mental health at Johns Hopkins University, Baltimore. “Data have shown significant mental health challenges for adults during the pandemic, and it is not surprising that children and youth would experience that as well, especially for those whose daily routines and structures changed dramatically and who were not able to be interacting in-person with teachers, staff, and classmates. This is an important reminder that schools provide not just academic instruction for students, but that the social interactions and other services (such as behavioral health supports, meals, and connections with other social services) students might receive in school are crucial.
“It has been heartening to see a stronger commitment to getting students safely back into school this fall across the country, and that the Centers for Disease Control and Prevention highlighted the benefits of in-person schooling in their COVID-19–related guidance for schools.”
Dr. Stuart added that, as students return to classes, it will be important for schools to tackle ongoing mental health challenges.
“Some students may be struggling in obvious ways; for others it may be harder to identify. It will also be important to continue to monitor children’s and youth mental health … as returning to in-person school may bring its own challenges. ”
Dr. Hawrilenko agreed.
“From a policy perspective, I am quite frankly terrified about how these inequities – in particular, learning loss – might play out long after school closures are a distant memory,” he said. “It is critical to provide schools the resources not just to minimize risk when reopening, but additional funding for workforce augmentation – both for mental health staffing and for additional educational support – to help students navigate the months and years over which they transition back into the classroom.”
Dr. Hawrilenko and Dr. Stuart had no disclosures.
Back-to-school jitters are heightened this year, as children head back to the risk of COVID transmission in class, but one upside to the return of in-person school may be better mental health for students.
New research shows that virtual schooling, which dominated in many districts last year, was associated with worse mental health outcomes for students – especially older ones – and youth from Black, Hispanic, or lower-income families were hit hardest because they experienced the most closures.
“Schools with lower funding may have had more difficulty meeting guidelines for safe reopening, including updates to ventilation systems and finding the physical space to create safe distancing between children,” explained lead author Matt Hawrilenko, PhD, of the department of psychiatry and behavioral sciences at the University of Washington, Seattle, in an interview.
“In the context of complex school reopening decisions that balance competing risks and benefits, these findings suggest that allocating funding to support safe in-person instruction may reduce mental health inequities associated with race/ethnicity and income,” he and his coauthors noted in the study, published in JAMA Network Open. “Ensuring that all students have access to additional educational and mental health resources must be an important public health priority, met with appropriate funding and work force augmentation, during and beyond the COVID-19 pandemic.”
The study used a cross-sectional population-based survey of 2,324 parents of school-age children in the United States. It was administered in English and Spanish via web and telephone between Dec. 2 and Dec. 21, 2020, and used the parent-report version of the Strengths and Difficulties Questionnaire (SDQ) to assess mental health difficulties of one child per family in four domains: emotional problems, peer problems, conduct, and hyperactivity. Parents were also asked about what kind of schooling their child had received in the last year (remote, in-person, or hybrid) and about demographic information such as child age, gender, household income, parent race and ethnicity, and parent education.
The results showed that, during the 2020 school year, 58.0% of children attended school remotely, 24% attended fully in person, and 18.0% attended in a hybrid format. “Fully remote schooling was strongly patterned along lines of parent race and ethnicity as well as income,” the authors noted. “Parents of 336 children attending school in person (65.8%) but of 597 children attending school fully remotely (44.5%) were White, whereas all other racial/ethnic groups had larger proportions of children attending school fully remotely (P < .001).”
In terms of mental health, the findings showed that older children who attended school remotely had more difficulties, compared with those who attended in-person – but among younger children, remote learning was comparable or slightly better for mental health.
Specifically, “a child aged 17 years attending school remotely would be expected to have a total difficulty score 2.4 points higher than a child of the same age attending school in person, corresponding to a small effect size in favor of in-person schooling,” the authors wrote. “Conversely, a child aged 4 years attending school remotely would be expected to have a total difficulty score 0.5 points lower than a child of the same age attending school in person, corresponding to a very small effect size in favor of remote schooling.”
Age of child proves critical
“Our best estimate is that remote schooling was associated with no difference in mental health difficulties at age 6, and with slightly more difficulties with each year of age after that, with differences most clearly apparent for high school–aged kids,” explained Dr. Hawrilenko, adding the finding suggests that school reopenings should prioritize older children.
However, “what kids are doing at home matters,” he added. “In the youngest age group, the biggest work kids are doing in school and childcare settings is social and emotional development. … Finding opportunities for regular, safe social interactions with peers – perhaps during outdoor playdates – can help them build those skills.”
He emphasized with the anticipated starts and stutters of the new school year there is an important role that doctors can play.
“First, they can help families assess their own risk profile, and whether it makes sense for their children to attend school in person or remotely [to the extent that is an option]. Second, they can help families think through how school closures might impact their child specifically. For those kids who wind up with long chunks of remote schooling, scheduling in regular interactions with other kids in safe ways could make a big difference. Another driver of child anxiety might be learning loss, and this is a good place to reinforce that not every mental health problem needs a mental health solution.
“A lot of kids might be rightfully anxious about having fallen behind over the pandemic. These kids are preparing to transition to college or to the workforce and may be feeling increasingly behind while approaching these moments of transition. Pointing families toward the resources to help them navigate these issues could go a long way to helping quell child anxiety.”
Research helps fill vacuum
Elizabeth A. Stuart, PhD, who was not involved in the study, said in an interview that this research is particularly valuable because there have been very few data on this topic, especially on a large-scale national sample.
“Sadly, many of the results are not surprising,” said Dr. Stuart, a statistician and professor of mental health at Johns Hopkins University, Baltimore. “Data have shown significant mental health challenges for adults during the pandemic, and it is not surprising that children and youth would experience that as well, especially for those whose daily routines and structures changed dramatically and who were not able to be interacting in-person with teachers, staff, and classmates. This is an important reminder that schools provide not just academic instruction for students, but that the social interactions and other services (such as behavioral health supports, meals, and connections with other social services) students might receive in school are crucial.
“It has been heartening to see a stronger commitment to getting students safely back into school this fall across the country, and that the Centers for Disease Control and Prevention highlighted the benefits of in-person schooling in their COVID-19–related guidance for schools.”
Dr. Stuart added that, as students return to classes, it will be important for schools to tackle ongoing mental health challenges.
“Some students may be struggling in obvious ways; for others it may be harder to identify. It will also be important to continue to monitor children’s and youth mental health … as returning to in-person school may bring its own challenges. ”
Dr. Hawrilenko agreed.
“From a policy perspective, I am quite frankly terrified about how these inequities – in particular, learning loss – might play out long after school closures are a distant memory,” he said. “It is critical to provide schools the resources not just to minimize risk when reopening, but additional funding for workforce augmentation – both for mental health staffing and for additional educational support – to help students navigate the months and years over which they transition back into the classroom.”
Dr. Hawrilenko and Dr. Stuart had no disclosures.
Back-to-school jitters are heightened this year, as children head back to the risk of COVID transmission in class, but one upside to the return of in-person school may be better mental health for students.
New research shows that virtual schooling, which dominated in many districts last year, was associated with worse mental health outcomes for students – especially older ones – and youth from Black, Hispanic, or lower-income families were hit hardest because they experienced the most closures.
“Schools with lower funding may have had more difficulty meeting guidelines for safe reopening, including updates to ventilation systems and finding the physical space to create safe distancing between children,” explained lead author Matt Hawrilenko, PhD, of the department of psychiatry and behavioral sciences at the University of Washington, Seattle, in an interview.
“In the context of complex school reopening decisions that balance competing risks and benefits, these findings suggest that allocating funding to support safe in-person instruction may reduce mental health inequities associated with race/ethnicity and income,” he and his coauthors noted in the study, published in JAMA Network Open. “Ensuring that all students have access to additional educational and mental health resources must be an important public health priority, met with appropriate funding and work force augmentation, during and beyond the COVID-19 pandemic.”
The study used a cross-sectional population-based survey of 2,324 parents of school-age children in the United States. It was administered in English and Spanish via web and telephone between Dec. 2 and Dec. 21, 2020, and used the parent-report version of the Strengths and Difficulties Questionnaire (SDQ) to assess mental health difficulties of one child per family in four domains: emotional problems, peer problems, conduct, and hyperactivity. Parents were also asked about what kind of schooling their child had received in the last year (remote, in-person, or hybrid) and about demographic information such as child age, gender, household income, parent race and ethnicity, and parent education.
The results showed that, during the 2020 school year, 58.0% of children attended school remotely, 24% attended fully in person, and 18.0% attended in a hybrid format. “Fully remote schooling was strongly patterned along lines of parent race and ethnicity as well as income,” the authors noted. “Parents of 336 children attending school in person (65.8%) but of 597 children attending school fully remotely (44.5%) were White, whereas all other racial/ethnic groups had larger proportions of children attending school fully remotely (P < .001).”
In terms of mental health, the findings showed that older children who attended school remotely had more difficulties, compared with those who attended in-person – but among younger children, remote learning was comparable or slightly better for mental health.
Specifically, “a child aged 17 years attending school remotely would be expected to have a total difficulty score 2.4 points higher than a child of the same age attending school in person, corresponding to a small effect size in favor of in-person schooling,” the authors wrote. “Conversely, a child aged 4 years attending school remotely would be expected to have a total difficulty score 0.5 points lower than a child of the same age attending school in person, corresponding to a very small effect size in favor of remote schooling.”
Age of child proves critical
“Our best estimate is that remote schooling was associated with no difference in mental health difficulties at age 6, and with slightly more difficulties with each year of age after that, with differences most clearly apparent for high school–aged kids,” explained Dr. Hawrilenko, adding the finding suggests that school reopenings should prioritize older children.
However, “what kids are doing at home matters,” he added. “In the youngest age group, the biggest work kids are doing in school and childcare settings is social and emotional development. … Finding opportunities for regular, safe social interactions with peers – perhaps during outdoor playdates – can help them build those skills.”
He emphasized with the anticipated starts and stutters of the new school year there is an important role that doctors can play.
“First, they can help families assess their own risk profile, and whether it makes sense for their children to attend school in person or remotely [to the extent that is an option]. Second, they can help families think through how school closures might impact their child specifically. For those kids who wind up with long chunks of remote schooling, scheduling in regular interactions with other kids in safe ways could make a big difference. Another driver of child anxiety might be learning loss, and this is a good place to reinforce that not every mental health problem needs a mental health solution.
“A lot of kids might be rightfully anxious about having fallen behind over the pandemic. These kids are preparing to transition to college or to the workforce and may be feeling increasingly behind while approaching these moments of transition. Pointing families toward the resources to help them navigate these issues could go a long way to helping quell child anxiety.”
Research helps fill vacuum
Elizabeth A. Stuart, PhD, who was not involved in the study, said in an interview that this research is particularly valuable because there have been very few data on this topic, especially on a large-scale national sample.
“Sadly, many of the results are not surprising,” said Dr. Stuart, a statistician and professor of mental health at Johns Hopkins University, Baltimore. “Data have shown significant mental health challenges for adults during the pandemic, and it is not surprising that children and youth would experience that as well, especially for those whose daily routines and structures changed dramatically and who were not able to be interacting in-person with teachers, staff, and classmates. This is an important reminder that schools provide not just academic instruction for students, but that the social interactions and other services (such as behavioral health supports, meals, and connections with other social services) students might receive in school are crucial.
“It has been heartening to see a stronger commitment to getting students safely back into school this fall across the country, and that the Centers for Disease Control and Prevention highlighted the benefits of in-person schooling in their COVID-19–related guidance for schools.”
Dr. Stuart added that, as students return to classes, it will be important for schools to tackle ongoing mental health challenges.
“Some students may be struggling in obvious ways; for others it may be harder to identify. It will also be important to continue to monitor children’s and youth mental health … as returning to in-person school may bring its own challenges. ”
Dr. Hawrilenko agreed.
“From a policy perspective, I am quite frankly terrified about how these inequities – in particular, learning loss – might play out long after school closures are a distant memory,” he said. “It is critical to provide schools the resources not just to minimize risk when reopening, but additional funding for workforce augmentation – both for mental health staffing and for additional educational support – to help students navigate the months and years over which they transition back into the classroom.”
Dr. Hawrilenko and Dr. Stuart had no disclosures.
FROM JAMA NETWORK OPEN
COVID-19 linked to rise in suicide-related ED visits among youth
After a steep decline in the first months of the COVID-19 pandemic, youth with suicidal thoughts and behaviors visiting an emergency department (ED) resurged with an overrepresentation among girls and children without a prior psychiatric history, according to a cross-sectional study conducted at Kaiser Permanente Northern California.
The latest findings, published in JAMA Psychiatry, are highly consistent with Centers for Disease Control and Prevention data published a few months earlier in the Morbidity and Mortality Weekly Report that looked at these trends among young people aged 12-25 before and during the pandemic. In addition, the new data suggest that prevention efforts might be particularly helpful for these young people and their families.
“As suicide-related encounters have made up more ED volume during the pandemic, increasing ED-based interventions, staff trained in addressing emergency mental health needs, and aftercare resources may also be valuable in addressing the needs of this population,” wrote Kathryn K. Erickson-Ridout, MD, PhD, first author of the more recent study and an adjunct investigator with the Kaiser Permanente Division of Research, Oakland, Calif.
“While these results suggest many of our youth are coping well through the pandemic, we need to be vigilant as health care workers,” she said in an interview.
Dr. Ridout and associates evaluated suicide-related ED visits among children aged 5-17 years presenting to EDs in the Kaiser Permanente Northern California system. Four periods in 2020 were compared with the same four periods in 2019.
In the first period, March through May 2020, the incidence rate ratio (IRR) of suicide-related ED visits among children and adolescents fell more than 40% (IRR, 0.53; P < .001) relative to the same months in 2019. This is consistent with a broader decline in other types of ED visits during the beginning of the COVID-19 pandemic.
In the periods of June through August and September to Dec. 15, suicide-related ED visits increased, reaching prepandemic levels overall but with differences between genders. In girls, an increase in the first period reached significance (IRR, 1.19; P = .04) and then climbed even higher in the second (hazard ratio, 1.22; P < .001).
Youth present with no prior psychiatric history
Among boys, the increase relative to 2019 in the first period was modest and nonsignificant (IRR, 1.05; P = .26) In the second period, suicide-related ED visits fell and the difference relative to the same period in 2019 reached statistical significance (IRR, 0.81; P = .02).
Other characteristics of suicide-related ED visits during the pandemic were also different from those observed in 2019. One was an increase in visits from youth with no prior history of mental health or suicide-related outpatient visits.
“This finding may suggest that a youth’s first presentation to the ED for suicidal thoughts and behaviors differed during the pandemic, compared to prior to the pandemic,” Dr. Erickson-Ridout explained. “Mental health comorbidities first diagnosed at the ED encounter may suggest an increased complexity at first presentation.”
These data are remarkably similar to ED visits for suicide attempts that were reported by the CDC several months earlier. The CDC data were drawn from the National Syndromic Surveillance Program, which captures data from 71% of the EDs in the United States.
Measured from March 29 to April 25, 2020, ED visits for a suicide attempt declined by more than 25% in both girls and boys, but by early May, those visits were already starting to return to prepandemic levels, particularly among girls, according to the CDC report. When evaluated from July 26 through Aug. 22, 2020, the mean weekly ED visits for suspected suicide attempts had increased 26.2% among girls but only 10.8% among boys, compared with the same period in 2019.
‘More severe distress’ found among girls
In the most recent period evaluated, starting Feb. 21, 2021, and extending to March 20, , compared with the same period in 2019. For boys, the increase was 3.7%.
Higher rates of suicide attempts among girls have been reported by others independent of the COVID-19 pandemic, but the CDC investigators led by Ellen Yard, PhD, a researcher in the CDC’s National Center for Environmental Health, Chamblee, Ga., reported that others have also found greater suicide ideation and attempts by girls during the pandemic.
Neither study was designed to isolate the reason or reasons for an increase in suicide-related ED visits overall or among girls specifically, but Dr. Yard and her coinvestigators speculated that social distancing and isolation during the COVID-19 pandemic might be affecting girls more.
The faster increase in suicide attempts among girls compared with boys “speaks to the importance of upstream prevention to prevent this group from becoming suicidal in the first place as well as improving suicide care both during and after ED visits,” said Dr. Yard, who was interviewed about this research.
For clinicians, she recommended “scaling up adoption of evidence-based best practice.” She cited two such resources from the National Action Alliance for Suicide Prevention (NAASP). One resource is the Best Practices in Care Transitions for Individuals with Suicide Risk: Inpatient Care to Outpatient Care; the other is called Recommended Standard Care. Both are available online for free from the NAASP.
Dr. Erickson-Ridout and Dr. Yard reported no potential conflicts of interest.
After a steep decline in the first months of the COVID-19 pandemic, youth with suicidal thoughts and behaviors visiting an emergency department (ED) resurged with an overrepresentation among girls and children without a prior psychiatric history, according to a cross-sectional study conducted at Kaiser Permanente Northern California.
The latest findings, published in JAMA Psychiatry, are highly consistent with Centers for Disease Control and Prevention data published a few months earlier in the Morbidity and Mortality Weekly Report that looked at these trends among young people aged 12-25 before and during the pandemic. In addition, the new data suggest that prevention efforts might be particularly helpful for these young people and their families.
“As suicide-related encounters have made up more ED volume during the pandemic, increasing ED-based interventions, staff trained in addressing emergency mental health needs, and aftercare resources may also be valuable in addressing the needs of this population,” wrote Kathryn K. Erickson-Ridout, MD, PhD, first author of the more recent study and an adjunct investigator with the Kaiser Permanente Division of Research, Oakland, Calif.
“While these results suggest many of our youth are coping well through the pandemic, we need to be vigilant as health care workers,” she said in an interview.
Dr. Ridout and associates evaluated suicide-related ED visits among children aged 5-17 years presenting to EDs in the Kaiser Permanente Northern California system. Four periods in 2020 were compared with the same four periods in 2019.
In the first period, March through May 2020, the incidence rate ratio (IRR) of suicide-related ED visits among children and adolescents fell more than 40% (IRR, 0.53; P < .001) relative to the same months in 2019. This is consistent with a broader decline in other types of ED visits during the beginning of the COVID-19 pandemic.
In the periods of June through August and September to Dec. 15, suicide-related ED visits increased, reaching prepandemic levels overall but with differences between genders. In girls, an increase in the first period reached significance (IRR, 1.19; P = .04) and then climbed even higher in the second (hazard ratio, 1.22; P < .001).
Youth present with no prior psychiatric history
Among boys, the increase relative to 2019 in the first period was modest and nonsignificant (IRR, 1.05; P = .26) In the second period, suicide-related ED visits fell and the difference relative to the same period in 2019 reached statistical significance (IRR, 0.81; P = .02).
Other characteristics of suicide-related ED visits during the pandemic were also different from those observed in 2019. One was an increase in visits from youth with no prior history of mental health or suicide-related outpatient visits.
“This finding may suggest that a youth’s first presentation to the ED for suicidal thoughts and behaviors differed during the pandemic, compared to prior to the pandemic,” Dr. Erickson-Ridout explained. “Mental health comorbidities first diagnosed at the ED encounter may suggest an increased complexity at first presentation.”
These data are remarkably similar to ED visits for suicide attempts that were reported by the CDC several months earlier. The CDC data were drawn from the National Syndromic Surveillance Program, which captures data from 71% of the EDs in the United States.
Measured from March 29 to April 25, 2020, ED visits for a suicide attempt declined by more than 25% in both girls and boys, but by early May, those visits were already starting to return to prepandemic levels, particularly among girls, according to the CDC report. When evaluated from July 26 through Aug. 22, 2020, the mean weekly ED visits for suspected suicide attempts had increased 26.2% among girls but only 10.8% among boys, compared with the same period in 2019.
‘More severe distress’ found among girls
In the most recent period evaluated, starting Feb. 21, 2021, and extending to March 20, , compared with the same period in 2019. For boys, the increase was 3.7%.
Higher rates of suicide attempts among girls have been reported by others independent of the COVID-19 pandemic, but the CDC investigators led by Ellen Yard, PhD, a researcher in the CDC’s National Center for Environmental Health, Chamblee, Ga., reported that others have also found greater suicide ideation and attempts by girls during the pandemic.
Neither study was designed to isolate the reason or reasons for an increase in suicide-related ED visits overall or among girls specifically, but Dr. Yard and her coinvestigators speculated that social distancing and isolation during the COVID-19 pandemic might be affecting girls more.
The faster increase in suicide attempts among girls compared with boys “speaks to the importance of upstream prevention to prevent this group from becoming suicidal in the first place as well as improving suicide care both during and after ED visits,” said Dr. Yard, who was interviewed about this research.
For clinicians, she recommended “scaling up adoption of evidence-based best practice.” She cited two such resources from the National Action Alliance for Suicide Prevention (NAASP). One resource is the Best Practices in Care Transitions for Individuals with Suicide Risk: Inpatient Care to Outpatient Care; the other is called Recommended Standard Care. Both are available online for free from the NAASP.
Dr. Erickson-Ridout and Dr. Yard reported no potential conflicts of interest.
After a steep decline in the first months of the COVID-19 pandemic, youth with suicidal thoughts and behaviors visiting an emergency department (ED) resurged with an overrepresentation among girls and children without a prior psychiatric history, according to a cross-sectional study conducted at Kaiser Permanente Northern California.
The latest findings, published in JAMA Psychiatry, are highly consistent with Centers for Disease Control and Prevention data published a few months earlier in the Morbidity and Mortality Weekly Report that looked at these trends among young people aged 12-25 before and during the pandemic. In addition, the new data suggest that prevention efforts might be particularly helpful for these young people and their families.
“As suicide-related encounters have made up more ED volume during the pandemic, increasing ED-based interventions, staff trained in addressing emergency mental health needs, and aftercare resources may also be valuable in addressing the needs of this population,” wrote Kathryn K. Erickson-Ridout, MD, PhD, first author of the more recent study and an adjunct investigator with the Kaiser Permanente Division of Research, Oakland, Calif.
“While these results suggest many of our youth are coping well through the pandemic, we need to be vigilant as health care workers,” she said in an interview.
Dr. Ridout and associates evaluated suicide-related ED visits among children aged 5-17 years presenting to EDs in the Kaiser Permanente Northern California system. Four periods in 2020 were compared with the same four periods in 2019.
In the first period, March through May 2020, the incidence rate ratio (IRR) of suicide-related ED visits among children and adolescents fell more than 40% (IRR, 0.53; P < .001) relative to the same months in 2019. This is consistent with a broader decline in other types of ED visits during the beginning of the COVID-19 pandemic.
In the periods of June through August and September to Dec. 15, suicide-related ED visits increased, reaching prepandemic levels overall but with differences between genders. In girls, an increase in the first period reached significance (IRR, 1.19; P = .04) and then climbed even higher in the second (hazard ratio, 1.22; P < .001).
Youth present with no prior psychiatric history
Among boys, the increase relative to 2019 in the first period was modest and nonsignificant (IRR, 1.05; P = .26) In the second period, suicide-related ED visits fell and the difference relative to the same period in 2019 reached statistical significance (IRR, 0.81; P = .02).
Other characteristics of suicide-related ED visits during the pandemic were also different from those observed in 2019. One was an increase in visits from youth with no prior history of mental health or suicide-related outpatient visits.
“This finding may suggest that a youth’s first presentation to the ED for suicidal thoughts and behaviors differed during the pandemic, compared to prior to the pandemic,” Dr. Erickson-Ridout explained. “Mental health comorbidities first diagnosed at the ED encounter may suggest an increased complexity at first presentation.”
These data are remarkably similar to ED visits for suicide attempts that were reported by the CDC several months earlier. The CDC data were drawn from the National Syndromic Surveillance Program, which captures data from 71% of the EDs in the United States.
Measured from March 29 to April 25, 2020, ED visits for a suicide attempt declined by more than 25% in both girls and boys, but by early May, those visits were already starting to return to prepandemic levels, particularly among girls, according to the CDC report. When evaluated from July 26 through Aug. 22, 2020, the mean weekly ED visits for suspected suicide attempts had increased 26.2% among girls but only 10.8% among boys, compared with the same period in 2019.
‘More severe distress’ found among girls
In the most recent period evaluated, starting Feb. 21, 2021, and extending to March 20, , compared with the same period in 2019. For boys, the increase was 3.7%.
Higher rates of suicide attempts among girls have been reported by others independent of the COVID-19 pandemic, but the CDC investigators led by Ellen Yard, PhD, a researcher in the CDC’s National Center for Environmental Health, Chamblee, Ga., reported that others have also found greater suicide ideation and attempts by girls during the pandemic.
Neither study was designed to isolate the reason or reasons for an increase in suicide-related ED visits overall or among girls specifically, but Dr. Yard and her coinvestigators speculated that social distancing and isolation during the COVID-19 pandemic might be affecting girls more.
The faster increase in suicide attempts among girls compared with boys “speaks to the importance of upstream prevention to prevent this group from becoming suicidal in the first place as well as improving suicide care both during and after ED visits,” said Dr. Yard, who was interviewed about this research.
For clinicians, she recommended “scaling up adoption of evidence-based best practice.” She cited two such resources from the National Action Alliance for Suicide Prevention (NAASP). One resource is the Best Practices in Care Transitions for Individuals with Suicide Risk: Inpatient Care to Outpatient Care; the other is called Recommended Standard Care. Both are available online for free from the NAASP.
Dr. Erickson-Ridout and Dr. Yard reported no potential conflicts of interest.
FROM JAMA PSYCHIATRY
Medical education must takes broader view of disabilities
“All physicians, regardless of specialty, will work with patients with disabilities,” Corrie Harris, MD, of the University of Louisville (Ky.), said in a plenary session presentation at the 2021 virtual Pediatric Hospital Medicine conference.
Disabilities vary in their visibility, from cognitive and sensory impairments that are not immediately obvious to an obvious physical disability, she said.
One in four adults and one in six children in the United States has a disability, said Dr. Harris. The prevalence of disability increases with age, but occurs across the lifespan, and will likely increase in the future with greater improvements in health care overall.
Dr. Harris reviewed the current conceptual model that forms the basis for the World Health Organization definition of functioning disability. This “functional model” defines disability as caused by interactions between health conditions and the environment, and the response is to “prioritize function to meet patient goals,” Dr. Harris said at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
This model is based on collaboration between health care providers and their patients with disabilities, and training is important to help providers make this collaboration successful, said Dr. Harris. Without training, physicians may be ineffective in communicating with patients with disabilities by not speaking directly to the patient, not speaking in a way the patient can understand clearly, and not providing accessible patient education materials. Physicians also tend to minimize the extent of the patient’s expertise in their own condition based on their lived experiences, and tend to underestimate the abilities of patients with disabilities.
However, direct experience with disabled patients and an understanding of the health disparities they endure can help physicians look at these patients “through a more intersectional lens,” that also takes into account social determinants of health, Dr. Harris said. “I have found that people with disabilities are the best teachers about disability, because they have expertise that comes from their lived experience.”
Patients are the best teachers
Several initiatives are helping physicians to bridge this gap in understanding and reduce disparities in care. One such program is FRAME: Faces Redefining the Art of Medical Education. FRAME is a web-based film library designed to present medical information to health care providers in training, clinicians, families, and communities in a dignified and humanizing way. FRAME was developed in part by fashion photographer Rick Guidotti, who was inspired after meeting a young woman with albinism to create Positive Exposure, an ongoing project featuring children and adolescents with various disabilities.
FRAME films are “short films presenting all the basic hallmark characteristics of a certain genetic condition, but presented by somebody living with that condition,” said Mr. Guidotti in his presentation during the session.
The National Curriculum Initiative in Developmental Medicine (NCIDM) is designed to incorporate care for individuals with disabilities into medical education. NCIDM is a project created by the American Academy of Developmental Medicine and Dentistry (AADMD).
“The need for this program is that there is no U.S. requirement for medical schools to teach about intellectual and developmental disabilities,” Priya Chandan, MD, also of the University of Louisville, said in her presentation during the session. “Approximately 81% of graduating medical students have no training in caring for adults with disabilities,” said Dr. Chandan, who serves as director of the NCIDM.
The current NCIDM was created as a 5-year partnership between the AADMD and Special Olympics, supported in part by the Centers for Disease Control and Prevention, Dr. Chandan said. The purpose was to provide training to medical students in the field of developmental medicine, meaning the care of individuals with intellectual/developmental disabilities (IDD) across the lifespan. The AADMD has expanded to 26 medical schools in the United States and will reach approximately 4,000 medical students by the conclusion of the current initiative.
One challenge in medical education is getting past the idea that people living with disabilities need to be fixed, said Dr. Chandan. The NCIDM approach reflects Mr. Guidotti’s approach in both the FRAME initiatives and his Positive Exposure foundation, with a focus on treating people as people, and letting individuals with disabilities represent themselves.
Dr. Chandan described the NCIDM curriculum as allowing for flexible teaching methodologies and materials, as long as they meet the NCIDM-created learning goals and objectives. The curriculum also includes standardized evaluations. Each NCIDM program in a participating medical school includes a faculty champion, and the curriculum supports meeting people with IDD not only inside medical settings, but also outside in the community.
NCIDM embraces the idea of community-engaged scholarship, which Dr. Chandan defined as “a form of scholarship that directly benefits the community and is consistent with university and unit missions.” This method combined teaching and conducting research while providing a service to the community.
The next steps for the current NCIDM initiative are to complete collection of data and course evaluations from participating schools by early 2022, followed by continued dissemination and collaboration through AADMD.
Overall, the content of the curriculum explores how and where IDD fits into clinical care, Dr. Chandan said, who also emphasized the implications of communication. “How we think affects how we communicate,” she added. Be mindful of the language used to talk to and about patients with disabilities, both to colleagues and to learners.
When talking to the patient, find something in common, beyond the diagnosis, said Dr. Chandan. Remember that some disabilities are visible and some are not. “Treat people with respect, because you won’t know what their functional level is just by looking,” she concluded.
The presenters had no financial conflicts to disclose.
“All physicians, regardless of specialty, will work with patients with disabilities,” Corrie Harris, MD, of the University of Louisville (Ky.), said in a plenary session presentation at the 2021 virtual Pediatric Hospital Medicine conference.
Disabilities vary in their visibility, from cognitive and sensory impairments that are not immediately obvious to an obvious physical disability, she said.
One in four adults and one in six children in the United States has a disability, said Dr. Harris. The prevalence of disability increases with age, but occurs across the lifespan, and will likely increase in the future with greater improvements in health care overall.
Dr. Harris reviewed the current conceptual model that forms the basis for the World Health Organization definition of functioning disability. This “functional model” defines disability as caused by interactions between health conditions and the environment, and the response is to “prioritize function to meet patient goals,” Dr. Harris said at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
This model is based on collaboration between health care providers and their patients with disabilities, and training is important to help providers make this collaboration successful, said Dr. Harris. Without training, physicians may be ineffective in communicating with patients with disabilities by not speaking directly to the patient, not speaking in a way the patient can understand clearly, and not providing accessible patient education materials. Physicians also tend to minimize the extent of the patient’s expertise in their own condition based on their lived experiences, and tend to underestimate the abilities of patients with disabilities.
However, direct experience with disabled patients and an understanding of the health disparities they endure can help physicians look at these patients “through a more intersectional lens,” that also takes into account social determinants of health, Dr. Harris said. “I have found that people with disabilities are the best teachers about disability, because they have expertise that comes from their lived experience.”
Patients are the best teachers
Several initiatives are helping physicians to bridge this gap in understanding and reduce disparities in care. One such program is FRAME: Faces Redefining the Art of Medical Education. FRAME is a web-based film library designed to present medical information to health care providers in training, clinicians, families, and communities in a dignified and humanizing way. FRAME was developed in part by fashion photographer Rick Guidotti, who was inspired after meeting a young woman with albinism to create Positive Exposure, an ongoing project featuring children and adolescents with various disabilities.
FRAME films are “short films presenting all the basic hallmark characteristics of a certain genetic condition, but presented by somebody living with that condition,” said Mr. Guidotti in his presentation during the session.
The National Curriculum Initiative in Developmental Medicine (NCIDM) is designed to incorporate care for individuals with disabilities into medical education. NCIDM is a project created by the American Academy of Developmental Medicine and Dentistry (AADMD).
“The need for this program is that there is no U.S. requirement for medical schools to teach about intellectual and developmental disabilities,” Priya Chandan, MD, also of the University of Louisville, said in her presentation during the session. “Approximately 81% of graduating medical students have no training in caring for adults with disabilities,” said Dr. Chandan, who serves as director of the NCIDM.
The current NCIDM was created as a 5-year partnership between the AADMD and Special Olympics, supported in part by the Centers for Disease Control and Prevention, Dr. Chandan said. The purpose was to provide training to medical students in the field of developmental medicine, meaning the care of individuals with intellectual/developmental disabilities (IDD) across the lifespan. The AADMD has expanded to 26 medical schools in the United States and will reach approximately 4,000 medical students by the conclusion of the current initiative.
One challenge in medical education is getting past the idea that people living with disabilities need to be fixed, said Dr. Chandan. The NCIDM approach reflects Mr. Guidotti’s approach in both the FRAME initiatives and his Positive Exposure foundation, with a focus on treating people as people, and letting individuals with disabilities represent themselves.
Dr. Chandan described the NCIDM curriculum as allowing for flexible teaching methodologies and materials, as long as they meet the NCIDM-created learning goals and objectives. The curriculum also includes standardized evaluations. Each NCIDM program in a participating medical school includes a faculty champion, and the curriculum supports meeting people with IDD not only inside medical settings, but also outside in the community.
NCIDM embraces the idea of community-engaged scholarship, which Dr. Chandan defined as “a form of scholarship that directly benefits the community and is consistent with university and unit missions.” This method combined teaching and conducting research while providing a service to the community.
The next steps for the current NCIDM initiative are to complete collection of data and course evaluations from participating schools by early 2022, followed by continued dissemination and collaboration through AADMD.
Overall, the content of the curriculum explores how and where IDD fits into clinical care, Dr. Chandan said, who also emphasized the implications of communication. “How we think affects how we communicate,” she added. Be mindful of the language used to talk to and about patients with disabilities, both to colleagues and to learners.
When talking to the patient, find something in common, beyond the diagnosis, said Dr. Chandan. Remember that some disabilities are visible and some are not. “Treat people with respect, because you won’t know what their functional level is just by looking,” she concluded.
The presenters had no financial conflicts to disclose.
“All physicians, regardless of specialty, will work with patients with disabilities,” Corrie Harris, MD, of the University of Louisville (Ky.), said in a plenary session presentation at the 2021 virtual Pediatric Hospital Medicine conference.
Disabilities vary in their visibility, from cognitive and sensory impairments that are not immediately obvious to an obvious physical disability, she said.
One in four adults and one in six children in the United States has a disability, said Dr. Harris. The prevalence of disability increases with age, but occurs across the lifespan, and will likely increase in the future with greater improvements in health care overall.
Dr. Harris reviewed the current conceptual model that forms the basis for the World Health Organization definition of functioning disability. This “functional model” defines disability as caused by interactions between health conditions and the environment, and the response is to “prioritize function to meet patient goals,” Dr. Harris said at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
This model is based on collaboration between health care providers and their patients with disabilities, and training is important to help providers make this collaboration successful, said Dr. Harris. Without training, physicians may be ineffective in communicating with patients with disabilities by not speaking directly to the patient, not speaking in a way the patient can understand clearly, and not providing accessible patient education materials. Physicians also tend to minimize the extent of the patient’s expertise in their own condition based on their lived experiences, and tend to underestimate the abilities of patients with disabilities.
However, direct experience with disabled patients and an understanding of the health disparities they endure can help physicians look at these patients “through a more intersectional lens,” that also takes into account social determinants of health, Dr. Harris said. “I have found that people with disabilities are the best teachers about disability, because they have expertise that comes from their lived experience.”
Patients are the best teachers
Several initiatives are helping physicians to bridge this gap in understanding and reduce disparities in care. One such program is FRAME: Faces Redefining the Art of Medical Education. FRAME is a web-based film library designed to present medical information to health care providers in training, clinicians, families, and communities in a dignified and humanizing way. FRAME was developed in part by fashion photographer Rick Guidotti, who was inspired after meeting a young woman with albinism to create Positive Exposure, an ongoing project featuring children and adolescents with various disabilities.
FRAME films are “short films presenting all the basic hallmark characteristics of a certain genetic condition, but presented by somebody living with that condition,” said Mr. Guidotti in his presentation during the session.
The National Curriculum Initiative in Developmental Medicine (NCIDM) is designed to incorporate care for individuals with disabilities into medical education. NCIDM is a project created by the American Academy of Developmental Medicine and Dentistry (AADMD).
“The need for this program is that there is no U.S. requirement for medical schools to teach about intellectual and developmental disabilities,” Priya Chandan, MD, also of the University of Louisville, said in her presentation during the session. “Approximately 81% of graduating medical students have no training in caring for adults with disabilities,” said Dr. Chandan, who serves as director of the NCIDM.
The current NCIDM was created as a 5-year partnership between the AADMD and Special Olympics, supported in part by the Centers for Disease Control and Prevention, Dr. Chandan said. The purpose was to provide training to medical students in the field of developmental medicine, meaning the care of individuals with intellectual/developmental disabilities (IDD) across the lifespan. The AADMD has expanded to 26 medical schools in the United States and will reach approximately 4,000 medical students by the conclusion of the current initiative.
One challenge in medical education is getting past the idea that people living with disabilities need to be fixed, said Dr. Chandan. The NCIDM approach reflects Mr. Guidotti’s approach in both the FRAME initiatives and his Positive Exposure foundation, with a focus on treating people as people, and letting individuals with disabilities represent themselves.
Dr. Chandan described the NCIDM curriculum as allowing for flexible teaching methodologies and materials, as long as they meet the NCIDM-created learning goals and objectives. The curriculum also includes standardized evaluations. Each NCIDM program in a participating medical school includes a faculty champion, and the curriculum supports meeting people with IDD not only inside medical settings, but also outside in the community.
NCIDM embraces the idea of community-engaged scholarship, which Dr. Chandan defined as “a form of scholarship that directly benefits the community and is consistent with university and unit missions.” This method combined teaching and conducting research while providing a service to the community.
The next steps for the current NCIDM initiative are to complete collection of data and course evaluations from participating schools by early 2022, followed by continued dissemination and collaboration through AADMD.
Overall, the content of the curriculum explores how and where IDD fits into clinical care, Dr. Chandan said, who also emphasized the implications of communication. “How we think affects how we communicate,” she added. Be mindful of the language used to talk to and about patients with disabilities, both to colleagues and to learners.
When talking to the patient, find something in common, beyond the diagnosis, said Dr. Chandan. Remember that some disabilities are visible and some are not. “Treat people with respect, because you won’t know what their functional level is just by looking,” she concluded.
The presenters had no financial conflicts to disclose.
FROM PHM 2021
Atopic dermatitis doubles risk of mental health issues in children
, according to a newly published cohort study of more than 11,000 children between the ages of 3 and 18 years.
Along with previous studies that have also linked AD to depression and other mental health issues in children, these data highlight the need for “clinical awareness of the psychosocial needs of children and adolescents with AD,” reported a multicenter team of investigators from the University of California, San Francisco, the University of Pennsylvania, and the London School of Hygiene and Tropical Medicine.
Unlike some previous studies, in this study, published online in JAMA Dermatology on Sept. 1, children were evaluated longitudinally, rather than at a single point in time, with a mean follow-up of 10 years. For those with active AD, compared with children without AD, the odds ratio for depression overall in any child with AD relative to those without AD was not significant after adjustment for variables such socioeconomic factors.
However, among children with severe AD, the risk was more than twofold greater even after adjustment (adjusted OR, 2.38; 95% confidence interval, 1.21- 4.72), reported the investigators, led by senior author Katrina Abuabara, MD, associate professor of dermatology and epidemiology at UCSF.
Internalizing symptoms seen with mild to severe AD
Internalizing behavior, which is closely linked to depression and describes a spectrum of inward-focusing activities, such as social withdrawal, was significantly more common in children with any degree of AD relative to those without AD: After adjustment, the risk climbed from a 29% increased risk in those with mild AD (aOR, 1.29; 95% CI, 1.06-1.57) to a more than 80% increased risk in children with moderate AD (aOR, 1.84; 95% CI, 1.40-2.41) and in children with severe AD (aOR, 1.90; 95% CI, 1.14-3.16).
In the study, depression was measured with the Short Moods and Feelings Questionnaire (SMFQ). Parental response to the Emotional Symptoms subscale of the Strength and Difficulties Questionnaire (SDQ) was used to measure internalizing behaviors.
The data were drawn from the Avon Longitudinal Study for Parents and Children (ALSPAC), a cohort that enrolled pregnant women in a defined area in southwest England and then followed children born from these pregnancies. Of the 14,062 children enrolled in ALSPAC, data from 11,181 children were available for this study.
In a previous meta-analysis of studies that have documented a link between AD and adverse effects on mood and mental health, an impact was identified in both children and adults. In children, AD was associated with a 27% increase in risk of depression (OR, 1.27; 95% CI, 1.12 -1.45). In adults, the risk was more than doubled (OR, 2.19; 95% CI, 1.87-2.57). The same meta-analysis found that the risk of suicidal ideation among adolescents and adults with AD was increased more than fourfold (OR, 4.32; 95% CI, 1.93-9.66).
In the ALSPAC data, the investigators were unable to find compelling evidence that sleep disturbances or concomitant asthma contributed to the increased risk of depression, which is a mechanism proposed by past investigators.
In an interview, Dr. Abuabara said that these and other data provide the basis for encouraging clinical awareness of the psychological needs of children with AD, but she suggested there is a gap in understanding what this means clinically. “We need more data on how dermatologists can effectively screen and manage these patients before we try to set expectations for clinical practice,” she said.
In addition, these data along with previously published studies suggest that change in mental health outcomes should be included in the evaluation of new therapies, according to Dr. Abuabara. She noted that there are several tools for evaluating mental health in children that might be appropriate, each with their own advantages and disadvantages.
“Ideally, recommendations would be issued through a group consensus process with patients, clinicians, researchers, and industry representatives working together as has been done for other outcomes through the Harmonizing Measures for Eczema (HOME) group,” Dr. Abuabara said.
Mental health assessments recommended
Others who have looked at the relationship between AD and depression have also recommended adding mental health outcomes to an assessment of efficacy for AD therapies.
Jonathan I. Silverberg, MD, PhD, MPH, associate professor of dermatology, George Washington University, Washington, is one such investigator. He is already monitoring depression systematically with the Hospital Anxiety and Depression Scale (HADS).
“HADS has been validated in AD and provides very important information about the emotional burden of AD,” explained Dr. Silverberg, whose most recent article on this topic appeared earlier this year. In that study, the relationship between AD and depression was found to be more pronounced in White children from families with lower incomes.
“Just a few hours ago, one of my patients thanked me for asking about their mental health and recognizing the holistic effects of AD,” Dr. Silverberg said.
The recent study based on ALSPAC data add to the evidence that AD, particularly severe AD, produces deleterious effects on mental health in children, and Dr. Silverberg believes clinicians should be acting on this evidence.
“I strongly encourage clinicians to routinely assess mental health. It will elevate the quality of care they provide, and their patients will appreciate them more for it,” he said.
Dr. Abuabara and another author report receiving research funding from Pfizer to their universities for unrelated work; there were no other disclosures. Dr. Silverberg reports financial relationships with more than 15 pharmaceutical companies.
Commentary by Lawrence F. Eichenfield, MD
More severe atopic dermatitis (AD) carries with it significant mental health concerns in children, as well as adults. Multiple studies have shown significantly higher rates of depression, anxiety, and “internalizing behaviors” (discussed as social withdrawal and other inward-focused activities) as well as attention-deficit/hyperactivity disorder. The study by Dr. Abuabara and colleagues is important as it followed children over time (an average of 10 years) and adjusted the data for socioeconomic factors, showing a rate of depression in children with severe AD twice that of those without. It appears that we are in the midst of a mental health crisis in children and teens, with markedly higher rates of pediatric and adolescent depression and anxiety, certainly influenced by COVID-19 societal changes. As the literature has developed on depression and AD, we have appreciated the importance of addressing this as part of our assessment of the disease effect on the individual and family, and it is one factor we consider in selections of systemic vs. topical therapies.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children's Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. He disclosed that he has served as an investigator and/or consultant to AbbVie, Lilly, Pfizer, Regeneron, Sanofi-Genzyme, and Verrica.
A version of this article first appeared on Medscape.com.
This article was updated 6/18/22.
, according to a newly published cohort study of more than 11,000 children between the ages of 3 and 18 years.
Along with previous studies that have also linked AD to depression and other mental health issues in children, these data highlight the need for “clinical awareness of the psychosocial needs of children and adolescents with AD,” reported a multicenter team of investigators from the University of California, San Francisco, the University of Pennsylvania, and the London School of Hygiene and Tropical Medicine.
Unlike some previous studies, in this study, published online in JAMA Dermatology on Sept. 1, children were evaluated longitudinally, rather than at a single point in time, with a mean follow-up of 10 years. For those with active AD, compared with children without AD, the odds ratio for depression overall in any child with AD relative to those without AD was not significant after adjustment for variables such socioeconomic factors.
However, among children with severe AD, the risk was more than twofold greater even after adjustment (adjusted OR, 2.38; 95% confidence interval, 1.21- 4.72), reported the investigators, led by senior author Katrina Abuabara, MD, associate professor of dermatology and epidemiology at UCSF.
Internalizing symptoms seen with mild to severe AD
Internalizing behavior, which is closely linked to depression and describes a spectrum of inward-focusing activities, such as social withdrawal, was significantly more common in children with any degree of AD relative to those without AD: After adjustment, the risk climbed from a 29% increased risk in those with mild AD (aOR, 1.29; 95% CI, 1.06-1.57) to a more than 80% increased risk in children with moderate AD (aOR, 1.84; 95% CI, 1.40-2.41) and in children with severe AD (aOR, 1.90; 95% CI, 1.14-3.16).
In the study, depression was measured with the Short Moods and Feelings Questionnaire (SMFQ). Parental response to the Emotional Symptoms subscale of the Strength and Difficulties Questionnaire (SDQ) was used to measure internalizing behaviors.
The data were drawn from the Avon Longitudinal Study for Parents and Children (ALSPAC), a cohort that enrolled pregnant women in a defined area in southwest England and then followed children born from these pregnancies. Of the 14,062 children enrolled in ALSPAC, data from 11,181 children were available for this study.
In a previous meta-analysis of studies that have documented a link between AD and adverse effects on mood and mental health, an impact was identified in both children and adults. In children, AD was associated with a 27% increase in risk of depression (OR, 1.27; 95% CI, 1.12 -1.45). In adults, the risk was more than doubled (OR, 2.19; 95% CI, 1.87-2.57). The same meta-analysis found that the risk of suicidal ideation among adolescents and adults with AD was increased more than fourfold (OR, 4.32; 95% CI, 1.93-9.66).
In the ALSPAC data, the investigators were unable to find compelling evidence that sleep disturbances or concomitant asthma contributed to the increased risk of depression, which is a mechanism proposed by past investigators.
In an interview, Dr. Abuabara said that these and other data provide the basis for encouraging clinical awareness of the psychological needs of children with AD, but she suggested there is a gap in understanding what this means clinically. “We need more data on how dermatologists can effectively screen and manage these patients before we try to set expectations for clinical practice,” she said.
In addition, these data along with previously published studies suggest that change in mental health outcomes should be included in the evaluation of new therapies, according to Dr. Abuabara. She noted that there are several tools for evaluating mental health in children that might be appropriate, each with their own advantages and disadvantages.
“Ideally, recommendations would be issued through a group consensus process with patients, clinicians, researchers, and industry representatives working together as has been done for other outcomes through the Harmonizing Measures for Eczema (HOME) group,” Dr. Abuabara said.
Mental health assessments recommended
Others who have looked at the relationship between AD and depression have also recommended adding mental health outcomes to an assessment of efficacy for AD therapies.
Jonathan I. Silverberg, MD, PhD, MPH, associate professor of dermatology, George Washington University, Washington, is one such investigator. He is already monitoring depression systematically with the Hospital Anxiety and Depression Scale (HADS).
“HADS has been validated in AD and provides very important information about the emotional burden of AD,” explained Dr. Silverberg, whose most recent article on this topic appeared earlier this year. In that study, the relationship between AD and depression was found to be more pronounced in White children from families with lower incomes.
“Just a few hours ago, one of my patients thanked me for asking about their mental health and recognizing the holistic effects of AD,” Dr. Silverberg said.
The recent study based on ALSPAC data add to the evidence that AD, particularly severe AD, produces deleterious effects on mental health in children, and Dr. Silverberg believes clinicians should be acting on this evidence.
“I strongly encourage clinicians to routinely assess mental health. It will elevate the quality of care they provide, and their patients will appreciate them more for it,” he said.
Dr. Abuabara and another author report receiving research funding from Pfizer to their universities for unrelated work; there were no other disclosures. Dr. Silverberg reports financial relationships with more than 15 pharmaceutical companies.
Commentary by Lawrence F. Eichenfield, MD
More severe atopic dermatitis (AD) carries with it significant mental health concerns in children, as well as adults. Multiple studies have shown significantly higher rates of depression, anxiety, and “internalizing behaviors” (discussed as social withdrawal and other inward-focused activities) as well as attention-deficit/hyperactivity disorder. The study by Dr. Abuabara and colleagues is important as it followed children over time (an average of 10 years) and adjusted the data for socioeconomic factors, showing a rate of depression in children with severe AD twice that of those without. It appears that we are in the midst of a mental health crisis in children and teens, with markedly higher rates of pediatric and adolescent depression and anxiety, certainly influenced by COVID-19 societal changes. As the literature has developed on depression and AD, we have appreciated the importance of addressing this as part of our assessment of the disease effect on the individual and family, and it is one factor we consider in selections of systemic vs. topical therapies.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children's Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. He disclosed that he has served as an investigator and/or consultant to AbbVie, Lilly, Pfizer, Regeneron, Sanofi-Genzyme, and Verrica.
A version of this article first appeared on Medscape.com.
This article was updated 6/18/22.
, according to a newly published cohort study of more than 11,000 children between the ages of 3 and 18 years.
Along with previous studies that have also linked AD to depression and other mental health issues in children, these data highlight the need for “clinical awareness of the psychosocial needs of children and adolescents with AD,” reported a multicenter team of investigators from the University of California, San Francisco, the University of Pennsylvania, and the London School of Hygiene and Tropical Medicine.
Unlike some previous studies, in this study, published online in JAMA Dermatology on Sept. 1, children were evaluated longitudinally, rather than at a single point in time, with a mean follow-up of 10 years. For those with active AD, compared with children without AD, the odds ratio for depression overall in any child with AD relative to those without AD was not significant after adjustment for variables such socioeconomic factors.
However, among children with severe AD, the risk was more than twofold greater even after adjustment (adjusted OR, 2.38; 95% confidence interval, 1.21- 4.72), reported the investigators, led by senior author Katrina Abuabara, MD, associate professor of dermatology and epidemiology at UCSF.
Internalizing symptoms seen with mild to severe AD
Internalizing behavior, which is closely linked to depression and describes a spectrum of inward-focusing activities, such as social withdrawal, was significantly more common in children with any degree of AD relative to those without AD: After adjustment, the risk climbed from a 29% increased risk in those with mild AD (aOR, 1.29; 95% CI, 1.06-1.57) to a more than 80% increased risk in children with moderate AD (aOR, 1.84; 95% CI, 1.40-2.41) and in children with severe AD (aOR, 1.90; 95% CI, 1.14-3.16).
In the study, depression was measured with the Short Moods and Feelings Questionnaire (SMFQ). Parental response to the Emotional Symptoms subscale of the Strength and Difficulties Questionnaire (SDQ) was used to measure internalizing behaviors.
The data were drawn from the Avon Longitudinal Study for Parents and Children (ALSPAC), a cohort that enrolled pregnant women in a defined area in southwest England and then followed children born from these pregnancies. Of the 14,062 children enrolled in ALSPAC, data from 11,181 children were available for this study.
In a previous meta-analysis of studies that have documented a link between AD and adverse effects on mood and mental health, an impact was identified in both children and adults. In children, AD was associated with a 27% increase in risk of depression (OR, 1.27; 95% CI, 1.12 -1.45). In adults, the risk was more than doubled (OR, 2.19; 95% CI, 1.87-2.57). The same meta-analysis found that the risk of suicidal ideation among adolescents and adults with AD was increased more than fourfold (OR, 4.32; 95% CI, 1.93-9.66).
In the ALSPAC data, the investigators were unable to find compelling evidence that sleep disturbances or concomitant asthma contributed to the increased risk of depression, which is a mechanism proposed by past investigators.
In an interview, Dr. Abuabara said that these and other data provide the basis for encouraging clinical awareness of the psychological needs of children with AD, but she suggested there is a gap in understanding what this means clinically. “We need more data on how dermatologists can effectively screen and manage these patients before we try to set expectations for clinical practice,” she said.
In addition, these data along with previously published studies suggest that change in mental health outcomes should be included in the evaluation of new therapies, according to Dr. Abuabara. She noted that there are several tools for evaluating mental health in children that might be appropriate, each with their own advantages and disadvantages.
“Ideally, recommendations would be issued through a group consensus process with patients, clinicians, researchers, and industry representatives working together as has been done for other outcomes through the Harmonizing Measures for Eczema (HOME) group,” Dr. Abuabara said.
Mental health assessments recommended
Others who have looked at the relationship between AD and depression have also recommended adding mental health outcomes to an assessment of efficacy for AD therapies.
Jonathan I. Silverberg, MD, PhD, MPH, associate professor of dermatology, George Washington University, Washington, is one such investigator. He is already monitoring depression systematically with the Hospital Anxiety and Depression Scale (HADS).
“HADS has been validated in AD and provides very important information about the emotional burden of AD,” explained Dr. Silverberg, whose most recent article on this topic appeared earlier this year. In that study, the relationship between AD and depression was found to be more pronounced in White children from families with lower incomes.
“Just a few hours ago, one of my patients thanked me for asking about their mental health and recognizing the holistic effects of AD,” Dr. Silverberg said.
The recent study based on ALSPAC data add to the evidence that AD, particularly severe AD, produces deleterious effects on mental health in children, and Dr. Silverberg believes clinicians should be acting on this evidence.
“I strongly encourage clinicians to routinely assess mental health. It will elevate the quality of care they provide, and their patients will appreciate them more for it,” he said.
Dr. Abuabara and another author report receiving research funding from Pfizer to their universities for unrelated work; there were no other disclosures. Dr. Silverberg reports financial relationships with more than 15 pharmaceutical companies.
Commentary by Lawrence F. Eichenfield, MD
More severe atopic dermatitis (AD) carries with it significant mental health concerns in children, as well as adults. Multiple studies have shown significantly higher rates of depression, anxiety, and “internalizing behaviors” (discussed as social withdrawal and other inward-focused activities) as well as attention-deficit/hyperactivity disorder. The study by Dr. Abuabara and colleagues is important as it followed children over time (an average of 10 years) and adjusted the data for socioeconomic factors, showing a rate of depression in children with severe AD twice that of those without. It appears that we are in the midst of a mental health crisis in children and teens, with markedly higher rates of pediatric and adolescent depression and anxiety, certainly influenced by COVID-19 societal changes. As the literature has developed on depression and AD, we have appreciated the importance of addressing this as part of our assessment of the disease effect on the individual and family, and it is one factor we consider in selections of systemic vs. topical therapies.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children's Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. He disclosed that he has served as an investigator and/or consultant to AbbVie, Lilly, Pfizer, Regeneron, Sanofi-Genzyme, and Verrica.
A version of this article first appeared on Medscape.com.
This article was updated 6/18/22.
FROM JAMA DERMATOLOGY
Choosing Wisely campaign targets waste and overuse in hospital pediatrics
“Health care spending and health care waste is a huge problem in the U.S., including for children,” Vivian Lee, MD, of Children’s Hospital, Los Angeles, said in a presentation at the 2021 virtual Pediatric Hospital Medicine conference.
Data from a 2019 study suggested that approximately 25% of health care spending in the United States qualifies as “wasteful spending,” in categories such as overtesting, and unnecessary hospitalization, Dr. Lee said. “It is essential for physicians in hospitals to be stewards of high-value care,” she emphasized.
To combat wasteful spending and control health care costs, the Choosing Wisely campaign was created in 2012 as an initiative from the American Board of Internal Medicine Foundation. An ongoing goal of the campaign is to raise awareness among physicians and patients about potential areas of low-value services and overuse. The overall campaign includes clinician-driven recommendations from multiple medical organizations.
The PHM produced its first set of five recommendations in 2012, Dr. Lee said. These recommendations, titled “Five Things Physicians and Patients Should Question,” have been updated for 2021. The updated recommendations were created as a partnership among the Academic Pediatric Association, the American Academy of Pediatrics, and the Society of Hospital Medicine. A joint committee reviewed the latest evidence, and the updates were approved by the societies and published by the ABIM in January 2021.
“We think these recommendations truly reflect an exciting and evolving landscape for pediatric hospitalists,” Dr. Lee said. “There is a greater focus on opportunities to transition out of the hospital sooner, or avoid hospitalization altogether. There is an emphasis on antibiotic stewardship and a growing recognition of the impact that overuse may have on our vulnerable neonatal population,” she said. Several members of the Choosing Wisely panel presented the recommendations during the virtual presentation.
Revised recommendations
The new “Five Things Physicians and Patients Should Question” are as follows:
1. Do not prescribe IV antibiotics for predetermined durations for patients hospitalized with infections such as pyelonephritis, osteomyelitis, and complicated pneumonia. Consider early transition to oral antibiotics.
Many antibiotic doses used in clinical practice are preset durations that are not based on high-quality evidence, said Mike Tchou, MD, of Children’s Hospital of Colorado in Aurora. However, studies now show that earlier transition to enteral antibiotics can improve a range of outcomes including neonatal UTIs, osteomyelitis, and complicated pneumonia, he said. Considering early transition based on a patient’s response can decrease adverse events, pain, length of stay, and health care costs, he explained.
2. Do not continue hospitalization in well-appearing febrile infants once bacterial cultures (i.e., blood, cerebrospinal, and/or urine) have been confirmed negative for 24-36 hours, if adequate outpatient follow-up can be assured.
Recent data indicate that continuing hospitalization beyond 24-36 hours of confirmed negative bacterial cultures does not improve clinical outcomes for well-appearing infants admitted for concern of serious bacterial infection, said Paula Soung, MD, of Children’s Wisconsin in Milwaukee. In fact, “blood culture yield is highest in the first 12-36 hours after incubation with multiple studies demonstrating > 90% of pathogen cultures being positive by 24 hours,” Dr. Soung said. “If adequate outpatient follow-up can be assured, discharging well-appearing febrile infants at 24-36 hours after confirming cultures are negative has many positive outcomes,” she said.
3. Do not initiate phototherapy in term or late preterm well-appearing infants with neonatal hyperbilirubinemia if their bilirubin is below levels at which the AAP guidelines recommend treatment.
In making this recommendation, “we considered that the risk of kernicterus and cerebral palsy is extremely low in otherwise healthy term and late preterm newborns,” said Allison Holmes, MD, of Children’s Hospital at Dartmouth-Hitchcock, Manchester, N.H. “Subthreshold phototherapy leads to unnecessary hospitalization and its associated costs and harms,” and data show that kernicterus generally occurs close to 40 mg/dL and occurs most often in infants with hemolysis, she added.
The evidence for the recommendations included data showing that, among other factors, 8.6 of 100,000 babies have a bilirubin greater than 30 mg/dL, said Dr. Holmes. Risks of using subthreshold phototherapy include increased length of stay, increased readmissions, and increased costs, as well as decreased breastfeeding, bonding with parents, and increased parental anxiety. “Adding prolonged hospitalization for an intervention that might not be necessary can be stressful for parents,” she said.
4. Do not use broad-spectrum antibiotics such as ceftriaxone for children hospitalized with uncomplicated community-acquired pneumonia. Use narrow-spectrum antibiotics such as penicillin, ampicillin, or amoxicillin.
Michelle Lossius, MD, of the Shands Hospital for Children at the University of Florida, Gainesville, noted that the recommendations reflect IDSA guidelines from 2011 advising the use of ampicillin or penicillin for this population of children. More recent studies with large populations support the ability of narrow-spectrum antibiotics to limit the development of resistant organisms while achieving the same or better outcomes for children hospitalized with CAP, she said.
5. Do not start IV antibiotic therapy on well-appearing newborn infants with isolated risk factors for sepsis such as maternal chorioamnionitis, prolonged rupture of membranes, or untreated group-B streptococcal colonization. Use clinical tools such as an evidence-based sepsis risk calculator to guide management.
“This recommendation combines other recommendations,” said Prabi Rajbhandari, MD, of Akron (Ohio) Children’s Hospital. The evidence is ample, as the Centers for Disease Control and Prevention recommends the use of sepsis calculators to guide clinical management in sepsis patients, she said.
Data comparing periods before and after the adoption of a sepsis risk calculator showed a significant reduction in the use of blood cultures and antibiotics, she noted. Other risks of jumping to IV antibiotics include increased hospital stay, increased parental anxiety, and decreased parental bonding, Dr. Rajbhandari added.
Next steps include how to prioritize implementation, as well as deimplementation of outdated practices, said Francisco Alvarez, MD, of Lucile Packard Children’s Hospital, Palo Alto, Calif. “A lot of our practices were started without good evidence for why they should be done,” he said. Other steps include value improvement research; use of dashboards and benchmarking; involving other stakeholders including patients, families, and other health care providers; and addressing racial disparities, he concluded.
The presenters had no financial conflicts to disclose. The conference was sponsored by the Academic Pediatric Association, the American Academy of Pediatrics, and the Society of Hospital Medicine.
“Health care spending and health care waste is a huge problem in the U.S., including for children,” Vivian Lee, MD, of Children’s Hospital, Los Angeles, said in a presentation at the 2021 virtual Pediatric Hospital Medicine conference.
Data from a 2019 study suggested that approximately 25% of health care spending in the United States qualifies as “wasteful spending,” in categories such as overtesting, and unnecessary hospitalization, Dr. Lee said. “It is essential for physicians in hospitals to be stewards of high-value care,” she emphasized.
To combat wasteful spending and control health care costs, the Choosing Wisely campaign was created in 2012 as an initiative from the American Board of Internal Medicine Foundation. An ongoing goal of the campaign is to raise awareness among physicians and patients about potential areas of low-value services and overuse. The overall campaign includes clinician-driven recommendations from multiple medical organizations.
The PHM produced its first set of five recommendations in 2012, Dr. Lee said. These recommendations, titled “Five Things Physicians and Patients Should Question,” have been updated for 2021. The updated recommendations were created as a partnership among the Academic Pediatric Association, the American Academy of Pediatrics, and the Society of Hospital Medicine. A joint committee reviewed the latest evidence, and the updates were approved by the societies and published by the ABIM in January 2021.
“We think these recommendations truly reflect an exciting and evolving landscape for pediatric hospitalists,” Dr. Lee said. “There is a greater focus on opportunities to transition out of the hospital sooner, or avoid hospitalization altogether. There is an emphasis on antibiotic stewardship and a growing recognition of the impact that overuse may have on our vulnerable neonatal population,” she said. Several members of the Choosing Wisely panel presented the recommendations during the virtual presentation.
Revised recommendations
The new “Five Things Physicians and Patients Should Question” are as follows:
1. Do not prescribe IV antibiotics for predetermined durations for patients hospitalized with infections such as pyelonephritis, osteomyelitis, and complicated pneumonia. Consider early transition to oral antibiotics.
Many antibiotic doses used in clinical practice are preset durations that are not based on high-quality evidence, said Mike Tchou, MD, of Children’s Hospital of Colorado in Aurora. However, studies now show that earlier transition to enteral antibiotics can improve a range of outcomes including neonatal UTIs, osteomyelitis, and complicated pneumonia, he said. Considering early transition based on a patient’s response can decrease adverse events, pain, length of stay, and health care costs, he explained.
2. Do not continue hospitalization in well-appearing febrile infants once bacterial cultures (i.e., blood, cerebrospinal, and/or urine) have been confirmed negative for 24-36 hours, if adequate outpatient follow-up can be assured.
Recent data indicate that continuing hospitalization beyond 24-36 hours of confirmed negative bacterial cultures does not improve clinical outcomes for well-appearing infants admitted for concern of serious bacterial infection, said Paula Soung, MD, of Children’s Wisconsin in Milwaukee. In fact, “blood culture yield is highest in the first 12-36 hours after incubation with multiple studies demonstrating > 90% of pathogen cultures being positive by 24 hours,” Dr. Soung said. “If adequate outpatient follow-up can be assured, discharging well-appearing febrile infants at 24-36 hours after confirming cultures are negative has many positive outcomes,” she said.
3. Do not initiate phototherapy in term or late preterm well-appearing infants with neonatal hyperbilirubinemia if their bilirubin is below levels at which the AAP guidelines recommend treatment.
In making this recommendation, “we considered that the risk of kernicterus and cerebral palsy is extremely low in otherwise healthy term and late preterm newborns,” said Allison Holmes, MD, of Children’s Hospital at Dartmouth-Hitchcock, Manchester, N.H. “Subthreshold phototherapy leads to unnecessary hospitalization and its associated costs and harms,” and data show that kernicterus generally occurs close to 40 mg/dL and occurs most often in infants with hemolysis, she added.
The evidence for the recommendations included data showing that, among other factors, 8.6 of 100,000 babies have a bilirubin greater than 30 mg/dL, said Dr. Holmes. Risks of using subthreshold phototherapy include increased length of stay, increased readmissions, and increased costs, as well as decreased breastfeeding, bonding with parents, and increased parental anxiety. “Adding prolonged hospitalization for an intervention that might not be necessary can be stressful for parents,” she said.
4. Do not use broad-spectrum antibiotics such as ceftriaxone for children hospitalized with uncomplicated community-acquired pneumonia. Use narrow-spectrum antibiotics such as penicillin, ampicillin, or amoxicillin.
Michelle Lossius, MD, of the Shands Hospital for Children at the University of Florida, Gainesville, noted that the recommendations reflect IDSA guidelines from 2011 advising the use of ampicillin or penicillin for this population of children. More recent studies with large populations support the ability of narrow-spectrum antibiotics to limit the development of resistant organisms while achieving the same or better outcomes for children hospitalized with CAP, she said.
5. Do not start IV antibiotic therapy on well-appearing newborn infants with isolated risk factors for sepsis such as maternal chorioamnionitis, prolonged rupture of membranes, or untreated group-B streptococcal colonization. Use clinical tools such as an evidence-based sepsis risk calculator to guide management.
“This recommendation combines other recommendations,” said Prabi Rajbhandari, MD, of Akron (Ohio) Children’s Hospital. The evidence is ample, as the Centers for Disease Control and Prevention recommends the use of sepsis calculators to guide clinical management in sepsis patients, she said.
Data comparing periods before and after the adoption of a sepsis risk calculator showed a significant reduction in the use of blood cultures and antibiotics, she noted. Other risks of jumping to IV antibiotics include increased hospital stay, increased parental anxiety, and decreased parental bonding, Dr. Rajbhandari added.
Next steps include how to prioritize implementation, as well as deimplementation of outdated practices, said Francisco Alvarez, MD, of Lucile Packard Children’s Hospital, Palo Alto, Calif. “A lot of our practices were started without good evidence for why they should be done,” he said. Other steps include value improvement research; use of dashboards and benchmarking; involving other stakeholders including patients, families, and other health care providers; and addressing racial disparities, he concluded.
The presenters had no financial conflicts to disclose. The conference was sponsored by the Academic Pediatric Association, the American Academy of Pediatrics, and the Society of Hospital Medicine.
“Health care spending and health care waste is a huge problem in the U.S., including for children,” Vivian Lee, MD, of Children’s Hospital, Los Angeles, said in a presentation at the 2021 virtual Pediatric Hospital Medicine conference.
Data from a 2019 study suggested that approximately 25% of health care spending in the United States qualifies as “wasteful spending,” in categories such as overtesting, and unnecessary hospitalization, Dr. Lee said. “It is essential for physicians in hospitals to be stewards of high-value care,” she emphasized.
To combat wasteful spending and control health care costs, the Choosing Wisely campaign was created in 2012 as an initiative from the American Board of Internal Medicine Foundation. An ongoing goal of the campaign is to raise awareness among physicians and patients about potential areas of low-value services and overuse. The overall campaign includes clinician-driven recommendations from multiple medical organizations.
The PHM produced its first set of five recommendations in 2012, Dr. Lee said. These recommendations, titled “Five Things Physicians and Patients Should Question,” have been updated for 2021. The updated recommendations were created as a partnership among the Academic Pediatric Association, the American Academy of Pediatrics, and the Society of Hospital Medicine. A joint committee reviewed the latest evidence, and the updates were approved by the societies and published by the ABIM in January 2021.
“We think these recommendations truly reflect an exciting and evolving landscape for pediatric hospitalists,” Dr. Lee said. “There is a greater focus on opportunities to transition out of the hospital sooner, or avoid hospitalization altogether. There is an emphasis on antibiotic stewardship and a growing recognition of the impact that overuse may have on our vulnerable neonatal population,” she said. Several members of the Choosing Wisely panel presented the recommendations during the virtual presentation.
Revised recommendations
The new “Five Things Physicians and Patients Should Question” are as follows:
1. Do not prescribe IV antibiotics for predetermined durations for patients hospitalized with infections such as pyelonephritis, osteomyelitis, and complicated pneumonia. Consider early transition to oral antibiotics.
Many antibiotic doses used in clinical practice are preset durations that are not based on high-quality evidence, said Mike Tchou, MD, of Children’s Hospital of Colorado in Aurora. However, studies now show that earlier transition to enteral antibiotics can improve a range of outcomes including neonatal UTIs, osteomyelitis, and complicated pneumonia, he said. Considering early transition based on a patient’s response can decrease adverse events, pain, length of stay, and health care costs, he explained.
2. Do not continue hospitalization in well-appearing febrile infants once bacterial cultures (i.e., blood, cerebrospinal, and/or urine) have been confirmed negative for 24-36 hours, if adequate outpatient follow-up can be assured.
Recent data indicate that continuing hospitalization beyond 24-36 hours of confirmed negative bacterial cultures does not improve clinical outcomes for well-appearing infants admitted for concern of serious bacterial infection, said Paula Soung, MD, of Children’s Wisconsin in Milwaukee. In fact, “blood culture yield is highest in the first 12-36 hours after incubation with multiple studies demonstrating > 90% of pathogen cultures being positive by 24 hours,” Dr. Soung said. “If adequate outpatient follow-up can be assured, discharging well-appearing febrile infants at 24-36 hours after confirming cultures are negative has many positive outcomes,” she said.
3. Do not initiate phototherapy in term or late preterm well-appearing infants with neonatal hyperbilirubinemia if their bilirubin is below levels at which the AAP guidelines recommend treatment.
In making this recommendation, “we considered that the risk of kernicterus and cerebral palsy is extremely low in otherwise healthy term and late preterm newborns,” said Allison Holmes, MD, of Children’s Hospital at Dartmouth-Hitchcock, Manchester, N.H. “Subthreshold phototherapy leads to unnecessary hospitalization and its associated costs and harms,” and data show that kernicterus generally occurs close to 40 mg/dL and occurs most often in infants with hemolysis, she added.
The evidence for the recommendations included data showing that, among other factors, 8.6 of 100,000 babies have a bilirubin greater than 30 mg/dL, said Dr. Holmes. Risks of using subthreshold phototherapy include increased length of stay, increased readmissions, and increased costs, as well as decreased breastfeeding, bonding with parents, and increased parental anxiety. “Adding prolonged hospitalization for an intervention that might not be necessary can be stressful for parents,” she said.
4. Do not use broad-spectrum antibiotics such as ceftriaxone for children hospitalized with uncomplicated community-acquired pneumonia. Use narrow-spectrum antibiotics such as penicillin, ampicillin, or amoxicillin.
Michelle Lossius, MD, of the Shands Hospital for Children at the University of Florida, Gainesville, noted that the recommendations reflect IDSA guidelines from 2011 advising the use of ampicillin or penicillin for this population of children. More recent studies with large populations support the ability of narrow-spectrum antibiotics to limit the development of resistant organisms while achieving the same or better outcomes for children hospitalized with CAP, she said.
5. Do not start IV antibiotic therapy on well-appearing newborn infants with isolated risk factors for sepsis such as maternal chorioamnionitis, prolonged rupture of membranes, or untreated group-B streptococcal colonization. Use clinical tools such as an evidence-based sepsis risk calculator to guide management.
“This recommendation combines other recommendations,” said Prabi Rajbhandari, MD, of Akron (Ohio) Children’s Hospital. The evidence is ample, as the Centers for Disease Control and Prevention recommends the use of sepsis calculators to guide clinical management in sepsis patients, she said.
Data comparing periods before and after the adoption of a sepsis risk calculator showed a significant reduction in the use of blood cultures and antibiotics, she noted. Other risks of jumping to IV antibiotics include increased hospital stay, increased parental anxiety, and decreased parental bonding, Dr. Rajbhandari added.
Next steps include how to prioritize implementation, as well as deimplementation of outdated practices, said Francisco Alvarez, MD, of Lucile Packard Children’s Hospital, Palo Alto, Calif. “A lot of our practices were started without good evidence for why they should be done,” he said. Other steps include value improvement research; use of dashboards and benchmarking; involving other stakeholders including patients, families, and other health care providers; and addressing racial disparities, he concluded.
The presenters had no financial conflicts to disclose. The conference was sponsored by the Academic Pediatric Association, the American Academy of Pediatrics, and the Society of Hospital Medicine.
FROM PHM 2021
United States reaches 5 million cases of child COVID
Cases of child COVID-19 set a new 1-week record and the total number of children infected during the pandemic passed 5 million, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
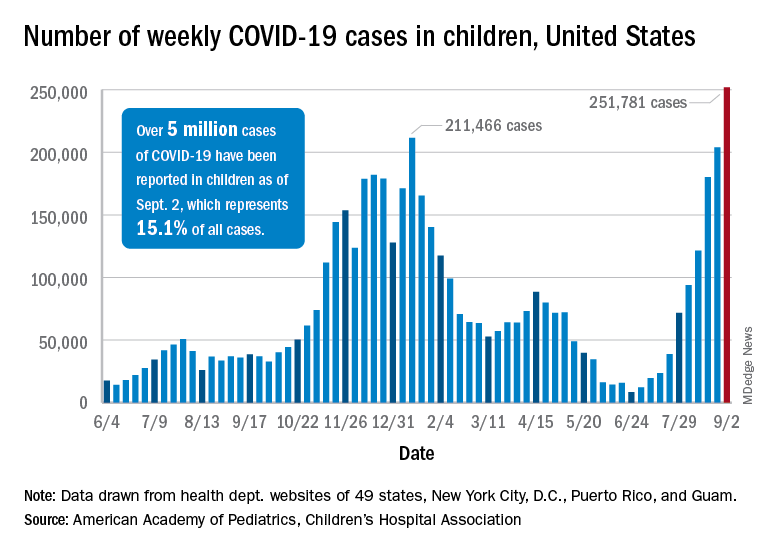
The nearly 282,000 new cases reported in the United States during the week ending Sept. 2 broke the record of 211,000 set in mid-January and brought the cumulative count to 5,049,465 children with COVID-19 since the pandemic began, the AAP and the CHA said in their weekly COVID report.
Hospitalizations in children aged 0-17 years have also reached record levels in recent days. The highest daily admission rate since the pandemic began, 0.51 per 100,000 population, was recorded on Sept. 2, less than 2 months after the nation saw its lowest child COVID admission rate for 1 day: 0.07 per 100,000 on July 4. That’s an increase of 629%, according to data from the Centers for Disease Control and Prevention.
Vaccinations in children, however, did not follow suit. New vaccinations in children aged 12-17 years dropped by 4.5% for the week ending Sept. 6, compared with the week before. Initiations were actually up almost 12% for children aged 16-17, but that was not enough to overcome the continued decline among 12- to 15-year-olds, the CDC said on its COVID Data Tracker.
Despite the decline in new vaccinations, those younger children passed a noteworthy group milestone: 50.9% of all 12- to 15-year-olds now have received at least one dose, with 38.6% having completed the regimen. The 16- to 17-year-olds got an earlier start and have reached 58.9% coverage for one dose and 47.6% for two, the CDC said.
A total of 12.2 million children aged 12-17 years had received at least one dose of COVID vaccine as of Sept. 6, of whom almost 9.5 million are fully vaccinated, based on the CDC data.
At the state level, Vermont has the highest rates for vaccine initiation (75%) and full vaccination (65%), with Massachusetts (75%/62%) and Connecticut (73%/59%) just behind. The other end of the scale is occupied by Wyoming (28% initiation/19% full vaccination), Alabama (32%/19%), and North Dakota (32%/23%), the AAP said in a separate report.
In a recent letter to the Food and Drug Administration, AAP President Lee Savio Beers, MD, said that the “Delta variant is surging at extremely alarming rates in every region of America. This surge is seriously impacting all populations, including children.” Dr. Beers urged the FDA to work “aggressively toward authorizing safe and effective COVID-19 vaccines for children under age 12 as soon as possible.”
Cases of child COVID-19 set a new 1-week record and the total number of children infected during the pandemic passed 5 million, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
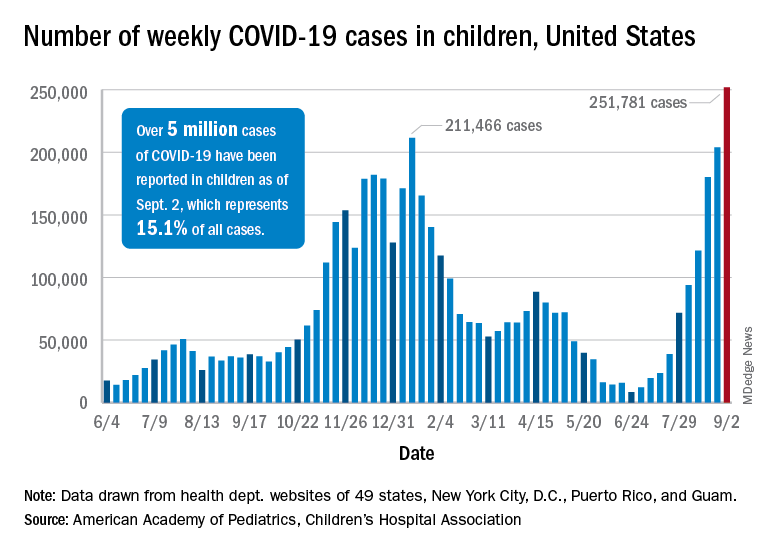
The nearly 282,000 new cases reported in the United States during the week ending Sept. 2 broke the record of 211,000 set in mid-January and brought the cumulative count to 5,049,465 children with COVID-19 since the pandemic began, the AAP and the CHA said in their weekly COVID report.
Hospitalizations in children aged 0-17 years have also reached record levels in recent days. The highest daily admission rate since the pandemic began, 0.51 per 100,000 population, was recorded on Sept. 2, less than 2 months after the nation saw its lowest child COVID admission rate for 1 day: 0.07 per 100,000 on July 4. That’s an increase of 629%, according to data from the Centers for Disease Control and Prevention.
Vaccinations in children, however, did not follow suit. New vaccinations in children aged 12-17 years dropped by 4.5% for the week ending Sept. 6, compared with the week before. Initiations were actually up almost 12% for children aged 16-17, but that was not enough to overcome the continued decline among 12- to 15-year-olds, the CDC said on its COVID Data Tracker.
Despite the decline in new vaccinations, those younger children passed a noteworthy group milestone: 50.9% of all 12- to 15-year-olds now have received at least one dose, with 38.6% having completed the regimen. The 16- to 17-year-olds got an earlier start and have reached 58.9% coverage for one dose and 47.6% for two, the CDC said.
A total of 12.2 million children aged 12-17 years had received at least one dose of COVID vaccine as of Sept. 6, of whom almost 9.5 million are fully vaccinated, based on the CDC data.
At the state level, Vermont has the highest rates for vaccine initiation (75%) and full vaccination (65%), with Massachusetts (75%/62%) and Connecticut (73%/59%) just behind. The other end of the scale is occupied by Wyoming (28% initiation/19% full vaccination), Alabama (32%/19%), and North Dakota (32%/23%), the AAP said in a separate report.
In a recent letter to the Food and Drug Administration, AAP President Lee Savio Beers, MD, said that the “Delta variant is surging at extremely alarming rates in every region of America. This surge is seriously impacting all populations, including children.” Dr. Beers urged the FDA to work “aggressively toward authorizing safe and effective COVID-19 vaccines for children under age 12 as soon as possible.”
Cases of child COVID-19 set a new 1-week record and the total number of children infected during the pandemic passed 5 million, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
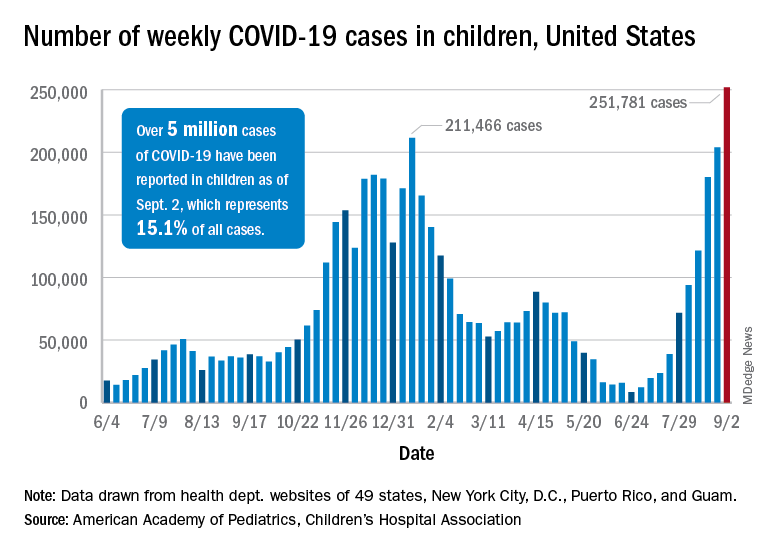
The nearly 282,000 new cases reported in the United States during the week ending Sept. 2 broke the record of 211,000 set in mid-January and brought the cumulative count to 5,049,465 children with COVID-19 since the pandemic began, the AAP and the CHA said in their weekly COVID report.
Hospitalizations in children aged 0-17 years have also reached record levels in recent days. The highest daily admission rate since the pandemic began, 0.51 per 100,000 population, was recorded on Sept. 2, less than 2 months after the nation saw its lowest child COVID admission rate for 1 day: 0.07 per 100,000 on July 4. That’s an increase of 629%, according to data from the Centers for Disease Control and Prevention.
Vaccinations in children, however, did not follow suit. New vaccinations in children aged 12-17 years dropped by 4.5% for the week ending Sept. 6, compared with the week before. Initiations were actually up almost 12% for children aged 16-17, but that was not enough to overcome the continued decline among 12- to 15-year-olds, the CDC said on its COVID Data Tracker.
Despite the decline in new vaccinations, those younger children passed a noteworthy group milestone: 50.9% of all 12- to 15-year-olds now have received at least one dose, with 38.6% having completed the regimen. The 16- to 17-year-olds got an earlier start and have reached 58.9% coverage for one dose and 47.6% for two, the CDC said.
A total of 12.2 million children aged 12-17 years had received at least one dose of COVID vaccine as of Sept. 6, of whom almost 9.5 million are fully vaccinated, based on the CDC data.
At the state level, Vermont has the highest rates for vaccine initiation (75%) and full vaccination (65%), with Massachusetts (75%/62%) and Connecticut (73%/59%) just behind. The other end of the scale is occupied by Wyoming (28% initiation/19% full vaccination), Alabama (32%/19%), and North Dakota (32%/23%), the AAP said in a separate report.
In a recent letter to the Food and Drug Administration, AAP President Lee Savio Beers, MD, said that the “Delta variant is surging at extremely alarming rates in every region of America. This surge is seriously impacting all populations, including children.” Dr. Beers urged the FDA to work “aggressively toward authorizing safe and effective COVID-19 vaccines for children under age 12 as soon as possible.”
COVID-19 continues to complicate children’s mental health care
The COVID-19 pandemic continues to impact child and adolescent mental health, and clinicians are learning as they go to develop strategies that address the challenges of providing both medical and mental health care to young patients, including those who test positive for COVID-19, according to Hani Talebi, PhD, director of pediatric psychology, and Jorge Ganem, MD, FAAP, director of pediatric hospital medicine, both of the University of Texas at Austin and Dell Children’s Medical Center.
In a presentation at the 2021 virtual Pediatric Hospital Medicine conference, Dr. Talebi and Dr. Ganem shared their experiences in identifying the impact of the pandemic on mental health services in a freestanding hospital, and synthesizing inpatient mental health care and medical care outside of a dedicated mental health unit.
Mental health is a significant pediatric issue; approximately one in five children have a diagnosable mental or behavioral health problem, but nearly two-thirds get little or no help, Dr. Talebi said. “COVID-19 has only exacerbated these mental health challenges,” he said.
He noted that beginning in April 2020, the proportion of children’s mental health-related emergency department visits increased and remained elevated through the spring, summer, and fall of 2020, as families fearful of COVID-19 avoided regular hospital visits.
Data suggest that up to 50% of all adolescent psychiatric crises that led to inpatient admissions were related in some way to COVID-19, Dr. Talebi said. In addition, “individuals with a recent diagnosis of a mental health disorder are at increased risk for COVID-19 infection,” and the risk is even higher among women and African Americans, he said.
The past year significantly impacted the mental wellbeing of parents and children, Dr. Talebi said. He cited a June 2020 study in Pediatrics in which 27% of parents reported worsening mental health for themselves, and 14% reported worsening behavioral health for their children. Ongoing issues including food insecurity, loss of regular child care, and an overall “very disorienting experience in the day-to-day” compromised the mental health of families, Dr. Talebi emphasized. Children isolated at home were not meeting developmental milestones that organically occur when socializing with peers, parents didn’t know how to handle some of their children’s issues without support from schools, and many people were struggling with other preexisting health conditions, he said.
This confluence of factors helped drive a surge in emergency department visits, meaning longer wait times and concerns about meeting urgent medical and mental health needs while maintaining safety, he added.
Parents and children waited longer to seek care, and community hospitals such as Dell Children’s Medical Center were faced with children in the emergency department with crisis-level mental health issues, along with children already waiting in the ED to address medical emergencies. All these patients had to be tested for COVID-19 and managed accordingly, Dr. Talebi noted.
Dr. Talebi emphasized the need for clinically robust care of the children who were in isolation for 10 days on the medical unit, waiting to test negative. New protocols were created for social workers to conduct daily safety checks, and to develop regular schedules for screening, “so they are having an experience on the medical floors similar to what they would have in a mental health unit,” he said.
Dr. Ganem reflected on the logistical challenges of managing mental health care while observing COVID-19 safety protocols. “COVID-19 added a new wrinkle of isolation,” he said. As institutional guidelines on testing and isolation evolved, negative COVID-19 tests were required for admission to the mental health units both in the hospital and throughout the region. Patients who tested positive had to be quarantined for 10 days, at which time they could be admitted to a mental health unit if necessary, he said.
Dr. Ganem shared details of some strategies adopted by Dell Children’s. He explained that the COVID-19 psychiatry patient workflow started with an ED evaluation, followed by medical clearance and consideration for admission.
“There was significant coordination between the social worker in the emergency department and the psychiatry social worker,” he said.
Key elements of the treatment plan for children with positive COVID-19 tests included an “interprofessional huddle” to coordinate the plan of care, goals for admission, and goals for safety, Dr. Ganem said.
Patients who required admission were expected to have an initial length of stay of 72 hours, and those who tested positive for COVID-19 were admitted to a medical unit with COVID-19 isolation, he said.
Once a patient is admitted, an RN activates a suicide prevention pathway, and an interprofessional team meets to determine what patients need for safe and effective discharge, said Dr. Ganem. He cited the SAFE-T protocol (Suicide Assessment Five-step Evaluation and Triage) as one of the tools used to determine safe discharge criteria. Considerations on the SAFE-T list include family support, an established outpatient therapist and psychiatrist, no suicide attempts prior to the current admission, or a low lethality attempt, and access to partial hospitalization or intensive outpatient programs.
Patients who could not be discharged because of suicidality or inadequate support or concerns about safety at home were considered for inpatient admission. Patients with COVID-19–positive tests who had continued need for inpatient mental health services could be transferred to an inpatient mental health unit after a 10-day quarantine.
Overall, “this has been a continuum of lessons learned, with some things we know now that we didn’t know in April or May of 2020,” Dr. Ganem said. Early in the pandemic, the focus was on minimizing risk, securing personal protective equipment, and determining who provided services in a patient’s room. “We developed new paradigms on the fly,” he said, including the use of virtual visits, which included securing and cleaning devices, as well as learning how to use them in this setting,” he said.
More recently, the emphasis has been on providing services to patients before they need to visit the hospital, rather than automatically admitting any patients with suicidal ideation and a positive COVID-19 test, Dr. Ganem said.
Dr. Talebi and Dr. Ganem had no financial conflicts to disclose. The conference was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The COVID-19 pandemic continues to impact child and adolescent mental health, and clinicians are learning as they go to develop strategies that address the challenges of providing both medical and mental health care to young patients, including those who test positive for COVID-19, according to Hani Talebi, PhD, director of pediatric psychology, and Jorge Ganem, MD, FAAP, director of pediatric hospital medicine, both of the University of Texas at Austin and Dell Children’s Medical Center.
In a presentation at the 2021 virtual Pediatric Hospital Medicine conference, Dr. Talebi and Dr. Ganem shared their experiences in identifying the impact of the pandemic on mental health services in a freestanding hospital, and synthesizing inpatient mental health care and medical care outside of a dedicated mental health unit.
Mental health is a significant pediatric issue; approximately one in five children have a diagnosable mental or behavioral health problem, but nearly two-thirds get little or no help, Dr. Talebi said. “COVID-19 has only exacerbated these mental health challenges,” he said.
He noted that beginning in April 2020, the proportion of children’s mental health-related emergency department visits increased and remained elevated through the spring, summer, and fall of 2020, as families fearful of COVID-19 avoided regular hospital visits.
Data suggest that up to 50% of all adolescent psychiatric crises that led to inpatient admissions were related in some way to COVID-19, Dr. Talebi said. In addition, “individuals with a recent diagnosis of a mental health disorder are at increased risk for COVID-19 infection,” and the risk is even higher among women and African Americans, he said.
The past year significantly impacted the mental wellbeing of parents and children, Dr. Talebi said. He cited a June 2020 study in Pediatrics in which 27% of parents reported worsening mental health for themselves, and 14% reported worsening behavioral health for their children. Ongoing issues including food insecurity, loss of regular child care, and an overall “very disorienting experience in the day-to-day” compromised the mental health of families, Dr. Talebi emphasized. Children isolated at home were not meeting developmental milestones that organically occur when socializing with peers, parents didn’t know how to handle some of their children’s issues without support from schools, and many people were struggling with other preexisting health conditions, he said.
This confluence of factors helped drive a surge in emergency department visits, meaning longer wait times and concerns about meeting urgent medical and mental health needs while maintaining safety, he added.
Parents and children waited longer to seek care, and community hospitals such as Dell Children’s Medical Center were faced with children in the emergency department with crisis-level mental health issues, along with children already waiting in the ED to address medical emergencies. All these patients had to be tested for COVID-19 and managed accordingly, Dr. Talebi noted.
Dr. Talebi emphasized the need for clinically robust care of the children who were in isolation for 10 days on the medical unit, waiting to test negative. New protocols were created for social workers to conduct daily safety checks, and to develop regular schedules for screening, “so they are having an experience on the medical floors similar to what they would have in a mental health unit,” he said.
Dr. Ganem reflected on the logistical challenges of managing mental health care while observing COVID-19 safety protocols. “COVID-19 added a new wrinkle of isolation,” he said. As institutional guidelines on testing and isolation evolved, negative COVID-19 tests were required for admission to the mental health units both in the hospital and throughout the region. Patients who tested positive had to be quarantined for 10 days, at which time they could be admitted to a mental health unit if necessary, he said.
Dr. Ganem shared details of some strategies adopted by Dell Children’s. He explained that the COVID-19 psychiatry patient workflow started with an ED evaluation, followed by medical clearance and consideration for admission.
“There was significant coordination between the social worker in the emergency department and the psychiatry social worker,” he said.
Key elements of the treatment plan for children with positive COVID-19 tests included an “interprofessional huddle” to coordinate the plan of care, goals for admission, and goals for safety, Dr. Ganem said.
Patients who required admission were expected to have an initial length of stay of 72 hours, and those who tested positive for COVID-19 were admitted to a medical unit with COVID-19 isolation, he said.
Once a patient is admitted, an RN activates a suicide prevention pathway, and an interprofessional team meets to determine what patients need for safe and effective discharge, said Dr. Ganem. He cited the SAFE-T protocol (Suicide Assessment Five-step Evaluation and Triage) as one of the tools used to determine safe discharge criteria. Considerations on the SAFE-T list include family support, an established outpatient therapist and psychiatrist, no suicide attempts prior to the current admission, or a low lethality attempt, and access to partial hospitalization or intensive outpatient programs.
Patients who could not be discharged because of suicidality or inadequate support or concerns about safety at home were considered for inpatient admission. Patients with COVID-19–positive tests who had continued need for inpatient mental health services could be transferred to an inpatient mental health unit after a 10-day quarantine.
Overall, “this has been a continuum of lessons learned, with some things we know now that we didn’t know in April or May of 2020,” Dr. Ganem said. Early in the pandemic, the focus was on minimizing risk, securing personal protective equipment, and determining who provided services in a patient’s room. “We developed new paradigms on the fly,” he said, including the use of virtual visits, which included securing and cleaning devices, as well as learning how to use them in this setting,” he said.
More recently, the emphasis has been on providing services to patients before they need to visit the hospital, rather than automatically admitting any patients with suicidal ideation and a positive COVID-19 test, Dr. Ganem said.
Dr. Talebi and Dr. Ganem had no financial conflicts to disclose. The conference was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
The COVID-19 pandemic continues to impact child and adolescent mental health, and clinicians are learning as they go to develop strategies that address the challenges of providing both medical and mental health care to young patients, including those who test positive for COVID-19, according to Hani Talebi, PhD, director of pediatric psychology, and Jorge Ganem, MD, FAAP, director of pediatric hospital medicine, both of the University of Texas at Austin and Dell Children’s Medical Center.
In a presentation at the 2021 virtual Pediatric Hospital Medicine conference, Dr. Talebi and Dr. Ganem shared their experiences in identifying the impact of the pandemic on mental health services in a freestanding hospital, and synthesizing inpatient mental health care and medical care outside of a dedicated mental health unit.
Mental health is a significant pediatric issue; approximately one in five children have a diagnosable mental or behavioral health problem, but nearly two-thirds get little or no help, Dr. Talebi said. “COVID-19 has only exacerbated these mental health challenges,” he said.
He noted that beginning in April 2020, the proportion of children’s mental health-related emergency department visits increased and remained elevated through the spring, summer, and fall of 2020, as families fearful of COVID-19 avoided regular hospital visits.
Data suggest that up to 50% of all adolescent psychiatric crises that led to inpatient admissions were related in some way to COVID-19, Dr. Talebi said. In addition, “individuals with a recent diagnosis of a mental health disorder are at increased risk for COVID-19 infection,” and the risk is even higher among women and African Americans, he said.
The past year significantly impacted the mental wellbeing of parents and children, Dr. Talebi said. He cited a June 2020 study in Pediatrics in which 27% of parents reported worsening mental health for themselves, and 14% reported worsening behavioral health for their children. Ongoing issues including food insecurity, loss of regular child care, and an overall “very disorienting experience in the day-to-day” compromised the mental health of families, Dr. Talebi emphasized. Children isolated at home were not meeting developmental milestones that organically occur when socializing with peers, parents didn’t know how to handle some of their children’s issues without support from schools, and many people were struggling with other preexisting health conditions, he said.
This confluence of factors helped drive a surge in emergency department visits, meaning longer wait times and concerns about meeting urgent medical and mental health needs while maintaining safety, he added.
Parents and children waited longer to seek care, and community hospitals such as Dell Children’s Medical Center were faced with children in the emergency department with crisis-level mental health issues, along with children already waiting in the ED to address medical emergencies. All these patients had to be tested for COVID-19 and managed accordingly, Dr. Talebi noted.
Dr. Talebi emphasized the need for clinically robust care of the children who were in isolation for 10 days on the medical unit, waiting to test negative. New protocols were created for social workers to conduct daily safety checks, and to develop regular schedules for screening, “so they are having an experience on the medical floors similar to what they would have in a mental health unit,” he said.
Dr. Ganem reflected on the logistical challenges of managing mental health care while observing COVID-19 safety protocols. “COVID-19 added a new wrinkle of isolation,” he said. As institutional guidelines on testing and isolation evolved, negative COVID-19 tests were required for admission to the mental health units both in the hospital and throughout the region. Patients who tested positive had to be quarantined for 10 days, at which time they could be admitted to a mental health unit if necessary, he said.
Dr. Ganem shared details of some strategies adopted by Dell Children’s. He explained that the COVID-19 psychiatry patient workflow started with an ED evaluation, followed by medical clearance and consideration for admission.
“There was significant coordination between the social worker in the emergency department and the psychiatry social worker,” he said.
Key elements of the treatment plan for children with positive COVID-19 tests included an “interprofessional huddle” to coordinate the plan of care, goals for admission, and goals for safety, Dr. Ganem said.
Patients who required admission were expected to have an initial length of stay of 72 hours, and those who tested positive for COVID-19 were admitted to a medical unit with COVID-19 isolation, he said.
Once a patient is admitted, an RN activates a suicide prevention pathway, and an interprofessional team meets to determine what patients need for safe and effective discharge, said Dr. Ganem. He cited the SAFE-T protocol (Suicide Assessment Five-step Evaluation and Triage) as one of the tools used to determine safe discharge criteria. Considerations on the SAFE-T list include family support, an established outpatient therapist and psychiatrist, no suicide attempts prior to the current admission, or a low lethality attempt, and access to partial hospitalization or intensive outpatient programs.
Patients who could not be discharged because of suicidality or inadequate support or concerns about safety at home were considered for inpatient admission. Patients with COVID-19–positive tests who had continued need for inpatient mental health services could be transferred to an inpatient mental health unit after a 10-day quarantine.
Overall, “this has been a continuum of lessons learned, with some things we know now that we didn’t know in April or May of 2020,” Dr. Ganem said. Early in the pandemic, the focus was on minimizing risk, securing personal protective equipment, and determining who provided services in a patient’s room. “We developed new paradigms on the fly,” he said, including the use of virtual visits, which included securing and cleaning devices, as well as learning how to use them in this setting,” he said.
More recently, the emphasis has been on providing services to patients before they need to visit the hospital, rather than automatically admitting any patients with suicidal ideation and a positive COVID-19 test, Dr. Ganem said.
Dr. Talebi and Dr. Ganem had no financial conflicts to disclose. The conference was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
FROM PHM 2021
Clinical genetic testing for skin disorders continues to advance
and families of pediatric patients to navigate the landscape.
“Testing options range from targeted variant testing and single-gene testing to exome and genome sequencing,” Gabriele Richard, MD, said at the annual meeting of the Society for Pediatric Dermatology. “It is not always easy to determine which testing is right.”
Increasingly, clinical genomic tests, including exome and genome sequencing, are used for patients with complex phenotypes, and possibly multiple disorders, who might have no diagnosis despite extensive prior testing, said Dr. Richard, medical director at Gaithersburg, Md.–based GeneDx., a molecular diagnostic laboratory that performs comprehensive testing for rare genetic disorders. These tests are also being used more for first-line testing in critically ill patients in the neonatal and pediatric intensive care units, and “have heralded a whole new era of gene and disease discovery,” she added.
Targeted variant testing is used for known familial variants, to test family members for carrier status and segregation, and to make a prenatal diagnosis, she said. Single-gene testing is available for most genes and has its place for conditions that can be clinically well-recognized, such as ichthyosis vulgaris, Darier disease, or Papillon-Lefèvre syndrome.
Specific tests for identifying gene deletions or duplications are exon-level microarrays, multiplex ligation-dependent probe amplification (MLPA), and chromosomal microarray analysis. “The latter has been successful in identifying diseases causing chromosomal abnormalities in over 10% of cases overall,” Dr. Richard said. An example of a skin disorder is X-linked ichthyosis caused by a deletion of the steroid sulfatase locus in more than 95% of affected males, she said.
“However, the current staple of molecular diagnostic testing is multigene next-generation sequencing (NGS) panels, which allow you to interrogate two to hundreds of genes concurrently, including sequencing and deletion duplication testing.” These tests are the most cost effective, she said, and are available for almost any genodermatosis or group of disorders with overlapping phenotypes, such as albinism or ichthyosis, epidermolysis bullosa and skin fragility, ectodermal dysplasia, or porphyria. According to Dr. Richard, the diagnostic outcomes of NGS panels mainly depend on test indication, panel size and gene curation, age of onset, and prevailing inheritance pattern of disorders.
Her recommended criteria for distinguishing the myriad of available NGS panels include checking gene content, technical sensitivity of sequencing and deletion/duplication analysis, quality of variant interpretation and reporting, turn-around time, and available familial follow-up testing. “If a family might consider future prenatal diagnosis, choose the lab that performs prenatal and diagnostic testing,” Dr. Richard said. “Equally important are client services such as ease of ordering, insurance coverage, and the ability to determine out-of-pocket cost to patients.”
Resources that enable consumers to compare panel content, methodology, turnaround time, and other parameters include the Genetic Testing Registry (GTR) operated by the National Center for Biotechnology Information, and Concert Genetics, a genetic testing company. The National Society of Genetic Counselors also offers a searchable database for finding a genetic counselor.
Exome sequencing includes the coding sequences of about 20,000 genes and has an average depth of 50 to about 150 reads. “It is a phenotype-driven test where only select variants are being reported fitting the phenotype,” Dr. Richard said. “The outcome of exome and genome sequencing much depends on optimization of bioinformatic pipelines and tools.” Besides small sequence variants, exome sequencing is able to identify a variety of different types of disease-causing variants, such as gene copy number variants seen in about 6% of positive cases, mosaicism, regions of homozygosity, uniparental disomy, and other unusual events and is cost effective.
Whole-genome sequencing, meanwhile, includes the entire genome, particularly noncoding regions, and has an average depth of more than 30 reads. “It’s based on single-molecule sequencing, has longer reads and more uniform coverage, compared to exome sequencing,” she said. “Higher cost, variant interpretation, and lack of coverage by payers are still presenting challenges for genome sequencing.” Genome sequencing can be done in a day or less.
According to diagnostic outcomes based on 280,000 individuals including 125,000 probands from GeneDx data, a definitive diagnosis was made in 26% of probands, of which 2.8% had more than one diagnostic finding and 1.8% had actionable secondary findings. In addition, 7% of the variants were found in candidate genes; 31% of probands had variants of uncertain significance, while 36% tested negative. “Nevertheless, the diagnostic yield of exome sequencing depends on the phenotype and cohort studied,” Dr. Richard continued.
At her company, she said, the highest positive rate is for multiple congenital anomalies (34%), skeletal system abnormalities (30%), and nervous system abnormalities (29%). Trio testing – the concurrent analysis of both biological parents and proband for all genes – “is a critical factor for success,” she added. “It not only improves the variant calling because we have three times the data and increases test sensitivity, it also provides more certain results, determines inheritance and allows for detection of parental mosaicism.”
According to Dr. Richard, trio testing has a one-third higher diagnostic rate than sequencing of the proband alone. Citing a published prospective study that compiled data from eight different exome- and genome-sequencing studies in critically ill neonates and children, trio testing made it possible to make a genetic diagnosis in up to 58% of children.
Whole-genome sequencing is estimated to have a 5%-10% higher diagnostic rate than exome sequencing. “However, we are still a ways away from using it as a routine diagnostic test for all test indications,” Dr. Richard said. “Automation, special bioinformatics algorithms and databases, and combination of genome sequencing with mRNA sequencing are being explored and built to further improve the diagnostic yield.”
Dr. Richard had no disclosures other than being an employee of GeneDx.
and families of pediatric patients to navigate the landscape.
“Testing options range from targeted variant testing and single-gene testing to exome and genome sequencing,” Gabriele Richard, MD, said at the annual meeting of the Society for Pediatric Dermatology. “It is not always easy to determine which testing is right.”
Increasingly, clinical genomic tests, including exome and genome sequencing, are used for patients with complex phenotypes, and possibly multiple disorders, who might have no diagnosis despite extensive prior testing, said Dr. Richard, medical director at Gaithersburg, Md.–based GeneDx., a molecular diagnostic laboratory that performs comprehensive testing for rare genetic disorders. These tests are also being used more for first-line testing in critically ill patients in the neonatal and pediatric intensive care units, and “have heralded a whole new era of gene and disease discovery,” she added.
Targeted variant testing is used for known familial variants, to test family members for carrier status and segregation, and to make a prenatal diagnosis, she said. Single-gene testing is available for most genes and has its place for conditions that can be clinically well-recognized, such as ichthyosis vulgaris, Darier disease, or Papillon-Lefèvre syndrome.
Specific tests for identifying gene deletions or duplications are exon-level microarrays, multiplex ligation-dependent probe amplification (MLPA), and chromosomal microarray analysis. “The latter has been successful in identifying diseases causing chromosomal abnormalities in over 10% of cases overall,” Dr. Richard said. An example of a skin disorder is X-linked ichthyosis caused by a deletion of the steroid sulfatase locus in more than 95% of affected males, she said.
“However, the current staple of molecular diagnostic testing is multigene next-generation sequencing (NGS) panels, which allow you to interrogate two to hundreds of genes concurrently, including sequencing and deletion duplication testing.” These tests are the most cost effective, she said, and are available for almost any genodermatosis or group of disorders with overlapping phenotypes, such as albinism or ichthyosis, epidermolysis bullosa and skin fragility, ectodermal dysplasia, or porphyria. According to Dr. Richard, the diagnostic outcomes of NGS panels mainly depend on test indication, panel size and gene curation, age of onset, and prevailing inheritance pattern of disorders.
Her recommended criteria for distinguishing the myriad of available NGS panels include checking gene content, technical sensitivity of sequencing and deletion/duplication analysis, quality of variant interpretation and reporting, turn-around time, and available familial follow-up testing. “If a family might consider future prenatal diagnosis, choose the lab that performs prenatal and diagnostic testing,” Dr. Richard said. “Equally important are client services such as ease of ordering, insurance coverage, and the ability to determine out-of-pocket cost to patients.”
Resources that enable consumers to compare panel content, methodology, turnaround time, and other parameters include the Genetic Testing Registry (GTR) operated by the National Center for Biotechnology Information, and Concert Genetics, a genetic testing company. The National Society of Genetic Counselors also offers a searchable database for finding a genetic counselor.
Exome sequencing includes the coding sequences of about 20,000 genes and has an average depth of 50 to about 150 reads. “It is a phenotype-driven test where only select variants are being reported fitting the phenotype,” Dr. Richard said. “The outcome of exome and genome sequencing much depends on optimization of bioinformatic pipelines and tools.” Besides small sequence variants, exome sequencing is able to identify a variety of different types of disease-causing variants, such as gene copy number variants seen in about 6% of positive cases, mosaicism, regions of homozygosity, uniparental disomy, and other unusual events and is cost effective.
Whole-genome sequencing, meanwhile, includes the entire genome, particularly noncoding regions, and has an average depth of more than 30 reads. “It’s based on single-molecule sequencing, has longer reads and more uniform coverage, compared to exome sequencing,” she said. “Higher cost, variant interpretation, and lack of coverage by payers are still presenting challenges for genome sequencing.” Genome sequencing can be done in a day or less.
According to diagnostic outcomes based on 280,000 individuals including 125,000 probands from GeneDx data, a definitive diagnosis was made in 26% of probands, of which 2.8% had more than one diagnostic finding and 1.8% had actionable secondary findings. In addition, 7% of the variants were found in candidate genes; 31% of probands had variants of uncertain significance, while 36% tested negative. “Nevertheless, the diagnostic yield of exome sequencing depends on the phenotype and cohort studied,” Dr. Richard continued.
At her company, she said, the highest positive rate is for multiple congenital anomalies (34%), skeletal system abnormalities (30%), and nervous system abnormalities (29%). Trio testing – the concurrent analysis of both biological parents and proband for all genes – “is a critical factor for success,” she added. “It not only improves the variant calling because we have three times the data and increases test sensitivity, it also provides more certain results, determines inheritance and allows for detection of parental mosaicism.”
According to Dr. Richard, trio testing has a one-third higher diagnostic rate than sequencing of the proband alone. Citing a published prospective study that compiled data from eight different exome- and genome-sequencing studies in critically ill neonates and children, trio testing made it possible to make a genetic diagnosis in up to 58% of children.
Whole-genome sequencing is estimated to have a 5%-10% higher diagnostic rate than exome sequencing. “However, we are still a ways away from using it as a routine diagnostic test for all test indications,” Dr. Richard said. “Automation, special bioinformatics algorithms and databases, and combination of genome sequencing with mRNA sequencing are being explored and built to further improve the diagnostic yield.”
Dr. Richard had no disclosures other than being an employee of GeneDx.
and families of pediatric patients to navigate the landscape.
“Testing options range from targeted variant testing and single-gene testing to exome and genome sequencing,” Gabriele Richard, MD, said at the annual meeting of the Society for Pediatric Dermatology. “It is not always easy to determine which testing is right.”
Increasingly, clinical genomic tests, including exome and genome sequencing, are used for patients with complex phenotypes, and possibly multiple disorders, who might have no diagnosis despite extensive prior testing, said Dr. Richard, medical director at Gaithersburg, Md.–based GeneDx., a molecular diagnostic laboratory that performs comprehensive testing for rare genetic disorders. These tests are also being used more for first-line testing in critically ill patients in the neonatal and pediatric intensive care units, and “have heralded a whole new era of gene and disease discovery,” she added.
Targeted variant testing is used for known familial variants, to test family members for carrier status and segregation, and to make a prenatal diagnosis, she said. Single-gene testing is available for most genes and has its place for conditions that can be clinically well-recognized, such as ichthyosis vulgaris, Darier disease, or Papillon-Lefèvre syndrome.
Specific tests for identifying gene deletions or duplications are exon-level microarrays, multiplex ligation-dependent probe amplification (MLPA), and chromosomal microarray analysis. “The latter has been successful in identifying diseases causing chromosomal abnormalities in over 10% of cases overall,” Dr. Richard said. An example of a skin disorder is X-linked ichthyosis caused by a deletion of the steroid sulfatase locus in more than 95% of affected males, she said.
“However, the current staple of molecular diagnostic testing is multigene next-generation sequencing (NGS) panels, which allow you to interrogate two to hundreds of genes concurrently, including sequencing and deletion duplication testing.” These tests are the most cost effective, she said, and are available for almost any genodermatosis or group of disorders with overlapping phenotypes, such as albinism or ichthyosis, epidermolysis bullosa and skin fragility, ectodermal dysplasia, or porphyria. According to Dr. Richard, the diagnostic outcomes of NGS panels mainly depend on test indication, panel size and gene curation, age of onset, and prevailing inheritance pattern of disorders.
Her recommended criteria for distinguishing the myriad of available NGS panels include checking gene content, technical sensitivity of sequencing and deletion/duplication analysis, quality of variant interpretation and reporting, turn-around time, and available familial follow-up testing. “If a family might consider future prenatal diagnosis, choose the lab that performs prenatal and diagnostic testing,” Dr. Richard said. “Equally important are client services such as ease of ordering, insurance coverage, and the ability to determine out-of-pocket cost to patients.”
Resources that enable consumers to compare panel content, methodology, turnaround time, and other parameters include the Genetic Testing Registry (GTR) operated by the National Center for Biotechnology Information, and Concert Genetics, a genetic testing company. The National Society of Genetic Counselors also offers a searchable database for finding a genetic counselor.
Exome sequencing includes the coding sequences of about 20,000 genes and has an average depth of 50 to about 150 reads. “It is a phenotype-driven test where only select variants are being reported fitting the phenotype,” Dr. Richard said. “The outcome of exome and genome sequencing much depends on optimization of bioinformatic pipelines and tools.” Besides small sequence variants, exome sequencing is able to identify a variety of different types of disease-causing variants, such as gene copy number variants seen in about 6% of positive cases, mosaicism, regions of homozygosity, uniparental disomy, and other unusual events and is cost effective.
Whole-genome sequencing, meanwhile, includes the entire genome, particularly noncoding regions, and has an average depth of more than 30 reads. “It’s based on single-molecule sequencing, has longer reads and more uniform coverage, compared to exome sequencing,” she said. “Higher cost, variant interpretation, and lack of coverage by payers are still presenting challenges for genome sequencing.” Genome sequencing can be done in a day or less.
According to diagnostic outcomes based on 280,000 individuals including 125,000 probands from GeneDx data, a definitive diagnosis was made in 26% of probands, of which 2.8% had more than one diagnostic finding and 1.8% had actionable secondary findings. In addition, 7% of the variants were found in candidate genes; 31% of probands had variants of uncertain significance, while 36% tested negative. “Nevertheless, the diagnostic yield of exome sequencing depends on the phenotype and cohort studied,” Dr. Richard continued.
At her company, she said, the highest positive rate is for multiple congenital anomalies (34%), skeletal system abnormalities (30%), and nervous system abnormalities (29%). Trio testing – the concurrent analysis of both biological parents and proband for all genes – “is a critical factor for success,” she added. “It not only improves the variant calling because we have three times the data and increases test sensitivity, it also provides more certain results, determines inheritance and allows for detection of parental mosaicism.”
According to Dr. Richard, trio testing has a one-third higher diagnostic rate than sequencing of the proband alone. Citing a published prospective study that compiled data from eight different exome- and genome-sequencing studies in critically ill neonates and children, trio testing made it possible to make a genetic diagnosis in up to 58% of children.
Whole-genome sequencing is estimated to have a 5%-10% higher diagnostic rate than exome sequencing. “However, we are still a ways away from using it as a routine diagnostic test for all test indications,” Dr. Richard said. “Automation, special bioinformatics algorithms and databases, and combination of genome sequencing with mRNA sequencing are being explored and built to further improve the diagnostic yield.”
Dr. Richard had no disclosures other than being an employee of GeneDx.
FROM SPD 2021
















