User login
Skinny-label biosimilars provide substantial savings to Medicare
Recent court rulings could put such saving under threat
Competition between five biologic drugs and their skinny-label biosimilars saved Medicare an estimated $1.5 billion during 2015-2020. But these savings accruing to Medicare and the availability of those and other biosimilars through skinny labeling is under threat from recent court rulings, according to a research letter published online in JAMA Internal Medicine.
The authors highlighted the need for such savings by noting that, while biologics comprise less than 5% of prescription drug use, their price tag amounts to about 40% of U.S. drug spending, Biologic manufacturers often delay the availability of biosimilars for additional years beyond the original patent expiration through further patents for supplemental indications. To provide a counterbalance, federal law allows the Food and Drug Administration to approve “skinny-label” generics and biosimilars that carve out patent-protected indications or regulatory exclusivities. But once a generic drug reaches the market through this process with a skinny label, it may often be substituted for indications that go beyond the ones listed on the skinny label. In fact, some state laws mandate that pharmacists substitute interchangeable generics for brand-name drugs, helping to decrease drug prices. In response to legal threats to the skinny-label pathway, Alexander C. Egilman and colleagues at Brigham and Women’s Hospital and Harvard Medical School, both in Boston, assessed the frequency of approval and marketing of skinny-label biosimilars from 2015 to 2021 and the resultant savings to Medicare.
The authors estimated annual Part B (clinician-administered) savings from skinny-label biosimilars through 2020 by comparing actual biologic and skinny-label biosimilar spending with estimated biologic spending without competition using the Medicare Dashboard. They assumed that the unit price of the biologic would increase at its 5-year compound annual growth rate prior to competition.
In that period, the FDA approved 33 biosimilars linked to 11 biologics. Among them, 22 (66.7%) had a skinny label. Of 21 biosimilars marketed before 2022, 13 (61.9%) were launched with a skinny label. Of the 8 biologics linked to these 21 biosimilars, 5 of the first-to-market biosimilars had skinny labels (bevacizumab, filgrastim, infliximab, pegfilgrastim, and rituximab), leading to earlier competition through 2021.
The estimated $1.5 billion in savings to Medicare from these skinny-label biosimilars over the 2015-2020 span represents 4.9% of the $30.2 billion that Medicare spent on the five biologics during this period. The researchers pointed out that once adalimumab (Humira) faces skinny-label biosimilar competition in 2023, savings will likely grow substantially.
In response to the research letter, an editor’s note by JAMA Internal Medicine Editorial Fellow Eric Ward, MD, and JAMA Internal Medicine Editor at Large and Online Editor Robert Steinbrook, MD, stated that, between 2015 and 2019, 24 (43%) of 56 brand-name drugs had competition from skinny-labeled generic formulations after first becoming available as generics.
The editors also referenced a JAMA Viewpoints article from 2021 that reviewed the most recent case challenging the skinny-label pathway in which GlaxoSmithKline sued Teva for its marketing of a skinny-label generic of the brand-name beta-blocker carvedilol (Coreg) that the plaintive claimed “induced physicians to prescribe carvedilol for indications that had been carved out by Teva’s skinny label, thus infringing GlaxoSmithKline’s patents.” A $235 million judgment against Teva was overturned by a district court and then reversed again by a Federal Circuit court that, after receiving criticism, reconsidered the case, and a panel affirmed the judgment against Teva.
“The Federal Circuit panel’s decision has the potential to put generic drugs that fail to adequately carve out indications from the brand name labeling at risk for damages related to infringement,” the authors wrote. Similar claims of infringement are being heard in other courts, they wrote, and they urged careful targeting of skinny-label carveouts, and suggest also that challenges to the arguments used against Teva focus on preservation of First Amendment rights as protection for lawful and accurate speech in drug labels.
“The legal uncertainties are likely to continue, as manufacturers pursue novel and complex strategies to protect the patents and regulatory exclusivities of brand-name drugs and biologics,” Dr. Ward and Dr. Steinbrook wrote, adding that “the path forward is for Congress to enact additional legislation that reaffirms and strengthens the permissibility of skinny labeling.”
The research letter’s corresponding author, Ameet Sarpatwari, PhD, JD, assistant professor at Harvard Medical School, and assistant director for the Harvard Program On Regulation, Therapeutics, And Law, echoed concerns over the Teva case in an interview. “There has certainly been concern that should the appellate decision stand, there will be a chilling effect. As the lone dissenter in that case noted, ‘no skinny-label generic is safe.’ I think many generic and biosimilar manufacturers are awaiting to see whether the Supreme Court will take the case.”
He added: “I do not believe the likelihood of skinny-label-supportive legislation making it through Congress will be greatly diminished in a divided Congress. Democrats and Republicans alike should seek to promote competition in the marketplace, which is what the skinny-labeling pathway accomplishes.”
The authors reported no relevant conflicts of interest. The research was funded by a grant from Arnold Ventures.
Recent court rulings could put such saving under threat
Recent court rulings could put such saving under threat
Competition between five biologic drugs and their skinny-label biosimilars saved Medicare an estimated $1.5 billion during 2015-2020. But these savings accruing to Medicare and the availability of those and other biosimilars through skinny labeling is under threat from recent court rulings, according to a research letter published online in JAMA Internal Medicine.
The authors highlighted the need for such savings by noting that, while biologics comprise less than 5% of prescription drug use, their price tag amounts to about 40% of U.S. drug spending, Biologic manufacturers often delay the availability of biosimilars for additional years beyond the original patent expiration through further patents for supplemental indications. To provide a counterbalance, federal law allows the Food and Drug Administration to approve “skinny-label” generics and biosimilars that carve out patent-protected indications or regulatory exclusivities. But once a generic drug reaches the market through this process with a skinny label, it may often be substituted for indications that go beyond the ones listed on the skinny label. In fact, some state laws mandate that pharmacists substitute interchangeable generics for brand-name drugs, helping to decrease drug prices. In response to legal threats to the skinny-label pathway, Alexander C. Egilman and colleagues at Brigham and Women’s Hospital and Harvard Medical School, both in Boston, assessed the frequency of approval and marketing of skinny-label biosimilars from 2015 to 2021 and the resultant savings to Medicare.
The authors estimated annual Part B (clinician-administered) savings from skinny-label biosimilars through 2020 by comparing actual biologic and skinny-label biosimilar spending with estimated biologic spending without competition using the Medicare Dashboard. They assumed that the unit price of the biologic would increase at its 5-year compound annual growth rate prior to competition.
In that period, the FDA approved 33 biosimilars linked to 11 biologics. Among them, 22 (66.7%) had a skinny label. Of 21 biosimilars marketed before 2022, 13 (61.9%) were launched with a skinny label. Of the 8 biologics linked to these 21 biosimilars, 5 of the first-to-market biosimilars had skinny labels (bevacizumab, filgrastim, infliximab, pegfilgrastim, and rituximab), leading to earlier competition through 2021.
The estimated $1.5 billion in savings to Medicare from these skinny-label biosimilars over the 2015-2020 span represents 4.9% of the $30.2 billion that Medicare spent on the five biologics during this period. The researchers pointed out that once adalimumab (Humira) faces skinny-label biosimilar competition in 2023, savings will likely grow substantially.
In response to the research letter, an editor’s note by JAMA Internal Medicine Editorial Fellow Eric Ward, MD, and JAMA Internal Medicine Editor at Large and Online Editor Robert Steinbrook, MD, stated that, between 2015 and 2019, 24 (43%) of 56 brand-name drugs had competition from skinny-labeled generic formulations after first becoming available as generics.
The editors also referenced a JAMA Viewpoints article from 2021 that reviewed the most recent case challenging the skinny-label pathway in which GlaxoSmithKline sued Teva for its marketing of a skinny-label generic of the brand-name beta-blocker carvedilol (Coreg) that the plaintive claimed “induced physicians to prescribe carvedilol for indications that had been carved out by Teva’s skinny label, thus infringing GlaxoSmithKline’s patents.” A $235 million judgment against Teva was overturned by a district court and then reversed again by a Federal Circuit court that, after receiving criticism, reconsidered the case, and a panel affirmed the judgment against Teva.
“The Federal Circuit panel’s decision has the potential to put generic drugs that fail to adequately carve out indications from the brand name labeling at risk for damages related to infringement,” the authors wrote. Similar claims of infringement are being heard in other courts, they wrote, and they urged careful targeting of skinny-label carveouts, and suggest also that challenges to the arguments used against Teva focus on preservation of First Amendment rights as protection for lawful and accurate speech in drug labels.
“The legal uncertainties are likely to continue, as manufacturers pursue novel and complex strategies to protect the patents and regulatory exclusivities of brand-name drugs and biologics,” Dr. Ward and Dr. Steinbrook wrote, adding that “the path forward is for Congress to enact additional legislation that reaffirms and strengthens the permissibility of skinny labeling.”
The research letter’s corresponding author, Ameet Sarpatwari, PhD, JD, assistant professor at Harvard Medical School, and assistant director for the Harvard Program On Regulation, Therapeutics, And Law, echoed concerns over the Teva case in an interview. “There has certainly been concern that should the appellate decision stand, there will be a chilling effect. As the lone dissenter in that case noted, ‘no skinny-label generic is safe.’ I think many generic and biosimilar manufacturers are awaiting to see whether the Supreme Court will take the case.”
He added: “I do not believe the likelihood of skinny-label-supportive legislation making it through Congress will be greatly diminished in a divided Congress. Democrats and Republicans alike should seek to promote competition in the marketplace, which is what the skinny-labeling pathway accomplishes.”
The authors reported no relevant conflicts of interest. The research was funded by a grant from Arnold Ventures.
Competition between five biologic drugs and their skinny-label biosimilars saved Medicare an estimated $1.5 billion during 2015-2020. But these savings accruing to Medicare and the availability of those and other biosimilars through skinny labeling is under threat from recent court rulings, according to a research letter published online in JAMA Internal Medicine.
The authors highlighted the need for such savings by noting that, while biologics comprise less than 5% of prescription drug use, their price tag amounts to about 40% of U.S. drug spending, Biologic manufacturers often delay the availability of biosimilars for additional years beyond the original patent expiration through further patents for supplemental indications. To provide a counterbalance, federal law allows the Food and Drug Administration to approve “skinny-label” generics and biosimilars that carve out patent-protected indications or regulatory exclusivities. But once a generic drug reaches the market through this process with a skinny label, it may often be substituted for indications that go beyond the ones listed on the skinny label. In fact, some state laws mandate that pharmacists substitute interchangeable generics for brand-name drugs, helping to decrease drug prices. In response to legal threats to the skinny-label pathway, Alexander C. Egilman and colleagues at Brigham and Women’s Hospital and Harvard Medical School, both in Boston, assessed the frequency of approval and marketing of skinny-label biosimilars from 2015 to 2021 and the resultant savings to Medicare.
The authors estimated annual Part B (clinician-administered) savings from skinny-label biosimilars through 2020 by comparing actual biologic and skinny-label biosimilar spending with estimated biologic spending without competition using the Medicare Dashboard. They assumed that the unit price of the biologic would increase at its 5-year compound annual growth rate prior to competition.
In that period, the FDA approved 33 biosimilars linked to 11 biologics. Among them, 22 (66.7%) had a skinny label. Of 21 biosimilars marketed before 2022, 13 (61.9%) were launched with a skinny label. Of the 8 biologics linked to these 21 biosimilars, 5 of the first-to-market biosimilars had skinny labels (bevacizumab, filgrastim, infliximab, pegfilgrastim, and rituximab), leading to earlier competition through 2021.
The estimated $1.5 billion in savings to Medicare from these skinny-label biosimilars over the 2015-2020 span represents 4.9% of the $30.2 billion that Medicare spent on the five biologics during this period. The researchers pointed out that once adalimumab (Humira) faces skinny-label biosimilar competition in 2023, savings will likely grow substantially.
In response to the research letter, an editor’s note by JAMA Internal Medicine Editorial Fellow Eric Ward, MD, and JAMA Internal Medicine Editor at Large and Online Editor Robert Steinbrook, MD, stated that, between 2015 and 2019, 24 (43%) of 56 brand-name drugs had competition from skinny-labeled generic formulations after first becoming available as generics.
The editors also referenced a JAMA Viewpoints article from 2021 that reviewed the most recent case challenging the skinny-label pathway in which GlaxoSmithKline sued Teva for its marketing of a skinny-label generic of the brand-name beta-blocker carvedilol (Coreg) that the plaintive claimed “induced physicians to prescribe carvedilol for indications that had been carved out by Teva’s skinny label, thus infringing GlaxoSmithKline’s patents.” A $235 million judgment against Teva was overturned by a district court and then reversed again by a Federal Circuit court that, after receiving criticism, reconsidered the case, and a panel affirmed the judgment against Teva.
“The Federal Circuit panel’s decision has the potential to put generic drugs that fail to adequately carve out indications from the brand name labeling at risk for damages related to infringement,” the authors wrote. Similar claims of infringement are being heard in other courts, they wrote, and they urged careful targeting of skinny-label carveouts, and suggest also that challenges to the arguments used against Teva focus on preservation of First Amendment rights as protection for lawful and accurate speech in drug labels.
“The legal uncertainties are likely to continue, as manufacturers pursue novel and complex strategies to protect the patents and regulatory exclusivities of brand-name drugs and biologics,” Dr. Ward and Dr. Steinbrook wrote, adding that “the path forward is for Congress to enact additional legislation that reaffirms and strengthens the permissibility of skinny labeling.”
The research letter’s corresponding author, Ameet Sarpatwari, PhD, JD, assistant professor at Harvard Medical School, and assistant director for the Harvard Program On Regulation, Therapeutics, And Law, echoed concerns over the Teva case in an interview. “There has certainly been concern that should the appellate decision stand, there will be a chilling effect. As the lone dissenter in that case noted, ‘no skinny-label generic is safe.’ I think many generic and biosimilar manufacturers are awaiting to see whether the Supreme Court will take the case.”
He added: “I do not believe the likelihood of skinny-label-supportive legislation making it through Congress will be greatly diminished in a divided Congress. Democrats and Republicans alike should seek to promote competition in the marketplace, which is what the skinny-labeling pathway accomplishes.”
The authors reported no relevant conflicts of interest. The research was funded by a grant from Arnold Ventures.
FROM JAMA INTERNAL MEDICINE
Could this computer help you beat cancer?
The 1960s marked the arrival of computers in medicine. Expensive, cumbersome hunks of plastic and metal that could (maybe) get test results to a doctor faster. The 1980s saw the first real difference-making functions computers could offer – clinical, financial, administrative – and in 1991, the Institute of Medicine published the first manifesto on what electronic health records could (and would) be.
Since then, we’ve seen computer breakthroughs across all areas of medicine, with artificial intelligence (AI), virtual reality, and telemedicine brought to the fore. But something else is brewing that not a lot of people know about yet:
“Think of it as transitioning from getting light through fire and candles and now having electricity, and there’s a light bulb that is lighting it all,” said Lara Jehi, MD, Cleveland Clinic’s chief research information officer.
What is quantum computing?
Classical computers (aka binary computers), which are the foundation of today’s devices, including artificial intelligence and machine learning, work by using information known as bits. These appear as 0 or 1 (sometimes defined as off/on or false/true).
Quantum computers, on the other hand, use quantum bits known as qubits. And yes, the definition of “quantum” – as in: very, very small – applies.
International Business Machines, more commonly known as IBM, is currently leading this new tech. A common misconception about quantum computers is that they are “a next evolution of computers that will get faster,” said Frederik Flöther, PhD, life sciences and health care lead with IBM Quantum Industry Consulting. Instead, he wants us to look at quantum computing as something completely new “because it is fundamentally a different hardware, a different software, not just an evolution of the same.”
How does it work differently from existing computers? Quantum computing deals in nature. Therefore, qubits have to be based on the natural world. What does that mean? Nobel Prize-winning physicist Richard Feynman was famously quoted as saying: “Nature isn’t classical, dammit, and if you want to make a simulation of nature, you’d better make it quantum mechanical, and by golly it’s a wonderful problem, because it doesn’t look so easy.”
Nature, said Dr. Jehi, doesn’t work in black and white or fit into boxes.
“We have to convert it to zeros and ones because that’s what computers speak,” she explained. But quantum computing uses the principles of quantum mechanics. “It’s exactly how nature works, because it is based on the fundamental unit of everything in nature, which is atomic structure.”
Very, very small indeed. And that’s why quantum computing could be game-changing tech in medicine.
“Quantum computers can be used to represent a bunch of different solutions to a problem all at the same time, and then collapse down to the optimal solution, the one that actually works,” said Tony Uttley, president and chief operating officer with Quantinuum, a collaboration between Cambridge Quantum and Honeywell Quantum Solutions that is working to drive the future of quantum computing. “And the reason it does that is because of some fabulous properties of quantum physics.”
Establishing a quantum computing beachhead
Scientists around the globe are studying quantum computers looking for ways to harness this technology to make big gains in medicine.
IBM has created the IBM Quantum Network and is partnering with different organizations, from startups to Fortune 500 companies, to develop and test technology in various settings. One of these partnerships with the Cleveland Clinic is set to establish the “Discovery Accelerator,” focused on advancing health care through high-performance computing on the hybrid cloud, quantum computing technologies, and artificial intelligence.
Many people around the country are now using this technology on existing computers by tapping into the cloud, but with limited qubit access. IBM has researchers in places like Germany and Japan working on quantum computers and will be installing the country’s first of IBM’s next-generation 1,000+ qubit quantum systems on the Cleveland Clinic campus, which they are planning to use to help further investigate quantum computing’s many predicted benefits.
But what are those benefits?
Drug discovery and development
Quantum chemistry is one main area quantum computing is poised to help.
“The immediate application of that would be in drug discovery,” said Dr. Jehi. When scientists make drugs, they sit in a lab and develop different chemical formulas for what might constitute that drug.
“But for us to really know if it’s going to work, we need to be able to imagine how that chemical composition will translate into a structure,” she said.
Even in their most powerful form, today’s supercomputers are slow in their ability to change this chemical formula on paper to a simulation of what the chemical compound will look like. And in many cases, they can’t do this type of analysis.
“So, we end up making the drugs without knowing exactly how they’re going to look, which is not really the optimal way of creating a drug you expect to work” explained Dr. Jehi. “It’s a waste of time creating compounds that aren’t going to have any effect.”
Quantum computers will allow researchers to create and see these molecular structures and know how they bind and interact with the human body. In effect, they’ll know if a potential drug will work before ever having to physically make it.
Because of its differences from classic computing, quantum computers are not limited in their ability to simulate how different compounds can appear. Being able to simulate the compounds that drugs are made of can lead to a faster discovery of medications to treat a wide range of conditions.
Disease analysis
Eventually, this technology could assist with disease analysis, working on a molecular level to allow computers/AI to contemplate, for example, cancer molecules and gain a deeper understanding of how they function.
Dr. Jehi said quantum computing can also be used to study things like chronic illnesses. These are conditions that people must live with and manage, and how a person is feeling in this instance can vary day to day, based on things like what a person is eating, the weather, or medications they are taking.
“There are so many different possibilities for what could change a patient’s trajectory in one way versus another,” said Dr. Jehi.
She stressed that, if one has a group of patients, and everything that’s happened to them along their disease journey has been captured, it’s very challenging to mimic what that group looks like, and then study the effects of these different interventions on it using traditional computing.
“It just gets way too complicated, and the computers that we have can’t keep up with analyzing the effects of the different possibilities. It gets jumbled up,” Dr. Jehi said.
But quantum computing can offer quantum machine learning, meaning you use this special quantum ability to handle different simulations and different possibilities.
The Cleveland Clinic, for instance, is looking at how some patients who undergo general surgeries have heart complications after their procedures.
“It would be transformative if we could identify ahead of time who is at highest risk of having a heart attack after surgery, as so we could take care of those people better,” she said.
The clinic’s current data set includes records for 450,000 patients, and current AI/machine learning makes sifting through this very slow and complex. The clinic is using machine learning approaches to create a synthetic data set, a smaller group that is a replica of the much larger one. Quantum technology could improve and speed this analysis to produce models that better perform.
Disease detection
“Imagine you go get a CT scan,” said Mr. Uttley. “There are already AI solutions that you can run that set of images through and ask: ‘Does this look like something that would be cancer?’ ” This existing technology works well on things that are typical and have been identified before, because that’s how machine learning works. If AI has seen something 100,000 times, it can often find something else that looks like it.
But today’s classical computers aren’t equipped to identify something unfamiliar. “Those are places where quantum computers can be much better at thinking of images and being able to say: ‘I can detect rare cancers or rare conditions that you don’t have a huge library of things that look like that,’ ” Mr. Uttley said.
This is also where researchers can use a quantum computer to be able to figure out what things could look like.
“The beauty of quantum computing is that it is a bias formation in quantum physics, this more probabilistic design. And so you can take advantage of that probabilistic design to help them think about this,” Mr. Uttley said.
How far out are we?
Mr. Uttley said we’re in an emergent era of quantum computing. Quantum computers exist and that’s a big deal, but a lot of this technology is still in fairly early stages.
“It’s a little bit like we’re at the beginning of the internet and saying, how are things going to play out,” he explained.
Right now, companies like Quantinuum are striving to perform computations on both a quantum and classic computer, compare the results, and say: “We’re getting the same answer.”
“So, this is the era where we’re able to build trust and say these quantum computers are actually working correctly,” Mr. Uttley explained.
In the future, he said, we can possibly imagine something like a quantum MRI that is able to understand your body in a way that transmits that data to a quantum computer to detect what’s wrong, and be able to tell the difference between cancerous and noncancerous. That will allow faster treatments and tailoring them to specific patient populations.
“What we’re doing today might seem slightly less sexy than that, but is maybe even equally important,” said Mr. Uttley.
This is using quantum computers to make the best encryption keys that can be made. The medical community, which is already using quantum computing to execute this, is excited about this being a better means of keeping patient data as secure as possible.
In June, Quantinuum launched InQuanto, which is quantum computing software that is allowing computational chemists, who, until now, only had classical computers at their fingertips. The move created an opportunity to start thinking about the problems that they worked on and what they would do with a quantum computer. As quantum computers become higher performing over the years, Mr. Uttley said the software will go from tasks like isolating one molecule to solving larger problems.
“That will happen over this next decade, where I think we’ll see the first kind of real use cases come out in the next likely 2 to 3 years,” he said. For now, this technology will likely be used in tandem with classical computers.
Mr. Uttley said that progress in the quantum world and medicine will continue to grow at a slow and steady pace, and in years to come, we’ll likely see things start to click and then eventually take off “full force.”
A version of this article first appeared on WebMD.com.
The 1960s marked the arrival of computers in medicine. Expensive, cumbersome hunks of plastic and metal that could (maybe) get test results to a doctor faster. The 1980s saw the first real difference-making functions computers could offer – clinical, financial, administrative – and in 1991, the Institute of Medicine published the first manifesto on what electronic health records could (and would) be.
Since then, we’ve seen computer breakthroughs across all areas of medicine, with artificial intelligence (AI), virtual reality, and telemedicine brought to the fore. But something else is brewing that not a lot of people know about yet:
“Think of it as transitioning from getting light through fire and candles and now having electricity, and there’s a light bulb that is lighting it all,” said Lara Jehi, MD, Cleveland Clinic’s chief research information officer.
What is quantum computing?
Classical computers (aka binary computers), which are the foundation of today’s devices, including artificial intelligence and machine learning, work by using information known as bits. These appear as 0 or 1 (sometimes defined as off/on or false/true).
Quantum computers, on the other hand, use quantum bits known as qubits. And yes, the definition of “quantum” – as in: very, very small – applies.
International Business Machines, more commonly known as IBM, is currently leading this new tech. A common misconception about quantum computers is that they are “a next evolution of computers that will get faster,” said Frederik Flöther, PhD, life sciences and health care lead with IBM Quantum Industry Consulting. Instead, he wants us to look at quantum computing as something completely new “because it is fundamentally a different hardware, a different software, not just an evolution of the same.”
How does it work differently from existing computers? Quantum computing deals in nature. Therefore, qubits have to be based on the natural world. What does that mean? Nobel Prize-winning physicist Richard Feynman was famously quoted as saying: “Nature isn’t classical, dammit, and if you want to make a simulation of nature, you’d better make it quantum mechanical, and by golly it’s a wonderful problem, because it doesn’t look so easy.”
Nature, said Dr. Jehi, doesn’t work in black and white or fit into boxes.
“We have to convert it to zeros and ones because that’s what computers speak,” she explained. But quantum computing uses the principles of quantum mechanics. “It’s exactly how nature works, because it is based on the fundamental unit of everything in nature, which is atomic structure.”
Very, very small indeed. And that’s why quantum computing could be game-changing tech in medicine.
“Quantum computers can be used to represent a bunch of different solutions to a problem all at the same time, and then collapse down to the optimal solution, the one that actually works,” said Tony Uttley, president and chief operating officer with Quantinuum, a collaboration between Cambridge Quantum and Honeywell Quantum Solutions that is working to drive the future of quantum computing. “And the reason it does that is because of some fabulous properties of quantum physics.”
Establishing a quantum computing beachhead
Scientists around the globe are studying quantum computers looking for ways to harness this technology to make big gains in medicine.
IBM has created the IBM Quantum Network and is partnering with different organizations, from startups to Fortune 500 companies, to develop and test technology in various settings. One of these partnerships with the Cleveland Clinic is set to establish the “Discovery Accelerator,” focused on advancing health care through high-performance computing on the hybrid cloud, quantum computing technologies, and artificial intelligence.
Many people around the country are now using this technology on existing computers by tapping into the cloud, but with limited qubit access. IBM has researchers in places like Germany and Japan working on quantum computers and will be installing the country’s first of IBM’s next-generation 1,000+ qubit quantum systems on the Cleveland Clinic campus, which they are planning to use to help further investigate quantum computing’s many predicted benefits.
But what are those benefits?
Drug discovery and development
Quantum chemistry is one main area quantum computing is poised to help.
“The immediate application of that would be in drug discovery,” said Dr. Jehi. When scientists make drugs, they sit in a lab and develop different chemical formulas for what might constitute that drug.
“But for us to really know if it’s going to work, we need to be able to imagine how that chemical composition will translate into a structure,” she said.
Even in their most powerful form, today’s supercomputers are slow in their ability to change this chemical formula on paper to a simulation of what the chemical compound will look like. And in many cases, they can’t do this type of analysis.
“So, we end up making the drugs without knowing exactly how they’re going to look, which is not really the optimal way of creating a drug you expect to work” explained Dr. Jehi. “It’s a waste of time creating compounds that aren’t going to have any effect.”
Quantum computers will allow researchers to create and see these molecular structures and know how they bind and interact with the human body. In effect, they’ll know if a potential drug will work before ever having to physically make it.
Because of its differences from classic computing, quantum computers are not limited in their ability to simulate how different compounds can appear. Being able to simulate the compounds that drugs are made of can lead to a faster discovery of medications to treat a wide range of conditions.
Disease analysis
Eventually, this technology could assist with disease analysis, working on a molecular level to allow computers/AI to contemplate, for example, cancer molecules and gain a deeper understanding of how they function.
Dr. Jehi said quantum computing can also be used to study things like chronic illnesses. These are conditions that people must live with and manage, and how a person is feeling in this instance can vary day to day, based on things like what a person is eating, the weather, or medications they are taking.
“There are so many different possibilities for what could change a patient’s trajectory in one way versus another,” said Dr. Jehi.
She stressed that, if one has a group of patients, and everything that’s happened to them along their disease journey has been captured, it’s very challenging to mimic what that group looks like, and then study the effects of these different interventions on it using traditional computing.
“It just gets way too complicated, and the computers that we have can’t keep up with analyzing the effects of the different possibilities. It gets jumbled up,” Dr. Jehi said.
But quantum computing can offer quantum machine learning, meaning you use this special quantum ability to handle different simulations and different possibilities.
The Cleveland Clinic, for instance, is looking at how some patients who undergo general surgeries have heart complications after their procedures.
“It would be transformative if we could identify ahead of time who is at highest risk of having a heart attack after surgery, as so we could take care of those people better,” she said.
The clinic’s current data set includes records for 450,000 patients, and current AI/machine learning makes sifting through this very slow and complex. The clinic is using machine learning approaches to create a synthetic data set, a smaller group that is a replica of the much larger one. Quantum technology could improve and speed this analysis to produce models that better perform.
Disease detection
“Imagine you go get a CT scan,” said Mr. Uttley. “There are already AI solutions that you can run that set of images through and ask: ‘Does this look like something that would be cancer?’ ” This existing technology works well on things that are typical and have been identified before, because that’s how machine learning works. If AI has seen something 100,000 times, it can often find something else that looks like it.
But today’s classical computers aren’t equipped to identify something unfamiliar. “Those are places where quantum computers can be much better at thinking of images and being able to say: ‘I can detect rare cancers or rare conditions that you don’t have a huge library of things that look like that,’ ” Mr. Uttley said.
This is also where researchers can use a quantum computer to be able to figure out what things could look like.
“The beauty of quantum computing is that it is a bias formation in quantum physics, this more probabilistic design. And so you can take advantage of that probabilistic design to help them think about this,” Mr. Uttley said.
How far out are we?
Mr. Uttley said we’re in an emergent era of quantum computing. Quantum computers exist and that’s a big deal, but a lot of this technology is still in fairly early stages.
“It’s a little bit like we’re at the beginning of the internet and saying, how are things going to play out,” he explained.
Right now, companies like Quantinuum are striving to perform computations on both a quantum and classic computer, compare the results, and say: “We’re getting the same answer.”
“So, this is the era where we’re able to build trust and say these quantum computers are actually working correctly,” Mr. Uttley explained.
In the future, he said, we can possibly imagine something like a quantum MRI that is able to understand your body in a way that transmits that data to a quantum computer to detect what’s wrong, and be able to tell the difference between cancerous and noncancerous. That will allow faster treatments and tailoring them to specific patient populations.
“What we’re doing today might seem slightly less sexy than that, but is maybe even equally important,” said Mr. Uttley.
This is using quantum computers to make the best encryption keys that can be made. The medical community, which is already using quantum computing to execute this, is excited about this being a better means of keeping patient data as secure as possible.
In June, Quantinuum launched InQuanto, which is quantum computing software that is allowing computational chemists, who, until now, only had classical computers at their fingertips. The move created an opportunity to start thinking about the problems that they worked on and what they would do with a quantum computer. As quantum computers become higher performing over the years, Mr. Uttley said the software will go from tasks like isolating one molecule to solving larger problems.
“That will happen over this next decade, where I think we’ll see the first kind of real use cases come out in the next likely 2 to 3 years,” he said. For now, this technology will likely be used in tandem with classical computers.
Mr. Uttley said that progress in the quantum world and medicine will continue to grow at a slow and steady pace, and in years to come, we’ll likely see things start to click and then eventually take off “full force.”
A version of this article first appeared on WebMD.com.
The 1960s marked the arrival of computers in medicine. Expensive, cumbersome hunks of plastic and metal that could (maybe) get test results to a doctor faster. The 1980s saw the first real difference-making functions computers could offer – clinical, financial, administrative – and in 1991, the Institute of Medicine published the first manifesto on what electronic health records could (and would) be.
Since then, we’ve seen computer breakthroughs across all areas of medicine, with artificial intelligence (AI), virtual reality, and telemedicine brought to the fore. But something else is brewing that not a lot of people know about yet:
“Think of it as transitioning from getting light through fire and candles and now having electricity, and there’s a light bulb that is lighting it all,” said Lara Jehi, MD, Cleveland Clinic’s chief research information officer.
What is quantum computing?
Classical computers (aka binary computers), which are the foundation of today’s devices, including artificial intelligence and machine learning, work by using information known as bits. These appear as 0 or 1 (sometimes defined as off/on or false/true).
Quantum computers, on the other hand, use quantum bits known as qubits. And yes, the definition of “quantum” – as in: very, very small – applies.
International Business Machines, more commonly known as IBM, is currently leading this new tech. A common misconception about quantum computers is that they are “a next evolution of computers that will get faster,” said Frederik Flöther, PhD, life sciences and health care lead with IBM Quantum Industry Consulting. Instead, he wants us to look at quantum computing as something completely new “because it is fundamentally a different hardware, a different software, not just an evolution of the same.”
How does it work differently from existing computers? Quantum computing deals in nature. Therefore, qubits have to be based on the natural world. What does that mean? Nobel Prize-winning physicist Richard Feynman was famously quoted as saying: “Nature isn’t classical, dammit, and if you want to make a simulation of nature, you’d better make it quantum mechanical, and by golly it’s a wonderful problem, because it doesn’t look so easy.”
Nature, said Dr. Jehi, doesn’t work in black and white or fit into boxes.
“We have to convert it to zeros and ones because that’s what computers speak,” she explained. But quantum computing uses the principles of quantum mechanics. “It’s exactly how nature works, because it is based on the fundamental unit of everything in nature, which is atomic structure.”
Very, very small indeed. And that’s why quantum computing could be game-changing tech in medicine.
“Quantum computers can be used to represent a bunch of different solutions to a problem all at the same time, and then collapse down to the optimal solution, the one that actually works,” said Tony Uttley, president and chief operating officer with Quantinuum, a collaboration between Cambridge Quantum and Honeywell Quantum Solutions that is working to drive the future of quantum computing. “And the reason it does that is because of some fabulous properties of quantum physics.”
Establishing a quantum computing beachhead
Scientists around the globe are studying quantum computers looking for ways to harness this technology to make big gains in medicine.
IBM has created the IBM Quantum Network and is partnering with different organizations, from startups to Fortune 500 companies, to develop and test technology in various settings. One of these partnerships with the Cleveland Clinic is set to establish the “Discovery Accelerator,” focused on advancing health care through high-performance computing on the hybrid cloud, quantum computing technologies, and artificial intelligence.
Many people around the country are now using this technology on existing computers by tapping into the cloud, but with limited qubit access. IBM has researchers in places like Germany and Japan working on quantum computers and will be installing the country’s first of IBM’s next-generation 1,000+ qubit quantum systems on the Cleveland Clinic campus, which they are planning to use to help further investigate quantum computing’s many predicted benefits.
But what are those benefits?
Drug discovery and development
Quantum chemistry is one main area quantum computing is poised to help.
“The immediate application of that would be in drug discovery,” said Dr. Jehi. When scientists make drugs, they sit in a lab and develop different chemical formulas for what might constitute that drug.
“But for us to really know if it’s going to work, we need to be able to imagine how that chemical composition will translate into a structure,” she said.
Even in their most powerful form, today’s supercomputers are slow in their ability to change this chemical formula on paper to a simulation of what the chemical compound will look like. And in many cases, they can’t do this type of analysis.
“So, we end up making the drugs without knowing exactly how they’re going to look, which is not really the optimal way of creating a drug you expect to work” explained Dr. Jehi. “It’s a waste of time creating compounds that aren’t going to have any effect.”
Quantum computers will allow researchers to create and see these molecular structures and know how they bind and interact with the human body. In effect, they’ll know if a potential drug will work before ever having to physically make it.
Because of its differences from classic computing, quantum computers are not limited in their ability to simulate how different compounds can appear. Being able to simulate the compounds that drugs are made of can lead to a faster discovery of medications to treat a wide range of conditions.
Disease analysis
Eventually, this technology could assist with disease analysis, working on a molecular level to allow computers/AI to contemplate, for example, cancer molecules and gain a deeper understanding of how they function.
Dr. Jehi said quantum computing can also be used to study things like chronic illnesses. These are conditions that people must live with and manage, and how a person is feeling in this instance can vary day to day, based on things like what a person is eating, the weather, or medications they are taking.
“There are so many different possibilities for what could change a patient’s trajectory in one way versus another,” said Dr. Jehi.
She stressed that, if one has a group of patients, and everything that’s happened to them along their disease journey has been captured, it’s very challenging to mimic what that group looks like, and then study the effects of these different interventions on it using traditional computing.
“It just gets way too complicated, and the computers that we have can’t keep up with analyzing the effects of the different possibilities. It gets jumbled up,” Dr. Jehi said.
But quantum computing can offer quantum machine learning, meaning you use this special quantum ability to handle different simulations and different possibilities.
The Cleveland Clinic, for instance, is looking at how some patients who undergo general surgeries have heart complications after their procedures.
“It would be transformative if we could identify ahead of time who is at highest risk of having a heart attack after surgery, as so we could take care of those people better,” she said.
The clinic’s current data set includes records for 450,000 patients, and current AI/machine learning makes sifting through this very slow and complex. The clinic is using machine learning approaches to create a synthetic data set, a smaller group that is a replica of the much larger one. Quantum technology could improve and speed this analysis to produce models that better perform.
Disease detection
“Imagine you go get a CT scan,” said Mr. Uttley. “There are already AI solutions that you can run that set of images through and ask: ‘Does this look like something that would be cancer?’ ” This existing technology works well on things that are typical and have been identified before, because that’s how machine learning works. If AI has seen something 100,000 times, it can often find something else that looks like it.
But today’s classical computers aren’t equipped to identify something unfamiliar. “Those are places where quantum computers can be much better at thinking of images and being able to say: ‘I can detect rare cancers or rare conditions that you don’t have a huge library of things that look like that,’ ” Mr. Uttley said.
This is also where researchers can use a quantum computer to be able to figure out what things could look like.
“The beauty of quantum computing is that it is a bias formation in quantum physics, this more probabilistic design. And so you can take advantage of that probabilistic design to help them think about this,” Mr. Uttley said.
How far out are we?
Mr. Uttley said we’re in an emergent era of quantum computing. Quantum computers exist and that’s a big deal, but a lot of this technology is still in fairly early stages.
“It’s a little bit like we’re at the beginning of the internet and saying, how are things going to play out,” he explained.
Right now, companies like Quantinuum are striving to perform computations on both a quantum and classic computer, compare the results, and say: “We’re getting the same answer.”
“So, this is the era where we’re able to build trust and say these quantum computers are actually working correctly,” Mr. Uttley explained.
In the future, he said, we can possibly imagine something like a quantum MRI that is able to understand your body in a way that transmits that data to a quantum computer to detect what’s wrong, and be able to tell the difference between cancerous and noncancerous. That will allow faster treatments and tailoring them to specific patient populations.
“What we’re doing today might seem slightly less sexy than that, but is maybe even equally important,” said Mr. Uttley.
This is using quantum computers to make the best encryption keys that can be made. The medical community, which is already using quantum computing to execute this, is excited about this being a better means of keeping patient data as secure as possible.
In June, Quantinuum launched InQuanto, which is quantum computing software that is allowing computational chemists, who, until now, only had classical computers at their fingertips. The move created an opportunity to start thinking about the problems that they worked on and what they would do with a quantum computer. As quantum computers become higher performing over the years, Mr. Uttley said the software will go from tasks like isolating one molecule to solving larger problems.
“That will happen over this next decade, where I think we’ll see the first kind of real use cases come out in the next likely 2 to 3 years,” he said. For now, this technology will likely be used in tandem with classical computers.
Mr. Uttley said that progress in the quantum world and medicine will continue to grow at a slow and steady pace, and in years to come, we’ll likely see things start to click and then eventually take off “full force.”
A version of this article first appeared on WebMD.com.
Are nurses who pick up extra shifts at risk of harming themselves or others?
on a nurse’s physical and mental health. Plus, it can diminish quality of care and lead to patient errors.
Medscape’s RN/LPN Compensation Report 2022 found that more than half of RNs and LPNs don’t think they get paid enough. Even though many nurses saw pay increases over the past 2 years, many were still dissatisfied with their earnings. They blamed job stress, staffing shortages, and benefits that cut into their wages.
Why do nurses pick up extra shifts?
Most nurses work extra hours for the money. Incentives like getting paid time and a half or scoring a $200 bonus are hard to pass up.
“I’m a single mother with two kids,” said Cynthia West, a critical care nurse in Atlanta. “I want to be able to pay my bills and enjoy my life, too.” So, Ms. West picks up two to three extra shifts a month. She also works on-call for a sexual assault center, earning $350 per exam.
But money isn’t the only reason for some nurses. Trang Robinson travels from her home in Atlanta to Palo Alto, Calif., every other week for her job as a labor and delivery RN.
“If my unit needs extra help, I want to help,” she said. “It’s not about the extra money, although that helps my family; it’s that we’ve been so short-staffed. My colleagues are burned out. Staff members are burned out. When I’m there, I work as much as I can to help out my unit.”
Leslie Wysong, an Atlanta postanesthesia nurse, worked in intensive care during much of COVID. She said the chance to make level 3 pay was rewarding for many nurses, but most weren’t doing it for the money.
“We were doing it to alleviate the strain on our fellow nurses, to get closer to a 2:1 patient/nurse ratio rather than the 3:1 we were dealing with over the pandemic,” she said. “It was to help out our colleagues during a desperate situation.”
What are the risks?
The U.S. Occupational Safety and Health Administration states that a work shift that lasts more than 8 hours can disrupt the body’s sleep/wake cycle. It can also lead to physical and mental fatigue resulting in errors, injuries, and accidents.
And a study published in the American Association of Occupational Health Nurses found that extended shifts or shift work impacted nurses in many ways, including more medication errors, falling asleep during work hours, decreased productivity in the last 4 shift hours (of a 12-hour shift), increased risk of mistakes and near-errors associated with decreased vigilance, critical thinking impairment, and more needlestick injuries.
Another study, published in Rehabilitation Nursing Journal, found even more adverse effects, such as sleep disorders like insomnia and excessive sleepiness; cognitive impairment such as the reduced ability to concentrate, slower reactions times, and reduced ability to remember information; higher rates of injury while on the job; being more likely to engage in overeating and alcohol misuse; GI issues such as abdominal pain, constipation, and heartburn; higher rates of heart disease and high blood pressure; higher risk for breast and prostate cancers, and higher rates of depression and anxiety.
These are risks some nurses aren’t willing to take. For example, Caitlin Riley, a pediatric ED nurse in Ocala, Fla., only picks up extra shifts when she must, like when Hurricane Ian swept through Central Florida.
“I think working extra hours can compromise your quality of care,” she said. “You may make mistakes with things like math calculations or not catch something if you’re not totally ‘in’ it mentally. At the end of the day, it’s your nursing license. Sure, the money is great, but I won’t do anything to compromise losing my license or patient care.”
How can nurses boost pay without working extra shifts?
Instead, Ms. Riley returned to school and earned an MSN in health care leadership/management, knowing that an advanced degree could lead to higher-paying work. According to the Medscape report, RNs with master’s and doctoral degrees earned over $10,000 more than those with bachelor’s, associate’s, or RN diplomas.
The report also compiled the following earnings data. The data may help nurses find other ways to raise their salaries without taking on extra shifts.
- Salaried RNs and LPNs made more than hourly paid nurses.
- In-patient hospital RNs and skilled nursing facility LPNs got paid more than nurses in other settings.
- Specialty certifications helped RNs earn more money than nurses without specialty certificates.
- Union RNs and LPNs earned more than nonunion nurses.
- RNs and LPNs who work in big cities or suburbs make more money than those in rural areas.
How to prevent burnout and exhaustion when you work extra shifts
While burnout can happen in any profession, an investigation published in JAMA Network Open suggests it’s prevalent among US nurses. The study found that nurses who worked over 40 hours a week were more likely to experience burnout. However, researchers say that adequate staffing and limiting shift hours may alleviate the problem. Here’s how the nurses in the survey dealt with battle burnout:
- Change departments. Ms. Wysong stepped away from the ICU after COVID and switched to postanesthesia. “The move has made my work life much less stressful,” said Ms. Wysong. “They are all happy endings in postanesthesia.”
- Leave work at work. Ms. Riley said she mentally clocks out as she leaves the hospital. “When I put my papers in my shredder at the end of my shift, I let it go. I walk away knowing I did the best for my patients. Once I’m home, it’s time for me to be with the people I love and to refuel my own sense of happiness with the people that mean the most to me.”
- Take time off. “When I’m burned out, I just don’t come in,” said Ms. Robinson. “If I’m mentally or emotionally drained, I give myself a shift off to decompress, or I don’t pick up extra shifts.”
- Engage in relaxing hobbies. Kris Coleman, an ED nurse in Hardeeville, S.C., typically works three 12-hours shifts and only picks up an extra 4-hour shift once a week. When he’s off, he takes advantage of his time away from work. He said: “Do the things that help you relax on your time off. For me, it’s golfing, fishing, and spending time with my family.”
- Build a support system. “I have a group of friends at work,” said Ms. West. “We talk to each other and vent. Having a good support system, people that are in it with you who get what you’re going through is a helpful way to manage burnout.”
A version of this article first appeared on Medscape.com.
on a nurse’s physical and mental health. Plus, it can diminish quality of care and lead to patient errors.
Medscape’s RN/LPN Compensation Report 2022 found that more than half of RNs and LPNs don’t think they get paid enough. Even though many nurses saw pay increases over the past 2 years, many were still dissatisfied with their earnings. They blamed job stress, staffing shortages, and benefits that cut into their wages.
Why do nurses pick up extra shifts?
Most nurses work extra hours for the money. Incentives like getting paid time and a half or scoring a $200 bonus are hard to pass up.
“I’m a single mother with two kids,” said Cynthia West, a critical care nurse in Atlanta. “I want to be able to pay my bills and enjoy my life, too.” So, Ms. West picks up two to three extra shifts a month. She also works on-call for a sexual assault center, earning $350 per exam.
But money isn’t the only reason for some nurses. Trang Robinson travels from her home in Atlanta to Palo Alto, Calif., every other week for her job as a labor and delivery RN.
“If my unit needs extra help, I want to help,” she said. “It’s not about the extra money, although that helps my family; it’s that we’ve been so short-staffed. My colleagues are burned out. Staff members are burned out. When I’m there, I work as much as I can to help out my unit.”
Leslie Wysong, an Atlanta postanesthesia nurse, worked in intensive care during much of COVID. She said the chance to make level 3 pay was rewarding for many nurses, but most weren’t doing it for the money.
“We were doing it to alleviate the strain on our fellow nurses, to get closer to a 2:1 patient/nurse ratio rather than the 3:1 we were dealing with over the pandemic,” she said. “It was to help out our colleagues during a desperate situation.”
What are the risks?
The U.S. Occupational Safety and Health Administration states that a work shift that lasts more than 8 hours can disrupt the body’s sleep/wake cycle. It can also lead to physical and mental fatigue resulting in errors, injuries, and accidents.
And a study published in the American Association of Occupational Health Nurses found that extended shifts or shift work impacted nurses in many ways, including more medication errors, falling asleep during work hours, decreased productivity in the last 4 shift hours (of a 12-hour shift), increased risk of mistakes and near-errors associated with decreased vigilance, critical thinking impairment, and more needlestick injuries.
Another study, published in Rehabilitation Nursing Journal, found even more adverse effects, such as sleep disorders like insomnia and excessive sleepiness; cognitive impairment such as the reduced ability to concentrate, slower reactions times, and reduced ability to remember information; higher rates of injury while on the job; being more likely to engage in overeating and alcohol misuse; GI issues such as abdominal pain, constipation, and heartburn; higher rates of heart disease and high blood pressure; higher risk for breast and prostate cancers, and higher rates of depression and anxiety.
These are risks some nurses aren’t willing to take. For example, Caitlin Riley, a pediatric ED nurse in Ocala, Fla., only picks up extra shifts when she must, like when Hurricane Ian swept through Central Florida.
“I think working extra hours can compromise your quality of care,” she said. “You may make mistakes with things like math calculations or not catch something if you’re not totally ‘in’ it mentally. At the end of the day, it’s your nursing license. Sure, the money is great, but I won’t do anything to compromise losing my license or patient care.”
How can nurses boost pay without working extra shifts?
Instead, Ms. Riley returned to school and earned an MSN in health care leadership/management, knowing that an advanced degree could lead to higher-paying work. According to the Medscape report, RNs with master’s and doctoral degrees earned over $10,000 more than those with bachelor’s, associate’s, or RN diplomas.
The report also compiled the following earnings data. The data may help nurses find other ways to raise their salaries without taking on extra shifts.
- Salaried RNs and LPNs made more than hourly paid nurses.
- In-patient hospital RNs and skilled nursing facility LPNs got paid more than nurses in other settings.
- Specialty certifications helped RNs earn more money than nurses without specialty certificates.
- Union RNs and LPNs earned more than nonunion nurses.
- RNs and LPNs who work in big cities or suburbs make more money than those in rural areas.
How to prevent burnout and exhaustion when you work extra shifts
While burnout can happen in any profession, an investigation published in JAMA Network Open suggests it’s prevalent among US nurses. The study found that nurses who worked over 40 hours a week were more likely to experience burnout. However, researchers say that adequate staffing and limiting shift hours may alleviate the problem. Here’s how the nurses in the survey dealt with battle burnout:
- Change departments. Ms. Wysong stepped away from the ICU after COVID and switched to postanesthesia. “The move has made my work life much less stressful,” said Ms. Wysong. “They are all happy endings in postanesthesia.”
- Leave work at work. Ms. Riley said she mentally clocks out as she leaves the hospital. “When I put my papers in my shredder at the end of my shift, I let it go. I walk away knowing I did the best for my patients. Once I’m home, it’s time for me to be with the people I love and to refuel my own sense of happiness with the people that mean the most to me.”
- Take time off. “When I’m burned out, I just don’t come in,” said Ms. Robinson. “If I’m mentally or emotionally drained, I give myself a shift off to decompress, or I don’t pick up extra shifts.”
- Engage in relaxing hobbies. Kris Coleman, an ED nurse in Hardeeville, S.C., typically works three 12-hours shifts and only picks up an extra 4-hour shift once a week. When he’s off, he takes advantage of his time away from work. He said: “Do the things that help you relax on your time off. For me, it’s golfing, fishing, and spending time with my family.”
- Build a support system. “I have a group of friends at work,” said Ms. West. “We talk to each other and vent. Having a good support system, people that are in it with you who get what you’re going through is a helpful way to manage burnout.”
A version of this article first appeared on Medscape.com.
on a nurse’s physical and mental health. Plus, it can diminish quality of care and lead to patient errors.
Medscape’s RN/LPN Compensation Report 2022 found that more than half of RNs and LPNs don’t think they get paid enough. Even though many nurses saw pay increases over the past 2 years, many were still dissatisfied with their earnings. They blamed job stress, staffing shortages, and benefits that cut into their wages.
Why do nurses pick up extra shifts?
Most nurses work extra hours for the money. Incentives like getting paid time and a half or scoring a $200 bonus are hard to pass up.
“I’m a single mother with two kids,” said Cynthia West, a critical care nurse in Atlanta. “I want to be able to pay my bills and enjoy my life, too.” So, Ms. West picks up two to three extra shifts a month. She also works on-call for a sexual assault center, earning $350 per exam.
But money isn’t the only reason for some nurses. Trang Robinson travels from her home in Atlanta to Palo Alto, Calif., every other week for her job as a labor and delivery RN.
“If my unit needs extra help, I want to help,” she said. “It’s not about the extra money, although that helps my family; it’s that we’ve been so short-staffed. My colleagues are burned out. Staff members are burned out. When I’m there, I work as much as I can to help out my unit.”
Leslie Wysong, an Atlanta postanesthesia nurse, worked in intensive care during much of COVID. She said the chance to make level 3 pay was rewarding for many nurses, but most weren’t doing it for the money.
“We were doing it to alleviate the strain on our fellow nurses, to get closer to a 2:1 patient/nurse ratio rather than the 3:1 we were dealing with over the pandemic,” she said. “It was to help out our colleagues during a desperate situation.”
What are the risks?
The U.S. Occupational Safety and Health Administration states that a work shift that lasts more than 8 hours can disrupt the body’s sleep/wake cycle. It can also lead to physical and mental fatigue resulting in errors, injuries, and accidents.
And a study published in the American Association of Occupational Health Nurses found that extended shifts or shift work impacted nurses in many ways, including more medication errors, falling asleep during work hours, decreased productivity in the last 4 shift hours (of a 12-hour shift), increased risk of mistakes and near-errors associated with decreased vigilance, critical thinking impairment, and more needlestick injuries.
Another study, published in Rehabilitation Nursing Journal, found even more adverse effects, such as sleep disorders like insomnia and excessive sleepiness; cognitive impairment such as the reduced ability to concentrate, slower reactions times, and reduced ability to remember information; higher rates of injury while on the job; being more likely to engage in overeating and alcohol misuse; GI issues such as abdominal pain, constipation, and heartburn; higher rates of heart disease and high blood pressure; higher risk for breast and prostate cancers, and higher rates of depression and anxiety.
These are risks some nurses aren’t willing to take. For example, Caitlin Riley, a pediatric ED nurse in Ocala, Fla., only picks up extra shifts when she must, like when Hurricane Ian swept through Central Florida.
“I think working extra hours can compromise your quality of care,” she said. “You may make mistakes with things like math calculations or not catch something if you’re not totally ‘in’ it mentally. At the end of the day, it’s your nursing license. Sure, the money is great, but I won’t do anything to compromise losing my license or patient care.”
How can nurses boost pay without working extra shifts?
Instead, Ms. Riley returned to school and earned an MSN in health care leadership/management, knowing that an advanced degree could lead to higher-paying work. According to the Medscape report, RNs with master’s and doctoral degrees earned over $10,000 more than those with bachelor’s, associate’s, or RN diplomas.
The report also compiled the following earnings data. The data may help nurses find other ways to raise their salaries without taking on extra shifts.
- Salaried RNs and LPNs made more than hourly paid nurses.
- In-patient hospital RNs and skilled nursing facility LPNs got paid more than nurses in other settings.
- Specialty certifications helped RNs earn more money than nurses without specialty certificates.
- Union RNs and LPNs earned more than nonunion nurses.
- RNs and LPNs who work in big cities or suburbs make more money than those in rural areas.
How to prevent burnout and exhaustion when you work extra shifts
While burnout can happen in any profession, an investigation published in JAMA Network Open suggests it’s prevalent among US nurses. The study found that nurses who worked over 40 hours a week were more likely to experience burnout. However, researchers say that adequate staffing and limiting shift hours may alleviate the problem. Here’s how the nurses in the survey dealt with battle burnout:
- Change departments. Ms. Wysong stepped away from the ICU after COVID and switched to postanesthesia. “The move has made my work life much less stressful,” said Ms. Wysong. “They are all happy endings in postanesthesia.”
- Leave work at work. Ms. Riley said she mentally clocks out as she leaves the hospital. “When I put my papers in my shredder at the end of my shift, I let it go. I walk away knowing I did the best for my patients. Once I’m home, it’s time for me to be with the people I love and to refuel my own sense of happiness with the people that mean the most to me.”
- Take time off. “When I’m burned out, I just don’t come in,” said Ms. Robinson. “If I’m mentally or emotionally drained, I give myself a shift off to decompress, or I don’t pick up extra shifts.”
- Engage in relaxing hobbies. Kris Coleman, an ED nurse in Hardeeville, S.C., typically works three 12-hours shifts and only picks up an extra 4-hour shift once a week. When he’s off, he takes advantage of his time away from work. He said: “Do the things that help you relax on your time off. For me, it’s golfing, fishing, and spending time with my family.”
- Build a support system. “I have a group of friends at work,” said Ms. West. “We talk to each other and vent. Having a good support system, people that are in it with you who get what you’re going through is a helpful way to manage burnout.”
A version of this article first appeared on Medscape.com.
Patient safety in hospitals improved in past decade: Report
, according to the 10th annual report from nonprofit the Leapfrog Group, a national nonprofit organization focused on health care safety and quality.
For five outcome measures, the safety improvements saved an estimated 16,000 lives during the 10-year period, the report said. These included two “never” events that both declined by approximately 25%: incidents of falls and trauma and incidents of objects unintentionally left in a body after surgery.
There were also decreases in three health care–associated infections, including methicillin-resistant Staphylococcus aureus (MRSA), which decreased by 22%; central line–associated bloodstream infection (CLABSI), which fell by 43%; and Clostridioides difficile infection (C. Diff), which declined by 8%.
The patient safety record of U.S. hospitals improved over the past decade, according to the report.
“Never in history have we seen across-the-board improvement in patient safety until this last decade, coinciding with the history of the [Leapfrog] Hospital Safety Grade,” said Leah Binder, president and CEO of the Leapfrog Group, in a news release. “We salute hospitals for this milestone and encourage them to accelerate their hard work saving patient lives.”
During the past decade, the report noted, hospitals have widely adopted technology and staffing strategies that can protect patients from preventable harm and death. Leapfrog cited a nearly sevenfold increase in the adoption of computerized provider order entry, which can reduce medication errors by more than 40%.
However, federal health officials separately have reported that the pandemic may have eroded some of those gains.
The Leapfrog report also cited a recent study, published in JAMA, that found that the rates of preventable adverse events in hospitalized patients – including adverse drug events, hospital-acquired infections, postprocedure events, and hospital-acquired pressure ulcers and falls – significantly declined between 2010 and 2019.
That study pointed to specific decreases in the rates of adverse events for patients admitted for myocardial infarction, heart failure, pneumonia, and major surgical procedures. There were also significant drops in adverse events for all other conditions, the study found.
Quality improvement efforts targeting those four conditions might have partly accounted for the lower rates of adverse events in patients with the conditions, the study observed. But “similar interventions did not occur for most of the conditions represented in the ‘all other conditions’ group,” it said.
In a 2019 report by the U.S. Agency for Healthcare Research and Quality (AHRQ), the agency noted that from 2000 to 2017, there had been gains in nearly two-thirds of patient-safety measures in acute, post-acute, and ambulatory care. Hospital safety improved on nine metrics and was unchanged on three. For example, from 2014 to 2017, the number of some hospital-acquired conditions, including adverse drug events and C. Diff infections, dropped about 20%.
However, in an article this past February, officials of the Centers for Medicare & Medicaid Services (CMS) said they had observed deterioration on multiple patient-safety metrics since the start of the pandemic. For example, central line infections, which had dropped by 31% in the five years before the COVID-19 outbreak, jumped 28% in the second quarter of 2020, compared with the prior-year period.
Commenting on these developments, the CMS authors said “the fact that the pandemic degraded patient safety so quickly and severely suggests that our health care system lacks a sufficiently resilient safety culture and infrastructure.”
A version of this article first appeared on Medscape.com.
, according to the 10th annual report from nonprofit the Leapfrog Group, a national nonprofit organization focused on health care safety and quality.
For five outcome measures, the safety improvements saved an estimated 16,000 lives during the 10-year period, the report said. These included two “never” events that both declined by approximately 25%: incidents of falls and trauma and incidents of objects unintentionally left in a body after surgery.
There were also decreases in three health care–associated infections, including methicillin-resistant Staphylococcus aureus (MRSA), which decreased by 22%; central line–associated bloodstream infection (CLABSI), which fell by 43%; and Clostridioides difficile infection (C. Diff), which declined by 8%.
The patient safety record of U.S. hospitals improved over the past decade, according to the report.
“Never in history have we seen across-the-board improvement in patient safety until this last decade, coinciding with the history of the [Leapfrog] Hospital Safety Grade,” said Leah Binder, president and CEO of the Leapfrog Group, in a news release. “We salute hospitals for this milestone and encourage them to accelerate their hard work saving patient lives.”
During the past decade, the report noted, hospitals have widely adopted technology and staffing strategies that can protect patients from preventable harm and death. Leapfrog cited a nearly sevenfold increase in the adoption of computerized provider order entry, which can reduce medication errors by more than 40%.
However, federal health officials separately have reported that the pandemic may have eroded some of those gains.
The Leapfrog report also cited a recent study, published in JAMA, that found that the rates of preventable adverse events in hospitalized patients – including adverse drug events, hospital-acquired infections, postprocedure events, and hospital-acquired pressure ulcers and falls – significantly declined between 2010 and 2019.
That study pointed to specific decreases in the rates of adverse events for patients admitted for myocardial infarction, heart failure, pneumonia, and major surgical procedures. There were also significant drops in adverse events for all other conditions, the study found.
Quality improvement efforts targeting those four conditions might have partly accounted for the lower rates of adverse events in patients with the conditions, the study observed. But “similar interventions did not occur for most of the conditions represented in the ‘all other conditions’ group,” it said.
In a 2019 report by the U.S. Agency for Healthcare Research and Quality (AHRQ), the agency noted that from 2000 to 2017, there had been gains in nearly two-thirds of patient-safety measures in acute, post-acute, and ambulatory care. Hospital safety improved on nine metrics and was unchanged on three. For example, from 2014 to 2017, the number of some hospital-acquired conditions, including adverse drug events and C. Diff infections, dropped about 20%.
However, in an article this past February, officials of the Centers for Medicare & Medicaid Services (CMS) said they had observed deterioration on multiple patient-safety metrics since the start of the pandemic. For example, central line infections, which had dropped by 31% in the five years before the COVID-19 outbreak, jumped 28% in the second quarter of 2020, compared with the prior-year period.
Commenting on these developments, the CMS authors said “the fact that the pandemic degraded patient safety so quickly and severely suggests that our health care system lacks a sufficiently resilient safety culture and infrastructure.”
A version of this article first appeared on Medscape.com.
, according to the 10th annual report from nonprofit the Leapfrog Group, a national nonprofit organization focused on health care safety and quality.
For five outcome measures, the safety improvements saved an estimated 16,000 lives during the 10-year period, the report said. These included two “never” events that both declined by approximately 25%: incidents of falls and trauma and incidents of objects unintentionally left in a body after surgery.
There were also decreases in three health care–associated infections, including methicillin-resistant Staphylococcus aureus (MRSA), which decreased by 22%; central line–associated bloodstream infection (CLABSI), which fell by 43%; and Clostridioides difficile infection (C. Diff), which declined by 8%.
The patient safety record of U.S. hospitals improved over the past decade, according to the report.
“Never in history have we seen across-the-board improvement in patient safety until this last decade, coinciding with the history of the [Leapfrog] Hospital Safety Grade,” said Leah Binder, president and CEO of the Leapfrog Group, in a news release. “We salute hospitals for this milestone and encourage them to accelerate their hard work saving patient lives.”
During the past decade, the report noted, hospitals have widely adopted technology and staffing strategies that can protect patients from preventable harm and death. Leapfrog cited a nearly sevenfold increase in the adoption of computerized provider order entry, which can reduce medication errors by more than 40%.
However, federal health officials separately have reported that the pandemic may have eroded some of those gains.
The Leapfrog report also cited a recent study, published in JAMA, that found that the rates of preventable adverse events in hospitalized patients – including adverse drug events, hospital-acquired infections, postprocedure events, and hospital-acquired pressure ulcers and falls – significantly declined between 2010 and 2019.
That study pointed to specific decreases in the rates of adverse events for patients admitted for myocardial infarction, heart failure, pneumonia, and major surgical procedures. There were also significant drops in adverse events for all other conditions, the study found.
Quality improvement efforts targeting those four conditions might have partly accounted for the lower rates of adverse events in patients with the conditions, the study observed. But “similar interventions did not occur for most of the conditions represented in the ‘all other conditions’ group,” it said.
In a 2019 report by the U.S. Agency for Healthcare Research and Quality (AHRQ), the agency noted that from 2000 to 2017, there had been gains in nearly two-thirds of patient-safety measures in acute, post-acute, and ambulatory care. Hospital safety improved on nine metrics and was unchanged on three. For example, from 2014 to 2017, the number of some hospital-acquired conditions, including adverse drug events and C. Diff infections, dropped about 20%.
However, in an article this past February, officials of the Centers for Medicare & Medicaid Services (CMS) said they had observed deterioration on multiple patient-safety metrics since the start of the pandemic. For example, central line infections, which had dropped by 31% in the five years before the COVID-19 outbreak, jumped 28% in the second quarter of 2020, compared with the prior-year period.
Commenting on these developments, the CMS authors said “the fact that the pandemic degraded patient safety so quickly and severely suggests that our health care system lacks a sufficiently resilient safety culture and infrastructure.”
A version of this article first appeared on Medscape.com.
Meet the JCOM Author with Dr. Barkoudah: Neurosurgery Operating Room Efficiency During the COVID-19 Era
Meet the JCOM Author with Dr. Barkoudah: Quality of Life and Population Health in Behavioral Health Care



Nurse practitioner fined $20k for advertising herself as ‘Doctor Sarah’
Last month, the San Luis Obispo County, California, District Attorney Dan Dow filed a complaint against Sarah Erny, RN, NP, citing unfair business practices and unprofessional conduct.
According to court documents, California’s Medical Practice Act does not permit individuals to refer to themselves as “doctor, physician, or any other terms or letters indicating or implying that he or she is a physician and surgeon ... without having ... a certificate as a physician and surgeon.”
Individuals who misrepresent themselves are subject to misdemeanor charges and civil penalties.
In addition to the fine, Ms. Erny agreed to refrain from referring to herself as a doctor in her practice and on social media. She has already deleted her Twitter account.
The case underscores tensions between physicians fighting to preserve their scope of practice and the allied professionals that U.S. lawmakers increasingly see as a less expensive way to improve access to health care.
The American Medical Association and specialty groups strongly oppose a new bill, the Improving Care and Access to Nurses Act, that would expand the scope of practice for nurse practitioners and physician assistants.
Court records show that Ms. Erny earned a doctor of nursing practice (DNP) degree from Vanderbilt University, Nashville, Tenn., and that she met the state requirements to obtain licensure as a registered nurse and nurse practitioner. In 2018, she opened a practice in Arroyo Grande, California, called Holistic Women’s Healing, where she provided medical services and drug supplements to patients.
She also entered a collaborative agreement with ob.gyn. Anika Moore, MD, for approximately 3 years. Dr. Moore’s medical practice was in another county and state, and the physician returned every 2 to 3 months to review a portion of Ms. Erny’s patient files.
Ms. Erny and Dr. Moore terminated the collaborative agreement in March, according to court documents.
However, Mr. Dow alleged that Ms. Erny regularly referred to herself as “Dr. Sarah” or “Dr. Sarah Erny” in her online advertising and social media accounts. Her patients “were so proud of her” that they called her doctor, and her supervising physician instructed staff to do the same.
Mr. Dow said Ms. Erny did not clearly advise the public that she was not a medical doctor and failed to identify her supervising physician. “Simply put, there is a great need for health care providers to state their level of training and licensing clearly and honestly in all of their advertising and marketing materials,” he said in a press release.
In California, nurse practitioners who have been certified by the Board of Registered Nursing may use the following titles: Advanced Practice Registered Nurse; Certified Nurse Practitioner; APRN-CNP; RN and NP; or a combination of other letters or words to identify specialization, such as adult nurse practitioner, pediatric nurse practitioner, obstetrical-gynecological nurse practitioner, and family nurse practitioner.
As educational requirements shift for advanced practice clinicians, similar cases will likely emerge, said Grant Martsolf, PhD, MPH, RN, FAAN, professor at the University of Pittsburgh School of Nursing.
“Scope of practice is governed by states, [so they] will have to figure [it] out as more professional disciplines move to clinical doctorates as the entry to practice. Pharma, [physical therapy], and [occupational therapy] have already done this, and advanced practice nursing is on its way. [Certified registered nurse anesthetists] are already required to get a DNP to sit for certification,” he said.
More guidance is needed, especially when considering other professions like dentists, clinical psychologists, and individuals with clinical or research doctorates who often call themselves doctors, Dr. Martsolf said.
“It seems that the honorific of ‘Dr.’ emerges from the degree, not from being a physician or surgeon,” he said.
Beyond the false advertising, Mr. Dow alleged that Ms. Erny did not file a fictitious business name statement for 2020 and 2021 – a requirement under the California Business and Professions Code to identify who is operating the business.
A version of this article first appeared on Medscape.com.
Last month, the San Luis Obispo County, California, District Attorney Dan Dow filed a complaint against Sarah Erny, RN, NP, citing unfair business practices and unprofessional conduct.
According to court documents, California’s Medical Practice Act does not permit individuals to refer to themselves as “doctor, physician, or any other terms or letters indicating or implying that he or she is a physician and surgeon ... without having ... a certificate as a physician and surgeon.”
Individuals who misrepresent themselves are subject to misdemeanor charges and civil penalties.
In addition to the fine, Ms. Erny agreed to refrain from referring to herself as a doctor in her practice and on social media. She has already deleted her Twitter account.
The case underscores tensions between physicians fighting to preserve their scope of practice and the allied professionals that U.S. lawmakers increasingly see as a less expensive way to improve access to health care.
The American Medical Association and specialty groups strongly oppose a new bill, the Improving Care and Access to Nurses Act, that would expand the scope of practice for nurse practitioners and physician assistants.
Court records show that Ms. Erny earned a doctor of nursing practice (DNP) degree from Vanderbilt University, Nashville, Tenn., and that she met the state requirements to obtain licensure as a registered nurse and nurse practitioner. In 2018, she opened a practice in Arroyo Grande, California, called Holistic Women’s Healing, where she provided medical services and drug supplements to patients.
She also entered a collaborative agreement with ob.gyn. Anika Moore, MD, for approximately 3 years. Dr. Moore’s medical practice was in another county and state, and the physician returned every 2 to 3 months to review a portion of Ms. Erny’s patient files.
Ms. Erny and Dr. Moore terminated the collaborative agreement in March, according to court documents.
However, Mr. Dow alleged that Ms. Erny regularly referred to herself as “Dr. Sarah” or “Dr. Sarah Erny” in her online advertising and social media accounts. Her patients “were so proud of her” that they called her doctor, and her supervising physician instructed staff to do the same.
Mr. Dow said Ms. Erny did not clearly advise the public that she was not a medical doctor and failed to identify her supervising physician. “Simply put, there is a great need for health care providers to state their level of training and licensing clearly and honestly in all of their advertising and marketing materials,” he said in a press release.
In California, nurse practitioners who have been certified by the Board of Registered Nursing may use the following titles: Advanced Practice Registered Nurse; Certified Nurse Practitioner; APRN-CNP; RN and NP; or a combination of other letters or words to identify specialization, such as adult nurse practitioner, pediatric nurse practitioner, obstetrical-gynecological nurse practitioner, and family nurse practitioner.
As educational requirements shift for advanced practice clinicians, similar cases will likely emerge, said Grant Martsolf, PhD, MPH, RN, FAAN, professor at the University of Pittsburgh School of Nursing.
“Scope of practice is governed by states, [so they] will have to figure [it] out as more professional disciplines move to clinical doctorates as the entry to practice. Pharma, [physical therapy], and [occupational therapy] have already done this, and advanced practice nursing is on its way. [Certified registered nurse anesthetists] are already required to get a DNP to sit for certification,” he said.
More guidance is needed, especially when considering other professions like dentists, clinical psychologists, and individuals with clinical or research doctorates who often call themselves doctors, Dr. Martsolf said.
“It seems that the honorific of ‘Dr.’ emerges from the degree, not from being a physician or surgeon,” he said.
Beyond the false advertising, Mr. Dow alleged that Ms. Erny did not file a fictitious business name statement for 2020 and 2021 – a requirement under the California Business and Professions Code to identify who is operating the business.
A version of this article first appeared on Medscape.com.
Last month, the San Luis Obispo County, California, District Attorney Dan Dow filed a complaint against Sarah Erny, RN, NP, citing unfair business practices and unprofessional conduct.
According to court documents, California’s Medical Practice Act does not permit individuals to refer to themselves as “doctor, physician, or any other terms or letters indicating or implying that he or she is a physician and surgeon ... without having ... a certificate as a physician and surgeon.”
Individuals who misrepresent themselves are subject to misdemeanor charges and civil penalties.
In addition to the fine, Ms. Erny agreed to refrain from referring to herself as a doctor in her practice and on social media. She has already deleted her Twitter account.
The case underscores tensions between physicians fighting to preserve their scope of practice and the allied professionals that U.S. lawmakers increasingly see as a less expensive way to improve access to health care.
The American Medical Association and specialty groups strongly oppose a new bill, the Improving Care and Access to Nurses Act, that would expand the scope of practice for nurse practitioners and physician assistants.
Court records show that Ms. Erny earned a doctor of nursing practice (DNP) degree from Vanderbilt University, Nashville, Tenn., and that she met the state requirements to obtain licensure as a registered nurse and nurse practitioner. In 2018, she opened a practice in Arroyo Grande, California, called Holistic Women’s Healing, where she provided medical services and drug supplements to patients.
She also entered a collaborative agreement with ob.gyn. Anika Moore, MD, for approximately 3 years. Dr. Moore’s medical practice was in another county and state, and the physician returned every 2 to 3 months to review a portion of Ms. Erny’s patient files.
Ms. Erny and Dr. Moore terminated the collaborative agreement in March, according to court documents.
However, Mr. Dow alleged that Ms. Erny regularly referred to herself as “Dr. Sarah” or “Dr. Sarah Erny” in her online advertising and social media accounts. Her patients “were so proud of her” that they called her doctor, and her supervising physician instructed staff to do the same.
Mr. Dow said Ms. Erny did not clearly advise the public that she was not a medical doctor and failed to identify her supervising physician. “Simply put, there is a great need for health care providers to state their level of training and licensing clearly and honestly in all of their advertising and marketing materials,” he said in a press release.
In California, nurse practitioners who have been certified by the Board of Registered Nursing may use the following titles: Advanced Practice Registered Nurse; Certified Nurse Practitioner; APRN-CNP; RN and NP; or a combination of other letters or words to identify specialization, such as adult nurse practitioner, pediatric nurse practitioner, obstetrical-gynecological nurse practitioner, and family nurse practitioner.
As educational requirements shift for advanced practice clinicians, similar cases will likely emerge, said Grant Martsolf, PhD, MPH, RN, FAAN, professor at the University of Pittsburgh School of Nursing.
“Scope of practice is governed by states, [so they] will have to figure [it] out as more professional disciplines move to clinical doctorates as the entry to practice. Pharma, [physical therapy], and [occupational therapy] have already done this, and advanced practice nursing is on its way. [Certified registered nurse anesthetists] are already required to get a DNP to sit for certification,” he said.
More guidance is needed, especially when considering other professions like dentists, clinical psychologists, and individuals with clinical or research doctorates who often call themselves doctors, Dr. Martsolf said.
“It seems that the honorific of ‘Dr.’ emerges from the degree, not from being a physician or surgeon,” he said.
Beyond the false advertising, Mr. Dow alleged that Ms. Erny did not file a fictitious business name statement for 2020 and 2021 – a requirement under the California Business and Professions Code to identify who is operating the business.
A version of this article first appeared on Medscape.com.
Why your professional persona may be considered unprofessional
On one of the first days of medical school, Adaira Landry, MD, applied her favorite dark shade of lipstick and headed to her orientation. She was eager to learn about program expectations and connect with fellow aspiring physicians. But when Dr. Landry got there, one of her brand-new peers turned to her and asked, “Why do you wear your lipstick like an angry Black woman?”
“Imagine hearing that,” Dr. Landry, now an emergency medical physician in Boston, says. “It was so hurtful.”
So, what is a “standard-issue doctor” expected to look like? Physicians manage their appearances in myriad ways: through clothes, accessories, hair style, makeup; through a social media presence or lack thereof; in the rhythms and nuances of their interactions with patients and colleagues. These things add up to a professional “persona” – the Latin word for “mask,” or the face on display for the world to see.
While the health care field itself is diversifying, its guidelines for professionalism appear slower to change, often excluding or frowning upon expressions of individual personality or identity.
“Medicine is run primarily by men. It’s an objective truth,” Dr. Landry says. “Currently and historically, the standard of professionalism, especially in the physical sense, was set by them. As we increase diversity and welcome people bringing their authentic self to work, the prior definitions of professionalism are obviously in need of change.”
Split social media personalities
In August 2020, the Journal of Vascular Surgery published a study on the “prevalence of unprofessional social media content among young vascular surgeons.” The content that was deemed “unprofessional” included opinions on political issues like abortion and gun control. Photos of physicians holding alcoholic drinks or wearing “inappropriate/offensive attire,” including underwear, “provocative Halloween costumes,” and “bikinis/swimwear” were also censured. Six men and one woman worked on the study, and three of the male researchers took on the task of seeking out the “unprofessional” photos on social media. The resulting paper was reviewed by an all-male editorial board.
The study sparked immediate backlash and prompted hundreds of health care professionals to post photos of themselves in bathing suits with the hashtag “#medbikini.” The journal then retracted the study and issued an apology on Twitter, recognizing “errors in the design of the study with regards to conscious and unconscious bias.”
The researchers’ original definition of professionalism suggests that physicians should manage their personae even outside of work hours. “I think medicine in general is a very conservative and hierarchical field of study and of work, to say the least,” says Sarah Fraser, MD, a family medicine physician in Nova Scotia, Canada. “There’s this view that we have to have completely separate personal and professional lives, like church and state.”
The #medbikini controversy inspired Dr. Fraser to write an op-ed for the British Medical Journal blog about the flaws of requiring physicians to keep their personal and professional selves separate. The piece referenced Robert Louis Stevenson’s 1886 Gothic novella “The Strange Case of Dr. Jekyll and Mr. Hyde,” in which the respected scientist Dr. Jekyll creates an alter ego so he can express his evil urges without experiencing guilt, punishment, or loss of livelihood. Dr. Fraser likened this story to the pressure physicians feel to shrink or split themselves to squeeze into a narrow definition of professionalism.
But Dr. Landry points out that some elements of expression seen as unprofessional cannot be entirely separated from a physician’s fundamental identity. “For Black women, our daily behaviors and forms of expression that are deemed ‘unprofessional’ are much more subtle than being able to wear a bikini on social media,” she says. “The way we wear our hair, the tone of our voice, the color of our lipstick, the way we wear scrub caps are parts of us that are called into question.”
Keeping up appearances
The stereotype of what a doctor should look like starts to shape physicians’ professional personae in medical school. When Jennifer Caputo-Seidler, MD, started medical school in 2008, the dress code requirements for male students were simple: pants, a button-down shirt, a tie. But then there were the rules for women: Hair should be tied back. Minimal makeup. No flashy jewelry. Nothing without sleeves. Neutral colors. High necklines. Low hemlines. “The message I got was that we need to dress like the men in order to be taken seriously and to be seen as professional,” says Dr. Caputo-Seidler, now an assistant professor of medicine at the University of South Florida, Tampa, “and so that’s what I did.”
A 2018 analysis of 78 “draw-a-scientist” studies found that children have overwhelmingly associated scientific fields with men for the last 50 years. Overall, children drew 73% of scientists as men. The drawings grew more gender diverse over time, but even as more women entered scientific fields, both boys and girls continued to draw significantly more male than female scientists.
Not everyone at Dr. Caputo-Seidler’s medical school adhered to the environment’s gendered expectations. One resident she worked with often wore voluminous hairstyles, lipstick, and high heels. Dr. Caputo-Seidler overheard her peers as they gossiped behind the resident’s back, ridiculing the way she looked.
“She was good at her job,” Dr. Caputo-Seidler says. “She knew her patients. She had things down. She was, by all measures, very competent. But when people saw her dressing outside the norm and being forward with her femininity, there was definitely a lot of chatter about it.”
While expectations for a conservative appearance may disproportionately affect women, and particularly women of color, they also affect men who deviate from the norm. “As an LGBTQ+ person working as a ‘professional,’ I have countless stories and moments where I had my professionalism questioned,” Blair Peters, MD, a plastic surgeon and assistant professor at Oregon Health & Science University, Portland, wrote on Twitter. “Why is it ‘unprofessional’ to have colored hair? Why is it ‘unprofessional’ to have a visible tattoo? Why is it ‘unprofessional’ to wear bright colors and patterns?”
Dr. Fraser remembers a fellow medical student who had full-sleeve tattoos on both of his arms. A preceptor made a comment about it to Dr. Fraser, and then instructed the student to cover up his tattoos. “I think that there are scenarios when having tattoos or having different-colored hair or expressing your individual personality could help you even better bond with your patients,” Dr. Fraser says, “especially if you’re, for example, working with youth.”
Unmasking health care
Beyond the facets of dress codes and social media posts, the issue of professional personae speaks to the deeper issue of inclusion in medicine. As the field grows increasingly diverse, health care institutions and those they serve may need to expand their definitions of professionalism to include more truthful expressions of who contemporary health care professionals are as people.
Dr. Fraser suggests that the benefits of physicians embracing self-expression – rather than assimilating to an outdated model of professionalism – extend beyond the individual.
“Whether it comes to what you choose to wear to the clinic on a day-to-day basis, or what you choose to share on a social media account, as long as it’s not harming others, then I think that it’s a positive thing to be able to be yourself and express yourself,” she says. “I feel like doctors are expected to have a different personality when we’re at the clinic, and usually it’s more conservative or objective or aloof. But I think that by being open about who we are, we’ll actually help build a trusting relationship with both patients and society.”
A version of this article first appeared on Medscape.com.
On one of the first days of medical school, Adaira Landry, MD, applied her favorite dark shade of lipstick and headed to her orientation. She was eager to learn about program expectations and connect with fellow aspiring physicians. But when Dr. Landry got there, one of her brand-new peers turned to her and asked, “Why do you wear your lipstick like an angry Black woman?”
“Imagine hearing that,” Dr. Landry, now an emergency medical physician in Boston, says. “It was so hurtful.”
So, what is a “standard-issue doctor” expected to look like? Physicians manage their appearances in myriad ways: through clothes, accessories, hair style, makeup; through a social media presence or lack thereof; in the rhythms and nuances of their interactions with patients and colleagues. These things add up to a professional “persona” – the Latin word for “mask,” or the face on display for the world to see.
While the health care field itself is diversifying, its guidelines for professionalism appear slower to change, often excluding or frowning upon expressions of individual personality or identity.
“Medicine is run primarily by men. It’s an objective truth,” Dr. Landry says. “Currently and historically, the standard of professionalism, especially in the physical sense, was set by them. As we increase diversity and welcome people bringing their authentic self to work, the prior definitions of professionalism are obviously in need of change.”
Split social media personalities
In August 2020, the Journal of Vascular Surgery published a study on the “prevalence of unprofessional social media content among young vascular surgeons.” The content that was deemed “unprofessional” included opinions on political issues like abortion and gun control. Photos of physicians holding alcoholic drinks or wearing “inappropriate/offensive attire,” including underwear, “provocative Halloween costumes,” and “bikinis/swimwear” were also censured. Six men and one woman worked on the study, and three of the male researchers took on the task of seeking out the “unprofessional” photos on social media. The resulting paper was reviewed by an all-male editorial board.
The study sparked immediate backlash and prompted hundreds of health care professionals to post photos of themselves in bathing suits with the hashtag “#medbikini.” The journal then retracted the study and issued an apology on Twitter, recognizing “errors in the design of the study with regards to conscious and unconscious bias.”
The researchers’ original definition of professionalism suggests that physicians should manage their personae even outside of work hours. “I think medicine in general is a very conservative and hierarchical field of study and of work, to say the least,” says Sarah Fraser, MD, a family medicine physician in Nova Scotia, Canada. “There’s this view that we have to have completely separate personal and professional lives, like church and state.”
The #medbikini controversy inspired Dr. Fraser to write an op-ed for the British Medical Journal blog about the flaws of requiring physicians to keep their personal and professional selves separate. The piece referenced Robert Louis Stevenson’s 1886 Gothic novella “The Strange Case of Dr. Jekyll and Mr. Hyde,” in which the respected scientist Dr. Jekyll creates an alter ego so he can express his evil urges without experiencing guilt, punishment, or loss of livelihood. Dr. Fraser likened this story to the pressure physicians feel to shrink or split themselves to squeeze into a narrow definition of professionalism.
But Dr. Landry points out that some elements of expression seen as unprofessional cannot be entirely separated from a physician’s fundamental identity. “For Black women, our daily behaviors and forms of expression that are deemed ‘unprofessional’ are much more subtle than being able to wear a bikini on social media,” she says. “The way we wear our hair, the tone of our voice, the color of our lipstick, the way we wear scrub caps are parts of us that are called into question.”
Keeping up appearances
The stereotype of what a doctor should look like starts to shape physicians’ professional personae in medical school. When Jennifer Caputo-Seidler, MD, started medical school in 2008, the dress code requirements for male students were simple: pants, a button-down shirt, a tie. But then there were the rules for women: Hair should be tied back. Minimal makeup. No flashy jewelry. Nothing without sleeves. Neutral colors. High necklines. Low hemlines. “The message I got was that we need to dress like the men in order to be taken seriously and to be seen as professional,” says Dr. Caputo-Seidler, now an assistant professor of medicine at the University of South Florida, Tampa, “and so that’s what I did.”
A 2018 analysis of 78 “draw-a-scientist” studies found that children have overwhelmingly associated scientific fields with men for the last 50 years. Overall, children drew 73% of scientists as men. The drawings grew more gender diverse over time, but even as more women entered scientific fields, both boys and girls continued to draw significantly more male than female scientists.
Not everyone at Dr. Caputo-Seidler’s medical school adhered to the environment’s gendered expectations. One resident she worked with often wore voluminous hairstyles, lipstick, and high heels. Dr. Caputo-Seidler overheard her peers as they gossiped behind the resident’s back, ridiculing the way she looked.
“She was good at her job,” Dr. Caputo-Seidler says. “She knew her patients. She had things down. She was, by all measures, very competent. But when people saw her dressing outside the norm and being forward with her femininity, there was definitely a lot of chatter about it.”
While expectations for a conservative appearance may disproportionately affect women, and particularly women of color, they also affect men who deviate from the norm. “As an LGBTQ+ person working as a ‘professional,’ I have countless stories and moments where I had my professionalism questioned,” Blair Peters, MD, a plastic surgeon and assistant professor at Oregon Health & Science University, Portland, wrote on Twitter. “Why is it ‘unprofessional’ to have colored hair? Why is it ‘unprofessional’ to have a visible tattoo? Why is it ‘unprofessional’ to wear bright colors and patterns?”
Dr. Fraser remembers a fellow medical student who had full-sleeve tattoos on both of his arms. A preceptor made a comment about it to Dr. Fraser, and then instructed the student to cover up his tattoos. “I think that there are scenarios when having tattoos or having different-colored hair or expressing your individual personality could help you even better bond with your patients,” Dr. Fraser says, “especially if you’re, for example, working with youth.”
Unmasking health care
Beyond the facets of dress codes and social media posts, the issue of professional personae speaks to the deeper issue of inclusion in medicine. As the field grows increasingly diverse, health care institutions and those they serve may need to expand their definitions of professionalism to include more truthful expressions of who contemporary health care professionals are as people.
Dr. Fraser suggests that the benefits of physicians embracing self-expression – rather than assimilating to an outdated model of professionalism – extend beyond the individual.
“Whether it comes to what you choose to wear to the clinic on a day-to-day basis, or what you choose to share on a social media account, as long as it’s not harming others, then I think that it’s a positive thing to be able to be yourself and express yourself,” she says. “I feel like doctors are expected to have a different personality when we’re at the clinic, and usually it’s more conservative or objective or aloof. But I think that by being open about who we are, we’ll actually help build a trusting relationship with both patients and society.”
A version of this article first appeared on Medscape.com.
On one of the first days of medical school, Adaira Landry, MD, applied her favorite dark shade of lipstick and headed to her orientation. She was eager to learn about program expectations and connect with fellow aspiring physicians. But when Dr. Landry got there, one of her brand-new peers turned to her and asked, “Why do you wear your lipstick like an angry Black woman?”
“Imagine hearing that,” Dr. Landry, now an emergency medical physician in Boston, says. “It was so hurtful.”
So, what is a “standard-issue doctor” expected to look like? Physicians manage their appearances in myriad ways: through clothes, accessories, hair style, makeup; through a social media presence or lack thereof; in the rhythms and nuances of their interactions with patients and colleagues. These things add up to a professional “persona” – the Latin word for “mask,” or the face on display for the world to see.
While the health care field itself is diversifying, its guidelines for professionalism appear slower to change, often excluding or frowning upon expressions of individual personality or identity.
“Medicine is run primarily by men. It’s an objective truth,” Dr. Landry says. “Currently and historically, the standard of professionalism, especially in the physical sense, was set by them. As we increase diversity and welcome people bringing their authentic self to work, the prior definitions of professionalism are obviously in need of change.”
Split social media personalities
In August 2020, the Journal of Vascular Surgery published a study on the “prevalence of unprofessional social media content among young vascular surgeons.” The content that was deemed “unprofessional” included opinions on political issues like abortion and gun control. Photos of physicians holding alcoholic drinks or wearing “inappropriate/offensive attire,” including underwear, “provocative Halloween costumes,” and “bikinis/swimwear” were also censured. Six men and one woman worked on the study, and three of the male researchers took on the task of seeking out the “unprofessional” photos on social media. The resulting paper was reviewed by an all-male editorial board.
The study sparked immediate backlash and prompted hundreds of health care professionals to post photos of themselves in bathing suits with the hashtag “#medbikini.” The journal then retracted the study and issued an apology on Twitter, recognizing “errors in the design of the study with regards to conscious and unconscious bias.”
The researchers’ original definition of professionalism suggests that physicians should manage their personae even outside of work hours. “I think medicine in general is a very conservative and hierarchical field of study and of work, to say the least,” says Sarah Fraser, MD, a family medicine physician in Nova Scotia, Canada. “There’s this view that we have to have completely separate personal and professional lives, like church and state.”
The #medbikini controversy inspired Dr. Fraser to write an op-ed for the British Medical Journal blog about the flaws of requiring physicians to keep their personal and professional selves separate. The piece referenced Robert Louis Stevenson’s 1886 Gothic novella “The Strange Case of Dr. Jekyll and Mr. Hyde,” in which the respected scientist Dr. Jekyll creates an alter ego so he can express his evil urges without experiencing guilt, punishment, or loss of livelihood. Dr. Fraser likened this story to the pressure physicians feel to shrink or split themselves to squeeze into a narrow definition of professionalism.
But Dr. Landry points out that some elements of expression seen as unprofessional cannot be entirely separated from a physician’s fundamental identity. “For Black women, our daily behaviors and forms of expression that are deemed ‘unprofessional’ are much more subtle than being able to wear a bikini on social media,” she says. “The way we wear our hair, the tone of our voice, the color of our lipstick, the way we wear scrub caps are parts of us that are called into question.”
Keeping up appearances
The stereotype of what a doctor should look like starts to shape physicians’ professional personae in medical school. When Jennifer Caputo-Seidler, MD, started medical school in 2008, the dress code requirements for male students were simple: pants, a button-down shirt, a tie. But then there were the rules for women: Hair should be tied back. Minimal makeup. No flashy jewelry. Nothing without sleeves. Neutral colors. High necklines. Low hemlines. “The message I got was that we need to dress like the men in order to be taken seriously and to be seen as professional,” says Dr. Caputo-Seidler, now an assistant professor of medicine at the University of South Florida, Tampa, “and so that’s what I did.”
A 2018 analysis of 78 “draw-a-scientist” studies found that children have overwhelmingly associated scientific fields with men for the last 50 years. Overall, children drew 73% of scientists as men. The drawings grew more gender diverse over time, but even as more women entered scientific fields, both boys and girls continued to draw significantly more male than female scientists.
Not everyone at Dr. Caputo-Seidler’s medical school adhered to the environment’s gendered expectations. One resident she worked with often wore voluminous hairstyles, lipstick, and high heels. Dr. Caputo-Seidler overheard her peers as they gossiped behind the resident’s back, ridiculing the way she looked.
“She was good at her job,” Dr. Caputo-Seidler says. “She knew her patients. She had things down. She was, by all measures, very competent. But when people saw her dressing outside the norm and being forward with her femininity, there was definitely a lot of chatter about it.”
While expectations for a conservative appearance may disproportionately affect women, and particularly women of color, they also affect men who deviate from the norm. “As an LGBTQ+ person working as a ‘professional,’ I have countless stories and moments where I had my professionalism questioned,” Blair Peters, MD, a plastic surgeon and assistant professor at Oregon Health & Science University, Portland, wrote on Twitter. “Why is it ‘unprofessional’ to have colored hair? Why is it ‘unprofessional’ to have a visible tattoo? Why is it ‘unprofessional’ to wear bright colors and patterns?”
Dr. Fraser remembers a fellow medical student who had full-sleeve tattoos on both of his arms. A preceptor made a comment about it to Dr. Fraser, and then instructed the student to cover up his tattoos. “I think that there are scenarios when having tattoos or having different-colored hair or expressing your individual personality could help you even better bond with your patients,” Dr. Fraser says, “especially if you’re, for example, working with youth.”
Unmasking health care
Beyond the facets of dress codes and social media posts, the issue of professional personae speaks to the deeper issue of inclusion in medicine. As the field grows increasingly diverse, health care institutions and those they serve may need to expand their definitions of professionalism to include more truthful expressions of who contemporary health care professionals are as people.
Dr. Fraser suggests that the benefits of physicians embracing self-expression – rather than assimilating to an outdated model of professionalism – extend beyond the individual.
“Whether it comes to what you choose to wear to the clinic on a day-to-day basis, or what you choose to share on a social media account, as long as it’s not harming others, then I think that it’s a positive thing to be able to be yourself and express yourself,” she says. “I feel like doctors are expected to have a different personality when we’re at the clinic, and usually it’s more conservative or objective or aloof. But I think that by being open about who we are, we’ll actually help build a trusting relationship with both patients and society.”
A version of this article first appeared on Medscape.com.
Quality of Life and Population Health in Behavioral Health Care: A Retrospective, Cross-Sectional Study
From Milwaukee County Behavioral Health Services, Milwaukee, WI.
Abstract
Objectives: The goal of this study was to determine whether a single-item quality of life (QOL) measure could serve as a useful population health–level metric within the Quadruple Aim framework in a publicly funded behavioral health system.
Design: This was a retrospective, cross-sectional study that examined the correlation between the single-item QOL measure and several other key measures of the social determinants of health and a composite measure of acute service utilization for all patients receiving mental health and substance use services in a community behavioral health system.
Methods: Data were collected for 4488 patients who had at least 1 assessment between October 1, 2020, and September 30, 2021. Data on social determinants of health were obtained through patient self-report; acute service use data were obtained from electronic health records.
Results: Statistical analyses revealed results in the expected direction for all relationships tested. Patients with higher QOL were more likely to report “Good” or better self-rated physical health, be employed, have a private residence, and report recent positive social interactions, and were less likely to have received acute services in the previous 90 days.
Conclusion: A single-item QOL measure shows promise as a general, minimally burdensome whole-system metric that can function as a target for population health management efforts in a large behavioral health system. Future research should explore whether this QOL measure is sensitive to change over time and examine its temporal relationship with other key outcome metrics.
Keywords: Quadruple Aim, single-item measures, social determinants of health, acute service utilization metrics.
The Triple Aim for health care—improving the individual experience of care, increasing the health of populations, and reducing the costs of care—was first proposed in 2008.1 More recently, some have advocated for an expanded focus to include a fourth aim: the quality of staff work life.2 Since this seminal paper was published, many health care systems have endeavored to adopt and implement the Quadruple Aim3,4; however, the concepts representing each of the aims are not universally defined,3 nor are the measures needed to populate the Quadruple Aim always available within the health system in question.5
Although several assessment models and frameworks that provide guidance to stakeholders have been developed,6,7 it is ultimately up to organizations themselves to determine which measures they should deploy to best represent the different quadrants of the Quadruple Aim.6 Evidence suggests, however, that quality measurement, and the administrative time required to conduct it, can be both financially and emotionally burdensome to providers and health systems.8-10 Thus, it is incumbent on organizations to select a set of measures that are not only meaningful but as parsimonious as possible.6,11,12
Quality of life (QOL) is a potential candidate to assess the aim of population health. Brief health-related QOL questions have long been used in epidemiological surveys, such as the Behavioral Risk Factor Surveillance System survey.13 Such questions are also a key component of community health frameworks, such as the County Health Rankings developed by the University of Wisconsin Population Health Institute.14 Furthermore, Humana recently revealed that increasing the number of physical and mental health “Healthy Days” (which are among the Centers for Disease Control and Prevention’s Health-Related Quality of Life questions15) among the members enrolled in their insurance plan would become a major goal for the organization.16,17 Many of these measures, while brief, focus on QOL as a function of health, often as a self-rated construct (from “Poor” to “Excellent”) or in the form of days of poor physical or mental health in the past 30 days,15 rather than evaluating QOL itself; however, several authors have pointed out that health status and QOL are related but distinct concepts.18,19
Brief single-item assessments focused specifically on QOL have been developed and implemented within nonclinical20 and clinical populations, including individuals with cancer,21 adults with disabilities,22 individuals with cystic fibrosis,23 and children with epilepsy.24 Despite the long history of QOL assessment in behavioral health treatment,25 single-item measures have not been widely implemented in this population.
Milwaukee County Behavioral Health Services (BHS), a publicly funded, county-based behavioral health care system in Milwaukee, Wisconsin, provides inpatient and ambulatory treatment, psychiatric emergency care, withdrawal management, care management, crisis services, and other support services to individuals in Milwaukee County. In 2018 the community services arm of BHS began implementing a single QOL question from the World Health Organization’s WHOQOL-BREF26: On a 5-point rating scale of “Very Poor” to “Very Good,” “How would you rate your overall quality of life right now?” Previous research by Atroszko and colleagues,20 which used a similar approach with the same item from the WHOQOL-BREF, reported correlations in the expected direction of the single-item QOL measure with perceived stress, depression, anxiety, loneliness, and daily hours of sleep. This study’s sample, however, comprised opportunistically recruited college students, not a clinical population. Further, the researchers did not examine the relationship of QOL with acute service utilization or other measures of the social determinants of health, such as housing, employment, or social connectedness.
The following study was designed to extend these results by focusing on a clinical population—individuals with mental health or substance use issues—being served in a large, publicly funded behavioral health system in Milwaukee, Wisconsin. The objective of this study was to determine whether a single-item QOL measure could be used as a brief, parsimonious measure of overall population health by examining its relationship with other key outcome measures for patients receiving services from BHS. This study was reviewed and approved by BHS’s Institutional Review Board.
Methods
All patients engaged in nonacute community services are offered a standardized assessment that includes, among other measures, items related to QOL, housing status, employment status, self-rated physical health, and social connectedness. This assessment is administered at intake, discharge, and every 6 months while patients are enrolled in services. Patients who received at least 1 assessment between October 1, 2020, and September 30, 2021, were included in the analyses. Patients receiving crisis, inpatient, or withdrawal management services alone (ie, did not receive any other community-based services) were not offered the standard assessment and thus were not included in the analyses. If patients had more than 1 assessment during this time period, QOL data from the last assessment were used. Data on housing (private residence status, defined as adults living alone or with others without supervision in a house or apartment), employment status, self-rated physical health, and social connectedness (measured by asking people whether they have had positive interactions with family or friends in the past 30 days) were extracted from the same timepoint as well.
Also included in the analyses were rates of acute service utilization, in which any patient with at least 1 visit to BHS’s psychiatric emergency department, withdrawal management facility, or psychiatric inpatient facility in the 90 days prior to the date of the assessment received a code of “Yes,” and any patient who did not receive any of these services received a code of “No.” Chi-square analyses were conducted to determine the relationship between QOL rankings (“Very Poor,” “Poor,” “Neither Good nor Poor,” “Good,” and “Very Good”) and housing, employment, self-rated physical health, social connectedness, and 90-day acute service use. All acute service utilization data were obtained from BHS’s electronic health records system. All data used in the study were stored on a secure, password-protected server. All analyses were conducted with SPSS software (SPSS 28; IBM).
Results
Data were available for 4488 patients who received an assessment between October 1, 2020, and September 30, 2021 (total numbers per item vary because some items had missing data; see supplementary eTables 1-3 for sample size per item). Demographics of the patient sample are listed in Table 1; the demographics of the patients who were missing data for specific outcomes are presented in eTables 1-3.
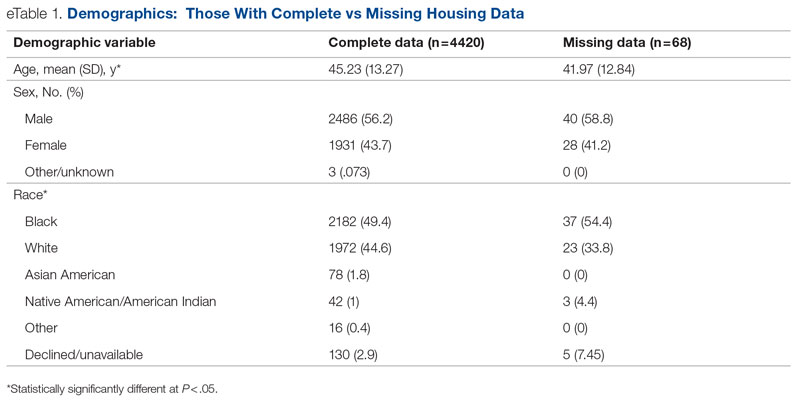
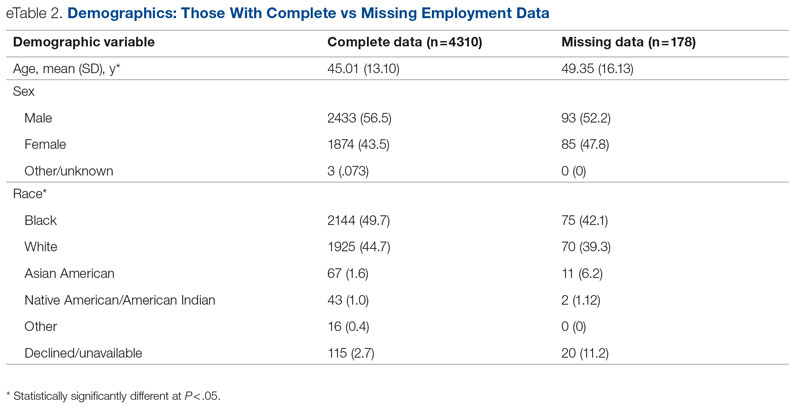
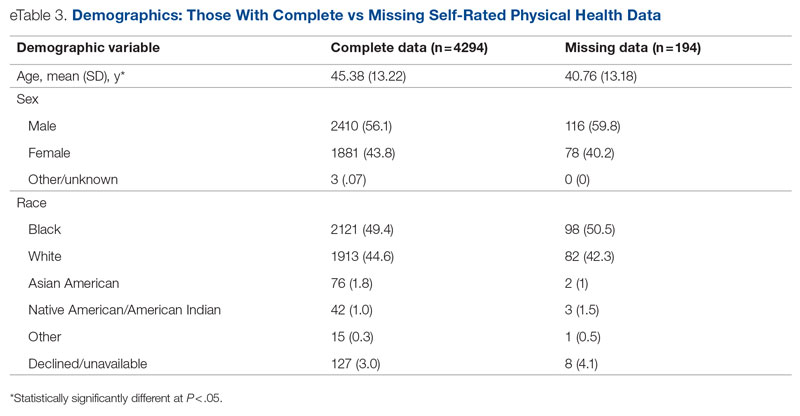
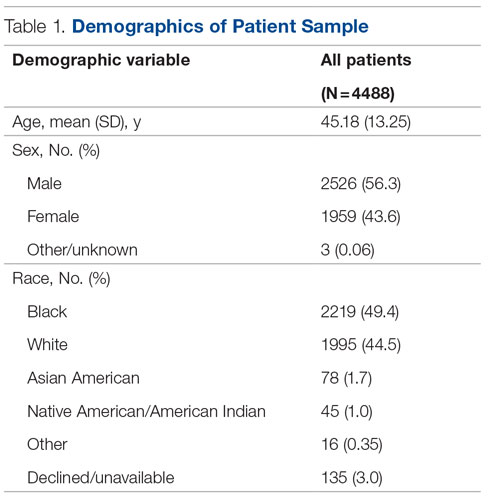
Statistical analyses revealed results in the expected direction for all relationships tested (Table 2). As patients’ self-reported QOL improved, so did the likelihood of higher rates of self-reported “Good” or better physical health, which was 576% higher among individuals who reported “Very Good” QOL relative to those who reported “Very Poor” QOL. Similarly, when compared with individuals with “Very Poor” QOL, individuals who reported “Very Good” QOL were 21.91% more likely to report having a private residence, 126.7% more likely to report being employed, and 29.17% more likely to report having had positive social interactions with family and friends in the past 30 days. There was an inverse relationship between QOL and the likelihood that a patient had received at least 1 admission for an acute service in the previous 90 days, such that patients who reported “Very Good” QOL were 86.34% less likely to have had an admission compared to patients with “Very Poor” QOL (2.8% vs 20.5%, respectively). The relationships among the criterion variables used in this study are presented in Table 3.
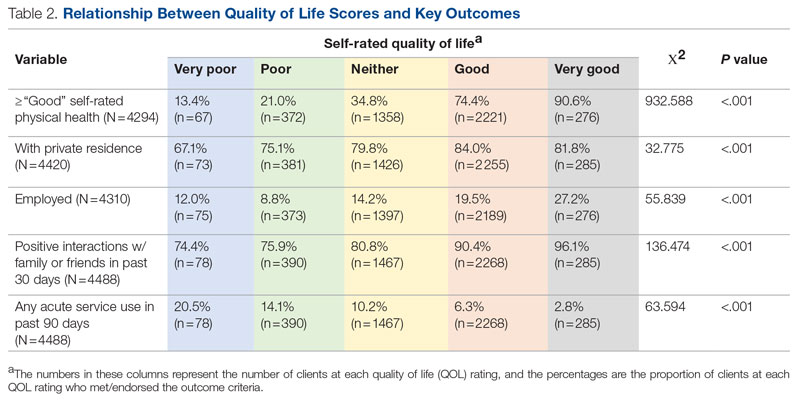
Discussion
The results of this preliminary analysis suggest that self-rated QOL is related to key health, social determinants of health, and acute service utilization metrics. These data are important for several reasons. First, because QOL is a diagnostically agnostic measure, it is a cross-cutting measure to use with clinically diverse populations receiving an array of different services. Second, at 1 item, the QOL measure is extremely brief and therefore minimally onerous to implement for both patients and administratively overburdened providers. Third, its correlation with other key metrics suggests that it can function as a broad population health measure for health care organizations because individuals with higher QOL will also likely have better outcomes in other key areas. This suggests that it has the potential to broadly represent the overall status of a population of patients, thus functioning as a type of “whole system” measure, which the Institute for Healthcare Improvement describes as “a small set of measures that reflect a health system’s overall performance on core dimensions of quality guided by the Triple Aim.”7 These whole system measures can help focus an organization’s strategic initiatives and efforts on the issues that matter most to the patients and community it serves.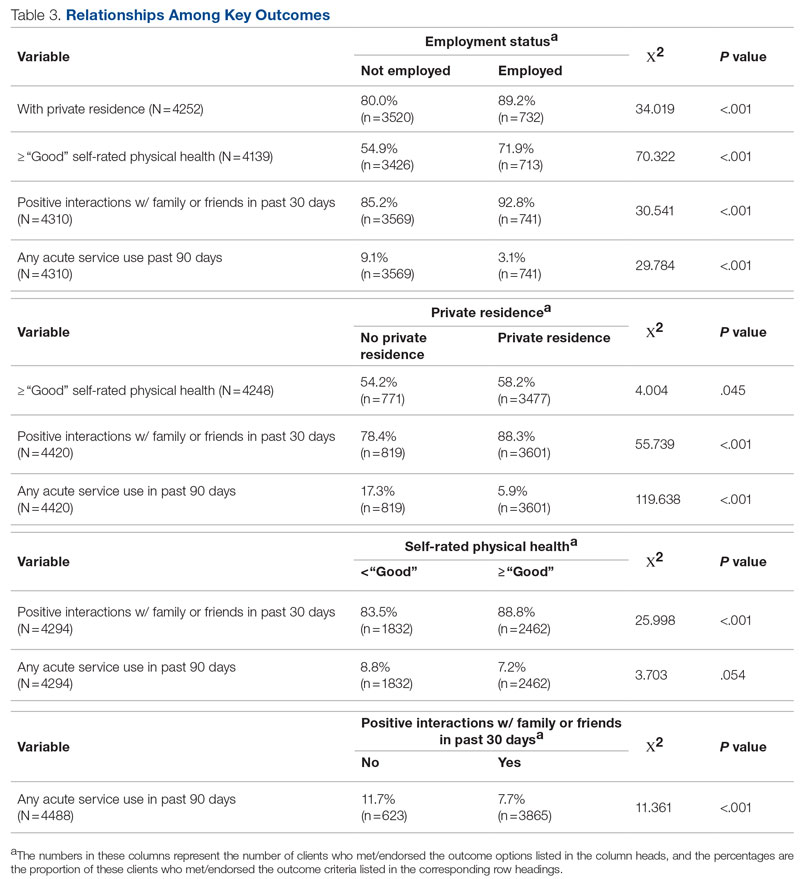
The relationship of QOL to acute service utilization deserves special mention. As an administrative measure, utilization is not susceptible to the same response bias as the other self-reported variables. Furthermore, acute services are costly to health systems, and hospital readmissions are associated with payment reductions in the Centers for Medicare and Medicaid Services (CMS) Hospital Readmissions Reduction Program for hospitals that fail to meet certain performance targets.27 Thus, because of its alignment with federal mandates, improved QOL (and potentially concomitant decreases in acute service use) may have significant financial implications for health systems as well.
This study was limited by several factors. First, it was focused on a population receiving publicly funded behavioral health services with strict eligibility requirements, one of which stipulated that individuals must be at 200% or less of the Federal Poverty Level; therefore, the results might not be applicable to health systems with a more clinically or socioeconomically diverse patient population. Second, because these data are cross-sectional, it was not possible to determine whether QOL improved over time or whether changes in QOL covaried longitudinally with the other metrics under observation. For example, if patients’ QOL improved from the first to last assessment, did their employment or residential status improve as well, or were these patients more likely to be employed at their first assessment? Furthermore, if there was covariance, did changes in employment, housing status, and so on precede changes in QOL or vice versa? Multiple longitudinal observations would help to address these questions and will be the focus of future analyses.
Conclusion
This preliminary study suggests that a single-item QOL measure may be a valuable population health–level metric for health systems. It requires little administrative effort on the part of either the clinician or patient. It is also agnostic with regard to clinical issue or treatment approach and can therefore admit of a range of diagnoses or patient-specific, idiosyncratic recovery goals. It is correlated with other key health, social determinants of health, and acute service utilization indicators and can therefore serve as a “whole system” measure because of its ability to broadly represent improvements in an entire population. Furthermore, QOL is patient-centered in that data are obtained through patient self-report, which is a high priority for CMS and other health care organizations.28 In summary, a single-item QOL measure holds promise for health care organizations looking to implement the Quadruple Aim and assess the health of the populations they serve in a manner that is simple, efficient, and patient-centered.
Acknowledgments: The author thanks Jennifer Wittwer for her thoughtful comments on the initial draft of this manuscript and Gary Kraft for his help extracting the data used in the analyses.
Corresponding author: Walter Matthew Drymalski, PhD; [email protected]
Disclosures: None reported.
1. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759-769. doi:10.1377/hlthaff.27.3.759
2. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-576. doi:10.1370/afm.1713
3. Hendrikx RJP, Drewes HW, Spreeuwenberg M, et al. Which triple aim related measures are being used to evaluate population management initiatives? An international comparative analysis. Health Policy. 2016;120(5):471-485. doi:10.1016/j.healthpol.2016.03.008
4. Whittington JW, Nolan K, Lewis N, Torres T. Pursuing the triple aim: the first 7 years. Milbank Q. 2015;93(2):263-300. doi:10.1111/1468-0009.12122
5. Ryan BL, Brown JB, Glazier RH, Hutchison B. Examining primary healthcare performance through a triple aim lens. Healthc Policy. 2016;11(3):19-31.
6. Stiefel M, Nolan K. A guide to measuring the Triple Aim: population health, experience of care, and per capita cost. Institute for Healthcare Improvement; 2012. Accessed November 1, 2022. https://nhchc.org/wp-content/uploads/2019/08/ihiguidetomeasuringtripleaimwhitepaper2012.pdf
7. Martin L, Nelson E, Rakover J, Chase A. Whole system measures 2.0: a compass for health system leaders. Institute for Healthcare Improvement; 2016. Accessed November 1, 2022. http://www.ihi.org:80/resources/Pages/IHIWhitePapers/Whole-System-Measures-Compass-for-Health-System-Leaders.aspx
8. Casalino LP, Gans D, Weber R, et al. US physician practices spend more than $15.4 billion annually to report quality measures. Health Aff (Millwood). 2016;35(3):401-406. doi:10.1377/hlthaff.2015.1258
9. Rao SK, Kimball AB, Lehrhoff SR, et al. The impact of administrative burden on academic physicians: results of a hospital-wide physician survey. Acad Med. 2017;92(2):237-243. doi:10.1097/ACM.0000000000001461
10. Woolhandler S, Himmelstein DU. Administrative work consumes one-sixth of U.S. physicians’ working hours and lowers their career satisfaction. Int J Health Serv. 2014;44(4):635-642. doi:10.2190/HS.44.4.a
11. Meyer GS, Nelson EC, Pryor DB, et al. More quality measures versus measuring what matters: a call for balance and parsimony. BMJ Qual Saf. 2012;21(11):964-968. doi:10.1136/bmjqs-2012-001081
12. Vital Signs: Core Metrics for Health and Health Care Progress. Washington, DC: National Academies Press; 2015. doi:10.17226/19402
13. Centers for Disease Control and Prevention. BRFSS questionnaires. Accessed November 1, 2022. https://www.cdc.gov/brfss/questionnaires/index.htm
14. County Health Rankings and Roadmaps. Measures & data sources. University of Wisconsin Population Health Institute. Accessed November 1, 2022. https://www.countyhealthrankings.org/explore-health-rankings/measures-data-sources
15. Centers for Disease Control and Prevention. Healthy days core module (CDC HRQOL-4). Accessed November 1, 2022. https://www.cdc.gov/hrqol/hrqol14_measure.htm
16. Cordier T, Song Y, Cambon J, et al. A bold goal: more healthy days through improved community health. Popul Health Manag. 2018;21(3):202-208. doi:10.1089/pop.2017.0142
17. Slabaugh SL, Shah M, Zack M, et al. Leveraging health-related quality of life in population health management: the case for healthy days. Popul Health Manag. 2017;20(1):13-22. doi:10.1089/pop.2015.0162
18. Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics. 2016;34(7):645-649. doi:10.1007/s40273-016-0389-9
19. Smith KW, Avis NE, Assmann SF. Distinguishing between quality of life and health status in quality of life research: a meta-analysis. Qual Life Res. 1999;8(5):447-459. doi:10.1023/a:1008928518577
20. Atroszko PA, Baginska P, Mokosinska M, et al. Validity and reliability of single-item self-report measures of general quality of life, general health and sleep quality. In: CER Comparative European Research 2015. Sciemcee Publishing; 2015:207-211.
21. Singh JA, Satele D, Pattabasavaiah S, et al. Normative data and clinically significant effect sizes for single-item numerical linear analogue self-assessment (LASA) scales. Health Qual Life Outcomes. 2014;12:187. doi:10.1186/s12955-014-0187-z
22. Siebens HC, Tsukerman D, Adkins RH, et al. Correlates of a single-item quality-of-life measure in people aging with disabilities. Am J Phys Med Rehabil. 2015;94(12):1065-1074. doi:10.1097/PHM.0000000000000298
23. Yohannes AM, Dodd M, Morris J, Webb K. Reliability and validity of a single item measure of quality of life scale for adult patients with cystic fibrosis. Health Qual Life Outcomes. 2011;9:105. doi:10.1186/1477-7525-9-105
24. Conway L, Widjaja E, Smith ML. Single-item measure for assessing quality of life in children with drug-resistant epilepsy. Epilepsia Open. 2017;3(1):46-54. doi:10.1002/epi4.12088
25. Barry MM, Zissi A. Quality of life as an outcome measure in evaluating mental health services: a review of the empirical evidence. Soc Psychiatry Psychiatr Epidemiol. 1997;32(1):38-47. doi:10.1007/BF00800666
26. Skevington SM, Lotfy M, O’Connell KA. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. Qual Life Res. 2004;13(2):299-310. doi:10.1023/B:QURE.0000018486.91360.00
27. Centers for Medicare & Medicaid Services. Hospital readmissions reduction program (HRRP). Accessed November 1, 2022. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program
28. Centers for Medicare & Medicaid Services. Patient-reported outcome measures. CMS Measures Management System. Published May 2022. Accessed November 1, 2022. https://www.cms.gov/files/document/blueprint-patient-reported-outcome-measures.pdf
From Milwaukee County Behavioral Health Services, Milwaukee, WI.
Abstract
Objectives: The goal of this study was to determine whether a single-item quality of life (QOL) measure could serve as a useful population health–level metric within the Quadruple Aim framework in a publicly funded behavioral health system.
Design: This was a retrospective, cross-sectional study that examined the correlation between the single-item QOL measure and several other key measures of the social determinants of health and a composite measure of acute service utilization for all patients receiving mental health and substance use services in a community behavioral health system.
Methods: Data were collected for 4488 patients who had at least 1 assessment between October 1, 2020, and September 30, 2021. Data on social determinants of health were obtained through patient self-report; acute service use data were obtained from electronic health records.
Results: Statistical analyses revealed results in the expected direction for all relationships tested. Patients with higher QOL were more likely to report “Good” or better self-rated physical health, be employed, have a private residence, and report recent positive social interactions, and were less likely to have received acute services in the previous 90 days.
Conclusion: A single-item QOL measure shows promise as a general, minimally burdensome whole-system metric that can function as a target for population health management efforts in a large behavioral health system. Future research should explore whether this QOL measure is sensitive to change over time and examine its temporal relationship with other key outcome metrics.
Keywords: Quadruple Aim, single-item measures, social determinants of health, acute service utilization metrics.
The Triple Aim for health care—improving the individual experience of care, increasing the health of populations, and reducing the costs of care—was first proposed in 2008.1 More recently, some have advocated for an expanded focus to include a fourth aim: the quality of staff work life.2 Since this seminal paper was published, many health care systems have endeavored to adopt and implement the Quadruple Aim3,4; however, the concepts representing each of the aims are not universally defined,3 nor are the measures needed to populate the Quadruple Aim always available within the health system in question.5
Although several assessment models and frameworks that provide guidance to stakeholders have been developed,6,7 it is ultimately up to organizations themselves to determine which measures they should deploy to best represent the different quadrants of the Quadruple Aim.6 Evidence suggests, however, that quality measurement, and the administrative time required to conduct it, can be both financially and emotionally burdensome to providers and health systems.8-10 Thus, it is incumbent on organizations to select a set of measures that are not only meaningful but as parsimonious as possible.6,11,12
Quality of life (QOL) is a potential candidate to assess the aim of population health. Brief health-related QOL questions have long been used in epidemiological surveys, such as the Behavioral Risk Factor Surveillance System survey.13 Such questions are also a key component of community health frameworks, such as the County Health Rankings developed by the University of Wisconsin Population Health Institute.14 Furthermore, Humana recently revealed that increasing the number of physical and mental health “Healthy Days” (which are among the Centers for Disease Control and Prevention’s Health-Related Quality of Life questions15) among the members enrolled in their insurance plan would become a major goal for the organization.16,17 Many of these measures, while brief, focus on QOL as a function of health, often as a self-rated construct (from “Poor” to “Excellent”) or in the form of days of poor physical or mental health in the past 30 days,15 rather than evaluating QOL itself; however, several authors have pointed out that health status and QOL are related but distinct concepts.18,19
Brief single-item assessments focused specifically on QOL have been developed and implemented within nonclinical20 and clinical populations, including individuals with cancer,21 adults with disabilities,22 individuals with cystic fibrosis,23 and children with epilepsy.24 Despite the long history of QOL assessment in behavioral health treatment,25 single-item measures have not been widely implemented in this population.
Milwaukee County Behavioral Health Services (BHS), a publicly funded, county-based behavioral health care system in Milwaukee, Wisconsin, provides inpatient and ambulatory treatment, psychiatric emergency care, withdrawal management, care management, crisis services, and other support services to individuals in Milwaukee County. In 2018 the community services arm of BHS began implementing a single QOL question from the World Health Organization’s WHOQOL-BREF26: On a 5-point rating scale of “Very Poor” to “Very Good,” “How would you rate your overall quality of life right now?” Previous research by Atroszko and colleagues,20 which used a similar approach with the same item from the WHOQOL-BREF, reported correlations in the expected direction of the single-item QOL measure with perceived stress, depression, anxiety, loneliness, and daily hours of sleep. This study’s sample, however, comprised opportunistically recruited college students, not a clinical population. Further, the researchers did not examine the relationship of QOL with acute service utilization or other measures of the social determinants of health, such as housing, employment, or social connectedness.
The following study was designed to extend these results by focusing on a clinical population—individuals with mental health or substance use issues—being served in a large, publicly funded behavioral health system in Milwaukee, Wisconsin. The objective of this study was to determine whether a single-item QOL measure could be used as a brief, parsimonious measure of overall population health by examining its relationship with other key outcome measures for patients receiving services from BHS. This study was reviewed and approved by BHS’s Institutional Review Board.
Methods
All patients engaged in nonacute community services are offered a standardized assessment that includes, among other measures, items related to QOL, housing status, employment status, self-rated physical health, and social connectedness. This assessment is administered at intake, discharge, and every 6 months while patients are enrolled in services. Patients who received at least 1 assessment between October 1, 2020, and September 30, 2021, were included in the analyses. Patients receiving crisis, inpatient, or withdrawal management services alone (ie, did not receive any other community-based services) were not offered the standard assessment and thus were not included in the analyses. If patients had more than 1 assessment during this time period, QOL data from the last assessment were used. Data on housing (private residence status, defined as adults living alone or with others without supervision in a house or apartment), employment status, self-rated physical health, and social connectedness (measured by asking people whether they have had positive interactions with family or friends in the past 30 days) were extracted from the same timepoint as well.
Also included in the analyses were rates of acute service utilization, in which any patient with at least 1 visit to BHS’s psychiatric emergency department, withdrawal management facility, or psychiatric inpatient facility in the 90 days prior to the date of the assessment received a code of “Yes,” and any patient who did not receive any of these services received a code of “No.” Chi-square analyses were conducted to determine the relationship between QOL rankings (“Very Poor,” “Poor,” “Neither Good nor Poor,” “Good,” and “Very Good”) and housing, employment, self-rated physical health, social connectedness, and 90-day acute service use. All acute service utilization data were obtained from BHS’s electronic health records system. All data used in the study were stored on a secure, password-protected server. All analyses were conducted with SPSS software (SPSS 28; IBM).
Results
Data were available for 4488 patients who received an assessment between October 1, 2020, and September 30, 2021 (total numbers per item vary because some items had missing data; see supplementary eTables 1-3 for sample size per item). Demographics of the patient sample are listed in Table 1; the demographics of the patients who were missing data for specific outcomes are presented in eTables 1-3.
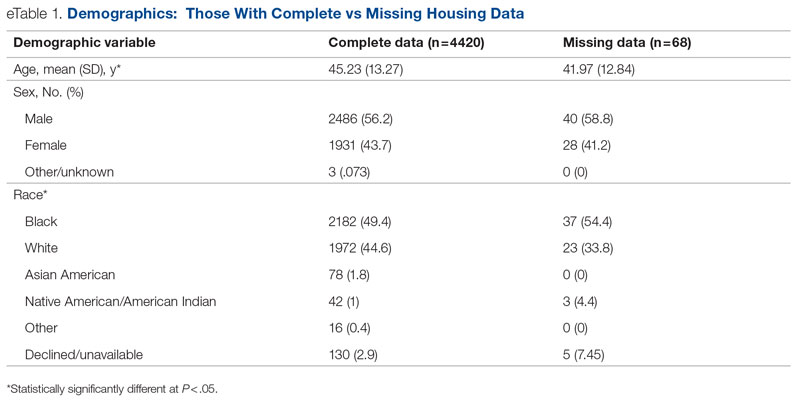
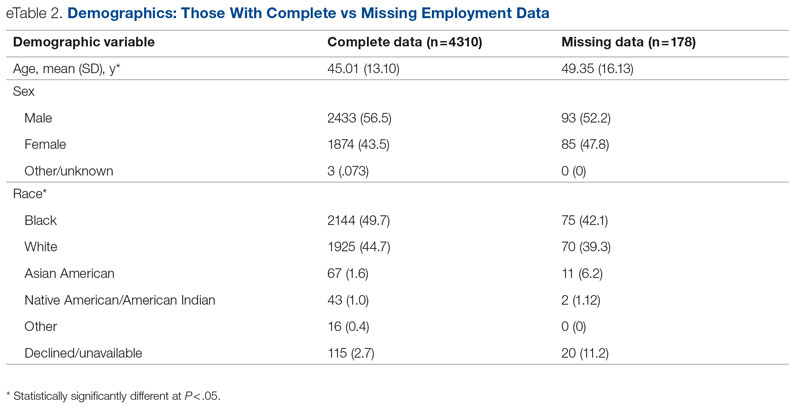
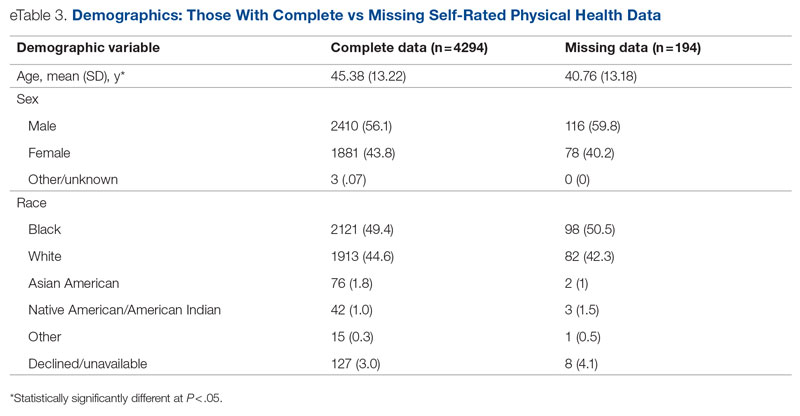
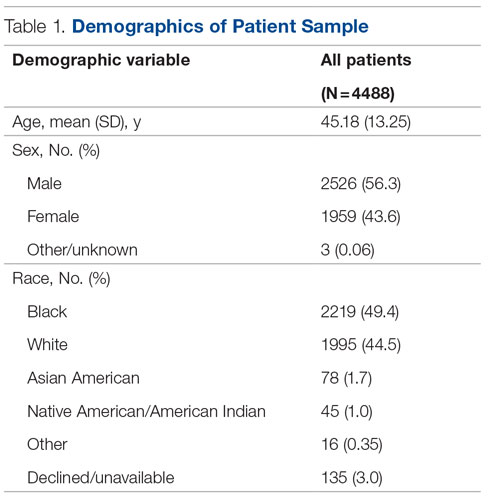
Statistical analyses revealed results in the expected direction for all relationships tested (Table 2). As patients’ self-reported QOL improved, so did the likelihood of higher rates of self-reported “Good” or better physical health, which was 576% higher among individuals who reported “Very Good” QOL relative to those who reported “Very Poor” QOL. Similarly, when compared with individuals with “Very Poor” QOL, individuals who reported “Very Good” QOL were 21.91% more likely to report having a private residence, 126.7% more likely to report being employed, and 29.17% more likely to report having had positive social interactions with family and friends in the past 30 days. There was an inverse relationship between QOL and the likelihood that a patient had received at least 1 admission for an acute service in the previous 90 days, such that patients who reported “Very Good” QOL were 86.34% less likely to have had an admission compared to patients with “Very Poor” QOL (2.8% vs 20.5%, respectively). The relationships among the criterion variables used in this study are presented in Table 3.
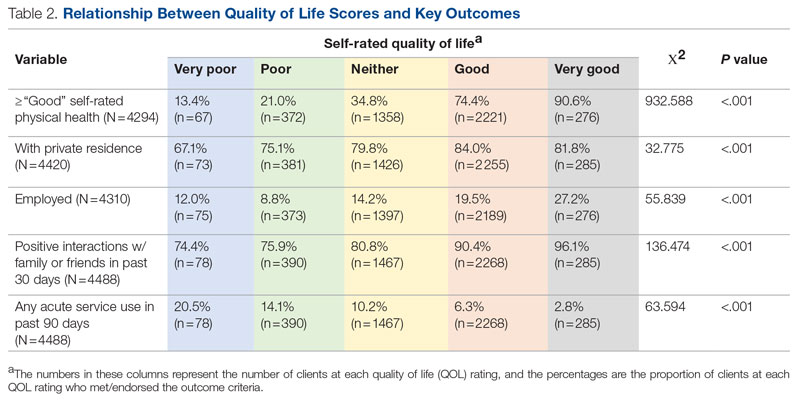
Discussion
The results of this preliminary analysis suggest that self-rated QOL is related to key health, social determinants of health, and acute service utilization metrics. These data are important for several reasons. First, because QOL is a diagnostically agnostic measure, it is a cross-cutting measure to use with clinically diverse populations receiving an array of different services. Second, at 1 item, the QOL measure is extremely brief and therefore minimally onerous to implement for both patients and administratively overburdened providers. Third, its correlation with other key metrics suggests that it can function as a broad population health measure for health care organizations because individuals with higher QOL will also likely have better outcomes in other key areas. This suggests that it has the potential to broadly represent the overall status of a population of patients, thus functioning as a type of “whole system” measure, which the Institute for Healthcare Improvement describes as “a small set of measures that reflect a health system’s overall performance on core dimensions of quality guided by the Triple Aim.”7 These whole system measures can help focus an organization’s strategic initiatives and efforts on the issues that matter most to the patients and community it serves.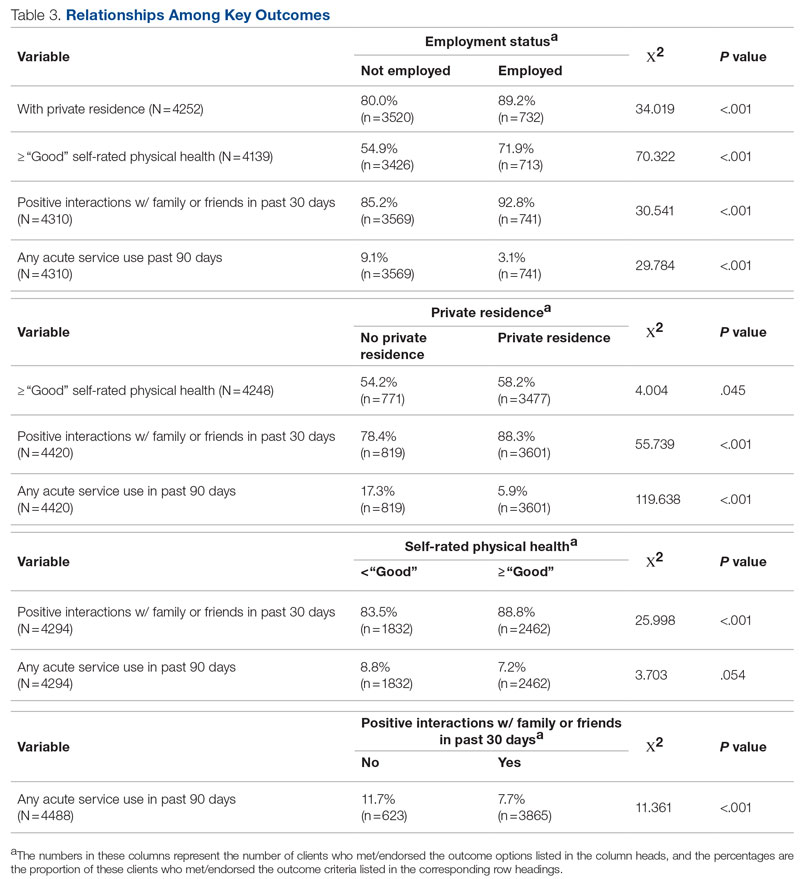
The relationship of QOL to acute service utilization deserves special mention. As an administrative measure, utilization is not susceptible to the same response bias as the other self-reported variables. Furthermore, acute services are costly to health systems, and hospital readmissions are associated with payment reductions in the Centers for Medicare and Medicaid Services (CMS) Hospital Readmissions Reduction Program for hospitals that fail to meet certain performance targets.27 Thus, because of its alignment with federal mandates, improved QOL (and potentially concomitant decreases in acute service use) may have significant financial implications for health systems as well.
This study was limited by several factors. First, it was focused on a population receiving publicly funded behavioral health services with strict eligibility requirements, one of which stipulated that individuals must be at 200% or less of the Federal Poverty Level; therefore, the results might not be applicable to health systems with a more clinically or socioeconomically diverse patient population. Second, because these data are cross-sectional, it was not possible to determine whether QOL improved over time or whether changes in QOL covaried longitudinally with the other metrics under observation. For example, if patients’ QOL improved from the first to last assessment, did their employment or residential status improve as well, or were these patients more likely to be employed at their first assessment? Furthermore, if there was covariance, did changes in employment, housing status, and so on precede changes in QOL or vice versa? Multiple longitudinal observations would help to address these questions and will be the focus of future analyses.
Conclusion
This preliminary study suggests that a single-item QOL measure may be a valuable population health–level metric for health systems. It requires little administrative effort on the part of either the clinician or patient. It is also agnostic with regard to clinical issue or treatment approach and can therefore admit of a range of diagnoses or patient-specific, idiosyncratic recovery goals. It is correlated with other key health, social determinants of health, and acute service utilization indicators and can therefore serve as a “whole system” measure because of its ability to broadly represent improvements in an entire population. Furthermore, QOL is patient-centered in that data are obtained through patient self-report, which is a high priority for CMS and other health care organizations.28 In summary, a single-item QOL measure holds promise for health care organizations looking to implement the Quadruple Aim and assess the health of the populations they serve in a manner that is simple, efficient, and patient-centered.
Acknowledgments: The author thanks Jennifer Wittwer for her thoughtful comments on the initial draft of this manuscript and Gary Kraft for his help extracting the data used in the analyses.
Corresponding author: Walter Matthew Drymalski, PhD; [email protected]
Disclosures: None reported.
From Milwaukee County Behavioral Health Services, Milwaukee, WI.
Abstract
Objectives: The goal of this study was to determine whether a single-item quality of life (QOL) measure could serve as a useful population health–level metric within the Quadruple Aim framework in a publicly funded behavioral health system.
Design: This was a retrospective, cross-sectional study that examined the correlation between the single-item QOL measure and several other key measures of the social determinants of health and a composite measure of acute service utilization for all patients receiving mental health and substance use services in a community behavioral health system.
Methods: Data were collected for 4488 patients who had at least 1 assessment between October 1, 2020, and September 30, 2021. Data on social determinants of health were obtained through patient self-report; acute service use data were obtained from electronic health records.
Results: Statistical analyses revealed results in the expected direction for all relationships tested. Patients with higher QOL were more likely to report “Good” or better self-rated physical health, be employed, have a private residence, and report recent positive social interactions, and were less likely to have received acute services in the previous 90 days.
Conclusion: A single-item QOL measure shows promise as a general, minimally burdensome whole-system metric that can function as a target for population health management efforts in a large behavioral health system. Future research should explore whether this QOL measure is sensitive to change over time and examine its temporal relationship with other key outcome metrics.
Keywords: Quadruple Aim, single-item measures, social determinants of health, acute service utilization metrics.
The Triple Aim for health care—improving the individual experience of care, increasing the health of populations, and reducing the costs of care—was first proposed in 2008.1 More recently, some have advocated for an expanded focus to include a fourth aim: the quality of staff work life.2 Since this seminal paper was published, many health care systems have endeavored to adopt and implement the Quadruple Aim3,4; however, the concepts representing each of the aims are not universally defined,3 nor are the measures needed to populate the Quadruple Aim always available within the health system in question.5
Although several assessment models and frameworks that provide guidance to stakeholders have been developed,6,7 it is ultimately up to organizations themselves to determine which measures they should deploy to best represent the different quadrants of the Quadruple Aim.6 Evidence suggests, however, that quality measurement, and the administrative time required to conduct it, can be both financially and emotionally burdensome to providers and health systems.8-10 Thus, it is incumbent on organizations to select a set of measures that are not only meaningful but as parsimonious as possible.6,11,12
Quality of life (QOL) is a potential candidate to assess the aim of population health. Brief health-related QOL questions have long been used in epidemiological surveys, such as the Behavioral Risk Factor Surveillance System survey.13 Such questions are also a key component of community health frameworks, such as the County Health Rankings developed by the University of Wisconsin Population Health Institute.14 Furthermore, Humana recently revealed that increasing the number of physical and mental health “Healthy Days” (which are among the Centers for Disease Control and Prevention’s Health-Related Quality of Life questions15) among the members enrolled in their insurance plan would become a major goal for the organization.16,17 Many of these measures, while brief, focus on QOL as a function of health, often as a self-rated construct (from “Poor” to “Excellent”) or in the form of days of poor physical or mental health in the past 30 days,15 rather than evaluating QOL itself; however, several authors have pointed out that health status and QOL are related but distinct concepts.18,19
Brief single-item assessments focused specifically on QOL have been developed and implemented within nonclinical20 and clinical populations, including individuals with cancer,21 adults with disabilities,22 individuals with cystic fibrosis,23 and children with epilepsy.24 Despite the long history of QOL assessment in behavioral health treatment,25 single-item measures have not been widely implemented in this population.
Milwaukee County Behavioral Health Services (BHS), a publicly funded, county-based behavioral health care system in Milwaukee, Wisconsin, provides inpatient and ambulatory treatment, psychiatric emergency care, withdrawal management, care management, crisis services, and other support services to individuals in Milwaukee County. In 2018 the community services arm of BHS began implementing a single QOL question from the World Health Organization’s WHOQOL-BREF26: On a 5-point rating scale of “Very Poor” to “Very Good,” “How would you rate your overall quality of life right now?” Previous research by Atroszko and colleagues,20 which used a similar approach with the same item from the WHOQOL-BREF, reported correlations in the expected direction of the single-item QOL measure with perceived stress, depression, anxiety, loneliness, and daily hours of sleep. This study’s sample, however, comprised opportunistically recruited college students, not a clinical population. Further, the researchers did not examine the relationship of QOL with acute service utilization or other measures of the social determinants of health, such as housing, employment, or social connectedness.
The following study was designed to extend these results by focusing on a clinical population—individuals with mental health or substance use issues—being served in a large, publicly funded behavioral health system in Milwaukee, Wisconsin. The objective of this study was to determine whether a single-item QOL measure could be used as a brief, parsimonious measure of overall population health by examining its relationship with other key outcome measures for patients receiving services from BHS. This study was reviewed and approved by BHS’s Institutional Review Board.
Methods
All patients engaged in nonacute community services are offered a standardized assessment that includes, among other measures, items related to QOL, housing status, employment status, self-rated physical health, and social connectedness. This assessment is administered at intake, discharge, and every 6 months while patients are enrolled in services. Patients who received at least 1 assessment between October 1, 2020, and September 30, 2021, were included in the analyses. Patients receiving crisis, inpatient, or withdrawal management services alone (ie, did not receive any other community-based services) were not offered the standard assessment and thus were not included in the analyses. If patients had more than 1 assessment during this time period, QOL data from the last assessment were used. Data on housing (private residence status, defined as adults living alone or with others without supervision in a house or apartment), employment status, self-rated physical health, and social connectedness (measured by asking people whether they have had positive interactions with family or friends in the past 30 days) were extracted from the same timepoint as well.
Also included in the analyses were rates of acute service utilization, in which any patient with at least 1 visit to BHS’s psychiatric emergency department, withdrawal management facility, or psychiatric inpatient facility in the 90 days prior to the date of the assessment received a code of “Yes,” and any patient who did not receive any of these services received a code of “No.” Chi-square analyses were conducted to determine the relationship between QOL rankings (“Very Poor,” “Poor,” “Neither Good nor Poor,” “Good,” and “Very Good”) and housing, employment, self-rated physical health, social connectedness, and 90-day acute service use. All acute service utilization data were obtained from BHS’s electronic health records system. All data used in the study were stored on a secure, password-protected server. All analyses were conducted with SPSS software (SPSS 28; IBM).
Results
Data were available for 4488 patients who received an assessment between October 1, 2020, and September 30, 2021 (total numbers per item vary because some items had missing data; see supplementary eTables 1-3 for sample size per item). Demographics of the patient sample are listed in Table 1; the demographics of the patients who were missing data for specific outcomes are presented in eTables 1-3.
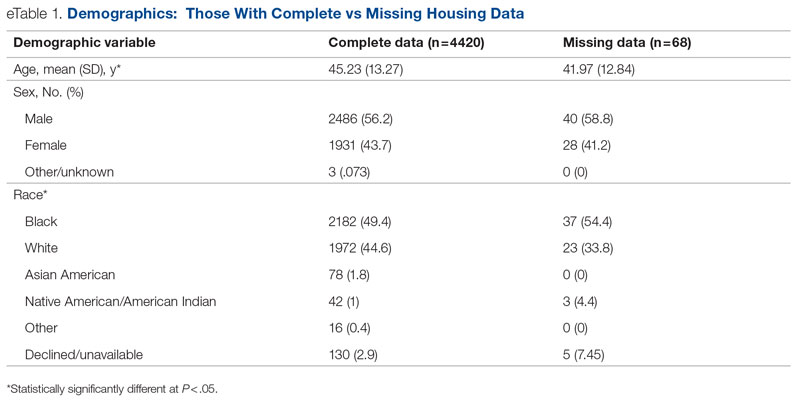
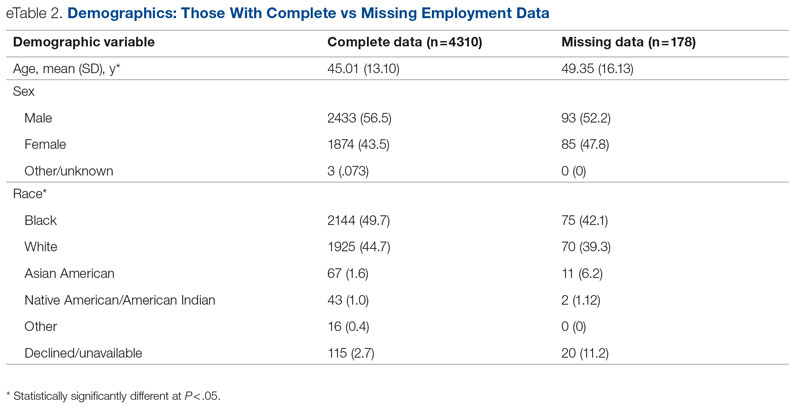
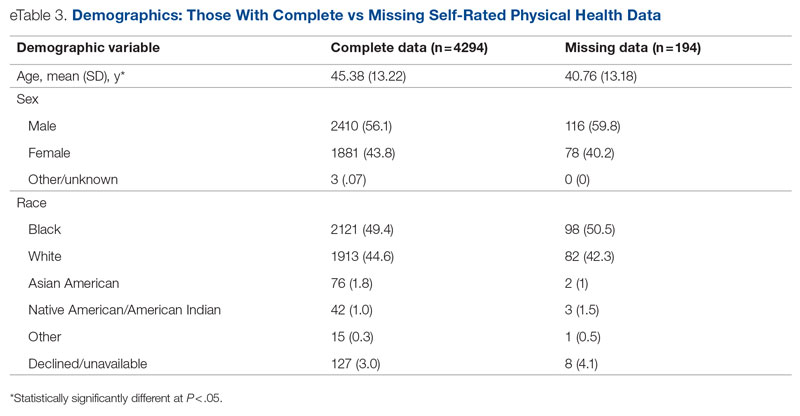
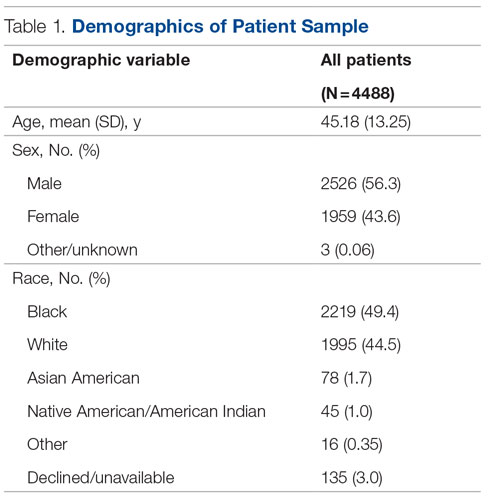
Statistical analyses revealed results in the expected direction for all relationships tested (Table 2). As patients’ self-reported QOL improved, so did the likelihood of higher rates of self-reported “Good” or better physical health, which was 576% higher among individuals who reported “Very Good” QOL relative to those who reported “Very Poor” QOL. Similarly, when compared with individuals with “Very Poor” QOL, individuals who reported “Very Good” QOL were 21.91% more likely to report having a private residence, 126.7% more likely to report being employed, and 29.17% more likely to report having had positive social interactions with family and friends in the past 30 days. There was an inverse relationship between QOL and the likelihood that a patient had received at least 1 admission for an acute service in the previous 90 days, such that patients who reported “Very Good” QOL were 86.34% less likely to have had an admission compared to patients with “Very Poor” QOL (2.8% vs 20.5%, respectively). The relationships among the criterion variables used in this study are presented in Table 3.
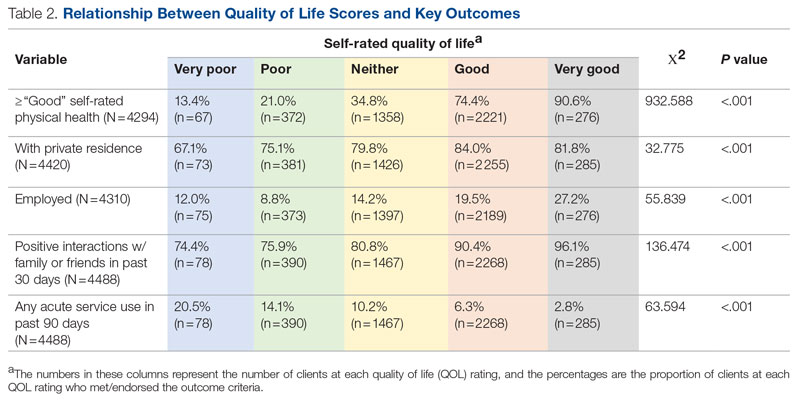
Discussion
The results of this preliminary analysis suggest that self-rated QOL is related to key health, social determinants of health, and acute service utilization metrics. These data are important for several reasons. First, because QOL is a diagnostically agnostic measure, it is a cross-cutting measure to use with clinically diverse populations receiving an array of different services. Second, at 1 item, the QOL measure is extremely brief and therefore minimally onerous to implement for both patients and administratively overburdened providers. Third, its correlation with other key metrics suggests that it can function as a broad population health measure for health care organizations because individuals with higher QOL will also likely have better outcomes in other key areas. This suggests that it has the potential to broadly represent the overall status of a population of patients, thus functioning as a type of “whole system” measure, which the Institute for Healthcare Improvement describes as “a small set of measures that reflect a health system’s overall performance on core dimensions of quality guided by the Triple Aim.”7 These whole system measures can help focus an organization’s strategic initiatives and efforts on the issues that matter most to the patients and community it serves.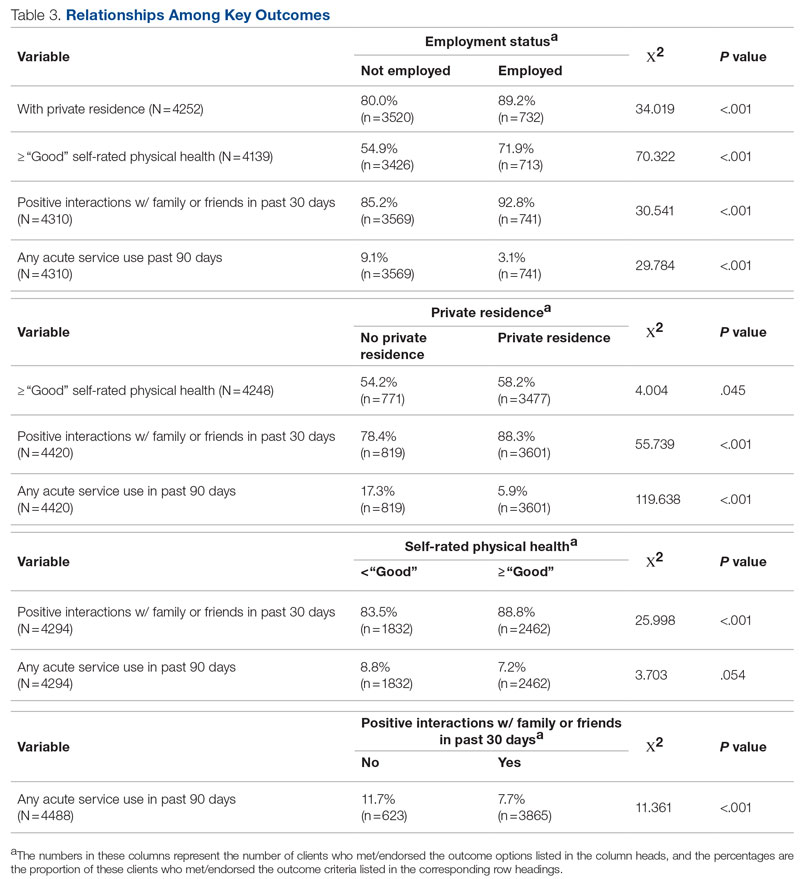
The relationship of QOL to acute service utilization deserves special mention. As an administrative measure, utilization is not susceptible to the same response bias as the other self-reported variables. Furthermore, acute services are costly to health systems, and hospital readmissions are associated with payment reductions in the Centers for Medicare and Medicaid Services (CMS) Hospital Readmissions Reduction Program for hospitals that fail to meet certain performance targets.27 Thus, because of its alignment with federal mandates, improved QOL (and potentially concomitant decreases in acute service use) may have significant financial implications for health systems as well.
This study was limited by several factors. First, it was focused on a population receiving publicly funded behavioral health services with strict eligibility requirements, one of which stipulated that individuals must be at 200% or less of the Federal Poverty Level; therefore, the results might not be applicable to health systems with a more clinically or socioeconomically diverse patient population. Second, because these data are cross-sectional, it was not possible to determine whether QOL improved over time or whether changes in QOL covaried longitudinally with the other metrics under observation. For example, if patients’ QOL improved from the first to last assessment, did their employment or residential status improve as well, or were these patients more likely to be employed at their first assessment? Furthermore, if there was covariance, did changes in employment, housing status, and so on precede changes in QOL or vice versa? Multiple longitudinal observations would help to address these questions and will be the focus of future analyses.
Conclusion
This preliminary study suggests that a single-item QOL measure may be a valuable population health–level metric for health systems. It requires little administrative effort on the part of either the clinician or patient. It is also agnostic with regard to clinical issue or treatment approach and can therefore admit of a range of diagnoses or patient-specific, idiosyncratic recovery goals. It is correlated with other key health, social determinants of health, and acute service utilization indicators and can therefore serve as a “whole system” measure because of its ability to broadly represent improvements in an entire population. Furthermore, QOL is patient-centered in that data are obtained through patient self-report, which is a high priority for CMS and other health care organizations.28 In summary, a single-item QOL measure holds promise for health care organizations looking to implement the Quadruple Aim and assess the health of the populations they serve in a manner that is simple, efficient, and patient-centered.
Acknowledgments: The author thanks Jennifer Wittwer for her thoughtful comments on the initial draft of this manuscript and Gary Kraft for his help extracting the data used in the analyses.
Corresponding author: Walter Matthew Drymalski, PhD; [email protected]
Disclosures: None reported.
1. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759-769. doi:10.1377/hlthaff.27.3.759
2. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-576. doi:10.1370/afm.1713
3. Hendrikx RJP, Drewes HW, Spreeuwenberg M, et al. Which triple aim related measures are being used to evaluate population management initiatives? An international comparative analysis. Health Policy. 2016;120(5):471-485. doi:10.1016/j.healthpol.2016.03.008
4. Whittington JW, Nolan K, Lewis N, Torres T. Pursuing the triple aim: the first 7 years. Milbank Q. 2015;93(2):263-300. doi:10.1111/1468-0009.12122
5. Ryan BL, Brown JB, Glazier RH, Hutchison B. Examining primary healthcare performance through a triple aim lens. Healthc Policy. 2016;11(3):19-31.
6. Stiefel M, Nolan K. A guide to measuring the Triple Aim: population health, experience of care, and per capita cost. Institute for Healthcare Improvement; 2012. Accessed November 1, 2022. https://nhchc.org/wp-content/uploads/2019/08/ihiguidetomeasuringtripleaimwhitepaper2012.pdf
7. Martin L, Nelson E, Rakover J, Chase A. Whole system measures 2.0: a compass for health system leaders. Institute for Healthcare Improvement; 2016. Accessed November 1, 2022. http://www.ihi.org:80/resources/Pages/IHIWhitePapers/Whole-System-Measures-Compass-for-Health-System-Leaders.aspx
8. Casalino LP, Gans D, Weber R, et al. US physician practices spend more than $15.4 billion annually to report quality measures. Health Aff (Millwood). 2016;35(3):401-406. doi:10.1377/hlthaff.2015.1258
9. Rao SK, Kimball AB, Lehrhoff SR, et al. The impact of administrative burden on academic physicians: results of a hospital-wide physician survey. Acad Med. 2017;92(2):237-243. doi:10.1097/ACM.0000000000001461
10. Woolhandler S, Himmelstein DU. Administrative work consumes one-sixth of U.S. physicians’ working hours and lowers their career satisfaction. Int J Health Serv. 2014;44(4):635-642. doi:10.2190/HS.44.4.a
11. Meyer GS, Nelson EC, Pryor DB, et al. More quality measures versus measuring what matters: a call for balance and parsimony. BMJ Qual Saf. 2012;21(11):964-968. doi:10.1136/bmjqs-2012-001081
12. Vital Signs: Core Metrics for Health and Health Care Progress. Washington, DC: National Academies Press; 2015. doi:10.17226/19402
13. Centers for Disease Control and Prevention. BRFSS questionnaires. Accessed November 1, 2022. https://www.cdc.gov/brfss/questionnaires/index.htm
14. County Health Rankings and Roadmaps. Measures & data sources. University of Wisconsin Population Health Institute. Accessed November 1, 2022. https://www.countyhealthrankings.org/explore-health-rankings/measures-data-sources
15. Centers for Disease Control and Prevention. Healthy days core module (CDC HRQOL-4). Accessed November 1, 2022. https://www.cdc.gov/hrqol/hrqol14_measure.htm
16. Cordier T, Song Y, Cambon J, et al. A bold goal: more healthy days through improved community health. Popul Health Manag. 2018;21(3):202-208. doi:10.1089/pop.2017.0142
17. Slabaugh SL, Shah M, Zack M, et al. Leveraging health-related quality of life in population health management: the case for healthy days. Popul Health Manag. 2017;20(1):13-22. doi:10.1089/pop.2015.0162
18. Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics. 2016;34(7):645-649. doi:10.1007/s40273-016-0389-9
19. Smith KW, Avis NE, Assmann SF. Distinguishing between quality of life and health status in quality of life research: a meta-analysis. Qual Life Res. 1999;8(5):447-459. doi:10.1023/a:1008928518577
20. Atroszko PA, Baginska P, Mokosinska M, et al. Validity and reliability of single-item self-report measures of general quality of life, general health and sleep quality. In: CER Comparative European Research 2015. Sciemcee Publishing; 2015:207-211.
21. Singh JA, Satele D, Pattabasavaiah S, et al. Normative data and clinically significant effect sizes for single-item numerical linear analogue self-assessment (LASA) scales. Health Qual Life Outcomes. 2014;12:187. doi:10.1186/s12955-014-0187-z
22. Siebens HC, Tsukerman D, Adkins RH, et al. Correlates of a single-item quality-of-life measure in people aging with disabilities. Am J Phys Med Rehabil. 2015;94(12):1065-1074. doi:10.1097/PHM.0000000000000298
23. Yohannes AM, Dodd M, Morris J, Webb K. Reliability and validity of a single item measure of quality of life scale for adult patients with cystic fibrosis. Health Qual Life Outcomes. 2011;9:105. doi:10.1186/1477-7525-9-105
24. Conway L, Widjaja E, Smith ML. Single-item measure for assessing quality of life in children with drug-resistant epilepsy. Epilepsia Open. 2017;3(1):46-54. doi:10.1002/epi4.12088
25. Barry MM, Zissi A. Quality of life as an outcome measure in evaluating mental health services: a review of the empirical evidence. Soc Psychiatry Psychiatr Epidemiol. 1997;32(1):38-47. doi:10.1007/BF00800666
26. Skevington SM, Lotfy M, O’Connell KA. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. Qual Life Res. 2004;13(2):299-310. doi:10.1023/B:QURE.0000018486.91360.00
27. Centers for Medicare & Medicaid Services. Hospital readmissions reduction program (HRRP). Accessed November 1, 2022. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program
28. Centers for Medicare & Medicaid Services. Patient-reported outcome measures. CMS Measures Management System. Published May 2022. Accessed November 1, 2022. https://www.cms.gov/files/document/blueprint-patient-reported-outcome-measures.pdf
1. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759-769. doi:10.1377/hlthaff.27.3.759
2. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-576. doi:10.1370/afm.1713
3. Hendrikx RJP, Drewes HW, Spreeuwenberg M, et al. Which triple aim related measures are being used to evaluate population management initiatives? An international comparative analysis. Health Policy. 2016;120(5):471-485. doi:10.1016/j.healthpol.2016.03.008
4. Whittington JW, Nolan K, Lewis N, Torres T. Pursuing the triple aim: the first 7 years. Milbank Q. 2015;93(2):263-300. doi:10.1111/1468-0009.12122
5. Ryan BL, Brown JB, Glazier RH, Hutchison B. Examining primary healthcare performance through a triple aim lens. Healthc Policy. 2016;11(3):19-31.
6. Stiefel M, Nolan K. A guide to measuring the Triple Aim: population health, experience of care, and per capita cost. Institute for Healthcare Improvement; 2012. Accessed November 1, 2022. https://nhchc.org/wp-content/uploads/2019/08/ihiguidetomeasuringtripleaimwhitepaper2012.pdf
7. Martin L, Nelson E, Rakover J, Chase A. Whole system measures 2.0: a compass for health system leaders. Institute for Healthcare Improvement; 2016. Accessed November 1, 2022. http://www.ihi.org:80/resources/Pages/IHIWhitePapers/Whole-System-Measures-Compass-for-Health-System-Leaders.aspx
8. Casalino LP, Gans D, Weber R, et al. US physician practices spend more than $15.4 billion annually to report quality measures. Health Aff (Millwood). 2016;35(3):401-406. doi:10.1377/hlthaff.2015.1258
9. Rao SK, Kimball AB, Lehrhoff SR, et al. The impact of administrative burden on academic physicians: results of a hospital-wide physician survey. Acad Med. 2017;92(2):237-243. doi:10.1097/ACM.0000000000001461
10. Woolhandler S, Himmelstein DU. Administrative work consumes one-sixth of U.S. physicians’ working hours and lowers their career satisfaction. Int J Health Serv. 2014;44(4):635-642. doi:10.2190/HS.44.4.a
11. Meyer GS, Nelson EC, Pryor DB, et al. More quality measures versus measuring what matters: a call for balance and parsimony. BMJ Qual Saf. 2012;21(11):964-968. doi:10.1136/bmjqs-2012-001081
12. Vital Signs: Core Metrics for Health and Health Care Progress. Washington, DC: National Academies Press; 2015. doi:10.17226/19402
13. Centers for Disease Control and Prevention. BRFSS questionnaires. Accessed November 1, 2022. https://www.cdc.gov/brfss/questionnaires/index.htm
14. County Health Rankings and Roadmaps. Measures & data sources. University of Wisconsin Population Health Institute. Accessed November 1, 2022. https://www.countyhealthrankings.org/explore-health-rankings/measures-data-sources
15. Centers for Disease Control and Prevention. Healthy days core module (CDC HRQOL-4). Accessed November 1, 2022. https://www.cdc.gov/hrqol/hrqol14_measure.htm
16. Cordier T, Song Y, Cambon J, et al. A bold goal: more healthy days through improved community health. Popul Health Manag. 2018;21(3):202-208. doi:10.1089/pop.2017.0142
17. Slabaugh SL, Shah M, Zack M, et al. Leveraging health-related quality of life in population health management: the case for healthy days. Popul Health Manag. 2017;20(1):13-22. doi:10.1089/pop.2015.0162
18. Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics. 2016;34(7):645-649. doi:10.1007/s40273-016-0389-9
19. Smith KW, Avis NE, Assmann SF. Distinguishing between quality of life and health status in quality of life research: a meta-analysis. Qual Life Res. 1999;8(5):447-459. doi:10.1023/a:1008928518577
20. Atroszko PA, Baginska P, Mokosinska M, et al. Validity and reliability of single-item self-report measures of general quality of life, general health and sleep quality. In: CER Comparative European Research 2015. Sciemcee Publishing; 2015:207-211.
21. Singh JA, Satele D, Pattabasavaiah S, et al. Normative data and clinically significant effect sizes for single-item numerical linear analogue self-assessment (LASA) scales. Health Qual Life Outcomes. 2014;12:187. doi:10.1186/s12955-014-0187-z
22. Siebens HC, Tsukerman D, Adkins RH, et al. Correlates of a single-item quality-of-life measure in people aging with disabilities. Am J Phys Med Rehabil. 2015;94(12):1065-1074. doi:10.1097/PHM.0000000000000298
23. Yohannes AM, Dodd M, Morris J, Webb K. Reliability and validity of a single item measure of quality of life scale for adult patients with cystic fibrosis. Health Qual Life Outcomes. 2011;9:105. doi:10.1186/1477-7525-9-105
24. Conway L, Widjaja E, Smith ML. Single-item measure for assessing quality of life in children with drug-resistant epilepsy. Epilepsia Open. 2017;3(1):46-54. doi:10.1002/epi4.12088
25. Barry MM, Zissi A. Quality of life as an outcome measure in evaluating mental health services: a review of the empirical evidence. Soc Psychiatry Psychiatr Epidemiol. 1997;32(1):38-47. doi:10.1007/BF00800666
26. Skevington SM, Lotfy M, O’Connell KA. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. Qual Life Res. 2004;13(2):299-310. doi:10.1023/B:QURE.0000018486.91360.00
27. Centers for Medicare & Medicaid Services. Hospital readmissions reduction program (HRRP). Accessed November 1, 2022. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program
28. Centers for Medicare & Medicaid Services. Patient-reported outcome measures. CMS Measures Management System. Published May 2022. Accessed November 1, 2022. https://www.cms.gov/files/document/blueprint-patient-reported-outcome-measures.pdf
Neurosurgery Operating Room Efficiency During the COVID-19 Era
From the Department of Neurological Surgery, Vanderbilt University Medical Center, Nashville, TN (Stefan W. Koester, Puja Jagasia, and Drs. Liles, Dambrino IV, Feldman, and Chambless), and the Department of Anesthesiology, Vanderbilt University Medical Center, Nashville, TN (Drs. Mathews and Tiwari).
ABSTRACT
Background: The COVID-19 pandemic has had broad effects on surgical care, including operating room (OR) staffing, personal protective equipment (PPE) utilization, and newly implemented anti-infective measures. Our aim was to assess neurosurgery OR efficiency before the COVID-19 pandemic, during peak COVID-19, and during current times.
Methods: Institutional perioperative databases at a single, high-volume neurosurgical center were queried for operations performed from December 2019 until October 2021. March 12, 2020, the day that the state of Tennessee declared a state of emergency, was chosen as the onset of the COVID-19 pandemic. The 90-day periods before and after this day were used to define the pre-COVID-19, peak-COVID-19, and post-peak restrictions time periods for comparative analysis. Outcomes included delay in first-start and OR turnover time between neurosurgical cases. Preset threshold times were used in analyses to adjust for normal leniency in OR scheduling (15 minutes for first start and 90 minutes for turnover). Univariate analysis used Wilcoxon rank-sum test for continuous outcomes, while chi-square test and Fisher’s exact test were used for categorical comparisons. Significance was defined as P < .05.
Results: First-start time was analyzed in 426 pre-COVID-19, 357 peak-restrictions, and 2304 post-peak-restrictions cases. The unadjusted mean delay length was found to be significantly different between the time periods, but the magnitude of increase in minutes was immaterial (mean [SD] minutes, 6 [18] vs 10 [21] vs 8 [20], respectively; P = .004). The adjusted average delay length and proportion of cases delayed beyond the 15-minute threshold were not significantly different. The proportion of cases that started early, as well as significantly early past a 15-minute threshold, have not been impacted. There was no significant change in turnover time during peak restrictions relative to the pre-COVID-19 period (88 [100] minutes vs 85 [95] minutes), and turnover time has since remained unchanged (83 [87] minutes).
Conclusion: Our center was able to maintain OR efficiency before, during, and after peak restrictions even while instituting advanced infection-control strategies. While there were significant changes, delays were relatively small in magnitude.
Keywords: operating room timing, hospital efficiency, socioeconomics, pandemic.
The COVID-19 pandemic has led to major changes in patient care both from a surgical perspective and in regard to inpatient hospital course. Safety protocols nationwide have been implemented to protect both patients and providers. Some elements of surgical care have drastically changed, including operating room (OR) staffing, personal protective equipment (PPE) utilization, and increased sterilization measures. Furloughs, layoffs, and reassignments due to the focus on nonelective and COVID-19–related cases challenged OR staffing and efficiency. Operating room staff with COVID-19 exposures or COVID-19 infections also caused last-minute changes in staffing. All of these scenarios can cause issues due to actual understaffing or due to staff members being pushed into highly specialized areas, such as neurosurgery, in which they have very little experience. A further obstacle to OR efficiency included policy changes involving PPE utilization, sterilization measures, and supply chain shortages of necessary resources such as PPE.
Neurosurgery in particular has been susceptible to COVID-19–related system-wide changes given operator proximity to the patient’s respiratory passages, frequency of emergent cases, and varying anesthetic needs, as well as the high level of specialization needed to perform neurosurgical care. Previous studies have shown a change in the makeup of neurosurgical patients seeking care, as well as in the acuity of neurological consult of these patients.1 A study in orthopedic surgery by Andreata et al demonstrated worsened OR efficiency, with significantly increased first-start and turnover times.2 In the COVID-19 era, OR quality and safety are crucially important to both patients and providers. Providing this safe and effective care in an efficient manner is important for optimal neurosurgical management in the long term.3 Moreover, the financial burden of implementing new protocols and standards can be compounded by additional financial losses due to reduced OR efficiency.
Methods
To analyze the effect of COVID-19 on neurosurgical OR efficiency, institutional perioperative databases at a single high-volume center were queried for operations performed from December 2019 until October 2021. March 12, 2020, was chosen as the onset of COVID-19 for analytic purposes, as this was the date when the state of Tennessee declared a state of emergency. The 90-day periods before and after this date were used for comparative analysis for pre-COVID-19, peak COVID-19, and post-peak-restrictions time periods. The peak COVID-19 period was defined as the 90-day period following the initial onset of COVID-19 and the surge of cases. For comparison purposes, post-peak COVID-19 was defined as the months following the first peak until October 2021 (approximately 17 months). COVID-19 burden was determined using a COVID-19 single-institution census of confirmed cases by polymerase chain reaction (PCR) for which the average number of cases of COVID-19 during a given month was determined. This number is a scaled trend, and a true number of COVID-19 cases in our hospital was not reported.
Neurosurgical and neuroendovascular cases were included in the analysis. Outcomes included delay in first-start and OR turnover time between neurosurgical cases, defined as the time from the patient leaving the room until the next patient entered the room. Preset threshold times were used in analyses to adjust for normal leniency in OR scheduling (15 minutes for first start and 90 minutes for turnover, which is a standard for our single-institution perioperative center). Statistical analyses, including data aggregation, were performed using R, version 4.0.1 (R Foundation for Statistical Computing). Patients’ demographic and clinical characteristics were analyzed using an independent 2-sample t-test for interval variables and a chi-square test for categorical variables. Significance was defined as P < .05.
Results
First-Start Time
First-start time was analyzed in 426 pre-COVID-19, 357 peak-COVID-19, and 2304 post-peak-COVID-19 cases. The unadjusted mean delay length was significantly different between the time periods, but the magnitude of increase in minutes was immaterial (mean [SD] minutes, 6 [18] vs 10 [21] vs 8 [20], respectively; P = .004) (Table 1). 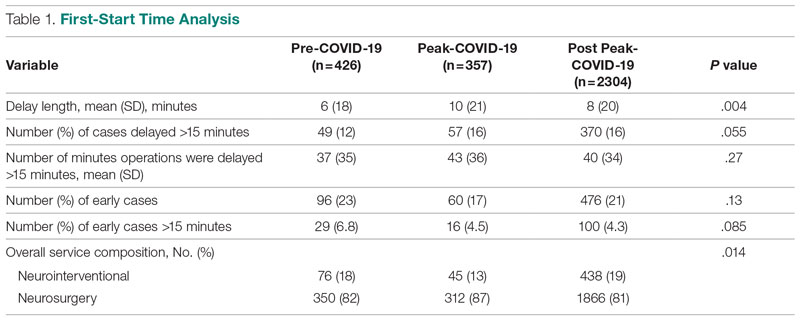
The adjusted average delay length and proportion of cases delayed beyond the 15-minute threshold were not significantly different, but they have been slightly higher since the onset of COVID-19. The proportion of cases that have started early, as well as significantly early past a 15-minute threshold, have also trended down since the onset of the COVID-19 pandemic, but this difference was again not significant. The temporal relationship of first-start delay, both unadjusted and adjusted, from December 2019 to October 2021 is shown in Figure 1. The trend of increasing delay is loosely associated with the COVID-19 burden experienced by our hospital. The start of COVID-19 as well as both COVID-19 peaks have been associated with increased delays in our hospital.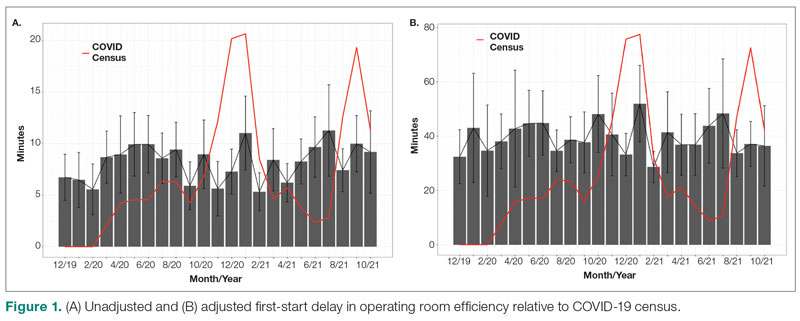
Turnover Time
Turnover time was assessed in 437 pre-COVID-19, 278 peak-restrictions, and 2411 post-peak-restrictions cases. Turnover time during peak restrictions was not significantly different from pre-COVID-19 (88 [100] vs 85 [95]) and has since remained relatively unchanged (83 [87], P = .78). A similar trend held for comparisons of proportion of cases with turnover time past 90 minutes and average times past the 90-minute threshold (Table 2). The temporal relationship between COVID-19 burden and turnover time, both unadjusted and adjusted, from December 2019 to October 2021 is shown in Figure 2. Both figures demonstrate a slight initial increase in turnover time delay at the start of COVID-19, which stabilized with little variation thereafter.
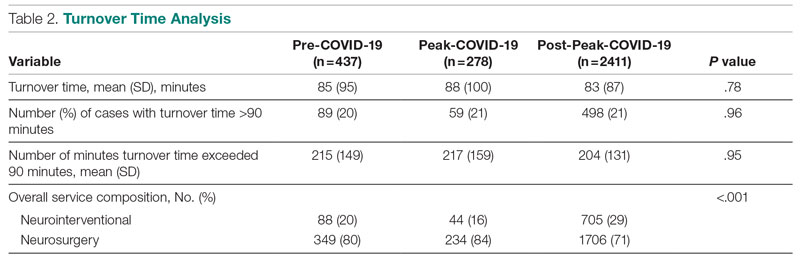
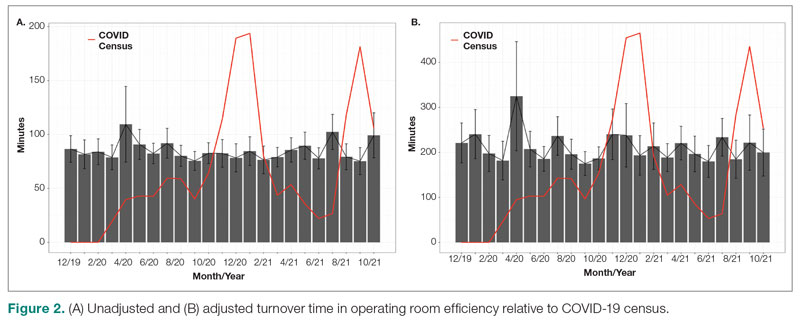
Discussion
We analyzed the OR efficiency metrics of first-start and turnover time during the 90-day period before COVID-19 (pre-COVID-19), the 90 days following Tennessee declaring a state of emergency (peak COVID-19), and the time following this period (post-COVID-19) for all neurosurgical and neuroendovascular cases at Vanderbilt University Medical Center (VUMC). We found a significant difference in unadjusted mean delay length in first-start time between the time periods, but the magnitude of increase in minutes was immaterial (mean [SD] minutes for pre-COVID-19, peak-COVID-19, and post-COVID-19: 6 [18] vs 10 [21] vs 8 [20], respectively; P = .004). No significant increase in turnover time between cases was found between these 3 time periods. Based on metrics from first-start delay and turnover time, our center was able to maintain OR efficiency before, during, and after peak COVID-19.
After the Centers for Disease Control and Prevention released guidelines recommending deferring elective procedures to conserve beds and PPE, VUMC made the decision to suspend all elective surgical procedures from March 18 to April 24, 2020. Prior research conducted during the COVID-19 pandemic has demonstrated more than 400 types of surgical procedures with negatively impacted outcomes when compared to surgical outcomes from the same time frame in 2018 and 2019.4 For more than 20 of these types of procedures, there was a significant association between procedure delay and adverse patient outcomes.4 Testing protocols for patients prior to surgery varied throughout the pandemic based on vaccination status and type of procedure. Before vaccines became widely available, all patients were required to obtain a PCR SARS-CoV-2 test within 48 to 72 hours of the scheduled procedure. If the patient’s procedure was urgent and testing was not feasible, the patient was treated as a SARS-CoV-2–positive patient, which required all health care workers involved in the case to wear gowns, gloves, surgical masks, and eye protection. Testing patients preoperatively likely helped to maintain OR efficiency since not all patients received test results prior to the scheduled procedure, leading to cancellations of cases and therefore more staff available for fewer cases.
After vaccines became widely available to the public, testing requirements for patients preoperatively were relaxed, and only patients who were not fully vaccinated or severely immunocompromised were required to test prior to procedures. However, approximately 40% of the population in Tennessee was fully vaccinated in 2021, which reflects the patient population of VUMC.5 This means that many patients who received care at VUMC were still tested prior to procedures.
Adopting adequate safety protocols was found to be key for OR efficiency during the COVID-19 pandemic since performing surgery increased the risk of infection for each health care worker in the OR.6 VUMC protocols identified procedures that required enhanced safety measures to prevent infection of health care workers and avoid staffing shortages, which would decrease OR efficiency. Protocols mandated that only anesthesia team members were allowed to be in the OR during intubation and extubation of patients, which could be one factor leading to increased delays and decreased efficiency for some institutions. Methods for neurosurgeons to decrease risk of infection in the OR include postponing all nonurgent cases, reappraising the necessity for general anesthesia and endotracheal intubation, considering alternative surgical approaches that avoid the respiratory tract, and limiting the use of aerosol-generating instruments.7,8 VUMC’s success in implementing these protocols likely explains why our center was able to maintain OR efficiency throughout the COVID-19 pandemic.
A study conducted by Andreata et al showed a significantly increased mean first-case delay and a nonsignificant increased turnover time in orthopedic surgeries in Northern Italy when comparing surgeries performed during the COVID-19 pandemic to those performed prior to COVID-19.2 Other studies have indicated a similar trend in decreased OR efficiency during COVID-19 in other areas around the world.9,10 These findings are not consistent with our own findings for neurosurgical and neuroendovascular surgeries at VUMC, and any change at our institution was relatively immaterial. Factors that threatened to change OR efficiency—but did not result in meaningful changes in our institutional experience—include delays due to pending COVID-19 test results, safety procedures such as PPE donning, and planning difficulties to ensure the existence of teams with non-overlapping providers in the case of a surgeon being infected.2,11-13
Globally, many surgery centers halted all elective surgeries during the initial COVID-19 spike to prevent a PPE shortage and mitigate risk of infection of patients and health care workers.8,12,14 However, there is no centralized definition of which neurosurgical procedures are elective, so that decision was made on a surgeon or center level, which could lead to variability in efficiency trends.14 One study on neurosurgical procedures during COVID-19 found a 30% decline in all cases and a 23% decline in emergent procedures, showing that the decrease in volume was not only due to cancellation of elective procedures.15 This decrease in elective and emergent surgeries created a backlog of surgeries as well as a loss in health care revenue, and caused many patients to go without adequate health care.10 Looking forward, it is imperative that surgical centers study trends in OR efficiency from COVID-19 and learn how to better maintain OR efficiency during future pandemic conditions to prevent a backlog of cases, loss of health care revenue, and decreased health care access.
Limitations
Our data are from a single center and therefore may not be representative of experiences of other hospitals due to different populations and different impacts from COVID-19. However, given our center’s high volume and diverse patient population, we believe our analysis highlights important trends in neurosurgery practice. Notably, data for patient and OR timing are digitally generated and are entered manually by nurses in the electronic medical record, making it prone to errors and variability. This is in our experience, and if any error is present, we believe it is minimal.
Conclusion
The COVID-19 pandemic has had far-reaching effects on health care worldwide, including neurosurgical care. OR efficiency across the United States generally worsened given the stresses of supply chain issues, staffing shortages, and cancellations. At our institution, we were able to maintain OR efficiency during the known COVID-19 peaks until October 2021. Continually functional neurosurgical ORs are important in preventing delays in care and maintaining a steady revenue in order for hospitals and other health care entities to remain solvent. Further study of OR efficiency is needed for health care systems to prepare for future pandemics and other resource-straining events in order to provide optimal patient care.
Corresponding author: Campbell Liles, MD, Vanderbilt University Medical Center, Department of Neurological Surgery, 1161 21st Ave. South, T4224 Medical Center North, Nashville, TN 37232-2380; [email protected]
Disclosures: None reported.
1. Koester SW, Catapano JS, Ma KL, et al. COVID-19 and neurosurgery consultation call volume at a single large tertiary center with a propensity- adjusted analysis. World Neurosurg. 2021;146:e768-e772. doi:10.1016/j.wneu.2020.11.017
2. Andreata M, Faraldi M, Bucci E, Lombardi G, Zagra L. Operating room efficiency and timing during coronavirus disease 2019 outbreak in a referral orthopaedic hospital in Northern Italy. Int Orthop. 2020;44(12):2499-2504. doi:10.1007/s00264-020-04772-x
3. Dexter F, Abouleish AE, Epstein RH, et al. Use of operating room information system data to predict the impact of reducing turnover times on staffing costs. Anesth Analg. 2003;97(4):1119-1126. doi:10.1213/01.ANE.0000082520.68800.79
4. Zheng NS, Warner JL, Osterman TJ, et al. A retrospective approach to evaluating potential adverse outcomes associated with delay of procedures for cardiovascular and cancer-related diagnoses in the context of COVID-19. J Biomed Inform. 2021;113:103657. doi:10.1016/j.jbi.2020.103657
5. Alcendor DJ. Targeting COVID-19 vaccine hesitancy in rural communities in Tennessee: implications for extending the COVID- 19 pandemic in the South. Vaccines (Basel). 2021;9(11):1279. doi:10.3390/vaccines9111279
6. Perrone G, Giuffrida M, Bellini V, et al. Operating room setup: how to improve health care professionals safety during pandemic COVID- 19: a quality improvement study. J Laparoendosc Adv Surg Tech A. 2021;31(1):85-89. doi:10.1089/lap.2020.0592
7. Iorio-Morin C, Hodaie M, Sarica C, et al. Letter: the risk of COVID-19 infection during neurosurgical procedures: a review of severe acute respiratory distress syndrome coronavirus 2 (SARS-CoV-2) modes of transmission and proposed neurosurgery-specific measures for mitigation. Neurosurgery. 2020;87(2):E178-E185. doi:10.1093/ neuros/nyaa157
8. Gupta P, Muthukumar N, Rajshekhar V, et al. Neurosurgery and neurology practices during the novel COVID-19 pandemic: a consensus statement from India. Neurol India. 2020;68(2):246-254. doi:10.4103/0028-3886.283130
9. Mercer ST, Agarwal R, Dayananda KSS, et al. A comparative study looking at trauma and orthopaedic operating efficiency in the COVID-19 era. Perioper Care Oper Room Manag. 2020;21:100142. doi:10.1016/j.pcorm.2020.100142
10. Rozario N, Rozario D. Can machine learning optimize the efficiency of the operating room in the era of COVID-19? Can J Surg. 2020;63(6):E527-E529. doi:10.1503/cjs.016520
11. Toh KHQ, Barazanchi A, Rajaretnam NS, et al. COVID-19 response by New Zealand general surgical departments in tertiary metropolitan hospitals. ANZ J Surg. 2021;91(7-8):1352-1357. doi:10.1111/ ans.17044
12. Moorthy RK, Rajshekhar V. Impact of COVID-19 pandemic on neurosurgical practice in India: a survey on personal protective equipment usage, testing, and perceptions on disease transmission. Neurol India. 2020;68(5):1133-1138. doi:10.4103/0028- 3886.299173
13. Meneghini RM. Techniques and strategies to optimize efficiencies in the office and operating room: getting through the patient backlog and preserving hospital resources. J Arthroplasty. 2021;36(7S):S49-S51. doi:10.1016/j.arth.2021.03.010
14. Jean WC, Ironside NT, Sack KD, et al. The impact of COVID- 19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir (Wien). 2020;162(6):1229-1240. doi:10.1007/s00701-020- 04342-5
15. Raneri F, Rustemi O, Zambon G, et al. Neurosurgery in times of a pandemic: a survey of neurosurgical services during the COVID-19 outbreak in the Veneto region in Italy. Neurosurg Focus. 2020;49(6):E9. doi:10.3171/2020.9.FOCUS20691
From the Department of Neurological Surgery, Vanderbilt University Medical Center, Nashville, TN (Stefan W. Koester, Puja Jagasia, and Drs. Liles, Dambrino IV, Feldman, and Chambless), and the Department of Anesthesiology, Vanderbilt University Medical Center, Nashville, TN (Drs. Mathews and Tiwari).
ABSTRACT
Background: The COVID-19 pandemic has had broad effects on surgical care, including operating room (OR) staffing, personal protective equipment (PPE) utilization, and newly implemented anti-infective measures. Our aim was to assess neurosurgery OR efficiency before the COVID-19 pandemic, during peak COVID-19, and during current times.
Methods: Institutional perioperative databases at a single, high-volume neurosurgical center were queried for operations performed from December 2019 until October 2021. March 12, 2020, the day that the state of Tennessee declared a state of emergency, was chosen as the onset of the COVID-19 pandemic. The 90-day periods before and after this day were used to define the pre-COVID-19, peak-COVID-19, and post-peak restrictions time periods for comparative analysis. Outcomes included delay in first-start and OR turnover time between neurosurgical cases. Preset threshold times were used in analyses to adjust for normal leniency in OR scheduling (15 minutes for first start and 90 minutes for turnover). Univariate analysis used Wilcoxon rank-sum test for continuous outcomes, while chi-square test and Fisher’s exact test were used for categorical comparisons. Significance was defined as P < .05.
Results: First-start time was analyzed in 426 pre-COVID-19, 357 peak-restrictions, and 2304 post-peak-restrictions cases. The unadjusted mean delay length was found to be significantly different between the time periods, but the magnitude of increase in minutes was immaterial (mean [SD] minutes, 6 [18] vs 10 [21] vs 8 [20], respectively; P = .004). The adjusted average delay length and proportion of cases delayed beyond the 15-minute threshold were not significantly different. The proportion of cases that started early, as well as significantly early past a 15-minute threshold, have not been impacted. There was no significant change in turnover time during peak restrictions relative to the pre-COVID-19 period (88 [100] minutes vs 85 [95] minutes), and turnover time has since remained unchanged (83 [87] minutes).
Conclusion: Our center was able to maintain OR efficiency before, during, and after peak restrictions even while instituting advanced infection-control strategies. While there were significant changes, delays were relatively small in magnitude.
Keywords: operating room timing, hospital efficiency, socioeconomics, pandemic.
The COVID-19 pandemic has led to major changes in patient care both from a surgical perspective and in regard to inpatient hospital course. Safety protocols nationwide have been implemented to protect both patients and providers. Some elements of surgical care have drastically changed, including operating room (OR) staffing, personal protective equipment (PPE) utilization, and increased sterilization measures. Furloughs, layoffs, and reassignments due to the focus on nonelective and COVID-19–related cases challenged OR staffing and efficiency. Operating room staff with COVID-19 exposures or COVID-19 infections also caused last-minute changes in staffing. All of these scenarios can cause issues due to actual understaffing or due to staff members being pushed into highly specialized areas, such as neurosurgery, in which they have very little experience. A further obstacle to OR efficiency included policy changes involving PPE utilization, sterilization measures, and supply chain shortages of necessary resources such as PPE.
Neurosurgery in particular has been susceptible to COVID-19–related system-wide changes given operator proximity to the patient’s respiratory passages, frequency of emergent cases, and varying anesthetic needs, as well as the high level of specialization needed to perform neurosurgical care. Previous studies have shown a change in the makeup of neurosurgical patients seeking care, as well as in the acuity of neurological consult of these patients.1 A study in orthopedic surgery by Andreata et al demonstrated worsened OR efficiency, with significantly increased first-start and turnover times.2 In the COVID-19 era, OR quality and safety are crucially important to both patients and providers. Providing this safe and effective care in an efficient manner is important for optimal neurosurgical management in the long term.3 Moreover, the financial burden of implementing new protocols and standards can be compounded by additional financial losses due to reduced OR efficiency.
Methods
To analyze the effect of COVID-19 on neurosurgical OR efficiency, institutional perioperative databases at a single high-volume center were queried for operations performed from December 2019 until October 2021. March 12, 2020, was chosen as the onset of COVID-19 for analytic purposes, as this was the date when the state of Tennessee declared a state of emergency. The 90-day periods before and after this date were used for comparative analysis for pre-COVID-19, peak COVID-19, and post-peak-restrictions time periods. The peak COVID-19 period was defined as the 90-day period following the initial onset of COVID-19 and the surge of cases. For comparison purposes, post-peak COVID-19 was defined as the months following the first peak until October 2021 (approximately 17 months). COVID-19 burden was determined using a COVID-19 single-institution census of confirmed cases by polymerase chain reaction (PCR) for which the average number of cases of COVID-19 during a given month was determined. This number is a scaled trend, and a true number of COVID-19 cases in our hospital was not reported.
Neurosurgical and neuroendovascular cases were included in the analysis. Outcomes included delay in first-start and OR turnover time between neurosurgical cases, defined as the time from the patient leaving the room until the next patient entered the room. Preset threshold times were used in analyses to adjust for normal leniency in OR scheduling (15 minutes for first start and 90 minutes for turnover, which is a standard for our single-institution perioperative center). Statistical analyses, including data aggregation, were performed using R, version 4.0.1 (R Foundation for Statistical Computing). Patients’ demographic and clinical characteristics were analyzed using an independent 2-sample t-test for interval variables and a chi-square test for categorical variables. Significance was defined as P < .05.
Results
First-Start Time
First-start time was analyzed in 426 pre-COVID-19, 357 peak-COVID-19, and 2304 post-peak-COVID-19 cases. The unadjusted mean delay length was significantly different between the time periods, but the magnitude of increase in minutes was immaterial (mean [SD] minutes, 6 [18] vs 10 [21] vs 8 [20], respectively; P = .004) (Table 1). 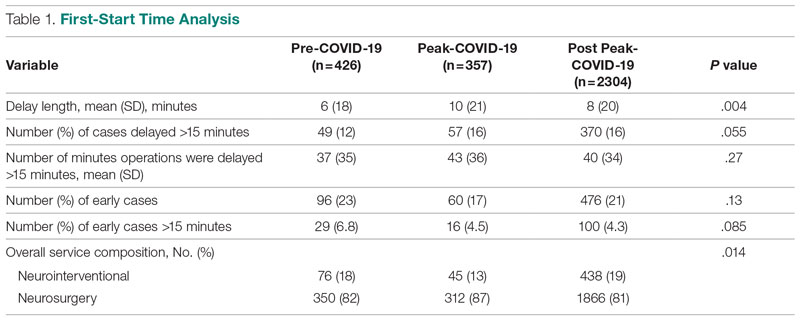
The adjusted average delay length and proportion of cases delayed beyond the 15-minute threshold were not significantly different, but they have been slightly higher since the onset of COVID-19. The proportion of cases that have started early, as well as significantly early past a 15-minute threshold, have also trended down since the onset of the COVID-19 pandemic, but this difference was again not significant. The temporal relationship of first-start delay, both unadjusted and adjusted, from December 2019 to October 2021 is shown in Figure 1. The trend of increasing delay is loosely associated with the COVID-19 burden experienced by our hospital. The start of COVID-19 as well as both COVID-19 peaks have been associated with increased delays in our hospital.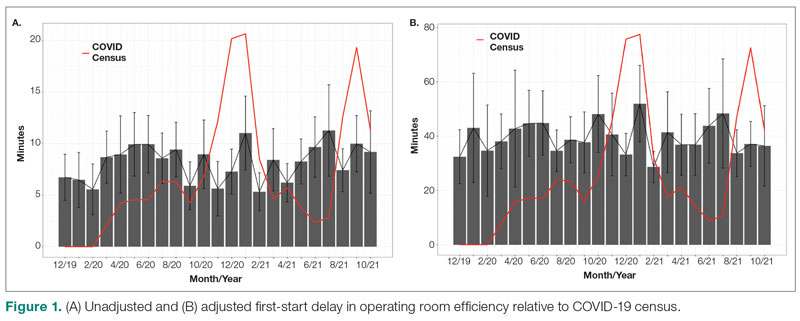
Turnover Time
Turnover time was assessed in 437 pre-COVID-19, 278 peak-restrictions, and 2411 post-peak-restrictions cases. Turnover time during peak restrictions was not significantly different from pre-COVID-19 (88 [100] vs 85 [95]) and has since remained relatively unchanged (83 [87], P = .78). A similar trend held for comparisons of proportion of cases with turnover time past 90 minutes and average times past the 90-minute threshold (Table 2). The temporal relationship between COVID-19 burden and turnover time, both unadjusted and adjusted, from December 2019 to October 2021 is shown in Figure 2. Both figures demonstrate a slight initial increase in turnover time delay at the start of COVID-19, which stabilized with little variation thereafter.
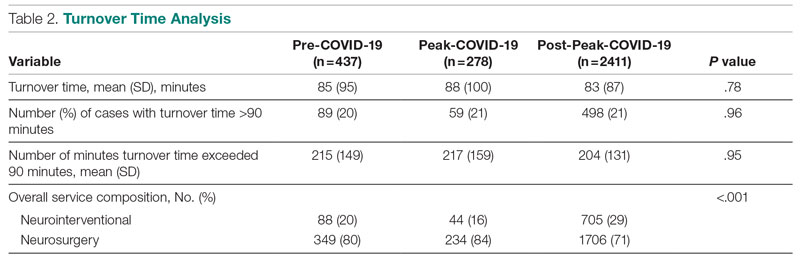
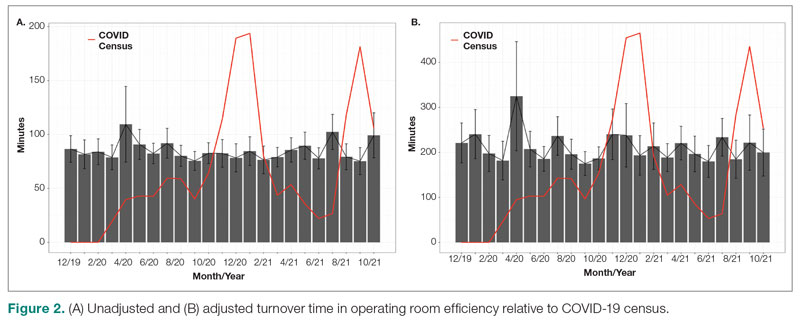
Discussion
We analyzed the OR efficiency metrics of first-start and turnover time during the 90-day period before COVID-19 (pre-COVID-19), the 90 days following Tennessee declaring a state of emergency (peak COVID-19), and the time following this period (post-COVID-19) for all neurosurgical and neuroendovascular cases at Vanderbilt University Medical Center (VUMC). We found a significant difference in unadjusted mean delay length in first-start time between the time periods, but the magnitude of increase in minutes was immaterial (mean [SD] minutes for pre-COVID-19, peak-COVID-19, and post-COVID-19: 6 [18] vs 10 [21] vs 8 [20], respectively; P = .004). No significant increase in turnover time between cases was found between these 3 time periods. Based on metrics from first-start delay and turnover time, our center was able to maintain OR efficiency before, during, and after peak COVID-19.
After the Centers for Disease Control and Prevention released guidelines recommending deferring elective procedures to conserve beds and PPE, VUMC made the decision to suspend all elective surgical procedures from March 18 to April 24, 2020. Prior research conducted during the COVID-19 pandemic has demonstrated more than 400 types of surgical procedures with negatively impacted outcomes when compared to surgical outcomes from the same time frame in 2018 and 2019.4 For more than 20 of these types of procedures, there was a significant association between procedure delay and adverse patient outcomes.4 Testing protocols for patients prior to surgery varied throughout the pandemic based on vaccination status and type of procedure. Before vaccines became widely available, all patients were required to obtain a PCR SARS-CoV-2 test within 48 to 72 hours of the scheduled procedure. If the patient’s procedure was urgent and testing was not feasible, the patient was treated as a SARS-CoV-2–positive patient, which required all health care workers involved in the case to wear gowns, gloves, surgical masks, and eye protection. Testing patients preoperatively likely helped to maintain OR efficiency since not all patients received test results prior to the scheduled procedure, leading to cancellations of cases and therefore more staff available for fewer cases.
After vaccines became widely available to the public, testing requirements for patients preoperatively were relaxed, and only patients who were not fully vaccinated or severely immunocompromised were required to test prior to procedures. However, approximately 40% of the population in Tennessee was fully vaccinated in 2021, which reflects the patient population of VUMC.5 This means that many patients who received care at VUMC were still tested prior to procedures.
Adopting adequate safety protocols was found to be key for OR efficiency during the COVID-19 pandemic since performing surgery increased the risk of infection for each health care worker in the OR.6 VUMC protocols identified procedures that required enhanced safety measures to prevent infection of health care workers and avoid staffing shortages, which would decrease OR efficiency. Protocols mandated that only anesthesia team members were allowed to be in the OR during intubation and extubation of patients, which could be one factor leading to increased delays and decreased efficiency for some institutions. Methods for neurosurgeons to decrease risk of infection in the OR include postponing all nonurgent cases, reappraising the necessity for general anesthesia and endotracheal intubation, considering alternative surgical approaches that avoid the respiratory tract, and limiting the use of aerosol-generating instruments.7,8 VUMC’s success in implementing these protocols likely explains why our center was able to maintain OR efficiency throughout the COVID-19 pandemic.
A study conducted by Andreata et al showed a significantly increased mean first-case delay and a nonsignificant increased turnover time in orthopedic surgeries in Northern Italy when comparing surgeries performed during the COVID-19 pandemic to those performed prior to COVID-19.2 Other studies have indicated a similar trend in decreased OR efficiency during COVID-19 in other areas around the world.9,10 These findings are not consistent with our own findings for neurosurgical and neuroendovascular surgeries at VUMC, and any change at our institution was relatively immaterial. Factors that threatened to change OR efficiency—but did not result in meaningful changes in our institutional experience—include delays due to pending COVID-19 test results, safety procedures such as PPE donning, and planning difficulties to ensure the existence of teams with non-overlapping providers in the case of a surgeon being infected.2,11-13
Globally, many surgery centers halted all elective surgeries during the initial COVID-19 spike to prevent a PPE shortage and mitigate risk of infection of patients and health care workers.8,12,14 However, there is no centralized definition of which neurosurgical procedures are elective, so that decision was made on a surgeon or center level, which could lead to variability in efficiency trends.14 One study on neurosurgical procedures during COVID-19 found a 30% decline in all cases and a 23% decline in emergent procedures, showing that the decrease in volume was not only due to cancellation of elective procedures.15 This decrease in elective and emergent surgeries created a backlog of surgeries as well as a loss in health care revenue, and caused many patients to go without adequate health care.10 Looking forward, it is imperative that surgical centers study trends in OR efficiency from COVID-19 and learn how to better maintain OR efficiency during future pandemic conditions to prevent a backlog of cases, loss of health care revenue, and decreased health care access.
Limitations
Our data are from a single center and therefore may not be representative of experiences of other hospitals due to different populations and different impacts from COVID-19. However, given our center’s high volume and diverse patient population, we believe our analysis highlights important trends in neurosurgery practice. Notably, data for patient and OR timing are digitally generated and are entered manually by nurses in the electronic medical record, making it prone to errors and variability. This is in our experience, and if any error is present, we believe it is minimal.
Conclusion
The COVID-19 pandemic has had far-reaching effects on health care worldwide, including neurosurgical care. OR efficiency across the United States generally worsened given the stresses of supply chain issues, staffing shortages, and cancellations. At our institution, we were able to maintain OR efficiency during the known COVID-19 peaks until October 2021. Continually functional neurosurgical ORs are important in preventing delays in care and maintaining a steady revenue in order for hospitals and other health care entities to remain solvent. Further study of OR efficiency is needed for health care systems to prepare for future pandemics and other resource-straining events in order to provide optimal patient care.
Corresponding author: Campbell Liles, MD, Vanderbilt University Medical Center, Department of Neurological Surgery, 1161 21st Ave. South, T4224 Medical Center North, Nashville, TN 37232-2380; [email protected]
Disclosures: None reported.
From the Department of Neurological Surgery, Vanderbilt University Medical Center, Nashville, TN (Stefan W. Koester, Puja Jagasia, and Drs. Liles, Dambrino IV, Feldman, and Chambless), and the Department of Anesthesiology, Vanderbilt University Medical Center, Nashville, TN (Drs. Mathews and Tiwari).
ABSTRACT
Background: The COVID-19 pandemic has had broad effects on surgical care, including operating room (OR) staffing, personal protective equipment (PPE) utilization, and newly implemented anti-infective measures. Our aim was to assess neurosurgery OR efficiency before the COVID-19 pandemic, during peak COVID-19, and during current times.
Methods: Institutional perioperative databases at a single, high-volume neurosurgical center were queried for operations performed from December 2019 until October 2021. March 12, 2020, the day that the state of Tennessee declared a state of emergency, was chosen as the onset of the COVID-19 pandemic. The 90-day periods before and after this day were used to define the pre-COVID-19, peak-COVID-19, and post-peak restrictions time periods for comparative analysis. Outcomes included delay in first-start and OR turnover time between neurosurgical cases. Preset threshold times were used in analyses to adjust for normal leniency in OR scheduling (15 minutes for first start and 90 minutes for turnover). Univariate analysis used Wilcoxon rank-sum test for continuous outcomes, while chi-square test and Fisher’s exact test were used for categorical comparisons. Significance was defined as P < .05.
Results: First-start time was analyzed in 426 pre-COVID-19, 357 peak-restrictions, and 2304 post-peak-restrictions cases. The unadjusted mean delay length was found to be significantly different between the time periods, but the magnitude of increase in minutes was immaterial (mean [SD] minutes, 6 [18] vs 10 [21] vs 8 [20], respectively; P = .004). The adjusted average delay length and proportion of cases delayed beyond the 15-minute threshold were not significantly different. The proportion of cases that started early, as well as significantly early past a 15-minute threshold, have not been impacted. There was no significant change in turnover time during peak restrictions relative to the pre-COVID-19 period (88 [100] minutes vs 85 [95] minutes), and turnover time has since remained unchanged (83 [87] minutes).
Conclusion: Our center was able to maintain OR efficiency before, during, and after peak restrictions even while instituting advanced infection-control strategies. While there were significant changes, delays were relatively small in magnitude.
Keywords: operating room timing, hospital efficiency, socioeconomics, pandemic.
The COVID-19 pandemic has led to major changes in patient care both from a surgical perspective and in regard to inpatient hospital course. Safety protocols nationwide have been implemented to protect both patients and providers. Some elements of surgical care have drastically changed, including operating room (OR) staffing, personal protective equipment (PPE) utilization, and increased sterilization measures. Furloughs, layoffs, and reassignments due to the focus on nonelective and COVID-19–related cases challenged OR staffing and efficiency. Operating room staff with COVID-19 exposures or COVID-19 infections also caused last-minute changes in staffing. All of these scenarios can cause issues due to actual understaffing or due to staff members being pushed into highly specialized areas, such as neurosurgery, in which they have very little experience. A further obstacle to OR efficiency included policy changes involving PPE utilization, sterilization measures, and supply chain shortages of necessary resources such as PPE.
Neurosurgery in particular has been susceptible to COVID-19–related system-wide changes given operator proximity to the patient’s respiratory passages, frequency of emergent cases, and varying anesthetic needs, as well as the high level of specialization needed to perform neurosurgical care. Previous studies have shown a change in the makeup of neurosurgical patients seeking care, as well as in the acuity of neurological consult of these patients.1 A study in orthopedic surgery by Andreata et al demonstrated worsened OR efficiency, with significantly increased first-start and turnover times.2 In the COVID-19 era, OR quality and safety are crucially important to both patients and providers. Providing this safe and effective care in an efficient manner is important for optimal neurosurgical management in the long term.3 Moreover, the financial burden of implementing new protocols and standards can be compounded by additional financial losses due to reduced OR efficiency.
Methods
To analyze the effect of COVID-19 on neurosurgical OR efficiency, institutional perioperative databases at a single high-volume center were queried for operations performed from December 2019 until October 2021. March 12, 2020, was chosen as the onset of COVID-19 for analytic purposes, as this was the date when the state of Tennessee declared a state of emergency. The 90-day periods before and after this date were used for comparative analysis for pre-COVID-19, peak COVID-19, and post-peak-restrictions time periods. The peak COVID-19 period was defined as the 90-day period following the initial onset of COVID-19 and the surge of cases. For comparison purposes, post-peak COVID-19 was defined as the months following the first peak until October 2021 (approximately 17 months). COVID-19 burden was determined using a COVID-19 single-institution census of confirmed cases by polymerase chain reaction (PCR) for which the average number of cases of COVID-19 during a given month was determined. This number is a scaled trend, and a true number of COVID-19 cases in our hospital was not reported.
Neurosurgical and neuroendovascular cases were included in the analysis. Outcomes included delay in first-start and OR turnover time between neurosurgical cases, defined as the time from the patient leaving the room until the next patient entered the room. Preset threshold times were used in analyses to adjust for normal leniency in OR scheduling (15 minutes for first start and 90 minutes for turnover, which is a standard for our single-institution perioperative center). Statistical analyses, including data aggregation, were performed using R, version 4.0.1 (R Foundation for Statistical Computing). Patients’ demographic and clinical characteristics were analyzed using an independent 2-sample t-test for interval variables and a chi-square test for categorical variables. Significance was defined as P < .05.
Results
First-Start Time
First-start time was analyzed in 426 pre-COVID-19, 357 peak-COVID-19, and 2304 post-peak-COVID-19 cases. The unadjusted mean delay length was significantly different between the time periods, but the magnitude of increase in minutes was immaterial (mean [SD] minutes, 6 [18] vs 10 [21] vs 8 [20], respectively; P = .004) (Table 1). 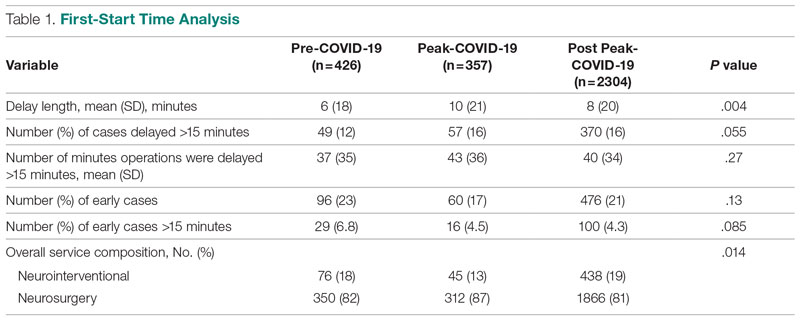
The adjusted average delay length and proportion of cases delayed beyond the 15-minute threshold were not significantly different, but they have been slightly higher since the onset of COVID-19. The proportion of cases that have started early, as well as significantly early past a 15-minute threshold, have also trended down since the onset of the COVID-19 pandemic, but this difference was again not significant. The temporal relationship of first-start delay, both unadjusted and adjusted, from December 2019 to October 2021 is shown in Figure 1. The trend of increasing delay is loosely associated with the COVID-19 burden experienced by our hospital. The start of COVID-19 as well as both COVID-19 peaks have been associated with increased delays in our hospital.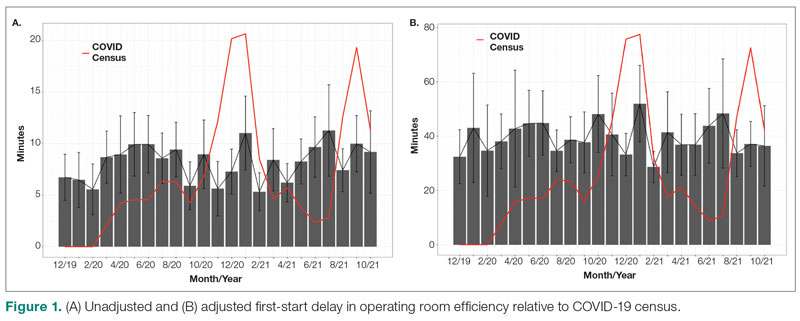
Turnover Time
Turnover time was assessed in 437 pre-COVID-19, 278 peak-restrictions, and 2411 post-peak-restrictions cases. Turnover time during peak restrictions was not significantly different from pre-COVID-19 (88 [100] vs 85 [95]) and has since remained relatively unchanged (83 [87], P = .78). A similar trend held for comparisons of proportion of cases with turnover time past 90 minutes and average times past the 90-minute threshold (Table 2). The temporal relationship between COVID-19 burden and turnover time, both unadjusted and adjusted, from December 2019 to October 2021 is shown in Figure 2. Both figures demonstrate a slight initial increase in turnover time delay at the start of COVID-19, which stabilized with little variation thereafter.
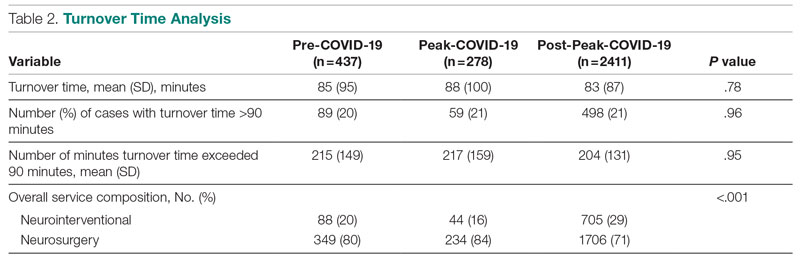
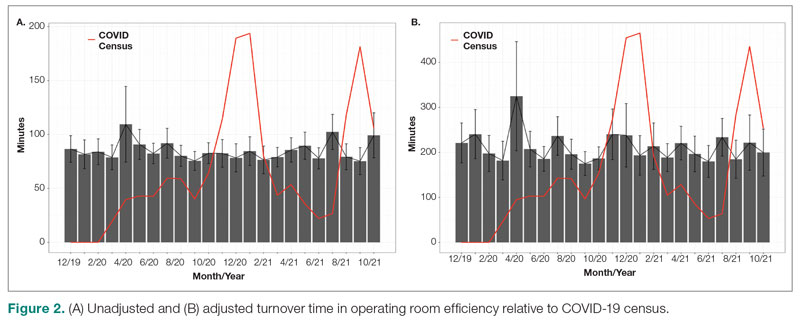
Discussion
We analyzed the OR efficiency metrics of first-start and turnover time during the 90-day period before COVID-19 (pre-COVID-19), the 90 days following Tennessee declaring a state of emergency (peak COVID-19), and the time following this period (post-COVID-19) for all neurosurgical and neuroendovascular cases at Vanderbilt University Medical Center (VUMC). We found a significant difference in unadjusted mean delay length in first-start time between the time periods, but the magnitude of increase in minutes was immaterial (mean [SD] minutes for pre-COVID-19, peak-COVID-19, and post-COVID-19: 6 [18] vs 10 [21] vs 8 [20], respectively; P = .004). No significant increase in turnover time between cases was found between these 3 time periods. Based on metrics from first-start delay and turnover time, our center was able to maintain OR efficiency before, during, and after peak COVID-19.
After the Centers for Disease Control and Prevention released guidelines recommending deferring elective procedures to conserve beds and PPE, VUMC made the decision to suspend all elective surgical procedures from March 18 to April 24, 2020. Prior research conducted during the COVID-19 pandemic has demonstrated more than 400 types of surgical procedures with negatively impacted outcomes when compared to surgical outcomes from the same time frame in 2018 and 2019.4 For more than 20 of these types of procedures, there was a significant association between procedure delay and adverse patient outcomes.4 Testing protocols for patients prior to surgery varied throughout the pandemic based on vaccination status and type of procedure. Before vaccines became widely available, all patients were required to obtain a PCR SARS-CoV-2 test within 48 to 72 hours of the scheduled procedure. If the patient’s procedure was urgent and testing was not feasible, the patient was treated as a SARS-CoV-2–positive patient, which required all health care workers involved in the case to wear gowns, gloves, surgical masks, and eye protection. Testing patients preoperatively likely helped to maintain OR efficiency since not all patients received test results prior to the scheduled procedure, leading to cancellations of cases and therefore more staff available for fewer cases.
After vaccines became widely available to the public, testing requirements for patients preoperatively were relaxed, and only patients who were not fully vaccinated or severely immunocompromised were required to test prior to procedures. However, approximately 40% of the population in Tennessee was fully vaccinated in 2021, which reflects the patient population of VUMC.5 This means that many patients who received care at VUMC were still tested prior to procedures.
Adopting adequate safety protocols was found to be key for OR efficiency during the COVID-19 pandemic since performing surgery increased the risk of infection for each health care worker in the OR.6 VUMC protocols identified procedures that required enhanced safety measures to prevent infection of health care workers and avoid staffing shortages, which would decrease OR efficiency. Protocols mandated that only anesthesia team members were allowed to be in the OR during intubation and extubation of patients, which could be one factor leading to increased delays and decreased efficiency for some institutions. Methods for neurosurgeons to decrease risk of infection in the OR include postponing all nonurgent cases, reappraising the necessity for general anesthesia and endotracheal intubation, considering alternative surgical approaches that avoid the respiratory tract, and limiting the use of aerosol-generating instruments.7,8 VUMC’s success in implementing these protocols likely explains why our center was able to maintain OR efficiency throughout the COVID-19 pandemic.
A study conducted by Andreata et al showed a significantly increased mean first-case delay and a nonsignificant increased turnover time in orthopedic surgeries in Northern Italy when comparing surgeries performed during the COVID-19 pandemic to those performed prior to COVID-19.2 Other studies have indicated a similar trend in decreased OR efficiency during COVID-19 in other areas around the world.9,10 These findings are not consistent with our own findings for neurosurgical and neuroendovascular surgeries at VUMC, and any change at our institution was relatively immaterial. Factors that threatened to change OR efficiency—but did not result in meaningful changes in our institutional experience—include delays due to pending COVID-19 test results, safety procedures such as PPE donning, and planning difficulties to ensure the existence of teams with non-overlapping providers in the case of a surgeon being infected.2,11-13
Globally, many surgery centers halted all elective surgeries during the initial COVID-19 spike to prevent a PPE shortage and mitigate risk of infection of patients and health care workers.8,12,14 However, there is no centralized definition of which neurosurgical procedures are elective, so that decision was made on a surgeon or center level, which could lead to variability in efficiency trends.14 One study on neurosurgical procedures during COVID-19 found a 30% decline in all cases and a 23% decline in emergent procedures, showing that the decrease in volume was not only due to cancellation of elective procedures.15 This decrease in elective and emergent surgeries created a backlog of surgeries as well as a loss in health care revenue, and caused many patients to go without adequate health care.10 Looking forward, it is imperative that surgical centers study trends in OR efficiency from COVID-19 and learn how to better maintain OR efficiency during future pandemic conditions to prevent a backlog of cases, loss of health care revenue, and decreased health care access.
Limitations
Our data are from a single center and therefore may not be representative of experiences of other hospitals due to different populations and different impacts from COVID-19. However, given our center’s high volume and diverse patient population, we believe our analysis highlights important trends in neurosurgery practice. Notably, data for patient and OR timing are digitally generated and are entered manually by nurses in the electronic medical record, making it prone to errors and variability. This is in our experience, and if any error is present, we believe it is minimal.
Conclusion
The COVID-19 pandemic has had far-reaching effects on health care worldwide, including neurosurgical care. OR efficiency across the United States generally worsened given the stresses of supply chain issues, staffing shortages, and cancellations. At our institution, we were able to maintain OR efficiency during the known COVID-19 peaks until October 2021. Continually functional neurosurgical ORs are important in preventing delays in care and maintaining a steady revenue in order for hospitals and other health care entities to remain solvent. Further study of OR efficiency is needed for health care systems to prepare for future pandemics and other resource-straining events in order to provide optimal patient care.
Corresponding author: Campbell Liles, MD, Vanderbilt University Medical Center, Department of Neurological Surgery, 1161 21st Ave. South, T4224 Medical Center North, Nashville, TN 37232-2380; [email protected]
Disclosures: None reported.
1. Koester SW, Catapano JS, Ma KL, et al. COVID-19 and neurosurgery consultation call volume at a single large tertiary center with a propensity- adjusted analysis. World Neurosurg. 2021;146:e768-e772. doi:10.1016/j.wneu.2020.11.017
2. Andreata M, Faraldi M, Bucci E, Lombardi G, Zagra L. Operating room efficiency and timing during coronavirus disease 2019 outbreak in a referral orthopaedic hospital in Northern Italy. Int Orthop. 2020;44(12):2499-2504. doi:10.1007/s00264-020-04772-x
3. Dexter F, Abouleish AE, Epstein RH, et al. Use of operating room information system data to predict the impact of reducing turnover times on staffing costs. Anesth Analg. 2003;97(4):1119-1126. doi:10.1213/01.ANE.0000082520.68800.79
4. Zheng NS, Warner JL, Osterman TJ, et al. A retrospective approach to evaluating potential adverse outcomes associated with delay of procedures for cardiovascular and cancer-related diagnoses in the context of COVID-19. J Biomed Inform. 2021;113:103657. doi:10.1016/j.jbi.2020.103657
5. Alcendor DJ. Targeting COVID-19 vaccine hesitancy in rural communities in Tennessee: implications for extending the COVID- 19 pandemic in the South. Vaccines (Basel). 2021;9(11):1279. doi:10.3390/vaccines9111279
6. Perrone G, Giuffrida M, Bellini V, et al. Operating room setup: how to improve health care professionals safety during pandemic COVID- 19: a quality improvement study. J Laparoendosc Adv Surg Tech A. 2021;31(1):85-89. doi:10.1089/lap.2020.0592
7. Iorio-Morin C, Hodaie M, Sarica C, et al. Letter: the risk of COVID-19 infection during neurosurgical procedures: a review of severe acute respiratory distress syndrome coronavirus 2 (SARS-CoV-2) modes of transmission and proposed neurosurgery-specific measures for mitigation. Neurosurgery. 2020;87(2):E178-E185. doi:10.1093/ neuros/nyaa157
8. Gupta P, Muthukumar N, Rajshekhar V, et al. Neurosurgery and neurology practices during the novel COVID-19 pandemic: a consensus statement from India. Neurol India. 2020;68(2):246-254. doi:10.4103/0028-3886.283130
9. Mercer ST, Agarwal R, Dayananda KSS, et al. A comparative study looking at trauma and orthopaedic operating efficiency in the COVID-19 era. Perioper Care Oper Room Manag. 2020;21:100142. doi:10.1016/j.pcorm.2020.100142
10. Rozario N, Rozario D. Can machine learning optimize the efficiency of the operating room in the era of COVID-19? Can J Surg. 2020;63(6):E527-E529. doi:10.1503/cjs.016520
11. Toh KHQ, Barazanchi A, Rajaretnam NS, et al. COVID-19 response by New Zealand general surgical departments in tertiary metropolitan hospitals. ANZ J Surg. 2021;91(7-8):1352-1357. doi:10.1111/ ans.17044
12. Moorthy RK, Rajshekhar V. Impact of COVID-19 pandemic on neurosurgical practice in India: a survey on personal protective equipment usage, testing, and perceptions on disease transmission. Neurol India. 2020;68(5):1133-1138. doi:10.4103/0028- 3886.299173
13. Meneghini RM. Techniques and strategies to optimize efficiencies in the office and operating room: getting through the patient backlog and preserving hospital resources. J Arthroplasty. 2021;36(7S):S49-S51. doi:10.1016/j.arth.2021.03.010
14. Jean WC, Ironside NT, Sack KD, et al. The impact of COVID- 19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir (Wien). 2020;162(6):1229-1240. doi:10.1007/s00701-020- 04342-5
15. Raneri F, Rustemi O, Zambon G, et al. Neurosurgery in times of a pandemic: a survey of neurosurgical services during the COVID-19 outbreak in the Veneto region in Italy. Neurosurg Focus. 2020;49(6):E9. doi:10.3171/2020.9.FOCUS20691
1. Koester SW, Catapano JS, Ma KL, et al. COVID-19 and neurosurgery consultation call volume at a single large tertiary center with a propensity- adjusted analysis. World Neurosurg. 2021;146:e768-e772. doi:10.1016/j.wneu.2020.11.017
2. Andreata M, Faraldi M, Bucci E, Lombardi G, Zagra L. Operating room efficiency and timing during coronavirus disease 2019 outbreak in a referral orthopaedic hospital in Northern Italy. Int Orthop. 2020;44(12):2499-2504. doi:10.1007/s00264-020-04772-x
3. Dexter F, Abouleish AE, Epstein RH, et al. Use of operating room information system data to predict the impact of reducing turnover times on staffing costs. Anesth Analg. 2003;97(4):1119-1126. doi:10.1213/01.ANE.0000082520.68800.79
4. Zheng NS, Warner JL, Osterman TJ, et al. A retrospective approach to evaluating potential adverse outcomes associated with delay of procedures for cardiovascular and cancer-related diagnoses in the context of COVID-19. J Biomed Inform. 2021;113:103657. doi:10.1016/j.jbi.2020.103657
5. Alcendor DJ. Targeting COVID-19 vaccine hesitancy in rural communities in Tennessee: implications for extending the COVID- 19 pandemic in the South. Vaccines (Basel). 2021;9(11):1279. doi:10.3390/vaccines9111279
6. Perrone G, Giuffrida M, Bellini V, et al. Operating room setup: how to improve health care professionals safety during pandemic COVID- 19: a quality improvement study. J Laparoendosc Adv Surg Tech A. 2021;31(1):85-89. doi:10.1089/lap.2020.0592
7. Iorio-Morin C, Hodaie M, Sarica C, et al. Letter: the risk of COVID-19 infection during neurosurgical procedures: a review of severe acute respiratory distress syndrome coronavirus 2 (SARS-CoV-2) modes of transmission and proposed neurosurgery-specific measures for mitigation. Neurosurgery. 2020;87(2):E178-E185. doi:10.1093/ neuros/nyaa157
8. Gupta P, Muthukumar N, Rajshekhar V, et al. Neurosurgery and neurology practices during the novel COVID-19 pandemic: a consensus statement from India. Neurol India. 2020;68(2):246-254. doi:10.4103/0028-3886.283130
9. Mercer ST, Agarwal R, Dayananda KSS, et al. A comparative study looking at trauma and orthopaedic operating efficiency in the COVID-19 era. Perioper Care Oper Room Manag. 2020;21:100142. doi:10.1016/j.pcorm.2020.100142
10. Rozario N, Rozario D. Can machine learning optimize the efficiency of the operating room in the era of COVID-19? Can J Surg. 2020;63(6):E527-E529. doi:10.1503/cjs.016520
11. Toh KHQ, Barazanchi A, Rajaretnam NS, et al. COVID-19 response by New Zealand general surgical departments in tertiary metropolitan hospitals. ANZ J Surg. 2021;91(7-8):1352-1357. doi:10.1111/ ans.17044
12. Moorthy RK, Rajshekhar V. Impact of COVID-19 pandemic on neurosurgical practice in India: a survey on personal protective equipment usage, testing, and perceptions on disease transmission. Neurol India. 2020;68(5):1133-1138. doi:10.4103/0028- 3886.299173
13. Meneghini RM. Techniques and strategies to optimize efficiencies in the office and operating room: getting through the patient backlog and preserving hospital resources. J Arthroplasty. 2021;36(7S):S49-S51. doi:10.1016/j.arth.2021.03.010
14. Jean WC, Ironside NT, Sack KD, et al. The impact of COVID- 19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir (Wien). 2020;162(6):1229-1240. doi:10.1007/s00701-020- 04342-5
15. Raneri F, Rustemi O, Zambon G, et al. Neurosurgery in times of a pandemic: a survey of neurosurgical services during the COVID-19 outbreak in the Veneto region in Italy. Neurosurg Focus. 2020;49(6):E9. doi:10.3171/2020.9.FOCUS20691


